In this issue:
3 Training Integrated residency, wellness and attrition
6 Advocacy VAM 2023 is in the room where it happens!
9 TAAA Video: Endovascular thermal septotomy
PRESIDENT-ELECT ZEROES IN ON COMPLEXITY OF ISSUES WITHIN VASCULAR SURGERY PIPELINE






The Vascular Annual Meeting

(VAM) E. Stanley Crawford Critical Issues Forum this year probes the problems and the challenges facing the vascular surgery workforce pipeline. The opening day highlight—the domain of the incoming SVS president, Joseph Mills, MD—seeks to unravel the multi-faceted, multi-directional nature of the issues contained within this complex structure.
See page 2
Award-winning vascular resident talks about the science behind her work, which her mentor says is
 By Éva Malpass
By Éva Malpass
University of Toronto surgeon-scientist trainee
Sneha Raju, MD, has been awarded the SVS Foundation Resident Research Award for 2023 for her work on a “new paradigm” of endothelial cell-cell communication and its invaluable implications for atherosclerotic plaque development. Her work delves into the “critical” bidirectional interface that endothelial cells (ECs) inhabit, in the hopes that manipulating
the mechanism might lead to mitigation of disease progression. Created to encourage early-career physicians to become involved in basic science research, the annual award centers on explorations of the biology of vascular disease and potential translational therapies. Abstracts
See page 3
13 Reintervention CEA more durable out to six months
14 BEST-CLI Restoring limb perfusion

19 Career Fair SVS stages recruiting event at VAM
SPOT LIGHT
WHAT’S UP ON OPENING DAY
AFTER A FULL YEAR OF preparation, the SVS anticipates the day we have all been waiting for: opening day 2023. Here are just some of the activities on tap: Registration will be open from 6 a.m.–5 p.m. (all times EDT) on the Ballroom Level of the Gaylord National Resort and Convention Center.
The rest of the day is jampacked with educational and scientific sessions, the annual meetings for the Vascular Quality Initiative (today is the final day) and the Society for Vascular Nursing (first of two days), receptions, industry sessions and more. It ends with a chance for attendees to put on their comfy jeans and casual shirts, and celebrate opening day with a free party for all ages.
SVS Connect@VAM: Building Community is from 7–9 p.m. on the atrium level.
Registrants will want to catch the Opening Ceremony from 7:30–8:30 a.m. in the main session room, Potomac A/B. That will be followed immediately by the William J. von Liebig Forum, presenting the first sets of plenaries. Also up, the Registered Physician Vascular Interpretation Exam Review, in two sessions, four “lunch and learn” sessions and more scientific sessions.
The day winds down with receptions for residents and medical students..—
Beth Bales
www.vascularspecialistonline.com THE OFFICIAL NEWSPAPER OF THE WEDNESDAY, JUNE 14, 2023 | CONFERENCE EDITION 1 Introducing the NEW Shockwave L6 Peripheral IVL Catheter Available in 8.0, 9.0, 10.0 and 12.0mm diameter sizes BE LARGE & IN CHARGE Rx Only. Visit Shockwavemedical.com for Important Safety Information Before Use. SPL-68921 Rev. A Shockwave-VAM L6 Print Ad-9.5x1.833-PRINTER.indd 1 5/22/23 2:05 PM
‘First’ study to identify endothelial cell-cell communication via bidirectional secretion of extracellular vesicle cargo wins SVS Foundation award, place on VAM stage
“moving the needle on every front.”
CRAWFORD FORUM
Joseph Mills
Dawn M. Coleman
Lee Kirksey
Michel S. Makaroun
Peter R. Nelson
Malachi Sheahan III
Laura Marie Drudi
WelcometoTurntopage10fordailyplanner
VAM VAM23
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek
MD, RPVI, FACS | Professor HansHenning Eckstein, MD | John F. Eidt, MD
| Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS
| Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray
L. Shames, MD | Niten Singh, MD | Frank
J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Director of Marketing & Communications Bill Maloney
Managing Editor SVS Beth Bales
Marketing & Social Media Manager
Kristin Crowe
Communications Specialist
Marlén Gomez
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Roger Greenhalgh
Content Director Urmila Kerslake
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution
Jocelyn Hudson, Will Date, Jamie Bell, Clare Tierney, Éva Malpass, Adam
Pearce and Benjamin Roche
Design Terry Hawes and Wes Mitchell
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. | The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | POSTMASTER: Send changes of address (with old mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. | Printed by Ironmark
©Copyright 2023 by the Society for Vascular Surgery
FROM THE COVER: PRESIDENT-ELECT ZEROES IN ON COMPLEXITY OF ISSUES WITHIN VASCULAR SURGERY PIPELINE
continued from page 1
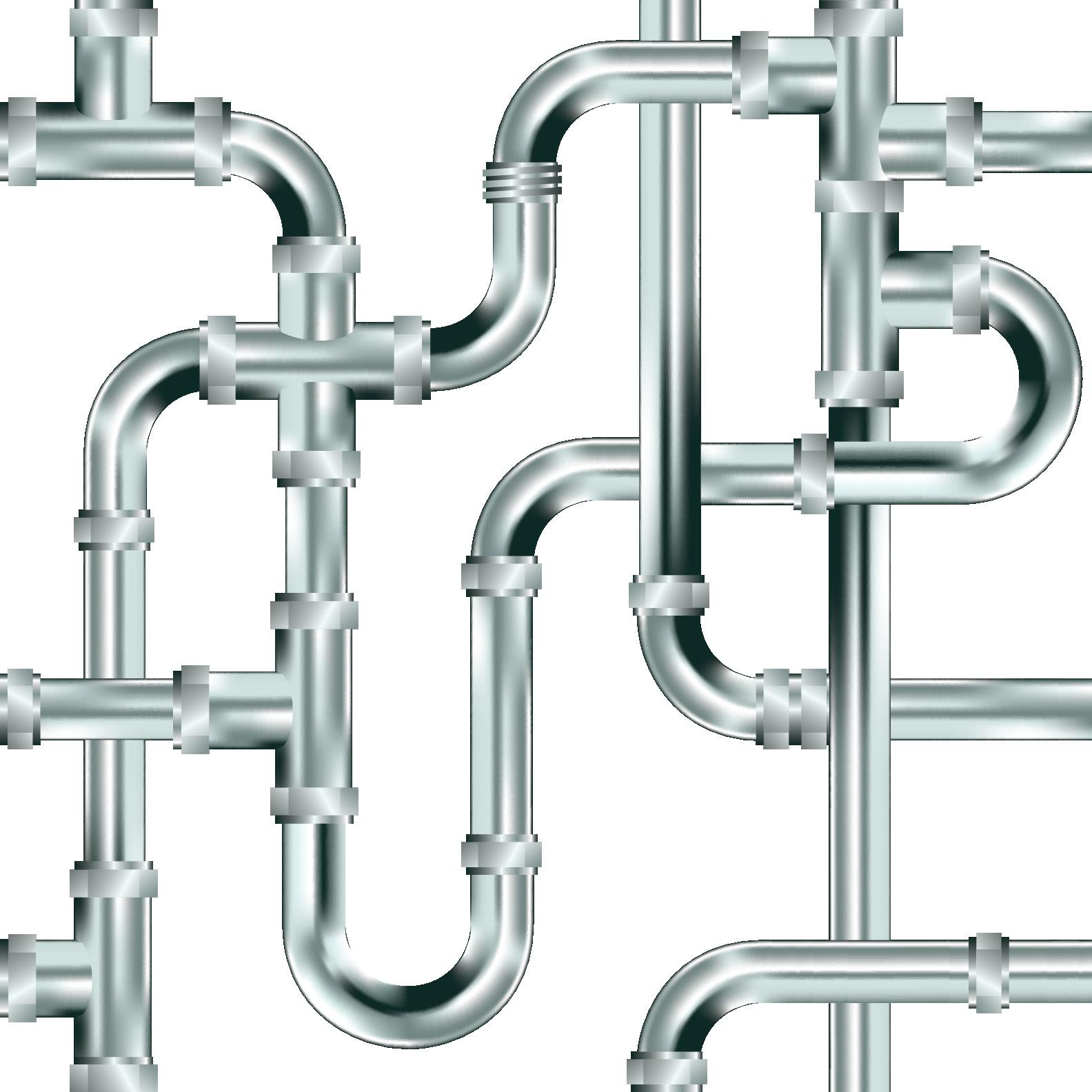
Joseph Mills describes it as having become something of an overused, one-dimensional trope. For the SVS president-elect, who takes over as president at the close of VAM 2023, the pipeline is far more complex than that: The issues surrounding, feeding into, emerging out of— and, potentially, clogging up—the vascular surgery workforce pipeline are myriad and far more difficult to pin down than to a simple, singular pipe. “The pipeline is not one line,” the professor and chief of vascular surgery at Baylor College of Medicine in Houston, Texas, tells VS@VAM “It has multiple connections that come from multiple places and go to multiple places.”
That’s why Mills planned this year’s Crawford Forum—traditionally the preserve of the incoming Society president to focus on the direction of vascular surgery—with a title reflecting one of the specialty’s most existential issues: The State and Future of Our Specialty—Extending, Repairing and Maintaining the Vascular Surgery Pipeline. The session will take place in Potomac A/B today (11 a.m.–12:15 p.m.).
The Forum’s panel captures three main areas of focus: sources of future vascular surgeons, the existing workforce, and the distribution of that workforce. To that end, Mills hand-picked six speakers to deal with the issues at hand. Lee Kirksey, MD, from the Cleveland Clinic in Ohio looks at outreach to high school and college students and Malachi Sheahan III, MD, from Louisiana State University in New Orleans, deals with outreach to medical students and
RADIATION SAFETY
residents in training. And while Dawn M. Coleman, MD, from Duke University Medical Center in Durham, North Carolina, will address vascular surgeon wellness, Laura Marie Drudi, MD, from Centre Hospitalier de l’Universite de Montreal in Canada, will discuss solutions for burnout in vascular surgery. Meanwhile, former SVS President Michel S. Makaroun, MD, from University of Pittsburgh Medical Center, is set to hone in on the question of insufficient supply or maldistribution in vascular surgery, as Peter R. Nelson, MD, from the University of Oklahoma in Tulsa, rounds out the panel with a talk on prophylactic measures to improve the workforce crisis.
‘It’s complicated’
Mills wants his colleagues to grasp the complexity of the issues facing the vascular surgery workforce. That is what his lineup of speakers and their topics are set up to elucidate. “The pipeline meme has become a bit of a tired one,” he says. “The pipeline that people traditionally think about—that there are not enough people coming into the pipeline; we need more people to pour out the end of the pipeline—I think it’s much more complicated than that. It’s an interconnected network of pipes, which is how I want to think about this problem.”
It’s as the title portends, Mills continues: “Extending, repairing and maintaining the pipeline; so it’s not just a matter of getting more people in so we can get more people out. It’s how we treat the people inside the pipeline to prevent them from clogging or from leaking out of the pipeline. And then how do we supply—think about an irrigation network supplying water to farmland. We have a maldistribution of vascular surgeons, and probably an insufficient supply also, although those two things interact.”
The first two talks—concerning recruitment—are about sparking interest. And it purposely goes beyond what might be thought of as the traditional realms of trainee origin, Mills says. “For years, we
took all our trainees from a general surgery program. As the specialty split off, it became obvious we needed to reach out to medical students.”
But to get the right mix, the specialty needs to reach even further back into the pipeline—even middle school students—to try to develop broad interest in medicine, Mills explains. “If you believe—and most of us do—that patients like to see doctors who are like them and understand them, then if you don’t recruit people from smaller and unrepresented communities, and you don’t recruit people who look like your patients, you’re going to perpetuate inequitable access to and distrust in our healthcare delivery system.”
Then there are concerns around maintenance of the existing workforce, and the specter of wellness, burnout and moral injury. That means keeping vascular surgeons in the pipeline so that they don’t retire too early because they get “burned out” amid some of the automated aspects of modern practice, says Mills. “There probably are too few vascular surgeons and a large proportion of us are over 55. If we start retiring earlier, and a large number of our specialists are over 55, that’s going to accentuate the lack of vascular surgeons. What will happen is other specialties will try to fill the gap.”
The other two talks ponder whether there are enough vascular surgeons currently practicing, or if they “are just in the wrong places,” Mills says. “My own take is that it is both.” His theme of a workforce pipeline is not meant to be “the tired” analogy of: “You’ve got to pour more people through to get more people out of the end.” The questions center on: “Are we attracting people from diverse backgrounds,” Mills concludes. “And if we do that, can we solve some of the distribution problems? Texas is an oil state. Pipelines burst and corrode. And they get obstructed. So how do you maintain what you have and, by design, even extend service to areas and people that aren’t being served.”—
Bryan Kay
A STUDY SET TO BE PRESENTED in today’s Plenary Session 2 (9:45–11 a.m.) in Potomac A/B has found that the long-term outcomes of transcarotid artery revascularization (TCAR) are “not significantly affected” by prior head and neck radiation. Owing to substantially increased risks of mortality with transfemoral carotid artery stenting (CAS), as well as both stroke and mortality with carotid endarterectomy (CEA), researchers believe TCAR “may be the preferred treatment modality for patients with radiation-induced carotid stenosis.”
Bala Ramanan, MBBS, MS, a vascular
surgeon at University of Texas (UT) Southwestern Medical Center in Dallas, will deliver these findings from a study that sought to evaluate the effect of radiation on long-term outcomes after various carotid revascularization techniques—TCAR, CAS and CEA—based on patients (≥65 years old) in the Society for Vascular Surgery’s (SVS) multicenter Vascular Quality Initiative (VQI) linked to the Vascular Implant Surveillance and Interventional Outcomes Network (VISION) database.
Ramanan et al found no significant differences in 30-day outcomes for death,
stroke, or major adverse cardiovascular events, across all three procedures— although the priorradiation group had higher rates of cranial injury (3.7% vs. 1.8%) and 90-day readmission (23.5% vs. 18.3%) after CEA.
Prior radiation significantly increased mortality risks after CEA and CAS, and the three-year risk of stroke associated with CEA was also significantly higher in radiated patients compared to non-radiated patients. Prior radiation did not, however, significantly affect death or stroke in patients undergoing TCAR. The researchers also found that prior radiation did not impact the rates of shortand long-term reintervention after any of the three procedures.—Jamie Bell
2 VS@VAM | Wednesday, June 14, 2023
Safety benefits mean TCAR may be preferable approach in radiationinduced carotid stenosis
TCAR
FROM THE COVER: ‘FIRST’ STUDY TO IDENTIFY ENDOTHELIAL CELL-CELL COMMUNICATION VIA BIDIRECTIONAL SECRETION OF EXTRACELLULAR VESICLE CARGO WINS SVS FOUNDATION AWARD
are submitted by the applicant alongside an SVS senior collaborator, and on winning, are given the opportunity to present their research at VAM. Said to be “moving the needle on every front” by her mentor and collaborator Kathryn L. Howe, MD, PhD, at the University of Toronto, Toronto, Canada, Raju is set to present her research during the first plenary—William J. von Liebig session—on Wednesday June 14, 8–8:10 a.m. in Potomac A/B).
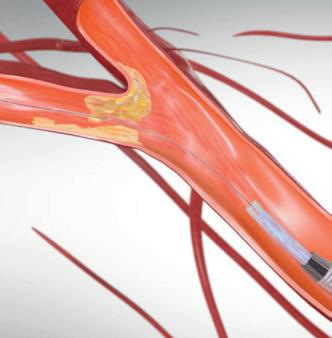
The research is founded on a central tenet—ECs can release extracellular vesicle (EV)-encapsulated miRNAs and proteins to mediate cell-cell communication. Seeking to expand on this, Howe and Raju hypothesized that EC-EV release is altered by activation state and drives functional changes in surrounding cells via bidirectional release.
In conversation with VS@VAM prior to her presentation, Raju reflects on how the research was borne out of a deficit in knowledge surrounding plaque burden and its progression. Approaching Howe who runs a laboratory focused on endothelial communication and carotid disease, Raju found that their interests blended, and they began investigating this question through an endothelial and vesicle perspective, specifically looking at the bidirectional interface where these cells communicate.
“The idea in both of our minds,” Howe tells VS@ VAM, “is that atherosclerosis does not form overnight—it is not a single moment in time, it takes decades to form. So, if you envision a cell that has lived at this interface for a time where it is constantly irritated or activated by non-laminar or turbulent flow, you can imagine how it may be constantly sensing and communicating back this distressed environment response.” With this information, Raju alongside Howe investigated what drives atherosclerosis and plaque build-up in target zones, considering what influences shifts in cell activation state from stable to vulnerable to rupture.
These activation states, Raju describes, can be “happy” or “angry”, denoting the either quiescent or inflammatory vesicle packages the EC contains. “We wanted to see how the EC modulates vesicle release in conditions that are quiet and happy—and in conditions where we have made them angry, as is seen in patients who have vascular diseases like atherosclerosis,” Raju outlines. Interestingly, when relevant cells are treated with EC-derived vesicles, they found that vesicles were able to modulate or change conditions in cells found in both the vessel wall and the
blood, raising new questions on the mechanism behind this.
“We were the first to show that ECs can load specific cargo and secrete it in both the apical and basolateral directions”, Raju says, their findings uncovering the “critical interface” ECs reside in. “Not only are they able to sense what is going on in the environment, but they are able to change the vesicular cargo” said Raju, which can then
continued from page 1
Making continued progress, Raju is interested in exploring this from a biomarker perspective so that she can get ahead of plaque progression before a patient becomes symptomatic. “As vascular surgeons we operate on patients who have symptomatic carotid atherosclerosis which leads to stroke.” However, without a “good biomarker” to indicate plaque progression in asymptomatic patients, predicting and preventing later clinical events can be difficult.
induce the happy or angry cell activation states. Importantly, they also found that ECs can polarize vesicle release bidirectionally, which may specifically govern functional changes in circulating and resident vascular cells.
“This has broad-ranging applications” Raju states, “although it builds on a fundamental principle of vascular biology—we know that these ECs are secreting vesicles that are going into the vessel wall and communicating with cells there. If we can find a way to harness and
Understanding the communication between ECs and progression to rupture or stroke formulates the translational aspect to Raju’s research, which is a key element in the Resident Research Award’s parameters. To explore this, Raju’s team have been collecting carotid plaques and plasma to see if this information can be corroborated with their patient cohort. From a therapeutic perspective, Raju states, they want to better understand the mechanism by which ECs are releasing vesicles in a basolateral direction and driving the biology of the disease, so that they can design therapeutics or small molecules that can “inhibit or enhance” the mechanism and find ways of reverting it into a quiescent phenotype. “I think we have unearthed a basic biological tenet that can be applied to several vascular pathologies, which is promising,” Raju concludes. “Beyond a vascular surgical viewpoint, it could also be applied to other areas such as cerebral aneurysms or cancer biology.”
On winning the award, Raju reflects on the “motivation and inspiration” gaining this recognition has instilled: “It is great that the committee thought this work deserving of the award, I am very grateful for this international platform to showcase my research and establish international collaborations with fellow vascular surgeons and scientists to advance some of these questions together.”
On her involvement in research projects of the future, Raju details that in the year before she returns to residency, she hopes to dedicate time to the translational side of the current research. “I hope to stay involved in this project as it progresses and develops, and use this skill set to ask vascular biology related questions as a future surgeon-scientist in my own independent lab—that would be the dream.”
change that communication to make it happier, then we can hopefully circumvent, reverse or rescue some of the negative cell-cell communication happening in disease states to mitigate plaque progression.”
Looking ahead to Raju’s presentation at VAM 2023, Howe believes it is an exciting chance to “lift the lid” on the progressions being made in research and “bring this into the space of the clinician.”
Today’s program will feature the presentation of an abstract by R. Debbie Li, MD, Loyola University Medical Center, Chicago, on the divergent perceived experiences of the shared learning environment by vascular and general surgery residents.


gent mixed-methods study which included the use of cross-sectional surveys following the 2020 ABS In-Training Examination (ABSITE) and Vascular In-Training Examination (VSITE). This survey looked at eight domains of the learning environment and resident wellness, while multivariable logistic regression models were used to compare thoughts of attrition between postgraduate year (PGY) 1–3 residents in general and vascular surgery across 57 institutions. Focus groups were also conducted at last year’s VAM.
expressed that early specialization and a smaller, more invested faculty allows for an apprenticeship model” that facilitates “frequent feedback, and thus early skill acquisition” as well as “closer relationships with co-residents and faculty.” This relationship in turn allowed vascular trainees to be more comfortable in reporting mistreatment.
T
he research, led by Dawn M. Coleman, MD, Duke University Medical Center, Durham, North Carolina, and Malachi Sheahan III, MD, on behalf of the Vascular Arm of the SECOND Trial was carried out in the belief that “an enriching learning environment is integral to resident wellness”
per the abstract. The study team aimed to identify differences in the experience of vascular and general surgery residents with a view to finding “practical levers for change” in improving resident wellness and addressing rates of attrition.
Li and colleagues conducted a conver-
In total, 205 vascular residents and 1,198 general surgical residents responded, with general residents found to be more likely to experience mistreatment and consider leaving their program. Coleman, Li and colleagues highlight the qualitative data they collected, stating: “Vascular trainees
These differences, the study authors suggest, may be the result of “intrinsic features of the integrated training paradigm that are not easily replicated” by larger surgical training programs. Li et al say they are “thrilled” with these results, and propose in conclusion that “optimization of differential aspects of the learning environment is crucial to continue to enhance the next generation of our surgical workforce.” —
Benjamin Roche
3 www.vascularspecialistonline.com
“I think we have unearthed a basic biological tenet that can be applied to several vascular pathologies, which is promising ”
SNEHA RAJU
Sneha Raju Kathryn Howe
INTEGRATED VASCULAR SURGERY PROGRAM FEATURES MAY OPTIMIZE TRAINEE WELLNESS AND DECREASE ATTRITION
RESIDENCY
not just for what providers care about, but for what patients care about as well.
VS: and efficacy findings of the study?
By Jamie Bell Misty Humphries
EARLIER THIS YEAR, RESEARCHERS debuted single-center experiences indicating that intravascular lithotripsy (IVL) may be able to expand transcarotid artery revascularization (TCAR) into patients with traditionally prohibitive calcific disease.
With a multicenter case series now further suggesting IVL’s utility, but also revealing potential safety concerns versus conventional TCAR or carotid endarterectomy (CEA), principal investigator Misty Humphries, MD, MAS, associate professor of surgery at UC Davis in Sacramento, California, gives VS@VAM the lowdown on these findings.
VS: Could you very briefly outline the motives behind this research?
MH: TCAR has been shown to be highly effective and safe, but there are still anatomic exclusion criteria—specifically, severe calcification. There are also many patients who are just not a candidate for traditional CEA for various reasons. The use of IVL has the potential to open TCAR technology up to more patients.
VS: How do these more recent, multicentric findings build on your publication from earlier in the year?
MH: With our initial presentation, we discussed how we do the procedure. That presentation was our own institutional data. When we analyzed our own experience, we had no complications, and the technology appeared safe. But, in this larger, multicenter cohort, we see a risk of transient ischemic attack (TIA) post-procedure that was not present. Multicenter studies like this demonstrate what can happen when technology is expanded to more practitioners of various skill levels.
VS: Why was freedom from stroke/TIA selected as the study’s primary safety endpoint?
MH: Stroke and TIA are the two outcomes patients care about most. We saw this with the CREST trial data that were analyzed. All of my research is patient-centered and, for me to use technology, I want to know that it is safe—

MH: be highly effective, allowing full stent ex pansion. The safety of the combined treat ment needs to be studied in a prospective trial. There are not a significant amount of known data on the risk of stroke and TIA in patients with severe calcium after carotid artery stenting (CAS) because these patients are typically excluded from trials. The best data we have were presented at the Society for Clinical Vascular Surgery (SCVS) meet ing earlier this year. In a review of Vascular Quality Initiative (VQI) patients who under went TCAR and CAS, patients with severe calcium had a higher risk of stroke/TIA than those who did not. This tells us that it is the disease process, and we need to learn more about this.
VS: technical success rate of 100% was achieved?
MH: can do the procedure. The real question is
Presenter Neeta Karani, MD, from Bronson Healthcare, Kalamazoo, Michigan, is set to elucidate findings that consider the incidence of carotid stent fractures and their impact on carotid stent durability during Plenary Session 2 (9:45–11 a.m.) in Potomac A/B. By Éva Malpass
Research from Karani and colleagues—including senior author Robert Molnar, MD, from Michigan Vascular Center—comes against the backdrop of the recent approval of transcarotid artery revascularization (TCAR) for asymptomatic patients by the Centers for Medicare and Medicaid Services (CMS), which, by proxy, has increased the number of carotid artery stenting (CAS) procedures being performed today. Subsequently, Karani, alongside co-
author Subbaiah Perla, a professor of statistics at Oakland University in Rochester, Michigan, identified a number of carotid stent fractures in their practice, and so set about investigating the prevalence of this condition and its influence on the efficacy of CAS.
Conducting a prospective trial, the researchers enrolled 200 patients who had undergone CAS between January 2002 and November 2021. Karani these patients for stent fractures via anterior-posterior (AP) and lateral cervical X-rays. These X-rays were independently reviewed by three vascular surgeons, who, upon complete consensus, identified those patients who had definitive stent fractures. Additionally, Karani and colleagues applied a modification to their study that allowed for a second X-ray to be obtained at a later date to assess the potential for late fracture development in their patient cohort.
Their primary outcome measure was defined as the incidence of carotid stent fracture, followed by a secondary measure which was an evaluation of the clinical implications associated with the condition upon confirmed identification.
In the 200 patients who consented and were enrolled in the study, a total of 227 stent procedures were performed over the duration of Karani and her team’s investigation. In the first wave of X-rays obtained by the team, they identified 18 stent fractures, amounting to a stent fracture rate of 7.9%. Karani will go on to report that 103 patients additionally received a second/delayed X-ray, which
4
MORE RESEARCH NEEDED BUT LITHOTRIPSY PLUS TCAR ‘AN ANSWER’ IN CERTAIN CAROTID DISEASE PATIENTS
Study finds carotid stent fracture rate to be negligible but long-term research needed
CALCIFICATION CAS
“There are some patients that cannot undergo CEA and, in those patients, IVL with TCAR is an answer”
1 The Venovo Venous Stent System was studied in the global VERNACULAR clinical trial, which was a prospective, multi-center, non-randomized, single-arm study of 170 patients. The primary effectiveness endpoint of the study was primary patency (PP) at 12 months post-index procedure, defined as: freedom from TVR and freedom from thrombus occlusion and stenosis > 50% as measured by DUS. Patients who received a Venovo Venous Stent had a weighted PP rate of 88.6%, demonstrating a statistically significant difference from a literature-derived performance goal (PG) of 74%. At 36 months, patients who received the Venovo™ Venous Stent had an unweighted PP of 79.5% (84.0% K-M) (N=141). The primary safety endpoint was freedom from major adverse events (MAE), including stent migration, through 30 days post-index procedure. Freedom from MAE was 93.5%, demonstrating a statistically significant difference from a literature-derived PG of 89%. Stents were evaluated at the 36-month follow-up for fracture analysis. An anteroposterior and lateral x-ray for each evaluated stent were sent to an independent core lab for analysis. 98 subjects’ x-rays were analyzed and no stent fractures were reported. Missing x-ray analyses were recorded as protocol deviations. Dake, Michael D, et al. “Three-Year Results from the Venovo Venous Stent Study for the Treatment of Iliac and Femoral Vein Obstruction.” Cardiovasc Intervent Radiol, vol. 44, no. 12, Dec. 2021, https://doi.org/10.1007/s00270-021-02975-2. Epub 2021 Sep 20.
The Venovo Venous Stent System is indicated for the treatment of symptomatic iliofemoral venous outflow obstruction. The Venovo Venous Stent System is contraindicated for use in patients with a known hypersensitivity to nitinol (nickel-titanium) and tantalum and patients
who cannot receive intraprocedural anti-coagulation therapy. The stent is not designed for repositioning or recapturing. Potential Adverse Events include, but are not limited to: Allergic/anaphylactic reaction · Death related/unrelated to procedure · Dissection · Embolization Extravasation · Hematoma, puncture site ·Hypotension/hypertension Incorrect positioning of the stent requiring further stenting or surgery · Intimal injury/dissection · Ischemia/infarction of tissue/organ · Malposition (failure to deliver the stent to the intended site) · Open surgical repair · Pulmonary embolism · Stent Fracture Stent Migration Venous occlusion/thrombosis/restenosis Please consult product labels and instructions for the use of indications, contraindications, hazards, warnings, and precautions BD, the BD logo, and Venovo are property of Becton, Dickinson and Company or its affiliates. © 2022 BD. © 2022 Illustrations by Mike Austin. All Rights Reserved. BD-70896 bd.com BD, Tempe, AZ, USA, 1 800 321 4254 PROVEN RESULTS BACKED BY 36-MONTH DATA1 84% PRIMARY PATENCY In the VERNACULAR Trial ZERO STENT FRACTURES In the VERNACULAR Trial ZERO STENT MIGRATIONS In the VERNACULAR Trial
VASCULAR SCIENCE
Special invited research presentations offered at VAM
 By Beth Bales
By Beth Bales
VAM traditionally includes presentations from specially invited translational researchers that are performing cutting-edge work focused on vascular disease. All are held during plenary sessions.


“These presentations inform the larger VAM audience about cutting-edge translational science performed by our members and, very importantly, how that research can, will and does translate to the care of the vascular patient,” said Katherine Gallagher, MD, chair of the Basic and Translational Research Committee.
“Our vascular surgeon-scientists look to the future as they evaluate molecular mechanisms and gain valuable information from human tissues and animal models. Research today could lead to breakthroughs in the coming years, and it’s important to tell our members about treatment possibilities from the exciting research that is going on,” she said.
“No one is more interested in identifying new treatments for vascular disease than vascular surgeons, who know and
“The endothelial cell is the superhero of the vascular system,” by Kathryn L. Howe, MD, PhD, University of Toronto, Toronto, Ontario, Canada; Discussant, Dr. Andrea Obi; 10:37–10:47 a.m.


Wednesday, during Plenary 2
“Cellular mechanisms of tissue repair in the ischemic limb,” Kevin Southerland, MD, Duke University Medical Center; Discussant, Dr. Gale L. Tang;
8–8:10 a.m.
Thursday, during Plenary 3
“The effect of physical activity on aneurysm and dissection: Insights from animal models,” by Areck Ucuzian, MD, PhD; University of Maryland School of Medicine; Discussant, Jean Marie Ruddy, MD; 8–8:10 a.m.

Friday, during Plenary 5
GREENBERG LECTURE
GROUNDBREAKING RESEARCH INTO AAAs SET TO TAKE CENTER STAGE SATURDAY
CUTTING-EDGE RESEARCH INTO THE prevention of both formation and progression of abdominal aortic aneurysms (AAA) will highlight this year’s Roy Greenberg Distinguished Lecture, set for 10:45–11:15 a.m. Saturday.
Michael P. Murphy, MD, of Indiana University, will deliver the lecture, “Modulating Patient Immune Responses to Prevent Abdominal Aortic Aneurysm Initiation and Expansion.” AAAs are a topic of particular focus for Murphy; his laboratory, funded by the National Institutes of Health, concentrates on defining the immune mechanisms pathogenic in the formation of abdominal aortic aneurysms. SVS President Michael Dalsing, MD, also of Indiana University and a past co-researcher of Murphy’s, will moderate the lecture.
“This is very cutting-edge research into the epigenetic events that lead to immune dysregulation and the formation of aortic aneurysms,” said Dalsing. “Based on the premise that unregulated T-cell mediated immune responses target elastin in the aortic wall, Dr. Murphy has developed a nanoparticle ‘reverse vaccine’” that will help prevent aneurysms.”
The late Roy Greenberg himself also was a pioneer in his research, said Dalsing. “It’s appropriate Dr. Murphy is giving the lecture named for Roy Greenberg, who we lost way too soon.” Murphy is the Cryptic Masons Medical Research Foundation professor of vascular biology research at the Indiana University School of Medicine in Indianapolis.—Beth
Katherine Gallagher
Bales
6 VS@VAM | Wednesday, June 14, 2023
“These presentations inform the larger VAM audience about cutting-edge translational science performed by our members and, very importantly, how that research can, will and
VAM IS ‘IN THE ROOM WHERE IT HAPPENS’
To borrow from the hit musical “Hamilton,” VAM 2023 takes place right near Washington, D.C., the seat of power, and “the room where it happens.”
By Beth Bales
WHILE THE SONG REFERS TO A particular room and a particular deal, “it,” can also refer to the art of the deal and the place where lawmakers make decisions that impact the country.
“Because of our Washington, D.C., location, advocacy and government relations have a much larger presence at this year’s VAM than is typical,” said Margaret C. Tracci, MD, vice chair (and soon chair) of the Society for Vascular Surgery’s Advocacy Council. The council oversees the work of four committees, including the Coding, Government Relations, Political Action Committee Steering and VA Vascular Surgeons committees.

“Fifty of us are going to the Hill (Capitol Hill) Tuesday to meet with lawmakers and staff. This is an incredible opportunity to drive home to legislators our issues with Medicare reimbursement, the extensive cuts our members have endured in the past several years and they will be facing going forward and the fact that the system is, essentially, broken,” she said. SVS members won’t just present problems but will also offer solutions to some of these issues, Tracci said.
SVS has been busy in the advocacy sphere recently, spearheading the introduction of H.R. 3674, the “Providing Relief and Stability for Medicare Patients Act,” in collaboration with its Clinical Labor Coalition.
The legislation is designed to mitigate cuts to office-based specialists for a targeted group of services for two years, thereby helping to avoid significant disruptions in patient access to care while overall concerns regarding the future of Medicare physician payments are addressed.
SVS is partnering with prominent members of both the House Energy and Commerce, and Ways and Means committees in introducing this critical legislation. “Using this bipartisan and dual-committee approach provides a strong foundation for the Society’s continued work to secure additional support for the bill and identify opportunities for advancement,” said Tracci.
The council asks SVS members to contact their lawmakers to urge them to co-sponsor H.R. 3674. The proposal will be a topic of conversation with lawmakers Tuesday, Tracci said.
VAM itself will feature two separate educational sessions highlighting the full breadth of SVS’ advocacy-related efforts: Member Perspectives on Advocacy—Myths, Facts and Reasons Why all SVS Members Should Engage, takes place from 12:30–1:30 p.m. Wednesday, June 14, while Tracci will first present the Elements of Effective Advocacy, followed by Advocacy Council Chair Matthew Sideman, MD, providing a primer of sorts on SVS’ advocacy and policy priorities.
A panel discussion will follow. Using the Slido live Q&A platform, audience members will be able to ask questions and provide comments to the panel in real time, which could well revolve around the visit to Capitol Hill the previous day.
A Friday breakfast session, from 6:45–8 a.m., will give participants an overview on the foundations of SVS’ advocacy and policy work, SVS Advocacy in Action: Work Being Done, Issues on the Horizon and How to Become Involved.
Sean Lyden, MD, and Peter Connolly, MD, will moderate. Both are heavily involved in SVS advocacy and government relations activities.
Presentations will include Lyden discussing
COMMENT& ANALYSIS CORNER STITCH
“Tell it to me straight: What does ‘Advocacy’ mean for SVS.”
Then Mounir Haurani, MD, will present “If You’re Not at the Table, You’re on the Menu: Why SVS Needs a Culture of Advocacy Engagement,” followed by payment reform with Tracci. Mark Mattos, MD, cochair with Connolly of the SVS PAC Steering Committee will present “Advocacy Ways and Means: The Important of SVS PAC.” Advocacy can include downtime as well!
Anyone who has contributed to the SVS Political Action Committee may attend a casual PAC Steering Committee-sponsored reception from 6:30 to 7:30 p.m. Wednesday, June 14, at the Harbor Social Restaurant, located in the Gaylord National Resort and Convention Center.
For information on any advocacyrelated question, contact advocacy@ vascularsociety.org.
Resident/fellow editor, Christopher Audu, MD, looks over the VAM program to pick out his 2023 highlights.
There are many exciting things to look forward to as a student, resident or trainee at VAM 2023. Starting from the very first talk today, by Dr. Sneha Raju—on her groundbreaking work linking endothelial cell communication with vascular disease—to understanding the perceptions of
shared learning environments between vascular and general surgery residents, this year’s meeting is shaping up to have trainees front and center presenting their amazing work with their mentors.
Personally, the E. Stanley Crawford Forum seems in teresting because it is about recruiting and retaining tal ent in vascular surgery. I’m looking forward to finding more effective ways to alleviate burnout, out reach to high school students, and retaining res idents in the field. With the multiple options and treatment beds shared by vascular and other specialties (some with less oner ous hours of work and a larger shared call pool), the vascular surgery career pathway, as we know, needs solutions to attract, recruit and retain talent for the next decades.
Of course, it goes without saying
that the major draw for VAM is to learn more about vascular disease and pathology and novel or creative ways to solve unusual problems. To this end, the video sessions highlighting how masters of the craft perform their operations is always a highlight.
There’s a potpourri of interesting clinical topics in the VESS sessions that I’m looking forward to learning from. What’s even more interesting is that most of the abstracts are being presented by trainees in differing stages of training . I always walk away from here with ideas for transforming my clinical care. There’s so much more to enjoy. Did you know that there are > 200 trainees registered for VAM? Welcome!

www.vascularspecialistonline.com
Seeking out novel, creative ways to solve unusual problems
ADVOCACY
“This is an incredible opportunity to drive home to legislators our issues with Medicare reimbursement, the extensive cuts our members have endured in the past several years and they will be facing going forward”
7
MARGARET C. TRACCI
Margaret C. Tracci
Christopher Audu
Vascular trauma session to highlight the current role of endovascular therapy

A focused session on vascular trauma, taking place
Wednesday afternoon (3:30–5:00 p.m.) in Potomac D, takes a deep dive into emerging issues and controversies in the field.
 By Will Date
By Will Date
MODERATED BY SHERENE
Shalhub, MD, of Oregon Health & Science University, Portland, Oregon, and Rishi Kundi, MD, of the R Adams Cowley Shock Trauma Center, Baltimore, Maryland, attendees can expect a series of presentations and discussions geared towards building a comprehensive update on the management of vascular injury.
The current role of endovascular therapy is a key theme running through the core of the session, moderator Shalhub
tells VS@VAM, pointing out a number of the important learning points attendees can expect to be covered by the course.
“Endovascular and hybrid techniques are increasingly dominant in the treatment of vascular trauma, and in some cases are the standard of care,” adds Kundi, touching on the significance of the session. “Vascular surgeons should work to not only familiarize themselves with vascular trauma surgery, but to seize the opportunity that trauma presents. There is nobody better to lead the discussion of vascular injury than vascular surgeons.”
Elina Quiroga, MD, opens the session with a presentation on thoracic endovascular aortic repair (TEVAR) for blunt thoracic aortic injury (BTAI)—taking the audience through what we know now that wasn’t known five years ago. Following Quiroga, Kathryn E. Bowser,

MD, will give attendees an overview of the principles of blunt arterial injury management.
Among other key learning objectives, Shalhub pinpoints that attendees of the session should take away an understanding of the state-of-the-art in both the open surgical and medical management of arterial injuries. In this arena, Anna Romagnoli, MD, addresses controversies in peripheral arterial vascular injuries— taking in both endovascular and open surgical approaches.
Another area of focus in the session, according to Shalhub, is a review the management of major venous injuries, with a particular focus on those to the inferior vena cava. This is a topic covered in depth by Adenauer Goes Jr., MD, whose presentation touches on injuries to the inferior vena cava and iliac veins.


PA SECTION
PAs PLAN EDUCATION, VASCULAR ‘JEOPARDY’ AT VAM


CALL IT “JEOPARDY! VISITS VAM,” complete with Daily Doubles and buzzers. But instead of “geography” or “famous artists,” all five categories will be vascular-related.

The session, “Jeopardy Cases Over Cocktails,” is for both members of the Society for Vascular Nursing and the Society for Vascular Surgery’s Physician Assistant (PA) section during this year’s VAM and the SVN Annual Conference.
Using the format of the popular Jeopardy! game show, contestants from the Society for Vascular Nursing and the Society for Vascular Surgery’s Physician Assistant (PA) Section, the contestants will compete from 3–4 p.m. Wednesday in Maryland D. “We have teams and buzzers. We have Daily Doubles and referee shirts. It should be great fun,” said Holly Grunebach, PA-C, section chair.
Then, from 12–1 p.m. Thursday, the two groups will talk about the vascular team and other topics during a lunchtime panel discussion with PAs Ricardo Morales, Erin Hanlon and Abby Keen, and nurses Katherine Hays, Gabriell Grayson and Stacy Hosenfeld. Audience members are asked to bring their questions.—Beth Bales
8 VS@VAM | Wednesday, June 14, 2023
THERAPY Subscribe today Available in print and digital formats and through our social channels *Available for US and EU readers only **Available worldwide Visit vascularspecialistonline.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** An official publication of the Society for Vascular Surgery (SVS) A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders Editorially independent
Sherene Shalhub
Prediction model offers new option for forecasting AAA growth
A predictive model incorporating 3D shape features such as aneurysmal flow lumen and outer wall structure extracted from computed tomography (CT) imaging can improve the ability to predict the growth of abdominal aortic aneurysms (AAAs). By Will Date
This is according to research to be presented during this morning’s William J. von Liebig Forum (8:00–9:30 a.m., Potomac A/B) by
Anirudh Chandrashekar, DPhil, of Stony Brook Medicine, Stony Brook, New York,
who tells VS@ VAM that the research has the potential to add to existing metrics for predicting aneurysmal growth, used to inform surveillance intervals and timing for surgical intervention.
Alongside senior author Regent Lee, PhD, from University of Oxford, England, Chandrashekar and colleagues set out to develop a means of predicting aneurysm growth beyond the current gold standard—namely assessment of the diameter of the aneurysmal sac. “What we wanted to do was to develop a prediction paradigm to individualize the follow-up and risk factor management for these patients,” Chandrashekar comments. “This may better inform the timing of surgery down the line.”
The first arm of the project saw the researchers develop a deep learning process to extract and categorize geometric features of the aneurysmal sac that may be associated with AAA-growth, including curvature of the sac and surface irregularity.
The latest step of their research, which will be presented here at VAM, looks at both the lumen and outer aneurysmal wall, and how these correlate with AAA growth. “The methodology is extremely novel, and this is the first time we are incorporating the lumen in this whole decision model,” says Chandrashekar.
To test their model, the researchers have conducted a retrospective analysis of serial CT images taken during surveillance in 192 patients with infrarenal AAAs, categorising
COMMENT& ANALYSIS
TAAA
ENDOVASCULAR THERMAL SEPTOTOMY FOR CHRONIC POST-DISSECTION AORTIC ANEURYSM
Aidin Baghbani-Oskouei, MD, and Gustavo S. Oderich, MD, from the University of Texas Health Science Center at Houston, Texas, detail the endovascular thermal septotomy technique for chronic post-dissection thoracoabdominal aortic aneurysms (TAAAs), which is set to feature as a video presentation at the end of the William J. von Liebig Forum today (9:15–9:24 a.m.).
patients into either “slow” or “fast” cohorts based upon the progression of their aneurysm.
Chandrashekar will report that integrating the lumen and outer wall structure as unique components within the 3D statistical shape model captured the lumen-thrombus interface, marking this as superior to max diameter, undulation index and radius of curvature in the prediction of AAA growth phenotype, with a p-value of <0.001.
“We can take a CT image, isolate the aneurysm section, extract out the aneurysm shape and extract measurements from the defined shape to a level that is clinically acceptable, and we can do this automatically,” says Chandrashekar of the top line messages of the research.

“Secondly, we are able to improve on already published
“We can take a CT image, isolate the aneurysm section, extract out the aneurysm shape and extract measurements from the defined shape to a level that is clinically acceptable, and we can do this automatically”
metrics to predict aneursymal growth, by incorporating not only the aneurysmal sac, but also how the flow lumen interacts with the surrounding thrombus and the surrounding aneurysmal wall,” he adds, commenting that this is “extremely novel in itself.”
Further work has been conducted to validate the model in an independent cohort of patients, which “excitingly,” according to Chandrashekar, shows that the growth model still holds to be predictive.
“Going on from there the next step is to try to establish a prospective study, a longitudinal study following aneurysm patients over time, extracting out additional clinical metrics, for example blood pressure, medication regimen and all those metrics that you would obtain in a randomized controlled study, to see whether this model truly is effective.”
Senior author Regent Lee told VS@VAM: “I congratulate Dr. Chandrashekar in spearheading this international collaborative project and for delivering refinement of our AAA growth prediction model as an independent postdoctoral researcher.”
“The results presented here further highlight the concept of CT image-derived indices as ‘standalone’ biomarkers to predict AAA growth. With appropriate regulatory approvals, this can be further field validated at scale by utilizing existing data already stored in the clinical picture archiving and communication systems (PACS) archives. We look forward to hearing from colleagues who are interested to participate in such collaborative studies.”
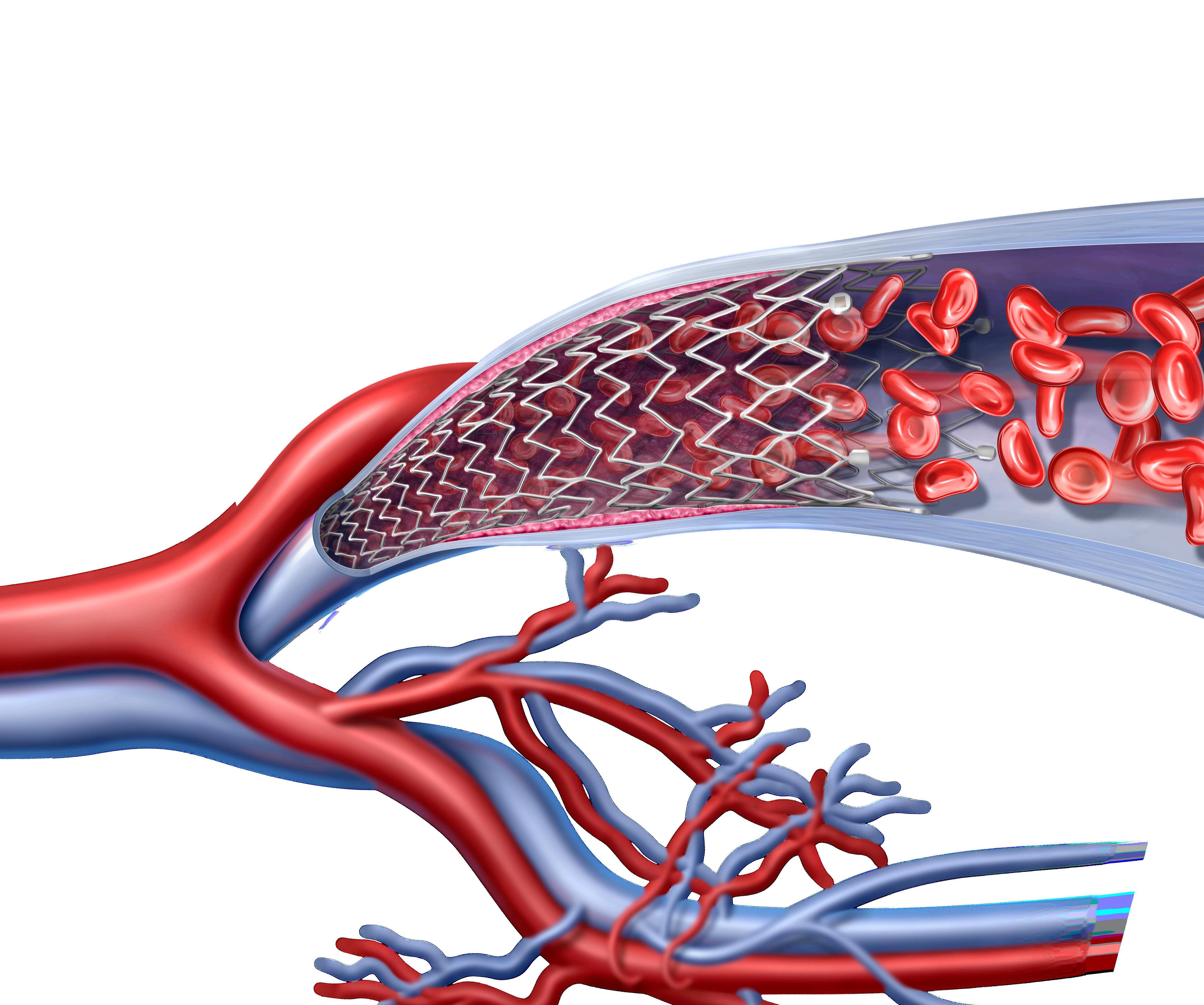
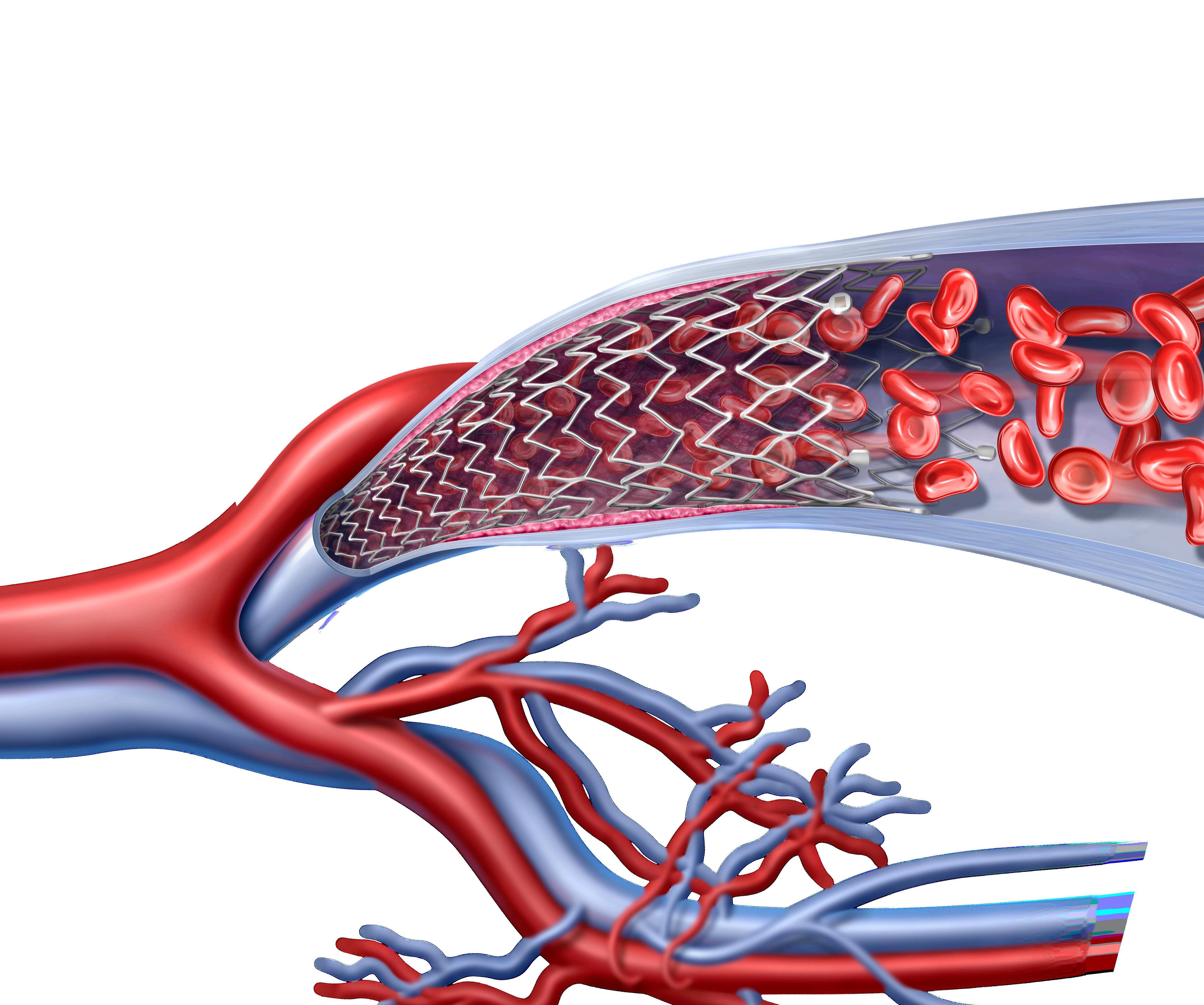
AORTIC DISSECTION OFTEN
results in chronic aneurysmal degeneration due to progressive false lumen expansion. Thoracic endovascular aneurysm repair (TEVAR) and other techniques of vessel incorporation—such as fenestrated-branched or parallel grafts—have been increasingly utilized to treat chronic post-dissection aneurysms. Even in patients with severe true lumen compression, or when vessels originate from the false lumen, this poses technical difficulties.
In these cases, the limited space from a compressed true lumen may result in inadequate stent-graft expansion or restrict the ability to reposition the device or manipulate catheters. Reentrance techniques may be used selectively to assist with target vessel catheterization. Thermal electrocautery septotomy is a novel technique that has evolved from the cardiology experience with trans-septal or trans-catheter aortic valve procedures. This technique has been applied in select cases to facilitate the creation of proximal and distal landing zones, to disrupt the septum in patients with an excessively compressed true lumen or with vessels that have separate origins from true and false lumens.
At VAM, we present a video that details the technical pitfalls of thermal electrocautery septotomy in a patient with chronic
post-dissection aortic aneurysm. The patient presented with isolated enlargement of the iliac artery and modest enlargement of the descending thoracic aorta (3.8 cm). To decrease the risk of spinal cord injury, we recommended endovascular repair of the infrarenal aortic enlargement with left internal iliac preservation using iliac branch endoprosthesis (IBE). The septotomy procedure was used as an adjunct technique to create a suitable proximal landing zone in the infra-renal aorta.
The procedure requires a standard percutaneous approach using perclose technique. Access is established into the true and false lumen and confirmed with intra-vascular ultrasound (IVUS). A 6F Oscor steerable guiding sheath is positioned in the intended area of septotomy, which due to excessive angulation was at the level of the celiac axis (CA). A 35-mm Amplatz Goose Neck Snare kit is advanced via the ipsilateral approach into the false lumen and opened opposite to the steerable sheath to facilitate orientation during guidewire crossing of the dissection septum. The orientation between the steerable sheath and snare is confirmed under fluoroscopy in the anteroposterior, lateral, and oblique views. Once the orientation is optimized, a 0.018 NaviCross catheter and 0.018 Astato hydrophilic guidewire are prepared by removing the guidewire
coating and connecting the guidewire to the electrocautery. With the electrocautery set on cut mode at 80 Watts, the guidewire is gently advanced across the dissection membrane without difficulty and promptly snared. The through-and-through guidewire is retracted along with the NaviCross catheter to allow the creation of a 5mm trapeze-shaped area which is denuded from the coating and readvanced into position.
A second 0.018 NaviCross catheter is advanced via the other end of the 0.018 Astato guidewire to protect structures from thermal injury, allowing only the 5-mm trapeze segment to be exposed. The Astato guidewire is again reconnected to the electrocautery and septotomy is performed extending to the distal end of the septum membrane in the external iliac artery. The septotomy is guided by fluoroscopy and confirmed with IVUS. Once the septotomy was completed, the infrarenal EVAR was performed in standard fashion using Gore Excluder Conformable with bilateral iliac limb extensions and a left Gore IBE device.
This adjunctive technique is useful to facilitate endovascular repair in patients with subacute or post-dissection aneurysms but has not been used in the acute setting where the friable membrane may be more prone to disrupt or detach from the aortic wall.
9 www.vascularspecialistonline.com
ANIRUDH CHANDRASHEKAR
ANEURYSMAL GROWTH
Welcome to VAM 2023
to
Education Session: Transition to
Education Session: Embolization for Vascular Surgeons: Techniques, Tips and Tricks
Lunchtime Education Session: Bringing What’s New in Deep Venous Thrombosis Treatments to You in 2023! (In collaboration with the American Venous Forum)
Lunchtime Education Session: Member Perspectives on Advocacy - Myths, Facts and Reasons Why all SVS Members Should Engage

10 VS@VAM | Wednesday 14 June 2023
12
5 p.m. VQI@VAM
2
6 p.m. Registration 5
6:30 p.m. VQI Poster
6 a.m. to 5 p.m. Registration 6:30 to 7:30 a.m. World
Educational Session 7:30 to 8 a.m. Opening Ceremony 8 to 9:30 a.m. Plenary 1: William J. von Liebig Forum 8 a.m. to 5 p.m. SVN Annual Meeting 8 a.m. to 5 p.m. VQI Annual Meeting 9:30 to 9:45 a.m. Coffee Break 9:45 to 11 a.m. Plenary 2 11 a.m. to 12:15 p.m. E.
12:15 to 12:30 p.m. Break 12:30 to 1:30 p.m.
Retirement 12:30 to 1:30 p.m.
12:30 to 1:30 p.m.
12:30
1:30 p.m.
Tuesday, June 13, 2023
to
(VQI Annual Meeting)
to
to
Networking Reception Wednesday, June 14, 2023
Federation of Vascular Societies
Stanley Crawford Critical Issues Forum
Lunchtime
Lunchtime
12:30 to 1:30 p.m. VESS Industry-supported Lunch Symposium 1:30 to 3 p.m. SVS-VESS Scientific Session@VAM: Session 1 1:30 to 3 p.m. ES: Aortic Dissection: From A to C (Acute to Chronic) 1:30 to 3 p.m. ES: Maximizing the Value of Wound Care in Your Practice 1:30 to 3 p.m. Registered Physician Vascular Interpretation Exam Review, Session 1 3 to 3:30 p.m. Coffee Break 3:30 to 5 p.m. SVS-VESS Scientific Session@VAM: Session 2 3:30 to 5 p.m. ES: The Roles of Vascular Surgeons in Managing Acute Strokes
Comprehensive Stroke Centers 3:30 to 5 p.m. ES: Emerging Issues and Controversies in Vascular Trauma:
in
Comprehensive Management of Vascular Injury 3:30 to 5 p.m. Registered Physician Vascular Interpretation Exam Review, Session 2 3:30 to 5 p.m. International Young Surgeons Competition 5 to 6 p.m. SVN Welcome Reception 5:15 to 6:15 p.m. General Surgery Resident/Medical Student Reception 5:15 to 6:15 p.m. International Guest Reception 5:15 to 6:30 p.m. Industry Evening Symposia 7 to 9 p.m. SVS Connect@VAM: Building Community Key: ES: Educational Session
in
Updates
the
Wednesday schedule ata-glance
Tuesday/
SVS Central provides a hub of information
As its name implies, “SVS Central” will be one of the places to be at the SVS Vascular Annual Meeting for help and information about anything SVS-related. SVS Central will be open for much of VAM, offering attendees a chance to connect with staff and faculty, gather information, grab some memorabilia and learn about the Society’s ongoing initiatives.
SVS Central will be open from 12–5 p.m. Wednesday, 10 a.m.–6:30 p.m. on Thursday and 9:30 a.m.–5 p.m. Friday.
Representatives from different SVS departments, including Education, Membership/ Marketing, Journal of Vascular Surgery (JVS), Vascular Quality Initiative, SVS Political Action Committee (PAC), SVS Foundation, SVS/Phairify Compensation Study and the American College of Surgeons/ SVS Vascular Verification Program all will have a presence at SVS Central.
Vascular surgeons can also get their SVS Fellow (FSVS™) ribbons, get help with the VAM mobile app, update their membership information and receive information on upcoming SVS educational courses and products.
SVS Central provides a convenient opportunity for attendees to donate to the SVS Foundation and SVS PAC. And, those planning to attend the Foundation’s “Great Gatsby Gala” Friday evening can save time on the big night by taking advantage of early check-in (see page 19).
VAM attendees can also channel their competitive side—and get some exercise in—by stopping at SVS Central to register for the 2023 SVS Foundation’s Vascular Health Step Challenge. Top walkers during the meeting will win prizes and will automatically be registered for the September month-long challenge. Following VAM, registration will open in July at vascular.org/Step23
SVS Central is also valuable for attendees seeking information about JVS and resolving subscription issues. Individuals can also learn more about the Vascular Verification Program and the Pharify/SVS Compensation Study, with representatives from both available to answer questions.—Marlén Gomez
Learn at lunchtime
The Society for Vascular Surgery has added four lunchtime learning sessions to the VAM opening day.
Topics are both clinical and non-clinical, ranging from planning for retirement, embolization tips and tricks, new deep vein thrombosis treatments and a session on the importance of advocacy from member perspectives.
All sessions are Wednesday from 12:30–1:30 p.m. and will include box lunches for attendees.
All are also part of the non-plenary educational sessions that are an important part of VAM. “We have something for everyone, at every career stage,” said Will Robinson, MD, chair of the Postgraduate Education Committee, which develops these sessions. “All these programs are terrific—they’re innovative and they’re current.”
Embolization for Vascular Surgeons: Techniques, Tips and Tricks (Maryland A) will cover an overview of a surgeon’s “embolization arsenal,” management of type II endoleaks, visceral artery aneurysms and embolization in trauma, followed by a panel discussion.
Case studies submitted by vascular residents will be a part of Bringing what’s New in Deep Venous Thrombosis Treatments to You in 2023 in Potomac C. The session, in cooperation with the American Venous Forum, will cover patient selection issues, the many options for deep venous thrombectomy therapies, tips and tricks for aggressive thrombus removal and what works when it comes to IVC thrombosis.
With the pronounced aging of the vascular surgery workforce, help with Transition to Retirement: What I Wish I Would have Known takes on new importance. Topics include ways to wind down, including opportunities beyond the operating room, staying fit despite ergonomic challenges while aging, financial considerations, including transitioning from growth to an income stream, asset protection and whether a surgeon has enough assets to call it quits. The session will be in National Harbor 4/5.
Two stalwart SVS supporters for advocacy will provide Member Perspectives on Advocacy—Myths, Facts and Reasons Why all SVS Members Should Engage in Potomac D.—Beth Bales
WHAT TO DO
Explore National Harbor while at VAM

The Gaylord National Resort and Convention Center in National Harbor, Maryland, sits abreast a beautiful waterfront location, providing a perfect setting for the top educational event in the world of vascular surgery. Guests will have ample chances to explore the surrounding area while here. The National Harbor tourism website labels “National Harbor as more than a destination. It’s an experience full of sights, sounds and tastes that will immerse you.” Besides the jam-packed meeting agenda, take in some of National Harbor’s attractions:
● Spirit Park, a modern tribute to the American flag: For patriots, this is a must-see location that showcases inspirational art in honor of the soldiers donning red, white and blue. Spirit Park is also home to one of the most enormous flying flags in the United States that is sure to impress VAM 2023 attendees and their guests.
SVS Connect@ VAM social event is tonight
As part of its ongoing commitment to foster collaboration and strengthen the vascular community, the SVS will host the inaugural SVS Connect@VAM: Building Community Wednesday evening, to close out the first day of VAM. This event allows attendees a unique opportunity to connect, relax and recharge in a festive atmosphere with colleagues, friends and family. Dress style is strictly casual.
Thanks to the sponsorship of Terumo Aortic and Philips, the event—which SVS leaders hope becomes an annual one—is free. However, because space is extremely limited, attendees are strongly encouraged to reserve their spots early by visiting vascular.org/ SVSConnectVAMBuildingCommunity.
From 7–9 p.m., attendees will gather on the lawn of the Gaylord National Resort and Convention Center, on the banks of the Potomac River. SVS Connect@VAM will feature interactive activities, food stations, games and entertainment designed to create an environment of camaraderie and fun for attendees and their families.—Marlén Gomez
● The Capital Wheel, to stop by and fly: One of the more popular attractions in National Harbor is the Capital Wheel. This Ferris wheel has 42 climate-controlled gondolas that take passengers 180 feet above the ground for breathtaking views of the Potomac River, the Washington Monument, the City of Alexandria, the Masonic Temple, Georgetown and more. After the ride, attendees can relax at the Flight Deck, an outdoor bar and lounge by the water. There’s also a carousel nearby for some family-friendly fun. Remember to snap some pictures for social media!
● Water Taxis to explore the area in style: Easily reach Washington, D.C., via the Potomac Water Taxi. This convenient mode of transportation connects National Harbor (145 National Plaza) to the Wharf in Washington, D.C., Georgetown and Old Town Alexandria. First, enjoy a scenic boat ride that lasts less than an hour. Then, take a 12-mile trip down the Potomac River to see Mount Vernon, the historic home of George and Martha Washington.—Marlén Gomez
Email svsmeetings@vascularsociety. org with any questions.
Get your free headshots!
The SVS is again providing a valuable opportunity for VAM attendees to obtain free professional headshots. These high-quality headshots are an excellent addition to any professional’s career portfolio, allowing vascular surgeons to enhance their online presence as well as their professional materials.
The headshot booth will be open from 10 a.m.–2 p.m. on Thursday and Friday, conveniently located near SVS Central, the Society’s member resource at VAM.
Both the booth and SVS Central will be situated just outside the entrance to the VAM Exhibit Hall.
A professional photographer will be available to ensure that the headshots capture the best possible image of attendees, helping professionals establish their professional identity and elevate their profiles within the vascular field.
For more information and updates on the free headshots, attendees should visit SVS Central for more information.—Marlén Gomez
www.vascularspecialistonline.com 11
Patients have spoken.
TCAR is preferred over CEA.
The Less Invasive Standard in Stroke Prevention

Designed to give the vascular specialist more options when treating carotid artery disease, TCAR is a less invasive treatment option that takes less time to perform and results in significantly less risk of CNI and in-hospital MI in comparison to CEA.* All while protecting the patient from surgery-related stroke with freedom from stroke rates as high as 99.4%.** With indisputable clinical and patient benefit
Come see the new ENROUTE Enflate® RX Balloon Specifically designed for TCAR
ASSOCIATED WITH LESS REINTERVENTION THAN STENTING IN FIRST SIX MONTHS–STUDY REINTERVENTION
By Bryan Kay
A DURABILITY STUDY THAT LOOKS at reintervention risk among patients treated with carotid endarterectomy (CEA) versus carotid artery stenting (CAS) procedures established that CEA demonstrated the lowest risk up to six months after surgery. A subgroup analysis between stenting procedures—transfemoral stenting versus transcarotid artery revascularization (TCAR)—further showed the latter stenting modality was superior after six months.
The data are to be delivered during Plenary Session 2 today (9:45–11 a.m.) in Potomac A/B by first author Shaunak Adkar, MD, a vascular surgery resident at Stanford Medicine in Stanford, California.

The point was to understand the as-yet lesser-understood nature of procedural durability, explains senior author Jordan R. Stern, MD, clinical associate professor of vascular surgery at Stanford, in an interview with VS@VAM ahead of this year’s meeting. “We don’t really know about the durability of each of the procedures,” he says.
The study team used the Vascular Quality Initiative (VQI), matching it to Medicare claims via the Vascular Implant Surveillance and Implantation Network (VISION) database.

They identified patients who had primary carotid revascularization from December 2016 to December 2019. The primary outcome was ipsilateral reintervention, while secondary outcomes included stroke and mortality. After propensity match-
DEPRESSION
ing, patients who underwent CEA and CAS were compared within six months following the index procedure, and from six months to three years separately. A separate propensity-matched analysis was then performed to compare transfemoral stenting and TCAR.
“Like many endovascular procedures, we had a presumption that reintervention may be significantly higher among stenting-type procedures versus endarterectomy—analogous to lower-extremity or aortic work,” explains Stern.
“When we looked at reintervention, which was what we were primarily interested in, we found a difference between endarterectomy and all stenting. CEA was superior up to six months, but that was not maintained in the long run. Over time, the reintervention rates merge and it’s no longer statistically significant.
“In terms of TCAR versus transfemoral stenting, I had the presumption that things would be equal,” Stern continues. “A stent is a stent, and, once you get through the perioperative risk of transfemoral stenting, I thought that, probably in the long run, the stents would be equally durable.
“But, actually, we did not find that—we found that TCAR was associated with a lower risk of reintervention than transfemoral stenting. That was after six months. So CEA is better than all stents within six months, and TCAR is better than transfemoral stenting after six months.”
The data were based on some 27,944
patients undergoing CEA (n=21,256) or CAS (n=6,688). After propensity matching, 4,705 patients were compared in each group.
They showed an increased risk of reintervention within six months for CAS, with a hazard ratio (HR) of 1.97 (confidence interval [CI] 1.11–3.50; p<0.05), but not beyond (HR: 1.08; CI: 0.62-1.89; p=0.79).
For Stern, the findings paint a broad
picture, between well-defined perioperative outcomes and reintervention risk.
“For me personally, transfemoral stenting has been relegated to a secondary procedure because of the perioperative stroke risk,” he says.
“I think, then, that when I’m looking at durability, if reinterventions are lower with CEA within the first six months, that would probably push me towards CEA even more than I already am. The finding of TCAR being lower than transfemoral stenting I think provides more evidence that TCAR is a superior procedure in most ways compared to transfemoral stenting.”
Ultimately, says Stern, “what we really want to know is what is good for patients long-term.”
To that end, further analyses carried out by the research team uncovered additional findings set to be elaborated upon during the VAM talk today.
“In the unmatched set, transfemoral stenting was an independent predictor of reintervention,” Stern reveals. “And we did an additional analysis of TCAR versus CEA, since those seem to be the superior modalities, and did not find a difference.”
Back on the core analysis, presenting author Adkar, on behalf of Stern and colleagues is set to tell VAM 2023: “CEA portends a lower risk of reintervention than CAS, particularly within the first six months after intervention. We also confirm prior data suggesting lower rates of ipsilateral stroke and death with CEA compared to CAS.
“On subgroup analysis of stenting modalities, TCAR had a lower rate of reintervention than transfemoral stenting. CEA appears to be the most durable carotid revascularization strategy, with TCAR being more durable among stenting procedures.”
Carotid revascularization capable of improving mood in depressed patients with carotid atherosclerosis
Aprospective study has demonstrated that carotid intervention can improve mood in depressed patients with advanced carotid disease, in addition to enabling cognitive improvements irrespective of baseline depression.
These findings are set to be presented during today’s Plenary Session 1: William J. von Liebig Forum by Bahaa Succar, MD, a postdoctoral research fellow at the University of Arizona in Tucson (8:23–8:34 a.m)
Speaking to VS@VAM, Succar said: “This study provides valuable information regarding the use of carotid interventions, particularly for patients with asymptomatic carotid artery stenosis. Since stroke and mortality rates are relatively low for carotid interventions and best medical therapy, mood and cognitive assessments could offer an additional perspective to help clinicians tailor the treatment approach when counselling a patient.”
Outlining the backdrop to their work, the researchers note that the impact carotid interventions may have on neurocognitive function in patients with advanced carotid atherosclerosis has not yet been fully elucidated. In addition, little is currently known about the impact carotid interventions
can have on mood.
As such, they set out to investigate this phenomenon in a “well-defined cohort of patients”, prospectively recruiting a total of 158 people undergoing carotid revascularization. Screening for depression was performed preoperatively, and at one, six and 12 months post-intervention using the long form of the geriatric depression scale (GDS) questionnaire. The cohort was divided into ‘depressed’ and ‘non-depressed’
based on preoperative GDS scores >9 and ≤9, respectively. Patients also received other neuropsychometric tests to assess memory and executive function concurrently at the designated timepoints—with scores being adjusted against age and education to generate scaled comparisons.
Succar is set to report the following results at VAM 2023: At baseline, depression (GDS >9) was observed in 49 subjects (31%), whereas 109 (69%) were not depressed (GDS score ≤9), and the average preoperative GDS scores were 15 and 4 in the depressed and non-depressed groups, respectively. A “significant improvement” in average GDS scores was observed within the depressed group at one month (13), six months (13.2) and one year (11.6) post-intervention compared to preoperatively, whereas the non-depressed group had similar postoperative GDS scores at all timepoints compared to baseline.
“Improvements in mood are only among those who had baseline depression,” the researchers conclude. “Further studies with larger sample sizes are warranted to investigate the association between depression, carotid disease, and carotid intervention.”—Jamie Bell
13 www.vascularspecialistonline.com
CEA
“We found that TCAR was associated with a lower risk of reintervention than transfemoral stenting. That was after six months”
JORDAN R. STERN
“Mood and cognitive assessments could offer an additional perspective to help clinicians tailor the treatment approach when counselling a patient”
BAHAA SUCCAR
Jordan R. Stern
BASE REVASCULARIZATION STRATEGY ON EFFECTIVENESS IN RESTORING ADEQUATE AND DURABLE LIMB PERFUSION, BEST-CLI SUBANALYSIS ADVISES
The results of a subanalysis of the BEST-CLI trial found that patients with chronic limb-threatening ischemia (CLTI) who were deemed suitable for open lower-extremity bypass surgery “have similar periprocedural complications following either open or endovascular revascularization.”
By Jocelyn Hudson
infarction, stroke and death— non-serious (non-SAE) and serious adverse events (SAE) 30 days after revascularization. The investigators share that they used a per-protocol analysis, which in this case was intervention received without crossover.

30-DAY mortality
The finding led researchers to assert that choice of revascularization strategy should be based primarily on effectiveness in restoring adequate and durable limb perfusion.
Submitting and presenting author Jeffrey J. Siracuse, MD, of the Boston University School of Medicine in Boston, is due to present the results of this study during the first of today’s two SVS-VESS (Vascular and Endovascular Surgery Society) Scientific Sessions (1:30–3 p.m.) in Potomac C.
In the abstract for their study, Siracuse et al note that perioperative morbidity is a “major deciding factor” for choosing a revasculariza-
tion method for CLTI. It was the objective in this study, they communicate, to assess systemic perioperative complications in the BEST-CLI trial.
By way of context, the authors write that the BEST-CLI trial was a prospective randomized trial comparing open and endovascular revascularization strategies. They detail that there were two cohorts, with cohort 1 including patients with adequate single-segment great saphenous vein (SSGSV) and cohort 2, those without SSGSV.
Data from the trial were analyzed for major adverse cardiovascular events (MACE)— defined as a composite of myocardial
Siracuse and colleagues relay that there were 1,367 (662 open, 705 endovascular) patients in cohort 1 and 379 (188 open, 191 endovascular) in cohort 2 who met their inclusion criteria. Sharing the results in their study abstract, the authors report that 30-day mortality was low—1.5% in cohort 1 (open 1.8%; endovascular 1.3%) and 1.3% in cohort 2 (2.7% open; 0% endovascular).

They add that the rate of MACE in cohort 1 was 4.98% for open vs. 3.3% for endovascular (p=0.12) and in cohort 2 was 4.3% for open and 1.6% for endovascular (p=0.16). The authors specify that on multivariate analysis, there was no difference in 30-day mortality MACE for open vs. endovascular for either cohort 1 (hazard ratio [HR] 1.49, 95% confidence interval [CI] 0.85–2.62, p=0.17) or cohort 2 (HR 2.25, 95% CI 0.49–10.4, p=0.3).
Acute renal failure was found to be similar by intervention, Siracuse et al state, detailing that the rates in cohort 1 were 3.6% for open vs. 2.1% endovascular (HR 1.6, 95% CI 0.85–3.12, p=0.14) and cohort 2, 4.2% vs. 1.6% (HR 2.86, 95% CI 0.75–10.8, p=0.12). In addition, they note that venous thromboembolism (VTE) rates were low, with cohort 1 at 0.7% (open 0.9%; endovascular 0.4%) and cohort 2 at 0.3% (open 0.5%; endovascular 0%).
Other results from the study include the fact that patients with non-SAE in cohort 1 were 23.4% for open and 17.9% for endovascular (p=0.06), and in cohort 2 were 21.8% for open and 19.9% for endovascular (p=0.71). Furthermore, the investigators share that patients with SAE in cohort 1 were 35.3% for open and 31.6% for endovascular (p=0.57), and cohort 2 were for 25.5% open and 23.6% endovascular (p=0.72). Siracuse and colleagues detail that the most common etiologies for nonSAE and SAE were infectious, procedural complications, and related to underlying peripheral vascular disease.
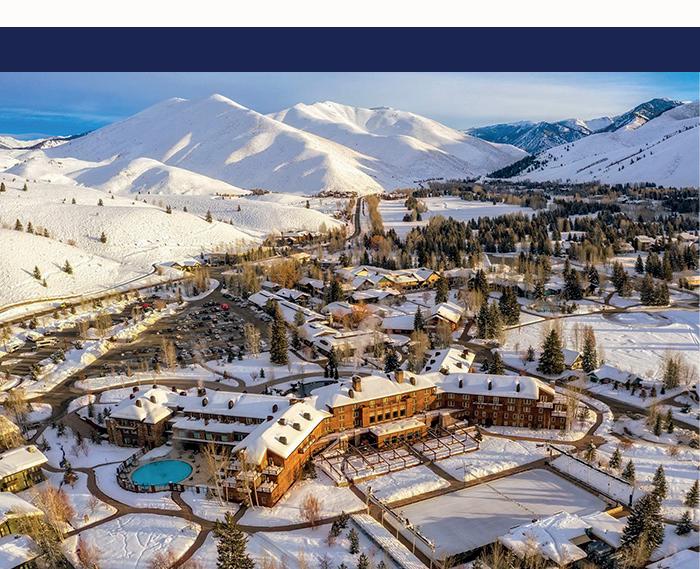
14 VS@VAM | Wednesday, June 14, 2023 Vascular and Endovascular Surgery Society SAVE THE DATE vesurgery.org 48th ANNUAL MEETING | January 18-21, 2024 | Sun Valley Resort | Sun Valley, ID Call for Abstracts now Open! Submission Deadline: September 6, 2023
CLTI COHORT 1: 1.5% OPEN 1.8% ENDOVASCULAR 1.3% COHORT 2: 1.3% OPEN 2.7% ENDOVASCULAR 0%
EDUCATION Global perspectives take center stage in second annual WFVS session at VAM

“The intellectual exchange of information and a better understanding of unique global perspectives has brought the leading societies closer,” Palma Shaw, MD, MBA, secretary general of the World Federation of Vascular Societies (WFVS) says of the success of this international organization ahead of its second annual Educational Session to be held at VAM, due to take place this morning (6:30–7:30 a.m.) in Maryland
A. By Jocelyn Hudson
IN AN INTERVIEW WITH VS@VAM AHEAD OF THE session, Shaw, of Upstate Medical University in Syracuse, New York, states that the key role of the WFVS is to “help form a bridge” between its various partner societies from across the globe. The organization’s goals, she continues, include “fostering international scientific discourse for the purpose of the understanding of vascular disease” and “shar-
ing knowledge in the development of effective therapies and interventions to treat vascular disease and strategies for training vascular specialists” for the benefit of vascular patients worldwide.
The VAM audience will hear from representatives of all member societies. On behalf of the Society for Vascular Surgery (SVS), Wei Zhou, MD, of the University of Arizona in Tucson, Arizona, is due to speak on tailoring carotid endarterectomy (CEA), transcarotid artery revascularization (TCAR) and transfemoral carotid artery stenting (TF-CAS) to improve clinical and cognitive outcomes.
“Although multiple randomized controlled trials and the most recent SVS carotid guideline endorse CEA over medical therapy in patients with carotid artery stenosis,” she tells this newspaper, “studies have shown that aggressive risk factor modification is just as effective in stroke prevention in asymptomatic patients.” Meanwhile, she notes that there has been a rapid increase in TCAR adoption in the US, and that TF-CAS continues to be widely accepted with stent innovation.
Speaking on behalf of the Latin American Association for Vascular Surgery (ALCVA), Nelson De Luccia, MD, of the University of Sao Paulo in Sao Paulo, Brazil, will focus on the topic of hybrid operations for aortic arch aneurysms. He describes this treatment option to VS@VAM as a “less invasive and effective solution” for many patients with aortic arch aneurysms at a time when total endovascular solutions are not yet available on a regular basis.
Mark J. Jackson, MD, MBBS, of Gold Coast Hospital in Southport, Australia, will be giving a presentation on behalf of the Australia and New Zealand Society for Vascular Surgery (ANZSVS) looking at challenges for the provision of vascular surgical services in remote Australia.
“The ANZSVS has proposed a model for a more reliable and sustainable vascular service in Australia’s remote regions,” he shares in an interview prior to VAM. However, he notes multiple jurisdictions and organizational barriers make this a “challenging” task.
On behalf of the Asian Society for Vascular Surgery (ASVS), Stephen W. K. Cheng, MBBS, MS, of the Univer-
Venous Forum, International Union of Angiology, World Federation of Vascular Societies, Society for Clinical Vascular Surgery, among others. His name is included in 501 peer-reviewed publications, he has authored or co-authored 250 book chapters and eight textbooks, and he has 26,874 citations to his name, plus he has just received an honorary doctorate title at the University of Padua, Italy—the list could continue.
sity of Hong Kong will give some insights from endovascular repair of the arch using custom-branched endografts. “Endovascular treatment of diseases of the arch, like aneurysms, dissections, and infections, had been the pinnacle of challenge in vascular surgery,” he says. “The WFVS session will be a good opportunity to showcase our results and share tips and tricks specific to pathology and anatomy of this region.”
Elsewhere in the session, Philippe H. Kolh, MD, PhD, of the University of Liege in Liege, Belgium—who is current president of the WFVS—will be speaking on behalf of the European Society for Vascular Surgery (ESVS). VAM delegates will also hear from Nihar Pradhan, MBBS, MS, of Apollo Health City in Hyderabad, India, representing the Vascular Society of India (VSI); Takahiro Suzuki, MD, of the University of Miami in Miami, Florida, representing the Japanese Society for Vascular Surgery (JSVS); and Asha Malan, MD, of the Universitas Academic Hospital in Bloemfontein, South Africa, representing the Vascular Society of Southern Africa (VASSA).
REFLECTING ON THE POSITIVES
and negatives of retirement, Peter Gloviczki, MD, from the Mayo Clinic, previously in Rochester, Minnesota, now in Scotlssdale, Arizona, and editor-inchief emeritus of the Journal of Vascular Surgery (JVS) is set to regale attendees of his “Lessons learned: What I wish I would have known before I retired” as part of the Transition to Retirement session taking place today from 12:52–12:58 p.m., Ballroom Level, National Harbor 4/5.
The annals of Gloviczki’s clinical practice show a brimming career spanning all areas of vascular surgery— arterial, venous and lymphatic—while having performed over 10,000 surgeries throughout his time with Mayo Clinic. He stood as the past president of the Society for Vascular Surgery, American

Gloviczki’s presentation details his life after retirement, denoting areas of major change in areas such as professional activities, personal life, healthcare, income and residency, describing the tectonic shifts these can bring for a physician accustomed to the busy fluctuations of healthcare.
Placing emphasis on loss, he describes the lack of access to clinical and patient data, and isolation from a team, be it surgical or research. He adds that retirement means a certain detachment from your previous institution, asserting that “emeritus status is not equivalent to being a full member of an institution”.
Looking at the glass half-full however, he pauses on the positive changes that occur in your personal life after retirement. Extending a new lease of agency, Gloviczki portends that getting up when you would
like and being home for lunch top the list for retirement bliss: “Your home is your castle, cafeteria, lounge, call-room and office.” Although, he ambiguously warns that being home much more may affect relationships with family members, leaving plausible room for the VAM 2023 audiences’ individual interpretation.
Customary to many who have retired from lengthy careers in healthcare, Gloviczki describes the procedures, patients, daily team interactions and the distancing from community that is felt. He does, however, caveat this with a reminder that there is “more work inside your house than [one] could have ever imagined” and weight can be
latter perhaps being dependent on the former.
More light-hearted discussions aside, Gloviczki brings awareness to the difficult questions that retirement can pose. What health, dental and eye-glass insurance should you buy? Should you take a lumpsum or monthly installments? What is the best time to start receiving Social Security? These are all among the dilemmas faced by retirees, and as Gloviczki notes with inflation rising and individual retirement account (IRA) decreases of more than 10%, making confident decisions can be a minefield.
Tailoring his final remarks to his personal experience, Gloviczki details the tribulations he experienced changing residence during retirement. Working full-time in a hospital did not prepare him for the “freezing cold” Minnesota, nor did his prolific involvement in vascular surgery prepare him for “how long it takes to dig a swimming pool” after his definitive retirement and subsequent move to Arizona. He adds that to top off the resounding joy that is retirement, “not all animals will make you feel less lonely” throughout—Arizona being home to a generous swath of scorpions and rattlesnakes.—Éva Malpass
15 www.vascularspecialistonline.com
‘WHAT I WISH I KNEW BEFORE RETIREMENT’ TALK GIVES INSIGHT INTO ADAPTATION AND EMERITUS LIFE
TRANSITION
“Studies have shown that aggressive risk factor modification is just as effective in stroke prevention in asymptomatic patients”
WEI ZHOU
Palma Shaw
Peter Gloviczki
Sponsored events cover vasculature, practice matters
Each year, companies sponsor several presentations at VAM, including breakfast sessions, evening symposia and Vascular Live presentations.
These sessions are not eligible for Continuing Medical Education credits. This year’s presentations include:
EVENING INDUSTRY SYMPOSIA 5:15–6:30 p.m. Wednesday
Session 1, Sponsored by W.L. Gore & Associates
Location: Potomac 1–3
Vascular Fellows: Preparing for Practice
Speakers/moderators: An experienced physician panel will populate the session
Session 2, Sponsored by 3M
Location: Potomac D
Reducing Surgical Site Complications: Innovative Techniques and Technologies
Speaker: Ellen Dillavou, MD
BREAKFAST SESSIONS 6:45–8 a.m. Thursday
B1: BEST-CLI, BASIL-2 and Data from Modern DrugEluting Technologies: What Conclusions Can We Draw?
Sponsored by Boston Scientific
B2: Translating the IVUS Expert Consensus to Real World Procedural Use, Sponsored by Philips
B3: Clinical Insights in PAD: Reducing the Risk of Major
Thrombotic Vascular Events, Sponsored by Janssen Pharmaceuticals
Location: National Harbor 3/4
VASCULAR LIVE: THURSDAY AND FRIDAY
Be sure to save time for the Vascular Live theater-in-theround presentations, with exhibitors presenting new ideas, showcasing new technologies and discussing the latest trends in vascular surgery. All Vascular Live events take place at the Vascular Live stage in Exhibit Hall C.
Thursday, June 15 10–10:25 a.m.
Sponsored by W.L. Gore & Associates
Optimizing Therapy Solutions with Gore Branched Technology
Speaker: Kendal M. Endicott, MD
12:15–12:40 p.m.
Sponsored by CVRx
Baroreflex Activation Therapy: A Novel Extravascular Procedure for Heart Failure
1–1:25 p.m.
Sponsored by Shockwave Going Big with IVL: The New Shockwave L6 in the Treatment of Calcified Iliac and Common Femoral Arteries
Speakers: Karan Garg, MD, and Michael Siah, MD
3–3:25 p.m.
Sponsored by 3M
Exploring the Current State of Amputation Site Management: Strategies to Prevent Surgical Site Complications
Speaker: Ellen Dillavou, MD
5:15–5:40 p.m.
Sponsored by Penumbra
Lightning Bolt 7 and 30-Day Results of the STRIDE Study on Thrombectomy for Acute Limb Ischemia
5:50–6:15 p.m.
Sponsored by Teleflex
MANTA® Vascular Closure Device
Friday, June 16 9:30–9:55 a.m.
Sponsored by Abbott
JETi Hydrodynamic Thrombectomy: A Dual-action Design for Efficient Clot Removal
Speaker: Kevin Onofrey, MD
12:15–12:40 p.m.
Sponsored by W.L Gore & Associates
Treating Complex PAD: Evolving Evidence Informing my Approach
Speakers: Steve Abramowitz, MD, and Caitlin Hicks, MD
1–1:25 p.m.
Sponsored by Shockwave Going Big with IVL: The New Shockwave L6 for Large Bore Access and the Treatment of Calcified Iliac Arteries
Speakers: Nicolas Mouawad, MD, and Leigh Ann O’Banion, MD
3 to 3:25 p.m.
Sponsored by Abbott
Unlocking Potential: Maximizing the Benefits of the Interwoven Supera Stent
Thank You to Our Sponsors!
Vascular Annual Meeting Sponsorships: 3M, Abbott, Boston Scientific Corporation, CompHealth, CVRx, Janssen Pharmaceuticals, Medtronic, Philips, Penumbra, Shockwave, Surmodics, Teleflex, Terumo Aortic and W L Gore & Associates, Inc
Educational Grants: Abbott, Boston Scientific Corporation, Cook Medical, Cordis®, Medtronic and W L Gore & Associates, Inc
16 VS@VAM | Wednesday, June 14, 2023 INDUSTRY@VAM Exhibitor Booth No 3M Health Care 902 3M Health Care Meeting Suite 1333 Abbott 517 Advanced Oxygen Therapy Inc 611 Aidoc 1011 ALPINION USA 1028 Amputee Associates 1006 AngioAdvancements 502 AngioDynamics 516 Aroa 1126 Artivion 1102 BD 827 BIBA Medical 1128 Bipore Medical Devices, Inc 1027 BLOXR Solutions 631 Boston Scientific 527 Cardiovascular Systems Inc 606 Cedaron Medical 533 Centerline Biomedical Inc 513 CompHealth 931 Cook Medical 711 Cordis® 806 Exhibitor Booth No Teleflex 534 Terumo Aortic 817 The Permanente Medical Group 511 Thompson Surgical Instruments Inc 834 TRUVIC Medical 632 UltraLight Optics Inc 1116 Vascular Technology Inc 602 Viz ai 910 VQI (Vascular Quality Initiative) 512 Wexler Surgical Inc 707 Ziehm Imaging 903 Exhibitor Booth No Core Sound Imaging 1010 CutisCare 911 CVRx 503 CVSUSTAIN 1026 Designs for Vision Inc 627 Elsevier Inc 706 Endologix Meeting Suite 629 Endovascular Today 807 Fivos (formerly Medstreaming) 803 Forme Financial 804 Getinge 1127 Gore & Associates 717 Hackensack Meridian Health 1131 Hayes Locums 1106 Humacyte Inc 610 Inari Medical 703 iThera Medical 1012 Janssen Pharmaceuticals, Inc 506 Janssen Scientific Affairs LLC 1115 Koya Medical 1103 LeMaitre 811 LifeNet Health 1002 Exhibitor Booth No Medistim 1118 Medtronic 917 Mercy Clinic 528 MiMedx Group, Inc 1107 Mindray 1112 Nectero Medical 1105 Penumbra, Inc 727 Philips 802 ProgenaCare 1121 Remington Medical Inc 927 Ronin Surgical Corp 514 Rooke Products by Osborn Medical 906 Scanlan International, Inc 907 Shape Memory Medical 526 Shape Memory Medical Meeting Suite 1337 Shockwave Medical 702 Silk Road Medical 603 Society for Vascular Ultrasound 1117 Softek Illuminate 1003 SurgiTel 1007 Surmodics Inc 507 Tactile Medical 505 A-Z EXHIBITOR LIST
INDUSTRY@VAM
INTERVIEW
CROSS-SPECIALTY
APPROACH TO EMBOLIZATION ‘PROVIDES THE BEST CARE FOR PATIENTS’

Shang Loh, MD, is chief of vascular surgery and endovascular therapy at Penn Presbyterian Medical Center in Philadelphia and professor of clinical surgery at the University of Pennsylvania. Ahead of the Embolization for Vascular Surgeons: Techniques, Tips and Tricks lunch session today (12:30–1:30pm in Maryland A), he spoke to VS@VAM about the embolization-related challenges vascular surgeons can come up against in their practice, and how cross-specialty partnership is key for maximizing the quality of this type of therapy. By Clare
VS@VAM: Would you be able to outline the embolization procedures that fall into the vascular surgery wheelhouse?
SL: I don’t think that any embolization procedure is necessarily out of the wheelhouse for a vascular surgeon if they have the desire to learn the skills. However, traditionally, the majority of embolization work falls into the following categories: primary treatment of aneurysms such as splenic, mesenteric, and pseudoaneurysms; adjuncts to aortic aneurysm treatment including embolization of branch vessels and accessory vessels; endoleak treatment; chronic dissection management; venous disease; arteriovenous (AV) or venous malformations; trauma and bleeding.
VENOUS DISEASE
VS@VAM: What does your vascular surgery practice focus around, particularly from an embolization perspective?
SL: My practice involves all areas of vascular surgery but primarily on the arterial side. My practice is mostly focused on aortic diseases but I also do aneurysm work in other areas, as well as peripheral and cerebrovascular work. I perform all my own embolizations except for venous disease and AV/venous malformations. Trauma is handled mostly by interventional radiology (IR) at our hospital but I will perform my own trauma embolizations if I am already involved in their care. The majority of my embolization work revolves around adjunct treatments for aortic aneurysms (such as
branch or accessory vessel occlusion), embolization for type II endoleaks, embolizations for aortic dissections, and embolization as primary treatment for other peripheral aneurysms. I also teach courses, along with Dr. Darren Schneider, on various techniques for embolizations of type II endoleaks and speak about embolization techniques.
VS@VAM: What are some of the challenges that vascular surgeons may face when doing these procedures?
VS@VAM: In your experience, what does this cross-disciplinary approach to caring for patients who require an embolization entail?
Shang Loh
SL: One of the main challenges is acquiring the proper skill set. This is heavily dependant on prior training with older surgeons not necessarily having been trained in this. As a corollary, surgeons starting out in the embolization realm may find challenges in getting the proper inventory in place— and having the right imaging equipment. However, the focus of sessions such as Wednesday’s is to help bridge that gap and allow them to incorporate these elements into their practice if they desire. The other main challenge is that other specialties, such as interventional radiology, perform similar procedures. It is critically important to discuss this from a multidisciplinary perspective in order to determine everyone’s role in treating the different types of patients. I strongly believe in cross-specialty participation in embolization and believe a partnership provides the best care for patients.
Learn the who, the when and the what of treating deep vein thrombosis
BETWEEN ADDITIONAL AVAILABLE THERAPIES, multiple new devices now on the market and evolving research supporting thrombus removal, Patrick Muck, MD, and Madhavi Meka, MD, anticipate an informative session on deep vein thrombosis (DVT) at lunchtime Wednesday.
The two surgeons will co-moderate Bringing What’s New in Deep Venous Thrombosis Treatments to You in 2023, from 12:30–1:30 p.m. in Potomac C. Box lunches will be available. The American Venous Forum (AVF) is collaborating with the SVS on both this program and Deep Venous Stenting Summit: Tips and Tricks for Success, from 1:30 to 3 p.m. Friday in the same location.
“Attendees will leave with thrombus removal strategies, coupled with several new DVT therapeutic options in their armamentariums,” said Muck. “Dr. Meka and I view this session as one to help to guide vascular surgeons on who to treat, when to treat and what device to use.”
Topics and speakers for the session include “Deep Venous Thrombosis Interventions: Who Do We Treat and Why,” with Alessandra Puggioni, MD; the many therapeutic DVT options available, presented by Angela Kokkosis, MD; tips and tricks for aggressive thrombus removal, with William Marston, MD; and “IVC (inferior vena cava) thrombosis: What works,” with Glenn R. Jacobowitz, MD.
Deep vein thrombosis is a “hot topic,” said Muck. “It’s an area of vascular surgery practice that’s growing, and it’s really an exciting session.”
Meka agreed. “There has been a paucity of literature over the past few years regarding thrombectomy/thrombolysis of large veins,” she said.
“In the past, the emphasis for treatment of acute iliac and venacaval thrombosis was on clot resolution using catheter-directed thromboslysis with percutaneous mechanical thrombectomy adjuncts such as Angiojet, EKOS and Trellis Thrombolysis systems. Prolonged infusion of lytics comes with the risk of hemorrhage, particularly intracranial. With emerging technology for enbloc clot removal (AngioVac, Inari, QuickClear, Penumbra, Jeti) infusion of lytics is becoming obsolete. The session intends to discuss some of these available techniques and gadgets.”
The presentations by Marston and Jacobowitz represent exciting topics. “There is more research now and more tools to choose from, along with information on which tool works where,” he said.—Beth Bales
SL: As I previously mentioned, I strongly believe in a partnership with a cross-specialty approach to embolization. This skill set is present in a few different specialties. The most important step is to have representation from all the specialties at the table and to formally outline areas that are treated by one specialty versus areas treated by more than one. This can also include how patients will be referred. It is also important to decide how the emergency cases will be handled and whether there should be a shared call schedule for these. This is most important in the trauma setting. This removes any confusion when referring patients and when patients need emergent treatment.
CARE DELIVERY
THE ESSENTIAL ‘NEED’ FOR VASCULAR SURGEONS IN PULMONARY EMBOLISM TREATMENT PARADIGM
VASCULAR SURGEONS WHO ARE SVS MEMBERS from pulmonary embolism response teams (PERTs) or busy PE programs at six large institutions will discuss advances in care and the role played by vascular surgeons in the current PE landscape in the VAM breakfast session, Management of Pulmonary Embolism: Fundamentals and Advances, taking place on Friday (6:45–8:00 a.m.).
The importance of a multidisciplinary team for treatment of PE patients that includes vascular surgery offers the best opportunity for improved patient outcomes, attendees will hear.
The addition of artificial intelligence (AI) in PE diagnosis, as well as the necessary role of vascular surgeons in PERT care form some of the central themes set to be discussed by Dennis R. Gable, MD, a vascular surgeon at Texas Vascular Associates in Plano, Texas. His talk will lead off the program. His talk takes place from (6:45–6:55 a.m.)
Fundamentally, Gable tells VS@VAM, venous thromboembolism (VTE), including PE, has always been considered a “peripheral vascular” diagnosis and, “we, as peripheral vascular specialists, need to be involved in this treatment paradigm and pathophysiology.”—
Bryan Kay
17 www.vascularspecialistonline.com
“It is critically important to discuss this from a multidisciplinary perspective to determine everyone’s role in treating the different types of patients”
SHANG LOH
Tierney
“There has been a paucity of literature over the past few years regarding thrombectomy/ thrombolysis of large veins”
MADHAVI MEKA
Make those VAM steps count: Compete to be the meeting’s top walker
 By
By


Any past VAM attendee knows he or she will put in a lot of steps on the way to educational sessions, the Exhibit Hall, receptions, plenaries and dancing the night away at the Gala.
This year those steps will count for more than just good health, with a competition to become VAM’s “Top Walker.” Register for the upcoming 2023 SVS Foundation’s Vascular Health Step Challenge and participate in two exciting challenges with just one registration.
“What better way to get people excited about stepping up to improve vascular health than during our annual meeting, where people are already logging thousands of steps?” asked SVS Secretary William Shutze, MD, an enthusiastic stepper himself.
Registration for the VAM Step Challenge, held from June 14 to 17, includes automatic registration for the Foundation’s second annual Vascular Health Step Challenge.


The Step Challenge – walking 60 miles to represent the 60,000 miles of blood vessels in the human body – is held throughout September, National Peripheral Arterial Disease

(PAD) Awareness Month. This month-long campaign urges patients and supporters to get moving in order to improve their vascular health.
In 2022, the Foundation raised more than $90,000 from more than 450 walkers, walking both individually and in teams. Proceeds helped the Foundation amplify the impor tance of vascular health and promote healthy vascular health habits in communities across the country. “Last year was our inaugural challenge and we were pleased and proud of the outcome,” said Shutze. “We’re aiming higher this year, to raise more money and help more people develop the walking habit and improve their health.”
New this year is a “Pay-it-Forward” plan. Participants can register themselves and fund the $60 registration for a low-in come PAD patient to participate in the challenge as well. Top walkers and Pay-it-Forward registrants may be recognized at VAM 2023 and on SVS social media accounts.

VAM attendees can register at vascular.org/Step23 or at “SVS Central,” which will be located just outside the Exhibit Hall on the lower level. SVS Central will be open from 12 to 5 p.m. Wednesday, 10:30 a.m. to 6:30 p.m. Thursday and from 9:30 a.m. to 5 p.m. Friday. Following VAM, registration will be open at vascular.org/Step23

18
PAD
Platinum Gold Silver Bronze Booth No. 527 Booth No. 717 Booth No 503 The Society for Vascular Surgery would like to thank the following companies for their support of the 2023 Vascular Annual Meeting and participation in the SVS Industry Alliance Program. Thank You SVS Industry Alliance Partners! Booth No 917 Booth No. 517 Booth No. 711 Booth No. 611 Abbott Shockwave Medical Philips Janssen Pharmaceuticals, Inc. 3M Health Care Cook Medical Advanced Oxygen Therapy Inc. From 2022 Challenge:
from more
Beth Bales
$90,000
than 450 walkers
“What better way to get people excited about stepping up to improve vascular health than during our annual meeting, where people are already logging thousands of steps?”
WILLIAM SHUTZE
Compiled by Beth Bales and Marlén Gomez
SVS Foundation: Gala offers early check-in option for guests
QUELL YOUR ANTICIPATION FOR the upcoming Great Gatsby Gala by skipping the registration lines Friday evening and heading straight to the night’s festivities. This year, the SVS Foundation offers guests early check-in for a no muss/no-fuss experience.
Registrants should already have received an email with check-in instructions, from live@classy-mail.org (check your spam folder!). Emails were sent to the registrant’s address. Those who did not receive the email and need it resent should contact kbrewer-smith@ vascularsociety.org
Guests must provide their cell numbers for updates and have a credit card number on file. This information will link guests’ registrations with their attendance. Those who do not want to provide their information will need to check on the day. Early check-in expires at 2 p.m. Friday.
Great Gatsby Gala announces After-Party
KEEP THE PARTY GOING AT THE Great Gatsby Gala after-party. New this year, enjoy two additional hours of Prohibition-era festivities by purchasing a ticket for $150. Gala tickets do not include access to the After-Party.
Also, get “Glam” before the Gala: The SVS Foundation is pleased to offer a limited number of hair and makeup sessions ahead of the Gala. Treat yourself to a pre-Gala makeover and champagne. Learn more and book your appointment by emailing crobb@ vascularsociety.org
Earn credits, contact hours at VAM, VQI@VAM and SVN meetings
ATTENDEES AT THE SOCIETY for Vascular Surgery Vascular Annual Meeting, the Vascular Quality Initiative meeting—VQI@VAM—and the Society for Vascular Nursing Annual Conference all can receive credits or project hours for their participation in the meetings.
The Accreditation Council for Continuing Medical Education (ACCME) has accredited SVS to provide CME for physicians. VAM has been designated for a maximum of 27 AMA PRA Category 1 Credit(s)™. VAM also includes a selfassessment component. Claim by July 17.
Each plenary to end with “how-to” video
AT THIS YEAR’S VAM, ORGANIZERS have planned even more “how-to” videos. As always, videos take center stage during the “How I Do It” video session. That session will be from 3:30 to 5 p.m. Thursday in Potomac D.
For this year, each of the eight plenary sessions, all in Potomac A/B, will end with a video presentation on performing a complex surgical procedure, said SVS Program Committee Chair Andres Schanzer, MD. They were selected from the approximately 50 videos submitted for consideration for VAM presentation. “These are all on different procedures and will be very educational to the audiences,” he said.
Topics include explant of an embolized left atrial appendage occlusion device and more. All sessions can be found on the Online Planner (vascular.org/OnlinePlanner23) and the mobile app, within each plenary description.
SVS PUTS ON CAREER FAIR AT VAM
ARE YOU INTERESTED IN STARTING OR ADVANCING YOUR CAREER in vascular surgery? This year, the SVS will host a Career Fair in Exhibit Hall E of the Convention Center from 9–3 p.m., Friday, June 16. This event is the top destination for those seeking opportunities in the specialty. As an extension of the SVS Job Bank, the Career Fair is free for conference attendees and will allow vascular surgery professionals to meet with potential employers in person.

With more than 1,000 attendees at all stages of their careers at VAM 2023, the Career Fair is an excellent opportunity for everyone. Attendees and professionals are invited to explore the Fair at their leisure. Recruiters from around the country will be present to meet with VAM guests.
Graduating trainees ready to take the next steps in their vascular careers will find the Career Fair an effective way to connect directly with recruiters rather than simply submitting their resumes and hoping for the best.
Even if you’re attending educational sessions, you can stop by the fair and discover new career opportunities from leading employers eager to hire. The Career Fair will helps build professional networks by allowing attendees to continue conversations with organization representatives for weeks or even months after the event.
Learn more at vascular.org/careerfair.
Bring your Twitter ‘A’ game
WHO ENJOYS TWITTER AS PART of their daily routine? The Society for Vascular Surgery Social Media Subcommittee plans a challenge during the Vascular Annual Meeting that’s right up their alley.
The #VAM23 Twitter Challenge, “You’re So Vein,” will test the prowess of all the Twitter users in attendance. In “Vein,” participants must meet challenges presented via Twitter with #VAM23. Participants’
Who will take home the award?
JOIN THE SVS AT THE AWARDS Ceremony, 10:30 to 10:45 a.m. Thursday in Potomac A/B for the presentation of the Lifetime Achievement Award. This award recognizes an individual’s outstanding and sustained contributions to both the profession of vascular surgery and the Society as a whole. It also honors an individual’s exemplary practice and leadership. Jonathan B. Towne, MD, received the award in 2022.
Voting to close Thursday
VOTING FOR THE NEW SVS VICE president and treasurer will close at 3 p.m. Thursday (EDT). Candidates are Kellie Brown, MD, and Keith Calligaro, MD, for vice president; and Thomas Forbes, MD, and Palma Shaw, MD, for treasurer.
tweets must be tagged with @VascularSVS and use #VAM23
The challenge opens Wednesday and closes at 4 p.m. Friday. The first three people to complete all challenges will receive a $100, $75 and $50 VISA gift card, respectively.
Winners must claim their prizes at the meeting.
Twitter profiles will need to be “public” during VAM so committee members can monitor results.
Questions? Send a tweet to @VascularSVS! Participants can also stop by SVS Central, outside the Exhibit Hall, to ask questions.
This year, voting has been open for an extended period of time, beginning in midMay and staying open into VAM. By the end of May, voting had already exceeded last year’s totals, to the satisfaction of SVS leaders who want to ensure all members, if they choose, have their voices heard. Members may vote by scanning the QR code at vascular.org/ vote2023
The QR code and website link will be included on signs throughout the Gaylord National Resort and Convention Center, site of this year’s meeting.
Learn more about the candidates at vascular. org/23_24Candidates.
www.vascularspecialistonline.com

DEEPLY COMMITTED TO INNOVATION SEEING OPPORTUNITY WHERE OTHERS DON’T. W. L. Gore & Associates, Inc. Flagstaff, Arizona 86004 goremedical.com Products listed may not be available in all markets. GORE, Together, improving life and designs are trademarks of W. L. Gore & Associates. © 2023 W. L. Gore & Associates, Inc. 231001708-EN MAY 2023 See the latest innovation in aortic branch technology We are continuously innovating to overcome yesterday’s limitations, creating new possibilities in care for your patients.






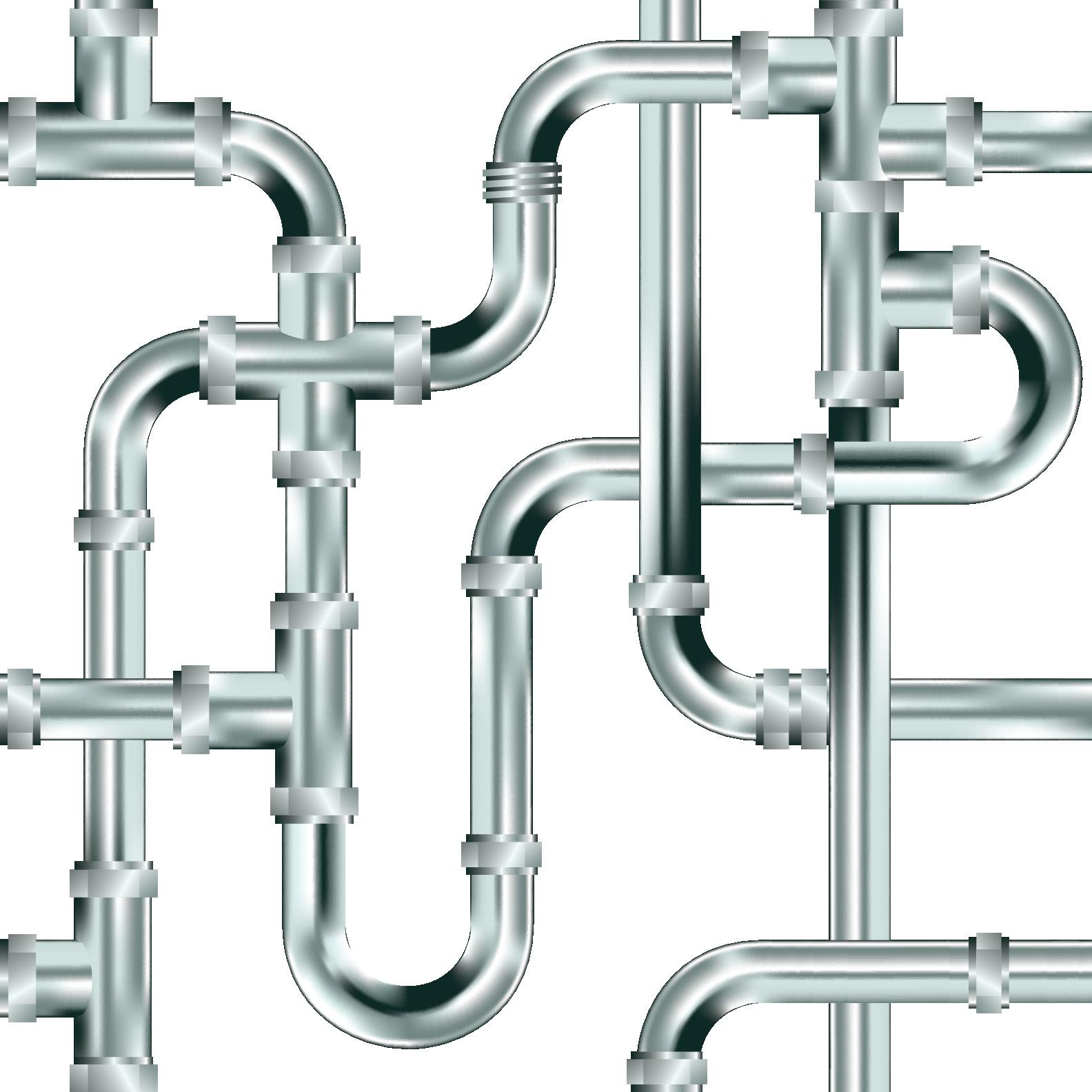

 By Éva Malpass
By Éva Malpass


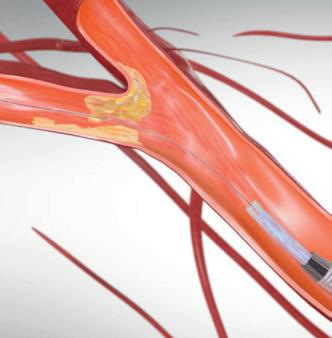



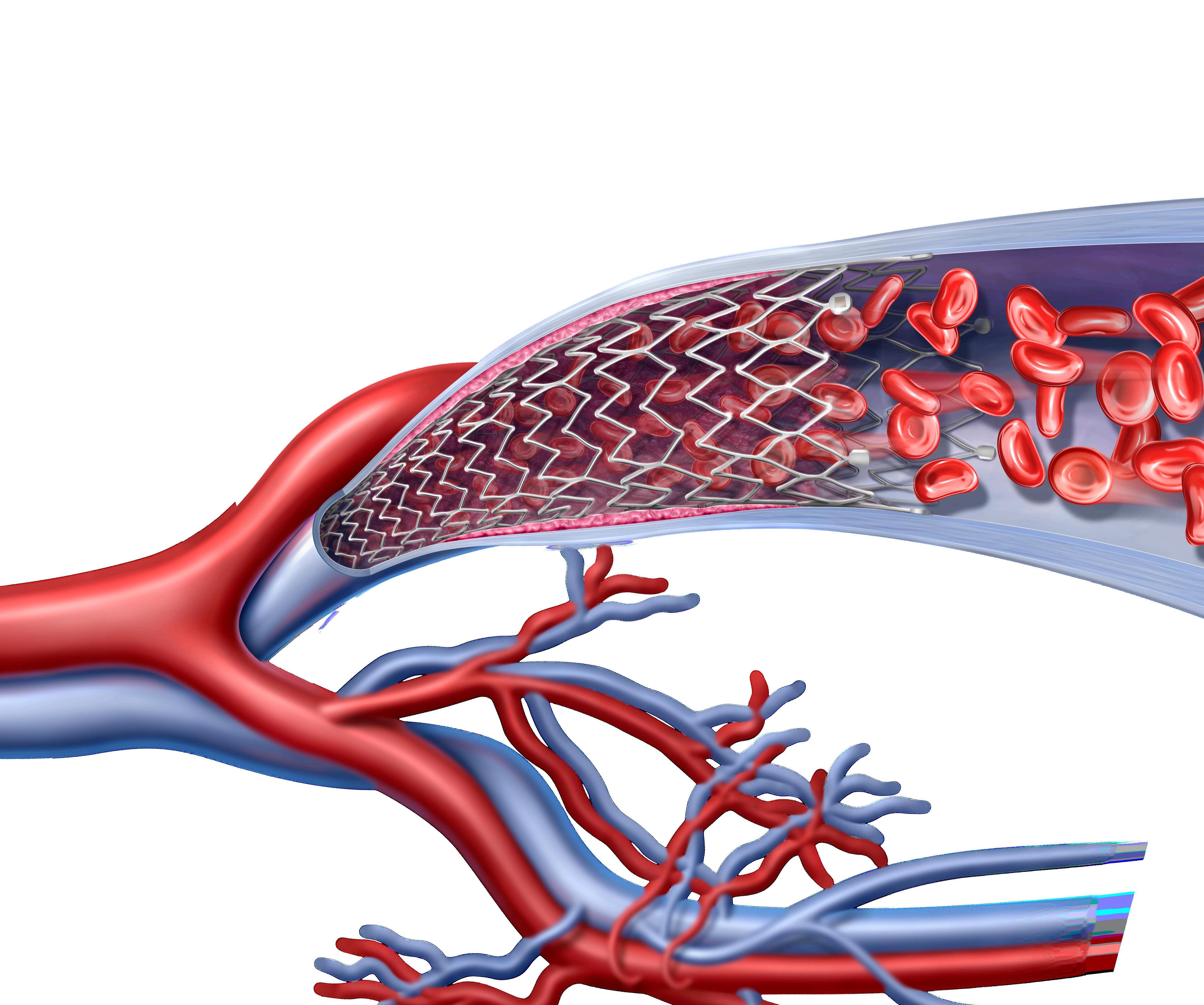
 By Beth Bales
By Beth Bales







 By Will Date
By Will Date












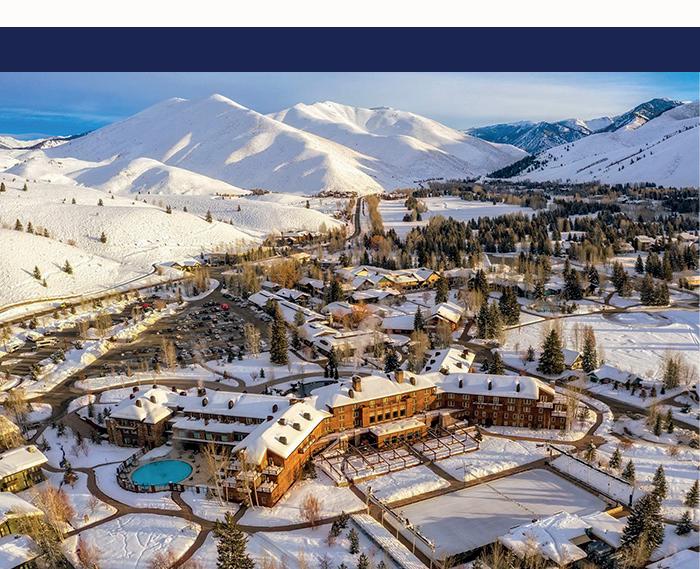




 By
By




















