

VOL. 73 NO.3 Summer 2022
Sarah E. Scher, JD Chief Executive Officer

More than 12,500 physicians rely on the Cooperative of American Physicians (CAP) to protect their practices every day.
Physician-founded and physician-governed, CAP provides superior medical malpractice coverage and solutions to help California physicians realize professional and personal success.
CAP members also receive risk management services, claims support and a dedicated in-house defense firm, practice management resources, and so much more. Find out what makes CAP different.
CAPphysicians.com 800-252-7706
Medical
“We want to make sure that California’s finest physicians are properly protected.”
A Team Approach to Medical Malpractice Coverage is a Winning Approach for Physicians
professional liability coverage is provided to CAP members by the Mutual Protection Trust (MPT), an unincorporated interindemnity arrangement organized under Section 1280.7 of the California Insurance Code.
•
curriculum with

A place to call home.
Our not-for-profit clinic network is looking for top-quality health care professionals who are truly committed to the core values and mission of the Community Health Center movement.

Established in 1978, CHC now operates more than thirty state-licensed health centers on California’s Central Coast. Spanning 120 miles of prime coastline, our service area is an ideal place to live, raise a family, and thrive. We support 150,000 unduplicated patients, 450,000 annual encounters, 900+ employees and a $120M annual budget. Priority one is caring for our patients and providers, so CHC commits itself to operating a nimble, diverse and sustainable agency that’s here to stay.
CHC is an Equal Opportunity Employer. We strongly support a smoke and drug free environment. To apply, contact: Madisyn Masatani at mmasatani@chccc.org or 1(805)346-3975

Community Health Centers of the Central Coast, Inc. (CHC)



A complete list of career opportunities at: communityhealthcenters.org/careers
•
in
2019-10_CHC+CFP-recruitment-ad_FINAL.pdf 1 10/1/2019 3:00:37 PM
JOIN OUR TEAM! See current openings at chsu.edu/careers • Make an impact on the Central Valley by serving the health care needs of our underserved and rural populations
Develop
whole-person approach to treatment and care, utilizing cutting-edge technology and hands-on experiences
Enjoy living
Central California’s diverse community culture with over 70 distinct ethnic groups • Find a family-friendly community with highly ranked educational institutions Now Hiring Primary Care Chair and Faculty For Advertising Information, contact: Michelle Gilbert mgilbert@pcipublishing.com 1-800-561-4686 ext. 120
816 21st Street
Phone (415) 345-8667
Officers and Board Staff
President
Lauren Simon, MD, MPH, FAAFP
Immediate Past President
Shannon Connolly, MD, FAAFP
President-elect
Raul Ayala, MD, MHCM
Speaker
Alex McDonald, MD, FAAFP
Vice-Speaker
Anthony "Fatch" Chong, MD
Secretary/Treasurer
Brent Sugimoto, MD, MPH, FAAFP
Chief Executive Officer
Lisa Folberg, MPP
Foundation President
Ron Labuguen, MD, FAAFP
AAFP Delegates
Jay Won Lee, MD, MPH, FAAFP
Lee Ralph, MD
AAFP Alternates
Michelle Quiogue, MD
Lisa Ward, MD, MPH, FAAFP
CMA Delegates
Kimberly Buss, MD Felix Nunez, MD
Sumana Reddy, MD, FAAFP Kevin Rossi, MD, FAAFP
CMA Alternate Delegates
Raul Ayala, MD, MCMH
Noemi Doohan, MD, PhD
Adia Scrubb, MD, MPP
David Tran, MD
Sacramento, California 95811
Fax (415) 345-8668
www.familydocs.org
E-mail: cafp@familydocs.org
Lisa Folberg, MPP
Chief Executive Officer lfolberg@familydocs.org
Karen Alvarado
Advocacy Assistant kalvarado@familydocs.org

Anita Charles Program Assistant acharles@familydocs.org
Morgan Cleveland
Manager of Operations & Governance mcleveland@familydocs.org

Jerri Davis, CHCP
Vice President, Professional Development, CME/CPD jdavis@familydocs.org
Christine Lauryn
Manager, Member Communications clauryn@familydocs.org
Josh Lunsford
Vice President, Membership & Communications jlunsford@familydocs.org
Pamela Mann, MPH E xecutive Director, CAFP Foundation pmann@familydocs.org
Catrina Reyes, Esq.
Vice President, P olicy and Advocacy creyes@familydocs.org
Jonathan Rudolph Manager, Finance jrudolph@familydocs.org
Tiyesha Watts
Legislative & Policy Advocate trwatts@familydocs.org
Brent Sugimoto, MD, Editor
Josh Lunsford, Managing Editor
The California Family Physician is published quarterly by the California Academy of Family Physicians. Opinions are those of the authors and not necessarily those of the members and staff of the CAFP. Non-member subscriptions are $35 per year. Call 415-345-8667 to subscribe.

pcipublishing.com
Created by Publishing Concepts, Inc. David Brown, President • dbrown@pcipublishing.com 800.561.4686 ext 103
For Advertising info contact Michelle Gilbert • 800.561.4686 ext 120 mgilbert@pcipublishing.com
4 California Family Physician Summer 2022
•
•
•
•
EDITION 42





Summer 2022 features departments 20 Make a Difference: Take Breaks at Work K aren Muchowski, MD, FAAFP 21 Implementing High-Quality Primary Care – A Leadership Opportunity for California D iane Rittenhouse, MD, MPH 22 Female Physicians Experience More Burnout K aren Muchowski, MD, FAAFP 23 Interview with Lauren Simon, MD, MPH, FAAFP 25 Interview with Jasmeet Bains, MD, Family Physician and Candidate for Assembly District 35 26 Districts II and IX Elect New Leaders 28 CAFP Members Receive State and National Recognition 6 Editorial I t Came from California B rent Sugimoto, MD, MPH, FAAFP 8 President’s Message P aving the Way to Wellness Through Title IX L auren Simon, MD 1 0 Poli tical Pulse Fin al 2022-23 Budget Preserves Key Health Care Investments Je ff Luther, MD, FAAFP 12 L egislative Update 2 022 Family Medicine Advocacy Summit: The Return of the FM Revolution Ti yesha Watts 16 CAFP Foundation C AFP Foundation: Another Successful Procedures Workshop P amela Mann, MPH 18 Trauma-Informed Family Medicine I mportance of ACEs in Adults: Out about ACEs A manda Wallner Your Online Resource for Continuing Medical Education. Visit education.familydocs.org
It Came from California
I am writing this somewhere high over Utah flying back from Kansas City, Missouri, where I went on my semiannual pilgrimage to the AAFP Summer Cluster. At this meeting, the Academy’s commissions gather for an intense weekend to help advise the work of the Board of Directors in areas such as membership, practice issues, public health, professional development, education, federal and state policy, Academy finances, and the newest focus: diversity, equity and inclusiveness in Family Medicine. For me, this is a great meeting of minds, where one can take the pulse of family medicine and exchange ideas with fellow colleagues throughout the nation.
One thing I learned there was existence of a phrase, “It came from California.” It can be delivered in various flavors. Sometimes it has a pejorative ring, as in an idea that could have only come from that hippy-dippy blue state on the West Coast. But on this past trip, I learned how “It came from California” could be heard as a call to action and an idea whose time has come.
A chapter executive from another state related how the CAFP’s adopted position on medical aid in dying (MAID) was the impetus for change in her own state.
In 2015, CAFP had modified its opposing position on MAID to a neutral one ahead of passage of California’s End of Life Option Act. This vital change allowed our academy to provide family medicine input to ensure policy met the needs of our practice and our patients.
This executive’s chapter had experienced resistance from some key members to adopt policy that would allow their chapter to engage with policymakers similarly. She pointed to our state and successfully made her closing pitch with, “It came from California.”
We have a dynamic membership in a state as large as ours, with interests as diverse as our colleagues’ backgrounds.
There are few problems in patient care, medical education, research, policy, public health and many other sectors that are not being tackled by a California family physician. It is not surprising that we are a birthplace of problem solving and innovation, and many look to us for solutions.

Yet, it is important to remember that diversity only serves us when we recognize and acknowledge the value that each family physician brings to our specialty. Our diversity is one source of the dynamism that
attracts others to our example. Even so, our academy has been self-reflective enough to recognize that we can always be better. Thus, I am very proud that the CAFP adopted the strategic goal of prioritizing justice through equity, diversity and inclusion (JEDI).
Furthermore, Academy’s strategic plan specified that it will use a trauma-informed lens in its JEDI initiatives. If injustice is a fundamental cause of the health disparities and inequity many of our patients experience, then trauma is an important medium for perpetrating that injustice within communities.
Consider one type of trauma: Adverse Childhood Experiences (ACEs). In a national sample of the Centers for Disease Control 2017 Behavioral Risk Factor Surveillance System (BRFSS), women were more likely to have had exposure to at least four ACEs (17.1% vs. 13.9% in men). Similarly, Black and especially Native American individuals were more likely to have had a high exposure of at least four ACEs compared to Whites (17.7% and 28.3% respectively vs. 15%).
It is relatively novel to apply a trauma-informed lens to issues of diversity, equity and inclusion within medicine. Nevertheless, our academy has decided a trauma-informed lens will be a useful tool to address health inequities. But as the CAFP is trailblazing its own path to JEDI, our academy will rely on its nearly 11,000 members to help it find the right path.
Towards that end, you will see in this issue a new department, Trauma-Informed Family Medicine. The articles will feature topics related to trauma and JEDI work. I hope this feature will help spark a fruitful conversation for how a trauma-informed lens will make us more effective family doctors for our most vulnerable patients.
Our work in trauma and JEDI could be yet another reason other states say, “It came from California.”
References
Merrick MT, Ford DC, Ports KA, et al. Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. MMWR Morb Mortal Wkly Rep 2019;68:999-1005.
DOI: http://dx.doi.org/10.15585/mmwr.mm6844e1
Brent K. Sugimoto, MD, MPH, AAHIVS, FAAFP editorial
6 California Family Physician Summer 2022
HIV TREATMENT AS PREVENTION
Talk to Your Patients With HIV About the Benefits of Becoming Undetectable.
Getting your patients with HIV on treatment and helping them achieve and maintain an undetectable viral load are critical steps toward ending the HIV epidemic. People with HIV who take antiretroviral therapy as prescribed and become undetectable:

• Can live longer, healthier lives.
• Have effectively no risk of transmitting HIV through sex.
Talk to your patients with HIV about the benefits of becoming undetectable to keep themselves and their partners healthy.
To access resources from the Centers for Disease Control and Prevention on HIV treatment as prevention, visit: cdc.gov/HIVCareIsPrevention.
Lauren Simon, MD, MPH, FAAFP, CAFP President

Paving the Way to Wellness through Title IX

On June 23, 2022 as hundreds of diverse Family Medicine resident physicians throughout California prepared to complete their last week of residency education, we celebrated the 50th Anniversary of the landmark legislation of Title IX of the Education Amendments Act of 1972 which included 37 words that changed the landscape for individuals then and for those of us who followed: "No person in the United States shall, on the basis of sex, be excluded from participation in, be denied the benefits of, or be subjected to discrimination under any educational program or activity receiving Federal financial assistance”. At its core, the impact of Title IX shows the vital importance of CAFP’s use of a Justice, Equity, Diversity, and Inclusion (JEDI) lens to plan all of our programs and policy which we validated as part of our current CAFP strategic plan. Title IX legislation provided choice rather removed it. It provided a basis for equitable treatment.
I was one of the women who benefited from the legacy of Title IX. It gave me the choice to pursue intercollegiate athletics due to the opportunities it provided. Due to Title IX, women’s swimming was added to my university’s varsity sports to balance men’s and women’s sports teams. That legacy enabled me to, not only compete on the Swimming Team at Colgate University, but also planted the seeds for my personal wellness. I competed in distance swimming, probably genetically determined by my endurance muscle fibers (although, I secretly had the desire to be a sprinter). While spending hours swimming, training for my events, although I did not know it then, I was practicing
personal wellness. Swimming numerous laps provided me the opportunity to be mindful and reflective of life while I swam (in addition to stimulating term paper ideas in my head).
Being part of the swim team provided me with wonderful social relationships, and opportunities to celebrate and express gratitude. It also provided me with great regular exercise, a focus on consuming a healthy diet and getting adequate sleep, all of which are core components of personal wellness which I strive to continue. Being part of the CAFP team surrounded by wonderfully talented and passionate physicians and CAFP staff has mutually increased all our wellbeing.
It can be difficult to focus on physician personal wellness during these challenging times in our country and when faced with large amounts of administrative burden and electronic health record tasks that accompany our care of patients. However, finding well-being strategies that prioritize caring for oneself is an important factor in caring for others. Focusing on wellness improves the joy we experience of being a Family Physician.
I am deeply humbled that you have entrusted me with serving as your CAFP President. I will advocate for you and our patients with a JEDI lens and will promote member wellness and joy in medicine for our learners and for early, middle, and late career physicians. I encourage you to choose your path to develop or augment your personal wellness. Consider eating healthy food each day, increasing exercise or sleep, learning something new or other techniques discussed in this issue of California Family Physician. You can find well-being resources through our Academy at www.familydocs.org/wellness. Just remember that if your wellness plan includes educational programs or activities, Title IX paved the way.
8 California Family Physician Summer 2022 president’s message
Personal Health Improvement Plan template https://www.aafp.org/dam/AAFP/documents/journals/fpm/personal_health_improvement_plan.pdf
VA Northern California Health Care System
WE ARE HIRING!
Primary Care Physicians - Supervisory and Staff Opportunities
Modesto, CA - Sonora, CA - Yuba City, CA - Stockton, CA Chico, CA - Redding, CA - Fairfield, CA
To apply, email current CV to: Crystal.Keeler @va.gov
The Department of Veterans Affairs (VA) needs primary care professionals who possess the energy, compassion, and commitment to serve those who served our country. Eligible applicants must be able to provide comprehensive general primary care and comprehensive women’s health care.

Whether your a new graduate or an experienced professional, physicians are always needed at the VA.

These locations have a lot to offer to those seeking good weather and an abundance of outdoor activities such as hiking, snow skiing, boating, hunting and fishing. Enjoy the area’s beautiful rural settings with access to many national parks, rivers, and lakes at your fingertips. Whether you’re interested in work/life balance, research or academics you will find that working for the VA offers many benefits not to mention the great honor we have in serving our nation's heroes.
Available benefits:
• Insurance for Medical, Dental, Vision and Long
• Term Care Sick and Annual Leave accrual starting on day one Education Debt Reduction Program
• Recruitment/Relocation Incentives
• Some positions offer partial tele-work opportunities, but are not virtual assignments
Candidates must: 1) be US Citizen or Green Card Holder; 2) BE/BC Family Medicine or Internal Medicine; 3) have a medical license in any State; and 4) confirm vaccination for seasonal influenza and Coronavirus Disease 2019 (COVID-19), which are both requirements for all Health Care Personnel (HCP) employed by Department of Veterans Affairs. Supervisory candidates should: have demonstrated leadership experience or demonstrate informal leadership training, experience and skills.
Summer 2022 9
political pulse
Final 2022-23 Budget Preserves
Key Health Care Investments
The Legislature and the Governor have reached agreement on the Budget Act of 2022. The 2022-23 budget includes total spending of just over $300 billion and total reserves of $37.2 billion in 2022-23. The budget preserves key investments to expand Medi-Cal to all eligible Californians regardless of immigration status, reproductive rights, and health workforce investments. See further details below:
• Medi-Cal for All, Regardless of Immigration Status. Expands Medi-Cal to all eligible Californians regardless of immigration status. Currently, income eligible young adults 25 and younger and those 50 and older have access to full scope Medi-Cal. The budget will expand access to ages 26 through 49 beginning no later than January 1, 2024.
• Reproductive Rights Investments. $200 million in key reproductive rights investments to assist California continue to lead in protecting reproductive rights. These include:
◊ $40 million for Uncompensated Care Fund.
◊ $30 million for Equity and Infrastructure payments for Clinic Abortion providers.
◊ $20 million for Reproductive Health Care Services Scholarships/Loan Repayments.
◊ $20 million Reproductive Health Care Facilities Security.
◊ $20 million for Premium Subsidy Payments.
$20 million for the California Abortion Support Fund.
$20 million for LA County Reproductive Health Pilot.
◊ $15 million for the Reproductive Justice and Freedom Fund.
◊ $10 million to backfill lost Title X Family Planning funds.
◊ $8 million for Family Planning, Access, Care and Treatment, and HPV Vaccine Coverage.
◊ $2 million for Reproductive rights website and research on unmet reproductive health care needs.
Jeff Luther, MD, FAAFP Chair, Legislative Affairs Committee

•
Song-Brown Program. $30 million allocated over three
years to the Song-Brown program for primary care graduate medical education (GME) programs, which is a portion of CAFP’s budget request.
• Workforce Development. $351.6 million over four years for workforce development, including:
◊ $200 million for the behavioral health workforce.
◊ $75.6 million for the public health workforce.
◊ $76 million for the primary care, clinic and reproductive health workforce.
• Public Health Infrastructure. $300 million ongoing investment in state and local health departments to address vital public health priorities.
• End the Epidemics One-Time Funding. $38 million over three years to prevent and treat sexually transmitted infections, including for syphilis, congenital syphilis, and hepatitis B.
• Restores the Covered California State Premium Subsidy. $304 million restoration of the state premium subsidy program in Covered California and modifies trailer bill language to eliminate deductibles and reduce copays if federal subsidies are renewed.
• Reduce Share of Cost Requirements for Seniors in Medi-Cal. Adopts trailer bill language to reduce share of cost requirements for seniors and persons with disabilities by increasing the Medi-Cal Maintenance Need Income Level, beginning January 1, 2025, subject to budget contingency language.
• Continuous Medi-Cal Coverage for Children Zero to Five. Adopts trailer bill language to provide continuous Medi-Cal coverage for children zero to five years of age, beginning January 1, 2024, subject to budget contingency language.
CAFP’s Key Contacts receive these updates through the weekly Legislative Update. To receive information on what’s happening in Sacramento, sign-up to be a Key Contact at www.tfaforms.com/379954.
10 California Family Physician Summer 2022
◊
◊
OCTOBER 7-11, 2022



HealthRIGHT 360 is Hiring



Medical Director- Integrated Care Center, San Francisco
https://www.healthright360.org/job/medical-directoricc-hafcmedical-0
Southern CA Associate Medical Director (Psychiatrist)

https://www.healthright360.org/job/socal-associatemedical-director-prototypes
Associate Medical Director, San Diego (Primary Care with Addiction Medicine experience or Board Certification)



https://www.healthright360.org/job/primary-careassociate-medical-director-ncsh
Also seeking Physicians, NPs, PAs, and RNs for our programs statewide
Please visit our website to view our openings, benefits, and more about organization.
https://www.healthright360.org/jobs recruiting@healthright360.org

Register today!
Join us in Anaheim for the 2022 National Conference & Exhibition, October 7-11.
We can’t wait to welcome you in person to network with colleagues, participate in worldclass education sessions, attend exciting special events, visit the exhibit hall, and much more! A limited virtual attendee experience will also be available.

The Leading Vaccine Buying Group for Family Physicians
JOIN TODAY FOR:
• Best pricing and terms for all vaccine manufacturers, including a new contract for Pfizer’s Prevnar 13® vaccine.






• Comprehensive flu program including Sanofi, Seqirus, GlaxoSmithKline, and AstraZeneca products.
• Excellent customer support for all vaccine-related issues, including ordering, reimbursement support, and advocacy.
• Enrollment is easy and there is no cost to join.
(800) 741-2044

info@atlantichealthpartners.com
www.atlantichealthpartners.com
For more information and to register, visit AAPexperience.org.
TARGETED ADVERTISING FOR THE MEDICAL
Contact Michelle Gilbert at 501-725-3561 mgilbert@pcipublishing.com
AAPexperience.org#AAP2022
PROFESSIONAL
legislative update
Tiyesha Watts Legislative and Policy Advocate

2022 Family Medicine Advocacy Summit: The Return of the FM Revolution
After two years of being virtual, more than 240 family physicians, residents, and medical students from across the country gathered at our nation’s Capital from May 22-May 24 for AAFP’s Family Medicine Advocacy Summit (FMAS). FMAS provides a unique opportunity for family physicians to directly lobby members of Congress and their staff on issues important to family medicine. This year during FMAS, family physicians attended informational sessions where they learned about the legislative process, gained insight into federal and state advocacy, and attended briefings on policy priorities for family medicine. CAFP members showed up and showed out in numbers at the summit and won the Extra-Large Chapter Award in recognition of our members’ outstanding support for FamMedPac.
After reconnecting and building their advocacy knowledge, CAFP and other chapter delegations walked the halls of the Capitol to put their advocacy skills into practice and lobbied 220 members of Congress and their staff on three top AAFP policy priorities: increasing access to telehealth, addressing the mental health crisis, and ensuring Medicaid payment parity. In these meetings, family physicians were able to remind lawmakers and their staff that family physicians are often the first point of contact for patients navigating the health care system, and shared personal stories about the impact they have on patients.
Below are the key topics and bills lobbied by members in their legislative meetings:
• Increasing Access to Telehealth - AAFP urges Congress to enact legislation to permanently remove Medicare geographic and originating site restrictions to allow all Medicare patients to access virtual care and to enact legislation to allow federally qualified health centers and rural health clinics to permanently provide telehealth services. AAFP endorses the following legislation to increase access to telehealth: Protecting Access to Rural Telehealth Act (S. 1988/ H.R. 5425), Evaluating Disparities and Outcomes During the COVID-19 Emergency Act (H.R. 4770), and Primary and Virtual Care Affordability Act (H.R. 5541)
• Behavioral Health Integration in Primary Care - AAFP supports the integration of behavioral health services within a patient’s medical home, which can include consistent coordination of referrals and exchange of information, colocation of services in the primary care setting, or full integration of treatment plans shared between primary care and behavioral health clinicians. AFFP urges Congress to pass legislation to improve the uptake of behavioral health integration models: such as the Collaborate in an Orderly and Cohesive Manner (COCM) Act (H.R. 5218). This bipartisan bill would provide grants to primary care practices covering start-up costs, technical assistance in implementing the Collaborative Care Model, and promote research to identify additional evidence-based models of integrated care. In addition, Congress should pass the Supporting Children’s Mental Health Access Act (H.R. 7076/S. 3864) to reauthorize the Pediatric Mental Health Care Access program for five years and expand it to all states.
• Access to Primary Care in Medicaid - AAFP recommends that Congress increase Medicaid payment rates to at least Medicare levels to ensure timely and equitable access to comprehensive primary care for Medicaid enrollees and to guarantee primary care clinicians have adequate resources to meet their complex needs. Additionally, Congress should ensure CMS enforces existing state reporting requirements and support the implementation of a more robust national access monitoring approach to ensure Medicaid beneficiaries have timely access to primary care. AAFP urges Congress to pass the Kids Access to Primary Care Act (H.R. 1025) and the Ensuring Access to Primary Care for Women and Children Act (S.1833).
CAFP is proud to see all the advocacy work, time, and, dedication our members put into attending FMAS and can’t wait to see our members continue to advocate for issues important to family medicine!
12 California Family Physician Summer 2022
continued on page 14


We Too Believe... Healthcare is a Fundamental Human Right! Join our team! Visit our Careers page at srhealth.org phone: 707.303.3600 ext. 2587
Photos from the 2022 Family Medicine Advocacy Summit




 Pictured: Dr. Tana Parker, Dr. Harnek Singh, Dr. Serena Liu, Dr. Tricia Bautista, Dr. Dylan Hanami, Dr. Fari Valji, and Dr. Samuel Huang at AAFP 2022 Family Medicine Advocacy Summit
Pictured: Tiyesha Watts, CAFP Legislative and Policy Advocate, Dr. Serena Liu, Dr. Fari Valji, Dr. Tricia Bautista, Dr. Harnek Singh, and Dr.Jay Lee at AAFP 2022 Family Medicine Advocacy Summit
CAFP Chapter Delegation at the Nation’s Capital
Pictured: Dr. Samuel Huang, Dr. Tricia Bautista, Dr. Harnek Singh, and Dr. Tana Parker lobbying U.S Representative Young Kim, California’s 39th Congressional District.
Pictured: Dr. Catherine Marks, Dr. Fari Valji, Dr. Dylan Hanami, and Dr. Jay Lee lobbying U.S Representative Michele Park Stele, California’s 48th Congressional district
Pictured: Dr. Tana Parker, Dr. Harnek Singh, Dr. Serena Liu, Dr. Tricia Bautista, Dr. Dylan Hanami, Dr. Fari Valji, and Dr. Samuel Huang at AAFP 2022 Family Medicine Advocacy Summit
Pictured: Tiyesha Watts, CAFP Legislative and Policy Advocate, Dr. Serena Liu, Dr. Fari Valji, Dr. Tricia Bautista, Dr. Harnek Singh, and Dr.Jay Lee at AAFP 2022 Family Medicine Advocacy Summit
CAFP Chapter Delegation at the Nation’s Capital
Pictured: Dr. Samuel Huang, Dr. Tricia Bautista, Dr. Harnek Singh, and Dr. Tana Parker lobbying U.S Representative Young Kim, California’s 39th Congressional District.
Pictured: Dr. Catherine Marks, Dr. Fari Valji, Dr. Dylan Hanami, and Dr. Jay Lee lobbying U.S Representative Michele Park Stele, California’s 48th Congressional district
continued from page 12
County of Santa Cruz Invites You To Apply for the Position of:


Clinic Physician Health Services Agency

• Bilingual (English/Spanish) Candidates Encouraged to Apply
• Salary: $247,333 - 267,488 Annually

• Sign-on incentive pay
• Comprehensive benefits to eligible employees and their dependents
To apply and for more information, visit: www.santacruzcountyjobs.com
You may contact us by phone at (831) 454-2600 or e-mail at personnel@Santacruzcounty.us
California Family Physician
LIVE Here. WORK Here. PLAY Here.
Summer 2022 15
Join our team! Now Recruiting for: Nurse Practitioner: $101,422-$123,606* Physician Assistant: $101,421-$123,605* Primary Care Practitioner: $165,484-$201,680* *These positions will receive an 8% salary increase adjustment effective 7/3/22 •Encounter bonus in additionto basesalary Benefits of Working at Tulare ounty: • Flexible work schedules • Stability •Tuition reimbursement • Vacation • Employee discounts • 13 Paid holidays •Team environment • Retirement • Giving back to the community • Life insurance • Locations throughoutTulare County • Health insurance Apply online at: www.governmentjobs.com/careers/tulare Touro University California COM is looking for Family Medicine or Internists interested in teaching first and second year students on its Vallejo campus as well as delivering patient care. Assistant or associate professor rank, benefits and Northern California lifestyle await you! Contact Gail Feinberg, DO, chair at gfeinber@touro.edu COLLEGE OF OSTEOPATHIC MEDICINE
CAFP Foundation: Another Successful This Time, With More Offerings and More

The CAFP Foundation (CAFP-F) strives to meet the special interests of students and residents, particularly through the work of the CAFP Student-Resident Council (the Council). The Council is a 30-member group, made up of highly engaged medical students and family medicine residents who strategize and implement activities important to/relevant for the future generation of family physicians.
One of these signature activities is the Procedures Workshop. Since 2014, the CAFP-F Procedures Workshop has been designed by California medical students and family medicine residents for medical students and residents. Over the years, the workshops have evolved to include a greater variety of procedures and have grown to welcome more attendees. In 2020, the workshop averaged close to 80 participants, including family medicine residents, first to fourth year medical students and even nursing students.
During the 2020-21 academic year, the Council identified a pressing, priority need for medical students and residents to practice office-based procedures. Since the onset of the COVID-19 pandemic, opportunities to develop these essential skills have been less available/put on hold. Therefore, the goals of the 2022 Procedures Workshop were to 1) introduce medical students to the family medicine specialty through hands-on procedures practice, and 2) remediate missed training/clinical setbacks for procedural practice among FM residents.
The 2022 Procedures Workshop was the first of its kind for the CAFP Foundation - we added an advanced track for residents along with the medical student track. The expanded procedure offerings included: pap, MSK joint injections, POCUS, suturing, IUD insertion/removal, colposcopy, endometrial biopsy, toenail removal, and shave/punch biopsies.
This year’s energetic, half-day event brought in more than 110 participants and 8 procedural sessions, making it the largest Procedures Workshop for the CAFP Foundation. We are hopeful it inspired medical students to pursue family medicine, gain insights into the full-spectrum nature of our field, and build

connections with FM residents and faculty. We are also hopeful that residents further perfected their techniques and gained confidence in common office-based procedures.
We’d like to say a special thanks to the Los Angeles AFP chapter and the AAFP Foundation for providing funding for essential supplies and models necessary to implement this workshop. This equipment will be used for future procedures workshops and will contribute to the sustainability of this legacy project.
We’d also like to recognize two members of the CAFP StudentResident Council for organizing this activity. Drs. Nadine GraceAbraham and Juliana Jones (both rising third year residents at the time of this publication) joined the planning committee when they were medical students. As residents, they continue helping to improve the procedures workshop experience for current and future family physicians.
CAFP Foundation
Pamela Mann, MPH, Executive Director, CAFP Foundation


Successful Procedures Workshop. More Participants




Importance of
Amanda Wallner Deputy Director, Health Access California
in Adults:
Amanda Wallner is currently Deputy Director of Health Access California. She most recently served as Director of Health Access California’s LGBTQ Health and Human Services Network Ms. Wallner talks about the disproportionate impact that trauma—particularly ACEs— has had on the LGBTQ+ community, and the indispensable role that family physicians can have in healing this community through Trauma-Informed Care.
Adverse Childhood Experiences (ACEs) and toxic stress represent a public health crisis that has been, until recently, largely unrecognized by our health care system and society. Appointed as California’s Surgeon General in 2019, Dr. Nadine Burke Harris† had made ACEs education the centerpiece of her agenda. For the last three years, the ACEs Aware campaign educated providers about the role of ACEs in overall health, how to conduct ACEs screenings, and implementing trauma-informed approaches into their daily practice. The California LGBTQ Health and Human Services Network (The Network) is proud to have played an important role in these efforts; specifically uplifting how ACEs impact LGBTQ Californians. The Network, with Cal
Voices launched Out About ACEs in December 2021. This initiative, under the umbrella of ACEs Aware, includes a webpage, videos, social media toolkit, research and other resources to help spread the word about ACEs in the LGBTQ community.
LGB, Transgender, and Questioning adolescents are statistically more likely to have experienced polyvictimization and psychological and/or physical abuse when compared with their straight or cisgender adolescent counterparts. The more ACEs a person has, the higher the cumulative risk of negative health consequences such as poorer self-rated health and life satisfaction, heart disease, lung cancer, diabetes and many autoimmune diseases, as well as depression, violence, being a victim of violence, and suicide.
The LGBTQ+ community is already at an elevated risk for these negative health consequences compared to the general population due to stigma, family rejection, and lack of access to affirming health care. When you take ACEs and their contribution, it's likely that it makes this risk even higher in the LGBTQ+ community. For example, in a quantitative study done by Smith College
 Trauma-Informed
Trauma-Informed
18 California Family Physician Summer 2022
Family Medicine
ACEs
Out about ACEs Together, we can get to the root cause of some of the most harmful, persistent, and expensive health challenges LGBTQ+ people deal with. Make your practice ACEs Aware and take the free, two-hour Becoming ACEs Aware in California Training to ensure LGBTQ+ Californians receive the support and care they deserve. “ “
(https://bit.ly/CFP22smithcollege) on the relationship between gender identity and ACEs, it found that 41.6% of LGB individuals report having 4 or more ACEs compared to 25.3% of straight individuals who reported having 4 or more ACEs.
When a healthcare provider is ACEs Aware and trained in trauma-informed care, they are better able to treat the whole person. The more healthcare providers become ACEs Aware, the more lives improved and saved. Screening for ACEs, assessing for toxic stress, and responding with evidencebased interventions, can significantly improve the health and well-being of LGBTQ+ individuals and families.
Family physicians can use trauma-informed care to help heal the LGBTQ+ community. Trauma-informed approaches can be helpful in treating LGBTQ patients, even if they don’t have a high ACEs score. As the Family Acceptance Project (https:// familyproject.sfsu.edu) points out, LGBTQ people may experience so-called invisible ACEs that aren’t captured on the 10-question screening instrument. Family rejection – everything from avoiding talking about LGBTQ issues to trying to change a child’s sexual orientation or gender identity – is a type of trauma that leads to significantly worse health outcomes for LGBTQ youth. However, we have interventions to work with LGBTQ youth and their families to improve their health now and in the future.
Together, we can get to the root cause of some of the most harmful, persistent, and expensive health challenges LGBTQ+ people deal with. Make your practice ACEs Aware and take the free, two-hour Becoming ACEs Aware in California Training to ensure LGBTQ+ Californians receive the support and care they deserve.
To learn more about Out About ACEs, visit bit.ly/outaboutaces.
† n.b., Dr. Burke-Harris resigned as California Surgeon General effective February 11, 2022
MemorialCare Medical Group Family Medicine Physician Job Opening

MemorialCare Medical Group is an award-winning team of healthcare professionals consisting of over 350 physicians dedicated to providing quality compassionate care to patients in Orange and Los Angeles counties. With multiple locations throughout the Southland, MemorialCare Medical Group offers a broad scope of multi-specialty services including primary care, specialty and ancillary care, laboratory and radiology services. MemorialCare Health System is listed among the top 20 percent of health systems nationwide by Thomson Reuters, one of the top 100 integrated healthcare networks nationwide, and the top 10 in the west region by IMS. In addition to multiple primary care locations throughout Long Beach and Orange County, MemorialCare Medical Group offers Urgent Care Centers that are open 365 days a year, virtual urgent care visits available around the clock; and Lab and X-ray services available onsite at most locations.
· Employed position with MemorialCare Medical Group

· Competitive base salary plus incentives
· 4.5 day workweek
· Outpatient only practice
· Epic EMR system
· Continuing medical education reimbursement fund and reimbursement for license and DEA renewals.
· Generous paid time off (PTO) benefit
· Full and comprehensive benefits for physician and family
· Malpractice insurance provided
· Mentoring program
· Two year shareholder track
Medical Group
To learn more, please contact: Keith Vo, Physician Recruiter Kvo@memorialcare.org careers.memorialcare.org (search: Physician Jobs at MemorialCare)
California Family Physician Summer 2022 19
Make a Difference:
Take Breaks at Work
The science behind the benefits of taking breaks at work is abundant (Seiter 2014). In any profession that is mentally complex, not taking time to recharge can make one less efficient, which can lead to more mistakes. Over time, this can make us less engaged which is one of the hallmarks of burnout (Seiter 2014). In other high-stress occupations like aviation, breaks are mandated. But this approach has not routinely been adopted in medicine. A search of the literature finds few studies on physician breaks.
One study of inpatient physicians found that on average they took 0.8 breaks a day (meaning some physicians never took a break in their day!) (Blasche 2022). Studies of surgeons taking pauses during their surgeries show no change in surgery times and decreases in physical and emotional fatigue (Dorion 2013, Engelmann 2011). A study employing 5-minute breaks every 30 minutes in 2-hour surgeries found a 22% decrease in salivary cortisol levels and significantly decreased intraoperative events and errors (Engelmann 2011). Imagine translating these findings to your clinic day. In any given clinic session, we make hundreds of complex decisions in different clinical scenarios that change every

day. How would we fare if we took scheduled breaks every 30 minutes? If this seems like a ridiculous notion, try starting smaller…try any of the below options for 5-10 minutes once a day. You (and your patients) will notice the difference!
• Take a walk (outside preferably)
• Read (something not work-related)
• 5-minute office yoga (https://youtu.be/6fnLKyRJsrs)
• Doodle/Color (free worksheets at https://www.doodleart-alley.com/free-coloring-pages.html)
• Listen to music
• Nap (even 10 minutes increases cognitive function and decreases fatigue)
• Talk to a friend
• 5-minute meditation (https://youtu.be/ssss7V1_eyA)
References
Blasche, Gerhard, Anna Arlinghaus, and Richard Crevenna. "The impact of rest breaks on subjective fatigue in physicians of the General Hospital of Vienna." Wiener klinische Wochenschrift 134.3 (2022): 156-161.
Dorion, Dominique, and Simon Darveau. "Do micropauses prevent surgeon's fatigue and loss of accuracy associated with prolonged surgery? An experimental prospective study." Journal of Vascular Surgery 57.4 (2013): 1173.
Engelmann, Carsten, Schneider Mischa, Kirschbaum Clemens, et al.. "Effects of intraoperative breaks on mental and somatic operator fatigue: a randomized clinical trial." Surgical endoscopy 25.4 (2011): 1245-1250.
Seiter, C. “The science of taking breaks at work: How to be more productive by changing the way you think about downtime. Retrieved from https://open.buffer.com/ science-taking-breaks-at-work/
Karen Muchowski, MD, FAAFP
20 California Family Physician Summer 2022
Implementing High-Quality Primary Care –
Diane Rittenhouse, MD, MPH, Senior Fellow, Mathematica

A Leadership Opportunity for California
A lot has happened over the past year on the front lines of family medicine, across the nation and around the globe. So, it is completely understandable if you missed the 2021 release of the National Academies of Sciences, Engineering, and Medicine (NASEM)’s report Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care1 Here I will briefly recap the contents of the report and highlight the significance of the report to California family physicians.
Implementing High-Quality Primary Care is the first NASEM consensus study report on primary care in 25 years. It is the culmination of two years of work by a special 20-member NASEM committee that was co-chaired by a family physician, included three California representatives, and was sponsored in part by the American Academy of Family Physicians and Blue Shield of California. The 400-page report takes a comprehensive view of primary care policy, addressing topics such as payment, accessibility, education and training, information technology, measurement, and research. The report also calls for specific actions, including leadership and accountability, on the part of many partners at multiple levels within the health care system. An implementation plan includes five plain language objectives to make high-quality primary care available for everyone in the United States:
1. Pay for primary care teams to care for people, not doctors to deliver services.
2. Ensure that high-quality primary care is available to every individual and family in every community.
3. Train primary care teams where people live and work.
4. Design information technology that serves the patient, family, and interprofessional care team.
5. Ensure that high-quality primary care is implemented in the United States.
So why does this report matter to California’s family physicians?
First, the report provides an updated consensus-driven definition, context, and vision for primary care in the United States, issued by a highly respected, high-profile national scientific body. This allows for alignment of efforts – public and private, state, and federal, purchasers, payers and providers. Second, California has not achieved any of the objectives outlined in the report – so there is much work to be done. Third, the report has led to new federal leadership such as the Initiative to Strengthen Primary Health Care2 launched by the U.S. Office of the Assistant Secretary for Health in September 2021, and increased accountability such as the new Health of U.S.
Primary Care Scorecard3 launched by Milbank Memorial Fund, The Physicians Foundation, and the Robert Graham Center in January 2022, that can assist California in its efforts. Fourth, and perhaps most important, the report provides for California a vision of primary care as a common good– and I believe California is poised to lead the nation in realizing this vision – not for primary care’s sake, but for the sake of equitable health outcomes for over 39 million Californians.
“Primary care is the only health care component where an increased supply is associated with better population health and more equitable outcomes. For this reason, primary care is a common good, making the strength and quality of the country’s primary care services a public concern.”
As California family physicians we can sometimes feel like Sisyphus eternally rolling the boulder uphill. But I believe a) we are not alone; and b) this moment is different. Take a look at the recent efforts by the California Health Care Foundation4, the Purchaser’s Business Group on Health5, and Blue Shield of California6 to see that other powerful players are working alongside us to promote high-quality primary care for all Californians. Leaders at the new California state Department of Health Care Access and Information, the Department of Health Care Services, the California Public Employees Retirement System, and Covered California are all investing in primary care. With improved coordination, leadership, and accountability –and with family physicians playing important roles in health care delivery and policy — I am optimistic that California can lead the country in realizing the vision of Implementing High-Quality Primary Care: Rebuilding the Foundation of Health Care.
1https://www.nationalacademies.org/our-work/implementing-high-qualityprimary-care
2https://www.hhs.gov/about/news/2022/06/27/fact-sheet-hhsinitiative-to-strengthen-primary-health-care-seeking-public-comment.
html#:~:text=The%20HHS%20Initiative%20to%20Strengthen,practice%20 of%20primary%20health%20care
3https://www.milbank.org/news/milbank-memorial-fund-collaborates-withthe-physicians-foundation-and-robert-graham-center-on-new-us-primarycare-scorecard/
4https://www.chcf.org/resource/primary-care-matters/
5https://www.pbgh.org/initiative/advanced-primary-care/
6https://news.blueshieldca.com/to-strengthen-primary-care-blue-shield-ofcalifornia-joins-milbank-memorial-fund-and-bluepath-health-to-improvepayments
California Family Physician Summer 2022 21
Karen Muchowski, MD, FAAFP

Female Physicians Experience More Burnout
Being a family physician can be an amazingly rewarding profession. We establish connections with patients and allow them to make changes in their lives that can have a dramatic impact on their well-being. But it can also be draining, empty our empathy buckets and sometimes make us wonder, did we choose the right career? Although rates of burnout are high for all physicians, there is data to show that female physicians (including family physicians) have higher rates of burnout than do male physicians (Willard-Grace 2019, Eden 2020). It is a complex picture, with many things competing for our time likely playing a role (taking care of children, family members, work demands, lack of self-care). I have often described myself as an octopus that needs more than 8 arms to do all I am supposed to do. Yet male physicians have work-balance issues as well…why are burnout rates higher in women? The below studies answer part of that question.
Female physicians spend more time with patients per patent encounter, but we generate equal revenue (meaning, we are not billing for our time). (Ganguli 2020, Jefferson 2013)
Female physicians spend up to 30% more time in the Electronic Health Record (EHR)(Rittenberg 2022, Tait 2021). Tait et al showed that this extra time equaled an added three 40-hour work weeks a year!!! And there was NO difference in patient satisfaction scores, or the number of health records closed by the end of the day.
Is burnout a systemic issue? Yes, all the way from how our clinics are structured, the use of EHR for documentation to how
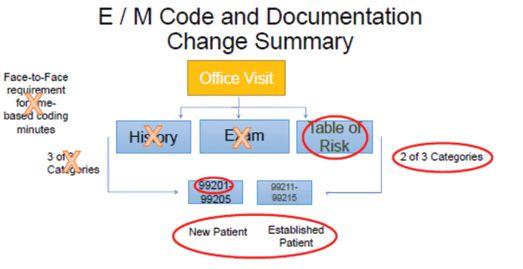
2021 E/M Code Documentation Changes
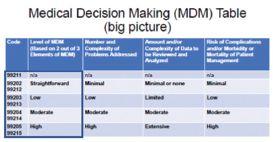
we are paid as a profession. Are there cultural and societal forces at play that make it harder for women to set work/ life boundaries? Certainly. But are there things we can do as individuals that could help us increase the time we spend outside of work? Absolutely.
If the excessive amount of time you spend with the EHR is one of the reasons you are tired, take a look at these resources on how to decrease your time with the electronic beast.
“Increasing Physician Efficiency: Eliminating the WAC” presentation in CAFP’s Homeroom – education.familydocs.org
Ten EHR Strategies for Efficient Documentation, https://www. aafp.org/pubs/fpm/issues/2020/0700/p5.html
Follow a “super user” in your clinic/group and have them show you why they are more efficient.
If you spend more time with patients, then bill for it. The 2021 E/M Code documentation changes in billing make this much easier.

Obviously, this is a topic that cannot be fully addressed in a small article and the causes of burnout in male and female physicians are multiple. But I am hoping that these few resources will help.
Finally, be kind to yourself. Remember that the work that you do is impactful and worth continuing.
Resources
Eden, Aimee R., et al. "Burnout among family physicians by gender and age." The Journal of the American Board of Family Medicine 33.3 (2020): 355-356.
Ganguli, Ishani, et al. "Physician work hours and the gender pay gap—evidence from primary care." New England Journal of Medicine 383.14 (2020): 1349-1357.
Jefferson, Laura, et al. "Effect of physicians’ gender on communication and consultation length: a systematic review and meta-analysis." Journal of health services research & policy 18.4 (2013): 242-248.
Rittenberg, Eve, Jeffrey B. Liebman, and Kathryn M. Rexrode. "Primary care physician gender and electronic health record workload." Journal of General Internal Medicine (2022): 1-7.
Tait, Sarah D., et al. "Electronic health record use by sex among physicians in an academic health care system." JAMA Internal Medicine 181.2 (2021): 288-290.
Willard-Grace, Rachel, et al. "Burnout and health care workforce turnover." The Annals of Family Medicine 17.1 (2019): 36-41.
Winner, Jay. "Ten EHR strategies for efficient documentation." Family Practice Management 27.4 (2020): 5-10.
22 California Family Physician Summer 2022
An Interview with your new President, Lauren Simon, MD, MPH, FAAFP


Why family medicine for you? Who were the role models who inspired you to go into family medicine?
One of my physician role models was my father. Some of my earliest recollections were my dad caring for people in our community in his Family Medicine clinic that was located in our basement. We lived on the end of a block of row houses so we had an additional entrance to the basement where the patients would enter the clinic. Many of the patients could not afford health care and my dad would see them without charge, always treating each patient with immense respect. He told me often that “everyone deserves care.” That was my introduction to what we currently refer to as social determinants of health. My siblings and I loved running down the stairs to greet the patients. Sometimes the patients brought us delicious homemade soup and bread. As I grew up, I found out that often the food was the patients’ unsolicited way of “paying” for the care or saying thank you. I also thought it was great that my dad cared for entire families in one space.
What piqued your interest in becoming active with your county and state AFP chapters?
I did an elective rotation with a local Family Physician named Dr. Ron Bangasser who was very involved in organized medicine and volunteered doing sports medicine in the community and he inspired me to get involved in CAFP. He also had done work in “undersea” medicine for the military and was a scuba instructor who taught me and fellow residents and faculty to scuba dive. When I went to a CAFP sponsored resident event I met two incredibly dynamic women: CAFP’s then Deputy EVP Shelly Rodrigues and Dr. Mary Frank (AAFP’s first female President who is from our great state of California) and I knew that I wanted to be actively involved in CAFP. Shelly told me about CAFP residents’ council which I really enjoyed, and I was elected president of the council and that is where my path to CAFP leadership began. I, like so many of my colleagues in CAFP leadership, got involved when someone told us about how great an organization CAFP is and how we could get engaged in the Academy and pursue our varied interests on CAFP committees and projects and make a difference. In turn, I am encouraging you to also get actively involved in your local chapter and our California chapter and be inspired.
Is now the best time ever to be a family physician, in your estimation?
From a service perspective, now is the best time to be a Family Physician as there is so much need in our communities for people of all ages to get access to holistic, compassionate medical care provided by our well-trained Family physicians, who have a strong fund of medical knowledge and are versatile and can provide that care through both in-person and virtual settings.
What are the most important challenges confronting CAFP?
One of the most important challenges facing CAFP involves advocacy at the state and Federal level. As our elected government and appointed judges make decisions which directly affect our patients’ lives and interfere with health care choices which should be made by physician- patient shared medical decision making, and not by government, or legislate items which increase physician administrative burden and/ or cost CAFP will continue to review legislation for items that may affect our physicians and patients and advocate with government on these issues and advocate for legislation for issues that come from our membership.
Another challenge for CAFP encompasses funding and
California Family Physician Summer 2022 23
continued on page 24
continued from page 23
provision of continuous medical education for our members.
Opportunities for nonprofit organizations to get grant funding for education has drastically decreased. CAFP has a broad generational
spectrum of learners who have different learning preferences such as in-person or various virtual formats and choice of where to obtain CME. Finding optimal formats for educational offerings for our members and sustainable funding sources for these projects as we move forward is a challenge which CAFP is actively addressing.
What has been the best part of being an officer in CAFP so far?
So far, the best part of being an officer for CAFP is being part of the “family” of Family Medicine leaders. I have learned a great deal of experiential and procedural knowledge from other CAFP and AAFP leaders and staff to help me guide our Board of Directors and serve our members. My fellow leaders share their wisdom, emotional support, constructive thoughts, and love of family medicine with me and each other and it truly feels like a family.
How do you maintain what former President Jay Lee calls “the joy” of family medicine?


I maintain the joy of family medicine by listening to my patients and learning from each of them. Each day I treasure the “stories” that my patients share of their lives: the successes, the challenges, the decisions they are pondering, the family relationships they have, whether functional or dysfunctional, and the dreams they have for their future. We, as family physicians, have the most incredible privilege to listen to our patients share the most intimate details of their lives with us and the awesome responsibility to be good stewards of that information and provide whole-person care.
How do you maintain work-life balance?
I have an incredibly supportive husband and children who help me maintain work-life balance. I enjoy exercising as a
family and individually, and attending the variety of school and extracurricular athletic, musical, religious, and scouting events that my family is involved with. Also, volunteering in my community recharges my energy.
What do you see as the best ways CAFP can help its members maintain the joy?
CAFP provides opportunities to encourage and promote one’s passion. CAFP provides additional opportunities for in-person events that are hybrids of social interaction and advocacy/ educational purposes.
Where will family medicine be in 10 years and what role will CAFP have played in it?
In ten years, there will be a lot more artificial intelligence being used to provide or augment patient care and more outcomesbased care. CAFP will provide resources and training along the way to keep our members current on technologic advances and medical advances to help us care for patients.
There will also be more focus on advocacy and CAFP will be prominently engaged in that from our headquarters in Sacramento near the state Capitol and with our members’ local advocacy throughout the state.

There will be even more Family Medicine residency training programs in California and our CAFP and CAFP Foundation will have assisted those residents in their training programs and in their transition to their desired practice.
What is your message to the next generation of family physicians – what will sustain them?
Find your passion both in Family Medicine and your personal life. Surround yourself with others who share your passion. Cultivate and nurture the personal relationships that will sustain you and help you grow.
Finally, what is one fun thing that CAFP members should know about you?
I was a Geology major in college and did my field research in the New England States which was an amazing experience stepping back in time through the lens of the rock record. I still really like to look at rock strata. If you are traveling with me, perhaps to visit our local CAFP chapters throughout the state, be prepared, I may pull over to explore a roadcut and look for historical clues in the rock record or search for fossils!
24 California Family Physician Summer 2022
Interview with Jasmeet Bains, MD,

Family Physician and Candidate for Assembly District 35
What inspired you to become a family physician?
Being a doctor was not something I ever imagined possible for myself. I grew up in Delano, California, a very rural area of the Central Valley. Access to health care has always been a struggle here. I witnessed it as a child. Not just access to care but access to social services and after school activities were very limited. It was this lack of health care access that inspired me to become a doctor and return to my hometown to provide health care. Every day I work it reminds me of the importance of this commitment. Times might have changed from when I was a child, but one thing is for sure, health care access was a struggle when I was growing and still is and in a lot of ways even harder now as the population has grown.
Can you tell us how you think by being a physician you may have a unique perspective on issues that aren’t traditionally thought of as health care issues, like social justice, police reform and education?
I see things through the eyes of a physician, this will never change as I spent a good portion of my life being educated and trained to become a doctor. The training of a doctor is not easy, you are forged into being a critical and fast thinker. And especially as a family medicine physician we are trained to be not only fast but in a way that takes the entire picture into account. The uniqueness of the training of a family Doctor is understand communities and what affects them. This is why family doctors make excellent leaders because we have developed a unique set of critical thinking skills that takes total pictures of the community, not just the patient in front of us. We are thinking how did that get here, who is here with them, what is their home environment like and how is that affecting their health?
A lot of physicians do not feel that they have time to get involved in the political process, or that “politics is dirty business.” What is your message to them?
Politics is what we allow it to be, stop voting for politicians who you believe are not sincere and support those that are. Everything comes down to our actions. We can either complain about how we are treated, or we can choose to change it or support those that can. It’s in our hands. Physician organizations are key to this.
If you’re elected, will you continue to practice medicine while in office?
Yes, I will continue practicing while in office, I have to as it is what gives me perspective onto things we need to change. I can’t lose that.
What is your advice to a physician who is thinking about running for office?
Running for office can seem daunting, but it's necessary. If we want change, we have to demand it and that will only happen if we seize the moment and either run or work hard to support those that are running. California has never had a Family Doctor in office and yet it is looked to as the state that is going to revolutionize healthcare for the country, we HAVE to be at the table when it comes to defining and cultivating our primary care healthcare.
What is the best way for family physicians to reach out to you if they are interested in connecting?

Send me an email at: info@drjasmeeetbains.com or follow me on SM at Dr Jasmeet Bains for State Assembly on FB, twitter, or instagram.
The Addiction Medicine Fellowship at Ventura County Medical Center is currently recruiting for an additional fellow. This ACGME accredited fellowship is located in the coastal city of Ventura, CA. Learn full spectrum ADM from some of the best in the field!

Contact Dr. Tipu Khan for more details: tipu.khan@ventura.org
https://www.venturafamilymed.org/addictionmedicine-fellowship
Dr. Bains needs your support. Donate to support her campaign at bit.ly/3RmRObg or scan the QR code.
California Family Physician Summer 2022 25
the
CAFP Welcomes New District II and IX Directors
Congratulations to Jorge Galdamez, MD (District II, Orange County, second term) and Lalita Abhyankar, MD (District IX, Humbolt, Del Norte, Mendocino, Lake, Marin, Napa, San Francisco, Solano and Sonoma counties) who were recently elected to serve on CAFP’s Board of Directors.
seen mountains move at the state level and know that there is more to do as we collectively advocate for our patients, our physicians, and our state.”
Health, a clinical start up focused on using technology to improve access to high quality patient care. Her personal mission is to ensure that we are creating a robust environment for family medicine to thrive by building and using the tools that we need with the end goal of improving the health and well-being of our patients and communities.”
Congratulations Drs. Galdamez, Abhyankar, Nguyen, and Lossy. Thank you for your commitment to serve!
Jorge Galdamez, MD was recently elected to a second term as District II Director on the CAFP Board. He describes his journey to state leadership in this way, “Inside the exam room, I feel that I can do anything for my patients. It is here where conversation, treatment plans, and better health begins. At least, that is what I felt when I first started practice. Then came the realization that there is more to it than that. Once my patient leaves the room, I knew that anything could happen, and it is out of my control. That feeling that I could not do anything outside the room led me to pursue leadership and to advocate for my patients outside the exam room, initially as a leader within my clinic, then my medical group, and for the past 10 years, within CAFP. I have
A recent transplant to California from New York, Lalita Abhyankar, MD, is excited to be an active member of the CAFP. In her previous roles, she was a family physician at an FQHC in Brooklyn, NY, worked with the NYAFP as a Board Member and Chair of the Advocacy Commission and was deeply involved in the academy’s strategic planning and development. “My interests include storytelling (especially on behalf of family physicians), improving and innovating technology to support primary care, and education of the next generation of family docs! I recently produced, scripted, and hosted a six-episode podcast series for Health Affairs, the health policy journal, on how market consolidation is affecting independent primary care practices and am a contributing author to the AAFP Fresh Perspectives Blog.”
Dr. Anhyankar currently works as a Clinician Manager for Carbon

Duy Nguyen, MD, Immediate Past President of the Orange chapter was elected to serve as District II Alternate.

Panna Lossy, MD, President of the North Bay chapter, was elected to serve as District IX Alternate.


26 California Family Physician Summer 2022
In
News
Vista Community Clinic has outstanding opportunities for Full-Time and Part-Time Physicians. We are looking for dedicated, motivated and enthusiastic team players who want to make a difference in the community.
Vista Community Clinic is a federally qualified, not-for-profit healthcare clinic with more than 800 employees and nine state-of-the-art clinics treating more than 69,000 patients every year. We provide healthcare throughout the Southern California regions of North San Diego, Orange and Riverside Counties.

Our compensation and benefits program includes: Competitive compensation, sign-on bonus, relocation bonus, health, dental, vision, company-paid life, long-term disability, flexible spending accounts, 403(b) retirement plan, malpractice coverage, NHSC loan repayment eligible organization, CME allowance, and no on-call hours

For more information visit www.vcc.org or email hr@vcc.org EEO/AA/M/F/Vet/Disabled
years
www.naspcc.org

Join a team that’s been helping to redefine what it means to be a community clinic for 50 years.
50
1972-2022
Help Your Patients Make Better Informed Decisions About Their Care The California Prostate Cancer Coalition, founded in 1997 as a 501(c)(3) not-for-profit organization, is dedicated to savings men’s lives www.prostatecalif.org https://naspcc.org/docs/informed-decision-9-11-17.pdf
To find out how contact... SINCE 1993 REACH THOUSANDS OF MEDICAL PROFESSIONALS EVERY QUARTER MICHELLE GILBERT 501-725-3561 mgilbert @pcipublishing.com
CAFP Members Receive State and National Recognition
Congratulations Dr. Monica Hahn on Receiving AAFP’s 2022 Public Health Award
The AAFP Board of Directors has selected Monica Hahn, MD as the recipient of the 2022 AAFP Public Health Award. This award was developed to recognize individuals who have made or are making extraordinary contributions to the health of the American public. Congratulations on this great honor.

Dr. Hahn is a physician, researcher, and champion of familycentered HIV primary and perinatal care. She demonstrates incredible compassion and evidence-based knowledge to carry the torch for the next generation of family physicians and public health leaders. Her passion for advancing social justice and health equity is exemplified by her leadership of the Pacific AIDS Education and Training Center (PAETC). By serving as co-principal investigator and clinical director, Dr. Hahn has led PAETC to adopt an anti-oppression and antiracism framework in the center’s HIV programming and curricular materials. Family medicine and other health providers caring for patients with HIV would gain valuable insight into helping patients living with HIV by adopting materials you have led the creation of, including your “Practicing Antiracism: A Curriculum for the HIV Workforce.”
Alex McDonald, MD Awarded 2022 Immunization Champion
Congratulations Alex McDonald, MD on being selected as the 2022 Association of Immunization Manager’s (AIM) Immunization Champion for California, by the California Department of Public Health (CDPH). Robert Schechter, MD, MPH, Chief, Immunizations Branch, CDPH said, “For your contributions to public health in promoting COVID-19 immunization, the California Department of Public Health Immunization Branch is proud to announce that you have been selected as the 2022 Association of Immunization Manager’s (AIM) Immunization Champion for California. Your selection comes from a pool of health professionals, community advocates, and other immunization leaders. We are honored to present you with this well-deserved award.”
For more information on the award please visit: https://eziz.org.
AAFP Program of Excellence Award Winners 2022
The American Academy of Family Physicians has named 14 family medicine interest groups (FMIGs) as the 2022 Program of Excellence Award winners for their exemplary efforts generating interest in family medicine. The University of California Irvine School of Medicine Family Medicine Interest Group is among those recognized. During the recent AAFP National Conference of Family Medicine Residents and Medical Students awards were presented. Congratulations UC Irvine, University of California, Riverside Family and Preventative Medicine Interest Group, and University of Southern California Keck School of Medicine.
28 California Family Physician Summer 2022





I n this one-day diabetes symposium the learners will gain key skills and insights to take to their practice immediately. Topics include the use of continuous glucose monitoring, the gut microbiome, and patientcentered language and approaches. Join national experts in person or virtually. Approved for 7.25 AAFP Prescribed Credits, AMA PRA, and AOA 1-A. SUNDAY | 11.06.22 | FAIRFIELD, CA | HYBRID | http://www.eeds.com/live/148518 Buzzed. Busted. Broke. Get caught, and you could be paying around $10,000 in fines, legal fees and increased insurance rates. YOU JUST BLEW $10,000. buzzeddriving.adcouncil.org Buzzed driving is drunk driving. S:4.625” S:10”
Incorporating Lifestyle Medicine Into Everyday Practice

Free Lifestyle Medicine Resources for Physicians

Read The Journal of Family Practice’s A Family Physician’s Introduction to Lifestyle Medicine supplement.

Use the American Academy of Family Physicans’ Lifestyle Medicine Toolkit.


Prescribe free plant slanted nutrition programs available online on demand.
Access these and more resources at: ardmoreinstituteofhealth.org/resources

A leader and innovator in the future of health care
Adult & Family Medicine Physician Opportunities
Northern & Central California - Ask us about our enhanced compensation!

The Permanente Medical Group, Inc. (TPMG) has a longstanding reputation for progress and quality service that not only o ers you the stability you need for a fulfilling career, but also the freedom to explore innovative ideas. We invite you to join our over 9,000 physicians at one of our 22 medical centers or numerous clinics throughout Northern and Central California and become part of our 75-year tradition.
When you join Kaiser Permanente in Northern or Central California, you'll enjoy the best of both big city and small town amenities. Our locations o er family-oriented communities, spacious parks, tree-lined streets, excellent schools, great shopping, outstanding restaurants, and a multitude of cultural activities. You’ll also enjoy nearby destinations such as the Napa Valley wine country, San Francisco, Lake Tahoe, and the stunning shoreline of the Pacific Coast.
To learn more and to apply, please visit: tpmg.permanente.org/careers
FAMILY MEDICINE: Contact Bianca Canales at: Bianca.Canales@kp.org or 510-421-2183
INTERNAL MEDICINE: Contact Harjit Singh at: Harjit.X.Singh@kp.org or 510-295-7857
Ask us about our enhanced compensation for AFM Physicians!
CONNECT WITH US:
We
A FEW REASONS TO PRACTICE WITH TPMG:
• Work-life balance focused practice, including flexible schedules and unmatched practice support.
• We can focus on providing excellent patient care without managing overhead and billing. No RVUs.
• We demonstrate our commitment to a culture of equity, inclusion, and diversity by hiring physicians that reflect and celebrate the diversity of people and cultures.

• Amazing benefits package, including comprehensive medical and dental, moving allowance and home loan assistance (up to $200,000 - approval required), and more!
$200,000-$325,000
LOAN PROGRAM
(based on location and experience)
Available exclusively to Internal Medicine and Family Medicine Physicians, the Forgivable Loan Program is just one of many incentives we o er in exchange for our Primary care Physician’s dedication and expertise.
are an EOE/AA/M/F/D/V Employer. VEVRAA Federal Contractor.
FORGIVABLE
Ever y physician deserves to be insured by a company like MIEC.
As a reciprocal exchange, MIEC is entirely owned by the policyholders we protect. Our mission to protect physicians and the practice of medicine has guided us over the past 47 years. Our Patient Safety and Risk Management team continues to provide policyholders timely resources and expert advice to improve patient safety and reduce risk. To learn more about the benefits of being an MIEC policyholder, or to apply, visit miec.com or call 800.227.4527.
Presorted Standard U.S. POSTAGE PAID Fayetteville, AR Permit No. 986 CALIFORNIA ACADEMY OF FAMILY PHYSICIANS 816 21st Street Sacramento, California 95811 Insurance by physicians, for physicians.™ miec.com | 800.227.4527 Get a quote today.
Medical Malpractice coverage for individuals, groups and facilities. Acupuncture, Psychiatry, and other specialty coverages available.
miec_2022_CAFP_bleed.pdf 1 4/15/22 10:52 AM
