Drug-coated balloon beats plain balloon in ABISS trial perprotocol analysis
Data have been presented for the first time at the Paris Vascular Insights (PVI) conference (23–25 November, Paris, France) from the ABISS trial, which compared drug-coated balloon (DCB) with plain-balloon angioplasty for arteriovenous fistula (AVF) stenosis.
ABISS WAS A PHYSICIAN-DESIGNED prospective, randomised, double-blind trial that included 12 centres in France. The study enrolled 150 adult patients who had a native autologous AVF stenosis already punctured for haemodialysis. Following predilatation, patients were randomised 1:1 between DCB (Lutonix, BD) and placebo balloon application. The study was mainly funded by the French government clinical research programme (PHRC).
The primary outcome of the study was cumulated incidence of loss of primary patency of AVF at six months. The study authors, led by Raphaël Coscas (Ambroise Paré Hospital and Paris-Saclay Univer sity, Paris, France) found in an intention-to-treat analysis DCB was superior to plain-balloon angioplasty at six months but not in a statistically significant way, with a p value of 0.09. It was, however, statistically significant at three months (p=0.002). In a prespecified per-protocol analysis, the DCB was superior to a statistically significant degree at the intervals of three (p=0.0004), six (p=0.008), and 12 months (p=0.029) for the main outcome.
Drug-coated balloon disadvantaged?
Drawing attention to the difference between the intention-to-treat analysis results and those of the per-protocol analysis, Coscas said that “the way data of the study were analysed will need to be discussed because, in the intention-to-treat analysis, patients lost to follow-up or who waived consent were imputed to the worstcase scenario (loss of patency if in the DCB arm and to patency if in the placebo arm),” suggesting a “disadvantage” for the DCB in the intention-to-treat results. “This was less the case in the per-protocol analysis—I think we will discuss that later on”.
Steal syndrome
Percutaneous endovascular arteriovenous fistula (endoAVF) procedures carry a lower risk of certain complications than surgical arteriovenous fistula (sAVF) creation, a new study has suggested. Published in the Journal of Vascular Surgery (JVS), the review of existing data on the two approaches examines whether endoAVF improves on sAVF’s patency and complication rates.
Beginning by outlining the “numerous complications and modest patency rates” of sAVF, which they note has “served for decades as the preferred method” for vascular access for haemodialysis, the study authors, led by Alkis Bontinis (AHEPA University Hospital, Thessaloniki, Greece), then turn their attention to endoAVF. They cite results of other recent studies stat ing that endoAVF may improve outcomes, but are keen to point out that those studies are limited by their number of included patients.



The study authors have sought to build on these investigations with a systematic review and aggregated data meta-analysis of 17 endoAVF and sAVF studies. Some 1,118 endoAVFs were considered in this analysis. Studies were considered for relevance before their data were used according to the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Primary endpoints were primary and secondary patency at a maximum follow-up of one year after the procedures. For the primary endpoint, the authors say they “failed to identify statistically significant differences between sAVF and endoAVF”. Randomised controlled trials as well as “prospective and retrospective data depicting endoAVF creation” were included.

The secondary endpoints included reintervention at the end of follow-up, technical success and incidence of
major complications. Steal syndrome and wound infection are two of the complications most associated with AVF procedures—and the study authors’ comparison of sAVF and endoAVF finds that there was “an almost sixfold increased risk for steal syndrome occurrence” when a fistula is created surgically instead of percutaneously. EndoAVF showed a lower rate of wound infection, risk ratio (RR) 4.19 (95% [confidence interval] CI: 1.04-16.88).
The researchers suggest that it is endoAVF’s standardisation of the size of the fistula that accounts for these differences, contrasting with sAVF’s reliance on “the surgeon’s subjective perception” of appropriate size. SAVF also demonstrated low primary patency rates and a higher rate of reintervention. The primary endpoints did not show statistically significant differences between the two types.
Three studies examined by Bontinis et al, including 314 patients, reported technical success rates regarding endoAVF and sAVF “with a pooled odds ratio (OR) of 2.68 (95% CI:0.51-13.97) (I2=0%, p=0.66) favouring sAVF”. Two studies compared the procedures for reintervention rates, “producing an incidence rate ratio (IRR) of 1.28 (95% CI:0.94-1.75) (I2=0%, p=0.85) favouring surgery”.
The statistically insignificant primary patency superiority of sAVF in this analysis may be attributable, they suggest, to “the high percentage of distal (brachiocephalic) AVFs which comprised 48.3% (253/524) of the total population in the sAVF”. They note that the majority of the study population who received endoAVF did so in the proximal forearm, pointing to other studies suggesting that these yield inferior outcomes compared to brachiocephalic AVF creation.
The medium quality of the studies used in the authors’ meta-analysis is described as a limitation. Others included the use of retrospective studies and the fact that only five of the total 18 analysed directly compared the two procedures. The authors also note that “the high heterogeneity presented in our results reflects variation in surgical strategies, anatomic locations, learning curve requirements and individual surgeons’ abilities.”
In this issue:
Cannulation innovation explored page 4
Profile: Robert Jones page
12
9 Home dialysis in depth page 6 February 2023 Issue 06 www.renalinterventions.net Follow Renal Interventions on all our social media platforms for the latest news, insight and events in kidney care
Dirk Hentschel on wearable dialysis
page
and wound infection less likely with percutaneously-created arteriovenous fistulas
Alkis Bontinis
Raphaël Coscas
Charing Cross programme seeks new avenues in vascular access and renal care
The role of drug-coated balloons (DCBs) within dialysis access treatment paradigms will be a central focus at this year’s Charing Cross (CX) symposium (25–27 April 2023, London, UK)—while device-created arteriovenous fistulas (AVFs), the latest in vascular access graft technology, and the management of renal artery aneurysms, are all likely highlights from the programme.
The morning section of the CX 2023 programme on Tuesday 25 April— which is set to kick off with the Vascular Access CX Masterclass—will see Ounali Jaffer (Barts Health NHS Trust, London, UK) and Narayan Karunanithy (Guy’s and St Thomas’ NHS Foundation Trust, London, UK) present on the topic of DCBs. The former will query whether there is “too much evidence” in this space, while the latter will broach “the need for more evidence”.
The treatment of arteriovenous access dysfunction in haemodialysis patients will be further examined during later talks by Andrew Holden (Auckland City Hospital, Auckland, New Zealand). Holden is scheduled to present on percutaneous transluminal angioplasty (PTA), an “older technology with newer outcomes”, and will also deliver the latest findings from IN.PACT AV Access trial (Medtronic) following his disclosure of three-year data at last year’s CX symposium.
Elsewhere in vascular access
The Vascular Access CX Masterclass is set to disseminate real-world experiences for physicians looking to integrate endovascular AVF (endoAVF) systems into their care protocols. CX Executive Board member Kate Steiner (East and North Hertfordshire NHS Trust, Stevenage, UK) will discuss “a case-based look at how I have refined my endoAVF creation practice and algorithm”, with a particular focus on patient selection and procedures, followed by Jaffer’s advice on how to add endoAVF creation into a dialysis practice.
Other presentations during the vascular access programme will outline novel technologies and approaches for dialysis patients. Frans Moll (University Medical Center Utrecht, Utrecht, The Netherlands)
is scheduled to present Podium First results with “a new kind of graft”, while Matteo Tozzi (University of Insubria, Varese, Italy) will discuss early-cannulation arteriovenous grafts (AVGs) and their role in high-risk failure-to-mature patients. In addition, Gavin Pettigrew (University of Cambridge, Cambridge, UK) will provide CX attendees with an update from
the SONAR study—a prospective, observational cohort study intended to determine whether ultrasound surveillance can reliably predict AVF failure in patients with chronic kidney disease.
Dialysis, transplants and aneurysms
The later portion of the first day of CX 2023 will see the programme’s focus expand beyond vascular access to incorporate more general discussions around dialysis, as well as kidney transplantation and renal artery aneurysms.




Peritoneal dialysis (PD)—a modality that has been the subject of ever-increasing interest as many healthcare systems and regions attempt to prioritise home therapies—will be explored by Frank Dor (Imperial College Healthcare NHS Trust, London, UK). Another presentation that looks set to unpack recent changes in kidney care will be delivered by Charmaine Lok (University of Toronto, Toronto, Canada), who plans to examine the evidence surrounding patient-based choices and other aspects of the vascular access treatment algorithm.
The afternoon’s Renal Interventions sessions will also provide an educational element—for example, through Andrew Garnham’s (The Royal Wolverhampton NHS Trust, Wolverhampton, UK) presentation on “training the vascular surgeon
for renal patients”. In two separate talks, Robert Jones (Queen Elizabeth Hospital, Birmingham, UK) and Tozzi will further advise their peers on how best to optimise the management and treatment of cephalic arch stenosis, while Jeremy Crane (Imperial College Healthcare NHS Trust, London, UK) is set to posit that “cost effectiveness should be the priority” in this space.
Once again, the latest technologies designed to advance kidney care will feature, with Dirk Hentschel (Brigham and Women’s Hospital, Boston, USA) delivering insights on an implantable, continuous haemofiltration device for dialysis that has also been covered in this issue of Renal Interventions. Turn to page 9 to read more.
Jones will later return to the podium as part of a Masterclass session on “Managing the Renal Artery”. He is set to present the interventional radiology (IR) perspective on renal artery aneurysms, and will be followed by David Kingsmore (Queen Elizabeth University Hospital Trust, Glasgow, UK) outlining the surgical standpoint on this topic. Tuesday’s programme will close with Andrew Willis (Queen Elizabeth Hospital, Birmingham, UK) discussing “Vascular issues with kidney transplant”, with panel discussions and audience participation ultimately seeking to reach a consensus on this subject.
David Kingsmore (L) debates with CX Executive Board member Nicholas Inston
Vascular Access Consensus: Full Day 25th April

Podium First Vascular Access data
“Podium First: IN.PACT AV access trial – 3 year subanalysis data”

Andrew Holden, Auckland, New Zealand
“Podium First: A new kind of graft” Frans Moll, Utrecht, Netherlands
A global perspective
Over 30 expert Faculty members from over 11 countries worldwide
Active audience participation, interaction and polling encouraged – have your say!

“Best of Abstracts” from around the world will be showcased
A new Renal Interventions session
highlighting
Lessons learned using stents and balloons
The latest dialysis technology
Training vascular surgeons for renal patients
Masterclass on managing the renal artery

Hands-on practical experience
Hone your skills on Tuesday 25th April within the Vascular Access Workshop, located in the Workshop Wing
Learn from expert demonstrators and get handson time with the latest Vascular Access devices

INNOVATION EDUCATION EVIDENCE CONTROVERSIES CHALLENGES CONSENSUS CXSYMPOSIUM.COM Peripheral Arterial Consensus Aortic Consensus Acute Stroke Consensus Venous & Lymphatic Consensus Vascular Access Consensus The Hurting Leg Consensus EXPLORE THE PRELIMINARY PROGRAMME ONLINE EARLY BIRD RATES AVAILABLE UNTIL 27 FEBRUARY 2023
Cannulation
The 40-year lack of progress in haemodialysis access cannulation
Deborah J Brouwer-Maier is the vascular access marketing manager for Transonic (Ithaca, USA) and a haemodialysis nurse of 40 years. In this opinion piece, she explores how her experience has shaped her views on access, outlines its problems, and argues for longoverdue remedies.

In the spring of 2023, I will be celebrating my 40th anniversary as a nephrology nurse. I have focused most of my career on haemodialysis vascular access, including cannulation, which captured my interest during my orientation as a haemodialysis nurse for a large US dialysis provider. The vascular access education and training was on-the-job training with limited theory and skills practice. I learned cannulation with a preceptor showing me how to cannulate several arteriovenous (AV) accesses, before I was then handed the needles and expected to successfully cannulate the subsequent AV accesses. The lack of a proper fake arm for initial cannulation training led to a different training model: individuals requiring haemodialysis. I found this unacceptable, and have worked for years to help innovate cannulation training methods, techniques, and devices to improve the cannulation experience for both dialysis staff and the individuals requiring cannulation of their vascular access to receive haemodialysis.
There are a number of areas that show promise for yielding this improvement, but need more effort to bring innovation to all individuals requiring haemodialysis. Improved fake arms and simulators to help train staff on cannulation would be an excellent start, as would providing meaningful assessment and feedback on the specific element of their cannulation method to adjust to improve outcomes. This includes elements such as the angle of entry of the needle into the skin and vessel to successfully reach the centre of the target vessel without infiltration, as well as measurement of the pressure exerted on the needle, and adjustment of the needle angle to advance the needle into the vessel. The simulator devices need to be low-cost to allow utilisation by global dialysis facilities to train new staff as well as ongoing skills assessments to further the capabilities of experienced dialysis staff. Ideally, the simulators could also be utilised to train any individual requiring haemodialysis that wants to learn self-cannulation for in-centre or home haemodialysis.
We also need a standardised cannulation training programme that includes
both theory and skills practice. The recent work by the Managing Access by Generating Improvements in Cannulation (MAGIC) group is supported by the UK Kidney Quality Improvement Partnership and can serve as a template for a global training process. The training also needs to expand to any individual that wants to learn self-cannulation.
Point of Care Ultrasound (POCUS) for cannulation mapping and ultrasound-guided cannulation availability globally for initial and difficult cannulation procedures by dialysis staff are also required. The POCUS allows the cannulator to measure the vessel depth from the skin to determine the proper cannulation angle, selection of the appropriate cannulation sites, improve needle site rotation for the rope
ladder cannulation method, and needle advancement without infiltration. The POCUS usability has reached a level that allows any trained cannulator to use the devices for cannulation mapping and with skills training for ultrasound-guided cannulation.
We need to see advancements in the needle or cannula designs. Safety needles and buttonhole needles have been the two major innovations in the standard metal AV fistula needle design, while plastic cannula utilisation has been standard practice in Japan for many years. More recently, the utilisation of plastic cannulas has spread in Europe.
The cost and the training required for staff to adjust to the plastic cannula have limited the adoption. Currently, no device is cleared by the US Food and Drug Administration (FDA) for use. This is a promising area that needs more focus by the kidney community for the adoption of an innovative needle design to become the standard of care.
Cannulation research needs to continue to advance. The various elements of the actual cannulation procedure need more clinical research, including the arterial needle direction (antegrade or retrograde), bevel orientation (up or down), angle of entry based on vessel depth, advancement of the needle, and needle design impacting the cannulation procedure. In addition, studies have investigated general cannulation methods such as area puncture (not to be used but still commonly practised), rope ladder, and buttonhole cannulation. A cannulation simulator could allow for the various elements of cannulation to be documented and then used to analyse the clinical cannulation outcomes of the same cannulator.
I served on the 1997, 2000, and 2006 National Kidney Foundation (NKF) Kidney
for future research
Test the safety, efficacy, and impact on health care resources and patient outcomes of ultrasoundguided cannulation in busy, operating dialysis units
Assess impact of manual compression versus mechanical clamp use after needle withdrawal on access patency/stenosis (AV access flow dysfunction)
Test effectiveness of simulation models and other techniques for improving cannulation success, reducing complications and improving patient satisfaction
Define expert cannulator and determine how such expert cannulators can maintain their expertise and be best used to improve overall cannulation success within a unit and for individual patients
Identify obstacles to achieving complication-free cannulation and strategies to mitigate such obstacles
RCTs to assess standard needles versus plastic cannulas in preserving AV access patency and reducing complications
RCTs to assess impact of needle size and pump speed on long-term AV access patency
Identify best practices for mechanics of cannulation, including needle type and size, angle of insertion, and graduated flow rates
Evaluate outcomes associated with alternative cannulation devices
Evaluate the safety, efficacy, and patient satisfaction with using plastic cannulas
Disease Outcomes Quality Initiative (KDOQI) VA Guideline Work Groups, and sadly so many of the questions they raised remain unanswered. Real future improvements in cannulation-related outcomes will require the 2019 KDOQI VA Guideline’s recommended research areas to be properly addressed. I remain optimistic that the kidney community is willing and able to keep improving cannulation with more progress in the next 5–10 years than I have witnessed in my 40 years of nephrology nursing.
References:
Liu Z, Zhang Z, Kunkel D, et al. Is experience in haemodialysis cannulation related to expertise? A metrics-based Investigation for skills assessment. Ann Biomed Eng. 2021 Jul;49(7):1688-1700. doi: 10.1007/s10439-020-02708-5. Epub 2021 Jan 8. PMID: 33417054; PMCID: PMC8263797.
Liu Z, Bible J, Petersen L, et al. Measuring cannulation skills for haemodialysis: Objective vs. subjective assessment. Front Med (Lausanne). 2021 Nov 30;8:777186. doi: 10.3389/fmed.2021.777186. PMID: 34917637; PMCID: PMC8669158.
Singapogu R, Chowdhury A, Roy-Chaudhury P, et al Simulator-based haemodialysis cannulation skills training: a new horizon? Clin Kidney J. 2020 Dec 6;14(2):465-470. doi: 10.1093/ckj/sfaa206. PMID: 33623670; PMCID: PMC7886575.
Zhang Z, Liu Z, Singapogu R. Extracting subtask-specific metrics toward objective assessment of needle insertion skill for haemodialysis cannulation. J Med Robot Res. 2019 Sep-Dec;4(3-4):1942006. doi: 10.1142/s2424905x19420066. Epub 2020 Apr 14. PMID: 33681506; PMCID: PMC7932179.
Niyyar VD. Ultrasound-based simulation for cannulation in outpatient haemodialysis units: An educational protocol. J Vasc Access. 2021 Jul;22(4):585-589. doi: 10.1177/1129729819891530. Epub 2019 Nov 29. PMID: 31782682.
Schoch M, Bennett PN, Currey J, et al. Point-of-care ultrasound use for vascular access assessment and cannulation in haemodialysis: A scoping review. Semin Dial. 2020 Sep;33(5):355-368. doi: 10.1111/ sdi.12909. Epub 2020 Aug 3. PMID: 32744355; PMCID: PMC7496621.
Smith V, Schoch M, Andie Xu Q, et al. The use of haemodialysis plastic cannula in prevalent patients with kidney failure: A feasibility crossover randomised trial study. J Ren Care . 2022 Dec;48(4):253-261. doi: 10.1111/jorc.12411. Epub 2022 Feb 4. PMID: 35119213.
Marticorena RM, Dacouris N, Donnelly SM. Randomised pilot study to compare metal needles versus plastic cannulae in the development of complications in haemodialysis access. J Vasc Access. 2018 May;19(3):272-282. doi: 10.1177/1129729817747535. Epub 2018 Feb 28. PMID: 29772982; PMCID: PMC6161775.
Nalesso F, Garzotto F, Muraro E, et al. Fistula cannulation with a novel fistula cannula: A review of cannulation devices and procedures. Blood Purif 2018;45(1-3):278-283. doi: 10.1159/000485594. Epub 2018 Jan 26. PMID: 29478068.
Smith V, Schoch M. Plastic cannula use in haemodialysis access. J Vasc Access. 2016 Sep 21;17(5):40510. doi: 10.5301/jva.5000521. Epub 2016 Mar 10. PMID: 26980628.
4 February 2023 – Issue 6 Cannulation
Deborah J Brouwer-Maier
NKF 2019 KDOQI Guideline recommendations
Vasc-Alert, a pioneer in vascular access surveillance, has announced the publication of a study in the Journal of Vascular Access (JVA) validating its Vasc-Alert surveillance technology for dialysis patients.
THE STUDY SHOWS THAT THE technology reliably predicts which patients may suffer from stenosis, or blockage, in their access—and may even be better than clinical monitoring alone. “We knew the Vasc-Alert technology was effective, but these results showed that it performs even better than we anticipated,” said study co-author Robert Provenzano (Ascension St John Hospital, Detroit, USA).
The study, at Henry Ford Hospital in Detroit, examined 38 patients who were receiving dialysis through an arteriovenous (AV) access. Researchers performed a physical and ultrasound exam on all these patients, comparing the results to the access risk score produced by Vasc-Alert’s proprietary algorithm that predicts how likely the patients were to suffer from access complications.
The technology works by using data that is already collected by the dialysis machines, such as arterial and venous pressures, to derive the pressures in the vascular access. This means that it requires no additional staff effort or time to test the access, reducing the burden on overworked dialysis personnel, Vasc-Alert argue. These results are then reduced to a simple one to 10 access risk score. The higher the score, the more likely it is that patients will experience stenosis and require an intervention to prevent complications.
In the study, half of the patients had scores of one, two, or three (meaning low risk) and half had scores of eight, nine, or 10 (high risk). The researchers evaluated both groups of patients for access stenosis by both physical and ultrasound examinations, or what is called clinical monitoring. Patients identified with high risk scores were seven times more likely to experience stenosis than patients with low risk scores.
Lalathaksha Kumbar (Henry Ford Hospital, Detroit, USA), lead author of the study, estimates that the technology can decrease the incidence of thrombosis by “at least 30–40%”.
Music during cannulation cuts patient pain, study indicates
Eight minutes of Mozart have been found to reduce the pain of cannulation for haemodialysis patients, though not their level of anxiety, in a recent study published in the Clinical Journal of the American Society of Nephrology (CJASN). The Japanese randomised controlled trial suggests the use of music can, at the very least, make for an effective and affordable adjunct to existing analgesic measures during what is often a painful procedure for patients.
High levels of pain during cannulation are associated with patients skipping dialysis sessions, while missing just one over several months has been associated with a 68% higher rate of mortality. This risk, as well as the cost associated with existing treatments for cannulation pain, prompted the study authors, including lead author Emi Inayama (Mihama Narita Clinic, Chiba, Japan) and corresponding author Yosuke Yamada (Shinshu University School of Medicine, Nagano, Japan), to investigate methods for its management.
Building on a study by Jin Hyung Lee (Ewha Womans University, Seoul, South Korea) that has suggested music is an effective reliever of pain in other medical settings, Inayama et al designed their own that explored its capacity for doing the same in a haemodialysis setting. It was a prospective, multicentre, single-blind, crossover, randomised controlled trial taking place across five dialysis facilities in Japan. There, 121 patients were selected who were over the age of 20 and who had been undergoing dialysis for more than six months at the beginning of the trial. Of these, 86 were men and 35 were women, while
Plastic cannulas “vital” for patients at risk of needle infiltration
Dori Schatell (Medical Education Institute, Madison, USA) has spoken at VEITHsymposium (15–19 November 2022, New York City, USA) extolling the advantages of plastic cannulas and their flexibility. Though not yet approved by the US Food and Drug Administration (FDA), Schatell argued that they present several opportunities for clinicians.
PLASTIC CANNULAS HAVE BEEN USED for 30 years or more in Japan, and 15 years in Europe, Australia, and New Zealand, but are not yet FDA-approved in the USA. That may be changing, Schatell said. She argued that plastic cannulas should be considered for patients requiring more flexible access. Needle infiltration, which occurs more frequently with metal cannulas, can disrupt treatment and create a requirement for new procedures. A flexible cannula may reduce the risk of infiltration, she said, while also drawing attention to other scenarios in which plastic cannulas may be useful, such as for nocturnal haemodialysis during sleep, in restless patients and children, as well as those with endovascular arteriovenous fistulas (endoAVFs) or metal allergies.
A direct statistical comparison was drawn by Schatell between plastic and steel. Referring to a study in the Journal of Vascular Access led by Sun Ryoung Choi (Hallym University Medical Center, Seoul, South Korea), she noted that there was “no optimal flow, angle, depth or needle eye” to prevent wall

their median age was 64 years. Those with impaired hearing were excluded.

Enrolled patients were randomly allocated to two groups, both of which experienced haemodialysis twice with no sound, once with white noise played as a control and once with Mozart’s “Sonata for Two Pianos in D Major, K.448”, which has been selected for other studies exploring music’s analgesic properties including James Stephen Jenkins’ (Ochsner Medical Center, New Orleans, USA) into the “Mozart effect”. The patients also experienced the white noise and music for eight minutes before cannulation. The primary endpoint was visual analogue scale (VAS) pain score reported by patients immediately after cannulation, while their VAS anxiety score was among the secondary endpoints.
The VAS pain score for patients who heard Mozart was 12% lower than for those who heard the control of white noise, which the authors describe as “significantly lower”. The 8% reduction on the VAS anxiety scale, meanwhile, they call “not significant”, while “the per-protocol set results were similar”. The study design had its limitations, including its gender imbalance, notable given that female gender has been associated with fear of needles by other studies. It was also not considered whether the analgesic effect of Mozart in particular is dependent on a patient’s cultural background and personal enjoyment of the genre or composer. Inayama et al call their study “well-designed” while demonstrating an analgesic effect. Their final remark states that “the effect size of music alone might not be clinically sufficient to control pain”, but that as a “safe and inexpensive adjunct pain relief method” alongside others it shows promise.
sheer stress with steel cannulas, while plastic cannulas were associated with more stable arterial and venous pressures. Cannulation success generally was higher with a plastic rather than metal needle, and plastic use resulted in “less AVF injury, failure [and] haemostasis time.”
There was, however, a “learning curve” associated with plastic, Schatell suggested. Cannulation pain was generally found to be higher than with metal cannulas, but can be addressed with topical anaesthetics. Nurses also found cannulation more difficult at first [p=0.084]. Despite these drawbacks, she said, plastic cannulas “save lives” by allowing earlier cannulation.
Though plastic cannulas initially cost more, Schatell said, their advantages resulted ultimately in savings for healthcare providers. She concluded by stating that they were “cheaper per patient” in part because they were both “less likely to harm the access” and “able to be used faster,” reducing the need to start haemodialysis with a risky central venous catheter.
“Blood vessels are flexible—but metal needles are rigid,” noted Schatell. “Getting plastic cannulas FDA-approved and in regular use is vital to reduce the fear, pain, and potential damage from metal needles and to help make home haemodialysis more possible for many.”
5 Issue 6 – February 2023 Cannulation Cannulation
Vasc-Alert data shows promise for stenosis prediction technology
Yosuke Yamada
Dori Schatell
“Getting plastic cannulas FDAapproved and in regular use is vital to reduce the fear, pain, and potential damage from metal needles, and to help make home haemodialysis more possible for many.”
Home haemodialysis brings its own “major challenges and barriers”
(Royal
and
Recent years have brought a change to the landscape of dialysis. With the COVID-19 pandemic, we have seen reignited efforts to support home dialysis options for patients, including HHD. The risk of contagion during in-centre dialysis is one factor that has accelerated this trend, but other, significant benefits of HHD uptake have also garnered increased attention. Patient preferences for HHD mainly relate to the clinical benefits achieved through high-intensity dialysis at home alongside what is often an improved quality of life. Many patients find it easier to manage HHD treatment with competing commitments such as employment and childcare. The HHD option also reduces the burden of travel, particularly for those with mobility problems and multimorbidities. On a broader level, reduced transportation needs and fewer demands for in-centre dialysis services can translate into greater public health cost savings. The advantages of HHD extend beyond the individual patient.
Whilst these represent considerable benefits, there are also major challenges and barriers associated with HHD for patients, families and clinicians, particularly for older patients who may find it more difficult to maintain the technical demands required to deliver home dialysis as effectively as their younger counterparts. Challenges are already apparent from the selection and training phases prior to HHD initiation. Patient fears relating to illness intrusiveness and being isolated from well-supported care are barriers when they consider selecting HHD as their dialysis modality.
There is uncertainty deciding upon an optimal length of training time before HHD commencement. Whether there is the capacity and infrastructure to support training needs for patients needs to be factored in, too. With previous studies demonstrating the length of training time required for competency in HHD being correlated with age, there is more difficulty training older adults, especially those with cognitive impairment. Greater frequency of retraining opportunities is ideal for older patients, though this may not be practically and financially viable to continuously promote over time. If caregiver support is not available and a patient is deemed incapable to continue HHD independently, they are more suited for in-centre dialysis.
Another conundrum relates to vascular access within the home setting. Many kidney failure patients have cardiac and vascular comorbidities, and it can be challenging for them to acquire
adequate vascular access consistently. Older patients tend to have reduced manual dexterity, reduced vision, and increased tremors—they will therefore find it even more difficult without caregiver or healthcare professional support. In remote environments where specialist services are not readily accessible, there could be greater challenges in managing vascular access complications such as infections, acute bleeding and thromboembolism.
Cardiovascular complications during HHD are important to consider and potentially tricky to manage. There may be difficulties in finding a strategy to optimise HHD intensity and session frequencies to control circulatory volume overload in some patients. Outside of dialytic factors, an often-underestimated component of care is patient compliance towards fluid intake restrictions and patient discipline of maintaining low-salt dietary intake patterns. Another challenge is tackling blood pressure (BP) instability. Whilst avoiding symptomatic hypotension or overtly low BP is vital, how best to decide on personalised BP target ranges remain uncertain. Accurate measurement of BP could be challenging, and there is debate over whether automated or manual measurement devices are better within the HHD context. Other treatment-related complications that are complex to manage holistically include protein-energy wasting, malnutrition and electrolyte abnormalities.
The physical practicalities of administering HHD are not the only potential challenges. Socioeconomic barriers of HHD implementation could occur in health systems where there is a lack of government-funded initiatives and financial reimbursement for patients and caregivers. Patients could find it very difficult to perform HHD adequately with limited housing space and increased utilities costs, while caregivers may need to find full-time employment to achieve financial sustainability for the family. They may also need to sacrifice other commitments to care for their loved one receiving HHD, which can increase caregiver stress and psychological burden.
There have been advances to ease some of these challenges, not least in telehealth platforms, which have brought new avenues for HHD care. They eradicate the pressures around maintaining social distancing that come with in-person consultations, and they enhance regular HHD care for those living in rural locations. However, the inability to perform physical examination (i.e. examination of an arteriovenous
fistula), concerns relating to patient privacy, and the magnification of socio-economic inequalities in dialysis care are noticeable issues. Poorer patients may not have access to updated electronic devices and broadband internet to receive a high-quality HHD service through telehealth, and it has been highlighted that ethnic minorities receiving home dialysis are underrepresented in the uptake of telehealth.
Despite these challenges, there are a host of other potential strategies to overcome the challenges and barriers of HHD beyond telehealth services. First, it is important to deliver educational initiatives for a wider community of patients and their families, addressing misconceptions regarding HHD and providing reassurance that they are not alone without healthcare staff support during therapy if this is required. At present, increased government funding to improve the capacity, infrastructure and quality of healthcare staff training in delivering HHD is planned for many parts of the world. An enhanced training programme for patients to practice performing HHD, initially with guidance from staff and caregivers before doing so independently (if they can) will hone their preparedness and competency, and increase their confidence. It may be helpful to set up annual retraining or refresher training courses for patients and caregivers, to ensure competency is maintained.
Clinicians should determine an optimal vascular access option for each patient during consultation to ensure safe and effective HHD delivery. Older patients, and those with pre-existing vascular disease, where a greater likelihood of challenges exist regarding vascular access, should be most carefully considered. Continuation of multicentre quality improvement initiatives aimed at minimising symptom burden and ensuring early identification and intervention of HHD complications and comorbidities is required, too. It should come in conjunction with the development of a robust support service in the community involving multidisciplinary teams to respond quickly and adequately could improve patient outcomes, should treatment-associated complications occur.
Disclosures: Henry Wu is supported by the Australian Government Research Training Program. Sandip Mitra is supported by the National Institute for Health Research at Manchester, UK, and Devices for Dignity MedTech & In Vitro Diagnostics Co-operative, Sheffield, UK. Both Henry Wu and Sandip Mitra do not have competing interests to disclose for the contents presented in this article.


Assisted HHD care models are another answer being developed for those having to chronically care for the family member receiving HHD. Cost-effective respite care may bring benefits in patient outcomes, as well as alleviation of caregiver burnout and psychological stress. Creation of financial reimbursement schemes, usually collaborations between governments and industry, could find solutions in addressing financial concerns for patients and their caregivers. Regarding telehealth, it would be important to identify areas for continued innovation and industry collaboration to improve existing and new technological platforms (such as virtual ward, digital rehabilitation programs) in HHD. As well as reducing the attrition of care for patients and caregivers, we should explore ways to widen participation of telehealth services in HHD to encompass a greater diversity of socioeconomic and ethnic groups.
A review like this therefore alerts us to the variety and scale of barriers to performing HHD, important considerations despite the advantages of pursuing this dialysis modality. There is increased awareness from the nephrology community on these issues and the need to address them. With concerted efforts in establishing more consensus guidance, health policies and government backing to support HHD care as well as creating opportunities to enable advances in technology for a wider population, we are confident in finding solutions to tackle these challenges and barriers going forward.
6 February 2023 – Issue 6 Home Dialysis Dialysis
Henry Wu
North Shore Hospital, Sydney, Australia)
Sandip Mitra (Manchester Royal Infirmary, Manchester, UK) write for Renal Interventions to evaluate some of the challenges associated with the expansion of home haemodialysis (HHD), as well as the strategies being devised to deal with them.
“Older patients tend to have reduced manual dexterity, reduced vision, and increased tremors— they will therefore find it even more difficult without caregiver or healthcare professional support.”
Sandip Mitra
Henry Wu
New US financial incentive fails to increase rates of home dialysis
The financial incentives offered by a recent US government programme for hospitals and clinicians to utilise home dialysis for end-stage kidney disease (ESKD) have not caused statistically significant changes in usage of the treatment. This is the conclusion of a study published by Yunan Ji (Georgetown University, Washington DC, USA) and colleagues to the JAMA Health Forum last month.
Estimates suggest that 85% of Medicare patients with ESKD are eligible for home dialysis, which is cheaper and equally or more effective than facility dialysis, but only 12.6% of those actually receive it. In an effort to increase this number to a target of 80%, the US Centre for Medicare and Medicaid Innovation (CMMI) employed a new payment incentive system, the End-Stage Renal Disease Treatment Choice (ETC) programme, to encourage clinicians to adopt home dialysis.
The ETC incentive system works
through two methods. The first increases the reimbursement rate for home dialysis in the first three years of the programme, while the other increases or decreases the rate for home and facility treatment based on the rate of home dialysis and treatment. The authors of the study followed the ETC specifications with some minor adjustments to eligibility criteria.
In the randomised clinical trial, researchers examined the statistics from 302 hospital referral regions (HRRs) in the USA, including 91 randomised to the treatment group where financial incen-
US adoption of peritoneal dialysis limited by “misconceptions” of clinicians, study suggests
The use of peritoneal dialysis (PD) in treating chronic kidney disease (CKD) patients is limited in the USA by the mistaken assumptions of clinicians, in part a result of insufficient education by healthcare providers, claims a new study published in the Cureus Journal of Medical Science.
DESPITE AN “ENCOURAGING” programme from the US government aimed at improving public understanding of end-stage kidney disease (ESKD), the study authors say that “misconceptions and differing attitudes about PD among physicians” remain “important barriers” to its further implementation.
The study, led by Hussan S Lalani (Brigham and Women’s Hospital, Boston, USA) and assisted by corresponding author Ramesh Saxena (UT Southwestern Medical Center, Dallas, USA), employed a survey of 10 questions “to assess the knowledge and attitudes around peritoneal dialysis and haemodialysis among internal medicine faculty at the University of Texas Southwestern Medical Center” in Dallas, USA. Lalani et al stress that, despite the “well-established benefits of PD”, including a “lower adjusted mortality rate” and its lower cost compared to in-centre haemodialysis, it is still unclear why PD has not further supplanted in-centre.
Lalani et al distributed their survey to both nephrologists and non-nephrologists, with 83 recipients fully completing it. Of those, 10 were nephrologists and the remaining 73 were from other disciplines. Both groups reported “increased perceived knowledge and comfort with
caring for patients on haemodialysis compared to patients on PD”. Nephrologists “scored 30% correct responses regarding medical contraindications and 48% regarding psychosocial contraindications to PD”. The authors describe it as “interesting”, meanwhile, that “non-nephrologists scored higher regarding medical contraindications” even though they reported “lower comfort and perceived knowledge (42.5% and 20.5%) of PD”.
In their discussion, the authors state that the results suggest there is a clinician “knowledge gap” between haemodialysis and PD. They state the results suggest “disproportionate hesitancy” towards PD among nephrologists, though are quick to stipulate that their study had its limitations, including its small sample size. The subject requires further study on a larger scale, they argue.
The authors are firm in their concluding emphasis on “the importance of basic education regarding PD candidacy and the subversion of misconceptions regarding PD” among both nephrologists and non-nephrologists. Finally, they propose a solution to the issues they raise in the form of regional centres of excellence dedicated to training physicians and other health professionals on PD.
tives were implemented and 211 to a control group where they were not. The primary outcome was the percentage of patients receiving home dialysis in their
first 90 days of treatment.
The study’s analysis found no meaningful difference in rates of home dialysis after those first 90 days between the two groups. The control HRRs saw a rate of 20.60% while the treatment group saw one of 20.72%.
This lack of difference leads the study authors to suggest that larger financial incentives may be required to deliver a significantly higher uptake of home dialysis treatment. It is noted that the 90-day period examined by the study limited it from assessing the effect of larger incentives, which were implemented in later years of the programme.
An accompanying editorial on the study led by Sri Lekha Tummalapalli (Cornell University, New York, USA) suggests that lack of increase in home dialysis rates may be a result of the fact that “care redesign to shift dialysis into the home is complex and time-consuming,” while “many frontline nephrologists may still be unaware of the ETC model.” Future studies, the editorial states, should also account for the fact that “randomised payment models operate pragmatically in real-world settings that are not fully controlled.”

Haematuria associated with incident CKD in new AJKD study
Patients with haematuria may be at increased risk of chronic kidney disease (CKD)—that is the conclusion of a new study in the American Journal of Kidney Diseases (AJKD). Led my Yoo Jin Um (Seoul National University Hospital, Seoul, South Korea), the study authors performed a retrospective cohort analysis to investigate the risk of developing CKD associated with microscopic blood in a patient’s urine.
THE RETROSPECTIVE COHORT STUDY EXAMINED THE DATA OF 232,220 patients from the Kankbuk Samsung Health Study. The patients received “comprehensive health examinations” at least twice between 2011 and 2018, with a follow-up before the end of 2020. This examination included blood pressure, estimated glomerular filtration rate (eGFR), serum creatinine and other measurements. Urinalysis of protein and blood cells was performed of “fresh and midstream spot urine samples” of all patients, and haematuria changes were determined at baseline and follow-up. The primary endpoint of the study was incident CKD, while secondary endpoints included decreased eGFR and proteinuria.

The results showed a statistically significant association. Male patients who experienced persistent haematuria had an 8.3-fold increased risk of developing CKD, while those who developed it had a 4.4-fold increased risk and those whose haematuria regressed had a 2.2-fold increased risk. Women with persistent haematuria had a 4.4-fold increased risk and those who developed it had a 2.5-fold increased risk. Both were statistically significant, and the authors said it reflected that microscopic haematuria was “significantly associated with subsequent CKD incidence[…] in both sexes,” despite a stronger association for men.
One point the team noted is those microscopic haematuria in premenopausal women was “commonly considered a benign finding,” something brought into question by the results of their study. They call the reason for the sex-based differences “unclear,” requiring exploration in further studies. Finally, they note limitations, including the lack of renal biopsies among the patient cohort, which limited their data, as well as the overall low number of incident CKD in their study, something which they suggested should prompt further study. Nevertheless, they say such further study could build on the strengths of their own to determine “whether appropriate management of haematuria can help decrease subsequent CKD risk and progression to renal failure”.
7 Issue 6 – February 2023 Dialysis Research Dialysis
Ramesh Saxena
Yunan Ji

Miniaturised Holly implantable dialysis device offers patients greater freedom
Dirk M Hentschel (Harvard Medical School, Cambridge, USA), president of the Vascular Access Society of the Americas (VASA), has presented on the new Holly portable device (Nephrodite) for haemodialysis. Designed as an “implantable continuous dialysis haemofiltration device blending haemodialysis and peritoneal dialysis in one device,” it purports to offer patients more freedom than both in-centre and home dialysis treatments.
THE PRESENTATION AT VEITHSYMPOSIUM (15–19 November, New York City, USA) began with a question—“why bother?” What makes an implantable device worth the investment for clinicians and their patients? The answer was multipronged, with Hentschel acclaiming the mobility gained and time saved by utilising products like Holly. The core of Holly’s utility is the freedom it gives to patients, he said. The ambition behind the device is to provide something “approaching continuous dialysis,” he continued, and that patients using the device “should reach stage 4 CKD kidney function (eGFR > 15ml/min)”. He outlined the core concepts behind the device, including miniaturisation of dialysis technology to allow it to be portable as well as the reuse of dialysate.
Hentschel was not afraid to outline the many challenges in designing a successful implantable dialysis device. Building a body-device connection was among them, as were the multiple risks associated with use of the device, which included both thrombosis and infection. There were also questions, Hentschel said, about how best to control the parameters of dialysis on the device after implantation.
He had answers to these questions, however. For controlling dialysis, he mooted the twin possibilities of an external device for controlling dialytic parameters as well as an internal one requiring a “biological kidney equivalent.” Holly itself, he said, operates on a hybrid system blending both of these approaches. Using a catheter coming out of the skin, it will connect to a wearable bag of dialysate fluid which patients can change themselves every four to six hours. This will give patients a new level of freedom even compared to existing home dialysis systems, Hentschel suggested.

Holly’s system brings its own challenges, however. Hentschel sketched a few of them, including those brought by the external reservoir connected to the system. The membrane of the device is subject to ageing and may mean it needs to be replaced, he said, while control of the micropump at the centre of Holly’s design also demands a solution and the dialysate needs to be monitored.
Disclosures: Dirk M Hentschel is a member of Nephrodite’s advisory board and has held equity in the company, as well as in BluegrassVascular.

GIANT steps for renal technologies hailed at 2022 conference
Rajesh Sivaprakasam (Barts Health NHS Trust, London, UK) was among several clinicians and industry speakers who recently spoke on a variety of new technologies in the renal space at the Global Innovation and New Technology (GIANT) summit (6–7 November, London, UK) for 2022. The conference’s Future Hospital debate and presentation programme offered a glimpse at the future of surgery and remote patient monitoring.
Wearables were evaluated in a morning discussion on non-invasive, remote monitoring technology. This included Alio’s SmartPatch device, wearable technology that monitors the vitals, blood pressure and other biomarkers of chronic kidney disease (CKD) and end-stage kidney disease (ESKD) patients. It was chaired by Sivaprakasam and featured CEO and co-founder of Alio, David Kuraguntla, Ken Callahan of the Hargan Group, former Senior Official at the US Department of Health and Human Services, and Deborah Duval, managing editor of Kidney Care UK, as well as lead nurse for dialysis at Barts Health, Joanna Dapatnapo (Barts Health NHS Trust, London, UK).
Dapatnapo opined that “we need remote, dynamic and non-invasive tools” such as the SmartPatch for monitoring the condition of haemodialysis patients. “Currently, dialysis patients require a blood test to confirm the adequacy of their access, and require the puncture of the fistula three times a week.” She said remote monitoring technology would relieve them of this need.
Callahan, meanwhile, outlined how KidneyX, a major partnership between the US Department of Health and kidney organisations, was assigning US$100 million to those innovating in kidney care. Alio, who received a US$1 million grant, also brought in US$18 million in its recent Series C funding round, and Kuraguntla stated that its SmartPatch would enable CKD patients of lower

socioeconomic status to be monitored with more attention than existing smartphone-based solutions. They expressed confidence, however, that it could benefit all CKD patients.
Sivaprakasam also participated in a lively panel discussion with Iain Hennessey (Alder Hey Children’s Hospital, Liverpool, UK) chaired by Shafi Ahmed (Barts Health NHS Trust, London, UK) on the prospects for surgery presented by developing technologies, as well as the existing issues with surgery in the National Health Service (NHS) they may help to solve. Sivaprakasam argued that the NHS was currently failing to fully adopt technologies that would make surgery more efficient. Allowing students to learn to perform surgeries using virtual reality simulation, for example, would make them “better prepared”, he said. Hennessey, meanwhile, suggested NHS procedures were not currently optimally assigned.
9 Issue 6 – February 2023 Renal technologies
“Currently, dialysis patients require a blood test to confirm the adequacy of their access... We need remote, dynamic and non-invasive tools.”
Joanna Dapatnapo
Dirk M Hentschel
Left, David Kuraguntla; right, Rajesh Sivaprakasam
Ultrasound as an “objective adjunct” can improve outcomes of cannulation

Ultrasound is a powerful tool for assessing haemodialysis (HD) access for maturity, but may also be used to guide HD access cannulations and has the potential to “actually change the process of care” according to Vandana Dua Niyyar (Emory University, Atlanta, USA). The president of the American Society of Diagnostic and Interventional Nephrology (ASDIN) has spoken to Renal Interventions about her view of the field of renal ultrasonography.

Niyyar emphasises the value of ultrasound throughout the spectrum of kidney disease, right from the first visit of the patient to the nephrologist, while also noting its wider variety of applications including assessment and cannulation of dialysis access. Cannulation has traditionally been done by experienced dialysis staff, she says, but with the increased turnover in dialysis staff after the COVID-19 pandemic, combined with the subjective nature of cannulation criteria, there is plenty of room for the extra objectivity provided by ultrasound. As an “adjunct to physical examination and experience”, she argues, it can transform the patient experience.
Addressing the changing landscape of fistula creation, Niyyar praises the influence of new technology in the field. While technology is already being used in the creation of fistulas, it is also worth putting it to use for the end user. She references patients with complex anatomy that she doubted would have been successfully cannulated without ultrasound. Niyyar says the technology is able to transform care of patients with arteriovenous fistula (AVF), which she stated had been “stagnant for quite a few years” despite technological advances in AVF creation. Ultrasound and other new technologies offer an opportunity to review how care is provided and a chance to “challenge the status quo”.
“I do not think an ultrasound should replace anything,” Niyyar stipulates, “but the ultrasound in combination with experience and physical examination can change the trajectory of what the patient experiences at the end point”. She repeatedly stresses the importance of the patient experience, in fact, saying that is “ultimately what we are here for”. Ultrasound has its limitations, she conceded. Though the ultrasound she uses is handheld, easy to “carry directly to the patient, and “relatively inexpensive”, she notes that it lacks flow measurements. She does also point out, however, that this is due to be remedied in future versions of the point-of-care ultrasound.
A study recently published in Kidney International Reports (KIR) has found that urinary peptidome (UP) analysis can help predict a patient’s risk of developing kidney failure. It also describes the “potential” for the process to “uncover new pathophysiological chronic kidney disease (CKD) progression pathways”.
THE STUDY AUTHORS, including lead authors Ziad A Massy (Paris West University, Paris, France) and Oriane Lambert (University Versailles-Saint Quentin, Villejeuf, France), as well as corresponding author Julie Klein (Institute of Metabolic and Cardiovascular Disease, Toulouse, France), drew attention first to the existing risk equations for predicting kidney failure, one of which, that devised by Tangri et al, uses urinary albumin-to-creatinine ratio as part of its formula. They argued that previous attempts to assess urinary proteins as biomarkers had demonstrated “inconsistent or still limited findings”. Their study, meanwhile, would compare the performance of a risk equation that also analysed peptides.
In designing the trial, the authors sought to “describe the urinary peptidome diversity” in CKD patients to “better characterise” their patient profile, while also uncovering whether it could “predict their progression to kidney failure.” It was carried out over 40 nephrology clinics across France, examining 1,000 adult CKD patients of stages 3–5 from the CKD-REIN study cohort. Fasting blood and second morning urine samples were taken at baseline, and patients were subsequently followed up annually over five years. The primary outcome was kidney failure, which was defined as beginning dialysis or receiving a pre-emptive transplantation.
Machine learning was used in the analysis of the data which was collected. A “clustering algorithm” was used to “classify patients at baseline,” dividing them into three groups of different CKD severity. Then, 5,000 peptides were sequenced with peptidome analysis and their abundances were compared with rates of kidney failure. Kidney failure prediction models were developed based on the results, with sets of predictors including the sequenced peptides as well as other risk factors.
A 90-peptide sequence was discovered which “achieved excellent discrimination in predicting the risk of progression” to kidney failure. However, it did not improve on the predictive capabilities of the kidney failure risk equation provided by Tangri et al. In their discussion, the study authors suggested that “in moderate to advanced CKD, the information contained in the urine peptidome, analysed with an untargeted holistic approach, is redundant with those captured by age, sex” and other variables. However, they did note that it may in fact be a “good predictor” for CKD itself in patients with type 2 diabetes and normoalbuminuria. Conceding that the study had limitations, the authors said it may have been improved by also examining earlier-stage CKD, rather than only looking at patients with stage 3–5 disease. Nevertheless, they concluded, the urinary peptidome “appears to represent a useful tool for the detection of new pathophysiological pathways” that are involved in progression to kidney failure, even though its purely predictive capabilities do not outstrip existing risk equations.
February 2023 – Issue 6 10 Ultrasound
Vandana Dua Niyyar
Urinary peptidome analysis may predict ESKD, claims study
Julie Klein
“I do not think an ultrasound should replace anything, but ultrasound in combination with experience and physical examination can change the trajectory of what the patient experiences at the end point.”
Procedures during nephrology training— time to reconsider?
Mukesh Sharma (University of Nevada Reno School of Medicine, Reno, USA) is a faculty member and Fellows Education Committe chair at the American Society of Diagnostic and Interventional Nephrology (ASDIN). In this opinion article, he writes to examine the unique capabilities of the interventional nephrologist, and the importance of nephrologists learning procedures such as catheterisation during their training.

Nephrology as a medical subspecialty blends intricate knowledge of physiology with clinical reasoning, encompasses building long-term patient relationships, and offers a gamut of surgical procedures for diagnostic and therapeutic implications for patients with kidney disease. The emergence, evolution, and establishment of interventional nephrology as a subspecialty has added further credence to the claim that nephrologists, adequately trained, are uniquely well-equipped to provide dialysis access services to patients with whom they already have long-term care relationships. Whereas a case can be made that promoting procedural training during fellowship may help lure more applicants to lift the sagging number of applications for the US Nephrology fellowship programmes, a hot debate has emerged regarding whether future generations of nephrologists should even be required to do a certain number of procedures during their training. These requirements
currently include temporary vascular access placement for haemodialysis and kidney biopsy.
Such questions about the utility of busy clinical nephrologists doing procedures gained prominence after the American Board of Internal Medicine (ABIM) 2021 procedural frequency survey results. The survey was sent to over 10,000 nephrologists asking them if they were performing procedures like kidney biopsy and temporary dialysis catheters in their day-today practice. Of these, 70.9% of the respondents said that they no longer performed temporary vascular access, and 14.7% performed between one and five procedures per year. For kidney biopsy, 83.1% of respondents no longer performed kidney biopsies, and only 6.9% performed between one and five biopsies per year.
In my opinion, the results of the ABIM survey need to be analysed carefully
before conclusions are drawn. First, the response rate on this survey was quite low (19.7%) and should not be generalised to the entire nephrology community. The views and opinions of the rest of the nephrologists who did not respond to the survey (81.3%) are hard to predict based on the lukewarm response to the survey. Even if the survey results are to be generalised, 30% of nephrologists still place an emergent temporary dialysis catheter at least once a year. On a national level, there are an estimated 10,000 adult nephrologists in the USA, and extrapolating this data reveals 3,000 nephrologists that place a temporary dialysis catheter usually in emergent situations.
As such, it is imperative that the nephrology fellows get adequate training during fellowship to gain the competency and confidence to place a temporary dialysis catheter to deal with emergent lifesaving scenarios and perform a kidney biopsy when required. This sentiment is shared and supported by nephrology fellows in general as well. The American Society of Nephrology (ASN) established a taskforce in April 2022 to deliberate on all aspects of future nephrology including the procedural requirements for nephrology fellowship programmes. The nephrology fellows themselves feel and have conveyed to the ASN taskforce that they should continue to do such procedures. To quote directly from the ASN taskforce discussion, the current nephrology fellows felt that they are “giving away procedures when other specialties were not”. They also felt that it was important for nephrologists to perform procedures because it was best for patients and avoided frag-
DART decision aid allows for better treatment decisions and reduces conflict for renal patients, study finds
A web-based decision aid can improve the quality of treatment decisions made by patients over 70 with chronic kidney disease (CKD)—that is the conclusion of a new study in the Annals of Internal Medicine (AIM).
THE DECISION AID FOR RENAL THERAPY (DART) is an educational aid accessible online that looks to remedy the issues with existing renal patient education materials outlined by the study authors, led by Keren Ladin (Tufts University, Medford, USA), which included that they are “generally not tailored for older adults”. It does this by “allow[ing] patients to control the pace of information” and providing accessible multimedia content for those with “limited health literacy”.

Older adults are also often educated on renal disease in single-session group classes, Ladin et al noted, which can be challenging for them due to hearing impairments, and which may not address their specific concerns. “Although decision aids improve decisional quality,” they added, “none have been specifically designed to meet the unique needs of older patients facing dialysis decisions”.
Keren Ladin
DART was a pre-existing tool for informing renal patients that was adapted by the study authors for older adults. The DART trial also addresses another gap—existing research on decision-making in dialysis patients has mostly focused on decisions made by those receiving maintenance dialysis, they have said, rather than those with advanced CKD who were yet to decide on treatment.
In total, 400 patients were recruited across nephrology clinics in four US cities for the trial, of whom 37 dropped out. These were patients who had not yet received dialysis but had stage four or five CKD with an estimated glomerular filtration rate <30mL/min/1.73m 2 It was a “non-blinded, site-level, 1:1 randomised trial”. Designing the trial around multiple centres was intended to account for “potential differences in site culture and patient education about kidney failure treatment choices”. Patients were followed for up to 18 months, and 183 were asked to use the DART tool at three months, the results of which were passed on to their clinician. The remaining 180 received “usual care”. The primary outcome was “change in deci -
menting care, and procedures were one way to attract future applicants. As ‘value-based care’ models gain wider acceptance across different payers, it is likely to add more disincentives for referring patients to other specialists for common procedures. The literature supports that nephrologists can competently perform common dialysis access procedures with outcomes comparable and in some cases better than those performed by their colleagues from other subspecialties. Being proficient and competent to do procedures will help the next generation of nephrologists survive and thrive in the evolving value-based healthcare ecosystem. We must continue to equip and train future nephrologists with proper procedural training, and American Society of Diagnostic and Interventional Nephrology (ASDIN) can play a major role, along with ASN, in helping to form our future nephrologists.
References:
1. Update on the Task Force on the Future of Nephrology. Reimagining nephrology fellowship training. Mark Rosenberg. Kidney News, Volume 14, Issue 7, Publication date: 01 July 2022, pp 10–11
2. The Nephrology Workforce 2016, ASN, 2016, Exhibit 1, p7. Available at https://www.asnonline. org/education/training/workforce/Nephrology_ Workforce_Study_Report_2016.pdf
3. The ASN Task Force on the Future of Nephrology: What have we been hearing? Kidney News, Volume 14: Issue 9, Publication Date: 01 Sep 2022 Page: 14
4. Effectiveness and safety of dialysis vascular access procedures performed by interventional nephrologists. Gerald A. Beathard, Terry Litchfield. Kidney International, Volume 66, Issue 4, October 2004, Pages 1622-1632. https://doi.org/10.111 1/j.1523-1755.2004.00928.
sional conflict from baseline to the three-month follow-up assessed using the decisional conflict scale (DCS)”.
DCS scores improved to a statistically significant degree for those patients in the DART-assigned group at three- and six-month assessments. At three months, the mean difference from the control group was -7.9 and at six it was -8.5 on the DCS scale. Those in the DART group were also found to “perform better with respect to implementing decisions” and were less likely to delay a decision.
Dialysis decisions
Patient knowledge increase within control group: 5.5%
Patient knowledge increase within DART group: 10.9%
Statistically significant change was also present in measures of patient knowledge. On mean test performance, the control group improved over the course of the study period from 57.0% to 62.5%, while those who used DART went from 59.4% to 70.3%.
The study authors dubbed DART “an effective, patient-centred intervention that can improve decisional quality and knowledge of prognosis”, while reducing the burden on clinicians by allowing patients to educate themselves at home. The effect of DART was particularly strong up to six months, they said, and was still positive but “attenuated” after 18 months. Most studies, they said, examine the effects of decision aids after one week or one month.
The authors noted a few limitations, including that “enrolment among Latinx patients was low”, which was “possibly because DART was only offered in English”. There was also no supervision over how DART was used by patients. Ladin et al neverthless called DART a “consistent and accessible” tool that cuts conflict and improves knowledge for older CKD patients. Their final note was constructive, suggesting patients should be encouraged to revisit DART to improve outcomes after 18 months.
Issue 6 – February 2023 11 Interventional Nephrology
Mukesh Sharma
Robert Jones
“More than in any other medical discipline,” says Vascular Access Society of Britain and Ireland (VASBI) president Robert Jones, “interventional radiology (IR) is where medicine meets technology”. A consultant interventional radiologist at Queen Elizabeth Hospital Birmingham, he is now looking to expand the society’s reach to patients, and help it stoke more interest in arteriovenous (AV) access from interventional radiologists. Speaking to Renal Interventions on IR its future, he describes its unique challenges, his mentors and the music that makes it onto his playlist.
What drew you to a career in medicine and in IR?
As a teenager, I spent some time in hospital as a patient and became fascinated with what was going on around me—I guess my interest in medicine developed from there. What drew me to IR was the idea of not only being able to confidently diagnose a condition, but also having the ability to treat it with state-of-the-art technology. IR really is where technology and medicine interact more than in any other medical discipline.
Who are your mentors and who has inspired you in your career?
I am exceptionally grateful to everyone who has ever taught me and invested time in my training. Whilst doing the IR fellowship in Vancouver in 2007/8, I was really inspired by Chris Morris, who was a senior interventional radiologist at the time. He had decades of experience and had seen IR evolve from a fledgling discipline in the 1970s to what it is today and it was fascinating hearing about his career. Even in the twilight of his career he would be there on call at two in the morning, enthusiastic to teach and impart his knowledge—his perseverance was really inspirational. Also, Gerald Legiehn taught me it is okay to be pedantic and to always maintain high standards, while the late Peter Riley, who trained me in Birmingham, taught me to weigh up the risks of everything before you do it. He was measured, but not afraid of a challenge—he also taught me some off-piste skiing and had a wicked sense of humour. When I was a registrar, I was doing a nephrostomy with him and I was making a hash of it. He elbowed me and said, “I tell you what, why don’t you let me finish up here? There’s a shopping list over there, in the control room. Just wander up to Marks and Spencer and get me a few bits and pieces”. He was old-school.
Which recent developments most interest you?
Endovascular arteriovenous fistula (endoAVF) is up there on that list. I have been involved in it for six years and it is still relatively early days, and we have got so much more to learn and understand, which will only come with more research, and everyday clinical use and exposure. There are many other developments in IR outside vascular access. There is an ever-expanding development of embolic materials, which allows us to carry out safer and more effective embolisation procedures (particularly in arteriovenous malformations [AVMs], which I also have an interest in). Watching this technology evolve is very interesting.
What is the most important thing you think can be done to improve IR provision for patients with kidney disease?
In the UK, vascular access is not necessarily the most popular domain of IR services. While many centres provide excellent IR support for dialysis patients, there are others where this is not necessarily present to the required level. There is concern within the vascular access community, judging from the results of national surveys, that some areas in the country are not getting the service they require. To improve on this, we need to enthuse colleagues and trainees around the country and demonstrate this field is not just about that heart-sink moment when you get a call at five o’clock on a Friday to de-clot a fistula or a graft, or just treat a simple fistula stenosis. Rather, it is an exciting area that poses many challenges that require prompt action and intervention to get the patient to their next dialysis session. Vascular access is also an area that allows you to build a rapport with patients through their regular visits to IR and become aware of their specific dialysis access circuit issues and requirements.
How does your work with VASBI affect your view of the field of vascular access?
It makes me realise that caring for dialysis patients is probably more multidisciplinary than other areas, with IR playing a vital role in not only maintaining and salvaging vascular access but, nowadays, creating it too. The fact that I interact frequently with colleagues in other specialties such as nephrology and surgery, provides a more holistic view of vascular access and makes me realise how important it is to read around the subject from all angles and keep up to date.
What are your goals as VASBI president?
What has been lacking from VASBI for many years is patient involvement, both in the society and the meetings. As we speak, we are developing a patient area on our website. This is a vital aspect to any society, and we are aiming for it to go live later this year. While it is still early in development, the concept is to provide patients with an easy-to-access and easy-to-use information database that includes all aspects of dialysis. This will be of huge benefit to both new and established dialysis patients. The website overall needs some maintenance and polish, and this is being looked at at present. Beyond this we want to attract more colleagues from around the country—and internationally too—to participate in the meetings and aim to offer more to membership such as focused one-day courses.
Are there any new technologies that you think will be especially effective in kidney care?
Artificial intelligence is coming into kidney care. Wearable devices to monitor dialysis access are a reality and the idea of artificial kidneys is fascinating—it is where science fiction meets medicine. With the tech boom progressing the way it has over the past 10–20 years, we may see some of these concepts pan out into reality sooner than we think. What we have to bear in mind is that a lot of kidney patients spend many hours, three or four days a week hooked up to a dialysis machine, so if technology can optimise or limit this in some fashion, it would be really effective for improving kidney care across the board.
What upcoming trial results in the space would you like to get a look at?
Beyond any specific trials, the drug-coated balloon space needs more work and understanding. While we know there is good evidence to support the use of certain drug-coated balloons in treating vascular access stenosis, there are other reports that are conflicting. There is a lot of evidence but it is very heterogeneous. To date, the main focus has been on paclitaxel, but at the Charing Cross Symposium last year there were results on sirolimus-coated balloon trials presented. It would be interesting and exciting to compare plain, paclitaxel and sirolimus balloons for the treatment of vascular access stenosis in a single trial.
How do you think the introduction of endovascular fistulas has impacted and will continue to impact dialysis care?
There is no doubt this is an exciting development with many benefits, but there are still so many unanswered questions, especially regarding realworld results outside of research studies. There is a lot of debate around patient selection, which is a vital consideration for improving results. Understanding which patients will benefit from endoAVF is key. We also have to think about how to deal with a dysfunctional endoAVF, as they
Current appointments: Consultant interventional radiologist, Queen Elizabeth Hospital Birmingham (QEHB), UK
Education:
1997: MBChB Leicester Medical School, UK
2002: MRCP (Member of Royal College of Physicians)
2005: FRCR (Fellow of Royal College of Radiologists)
2002–07: West Midlands Radiology training programme, UK
2007–08: Vascular IR Fellowship, VGH/UBC, Vancouver, Canada
Honours (selected):
2011–14: Lead for IR at QEHB
2014–17: Clinical Service Lead for Radiology, QEHB
2017–22: VASBI Treasurer
2022–24: VASBI President
2016: DeVA trial principal investigator (PI)
2016: EverlinQ EU trial, site co-investigator, QEHB
2022: WAVE Wrapsody trial PI
Profile 12 February 2023 – Issue 6
Fact file
Q&A
Illustration by: Andy Watt / NB Illustration
do require maintenance procedures, and the technical approach is very different to a standard surgical AVF (sAVF). Patient choice is a big consideration when patients become more aware of these more cosmetically acceptable fistulas created via a minimally invasive procedure. In the UK there is no lack of enthusiasm for endoAVF, but evidence on reinterventions is scarce and the device cost is prohibitive. Without a national tariff and National Institute for Health and Care Excellence (NICE) guidance, it is difficult to convince hospital administration of their value in the UK, and more robust health economics would help.

What are the fundamental questions you ask, and what is your philosophy as a physician, when you approach each patient?
If I am teaching a registrar, I encourage them to first of all gather as much information on a patient’s history as they can, even before they meet them—and not just imaging history, but also clinical notes and letters. Get a feel for the patient’s condition before you meet them. Focus on their current issues, but keep the whole
patient in the background. Communication is massive, irrespective of your specialty. Put the patient at ease and show them you are human too while still maintaining a gap—get the balance. I have conversations with patients during procedures, and it is easy to find something to talk about. Seeing as most of our patients are awake or under light sedation in IR, maintaining that line of communication during a procedure is particularly important to reduce their stress
levels. Constantly balance the risk and benefit of each action you take during a procedure.
What advice would you give to young physicians and students looking to focus on vascular access?
Whatever you do, do it to the best of your ability irrespective of your specialty. Stay up to date with the evidence. Be interested in your work and enjoy it, and this will reflect in the treatment of your patients. This is universal across medicine.
What are your interests outside of medicine?
I cycle (road and mountain bike) and hike all year round, and ski in the winter. I visit my native Wales as much as possible. When I can find the time, I tinker with my classic Ford.
What music is on your IR suite playlist ?
Anything from the 60s through the 90s of any genre is typical, particularly rock based. Even more esoteric and recent rock or blues-type stuff is there—if it is not met with too much objection from the staff.
Profile 13 Issue 6 – February 2023
“The drug-coated balloon space needs more work... There is a lot of evidence but it is very heterogenous.”
Steal syndrome solutions proposed amid assessment of ischaemia risks
VIETHsymposium (15–19 November, New York City, USA) has played host to a “mini-symposium” on the risk of steal syndrome and distal ischaemia posed by vascular access for haemodialysis. Moderated by John E Aruny (Dialysis Access Institute, Orangeburg, USA) and Clifford M Sales (Mount Sinai School of Medicine, Summit, USA), it saw prominent vascular access voices tackle the issue and propose means of mitigating it.
First to speak was William Jennings (University of Oklahoma School of Community Medicine, Tulsa, USA), who gave a presentation reviewing his published findings that even patients “at high risk of hand ischaemia” can have “a safe and functional arteriovenous fistula (AVF) established” for vascular access. Haemodialysis access-induced distal ischaemia (HAIDI) is a particular risk, he said, for individuals with peripheral vascular disease, diabetes, a history of any amputation, previous steal syndrome, females, and older patients, among others. Jennings set about outlining methods for minimising the risk of HAIDI, including “more (and more successful) distal radiocephalic AVFs” as well as proximal radial artery inflow. He noted too that “reports of percutaneous AVFs all note a very low incidence of HAIDI,” referencing the 2020 study by Alexandros Mallios (Hôpital Paris Saint-Joseph, Paris, France) et al on the
Ellipsys (Medtronic) system and the 2017 NEAT trial of WavelinQ (BD) published by Charmaine Lok (University of Toronto, Toronto, Canada) et al in the American Journal of Kidney Diseases (AJSN)
Following Jennings came Matthew J Dougherty (Pennsylvania Hospital, Philadelphia, USA), who explored strategies for managing steal syndrome and neuropathy related to dialysis access. Dougherty provided statistics on the prevalence of


steal, which affects 10–20% of dialysis patients. Of those, 4–6% require intervention, he said, while also noting that while neuropathy of various aetiologies was experienced by between 10 and 40% of dialysis patients, ischaemic monomelic neuropathy (IMN) affects fewer than 1%.
He differentiated the two conditions, noting that steal has a slower, less conspicuous onset than IMN which is “immediate.” Steal, he said, is associated more with vascular access at the distal brachial level, while IMN is almost exclusively associated with diabetes. Dougherty proposed an algorithm for the work-up and management of neuropathy and steal syndrome, with a diminished emphasis on the distal revascularisation and interval ligation (DRIL) procedure as the dominant option, which was shared by the panel.
Outlining treatment options, Dougherty pointed to ligation, which he described as “simple” and a way of restoring a patient’s baseline anatomy. Banding, meanwhile, he described as “a poor choice for low flow” and “less predictable” than alternative treatments, but said it was better for veins than prosthetics. For low-flow patients, he did suggest DRIL.
He also examined revision using distal inflow (RUDI) but said it shared problems with banding and that clinical data on the procedure were limited. He advocated perhaps most strongly for minimally invasive limited ligation endoluminal-assisted revision (MILLER) as a steal treatment, referring to Gregg Miller (American Access Care of Brooklyn, Brook-
Hypotension and AV access thrombosis: causation or just association?
Aisha Shaikh (Memorial Sloan Kettering Cancer Centre, New York, USA) has staked a claim that, though hypotension is “associated” with arteriovenous access (AV) thrombosis, it should be far from the only consideration in choosing an access modality. She did so while presenting at VEITHsymposium (15–19 November, New York, USA).


SHAIKH BEGAN BY DRAWING ATTENTION TO THE fact that chronic hypotension in ESKD patients is often caused by poor cardiac function, autonomic dysfunction or a combination of both. Chronic hypotension is associated with increased risk of AV access thrombosis, and AV access thrombosis in turn is associated with poor outcomes, Shaikh said. She stated that high AV access flow can lead to heart failure especially in the setting of poor myocardial reserve, which can in turn can lead to hypotension. Therefore, she argued, in patients with chronic hypotension it is peritoneal dialysis (PD) that is the preferred dialysis modality as it causes less blood pressure variability.
She stressed that it is nevertheless important to assess whether a patient is a candidate for PD—as well as whether they are a candidate for a kidney transplant. If they are, then their clinician must also “determine living donor availability and transplant wait-time”. All of these considerations must be taken into account when making modality decisions.
With all of this in mind, she reminded the audience of the three vascular access options for the chronically hypotensive ESKD patients who are not candidates for PD: an arteriovenous fistula (AVF), an arteriovenous graft
(AVG) or a central venous catheter (CVC). Functional AV fistulae carry lower risk of thrombosis and infection compared to AV grafts and CVCs.
Next, Shaikh discussed the findings of a study led by Tara I Chang (Stanford University, Palo Alto, USA) that investigated the association between intradialytic
lyn, USA) et al’s 2009 retrospective analysis study in Kidney International which described the “minimally invasive” procedure as “effective and durable.”
Yana Etkin (Zucker School of Medicine at Hofstra/Northwell, Hempstead, USA) followed this with her own presentation examining a modified banding technique as a treatment option for distal ischaemia. She distinguished first between high flow rate steals, adequate and low flow rate steals and severe ischaemia, all of which demand different treatments. Modified banding is only appropriate as a treatment for high flow rate steals, she said, echoing Dougherty.
She stated that overall banding is associated with a “high rate of failure” and complications. Drawing on a Journal of Vascular Surgery (JVS) study by Andrew E Leake (Vascular Surgery Associates of Richmond, Henrico, USA) et al from 2015, Etkin made the claim that banding could benefit from “intraoperative measurement of distal perfusion” as a “simple and effective adjunct” that could be easily performed, requiring no “special equipment or personnel.”
“HAIDI could lead to devastating complications including loss of digits or even limbs in a small group of patients,” Etkin said later to Renal Interventions. “We are continuing to improve our techniques to manage this challenging problem.”
The symposium explored a variety of treatments for steal and neuropathy, before a concluding presentation which diverged into vascular access haemorrhage.
hypertension and the risk of AV access thrombosis. In this study, intra-dialytic hypotension increased the risk of AVF thrombosis. Low predialysis and postdialysis systolic blood pressure were associated with increased risk of AVF and AVG thrombosis. Furthermore, patients in the higher quartiles of intradialytic hypotension were older, tended to use AVG more than AVF and were more likely to have heart disease.
She also alluded to another recent study by Mu-Yang Hsieh et al that showed an association between blood pressure variability and higher risk of AVF and AVG thrombosis. Although she said intra-dialytic hypotension, pre- and post-hypotension, as well as blood pressure variability, are all “associated” with increased risk of AV access thrombosis, she was careful to note that “association does not establish causation.” She insisted that, though it is “reasonable” to employ treatment of intra-dialytic hypotension and chronic hypotension for patients with recurrent AV thrombosis, such interventions have not been proven to lower the risk of AV access thrombosis.
In patients with heart failure and chronic hypotension, Shaikh described it as preferable to create a radial arterybased AV fistula. If a brachial artery-based AV fistula is created then AV fistula flow rate should be monitored and flow reduction must be considered if the flow rate exceeds 1.5 L/min. In patients who are at high risk of AV fistula failure, an AV graft is a reasonable AV access choice. In patients with poor life expectancy, a CVC can be used as a permanent vascular access.
Shaikh concluded by stressing that, “association between hypotension and AV access thrombosis… does not establish causation,” The final decision on AV access choice should not solely be based on presence of hypotension. Other factors, including “comorbidities, symptoms, frailty status, life expectancy and patient preference” should all be considered.
14 February 2023 – Issue 6 VEITHsymposium
“Even patients at high risk of hand ischaemia can have a safe and functional AVF established.”
William Jennings
William Jennings
Yana Etkin
Matthew J Dougherty
Aisha Shaikh
Most rejected donor kidneys found to be viable in new study
The “overwhelming majority” of previously-rejected deceased donor kidneys that have later been used for transplantation have been found viable by a new study published in Transplantation. According to its authors, the results suggest that more consideration should be given to high-risk donors for use in selected patients in need of a kidney transplant. The study focused on kidneys that were specifically rejected for donor or organ-related reasons (DORR).
Kidney transplantation has been found in numerous studies to be a more effective long-term procedure for kidney disease than dialysis in terms of both survival and quality of life, yet “there are concerns that some kidneys are discarded unnecessarily” each year by patients and clinicians who deem some to be high-risk. The uncertainty underpinning the decision of clinicians to reject some donor kidneys has previously been explored by David Howard (Emory University, Atlanta, USA) et al, but this study, led by Maria Ibrahim (Guy’s and St Thomas’ NHS Foundation Trust, London, UK), is the first outside of the USA to compare on a large scale the difference in outcomes between those who accept a higher-risk donor kidney and those who remain on the waiting list.
That distinction is crucial—the transplant community of the UK, where this study’s patients were enrolled, “implants kidneys from older, more marginal donors than the USA” while also offering chronic kidney disease (CKD) patients more kidneys from donation after circulatory death (DCD) donors. US kidney disease patients on the waitlist for a transplant reject a median of 16 offers, yet they have an eight-year cumulative mortality of 42%. UK patients, meanwhile, still reject over 40% of initial deceased donor kidney offers, but “the nation’s organ utilisation practices” remain “generally more aggressive than many other countries”. This makes it a particularly worthwhile
site for comparing outcomes for those who remain on the waitlist with those who accept a kidney they perceive as suboptimal, such as those from aged donors or those with comorbidities.
In the UK, kidneys declined for a named patient are either offered to another or entered into the UK Kidney Fast Track Scheme (KFTS), which is run by NHS Blood and Transplant (NHSBT). The study was performed “within NHSBT as a service evaluation project to monitor the national transplant programme” and included kidneys offered to named patients over the age of 18. Kidneys that were finally deemed nonviable were excluded, with only those that were eventually used in a single-kidney transplant accepted.
The kidneys came from donation after brain death (DBD) donors only. This study aimed to look at outcomes of both patients who declined deceased donor kidney offers and those who received the declined organ. Of patients who received a previously-rejected kidney, 1,718 were examined, while 2,805 patients who rejected a kidney and later received one were also included. Kidney quality was measured using the US Kidney Donor Risk Index (KDRI).
Outcomes for those implanted with a previously-rejected kidney included
“all-cause graft failure, death-censored graft survival (DCGS), and patient survival at one and five years post-transplant”. At one year after their transplant, 91% remained alive with a functioning graft with 4% dying, while 81% survived with a functioning graft at five years. Survival outcomes for those who rejected a transplant and eventually received a later one were “comparable”, and “4% of patients were either removed from the list or died while on the [waiting] list”.
In their discussion, the authors are keen to stress the point that improved outcomes were not found for those who rejected a kidney “despite waiting for an additional 174 days, on average, before being transplanted”. Waiting for a “better” offer did not then, they say, improve patient or graft survival, while “there may well be a quality-of-life advantage associated with early transplantation for many patients”. Accepting rather than rejecting a kidney would at the very least offer “six months of dialysis-free patient survival” to those on the waiting list.
It is noted that such advantages may be more pronounced under the UK system of kidney allocation, whereas in countries like the USA, where waiting times are typically longer, “the morbidity and mortality associated with remaining on the list may well be higher”. The patients in the study who did receive a previously-rejected organ had also been on the waiting list a median of 10 months longer—suggesting “they were more willing to accept kidneys perceived to be of higher risk”.
The study stratified its results by centre, with 23 examined. Of those, four demonstrated a statistically significantly higher rate of organ refusals, echoing the “disparity in risk-appetite” found in studies in the USA. However, these centres did not ultimately show significantly different rates of functioning in the subsequent use of declined kidneys. Ibrahim et al argue that this suggested that these centres “are no better at discriminating between higher- and lower- quality kidneys” than others. They also remark
Royal Free Hospital’s first day-case robotic nephrectomy complemented by remote monitoring
Ravi Barod (Royal Free Hospital, London, UK) performed the day-case procedure, which has previously been performed in the United States. The technology has been utilised for different forms of nephrectomy at the New Cross Hospital in Wolverhampton (UK). Barod spoke exclusively to Renal Interventions, diving into its outcome and the opportunities the technology presents for clinicians to perform effective non-invasive surgeries as day cases.

AROUND 450 NEPHRECTOMIES ARE PERFORMED each year at the Royal Free Hospital, Barod said. The pressures in the UK’s National Health Service (NHS) during the winter, as well as a desire “to improve the patient experience”, sparked Barod’s decision to try day-case robotic nephrectomy for the first time at the hospital, for select patients. He outlined how robotic surgery was the
most common type the hospital performed.
That team has also developed an “enhanced recovery programme” to accompany these surgeries, which reduced hospital stays from around five days with open surgery to around two days with robotics. “The natural progression of this,” Barod suggested, “was for some of those patients to go home and sleep in their own bed. We know that patients who are mobilised early and have a much quicker initial recovery after surgery then have a quicker return to their normal activity. The shorter you are in hospital, the quicker your recovery and return to normal.”
The surgery was performed on 26 November 2022 with no catheter and one Venflon (BD) cannula on a young adult male patient with very few other medical problems, besides a failed kidney. He also lived near to the Royal Free Hospital; Barod said that it was important “early on to select for patients with no comorbidities who have
that the similar survival of patients who rejected the deceased donor kidney offer and remained on the list compared to those who accepted a declined kidney marked a difference to US studies in the area, but that this may be explained by “longer waiting times for deceased donor kidney transplantation in the USA than in the UK” along with “comparatively higher rates of mortality on the list in the USA”.
The authors suggest that their study demonstrates a potential issue of needlessly discarded kidneys, though they also say it is important to note that each kidney offer required a highly individualised and complex decision-making process. They described too the “benefit of organ transplantation to the families of deceased donors” that is foregone when deceased donor kidneys are discarded. Existing risk stratification tools for patients and clinicians considering a transplant, meanwhile, are “not sufficiently accurate to inform patient-level decisions for organ acceptance or decline”, and organ-offering schemes need to be improved.
Patients were also included in the discussion. They needed “detailed education” on an “individualised” level, catered to those with various degrees of health literacy. The authors’ study itself, they suggest, may be useful in demonstrating that “selected kidneys can function well even when initially declined for donor- or organ-related reasons (DORRs)”.
Reviewing the study’s limitations, the authors point to the data’s lack of detailed explanation for each decline of an organ offer. It is also impossible to say, they add, whether the kidneys which eventually functioned well in one patient may have functioned equally as well in those who declined it. They also state that registry data cannot account for the “all-important quality of life advantages (or disadvantages) that may be involved in kidney transplantation.”
The issues around organ selection remain complex, Ibrahim et al conclude. Their study suggests the great majority of rejected kidneys declined for DORR in fact go on to be viable if used in transplantation, and “encourages the improved utilisation of organs perceived to be of higher risk”. They say it remains important still to judge each case on its specifics.
the ability to get back to the hospital within a short period of time in case we had any concerns.”
With the nephrectomy performed, he was “in and out of hospital within twelve hours,” after which Barod used a variety of remote monitoring tools after the surgery to maintain awareness of his condition. The patient was also able to keep track of his own electrocardiogram (ECG) readings and pulse rate, and was given the opportunity to ask Barod any questions via video call. Barod said that the most important use of remote monitoring technology, when combined with the ability to quickly get back in touch with their doctor, was to improve “patient confidence and motivation,” breaking the misplaced conviction among some patients that surgery had to be recovered from in hospital.
Distinguishing between nephrectomies for kidney failure and tumours, Barod stated that “there is no reason that [robotic nephrectomy] cannot be rolled out for patients with cancer,” but that it is more appropriate for cancers that “are not too complex to remove.” Comorbidities may also make the procedure inappropriate for some patients. Most of those who can undergo it, however, would likely be day cases, he said.
Issue 6 – February 2023 15 Transplantation
Ravi Barod
“Our study encourages the improved utilisation of organs perceived to be of higher risk.”
Early plan for “crash-landers” during tunnelled dialysis catheter placement crucial
The fourth annual Hamburg Dialysis Access Symposium (23–24 September, Hamburg, Germany) was recently organised and moderated by Robert Shahverdyan (Asklepios Clinic Barmbek, Hamburg, Germany), who also presented. He reports for Renal Interventions on the event, which also included a hands-on workshop including live transmission of three endovascular arteriovenous fistula (endoAVF) creation cases with the Ellipsys (Medtronic) and WavelinQ (BD) devices. He writes here on the most salient takeaways from the presentations.
This year’s symposium included speakers not only renowned in Germany but also internationally. The symposium was opened by a presentation from Maurizio Gallieni (University of Milan, Milan, Italy), who gave a talk on the importance of guidelines in dialysis access. He noted that there were guidelines available from several different societies, including the European Society for Vascular Access (ESVS) guidelines from 2018 and the updated Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines from 2019, but said that there were slight differences between them.
The available evidence in dialysis access in general is scarce, he said, especially with regards to the randomised controlled trials and number of patients included in the publications, and he advised everyone to collect and submit high quality data from their experience to related journals. One journal highly associated with dialysis access, is, of course, the Journal of Vascular Access (JVA), which is distinguished by a relatively fast review process.
Followed by several talks about the low incidence of home haemodialysis and relatively low incidence of peritoneal dialysis, Clemens Weinberg (Asklepios Clinic
Barmbek, Hamburg, Germany) talked about the incidence and prevalence of tunnelled dialysis catheters (TDC) in Hamburg, Germany. The key message he gave was that, even though around 50% of patients referred to dialysis access creation in Hamburg are end-stage kidney disease (ESKD) patients with an indwelling tunnelled dialysis catheter, having an early plan for “crash-landers” already at the time of the TDC placement is crucial: saving the veins, creating an early vascular access, starting early cannulations. These are vital to remove the TDC as soon as possible to reduce the unnecessary risk of catheter associated infections and central venous obstructions. In addition to that, Theodore Saad (Nephrology Associates, Newark, USA) talked about the implications of volume flow and long-term dialysis access on a patient’s heart. Whether the vascular access should be preserved or abandoned, or whether flow reduction should be performed after successful kidney transplant in ESKD patients, remains an open debate.
I was among those who spoke at the second session, which started with presentations about the role and importance of innovations in dialysis access such as the VasQ external support device (Laminate Medical), early cannulation grafts and endoAVFs. President of the Vascular Access Society, David Shemesh (Shaare Zedek Medical Center, Jerusalem, Israel), and Dominik Liebetrau (University Hospital Augsburg, Augsburg, Germany) also spoke, before a keynote lecture of the Symposium was presented by Julius Kunow (Diaverum Alter Teichweg, Hamburg, Germany). Talking about the challenges and difficulties of adapting endoAVFs for cannulations at his dialysis center, Kunow remarked that being open
to innovations, showing trust in vascular access surgeons in the choice of creating the best possible dialysis access for the patients, as well as the role of ultrasound-guided cannulations in the first stage of endoAVF cannulations, have lead to successful cannulations and more satisfied patients and clinicians.

Building on the previous presentation, one whole session was dedicated to the importance of the cannulations of arteriovenous fistulas (AVFs). Pascal Kopperschmidt (Fresenius Medical Care, Bad Homburg, Germany), himself a dialysis patient of decades, reported on his experience of buttonhole cannulations, the challenges associated with learning how to cannulate, and, mostly importantly, the hygienic perspective of avoiding the risk of infection.
Getting the right angle of cannulation for dialysis access, as well as routine use of point-of-care-ultrasound (POCUS) during cannulation, can reduce the risk of associated backward penetration, hematomas and eventually dialysis access failure, said experienced dialysis nurses Kathleen Rickert (Asklepios Clinic Barmbek, Hamburg, Germany) and Beate Spindler (Nephro Experts, Bad Homburg, Germany). Rickert stressed during the
post-presentation discussion that adopting ultrasound-guided cannulations in every dialysis unit should be the expectation and not the exception.
In the next session, I spoke on getting the right access for the right patient alongside nephrologist Haimanot Wasse (RUSH Medical College, Chicago, USA), and dialysis patient Stefanie Neuhäuser from Cologne, Germany. One of our key messages was that the patient’s decision should always be considered by a multidisciplinary team prior to any decision on dialysis access modality.
Finally, a whole session was dedicated to the maintenance of dialysis access dysfunction. Wasse presented again, this time on access dysfunction caused by cephalic arch stenosis. She examined the challenges of both endovascular and surgical treatments, their possible treatment algorithms, as well as tips and tricks on using balloons or stent grafts.
All presentations were followed by individual discussions and questions and answers. I found the symposium both educational and interactive for its more than 80 participants from Hamburg and across Germany. They were exposed to presentations on both conventional and innovative dialysis access modalities, while we also explored cannulation and the maintenance of several complex problems related to dialysis access. We look forward to our next symposium, on 8 and 9 September 2023.
Disclosures: Receipt of honoraria or consultation fees from BD, Bluegrass Vascular Technologies, Laminate Medical and Medtronic, participation in a company-sponsored speaker’s bureau: W L Gore, BrosMed Medical
February 2023 – Issue 6 16 Dialysis Access
“The patient’s viewpoint should always be considered by a multidisciplinary team prior to any decision on dialysis access modality.”
Robert Shahverdyan
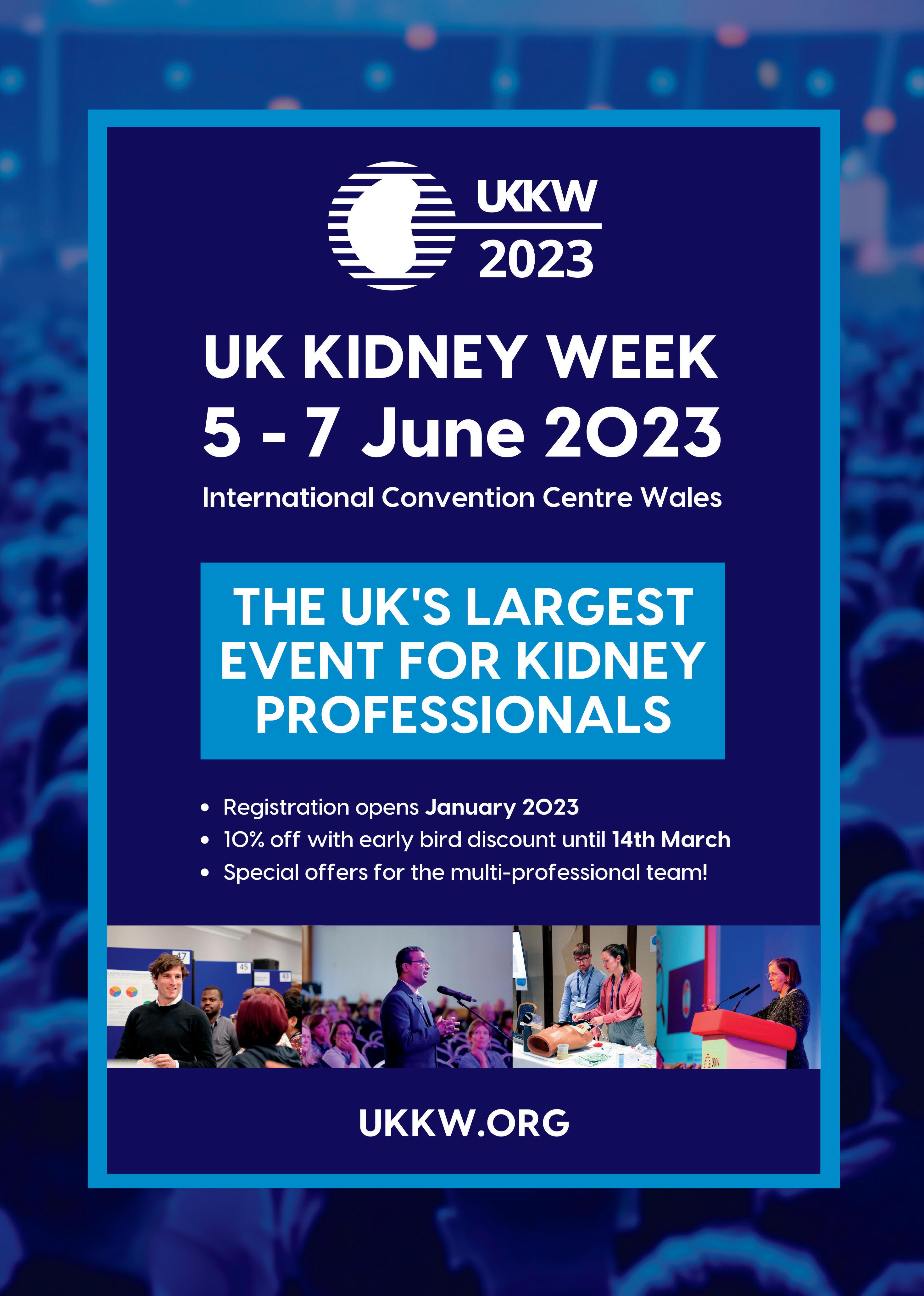
Miniaturised portable kidney device proposed to improve quality of life for dialysis patients
Buddy Ratner (University of Washington, Seattle, USA) has given a presentation on the prospect of miniaturised haemodialysis for chronic kidney disease (CKD) patients at VEITHsymposium (15–19 November, New York City, USA).
BEGINNING BY ASSESSING
the recent history of haemodialysis, he reminded his audience of the advances made in the world of dialysis between 1958 and 1962, including the landmark development by Belding H Scribner and Wayne Quinton of their Teflon Quinton-Scribner shunt. “Sixty years have passed since these pioneering efforts,” Ratner said, but followed this by asking of the years since: “Where is the progress?” Kidney dialysis today, he added, is “quite similar to what we were doing in 1960.”
More than four million people are on dialysis across the world, Ratner was keen to note. He pointed to the environmental impact of this treatment, noting that it used 129 billion litres of water as well as 770 million kWh of electricity per year globally, all while producing two million miles of PVC tubing waste. The “expensive, inconvenient” practice of in-clinic dialysis, Ratner suggested, could be supplanted by a wearable artificial kidney which would also improve quality of life for patients inconvenienced by clinic-based dialysis.
To help pioneer such an invention, Ratner and nephrologist Jonathan Himmelfarb (Universty of Washington, Seattle, USA) founded the Center for Dialysis Innovation, which aims to improve the quality of dialysis. Its solution to the problems Ratner diagnosed is the Ambulatory Kidney to Increase Vitality (AKTIV). Not only miniaturised and portable, it is also “greener, cost-effective [and] patient-centred,” Ratner said. Its firstgeneration is portable, fitting in a suitcase; the second is planned to be wearable.
Developing a miniaturised haemodialysis device to facilitate these innovations means “rethink[ing] every component of the haemodialysis system,” Ratner claimed, from the device’s “membranes” and “sensors” right up to its commercialisation. This has driven Ratner’s team to develop a novel solution to a number of the problems developing the device: photo-oxidation of urea. This, they argue, allows for far more water-efficient haemodialysis through its light-sensitive dialysis regeneration module.
The AKTIV also boasts “much improved blood compatibility” due to its “zwitterionic coating or a unique fluoropolymer coating,” Ratner claimed. He also detailed its AKTIV Connection system, which allows for “painless, safe blood access” without needles or even touch, with “integrated skin healing,” which he said will further help enable home dialysis.
Ratner concluded by hailing the reduced costs that would come with a wide rollout of such technology, while conceding that it remained a challenge to “get a university development to patients.” Nevertheless, he said, the inclusion of patients in the decision-making around AKTIV’s design and implementation would help it to fulfil the “promise” of kidney disease rehabilitation.

KDIGO clinical practice guideline update outlined
The Kidney Disease: Improving Global Outcomes (KDIGO) Work Group has issued a 2022 update to its 2020 guideline for the management of diabetes in chronic kidney disease (CKD). KDIGO, which develops and publishes guidelines, said the update was an endorsement of “a layered approach to care” integrating lifestyle changes and clinically proven “first-line pharmacotherapy” as the starting point for treatment.
Asynopsis of the update, led by Sankar Navaneethan (Baylor College of Medicine, Houston, USA), Sophia Zoungas (Monash University, Melbourne, Australia) and Kamlesh Khunti (University of Leicester, Leicester, UK) has been published in the Annals of Internal Medicine Basing the changes on a review of new evidence up to February 2022, the Work Group, co-chaired by Ian de Boer (Kidney Research Institue, Seattle, USA) and Peter Rossing (Steno Diabetes Center, Copenhagen, Denmark) encompassed “nephrologists, endocrinologists, cardiologists, primary care physicians, registered dietitians, and patients”. They employed the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system to assess the quality of the evidence and conclusions of a variety of studies, before using them to formulate graded recommendations and “consensus practice points”.

The evidence for the update was taken exclusively from randomised controlled trials. The “overall scope and systematic literature search for the update” have remained unchanged from the 2020 guideline, and it continues to address treatment of type 1 and type 2 diabetes, as well as CKD, kidney transplant, and both peritoneal and haemodialysis patients.
Primary among the change in recommendations is a renewed focus on employing a “holistic approach to patient care,” which includes “control of multiple risk factors” as well as a more “collaborative partnership among patients with CKD” from clinicians. There have been changes to the stage at which KDIGO recommends use of certain pharmacologic therapies, with SGLT2 inhibitors, in combination with metformin, now “the preferred first-line pharmacologic therapy for patients with type 2 diabetes and CKD”.
In the 2020 guideline, SGLT2 inhibitors were recommended for CKD patients with an estimated glomerular filtration rate (eGFR) of at least 30mL/min/1.73m2, while the update recommends them for those with and eGFR of 20mL/ min/1.73m2. This change is based on the findings of seven large trials “examining the cardiovascular and kidney effects of various SGLT2 inhibitors”, four of which “demonstrated benefits for cardiovascular events and kidney disease progression as a pre-specified secondary endpoint”.
with type 2 diabetes, eGFR ≥25mL/min/1.73m2, normal serum potassium, and albuminuria ≥30 mg/g [≥3mg/mmol].
The KDIGO Work Group supports starting each new treatment one at a time, adjusting for any resulting changes in a patient’s condition. They strongly advocate “ongoing monitoring” as “critical” to tracking these changes. Given the new therapies for CKD and limitation of cardiovascular disease burden, healthcare providers should, the guideline suggests, “focus on preserving kidney function and maintaining wellbeing rather than replacing kidney function”. Wide implementation of the new therapies for CKD and diabetes demands engagement from “health systems, payers, regulators, and life science industries” as well as patients, the Work Group states. Similar widespread action is also required for earlier detection of CKD.
Obstacles to such implementation are acknowledged by the guideline, which points to the high initial cost of the new treatments it includes. That cost is offset, the Work Group says, by the eventual savings provided by earlier and more effective treatment of CKD, limiting its later demands on healthcare providers. It may be more cost-effective “to implement new therapies while we await more data to support broader access” to them, while “team-based, integrated care focused on risk evaluation and patient empowerment” can help to improve quality of life for patients.

In its conclusion, the report directly tackles the issue of confusion caused by multiple sets of guidelines from various professional societies. The “appearance of inconsistency” it projects, say Navaneethan, Zoungas et al, is a “concern”, but one that KDIGO has addressed by partnering with the American Diabetes Association to issue “a consensus report on the diagnosis and management of diabetes and CKD”. In this report, the two societies together offer “aligned, evidence-based recommendations” while also alerting clinicians to the most “high-priority interventions” for each condition and addressing “CKD prevention, screening, and diagnosis”, which the KDIGO report does not.

Disclosures: Buddy Ratner is founder of both Kuleana Technology and Healionics
The second-line class of drug the guideline recommends for lowering glucose in type 2 diabetes and CKD patients who have not achieved individualised glycaemic targets despite the use of metformin and SGLT2i or those who are unable to use those medications, meanwhile, is GLP-1 RAs, which was justified with reference to the AMPLITUDE-O trial. Nonsteroidal mineralocorticoids (MRAs) are also recommended for patients
18 February 2023 – Issue 6 Guidline updates
Sankar Navaneethan
Kamlesh Khunti
Sophia Zoungas
Primary among the changes is a focus on a “holistic approach to patient care [including] control of multiple risk factors.”
Buddy Ratner
Cooler dialysate fails to cut major cardiovascular event or death, MyTEMP trial suggests
Haemodialysis has traditionally been conducted with dialysate of a temperature of 36.5°C, but the use of a personalised, lower-temperature dialysate is experiencing “rising popularity” with clinicians. Amit Garg (Western University, London, Canada) is corresponding author of the MyTEMP trial, an investigation into lower-temperature dialysate’s effectiveness, who recently presented at American Society of Nephrology (ASN) Kidney Week. The full results of the trial have now followed, published in The Lancet.

The study was performed across 84 haemodialysis centres across Ontario, Canada. Of these, half were assigned to use dialysate set to a standard temperature (36.5°C), while the other half used dialysate at a personalised lower temperature, 0.5–0.9°C cooler than the patient’s body temperature—as determined before the therapy—with a minimum temperature of 35.5°C.
In total, more than 15,000 patients’ outcomes were recorded by the study, making this the largest haemodialysis care study to date in terms of number of participants. The trial was not double-blind. Instead, the primary outcomes were collected as part of routine care “by medical coders who were unaware of the trial or the centres’ group assignment.”
The primary outcome after the four-year trial period was a composite one including “cardiovascular-related death or hospital admission with myocardial infarction, ischaemic stroke, or congestive heart failure.” The composite outcome occurred in 22.4% of patients in the standard temperature dialysate group and 21.4% in the cooler dialysate group—a finding which was not considered statistically significant. The team also found no significant difference in the average drop in systolic blood pressure during dialysis between the two groups, with “26.6 mm Hg in the cooler dialysate group and 27.1 mm Hg in the standard temperature group.”
The study authors concluded that “centrewide delivery of cooler dialysate” did not offer better outcomes to patients on the evidence they found. They said that the trend of increasing use of cooler dialysate may do little to prevent cardiovascular events, and that “the risks and benefits of cooler dialysate in some patient populations should be clarified in future trials.”
Speaking to Renal Interventions, Garg said that “what is remarkable about the MyTEMP trial is the tremendous support of our community and the methods we used. With this support we embedded the trial into existing healthcare at nearly all haemodialysis centres in Ontario, we were able to determine whether the intervention would improve outcomes in a real-world setting that represented all patients who receive haemodialysis in routine care. The trial was strongly supported by the Ontario Renal Network and helps realise the goal of a learning healthcare system.”
suggested incremental implementation did not change the risk of patient hospitalisation, while two randomised controlled trials suggested it decreased it, and one study suggested it increased it.

Haemodialysis (HD) is traditionally implemented in four-hour sessions, three times a week. The efficiency of this approach has been questioned, however, by the authors of a new study published in Nephrology Dialysis Transplantation. Led by Emma Caton (School of Life and Medical Sciences, Hatfield, UK), it looked at whether it benefitted end-stage kidney disease (ESKD) patients to have their dialysis sessions gradually increased in line with the progression of their condition.
HD PATIENTS OFTEN SHOW disproportionately high rates of mortality in the first few months of treatment, said the study authors. The prevailing style of HD implementation poses difficulty in adjusting to the treatment for patients, who “may benefit from a gentler start to dialysis.”
Incremental HD starts patients on lower doses tailored to the specific stage of their illness, measured in residual kidney function (RKF). This normally entails an initial reduction in sessional frequency from thrice to twice weekly. Not only does this offer “cost benefits for the healthcare service,” the study suggested, but it also “is likely to appeal to the HD popula-
tion,” who often prioritise “dialysis-free time” according to the Standardised Outcomes in Nephrology-Haemodialysis (SONG-HD) initiative.
The study was a retrospective meta-analysis of studies, drawing on existing research comparing incremental with traditional implementation, and looking at some 644 records. Its primary endpoint was mortality, while secondary endpoints included “treatment-emergent adverse events, loss of RKF, quality of life and cost effectiveness.”
There was no significant difference in mortality between the groups who experienced traditional or gradual HD implementation. Most studies examined
No significant differences in quality of life emerged. The authors were keen to note that the 44% reduction in individual dialysis sessions performed by participating hospitals compared with traditional implementation resulted in significant cost reduction. They pointed to a study by Vilar et al that indicated incremental HD could cause a more than 20% reduction in costs per patient per year.
There remain questions about incremental HD, the authors stated. The studies they reviewed included “patients [who] did not have fair or equal access to dialysis treatment and were initiated on less frequent HD as a result of financial pressures or a lack of adequate healthcare services.” This may have affected the find-
ings, while further limitations included the researchers’ exclusion of studies who did not report on mortality at all, instead only including data points on secondary endpoints. Nevertheless, the authors concluded, the review “lend[s] support to the safety of incremental HD as a treatment for ESKD.”
19 Issue 6 – February 2023 Dialysis Practice
ESKD patients “may benefit from a gentler start to dialysis”
44%
Reduction of individual dialysis sessions performed compared with traditional implementation
“This lends support to the safety of incremental haemodialysis as a treatment for ESKD.”
“The risks and benefits of cooler dialysate in some patient populations should be clarified in future trials.”
Emma Caton
Sugar may accelerate cyst growth in polycystic kidney disease patients
A new study in Nature Communications has associated sugar with the development of the cysts that characterise polycystic kidney disease (PKD), with implications for how the condition should be treated. Co-lead authors Sienna Li and Ramila Gulieva (University of Washington School of Medicine, Seattle, USA) performed the experiments, which concluded that glucose absorption “can mediate PKD cyst growth in human organoids”, which may influence the development of treatments.


PKD is an inherited disorder, usually through “heterozygous, loss-of-function mutation” in either of the genes PKD1 or PKD2. It results in the growth of cysts from the kidney, while the recently-approved therapeutic for the condition, Tolvaptan, is described by the study authors as having efficacy and safety limitations. This investigation builds on the conclusions of a study by Isaline Rowe et al (San Raffaele Scientific Institute, Milan, Italy) from 2013 which found that “defective glucose metabolism is intimately involved in the pathobiology” of PKD.
Li, Gulieva et al have developed kidney organoids as part of an in vitro human model in order to explore other treatments. In this study, the organoids were gene-edited to “strikingly recapitulate the genotype-phenotype correlation in PKD”.
To do this, they exposed such organoids “to fluid shear stress in a PKD-on-a-chip microphysiological system”, allowing for measurement of fluid flow, “which is difficult to assess in vivo” but is commonly associated with cystic expansion. This study examined how flow of glucose-rich fluid can modulate such development.
While they describe kidneys as “highly reabsorptive organs”, the authors note that it is in fact unclear whether PKD cysts absorb glucose
in particular. Flow of fluid rich in glucose, which the authors call “an abundant renal solute and transport cargo”, was measured using time-lapse imaging of “a fluorescent glucose analogue, NBD glucose”.
While the authors anticipated that fluid flow generally would exacerbate cyst development, they unexpectedly discovered that the cysts formed by absorbing glucose-rich fluid, rather than releasing fluid as was anticipated. In their discussion, they state that their findings “indicate that flow, volume, and solute concentrations are positive regulators of cyst expansion,” noting that it can be accelerated via “glucose transport”.
They describe glucose and “its transport into cyst structures” as “a driver of cystic expansion in proximal nephron-like structures”. “Absorption,” they conclude, “can mediate PKD cyst growth in human organoids”. Finally, they offer the suggestion that therapeutic treatments that may limit reabsorption of glucose could be “beneficial in reducing cyst growth in specific nephron segments”. Future studies into the mechanics of PKD, they say, may build on these findings.
New study examining UK Biobank data associates retinal age gap with ESKD
Patients likely to develop end-stage kidney disease (ESKD) may first exhibit ageing in the eye, a study in the American Journal of Kidney Disease (AJKD) has suggested. Retinal age gap, a measure which comprises retina-predicted age minus the patient’s actual age, was “significantly associated with incident ESKD,” said the study authors, led by Zhuoting Zhu (University of Melbourne, Melbourne, Australia).
THEY NOTED THAT PATIENTS WITH THE SAME chronological age could exhibit different biological ages, highlighting the “growing evidence showing the relationship between ageing biomarkers” and chronic kidney disease (CKD) and ESKD. Discovering markers that may indicate the onset of ESKD early may allow clinicians to make earlier interventions to prevent progression of the condition. The study authors stipulated that existing studies on the utility of biomarkers were sometimes limited by “cross-sectional designs and small sample sizes.” Their study sought to change that for the health of the retina, which “has long been considered as a window to
the kidney,” and to explore whether the retinal age gap could predict for ESKD.
The study utilised the data of the UK Biobank, which includes those of over 500,000 patients aged 40–69. Employing a deep learning model, they used fundus images of the eyes of 46,969 patients to predict their retinal age gap. Those patients’ ESKD status and diagnosis date were obtained from National Health Service (NHS) Digital. The follow-up period was from the date of fundus image acquisition to “the first occurrence of ESKD or lost to follow-up or death, whichever came the earliest.”
The results showed a statistically significant association between retinal age gap and ESKD occurrence. For each one-year increase in the retinal age gap, patients were 9% more likely to experience incident ESKD. There was also a notable difference in retinal age gap’s association with ESKD between male and female patients, with an 8 and 13% risk increase respectively with each one-year increase. A “trend of increasing association was noted with incident ESKD across different quartiles of retinal age gaps,” and those in the fourth quartile were at a significantly greater risk of ESKD compared to those
NEXTKIDNEY, A NETHERLANDS-BASED company that has developed the world’s first fully-portable haemodialysis device in the form of the NeoKidney, has raised €4.1 million in a new crowdfunding effort.

Carried out on the Oneplanetnow Dutch fundraising platform, and co-led by the Generous Minds initiative, the funding is a major step in the development of the device. Planned to utilise only four litres of fluid per dialysis session, the device promises chronic kidney disease (CKD) patients “more freedom and a significant improvement in quality of life”.
The portable dialysis project “stems from the initiative of the Dutch Kidney Foundation and health insurers CZ, ZilverenKruis and Menzis”. The company describe the device as being in “the final stages of development”, with a working prototype already complete. Safety testing went underway in Singapore in April 2022, while clinical trials will take place in 2023 in both France and The Netherlands.
“We are investing in the portable artificial kidney and its introduction into healthcare because we believe that the portable artificial kidney dramatically improves the lives of kidney patients,” Joep de Groot, CEO of CZ, said. “The portable artificial kidney also contributes to a reduction in healthcare costs, partly because it requires less deployment of scarce medical staff. Thereby, this unique dialysis machine helps to keep healthcare in The Netherlands widely acces-
in the first (p=0.002).
The study authors made the case in their discussion that retinal age gap is thus “a promising biomarker of future occurrence of ESKD independent of traditional risk factors.” They cited a Mendelian randomisation study into the link between ageing and kidney disease led by Sehoon Park (Seoul National University, Seoul, South Korea), stating that “telomere attrition was significantly associated with a higher risk of kidney function decline,” but made the case for retinal age gap as a biomarker, not least due to “its non-invasive nature, ease of calculation and accuracy.” Finally, they speculated about the mechanisms explaining the association, citing the retina and kidneys’ “common developmental pathway.” These included inflammation, endothelial dysfunction and oxidative stress. While previous studies, they said, have found retinal age gap an effective biomarker for “vascular stiffness and vascular ageing,” their study may pave the way for it to play a larger role—and increase the compliance rate—in kidney disease screening.
February 2023 – Issue 6 20 Latest Advances
Portable haemodialysis company raises €4.1m from crowdfunding
“Limiting reabsorption of glucose could be beneficial in reducing cyst growth.”
Ramila Gulieva
Sienna Li
“A promising biomarker of future ESKD [that is] noninvasive, with ease of calculation and accuracy.”
Nextkidney
IceCure releases preliminary data on ProSense cryoablation system
IceCure Medical, developer of the minimally-invasive ProSense System for cryoablation, which destroys tumours by freezing, has announced interim results from the ICESECRET study for the treatment of patients with small renal masses (SRM) who cannot be offered kidney-preserving surgery. Data were presented at the Urological Association Conference (14 December, Eilat, Israel). The presentation, titled “Renal Mass Cryoablation - Interim Analysis ICESECRET Study”, was delivered by Nasir Said (Bnai Zion Medical Center, Haifa, Israel).
According to the presentation, out of the 115 patients enrolled, 107 patients (112 lesions) returned for follow-up with a mean duration of 22.8 months and a range 12-60 months. In a subgroup of patients with no previous history of kidney cancer on the same kidney and a lesion ≤3cm, an 89.5% recurrencefree rate was observed at a mean follow-up time of 22.2 months when the procedure protocol was followed.
The recurrence-free rate was 85.1% for the 107 patients (91 patients, including 13 patients who underwent a second cryoablation), at a mean followup period of 16.5 months. Five serious adverse events were reported, four of which were of mild severity and were treated conservatively and resolved within one to five days, with one severe complication of a new onset of ipsilateral hydronephrosis seven months after the cryoablation procedure that led to nephrectomy.
Cryoablation time and hospitalisation time were relatively short, up to approximately 25 minutes and two days, respectively. The presentation concluded that, based on these interim results, cryoablation is safe and effective for treating renal masses under five centimetres.
Medtronic announces first patient enrolled in Expand URO trial for Hugo roboticassisted surgery
Medtronic has announced the first patient enrolled in the Expand URO US clinical trial for the Hugo roboticassisted surgery (RAS) system. The robotic-assisted prostatectomy procedure was performed by Michael R Abern (Duke University Hospital, Durham, USA) at Duke University Hospital in North Carolina, USA.
Minimally invasive surgery, including robotic-assisted surgery, offers fewer complications, shorter hospital stays, faster return to normal activities, and smaller scars. Urologic procedures are one of the most commonly performed with the assistance of a surgical robot. The Hugo RAS system is intended to be used in this study for urologic surgical procedures including radical prostatectomy, radical cystectomy, and nephrectomy (partial or radical) procedures at sites in the USA.
The Expand URO clinical trial is being conducted pursuant to an Investigational Device Exemption from
the US Food and Drug Administration (FDA). Up to 122 patients will be enrolled in the study at six sites in the US. The Hugo RAS system, combined with Touch Surgery Enterprise, purports to offer a “smart, digitally enabled surgical experience”. Outside the US, it is in use at hospitals across three continents in a range of procedures within urology, gynaecology, and general surgery.
A Medtronic press release detailed that the system is commercially available in certain geographies. Regulatory requirements and status in individual countries and regions will determine market availability of the Hugo RAS system and approved indications. In the USA, the Hugo RAS system is an investigational device not for sale.
Nephroflow as good as Transonic for measuring VA flow, finds JVA study

NephroFlow device is as effective for ultrasound dilution (UD) for vascular access (VA) as existing devices such as the Transonic VA flow measurement technology, according to a Spanish study comparing the two led by Jose L Merino (Hospital University del Henares, Madrid, Spain) and published in the Journal of Vascular Access (JVA). NephroFlow meets the standard set by Transonic and demanded by current Spanish guidelines for UD-based assessment of the complication risks associated with arteriovenous fistula (AVF) for haemodialysis (HD).
The study was conducted with 44 patients with a mean age of 67 ± 12 years who had been on VA for at least three consecutive months. Patients were studied on the second day of their HD if they received three or more sessions, or the first day of the week if they received two.
It was found that the mean flow for Transonic was 1222±805 ml/min while for NephroFlow it was 1252±975 ml/ min. The authors described this as a representing a result “comparable to the accepted gold standard method” for VA flow surveillance. They claim that, upon review of other studies, “there is no method with better evidence than classic UD methods for VA surveillance.” Other methods such as duplex ultrasonography (DUS), they argue, take longer to achieve a measurement, as suggested for DUS in the study of Karava et al. The “speed for measurement could be a favourable aspect of the NephroFlow method,” they added.
With all this considered, the authors maintained that “as far as we know, this is the first study comparing both methods [of UD assessment of VA].” They concluded by suggesting that the NephroFlow device “could be applied in the surveillance of VA in the detection of VA at risk, as recommended by the [Spanish] guidelines.”
Speaking exclusively to Renal Interventions, Merino supplemented this conclusion by saying that “we continue to use the device in our daily routine and its speed allows us
to optimise nursing times. Although several guidelines question the benefit of routine surveillance, the Spanish Multidisciplinary Group on Vascular Access (GEMAV) guidelines and we believe low-cost and easily applicable devices can improve vascular access survival.”
“Impressive” 12-month Flex vessel prep data presented at VEITHsymposium
VentureMed Group, a privately held medical device innovator in access management for arteriovenous (AV) fistulas and grafts and vessel preparation for interventional treatment of peripheral arterial disease (PAD), recently presented new data at the VEITHsymposium, (15–19 November, New York, USA). Overall, the data presented demonstrated that Flex vessel prep used prior to balloon angioplasty improves 12-month outcomes both in PAD and AV fistulas and grafts.
“AV Access management is a critical component of successfully treating AV patients over time,” said John Aruny (Dialysis Access Institute, Orangeburg, USA), primary investigator of the Flex Vessel Prep AV registry clinical study, the 12-month outcomes of which he presented at VEITH. “The FLEX AV Registry 12-month outcomes
Management programmes. The majority of patients were being treated by their primary care physician.
The study was conducted in collaboration with the Mount Sinai Health System’s Population Health Ambulatory Pharmacy and Condition Management programmes and included 1,686 patients seen by 75 providers at 20 clinical sites. The real-world evidence study demonstrated that patients with early-stage DKD and a high risk KidneyIntelX score received higher frequency of clinical management visits, introduction to guideline-recommended medications, and specialist referral for disease management compared to those who were identified as low- or intermediate-risk patients.
When evaluating new or modified prescriptions for hypertension at six months, both angiotension-convertingenzyme inhibitors and angiotensin receptor blockers achieved a greater than 20% change in patients with hypertension in the high risk group vs. the low risk group. Medication management for use of SGLT2 inhibitors was even more pronounced; 25% of patients in the high risk group received new SGLT2 inhibitor prescriptions vs. 7% in the low risk group, a 4.5fold increase. Thus, KidneyIntelX enabled physicians to take guidelinerecommended clinical actions in high risk, early stage (stage 1-3b) diabetic kidney disease patients. New referrals by risk group were 6% for low risk, 12% intermediate risk and 15% high risk.
Thulium fibre laser found to be clinically comparable to ‘gold-standard’ kidney stone treatment
shows that utilising Flex vessel prep provides more time between interventions and continues to excel in the very difficult cephalic arch lesions.”
The study was a single-arm, prospective study conducted in eight centres in the USA with 114 real world patients. The Flex AV Registry 12-month outcomes demonstrate sustained patency across most patients and particularly good results specifically in the cephalic arch, with no observed serious adverse events.
Renalytix share new data suggesting their KidneyIntelX bioprognostic test improves decision-making

Renalytix has announced the publication of new real-world evidence in Primary Care and Community Health demonstrating the company’s KidneyIntelX bioprognostic test resulted in changed clinical decision-making for patients in the early-stage of diabetic kidney disease (DKD) being cared for within the Mount Sinai Health System’s Population Health Ambulatory Pharmacy and Condition
The recently introduced thulium fibre laser (TFL) does not improve the clinical outcomes of laser treatment for urinary stones compared to the standard for laser stone therapy, reports a randomised trial in the Journal of Urology, an official journal of the American Urological Association (AUA).
Despite its theoretical technical advances, the new study shows TFL has no significant clinical advantage over a modern high-power pulsemodulated holmium-yttrium aluminium garnet (Ho:YAG) laser in ureteroscopic lithotripsy of stones. “Our findings suggest that either of these currently available laser systems can provide excellent clinical outcomes treating non-staghorn renal and ureteral calculi in skilled hands,” comments lead author Christopher R Haas (University of Wisconsin, Madison, USA).
Approved by the US Food and Drug Administration (FDA) in 2019, the TFL is a relatively new alternative to Ho:YAG energy for laser lithotripsy of urinary stones. The Ho:YAG laser has been the “gold standard” of care for laser lithotripsy since the 1990s.
In this minimally invasive procedure, laser energy is delivered through a fibre passed through a ureteroscope directly to the visualised stone to break up or “dust” stones into pieces small enough to pass down the ureter.
The results showed that the two lasers required similar time to break up stones into passable fragments of 1mm or less: an average of 19.9 minutes with the TFL and 21.4 minutes with the Ho:YAG laser. Haas et al concluded that the trial “suggests no significiant clinical advantage” for either technology.
Latest News 21 Clinical News Issue 6 – February 2023
John Aruny
Genetically-modified pig patent promises expansion of kidney xenotransplantation
Makana Therapeutics, a global leader in the field of xenotransplantation, was granted an important European patent that will catalyse xenotransplantation efforts abroad, the company has announced. Makana is working to solve the organ shortage crisis by making genetically modified pigs for use as organ donors for human recipients. The patent was granted on the TKO pig, or “Triple Knockout,” which is a combination of three xenoantigen gene knockouts in the pig that effectively camouflage the cross-species grafts from the human recipient’s immune system.
Makana has demonstrated compelling results in xenotransplantation. “Our knockout pigs combined with our advancements in immunosuppression and patient matching have resulted in the longest and most consistent preclinical survival data in the xenotransplantation field,” said Mark Platt, the company’s president and chief executive officer.
The Triple Knockout Pig was discovered in the lab of Joe Tector (University of Miami Medical School, Miami, USA), who is also the founder of Makana. “The Triple Knockout Pig has fundamentally changed the xenotransplantation field,” Platt said. “The organs from this animal have been shown to be an acceptable match to more than 30% of patients waiting for a kidney transplant, and likely more than 70% of patients can benefit from these organs with available pretransplant treatment.”
Makana is in talks with the US Food and Drug Administration (FDA) regarding next steps to conduct the first-ever human clinical trial in kidney transplant. This recent development will add to Makana’s portfolio of intellectual property, which they say “will help the company to serve patients in Europe who are in desperate need of a transplant”.
Lydus Medical announces US FDA clearance of microvascular anastomosis aid device

Lydus Medical has announced that its Vesseal device has received US Food and Drug Administration (FDA) 510(k) clearance. The Vesseal is a microvascular anastomosis suture deployment system, for standardised omnivessel anastomoses, enabling “simple, fast, safe, and effective procedures”.
Until now, microvascular anastomoses have been performed manually. Manual microanastomoses are time- and labour-intensive, require a long learning curve, a unique skill set and great surgical dexterity. The Vesseal is designed to mimic the skill set and dexterity needed to deliver quality patient care in microsurgical anastomoses. It is described as offering “simple, accurate, dependable and consistent results” through symmetrical placement of eight microsutures at the anastomosis site.
“FDA clearance of the Vesseal is a significant milestone both for innovation in microvascular anastomoses, and for Lydus Medical. It is common knowledge that there are large clinical unmet needs around microvascular anastomosis,” said Jessica Weiss, CEO of Lydus Medical. “Clinicians who used the Vesseal stated that it shows a significant advantage over the manual anastomosis and provides more consistency in the procedure. We believe that the Vesseal will support enhanced outcomes in microsurgical procedures, as well as improved patient care”.
Baxter restructures renal unit into independent company amid new strategy to increase innovation
Baxter International has announced a new strategic roadmap designed to accelerate innovation and improve its “operational effectiveness” and long-term performance. These changes include a plan to spin off the company’s Renal Care and Acute Therapies global business units into an independent, publicly traded company; a simplified commercial and manufacturing footprint to enhance underlying business performance; and further portfolio actions to improve Baxter’s capital structure, including a review of strategic alternatives for the BioPharma Solutions business.
The new kidney care company will benefit from its existing product portfolio and “robust service capabilities that support its therapies delivered in the home, clinics, and intensive care unit (ICU)”. As a standalone entity with its own investment priorities and enhanced management focus, the new kidney care company is intended to be better positioned to pursue growth opportunities and invest in innovation.
Over the past several years, Baxter has executed many initiatives to strengthen its ability to deliver on its vision to transform healthcare. To better achieve these goals, the company is working to finalise a new operating model that it will begin to implement in parallel with its planning for the proposed spinoff of the Renal Care and Acute Therapies businesses.
Digital dialysis device from liberDi receives FDA approval liberDi has announced that it has received regulatory clearance from the US Food and Drug Administration (FDA) for its digital dialysis clinic, which allows patients to perform dialysis at home or at the workplace, by themselves, monitored by their physician using the advanced telemedicine capabilities of the system.

liberDi CEO, Hezkiah Tsoory remarked, that “receiving FDA clearance for our state of the art digital dialysis clinic technology, is a huge achievement for liberDi. liberDi’s system is designed to provide these patients with ease of use, freedom of movement, automatic catheter connection flush technology and patient monitoring, while performing their daily dialysis activities from the comfort of their home or workplace”.
liberDi conducted two initial clinical studies to demonstrate the safety and effectiveness of the portable peritoneal dialysis system on patients requiring dialysis. For this, 42 subjects used the system for dialysis under the supervision of three medical centres in Israel. liberDi also performed a human factor validation study evaluating all user groups: people requiring dialysis and their caregivers, as well as healthcare professionals such as nephrologists and dialysis nurses. The study simulated a real-world environment and were said to prove that anyone can operate the system following a single 90-minute proper training session.
XORTX submits patent application for methods for early detection of kidney disease
XORTX Therapeutics, a late-stage clinical pharmaceutical company focused on developing innovative

requiring renal replacement therapy. Two genes are associated with ADPKD, PKD1 and PKD2, with mutation of PKD1 having a higher prevalence (85% of cases), an accelerated progression and more severe renal disease. Mutations are inherited in an autosomal dominant manner and display a vast spectrum of clinical disease severity depending on the inherited mutation and other factors, including age and sex.
EU Commission to propose delay to MDR implementation
Europe’s health commissioner, Stella Kyriakides, has announced that proposals to extend the transition period for the implementation of the European Union’s (EU) Medical Device Regulation (MDR) will be put forward in early 2023.
Kyriakides informed health ministers from the EU’s 27 Member States of the plan at a meeting of the Employment, Social Policy, Health and Consumer Affairs Council in Brussels on Friday (9 December), where the council members discussed the current status of the implementation of the MDR.
The regulation—which changes the way that medical devices are certified for use in the European market—first came into effect in 2021 with an initial three-year transition period, having been delayed by one year in 2020 due to the onset of the COVID-19 pandemic.
Concerns have been raised over the impact of the transition to the new regulatory regime, with the European Society of Cardiology (ESC) previously calling upon ministers to act to prevent a “shortfall of essential medical devices for cardiovascular patients”, which the Society warned could include diagnostic and ablation catheters and some stents.
“Patients rightly expect to have safe and high-quality medical devices,” Kyriakides told journalists at a press conference that followed the council meeting, where she acknowledged it is now a “crucial time” for the transition to the new rules. She described the policy shift as a response to global supply shortages of medical devices.
FDA grants Breakthrough Device Designation for RenalGuard AKI prevention technology
therapies to treat progressive kidney disease, has submitted a Patent Cooperation Treaty (PCT) patent application seeking international patent protection for the patent entitled “Compositions and Methods for Diagnosis, Treatment and Prevention of Kidney Disease”.
Recent discoveries at XORTX and by its independent research laboratories, suggests that certain individuals, most at risk for accelerated kidney disease progression, may be identified, diagnosed, and treated based upon a novel risk profile. This new patent application proposes proprietary diagnostic methods, and potential therapeutic approaches for personalising the medicines used to treat those most at risk of health consequences of aberrant purine metabolism in cystic kidney diseases.
Autosomal dominant polycystic kidney disease (ADPKD) is a genetically linked nephropathy and the fourth most common cause of kidney failure
CardioRenal Systems have announced that the US Food and Drug Administration (FDA) has granted Breakthrough Device Designation for its RenalGuard Therapy device for the prevention of Acute Kidney Injury (AKI) in patients at risk for Cardiac Surgery Associated AKI (CSA-AKI).
“The high prevalence of acute kidney injury in cardiac surgery today is a well-known risk. We look forward to building further clinical validation that RenalGuard Therapy can provide the solution to reduce the prevalence of CSA-AKI,” said Ilya Budik, CEO of CardioRenal Systems.
The FDA’s Breakthrough Device Designation is a federally legislated programme is designed to expedite the review process and to facilitate the clinical trial development of devices that treat life-threatening conditions or irreversibly debilitating human disease or conditions. Budik commented that “we are looking forward to the initiation of the upcoming US pivotal study”.
Latest News 22 February 2023 – Issue 6
Industry News
Lydus Medical Vesseal
liberDi Intellgient Dialysis Assistant (IDA)
Conference Calendar
17–19 February
American Society of Diagnostic and Interventional Nephrology (ASDIN) 19th Annual Scientific Meeting Orlando, USA asdin.org/mpage/19thannual
01–03 March
British Transplantation Society (BTS)NHS Blood and Transplant (NHSBT) Joint Congress Edinburgh, UK bts.org.uk/events-meetings/bts-nhsbt-jointcongress-2023
04–09 March
Society of Interventional Radiology (SIR) 48th Annual Scientific Meeting Phoenix, USA www.sirmeeting.org
Meet our editorial board
Nicholas Inston
Chairman of the Editorial Board
Nicholas Inston is a transplant and vascular access surgeon, and the clinical service lead for renal surgery, at Queen Elizabeth Hospital in Birmingham, UK.





30 March–02 April





World Congress of Nephrology (WCN’23) Bangkok, Thailand theisn.org/wcn
11–15 April
National Kidney Foundation (NKF) Spring Clinical Meetings Austin, USA kidney.org/spring-clinical
25–28 April
Charing Cross (CX) Symposium 2023 London, UK cxsymposium.com
26–29 April
13th International Congress of the Vascular Access Society (VAS) Porto, Portugal vas2023.com

07–10 May
American Nephrology Nurses Association (ANNA) National Symposium Palm Springs, USA annanurse.org/events/2023-national-symposium
19–21 May
Vascular Access Society of the America (VASA) Hands-On Practicum on Hemodialysis Access Houston, USA vasamd.org/events/2023-practicum
Ziv Haskal Board Member

Ziv Haskal is a professor of radiology, and an interventional radiologist and interventional oncologist, at the University of Virginia School of Medicine in Charlottesville, USA.

Stephen Hohmann
Board Member
Stephen Hohmann is a vascular and general surgeon at the Texas Vascular Associates clinic in Dallas, USA.

Robert Jones
Board Member
Robert Jones is an interventional radiologist at Queen Elizabeth Hospital in Birmingham, UK.

Issue 6 – February 2023 23 Upcoming conferences *Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the field of renal disease management Editorially independent Subscribe today Available in print and digital formats and through our social channels Visit renalinterventions.net and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** this issue: Wrapsody results dialysis care the spotlight and the American Society of Nephrology (ASN) have jointly released report outlinNKF-ASN Task Force on Reassessing the the new estimated glomerular ltration creatinine equation that estimates kidney T patients and family members, medical students and other this new approach as rapidly possible so that we can creatinine equation without the race variable, the task the USA, more than million adults have kidney “unacceptable” health disparities and inequities healthasserting that race modi ers Bioarti cial device receives KidneyX award after reaching preclinical testing kidney device (iBAK) has moved closer oration led by Shuvo Roy (University tested the two essential components kidney functions, to provide continuous renal replacement cial Kidney Prize—becoming one six “The NKF and ASN urge all laboratories and healthcare systems nationwide to adopt this new approach as rapidly as possible so that we can move diagnosing kidney diseases that is independent of race.” Paul Palevsky Renal community reckons with removal of race variable in kidney disease diagnosis