2 Guest Editorial The Golden Larva Syndrome: Is it real?
4 Comment & Analysis Congress considers incremental steps towards Medicare payment reform


2,300

7 Presidential Address From rural America to the vanguard of a revolutionary surgical specialty
13 Vascular Leaders SVS honors two vascular surgeons with Lifetime Achievement Award




See page 6
By Beth Bales

JULY 2023 Volume 19 Number 07
this issue:
THE OFFICIAL NEWSPAPER OF THE ascularV pecialists CHANGE SERVICE REQUESTED 9400 W. Higgins Road, Suite 315 Rosemont, IL 60018 Presorted Standard U.S. Postage PAID Permit No. 384 Lebanon Jct. KY
In
www.vascularspecialistonline.com
numbers are in: VAM 2023 adds up to another SVS classic
The
SAVE THE DATE
nearly 1,400
the needle with program
slew of new
agenda. 23 VAM REVIEW EDITION
Landmark meeting (June 14-17) with
vascular professionals moves
innovations,
science and jam-packed
total
Nearly
attendees
GUEST EDITORIAL
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William
Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek
MD, RPVI, FACS | Professor Hans-

Henning Eckstein, MD | John F. Eidt, MD
| Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS
| Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray
L. Shames, MD | Niten Singh, MD | Frank
J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Director of Marketing & Communications Bill Maloney
Managing Editor SVS Beth Bales
Marketing & Social Media Manager
Kristin Crowe
Communications Specialist
Marlén Gomez
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Roger Greenhalgh
Content Director Urmila Kerslake
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution Jocelyn Hudson, Will Date, Marni Davimes, Clare Tierney, Éva Malpass and Benjamin Roche
Design Terry Hawes and Wes Mitchell
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. | The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | POSTMASTER: Send changes of address (with old mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. | Printed by Vomela
Commercial Group ©Copyright 2023 by the Society for Vascular Surgery
Failure is part of the process that leads to success. Occasional failures may sting but we must recognize the adage that failure is a “bruise, not a tattoo.”
Iknew a mid-career faculty member some years ago who was rapidly progressing up the leadership ladder until they were not. There were no apparent personal or health issues, or any other roadblocks, but gradually, over a period of six to 12 months, the brakes went on. There were some inexplicable decisions, beyond just humility or caution, which made me wonder if professional advancement was even a priority.
My experience with a few underachieving physicians has been more in the academic sphere than the private-practice world. Although there were some private practitioners who wished to climb the administrative ladder, most were focused on patient care, some academic work, and activities outside work.
Academic physicians have specific targets, such as promotion, climbing the administrative ladder, and moving up the national and international specialty society hierarchy. These steps are linked with financial rewards and professional recognition. The behavior of underachieving, resulting in a failure to advance, is seen in many professions, including sports and business, and is said to be part of the “Golden Larva syndrome.”
The Golden Larva syndrome: Is it real?
Suzanne Imes in professional women.2 They initially described women as feeling like frauds and lacking confidence, but later determined that the syndrome occurred in both sexes equally. People with imposter syndrome doubt their abilities, don’t like attention, feel unworthy or less deserving of any success, and give credit to factors other than themselves. Success may also be avoided because one feels unfit or fearful of being under the spotlight in society and taking the place of more deserving people. Some consider this is “success phobia,” part of an ever-increasing number of phobias. There is no joy if and when success does come. Psychologists say that the syndrome is not a medical diagnosis but viewed as “cognitive distortions,” or biased on irrational thoughts and beliefs that we choose to self-reinforce over time.2 There are some who think that imposter syndrome is an excuse to cover up systemic failures. Ruchika Tulshiyan and Jodi-Ann Burey believe it is a result of bias and exclusion, and that women especially are made to feel that it is a lack of self-confidence that causes them to fail rather than system or organizational issues.3
By Bhagwan Satiani, MD
Robert F. Kennedy is supposed to have said, “Only those who dare to fail greatly can ever achieve greatly.” In a business, entrepreneurial and leadership context, failing is part of the process that leads to success. Famous founders of companies like Google and Apple are cited. New, successful writers are a good example. They ask themselves, “Can I succeed again?” And fear failure. Similarly, the fearful leader may freeze and be unable to make any decisions. Carried to an extreme, an irrational fear of failure or atychiphobia occurs often in perfectionists. Fear of failure can sometimes be crippling. Paulo Coelho, the writer, is reputed to have said: “There is only one thing that makes a dream impossible to achieve: the fear of failure.” If enough self-doubt creeps in, most will either not attempt a “stretch” goal, or, if they do, they make it known that their expectations are low.
Self-doubt is common before we develop enough self-awareness and discover our own capabilities. However, achievements are not always under our control. In my case, I know that there were some events beyond my control, such as timing, bias, or cultural upbringing, where boasting about accomplishments was considered gauche. My deliberate choice of family time versus work and travel was also a factor. It was never a fear of failure. Later, there were health issues that would have prevented me from being competitive and successful, but I wonder if there was, at times, a touch of the Golden Larva syndrome.
The behavioral hodgepodge of underachievement, negative thinking, sometimes self-sabotage, fear of failing, or even fear of success, falls under the Golden Larva syndrome. Educator and psychoanalyst Manfred Kets de Vries describes one extreme when there is selfsabotage as being akin to a caterpillar that does not fulfill its potential, and therefore fails to flourish into a butterfly. People possess the promise of a bright future, but get in their own way and hinder their ability to thrive. Hence, the term Golden Larva syndrome. This includes manifestations such as imposter syndrome and Peter Pan syndrome.
Imposter syndrome is the most wellknown and was first described in 1978 by psychologists Pauline Rose Clance and
Another reason why some may selfsabotage is a reluctance to grow up and take on responsibilities, otherwise known as Peter Pan syndrome. Dan Kiley described this phenomenon in his book, The Peter Pan Syndrome: Men Who Have Never Grown Up. This is also not a medical diagnosis, but a term psychologists use to describe adults, most often males, who decline to shoulder responsibilities and are unable to have healthy personal relationships. In another book, Men Who Never Grow Up, Dan Kiley describes these men as unable to “grow up.” Other traits include a fear of loneliness, a tendency of being self-centered or narcissistic, and impulsive behavior.
As surgeons, we sometime fail even after performing a “perfect” operation, and although cumulatively these failures take a toll, few of us feel like failures ourselves and stop helping our patients.4 In a clinical context, I know I have had, at one time or another, a fear of failing but in the context of causing harm to patients. We fight through this. We have faith in our training and experience. But the most valuable asset we have are the people around us who believe in us and our abilities, at home and work.
Given a difficult surgical problem, we have the luxury of leaning on colleagues and members of our society to seek other opinions. I have never had anyone refuse to assist me or decline a call for help when I needed another opinion. Nor have I ever declined to help, including desperate calls from the operating room. This is another reason why we can reach out to members of our society, as extended family, to give our patients the very best care that they deserve. Occasional failures do sting, but family, faith, friends, work-related teams and, yes, our colleagues are powerful antidotes. As the poet and writer John Sinclair said: “Failure is a bruise, not a tattoo.” Healers need other healers to take care of each other. We should try this more often.
Occasional failures do sting, but family, faith, friends, work-related teams and, yes, our colleagues are powerful antidotes
References
1. De Vries KMFR. Breaking the Cycle of Self-Sabotage: How to Overcome the “Golden Larva Syndrome.” https:// knowledge.insead.edu/career/breaking-cycle-self-sabotagehow-overcome-golden-larva-syndrome
Saymeh A. What is imposter syndrome? Learn what it is and 10 ways to cope. https://www.betterup.com/blog/what-is-impostersyndrome-and-how-to-avoid-it#:~:text=Imposter%20syndrome%20 is%20the%20condition,phony%22%20and%20doubting%20 their%20abilities
3. Tulshyan R, Burey JA. Stop Telling Women They Have Imposter Syndrome. https://hbr.org/2021/02/ stop-telling-women-they-have-impostersyndrome?ref=charterworks.com
2
Vascular Specialist | July 2023
AMNIOFIX® and AMNIOEFFECT®: Placental-based sheet allografts provide a protective barrier to support the healing cascade and the development of granulation tissue.


AXIOFILL®: Acellular human placental ECM particulate used in the replacement or supplementation of damaged or inadequate integumental tissue.

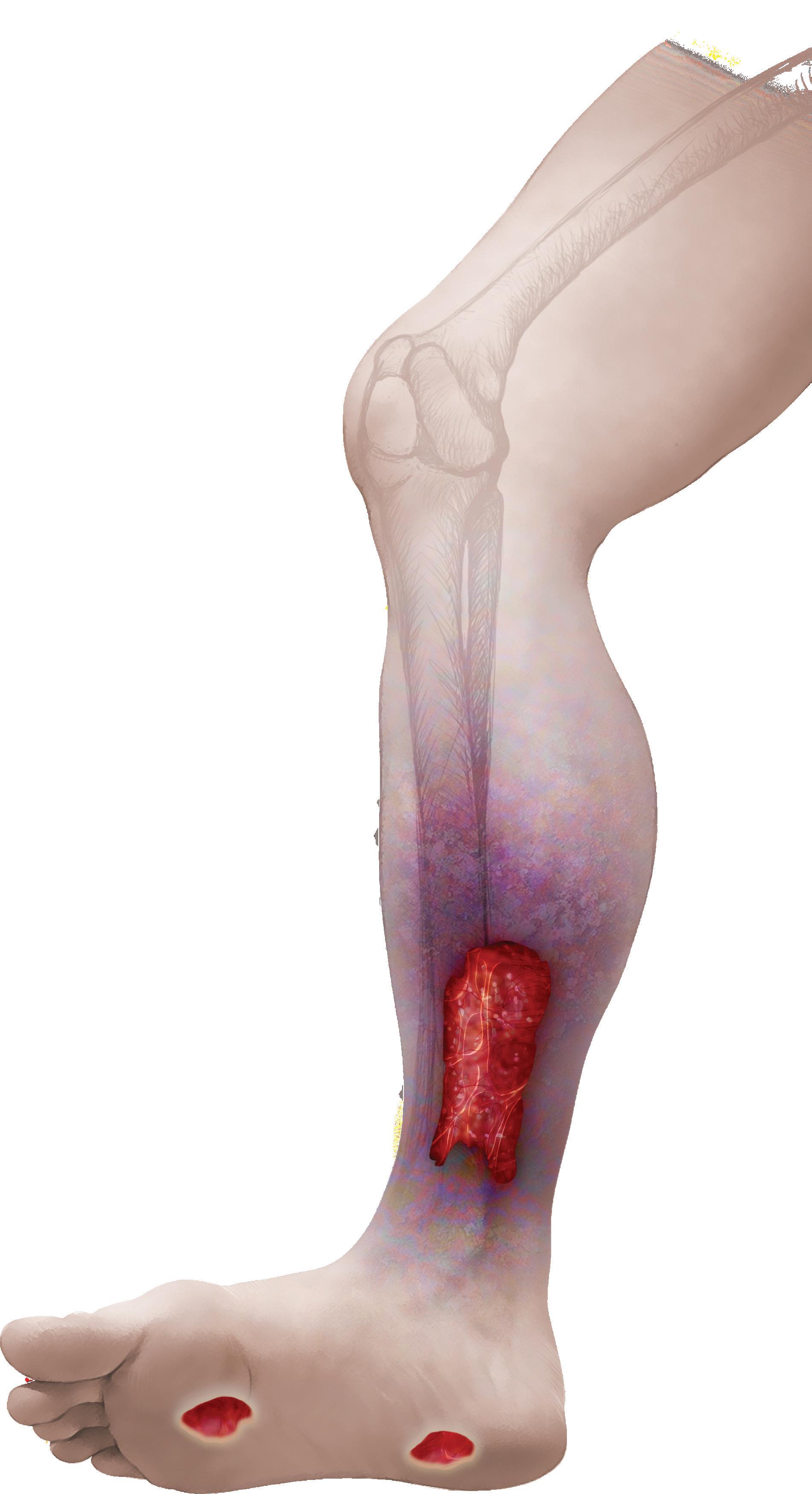
RCT Outcomes with DHACM Scan to learn more or contact us: 888.543.1917 customerservice@mimedx.com DHACM = Dehydrated Amnion/Chorion Membrane, DFU = Diabetic Foot Ulcer, VLU = Venous Leg Ulcer, SOC = Standard of Care * 2x = based on mean time and 3.8x = based on median time, ^ Per Protocol group VLUs DFUs defect closure vs. SOC at 16 weeks3,4^ 1.6x rate of
2x to 3.8x faster defect closure vs. SOC1,2* Patents and patents pending see: www.mimedx.com/patents. AMNIOFIX, AMNIOEFFECT, AXIOFILL, and MIMEDX are trademarks of MIMEDX Group, Inc. ©2023 MIMEDX Group, Inc. All Rights Reserved. www.mimedx.com US-AC-2300002 v1.0 REFERENCES: 1. Zelen CM, et al. Int Wound J. 2013;10(5):502-507. 2. Zelen CM, et al. Int Wound J. 2015;12(6):724-732. 3. Bianchi C, et al. Int Wound J. 2018;15(1):114-122. 4. Bianchi C, et al. Int Wound J. 2019;16(3):761-767. THINK ASAP. Before
defects lead to amputation, Advanced Surgical Allograft Products
limb
ADVICE FROM A SEASONED NURSE PRACTITIONER TO VASCULAR SURGERY INTERNS
By Rachel Scheich, NP
YOU’VE MADE IT THROUGH medical school and now you’re a new doctor on the wards! As you enter this new chapter in your life, I have some advice to share from more than 20 years of observing new doctors as they enter their intern year.
I share in the hope that it improves the next year of your lives as vascular interns. Here are my top-10 tips to improve your internship.
1) Be present in the patient’s room: You
probably already know this, but once that pager starts going it can be overwhelming at times to remember this. In addition, you learn so much from the patient and their family, and find out what’s most important to them and what their goals of care can be. The best interns I’ve observed build this rapport with the patients, making for a true therapeutic alliance.
2) Always check the patient’s pupil and pulse exams yourself—even immediately postop. Sometimes, you’re the only continuous eye on the patient over multiple staff shift changes. You will never regret having a baseline in case something changes. In addition, this may help to save you a phone call to a senior in the middle of the night.
3) If a nurse comes to you with a concern, always go evaluate the patient. You will earn their respect and may just identify a problem earlier. “Care from the chair” is never as effective.
4) Work with others as part of a team! Remember that it is called a “team”
GOVERNMENT GRAND ROUNDS
payment reform
By Jill Rathbun
THERE IS NO DOUBT THAT THE MEDICARE payment system needs reform. At this moment, the SVS is aiming to inspire reform through all facets of effective advocacy. This takes place incrementally by raising Congressional awareness of the issues that physicians face.

Following its enactment in 2015, Congress has not conducted rigorous oversight of the implementation of the Medicare Access and CHIP Reauthorization Act (MACRA) law. But that changed this summer with the Energy and Commerce Committee Subcommittee on Oversight and Investigations convening a hearing in June titled “MACRA Checkup: Assessing Implementation and the Challenges that Remain for Patients and Doctors.” The hearing’s intent was to give members of Congress the opportunity to hear from experts, evaluate the implementation of the law and better understand what challenges remain.
In addition, Congressional committees with jurisdiction over healthcare matters are conducting hearings to examine the drivers of escalating healthcare costs, including consolidation and price transparency. The House Energy and Commerce, and Ways and Means committees, and the Senate Finance Committee, have held hearings on healthcare system consolidation resulting from hospital mergers, and corporate and private equity acquisition of independent physician practices. Witnesses have discussed how this practice of consolidation has
because it is just that. No one member in the group is more important than another. Each provider brings something special to the patient’s care.
5) Never be afraid to take a concern up the appropriate chain of command, because it just may improve a patient outcome. As always, the patient comes first. The best interns I’ve worked with over the years always ask, “What’s best for the patient in this situation?”
6) Sometimes, with patient care, it’s the little things. For example, consider returning to a patient’s bedside to see if one of your interventions worked. You would be surprised how much the patient values their doctor talking to them and giving them their time.
7) Always know your patient’s IV access when you take over their care. That way when a problem arrives you will be able to safely intervene. (This also could be said for confirming that you have a current type and screen.)
8) Always remain approachable. This,
demonstrated increased healthcare spending without corresponding improvements in quality of care.
Inadequate physician payments and the instability of the Medicare physician fee schedule are factors that have led to health system consolidation. For some independent physician practices, an employment arrangement through merger with a hospital system is the only viable financial option to remain in business.
There are many flaws in the Medicare physician fee schedule that need to be addressed so physicians receive predictable, sustainable payment. While solving these issues will necessitate a broad approach to physician payment reform, the SVS has led the Clinical Labor Coalition to advocate for the introduction of legislation providing payment relief to clinicians who provide specialty care using high-cost supplies and equipment in community-based independent practices.
The Providing Relief and Stability for Medicare Patients Act (H.R. 3674), introduced by Reps. Gus Bilirakis (R-12FL), Tony Cardenas (D- 29-CA), Greg Murphy (R-3-NC) and Danny Davis (D-7-IL), mitigates the reduction in payments for office-based specialty procedures due to budget neutrality and the update in clinical labor costs that the Centers for Medicare & Medicaid Services (CMS) began in 2022 and is phasing in over a four-year period.
H.R. 3674 will provide two years of targeted relief for specialist providers who have been most adversely affected by the update of the clinical labor costs by increasing the non-facility practice expense relative value units (PE
of course, is easier said than done, particularly after a long and busy shift. However, this effort is not wasted.
9) Trust but verify. Lots of information can pass through providers every day, but unless you have seen something with your own eyes, you cannot speak your truth. Information can easily get lost in translation.
10) Don’t let any job in the hospital be beneath you. Always remember that these are patients we care for, and sometimes the task at hand is not appealing. Try to place yourself or a loved one in their situation. This can help you develop your empathy and compassion for your patients.
Lastly, welcome to the field of vascular surgery. You have chosen a career that gives you the opportunity to change the lives of your patients. This will be a whirlwind of a year, but it will be worth it.
The clinical and personal growth I have seen after intern year is incredible!
RACHEL SCHEICH is a vascular surgery nurse practitioner at the University of Michigan.

RVUs) for those procedures performed in an office-based setting that need an expensive medical device or piece of medical equipment.
Although the SVS continues to pursue systemic physician payment reform, passage of H.R. 3674 will provide some modest relief from payment cuts that are eroding patient access to vascular care and the viability of the community-based vascular practice. This seemingly small step is a crucial piece of an effort to influence massive reform of how healthcare is funded at the federal level.
These efforts over time can help raise awareness of the issues our specialty and physicians face, and along the way inspire reform to a more sustainable and competitive system.
For more information on how the SVS inspires reform at the federal level, visit vascular.org/advocacy or contact svsadvocacy@vascularsociety.org
COMMENT& ANALYSIS CORNER STITCH 4 Vascular Specialist | July 2023
“There are many flaws in the Medicare physician fee schedule that need to be addressed so physicians receive predictable, sustainable payment”
JILL RATHBUN is a member of the SVS Washington, D.C., office.
Congress considers incremental steps towards Medicare
VAM 2024
This call for proposals is not the same as the call for scientific abstracts. That submission process will open in November.
The SVS Postgraduate Education Committee (PGEC) reviews and selects topics from among those submitted. Members then will work with the submitters to develop and flesh out the content. Notifications of further development will be made by the end of September.
Proposals will be accepted only through the online submission site; the PGEC will not review text documents submitted via email.
Those who have ideas for sessions they’d like to see covered at VAM should consider: What is the educational need the proposal is attempting to address? What are the goals of the proposal/session? Can an “innovative” format be utilized (such as a call for cases or engagement via social media)? What would the program outline look like? What topics and suggested speakers would be included?

Representatives of the Society’s special membership sections (Community Practice, the Subsection on Outpatient and Office Vascular Care [SOOVC], Women’s and Young Surgeons) do not need to submit proposals. Each section will have a committee member assigned to co-moderate each session.
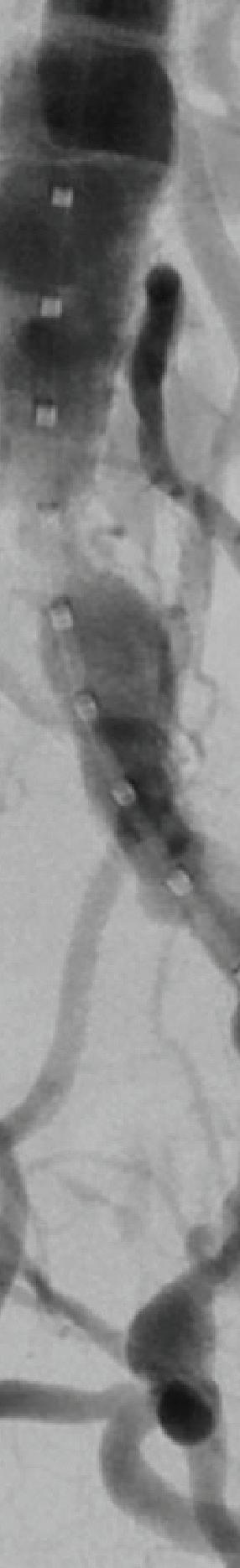
BEST-CLI LOOMS LARGE OVER VAM 2023 PROGRAM
The landmark BEST-CLI randomized-controlled trial (RCT) was featured in multiple scientific and invited sessions dotted across the program in National Harbor.

Two of the headline points of interest—the inaugural Frank J. Veith Distinguished Lecture and a session dedicated to debate and analysis of both BEST-CLI and BASIL-2, another landmark RCT looking at chronic limbthreatening ischemia patients— saw attendees flock to the main plenary hall for a series of talks around the hot topic.
With the curtain down on VAM 2023, another is already rising for VAM 2024. Proposals for educational sessions for the 2024 meeting, June 19–22, 2024, in Chicago, can be submitted from July 26–Aug. 23. These sessions cover both clinical and non-clinical topics. VAM 2023 included 21 educational sessions, covering a range of topics, from planning for retirement, advocacy, embolization tips and tricks, managing acute limb ischemia and optimizing vascular reconstruction in oncology, to how to develop a successful clinical research program to improve patient care.



Submission guidelines will be released in midJuly, and more information on the process will be publicized online and in Pulse, the SVS’ weekly electronic newsletter. —Beth Bales
During the Veith lecture, BEST-CLI lead investigators Alik Farber, MD, and Matthew Menard, MD, struck a conciliatory tone as they laid bare the blood, sweat and tears shed on their journey to complete the study. “We hope our story encourages others to pursue their research ambitions, even in the face of obstacles, self-doubt and judgment of others,” Farber told VAM.
“Turf battles in the vascular community have been, and still are distracting, destructive,
highly counter-productive and of very little service to our patients,” added Menard.
During the session addressing both BEST-CLI and BASIL-2 together, Farber and Menard reiterated their message that the former trial “supports a complementary role for open and endovascular revascularization strategies” and the need for expertise in both. The session also heard from BASIL-2 lead investigator Andrew Bradbury, MD, from the University of Birmingham in Solihull, England, who addressed the question of whether the trial would change practice in the UK. He said that in around 50% of patients it is not “obvious” that infrapopliteal vein bypass or best endovascular therapy is preferable.—
Bryan Kay
HEALING
FASTER SUSTAINED HEALING for Venous Leg Ulcers
Pain score dramatically dropped from 8 to 3 in 13 days
5 www.vascularspecialistonline.com
REFERENCE: 1. Tawfick WA, Sultan, S. Technical and Clinical Outcome of Topical Wound Oxygen in Comparison to Conventional Compression Dressings in the Management of Refractory Nonhealing Venous Ulcers Vascular and Endovascular Surgery, 2012. LEARN MORE
MB1090-A
DELIVERING EXCEPTIONAL OUTCOMES
FASTER
1 2X LOWER RECURRENCE1 8X
Already on deck: Submit session ideas for next year
Matthew Menard addresses VAM
FROM THE COVER: THE NUMBERS ARE IN: VAM 2023 ADDS UP TO ANOTHER SVS CLASSIC
With more content presented than ever before, a family-friendly Wednesday night gathering, the inaugural Frank J. Veith Distinguished Lecture, a hugely successful gala and the vascular surgery community more than happy to be together, the 2023 Society for Vascular Surgery (SVS) Vascular Annual Meeting (VAM) was heralded as another big success.
“Overall, it was really well-received,” declared Andres Schanzer, MD, chair of the SVS Program Committee, which oversees the scientific content at the meeting. “People really enjoyed themselves,” he said.
“The quality and impact of the science was really high. It was diverse across the whole array of vascular surgery procedures and medical management.”
And, not only was the science and research
important, “but I think people really enjoyed the opportunity to connect with colleagues. People are enjoying interacting with each other in a meaningful way around vascular surgery,” Schanzer continued.
“And most importantly, we are being as inclusive as possible with the hope that our meeting participants look more like the patients we take care of.”
Some of the highlights of VAM 2023 by the numbers include:
● More than 800 abstracts submitted

● Fifty-two abstracts at eight plenaries
● Twenty-one educational sessions
● Four SVS special section sessions
● Hands-on learning for the Physician Assistant Section
● Five international sessions
● A total of 271 posters
● Eleven abstracts presented simultaneously with publication in the Journal of Vascular Surgery
● The move of officer voting into VAM’s first few days
This year’s meeting also included a number of new initiatives and events, which proved quite popular, Schanzer said.
Attendees enjoyed an opening night, family-friendly SVS Connect@VAM: Building Community party that was open to all, with food, games and activities. With a successful debut, it will return in 2024 and afterwards as an annual event, Schanzer said.
The inaugural Frank J. Veith Distinguished Lecture, announced at the close of VAM 2022—which focused on the results of the BEST-CLI trial—drew a healthy crowd, as

caregivers and communities whom we serve, and they hold surgeons in such high regard, they are waiting for us to take a leadership role in galvanizing the resources and continuing to address the important issue of shaping a multi-dimensional, diverse healthcare workforce.”
Malachi Sheahan III on medical education and training…
continued from page 1
did several other BEST-CLI-focused content.
Organizers moved the championship round of the Poster Competition to the plenary room on Saturday morning, leading to a robust audience and more recognition for the 10 finalists.
Highlighting sessions that included topics related to diversity, equity and inclusion, plus including “invited discussants” for many of those sessions, also was well-received.
The Program Committee and Postgraduate Education Committee are reviewing the feedback obtained via the VAM 2023 evaluation, Schanzer said.
“So, if you have not completed the evaluation please do so no later than July 14. It is critical we hear from you so we can continue to meet your educational needs going forward,” he added.
sleep disruptions, insomnia, isolation, etc. Moral distress matters, which can intersect with burnout, and I am positive all of us feel this at some point.”
Laura Marie Drudi on burnout solutions…
This year’s E. Stanley Crawford Critical Issues Forum zeroed in on the pipeline of sources feeding the vascular surgery ranks. Incoming SVS President Joseph Mills, MD, assembled an expert panel to look at many of the key issues at the heart of efforts to address workforce-related concerns.

The panel captured three main areas of focus: the root sources of future vascular surgeons, the existing workforce, and the distribution of that workforce. Lee Kirksey, MD, from the Cleveland Clinic in Ohio, looked at outreach to high school and college students and Malachi Sheahan III, MD, from Louisiana State University in New Orleans, dealt with efforts to attract medical students and residents in training. Dawn M. Coleman, MD, from Duke University Medical Center in Durham, North Carolina, addressed vascular surgeon wellness, followed by Laura Marie Drudi, MD, from Centre Hospitalier de l’Universite de Montreal in Canada, on burnout solutions. The panel was rounded out by former SVS President Michel S. Makaroun, MD, on workforce supply or maldistribution, and Peter R. Nelson, MD, from the University of Oklahoma in Tulsa, on measures to improve the workforce crisis.
Lee Kirksey on the early years…
“Not everyone is capable of, or wants, to be a physician. I know it’s hard for us in this room to believe that, but not everyone wants to be a physician or vascular surgeon. However, there is a broad range of healthcare ecosystem jobs that provide family-sustaining wages and opportunities for a rewarding career. Much investigation is needed to better understand the student- and familyperceived barriers in pursuing health science careers. We think we know, but when we talk to parents we actually are probably missing the point. And in every community, whether it is urban, indigenous American, rural, White, Black or brown, there are motivated
“It is time to establish ourselves as the expert on vascular disease at the medical school level. If we don’t, there are other specialties very interested. In a [2016] editorial by the leaders of the American Heart Association and the American College of Cardiology, they say they need an American Board of Internal Medicine-certified specialty focused on patients with peripheral arterial disease [PAD] because their care has been undermined. So if we don’t establish ourselves as the expert, other people will.”
Dawn M. Coleman on surgeon wellness…
“Physician burnout is a public health crisis. Frankly, it is a workforce crisis for us. It is a chronic condition in which your perceived demands outweigh perceived resources. There are staggering personal and professional repercussions of physician burnout. In 2019, burnout was reclassified as an occupational phenomenon by the ICD-11 classification of diseases. And there are also staggering personal and professional ramifications that are associated with work-related stress—which is a precursor for burnout—that have really impressive medical sequelae, including cognitive dysfunction, increased risk of heart disease, type-2 diabetes, fertility challenges,
“Addressing physician burnout and well-being requires a multi-level, multi-pronged approach that involves both individual and organizational factors. Although burnout is rooted in the environment and systems in which we work, I do believe we have to first turn inwards to fill our own cup before we serve others. For those of you who are experiencing burnout and feel isolated, you’re not alone. Through support, connection and engagement, I am confident we will make progress in this space together.”
Michel S. Makaroun on workforce supply…
“In the last three years, approximately 170 vascular certificates have been issued every year, but we are still far behind the interventional radiologists and interventional cardiologists. So, is the funnel looking a little bit better? It is. We are now producing about 58 new vascular surgeons per year, but it is still inadequate. I will leave with you with this statement from a paper about the county-level maldistribution. ‘Although encouraging vascular surgeons to practice in underserved areas would be an ideal solution, it is not pragmatic.’ Developing alternatives is essential to get new methods of providing vascular care to geographically isolated populations.”
Peter R. Nelson on prophylactic measures to address the workforce crisis…
“We really need to work toward regional systems for efficient education, communication and delivery of multidisciplinary team healthcare. Patients want access to vascular healthcare close to home. They don’t want to come to Tulsa or Oklahoma City to get care. Vascular surgeons can and should lead in these efforts by recruiting vascular surgeons to work in these underserved areas with support from the tertiary referral centers—but, more importantly, to think broadly of how we define workforce, empower other physicians who are already in those communities—primary care providers, podiatrists, general surgeons, cardiologists—to feel more comfortable and confident taking care of vascular disease.” Bryan Kay
6 Vascular Specialist | July 2023
23
Crawford panel looks at opportunities to plug and extend vascular surgery workforce pipeline
VASCULAR FUTURE
The Crawford Forum panel takes questions
From rural America to the vanguard of a revolutionary surgical specialty
The Friday morning of VAM 2023 saw Michael C. Dalsing, MD, deliver what is an annual hallmark of the VAM program— the SVS Presidential Address.
 By Jocelyn Hudson and Marni Davimes
By Jocelyn Hudson and Marni Davimes
DALSING CHARTED HIS PERSONAL journey from “small-town boy with some big dreams” to president of the SVS, as well as the history of the Society and that of the vascular surgery specialty in general, all the while delivering the salient message that “the annual meeting is only part of our story.”
Rural America was the opening scene for Dalsing’s address. This is where he grew up, with parents who were “deeply affected by World War II and the Depression,” with his mother— who, Dalsing said, would have traveled widely given the chance—“convinced that education would open doors to the world.”
“I remember insensitive people making remarks about our lack of material worth –they didn’t understand a family’s true value,” Dalsing remarked. “What you ‘have’ does not define you.”
Dalsing took this set of values to heart, refusing to let his humble upbringing prevent him from achieving his goals, especially when it came time to consider higher education. “Not wanting to spend [his] life farming,” Dalsing was quick to accept the opportunity to attend college on a full-ride scholarship when given the chance.
Against this backdrop, Dalsing moved away to attend a small college, majoring in biology and expecting to be a scientist, before making “potentially one of the most consequential decisions of [his] life” and taking the Medical College Admissions Test (MCAT), thus launching a long and celebrated career in vascular surgery.
“Destiny, maybe, but they say you make your own,” he teased.
Before delving into his introduction to the world of vascular surgery, Dalsing took the opportunity to touch on the impact his personal life has had on his professional success, not hesitating to declare that “the most important event in [his] life was meeting and marrying [his] wife, Rosa, just before [his] surgical internship.” He credited Rosa as the “emotional strength” in his life and “a pillar of acceptance, joy, and safety.”
Vascular influences
Jumpstarting his journey into vascular surgery was achieved by observing Victor Bernhardt, MD, and Jonathan Towne, MD, during his time at Marquette. But, Dalsing observed, his interest in vascular surgery was really awoken by Russell Dilley, MD, and John Glover, MD.
Completing a one-year fellowship at Northwestern, where he was greatly influenced by John Bergan, MD, James Yao, MD,
and Bill Flynn, MD, Dalsing admitted that this time in his life was a “blur of hard work and long hours, convincing [him] that no one is ‘entitled to anything,’ but hard work can win the day if given the opportunity.”
Alongside his personal and professional journey to SVS president, Dalsing delivered a sweeping history of vascular surgery and outlined how the twists and turns of certain decades were pivotal in defining it as the distinct specialty that it is today, as well as some
ship by establishing criteria for endovascular credentials nationwide.” As “established vascular surgeons gained endovascular experience,” he continued, sometimes spending months undergoing further training, by 2009, upwards of 80% of endovascular resident training was being provided by vascular surgeons.—an experience that would foreshadow a “complex and, in some cases, contentious” relationship with those who would “encroach on our discipline.”
Despite describing vascular pathology as an “unrelenting foe requiring special attention to proper timing and intensity of care,” Dalsing went on to note that “we are the only specialty who can correct the interventional misadventures of others, or enable others to provide complete trauma, orthopedic, or cancer care. This central role highlights our position as champions for quality vascular care.”
The president, who is professor emeritus in the Division of Vascular Surgery at Indiana University School of Medicine in Indianapolis, reflected on his current position within the vascular surgery field, paying
stated, with its role extending far beyond the calendar highlight that is VAM. “SVS is literally reinventing itself as it evolves and moves forward to integrate dozens of new innovative ideas currently under consideration for implementation. This process happens year over year. We are coming of age as a mature organization,” he told attendees.
SVS: Vascular surgery’s advocate
And who but the SVS will advocate for the interests of vascular surgeons? Dalsing asked. “No one!” He stressed that the SVS is a small group that “must speak with a strong and unified voice to be heard,” all in the interest of vascular patients, as well as members’ well-being.
of the challenges that it presently faces.
In the 1940s, he said, vascular surgery was “coming of age.” In the 1970s and early 80s, training, certification, and defining the specialty took “center stage.” And the endovascular revolution of the 1990s and 2000s, he continued, saw a vascular surgery field that was “changing fast.”
Alongside mounting changes, the space was also being confronted by new challenges on the horizon. As “radiologists and cardiologists were embracing endovascular interventions” due to the access they had to appropriate imaging facilities, vascular surgeons didn’t get the same privilege.
A ‘unique’ specialty
“Vascular surgeons were pushing the envelope in the endovascular treatment of aortic aneurysms,” Dalsing said. “Some were trying to incorporate an endovascular suite in the operating room with some success. But we would have to catch up—take ownership—or be left behind. We righted our
honorable mention to a “long list” of individuals who have influenced his career over the years. He also described the “immense joy” at seeing the next generation of vascular surgery residents and fellows serve their communities as “compassionate and skilled vascular surgeons,” in addition to being “exceptional people.”
Dalsing’s talk argued that vascular surgery is “unique” as a specialty, in that it involves the care of a patient from initial contact to the end of their life. As a result, specialists “must master several dissimilar skillsets requiring years of training.”
The specialty is, however, a “hidden gem,” Dalsing said, which he highlighted as a problem. “In general, people do not know what we do,” meaning the specialty risks being “overlooked as a needed partner in discussions about our patients’ care.”
And this is all in the context of an aging population and its “increasing demands,” being served by a “finite” number of providers.
This is where the SVS comes in, Dalsing
“We are the champions of quality vascular care. We must embrace this role and encourage those who want to be on the vascular team,” Dalsing said. He expressed his belief in the need to market to the general population—a seemingly “unattainable” goal, but one he feels is the “endgame” if there is a desire to be recognized as the “undisputed champions of quality vascular care.”
He defined the scope, the added value the specialty brings, and a general impression of the players involved. The next steps? According to Dalsing, they are “defining the rules of engagement and tactics to be used for success,” with education a “centerpiece” of this effort.
As his “musings [came] to an end,” Dalsing expressed thanks to everyone who gave a once “small-town boy with some big dreams” the chance to represent the SVS as president. It has been, he said, a “distinct privilege and honor” to serve in the role—one he described as “unexpected but dearly cherished.”
“Our society is you, a collection of diverse individuals reflective of our general population, but one in dedication and purpose for our patients,” Dalsing concluded. “I admire what you do daily, I am proud to be a vascular surgeon, and will miss the personal interactions I have had with many as I filled this role. Good luck and the best to us all as we face the world together.”
PRESIDENTIAL ADDRESS www.vascularspecialistonline.com 7
“We are the only specialty who can correct the interventional misadventures of others, or enable others to provide complete trauma, orthopedic, or cancer care”
MICHAEL C. DALSING
By Marni Davimes and Bryan Kay
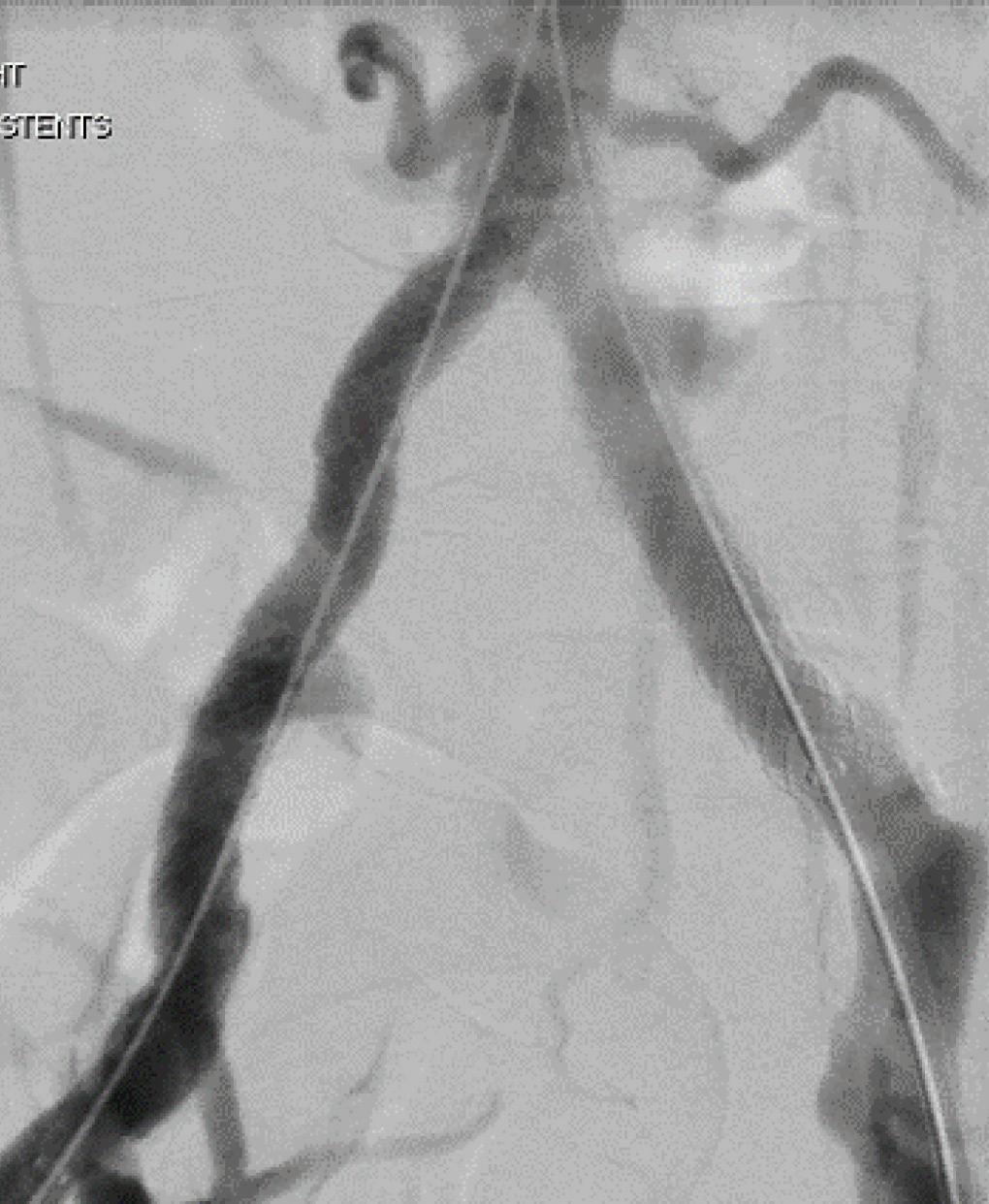
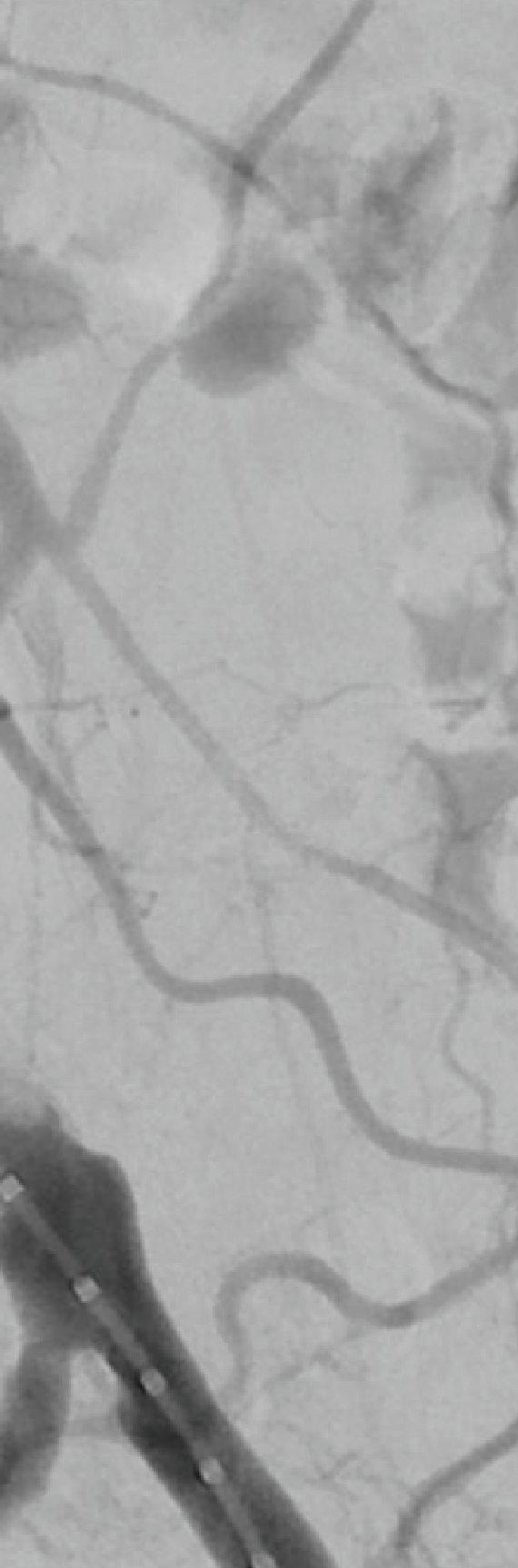
THE SAFE MANAGEMENT OF AORTOiliac graft infections has proven possible by utilizing either cryopreserved arterial allografts (CAA) or rifampin-soaked Dacron (RSD) for select in-situ reconstruction based on the findings of a recent study conducted by the Mayo Clinic and Karolinska Institutet.
While it was found that reinfection rates among the RSD group were lower compared to the CAA group, it was not statistically significant, making both interventions viable options for infected patients.
Armin Tabiei, MS, a vascular surgery research trainee and medical student at the Mayo Clinic in Rochester, Minnesota, and Karolinska Institutet in Stockholm, Sweden, shared these findings at VAM 2023 in National Harbor, Maryland.

Although a single-center retrospective cohort study, said Tabiei, results showed “comparable early and long-term morbidity and mortality between the groups.”
While rates were higher in the CAA group and there was a trend toward higher reinfection rates in the RSD group, Ta-
biei expressed confidence in both as viable options for in-situ reconstruction patients and conveyed that they “need to be customized for each patient’s characteristics.”
Tabiei et al’s objective was to compare the safety and effectiveness of CAA and RSD as options for in-situ reconstruction in aorto-iliac graft-infected patients.
Data collected from aortic and iliac graft-infected patients undergoing in-situ reconstruction with either CAA or RSD from January 2002 through August 2022 were analyzed retrospectively to assess overall survival rates as well as secondary outcomes such as graft-related intervention, reinfection, perioperative mortality, and major morbidity, The study included 149 subjects, 80 of which received RSD intervention and 60 who underwent CAA, with a mean age of 68.9 and 69.1, respectively. Moreover, endovascular stent grafts were infected in 60 patients, 41 of which were in the CAA group, with the remaining 19 patients in the RSD group.
With respect to graft-enteric fistulas, they were significantly more common in the RSD group, and management included complete resection of the infected graft. Aortic reconstructions were covered in omentum in 57 CAA patients and 63 patients in the RSD group.
There was a median follow-up of 20.5 months in the CAA group and 21.5 months in the RSD group, with
FROM THE FLOOR
overall survival at five years similar between the two cohorts, with 59.2% in the RSD group and 59% in the CAA group. Freedom from graft-related reintervention at one and five years was 81.3% and 66.2% in CAA patients compared to 95.6% and 92.5% in RSD patients.
Tabiei went on to describe that indications for reintervention in the CAA group included five patients with stenosis, four with pseudoaneurysm, two occlusion patients, one with graft-limb kinking, and one patient who experienced rupture.
Keith Calligaro, MD, Philadelphia: “I applaud your effort but I don’t know if we’re ever going to get a good answer on this—it’s all retrospective … I personally take a different attitude about the use of cryograft. When it's a younger patient, I tend to use the cryograft because I'm more worried about recurrent infection, but every series has shown that cryograft is more likely to develop recurrent stenosis. That's the advantage of rifampin—you're

In the RSD group, indications for reintervention included three patients with reinfection, one occlusion patient, one endoleak patient, one with omental coverage, and one incidence of rupture. Freedom from reinfection at one and five years was 98.3% and 94.9% in the CAA cohort compared to 92.5% and 87.2% for the RSD group.
Wrapping up, Tabiei concluded that the study found both CAA and RSD to be suitable interventions, but noted that reintervention was more common with CAA—ultimately reaffirming that individualized treatment and long-term follow-up are most appropriate with aortic and iliac graft-infected patients.
Tabiei added that at his institution, CAA are considered in older patients, and in cases of highly virulent microorganisms and such instances as intra-abdominal abscesses. RSD tends to be used in younger patients and in urgent cases.
pain or follow-up of an unrelated pathology.
Of the patients with imaging follow-up, 23% experienced growth, with an average increase of 2.5mm. The most common size of aneurysm was between 10mm and 19mm, with an annual growth rate of 0.17mm. Notably, there was no difference between the size cohorts.
referred to a vascular surgeon. We found these aneurysms through the radiology report, which we then verified. So, most of the women who had aneurysms actually never saw a vascular surgeon,” Zhang noted when asked about the current guidelines for aneurysm treatment in women of childbearing age.
DESPITE RECENT GUIDELINES recommending that women of childbearing age have interventions on their splenic aneurysms, only a minority in a recent study did so, according to first-named author Jason Zhang, MD, an integrated vascular surgery resident at New York University Grossman School of Medicine, who raised the need for inquiry into prior smoking history in the patient cohort. Zhang was presenting at VAM 2023, shedding light on the findings of a retrospective analysis of splenic aneurysms in pregnant women.
“Splenic-type aneurysms are the most common type of visceral aneurysms, and pregnancy is a known risk factor, with pregnant women having a higher mortality rate from rupture,” Zhang began. The
headline findings, he said, suggested the guidelines “might not be known among the greater medical community.”
To achieve better outcomes for this patient cohort, Zhang argued that the vascular specialty as a whole must work on updating guidelines across the board.
To better understand the study group, Zhang explained that the analysis focused on the incidence of enlargement, intervention, and rupture of aneurysms. Pulling from the New York University Grossman School of Medicine’s radiology database from 2015 to 2020, a total of 853 patients were analyzed, with 514 having had both clinical and imaging follow-ups at a mean of 3.8 years.
Zhang noted that the most common indications for imaging were abdominal
Shifting focus to the childbearing cohort of the analysis, Zhang explained that 37 women of childbearing age were included in the study, with a mean aneurysm size of 16mm. In the entire study, only one patient presented with a rupture, measuring 23mm in size, and the aneurysm was closed successfully.
“What we found, actually, was that the large majority of these patients were never
Zhang was also asked about incidental diagnoses and the opportunity for those patients to be referred sooner to a vascular surgeon by Dawn Coleman, MD, chief of vascular surgery at Duke University in Durham, North Carolina. “What are you going to do about that at a local level?” she added.
Zhang referred to potential “quality initiatives”—such as an automatic flag in the electronic medical record (EMR) when a patient has an aneurysm—but said the point was a “good consideration.”
The real conclusion, Zhang said, is that there needs to be more research done on splenic aneurysms in this patient cohort, and his team’s retrospective analysis is “just a starting point.”
To better treat women of childbearing age, the vascular community must prioritize the creation of uniform guidelines and follow up with continued research and analysis, he added.—Marni Davimes and Bryan Kay
8 Vascular Specialist | July 2023
VISCERAL ARTERIES PRIORITIZING CREATION OF UNIFORM GUIDELINES IN THE TREATMENT OF SPLENIC ARTERY ANEURYSMS IN CHILDBEARING WOMEN FOR THE VASCULAR COMMUNITY
RECONSTRUCTION
Both cryopreserved allografts and rifampin-soaked Dacron prove feasible for infected aorto-iliac grafts, study finds
“What we found, actually, was that the large majority of these patients were never referred to a vascular surgeon”
JASON ZHANG
Armin Tabiei
less likely to get recurrent infection.”
GAVEL PASS
SVS UNVEILS 2023–24 SLATE OF OFFICERS
By Beth Bales
WITH NEARLY 940 VOTES CAST, Keith Calligaro, MD, was elected vice president of the SVS and Thomas Forbes, MD, its treasurer following the conclusion of the 2023 officer elections. Results were announced during the SVS Annual Business Meeting, held Saturday, June 17, during VAM 2023.

“Each of these newly elected officials is incredibly deserving and I am excited to work with them going forward,” said SVS President Joseph Mills, MD. “They will provide strong voices to the SVS in their roles. Please join me in celebrating their new leadership roles.”
Candidates included Kellie Brown, MD, and Calligaro for vice president, and Forbes and Palma Shaw, MD, for treasurer. Mills thanked
MEMBERSHIP
both Brown and Shaw, calling them “strong leaders within the Society and their respective institutions. I look forward to continuing to work with them within SVS; there’s no doubt we will continue to see great things from them.”
Voting opened in mid-May and closed June 15, during VAM itself. “We left no stone unturned to stress the importance of voting to all voting-eligible members, which resulted in a record turnout with 939 votes [30% of eligible voters],” said Mills. The push resulted in a 50% increase in voting in just one year. In the 2022 election, slightly more than 600 voting-eligible members voted.
In late 2022, Society members approved three revisions to Article X of the SVS bylaws to restructure the Nominating Committee. These revisions resulted in increased committee diversity, adding the chair or vice chair of the SVS Diversity, Equity and Inclusion (DEI) Committee and of the Young Surgeons Section as full, voting members.
The Nominating Committee, said Mills, “selected outstanding candidates for this year, all of whom are incredible leaders for our specialty.” He added that the SVS will continue to re-examine, review and explore whether the current process could be further optimized to meet the Society’s strategic and governance
needs. At the close of the meeting, Immediate Past President Michael Dalsing, MD, passed the presidential gavel on to Mills.
OFFICER CLASS OF 2023–24
Michael Dalsing and
After thanking the crowd as well as outgoing President Dalsing, Mills undertook his first official action. After a motion and a second, he declared the meeting adjourned, asking “all of you to assemble in June 2024 in Chicago!”
The 2023-24 slate of officers are as follows: President Joseph Mills; PresidentElect Matthew Eagleton, MD; Vice President Keith Calligaro; Secretary William Shutze, MD (in the second of a three-year term); Treasurer Thomas Forbes (first of a threeyear term); and outgoing President Michael Dalsing Audra Duncan, MD, Kwame Amankwah, MD, and Kellie Brown, MD, have accepted presidential appointments as liaison members of the Executive Board.
Three SVS members receive honors for service to community practice
Patricia Furey, MD, Clifford Sales, MD, and G. Stephen (Steve) Vincent, MD, received the SVS Excellence in Community Practice Award during VAM 2023.
This honor is bestowed upon members who have exhibited outstanding leadership within their communities as practicing vascular surgeons.
Furey practices in Bedford, New Hampshire, as director of Vein and Vascular Specialists at Catholic Medical Center and as an associate director of surgical services at the New England Heart and Vascular Institute, which includes work in promoting and integrating vascular and cardiac surgeons and cardiologists in order to help advance endovascular service lines.
She has been integral in developing, planning and implementing a state-of-the-art outpatient interventional suite with a full-time vascular lab on-site, and is participating in the planning and oversight of a new cardiovascular construction scheduled to open in 2025.
She has held numerous leadership positions, including within her medical center plus within the specialty, such as vice president for the New England Society for Vascular Surgery. She was an inaugural member of the SVS Women’s Section Steering Committee.
Sales is a vascular surgeon, managing partner and CEO of the Cardiovascular Care Group in West field, New Jersey.

He is former chief of vascular surgery and director of the noninvasive vascu lar lab at Overlook Hospital and, since 1998, he also has been clinical assis tant professor of surgery at Mount Sinai School of Medicine.




Sales is currently vice president, vascular services, RWJBarnabas Health Care System—the largest healthcare system in the state of New Jersey.
His society memberships have include the Eastern Vascular Society, Society for Clinical Vascular Surgery, the Vascular Society of New Jersey, American Venous Forum and the Frank J. Veith Society (founding member). He also has been involved with the SVS Community Practice Section, which was founded in 2021.

Sales also runs an annual program for 15–20 college students who spend one month at his institution rotating through different specialties, including vascular surgery. The program has become nationally recognized, and Sales receives hundreds of applications each year for the limited number of positions.
Vincent has spent his career in Ohio. When he began practice in the Columbus area, he collaborated with a community hospital in an underserved area to begin an outreach vascular program to patients that lacked access to vascular care. This initially began with development of a vascular office practice and simple procedures, but has progressed to provide full-service vascular care, with angiography, angioplasty, stenting, bypass procedures, endarterectomy, aneurysm and
dialysis-access procedures.
He was instrumental in building the local wound care service line, which offers extensive services for a rural community, including the availability of two hyperbaric treatment chambers.
Vincent is on the staffs of several hospitals, some for 35 years, and is medical director for the non-invasive vascular laboratories at two.
He volunteered to help organize and start the Society of Black Vascular Surgeons (SBVS). Vincent serves as vice president. He “had a significant amount of history of the denigrating issues facing Black vascular surgeons who were either in private or academic practice in the 80s and 90s,” said a colleague also involved in forming the SBVS.
“His insight, leadership and support were crucial to getting a more comprehensive understanding as to the mission of the organization. Because of his influence we were able to form an organization that focused on mentoring those currently in practice and those following our footsteps.”
Vincent also has been a medical leader within the community, been involved with 17 medical societies and been chapter president of the National Medical Association. His community activities include the Park Foundation, as well as extensive involvement with the Boy Scouts of America.—Beth Bales

9 www.vascularspecialistonline.com
“We left no stone unturned to stress the importance of voting to all voting-eligible members which resulted in a record turnout with 939 votes”
JOSEPH MILLS
Joesph Mills
“[Vincent] had a significant amount of history of the denigrating issues facing Black vascular surgeons who were either in private or academic practice in the 80s and 90s”
Clifford Sales, G. Stephen Vincent and Patricia Furey with Robert Molnar
INTERNATIONAL AORTIC SUMMIT |

October 19-21, 2023 | Hilton Aruba

Learn about modern trends in aortic surgery with the world’s experts!

Join us October 19-21, 2023, as the key opinion leaders in Aortic Surgery convene in Aruba to present and discuss the endovascular techniques.

COURSE DIRECTORS
Joseph V. Lombardi, MD, MBA, FACS
Professor and Chief, Division of Vascular & Endovascular Surgery Cooper Medical School of Rowan University
Director, Cooper Aortic Center Camden, NJ
Joseph J. Ricotta, MD, MS, FACS
National Medical Director, Vascular Surgery and Endovascular Therapy Tenet Healthcare Corporation
Professor of Surgery, Charles E. Schmidt College of Medicine
Program Director, Vascular Surgery Fellowship Florida Atlantic University
Boca Raton, FL
PROGRAM COMMITTEE
Ali Azizzadeh, MD Cedars-Sinai Medical Center, Los Angeles, CA
James H. Black, III, MD
The Johns Hopkins University School of Medicine, Baltimore, MD
G. Chad Hughes, MD Duke University Medical Center, Durham, NC
James F. McKinsey, MD
Jacobson Aortic Center Mount Sinai Medical System, New York, NY
Darren B. Schneider, MD
The Hospital of the University of Pennsylvania, Philadelphia, PA
Provided by:
Program Highlights Include:
AAA Repair
Aortic Dissection
Aortic Emergencies
Aortic Occlusive Disease
Fenestrated Branch Endografts
Graft Infections
New Endovascular and Thoracoabdominal Repair
And more!
Vascular Fellows and Residents Competition:
Submit an interesting aortic case in abstract format. The Best 10-15 cases will be submitted for presentation in the IAS 2023 program. Fellows/Residents whose abstracts are selected for presentation in the Case Competition will receive the following:
Complimentary registration
Up to a maximum of two (2) nights hotel accommodations at the Hilton Aruba



Economy airfare to Aruba (to be reimbursed)

Deadline to submit is August 1, 2023. Scholarships are limited!

aorticsummit.org
305.928.4669 | info@aorticsummit.org | 9737 NW 41st Street | Suite 1018 | Doral FL 33178
Hilton Aruba
PATIENT SAFETY
VQI launches ‘CAN DO’ smoking cessation drive at VAM 2023
The SVS Patient Safety Organization (PSO) has launched a national smoking cessation initiative.
By Beth Bales
THE SVS PATIENT SAFETY ORGANIZATION (PSO) has launched a national smoking cessation initiative.
SVS PSO Associate Medical Director Gary Lemmon, MD, and SVS PSO Director of Quality Betsy Wymer introduced the program during the PSO’s Vascular Quality Initiative (VQI) Annual Meeting, which took place during VAM 2023.
CAN-DO (Choosing Against Combustible Nicotine Despite Obstacles) joins two existing national initiatives on discharge medications and sac diameter reporting, with imaging, in connection with endovascular aneurysm repair (EVAR) for aortic aneuryms.
“Smoking is the leading cause of preventable death and disability—10 times more than the premature deaths from all wars fought by the U.S.,” said Lemmon.
It’s a major cause of cardiovascular disease and more than 90% of cancer of the lungs and other organs. Moreover,
POSTER COMPETITION
COMPLICATIONS
ascular surgery plays an essential role in assisting other surgical services with iatrogenic vascular complications—“something that must be considered when assessing the value proposition of a vascular surgery service line”—the first author of the winning entry in the VAM 2023 Poster Competition told attendees. “Oftentimes, vascular surgery is called for urgent or emergent assistance for patients who are critically ill at non-peak hours when there are less resources available,” Abhishek Rao (pictured center), MD, a vascular surgery integrated resident at Columbia University Medical Center in New York University, said.
He was outlining the main takeaways from his first-place paper, “The significant burden of iatrogenic vascular injury on the vascular surgery workforce at an academic medical center,” for which he took home a $1,500 award.

Rao and colleagues identified all vascular surgery consultations for iatrogenic vascular complications at a single tertiary care center—retrospectively during a seven-
secondhand smoke increases the risk of death and disability to those who do not smoke themselves.
CAN-DO includes three components to increase smoking quit rates, including smoking cessation variables (preop smoking in elective procedures only, and smoking cessation for elective, urgent and emergent cases) in the VQI’s arterial registries; physician and patient toolkits; and revising the smoking cessation section on the SVS website in order to make it more patient-centered and increase its visibility.
The VQI currently captures some variables, but the new initiative expands upon them to include smoking status, history and demographics prior to surgery, and in post-op care and long-term follow-up.
Simplicity is stressed. “We’re trying to minimize the burden” on VQI members in terms of the additional variables, Wymer said.
The physician toolkit includes many elements physicians and surgeons will find useful, including results and efficacy from a clinical trial of a brief smoking cessation intervention, a “visual dictionary” on electronic cigarettes and vaping products, an educational library of useful resource documents, the patient-facing document housed on the SVS site and, importantly in a billable world, billable smoking cessation codes.
“We can receive reimbursement for talking to patients about quitting smoking,” said Lemmon. He discussed key phrases and elements to be included to meet the threshold for reimbursement.
The patient toolkit, meanwhile, includes links to many resources on quitting smoking. Patient education is another important component, said Wymer. In the U.S., 30.8 million adults smoke cigarettes, 3.08 million middle and high school
students use tobacco products, one in four people who don’t smoke are exposed to secondhand smoke, and more than $240 billion a year goes to treat smoking-related diseases.
Moreover, tobacco companies target specific populations, including people of lower income, and spend $9.1 billion in marketing annually in the U.S.
“There are nearly five times more tobacco retailers per square mile in neighborhoods with the lowest income compared to neighborhoods with the highest income,” she said.


Lemmon also noted that simply asking a patient, “Do you smoke?” is insufficient. Surgeons and doctors should instead extend the conversation to the “3 As”: ask if the patient wants to quit and when the patient smokes that first cigarette of the day; assist by offering liberal use of nicotine replacement therapy and medications, but also add that the patient should not combine e-cigarettes as a crutch while also smoking; and give advice by referring patients to professional counseling, apps and other tools.
Other useful information includes a quick guide to treatment options, including nicotine patches, lozenges, nasal spray, gum and inhalers, and the use of counseling via text messaging, smartphone apps and web-based services.
Wymer and Lemmon also stressed the deleterious effects of smoking on health: increased risk for peripheral artery disease and plaque-building in arteries. Smoking narrows, and thus damages, blood vessel walls; it increases blood pressure and heart rate; affects cholesterol; and increases triglyceride levels, a type of fat found in the blood.
Both the SVS and the American Heart Association advise patients to quit smoking before they undergo surgery.
Learn more at www.vqi.org/smoking-cessation.
GREENBERG LECTURE
Immune responses and the prevention of AAAs
and-a-half-month period and prospectively from the following three-month timeframe—for a total of 63 patients.
They found that the most common consulting service was cardiology (32%), immediately followed by cardiothoracic surgery (27%). Rao said 25% were intraoperative, 19% related to ECMO cannulation, and another 19% to ventricular assist devices. The research team noted a particular peak for consult timings from 6–7 p.m. Most involved uncontrolled hemorrhage (42%), followed by ischemia (32%) and pseudoaneurysm (27%). “Emergent or urgent intervention was required in 75% of cases,” he said, “typically requiring open surgical repair, with a significant proportion—15%—requiring endovascular intervention.”
In second place ($1,000) was Raaz Samra (middle left), MD, of Indiana University School of Medicine. In third ($500) was Hanaa Dakour-Aridi (middle right), MD, of the University of California, San Diego. The top 10 posters were presented in the main plenary hall.—Bryan Kay

DATA ON THE ROLE OF ALLOGENEIC MESENCHYMAL STROMAL CELLS obtained from a young healthy female donor—in inducing Tr1 and reducing Th17 cells in the context of abdominal aortic aneurysms (AAAs) formed a key part of the message of the 2023 Roy Greenberg Distinguished Lecture at VAM. “There is very preliminary evidence that mesenchymal stromal cells may prevent aneurysm expansion,” this year’s lecturer, Michael Murphy, MD, told those gathered. “Given this body of data, we are going to move forward with a multicenter, multi-dosing, randomized, placebo-controlled study to see if there is true efficacy in preventing or decreasing overall aneurysm expansion, measured either by diameter, or preferably by volume, because I think it’s a much more sensitive measure as it contains three dimensions rather than just two, at one and two years.” Murphy, a professor of vascular biology at Indiana University School of Medicine in Indianapolis, was giving a talk built around the title, “Modulating patient immune responses to prevent AAA initiation and expansion.”
Murphy also told attendees how he and colleagues had demonstrated how nanoparticles loaded with elastin degradation products demonstrate efficacy in preventing aneurysm initiation. “We developed a skin test that can determine a response to immunotherapy, but it may also be able to identify patients who may be at risk for developing an aneurysm,” he said, explaining, “somebody who may have had a father who had an aortic aneurysm—young, Caucasian, cigarette smoker, obviously in their 40s, and doesn’t have an aneurysm yet—but if they have a positive skin reaction, it might be somebody who we would follow more closely.

“Better yet, if we have an effective reverse vaccine, we can start administering immunotherapy.”
With data obtained from a mice model, Murphy and colleagues aim to move to a phase I safety study in a clinical setting, following Food and Drug Administration (FDA) approval, of a nanoparticle vaccine.—Bryan Kay
11 www.vascularspecialistonline.com
V
ESSENTIAL ROLE OF VASCULAR SURGERY IN SETTING OF IATROGENIC
Michael Murphy
Learn valuable compensation information by completing survey
MEMBERS FREQUENTLY WONDER HOW
THEIR financial compensation compares to other vascular surgeons in their geographic area. How about to those in academics versus private practice? To those of a different gender, race or age? Do others get compensated for being on-call?
The SVS Financial Compensation Task Force created a survey to answer these questions; participants can gain knowledge of the vascular surgery compensation market as they negotiate personal compensation packages.

The initiative launched in June at VAM 2023 and is a response to pressing requests from SVS members. The Task Force created a survey to answer these questions, partnering with Phairify, a firm devoted to creating valid survey data, to ensure reliable results. The committee met virtually bi-weekly from January through May to fulfill the mandate of completing the survey form to distribute to SVS members at VAM. The committee and Phairify also developed templates for those participants who wished to learn more about a particular issue, such as compensation for medicolegal expert billing, medical industry relations and being on-call.
Study participants must be residents of the U.S. in the Active member category. Participants will receive immediate access to compensation benchmark data based on anonymous information submitted from other SVS members for all data fields that meet the threshold of at least 10 responses. Participants can gain knowledge of the vascular surgery compensation market as they negotiate personal compensation packages.
There is no cost to participate. Members must enter data in a short 15-minute survey to review the results. The data are
completely de-personalized and no identifiable information is accessible to any external agency. A strict application process must be followed to publish any data based on survey results.
SVS members can participate in the survey at any time going forward. “Do it now!” said Task Force Chair Keith Calligaro, MD, now SVS vice president. “Please participate in this vitally important survey and learn how your financial package compares to that of other SVS members.”
To access the survey, visit vascular.org/Compensation Study2023. Select “Society for Vascular Surgery” from the menu and enter the email address associated with your SVS membership to set up an account and access the sur vey. After completing the survey, members can log in at any time at www.phairify.com. Email questions or concerns to SVSQuality@vascularsociety.org
Besides Calligaro, Compensation Task Force members include Bernadette Aulivola, MD, Ali Azizzadeh, MD, Sira Duson, MD, Geetha Jeyabalan, MD, Judith Lin, MD, Joseph Lombardi, MD, Dan McDevitt, MD, Richard Powell, MD, and Matthew Smeds, MD. Beth Bales
12 Vascular Specialist | July 2023
CAREER
“Please participate in this vitally important survey and learn how your financial package compares to that of other SVS members”
KEITH CALLIGARO
SVS HONORS TWO WITH LIFETIME AWARD
By Beth Bales
The SVS has honored two surgeons—instead of the traditional one—with its highest accolade, the Lifetime Achievement Award. It’s only the third time the Society has done so in the award’s history, said outgoing SVS President Michael Dalsing, MD, who added that presenting this award is “one of my biggest honors” as president. He presented the honorees—Enrico Ascher, MD, professor of surgery at NYU Langone School of Medicine, and Julie Freischlag, MD, formerly dean of Wake Forest University School of Medicine and now chief academic officer of Advocate Health and chief executive officer of Atrium Health Wake Forest Baptist— during VAM 2023. Freischlag is the SVS’ first, and only, woman president to date. Ascher, too, is a former SVS president.

Both Ascher and Freischlag are “exceptionally deserving of this prestigious distinction,” added Dalsing. The award recognizes an individual’s outstanding and sustained contribution to both the profession and the Society.
Enrico Ascher
Ascher has been involved in regional, national and international societies, including as president of the Eastern Vascular Society, the Society for Clinical Vascular Surgery (SCVS), SVS and the World Federation of Vascular Societies (WFVS), which he co-founded. His service to the vascular surgery specialty in general and the SVS in particular, said a longtime colleague, “has been nothing short of spectacular; he has given and continues to give time, effort and resources to our specialty.”
Professor of surgery at New York University Langone School of Medicine, Ascher also has written approximately 340 peer-reviewed publications, including as first, senior and mentoring author to residents and fellows. He has written more than 80 book chapters and served as editorin-chief for the fifth and sixth editions of Haimovici’s
Vascular Surgery
He is considered on the forefront of the endovascular wave, defining the practice in using ultrasound guidance—a low-risk methodology to the patient and operators, said his colleague. Under his leadership, his group published many articles encouraging this technique.
“This innovative technique and others, as indicated by his bibliography, illustrate his innovative approach to issues that plagued vascular surgeons. His academic achievements earned him the respect of his peers, which led to his service on editorial boards and in editorial leadership positions for peer-reviewed
journals. Ascher’s extensive list of invited national and international presentations, membership on editorial boards, and book chapters is indicative of his stature in the vascular surgery community and sustained impact on the specialty for about 40 years.”
For nearly 35 years, he has been involved as a vascular fellowship program director who has founded many annual meetings at which fellows present their research. One of his most important achievements in research presentation is as co-chair—since 2005—of the annual VEITHsymposium, introducing many innovations to the meeting. He recently founded the Frank J. Veith International Society in honor of Frank Veith, MD, his mentor; the Society is holding annual postgraduate meetings and annual competitions for young vascular surgeons from all over the world. Another colleague focused on his mentorship of her, as well as other young vascular surgeons. She met Ascher at a vascular meeting while a general surgery chief resident in the late 1990s, which
“left me completely inspired to pursue a career in vascular surgery.” Ascher has been a mentor and close friend ever since, she added. Through him, she has had numerous opportunities to moderate and present at the Veith Associate Faculty program and to speak at the Frank J. Veith International Society annual meeting. “I can sincerely say that no one else has made such an effort for me as a female in vascular surgery—to give me exposure and support my advancement in the field,” she said. “He makes a person feel valued and inspired at the same time.”
His important contributions to the SVS include using his international ties and position as a world-renowned leader to initiate and later expand the international sessions at VAM. He also supported the development of and co-chaired the WFVS session initiative at the VEITH meeting.
In accepting his award, Ascher thanked “this great society” for this singular recognition. He finalized his brief comments by calling on the vascular community to consider the creation of a network of vascular services that are “able and willing” to serve as regional referral centers. “Think regionalization for complex vascular care,” said Ascher. He also wondered whether it is time to study the possibility of sub-specialization in vascular surgery since the specialty has expanded and matured, and called for better assessment of candidates for vascular residency, including psychological tests.
Julie Freischlag
Freischlag has worn a great many hats in her career: mentor of many, vascular surgeon, researcher, guest speaker, editor, writer, professor, vice chancellor, medical school dean, member of many societies, SVS president, American College of Surgeons president, wife, mother. Currently: chief academic officer of Advocate Health and chief executive officer of Atrium Health Wake Forest
Lifetime Achievement Award recipient. Freischlag is one of the first women in the country to be board-certified in vascular surgery.
“She has impressive leadership skills and, through her various leadership positions in different institutions, exemplifies the vascular surgeon as leader,” said Dalsing. He added that he hoped he could speak for her in saying “she is proud to be one of the first women in vascular surgery, but is even more proud of all the women who have entered the field … since then. She’s been an impressive mentor for so many.”
Said one SVS member: “Dr. Freischlag has also been an active researcher contributing to a large output of manuscripts and receiving several grants. She has also been a sought-after surgeon in her area of expertise of thoracic outlet evaluation and management. Thinking about her contributions, however—her most influential role has been in serving as a role model to numerous women in vascular surgery, making them ‘believe’ in their abilities to reach leadership positions in our field.” He added, “For an award named for ‘Lifetime Achievements,’ it would be hard to find anyone who has achieved more.”
Said another colleague, “Many of the changes that have occurred in the field of vascular surgery, including the increasing role of members of underserved groups in SVS leadership positions, have occurred, in my opinion, because of Julie’s advocacy for them—nominating a diverse group of individuals to leadership positions. Although our Society has a long way to go in becoming fully inclusive, Julie will continue to be their advocate and mentor.”
Another called her “unique with her outsized impact on our specialty of vascular surgery and surgery in general. Julie Freischlag has inspired many women (as well as men) to enter the field of vascular surgery when it was seen primarily as a field for men. She has made major contributions in her area of special clinical interest, thoracic outlet syndrome, and she has been selected to major leadership roles as the dean and vice president of two medical schools, as well as being selected to the highest elected position in American surgery as the president of the ACS.”
Freischlag told the audience that a young woman had asked her the previous day how she stayed in contact with other surgeons and professionals before cell phones and texting, and how they helped each other. “It was the meeting and the connections we made there!” she said. “It was meeting all of you who inspired me to carry on and stay in vascular surgery.”
She advised others to reach for the stars and to “make sure you’re always learning something, you’re making an impact and you’re trying to make [a situation] better and do a good job. Make sure you’re an excellent boss and you’re part of an excellent team.”
13 www.vascularspecialistonline.com
“[Julie Freischlag] has impressive leadership skills, and through her various leadership positions in different institutions exemplifies the vascular surgeon as leader”
MICHAEL DALSING
VASCULAR LEADERS
Michael Dalsing is flanked by awardees Julie Freischlag and Enrico Ascher
VAM 23 THROUGH THE LENS »







14 Vascular Specialist | July 2023
For four days, attendees reveled in the sights and sounds of science, education and fun at VAM 2023 in National Harbor, Maryland. Going clockwise from the far left, Palma Shaw, MD, welcomes her colleagues at the Women’s Leadership Dinner, and then-SVS President Michael Dalsing, MD, and Andres Schanzer, MD, chair of the SVS Program Committee, officially begin the meeting at Wednesday’s Opening Ceremony.








Clockwise from the right, former SVS President Peter Gloviczki, MD, discusses his own transition to retirement; President Dalsing’s grandson, Elliott, points to a familiar, well-loved figure— Opa—up on stage delivering his Presidential Address; Peter Nelson, MD, listens carefully during the E. Stanley Crawford Critical Issues Forum; and Matthew Menard, MD, discusses the BEST-CLI clinical trial results. Wednesday evening’s family-friendly Connect@VAM party drew a crowd—including this group of medical students—happy to have fun after a full day of education; and the large VAM sculptured sign proved a popular “selfie” spot. Wanda Rogers, BSN, RN, CPHQ, of Houston, discusses her Aorta Diagram Project during the Vascular Quality Initiative’s poster and networking reception; representatives of Indiana University healthcare institutions receive VQI Certificates of Achievement from Adam Beck, MD (second from right); and crowds stream downstairs to the opening of the Exhibit Hall.

15 www.vascularspecialistonline.com
Photography by Martin Allred/ Nationwide Photographers
“We are being as inclusive as possible with the hope that our meeting participants look more like the patients we take care of”
ANDRES SCHANZER
SVS FOUNDATION

‘Great Gatsby Gala’ adds flair to Vascular Annual Meeting


 By Marlén Gomez
By Marlén Gomez
THE HIGHLY ANTICIPATED “GREAT GATSBY GALA,” hosted by the SVS Foundation, added a whirlwind of excitement and philanthropy to VAM 2023. The event, held at the same Gaylord National Convention Center venue as VAM, transported attendees back to the era of the legendary literary classic, The Great Gatsby, emulating the parties of the Roaring Twenties.
Gala Committee Co-Chairs Venita Chandra, MD, and Leigh Ann O’Banion, MD, announced during the evening that the third annual Foundation Gala of recent times raised more than $200,000 in support of vascular health.
“An inspiring moment occurred towards the end of the night when everybody raised their paddles and pledged to donate $100,” said O’Banion.
“I didn’t expect to see so many raised, and it was amazing to witness everyone’s willingness to donate once again and support the mission we aimed to accomplish that evening.”
As in previous years, the event was sold out. Chandra noted that ticket sales sold out even earlier than last year’s Gala, serving as a testament to the importance of this event for the Foundation as well as to people’s enjoyable experience in previous years.
The festivities began with a pre-event reception, the Sur-
geon Speakeasy. Attendees enjoyed an open bar, hors d’oeuvres, a jazz band, a photo booth and flapper-girl entertainment. The ambiance complemented the guests’ attire as they embraced the time’s fashions.

“The 1920s theme was a tremendous success,” said Chandra. “It was delightful to see people inspired and dressed appropriately for the occasion, which set a festive atmosphere for the entire Gala. Many got into the theme, but everyone came ready to immerse themselves in the spirit of the Foundation and its mission.”
The evening included a Live Auction, with participants competing for an array of exclusive items and experiences. The night’s most competitive bidding war was for a spot on the annual University of Florida and Women’s Vascular Surgery fishing trip weekend, which was donated by Keith Ozaki, MD.
The Vascular Hero video screening, during which loved ones delivered heartfelt messages to the vascular surgeons in the room, was a standout, emotional moment of the night.
“It served as a reminder that, despite our role as vascular surgeons dedicated to advancing science, we are also children of parents and cherished by our families,” said O’Banion. “The video left many in the room in tears, highlighting
the genuine humanity of vascular surgeons, and honoring their dedication.”
A DJ took the stage to sustain the energetic atmosphere, setting the tone for a night of dancing and merriment. Attendees showcased their best dance moves, bringing the spirit of the 1920s to life and fostering an atmosphere of joy and camaraderie among the vascular surgery ranks.
The festivities continued at another sold-out after-party, with saxophonists and an assortment of other forms of entertainment.
Reflecting on the night’s success, Chandra and O’Banion expressed their deep appreciation to everyone who attended, supported and contributed to the Gala.
“We couldn’t have done it without the collective effort of our amazing Gala Committee,” said Chandra. “Everyone played a vital role in advancing the Foundation’s mission and ensuring a brighter future for vascular health.”
SVS Foundation Vascular Innovation Partners (VIP)
There has been a long history of engagement, leadership and volunteerism of the Stanford Division of Vascular Surgery within the Society for Vascular Surgery We share a common goal of compassionate care for all patients, cutting-edge innovation and research, improving surgical care, and training the next generation of surgeons.

As the SVS seeks to advance excellence and innovation in vascular health around the globe, Stanford Vascular Surgery works to achieve similar values through accomplishments in research, clinical practices, and education Being part of this organization allows our Division to excel to achieve the best outcomes for all vascular care on a much larger scale.

16 Vascular Specialist | July 2023
Learn more at vascular.org/VIP
The Vascular Innovation Partners (VIP) program, a new initiative of the SVS Foundation, consists of institutional partners whose values align with the mission of the Foundation
“An inspiring moment occurred towards the end of the night when everybody raised their padles and pledged to donate $100”
LEIGH ANN O’BANION
Left: Venita Chandra hosts the 2023 Gala, which was also presided over by Leigh Ann O’Banion (top left)
PRESIDENTIAL CITATIONS TRAINING
SVS ANNUAL BUSINESS MEETING WITNESSES SLEW OF AWARDS
 By Beth Bales
By Beth Bales
PART OF THE “BUSINESS” AT THE SVS ANNUAL Business Meeting at VAM includes a large number of honors and recognition. The list for 2023 honors features a slew of Presidential Citations, as each SVS president gets the opportunity to recognize service to the Society during the his or her term of service.
This year’s honorees are: Bernadette Aulivola, William Baker, Nilesh Balar, Bernard (Tim) Baxter, the late Dolores Cikrit, Dawn Coleman, Peter Connolly, William Flynn, Robert Kistner, Timothy Kresowik, Joann Lohr, Elna Masuda, Mark Mattos, Afshin Molkara, Peter Nelson, Vincent Rowe, Palma Shaw, Matthew Sideman, Michael Singh, Malachi Sheahan III and Sunita Srivastava. Learn more about these members’ contributions at vascular.org/PrezCitations23
Sheahan, Vascular Specialist medical editor, was recognized for his “dedication and wit” as editor-in-chief of the SVS monthly newspaper as well as its sister title, VS@VAM, the daily newspaper published at VAM.

The SVS Foundation Mentored Research Career Development Awards (K awards): This program has provided $13 million in funding to 45 vascular surgeon-scientists since 1999. The 2023 awardees are: Samir Shah, K23, University of Florida, for “Outcomes and perspectives on treatment for critical limb ischemia in patients with end-stage renal disease,” and Tammy Nguyen, K08 Award, co-sponsored by the American College of Surgeons, for “Dissecting the human diabetic bone marrow niche.”
Also honored was the 2022 K23 awardee, selected at VAM 2022 in Boston, Jesse Columbo, of Dartmouth Hitchcock
APPROPRIATENESS
Medical Center, for “Comparative effectiveness of procedures for carotid revascularization.”
The Clinical Research Seed Grant was awarded to Miranda Witheford, from the University of Toronto, “Deep learning models of aortic deformation after complex endovascular aneurysm repair to predict endograft failure.”
Distinguished Fellows: The 2023 SVS Distinguished Fellows are: Shipra Arya, Randall DeMartino, Caitlin Hicks, Jeffrey Jim, Grace Wang and Mohamed Zayed.
The Journal of Vascular Surgery presented “Reviewer of the Year” awards for four of its publications, JVS, JVS-Vascular and Lymphatic Disorders (JVS-VL), JVS Cases, Innovations and Techniques (JVS-CIT), and JVS-Vascular Science (JVS-VS) Recipients are:
● JVS: Michael Singh, MD, University of Pittsburgh Medical Center
● JVS-VL: Alvaro Orrego, MD, San Sebastian University, Viña del Mar, Chile
● JVS-CIT: Grayson Pitcher, MD, University of Rochester, Rochester, New York
● JVS-VS: April Boyd, University of Manitoba, Winnipeg, Canada
The Regional Society Political Action Committee Award: The Midwestern Vascular Surgery Society for the third straight year received this award for having the highest participation rate among the regional societies for contributions made in 2022.
Also honored were the five practices with 100% participation for contributions in 2023: Loyola University Medical Center, Indiana University Vascular Surgery, Nashville Vascular and Vein Institute, Midwest Aortic and Vascular Institute, and University of Massachusetts Vascular Surgery.
Physical pain found to be a risk factor for trainee burnout, new survey reveals
A RECENT SURVEY HAS INDICATED THAT PAIN is “prevalent” among vascular surgery trainees and represents a risk factor for burnout. Eric Pillado, MD, MBA, a vascular surgery resident at Northwestern University Feinberg School of Medicine in Chicago, shared this conclusion during the second Vascular and Endovascular Surgery Society (VESS) session at VAM 2023.
Pillado detailed that 527 trainees completed a confidential, voluntary survey, administered after the Vascular Surgery In-Training Examination (VSITE), representing an 82.2% response rate. He revealed that 38% reported moderate-to-severe discomfort/pain after a full day of working, among whom 73.6% reported using ergonomic adjustments and 67% over-the-counter medications. Pillado also communicated that more women tended to report moderate-to-severe pain than men (44.3% vs. 34.5%, p<0.01).
After adjusting for gender, training level, race/ethnicity, mistreatment, and lack of operative autonomy—which the authors describe in their abstract as a proxy for loss of meaning in work— moderate-to-severe pain (odds ratio [OR] 2.52, 95% confidence interval [CI] 1.48–4.26) and using physiotherapy as pain management (OR 3.06, 95% CI 1.02–9.14) were determined to be risk factors for burnout.
In light of these findings, the presenter suggested in his conclusion that programs “should provide ergonomic education and adjuncts, such as posture awareness and microbreaks during surgery, early and throughout training.”—Jocelyn
Hudson
New SVS-ACS Vascular Verification Program verifies first four hospitals
The American College of Surgeons (ACS), with the Society for Vascular Surgery (SVS), has verified the first four hospitals as part of the recently launched Vascular Verification Program (Vascular-VP). To receive verification, these hospitals have shown a commitment to improving outcomes and delivering the best treatment for patients receiving vascular surgical and interventional care in an inpatient setting.
Vascular-VP is an ACS Quality Program developed with the SVS, and leverages the strengths and expertise of the ACS and SVS to provide an evidence-driven, standardized pathway for instituting and growing a quality improvement and clinical care infrastructure within a hospital’s vascular program.
The newly verified hospitals are Albany Medical Center in Albany, New York; The Heart Hospital-Plano in Plano, Texas; Keck Hospital of University of Southern California, Los Angeles; and University of California San Francisco Medical Center in San Francisco.
These four hospitals are verified as comprehensive inpatient centers. The Vascular-VP offers two levels of participation for inpatient hospitals relative to the scope of care provided: comprehensive inpatient and verified inpatient.
“This verification has allowed us to have the support of the American College of Surgeons and the Society for Vascular Surgery in providing the best care to vascular patients,” said R. Clement Darling III, MD, chief of vascular surgery at Albany Medical Center, and chair of the inpatient subcommittee of the Vascular Standards Committee that helped develop Vascular-VP.
“The most important benefit patients get from this program is that they know the hospital in which they are receiv -
ing care is committed to quality and has demonstrated they meet clinical care standards for vascular surgery. It’s not just their own hospital evaluating itself, it’s outside institutions and surgeons who have expertise in evaluating centers.”
Meeting the highest standards of care
To become verified, these hospitals have met the standards outlined in the Optimal Resources for Vascular Surgery and Interventional Care (2023 Inpatient Standards), which addresses elements of vascular surgical care and quality.
standards in surgical quality. These four hospitals are ACS Quality Partners by participating in Vascular-VP.
“We welcome these centers into the ACS Quality Programs. They have shown their commitment to delivering the highest quality care, evaluating that care in a rigorous fashion, and dedicating themselves to continuous improvement,” said ACS Executive Director and CEO Patricia L. Turner, MD, MBA.
R. Clement Darling III
“These four hospitals have, first as pilot sites and now as verified centers, established themselves as leaders in vascular care. They have paved the way for many more hospitals to join us in their journey to continuous improvement by using data and ACS standards and resources to deliver the best possible patient care,” said Clifford Y. Ko, MD, director, ACS Division of Research and Optimal Patient Care.
Becoming an ACS Surgical Quality Partner
As a Vascular-VP verified hospital, these centers also become an ACS Surgical Quality Partner. Being such a quality partner signifies a hospital’s dedication to consistently improving procedures and approaches, while maintaining a critical eye on process at every step. The Surgical Quality Partner designation lets patients know a hospital is dedicated to quality and self-improvement and has been verified or accredited by the ACS. Patients can trust that the care they receive at Surgical Quality Partner hospitals adheres to the most rigorous
Hospitals interested in becoming a verified center and continuing the quality improvement journey of their vascular service are encouraged to apply online at vascular.org/VVPApplication
More information about Vascular-VP is available at vascular.org/VascularVP
17 www.vascularspecialistonline.com
“The most important benefit patients get from this program is that they know the hospital in which they are receiving care is committed to quality and has demonstrated they meet clinical care standards for vascular surgery”
R. CLEMENT DARLING III
Mark Mattos, a citation recipient
SOCIETY BRIEFS
SVS Foundation welcomes two to Board of Directors
BERNADETTE AULIVOLA, MD, AND Vikram Kashyap, MD, have been named to the SVS Foundation Board of Directors.
Aulivola is professor and director of the Division of Vascular Surgery and Endovascular Therapy and medical director of the Vascular Non-invasive Lab for Loyola University Health System’s Stritch School of Medicine near Chicago. She has made significant contributions to the field, particularly in venous disease and aortic aneurysms, and her research endeavors have resulted in numerous publications in medical journals.
Compiled by Beth Bales and Marlén Gomez
RESULTS OF VAM 2023 INTERNATIONAL EVENTS
VAM includes a number of competitive international events, recognizing top-scoring research.
International Young Surgeons Competition
All three tied for first place and received the 2023 Frank J. Veith Award. They are: George A. Ninkovic-Hall, England; “Small abdominal aortic aneurysms under surveillance in the over 80s—a step too far?”
Rodrigo Garza Herrera, MD, Mexico; “Relationship of mobbing and burnout in vascular surgeons”
Titia Sulzer, MS, Netherlands; “Aneurysm-sac dynamics and mid-term outcomes following fenestrated endovascular aneurysm repair after previous endovascular aneurysm repair”
International Poster Session
Leadership in challenging times
JULY’S “SVS PRESENTS” webinar will feature disaster preparedness and leadership challenges. This webinar, the first of two, will be from 7 to 8 p.m. CDT July 12 and will feature two experts discussing their experiences during mass-casualty incidents.
This interview-style webinar will include topics on how leaders can prepare their institution and lessons learned. Register at vascular.org/ SVSPresents071223
Kashyap is Frederik Meijer Endowed Chair of Meijer Heart and Vascular Institute and vice president of Cardiovascular Health for Corewell Health in Grand Rapids, Michigan. With several decades of experience, Kashyap has co-authored more than 200 articles and book chapters.
JVS presentations with simultaneous online publication a ‘hit’
FOR VAM 2023, THE JOURNAL OF Vascular Surgery expanded upon an earlier initiative, publishing 11 research papers as they were presented at VAM.
Program Committee Chair Andres Schanzer, MD, expanded the opportunity to feature not only those authors whose work was accepted for full-length plenary presentations but also rapid-pace plenary presenters as well, reaching out to all of them to encourage participation. The process involved expedited reviews and revisions.
Slides preceding plenaries and other sessions highlighted the program.
The program proved a “hit”and popular with investigators, he said.
Who logged the most steps at VAM?
WITH PLENARIES, SESSIONS AND receptions held throughout the Gaylord National Resort and Convention Center, VAM was the perfect place to hold a preview of sorts for the upcoming SVS Foundation Vascular Health Step Challenge. This was a short and sweet challenge; instead of the 60 miles participants in September will try to walk, the VAM challenge simply logged steps during the four-day meeting.
The top three walkers were Stephanie Vasquez, Melissa Meghpara, DO, and Edward Gifford, MD. All VAM Step participants are already registered for the September challenge, held to coincide with National Peripheral Arterial Disease Awareness Month.
First place: Shuhei Miur, MD, Sapporo, Japan; “Mid-term results of postoperative initial two-day blood-pressure management after endovascular aneurysm repair lowering the Incidence of type II endoleak”
Second place: Yasaswi Vengalasetti, Stanford–, California; “Understanding vascular trauma at a level-one trauma center on Long Island, New York, a protypical American suburb (2015–2021)”
Third place: Wei-Guo Ma, Shanghai, China; “Mid-term outcomes of open thoracoabdominal aortic aneurysm repair following thoracic endovascular aortic repair”
International Fast Talk
First place: Michele Piazza, MD, Padova, Italy; “Effect of narrow paravisceral aorta on target vessel instability after fenestrated-branched endovascular aortic repair”
Second place (tie): Keisuke Miyake, MD, PhD, Ashiya, Japan; “Importance of pedal microcirculation to wounds for wound healing after bypass surgery in chronic Llmbthreatening ischemia”
Second place (tie): Shinsuke Kikuchi, MD, Asahikawa, Japan; “Importance of limb severity on primary graft patency of ipsilateral single saphenous vein grafts for lower-extremity artery bypass in chronic limb-threatening ischemia”

CPVI course
ON OCT. 1 AND 2, THE SVS will host its second annual skills course focused on complex peripheral vascular intervention (CPVI). Medical professionals will gain the necessary skills to become familiar with the latest innovations and techniques in treating patients with peripheral arterial disease (PAD).
Coding workshop
THE SVS’ 2023 CODING AND Reimbursement Workshop will help particiapnts learn about accurate coding and reimbursement for vascular surgery. The intensive two-day program will review essential topics such as recent Current Procedural Terminology (CPT) code and Medicare changes.
An optional workshop on evaluation and management (E/M) codes is being offered to provide participants with a deeper understanding of E/M codes, which are crucial for accurately
Take review course before exams
THOSE PREPARING FOR Vascular Surgery Board examinations can attend the annual “Comprehensive Review and Update of What’s New in Vascular and Endovascular Surgery” from Aug. 23 to 26. Visit vascular.org/ UCLAReviewCourse23
ERIC T. CHOI, MD, has been appointed chairman of surgery at St. Joseph’s Health in Patterson, New Jersey. He joined the center in September 2022 as vice chair of the Department of Surgery for the Division of Vascular Surgery. Before, Choi served as the chief of the Division of Vascular and Endovascular Surgery, co-surgical director of the Temple Heart and Vascular Institute, and professor of surgery at Temple University.
As with last year’s course, participants will learn from expert faculty through a combination of didactic and case-based presentations, as well as hands-on experience. The two-day course will run from 7:30 a.m. to 5:30 p.m. Oct. 1 and from 7:30 a.m. to 4 p.m. on Oct. 2. Visit vascular.org/cpvi23
VESAP5 expires July 14
THE SVS’ FIFTH EDITION OF the Vascular Education and SelfAssessment Program (VESAP5) expires at 9 a.m. CDT July 14 and with it, the possibility of claiming continuing medical education credits.
documenting patient encounters and determining appropriate reimbursement.
The optional workshop will be held from 8 a.m. to 12 p.m. on Oct. 16. The main course will be conducted from 1 to 5 p.m. on Oct. 16 and from 7:30 a.m. to 4:30 p.m. on Oct. 17.
Both the CPVI Skills Course and the Coding and Reimbursement Workshop will be held at the OLC Education & Conference Center, 9400 W. Higgins Road, Rosemont, Illinois.
Visit vascular.org/coding23
Learners can earn credits and obtain certificates until then. Vascular surgeons and trainees can utilize the online program to prepare for qualifying, certification and recertification exams in vascular surgery and to keep up-to-date in the field.
The VESAP5 program was released on July 16, 2020. Those who purchase the VESAP5 comprehensive package—now at up to 50% off—before the expiration date will have access to a non-CME version from July 17 of this year through July 17, 2024.
The educational content will remain accessible even after the CME expiration. Learn more at vascular.org/VESAP5
18
Vascular Specialist | July 2023
SPOT LIGHT
SVS mourns death of Past President Kenneth Wayne Johnston
THE SOCIETY FOR VASCULAR SURGERY (SVS) mourns the death of Kenneth Wayne Johnston, an SVS member, former president and recipient in 2009 of the SVS’ highest honor, the Lifetime Achievement Award.
Barry Rubin, MD, chair and program medical director for the Peter Munk Cardiac Centre for the University Health Network in Toronto, writing with other colleagues, called Johnston “one of Canada’s preeminent and gifted academic surgeons … Dr. Johnston was a visionary leader, educator, researcher and tireless advocate for vascular surgery who cared for his patients with kindness and compassion. His surgical skills were outstanding and always carefully applied and he was a patient teacher of clinical skills to a large cohort of residents and fellows.
“Dr. Johnston’s work ethic was legendary, and he led by example, always contributing, learning and exploring new areas of research to apply to patients with vascular disease. He continuously questioned current dogma and used the scientific approach to develop new diagnostics and therapies and instilled this quest in the trainees who were privileged to work with him. Dr. Johnston set very high standards for himself and strove each day to meet them—we and many others were deeply influenced by watching Dr. Johnston reach those standards and are much better today because of it.”
In the U.S., Johnston played a critical role in brokering the merger of the two American vascular societies to become the SVS, overcoming strong resistance to the merger at the time. He served as vice president and then president, in 2008, leading the development of the SVS’ first strategic plan. He received the SVS Lifetime Achievement Award in 2009, to recognize his outstanding and sustained contributions to the profession of vascular surgery and to the Society itself. He is the only Canadian to ever have received this most prestigious award. He was also Vascular Specialist’s first-ever medical editor.
Said SVS Treasurer Thomas Forbes, MD, a colleague of Johnston: “Wayne was the ultimate vascular surgeon, scholar, leader and educator. More importantly he was a loving family man and trusted mentor, colleague and friend. We all looked to him for his sage advice and wisdom. He will be sorely missed, but we’ll all try to continue his legacy—locally, nationally and internationally.”
Johnston was a pioneer and driving force in the establishment of the Canadian Society for Vascular Surgery 40 years ago, and served as both its secretary and president.

At the University of Toronto, Johnston established the Division of Vascular Surgery and was its inaugural chair, a position he held for more than 20 years. As a teacher and mentor, he established the first vascular surgery training program in Canada and trained a generation of vascular surgeons, many of whom he inspired to go on to have distinguished careers in academic and community medicine. A strong proponent of multidisciplinary approaches to research, he supervised 43 masters and doctoral-level engineers.
Johnston played a major role in setting the standards for ac-
CLINICAL&DEVICENEWS
FDA approves study of ZFEN+ for treatment of aortic aneurysms
The Food and Drug Administration (FDA) has granted approval for Cook Medical to initiate an investigational device exemption (IDE) study on the Zenith fenestrated+ endovascular graft (ZFEN+).The clinical study will assess the safety and effectiveness of the ZFEN+ in combination with the Bentley InnoMed BeGraft balloonexpandable fenestrated endovascular aortic repair (FEVAR) bridging stent graft system for patients with aortic aneurysms involving one or more of the major visceral arteries.
The ZFEN+ is predicated on the commercially available Zenith fenestrated abdominal aortic aneurysm (AAA) endovascular graft, but extends the proximal margin of aneurysmal disease that can be treated endovascularly to include patients with more complex aortic disease. For patients with complex aortic disease, the only established treatment option is open repair.
The ZFEN+ study is prospective and singlearm and includes sites in the U.S. and Europe. The FDA has approved enrollment of the first 30 patients. The primary safety endpoint is a composite measure of device technical success and procedural safety within 30 days. Likewise, the primary effectiveness endpoint is a composite measure of freedom from aneurysmrelated mortality and freedom from clinically significant reintervention through 12 months post procedure.—Jocelyn Hudson
Surmodics receives FDA approval for the SurVeil drug-coated balloon
Surmodics has announced the receipt of FDA approval for the SurVeil drug-coated balloon (DCB).
A company press release notes that the SurVeil DCB may now be marketed and sold in the U.S. for percutaneous transluminal angioplasty after appropriate vessel preparation, of de novo or restenotic lesions (≤180mm in length) in femoral and popliteal arteries having reference vessel diameters of 4mm to 7mm.
“I am excited that the Surveil DCB will be available to treat patients in the U.S.,” said Kenneth Rosenfield, MD, an interventional cardiologist at Massachusetts General Hospital in Boston, co-principal investigator of the TRANSCEND clinical trial.
“The Surveil DCB is the nextgeneration DCB as established by results from the TRANSCEND trial, which is the only head-to-head pivotal study that has been conducted versus the market-leading DCB. The Surveil DCB successfully demonstrated non-inferior safety and effectiveness at two years posttreatment with a substantially lower drug dose.” Clare Tierney
creditation of training in vascular surgery that were adopted by the Royal College of Physicians and Surgeons of Canada. He co-edited the seventh and eight editions of Rutherford’s Vascular Surgery For seven years, he was editor-in-chief of SVS’ peer-reviewed scientific journal, the Journal of Vascular Surgery , and was the first Canadian to be honored with this responsibility.
As a clinical scientist, Johnston’s research greatly improved the care of patients with vascular disease, and his vascular research lab was one of the first in North America. His impact on the understanding and treatment of patients with vascular disease was unparalleled. Johnston published seminal papers detailing the results of the world’s first major prospective study of patients that established the role of balloon angioplasty of the arteries of the legs in treating patients with impaired circulation, preventing disabling pain and amputations. His research changed the way that patients with blocked arteries are treated. This procedure is now recognized internationally as the treatment of choice.
Additionally, in the late 1980s and early 1990s, Johnston led the first and largest Canadian-based multicenter study of abdominal aortic aneurysms in the world.
INDICATIONS FOR USE IN THE U.S.: The GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis is indicated for the treatment of de novo or restenotic lesions found in iliac arteries with reference vessel diameters ranging from 5 mm – 13 mm and lesion lengths up to 110 mm, including lesions at the aortic bifurcation.
CONTRAINDICATIONS: Do not use the GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II. Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available.
19 www.vascularspecialistonline.com
Consult Instructions for Use eifu.goremedical.com Products listed may not be available in all markets. GORE, VBX, VIABAHN and designs are trademarks of W. L. Gore & Associates. © 2021 W. L. Gore & Associates, Inc. 21100151-EN APRIL 2021 OBITUARY
GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis
“Wayne was the penultimate vascular surgeon, scholar, leader and educator”
THOMAS FORBES
Kenneth Wayne Johnston
LONG-TERM DURABLE CLINICAL OUTCOMES IN COMPLEX AORTOILIAC OCCLUSIVE DISEASE
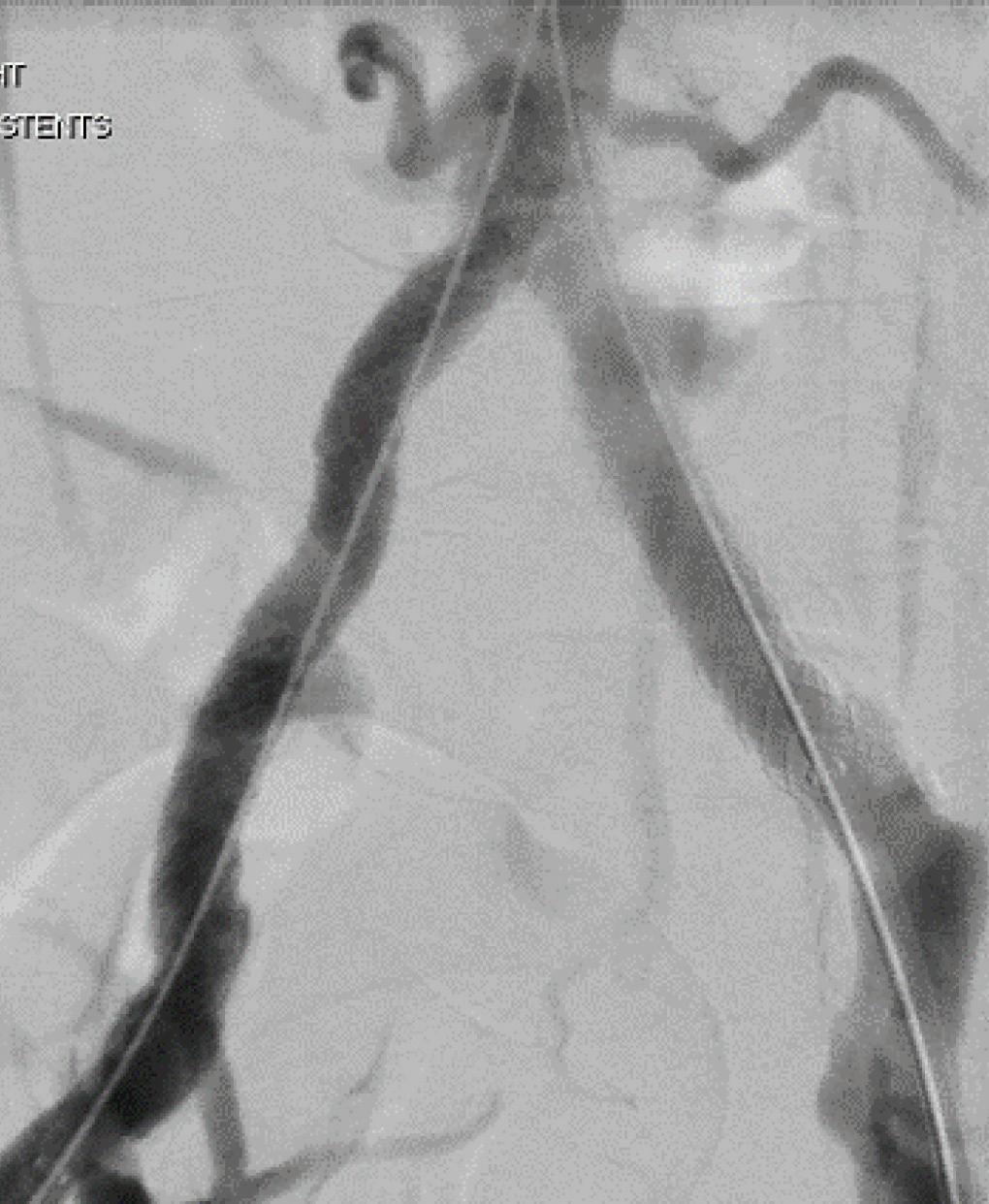
Sustained clinical effectiveness through five years1:

freedom from target lesion revascularization per subject 8.% primary patency per lesion .%


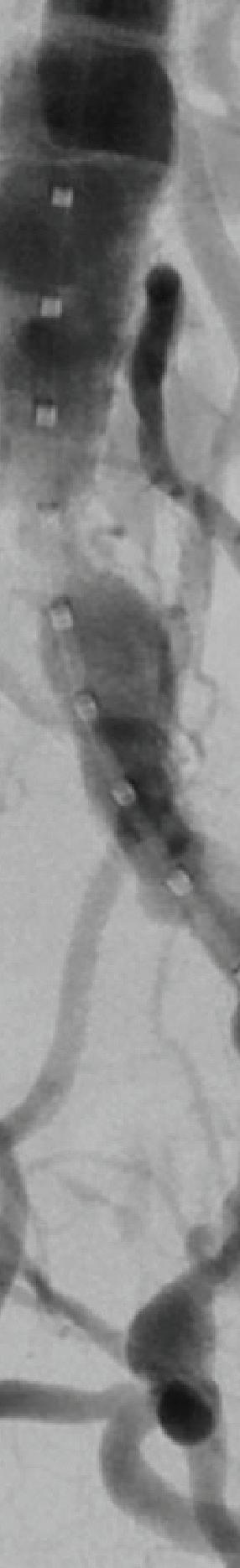
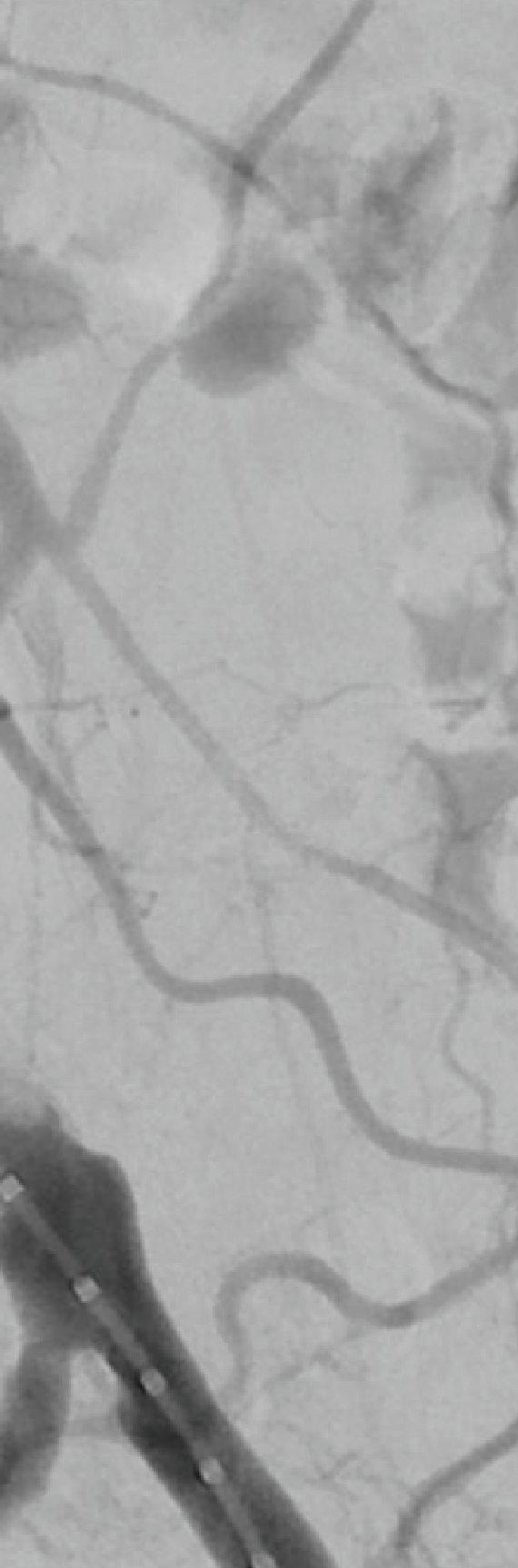
W.












Arizona 86004 goremedical.com
Please see accompanying prescribing information in this journal.
Products listed may not be available in all markets.
GORE, Together, improving life, VBX, VIABAHN and designs are trademarks of W. L. Gore & Associates.





























© 2023 W. L. Gore & Associates, Inc. 23938719-EN APRIL 2023
See the data
After Before
1. Holden A, Takele E, Hill A, et al. Long-term follow-up of subjects with iliac occlusive disease treated with the Viabahn VBX Balloon-Expandable Endoprosthesis. Journal of Endovascular Therapy. In press.
L. Gore & Associates, Inc. Flagstaff,
GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis













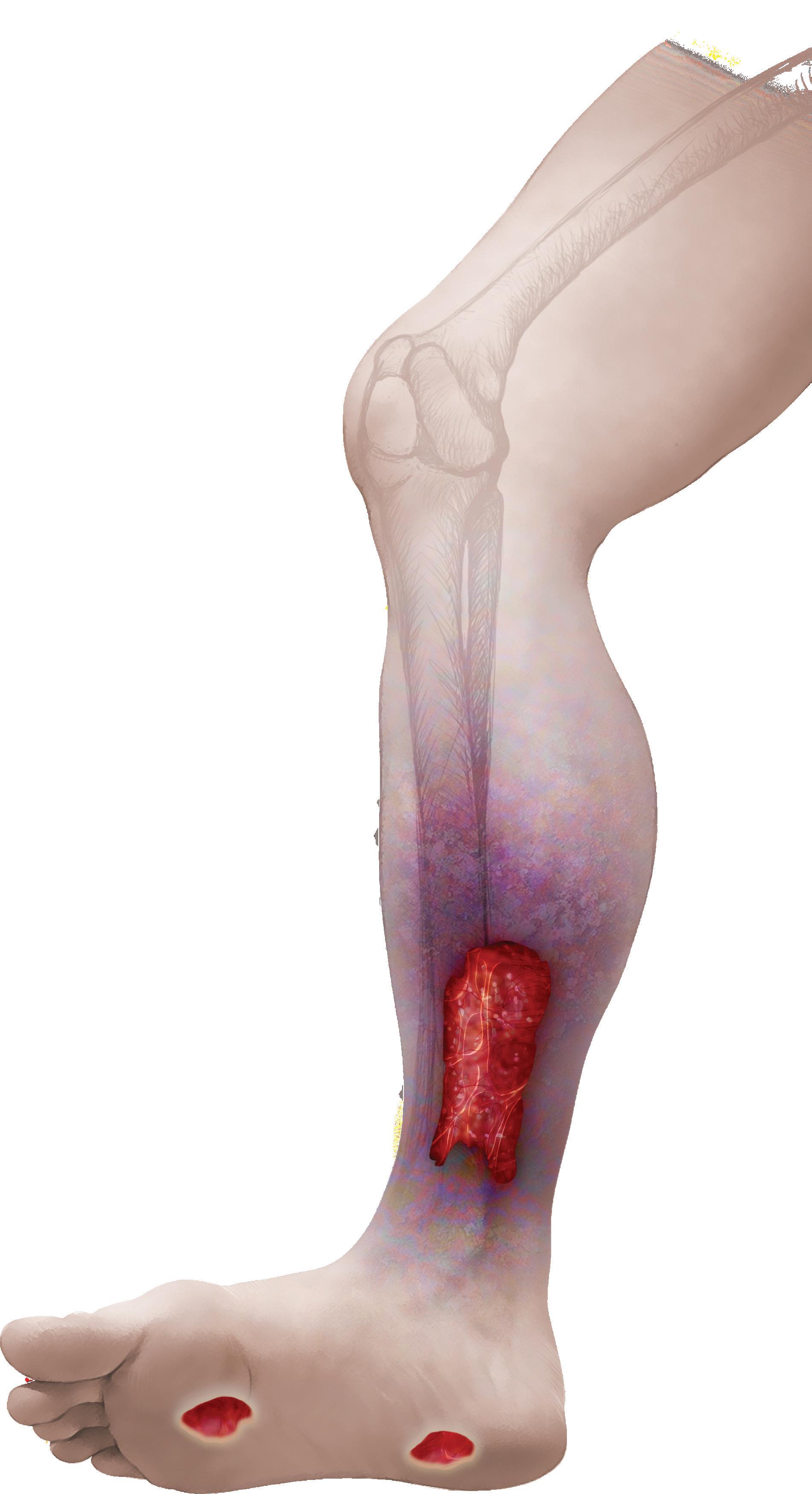










 By Jocelyn Hudson and Marni Davimes
By Jocelyn Hudson and Marni Davimes










































 By Marlén Gomez
By Marlén Gomez



 By Beth Bales
By Beth Bales