

Like cycling, don’t like cancer?
We’re delighted to welcome the Melbourne Pedalthon back to Sandown Racecourse, ready for you to ride and help those living with below the belt (kidney, bladder, testicular, penile and prostate) cancers.




Whether you’re an avid cyclist, new to the sport or just looking for a challenge, we invite you to ride to fight cancer below the belt.


The Pedalthon promises to provide a unique event to network with the community, promoting teamwork, healthy competition, plus some fun.
Every cent raised by the Pedalthon goes directly towards clinical trials research, which means straight into the hands of experts committed to improving treatments and outcomes for those living with below the belt cancer.
Since 2014:

What is ANZUP?
The Australian and New Zealand Urogenital and Prostate Cancer Trials Group was formed in 2008, bringing together a world-leading multidisciplinary team of doctors, nurses, other health care professionals, scientists, researchers, and community representatives, all working in areas related to urogenital cancer.
ANZUP has members in every state and territory in Australia and New Zealand, with an increasing international membership.
Urogenital cancers are those coming from the testicles, prostate, kidney, penis or bladder.
ANZUP aims to improve outcomes for people affected by these cancers. We do this by performing clinical trials to generate new evidence for better treatments, or ways of providing other support.
Our members and investigators are widely dispersed and busy, working in a range of disciplines. A trial idea only comes to fruition when we are able to provide opportunities for people to meet, work through the science, develop the trial concepts, and write and work through all the other documentation and processes. Then it is necessary to initiate, run, monitor and report the trial results. All of this relies on the volunteered time of our members and is separate from the other needs ANZUP has to source the much larger amounts of funding to support the trials themselves.
Australian Registered Charity: ACN 133 634 956
New Zealand
Registered Charity: CC51217

ANZUP acknowledges the Traditional Owners of the lands on which our company is located and where we conduct our business. We pay our respects to ancestors and Elders, past and present. ANZUP is committed to honouring the First Peoples’ unique cultural and spiritual relationships to the land, waters and seas and their rich contribution to society.
The paper used in this edition is called Maine Recycled Digital – Silk. It is made with fibre derived only from sustainable sources and produced with a low reliance on energy from fossil fuels. The purchase of carbon offsets compensates for emissions produced over an international supply chain, from seedling through to final delivery to the customer.
“Every meaningful advance in treatment has been the result of testing a new idea in a clinical trial.”
Professor Ian Davis, ANZUP Chair
About the front cover: “I grew up on a sheep, wheat and barley property in South Australia, 650 kilometres from Adelaide,” says Dr Kate Gunn. “From that community I watched people struggle with the challenges a diagnosis of cancer brings, particularly when it is accompanied by isolation and the need to travel for medical treatment. Which included my father when he went through treatment for prostate cancer”. Read more about cancer treatment for rural and remote patients on page 19.
What’s inside
Consumer Advisory Panel (CAP) Update
In the Media
The inaugural ANZUP Outstanding Leadership Award - Guy Toner
Friends of ANZUP

Improving Access to clinical trials for culturally and linguistically diverse (CALD) populations
Cancer treatment for rural and remote patients
International Clinical Trials Day with Dr Ciara Conduit
Survivorship Unmuted
Out with Cancer Toward LGBTQI+ inclusive cancer
Save the Date – Sydney Pedalthon 2023

ANZUP at the American Society of Clinical Oncology Meeting

ANZUP’s 2022 Below the Belt Research Fund Recipients
Research funding helping initial ideas progress
Do you have a story you could share with others?
Spotlight on prostate cancer
Thousands join research quest

Sydney Pedalthon: page 77.
The evolution of prostate cancer treatment ANZUP trials – prostate

In the News
ANZUP trials – prostate
Co-badged trials – prostate
Spotlight on bladder and urothelial cancer
Below the Belt Cancer Research Highlights: Professor Dickon Hayne
ANZUP trials – bladder
Spotlight on testicular cancer
Meet Associate Professor Ben Tran
ANZUP trials – testicular
Spotlight on kidney cancer
Treatment choices and decision making
ANZUP trials – kidney
Spotlight on penile cancer
Penile Cancer and Supportive Care
Trials in follow up
Below the Belt #YourWay
ANZUP Below the Belt Pedalthon – Sydney 2022
How does your donation make a difference?
Community Fundraising
Thanks to our Corporate Partners, Supporters and In-Kind Supporters

Welcome to this latest edition of “A little below the belt.”
Here’s a few things you may or may not have heard about:
• Penicillin
• Smallpox vaccination (leading to monkeypox and other vaccines)
• The first portable electrocardiograph
• Treatment of bipolar disorder with lithium
• Development of respirators
• Discovery of how the immune system works
• Development of life-saving drugs for cancer treatment
• The bionic ear
• Artificial heart valves
• Discovery of the bacterium that causes stomach ulcers
• Discovery of risk factors for sudden infant death syndrome
• In vitro fertilisation
• Spray-on skin
• Cervical cancer vaccine
Here’s a few more:
• Plastic surgery
• Disposable syringes
• John Clarke
All of those things in the first list (and many many more) are the result of research done by Australians. All the ones in the second list are from New Zealand, although Australia would like to claim at least one of those as its own. The population of Australia right now is about 27 million, which is about 0.3% of the world’s population, yet we produce 2.7% of the world’s research. Australia’s investment in research is 1.8% of its GDP, far lower than USA (2.9%) or China (2.4%). However, if you look over those partial lists, you’ll probably agree that what researchers produce in this part of the world is pretty impressive and literally life changing. And not only does it transform people’s lives, but it also actually shows a
fantastic return on investment: every dollar invested in this research returns somewhere between 5 to 10 dollars in value for the wider community, in terms of better health outcomes, more efficient health care, keeping people well and productive for longer, and support for the economy overall.

Other countries are bigger and better resourced. Some pharmaceutical companies have resources greater than many countries. Why do we do so well in research in this part of the world? I think it’s because we approach things in a different way. We can’t throw endless resources or people at a problem; we have to work much more intelligently than that. In the case of medical research, this usually means bringing together the people who care for those affected by the conditions with the scientists doing the research (sometimes they’re the same people); and importantly, with the affected people themselves. That means we can better understand what the clinical needs really are, what questions the community needs us to answer, and what the clinicians and scientists can learn from each other. We can design research to answer those questions, and we can work with industry without having to take on their additional complications and pressure of having to develop commercial products for stock market and shareholder success. As Harry S Truman said, “It is amazing what you can accomplish if you do not care who gets the credit.”
ANZUP is the Australian and New Zealand Urogenital and Prostate Cancer Trials Group. We are a group of over 2000 clinicians, researchers, and representatives of the community, all involved in the care of people affected by “below the belt” genitourinary cancers (prostate, kidney, bladder, testis, penis). Collectively these cancers make up an enormous proportion of the total number of cancers in Australia and New Zealand. We are here to try to improve the lives of people affected by these cancers.
ANZUP performs clinical trials to answer these questions, so that we can generate the evidence all of us need when making decisions for ourselves or our loved ones if we are affected by those cancers.
This is hard work, sometimes tedious, always time-consuming, frequently expensive. ANZUP members donate their time and expertise to make sure that the clinical trials we do are the best that they can be. We look for every opportunity to maximise the value we can get from a trial, and from the time / information / tissue and blood samples that people participating in these trials so generously provide. A clinical trial might be about testing a new treatment, but we also want to know answers to other questions: it’s more than “does this treatment shrink cancer?” We also want to know: Who is most likely to benefit? Who is least likely to benefit and should have some other treatment? Can we use known treatments more effectively? Can we study blood and tissue samples and see if there are any characteristics that match up with the clinical outcomes people experience on these treatments? Will these treatments be cost-effective and able to be used in broader clinical practice? What are the experiences of people affected by these cancers and receiving treatment? Are there better ways of supporting their needs? Are there special groups of people who might have very specific needs that would otherwise be overlooked?
We can’t all be experts at everything. I’m a medical oncologist and can barely tie my own shoelaces; you don’t want me doing your surgery, I’m probably pretty average at providing psychological support, and my lab staff get nervous when I pick up a pipette. We need all types of health care experts involved in design of these trials, just as we do for the best clinical care. Most importantly, I don’t have one of those cancers (yet; as far as I know), so I don’t have the personal lived experience of knowing what it’s like to have one. People like that are experts too, and ANZUP is very fortunate to have a great group of community representatives to advise us and steer our scientific direction. In fact, we are just about to start a new project based on an idea that came from one of our Consumer Advisory Panel members.
My unsympathetic and brutally honest mirror also tells me that we are all getting older, and the individuals involved won’t be doing this forever. ANZUP also looks for ways to support new people entering the research field, with practical support such as scholarships, prizes, grants, travel fellowships, and educational and training programs. We look for ways to involve any interested ANZUP members in the development and conduct of our research. Our Below the Belt Research Grant program, supported by ANZUP’s fundraising initiatives, has provided since 2014 over $1.96M in grants and funded 36 research projects that otherwise would have had no support, many of which have then led on to ANZUP trials. A lot of these grants have gone to early career researchers.
And it’s paying off.
ANZUP is leading or has been involved with over 20 clinical trials. Our trials have included over 7000 participants from nearly 700 sites around the world. One of our trials swept the pool of awards from the Australian Clinical Trials Alliance in 2020, winning Trial of the Year, as well as awards for the statistical quality of the research, and (we love this) for consumer engagement. We continue to develop and lead clinical trials that will help us all understand these diseases better and provide better treatments and support. Our work is being recognised on the global scale as being important and transformative.
But, like I said, clinical research takes a lot of time and a lot of money, and the sort of work ANZUP does could not happen without the extraordinary donations of time and expertise from its members. There are no free handouts. We have to find the resources to do every clinical trial we do, as well as keeping the lights on. We go through competitive grant application processes, but these can take up to a year for outcomes to be known, and the probability of getting grant funding in Australia is less than 10% even for work rated as “excellent” by the grant reviewers. We work with industry, making sure that the trials are designed, led, and overseen by ANZUP. And we are a charity registered right across Australia and New Zealand, allowing us to raise funds that all go back to supporting research; the actual costs of doing the fundraising are not paid for by the donations.
I’m amazed that you’ve read this far, but if you have then you’re either way more bored than you thought you were (sorry if I didn’t help with that), or more likely that you have some sort of personal interest in all this. Perhaps you or someone you love has been affected by one of these cancers. Perhaps you’ve been the beneficiary of research (almost certainly – look at those lists again). There are many ways that you can help. You can raise awareness of the importance of these cancers. You can encourage people to support and participate in research, including clinical trials, where they will get the best possible care available. Perhaps you’re thinking that you might be willing to donate to ANZUP or to participate in one of our fundraising activities, like a Pedalthon or #YourWay or one of the other initiatives you will read about in these pages. We would love to hear from you!
Maybe you’re thinking that anything you could contribute is too small to make a difference, in which case I have to close with a quote from the Dalai Lama: “If you think you are too small to make a difference, you haven’t spent the night with a mosquito.”
Let’s join together and show these cancers what determined mosquitoes can do.
Please enjoy this edition of “A little below the belt.”
IAN DAVIS CHAIR, ANZUPWe know there are too many unanswered questions about why these cancers behave the way they do, and what might be the best ways to treat them and to look after the people affected by them.
A message from the CEO, Margaret McJannett
ANZUP is a cancer co-operative clinical trials group that brings together a leading multi-disciplinary network of surgical, medical, radiation oncologists, nurses, psychologists and allied health professionals researching and treating patients with prostate and urogenital (bladder, kidney, testicular, penile) cancers.
Our mission is to improve treatment and outcomes for people affected by prostate and urogenital cancers. We do this by performing high quality clinical trials that generate the evidence that can make a difference to those impacted by these “below the belt” cancers.
Despite COVID-19 and the peak of an early winter flu season ANZUP has continued to achieve some significant milestones across our research activities.
In relation to our clinical trials, in July we opened our latest ground-breaking study, the EVOLUTION trial. This multimillion-dollar trial has been made possible through a partnership with the Prostate Cancer Foundation of Australia (PCFA) with support from Bristol Myers Squibb and Novartis. It aims to see whether Lu-PSMA combined with cancer immunotherapy is safe and can lead to clinically meaningful anti-cancer effects. This ANZUP-led study is a collaboration with the University of Sydney NHMRC Clinical Trials Centre (NHMRC CTC), our community of clinicians and researchers, the Australasian Radiopharmaceutical Trials Network (ARTnet), the Australian Nuclear Science and Technology Organisation (ANSTO), MiM and WIDEN. The EVOLUTION Study Chair is Professor Shahneen Sandhu.
We were excited to reach our recruitment target of 160 patients for the ENZA-p trial. This trial aims to determine if adding Lu-PSMA to enzalutamide overcomes resistance to treatment and prolongs treatment responses. ENZA-p was funded through a partnership with the Prostate Cancer Research Alliance (PCRA): An Australian Government, Movember Foundation and Cancer Australia alliance, St Vincent’s Clinic Foundation, GenesisCare and Roy Morgan Research. This ANZUPled study was a collaboration with the NHMRC Clinical
Trials Centre, ARTnet and with funding and product support from Novartis and Astellas. We look forward to reporting on the results of the trial in 2023. ENZAp’s Study Chair is Professor Louise Emmett.

Our BCG+MM trial is closing on its recruitment target of 500 participants. This trial is aiming to determine if the combination of BCG and mitomycin is more effective than BCG alone in the treatment of patients with aggressive bladder cancer that has not yet invaded the muscle of the bladder wall. This randomised trial will determine the effects of adding mitomycin on cure rates, survival, side effects and quality of life. This could potentially provide a simple and cost-effective treatment for patients who suffer from this cancer.
Earlier this year ANZUP was awarded two oral and two poster presentations at the American Society of Clinical Oncology (ASCO) Annual Meeting in Chicago, the largest oncology meetings in the world.
ANZUP’s Chair Professor Ian Davis presented the updated results from ANZUP’s ENZAMET (ANZUP 1304) trial – which showed a 30% survival benefit. TheraP (ANZUP 1603) Study Chair Professor Michael Hofman also presented the three-year results from ANZUP’s TheraP (ANZUP 1603) trial – the first randomised trial comparing Lutetium-177 PSMA-617 to standard of care chemotherapy.
The two trials in progress posters provided updates for our UNISoN trial and DASL-HiCAP. You can read more about this important meeting and ANZUP’s presence on page 28.
We are constantly looking at how we can improve access to our clinical trials for all people affected by these “below the belt” cancers. Each new trial is considered for suitability to include a teletrials model, to build capability at new regional and rural sites, increase the number and accessibility ANZUP trials, and provide better access for patients living in regional and rural Australia or New Zealand. As a consequence, we have reached out to new regional sites, utilising the
Teletrial model for several of our ANZUP trials and we will continue to look for opportunities to expand on this model where possible.
We continued to convene our highly successful Idea Generation Workshops, (previously known as Concept Development Workshops), albeit virtually, across all the diseases we represent, and also includes Quality of Life and Supportive care and Translational Research. These workshops are a forum for members to present research ideas that might be immature, in order to obtain advice on further development and input on the project’s scientific value, design, funding support and acceptability. All members are invited to submit concepts for discussion. This is particularly valuable for junior or early career researchers. Concepts that are approved for further development have a working group assigned including members from our consumer advisory panel (CAP). The workshops also provide a supportive environment for “brainstorming” and “horizon scanning” to generate new ideas and opportunities. Some concepts are recommended for applications for funding through the ANZUP Below the Belt Research Fund mechanism. You can read more about this on page 32.
After two years of virtual meetings, we finally held the ANZUP Annual Scientific Meeting (ASM) in-person from 10 – 12 July 2022 in Adelaide. This year’s ASM theme ‘No Longer on Mute: Patients, Carers and Our Research Community’ provided a platform to discuss the need for a voice for many groups – the patient, carers, vulnerable communities, other disciplines, and the research community – about clinical trials. It was exhilarating to be able to finally come together face-to face and network, debate, discuss and appreciate ANZUP’s truly multidisciplinary group.
In terms of fundraising: We held our virtual Below the Belt #YourWay Challenges during the month of May in 2022. Over 1,400 people throughout Australia registered and participated in either the 77 Crunches a Day in May Facebook Challenge or the 77km #YourWay in May Challenge acknowledging the 77 people every
day in Australia who are diagnosed with a below the belt cancer.
After three years off the track, we were delighted to welcome back riders, supporters and volunteers who joined us at Sydney Motorsport Park on Tuesday 22 November for the Sydney Pedalthon. The day was full of energy and competitive spirit; we witnessed grit, determination, and cycling prowess, as well as a lot of fun.
We are thrilled to announce that not only have we raised more than $53,000 but another milestone was made with the funds raised from this event ticking us over to more than $2 million raised since 2014. That is over $2 million going straight to ANZUP Cancer Trials Group to improve the lives of people affected by bladder, kidney, testicular, penile, and prostate cancers through practicechanging multidisciplinary collaborative clinical trials.
Thank you to everyone who participated or donated and helped raise awareness and funds for ANZUP’s clinical trials research which directly supports our members to develop research projects with the potential to lead to future ANZUP trials.

We are fortunate to have such a dedicated membership, now over 2,000, who help us deliver on our mission and keep pushing for better treatment and outcomes for our community. We are extremely grateful to our donors, funders and corporate supporters who continue to generously support our research endeavours. Finally, a heartfelt thanks to the many thousands of patients who participate in our ANZUP trials across Australia, New Zealand and internationally. Without every single one of you we would not be able to strive to achieve our mission: To improve the lives of people affected by “below the belt” cancers through practice-changing multidisciplinary collaborative clinical trials.
On behalf of the ANZUP team I hope you enjoy this edition of our magazine, ‘A little below the belt’.
MARGARET MCJANNETT CEO, ANZUPConsumer Advisory Panel (CAP) update
By Belinda Jago, CAP ChairThe ANZUP Consumer Advisory Panel, otherwise known as the CAP, consists of a group of people from the general community who have been touched by cancer. They may be a patient, cancer survivor, partner of someone who has had cancer or have been a carer to a family member or friend.


As the Chair of the CAP, I bring my own experience, as I was a carer to my daughter who died from kidney cancer at just 19 years old.
The CAP feels very privileged to provide consumer feedback to ANZUP, on behalf of the community, and we are made to feel welcome by the healthcare professionals on all the committees we are a part of. The CAP is integrated through all ANZUP’s research activities and participate in each of the disease specific subcommittees, the Scientific Advisory Committee, including strategic planning workshops and report regularly to the Board.
The CAP plays a significant role in reviewing the clinical trial Patient Information and Consent Forms for each ANZUP clinical trial. We give valuable feedback to the clinical trial investigators as these forms are an important part of the decision-making process for the patient and their participation on a clinical trial.
The CAP also takes part in ANZUP’s Below the Belt Research Fund reviews to ensure we provide community expectations around the research ideas put forward for funding by ANZUP members.
CAP members are supported through internal education sessions and other external training opportunities as they arise. Despite the difficulties of living through the COVID-19 pandemic we have continued in our roles using virtual technology and are pleased to see the return of face-to-face meetings and education sessions. I am delighted to advise that seven out of the ten CAP members were able to catch up in person at this year’s ANZUP Annual Scientific Meeting (ASM) held in July in Adelaide – and the event was aptly themed “no longer on mute.”

The ASM was a fabulous three days and highlighted that while we have “managed” virtually, the value of live conversations and interactions cannot be underestimated. This meeting provided a key opportunity for CAP members to take part in education sessions to provide constructive input into ANZUP clinical trial research from a consumer perspective. We were given the opportunity to participate in various sessions throughout the three days of the ASM.
Each year, a Sunday session at the ASM focuses on education sessions for specific interest groups. This year it included:
• The CAP’s half-day education session for all CAP members, and we warmly welcomed two new CAP members – Tuan Hoang and Paul Zawa. We then participated and presented in a new session titled ‘Clinical Trials Research Symposium’. This was a fabulous session concentrating on the life cycle of a clinical trial and included a segment on “Putting it in Perspective – The Role of Consumers “.
• Multidisciplinary Master classes for trainee medical clinicians and allied health professionals were also part of the ASM program. These sessions focused on case studies from each disease type. As cases are discussed, CAP members were invited to be part of the discussion panel to provide the patient perspective on cancer treatment.
• ANZUP’s Community Engagement Forum (CEF), was another part of the ASM program that required input from the CAP. The CEF offers up-to-date information on ANZUP clinical trials and the benefits of being a clinical trial participant. Leonie Young, a member of the CAP chaired the CEF.
• One of the highlights of the CEF was the inclusion of a powerful patient story. Juliet De Nittis shared her story about the benefits of considering a clinical trial as a treatment option. You can read more about Juliet’s cancer journey on page 62.
• Another highlight was the session, Getting the balance right with reliable information with CAP member Michael Twycross and Quality of Life Subcommittee Chair Associate Professor Haryana Dhillon, who discussed what to look for when dealing with a cancer diagnosis.
• CAP member Melissa Le Mesurier was part of a panel at the Sunday Evening Symposium, “Survivorship Unmuted” and spoke about her experience on a bladder cancer clinical trial, both the pros and cons. You can read more about this on page 22.
The following days of the ASM involved CAP members as session chairs to provide a CAP update to the delegates. These learning opportunities ensure the CAP have the best possible understanding of the technical design of trials, timing issues, and complexities around ethics and funding approvals.
Support for, and inclusion of the CAP at ANZUP ensures we are a committed and enthusiastic group, extremely interested in assisting with ANZUP clinical trials. As a CAP member, it is exciting to be part of this successful and growing organisation, turning an unwanted cancer experience into a positive outcome.
Please take the time to consider if you could be involved with ANZUP – share a story, your experience on an ANZUP clinical trial, or volunteer /participate at one of our fundraising events. We hope you enjoy this edition of the magazine.
 BELINDA JAGO CAP CHAIR
BELINDA JAGO CAP CHAIR

History in the making – Guy Toner
The inaugural ANZUP Outstanding Leadership Award
At the ANZUP Annual Scientific Meeting held in July 2022 the inaugural ANZUP Outstanding Leadership award was presented. Associate Professor Guy Toner was the extremely well-deserving recipient of this award.



There are many reasons Assoc. Prof. Toner was awarded this accolade. In addition to being an incredible clinician to many patients and their families, very few people display unwavering dedication and commitment over a lifetime, do not seek personal tributes, and always uplift and enable others. Throughout his stellar career he also made an incredible contribution and long-standing impact on ANZUP.
In 2021 Assoc. Prof. Toner announced he would be standing down from the ANZUP Board, as well as retiring from the Peter MacCallum Cancer Centre after 30 years of service. He played a crucial role in the establishment of ANZUP, having chaired one of its predecessor organisations, Australia New Zealand Germ Cell Tumour Group (ANZGCTG) and was then on the ANZUP Board as Deputy Chair since ANZUP’s inception in 2008. He has been the quiet but effective force behind many of ANZUP’S initiatives, including the highly successful Below the Belt Research Fund and more recently the Discretionary Funding Initiative. Assoc. Prof. Toner’s leadership has been instrumental, and he has been a trusted mentor to many in the clinical community.
Assoc. Prof. Toner was a Consultant Medical Oncologist at Peter MacCallum Cancer Centre and Associate Professor of Medicine at the University of Melbourne. He is a graduate of the University of Melbourne and undertook sub-specialty training in medical oncology at the Alfred Hospital before spending 3 years at Memorial Sloan-Kettering Cancer Centre in New York, where he worked in the genitourinary service. He developed a special interest in testicular cancer whilst in New York, and his research there formed the basis of his MD (Doctor of Medicine) thesis. He then returned to Melbourne to take up a full-time position at Peter MacCallum Cancer Centre in 1990. His clinical and research interests include all urological cancers, and he also has an interest in new drug development.
How was ANZUP started?
ANZUP began in 2008 and around that time Cancer Australia was founded. Professor Ian Davis had started a prostate and urogenital group, leaving germ cell cancers out because of the pre-existence of the germ cells trials group. And Cancer Australia said we are not going to fund two urological groups, so the groups needed to join together – and that is how ANZUP started.
Associate Professor Craig Gedye, Chair of ANZUP’s Renal Cell Subcommittee, recently sat down with Associate Professor Guy Toner to ask him about his career, cancer research and ANZUP.
Did you envisage ANZUP would be where it is today?
It is wonderful to see what ANZUP has been able to achieve over the last 14 years. It has grown dramatically well, and I never thought it would have done as well as this. It’s a great joy to see it functioning so well and see all the people involved.
What are you most excited about in below the belt cancer research?
It’s amazing to think where we have come from and where we are going. It is hard to see the future in terms of what we can achieve. The goal is still there to treat to cure prostate cancers in the future, but I think we are learning about having to live with cancer and reducing the side effects and morbidities.
How did you come to the idea of the Below the Belt Research Fund?
The idea was to encourage young investigators to be able to get some funding to do some simple things and generate data to then move to bigger ideas.
Often funding requires you to have some baseline data, something to move on with, and that first step is often very difficult for registrars, fellows, and junior faculty. The idea was to help that happen without making it too difficult for them. Below the Belt has really allowed us to do that.
Has the involvement of the Consumer Advisory Panel (CAP) been important for ANZUP?
The involvement of consumers has been one of the great strengths of ANZUP and it continues to work really well.
Having the CAP involved helps the healthcare professionals to remain focussed on what the mission is.
Is there any other ANZUP initiative you have had input into that makes you particularly proud?


I am most proud of the culture of the organisation. What I love about the organisation is that it is multidisciplinary. It is great to see surgeons and nuclear medicine physicians running trials within the group. Co-operative trials groups have been mainly medical oncologists, but ANZUP has been able to change that. The other thing I love about the organisation is its welcoming nature. It welcomes young clinicians into the group all the time and it is terrific to see people evolving their skills and becoming important researchers in their field.
What was your ‘biggest win’ over your career?
People might think I would say a certain publication or presentation at ASCO, but I think the greatest win from my perspective is actually seeing young people coming through. I have been very privileged to have registrars and fellows coming through Peter MacCallum, where I have been for many years, a great population of people come through and see their careers develop. And I think this is the thing I have enjoyed the most.
advice would you give to aspiring researchers?
Persistence is the most important thing. You need to be able to keep going. People will often give negative feedback or not be interested or suggest you can’t do something but keep persisting with something is the most important thing. It is not enough to come along with a good idea, you have actually got to convince your colleagues it’s a good idea, write the outlines and protocols, and just keep working at it and you can be successful.
In addition to all his clinical research, Assoc. Prof. Guy Toner has been an extraordinary clinician to many patients and their families, leaving a lasting, positive impression.
Dear Dr Toner, Laura and I (and my family and friends) would just like to say a massive thank you for everything you have done for me over the past five years.

You
Aside from
I was quite looking forward to celebrating (hopefully) the five-year mark with you this year and it honestly will not be the same experience without you.
The words ‘thank you’ are not enough and we hope you enjoy your retirement and whatever the future may hold.
Thanks again Dr Toner. Trav, Laura and Ivy.
Recognition and thank you to Guy Toner
The Consumer Advisory Panel’s (CAP) role is to provide advice from a community perspective to the ANZUP clinicians and researchers across a broad range of research proposals.
In doing this we are fortunate to have these discussions and input with leading experts in this field. The CAP would like to thank and acknowledge with gratitude A/Prof Guy Toner for the support he has offered the group since we all came together in 2012.
We have always been impressed by A/Prof Toner’s calm and unassuming manner. We have learned much from him over the years - particularly with the wise questions and thought-provoking comments he raised at the Scientific Advisory Committee meetings, Concept Development Workshops, and many other review panels we have been CAP members on.
We know he has provided much more than this to ANZUP, with outstanding leadership and guidance overall. In standing down from his position as Deputy Chair, he will be greatly missed for the valuable contribution he has made.
On a very personal note, I can’t thank A/Prof Toner enough for the very encouraging and caring role he played in looking after our daughter for 5 years. This was challenging not only from a cancer perspective but also in helping guide our family. When we first met A/ Prof Toner our daughter was a shy 13-year-old who had been diagnosed with a rare kidney cancer. He was then on a journey with us until she was a grown up 19-year-old who never complained.



We know A/Prof Toner looked after many patients and they were all very fortunate to have experienced his kindness, patience, respect, and expertise.
We hope to still see A/Prof Toner at some of the ANZUP meetings as he has much to offer in many ways, particularly in mentoring others. We wish A/Prof Toner all the best as he moves closer to a very well-deserved retirement after a rewarding but very challenging and successful career in medical oncology and research.
Thank you always.
BELINDA JAGO CAP CHAIR

have quite literally saved my life and given us the opportunity to have a now two-year old beautiful daughter, Ivy, with our second child expected in September.
being a brilliant and knowledgeable clinician, you have always been polite, respectful and most importantly honest and factual with us throughout my diagnosis, treatment and follow-up.
Connect with a community impacted by below the belt cancers and learn from clinical experts
Friends of ANZUP was established to connect people whose lives have been affected by prostate, kidney, bladder, penile and testicular cancer, ie below the belt cancers. If you are seeking more information about any of these cancers, would like to hear from people who have been faced with the same challenges, and if you have questions about clinical trials, what they are and if there is a clinical trial suitable for you – then this program could provide some answers.
Friends of ANZUP aims to provide:
• Information about the benefits of clinical trials and how to access them;
• Information about the clinical trials research conducted by ANZUP;
• Biannual community magazine ‘A little below the belt’ featuring regular updates and stories from health professionals, researchers, cancer survivors and cancer trial participants;
• Invitation to Community Engagement Forum/s;
• Practical information and e-news to help those living with below the belt cancers;
• Updates from the ANZUP clinical community
And remember, if you are wondering if a clinical trial is the correct treatment pathway then consider each point below:
• Participation in a clinical trial may increase the total number of treatment options available to you –even if you have not yet had all the standard (current) treatment options.

• You could have access to treatment not yet commercially available, which might work better or be safer than current treatment options.
• Making the decision to take part in a clinical trial may make you feel you have more control over your situation and that you are taking a more active role in your treatment.
• Your cancer care team will probably provide more attention and more careful monitoring of your condition and possible side effects of treatment if you take part in a clinical trial.
• And importantly, you might help others who have the same cancer type in the future by helping advance cancer research.
It’s only through clinical trials we can improve treatment options and outcomes for over 33,135 Australians diagnosed with “below the belt” cancers each year. By joining our community, you can take control of your treatment, be better informed, hopefully become an advocate for clinical trials and assist us in raising awareness of the benefits of clinical trials research and ultimately help us continue to fight cancer below the belt.
To find out more visit https://anzup.org.au/join-usfriends-of-anzup/
Improving Access to clinical trials for culturally and linguistically diverse (CALD) populations
Australia and Cultural Diversity
Australia is a multicultural society, with a population that includes many people born overseas, or who have a parent born overseas or speak a variety of languages. Together, these groups of people are known as culturally and linguistically diverse (CALD) populations.
The 2021 census showed that 27.6% of the Australian population were born overseas and the top 5 languages spoken in the home, other than English, were Mandarin (2.7%), Arabic (1.4%), Vietnamese (1.3%), Cantonese (1.2%) and Punjabi (0.9%). The figures from the Australian Bureau of Statistics (ABS) revealed that over 300 separate ethnic backgrounds were identified in the 2016 census, with over 300 separately identified languages spoken in Australian homes.*

Due to the large number of Australians belonging to CALD groups, research into cultural diversity has been attracting a lot of attention from researchers and policymakers in Australia. This diverse group of people have been reported to experience health inequalities and unique circumstances such as language barriers, prejudice, discrimination, and racism.
Access and participation on cancer clinical trials for CALD communities
Dr Abhijit Pal, a medical oncologist working as a staff specialist at Liverpool Hospital, recently presented some of the findings from his PhD. His study is looking at ways to improve the representation of patients from culturally and linguistically diverse backgrounds (CALD) on cancer clinical trials.

Dr Pal works in Liverpool, an area of southern Sydney that is extremely culturally diverse. One in two people are from a background other
than Australian and speak a language other than English. His research aimed to survey the cancer clinical trials workforce in Australia to understand the challenges facing recruitment of CALD patients to cancer clinical trials.
It is understood that patients with cancer from CALD backgrounds face challenges at every step of the patient journey from screening, diagnosis, standard of care and discussion about clinical trials.
“Inequity in cancer clinical trials has been a perennial issue and is becoming more noticeable this year. It is simply not fair that one sector of the community repeatedly does not get access to the wonderful advances that are being made every year in medical oncology through clinical trials – new anti-cancer therapies which offer better quality of life or longer survival are for everyone, not just a select few. We all need to do our part at the community, site and sponsor level to address this complex inequity and the many barriers that patients from CALD backgrounds face in being recruited to cancer clinical trials. At the very least, we need to measure properly and collect the correct data on CALD recruitment at site and sponsor level so we can benchmark the inequity for future years.”
Dr Abhijit PalPlenary: Raising your voice for equity in cancer care




(Current Resources)
Studies in Australia, UK and USA clearly demonstrate a systematic and consistent under representation of patients from ethnic minorities and CALD backgrounds on cancer clinical trials.
Cancer clinic appointments for
CALD patients:
• Prior to March 2020 – appointments provided an in-person interpreter but at least double the length of a consultation without an interpreter
• Last two years – all appointments have been provided via a phone interpreter which was even more difficult than in-person
Survey results
The survey developed by Dr Pal was distributed to the Clinical Oncology Society of Australia (COSA), the Medical Oncology Group of Australia (MOGA) and 14 cancer cooperative trials groups – which included ANZUP. The key questions, and some remarkable answers in the survey included:
• Question 1: Does the trial unit routinely collect data on preferred language or ethnic backgrounds of patients enrolled onto cancer clinical trials.
• Answer 1: 74% of respondents did not collect routine data
• Question 2: What services does your unit have available to assist CALD or CALD-PLNE (preferred language not English) patients to access and participate in cancer clinical trials?
• Answer 2: Only 43% of respondents said they had in person medical interpreters and 30% had nothing available at all. This then leads to a huge barrier to access to clinical trials.
For scientific purposes, it is important to have representation across cultural groups. Without a true cross-section of the population on trials there will be a limited understanding of how certain medications may affect people of different ethnicities. If participants in research reflect the true diversity of our society and culture, then evidence generated from investigator-led trials has the potential to be more generalisable and relevant for the broader Australian population, including the more vulnerable groups in need of high-quality care.

Interpreter services are one barrier to providing cancer clinical trials access to the CALD community. Often interpreters are unable to fully explain the intricacies of cancer treatments and the rationales of treatments, so patients do not end up fully informed about the clinical trial. In addition, face-to-face interpreter services have been restricted due to the pandemic. They are in high demand and not always available when required.
The survey results also demonstrated that many institutions do not have systematic processes in place to help CALD and CALD-PLNE patients gain access to partake in clinical trials.
Improving access to cancer clinical trials for patients from CALD backgrounds whose preferred language is not English –Results of a National Survey in AustraliaDr Abhjit Pal On behalf of Dr Ben Smith, Ms Christie Allan, Dr Deme Karikios, Professor Frances Boyle Chair: Associate Professor Haryana Dhillon
Next steps in cancer clinical trials
As trials evolve, the clinical trials teams should be required to report all the ethnicity, cultural and linguistic data, and also think more about future trial protocol development and how to collect information of patient populations systematically.
Crucially, interpreter services are pivotal in the delivery of clinical trials. Very few clinical trial sites and hospitals have specific CALD services. There is a clear need for more interpreters and interpreters trained in communicating clinical trials.


Taking cultural differences into account can help make trials and resources more accessible, inclusive, and responsive to the needs of all people who require assistance. In contrast, poor identification and communication with CALD populations might lead to ineffective resource allocation and interventions.
ANZUP plans to review their clinical trials to assess if they are accessible to all, regardless of ethnicity and preferred language.
References
* https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7830035/
Cancer treatment for rural and remote patients

About a third of Australians live in rural, regional, and remote areas of the country, for example outside metropolitan centres. People in these communities can have additional challenges with cancer care, such as having to travel for tests or treatment. For some people, this can cause financial and emotional stress. In addition, rural cancer patients have unique needs that should be recognised, so treatment may need to be adjusted in comparison to those living in big cities.

Dr Kate Gunn of the University of South Australia, Department of Rural Health, presented at the ANZUP Annual Scientific Meeting in July and provided an important insight into what should be kept in mind when working with, or undertaking research with rural people affected by cancer. Dr Gunn’s main research interests include addressing the psychosocial needs of rural people affected by cancer, rural help-seeking behaviour and online and telephone-based cancer support interventions.
“I grew up on a sheep, wheat and barley property in South Australia, 650 kilometres from Adelaide,” says Kate. “From that community I watched people struggle with the challenges a diagnosis of cancer brings, particularly when it is accompanied by isolation and the need to travel for medical treatment”.
https://www.adelaide.edu.au/lumen/issues/66602/ news66742.html
Dr Gunn explained the concerns of cancer treatment for a patient based in a metropolitan setting versus a rural patient are very different. The rural patient has additional burdens as outlined in the table below.
Concerns of the metropolitan versus rural cancer patient
Metropolitan cancer patient
• Treatment is tiring
• Side effects are unpleasant
• Parking is difficult
• Information provided is overwhelming
• Fear of cancer recurrence
Rural cancer patient
• Treatment is extra complicated due to being several hours from home and the support of family, friends, and support networks
• Self employed so have no sick leave
• Worries if a neighbour or wife/partner can manage the livestock or property
• Living away from home is expensive, lonely, and stressful
There are many reasons why rural cancer patients must travel for treatment. This can include:
• the closest town does not have the type of cancer specialists needed
• the type of treatment required (surgery, radiation therapy or chemotherapy) is not available near by
• if a rare cancer is diagnosed, or a cancer requires complex treatment, then certain hospitals will be recommended. People living with cancer in regional and rural areas also have poorer survival rates than those living in major cities, and the further from a major city cancer patients live, they are 35% more likely to die within five years of diagnosis.
Contributing factors which lead to lower survival rates for people with cancer in rural areas include:
• less availability of diagnostic and treatment services;
• later diagnosis;
• lower socioeconomic status;
• reduced rates of physical activity;
• increased rates of highrisk alcohol consumption;
• higher rates of smoking;
• the higher proportion of Aboriginal and Torres Strait Islander people; and
• increased sun exposure.
In addition, throughout her research, Dr Gunn found that rural cancer patients experience various key differences to urban based patients including:
• Poorer treatment outcomes
• Additional stressors, e.g., travel and financial burdens
• Later diagnosis – possibly due to access or the use of screening services
• Differences in treatment type – possibly to minimise the amount of time a rural patient spends away from home
• The further a patient lives from radiation therapy treatment, the less likely they are to receive it
• There is a higher incidence of some cancers in rural areas, particularly bowel, prostate, melanoma, cervical, lung and cancer of an unknown primary. This may be due to lifestyle factors, increased sun exposure and elevated rates of smoking
• In many areas of regional and rural Australia there are a lack of general practitioners, allied healthcare professionals and support services, clinical trialists and specialists with knowledge for follow-up
• The cost of accessing essential services is greater in the rural setting
• There are attitudinal barriers, such as stoicism and privacy, influence accessing of services
What can be done to reduce the gap in the diagnosis and treatment of rural cancer patients?

A patient’s preference to be treated close to their home and family should not compromise access to highquality care. In addition to providing better services in larger regional centres there is a need to utilise new technologies such as tele-oncology to enable improved access without compromising quality of care. The travel and accommodation schemes for cancer patients and their families in each state and territory are complex and
unsatisfactory. Reform is required to provide better assistance to cancer patients.
The burden of cancer in Australia is increasing as our population ages and there is evidence that people in rural and remote areas will continue to bear an unequal part of this burden. Addressing current shortcomings in rural and regional cancer services is vital to improving survival and outcomes for country people.
Urban-based healthcare professionals can improve the experience of a rural cancer patient by acknowledging:
• Being away from family, friends and support networks during treatment adds to levels of distress.
• Staff in small rural hospitals know their patients. The anonymity of large urban hospitals is overwhelming, impersonal, distressing, and difficult to navigate.
• The patient has travelled a long distance so help make the patient feel understood.
• Travelling is tiring and difficult so have appointments scheduled together and do not change appointments at the last minute.
• It is helpful to find ways to have tests and data collection done closer to home and offer telehealth if it is possible.
• Rural people find it difficult to ask for and/or accept help, especially to deal with emotional issues, so if making a referral or recommendation, point out that it is what most people in their situation do, i.e., normalise help-seeking.
Rural cancer patients and carers cancer treatment experiences can be made easier by improving health systems and coordination to ease the burden of travel, providing information about available support and what to expect throughout cancer treatment that is relevant to the rural context, and increasing access to quality health, community, and support services, including palliative care, in rural areas. More training on the specific needs of rural patients and their carers is needed for urban healthcare professionals. Peer support groups may have value for cancer carers in rural settings, where there are known to be multiple barriers to accessing professional sources of psychosocial support.
Rural cancer patients want their unique needs to be recognised and to be treated differently to their urban counterparts. There is a need for more targeted and rurally relevant information for rural cancer patients, both to inform them of, and change their attitudes towards diagnosis, treatment, and supportive care.
International Clinical Trials Day with Dr Ciara Conduit
International Clinical Trials Day falls on the 20th May each year. It is a day to highlight the importance of clinical trials research and also commemorate the day Scottish physician James Lind began his study to find a treatment for scurvy in 1747. He did this by dividing 12 sailors into separate groups. He tested the effect of providing different treatments to each group – some were given citrus fruit and some were not. Lind was then able to provide evidence of the link between citrus fruit and preventing scurvy. This was the first recorded controlled clinical trial.
Today, thousands of incredible researchers and clinicians across the world are working together in a global effort to pave the way for a better future through clinical trials. International Clinical Trials Day is about celebrating their work, shining a light on the results, and appealing to those considering medical research as a career.
Dr. Ciara Conduit touches on the importance of International Clinical Trials Day, the work of ANZUP, improving the treatments and outcomes for people affected by below the belt cancers, and an insight into what exciting developments are in the pipeline.

Can you please introduce yourself and tell us about your role?
I am a Clinical Research Fellow at the Australian and New Zealand Urogenital and Prostate (ANZUP) Cancer Trials Group helping develop and support clinical trials and other initiatives for patients with below the belt cancers.
By background, I am a specialist Medical Oncologist at Peter MacCallum Cancer Centre, with an interest in genitourinary cancers, particularly testicular cancer, as well as melanoma, new drug development, and communication.
Can you please tell me about some of the latest research projects you have been involved in?
In my role at ANZUP, I am fortunate to work with many brilliant Australian clinicians and researchers trying to help answer some of the tough questions that face us in the clinic each day.
Recently in this role, my focus has been on the role of immunotherapy in rare variant kidney cancers in ANZUP’s UNISoN clinical trial, as well as personalising chemotherapy for patients with advanced prostate cancer in the GUIDE trial. There are a lot of other exciting studies in the pipeline too!
From your personal standpoint, can you please tell us what International Clinical Trials Day means for you and what it represents?
To me, International Clinical Trials Day is an opportunity to celebrate those who strive to find answers to the tough clinical questions. Improvements in health outcomes because of clinical trials are vital, enabling the development of new interventions, helping to raise standards of treatment, and, crucially, benefiting patients by enabling faster access to the latest treatment. That’s why I do what I do.
The day also provides our community with a unique opportunity to raise awareness of clinical trials which they know a lot about after COVID!
In recent history, what do you think are some of the major breakthroughs that have come out of clinical trials for below the belt cancers?
There have been significant advances in treatment opportunities for patients with below the belt cancers in recent years, led by international collaborations.
In Australia and through ANZUP, we have been involved in many of these important advances including:
• ENZAMET / Prostate Cancer – The landmark Australian-led clinical trial, ENZAMET, showed that hormone therapy with a drug called enzalutamide can improve the survival of some people with advanced, hormone-sensitive prostate cancer.
• TheraP / Prostate Cancer – a new treatment for advanced prostate cancer using Lutetium-177 PSMA radionuclide therapy (Lu-PSMA). The primary endpoint of the study was to compare the effects of the two treatments on change in PSA, a blood biomarker of prostate cancer. A favourable response, defined by reduction of PSA by 50% or more, occurred in 66% of people assigned to receive 177Lu-PSMA-617 compared to 37% with cabazitaxel chemotherapy.
• Immunotherapy in kidney cancer – UNISoN tests whether new immune treatments can help people with rare kidney cancer (‘non-clear cell’ cancer).
• Bladder cancer – world first SUBDUE-1 trial, which saw the immune-stimulating cancer drug durvalumab injected directly into patients’ bladder tissue, rather than a vein, for the first time.
• Testicular cancer – Several decades ago testicular cancer was a disease with a very poor prognosis. But now, because of new treatments, tested carefully in clinical trials, it is almost always curable even when it has spread.
• ENZA-p/ Prostate Cancer – Precision medicine is the concept of targeting the right patient for the right treatment at the right time. ENZA-p is a clinical trial that aims to use new theranostic agents to allow more accurate prognostic decision making, and subsequently more effective personalised treatment with less side effects, for people confronting metastatic castrate resistant prostate cancer.
What sort of areas will clinical trials into below the belt cancers be focusing on in the future?
Oncology is a rapidly changing field, and it is sometimes hard to predict how different things may look in just a short period of time. At ANZUP, we’re excited about the future and focusing on blood-based and imaging biomarkers to help personalise care, as well as novel treatment approaches that might offer patients better cancer control and quality of life, amongst other things. We look forward to seeing how new LuPSMA therapies will transform care in prostate cancer after the results of the TheraP trial and other studies. The following are just some of the current and upcoming trials at ANZUP:
• GUIDE – A randomised non-comparative phase II trial of biomarker-driven intermittent docetaxel versus standard-of-care (SOC) docetaxel in metastatic castration-resistant prostate cancer (mCRPC).
• CLIMATE – Assessing the Clinical utility of miR-371a-3p as a marker of residual disease in Clinical Stage 1 Testicular Germ Cell Tumour, following orchidectomy.
• DIPPER – This clinical trial will use modern PET scanning (PSMA PET/CT) in people who have a rising PSA level after prostate surgery to select those who can potentially avoid or minimise additional (radiation, hormone) treatments safely.
• EVOLUTION – W ill test the effectiveness of using Lutetium-177-PSMA (Lu-PSMA) and cancer immunotherapy to treat metastatic castration resistant prostate cancer (mCRPC, or advanced prostate cancer).
• ZipUp – First in the world trial investigating a novel type of PET scan in bladder cancer. Aim is to improve scans and treatment planning for bladder cancer.

does Australia compare vs the rest of the world when it comes to trials and research into below the belt cancer?
This study was a key factor in enzalutamide being approved by the Food and Drug Administration (FDA) in America, for metastatic hormone-sensitive prostate cancer. This was a major milestone.
How
ANZUP has been extremely successful in a relatively short space of time with leading global pivotal studies in below the belt cancers. The data from these studies have had a major impact on clinical practice, as best evidenced by a study such as ENZAMET.CIARA CONDUIT AT THE 2022 ANZUP ASM
Survivorship Unmuted
The term “cancer survivor” is used for anyone who has been diagnosed with cancer, but what is survivorship and life after treatment really like?
engagement and patient empowerment–something sparked when her (now adult) son was diagnosed with cystic fibrosis in 1996 and strengthened when she was diagnosed with bladder cancer in 2017.
“I still laugh when I think of one person’s reaction when I told them I had bladder cancer and she said, “Is that even a thing?”.”
Channel 9 news presenter Will McDonald was in shock the day he was given a life-changing prostate cancer diagnosis at only 42 years of age.
In July at ANZUP’s Annual Scientific Meeting, we held our Evening Symposium, ‘Survivorship Unmuted’ and heard from a panel of cancer survivors, about their experiences and how life looks for them now. This session was led by Associate Professor Ben Tran.




Meet the Chair
Associate Professor Ben Tran is an Associate Professor within the Sir Peter MacCallum Department of Oncology at The University of Melbourne. He is also a Medical Oncologist at Peter MacCallum Cancer Centre and holds a Clinician Scientist appointment at the Walter and Eliza Hall Institute. His clinical focus lies entirely within the genitourinary (GU) tumour stream. Ben currently leads the GU clinical trials program at Peter MacCallum Cancer Centre and is Chair of the GU Tumour Group within Cancer Trials Australia, and Chair of the ANZUP Germ Cell Subcommittee.
Meet the Panel
Melissa Le Mesurier, originally trained as a journalist and has 25 years’ experience as a senior corporate affairs executive. Both professionally and personally, Melissa is passionate about medical research, consumer
“I’d started going through the ‘why me’ conversation with myself, but by the time I’d gotten home, I’d come to the realisation ‘why not me’.”
Ben: Melissa, tell me a bit about your cancer journey. Melissa: I was diagnosed in late 2017 and it was a bit of a surprise. I had been having bowel issues and I saw a bowel surgeon and I casually mentioned that I’d also been having trouble passing urine and it had got progressively worse, but I had ignored it as I thought it could have been a urinary tract infection.
My husband and I had been on holidays in Cairns, and we were about to get on the Sky rail when I realised, I hadn’t passed urine for 12 hours. As the Sky Rail was about two hours, I thought “I don’t think I can get on this gondola thing. If I’m busting and I need to go, we’re in the sky with the trees. And I thought, right, when I get home, I’m seriously doing something about this”.
My bowel surgeon referred me to Professor Shomik Sengupta, a urologist, as I was not a typical bladder cancer patient. It mainly affects people over 65, and smokers. I didn’t really fit the standard stereotype.
I had a cystoscopy, and it came back with small highgrade tumour which pretty much upended my life for about 12 months. I was put on the BCG + MM trial which was about nine months of treatment. I’m approaching the five-year mark now and feel like I should be touching wood.
Ben: In a nutshell; how did you find the whole process around being approached about a clinical trial and, and what went through your head?
Melissa: It was a quick decision. I have two children and my 25-year-old son has cystic fibrosis; he was diagnosed at four weeks old. From that day on, I was passionate about medical research, and we set up a trust foundation with the Royal Children’s Hospital. We raised money through sausage sizzles and helped to employ about 20 medical fellows for cystic fibrosis research.
I’d worked a little bit in health, and I consider myself quite health literate. My diagnosis didn’t spook me, and I read up about it and Shomik was very open about the clinical trial, that it may or may not help you. But in an altruistic way, I thought if it doesn’t help me, it may help somebody else.
Ben: A lot of my patients find that, during the treatment phase, it’s a lot of visits, a lot of consultations and then it’s done, and the consultations are very sparse, and they explain to me how things are very different and it’s sometimes adapting to that change is difficult. Did you find that difficult?
Melissa: Yeah, I think so. I think one of the beauties of the clinical trial, was that you felt you were being monitored a lot. And I like that. I like that there was somebody to ring. But yes, even now as I approach that magic five year, you think - what happens now?
I’m also on a few forums and I see patients that say it’s fabulous that you are cured, but you feel you are left in the wilderness a little bit. I know there’s a lot of resources you can access, but I also think its lacking for of the below the belt cancers, there’s not the breast cancer nurse support network.
Ben: How could we do better in that space? Do you think it’s just having that extra support, the nursing support, or is it more than that? Is it supporting you as appointments approach or is it better to kind of let you be?
Melissa: I think having access is a great support. I know there are patients that need a lot more love and reassurance, and I probably did, and I’d like to know that

the door was always open. I do honestly feel that I could ring Shomik’s office or when I was on the trial, I’d ring the trial coordinator. In my opinion, I think the greatest contact is through ANZUP and meeting other patients and people, who’ve been in similar circumstances and happy to share their stories.
I feel I’m quite resourceful. I will pick up the phone if I need to, but I’ve seen the other side as well, where other people go through their own journeys and even my son where the receptionist can put you off. They’re too busy, they’re in surgery and can only get back to you in four weeks.
I know they sound minor, but all those interactions can influence whether you will, or won’t get involved. That would be my request from my specialist, that there were contact numbers, collateral, and an understanding of the clinical trial process, and who is involved.
Ben: I’m interested to hear about your experience on the ANZUP Consumer Advisory Panel (CAP). And have you been involved in other groups?

Melissa: Yes, through my son, I’ve sat on the Alfred Hospital’s Consumer Committee and I’m a Board Director at the Lung Foundation however I feel my involvement is very valued at ANZUP. The CAP plays a part from the beginning with the trials. From Idea Generation Workshops, to discussing the trial with principal investigators and reviewing important paperwork, seen through the eyes of a patient.

I think ANZUP really are top shelf in this respect and would urge anyone to get involved. Your views as a patient are respected and the other CAP members, along with the whole of ANZUP.

Ben: I’ve heard through the grapevine; you’re writing a book. I’d love to hear more about it.
Melissa: Just to backtrack a little bit, the main side effect I had from the trial was tiredness. I was also driving an hour and a half each way to a primary health job in Melbourne. I was just too tired to be honest. I had my son to care for, he was quite ill, and my husband had an acute mental illness during that period. So twice in that year, three of us were in hospital at the same time. I learned through my son’s experience with hospital, my work, and then the bladder cancer situation, that not everything is easy to find. There’s very little that’s curated and it’s hard for people to even know about clinical trials. And if they don’t have a clinician that provides their patient with resources, or information, it can be very confusing and scary.
I took six months off work to start writing this book, sorry for the long preamble, but it’s how I have got to this point. Like a Barefoot investor book for cancer and health literacy, you could even call it a dummies guide. Like if things go pear shaped, here’s the five questions to ask on the first visit. Here’s what to do at this stage, without all the medical jargon.
lockdown. I went for a workout and my left hip joint went click and just didn’t feel right.
Over time it started to get a little bit worse, no matter what I did, including rest, it got worse. I used to have this joke that I was kind of like a low-level superhero, like Wolverine, as I used to heal well. I never had injuries that would persist. I could always push through it. It’d get better quickly. This one didn’t get better, it just kept getting worse and worse.
Five weeks later I went skydiving and this is the bit where I always say skydiving saved my life because I did about four jumps on a Friday, and I didn’t do anything wrong. I didn’t land badly. I didn’t do anything. But my left hip joint was so painful, and I was limping, but adrenaline and you know, thinking you’re bulletproof, you keep doing stuff. On the drive home I had this stabbing pain, and I thought oh no, I’m injured. Something’s wrong here. A week later I managed to get an MRI, and that’s when the alarm bells went off. The GP told me there were white spots on the scan, that could be cancer.
Shortly after the visit to the GP, I had blood tests which showed my PSA was 38. We found the culprit. It was a bit of a whirlwind from this point. I was quickly referred to a specialist, who I could see straight away. The specialist looked at my scans and said, “Your hip joint’s no good. You’ve cracked the outer casing of the acetabulum. But that’s not your problem. Your prostate’s your problem. You’ll need to see a urology colleague of mine straight away”.
Straight away was the next day. The urologist looked at my scans, reviewed my blood work and sat me down and he said, “okay, we’ve got surgery list this afternoon. You’re on it”.
The biopsy revealed advanced aggressive prostate cancer with a Gleason score of nine.
Ben: I think that’s so crucial. When I have family members who might be unwell, I say make sure you ask these questions, or this is what you need to do. It can be such a blur for patients and their families so your book sounds so valuable.
Melissa: I hope so. I’ll tell you when it’s out there. Questions about what the difference between the public system or the private system. What’s a resident, what’s a consultant. In research, it has been found 64% of people have the lowest form of health literacy and that’s English speaking. What does the indigenous person do with no internet access in rural areas.
Ben: Thanks Melissa, I’d now like to welcome Will McDonald. Will, we’d love to hear your story. Are you able to share with us how you are going?
Will: Absolutely. I have always been really fit and active. I remember the day clearly; it was the 1st June 2020 and the gyms reopened in Adelaide after our first COVID
The Gleason grading system is used to help evaluate the prognosis of people with prostate cancer using samples from a prostate biopsy. Together with other parameters, it is incorporated into a strategy of prostate cancer staging which predicts prognosis and helps guide therapy. Cancers with a higher Gleason score are more aggressive and have a worse prognosis. Pathological scores range from 2 to 10, with higher numbers indicating greater risks of recurrence or death.
I’m 44 and most people probably assumed that I’ve had kids, but I haven’t. So luckily, I mentioned to the specialist before I went on hormone therapy and visited the sperm bank.
I started hormone therapy straight away and my medical oncologist, who I was referred to, put me on six doses of chemotherapy. I said to them, turn the machine up to full blast and give me the maximum allowable human dosage. That was my method of what I was going to do to try and get through this was, do not leave any stone unturned.
During this time, I went to work every day, every time. I guess my attitude through that whole period was positive. My brain switched to the point of going no thanks cancer, you’re not going to ruin my life. That’s how I dealt with the treatment. Luckily after the six rounds of chemo, I had another PSMA PET scan, and everything had shrunk, and my PSA was dropping. However, the specialists decided to blitz me with radiotherapy.
I had 20 doses of external beam therapy. Now, my tough facade and positive attitude was tested during radiotherapy. It was the most difficult part of my treatment. Especially when out and about, you’re always looking for the bathroom in case you might wet yourself. Thankfully after the radiotherapy my PSA kept dropping. I think my last result was 0.1. It started at 38 and down to 0.1, and it’s never gone up. So that’s a good sign. My appointments are now every three months.
Ben: When you were going through treatment, it’s very intensive, a lot of visits and now it’s much less frequent. How have you adapted to that kind of shift?
Will: Yeah, it certainly is. I think I’ve adapted to it now. But there is that period when you get towards the end of the chemotherapy and radiotherapy treatments. A solid six months of seeing a doctor every three weeks, at least. And then at the end you walk out of it thinking, well, what do I do now? I’m not fighting anything, I guess. It’s that mental shift where you really must prepare yourself and, and come to terms with, accept this is life.
Ben: Is there anything the community or healthcare industry can do to help.

Will: I think partly it probably is what it is, but I probably come at it from a different point of view. I’ve been so lucky in terms of the networks that I have been able to establish quickly both personally but also during my cancer treatment, people from Cancer Council and Prostate Cancer Foundation of Australia.
I think that idea of just having a number to call, to be able to talk to someone during that time is invaluable. You’re not bothering anyone when you call. That’s why they’re there.
Ben: Have you been one to seek out prostate cancer support groups? I know young people with prostate cancer find it very hard, as there are a lot of older people in the groups, to find those in similar situations.

Will: Yes, very few. I don’t think I’ve met anyone in Adelaide around my age with prostate cancer. I have had one guy in Tasmania who has approached me, who’s only a little bit older and in a very similar situation. And another fellow on the Gold Coast in a similar situation when he was diagnosed. We emailed back and forth. We talk about how to combat the side effects of the hormone therapy and some of the challenges going through treatment.
Ben: Do you find talking to people who have been through it before or going through it at the same time helpful?
Will: Absolutely. I guess when you’re first diagnosed with prostate cancer or any cancer, and I know I did, you feel overwhelmingly alone. Like there was just this sense that no one else had any idea what I was going through, and you were just alone. That’s probably why I didn’t tell anyone to start with, but then you open up, and talk to people, and you know, you’re not alone, there’s other people going through it. I found it helpful to talk to a huge range of people to be fair, people who have come from all different scenarios, and different cancers.
Ben: Learning from others, right?
Will: By learning from others, you learn lots of things. There’s a lovely lady that I met through Cancer Council, she was a palliative care nurse in her working life. She’d had breast cancer and then she was diagnosed with an unrelated stomach cancer, which really knocked her about. When I met her, she was going okay. She said there are five stages of fighting it, of grief and dealing with it. She said, just skip straight to acceptance. It’s easier. That was one of the greatest pieces of advice that I’ve ever had – was a terrific one.

Out with Cancer
Toward LGBTQI+ inclusive cancer
By Dr Rosalie Power, Associate Research Fellow, Translational Health Research Institute carePeople with cancer who are lesbian, gay, bisexual, transgender, queer and/or intersex (LGBTQI+) often have unique experiences and needs. The Western Sydney University ‘Out with Cancer Study’, funded by the Australian Research Council (ARC), in partnership with PCFA, Cancer Council NSW, Canteen, BCNA, ACON and LGBTQI Health Alliance, explored these experiences with 430 LGBTQI+ people with cancer, 132 of their partners and carers, and 357 healthcare professionals.
Higher distress than the broader Australian cancer population
41% of LGBTQI+ people with cancer reported high or very high levels of distress, 3-6 times higher than previous non-LGBTQI+ cancer studies.

Higher levels of distress were reported by people were trans (binary and non-binary) compared to cisgender people, adolescents and young adults, compared to older people, those who were bisexual or queer, compared to lesbian or gay people, and those who lived in rural or regional areas, compared to urban areas.
Distress was associated with experiences of discrimination in life and during cancer care, feelings of discomfort being LGBTQI+, lower outness about being LGBTQI+ and lower social support.
Difficulties ‘coming out’ to cancer healthcare professionals
Less than 1 in 5 participants were out to all healthcare professional involved in their cancer care. For many people, deciding if, when and how to disclose being LGBTQI+ added to distress during cancer. Many patients and carers felt excluded or invisible in cancer care, due to cis-heteronormativity – the assumption that everyone is heterosexual and cisgender.
I don’t feel safe. I have
think ALL
TIME in medical situations if it’s safe to come out. Correcting, educating, making formal complaints – I am enraged that my energy has been taken up by this my whole life when I’m in pain; very sick; recovering; scared.
Queer femme, age 38, multiple cancers
Cancer impacted LGBTQI+ identities and body image
Our PCFA funded pilot research found that gay and bisexual men experienced greater distress than heterosexual associated with sexual changes after cancer. Loss of erectile function or ejaculate and reduced penis size threatened masculinity and gay identity. However, gay and bisexual men were more likely to use sexual aids or seek counselling for sexual changes. This enabled renegotiation of sex and intimacy
For some trans people, cancer treatment side effects erased gender affirmation. Loss of hair and weight loss exacerbated body dysphoria and resulted in participants being misgendered.
For some LGBTQI+ people cancer facilitated greater alignment of their body and identity. For example, cancer treatment which caused reduction in erectile function, penis and testicle size, or feminizing bodily changes, were affirming of identity for some trans women, as they mirrored the impacts of gender affirming hormonal therapy.
to
THE
The importance of LGBTQI+ community connection
LGBTQI+ partners and chosen family (often other LGBTQI+ people) buffered negative experiences during cancer including helping navigate discrimination in cancer care and cis-heteronormativity.
A number of participants mobilized around their cancer experiences and set up services including support groups to build connections between LGBTQI+ people with cancer. These groups reinforced LGBTQI+ identities, reduced social isolation and helped participants navigate their cancer journey.
Here we are at a pride march. We all had t-shirts and arrows saying different things about our sexualities, genders and interests. Showing that we as a community are completely diverse. I also wore a t-shirt that said, “know your prostate” and as we walked along, I handed out pamphlets about a prostate cancer support group for LGBT people. It felt really important to me to be involved in this activism around sexuality and prostate cancer.
Gay man, age 60, prostate cancer

I believe I am an open person and I am very happy to treat patients of the LGBTQI+ community but I acknowledge my knowledge is limited and I possibly carry some misconceptions about their lifestyle and needs. I would be very receptive to education on the issues that pertain to this community.
Medical professional, age 41
Signs of LGBTQI+ inclusive cancer care
1. You feel emotionally and physically safe with health care professionals.
2. Healthcare professionals do not assume you are heterosexual and/or cisgender: use your preferred name and pronouns.
3. Your partners or chosen support people, are included in your care
4. Patient records allow you to record your LGBTQI+ status.
5. Your healthcare professionals understand your sexual needs during cancer.
6. You have access to cancer information that is LGBTQI+ inclusive.
7. Healthcare environments signpost LGBTQI+ inclusivity (such as posters, flags and icons on resources).
8. Healthcare services have anti-LGBTQI+ discrimination policies.
9. You and your chosen support people have access to gender-neutral bathrooms.
More information
www.westernsydney.edu.au/outwithcancer
Ussher, JM, Perz, J., Rose, D., et al (2017) Threat of Sexual Disqualification: The Consequences of Erectile Dysfunction and other Sexual Changes for Gay and Bisexual Men with Prostate Cancer Archives of Sexual Behavior 46(7) 2043-2057. doi: 10.1007/ s10508-016-0728-0
Ussher, JM., Power, R., Perz, J., et al LGBTQI Inclusive Cancer Care: A Discourse Analytic Study of Health Care Professional, Patient and Carer Perspectives. Frontiers in Oncology. 2022; 12:832657. Ussher, JM., Allison, K., Perz, J., Power, R., et al LGBTQI Cancer Patients’ Quality of Life and Distress: A Comparison by Gender, Sexuality, Age and Cancer Type. Frontiers in Oncology. 2022. Doi 10.3389/fonc.2022.873642
Most healthcare professionals said they were comfortable treating LGBTQI+ patients but that they lacked confidence and wanted more education and training, particularly on the needs of patients with cancer who are trans or have intersex variation.
Power, R., Ussher, JM., Perz, J., Allison, K., et al “Surviving Discrimination by Pulling Together”: LGBTQI Cancer Patient and Carer Experiences of Minority Stress and Social Support. Frontiers in Oncology. 2022; 12:918016.
Ussher, J. M., Perz, J., Allison, K., Power, R. et al (2022). Attitudes, knowledge and practice behaviours of oncology health care professionals towards lesbian, gay, bisexual, transgender, queer and intersex (LGBTQI) patients and their carers. Patient Education and Counseling. 105(7), 2512-2523.
Cancer healthcare professionals want to provide LGBTQI+ inclusive cancer care but lack knowledge and confidence.







ANZUP at the American Society of Clinical Oncology Meeting
Each year more than 40,000 oncology professionals from around the world come together for 5 days in June in Chicago USA for the American Society of Clinical Oncology (ASCO) Annual Meeting. This meeting allows the oncology community to stay up to date on new clinical cancer advances in every area of cancer research, gain real-time insights from worldrenowned faculty, and connect with one of the largest, most diverse audiences in global oncology.
The ASCO Annual Meeting is one of the most important conferences for presenting the latest, most practice-changing research in cancer care. Through this conference, the cancer community learns how to better care for, support, and treat people with cancer.
At the most recent ASCO Annual Meeting held from 3 – 7 June, ANZUP was in attendance to give two oral presentations and two poster presentations. The presentations included updates on the prostate cancer ENZAMET and TheraP trials, and poster presentations for a kidney cancer trial called UNISoN, and another prostate cancer trial, DASL-HiCAP.
ENZAMET
At the ASCO 2022 Annual Meeting in Chicago, ANZUP presented the planned analysis results of the ENZAMET study, after patients had been followed on average for more than 5 years.

ENZAMET showed that people with advanced, hormone-sensitive prostate cancer who receive enzalutamide added to standard treatment are 30% less likely to die compared to people receiving standard treatment alone.
Study Co-Chair and Board Chair of ANZUP, Professor Ian Davis, said, “ENZAMET is a unique collaboration of clinicians and scientists from Australia, New Zealand, Ireland, UK, Canada, and the USA, all coming together to work with the community to find better ways of treating prostate cancer. ENZAMET won the 2020 Trial of the Year Award, as well as awards for community involvement, and for high quality statistical conduct. Now we have very mature results confirming that the benefit of enzalutamide treatment persists even after much longer followup, and we continue to see other informative results emerging from this very important trial.”
TheraP
Professor Michael Hofman presented the three-year follow-up results from ANZUP’s TheraP trial - the first randomised trial comparing 177Lu-PSMA-617 to standard of care chemotherapy.
TheraP is the first randomised trial comparing 177LuPSMA-617 (Lu-PSMA), a novel radioactive treatment, to the current standard-of-care chemotherapy called cabazitaxel for people with metastatic castrationresistant prostate cancer. These people had disease that had already progressed after standard chemotherapy.
This unique treatment involved two distinct parts. Firstly, a PET scan is used to ‘map’ the cancer. This is done by injecting a radioactive molecule called gallium-68 attached to a small molecule that rapidly localises to prostate specific membrane antigen (PSMA) on the surface of prostate cancer cells in the body. The result is the cancer cells ‘light up’, showing exactly where the disease is and enables identification of patients that may benefit from this new therapy. The second part is the therapy itself: the Lu-177 radionuclide is attached to a similar molecule used in the scanning process, and
Lu-PSMA is administered to the patient, targeting the tumours and killing the cancer cells while minimising damage to surrounding tissue.
Study Chair Prof. Michael Hofman said “Three-year follow-up of the TheraP study provides compelling evidence that Lutetium-177 PSMA-617 is a new treatment option for people with prostate cancer, providing an alternative to cabazitaxel chemotherapy with better patient reported outcomes and lower side effects.”
not met as a minority of participants benefited from treatment with ipilimumab and nivolumab after failure of nivolumab therapy alone. Whilst some participants did gain meaningful benefit from this approach, further research is required to explore other strategies.
UNISoN
The UNISoN trial aims to test whether new immune treatments can help people with rare kidney cancer (‘non-clear cell’ cancer). Non-clear cell cancer represents approximately 25% of people with kidney cancer; and because it is rare there are no treatments currently reimbursed in Australia.
The UNISoN trial will test immune treatments in two different ways; firstly, it will investigate how well one immune treatment (nivolumab) works alone. If this is unhelpful by itself, then people can continue taking nivolumab but also add in a 2nd immune treatment (ipilimumab). The trial hopes to discover how many people will benefit from one drug alone. By undertaking detailed laboratory testing of people’s cancer samples, it is hoped we also learn who will benefit from taking both treatments together.
The UNISoN study poster was presented at ASCO by ANZUP Chair, Professor Ian Davis and focussed on the final study report. The report demonstrated that the primary endpoint of the UNISoN study was


DASL-HiCAP
The purpose of the DASL-HiCAP prostate cancer trial is to see if a new tablet drug, darolutamide, combined with the current best treatments, can improve outcomes for people with high-risk prostate cancer that has not spread beyond the prostate area.
The Study Co-Chair, Professor Chris Sweeney presented a ‘Trial in Progress’ poster at ASCO. This poster was based on trial data taken as of 10 May 2022. The data was able to show that there are currently 530 patients enrolled in the study, which totals 50% of total patient recruitment. The study is also open at 56 participating centres and is recruiting internationally across Australia, New Zealand, Canada, USA, Ireland, and the United Kingdom.

Below the Belt Research
2022 Below the Belt Research Fund Recipients
Overview - Below the Belt Research Fund
The Below the Belt Research Fund was established to support ANZUP members in the development of investigator-initiated studies. The funds raised from Below the Belt events, and donations from our supporters, go directly towards clinical trial research via the Below the Belt Research Fund.
The Below the Belt Research Fund was established to provide much needed seed funding to support ANZUP members to progress new trial ideas to the point of becoming full scale studies.
Since 2015 the Below the Belt Research Fund has supported many members in the development of investigator-initiated studies and turn an idea into a fully-fledged trial.
At the ANZUP Annual Scientific Meeting the 2022 recipients of the Below the Belt Research Fund were announced. Congratulations to:
• Louise Emmett
• Chun Loo Gan
• Weranja Ranasinghe
• Shomik Sengupta
Professor Louise Emmett

Director of Theranostics and Nuclear medicine, St Vincent’s Hospital Sydney
The RE-SPECT project: Development of interim response biomarkers in Lu PSMA therapy.

Lu PSMA therapy is a new therapy for people with metastatic castrate resistant prostate cancer (mCRPC) that has been shown to be better tolerated than and equally effective to cabazitaxel chemotherapy
(TheraP). However, not all people respond to the treatment identically, with some people demonstrating dramatic responses and others progressing early.
Personalising treatment for the individual requires response bio-markers that can accurately measure dynamic changes in treatment response, allowing intensification or de-intensification of treatment. In people with exceptional response, treatment can be paused, while in people with cancer growth despite treatment, treatment can be intensified or changed.
Currently we use PSA, CT scans and bone scans to determine whether a person is responding well to treatment. However, Lu PSMA treatment emits a gamma wave that enables a whole-body image evaluating all tumour sites after each therapy injection (24 hours); this picture is called a SPECT scan. Work on the LUPIN trial at St Vincent’s has shown that any increase in tumour volume on Lu PSMA SPECT predicted cancers that were not responding to treatment, even when the PSA had not yet risen.
The concept of using images from the therapy itself (SPECT imaging) – is unique to theranostics approaches like Lu PSMA. The potential for these SPECT scans to provide dynamic treatment response information has not been fully assessed.
While this initial evaluation shows that Lu PSMA SPECT has the potential to be an effective response biomarker, many questions remain to properly validate its role and optimise its potential uses. ANZUP has unique clinical trials in Lu PSMA with stored SPECT data and the associated treatment response data for each patient. Analysing these data would allow us to fully evaluate the role and benefit of SPECT as an interim response biomarker – potentially further improving the lives of patients through better, faster clinical decision making.
Below the Belt Research
Dr Chun Loo Gan

Early career GU medical oncologist, Royal Brisbane and Women’s Hospital and Greenslopes Private Hospital
PREDICTing treatment response to first-line immunotherapy-based combinations with PSMA and FDG PET in advanced Renal Cell Carcinoma
More than 4000 people in Australia are diagnosed with kidney cancer each year. While anti-cancer medications such as oral tyrosine kinase inhibitors and intravenous immunotherapy have prolonged lives for patients with metastatic kidney cancer (cancer that has spread from the kidney to another part of the body), it is difficult for doctors to work out which patients will respond to which drug or drug combination. More research is needed to identify individual patient factors (biomarkers) that may provide additional information to determine the best treatment for patients with metastatic kidney cancer.
In some cancers, positron emission tomography or PET scans are better at identifying cancer deposits than computerised tomography (CT) and are commonly used. In some hospitals in Australia, PET scans are already being used to inform the management of patients with kidney cancer, but this approach is not well studied.
This research project aims to find out if PET scans can provide doctors with more information in selecting the best treatment for patients with metastatic kidney cancer. Using information from this study, we will develop a follow-up study using PET scans to help choose between available therapies for patients to achieve the best outcomes.
Dr WeranjaRanasinghe
Urologic-oncology surgeon, Monash Health
Utilising a pro-inflammatory gene signature and immune cell markers to identify non-muscle invasive bladder cancer patients at high risk of intravesical BCG failure.
Almost 80% of patients who are newly diagnosed with bladder cancers have tumours limited to the superficial layers of the bladder. The more aggressive forms of these superficial bladder cancers are commonly treated with an immunotherapy medication called BCG which is put into the bladder. This medication, an inactivated bacterium resembling tuberculosis (BCG), has been
used effectively for decades, reducing the likelihood of bladder cancer coming back or spreading outside the bladder. However, 30-45% of patients, this BCG treatment will fail with the cancer progressing into deeper layers or spreading outside the bladder despite treatment. If the cancer progresses to the bladder muscle despite BCG, even curative treatments such as removal of the bladder result in poor outcomes. Therefore, it is vital to identify patients who will not respond to BCG treatment early.
BCG works by activating our immune system to target cancer cells in the bladder. Studies suggest that recruiting more immune cells in the cancer environment can benefit patients receiving BCG treatment. However, in patients who have an exaggerated inflammatory response with a large number of immune cells present before BCG treatment, it can cause exhaustion of these immune cells rendering these cells dysfunctional and unable to mount a response when BCG is administered.
This study aims to utilise genetic pro-inflammatory gene markers and immunostaining to help identify which patients will not respond to BCG treatment. This will enable better selection of patients for this treatment and allow for future research to develop other therapies for bladder cancer.
Professor Shomik Sengupta

Professor of Surgery and Deputy Head of School at the Eastern Health Clinical School, Monash University & consultant urologist & Uro-Oncology lead at the Department of Urology, Eastern Health.
Non-muscle invasive bladder cancer registry
Bladder cancer is a common condition. Reliable sources of information on bladder cancer treatment and outcomes in Australian patients are not limited. This proposal is to develop a platform for collecting information on patients diagnosed and treated for bladder cancer. The main aim will be to utilise the information to improve treatment in the future. The platform would also allow us to plan and run some studies to compare and assess different ways of treating bladder cancer.
Below the Belt Research
Research funding helping initial ideas progress
What is Research Funding?
Research funding is defined as a grant obtained to undertake scientific research. A grant is a way ideas and projects can progress with financial assistance. Applications for a grant are usually done as part of a competitive process. Applying for grants and securing funding is an essential part of conducting research.
The two most important components of any research project are the idea and execution. The successful execution of a research project depends not only on the effort of the researcher but also the availability of infrastructure to conduct the research. The infrastructure includes research facilities, equipment and resources required to undertake the research, and the experts.
Once a research project begins, expenses are incurred for both the time of the researchers and the materials required for the research. Funding is essential to meet these monetary requirements.

When studies involve multiple participation centres, are randomised controlled trials, are an experimental or observational study with a large sample size, it may not be possible to conduct the study within the resources of the institution and a source of external funding will be needed. Lack of funding means many great ideas do not progress into good quality research projects.
Below the Belt Research Fund
Great ideas need funding. ANZUP decided to take on the challenge of seeding new projects through the Below the Belt Research Fund. The launch of the Below the Belt Research Fund was announced at the 2nd annual Below the Belt Pedalthon at Eastern Creek in September 2015. Since then, ANZUP and the Below the Belt Events have raised just over $1.96million and supported 36 members to progress their ideas.
Ciara Conduit, a medical oncologist at Peter MacCallum Cancer Centre in Melbourne, and Steve McCombie, a urologist at Fiona Stanley Hospital in Perth, are both recipients of the Below the Belt Research Fund.
Ciara is undertaking research with testicular cancer survivors who have had retroperitoneal lymph node dissection. Sometimes after retroperitoneal lymph node dissection (RPLND; surgery involving the lymph nodes at the back of the abdomen), important nerves controlling ejaculation can become disrupted. This results in retrograde ejaculation (RE), where sperm flows back into the bladder instead of through the penis after orgasm. The research being undertaken will investigate how this retrograde ejaculation affects people’s quality of life.
The research Steve is undertaking involves tumour and biopsy tissue samples being telescopically removed from patient’s bladders at several timepoints during their treatment whilst on the ANZUP BCG+MM trial. Along with the research team, Steve plans to perform extensive analyses on these samples to try and determine if it can be predicted which patients may do better with BCG treatment alone, combined BCG and mitomycin treatment, or those that may not be likely to respond to either BCG or the combination.
Below the Belt Research
Both Ciara and Steve acknowledged that it is difficult to obtain grants in hospitals and in the state systems – there are not a vast number available. So, the Below the Belt Research Fund grants provide a good opportunity for those working in urological cancers.
Ciara and Steve believe the Below the Belt Research Fund provides an exciting opportunity for all researchers as a grant can make a big difference and help identify preliminary data. Seed funding will help to propel the researchers to answer initial ideas which will then hopefully move them towards larger grant applications, answering the questions on a larger scale as a fully-fledged trial.
They both agree it is important to encourage peers and colleagues to apply for the Below the Belt Research Fund grants that are awarded each year at the ANZUP Annual Scientific Meeting in July. The grant provides an exciting opportunity to make a big difference in urological cancer research.

Steve went on to say, “I am often asked by people who have research ideas how can I bring them forward and I direct them to ANZUP when it is to do with urological cancers, and if it is, then the Below the Belt Research Fund is a really nice idea and a good opportunity for them.”

“Thank you to everyone who has raised funds for the Below the Belt Research Fund. It has really helped us do our projects.”
Steve McCombieCIARA CONDUIT AND STEVE McCOMBIE
DO
W
Share your story with us here anzup@anzup.org.au

Share your story with us here anzu
Create awareness and let other not alone
Create awareness and let others know they are not alone.
Spotlight on prostate cancer

The prostate is a walnut-sized gland located in front of the rectum, behind the base of the penis, and below the bladder. It surrounds the urethra, the tube-like channel that carries semen and urine through the penis. The main function of the prostate is to make seminal fluid, the liquid in semen that protects, supports, and helps transport sperm.
24,217+
estimated new diagnoses in Australia
In 2022: deaths in Australia
five year survival rate after diagnosis
95% 3,507
What is prostate cancer?
Prostate cancer begins when healthy cells in the prostate change and grow uncontrollably, forming a tumour. A tumour can be benign or cancerous. A cancerous tumour is malignant, meaning it can grow and spread to other parts of the body. A benign tumour means the tumour can grow but will not spread.
Prostate cancer is slightly unusual when compared with other cancer types. This is because many prostate tumours do not spread rapidly to other parts of the body. Some prostate cancers grow at a very slow rate and may not cause problems or symptoms for years, or sometimes ever. Even when prostate cancer has spread to other parts of the body often it can be managed for a long time. So people with prostate cancer, and even those with advanced prostate cancer, may live with good health and quality of life for many years. However, if the cancer cannot be well controlled with existing treatments, it can cause symptoms like fatigue and pain and sometimes can lead to death. An important part of managing prostate cancer is monitoring it for growth over time, in order to find out if it is growing slowly or rapidly. Based on the pattern of growth, your doctor can then decide the best available treatment options and when to give them.
Prostate cancer is the most common cancer diagnosed in Australia. By the age of 85, it is estimated one in six people will be diagnosed with prostate
cancer. It is more common in older people, with 63 per cent of cases diagnosed in people over 65 years of age.
In 2022, it was estimated that 24,217 new cases of prostate cancer will be diagnosed in Australia. The five-year survival rate for people diagnosed with prostate cancer has increased over the years from 60 per cent to 95 per cent. Nearly all patients who present with localised disease will live beyond five years.
In 2022, deaths from prostate cancer were estimated to be 3,507.
Prostate cancer symptoms
Symptoms are not usually seen with early prostate cancer. Advanced prostate cancer symptoms can include:
• Frequent urination, particularly at night;
• Pain on urination;
• Blood in the urine;
• A weak urine stream;
• Pain in the pelvis or back
• Weak legs or feet
If the disease becomes more widespread and found in the bones, it can cause unexplained pain, fatigue and weight loss.
Spotlight on prostate cancer
Causes of prostate cancer
Some of the risk factors for prostate cancer:
• Age, increasing greatly if you are aged over 50 years;
• Family history of prostate, breast or ovarian cancer, especially BRCA1 and BRCA2 gene mutations;
• A brother or father diagnosed with prostate cancer before the age of 60 years
• T here is also an association with high testosterone levels.
Treatment Options
If you do not have a family history of prostate cancer, you may want to consider tests for early detection after discussing the risks and benefits with your general practitioner (GP).
If you have a family history of prostate cancer, your GP should discuss the option for annual PSA testing.
Your general practitioner (GP) will assess your symptoms, conduct a physical examination and arrange blood tests if needed. Your GP should also discuss your needs (including psychological, physical, social and information needs) and suggest sources of reliable information and support.
Treatment and care of people with cancer is usually provided by a multidisciplinary team, i.e a team of health professionals, both medical and allied health. Your health care team will help decide the optimal course of treatment and take into consideration:
• the stage of the disease
• the location of the cancer
• the severity of symptoms
• your general health and wishes.
Treatment may take various forms and may not be recommended straight away. Options include:
1. Watchful waiting where you might be monitored in case symptoms develop or change.
2. Active surveillance when you will likely have regular blood tests to check your PSA level, regular digital rectal examinations, and maybe ultrasounds or biopsies. If the cancer starts to grow or there are signs it is worsening, you might begin treatment.
3. Surgery will become an option if the tumour has not spread outside the prostate. The prostate and some of the surrounding tissue will be removed, including the seminal vesicles. This is called a radical prostatectomy.
4. Radiotherapy can take two forms:
a. external beam radiation therapy – where a machine outside the body directs radiation towards the prostate gland
b. internal radiation therapy (brachytherapy) –where small radioactive ‘seeds’ are placed inside the prostate.
5. Hormone therapy involves reducing the levels of certain hormones in the body, so the cancer can slow its growth or even shrink. Hormone therapy for prostate cancer is also called androgen deprivation therapy (ADT).
7. Chemotherapy can also be used to treat prostate cancer.
Clinical Trials
New drugs and treatment approaches are constantly being developed and researched. New combinations of different strategies and therapies, as well as the development of new drugs, are constantly being trialled and tested to see if they can further improve treatment options and quality of life for people with advanced prostate cancer. Please talk with your doctor to see if there is a clinical trial suitable for you.
References:
https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/cancer-rankings-data-visualisation https://www.cancer.org.au/about-cancer/types-of-cancer/prostate-cancer/ https://www.prostate.org.au/awareness/for-recently-diagnosed-men-and-their-families/advanced-prostate-cancer/treatment/are-therenew-treatments/
Thousands join research quest
Every September for Prostate Cancer Awareness Month, thousands join The Long Run to raise vital funds for groundbreaking research and clinical trials to help make prostate cancer history.
As Prostate Cancer Foundation of Australia’s pinnacle event, The Long Run encourages Australians to run, walk or wheel 72km in an effort to collectively cover the distance to the moon (384,400km) and raise vital funds for support services and research.
With 66 people diagnosed every day, prostate cancer has overtaken breast cancer as Australia’s leading cause of cancer. This year alone, more than 24,000 people are expected to be diagnosed with the disease.
PCFA CEO Anne Savage said “The Long Run had already paved the way for vital research and will continue to provide funding for life-saving work”.
Lu-PSMA with immunotherapy, which we think will be a gamechanger in the treatment of advanced prostate cancer.”
“We are on the verge of a complete transformation in prostate cancer treatment, giving people with the most aggressive and deadly forms of this disease a greater hope of survival.”
More than 240,000 Australians have now been diagnosed with prostate cancer in their lifetime –a figure set to increase by 43 per cent by 2040.
“Funds raised from The Long Run are instrumental to our ongoing partnership with ANZUP - a cancer cooperative trials group - and the ground-breaking work we are achieving together.
“This includes the world-first ANZUP-led EVOLUTION Phase II Clinical Trial which commenced earlier this year.”
“This trial will go beyond where any other trial has gone before, exploring the next frontier in precision nuclear medicine for prostate cancer, combining
Australians can join The Long Run via thelongrun.org.au.

For information call PCFA on 1800 22 00 99 or go to www.pcfa.org.au.

“With increasing numbers of people being diagnosed and nearly 10 dying from prostate cancer every single day, we need to be taking action and investing in research that could save lives,” Ms Savage said.
“This work is only made possible with the support of the community so we’re asking those who want to take part in ‘The Long Run,’ to run, walk or wheel 72km during September to help make prostate cancer history.”
– Anne Savage
“We’ve come a long way –increasing survival rates to 95 per cent, but we will not stop until we defeat prostate cancer,” Ms Savage said.
The evolution of prostate cancer treatment
The first case of prostate cancer was discovered in 1853 by J. Adams, a surgeon in London. At the time the surgeon noted in his report - it was ‘a very rare disease’.
Today however, prostate cancer is not unusual. Prostate cancer is the most common cancer in Australians (apart from skin cancers). In 2022, it is estimated that 24,217 new cases of prostate cancer will be diagnosed in Australia. About 1 in 10 people will develop prostate cancer before the age of 75.
This increased incidence has led to remarkable changes in the diagnosis and treatment of prostate cancer over the past century.
A grading system for prostate cancer
In 1966, the Gleason grading system was developed to help doctors and patients understand if prostate cancer is low-risk, intermediate-risk, or high-risk. The scores indicate:
• Low-risk: Gleason score of 6 or below
• Intermediate-risk: Gleason score of around 7
• High-risk: Gleason score of 8 or above
History of Prostate Cancer Treatment
The first operation to surgically remove a man’s prostate gland, which is called a prostatectomy, was performed at Johns Hopkins Hospital.
Doctors began to implant radium directly into the prostate to treat cancer.
Doctors started to use a different surgical technique to remove the prostate gland.
Megavoltage radiation was used to treat prostate cancer. The treatment was for people whose cancer had not spread beyond the prostate gland.
Hormone treatments that block the production of male sex hormones (androgens) were developed. Doctors had learned that androgens can contribute to prostate cancer growth.
It became standard treatment to combine certain types of radiation and hormone therapy to treat prostate cancer.

Current Treatment Options
Most people diagnosed with prostate cancer will live a long time, but challenges remain in choosing the best treatments for individuals at all stages of the disease. Treatment for prostate cancer has evolved over time. Surgery, radiation, and hormone therapy are among the options.
Treatment for prostate cancer depends on various factors such as,
• the stage of the disease
• the location of the cancer
• the severity of symptoms
• the general health and wishes of the patient.
Treatment can vary and may include:
1. Watchful waiting – the patient is monitored in case symptoms develop or change.
2. Active surveillance – If the prostate cancer is regarded to be low-risk and localised to the prostate, then ‘active surveillance’ may be the form of treatment used. Regular blood tests to check PSA levels, regular digital rectal examinations, and possibly ultrasounds or biopsies will be undertaken. If there are signs the cancer is worsening treatment may then commence.
3. Surgery – If the tumour has not spread outside the prostate, you might have surgery to remove the prostate and some of the surrounding tissue. This is called a radical prostatectomy.
4. Radiotherapy – this can be used to treat prostate cancer. It can either be external beam radiation therapy or internal radiation therapy.

5. Hormone therapy – some types of cancer, including prostate cancer, need certain hormones to grow. By reducing the levels of these hormones in the body, the cancer can slow its growth or even shrink. Hormone therapy for prostate cancer is also called androgen deprivation therapy (ADT), and there are several types.
6. Chemotherapy – is a drug treatment that uses powerful chemicals to kill fast-growing cells in your body such as cancer cells.
7. Immunotherapy – uses substances made by the body or in a laboratory to boost the immune system and help the body find and destroy cancer cells.

The Future of Prostate Cancer Treatment
New drugs and treatment approaches are regularly being developed and researched. New combinations of different strategies and therapies, as well as the development of new drugs, are constantly being trialled and tested to see if they can further improve treatment options and quality of life for people.
A world first prostate cancer trial is now being led by ANZUP in partnership with the Prostate Cancer Foundation of Australia (PCFA). This trial is called the EVOLUTION (ANZUP 2001) trial – and hopefully it will add to the treatment arsenal for prostate cancer.

It will be the first clinical trial of its kind to test the effectiveness of a new generation of radiotherapy treatment with existing forms of immunotherapy. The EVOLUTION clinical trial will assess whether radiotherapy and immunotherapy combined can create a new pathway for combatting prostate cancer once and for all.
Two drugs that activate the body’s own immune response to kill cancer cells, (ipilimumab and nivolumab), will be combined with a type of treatment called radionuclide therapy (177Lu-PSMA). This radionuclide therapy can be used to treat prostate cancer by bringing radioactive atoms into the cancer cells. The trial will explore if the combination can further improve the anti-cancer effects already demonstrated by 177Lu-PSMA treatment.
This new treatment combination may lead to shrinkage or stabilisation of previously progressing tumours and therefore hopefully stop or reverse the growth of the cancer.
At present it is extremely difficult to defeat aggressive forms of prostate cancer. This form of cancer imposes an incredibly intense burden on people and their families, who commonly must endure the fear and distress of not knowing how quickly the cancer will spread. Patient enrolment on this study marks the start of the journey to recruit and follow up 100 eligible patients across 9 cancer centres throughout Australia. This trial may possibly lead to complete transformation in prostate cancer treatment, providing people with the most aggressive and deadly forms of this disease a greater hope of survival.
“We’re
opening the first ever study to test the effectiveness of combining 177Lu-PSMA with cancer immunotherapy. This study has the potential to lead to better and more durable responses for people with prostate cancer,” said Associate Professor Shahneen Sandhu, Principal Investigator.
and other genitourinary cancers. This great collaboration brings together ANZUP, PCFA, our community of clinicians and researchers, and people directly affected by prostate cancer, to learn from what has gone before and to take new steps forward together. Clinical trials like EVOLUTION are the only way we make true progress in medical care,” said Professor Ian Davis, ANZUP Chair.

excited to be
“EVOLUTION continues ANZUP’s mission of improving outcomes for people affected by prostateASSOCIATE PROFESSOR SHAHNEEN SANDHU, PRINCIPAL INVESTIGATOR PROFESSOR IAN DAVIS, ANZUP CHAIR
In the News!

Evolution revolution plan to beat a cancer
An ambitious plan to turbocharge the immune system to beat prostate cancer will be trialled at the Royal Adelaide Hospital (RAH) along with hospitals around Australia.
The multi-site EVOLUTION project has enrolled its first patient in Melbourne and comes as prostate cancer this week overtook breast cancer to become the nations leading cancer.
It will be the first clinical trial of its kind to test the effectiveness of a new generation radiotherapy treatment with existing forms of immunotherapy, which has previously failed in treating prostate cancers.
The trial will be led by Australia and New Zealand Urogenital and Prostate (ANZUP) Cancer Trials Group, with $1.6M in funding from Prostate Cancer Foundation of Australia.
ANZUP Chair Professor Ian Davis said there had been ‘tantalising hints’ some patients may be able to have their own immune system triggered to fight the cancer.
The trial will be expanded to key sites across the nation, including RAH in the hope it can help prevent the deaths of more than 3100 Australian people each year from the disease.
Prostate cancer remains an “awkward” topic for some people with vague references to “trouble with the waterwork”, Professor Davis said.
He hopes the ANZUP Community Engagement Forum at the Adelaide Convention Centre will remove stigma, clear up myths and show the importance of clinical trials as well as the impact a cancer diagnosis can have on a person and their family.
The ‘A little below the belt’ forum will also discuss bladder, kidney, testicular and penile cancers.
Professor Davis said prostate cancer did not get the funding or attention it may warrant for several reasons. “Historically, people have kept this sort of thing quiet,” he said.
“They get dragged to the doctor by their partners rather than seeking help themselves, but this is changing”, he said. “It’s a sensitive part of the body and some people don’t like to talk about it. It’s a bit awkward.”
Professor Davis said.
Each year during the ANZUP Annual Scientific Meeting, a free forum is held to provide the community with information about the importance of clinical trials and how research can improve treatments and outcomes for people diagnosed with prostate, bladder, kidney, penile or testicular cancer.
If you’re interested in future forums, please register your interest via https://anzup.org.au/join-us-friends-of-anzup/

“The treatment would wake up the immune system more effectively, so it recognises there is something foreign and says, ‘ I’m going to reject this’”
ANZUP trials - prostate


DASL-HiCaP
ANZUP 1801
Status: Open and recruiting
Location: Australia & Internationally
Activated sites: 76
Patients recruited: 794 • Patients required: 1100
The purpose of this study is to see if a new tablet drug, darolutamide, combined with the current best treatments, can improve outcomes for people with high risk prostate cancer that has not spread beyond the prostate area.
Previous studies have shown promising results for darolutamide preventing disease progression and improving survival for people with advanced prostate cancer.
DASL-HiCaP is being led internationally by ANZUP with another exciting opportunity to collaborate with our partners at the NHMRC Clinical Trials Centre, the Canadian Cancer Trials Group, Cancer Trials Ireland (Ireland and UK), and the Memorial Sloan Kettering Cancer Center and Prostate Cancer Clinical Trials Consortium in the US. The University of Sydney is the Sponsor and and the NHMRC Clinical Trials Centre is the global coordinating centre. We plan to enrol 1,100 people from Australia, New Zealand, Canada, US, Ireland, and the UK.
We thank and acknowledge Bayer for providing funding and product fo the DASL-HiCaP Trial.
For more information please refer to https://anzup.org.au/clinical-trial/dasl-hicap-trial/
Current locations for the DASL-HiCAP trial:
AUSTRALIA
NSW
• Northern Cancer Institute - St Leonards
• GenesisCare Newcastle
• Shoalhaven District Memorial Hospital
• Prince of Wales Hospital
• St Vincent’s Public Hospital - Sydney
• Chris O’Brien LifeHouse
• Liverpool Hospital
• Wollongong Hospital
• St George Hospital
• Gosford Hospital
• Calvary Mater Newcastle
• Sydney Adventist Hospital
• Campbelltown Hospital
VIC
• Peter MacCallum Cancer Centre
• The Alfred Hospital
• Box Hill Hospital
• Latrobe Regional Hospital
• Border Medical Oncology Research Unit
• Peter MacCallum Cancer Centre (Moorabbin Campus)
• Sunshine Hospital
• Peter MacCallum Cancer Centre - Bendigo Campus
• GenesisCare Cabrini
QLD
• Royal Brisbane and Women’s Hospital
• Princess Alexandra Hospital
• The Townsville Hospital
• Princess Alexandra Hospital - Radiation Oncology Services
• Mater Centre (ROPART)
• Icon Cancer Centre - Gold Coast University Hospital
SA
• Ashford Cancer Centre Research
WA
• Sir Charles Gairdner Hospital
• Fiona Stanley Hospital
TAS
• Royal Hobart Hospital
• Icon Cancer Centre Hobart
NEW ZEALAND
• Auckland City Hospital
• Christchurch Hospital
• Palmerston North Hospital
USA
• Memorial Sloan-Kettering Cancer Center (MSKCC)
• New York University Langone Medical Center
• Dana Farber Cancer Institute
• MSKCC - Commack
• MSKCC - Basking Ridge
• MSKCC - Nassau
• MSKCC - Westchester
• MSKCC - Monmouth
• MSKCC - Bergen
• New Mexico Cancer Center
• Greater Dayton Cancer Center
• Urology Cancer Center
• Lahey Hospital and Medical Center
• Dana Farber Cancer Institute – St. Elizabeth’s
• Dana Farber Cancer Institute – Milford
• New York University Langone Long Island
• Seattle Cancer Care Alliance
• Dana Farber Cancer Institute – St. Elizabeth’s,
• Dana Farber Cancer Institute – Milford
ANZUP trials - prostate
CANADA
• Queen Elizabeth II Health Sciences Centre
• Odette Cancer Centre - Sunnybrook Hospital
• Ottawa Health Research Institute
• Princess Margaret Cancer Centre
• CancerCare Manitoba
• Saskatoon Cancer Centre
• BC Cancer Agency (BCCA) Fraser Valley
• Allan Blair Cancer Centre
• Cross Cancer Institute
• Centre Hospitalier Universitaire de Sherbrooke
• Dr. H. Bliss Murphy Cancer Centre St. John’s
• CHUQ-Pavillon Hotel-Dieu de Quebec
• Western Manitoba Cancer Centre
• Jewish General Hospital
• Kingston Health Sciences Centre
• Centre Hospitalier de l’Universite de Montreal
• Centre hospitalier regional de Trois-Rivieres
• Regional Health Authority B - Zone 2 Saint John Regional Hospital
• Centre Integre de Sante et de Services Sociaux de la
• Monteregie-Centre
IRELAND
• Cork University Hospital
• Mater Misericordiae University Hospital
• Mater Private Hospital - Dublin
• St. Vincents University Hospital
• St. Luke’s Hospital
• Beacon Private Hospital Dublin
• Tallaght University Hospital
• Bon Secours Hospital Cork in association with UPMC Hillman Centre
UK
• Western General Hospital
• Beatson West of Scotland Cancer Centre
• Guys and St Thomas Hospital
• Royal Marsden Hospital (London)
• Velindre Hospital
• Aberdeen Royal Infirmary
• Royal United Hospital Bath
• Nottingham University Hospitals NHS Trust - Nottingham City Hospital
• Kent and Canterbury Hospital
• Charing Cross Hospital: Imperial College Healthcare NHS Trust
• Belfast City Hospital
• William Harvey Hospital
EVOLUTION
ANZUP 2001
Status: Open and recruiting
Location: Australia
Activated sites: 5
Patients recruited: 39 • Patients required: 100
The aim of this study is to see if combining ipilimumab and nivolumab (drugs that activate the body’s own immune response to kill cancer cells), with Lu-PSMA (a type of treatment called radionuclide therapy that can be used to treat prostate cancer by bringing radioactive atoms into the cancer cells), can further improve the anti-cancer effects of Lu-PSMA. It is thought that ipilimumab and nivolumab and Lu-PSMA may work together to treat prostate cancer. Lu-PSMA can potentially kill cancer cells and break up the tumour into small pieces that may be recognised by your immune system while ipilimumab and nivolumab help activate the immune system to find and attack the cancer. This new treatment combination may lead to shrinkage or stabilisation of previously progressing tumours and therefore hopefully stop or reverse the growth of the cancer.
Acknowledgments:
The EVOLUTION Trial is an investigator-initiated trial sponsored and led by ANZUP. This trial has received funding in partnership with the Prostate Cancer Foundation
Principal Investigator: Associate Professor Shahneen Sandu

of Australia, Bristol Myers Squibb and Novartis. This trial is a collaboration between ANZUP, the NHMRC Clinical Trials Centre at the University of Sydney and the Australasian Radiopharmaceutical Trials Network (ARTnet) with support from MIM Software Inc. and ANSTO.
For more information please refer to https://anzup.org.au/clinical-trial/evolution/
Current locations for the EVOLUTION trial:
NSW
• St Vincent’s Hospital Sydney
• Calvary Mater Newcastle Hospital
VIC
• Austin Health
• Austin Hospital
• Peter MacCallum Cancer Centre
SA
• Royal Adelaide Hospital
GUIDE
ANZUP 1903
Status: Open and recruiting
Location: Australia wide
Planner sites: 6
Patients recruited: 2 • Patients required: 120
The purpose of this study is to see if a prostate cancer marker in the blood (mGSTP1) can be used to guide chemotherapy treatment. Based on the level of this blood marker, some people may be able to have breaks in treatment rather than having chemotherapy continuously which is the current standard of care. This study will tell us if having these treatment breaks guided by mGSTP1 can improve how people feel during treatment while still treating the prostate cancer effectively.
GUIDE is an investigator-initiated study sponsored and led by ANZUP. The study is funded by ANZUP Discretionary Funding Initiative, ANZUP Below the Belt Research Fund and Chris O’Brien Lifehouse Philanthropic Fund.

For more information please refer to https://anzup.org.au/clinical-trial/guide/
Current locations for the GUIDE trial: AUSTRALIA
NSW
• Chris O’Brien Lifehouse
• Concord Repatriation General Hospital
• Dubbo Base Hospital
• Border Medical Oncology
VIC
• Goulburn Valley Health
• St Vincent’s Hospital - Melbourne
Co-badged trials - prostate
Principal Investigator: Associate Professor Arun Azad
#UpFrontPSMA
Status: Open & recruiting
Location: Australia wide
Activated sites: 10
Patients recruited: 121 • Patients required: 140
Most prostate cancer cells have a molecule on their surface called prostate cancer specific membrane antigen (PSMA). PSMA can be targeted with Lutetium-177 PSMA (Lu-PSMA), a radioactive drug that kills prostate cancer cells anywhere in the body. This investigational drug is not approved for use in Australia by the Federal Government’s Therapeutic Goods Administration (TGA). It is a new form of treatment that is effective in some patients with metastatic prostate cancer. It is a radioactive substance that, after injection into a vein, attaches to prostate specific membrane antigen (PSMA). The treatment enables delivery of highly targeted radiation to cancer cells. The emitted radiation only travels about 1mm, which means it mainly causes the death of cancer cells, while avoiding healthy cells, and seems to be well tolerated with few side effects. This is called radionuclide therapy or theranostic therapy. The purpose of this randomised controlled clinical trial is to compare the effectiveness of Lu-PSMA therapy followed by docetaxel chemotherapy versus docetaxel chemotherapy on its own. Previous clinical trials have shown promising activity of Lu-PSMA in treatment of patients with metastatic prostate cancer. Docetaxel is a chemotherapy drug that is approved by the TGA to treat prostate cancer and has been used for many years in the treatment of metastatic prostate cancer. Since Lu-PSMA radiotherapy and docetaxel chemotherapy are both effective in treating metastatic prostate cancer, it is possible that using Lu-PSMA in addition to standard docetaxel chemotherapy at the beginning of the treatment course may improve patient outcomes when compared to treatment with docetaxel alone.
A recent phase 2 clinical trial, showed the effectiveness of Lu-PSMA when used as a last treatment option and helped control disease progression.This study brings the use of Lu-PSMA forward as a first option to patients, with the hope of disease eradication and potential cure.
The trial is open and recruiting.
For more information please refer to https://anzup.org.au/clinical-trial/upfrontpsma-trial/
Current locations for the #UpfrontPSMA trial:
NSW
• Liverpool Hospital
• Royal North Shore Hospital
• St Vincent’s Hospital Sydney
VIC
• Alfred Health
• Peter MacCallum Cancer Centre
• Austin Hospital
QLD
• Royal Brisbane and Women’s Hospital
SA
• Royal Adelaide Hospital
WA
• Sir Charles Gardiner Hospital
• Fiona Stanley Hospital
is funded through the Prostate Cancer Research Alliance – a program jointly funded by the Australian Government and the Movember Foundation (Movember).
Co-badged trials - prostate


NINJA
Status: Open & recruiting
Location: NSW and VIC
Activated sites: 17
Patients recruited: 215 • Patients required: 474
The NINJA clinical trial aims to compare two emerging schedules of radiotherapy in the treatment of intermediate or high risk prostate cancer. Participants will be randomly assigned to one of two radiotherapy schedules as part of this study. In schedule 1 (called Stereotactic Body Radiotherapy) participants will receive 5 radiotherapy treatments over 2 weeks, and in schedule 2, (called Virtual High Dose Rate Boost), participants will receive Stereotactic Body Radiotherapy delivered in 2 treatments over 1 week followed by 12 treatments of conventional external beam radiotherapy over 2 and a half weeks. It is hoped this research will potentially improve the accuracy and quality of radiotherapy treatment in prostate cancer.
This study will include 474 people. Currently we have active sites across Australia and New Zealand with 120 patients currently enrolled.
This trial is open and recruiting. If you are interested in participating in the trial, please refer to https://anzup.org.au/clinical-trial/ninja/
This study is being led by the TransTasman Radiation Oncology Group and co-badged with ANZUP. The study is being funded by Cancer Australia, and we acknowledge MDI for providing the study drug.
Current locations for the NINJA trial:
NSW
• Blacktown Hospital
• Calvary Mater Newcastle
• Campbelltown Hospital
• GenesisCare Hurstville
• GenesisCare Newcastle
• Liverpool Hospitals
• Illawarra Cancer Centre
• St George Hospital
• Westmead Hospital
VIC
• Peter MacCallum Cancer Centre (Parkville)
QLD
• Princess Alexandra Hospital SA
• Genesis Care South Australia
• Royal Adelaide Hospital
WA
• 5D Clinics
• Genesis Care Fiona Stanley Hospital
• Sir Charles Gairdner Hospital
NEW ZEALAND
• Waikato Hospital NZ
Spotlight on bladder and urothelial cancer

What is bladder cancer?
The bladder is a hollow organ in the pelvis that holds urine before it is eliminated by the body during urination. This function makes the bladder a crucial part of the urinary tract. The urinary tract is also made up of the kidneys, ureters, and urethra. The renal pelvis is a funnel-like part of the kidney that collects urine and sends it into the ureter. The ureter is a tube that runs from each kidney into the bladder. The urethra is the tube that carries urine out of the body. The prostate gland is also part of the urinary tract.
The bladder, like other parts of the urinary tract, is lined with a layer of cells called the urothelium. This layer of cells is separated from the bladder wall muscles, called the muscularis propria, by a thin, fibrous band called the lamina propria.
Bladder cancer starts when healthy cells in the bladder lining – most commonly urothelial cells – change and grow uncontrollably, forming a mass called a tumour. Urothelial cells also line the renal pelvis and ureters. Cancer that develops in the renal pelvis and ureters is also considered a type of urothelial cancer and is often called upper tract urothelial cancer. In a lot of cases, it is treated similarly to bladder cancer. A tumour can be cancerous or benign. A cancerous tumour is malignant, meaning it can spread and grow to other parts of the body. A benign tumour means the tumour can increase in size but will not spread. Benign bladder tumours are quite rare.
Types of bladder cancer
Bladder cancer takes different forms*:
• urothelial carcinoma, formally known as transitional cell carcinoma, is the most common form of bladder cancer (80-90%) and starts in the urothelial cells in the bladder wall’s innermost layer
• squamous cell carcinoma begins in the thin, flat cells that line the bladder
• adenocarcinoma is a rare form which starts in mucusproducing cells in the bladder.
* other rarer variants are also found
Bladder cancer may be limited to the lining of the bladder (non-muscle invasive bladder cancer, NMIBC), invade the bladder wall (muscle invasive bladder cancer, MIBC) or spread further to lymph nodes or other organs (advanced or metastatic bladder cancer).
Bladder cancer was the 11th most commonly diagnosed cancer in Australia in 2022. In 2022, it was estimated 3,219 cases of bladder cancer would be diagnosed in Australia. This is equivalent to an estimated incidence rate of 9.3 cases per 100,000 persons. In addition, it was estimated there would be 1,043 deaths in Australia from bladder cancer but from 2014 - 2018 on average, 55.8% of people diagnosed with bladder cancer survived 5 years after diagnosis.*
Among Australia’s 15 most common malignancies, bladder cancer remains the only one with survival rates that have worsened over the past 30 years.
Bladder cancer can be treated effectively if found early and before it spreads outside the bladder.
Spotlight on bladder and urothelial cancer
Bladder cancer symptoms
The most common symptom of bladder cancer is blood in the urine (haematuria), which usually occurs suddenly and is generally not painful.
Other less common symptoms include:
• Problems emptying the bladder;
• A burning sensation when passing urine;
• Pain when urinating;
• Need to pass urine often;
• Back pain or lower abdominal pain.
Causes of bladder and urothelial cancer
Environmental risk factors are thought to be more important than genetic or inherited susceptibility when it comes to bladder cancer. Some factors that can increase the rise of bladder and urothelial cancer include:
• smoking;
• older age;
• family history;
• diabetes treatment using the drug pioglitazone;
• w orkplace exposure to certain chemicals used in dyeing in the textile, rubber and petrochemical industries;
• u se of the chemotherapy drug cyclophosphamide;
• c hronic urinary tract infections.
Common treatment approaches
Many times, the best option might include more than one of type of treatment. Surgery, alone or with other treatments, is used to treat most bladder cancers. Early-stage bladder cancers can often be removed. But a major concern in people with early-stage bladder cancer is that new cancers often form
in other parts of the bladder over time. Taking out the entire bladder (called radical cystectomy ) is one way to avoid this, but it causes major side effects. If the entire bladder is not removed, other treatments may be used to try to reduce the risk of new cancers. Whether or not other treatments are given, close follow-up is needed to watch for signs of new cancers in the bladder.
Depending on the stage of the cancer and other factors, treatment options can include:
Bladder cancer surgery - type of surgery done depends on the stage of the cancer.
Intravesical therapy - the doctor puts a liquid drug right into your bladder rather than giving it by mouth or injecting it into your blood.
Chemotherapy - it can be given in 2 different ways, either straight into the bladder or given in pill form or injected into a vein or muscle. The drugs then go into the bloodstream and travel throughout the body. Radiation therapy - uses high-energy radiation to kill cancer cells.
Immunotherapy - is the use of medicines to help a persons own immune system recognise and destroy cancer cells.
Targeted therapy - as researchers have learned more about the changes inside cells that cause cancer, they have developed newer drugs that target some of these changes. These targeted drugs work differently from other types of treatment, such as chemotherapy, and they may work in some cases when other treatments don’t.
Clinical trials - several ground-breaking bladder cancer trials using some of the therapies listed above, are currently underway in Australia. You can read more about ANZUP’s bladder cancer trials on pg 53.
The worsening bladder cancer survival rates over the past 30 years can mainly be attributed to Australia’s ageing population as the percentage of patients diagnosed with bladder cancer over the age of 80 years has gradually increased. Early identification and referral can lead to timely diagnosis. In addition, the hope is that novel approaches are identified through clinical trials and help reverse the trend of deteriorating survival rates in bladder cancer. * https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/summary
Below the Belt Cancer Research Highlights: Professor Dickon Hayne

Professor Dickon Hayne is a clinical academic who leads urological research and education in urology, at the University of Western Australia. He works as a consultant urological surgeon and is the Head of Urology for the South Metropolitan Health Service, WA. He is Chair of the Bladder, Urothelial and Penile (BUP) Cancer Sub-committee of the Australian & New Zealand Urogenital & Prostate Cancer Trials Group (ANZUP), a Scientific Advisory Committee (SAC) member, leads the BCG+MM trial and is widely engaged in other sub-committees, trials, and activities of ANZUP. His major clinical and research interests are urological cancer, in particular bladder cancer.
Professor Dickon Hayne touches on the importance of clinical trials, the work of ANZUP in improving the outcomes for people affected by below the belt cancers, and an insight into the future of medical practices.
Can you please tell us about some of the latest research projects that you have been involved in?
Perhaps one of the main ones that I am still very much involved in is the BCG Mitomycin (BCG+MM) trial, which is now the largest Australian initiated bladder cancer trial that has been undertaken. We’ve got over 415 patients on the study, 15 centres around Australia, and now also open in the UK.
This trial looks at standard treatment for non-muscle invasive bladder cancer and BCG treatment, comparing that with a combination treatment of BCG and a chemotherapeutic agent called Mitomycin.
I’m also leading SUBDUE-1, a study looking at a new route of administering the checkpoint inhibiting drug durvalumab for bladder cancer. It’s a drug used in metastatic bladder cancer, and we are trying to bring these drugs earlier into the treatment paradigm. In the study, increasing doses are injected directly into the bladder wall. In the future this may become a new treatment for early bladder cancer.
I’m also involved in the ZIPUP study, which is a new PET scan staging trial for bladder cancer. We are using an antibody that sticks to bladder cancer attached to a radioactive substance that shows up on a PET scan. It is important to try to see how far a cancer is spread to decide what the best treatment is for patients.
What do survival rates look like at the moment?
I’m going to answer about bladder cancer specifically. The most recent up to date data we have, indicates that we are going backwards and that survival rates in bladder cancer in Australia are getting worse. The whole impetus behind bladder cancer research is to try and reverse that alarming trend. We do have a number of new agents and therapies that are available for bladder cancer that are only just emerging and haven’t made it into clinical practice yet. This is where clinical trials come into effect.
What have been some of the major breakthroughs that came out of clinical trials for below the belt cancers?
It depends on how far back we look – we didn’t even have hormonal therapy for prostate cancer until Huggins and Hodges won a Nobel Prize for it in 1966. That may seem like a long time ago, but it was a gamechanger.
Platinum based chemotherapy for testicular cancer was another one that revolutionised treatment – metastatic testicular cancer was almost always fatal but with the arrival of platinum-based chemotherapy it’s now very unusual to die from. Those are two massive leaps in two of the below the belt cancers.
Checkpoint inhibitors are a type of immunotherapy. They block proteins that stop the immune system from attacking the cancer cells.PROFESSOR DICKON HAYNE PROFESSOR DICKON HAYNE
In recent years there have been a lot of advancements with immunotherapy, which is one of the new and exciting areas in oncology. The immunotherapeutic drugs and other new agents that are used are often targeted, appropriate for patients that have specific mutations in their DNA and require certain drugs suitable for their individual case.
Staging is a way to describe a cancer. The cancer’s stage tells you where a cancer is located and its size, how far it has grown into nearby tissues, and if it has spread to nearby lymph nodes or other parts of the body. Before starting any cancer treatment, doctors may use physical exams, imaging scans, and other tests to determine a cancer’s stage. Staging may not be completed until all the tests are finished.
The other thing that is changing the face of cancer therapy is theranostics, where you can image a patient with a pet scan and if the cancer is visible, you can add on a killer radioactive molecule that will hunt down, stick to the cancer, and kill it.
Theranostics
combination
diagnostics. Theranostics
Another recent trial, the proPSMA PET trial, implemented a new staging scan for prostate cancer showing that it was accurate and superior to conventional staging. It’s important to note that in terms of survival rates, prostate cancer is the second most common in terms of cancer deaths, so it’s important to be able to stage these patients properly.
We have been talking about targeted therapy and personalised medicine for years but now it is becoming a reality. The trials we are focusing on now will inform the basis of future treatments.
How does Australia stack up against the rest of the world when it comes to trials and research into below the belt cancers?
Australia punches above its weight in terms of clinical trials. With ANZUP as a coordinating centre for urogenital cancers and trials into below the belt cancers, we are starting to make some proper inroads to cancer care that are practice changing.

Immunotherapy is a type of cancer treatment. It uses substances made by the body or in a laboratory to boost the immune system and help the body find and destroy cancer cells.
is a
of the term’s therapeutics and
is the term used to describe the combination of using one radioactive drug to identify (diagnose) and a second radioactive drug to deliver therapy to treat the main tumor and any metastatic tumors.
ANZUP trials - bladder

This bladder cancer trial is currently being run by ANZUP. For more information about this trial, go to the ANZUP bladder cancer trials web page: https://anzup.org.au/clinical-trials/bladder-cancer-trials/
Principal Investigator: Professor Dickon Hayne

BCG + MM ANZUP
1301
Status: Open & recruiting
Location: Australia
Activated sites: 17
Patients recruited: 456
Patients required: Stage one: 130 / Stage two: 370
Non-muscle invasive bladder cancer is common and causes substantial suffering. It requires removal or irradiation of the bladder within five years in more than 30% of people with high-risk tumours, despite best current treatment.
Recent preliminary studies show promising results from adding mitomycin (MM), a chemotherapy drug, to current treatment with BCG (Bacillus Calmette-Guérin, a strain of modified bacteria which stimulates an immune response to early cancer cells).
This randomised trial will determine the effects of adding mitomycin on cure rates, survival, side effects and quality of life. This could potentially provide a simple and costeffective treatment for patients who suffer from this cancer. This study is currently active and recruiting. Please speak with your doctor if this is of interest to you or someone you know.
ANZUP collaborates with the University of Sydney through the National Health and Medical Research Council Clinical Trials Centre (NHMRC CTC).
This ANZUP investigator-initiated study is being funded by Cancer Australia and the National Health and Medical Research Council. We acknowledge Omegapharm and Merck Sharp & Dohme for providing the study drugs.
Current site locations for the BCG + MM trial are: NSW • Concord Repatriation General Hospital
John Hunter Hospital
Nepean Hospital
Northern Cancer Institute (GenesisCare)
SAN Clinical Trials Unit
Southside Cancer Care Centre
The Tweed Hospital
Westmead Hospital
• Austin Health
Epworth HealthCare (Richmond)
Footscray Hospital
Frankston Hospital
Royal Melbourne Hospital
The Alfred Hospital WA
Fiona Stanley Hospital
Redcliffe Hospital UK • Nottingham University Hospital
Spotlight on testicular cancer

The testicles are part of the reproductive system. There are normally 2 testicles, and they are located under the penis in a sac-like pouch called the scrotum. They can also be called gonads or testes. The testicles produce sperm and testosterone. Testosterone is a hormone that plays a role in the development of masculine characteristics and the reproductive organs.
964 estimated diagnoses
31 estimated deaths
What is testicular cancer?
Cancer that develops in a testicle is called testicular cancer or cancer of the testis. Usually only one testicle is affected, but in some cases both. About 90 to 95 per cent of testicular cancers start in the cells that develop into sperm - these are known as germ cells.
Compared with other types of cancer, testicular cancer is rare. But testicular cancer is the second most common cancer in young people (aged 18 to 39) excluding non-melanoma skin cancer. However, this form of cancer is highly treatable, even when cancer has spread beyond the testicle.
It was estimated only 964 people would be diagnosed with testicular cancer in Australia in 2022. This equates to 1% of all cancers. For Australians, the risk of being diagnosed with testicular cancer by the age of 85 is 1 in 202. The rate of people diagnosed with testicular cancer has grown by more than 50% over the past 30 years, however the reason for this is not known.
Germ cell tumours are the most common testicular cancers. Under a microscope there are two main types that are quite different when observed – seminoma and non-seminoma cells. Seminoma cells usually occur in people aged 25-45 but can also occur in people over the age of 60 or at any age. This form of testicular cancer develops more slowly than non-seminoma cancers. The faster developing, rarer form of testicular cancer occurs in younger people in their late teens and early 20s.
In 2022 a total of 31 deaths from testicular cancer were estimated. In 2014 - 2018, on average 97.3% of those diagnosed with testicular cancer survived 5 years after diagnosis.
Testicular cancer symptoms
Testicular cancer may cause no symptoms. The most common symptom is a painless swelling or a lump in a testicle.
Less common symptoms include:
• Feeling of heaviness in the scrotum;
• Change in the size or shape of the testicle;
• Pain or ache in the lower abdomen, the testicle or scrotum;
• Back pain;
• Feeling of unevenness;
• Tenderness or tenderness of the breast tissue (due to hormones created by cancer cells).
Self-checking is so important –because if found early, testicular cancer is one of the most curable cancers.
Spotlight on testicular cancer
Causes of testicular cancer
A couple of factors that may increase a person’s risk of testicular cancer include an undescended testicle as an infant, or family history, mainly having a close relative who has had testicular cancer.
In addition, personal history may contribute to testicular cancer. If you have had cancer in one testicle you are more likely to develop cancer in the other testicle. It is also found that infertility may be another possible cause. There is no known link between testicular cancer and injury to the testicles, hot baths, wearing tight clothes or sporting strains.
Testicular cancer treatment
Treatment for testicular cancer depends on the type of cancer you have and how far it has spread. Your medical team will advise the best treatment for you. They will consider various points:

• your general health
• the type of testicular cancer
• the size of the tumour
• the number and size of any lymph nodes involved
• if the cancer has spread to other parts of your body. If testicular cancer does spread, it most commonly spreads to the lymph nodes in the pelvic and lower abdominal regions.
Understanding testicular cancer, the treatments available and possible side effects can help you decide your treatment pathway. You may also want to talk to your doctor about how treatment for testicular cancer may affect your fertility.
In almost all cases if testicular cancer is suspected, the affected testicle is surgically removed in an operation called an orchiectomy. A laboratory will then examine the tissue to confirm the type of cancer and the stage it is at.
After the surgery, you may not need any further treatment but will be closely monitored. This is called surveillance. If other treatments are required they may include chemotherapy or radiotherapy to stop the spread of cancer cells to other parts of the body. Some people may require further surgery.
Testicular cancer clinical trials
Several decades ago testicular cancer was a disease with a very poor prognosis. But now, because of new treatments, tested carefully in clinical trials, it is almost always curable even when it has spread. However, even though there are excellent treatments available, we still need to do more. This can only happen through understanding the science and by performing clinical trials to see which treatments are most likely to help further improve outcomes. ANZUP is involved in clinical trials in testicular cancer through its clinical trials program.
Speak with your doctor if you would like to know more about testicular cancer clinical trials. You can also read about ANZUP’s trials on the following pages.
For more detailed information about these trials, go to the ANZUP testicular cancer trials web page: https://anzup.org.au/clinical-trials/testicular-cancer-trials/
References
https://www.cancer.org.au/about-cancer/types-of-cancer/testicular-cancer.html https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/cancer-summary-data-visualisation
Meet Associate Professor Ben Tran
 Chair of ANZUP Germ Cell (Testicular) Cancer Research Subcommittee
Chair of ANZUP Germ Cell (Testicular) Cancer Research Subcommittee
Who is Ben Tran?
Ben is a medical oncologist at Peter MacCallum Cancer Centre where he is the lead Genitourinary (GU) medical oncologist and GU clinical trials lead. Ben is also an Associate Professor within the Sir Peter MacCallum Department of Oncology at The University of Melbourne and is the Chair of ANZUP’s Germ Cell Subcommittee.
He is a passionate clinician and researcher, with special interests in below the belt cancers, Early Drug Development, and Real-World Data.
In this interview, we hear from Ben about testicular cancer, the latest in clinical trials research and his health advice to people.
Can you please provide an insight into why people should have regular check-ups?
People often neglect their health, but they should be seeing their general practitioner (GP), every 3 months for regular checks for things like cholesterol and blood pressure. Unfortunately, people who tend to look after themselves are those who have partners. Either they’re motivated to take better care of themselves, or their partners motivate them.
I treat people of all ages, across the spectrum and when I ask about their GP appointments they often say, “what GP? I don’t have one”. This means that many problems are going undiagnosed for too long. They’re only picked up once they become a real problem and this sometimes makes treatment more difficult.
According to the Australian Institute of Health and Welfare data, diagnosis of testicular cancer has increased by 50% over the last 30 years. Why is this the case?
Yes, testicular cancers are becoming more common.
There’s a genetic component that we don’t fully understand and perhaps multiculturalism has contributed to the increase we’re seeing in Australia.
Testicular cancer is more common in the 18-39yr group, so young people need to understand that if they feel a lump or mass, they need to have it checked immediately.
Should young people be regularly checking their testicles for lumps?
Absolutely. People over 18 years should be checking their testicles every month and going straight to their GP if anything feels irregular or they’re experiencing discomfort. What we find is that people procrastinate and wait too long before seeing a doctor and this makes the problem worse and the treatment more complex.
Is testicular cancer difficult to treat?
The good news is that testicular cancer is highly curable. Sometimes these cancers spread to other areas, but even then, it’s usually treatable.
Tell us about the testicular cancer clinical trial research you’re involved in?
We want people to be treated to live long healthy lives. Our research is helping us to know how to optimise treatments so there are fewer effects from our interventions.
We use a few approaches to treat testicular cancer; surgery, radiotherapy, and chemotherapy and these sometimes have unwanted effects on people either now or in the longer term. For example, chemotherapy can have effects on nerves, hearing, kidney function and the cardiovascular system and radiation therapy can affect the rate of other cancers developing.
Our research is working out how to reduce treatments as much as possible while keeping the cancer away.
Our latest trial is called the CLIMATE trial. CLIMATE aims to assess the clinical utility of the exciting new biomarker miR-371 in stage 1 testicular cancer.
a while and once they see their GP, things have happened quite quickly. They then wait a few more weeks to see me and their anxiety and distress have risen considerably. Also, the information they have been accessing online in that time is often pretty poor quality.
My opening line is often ‘My name is Ben, and you don’t have cancer. This comes as a surprise to them as they’re expecting the worst. I then go on to explain what must happen to keep them this way.
What do patients need to do to stay well?
They need to keep their appointments with their specialists. Young people find this hard as they may be working and traveling. We try our best to explain the importance of keeping this up without too much disruption to their lives. We don’t want people to be defined by this illness.
What’s involved for patients who participate in the trial?
It’s not much more involved than their usual appointments, it’s not very disruptive at all. People are usually very happy to participate because they want to help future research, to improve outcomes for people with testicular cancer.
You’re working with ANZUP Cancer Trials Group on the CLIMATE Trial. Tell me a little more about ANZUP?
ANZUP is a fantastic and vital organisation for people with cancers living with a below the belt (penile, bladder, kidney, prostate and testicular) cancer.
Testicular cancer is a highly curable disease, but many patients are over treated or over investigated unnecessarily, which can result in long term morbidity and increased anxiety.
We’re hoping to demonstrate that miR-371 can better identify patients who may need adjuvant chemotherapy and those who can have less frequent surveillance. This would maximise outcomes while minimising treatment in this young population.
We are aiming to recruit 200 people for the study, and we currently have 23 patients enrolled.
How do you discuss this trial with the young people you treat?
First of all, I usually see patients for the first time a few weeks after they’ve had a lump removed surgically. They’ve often procrastinated for quite
ANZUP is a network of medical researchers, clinicians, nurses, psychologists, scientists, allied health, and consumer representatives working to identify and close gaps in medical need and evidence.
ANZUP’s mission is to improve the lives of people affected by bladder, kidney, testicular, penile, and prostate cancers through practice-changing multidisciplinary collaborative clinical trials. ANZUP is globally recognised for its practice-changing research that genuinely improves patient outcomes.
If a patient has a below the belt cancer, will their treating doctors know about ANZUP trials?
Yes, they will, and, if applicable, they’ll be happy to talk to the patient about how they can participate in an ANZUP trial to contribute to medical knowledge and clinical care.
It’s about knowing what the right treatment for the right patient is, at the right time. Knowing who needs treatment and who we can just continue to monitor.
Biomarker testing is a way to look for genes, proteins, and other substances (called biomarkers or tumor markers) that can provide information about cancer. Each person’s cancer has a unique pattern of biomarkers. Some biomarkers affect how certain cancer treatments work.
ANZUP trials - testicular
Principal Investigator: Associate Professor Ben Tran

CLIMATE ANZUP 1906
Status: Open & recruiting
Location: Australia wide
Planned sites: 11
Patients recruited: 39 • Patients required: 200
Testicular cancer is the most common cancer diagnosed in people aged between 15 and 39 in Western countries, however it can occur at any age. Most people diagnosed with testicular cancer will have cancer confined to the testicle, without evidence of spread to other areas of the body. These people are highly likely to be cured following surgical removal of the testicle (orchidectomy) alone, and most will not require additional chemotherapy or radiotherapy. Sometimes, a person with testicular cancer may choose to undergo preventive chemotherapy or radiotherapy, which reduces the risk of their cancer coming back; however, this may result in long-term side effects for some people.
For this reason, most people in Australia are recommended “active surveillance,” which involves regular reviews with their doctor, computerised tomography (CT) scans and blood tests, but no chemotherapy or radiotherapy.
With this approach, most will be spared from unnecessary treatment and side effects. However, a small number of these will have recurrent cancer detected during active surveillance. Reassuringly, these people are also highly likely to have a positive outcome following additional treatment.
A new blood test, micro-ribonucleic acid (miRNA), which evaluates a protein commonly found in testicular cancer is under investigation. Early studies have found that miRNA is detectable in blood samples of people who have known testicular cancer.
CLIMATE is an investigator-initiated research project led by ANZUP in collaboration with the Walter and Eliza Hall Institute for Medical Research (WEHI). This study has been co-funded by the ANZUP Cancer Trials Group Discretionary Funding Initiative and WEHI.
For more information please go to the trials page on the ANZUP website: https://anzup.org.au/clinical-trial/climate/
Active site: NSW
• Calvary Mater Newcastle
Pending sites: NSW
• Chris O’Brien Lifehouse
• Southside Cancer Care Centre
• St Vincent’s Hospital - Sydney
• Sydney Adventist Hospital
VIC
• Austin Health
• Barwon Health
• Eastern Health
• Epworth Healthcare
• Peter MacCallum Cancer Centre
QLD
• Royal Brisbane & Women’s Hospital
ANZUP trials - testicular
Principal Investigator: Associate Professor Peter Grimison (ANZ)

P3BEP
ANZUP 1302
Status: Active & recruiting
Location: Australia wide & Internationally
Activated sites: 89
Patients recruited: 228 • Patients required: Stage 1 (150) Stage 2 (350)
The current standard practice for the treatment of germ cell tumours is the use of the chemotherapy combination called BEP, which consists of three chemotherapy agents – Bleomycin, Etoposide and Cisplatin – administered on a three-weekly cycle. BEP is given with a drug called pegylated G-CSF (or pegfilgrastim) that stimulates white blood cell production.
The purpose of this study is to determine whether giving the same dose of BEP on a two-weekly schedule will be more effective and better tolerated than a three-weekly schedule. The two-weekly schedule is called “accelerated BEP” and the three-weekly schedule is called “standard BEP”.
For more information, please go to the trials page on the ANZUP website: https://anzup.org.au/ clinical-trial/p3bep/.
ANZUP collaborates with the University of Sydney through the NHMRC CTC to conduct P3BEP Trial.
This ANZUP investigator initiated study is being funded by a Cancer Australia grant.
Current locations for the P3BEP trial: NSW
• Chris O’Brien Lifehouse
• Nepean Hospital
• Prince of Wales Hospital
• Calvary Mater Newcastle
• Concord Repatriation General Hospital
• Macquarie Cancer Clinical Trials
QLD
• Princess Alexandra Hospital
• Royal Brisbane & Women’s Hospital
• Queensland Children’s Hospital
SA
• Royal Adelaide Hospital
• Flinders Medical Centre
TAS
• Royal Hobart Hospital
VIC
• Peter MacCallum Cancer Centre
• Border Medical Oncology
• Austin Health
• Box Hill Hospital
WA
• Fiona Stanley Hospital
NEW ZEALAND
• Auckland Hospital
• Christchurch Hospital
• Starship Hospital – Paediatric
• Palmerston North Hospital
• Christchurch Children’s Haematology Hospital
UK
• Royal Marsden Hospital
• University Hospital Southampton
• St James’s Hospital – Leeds
• Cambridge University Hospital
Paediatric
• Royal Preston Hospital
• Beatson West of Scotland Cancer Centre
• Belfast City Hospital
• Nottingham University Hospital
• St Bartholomew’s Hospital
• Bristol University Hospital
• Velindre Hospital
• Derriford Hospital, Plymouth
• Northern General Hospital
• Aberdeen Royal Infirmary
• University College Hospital, London
• The Christie
USA
• Memorial Sloan Kettering Cancer Center
• Lucile Packard Children’s Hospital Stanford
• USC / Norris Comprehensive Cancer Care
• Washington University School of Medicine
• Rady Children’s Hospital
• Geisinger Medical Center
• University of Texas Science Center at San Antonio
• Carolinas Medical Center
• Advocate Children’s Hospital – Park Ridge
• Advocate Children’s Hospital – Oak Lawn
• Mayo Clinic
• Driscoll Children’s Hospital
• Wake Forest University Health Sciences
• UT Southwestern Simmons Cancer Center
• Dell Children’s Medical Center
• Augusta University Medical Center
• Vanderbilt University Medical Center
• Memorial Health University Medical Center
• University of Mississippi Medical Center
• Palmetto Health Richland
• Methodist Children’s Hospital of South Texas
• University of Wisconsin Hospital
• East Tennessee Children’s Hospital
• Miller Children’s and Women’s Hospital Long Beach
• Roswell Park Cancer Center
• Broward HealthCare
• Dana Farber Cancer Center
• LA Biomedical Research Institute at Harbor– UCLA
• Dayton Children’s Hospital
• Loma Linda University Medical Center
• University of Iowa
• Presbyterian Hospital New Mexico
• Saint Mary’s Hospital
• Hackensack University Medical Center
• Providence Sacred Heart Medical Center and Children’s Hospital
• University of Minnesota/Masonic Cancer Centre
• Tufts Children’s Hospital
• Dartmouth-Hitchcock Medical Center
• Children’s Hospital of Alabama
• Ann & Robert H. Lurie Children’s Hospital
• NYU Winthrop Hospital
• Kaiser Permanente Downey Medical Center
• Children’s Healthcare of Atlanta - Egleston
• Children’s Hospitals and Clinics of Minnesota
• Golisano Children’s Hospital of Southwest Florida
• Yale University
• Johns Hopkins University/Sidney Kimmel Cancer Center
• University of Alberta Hospital
• BI-LO Charities Children’s Cancer Centre
• Massachusetts General Hospital Cancer Center
• Rutgers Cancer Institute
Spotlight on kidney cancer
People usually have two kidneys, located in the abdomen above the waist on either side. These bean-shaped organs are each about the size of a small fist and are located closer to the back of the body than to the front. Each kidney works independently so the body can function with less than one complete kidney. The kidneys filter blood to remove excess minerals, salts and impurities, as well as extra water. Blood pressure, red blood cell production, and other bodily functions are controlled by hormones produced by the kidneys.
4,552
What is kidney cancer?

Kidney cancer has become increasingly more commonly diagnosed and survival rates continue to improve. This cancer is the 7th most diagnosed cancer in Australia and in 2022 it is estimated there will be 4,552 new cases of kidney cancer diagnosed. Kidney cancer is rare in people under 40 but risk does increase with age.
Kidney cancer generally refers to renal cell cancer, which develops in the lining of the small tubes in the kidney. There is usually just a single tumour in one kidney, but sometimes there may be more than one tumour, or tumours in both kidneys. Kidney cancer can be subdivided into several different types, based on the appearance of the cancer cells under a microscope as well as other genetic factors. About 90% of kidney cancers are renal cell cancer, and the most common subtype is clear cell renal cancer.
Other types of kidney cancers include:
• Urothelial carcinoma. This is also called transitional cell carcinoma. It constitutes 5% to 10% of the kidney cancers diagnosed in adults. Urothelial carcinoma begins in the area of the kidney where urine collects before moving to the bladder, called the renal pelvis. This type of kidney cancer is treated like bladder cancer because both types of cancer begin in the same cells that line the renal pelvis and bladder.
• Wilms tumour is most common in children and is treated differently from kidney cancer in adults. About 1% of kidney cancers are Wilms tumors. A different approach to treatment is used for this type of kidney cancer. This type of tumour is more likely to be successfully treated with radiation therapy and chemotherapy than the other types of kidney cancer when combined with surgery.
• Sarcoma of the kidney is rare. This type of cancer develops in the soft tissue of the kidney, i.e. the thin layer of connective tissue surrounding the kidney, called the capsule; or surrounding fat. This form of kidney cancer is usually treated with surgery. However, sarcoma commonly comes back in the kidney area or spreads to other parts of the body. After the first surgery additional surgery or chemotherapy may be recommended.
In 2022 it is estimated:
most diagnosed cancer in Australia
diagnoses of kidney cancer in Australia
Spotlight on kidney cancer
In 2022, it is estimated there will be 912 deaths from kidney cancer and the five year survival rate from 2014 - 2018, for Australians diagnosed with kidney cancer was 80.7%, although most people with kidney cancer localised only to the kidney can be cured.
Kidney cancer symptoms
In its early stages, kidney cancer often does not produce any symptoms. Many are diagnosed with the disease when they see a doctor for a different reason.
Symptoms may include:
• blood in the urine (haematuria);
• pain or a dull ache in the side or lower back that is not due to an injury;
• a lump in the abdomen;
• rapid, unexplained weight loss;
• constant tiredness;
• fever not caused by a cold or flu.
If you are experiencing some of these symptoms, please see your doctor.
Causes of kidney cancer
The causes of kidney cancer are not known, but factors that put some people at greater risk include:
• Obesity – Excess body fat may alter certain hormones that can lead to kidney cancer.
• Smoking – Up to one-third of all kidney cancers are thought to be related to smoking. People who smoke have almost twice the risk of developing kidney cancer as non-smokers.
• High blood pressure – Whether it is caused by another medical condition or due to being overweight, high blood pressure increases the risk of kidney cancer.
• Kidney failure – People with end-stage kidney disease have an increased risk of developing kidney cancer.
• Family history – People who have family members with kidney cancer, especially a sibling, are at a greater risk.
• Inherited conditions – About 3–5% of kidney cancers occur in people with particular inherited syndromes, such as von Hippel-Lindau disease, Birt-Hogg-Dubé syndrome, and hereditary papillary RCC.
• Exposure to toxic substances at work or in the environment – After regular exposure to certain chemicals, such as arsenic, cadmium or some metal degreasers, the risk of kidney cancer may be higher.
Treatment options
Treatment will depend on the type of kidney cancer, the stage of the cancer and your general health. The main treatment for kidney cancer is surgery alone or with radiotherapy and will depend on the stage of the cancer. All treatment has benefits and side effects, which need to be discussed with your multidisciplinary cancer care team.
Treatment for kidney cancer is provided by a multidisciplinary team, comprising a urologist, urologic oncologist, medical oncologist and radiation oncologist. This team will regularly meet and discuss the patient’s medical history, organise appropriate tests, assess the test results, and together determine the most appropriate treatment care plan.
Clinical trials
One treatment option is taking part in a clinical trial. A trial will help confirm whether novel medicines are safe and effective to introduce as new treatment for more kidney cancer patients. During a trial your health and progress is monitored extremely closely and as a participant in a trial you may also gain access to a treatment option that is not yet available to the wider public.
If you have already had one or more forms of cancer treatment and are looking for a new treatment option, you may be suitable for a clinical trial. Or, if you have just been diagnosed with cancer, the time to think about joining a trial is before you have any treatment.
Read more about kidney cancer trials: https://anzup.org.au/clinical-trials/kidney-cancer-trials/
Reference:
https://www.aihw.gov.au/reports/cancer/cancer-data-in-australia/contents/cancer-summary-data-visualisation
Treatment choices and decision making
Associate Professor David Pook and Juliet De NittisAt ANZUP’s recent Community Engagement Forum, Associate Professor David Pook and his patient Juliet De Nittis discussed Juliet’s cancer, and the trial she went on under the guidance and support of David.
Who
I received from an ANZUP clinical trial.
“I firmly believe a clinical trial saved my life” Juliet says.

There is no good day to hear ‘you have cancer.’ But for Juliet it was the worst possible timing. On the eve of her daughter’s 16th birthday, she was diagnosed with kidney cancer.
Juliet put on a brave face to avoid upsetting her daughter, her heart was silently breaking. Doctors only gave her a year or two to live, at the most. As more results came back, that was reduced to just 8 months. “It was a shock,” Juliet says. “I wanted to live.”
While Juliet had stomach and back pain, for many, kidney cancer has no symptoms at all. And the disease is increasingly common.
Juliet’s type of kidney cancer was aggressive and considered untreatable. It covered her whole kidney and had already spread to her lungs.
The opportunity to be on the ANZUP’s UNISoN trial gave her some hope to cling to. For the trial, Juliet took an immunotherapy drug, nivolumab, which primed her immune system to recognise and destroy her cancer cells.
‘Now, incredibly, after 2 years of immunotherapy treatment and another year of treatment free, my cancer is still in remission, stable and the latest scan unbelievably revealed: “Lungs Clear!!”; my expiry date has expired!’
About David
Associate Professor David Pook specialises in the treatment of prostate, kidney, bladder, and testicular cancers. He is the principal investigator on multiple international clinical trials treating urological cancers with experimental drugs including novel combinations of immune therapy.

He is a clinical research fellow in the Prostate Cancer Research Group at Monash University where he helps develop prostate cancer models which can be used to test novel treatments. He is also the Deputy Chair of the Kidney Cancer Subcommittee of the Australia and New Zealand Urological and Prostate Cancer Trials Group.
Q: What treatment plan did you put in plan did you put in place for Juliet?
DP: Juliet was an easy one, but not for a good reason, as she had non-clear cell kidney cancer. The standard treatment was palliative care, which was not an option. The ANZUP UNISoN clinical trial had opened for nonclear cell rare cancer, so we offered this to Juliet.
Q: Juliet, when you were given this information, what went through your mind when David was explaining it all?
JDN: I think like anyone would, if you have a chance, if there is some hope you take it. That was the first thing I thought, and if it didn’t work for me, it may work for the next person.
DP: Juliet said that it might not work for you, but it might for the next patient. This is the reason a lot of us do medicine. Juliet came to the clinic, and she was scared and worried that her cancer has spread. Juliet was going through the worst time of her life, and she was still thinking about other people.
is Juliet De Nittis?
I am a success story. I would not be here today without the immunotherapy treatment
Q: What information did you look at when you were trying to decide what to do?
JDN: I did what most did. I went to google search, which can be incredibly depressing. I found asking David and the trials coordinators for information helped. I then read all the information and wrote down many questions to ask, so I felt prepared. I also felt part of the decision-making process.
Q: What has your experience of the trial been like?
JDN: I was placed on the UNISoN trial and given a new immune treatment to see if it helped me.
When I discussed my options with my specialist, David, he said because of the type of cancer I had, if we had nothing to treat me with, I would be dead.
The medical staff, all of them; doctors, study coordinators, and incredible, competent, endlessly patient, fabulous nurses and auxiliary staff at Monash Clayton Clinical Trials Centre are brilliant, kind, and professional – vitally important and have helped me and fellow patients through our trial experience.
Currently, I am testing another drug called cabozantinib in non-clear-cell kidney cancers like Juliet’s which are no longer responding to immunotherapy.
I am also involved in testing immunotherapy as a preventer of cancer returning after surgery. This is exciting as a recent trial has shown that this is effective. It is a positive time with kidney cancer treatment now at a transition point.
For a while, treatment options for kidney cancer included surgery alone. We now have more to offer as a standalone treatment or in combination. Targeted therapies are now being used and target specific molecules in cells to block cell growth.
We are also aware of the role immunotherapy plays in cancer treatment and are excited to be part of clinical trials of immunotherapy in kidney cancer.
DP: I am the principal investigator for ANZUP on multiple international clinical trials treating urological cancers (including kidney cancer) with new drugs and combinations of immunotherapy.
Symptoms of kidney cancer are blood in the urine, a pain or dull ache in the side of the lower back that is not due to an injury, a lump in the abdomen, rapid, unexplained weight loss, constant tiredness, and fever not caused by a cold or flu. But many people with kidney cancer have no symptoms. Many are diagnosed with the disease when they see a doctor for a different reason.
Juliet has a type of kidney cancer called non-clearcell kidney cancer. In Australia there are no treatment options for this type of cancer funded by the PBS.
Juliet agreed to take part in an ANZUP trial evaluating the immunotherapy drug, nivolumab. In doing this, she is helping future patients who develop this disease, by allowing us to assess how well this drug works in this situation.
We are eager to explore how immunotherapy can be integrated with existing therapies and current treatment combinations.
Current trials will allow us to understand how this form of treatment will benefit patients with kidney cancer –both the rare and common forms of the disease.
I was completely surprised by the success I have had. You wish for it, but you cannot allow yourself to truly belief it!
Q: David, what are some of the clinical trials you are working on?
Immunotherapy works to enhance the immune system of your body… to take ‘the handbrake’ off the immune system by blocking so-called checkpoints. This allows the immune system to attack kidney cancer and for the first time we have seen kidney cancer disappear in some patients.
At the same time, it is likely that more targeted immunotherapy treatments that are now being tested in other cancers will be modified for use in kidney cancer and enter clinical trials – further improving outcomes in the years to come.
Q: What advice would you give other people in a similar situation?
DP: If anyone is thinking about participating in a clinical trial, you should ask your clinician any of your concerns, questions, and queries. It is also important to get a good picture of what the standard treatments options are, and to ask your clinician if there are any clinical trials suitable for you.
JDN: First, I would ask the question ‘is there a trial suitable for me?’ I felt extremely lucky to be eligible for a trial, as it was an incredible opportunity to have the best outcome you can have.
I joined the trial not just with the hope the treatment may help me in some way but also to contribute to research for future cancer patients, and with enormous gratitude for previous cancer patients who have participated in trials that have led to my current treatment.

Make a difference with ANZUP
Any donation, large or small, goes straight into the hands of experts
To find out more or to donate please go to https://anzup.org.au/donate/
All the research being undertaken suggests we will witness a rapid increase in the number of available kidney cancer treatments soon leading to some people having incredibly positive outcomes from their kidney cancer treatment.JULIET AND HER DAUGHTER
We need your help to improve outcomes for people affected by these below the belt (prostate, testicular, penile, bladder, and kidney) cancers and for future generations.
to find the answers we need.
ANZUP trials – kidney
ANZUP is currently running a number of kidney cancer trials. For more details information about these trials, go to the ANZUP kidney cancer trials web page: https://anzup.org.au/clinical-trials/kidney-cancer-trials/
RAMPART
ANZUP 1606
Status: Open & recruiting
Location: Australia & Internationally
Activated sites: 9 (Australian)
• Patients recruited: 24
Patients required: Australian recruitment target - 200pts (total international recruitment 1750pts)
Removing the kidney (or part of a kidney) by surgery is currently the best treatment if you have kidney cancer. The current standard treatment after surgery is ‘active monitoring’. This means no further treatment, but having regular checks so that if the cancer does come back further treatment options can be considered as early as possible.
Surgery, together with ongoing regular follow-up and observation, is the standard approach for people diagnosed with kidney cancer that has required removal of the kidney (or part of a kidney) by surgery. For some people the cancer may return which is when other treatment is offered. We are aiming to find out whether taking one drug (durvalumab) or a combination of two drugs (durvalumab and tremelimumab) can prevent or delay kidney cancer coming back.
For more information, please refer to https://anzup.org.au/clinical-trial/rampart/
Current locations for the RAMPART trial:
NSW
• Calvary Mater Newcastle • Campbelltown Hospital
• Concord Repatriation General Hospital
VIC
• Eastern Health (Box Hill Hospital)
• Monash Health
• St Vincent’s Hospital Melbourne
QLD
• Mater Cancer Care Centre, Mater Misericordiae Ltd • Sunshine Coast University Hospital

SA
• Royal Adelaide Hospital
Spotlight on penile cancer

The penis is the external genital organ. It is composed of three chambers of spongy tissue that contain smooth muscle and many blood vessels and nerves. The corpora cavernosa makes up two of the chambers located on both sides of the upper part of the penis. The corpus spongiosum is located below the corpora cavernosa and surrounds the urethra. The urethra is the tube through which semen and urine exit the body at an opening called the meatus.
What is penile cancer?
Penile cancer is a rare type of cancer and occurs on the foreskin, on the skin of the penile shaft, or the glans (head) of the penis. It occurs mostly in uncircumcised people (who still have foreskin around the head of the penis). Circumcision is the removal of the foreskin and may reduce the risk of penile cancer.
The stats *
Penile cancer is rare. In 2022 there will be an estimated 183 cases of penile cancer diagnosed and 29 deaths from this disease. In 2014 - 2018, on average, 74.5% diagnosed with penile cancer survived 5 years after diagnosis. In 2022, the estimated age-standardised incidence rate of penile cancer is 1.2 cases per 100,000 people.
Penile cancer symptoms
People with penile cancer may experience a variety of symptoms. Symptoms may include:
• a growth or sore on the head of the penis (the glans), the foreskin or on the shaft of the penis that doesn’t heal in a couple of weeks
• bleeding from the penis or under the foreskin
• a hard lump on or under the foreskin
• an odorous discharge under the foreskin
• changes in the colour of the skin on the penis or foreskin
• thickening of the skin on the penis or foreskin that makes it hard to pull back the foreskin
• pain in the shaft or tip of the penis
• swelling at the tip of the penis
• a rash on the penis or a constant red patch of skin that does not resolve
• lumps in the groin due to swollen lymph nodes.
Are estimated to be affected by penile cancer in Australia in 2022.

Spotlight on penile cancer
Causes of penile cancer
The cause of penile cancer is not known in most cases. However, there are several risk factors.
Infection with human papilloma virus is a risk factor for cancer of the penis. Some other conditions that affect the appearance of the skin of the penis can lead to cancer, so it’s important to see your doctor if you notice white, red or scaly patches.
Other risk factors for penile cancer include:
• not being circumcised
• smoking tobacco
• increasing age
• certain skin conditions such as psoriasis
• HIV/AIDS
• premalignant lesions/conditions
• exposure to ultraviolet (UV) radiation.
Who treats penile cancer?
Based on your treatment options, you might have different doctors of various specialties on your treatment team. For penile cancer, the multidisciplinary team often includes a surgeon, a doctor called a urologist who specialises in urinary tract problems, a medical oncologist, and a radiation oncologist. Your healthcare team may also include a variety of other health care professionals, oncology nurses, social workers, pharmacists, counsellors and psychologists, dietitians, and others.
How is penile cancer treated?
Surgery is the main treatment for most people with penile cancers, but sometimes radiation therapy may be used, either instead of or in addition to surgery. Other local treatments might also be used for early-stage cancer. Chemotherapy may be given for some larger tumours or if the cancer has spread.
As well as medical treatment for penile cancer it is also important to adjust to living with the diagnosis. A specialist nurse, psychologist, social worker, a GP and support groups can all help and provide ways of coping.
Thinking about taking part in a clinical trial
Progress in treating penile cancer has been hindered by its rarity so it is difficult to recruit enough patients to penile cancer clinical trials.
Clinical trials are carefully controlled research studies that are done to get a closer look at promising new treatments or procedures. Clinical trials are one way to receive state-of-the art cancer treatment, management and care that is not yet available to the wider public. Clinical trials are also the best way for a multidisciplinary team to learn better methods to treat this rare form of cancer.
If you would like to learn more about clinical trials that might be right for you, start by asking your doctor or contact ANZUP.
Although penile cancer is a relatively rare disease, its consequences can have profound effects for the people who experience it.
Evidence supports the view that factors such as embarrassment, fear, the potential impact on sexuality and a cancer in a sexual organ all impact on patients’ seeking help, resulting in a delay in going to a healthcare professional. See your doctor early and ensure you talk about treatment and the effects on sexual health and fertility.
Penile Cancer and Supportive Care
Associate Professor Catherine PatersonRare cancers – an overview
Any cancer diagnosis can cause anxiety but when someone is diagnosed with a rare, or less common cancer, it can be overwhelming and challenging, leading to feelings of isolation and vulnerability.
A rare cancer is one that has an incidence rate of less than 6 cases in 100,000 Australians per year. Less common cancers are those that occur in between 6 and 12 (inclusive) people per 100,000 Australians annually. These statistics might seem relatively low, but collectively rare and less common cancers are the cause of 50% of all cancer deaths.
Due to the low number of people with rare cancers, the amount of research and clinical trials being undertaken is remarkably less than those with common cancers.
Penile cancer - treatment
There are a range of treatment options for penile cancer depending on the stage of disease. Treatment options range from minor surgery, chemotherapy, radiation, circumcision and amputation (penectomy). All treatments can be disfiguring and have a profound negative impact on the patient’s sexual function, quality of life (QOL), social interactions, self-esteem and self-image. Different types of treatment are all associated with their own individual challenges for patients including complications, unique psychological burden, and often unmet supportive care needs.
With less research, there is less information about these cancers, reduced community awareness, diagnosis remains slow and treatment availability is reduced. All of this adds to the increased mortality rates for rare cancers.
Penile cancer – the stats

Penile cancer affects people over 18 years of age with the average age of 55 years at the time of being diagnosed. Penile cancer can affect anyone with a penis – including men, teenagers, transgender women, non-binary individuals, and intersex people.

Penile cancer and supportive care
People diagnosed with penile cancer, and their partners, can experience a series of unmet physical and psychological supportive care needs whilst being treated for this rare cancer. Globally, the delivery of supportive care for patients and their families affected by penile cancer remains less than ideal. Evidence demonstrates that often patients and their partners require many forms of supportive care that focusses on improving quality of life and addresses what matters most to them.
Currently, in Australia researchers and healthcare professionals don’t know what is actually required to support the needs of penile cancer patients and their families. To try and address this gap in knowledge and support, a study funded by ANZUP is now being undertaken. The study is titled, ‘What are the barriers and facilitators to multidisciplinary models of personcentred supportive care in the context of penile cancer?’ The study is being led by Professor Catherine Paterson, University of Canberra, School of Nursing, Midwifery and Public Health.
Patient involvement
Patients will be consulted when collecting and analysing data to make sure the best quality questions are asked to patients and the partners taking part in the study. The patients consulted will provide feedback on the materials produced for the study, such as, information leaflets and educational materials. They will also support the sharing of the results of the research with the wider public, as well as with scientists, and healthcare professionals.
Research Questions
The study will ask and focus on the questions below:
1) W hat are the most frequently reported areas of unmet supportive care needs in people affected by penile cancer and their partners?
2) W hat are the self-reported levels of anxiety, depression, health-related quality of life, distress and perceptions of person-centred care experienced by people affected by penile cancer and their partners?
3) W hat are the barriers and facilitators of multidisciplinary penile cancer models of personcentred supportive care delivery?
ANZUP and penile cancer
Penile cancer and supportive care study
The study will be conducted over 24 months and aims to help improve the lives of people diagnosed with penile cancer, as well as their partners. The research team seeks to propel service improvements, develop information to assist and support patients and their families, and help clinical teams choose the most suitable model of person-centred supportive care. This study will hopefully provide the much-needed information required that will lead to a future, fullyfledged supportive care intervention trial.
Development of the research proposal for this study has included consumer involvement. This input has been fundamental as the aim has been to obtain patient engagement, so the study adequately identifies, prioritises, designs, conducts the study and disseminates the findings and results.
Another vital aspect of this study will involve working collaboratively with patient coalition partners such as ‘checkyourtackle’. This alliance aims to ensure the study is in line with patients’ perspectives, experiences and needs, and is informed by the best available clinical evidence and capability, throughout the lifetime of the project.
ANZUP is committed to improving treatments, supportive care and outcomes for penile cancer patients and their families, but we need your help in doing so.
Here are some ways you can help:
• If you have, or know someone who has, penile cancer – get in touch with ANZUP today via anzup@anzup.org.au We are always looking for people who are willing to be a part of research. Patients who take part in clinical trials and research help improve the way cancer will be treated in the future.

• Share this article with your networks and your local GP – this will help increase awareness of penile cancer.
• Donate to ANZUP – ANZUP funds not only cancer trials, but all types of cancer research that aims to improve the lives of those with cancer. Your donation will help us get one step closer to a full trial for penile cancer.
“Moderate evidence exists that people affected by penile cancer experience a range of unmet supportive care needs across the international literature.
This study will provide the muchneeded information to address the complex unmet personcentred needs of people and their intimate partner affected by this rare cancer”
ANZUP trials in follow up
Trials in follow up
Once a clinical trial is finished, researchers scrutinise all the information collected during the course of the study. Reviewing all the data allows researchers to decide whether the results mean the new drug or device should continue to the next phase of clinical trial, or, when applicable, seek approval for broader use by the appropriate authorities. Once a new drug or device has been proven to be effective and safe, it may become part of standard treatment for the condition or disease.
Review and analysis of the information can take an extended period of time. So there may be a delay before the results of a clinical trial are known. This is definitely the case with larger trials that can involve thousands of people from many hospitals both in Australia and overseas. In large multi-centre trials, the examination of the data and outcomes may take place over several years.
If you have taken part in a trial and specified you wish to know the overall results of the trial, the researchers should make them available to you directly. Usually results of all completed studies will also be made available in papers or reports published in scientific journals.

ANZUP now has nine trials in follow-up across four of the below the belt cancer types – bladder, testicular, prostate and kidney cancer.
ANZUP Trials
1. ENZAMET – Prostate Cancer ANZUP 1304
Enzalutamide is a new hormone treatment taken as tablets. Previous trials have proven that enzalutamide improves survival and quality of life in people with prostate cancer that has stopped responding to standard hormone treatments and chemotherapy.
This large, international randomised trial was undertaken to determine if treatment with enzalutamide can improve survival and quality of life in people starting hormone treatment for newly diagnosed prostate cancer that has spread beyond the prostate. The trial was led from Australia by ANZUP in collaboration with the NHMRC Clinical Trials Centre. It involved 1,125 people from Australia, New Zealand, Canada, the US, Ireland, and the UK.
In 2020 the ENZAMET trial won all three of the Australian Clinical Trials Alliance (ACTA) Awards. The ENZAMET trial was awarded the 2020 ACTA Trial of the Year Award, the ACTA STInG Award for Excellence in Trial Statistics and the Consumer Involvement Award.
This landmark Australian led clinical trial, ENZAMET, has now shown that hormone therapy with a drug called enzalutamide can improve the survival of some people with advanced, hormone-sensitive prostate cancer.
Findings from the ENZAMET trial, led by ANZUP, have shown that people with this sort of cancer who receive enzalutamide with standard treatment have a 33% improvement in survival compared to people receiving standard treatment alone and a 60% improvement in the time it takes to detect the cancer growing again. These results were much better than it was thought they might be when the trial began.
The ANZUP investigator initiated studies were financially supported by Astellas, who also provided enzalutamide.
ANZUP trials in follow up
2. ENZARAD – Prostate Cancer ANZUP 1303
ENZARAD is a randomised phase 3 trial of enzalutamide in androgen deprivation therapy with radiation therapy for high risk, clinically localised, prostate cancer.
Enzalutamide is a new hormone treatment taken as tablets. Previous trials have proven that enzalutamide improves survival and quality of life in patients with prostate cancer that have stopped responding to standard hormone treatments and chemotherapy. This large, international randomised trial will determine if treatment with enzalutamide can improve survival and quality of life in people starting radiation and hormone therapy for prostate cancer that does not seem to have spread beyond the prostate.
The trial has been led from Australia by ANZUP in collaboration with the NHMRC Clinical Trials Centre. The trial accrued 802 people from 69 sites across Australia, New Zealand, Canada, the US, Ireland, and the UK. Recruitment closed on 30th June 2018.
The ANZUP investigator initiated studies were financially supported by Astellas, who also provided enzalutamide.
3. TheraP –
Prostate Cancer
ANZUP 1603
Lutetium-177 PSMA radionuclide therapy (Lu-PSMA) is a new treatment for advanced prostate cancer. Lu-PSMA is a radioactive molecule that specifically attaches to cells with high amounts of PSMA on the surface of the cells. This allows the radioactivity to be delivered mainly to the prostate cancer cells wherever they have spread, while sparing most normal tissues. Previous small studies of Lu-PSMA showed promising activity in patients with advanced prostate cancer.
This randomised study has compared Lu-PSMA, with a type of chemotherapy called cabazitaxel, which is the standard treatment for advanced prostate cancer when other treatments have stopped working. Half the participants received Lu-PSMA and half received cabazitaxel. This trial enrolled 200 participants in Australia.
ANZUP was able to report interim results of the TheraP clinical trial at the American Society of Clinical Oncology (ASCO) Annual Scientific Virtual Meeting on Friday 29 May 2020.
A favourable response, defined by reduction of PSA by 50% or more, occurred in 66% of people assigned to receive Lu-PSMA compared to 37% with cabazitaxel. Results of the trial also demonstrated the treatment had less severe side effects than chemotherapy.
Patient follow-up is ongoing with initial results suggesting the new treatment may delay progression of prostate cancer.
TheraP is a partnership between ANZUP Cancer Trials Group and the Prostate Cancer Foundation of Australia (PCFA) with support from the Australian Nuclear Science and Technology Organisation (ANSTO), Endocyte, It’s a Bloke Thing, Movember and CAN4CANCER.
4. ENZA-p – Prostate Cancer ANZUP 1901
Enzalutamide is a potent hormone therapy that prevents testosterone from reaching prostate cancer cells, thereby stopping cancer growth. It is already widely used in people with prostate cancer that has stopped responding to standard hormone treatments (castration-resistant prostate cancer). However, most cancers become resistant to enzalutamide over time, with almost 1 in 4 being resistant from the start of treatment.
Many prostate cancers, in particular those that have spread or become resistant to hormonal therapies, have a substance on their cell surface called prostate specific membrane antigen (PSMA). Lutetium-177 PSMA (LuPSMA for short) is a new treatment in advanced prostate cancer. Lu-PSMA is a radioactive molecule that attaches to the surface of prostate cancer cells throughout the body. This drug is given as an injection through the vein and allows targeted radiation to be delivered directly to prostate cancer cells.
Smaller pre-clinical studies have demonstrated synergistic effects by combining Lu-PSMA with enzalutamide. It is possible that Lu-PSMA can prevent early resistance to enzalutamide, extending the time that people benefit from treatment.
The ENZA-p clinical trial aims to compare the effectiveness of enzalutamide in combination with LuPSMA, versus enzalutamide alone for the treatment of prostate cancer. This is a randomised study, so half the people in this trial were randomly allocated to receive Lu-PSMA and enzalutamide, and the other half were randomly allocated to receive enzalutamide alone. There are 160 participants enrolled in this trial across Australia.
ANZUP trials in follow up
5. PCR-MIB – Bladder Cancer ANZUP 1502
Opened in mid-2016, this trial is aimed at managing bladder cancer that has spread into the wall of the bladder. A combination of chemotherapy and radiotherapy is the current standard treatment.
This study aims to assess if it is safe and effective to add an additional new drug called pembrolizumab to the standard therapy of chemotherapy and radiation therapy. Pembrolizumab is a new treatment that “takes the brakes off” the immune system, allowing it to attack cancers more effectively. Studies of pembrolizumab in widespread bladder cancer have shown benefit, with cancer shrinkage observed in about two thirds of people, and in some cases long periods of disease control. At present, pembrolizumab, is approved for use in Australia for the treatment of advanced melanoma in adults.
6. UNISoN – Kidney Cancer ANZUP 1602
In this clinical trial ANZUP will test whether new immune treatments can help people with rare kidney cancer (‘nonclear cell’ cancer).
Non-clear cell kidney cancer represents approximately 25% of people with kidney cancer; and because it is rare there are no treatments currently reimbursed in Australia.
The UNISoN trial is now closed to recruitment and is in follow up. This trial is investigating immune treatments in two different ways; firstly the trial is investigating how well one immune treatment (nivolumab) works alone. If this is unhelpful by itself, then people can continue taking nivolumab but also add in a 2nd immune treatment (ipilimumab). The trial will also discover how many people will benefit from one drug alone, and by doing detailed laboratory testing of people’s cancer samples, we hope to also learn who will only benefit from taking both treatments together.
Nivolumab and ipilimumab have been used alone or together in many cancers, so the side-effects are well known and should be manageable. Immune treatments help some people with cancer, especially those with melanoma, common (clear cell) kidney cancer, lung and bladder cancer. Unfortunately they are much less effective in other cancers (like pancreas, prostate and brain cancers). Nivolumab and ipilimumab have not been tested in people with non-clear cell kidney cancers, so ANZUP is delighted to ask this question, and hopes to help people with this rare disease.
We thank and acknowledge BMS for providing the study drug and funding to conduct the UNISoN trial.
7. KEYPAD – Kidney Cancer ANZUP 1601
Renal cell carcinoma (RCC) is the 7th most diagnosed cancer in Australia and the 14th most common cancer in Western populations. Approximately 90% of kidney cancers are renal cell carcinomas (RCC). At the moment the five-year survival rate for Australians diagnosed with kidney cancer is 78.5%, although most people with kidney cancer localised only to the kidney can be cured.
Immune therapies have been shown to be effective in about a quarter of patients with clear cell renal cell carcinoma after the standard treatment (sunitinib or pazopanib) has failed.

This study will test if denosumab, a drug frequently used to treat osteoporosis, (thinning of the bones), can team up with immune therapy to improve survival and increase the chance of the cancer shrinking for people with clear cell kidney cancer.
In the trial, people with advanced clear cell kidney cancer were offered treatment with two antibodies (a type of protein). This trial will investigate if these drugs taken together can increase the ability of the body’s immune system to attack kidney cancer cells.
It is hoped that by combining pembrolizumab with denosumab, it will stimulate the immune system, so that the immune therapy will work better in the tumours.
ANZUP collaborated with the University of Sydney through the NHMRC CTC to conduct the KEYPAD Trial.
ANZUP trials in follow up
8. TIGER – Testicular Cancer ANZUP 1604
This randomised phase III trial will study how well standard-dose combination chemotherapy works compared to high-dose combination chemotherapy and stem cell transplant in treating patients with germ cell tumours that have returned after a period of improvement or did not respond to treatment.
Drugs used in chemotherapy, such as paclitaxel, ifosfamide, cisplatin, carboplatin, and etoposide, work in different ways to stop the growth of tumour cells. They either kill the cells by stopping them from dividing or stop them from spreading. Giving chemotherapy before a stem cell transplant halts the growth of cancer cells by stopping them from dividing or by killing them. Giving colonystimulating factors, such as filgrastim or pegfilgrastim, and certain chemotherapy drugs, helps stem cells move from the bone marrow to the blood so they can be collected and stored. Chemotherapy is then given to prepare the bone marrow for stem cell transplant. The stem cells are then returned to the patient to replace the blood-forming cells that were destroyed by the chemotherapy.
It is not yet known whether high-dose combination chemotherapy and stem cell transplant are more effective than standard-dose combination chemotherapy in treating patients with refractory or relapsed germ cell tumours.
Up to 420 patients were enrolled in Australia, New Zealand and other countries.
ANZUP is collaborating with the Alliance for Clinical Trials in Oncology (USA) and EORTC (Europe) and the NHMRC Clinical Trials Centre. We thank and acknowledge the Movember Foundation for their funding support to conduct the TIGER trial.

9. UNICAB - Kidney
ANZUP 1802
Cancer
This study aims to find how safe, tolerable and effective a new treatment called Cabozantinib is for non-clear cell kidney cancer.
All patients will take cabozantinib orally every day, until the medication is no longer effective. There is no placebo (inactive treatment), which means that everyone who takes part in the trial will receive the active cabozantinib drug. Cabozantinib is an anti-cancer drug that works by blocking cancer cell growth. Cabozantinib has previously been used in the treatment of many cancers, including clear cell kidney cancer and thyroid cancer.
However, it has not been tested in people with non-clear cell kidney cancer. 48 participants with non-clear cell kidney cancer participated in this study, from Australia.
Trials in follow up
Co-badged Trials
9. proPSMA – Prostate Cancer
Prostate cancer is the most commonly diagnosed cancer in Australian people. If detected early, when disease has not spread, there is a high chance of cure. Relapse, however, is not uncommon despite careful selection of patients prior to surgery or radiotherapy. This, in part, reflects a failure to detect disease spread at baseline due to limited accuracy of current scanning techniques. More accurate scanning may improve outcomes by redirecting patients with disease spread from unsuccessful local treatments to more appropriate management.
This clinical trial will investigate a new type of scan which provides whole body images of prostate cancer spread. Early experience suggests that this new technology, called PSMA PET/CT (prostate specific membrane antigen positron emission tomography/computed tomography), is superior to current scanning techniques. PSMA PET/CT has capacity for wide availability at relatively low cost. Performing a single better test rather than several less accurate scans will also be cheaper, improve patient experience and expose patients to lower amounts of radiation.
This is a randomised study at multiple centres around Australia comparing PSMA-PET/CT to conventional imaging. If the initial work-up does not demonstrate tumour spread, patients will cross-over to the other imaging arm. We hope to prove that PSMA-PET/CT has superior diagnostic performance, should be used as a firstline test for staging prior to surgery or radiotherapy and will result in significant changes to patient management. Results of this trial will be used to support funding of this new technology in Australia and internationally.
The trial has now closed to recruitment and enrolled 300 participants in Australia.
10. FASTRACK II – Kidney Cancer
Surgery is the standard treatment for primary kidney cancer. However, in some cases, surgery is either not possible or other health problems make surgery high risk. This study involves a relatively new, highly precise multidirectional radiotherapy technique called Stereotactic Ablative Body Radiotherapy (SABR) which will be applied to all participants.
The aim of the study is to test the ability of the technique to control cancer within the kidney for those people for whom surgery is not an option, and to examine the side effects of the treatment, including how it may affect your kidney’s function.
This study is led by TROG and co-badged by ANZUP Cancer Trials Group and is now closed to recruitment and is in follow up.
11. NMIBC-SI – Bladder Cancer
Non-muscle invasive bladder cancer (NMIBC) makes up approximately 70-80% of all bladder cancer diagnoses. NMIBC is bladder cancer that has not yet invaded through the wall of the bladder. Treatment is generally intended to reduce the risk of the bladder cancer recurring or progressing to muscle invasive disease. Treatment involves endoscopic resection to the bladder tumours followed by potential intravesical chemotherapy or immunotherapy.
Although treatments can significantly reduce the risk of recurrence and progression, there are both benefits and harms that are likely to vary between treatment options. However, little is known about the impact of these treatments on patients’ quality of life.
Phase I of the project involved qualitative research to develop a draft Non-Muscle Invasive Bladder Cancer Symptom Index (NMIBC-SI). The second phase of the project aims to evaluate the psychometric properties of the NMIBC-SI. This was conducted across two field tests:
• Field Test 1 was a cross-sectional study design asking participants to complete the draft NMIBC-SI questionnaire either on paper or lectronically. The purpose of Field Test 1 is to produce a shorter version of the NMIBC-SI by eliminating items with poor psychometric properties.
• Field Test 2 used a prospective longitudinal study design to evaluate the clinical validity of the final version of the NMIBC-SI. Participants were asked to complete the NMIBC-SI along with comparative questionnaires at different time-points during their treatment. The purpose of Field Test 2 is to assess the reliability, validity and responsiveness of the final version of the NMIBC-SI to ensure it is fit for purpose in clinical research.
ANZUP was running this trial in collaboration with Cancer Australia and Cancer Council NSW. This study is being sponsored by the University of Sydney.
For more information on our trials in follow up, go to our website https://anzup.org.au/clinical-trials/follow-up/
In May, we did things differently for our annual Below the Belt #YourWay Challenge, focusing on the 77 people diagnosed with a below the belt cancer every day. This included the 77 crunches in May #YourWay Challenge that was run through the Facebook Challenge Platform and the 77km #Your Way in May Challenge via our below the belt website.

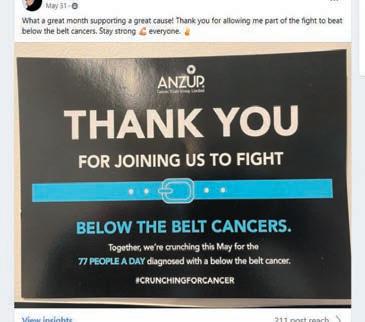


We welcomed over 1,300 challengers, raised $60,000, undertook 7,743 kms and achieved over 2,387 crunches each. Whether they were walking, running, cycling, or crunching, all challengers were raising awareness and funds to improve the lives of people affected by bladder, kidney, testicular, penile and prostate cancers through practicechanging multidisciplinary collaborative clinical trials.



Below the belt cancers –testicular, penile, prostate, bladder, and kidney – affect 77 new people every day in Australia and New Zealand.


















It’s back!
The return of the Sydney Pedalthon

7 Sydney Pedalthons, 5 cancers, 1038 laps, 4079 kilometers (that’s from Sydney to Perth!), an extraordinary $53,000 raised and the funds are still rolling in!

After three years off the track, we thank every rider, supporter and volunteer who joined us at Sydney Motorsport Park on Tuesday 22 November, for the energy and commitment to making it a fantastic day, as well as the amazing efforts in raising vital funds for testicular, prostate, penile, kidney and bladder cancer research!


The day was full of energy and competitive spirit; we witnessed grit, determination, and cycling prowess, as well as a lot of fun.
A special thank you to ANZUP’s Researchers, Professor Lisa Horvath and Associate Professor Kate Mahon, thank you for riding and reminding us why the Pedalthon is so important. And to Associate Professor Peter Grimison for riding every year in support of the Pedalthon’s founder Simon Clarke and ANZUP and representing ANZUP on the day.






Champions of the track
Congratulations to Macquarie Bank Pedallers who won the 2022 Below the Belt Champions and got to take home the coveted trophy.





Congratulations to our other winners of the day:
Fastest lap: Jamie Kennell - Webb
Champion of the mountain - Female: Alana Rados
Champion of the mountain - Male: Jonny Harrision
Most laps - Female: Annett Happich
Most laps - Male: Nick Johnston
Winner fastest 2 laps: Tom Bills
Below the Belt Pedalthon 3rd Place Champions: Origin Energy
Below the Belt Pedalthon 2nd Place Champions: Lion Hearts
Bronze Sponsor – Pfizer Oncology

Thank you to our wonderful Bronze Sponsor Pfizer for their amazing support.


Pfizer Oncology has been a regular face at the Sydney Pedalthon both on and off the track since its inception in 2014. This year, Pfizer generously returned for the fourth time as Bronze Sponsor for the event.



Not only that, but 2022 was their seventh time as riders – which means that they have supported and pedalled with us at every Sydney event.
We would also like to extend our thanks to our 21 incredible supporters for their donations on the day helping to sustain our riders across the 3 hours.
With thanks to our sponsors and supporters!
How does
All contributions, large or small, get us closer to finding better treatments for cancer. Clinical trials are a costly exercise, but the outcomes are so worthwhile. This is where your donated funds go:
Will support the attendance of an ANZUP multidisciplinary member at a conference or scientific meeting.
Will allow us to hold face-to-face Ideas Generation Workshops to discuss new research ideas and concepts to consider developing into a future grant applications.

Will allow us to invest in a pilot study to test the feasibility of promising drug therapies, surgical methods, post-operative care and palliative care options.


Fundraising for ANZUP
Community fundraising
City2Surf
The City2Surf returned in style, with 60,000 participants running, walking, and dancing their way through the city to the sun-drenched Bondi Beach, after two years of virtual races on Sunday 14 August.

Steven Guy was one of those walkers and fundraisers, whose mission was to walk for cancer.
“My name is Steve, and I was first diagnosed with kidney cancer in April 2019, it rapidly metastasized. Now, after 3 years where I have had 3 major surgeries, numerous procedures and ongoing treatments and tests, I have decided to try to give something back by raising money from walking the 14km City2Surf in August 2022 in under 3 hours”.

Steven raised an incredible $1,441.50 for ANZUP and below the belt cancer research and walked 14 kilometres in 2 hours and 21 minutes. An incredible effort and commitment to raising funds and awareness to improve outcomes for kidney cancer.

Interested in joining a public event and raising funds for ANZUP? Go to belowthebelt.org.au/event-listings for current event listings.
Breakfast Point Men’s Shed
John and the Breakfast Point Men’s Shed team have been great supporters of ANZUP since 2018 at our Pedalthon events, and local community events to raise funds and awareness for below the belt cancer.

In August the Men’s Shed with the support of IGA Breakfast Point put on a community sausage sizzle. Despite a windy morning, the sausage sizzle welcomed over 100 people and raised over $1,300 funds to go towards the Sydney Pedalthon and below the belt clinical trials research.
Many thanks to the Breakfast Point Men’s Shed for their outstanding efforts to raise awareness and funds for the Sydney Pedalthon. They raised over $20,000!!!!

Fundraising for ANZUP
Dry-Gust
In August, ANZUP encouraged supporters to go dry and make a difference to the lives of people affected by below the belt cancers.
Charlie Harris put his hand up for the challenge and raised $234. Charlie went booze free throughout the month of August and feeling the benefits!
Host your own fundraiser and help us fight cancer, below the belt
Rum, ride, go without your daily coffee, host a garage sale, or bake your heart out. The sky is the limit when it comes to hosting your own fundraiser.
No matter where you are across Australia or New Zealand, or around the world, you can use your skills and interests to get involved and help fight below the belt cancers.

So far, through our Below the Belts events we have raised over $1.96 million and funded 36 new cancer research projects.
Get involved today and help support more projects to improve the lives and outcomes for those living with below the belt cancers.
https://www.belowthebelt.org.au/funraiseyourway
Perpetual’s
2022 IMPACT Philanthropy Program: ANZUP awarded two grants

We are pleased to announce that in the recent funding round for Perpetual’s 2022 IMPACT Philanthropy Program, ANZUP was awarded two grants.
1. TheraP Translational Research.
ANZUP’s TheraP trial showed that Lu-PSMA is more effective than chemotherapy in advanced prostate cancer. Although this is very promising and exciting, we know that not all people benefit from Lu-PSMA and after a period, the treatment stops working in all people. We have developed technology to pick up tiny amounts of DNA (the genetic blueprint) released by cancer cells into the bloodstream. This is also referred to as circulating tumour DNA (ctDNA).
By testing ctDNA in the laboratory from blood samples collected on the TheraP trial, we will try to understand which people get excellent responses to treatment, which people never respond to treatment, and also what causes Lu-PSMA to stop working.
Many thanks to the Centenary Foundation – Betty Lowe Memorial, Centenary Foundation – Robert William Alfred Blackburn, Hillcrest Foundation and James & Barbara Quinn & Family Foundation for their funding towards this important work.
2. UNISoN Kidney Cancer Genetic Analysis.
By reviewing kidney cancer samples and blood tests donated by the people on the UNISoN kidney cancer clinical trial, we hope to learn if we can predict which people who have rare variant kidney cancer are most likely to benefit from treatment, who needs one drug and who needs two. We have planned a suite of different scientific experiments to test these samples and compare them to the outcomes of people on the UNISoN trial.
Many thanks to the Hillcrest Foundation for their generous funding.

Thanks to our Partners, Corporate and In-kind Supporters

Corporate Supporters

We are very fortunate to have our corporate supporters and partners who enable ANZUP to better support our members and ultimately, patients and their families. Our 2022 corporate supporters include: Astellas, AstraZeneca, Bayer, Bristol Myers Squibb, Ipsen, and Pfizer Oncology.


In-Kind Supporters
We acknowledge and thank the following organisations for the generosity they have shown by providing their services pro-bono.
AFI Branding, The Saturday Paper, and FC Lawyers.





