
17 minute read
Healthcare
from AZRE May/June 2020
by AZ Big Media
How COVID-19 will change healthcare facility design RIPPLE EFFECT
When the COVID-19 virus began spreading throughout the globe, the call to action rose up in the medical world. Healthcare professionals did their best to prepare for an expected wave of patients in need of treatment, some requiring standard levels of care, while many others requiring intensive care, including intubations. By and large, the healthcare community in the United States rose up to meet the challenge.
Part of the way healthcare professionals prepared for what was coming, was by taking a hard look at the space they had available and how they can make better use of it to treat the maximum amount of patients.
Some communities converted convention centers into treatment facilities. In Arizona, a closed hospital, St. Luke’s Medical Center in Phoenix, was activated and utilized by the Army Corps of Engineers to ensure there were enough beds to meet the growing demand.
Valley architects sprung into action, as well, to help local facilities make the best use of their space.
“Here locally, our focus has been on helping Banner Health,” said Craig Passey, vice president and health studio leader for SmithGroup. “Banner has reached out to their architectural and engineering partners in the community to help maximize their ability to accommodate as many patients as possible.”
Passey said his firm helped Banner look into non-clinical spaces, such as conference rooms, dining areas or cafeterias, to see if they could be By STEVE BURKS
activated as treatment areas.
“The intent is to see how we can perhaps repurpose and maximize the number of beds they can get into their existing footprint,” Passey said.
SmithGroup was also part of a group of firms that were contacted by the City of Los Angeles mayors office. The group looked into converting the Los Angeles Convention Center into a space to treat patients if the need arose.
“The study was to understand how to work with the existing facilities and create a M.A.S.H. unit in the facility,” Passey said. “It yielded about 1,600 bays or stations. It also looks at some of the necessary support provisions that would be required.”
Passey agrees that the COVID-19 pandemic and the stress it put on healthcare facilities around the country will be something that healthcare design firms like his will be examining closely. AZRE Magazine reached out to Valley architecture firms to get their perspective on what the pandemic revealed as issues with healthcare facility design and what architects can do to make sure the facilities are better prepared for the next pandemic. Below are some of their answers. For complete responses, visit azbigmedia.com.
AZRE: From a design and function standpoint, what are healthcare operators and engineers and designers learning about the limitations of their facilities during this pandemic? STEVEN STACK, president of Devenney Group Ltd., Architects: Air distribution systems are not designed to provide the amount of negative pressure required to create isolation spaces for COVID-19 influx. Negative pressure rooms are distributed across hospital units by design, to deal with the need across different clinical specialties. What is needed with COVID-19 is a large cohort of negative pressure rooms, notdistributed. CARL NELSON, partner, healthcare leader at Orcutt | Winslow: Most facilities or organizations are realizing they are ill-prepared to handle the surges they are experiencing especially when it comes to converting existing spaces into temporary ones. Acuity has a tremendous impact on what spaces can be converted more readily than others. We are finding that it is difficult to convert large open areas such as conference and training rooms into high-acuity spaces. However, they can more easily be converted into non-COVID holding or observation units fairly quickly. Another major limiting factor is just availability of any unoccupied space. We are seeing the lack of space resulting in temporary “tent structures” or make-shift structures. JOHN CANTRELL, principal, design leader at Orcutt | Winslow: One of the biggest concerns of hospitals is managing the flow of visitors to the right service line for care. Hospital facilities managers and administrators are telling us that people infected with COVID-19 are showing up at any entrance to the campus and wandering around until they find someone to assist them. Two observations are being made regarding this: One is
Every bank has business accounts.

Ours come with accountability.
Our commitment to you is based on more than just numbers. At Alliance Bank of Arizona, we’re invested in your business as much as you are.
Bank on Accountability
that medical campuses have too many uncontrolled access points; and two, the emergency department needs to be expanded virtually (think telemedicine) or via remote screening areas outside of the emergency department proper.
AZRE: To your knowledge, what are some creative ways healthcare facilities are currently adapting (or preparing to make adaptations) to accommodate the expected spike in patients? ASHLEY MULHALL, senior associate, high performance and sustainability leader at Orcutt | Winslow: Most large facilities have in-house 3D printing capabilities and we are seeing these reconfigured to manage shortages of personal protection equipment (PPE) and other equipment such as ventilator parts. This out of the box thinking could transform supply chain going forward. J.C.: To comply with the Department of Health’s requirement to increase bed capacity by 25 percent, with a 50 percent capacity increase by late April, we’re working with Honor Health to assess their current facilities and specifically how we can repurpose underutilized space to accommodate general patient rooms. This will free up beds within

the hospital for COVID-19 patients. A rehab gym space has been identified at the North Mountain Campus of Honor Health that can fill the need to increase capacity to 50 percent. S.S.: Moving triage of patients to tents outside of emergency department. Current facility examples of parking lots and public spaces being empty and reducing overall parking need. This allows for patients to be “pre-screened” prior to entering the hospital and infecting others or getting infected.
AZRE: Once we are clear of this current crisis, what do you feel will be the first design change we will start seeing more of in healthcare facilities? J.C.: One immediate change we expect to see is the concept of “Social Distancing” designed into all healthcare waiting areas. The days of one large waiting area may be a thing of the past. Smaller enclave waiting space that separate sick from well visitors. Private spaces within emergency departments or doctors’ offices where you can wait as a care giver to a child or parent. S.S.: Health systems will need to plan more strategically around which facilities in their systems should house “routine patient care” and which are equipped for disaster protocols. Patients could be better triaged across a healthcare system by allowing for routine day to day operations to function at a “non-disaster” facility. Put a higher focus on capabilities of the lab and enhancing or expanding capabilities in order to handle increased testing.
JENNIFER WILCYNSKI, interior designer at Orcutt | Winslow: I believe one of the things that will come out of this pandemic is more physical barriers between our caregivers and the public. We are now seeing acrylic screens at the grocery store while we check out. We will need to consider the psychological impact of all involved – consider going from open nurse stations to enclosing them in “glass bubbles”. Do we prioritize our staff’s personal safety over open communication? I think the answer to that is a resounding “YES!” We are likely to see more ancillary pieces of furniture to house personal protection equipment (PPE) for the professional and public alike. And, we’ll need a supply chain to ensure they are available to all our healthcare facilities.
BUILT TO EXPAND HORIZONS
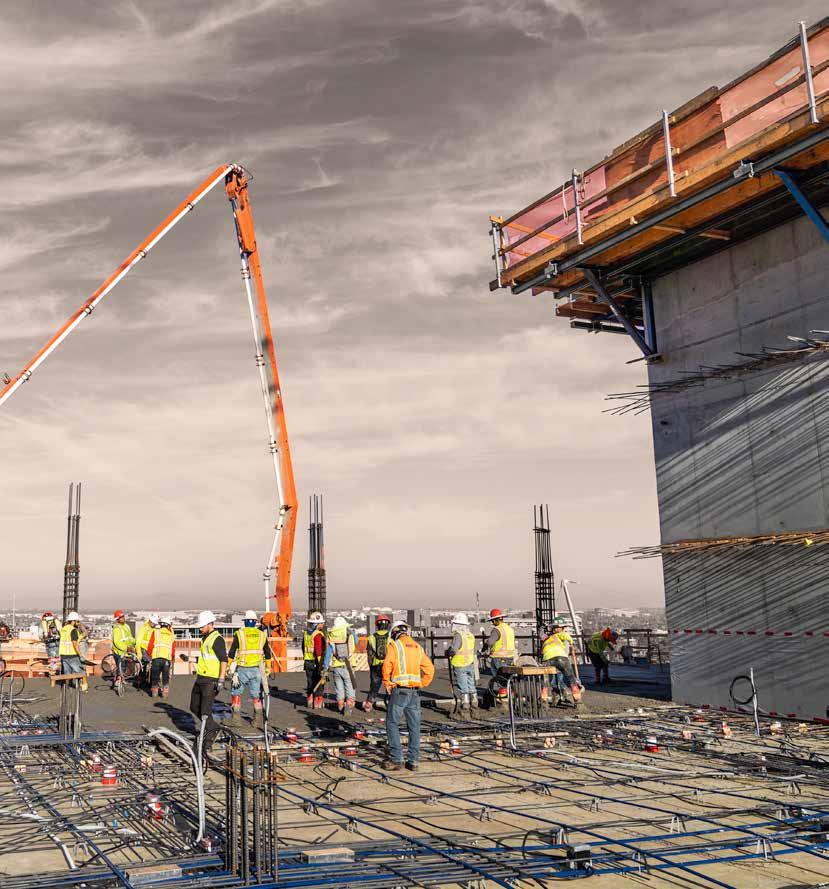


Akara, Phoenix
GRIT

PERSEVERANCE GETS THE JOB DONE RIGHT.
AJ Thomas Ashley Mulhall Carl Nelson
Craig Passey Jennifer Wilcynski John Cantrell Steve Stack
AZRE: How do you expect architects will approach coming up with creative solutions to facility issues that arose during this current pandemic? J.C.: Architects and designers generally apply their skill sets to solving existing problems that they can see, when in fact, we need to expand our design processes to look ahead and predict problems we need to solve before they happen. In a Design Intelligence article by Michael Lefevre on Foresight he writes: “Foresight is intentional and can be developed as a form of intuition and data-enriched visibility. Those who have it, start by pausing to look. Where are the beneficial Black Swans of our industry – and who can see them coming?” He goes on to suggest that by pooling our intelligence to see collectively can we plan for unpredictability. The message is clear – to solve these problems and those in the future it will take the collective thinking of healthcare providers, architects, designers, medical simulation modelers, construction experts and manufacturing industries to come together and to look ahead. To see the next Black Swan coming we must be looking. S.S.: As a Joint Commission requirement, every hospital must regularly conduct a hazard vulnerability and risk assessment relative to their catchment area. This includes public health emergencies such as a pandemic. There are three key essentials necessary for maintaining access to healthcare during disasters or emergencies: safeguarding human resources, maintaining business continuity and protecting physical resources. Required disaster planning includes emergency management training and coordination with local officials and first responders in a proactive, drill/planning scenario. We would expect architects and contractors to play a role in future drills and planning; in addition to seeing revisions made to individual healthcare facilities’ emergency management plans as a result of lessons learned through the COVID-19 pandemic. C.N.: In a way, healthcare architecture has been searching for the next trend. Previous trends include BIM, Evidence Based Design, LEAN / IPD and most recently Behavioral Health. You will find that every healthcare architect will likely proport that they have been involved with surge projects and will find angles to leverage that experience. What we really need to focus on is how we take the lessons learned and apply them to future events AND other areas within healthcare design.
HEALTHCARE FACILITY CHANGES
AJ Thomas serves as principal and healthcare sector leader for Corgan. He provided the following five examples of how healthcare facility design and function may evolve due to the COVID-19 pandemic.
1. Manage safety and infections ( through operations)
• Eliminate Lobby waiting. Enable patients to wait in their car in the parking lot, implementing just-in-time operations. • Increase use of telemedicine for follow-up patients. CMS has loosened the regulations for telemedicine in response to the COVID-19 pandemic. Telehealth services may now be delivered to Medicare beneficiaries by phone as long as video capability is available. • Install temperature screening devices at entry doors for ambulatory facilities.
2. Manage safety and infections ( through design and 3D print)
• Hands free door opener, we have the ability to 3D print these hands-free door openers. One less touch point for our caregivers.
3. Increase bed capacity
• Convert a single patient room to “manage” multiple patients. • Rapid prefab construction for emergency response through a partnership with DIRTT for temporary and new facilities. • Identifying and converting building typologies in the community (motels, dorms, and office buildings) to manage overflow capacity. We are currently working on a feasibility study with a developer and the Governor’s office in Texas to relocate less acute care to nontraditional spaces (office building) to free up hospital bed capacity.
4. Increase Isolation rooms
• Change in HVAC systems and filtration protocols. Shared air is a problem. We have seen our clients retrofit window A/C’s to patient rooms, to temporarily convert hospital rooms to isolation rooms. We can help facilitate an engagement with our MEP partners to work out the ideal solution.
5. Address shortage of medical equipment
• With the looming threat of medical equipment shortages during this pandemic, 3D printing is emerging as a potential solution. Corgan has a fabrication shop with 3D printing capabilities to assist with emergent prototyping and production for critical shortages.

Over 75 Years of Working Hard for Arizona
SPECIALTY HEALTHCARE

SENIOR LIVING
Pete King is committed to providing an environment where employees are treated like family, careers are built and safety is a top priority.
11040 North 19th Avenue Phoenix, Arizona 85029 | 602.944.4441 • petekingaz.com
COMPANY TRADITION

TEAMWORK 24/7 SERVICE


IN-HOUSE EDUCATION
BUILDING FOR THE NEXT GENERATION
Senior living facilities changing with the times
By STEVE BURKS
Much of the focus for modern product design is on how the next generation will embrace a product or concept. Terms like Millennial or Gen Z are thrown around when retailers talk about attracting new customers, and their needs and wants are often at the forefront of how something is designed.
The changing demands of the customer are also at the front of mind for developers of senior living communities. As Americans age, the needs and preferences of those moving into senior living facilities change. The challenge for the modern senior living designer and builder is to anticipate what the next generation will want.
“If you think about our original communities, they were 100 percent independent living,” said Nicolle Blais, chief operating officer for Statesman USA, part of The Statesman Group of Companies. “When we started to see a changing need in our existing resident and incoming resident, we said, lets make some adaptations within the building and let’s offer assisted living. And then, let’s offer memory care and then let’s get creative with some of the lifestyle offerings that we have.
“We’re very adaptable and we try to design the building to give us that flexibility for adaptability as we change our programs along the way.”
Blais leads the Statesman USA team that is currently building the company’s latest senior living community, The Manor Village at Desert Ridge, which is located in the highly sought after North Phoenix submarket, along Deer Valley Dr., west of 56th St.

The Statesman Group has been a developer and builder since 1976, starting in Canada and operating in Arizona for the past 25 years. The company specializes in single-family, multi-family, resort and senior living communities. The Manor Village brand is the company’s senior living component.
The Manor Village at Desert Ridge facility is expected to be completed by the end of 2020, with independent living residents moving in first. After getting all of its licenses secured, Blais said the facility hopes to begin welcoming assisted living and memory care residents by Summer of 2021.
Blais and the Statesman team is very excited to bring this new community to market and she feels that the company’s reputation might be its biggest selling point. Statesman handles all facets of the planning, development and building of the community, as well as its operations, in house.
“We know that in the senior living industry a lot of owners will outsource the operations and the food service and the care, we do everything ourselves,” said Blais. “So, being our own developer, our own general contractor and our own operator, we really focus the time and attention on
33 BUILDING SUCCESSFUL
ARIZONA PROJECTS FOR 33 YEARS

EXCELLENCE.
480.497.2300 • fax: 480.497.9610 www.bjerkbuilders.com Not only will Bjerk Builders perform at the top of their game, but well above the competition. Consistently on target in completing your project on time, within budget and with the utmost level of quality. License B1-088897
Bjerk-Excellence33-7.125x4.75-HfPg.indd 1

10/25/19 8:30 AM
the design of the communities from an operations perspective, but also from a resident perspective.”
Blais also believes that Statesman’s all-around focus on the community makes it an attractive option for seniors and their families when they are looking for a place to live.
“We’re family owned and operated, so to our future residents and their families, that’s really important to them. We’re not a merchant-style builder, where we build the building, fill it and then flip it,” Blais said. “You see it many times, senior facilities change hands multiple times, which means new management, fee increases, ect., ect. So, they have peace of mind knowing that it’s family owned and operated, and we’ve been doing it for 25 years and we bring all of that knowledge to this project.
“We put our blood, sweat and tears into this community, and our hearts as well. So I think that is a sure value-add for our future residents.”
The modern senior living facility serves three unique functions for its residents as they age. First, it serves as a new home for seniors who are still active and independent and don’t require any additional care to go about their daily life. Second, it serves as an assisted living facility for seniors who require special care due to physical limitations. And finally, it serves as a place that seniors with cognitive or memory issues can live and receive the kind of care that helps them remain active and aging gracefully.
The challenge for the modern senior living facility is to incorporate all three of those facets into a facility, without losing the sense of it being first and foremost, someone’s home.
“We want it to be graciously appointed, we want it to be beautiful, but it has to be warm and inviting and home-like,” Blais said. “Our owner (Dr. Garth Mann) has been very involved in the design of the Manor Villages, and he’s created magic. Every community has a beautiful, warm, home-like feel.
“You recognize that it’s someone’s home, but it still allows us to function as an operating entity and provide the care and the services, because it’s a balancing act, for sure.”
The Manor Village at Desert Ridge

will feature suites that range from 700 square feet up to more than 1,000 square feet for the independent living residents. The Manor Village is not a buy-in community, instead, residents are on month-to-month rental leases and all expenses, from utilities to housekeeping to even a meal plan, are included in the rental price.
The suites will have high-end finishes and full kitchens. The residents will be encouraged to decorate their homes as they wish. The layout of the suite is easy to navigate for the residents, making their day-to-day activities easier as they age.
Outside of the individual suites, the facility will have many community spaces to encourage socialization, a large community dining room, a bistro and general store-like space, as well as a pool, outdoor dining area, rooftop patios, a 50-seat theater and a fireside lounge for enjoying a drink and socializing before or after dinner. The facility will also have underground parking for those residents who are still driving, as well as a 5,000 square foot spa and salon that will offer massages, manicures, pedicures, haircuts and more. Residents will also have access to facilities at the neighboring Montreaux luxury apartment complex, which is also owned and operated by Statesman.
All told, the senior residents at Manor Village will be living at a luxury apartment complex, with all of the amenities that come with it.
“We will have 196 suites, total, with the third floor being independent living, the second floor is assisted living and we will have two neighborhoods of Our Hearts Memory Care on the main floor,” Blais said of the layout.
Another challenge of the modern senior living facility is making sure they have the staff to provide services to the residents, be they independent living, assisted living or memory care resident. Blais said that Statesman puts a lot of time and energy in attracting and retaining the best staff in the industry. They will have a wellness director that is a registered nurse (RN) and the facility will also have at least one Licensed Practical Nurse (LPN) on site at all times, sometimes multiple LPNs.
For residents in the memory care communities at Manor Village, there will be a full-time recreation director, a recreation therapist and an activity coordinator. They will also have a part-time musical therapist providing programming for residents.
“We know the impact that music therapy can have on our residents and it’s an important thing for us,” Blais said. “We’re very focused on providing lifestyle enrichment activities within the memory care community. We do regular personalized wellness evaluations and we want to make sure that the care that we’re providing is personalized for that individual.”
Building exceptional work.
One project, one team at a time.
602.296.1496 HAYDONBC.COM
LIC#A ROC108937 | B-01 ROC108085

SUMMIT HEALTHCARE OUTPATIENT CAMPUS SHOW LOW, AZ
DONATE AT MEALSONWHEELSAMERICA.ORG/COVID19











