5
NEW TO SOCIAL MEDIA?
Connect with the global GI community on social media.
20 NEW MASTERS HONORED
Six members earn the distinction of MACG.

Connect with the global GI community on social media.
Six members earn the distinction of MACG.
Learn about the Fellows-focused events.
Hands-On Workshop sessions run from Sunday through Tuesday.
There is always plenty to see and do in the Exhibit Hall.

On Monday evening October 24, 2022 at the ACG Business Meeting, Daniel J. Pambianco, MD, FACG, will become the next President of the ACG. We asked Dr. Pambianco to share with us some of his ideas and aspirations for the coming year.
One of the hallmarks of the American College of Gastroenterology is to make sure there is representation of private practice clinicians throughout all aspects of the organization, including the Board of Trustees. As a private practitioner in Charlottesville, VA, what led you to make the College your professional home?

I gave my first presentation as a UVa fellow at an ACG meeting in Dallas and was impressed by depth and breadth of its iconic members and the organization. When I transitioned from academics, it became apparent that the ACG was a clinically focused association promoting clinically relevant education and research to advance patient care that I felt I could contribute despite being in private practice. Since my initial committee appointment, the College has been a vibrant and progressive home for professional growth and opportunity through unparalleled mission-driven collegiality.
As you prepare to assume the Presidency of the American College of Gastroenterology, do you have specific goals in mind for this year that you would like to share with the membership?
My overarching goal is to facilitate and highlight the brilliant creative minds and leadership that exist in the administration of the College organizationally and academically.
I would also hope to bring a greater focus on achieving and maintaining high performance private practice as a continued vocation in these challenging times. The landscape for private practitioners to remain independent is increasingly fraught and everchanging with the necessity for business acumen and work-life balance to mention a few areas where the College is working vehemently.
We have all seen that the country, GI practices and the College continue to navigate COVID variants while working to support organized medicine and clinical GI and our collective patients. How have your goals for this year been impacted both for the College and even your own practice?
Foremost, it must be noted that the pandemic presented formidable challenges for the College staff and previous presidents in continuing the paramount educational programing and developing novel COVID education to our members, but these efforts were highly successful! We need to celebrate the incredible leadership the College brought to providing clinicians with continuing education allowing effective and safe care to our patients with the utmost urgent and rapid information. Having made that acknowledgement, while hopefully the pandemic is winding down, there are ongoing challenges that continue to impact conducting meetings as hybrids of on-site and remote learning, and there remains a need for vigilance for resurgence. My goals for the College will be to continue to monitor our live meetings based on current CDC and state guidelines for vaccination and masking. In my practice protective personal equipment and patient and staff symptom screening is a mainstay.
Medical practice structures across medicine and GI in particular have been changing profoundly in recent years. Introduction of venture funding, mega groups, increased use of hospitalists and employed physicians are among those changes. As someone who has spent his entire career in private practice, what do you make of these changes and what, if anything, does it mean for what the College does for its members?
I believe we are in the most challenging times for the practice of medicine in general and particularly GI for the following reasons: we will be facing a critical shortage of gastroenterologists in the next 5 to 7 years between age attrition, forced retirement due to COVID, increasing U.S. population and colorectal cancer screening demands, the economic demands of increased non-reimbursable cost of practice due to COVID, increased cost of




ACG 2022 once again set a record for abstract submissions and attendees will benefit with nearly 90 exceptional oral presentations and more than 3,600 poster presentations. The oral presentations are in addition to the simultaneous symposia, optional bonus sessions (previously the breakfast sessions), featured lectures, and hands-on sessions that will be offered.
Monday kicks off with “Meet the Experts” Breakfast Sessions. Faculty from Annual Scientific Meeting Bonus Sessions A-E will be available to discuss their topics and continental breakfast will be served. These Meet the Expert sessions are open to all Annual Scientific Meeting attendees.
The breakfast “Meet the Experts” will be followed by 2 presidential plenary sessions. Between plenary sessions, ACG President Samir A. Shah, MD, FACG, will deliver the ACG President’s Address. Don’t miss it!
The Exhibit Hall opens at 10:00 am Monday and will remain open until 4:45 pm. Visit with exhibitors, attend an Exhibitor Theater presentation, or participate in a Hands-On Endoscopy Workshop session!
NEW FOR 2022! A separate Poster Hall has been added. From 10:00 am on Monday until Noon, posters from Scientific Poster Session B will be on display in the Crown Ballroom. Stop by to see the latest in scientific advanced and meet the authors from 10:30 am -11:30 am.
Three simultaneous symposia are offered Monday morning, including IBD Partners in Crime: Management of Concurrent Conditions (1A), ACG Past Presidents’ Symposium 2022 (1B), and The Changing Landscape in the Management of Esophageal Disorders(1C). Join the experts as they discuss these hot topics!
THE AMERICAN JOURNAL OF GASTROENTEROLOGY LECTURE Patrick S. Kamath, MD October 24 3:05 pm – 3:35 pm

At 3:05 pm, learn how clinicians can participate in research that moves the fields of gastroenterology and hepatology forward when Dr. Patrick S. Kamath, MD presents The American Journal of Gastroenterology Lecture on “The Transformative Power of Research Carried out by Busy Clinicians.”
If you have burning questions about how to get your research published, there will be a special Tuesday morning “Meet the Experts” Breakfast session on How to Get Published: An ACG Journal Editors’ Roundtable. The session is free to all and perfect for GI fellows or anyone new to publishing.
Scientific Poster Session C will take place in the Crown Ballroom from 3-5pm with authors presenting their work from 3:45 pm – 4:45 pm.
Two additional simultaneous plenary sessions discussing Esophagus, and Functional / Practice Management / Obesity are offered on Monday afternoon, plus 3 simultaneous symposia sessions on Common Liver Consults (2A), C. difficile Controversies (2B), and Live From Charlotte!: The 10th Annual Endoscopy Video Forum (2C).
The 10th Annual Endoscopy Video Forum (2C). Attendees at the Endoscopy Video Forum can vote, along with the moderator and a panel of judges, for the winning video.
Following the educational agenda, ACG will hold its Annual Business Meeting at 6:00 pm. All members and Fellows (FACG) are invited to attend.
Tuesday will once again begin with “Meet the Experts” Breakfast Sessions. Faculty from Annual Scientific Meeting Bonus Sessions F-J plus a special session on “How to Get Published: An ACG Journal Editors’ Roundtable” will be available to discuss their topics and continental breakfast will be served. These Meet the Expert sessions are open to all Annual Scientific Meeting attendees.
The breakfast “Meet the Experts” will be followed by 2 simultaneous plenary sessions discussing Liver / Pancreas-Biliary and Endoscopy / Stomach / GI Bleeding. After the plenary sessions, Bruce E. Sands, MD, MS, FACG, will deliver the J. Edward Berk Distinguished Lecture entitled, "The Promise and Progress of New Approaches to Treating Inflammatory Bowel Diseases."
The Exhibit Hall opens at 10:35 am. Visit with exhibitors, attend an Exhibitor Theater presentation, or participate in a Hands-On Endoscopy Workshop session.
Scientific Poster Session D will take place in the Crown Ballroom from 10:00 am - Noon with authors presenting their work from 10:30 am – 11:30 am.
Three simultaneous symposia are offered on Tuesday morning, including sessions on Applying the Latest Antithrombotic Guidelines to Your Practice: A Case-Based Approach (3A), NonInflammatory Bowel Disease Colonic Disorders (3B), and Case-Based Tours of Recent Advances in the Diagnosis and Management of Esophageal Disorders3C). Join the experts as they discuss these hot topics!
In the afternoon 2 additional simultaneous plenary sessions will take place discussing IBD / Late Breaking Abstracts and Colorectal Cancer Prevention / IBD. After these plenary sessions, Aasma Shaukat, MD, MPH, FACG, will present the Emily Couric Memorial Lecture entitled, "Colon Cancer Screening: What Do We Need to Build and Who Will Come?"
Scientific Poster Session E will take place in the Crown Ballroom from 3-5pm with authors presenting their work from 3:45 pm – 4:45 pm.
Be sure to visit the Exhibit Hall one last time before it closes at 5:10 pm Tuesday, then attend one of 2 afternoon simultaneous symposia sessions, including It’s No Longer Obscure! Small Bowel Bleeding in 2022 (4A), and Just Because They’re Common Doesn’t Make Them Easy: Management of Common GI Issues (4B). Don’t miss these important practical topics.
Wednesday kicks off with 2 simultaneous plenary sessions focusing on Colon and IBD and Liver. After the plenary sessions, Emeran A. Mayer, MD, will deliver the David Y. Graham Lecture entitled, "Why Do All Diseases Start in the Gut?"
Two simultaneous symposia wrap up the educational agenda for the meeting, including sessions on New Kids on the Block: Approved Therapies in the Expanding Medicine Cabinet (5A), and Artificial Intelligence in Gastroenterology and Endoscopy (5B). Be sure to arrange your schedule so you can stay for these great closing topics.
personnel, decreased reimbursements from government and insurers, and diminishing interest in graduating trainees to enter practice with the forementioned issues and burdened with unprecedented educational debt. As such, approximately 50% of GIs are currently employed by hospitals or healthcare organizations and this number is rising. Due to the decreasing ability for private practice self-capitalization, there is increasing interest in consolidation with other GI groups and an environment of increased interest by healthcare private equity groups in GI practices. My goal as president is to broaden our educational support for our members to help understand this current phenomenon and prepare our trainees and practices to make the most intelligent decisions for the betterment of our patient care.

You have been very involved in debates over the American Board of Internal Medicine (ABIM) Maintenance of Certification (MOC) program. Indeed, you, along with Dr. Amy Oxentenko, represented the College in its efforts to develop an alternative that was less burdensome and more clinically relevant with our colleagues in the other GI societies. This year the ABIM has introduced the Longitudinal Knowledge Assessment (LKA) which seems to seek to adopt many of the elements of the joint GI plan. What do you think about this and where do you think MOC is headed?
To the credit of the ABIM, in their current LKA they have adopted many elements of the proposed GOAL (Gastroenterology Ongoing Assessment and Learning) MOC program developed by the ACG and brought to fruition along with the other GI societies. However, the current limitations of ABIM’s LKA continue to be the modularity in testing, i.e., being assessed in the subspecialty of your practice such as interventional endoscopy or hepatology, etc. Also, there continues to be a prescribed fail rate which for adult learning is not a productive incentive. The ABIM vows to continue to improve its testing acumen and prove its validity as a hallmark of practice competence, however without a specific timeline. Until then, given the current practice demands of time, cost, added emotional stressors as demonstrated by a precipitous increase physician burnout and suicide, I am concerned that this may be too little, too late for the ABIM to maintain its desired monopoly on MOC.
You served as ACG Governor for Virginia as well as Vice Chair and Chair of the Board of Governors as did your immediate predecessor, Dr. Shah. Can you share your thoughts on the Board of Governors and its role within the life of the College and beyond?
The Board of Governors is a unique aspect of the ACG which creates an interconnectedness with the membership and patients’ representation, needs, issues, and solutions, fostering communication from the local level to the Board of Trustees. This integral apparatus is ever evolving to provide a collective voice to the College’s advancement and success as well as advocacy with state and federal governments, and insurers. The BOG serves also as a resource for attracting new members and a laboratory for future College leaders. I am proud to have had the opportunity to be a part of the BOG!
As part of your Board service, you had the opportunity to sit on the ACG Institute for Clinical Research and Education. From your perspective as a private practitioner, what is the most meaningful work the ACG Institute does?
If the BOG is the jewel of the ACG, the Institute is the crown! Witnessing the function of the Institute Board and its leaders conjure the level of creativity and stewardship to insure not just the future of the College but the future of gastroenterology, through research funding for teaching, programs, and career development, was truly inspiring.
Like many of your colleagues in independent practice, practice management has been an area of focus for you. You have been involved in the College’s efforts to develop GI OnDEMAND which provides high quality, GI specific resources to ACG members in areas including genetic screening, nutrition and mental health to benefit their patients. What led you to become engaged in this particular initiative?
In practice while opting to be a master of all of that gastroenterology has to offer patients, the reality is that, either because of time constraints or the patient’s need for greater depth of care, we also need to be an effective conduit for our patients to additional resources. Moreover, COVID has revealed a distinct unmet need for patient access to care through telemedicine. Hence, my interest to contribute to the development of the GI OnDEMAND platform which allows the opportunity to for clinicians to connect much more seamlessly with patients and also allows patients to connect with experts in nutrition, genetic screening, brain-gut psych counseling, etc.– in effect bringing tertiary care opportunities to our office practices.
At its core, the College is an education organization. There is a long-standing commitment to a wide variety of educational programs in addition to the largest clinical postgraduate GI course in the country, regional courses, and innovative programs like the IBD, Hepatology, Functional GI Schools and the newest addition – Endoscopy School. As someone from Virginia where the College has long held a regional course in partnership with the Virginia Gastroenterology Society and the Old Dominion Society of Gastroenterology Nurses & Associates, how would you assess the state of the College’s educational program portfolio?
The state of the College’s educational portfolio is outstanding. I am especially excited about the addition of the Endoscopy School program. The VGS-ODSGNA course with ACG has been highly successful and a model for other states. This year Williamsburg course will be particularly opportune given the first in-person meeting since COVID as well as the conjoint IBD School. The add-on Hepatology, IBD and Endoscopy Schools I believe to be an advantageous offering to ACG’s regional courses, offering a more concentrated and wellrounded educational opportunity.
You worked very closely this year with our outgoing ACG President, Dr. Shah, during these uncertain and tumultuous times. What lessons have you learned through this process that will impact your approach to serving in this role and what other thoughts would you like to share with the membership as you prepare to undertake this position?
Dr. Shah has been an exemplary mentor and has had his share of turbulent times. The lesson I have learned is to expect the unexpected and the formula I hope to emulate encompasses the necessity for rationale plasticity, the prudence of timing, a large aliquot of the ACG Board of Trustees, the sagacity of Brad Stillman, and the swaddling of the ACG staff!
As the
How It
a
Increasingly, physicians are engaging on social media to stay abreast of trends, news, and research in the medical profession. Some GI physicians are leading the way when it comes to sharing links to clinical resources and interesting news. For others, platforms like Twitter are a way to network with other physicians, establish collaborative relationships, and keep abreast of happenings at conferences such as the ACG Annual Scientific Meeting.
If you have been tentative about exploring social media, here are some practical tips to connect on the major social media channels: Twitter, Facebook, Instagram and LinkedIn.
Certain ACG members have an active presence on Twitter. As you follow more people in the GI space, you will see recommendations from Twitter for accounts you may be interested in following. You can also search ACG-affiliated hashtags to make connections, including the ACG meeting (#ACG2022), Diversity in GI (#DiversityinGI), and ACG virtual learning (#GIhomeschooling) hashtags. Using these is a convenient way to aggregate social media posts from those in ACG’s GI community.

In an article in the Red Section of The American Journal of Gastroenterology, “The Impact of Twitter: Why Should You Get Involved, and Tips and Tricks to Get Started,” Dr. Mohammad Bilal and Dr. Amy Oxentenko share the impacts and benefits of using Twitter in the GI community and provide tips and tricks for getting started. They suggest, “Twitter can feel daunting when getting started, but akin to professional success, ‘slow and steady’ is a safe approach. Similar to Bloom’s taxonomy for learning theory, we suggest a similar ‘taxonomy of tweeting’ for those new to Twitter.”
1. Start with liking tweets
2. Retweet tweets of others
3. Retweet with comment, adding your own thoughts on another’s tweet
4. Create your own original tweets Read the article at bit.ly/AJG-TwitterImpact.
The hashtag for the meeting is #ACG2022. Follow the hashtag by searching #ACG2022 on Twitter, Facebook, and Instagram. Insert #ACG2022 into meeting-related posts on all social media platforms so others can find and engage with your posts.
Share and Discuss Journal Science on Twitter with @AmJGastro, @ACG_CTG and @ACGCRJ


The College launched Twitter accounts for The American Journal of Gastroenterology, Clinical and Translational Gastroenterology, and ACG Case Reports Journal to share emerging science from the journals. Be sure to follow:
Sign Up: Sign up online at twitter.com. On the site, you can set up a username and password and add a photo and brief description to your profile. Follow ACG: Visit twitter.com/AmCollegeGastro
Sign Up: Sign up online at facebook.com. Once you have signed up, you can add a photo and background information that you feel comfortable sharing. Follow ACG: Visit facebook.com/AmCollegeGastro
Sign Up: Download the Instagram app from your mobile phone’s app store. Open the app, click “Sign Up,” enter your information, and create a username and password. Follow ACG: With the Instagram app open, click the icon at the bottom of the screen. In the search bar, type “AmCollegeGastro.” You will see the ACG logo pop up. Tap that logo and click “Follow.”
Sign Up: Sign up online at linkedin.com. On the site, you can add a photo, your professional, educational, and volunteer experience, skills you possess, and more. Follow ACG: Visit bit.ly/ACG-Linked-In and click “Follow.”
Two distinguished ACG Past Presidents are the recipients of this year's Distinguished Mentorship and Teaching Award: Dr. Lawrence J. Brandt and Dr. Christina Surawicz. Among their many contributions to the College and to the field of gastroenterology, these two stand out for their dedication to cultivating the skills and talents of future generations of gastroenterologists.
Lawrence J. Brandt, MD, MACG, earned his bachelor’s degree with honors from The College of the City of New York and his medical degree from The State University of New York Downstate Medical Center. He then did his postgraduate medical education, including a fellowship in gastroenterology, at The Mount Sinai Hospital in New York, after which he served in the Army as a gastroenterologist stationed in Stuttgart, Germany. After his military discharge, Dr. Brandt joined the staff of Montefiore Medical Center in the Bronx, New York, where he currently is the Emeritus Chief of Gastroenterology and Professor of Medicine and Surgery at Albert Einstein College of Medicine.
Dr. Brandt’s main areas of interest are vascular and ischemic disorders of the gastrointestinal tract, especially ischemic colitis, and C. difficile colitis. Dr. Brandt was one of the pioneers of fecal microbiota transplantation to treat recurring C. difficile colitis. He also has had a long-standing interest in irritable bowel syndrome, the patientdoctor relationship, and how a patient’s psychological makeup influences his/her illnesses and treatments.
The author or editor of more than 850 publications and 10 books, Dr. Brandt was one of the three editors of the standard textbook in gastroenterology (Sleisenger and Fordtran’s Gastroenterology and Liver Disease) for 15 years; he also served for ten years as Associate Editor for the Focal Points section of Gastrointestinal Endoscopy Dr. Brandt is a Master of the American College of Gastroenterology (ACG) and has received many awards and honors, including the Distinguished Educator Award from both the AGA and ASGE; the ACG Berk/Fise Clinical Achievement Award; and the William Dock M.D. Master Teacher Award in Medicine of SUNY (Downstate). In 2018, Dr. Brandt was awarded the Alumni Association Achievement Medallion for Distinguished Service to American Medicine by Downstate Medical Center. He served on ACG’s Board of Trustees for 13 years before being elected President of the ACG (1992-1993). He served three terms as a member of the ABIM subspecialty section in gastroenterology. Dr. Brandt has been Visiting Professor at many institutions throughout the United States and has given over 600 lectures nationally and internationally. He is an honorary member of the Puerto Rican, Argentine, and Dominican Republic’s Societies of Gastroenterology. Dr. Brandt is a member of the Albert Einstein’s Leo M. Davidoff Society for excellence in teaching of medical students and was named the Montefiore Staff and Alumni Association's Honoree in 1999. Since 1994, he has been listed every year in Best Doctors in America and since 1998 in Who’s Who. Dr. Brandt is also an Honorary Police Surgeon for the New York Police Department.
Christina M. Surawicz, MD, MACG, is Emeritus Professor of Medicine at the University of Washington School of Medicine in Seattle. She graduated with honors from the University of Kentucky College of Medicine in 1973. She completed internal medicine residency and a gastroenterology fellowship (the first woman fellow) at the University of Washington, following which she joined the faculty in the Gastroenterology Division (the first woman faculty member). She spent her entire academic at UW, based at the county hospital, Harborview Medical Center, where she served as Chief of Gastroenterology for 20 years. For many years she chaired the medical school’s Committee on Women in Medicine and Science and set up programs for career advancement and professional and personal satisfaction for all faculty. In 2002, she was appointed the inaugural Assistant (then Associate) Dean for Faculty Development, a position she held until retiring in 2018.

Her research interests included the role of colorectal biopsy in inflammatory bowel disease and infectious colitis, the role of HPV in anal cancer, clinical trials of the probiotic S. boulardii in antibiotic associated diarrhea and recurrent C. difficile infection (CDI), and the use of fecal microbiota transplant in recurrent CDI. While she has been active in other societies, and was President of the Western Association of Physicians, it is her involvement in the American College of Gastroenterology (ACG) that has been most meaningful. She served as ACG President in 1998-1999. Dr. Surawicz also served as ACG Governor for Washington from 1989-1992 and on the Board of the ACG Institute for Clinical Research and Education from 1995-2000 and 2004-2011. In addition, she served and chaired several ACG Committees including the Awards and Professionalism Committees and was a Senior Associate Editor of The American Journal of Gastroenterology. She is proud of the accomplishments of her many mentees and students, and grateful for the support given by her husband and children over these many years.
In 2021, the College established a new Distinguished Mentorship and Teaching Award to recognize ACG members who have provided meaningful and sustained contributions to trainees/colleagues in gastroenterology. The vision for this award is to celebrate mentorship or teaching that helps develop the mentees’ overall scientific growth and career or life planning; supports their practice of high-level clinical gastroenterology; imparts skills to perform high quality clinical research; encourages those skills necessary to present and publish results of clinical research or quality improvement; and inspires mentees’ involvement in professional society, healthcare organization or leadership development.
The spirit of the award is to honor those mentors and teachers who have made contributions over a significant period of time in gastroenterology. Such contributions may be via academic affiliation as well as in private practice or an integrated (government or non-government) health system. Recognizably, each of these specific pathways has provided impactful mentorship to many individuals, hence any of these backgrounds would be suitable for this award. The decision to grant any award within a given year, as well as the selection of the award winner, is at the discretion and recommendation of the ACG Awards Committee, and upon approval of the ACG Board of Trustees. This award is not necessarily given annually.

OCTOBER 21
OCTOBER 24
OCTOBER 25
OCTOBER 26
1. FIND THE CODE for your session below
2. TEXT THE CODE AND YOUR QUESTION TO 22333 during the session
3. You MUST TEXT "LEAVE" to 22333 AT THE END OF EACH SESSION in order to participate in subsequent sessions.
FOR EXAMPLE: if you have a question during Saturday’s Postgraduate Course Session 1A: Colorectal Cancer, you would send a text to 22333 with the code ACGPG1A and your question.
GI Pathology & Imaging Course
7:00 am - 12:30 pm
Richardson Ballroom A Code: ACGPATH What's New in GI Pharmacology Course 1:45 pm - 5:20 pm
Richardson Ballroom A Code: ACGPHARM Practice Management Summit 1:45 pm - 5:30 pm E219AB Code: ACGPM Networking, Negotiating and Leadership Skills 5:45 pm - 9:00 pm E216AC Code: ACGNET
Postgraduate Course Session 1A 8:00 am - 9:40 am Exhibit Hall C
Code: ACGPG1A Postgraduate Course Session 1B 10:30 am - 12:10 pm Exhibit Hall C Code: ACGPG1B
Women in GI Luncheon 12:20 pm - 1:35 pm E212 Code: ACGWOMEN
Postgraduate Course Simultaneous Session A 1:45 pm - 3:00 pm Richardson Ballroom Code: ACGPGSSA
Postgraduate Course Simultaneous Session B 1:45 pm - 3:00 pm Exhibit Hall C1 Code: ACGPGSSB
Postgraduate Course Simultaneous Session C 1:45 pm - 3:00 pm Exhibit Hall C2
Code: ACGPGSSC
Postgraduate Course Session 1C 3:35 pm - 5:15 pm Exhibit Hall C Code: ACGPG1C
Postgraduate Course Session 2A 8:00 am - 9:40 am Exhibit Hall C Code: ACGPG2A
Postgraduate Course Session 2B 10:00 am - 12:00 pm Exhibit Hall C Code: ACGPG2B
Trainees Luncheon 12:20 pm - 1:35 pm E212 Code: ACGTRAINL
Postgraduate Course Simultaneous Session D 1:45 pm - 3:00 pm Exhibit Hall C2 Code: ACGPGSSD Postgraduate Course Simultaneous Session E 1:45 pm - 3:00 pm Exhibit Hall C1 Code: ACGPGSSE
Postgraduate Course Simultaneous Session F 1:45 pm - 3:00 pm Richardson Ballroom Code: ACGPGSSF
Postgraduate Course Session 2C 3:35 pm - 5:15 pm Exhibit Hall C Code: ACGPG2C
Presidential Plenary Session 1 8:00 am - 9:00 am Exhibit Hall C2 Code: ACGPRES1
Presidential Plenary Session 2 9:30 am - 10:30 am Exhibit Hall C2 Code: ACGPRES2
Resident Session - Applying for GI Fellowship 10:30 am - 11:30 am Richardson Ballroom Code: ACGRES
Simultaneous Symposium 1A 11:30 am - 12:45 pm Exhibit Hall C2 Code: ACGAM1A
Simultaneous Symposium 1B 11:30 am - 12:45 pm Exhibit Hall C1 Code: ACGAM1B
Simultaneous Symposium 1C 11:30 am - 12:45 pm Richardson Ballroom Code: ACGAM1C Plenary Session 1A 2:15 pm - 3:00 pm Exhibit Hall C2 Code: ACGPL1A
Plenary Session 1B 2:15 pm - 3:00 pm Exhibit Hall C1 Code: ACGPL1B
Simultaneous Symposium 2A 4:45 pm - 6:00 pm Exhibit Hall C2 Code: ACGAM2A
Simultaneous Symposium 2B 4:45 pm - 6:00 pm Exhibit Hall C1 Code: ACGAM2B
Simultaneous Symposium 2C 4:45 pm - 6:00 pm Richardson Ballroom Code: ACGAM2C
Journal Editors Roundtable 7:30 am - 8:15 am E220 Code: ACGJER
Plenary Session 2A 8:30 am - 10:00 am Exhibit Hall C2 Code: ACGPL2A
Plenary Session 2B 8:30 am - 10:00 am Exhibit Hall C1 Code: ACGPL2B
Simultaneous Symposium 3A 11:30 am - 12:45 pm Exhibit Hall C2 Code: ACGAM3A
Simultaneous Symposium 3B 11:30 am - 12:45 pm Exhibit Hall C1 Code: ACGAM3B
Simultaneous Symposium 3C 11:30 am - 12:45 pm Richardson Ballroom Code: ACGAM3C
Plenary Session 3A 2:15 pm - 3:45 pm Exhibit Hall C2 Code: ACGPL3A
Plenary Session 3B
2:15 pm - 3:45 pm Exhibit Hall C1 Code: ACGPL3B
Simultaneous Symposium 4A 5:10 pm - 6:25 pm Exhibit Hall C2 Code: ACGAM4A
Simultaneous Symposium 4B 5:10 pm - 6:25 pm Exhibit Hall C1 Code: ACGAM4B
Plenary Session 4A
8:30 am - 10:15 am Exhibit Hall C2 Code: ACGPL4A
Plenary Session 4B 8:30 am - 10:15 am Exhibit Hall C1 Code: ACGPL4B
Simultaneous Symposium 5A 11:00 am - 12:15 pm Exhibit Hall C2 Code: ACGAM5A
Simultaneous Symposium 5B 11:00 am - 12:15 pm Exhibit Hall C1 Code: ACGAM5B
ACG is pleased to offer MOC points for all of its ACG 2022 CME courses. Attendees can earn MOC credit in the American Board of Internal Medicine’s (ABIM) and American Board of Pediatrics’ (ABP) MOC programs commensurate with the number of AMA PRA Category 1 Credits™ for each activity, at no additional cost or extensive time commitment!
STEP 1: Complete the course evaluation at https://evals.gi.org/am/2022
Participants who wish to receive MOC points for their participation must FIRST complete their meeting evaluation and claim the CME credit commensurate with their participation in the course. Evaluations can only be completed online at https://evals.gi.org/am/2022
STEP 2: Access the MOC link on the evaluation site (ABIM diplomates only) Once the CME evaluation has been submitted, the MOC link will be displayed for the course. Click the link next to the activity to complete the required assessment and submit your personal information to ACCME for the purpose of granting ABIM MOC credits.
You must complete the CME evaluation and claim your CME credits prior to accessing the MOC site. MOC is available for a limited time. Attendees should complete the MOC assessment soon after the course. Full details are provided online before beginning the assessment.
Please allow 72 hours for your MOC points to appear on your ABIM or ABP record. Contact ACG if you receive a message on the submission page that indicates an error with logging your credits or if points are not applied to your profile.
ABIM Board Certified physicians with a 2022 year-end MOC deadline will need to complete their MOC submission by December 31, 2022 in order for the MOC points to count for 2022. No MOC credit will be awarded after April 28, 2023 for these activities.

ABP DIPLOMATES: AFTER completing your CME evaluation and submitting for CME credits for an individual course, ABP MOC can be claimed by emailing education@gi.org to obtain the required forms for completion. ABP diplomates may NOT use the MOC link on the evaluation site to claim MOC points. ABP learner completion data should be submitted within 30 days of activity completion.
REMINDER ON ABIM 2021 MOC EXTENSION: In light of the COVID-19 pandemic, ABIM extended 2021 MOC requirements to December 31, 2022. You may have Maintenance of Certification program requirements to complete before the end of the year. To see due dates for your specific requirements, sign in to your ABIM Physician Portal.
ACG Past President Dr. Delbert Chumley is honored for his leadership, generosity, wise counsel, and passionate support for the College with the Samuel Weiss Award, a service award in commemoration of ACG’s founding father, Dr. Samuel S. Weiss, presented periodically, and not necessarily annually, to a Fellow of the College in recognition of outstanding career service to ACG.
Dr. Chumley has demonstrated steadfast dedication in all of his many important ACG roles over the decades. While growing and managing a thriving private practice in San Antonio, TX, Dr. Chumley carved out a path in ACG that included service on the Board of Governors, committee leadership, and roles as a Trustee and Officer, including ACG President from 2010 to 2011. His extraordinary devotion to ACG is typified by his six years of service as the Administrative Trustee, selflessly representing ACG to the College’s administrative staff as liaison for the Board of Trustees from 2013 to 2019.
Notable among his decades of exemplary contributions to ACG is Dr. Chumley’s instrumental role encouraging charitable support from ACG members and GI practices for the ACG Institute for Clinical Research and Education in its early history, helping to ensure the success of the Institute’s capital campaign and its ongoing financial strength. Dr. Chumley currently serves as a member of the Board of the ACG Institute.
As a Governor and ACG Trustee, Dr. Chumley was an effective advocate on Capitol Hill and interfaced with the key members of the Texas congressional delegation in Washington on behalf of ACG and the interests of gastroenterologists in clinical practice. In recognition of his many professional accomplishments, Dr. Chumley became a Master of the American College of Gastroenterology (MACG) in 2020.
Dr. Chumley’s engagement with the College is marked by a keen dedication to protecting and advancing ACG’s interests and for the many enduring friendships and connections he has forged over the years, which have made him such an effective and outstanding leader. For his loyal commitment to the advancement, security, and success of the College, Dr. Chumley is recognized with the College’s highest honor, the Samuel Weiss Award.
Delbert L. Chumley, MD, MACG, was born and raised in San Antonio, TX, where he attended Central Catholic High School and has spent the last four decades in private practice. After graduating from Texas A&M University, he received his medical degree from The University of Texas Medical Branch, Galveston, where he remained for his post-graduate education serving as Chief Resident in internal medicine and completing a fellowship in gastroenterology in 1976. Afterwards, he moved back to his hometown and established Gastroenterology Consultants of San Antonio which has grown into a 28-physician group.
Dr. Chumley is a Fellow of the American College of Physicians (ACP), a Master of the American College of Gastroenterology (ACG), and continues to maintain a clinical faculty appointment of Professor of Medicine at The University of Texas Health Science Center, San Antonio.
He has held several hospital and professional appointments and remains very active in organized medicine, legislative affairs, and development of medical education programs. In recent years, Dr. Chumley has served as President of the Texas A&M Medical and Dental Society, President of the Texas Society of Gastroenterology and Endoscopy, President of the Bexar County Medical Society, and President of the ACG (2010-2011). He also served as ACG Governor for Southern Texas from 1990 to 1996 and served and chaired several ACG Committees including the Nominating, Finance and Budget and Membership Committees. He is currently serving on the Board of the ACG Institute for Clinical Research and Education.
Dr. Chumley has received numerous honors and awards including: ACG Governor’s Award, 1996; ACG William D. Carey Award, 2000; Texas Society of Gastroenterology and Endoscopy Marcel
Patterson – Robert Nelson Award, 2002; ACP Texas Chapter Laureate Award, 2007; San Antonio Business Journal Healthcare Heroes Lifetime Achievement Award, 2013; University of Texas Medical Branch Ashbel Smith Distinguished Alumnus Award, 2016; Texas Society of Gastroenterology and Endoscopy Patient Advocacy Award, 2019; and Bexar County Medical Society Golden Aesculapius Award, 2020.

He and his wife of 48 years, Louise, have remained active in community affairs supporting numerous nonprofit organizations including serving as co-chairs for the American Cancer Society Cattle Barons Gala. Dr. Chumley most recently served on the Board of Directors for BioMedSA which focuses on the growth of biomedical research in San Antonio and as Trustee for Administrative Affairs on the ACG Board of Trustees.
He and Louise enjoy spending time at their second home in Rockport, fishing in Aransas Bay, attending Texas A&M home football games, and supporting the San Antonio Spurs. They obtain the greatest pleasure, however, enjoying their three adult children and their spouses and their five grandkids.
The Samuel S. Weiss Award was established as a service award in commemoration of the founding father of the ACG, Samuel S. Weiss, MD, whose efforts and initiative resulted in the establishment of the College in 1932. Since its inception in 1972, it has been presented periodically (not always annually) to a Fellow of the College in recognition of outstanding career service to the American College of Gastroenterology. Nominations are solicited and reviewed by the Awards Committee and the recipients must be approved by the ACG Board of Trustees.
Jean S. Wang, MD, PhD, FACG, is recognized by the College for her commitment to colorectal cancer awareness efforts and consistent advocacy in Missouri. In addition to her engagement with state-level policymakers, Dr. Wang regularly volunteers with members of her community to raise awareness of colorectal cancer screening and prevention. For her sustained local and state outreach to improve CRC screening rates, Dr. Wang is the recipient of the 2022 ACG Community Service Award..
Jean S. Wang, MD, PhD, FACG, is a Professor of Medicine at Washington University in Saint Louis where she serves on the Community Outreach and Engagement Leadership Team and the Program for the Elimination of Cancer Disparities Leadership Team at the Alvin J. Siteman Comprehensive Cancer Center.
Dr. Wang has been a passionate advocate for colorectal cancer screening throughout her career and has been very active in statewide and regional efforts to increase screening. She has been interviewed numerous times on local television and radio stations and has also given many talks to local churches and community groups over the years. Dr. Wang volunteers her time on the weekends at health fairs throughout Missouri where she often travels with the inflatable colon to educate the community on colorectal cancer and the importance of screening. Working with Siteman Cancer Center, she has trained community health workers and established a free colorectal cancer screening program utilizing FIT tests in the most underserved areas of the Saint Louis region. She has served on the ACG Patient Care Committee since 2017.
In 2018, Dr. Wang co-founded the Missouri Colorectal Cancer Roundtable in collaboration with the Missouri Cancer Consortium, American Cancer Society, and the Missouri
Department of Health. This statewide group is modeled after the National Colorectal Cancer Roundtable, with the mission of increasing colorectal cancer screening rates in the state of Missouri. The Missouri Colorectal Cancer Roundtable was instrumental in fostering collaborations among university academic centers and the Missouri Department of Health which led to Missouri receiving grant funding from the CDC National Colorectal Cancer Control Program to increase colorectal screening rates across the state. Through this work, the Missouri Roundtable has been involved with multiple Federally Qualified Healthcare Center networks across the state of Missouri to implement evidence-based interventions to increase colorectal cancer screening. In addition, Dr. Wang is working with the Missouri Department of Health on a statewide colorectal cancer screening campaign targeting over 40,000 Missouri state employees. Dr. Wang has also served on the Missouri Cancer Consortium Executive Committee, where she has worked with other community organizations and the Missouri Department of Health to develop and implement the State Cancer Action Plan, where colorectal cancer screening was made a state priority. Through her role leading the Missouri Colorectal Cancer Roundtable, she has also advocated for the importance of colorectal cancer screening through meetings with state legislators
and the Missouri Governor. She was honored to receive the ACG SCOPY Effective Advocacy Award in 2019 for her efforts.
Dr. Wang received her undergraduate and medical degrees from Brown University. She then completed her residency in internal medicine and fellowship in gastroenterology at the Johns Hopkins Hospital. She subsequently completed a PhD in Clinical Investigation at the Johns Hopkins Bloomberg School of Public Health. She lives in Saint Louis, Missouri, with her husband Michael and children, Matthew and Madeline.

The Community Service Award is bestowed upon an ACG Allied Health Member, Resident Member, Trainee Member, Member, Fellow, or Master who has initiated or has been involved in volunteer programs or has provided extensive volunteer service post-training. The service must have been performed on a completely voluntary basis and not for the completion of training or position requirements. Such service may include but is not limited to the following: community education programs (e.g., colon cancer awareness); working in free clinics; mentoring advocacy groups or local government committees; teaching in under-served schools related to health education; and political work on committees for comprehensive health insurance or other issues.
Rachel Issaka, MD, is awarded the 2022 ACG Diversity, Equity, and Inclusion Award for her dedication to improving health equity and prioritizing health disparities, reinforcing them as key areas of focus for the GI community. Dr. Issaka has emerged as a leader in healthcare disparities research, particularly for her commitment to addressing CRC screening among medically underserved populations. She has also assumed advisory roles at the national level to address this critical public health issue and has worked to bolster the pipeline of Black gastroenterologists and hepatologists and advance opportunities for scholarship and leadership.
Rachel Issaka, MD, is a gastroenterologist, Assistant Professor, and the Kathryn Surace-Smith Endowed Chair in Health Equity Research at the Fred Hutchinson Cancer Research Center (FHCRC) and the University of Washington (UW). She is the Director of the FHCRC/UW Medicine Population Health Colorectal Cancer Screening Program. Dr. Issaka’s research focuses on decreasing colorectal cancer mortality through increased screening in medically underserved populations. Her work has been funded by the National Institutes of Health and the Centers for Medicare and Medicaid Services.
Dr. Issaka has contributed to national medical practice guidelines for the Centers for Disease Control, the National Comprehensive Cancer Network, and the National Colorectal Cancer Roundtable. In 2020, she was selected to serve on an expert panel advising the President’s Cancer Panel and the COVID-19 Prevention Network, a group formed to provide oversight for National Institutes of Health funded COVID-19 vaccine trials. Dr. Issaka has published in high-impact journals
including the Journal of the American Medical Association, Lancet Gastroenterology & Hepatology, and The American Journal of Gastroenterology on topics varying from, pandemicrelated disparities in cancer care and options for CRC screening. Her research and contributions in these spheres have also been featured in the New York Times, Reuters, and Scientific American and quoted in media outlets including NPR, Time Magazine, and U.S. News & World Reports.
In addition to her scholarly work, Dr. Issaka is a leader in Diversity, Equity, and Inclusion efforts nationally and in her local community. She is a co-founder and board member of the Association of Black Gastroenterologists and Hepatologists, an organization that aims to improve gastrointestinal health outcomes in Black communities, foster networking, and scholarship among its members, develop the pipeline of Black gastroenterologists and hepatologists, and promote health equity in the fields of gastroenterology and hepatology. She is involved in efforts to improve the health of Black and other racial/ethnic

minority communities and does so by partnering with local organizations, churches in minority communities, and serving on the Board of Directors of the Urban League of Metropolitan Seattle.
Dr. Issaka completed her gastroenterology fellowship at the University of California, San Francisco where she also earned a master’s degree in clinical research. She completed her internal medicine residency at Northwestern University Feinberg School of Medicine, where she served as chief resident and obtained her medical degree from the University of Michigan Medical School.
The Diversity, Equity and Inclusion Award is awarded to an ACG member, in recognition of outstanding work in the areas of clinical practice, research, teaching and/ or leadership which has demonstrated an emerging or sustained commitment to the values of diversity, health equity and inclusion.
BAG
continue participating in
Charlotte.
For commitment to improving health outcomes among medically underserved populations, RACHEL ISSAKA, MD, RECEIVES THE DIVERSITY, EQUITY, AND INCLUSION AWARD
Monday,
Join Dr Patrick Kamath as he explores how clinicians can participate in research that moves the fields of gastroenterology and hepatology forward during Monday’s The American Journal of Gastroenterology lecture.

Patrick S. Kamath, MD, is a Professor of Gastroenterology and Hepatology at the Mayo Clinic in Rochester, Minnesota. Dr Patrick completed his MBBS from St. John's Medical College, Bangalore University and both his DM in Gastroenterology and MD in Internal Medicine from Postgraduate Institute of Medical Education & Research in Chandigarh, India, where he also completed his residency and fellowship in Gastroenterology. He then completed three fellowships at the Mayo Clinic.
His research focuses on acute-on-chronic liver failure, nonalcoholic fatty liver disease, polycystic liver disease, Budd-Chiari syndrome and hereditary hemorrhagic telangiectasia. Dr. Kamath also studies alcoholic hepatitis, cirrhosis and the complications thereof, including portal hypertension, variceal hemorrhage, ascites and hepatic encephalopathy. He works to improve understanding of the mechanisms and complications of liver disease, in the hopes of developing new strategies of prevention and treatment that will improve quality of life and overall outcomes for patients with various liver diseases. He and his co-workers were instrumental in developing the Model for End-Stage Liver Disease (MELD) score, which is used worldwide to determine prognosis in liver disease and prioritize organ allocation for liver transplantation. He also serves as a co-investigator in the Translational Research and Evolving Alcoholic Hepatitis Treatment (TREAT) consortium. His current focus is on finding ways to improve survival in patients with acute-on-chronic liver failure, and he is also dedicated to the education of the next generation of physicians, who will further advance this work.
Dr. Kamath has contributed to recently published research on management of acute-on-chronic liver failure and on prevention and treatment of cirrhotic complications, including management of hepatic encephalopathy in the hospital, primary prophylaxis of variceal bleeding, and prevalence and prediction factors of infections in patients with cirrhosis. He has published over 300 articles in peer reviewed journals, including four ACG guidelines. As a busy clinician, lecture attendees will learn much from Dr. Kamath’s experiences as an academic and very busy clinician.
Tuesday, October 25
10:05 am – 10:35 am
Exhibit Hall C2
At this year’s J. Edward Berk Distinguished Lecture, Dr. Sands will describe the efficacy and safety of newer agents for IBD, and the potential for combination therapy and precision medicine approaches to treat Crohn's disease and ulcerative colitis.

Dr. Sands is the Chief of the Dr. Henry D. Janowitz Division of Gastroenterology at the Mount Sinai Medical Center, and the Dr. Burrill B. Crohn Professor of Medicine at the Icahn School of Medicine at Mount Sinai. He was awarded his MD at Boston University School of Medicine and completed an internship and residency at the Hospital of the University of Pennsylvania in Philadelphia. He received his fellowship training in gastroenterology at the Massachusetts General Hospital and also completed a Master of Science in Epidemiology at the Harvard School of Public Health. Dr. Sands was a faculty member at Harvard Medical School and Medical Co-Director of the Massachusetts General Hospital Crohn's and Colitis Center, and then served as the Acting Chief of the Gastrointestinal Unit at Massachusetts General Hospital before moving to Mount Sinai in 2010. Dr. Sands is a Fellow of the ACG and AGA. Additionally, he has served as the Chair of the Crohn's & Colitis Foundation of America's Clinical Research Alliance, and Chair of the Immunology, Microbiology and IBD Section of the AGA. He served as an Associate Editor for the journal Gastroenterology. Dr. Sands is widely published in the area of inflammatory bowel diseases, with numerous publications in journals such as Gastroenterology, Gut, and the New England Journal of Medicine. In addition to his extensive research background, Dr. Sands is internationally renowned for his expert care of complex inflammatory bowel disease.
J. Edward Berk Distinguished Lecture is awarded to individuals prominent in gastroenterology or a related area. The lecturer is nominated by the ACG President and the appointment is subject to approval by the ACG Board of Trustees. The lectureship was established in recognition of the significant contributions made by J. Edward Berk, MD, MACG, to clinical gastroenterology during his long and distinguished clinical and academic career.
Tuesday, October 25
4:30 pm – 5:00 pm
Exhibit Hall C2
Join Dr. Shaukat as she delivers the Emily Couric Memorial Lecture and discusses current colon cancer screening tests and strategies to increase screening uptake in all populations.

Aasma Shaukat, MD, MPH, FACG serves as the Director of Outcomes Research in the Division of Gastroenterology and Hepatology at NYU Langone Health. Dr. Shaukat also has dual appointments as the endowed Robert M. and Mary H. Glickman Professor of Medicine and Gastroenterology in the Department of Medicine and Professor in the Department of Population Health. In addition to her role within the division, she serves as co-director of translational research education and careers in the Clinical and Translational Science Institute and is a staff physician at the New York Harbor VA Medical Center. Before joining NYU Langone, Dr. Shaukat served on the faculty at the University of Minnesota Medical School, where she was a professor of medicine and public health and section chief of gastroenterology service at the Minneapolis VA Health Care System. An alum of the Aga Khan University Medical College in Karachi, Pakistan, Dr. Shaukat obtained a Master of Public Health in international health and epidemiology from Johns Hopkins School of Public Health. She went on to complete her residency in internal medicine at the State University of New York School of Medicine in Buffalo, New York, and a fellowship in gastroenterology at Emory University.
A highly regarded clinician, distinguished epidemiologist, and prolific researcher, Dr. Shaukat has published extensively on colorectal cancer screening, prevention, and quality indicators for colonoscopy. She has pioneered some of the foundational studies on the reduction in morbidity and mortality related to colon cancer screening and, most recently, served as first author on the newly updated ACG Clinical Guidelines: Colorectal Cancer Screening 2021 published in The American Journal of Gastroenterology. Her research has been consistently funded by organizations such as the National Institutes of Health, Department of Veterans Affairs, American College of Gastroenterology, and American Society for Gastrointestinal Endoscopy.
Dr. Shaukat has published more than 180 peer-reviewed articles in numerous toptier medical publications, authored a number of textbook chapters, and serves on multiple editorial boards, including the position of Senior Associate Editor of AJG. She is a thought leader and has given numerous keynote presentations both nationally and internationally. She has served on several review panels and holds leadership roles with numerous professional organizations and task forces, including the U.S. Multi-Society Task Force on Colorectal Cancer, the American Society of Clinical Investigation, chair of the Young GI Members Committee for the WGO, chair of the GI field advisory board for the Veterans Healthcare Administration, the American Society for Gastrointestinal Endoscopy Quality and Safety Committee, and the American Gastroenterological Association Clinical Practice Updates Committee.
Aasma Shaukat, MD, MPH, FACG
THE PROMISE AND PROGRESS OF NEW APPROACHES TO TREATING THE INFLAMMATORY BOWEL DISEASES
What Do We Need to Build and Who Will Come?
Wednesday, October 26
10:20 am – 10:50 am
Exhibit Hall C2
Attend Dr. Mayer’s David Y. Graham Lecture and gain a better understanding of how the gut connectome translates microbial signals into health and disease.
Emeran A. Mayer, MD, is a Distinguished Research Professor in the Department of Medicine at the David Geffen School of Medicine at UCLA with joint appointments in Psychiatry and Physiology. He is the Executive Director of the G. Oppenheimer Center for Neurobiology of Stress and Resilience and Founding Director of the UCLA Microbiome Center at UCLA. He is one of the pioneers and leading researchers in the role of brain-gut interactions in health and chronic disease. He has been continuously funded by the NIH for the past 30 years and has published close to 400 scientific papers, co-edited three books, published the best-selling The Mind Gut Connection book in 2016 and The Gut-Immune Connection book in June 2021. He is the recipient of the 2016 David McLean award from the American Psychosomatic Society and the 2017 Ismar Boas Medal from the German Society of Gastroenterology and Metabolic Disease. His most recent work has focused on alterations in the bidirectional communications within the braingut microbiome system and their role in chronic inflammatory and functional diseases of the gut, obesity, and cognitive decline.
October
The Endoscopy Video Forum Symposium will feature the best video presentations submitted by colleagues from across the U.S. and around the world. Submitted during the Call for Abstracts and peer-reviewed and selected for oral presentation, the cases will feature interesting endoscopic techniques and challenging or unique cases encountered in daily clinical practice. At the end of the session, the audience, along with the judges, will vote to select the best video of ACG 2022.
Moderators: Seth A. Gross, MD, FACG
Vivek Kaul, MD, FACG
Judges: Jodie A. Barkin, MD
Rabia A. de Latour, MD
Alexandra Guillaume, MD
Immanuel K. H. Ho, MD, FACG
Laith H. Jamil, MD, FACG
Kenneth J. Vega, MD, FACG
Presenting Authors are underlined
V1. (S346) Gallbladder to the Rescue: Transcystic Endoscopic Ultrasound-Guided Rendezvous Ramzi Mulki, MD1, Samuel Fernandez Prada, MD2, Antonio Martinez Ortega, MD2, Ramon Sanchez-Ocana, MD2, Carlos De la Serna Higuera, MD2, Manuel Perez-Miranda, MD2; 1University of Alabama at Birmingham, Birmingham, AL, 2Universitay Hospital
Rio Hortega, Valladolid, Castilla y Leon, Spain
V2. (S347) Endoscopic Suture Repair of a Transmural Esophageal Perforation
Munraj Singh, MD, Catherine Hudson, MD, MPH; Louisiana State University Health Sciences Center, New Orleans, LA
V4. (S349) Cholangioscopic Recanalization of a Completely Obstructed Post-Transplant
Anastomotic Stricture
Ghada Mohamed, MBChB1, Andrew Gilman, MD2, Todd H. Baron, MD3; 1Duke University Medical Center, Durham, NC, 2University of North Carolina, Chapel Hill, NC, 3University of North Carolina at Chapel Hill, Chapel Hill, NC
V5. (S350) Successful Endoscopic Drainage of Acute Duodenal Diverticulitis Complicated by Abscess
Billy-Joe Liane, MD1, John Quiles, MD2; 1Brooke Army Medical Center, San Antonio, TX, 2San Antonio Military Medical Center, Fort Sam Houston, TX
V6. (S351) Peroral Endoscopic Myotomy in the Presence of Esophageal Varices
Hyun Jae Kim, MD, Billy Zhao, BSc, Neal Shahidi, MD, Eric Lam, MD; University of British Columbia, Vancouver, BC, Canada
Graham Lecturer is chosen
by
President and is
Board of Trustees. Established in 2004 in
of
many contributions to clinical gastroenterology made by David Y. Graham, MD, MACG, this named lectureship was made possible through a donation by Otsuka Pharmaceutical Co., Inc., and Meretek Diagnostics,
V3. (S348) Creating Your Own Paths: EUS-Guided Transjejunal Gallbladder Drainage and ERCP, Cholecystoscopy, and Electrohydraulic Lithotripsy for Choledocholithiasis and Cholelithiasis in a Patient With Roux-en-Y Gastric Bypass Jason Nasser, MD1, Arjun Chatterjee, MD1, Mohannad Abou Saleh, MD1 Donald Kirby, MD1, Prabhleen Chahal, MD2; 1Cleveland Clinic Foundation, Cleveland, OH, 2Cleveland Clinic, Cleveland, OH


Hours are:
Friday, October 21
8:00 am - 5:00 pm
Saturday, October 22 8:00 am - 5:00 pm
Sunday, October 23 8:00 am - 5:00 pm
Monday, October 24 8:00 am - 5:00 pm
Tuesday, October 25 8:00 am - 5:00 pm
The ACG Junior Governor’s Award is given to an ACG Governor in the first term of service. Nominees demonstrate a clear commitment of service to the Board of Governors and show potential for future growth within the organization. Awardees have demonstrated service on ad hoc committees, national affairs, local and state legislative efforts, recruitment, correspondence with constituents, participation in regional meetings, speakers bureau or other special projects.
This year’s award is presented to Vonda G. Reeves, MD, MBA, FACG. Dr. Reeves is ACG Governor for Mississippi. She is in private practice in Flowood, is the CoFounder of the Mississippi Colorectal Round Table, and mother of three entertainment industry executives and one researcher.

A graduate of Meharry Medical College in Nashville, TN, Dr. Reeves completed her medical residency in Internal Medicine and her fellowship in gastroenterology at the University of Texas Medical Branch in Galveston.
Dr. Reeves is passionate about advocating for her patients and profession on a state and national level and has been an instrumental advocate since beginning her tenure. She has attended the ACG Governor’s fly-in to advocate for her patients and practices across her home state of Mississippi. She is a Course Director for the ACG Practice Management Summit at ACG’s 2022 Annual Scientific Meeting and is a current member of the ACG Awards Committee.
The ACG Senior Governor’s Award is given to an ACG Governor in the second or third term of service. Awardees have demonstrated a strong commitment to the Board of Governors in various areas such as service on ad hoc committees, national affairs, local and state legislative efforts, recruitment, correspondence with constituents, participation in regional meetings, speakers bureau or other special projects.
This year’s award is presented to Tauseef Ali, MD, FACG. Dr. Ali has been the ACG Governor for Oklahoma since 2017 and is currently a member of the ACG Constitution and Bylaws Committee, Legislative and Public Policy Council, Membership Committee, and Nominating Committee, and is the current chair of the Public Relations Committee. Since becoming ACG Governor for Oklahoma, he has advocated tirelessly on behalf of patients and practices throughout his home state, emphasizing the importance of laws minimizing prior authorization and step therapy requirements for patients. Dr. Ali graduated from King Edward Medical College, Pakistan. He completed his residency and fellowship at the University of Oklahoma Health Sciences Center. He was a CCFA visiting IBD fellow at the University of Chicago. Dr. Ali is a gastroenterologist and IBD specialist at SSM Health Saint Anthony Hospital, Oklahoma. He is the executive medical director of SSM Health Digestive Institute and the director of the Crohn’s and Colitis Center. He also serves as the clinical faculty at the University of Oklahoma and adjunct faculty at Oklahoma State University. He is the author of Crohn’s and Colitis for Dummies by Wiley Publishers. He regularly tweets through his educational Twitter account @ibdtweets, using it to further advocate and to further educate colleagues.

Dr. William D. Carey was elected Governor for Northern Ohio in 1987 and served as Chairman of the Board of Governors from 1988-1990. He has served the College as Treasurer and Trustee, and has chaired numerous College Committees. Dr. Carey is the first Chairman of the Board of Governors to be elected as President of the American College of Gastroenterology (1993). In honor of his years of distinguished service and because of the example he has set for other Governors an award will be given in his name.
This year’s award is presented to James C. Hobley, MD, MSc, FACG. Dr. Hobley is a Trustee on the ACG Board of Trustees, a past member of the Legislative and Public Policy Council and previous Chair of the committee from 2020-2021, as well as a former member of the ACG Membership Committee, Credentials Committee, and Minority Affairs and Cultural Diversity Committee. Following in the footsteps of Dr. Carey and other previous Award winners, Dr. Hobley served as the ACG Governor for Louisiana from 2014-2020. Dr. Hobley is incredibly active in advocacy for patients on the state level in Louisiana on behalf of ACG and other patient advocacy organizations, and nationally by participating in numerous virtual “Governors Advocacy Series” meetings with members of Congress and their staff and ACG Advocacy Fly-ins.
Dr. Hobley has been in private practice at GastroIntestinal Specialists in Shreveport, Louisiana, since 2006 and is on the Board of Directors for GI Specialists. He practices general gastroenterology and is a past President of the Louisiana Gastroenterology Society. Dr. Hobley completed his undergraduate education at Tulane University in New Orleans, LA, and received his Doctor of Medicine degree from Pennsylvania State University College of Medicine in Hershey, PA. He completed his residency at Milton S. Hershey Medical Center in Hershey, PA, in Internal Medicine, and his fellowship at Milton S. Hershey Medical Center in Hershey, PA, in Gastroenterology/Hepatology.
Dr. Hobley is married to his best friend, Marie-Alice, and together they share six wonderful children.
Raquel Croitoru, MD, FACG
LONG ISLAND
Frank G. Gress, MD, FACG
NORTH CAROLINA
Thomas M. Swantkowski, MD, FACG
NORTHERN NEW YORK Shivangi T. Kothari, MD, FACG
Guilherme G. Macedo, MD, PhD, FACG
SOUTHERN CALIFORNIA A Brennan M. Spiegel, MD, MSHS, FACG
SOUTHERN NEW YORK
Thomas A. Ullman, MD, FACG
SOUTHERN OHIO Andrew B. Chun, MD, FACG
Rathi Narayan, MD, FACG WASHINGTON
Kunjali Padhya, MD, FACG

The ACG Nominating Committee, composed of ACG Past Presidents, David A. Greenwald, MD, FACG; Mark B. Pochapin, MD, FACG; and Sunanda V. Kane, MD, MSPH, FACG; and ACG Governors, Tauseef Ali, MD, FACG; and Russell D. Cohen, MD, FACG; met by telephone conference call on June 12 and 14, 2022, and proposed the following slate of Officers for 2022 – 2023 and the following slate of Trustees for 2022 – 2024:
OCTOBER 2022 - 2023
• President: Daniel J. Pambianco, MD, FACG
• President-Elect: Jonathan A. Leighton, MD, FACG
• Vice President: Amy S. Oxentenko, MD, FACG
• Secretary: Costas H. Kefalas, MD, MMM, FACG
• Treasurer: William D. Chey, MD, FACG
OCTOBER 2022 - 2024
• Jean-Paul Achkar, MD, FACG
• David J. Hass, MD, FACG

• Nicholas J. Shaheen, MD, MPH, MACG
• Aasma Shaukat, MD, MPH, FACG
• Renee L. Williams, MD, MHPE, FACG
• Patrick E. Young, MD, FACG
ACG’s Secretary, William D. Chey, MD, FACG, has announced that the College’s 2022 Annual Business Meeting will be held on Monday, October 24, 2022, at 6:00 pm in Exhibit Hall C2 at the Charlotte Convention Center in Charlotte, NC. The Nominating Committee will present its proposed slate of officers and trustees at that time, and all Fellows and Members are encouraged to attend and to vote on this and all other items of business at the meeting.

Distinguished careers in gastroenterology and contributions to the College through service, leadership and education have earned six colleagues the distinction of Master of the American College of Gastroenterology (MACG).
Neena Abraham, MD, MSc (Epid), MACG, is a Professor of Medicine at Mayo Clinic and a Consultant in the Division of Gastroenterology & Hepatology and Health Care Policy Research. She completed her medical school training at Dalhousie University, Halifax, Nova Scotia, Canada (1994), internal medicine residency at the University of Alberta (1997), GI fellowship (1999), advanced therapeutic endoscopy fellowship (2000), and post-doctoral research training (2001) at McGill University Montreal, Quebec, Canada.
Dr. Abraham is the Medical Director of the Mayo Clinic CardioGastroenterology Clinic, which uses a multi-specialty collaborative care model to improve clinical outcomes for cardiac patients at risk of gastrointestinal bleeding. She is the primary author of the 2022 ACG-CAG Clinical Practice Guideline: Management of Anticoagulants and Antiplatelets During Acute Gastrointestinal Bleeding and the Periendoscopic Period, and since 2008 she has authored an additional seven national and international practice guidelines related to antithrombotic drug management and acute gastrointestinal bleeding. She is a federally funded investigator at the intersection of cardiology and gastrointestinal disorders, investigating how antithrombotic drugs contribute to gastrointestinal bleeding in cardiac patients, the elderly, and highly co-morbid.
Dr. Abraham is the first female Director of the American College of Gastroenterology Institute for Clinical Research and Education (2020-ongoing) and a member of the ACG Board of Trustees (BOT) and ACG BOT Executive Committee. Under her leadership, the ACG Institute has surpassed the $2 million mark in annual funding for competitively awarded clinical research, and in 2021 she launched the ACG Institute Center for Leadership, Ethics, and Equity (LE&E Center). This new Institute Center develops and funds programs promoting ethical physician-leadership and leadership training (the Young Physician Leadership Scholars Program, the Early Career Leadership Program, and the Advanced Leadership Development Program); scientific discovery to reduce health disparities and advance health equity (the Health Equity Research Awards); and educational activities that support the College's commitment to increasing diversity, equity, and ethical care in our profession (the ACG Institute Visiting Scholars in Equity, Diversity, and Ethical Care, and the Prescriptions for Success High School Program). In 2023, the LE&E Center will launch the Clinical Research Leadership Program designed to ensure funded ACG investigators have the leadership skills to maintain successful research programs and mentor the next generation of clinical investigators.
Dr. Abraham was a member of the ACG Research, Women's, and Public Relations Committees before serving as a Trustee of the ACG (2009-2015) and on the ACG Institute Board (2017-2020). She was the Course Director for the ACG Postgraduate Course (2008), the ACG ABIM Recertification and Maintenance of Competence course (2011-2014), and the first ACG Women in Gastroenterology Forum (2014). At the 2020 ACG Annual Postgraduate Course, Dr. Abraham was honored to deliver the David Sun Lecture on CardioGastroenterology, and in 2021 she was recognized as the Healio & American College of Gastroenterology Disruptive Innovator in Clinical Medicine.

Qiang Cai, MD, PhD, MACG, is a graduate of Jiangxi Medical College (1982) in China. After graduating from the medical college, he worked in Peking Union Medical College Hospital, one of the best hospitals in China, where he began his career in gastroenterology under the tutorship of Drs. Xiao-Qian Zhang, Min-Zhang Chen, Shou-Po Chen, and Yuan-Fang Chen. There, he obtained his master’s degree in gastrointestinal physiology in 1986 and served as a junior faculty member in the Division of Gastroenterology and Hepatology before moving to the United States in 1987.
In 1992, Dr. Cai obtained his PhD in gastrointestinal physiology from Cornell University, where he studied intestinal calcium absorption under the guidance of Dr. Robert H. Wasserman, the father of intestinal calcium binding protein. He completed his second internal medicine residency training at Marshfield Clinic, one of the training facilities of the University of Wisconsin, and his second gastroenterology fellowship at Emory University School of Medicine. Dr. Cai joined the faculty team at the Division of Digestive Diseases, Department of Medicine, Emory University School of Medicine in July 2001. He was a Professor of Medicine and the only master physician then in the division. He also directed the advanced endoscopy fellowship program for 10 years before he was invited as a Professor of Medicine and the Director for the Division of Gastroenterology and Hepatology at Louisiana State University Health Science School of Medicine, Shreveport, Louisiana in April 2021.
Dr. Cai’s main research interests are therapeutic endoscopic procedures. He is an author of more than a hundred peer-review journal papers and an editor for three books.

Dr. Cai has been a member of ACG for 24 years, and a fellow of ACG for 17 years. He was an invited speaker for many ACG regional courses and national annual scientific meetings. Dr. Cai has served on many ACG Committees including the Research Committee, Training Committee, International Relations Committee, Educational Affairs Committee, and Credentials Committee. He also chaired the International Relations Committee from 2010-2013 and served as ACG Governor for Georgia from 2017-2021. He was a Director of both ACG’s regional and national hands-on endoscopy courses and a Director of a regional ACG Postgraduate Course. In addition, Dr. Cai was an Associate Editor for The American Journal of Gastroenterology for 6 years.
In 2015, Dr. Cai, together with the ACG International Relations Committee and ACG staff, established the “ESD with Asian Experts” as a session at ACG’s national hands-on endoscopy course. The session has been offered every year since.
W. Elwyn Lyles, MD, MACG, was born and raised in Mangham, Louisiana. After graduating from Northeast Louisiana University with a Bachelor of Science, he attended Louisiana State University School of Medicine Shreveport where he was awarded his medical degree. He completed his internal medicine internship at the University of Florida in Jacksonville. Dr. Lyles completed his residency in internal medicine at the University of Tennessee – Memphis, and later completed a gastroenterology fellowship at the University of Florida –Jacksonville. Following his fellowship, Dr. Lyles joined the United States Air Force as a commissioned officer at Eglin Air Force Base where he served for two years. He began his private practice in Alexandria, Louisiana, in 1994, where he served the Central Louisiana region for twenty years. Since 2014, Dr. Lyles has been employed as a gastroenterologist by Blount Memorial Physician Group in Maryville, Tennessee. Dr. Lyles is currently a Fellow of the American Society of Gastrointestinal Endoscopy and serves on the American College of Gastroenterology (ACG) Institute Board. He served on the ACG Board of Trustees from 2006-2012, as ACG Governor for Louisiana from 2005-2008, and on multiple Committees including the ACG Patient Care Committee and Publications Committee which he chaired from 2004-2006. Dr. Lyles has represented the ACG on the Accreditation Association for Ambulatory Health Care Board of Directors. He has received several honors including the ACG Board of Governors (BOG) William D. Carey Award in 2011 and ACG BOG Service Awards in both 2005 and 2006.
Dr. Lyles was a founding member of the Louisiana GI Society and served the institution as its inaugural President. At the regional level, he served as President of the Rapides Parish Medical Society. Currently, Dr. Lyles serves as an Adjunct Professor and lecturer at the Lincoln Memorial University –DeBusk College of Osteopathic Medicine.
The years with the ACG have produced many life-long friendships which Dr. Lyles enjoys to this day. In his free time, he enjoys fishing, football, and hiking in the beautiful mountains of eastern Tennessee with his wife Rhonda. They enjoy spending time with their children and many grandchildren.
Professor Guilherme Macedo, MD, PhD, MACG, is the Director of the Gastroenterology Department of Centro Hospitalar Universitario São João Porto, Portugal, and an invited full Professor at the Faculty of Medicine at the University of Porto. He also leads the World Gastroenterology Organisation Gastroenterology and Hepatology Training Center in Porto.
After his GI fellowship, he received advanced training in hepatology in Paris, France, and Freiburg, Germany, and began his academic career at the Faculty of Medicine in 1994. That year he attended his first ACG Annual Scientific Meeting, in San Francisco. During the following years, Prof. Macedo was awarded fellowships in ACG, AASLD, and AGA, while he actively produced intensive clinical work, especially in the fields of hepatology and endoscopy, locally pioneering the endo-hepatology concept in recent years. Throughout his career he has received numerous national awards and honors and was distinguished with the ACG International Leadership Award in 2015.
Prof. Macedo has served as President of the Portuguese Association for the Study of Liver Disease, President of the Portuguese Society of Endoscopy, and he is currently the President of Portuguese Society of Gastroenterology. He served as ACG Governor for Portugal for 2 terms (20072013) and was a member of the ACG International Relations Committee (2013-2019). Included in his clinical work he is actively involved in community health programs and fostered several ongoing projects, particularly with vulnerable populations (prisoners, homeless, and substance abuse organizations).

He has more than 400 publications to his credit in indexed journals and has lectured extensively on many clinical and training aspects of gastroenterology. His passion for teaching and mentoring underlies his commitment with the WGO Train the Trainers Program, over the last 15 years, nurturing and organizing several standard and advanced courses on leadership and management. After serving as Chair of the WGO Foundation, he is the current President of the World Gastroenterology Organisation.
He has very eclectic personal interests, with a special focus on movies, music, pop art, and soccer, in accordance with his role at the Board of the Superior Council of FCPorto over the last 20 years. Prof. Macedo has been blessed with everlasting support from his family (wife, three children, and grandson), faithful friends, and a Bernese Mountain dog.
MITCHELL L. SHIFFMAN, MD, MACG Mitchell L. Shiffman, MD, MACG, received his MD from the State University of New York Upstate Medical Center in Syracuse. He then traveled south to Richmond for training in Internal Medicine and Gastroenterology at the Virginia Commonwealth University Medical College of Virginia, many years before any formal training in hepatology ever existed.
Dr. Shiffman joined the faculty at VCU/MCV in 1989 and became Chief of Hepatology and Medical Director of the Liver Transplant Program 6 months later. Over the next 20 years he directed clinical trials at VCU which helped define treatments for chronic viral hepatitis B and C viruses, issues related to liver transplantation, TIPS, and many other liver diseases. He co-chaired 2 NIH consensus conferences, one on TIPS and the other on living donor liver transplant and received 5 NIH-sponsored grants to define treatments for PBC, PSC, HCV, HBV, and living donor liver transplantation. During this time, he became recognized as an international hepatology key opinion leader and was a frequent speaker at national and international meetings. He has given lectures in 42 states, 35 countries, 6 continents, has published over 360 articles in peer-reviewed journals, and edited 5 books and/or journal supplements on liver disease.
Dr. Shiffman left the VCU Medical Center in 2009 to join Bon Secours Mercy Health and start the Liver Institute of Virginia. This community practice has grown to 7 providers in 2 Virginia cities 70 miles apart, and cares for patients with all types of liver diseases, provides pre-transplant assessment and management, post-liver transplant care, treatment for hepatocellular carcinoma, and conducts numerous clinical research trials.
Of all his professional accomplishments, Dr. Shiffman is most proud of the work he has done with and for the ACG. He joined the College and attended his first meeting in 1990. He served on several committees including Membership and Educational Affairs where he promoted the growth of hepatology membership and liver disease topics at ACG
meetings. He was co-director of the Postgraduate Course in 1995, the last ACG Annual Scientific Meeting held in New York City. He conceived and has co-directed Hepatitis School, a one-day program held in conjunction with an ACG Postgraduate Regional Course. Hepatitis School began its run in May 2013, morphed into Hepatology School in August 2018 and spawned the equally successful IBD and Functional GI Disorders Schools. Dr. Shiffman had the great honor to serve as a Trustee of the College between 2004 and 2009. He is married to Lori, and they have 4 children, Josh, Ben, Rachel, and Nathan and 2 grandchildren Aubree Briggs, age 2, and Jackson Shiffman, age 1.
Dr. Shiffman’s secret claim to fame is that he grew up in the small town of Bethel, New York, 2 miles from the Woodstock Festival site of 1969, attended the Festival all 3 days and retains his original unused ticket in perfect condition.

Stuart J. Spechler, MD, MACG, has been Chief of the Division of Gastroenterology and CoDirector of the Center for Esophageal Diseases at Baylor University Medical Center at Dallas, and Co-Director of the Center for Esophageal Research at the Baylor Scott & White Research Institute since January 2017. From July 1997 to December 2017, Dr. Spechler was the Chief of the Division of Gastroenterology for the VA North Texas Healthcare System, Professor of Medicine, and holder of the Berta M. and Cecil O. Patterson Chair in Gastroenterology at the University of Texas Southwestern Medical Center. He also had been the Director of the Center for Swallowing Disorders at the Beth Israel Deaconess Medical Center and Harvard Medical School in Boston, Massachusetts, from July 1990 to June 1997.
Dr. Spechler’s research has focused primarily on disorders of the esophagus, especially GERD, Barrett’s esophagus, eosinophilic esophagitis, and esophageal motility disorders. He has chaired three VA Cooperative Studies on medical and surgical treatments for gastroesophageal reflux disease and published the results of those studies in JAMA and in The New England Journal of Medicine. He described the condition known as “short-segment Barrett’s esophagus” in 1994. He has made important contributions to understanding the complex relationship between GERD and eosinophilic esophagitis and was the first to propose the notion that a clinical response to PPIs neither rules in GERD nor rules out eosinophilic esophagitis. Dr. Spechler was also the first to propose that achalasia and other esophageal motility disorders might have an allergic etiology, and that eosinophilic esophagitis might have mucosal-predominant and muscle-predominant forms.
He has published more than 400 scientific reports, editorials, review articles, and book chapters on esophageal disorders. He is best known for his work in the areas of GERD, Barrett’s esophagus, eosinophilic esophagitis, and esophageal motility disorders. Dr. Spechler has served on the editorial boards of numerous journals including Gastroenterology, Gut, Alimentary Pharmacology and Therapeutics, Nature Reviews in Gastroenterology, Current Opinion in Gastroenterology, Digestive Diseases and Sciences, Diseases of the Esophagus, and Foregut.
Dr. Spechler served as the American College of Gastroenterology (ACG) Governor for Massachusetts (1992-1994) and was the senior author of the 2021 ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease.


Professor Seshadri T. Chandrasekar, MD, FACG has an extensive history of mentoring GI trainees in India and providing clinical education, adapting his training efforts to a virtual format during the COVID-19 pandemic. He has also developed a number of community education tools to address health care access, obesity, and liver health. For his work expanding educational offerings to physicians and trainees in India, Dr. Chandrasekar is the recipient of the 2022 International Leadership Award.
Professor Seshadri T. Chandrasekar, MD, FACG, fondly called TSC, is the Chairman and Chief Gastroenterologist of MedIndia Hospitals, a stand-alone GI institution in Chennai, India, affiliated with The Tamilnadu State Dr. M. G. R. Medical University, where he sits as a distinguished Professor. A multi-gold medalist from his graduate medical school, Madurai, India, he took his MD and gastroenterology fellowship at the prestigious Post Graduate Institute (PGIMER), Chandigarh. Then, after serving as faculty at the Madras Medical College, he established a new department of gastroenterology at the Coimbatore Medical College, Coimbatore, India.
Dr. Chandrasekar pioneered many cutting-edge endoscopic procedures since 1990 and demonstrated many of these interventional endoscopy procedures live in gastroenterology workshops across India, South Asia, and Africa. He has organized several international and national conferences and delivered many prestigious orations and invitational lectures at numerous international conferences. He is credited with noteworthy scientific publications in peer-reviewed journals and serves on the editorial boards of the Journal of Digestive Endoscopy, the Indian Journal of Gastroenterology, and Hepatology
He created teaching CD-ROMs on 14 GI Endoscopy topics and donated them to medical colleges across India. He has trained hundreds of gastroenterology fellows, and many of his mentees have become leaders in India and other South Asian countries. He served as the President of the Indian Society of Gastroenterology (ISG) in 2016 and introduced ACG-ISG collaborative lectures in the national ISG conference.
Undeterred by the pandemic, he passionately organized sixteen international webinars endorsed by ACG and ASGE and witnessed the attendance of several thousand delegates worldwide. He also launched consultdocnow.com, Liver doorbell, and Obesity preventive kit — all web-linked network initiatives — as well as an emergency digital medical care card and COVID-19 hygiene app for public benefit.
Dr. Chandrasekar created “Braille Charts on Hygiene” and distributed them in several health camps organized for the blind. His pilot projects, on assessment of nutrition and IQ for career counselling for school children with visual and hearing impairments, were later converted into statefunded projects. A TEDx invited speaker, Dr. Chandrasekar, continues to guide young professionals worldwide in the art of interventional Gastroenterology.
The Hon’ble President of India bestowed him the ‘Best Individual’ award and Padma Shri award, one of the highest civilian awards, for his outstanding services to gastroenterology and humanity. He has been awarded the ACG Community Service Award, the ASGE International Service Award, and Master award by the World Gastroenterology Organisation (MWGO). He also received the Fellowships (FRCP) of the Royal Colleges of Physicians of Edinburgh, London, Glasgow and Ireland. He was awarded a DSc by the state medical university in Chennai.
He is thankful for the unrelenting support by his wife, Sharmila, and married son, Dr. Viveksandeep, a gastroenterologist at Augusta University Hospital in the USA, and daughter, Rashmica, an engineer living with her husband in Germany.
The International Leadership Award is given to a Fellow or Master of the ACG in recognition of outstanding and substantial contributions to gastroenterology, to the College, and to the international gastroenterology community. Substantial contributions internationally may include, but are not limited to the following: The training of individuals from other countries who have gone on to become leaders in gastroenterology in their community; leadership in international organizations that has resulted in improvement in the care of patients; and participation in humanitarian efforts.
Throughout her career, Dr. Kane has been dedicated to excellence in clinical care, education and clinical/ epidemiological outcomes in gastroenterology with a focus on IBD. Her research spans the breadth of IBD clinical science and she has developed and important niche in the fields of women’s health and pregnancy in IBD.
Dr. Kane has distinguished herself as a preeminent clinician, educator, mentor, and leader. Her presence in the College has been graced with accomplishments and unwavering support for ACG’s role in research, education, and patient care.
Her colleagues describe her as a gifted diagnostician and note her incredible and obvious compassion towards her patients and ability to establish trust with them through genuine empathy. One of Dr. Kane’s nominators reflected that, “anyone who knows Dr. Kane is immediately impressed by her kindness and humanistic qualities. She transmits these into her clinical care where she is a consummate and adored clinician, while at the same time she has assumed leadership positions at every step of the way where she maintained the humanism, enthusiasm, and optimism that only she can confer.”
Dr. Kane is recognized for the breadth and depth of her efforts in teaching, quality, clinical research, and clinical care. She was described as a leader who “gives her all and beyond, yet remains humble, collegial, and indefatigable.”
On the merits of her stellar contributions to clinical practice, passion for education, innovation in clinical research, and outstanding dedication to the College, Dr. Kane fulfills the qualifications and embodies the spirit of the Berk/Fise Clinical Achievement Award.
Dr. Kane is a Professor of Medicine at the Mayo Clinic in Rochester, Minnesota. She has a busy clinical practice that reflects her expertise in IBD, which is also the focus of her research work encompassing new therapies, gender-specific issues, and medication adherence.
Dr. Kane is a prolific researcher and writer, having published over 200 original articles, reviews, and book chapters along with the first two editions of a book for patients on selfmanagement of IBD. She is a passionate teacher, not just to students in the medical school, trainees, and colleagues, but also to patients in her previous role as Chair of the National Patient Education Committee for the Crohn’s and Colitis Foundation. She was the first female Associate Editor for Alimentary Pharmacology and Therapeutics and serves in editorial roles for other journals and is the Section Editor for IBD for UpToDate as well.
Amongst many leadership positions that Dr. Kane holds within Mayo Clinic is the Associate Chair of Patient Experience within the Division of Gastroenterology and Hepatology, and Physician Chair of the Mayo Quality
Academy Fellow Subcommittee. The pinnacle of her leadership journey was being President of the American College of Gastroenterology (ACG) in 2018-2019. Dr. Kane also served on and chaired several ACG Committees including Finance and Budget, Nominating, and Women in Gastroenterology, and served on the Board of the ACG Institute for Clinical Research and Education. She also just completed a 5-year service on the Gastroenterology Specialty Council of the American Board of Internal Medicine.

For all those academic pursuits, her first love remains the clinic. She has a large practice of IBD patients with whom she has formed long lasting bonds. Her office is filled with presents, cards, and tokens of appreciation that she treasures as reminders of her responsibility and duty to her patients.
The Berk/Fise Clinical Achievement Award, formerly the ACG Clinical Achievement Award, is presented to no more than one member/Fellow of the College in any year, and is made in recognition of distinguished contributions to clinical gastroenterology over a significant period of time. In addition to a career of distinguished clinical practice of gastroenterology, specific criteria include contributions in patient care, clinical science, clinical education, technological innovation, and public and community service.

THE NP/PA AWARD FOR CLINICAL EXCELLENCE recognizes a distinguished nurse practitioner or physician assistant who is an ACG Advanced Practice Provider Member and has shown long-standing contributions to advancing clinical practice in the field of gastroenterology and hepatology. These efforts are demonstrated by the awardee’s substantial contributions in GI in the areas of practice expertise, leadership, mentoring, and collaborative activities that have an impact at the state, regional, national or international level. This award is being given for the first time in 2022 to the following two individuals.

Kim Orleck, PA-C, received her undergraduate degree from Emory University in Atlanta, GA, and attended Emory University School of Medicine Physician Assistant Program for a Masters in Medical Science. She also holds a Master’s in Public Health in nutrition from the University of North Carolina at Chapel Hill and she is a registered dietician.
She began her career in gastroenterology upon joining Atlanta Gastroenterology Associates in 2009. Over the last 12 years, her role has evolved from primarily clinical to a mix of clinical and administrative. She has practiced both inpatient and outpatient GI at Atlanta Gastroenterology’s Emory Midtown Hospital location. In 2015 she took on the role of Advanced Practice Provider (APP) Supervisor for Atlanta Gastroenterology Associates. In that position, Ms. Orleck developed a successful recruiting, onboarding, training, and continuing education program for their then 35 APPs. As the practice has grown and partnered with United Digestive, she has been instrumental in leading the practice in the utilization of APPs and subsequently was promoted to Director of Advanced Practice Providers for United Digestive in 2021. Ms. Orleck now leads a team of 80 APPs in 3 states (and growing).
In addition to her clinical and administrative position with Atlanta Gastro/United Digestive, she also holds a part-time faculty position with the Emory University Physician Assistant Program. She teaches at both Emory University and Mercer University PA programs in addition to precepting PA students from Emory, Mercer, and Augusta University. She also leads Emory University’s GI board review annually. She is the chair of education for GHAPP (Gastroenterology and Hepatology Advanced Practice Providers) and on the Advanced Practice Providers and Practice Management Committees for ACG.
Ms. Orleck is passionate about APP education, professional growth, development, and leadership. In her free time, she loves spending time with her 8-year-old twins (boy/girl), 5-year-old son, and husband. She is a fitness enthusiast, a loyal Peloton rider, and avid runner. She has completed over 10 half and full marathons and is looking forward to her next half marathon this fall.

Monica Nandwani, DNP, RN, FNP-BC, began her gastroenterology advanced practice provider career at Johns Hopkins where she completed a year-long gastroenterology nurse practitioner fellowship, the first of its kind, in 2011. She worked at the Center for Neurogastroenterology and Motility at Johns Hopkins until 2016 when she moved to Northern California to assume the role as the first nurse practitioner at the Stanford Esophagus Center. She has provided motility interpretation education to physician and advanced practice provider trainees during her time at Hopkins and at Stanford. In 2019, she was promoted to Manager of Advanced Practice Providers at Stanford Health Care’s Center for Advanced Practice providing administrative and programmatic support for the organization’s over 600 APPs.
Originally from Bacolod City, Philippines, also known as the “City of Smiles,” she came to the United States after high school to spend the year as a foreign exchange student and ended up pursuing a career in nursing. She completed her Bachelor’s and Master’s degrees in Nursing at the Johns Hopkins University School of Nursing and completed her Doctor of Nursing Practice degree at the Duke University School of Nursing.
Passionate about education, APP professional development, quality improvement, and evidencebased practice, she is a member of the ACG Advanced Practice Providers Committee. She has presented at various national GI conferences and co-authored a variety of publications including an article on ‘Incorporating Advanced Practice Providers into Gastroenterology Practice.’.
In her free time, she enjoys hiking, exploring new restaurants, and travelling with her family. She is grateful to her physician and APP mentors in gastroenterology who have guided and supported her through the years and to the College and Awards Committee for their work and advocacy in creating an award that recognizes and highlights the contributions of APPs in gastroenterology and hepatology.

These sessions are available for in-person attendees only
THE AMERICAN COLLEGE OF GASTROENTEROLOGY IS COMMITTED TO SERVING THE SPECIFIC NEEDS OF GI TRAINEES. ACG 2022 includes elements designed with this aim in mind.


Sunday, October 23
Monday, October 24
Monday, October 24
Exhibit Halls AB
4:00 pm
10:30 am
3:45 pm
5:00 pm
11:30 am
4:45 pm
Residents will be able to get hands-on endoscope training in our residentsonly training sessions. Experts will be available to guide residents on the use of the scopes as they navigate tasks using the Thompson Endoscopic Skills Trainer (T.E.S.T)
Monday, October 24
7:45 am
9:30 am
Exhibit Halls AB
The always popular FREE Hands-on Endoscopy Workshop Center sessions will again be offered in the Exhibit Hall. Expert faculty will demonstrate techniques using a wide variety of equipment and products. Attendees will then have an opportunity to practice using the equipment.
Monday, October 24
10:30 am
11:30 am
Richardson Ballroom
The American College of Gastroenterology is introducing a special session for internal medicine residents who are interested in pursuing a career in gastroenterology. Gastroenterology & Hepatology fellowship continues to be one of the most competitive internal medicine subspecialities. This session will focus on answering questions that prospective GI fellowship applicants may have. In addition, a panel of GI fellowship program directors and current GI fellows will share their experiences and tips regarding the application process.
This free session is open to all residents attending the Annual Meeting. No pre-registration is required.
Tuesday, October 25 |
7:30 am - 8:15 am
Room E220
ACG’s journal editors frequently receive questions about how best to get published, how they assess submissions, how to best format a manuscript, and the peer review process. In this session, the editors discuss the most commonly asked questions they receive about the publication process and share pearls of wisdom about what works—and what doesn’t—when submitting papers for publication. If you want to start or improve your publishing career, then don’t miss this valuable opportunity to hear directly from the editors who are eager to help!
This session is free and open to all in-person attendees.
Gain insight from leading experts and learn about the latest tools and techniques when you participate in one or more of the numerous sessions to be offered.
\ GI Fellows-only sessions will be offered on Monday, October 24.

\ Resident Training sessions will be offered on Sunday, October 23, and Monday, October 24.
Please note: All Hands-on Workshop registration will be done via the meeting app; registration for a session will open in the app the day before the session. Space is limited.
am
/ Polypectomy Faculty Leader: Vinay Chandrasekhara,
Foreign Body Removal Faculty Leader: Julie Yang, MD,
Hemostasis Faculty Leader:
J. Qumseya,
CHALLENGE!
ERCP Faculty Leader: Michelle A. Anderson, MD,
EMR / Polypectomy Faculty Leader: Saowanee Ngamruengphong, MD
1:05 pm Stenting Faculty Leader: Mohamed O. Othman, MD Hemostasis Faculty Leader: John R. Saltzman, MD, FACG
4:30 pm
4:40 pm
EUS Faculty Leader: Vanessa M. Shami, MD, FACG ESD with Asian Experts Faculty Leader: Norio Fukami, MD, FACG
Mucosal Ablation Faculty Leader: Prasad G. Iyer, MD, MSc, FACG Hemorrhoid Therapy Faculty Leader: Harry E. Sarles Jr., MD,
ERCP Faculty Leader: Vivek Kaul, MD,
Enteroscopy Faculty Leader: Carol E. Semrad, MD,
Mucosal Ablation Faculty Leader: V. Raman Muthusamy, MD, MAS,
Capsule Endoscopy Faculty Leader: Shabana F. Pasha, MD,
Hemorrhoid Therapy Faculty Leader: Stephen
Hands-On
The College takes great pride in the GI community’s passionate and unwavering commitment to support colorectal cancer (CRC) prevention. In 2015, ACG introduced a prize to recognize the most innovative and impactful CRC awareness efforts: SCOPY—Service Award for Colorectal Cancer Outreach, Prevention & Year-Round Excellence.
THIS YEAR’S JUDGES AWARDED A TOTAL OF 26 SCOPY AWARDS TO AN OUTSTANDING SLATE OF CRC AWARENESS CHAMPIONS. Their initiatives demonstrated a dedication to reaching underserved communities, increasing screening among patients who delayed due to the COVID-19 pandemic, creativity in leveraging new forms of media and integrating pop culture to grow awareness among new audiences, and an understanding that collaboration is key in raising CRC awareness and increasing screening rates.
26 winners were selected by the 2022 SCOPY Awards judges: Tauseef Ali, MD, FACG
Chair, ACG Public Relations Committee
Chief, Gastroenterology Section, SSM Health St. Anthony Hospital; Clinical Assistant Professor, University of Oklahoma; Oklahoma City, OK
Maham Hayat, MD University of Oklahoma Health Sciences Center
Nizar H. Senussi, MD University of New Mexico
Best Comprehensive Digital Production: Kaiser Permanente Center for Health Research and AltaMed Health Services Institute for Health Equity; Portland, OR; Developing Patient-Refined Messaging and Culturally Relevant Materials for Follow-Up Colonoscopy After Abnormal Fecal Testing
Best Foreign Language Patient Outreach: Mayo Clinic Rochester Internal Medicine Residency; Circumventing Gut Reactions: Addressing Myths & Barriers in Colorectal Cancer Screening in the Somali Community
Best Foreign Language Print Media: University Hospital Center; Centre Hospitalier Universitaire Ibn Rochd, Maarif, Casablanca, Morocco; For Optimal Bowel Preparation
Best Foreign Language Video: Ghulam Mujtaba, MD; Suleman Roshan Medical College, Shahdadpur, Sanghar, Sindh, Pakistan; Awareness Video Regarding Colorectal Cancer
Best International Outreach & Education: Akwi W. Asombang, MD, MPH, FACG, FASGE; Massachusetts General Hospital/Harvard Medical School; Colorectal Cancer Patient Education Webinar Series
Best Innovative Multilingual Messaging: Allegheny Health Network, Division of Gastroenterology, Hepatology, and Nutrition; Pittsburgh, PA; Coming Together for Your Health
Best Print Media Tactic to Advance Engagement and Education: Muhammad Sayedul Arefin, MD; Sheikh Russel National Gastroliver Institute and Hospital, Uttara Model Town, Dhaka, Bangladesh; Writing in a Daily Newspaper
Best Public Service Announcements Written and Delivered by Gastroenterologists: Memorial Hermann Health System, Houston; Colon Cancer Awareness Marketing Campaign 2022
Best Screening Initiative with Nurse Navigation: University of Virginia Health; UVA Health Employee Colorectal Cancer Screening Campaign
Best Spanish Language Patient Education Video: Stony Brook Hospital; Stick with Me, and Get Your CRC Screening!
GRAND SCOPY: University of Chicago Medicine & Benjamin Levy, MD; Tune It Up: A Concert To Raise Colorectal Cancer Awareness
Most Creative Community Awareness Initiative: Texas Digestive Disease Consultants & Gastroenterology Consultants of San Antonio (GI Alliance); Gut in the Museum
Most Far-Reaching and Impactful Initiative: GI Alliance (Texas Digestive Disease Consultants, Digestive Health Associates of TX, Gastroenterology Consultants of San Antonio, San Antonio GI Associates, Arizona Digestive Health, Illinois Gastroenterology Group and Utah Gastroenterology); Ad Campaign, "Drama"
SCOPY Best Culturally Conscious Patient Outreach Initiative: Cleveland Clinic, Abu Dhabi; For Women, By Women Endoscopy Team
SCOPY Best Targeted Community Outreach (1 of 2): SBH Health System; Bronx, NY; Increasing Colorectal Cancer Awareness and Screening Tests for the Albanian Community in Bronx, New York
SCOPY Best Targeted Community Outreach (2 of 2): Subhankar Chakraborty, PhD; The Ohio State University Wexner Medical Center; Outreach on Colorectal Cancer Awareness Among the Bhutanese and Nepalese Community in Columbus, Ohio
SCOPY Consistent Creativity & Commitment Award: Ronald Hsu, MD, FACG; Bridging Medicine & Music Seminar and Concert 2022
SCOPY CRC Superheroes Award: Brian L. McGee, MD; Arkansas Diagnostic Center; CHAD: Colorectal Health Advocates & Doctors
SCOPY Creative Vision Award: Vladimir Lamm, MD; Washington University in St. Louis School of Medicine; Route #2: Improving the Bowel Preparation Experience for Patients, Caregivers, and Hospitals with Comics
SCOPY Culture of Creativity Award: Connecticut GI; Dress in Blue Day!
SCOPY Early Advocacy & Artistry Award: Mohid Ali; student, Casady School, Oklahoma City, OK; Abstract Art by High School Art Student for Colon Cancer Awareness
SCOPY Global Outreach Award: Massachusetts General Hospital (MGH) Division of Gastroenterology, MGH Center for Global Health, Pan-African Organization for Health, Education and Research, African Association of Future Gastroenterologists, Society of Gastroenterology and Hepatology in Nigeria, World Gastroenterology Organisation Training Center Lagos and Lagos University Teaching Hospital; Colorectal Cancer in Africa Virtual Symposium: Updates
SCOPY Healthy Living Award: Fred Hutchinson Cancer Center/UW Health; UW Medicine/Fred Medicine Population Health Colorectal Cancer Screening Program 2022 Community Education Event
SCOPY High Impact Media Placements Award: Jinnah Postgraduate Medical Centre, Karachi, Sindh, Pakistan; Screening and Awareness of Colorectal Carcinoma, Identifying Risk Factors and 45 is the New 50 for Screening Colonoscopy
SCOPY Mythbusters Award: Mayo Clinic Rochester; Division of Gastroenterology and Hepatology; Colorectal Cancer Awareness—Fact or Fiction?
SCOPY Polyp Poetry Award: John K. Corless, MD, AGAF; South Carolina Gastroenterology Association; Polypoetry: A New Genre for Colorectal Cancer Awareness














JOIN YOUR ACG COLLEAGUES AND THE GI COMMUNITY FOR THE DIVERSITY IN GI VIRTUAL 5K to celebrate the diversity of the GI profession, shine a light on a critical issue in gastroenterology and medicine, and create a fun, healthy, and thoughtful event with potential for widespread social media visibility and engagement – not to mention enthusiasm from a vocal core constituency of ACG members who run!

Registrants will run or walk on their own, log their activity online, take photos in race “swag” and celebrate via social media during ACG 2022 Annual Scientific Meeting in October. The Virtual 5K is a chance for the entire GI community to show their support, get some exercise, and connect via social media in the weeks surrounding the ACG 2022 Annual Scientific Meeting (October 21 – 26, 2022).
There is a small registration fee but thanks to generous sponsorships from Ironwood and Takeda, proceeds of the event will benefit the ACG Summer Scholars mentorship program for medical students and residents from groups under-represented in medicine.
HOW IT WORKS: Registrants will run or walk on their own, log their activity online, take photos in race “swag” and celebrate via social media using #DiversityinGI during the ACG 2022 Annual Scientific Meeting.


After you run/walk wearing your #DiversityinGI 5K race tee shirt, importantly, be sure to post photos on social media! Encourage your colleagues, friends and family to participate and celebrate the diversity of the GI profession. Support this event by conveying with your words and actions how diversity drives excellence and innovation. REGISTER: bit.ly/ACG-DiversityinGI-22


On Monday, October 24, and Tuesday October 25 at 7:00 am EST plan to meet up with other avid runners outside the South College Street Entrance of the Charlotte Convention Center for a morning run to support #DiversityinGI. This is the entrance near ACG Meeting Registration.

Under the leadership of ACG DEI Committee Chair Dr. Sophie Balzora -- and with inspiration and commitment from numerous College leaders -- ACG continues to strengthen and deepen its longstanding commitment to diversity, equity and inclusion through meaningful action. ACG has launched a "Health Equity and DEI in Gastroenterology" educational module via the ACG Education University. An ongoing collaboration with sister GI organizations as part of the Intersociety Group on Diversity means that ACG is well-positioned in the GI profession as a catalyst for action. Through the ACG Institute, the College is proud to offer a Health Equity Resarch Award of $50,000 to fund research to produce actionable science that will translate to reducing health and/or healthcare disparities, thereby promoting health equity.
Dr. Balzora hopes this virtual 5K event will be celebrate the spirit of inclusion, representation and community that is at the center of the life of the College and offer a dose of healthy activity as we gather for the ACG 2022 Annual Scientific Meeting.
THE UPDATED ACG MONOGRAPH IS A SUPPLEMENT TO THE AMERICAN JOURNAL OF GASTROENTEROLOGY and includes state-of-the-art recommendations that help guide readers to provide the highest quality, evidence-based care for their patients with GI disorders during pregnancy and the postpartum period.
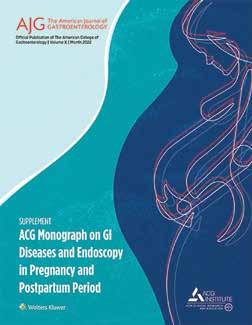
Gastroenterology and hepatology, along with endoscopic practice, have evolved significantly over the past few decades. Similarly, maternal fetal medicine and the care of the pregnant person has become increasingly sophisticated. Gastroenterologists are frequently called upon to provide consultative input and/or perform endoscopy during pregnancy. In order to be able to provide the best possible care to these patients, gastroenterologists need to be aware of (and familiar with) the various nuances and caveats related to the care of pregnant patients presenting with GI and liver disorders.
ACG first published a monograph on the treatment of gastrointestinal disorders during pregnancy in 1994. A subsequent revised monograph was published in 2007. Given the significant advances in both specialties since then, the ACG, under the auspices of the Women in GI Committee and in collaboration with the ACG Institute for Clinical Research and Education commissioned a newly updated third edition of the monograph. The objective of this compendium is to provide the current best practice approaches and guideline-based recommendations in the treatment of various GI and liver disorders and endoscopy practice in pregnancy and the postpartum period.
The editors and authors hope that this information will help gastroenterologists, obstetricians, and non-gastroenterologists understand and manage gastrointestinal problems that can occur or worsen during pregnancy (or are unique to pregnancy). The monograph has been a collaborative effort between various subject matter experts from the fields of gastroenterology, hepatology, obstetrics/gynecology, maternal-fetal medicine, and nutrition. This monograph would not have been possible without the hard work, time, and effort of all the contributing authors.
Linda Anh B. Nguyen, MD
Jaclyn Elkins, RD
Amy S. Oxentenko, MD, FACG

Kerry Dunbar, MD, PhD
Vani J. A. Konda, MD, FACG
Rena Yadlapati, MD, MSHS, FACG
Stacy B. Menees, MD
Aline Charabaty, MD, FACG
Anthony J. Lembo, MD, FACG

David L. Hepner, MD, MPH

Uzma D. Siddiqui, MD, FACG
Amrita Sethi, MD
Subhas Banerjee, MD
Prabhleen Chahal, MD, FACG


Nancy S. Reau, MD, FACG

Santiago J. Munoz, MD, FACG Thomas D. Schiano, MD
Biotech, Inc.
Amy Lightner, MD
Kellie L. Mathis, MD
IBD
Eugenia Shmidt, MD
Marla C. Dubinsky, MD
Satish S.C. Rao, MD, PhD, FACG
David A. Johnson, MD, MACG
Waqar A. Qureshi, MD, FACG
Yun Yan, MD, PhD

Shivangi T. Kothari, MD, FACG Chair, ACG Women in GI Committee
Sunanda V. Kane, MD, MSPH, FACG ACG Past President
Vivek Kaul, MD, FACG Chair, ACG Innovation & Technology CommitteeASSOCIATE EDITORS Lori M. Gawron, MD, MPH, FACOG Martha B. Kole-White, MD, FACOG Jason Sauberan, PharmD BOARD OF TRUSTEES LIAISON Mark B. Pochapin, MD, FACG
always plenty
on
Inc. 1535
735
635
Health 942 Boston Scientific 519
- A Part of Sebela Pharmaceuticals 825* Bristol Myers Squibb 425
Diagnostics 744
Inc. 339 CapsoVision, Inc. 1234
Biosciences 2209*
Diagnostics 1525
Mercy Health 1441 ChiRhoClin, Inc.
Collaborative Medical Solutions 1940
of Crohn's and Chronic Illness 2037* Colorectal Cancer Alliance 1141 ColoWrap 342
Commonwealth Diagnostics International, Inc. 2229* CompHealth 430 Concord Hospital 1243 Cook Medical 1119 Creo Medical 325
CRH Medical Corporation 1019*
Definitive Healthcare 636 Digestive Care, Inc. 918
DRW Healthcare Staffing
Health
Lilly & Co.
Pharmaceuticals
GI medical
EndoGastric Solutions
EndoSoft
Endo-Therapeutics, Inc.
Enterra Medical 1342
USA
Evoke Pharma 1041
Sciences
ExeGi
Corporation
Gastroenterology
Laboratory Management,
Division
Sciences
Guthrie Medical Group
Foods
LOCUMS
Healix Infusion Therapy,
Foundation
Inc.
Hologic
Inc.
Inc.
University Health
Intercept Pharmaceuticals, Inc. 1235
Intermountain Healthcare 329 International Foundation for Gastrointestinal Disorders 1135
Interpace Diagnostics 925
Intra-Sana Laboratories 230
IntroMedic America, Inc. 843
Iterative Health 1341* Jackson & Coker 2135
Janssen Biotech, Inc. 1625*, 1817
Konsyl Pharmaceuticals, Inc. 1937 Laborie 1618
Lynx.MD 2134
Madrigal Pharmaceuticals 2213
Mahana Therapeutics 343
Mallinckrodt Pharmaceuticals 501 Medspira, LLC 1240
Medtronic 801
Merck & Co., Inc. 634, 713
Meridian Bioscience, Inc. 1044
Merit Medical Endotek 916
Micro-Tech Endoscopy USA 224
Mindset Health 240
Modernizing Medicine 1209
Mother to Baby Pregnancy Studies Conducted by the Organization of Teratology Information Specialists 1205
Motus GI 2035
Neptune Medical Inc. 1541
Nestle Health Science 1140
Nestle Health Science (US Pharmaceuticals) 1307
Nextservices 1014
Northwell Health 1836
Norton Medical Group 438
NYU Langone Health 1843
Officite 434
Olympus America Inc. 1005
Omega Medical Imaging 328
One GI 2234
OSF Healthcare 340
Ovesco Endoscopy 812
Palmetto Infusion 943
PE GI Solutions 1304
PENTAX Medical 1616
Perspectum Ltd. 234
Pfizer 1325*
Pfizer - Medical Information 2015
Phathom Pharmaceuticals 835
Pinnacle GI Partners 439 PracticeLink 1521
Prisma Health 1841*
Prometheus Laboratories 1308
Provation 1335, 1339
Provider Solutions & Development 2136
QDX Pathology Services 903
Qleanse 538
QOL Medical, LLC 927 Quad A 337 ResiCal, Inc. 1434
Rockett Healthcare, LLC 225
Rocky Mountain Gastroenterology 1439
RosmanSearch 944
Salix Pharmaceuticals, Inc. 1615
Sandoz 1035
Saneso Inc. 625
Sanford Health 335
Sanofi and Regeneron 809*
Seagen 436
Seres Therapeutics, Inc. 327
Seres Therapeutics/Aimmune Therapeutics 227
Smart Medical Systems Ltd. 1002
SML Med-Tech Solutions Limited 1042
Sonic Healthcare USA, Anatomic Pathology 1634
South Georgia Medical Center 228
SpaceBander Corp 2207 Staff Care, Inc. 334
STERIS Endoscopy 719
Takeda Pharmaceuticals U.S.A., Inc. 1024, 1025, 1028, 1225, 1313
The Delta Companies (Delta Physician Placement & Delta Locum Tenens) 845
The Permanente Medical Group/ Kaiser Permanente 1244
The Rome Foundation 336
United Porphyrias Association 1144
Veterans Health Administration 1440 Vial 1438*
Virtua Health 1238
Weatherby Healthcare 631
Wellstar Medical Group 1242
World Gastroenterology Organisation (WGO) 1143
* Virtual booth upgrade with additional company information.
Industry-sponsored satellite symposia provide additional educational opportunities for attendees. These programs are independent of the ACG 2022 Annual Scientific Meeting and Postgraduate Course programs. The ACG is not the continuing medical education provider of these programs. Unless otherwise noted, all symposia will take place at the Westin Charlotte. For more information, see the company sponsor.
*Assessing Ulcerative Colitis: Is There Something Your Patient Isn’t Telling You?
5:30 am - 7:30 am
ACG Junior Faculty Development Award $150,000 a year for three years
Established Investigator Bridge Funding Award up to $150,000 a year for two years




Health Equity Research Award up to $75,000 ($50k year-one, $25k year-two based on progress)
ACG/ASGE Epidemiologic Research Award in Gastrointestinal Endoscopy up to $50,000 for research utilizing the GIQuIC database
NOTE: Deadline Friday, December 9, 2022 Clinical Research Award up to $50,000 for clinical research
Clinical Research Pilot Award up to $15,000 for pilot projects

Resident Clinical Research Award up to $10,000
Medical Student Research Award up to $5,000 for 6–10 week summer project
Charlotte Convention Center Room E217
Join us for this hybrid interactive case-based discussion exploring unmet patient needs related to ulcerative colitis assessment and management. The symposium will take place on Monday, October 24th from 6:30–7:30 AM (EST). Breakfast will be served starting at 5:30 AM. This program is sponsored by Eli Lilly.
*Exploring Cholestatic Pruritus in PBC—are we even scratching the surface? Alan Bonder, MD; Robert G. Gish, MD; Binu V. John, MD, MPH, FACG
7:00 pm – 9:00 pm
Uptown Ballroom I
Previous studies have demonstrated low understanding of the mechanism of disease for cholestatic pruritus in PBC, as well as mismatch in the burden of disease experienced by the match compared to the physician perception of that burden. This symposium will review the definition diagnosis of PBC and cholestatic pruritus (CP), as well as the patient journey and course of illness, mechanism of disease, disease burden, and current treatment options.
This program is sponsored by GlaxoSmithKline.
Most Patients With Ulcerative Colitis ‘Can’t Wait’:
The Impact and Clinical Assessment of Bowel Urgency
Marla C. Dubinsky, MD; David T. Rubin, MD, FACG; Subrata Ghosh, MD, FMedSci
7:00 pm - 9:00 pm
Grand Ballroom C Prof. Marla C. Dubinsky, Prof. David T. Rubin and Prof. Subrata Ghosh will discuss the impact and clinical assessment of bowel urgency.
This activity is supported by an educational grant from Lilly.
Marla C. Dubinsky, MD; Miguel D. Regueiro, MD, FACG
6:00 am - 8:00 am
Charlotte Convention Center - Room E217
This program is sponsored by Pfizer.
Cutting-Edge Therapies and Cross-Disciplinary Approaches for Crohn’s Perianal Fistulas Mahmoud Al-Hawary, MD, FSAR; Tina Aswani-Omprakash; David P. Hudesman, MD, FACG; Amy Lightner, MD; Kelsey N. Trull, PA-C
7:00 pm - 9:00 pm
Grand Ballroom AB
Review the latest advances in care for patients with Crohn's perianal fistulas (CPF), including emerging clinical evidence, novel treatments, stem cell therapies, and evolving approaches for multidisciplinary coordination of care. Firsthand perspectives from patients with CPF will provide a window into the need for patient-centric care in daily practice.
This activity is supported by an educational grant from Takeda Pharmaceuticals U.S.A., Inc.
*Partnering With Patients: Personalizing Care for IBS-C Brooks D. Cash, MD, FACG; Amol Sharma, MD, FACG
7:00 pm - 9:00 pm
Grand Ballroom C
Irritable bowel syndrome with constipation (IBS-C) is a chronic disease that substantially impacts patients’ physical and psychosocial well-being. Many patients go years before being diagnosed, and a significant proportion remain undiagnosed and untreated. In this live symposium, expert faculty will discuss the latest clinical evidence and best practices for the diagnosis and treatment of IBS-C. Presentations will be aided by a clinical whiteboard to illustrate key concepts in the complex pathophysiology of IBS-C that now be targeted by FDA-approved treatments. In addition, a patient with IBS-C will join the panel and provide her perspective on the diagnostic and treatment journey, as well as tips for improving dialogue with patients to optimize care of patients with this burdensome condition.
This program is supported by an independent educational grant from Ardelyx
*Session will be recorded and will be made available on the ACG Virtual Conference Platform after the live program.
OPEN TO ALL IN-PERSON ACG 2022 ATTENDEES. These presentations provide additional educational opportunities for attendees. No CME is provided for Theater presentations. The Exhibitor Product Theater is located in booth 2117 in Exhibit Hall AB.
Could It Be More Than Occasional Constipation? Time To Have A Deeper Conversation With Your Patient
Darren M. Brenner, MD, FACG
10:30 am – 11:30 am
IBS-C impacts nearly 11.5 million Americans. It’s a condition that is characterized by constipation, as well as chronic and burdensome symptoms like pain, bloating, and discomfort. Research shows many patients are uncomfortable discussing the totality of their symptoms with their healthcare provider. Come to a clinical review to learn more about a treatment that may help adults with IBS-C.
This program is sponsored by Ironwood Pharmaceuticals.
From Diagnosis to Treatment: Assessing Moderately to Severely Active Crohn’s Disease
Anita Afzali, MD, MPH, MHCM, FACG
11:45 am – 12:15 pm
An interactive case study discussing a hypothetical Crohn’s disease patient. This case will cover patient presentation, biomarker and imaging findings, treatment options, and follow-up.
Sponsored by Takeda Pharmaceuticals U.S.A., Inc.
Emerging Concepts in Nonalcoholic Steatohepatitis (NASH) Naim Alkhouri, MD, and Kimberly A. Brown, MD
12:30 pm – 1:00 pm
This session will explore several emerging concepts in NASH including: (1) epidemiology and comorbidities, (2) pathophysiology and the role of lipotoxicity in the liver, (3) morbidity and mortality, (4) patient identification and monitoring approaches, and (5) disease management strategies.
This program is sponsored by Madrigal Pharmaceuticals.
UC Powerful Evidence: A therapy that helps deliver clinical remission and histologic and endoscopic outcomes for adult TNFi-IR patients with moderate to severe ulcerative colitis (UC) Miguel D. Regueiro, MD, FACG 1:15 pm – 1:45 pm
The program is sponsored by AbbVie.
Eosinophilic Esophagitis: Discover a New Treatment Option for Your Appropriate Patients
Ikuo Hirano, MD, FACG
2:00 pm – 2:30 pm
Take an afternoon break with us to learn about an exciting new advancement in the treatment of eosinophilic esophagitis. An expert will walk us through clinical data, an example of an appropriate patient, and answer your questions!
This program is sponsored by Regeneron Pharmaceuticals, Inc. and Sanofi.
An Innovative Approach to the Treatment of Adults with Irritable Bowel Syndrome with Constipation (IBS-C)
Susan L. Lucak, MD 2:45 pm – 3:15 pm
Please join us for an engaging session about an innovative approach to treat adults with Irritable Bowel Syndrome with Constipation (IBS-C).
This program is sponsored by Ardelyx.
The Power of the Microbiome: Can it be harnessed to break the cycle of recurrent Clostridioides difficile infection (rCDI)?
Paul Feuerstadt, MD, FACG
3:45 pm - 4:45 pm
Understand the role of the microbiome in overall health and the essential, symbiotic roles of Bacteroidetes and Firmicutes
• Explore the relationship between the gut microbiome, pathogenesis of Clostridioides difficile infection (CDI), and the cycle of recurrence • Describe the profound burden of rCDI during and beyond acute infection • Evaluate the potential of microbiome-based therapeutics in the management of rCDI.
This program is sponsored by Ferring Pharmaceuticals, Inc.
The Power to Eradicate H. pylori Infection in Adults
Colin W. Howden, MD, FACG
10:35 am – 11:30 am
Join Dr. Colin Howden for an engaging session on a new therapeutic option in the treatment of H. pylori infection and the role of acid suppression in enhancing antibiotic effectiveness.
This product theater is sponsored by Phathom Pharmaceuticals and is not a continuing medical education program.
Long-term Safety and Efficacy Data for a Chronic Hepatitis B (CHB) Treatment Option
11:45 am – 12:15 pm
During this presentation, we will discuss the prevalence of chronic hepatitis B, the burden of disease, and the current treatment guidelines. We will also share the latest updated efficacy and safety data for a CHB treatment.
Sponsored by Gilead Sciences, Inc.
Presenting New 4-Year Data in UC and 5-Year Data in CD Anita Afzali, MD, MPH, MHCM, FACG, and Jennifer Seminerio, MD 12:30 pm – 1:00 pm
New 4-year efficacy and safety data in UC. Join a peer discussion on Lasting* Remission at the STELARA® Product Theater *In both the CD and UC studies, many patients achieved clinical remission at 1 year with STELARA®
This program is developed and sponsored by Janssen Biotech, Inc.
Eosinophilic Esophagitis: Discussing the Clinical Implications of Disease Progression Joy W. Chang, MD 1:15 pm – 1:45 pm
Join us as we bring type 2 inflammation to the discussion in a way that is meaningful to your patients with eosinophilic esophagitis and clinical practice. Hear about the clinical implications of uncontrolled type 2 inflammation on the chronic and progressive nature of this disease.
Sponsored by Regeneron Pharmaceuticals, Inc. and Sanofi.
How Race Affects the Treatment and Diagnostic Journey in IBD
Evelyn Lewis, MD, MA, FAAFP, DABDA; Marie L. Borum, MD, EdD, MPH, FACG; and Melodie Narain-Blackwell 2:00 pm – 2:30 pm
Join Dr. Marie Borum, a gastroenterologist with expertise treating patients from minority groups, and Melodie Narain-Blackwell, a Black patient with Crohn's disease, for a discussion about disparities in diagnosis and healthcare resource utilization across racial and ethnic groups in inflammatory bowel disease (IBD).
This panel discussion aims to help raise awareness about current challenges and how they can be addressed with the goal of improving patient outcomes.
This program is sponsored by Takeda Pharmaceuticals U.S.A., Inc.
December 2–4, 2022
Grand Hyatt | Nashville, TN
January 27–29, 2023
Caesars Palace | Las Vegas, NV
February 24–26, 2023
Hilton New Orleans Riverside | New Orleans, LA
March 10–12, 2023
June 2–4, 2023
Washington,
A0632. Increasing Inpatient Endoscopy Volumes Using the Model for Continuous Improvement A0635. Second Primary Malignancy in Gastrointestinal Stromal Tumors: Insights From a Population-Based Analysis A0651. A Case of Systemic Mastocytosis Diagnosed Endoscopically A0685. Pooled Efficacy Analysis of Tradipitant in Idiopathic and Diabetic Gastroparesis Study VP-VLY-686-3301 and VPVLY-686-2301
A0687. The Epidemiology of Gastric Cancer in the United States: A Population-Based Study A0696. Malignant Transformation of a Gastric Duplication Cyst: A Rare Entity
A0708. Gastric Adenocarcinoma of the Remnant Stomach After Roux-en-Y Diagnosed by EDGE A0726. From Zero to Gyro: A 12-Month Trial of a LumenApposing SEMS on a Benign Recalcitrant Post Surgical Stricture
A0729. Gastric Metastasis of Merkel Cell Carcinoma: A Rare Cancer A0735. Pylorus-Directed Therapy for Gastroparesis Using EsoFLIP
NEW FOR 2022! With a record number of abstracts submitted to ACG, we have added a dedicated Poster Hall in the Crown Ballroom in order to display the 3,675 posters accepted for presentation, and have expanded the poster sessions from 3 to 5 sessions. Learn about the latest clinical research from colleagues from across the U.S. and around the world when you visit the ACG 2022 Poster Hall. Posters will be presented beginning Sunday afternoon through Tuesday. Over 220 of the more than 3,600 posters presented this year have been honored with a Presidential Poster Award. Determined by the ACG Abstract Selection Committee, approximately 5% of accepted abstracts annually receive this distinction for high-quality, novel, unique and interesting research. Listed below are this year’s Presidential Poster Award recipients, which will be recognized with a blue Presidential Poster ribbon pinned to the poster during the ACG 2022 poster sessions. Additionally, all posters will be viewable online as ePosters on the ACG 2022 Conference Platform beginning at 12:00pm (Eastern time) October 23, and will be accessible until March 31, 2023 when the platform closes. Presidential Poster Award recipients will be recognized in the ePoster Hall by a blue ribbon icon.
SCIENTIFIC POSTER SESSION A Sunday, October 23 • 3:00 pm - 5:00 pm
P0002. A0017. Mortality in Acute Necrotizing Pancreatitis at Baseline (MANP)-B Scoring for the Inpatient Mortality of Acute Necrotizing Pancreatitis A0060. Pancreatitis-Related Purtscher's-Like Retinopathy Presenting With Visual Hallucinations
A0084. Outcomes of Patients Receiving Bezlotoxumab for the Prevention of Recurrent Clostridioides difficile Infection –A Multicenter Study
A0125. Extramammary Perianal Paget Disease, Colonoscopy Findings That Led to the Diagnosis of a Genitourinary Mass A0137. Isolated Cardiac Metastasis as an Initial Presentation of Colorectal Cancer in a Young Male Due to Lymphatic Spread
A0150. A Rare Association of Colonic Malakoplakia With Type 2 Diabetes Mellitus
A0168. Serrated Polyps in Patients With Positive FIT or MtsDNA, or Colonoscopy Only: Data From the New Hampshire Colonoscopy Registry
A0169. What Do "False-Positive" Stool Tests Really Mean? Data From the New Hampshire Colonoscopy Registry
A0192. Health Care Resource Utilization and Costs Among Eosinophilic Esophagitis Patients in the United States A0198. Esophageal Cytology Collection Device for Assessment of Esophageal Eosinophilia in Eosinophilic Esophagitis: Real World Experience
A0199. Cannabis Interferes With Deglutitive Inhibition Assessed by Response to Multiple Rapid Swallows During High-Resolution Esophageal Manometry
A0202. Dramatic Stabilization of Trend of Esophageal Adenocarcinoma (EAC) in the United States: A PopulationBased Time-Trend Analysis of Surveillance, Epidemiology and End Results Program Database (SEER), 2001-2018
A0213. Oral Viscous Budesonide Ameliorates PPIRefractory Lymphocytic Esophagitis: A Longitudinal Clinical, Endoscopic, and Histologic Outcome Case Report A0224. Esophageal Perforation Following Atrial Fibrillation Ablation: A Review of Ablation-Associated Esophageal Injury A0236. Vape-Induced Herpes Simplex Esophagitis in an Immunocompetent Host
A0247. Impact of COVID-19 on Motility Practices: New Onset Gastrointestinal and Autonomic Dysfunction After COVID-19 and the Effects of Vaccination in a Nationwide Cohort Study
A0250. Development and Validation of Brain Fog Questionnaire in Patients and Healthy Volunteers
A0255. A Case Series of 25 Auto-Brewery Syndrome Patients: A Single Community Hospital Experience A0268. Rubber Band Ligation versus Infrared Coagulation in the Management of Hemorrhoidal Disease: A Systematic Review and Meta-Analysis A0293. Efficacy and Safety of Hemorrhoid Energy Therapy in Hemorrhagic Internal Hemorrhoids: A Single Center Retrospective Study
A0295. Comparison of Over-the-Scope Clips and Standard Therapy for Management of Non-Variceal Upper GI Bleed: A Systematic Review and Meta-Analysis A0296. Trend Analysis of Lower Gastrointestinal Bleeding Over a Decade: A Population-Based Study
A0324. Not Your Everyday Duodenal Ulcer: Massive GI Bleed Secondary to Extramedullary Plasma Cell Myeloma
A0403. A Slippery Slope: Inflammatory Bowel Disease and Transitions in Care A0414. Multifocal Small Bowel Adenocarcinoma as Primary Presentation of Crohn's Disease in a Patient With a Remote History of Celiac Disease
A0428. Outcomes and Trends of Endoscopic Retrograde Cholangio-Pancreatography in Bariatric Surgery Patients - A National Inpatient Sample (NIS) Study
A0431. Closure of an Iatrogenic Duodenal Perforation Using a Novel Tack and Suturing System
A0438. Diagnosis and Correction of Afferent Limb Reflux After Single Anastomosis Duodenoileostomy: A Novel Endoscopic Approach
A0520. Transjugular Intrahepatic Portosystemic Shunt as a Cure for Macrohematuria
A0534. The Spectrum of Spontaneous Bacterial Empyema: An Elusive Disease A0540. Tocilizumab as an Effective Steroid-Sparing Agent for the Treatment of Recurrent and Steroid-Dependent Immune Checkpoint Inhibitor-Mediated Hepatotoxicity: A Case Study and Insight into Pathophysiology A0542. COVID-19 Vaccine-Induced Liver Injury: A Case Series A0583. Clinical Course and Diagnostic Challenge of Jamestown Canyon Virus Infection in Post Liver Transplant Recipient With Altered Mental Status A0596. Monoclonal Antibodies (mAbs) to GlucoseDependent Insulinotropic Polypeptide (GIP) Prevent and Treat Obesity in Wild-Type (wt) and Leptin-Deficient (ob/ob) Mice A0600. Metatranscriptomic Analysis of Pediatric Esophageal Epithelium and Microbiome Response to Proton-Pump Inhibitors
SCIENTIFIC POSTER SESSION B Monday Morning, October 24 10:00 am - 12:00 pm
B0005. Incidence and Risk Factors for Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE) in Necrotizing Pancreatitis (NP) - An Underappreciated Sequalae B0012. Short- and Long-Term Outcomes of Necrotizing Pancreatitis After Endoscopic, Percutaneous and Surgical Management
B0065. A Rare Case of Intraductal Papillary Mucinous Neoplasm of the Biliary Ducts With Malignant Degeneration into Cholangiocarcinoma B0105. Real World Validation of an Artificial Intelligence Characterization Support System for Prediction of Polyp Histology in Colonoscopy: Interim Analysis of a Prospective Multicenter Study
B0118. Colonic Mucormycosis as a Complication of COVID Pneumonia: A Case Report B0133. When GI Endoscopy Shines a Light on the Endometrium B0171. Risk Factors of Colorectal Cancer in Africa: A Systematic Review and Meta-Analysis B0178. Improving Adherence to Colorectal Cancer Screening Recommendations for First-Degree Relatives of Patients With Advanced Adenomas B0184. Solitary Penile Lesion: A Peculiar Presentation of Colorectal Cancer Recurrence and Metastasis B0185. Taking Caution at Road’s End: Incidental Finding of Appendiceal Goblet Cell Tumor on Colonoscopy B0186. Light at the End of the Tunnel: Pipeline to the Jejunum
B0188. Recurrent Obstruction After Surgical GJ in a Rare Case of Gastric Outlet Obstruction: EUS to the Rescue B0194. Mushroom Sign: Complete Esophageal Obstruction Following Endoscopic Variceal Band Ligation B0202. Dupilumab Treatment Leads to Rapid and Sustained Improvements in Dysphagia B0229. A Rare Case of Metastatic Muscle Invasive Bladder Cancer to the Esophagus B0230. Use of Upadacitinib in Refractory Esophageal Lichen Planus: Endoscopic Improvement in "Planus" Sight B0274. IgG-based Elimination Diets for Patients with IBS: Results From a Prospective, Multi-Center, Double-Blind, Placebo-Controlled Trial B0318. Prophylactic Epinephrine Injections for the Prevention of Postpolypectomy Bleeding: A Meta-Analysis B0331. GI Bleeding From an Unusual Cause in an Unusual Place B0332. Intestinal Endometriosis Leading to Recurrent Hematochezia B0333. Don’t Get Fooled: Scurvy Can Mimic Portal Hypertensive Gastropathy Bleeding B0347. An Unusual Cause of Obscure Gastrointestinal Bleeding B0363. Serum Ustekinumab Concentrations Are Associated With Improved Outcomes With the Magnetic Resonance Index of Activity for Crohn's Disease B0372. Endoscopic Disease Activity and Biologic Therapy Are Independent Predictors of Suboptimal Bowel Preparation in Patients With Inflammatory Bowel Disease Undergoing Colonoscopy: A Multicenter Analysis B0414. Insurance Companies’ Poor Adherence to ACG/AGA Guidelines for Moderate to Severe Ulcerative Colitis and Crohn’s Disease Management B0428. A New Protein Losing Enteropathy: Autoimmune Cryptolytic Enterocolitis
B0445. Are Advanced Endoscopy Fellows in the United States Achieving Adequate ESD Experience?
B0465. Closing the Gap: First Report of Endoscopic Suture Closure of Malignant Gastric Hemorrhage
B0503. Mild Thrombocytopenia as a Predictor of Surgical Outcomes Following Cholecystectomy: A Tool for Perioperative Assessment in Patients With Non-Alcoholic Fatty Liver Disease?
B0517. Beta-Blockers Protective of Decompensated Congestive Heart Failure (dCHF) in Patients With Cirrhosis After Transjugular Intrahepatic Shunt (TIPSS) B0546. A Rare Case of Refractory Drug Induced Liver Injury Following Ocrelizumab Use for Multiple Sclerosis
B0564. Acute Alcoholic Hepatitis With Portal Hypertension Complicated by Tuberculous Peritonitis and Ascites B0629. Effects of Heterozygous Variants in the LeptinMelanocortin Pathway on Transoral Outlet Reduction After Roux-en-Y Gastric Bypass
B0634. Effect of Probiotics on Mental Health and Their Association With Serum Neurometabolites in Adults With Depression or Anxiety: A Systematic Review and MetaAnalysis
B0666. A Case of Progressive Refractory Diarrhea due to Zollinger-Ellison Syndrome
B0670. A Case of Invasive Gastrointestinal Mold Infection B0681. Females May Be at Higher Risk of Severe and Dysplastic Fundic Gland Polyposis: An 844-Patient Analysis B0711. Cellulase With Prokinetics Is an Effective Dissolution Therapy for Gastric Phytobezoars
B0714. See Something, Say Something: GPS Tracker Foreign Body Ingestion as a Unique Presentation of Human Trafficking B0733. Unique Approach to Refractory Nausea With Ketamine Infusion
SCIENTIFIC POSTER SESSION C Monday Afternoon, October 24 3:00 pm - 5:00 pm
C0005. Impact of Pancrelipase on Stool Frequency and Consistency in Patients With Exocrine Pancreatic Insufficiency Due to Chronic Pancreatitis or Pancreatic Surgery: Analysis of Randomized Trial Patient-Reported Daily Symptoms
C0011. Development of a Clinical Screening Tool for Exocrine Pancreatic Insufficiency in Patients With Chronic Pancreatitis C0040. A Novel Approach to Obtaining Tissue in a Difficult to Access Indeterminate Biliary Stricture: Percutaneous Cholangioscopy and Biopsy
C0053. Isolated Intramural Gastric Metastasis of Pancreatic Ductal Adenocarcinoma (PDAC) Detected on Surveillance Esophagogastroduodenoscopy (EGD) Before Endoscopic Ultrasound (EUS) Guided Biopsy
C0072. Sarcoidosis Masquerading as Pancreatic Adenocarcinoma: A Case Report
C0084. Hypertriglyceridemia Independent Propofol-Induced Acute Pancreatitis – A Rare and Unusual Complication
C0085. Incidence and Outcomes of C. difficile Infection Following Colon Ischemia
C0089. Long-Term Risk of Colorectal Cancer in Patients With Prediabetes: A Systematic Review and Meta-Analysis C0093. Examining Colorectal Cancer (CRC) Stage at Initial Diagnosis Before and During the COVID-19 Pandemic in the United States
C0099. Impact of Socioeconomic Status on Colorectal Cancer Survival in the United States: A Population-Based Study 2010–2018
C0135. McKittrick-Wheelock Syndrome: A Case Report and Review of Literature
C0144. Metastatic Melanoma to the Cecum 10 Years After Surgical Resection of the Primary Cutaneous Tumor
C0156. Treatment of Refractory ICI-Associated Colitis With Fecal Microbiota Transplant
C0183. Screening With FIT-DNA: Impact on Colonoscopy Withdrawal Time, Adenoma Detection and Endoscopist’s Recommendation for Follow-Up
C0184. Colorectal Cancer Screening Rates at Federally Qualified Health Centers in 2019 and 2020 Varied Based on Urban-Rural Status and Predominant Racial/Ethnic Group C0211. Anesthesia Choice Can Affect EndoFLIP®
Measurements and Thereby Misdiagnose Esophageal Motility Disorders C0220. Co-Localization of Immunoglobulin G4 (IgG4) and Milk Proteins Is Associated With Eosinophilic Esophagitis Disease Activity
C0225. Higher Rates of Dysphagia Incidence Among Patients With Malignant Primary Brain Tumors Compared to Brain Metastases: A National Study of Medicare Beneficiaries
C0235. A Rare Case of Esophageal Carcinoma After Tracheoesophageal Fistula Repair
C0242. Achalasia as a Sequelae of COVID-19
C0244. The Efficacy and Safety of Treatment Outcomes for Refractory Benign Esophageal Strictures Using a Novel Combination of Needle-Knife Stricturoplasty, Balloon Dilation, and Steroid Injection
C0276. Virtual Visits for Initial Evaluation of Constipation Are Associated With Reduced Outpatient Order Compliance
C0289. Efficacy and Safety of the Push and Pull Method for Treatment of Food Bolus Impaction: A Systematic Review and Meta-Analysis
C0290. Cap-Assisted Endoscopy for Esophageal Foreign Bodies: A Meta-Analysis
C0333. EUS-Guided Coil Embolization and Absorbable Hemostatic Gelatin Sponge Is a Safe and Efficacious Treatment of Rectal Varices
C0338. Tacrolimus-Induced Esophageal and Colon Ulcers: A Case Report
C0344. An Unusual Cause of Upper Gastrointestinal Bleed: Temporary Epicardial Pacing Wire
C0393. Clinical Utility of Precision-Guided Dosing Tool for Infliximab During Maintenance Therapy of Inflammatory Bowel Disease
C0425. Endoscopic Management of Obstructing Pouch Twist C0429. Lactobacillus Sepsis, Endocarditis, and Septic Emboli in a Patient with Ulcerative Colitis Taking Probiotics
C0451. Endoscopic Sleeve Gastroplasty in Class III Obesity (BMI>40): A Propensity-Matched, Retrospective Comparison of Short-Term Safety and Efficacy vs Bariatric Surgery
C0465. Disseminated Cryptococcosis Masquerading as Large Abdominal Mass Concerning for Pancreatic Malignancy in HIV-Positive Patient
C0468. Relief of Malignant Gastric Outlet Obstruction With Lumen Apposing Metallic Stent-Assisted Percutaneous Endoscopic Gastrostomy Tube After Roux-en-Y Gastric Bypass
C0470. Refractory Bleeding From Nodular Gastric Antral Vascular Ectasia (GAVE): Is Combination Therapy of Sclerotherapy and Band Ligation the Solution?
C0479. Endoscopic Ultrasound Guided Drainage of a Massive Right Sided Hemorrhagic Liver Cyst: The Rapidly Evolving Field of Endo-Hepatology
C0482. Spiration Valve to Manage Esophago-Bronchial/ Pleural Fistulas: A Novel Approach
C0483. Novel Use of Lumen Apposing Metal Stent for Management of Gastrointestinal Perforations
C0500. NAFLD Prevalence in BMI Subclass and Outcomes in 2019
C0518. Mortality in Patients With Lean NAFLD: A Systematic Review and Meta-Analysis
C0530. Assessment of Hospital Readmissions in Decompensated Cirrhosis: Are We Doing Enough?
C0552. A Superfood With a Dark Side: A Case of Severe Liver Injury Due to Turmeric
C0594. Metastatic Ocular Melanoma Mimicking Budd-Chiari Syndrome
C0597. Liver Transplant for Management of Neurological Wilson Disease in a Patient With Preserved Liver Function
C0642. Clinicopathologic Characterization and Genotype Correlation of Duodenal Polyposis Among Hispanics With Familial Adenomatous Polyposis
C0653. Diaphragm Disease: A Crohn's Mimicker?
C0730. Herpes Gastritis: A Rare Cause of Gastric Outlet Obstruction
SCIENTIFIC POSTER SESSION D Tuesday Morning, October 25 10:00 am - 12:00 pm
D0001. Endoscopic Ultrasound-Guided Pancreatic Duct Drainage: A 10-Year Single-Center Experience
D0005. Pilot Trial of Endoscopic Ultrasound-Guided Fiducial Marker Placement to Facilitate Intraoperative Management of Pancreas Tumors
D0009. Partially-Covered versus Uncovered: SelfExpandable Metal Stents in the Palliative Treatment of Malignant Distal Biliary Obstruction
D0060. Hepatolithiasis Caused by Right Hepatic Artery Branches Forming an Arterial Ring Compressing the Common Hepatic Duct
D0070. Acute Pancreatitis Secondary to PembrolizumabInduced Hypertriglyceridemia: First Clinical Experience
D0076. Diagnosis of Biliary Varices Using Digital Cholangioscopy: Uncommon Cause of Biliary Obstruction and Bleeding
D0097. Low Volume Preparation Regimen for Colon Capsule Endoscopy – Clinical Study
D0107. Metastatic Renal Cell Carcinoma Involving the Colon: An Unusual Cause of Lower Gastrointestinal Bleeding D0143. Pregnancy With a Twist: A Case of Sigmoid Volvulus in the Third Trimester
D0149. Waldenstrom Macroglobulinemia: A Malignant Mimicker of IBD
D0187. With a Little Help From My Friends: PercutaneouslyAssisted Biliary Drain Internalization
D0221. Treatment of Achalasia With Endoscopic Ultrasound-Guided Botulinum Injection in the Setting of Esophageal Varices
D0226. A Case of Cervical Esophageal Adenocarcinoma Arising From Gastric Inlet Patch: A Benign Lesion With Malignant Potential
D0240. Cirrhosis, Varices, and Barrett’s Esophagus: WATS3D-only Surveillance and Band Ligation in the Management of Nondysplastic Barrett’s Esophagus Progressing to High Grade Dysplasia With Underlying Esophageal Varices
D0260. Clinical Utility of Anorectal Manometry and Balloon Expulsion Testing to Predict Outcomes With CommunityBased Pelvic Floor Physical Therapy: A Pragmatic Clinical Trial of Patients With Chronic Constipation D0282. Comparing Left Colon Mucus Production by Water versus Saline Infusion During Water Exchange Colonoscopy: A Prospective Randomized Controlled Trial D0293. Outside In: Endometriosis of the Appendix, Cecum, and Ileum Masquerading as Suspected Crohn’s Disease D0303. Improving the Quality of Esophagogastroduodenoscopy Using Prokinetic in Upper Gastrointestinal Bleeding: A Network Meta-Analysis D0328. Gone to Guts: A Case of Osteosarcoma With Metastasis to Upper and Lower Gastrointestinal Tract Presenting as Recurring Bleeding D0397. Fecal Transplantation Improved Patients’ Reported Outcome After Immune Checkpoint Inhibitor Colitis D0413. Economic Costs and Trends in Inflammatory Bowel Disease-Related Hospitalizations and Surgery in the United States
D0418. Fecal Microbiota Transplantation as First-Line Treatment for Immune-Mediated Colitis D0430. Anesthesia Care Provider Sedation (ACPS) Is Superior to Conscious Sedation (CS) for Successful Diagnostic Tissue Acquisition in Endoscopic Ultrasound Fine Needle Aspiration and/or Biopsy (EUS FNA/B) D0432. Safety of Endoscopic Pancreatic Necrosectomy Compared With Radiologic or Surgical Necrosectomy: A Nationwide Inpatient Analysis D0433. Early ( < 4 Weeks) vs Standard (≥ 4 Weeks) Endoscopic Drainage of Pancreatic Walled-Off Fluid Collections: A Systematic Review and Meta-Analysis D0437. Assessment of Pathogenic Enteric Flora Contaminating Novel Duodenoscopes With Disposable Tips D0443. Concomitant Transoral Incisionless Fundoplication Outcomes and Efficacy for Gastroesophageal Reflux Disease: A Retrospective Analysis D0501. Clinical and Economic Burden of Patients With HRSAKI Treated With Current Standard of Care: Retrospective Analysis of Real World Data D0519. Safety and Efficacy of Oral TLR8 Agonist, Selgantolimod, in Viremic Adult Patients With Chronic Hepatitis B D0535. Transcatheter Aortic Valve Replacement Restoring Candidacy for Liver Transplant in Cirrhotic Patients D0561. A Case Report of Ivermectin-Induced Liver Failure D0613. Outcomes of Endoscopic Sleeve Gastroplasty in the Elder Population D0626. Gastroenterology Consults Had Little Utility Prior to Transesophageal Echocardiograms in a Prospective Cohort Study
D0639. Algorithmic Approach to Differentiate Between NonSpecific and Specific Etiologies of Chronic Terminal Ileitis D0651. Exploring Probe-Based Confocal Laser Endomicroscopy as a Novel Tool in Graft Monitoring After Small Bowel Transplantation D0671. Liposarcoma Masquerading as IgG4-Related Disease D0689. Gastroparesis Is Associated With More Psychiatric Disorders Than Functional Dyspepsia
D0691. Effects of Surgical Pyloroplasty on Pyloric EndoFLIP Measurements and Gastric Emptying in Patients With Refractory Gastroparesis and Identification of Pyloric Sphincter Smooth Muscle Pathology
Tuesday Afternoon, October 25 3:00 pm - 5:00 pm
E0001. Early Feeding Rates in Acute Pancreatitis Is Associated With Decreased Length of Hospitalization E0010. Index Admission Cholecystectomy in Uncomplicated Acute Biliary Pancreatitis E0030. Intrahepatic Biliary Colloid Carcinoma: A Rare Site for Recurrence E0033. Icteric Leptospirosis Leading to Multiorgan Failure and Concomitant Pancreatitis E0037. An Unusual Cause of Septic Shock Secondary to Lemmel Syndrome E0113. A Case of Isolated Colonic MALT Lymphoma and Synchronous Celiac Disease E0115. Management of a Retracted Colostomy With Esophageal Stent E0120. A Diagnosis Rarer Than My Steak: The Challenges Behind Alpha-Gal Syndrome
E0128. A Percutaneous Endoscopic Colostomy (PEC) Tube to the Rescue E0132. Pre-Operatively Confirmed Idiopathic Myointimal Hyperplasia of the Mesenteric Veins E0142. Anorectal Mucosal Melanoma: A Case Series Demonstrating the Importance of Maintaining a High Index of Suspicion for This Deadly Disease E0156. A Rare Case of McKittrick Wheelock Syndrome E0169. Colorectal Cancer Screening Rates at Federally Qualified Health Centers in California During the COVID-19 Pandemic: Insights From National Health Resources and Services Administration Data E0178. Assessing the Impact of a Multi-Component Health System Intervention to Address Low Colorectal Cancer Screening Participation in Patients With a Family History of Colorectal Cancer E0182. A Step-by-Step Endoscopic Tour of the Primary Obesity Surgery Endoluminal (POSE 2.0) Procedure E0184. Pancreatoscopy Using Adult Gastroscope as a Diagnostic Method for Main Duct IPMN E0196. The Impact of Centralized Care in the Management of Barrett’s Related Neoplasia: A Systematic Review and Meta-Analysis E0233. Subcutaneous Emphysema of the Penile Shaft: A Rare Complication of Peroral Endoscopic Myotomy E0246. A Case of Progressive Untreated Eosinophilic Gastrointestinal Disorder Complicated by Eosinophilic Myocarditis E0251. Multifocal Pyloric Gland Adenoma of the Esophagus Treated by Circumferential Endoscopic Submucosal Dissection E0252. Evaluation of Probiotic Use, SIBO, and Lactatemia in Patients With Brain Fogginess, Gas, and Bloating E0277. Development and Validation of a Convolutional Neural Network for the Automatic Detection of Multiple Gastric Lesions in Multi-brand Capsule Endoscopy Videos: A Pilot Study E0279. Outcomes and Complications of Radiologic Gastrostomy vs Percutaneous Endoscopic Gastrostomy for Enteral Feeding - An Updated Systematic Review and MetaAnalysis
E0307. Early Feeding vs Delayed Feeding After Therapeutic Endoscopic Intervention in Upper GI Bleeding: A Systematic Review and Meta-Analysis E0309. Early Colonoscopy Is Associated With Lower Mortality in Stable Diverticular Bleeding: A National Database Study
E0310. Safety and Efficacy of Hemorrhoidal Artery Embolization in Patients Refractory to Conservative Management
E0311. Gastric Variceal Bleed Secondary to Acute Portal Vein Thrombosis and Chronic Splenic Vein Thrombosis in the Setting of Paroxysmal Nocturnal Hematuria E0393. Risk of Avoidant/Restrictive Food Intake Disorder Prevalence Among Underrepresented Minority Patients With Inflammatory Bowel Disease
E0442. Novel Through the Scope Steerable Grasper Reduces Dissection Time and Technical Demand in Endoscopic Submucosal Dissection in Novice Endoscopists Compared to Clip and Line Traction Method: An Ex Vivo Randomized Study
E0451. Mucosal Ablation Salvage Therapy After Prior TIF for Recurrent GERD E0461. Combined Antegrade Retrograde Dilation of Radiation-Induced Benign Esophageal Obstruction With Septum Formation: A Case Report
E0471. Females Are at Lower Risk of Mortality as Compared to Males When Admitted for Esophageal Variceal Bleeding: A National Inpatient Sample Analysis
E0574. Severe Immune-Mediated Liver Injury Following COVID-19 Vaccination Necessitating Liver Transplantation in a Patient With Cirrhosis
E0601. HBV-Host Junctional Sequences: A Novel Urine Tumor Marker for Recurrent Hepatitis B-Associated Hepatocellular Carcinoma With Low Alpha-Fetoprotein
E0607. Cost-Effectiveness Analysis of Endoscopic Sleeve Gastroplasty
E0609. Depression Is Highly Prevalent in Patients Treated With Intragastric Balloon Therapy but Does Not Correlate With Weight Loss Efficacy
E0613. Rates of Gastrointestinal Hospitalizations in Adults With Chronic Kidney Disease
E0629. Health Disparities in Gastroenterology in LGBTQ+ Individuals: A Rochester Pride 2022 Survey
E0630. Paracentesis Team: An EPIC Chat Opt-In Group for Hospital Procedures
E0633. Characteristics and Healthcare Patterns of SuperUtilizers Among Patients Hospitalized With a GI Diagnosis E0636. Iron Deficiency and the Development of Celiac Disease
E0637. Celiac Disease Is Associated With Cardiac Pathology: Results From a National Database
E0650. MEN2B-Associated Chronic Intestinal PseudoObstruction
E0662. Laparoscopic-Assisted Enteroscopy with “Shar Pei” Technique for Resection of Deep Small Bowel Polyps E0694. Does Aortic Stenosis Impact the Prevalence and Outcomes of Gastric Antral Vascular Ectasia? A Retrospective Study of 85,000 Patients
E0725. Gastric Syphilis: An Unusual Etiology of Melena in a Patient With AIDS
E0729. Transcatheter Arterial Radioembolization (TARE)Induced Gastric Ulcer in an Excluded Stomach After Rouxen-Y Gastric Bypass
E0735. Angiotensin Receptor Blockers-Associated Lymphocytic Gastritis: A Case Series and Review of the Literature

The College is pleased to once again provide recognition for “Outstanding Poster Presenter” at this year’s Annual Scientific Meeting. ACG hopes to cultivate the ability of clinical GI researchers to use critical storytelling and presentation skills essential for a career as a clinical investigator and scientific communicator.
During the daily Poster Rounds with the experts, poster presenters may be invited to give a succinct and informative two-minute briefing on their research, followed by one minute of Q&A with a faculty judge. Each judge will select one or more presenters within a poster category who are best able to communicate their key findings, the significance of their data, and articulate the potential impact of their work for clinicians and patients, to receive an “Outstanding Poster Presenter” distinction. Recipients of this designation will be recognized with a red ribbon and will receive a certificate.
Poster Rounds with the experts will take place on Sunday (5:30 pm - 6:30 pm), twice on Monday (10:30 am - 11:30 am, and 3:45 pm - 4:45 pm), and twice on Tuesday (10:30 am - 11:30 am, and 3:45 pm - 4:45 pm). Attendees who wish to attend these rounds can join the Experts at the Poster Counter in the Crown Ballroom Foyer 10 minutes before the start time.
Learn how the ACG Institute for Clinical Research and Education supports clinical GI investigators, leadership development, and education for physicians and patients in the NEW Institute in Focus This new booklet shares important application deadlines and opportunities for leadership, clinical research, and educational growth for you and your colleagues.
The LE&E Center addresses the contemporary need for leadership training, equitable delivery of care, and ethically based decision-making with a suite of training programs and activitiesto provide transformational tools and experiences to GI clinicians. The programs under the LE&E Center include:
NEW — The ACG Clinical Research Leadership Program
The ACG Early Career Leadership Program

ACG Advanced Leadership Development Program
The ACG Health Equity Research Award
The ACG Visiting Scholar in Equity, Diversity & Ethical Care

Scholarships for High School Students Through the Prescriptions for Success: Careers in Medicine High School Visit
The ACG Institute supports a robust clinical research program in gastroenterology and hepatology. This upcoming year, the ACG Institute is funding eight different award types, supporting researchers throughout their careers from medical school to established investigators. Notably, funding for the ACG Health Equity Research Award has been increased to $75,000 ($50,000 year-one and $25,000 year-two based on progress).
Junior Faculty Development Award ($450,000 total / $150,000 per year)
Investigator Bridge Funding Award ($300,000 total / $150,000 per year)
Epidemiologic Award in Gastrointestinal Endoscopy ($50,000 / 1 or 2-year)
Deadline for this award is Friday, December 9, 2022
Health Equity Research Award ($75,000 /50k year-one, 25k year-two based on progress)
Clinical Research Award ($50,000 / 1-year)
Pilot Research Award ($15,000 / 1-year)
Resident Clinical Research Award ($10,000 / 1-year/ travel to ACG 2022)
Medical Student Research Award ($5,000 / 6-10 weeks/travel to ACG 2022)
Deadline for all awards: MONDAY, DECEMBER 5, 2022
This new signature program of the ACG Institute's Center for Leadership, Ethics & Equity will help train clinical investigators as scientific leaders, team managers, financial stewards of research dollars, and mentors. This unique interactive program will provide funded ACG clinician investigators with the skill set to start, grow, and successfully maintain an independent research program.
The program aims to provide leadership training for early to mid-career clinical investigators who are US-based ACG member physicians (between 2-15 years out of fellowship training) with active or recent ACG or federal funding as a Principal Investigator or Co-Principal Investigator.
The ACG Institute is developing a program for outstanding 3rd and 4th-year fellows to explore their leadership potential. Look for more information on The LE&E Center's website in 2023!
The Early Career Leadership Program (formerly the Young Physician Leadership Scholars Program) develops future leaders in clinical gastroenterology by providing leadership and policy training to early career physicians. These physicians have completed one full year of practice after their terminal GI or hepatology fellowship and are in their first five years of clinical practice.
The Early Career Leadership Program includes:
Pre-course learning
Friday course at ACG 2022
Participate in the ACG Governors’ Washington, DC Fly-in April 2023
Participants will be immersed in coursework covering effective leadership, impactful networking, emotional intelligence, group dynamics, and team building. The ACG Institute is excited to welcome the fifth cohort of Early Career Leadership Scholars in 2022.
Allon Kahn, MD, and Elizabeth R. Paine, MD, FACG
The Advanced Leadership Development Program aims to develop a cohesive group of peer leaders who will serve as problem-solving consultants for each other and the College. This program offers mid-career physicians (10-20 years post-fellowship completion) the opportunity to develop comprehensive leadership skills and provides advocacy training. The program will enhance the ability of these individuals to:
Broaden their leadership skills
Learn how to embrace and become agents of change
colleagues and trainees through mentorship and sponsorship
practice and policy development on a local, regional, and national level
their flexibility and adaptability
how
strategic thinking
the importance of work-life
Course Directors: David J. Hass, MD, FACG, Sunanda V. Kane, MD, MSPH, FACG, and Mark B. Pochapin, MD, FACG
This program, which honors former ACG Institute Director Edgar Achkar, MD, MACG, enables GI fellowship programs to host highquality visiting professors to enhance the training program by providing lectures, small group discussions, and one-on-one visits with trainees and faculty. Additionally, this program allows community gastroenterologists to learn from an expert through an evening event or medical grand rounds. New in 2022, the LE&E Center supported six ACG Visiting Scholars in Equity, Diversity, and Ethical Care.

The ACG Visiting Scholars in Equity, Diversity, and Ethical Care help institutions create awareness around the issues and challenges of delivering equitable care, respecting diversity, and instilling ethical decision-making. These visits provided an impactful learning opportunity for fellows, faculty, leadership, and Diversity, Equity, and Inclusion (DEI) leadership, as physicians seek to improve care and communication for their diverse patient populations. Topics to date have included DEI & colorectal cancer screening; hepatology/ ethical issues in the care of patients with liver diseases; how implicit bias affects healthcare outcomes, health disparities in GI, and diversity in GI, with additional talks planned.
LEARN MORE: GI.ORG/EAVP
In partnership with the ACG Women in GI Committee, the ACG Institute has published a third monograph to address the current best approaches to treating GI diseases and endoscopy during pregnancy and postpartum. The comprehensive monograph was released as a supplement to the October 2022 issue of The American Journal of Gastroenterology and has an editorial team of gastroenterologists, OB/GYNs, and a neonatal pharmacologist. Topics covered include liver disease during pregnancy, IBD during pregnancy, and advanced endoscopic procedures in pregnancy.







The G.U.T. Fund is the ongoing campaign that makes possible innovative Institute programs such as the ACG Visiting Scholar in Equity, Diversity & Ethical Care, Junior Faculty Development Awards, the Early Career Leadership Program, the Advanced Leadership Development Program, the Clinical Research Leadership Program, Scholarships for High School Students through the Prescriptions for Success High School Visit initiative, and much more.
The G.U.T. Fund is supported by the ACG community, individual and legacy gifts, and industry contributions. Thousands of ACG members and supporters annually make philanthropic gifts that take the programs of the ACG Institute from GOOD to GREAT. To learn more about the ACG Institute programs or to support the work of the Institute through the GUT fund, please visit: gi.org/ acg-institute or read the new report - Institute in Focus online or at ACG 2022.
EDGAR READ THE ACG PREGNANCY MONOGRAPH: AMJGASTRO.COM









Founded by the American College of Gastroenterology (ACG) and the American Society for Gastrointestinal Endoscopy (ASGE), the GI Quality Improvement Consortium (GIQuIC) recently expanded its board of directors to include seven prestigious members. Representing the interests and vision of gastroenterologists, it is under the board’s direction and guided by its leadership that GIQuIC continues to evolve the registry to expand beyond colonoscopy and EGD. Clinical experts are working to develop additional modules, including inflammatory bowel disease (IBD), Endoscopic Bariatric Therapies (EBT), and ERCP clinical modules.

For the ninth year in a row, CMS has approved GIQuIC as a Qualified Clinical Data Registry (QCDR) for reporting to the Meritbased Incentive Payment System (MIPS). As a result, GIQuIC participants have the option of reporting to the Quality, Promoting Interoperability (PI), and Improvement Activities (IA) performance categories to decrease negative payment adjustments and even increase CMS payouts.
For more information about utilizing GIQuIC as a QCDR to report to MIPS or to inquire about the benefits of implementing GIQuIC as a performance benchmarking registry, please email Therese Basham, Member Relations Manager, at tbasham@gi.org
Participating in GIQuIC contributes valuable data that is being used to conduct vital research, including a study that was recently published in The American Journal of Gastroenterology



It examined the impact on endoscopist adenoma detection rate (ADR) of conducting screening colonoscopies on individuals beginning at age 45 instead of 50. By examining the procedure data of more than 2.8 million colonoscopies in the registry, the authors, including GIQuIC Board Member Dr. Aasma Shaukat, found the mean ADR was:



• 45 - 49 years old 28.6%
• 50 - 54 years old 31.8%
• 50 - 75 years old
36.3%
Visit bit.ly/ajg-podcast-giquic to listen as Co-Editor-in-Chief of The American Journal of Gastroenterology, Jasmohan Bajaj MD, FACG, and author Aasma Shaukat, MD, MPH, FACG , FASGE discuss the implications of this study You can view the study here: bit.ly/ajg-bilal-giquic-adr-45-49

ACGCRJ is a fully open access journal. View all published case reports for free. acgcasereports.com



Thanks to outgoing
thank
Judy Trieu, MD, MPH
Katherine Falloon, MD


Abhishek Agnlhorti, MBBS, MD
of
Board
continued
Amber Charoen, MD


Anthony Horton, MD



Fredy Nehme, MD, MS Hirsh Trivedi, MD



for their
in
Malav Parlkh, MD
Mike Wei, MD

Phillip Gu, MD










































































































































































































BRIEF SUMMARY: Before prescribing, please see Full Prescribing Information and Medication Guide for SUTAB® (sodium sulfate, magnesium sulfate, potassium chloride) tablets for oral use.
INDICATIONS AND USAGE: An osmotic laxative indicated for cleansing of the colon in preparation for colonoscopy in adults.
DOSAGE AND ADMINISTRATION: Split Dose (2-Day) Regimen: Dose 1 – On the day prior to colonoscopy: A low residue breakfast may be consumed. After breakfast, only clear liquids may be consumed until after the colonoscopy. Early in the evening prior to colonoscopy, open one bottle of 12 tablets. Fill the provided container with 16 ounces of water (up to the fill line). Swallow each tablet with a sip of water and drink the entire amount over 15 to 20 minutes. Approximately one hour after the last tablet is ingested, fill the provided container a second time with 16 ounces of water (up to the fill line) and drink the entire amount over 30 minutes. Approximately 30 minutes after finishing the second container of water, fill the provided container with 16 ounces of water (up to the fill line) and drink the entire amount over 30 minutes. Dose 2 - Day of colonoscopy: Continue to consume only clear liquids until after the colonoscopy. The morning of colonoscopy (5 to 8 hours prior to the colonoscopy and no sooner than 4 hours from starting Dose 1), open the second bottle of 12 tablets. Fill the provided container with 16 ounces of water (up to the fill line). Swallow each tablet with a sip of water and drink the entire amount over 15 to 20 minutes. Approximately one hour after the last tablet is ingested, fill the provided container a second time with 16 ounces of water (up to the fill line) and drink the entire amount over 30 minutes. Approximately 30 minutes after finishing the second container of water, fill the provided container with 16 ounces of water (up to the fill line) and drink the entire amount over 30 minutes. Complete all SUTAB tablets and required water at least 2 hours before colonoscopy. CONTRAINDICATIONS: Use is contraindicated in the following conditions: gastrointestinal obstruction or ileus, bowel perforation, toxic colitis or toxic megacolon, gastric retention, hypersensitivity to any ingredient in SUTAB. WARNINGS AND PRECAUTIONS: Serious Fluid and Electrolyte Abnormalities: Advise all patients to hydrate adequately before, during, and after the use of SUTAB. If a patient develops significant vomiting or signs of dehydration after taking SUTAB, consider performing post-colonoscopy lab tests (electrolytes, creatinine, and BUN). Fluid and electrolyte disturbances can lead to serious adverse events including cardiac arrhythmias, seizures and renal impairment. Correct fluid and electrolyte abnormalities before treatment with SUTAB. Use SUTAB with caution in patients with conditions, or who are using medications, that increase the risk for fluid and electrolyte disturbances or may increase the risk of adverse events of seizure, arrhythmias, and renal impairment; Cardiac arrhythmias: Use caution when prescribing SUTAB for patients at increased risk of arrhythmias (e.g., patients with a history of prolonged QT, uncontrolled arrhythmias, recent myocardial infarction, unstable angina, congestive heart failure, or cardiomyopathy). Consider pre-dose and post-colonoscopy ECGs in patients at increased risk of serious cardiac arrhythmias; Seizures: Use caution when prescribing SUTAB for patients with a history of seizures and in patients at increased risk of seizure, such as patients taking medications that lower the seizure threshold (e.g., tricyclic antidepressants), patients withdrawing from alcohol or benzodiazepines, or patients with known or suspected hyponatremia; Use in Patients with Risk of Renal Injury: Use SUTAB with caution in patients with impaired renal function or patients taking concomitant medications that may affect renal function (such as diuretics, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, or non-steroidal anti-inflammatory drugs). These patients may be at risk for renal injury. Advise these patients of the importance of adequate hydration with SUTAB and consider performing baseline and post-colonoscopy laboratory tests (electrolytes, creatinine, and BUN) in these patients; Colonic Mucosal Ulcerations and Ischemic Colitis: Osmotic laxative products may produce colonic mucosal aphthous ulcerations, and there have been reports of more serious cases of ischemic colitis requiring hospitalization. Concurrent use of stimulant laxatives and SUTAB may increase these risks. Consider the potential for mucosal ulcerations resulting from the bowel preparation when interpreting colonoscopy findings in patients with known or suspect inflammatory bowel disease (IBD); Use in Patients with Signifcant Gastrointestinal Disease: If gastrointestinal obstruction or perforation is suspected, perform appropriate diagnostic studies to rule out these conditions before administering SUTAB. Use with caution in patients with severe active ulcerative colitis. Hypersensitivity Reactions: Serious hypersensitivity reactions, including anaphylaxis, angioedema, dyspnea, rash, pruritis and urticaria have been reported with SUTAB. Inform patients of the signs and symptoms of anaphylaxis and instruct them to seek immediate medical care should signs and symptoms occur. ADVERSE REACTIONS: Most common gastrointestinal adverse reactions are: nausea, abdominal distension, vomiting and upper abdominal pain. Postmarketing Experience: Gastrointestinal: gastric ulceration, gastritis; Hypersensitivity: anaphylaxis, angioedema, dyspnea, rash, pruritus, urticaria. POTENTIAL FOR DRUG ABSORPTION: SUTAB can reduce the absorption of other co-administered drugs. Administer oral medications at least one hour before starting each dose of SUTAB. Administer tetracycline and fluoroquinolone antibiotics, iron, digoxin, chlorpromazine, and penicillamine at least 2 hours before and not less than 6 hours after administration of each dose of SUTAB to avoid chelation with magnesium. Pregnancy: There are no available data on SUTAB use in pregnant women to evaluate for a drug-associated risk of major birth defects, miscarriage, or adverse maternal or fetal outcomes. No reproduction or developmental studies in animals have been conducted with sodium sulfate, magnesium sulfate, and potassium chloride (SUTAB). Lactation: There are no available data on the presence of SUTAB in human or animal milk, the effects on the breastfed child, or the effects on milk production. Pediatric Use: Safety and effectiveness in pediatric patients has not been established. Geriatric Use: Of the 471 patients who received SUTAB in pivotal clinical trials, 150 (32%) were 65 years of age or older, and 25 (5%) were 75 years of age or older. No differences in safety or effectiveness of SUTAB were observed between geriatric patients and younger patients. Elderly patients are more likely to have decreased hepatic, renal or cardiac function and may be more susceptible to adverse reactions resulting from fluid and electrolyte abnormalities. STORAGE: Store at 20º to 25°C (68º to 77°F). Excursions permitted between 15º to 30°C (59º to 86°F). See USP controlled room temperature. Rx only. Manufactured by Braintree Laboratories, Inc. Braintree, MA 02185
See Full Prescribing Information and Medication Guide at SUTAB.com.
Packaging and tablets not shown actual size.
References: 1. SUTAB® [package insert]. Braintree, MA; 2020. 2. Di Palma JA, Bhandari R, Cleveland M, et al. A safety and efficacy comparison of a new sulfate-based tablet bowel preparation versus a PEG and ascorbate comparator in adult subjects undergoing colonoscopy. Am J Gastroenterol. 2021;116(2):319-328. doi:10.14309/ajg.0000000000001020 3. Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM; ACG. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol. 2009;104(3):739-750.
For additional information, please call 1-800-874-6756
©2022 Braintree Laboratories, Inc. All rights reserved. 201-289-v4-D February 2022




– Two SUTAB doses are required for a complete preparation1





Dose 1 consists of 12 tablets and 16 oz of water
Dose 2 consists of 12 tablets and 16 oz of water Each dose is followed by two additional 16 oz of water




91% OF PATIENTS IN ONE PIVOTAL TRIAL RATED SUTAB AS TOLERABLE TO VERY EASY TO CONSUME2†




• 52% of all SUTAB and MoviPrep® patients reported at least one selected gastrointestinal adverse reaction1,2‡
• More SUTAB patients reported experiencing nausea and vomiting than competitor, with ≤1% of these reports considered severe2‡
*Success was the primary endpoint and was defined in non-inferiority trials as an overall cleansing assessment of 3 (good) or 4 (excellent) by the blinded endoscopist; scores were assigned following completion of the colonoscopy. †Patients completed a preference questionnaire following completion of study drug to capture their perceptions of the preparation experience. This questionnaire has not undergone formal validation. ‡Patients were queried for selected gastrointestinal adverse reactions of upper abdominal pain, abdominal distension, nausea, and vomiting following completion of study drug, rating the intensity as mild, moderate, or severe.1,2
ACG=American College of Gastroenterology
MoviPrep is a registered trademark of Velinor AG.
Packaging and tablets not shown actual size.
SUTAB® (sodium sulfate, magnesium sulfate, potassium chloride) tablets for oral use is an osmotic laxative indicated for cleansing of the colon in preparation for colonoscopy in adults. DOSAGE AND ADMINISTRATION: A low residue breakfast may be consumed. After breakfast, only clear liquids may be consumed until after the colonoscopy. Administration of two doses of SUTAB (24 tablets) are required for a complete preparation for colonoscopy. Twelve (12) tablets are equivalent to one dose. Water must be consumed with each dose of SUTAB and additional water must be consumed after each dose. Complete all SUTAB tablets and required water at least 2 hours before colonoscopy. CONTRAINDICATIONS: Use is contraindicated in the following conditions: gastrointestinal obstruction or ileus, bowel perforation, toxic colitis or toxic megacolon, gastric retention, hypersensitivity to any ingredient in SUTAB. WARNINGS AND PRECAUTIONS: Risk of fluid and electrolyte abnormalities: Encourage adequate hydration, assess concurrent medications and consider laboratory assessments prior to and after each use; Cardiac arrhythmias: Consider pre-dose and postcolonoscopy ECGs in patients at increased risk; Seizures: Use caution in patients with a history of seizures and patients at increased risk of seizures, including medications that lower the seizure threshold; Patients with renal impairment or taking concomitant medications that affect renal function: Use caution, ensure adequate hydration and consider laboratory testing; Colonic mucosal ulcerations: Consider potential for mucosal ulcerations when interpreting colonoscopy findings in patients with known or suspected inflammatory bowel disease. Suspected GI obstruction or perforation: Rule out the diagnosis before administration. Hypersensitivity reactions, including anaphylaxis: Inform patients to seek immediate medical care if symptoms occur. ADVERSE REACTIONS: Most common gastrointestinal adverse reactions are: nausea, abdominal distension, vomiting and upper abdominal pain. DRUG INTERACTIONS: Drugs that increase risk of fluid and electrolyte imbalance.
Please see Brief Summary of Prescribing Information on reverse side. See Full Prescribing Information and Medication Guide at SUTAB.com
