JOURNEYS



ON THE COVER
Ryan King, a former triathlete, has stayed active while persevering through treatment for stage IV lung cancer. Read his story on Page 2.
We welcome your comments. For more information about Journeys, contact the Advancement team by calling 402-481-8674.
To learn more about Bryan programs and services, visit us online at bryanhealth.org.
Russ Gronewold
President & CEO, Bryan Health
John Woodrich
Executive Vice President and COO, Bryan Health
Eric Mooss
President & CEO, Bryan Medical Center
Robert Oakes, MD
Chief of Staff, Bryan Medical Staff
Bob Ravenscroft
System Vice President, CMO & CDO
Kevin Rummel, MD Medical Editor
David Berman Editor





22 Positive attitude, exceptional care help triathlete endure stage IV cancer
25 Headed toward liver transplant, Bryan Independence Center helps Jenny reverse course
28 Welcome these physicians to the Bryan medical community
Bryan Health Annual Report on Giving 12 First Focus Program class sets standard 13 NICU support helps keep their child’s memory alive
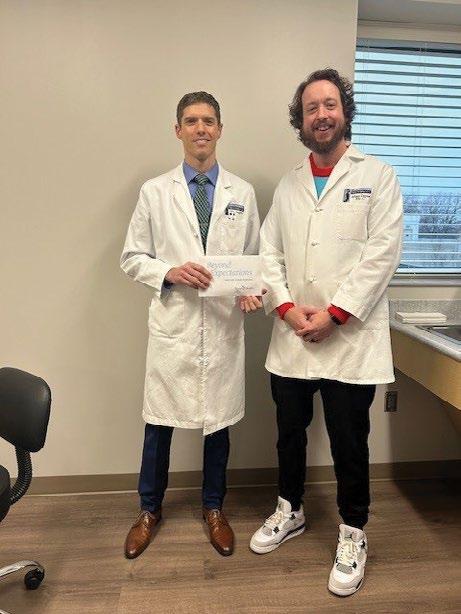
14 Beyond Expectations honorees
15 Community Benefits
18 Bryan partnered with these community organizations throughout 2023 19 Bryan Heart physician a “life saver” during waiting room cardiac arrest 22 Ask the Doctor: What to know about leading-edge AFib treatment
Trustees and Leaders Meet new CEOs Douglas Koch and Jodi Mohr
Just weeks after surgery, Carolyn attends son’s wedding thanks to innovative procedure
know new Bryan College of Health Sciences President
Presenting partners:
Bank & Trust Sampson Construction CDW
Nick & Ann Cusick Davis Design
DuTeau Chevrolet-Subaru
Eakes Office Solutions
“The greatness of a community is most accurately measured by the compassionate actions of its members.”
– Coretta Scott King
At Bryan Health, it takes all of us.
It took a village to open the April Sampson Cancer Center this spring. From our dedicated staff and providers to our passionate donors, the sparkling new facility is here thanks to countless individual efforts.
Ultimately, that’s what health care is all about: many parts leading to a healthy whole. We are honored to be a small part of what makes this big community so special.
As a nonprofit, Bryan Health gives back to those who have given so much to us. In
We are also eternally grateful to those who donated to the Bryan Foundation in 2023. Your gifts added up to over $7 million—dollars that will go right back into our healthcare mission.
We look forward to beginning the celebration of our 100th anniversary in 2025. Recognizing the past, cherishing the present and looking toward the future will be on our minds as we enter our centennial year.
Bryan Health. Forward. Together.


Ryan King is an exceptionally positive person. He’s an engaging, energetic man who will put you in a good mood just by talking to him. You would never guess what he is going through.
More than two years ago, Ryan, 50, was diagnosed with stage IV lung cancer that had spread to his brain. The five-year relative survival rate of this diagnosis is less than 10 percent. But Ryan has tried to maintain an upbeat attitude despite what he faces.
“From what I see, I think there are a lot of people who get a diagnosis and they go home and wait to die,” he said. “That would not be what I recommend.”
Ryan is a lifelong Lincolnite who just celebrated his 20th year at Mapes Industries. Shortly after he quit smoking about 10 years ago, he started running for fun. His hobby ballooned from competing in 5- and 10-kilometer races to becoming a passionate triathlete.
In fall 2021, he was training for two Ironman triathlons and started to experience headaches. He went to his primary care and eye doctors, who couldn’t find anything wrong. He was told to go to the emergency room if it didn’t improve, which he ended up doing in early January 2022 after an episode of blurry vision.
Within minutes of arriving, a CT scan raised alarm bells for the doctors. Once neurosurgeon Steven Gogela, MD, stepped into the room, Ryan knew something must be wrong.
Dr. Gogela told Ryan he had a tumor the size of a golf ball in the back left part of his brain. He quickly had surgery to remove the tumor and that summer began chemotherapy with Dr. Steven Dunder, and radiation with radiation oncologist Dr. Mark Stavas.
While receiving treatment, Ryan was unable to maintain the rigorous training needed to compete in the triathlon circuit. However, once his treatment slowed down, he decided he wanted to run in one more triathlon.
In April 2023, he completed an Ironman triathlon in Oceanside, California, which consisted of a 1.2-mile swim, a 56-mile bike ride and a 13.1-mile run. His placement didn’t matter to him; all he wanted to do is say that he finished.


Once he returned home from California, he contemplated what to do with his recently earned medal. Dr. Stavas had been his “biggest cheerleader” during his treatment and training, so Ryan decided to give the medal to him as a token of his appreciation.
He told one of Dr. Stavas’ nurses his plan, and she told him Dr. Stavas had attempted to secure a spot in the race to run with Ryan. The pair had thought of a way to support and appreciate each other without the other knowing.
“The medal meant a lot to me, but I think it maybe meant as much to him because he’s just a great guy,” Ryan said. “He’s talked me off a ledge many times the last couple years.”
Dr. Stavas said Ryan embraces the best of what it means to live life with uncertainty.
“He has been a wonderful teacher to me, as I’ve realized that each of us can be as healed as those we are healing,” Dr. Stavas said.
Ryan had been feeling well, keeping tabs with Drs. Stavas and Dunder to prevent any recurrence. In December 2023, he was driving home from work. One second, he was driving normally down I-80. The next, he realized he had veered all the way to the shoulder without realizing it.
“I didn’t get dizzy or anything,” he said. “It was just like I was there, then I wasn’t, and then I came back.”
Ryan and Dr. Stavas embrace at the April Sampson Cancer Center.
He went in for a CT scan the next day. There was a much bigger tumor than before, this time on the back right of his brain.
He had the second tumor removed on January 9. Ryan said his recovery was much harder this time since he was less physically fit than before. He was told it often takes six to eight weeks to feel normal after a craniotomy. While he bounced back only a few weeks after the first surgery, he said it took closer to the higher end of that range the second time. He also got bronchitis and COVID during his recovery.
After other small recurrences, Ryan has undergone two Gamma Knife stereotactic radiosurgeries in the last six months by Drs. Stavas and Gogela.
During the last few years, Ryan has struggled with anxiety and depression, especially surrounding his health. Every mundane headache brings fears that his cancer may be back.
Despite this, he strives to be positive and take each day one step at a time. He said his wife, Kim, and his two stepchildren have surrounded him with support. The entire staff at the April Sampson Cancer Center has made him feel comfortable and welcomed.
“When I walk into the cancer center, it’s like everybody gives me a big hug,” he said. “Everybody knows my name. They know what you’re going through because they see it every day, and they’re compassionate.”
Ryan hopes his story helps others with cancer find the positivity in their lives. Despite the difficulties of the last few months, he’s grateful for his home, work and family.
Now, Ryan lives three months at a time, which is the frequency of his brain scans. He knows the length of his life is uncertain, which has altered his perspective. He tries to squeeze as much out of each day as he can.
“I’ll go to the ends of this earth just to get one more day.”
To support cancer care, call the Bryan Foundation at 402-481-8605.

Jenny Quicke said her experience at the Independence Center helped her rediscover her true self. “I didn’t have to hide who I was anymore,” she said.

Concerned about alcohol or drug use?
Scan QR code to take a free, confidential screening or call Bryan Independence Center at 402-481-5268.
The day after Easter in 2023, Jenny Quicke found herself in the emergency room. She was severely dehydrated and anemic, and suffering from catastrophic liver damage. Doctors told her that if she had kept drinking for just three more days, she would have died.
Alcohol was never a part of her life growing up. Born in Gering, Nebraska, she grew up in a Catholic family with three brothers. She was a high achiever in school who competed in multiple sports.
After graduating high school in 2003, she went to Western Nebraska Community College and played volleyball on scholarship. A few months after turning 21, she decided to move in with two of her brothers in Lincoln and attend the University of Nebraska-Lincoln.
Her newfound adulthood and Lincoln nightlife became a dangerous combination. Looking back now, 20 years later, Jenny calls that first year of legal drinking “addicting.” She started going out to bars a few days a week to socialize while at UNL.
It was only the beginning.
Over time, Jenny’s drinking steadily increased. She started working at a local bar and grill as a bartender. After quickly working her way to a management position, she dropped out of school to focus on her job.
With her nights spent around people drinking and having a good time, it was hard for her to resist joining in.
She would stick around work after her shift and grab a few drinks. Often, she would wake up hungover.
“I just thought I was young, so it was fine.”
She was still steady at work and in her social life, but behind closed doors, her drinking intensified.
“In front of everybody else, I was smiling. I was a bartender, so patrons would ask me how my day was, and I would say I was doing great.”
But deep down, she was far from OK.
The COVID-19 pandemic only made her drinking worse. She was already drinking every day, but during the pandemic she would drink before, during and after work. It was easier to get away with this during a period of reduced contact with friends and family.
Looking back, she calls herself a functional alcoholic. She had become dependent on alcohol—drinking around a bottle of hard alcohol a day—but was still able to juggle day-to-day responsibilities and relationships.
But eventually, she didn’t have an appetite. She could barely swallow food, so she was constantly drinking on an empty stomach. There were days where she would throw up one shot of alcohol and then take another until it stayed down.
“I knew my health was not in a good place, but at that point, I also thought that alcohol was the only way I could feel better,” she said.
Easter weekend of 2023, her parents came to town, but Jenny was too weak to make it to Easter dinner. When her parents came by to check on her, they could tell she was sick and wanted her to seek medical attention. But it wasn’t until they walked outside that they knew she was in serious trouble.
“I stepped into the sunlight, and my mom goes ‘Oh my gosh— you’re yellow. You’re completely yellow.’ They took me right to the emergency room.”
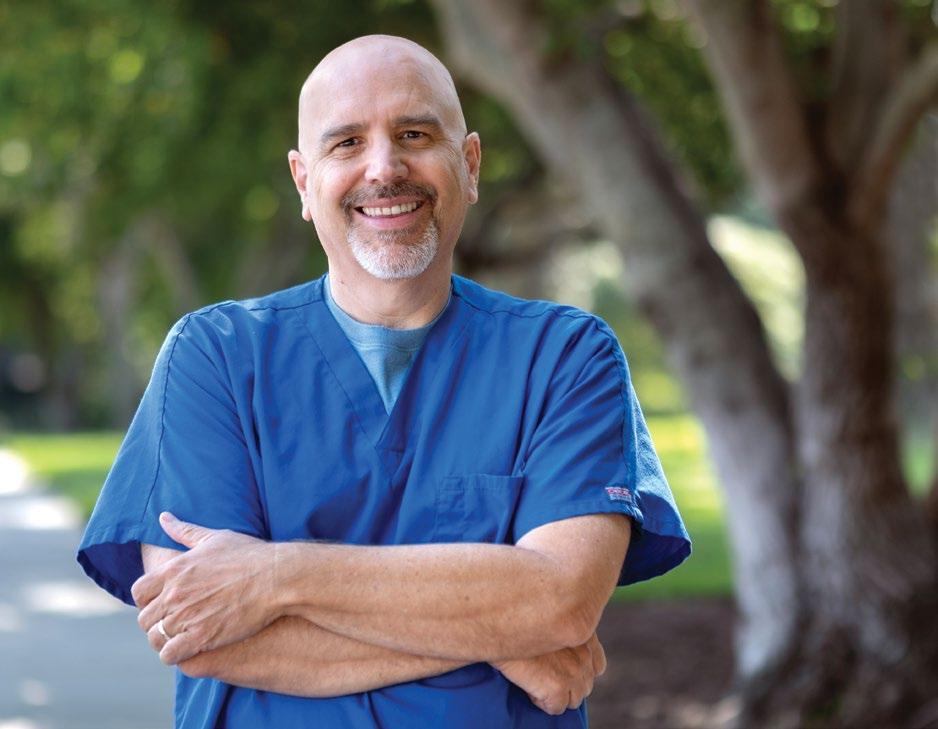
Dave Dermann has worked at Bryan Health for over two decades, helping countless patients like Jenny.
MELD scores estimate the severity of a patient’s liver disease and the likelihood of survival over the next three months. The range of scores is from six to 40; the higher the number, the more urgent the need for a transplant. When she was hospitalized, her score was 31.
Jenny had reached rock bottom and was open to whatever was necessary to get better. In the emergency room, at this turning point in her life, she met Dave Dermann.
Dave is an intervention nurse at the Bryan Independence Center, which has provided alcohol and drug treatment services since 1971. He visits patients at hospitals around Lincoln to help sort through treatment options for substance use. The Independence Center offers various levels of care, including short-term residential, partial care and intensive outpatient services.
When Dave meets with patients, all his recommendations are voluntary on the patient’s part. If somebody doesn’t want to receive treatment, he will leave his card and periodically check in on them.
“What I’ve found is that when you honor those choices, more often than not that person will eventually call you,” Dave said. “They now know that somebody cares.”
Jenny didn’t need much convincing to use the resources at the Independence Center. After almost a week in the ICU, she was admitted into short-term residential care on April 24.
Jenny said her first few days were rough. She still felt very sick and was nervous about the entire experience. Inpatient care at the center is rigorous, with eight to 10 hours of programming a day.
“Even on a good day, it’s pretty exhausting,” Dave said.
But the programming soon captured her attention.

I was fighting for other aspects of my life. I’m the kind of person that, if I’m going to do something, I want to be the best.”
She took detailed notes during each class and found herself staying up late every night researching her disease. She had a strong sense that the Independence Center was where she was meant to be.
Jenny said she also benefitted from the structure of the center. She established routines for herself and ate three good meals a day. Everybody at the Independence Center has a roommate to encourage accountability.
Jenny said the busy schedule helped take her mind off her addiction.
“The crazy thing is that I wasn’t thinking about wanting to drink, but I was sitting there talking about alcohol.”
Like many Independence Center patients, Jenny slowly moved from the most intensive care to the least. She “graduated” from the Independence Center last July, but her recovery will be constant. She’s currently on Step 11 of the 12-Step Addiction Recovery Program and attends a women’s recovery group every weekend.
Jenny said her experience at the center helped her re-discover her true self.
“I didn’t have to hide who I was anymore,” she said. “I didn’t have to put that fake smile on—I have a real smile now.”
In November 2023, Jenny underwent a pre-evaluation for a liver transplant. At the time, it was believed her liver was still too damaged to function long-term. The test results came as a shock to her.
“It was three days of testing, and after everything, they tell me ‘Oh wow, you’re looking good.’”
Her MELD score had dropped all the way to an eight. Her commitment to recovery, bolstered by her time at the Independence Center, had saved her life.
Dave believes Jenny’s desire to get better is a major reason for her success. A patient’s mindset, starting at their first meeting with an intervention nurse, plays a major role in their recovery.
“We empower people who initially say no and tell them that it’s their decision,” Dave said. “It’s your story. It’s not our story, but we’re here and available to help you.”
One teaching from the center that Jenny has especially held onto is the idea of creating a mental toolbox. She was told the journey she is on is not a luxury cruise—it can be a bumpy voyage.
With support from her family and determination to be healthier, she has developed the right tools to stay above water.
“The Independence Center got my foot in the door of sobriety,” Jenny said. “It is the best thing I’ve ever done, and in a lot of ways, it saved my life.”
To support Bryan Independence Center, call the Bryan Foundation at 402-481-8605.



Akshay Agrawal, MD, Prairie Center Internal Medicine & Nephrology, part of Bryan Physician Network
Specialty: Internal Medicine
Medical Education: Lokmanya Tilak
Municipal Medical College and Sion Hospital, Mumbai, India
Residency: St. Barnabas Hospital, Bronx, New York
Zane Atkins, MD, Platte Valley Medical Clinic
Specialty: Cardiothoracic Surgery
Medical Education: Duke University School of Medicine, Durham, North Carolina
Residency: Duke University School of Medicine


Antonio Beltran, MD, Urology Partners of Nebraska
Specialty: Urology
Medical Education: University of Cincinnati, Ohio
Residency: Tulane University School of Medicine, New Orleans, Louisiana

Taryn Boik, MD, associated with Lincoln Pediatric Hospitalists
Specialty: Pediatrics
Medical Education: University of Nebraska Medical Center
Residency: University of Minnesota, Minneapolis
Dalan Brown, MD, Madonna Rehabilitation Physicians
Specialties: Pediatrics, Internal Medicine
Medical Education: University of Washington, Seattle
Residency: University of Arizona, Phoenix
Daniel Cybulski, MD, associated with Consultants in Infectious Disease
Specialties: Infectious Disease, Internal Medicine
Medical Education: Uniformed Services
University of the Health Sciences, Bethesda, Maryland
Residency: Wright State University, Dayton, Ohio
Fellowship: San Antonio Uniformed Services Health Education Consortium, Texas

Robert Harrold, MD, Lincoln Radiology Group
Specialty: Radiology
Medical Education: University of Queensland with Ochsner Clinical School, New Orleans
Residency: Ochsner Medical Center Fellowship: Alabama Orthopedic Imaging, Mobile




Matthew Hoffman, DO, Nebraska Emergency Medicine
Specialty: Emergency Medicine
Medical Education: Western University of Health Sciences, Pomona, California
Residency: St. Barnabas Hospital

Brian Kim, MD, Platte Valley Medical Clinic
Specialties: Cardiology, Electrophysiology
Medical Education: Medical College of Pennsylvania, Philadelphia
Residency: Medical College of Pennsylvania
Fellowships: University of Miami, Florida; UCLA/West LA Veterans Hospital, California
Adam Mues, MD, Urology Partners of Nebraska
Specialties: Urologic Oncology, Urology
Medical Education: University of Nebraska College of Medicine
Residency: Ohio State University College of Medicine, Columbus
Fellowship: Columbia University New York Presbyterian Hospital


Matthew Schukar, DO, Nebraska Emergency Medicine
Specialty: Emergency Medicine
Medical Education: Edward Via College of Osteopathic Medicine, Spartanburg, South Carolina
Residency: ProMedica, Monroe, Michigan

Jon Steinhauer, MD, Pathology Medical Services
Specialty: Pathology
Medical Education: University of North Dakota School of Medicine, Grand Forks
Residency: University of Alabama at Birmingham
Fellowship: University of Texas MD Anderson Center, Houston
Adam Streit, DO, Nebraska Orthopaedic Center
Specialty: Orthopedics
Medical Education: Kansas City
University of Medicine and Bioscience
Residency: Ohio University, Athens
Jeremy Strom, MD, Prairie Center
Internal Medicine & Nephrology, part of Bryan Physician Network
Specialties: Pulmonology, Critical Care Medicine
Medical Education: Ross University
School of Medicine, West Indies
Residency: University of Kansas
Medical Center, Kansas City
Fellowship: University of Kansas Medical Center
Jaci Timmons, MD, associated with Lincoln Pediatric Hospitalists
Specialty: Pediatrics
Medical Education: Rush Medical College, Chicago
Residency: Rush University
Medical Center
Jana Van Wie, MD, Prairie Center
Internal Medicine & Nephrology, part of Bryan Physician Network
Specialty: Family Practice
Medical Education: University of Nebraska Medical Center
Residency: University of Nebraska
Medical Center
Fellowship: Michigan State University, Lansing
These APPs are working within the Bryan Health system:
Lexi Askey, CRNA, Associated Anesthesiologists
Chelsea Baird, APRN-NP, Capital Foot & Ankle, part of Bryan Physician Network
Kelsey Baxa, APRN-NP, CAMC Family Practice
Kent Cannon, PhD, Bryan Counseling Center
Lisa Cleveland, APRN-NP, Lincoln Nephrology and Hypertension
Amanda Coleman, CRNA, Associated Anesthesiologists
Kristina Draper, CRNA, Associated Anesthesiologists
Zoryana Dubina, PA-C, Bryan Neurology, part of Bryan Physician Network
Amanda Dunn, APRN-NP, Bryan Heart
Kerry Emeigh, APRN-NP, Plaza West Psychiatry, part of Bryan Physician Network
Esthefany Estrada, APRN-NP, Bryan Trauma and Acute Care Surgery, part of Bryan Physician Network
Michelle Fedon, APRN-NP, Lincoln Nephrology and Hypertension
Sarah Frischmeyer, PA-C, Bryan Trauma and Acute Care Surgery, part of Bryan Physician Network
Paulina Gossman, APRN-NP, Nebraska Hematology Oncology Cancer Center
Brad Greisen, CRNA, Associated Anesthesiologists
Jill Hobelman, PA-C, CAMC Family Practice
Rachel Karr, PA-C, Capital Foot & Ankle, part of Bryan Physician Network
CallieAnn Kohout, PA-C, Lincoln Pediatric Hospitalists
Jennifer Kramer, APRN-NP, Bryan Psychiatry, part of Bryan Physician Network
Breanne Kuntz, PA-C, Bryan Orthopedic Trauma, part of Bryan Physician Network
Libby Lewandowski, APRN-NP, CAMC Family Practice
Lindsey Maas, APRN-NP, Women’s Healthcare Center of Williamsburg
Kasha Meyer, PA-C, Nebraska Emergency Medicine
Denise Murry-Porter, CRNA, KRMC Anesthesiology
H. Summer Nguyen, PA-C, Nebraska Hematology Oncology Cancer Center
Michelle Oehm, APRN-NP, Bryan Neurology, part of Bryan Physician Network
Jackie Oden, APRN-NP, Women’s Clinic of Lincoln, part of Bryan Physician Network
Kevin Ourada, CRNA, Associated Anesthesiologists PC
Jacqueline O’Doherty, PA-C, Urology PC
Jason Peterson, APRN-NP, CAMC Emergency Department
Kendra Piening, APRN-NP, Bryan Palliative Care, part of Bryan Physician Network
Paula Railsback, APRN-NP, Women’s Clinic of Lincoln, part of Bryan Physician Network
Danielle Reuter, APRN-NP, Bryan Heart Vascular Surgery
Andrea Roberts, APRN-NP, Women’s Clinic of Lincoln, part of Bryan Physician Network
Jessica Rowell, APRN-NP, Nebraska Orthopaedic Center
Courtney Sams, APRN-NP, Women’s Clinic of Lincoln, part of Bryan Physician Network
Adam Schapmann, PA-C, KRMC Cath Lab
Kristin Schellpeper, CNM, Lincoln OB/GYN
Taylor Schendt, PA-C, Plaza West Psychiatry, part of Bryan Physician Network
Michael Sebek, PA-C, Nebraska Orthopaedic Center and Nebraska Emergency Medicine
Molly Snow, APRN-NP, Women’s Clinic of Lincoln, part of Bryan Physician Network
Maudine St. Onge, PA-C, Bryan Plastic and Reconstructive Surgery, part of Bryan Physician Network
Jodi Wegner, APRN-NP, Women’s Clinic of Lincoln, part of Bryan Physician Network
Nathan Weiss, APRN-NP, Nebraska Emergency Medicine
Carrie Wiechmann, APRN-NP, Bryan Trauma and Acute Care Surgery, part of Bryan Physician Network
Julie Wilson, APRN-NP, Urology PC
Jessica Wollberg, APRN-NP, Lincoln Pediatric Hospitalists
David Zink, PA-C, Nebraska Orthopaedic Center
Gift and pledges from individuals, corporations and foundations $6,153,302

*562 volunteers served throughout Bryan Health and contributed 34,195 hours of service in FY 2023, valued at $1,008,753. The Institute of Philanthropy quantifies the value of each hour of service at $29.50.







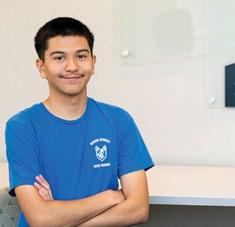
Alex Ibarra Juarez took a huge leap of faith heading into his junior year of high school.
Having attended Lincoln Southwest High School for his first two years, he saw an opportunity he couldn’t refuse – transferring to the newly-opened Lincoln Northwest High School to participate in the Bryan College of Health Sciences Medical Sciences Focus Program.
The program allows juniors and seniors at Lincoln Northwest to earn up to 20 early college credits from the college with reduced tuition. Students eligible for free and reduced lunch can apply for free tuition through the Nebraska ACE scholarship program. Bryan Foundation also offers scholarships and certification support.
“I always knew I wanted to help people, but I didn’t know how,” Alex said. “So, I thought I’d try the Focus Program and see what health care is all about.”
Alex, along with seven peers, was in the first class of students to complete the program. He graduated in May and will attend the college in the fall to pursue a career in cardiovascular sonography. This summer, he’s working as a patient care technician at Bryan Medical Center in the progressive cardiac care unit and will continue this position once classes begin.
Jason States, the first director of high school outreach programs, worked closely with Lincoln Public Schools officials to develop the program. He moved to a dean position at the college in July.

“Students get lots of good hands-on experiences and get to see different aspects of health care,” Jason said of the program. “A lot of people think you can either be a nurse or a doctor, but there are so many more people on the team who make everything work.”

Alex and his cohort are the first to have their names displayed as graduates of the Focus Program.
Alex said the program helped cement his interest in sonography. He and his peers took classes such as introduction to health professionals and anatomy and physiology. The program also offered opportunities for him to shadow professors and students at the college during Blue Healer Days and listen to guest speakers from many medical disciplines.
One of Jason’s favorite elements of his job is watching students grow. Alex’s cohort was brought to the college for a “signing day” before they even began the program. Jason said the students barely said two words to each other that day, but they since have formed strong bonds. Alex said they have a group chat to keep in touch. Half of his cohort will join him at the college in the fall.
“The connections I made through this program were great,” Alex said. “We went from not saying a word to each other to calling each other for help with homework.”
Jason said he’s excited to see the program continue to grow heading into its third year. Many more students will pass through the program in the years to come, but Alex and his classmates will always be the first. A large display board at Lincoln Northwest dedicated to graduates of the program will forever show their names.
“It feels great,” Alex said. “We made the first step, and we have set the bar really, really high for everyone else.”
Jen Wallin and her husband, Josh, had one of the worst moments of their lives at the Bryan Medical Center neonatal intensive care unit (NICU). Their son, Thomas, died of a genetic disorder a few days after his birth. That was over a decade ago; they have since worked tirelessly to support the NICU.
“I remember the staff taking such great care of Thomas while he was alive,” Jen said. “Giving back to them was something we could do that would hold a lot of meaning.”
Jen and her husband have two more children – Noah, 7, and Bentley, 5. Bentley also was born with medium-chain acyl-coenzyme A dehydrogenase (MCAD), the disorder that claimed his brother’s life. MCAD is an inherited disorder that prevents the body from breaking down certain fats and turning them into energy. It is present from birth and is a lifelong condition.
The family celebrates Thomas’ birthday every year in various ways, including family trips and bringing birthday cake to the NICU. The family also has put on a “Run for Thomas” for the last 10 years at Holmes Lake to raise awareness about MCAD and remember Thomas.
Proceeds from the run go toward care packages that the Wallins donate to the NICU and pediatric unit. The packages include items such as baby blankets, stuffed animals, coloring books, lotion and snacks. Jen also handwrites notes for each package letting the family know that they are not alone on their journey. Finally, a card explains the meaning behind the package and informs each family of Thomas’ story.


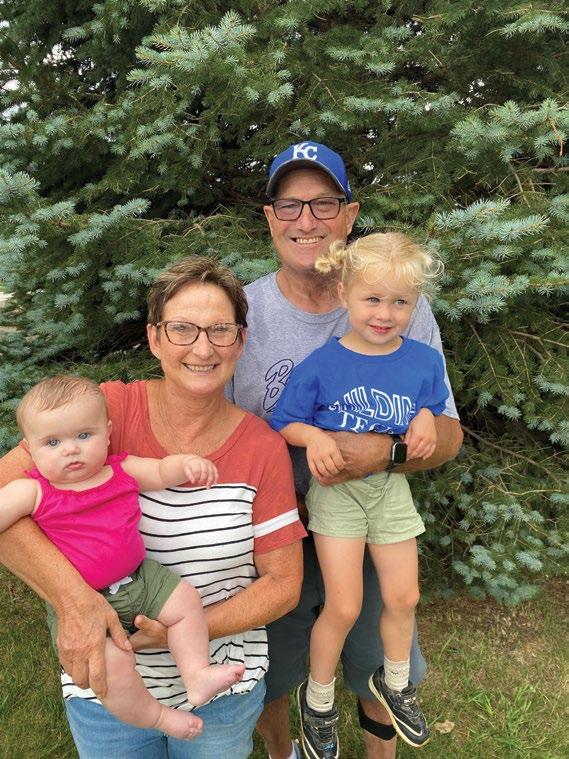
The Wallin family at the “Run for Thomas” event.
One of the trees in the NICU healing garden was donated in memory of Thomas. And every year, the family donates items from the NICU’s wish list, such as artwork and mobiles.
Jen said she and her husband are so involved with the NICU for many reasons, including feeling close to Thomas and helping other families facing the uncertain health of their newborns. The couple experienced that uncertainty firsthand during Thomas’ few days on Earth.
After a C-section, medical staff conducted standard newborn screenings on Thomas with all looking well. But then Thomas stopped breathing on his third night in the hospital.
He was rushed to the NICU, where he was revived. After further testing, he was diagnosed with MCADD.
He began breathing on his own again, and by the next day, he seemed to have stabilized. The couple were resting elsewhere when they were asked if they wanted to hold Thomas for a while. By the time they arrived back at the NICU, staff were performing CPR on their newborn. He passed away a few hours later.
Bentley struggles to maintain his body temperature in the heat, and he drinks a lot of Gatorade to keep his sugar level high. Otherwise, he is a normal, happy-go-lucky 5-year-old, his mom said.
“He’s full of the bumps and bruises from the playground that a normal 5-year-old has,” she said.
Jen is still in touch with many of the NICU nurses from those tragic few days. They often text photos of Thomas’ tree glowing through the night and ask her how she and her family are doing.
Her family’s connection to Bryan Medical Center keeps her tethered to her beloved first child.
“I always think to myself, ‘What am I doing for Thomas today?’” she said. “We’ve always said we’ll do something good throughout the day to honor and cherish him.”
Our patients and their families made Beyond Expectations gifts in honor of these physicians and employees who went beyond expectations to provide exceptional services in 2023.
Edie Aman
Kelsey Arner
Ian Baker
Katie R. Barnes
Shannon Becher-Kulwicki
Stacey Bostwick
Brandie Campbell
Trina Casey
Wanda Dos Santos
Stephanie Everett
Tessa Falos
Bobbi Ferguson
Mary Garner
Dr. Steve Gogela
Nancy Grant
Megan Groathouse
Briley Hannaford
Megan Hatch
Jacqueline Hemmingsen
Cindy Jaimes
Dr. Rachel Jendro
Jacki Jimenez
Riley Johnson
Gabbie Karpisek
Alauna Lammermann
Madison Lechner
Lindsey Lempka
Alyssa Long
Dr. Daisy Madathil
Sian Maxwell
Rhondel McCann
Alex Mcintire
Mindy Mcintire
Samantha Mlinar
Cassie Nguyen
Bailey Novak
Carmen Orr
Katherine Ortega Navarro
Dr. Robert Pitsch
Cece Podraza
Crystal Porter
Mariclaire Prill
Carrie Reed
Dr. Eric Riddle
Michael Roberts
Brandey Ryan

Dr. RoseAnn Schwaninger
Erin Skolil
Amanda Smith
Stefanie Staab
Crystal Stech
Lori Stewart
Samantha Strain
Zarifa Tucovic
Cornel Tuns
Mary Turner
Susie Vavra
Barbara Wagner
Lauretta Yuma
Rodney Zach

This is the total cost of community benefits provided by the entities of Bryan Health in Fiscal Year 2023—an increase of $18 million from the previous year. The total breaks down like this:

$23 million in charity care. These free or discounted health services are provided to patients who can’t afford to pay and who meet criteria for financial assistance.
$186 million in unreimbursed cost of Medicare, Medicaid and other public programs. This represents the shortfall between the actual cost of providing care and payments received from the government.
$20 million to fund other community programs and subsidized services. These activities and programs improved community health and wellness, and we subsidized healthcare services that met identified needs in the community.
$6 million for health professionals education. This is how much it cost to provide accredited training and education programs for doctors, nurses and other health professionals through residency education and continuing medical education, plus financial support of the Bryan College of Health Sciences.
$600 thousand in partnership with other nonprofit organizations for charitable purposes.
Having trouble paying your bill? You may be eligible for financial assistance if you have limited or no insurance and can demonstrate financial need. Complete a Bryan financial assistance application and submit with required federal financial documents. Get an application at bryanhealth.org/financial-assistance or call our financial counselors at 402-481-5791 (toll free 977-577-9277).


Throughout Nebraska, Bryan Health provided $236 million in community benefits during Fiscal Year 2023
Grand Island
Regional Medical Center
Charity care: $4 million
Unreimbursed cost of Medicare/Medicaid: $15 million
Community programs: $600 thousand

Charity care: $330 thousand
Community programs: $230 thousand
Bryan Medical Center, Bryan Heart and Bryan Physician Network
Charity care: $14 million
Unreimbursed cost of Medicare/Medicaid: $140 million
Health professionals education: $6 million
Community programs and partnerships: $3 million
Kearney Regional Medical Center
Charity care: $4 million
Unreimbursed cost of Medicare/Medicaid: $31 million
Community programs and partnerships: $40 thousand
Charity care: $850 thousand
Community programs and partnerships: $333 thousand
*$17 million in community programs and partnerships came from Bryan Health.
American Heart Association
Arc of Lincoln
Asian Community & Cultural Center
Association of Fundraising Professionals
Black African Family
Boy Scouts of AmericaCornhusker Council
Camp Kesem – Nebraska
Center for People
CenterPointe
Child Advocacy Center
City of Lincoln
Civic Nebraska
Clinic with a Heart
Family Service Lincoln
Crete Area Health
Care Foundation
Educare of Lincoln
El Centro de las Américas
First Plymouth Congregational Church, UCC
Good Neighbor
Community Center
Gravel Adventures
Great Plains Trails Network
Heartland Cancer Foundation
HopeSpoke
Houses of Hope of Nebraska
Indian Center, Inc.
Junior Achievement
Karen Society of Nebraska
Kearney Chamber of Commerce
Kim Foundation
Lighthouse
Lincoln Arts Council
Lincoln City Libraries
Lincoln Community Foundation
Lincoln Homeless Coalition
Lincoln Literacy
Lincoln Public
Schools Foundation
LMEP - SCIP
Lutheran Family Services
Madonna
Make-A-Wish Nebraska
Malone Community Center
Matt Talbot Kitchen & Outreach
Memories for Kids
Mourning Hope
NAMI Nebraska
Nebraska Breastfeeding Coalition
Nebraska Commission on Latino-Americans
Nebraska Cures

Nuer Community Development Services
Partnership for Healthy Lincoln
Pius X High School
Ponca Health Services – Lincoln Health & Wellness Center
Postpartum Support International
Project Pink’d Inc.
ROSS Leaders
Seniors Foundation
Nebraska Department of Health & Human Services - Office of Health
Disparities & Health Equity
Nebraska Folklife
Nebraska Hospital Association
Nebraska Medical Association
Nebraska Nurses Association
Nebraska Stroke Association
New Americans Task Force (Lincoln)
No Footprint Too Small
Sewing for Babies, Inc.
Sunrise Communications - KZUM
Tabitha
United Way of Lincoln & Lancaster County
University of NebraskaLincoln
University of Nebraska Foundation
Visionary Youth
YWCA

Doug and Dianne Weishahn pose with Dr. Isaac Meier and some of the Beatrice Community Hospital staff who saved Doug’s life that December day.
Dr. Isaac Meier had just started his day. The Bryan Heart interventional cardiologist had driven down to Beatrice last December for his usual monthly clinic while remotely attending a morning meeting. He walked into Beatrice Community Hospital, headphones in his ears as he listened to the meeting and mentally prepared for the day’s workload. That’s when he heard the cries for help.
“I heard what you wouldn’t expect to hear when you walk into the waiting room—stressful cries,” Dr. Meier said.
The source of the cries was a woman whose husband had slumped over in his chair, completely unresponsive. Dr. Meier quickly checked for a pulse. There wasn’t one; the man had gone into cardiac arrest.
The man, Doug Weishahn, is a farmer from the village of Western, Nebraska, where he has lived most of his life. His wife, Dianne, has worked as a patient concierge at the Beatrice Community Hospital for the past 13 years. The couple met on a blind date and have been married for 43 years.
While recovering from a 10-hour back surgery in October, Doug experienced atrial fibrillation—a type of irregular heart rhythm that can be a common occurrence after a surgery. Doug and Dianne were at the Beatrice hospital that December day for an appointment with Dr. Meier in their specialty clinic space.
Doug had been cleared to drive, so he drove himself to the hospital. Dianne, who had to work after the appointment, followed him. They walked up stairs to the clinic waiting room when Dianne said he broke out in a sweat and started to shake.
Dianne sat him down, thinking he was about to faint. He soon did, and Dianne ran up to the front desk to call a rapid response team. As she turned around, she saw Dr. Meier walk into the room.
Dr. Meier didn’t realize that Doug was his first patient of the day—they had never met before. But Dianne knew what Dr. Meier looked like from his Bryan Heart profile page. Once she saw him walk into the waiting room, she immediately went to him for help.
Dr. Meier rushed over to examine Doug. A back brace he was wearing to help with his recovery kept him upright. With the help of the reception desk staff and nearby nurses, he lowered Doug to the floor, removed his brace and started CPR.
Doug has recovered well, allowing him and Dianne to do what they love: spending time with their grandchildren.
While Doug was lucky to experience this episode while in a healthcare setting, he wasn’t around the typical live-saving equipment found in an emergency room or intensive care unit (ICU).
Thankfully, the clinic did have an Automated External Defibrillator, or AED. Dr. Meier applied the AED to Doug’s chest. He was taken to the emergency room at Beatrice and then was transported to Bryan Medical Center, where he was diagnosed with multivessel coronary disease. Dr. Ryan Shelstad, a cardiothoracic surgeon with Bryan Heart, performed open heart surgery to bypass three blockages.
Dr. Meier said he had never experienced anything quite like that moment. One second, he was focusing on a meeting and preparing himself for his day. The next, he was thrown into life-saving mode.
“It’s one of those things where we deal with it frequently, but this was just in a completely different environment,” he said. “We had to take a step back and say, ‘well, what’s available to us right now?’ You feel a little helpless because, in my role, you’re used to having so many tools in these situations.”
Fortunately, Doug’s heart was stopped only for around a minute, so he suffered no heart damage. The proximity of an AED is a major factor in this outcome, Dr. Meier said. He is a strong advocate for AED accessibility, as he has one on hand in his car and house.

“I think AEDs should be everywhere,” he said. “It’s a necessity in sports venues and in most health clinics. Most public places should probably have one. The more people there are, the more likely you’ll need one.”
Dr. Meier sees the message about the importance of AEDs getting to the public but feels it’s one that still needs to be promoted. People can get uncomfortable when thinking about cardiac episodes, but Dr. Meier said they need to get over this hump.
“You have to do chest compressions, get the AED on and call 911,” he said. “If you do those things, I think you can walk away feeling like you did everything you could.”
Once Doug was stabilized, he met Dr. Meier in the capacity which he was originally intended—as his cardiologist. He will see Dr. Meier every three months for the foreseeable future for routine check-ins. Doug’s heart-health maintenance plan is standard, which is remarkable considering the severity of his recent episode.
“It’s almost a little weird in the sense that you connect him with a different outcome because of that day, but in terms of care, it’s actually very standard,” Dr. Meier said.
Doug said he doesn’t remember much about that day in December—only getting to the hospital and feeling warm in the waiting room. But he and his wife will always remember what Dr. Meier did for them.
When the couple attended Doug’s first follow-up appointment, returning to the spot where he collapsed just weeks earlier, they brought Dr. Meier a token of gratitude: a bag of Life Savers® candies.
Dr. Meier paused to collect himself as he reflected on this gesture.
“It’s not that it was some big gift,” he said through tears. “I just felt so appreciated. I didn’t end up opening it in front of them, which I wish I had.
“In hindsight, it’s probably good because I would have cried.”
To support cardiac services, call the Bryan Foundation at 402-481-8605.
Over 12 million people are projected to have atrial fibrillation (AFib) by 2030. In this issue’s “Ask the Doctor” segment, electrophysiologists Dr. Peter Gallagher and Dr. Grant Wallace discuss a new treatment for AFib –pulsed field ablation – available at Bryan Health.
What is an electrophysiologist?
An electrophysiologist is a cardiologist who specializes in electrophysiology or the electrical component of the heart that controls the rhythm of your heart beats (also known as arrhythmias). As an electrophysiologist, you receive extensive training to diagnose and treat irregular heart rhythms. The training required to become an electrophysiologist is lengthy and requires eight years after medical school – including three years of internal medicine residency, three years of clinical cardiology fellowship and two years of clinical cardiac electrophysiology fellowship.
What is AFib?
AFib is a type of arrhythmia or irregular heartbeat that causes the upper chambers of the heart to beat very fast and irregularly. For people experiencing AFib, their heart’s upper chambers (atria) can beat as fast as 500-600 beats per minute, when a normal resting heart rate beats about 1 time per second or 60 times per minute.
Why is AFib important to treat?
The quivering or irregular heartbeats of AFib don’t allow your heart to pump blood like it should which results in blood pooling in the atria. This pooling of blood can lead to blood clots, stroke, heart failure and other heart-related complications.
How do you treat AFib?
Treatment for AFib often includes ablation (or destroying) of the heart tissue that is causing abnormal electrical signals resulting in irregular heartbeats. Historically there have been two different types of ablation techniques—radiofrequency (using heat waves) and cryoablation (using freezing cold temperatures) to ablate or destroy the heart tissue. However, a new technique has recently emerged, called pulsed field ablation. This new technology involves a state-of-the-art catheter that ablates the various areas of the pulmonary vein using short pulses of energy directly to the AFib sites.


The shape of the pulsed field ablation catheter, pictured above, drastically shortens the procedural time for the patient compared to previous methods.




Pulsed field ablation uses tissue-selective, non-thermal electric fields to ablate heart tissue and avoid damage to surrounding areas of the heart.
This new technology has been proven to deliver as safe and effective results as the more traditional thermal (radiofrequency and cryoablation) applications without causing additional damage to surrounding areas of heart tissue. The shape of the pulsed field ablation catheter and delivery method of the energy drastically shortens the procedural time for the patient, meaning less anesthesia is used, and recovery is quicker.
In May, we became the first team to perform pulsed field ablation in Lincoln.
Bryan Heart electrophysiologists and Bryan Medical Center are one of only two programs in the region that perform this procedure.
With the incidence of AFib on the rise, pulsed field ablation allows Bryan Heart electrophysiologists another effective and efficient therapy to treat more patients, reduce complications and improve the quality of life for our patients and their families.
For more information, please contact your physician’s office.

The first pulsed field ablation in Lincoln was performed in May at Bryan Medical Center.
Dr. Gallagher grew up in Omaha and has been actively practicing in Lincoln and the surrounding communities since 2008. Dr. Gallagher has a special interest in complex ablations, atrial fibrillation and flutter, pacemakers and defibrillators as well as clinical research.
Dr. Gallagher was fortunate to be involved in some of the pre-clinical research involving the Farapulse™ system (the pulsed field ablation technology) before it was made available to the public. He is excited about what this new treatment means for his patients and their loved ones.
Dr. Wallace is a native of Oakland, Nebraska. Upon joining Bryan Heart in September 2023, Dr. Wallace brought with him a unique perspective with his combined internal medicine and pediatrics background prior to continuing his training in cardiovascular disease and cardiac electrophysiology.
Dr. Wallace specializes in complex ablations, atrial fibrillation and flutter, and device-based therapies with a focus on conduction system pacing, congenital heart disease related to arrhythmias, and clinical research. His goal with every patient is that they feel included in their care plan and informed about the treatment options available to them.
Bryan College of Health Sciences
Kelsi Anderson, PhD
Laurie Bellows, PhD
Cedric Cooper, MEd
Pete Ferguson
David Griffiths
Russell R. Gronewold
Beth Lau, MD, Chair
Melissa Newton
Sydney Parsons
Katie Sladky, EdD
Lisa Vail, RN, DNP, NEA-BC
Carrie Weber
Karen White
Bryan Foundation
Preeta Bansal
Loel Brooks
Joseph Kam Chiu, MD
Jill Davis
Michael Dewerff
Greg Dynek, Chair
Dan Grasso
Russell Gronewold
Jennifer Hilkemann
Chris Hove
Nelle Jamison Woods
Ben Kiser
Reg Kuhn
John Laflin
Quinn Lawton
Judy Lichti
Crystal Livingston
Scott McHam, DO
Jake Muhleisen
John Olsson
Trey Pittenger
Bob Ravenscroft
Deb Schorr
Layne Sup
Eric Sutton
Mike Works
Bryan Health
Bob Caldwell
John Decker, Jr.
Stephanie Dinger
Greg Dynek
Kathy Farrell, Treasurer
Tony Goins
Russell Gronewold
Ken Gross, MD
Tom Heacock
Jasmine Kingsley, Secretary
Gail Perry
Beau Reid
Chris Roth, Vice Chair
H. Russell Semm, MD
Aina Silenieks, MD, Chair
Clay Smith
John Woodrich
Bryan Heart Board of Managers
Mathue Baker, MD
Michael Dewerff, Treasurer
Jack Huck
Matthew Johnson, MD, Chair
Aina Silenieks, MD
John Steuter, MD, Secretary
John Woodrich, Vice Chair
Bryan Medical Center
Lorenzo Ball
Pablo Cervantes
Janet Chung
Alissa Clough, MD
Connie Edmond, Treasurer
Russell Gronewold
Ken Gross, MD, Chair
Shannon Harner
Jack Huck, Vice Chair
William Johnson, MD
Michaella Kumke
Beth Lau, MD
Eric Mooss
Robert Oakes, MD
Gayle Page
Erin Pemberton, JD, MSN, Secretary
Max Rodenburg
Krystal Siebrandt
Aina Silenieks, MD
Lisa Vail, RN, DNP, NEA-BC
Bryan Physician Network
John Dittman, Chair
Patrick Ganyo
Jessica Heckman, MD
Rubab Husain, MBBS
Torri Janecek, DO
Joe Mangiameli, President
Ben Pankonin
Matt Wittry, DO, Vice Chair
Crete Area Medical Center
Lupe Avelar, Secretary
Stephanie Boldt
Patrick Ganyo
Jason Hesser, MD
Maria Isquierdo
Justin Kozisek, Vice Chair
Dave Newmyer
Eric Post, DVM, Chair/Treasurer
Grand Island Regional Medical Center
Eric Barber
Luke Biggs, Secretary-Treasurer
Ryan Crouch, DO, Chair
Teresa Grabowski
Russell Gronewold
Cindy Johnson, Vice-Chair
Molly Johnson, MD
Greg Sextro, MD
Krista Stoecker, MD
Tom Werner, MD
John Woodrich
Kearney Regional Medical Center
David Benavides, MD, Secretary
Brenda Benjamin
Joey Cochran, Treasurer
Sean Denney, MD
Russell Gronewold
Jeff Hinrichs, Chair
Mike Morgan
Kari Nickman
Scott Smith, MD, Vice Chair
Merlin Wehling, MD
John Woodrich
Merrick Medical Center
Nathan Perry, Chair
Shannon Hannappel, Vice Chair
Patrick Ganyo, Secretary
Rich Lloyd, Phd
Jodi Mohr
Blake Cover, MD

Douglas Koch, MHA, has been named CEO at Kearney Regional Medical Center (KRMC) and assumed these responsibilities on Aug. 5, 2024.
From 1993 to 2001, Koch held clinical and leadership positions at Avera Health and Sanford Health in South Dakota. From 2001 to 2018 he held executive positions at Aurora Healthcare, an integrated nonprofit healthcare system in eastern Wisconsin and northern Illinois, with 17 hospitals, more than 150 clinics, and 70 pharmacies in 30 communities. In 2018 he returned to South Dakota, serving for three years as vice president of operations for Monument Health in Rapid City. For the last three years, he has served as chief executive officer for Governor Juan F. Luis Hospital and Medical Center in Saint Croix, U.S. Virgin Islands.

On June 24, 2024, Jodi Mohr began her role as the chief executive officer at Merrick Medical Center (MMC).
Mohr lives in Central City and has served as the director of clinic operations at Mary Lanning Healthcare in Hastings since 2017.
In this position, she has overseen multiple primary care and specialty clinics, collaborated with providers and used metrics and data to initiate improvements.
Mohr has a master’s degree in healthcare administration and has had significant experience in imaging leadership at two critical access hospitals and CHI St. Francis in Grand Island.
Prior to living in Central City, Mohr and her husband, Kevin, lived in Aurora for 22 years. The Mohr family includes Andrew, Molly and Zac.
Mohr’s interest in health care sparked from an unusual encounter. In the fifth grade, she had a CT scan. She told the doctor that she enjoyed it, so he showed her around the radiology department. From that moment, she knew she wanted to work in this environment.
Mohr is excited about the opportunity to work closer to home and make an impact in her community.
“Doug’s Midwestern roots, education and vast operational experience are an ideal fit to join the Bryan Health administrative leadership team and lead KRMC as it enters its second decade of operation,” said John Woodrich, Bryan Health executive vice president and chief operating officer.
During the extensive national search, leaders from KRMC and Bryan Health said Doug clearly emerged as the ideal candidate to lead Kearney Regional Medical Center.
“Doug is someone who likes to see communities thrive,” Woodrich said. “He will be an outstanding leader for Kearney Regional Medical Center and will help Bryan Health bring the most benefit to central Nebraska and the Kearney community.”
Koch said he’s excited to engage in the Kearney community in his new role. With KRMC recently celebrating its 10th anniversary, he’s eager to help usher the center into its second decade.
“Living in Central City, I’ve seen first-hand Bryan’s commitment to the people of our community and Merrick Medical Center,” Mohr said. “I’m honored and humbled to now lead the outstanding team at MMC. Between our new facility and outstanding providers and staff, we have everything we need to be successful. Every day, we’ll be working together to provide better health care for the people we serve.”
As she transitions into her new role, Mohr said the staff has already made her feel welcome, and she looks forward to working with them every day.
“Jodi will be an outstanding leader for Merrick Medical Center, and we’re excited to welcome her to the Bryan family,” said Patrick Ganyo, system vice president of rural services at Bryan Health. “She has a tremendous passion for making a positive impact on local patient care. Her drive will greatly benefit Central City and the surrounding communities.”
Mohr’s initial goals during her first few months at MMC are to get to know the staff and evaluate opportunities for growth in surgical services and specialty clinics.
In her free time, Mohr enjoys spending time outside, often in and around the Platte River. She also has interests in photography and traveling.

Carolyn Mach knew something was wrong immediately after the fall. The pain in her lower torso was debilitating, and she couldn’t get herself off the ground.
Emergency department doctors at Crete Area Medical Center (CAMC) performed an X-ray, discovering a fracture in Mach’s pelvis. She was kept overnight for observation as a precaution; the next day, her blood pressure began to drop.
CAMC doctors called Dr. Alesha Scott, medical director of orthopedic trauma at Bryan Medical Center, who recommended a CT scan. Soon after, Mach was in an ambulance on her way to Lincoln, with surgery scheduled for the next day.
The CT scan determined that Mach did indeed have a pelvic ring injury with multiple fractures, two in the front and one in the back. Dr. Scott, who was recruited by Bryan Health in 2017 to build the orthopedic trauma
program, said it’s common for the pelvis to break in multiple areas due to its rigid nature. The break in the back of the pelvis is why the injury hurt too much for Mach to walk on it.
Dr. Scott operated on Mach in January through percutaneous—or very small—incisions in the skin. The surgeon uses wires and a live X-ray machine to tunnel through safe corridors in the bone and insert screws to stabilize the bones. The process is minimally invasive and has a much shorter recovery time compared to an “open” procedure.
Dr. Scott learned the procedure through her orthopedic trauma fellowship at the University of Kentucky and has performed it “more times than I can count.” She was the first orthopedic surgeon to bring fully percutaneous pelvic fixation to Lincoln.
Before bringing this surgery to Lincoln, patients with this type of injury had limited treatment options. There is too much pain to move or do physical therapy. This meant weeks of bed rest while trying to manage the pain, as it takes at least six weeks for the bone to heal. For many older adults, this becomes an injury from which they are not able to recover; it can be a death sentence.
With this specialized surgery, patients get their life back, Dr. Scott said. They have significantly reduced pain and can participate in physical therapy and other activities to regain strength and mobility.
Mach said she was relieved to learn she was going to have surgery instead of multiple weeks in bed.

“I just thought, it’s got to be better than the way I was,” she said with a laugh. “And it was a night and day difference after the surgery.
“I was in surgery, and then Dr. Scott came in and said, ‘Can you imagine not having the surgery?’ And I said ‘no.’ Everything was great. They did well by me.”
Mach said she had a compassionate experience under Dr. Scott and her team’s care.
“Everything went smoothly,” Mach said. “They took care of me. I was amazed by Bryan’s emergency room, how all these people were doing their jobs so fast, getting me taken care of.”
Mach, a lifelong Nebraskan, was walking with the assistance of a physical therapist and a walker the same day as her surgery. She was able to go right home with her husband of 53 years, Dean, and has continued with outpatient physical therapy twice a week at CAMC. A few weeks after the surgery, Mach attended her son’s wedding. She is positive she would not have been able to be there without the successful surgery.
Though she’s still in some pain, she said it’s far more bearable than before the surgery, and that she has steadily made progress ever since.
“I’m still going with the walker, but it’s getting better,” Mach said. “Every day it’s a little easier.”
Dr. Scott and the Bryan Medical Center orthopedic trauma department have Carolyn back on her feet and enjoying life after a scary fall.
Dr. Scott said she most often sees pelvic fractures like Mach’s in older patients who have lower bone density to begin with and may also have osteoporosis. Such patients also are more likely to have undiagnosed injuries. Pelvic fractures in younger patients come from more obvious injuries, like a car accident or a fall from a ladder, Dr. Scott said, whereas older patients may seriously hurt themselves without even knowing.
“The patients who can fall through the cracks are those who just slip and fall, or maybe even slip off of their recliner and bump their hip and think it’s nothing, and then it just doesn’t feel better,” she said.
Dr. Scott provided some warning signs for patients who have had a recent fall. Hip, groin, lower back and pelvis pain is common after a minor fall and may go away after a day or two, she said. However, if they’re not able to take a step or sit without pain, they should go see their doctor and get an X-ray. If an X-ray doesn’t show a break and they’re still in major discomfort, Dr. Scott said they can call her office, Bryan Orthopedic Trauma, part of Bryan Physician Network.
Mach said she hopes her story helps others with similar traumatic injuries, as she encourages people to be aware that this treatment option exists in Nebraska.
“Do it,” Mach said. “Definitely do it. It’ll get you going faster, and you’ll be on the mend sooner. You hear people not having this surgery, and a lot of them die. I feel fortunate that they were able to do this for me.”
First remote surgery in space
“The adrenaline was pumping, and I could feel my heart pounding.”
Dr. Michael Jobst, a colorectal surgeon on the Bryan medical staff, made national news in February after performing a surgery that was out of this world.
Using the tiny surgical robot, spaceMIRA, Dr. Jobst remotely operated on simulated tissue 250 miles above Earth, orbiting on the International Space Station.

The 2-pound robot uses two arms to mimic the movements of a human surgeon—the left arm grasps, and the right arm cuts. The demonstration in February called for Dr. Jobst to control
The work of the Bryan Health Perinatal Simulation Outreach Team (PSOT), which has strived to overcome maternal health care and education disparities in Nebraska, was featured in a recent article published in the medical journal “Clinical Simulation in Nursing.”
Three of the five authors of the article are current Bryan employees—Marisa Schaffer, maternal child education coordinator; Beckie Trevino, clinical educator; and Jayne Van Asperen, rural division quality officer. A fourth author, Barbara Sittner, retired in 2023 after four years as Simulation Center director at Bryan College of Health Sciences.
the robots’ hands to hold the tissue, made of rubber bands, and dissect it with scissors. The demonstra tion was deemed a success.
This was the first time the robot was used in space. Dr. Jobst previously used spaceMIRA on several cases at Bryan Medical Center. This technology could make a profound impact on our own planet, allowing patients to undergo procedures in remote locations.

Dr. Jobst’s experience was featured on CNN’s “The Situation Room with Wolf Blitzer.”


Allen Ray Hohensee, MD, died May 24 at age 81 after 10 years with Myelodysplastic syndrome.
After attending medical school at the University of Nebraska Medical Center, Dr. Hohensee spent his career practicing family, emergency and internal medicine. He practiced emergency medicine at Bryan Memorial Hospital for eight years.
A pilot, Dr. Hohensee loved navigating the skies with his wife of 55 years, Susan. They also enjoyed planting trees and cheering on Husker volleyball together.
The Lincoln native is survived by his wife, Susan, two children and three grandchildren.

Thomas Dale Calvert, MD, died June 19 at age 90. He was a graduate of Nebraska Wesleyan University and the University of Nebraska Medical Center. Dr. Calvert completed his internship at Nebraska Methodist Hospital and his pediatric residency at Children’s Memorial Hospital. Dr. Calvert worked in pediatric medicine for 36 years with Lincoln Pediatric Group before his retirement in 2000. He was instrumental in the passing of a bill that advanced child car seat safety.
Dr. Calvert enjoyed fishing, biking, hiking and being with friends and family. He is survived by his wife of 67 years, Nancy, four children and nine grandchildren.
On July 1, Kelsi Anderson, PhD, became the president of Bryan College of Health Sciences, succeeding Rich Lloyd, PhD.
Dr. Anderson was born in Lincoln, graduating high school from Lincoln Christian School. She went to North Park University in Chicago for her undergraduate degree and returned to Nebraska for graduate school at the University of Nebraska Medical Center, earning a PhD in microbiology. She completed a postdoctoral fellowship at the University of Michigan and then spent six years at Concordia University in Ann Arbor, Michigan, teaching in the biology department and working in administration.
She came home to Lincoln in 2016 and began work at Bryan College of Health Sciences as program director of the biomedical sciences department. She became provost in 2018.
In her first months as president, Dr. Anderson hopes to connect with individuals within the college and work with them on the college’s strategic plan in tandem with the Bryan Health overall plan.
Dr. Anderson said there are four goals in place for the start of her tenure:
• Life cycle enrollment: Engage with students from recruitment all the way through graduation and alumni status.
• Comprehensive support: Provide aid to students on a variety of needs, including academics, mental health and food insecurity.
• Build the workforce: Bolster the healthcare workforce at Bryan Health and in Nebraska.
• Connect with alumni: Re-establish relationships with alumni, increasing their engagement with the student body.
“I’m so honored to be entrusted with this position,” Dr. Anderson said. “I see it as a huge responsibility. We have an almost 100-year reputation as being a high quality education leader in health sciences, and I want that to continue.”

Dr. Anderson said she is excited to welcome students back to campus in August, especially new students who will experience college for the first time. She encourages all students to use the many resources in the college and know they are not alone on their journey.
“It’s so important for students to know that we have resources here to help them, no matter what it is,” she said. “They may need tutors, peer mentors, private testing, you name it, but we don’t necessarily know they need it unless they ask. That help will be given to them in any way they need, and we are all here to support them and see them be successful.”
Fun Fact: Dr. Anderson loves watching game shows and dreams of being a contestant.
In her free time, Dr. Anderson loves spending time with her husband, Dirk, and their daughter, Sydney, and son, Jafar. She enjoys being outdoors, especially in the summer, and traveling around the country.
To support the college, call the Bryan Foundation at 402-481-8605.




