7 Career SVS calls on members to participate in financial compensation survey— and help bolster results
13 Elections
The SVS Executive Board breaks down the demographics
15 Venous Disease
Venous valve technologies set to address “large unmet need worldwide”

www.vascularspecialistonline.com
SVS MEMBERS RALLY TO RESPOND TO CMS STENTING COVERAGE EXPANSION

Nearly one-third of the public comments submitted to the Centers for Medicare & Medicaid Services (CMS) on a controversial proposed coverage decision affecting carotid stenting were submitted by SVS members. “We could not have been more pleased with our members’ response to a proposal that we, as a Society, believe will negatively impact patient care, result in unnecessary procedures, and increase the number of strokes across the vascular patient spectrum,” said SVS President Joseph Mills, MD.
Of approximately 760 responses, at least 237 were initially identified as being from SVS members, he said. “There may well be even more.”
e would have fewer untoward side effects, fewer drugs removed from the market by the FDA [Food and Drug Administration], and, ultimately, better outcomes in women,” states Melina R. Kibbe, MD, dean at the University of Virginia School of Medicine, Charlottesville, Virgina, as she reflects on two decades of missed opportunities, the underrepresentation of women as clinical principal investigators (PIs), and women’s under-enrollment as participants in vascular trials. Her statement is far from isolated—underpinned by a growing body of research which addresses key gender inequities in study leadership and participation. Vascular Specialist spoke to prominent names across the global vascular space on their experiences as a PI, meditations on the barriers to access, and the vital work needed to improve diversity across the board.
Mounting data from recent research has spurred widespread review of women’s progression in the vascular field to date. In particular, focus has been placed on how the gender of PIs has affected the balance of male and female participants enrolled in trials. Conducted in April this year, Kibbe et al evaluated 1,427 clinical trials published in the Journal of the American Medical Association (JAMA), The Lancet, and the New England Journal of Med-
See pages 10–11
In July, CMS released a proposed decision that would significantly broaden coverage for percutaneous transluminal angioplasty (PTA) of the carotid artery concurrent with stenting. The proposal would expand Medicare coverage of the procedure to individuals previously only eligible for coverage in clinical trials, remove the limitation of coverage to only high surgical risk individuals, and remove facility standards and approval requirements. The proposal adds shared decision-making with the patient prior to the procedure and allows Medicare Administrative Contractors (MAC) discretion for all other coverage of carotid artery PTA concurrent with stenting not otherwise addressed in the national coverage determination.
Comments were due by Aug. 10. In the weeks prior to that, SVS leaders wrote the Society’s formal comment and embarked on a careful campaign to solicit
See page 4

SEPTEMBER 2023 Volume 19 Number 09
THE OFFICIAL NEWSPAPER OF THE ascularV pecialists CHANGE SERVICE REQUESTED 9400 W. Higgins Road, Suite 315 Rosemont, IL 60018 Presorted Standard U.S. Postage PAID Permit No. 384 Lebanon Jct. KY
2 Guest Editorial Expiation, Karl Wallenda, Oppenheimer and us
In this issue:
“Multifactorial” issues persist in gender representation in vascular leadership and trial enrollment, reports Éva Malpass
“W
CLINICAL TRIALS
When women are PIs: A story foretold on the vascular frontlines
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William
Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek
MD, RPVI, FACS | Professor Hans-
Henning Eckstein, MD | John F. Eidt, MD
| Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS
| Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray
L. Shames, MD | Niten Singh, MD | Frank
J. Veith, MD | Robert Eugene Zierler, MD

Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Director of Marketing &
Communications Bill Maloney
Managing Editor SVS Beth Bales
Marketing & Social Media Manager
Kristin Spencer
Communications Specialist
Marlén Gomez
Expiation, Karl Wallenda, Oppenheimer and us
By Arthur E. Palamara, MD
On March 22, 1978, Karl Wallenda went up on a high wire in Puerto Rico strung between two high-rise buildings. There was no safety net. The winds were blowing hard. A crowd was massed below, awaiting the event. As a seasoned circus performer, he knew that a star never disappoints the crowd. Even at the risk of his own death. He was the founder of the world-renowned family circus troupe called The Great Wallendas, famous for performing daredevil acts without a safety net.
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Roger Greenhalgh
Content Director Urmila Kerslake
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution Jocelyn Hudson, Will Date, Jamie Bell, Éva Malpass and Benjamin Roche
Design Terry Hawes and Wes Mitchell
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe

526 Fulham Road, London SW6 5NR, United Kingdom BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. | The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | POSTMASTER: Send changes of address (with old mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com | For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. | Printed by Ironmark |
©Copyright 2023 by the Society for Vascular Surgery
In 1962, The Great Wallendas began forming their “human pyramid,” a stunt they had been performing for many years. As they made their way to the wire, the pyramid collapsed. Two family members were killed and one was paralyzed. Karl, the patriarch of the family, managed to catch one performer with his legs, saving his life. Karl ultimately fell, broke his ribs, but miraculously survived. Although he continued to perform, the memory of that tragic day haunted him incessantly.
On that day in 1978, standing ringside at Madison Square Garden, I was watching Tito Gaona, renowned aerialist for the Barnum and Bailey Circus, attempt his quadruple somersault. He was a master in his own right, performing the triple somersault so effortlessly that it became boring. He came out of the rotation easily, but his catcher, his cousin Laio Murillo, could not hold on, and Tito fell to the net. As show time approached, they tried four times and gave up.
Tito and his cousin went to their dressing room to change into their costumes. The ringmaster could be heard in the background starting the show. “Ladies and Gentlemen, and children of all ages…” bellowed in the distance. The show had begun. Tito and his cousin came into the doctor’s office, a few paces from the Madison Square Garden arena, waiting for their event. The office was a hangout for entertainers, security guards, executives and whoever passed by to chew the fat, and often to receive a vitamin B shot, which they thought was universally curative. A cheap black-and-white television, perched on the desk, droned mindless blather. As Tito and his cousin entered, programming was interrupted to announce a tragedy that had just occurred in Puerto Rico: the great Karl Wallenda had fallen to his death.
We stood there in stunned silence. The reporter described the scene and attempted to attribute cause. “Karl should have never been up there in the first place; the wire had not been set properly; the winds were too high; he was too old.”
He was a great performer for the ages, he continued.
After several minutes of reflection, Tito broke the silence remarking: “Karl has finally paid for his sin.” It was a statement that seemed incongruous with those offered by the television reporter a few moments earlier. The group standing around the TV performed similar tricks and risked their lives nightly. Clearly their protective confidence had been penetrated by Karl’s death.
Afraid to break reverence of the moment, I mindlessly blurted, “What sin?”
Tito replied, “Karl never dropped his pole. Doing so, he may have killed spectators below. But, had he done that,
he could have pulled himself back onto the wire and saved himself. He knew it was time to pay for his sin”: the human pyramid that had killed members of his family, for which he had never forgiven himself.
Self-reproach takes many forms.
Oppenheimer—both the film and the individual—is a complex depiction of existential choices faced by imperfect men at critical junctures in human history. “Oppie,” as he was called by his friends, was a Jewish scientist and an expert in quantum physics, tasked with the responsibility of creating the atom bomb. He was selected because of his intense desire to avenge the death of Jews in the Nazi concentration camps. J. Robert Oppenheimer was offered the responsibility of creating a weapon so powerful it would redefine warfare. It would also instill existential fear. Like Prometheus, who brought both salvation and fiery destruction to humanity, this weapon would bring hope for ending the war in Japan—but bore the potential of causing cataclysmic destruction to end humanity.
“Could this bomb vaporize the atmosphere?”
Oppenheimer was asked.
“We don’t know, but almost zero probability,” was his reply. Almost zero? Is that the best we can do?
Back then, as Oppenheimer discovers the purpose of the project is to bomb two Japanese cities and end the war, he becomes increasingly despondent. Aware that the 200,000 Japanese casualties will be comprised of combatants and innocents alike, he vigorously opposes creating the far more lethal hydrogen bomb. Rich in symbolism, he names the site for the first detonation, Trinity.
E. Palamara
Oppenheimer has now become the angel of death. Unlike Prometheus, his liver will not be eaten daily by an eagle sent as punishment by Zeus, but his conscience will perpetually search for moral relief. Prometheus’ liver regenerated at night. Oppenheimer woke every day to face the same selfreproach. President Harry S. Truman offered him respite by saying that he didn’t make the decision to drop the bomb and kill those people: “I did! “You only made it!” In that confrontational meeting, an exasperated Truman yelled at his Secretary of War, Henry L. Stimson, to “get that crybaby out of here!” He was referring to Oppenheimer.
As a means of seeking vindication, he appealed to a committee arranged to decide if Oppenheimer should continue his leadership of the Atomic Energy Commission. The committee was ostensibly centered on national security and support for the even deadlier hydrogen bomb. Its real purpose was to get rid of Oppenheimer, a troubled human who realized what he had released into the world.
Before Oppenheimer’s appearance, he bellowed to his wife, “They [the people] must hear this.” The hostile meeting was a surrogate for his anguish. Members of the committee were selected to prevent his continued leadership since he realized that further development of weapons of mass destruction would only hasten mankind’s demise. Anticipating the committee’s decision, his wife said: “They will never give it to you.” What she meant was: they will grant you neither the chairmanship, nor forgiveness.
continued on page 4
2 Vascular Specialist | September 2023
Arthur
GUEST
EDITORIAL
Truman offered him respite by saying that he didn’t make the decision to drop the bomb and kill those people: ‘I did!’

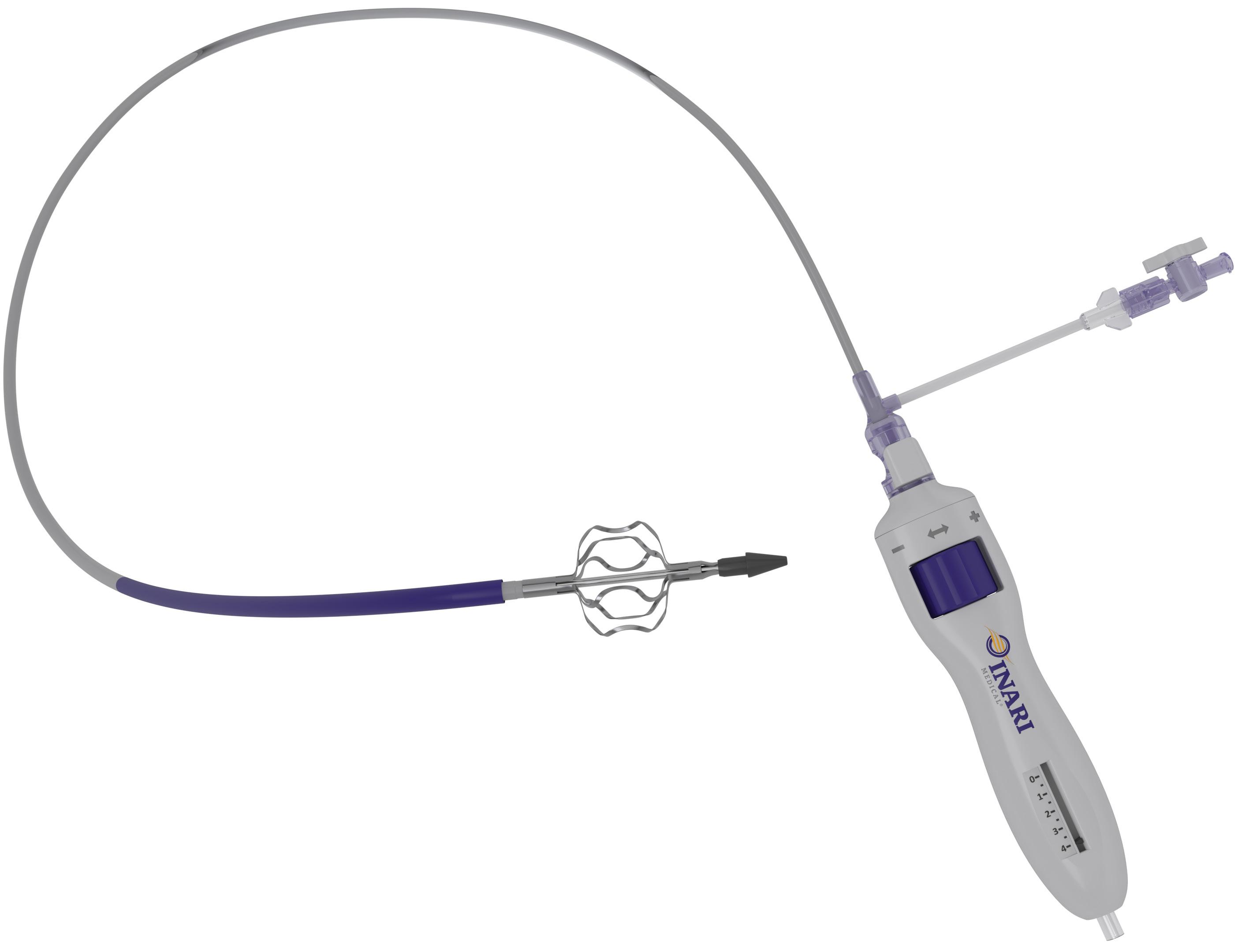
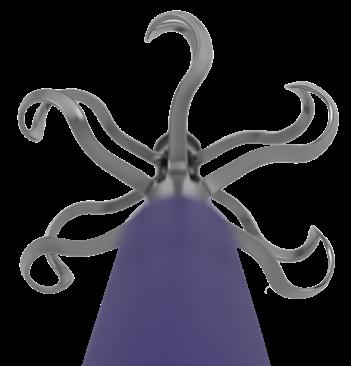
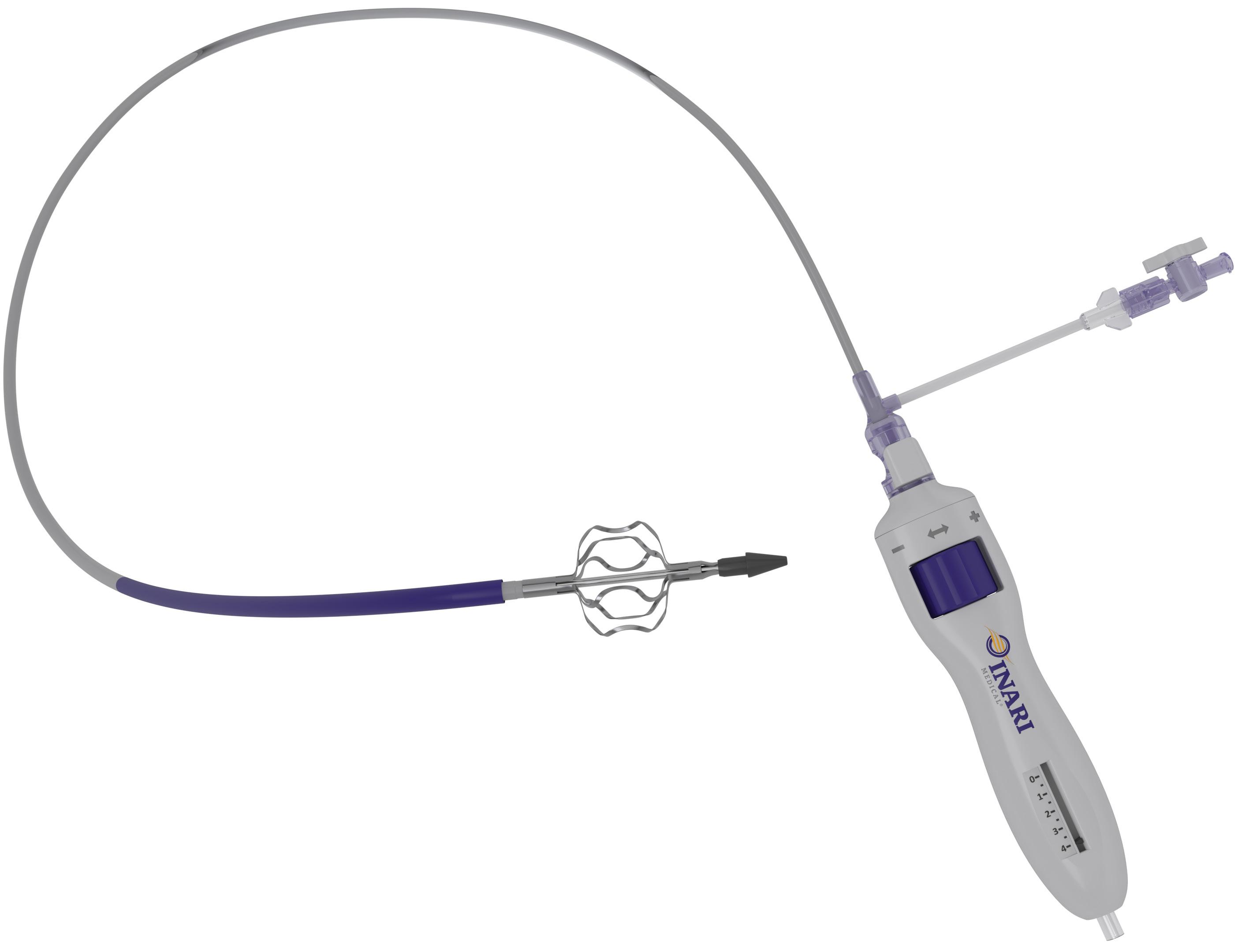
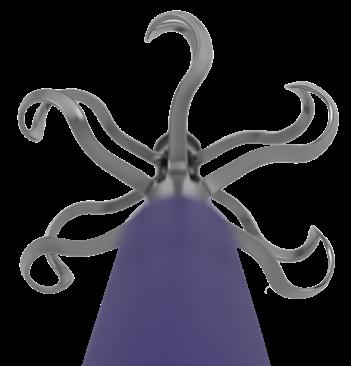
RevCore™
The First Mechanical Thrombectomy Device for Venous Stent Thrombosis Scan to learn more Indications For Use: The RevCore Thrombectomy Catheter is indicated for (1) The non-surgical removal of thrombi and emboli from blood vessels (2) Injection, infusion, and/or aspiration of contrast media and other fluids into or from a blood vessel. The RevCore Thrombectomy Catheter is intended for use in the peripheral vasculature. Refer to IFU for complete Indications for Use, contraindications, warnings, and precautions. Caution: Federal (USA) law restricts this device to sale by or on the order of a physician. All trademarks are property of their respective owners. MM-01624_Rev. B_EN_2023-08-16 6001 Oak Canyon, Suite 100 Irvine, CA 92618-5200 | InariMedical.com
Right Size, Every Time Expandable element to treat vessels 6 - 20 mm in diameter Accurate and immediate torque response in targeted segment
Thrombectomy Catheter
Complete Control
FROM THE COVER: SVS MEMBERS RALLY TO RESPOND TO CMS STENTING COVERAGE EXPANSION
members to add their voices to the discussion.
“We focused on patient safety, because we believe it is at risk if NCD 20.7 is finalized without our issues addressed,” Mills said.
A CMS decision is expected on or before Oct. 6. In its formal response, SVS made three recommendations.
First, mandate utilization of a standardized “shared decision-making” tool that would be designed in collaboration with applicable medical specialty societies and/or other relevant stakeholders.
“Shared decision-making is a vital component of allowing patients to receive a carotid treatment plan that best aligns with their wishes and values. Unfortunately, currently there is no validated carotid decision tool that captures the options offered in contemporary practice that are the subject of this NCD,” the Society said.
Second, revise the proposed decision memo to emphasize the collection of realtime data, paired with the continuation of the credentialing process and requirements for reporting standards. “These elements are critical for ensuring a high degree of patient safety,” the Society commented.
Third, revise the proposed decision memo to include a definition of a “qualified physician” with demonstrated core competency standards relating to carotid stenting. “CMS should work

with relevant stakeholders to develop the core competency standards.”
In its conclusion, the response states the SVS believes the coverage expansion is “premature and jeopardizes patient safety.” If CMS finalizes the proposed expansion of coverage, the letter states, the “finalized memorandum should reflect the outlined recommendations.”
“SVS will continue to actively promote quality and safety for vascular patient care through its published guidelines, appropriate use criteria (AUC) documents, PSO-VQI Registry and other major initiatives such as the Vascular Verification Program. All practitioners caring for patients with vascular disease are encouraged to become familiar with these tools and to utilize them. SVS will continue to develop these resources and make them available.”
Mills pointed out that, among other concerns, clinical trial data from the Carotid Revascularization and Medical Management for Asymptomatic Carotid Stenosis (CREST-2) trial have yet to be released, and such a major expansion of coverage should not be implemented until data have been released and analyzed.
“Our primary focus remains, as it always has been, patient safety,” he said. “We are not anti-stent in the appropriate patient and setting. The sheer number and depth of responses from our members demonstrate the firm commitment of SVS members to quality and safety in the care of patients with vascular disease.”—Beth
Bales
Read about the proposed decision at vascular. org/CarotidNCD. Read the formal response at vascular.org/NCDResponse
GUEST EDITORIAL EXPIATION, KARL WALLENDA, OPPENHEIMER AND US
continued from page 2
continued from page 1
SVS MEMBERS CONTRIBUTE INDIVIDUAL COMMENTS
Members of the Society were among the individuals and organizations who contributed comments to the proposed carotid stenting coverage expansion by CMS. A sample follows:
Edward Gifford, MD, Hartford HealthCare, Hartford, Connecticut
“As a young vascular surgeon, I feel this proposed decision does not do enough to monitor for the safety of patients after removing previous guardrails for carotid artery stenting. I feel that transfemoral stenting (TF-CAS] has a role in carotid stenosis. However, on the whole, our threshold to intervene on asymptomatic disease has only increased as medical therapy advances.”
Katharine McGinigle, MD, University of North Carolina at Chapel Hill
“Before the new level 1 data is available, I do not think that it is appropriate to change practice patterns. I am in agreement with the Society for Vascular Surgery that the coverage expansion in CMS’ proposed decision memo regarding NCD 20.7 is premature and jeopardizes patient safety.”
Robert Molnar, MD, Michigan Vascular Center, Flint, Michigan
“Not only is [NCD 20.7] premature, given the pending CREST-2 trial, which specifically will address the outcomes of TF-CAS with best medical therapy, but it completely removes common sense safeguards needed to allow for all-inclusive TF-CAS.”
Elsie Gyang Ross, MD, University of California San Diego (UCSD)
“With the expansion, we will likely see new outpatient ‘stroke prevention centers’ whereby a number of specialists who can navigate to the carotid and place a stent will do so, without the true consideration of patient risk. It is an unfortunate byproduct of healthcare today in the U.S.”
Ali Azizzadeh, MD, Cedars-Sinai Medical Center, Los Angeles
“Since the level 1 evidence regarding the use of TF-CAS, particularly in standard-risk patients, is evolving, it seems that it is too premature to jump to approval of TF-CAS, even in high-risk patients, and I would disagree with the decision memo.”
Predictably, he was rejected. How does this apply to vascular surgery? Some years ago, my partner and I performed an open aneurysm repair on a healthy 60-year-old male. The patient worked out every day and was a prominent lawyer in the community. The operation went along flawlessly: the graft was sewn in and the retroperitoneum closed. Heparin was reversed with protamine with no issue. Vital signs were stable. My partner scrubbed out to enter post-op orders. The anesthesiologist asked if I wanted to return the cell-saved blood. Although we had not lost much, I reasoned that it was his blood and would make his recovery that much easier. I agreed and the perfusionist spun down the blood and began the infusion. At that moment, disaster struck.
His blood pressure and saturation fell to zero. We immediately performed a transesophageal echocardiogram. The
images were staggering. Both atria and ventricles were filled with clot, as were the pulmonary artery and aorta. The patient had suddenly clotted his vascular system for no apparent reason. We thought of extracorporeal membrane oxygenation (ECMO), but there was literally nothing to be done.
We called around the country seeking information or if anyone had ever experienced a similar complication. A professor at Emory in Atlanta suggested antiphospholipid antibody syndrome or pre-formed anti-heparin antibodies. Our hospital did an investigation and came up with nothing. We met with the widow multiple times and tried (but failed) to give her an explanation.
Understandably, the wife obtained the best malpractice law firm in the area. When I received the intent-to-sue letter, I did something I had never done before and called the attorney. I told him that I had no
idea why that patient clotted his heart, that I had never seen that happen before, and that I hoped to never see it again. I told him of the research that we did and that, if his experts had any insight, to please share it. We never heard from him again.
The renowned Boston vascular surgeon, Alan Callow, used to say that the ghosts of our failures parade around our bed at night. Yet, every patient we place on the operating table is put at risk. It takes a special person to accept this heavy responsibility, and we all carry the emotional burden of our failures. How we seek expiation is a matter of personal accommodation. A resident who worked with Dr. Charles Bailey, a pioneer in pediatric cardiac bypass surgery in the 1950s, told me that Bailey lost his first 74 patients. The resident approached Dr. Bailey, asking: “Dr. Bailey, don’t you think we should stop?” Bailey responded: “No! We are close!” The 75th patient survived.
I’m not sure that many of us would have had the callousness to continue after losing 74 patients, nor would it even be possible today. But we surgeons all face similar responsibilities and bear the weight of our failures. And somehow, we return to the operating room the next day wizened, but humbled. To survive, we either develop emotional callousness, or realize that the good we do for most patients outweighs our failures. Or both.
Before he accepted the leadership of the atom bomb project, Albert Einstein asked Oppie: “Do you think you will be able to handle the consequences?” Oppenheimer did not answer.
As each practitioner seeks their own reconciliation, we acknowledge that our choice is not an easy profession—replete with gratification but often humbling.
4 Vascular Specialist | September 2023
ARTHUR E. PALAMARA, MD, is a vascular surgeon in Hollywood, Florida.
➽








EXPAND YOUR PAD TREATMENT OPTIONS T: +86.755.8358.0181 F: +86.755.8358.0169 www.OrbusNeich.com 1 Jinkui Road, Futian Free Trade Zone, Shenzhen, 518038, China *Manufactured by: T: 651.259.1600 F: 612.677.3355 877.274.0901 www.csi360.com 1225 Old Hwy 8 NW St. Paul, MN 55112 Distributed by: CSI®, Diamondback 360®, Shepherd®, ViperCath , and ViperCross are trademarks of Cardiovascular Systems, Inc. © 2023 Cardiovascular Systems, Inc. MAT-0348 0723. JADE, Sapphire and OrbusNeich are registered trademarks of OrbusNeich Medical Group Holdings Limited or its affiliates. © 2023 OrbusNeich Medical Group Holdings Limited or its affiliates. All Rights Reserved. Diamondback 360® Peripheral Orbital Atherectomy System Diamondback 360® Peripheral Orbital Atherectomy System ViperCath™ XC Peripheral Exchange Catheter JADE® PTA Balloon Catheters* Sapphire® II PRO 1.00 mm Balloon* ViperCross™ Support Catheter 2.00 mm Max Crown Shepherd® Peripheral Guidewires Available in radial and standard length. Exchangeable Series CSI IS NOW ABBOTT.

SVS URGES MEMBERS TO TAKE PART IN COMPENSATION SURVEY— AND BOLSTER RESULTS
By Bryan Kay
Organizers behind an SVS-commissioned financial compensation survey are calling on more members to fill out the short list of questions so that they can break a key 20% response-rate target and begin to publish data gleaned from participants. Any member completing the survey can learn the results, but the goal is to inform the entire membership of the results, they emphasized.
Keith Calligaro, MD, chair of the SVS Compensation Task Force that developed the survey, highlighted the potential value of the data the survey is designed to produce: robust demographic statistics around vascular surgeon salaries and employment conditions. Calligaro also sought to allay confidentiality concerns expressed by some members related to the information they provide in the survey, which is being carried out in partnership with Phairify, a medical profession-focused data collection platform.
“Over the last few years, many SVS members have noted that when vascular surgeons apply for a job somewhere—whether after completing a fellowship or a mid-career move—they are not sure what to expect in terms of financial compensation. This survey will help in terms of dealing with future employers, what to expect
SVS FOUNDATION

and maybe even what to ask for,” he explained.
“We want to emphasize this is confidential information. There is no way anyone can find out which individual is filling out the survey. That’s been one concern we have heard about. People are concerned their responses will somehow be public information, which is not true.”
The point of the survey is to ask questions in key areas around annual salaries, Calligaro said. “What is your annual salary? How old are you? Salaries might vary on age. How many years have you been in clinical practice? Do you identify as a man or a woman? Where do you work? If you work in Philadelphia, do you get paid less or more than if you work in a small hospital in Iowa?
“There are about 25 questions, which are very basic and preliminary. We also created templates for those wishing to learn more about particular issues, such as being on call or serving as a medicolegal expert. If you fill out that template, you get access to the results.”
The crux is this, continued Calligaro: “Twenty percent of the members have to fill out the survey before we can publish anything and allow all members to know the results.”
In essence, in order for
the SVS to publish any type of results, a 20% completion rate is required for scientific validity in the publication environment—and filling out the list of questions should take no longer than 10–15 minutes, Calligaro added.
Phairify is working on the logistics to have office hours available to help each individual completing the survey access the data, the SVS pointed out. Once the process is ready, the Society will make an announcement.
“Our members get inundated with surveys, and we understand that,” Calligaro
said. “However, the latest figure we have is that only 10% of members have completed the survey, and we’re trying to build that up to at least 20%. If so, then I see the number of participants exploding because then we can start showing the results to all of the members.”
The survey was launched at VAM 2023, which took place at National Harbor, Maryland, in June. Members can participate by visiting vascular.org/CompensationStudy2023

Members of the Compensation Task Force include Calligaro as chair; Bernadette Aulivola, MD; Ali Azizzadeh, MD; Sara Duson, MD; Geetha Jeyabalan, MD; Judith Lin, MD; Joseph Lombardi, MD; Dan McDevitt, MD; Richard Powell, MD; Matthew Smeds, MD; Mark Kristiansen, co-founder and CEO at Phairify; G. Randall Green, MD, of Phairify; Reva Bhushan, SVS director of clinical guidelines and quality practice; Carrie McGraw, SVS manager of quality improvement and practice; and Jim Wadzinski, SVS assistant executive director.
‘Voices of Vascular’ attracts national recognition with diversity award
“VOICES OF VASCULAR,” AN INITIATIVE TO highlight the diverse voices within the SVS, has earned the Society and the SVS Foundation a Profile of Excellence Award from the American Association of Medical Society Executives.


Catherine Lampi, the Foundation’s director of development, accepted the award on behalf of the Society, in the “diversity, equity and inclusion” (DEI) category, at the AAMSE conference, which took place in mid-July.
The annual awards program recognizes member organizations that have achieved excellence in one of several categories: DEI, advocacy, communications, education, membership and leadership.
Voices of Vascular honors several months of diversity throughout the year, including Black History Month in February; Women’s History Month in March; Asian Ameri-

can and Pacific Islander Heritage Month in April; Pride Month in June; and National Hispanic Heritage Month, which runs from Sept. 15 through Oct. 15.
During each of the given months, the SVS and the Foundation share important facts about the groups to spread awareness. The campaign also involves posting profiles of SVS members and, on occasion, patients too.
“Every person has a story,” said Foundation Chair and Immediate Past President Michael Dalsing, MD. “Voices of Vascular shares our members’ stories and experiences, not only as a vascular surgeon, but

also as a member of a particular group. The initiative has proved very popular and insightful.”
During June, Pride Month, Eric Pillado, MD, an integrated vascular surgery resident at Northwestern University in Chicago, shared his life’s story.
“I think the future of vascular involves Pride Month, making sure all our patients, regardless of their background, are included, and the future of vascular surgery involves providers of various backgrounds being included in our specialty.”—Beth Bales
Visit Voices of Vascular at vascular.org/ VoicesofVascular.
7 www.vascularspecialistonline.com
“The latest figure we have is that only 10% of members have completed the survey, and we’re trying to build that up to at least 20%”
KEITH CALLIGARO
CAREER
I think the future of vascular involves Pride Month making sure all our patients regardless of the r background are inc uded and the future of vascular surgery involves providers of var ous backgrounds being included in our specialty
Eric Pillado, MD
A Voices of Vascular posting % of SVS members who have responded so far: 10% % required for scientific validity: 20%
Keith Calligaro
‘FDA’S MISSION TO BRING SAFE AND EFFECTIVE VASCULAR SURGERY DEVICES TO MARKET REMAINS STEADFAST’
The Vascular and Endovascular Devices Team (VEDT) in the Food and Drug Administration (FDA) Office of Cardiovascular Devices appreciates the Vascular Specialist editorial board’s offer to provide an update to the vascular community to enhance regulatory transparency and communication. In this commentary, Ronald M. Fairman, MD, Gordon Bryson, Carmen Gacchina Johnson, PhD, and Andrew Farb, MD, cover COVID-19’s impact on the team’s work, pre- and post-market data collection, physician-sponsored investigational device exemption (PS-IDE) studies, and ongoing collaborations to support timely access of innovative devices to U.S. patients. The authors are responding to a report—“Getting medical devices to market: The future might not be now, says regulatory expert”—carried in the April issue of Vascular Specialist.
The COVID-19 pandemic broadly impacted the vascular community, notably numerous challenges to initiating new and conducting ongoing medical device studies. One important example was the difficulty investigators and device manufacturers faced maintaining subject follow-up compliance to collect complete and meaningful information in support of future device marketing applications. Despite the challenges during this time, sustained collaboration between FDA review staff and study sponsors helped assure access to innovative vascular surgery devices (e.g., ascending, aortic arch, descending thoracic and thoracoabdominal aortic devices).
Two recent examples include FDA approval of the first frozen elephant trunk platform, and the first single-branch thoracic endoprosthesis for endovascular repair of descending thoracic aortic lesions that maintains blood flow into the left subclavian artery.
Despite the challenges posed by COVID-19, the Office of Cardiovascular Devices worked diligently with industry sponsors to ensure novel, safe and effective devices reached the U.S. patients. In addition, there are multiple actively enrolling studies at U.S. sites for devices placed in the ascending aorta, aortic arch and thoracoabdominal aorta to treat diverse aortic pathologies.
Given the limitations in maintaining patient follow-up compliance during the
COVID-19 pandemic, as well as experience with prior studies (e.g., challenges in longer-term data collection, strict selection criteria in studies not reflecting real-world device use), and in consideration of our commitment to commercialize lifesaving new therapies in a timely manner, VEDT re-evaluated our approach to postmarket studies.
Applying the appropriate pre-market and post-market data collection balance facilitates timely patient access to important new technology without undermining patient safety. As such, there have been new efforts to identify areas for improvement in post-market data collection.
Long-term safety
On Nov. 3, 2021, the FDA held a public meeting of the Circulatory System Devices Panel of the Medical Devices Advisory Committee to obtain advice and recommendations on the long-term safety and effectiveness of endovascular aneurysm repair (EVAR). This meeting included industry sponsors, investigators, patient advocate organizations, and physician experts.
After the panel meeting, the FDA issued a letter to healthcare providers in February 2022 and has been involved in dedicated efforts to gain alignment with stakeholders on ways to strengthen post-market data collection, which are intended to allow
for a better understanding of long-term outcomes with EVAR devices, help identify safety signals, and potentially support labeling expansions.
Independent of these post-market activities, it is important to address concerns regarding PS-IDEs evaluating the performance of devices in the thoracoabdominal aorta. These PS-IDEs typically study commercially available devices that are physician-modified or used for a new intended use, or devices that are commercially available outside of the U.S. If physician modification of a commercial aortic device or use of a commercial device for a new indication is being done on a routine basis, we continue to recommend an IDE should be submitted.
We recognize that there are patients with complex life-threatening aortic pathologies, and PS-IDEs are an option that has been utilized to allow access to new devices or approved devices for new indications, particularly for treatment of thoracoabdominal aortic aneurysms. PSIDEs have helped advance device design, management of bridging stent instability, patient selection, management, and prevention of spinal cord ischemia.
PS-IDEs have also refined strategies to reduce radiation exposure, improve imaging, and guide accessory device use. The results of many of these studies have been published in the Journal of Vascular Surgery (JVS) and presented at the SVS’ Vascular Annual Meeting (VAM). VEDT currently has over 30 approved PS-IDEs, and the number has been growing annually.
There are some regulatory concerns regarding PS-IDEs that can impact the availability of new beneficial therapies for patients. Typically, PS-IDEs are of limited
performance, the devices studied (and their physician modifications) remain investigational, and the devices are not available to treat many U.S. patients with the target clinical condition.
To address this issue, we are collaborating with investigators and manufacturers on physician-sponsored and industry-sponsored feasibility and pivotal IDE studies that will support device approval so that new safe and effective devices are available to all U.S. patients.
There has been communication with industry and physician sponsors to discuss the future of PS-IDEs and alignment on plans to bring these life-saving aortic devices to market in a timely manner. These plans include the following:
The FDA continues to consider access to devices through PS-IDEs as long as adequate information is provided to support the IDEs (e.g., non-clinical information, individual investigator experience). When there is significant interest in device access, efforts are underway to pursue manufacturersponsored studies and/or marketing applications in a timely manner.
Device manufacturers and the FDA are working together to limit the number of PS-IDEs so as not to create situations that would in effect constitute commercializing an investigational device.
Stakeholders are collaborating to determine if existing data are adequate to support pivotal studies or marketing applications.
Emerging technology
The FDA is encouraging physicians treating patients with unmet clinical needs to engage in pivotal studies for nextgeneration devices.
As illustrated in the above framework, the FDA remains committed to promoting timely access to safe and effective devices. The FDA remains supportive of PSIDEs when appropriately justified, and we would like to assure the community that there have been no measures to halt existing PS-IDEs provided the results are encouraging.
We are regularly accessible to practicing physicians to discuss unmet needs of their patients and how we may work together to address them, and we encourage engagement with the FDA on such proposals through the Q-submission process.
size and scope and do not collect the definitive data needed for device approval (a reasonable assurance of safety and effectiveness).
Further, PS-IDEs may have little or no industry support, such that non-clinical testing and manufacturing requirements are not met to support a marketing application. As a result, although PS-IDEs can provide important insights into device
We are also currently working with the SVS on updates to the PS-IDE template for treatment of complex aortic pathologies. We encourage physicians who may pursue a PS-IDE to obtain the template from the Society (vascular@vascularsociety.org) as it provides a clear outline, pre-populated content, and suggestions for providing study-specific information.
We acknowledge there are increasing numbers of well-trained physicians with experience and sophisticated skills treating patients with complex aortic pathologies
8 Vascular Specialist | September 2023
COMMENT& ANALYSIS FOOD AND DRUG
ADMINISTRATION
We recognize that there are patients with complex life-threatening aortic pathologies, and PS-IDEs are an option that has been utilized to allow access to new devices or approved devices for new indications
using investigational or modified devices. Yet, after leaving their training programs where they may have used devices under an IDE, physicians may experience limitations to access investigational devices and techniques for endovascular treatment of complex cases.
The FDA does not encourage physician modifications of commercialized

endovascular grafts, but notes that the routine practice of physician modification of devices should be conducted under an IDE.
VEDT is hopeful that the need for physician-modified devices will be substantially decreased as device manufacturers pursue clinical studies for devices meeting patient needs and as
devices currently under study come to market with data to support a reasonable assurance of safety and effectiveness.
Steadfast commitment
In summary, the FDA Office of Cardiovascular Devices is focused on supporting and enhancing patients’ timely access to safe and effective cardiovascular devices. The FDA’s mission, enthusiasm, and the commitment of VEDT to advance medical device innovation to bring safe and effective vascular surgery devices to market—thereby supporting and improving public health—remain steadfast.

We seek efficient clinical studies and commercialization of innovative technology addressing unmet needs for U.S. patients, and we are engaged with external stakeholders to navigate paths to achieve these goals.
Continued stakeholder collaboration on pivotal studies, marketing applications, and robust post-market data collection plans are critical to get devices to market to address unmet needs.
We are dedicated to working with all stakeholders in order to bring life-saving and innovative devices to the U.S. market to benefit patients.
It was a pleasure for many VEDT reviewers to participate in the recent VAM 2023 and engage with many of you. We look forward to the ongoing collaborations. Thank you again for this opportunity to reach out to the broader vascular community with this update.
DISCLAIMER: This article reflects the views of the authors and should not be construed to represent the FDA’s views or policies. Ronald M. Fairman is the FDA’s VEDT medical officer and a former SVS president. Gordon Bryson is an FDA biomedical engineer; Carmen Gacchina Johnson the organization’s assistant director for vascular and endovascular devices; and Andrew Farb its chief medical officer in the Division of Cardiovascular Devices.
www.vascularspecialistonline.com 9
We seek efficient clinical studies and commercialization of innovative technology addressing unmet needs for U.S. patients, and we are engaged with external stakeholders to navigate paths to achieve these goals
The FDA encourages physicians treating patients with unmet clinical needs to engage in pivotal studies for next-generation devices
icine (NEJM), from January 1, 2015, to December 31, 2019, to determine if women’s enrollment in research correlated with the gender of first and/or senior authors. Their results showed a positive correlation between female enrollees and female first and senior authors (51.7% vs. 48.3%, p≤0.0001)—an association which endured in subset analyses by funding source, phase, randomization for study participants, drug and/or device trial, and geographic location.

Kibbe et al’s results uncover a deficit in both leadership and enrollment which poses crucial challenges to obtaining accurate research outcomes for women and underrepresented minorities (URMs). Adding detail to this, Kathleen Ozsvath, MD, president-elect of the Eastern Vascular Society (EVS), from St Peters Health Partners in Albany, New York, tells Vascular Specialist of the fundamental anatomical differences, presentation to care, and symptom manifestation—such as acute myocardial infarction, she adds— that differ between women and men in vascular treatment. Ozsvath notes that “these differences are yet to be better understood,” a statement echoed by Caitlin Hicks, MD, associate fellowship program director at Johns Hopkins in Baltimore, Maryland, who says that gender-based differences have “only just” begun to gain attention in vascular surgical outcomes, “despite being present for decades.”
Considering the results of her review, “no,” is Kibbe’s resounding response when reflecting on whether current journal and society efforts are sufficient in promoting diversity and inclusion. Hicks observes the SVS’ “concerted effort over the last few years to improve equity in a wide range of vascular-related initiatives,” but there remains, she adds, a “persistent gender gap in clinical trial PIs,” despite how “critically important” rectification of enrollment inequities is. Moreover, Palma Shaw, MD, professor of surgery at the State University of New York in Albany, New York, and president-elect of the International Society for Endovascular Specialists (ISEVS), delineates that “opportunities for women’s advancement differs in each society, but regional vascular societies have been more progressive”—although when looking nationally, progression is “much slower.” Shaw continues: “Some journals have made an intentional effort to increase the number of female and underrepresented minorities as reviewers and editors. The #Medbikini movement triggered a much-needed change.”
A watershed dressed in a bikini
In 2020, #Medbikini marked a watershed, exposing the deepening inequities that have been slow to change. The hashtag arose after an abstract, entitled “Prevalence of unprofessional social media content among young vascular surgeons,” published in the Journal of Vascular Surgery (JVS), was shared online. Labeling bikinis “inappropriate attire,” the study warned that posting pictures wearing one could be viewed as “potentially unpro-
continued from page 1
fessional.” This ignited a viral response on Twitter and Instagram under the hashtag #Medbikini, seeing women and men across specialties post themselves in bikinis or casual attire in shared criticism of biased targeting of women in vascular surgery.
The virality of the movement undoubtedly reflected back an uncomfortable truth for vascular societies and institutions, which
tems in Vascular Surgery at the 2022 Vascular Annual Meeting (VAM) given by Imani E. McElroy, MD, from Harvard University, in Cambridge, Massachusetts and Carla C. Moreira, MD, from Brown University in Providence, Rhode Island, “shockingly low attendance” by both members and leaders was reported, leaving the few attendees feeling as if they had “witnessed a fumble at a one-yard line.” The subsequent social media backlash drew a brief statement from the SVS committing to continued prioritization of DEI principles to address shortcomings.
This year, at VAM 2023, the E. Stanley
are still “a fraction of the membership within vascular societies” today. This detail sits amid an international rise in the number of women in the vascular field, yet runs parallel to a wealth of new research which reports how this increase does not translate to equitable gender distribution in roles of high-level seniority or decision-making in both academia and clinical care.
A retrospective review conducted in 2021 by Misty D. Humphries, MD, of UC Davis Health in Sacramento, California, et al—including Julie A. Freischlag, MD, the first and still only ever woman SVS president, and
began installing strategies to support women and URMs seeking equal opportunities in research and clinical progression. In 2019, Kim Hodgson, MD, then SVS president, established the SVS Diversity, Equity and Inclusion (DEI) Task Force. Late in 2020, as the Task Force was morphing into a committee, leaders asked members to complete a census to survey demographics and member priorities.
In a review of the dedicated DEI session named Building Diversity and Equitable Sys-
Crawford Critical Issues Forum raised continued concerns over workforce maldistribution relating to the SVS’ DEI declaration, which states support of “a diverse workforce with equal opportunities.” Addressing the panel, Rana Afifi, MD, associate professor of vascular surgery at McGovern Medical School, University of Texas Health Houston in Houston, Texas, maintained how data presented by former SVS president Michel S. Makaroun, MD, from the University of Pittsburgh Medical Center in Pittsburgh, Pennsylvania—whose talk concerned insufficient numbers in the workforce pipeline—do not represent her.
After graduating from her residency-fellowship outside of the U.S., Afifi was told after “PGY-11 years” to repeat her residency when seeking a path toward U.S. Board certification, she related from the VAM floor. Afifi asserted that others too must be “struggling,” and “are broken because they feel inadequate,” highlighting key “problems” in the handling of DEI matters relating to the vascular workforce.
Slow progress to seniority
“Times are changing with an interest and awareness of DEI,” Ozsvath asserts, punctuating her optimism with the fact that women
CEO of Atrium Health Wake Forest Baptist, Winston-Salem, North Carolina—found that between 1999–2009 and 2010–2019, the mean percentage of women who presented abstracts at five U.S. regional and national societies “increased significantly” from 10.9% to 20.6%. However, increases in the number of women as senior authors and committee chairs remained statistically insignificant throughout both early and late periods. Humphries et al commented that efforts to recruit women into the field of vascular surgery, and support for their professional development, are “facilitated” by women in leadership roles. Speaking to Vascular Specialist, Freischlag emphasizes that the progression of women and people of color to these positions is “key” to more accurate enrollment and results in clinical research.
In Europe too, the unequal representation of women pervades. “It’s a male community,” Marianne Brodmann, MD, head of clinical research in the division of angiography at Medical University of Graz in Graz, Austria, tells Vascular Specialist, “especially in the endovascular and [vascular] surgical [space].”
Weighing in, Janet Powell, MD, professor of vascular biology and medicine at Imperial College in London, England, and co-investigator in the widely endorsed WARRIORS
10 Vascular Specialist | September 2023
FROM THE COVER: WHEN WOMEN ARE PIS: A STORY FORETOLD ON THE VASCULAR FRONTLINES
“Some journals have made an intentional effort to increase the number of female and underrepresented minorities as reviewers and editors. The #Medbikini movement triggered a muchneeded change”
PALMA SHAW
(Women’s abdominal aortic aneurysm research: repair immediately or routine surveillance) trial, says that Europe’s advancement in this arena is “further behind” that of the U.S., which boasts the likes of Linda M. Harris, MD, who, to Powell, represents a “leading light in making life easier for women [in clinical research].” Harris set up the Women’s Vascular Summit, an annual meeting dedicated to reviewing how vascular disease presents and is treated in women.

However, for Powell, “better representation” of women only gained significant ground around nine months ago, while the inclusion of people from minorities and lower socioeconomic groups has not yet been addressed, she adds. In particular, Powell raises concerns over the underenrollment of women and URM groups in the recent BASIL-2 and BEST-CLI trials for the management of chronic limb-threatening ischemia (CLTI). Women made up just 28% and 19% of participants in the trials, respectively, while 72% and 91% of enrollees were white. In Powell’s words, this reveals how contemporary enrollment disparities are perhaps “worse in Europe” currently, but shows a global need to urgently re-evaluate enrollment processes.

Industry responsibility and stimulating change
For Harris, who is a professor of vascular surgery at the University at Buffalo in Buffalo, New York, and a past president of the EVS, slow progression of diversity in PI positions and leadership roles in the vascular field is “multifactorial.”

“Some of it is seniority, but much of it is relationships cultivated with industry in a previously more nepotistic system,” she tells Vascular Specialist. “Breaking in as a PI, especially for women, is the hard part. Once established, it is much easier to continue work with industry, and sponsorship helps immensely—or having partners from the same or different institutions.”
However, cultivating these relationships
LAUNCHES
THE JOURNAL OF VASCULAR Surgery: Venous and Lymphatic Disorders (JVS-VL) has launched its first virtual special issue on diversity, equity and inclusion in (DEI) vascular surgery.
“DEI issues have come to the forefront and affect multiple aspects of the care we render our patients every day,” said Anil Hingorani, MD, JVS-VL associate editor and DEI officer. “This peer-reviewed collection is meant to be a living set of articles focused on DEI, and more articles will be added in the future.”
Hingorani likened the virtual issue to print supplements of previous years, which “really drill down into a topic important
with limited experience of the process may be “hard,” Hicks opines, and “initiative typically falls on the woman,” rather than on the industry partner’s outreach efforts. “Our industry partners need to play a role in this— many vascular trials are industry sponsored and, therefore, medical device companies need to recognize and acknowledge the lack of women PIs included in prior trials, and make a conscious effort to include women moving forward,” Hicks says.
The rise in research concerning gender equity within vascular specialties in recent years has created a wealth of visible evidence. Hopes abound that industry and institutions will now do more. However, in a male-dominated field, fears exist that research of this nature could spark a backlash and/or result in researchers being ostracized.

A study carried out by Matthew R. Smeds, MD, et al, titled “Gender disparity and sexual harassment in vascular surgical practices,” found—through an anonymous survey sent to vascular surgery faculty members at 52
training sites in the U.S. — that 32% of respondents believed that harassment most commonly occurred in surgical specialties that are historically male-dominated due to purposeful ignorance of hierarchy/ power dynamics in the field. Of the study’s conclusions, perceptions of workplace gender disparities “differed significantly” between the genders.
Better strategies are needed
Research such as this makes clear that alignment on gender inequities among vascular professionals must be present to affect change—in Ozsvath’s words “awareness of this deficit will encourage industry to find more diverse PIs” and support DEI initiatives more broadly. Positively, initiatives are being taken up by more institutions to improve gender disparities, such as the Athena Swan Charter—a framework used globally to support the advancement of women in higher education and research. “The initiative is taken very seriously and is supported by annual Athena Swan lectures,” Powell notes of her institution in the UK.

For women in the vascular field, deciding to pursue academic progression can be “complex,” Harris explains, as, for women beginning down this career path, most are “also at an age when they often have young children.” Although this “does not preclude them from running studies or being academic surgeons, the work-life balance issues are still


different and more complex for women than for men based on assessments of division of labor for home obligations,” she states.
Yet, Harris believes that this is “starting to change” as the younger generations “[embrace] more of a work-life balance for all.”
When speaking to Vascular Specialist, all interviewees coalesced around the idea that women’s representation in academic and clinical leadership, as well as in research enrollment, must be addressed collectively to accelerate progression to gender equity. Most vitally, through better representation, Powell says, women who have previously been “underrepresented and underserved” in clinical research can be more accurately assessed and treated with improved knowledge of their crucial vascular variations.

For Shaw, the positioning of women in these roles and the targeted enrollment of women need to be “deliberate and established at the time of the proposal for the trial.” This approach must include women from “diverse backgrounds,” Ozsvath says, “so we can better understand how these patient populations differ in presentation and what best treatment options exist specific to them.” By measuring the impact of women’s vascular differences, including “size, biologic responsiveness, hormonal issues, social determinants and trust issues,” Harris finishes, “we will be successful in moving the needle in our understanding and care of women vascular patients.”
to vascular surgery and really get into the weeds. This is a modern version.”
DEI issues are “sort of the elephant in the room,” pointing out many parts of the country will be majority non-white in the foreseeable future, he said. “As diversity spreads across the nation, we all need to be aware of this.”
In healthcare, diversity packs an impact, Hingorani continued. “It directly affects how patients present, how they’re diagnosed, treatment algorithms and support. Everything we do is affected by the patient’s identity.”
The collection currently includes four articles: “Race, sex and socioeconomic disparities affect the clinical stage of patients presenting for treatment of superficial venous disease”; “Black or African American patients undergo great
saphenous vein ablation procedures for advanced venous disease and have the least improvement in their symptoms after these procedures”; “Importance of sensitivity to patients’ individual background in venous care”; and “A review of the current literature of ethnic, gender, and socioeconomic disparities in venous disease.” The fourth article is available via open access at vascular.org/JVSVL-
DEIdisparitiesReview
Each takes a slightly different tack.
“It’s not just patient outcomes and presentations; DEI affects a lot more than patient-centered outcomes,” said Hingorani.
Four more, presented at the 2023 American Venous Forum and Society for Clinical Vascular
Surgery (SCVS) meetings, are in the process of being added to the site.
The journal website permits JVS-VL to “bring together the best and most recent articles—top-notch, state-of-the-art ideas from around the world,” Hingorani said. The work to update the site, as opposed to a print journal, is simple, he added. It’s all part of the transition to open access and the online world, he said. “It’s something that’s happening, and I think it will continue. This is part of that process.”
Editors are always looking for new articles, he said, as he invited researchers to submit their work. Those who are submitting papers are excited about the new initiative. “There is a lot of enthusiasm to have a focus on DEI issues,” Hingorani said.—Beth Bales
Visit www.jvsvenous.org/ DEIinvascularsurgery to read the collection.

11 www.vascularspecialistonline.com
“Our industry partners need to play a role in this—many vascular trials are industry sponsored and, therefore, medical device companies need to recognize and acknowledge the lack of women PIs included in prior trials, and make a conscious effort to include women moving forward”
CAITLIN HICKS
JVS-VL
VIRTUAL SPECIAL ISSUE ON DEI TOPICS
PEER REVIEW
Top to bottom (right to left): Julie A. Freischlag, Caitlin Hicks; Janet Powell, Melina R. Kibbe; Linda M. Harris, Marianne Brodmann; Kathleen Oszvath and Palma Shaw
Anil Hingorani
YOUR SVS SVS EXECUTIVE BOARD SETS COURSE FOR THE YEAR AHEAD
PHASE II OF A NATIONAL BRANDING campaign for vascular surgery and three new task forces are just a couple among several initiatives the SVS Executive Board (EB) highlighted for further action and attention during a recent retreat.
The SVS Strategic Board meets each January to review the Society’s Strategic Plan and develop priorities for the coming year. Each July, the EB meets to accelerate implementation of those key priorities. The SVS EB met July 27–29 under the leadership of SVS President Joseph Mills, MD, and took action to move multiple priorities forward:
● Establish a Bylaws Subcommittee to deliberate and recommend any further changes regarding selection and election of SVS officers and EB members
● Approve and agree to provide resources for phase II of a major national branding campaign for vascular surgery
● Establish three new task forces to fast-track strategy development: A Research Clinical Trials Task Force, which will foster and accelerate new trials; an Innovation Task Force, which will provide education and resources to help member entrepreneurs; and a Patient Engagement Task Force, to optimize patient engagement in SVS’ work

● Agree to develop a new standalone Advocacy/Health Policy Leadership Conference
● Approve methodology/terminology to move forward with appropriate use criteria (AUC) on carotid disease
● Establish a private practice peer review process to augment the upcoming launch of the Vascular Verification Outpatient Program
The board has vowed to keep members abreast of developments—and reach out to seek volunteers—across SVS communications channels in Pulse, Vascular Specialist, social media, SVSConnect and via email.
“These are just a few of the key discussions we had and actions we took,” said Mills. “We will keep members informed—and ask for volunteers to help these plans progress.”
Beth Bales
‘SVS Presents’ to focus on leadership during natural disasters
The upcoming “SVS Presents” webinar, Leadership During Challenging Times, will focus on leadership during major national disasters such as hurricanes and earthquakes.
This second installment of the leadership webinar series will be held from 7–8 p.m. Central time on Oct. 4.
Four experts in the field of disaster preparedness will speak about their experiences during these major catastrophes.
The webinar will be held in an interview style and include topics on how people can prepare their institutions, lessons learned, posttraumatic stress syndrome, and how to involve trainees in preparedness. The SVS will also provide resources related to disaster preparedness.
SVS member Caitlin Hicks, MD, is set to moderate the session.
Fernando L. Joglar, MD, and Pablo Rodriguez-Ortiz, MD, will discuss hurricanes in a country with limited resources, including what occurred and what was learned. Magdiel Mayol, MD, and Gerd Daniel Pust, MD, will cover the same topics with regards to earthquakes.
Fernando L. Joglar, MD, an
associate professor of surgery at the University of Puerto Rico School of Medicine, is a course director on disaster management and emergency preparedness and advanced trauma life support. Board-certified in both general and vascular surgery, he currently specializes in vascular surgery and vascular trauma, and is the vice chair of the Puerto Rico American College of Surgeons Committee on Trauma PR Chapter.
Magdiel Mayol, MD, is a lieutenant colonel in the U.S. Army, a sports medicine specialist and auxiliary professor at the University of Puerto Rico School of Medicine.
Gerd Daniel Pust, MD, is an associate professor of surgery at Ryder Trauma Center, University of Miami, director of the surgical intensive care unit and associate program director of the surgery residency program. Pust completed his general surgery residency and subsequent fellowship in critical care and trauma surgery at Jackson Memorial Hospital/Ryder Trauma Center in Miami.
Pablo Rodriguez-Ortiz, MD, is chair for Puerto Rico of the Committee on Trauma of the American College of Surgeons, and the medical director for the Puerto Rico Trauma Center.—Beth Bales
Visit vascular.org/SVSPresents for more information and to register.

12 Vascular Specialist | September 2023
“We will keep members informed—and ask for volunteers to help these plans progress”
JOSEPH MILLS
DEMOGRAPHICS 2023 SVS officer election: A look behind the curtain at the electorate
The SVS Executive Board highlights details of the most recent SVS elections in order to inform members and further strengthen the process.
DRIVEN BY COVID-19 TRAVEL LIMITATIONS AND a desire to increase member engagement in selection of SVS leadership, in 2020, SVS leadership proposed, and SVS members resoundingly approved with a 97.7% majority (1704), a bylaws change affecting officer elections. The change mandated that the SVS Nominating Committee propose two candidates for each open officer position and that voting be open to all eligible SVS members, regardless of their ability to be present at the Annual Business Meeting (ABM).
The prior bylaws permitted the Nominations Committee to advance a single slate of officers, which had become increasingly challenged and was tending toward annual multiple run-off elections at the ABM. The SVS leadership proposed the bylaws change to ensure that members would always have a choice in the election of their officers.
The second facet of the bylaws change—opening up the election to all qualified SVS members—required a transition to electronic voting. This change permitted 10 times more SVS members to actively participate and vote than usually attend the ABM. The results of this change were immediately evident as the inaugural internet election in 2020 engaged 482 voters, substantially more than the 250 typically present. In 2021 and 2022 the number of members who voted grew to 611 and 602, respectively. In 2023, that number rose to 939.
The Nominating Committee continues to carry out its crucial charge in identifying, vetting and advancing highly qualified nominees based on commitment and service to the SVS, time availability, track record of leadership success, strategic vision, and a growing awareness and mindfulness of SVS diversity, equity, and inclusion (DEI) principles.
The 2023 election for SVS officers was held May 11 to June 15, during which time 939 members cast their votes for vice president and treasurer. The election was well publicized with SVS members, who received 75-plus reminders and prompts to vote via various media and social media channels.
The transition to internet voting was initiated to engage every voting-eligible member across the country to participate.
There are approximately 2,900 eligible members in the SVS. Compared to other medical societies that hold internet elections, a 20% voter turnout is considered healthy and above average.
The goal of the Nominating Committee and the Executive Board is to achieve at least 1,000 votes, or 33% of eligible voters; 2023’s 939 votes hit that 33% on the nose.
In the 2023 election, the demographics of the voter pool largely parallel the demographics of the overall SVS membership, although there are some differences.
With regard to gender, 77.7% of those who voted identified as male (compared to 80% in 2022), 21% female (compared to 18% in 2022), and 2% undisclosed in both 2023 and 2022. This compares to 84%, 11%, and 5% in the overall SVS membership. The percentage of female voters was slightly larger than the general SVS membership, 21% vs. 11%; and
COMMENT& ANALYSIS CORNER STITCH
SELF-MOTIVATION TIPS FROM THE TRAINEE TRENCHES
By E. Hope Weissler, MD
The new academic year usually feels exciting—new responsibilities! new co-residents!—but it can also be a daunting reminder of how much training remains ahead. In those moments, training can feel more like a grind than an opportunity.
We are all intrinsically motivated by hopes of helping patients and being excellent surgeons, teachers and colleagues, but, sometimes, those altruistic motives don’t feel immediate enough. In those moments, I often find myself looking to extrinsic motivators instead, like the thought of a truly giant meal after a long case, or pride in my step count after running around chasing
consults all day. Those short-term rewards can be helpful and even healthy, but they don’t provide the same direction and propulsion as more high-minded motivations.
One way I’ve found to short-circuit this issue is what I call the “myth of self.” A myth of self is a story you tell yourself about what type of person you are that can then be used to provide extrinsic motivation that aligns with your more altruistic (and esoteric) intrinsic goals.
There are a few helpful features of the myth of self. It should be aspirational. You can tell yourself that you’re the sort of person who does “X” when you have, in fact, done “Y” many times in the past, because telling yourself that you’re an “X” person makes “Y” more difficult and less likely. Think of the senior residents you’ve wished you could be “when you grew up” and your most slick/smart/steady attendings. Take the qualities of those people and adapt them to your own purposes.
It should induce a growth mindset. One of the things that makes a myth mythic is the journey. You probably remember
the percentage of males slightly lower, 78% vs. 84%.
With regard to age, 31% of voters were 60+ years of age (28% in 2022), followed by 27% for those 51–60 (same as 2022) and 29% for 41–50 (27% in 2022). Finally, 9% were under 40 years of age, the same as in 2022. This compares to 42% over 60 in the overall membership, 17% 51–60; 19% 41–50; and 4% 31–40. In general, those who voted were slightly younger than represented in the general membership with 36% of the vote from members under age 40, compared to 22% in the overall membership.
With regard to geographic location, the population of voters was very close in parallel to the overall SVS membership with the South Atlantic at 19% (21% in 2022); Mid-Atlantic 19% (17% in 2022), East North Central at 16% (same as 2022); Pacific 14% (13% in 2022), New England 9% (10% in 2022) West South Central identical with 8% (same as 2022); East South Central, 4%; West North Central, 4%; and Mountain, 3%.
Lastly, with regard to ethnicity, it is difficult to make comparisons as the percentages of members who identify as minorities underrepresented in medicine (URiM) are small. Overall, the percentage of voters who represent as non-Caucasian ethnicities appears slightly higher than in the general membership, 29% vs. 25% (same as 2022), but this may be due to more non-Caucasian members identifying as a different ethnicity compared to the general membership profile.
The transition to open internet elections has just completed its third full year. Following the 2023 election, SVS President Joseph Mills, MD, convened a special input session and established a subcommittee to evaluate whether the current SVS election process can be further strengthened. The work of the Nominating Committee is challenging because the SVS is blessed with an abundance of qualified nominees, and likely due to this quality, elections will be predictably close, so every vote matters.
The SVS Executive Board and Nominating Committee are currently deliberating further improvements to broaden diversity and choice in candidates and increase member engagement. Those who have comments or suggestions are asked to email them to president@vascularsociety.org
the three stages of the hero’s journey according to Joseph Campbell from middle school: departure; initiation, in which the hero ventures into the unknown and overcomes various obstacles and challenges; and return (in triumph) to a more familiar world. Sounds a bit like training, right?
Your myth of self should include not only static characteristics (“I am a person who stays calm under pressure”), but also beliefs about how you respond to adversity (“I am a person who takes criticism well because I want to get better”).
It should be very personal and portable. Your myth of self will be shaped by your personality, your strengths and weaknesses, and your values. Your myth of self will not work for me (and vice versa) because it needs to feel like a possible version of you in order to be effective. That self will change with you as you encounter new experiences and challenges over time.
Here’s how I use my myth of self: I am (like maybe some of you) a flawed human
who can be impatient, defensive and insecure. But I tell myself that I am a person who is steady, generous and open-minded. When I get out of a late case and have a patient in the ICU who is doing a bit marginally, I could rationalize going home, because that patient is already in the best place for them, so my checking on them won’t make a difference. But then I ask myself if I’m a person who doesn’t check on patients because I’m tired. When you phrase the wrong option as an ego transgression, it gets a lot harder to choose. Conversely, when you choose the right option, you get a nice little dopamine surge as a reward for affirming your ego.
This may sound like a crazy approach, but it has supported me through six years of training, helping me feel the joys of my successes while softening the blows of my failures.
13 www.vascularspecialistonline.com
Aspirations of the SVS Nominating Committee and Executive Board are set on achieving 1,000 votes amongst eligible voters in the election
E. HOPE WEISSLER is a vascular resident at Duke University in Durham, North Carolina.
E.
Hope Weissler 482 2020 939 2023 GROWTH IN TURNOUT:
PTS
VENOUS STENTING AND THE IVC: ‘PERSISTENT PROBLEMS’ IN THE SETTING OF POSTTHROMBOTIC SYNDROME
By Bryan Kay
THE QUESTION OF “PERSISTENT
problems” with venous stenting among post-thrombotic syndrome (PTS) patients emerged as a key talking point during the recent Deep Venous Stenting Summit that took place at VAM 2023 in National Harbor, Maryland (June 14–17).
The issue was raised by venous disease titan Peter Gloviczki, MD, professor and chair emeritus of vascular surgery at the Mayo Clinic in Scottsdale, Arizona, after a talk by Erin Murphy, MD, director of Sanger Heart & Vascular Institute’s venous and lymphatic program in Charlotte, North Carolina, drilled into the management of stent complications—pondering whether to recanalize, explant or bypass.
Prior speaker, Mark D. Iafrati, MD, a professor of vascular surgery at Vanderbilt University Medical Center in Nashville, Tennessee, had in a prior talk on best medical treatment and surveillance protocols already provided the data behind Gloviczki’s point— published in 2013 in the Journal of Vascular Surgery by Seshadri Raju, MD, a vascular surgeon at the Rane Center in Jackson, Mississippi, and colleagues showing 90–100% patency in the setting of non-thrombotic disease and 74–89% in PTS at three to five

PERT CARE
years, outcomes which he said hold up today.
“Dr. Raju’s results are excellent, but let’s face it, about one-in-four post-thrombotic patients has problems with stents, and there are persistent problems,” Gloviczki commented from the floor during questions. “One, for instance, is if you have a lesion very close to the IVC [inferior vena cava].
“We really don’t have a beveled stent in this country,” he continued, referring to the CE-marked sinus-Obliquus device. “Even the dedicated stents extend, at least in part, in these patients into the vena cava. So, I wanted to ask Erin if you still use the technique of combined stenting and have you had problems with the penetration of the wall by the Z-stent?”
Murphy related her early experience navigating venous dedicated stents to her intended landing spot.
With the coming of more advanced stents, “initially, I encountered some challenges in precisely posi tioning them at the cava and effectively addressing the cra nial disease,” she said. “This
predicament led me to consider reverting to the use of combined stenting with Z-stents. However, over time, I have managed to refine the technique of accurate placement without covering the contralateral vein.”
It is a different story among already stented patients who land in Murphy’s practice, she continued. “I do see patients come into my practice after being stented elsewhere, and many of these stents are extended into the IVC, effectively jailing the contralateral iliac vein. While I recognize that our understanding is still evolving, it took us a span of 10 to 15 years of Wallstent use to conclusively identify this as a problem. While there are bigger interstices on the newer-generation stents, suggesting that jailing may be safer, isolated instances of contralateral deep vein thromboses hint at the possibility of its eventual prevalence.”
Regarding Z-stent use, Gloviczki inquired whether Murphy is seeing these stents erode through the caval wall over time. Murphy stated that “proper technique using these stents within a Wallstent, with only a quarter of the stent extending cranially from the Wallstent edge, often prevents this complication.”
She further admitted that “in cases of unsupported Z-stenting, particularly after cutting the cranial Z-stent suture,” she has seen this occur in
a few patients, “albeit without consequences thus far.”
Gloviczki further pondered the external iliac vein. “We never talk about it but most of the time we stent into the external iliac vein, and mostly we do so because some of the common iliac veins are so big, but practically every time we jail the internal iliac vein, and I wonder if in the long run this is not going to be an issue.”
Murphy referred to the use of Wallstents in this setting: “I don’t recall seeing a consequence of that. The internals are so well collateralized, but maybe we’re just not looking.”
Fellow panelist Lorena DeMarco-Garcia, MD, chief of vascular surgery at Plainview Hospital, Northwell Health in Syosset, New York, who spoke on stenting for non-thrombotic iliac vein lesions (NIVLs), concurred: “The pelvic floor drains contralaterally and that is it. But I’m sure we are probably eventually causing future ostium occlusion, for sure,” she said.

“PERT CARE IS THE COALITION OF THE willing,” quipped Dennis Gable, MD, a vascular surgeon at Texas Vascular Associates in Plano, Texas. He was referring to team-based care for pulmonary embolism (PE) patients and how, unlike acute stroke intervention and ST-elevation myocardial infarction (STEMI) care, PE lacks a clear owner specialty in the setting of pulmonary embolism response teams (PERTs), which represent multidisciplinary care characterized by easy accessibility, rapid response and individualized consensus-driven treatment. Gable was making the case that vascular surgeons are well poised to assume the mantle of a pivotal role during Management of Pulmonary Embolism: Fundamentals and Advances, a special session that took place during the Society for Vascular Surgery’s 2023 Vascular Annual Meeting (VAM) in National Harbor, Maryland (June 14–17).
“There is no specialty that has really stepped up and said we are going to own the right heart and lung, and a lot of people don’t want to deal with PE altogether—they want to send that to the specialty centers of which we are growing in number,” he told attendees.
PE is a problem whose scope is significant, with many centers lacking the ability to treat this patient population, Gable observed. The importance of “team” in PERTs is paramount, he emphasized. “That entails not only vascular surgery, which is an important part of this and a key member, but also cardiology, interventional radiology, your ER
[emergency room] physicians, pulmonary critical care and CT [cardiothoracic] surgery.”
Based on his team’s institutional experience, the establishment of a PERT was associated with “significantly higher utilization” of catheter-directed interventions, less major bleeding events and reduced in-hospital and 30-day mortality, Gable said. “Overall, our data suggest a definite advantage for a full multidisciplinary team to treat these patients.”
Data from 2016 demonstrated that vascular surgery involvement in PERTs was not among the top contributors to PE care teams. Gable said he was not aware of more recently published data mapping out the specialty’s current role but believes it likely now is the second or third top contributor.
He contrasted this with an allusion to CT surgery’s diminished role in cardiac catheterization: “Our CT colleagues, when cardiac catheterization came out, they were so busy with development and initiation of cardiac surgery, they gave up the cardiac catheterization to cardiology primarily,” Gable explained. “They took a role of standby operator backing up the interventionalists—but currently that is no longer existent in most centers.”
“PERTS have demonstrated the value for patient survival and decreased utilization of critical care resources,” Gable concluded. “Vascular surgeons have demonstrated expertise in this arena and treatment space. Vascular sur-
gery is, and should be, a key member of the PERT team. And, to maintain branding as a vascular specialist and for our specialty overall, should remain and strive to be leaders in the area.”
Elsewhere, Gable also referenced the emerging role of artificial intelligence (AI) in PE care, and how machine learning can shave considerable time off the process of determining management for individual patients. AI algorithms allow treatment determinations to be established in “a more rapid fashion,” he noted.—Bryan Kay
14 Vascular Specialist | September 2023
“Dr. Raju’s results are excellent, but let’s face it, about one-in-four postthrombotic patients has problems with stents, and there are persistent problems”
PETER GLOVICZKI
Peter Gloviczki
‘Vascular surgery should be a key member of pulmonary embolism response teams’
The VAM pulmonary embolism session panel featuring Dennis Gable (seated, third from left)
DEEP VENOUS VALVE TECHNOLOGIES SET TO ADDRESS ‘LARGE UNMET NEED WORLDWIDE’
The pursuit of a cure for deep venous valvular reflux—long considered to be the “holy grail” of deep venous disease—is underway, with new technologies set to address a longstanding unmet clinical need across the globe.
By Jocelyn Hudson and Bryan Kay
Chronic venous disease affects nearly 25 million in the U.S. alone, and among those patients, the deep venous reflux population is close to two million people. Erin Murphy, MD, director of the venous and lymphatic program at Atrium Health’s Sanger Heart & Vascular Institute in Charlotte, North Carolina, and Marc Glickman, MD, the senior vice president and chief medical officer at Envveno Medical, put forward these figures to set the scene for a deep dive into deep venous valvular reflux during a recent CX Vascular Live discussion. They were joined by Ramon Varcoe, MBBS, director of operating theaters at Prince of Wales Hospital in Sydney, Australia, to outline the scale of the issue, as well as potential solutions in the pipeline.
“The population is large, it is being treated most of the time with conservative therapy, so I think there is a large demand—untreated, unmet and underdiagnosed,” said Glickman in summary of the overarching issue. “This is a large unmet need worldwide.” He stressed that countries such as India, China and Brazil have even larger patient populations with deep venous reflux.
Varcoe concurred that deep venous reflux represents an “enormous global burden,” not only in terms of healthcare costs, but also in patients’ livelihoods. To this point he described the difficulties associated with living with venous ulcers, and the fact that vascular surgeons “really struggle” with these patients in terms of applying compression therapy and using other conservative measures.
Murphy noted that there has been “considerable progress” over the last 10 years in treatment options for patients with reflux in the superficial system, and also in the deep venous obstruction space, with various new stents now available. “Why do you think it is taking so long to establish new technology in the deep venous valve realm?” she asked the assembled panel.
“For the last 50 to 60 years, everyone has considered finding a cure for deep venous valvular reflux as the holy grail of deep venous disease,” remarked Glickman, highlighting the importance of—and difficulty associated with—finding a solution to the problem.
He put forward two issues at play here—one is the challenging nature of correctly diagnosing deep venous valvular insufficiency and, the other, a lack of standardization in making that diagnosis, resulting in the severity of the disease being “missed throughout the medical community.”
Varcoe stressed the “huge variability” in how this disease is diagnosed, and noted another issue—that surgery in these patients is “next to impossible” due to challenging anatomical conditions.
Glickman, too, noted another challenge for the venous space: the fact that vascular surgery training tends to focus on the arterial side of vascular disease and less on the venous world, which has resulted in only “very minor” innovation in the latter.

New technologies “on the horizon”

Glickman expressed his belief that the potential for growth in the deep venous valve market is “enormous,” moving the focus of the conversation towards two new technologies that could improve patient outcomes in this challenging space. On this note, Varcoe expressed his excitement that there are some new technologies “on the horizon” that “might make a huge difference to patients’ lives.”
Glickman, of Envveno Medical, the company behind the VenoValve, and shared that his training as a vascular surgeon informed him that “most of our endovascular procedures have started out as open procedures that have worked and that have migrated to endovascular,” citing the examples of carotid stenting, ablation and stripping, and the treatment of abdominal aortic aneurysms. In the deep venous reflux space, however, he noted that an open surgical technique is missing.
About seven years ago, Glickman recalled, the VenoValve was developed. He detailed that it is made from a porcine aortic monocusp on a stainless steel frame that is surgically implanted into the femoral vein in the mid-thigh region. The procedure takes about an hour and 15 minutes.
Glickman noted that three-year data from a first-in-human trial conducted in Colombia, which were recently shared at the 2023 American Venous Forum, showed improvement in reflux time, improvement and consistency of the Venous Clinical Severity Score (VCSS), and a reduction in pain. The team are presently conducting another trial—SAVVE at 24 sites in the U.S. He highlighted that the company is now working on a transcatheter version of their VenoValve device, with the plan being to commence a first-in-human study.
Varcoe, who has been involved in clinical studies on the BlueLeaf (InterVene), shared that this novel device is “completely different” to the VenoValve. “What we do with this device is we make a valve leaflet from the blood vessel wall itself— so we leave nothing behind, we are not transplanting anything, we are literally creating a flap-like valve, which can be either monocuspid or bicuspid and it can be done multiple times in the same vein segment,” he explained. The device is percutaneous, Varcoe added, and is therefore inserted over a guidewire, with the procedure guided by both intravascular ultrasound and fluoroscopy. “It takes around an hour and a half to make a series of valves and we hope that over time those valve cusps endothelialize and become part of the native structure of the vein wall,” he said.
In terms of data, Varcoe noted that 41 patients have now been enrolled in a global clinical trial of the technology. The data demonstrate the safety and efficacy of the device in its early stages, Varcoe reported, and that the procedure can be done without creating deep vein thromboses, which was an “initial fear.” He added that the data have shown some “dramatic, remarkable improvement” in VCSS scores. “Patients I have seen who have had ulcers for 20 years have had them healed within six weeks, and that is extremely satisfying,” he shared.
In addition to VenoValve and BlueLeaf, Cook Medical announced earlier this summer that the first patient has been treated in a clinical study to evaluate a new venous valve designed for treating chronic venous insufficiency (CVI).
The patient was treated by principal investigator Mauricio Alviar, MD, of Clinica de la Costa in Barranquilla, Colombia.
The valve’s safety and efficacy are now being tested in a global, multi-site clinical trial. The global principal investigator of the study is Paul Gagne, MD, of Vascular Care Connecticut in Darien, Connecticut.
“When leg veins function poorly, patients suffer with leg
swelling, leg pain, leg ulcers, disability, and possible amputation. Therefore, it is important to restore blood flow out of the leg veins, back to the heart. Part of doing this successfully required restoring the function of the venous valves,” Gagne said in a press release at the time.
What is next?
While these technologies are in their infancy, both Glickman and Varcoe are cautiously optimistic about the future. Glickman noted that the focus at Envveno Medical will be finishing up the trial for Food and Drug Administration (FDA) approval by the end of this year, after which it will take six months to get the approval. The plan is to conduct a large trial in the U.S. He summarised that the percutaneous device is probably five years out, and VenoValve “probably two years out from being in people’s hands.”
Jorge Ulloa, MD, of Fundacion Santa Fe-Universidad de los Andes, Bogota, Colombia, one of the key figures behind research of the surgical VenoValve, said the future looks bright in the venous valve space following 65 years of development. “So far, we are at the pivotal phase of the study [of the surgical version of the valve],” he said, relating how more than 50 cases have now been performed in the U.S. so far. This follows the first-in-human trial carried out at Ulloa’s institution in Bogota. The surgical valve “seems to have a promising future, due to the length and results from the follow-up, that we have presented extensively in the last three years,” he continued. “There is another player from Cook Medical, which has already implanted a first device via endovascular deployment, and we are on the way to migrating to [an endovascular device] also.”
Ulloa is similarly involved in the first-in-human trial of the endovascularly delivered version of the valve. In the meantime, continuing study of the surgical valve is showing “a plateau in terms of stabilization in pain, VCSS and reflux time,” he said. “It means that there is no tendency to return to baseline at 36 months of follow-up. That is something that has never happened in previous series, and everything looks like it will continue this way. Of course, only time and follow-up of these cases will show us the path to continue.”
Ulloa believes more new technology will emerge in the coming years. “I envision a myriad of new devices that will emulate our experience,” he said. “Some will work, some won’t. So far, there are more than four major companies designing their own concepts, and they will have to run through all the necessary stages in order to prove that they are safe and functional. All of these efforts will only benefit PTS [post-thrombotic syndrome] patients—and that is a good thing.”
Regarding BlueLeaf, Varcoe stated that the team involved is “in a process of innovating and iterating the device.” They are about to launch the fourth generation of the device, which allows for the treatment of larger veins and the creation of more circumferential valve cusps. Varcoe added that they are going through the pre-submission process with the FDA about what an investigational device exemption trial might look like, which they hope to be able to start soon. “I see a future where this technology is successful,” he said, whichever technologies “end up being available to us.”
Glickman acknowledged that paradigm shifts in medicine “take time,” emphasizing the complexity of the regulatory environment. He also pointed out the importance of continued education in this space to address a lack of understanding of deep venous insufficiency within the medical and vascular surgical community.
“I am seeing huge interest in venous disease now and it is a really great time to be involved in the field,” Varcoe added.
15 www.vascularspecialistonline.com
“I envision a myriad of new devices that will emulate our experience. Some will work, some won’t.”
JORGE ULLOA
VENOUS REFLUX
Erin Murphy Jorge Ulloa
Exercise key to surgeons living well, healthy in retirement
Vascular surgeons may not realize it, said Samuel Money, MD, “but we’re doing physical labor.” Here, Beth Bales reports on retirement and how ergonomic challenges can impact vascular surgeon longevity.

Some 50–80% of surgeons suffer work-related pain during their career and 40% report current pain. “Most of us are in great shape, but my lower back is letting me know it’s there.”
He presented “ergonomic challenges” as part of an education session at the VAM 2023 on “Transition to Retirement: What I Wish I Would Have Known.”
Previous studies have shown surgeons experience pain in the neck (45%), lower back (39%) and the lower extremities (18%).
He told attendees to “look at the big picture: Am I going to live long and am I going to live healthy?” Genetics, the environment and local behavior all impact longevity, he said.
He stressed that people 60 and older who exercise more than 180 minutes per week “live longer and have a better quality of life. If I could leave you with one point, that’s the
one,” Money said. To be stronger and live longer, older people need muscular resistance, aerobic and balance training, and flexibility, Money continued.
He suggested muscular resistance training two to three times per week, with weight-lifting, free weights or ma chines, targeting both the upper and lower body. “Older people do better with machines,” he noted. Resistance training is vital to build bone health, as people lose significant amounts of muscle mass as they age. “Exercise isn’t just walking, biking or running,” he emphasized. “You have to hit the gym … you have to do muscular resistance training.”


And because older people who do aerobic exercise live longer, such exercise should be undertaken three to seven times a week, at 30 to 60 minutes a session, Money continued. Balance also is critical, as falls are the third leading cause of death in senior citizens and the third leading expense in terms of medical expenditures, he said. Nearly 30% of Americans over 65 fall once a year. He related a statistic he found surprising and worth noting: “If you fall and break a hip, it’s similar to you having an acute MI [myocardial infarction] in terms of one-year survival.”
“Most of us as we age do not have good balance; you have to practice,” Money added. He recommended a short balance test: standing on one leg for 15 seconds without holding on to anything. “This is a predictor of longevity,” he said. “If you can do that, you will live longer. My guess is a third of you can’t do it for 10 seconds.”
He recommended yoga and stretching for flexibility, two to five times a week.
Money went over a number of exercises people can do at home, without necessarily going to a gym or fitness center. “All this can be done at home. Basic exercises like that are not that hard and will keep you in shape forever.”
His bottom line is that a week contains 168 hours. “If you spend six hours in a week—3.6% of your time—you will live longer and be happier. Is it worth it?” He echoed the Nike slogan as his final summary: “Just do it!”
During the comments phase, one attendee pointed out that the audience for Money’s presentation was not those near retirement age, but members of the Young Surgeons Section. “This talk is better for them so they don’t get into trouble the way I did and others in the room did.”
Money agreed that it is important for younger surgeons to know what lies ahead, but said he’s not sure how the message would be received by, say, a 32-yearold. “You’re invincible at 32. Take Motrin!”
The full session is available to VAM registrants at vascular.org/ OnlinePlanner23

16 Vascular Specialist | September 2023 #IAMSVN V A S C U L A R N U R S E S W E E K S E P T . 1 0 - 1 6 , 2 0 2 3 Celebrating L E A R N M O R E A T B I T L Y . V A S C U L A R . O R G / V N W
WELLNESS
“Exercise isn’t just walking, biking or running. You have to hit the gym … you have to do muscular resistance training”
SAMUEL MONEY
Samuel Money
Register for CPVI course before it fills up
By Beth Bales
TIME IS RUNNING OUT TO REGISTER for the SVS’ Comprehensive Peripheral Vascular Interventions (CPVI) Skills Course, set for Oct. 1–2 in Rosemont, Illinois.

The course focuses on treating patients with peripheral aterial disease (PAD), the largest clinical area for vascular surgeons in the United States. Registrants will learn
the latest innovations and techniques in treating patients with PAD, through a mix of didactics, case-based learning and extensive hands-on training using cadavers and benchtop models.
Areas covered include retrograde tibial and pedal access, pedal loop imaging and techniques, deep venous arterialization, IVUS
axial imaging, atherectomy devices, aspiration/peripheral thrombectomy catheters, re-entry devices and closure devices.
In response to feedback after the inaugural 2022 course, the handson portions have been spread over the two days. Those sessions are not accredited for continuing medical education credit.
Course co-directors are Patrick Geraghty, MD, Vikram Kashyap, MD, and Daniel McDevitt, MD. Sixteen additional surgeons comprise the faculty. Elizabeth Genovese, MD, is vice co-director.
“One of the factors that sets the CPVI course apart from other offerings is that we charge our world-class faculty to provide attendees with the whole story,” said Geraghty. “In their lectures, their debates and their hands-on sessions, the CPVI faculty leverage their experience to describe the optimal uses of certain devices or modalities—but they also speak frankly about the complications specific to those therapies, and the anatomic characteristics or other factors might lead them to use alternative approaches.”
The faculty all are well-versed in treating PAD, from simple to complex, course directors said.
A participant called the inaugural 2022 course “very helpful,” overall, adding it
STEP CHALLENGE
“opened my eyes about alternative access and pulled back the curtain. (I’m) much more confident to use these in my practice.”
Geraghty said the low 5:1 ratio of attendees to faculty also sets the SVS CPVI course apart. “We purposefully designed this course to optimize the interaction of our attendees with our faculty, particularly in the extensive hands-on sessions,” he said. “Working through a planned sequence of intimate, small-group sessions allows the course attendees to absorb the greatest amount of learning from these tremendously experienced surgeons. I was honestly amazed at how successful this format was in our inaugural course.”
He said he pulled aside an instructor at last year’s course, asking him to look around the massive lab space. “I wanted him to notice that of our 75 attendees, every last one was completely focused on their small-group faculty leader,” said Geraghty. “To me, that moment confirmed the high value of the instruction at the CPVI course, and I was really pleased to see that reflected in the outstanding feedback we received from our attendees.”
Learn more, register and view the recap video from 2022 at vascular.org/CPVI23
FOR VASCULAR SURGEONS TO BE reimbursed for their work, proper coding is essential. In the vascular surgery world, it’s also complicated.
To help surgeons or their coding staff members keep pace with the various complexities in the process, the SVS will hold its annual Coding and Reimbursement Workshop, plus an optional workshop on Evaluation and Management (E/M) codes, Oct. 16–17 at the OLC Education and Conference Center, 9400 W. Higgins Road, Unit 100, in Rosemont, Illinois. The building also houses the SVS headquarters office. The workshop will provide a comprehensive review of current coding and reimbursement information, including critical updates to those who want to be well versed in vascular coding.
Attendees will learn about changes in Medicare and the Current Procedural Terminology (CPT) codes, how to apply the application of modifiers for streamlined
reimbursement, define the Global Surgical Package and how it impacts billing and reimbursement, the principle of component-coding and the correct coding for key endovascular and open vascular procedures.
The 2023 update in E/M guidelines includes information on whether time or medical decision-making (MDM) works better for vascular surgeons and the opportunities and limitations of using “time.”
The E/M session will be from 8 a.m. to 12 p.m. Central time on Oct. 16. The Coding and Reimbursement Workshop will be from 1 to 5 p.m. Central on Oct. 16 and from 7:30 a. m to 4:30 p.m. Central on Oct. 17.
Office staff, including practice managers, nurse practitioners, physician assistants, nurses, surgery schedulers, coders, and others, would benefit from the workshop.
The faculty includes Sean Roddy, MD; Robert Zwolak, MD, PhD; Sunita Srivastava, MD; and Teri Romano, RN, MBA, CPC. All faculty members are experts on coding for vascular surgeons. Beth Bales
Register at vascular.org/Coding23
PARTICIPANTS ARE PREPARING TO LACE UP THEIR RUNNING SHOES in support of vascular health, committed to both talking the talk and also walking the walk.
“The walk” is the SVS Foundation’s Annual Vascular Health Step Challenge: walking 60 miles during September, National Peripheral Artery Disease (PAD) Awareness Month. The distance represents the 60,000 miles of blood vessels in the human body. The SVS Foundation’s goal is to raise $60,000, which will support low-income patients in exercise therapy programs.
According to estimates, more than 12 million people in the United States suffer with PAD, caused by buildup of plaque in the lower extremities, which narrows the arteries and causes them to become stiff. In the most severe cases, PAD can lead to amputation.

Exercise therapy—such as walking—is a first-line response to PAD, and numerous studies have confirmed the health benefits of putting one foot in front of the other. The SVS Foundation lists a number of walking benefits on its Step Challenge information page, vascular.org/FoundationStep23. And a recent meta-analysis of 17 studies study showed people who walk at least 4,000 steps a day can lower their risk of death from any cause. Those who walk only 2,337 steps a day lower their risk of death from cardiovascular disease.
Beyond mere bragging rights are prizes: a Sport backpack for those who meet the 60-mile goal; a Stanley drink cup for those who raise $600; a Step Challenge hat for team members who meet the $6,000 team goal; and an outdoor blanket for the top individual walker and fundraiser.
New this year is a “Pay it Forward” initiative in which registrants offer to pay the $60 sign-up fee for low-income patients. Sponsors for this year’s Step Challenge are: AOTI, Gore, The Way to My Heart organization, Medtronic, 3M and the Society for Vascular Nursing (SVN).—Beth Bales
Learn more and register now at vascular.org/Step23
17 www.vascularspecialistonline.com
“One of the factors that sets the CPVI course apart from other offerings is that we charge our world-class faculty to provide attendees with the whole story”
COMPLEX PAD
PATRICK GERAGHTY
REIMBURSEMENT UNLOCK PROPER CODING AT OCTOBER WORKSHOP
OCT. 16TH –17TH OCT. 1ST –2ND
READY, SET, WALK
SOCIETY BRIEFS
Compiled by Beth Bales and Marlén Gomez
AMPLIFYING ADVOCACY: SVS TOOL FOR VASCULAR INFLUENCE ON THE FEDERAL STAGE
By Sean Lyden, MD
Vascular Nurses Week shines spotlight on vital role in patient care and innovation
IN A WORLD IN WHICH BOTH MEDICAL breakthroughs and technological advancements seem to dominate the healthcare landscape, it’s easy to overlook the unsung heroes who work tirelessly to ensure that patients receive the specialized care they need. Vascular Nurses Week—Sept. 10–16—serves as a reminder of the role vascular professionals play in patient care, education and research.
Kristen Alix, MS, ANP-BC, AGACNP-BC, CVN, a vascular nurse since 1997 and the president of the Society for Vascular Nursing (SVN), emphasizes that this celebratory week is about more than receiving recognition. It’s also a platform for education, advocacy and a call to raise awareness about vascular health.
Alix’s interest in vascular nursing stems from the challenges posed by this specialty. “The vascular patient as a whole is a big medical puzzle for people to solve,” she said. “Such patients present a variety of comorbidities, including hypertension, cardiac disease, renal disease or diabetes, not to mention the complicated social challenges. The vascular nurse is an individual contributor to the patient’s success before, after and sometimes during the surgery.”
Alix noted that vascular nursing is a vocation not for the faint of heart, as it places vascular nurses at the forefront of patient care.
Founded in 1982, the SVN emerged as a society that formally acknowledged vascular nursing as a specialized field.
The society is not composed solely of nurses, but incudes a diverse assembly of providers, researchers and leaders, spanning the spectrum of healthcare contributors.

“My attraction to vascular nursing stems from the critical thinking and the creativity needed to help solve the patient’s issue,” she said.
As Vascular Nurses Week neared, Alix and the SVN invited everyone to take a moment and express appreciation for the dedication, compassion and expertise of these healthcare professionals. Throughout the celebratory week, the SVN urges individuals to amplify the message by sharing the hashtag #IAMSVN across social media platforms.
The SVN also advocates for individuals to consider offering the gift of membership to their nurse practitioners and nursing teams.
To give the gift of membership and join in this movement, visit https://www.svnnet.org/page/ GIFTOFMEMBERSHIP
IN THE DYNAMIC ARENA OF HEALTHCARE ADVOCACY, THE SVS stands as a champion, harnessing the power of amplification to thrust the voices of vascular surgeons into the forefront of federal decision-making. Over the past year, the SVS has orchestrated three compelling “Week of Action” campaigns, underscoring the Society’s commitment to advancing legislative priorities on Capitol Hill and invigorating advocacy participation within its membership.
Recognizing the evolving landscape of advocacy, the SVS has embraced a multi-pronged approach to the “Week of Action,” aimed at advancing the interests of vascular surgery.

Grassroots campaigns: Embracing the strength of collective voices, SVS empowers its members to actively participate in grassroots campaigns via the “Voter Voice” platform. This digital rallying cry amplifies the concerns of vascular surgeons, magnifying their impact on pivotal issues. By channeling the diversity and energy of its membership, the SVS cements its position as an influential force.
Supporting candidate and incumbent lawmakers through the SVS Political Action Committee (PAC): the SVS not only raises its voice, but also invests in the future of advocacy for vascular surgery. The SVS PAC serves as a pivotal tool, bolstering the campaigns of lawmakers who champion healthcare policies aligned with the SVS’ overarching mission. Through backing candidates who resonate with the principles of vascular surgery, the SVS proactively shapes a legislative landscape conducive to the field’s growth.
Traditional legislative advocacy and lobbying: Capitol Hill has borne witness to the presence of SVS representatives as they advocate for policies that resonate with the core of vascular surgery. Through deliberate engagements with federal lawmakers, the SVS ensures that the intricacies and concerns of vascular surgeons are not only acknowledged but also deeply understood. This timeless approach remains a cornerstone of the SVS’ advocacy efforts, forging relationships that pave the way for well-informed decision-making.
Amplification transcends mere volume: The SVS has wielded this principle to increase our level of influence, ensuring that the aspirations and concerns of vascular surgeons are heard at the federal level. The “Week of Action” campaigns further underscore the SVS’ dedication, showing how a collective voice can serve as an agent of transformation.
As the SVS charges ahead, the tool of amplification remains a central pillar of its advocacy strategy. With every campaign, each engagement, and participation of its members, the SVS fortifies its position as a resounding voice, propelling change in the healthcare landscape and securing a positive future for vascular surgery.
To learn more about SVS advocacy efforts, or catch up on previous “Week of Action” campaigns, visit vascular.org/advocacy
SEAN LYDEN is a member of the SVS Advocacy Council.
SVS member RONALD KLINE, MD, has been appointed the head of St. Claire HealthCare’s new Vascular Surgery Clinic in Morehead, Kentucky. In coming weeks, the hospital plans to offer a full vascular service line; in the past area patients often had to travel to Lexington for specialized cardiovascular care. Kline previously practiced in Arizona and is founder and director of the S.A.V.E Foundation, which promotes education and research in vascular disease and wound care.
SVS History Digital Archive Task Force calls for notabilia
THE SVS HISTORY DIGITAL
Archives Task Force is soliciting contributions as it aims to present a curated collection to SVS members and the medical community. The initiative came from the SVS Executive Board earlier this year as members saw a need to foster a comprehensive digital repository of the specialty.
Task Force Co-Chairs Jerry Goldstone, MD, and Craig Miller, MD, have outlined a list of topics of potential interest. These include historical figures, technological advancements, scientific discoveries and novel procedures of significant clinical impact. Miller emphasized that members with primary-source items are encouraged to submit.
“One of the things we’re doing right now is assembling documents that we’ve created ourselves ... We aim to assemble these items to create a cohesive narrative. This is a project that should be ongoing. Moving forward, what is present will become past. As another generation comes along, there are things that will turn out to be of historical significance.” Submit at vascular.org/DigitalArchive
SVS COMMEMORATES NATIONAL APP WEEK
THE SVS HONORS THE dedication and contributions of advanced practice providers (APPs) in vascular health both before and during National Advanced Practice Provider Week. The week, celebrated the fourth week of September, serves as a beacon of recognition for the role healthcare professionals take in revolutionizing patient outcomes. Professionals honored during this celebration include nurse practitioners, physician assistants, nurse anesthetists and clinical nurse specialists who play a vital role in delivering high-quality patient care across various medical specialties.
Holly Grunebach, MMS., MSPH, PA-C, chair of the SVS Physician Assistant Section, shared her insights and perspectives on the celebratory week as a physician assistant with more than 13 years of experience in vascular surgery.
“National Advanced Practice Provider Week is a time to reflect on the incredible progress that advanced practice providers have made in our healthcare system,” said Grunebach. “We have evolved from being supportive members of healthcare teams to being integral components of patient-centered care.”
18
Vascular Specialist | September 2023
SPOT LIGHT In memoriam ALLAN
R. DOWNS, MD, of Winnipeg, Manitoba, Canada, Jan. 12.
Publications: Newest JVS peer-review title appoints editor-in-chief
The Journal of Vascular Surgery (JVS) announced the appointment of Anahita Dua, MD, as the editor-in-chief of the Journal of Vascular Surgery-Vascular Insights (JVS-VI), the newest title in the JVS stable. By Marlén Gomez
DUA, AN SVS MEMBER, IS AN ASSOCIATE professor of surgery at the Massachusetts General Hospital (MGH) and Harvard Medical School in Boston. She has authored more than 180 peer-reviewed papers and has edited five vascular surgery medical textbooks. Dua also runs a National Institute of Health (NIH)-funded coagulation lab at MGH and a vascular surgery practice focusing on complex peripheral arterial disease (PAD) and limb salvage. Her appointment became effective Aug. 1.
“It’s crucial to provide fellow vascular professionals with the most up-to-date data to make well-informed decisions in their daily practice,” Dua told Vascular Specialist. “I believe this position allows me to be part of shaping the landscape of vascular surgery by delivering high-quality data through an evidence-based journal that focuses on the ‘other’ crucial parts of success in vascular surgery in 2023, including aspects such as quality, research, DEI [diversity, equity and inclusion] efforts, innovation, administration/business and health policy.”
JVS-VI launched in early January, coinciding with the renewal of the SVS’ publishing contract with Elsevier. In response to the changing landscape of academic
publishing, JVS-VI was introduced as an online-only, openaccess (non-subscription) journal, allowing for broader accessibility to the latest research and developments in the field.
Ronald Dalman, MD, executive editor of the JVS group, was editor-in-chief for JVS-VI upon its creation. However, recognizing the need for a dedicated editor to lead the journal, he noted how the its success depended on someone with a vision and passion.
“Establishing a dedicated editor-in-chief for this journal became our goal, and during the interview process, it became clear that Dr. Dua’s compelling vision made her an excellent fit for the role,” said Dalman.
The JVS editorial team integrated the journal into its portfolio of publications to capture exceptional work that other journals might have overlooked. Dua believes that JVS-VI will ensure that significant topics receive the recognition they deserve.
Under Dua’s leadership, the JVS-VI editorial team will give priority to high-quality research manuscripts that generate hypotheses and provide background information, along with review articles, single-center
CLINICAL&DEVICENEWS
IMAGING
FIRST PATIENT TREATED IN GLOBAL STRATEGIC COLLABORATION BETWEEN CYDAR MEDICAL AND MEDTRONIC

Cydar Medical has announced the successful treatment of the first patient in a strategic collaboration with Medtronic. The collaboration, which spans 40 sites across the U.S., UK and Europe, involves the integration of the company’s Cydar Maps software with Medtronic’s services and case support, with the aim of improving patient care and the efficiency of medical professionals by introducing unique artificial intelligence (AI) solutions into the clinical environment.
The first patient in the pilot program was treated using Cydar Maps at Edward Hospital in Naperville, Illinois, by vascular and endovascular surgeon George Pontikis, MD.
Cydar Maps is the first product from Cydar’s AI technology platform and, according to the company, transforms the way information is provided to clinicians undertaking image-guided minimally invasive surgery simplifying complexities within operating theatres at leading hospitals across the globe.
The company explains that Cydar Maps generates a 3D map of patient soft tissue to support and integrate preoperative
planning, intraoperative guidance and postoperative review of endovascular minimally invasive surgery, using AI to update the map throughout the patient journey. Cydar Maps has been shown to offer a number of benefits, a company press release reports, including halving the radiation exposure for patients and the clinical team, simplifying the clinical workflow and increasing clinician confidence, which in turn can significantly reduce procedure times.
quality improvement projects and discussions on practice management, business, ethics topics, commentaries and historical vignettes.
Dua emphasized that the move towards open access ensures that a wider audience can access crucial research discoveries globally without charge immediately upon publication, fostering collaboration, creativity and equity within the vascular surgery field.
“This journal is dedicated to modern vascular surgeons practicing in 2023 faced with not only ensuring optimal surgical technique but also maintaining the other parts of vascular surgery practice—quality, logistics, education, research—that support excellent patient outcomes,” she said.
“We aim to address various aspects of vascular surgery in this day and age, and I feel a great responsibility to our readership to present quality articles that discuss these topics. I’m very excited to bring fresh new ideas to our portfolio, starting with a diverse editorial board with national and international representation.”
Read JVS-VI at www.jvsvi.org.
Compiled by Bryan Kay
VASCULAR TRAUMA
Clinical performance of Human Acellular Vessel amid war in Ukraine presented at military research symposium
Clinical outcomes of Humacyte’s investigational Human Acellular Vessel (HAV) were presented at the Military Health System Research Symposium in Kissimmee, Florida (Aug. 14–17), following a yearlong program in Ukraine.
The bioengineered, implantable human tissue-based device was provided to five hospitals on the frontlines of the Ukrainian war to treat traumatic vascular injuries beginning in June 2022.
The pilot program is also expected to inform the ongoing development of Cydar Maps, which will include predictive analytics to support optimized procedure planning based on the use of AI to compare patient anatomy and procedure outcomes from a global dataset. Pontikis said: “This cutting-edge technology empowers us with the ability to navigate complex vascular procedures with greater precision—ensuring optimal outcomes for our patients. We are honored to be a part of this innovative program and are eager to contribute to the advancement of endovascular aortic surgery.”
War injuries in Ukraine have led to tens of thousands of amputations, many of which occur because blood flow cannot be restored after the injury, the company outlined in a press release. As of July 2023, the HAV has been used to treat 19 patients in the eastern European country suffering from a range of traumatic vascular injuries, including gunshots, shrapnel, blasts and industrial accidents.
Clinicians reported that the rate of success in treating patients with the HAV was high, Humacyte reported, with an observed 30-day HAV patency (presence of blood flow) of 95%. At 30 days after treatment with the HAV, the limb salvage rate was 100%, meaning no amputations
occurred in patients treated with the bioengineered vessel. In addition, there was 100% patient survival and no cases of infection of the HAV. There was one patient whose HAV had to be removed due to shrapnel-related bleeding.
“The novel bioengineered, off-the-shelf HAV provides time to the surgeon and patient,” said Oleksandr Sokolov, MD, a Ukrainian vascular surgeon and HAV implanter in the humanitarian program.
Humacyte’s humanitarian program was initiated in May 2022, when the company provided investigational HAVs to hospitals in Vinnytsia, Dnipro, Odessa, Kyiv and Kharkiv. The new data from the frontlines in Ukraine will be included as part of Humacyte’s Biologics License Application (BLA) to the Food and Drug Administration (FDA). It is an investigational product and has not been approved for sale by the FDA or any other regulatory agency.
19 www.vascularspecialistonline.com

DEEPLY COMMITTED TO INNOVATION SEEING OPPORTUNITY WHERE OTHERS DON’T. W. L. Gore & Associates, Inc. Flagstaff, Arizona 86004 goremedical.com Products listed may not be available in all markets. GORE, Together, improving life and designs are trademarks of W. L. Gore & Associates. © 2023 W. L. Gore & Associates, Inc. 231001708-EN MAY 2023 See the latest innovation in aortic branch technology We are continuously innovating to overcome yesterday’s limitations, creating new possibilities in care for your patients.