CX 2023 heralds new era of yearround education for the vascular community


DELEGATES CAN EXPECT another full programme of sessions and additional events on the third and final day of the 45th CX meeting. Stay tuned for the announcement of the winner of the Hurting Leg competition—a new feature of the 2023 programme—as well as a full-day venous and Hurting Leg workshop, audience polling in this morning’s thoracic session, and a Podium First in the CX Innovation Showcase later today. As the meeting draws to a close, the time has also come to look ahead at what is in store for 2024.


Following this landmark anniversary symposium, headlined by the first-time BASIL-2 presentation on Tuesday, the CX Symposium is set
to return in 2024 with a controversies update. Next year, the meeting will take place in a new venue, the international ExCeL centre, with the aim of offering more space for the plenary programme, as well as larger exhibition and workshop spaces.





The in-person and virtual CX 2023 event might be drawing to a close, but the education does not end here. All presentations, as well as CX materials from previous years, will be available to members of the online community at CXVascular.com after the event. Stay up to date with the latest updates in the vascular and endovascular world year-round with this new interactive platform, ahead of next year’s CX 2024 in-person and virtual event.
CX Podium First: Statins save lives after aortic repair regardless of dose

Statin treatment after aortic repair is associated with improved long-term survival, while dose does not matter. This was the key message from a Podium First presentation delivered by Kevin Mani (Uppsala, Sweden) during yesterday’s abdominal aortic session in Kensington 1. The CX audience showed their support for this conclusion, with 89% agreeing with the statement ‘Statins save lives’ during discussion time.
Continued on page 4
Mani began by underlining the fact that abdominal aortic aneurysm (AAA) is a cardiovascular disease that shares risk factors with atherosclerotic cardiovascular disease (ASCVD). According to the American Heart Association (AHA), the presenter detailed, AAA is in fact classified as one of the ASCVDs.
“AAA patients have a higher mortality than the general
Continued on page 2
population due to cardiovascular disease,” Mani noted, adding that statin treatment is associated with improved survival in patients with ASCVD.
The presenter detailed that current European Society for Vascular Surgery (ESVS) guidelines on the management of abdominal aortoiliac artery aneurysms, published in 2019, suggest that patients with AAA should have blood pressure control, statins and antiplatelet therapy.

“This is a class IIa recommendation with level B evidence,” the presenter specified, which he said indicates that “probably all patients” with AAA should have statin treatment.
The AHA guidelines, Mani highlighted, split statin treatment into high dose and moderate to low dose. “The suggestion is that patients with ASCVD including those with AAA should have high-dose statin treatment,” the presenter shared with the Kensington 1 audience. “However,” he said, “the evidence for what dose should be given to AAA patients is non-existent, and the vascular surgical guidelines do not recommend a specific dose for AAA patients.”
To address this gap in the literature, Mani
CX 2023 OVERVIEW DAY
Thoracic Aortic Thursday, 08:00–18:00 Kensington 1 Chronic Limb-Threatening Ischaemia (CLTI) & Hurting Leg Thursday, 08:00–18:00 Kensington 2 CX Innovation Showcase Thursday, 08:00–18:00 Admiral CX Innovation Showcase CLTI & Hurting Leg Consensus Thoracic Aortic Consensus Thursday 27 April 2023
THREE
Join the community #CX2023
REPAIR
AORTIC
ON-DEMAND CATCH UP NOW WITH Scan here to view
2024
CXVascular.com
IT LIVE?
MISSED
Kevin Mani
Continued from page 1
and colleagues conducted a national study assessing the potential benefit of statin treatment in AAA patients and assessed whether dose has an effect. The team used four national registries and then cross-matched these to identify all AAA repairs performed in Sweden between the years of 2006 and 2018, the presenter explained. The team then assessed statin treatment by combining patient data and the national prescribed drug registry, looking at outcomes in terms of death, cause of death and rehospitalisation, also using national registries.
Mani detailed that the researchers performed three analyses, the first looking at 90-day mortality for patients who had statin treatment preoperatively, the second assessing statin versus no statin treatment postoperatively, and the final one examining high-dose versus low-to-moderate-dose statin treatment postoperatively, considering overall survival, aortic-related survival and freedom from cardiovascular events. Propensity score matching was used to ensure that the groups were comparable in terms of baseline comorbidities and characteristics.
The presenter revealed that approximately 60% of the 11,000 patients who underwent AAA repair in the national study had statin treatment prior to undergoing repair. Postoperatively, he added, half of the patients had continuous statin treatment 80% of the time after the operation. In both instances, the rates were higher among men compared to women.
Looking at perioperative mortality, Mani reported that this was the same in the group on statin treatment versus no statin treatment and was equal for the endovascular aneurysms repair (EVAR) and open repair cohorts, with an overall 90-day mortality of just under 3%.
The presenter also shared the finding that patients on
Acute Stroke Consensus
statin treatment had an improved survival in the long term, and that overall survival was “significantly improved” in a propensity score-matched group of patients with or without continuous statin treatment after AAA repair. Aortic-related survival was improved with statin treatment, he stated, as was freedom from cardiovascular events, if the patients were on statin treatment.
Finally, the team assessed the high-dose statin group versus the low-to-moderate-dose group. “There was no effect of the dose of statins, neither on overall survival nor on aortic-related survival or cardiovascular events,” he communicated. “These were equal, irrespective of dose.”
“In conclusion,” the presenter summarised, “statin treatment is beneficial in AAA patients with improved longterm survival, as well as improved freedom from aorticrelated complications and cardiovascular events.” However, he added the caveat that there is no support in the study for high-intensity statin treatment after AAA repair, and that perioperative mortality was not affected by statin treatment.
In a subsequent discussion, panellist Janet Powell (London, United Kingdom) asked whether the study results are independent of low-density lipoprotein (LDL) cholesterol levels. Mani responded that the team does not have such data. However, he highlighted the fact that the AHA recommendation for high-dose statins for patients with AAA below the age of 75 is irrespective of their LDL levels. “Clearly, this is an area where we need to work more on how we achieve the adequate effect of statins by looking at LDL levels,” he remarked, considering future research in this space.
Discussion continues at the CX Live studio
Vascular community split over “death”
of traditional
carotid stenting
A CX debate between two prominent carotid interventionists— Peter Schneider (San Francisco, United States) and Domenico Valenti (London, United Kingdom)—yesterday revealed that the vascular community is currently divided over the benefits of transcarotid artery revascularisation (TCAR), as compared to percutaneous carotid artery stenting (CAS).


SCHNEIDER KICKED OFF
the debate by arguing in favour of TCAR, initially outlining some of the limitations of percutaneous CAS that prior studies have demonstrated—for example, unwanted events relating to manipulation of the aortic arch as well as incomplete particulate capture. He went on to query if there is a “better way” to treat carotid artery disease, positing that TCAR may offer a solution that overcomes these limitations. Once again referring to the current literature in this space, he noted that TCAR can enable greater neuroprotective capabilities; improved safety in symptomatic patients and octogenarians; and carries a more efficient learning curve, versus
percutaneous stenting.
After reiterating the “unresolved challenges” CAS faces, including those relating to the aortic arch and particulate capture, Schneider concluded that prospective TCAR studies and his own experiences have shown both safety and efficacy with the procedure, demonstrating outcomes that are “competitive” with carotid endarterectomy (CEA) and “substantially better” than with percutaneous stenting.
Offering a riposte to these assertions, Valenti stated that TCAR—in essence, at least—has been around for many years, and is therefore not the “disruptive technology” within carotid interventions it is sometimes presented
as, also claiming that his opponent and other TCAR advocates have been “mesmerised” by the existing data. Homing in on said data, Valenti challenged positive conclusions drawn from the results of the ROADSTER 2 trial, noting its non-randomised nature, low proportion of symptomatic patients and, “more importantly”, lack of stratified data on delay to treatment. Additionally, he told attendees that findings from the Society for Vascular Surgery’s (SVS) Vascular Quality Initiative (VQI) are also limited by selection biases, gaps in the data, and the fact they come from a nonrandomised trial. Finally, Valenti noted that CAS
Following his Podium First presentation ‘Statin treatment after aortic repair’ during the abdominal aortic session on Wednesday morning, Kevin Mani (Uppsala, Sweden) joined Janet Powell (London, United Kingdom) at the new CX Vascular Live studio to discuss the new data, its implications and potential further research in the space. Powell had also given a presentation during the same session, speaking on a core outcome set for abdominal aortic aneurysm (AAA) repair.
“Statin treatment did not affect perioperative mortality, but it did significantly affect improved long-term survival,” Mani stated in the studio, sharing one of the key findings from his presentation on a national study of patients undergoing aortic repair. However, he stressed that the dose of statin “did not affect mortality in-andof itself”.
has been subject to far more “intense scrutiny” than TCAR to date—for example, in the CREST, ICSS and SPACE randomised controlled trials (RCTs). And, while he commented that TCAR may yet prove useful in certain patients, they are yet to be identified, and the lack of RCT-derived evidence supporting it means the “death” of percutaneous stenting is not imminent. A subsequent audience poll produced a very close result, but ultimately saw more CX attendees concur with Valenti’s closing gambit that “TCAR is not about to send CAS to oblivion”, as 52% voted against the statement that ‘TCAR is better than percutaneous carotid stenting’.
Thursday 27 April 2023 2 THIRD EDITION #CX2023 Consensus Update
CX Podium First: Statins save lives after aortic repair regardless of dose
The vascular surgical guidelines do not recommend a specific [statin] dose for AAA patients.”
Left to right: Peter Schneider, Maarit Venermo, Alexander Zimmermann and Domenico Valenti






Join the CX Vascular platform today to connect and engage with the global vascular community, share expertise and experiences, and stay up-to-date with the latest education and news in the vascular world. Members will also have access to exclusive content including live discussions on the latest advances in the vascular field and interviews with key thought leaders in the space. Register now Education, News, Insights Join the community at https://cxvascular.com
Hence Verhagen
Endurant stent graft proves efficacious and durable in ENGAGE 10-year data
Yesterday’s Podium First presentation from Hence Verhagen (Rotterdam, Netherlands) saw him present unique 10-year data from the ENGAGE OUS registry on the Endurant abdominal aortic aneurysm (AAA) stent graft (Medtronic). “Ever since we started doing endovascular aneurysm repair (EVAR) about 30 years ago, there have been concerns about durability,” Verhagen stated at the opening of the talk. “What we have revealed is that the survival between open and endovascular patients is the same in the long term.”


VERHAGEN DIRECTED HIS AUDIENCE’S attention to previous randomised controlled trials such as EVAR1 and DREAM, which “raise[d]
concern” around durability. The latter in particular showed patients in its EVAR group had “many more secondary interventions after about four years”. He also said that, though there were some other studies with long-term data (≥10 years), many of these have “strict limitations”, leading to a “paucity of long-term data” with a large stenting sample size. The reason, he said, was the high mortality in such trials— meaning that, after 10 years, “there are not that many patients left […] You need a very large group to start off with to have survival and results after 10 years.”
Setting out some details of the registry, Verhagen detailed it included 1,260 patients from 79 sites in 30 countries. The patients initially enrolled only consented to five-year follow-up, however, which
Hands-on aortic course opens up new options in physician-modified F/BEVAR
Wednesday’s aortic course gave attendees the opportunity for hands-on learning on physician-modified grafts for fenestrated and branched endovascular aneurysm repair (F/BEVAR).
Course director Alexander Zimmermann (Zürich, Switzerland) guided participants through a series of interactive sessions in which they were instructed on key objectives including measurement and modification of modified grafts.
“For thoracoabdominal aneurysms you have branched, offthe-shelf stent grafts, and for infrarenal aneurysms you have standard devices that you can use in emergency or urgent situations,” Zimmermann tells CX Daily News, outlining the rationale for the course. “For aneurysms that are at the level of the renal visceral arteries, there is a lack of off-the-shelf devices to treat emergency or ruptured cases.”
Having the option to use a physician modified graft in these cases offers a route outside of open surgery or parallel grafts, Zimmermann explains, closing the gap between the thoracoabdominal and infrarenal emergent cases.
The CX aortic course is unique as many physicians will not have had the opportunity for instructor-led education on this subject to date, says Zimmermann. “To lower the fear for using this kind of device and to do something hands on and to experience how easy it can be done will help to widen the indication in emergency cases,” he says.
“The goal is that when they leave this course, they are capable of doing these physician modifications by themselves and with the next emergency that they experience in their hospital, they have another option besides parallel grafts or open surgery.”
required a reconsent process for 10-year followup—with only 49 of the initial 79 centres agreeing. This, combined with patient refusals, reduced the total cohort for long-term results to around 390 patients. “Not surprisingly, these patients were a little younger than the original and had generally fewer comorbidities,” Verhagen added.
All-cause mortality up to 10 years was analysed, revealing a survival rate of about 42%. There was no steep decline after five years, something which also held for aneurysm-related mortality (around 5% of patients). Reinterventions, “the Achilles’ heel of EVAR,” were also not found to accelerate after five years’ follow-up, with around 70% of patients free from secondary interventions. Stratified into groups undergoing reintervention at 0–5 years and at 6–10 years, Verhagen and colleagues found “very, very few” type 3 endoleaks “in the first seven years or so”, he stated, “with a slight increase at 10 years”.
Patients with a type 1a endoleak, Verhagen noted, increased in number by 4.1% at 10 years. Of those, however, 40% “started off with well-known risk factors”. Clinical events were also examined, with aneurysm rupture—“the ultimate failure”—occurring “very, very little”, increasing at a rate of 1.5% at 10 years.
Setting out a few limitations, Verhagen reminded his audience of the loss of patients during the reconsenting process, leaving a healthier cohort, as well as the fact that it was a single-arm observational registry. The take-home message, Verhagen stated, was that these were “probably unique data” up to 10 years, and that they “confirm the long-term efficacy and the durability of the Endurant stent graft with these numbers of aneurysms and mortality”. There was “no big decline” in patient outcomes at this longer follow-up point, with consistent 60% sac regression. Reviewing the most frequent causes of late adverse events, he put forward that initial hostile anatomy was a particularly influential factor. Finally, he said that “lifelong surveillance is critical for EVAR patients”.
Thursday 27 April 2023 4 THIRD EDITION #CX2023 Aortic Update
Lifelong surveillance is critical for EVAR patients.”
Alexander Zimmermann
Advanta V12

balloon expandable covered stent

Right from the start Still going strong
Advanta V12 is a balloon expandable, fully encapsulated PTFE stent with first to market covered balloon expandable stent technology that has served more than 700,000 patients. Known for its precision and predictability – the versatile Advanta V12 has been meeting the needs of surgeons and patients for 20 years and is the only durable solution backed up by decades of real-world evidence and more than 550 publications.
getinge.com
Getinge, and , are trademarks or registered trademarks of Getinge AB, its subsidiaries, or affiliates in the United States or other countries. Copyright 2023 Atrium Medical Corp. All rights reserved. PN011928 Rev AA 03/2023
CX 2023: Through the lens
A packed day of presentations, edited cases and workshops covering aortic, venous, acute stroke and vascular trauma domains dominated the three main CX auditoria on day two. The exhibition area was also abuzz with delegates eager to see the latest innovation in the space.






6 #CX2023 Thursday 27 April 2023 THIRD EDITION








7 #CX2023 Thursday 27 April 2023 THIRD EDITION
“Passion about the patients, passion about the team you are working with, about research, about education—this is all very important.”
MARIANNE DE MAESENEER
Deep venous consensus: Multidisciplinary faculty address key issues in the pelvic venous disease space
Wednesday’s deep venous consensus update covered a range of key topics in the field, including issues associated with pelvic venous lesions. Anchor Erin Murphy (Charlotte, United States) was joined by moderators Armando Mansilha (Porto, Portugal) and Manj Gohel (Cambridge, United Kingdom) to oversee various presentations and edited cases over the course of the afternoon.
THE SESSION OPENED WITH A series of presentations on the pelvic veins, starting with one from Kathleen Gibson (Bellevue, United States) on optimal work-up before intervention for patients with pelvic venous reflux. “This is going to be one of these talks that is full of my opinions and not data,” she said in opening, explaining that this is an area in which there is, as yet, no consensus. Among Gibson’s conclusions was the message that patient history and presentation are important in patients with pelvic venous reflux, urging audience members to “treat the patient, not the imaging”. On the topic of imaging,
however, she did note that duplex ultrasound, cross-sectional imaging and venography/intravascular ultrasound “all have important diagnostic roles” and that confirmatory imaging is “very important” to make a definitive diagnosis prior to treatment.
Subsequently, Aleksandra JaworuckaKaczorowska (Gorzow Wielkopolski, Poland) outlined three edited cases on ‘bottom-up’ treatment for pelvic origin varicose veins. She explained that, in her experience, ‘top-down’ treatment does not give good results and that very often multiple embolisation sessions are required. The results of ‘bottomup’ treatment, on the other hand, she

has found to be good. This is also a less invasive treatment, she pointed out, adding that it can be repeated if required and is cost-effective.
Moderator Manj Gohel (Cambridge, United Kingdom) noted that the presenter was able to offer a “unique perspective” on this topic due to the fact she is a trained gynaecologist, and, in the discussion following her presentation, Jaworucka-Kaczorowska shared some insights from her practice with an audience of vascular surgeons.
Later in the session, Karen Breen (London, United Kingdom), a consultant haematologist, spoke on the implications of pelvic venous and iliac venous interventions of future pregnancies. She advised delegates to discuss acceptable forms of contraception with these patients and highlighted the importance of pre-conception counselling. Breen also underscored the significance of a multidisciplinary team approach “where practical” and stressed that “more data on outcomes are needed”.
Gibson presented another edited case, focusing on the
Venous, we have a perception problem
Venous disease care has a problem with optics in the context of growth in the number of venous procedures and the spectre of inappropriate care, the CX superficial venous and lymphatic consensus update session heard yesterday morning.
THE CONVERSATION THREAD EMERGED in a question from co-moderator Stephen Black (London, United Kingdom), posed to presenter Erin Murphy (Charlotte, United States), who had just presented possible solutions that can be targeted at not only discouraging inappropriate venous care but also encouraging appropriately administered procedures.
Having trained and carved out a career as a venous specialist, said Black, if he were to suddenly decide “to now go and do a coronary angiogram and stent, I would get absolutely obliterated”.
So, he asked Murphy: “Why is it that it is so easy for people who have never trained in veins just to crack on and treat veins without any consequences?”
Murphy pointed to a problem with misperception—”that this is an easy patient subset to treat, and I think those of us who are in this room treating these patients know that there is actually very complex decision-making [involved] in order to get the right outcomes for our patients,” she said. “We need to change that perception.”
Murphy had outlined several ways she sees of helping to curb the problem, building on a talk Manj Gohel (Cambridge, United Kingdom) gave last year. They included defining appropriate care through research initiatives, consensus statements and guideline data; educating and disseminating such
data; holding practices accountable for decisions to carry out inappropriate care; and establishing correct financial incentives.
The biggest of these challenges currently involves
optimum technique for pelvic venous embolisation for pelvic congestion.
Another topic in the spotlight yesterday afternoon was venous stenting, with faculty including Gerard O’Sullivan (Galway, Ireland), Houman Jalaie (Aachen, Germany) and Marie Van Rijn (Nijmegen, Netherlands), as well as anchor Murphy, speaking on topics including strategies for avoiding venous stent migration and trends and disparities in US venous investigational device exemption trials.
There was also an edited case in this part of the programme on endophlebectomy to optimise inflow for iliac venous stenting from Steven Abramowitz (Washington, United States) and another from Stephen Black (London, United Kingdom) on reintervention for a chronically occluded venous stent.
educating a sprawling array of providers who treat venous disease patients, Murphy said. Are the right doctors treating the venous disease population? Vascular surgeons, for instance, “have no requirement in their board certification to be treating venous patients,” Murphy said, asking whether they are well-enough trained in the venous area. “Coming out of training, they have done about 40 venous cases overall.” Similarly, for interventional radiology, the situation is not any better, she reasoned. “Cardiology has no required training. So, what we do?”
The answer might be dedicated providers who undertake training and fellowship requirements specific to venous disease, as well as specific board certification, and accreditation. “This is in progress,” Murphy pointed out. “This is probably a direction that we need to go.”
In terms of accountability, she queried whether the venous space should be auditing for decisionmaking when people are trained appropriately. “We have seen when we identify practices that are doing things outside the norm,” Murphy explained, drawing attention to example of practices carrying out more ablations per patient compared to the average practitioner treating venous disease, “when we notified the practice of their outside-the-box numbers, they actually self-corrected to an extent.” The implication here is that they had been educated, she added.
“Underdiagnosis and undertreatment probably affect more patients than overtreatment, particularly over time,” Murphy said. “So, we do not want to disincentivise. But a multimodal effort to address inappropriate care is needed, and, probably, educating providers is our number one thing.”

Venous &
8 #CX2023 Thursday 27 April 2023 THIRD EDITION Venous Update
Lymphatic Consenus
Kathleen Gibson
Underdiagnosis and undertreatment probably affect more patients than overtreatment, particularly over time,”
SUPERFICIAL VENOUS
De Maeseneer receives CX award for dedication to specialist venous care
Marianne De Maeseneer (Rotterdam, Netherlands) was at the podium to dispense tips for success and longevity as a venous specialist. For CX executive board member Manj Gohel (Cambridge, United Kingdom), no one is better placed to deliver such advice than De Maeseneer, he told symposium attendees.

DE MAESENEER WAS GIVING THE penultimate talk in yesterday’s superficial venous and lymphatic consensus update session, and Gohel, as co-moderator, was welcoming her to the podium. She kicked off her message by recasting the title as ‘How to be a good and happy venous specialist’, shortlisting the keys as curiosity, exchange of ideas, commitment to clinical practice, research and scientific societies, worklife balance and passion.
“Passion about the patients, passion about the team you are working with, about research, about education—this is all very important to become and stay a happy and good working venous surgeon, and
hopefully long-living venous specialist,” she said.
Co-moderator Stephen Black (London, United Kingdom), also a CX executive board member, invited De Maeseneer to remain at the podium to receive the CX Lifetime Achievement Award. Presented by Armando Mansilha (Porto, Portugal), another member of the CX executive board, she becomes the secondever recipient. “I do not think anyone has put more into defining how we treat our specialty,” said Black.
“If any of you can emulate a career in veins, and put veins on the map, Marianne is a great role model to follow.”
Benefits of Clinical Longevity Through Custom Solutions

Thursday 27th April 2023 • 09:40 - 10:10 • Kensington 1
Moderator: Tilo Kolbel, Germany
The Clinical Importance that Relay Branched Platform Offers

Maani Hakimi, Switzerland
Simplifying Complex Thoraco Abdominal Challenges with Two Devices: Fen Anaconda & Fen TREO



Florian Elger, Germany
Treating the Untreatable Complexities: CM
ThoracoFlo
Alexander Zimmerman, Switzerland
The Clinical Benefits of Physician Modified TREO Platform: IDE Results So Far
Dean Aranoutakis, United States
9 #CX2023 Thursday 27 April 2023 THIRD EDITION Venous Update
SYMPOSIUM
TERUMO AORTIC
terumoarotic.com/custom-solutions
Please visit us at booth 28 & 30 to discuss our wide range of Custom Solutions. Discover Custom Solutions
From left: Stephen Black, Manj Gohel, Marianne De Maeseneer, Erin Murphy and Armando Mansilha
If any of you can emulate a career in veins, and put veins on the map, Marianne is a great role model to follow.”
Stephen Black




Thursday 27 April 2023 10 THIRD EDITION #CX2023 LIFT LIFT LIFT1 LIFT2 LIFT LIFT4 FT RECEPTIONMAIN LOBBYAND MAIN ENTRANCE MAIN ENTRANCE BOWBAR BOWBAR SEMI-PRIVATE WEST WING LOBBY HOXTONROOM SPEAKER READY ROOM ORGANISERS OFFICE TYBURNMARKET TYBURN BAR TYBURN RESTAURANT HYBRID MEETING ROOMS 1 HYBRID MEETING ROOMS 2 HYBRID MEETING ROOMS 3 KENSINGTON 2 KENSINGTON 1 CATERING CATERING A27 A29 A23 A21 B24 A25 D38 B36 B38 C36 C32 B28 B32 C28 D24 E40 D40 E38 D38 E36 D36 E32 D28 D32 F33 F27 F25 F19 D20 B20 A19 A15 F23 G12 G13 G14 G11 G10 A30 F35 MEZZANINE BALCONY 26 SQM 26 SQM 56 SQM 66 SQM 45 SQM 45 SQM WORKSHOPS & Abstracts ADMIRAL PLENARY 55 SQM 57 SQM
Day 3: Thursday 27 April
Kensington 1
Thoracic Aortic
Thoracic Arch Consensus Update
Time: 08:00–09:10
Anchor: Roger Greenhalgh, London, United Kingdom
Moderators: Afshin Assadian, Vienna, Austria and Tilo Kölbel, Hamburg, Germany
Thoracic Dissection Consensus
Update
Time: 09:10–09:40
Anchor: Roger Greenhalgh
Moderator: Gustavo Oderich, Houston, United States
Sponsored Education
Time: 09:40–10:10
Thoracic Dissection Consensus
Update Continued
Time: 10:30–11:20
Anchor: Roger Greenhalgh
Moderators: Gustavo Oderich and Tilo Kölbel
Thoracoabdominal Consensus Update
Time: 11:20–12:30
Anchor: Tilo Kölbel
Moderators: Gustavo Oderich and Timothy Resch, Copenhagen, Denmark
Sponsored Education
Time: 12:30–13:00
Thoraco-abdominal Consensus Update
Continued
Time: 13:30–14:20
Anchor:Tilo Kölbel
Moderator: Gustavo Oderich
Thoracic Consensus Update
Time: 14:20–15:20
Anchor: Andrew Holden, Auckland, New Zealand
Moderators: Gustavo Oderich and Tilo Kölbel
Best of Abstracts
Time: 15:20–15:50
How To Do It (HTDI)
How To Do It: Open, Hybrid & Endo Management of Complex Post-dissection Aortic Aneurysms
Time: 16:10–17:20
Anchor: Roberto Chiesa, Milan, Italy
Kensington 2
Admiral
Chronic
Limb-Threatening Ischaemia (CLTI) & Hurting Leg
Chronic Limb-Threatening Ischaemia (CLTI)
Consensus Update
Time: 08:00–10:10
Anchor: Sophie Renton, London, United Kingdom
Moderator: Robert Hinchliffe, Bristol, United Kingdom
Best of Abstracts: Rising Stars
Time: 10:30–12:00
Anchor: Sophie Renton, London, United Kingdom
Moderator: Jonathan Boyle, Cambridge, United Kingdom
Rouleaux Club
Time: 12:00–12:30
Chairing: Sophie Renton and Leanna Erete (Middlesborough, United Kingdom)
Best of Abstracts
Time: 12:30–13:00
Anchor: Gunnar Tepe, Rosenheim, Germany
Moderator: Marianne Brodmann, Graz, Austria
CLTI & Hurting Leg Consensus Update
Continued
Time: 13:30–15:20
Anchor: Roger Greenhalgh
Moderator: Sophie Renton
Sponsored Education
Time: 15:20–15:50
CLTI & Hurting Leg Consensus Update
Continued
Time: 16:10–18:00
Anchor: Roger Greenhalgh
Moderators: Robert Hinchliffe and Sophie Renton
Hurting Leg Roundtable Discussion: Can we use existing screening programmes like aneurysm and breast screening to opportunistically identify ‘the hurting leg’?
Time: 17:10–18:00
Innovation Showcase
Chairing: Frans Moll, Utrecht, Netherlands
Innovation Consensus
Time: 08:00–09:20
Complex Abdominal Aortic Aneurysm
(AAA) Innovation Consensus
Time: 09:20–10:10
AAA Prevention Innovation Consensus
Time: 10:30–11:10
Vascular Access & Renal Innovation
Consensus
Time: 11:10–12:00
Venous Innovation Consensus
Time: 12:00–13:00
Peripheral Innovation Consensus
Time: 13:30–15:00
Artificial Intelligence Deep Learning
Time: 15:00–15:50
Dragon’s Den
Time: 16:10–18:00
Chairing: Stephen Greenhalgh, London, United Kingdom
Panel: Bob Mitchell, Park City, United States
Frans Moll
Kieran Murphy, Toronto, Canada
Chas Taylor, United Kingdom
George Adams, Chapel Hill, United States
Jeffrey Jump, Nyon, Switzerland
Patrick Kelly, Sioux Falls, United States
Tom Carrell, Barrington, United Kingdom
Peter Hinchliffe, United States
Thoracic Consensus Update Continued
Time: 17:20–18:00
Anchor: Alexander Zimmermann, Zürich, Switzerland
11 Thursday 27 April 2023 THIRD EDITION #CX2023 Programme
Key: Aortic How To Do It Hurting Leg Innovation Showcase
PROGRAMME
AT A GLANCE
INNOVATION SHOWCASE
Innovation Showcase to feature vascular technologies of tomorrow


The CX Innovation Showcase will take place once again at this year’s symposium, with demonstrations of some of the most novel and potentially practice-changing techniques, technologies and trials in vascular surgery taking place. The session runs throughout day three in Admiral.
The session’s opening section focuses on innovation consensus—chaired by Frans Moll (Utrecht, Netherlands)—and will see speakers from



across the globe offer a wide range of industry perspectives.
Later the same morning, innovations in complex abdominal aortic aneurysm (AAA) treatment and prevention will be delivered. These include custom-made fenestrated and branched endovascular aneurysm repair (EVAR) solutions, presented by Tilo Kölbel (Hamburg, Germany); and preliminary experience with a new, self-expandable stent graft in complex aortic repair, presented by Giacomo Isernia (Perugia, Italy). Additionally, a Podium First will see Andrew Holden (Auckland, New Zealand) present first-in-human experiences with the Suture-Tight device (Vesteck).
In the vascular access and renal innovation portion of the programme, novel technologies like the Holly implantable device (Nephrodite) for continuous haemodialysis, and a wearable device for non-invasive, remote monitoring and classification of access patency and flow characteristics in haemodialysis patients, will be presented by Nikhil Shah (Atlanta, United States) and John Aruny (Orangeburg, United States), respectively.
Five-year data on GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis “raise the bar” in aortoiliac occlusive disease therapy
At this year’s CX Symposium, Andrew Holden (Auckland City Hospital, Auckland, New Zealand), presented results from the longest follow-up study to date evaluating the GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis (VBX Stent Graft; Gore) in aortoiliac occlusive disease (AIOD). Here, he details how these new data “raise the bar” for durable, robust AIOD treatments.
AIOD is an “increasingly common problem”, Holden asserts, with around a third of all peripheral arterial disease (PAD) cases involving the iliac arteries. Discussing the backdrop to the VBX FLEX Clinical Study, he notes that—with endovascular treatments growing in prevalence over the past 15 years—balloon-expandable covered stents represent a “very appealing” option for this indication, theoretically providing lower rates of serious complications as well as improvements in long-term patency outcomes.
Results from the original VBX FLEX Study appeared to bear out these benefits, with the VBX Stent Graft demonstrating high one-year rates of primary (94.5%), primary-assisted (99%) and secondary (99.5%) patency, in addition to a 98.1%

rate of freedom from clinically driven target lesion revascularisation (fCD-TLR) at three years. However, in an attempt to further elucidate the durability of these positive findings, Holden led a physician-initiated follow-up in a subset of these patients out to five years.
“The concept of durable patency in aortoiliac disease is really important,” he says. “The vast majority of these patients are ‘claudicants’ [who] have a much longer life expectancy than patients with critical limb ischaemia—often living for 10 years or longer—so durability of treatment is something that has come into focus. But, until recently, we really had very little useful information on how durable these covered stents are, in particular in the iliac arteries.”
The five-year follow-up with the
Prior to the day’s lunch break, Stephen Black (London, United Kingdom) will deliver a talk titled, “Early clinical optimisation with microinfusion device and DEXTERITY study update”, as part of the venous innovation consensus session. Following this, Ramon Varcoe (Sydney, Australia) will present first-in-human experiences with a percutaneous valve for venous insufficiency. A packed afternoon session on peripheral innovations will see further updates on vascular trials—for example, the RESOLV study, set to be delivered by Marianne Brodmann (Graz, Austria). A number of presentations are also scheduled to examine the role more novel drugs like sirolimus and everolimus can play in below-the-knee treatments. Eric Secemsky (Boston, United States) will also discuss “the next frontier” in peripheral therapies: the role of micro-incisions in preparing the vessel for drug-coated balloons (DCBs).
Artificial intelligence (AI) and deep learning will be the centre of focus during the penultimate session of the day, with presentations from Guy Martin (London, United Kingdom) and Tomas Baltrunas (Vilnius, Lithuania) on robotic endovascular surgery leading the agenda. This is set to be followed by a talk from Richard Linder (Sandy, United States) on the impact of “the first global wireless network for vascular imaging and physiology”.
Chaired by Stephen Greenhalgh (London, United Kingdom), the CX Innovation Showcase will close with a Dragon’s Den-style competition. Among these innovations are a remote vascular connection technique for distal bypass surgery; the non-invasive, distant and lifelong monitoring of arteriovenous fistulas (AVFs); a prophylactic sac management system; and an electrocardiogram (ECG) “anytime, anywhere, in 60 seconds”.
VBX Stent Graft saw 59 patients enrolled from the original study’s three highest-participating centres—Holden’s own centre in Auckland, as well as Prisma Health (Greenville, USA) and Wellmont Holston Valley Medical Center (Kingsport, USA). A total of 28 patients completed the five-year follow-up and could be assessed as per the study’s primary durability endpoint of long-term primary patency. An important detail Holden highlights here is that this patient cohort was representative of the full spectrum of disease seen in AIOD patients, with about one third of patients having more complex lesions (Trans-Atlantic InterSociety Consensus [TASC] C or D).
Arriving at the crux of the study’s findings, he reports sustained long-term durability with the VBX Stent Graft, indicated by an “excellent” 84.4% primary patency rate per subject, and an 89.5% primary patency rate per lesion (n=94)—an “incredible, unrivalled performance”—at five years.
“To put that into context, there had only been one other publication reporting five-year patency—74.7% with the iCAST/Advanta V12 [Getinge] in COBEST,” Holden states, “so to really raise the bar and report a patency of 89.5% was extremely pleasing.”
He goes on to note that the persubject primary-assisted and secondary patency rates were the same (93.3%) at five years, as was the per-lesion rate (96.1%) for both. Additionally, there was a five-year, per-subject fTLR rate of 89.1%—also a “very high figure”, according to Holden—and 12 deaths (20.3%), none of which were found to have been device-related. Finally, he outlines sustained improvements in Rutherford classification scores and walking impairment, as well as on quality-of-life questionnaires.
“For these patients, we hope to provide a durable treatment, and it is very difficult to imagine any treatment for aortoiliac disease that could achieve superior patencies to this—particularly a minimally invasive therapy like an endovascular covered stent,” Holden concludes. “To be able to tell patients they are going to get a durable patency, and the vast majority will never need to have another intervention related to this treatment; those are the most compelling outcomes for me.”
The CX Symposium also saw Holden announce a “very exciting” next step in evaluating the VBX Stent Graft: a multicentre randomised controlled trial, with long-term follow-up, comparing the device to bare metal stenting in complex iliac occlusive disease.

12 #CX2023 Thursday 27 April 2023 THIRD EDITION Innovation
THIS ADVERTORIAL IS SPONSORED BY GORE
Andrew Holden
Frans Moll (second from left) chairs
JOIN THE NEXT GENERATION OF CARE

























































GORE® VIABAHN® Device family GORE® VIABAHN® Endoprosthesis with PROPATEN Bioactive Surface* In the treatment of aortoiliac occlusive disease. The GORE® VIABAHN® Device family† of covered stent grafts gives you the flexibility and conformability to safely and confidently address even the most complex cases.1,2 See the data at goremedical.com/eu/viabahn/device-family *As used by Gore, PROPATEN Bioactive Surface refers to Gore’s proprietary CBAS Heparin Surface. † The GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis indication includes de novo or restenotic lesions in iliac arteries, including those at the aortic bifurcation. The GORER VIABAHNR Endoprosthesis indication includes lesions in the iliac arteries only. 1. Piazza M, Squizzato F, Dall’Antonia A, et al. Outcomes of self expanding PTFE covered stent versus bare metal stent for chronic iliac artery occlusion in matched cohorts using propensity score modelling. European Journal of Vascular & Endovascular Surgery. 2017;54(2):177-185. 2. Panneton JM, Bismuth J, Gray BH, Holden A. Three-year follow-up of patients with iliac occlusive disease treated with the Viabahn BalloonExpandable Endoprosthesis. Journal of Endovascular Therapy. 2020;27(5):1. Products listed may not be available in all markets. GORE, Together, improving life, PROPATEN, VBX, VIABAHN and designs are trademarks of W. L. Gore & Associates. © 2022 W. L. Gore & Associates GmbH 22443002-EN FEBRUARY 2022 GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis
Long-term data demonstrate efficacy of bridging stent for F/BEVAR
In a review of 20 years of real-life experience, the Advanta V12 balloonexpandable covered stent (Getinge) has been labelled “excellent” in fenestratedbranched endovascular aortic repair (F/ BEVAR). This is according to “proven and reliable” eight-year clinical data which compared outcomes including target vessel patency, freedom from reintervention and endoleak.
AMONG SEVERAL FIRST-TIME DATA presentations at this year’s CX Symposium, Eric Verhoeven (Nuremberg, Germany) delivered the findings during the afternoon juxtarenal aortic session on Wednesday. First providing a product overview of Advanta V12, Verhoeven cast an eye back over the previous 15 years of use and design evolution, which have provided “increased flexibility, greater radial strength and lower recoil” for the restoration of iliac and renal arteries.
Covered stents “should be preferred” in chronic mesenteric ischaemia
Providing insight on the pivotal and parallel evolution within aneurysmal disease treatment, Verhoeven emphasised the move toward fenestrated and branched grafts for complex aortic aneurysms, focusing on covered stent use for FEVAR. Elaborating further, he referenced a 2009 renal fenestration study conducted by Walid Mohabbat (Sydney, Australia) et al which found that covered renal stents are associated with lower incidence of in-stent stenosis, and so are recommended for use in fenestrated or branched endografts.

Using Mohabbat as a jumping-off point, Verhoeven then moved ahead to 2015, developing the Advanta V12 timeline for the audience. Referencing his own research, he discussed a previous review of ten-year thoracoabdominal aortic aneurysm (TAAA) repair, which, of 600 target vessels, 553 (92.2%) were treated using Advanta V12, and seen to be preferable and “effective” in a high-risk patient cohort. Then, making the short leap to 2016, Verhoeven detailed his continued research into FEVAR as a first-line treatment strategy at his institution in Nuremberg. Using Advanta V12 for 99.7% of target vessels, their results showed FEVAR to be associated with “high” technical success—Verhoeven setting a salient course to contextualise their later conclusions.
Broadly looking between 2010–2020, Verhoeven proceeded to review the experience of Advanta V12 at his institution, observing its successful deployment in 83.2% of procedures. Furthermore, when relaying more granular data to the CX 2023 audience, Verhoeven highlighted the target-vessel patency rates, which were 99.1±0.2% at one year, 96.9±0.5% at five and 96.2±0.7% at eight years follow-up, respectively.
Verhoeven, dissecting these figures further, then compared patency rates between fenestrations and branches. This revealed lower patency among branches when measured against fenestrations, particularly when concerning renal arteries, which were 98.2 ±0.5% at eight years for fenestrations and 77.3±5.9% for branches.
83.2% SUCCESSFUL DEPLOYMENT
Concluding, Verhoeven made clear that despite disparities in the data, Advanta V12 has persisted as an invaluable device, which has provided “excellent” handling and flaring over the course of 20-plus years of use. Placing emphasis on the long-term patency rates that have made the Advanta V12 an invaluable tool within F/BEVAR he says, Verhoeven concluded by alluding to its steadfast place within the future of treatment.
Bridging covered stents and selfexpanding grafts “similar” in terms of primary patency and branch related endoleak
The late afternoon juxtarenal aortic consensus update session on bridging stents offered salient conclusions to the CX audience, through Luke Terlouw’s (Rotterdam, Netherlands) presentation of long-term results of a randomised controlled trial comparing covered with bare-metal stenting of the mesenteric arteries in patients with chronic mesenteric ischaemia (CMI).
Terlouw described the details of the multicentre patient- and investigator-blinded trial, noting that the study included patients undergoing endovascular treatment of atherosclerotic CMI with a stenosis length of <25mm.
He defined the trial’s primary endpoint as 24-month primary patency and specified subsequent patency loss to be luminal surface area reduction ≥75% or performance of a reintervention to maintain patency. Patency was assessed by two interventional radiologists with 15 and 19 years of experience.
Presenting the findings, Terlouw confirmed that, considering the follow-up data show “significantly” better primary patency and lower reintervention rates, the covered stent should be regarded as the preferred stent when treating patients with atherosclerotic CMI.
KONSTANTINOS SPANOS (LARISSA, GREECE) PRESENTED META-ANALYSIS DATA of comparative studies evaluating balloon-expandable bridging covered stent versus self-expanding stent grafts for branched endovascular aneurysm repair (BEVAR) in a Podium First on Wednesday afternoon. The findings show that bridging covered and self-expanding stents perform “similarly” when compared via primary patency and branch-related endoleak during mid-term follow-up.
Addressing the CX 2023 audience, Spanos explained that currently available stent grafts— bridging covered stents or self-expanding grafts—are not originally designed as bridging stents for complex aortic repair with branched devices. Continuing, he outlined the aim of the current review was to evaluate the impact of each type of bridging stent graft on target vessel outcomes during the mid-term follow-up after BEVAR.
In total, Spanos stated, 96% of target vessels remained patent using bridging covered stents and 97% using self-expanding grafts, and he added the overall pooled primary patency rate did not differ between groups. Concerning revascularisation, Spanos also asserted that no significant differences were found between the two groups, showing 97% for bridging covered stents and 99% for selfexpanding grafts, respectively.
Of note however, Spanos confirmed that the researchers found a lower risk for target vessel instability using self-expanding stent grafts during revascularisation when compared to bridging covered stents, which he defined as any death or rupture related to a side-branch complication.
Concluding his presentation, Spanos conveyed that although performance of bridging covered stents versus self-expanding stent grafts was similar, current data from retrospective studies suggest that overall target vessel instability and reintervention rates are favourable for self-expanding grafts as bridging stent grafts in BEVAR. Finally, Spanos remarked that further research in the form of randomised controlled trials may be needed in this area.
Thursday 27 April 2023 14 THIRD EDITION #CX2023 New Juxtarenal Data
Eric Verhoeven
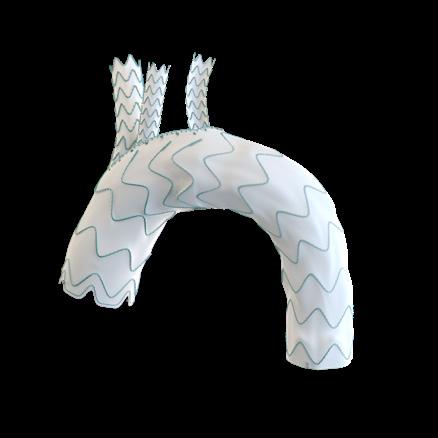
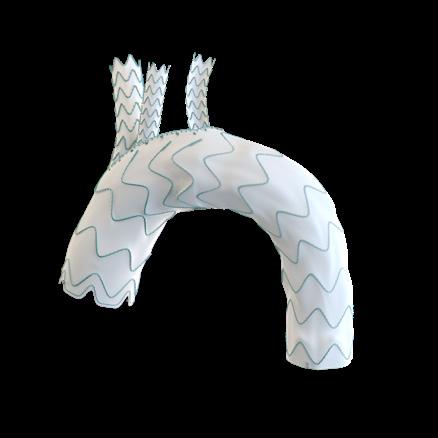
• Small aortic bifurcations
• Excellent control of distal alignment
• 0-90o infrarenal angle
• Pararenal sealing
• Conformable leg extension design
• Ultra-low profile 14Fr delivery system



• Fully re-positional for accurate placement









• Trimodular design

• Helical leg extension design




• Ultra-low profile
• Leave-behind sheath
Every AAA patient deserves the most appropriate treatment... ... and we have the right solution for each one of them.
most complete portfolio for EVAR
F19 ©2023 Lombard Medical. All rights reserved
The
Come visit us at booth
Abstracts session to feature up-and-coming vascular surgeons
Making up part of the chronic limb-threatening ischaemia (CLTI) and hurting leg programme today will be a special ‘best of abstracts’ session dedicated to showcasing the vascular world’s ‘rising stars’—early-career and trainee vascular surgeons. There will be an opportunity following each presentation for the audience to ask questions and participate in stimulating discussion.
ANCHOR SOPHIE RENTON (LONDON, United Kingdom) and moderator Jonathan Boyle (Cambridge, United Kingdom) oversee the session, and Boyle spoke to CX Daily News ahead of the presentations on what it means to be a vascular surgery ‘rising star’, and what they are looking forward to in tomorrow’s session, taking place 10:30–12:00 in Kensington 2. For Boyle, “it is vital that young researchers get an opportunity to present their work at prestigious international meetings such as [CX] to support their academic development”. The moderator added that the delegates benefit too—from learning about cutting-edge and innovative vascular research topics. Asked what he was most looking forward to about the session, Boyle said it was the “innovative research into peripheral arterial disease [PAD]”.
Zhi Xuan Low from Singapore will be first to step up to the podium, presenting ‘Outcomes of maggot debridement therapy as adjunctive wound care for peripheral arterial wounds: Observations from a single-centre, multi-ethnic population’.
Second to speak on her abstract will be Alice
SATELLITE PREVIEW
Camagni (Forli-Cesena, Italy), who has evaluated the impact of retrograde revascularisation techniques in endovascular treatment of infrapopliteal lesions in diabetic patients with CLTI. On a similar topic will be Elisa Piccolo’s (Abano Terme, Italy) presentation of the clinical and technically successful results of
endovascular revascularisation for diabetic patients with CLTI and high-grade medial arterial calcification. Some of the further abstracts featuring in the session will shed light on ‘Predicting functional outcomes after major lower limb amputation’, on which Arsalan Wafi (London, United Kingdom) will present, as well as operator-performed peripheral nerve blocks for pain management during endovascular interventions, and whether female gender is associated with longer hospital stays postinfrainguinal bypass for PAD.
The conclusion of the ‘best abstracts’ session will bring the Hurting Leg Competition for trainees and medical students, organised in collaboration with the Rouleaux Club (the Vascular Society of Great Britain and Ireland’s trainee association). Renton will chair alongside Rouleaux Club president Leanna Erete (Middlesbrough, United Kingdom). The audience will be able to vote for whichever of the five infographic and two infomercial entries they deem to best meet the brief of educating members of the public on CLTI and the need to present early to their general practitioner (GP) or family doctor. Among the messages of the shortlisted entries are “listen to your legs” and “arterial disease can
All times are London time BST (British Summer Time), which is GMT+1. The organisers reserve the right to alter timings if necessary.
Thursday 27 April: Satellite symposia
Benefits of clinical longevity through custom solutions
09:40–09:45
The clinical importance that relay branched platform offers

Speaker: Maani Hakimi, Luzern, Switzerland
09:45–09:50
Simplifying complex thoraco-abdominal challenges with two devices: Fen Anaconda & Fen Treo
Speaker: Florian Elger, Göttingen, Germany
09:50–09:55
Treating the untreatable complexities: CM ThoracoFlo
Speaker: Alexander Zimmermann, Zürich, Switzerland

09:55–10:00
The clinical benefits of physician-modified Treo platform: IDE results so far
Speaker: Dean Arnaoutakis, Tampa, United States
10:00–10:10
Audience participation & discussion
Sirolimus-coated balloon: The next step in PAD treatment
15:20–15:21
Introduction and session objectives
15:21–15:31
Thirty six-month result from XTOSI and updates from FUTURE BTK and SFA
Speaker: Edward Choke, Bukit Merah, Singapore
15:31–15:41
Debate BTK Duell—Case presentations
Speaker: Francesco Liistro, Arezzo, Italy
15:41–15:50
Discussion and conclusion
Treating thoracoabdominal aorta; what are the options?
Moderator: Tilo Kölbel, Hamburg, Germany
Faculty: Luca Bertoglio, Brescia, Italy; Tomasz Jakimowicz, Warsaw, Poland; Timothy Resch, Copenhagen, Denmark
12:30–12:33
Introduction
Speaker: Tilo Kölbel, Hamburg, Germany
12:33–12:39
How do you address renal patency issues at the planning stage?
12:39–12:45
When do you choose an inner branch vs an inner/ outer branch?
12:45–12:51
What is your design preference when treating chronic dissections?
12:51–12:57
When do you use a t-Branch in thoracoabdominal repair?
12:57–13:00
Audience participation & discussion
Thursday 27 April 2023 16 THIRD EDITION #CX2023
Kensington 1 — 09:40–10:10
Kensington 1 — 12:30–13:00
Kensington 2 — 15:20–15:50
It is vital that young researchers get an opportunity to present their work at prestigious international meetings such as CX, to support their academic development.”
FUTURE LEADERS
Jonathan Boyle
Vascular Trauma Consensus
Vascular trauma session offers ischaemia insights
Among the highlights from yesterday’s vascular trauma session were two initial presentations on resuscitative endovascular balloon occlusion of the aorta (REBOA), as well as several short presentations and discussions on blunt cerebrovascular injuries. A concluding talk on opportunities for training in emergency open approaches given by Inova Lee (London, United Kingdom).
Robert Lendrum (London, United Kingdom) opened proceedings with
a presentation on the refinement of REBOA for major vessel injury. After this came Megan Foley (Dublin, Ireland), who highlighted the potential complications of REBOA and suggested that further research is needed on what subset of patients benefit from the intervention. She presented a systematic review and meta-analysis of lower extremity vascular complications after arterial access for REBOA.
The analysis drew on 28 studies with 887 patients from 11 countries—though no randomised controlled trials were included. Of those 28, 13 studies had previously been employed in another metaanalysis led by Ramiro ManzanoNunez (Cali, Colombia). Foley et al’s analysis found that up to 10% of patients who undergo REBOA will experience a lower extremity vascular complication. Foley noted the study’s focus on lower limb complications and some source data’s heterogeneity and methodological quality as limitations, and concluded that future research should home in on trauma patients most likely to benefit from REBOA.
Following Foley was Deborah Low (London, United Kingdom), who evaluated endovascular management of penetrating limb trauma, and whose take-home message drew on experience of

lower limb trauma in an urban trauma centre. Overall, a small proportion (6%) of all lower limb injuries were suitable for endovascular management. She said that computed tomography angiography (CTA) should be the initial imaging modality for assessing them, before giving examples of endovascular management in pseudoaneurysm and arteriovenous fistula (AVF), the main forms of management for which she outlined as embolisation and stent grafts. A poll after Low’s presentation asking the audience to agree or disagree with the statement “REBOA is an essential tool for vascular trauma management” found 77% agreed and 23% disagreed. Speaking as part of the cerebrovascular trauma phase of the session, Morgan McMonagle (Waterford, Ireland) delivered a talk on the management of penetrating carotid and vertebral injuries. His concluding message was “keep it simple!”, and he advised his audience to focus on protecting the airway, and to consider the zones of the neck with a “no zone” approach. “Always prepare the chest in the
field,” he urged, in case proximal control cannot be obtained in the neck itself.
Ligation, meanwhile, was best avoided except when strictly necessary, while repair “will almost always require an interposition graft”, which he said can be a synthetic rather than autologous graft. Finally, he suggested that interventional radiologists may have a role in the management of vertebral injuries, if the patient is well enough.
“Otherwise,” he said, “familiarise yourself with dissecting the vertebral vessels.”
Rounding out the vascular trauma session was a ‘best of abstracts’ section, in which Hannah O’Neill (Aberdeen, United Kingdom) put forward details of a systematic review into endovascular techniques’ role in the management of blunt popliteal artery injury. Considering the popliteal artery’s “relative inaccessibility” and is proximity to neurovascular structures, O’Neill drew on the findings of the review, which analysed data from seven studies, to suggest that open repair “remains the gold standard,” though she said there is a “potential role for endovascular therapy”.

FlowTriever ®
Join our experts at the Venous Workshop to
FlowTriever® and ClotTriever® systems
Discuss DVT and acute PE case studies
The latest clinical studies: CLOUT, FLASH & FLAME
ClotTriever ®
Thursday 27th April 10:00 - 16:00
East Wing (Level –2) Workshop area next to the 3rd auditorium:
The Admiral Dr Emma Wilton Vascular Surgery (UK)
The FlowTriever® Retrieval/Aspiration System is indicated for (1) the non-surgical removal of emboli and thrombi from blood vessels; and (2) injection, infusion and/or aspiration of contrast media and other fluids into or from a blood vessel. The FlowTriever system is intended for use in the peripheral vasculature and for the treatment of pulmonary embolism. Indications, Contraindications, warnings and instructions for use can be found in the product labeling supplied with each device. Caution: Federal (USA) law restricts this device to sale by or on the order of a physician. All trademarks are property of their respective owners.


Dr Nicolas Mouawad Vascular Surgery (USA)

The
with each device. Caution: Federal (USA) law restricts this device to sale by or on the order of a physician.
Thursday 27 April 2023 18 THIRD EDITION #CX2023 Vascular Trauma
Remove clot. Restore flow. Lytic-free approach.
ClotTriever® Thrombectomy System is indicated for the non-surgical removal of thrombi and emboli from blood vessels, and for injection, infusion, and/or aspiration of contrast media and other fluids into or from a blood vessel, for use in the lower peripheral vasculature, including Deep Vein Thrombosis. Indications, Contraindications, warnings and instructions for use can be found in the product labeling supplied
• • •
about:
learn more
Megan Foley
The next fenestrated device: A gamechanger in the aortic space?
Inter-hospital transfers of patients with ruptured AAA influence outcomes
TCAR is better than percutaneous carotid stenting
Vascular trauma
REBOA is an essential tool for vascular trauma management
Aneurysm sac change can be used to develop a dynamic personalised risk prediction model of long-term endograft complications after EVAR Agree % Agree %
19 Thursday 27 April 2023 THIRD EDITION #CX2023 89% 11
Statins save
57 43 AAA
%
lives CX audience members have their say on statins in the setting of aortic repair
Ruptured
AAA
Aortic abstracts
Acute stroke Agree % Disagree % Agree % Disagree % For the motion % Against the motion %
Juxtarenal aortic
Agree Disagree POLL RESULTS 48 52 29 71
Disagree % Disagree % 77 90 23 10
EnChEVAR with Endurant™ II/IIs stent graft system + Radiant™ balloon-expandable covered stent

EnChEVAR. Elevating ChEVAR therapy.
1.6 % late new onset of type Ia endoleak 1
95.7 % chimney graft patency 1
Tested, proven, for ChEVAR
See the device manual for detailed information regarding the instructions for use, indications, contraindications, warnings, precautions, and potential adverse events. For further information, contact your local Medtronic representative and/or consult the Medtronic website at medtronic.eu.
1 Donas KP, et al. J Vasc Surg. 2016;63:1-7.
Medtronic.com/aorticpartnerglobal
UC202312111-01 EE ©2023 Medtronic. Medtronic and the Medtronic logo are trademarks of Medtronic. All other brands are trademarks of a Medtronic company. Not for distribution in the USA and France. 04/2023