CIRSE curriculum update targets greater harmonisation and improvement in global IR training standards
In February 2023, the Cardiovascular and Interventional Radiological Society of Europe (CIRSE), in conjunction with the European Union of Medical Specialists (UEMS) Interventional Radiology (IR) division, published a new curriculum and syllabus, an update to the previous version released five years prior. According to the CIRSE website, the society provides interventional radiologists with the curriculum and syllabus so they have access to “a standardised IR training guideline that covers the breadth of clinical and technical skills that are needed to perform safe and effective treatments”.
Different countries have different requirements when it comes to declaring interventional radiologists ‘qualified’, and therefore, there can be variation in knowledge and skill bases from one country to another. However, CIRSE’s European Board of Interventional Radiology (EBIR) qualification is one example of a “voluntary and supplemental” certification that has widespread recognition, and is designed to demonstrate holders’ commitment to, and competency in IR. The updated European Curriculum and Syllabus for Interventional Radiology “serves as the framework for the EBIR examination” and is the basis for the ‘blueprint’ used to create examination questions.
In December 2021, CIRSE created a task force for updating the curriculum, which the website states is “the most comprehensive” of all available IR curricula. Between then and February this year, chairperson Raman Uberoi (Oxford University Hospitals, Oxford, UK) and 17 international task force members have adapted the latest version. Mick Lee (University of Medicine and Health Sciences, Royal College of Surgeons, Dublin, Ireland), who led the European Training Requirements (ETR) group, also succeeded in getting the new version included among the European Training Requirements (ETR) at the UEMS. They did this by rewriting large sections of the document to reflect the advancements in IR that have occurred in the last five years, as well as the new quality standards necessary for modern IR training.
Curriculum task force chairperson on the updates
Speaking to Interventional News, Uberoi provided insight into the importance of the syllabus—“in 2006, the CIRSE board recognised the need to standardise IR training and assessment across Europe so that patients get the best treatments possible regardless of geography by well trained IR clinicians. In
2

Profile: Farah Gillan Irani

page 20
CRLM: Bridging to transplant


page 28
New report returns to issue of improving UK’s paediatric IR provision
IN 2010, THE UK ROYAL COLLEGE of Radiologists (RCR) with the Royal College of Paediatrics and Child Health (RCPCH) published a report focused on how to improve paediatric interventional radiology (PIR) services. In June 2023, an updated report was published, this time by the RCR on its own. The purpose of the report is to “identify how PIR services can be expanded and improved” and “suggest solutions” that can be enacted by commissioners, healthcare leaders and hospitals. The conclusion of the 2023 report states that “the 2010 report recognised the value and importance of PIR to the National Health Service (NHS) and made recommendations to grow and support PIR but has not driven change”. In light of this, what do the updated recommendations suggest is needed to drive change successfully this time round?
other words, this means that no matter where future young IR trainees practice, they would achieve the same fundamental competencies.” He went on to explain that this led to the first European curriculum being published in 2013, with this latest edition the third iteration. In Uberoi’s words, “it sets out the objectives, learning methods, outcomes, supervision and assessment of IR training, forming the basis of the syllabus used to blueprint the EBIR (European Board of Interventional Radiology) examination, a high-level professional global examination of IR competence”. There are now almost 1,500 EBIR holders across the world, he added.
What has changed in this version?
When asked about the major changes from the last version of the curriculum, Uberoi clarified that the amendments and additions as a whole “[ensures] that IR education continues to adapt to the changing environment, work practices and needs of current and future interventional radiologists”. Specifically, the changes include a “greater emphasis on clinical responsibility and training requirements for new procedures,” a more “streamlined format”, and creation of four chapters dedicated

The introduction to the report seeks to clarify that “PIR is more than just IR in children, and requires specific skills, staff and infrastructure to be done right”. In spite of this, according to the latest RCR workforce census, the UK has 743 consultant interventional radiologists, but less than 20 of those are formal PIR posts. The report goes on to state how the majority of these posts are in London, meaning children and families across most of the UK do not have easy access to PIR services. The RCR’s goal in providing an update to the joint report is to finally “bring PIR service provision into the 21st century”.
PIR in the UK in 2023
The main body of the report begins by listing the advantages to making PIR services fit for purpose, which will bring about faster recovery times through less invasive procedures, and therefore the use of fewer inpatient beds and other resources, as well as a more manageable experience for the patient and their family. The report further informs readers that there is, roughly, only one paediatric interventional radiologist per million children in the UK, to the USA’s one per 342,000 children. Moreover, it states, there is roughly one adult interventional radiologist per 74,000 adults in the UK, yet even this is jeopardised by the “[worrying]” shortage of radiologists generally.
Continued on page 5
Continued on page 4
www.interventionalnews.com
It is another step on the road for interventional radiologists in forging their own destiny.”
Mick Lee
September 2023 | Issue 91
Brian Stainken: Editorial opinion page
What’s better, what’s not, and what’s next
Interventional News began more than 20 years ago as an effort to better cover the global interventional space, selecting news stories and other content that is not the province of peer-reported journals, but still important to the practising interventionalist. We focus on content that is relevant and on conversations that you might not hear on other channels.
Iam a newly retired, USA-based interventional radiologist. I finished fellowship training in 1992 and enjoyed a practice in both clinical and academic environments. It has been a privilege and an education to watch our profession evolve over the past half-century (yes, the Society of Interventional Radiology [SIR] turns 50 this year!) As a past leader in SIR, with a leadership focus on international interventional radiology (IR), I have had a front row seat for at least half of that time, so I thought I would offer one man’s perspective on what’s better, what’s not, and what’s next. When you read this, understand my focus is our global IR community and that my opinions are not necessarily Prof Adam’s (my co-editor-in-chief), Interventional News’, or those of our representative societies. Let us start with the good news:
What’s better:
1. Our tools. Frankly, IR is a lot easier now because the random stent migrations, wire fractures, ‘stuck’ devices and oversized introducers are mostly a thing of the past. We even have devices for haemostasis! As a fellow, after a long lytic case, I still remember holding groins for days…This evolution in equipment has allowed our field to advance into progressively more novel and technically demanding approaches, solving more problems with less risk compared with the alternatives. But we should never fall for the fallacy that there is any relationship between introducer size and risk. As many of us know based on first-hand experience, one disadvantage of IR access approaches when compared with predicate open procedures is potential for loss of control. A poorly trained provider can do a lot of harm through a small hole. As IR becomes ever more complicated, we need to accept that our training and certification systems must evolve in parallel, on a global scale.
2. Our culture. Dotter’s vision has arrived. IR is for patients, not procedures. This culture becomes a progressively
important bedrock as our techniques mature and tools improve. It is all too easy to apply low- or no-risk solutions. It is not just risk/benefit that matters, it is also about alternatives. Like any surgeon, when we can avoid a procedure, we must. A great example is supervised exercise for claudication. Many patients do not want it over a simple percutaneous transluminal angioplasty [PTA], but unless and until there is a proven benefit for superficial femoral artery interventions over no intervention for claudicants, we must stand down. Yes, the data may say others do it more and we will lose market share, yes the patient may go to the ‘competition’, but our culture must be about standards of practice, clinical integrity, rigorous training and professional certification. Our superpower is a cautious culture that maximises the public benefit of our tools because we put our patients first.
3. Imaging. Am I the only one who remembers Dr McCoy solving problems on Star Trek with his ‘wand’ thing? Look like an ultrasound probe to anyone else? I bet that McCoy had at least four years of training and demonstrated clinical imaging competency before they let him apply it to the crew of the Enterprise. In the USA, IR is the primary specialty that delivers image-guided care. As the imaging tools used to guide our solutions evolve, the fundamental need for demonstrable core imaging competency among IR providers will grow. Advances in imaging have made IR better, for sure, but that is only evident and possible if you understand what you are looking at. Excellence in IR requires excellence in imaging.
What’s not:
Brian Stainken
1. We can’t do it all. It was amazing to learn IR in a time when the specialty had no boundaries other than solving a problem in a better way. I am not sure what I will do with the skill sets like building endografts, cannulating pedal lymphatics, freezing prostates with five 24Fr probes, or mounting stents on balloons—by hand. At the time, it was what we had to work with. For the future, we must accept that core IR requires advanced training and certification. Subspecialised IR requires even more to establish clinical equipoise and meet our specialty’s culture of excellence. You cannot do it all. When it is outside your wheelhouse, refer. Embrace subspecialised practice. Be the best.
2. We are no longer alone. We should do a better job looking at the macroeconomics of disease state management. What are the least expensive, most efficacious solutions? In the USA, our payment structures and departmental hospital structures can interfere with closer collaboration among professional peers. Globally, regulators and payors or hospitals often restrict less invasive advances in care because of bias, or overly simplistic/outdated thinking. The result is that far too
The latest stories from the interventional world

n CIRSE PUBLICATION, PREDATING US FDA LETTER, SUPPORTS USE OF PACLITAXELCOATED DEVICES:
The Cardiovascular and Interventional Radiological Society of Europe (CIRSE) editorial, written and accepted for publication in CardioVascular Interventional Radiology (CVIR) before the US Food and Drug Administration (FDA) letter, refutes a mortality signal for paclitaxel. The editorial coincided with the publication of the US FDA letter in July, stating that the data do not show excess mortality risk.
For more on this story go to page 6.
n NEW RENAL TECHNOLOGIES: FROM RADIAL ACCESS TO CT ANGIOGRAPHY:
Olivier Pellerin (Université de Paris, Paris, France) presented on technological updates in the renal space at the Global Embolization Symposium Technologies meeting GEST, 18–21 May, New York City, USA).
During his presentation, he delved into radial access, computed tomography (CT) angiography, among other advancements in the space.
For more on this story go to page 11.
n COMMENT: ADVANCES IN PANCREATIC CANCER THERAPIES:
Ripal Gandhi is a vascular and interventional radiologist at Miami Cardiac and Vascular Institute and Miami Cancer Institute (Miami, USA) and writes on the intra-arterial approach to locally advanced pancreatic cancer for Interventional News. He describes the procedure of transarterial microperfusion and a current study comparing its efficacy to the standard of care in patients with pancreatic cancer.

For more on this story go to page 26.
Andreas Adam


Continued on page 4
Editors-in-chief: Professor Andy Adam, Dr Brian Stainken | Publisher: Roger Greenhalgh | Content director: Urmila Kerslake | Head of Global News: Sean Langer

Editor: Clare Tierney | Editorial contribution: Jocelyn Hudson, Will Date, Bryan Kay, Jamie Bell, Benjamin Roche, Eva Malpass and Adam Pearce
Design: Terry Hawes, Wes Mitchell and David Reekie
Advertising: Michael Broughton michael@bibamedical.com
Subscriptions: subscriptions@bibamedical.com
write
September 2023 | Issue91 2 EDITOR’S LETTER interventionalnews linkedin.com/company/interventional-news/ @in_publishing Published by: BIBA News, which is a subsidiary of BIBA Medical Ltd | BIBA Medical, Europe, 526 Fulham Road, Fulham, London, SW6 5NR, United Kingdom Tel: +44 (0) 20 7736 8788 BIBA Medical, North America, 155 North Wacker Drive, Suite 4250, Chicago, IL 60606, United States Tel: +1 708-770-7323 Printed by: Buxton Press Reprint requests and all correspondence regarding the newspaper should be addressed to the editor at the United Kingdom address. © BIBA Medical Ltd, 2023. All rights reserved.
clare@bibamedical.com
If you have comments on this issue or suggestions for upcoming editions
to
News in brief


MORE OPTIONS. MORE INDIVIDUALIZED TREATMENT. Our innovative product portfolio provides expanded options to individualize HCC treatments. IS1540GB0623MVII Not all products are available for sale in all countries. This information is provided only in respect to markets where these products are approved or cleared. Not all products are cleared or approved in the U.S.A. by the Food and Drug Administration. Please contact your Terumo local sales representative for more information. www.terumo-europe.com
Continued from page 2
COVER
continued
CIRSE curriculum update targets greater harmonisation and improvement in global IR training standards
Continued from page 1 many open procedures are done around the world simply because the local system favours sutures over devices! We need to work together to educate stakeholders about the economics of the solutions we bring. IR is more flexible, and it is cheaper and safer when delivered by well trained providers. We need to make our case and champion a right of access to IR care around the world.
What’s next:
1. Grow global training. Our existing national societies are busy working on the needs of their members as they should. But we need to accept that the ultimate success of IR as a specialty, to some degree, rests in the development of skilled providers worldwide. There are not enough interventional radiologists, and far too few training options for most young doctors interested in the field. This is not insurmountable, but our strategy must change. Rather than funnelling trainees through a few excellent centres located far from home, we must build our in-country ‘national’ training centres. Training concepts and best practice strategies should be shared among centres. Other national groups should mentor, endorse, and provide needed faculty. To do this we need money! This is where our major societies need to join with industry to create a fund/ foundation focused on improving access to quality IR worldwide through the development of in-country training centres.
2. Demand recognition/access/payment. Show me a country that does not recognise our peers in cardiology or vascular surgery. IR is a primary specialty with a unique competency that must be recognised. We need to focus and drive this message home, worldwide. It is time to collaborate to achieve the global goal of professional recognition.
to interventional oncology (IO). Uberoi also mentioned that the curriculum specifies the level trainees must have reached in core competencies by different points in their training. Regarding regulatory bodies, the chairperson noted that the curriculum reflects what national IR accreditation boards expect of their interventional radiologists, in addition to the UEMS.
The curriculum goes beyond requirements for trainees, it also sets out the requirements for trainers and training centres too, Uberoi continued, “to ensure that trainers are appropriately qualified to train and that training centres have the right infrastructure to support training”. An example of these requirements is that, depending on the centre, trainees may need to rotate between hospitals to gain sufficient exposure to, and practice in, different procedures.
Finally, Uberoi touched on how the curriculum pertains to EBIR examinations, “the traffic light system has also been updated to make it easier for candidates to focus on the most commonly assessed areas of IR practice” when preparing for assessment. “The objective is always to improve the training and quality of interventional radiologists in Europe and globally, and ultimately patient outcomes and care,” Uberoi concluded.
The importance of inclusion in the ETR

As referred to above, being included in the ETR is a significant achievement. The stringent requirements are set out by the body responsible for standardising medical training across European countries: the UEMS. Recognition by the UEMS represents a “strong recommendation for national medical authorities all over Europe” to adopt these requirements and the corresponding assessment for national IR training pathways. This will increase the likelihood that interventional radiologists in different countries, at least in Europe, will have harmonised training and achieve common standards and competencies, leading to greater uniformity in IR care provisions across the continent.
The longer-term impact?

Asked to elaborate on the mid- to long-term impact of the UEMS approval, Lee opined that with “this IR training curriculum, and with competency assessment through the EBIR, patients will be treated safely and effectively throughout Europe, and perhaps, in the fullness of time, the putative goal of harmonisation of training across Europe, and the free movement of IR professionals across borders, will become a reality”.

Like Uberoi, Lee emphasised the significance of the curriculum including the resources and requirements for trainers and training institutions, as this has not been done in previous versions. This will enable “robust training”, he added, the product of which will be “doctors who are fit for purpose”. Moreover, Lee underlined how important it is that the curriculum and UEMS endorsement break new ground—“it is another step on the road for interventional radiologists in forging their own destiny”.
Benefits of multilingual curriculum and syllabus “manifold”

Maria Weren, head of certification and accreditation at CIRSE, added her voice to the discussion on the latest curriculum update. She began by outlining how this comprehensive training programme consisting of a curriculum, an examination, an article and structured learning resources can be “easily, fully or partially, adopted by, or integrated into, national training and certification pathways, which will push clinical services in IR and support the further development of IR as an established and growing medical field”. The ultimate goal off the back of this is that, with more trained practitioners, more patients can access IR services, she expanded. Regarding access to the curriculum itself, Weren averred that there are plans to publish it in additional languages, “not least because the [EBIR] examination is offered in German and Spanish through collaboration with national IR societies”. Probed as to the potential global reach of a multilingual curriculum and EBIR, Weren set out benefits to interventional radiologists in and outside of Europe using them. “All areas of the broad medical field are covered, [meaning] an interventional radiologist [can] expand their general IR knowledge and have this excellent knowledge base attested to through EBIR certification. Widespread recognition also allows greater job mobility and can be a real career boost for young doctors. In countries like Switzerland or Germany, the qualification has found its way into hospital accreditation, which means it is a prerequisite for centres to employ certified interventional radiologists.”
If you have made it to this point, thanks. I would love to hear your thoughts. Email me via the editor at eva@ bibamedical.com.
Lee, the aforementioned leader of the group dedicated to achieving this milestone, and president of the UEMS’s IR division, weighed in on why UEMS endorsement matters: “For the first time, the Division of IR of the UEMS Radiology section and CIRSE collaborated to produce this third edition of the curriculum and syllabus. The IR curriculum underwent a rigorous appraisal by all of the other UEMS medical specialties and was eventually approved by the UEMS Council in October 2022 with universal support. This is a landmark achievement for European IR and potentially a potent mechanism for achieving the necessary resources to structure and run competent IR training programmes across Europe.”
Supplementing this, Weren mentioned that EBIR diploma holders “can also gain advanced certification in the field of endovascular therapy, as CIRSE also offers the European Certification for Endovascular Specialists”. She explained that this is a documented-experience certification that aims to further recognition of interventional radiologists as experts in minimally invasive and image-guided endovascular treatment.
Weren’s final note summarises the importance of the new curriculum and syllabus and its endorsement by over 40 national IR societies, within and outside Europe, “whose common goal is to strengthen IR and help many patients with its minimally invasive therapy options”.

4 September 2023 | Issue91 Editor’s Letter/Cover Story
STORY
BRIAN STAINKEN is joint editor-inchief of Interventional News
EDITOR’S LETTER continued
What’s better, what’s not, and what’s next
Maria Weren
Raman Uberoi Mick Lee
Far too many open procedures are done around the world simply because the local system favours sutures over devices!”
New report returns to issue of improving UK’s paediatric IR provision
Continued from page 1
The report also outlines how PIR services are currently delivered, and that a variety of models are used. In a small number of hospitals, the entire PIR service is delivered by paediatric interventional radiologists. In others, some procedures are carried out by adult interventional radiologists, some by paediatric diagnostic radiologists, and others by paediatric interventional radiologists. There are further centres where PIR services are either carried out by adult interventional radiologists, or commissioned to a paediatric specialist at another centre. Beyond this, there are centres where there is no provision in the wider region beyond an adult IR, which can take care of some procedures, but not all.

Acknowledging that some progress has been made

Although the report laments that the 2010 RCR/RCPCH document “has not

driven change”, it acknowledges that the latter may have had a hand in bringing about certain recent advances that the RCR “welcome[s]”. These include a new IR training post at Birmingham Children’s Hospital (Birmingham, UK), the second national PIR training post in the UK, and the recent integration of PIR into the adult IR training programme at Guy’s and St Thomas’ and the Evelina London Children’s Hospitals (London, UK). Recently, additional PIR posts have been created at Leeds Children’s Hospital (Leeds, UK), Alder Hey Children’s Hospital (Liverpool, UK), and The Royal Hospital for Children (Glasgow, UK). Beyond this, the RCR has collaborated with the British Society of Interventional Radiology (BSIR)’s PIR special interest group on “the development of a rolling PIR cross-skilling programme, aimed at adult IRs, paediatric diagnostic radiologists, surgeons and anaesthetists”. Nevertheless, the report proceeds to question whether PIR can become centrally funded “so organisations do not view it as an unfeasible financial burden”, which is a current barrier to these positive steps being more widespread.
Solutions set out in the report
In terms of recommended action from various colleges and governmental bodies, the 2023 report echoes much of that which was stipulated 13 years prior. Firstly, to address the

shortfall in numbers of PIR consultants, the report advocates for doubling the PIR consultant posts available every five years, so that there are 96 in the UK by 2038. Linked to this, crossskilling, such as has been discussed in collaboration with BSIR, is also key, the RCR believes, as there are insufficient numbers of doctors across radiology and IR, among other specialties, which can impact existing PIR care offered under the various models enumerated above. Adult IR, paediatric surgeons, anaesthetists, radiographers, and nurses could be trained in certain areas of PIR care provision to help compensate for inadequate numbers of PIR serviceproviding consultants.
The report further recommends that national training bodies such as Health Education England could provide funding for PIR trainee posts, open to final-year (ST6) trainees in IR or paediatric radiology. There is also a need “to consider how to better integrate PIR into existing training curricula” to address the problem of the “relative invisibility” of PIR to medical students and junior doctors.

Regarding how to deliver a PIR service, the report emphasises the need for a “clear PIR service delivery policy in all hospitals that offer care to children”. It adds that “unambiguous arrangements must be in place for the early referral of
children requiring PIR care that cannot be provided locally in a timely manner”. In order to achieve this, PIR must be included in treatment algorithms, local service models and referral pathways, in cooperation with other specialties such as anaesthesia and paediatric surgery.
Speaking to Interventional News, report author and PIR consultant at Great Ormond Street Hospital (London, UK), Alex Barnacle, gave her take on which recommendations will be the easiest to achieve. She believes that PIR in the UK is most likely to see an increase soon in the number of PIR practitioners through cross-skilling of healthcare professionals, and training capacity in PIR, as well as some refinements in how data is collected. On the flip side, substantially increasing PIR consultant post numbers poses the greatest challenge.
Asked to comment on the issues outlined in the report, president of the RCR, Katharine Halliday said: “For some of our sickest children, PIR can be a lifeline, providing minimally invasive treatment and reducing lengthy hospital visits. But too few children, whose lives could be improved through these life-changing procedures, do not have access. We are urging the [UK] Government and trusts to take note: this is highly effective, cost-saving care that desperately needs to be resourced.”
5 Issue91 | September 2023 Paediatric IR in the UK Isolis cryoprobe
isotherms and laser-guided precision. Accelerate procedures and optimize results with innovations designed to facilitate greater accuracy, efficiency, and patient safety. Isolis NEW 510(k) cleared. Currently not available for sale outside the U.S. Scan to discover Isolis and its availability in your market.
Large
Left: Alex Barnacle
Right: Kath Halliday
Organisations [should] not view [PIR] as an unfeasible financial burden.”
FDA removes red flag for paclitaxelcoated devices after review finds data do not support mortality risk
In a letter to healthcare providers dated 11 July 2023, the US Food and Drug Administration (FDA) communicates that the risk of mortality associated with paclitaxel-coated devices to treat peripheral arterial disease (PAD) is no longer supported based on the totality of the available data and analyses.
THIS UPDATE SIGNALS A lowering of the red flag raised in a 2019 letter from the Administration— published in response to a metaanalysis that indicated a late mortality signal—warning that treatment of PAD with paclitaxel-coated balloons
and paclitaxel-eluting stents was “potentially associated with increased mortality”.
Alongside the letter, the US FDA has updated its recommendations for healthcare providers regarding the use of paclitaxel-coated balloons and stents for PAD. As well as removing reference to the possibility of increased mortality with these devices, the amended guidance softens the language around the monitoring of patients who have been treated with paclitaxelcoated stents and balloons, stating that healthcare providers should continue ‘routine’ rather than ‘close’ monitoring of these patients, as had previously been stated.
The safety of paclitaxel—used in peripheral interventions to prevent restenosis—was called into question by data put forward in 2018 by Konstantinos Katsanos (University of Patras, Patras, Greece) et al that pointed to an increased risk of death at two and five years following the use of paclitaxel-coated balloons and paclitaxel-eluting stents in the femoropopliteal artery.
The FDA responded, notifying healthcare providers in early 2019 about a late mortality signal in patients treated for PAD in the femoropopliteal artery with paclitaxelcoated balloons and paclitaxel-eluting
stents. Their most recent update on the topic, prior to that shared on 11 July 2023, was posted in August 2019.
In its new update, the FDA notes that “additional data from the pivotal randomised controlled trials (RCTs) has become available,” and that the Administration has worked with device manufacturers and external stakeholders to develop the protocol and analysis plan for new data generation.
The FDA references the fact that device manufacturers collaborated in an updated meta-analysis, which included “additional studies, more complete vital status information, and longer-term follow-up compared to prior studies”. Patient follow-up in these studies ranged from two to five years, the Administration notes, and led it to conclude that the updated RCT meta-analysis “does not indicate that the use of paclitaxel-coated devices is associated with a late mortality signal”.
BARMER Health Insurance study, the US Veterans Health Administration study and the Medicare SAFE-PAD study. “None of these studies, with mean or median follow-up ranging from 1.7 to 3.5 years, found a risk for late mortality associated with paclitaxel-coated devices,” the FDA communicates, adding that longer-term follow-up in several of these studies is ongoing.
NONE of these studies, with mean or median follow-up ranging from
1.7 3.5
YEARS
found a risk for late mortality associated with paclitaxel-coated devices
Furthermore, the FDA states that it also reviewed additional analyses of the risk for late mortality, including the SWEDEPAD trial interim analysis, the VOYAGER PAD study, the German
CIRSE publication, predating US FDA letter, supports use of paclitaxel-coated devices
The Cardiovascular and Interventional Radiological Society of Europe (CIRSE) editorial, written and accepted for publication in CardioVascular Interventional Radiology (CVIR) before the US Food and Drug Administration (FDA) letter, refutes a mortality signal for paclitaxel. Written on behalf of CIRSE’s Endovascular Subcommittee, the authors “advocate that the benefits of paclitaxel-coated device use in the femoropopliteal segment in terms of increased primary patency and reduced TLR [target lesion revascularisation] warrant their use in the routine treatment of patients with femoropopliteal disease”. The editorial coincided with the publication of the US FDA letter in July, stating that the data do not show that paclitaxel-coated devices come with an excess mortality risk.
THE AUTHORS, INCLUDING corresponding author Robert Morgan (St George’s University Hospitals NHS Foundation Trust, London, UK) begin their editorial by outlining the background to the controversy around use of paclitaxel-coated balloons and paclitaxel-eluting stents. They reference initial “encouraging data” that led to “increasingly widespread” recourse to drug-based therapies to treat peripheral arterial disease (PAD) in femoropopliteal disease up until Katsanos et al published their meta-analysis in 2018. The findings of this meta-analysis—that all-cause mortality following treatment with paclitaxelcoated balloons and paclitaxel-eluting stents in the femoropopliteal segment in claudicants was 14.7% at five years, with the rate post-percutaneous transluminal angioplasty (PTA) calculated as 8.1%—“resulted in a metaphorical tsunami destroying confidence worldwide in paclitaxel” as safe for preventing restenosis.

Morgan et al outline that after the Katsanos meta-analysis was published, the US FDA created
an expert panel to provide updates to healthcare providers. Other national medical regulators also made recommendations in light of the findings to be “[cautious]” in using paclitaxel, with the UK Medicines and Healthcare Products Regulatory Agency (MHRA) among those advocating for limiting its use to patients with chronic limb-threatening ischaemia (CLTI) only. This reduction in use of paclitaxel in these settings led to the “loss of the proven benefits of drug-based device therapies to patients in terms of reduced patency of femoropopliteal angioplasty and stenting using non-paclitaxel-coated devices, and probably an associated increase in the need for hospital readmission rates for repeat revascularisation procedures”.
The editorial proceeds to highlight the findings of a subsequent meta-analysis based on the same randomised trials included by Katsanos et al: “There is a minimal or no increase in mortality associated with paclitaxel-coated devices. Moreover, when the
In a video interview with Interventional News in the wake of the FDA letter, Andrew Holden (Auckland City Hospital, Auckland, New Zealand) described receiving the news with excitement as now, “globally, patients can really benefit from [paclitaxel]-coated devices […] and we can look forward to an era where [unnecessary reintervention and morbidity] no longer occurs”. He also conveyed his pride, “I cannot remember another time in my career where physicians and industry leaders have worked so tirelessly and responsively to achieve such a good outcome”. Finally, he admitted to feeling “challenged”, thinking about how since 2019, in addition to the cost to patients, there has been a significant time and resource cost to physicians and industry.
patient-level data of the trials used for the Katsanos meta-analysis were assessed, the absolute increased mortality risk associated with paclitaxel use at five years decreased from 14.7 to 4.6%.” Morgan et al suggest that the difference in these reported outcomes could be attributed to different study designs and data sources, among other factors.
“One major flaw” in the conclusions reached by Katsanos, the CIRSE editorial opines, is that “none of [the trials included in the meta-analysis] were designed to assess for a difference in mortality between the patient groups”. Morgan et al also list various studies post-Katsanos that suggest paclitaxel to be “associated with improved efficacy but was not associated with increased mortality” (the full list can be found in the footnotes of the CVIR publication).
Rounding off, the CIRSE authors point out that “a robust body of evidence now exists to refute the existence of a long-term mortality signal associated with paclitaxelcoated devices i.e. any mortality risk is negligible or absent”. They conclude that “all efforts to find a link and a causal explanation for the perceived mortality risk between paclitaxel dose and mortality have failed”. Looking to the future, Morgan et al urge that “endovascular trial designs must incorporate strategies and methods to maximise patient retention and facilitate long-term assessment and reporting of vital statistics, including mortality”. In addition, they express their interest in seeing data on the efficacy of sirolimus-eluting devices and on the efficacy of paclitaxel-coated versus sirolimus-eluting devices. For the time being, the authors support using paclitaxel-coated devices in the femoropopliteal segment to increase primary patency and reduce TLR in patients with femoropopliteal disease.
6 September 2023 | Issue91 Paclitaxel Update
PACLITAXEL
Robert Morgan
Embo ASSIST AI
Artifical Intelligence, Augmented Imaging
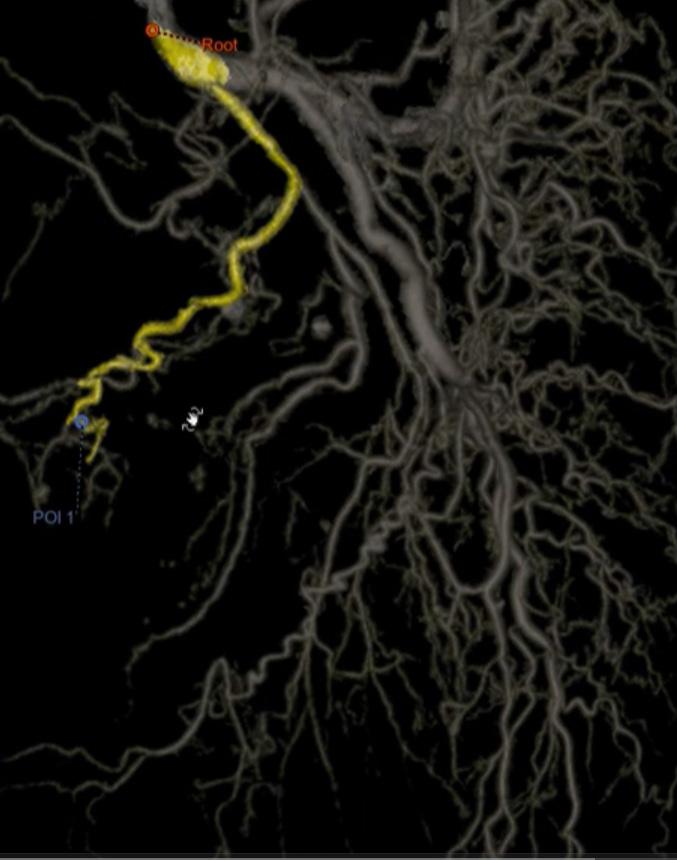
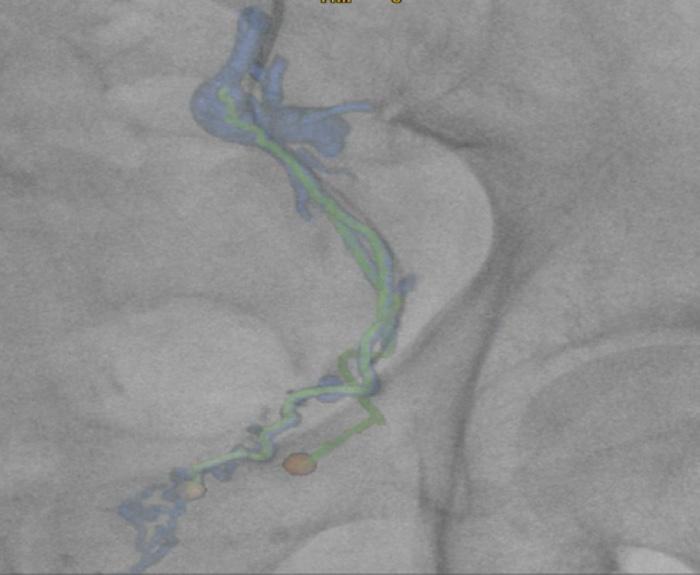
Embo ASSIST AI 1 provides an automated, click-less segmentation of vascular structures from a CBCT and provides easy access to unique Virtual Injection technology to simulate your embolization procedure before you treat
Plan
Automatically segment vascular structures to facilitate embolization workflow planning
Simulate injection points and extract vessels in one click
Guide
Export the 3D-model of selected potential embolization pathways for 3D-fusion guidance
Navigate through tortuous anatomies with the help of Digital Zoom 2
Assess
Visualize distal vessels and blushes with 3DCT HD to confirm catheter location before embolization
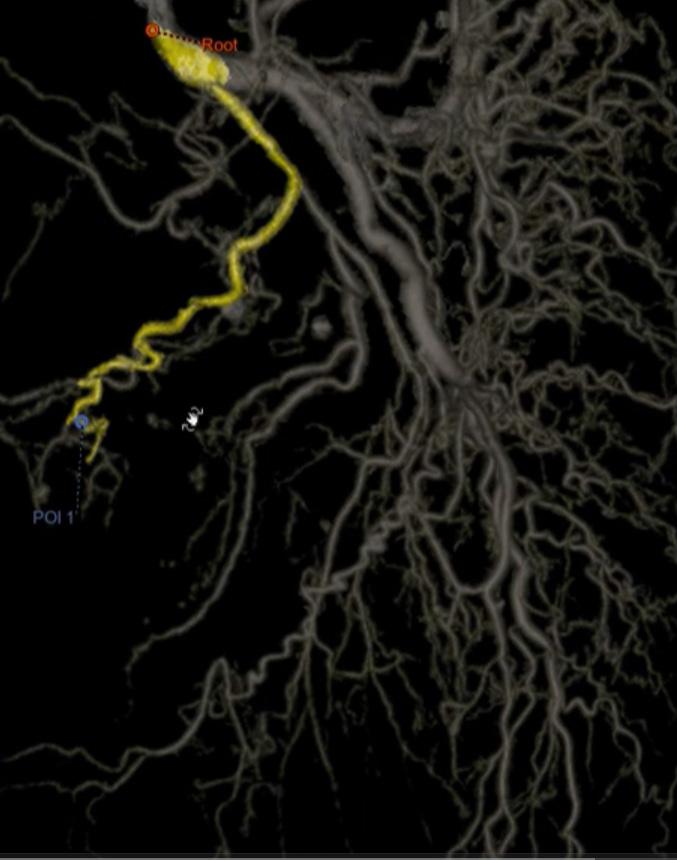
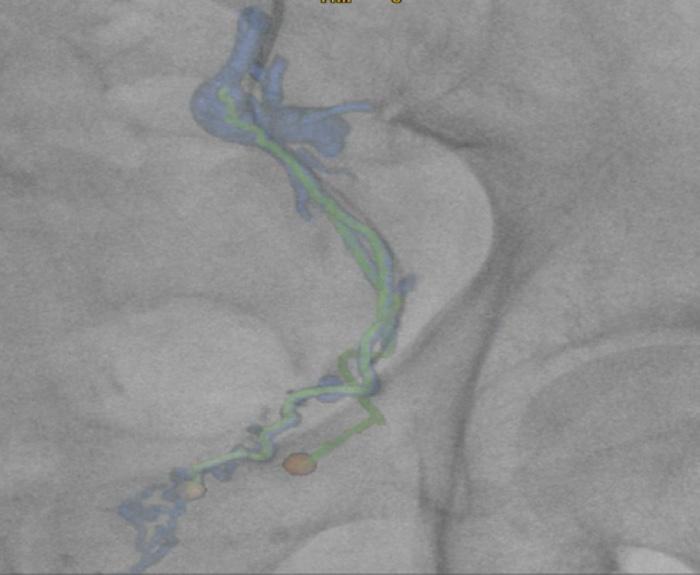

1. Embo ASSIST AI solution includes FlightPlan for Embolization with AI Segmentation option and requires AW workstation with Volume Viewer, Volume Viewer Innova, Vision 2, VesselIQ Xpress, Autobone Xpress. These applications are sold separately. FlightPlan for Embolization with AI Segmentation may not be available in all countries. Refer to your sales representative for more information. 2. The live image display screen of the IGS x-ray system is the reference screen for fluoroscopy during an interventional procedure © 2023 GE HealthCare. GE is a trademark of General Electric Company used under trademark license. JB06680XE

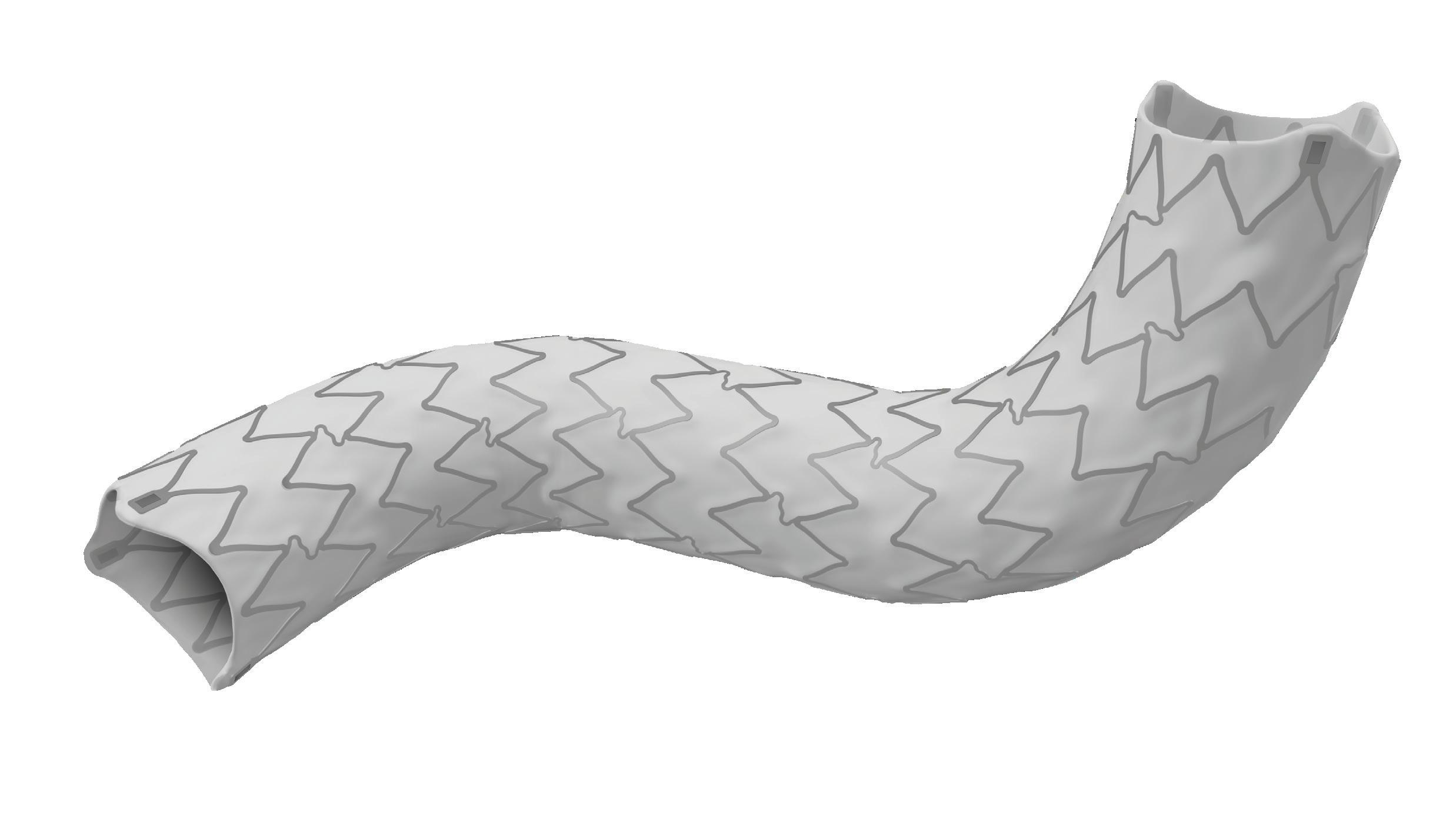

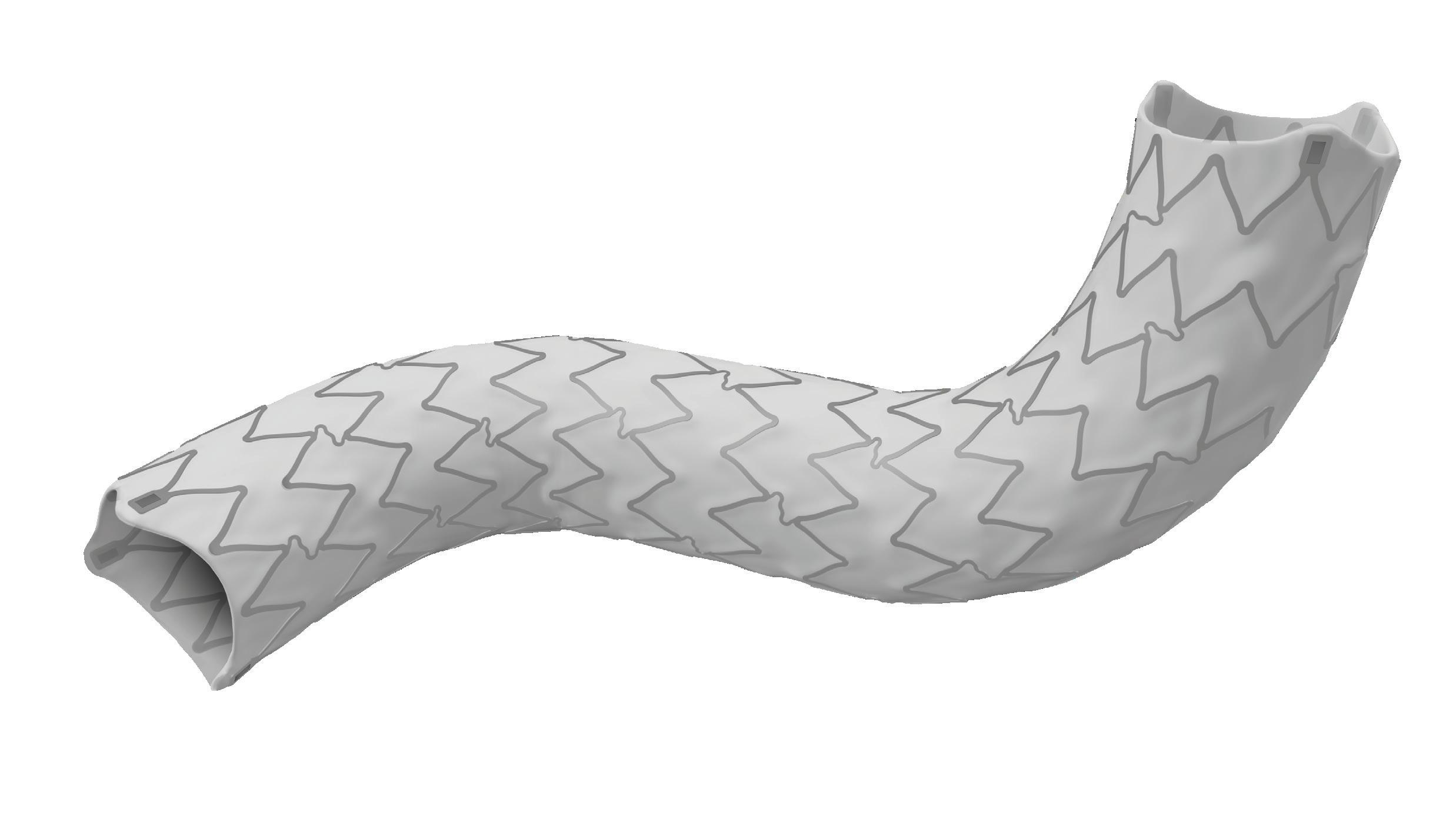
*6F up to 8x17 mm and 7F from 8x27mm up to 10 mm. www.ivascular.global iCover BX ePTFE covered stent The visibility you deserve Smallest profiles 6F introducer compatibility up to 8mm* High flexibility Enhanced visibility Unique stent with radiopaque markers to facilitate the implantation To arrive and treat the most angled arteries Proprietary technology to encapsulate the stent into an inner and outer ePTFE layer TechCover
SIR and Congressional Men’s Health Caucus collaborate on PAE briefing
On 5 June, the Society of Interventional Radiology (SIR) held a briefing in Washington DC, USA, which focused on benign prostate hyperplasia (BPH). The briefing took place in conjunction with the US Congressional Men’s Health Caucus. Shivank Bhatia (University of Miami, Miami, USA) took to the podium to introduce prostate care as an “issue of great importance to men’s health”— all the more relevant the week before National Men’s Health Week (12–18 June) in the USA. His talk during the session centred around prostate artery embolization (PAE).
It was Bruce Kava, professor of urology at the University of Miami, who presented first during the session, outlining what BPH is—“bigger is not always better, and at some point [around the age of 30 for most men], the prostate begins to grow”. The more severe consequences of an enlarged prostate, the audience heard, can include “urinary retention, recurrent infection, bladder stones, or [even] kidney failure”. The symptoms as a whole are classified as lower urinary tract symptoms, or “LUTS”, Kava explained—“the burden of LUTS for people with BPH is immense”. The symptoms are not usually life-threatening, Kava went on, but they create bother, “which translates to lower quality of life, [including] anxiety, depression, and loss of productivity”. Kava then informed his audience that around 25% of men over the age of 50 have LUTS of “at least moderate severity”.
Access to care for BPH—namely medication or surgical procedures— differs based on race, Kava lamented, stating that it is “less for African American and Hispanic males”.
Members of these groups, therefore, “present to the emergency room much more frequently than caucasians do”.
Treatment, when it is accessible, centres on reducing symptom severity, namely improving urinary flow,
reducing urinary tract infections, and improving renal insufficiency. Kava also noted that BPH treatment is designed to slow the growth of the prostate. However, he pointed out that medications show only “modest effects” in terms of International Prostate Symptom Score [IPSS] reduction. The minimally invasive surgical treatment transurethral resection of the prostate (TURP) can be an outstanding option, Kava suggested, but side-effects, which include an overnight hospital stay, occasional bleeding (in particular for larger prostate glands), and ejaculatory dysfunction may mean it is not always the perfect option for some men.
Nowadays, Kava explained that in urology, they have been offering treatment via other modalities, including a number of laser procedures, prostatic urethral lift, water vapor thermotherapy, and aquablation. Size of the prostate is often the key determinant of success with these modalities. For instance, prostatic urethral lift and water vapour thermotherapy are more efficacious with smaller prostate glands. There is demand for a minimally invasive modality that is highly effective in patients with larger prostates, offering rapid recovery and reduces the risk of transfusion and other adverse effects.
The UK’s National Institute for Health and Care Excellence (NICE) announced on 28 June that it recommends the use of radiofrequency ablation (RFA) for the treatment of osteoarthritic knee pain


OSTEOARTHRITIS IS THE MOST COMMON form of arthritis, and for patients who are not yet ready for surgery, RFA pain management products provide minimally invasive relief without the use of opioids by denervating the nerves in the area causing the patient pain.
Bhatia, who is chair of the Department of Interventional Radiology and professor of urology, then took to the podium to speak about prostatic artery embolization (PAE) as the answer to other treatments’ size-related limitations. Bhatia first set out how image-guided interventions—such as PAE—are largely unknown to the public. He then explained that PAE involves using small microsphere to cut off blood flow to large prostates, causing them to shrink.

“Ninety-nine per cent of men eligible for treatment for BPH do not receive invasive therapy,” Bhatia shared, adding that for some, their reason for avoiding treatment will be that they do not like the options available—such as resection. This is where minimally invasive options such as PAE come in. PAE has been US Food and Drug Administrationapproved since 2016.
Bhatia relayed that advantages of PAE over surgical treatment are that it does not require general anaesthesia, is a same-day, outpatient procedure, with no size limit of the prostate. He explained that one can avoid the risk of bleeding and adverse impact on sexual function associated with surgical procedures.
From the patient’s perspective, PAE offers a “90% success rate”, the benchmark for which Bhatia described as around a “50% improvement in symptoms [according to the IPSS]”. After PAE, he went on, the prostate will keep shrinking and will not start growing again “for three to five years”.
Bhatia then shared his centre’s experience treating over 1,000 patients over six years, as presented at the SIR 2023 annual scientific meeting (4–9 March, Phoenix, USA), before thanking his patients for having put “their trust in [him]” to have the PAE procedure. Among the study’s notable findings was a persistent, years-long reduction in prostate size among the patients, he underlined,
From the NICE announcement: “Radiofrequency energy is used to denervate the target nerves. The radiofrequency energy can be delivered as conventional radiofrequency, cooled radiofrequency or pulsed radiofrequency. The aim is to reduce pain and delay the need for knee arthroplasty. There is good evidence to show that this procedure relieves pain in the short term. There are no major safety concerns, and the complications, including numbness, are well recognised.”
“The new interventional procedure recommendations published by NICE is a great
well as dramatic decreases in patients’ IPSS and self-reported quality of life. Bhatia mentioned that one of the most crucial limitations of PAE was the lack of awareness about this procedure.
Following this, one of the first 25 patients treated by Bhatia, Roland Klein, spoke from his point of view on the merits of PAE. “I started having symptoms long before PAE existed,” Klein conveyed, adding how he began researching the various treatments available to him. “I decided I was going to fly to Brazil to try PAE,” he explained, “because it was the least invasive treatment you could possibly get”. As he was continuing to read up on PAE, Klein reported that he saw that the University of Miami was starting a trial programme, “so [he] contacted Dr Bhatia […] was told [he] would be a candidate, and [he then] had the procedure”. In Klein’s eyes, “the procedure is a ‘nothing’ procedure”, involving only a “pinhole” incision and
a few hours in the hospital pre-, during and post-procedure. He reported how he experienced a little pain when urinating for “about three to five days” before returning to work. “It has been nine years, and I still do not have any issues with urination,” he concluded.
In summary, Bhatia and Kava delivered a briefing to the Congressional Men’s Health Caucus, explaining different options available to treat symptoms related to enlarged prostate, with an emphasis on PAE, a minimally invasive option with no risks of sexual side-effects or leakage, no need for a urinary catheter.
step forward to help adopt radiofrequency ablation therapy for the treatment of osteoarthritic knee pain,” said Robin Correa, consultant in Pain Management and Anaesthetics, University Hospitals Coventry and Warwickshire NHS Trust (Coventry, UK). “Having observed the transformation in the quality of life of patients under my care using this treatment, I am delighted to see the publication of the NICE recommendations. I hope this will now help to increase awareness of this innovative therapy leading to improved outcomes for many more patients.”
9 Issue91 | September 2023 SIR at the US Capitol
Ninety-nine per cent of men eligible for treatment for BPH do not receive invasive therapy.”
Shivank Bhatia



CONTROVERSIES CHALLENGES CONSENSUS INNOVATION EDUCATION EVIDENCE Controversies Update Vascular & Endovascular REGISTER NOW CXSYMPOSIUM.COM 23–25 APRIL 2024 TUESDAY-THURSDAY NEW VENUE, E xCeL LONDON, UNITED KINGDOM Peripheral Arterial Controversies Aortic Controversies Acute Stroke Controversies Vascular Trauma Controversies Venous & Lymphatic Controversies Vascular Access Controversies The Hurting Leg Controversies
New renal technologies: From radial access to angio-CT
Olivier Pellerin (Université de Paris, Paris, France) presented on technological updates in the renal space at the Global Embolization Oncology Symposium Technologies meeting (GEST; 18–21 May, New York City, USA). He set out to provide a “broad overview” of radial access, navigation and computed tomography (CT) angiography for the audience.
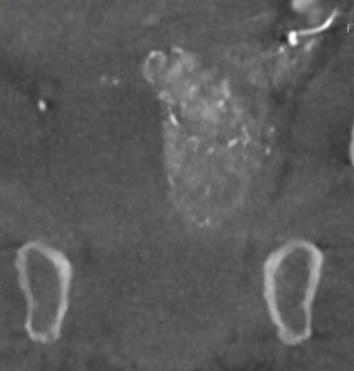
PELLERIN STARTED HIS PRESENTATION by outlining what is necessary for “optimal” renal tumour treatment. He listed among these requirements treatment planning and assessment, the visibility of the tumour, access to the patient intervention site and tumour, the radiation dose to patient and operator, and the procedure morbidity.
Moving on to focus on radial access, Pellerin questioned rhetorically whether the “big push” towards the approach in the last five to 10 years is solely down to industry, or whether it is because it actually offers a “real advantage” when it comes to achieving optimal renal tumour treatment. He made the point that this approach is “widely used and accepted” by cardiologists. The evidence from the last decade comparing femoral with radial access, Pellerin detailed, spans transarterial chemoembolization (TACE), yttrium-90, angioplasty of the superior mesenteric or renal arteries, and renal embolization. This evidence shows that the technical success between the two access approaches is “similar, but it is probably one point to renal access”.
Continuing, Pellerin stated that a radial approach can lower access site complications, based on the existing literature, however, this is “cardiology literature”, he conceded. He then stated that where patient comfort is the concern, radial access is “preferred”, as it only requires “a small puncture under local anaesthesia”. Possible limitations with radial access, Pellerin stipulated, include for procedures where the objective of the intervention is to control
What exactly is tumour temperature?
Erik Cressman (MD Anderson Cancer Center, Houston, USA) took to the podium, also at GEST, to dive into why tumour ‘temperature’ matters— explaining what the terminology refers to, and its significance for patient treatment.

HE FIRST ADDRESSED HOW cancer is “eventual failure of the immune system”—depending on the source, Cressman explained that a single cell’s DNA can take “10,000 hits per day”. Of our roughly 100 trillion cells, five billion are replaced every day, leading the presenter to posit that “on the one hand, it is amazing that we are not all sitting here with cancer, while on the other hand, it is amazing that the immune system works as well as it does”. Not all the cell damage that occurs leads to a tumour, but unfortunately, natural selection is at work in damaged or unregulated cells, and Cressman added how the selection process favours scenarios that evade or

a symptom which itself “does not involve the vital prognosis of the patient”, as is the case for uterine artery embolization for symptomatic fibroids, or prostate artery embolization for dysuria management.
The choice of vascular access, the speaker set out, “must be guided by a detailed study of risks versus benefit in relation to complications linked to vascular access”. In other words, Pellerin invited the audience
it has become “more and more stereotactic”, Pellerin noted. Artificial intelligence also assists with needle planning, simulating the ablation zone, and predicting success. It is also possible now to optimise targeting, which means “finding the best option for insertion into the lesion, avoiding critical structures,” Pellerin explained. Robotic arms can also aid in delivery, and there is also confirmation software to help ascertain whether the target has been reached.
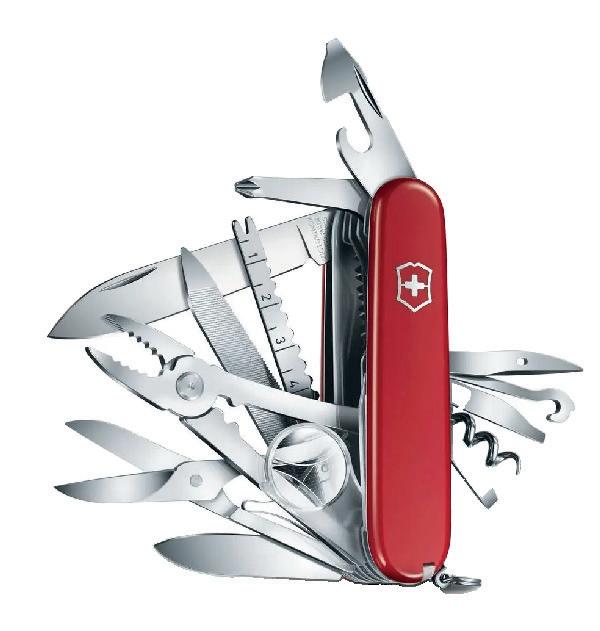
Lastly, Pellerin touched on angio-CT which he likened to a Swiss army knife as it “expands your possibilities a lot—you have a very high level of imaging quality”. He then referenced the emerging CT technologies, including spectral CT, which can “totally change the vision of the work we do [by] making possible the comparison of multiple functional parameters”. For example, it can “improve visualisation of lesions to facilitate procedure planning and enable accurate assessment of ablation margins”, while also “characterising tissue to better guide procedures and facilitate clinical decision-making, and analysing quantities such as iodine concentration to help determine procedural success”.
to question whether “a haematoma at the puncture site is preferable to a stroke” and similarly, these types of questions “must also be addressed with regard to cancer management”. Whether there is increased morbidity linked to longer procedures has “not yet been studied”, Pellerin added.
Moving on to address navigation, the presenter defined it as “performing the ideal placement of probes based on a predefined trajectory”. Compared to in the past, navigation is “different”, as
suppress immune surveillance.
Next, the speaker alluded to the “mixed bag” that is immunotherapy, which, while yielding “some inspiring success stories”, it also fails, which can be for a number of reasons. “It is a complicated thing,” he summarised, elaborating that some of the failures are “spectacular” in how they “unleash the immune system”. The older immunosuppressant drugs such as steroids are often not specific enough in responding to unregulated cell proliferation. Now, Cressman expanded, “we have these very highly specific antibodies that have a long-circulating half-life, [which you might only need] once every month or once every three months”. The downside of this type of immunotherapy is that “you are going to be hit with a high bill.
“The concept of an immunoscore to assess the tumours when we are talking about hot and cold” is well over a decade old, Cressman continued, coming to the pivotal focus of his presentation. The speaker referred to Galon and Bruni’s 2019 review to unpack this concept and “look at what is going on at the centre of the tumour and at the margin”. A low immunoscore correlates with a low response to T-cell checkpoint inhibition, Cressman stated, proceeding to celebrate that
the prognostic value of immunoscore is “better than much of what we were taught”.
The presenter then showed delegates microscope images of hot versus cold tumours, where hot means a lot of immune cells throughout and cold, not being able to see any. He also showed the audience how “excluded” tumours are those that have a lot of immune cells, but which are yet to penetrate the tumour itself. “Suppressed” means there are some immune cells, “not particularly excluded”, but which do not function as typical immune cells.
“To summarise, the hot tumours have a high degree of T-cell and cytotoxic T-cell infiltration, and checkpoint activation is clearly going on”. Checkpoint inhibitors have a “greater likelihood of success” in these tumours, Cressman set out. Immunosuppressed tumour cells with an intermediate immunoscore have “poor, albeit not absent” T-cells and cytotoxic T-cell infiltration, and the presence of soluble inhibitory mediators, as well as T-cell checkpoints. There is a “modest response to immunotherapies” in these tumours. Immune-excluded tumours have “no T-cell infiltration inside
the tumour bed and accumulation of T-cells at the tumour border”, as well as abnormal vasculature and hypoxia, and they yield a poor response when immunotherapies are used. “Cold” tumours have no T-cells either within or at the tumour edges, and there is failed T-cell priming, leading to poor response from immunotherapies.
“So, what can you do to improve outcomes? You can use imageguided injection of some of these antibodies to ramp up the immune system locally”, Cressman suggested, listing normalising the vascularity by triggering angiogenesis, addressing metabolism, restoring a normal pH as acidity is immunosuppressive, depleting immune-suppressive cell populations, and implementing a “combination of all of the above”, as additional strategies.
11 Issue91 | September 2023 GEST 2023
Hot tumours have a high degree of T-cell and cytotoxic T-cell infiltration.”
Erik Cressman
Olivier Pellerin
CT angiography expands your possibilities a lot.”
A window into IR training in the USA
Oluwatoyin (Toyin) Dada is a current fifth-year postgraduate trainee (resident) in interventional radiology (IR) and diagnostic radiology (DR), and Ariana Mills, a first-year resident. Both are based at the Icahn School of Medicine at Mount Sinai (New York City, USA) and have answered some questions for Interventional News about their journeys into IR from their US perspective.
IN: What led you into medicine? What has since led you to pursue IR?
OD: Some of my greatest influences growing up were my mom, who was a health aide for a short time, and my older sister, who pursued medicine. Naturally, I wanted to be like them, so medicine was always something I had at the back of my mind. I also had the opportunity to work with a child who had autism and volunteered at our community hospital during high school. Being in those environments gave me a deep appreciation for medicine. In medical school, I knew I wanted to go into a field that had a lot of variety and allowed me to do procedures, as I already loved hands-on activities. I went to a Latino Medical Student Association conference as a second-year student and met an IR attending who chatted with me about the variety of cases in IR, their complexity, and what they were able to offer patients. After that interaction, I made it my mission to learn more about the field of IR, and the rest is history!
AM: I wanted to become a doctor after taking a human biology class in sixth grade. I loved science and admired the tremendous commitment to helping patients inherent in medicine. After seriously exploring that childhood dream through shadowing, I was certain I wanted to begin the path to applying to medical school by the time I started college. I learned about IR from an attending physician on a panel during my first semester of medical school. After shadowing that physician, I was drawn to the specialty. I liked the field’s procedural nature, the ability to treat various pathologies, the countless opportunities for research, the supportive professional community, and the novelty of devices and interventions. After leading a research project on fertility after transcatheter arterial embolization for obstetric haemorrhage, I was certain I wanted to train in IR because the field constantly identifies safe and innovative alternatives for patients.
IN: What did you do to prepare for your application to IR? What was the greatest challenge?
OD: I did a two-week IR rotation at the beginning of my clinical years and did a quality improvement project with the IR faculty at my institution. I also tried to attend conferences and symposia geared toward medical students, which provided a window into other IR departments across the country. I would say the biggest challenge when applying was the number of people telling me not to pursue IR/ DR for fear of poor work-life balance, artificial intelligence taking over, turf wars, radiation exposure, etc. I decided to apply anyway and have been extremely happy with my choice thus far.
AM: I prepared for my application by exploring my interest in IR. Specifically, I shadowed during preclinical years, participated in multiple clinical
rotations, completed two visiting student electives, attended and presented at academic conferences and symposia, and volunteered with the Society of Interventional Radiology (SIR) Medical Student Council. Not only was this process helpful for building my application, but it gave me a multifaceted view of IR that informed my decision to apply to the specialty. I wanted to remain open-minded about other specialties during medical school too, so my greatest challenge was maintaining a strong involvement with IR while also exploring other fields.
IN: Toyin, what has been the highlight of your residency so far? The biggest challenges? Ariana, what are you most looking forward to, and what do you think the greatest challenge will be?
OD: The biggest highlight of residency was finding that I was staying at my current institution for IR training! It felt like all the hard work finally paid off. Because IR/DR is a rapidly evolving field and there is not much exposure as medical students, I found that the learning curve was incredibly steep. Thankfully, with repetition and experience, I am finding it much easier now to grasp concepts. Additionally, there are multiple amazing resources (SIR Learning Center, the Backtable podcast, etc.) that are available to trainees to make learning IR concepts much easier.
AM: I am most looking forward to being even more involved in patient care as a resident physician. I am also excited to spend more of my time learning experientially, working towards a collective goal as a part of a team, and contributing to a rapidly growing specialty. Given that residents are learning at such


have!) amazing mentors, I find that not many people in IR look like myself—a black woman. I feel it is important to be visible and show others like me that we are here, and that there is plenty of room for them at the table too.
AM: Dr Daryl Goldman started an elective called ‘Introduction to IR and Minimally Invasive Procedures’ that was offered to students at our institution. During the pandemic, she recognised that the widespread adoption of virtual education could enable the department to expand the elective to any student worldwide interested in IR. She kindly reached out to me to see if I would like to help her facilitate this iteration of the course, and I was subsequently co-course director for two years. It was very impactful to witness that the course fostered excitement in students, and I look forward to working on similar initiatives in residency.
IN: What words of advice would you give to current medical students trying to decide what specialty to go into?
OD: The best advice I received as a medical student is to stay open to all possibilities and treat each rotation as if that is the specialty you are going into. I took that advice very seriously and I am in a completely different field than the one I first thought I would pursue. I am very happy with my choice and would gladly choose IR all over again.
AM: Deciding on a specialty involves a lot of reflection. It is helpful to be extremely honest with yourself about who you are, including your proclivities, strengths, areas for growth, limitations, and professional and personal aspirations. As you learn about different fields, consider what is required in the training and especially what is required as an attending. Through this process, you can evaluate whether you see yourself being successful professionally in this field, whether you are excited about what the field can add to your life, and what you believe you can offer to the field.
IN: How well is IR introduced to med students in the USA? What, if anything, do you think med schools in the USA could do to better inform students of opportunities in IR, or what a career in IR entails?
a fast pace and being pushed to their full potential, I think the greatest challenge for me will be to keep in mind how much progress I have made without harping on how much I still cannot do and how much I still do not know.
IN: I can see from Twitter etc. that you are involved in IR outreach)—what made you want to be involved in this?
OD: Many people invested time in me as a medical student and resident, and it has paid off greatly. I feel that it is my duty to pay it forward to those coming up behind me. Additionally, while I have had (and still
OD: Depending on the institution, IR is not readily offered as an elective or is often limited to a small number of students. A strategy that I have seen work really well, especially at Mount Sinai, is that it is offered as a subspecialty elective within the required surgery rotation. Speaking from my own experience, I learned about IR at a non-IR conference, and that was pivotal in my career path. Symposia and conferences geared towards medical students are fantastic ways to reach potential recruits early on.
AM: It is well established that students do not have much exposure to IR in medical school, and in my experience it is not for lack of enthusiasm from the IR community. I hope the general medical education teams can do more to reduce barriers to exposing students to IR. For example, schools could invite interventional radiologists to be involved in preclinical education, such as around IR procedures like uterine fibroid or prostate artery embolization during relevant lectures, and schools could allow rotations in IR to meet acting internship requirements.
12 September 2023 | Issue91 US Trainees’ Perspective
Oluwatoyin Dada
Ariana Mills
IO of the past, present and future: presentation predicts what is to come in the next five years
Setting the audience’s sight on the horizon at the 2023 Global Embolization Oncology Symposium Technologies (GEST, 18–21 May, New York City, USA) meeting, Daniel Sze (Stanford University, Stanford, USA), editor-in-chief of the Journal of Vascular and Interventional Radiology, gave his predictions on what the interventional oncology (IO) space will look like in five years. His forecast identified the important research changing the landscape of IO, the developments that have brought us to present day, and the current areas with unmet medical needs that are receiving the most investment.
OPENING HIS PRESENTATION
with the words of Søren Kierkegaard: “Life can only be understood by looking backward; but it must be lived looking forward”, Sze began by describing recently published research articles with important implications for future practice which have been selected for editor’s awards by the Journal of Vascular and Interventional Radiology Delving into the content of these research papers, Sze discovered dialysis access to be the most prevalent topic to appear among award-winning papers, because of large, prospective, randomised, industry-sponsored trials.
Of the most frequently awarded research within IO, Sze identified papers that explored the interactions between locoregional therapies and the immune system or immunotherapy, a topic more frequently awarded than transarterial radioembolization (TARE), transarterial chemoembolization (TACE), and ablation research publications.
Reflecting on changes that have occurred in the last five years, Sze outlined the treatments carried out now that were not performed, or as much, five years ago. Compiling a list of six treatments, Sze included musculoskeletal ablation and
GEST speakers make predictions on the future of embolization

Speaking in the Vanguard session on the first day of the 2023 Global Embolization Oncology Symposium Technologies (GEST, 18–21 May, New York City, USA), Lindsay Machan (University of British Columbia, Vancouver, Canada) gave a comprehensive outlook on the next five years in embolization, outlining procedures that will be characteristic of the period ahead and the advancements that are needed to propel practice into the future.
MACHAN BEGAN BY DESCRIBING the first therapeutic embolization in 1972, defining the achievement via the radiologists’ “conviction”, the equipment of the time, the research that was carried out and the comparisons drawn with existing treatment options which enacted its success.
Skipping ahead to present day, Machan introduced the current and future expansion of therapeutic embolization, briefly listing the areas he predicts to be of note including musculoskeletal (MSK) embolization, granulomatous amoebic encephalitis (GAE),
stabilisation, ablative dose TARE, pressure-augmented TACE, thyroid ablation, genomics biopsy and venous deprivation. Applying a set of probing questions for each, Sze interrogated the procedures respectively, asking—“why not use the concept of future liver remnant?” for ablative dose TARE, “what is the pressure endpoint?” when performing pressure-augmented TACE, and “how can we block accelerated tumour growth without blocking hepatocyte growth?” in venous deprivation.
Pivoting, Sze addressed the unmet medical needs which are receiving the most investment today. First, he described new ablative technologies such as sonication, being explored by HistoSonics with their Edison histotripsy system. Additionally, Sze included the Galvanize Aliya pulsedelectric-field technology and Erik Cressman’s (MD Anderson Cancer Center, Houston, USA) development of thermochemical ablation.
Continuing, Sze outlined new anatomical targets that are receiving greater investment, such as bronchial and pulmonary TACE and renal, prostate and intracranial TARE. Alongside these, he noted new radionuclides that have received contemporary attention, for example radio-opaque TARE from ABK
shoulder/elbow enthesopathy/tendinopathy, osteoarthritis (OA) hand, lumbar facet disease and acute sporting injuries.
Observing the applications of MSK embolization, Machan stated that complex knee pain, pelvic congestion syndrome and neural mechanisms are key areas which would benefit most from the advancement of MSK embolization. Interrogating what is needed to advance the field, Machan emphasised that improved data sought through large, prospective, multicentre trials, as well as smaller and resorbable embolics are the pathways to take to do so.
Next, addressing lymphatic interventions such as peripheral lymphatic embolization, retrograde transvenous and transcervical accesses and mesenteric lymphangiography, Machan moved on to explore future opportunities within embolization. Referencing titled ‘Imaging and interventions for lymphatic and lymphaticrelated disorders’, Machan explained that the lymphatic system is involved in all disorders that present with fluid accumulation. For this reason, he opined that more evolved imaging, better access tools and new embolic agents are essential to continued progression in the specialty.
Acknowledging two pivotal changes, the speaker then recognised the seismic shifts artificial intelligence (AI) and consumerism have made in healthcare delivery.
Discussing the role of
Biomedical and holmium-166 TARE developed by Quirem Medical, among others. Finally, Sze highlighted new immunotherapies and combination treatments that have received investment to help meet unmet medical needs, citing the large variety of non-PDL and non-CTLA4 immunotherapies in development. He foresees increased involvement of IR with in-situ vaccination, since practitioners in the field are uniquely qualified in drug delivery and local tumour environment modulation.
Looking ahead, Sze concluded his presentation by stating that “five years is not a long time”, emphasising that physicians should be looking ahead not just five, but 15 and 50 years, to identify ways that interventional radiology can lead the fight against cancer, and possibly for patients in earlier stages rather than salvage settings. Wrapping up his premonitions for future practice, Sze predicted that in five years, interventional radiologists should expect to be performing incrementally improved ablation, TACE, and TARE, combining locoregional therapies “more rationally” with immunotherapy, increasingly informed by tumour genetics, and most importantly, he added, continuing the pursuit of the elusive abscopal response, the holy grail of IO.
AI in embolization, Machan noted a preliminary study—published in the Annals of Vascular Surgery that concerned AI-assisted microcatheter shaping for intracranial aneurysm coiling by Changya Liu (Huazhong University of Science and Technology, Wuhan, China). Applying this example, the speaker then used the increasing prevalence of AI’s deployment within treatment to draw attention to the growing imbalance between healthcare—which makes up a sixth of US gross domestic product (GDP)—and the economy, which is expanding at a much slower rate. Additionally, he stated that medical errors are the eighth leading cause of death in the USA, while too making note of the “easily tracked” cost versus outcome dichotomy in contemporary treatment.
Concluding his presentation, Machan painted a clear picture of the future of embolization, making particular mention of more frequent MSK embolization and lymphatic procedures to come, alongside reduced usage of glue. He averred that healthcare professionals in this space will “continue to be referred patients that no one else wants to treat”, however he affirmed that it is essential that time is used advantageously to create data and exploit the pervading “digitisation of everything”.
13 Issue91 | September 2023 GEST 2023
Healthcare professionals in this space will “continue to be referred patients that no one else wants to treat.”
Daniel Sze
Lindsay Machan
Evaluation of transpulmonary chemoembolization (TPCE) Thomas Vogl
Point of View
The incidence of lung cancer has increased considerably in the last few decades with the lung as the most common site of metastatic involvement. Despite the improvements in the diagnosis and treatment for malignant lung tumours, the prognosis of the patients is still unsatisfactory.1 Currently, locoregional chemotherapeutic techniques such as transpulmonary chemoembolization (TPCE) for the treatment of lung malignancies have gained increasing importance. The purpose of this retrospective study was to evaluate local tumour response and patient survival after the treatment of pulmonary metastases using TPCE as a palliative treatment method.
In TPCE, a 5 French (Fr) endovascular sheath and 5Fr headhunter catheter are routinely placed transfemorally under fluoroscopy until the pulmonary artery and subsequently the tumourfeeding segmental pulmonary branch are reached. A balloon catheter (up to 7mm in diameter) is optionally placed for better results.2 This selective pulmonary artery catheterisation results in a blockage of the arterial supply to the tumour tissue, resulting in regional ischaemic necrosis in the target tumour tissues while reducing damage to the surrounding normal lung parenchyma. Thereafter, mitomycin
and gemcitabine as chemotherapeutic agents are administered in combination with an embolization of lipiodol and microspheres. This extends the storage time of the injected cytostatics in the tumours and reduces the outflow into
AI enables “more effective” research and practice development
Discussing the role of artificial intelligence (AI) in improving outcomes within research and practice development, Hamid Mojibian (Yale School of Medicine, New Haven, USA) explicated the ways in which AI is changing interventional radiology (IR) at the 2023 Global Embolization Oncology Symposium Technologies (GEST, 18–21 May, New York City, USA).
“AI IS HERE” WAS MOJIBIAN’S introductory statement, pointing to the definite AI integrations that are already occurring in radiology. Expanding on this, he described an AI-based workflow that can identify critical findings through image acquisition, automatic AI application and prioritisation of key findings. These findings can then trigger an alert which connects patients with the most appropriate care teams, and automate patient follow-up.
Using pulmonary embolism (PE) as
an example, Mojibian drew parallel comparison between the workflow with and without AI—with more steps and a less direct pathway to treatment in the non-AI roadmap, Mojibian highlighted how AI can enable a “more effective” care system.
Following this, he discussed disease discovery modules that utilise natural language processing (NLP) to analyse radiology reports. Potential uses for this technology span from uterine fibroids, spine compression fractures and detecting inferior vena cava (IVC)
the circulatory system.3 Consequently, the frequency and severity of systemic effects are limited. Other occlusion materials used are coils, polyvinyl alcohol, degradable starch microspheres, and gelatin sponges.
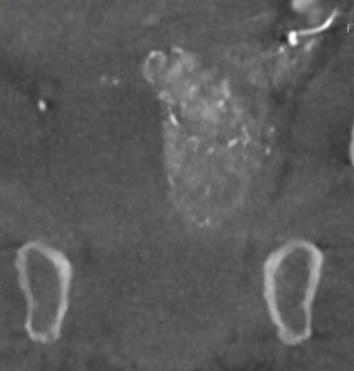
In our study, 223 patients (138 women, 85 men; mean age: 59.3±11.9 years) with unresectable lung metastases and/or not responding to systemic chemotherapy received repetitive TPCE (mean number of sessions 4.7±3.7) between January 1990 and May 2021. Patients had predominant lung metastases and in most cases with bilateral lung involvement. Origin of the metastases were either colorectal carcinoma (n=139) or breast cancer (n=84). Tumour-supplying vessels were catheterised selectively in order to apply chemotherapeutic agents locally, combined with lipiodol and microspheres. The response was assessed according to the revised RECIST criteria.
Of the evaluated 183 cases, partial response was achieved in 4.9% (n=9), stable disease in 62.3% (n=114), and progressive disease in 32.8% (n=60) of the patients. Mean and median overall survival time were 23.5 and 14 months, respectively.
TPCE can be used as a palliative treatment in unresectable lung malignancies to reduce the tumour burden or to achieve local tumour control,4 or as a neoadjuvant or curative treatment option combined with thermal ablation such as radiofrequency ablation (RFA) and microwave ablation (MWA) (Figure 1).5,6
A multicentre study may include a larger population of patients and combine expertise from different institutes. Although TPCE has the potential to improve local tumour control and to prolong survival, randomised controlled trials are still needed.
Thomas Vogl is director of the Institute for Diagnostic and Interventional Radiology at University Hospital Frankfurt (Frankfurt, Germany).
References:
1. Lemjabbar-Alaoui H, Hassan OU, Yang Y-W et al Lung cancer: Biology and treatment options. Biochim Biophys Acta 2015; 1856: 189-210.
2. Vogl, TJ, Herzog C, Zangos S, Lindemayr S. Transpulmonale Chemoembolisation (TPCE) als palliatives Behandlungskonzept bei primären Lungentumoren. Fortschr Rçntgenstr 2007; 179: 300-307
3. Vogl TJ, Mekkawy AIA, Thabet DB, et al. Transvenous pulmonary chemoembolization (TPCE) for palliative or neoadjuvant treatment of lung metastases. Eur Radiol 2019, 29: 1939-1949

4. Vogl TJ, Shafinaderi M, Zangos S et al. Regional chemotherapy of the lung: transpulmonary chemoembolization in malignant lung tumors. Semin Interven Radiol 2013; 30: 176-184
5. Smith SL, Jennings PE. Lung radiofrequency and microwave ablation: A review of indications, techniques and post-procedural imaging appearances. Br J Radiol 2015; 88, 20140598
6. Vogl TJ, Hammann L, Adwan H. Transvenous Pulmonary Chemoembolization and Optional Microwave Ablation for Colorectal Lung Metastases. J Clin Med 2023; 12(10):3394
Disclosures: The author shared no relevant disclosures.
1a: Axial CT diagnosis with documentation of two colorectal carcinoma lung metastases (T3N0M1) in the right middle and upper lung field with 13mm and 18mm in diameter (arrows). Post-inflammatory subpleural lesion on the left.


1b: Transpulmonary chemoembolization (TPCE) via a transpulmonary-arterial catheter into the right pulmonary artery supplying the middle lobe. Injection of perfusion using mitomycin, cisplatin, irinotecan. Embolization was performed using Embocept (PharmaCept).
1c: Partial response with massive volume reduction of the intrapulmonary lesions. Here the size of lesions remained constant over a total of six months (arrows).
filters that are eligible for removal— Mojibian stated in a single month they identified 91 filters that were eligible. Furthermore, he added that in deep venous thrombosis cases, NLP systems have the potential to increase patient recruitment for randomised trials.
Continuing to outline the effectiveness of AI’s employment within healthcare, Mojibian explained a prospective research workflow enabled by the technology. Initiated by a notification, he described how AI can then enable patient stratification and inclusion through integration with electronic medical records. He opined that this system improves efficiency and maximises collaboration throughout the research process, while also incorporating advanced image processing benefitting classification, segmentation and quality control.
Concluding his presentation, Mojibian’s final thoughts emphasised his belief that AI will not replace clinicians, but clinicians who do not
take up AI technology will be replaced by those who do. Now is the time to plan and act, he stated, underlining that greater awareness is needed to spot and capitalise on opportunities to lead and co-innovate alongisde fellow healthcare professionals.

14 September 2023 | Issue91 Point of View
In deep venous thrombosis cases, natural language processing systems have the potential to increase patient recruitment for randomised trials.”
1a 1b 1c
The Confi dent Choice










Designed for Superior Performance
Highest Kink Resistance with up to 50% greater kink resistance, SKATER’s soft catheter material helps maintain catheter patency and provide patient comfort
















Easier Inser tion
SKATER’s SLIP-COAT ™ hydrophilic coating and internal locking tip allow for an accurate and easy insertion




Maximum Drainage





SKATER offers the largest, oval drainage holes, resulting in greater drainage flow and volume

argonmedical.com *Data on File. Scan here to read the full results!
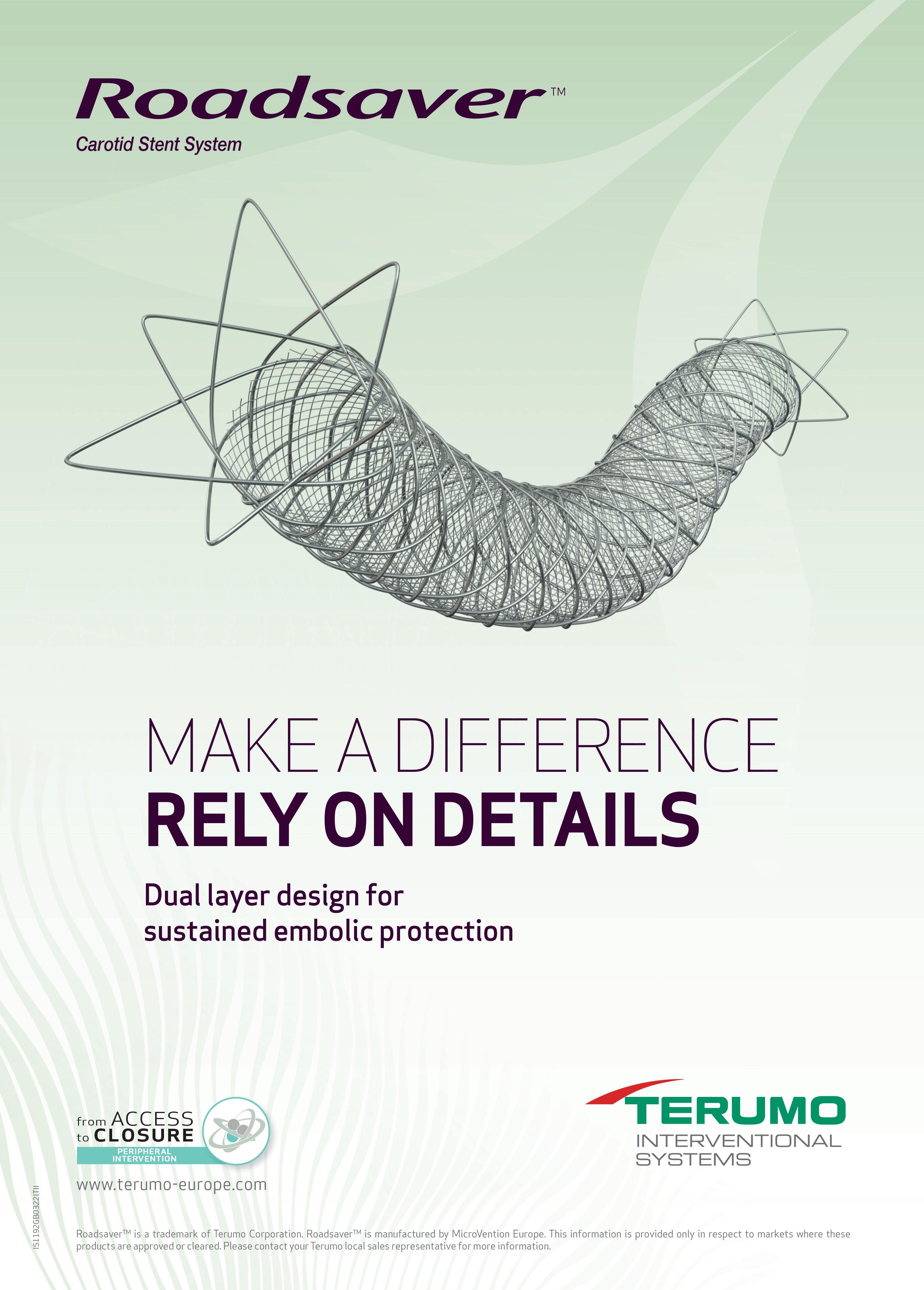
Rectal embolization shows “similar clinical success” to transanal haemorrhoidal dearterialisation
Silvia Busó Gil (Hospital Universitario de la Ribera, Alzira, Spain) presented at the scientific papers session, on the difference in outcomes between patients undergoing rectal embolization for haemorrhoids over transanal haemorrhoidal dearterialisation. She and colleagues carried out a study to examine exactly this, finding “similar clinical success and rebleeding rates”.
BUSÓ GIL BEGAN BY CREDITING
Aigner’s study from 2006 with determining that, in cases of pathological haemorrhoids (those which cause symptoms), there was high arterial flow, and hence, to treat haemorrhoids, the arterial “hyperflow” needs to be stopped.
She continued by explaining that the literature shows that “despite no difference in outcomes, embolization of the superior rectal arteries […] showed pain levels lower than those observed after surgical treatment”.

For her group’s study, Busó Gil detailed that they compared embolization with one of the “less invasive” surgery options—transanal haemorrhoidal ligation (THD). For the rectal artery embolization, the speaker shared that they used 300–500-micrometre particles and 2–3mm microcoils, before using angiography to confirm the occlusion. The study was retrospective and observational, and included 40 patients who received embolization and 69, THD, between the years 2016 and 2022.
Busó Gil then elaborated on the two groups’ demographics, explaining that the mean age of the embolization group (61.7 years) was greater than that of the THD group (51.3 years), as the patients referred for embolization tended to have more comorbidities, included those
A dive into sports injuries from an embolization perspective
which contraindicated anaesthesia and THD itself.
Regarding the results, the speaker communicated that in terms of the French Bleeding Score (FBS), there was “no significant difference” between the two groups: the embolization group’s reduced from a mean of 5.93 to 1.75, and the THD group, from 4.23 to 1.23. Clinical success was defined as a decrease of two points in the FBS, meaning that 92.8% of the embolization group and 76.9% of the THD group, respectively, underwent a clinically successful procedure. This was calculated as not being “clinically significant”, as was the rebleeding rate between the groups. The other outcomes assessed were postoperative symptoms and hospitalisation.
Concluding, Busó Gil reiterated that the study demonstrated “similar clinical success and rebleeding rates”. There were lower rates of postoperative complications in the embolization group, in seven patients vs. 43 in the THD groups. The main factor when determining which procedure a patient undergoes is whether they are experiencing high levels of bleeding or anaemia (in which cases, embolization is preferred), prolapse (in which case, THD), and also patient preference and resource availability.
High-dose dexamethasone for post-embolization syndrome in PAE “ineffective”
Petra Svarc (Rigshospitalet, Copenhagen, Denmark) presented during the scientific paper session at ET 2023. She imparted on the audience the results of hers and colleagues’ double-blinded randomised controlled trial (RCT) of high-dose dexamethasone to reduce the symptoms of post-embolization syndrome (PES) in patients who had undergone prostate artery embolization (PAE; the DEXAPAE trial). The group’s findings were that 24mg of dexamethasone is “safe”, as the participants reported no sideeffects, but that “it does not reduce PES following PAE” any more than “our standard treatment, which is paracetamol”.
PES is “an umbrella term for the systemic response to tissue necrosis,” Svarc began, detailing that it can include fever, influenza-like symptoms, local pain, and a worsening of lower urinary tract symptoms (LUTS). In a small number of PAE patients, PES can be severe and “mimic” urinary tract sepsis.
Theirs is the “first trial that examined [steroid’s] efficacy” in reducing the
inflammatory response of PES in PAE patients, Svarc went on. It was a single-centre, double-blinded RCT, where 31 participants were allocated 1:1 to receive either 24mg of dexamethasone or a placebo. Inclusion criteria included having LUTS secondary to benign prostate hyperplasia (BPH), a prostate volume >80ml,
Yuji Okuno (Okuno Clinic, Tokyo, Japan) shared with delegates at the European Conference on Embolotherapy (ET; 21–24 June, Valencia, Spain) an analysis of the best embolization approaches to certain sports injuries associated with overuse.

Okuno began his presentation by defining overuse sports injury as “an injury occurring in the absence of a single, identifiable traumatic cause”. The priorities when it comes to treating these injuries are achieving reliable results and the patient being able to return to their activity quickly, as often, it is high-level athletes who are affected. However, these injuries are usually quite difficult to manage with usual conservative treatment, such as steroid or stem cell injections, and therefore “good indications” for musculoskeletal (MSK) embolization. This is because of the treatment’s minimally invasive nature, which limits patients’ recovery time, Okuno clarified.
Among the overuse sports injuries that can be best treated with embolization, according to Okuno, are tennis elbow, jumper’s knee, Achilles tendonitis, hip pain as a result of hamstring injury, and pain in the lumbar region from spondylolysis. To begin treating these patients, Okuno set out that first, he will evaluate using
an International Prostate Symptom Score (IPSS) of eight or more, being eligible for catheter-based intervention, and having no contraindication to dexamethasone.
The primary outcomes assessed in the trial, Svarc noted, were morning rectal temperature at two days following PAE and pain severity and interference scores on the Brief Pain Inventory used for the first five days post-PAE. Secondary outcomes included hospital admission, levels of c-reactive protein (CRP) and acute urinary retention.
“Most patients in both groups were subfebrile for all of the five days,” Svarc shared. Regarding pain, the scores were “generally low, and low means higher quality of life,” she added. The only significant difference regarding secondary outcomes, was the level of CRP—a mean of 108mg/l [range=54–161mg/l] in the control group vs. 10mg/l [5–33mg/l], p value<0.01 in the
magnetic resonance imaging (MRI) or ultrasound to “confirm the presence of the hypervascular region”. For the first three types of injury, Okuno shared with delegates that soluble gelatin microspheres (100–300 micrometres) are a good, “safe”, embolic choice. For the hip, lumbar region, and stress fractures, the speaker conveyed how he “always” uses imipenem/cilastatin. A permanent microsphere is an option for tennis elbow or jumper’s knee.
During the procedures, Okuno continued, there are two endpoints— the imaging endpoint and the physical endpoint, or the disappearance or decrease in localised “painful tenderness” at the injury site.
A key takeaway Okuno wished to give his audience was that the evidence shows that, when doing lumbar embolization, some particles can cause the nerve root or spinal cord to necrose. This is the case even for some temporary materials. Therefore, imipenem is the only embolic he would recommend.
Yuji Okuno
dexamethasone group.
Svarc then clarified for delegates why the trial ended after only 31 patients were randomised, when 60 had been recruited initially. The reasons were, she explained, that they saw no significant difference in primary outcomes and the control group had only mild PES symptoms.
Concluding, Svarc’s group found that 24mg of dexamethasone is safe, but does not help reduce PES symptoms following PAE. They also suggest based on their findings that mean temperature and pain may not warrant active treatment, “especially when we look at the control group”.
31 participants were allocated 1:1 to receive either 24mg of dexamethasone or a placebo
17 Issue91 | September 2023 ET 2023
Petra Svarc
placebo
dexamethasone
The Lancetpublished study finds “PAE provides more urinary and sexual symptom benefits” than combined medical therapy



A French group of interventional radiologists and urologists has recently published the results of its randomised, multicentre, open-label, phase 3 superiority trial of prostate artery embolization (PAE) versus medical therapy (PARTEM) in The Lancet. The group, of whom Marc Sapoval (Hôpital Européen Georges Pompidou, Paris, France) is the corresponding author, states in its publication that the PARTEM trial met its primary endpoint of clinically significant superior reduction of International Prostate Symptom Score (IPSS) after PAE at nine months compared to following combined medical therapy (CT), “in patients who failed to improve after single alpha-blockers therapy”.
THE AUTHORS DETAIL THAT “THE AIM OF the trial was to compare effect on lower urinary tract symptoms (LUTS) of PAE versus medical treatment in patients with symptomatic benign prostate hyperplasia
(BPH) who still complained of bothersome LUTS despite >one month of treatment with alpha blockers”.
Also noted in the introduction to the paper was the fact that, to the authors’ knowledge, “this is the first randomised trial showing that PAE provides a clinically significant benefit over [CT]”. Additionally, they found that embolization provided the PAE cohort with better sexual function compared to the CT arm.
The authors set out the background to their study as being that PAE is an “increasingly recognised treatment option” owing to its “good risk/efficacy profile”.
Sapoval et al carried out their study in 90 randomised patients (aged 50 to 85 years) between September 2016 and February 2020, of whom 44 and 23 patients were assessed for the primary endpoint in the PAE and CT groups, respectively. The study took place across 10 French hospitals and the population was selected based on having bothersome LUTS defined by an IPSS >11, quality of life >3 (according to the last question of the IPSS questionnaire), and BPH ≥50 ml resistant to alpha-blocker monotherapy.
The CT group received oral dutasteride 0.5mg/tamsulosin hydrochloride 0.4mg per day.
The authors also outline that four patients in the PAE group underwent unilateral embolization, of whom two underwent a second attempt at bilateral PAE. “Unilateral embolization was done when it was impossible to catheterise the prostatic artery selectively,” they elaborate, explaining that this was related to excessive
angulation, calcification or stenosis.
The PAE cohort’s nine-month change in IPSS was −10.0 (95% confidence interval [CI]: −11.8 to −8.3), versus −5.7 (95% CI: −7.5 to −3.8) in the CT group. The authors go on to note no treatment-related adverse events or hospitalisation for either group, and the respective number of invasive prostate retreatments in the PAE versus CT groups at nine months was five versus 18.
From their study, Sapoval et al have been able to conclude that “in patients with BPH ≥50ml and bothersome LUTS resistant to alpha-blocker monotherapy, PAE provides more urinary and sexual symptom benefits than CT up to 24 months”.
Moreover, as part of the study, the authors carried out an economic evaluation, as they recognise that “the choice of an optimal treatment strategy for BPH is also informed by economic data due to the high prevalence of the condition and the costs of surgery”. Sapoval et al add that “the selection outcome for the economic evaluation was driven by the clinical relevance of treatment success at nine months and the limited sensitivity of generic quality of life measures EQ-5D over a short period”.
Sapoval gave the following statement to Interventional News regarding the importance of his and colleagues’ findings: “This study helps to advise patients suffering from bothersome LUTS related to BPH >50ml that PAE may be a valid option able to provide significant symptom relief.”

18 September 2023 | Issue91 PAE Research
A study carried out in 90 randomised patients (aged 50 to 85 years) between September 2016 and February 2020
Guidelines for obstetric interventions in IR Lakshmi Ratnam
Point of View
The CIRSE 2020 Standards of Practice document for gynaecological and obstetric haemorrhage are among the most comprehensive guidelines in interventional radiology (IR) for obstetric interventions. The guidelines cover the use of IR for both elective and emergency procedures. The indications for IR are for postpartum haemorrhage and post-surgical bleeding in the emergency setting, and electively for the embolization of tumours either as a primary treatment or as an adjunct to surgery; embolization for arteriovenous fistulas and malformations; and the elective use of prophylactic occlusion balloons in abnormal placentation.
The guidelines cover the basics of anatomical knowledge required to perform an effective embolization. The operator must be aware of potential causes of failure of embolization including failure to search for and treat collateral supply to the uterus. Recommendations are made for appropriate imaging equipment which should ideally consist of an IR or hybrid theatre setting with digital subtraction angiography. However, it is recognised that lifesaving embolization may be required and can be performed successfully in an obstetric theatre using
portable image intensifiers. In such non-optimal settings, the operator must be aware of the higher potential for non-target embolization secondary to poor visualisation. The guidelines also suggest having available an ‘emergency haemorrhage control box’ which would have all the essential equipment needed to provide this procedure in a setting remote to the IR suite.
Active extravasation is only seen in 21–52% of cases and is mostly seen with uterine atony. In most cases of postpartum haemorrhage, a focal bleeding point is not identified. It is
London hospital’s positive 25year experience offering daycase IR service
Authors from King’s College Hospital (London, UK) have recently published a letter in Clinical Radiology detailing their centre’s experience after 25 years of day-case interventional radiology (IR) services. The King’s experience, according to the title of the response letter, has been “worth the effort”, which corresponding author Nuran Seneviratne et al explain is because day-case IR at King’s has proven to be “efficient, [to reduce] patient anxiety, [optimise] the role of the interventional radiologists in elective and emergency preassessment, [maintain] patient safety” and to pave the way for treating a “broader selection of patients” through a wider variety of procedures.
SENEVIRATNE AND COLLEAGUES responded to a paper published earlier in 2023, also in Clinical Radiology , by Lakshminarayan et al , which makes the case for providing IR care in a day-case setup. Their reasoning for advocating for this model is, as outlined in the paper’s introduction, that IR has, over time, become less invasive, which “[enables] rapid
recovery, [expediting] ambulation and [promoting] same-day discharge”. This model, Lakshminarayan et al detail, can improve patient experience and cost-effectiveness.
The authors of the King’s letter outline that they wish to “offer encouragement” to other hospitals motivated to establish or improve their day-case unit to profit from
important in this situation to perform bilateral empirical embolization of the uterine arteries. The embolic agent of choice in this situation is absorbable gelatine sponge. This allows for later recanalization of the artery when it has healed. In an emergency, patients usually require rapid catheter angiography and embolization. However in a more elective situation, for example where there is a slow bleed, but the patient is not unstable, a triple phase computed tomography (CT) scan may be useful in identifying a source of bleeding, thus enabling targeted embolization. If focal bleeding points are identified, for example, a pseudoaneurysm, permanent embolic agents can be used, such as coils. The choice of embolic agent is dependent on operator expertise and availability.
Approximately 5–10% of patients undergoing embolization may re-bleed. Causes of failure of embolization include development of arterial spasm, collateralisation after primary embolization of the uterine arteries, bleeding from non-uterine artery sources, previous surgical ligation or dilatation and curettage, unilateral embolization, and abnormal placentation. Potential complications from embolization include non-target embolization resulting in limb and buttock claudication, and necrosis of structures with pelvic arterial supply. These risks can be mitigated by using high-quality imaging, avoiding the use of very small particles, and being aware of collateral and cross-uterine blood supply.
The placement of prophylactic occlusion balloons in the management of patients with abnormally adherent placenta is also becoming more commonplace with the increase in incidence of abnormally adherent placenta and this is also discussed briefly in the guidelines.
Postpartum haemorrhage remains the
the advantages it can offer, as set out in Lakshminarayan’s paper. At King’s College Hospital, theirs is a “dedicated 10-bedded, nurse-led day-case interventional unit”, the letter conveys. It “initially focused on peripheral angiography, vascular access, liver biopsy, and percutaneous drainage work, [but] the service has now expanded to encompass a broad range of arterial and venous interventions, a large hepatobiliary service, and interventional oncology procedures”. The authors add that since its foundation in 1997, the unit has carried out over 2,500 percutaneous liver biopsies.
The letter goes on to include details of the vascular procedure data the unit gathered to assess the value of the unit. “The number of procedures increased steadily over time, and the proportion of interventional to purely diagnostic angiography also increased. There were also significant cost benefits compared to admission (£131.15 vs. £318.65 in 2007). The complication rate was well within
leading cause of maternal morbidity and mortality worldwide. In 2015, postpartum haemorrhage was reported to be responsible for more than 80,000 maternal deaths worldwide. The use of embolization in the treatment of obstetric haemorrhage was first reported in the 1970s. Since then, the use of IR in the treatment of both elective and emergency haemorrhage has increased and the success rates of embolization for postpartum haemorrhage are reported as being between 79% and 100%. Despite this, the rates of hysterectomy remain high and the use of IR for the treatment of postpartum haemorrhage is still significantly underutilised. Much more needs to be done to promote the availability and access to IR for patients. CIRSE’s 2020 guidelines and the 2022
International Federation of Gynaecology and Obstetrics guidelines both recommend the use of IR after failure of conservative measures to control haemorrhage, and before contemplating surgery. We need to move beyond these guidelines to make this a reality in practice for patients.
Lakshmi Ratnam is a consultant diagnostic and interventional radiologist at St George’s University Hospitals NHS Foundation Trust in London, UK.

Disclosures: The author declared no relevant disclosures.
the accepted Royal College of Radiologists’ standards at the time, with only 5.2% of cases requiring admission due to complications.”
Seneviratne and colleagues proceed to acknowledge that IR procedures are increasingly complex, and that, therefore, the day cases “now [require] more extensive input from interventional radiologists to ensure optimal patient selection, clinical optimisation, and effective coordination with other specialties”. As was the setup back in 1997, the authors state that “the nurse-led model for the organisation of the day-case unit, with pre-assessment conducted within the unit” today enables consultant interventional radiologists to work as efficiently as possible.
Finally, the authors go on to conclude their letter by sharing how their hospital is “poised to move into the next phase of day-case radiological intervention”, celebrating Lakshminarayan et al ’s paper once again as “a timely reminder of the potential of IR”.
19 Issue91 | September 2023 Point of View
Postpartum haemorrhage remains the leading cause of maternal morbidity and mortality worldwide.”
Farah Gillan Irani
“Even [in Singapore], healthcare costs are spiralling, so we are also learning how to be prudent.” Farah Gillan Irani is an Indian-born and educated interventional radiologist who has practised in Singapore since 2009. She has been a principal investigator in a drug-eluting balloon (DEB) angioplasty trial, a reviewer for CardioVascular Interventional Radiology and the Journal of Interventional Radiology for the last 10 years, and is vice chair of the cardiovascular interventional radiology (IR) subsection of the Singapore Radiological Society (SRS). She charts the progress in IR that she has observed in South East Asia and the Indian subcontinent to Interventional News, explains the value of fellowships abroad, and imparts her passion for extreme climbing and cycling pursuits.
What attracted you to a career in IR?
During my training, IR in India was a very nascent field and we did not have much exposure to its enormous potential. Having completed my finals, I happened to attend an IR conference where I heard Dr Sundeep Punamiya speak. The science he presented, his clarity of thought and depth of knowledge about this radiology subspecialty completely drew me in. Having wanted to be a surgeon, I wanted to work with my hands and have direct patient contact. In IR, I found the happy medium of being in one of the most rapidly innovating fields of medicine with the ability to alleviate patient suffering through minimally invasive procedures.
Who were your mentors?
Prof Andreas Adam and Dr Tarun Sabharwal from Guy’s and St Thomas’ Hospital (London, UK), Prof Afshin Gangi from the University of Strasbourg (Strasbourg, France), and Prof Bien Soo Tan from Singapore General Hospital (Singapore).
Could you describe a particularly memorable case of yours?
Sometimes it is not the most technically challenging case or the thrill of using a new device that stays with you, but the impact of the simplest procedure on a patient’s outcome. I was on call and the team got called in for a massive gastrointestinal bleed in a 62-year-old patient with a duodenal ulcer which, in spite of clipping, continued to bleed. The patient was in haemorrhagic shock with three inotropes and on his third round of the massive blood transfusion protocol. In the chaos of treating a very unwell patient, the IR nurse and radiographers maintained their calm and prepped the patient. A simple gastroduodenal artery embolization using glue and coils stopped the bleed 20 minutes after accessing the femoral artery to closure. Following a short hospital stay he was discharged home, and then came to see us in clinic ever so grateful. This case remains with me as it shows that our simple minimally invasive IR procedures are highly effective and that teamwork saves patients’ lives.
How does practising in India compare to practising in Singapore?
I have not worked as a consultant IR in India and hence, I cannot compare the practice in these two very different countries. India is a huge country with great disparities in wealth and access to healthcare. In rural India, the health infrastructure mainly caters to family medicine with just basic services available. While, in large urban cities, state-of-the-art IR services are available, however affordability of IR kit can put many procedures out of reach. This is in contrast to Singapore, which has a small population and one of the best healthcare systems in the world. The latest imaging equipment is readily available, and we are
able to use these expensive devices in our patients. Yet, even here, healthcare costs are spiralling, so we are also learning how to be prudent. Luckily, IR is also now starting to be recognised as a speciality in its own right in India and there are several IR fellowships available to train the next generation.
What are the priorities for the IR subsection of the Singapore Radiological Society (SRS), of which you are currently vice chair? What challenges does IR face in Singapore and your wider region?

Minimally invasive IR procedures are front and centre and critical to the running of any major acute hospital, but many of the public do not know who we are and what IR is about. As part of the IR subsection, public education has been part of our goal. This year, we want to extend that outreach to medical students early in their career so that our field is recognised, and we can attract the brightest and most talented young people into our fold.
IR is also now recognised as a Chapter in the Singaporean College of Radiologists (CRS) under the Academy of Medicine Singapore. We are working with the College to get subspecialty recognition by the Singapore Medical Council and Ministry of Health. On a related note, it is gratifying to see that IR is now practised at a high level in Thailand, Malaysia, Vietnam and has a presence in Bangladesh, Myanmar, Mongolia, and even Cambodia. The latter is thanks to the outreach programmes organised by the Asia Pacific Society of Cardiovascular and Interventional Radiology.
You have been a reviewer for CVIR for the last 10 years? What have you learned through doing this?
It has been an amazing journey. As a reviewer, you get a ring-side seat observing the amazing innovation in your field and delve into the depths of various aspects of anatomy, physiology, imaging and new devices. Being a reviewer carries responsibility. As a gatekeeper for the wider IR community, you need to make sure that the science is sound, safe, truthful, verifiable and beneficial to patients, doctors and healthcare systems. As a reviewer, I have gained immense knowledge and it has inspired me to undertake research of my own.
You were principal investigator for a randomised trial comparing drug-eluting balloon angioplasty with conventional angioplasty for haemodialysis arteriovenous fistula or arteriovenous graft stenoses. What led you to become involved and what did you take away from the trial?
In Singapore, we have a very high incidence of renal failure for which many patients depend on long-term haemodialysis, as our renal transplantation numbers are low due to a lack of organs. Repeated and frequent interventions to maintain access circuit patency is costly. Hence, when drug-eluting balloons were introduced, our team decided to evaluate whether these devices truly increased duration of lesion and circuit patency and reduced healthcare costs. Along with our renal medicine physicians and vascular surgery
20 Interview September 2023 | Issue91
It is gratifying to see that IR is now practised at a high level in Thailand, Malaysia, Vietnam.”
PROFILE
Andy Watt/NB Illustration
Current Appointments
2020–present: IR lead, Department of Diagnostic Radiology, Sengkang General Hospital, Singapore
2017–present: Senior consultant, associate professor and deputy head, Department of Vascular and Interventional Radiology, Singapore General Hospital, Singapore
Selected past appointments
2009–2017: Consultant, Department of Vascular and Interventional Radiology,
Singapore General Hospital
2008–2009: Clinical associate, Ruby Hall Clinic, Pune, India
2007–2008: Fellow, University of Toronto, Toronto, Canada
2006–2007: Fellow, Hôpital Civil Strasbourg, Strasbourg, France
Society positions/memberships
2022–present: Vice chair, Cardiovascular IR subsection, SRS and CRS

2010–present: Member, CIRSE
2009–present: Member, SRS and CRS
colleagues, we designed and undertook this trial. Running trials is hard work and requires input from many people. Research co-ordinators, statisticians and allied health staff are just as important as the clinicians. As principal investigator, I was but a representative of the amazing and dedicated team. The adage “it takes a village to raise a child” is very applicable.
You undertook fellowships in London, Strasbourg and Toronto. What advice would you give to (interventional) radiologists-in-training who are considering spending time in hospitals abroad?
I would highly recommend that everyone does a fellowship abroad. The wealth of experience gained is immeasurable. You are exposed to a different system of medicine and are able to take ideas back to your own practice. It also helps you appreciate the attributes of your own system. You learn different ways of doing the same procedure and these experiences help you formulate your own best way of doing it. On a personal level, you are exposed to a different culture which you need to respect, and you are out of your comfort zone, so the experience teaches you about your own strengths and weaknesses. It is an important lesson in life and just not medicine.
What are your hobbies and interests outside of medicine?
I enjoy sports, and these days, I am into cycling, the gym and golf (which I have recently taken up). Singapore General Hospital celebrated its bicentenary in 2021, and as part of the celebrations, we cycled 200km around Singapore to raise funding for our patients. I also enjoy hiking and trekking and have been lucky to have undertaken trips in the Americas, Africa, Europe and Asia. I was recently introduced to via ferratas, which I find thrilling; I have done the one in Kinabalu and one in the Dolomites. Being a Parsee, food is an integral part of our culture. Living in Singapore—a food lover’s paradise—I enjoy discovering, and eating at, amazing Hawker Centre stalls as well as the gourmet Michelin Star restaurants. I enjoy cooking and one of my goals is to do a gourmet cookery course.
Medical education
2005: Fellowship, Royal College of Radiologists London, UK
1999: Medical degree, BJ Medical College, Pune, India
1992: Honours in Science, Vidya Bhavan Junior College Pune, India
21 Interview Issue91 | September 2023
Copenhagen, Denmark
September 9-13
CIRSE 2023
featuring
CIRSE 2023 will feature the best of interventional radiology through 251 sessions, 1,590 presentations, 523 faculty members, 876 scientific paper and poster presenters and a multitude of hands-on learning opportunities.
It’s not too late to join us in Copenhagen! Secure your spot at CIRSE 2023 today.
All-Access Pass
For even more savings and to gain access to all of CIRSE’s online educational offerings, get the 2023 All-Access Pass!
Catch a sneak peek
Get a first glimpse at some of this year’s programme highlights with sneak peek articles from the lecturers!
Your stay in Copenhagen
Browse our interactive hotel map to find the perfect accommodation for your stay in the beautiful Danish capital! All offered hotels have been hand-selected to offer great value for competitive prices as well as convenient locations close to the congress centre.
BUILDING BETTER CARE cirsecongress.cirse.org Cardiovascular and Interventional Radiological Society of Europe
The world’s largest IR meeting is just around the corner !
“Doing better” for IR in Australia and New Zealand, from specialty status to qualification
Interventional radiologist Nick Brown is clinical director of the radiology service at The Wesley Hospital (Auchenflower, New Zealand) and associate professor at the University of Queensland (Brisbane, Australia). He sat down with Interventional News at the European Conference on Interventional Oncology (ECIO; 16–19 April, Stockholm, Sweden) to discuss the current picture of interventional radiology (IR) and interventional oncology (IO) in Australasia—the progress that has been made recently, and how far they still need to go to achieve specialty status, alongside a programme of IR training, education and ultimately, a qualification unique to the region.
“WE ARE CERTAINLY VERY
proud to be the first site in Australia and New Zealand to be accredited,” Brown begins, referring to the International Accreditation System for Interventional Oncology Services (IASIOS) certification that I-MED at The Wesley Hospital gained back in September 2021. “There are two other enrolled sites, and possibly some more about to be,” he continues, highlighting how the programme is gaining traction among hospitals in his region as centres seek to be able to demonstrate to referring clinicians that their IO service is high performing. Showing this to patients as well is key, as understanding of IR and IO among the public is often minimal, he explains. “It is always better to have a team working together to promote [IO].”
IASIOS certification improves IO recognition
In Australia and New Zealand, as elsewhere in the world, Brown clarifies, “there are challenges—getting recognition for IO and getting a seat at the MDT [multidisciplinary team] table, having the value of what we do recognised by the hospitals in which we work, by the referring physicians, and by the patients themselves”. Therefore, Brown defines “true success” with IO standards as having a “network of IASIOS sites across Australia and New Zealand and throughout Asia”. This is advantageous, he elaborates, because the centres will be able to “support each other and learn from each other”, rather than having the nearest reference points and collaborators in Europe “on the other side of the world” and in different time zones. Brown adds that the Royal Australian and New Zealand College of Radiologists (RANZCR) does already have a relationship with Singapore “and hospitals in Singapore have been accredited”. The next step towards “a great foundation on which to build”, he stipulates, would be for a hospital in New Zealand to become accredited—“Auckland Hospital may be on the cards”.
Next, Brown turns to address the
impact accreditation has had on the service his centre provides, nearly two years on. “We have the IASIOS symbol at the bottom of all our reports, letters, and emails,” he relays, notwithstanding having it prominently displayed in clinic. This prompts some patients to ask about the value of the certification, which Brown sees as a positive thing. However, he says the “real value” lies in how it has informed referrers. “We can say that we are a clinic that has most of our interventional radiologists EBIR [European Board of Interventional Radiology]-certified and we are now accredited with IASIOS—we can explain what this means and why it matters,” Brown details. This has led to an increase in referrals for several key IR procedures, he says.
Striving for better as both a hospital and discipline

“It was a lot of work to get to this standard—we needed dedicated staff and time set aside,” Brown wishes to underline, but nonetheless, he believes his centre has ‘IASIOS Centre of Excellence’ status “within [its] reach”. He then emphasises how important it is that they, at his hospital, “do what we do knowing that it is the best we can do and meets the highest expectations”. Quality assurance in IR and IO has been, and can be, more difficult to achieve than for other specialties like radiation oncology, with quality control “inbuilt”. Wanting to “do better” is what Brown thinks IR, as a whole, should keep at the heart of its practice, in order to bring about better outcomes.
Accreditation, such as IASIOS, is one aspect of the solution to the lack of public recognition of IR, Brown says, moving on to examine the bigger picture—there is a problem everywhere in that people are not familiar with IR. He laments the fact that there are “limitations to what individual interventional radiologists can do” to resolve this issue, so there needs to be a set of strategies at

a college, society and government level in all countries for realising better IR recognition through avenues such as policy.
A region-specific training programme is key
Training is another aspect Brown mentions, citing RANZCR’s new training programme currently in development for interventional radiologists and interventional neuroradiologists, as well as a new qualification which will be recognised in Australia and New Zealand. This is superior to relying on certification such as from EBIR and IASIOS, as it is purpose-built, with the locoregional health system and accreditation processes in mind. In addition, Brown stipulates the need to train more interventional radiologists to achieve
change for the better, he adds, would be for consultants to make an effort to do ward rounds themselves, even if this strays from the status quo. “We all need to be the change that we want to see in the world”—this will help enormously in the effort to increase IR awareness through delivering services of the highest possible standard.
Why specialty status matters
Another “really important part” of resolving the lack of recognition, Brown then notes, is achieving specialty status for IR—and this is true of many countries where this is not already the case. Not having IR recognised as a full specialty accompanies the further problem of not having an official IR training programme and qualification. “EBIR is very good in that respect […] as a platform to launch from,”
a workforce of adequate size and quality, as part of the solution to underrecognition of IR is “a numbers game”.
Brown then makes a point about the onus that rests on the shoulders of individual clinicians, who can
Brown admits, but “long-term structural change” spearheaded by colleges and societies working together is the only way to ensure uniformity of recognition and a high standard of IR training, he avers. It has taken time for RANZCR, the Interventional Radiology Society of Australasia, and the Australian and New Zealand Society of Neuroradiology to collaborate on advancing the cause of IR and interventional neuroradiology (INR) and to “support a plan specific to [the region]”, learning from European and North American experiences where specialty status has either already been obtained, or is in progress.
Concluding, Brown first sums up the impact of achieving IR specialty status on him—he is looking forward to “no longer being just a diagnostic radiologist, but a dual-trained specialist interventional radiologist as well, with hospital managers and colleagues knowing exactly what that means”. At a national and regional level, Brown then summarises that “we have to stand on our own two feet in our jurisdiction […] as the international standards are not sufficient to create that change for us” in Australia and New Zealand, as regards specialty status, training programmes and qualifications.
23 Issue91 | September 2023 IR in Australasia
We all need to be the change that we want to see in the world.”
Nick Brown
The Wesley Hospital, the first site in New Zealand and Australia to receive IASIOS certification
BSIR 2023 Annual Scientific Meeting
NOVEMBER 8-10 |
NEWPORT, WALES
The annual scientific meeting of the British Society of Interventional Radiology provides a platform for knowledge exchange and networking for interventionalists throughout Britain and beyond.
BSIR 2023 will showcase cutting-edge content from across our interventional radiology community, offering fresh ideas suited for every stage of IR. We hope to see you this autumn in Newport, Wales !
Register
BSIR 2023 registration includes both onsite and on-demand access to scientific content. It’s not too late to catch the early fee ! Register before August 31 to enjoy a discounted rate.
Programme
CATCH THE EARLY FEE!
BSIR highlights will include sessions on peripheral and visceral interventions, aortic and venous interventions, embolisation, interventional oncology, non-vascular interventions, clinical effectiveness, quality improvement and much more. Scan the QR to browse the programme.
Accommodation
BSIR’s official travel partner has secured a number of hotel rooms in the Newport area for the benefit of meeting participants. Use the interactive booking map to find your perfect room.
Spread the word
BSIR 2023 posters, social media graphics, wallpapers and more are available for download. Help us to promote the event by sharing with your colleagues.
www.bsirmeeting.org
British Society of Interventional Radiology
A new age in fertility: Remastering fallopian tube recanalisation
blocked tube, sperm can reach the egg, potentially leading to successful fertilisation and pregnancy. This can be particularly meaningful for couples who desire to conceive without the assistance of assisted reproductive technologies. Moreover, FTR is a less invasive procedure compared to major surgeries like tubal ligation reversal or in vitro fertilisation. This makes it an appealing option for those who would prefer a natural approach to conception. Additionally, FTR is often considered a cost-effective alternative, as other approaches can be costly.
Point of View
Each woman is unique, and a one-size-fits-all approach is not appropriate for addressing what can be extremely complex reproductive health issues. Natural Procreative (NaPro) technology, is a groundbreaking medical approach that focuses on understanding and treating the underlying causes of women’s health issues rather than merely addressing symptoms.
Developed by Dr Thomas Hilgers in the 1990s, NaPro combines the best aspects of reproductive medicine and natural fertility awareness methods to provide personalised and effective care for women. This involves identifying and treating the root causes of infertility, irregular cycles, and other male and female conditions. NaPro’s effectiveness is supported by extensive research and a growing body of evidence. Studies have shown that NaPro can significantly improve fertility rates,
with success rates rivalling or surpassing those of conventional treatments.
Up to 67% of all infertility cases can be attributed to fallopian tube disease. In cases where infertility is caused by blockage of the fallopian tubes, a simple and obvious alternative might seem to be to try unblocking the tubes in question. Fallopian tube recanalisation (FTR) is a procedure that aims to reopen blocked or damaged fallopian tubes, allowing the possibility of restoring natural conception. By reopening the
The American Society for Reproductive Medicine recommends that patients who have proximal tubal obstruction undergo selective salpingography and tubal recanalisation before considering more invasive and costly treatments. Since hysterosalpingography followed by FTR could potentially be considered for any woman undergoing infertility investigation, it is unfortunate that numerous infertility clinics remain unaware of this procedure, or they may have knowledge of it but lack access to an interventional radiologist capable of performing it. Consequently, several interventional radiologists may also lack awareness regarding the procedure and the number of potential patients who could benefit from it.
In this context, several controversial questions may arise. Within this straightforward procedure, over 85% of patients are discharged with a satisfactory outcome (successful tubal recanalisation), and more than 30% achieve pregnancy within the first year following the procedure. However, if tubal recanalisation (FTR) is indeed a
simple, safe, and cost-effective method, why is it seldom utilised? Why are other more invasive techniques, which are not free of side-effects and considerably more expensive, routinely employed? Why do insurance companies include the tubal recanalisation as any other artificial fertility treatments and fail to provide coverage for this treatment of a straightforward condition such as tubal obstruction? Even when development of new materials and kits for this purpose should be considered, the industry appears to be blind to this.
When talking about fertility, a tailored treatment plan to meet the specific needs of each patient should be performed in the fertility unit and an interventional radiologist should play an active part in this.
DIMITRIOS FILIPPIADIS (NATIONAL AND Kapodistrian University of Athens [ATTIKON], Athens, Greece) was the final speaker to take to the podium at the European Conference on Interventional Oncology’s (ECIO; 16–19 April, Stockholm, Sweden) advanced musculoskeletal (MSK) session. His presentation drew on the subtopics within MSK oncology addressed by previous speakers to underline the importance of multidisciplinary collaboration to treat a range of MSK tumours or metastatic disease. Echoing the takeaways of preceding sessions, Filippiadis underlined that, despite the good work already being done to prove the value of a multidisciplinary approach to treating patients with MSK tumours or metastatic disease, gaps in the data persist from a clinical evidence point of view.
Filippiadis began by advocating for cancer patients being managed at multidisciplinary tumour board meetings, “ideally with orthopaedic and neurosurgeons, medical and radiation oncologists, and, of course, interventional radiologists”.
The speaker then homed in on the value of shared terminology, and mutual understanding of what keywords mean—in the National Comprehensive Cancer Network (NCCN) 2023 guidelines, in relation to management of pain in adult cancer patients,
‘interdisciplinary’ was replaced by ‘multidisciplinary’, Filippiadis detailed. “We need to have both—to be able to offer a patient-tailored, or, even better, a lesion- or tumour-tailored approach.” The presenter elaborated how “everything in theory seems to work if you can have a multidisciplinary approach, but there are practical gaps that we need to fill in”.
Moving on to focus on a location-specific example of where multidisciplinary treatment has worked well, Filippiadis suggested that “we can all agree that [Wallace et al’s paper in The Oncologist on treating metastatic spine disease in a multidisciplinary manner] was a success”. The essence of this, the speaker summarised, is having “therapies proposed from different disciplines”, adding that it “goes without saying that interventional radiology [IR] was at the core of these multidisciplinary approaches”. Filippiadis listed the advantages of IR treatments which render it so well suited to featuring in the multidisciplinary approach— “it is minimally invasive; well tolerated even in patients with comorbidities or extensive disease; the overall morbidity of the procedures is low; and there is impressive and reliable pain relief in the vast majority of cases”.
Alberto Alonso-Burgos is head of the Interventional Radiology Unit


Luis Chiva de Agustín is director of the Department of Obstetrics and Gynecology at the University of Navarra, Pamplona, Spain.
Disclosures: The authors declared no relevant disclosures.
Furthermore, Filippiadis mentioned, among other examples of specific treatments for specific tumour types, or systemic therapies to treat desmoid tumours or sarcoma metastatic disease, it is a “good example of how you can combine with local treatments”.
However, the speaker made sure to note “clear gaps” in knowledge surrounding a multidisciplinary approach to treating MSK tumours or metastatic disease. Yet Filippiadis outlined how data on the immuno-oncological effect of ablation on a tumour, including when combined with immunotherapy, plus the interplay and timing between systemic therapy and MSK oncology interventions and techniques”, is coming to “[fill] these gaps”.
Filippiadis then took the opportunity to recommend distinct approaches depending on “whether the goal of your therapy is local tumour control or pain palliation”—the time interval between treatments can be adjusted accordingly. A pain palliation specific knowledge gap is around “the effect of ablation combined with radiation therapy for pain palliation”.
A phase I or II trial for painful skeletal metastases could be a first step, he suggested. To conclude, Filippiadis reiterated that IR treatments for MSK tumours have a “significant role to play because they are simple and effective and afford great benefits to practitioners, to the cancer patients and to the wider field of oncology, including the healthcare system and its economics”. As the presenter sees it, “high-quality data [can] fill in these gaps, [but] the prerequisite for this is that people from different specialties are speaking the same language”.
25 Issue91 | September 2023 Point of View
Alberto Alonso-Burgos & Luis Chiva de Agustín
A tailored treatment plan to meet the specific needs of each patient should be performed.”
Multidisciplinary approach to MSK cancer treatment needs “theoretical and practical gaps” filled
Dimitrios Filippiadis
Intra-arterial approach to locally advanced pancreatic cancer Ripal Gandhi
Point of View
The use of catheter-based localised delivery of drugs for treatment of cancer patients has proven to be effective and provides the benefit of reduced systemic toxicity. A critical prerequisite for these modalities is the angiographic identification and engagement of feeder vessels of appropriate size into the tumours in order to deliver the designated therapy. Therefore, hypovascular tumours are not optimally treated with these catheter-based techniques. For instance, pancreatic tumours, unlike their liver counterpart, are generally hypovascular, and are without any obvious arterial feeder vessels. Novel approaches to overcome this obstacle for drug delivery in these tumours has the potential to significantly improve outcome and potentially survival in these patients.
One such approach currently being investigated is trans-arterial micro-perfusion (TAMP). TAMP first isolates an artery of interest using a double balloon catheter to occlude the proximal and distal part of the
vessel, followed by exclusion of major side branches. Upon infusion of drugs between the balloons in this isolated section, the increased intravascular pressure permits active diffusion of infusate directly across the vessel wall
SIR position statement outlines appropriate use of endovascular management for chronic iliofemoral venous occlusions
The Society of Interventional Radiology (SIR) has published a position statement offering recommendations on the management of chronic iliofemoral venous obstruction with endovascular placement of metallic stents. The statement, published online in the Journal of Vascular and Interventional Radiology, is a companion to the 2022 statement on the treatment of acute iliofemoral deep vein thrombosis.
IN THE NEW STATEMENT, a multidisciplinary group of experts from interventional radiology (IR), vascular medicine, and vascular surgery indicated that among patients with chronic venous disease and iliofemoral venous obstruction, those who are experiencing life-disrupting symptoms or disability
into the surrounding tissue. Early studies of TAMP using gemcitabine chemotherapy in patients with locally advanced pancreatic cancer (LAPC), has shown the approach to be safe with no obvious local toxicity.1
Currently, a phase III clinical trial, TIGeR-PaC, is comparing the efficacy of this approach using intra-arterial gemcitabine (IAG) versus standard of care IV gemcitabine/nab-paclitaxel (GN) for patients with LAPC. The trial is designed with an induction phase for all patients of upfront systemic chemotherapy and radiation prior to randomisation to IAG or continuation of GN. LAPC patients receive three cycles of GN and one cycle of radiation (stereotactic body radiation therapy; 33Gy in five fractions). Following induction, patients with non-progressive disease are randomised to receive IAG (eight treatments biweekly for 16 weeks) or continuation of GN for four cycles over 16 weeks. After the 16 weeks of randomised therapy, patients with non-progressive disease receive continuation systemic therapy of GN or low-dose oral capecitabine, per investigator’s preference until disease progression and are followed for survival only.
Recently, the first interim analysis of the trial was presented at the World Congress on Gastrointestinal Cancer (28 June–1 July, Barcelona, Spain).2 At the time, 45 patients had been randomised in the trial; the survival, progressionfree survival (PFS) and the adverse events data (AE) comparing the two arms were presented. Of the 45 patients randomised, 23 were randomised to IAG and 22 to GN. There were equal number of primary events (13) in each
and who have anatomic features that favour long-term patency, may be more likely to benefit from stenting as an adjunct to conservative management. Most other patients with chronic iliofemoral venous occlusions would be better served with conservative management alone, such as use of medical therapy and compression garments, and re-evaluated over time.
“There is strong consensus on the panel that excellent clinical decision-making around venous stent placement will be most likely when the treating physician has strong familiarity with key clinical considerations around optimal diagnosis and evaluation of iliac vein obstruction, as well as assessment of its clinical severity and life impact,” said Suresh Vedantham, interventional radiologist and professor at Washington University School of Medicine (St Louis, USA), who is the lead author of the statement. “The statement provides a framework against which IR physicians can review their practices, address knowledge gaps, deliver treatment effectively, and ensure that patients selected for stent placement are likely to benefit from it.”
The statement authors note that additional research is needed to better guide the use of stents in this patient population. If completed, two ongoing multicentre randomised controlled trials—C-TRACT and BEST—can enable a strong and unbiased understanding of the treatment effects associated with the addition of venous stent placement to standard care, Vedantham said.
“For both studies, success will depend on whether providers make it a priority to refer patients to study sites,” he said. “It is hoped that physicians will
arm. Patients enrolled in the study were randomised after the induction phase that lasted, on average, 5.5 months.
After randomisation, the median survival in the control arm is 10 months, vs. 16 months in the IAG arm. The p values based on Wilcoxson nonproportional hazard ratio (HR) is 0.08 between the two arms. The PFS in control arm was seven months vs. 15 months in IAG (HR 0.55; confidence interval [CI]: 0.21–1.47). There was a threefold increase in AE in the control arm versus IAG (245 vs. 85); most of difference in AE were haematological (neutropaenia and thrombocytopaenia), followed by transaminitis. Lastly, in term of tolerability of completing all four cycles of active treatment without treatment modification, 61% of patients in IAG completed all intended treatment vs. 18 % of the patients in GN. The first interim look at the trial results is very encouraging in favour of IAG. Currently, the trial continues to enrol in 17 centres in the USA, with a second interim look at the data expected at end of 2024.
Ripal Gandhi is a vascular and interventional radiologist at Miami Cardiac and Vascular Institute and Miami Cancer Institute (Miami, USA).
References:
1. Rosemurgy AS, Ross SB, Vitulli PL, et al. Safety Study of Targeted and Localized Intra-Arterial Delivery of Gemcitabine in Patients with Locally Advanced Pancreatic Adenocarcinoma. J Pancreat Cancer. 2017 Aug 1;3(1):58-65.
2. Pishvaian M, Zureikat A, Novelli P, et al. The Phase 3 Study: Targeted Intra-Arterial Gemcitabine vs. Continuation of IV Gemcitabine plus Nab-Paclitaxel Following Induction with Sequential IV Gemcitabine plus Nab-Paclitaxel and Radiotherapy for Locally Advanced Pancreatic Cancer (TIGeR-PaC) Ann Oncol 2023 Jun 34(1): S1-S186
Disclosures: Gandhi is his site’s principal investigator for the TIGeR-PaC trial.

promote the welfare of future venous disease patients by actively choosing now to enrol eligible patients in ongoing clinical trials that are designed to generate high-quality evidence on the benefits, risks, and best practices around venous stent placement.”
While this research proceeds, SIR believes that adherence to the statement’s recommendations will enable judicious use of endovascular therapy in a manner that optimises benefit and minimises harm.
“The new statement provides the best assessment
of the current evidence we have to date, and SIR is grateful to the authors for their time and energy in ensuring that we have evidence-based guidance for the treatment of chronic venous occlusions,” said SIR President Alda L Tam, interventional radiologist and professor at the University of Texas MD Anderson Cancer Center (Houston, USA). “SIR remains committed to supporting ongoing and future research in this area to ensure that physicians have the information they need to optimise patient care now and in the future.”
26 September 2023 | Issue91 Point of View
IR physicians can review their practices, address knowledge gaps, deliver treatment effectively.”
Suresh Vedantham
PRIZER study to put the spotlight back on bare metal stents

Koen Deloose (Sint Blasius Hospital, Dendermonde, Belgium) talks to Interventional News about the importance of treating femoropopliteal disease patients and why some of the new generation bare metal stents are more advantageous for those complex lesions. He also discusses the PRIZER study, currently under enrolment, which aims to confirm the safety and efficacy of the RenzanTM peripheral stent system (Terumo Interventional Systems).
How prevalent is femoropopliteal disease and what is the impact of non-treatment for both patients and wider healthcare systems?
I think we are all aware of the fact that today the prevalence of peripheral arterial disease (PAD) in people over the age of 70 is around 15% and one out of every three of these definitely needs treatment. Interventional treatment can include supervised walking exercises as well as medicament therapy. My experience, and indeed my preference, is a combination of treatments. It is important for the patient that they are on the right drugs, that they are doing sufficient exercises but also that they are revascularised, whether with a bypass or, our preference, with a minimally invasive endovascular approach.
There are two categories of PAD patients—on one side you have the claudicants, and on the other the chronic limb-threatening ischaemia (CLTI) patients. We know that 5% of the severe claudicants are also evolving towards becoming CLTI patients. However, in a lot of countries they do not treat the claudicants with anything other than a conservative approach. In Belgium and in many other European countries we have noticed that there is definitely a space for the treatment of claudicants, especially as severe claudication has a very profound impact on the quality of life of the patient, and on their independent wellbeing.
These patients (Rutherford 4+) have rest pain or they have a lot of tissue loss and so if you stick to just a conservative approach these people are definitely going to end up with major amputation or death. Lack of treatment thus can have a huge impact on the social life of patients and ultimately a financial impact on healthcare systems as well. So we need to avoid this and we need to intervene, on time, in this category of patients.
How can the use of different stents to treat calcified lesions help resolve the unmet needs of these patients?
I noticed in my own practice in Dendermonde that the idea of ‘leaving nothing behind’ just did not work. It only worked for the straightforward, easy, noncalcified, stenotic, relatively short lesions, where it was feasible to treat these patients with angioplasty alone or a drug-coated balloon (DCB). But the vast majority of lesions that, as a vascular surgeon, I come across are chronic total occlusions. They tend to be more than 15cm TASC C and D severely calcified lesions. And so I noticed that the dream of leaving nothing behind remained a dream.
Because of this, in more than 50% of these patients, we need a scaffold. So I think there should be a greater focus on the need for bare metal stents, because a lot of interventionalists have almost
forgotten the existence of bare metal stents. But in this category of patients, DCB alone or angioplasty alone is insufficient and we need bail-out scaffolding.
There are currently a wide range of stents available. For example, we have stents with very low chronic outward force that we use to scaffold a flow limiting dissection in the less calcified lesions. But then we also have the severely calcified lesions where we need bare metal stents with a very high radial resistive force and crush resistance such as the Renzan stent which is the new kid on the block.
It is definitely important to select the right bare metal stent for the right indication and that is the challenge we need to overcome today.
How have stents evolved over time and why is it important to have nextgeneration stents like self-expandable micro-mesh stents available on the market?

In my mind and in my hands there are some essential requirements when it comes to the ideal bare metal stent. For me, as a pragmatic vascular surgeon, it first of all needs to be easy to use. If it is too complex, takes too many steps to implant, forget it. And of course accuracy of deployment. For example, if you really want to end up at the ostium of your superficial femoral artery for instance you need 100% accuracy. The nice thing about the Renzan stent is the fact that it is repositionable. So if you make a mistake, if you did not take into account tortuosity in the access towards the vessel and you made an error, you can reposition and try again.
When we are talking about the femoropopliteal area, visibility, flexibility, and conformability to
the vessel anatomy are also extremely important. You need the right chronic outward or radial forces. I notice that especially in the USA, a lot of physicians are using distal embolic protection devices to avoid distal embolization. These definitely have some disadvantages, including additional steps to the procedure that come with their own potential difficulties and complications. However, we now have a bare metal stent available with dual layer micro mesh technology, which aims to prevent plague prolapse and distal embolization based on experience in other therapeutic areas.
What is the PRIZER study and what do you expect or hope to see?
The PRIZER study is a prospective multicentre postmarket single-arm study which is looking to assess the performance of the Renzan stent in femoropopliteal disease treatment. There are two endpoints, a safety endpoint—defined as freedom from deaths, TLR and any amputation of the index limb at 30 days—and then we have an efficacy endpoint which is defined as primary patency at one year. We plan to enrol 135 patients in this study with follow-up of 36 months. There are 13 centres enrolling patients across five European countries: Germany, The Netherlands, Belgium, France and Spain.
I am actually excited about the spotlight again being on bare metal stents. I have mentioned that the dream of leaving nothing behind with a DCB has remained, in 2023, a dream, especially for the more complex lesions. On the other side of the spectrum if we are talking about drug-eluting stents, which have a lot of advantages but also some disadvantages such as the short lengths of some devices, so when treating a 30cm lesion I might need three stents which, in the Belgian healthcare system, is unpayable. There is also data showing signs that in the long run there can be some toxicity of paclitaxel.
On the other hand, we have access today to a completely new generation dual-layer micro-mesh
vessel preparation before implanting the stent. There is also a learning curve that you need to overcome in order to be an expert at Renzan implantation.
I am happy about this device, and I hope that the PRIZER study with the Renzan stent will confirm my enthusiasm.
Disclaimer: The Renzan Peripheral Vascular Stent System is indicated for use in patients with Peripheral Vascular Disease. Refer to instructions for use, contraindications and warnings for additional information. Renzan is manufactured by MicroVention Europe and distributed by Terumo Europe N.V. All brand names are a Trademark or registered trademarks of TERUMO CORPORATION, its affiliates, or unrelated third parties.
27 Advertorial Issue91 | September 2023
THIS ADVERTORIAL IS SPONSORED BY TERUMO INTERVENTIONAL SYSTEMS
Koen Deloose
It is definitely important to select the right bare metal stent for the right indication and that is the challenge we need to overcome today.”
thrombectomy in medium vessel occlusions
WHEN UTILISED AS A FIRST-LINE technique for medium vessel occlusion (MeVO) stroke, aspiration and stent-retriever thrombectomy have demonstrated “no significant difference” in imagingrelated or clinical outcomes. That is according to a multicentre, propensity score-matched analysis including more than 400 patients, the results of which have been published in the journal Stroke: Vascular and Interventional Neurology
“Altogether, these findings do not suggest one technique […] to be associated with any greater probability of technical success, safety, or better long-term functional outcomes,” write authors Adam A Dmytriw (Massachusetts General Hospital, Boston, USA) et al. “The technical success rates with either technique were high (80–90%) and are consistent with those reported from secondary analyses of clinical trials.”
Led by first author James Siegler (Cooper Neurological Institute, Camden, USA), the researchers initially note that, due to the lack of data regarding MeVO thrombectomy, they set about evaluating outcomes according to first-line techniques in a large, multicentre registry referred to as ‘MAD-MT’. This
consortium was founded by Dmytriw and Adrien Guenego (Erasme University Hospital, Brussels, Belgium). Imaging, procedural and clinical outcomes were assessed, with acute proximal or distal MeVO patients being treated at 37 sites across 10 countries and analysed according to the first-line thrombectomy technique they received—aspiration or stent retriever.
Multivariable logistic regression and propensityscore matching were used to estimate the odds of the primary outcome—expanded thrombolysis in cerebral infarction (eTICI) scores of 2b–3, defined as ‘successful recanalisation’—between the two treatment groups. Secondary outcomes included the ‘first-pass effect’, eTICI scores of 2c–3, intracerebral haemorrhage, 90-day modified Rankin scale (mRS) scores, and 90-day mortality.
Of 440 included patients, 55.5% were treated with aspiration thrombectomy versus 44.5% with a stent retriever. Dmytriw et al report those treated via stentretriever thrombectomy as having lower baseline Alberta stroke programme early computed tomography scale (ASPECTS) scores (median=8 vs 9); higher National Institutes of Health stroke scale (NIHSS) scores (median=13 vs 11); and non-significantly fewer medium-distal occlusions (M3, A2, P2 or other; 17.4% vs 23.8%).
Use of a stent retriever was associated with a 15% reduction in the likelihood of successful recanalisation (odds ratio [OR]=0.85)—but this difference was not found to be significant after multivariable adjustments
Severe obesity linked to lower AVF maturation rates
Researchers behind a new study published in the Annals of Vascular Surgery, among them lead author Laura Anderson and corresponding author Benjamin Brooke (both University of Utah Health, Salt Lake City, USA), have found that severe obesity risks a greater likelihood of maturation failure in the arteriovenous fistulas (AVFs) of patients looking to start dialysis.

THEIR WORK CITES A 2008
Kidney International-published metaanalysis by Y Wang (Johns Hopkins University, Baltimore, USA) et al, which suggested that 33% of all US cases of end-stage kidney disease (ESKD) are associated with obesity and metabolic syndrome. Anderson and colleagues further aver that there has been a 42% increase in ESKD cases in the USA, which significantly includes a sevenfold increased risk of developing the condition for those with a body mass index (BMI) ≥35.
In reviewing the existing literature, the authors of this study note that, while some research has found higher AVF patency rates for obese patients, other research has found higher rates of failure and stenosis. Anderson and colleagues sought to clarify the effect of a BMI ≥35, “the most severe classes of obesity”, with a view to facilitating better clinical decision-making.
They conducted a retrospective cohort study, analysing the data from patients
who received either a radiocephalic, brachiocephalic, or brachiobasilic AVF at a single centre during the period 2016–2019. The primary outcome was functional maturation following AVF creation, defined as use of the AVF with two needles for 75% of dialysis sessions in a continuous four-week period. Secondary outcomes included AVF depth and diameter, as well as flow volume, which was measured using a postoperative ultrasound examination. A total of 426 AVF procedures were performed during the study period, with 202 available for analysis following the exclusion criteria. Among these were 49 (24%) with radiocephalic, 87 (43%) with brachiocephalic, and 66 (33%) with brachiobasilic AVFs. Stratification by BMI yielded 53 patients (26%) in the severely obese group and 149 (74%) in the remaining categories. There were “no significant differences” between the groups on other factors, apart from a higher percentage of female patients in the former group.
across the total cohort (adjusted OR=0.88), or in the propensity score-matched cohort, in which both groups included a total of 105 patients (adjusted OR=0.94). Furthermore, there was no significant association between thrombectomy technique and secondary outcomes in the propensity score-matched, adjusted models, the authors relay.
As such, they conclude that—in this large, heterogenous, multinational cohort of MeVO patients—no significant differences in imagingrelated or clinical outcomes were observed between aspiration and stentretriever thrombectomy. Dmytriw et al go on to assert that there appears to be “no significant technical or functional advantage” to using either specific technique.
However, despite this cohort being “one of the largest to date” to report outcomes associated with first-line aspiration versus stent-retriever thrombectomy in MeVO/distal vessel occlusions, they acknowledge the non-randomised allocation of the techniques; the influence of unmeasured confounding factors; and some missing reperfusion data as well as between-site variations, as limitations of the analysis.
“Other clinical and imaging predictors, such as clot composition or hyperdense vessel sign, warrant further exploration to better understand the selective vulnerability of certain occlusions to one device or another,” they add, also noting that multiple ongoing randomised trials are “anticipated to shed light on these treatment considerations”.
The authors found a “significantly lower rate of functional maturation” in the severely obese group (58% severe obesity vs. 80% non-severe obesity; p=0.002). A subanalysis by fistula type found that differences in primary and assisted maturation between obesity groups on brachiocephalic AVFs were significant, but were not so for those with radiocephalic and brachiobasilic AVFs.
significant differences in flow volume for any AVF type between any of the study groups.
The data suggest that obesity is of greatest concern in fistula maturation for severely obese patients with a brachiocephalic fistula, the authors say in their discussion, adding that it can also impact brachiobasilic AVFs “even after transposition”. Drawing attention to the “obesity paradox”, the finding of some studies that patients with higher BMIs have better survival rates with ESKD, sometimes attributed to “nutritional preserve and protection against wasting in the setting of acute illness”, they argue that their results indicate that this does not extend to fistula maturation. For treatment of severely obese patients with an AVF who cannot be cannulated, Anderson et al note that transposition and superficialisation of the fistula are established options.
On the secondary outcomes, outflow average vein depth was “significantly increased” in severely obese patients compared to the other groups, with the difference marked across all three types of AVF (p<0.05 for all comparisons). There was also a statistically significant larger average vein diameter for those severely obese patients with brachiocephalic AVFs (6.8mm severe obesity vs. 5.9mm non-severe obesity; p=0.007). The authors did not find
Outlining some limitations, including the retrospective cohort design of their study and its focus on functional maturation outcomes rather than primary or secondary patency, the authors nevertheless conclude that their results support the claim that BMI ≥35 reduces functional maturation rates. “These data,” they state finally, “can help guide decision making when planning AVF placement in severely obese patients, which should include scheduling adjuvant superficialisation procedures on appropriate patients.”
28 September 2023 | Issue91
“No significant difference” between aspiration and stent-retriever
Stroke Thrombectomy
were treated with aspiration thrombectomy
55.5%
44.5% with a stent retriever
Of 440 included patients
Patients undergoing dialysis
How does a lytic-free approach in DVT treatment help in building a successful venous practice?
A recent Inari Medical roundtable webinar examined how to build a venous practice effectively—three experts from different specialties discussed the importance of forming and maintaining internal and external networks; what to consider when building a deep vein thrombosis (DVT) pathway; and how to choose the right treatment for each DVT patient. The webinar is part of the first edition of the ClotWarrior Academy DVT Webinar Programme set up by Inari Medical to initiate further education and conversation around the effective management and treatment of the full range of DVT chronicity.
Stephen Black, vascular surgeon at Guy’s and St Thomas’ NHS Foundation Trust (London, UK) began proceedings, focusing on “the power of the multidisciplinary team”. Black also pinpointed how crucial it is to know the data and the literature relating to venous work, as well as to spend time with “people who have done it” before and “utilise their skill”—namely, those with established practices. In terms of data, there are more to come, Black added. “We have launched DEFIANCE, a randomised controlled trial (RCT) evaluating its clinical outcome in DVT treatment. Its goal is to demonstrate that mechanical thrombectomy is superior to anticoagulation alone. Other RCTs in the DVT space have all focused on catheter-delivered lytics and we know that the downside of lytics is bleeding, which was a significant outcome of the ATTRACT study. Trying to find something that avoids lytics is going to be really useful for this therapy.”
In terms of building the team, Black made the point that venous patients can be “more needy than their arterial [counterparts]”, and so lots of staff from different departments need to be involved in their care, including in theatre, interventional radiology (IR), haematology, ultrasonic angiology, and research. Black emphasised that even the intervention itself can be multidisciplinary depending on circumstances, with “another member of the team finishing it off”. He then touched on the protective, supportive aspect of working as a team—“if something goes wrong, […] and it will, you are very vulnerable if you are by yourself […]”, whereas as part of a team, this is guarded against.
Next, Black addressed how introducing pathways into the hospital is key “because you cannot be there all the time” to oversee every patient’s referral and care. These pathways enable smooth follow-up and decision-making around “who to treat and who not to treat”. Having an eye for detail is also important, he continued, stating that “it is not good enough to [just] hope for the best”.
After the procedure, Black advocates for duplex follow-up, then reflecting on the outcome, and repeating this after every procedure, having considered the success of factors such as “stent choice and placement, errors, and IVUS”. Moreover, he suggested that “most errors of a technical nature are the fault of the user, not the product”. Returning each time to consider outcomes will ensure that they keep getting “better and better”, Black averred.
Michael Piorkowski, interventional angiologist and cardiologist at CCB Frankfurt (Frankfurt, Germany) was next to speak, first outlining how the interventional DVT programme at his centre started.
He described his hospital’s large cardiovascular outpatient service and how “every day, there are up to ten patients referred from general practice with suspected DVT”. The programme has office hours of 8am to 6pm Monday to Friday, with various lab testing capabilities as well as those for other types of imaging, including several vascular ultrasound machines and computed tomography (CT) and magnetic resonance imaging (MRI) with cardiovascular-specialised radiologists.
“When I started here in 2014, the majority of patients, even those with iliofemoral DVT, were treated with compression stockings and oral anticoagulation,” Piorkowski relayed, going on to say that when he first treated acute DVT in 2012, he used a rotational thrombectomy device. He then switched to a pharmacomechanical aspiration device but “most patients still also had some form of lysis”. This limited the indication, Piorkowski went on, adding that the research at the time was also not really venturing beyond chronic venous disease.
Nowadays, he noted that they still see patients who underwent DVT treatment 10 or 15 years ago—“there is a high patient loyalty”. They have started to treat chronic venous occlusions, especially in middle-aged women who experienced an iliofemoral DVT in their twenties or following childbirth. “There is a growing recognition of the need for a treatment with high thrombus removal and without lytics,” Piorkowski then affirmed. “We were one of the first centres outside of the US to introduce the ClotTriever system and in my opinion this is the most efficient way to remove acute and chronic clots. I faced the problems of patients developing PTS over the long term, including problems with varicose veins, leg ulceration, constant heaviness and swelling of the legs. By removing all of the clot, in the acute phase, we can prevent all of this.
Gerd Grözinger, interventional radiologist at the University of Tübingen (Tübingen, Germany) followed Piorkowski, sharing his experience of how he takes on DVT referrals. Firstly, he outlined an example of a case he has seen—a 30-year-old woman with five-day-old leg pain, who had never had thrombosis before nor had a family history of it. She took the contraceptive pill and was a smoker, Grözinger shared. She received an ultrasound, which confirmed the DVT, and she was then referred to Tübingen. This led Grözinger to make the point that networks of hospitals including specialist centres are crucial in providing adequate care for DVT, so that hospitals in rural areas that may not have the required expertise can work with bigger, more specialised hospitals to refer their patients over if necessary.



“The team is very important,” he continued, expanding on this to describe his hospital’s vascular centre, which has all the specialties combined, including vascular surgery, cardiology, angiology, IR and dermatology. There are two vascular board team meetings each week, at which DVT patients are discussed, and a 24/7 service for vascular emergencies, Grözinger detailed. Different external specialists refer DVT patients to the vascular centre, including internal medicine and emergency departments, and primary care physicians.
Grözinger then highlighted a “holistic approach” as key, which, at his centre, means they have a linked pulmonary embolism (PE) team, and often see patients who are being seen, for example, by oncology for metastatic lymph nodes in the pelvis, which has gone on to cause compression disease and subsequently DVT. Standardised treatment pathways for DVT and PE are necessary, he stipulated. Grözinger shared that, at his hospital, their DVT pathway is mostly based on the European Society of Cardiology guidelines. “All patients with a proximal DVT have cross-sectional imaging with MRI, as it is the only modality that can assess the real age of the thrombus”.
“I think we all have to consider that DVT is not a life-threatening condition,” Grözinger then mused, reflecting on how the bleeding risk with treatments including catheter-directed thrombolysis (CDT) may not be worth it. Therefore, there is “a need for a mechanical thrombectomy system without CDT”—ClotTriever (Inari Medical) is an answer to this need, he put forward. “The system is a mechanical thrombectomy system designed to remove large thrombi from large vessels in a single session, without the need for thrombolytic drugs or consequent intensive care stay. The patient I mentioned earlier, who was referred to us, was also treated with ClotTriever system. She had a complete occlusion and the clot which we removed during the intervention was organised thrombus. This is what we experience in a number of patients—they develop chronic DVT and thrombolysis would not work in those cases.”
Grözinger’s last word was on increasing the visibility of this “undertreated disease”, which he believes can be achieved with “satisfied patients with quick improvement of symptoms”. He would also advise good communication about cases with the referring centre beforehand, and offering lectures and educational material to these referring physicians to “raise awareness”.
To learn more about the lytic-free mechanical thrombectomy ClotTriever and FlowTriever systems, join Inari’s symposium at CIRSE 2023 on Sunday 10 September at 1pm (Auditorium 15).
29 Advertorial Issue91 | September 2023 2023
THIS ADVERTORIAL IS SPONSORED BY INARI MEDICAL
There is a growing recognition of the need for a treatment with high thrombus removal and without lytics.”
Michael Piorkowski
Stephen Black
Gerd Grözinger
Michael Piorkowski
“The PAIRS IR curriculum […] will be published by the 2024 annual meeting”
Ayman Al Sibaie is a consultant interventional radiologist currently working at Rashid Hospital (Dubai, UAE), and has been the president of the Pan Arab Interventional Radiology Society (PAIRS) since 2019. Interventional News interviewed him to delve into his practice in Dubai, to get his take on how interventional radiology (IR) practice varies between the Middle East-North African (MENA) region and the Western world, and his perspective on PAIRS’ work, having been president for the past four years.
Would you be able to provide some insight into your background and IR training?
I am originally Syrian and have German nationality. I studied medicine in Germany and graduated from Friedrich Schiller University Medical School (Jena, Germany) in 1992. Then I did my radiology residency in the same university hospital and finished my postgraduate studies in 1997. I have been in love with IR since the very beginning and I worked as an interventional radiologist in many German cities like Jena and Gera before becoming a consultant of IR in 1998. In 2005, I decided to go to Dubai to start a new career there.

How was it starting a new IR career in Dubai?
It was far from an easy ride. When I first came to Dubai there was nothing—IR was rather a new specialty so I had to start from scratch. The infrastructure was good and the hospital authorities were willing to do anything to help the patients, however I had to talk to companies from my connections in Germany to get the tools. I then started recruiting residents who could help me with cases, and talking to doctors from other specialties to send patients. Fortunately, after 18 years, I can definitely say we have a practice in Dubai that is not at all inferior to those in Europe and the USA.
What is your special interest within IR?
Practising IR in the MENA region requires you to cover a wide spectrum of procedures. For example, the hospital I work in is a trauma centre—one of the biggest emergency and trauma centres in the Middle East—that has different specialties like neuro and vascular, and I am the only IR consultant. This means I have
to cover almost all IR procedures, including for aneurysms, arteriovenous malformations, stroke, the aorta, critical limb ischaemia, pulmonary embolism and deep vein thrombosis. Also emergency embolization for bronchial, gastrointestinal bleeds, and renal, as well as elective embolization for uterine fibroids, prostate, and varicose vein management.
What are the key differences in IR practice between the MENA region and Europe? There are substantial differences on many levels. For example, the regulations are much more flexible in our region, allowing us to use a wide range of supplies from all over the world. There is a lot of variation in diseases in my region due to the difference in weather and our younger population, not to mention the difference in health insurance coverage and a bigger private sector with self-payors in the MENA region compared to in the Western hemisphere.
I would also like to add that there is huge heterogeneity in my region when it comes to IR, from countries with a remarkably advanced IR practice like UAE, Egypt and Saudi Arabia, to countries with no access to IR services at all. Even if there is IR provision in a country, it will tend to be centralised in the major cities, depriving the rural areas. So, in a country like Egypt, of 120 million people, with a high-volume IR practice, almost 90% of trained interventional radiologists are in Cairo.
Talking now about PAIRS, how much progress have you seen in the past few years with the society? What are the challenges, and for the specialty overall? What is your vision for the future?
In 2018, PAIRS had 30 active members.
In 2023, we now have more than 1,000. In 2014, the annual meeting was attended by 150 people, whereas in 2023 it was attended by 4,300 people. Now, we are collaborating with all the big IR societies and meetings worldwide like the Cardiovascular and Interventional Radiological Society of Europe, Leipzig Interventional Course, Global Embolization Symposium Technologies, as well as being the regional hub for the different national societies in the MENA region.
As for my vision (although this vision belongs to the whole of the current board), I remember having an eighthour board meeting in Dubai in the holy month of Ramadan in 2019, when we planned for the years ahead. Our main goal was to transform PAIRS from a successful annual meeting to a fully functioning multicommittee society, working to face challenges, and help doctors and patients in the region to access IR. If you look now, we have a decent website with a big academy, housing hundreds of lectures accessible to all members. We have the Arab Journal of Interventional Radiology growing every day led by Mohammad Arabi as editor-in-chief; we also have the educational committee led by Refaat Salman doing dozens of webinars, which has also started our hands-on courses.
The board has a vision of investing in the younger generation, so we formed the very active residents, fellows and students (RFS) committee led by Rana Khafagy, who initiated the Global IR Juniors Summit organised
in collaboration with the Society of Interventional Radiology RFS, the European Trainees Forum, and the British Society of Interventional Radiology. It will be its fourth year in PAIRS next year, and the RFS committee has been also working on the PAIRS IR curriculum, which will be published by the 2024 annual meeting. Regarding PAIRS’s vision to further promote IR training in the region and to recruit more and more young minds to join IR, PAIRS initiated the #I_AM_ PAIRS IR awareness campaign led by our secretary Karim Abd El Tawab, and it took place in six medical schools in Egypt, Morocco, Saudi Arabia, Tunisia, UAE, and Syria, with almost 1,000 total attendees. Finally, we have the Women in IR committee headed by Noha Guzaiz (King Abdullah Medical City, Makkah, Saudi Arabia), which is dedicated to boosting numbers of female interventional radiologists in the region. Five or six years ago, none of these committees even existed.
What advice do you have for interventional radiologists just starting out?
My advice would be this: you are an interventional radiologist, so you are a hero, as every day you will save lives and can treat disease all over the body. The important thing you have to learn is when not to do cases, where to stop and say “I should not do this case” or “there is a better option for this patient”. As long as you are developing your clinical skills, you should concentrate on making the best decisions for your patients.
In a country like Egypt, of 120 million people, with a highvolume IR practice, almost 90% of trained interventional radiologists are in Cairo


30 September 2023 | Issue91 IR in the Middle East Interview:
90%
Ayman Al Sibaie
THIS ADVERTORIAL IS SPONSORED BY TERUMO INTERVENTIONAL SYSTEMS
Pooled analysis data from 580 patients with unresectable HCC reinforce positive outcomes of LifePearlTM microsphere
TACE procedures
LifePearl microspheres (Terumo) are polyethylene glycol (PEG) embolization microspheres that can be loaded with chemotherapeutic drugs including doxorubicin, irinotecan, idarubicin and epirubicin.1 Philippe Pereira (SLK-Kliniken GmbH, Heilbronn, Germany) speaks to Interventional News about his experience using LifePearl microspheres in his interventional oncology practice. He shares his knowledge on how to achieve the optimal transarterial chemoembolization (TACE) procedure, and how the latest pooled analysis data from hepatocellular carcinoma (HCC) patients reinforce the evidence on efficacy and safety of drug-eluting microspheres (DEM) TACE with LifePearl microspheres in patients with HCC.
Pereira begins by outlining some of the current challenges of TACE. “Having a personalised approach to chemoembolization is very important and one of the main advantages of local therapies,” he stipulates, “and every chemoembolization is different—regarding the dose, the vessel anatomy, etc. He also stipulates the need to preserve the patient’s liver function following TACE. Altogether, you need a very high level of experience, and for the large majority of tumours, a superselectivity of your catheterisation is absolutely required”.
How do you perform your TACE procedures for HCC?
Next, Pereira details the advantages of using LifePearl microspheres as a means of overcoming the challenges often associated with TACE, drawing on his own experience, having used it for eight years. “In Germany, the preparation [for TACE] with cytotoxic drugs is no longer done in the radiology department, but in the pharmacies. As our pharmacists have said to me, it is really easy to load them with only few preparation steps required”. Another advantage, according to Pereira, is that the LifePearl microspheres are available in a variety of sizes, including “a very small size (100µm) for the treatment of primary and secondary liver tumours”. This is coupled with a narrow size distribution for targeted treatment. The third benefit, he continues, is the “long time stability” of LifePearl microspheres mixed with contrast medium allowing a smooth delivery.2,3
Furthermore, Pereira explains that he uses “a 2.4Fr Progreat microcatheter for TACE procedures and in some more difficult situations where you have a complex intrahepatic arterial anatomy, you should be very selective and we sometimes go to a 2.0Fr microcatheter”. OcclusafeTM micro balloon microcatheter can also allow for blood flow redistribution during TACE, which is not possible with a standard microcatheter and can be beneficial for some types of tumours.
What are the highlights of the latest clinical evidence with LifePearl microspheres from your perspective?
Pereira then outlines some of the key findings from the pooled analysis of 580 patients with unresectable HCC treated with LifePearl microspheres, first highlighting the “median overall survival of 50.8 months, which appears to be much more than 25–37 months usually obtained with [conventional] TACE”, although this figure can vary depending on the patient’s Barcelona
Clinic Liver Cancer (BCLC) stage.
Also, of interest to Pereira is the “stratification following the ALBI [albumin-bilirubin] scores, allowing maybe a better selection of patients or a more personalised approach with DEM-TACE”.
In addition, he notes “the importance of a low level of liver damage” observed in the patients treated with LifePearl microspheres, and that “a low level of hepatic damage is extremely important for continued targeted therapy with TACE or for allowing a stage migration with systemic treatment.”
In a similar vein, Pereira suggests some of the reasons why LifePearl microspheres achieved a greater median overall survival rate as compared to previous reports—“maybe because they have a higher elution rates as demonstrated in in vitro comparative testing, maybe in relation to the tighter size calibration of microspheres allowing a more targeted embolization, maybe both, since there is better standardisation for TACE with microspheres versus conventional TACE.”
The improvement of the TACE technique over the years (with superselectivity, improved images etc) can also explain these latest outcomes.
What would be your recommendations for performing an optimal TACE procedure?
Pereira proceeds to speak about recommendations for carrying out an optimal TACE procedure in HCC patients, where superselectivity is key. In the German guidelines, Pereira states, it says that for HCC, “if you cannot be superselective, it is not recommended to perform TACE”. Moreover, in his opinion, Pereira says that this is true “independent of the size of the tumour”—even if there are “satellite” tumours surrounding it, “you should address each tumour-feeding artery in a selective way”. Another reason why selectivity matters so much for HCC, he elaborates, is to reduce the toxicity of the TACE, especially for patients with the beginnings of liver insufficiency. “It is very important because the TACE will be repeated and you keep, also, the possibility to move to another treatment.” In summary, Pereira states that, with selectivity, “you increase efficacy, and you reduce the adverse effects”.
Pereira returns next to his personal experience, and what is, for him, crucial for an optimal TACE procedure. “Imaging is important—good quality will reduce radiation,” he says. Going into more detail on imaging, Pereira specifies that real-time monitoring can help to analyse the perfusion of HCC tumours in some more tricky cases. “As HCC is mostly a highly
perfused tumour, this online monitoring may work very well. It is not necessary for all patients, but in some cases, we use it if we are not sure whether there might be another tumour-feeding artery that we would need to perform TACE on.”
What do you think can be done to further improve clinical outcomes for TACE?
First of all, Pereira suggests that “to improve clinical outcomes, we need to improve training of interventional oncologists on performing TACE procedures—it is a prerequisite”.

Looking ahead to the potential for further innovation, Pereira suggests that “perhaps we need, in the future, resorption of the microspheres to be able to repeat the treatment”. BioPearlTM microspheres (Terumo) are an example of this technology to which Pereira refers to reinforce this point. Access to the tumour over time can become problematic due to “changes in morphology in the alreadytreated tumour-feeding artery, such as if you need to treat the same tumour multiple times”. Resorbable microspheres can guard against this, Pereira underlines, but that how quickly different embolic agents are resorbed remains a question to be answered through future research.
Staying on the subject of future developments, Pereira suggests that we should also improve the possibility of loading DEM-TACE microspheres with different cytotoxic drugs or even immunotherapies, such as immune checkpoint inhibitors.” Pereira points out that there is some preliminary experience of loading embolic microspheres with immunotherapies and treating locally, but that this should be also studied further.
Summarising, Pereira believes that the first way to improve TACE procedures is for the interventional oncologist to develop and standardise the technical aspects, including use of imaging and microcatheters, but that another possible means of achieving better procedural outcomes is to better select the patients and “work together with hepato-oncologists to improve the treatment strategy by combining local and systemic therapies”.
References:
1. Terumo. LifePearl microspheres. 2023. https://www.terumo-europe.com/ en-emea/products/lifepearl%E2%84%A2-drug-elutable-microspheres
2. De Baere T, Plotkin S, Yu R, et al. An In Vitro Evaluation of Four Types of Drug-Eluting Microspheres Loaded with Doxorubicin. J Vasc Interv Radiol. 2016;27:1425–31.
3. Pereira P, Plotkin S, Yu R, et al. An in-vitro evaluation of three types of drug-eluting microspheres loaded with irinotecan. Anti-Cancer Drugs 2016;27:873–878.
Disclaimer: Intended purpose: LifePearlTM microspheres are indicated for embolization of blood vessels supplying primary hypervascular tumours or metastases in the liver. Note: LifePearlTM microspheres can be loaded with chemotherapeutic drugs. When used for drug loading, drug loading should be done under a physician’s direction, choice and responsibility, based on type and dose of drug most beneficial to the patient. LifePearlTM microspheres are compatible with doxorubicin, epirubicin, idarubicin and irinotecan. LifePearlTM microspheres can be drug loaded prior to embolization and then, as a secondary action, elute a local, controlled, and sustained dose to the targeted tumour sites after embolization.
OcclusafeTM temporary occlusion balloon microcatheter is intended for use in the peripheral vasculature where temporary occlusion is desired. It provides temporary vascular occlusion, which is useful in selectively stopping or controlling blood flow. For use in the peripheral vasculature for the infusion of contrast media, drugs and embolic materials.
Progreat™ is intended for the infusion of contrast media into all blood vessels. The catheter is also intended for drug infusion in intra-arterial therapy and for the infusion of embolic materials for haemostasis. Do not use this product in coronary and cerebral blood vessels.
LifepearlTM microsphere and OcclusafeTM temporary occlusion balloon microcatheter are not available for sale in all countries. This information is provided only in respect to markets where these products are approved or cleared. The use of the LifePearlTM microspheres device is not cleared or approved in the U.S.A. by the Food and Drug Administration. LifepearlTM microspheres are not approved in Canada. Please contact your Terumo local sales representative for more information. LifePearlTM microspheres are manufactured by MicroVention Europe SARL and exclusively distributed by Terumo Europe NV in EMEA region.
All brand names are trademarks or registered trademarks of TERUMO CORPORATION and their respective owners. Scientific and clinical data related to this document are on file at MicroVention and at Terumo Clinical Supply Co., Ltd. Refer. Refer to Instructions for Use for Contraindications, Warnings and Precautions.
© 2023 Terumo Corporation. CE0297 – Manufacturer MicroVention Europe
SARL – 30 bis, rue du Vieil Abreuvoir 78100 Saint-Germain-en-Laye FRANCE – Tel: +33(0)1 39 21 77 64 – Fax: +33(0)1 39 21 16
© 2023 Terumo Clinical Supply. CE0344 – Manufacturer TERUMO CLINICAL SUPPLY CO., LTD. – 3, Kawashima-Takehamachi, Kakamigahara, Gifu, 501-6024, JAPAN
31 Advertorial Issue91 | September 2023 2023
Philippe Pereira
ESKD Summit 2023: What matters to patients gains momentum with input from multidisciplinary experts
Focusing on the disease through the patient’s lens, establishing well-functioning multidisciplinary teams, to potentially enhance both the patient’s journey and clinical outcomes got top billing at BD’s second EMEA End-Stage Kidney Disease (ESKD) Summit (9–10 May 2023, Milan, Italy). With a multispecialty faculty comprising 22 leading voices including nephrologists, vascular and transplant surgeons, and interventional radiologists (with a combined knowledge of over 400 years), selected from 12 countries, BD’s second edition of “The Changing Face of a Dialysis Patient” showed commitment to a new format of scientific peer-to-peer communication, characterised by open interaction and vibrant discussion. More than 30 presentations including challenging cases, 14 hands-on workshops and the participation of 200 attendees marked the event.
Scientific directors of the summit, interventional radiologist Fabrizio Fanelli (Florence, Italy) and vascular access and transplant surgeon Nicholas Inston (Birmingham, UK), welcomed delegates to a programme that encouraged placing patients at the heart of care in dialysis access creation, restoration and maintenance.
Disease overview and patient journey
Charting the various difficult terrains of end-stage kidney disease (ESKD) in the renal patient pathway, Inston said each person’s course depends on age, comorbidities, “events” and interventions that were influenced by decisions made by clinicians, and importantly, by patients. Even simple clinical decisions can have a disproportionate, and sometimes uncaptured, impact on a patient’s life, he underscored. “When a fistula does not work, clinicians may simply plan to create another one, but this might have major disruption on a patient’s life and can potentially create a very negative loop for patients as they have likely gone through six to 12 months of other procedures to get to this point,” he said.
Based on his clinical experience, Inston referenced the concept of “much more tailored” minimally disruptive medicine (MDM). In this context, “the appropriate focus of treatment is the situation and the individual tackled as a whole”. MDM aims to reduce workload and individualise treatment, taking into account the effects of, for instance, “12 hours of dialysis per week, transport, maintenance interventions, clinical appointments and possible surveillance on a person’s life and calendar”.
Is there a case for rebooting questionnaires?
Inston kickstarted a discussion of wide-ranging quality of life issues with questions such as: “Is measuring patients’ quality of life via questionnaires of any use? Are they representative or do they misguide us? Do we add to the patients’ workload with more surveys/ questions/studies? Are we considering what we can do to tailor care to the patient and reduce workload? And can minimally disruptive medicine be applied to dialysis care?”
Daniel Gallego, a patient advocate and president of the European Kidney Patient’s Federation, has been a kidney patient since 1993, undergoing haemodialysis since 1995. To Inston’s points, he responded: “Twenty years of in-centre haemodialysis is different from home haemodialysis or peritoneal dialysis. Health questionnaires have been decided by clinical professionals and they do not include components on self-esteem, physical appearance, or things that really matter to us. […] Many aspects that might improve the life or quality of life of patients are not really captured in the outcomes. […] And sometimes these are misguiding us.” He called for a redesign of the
questions asked and the management of information gathered so that the right decisions for patients can be made. Gallego also placed the spotlight on including the perspective of care-partners and families who influence the quality of life experiences for patients.
Responding to a question from the audience on whether a patient can influence the final decision on treatment modality, Gallego pressed on to say that with enough information and involvement at every stage, yes, patients can be responsible for both the choice and consequences of that choice for their access.
Külli Kuningas, lead renal research nurse, Queen Elizabeth Hospitals, Birmingham, UK, then outlined the “Our Arteriovenous Fistula (AVF) Lives” project, a patient-led ethnographic research undertaking run by the hospital to capture more in-depth patient perspectives on living with vascular access for dialysis. Relying on primary source material in the form of video diaries and the filming of patients in their own environments without the use of questionnaires, researchers aim to analyse how patients describe their conditions and what is important to them, to capture a repository of “true patient perspective”.
Gallego stressed that patient-reported outcomes were received usually from articulate, perhaps educated respondents who have the luxury of time. A critical component will be to validate these responses so that they become applicable to patients who might have poor language skills, come from populations with different cultures and languages and to those who might never answer questionnaires. He also addressed the discussion point of disparities in guidelines by stating that a consensus was needed, without bias, on the right treatment. This sparked the question: should care be “guideline-driven” or “tailored to the individual patient”? “We need to adapt, because every single patient is unique,” said Gallego.
The ensuing panel discussion on harnessing

multidisciplinary expertise into the care of patients with kidney disease painted the picture of a changing paradigm. In “the old days”, and according to the panel’s experience, the “thinkers” were the nephrologists and the “doers” interventionalists and surgeons. With nephrologists also embracing interventional skills, there is a merging of the “thinkers” and “doers” responsible for a patient’s access, but this varies considerably based on local expertise, the panel said. According to their experience, there was acceptance that the nephrologists and nurses were ‘closer’ to the kidney patient’s journey and pivotal in coordinating care within multidisciplinary teams. Longstanding relationships with the patient, underpinned by trust and time were also identified as central to the patient’s experience of care. The panel agreed that a close connection in the discussion
between patients, nephrologists and vascular access teams was core to good patient care. “More than the specialties of clinicians, communication is the key, and having one person in charge, potentially a nurse or dialysis access coordinator, who communicates in simple language along the whole journey with patients, is vital,” offered Gallego.
Ounali Jaffer (interventional radiologist, London, UK), Fien Gryffoy (vascular surgeon, Antwerp, Belgium), Gürkan Sengölge (interventional nephrologist, Vienna, Austria) and Ioannis Griveas (nephrologist, Athens, Greece) contributed to the discussion.
Looks as well as books
Panos Kitrou (interventional radiologist, Patras, Greece) detailed the importance of the Haemodialysis Arteriovenous Access Cosmesis Scale (AVACS), which is a new measure for vascular access. While clinical decision-making is often based on the twin-pillars of safety and effectiveness, the impact that vascular access has on the patient is also very important, he said.
Research has shown that lumps, bulging and related tortuosity, “mega access”, access-related scarring and number of scars, and the noticeability of the vascular access have been identified as some issues that play on patients’ minds.
Kitrou noted that there is a paucity of reports about the effect of AV access cosmesis on patients’ quality of life, dialysis experience, and decision-making about choice of vascular access type and creation.
“The cosmetic effect has an influence on patients’ psychology and therefore on the type of vascular access selected,” Kitrou posited.
“Cosmesis in the context of access is defined as the preservation of, or change in, limb physical appearance after AV access creation. It is one of many important
32 Advertorial September 2023 | Issue91
THIS ADVERTORIAL IS SPONSORED BY BD
The multidisciplinary panel discussions were characterised by lively interaction
factors to be considered in choosing vascular access within the context of the patient’s ESKD Life-Plan. By creating a scoring instrument that allows stratification of cosmesis of AV accesses, factors that affect cosmesis can be assessed,” he informed delegates. “In doing so, both clinicians and patients will be better informed to make access decisions in line with a patient’s priorities,” he concluded.
New guidelines signal change
Narayan Karunanithy (interventional radiologist, London, UK) and José Ibeas (interventional nephrologist, Barcelona, Spain) then delved into the updates on the most recent guidelines.
The former unpicked the latest UK Kidney Association (UKKA) guidelines to point out that these guidelines, from the oldest continuously active nephrology society in the world, are not funded by any external organisation, commercial company or charity.



The recent haemodialysis access guideline update marks a considerable shift in how the organisation recommends that clinicians approach choices in vascular access for patients and does away with the idea of targets to place patient choice at the heart of vascular access creation and care. The team behind the guidelines have said it is a pragmatic guideline that had active representation from a variety of specialties but also three active patient representatives. “The guideline emphasises different patient characteristics rather than just saying: ‘This is the best access for you,” Interventional News was informed.

Karunanithy noted the endovascular-first approach to access dysfunction and that the additional value of covered stents and drug-coated balloons was discussed. Despite high-quality data in many areas, evidence gaps still exist, he pointed out.





Ibeas then turned to the most recent guidelines from the European Renal Association (ERA), European Society for Vascular Surgery (ESVS), Kidney Disease Outcomes Quality Initiative (KDOQI) and El Grupo Español Multidisciplinar del Acceso Vascular (GEMAV) to distil the areas of commonality and dissonance in their recommendations.
“According to my experience, evidence-based medicine is subject to the influence of several factors, that is, the methodology, perspective of the specialty, geographical area or health management system; and the values and circumstances of the patient […] and to
their interpretation,” he said.
“[…] the most important point is the effort for consensus on the one hand and generating evidence in the areas of conflict on the other. When reading the guidelines, it is convenient to understand how each recommendation in each guide is justified. In this way, the clinician can generate his own critical judgment and contribute to the implementation of the guidelines
in his environment in the most rational way. That can benefit the ultimate recipient of the guidelines, the patient,” Ibeas said.
Lean, clean and controlled: New tools for healthcare






Fanelli then brought to the fore an award-nominated project at the Careggi University Hospital, Florence, Italy, that applied lean management concepts to the patient’s journey. This approach seeks to define the process and the problem; measure performance; analyse the process for issues and root causes; improve by determining and implementing actions; and exercise control to maintain the improvement. When applied to endovascular procedures, lean management resulted in improved capacity and productivity; reduced procedure time; lowered operator stress; improved quality and reduced hospital stay.
“Lean healthcare is used in a growing number of hospitals to increase efficiency and quality of care. In healthcare organisations, it attempts to empower staff to generate continuous improvement through incremental but regular improvements in work processes. Periodic, detailed and specific feedback is extremely important to decrease complication rates and increase the service quality,” he shared.
Innovative highlights
Within the endoAVF creation session, Matteo Tozzi (vascular surgeon, Varese, Italy) presented a novel case report of Wavelinq endoAVF creation using carbon dioxide (CO2) contrast.


Detailing the clinical benefit of preserving residual renal function (RRF) in dialysis patients, Tozzi commented that those with residual renal function had better control of serum potassium and sodium, acid-

33 Advertorial Issue91 | September 2023
Fabrizio Fanelli
Panos Kitrou
Ioannis Griveas
Yousof Al Zahrani
Nicholas Inston
Ounali Jaffer
Narayan Karunanithy
Jose Maria Abadal
Daniel Gallego
Fien Gryffroy
Jose Ibeas
Joseph Touma
Külli Kuningas
Gürkan Sengölge
Tobias Steinke
Above:
Interventional radiologist Noha Guzaiz (Makkah, Saudi Arabia) leads a hands-on session
Interventional radiologist Shagran Binkhamis (Riyadh, Saudi Arabia) leads a hands-on session
BD ESKD Summit 2023: What matters to patients gains momentum with input from
device-related complications and reinterventions were needed in five patients (18%),” he detailed.



Continued from page 33
base status and volemia.
Outlining his goals for the case, Tozzi explained that he planned distal injection through a drug-coated balloon or plain balloon to use CO2-viscosity wisely and enable a faster procedure with reduced risk and complexity.

His take-home message from this innovative approach to imaging: There was no damage on kidney residual function in chronic kidney disease patients and no damage on kidney residual function in kidney replacement therapy patients. “Noniodinated contrast can be used in the implementation of [an] endovascular approach for vascular access creation,“ he submitted.

Tobias Steinke (vascular surgeon, Düsseldorf, Germany) then doubled down on the reasons for pursuing an endovascular creation strategy. He stated: “EndoAVF systems are designed to be less invasive and maybe to last longer; reduce the rate of primary failure and enable more medical specialties to participate in the creation of AVF, which can be relevant in areas underserved by vascular surgery.”
“Based on my experience, attempts to optimise perioperative haemodynamic conditions, regional blocks and endovascular technique modifications are worthwhile to improve fistula outcome and have the potential to increase the number of functional endoAVFs,” he underlined.
Yousof Al Zahrani (interventional radiologist, Riyadh, Saudi Arabia) then detailed the simplicity of his experience from learning to mastering WavelinQ in a hospital setting that caters for 2,100 beds with the expertise of 12 interventional radiologists, four neuroradiologists, two paediatric interventional radiologists and six fellows.
In pursuing an endoAVF creation programme, the team has performed 32 percutaneous procedures, with the majority of patients undergoing a WavelinQ procedure under regional anaesthesia.
“Procedural success was 85%, with successful cannulation achieved in 88% with a time to cannulation of four to eight weeks. There were no
In a session examining restoration of dysfunctional AVF, Jose M Abadal, president of the Spanish Interventional Radiology society (SERVEI; Madrid, Spain) shared his approach to percutaneous angioplasty (PTA) balloon selection based on the type of stenosis. He exhorted that the degree of stenosis was not enough of a measure, but that the type of stenosis is vital in determining the choice of device. In his centre, choice rests on a combination of medical evidence, cost containment and a clinical practice that is heavily reliant on Doppler ultrasound use. He reminded delegates that the technique of PTA is still variable, quipping “standardisation is clearly reserved for cardiologists”. Abadal stated that plain balloon angioplasty is the first choice followed by a double whammy of angioplasty then drug-eluting balloon. Ultra-high pressure balloons are the
plenary with a general introduction around the pathology of lesions making the point that “veins are not arteries”. It is important to drill-down into why stenoses occur, he said. “Lesion characteristics can be complex. A UK expert consensus approach for managing symptomatic arteriovenous fistula (AVF) stenosis in haemodialysis
haemodialysis patients remain alive after five years of treatment, Kolasa pointed out that these survival rates remain worse than those for many common cancers.
AVF is the preferred access choice, and vascular access-related complications and interventions account for almost one-third of hospital admissions among patients receiving dialysis, she said.
To mitigate against the high economic burden associated with AVF stenosis, early consideration of additional procedures along with angioplasty in the course of treatment and postponing additional procedures until it is absolutely necessary have the greatest potential to produce long-term savings, she commented.

first choice and in case of recoil either these or scoring balloons are applied, with stent grafts only selected if there is a clear indication. “Ultrasound is mandatory for sizing and new Doppler ultrasound criteria will be used to determine technical success,” he noted.
Joseph Touma (vascular surgeon, Paris, France) spoke on his centre’s experience of drug-coated balloon in fistula maintenance and Luka Novosel (interventional radiologist, Zagreb, Croatia) updated on the AVF cohort of the Lutonix AV Global registry, drawing out the patient and procedural variables of the study.
In the maintenance session for dysfunctional AVF, Griveas described the access life circuit that begins with vascular access stenosis. “Drugreleasing balloons can be a useful therapeutic option for patients with AVF stenosis due to accelerated endothelial hyperplasia. The use of paclitaxel-coated balloons helps reduce the risk of restenosis of arteriovenous anastomoses and is a safe, minimally invasive and immediate solution to AVF management,” he quoted from a paper published by his group in Nephrology Dialysis Transplantation in 2020.
Jaffer opened the second day’s
patients, published in CardioVascular and Interventional Radiology in 2021, recommends that if a patient requires four or more interventions for the same stenosis in a 12-month period (or three or more in a six-month period), a multidisciplinary meeting and patient discussion on access options should be triggered. For de novo stenosis, plain balloon or high-pressure balloon angioplasty are acceptable first interventions. Bare metal stents have a place only for central region stenosis and if there is recurrence between three and 12 months, consider a drug-coated balloon,” he reported.
This was followed by Kitrou presenting on endovascular treatment of dysfunctional AVF including an algorithm option and Jamal Al Koteesh (interventional radiologist, Al Ain, United Arab Emirates) presenting cases of complex AVF lesions.

Karunanithy then described to delegates why covered stents are key to haemodialysis access salvage.
Katarzyna Kolasa (health economist, Warsaw, Poland) presented findings from a literature review to examine whether covered stents are a costeffective choice to treat AVF stenosis in haemodialysis patients.
Setting out that only 35% of
Identifying the clinical evidence required for budget holders to ensure funding of covered stents for AVF stenosis, Kolasa said real-world data confirming that the covered stents lower the risk of reintervention, economic modelling data showing the same findings and more such data verifying long-term outcomes for patients would be valuable tools.
“As the outcomes of haemodialysis patients are variably monitored, there is a need for country-specific data collection efforts to inform reimbursement decisions in order to improve access to treatment,” she said.
Inston and Fanelli summed up the discussions when they told Interventional News: “The ESKD summit brings together the multidisciplinary team to consider more than just procedures and devices. It approaches treatments as more than just isolated procedures, and consciously reframes these in the context of a patient’s journey. This journey may have one clinician at the centre or have multiple inputs into treatments, but it is one that has a profound impact on each individual patient and their families. We feel that the summit achieved this vision by using a patientcentred approach.”
34 September 2023 | Issue91 Advertorial
THIS
ADVERTORIAL IS SPONSORED BY
multidisciplinary experts
Vascular surgeon Robert Shahverdyan (Hamburg, Germany) leads a hands-on session
Luka Novosel Katarzyna Kolasa
Disclaimer: Please consult Becton, Dickinson and Company product labels and inserts for any indications, contraindications, hazards, warnings, cautions and instructions for use. The opinions and clinical experiences presented herein are for informational purposes only. The results from this case report may not be predictive for all patients. Individual results may vary depending on a variety of patient specific attributes. The clinicians have been compensated by Becton, Dickinson and Company to participate in this advertorial. BD Switzerland Sarl, Terre Bonne Park – A4, Route De Crassier, 17, 1262 Eysins, Vaud. Switzerland, Tel: +41 21 556 30 00. Fax: +41 44 722 5370. bd.com. BD, the BD logo and Aspirex trademarks are the property of Becton, Dickinson and Company or its affiliates. © 2023 BD. All rights reserved. Straub has joined BD. All rights reserved. BD-94938 2797 0344 0483
Jamal Al Koteesh
Promising future previewed for PAD treatment at Riga summit
There has been major progress in the treatment of peripheral arterial disease (PAD) globally in the last few years, “but there are still issues that need to be addressed”, Marianne Brodmann (Medical University of Graz, Graz, Austria) told Interventional News, reviewing her experience as co-director of the recent BD PAD Summit (20–21 June, Riga, Latvia). She said the event highlighted the “consensus and strong will” among physicians to “improve” the picture when it comes to fighting the disease.
The summit was led by course chair Bruno Migliara (Pederzoli Hospital, Pescheria del Garda, Italy), alongside co-directors Brodmann, Koen Deloose (AZ Sint-Blasius Hospital, Dendermonde, Belgium), and Marco Manzi (Policlinico Abano Terme, Abano Terme, Italy).
Aimed at “shaping the future of PAD patient care”, its programme was divided into five sections. Sessions on diagnostic tools and algorithms were complemented by presentations on access and crossing lesions, treating lesions and optimising patency, and finally, on the future of PAD treatment. Across a day and a half, over 170 attendees were offered 24 hours of hands-on sessions, as well as the opportunity to hear 31 presentations by 20 key opinion leaders in the field. Rapid-fire debates followed most presentations, while a research and development session offered education on further new advances.
Brodmann opened the conference by addressing what she called the historical underappreciation of the problem of PAD—236 million adults worldwide have the condition—when compared with other conditions such as coronary artery disease and stroke.
More recently, she said, there has been “increasing recognition that PAD is an important cause of cardiovascular morbidity and mortality”, with particular attention given to its status as a “leading cause of physical disability”, especially when it progresses to critical limb ischaemia (CLI).
The problem is growing, she suggested, noting a study which found that the prevalence of the disease jumped by 45% globally between 2000 and 2015. “It can only be changed by awareness campaigns […] from healthcare providers as well as the general population,” she told Interventional News
Part of the issue, Brodmann suggested, lies with difficulties in diagnosing PAD. This set the stage for the beginning of the first session on diagnostic tools, where Christos Rammos (University of DuisburgEssen, Essen, Germany) highlighted a selection of new options in angiography, among them carbon dioxide angiography. Following him came Daniel van den Heuvel (St Antonius Hospital, Nieuwegein, The Netherlands), who assessed duplex ultrasound as a method for developing an “objective endpoint” in
the definition of optimal results from revascularisation procedures.
Algorithms came to the forefront next, with Brodmann stepping in to deliver the absent Maria Ruffino’s (Institute of Imaging of Southern Switzerland, Lugano, Switzerland) presentation on the need for clarity on the best aortoiliac lesion treatment. A compelling discussion followed, where it was suggested by one audience member that lack of evidence-based treatment in this area could be due to physicians’ preference. In conversation with Interventional News, Brodmann said: “This is indeed the case. Therefore, there is a need for creating strong treatment algorithms in different areas.” This, she suggested, was a need that could be met by physicians.

Deloose, meanwhile, also contributed to the session by telling the audience to base their treatment algorithms on their prepping algorithms—which should in turn be based on how you pass the lesion. PAD below the knee (BTK) was addressed during this session by Marc Sirvent (General University Hospital of Granollers, Granollers, Spain), who, in an assessment of different strategies, highlighted the “essential” nature of good angioplasty technique.
Next up came a set of talks on access and crossing lesions. Ralf Langhoff (Sankt Gertrauden Hospital, Berlin, Germany) set the tone by alerting listeners to the fact that up to 11% of peripheral vascular interventions result in access complications, underscoring the importance of addressing them. Also speaking in this session was Giacomo Isernia (Azienda Ospedaliera di Perugia, Perugia, Italy), who outlined why the guidewire is “essential” in complex occlusion cases. Yann Gouëffic (University Hospital of Nantes, Nantes, France) addressed the audience too, stating on the subject of vessel preparation
Bruno Migliara (pictured right) leads one of the 31 presentations that made up the summit. A total of 20 key opinion leaders were among those who took the stage

devices that “no studies have shown” that they offer a decisive advantage in cutting intimal hyperplasia.
Following one packed day of presentations came another, with the session on lesion treatment opening with further discussion from Rammos, who presented on a rotational atherothrombectomy device. In the subsequent talks on lesions, Mercedes Guerra (University Guadalajara Hospital, Guadalajara, Spain) gave a strong presentation on the need for better classification of extremely calcified lesions, which she said require their own treatment approach.
Migliara spoke to Interventional News following the summit to praise Guerra’s talk, which he said “analysed very well and deeply one of the most challenging and discussed questions: how to treat calcium”. The presentation and discussion which followed illuminated the need to “better define the best treatment choice for every different type of lesion”, he added.
Migliara himself presented during this session, returning to the rotational atherothrombectomy device explored by Rammos, which he said held particular promise for the treatment of in-stent restenosis. Its advantage, he averred to Interventional News, was that it “allow[s] retreatments without increasing their complexity”. In the debate following his talk, he suggested its repeated use for debulking poses fewer risks than bypass.
One highlight of the conference was what Migliara described as its “best debate”, between Deloose and Sherif El Kerdawy (Wadi El Neel Hospital, Cairo, Egypt) on the benefits of covered and uncovered stents in iliac artery treatment. Through this “scientific but also friendly debate”, Migliara said, “we understood better where the best choice is uncovered and where [it is] covered.” The audience swayed to the side of El Kerdawy: a post-debate poll found 42.9% on the side of the covered stent and 57.1% on the side of the uncovered.
“I learned many new ideas not only about techniques, but also about new materials and devices,” Migliara said of the concluding session on the future of PAD. Drawing special attention to vessel preparation and resorbable stents for BTK, he also praised a talk by Marta Lobato (Hospital de Cruces, Barakaldo, Spain) on new arterialisation techniques.
Migliara thanked those who spoke at the summit. Their “interesting presentations” and “active discussions” provided opportunities for learning, he said in review, and allowed him and his co-directors “to achieve the aim of this meeting”.
Disclaimer: The opinions and clinical experiences presented herein are for informational purposes only. The results from this Advertorial may not be predictive for all patients. Individual results may vary depending on a variety of patient specific attributes. The clinicians have been compensated by Becton, Dickinson and Company to participate in this advertorial. BD Switzerland Sarl, Terre Bonne Park – A4, Route De Crassier, 17, 1262 Eysins, Vaud. Switzerland, Tel: +41 21 556 30 00. Fax: +41 44 722 5370. bd.com. BD, the BD logo are the property of Becton, Dickinson and Company or its affiliates. © 2023 BD. All rights reserved. BD-94905
35 Advertorial Issue91 | September 2023
THIS ADVERTORIAL IS SPONSORED BY BD
Product News
clearance for MediView, but it is the first 510(k) clearance for an augmented reality device utilising live imaging combined with 3D extended reality (XR) visualisation for pre- and intraoperative indications for use, which sets the stage for further advancements in augmented reality in the healthcare space.” said Adam Cargill, director of Quality, Regulatory and Clinical Affairs at MediView.
Health Canada approves IceCure Medical’s ProSense cryoablation system
IceCure Medical has announced in a press release that Health Canada, the Canadian government’s regulatory agency, has approved its ProSense system, disposable cryoprobes, and introducers as cryosurgical tools for various indications.

These include tumours, for ablation of benign and malignant tumours of the lung, liver, kidneys, and musculoskeletal system, and benign tumours of the breast; general surgery; palliative intervention; and other surgeries.
“As we continue to gain traction in the USA, this approval in Canada will create synergies for us in the broader North American market. We have been directly engaging with healthcare providers through education, hands-on training seminars, marketing, and sales in the USA and we will expand these activities into Canada. We have already been contacted by multiple Canadian healthcare providers with requests to purchase and implement ProSense,” stated IceCure chief executive officer Eyal Shamir.
IceCure’s cryoablation system currently has regulatory approval for various indications in 15 countries, including in the USA, Europe, and China.
XR90 is a diverse imaging tool providing a new way to view patient anatomy and visualise instrumentation pathway while maintaining natural alignment of senses. Clinicians at remote locations can also collaborate real-time with shared visualisation, communication, and the ability to provide guidance during procedures for collaborative patient care. These features can provide increased support for understaffed facilities, rural or underserved populations and a distinct ability to limit caregiver and patient exposure to COVID-19 while maintaining care levels.
first performed at Cleveland Clinic’s Sydell and Arnold Miller Family Heart, Vascular & Thoracic Institute (Cleveland, USA) and at Salinas Valley Health Medical Center (Salinas, USA).
“We are delighted to be able to introduce PTAB using the Detour system into clinical use,” said Matt Thompson, president, and CEO of Endologix. “The Detour system is a pivotal addition to our product portfolio, which now offers differentiated therapies for both abdominal aortic aneurysms and PAD.”
Boston Scientific receives 510k clearance for Embold soft and packing coils
Boston Scientific has received US Food and Drug Administration (FDA) 510(k) clearance for its Embold soft and packing coils, the company has announced in a press release. The coils are designed for use in a variety of embolization procedures.
These coils further strengthen Boston Scientific’s embolic portfolio by creating a single platform consisting of just three coils, which is designed to make it simpler for physicians to address a variety of different patient needs and anatomies, while also streamlining hospital inventory, the company states. The soft and packing coils complete the trio by building on the success of the Embold fibred coil, which launched last year and is currently available in the USA, Canada and Japan.
Endologix announces first patients treated with the Detour system
Endologix has shared in a press release that the first patients underwent percutaneous transmural arterial bypass (PTAB) using the Detour system since US Food and Drug Administration (FDA) approval of the system was granted. This marks the official start of its US targeted market release.
MediView receives FDA
510(k) clearance for XR90 augmented reality-based visualisation and navigation platform
MediView announced it has received 510(k) clearance from the US Food and Drug Administration (FDA) for its XR90 augmented reality-based surgical visualisation and navigation platform. XR90 is intended to be used adjunctively for minimally invasive ultrasound and computed tomography (CT)-guided needle-based procedures for soft tissue and bone.
“This is not only the first 510(k)
PTAB with the Detour system offers a disruptive, novel approach to treating complex peripheral arterial disease (PAD), enabling physicians to bypass lesions in the superficial femoral artery, by using stents routed through the femoral vein to restore blood flow to the leg. This approach is effective for patients with long lesions (20–46cm in length), those that have already undergone failed endovascular procedures, or those that may be suboptimal candidates for open surgical bypass.

For the rollout, Endologix collaborated with two healthcare systems known for clinical excellence. PTAB using the Detour system was
“The addition of the soft and packing coils now completes the Embold platform, and is expected to build upon the success we have already seen with the launch of our fibred coil last year,” said Peter Pattison, president, Interventional Oncology and Embolization, Boston Scientific. “With the full platform of Embold coils, along with our conformable embolic, Obsidio, we will be able to offer our customers a complementary and highly differentiated portfolio of embolics, enabling them to provide highly personalised care to address the unique needs of their patients.”
importance of supporting healthcare professionals in their daily tasks, the company has said in a press release.
The introduction of Aplio flex and Aplio go aims to revolutionise the healthcare market by providing compact, manoeuverable, and technologically advanced ultrasound systems that meet the evolving needs of medical practitioners.

The redesigned control panel of Aplio flex and Aplio go ensures efficient and intuitive operation from the moment the systems are installed, the company states. With this new control panel, direct operation is simplified, promoting ease of use and productivity.
Both Aplio flex and Aplio go are equipped with ApliGate, a technology that enhances collaboration. Whether you work at a large university or local hospital, in a private practice or imaging centre, or even outside the hospital, this tool for remotely sharing images enables you to directly connect with fellow professionals or Canon experts. You can seek advice, share discoveries, and engage in online collaboration with subject, the company says.
Terumo Aortic announce Thoraflex device approval in Japan
Terumo Aortic has announced that the Japanese Pharmaceuticals and Medical Devices Agency (PMDA) has granted approval of the Thoraflex Hybrid Frozen Elephant Trunk (FET) device for commercial sale in Japan for the treatment of patients with complex aortic arch disease.
Thoraflex Hybrid is a single use medical device combining a Gelweave polyester graft with a Nitinol self-expanding stent graft and is indicated for the open surgical repair or replacement of damaged or diseased vessels of the aortic arch and descending aorta with or without involvement of the ascending aorta in cases of aneurysm and/or dissection.
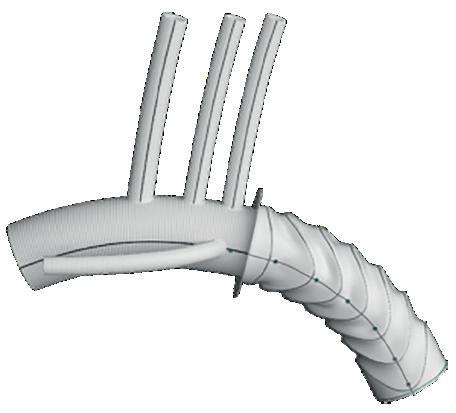
Kotaro Yoshida, senior vice president of Asia Pacific added: “The PMDA approval of Thoraflex Hybrid is a fantastic opportunity for Terumo Aortic in Japan. This innovative hybrid device complements our open surgical graft and endovascular portfolio currently available in Japan; the approval of this device will contribute significantly in the delivery of our commitment to providing solutions for every aorta.”
Canon Medical introduces Aplio flex and Aplio go ultrasound systems in Europe
Canon Medical has announced the commercial availability of its two latest ultrasound systems, Aplio flex and Aplio go, in Europe. With the growing challenges faced by medical staff, including high workload and work-related musculoskeletal disorders, Canon Medical recognises the
Thoraflex Hybrid received CE mark approval in 2012 and US Food and Drug Administration (FDA) approval in 2022 with more than 13,000 devices sold around the world.

36 Market Watch September 2023 | Issue91
Aplio flex and Aplio go
Thoraflex Hybrid
XR90 platform
ProSense cryoprobe
Depiction of PTAB
FDA update: Paclitaxelcoated devices for PAD cleared of excess mortality risk, proven safe and effective
Data on hundreds of thousands of patients who have received lower limb endovascular treatment provide confidence in paclitaxel safety. This central message from a Boston Scientific symposium at the recent Leipzig Interventional Course (LINC 2023; 6–9 June, Leipzig, Germany) was delivered a month before the US Food and Drug Administration (FDA) removed restrictions on use of paclitaxel in peripheral arterial disease (PAD) treatment.
The LINC 2023 symposium—moderated by Marianne Brodmann (University of Graz, Graz, Austria) and Koen Deloose (AZ Sint-Blasius, Dendermonde, Belgium)—saw various speakers outline existing and new data concerning the use of the Eluvia drug-eluting stent (DES) and the Ranger drugcoated balloon (DCB) in the superficial femoral artery (SFA), including four-year data from the Ranger II SFA randomised controlled trial (RCT) and several registries.
that they “provide more evidence of Eluvia DES and Ranger DCB successful outcomes”.
The presenter outlined that in the CAPSICUM registry (1,097 patients), three-year follow-up showed acceptable restenosis rates for the Eluvia DES, and decreasing annual event rates for restenosis, reocclusion and stent thrombosis.
Iida also addressed the CAPRICORN propensitymatched cohort (1,456 patients), which demonstrated significantly lower one-year restenosis rates for the Eluvia DES versus the IN.PACT DCB. He noted that this was the first study to demonstrate superiority of DES over DCB in real-world practice.
Finally, Iida shared that the PROSPECT MONSTER study (581 patients) showed that the low-dose Ranger DCB performed similarly to the high-dose IN.PACT DCB. This result was also observed in the COMPARE RCT, as Brodmann had previously noted.
Big data from big databases— PTX safety
The role of
RCTs in shaping clinical practice
Brodmann opened the session with a presentation on RCT data, which she described as “the pinnacle of proof”, stressing their importance in proving device performance against standard of care, and in shaping clinical guidelines.
The first RCT discussed was the Ranger II SFA RCT that assessed the Ranger DCB versus standard percutaneous transluminal angioplasty (PTA). In this single-blind, superiority trial, 376 patients were randomised 3:1.
Brodmann shared long-term follow-up results, revealing specifically three-year patency and four-year clinical safety results. The investigators “demonstrated outstanding three-year primary patency of 77% for the [Ranger] DCB and four-year freedom from clinically driven target lesion revascularisation [CD-TLR] which is greater than [that] reported in other DCB studies previously published,” she summarised.

Aside from the Ranger II results, Brodmann also informed the LINC 2023 audience about three other RCTs—COMPARE, IMPERIAL and EMINENT— and relayed their positive outcomes.
COMPARE showed similar primary patency between the low-dose Ranger and the high-dose IN.PACT DCB (Medtronic), the presenter outlined, while IMPERIAL demonstrated superior primary patency for Eluvia over Zilver PTX (Cook Medical) at 12 months, a “significant” TLR advantage at 24 months and similar safety outcomes out to five years. Brodmann continued that, in the EMINENT RCT, the Eluvia DES showed superiority in terms of efficacy compared to bare metal stents (BMS) and is the first and only DES to do so in SFA intervention.
Real-world evidence: Registries complement, and do not replace RCTs
Giovanni Torsello (St Franziskus Hospital, Münster, Germany) then shared real-world evidence on the Eluvia DES. “The real-world data are consistent with RCT results for Eluvia DES despite markedly increased lesion


complexity and patient comorbidities,” he remarked.
Torsello spoke on several registries studying the Eluvia DES, including Auckland, DESAFINADO, Regal, and Münster. The studies all demonstrated around 90% primary patency for the Eluvia DES at 12 months despite often involving long lesions and high patient comorbidity. According to Torsello, the available registry data “provide more evidence and more confidence that the Eluvia RCT results are generalisable and repeatable”.
Osamu Iida (Osaka Police Hospital, Cardiovascular Division, Osaka, Japan) then shared real-world data on drug-eluting therapies from Japan, concluding
Join Boston Scientific’s symposium at CIRSE 2023 to continue the discussion
Lessons learned; insights gained. Drug-eluting technologies for endovascular interventions in PAD
Saturday September 9 1–2pm CEST, Auditorium 2
Moderator: Marianne Brodmann

Speakers: Sabine Steiner, Yann Gouëffic, Koen Deloose
Yann Gouëffic (Groupe Hospitalier Paris Saint Joseph, Paris, France) addressed the topic of paclitaxel safety with an overview of studies that included more than 180,000 patients, such as SWEDEPAD, VOYAGER PAD, and SAFE-PAD. He detailed that these studies all refute the findings of the 2018 Katsanos metaanalysis, by showing no difference in mortality between patients treated with either a drug-coated device or a non-drug-coated device. He closed by introducing the DETECT study, based on French national healthcare data. This study includes ~260,000 patients and, as reported by Gouëffic, it confirmed the conclusion on paclitaxel safety. The final analysis is expected later this year.
On 11 July, soon after LINC 2023, the US Food and Drug Administration (FDA) updated its guidance on the use of paclitaxel-coated devices to treat PAD, determining that additional long-term clinical data from the pivotal RCTs do not support an excess mortality risk for paclitaxel-coated devices.1
In a Boston Scientific statement released following the FDA announcement, chief medical officer Michael Jaff commented that the update recognises the safety and efficacy of devices such as Eluvia and Ranger, “both of which have demonstrated excellent safety profiles and very low revascularisation rates in the hundreds and thousands of patients treated worldwide with these devices”.2
The Cardiovascular and Interventional Radiological Society of Europe (CIRSE) added to the subject in an online editorial dated 12 July, underscoring that re-analysis of old data and new outcomes data do not support a link between paclitaxel-coated balloons and paclitaxel-eluting stents and mortality. On this basis, CIRSE encourages the use of these devices for treating PAD in femoropopliteal disease, relying on their published efficacy.3
References:
1. UPDATE: Paclitaxel-Coated Devices to Treat Peripheral Arterial Disease
Unlikely to Increase Risk of Mortality - Letter to Health Care Providers | FDA
2. News Releases - Boston Scientific: Boston Scientific Position on FDA
Update About Use of Paclitaxel-Coated Devices to Treat Peripheral Arterial Disease
3. Müller-Hülsbeck S, Fanelli F, Haage P, et al. Re-analysis of old data and new outcomes data do not support a link between paclitaxel-coated balloons and paclitaxel-eluting stents and mortality: these devices should be used in PAD (peripheral arterial disease) treatment in femoropopliteal disease on the basis of their published efficacy. Cardiovasc Intervent Radiol. 2023;46:977–980. https://doi.org/10.1007/s00270-023-03507-w
Disclaimer: CAUTION: The law restricts these devices to sale by or on the order of a physician. Indications, contraindications, warnings and instructions for use can be found in the product labelling supplied with each device. Products shown for INFORMATION purposes only and may not be approved or for sale in certain countries. This material not intended for use in France. 2023 Copyright © Boston Scientific Corporation or its affiliates. All rights reserved. (copyright statement only required if not otherwise on material) For information purposes only. The content of this article/publication is under the sole responsibility of its author/publisher and does not represent the opinion of BSC. PI-1656303-AA
37 Advertorial Issue91 | September 2023
THIS ADVERTORIAL IS SPONSORED BY BOSTON SCIENTIFIC
Koen Deloose Yann Gouëffic
Sabine Steiner Marianne Brodmann
Industry News




EIBIR and ESR announce changes to leadership
The European Institute for Biomedical Imaging Research (EIBIR) has announced the appointment of Regina Beets-Tan as its new scientific director. Beets-Tan, EIBIR states, will contribute to further enhancing the organisation’s support for European biomedical imaging research and networking between institutes and disciplines.
Beets-Tan chairs the department of Radiology at the Netherlands Cancer Institute and is professor of Radiology at the University of Maastricht, The Netherlands and adjunct professor of Abdominal and Oncological Radiology at the University of Southern Denmark.
Adrian Brady from Ireland assumes the position of chairperson of the European Society of Radiology (ESR) board of directors, the highest governing role within the society. Carlo Catalano from Italy takes on the esteemed position of ESR president and will also chair the ECR 2024 Programme Planning Committee. The ESR extends a warm welcome to Minerva Becker, who joins the ESR board of directors following her successful election.
Conference calendar
9–13 September
Cardiovascular and Interventional Radiological Society of Europe (CIRSE) 2023 Copenhagen, Denmark cirsecongress.cirse.org
22–24 September
Symposium on Clinical Interventional Oncology (CIO) 2023 Orlando, USA theiomeeting.com
Boston Scientific announces position on FDA update about use of paclitaxel-coated devices to treat PAD
Following the news that the US Food and Drug Administration (FDA) has changed its stance on the use of paclitaxel-coated devices to treat peripheral arterial disease (PAD), Boston Scientific has announced its position on the update. The company’s full statement reads as follows:
On 11 July 2023, the FDA published a letter to healthcare providers stating that, based on its review of the totality of the available data and analyses, the excess risk of mortality associated with paclitaxel-coated devices to treat PAD is no longer supported. The letter recognises the safety of paclitaxel-coated devices and provides updated guidance that eliminates the requirement for device manufacturers to include specific warning language within device labelling.
“We are pleased that, after continued analysis of data and collaboration among a broad set of stakeholders, the FDA has determined the large body of
long-term clinical data do not support an excess mortality risk for paclitaxelcoated devices used to treat patients with PAD,” said Michael R Jaff, chief medical officer and vice president, Peripheral Interventions, Boston Scientific. “We remain dedicated to helping physicians provide the best care possible for their patients through access to life-changing technologies, including the Eluvia drug-eluting vascular stent (DES) system and the Ranger drug-coated balloon (DCB).”
US FDA seeks to “modernise” clinical trials with new draft guidance
The US Food and Drug Administration (FDA) has released draft guidance with updated recommendations for good clinical practices (GCPs) aimed at modernising the design and conduct of clinical trials.
In a statement, the regulator said that the updates are intended to help pave the way for more efficient clinical trials to facilitate the development of medical products, aiming to be “more agile without compromising data integrity or participant protections”.
The draft guidance is adopted from the International Council for Harmonisation’s (ICH) recently updated E6(R3) draft guideline that was developed to enable the incorporation of rapidly developing technological and
methodological innovations into the clinical trial enterprise.


“A more robust clinical trial ecosystem that is capable of producing reliable evidence more efficiently may support more informed decisionmaking in developing medical products to help patients,” said FDA commissioner Robert M Califf. “These draft recommendations propose a major step forward in this work. Building quality into the design and conduct of trials and encouraging the use of innovative trial designs and health technologies are essential to truly advance clinical trials and generate meaningful results.”
GCPs ensure the safety of trial participants, as well as the integrity of trial data. Over the years, the clinical trial enterprise has been viewed as costly, inefficient and constrained by inadequate collaboration and insufficient utilisation of technology, data sources and innovations in design and conduct. The COVID-19 pandemic highlighted many of these challenges, while also spurring the development of new approaches, FDA’s statement adds.
The draft guidance will be open for public comment for 60 days. The ICH Expert Working Group will review and consider comments on this draft guidance, as well as feedback from other ICH member countries before finalising the ICH guideline.

8–10 November
British Society of Interventional Radiology (BSIR) 2023 Newport, UK bsir.org/meetings/bsir-asm-2023
25–29 January
Society of Interventional Oncology (SIO) 2024 Long Beach, USA sio-central.org
10–13 February
Pan Arab Interventional Radiology Society (PAIRS) 2024 Dubai, UAE pairscongress.com
23–28 March


Society of Interventional Radiology (SIR) 2024 Salt Lake City, USA sirmeeting.org
11–13 April
International Multidisciplinary Endovascular (IM Endo) Forum 2024 Florence, Italy mendoforum.com
23–25 April
Charing Cross (CX) Symposium 2024 London, UK cxsymposium.com
28 April–1 May
European Conference on Interventional Oncology (ECIO) 2024 Palma de Mallorca, Spain ecio.org/attend/ecio-2024
16–19 May
Global Embolization Symposium Technologies (GEST) 2024 New York, USA thegestgroup.com
September 2023 | Issue91 38 Market Watch Sign up for a free print subscription* and e-newsletter subscription** www.interventionalnews.com Interventional News is a trusted, independent source of news and opinion in the interventional world. *Available for US and EU readers only ** Available worldwide
Clinical News
Humacyte completes enrolment in Phase II/III trial of Human Acellular Vessel for vascular trauma repair
Humacyte has announced completion of enrolment in its Phase II/III vascular trauma trial (V005) that is expected to support a Biologics License Application (BLA) filing for the company’s Human Acellular Vessel (HAV) in vascular trauma repair.
A press release details that the HAV is designed to provide surgeons with an off-the-shelf bioengineered human artery that has been observed to repopulate with the patient’s own cells to provide a durable, infection-resistant replacement for damaged and diseased arteries. The HAV has the potential to assist healthcare professionals in saving life and limb in some of the most difficult circumstances. The results from the Phase II/III vascular trauma trial are intended to support a BLA filing with the US Food and Drug Administration (FDA), planned for the fourth quarter 2023.
The V005 trial is a single-arm, open-label, pivotal study of patients suffering from vascular trauma injuries, conducted at Level I trauma centres in the USA and Israel. The primary efficacy assessment will be based on a 30-day HAV patency (presence of blood flow) in patients who have vascular trauma of the extremity, as compared to historic benchmarks reported in literature. Humacyte, the clinical trial sites, and contracted service providers are preparing for locking of the trial database in order to report the V005 results. The company currently expects to complete these activities and report top-line results from the trial before the end of the third quarter 2023.
“We believe that the HAV could revolutionise the ability of surgeons to save the lives and limbs of patients suffering vascular injuries, not only in civilian settings, but also in more challenging environments like the battlefield,” said Laura Niklason, CEO of Humacyte.
efficacy of 0.05mmol/kg gadopiclenol (Vueway) with 0.1mmol/kg gadobutrol (Gadavist) in 273 adult patients referred for contrast-enhanced magnetic resonance imaging (MRI) of head and neck, thorax (including breast), abdomen (including liver, pancreas, and kidneys), pelvis (including ovaries, uterus, and prostate), and musculoskeletal (including extremities).
Despite being administered at half the dose of gadobutrol, gadopiclenol provided a comparable degree of contrast enhancement and quality of morphologic assessment of lesions.
The type and severity of adverse events (AEs) were similar with the two gadolinium-based contrast agents, with Vueway (4.2%) having a slightly lower rate to that of Gadavist (5.5%).
The publication of the results of the PROMISE study comes on the heels of those of the PICTURE clinical trial, which were published in Investigative Radiology and showed non-inferior quality of morphologic assessment of lesions of the brain and spine with 0.05mmol/kg Vueway compared with 0.1mmol/kg gadobutrol (Gadavist).
The combined results of the PROMISE and PICTURE trials, and additional clinical evidence, supported the regulatory application for gadopiclenol submitted to the US Food and Drug Administration (FDA), resulting in priority review and subsequent approval in 2022.
from Johns Hopkins (Baltimore, USA) and Samir Taneja from NYU Langone (New York, USA) are co-principal investigators on the study, and the first patient procedure was successfully completed by Naveen Kella of The Urology Place in San Antonio, USA.

Francis Medical’s Vanquish water vapour technology applies the thermal energy stored in a few drops of sterile water to deliver targeted treatments to the cancerous tissue through a simple transurethral procedure. The therapy is designed to ablate cancer cells while protecting surrounding structures, lessening the likelihood of side-effects common with other prostate cancer treatments.
The company anticipates using the one-year follow-up data from the VAPOR 2 study in support of a US Food and Drug Administration (FDA) submission for US market clearance. VAPOR 2 patients will be followed for a period of five years to gather longerterm cancer outcomes.
Biotronik announces oneyear subgroup results from
through 12 months post-index procedure. It showed no statistically significant difference between balloons for the full data set and across subgroups.
Approval granted to commence study of renal pelvis denervation system
Verve Medical has received approval from the US Food and Drug Administration (FDA) to initiate its Natural Orifice via renal pelvis denervation (NOVEL-Denervation) pivotal investigational device exemption (IDE) trial for the treatment of uncontrolled hypertension to lower blood pressure.
The Verve RPD, NOVEL pivotal trial will enrol up to 300 patients, and will be a 2:1 randomised, sham-controlled, double-blinded study to determine the safety and efficacy of the Verve RPD minimally invasive, non-vascular renal pelvic denervation system to treat hypertension.
In contrast to other renal denervation approaches in the renal artery, Verve’s method accesses the renal nerves through the natural orifice of the urethra, like a common urology procedure. The Verve RPD system ablates afferent and efferent nerves in the renal pelvis and is likely more effective due to the increased density of innervation in the renal pelvis, where easier access can be obtained versus the traditional arterial renal denervation approach, Verve Medical says in a press release.
BIOPACT RCT
Biotronik has announced one-year subgroup results from the investigatorinitiated BIOPACT randomised controlled trial (RCT), which were presented by principal investigator Koen Deloose (AZ Sint-Blasius, Dendermonde, Belgium) at this year’s Leipzig Interventional Course (LINC 2023, 6–9 June, Leipzig, Germany).
First patient treated in VAPOR 2 pivotal study for water vapour ablation of prostate cancer
The randomised controlled noninferiority trial evaluated the safety and efficacy of the Passeo-18 Lux drug-coated balloon (DCB) catheter compared to the In.Pact Admiral DCB (Medtronic) and showed excellent results for both balloons through 12 months across a variety of sub-cohorts, Biotronik reports.

Data reinforcing efficacy and safety of gadopiclenol in contrast-enhanced MRI published in Radiology
Bracco Imaging has announced the publication of the PROMISE trial in Radiology. The PROMISE study was a prospective, multinational, crossover (within-patient), doubleblind comparison of the safety and

Francis Medical, a privately held medical device company developing proprietary water vapour ablation therapy for the treatment of prostate, kidney, and bladder cancer, has announced the first patient has been treated in the company’s VAPOR 2 pivotal clinical study evaluating the safety and efficacy of its Vanquish minimally invasive water vapour ablation therapy for managing prostate cancer.
VAPOR 2 is a prospective, multicentre, single-arm study that will treat 235 patients with intermediaterisk, localised prostate cancer at up to 30 US clinical sites. Arvin George
The prospective, multicentre, core lab-adjudicated noninferiority study enrolled 302 patients in Austria, Belgium, France and Switzerland with Rutherford 2-4 disease. Patients were randomised 1:1 to either the Passeo-18 Lux DCB or In.Pact Admiral DCB for the treatment of stenotic, non-stented restenotic or occlusive lesions in the femoropopliteal artery. The primary safety endpoint was a composite of freedom from device- and procedurerelated death through 30 days postindex procedure, freedom from major target limb amputation and clinically driven target vessel revascularisation
Serranator demonstrates 49% less recoil than plain balloon angioplasty in BTK arteries
Cagent Vascular has announced the results of its below-the-knee (BTK) RECOIL study. This core lab-adjudicated Recoil analysis— the first of its kind, according to the company— evaluated vessel recoil in lesions treated with Serranator verses plain balloon angioplasty.
The study results demonstrated that lesions treated using serration angioplasty exhibited 49% less average recoil than plain balloon angioplasty. Stefan Stahlhoff (Arnsberg Clinic, Arnsberg, Germany) and Venita Chandra (Stanford University, Stanford, USA) led the RECOIL study as co-principal investigators.
The Serranator percutaneous transluminal angioplasty (PTA) serration balloon catheter is the first and only angioplasty balloon that is US Food and Drug Administration (FDA) cleared and CE-marked that embeds serration technology into a semi-compliant balloon for treating peripheral arterial disease (PAD). The device is designed to create multiple longitudinal lines of interrupted microserrations to aid arterial expansion.
39 Market Watch Issue91 | September 2023
(Left to right) Michael Hoey, Naveen Kella and Christopher Dixon
Serranator
Passeo-18 Lux