Above and Beyond the Call of Duty
Military service made these alumni better physicians, leaders, and people of purpose.
Page 28

Learn Critical Skills on the Other Side of the Bed BUMC Donates 50 Microscopes to 3 Boston High Schools

Military service made these alumni better physicians, leaders, and people of purpose.
Page 28

Learn Critical Skills on the Other Side of the Bed BUMC Donates 50 Microscopes to 3 Boston High Schools

Dear Alumni, Friends, and Colleagues, As we welcome the new academic year, we also welcome our new BU president, Dr. Melissa Gilliam, a member of our OB/GYN faculty.
Several other leadership transitions will occur over the next year. Dr. Tarik Haydar will return October 1 as chair of our anatomy and neurobiology department; Dr. Donald Lloyd-Jones will join BU on January 1 as director of the Framingham Center for Population and Prevention Science, PI of the Framingham Heart Study, and chief of the section of preventive medicine in the department of medicine; and we currently have search committees for department chairs of medicine, surgery, and dermatology.
At the end of May I announced my desire to step down as Medical Campus provost and dean of the Chobanian & Avedisian School of Medicine. A search committee should be constituted soon and will take time to find new leadership. Meanwhile, I will remain in these roles until the arrival of my successor, and then plan to take a year-long sabbatical before returning to the faculty.
Serving as dean and Medical Campus provost has been a privilege. Over the past two decades, we built the medical student residence, extensively renovated our other facilities, regularly revised the curriculum, invested in new faculty and staff, substantially increased endowments for scholarships and professorships, and named the school. I am grateful to all of you who have supported these initiatives and provided wise counsel over the years. Thank you.
The school is in a great place and I’m sure that the University will have many exceptional candidates to lead this outstanding school of medicine.
Meanwhile, this issue of BU Medicine has many excellent articles. Our cover story highlights alumni who have become military physicians. Some choose to make it a career while others leave after fulfilling their active-duty commitment, but all agree that the rewarding experience has made them better physicians and leaders.
Boston University Medicine
Boston University Medicine is published by the Chobanian & Avedisian School of Medicine Communications Office.
Maria Ober
Associate Dean, Communications design & production Boston University Creative Services
contributing writers
Lisa Brown, Gina DiGravio, Doug Fraser, Sarah Rowan
photography
Zoë Farr, Dave Green, David Keough, Jake Mackey, Sarah Rowan, School of Medicine Archival Photos, Sentara Health
Please direct any questions or comments to:
Maria Ober
Communications Office
Boston University Medical Campus
85 East Newton Street, M810H Boston, MA 02118
P 617-358-7869 | E mpober@bu.edu 0924
We showcase a unique program created by VA Boston Healthcare called The Other Side of the Bed, whereby medical students gain critical experience and skills from nurses and physicians who care for our veterans, and also tell you about a special gift of 50 labquality microscopes to three Boston secondary schools.
Our Giving section highlights the Third Annual Alan and Sybil Edelstein Professionalism & Ethics in Medicine Lecture, as well as stories on research supported by The PatientCentered Outcomes Research Institute, the Carol and Gene Ludwig Family Foundation, and the Edward N. and Della L. Thome Memorial Foundation, and features a profile on Mort Salomon, who credits the school for his satisfying, multifaceted career.
Our Alumni section announces our Alumni Award recipients. Louis Sullivan, MD’58, will receive the Dean’s Lifetime Achievement Award in Medicine and Biomedical Sciences in recognition of his outstanding career in medicine and healthcare leadership. Jennifer Luebke, PhD’90, and Christopher Andry, MPhil, PhD’94, will each receive the GMS Alumni Award in recognition of their scientific and leadership contributions to BU.
In addition to the always-popular Class Notes, the section also continues our Alumni Stories feature with a profile on Fredric Meyer, MD (CAMED’81).
Please enjoy this issue of BU Medicine
Best Regards,
Karen Antman, MD Provost, Medical Campus Dean, Chobanian & Avedisian School of Medicine

Five faculty members received Edward Avedisian Professorships in a March 12 ceremony in Hiebert Lounge that included online viewers both in the US and abroad. The professorships were funded out of the $25 million set aside from the transformational $100 million gift from the late Edward Avedisian and his wife Pamela in 2022, which resulted in the school being named the Aram V. Chobanian & Edward Avedisian School of Medicine.
Last April, Nancy Sullivan, ScD, director of the National Emerging Infectious Diseases Laboratories, and Venetia (Vanna) Zachariou, PhD, chair of pharmacology, physiology & biophysics, were installed as the initial recipients of Edward Avedisian Professorships.
“We’re abidingly grateful to Ed and Pamela Avedisian for their generosity and the recognition that a great medical school is a precious renewable resource for our society and for the world,” said Boston University President Ad Interim Kenneth Freeman.
Freeman noted that the five endowed chairs did not bear the Avedisian name but rather, had been selected to honor others.
“We chose to name these professorships to honor individuals who not only achieved great success in their medical careers but have continually used that success to help others,” said Pamela Avedisian. “We want them to inspire the current and future generations of medical students.”
“In medicine, we often say that we stand on the shoulders of giants. Today you will be introduced to 10 remarkable leaders in medical sciences,” said Dean and BUMC Provost Karen Antman, MD,
who emceed the installation ceremony.
Toby Chai, MD, professor and chair of urology, was named the inaugural Richard K. Babayan, MD, Professor of Urology. Babayan, professor emeritus and former chair of urology, retired in 2022 after 43 years at the school. He was honored with numerous awards and in 2005, was the first in Boston to do a robot-assisted radical prostatectomy.
“I’m humbled by this experience and very grateful,” said Babayan, who introduced Chai, the urologist-in-chief at Boston Medical Center and president of Boston Medical Center Urologists, Inc. Chai previously held the John D. Young Professorship in Urology at the University of Maryland School of Medicine and was vice chair of research in urology at Yale University School of Medicine. He titled his remarks, “Gratitude with a Purpose,” noting that the professorship was about more than one person: “It really is to help our department continue our academic mission to make it the best that it can be.”
Rachel Fearns, PhD, chair of virology, immunology & microbiology, was named the Ernest Barsamian, MD, Professor.
Barsamian grew up poor in Syria, became a professor of surgery and faculty dean at Harvard Medical School, invented one of the early heart-lung machines, and was the chair of cardiac and thoracic surgery, chair of surgical services, and chief of staff at the Boston Veterans Administration Medical Center.
“From the earliest days of his medical career, our father worked tirelessly to balance leading-edge prowess in medicine, particularly surgery, with the compassion and humanity that marks the successful physician,” said his son, Peter Barsamian.

Originally from the UK, Fearns holds a PhD from the University of St. Andrews. Her research focuses on the transcription and replication of RNA viruses, like respiratory syncytial virus and emerging pathogens including the Marburg, Ebola, and Nipah viruses. Fearns frequently works with the pharmaceutical industry on small molecule polymerase inhibitors that help fight diseases by inhibiting their functionality.
“It’s such an honor to be the inaugural Barsamian chair. I’m excited to take this on,” she said. “My parents are educators and imbued in me the sense that education allows you to make choices in life.” She thanked her mentors, including Ronald Corley, PhD, recently retired as chair of virology, immunology & microbiology, who “built a wonderful department here,” and the department faculty who have helped mentor her students and elevate her science.
Hee-Young Park, PhD, professor and chair of medical sciences and education, professor

of dermatology, and associate dean for faculty affairs, was named the Carolann S. Najarian, MD, Professor. Najarian (CAMED’80) spent most of her career in private practice. In response to the devastating 1988 Armenian earthquake, she established the Armenian Health Alliance, delivering medicine and medical supplies and establishing a primary care facility and a center for expectant women. She was also assistant medical director at Middlesex County Hospital and an instructor in clinical medicine at Harvard Medical School.
“We chose to name these professorships to honor individuals who not only achieved great success in their medical careers but have continually used that success to help others,” said Pamela Avedisian.
“I know this chair will add significantly to the education of students here, enriching their medical education and preparing them to go out into a culturally diverse world to care for patients,” Najarian said.
Park said it took a global community to raise her and get her to where she is today. Born in Korea, she credited her father with believing that education was for all—including women. Arriving alone in Arkansas at age 15 to pursue science education, Park expressed her gratitude to the Blyholder family in Fayetteville, Arkansas, who sponsored and hosted her.
“Today would not be possible without friends, families, and colleagues,” she said.
Andrew Taylor, PhD, associate dean of research and professor and vice chair of research in ophthalmology, was named the Sarkis J. Kechejian, MD, Professor. An internationally known researcher in ocular immune privilege, ocular autoimmune disease, and the role of melanocortin pathways in regulating inflammation and immunity, Taylor thanked the Avedisians, his family, students, colleagues, and research collaborators, and paid tribute to his mentors, J. Wayne Streilein, MD, and Joan Stein-Streilein, PhD.

Kechejian (CAMED’63) is the president of KClinic in Texas, CEO and chairman of Alliance Health, and president of the Kechejian Foundation. He said his mother taught him “the necessity of being involved in the community and instilled in me concern for helping others.”
He is a longtime advocate for increased scholarships for BU medical students, especially to ease the financial considerations that exacerbated a chronic shortage of primary care physicians and other nonsurgical specialties, and has received the school’s Distinguished Alumni Award. The Avedisian gift included $50 million for student scholarships. Kechejian said the scholarship fund has grown from $5 million in 1996 to $150 million today.
The Edgar Minas Housepian, MD, Professorship went to David Harris, MD, PhD, chair of biochemistry & cell biology since 2009. Harris studies molecular and cellular mechanisms underlying human neurodegenerative diseases. His work on infectious prion diseases—like mad cow disease, where brain proteins fold and can result in neurodegenerative effects—has helped research into other diseases like Alzheimer’s, Parkinson’s, and Huntington’s diseases.
“What I want to highlight here is the incredible foresight to use that endowment ($25 million of the Avedisian fund is dedicated to research and teaching) to support basic research which is…always at the root of great medical discoveries,” said Harris. “I am honored to be associated with a legacy that values the pursuit of knowledge and scientific excellence.”
Housepian was a renowned neurosurgeon at New York Presbyterian Hospital and professor of neurology at Columbia University Medical School, where he taught for 44 years.
His career began in labs, then evolved to surgery, but education remained his key concern and in his retirement years, he was an advocate for international educational affiliations for medical students. “He was a very creative person with a long-range vision,” said his daughter, Jean Housepian. ●

Karen Antman
as BU’s Medical School Dean and Medical Campus
Provost
Transformational leader oversaw new facilities and faculty & a new school name
“ Karen hired me 10 years ago and over this decade, I’ve had the privilege of learning many things from her—like why use 10 words when one will do, short bullets not long paragraphs, select the right font, do not use CAPS on slides or reports, run it by legal counsel, and make sure you know the policy and follow it to the letter.
But what I really learned is what ‘collaborative leadership’ looks like. I learned that questions are good and encouraged and will be answered with patience fueled by her sincere desire to share knowledge and skill. Differing views are valued and encouraged. I deeply admire her sense of fairness and her ability to make impossibly hard decisions and saw what integrity in action looks like, with 100% commitment to the students.
At the end of the day, the bottom line is that it is never about Karen herself; she is all about supporting the success of others and making the school better. And that is exactly what she has done. With deep admiration, thank you, Karen.”
ANGELA H. JACKSON, MD ASSOCIATE DEAN, STUDENT AFFAIRS ASSOCIATE PROFESSOR OF MEDICINE

I have had the pleasure of working with Dean Antman throughout her two-decade tenure. During this time, she has steadfastly supported the VA’s BU faculty, academic vitality, and mission of caring for those who have served.”
MICHAEL E. CHARNESS, MD CHIEF OF STAFF VA BOSTON HEALTHCARE SYSTEM
Karen Antman, who led two transformative decades as dean of Boston University’s Chobanian & Avedisian School of Medicine and provost of the Medical Campus, has announced plans to step down from those roles and return to the faculty at BU’s medical school as a professor of medicine when her successor is named.
Antman, a leading expert on breast cancer, mesotheliomas, and sarcomas, also presided over the construction of BU’s first medical student residence, throwing an affordable housing lifeline to students facing medical education bills. Antman oversaw the naming of the medical school in 2022 following a staggering $100 million gift from alum and philanthropist Edward Avedisian (CFA’59,’61, Hon.’22). She has led the Medical Campus since 2005 and says the pending inauguration of a fellow physician, Melissa Gilliam, as the new University president helped prompt her to step down from leadership.
“A new president—an MD—should pick their own new dean for the medical school,” Antman said. She also wants to spend more time with her family. “I plan to take a sabbatical. After a real vacation, I plan to “

collaboratively write infrastructure grants” for the medical school.
Kenneth Freeman, former BU president ad interim, said information about appointing her successor will be forthcoming in the next several months.
“Dr. Antman’s energetic leadership over the last 19 years has fostered a culture of excellence,” Freeman said, adding that under her leadership, the Chobanian & Avedisian School of Medicine “has gained in reputation and attracts outstanding faculty, staff, and students.”
“Dr. Antman has been consistently committed to facilitating faculty and student research,” he added. “Faculty members have particularly appreciated the establishment of the Proposal Development office, which assists faculty in writing grants.”
Robert Brown, BU president emeritus, who worked closely with Antman during his 18-year tenure, said she “has been a wonderful leader of our medical school, demonstrating time and again her unwavering commitment to our medical students and the quality of their education. Her work has been recognized nationally, and she leaves the school well positioned to excel.”
The Medical Campus provost oversees the South End complex, which includes the medical school, the Henry M. Goldman

“
Dean Antman’s leadership has made it possible to smoothly transition to the establishment of a new department, setting up new cores and technologies, and expanding to new directions.”
VANNA ZACHARIOU, PHD, EDWARD AVEDISIAN PROFESSOR AND CHAIR, PHARMACOLOGY, PHYSIOLOGY & BIOPHYSICS

“
Throughout her tenure as dean and Medical Campus provost, Karen Antman strongly supported the Framingham Heart Study and BU’s Framingham Heart Study Center. Her advocacy has been essential to ensuring that this groundbreaking study, now in its 75th year, continues to make vital research contributions to the prevention of heart disease, stroke, dementia, and other health conditions.”
JOANNE MURABITO, MD, AND GEORGE O’CONNOR, PHD, CO-INTERIM PI s
NICK DI PERSIO, FINANCIAL & ADMINISTRATIVE DIRECTOR
FHS CENTER AND FRAMINGHAM HEART STUDY
School of Dental Medicine, the School of Public Health, and the University’s collaborative role with Boston Medical Center, BU’s primary teaching hospital and New England’s largest safety net hospital.
Antman sums up her institution-changing tenure as “construction, fundraising, and recruiting the right leadership for the campus and school.”
The $100 million gift from Avedisian, an investor and for four decades a clarinetist with the Boston Pops and the Boston Ballet Orchestra, was a capstone to Antman’s tenure. He had suggested that the school be named after his lifelong friend Aram Chobanian (Hon.’06)—cardiologist, BU president emeritus, and dean emeritus of the medical school and provost of the Medical Campus. Neither man wanted his name on the school until they were persuaded to allow it to be named after both of them.
The gift enables $50 million for scholarships for medical students, $25 million to support endowed professorships, and $25 million to the Avedisian Fund for Excellence, paying for cutting-edge research and teaching.
Of the medical residence, Brown said at its 2010 groundbreaking, “This facility will make the burden of a medical education a little bit lighter to carry.” In recent years, MDs have been among the five degrees that account for most student debt.
Financial management of the medical school and campus involved more than the naming gift, especially during the first decade of Antman’s tenure, a time of flat budgets at one critical funding source, the National Institutes of Health. Antman says she nevertheless managed to recruit “outstanding, grant-funded faculty to new and renovated campus facilities, paid for by moving faculty to campus from off-campus rental space, thus decreasing costs and significantly increasing our research funding.”
She is proud of the “exceptionally prepared and accomplished medical and graduate students” that the medical school has attracted during her tenure. “We are now the top choice for many and turned down for only the most competitive medical schools.”
She led in opening more than 20 new research cores (shared research facilities) “to

“
The Boston University Genome Science Institute (GSI) is a vibrant research center that Dean Karen Antman played a key role in establishing at the beginning of her deanship to foster cutting-edge genetics and genomics research here on the Medical Campus as well as extending to researchers on the Charles River Campus. We are indebted to Dean Antman’s commitment to supporting the GSI research community, including delivering her address every year at our annual research symposium. We hope to continue her research support legacy in genetics and genomics for years to come.”
NELSON LAU, PHD
ASSOCIATE PROFESSOR, BIOCHEMISTRY & CELL BIOLOGY
GENOME SCIENCE INSTITUTE DIRECTOR
“
During my eight years as an associate dean, I had the privilege of working closely with Dr. Antman and witnessing her integrity, brilliant intellect, sharp wit, and dedication to educating future physicians and researchers. Her numerous accomplishments have left an indelible mark on our institution. While I am confident that we will be able to recruit a highly qualified successor, Dr. Antman’s legacy will be difficult to match.”
RAFAEL ORTEGA, MD, FASA PROFESSOR & CHAIR, ANESTHESIOLOGY
provide access to expensive, state-of-theart equipment,” she said, including the $8 million Center for Biomedical Imaging and the $4 million Cryogenic Electron Microscopy (Cryo-EM) Core Facility, opening this summer with a state-of-the-art electron microscope. Antman also cites the establishment of an office to assist faculty with grant writing.
BU’s Chronic Traumatic Encephalopathy (CTE) Center, created on her watch in 2008, has garnered international recognition for its research into the debilitating effects of repeated head traumas, in athletes and military especially. The center says its bank of 1,250-plus donated brains for study is “the largest tissue repository in the world focused on traumatic brain injury and CTE.”
Beyond new facilities, Antman supported the medical education faculty’s revised, team-based MD curriculum that necessitated “substantial renovations of every floor,” she said, in the Instructional Building—“including a 250-seat testing center, a 6,000-square-foot Team-Based Learning Lab, and completely renovated library floors.”
Before her BU service, Antman was deputy director of translational and clinical sciences at the National Cancer Institute. She also has served as the cancer center director at Columbia University College of Physicians and Surgeons (where she earned her MD
“ I became Chair of Pathology & Laboratory Medicine in 2019. The dean was extremely supportive of my candidacy and our department. Dean Antman provided mentorship and guidance along the way. We worked very well together over the past 4.5 years. I always found her open to discussion and forthright, judicious and thoughtful, available and supportive.”
CHRISTOPHER ANDRY, MPHIL, PHD, PROFESSOR AND CHAIR, PATHOLOGY & LABORATORY MEDICINE


“ Dean Antman has been a force at the School of Medicine over the past 19 years. Her creativity, vision, and dedication are why the school has the exceptional reputation it enjoys. I have learned so much from her about leadership and am grateful for all she has done to support me and the Department of Otolaryngology.”
GREGORY A. GRILLONE, MD, FACS, M. STUART STRONG AND CHARLES W. VAUGHAN PROFESSOR AND CHAIR, OTOLARYNGOLOGY-HEAD AND NECK SURGERY
and codirected the cancer care service line at New York–Presbyterian Hospital) and at Harvard Medical School from 1979 to 1993. At Harvard, she had hospital appointments at Brigham and Women’s Hospital and DanaFarber Cancer Institute.
She has edited five textbooks and monographs, authored or coauthored more than 300 publications, and written reviews and editorials on such topics as medical education, medical policy, and the effect that research funding and managed care have on clinical research.
Antman was elected a member of the National Academy of Medicine, an advisory group to the federal government, as dean, and chaired the American Association of Medical College Council of Deans. She also served as president of the American Society of Clinical Oncology and the American Association for Cancer Research. ●
“ In addition to an amazing career in academic medicine, you’ve been a truly excellent dean. The legacy you will leave behind is enormous and enduring. It’s been a privilege to serve as a chair under your leadership. Thank you, and best wishes for much good still to come.”
STEPHEN CHRISTIANSEN, MD, PROFESSOR AND CHAIR, OPHTHALMOLOGY


Focus should be on improving health beyond the healthcare system
“Healthcare is a basic human right, not a privilege. Our profession should focus on improving health beyond the healthcare system, in communities, with equal focus on prevention of disease and treatment of disease,” said convocation speaker Monica Bharel, MD (CAMED’94), MPH.
Medical Campus Provost and Chobanian & Avedisian School of Medicine
Dean Karen Antman, MD, addressed a celebratory crowd of students, faculty, and friends gathered at the BU Track & Tennis Center for the Chobanian & Avedisian School of Medicine convocation ceremony on May 16. Noting that graduation is one of the most joyous events of academic life, she also reminded the Class of 2024 that their degrees also confer considerable public trust.
With so much unrest around the world, natural disasters, and medical challenges on a global scale, “We hope that you will become leaders in solving these issues,” said Antman.
The school conferred 35 PhDs, 144 MDs, four MD/PhDs, three MD/MBAs, one MD/ JD, and two MD/OMFS (Oral Maxillofacial Surgery). Fifteen students earned cum laude honors and five, magna cum laude. Two students, Jonathan Berlowitz and Sarah Golden, graduated summa cum laude.
“The faculty know that you will use the knowledge, the research, and the clinical
skills that you have mastered here to make a difference in the world going forward,” said C. James McKnight, PhD, associate provost and dean of Graduate Medical Sciences.
“Humility reminds me of how far I’ve come and how much more there is to accomplish,” said PhD student speaker Josiane Fofana, who grew up in Senegal. After moving to Boston in 2011, Fofana completed an associate degree in biological sciences at Bunker Hill Community College, a BS in biochemistry at Brandeis University, and a PhD in virology, microbiology & immunology at BU.
Fofana urged students to look beyond their degrees. “In the pursuit of knowledge, we often overlook the importance of emotional intelligence. Brilliance devoid of empathy just renders us empty, contributing to the injustice in this world,” she said.
The mother of a toddler, Fofana founded a nonprofit that provides quality, STEM-based education to children in Dakar, Senegal. She is pursuing a postdoctoral position at the University of Ghana as a Fogarty Global Health Fellow.
“Do not think that the degree or leadership position you’re holding grants you the

ultimate wisdom on every issue,” she said. “Remain open to others’ experiences and embrace discomfort in order to grow.”
MD student speaker Bridgette Merriman grew up in Rochester, New York, graduated from Boston College, and will complete a pediatric residency at Cincinnati Children’s Hospital. A childhood cancer survivor, she was hooded by David Korones, MD, her pediatric oncologist at Golisano Children’s Hospital in Rochester.
“One of the most beautiful aspects of our journey together has been the friendships we’ve formed and the shared experiences that have strengthened our bond,” Merriman said. “From our first days of orientation to the challenges of clinical rotations, we’ve grown together, supporting each other every step of the way.”
“I know that you have the minds, the hearts, and the souls of change-makers,” she said.
Monica Bharel, MD (CAMED’94), MPH,
formerly chief medical officer at Boston Health Care for the Homeless and commissioner of the Massachusetts Department of Public Health and currently the clinical lead for public sector health at Google, encouraged students to consider global issues of health equity and socioeconomic impacts.
“Healthcare is a basic human right, not a privilege. Our profession should focus on improving health beyond the healthcare system, in communities, with equal focus on prevention of disease and treatment of disease,” Bharel said.
During patient interactions, Bharel advised students to turn away from their screens, look their patients in the eyes, and allow them to tell their story.
“Choose kindness and selflessness. Listen to your patients with humility. Connect your scientific endeavors to our most pressing health issues,” she said. ●


Told to make a difference with their education, training
On May 16, Graduate Medical Sciences (GMS) students, their families, friends, and faculty assembled at the BU Track & Tennis Center for the convocation ceremony marking a joyous passage in academic life. C. James McKnight, PhD, associate provost and GMS dean, urged graduates to make an impact on the world and in their own lives.
“You must continue to make a difference with the education and training you have received in your time here,” said McKnight. “Not just professionally; you should continue to make a difference in your families and your communities. Be involved, take care of the world, be engaged, and speak out.”
“The diploma you get today is the credential that grants you entry to the next stage of your life,” said Medical Campus Provost and Chobanian & Avedisian School of Medicine
Dean Karen Antman, MD. “The faculty have great confidence in your creativity, resilience, collaboration, and commitment.”
Student speaker Brent Leung of Toronto, Canada, graduated from the Master of Science in Medical Sciences (MAMS) program—one of the oldest and most successful special master’s programs in the US that has prepared more than 3,000 students for medical school since 1989—and is headed into the University’s MD program this fall.
He fondly recalled studying electron microscope slides on his laptop when friends and other MAMS students spontaneously gathered around to help him in one of the informal learning sessions that continued throughout his two years.
“Bonding over practice questions, writing out pathways on whiteboards, going out for drinks after an exam—these are the memories that come to mind when I reflect on the past two years,” said Leung. “While I don’t know what the future holds for all of us, I do know that we all have the capacity to succeed.”
Representing the Physician Assistant (PA) program, student speaker and Texas native Ellie McIntosh admitted fainting during the
first surgery she attended as a high school student and described an undergraduate journey that shifted through four majors until she graduated with a degree in finance.
Working at an OB/GYN clinic in Dallas brought her back into medical science and healthcare, which she will practice as a PA in Boston. Like Leung, she spoke of the support she received from her classmates, faculty, family, and friends.
“My charge to you is to not let this fervor for life dissipate on those grueling days that will inevitably come as we continue this roller coaster of life,” McIntosh said. “We can treat, heal, and interact with people of all different backgrounds and socioeconomic status and help them fight for a truly better tomorrow.”
MS student speaker Aris Desai, also a Texas native who will return there to do research, echoed iconic New England poet Robert Frost. “The road less traveled is often rugged, and less signposted perhaps, but it is ripe with the promise of personal growth and discovery,” he said.
“Each lab experiment, each patient case study, and each research project was an opportunity to choose resilience over resignation, curiosity over complacency, persistence over surrender,” he reflected. “It is a testament to the idea that success is not just in the destination, but also in the journey.”
Forty-three Master of Arts, 323 Master of Science, and 10 combined Master of Science/Master of Public Health degrees were awarded. ●

On May 3 in Hiebert Lounge, anatomy students celebrated those who donated their bodies to medical education in a memorial service featuring songs, music, poems, and prose dedicated to honoring and thanking them and their families.
“We should always remember and honor their sacrifice and the sacrifice their families made in supporting their decision to donate their bodies,” said first-year medical student Sophie Gray to the audience of donor families, students, faculty, and staff. “As students, we will strive to continue their legacies by using the knowledge and skills we have gained by learning from the donors to make a positive impact on the world.”
Each year, approximately 45 donor bodies are required for instruction of 310–370 medical, dental, physician assistant, and graduate medical science students studying in the Gross Anatomy Lab. This year’s ceremony honored the 23 donors whose bodies were studied in anatomy courses held in the past academic year, with 77 family members present among the audience of 200.
“The donors came from all walks of life, but what united them was their selflessness,” said Gray.
“I have lived inside this amazing creation for 91 years,” one donor wrote in a letter to students. “How I envy you the opportunity to learn and figure it all out.”
Nancilee Fuller signed on as a donor in 1990. She worked as a restaurant and office manager
and for 20 years as a medical secretary in her local hospital, finally retiring at 80. Fuller loved to garden and was a member of a synchronized skating team until she was 75.
“She just loved being in the medical environment and always knew she wanted to contribute her body to science and further medical knowledge,” said her daughter Heidi Finnegan.
“I didn’t realize how emotional this would be for me,” said Finnegan when she saw her mother’s photo and heard first-year medical student Aaron Ramtulla sing one of her mother’s favorite Adele songs.
“I wanted to show my appreciation for these people, these families, and the donors,” said Ramtulla.
When students first open the body bag of a donor, Jonathan Wisco (PhD’02), associate professor of anatomy & neurobiology, asks them to gently place their hands on the donor.
“This is the first time they have experienced the gift of death, so that they can learn how to preserve life,” said Wisco.
“As soon as I saw the body, I felt this immediate sense of honor by the fact that

I had the opportunity to learn from them,” said Ramtulla. “I was overwhelmed with those feelings.”
Until around 20 years ago, the end of anatomy classes for the school year was marked with a moment of silence before students zipped up the donor bags for the last time and the bodies were sent to the crematorium. But Robert Bouchie, manager of the Gross Anatomy Lab and director of the Anatomical Gift program, realized that students wanted more, and the memorial evolved into a nondenominational, student-run ceremony that over the past decade also has included donor families.
One of 14 students on the ceremony’s organizing committee, first-year medical student Giulio Cataldo said meeting donor families at the ceremony completes the circle that begins when they are introduced to the donor bodies and learn about their histories through the physical manifestations—such as an enlarged heart, gallstones, or overdeveloped muscles—that they accumulated during life. The families are key to helping them reunite the body with the person who inhabited it.
“We get to know them very intimately and
personally, seeing their internal organs and hearing about their past medical conditions,” said Cataldo. “We were really looking forward to meeting the families. I’m excited to hear the stories about their loved ones.”
“I like that [the ceremony] is studentdriven,” said keynote speaker Monica Pessina (PhD’05), clinical associate professor of anatomy & neurobiology. “I think the families are very touched. You hear about the value of the body donation, but they see it and feel it from the students who are there.”
A United Methodist minister in life, Jim Todd was an advocate for peace, social justice, and LGBTQ+ inclusion in the church. He and his wife Mary decided to donate their bodies to BU nearly 30 years ago. Mary attended the ceremony. “You put your whole self in, and that’s what Jim did,” she said.
“The music was just absolutely beautiful. It was a wonderful service that I felt truly healed by,” said Todd’s daughter Julie. “He would have loved every minute of it.”
The program included an opportunity for the donor families and students to meet and talk while sharing a meal. First-year medical
student Keven Cheung sat with the Todds. “Hearing what kind of man he was really touched me because of the things he was fighting for,” said Cheung. “Connecting with them makes me appreciate the gift that much more, and makes me realize that every one of the donors had decades of life and experiences—things they fought for; hopes and dreams—that live on in the people they knew, in their families, and in us.”
At the close of the ceremony, donor families privately receive the cremated remains of their loved ones, with Bouchie personally delivering them to families unable to attend the service.
Gillian Sanders attended the ceremony with her brother Michael. “I can’t wait to bring her home,” she said of her mother Doris Sanders, who will be reunited with her husband Charles, who donated his body eight years earlier. Doris and Charles met in Germany during WWII; she was German and he was an American soldier. “We were waiting to take them both back to Germany and sprinkle their ashes there.” ●

“Our goal is to increase physician/ nurse collaboration by helping medical students understand the role of nursing and the skills that nurses bring to healthcare,” says Cecilia McVey, MHA, RN, FAAN, associate director of nursing and patient care services at VA Boston Healthcare.
VA Vascular Access Nurse Kassidy Dias, RN, gently taps her forefinger on the blue vein in the arm of Vietnam War Army Veteran David Preston.
“Feel the bounce? That’s perfect,” Dias tells second-year medical student Juan Guerrero as he prepares to draw blood from Preston, a former sergeant in the 101st Airborne.
Guerrero is one of five second-year medical students from BU, along with a student from Harvard and another from Tulane, working on wards at the West Roxbury VA Medical Center, training in an innovative program known as The Other Side of the Bed. The six-week summer program, which began in 2009, has medical students undertaking many of the routine patient care tasks typically performed by the nursing staff.
“Our goal is to increase physician/nurse collaboration by helping medical students
understand the role of nursing and the skills that nurses bring to healthcare,” says Cecilia McVey, MHA, RN, FAAN, associate director of nursing and patient care services at VA Boston Healthcare System. She estimates that more than 200 medical students have participated over the past 15 years.
The program addresses what numerous studies have found: that an uneven power dynamic and issues around professional respect between doctors and nurses hinder collaboration, teamwork, and patient care.
VA Boston Chief of Staff Michael Charness, MD, believes the increased use of technology has exacerbated the problem.
“I think that as healthcare and medical education have evolved it’s harder for the different members of the team to understand and appreciate the skills each profession brings. And I think patient care can suffer from insufficient collaboration and communication,” says Charness.
Innovative program helps medical students understand the vital collaboration and communication between physicians and nurses

“I watch physicians as they are coming in for an hour, a half-hour, sometimes less, talking to patients, but there is a big difference being on the floor and being with patients the whole time,” says second-year medical student Rachel Kim.
Kim says nurses are continually asked to expand their responsibilities. On one of her first days on the ward, she watched a nurse juggle her patient load while taking time to accompany a veteran desperate for a walk, but who was a fall risk navigating with a walker while trailing an IV pole.
When a patient rapidly deteriorated and prognosis went from recovery to palliative care, Kim noticed nurses making careful observations of the changes. Although unconscious, the patient appeared to be experiencing pain. When the resident came on to the ward, Kim noted that he first turned to the nursing staff to ask what they had observed and what they thought should be done.
“One thing that really surprised me is how quickly you can make a valuable connection with a patient,” says second-year med student Douglass Bryant. “They are more than just their medical problems. They matter to so many other people and that’s all the more reason to do a great and respectful job.”
“It was the first time I saw one of the physicians take the time to get the full story from the nurses,” says Kim. “I saw that, and I said ‘okay, this is what I want to keep with me and emulate as I move forward in my training.’”
Studies also found that increasing reliance on technology, even just entering patient information and observations into a laptop, estranged physicians from patients. Students in The Other Side of the Bed said it was the opportunity to work directly and intensively with patients that drew them to the program.
“One thing that really surprised me is how quickly you can make a valuable connection with a patient,” says second-year med student Douglass Bryant. “They are more than just their medical problems. They matter to so many other people and that’s all the more reason to do a great and respectful job.”

“Throughout my first year [in medical school], I was afraid of having too much physical contact [with patients], too afraid of invading their privacy. It’s a hard line to walk, in how to provide hands-on care while still respecting their privacy and sense of personhood,” says Kim.

Working alongside nursing assistants (NAs) and nurses for eight- and sometimes 12-hour shifts, the medical students perform the most basic, but vital, tasks: bathroom assists, help with feeding and testing, and responding to call lights. Students shadow and learn skills from various teams, including vascular access, EKG, and respiratory therapy. There are weekly lunchtime lectures by a physician or researcher from the VA or BU.
Like most of the students, Guer rero was drawn to the intensive hands-on care experience, but found the reality of that work challenging.
“I thought I knew what I was getting into, but this was a lot more difficult; changing a patient for the first time, understanding how to move around a catheter, dealing with someone who feels really betrayed by the system and not knowing how to get through to them,” he says Sometimes, it’s the small details of care
that make patients’ lives in the hospital more bearable. Glucose testing is a daily ritual on many wards, and it involves pricking the patient’s finger with a needle to raise a drop of blood. No painkiller is used for this test and Kim found herself massaging patients’ hands to warm them and get the blood flowing.
“Throughout my first year [in medical school], I was afraid of having too much physical contact [with patients], too afraid of invading their privacy. It’s a hard line to walk, in how to provide hands-on care while still respecting their privacy and sense of personhood,” says Kim. “I learned a lot from [nurses] about how to do these really intimate tasks with dignity.”
Success is measured in achievements most people take for granted and patients provide life lessons that are humbling to students accustomed to accolades and success. When a patient started sharing his ignored
requests, Guerrero jumped in to express his sympathy, only to be rebuffed.
“He was very clear that he just wanted to be listened to. He didn’t want to be fixed; he wanted me to bear witness to his suffering,” says Guerrero.
Second-year medical student Jackson Wallner thought the most underrated aspect of the program was the opportunity to talk with patients and not feel rushed to move on to something else, a luxury he expects they won’t have as a physician. It’s why he knew that a shave was important to retired Army drill sergeant Robert “Rick” James. It’s a remedy that won’t be found in a medical textbook or that he’ll be expected to do on his future clinical rotations and residency, but Wallner grabbed shaving gear and fulfilled James’s request.
“He’s going to make a good doctor. He’s got the heart,” says James, a Vietnam War veteran. ●

Valeda Britton, BUMC executive director of community relations, presents one of 17 microscopes donated to New Mission High School to Head of School Will Thomas (Sargent’97, Wheelock’04) and his dedicated staff.
The Medical Campus recently donated 50 lab-quality micros copes to three schools in the Boston Public School (BPS) system.
The John D. O’Bryant School of Mathematics and Science in Roxbury, Dearborn STEM Academy in Roxbury, and New Mission High School in Hyde Park received Olympus CH series microscopes that were once used by Boston University Medical Campus (BUMC) students.
“This was a magnificent gift. We had the microscopes and the carrying cases, and the microscopes are in wonderful condition,” says Valeda Britton, BUMC executive director of community relations.
These 1970s-era Olympus CH series microscopes last a long time, but technology upgrades eclipse even the best performers eventually. Approximately a decade ago, the medical school and campus transitioned to virtual online microscope programs for teaching purposes. Eventually, the microscopes were placed in storage, with space limitations prompting plans to donate them.
“They were used less and less,” says Lucy Milne, director of education media. “Erita
Ikonomi, an educational technologist, maintained the scopes and kept them safe so they can now have a second life.”
The Medical Campus’s history of supporting Boston Public Schools includes establishing grants and other financial programs, offering the expertise of BUMC students and faculty, and donating excess equipment. BU also has specific initiatives—like the Summer Biomedical Research Internship and the Med-Science Program—that introduce underrepresented youth from Boston and other communities to postsecondary STEM-M (Science, Technology, Engineering, Mathematics and Medicine) programs.
As Medical Campus liaison to the surrounding communities, Britton and her colleagues visited the schools in advance of the donation.
“We casually brought up that we had these microscopes, and asked if they could use them in their science classes. And all three schools said yes,” she recalls. Within a few days, the 50 microscopes were loaded into a BU truck and driven to the schools, with two receiving 17 instruments and the third 16.
“The folks at the schools met us and they were really grateful to have these microscopes. I like the idea of those microscopes leading students to be more curious and more willing to explore,” Britton says.
“We said yes,” says Samuel Baker, an instructional coach at Dearborn STEM Academy focused on STEM and interdisciplinary pathways in health sciences, engineering, and advanced manufacturing and computer science. “The microscopes are of such good quality and very durable. They can take the wear and tear.”
In 2018, Dearborn moved into a brandnew, $70 million state-of-the-art STEM facility. Baker says the four-story school has microscopes in a lab on the second floor that had to be transported up to the biology lab floor when needed; the 16 Olympus microscopes allows them to have instruments in both labs.
Baker cites another benefit of institutions of higher learning interacting with BPS students—whether it’s university staff, faculty, or students who come to the high schools, they give students there the opportunity to broaden their everyday experiences by interacting with them. Dearborn’s student population is 90% African American, with many Cape Verdean families. Often, English is their second or even third language. “Students need to hear the college language, whether it’s a four-year or two-year college. We need to expose them to opportunities after high school,” he says. ●

Clinical Associate Professor of Anesthesiology
Robert J. Canelli, MD, has received the 2024 Leonard Tow Humanism in Medicine Award from the Arnold P. Gold Foundation. This award is presented to faculty who best demonstrate the foundation’s ideals of clinical excellence as well as outstanding compassion in the delivery of care and respect for patients, their families, and healthcare colleagues.
An anesthesiologist and intensivist at Boston Medical Center (BMC), Canelli demonstrates remarkable empathy for patients and their families, says a colleague. “His compassion is present in the perioperative arena, where Canelli strives to make his patients feel at ease prior to surgery. It extends into his practice in the intensive care unit, where he strives to care for critically ill patients and their families at their most vulnerable time. Canelli’s clinical expertise coupled with his caring bedside manner are an asset to BMC as he delivers high-quality anesthetic and intensive care to our most at-risk patients.”
Another colleague says Canelli not only excels as a clinician, working conscientiously and meticulously on behalf of patients in a wide range of clinical settings, but also as an enthusiastically involved educator who teaches and mentors medical students, residents, and junior faculty. “He is a role model who shows respect for everyone. As an accomplished academic clinician, he is constantly immersed in elucidating complex diagnoses and ethical dilemmas, always guiding trainees towards
the best management strategies for critically ill patients.”
Dedicated to fostering the next generation of physicians and healthcare providers, Canelli has developed a systems-based simulation curriculum for anesthesia trainees and introduced a point-of-care ultrasound initiative to teach this skill to medical students, residents, nurse practitioners, and fellows. “Not only is Dr. Canelli regularly going out of his way to teach trainees at the individual level, but he has also created an environment that allows and encourages them to gain knowledge in the use of ultrasound for the evaluation of cardiac, pulmonary, and gastric abnormalities,” says a colleague.
Canelli received his BS in chemistry from Villanova University and MD from St. George’s University School of Medicine. He completed his residency at the University of Massachusetts, UMass Memorial Medical Center, where he served as chief resident, and a fellowship in critical care from Harvard University, Beth Israel Deaconess Medical Center.

Ricardo Cruz, MD, MPH, MA, assistant professor of medicine (pictured), and Shamaila Khan, PhD, clinical associate professor of psychiatry, have each received the Diversity, Equity, Inclusion & Accessibility (DEIA) of the Year Award. The annual award recognizes faculty and staff who have done extraordinary work addressing and improving diversity and a culture of inclusion, equity, and accessibility throughout the school community.
Since joining the faculty in 2014, Cruz has focused his clinical work at Boston Medical Center (BMC) on primary care and treatment
of substance use disorders for vulnerable populations, including racial and ethnic minority communities and individuals with a history of criminal justice involvement. He is also a physician in the Faster Paths to Treatment clinic, BMC’s innovative, low-barrier, substance use disorder bridge clinic.
His research interests include clinical innovations to address health and treatment disparities among people with substance use disorder. He was the principal investigator of the Department of Health and Human Services Office of Minority Health–funded Project RECOVER (Referral, Engagement, Coaching, Overdose preVention Education in Recovery), which utilizes peer recovery coaches to assist in the engagement and retention of individuals with opioid use disorder into treatment and primary care services after completion of acute treatment services (detoxification). He also served as coinvestigator on National Institute on Alcohol Abuse and Alcoholism and National Institute on Drug Abuse–funded randomized clinical trials testing medications for alcohol and cocaine use disorders.
According to a nominator and colleague, “Dr. Cruz is a committed advocate for DEIA not only as a primary care clinician and addiction medicine specialist in the section of general internal medicine, but also as an educator and innovator of programs addressing health inequities. He provides exceptional care to Boston’s most underserved groups, many of whom face barriers to obtaining equitable healthcare.”
According to another, Cruz educates medical students and residents on the health impact and inequities driven by the criminal justice system: “Dr. Cruz is known as an excellent clinical teacher. His educational scholarship is deeply tied to the values of antiracism.”
A licensed clinical psychologist with a psychodynamic background and an interest in postcolonial theory, Khan’s clinical, academic, and research experience encompasses trauma and disaster relief work focused on

multiculturalism, decolonizing, and social justice. She treats those with individual trauma, community-based trauma, and immigration, racial, and postcolonial trauma. She travels globally to provide culturally significant disaster-relief services.
Khan also heads the Center for Multicultural Training in Psychology and the Center for Multicultural Mental Health and previously directed the Haiti SERG Program and served as clinical director of the Resilience Training Program at BMC. She was the first responder and director of behavioral health services at BMC’s Massachusetts Resiliency Center, serving the victims/survivors of the Boston Marathon bombings and led the Family Support Center, providing services to those impacted by the pandemic.
Khan is a member of both the Multicultural Concerns and the Professional Issues Committees of the American Psychological Association (APA) Division of Psychoanalysis, and the APA’s Committee on Accreditation multicultural expert and site visitor. She also serves on the Disaster Behavioral Health Advisory Committee of the Massachusetts Department of Mental Health and is cochair for the DEI Committee and diversity champion for the department of psychiatry.
“Dr. Khan embodies what this award is meant to honor. I can think of no one at the Medical Campus who is more deeply engaged in promoting diversity among students, trainees, staff, and faculty—and who is more deserving of this recognition,” said a nominator.
According to another colleague, Khan creates and implements programs designed to improve DEIA—including pathway programs such as the Black Lives Matter Training series— and has led a range of affinity groups, listening sessions, and healing circles at the Medical Campus and in the Boston community. “These efforts have made meaningful impacts as healing spaces related to the Boston Marathon bombing, COVID pandemic, George Floyd inci-
dent, anti-Asian hate incidents, LGBTQI hate crimes, and, most recently, in relation to Israeli/ Palestinian world events.”
Five Boston University Chobanian & Avedisian School of Medicine faculty have been honored as 2024 Educators of the Year by the school’s Awards Committee. The annual awards recognize Chobanian & Avedisian School of Medicine educators who demonstrate excellence in teaching and mentoring. Nominated by students and faculty, this year’s recipients are Molly Cohen-Osher, MD, MMedEd, Educator of the Year, Preclerkship; Christine Cary Cheston, MD, Educator of the Year, Clerkship; William Lehman, PhD, Educator of the Year, MA/MS Programs; Jeffrey L. Browning, PhD, Educator of the Year, PhD Programs; and Vanessa Villamarin, MD, Resident Educator of the Year.

Cohen-Osher is the assistant dean of medical education for curriculum and instructional design. Cohen-Osher joined BU in 2012 as the associate clerkship director of family medicine and assistant professor of family medicine. She completed a seven-year BA/MD program at Rutgers University/University of Medicine and Dentistry of New Jersey, Robert Wood Johnson Medical School and did her internship in family medicine at the University of Wisconsin-Madison, residency in family medicine at the MacNeal Family Medicine Residency Program in Berwyn, Illinois, and a master teacher fellowship at the Tufts University Family Medicine Residency
Program at Cambridge Health Alliance. She received her master’s in medical education at University of Dundee, Scotland.
Cohen-Osher focuses on creating learning experiences that foster active learning, teamwork, and the skills to build meaningful therapeutic alliances with patients, and supports faculty in implementing new instructional methods and curriculum.
According to a nominator, “Molly has been a model of professional behavior, dealing with students and faculty in a caring and compassionate way. She is an active listener and willing to make changes in response to feedback while holding fast to her principles as an educator. She is a superb role model for all educators at our institution. I cannot think of anyone more deserving.”

Cheston is an associate professor of pediatrics in hospital and newborn medicine and program director of the Boston Combined Residency Program (BCRP) at Boston Medical Center (BMC). Cheston received her undergraduate degree at the University of Virginia and her MD at the Johns Hopkins School of Medicine. She completed her pediatric residency in the Urban Health and Advocacy Track of the BCRP and received the Harvard Medical Student Teaching Award as a senior resident. She served as BMC chief resident prior to joining the faculty and in 2022, became an inaugural graduate of the BU Clinician Educator Leadership Program.
A student nominator cites Cheston as a model physician/educator who embodies a commitment to student growth, mentorship, and antiracism. “Dr. Cheston models compassionate, patient-centered care during rounds. She consistently prioritizes patient needs by requesting in-person interpreters,
finding chairs or squatting to maintain eyelevel communication, and offering nonjudgmental language suggestions to center the patient and minimize stigma. Moreover, Dr. Cheston empowers students to lead discussions and challenges our thought process to mitigate anchoring bias by asking for wide differential diagnoses and explanations for patient assessments based on their current clinical picture.”

Lehman is professor and vice chair of the Department of Pharmacology, Physiology & Biophysics and previously served as chair ad interim of physiology & biophysics. His research focuses on characterizing the role played by muscle thin filaments in regulating cardiac, skeletal, and smooth muscle contractility using a structural approach that combines molecular biology, cryoelectron microscopy, image processing, and computational tools such as molecular dynamics. His laboratory was the first to directly visualize and identify components of cardiac and skeletal muscle actin-containing thin filaments that respond to calcium and, in turn, control muscle activity. His molecular models of thin filaments provide a framework for investigating disease-bearing mutations leading to cardiomyopathies, and for drug discovery to counteract disease development.
Lehman received his BS from Stony Brook University, New York, and his PhD from Princeton. He spent three years as a postdoctoral fellow at Brandeis University and an additional year as a higher scientific officer at Oxford University before assuming his faculty position at BU in 1973.
“Dr. Lehman is a first-class professor who is immensely passionate about the education of his students and their success within the
healthcare field. His outstanding leadership has made each of his students exceptionally competent and knowledgeable, and we are extremely thankful to have had him guide us through such a challenging yet rewarding course,” said a nominator.

Browning received his PhD in biochemistry at the University of Wisconsin. He did postdoctoral work with Joachim Seelig, PhD, in the biophysics department of the University of Basel, using nuclear magnetic resonance methods to study membrane structure; and with Louis Reichardt, PhD, in the neurobiology department at the University of California-San Francisco, researching the neuromuscular junction. Beginning in 1984, for 28 years he was a research scientist in the immunobiology discovery group at the biotech firm Biogen in Cambridge, Massachusetts. His research interests center on the tumor necrosis factor family of regulatory molecules—notably the discovery of the lymphotoxin, BAFF, and TWEAK systems—and translation of modulators of the lymphotoxin pathway to the clinic in indications ranging from autoimmune disease and inflammatory bowel disease to oncology. A research professor in the Department of Virology, Immunology & Microbiology and the section of rheumatology since 2013, his current research focuses on altered vascular and stromal states in the perivascular compartment in the skin of systemic sclerosis and lupus patients, and their impact on the pathology.
One of his nominators said, “Jeff is a dedicated educator who is passionate about immunology and its role in health and disease, and who consistently strives to impart his vast knowledge and excitement for immunology to students. He pays a great deal of attention to each student’s research
and provides insightful comments as well as providing students with relevant papers and avenues for consideration. Importantly, he does not shy away from demanding the best of students but works hard to help them meet a high bar.”

Villamarin is a rising obstetrics & gynecology fourth-year resident at Boston Medical Center (BMC). Born in the Bronx, New York, Villamarin spent most of her early childhood in Ecuador before moving to central Massachusetts. After completing her BS in psychology on the neuroscience track at the University of Massachusetts, Amherst, she worked as the lead research coordinator for clinical postpartum depression studies at the University of Massachusetts Chan Medical School, where she earned her medical degree and was a student leader for the Worcester Healthy Baby Collaborative, working to address racial disparities in infant mortality. She also served on the executive board of the Latino Medical Student Association and Student National Medical Association chapters at UMass Chan.
Villamarin is passionate about social justice, equity in healthcare, and increasing diversity in medicine. According to a nominator, “She saw firsthand how dedicated BMC is to advocating for and providing equitable and excellent care to underserved communities when her mom received care at BMC as an uninsured patient.”
Her nominators describe her as kind, empathetic, and generous to students with her time. One said, “From day one, she was approachable and vested in my success. She always encouraged me to ask clarifying questions on rounds and in the OR, and shared constructive feedback in a way that encouraged my growth. Additionally, she taught me
how to approach challenging conversations with patients and the importance of always practicing shared decision-making. Her patients’ trust in her was palpable.”

Assistant Professor of Family Medicine Cheryl A. McSweeney, MD, MPH, has received the Chobanian & Avedisian School of Medicine’s highest teaching honor, the Stanley L. Robbins Award for Excellence in Teaching.
Established in recognition of the exceptional teaching and devotion to students exemplified by Stanley L. Robbins, MD, former professor and chair of pathology, the annual award recognizes an outstanding educator who represents the importance of teaching skills and demonstrates commitment to students and education.
McSweeney is director of the Learn, Experience, Advocate, Discover and Serve (LEADS) course, launched in 2022 to equip medical students with the skills necessary to recognize and engage with the social drivers of health. In LEADS, students examine the structures and systems that have resulted in health inequities both currently and historically, explore their roles as physician advocates for justice in service to others, and develop pragmatic skills to advance health equity.
“LEADS is a complex course, and similar to other brand-new courses, it has required constant evolution and refinement. Yet, somehow, Dr. McSweeney has found a way to maintain a calm and cheerful demeanor in leading our team and the course. Whether providing feedback to a draft of a self-learning guide or leading a workshop for students on advocacy skills, Dr. McSweeney’s dedication to LEADS, our team, and the students is constant and evident. She fills every gap
and ensures every detail is accounted for thoughtfully and intentionally,” said a colleague in recommendation.
“Cheryl is patient, thoughtful, and kind in everything she does. While the LEADS curriculum provided multiple challenges around logistics, moving parts, and clarity on goals since inception, Cheryl has been able to take every challenge presented and work with individuals in an open, kind, nonjudgmental manner. She never presented herself as all-knowing but as inclusive, open to suggestions, flexible, and accommodating to change. Cheryl was committed to creating a road map that was visible and usable for everyone, despite constant pivots. She embodies servant leadership at the highest level,” said another colleague.
Multiple faculty members noted that McSweeney helped orient and mentor them when they were new. “She fosters a culture of collaboration and continuous improvement. Furthermore, she empowers the faculty and administrative team to innovate. She considerately approaches new ideas, strengthening them and helping support their success. She thus creates space for faculty to develop unique didactics focused on health equity,” one said.
Another colleague noted that McSweeney is a vocal advocate for diversity, equity, inclusion, and belonging in the curriculum, saying, “She encourages our team to ensure that the students learn from an incredibly diverse set of speakers and that every learning objective promotes health equity. She values differences of opinion on our teams and seeks to provide a safe environment for students and faculty to express their challenges and frustrations.”
McSweeney’s outpatient family medicine practice is located in the East Boston Neighborhood Health Center, where she provides primary care to families and teaches third-year medical students.
Student evaluations describe her as “very engaging and knowledgeable”; “easy to get ahold of for questions and discussion”; “clear and passionate about equity and learning”;
and also as a mentor who “creates a very kind and comfortable learning environment” and “challenges students to think critically and apply concepts in her teaching.”
McSweeney received her undergraduate degree in brain and cognitive sciences from the Massachusetts Institute of Technology and MD from The Ohio State University, followed by an MPH in maternal child health from Boston University School of Public Health in 2013. She completed her residency at the University of Massachusetts Family Health Center in Worcester, Massachusetts. ●
The BU endocrinologist and department of medicine chair will remain on the medical school faculty

“I look forward to hearing from my colleagues across the hospital to build on their ideas and expertise to meet the health and social challenges of the patients we serve.”
Anthony Hollenberg, a nationally renowned endocrinologist and physician-in-chief at Boston Medical Center (BMC), as well as the chair of the Chobanian & Avedisian School of Medicine department of medicine, has been named the new president of BMC, Boston University’s primary teaching hospital and New England’s largest safety-net facility, serving disadvantaged patients.
Effective June 3, the appointment was made by BMC’s trustees, whose chair, Martha Samuelson, said that Hollenberg “will further cement our hospital and health system’s role as a national model in equitable care.”
BMC is one of six healthcare providers and plans in the Boston Medical Center Health System, which is creating a coordinated care system to give patients state-of-the-art treatments, while also conducting cutting-edge research.
“I’m truly honored to lead BMC and our world-class clinical, research, administrative, and operational team members as our health system reimagines the future of equitable, expert care for our patients and members,” Hollenberg says. “I look forward to hearing from my colleagues across the hospital to build on their ideas and expertise to meet the
health and social challenges of the patients we serve. Every role at the hospital is critical to helping our patients and communities thrive.”
A native of Toronto, Hollenberg is taking a newly created job as BMC’s president under the hospital’s restructuring as an integrated health system.
Hollenberg will remain a professor of medicine. BMC and the medical school will begin a search for both department of medicine chair and physician-in-chief.
Before joining BMC in 2022, Hollenberg chaired the department of medicine at Weill Cornell Medicine in New York City and was physician-in-chief at New York Presbyterian/ Weill Cornell Medical Center.
“Dr. Hollenberg’s extensive leadership background at academic medical centers, demonstrated experience as a highly accomplished physician-researcher, and his long-standing commitment to clinical innovation and health equity make him ideal to drive BMC forward as a premier academic medical center,” says Alastair Bell, president and CEO of Boston Medical Center Health System.
“As our health system rewrites how to best deliver care to our patients and members,” Bell says, “Dr. Hollenberg will further advance systems of care to ensure BMC remains a strong, trusted, and sustainable organization.”
Hollenberg’s research and clinical practice focus on thyroid disorders. He studies how thyroid hormones govern metabolism, including body weight, and also researches thyroid gland development. He has published more than 100 studies and 30 book chapters and reviews.
A graduate of Harvard University, he earned a medical degree from the University of Calgary. He served his residency in internal medicine at Boston’s Beth Israel Deaconess Medical Center, followed by a clinical and research fellowship at Massachusetts General Hospital.
“Tony is an accomplished physicianscientist and leader in academic medicine,” says Karen Antman, dean of the Chobanian & Avedisian School of Medicine and provost of the Boston University Medical Campus. “He is deeply committed to clinical excellence and health equity. We wish him great success and look forward to collaborating with him in his new role.”●
Donald M. Lloyd-Jones, MD, ScM, has accepted the position of director of the Framingham Center for Population and Prevention Science, principal investigator of the Framingham Heart Study, and chief of the section of preventive medicine within the department of medicine at the Chobanian & Avedisian School of Medicine and Boston Medical Center, effective January 1, 2025.
Lloyd-Jones is the chair of preventive medicine and Eileen M. Foell Professor of Heart Research and professor of preventive medicine, medicine and pediatrics at Northwestern University. He previously served as senior associate dean for clinical and translational research and PI/director of the Northwestern University Clinical and Translational Sciences (NUCATS) Institute from 2012–20. Lloyd-Jones also served as the national president of the American Heart Association from 2021–22.
He received a BA from Swarthmore College, an MD from Columbia University College of Physicians and Surgeons, and a master of science in epidemiology from Harvard TH Chan School of Public Health. He completed a residency in internal medicine at Massachusetts General Hospital (MGH) and served as chief medical resident. Following a cardiology fellowship at MGH, he joined the staff as an attending cardiologist and was an instructor and then assistant professor of medicine at Harvard Medical School and MGH. He joined the Framingham Heart Study as a research fellow in 1997 and was a research associate from 1999–2004. In 2004, he moved to Northwestern’s Feinberg School

of Medicine and became chair of preventive medicine in 2009.
Lloyd-Jones’ research interests include the study of the mechanisms and life course of cardiovascular health and healthy aging, and cardiovascular disease epidemiology, risk estimation and prevention. Other areas of interest include the use of novel biomarkers and imaging of subclinical atherosclerosis to improve prevention, and the epidemiology and outcomes of hypertension and dyslipidemia. His clinical and teaching interests lie in general cardiology with a focus on prevention.
He has been a national leader in public health and clinical approaches to promoting cardiovascular health and preventing cardiovascular diseases across the life course. He served as cochair of the Risk Assessment
Guidelines and a member of the Cholesterol Treatment Guidelines Panel for the 2013 ACC/ AHA Guidelines for Cardiovascular Disease Risk Reduction and was the lead member for risk assessment on the 2018 Cholesterol Guidelines Panel and the 2019 Primary Prevention Guidelines Panel. He has authored over 750 peer-reviewed scientific publications and has been a PI or coinvestigator on more than 120 grants, the majority from NIH.
Lloyd-Jones has been named a “Highly Cited Researcher” by Clarivate Analytics in each of the last 10 years for being in the top 1% of cited authors in the field of clinical medicine, a distinction that includes only ~420 investigators worldwide.
The recipient of numerous awards and honors, he is a fellow of the American Heart Association, the American College of Cardiology, and the American Society for Preventive Cardiology. ●
Also worked as part of a clinical team helping to treat injured athletes at the Summer Games.
As a basketball and tennis player of admittedly limited skills, Ali Guermazi, MD, PhD, MSc, would never be headed to the Olympics as an athlete. But as a radiologist and professor of radiology and medicine, Guermazi journeyed to his second Olympic games in eight years this summer when the Paris 2024 Organizing Committee for the Olympic and Paralympic Games named him codirector of radiology research for the Summer Games.
In the Olympic village from July 23 to August 12, Guermazi joined 32 radiologists and 36 radiographers, including Michel Crema, MD, an adjunct assistant professor of radiology at the school. For five of those days, he worked as a clinician, reading X-ray, ultrasound, and magnetic resonance imaging for athletes injured during the games. For the rest of the Olympics, he directed the collection of injury data with the goal of producing 20 research papers that the Olympic committee hopes will provide insight into training, injury prevention, and treatment.
“It’s all about best practice,” says Guermazi of the research. “The goal is to give [athletes, trainers, and coaches] an idea of why it happened and how to prevent it the next time.”
One of the papers from the 2016 Rio Olympics detailed the damage to muscles, connective tissue, and bone wrought by competition at the highest level, with more than 1,100 injuries diagnosed for 11,274 athletes. BMX cycling, with 38 percent of the athletes injured, and boxing, with 30 percent, topped the list.
“Thirty percent of the athletes who participated in the Rio de Janeiro Olympics had arthritis and were very young. Those were probably posttraumatic [injuries],” says Guermazi.

As chief of radiology at the VA Boston Healthcare System, he sees some similarities between military veterans and athletes.
“Almost every veteran has posttraumatic osteoarthritis because they went to war…and they do things that are very stressful on the joints,” he said.

“We’re looking for treatment because at this point, there is no treatment.”
When injuries occur, the impact of a correct diagnosis and treatment of an injury play out in real time in the medical clinic. Not just muscles and bones are torn and shattered, but Olympic dreams as well. Whether the athlete enters the clinic accompanied by a coach or trainer, or with an entourage of a dozen people, as happens with the Olympic stars, the images reveal the toll of the pursuit of excellence.
“We can say to the athletes how long it’s probably going to be for them to return; if it’s five or six days and you can continue [competition], or if their Olympics are over,” says Guermazi, who has worked in sports medicine for 30 years. The 2015 book he coedited and helped author, Imaging in Sports-Specific Musculoskeletal Injuries, factored into his invitation to the 2016 Olympic Games in Rio de Janeiro.
These high-performing athletes are not typical people, Guermazi says, and their injuries are often way beyond what he sees in his sports medicine practice. But when they finally get to the Olympics after years of training, their drive to win is often stronger than their fear of injury.
“They want to win. For them, it has to be first, not second or third,” he says. “When they get injured, it’s really big. You see the images and sometimes you say, ‘Oh my God, what’s this?’ It’s kind of mind-blowing.”
Guermazi is impressed by the athletes’ resilience and their capacity to endure pain and even risk long-term disability to succeed. He cites a champion judo athlete who has almost no rotator cuff on one arm—the rotator cuff holds the shoulder joint in place and
Ali Guermazi (right), a radiologist and professor of radiology and medicine, was part of a team of radiologists treating injured athletes at the 2024 Paris Summer Olympics. He previously served at the 2016 Rio de
allows movement of the arm and shoulder, which would seem essential in a sport like judo—yet the athlete continued to compete and win despite what should have been a career-ending condition.
According to Guermazi, preventing osteoarthritis in both athletes and the general public is a tough task, but it’s vital to ensure the least amount of trauma and microtrauma.
“Exhausting your body is not going to be okay,” he says.
NBA players, for example, who play 82 games over a seven-month schedule— roughly, a game every two and a half days— have little time for recovery.
“That’s really too much for the body,” he says. “I can assure you, there is no NBA player who has a normal body.”
These harsh realities have only deepened Guermazi’s appreciation for sports—and for the athletes.
“You and I go to work; we sit, we relax, we do our work. But they are working really hard, getting up at six in the morning, training all day long,” he says. “Sometimes it’s raining or snowing; sometimes they love it, sometimes they hate it—but they have to do it. There is no stop for them.”
Ideally, the payoff can be that moment of global triumph and acclaim. Guermazi especially admires the sprinters, whose years of training lead to just seconds of competition, with a margin of victory measured in milliseconds. The true picture of their greatness, he says, lies in the slow-motion replay.
“You see all the muscles, one after the other, going up and down…every single motion is calculated, measured to the millimeter,” he says. “It’s incredible.” ●

Military doctors receive financial benefits, travel, leadership training— and a sense of purpose
By Doug Fraser

Retired Two-Star Admiral Christine Hunter, MD (CAMED’80), on board her first posting, the USS Hunley.

Following her graduation with honors from Boston University’s six-year combined BA/MD program Christine Hunter, MD (CAMED’80), reported to the USS Hunley, a submarine tender watching over nuclear-armed submarines.
Fresh out of a postmedical school internship, Hunter found herself the only doctor taking care of 1,200 sailors and officers on the 600-foot-long ship.
Though self-confident, at 4’10” and just 24 years old, Hunter knew she was not the typical command figure. She was among the first cohort of female officers to serve aboard Navy vessels and would oversee a medical department of 20 enlisted men, ranging from 19-year-olds with just six months of training to experienced corpsmen—the Navy equivalent of medics—who were deployed far from home with limited access to help.
“When I got my orders, I called my recruiter and said, ‘What in the world am I supposed to do?’” recalls Hunter, who lacked a military background. The recruiter urged

her to simply show up and do her best.
Fortunately, the military has a longstanding policy of pairing inexperience with experience, regardless of rank.
“It was all on-the-job training, and God bless the corpsmen and my fellow officers because they trained me in all the things I needed to know to be successful,” Hunter says. Now retired from the Navy and a two-star admiral, she was the first woman to be named Pacific Fleet Surgeon, then served as commanding officer of Naval Medical Center San Diego before finishing her time in uniform as the senior military officer overseeing the TRICARE military healthcare program of 9.6 million subscribers. After retiring from active duty, she was named chief medical officer of the US Office of Personnel Management, overseeing healthcare delivery to 8.3 million members.
Each year, BU medical students choose to become military physicians. Some make it a career, as Hunter did, while others leave after they have fulfilled their active-duty commitments.

Anna Hohler, MD (CAMED’98), receives her first coin and salute from her brother
Staff Sergeant Gerald DePold in 1995.

All agree it was a rewarding, personally fulfilling experience that molded them into better physicians and healthcare leaders.
“I think the military provides you with an amazing framework for leadership, selfdiscovery, and service to our country,” says Anna Hohler, MD (CAMED’98), chair of neurology at St. Elizabeth’s Medical Center in Brighton, Massachusetts. Anna was active duty in the Army for eight years, including her time in the Reserve Officers’ Training Corps (ROTC) while in medical school. A tradition of service runs in Hohler’s family, with uncles, cousins, and two brothers in the military. “It was important to us to serve our country, and that was something we were always proud of,” she says.
The rewards of military service go beyond personal fulfillment.
“It’s a close-knit community. We all work off a shared sense of purpose,” says Lt. Colonel Sarah Bowe, MD (CAMED’08), an otolaryngologist who has been active duty in the Air Force for more than 15 years. Bowe also comes from a family tradition of military service, including a great uncle who was a decorated Navy veteran, a great aunt who was an Army nurse, and a grandfather who retired as a major in the Air Force and commissioned her when she entered the service.
BU’s strong links to the military include being one of only five universities in Massachusetts offering ROTC membership and training. The medical school established the Center for Military Health in 2015, which is dedicated to improving the health of veterans and service members by coordinating interdisciplinary research and developing clinical innovations and programming on medical issues particular to the military.
Kim Dever, MD (CAMED’92), after completing the Officers Basic Training course at Fort Sam Houston in San Antonio, Texas.
In addition to family history and a sense of duty, the financial benefits inspire some med students to enlist. “The reason I went in was completely about financial expediency. But I stayed for the opportunities and the camaraderie,” says Hunter.
“We didn’t have a lot saved for my college education,” says Kim Dever, MD (CAMED’92), whose father was a firefighter and mother, a homemaker.
Dever is now vice president of women’s health and chair of obstetrics & gynecology at South Shore Health in Weymouth,
Massachusetts. “Always in the back of my mind was that my parents were very concerned about the finances of four years in medical school,” she recalls.
When a college classmate went to talk to a military recruiter, she tagged along and enlisted.
The military financial package, known as the Health Professions Scholarship Program (HPSP), pays a signing bonus of $20,000 plus the cost of tuition, books, supplies and equipment, a monthly stipend of approximately $2,700, and officer’s pay while on active duty. HPSP students are considered reservists and must complete six weeks of active duty every year during medical school and residency; their years in residency are not covered by scholarships or stipend and the student is obligated to four years active duty. Further subsidized training in a specialty adds to the active-duty time obligation.
“I definitely thought I was going to be in that camp, you know, do my four years and out,” says Brian Norwood , MD (CAMED’03), a pediatrician at Sentara Health in Virginia who recently retired with the rank of captain after 20 years in the Navy. While the financial incentives were initially a factor, Norwood also enjoyed the travel.
His first active-duty posting was a large naval base in Yokosuka, Japan, a city of 400,000 surrounded by the sea and mountains and
blessed with a mild climate. Yokosuka proved the perfect home base for trips around Japan for Norwood, his wife, and their first child during the three years he was stationed there.
“We just loved it,” he says.
Norwood and his family next moved to Norfolk, Virginia, where he became the senior medical officer on the 833-foot amphibious assault vessel USS Nassau, which was capable of carrying as many as 3,000 personnel. There, he oversaw a 300-bed floating hospital and a staff of nine physicians. Layered on top of the daily rounds seeing patients, consulting with other physicians, and meetings was the routine of the ship, with jets and helicopters taking off and landing amid the ever-changing sea and exotic ports-of-call.
“It was probably the most fun job I ever had,” he says.
Like everyone else who serves in the military, Norwood has a fascinating story about the experience. He recalls an episode from a relief mission to Haiti following the devastating 2010 earthquake that killed 220,000 people. He was up on flight deck of the Nassau when a helicopter landed.
“There was a guy on a stretcher, and at the end of the stretcher there was a box with a hand-written message that said, ‘Baby in box, do not throw out.’ We looked inside and, sure enough, there’s a baby inside, probably a day
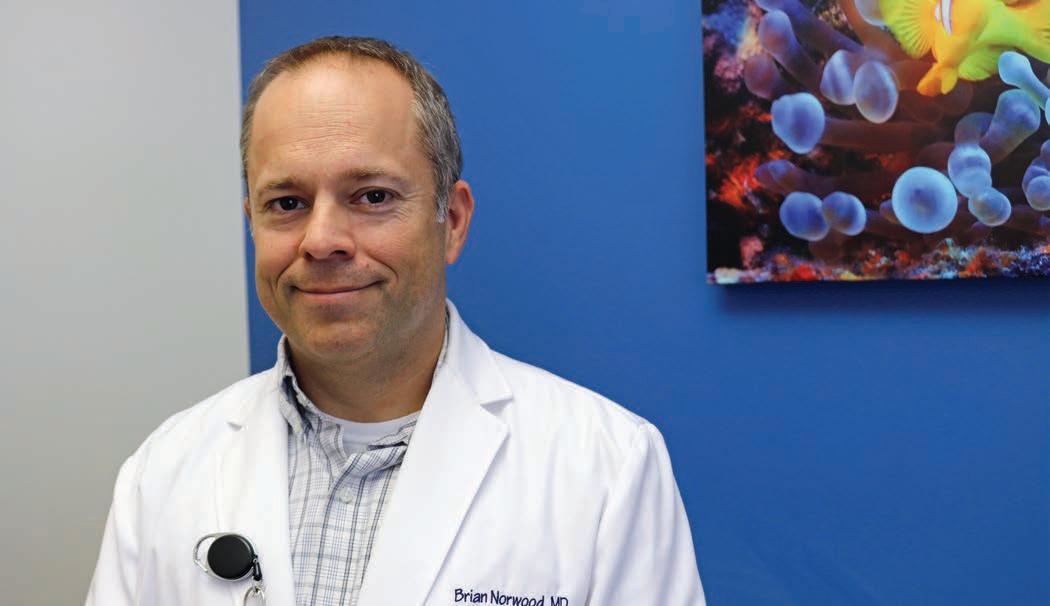
Retired Navy Captain Brian Norwood, MD (CAMED’03), is now a pediatrician at Sentara Health in Virginia.
old, with the umbilical cord still attached. You have a whole (medical) department of people who are away from their families, and everyone wanted to hold this baby and feed it,” he says.
In a happy ending, the baby was reunited with its mother, who was recovering on a nearby medical ship.
“This is what the military offers, these unique opportunities,” says Marisela Noorhasan , MD (CAMED’02), an endocrinologist and obesity medicine specialist who joined the Navy while she was attending BU and is now a captain in the Navy Selected Reserves.
Born in Guyana, Noorhasan moved with her family around the Caribbean before finally settling in the US Virgin Islands.
After graduating from the University of the Virgin Islands, she moved to Boston to study medicine through BU’s Early Medical School Selection Program.
Following medical school, Noorhasan went on active duty, completing an internal medicine residency and serving as senior medical officer at Camp Buehring, Kuwait, during Operation Enduring Freedom from 2009–2010. Other postings included responding to Hurricane Katrina in 2005 in New Orleans and working with the Brazilian Navy and local physicians treating tropical diseases along the Amazon River basin in 2008. She recently returned

from service on the USNS Mercy, a 1,000bed hospital ship on a disaster response preparedness mission in the Indo-Pacific.
“Joining the military opened many avenues for education, training, leadership, and career opportunities,” says Noorhasan. “In the military there is camaraderie, a sense of belonging, and a support structure to foster personal and professional growth.”
After eight years active duty, Noorhasan transitioned into the reserves and for the past 11 years has held various administrative positions, currently serving as chief medical officer at Navy Medicine Readiness and Training Command Corpus Christi, Texas. During her time on active-duty and in the naval reserves, Noorhasan has relocated many times for deployments, career opportunities, education, and training.
“I would like to say that you can choose your own destiny, but when you sign that contract, you are committing yourself to the US Navy or another branch of the service, and they have final say over where you’re going to be living,” says family physician Adrienne Parad , MD (CAMED’07), who served seven years in the Navy.
Parad’s first duty station was at the Navy hospital in Pensacola, Florida, tending to a flight community that included the Navy’s prestigious Blue Angels. Along with her husband Andrew Parad , MD (CAMED’06),

“It’s a close-knit community. We all work off a shared sense of purpose.”
–LT. COLONEL SARAH BOWE, MD (CAMED’08)
“I make sure they understand that there is risk,” says Glenn Markenson, MD, a retired Army colonel with nearly 26 years of service including active duty, reserves, and National Guard. “ They most likely will get deployed and it could be in a war zone.”
also a Navy physician, she deployed to US Naval Forces Central Command in Bahrain, where they witnessed the upheaval that took place during the Arab Spring. Following that, she was posted to Naval Submarine Base New London in Groton, Connecticut.
In military life, deployment to a combat zone is always a possibility.
“{Enlistment} is not a decision to be taken lightly,” says Air Force veteran Bowe, now an associate professor of surgery at the Uniformed Services University’s largest campus in San Antonio, Texas. “You have to be in line with the overall mission of the military and the underlying values of what it is to be a military officer—and be comfortable with the fact that you may be put into challenging situations and may be deployed overseas away from your family.”

Randolph Taylor II, MD (CAMED’06), in Iraq.

Joining the Army was “a sound business decision,” says family physician Randolph Taylor II, MD (CAMED’06).
Ending up “downrange,” military slang for a war zone, seemed only a slight possibility. But with ongoing conflicts in Iraq and Afghanistan, Taylor found himself worrying
about being deployed to a combat zone. He discussed his concerns with Jonathan Woodson, MD, former school of medicine associate dean of multicultural affairs (now the diversity & inclusion office), and professor of surgery.
“It’s our youngest men and women on the front lines, putting their lives on the line to protect us. And if something happens to them, they need the best medical care,” Taylor recalls Woodson saying.
Glenn Markenson, MD, professor of obstetrics & gynecology and director of the Center for Military Health, counsels between five and 10 medical students a year who are considering the military option; one or two each year decide to sign up.
“I make sure they understand that there is risk,” says Markenson, a retired Army colonel with nearly 26 years of service including active duty, reserves, and National Guard. “They most likely will get deployed and it could be in a war zone. If that’s something they think that they would not be able to handle, then the military wouldn’t be for them.”
Markenson, who served as a physician during operations Desert Storm and Iraqi Freedom, worked in an evacuation hospital during the Gulf War (1990–91), stabilizing soldiers for transport to hospitals in the US and elsewhere.
In February 1991, an Iraqi Scud hit a makeshift barracks in Dhahran, Saudi Arabia, killing 27 US troops and wounding 98. Many came to Markenson’s facility.
“A lot of them died. It’s serious stuff and [medical enlistees] must be ready for that,” he says.
Woodson retired from the Army reserves in 2022 as a major general after 36 years of service— including in Saudi Arabia, Kosovo, and Iraq—and is now president of the military’s Uniformed Services University (USU). Made up of four schools and colleges and 20 research centers spread across three campuses, USU serves the military medical professions with medical, dental, nursing, and allied sciences schools.
As an associate dean at BU’s medical school, he counseled students experiencing financial hardships, with military enlistment an option to ease the burden. He recalls students being concerned about two things: the active-duty commitment time and the impact of military service on their career development.
“I would tell them there’s a lot of opportunity to diversify in terms of a specialty, but, more importantly, that they would come out of their service with much broader skills than their peers because they were in an environment in which they had to understand leadership and commitment to mission,” he says.
Taylor believes that the exceptional training he received while in the Army, particularly trauma training to prepare him for deployment to a combat zone, carried over into his private practice. Deployed to Iraq, he would ride to a forward-operating base in a Humvee that jammed signals sent to Improvised Explosive Devices planted along their route.
“Combat injuries weren’t in the majority, but when they happened, they were very, very bad,” Taylor says. “We trained medically for mass casualties; we went through every scenario we could think of.”
After six years of active duty, he left the Army as a major in 2012 and entered sports and family medicine in Houston, Texas, serving as the ringside physician for the mixed martial arts Ultimate Fighting Championship and Top Rank Boxing. Taylor now lives in Atlanta, Georgia. He encourages medical students who ask him about joining the military to join up.
“I tell them ‘Do it!’—it made me a better doctor,” says Taylor. “I didn’t have X-rays downrange; I didn’t have all these fancy blood tests and stuff like that. All I had was the clinical knowledge I’d learned and the book knowledge to make a diagnosis. That allowed me to hone my skills. It’s a good thing to do, both professionally and financially.”
Many BU alumni agree that the most valuable skill they learned from their military experience was how to be a leader.
“I had so many opportunities as a young practicing physician to take on leadership roles,” says Parad. “When I transitioned out, I had all these leadership skills.”
Within two years of leaving the Navy, Parad was on the executive committee and ultimately became vice president of the medical staff at Lawrence & Memorial Hospital in New London, Connecticut. She is now a physician clinical reviewer with Evolent Health.
An OB/GYN, Dever completed four years of residency followed by four years active duty at a military hospital in Germany. She left the Army in 2000, but says the military’s emphasis on leadership and responsibility paved her way into hospital administration.
“A lot of what I learned was how to manage people. Being put in a leadership position, especially as a young woman, really gave me the opportunity to stand up for myself,” says Dever. “The military is very male-oriented, and so is medicine. I learned very early on that I’m going to have a voice and I need to represent my department and the patients.”
Dever’s military experience taught her the importance of being organized, knowing policy, and operating within the chain of command. She found employers valued those skills and had high levels of confidence in the leadership abilities of military physicians.
“Most people wait 10 or 20 years longer to have this opportunity,” says Hohler, reflecting on being named the first female chair of neurology at St. Elizabeth’s Medical Center in 2017 at age 45, after working at BU and BMC as the inaugural director of the Center for Military Health and assistant dean for strategic & affiliate relations. “A lot of my leadership positions in the military—and after—were due to the great training I had in the military.”
While on active duty in the Army, Hohler filled several leadership roles, including at the Madigan Army Medical Center in Tacoma, Washington, where she served as the neurology residency program director and the neurology clinic chief.
“I tell everyone that in the military, one of the big areas of focus is developing leadership skills. In my ROTC training at BU, I was instilled with all types of skills and tools to be able to lead effectively,” Hohler says. “There’s leadership when the waters are calm and there is leadership in choppy waters. The thing about the military is, they train you for both.” ●

Chemical hair relaxers are heavily marketed to, and commonly used by, Black women to straighten curly or tightly coiled hair. Only loosely regulated, these products are known to contain potentially harmful ingredients— including chemicals known as endocrine disruptors that can be absorbed via inhalation or through the skin. Prior studies have linked these chemicals to a wide range of women’s reproductive health outcomes.
A study in the journal Environmental Research has reported that long-term use of chemical hair relaxers by postmenopausal Black women is associated with increased risk of uterine cancer. Compared to women who never or rarely used hair relaxers, those who reported using hair relaxers more than twice a year, or for more than five years, had a greater than 50% increased risk of uterine cancer.
“Our study suggests that moderate and heavy use of chemical hair relaxers may be associated with higher risk of uterine cancer among postmenopausal Black women. In addition, there are major racial disparities
They found that, among postmenopausal women, rates of uterine cancer were statistically significantly higher for those who commonly used hair relaxers even after adjustment for other potential risk factors.
in uterine cancer. Compared to non-Hispanic white women, Black women have higher rates of aggressive subtypes of uterine cancer and are nearly twice as likely to die from their disease,” said corresponding author Kimberly Bertrand, ScD, associate professor of medicine. The researchers asked nearly 45,000 women in the Black Women’s Health Study who had no prior history of cancer and an intact uterus about their past use of chemical hair relaxers. They then followed the women for up to 22 years and compared rates of uterine cancer among women who reported frequent or long-term use of hair relaxers to rates among women who never (or rarely) used hair relaxers. They found that, among postmenopausal women, rates of uterine cancer were statistically significantly higher for those who commonly used hair relaxers even after adjustment for other potential risk factors. ●

New guidance has been issued for clinicians on the determination of brain death—also known as death by neurologic criteria—in the form of a consensus practice guideline, developed through a collaboration between the American Academy of Neurology (AAN), the American Academy of Pediatrics (AAP), the Child Neurology Society (CNS), and the Society of Critical Care Medicine (SCCM) and published in the journal Neurology
This guideline updates the 2010 AAN adult practice guidelines and the 2011 AAP/CNS/SCCM pediatric practice guidelines on the determination of brain death. Until now, there have been two separate guidelines for determining brain death, one for adults and one for children. This update integrates guidance for adults and children into a single guideline, providing clinicians with a comprehensive and practical way to evaluate someone who has sustained a catastrophic brain injury to determine if they meet the criteria for brain death.
“Brain death means that clinicians cannot observe or elicit any clinical signs of brain function,” said author David M. Greer, MD, FAAN, FCCM, professor and chair of neurology. “Brain death is different from comatose and vegetative states. People do not recover from brain death. Brain death is legal death.”
The consensus practice guideline outlines the standardized procedure for trained clinicians to evaluate people for brain death. As part of this procedure, clinicians perform an evaluation to determine whether there is any clinical functioning of the brain and brainstem, including whether the person breathes on their own. Brain death is declared if a person has a catastrophic brain injury, has no possibility of recovering any brain function, is completely unresponsive, does not demonstrate any brain or brainstem function, and does not breathe on their own. The guideline includes updates on the prerequisites for brain death determination, the examination and the examiners, apnea testing, and ancillary testing. ●
Black women who develop high blood pressure before age 35 and are on medication for hypertension may triple their odds of having a stroke, and those who develop high blood pressure before age 45 may have twice the risk, according to a preliminary study presented at the American Stroke Association’s International Stroke Conference 2024 by Hugo J. Aparicio, MD, MPH, associate professor of neurology.
“This research was motivated by the glaring disparity I have seen in my own practice. Strokes are occurring at younger ages among my patients who identify as Black and among women,” said Aparicio. “Early onset stroke, particularly at midlife, is even more tragic because these patients often have families or are caretakers for sick family members themselves.”
Researchers investigated how the development of high blood pressure at a younger stage in life among Black women may influence the risk of a potentially disabling stroke. They compared participants from the Black Women’s Health Study with and without treatment for hypertension before age 45, between ages 45 and 64, and within 10-year age intervals from 1999 to 2019.
Compared to Black women with no history of hypertension treatment:
● Black women who developed high blood pressure and began hypertension treatment between ages 24 and 34 had a 3.1 times higher risk of having a subsequent stroke;
● Black women who developed high blood pressure and were treated before age 45 had 2.2 times higher risk of stroke; and
● Black women who had high blood pressure and were treated between ages 45 and 64 had 1.69 times higher risk of stroke.
“We expected to see an association between having high blood pressure at a younger age and having a stroke during midlife and later life; however, we were surprised and concerned to see the magnitude of the relationship, especially for women who were taking antihypertension medications before age 35,” said Aparicio. ●
Social media platforms such as Snapchat and Instagram are pivotal in perpetuating “selfie” culture, whereby an individual takes and shares a photo of themselves. Globally, social media usage has been increasing, with at least 3.5 billion users on social media in 2019. As of 2018, the average adult was spending 6.3 hours per day on an internet-connected device. A particularly troubling consequence of an increase in social media usage is the effect it has on body perception and self-esteem.
The angle of the “selfie” photographs taken for social media often distorts facial features in a way that leads to dissatisfaction. Medical professionals have reported a phenomenon of “snapchat dysmorphia,” whereby patients seeking cosmetic procedures attempt to emulate filtered and edited versions of themselves.
A study in the Journal of Clinical and Aesthetic Dermatology found that time spent on social media and the use of photo-editing applications correlates with a
A particularly troubling consequence of an increase in social media usage is the effect it has on body perception and self-esteem.
person’s desire to undergo cosmetic procedures, and likely has led to the increase in cosmetic visits seen during the pandemic. They also found patients who followed and engaged with celebrities and influencers on social media, as well as following and engaging with plastic surgery, dermatology, or other accounts showing the results of cosmetic procedures on social media, were significantly more influenced to have a cosmetic procedure done.
“While there was an increase in cosmetic focus during the pandemic, until now there has not been data highlighting a clear link or factors that made patients more or less likely to participate in cosmetic treatments,” explained corresponding author Neelam Vashi, MD, associate professor of dermatology and director of the Boston University Cosmetic and Laser Center at Boston Medical Center.
According to Vashi, this study indicates that practitioners should discuss social media usage with their patients to better understand the desire to undergo cosmetic procedures. ●

“As exciting as cellfree DNA is as an opportunity to learn information about a pregnancy without invasive testing like amniocentesis that uses a needle to withdraw a sample of amniotic fluid, there are many challenges to this technology,” said Holland.
On March 25, panelists at the Third Annual Alan and Sybil Edelstein Professionalism & Ethics in Medicine Lecture described the ethical maze of laws, professional and personal responsibility, and societal values swirling around the rapidly evolving field of genetic testing. More than 100 viewers attended the online event, hosted by David Edelstein, MD (CAMED’80), and his sister Marcia Edelstein Herrmann, MD (CAMED’78). The lecture is named in honor of their parents.
Genetics has evolved from single-gene testing to exome and genome sequencing, which looks at all the DNA of our genetic code, said panelist Jodi Hoffman, MD, associate professor of pediatrics and Boston Medical Center’s (BMC) chief of medical genetics in pediatrics. This can lead to unexpected findings—like the discovery of a debilitating or fatal condition, or other information unrelated to the original reason for the testing—resulting in ethical dilemmas for patients and physicians.
“When we practice genetics, there are some additional principles that we have to keep in mind: informed consent, confidentiality, the duty to warn or inform, as well as fidelity or veracity,” said Hoffman. “We want to make sure that when people have genetic testing, they have the full capacity to understand what they are being offered, exactly what sort of testing we will be doing, and that they are able to choose to do this testing or not to do this testing.”
She said research has shown that most patients want to know all that is discovered by their genetic test.
“We test for 150 or so hearing loss genes,” said panelist Margaret Kenna, MD (CAMED’79), MPH, director of clinical research in otolaryngology and communication enhancement at Boston Children’s Hospital and professor of otolaryngology-head and neck surgery at Harvard Medical School. Kenna described an example of an ethical dilemma: the possibility that a deaf couple would use genetic testing to select for a deaf child.
“What is the duty of the physician? Is the mother the patient, or the baby? These are very big and new challenges for us,” Kenna said.
Panelist Daniel Faden, MD (CAMED’11), FACS, a head and neck surgical oncologist and scientist who practices at BMC and Mass Eye and Ear, and an assistant professor of otolaryngology-head and neck surgery at Harvard Medical School, urged caution in marketing genetic testing to the public as screenings for cancers, known as MultiCancer Early Detection (MCED) tests. He worried about the balance between causing patient anxiety and the benefits of catching a cancer early and treating it.
“I’m a big believer in the potential for MCEDs to revolutionize cancer screening, but I think we’ve gotten a little ahead of ourselves,” he said, pointing out that in the US, in the age group targeted for this testing, even a 1% inaccuracy rate yields nearly a million false positives. “That’s almost a million people you’d be telling had a cancer who actually don’t.”
Erica Holland, MD, assistant professor of obstetrics & gynecology and BMC director of maternal and fetal medicine, discussed the perils of patients putting too much faith in genetic testing.
“As exciting as cell-free DNA is as an opportunity to learn information about a pregnancy without invasive testing like amniocentesis that uses a needle to withdraw a sample of amniotic fluid, there are many challenges to this technology,” said Holland, including the possibility that the placental DNA does not match the DNA of the fetus.
Continued from previous page
Panelists said that surveys indicate that patients want to know what genetic tests reveal even if they are secondary in importance to other aspects of the medical examination and not the reason for the patient’s appointment.
Holland said the prenatal genetic counseling team at BMC, led by Philip Connors, MS’14, MPH’20, CGC, assistant professor of obstetrics & gynecology, is working to reduce societal and educational barriers in communicating the risks and rewards of genetic testing. Connors creates videos explaining the test for patients awaiting their first-trimester ultrasounds. High-risk patients speak directly with a genetics counselor.
Wendy Kuohung, MD, an associate professor of obstetrics & gynecology and director of reproductive endocrinology and infertility at BMC, spoke about the use of preimplantation genetic testing (PGT) in selecting embryos for transfer in the in vitro fertilization process. “There are cases where the provider may find the patient desire to use PGT ethically problematic,” Kuohung said.
PGT-A is used in 40% of all in vitro fertilization cycles in the US, most frequently to select embryos with the normal number of chromosomes as opposed to those with missing or extra chromosomes that are more likely to result in miscarriage, cycle failure, or a baby with birth defects. Another PGT test looks for changes in chromosome structure, indicative of complex diseases presenting later in life like diabetes, cancer syndromes, and cardiovascular disease.
“It isn’t as widely employed and is not as widely accepted,” said Kuohung, who also addressed the ethical dilemma inherent in choosing embryos based on their genetic predisposition to a disorder that does not manifest until adulthood.
Choices are not always as straightforward as adhering to an ethical barometer. Kuohung cited the case of an older patient with diminished ovarian reserve whose only available embryo tested positive for genes that might lead to Down syndrome, but who requested the transfer of the embryo anyway.
“Most fertility doctors will refuse to transfer the Down syndrome embryo due to the ethical mandate to do no harm, but they
may be depriving that patient of ever having a pregnancy if that embryo is the only one the patient has,” said Kuohung, adding that while there is no right answer that applies to every patient, there are guiding principles to help providers and patients make decisions.
She stressed that while patients have the right to reproduce and make decisions regarding their healthcare and treatments, at the same time, providers may exercise the freedom to grant or deny their services based on their own ethical principles.
Panelist Kathleen Swenson, MS, MPH, CGC, a clinical associate professor of medical sciences & education and director of the master’s program in genetic counseling, pointed out that many of these issues preexisted new genetic technologies and involved a similar decision process.
“Genetic counselors support patients, knowing they are resilient; that their emotions matter,” she said.
“We help our patients understand and apply information to make decisions, manage the conditions, and adapt to the situation.” ●

“This project was selected not only for its scientific merit and commitment to engaging patients and other healthcare stakeholders, but also for its conduct in real-world settings,” said PCORI Executive Director Nakela L. Cook, MD, MPH.
Professor of Psychiatry Casey Taft, PhD, has received a fiveyear, $2.8 million award from the Patient-Centered Outcomes Research Institute (PCORI) for his research study, “A Randomized Controlled Trial to Evaluate a Trauma-Informed Partner Violence Intervention Program.” An independent, nonprofit organization, PCORI is authorized by Congress to fund patient-centered comparative clinical effectiveness research that provides patients, their caregivers, and clinicians with the evidence-based information they need to make better informed health and healthcare decisions.
Taft, who also is a staff psychologist at the National Center for PTSD at VA Boston Healthcare System, is conducting a randomized controlled trial of Strength at Home—the only such program that has been shown to be effective in preventing partner violence in military veterans—to prevent and end intimate partner violence (IPV) in Rhode Island. Taft will examine whether this program is also effective within civilian populations.
IPV, specifically physical and psychological aggression toward an intimate partner, represents a public health crisis that affects millions of Americans each year, contributing to a range of mental and physical health conditions in survivors. Children exposed to IPV are at an increased risk for psychological, social, emotional, and behavioral problems and also are more likely to engage in IPV later in life.
“Presently there is little evidence from randomized controlled trials (the gold standard for determining effectiveness) showing that available interventions prevent and end perpetration of IPV in the general [civilian] population. This lack of demonstrated intervention effectiveness in existing programs is troubling, considering that approximately half a million people are court-mandated to these programs each year in the US,” says
Taft, the primary developer of the Strength at Home program.
“This project was selected for PCORI funding not only for its scientific merit and commitment to engaging patients and other healthcare stakeholders, but also for its conduct in real-world settings. It has the potential to answer an important question about intimate partner violence and fill a crucial evidence gap,” said PCORI Executive Director Nakela L. Cook, MD, MPH. “We look forward to following the study’s progress and working with Boston University to share the results.”
Taft has served as principal investigator on funded grants focused on understanding and preventing partner violence through the National Institute of Mental Health, the Department of Veterans Affairs, the Centers for Disease Control, the Department of Defense, the Blue Shield Foundation of California, the Bob Woodruff Foundation, and the Mother Cabrini Health Foundation.
The 2009 Linda Saltzman Memorial Intimate Partner Violence Researcher Award winner from the Institute on Violence, Abuse, and Trauma, Taft sits on the editorial boards of five journals and has published more than 125 academic articles and an American Psychological Association book on trauma-informed partner violence intervention.
Taft’s study was part of a competitive review process in which patients, caregivers, and other stakeholders join scientists to evaluate the proposals. It was selected for funding through a PCORI program designed to support research that produces results that are broadly applicable to a diverse range of patients and care situations and can be more quickly taken up in routine clinical practice.
Taft’s award has been approved pending completion of a business and programmatic review by PCORI staff and issuance of a formal award contract. ●

Using funds from both foundations, TCW will investigate mechanisms that are potentially targetable for therapeutic interventions.
Julia TCW, PhD, assistant professor of pharmacology, physiology & biophysics, and bioinformatics, has received a $420,000 Carol and Gene Ludwig Award for Neurodegeneration Research and $500,000 from the Edward N. & Della L. Thome Memorial Foundation Awards Program in Alzheimer’s Disease Drug Discovery Research. Using funds from both foundations, TCW will investigate mechanisms that are potentially targetable for therapeutic interventions for Alzheimer’s disease (AD).
AD research has largely focused on the disease endpoint pathologies, ß-amyloid (Aß) plaques and neurofibrillary tangles (tau). Studies have demonstrated that AD pathology begins to accumulate 10–20 years prior to clinical presentation, and molecular changes driven by disease-associated genetic variants likely occur even earlier.
Among significant variants identified in a genome-wide association study, Apolipoprotein E (APOE) is the most significant genetic risk factor for late-onset AD. First discovered in 1993, it is present in 64% of sporadic, late-onset AD and at least 80% of familial cases. The fundamental basis through which the APOE4 variant confers heightened risk for AD may be initiated as early as fetal brain development.
Astrocytes and microglia play critical roles in neural circuit formation during brain development. TCW’s group recently reported that APOE4 induces robust species-specific dysfunction in lipid metabolism in human astrocytes and microglia, but not astrocytes and microglia isolated from APOE targeted-replacement (APOE-TR) in experimental models.
As a Ludwig investigator, TCW proposes to investigate molecular and cellular mechanisms of protective Christchurch variant (a rare variant that helps protect the brain and dramatically slows the progression of AD) effects on astrocytes derived from human
AD patient-induced pluripotent stem cells (hiPSCs). “We expect this study will reveal protective mechanisms that could potentially be targetable for therapeutics,” she says.
Using funds from the Edward N. and Della L. Thome Memorial Foundation, TCW will study the role of cholesterol in neurodegeneration with the goal of developing pharmacological interventions targeting cholesterol that are accumulated in AD patient brains.
TCW received her PhD and AM in molecular and cellular biology from Harvard University. She pursued postdoctoral research in the department of neuroscience at the Ronald M. Loeb Center for Alzheimer’s Disease at Icahn School of Medicine at Mount Sinai, New York, ultimately joining the research faculty in the department of genetics and genomic sciences and neuroscience, where her focus was on the development of iPSC models and AD genetics.
The Carol and Gene Ludwig Family Foundation supports medical research with a focus on neurodegenerative disorders, especially Alzheimer’s disease, in addition to education and community engagement.
The Edward N. and Della L. Thome Memorial Foundation was created in 2002 to advance and support direct service projects and medical research on diseases and disorders affecting older adults. ●
Mort Salomon credits Boston University Chobanian & Avedisian School of Medicine for his satisfying, multifaceted career and is pleased to make a gift that will pave the way for future students.
Back when Mort Salomon, MD (CAMED’77), earned his first degree, a bachelor’s in history, his path to a successful medical career was anything but clear.
Salomon’s pursuit of a clinical psychology PhD at the University of Rochester was disrupted by the Vietnam War and the end of graduate-school exemptions and deferments. He was not drafted, but the hiatus in his education led him to look more closely at his goals—and a stint working in clinical group therapy made them clear. “I was looking for something that would be more definitively helpful to people, and medicine seemed like an obvious alternative to psychotherapy,” he says.
After a short period at Columbia University while working as a research assistant at New York Medical College, Salomon began his medical education at BU in 1973. With his family funding his tuition and his own savings covering living expenses, he found himself in a better position than many, but national politics came into play again. During his four years at BU, Congress reduced—and then ended—subsidies for medical training and tuition quintupled.
Amidst ballooning costs and antiwar demonstrations, Salomon forged strong bonds with his medical school classmates. He fondly remembers joining a student action to resist the sudden end of pass/fail grading by taking exams anonymously and withholding the identity key from faculty.
During his first year, Salomon heard advice from Pediatrics Chair Joel Alpert that he kept in mind throughout his career. Alpert described how, in the first two years of school, medical students are subject to a lot of scientific education, often causing those seeking to become clinicians to consider the emphasis on science irrelevant—a tension that’s long existed in medical schools. “Not
everything you’re going to learn is relevant. But, as first-year students, you’re not in a position yet to know what is relevant and what is not,” Alpert had said.
“I realized that Joel was correct about that,” Salomon reflects. “Lots of things that seem very esoteric for a first-year student actually come back to inform your thinking about patients later on.”
He also recalls formative memories of Dr. Eileen Ouellette. “She took a couple of evenings out of her personal life to shepherd us around the pediatric emergency department and talk to us about patients who were there, just to give us clinical exposure,” he says of his professor. “In the first months of our education, that was a wonderful gift.” His BU experiences led Salomon to his dual career path: pediatrics and emergency medicine.
“My educational opportunities allowed me to have a meaningful career that provides a lot of social benefit. I feel that helping the medical school fund the education of other developing doctors is a meaningful gift.”
MORT SALOMON
Salomon became board certified in emergency medicine a few years after it became a specialty in 1979 and then spent almost 20 years in the Bronx, which culminated in an academic promotion to professor of clinical emergency medicine at Albert Einstein College of Medicine. He was also appointed director of the emergency department at Montefiore Medical Center
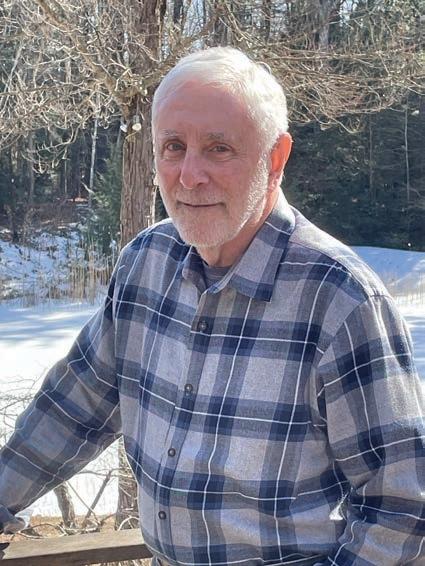
and executive vice chairman of the newly formed academic department of emergency medicine. Another decade followed at St. Vincent’s Medical Center in Bridgeport, Connecticut, where he served first as chairman of emergency medicine and then as hospital vice president.
Along the way, Salomon grew increasingly concerned by the rapid inflation of healthcare costs and wanted to help blunt the upward curve. As medical director of Cotiviti, a medical technology and data analytics company, he spent the last leg of his medical career focused on pricing accuracy in healthcare, finding it another concrete and rewarding way to help people. “My career in medicine has been extremely satisfying to me,” he says.
Salomon recently retired and moved with his wife Teri to western Massachusetts. When looking back on his life in medicine and ahead to the plans for his estate, he thought of the educational institutions that gave him his start and decided to provide both for BU and for his undergraduate alma mater. “My educational opportunities allowed me to have a meaningful career that provides a lot of social benefit,” he says. “I feel that helping the medical school fund the education of other developing doctors is a meaningful gift.” ●

THIS ISSUE OF OUR MAGAZINE HIGHLIGHTS THE STORIES AND ACCOMPLISHMENTS of alumni who have become military physicians. In the past year, I learned about the life of Dr. Almira Fifield, who graduated in 1859 from New England Female Medical College, a predecessor of Boston University Chobanian & Avedisian School of Medicine. As a female physician, Fifield was told to “bury in silence” her medical education and her degree to officially serve and care for sick and wounded soldiers during the Civil War. After catching an illness while working in a Kentucky hospital, Fifield died in 1863. She was 29.
The US Department of Veterans Affairs has recognized Almira Fifield’s service in the Civil War and is reviewing a request for a Civil War marker and headstone in her honor. Her story, along with those of the other featured alumni, brings to light the challenges and triumphs of providing quality healthcare in combat to those who serve our country.
At a June 2023 alumni board meeting, I asked, “What achievements and standards are valued in our distinguished alumni and recognized in our alumni awards? Are there notable alumni contributions that are not being recognized?”
Over the past year, a working group of our board members has met to discuss the criteria and aspects of medicine we’d like to highlight through new awards, thereby creating an environment that celebrates the career variation among our alumni.
Our new Emerging Leader Award honors professional accomplishments of those within 10 years of completing postgraduate training. Our Advocacy, Equity and Social Justice in Medicine Award recognizes those who work above and beyond their daily professional role to implement sustainable policies and processes that have demonstrated reduction in health disparities and advancement in health equity for patients and communities. Our Dean’s Lifetime Achievement Award celebrates those who have had a profound and lasting influence on the advancement of medicine and/or biomedical sciences through leadership, research, clinical practice, education, and advocacy.
During Alumni Weekend 2024, we will recognize Louis Sullivan, MD (CAMED’58) as the inaugural Dean’s Lifetime Achievement Award recipient in Medicine and Biomedical Sciences for his outstanding career in medicine and healthcare leadership.
To learn more about our new alumni awards, please visit the alumni pages of the school website.
This year, we experienced another successful Giving Day, with many donations to our network of scholarship programs. Led by Emeritus Professor of Medicine and former Associate Dean and Director of Admissions Robert Witzburg, MD (CAMED’77), our efforts to engage with potential donors led to 138 people contributing $65,483. It’s exciting to see how our alumni work together to advance our mission while easing the educational journey for current students and propelling their future endeavors.
The Alumni Association remains committed to fostering the relationship between the school and our alumni. To connect former and current students, we have developed a series of events called Alumni Pathways. With alumni sharing time and resources, students will have the opportunity to speak with them about their careers and the scope of their specialties, gain perspective and strategies, and learn about next steps for navigating their own future careers. We would like to extend special thanks to Lauren Lerner, MD (CAMED’80), Fredric Meyer, MD (CAMED’81), Carl Rosen, MD (CAMED’89), Linda Li, MD (CAMED’93), Akash Agarwal, MD (CAMED’00), Tyler Lazaro, MD (CAMED’17), Miguel Dorante, MD (CAMED’19), Benjamin Petrie, MD (CAMED’21), and Wali Sabuhi, MD (CAMED’23) for their expertise, time, and participation.
We hope we will continue to see you at alumni events. As always, we greatly value your depth of knowledge and professional insights. If you are interested in connecting with classmates by hosting a gathering or engaging with current students, please reach out to us! We appreciate you and look forward to staying connected.
Sincerely,
Heather Miselis,
MD, MPH (CAMED’00,’04, SPH’00)
Assistant
Dean for Alumni Affairs
BARBARA FIFIELD BRANDT, PHD, ADVOCATED FOR CIVIL WAR PHYSICIAN FIFIELD
In her time, Almira Fifield, MD, New England Female Medical College (NEFMC)
Class of 1859, was praised for her dutiful and skillful tending to sick and wounded Union soldiers during the Civil War, and for her sacrifice—she died in 1863 at age 29 from an illness caught while working at a Kentucky hospital.

News of her death was published in the Chicago Tribune, in her local newspaper in Valparaiso, Indiana, and other Indiana newspapers, and her name appeared in publications in Europe alongside other wellknown women physicians of the time.
But time erased nearly all traces of Fifield, and she lies buried in an unmarked grave in Valparaiso. Barbara Fifield Brandt, PhD, EdM, founding director of the National Center for Interprofessional Practice and Education in Minnesota, aims to rectify that.
Two years ago, Brandt learned that a Fifield had graduated from New England Female Medical College (which later became part of Boston University), had died in the Civil War while caring for Union soldiers, and was buried in the Valparaiso cemetery. Brandt determined that this person was Almira Fifield, who was born in New Hampshire in 1833 and related to her through her father’s family.
Brandt felt deeply obligated to advocate for a headstone to give Fifield the recognition she was due as a human being and as a doctor who died in service to her country. Due in large part to her sleuthing, the Indiana Historical Bureau recently approved a historical marker for Fifield in
Valparaiso. Brandt’s request for a Civil War marker and headstone is under review at the US Department of Veterans Affairs.
The Fifields moved from Enfield, New Hampshire, to Canada, then to Porter County, Indiana, to land inherited by Brandt’s paternal grandfather.
Historical records, including archives at the Medical Campus Alumni Medical Library, revealed that Fifield started out as a schoolteacher, but decided to become a physician at age 26.
At the time, her decision to travel across the country to attend medical school was a highly unusual one. Brandt found that Fifield was one of only six of the 98 NEFMC graduates between 1848 and 1874 who weren’t from New England or New York, and theorizes that there may have been a religious and abolitionist connection between the Fifields and NEFMC.
Perhaps because her brother, Zacheus Barnum Fifield, had recently been wounded while fighting with the Union Army— or perhaps due to her own abolitionist leanings—soon after her return home, she started campaigning to use her medical degree and skills to treat Union soldiers. US Representative from Indiana and 17th Vice President of the United States Schuyler Colfax, who led the drive for a constitutional amendment abolishing slavery, wrote a letter on Fifield’s behalf to Dorothea Dix, superintendent of nurses for the Union Army.
“I add my testimony to that of her other friends, knowing her to be capable, zealous,
worthy, robust & has a withal good knowledge of medicine,” Colfax wrote.
Both prejudice from male physicians and public sentiment were aligned against the 222 female physicians in the US at the time. Although 21,000 women volunteered as nurses, laundresses, and cooks, only 19 female physicians were allowed to treat soldiers during the war. Mary Walker, who won the Medal of Honor for her service, was the only woman officially listed as a doctor.
According to an article published soon after her death, Fifield was told to “bury in silence her medical education and her degree,” and agreed to serve as a nurse, proving herself so valuable and skillful that she was put in charge of a surgical ward at the Union Hospital in Paducah, Kentucky.
Life was extremely difficult for patients and staff in Civil War hospitals. Medicine at the time did not address germs or include the use of sterile dressings, antiseptic surgery, or sanitation and hygiene. Infectious diseases, like typhoid and dysentery, took nearly 225,000 lives on the Union side alone.
After only a year on the job, Fifield succumbed to “congestive chills,” likely tuberculosis or typhus, and was buried in the cemetery where her father, his three wives, and other relatives would eventually be interred. An article in the Valparaiso newspaper called Fifield a fallen martyr and praised her “skillful and continuous labors for the sick and wounded in different hospitals for many months, from all whose surgeons she received testimonials of the highest character.”
Last year, Brandt traveled to the cemetery, which is locked and closed to the public due to vandalism. Although some headstones remained, many were toppled or missing. “It was quite emotional for me,” she recalls.
The Valparaiso genealogy center records showed that 42 Civil War veterans were buried there, including Fifield and two other nurses.
Brandt hopes she soon will return to the cemetery to see Fifield honored in a manner befitting her service and sacrifice. “What I’m fighting for now,” she says, “is to have the MD included on her Civil War marker.” ●
Following his graduation from medical school, Fredric Meyer, MD (CAMED’81), steadily climbed the administrative and academic ranks at Minnesota’s Mayo Clinic, beginning his career as a neurosurgery resident, then becoming an assistant, associate, and full professor of neurosurgery before eventually achieving the position of neurosurgery chair.
In 2016, Meyer was named to his current positions of executive dean of education for the Mayo Clinic College of Medicine and Science and dean of the Mayo Clinic Alix School of Medicine.
In addition to these responsibilities, Meyer remains a practicing neurosurgeon specializing in brain tumors and travels between Mayo’s campuses located in Phoenix, Arizona, and Jacksonville, Florida. He also has been executive director of the American Board of Neurological Surgery since 2015.
Along the way, he and his wife Irene Meissner, MD, have raised six children.
Meyer attributes his success to the work ethic his father passed down and the lessons he learned during a decade working at a Martha’s Vineyard fish house and on fishing vessels.
“I would consider myself very unspecial from an academic perspective,” he says.
Meyer was drawn to BU by the rare pairing of a medical school and a hospital dedicated to the mission of providing healthcare to the poorer members of society.
“I thought it was pretty special and was much more consistent with the calling of medicine, where you are supposed to take care of everyone,” Meyer says. He praised Boston Medical Center’s Geriatric Home Care Program, which was founded in 1875 and is the oldest, continuously operating in-home medical service in the United States. The program offers diagnosis and treatment to homebound seniors over 70.
“That was so visionary, so unique. A lot of medical schools still don’t have that,” Meyer says. “To me, the mission was beautiful.”
Meyer was influenced by many outstanding faculty during his time at BU, particularly

William McNary, MD, professor of anatomy and the first dean of students at the medical school; Kenneth Edelin, MD, chair of obstetrics & gynecology from 1978 to 1989 and an outspoken advocate for women’s reproductive rights; and Edward Spatz, MD, professor of neurosurgery for more than 40 years.
“The impression they left on me was that the needs of the patient come first,” he says. He cites Spatz as his mentor and the
In addition to his administrative duties, he remains a practicing neurosurgeon specializing in brain tumors.
reason he became a neurosurgeon. “He was so devoted to his patients. To me he was a beautiful spirit; very humble, very modest.”
Meyer has lived in Minnesota for most of his life but has strong Massachusetts roots. He grew up in Springfield and family vacations were on Martha’s Vineyard, a tradition that continues to this day. At the family summer home in Aquinnah on the island, he fishes for striped bass and albacore.
After his first two choices for residency programs didn’t work out, Meyer flew to the Mayo Clinic medical center for an interview with the late Ross H. Miller and the late Thoralf M. Sundt Jr., who was then professor and chair of the department of neurologic surgery as well as program director. Sundt was also a distinguished brain surgeon who had once operated on President Ronald Reagan.
As the interview progressed, the conversation turned to fishing and Meyer’s work at the fish market and on a swordfishing boat. Meyer initially thought that perhaps he’d come up short on another interview, but the two neurosurgeons were impressed by his work ethic and Sundt called to offer him a residency position.
“We’ve decided to offer you a job because what we want are people who are going to work really hard,” Meyer recalls Sundt telling him.
Meyer took that to heart and, as a resident, was on call every other night for two years. “I never left the hospital,” he says.
He greatly admired Sundt, a pioneer in the development of microsurgery of the cerebrovascular system. Even when stricken with a cancer that made his bones brittle and caused him to become progressively weaker, Sundt continued operating almost right up to his death at age 62.
“He really cared about his patients,” Meyer says. “He was very sick and worked in a back brace in the operating room. He was in constant pain, but to see him suffer and yet adhere to the principles of patient care was inspiring.”
Meyer remembers Sundt telling him that “life is short, and it’s not all about work. It’s important to remember your family, your friends—particularly your family—and devote time to them.”
“I have six children and try really hard to be a good father,” Meyer says. Frequently, he’d leave after a day of surgery and go straight to his children’s swim meets.
It’s been eight years since Meyer was chosen to lead the College of Medicine and Science, which includes the medical school, graduate medical education, biomedical sciences, professional development, and health sciences education and involves more than 4,300 students and trainees in 450+ educational programs on three campuses. He is especially proud of raising the medical school ranking into the top 10 nationally and of the school’s increasing diversity— currently, one-third of their students are from underrepresented populations. ●
Sandra Kaplan of Pittsburgh, Pennsylvania, writes, “I’ll be 90 years old in a few months. I’ve lived in my own home for over 60 years and recently remarried; my husband’s name is Karl Brammer, who also is 90 years old. Our geriatric dog lives with us. I have become completely deaf but appear to be otherwise intact and functional. I’ve always maintained fond memories of the school but have lost contact with classmates.”
Gilles Monif of Bellevue, Nebraska, writes, “After stepping down as an assistant dean at Creighton University School of Medicine, using IDI (Intercultural Development Inventory) I entered into a strategic alliance with the University of Florida to look at the role a bovine mycobacterium possibly played in the pathogenesis of Crohn’s disease. In the ensuing 14 years, the means by which an infectious disease created an immune-mediated disease was delineated (Hruska Postulate). Knowledge of the event that combined to produce Crohn’s disease allows for delineation of its prevention, economic treatment, and probable disease termination. This was just published in a novella entitled The Prevention and Therapy of Crohn’s Disease.”


Meyer Lifschitz of Jerusalem, Israel, writes, “My wife and I are here about 21 years and virtually all of our children and grandchildren are here as well. I stopped practicing medicine when COVID came and now learn in Yeshiva Ohr Somayach full time and function there as the informal MD for minor questions. My wife still teaches math at Touro College, Neve Yerusaliyim and Meor Beis Yacov. This year we are fortunate enough to have five grandchildren getting married. One of the advantages of living past 80. If any classmates are here on a visit, I would be happy to get together.”
Geraldine Feldman of Naples, Florida, writes, “The school was well represented at the February wedding of Lauren Burdine Simon (CAMED’21). In attendance were Sara Feldman Jacobson (CAMED’00), Geraldine Feldman (CAMED’69), Lauren Burdine Simon (CAMED’21), and Zoe MacKay (CAMED’21).”
Michael Salcman of Baltimore, Maryland, writes, “I closed my medical office in 2019 a few months before COVID. Since then I have had three collections of poetry published by Spuyten Duyvil in New York. Shades & Graces: New Poems was the inaugural winner
of the Daniel Hoffman Legacy Book Prize, named for the late US poet laureate. Every poet dreams of producing a collection drawn from his previous books; Necessary Speech: New & Selected Poems came out during the pandemic and has an entire section of new poems devoted to COVID-19. My sixth collection of poems is called Crossing the Tape I am 77 years old and surprised that I am still producing new poems that find their way into literary journals; most good poems are written when poets are in their youth and I am already working on my seventh collection! I have stopped writing art reviews but still teach the history of modern and contemporary art at Towson University and other venues. Ilene (CAS’70) and I have started looking for an institution that wants to accept a gift of our art collection; she is still working part time as a financial advisor. The eldest of our three grandchildren in California is already a terrific ballet dancer and the middle one studies at a school named for brain function, Synapse. My anthology of classic and contemporary poems about doctors, patients, illness, and healing, Poetry in Medicine, is still selling. Ilene and I were very upset by the recent collapse of the Francis Scott Key Bridge in Baltimore, a structure beneath which we spent many happy years sailing Chesapeake Bay.”

Bob Friedman of Lakeville, Massachusetts, writes, “I practiced primary care internal medicine for 34 years in Middleborough, Massachusetts. I joined a large medical group in 2013—that didn’t work out and I kind of retired. Since then, I’ve had a house call job, did some telemedicine, worked as a jail doctor in Plymouth, and walked into a psychiatric hospital and got a job doing medical care on the patients. I soon learned about addiction medicine and have been working in substance use disorder clinics for the past seven years. I have continued my education in this field and am very happy that most of our patients are doing so well. It is a fact that 2/3 of people with opioid use disorders developed the problem due to medical issues or work-related injuries, and the other third often had major adverse childhood events. It has been a privilege to work in this field and I hope to continue for a while longer. It is part time and I have plenty of time for cycling—I’m now getting ready for my 24th Pan Mass Challenge ride.”
Russel Jaffe of Vienna, Virginia, writes, “Published a few books: Joy of Living the Alkaline Way, 36th edition; Thriving in the 21st Century, Bones Joints & Muscles. I am grateful to BU for my successes.”
Alan Peterson of Willow Street, Pennsylvania, writes, “I am the emeritus director of environmental and community medicine at
Lancaster General Health/Penn Medicine. As a family medicine doctor, I helped train over 500 resident physicians in 42 years teaching and caring for patients there. Recently I received the annual Societas Generalis Excellence in Medicine Award, the highest honor bestowed on physicians by the organization.”
Diane Jeffery of Cincinnati, Ohio, writes, “These are the most recent photos I have, taken on a Mediterranean cruise last month.”

Alice Rothchild of Seattle, Washington, writes, “Last year my Palestine-focused, young adult novel, Finding Melody Sullivan, and my Palestine-focused, middle grade novel, Old Enough to Know, were published. My memoir, Inspired and Outraged: The making of a feminist physician, is coming out at the end of 2024. I continue to write about health and human rights issues in Israel/

Palestine, documenting and working to end the genocide in Gaza. I was last in Gaza in August 2023 and had a subsequent op-ed in the New York Times and the Seattle Times Otherwise, I do childcare for my two grandchildren, and enjoy the glories of Pacific Northwest hiking and gardening.”
Robert Wolff of Boston, Massachusetts, writes, “As a proud member of the graduating class of ’74, I am now a few months away from completing my career as a pediatric neurologist at Boston Children’s Hospital (BCH); I was in a private practice for many years in the New York metropolitan area before joining the staff of BCH some 16 years ago. As a third-year medical student at the school I was inspired by Dr. Paul Rosman, who taught at Boston City Hospital. I feel so privileged to have been in a career which I have so thoroughly enjoyed. It has been gratifying to now see conditions, such as spinal muscular atrophy and many others to follow, for which we now may offer effective treatment based upon the advances of molecular biology. Thank you to my teachers and classmates at the school and a special thank you to Paul Rosman.”
Larry Nichter of Newport Beach, California, writes, “I am still trying to transition to ‘ gentleman surgeon’ status at the Pacific Center for Plastic Surgery rather than running a busy Newport Beach, California, practice. If only I could do surgery without the administrative hassles. I travel extensively, training surgeons in remote areas of great need. My NPO, Mission Plasticos, is celebrating its 25th anniver-

sary since I founded it; I still serve as medical director. I have been on more than 100 global missions training plastic surgeons in areas of need, focusing on development and capacity building. We have been unique in helping to establish and train advanced acute burn care in Nepal and postmastectomy reconstruction in Central and South American countries, as well as work in microsurgery, pediatric surgery, and congenital and acquired deformities. For these efforts, I was invited for an audience with the Dalai Lama in 2022, and have been named the 2024 Noordhoff Humanitarian Award winner by the American Society of Plastic Surgeons and The Plastic Surgery Foundation. Most importantly, I am a new grandparent, still enjoy my craft, and—when time permits—hiking, surfing, skiing, and snowboarding.”
David Saltzberg of Baltimore, Maryland, writes, “Recently hosted an alumni program at my home in Baltimore. There was lots of good conversation about the cost of medical education and the closure of the six-year medical program. I am enjoying retirement after 40 years of practice in gastroenterology.”
Karen Brown of New York, New York, writes, “After a 38-year career with the last three years spent at the University of Utah in Salt Lake City as chief of the interventional radiology section, I am now mostly retired and back in New York City. Currently working one day a week at New York Hospital, primarily focused on teaching radiology residents. Planning some traveling for next year and including Alumni Weekend at the school in my travel plans. Hope to see some former classmates then.”
David Edelstein of New York, New York, writes, “Last fall I received an award from the American Academy of Otolaryngology-Head and Neck Surgery. They give one ENT doctor the Board of Governors Practitioner of Excellence Award that ‘recognizes the prototypical clinical otolaryngologist one wishes to emulate, who, within the past 10 years, has practiced medicine in an exemplary manner and is sought out by other physicians because of personal and effective care. In addition


to clinical skills, the recipient demonstrates involvement in civic leadership, charitable activity, and leadership in state, regional or national medical organizations.’”
Martha (Marty) Gilpatrick of Concord, Massachusetts, writes, “Rough year—property damage, accounts hacked, broken leg—but most of all, lost my life partner. Still working part time as I adjust.”
Lauren Lerner of Plantation, Florida, writes, “After over 40 years practicing medicine, Keith and I, a class couple who graduated together, are loving retirement. He is enjoying tennis and reading; I’m doing a little medical legal work and volunteering with refugees. We’re traveling, and best of all, spending time with the grandkids. I wrote a novel about climate change and the legacy we are leaving for future generations called The Legacy, under the pen name Ilise Lauren. It’s on Amazon if you want to check it out.”
Melody T. McCloud of Roswell, Georgia, writes, “I was bestowed a Distinguished Alumni Award by Emory University School of Medicine last February. Such awards began in 1958, and prior to this year, only fourteen women had been recognized. Also, my latest book (with information for all women), Black Women’s Wellness, ranked #1 on Amazon’s Women’s Sexual Health and Health Policy lists. I’m a ‘Double Terrier’—CAS’77 and CAMED’81—so the book was recently fea-
tured in Bostonia. I trained at Emory, established hospital-wide endoscopic protocols, served on the Medical Executive Committee, and am active in the community. I’m retired from active practice, but I remain affiliated with Emory University Hospital Midtown. I write and give lectures, including at Chobanian & Avedisian School of Medicine.”
Paul Kalb of Washington, D.C., writes, “Three decades after leaving medicine for the practice of law in Washington, D.C., I am returning (sort of) to my roots, both professionally and geographically. In 2024, my wife and I will join the Harvard Advanced Leadership Initiative, a program for about 40 people from around the world ‘designed to unleash the potential of experienced leaders to help solve society’s most pressing challenges.’ I plan to focus on one or more public health challenges. At Harvard, I will have the pleasure of studying again with Dr. Howard Koh.”
David Sherer of Chevy Chase, Maryland, writes, “My seventh book, Hunger Hijack: how your eating habits are changing your brain and making you sick, has been released. It deals with the dangers of processed food and the problem of increasing body mass index in the developed world, and advocates for habit change and prevention over allopathic medicine for improving the health of people worldwide.”


Karen Bayle of Fairfax, California, writes, “Enjoying retirement after 30+ years as a primary care MD.”
Jai G. Parekh of Towaco, New Jersey, writes, “Living life to its fullest remains my biggest focus. In addition to a busy practice where we just partnered with BlackRock/Zenyth Capital, my best days are teaching at Mt. Sinai School of Medicine. I also became chief commercial officer of Nordic Pharma Eye Care to help bring innovative products to the marketplace. Swati and I are married 30 years now and are going to be empty nesters, as Bela matched at Wills Eye Hospital for Ophthalmology and Tej started in growth private equity at a top New York City firm. Sima is doing social impact/ fintech at MasterCard Corporate. What else? Rob Rothman (CAMED’93) and I may start a podcast together, and I was emcee at the Glaucoma Foundation featuring David Letterman!”
Kerry Girard of Bridgewater, Massachusetts, writes, “So my medical school baby, Matt, had a baby, Emily Jane Girard, and now I’m adding ‘Mimi’ to my credentials. Honestly, this is the BEST job.”
Amir Jaffer of New York, New York, writes, “It will be almost 30 years since graduating medical school. It has been an incredible journey professionally and personally. Blessed with a loving wife, Hajra, and two children, Saniya (28) and Salman (24), who are working in fashion and fintech, respectively. Professionally, I am enjoying my career transforming and improving care delivery as a chief medical officer at NewYork-Presbyterian in Queens. Would love to hear from medical school colleagues.”
Gayle Ryan of Manheim, Pennsylvania, writes, “I recently recommissioned in the Army National Guard and received my first salute from my West Point Graduate! Tim and I are proud parents of kind and overachieving children; all three exceeding our
wildest expectations! Wishing everyone the best life has to offer.”
Aaron Allen of Yad Binyamin, Israel, writes, “I am the chair of radiation oncology at the Helmsley Cancer Center at Shaare Zedek Medical Center in Jerusalem, Israel.”
Mark and Jessica (CAMED’03) Amorosino of Newburyport, Massachusetts, write, “After living and working in the Boston area for many years, we moved our family of six—including Steven (16), Maddie (14), Josi (10), and Chris (8)—to the Sunshine State and enjoy spending time between our hometown of Newburyport and new residence in Jupiter, Florida. Mark will be opening up a comprehensive medical weight loss center in Palm Beach County after successfully helping hundreds of people lose weight and learn to keep it off in Newburyport and Beverly, Massachusetts. Looking forward to bringing this innovative, first-of-its-kind medically supervised weight management program to a larger market with the opening of MetTrimMD Palm Beach slated for summer 2024. Jessica is enjoying her remote work from Florida at Wellsense, formerly known as BMC Health Plan, as a medical director in the field of utilization management after




many years in pediatric clinical practice in Massachusetts. We have been keeping up with many classmates over the years as they pass through Boston, and now through Florida, and are grateful for the memories and continued friendships.”
Rahul Anand of Fairfield, Connecticut, writes, “I am the president of the Connecticut Pain Society.”
Anjali Vaidya of Philadelphia, Pennsylvania, writes, “I am a professor of medicine, cardiologist, and codirector of pulmonary hypertension, right heart failure, and the CTEPH program at Temple University Lewis Katz School of Medicine in Philadelphia. Was honored by the Temple University Provost with the 2023–2024 Lindback Award for Distinguished Teaching, recognizing academic excellence, outstanding teaching, and exceptional achievements and accomplishments. The award honors faculty members who epitomize the highest levels of sustained teaching distinction.”
Luqman Dad of New York, New York, writes, “Following my time in Boston, I completed training in radiation oncology at Roswell
Park Cancer Institute, then took some of my passion for global health that was cultivated at Boston University and founded my specialty’s first-ever global health initiative, sending three trainees each year to an underserved region of the world for academic study and research. Following training, I returned home to Maryland, where I was a partner in private practice for more than 10 years. In 2023, I made the transition back to academics at Columbia University Irving Medical Center (CUIMC), serving as the codirector for head and neck cancer and director of global engagement and community outreach. My amazing medical school mentor, who is chair here at CUIMC, recruited me to New York City, and I feel blessed to be a part of the BU community and here today at Columbia University, working on things I am most passionate about—patient care, trainee education, and global health.”
Yesenia Greeff of Florence, Massachusetts, writes, “I completed residency at Beth Israel Deaconess Medical Center in Boston and GI fellowship at Brown University before joining the faculty at Baystate Medical Center in Springfield, close to my hometown of Amherst, Massachusetts. I’ve been an assistant program director for our medium-sized
internal medicine residency program since 2020, and will now be transitioning to the role of gastroenterology fellowship program director. I got married during fellowship and now get to spend my free time snuggling my son (4) and daughter (1.5).”
Michael Harrell of San Antonio, Texas, writes, “Since graduating, I’ve spent four years on active duty in the US Navy, traveling to Europe for a deployment. I returned to BMC for an ophthalmology residency from 2019 to 2022 and subsequently completed a medical diseases of the retina fellowship at Northwestern University. I’m now a new faculty member in the department of ophthalmology at UT Health San Antonio.”
Tyler Robinson of Folsom, California, writes, “After 15 years of school and training, I finally started practice as a general and minimally invasive surgeon in Sacramento, California. My wife Basia and I spend most weekends chasing around our two dirty-buthappy sons, four and one. My first children’s book, The Higgily Hospital, was just published on Amazon!” ●

Harold L. Osher of Portland, Maine, on December 23, 2023, passed away at the age of 99. He was born in Portland, Maine, on January 11, 1924, to Samuel and Leah (Lazarovich) Osher, immigrants from Russia and Lithuania. The middle child of five, after school he and his siblings worked at the family hardware store in Biddeford, Maine, alongside their parents, from whom they learned the values of education, hard work, and philanthropy.
Dr. Osher attended Bowdoin College and medical school at Boston University. He served his residency in internal medicine at Boston City Hospital and his fellowship in cardiology at Beth Israel Hospital in Boston, and also worked on the Framingham Heart Study from 1950 to 1953.
Although he’d imagined himself teaching at a medical center in Boston, when he married Peggy Liberman in 1950, they decided that Maine would be a better place to raise a family. He established a thriving private practice in Portland and was deeply devoted to his patients. In Maine, Dr. Osher thought he’d be trading an exciting medical career for a preferred lifestyle; during his 45 years of medical practice, he was delighted to discover otherwise. He contributed to the tremendous growth of the Maine Medical Center and Division of Cardiology with his gentle, astute care of patients and through innovation as the director of the Cardiac Catheterization Laboratory, chairman of the Research and Executive Committees, and ultimately, as the director of the Division of Cardiology for 16 years. He extended cardiac care to those in rural areas and was instrumental in starting a regional coronary care program so physicians could receive consultation remotely. Ever committed to education, Dr. Osher had faculty appointments at Boston University School of Medicine, Tufts University School of Medicine, and the University of Vermont College of Medicine and thoroughly enjoyed teaching and mentoring many young doctors.
Dr. Osher was president of the Maine affiliate of the American Heart Association and established the prestigious annual Eugene Drake Memorial Lecture, named after a beloved colleague and mentor. He attracted luminaries in the field of cardiology to speak at this event, including Dr. Paul Dudley White, Dr. Michael DeBakey, Dr. Denton Cooley, and Dr. Christiaan Barnard, who performed the world’s first successful heart transplant. In addition to holding leadership positions in many medical societies in Maine, Dr. Osher was a fellow and involved member of the American College of Cardiology, the American Cardiology Foundation, and the American College of Physicians, and served as vice president of
the American Heart Association. He received multiple awards for outstanding service and excellence in teaching.
Dr. Osher is survived by his children Susan Osher Epstein (William), Nancy Osher Blumberg, Judy Osher (Joel Bresler), and Sam Osher (Alana), grandchildren Joshua (Lorri), David (Heloisa Rutigliano), Daniel, Yoni Blumberg, Benjamin, Nathaniel, and William Osher, Abigail and Matthew Bresler, great-grandchildren Mason, Asher, Beatriz, and Leonardo Epstein, his brother Bernard (Barbro) and sister-in-law Dorothy Suzi Osher, and five nieces and nephews.
Charles Mahanor Jr., of Milton, Massachusetts, on February 18, 2024. Born in 1928 to Charles and Della Mahanor, he was the oldest of six children. He attended public schools in Brockton, graduating from Brockton High School. He was then accepted at Tufts University, where he received his bachelor of science. Charles also completed a master’s degree and enrolled in medical school at Boston University, graduating in 1954. He did his residency at St. Elizabeth’s Hospital, after which he enlisted in the United States Army from 1956 to 1958, serving as a captain. He was assigned to Korea, initially with the 44th Surgical Mobile Army Hospital. After three months, he was transferred and made Commanding Officer of the 43rd Surgical Mobile Army Hospital, where he led with distinction, receiving a commendation for his service from the Eighth United States Army.
Returning from his enlistment to St. Elizabeth’s Hospital, he met his future wife and love of his life, Marjorie. His career took him to the Carney Hospital, where he served on the medical staff from 1959 to 2015. He practiced general surgery with a specialty in hand surgery. A gifted surgeon, he healed and saved many lives, and made many friendships among the hospital staff. After retiring from his own practice, he “un-retired” to continue surgery in the hospital’s outpatient center, and after several years began treating patients at the Copeland Surgical Center for wound care at the hospital. He served in many roles at Carney Hospital, including secretary, vice president, and president of the hospital’s medical staff. He also served on the hospital’s development committee and was a founding member of the Carney Hospital Foundation and on the board of trustees.
Charles mentored and trained surgical residents through Boston University surgical training programs. He was also on the medical staff at St. Elizabeth’s Hospital, Milton Hospital, and the Youville Hospital (formerly the Holy Ghost Hospital), where he served as
president of the medical staff. During his time at St. Elizabeth’s and Carney, he treated patients at the Chelsea Soldier’s Home. For more than 20 years, he worked the 12-hour Friday shift in the Carney Hospital emergency room. He became the medical director at the Liberty Mutual medical unit in Boston, which treated and rehabilitated patients injured through employment, and was a member of the Massachusetts Medical Society and the Norfolk District Medical Society. He also served on the Guild of St. Luke in many roles, including president and was an active member in St. Agatha’s Parish in Milton and St. Theresa’s Chapel in Marshfield.
Charles was married for 37 years to his late wife Marjorie (Gorman). He is the beloved father of Charles, Susan, Elizabeth, and the late Richard. Dear, loving brother to Robert Mahanor, Beverly Jansen, Lawrence Mahanor, and the late Donald Mahanor and Alan Mahanor. He is also survived by many loving nieces and nephews. A man of great faith, spirituality, and ethics, he lived a long and productive life as a loving father, son, brother, uncle, colleague, friend, mentor, spiritual leader, and guide.

Murray Weinstock of Baltimore, Maryland, and Naples, Florida (formerly of Woodcliff Lake, New Jersey), on January 23, 2024.
Born on December 5, 1934, in Monasterzyska, Poland, his first language was Yiddish. He immigrated to the United States with his parents in 1937 and settled in West New York, New Jersey. Murray attended Memorial High School in West New York and later put himself through the Rutgers College of Pharmacy. He served in the US Army for six months and the Army Reserve for six years. Later, he put himself through medical school—starting at the University of Amsterdam (without knowing Dutch) and then finishing at Boston University, where a niece and nephew later followed in his footsteps. Murray did his internship at Boston University, his residency in internal medicine at Albert Einstein, his fellowship in cardiology at the Mount Sinai School of Medicine, and worked at the Bronx Veterans Administration Hospital. Murray enjoyed a long career as a practicing cardiologist beloved by his patients and staff, seeing patients until he was in his late 70s. He was an attending physician at Hackensack University Medical Center for more than 40 years and a US FAA designated senior aviation medical examiner and offered immigration medical exams. After he retired from his private practice, Murray worked as an expert witness for court cases with medical questions.
He is survived by his beloved wife, Gloria Weinstock, devoted children Abby (Shawn) Sefret and Judith (Craig) Bitman, loving sister Lenore (Spencer) Shaps, adoring grandchildren Jonah Luke Bitman, Eli Thomas Bitman, Grant Spencer Bitman, Shayna Eva Sefret, Aliza Rose Sefret, and Hannah Leah Sefret, and dear nieces, nephews, and their children.

Malcolm N. Joseph III, of Clarksville, Maryland, on November 26, 2023.
Malcolm was born in New York City to Malcolm and Essie Joseph in 1949. He graduated from Cardinal Hayes High School in 1967. In 1971, Malcolm became one of the first Black alumni of the College of the Holy Cross, graduating with a degree in biology and sociology. He then accepted a Reserve Officer Training Corps commission into the United States Air Force. After Malcolm earned his MD from Boston University, he completed his internship at Malcolm Grow Medical Center at Andrews Air Force Base and residency in occupational medicine at Johns Hopkins University. He also earned his MPH from Johns Hopkins.
In 1983, Malcolm married Pamela, whom he met while both were stationed at Andrews Air Force Base (AFB). After assignments at Robins AFB in Georgia, Elmendorf AFB in Alaska, Johns Hopkins University Hospital in Maryland, and the Pentagon, the Joseph family settled in Maryland. Together, Malcolm and Pamela raised four children, Natalie C. Zeigler, Malcolm N. Joseph IV, Margaret T. Joseph, and the late Elizabeth D. Joseph, who passed away at age four from bacterial meningitis.
After serving the country for over two decades as a chief flight surgeon, traveling the world providing medical staffing for three presidential administrations and serving on Air Force One as Vice President Walter Mondale’s physician, Malcolm retired in 1998 as a USAF Colonel. Then, he joined CareFirst, where he served as a medical director for nearly 20 years. ●
The Chobanian & Avedisian School of Medicine Alumni Association announces the 2024 Alumni Award recipients
Dean’s Lifetime Achievement Award in Medicine and Biomedical Sciences
Louis Sullivan, MD’58
In recognition of his outstanding career in medicine and healthcare leadership


Jennifer Luebke, PhD’90 Chair of Anatomy & Neurobiology
Christopher Andry, MPhil, PhD’94 Chair of Pathology & Laboratory Medicine
In recognition of their scientific and leadership contributions to BU

Alumni Award recipients will be recognized at an in-person ceremony and luncheon on Saturday, September 28, as part of our Alumni Weekend events.
Members of the Classes of 1969, 1974, and 1975 returned to the Medical Campus to celebrate their Golden Reunions May 17–18 with a reception, class dinner, and student-led campus tours.

Stuart Rhein, MD (CAMED’69), Judy Rhein, Lucas Brunelle, Robert Novelline, MD (CAMED’69), George Hines, MD (CAMED’69), and Helene Hines.

Paul Freedberg, MD (CAMED’74), Ruth Tuomala, MD (CAMED’74), Susan Davis, MD (CAMED’74), Rebecca Backenroth-Maayan, MD (CAMED’74), J. Kristin Olson-Garewal, MD (CAMED’75), Rosemary Sokas, MD (CAMED’74), and Robyn Karlstadt Meyeroff, MD (CAMED’74).

J. Kristin Olson-Garewal, MD (CAMED’75) and Nnaemeka Nwoke (CAMED’27).

Sara Achrati, MD (CAMED’17), Susan Davis, MD (CAMED’74), Rosemary Sokas, MD (CAMED’74), J. Kristin Olson-Garewal, MD (CAMED’75), and Karen Antman, MD.

Christopher Lietz (CAMED’27) and Judy Rhein.

It’s easy—and rewarding. Take the time now to make sure that your will reflects your intentions to care for your family and the people and causes that matter most to you.
If you include a gift for BU in your estate plans, you will have the satisfaction of knowing that future generations of students will benefit from your generous legacy.
To learn more about how you can make a gift in your will to support BU, contact Boston University Planned Giving at 800-645-2347 or opg@bu.edu, or visit bu.edu/plannedgiving.
Download a complimentary copy of our Estate Planning Guide at bu.edu/estateguide.