


























The magazine industry continues to go through significant changes as the industry transitions from print to digital over the past few years with readers, paid subscribers, and online formats all shifting. These shifts, driven by technological advancements, changes in consumer behavior, and the evolving media landscape, also required Cal Broker to adapt.
Our number one focus is to continue to enable life and health insurance professionals' access to the resources and connections they need to provide solutions for their clients.
Over the past 12 months, California Broker magazine made the move to a digital media company. We provide a growing number of digital tools and products, and offer our readers, authors, and advertisers, new tools and tips with immediate access through this new digital experience.
The Cal Broker team is focused on ways to enhance the reader’s ability to connect with our authors and advertisers.
The digital capabilities enable us to provide the most current industry related News and industry events to our subscribers. In 2025, our eCalendar will include more events, access to more recordings of key webinars, and links to access a range of content covering the key topics our readers must have. California licensed professionals will have one location to find CA solutions and CA resources they can use to help their CA life and health insurance clients.
Our goal is to provide quality content and attract support from advertisers looking to reach YOU, their “target” audience with tips and tools to help our 255,000 subscribers.
Since 1981, soon to be 44 years running, we continue to remain committed to our Mission. For our continuous improvement we would like your feedback.
Please be on the lookout for upcoming emails with survey feedback.
We look forward to helping you in the same way you have enjoyed our content, AND in new Digital ways as well.
•Balance of Special Issues and Short Snackable Content.
For 2025 we plan to offer more content in new formats. With the rise of mobile and on-the-go reading, we will tailor our content to be more concise, visually driven, and accessible for fast consumption. Many readers love short marketing emails with valuable resources and solid offers for subscribers.
A few changes under consideration--
•Our eNewsletters will be three times a month and have varied content. Industry News, Partner Resource Education, and both our eCalender and eDirectory.
•More recorded/Video content.
We plan to feature our partner’s content in several of our media tools.
•S avvy and Seasoned
Some of the best ideas come from seasoned professionals. This information will impact your career journey. Learn from industry subject matter experts and benefit from their sage wisdom available on our website and in select newsletters.
You are a valuable subscriber and as part of our 255,000 CA life and health licensed insurance professionals, we appreciate you.
Our digital media company, Cal Broker Media, continues to be the leading industry resource for CA brokers.
Thank You!
Cal Broker’s commitment is to be the leading source of news and information for California brokers and agents operating in the health, life, and annuity industry. We are committed to connecting Life and Health insurance professionals to valuable resources and solutions they can provide to their insurance clients.
Tracking Trends and Making Plans
Our digital media company, Cal Broker Media, continues to be the leading industry resource for CA brokers.
By Phil Calhoun
Health & Wellness in the Holiday Season
The holidays are on their way, and it’s no secret that eating healthily during these times can be difficult! Here are two California voices which provide some tips, tricks, and food options that will be helpful during the holiday season.
By Emma Peters
Six Considerations Before Selling Your Business
In our ten years of helping health brokers with commission planning, it is clear that seller’s remorse is real. This article covers SIX key reasons and signs to consider before selling your business.
By Phil Calhoun & David Ethington

The Cost of Waiting: A Personal Long-Term Care Story
Long-term care insurance (LTCi) isn’t just a financial tool—it’s a way to safeguard families from the emotional, physical, and financial toll of caregiving. Learn from this author’s personal experience which unfolded within their own family that caused them to truly grasp the human cost of delaying these crucial decisions.
By Marc Glickman FSA, CLTC, LTCP
Long-Term Care Insurance Equals Family Care
LTC is about protecting those we love from the physical, emotional and financial consequences they’ll face when a parent or loved one needs help. It’s important that caregivers understand the costs (financial, social, physical, psychological), because it’s never too early to plan for long term care.
By Diane Stoddart
First, Seek to Understand Long Term Care
For this article focuses on how long-term care coverage is and how insurance can help alleviate funding concerns by providing financial support for extended care services. By learning about the ins and outs of longterm care insurance, you’ll help your clients effectively plan for their future health needs.
By Gretchen Barry
26
What Happens if an Insurance Company Goes Out of Business? What happens if an insurance company is liquidated? Learn more from this author on how the liquidation of insurance companies is an incredibly rare phenomenon.
By Phyllis Shelton
28 BUDDY INSURANCE
The Hybrid Life Insurance with LTC Connection: A Valuable Benefit for Women
Working women face multiple responsibilities, including employment and caregiving challenges, while juggling various responsibilities. Learn why the dual-benefit option can be extremely beneficial for women and ease their families’ financial burdens.
By Wendy Boglioli
30 HEALTH & WELLNESS
Nutrition As We Age
From hormone fluctuations and metabolic shifts to skin and hair color changes, our body’s needs evolve over time. In this article we will review the main dietary areas of concern for aging and what we can focus on in our meals and snacks to maximize health in our older years.
By Megan Wroe, MS, RD, CNE, CLEC
32 LTCi
Long-Term Care Insurance Costs
As the aging population increases, you will likely see an uptick in long-term care needs for your clients. Knowing the average costs of long-term care can help you prepare your clients and choose the right long-term care insurance coverage for them as they enter their golden years.
By CalBroker Mag

34
LTCi
Long-Term Care Insurance Coverage
Insurance coverage for long-term care alleviates these concerns by providing financial support for extended care services. This insurance can give policyholders peace of mind and safeguard their financial futures. By learning about the ins and outs of longterm care insurance, you’ll help your clients effectively plan for their future health needs.
By CalBroker Mag
36
LTCi
Long-Term Care Insurance & Medi-Cal
Medi-Cal offers many benefits for Californians who need long-term care. However, residents must meet strict eligibility criteria and contribute a portion of their income. By understanding the relationship between MediCal and long-term care expenses, you can help your clients make strategic decisions about their financial and medical futures.
By CalBroker Mag
38
LTCi
Are your clients prepared for the “Silver Tsunami”?
Discussing future long-term care health needs and aging with Baby Boomers is tough. Yet, it’s important to have those delicate conversations about future care plans so you, your clients, and the people you love can live life on their own terms with significant difference in your cancer risk. Learn some topics to discuss with your clients so they’re fully prepared.
By Marcia Israel
Custodial & Skilled Care: What Medicare Pays
Medicare provides health coverage for more than 65 million Americans. Medicare, however, will only pay for short-term skilled nursing care. Read this article to consider certain medical situations to help your clients.
By Jennifer Turner
42
LTCi
The Case for a New Retirement Planning Model: The Missing 4th Phase
As retirees aged into the stage of life where they began to need some assistance and support, their best-laid ‘retirement plan’ was inadequate. Learn from this author’s retirement model which has more than a 3-phase model for retirement or wealth planning.
By Jon Thomas
Interview with Author Carroll Golden on: How Not to Pull Your Life Apart: Caregiving
Carroll S. Golden’s three simple steps in her newest book, How Not to Pull Your Life Apart: Caregiving, kickstarts critical conversations. In the following interview, we ask the author about the best ways to uncover a financially stable plan for you, your family, the people you love, and clients that are more likely than not going to deal with these issues at some point in their lives.
By Emma Peters

‘Tis the Season to Talk About Your Value During Holiday Social Gatherings
Let’s say you’re at a holiday party or other social event and someone asks, “What do you do?” How do you respond? Do you whip out your best elevator speech? Learn about how to best communicate your value at social events from this article.
By Bill Cates
PUBLISHER Phil Calhoun
Health Broker Publishing, LLC publisher@calbrokermag.com
PRODUCTION DIRECTOR Zulma Mazariegos Zulma@calbrokermag.com
DIGITAL DIRECTOR Carmen Ponce Carmen@calbrokermag.com
EDITOR ASSISTANT Emma Peters Emma@calbrokermag.com
CIRCULATION
zulma@calbrokermag.com
120,000 subscribers 12,000 monthly website visits
ADVERTISING
Health Broker Publishing 14771 Plaza Drive Suite C Tustin, CA 92780 714-664-0311
publisher@calbrokermag.com
publisher@calbrokermag.com
Subscriptions: U.S.: $15/issue Send change of address notification at least 20 days prior to effective date; include old/new address to:
Health Broker Publishing 14771 Plaza Drive Suite C • Tustin, CA 92780 714-664-0311
©2024 by Health Broker Publishing. All rights reserved. No part of this publication should be reproduced without consent of the publisher.
Patient advocates can help explain complex medical jargon, assist with billing, or even book appointments. Seniors living alone or juggling information about several conditions may find these advocates particularly useful. Learn more about patient advocates, their role within the health care system, and how they can help you navigate it.
In this article:
• What is a patient advocate?
• How do medical advocates support patient health?
• How can I get in contact with a patient advocate?
• What is a patient advocate?
The patient advocate definition changes depending on what is needed by the patient. Patient advocates generally answer health questions, educate patients and family members, and offer support according to the medical needs of the patient, as outlined by the University of Rochester Medical Center — Health Encyclopedia.
A patient advocate is also known as the following:
• Medical advocate
• Health advocate
• Ombudsman
• Patient liaison
• Care or case manager
Patient advocates don’t provide medical advice on their own, although sometimes physicians or nurses act as patient advocates and then provide medical advice. Generally, advocates help you to get the right advice from medical practitioners and understand it. Then, they help you manage the recommended care. Some patient advocates work as independent contractors or volunteers, while others are hospital or insurance employees.
How do medical advocates support senior health?
For aging seniors or busy caregivers, the reasons to consider working with a patient advocate are compelling.
READ FULL ARTICLE » https://bit.ly/3BJ1bPM
Long-term care (LTC) insurance primarily pays for supervision or assistance with everyday tasks (such as bathing or dressing) when you have a physical impairment or need supervision of these activities when you have a cognitive impairment such as dementia caused by Alzheimer’s disease. LTC takes place at home, in a community program, in an assisted living facility (ALF) or in a nursing home. LTC services are often provided by family members or nurses’ aides, and do not require the skilled care that nurses and doctors are licensed to provide.
LTC insurance benefits may be part of a life insurance or annuity policy or contained in a freestanding LTC policy.
More than 13,000 caregivers have enhanced or expanded their skills and confidence with CalGrows courses; Millions of dollars in incentives are available through August 30
Sacramento – California faces a looming shortage of caregivers for older adults and adults with disabilities over the next five to 10 years. The California Department of Aging (CDA) has committed to helping close the gap through the CalGrows direct care workforce training and career development program. CalGrows encourages, supports, and incentivizes home and community-based services (HCBS) caregivers. To date, more than 13,000 caregivers across the state have participated in more than 89,000 training courses, and qualified applicants have collected over $7 million in incentive payments.
READ FULL ARTICLE » https://bit.ly/3YxFIm8

By Don Thompson
SACRAMENTO — California Gov. Gavin Newsom will soon decide whether the most populous U.S. state will join 25 others in regulating the middlemen known as pharmacy benefit managers, or PBMs, whom many policymakers blame for the soaring cost of prescription drugs.
PBMs have been under fire for years for alleged profiteering and anticompetitive conduct, but efforts to regulate the industry at the federal level have stalled in Congress.
READ FULL ARTICLE » https://bit.ly/4hsZd6T

CMS and Medicare explain LTC and what Medicare beneficiaries can expect. Key take away is that none of the Medicare insurance or MAPD plans cover beyond what CAM and Medicare outline in this brochure.
READ FULL ARTICLE » https://search.app/uaL7VUSJymLonKGz6
By Jordan Rau
Video by Hannah Norman
Finding a nursing home for yourself or a parent can be daunting. Many facilities are understaffed, and the worker shortages have gotten worse since the start of the pandemic. KFF Health News senior correspondent Jordan Rau shares tips about finding nearby homes, evaluating staffing levels, what to look for when visiting, and more.
READ FULL ARTICLE » https://bit.ly/3A4a6Lt

California Medicaid Ballot Measure Is Popular, Well Funded — And Perilous, Opponents Warn
By Bernard J. Wolfson
The proponents of Proposition 35, a November ballot initiative that would create a dedicated stream of funding to provide health care for California’s low-income residents, have assembled an impressive coalition: doctors, hospitals, community clinics, dentists, ambulance companies, several county governments, numerous advocacy groups, big business, and both major political parties.
The Yes on Prop 35 campaign has raised over $48 million as of Sept. 9, according to campaign filings with the secretary of state. The measure would use money from a tax on managed-care health plans mainly to hike the pay of physicians, hospitals, community clinics, and other providers in Medi-Cal, the state’s version of Medicaid.
READ FULL ARTICLE » https://bit.ly/3YACIUX
Subject: Skilled Nursing Facility (SNF) care past 100 days
Medicare covers up to 100 days of care in a skilled nursing facility each benefit period. After Medicare coverage ends, you may consider these options.
Source: Medicare Interactive READ FULL ARTICLE » https://search.app/M6aWBcPw8sQodb486
With the annual Medicare open enrollment period now underway, KFF looks at the latest information about Medicare Advantage and Part D prescription drug plans and examines which beneficiaries are comparing their options--or not.
Additionally, in a new column, KFF’s President and CEO, Drew Altman, explores how Medicare, and other big health care programs, provide popular benefits valued by Americans from across the political spectrum even though the politics about them are partisan. And, we examine Vice President Harris’ recent proposal to broaden Medicare coverage of home care.
READ FULL ARTICLE » https://bit.ly/3YwkXqI
Medicare Part A Skilled Nursing Facility coverage is generally available to qualified individuals 65 years of age or older and individuals under age 65 who have been disabled for at least 24 months who meet the following 5 requirements: 1) the resident requires daily skilled nursing or rehabilitation services that can be provided only in a skilled nursing facility; 2) the resident was hospitalized for at least 3 consecutive days, not counting the day of discharge, before entering the skilled nursing facility; 3) the resident was admitted to the facility within 30 days after leaving the hospital; 4) the resident is admitted to the facility to receive treatment for the same condition(s) for which he or she was treated in the hospital; and 5) a medical professional certifies that the resident requires skilled nursing care on a daily basis.
Where these five criteria are met, Medicare will provide coverage of up to 100 days of care in a skilled nursing facility as follows: the first 20 days are fully paid for, and the next 80 days (days 21 through 100) are paid for by Medicare subject to a daily coinsurance amount for which the resident is responsible.
But beware: not everyone receives 100 days of Medicare coverage in a skilled nursing facility. Coverage will end within 100 days if the resident stops making progress in their rehabilitation (i.e. they “plateau”) and/or if rehabilitation will not help the resident maintain their skill level. Coverage will also be terminated if the resident refuses to participate in rehabilitation.
Written notice of this cut-off must be provided. When Medicare coverage is ending because it is no longer medically necessary or the care is considered custodial care, the health care facility must provide written notice on a form called “Notice of Medicare NonCoverage” to the resident and their designated representative. If you believe rehabilitation and Medicare coverage is ending too soon, you can request an appeal. Information on how to request this appeal is included in the Notice of Medicare Non-Coverage.
Don’t be caught off-guard by assuming your loved one will receive the full 100 days of Medicare. Be sure to have a plan in place to preserve assets while securing government benefits to help pay for long-term health care needs.
California law requires health plans to provide timely access to care. This means that there are limits on how long you have to wait to get health care appointments and telephone advice.
If you have a problem getting timely access to care, you should call your health plan. If your plan does not resolve your problem, contact the Help Center.
Wait Times from Date of Request for Appointment
Health plan members have the right to appointments within the following time frames:


Sutter Health’s systemwide agreement with Anthem Blue Cross (Anthem) expires on Dec. 31, 2024. For several months, we have actively engaged in good faith negotiations to renew this agreement. While discussions continue, we have not yet reached a resolution.
Unfortunately, Anthem recently informed us that it intends to send letters to their HMO members informing them they will be reassigned to non-Sutter doctors effective Jan. 1, 2025, if we do not have a renewal agreement by the end of this year. Anthem HMO members who are assigned to Sutter doctors may receive this notice as early as Nov. 1, 2024.
This action is concerning, as the current agreement includes a transition period that would allow patients to continue seeing their Sutter doctors after the expiration date for up to six months (June 30, 2025). This transition period is designed to avoid disruption in care while the parties continue to negotiate mutually acceptable rates and terms. It is unfortunate that it appears Anthem decided to opt out of using the transition agreement and instead intends to disrupt and cause concern with thousands of their HMO members — and our patients.
Note: the transition agreement between Sutter and Anthem also provides for Anthem EPO and PPO members to continue accessing their Sutter providers for up to six months (through June 30, 2025) as part of their in-network benefits, if the Sutter provider was a participating provider of the member’s plan on Dec. 31, 2024.
We remain hopeful that we can reach an agreement with Anthem and avoid any member or patient disruption in care.
Please note, the following Northern California payer agreements are renewed for 2025:
• Aetna – through June 30, 2025
• Alignment Health Plan, including Sutter Advantage HMO (Medicare Advantage)
• Blue Shield of California (Commercial and Medicare Advantage)
• Cigna Healthcare
• Health Net/Wellcare (Commercial and Medicare Advantage)
• Humana (Medicare Advantage)
• UnitedHealthcare (Commercial and Medicare Advantage)
Across the nation multiple insurance companies are making changes to the Medicare Advantage (MA) products, including MA product offerings in Northern California. We have confirmed that UnitedHealthcare will discontinue its MA PPO products across Northern California and will exit the MA HMO product in several counties. Wellcare by Health Net will exit its MA PPO products, and Humana will exit its MA HMO product in Contra Costa County. These changes are effective Jan. 1, 2025, and will impact many of our patients. Please review the following which you may find helpful for your clients:

Sutter Health patients who are affected by these changes will have the opportunity to review their plan options during Medicare’s Annual Enrollment Period (AEP), which runs from October 15 to December 7. During this period, patients can select a different MA plan (if available in their county) or return to Original Medicare.
We will support our affected MA HMO patients by sending them letters outlining the necessary steps to continue seeing their Sutter doctors in 2025. Additionally, insurance companies are required to inform their affected members about these MA changes.
If you’d like more information about any of the content in this update or have questions about Sutter Health, email us at brokers@sutterhealth.org.
For a complete list of the specific products that include Sutter Health's doctors, hospitals and other healthcare services, please check with the health plan directly or visit sutterhealth.org/health-plan.
Please note:
This notice is not applicable to Sansum Clinic serving the Greater Central Coast community.
About Sutter Health
Sutter Health’s integrated, not-for-profit system of aligned doctors and clinicians, employees and volunteers support approximately 3.5 million patients in communities across 22 counties. Headquartered in Northern California, Sutter Health provides access to highquality, affordable care through its network of hospitals, medical foundations, ambulatory surgery centers, urgent and walk-in care centers, telehealth, home health and hospice services. You can learn more by visiting us online.

» https://cahealthadvocates.org/
Available via an annual subscription, our 32 fact sheets cover 9 different Medicare and other health insurance topics. Those fact sheets pertaining to Long-Term Care include:
• Options for Financing Long-Term Care(H-001)
• An Overview of Long-Term Care Insurance (H-002)
• Frequently Asked Questions about Long-Term Care Insurance(H-003)
Websites and other resources:
AARP Report: Comparing Long-Term Care Insurance Policies: Bewildering Choices for Consumers
Authored by Bonnie Burns of California Health Advocates, this report reviews the long-term care (LTC) insurance options available to consumers and offers helpful recommendations.
Administration for Community Living
ACL advocates across the federal government for older adults, people with disabilities, and families and caregivers; funds services; manages programs; and invests in training, education, research and innovation.
Advance Planning Guides for People Living with Dementia
The National Alzheimer’s and Dementia Resource Center created a series of consumer guides to help people living with dementia and their family members or other care partners know what to plan for and how to get started. The guides cover 4 topics: 1) health care planning; 2) financial planning; 3) care planning; and 4) supporting someone living with dementia in making decisions.
California Advocates for Nursing Home Reform (CANHR)
1-800-474-1116 Offers consumer information on nursing homes, Medi-Cal, LTC, pre-placement counseling, quality of care and pension rights counseling.
California Association of Area Agencies on Aging (C4A) Services and programs for older adults and people with disabilities, including LTC services. Website includes each county’s Area Agencies on Aging
California Department of Aging
Oversees programs for older adults, people with disabilities, caregivers and LTC facility residents. Website includes Taking Care of Tomorrow, a booklet about LTC options. Available in English and Spanish.
California Department of Insurance
Offers consumer information on LTC insurance and a rate guide for companies selling LTC insurance.
California Medicare News
Variety of current articles on Medicare-related topics, including LTC.
California Nursing Home Guide
Provides information on all available nursing homes in California. This guide is produced and maintained by CANHR and was the first computerized nursing home information system in the country.
California Partnership for Long-Term Care
1-800-227-3445 Information on LTC insurance, including Partnership policies.
California Public Employees’ Retirement System (CalPERS)
1-800-982-1775 LTC insurance for California public employees, retirees, their spouses, parents, parents-in-law and adult siblings (age 18 and over).
California State Teachers’ Retirement System (CalSTRS)
1-800-228-5453 Information on retirement planning and benefits for California teachers.
CalQualityCare.org
Rates the care at nursing homes, hospice and home health agencies, and provides information on assisted living, retirement communities, and day care options. Also has a “Long Term Care Assistant” tool that uses 10 simple questions to help you choose among your long-term care options.
Federal Long Term Care Insurance Program (FLTCIP)
1-800-582-3337 LTC insurance for federal and postal employees, beneficiaries of annuities, members and retired members of the uniformed services, and qualified relatives.
Health Insurance Counseling & Advocacy Program (HICAP)
1-800-434-0222 Free counseling on Medicare and other healthrelated issues, including LTC and LTC insurance.
LongTermCare.gov
Provides tools and information on long-term care planning options and material on Medicaid eligibility for long-term care.
Long Term Care Ombudsman
1-800-231-4024; Sacramento: 916-323-6681 Offers information about nursing homes and resolves problems between nursing homes and residents or their families.
Network of Care
Comprehensive service directory for consumers, community-based organizations and municipal government workers. Provides links to pertinent websites and offers a comprehensive library, political advocacy tool and community message boards.
Nov 4-7 SHRM Inclusion 2024 Conference @ Aurora, CO
Nov 11-14 Becker's Healthcare 12th Annual CEO + CFO Roundtable @ Chicago, IL
Nov 11-14 SHRM The Women in Leadership Institute @ Orlando, FL & Virtual Nov 20 SHRM Workplace Law Forum 2024 @ Washington, D.C.
Feb 3, 2025 @9:30am-4:30pm CAHIP 2025 Innovation Expo @Long Beach, CA
Nov 6 @8:30am-9:30am BBSI Job Offer and Pre-Employment Best Practices @Long Beach, CA
Nov 6 @9:45am-10:45am BBSI Efficient New Hire Form Management and Effective Record Retention @Long Beach, CA Nov 6 @11-12pm
BBSI Create an Engaging and Efficient Onboarding Process @Long Beach, CA
Nov 7 @8:00am-12:30pm BBSI Red Cross Certification- Blended First Aid/CPR @Long Beach, CA
Nov 8 @8-11am BBSI Fall Protection Plan Workshop @Long Beach, CA
Nov 12 @ 8:00am-12:30pm BBSI Red Cross Instructor Led First Aid/CPR @Long Beach, CA
Nov 14 @9-10am BBSI Employee Anti-Harassment Training en Espanol @Long Beach, CA
Nov 19-Nov 20 @7:00am-12:30pm BBSI OSHA 10-Hour Construction Training Course @Long Beach, CA
Nov 14 @2:30-4:30pm EPI OC Chap Unlocking Hidden Value- Project Phoenix as a Sum of Its Parts @Costa Mesa, CA Nov 15
@5:30-7:00pm CAHIP Orange County It's A Pizza Party! @Irvine CA
Nov 20 @11:00am-1:00pm EPI Conejo Valley Optimizing After Tax Sale Proceeds @Westlake Village, CA
Nov 20 @2:30-4:30pm EPI Greater Los Angeles Chapter 2025 Pre-Election Economic Outlook @Los Angeles, CA
Nov 20 @ 2:30-4:30pm EPI San Diego Chapter Unlocking Hidden Value-Project Phoenix as a Sum of its Parts @Cardiff, CA Nov 21
@2:30-4:30pm EPI Inland Empire Chapter Inland Empire Case Study @Ontario, CA
VIRTUAL EVENTS
Nov 1 @10-11am The Real Fear of Missing Out: Coaching Clients Through Volatility
Nov 1 @12pm EST Live Call with David McKnight Brought to you by NAIFA
Nov 7 @11am EST Live Call with David McKnight Brought to you by NAIFA
Nov 12 @12pm EST Tax and Estate Planning Under a New Presidential Administration NAIFA-FSP WEBINAR SERIES
Nov 12 @1pm EST M&A Summit: Opportunity of a Lifetime Webinar In Partnership With NAIFA
Nov 12 @2-4:15pm BBSI Supervisor Anti-Harassment Training
Nov 14 @9-10:15am BBSI Employee Anti-Harassment Training
Nov 14 @11-12:15pm Webinar: Don't Be Scared of the Big Bad AI Wolf! NAIFA-Greater Bay Area
Nov 15 @9-11:15am BBSI Supervisor Anti Harassment Training en Espanol
Nov 20 @11am-6pm EST Trustworthy Selling
Nov 21 @10am EST Live Call with David McKnight Brought to you by NAIFA
RECORDED WEBINARS
Benefit Mall October Compliance Webinar w/ Misty Baker
Benefit Mall September Compliance Webinar
Benefit Mall August Compliance Webinar

By Emma Peters
Contributions from Sutter Health and the California Walnut Association
The holidays are on their way, and it’s no secret that eating healthily during these times can be difficult! Here are two California voices which provide some tips, tricks, and food options that will be helpful during the holiday season.
California is the healthiest state because of its lower smoking rate and higher amount of fitness and health locations.
California is the fittest state, with eight of the top 20 fittest cities.
By Meg Walker
The holidays are upon us! People are looking forward to spending time with friends and family. Along with the festive atmosphere and holiday cheer, comes tasty appetizers and big meals, and that can test your willpower and your waistline.
The truth is that a person can take in between 3,000 and 4,500 calories in a typical traditional Thanksgiving meal, according to Consumer Reports. Compare that to the calories a person generally consumes in a day: depending on your age, gender and level of exercise that can be from 1,800 to 2,500 calories, say dietitians at Northern California integrated health system Sutter Health.
Overeating happens all too quickly, and at this time of year Sutter nutritionists are counseling patients on how to handle holiday eating. Enjoy the events but take steps to practice healthy eating, they advise. “Food is a part of making connections with your family and friends,” says Kathy Solis, a registered dietitian and certified diabetes care and education specialist who works in the diabetes education program at Sutter Pacific Medical Foundation. “You want to be part of the group and enjoy the day, but still be cautious of food choices.”
Seema Karnik, manager for nutrition services for Mountain View Nutrition Services at Sutter’s Palo Alto Medical Foundation, adds: “Holidays are a time when we need to be mindful of how far we can go. We need to find a balance between healthy eating and having fun.”
Like most things, moderation and balance are key. To help you include healthy eating into your holidays, here are some tips from Sutter’s registered dietitians:
Don’t skip meals on the day of the big meal otherwise you will arrive at your holiday party hungry and risk making bad food choices.
Being active or exercising before and after a meal can help cut down calories.
Once you are at the event, concentrate on catching up with friends and family and having good conversations. Play games and spend time outdoors, if possible. Move around, especially if it’s a long, sit-down meal.
Start the meal with soup if that is offered, as it is a good way to cut down on your appetite. Focus on what you can add to your plate that is healthy and not calorie rich. Vegetables are king in this category as they are rich in fiber, which takes longer to digest and can help you feel full on less calories. And choosing colorful vegetables makes a plate look pretty and healthy at the same time. Some choices are squashes, green beans, beets, carrots and different colors of chard.
Also, go for these greens rather than grains such as bread or rolls. Some turkey is fine but go light on stuffing and sauces or gravy.
If you know you want to have dessert, cut down on other carbohydrates in the meal such as stuffing or bread.


Use the healthy plate method: half of your plate should be non-starchy vegetables (examples include broccoli, salad, asparagus, cauliflower, spinach, tomatoes); one quarter of your plate should be protein, including turkey or fish; and one third can be whole grains and starchy vegetables like sweet potatoes, corn or peas.
If you are going to drink alcohol, try to stick to a 5-ounce glass of wine or one beer or one cocktail. Consider not drinking alcohol if you can’t be moderate.
Consider bringing your own healthy dish, especially if you have food restrictions.


Now learn about a California-grown food that you might know the nutritional benefits of:
Consider incorporating these into your diet during this upcoming holiday season:
Food plays a big role in everyone’s identity, and those born between 1997-2012, commonly known as Gen Z, have been deemed the “foodie generation.” Gen Z is driven to a particular food by varied factors, but data suggests foods that support health and well-being by providing energy, managing weight, and fostering mental health are priorities.
Yet when it comes to choosing foods that support these needs, Gen Z, along with Millennials and beyond, often overlooks a convenient and important food group – tree nuts, including walnuts.
Nuts, including walnuts, are nutrient dense and considered a key component of many recommended dietary patterns, including the Mediterranean and vegetarian diets. They are also recommended for daily consumption in the latest U.S. Dietary Guidelines. Despite the recommendations, nuts remain under-consumed by the U.S. population, perhaps because nuts are calorie-dense, leading to potential concerns that including nuts in the diet could promote weight gain.
But new research suggests Gen Z and Millennials should reconsider nuts, like walnuts.
New Research Evaluates the Impact of Nuts on Weight Management for Gen Z and Millennials
In a recent observational study from Indiana University School of Public Health-Bloomington, funded by the California Walnut Commission, researchers observed that adolescents and young adults who consumed walnuts and other nuts had a lower prevalence of obesity when compared with those who consumed no nuts.
Researchers analyzed data from the National Health and Nutrition Examination Survey (NHANES) which included more than 19,000 adolescents (12 – 19 years old) and young adults (20 – 39 years old) to understand the associations between consumption of walnuts and other nuts with measures of obesity including relative fat mass (RFM), a validated tool for estimating body fat percent and regional fat composition.
Young women consuming only walnuts had a significantly lower prevalence of obesity when compared to non-nut consumers. However, this association was not found among young men, adolescent boys, or adolescent girls who consumed walnuts only. Researchers also observed that adolescent girls and young women who consumed walnuts only, or other nuts, had a significantly lower RFM compared to non-nuts consumers. Only young males in the walnut and other nut groups showed an inverse association with RFM compared to no nuts group, this was not found in adolescent boys.
These results are promising suggesting that there may be an association between the consumption of nuts, especially walnuts, with a lower prevalence of obesity and lower RFM within certain populations. However, cause and effect could not be determined, and additional research is needed to support these results.
“As a registered dietitian and a mom of a college student, I’m excited by the emerging research highlighting the potential cognitive, mental health, and metabolic benefits of walnuts for teens and young adults. Incorporating walnuts into kids’ daily lives is easy, delicious, and nutritious, and it’s a strategy that may help them thrive mentally and physically during these critical developmental years,” notes Samantha Cassetty, MS, RD.
Beyond Weight Management: Walnuts May Support Overall Physical and Mental Well-Being in Gen Z & Millennials
Teens and young adults crave food that supports both their physical and mental health, with over 30% seeking emotional and mental health benefits.1 Research suggests that daily walnut consumption could potentially support cognitive health and mental well-being in this unique population.
• Daily Walnut Consumption May Support Teens’ Focus and Attention –
In a multi-school randomized controlled trial of 771 healthy teenagers ages 11 to 16, those who consumed 30 grams of walnuts per day (1 ounce or 1 handful) for six months had improved scores for attention, fluid intelligence (i.e. problem solving, quick reasoning skills) and ADHD symptoms, when compared to the group not eating walnuts. The positive results in this study were only seen in those teenagers who consumed more than 3 servings of walnuts per week. While these results are positive it should be noted that less than half of the participants in the intervention group adhered to the protocol of

eating walnuts daily. Thus, the positive results of this study were only seen in the teenagers who regularly ate walnuts. While more research is needed, this study provides valuable insights and a basis for further research on the effect of walnuts on brain development in adolescents.
• Walnuts May Improve Mental Health and General Well-Being in University Students –
A novel study of 80 healthy university students ages 18 to 35 found that 2 ounces (or about 2 handfuls) of walnuts a day for 16 weeks prevented negative changes in self-reported mental health scores and scores of stress and depression during a stressful academic period, compared to those who did not eat walnuts. The group that ate walnuts experienced an increase in markers that protect against stress and a decrease in those that are linked with stress.
• Snacking on Walnuts May Improve Metabolic Health in Young Adults – In a recent study of 84 young adults, ages 22 to 36, with at least one metabolic syndrome risk factor, researchers found that snacking on 1 ounce of mixed unsalted tree nuts, including walnuts, twice daily, may improve metabolic health, when compared to carbohydrate-rich snacks. Among tree nut snack consumers, researchers observed a reduction in waist circumference and lipid markers in female participants and decreased blood insulin levels in male participants. Those consuming tree nut snacks also saw an effect on triglycerides and TG/HDL ratios with TG/HDL ratios reduced ~11% compared to those consuming carbohydrate-rich snacks.
These studies are not without limitations. While the findings cannot prove causality, they do shed light on how nuts, including walnuts, can be a part of a healthy diet that supports metabolic health and well-being. Additional research is needed to determine how these results apply to other populations.
Walnuts are tasty and versatile and can be added to meals and snacks to support optimal nutrition in Gen Z and Millennials, while also helping to close the gap in consumption.
Cassetty suggests toasting walnuts to toss into whole grain salads, roasted veggies like broccoli and green beans, and breakfast foods like yogurt bowls and oatmeal. “They also make green salads heartier and more enticing. Walnuts are also a natural fit for baked goods, and walnuts with dark chocolate is one of my favorite dessert pairings,” she added.
A 1-ounce serving of walnuts contains a powerhouse of nutrients for optimal health.
Simple ways to just add walnuts:
• Breakfast can be made easy with prep-ahead breakfasts, like a Banana Walnut Bread Overnight Oats recipe that eliminates the need to wake up extra early to make a meal or wait in line at a grab-and-go spot.
• Make snack time flavorful with a simple Rosemary and Sea Salt Walnut recipe. It’s also perfect for entertaining!
• Make lunch a time to refuel with nourishing meals, like this Walnut Balsamic Spinach Salad recipe that is tasty and filling to get through a busy afternoon.
• Dinnertime doesn’t need to be complex. A Walnut Mexican Street Corn Taco recipe makes the perfect weeknight dinner in just 18 minutes.
For more recipes and research on the health benefits of walnuts, visit walnuts.org.
There is a lot of temptation during the holiday season to eat poorly, but with these tips and tricks one can be mindful of what they eat and include healthy delicious recipes at the same time!
“ California is the healthiest state because of its lower smoking rate and higher amount of fitness and health locations.
California is the fittest state, with eight of the top 20 fittest cities. “

Emma Peters is the media assistant at California Broker Magazine. She recently graduated from Point Loma Nazarene University summa cum laude, with a Bachelor of Arts in Literature and a minor in Humanities.
Sources: SutterHealth https://vitals.sutterhealth.org/holiday-meals-can-pack-on-the-calories-nutritionists-give-tips-onmaintaining-healthy-eating/ Walnuts https://walnuts.org/blog/balanced-lifestyle/walnuts-may-be-a-key-ingredient-for-well-beingamong-gen-z-millennials/

By Phil Calhoun & David Ethington
The “Should I sell my business?” question comes to most business owners at some point. In our ten years of helping health brokers with commission planning, it is clear that seller’s remorse is real. In fact, 75% of business owners regret selling their company just one year after the transaction, according to a PwC research mentioned by the Exit Planning Institute
“From our experience we find some brokers have not kept current with technology and this is causing them to lose clients, miss out on finding leads, and experience difficulties with closing new business.”
This article covers SIX key reasons and signs to consider before selling your business.
As an experienced business owner, you may desire other opportunities of greater interest at some point. Starting a new challenge usually means you’ll need money or time, which leads to giving up your current business ownership. According to the Exit Planning Institute, 80-90% of business owners’ wealth is related to the value of their business. Taping into this value is tempting for some owners.
If you built your company early in your career, you might reach a point where you look for something that is more aligned with your current lifestyle.
Most of the brokers we work with are ready to retire. Few health brokers sell then get into a new industry. Some sell and stay in the industry. Working with carriers GAs or FMOs are considerations. Making an industry decision makes more sense and may bring more value both to the employer and their new employee, you. It is understandable for younger professionals to follow their desire to relocate as they have the drive to find a new opportunity and are willing to make more” dramatic” life changes than someone with family and significant local connections to lose.
When your business isn’t as profitable as it was before due to rising costs, a lack of growth in the industry, or a shift in market preferences, it’s a good sign to let go of it. It’s important to highlight that a lack of profitability alone doesn’t mean your business has no value.
There might be several different factors causing this issue and maybe you are not in the mood to turn things around.
With a commission-based business, unless you have added staff or have family in the business and need to share the success, profitability is not often a concern.
If you have a family business and there are no potential successors, planning the sale as a next step is the smart thing to do.
Doing exit planning allows you to train the next generation of the management team. It is common that as part of the transition and future of the business the seller will need to stay for a year or two to provide the experience the buyer needs.
We have found some sellers want out while others may complain but they have not looked at what is next. In the case where the seller is needed in a post-sale transition, this is ideal when the Buyer wants the Seller to gradually transition out.
Over the years it might be possible that the number of competitors in the industry and the risks of the business operations increase to a level with which you’re no longer feeling comfortable.
Relying too much on just a few referral sources in the local market can impact new business. Under these circumstances, some sellers decide to start the sales process.
When litigation risks can jeopardize the company’s future, sellers should disclose to potential buyers if there are any pending lawsuits or penalties. In most cases issues are discovered during due diligence.
In the state of CA there are many competitors who enter the state with advanced technology, unmatchable marketing resources, and new products that open the door open to catch the eye of your clients. More competition in health isnurance linesis forecasted in 2025 and beyond, so brokers not able to stay current with the competition will face an uphill battle.
If managing the business doesn’t feel any more like a challenge due to a lack of strategy for the future, then it’s possible that business owners feel like it’s time to move on. Additionally, through the year, entrepreneurs can face many new challenges. If there isn’t a contingency plan that can give some guidance and support against these potential issues, then the lack of business strategy can feel overwhelming.
Running a book of business is no easy job and can take a toll on the business owner’s health. This can lead to looking forward to retirement or simply taking time to rest. Whichever the reason, many business owners can always decide they’ve reached a point at which they should lay back and enjoy what they have worked so hard for.
From our experience we find some brokers have not kept current with technology and this is causing them to lose clients, miss out on finding leads, and experience difficulties with closing new business. The competition has the edge when they bring technology with CRM systems to service clients, methods to regularly touch clients, and marketing programs to reach out to more prospects. Consider today’s Medicare age ins are more tech savvy and most younger business owners and benefits decision makers look for technology solutions for their group benefits management. Brokers who do not have the ability to stay competitive will see their book of business shrink. And at some point, they are better off planning their exit.
Here’s situations where we can help:
• Have no idea about your future plan, Have family or employee(s) who will step in, we can help

Using your own money to cover operating expenses is not a plan but is a sign that funding new projects will be more difficult.
In our experience industry changes and challenges keep coming, 7 years with group benefits and nearly every other year with Medicare. Carriers change plans, federal and state laws drive change (ACA, CMS and Medicare marketing hurdles, DOI and DOL requirements, tax laws) and the cost of doing business. Partners can help (FMOs and GAs) bring resources to deal with industry changes and tech challenges. Finding advisors and mentors is also vitally important to build a successful business strategy.
Integrity Advisors is a health insurance agency which specializes in educating health brokers on the importance of commission protection. Commission Solutions is a program offered by Integrity Advisors.

Phil Calhoun MBA,is a board member of the Exit Planning Institute Orange County Chapter, he owns Integrity Advisors.
Click here to arrange a no obligation 15-minute coach session Phil@commissions.solutions 714-664-0311

David Ethington, is an expert in the process to acquire and transfer health commissions. He has trained many brokers in commission education and built the commission transfer planning module for Medicare commissions provided to our broker colleagues.
Click here to arrange a no obligation 15-minute coach session David@commissions.solutions 714-664-0605

By Marc Glickman FSA, CLTC, LTCP
Long-term care insurance (LTCi) isn’t just a financial tool—it’s a way to safeguard families from the emotional, physical, and financial toll of caregiving. As an actuary with over a decade of experience designing LTCi products, I’ve long understood the value of planning for longterm care. However, it wasn’t until a personal experience unfolded within my own family that I truly grasped the human cost of delaying these crucial decisions.
It all started with a simple phone call from my relative, Colin, a respected doctor and a family man, who was seeking advice on LTCi. Colin and his wife, Amy, were facing the same question that many families ponder: should they buy long-term care insurance, or could they afford to self-fund the costs? Although Colin was confident in their financial security, years of hesitation had kept them from moving forward with a plan. This phone call would lead us down a path of unexpected events that drove home the importance of timely planning for long-term care.
During our conversation, Colin reminded me of our family’s history with long-term care. My grandparents, whom we lovingly called Bubbe and Zedde, both needed extended care for many years. Zedde, a Holocaust survivor, had suffered severe trauma from his experiences during World War II, which led to mental health struggles later in life. He eventually suffered a stroke that left him physically incapacitated, and the family had to make difficult decisions about his care.
Bubbe also experienced a stroke, and I remember vividly how my mother took on the role of her full-time caregiver. For five years, my mother dedicated herself to caring for Bubbe, putting her own health and well-being aside. The burden was immense, both emotionally and physically. These memories stuck with me, and they were a driving factor in why I pursued a career in long-term care insurance. But for Colin and Amy, those memories were too painful, and the thought of repeating that experience with their own children gave them pause. However, decision and prediction algorithms aren’t yet ready for large-scale use without oversight. Recent lawsuits showcase issues with reliability, leading to common themes and complaints.
“Long-term
insurance (LTCi) isn’t just a financial tool—it’s a way to safeguard families from the emotional, physical, and financial toll of caregiving.”
Colin made it clear: “We don’t want our kids to suffer the way we did, caring for our parents.” Yet, despite this resolve, they had delayed purchasing LTCi, primarily because their financial advisor had suggested they could self-fund the risk. “He wasn’t sure if LTCi was worth the cost,” Colin admitted, echoing a sentiment I’ve heard from many clients over the years.
As an actuary, I’ve analyzed the self-funding argument extensively. While self-funding may seem like a viable option for affluent families, it’s fraught with risks. Market volatility, taxation, and the uncertainty of when care will be needed all complicate the notion of simply relying on personal savings. I explained to Colin that LTCi isn’t just about covering costs—it’s about leveraging insurance to provide peace of mind and, more importantly, protecting their children from the heavy burden of caregiving.
Colin and Amy had also delayed because of concerns about the cost of LTCi and potential rate increases. I reassured them that today’s LTCi market offers a variety of options, including prepaid plans and guaranteed premiums. There is even traditional lifetime payment plans that are more conservatively priced than in the past. Together, we could build a customized plan that fit their needs without breaking the bank.
Colin agreed to move forward, and over the next few days, we worked together to find the right LTCi product for them. Given their excellent health, I was able to secure a plan with superior longevity protection and excellent value. They were so pleased with the outcome that they even considered increasing their coverage to better prepare for future care costs.
However, as often happens in life, unexpected events soon intervened. Colin and Amy were traveling and wouldn’t be able to sign the application for another month and a half. I remember cautioning them: “Heaven forbids any health issue should happen before you return—you might not qualify for coverage.” At the time, it felt like a typical sales line, but it wasn’t long before that warning took on a much more personal significance.
Two weeks later, my mother called with a quiver in her voice. “Colin and Amy were at the gym, and Amy suddenly collapsed,” she told me. I was shocked to learn that Amy had suffered a brain aneurysm, a sudden and life-threatening condition. The first thought that crossed my mind was whether she would survive. Then, almost immediately, my mind shifted to the possibility of long-term care. What if Amy needed extended care? Would they still be able to qualify for LTCi? And then, I felt a deep sense of gratitude that I had spoken with them just two weeks prior.
Thankfully, Amy survived. She underwent a cuttingedge surgical procedure that repaired the aneurysm, and her recovery has been nothing short of miraculous. However, this close call underscored the reality that life’s unpredictable twists and turns can derail even the best-laid plans. Colin and Amy’s situation could have been much worse had they delayed their decision any longer.
This experience reinforced what I’ve always known: waiting to plan for long-term care is risky. For many families, it’s not just about the financial costs—it’s about ensuring that loved ones aren’t left to shoulder the burden of caregiving. Amy’s near-death experience highlighted the urgency of making decisions before it’s too late. While they may not have been able to move forward with their original LTCi Plan A, I was grateful to have a Plan B ready—one that still offers protection and peace of mind.
As I reflect on this personal story, I’m reminded of how powerful storytelling can be. It’s one thing to discuss insurance in terms of numbers, benefits, and features, but it’s another to share real-life experiences that demonstrate the importance of planning. Stories like these build trust with clients and help them connect on a deeper level with the products and services we offer.
For Colin and Amy, the story had a happy ending. But not every family is so fortunate. The lesson here is clear: don’t wait. Whether you’re considering LTCi for yourself or advising clients on their options, the best time to plan is now.


Marc Glickman,FSA, CLTC, is CEO and co-founder of BuddyIns, a leading long-term care insurance education, marketing and technology company. Marc is a licensed insurance agent in all 50 states and serves on the Board of Advisors for CLTC. Marc has over 15 years of experience as an actuary including as the chief investment officer and chief sales officer for a major LTC insurance company. Marc earned his degree in economics from Yale University. In 2019, he was named one of the top 20 innovators in the insurance brokerage space.
marc@buddyins.com 818-264-5464
By Diane Stoddart CLTC, LTCP

“Without LTC planning, many family members sacrifice their futures and savings for their own retirement years.”
Long-term care (LTC) planning has as much to do with the person needing care as it has to do with their caregivers’ wellbeing. LTC is about protecting those we love from the physical, emotional and financial consequences they’ll face when a parent or loved one needs help. About one (1) in five (5) of all adults (22 percent) will have a care need that extends beyond five (5) years.
November is long-term care awareness month. It’s important to understand the costs (financial, social, physical, psychological) to caregivers because it’s never too early to plan for long term care. Associated health costs continue to rise, and the expense of caring for patients for an undetermined number of days/weeks/months or years, can create significant financial difficulties.
In the 21st Century, people are living longer, and LTC can help make our senior years as comfortable and stress-free as possible. The incidence of memory disorders and cognitive decline is on the rise, and diagnoses of dementia create one of the most common needs for extensive long-term care.
Have you or a loved one said, “Please promise to never to put me in a nursing home…but I don’t want to be a burden…” Many try to keep those promises to their own detriment. Without LTC planning, many family members sacrifice their futures and savings for their own retirement years.
Case Study: I’ve witnessed families deplete their assets and sell their parents’ homes to pay for care. What happens when the money runs out? Without a home, the parents need to either move to a facility or move in with their kids. With that nursing home promise lingering in the background, discord among siblings results, and they frequently argue about costs of care or “a place for Mom.”
On the other hand, we meet seniors who planned and bought LTC insurance many years ago. Planning ahead provides time to discuss what kind of care they would like when care is needed. Some have already toured assisted living facilities/communities (ALFs) and decided where they would want to live, when they can no longer live independently.
Caregivers or adult children of senior parents, who purchased LTC insurance, are often able to couple the insurance proceeds + the patient’s income. With the combined funds, many can afford a nice ALF or 6-10 hours of in-home care per day.
Full-time or part-time (in-home) care enables caregivers and adult children to take care of their own families, knowing their parent is receiving appropriate care. Often, families select “step up” care that allows them to transition from the home until residential care in an ALF is needed.
Recognizing that there is no “one size fits all” plan (some clients prefer the idea of an ALF), it’s good that there is a wide assortment of LTC plan options today. Some use a lower premium that is paid over your lifetime, while others use a 1, 5, 10, 15 or 20 years paid-up funding strategy. Optimally, you will pay for the plan before reaching retirement.
New laws allow us to reposition cash value from life insurance and annuities to create LTC plans that pay tax-free benefits for care or pay your beneficiaries, if no care is needed. In fact, there are options for a full return of premium if a client changes their mind and cancels.
When we plan in our 40s and 50s, we often guarantee that both the LTC benefit, and the death benefit will pay significantly more than the premium paid.
With options, we need not feel like we are abandoning our loved ones to the nursing home. Nor do we need to feel like we will be abandoned. Instead, we can proactively plan, communicate, and carry out our loved ones wishes that were designed many years before care was needed.
We need to become more aware of what planning strategies and policy options are available today to help us prepare for tomorrow. Before you know it, we will be the ones living longer than we thought we would. It’s important that we protect our families from physical, financial and emotional devastation.
“With options, we need not feel like we are abandoning our loved ones to the nursing home. Nor do we need to feel like we will be abandoned. Instead, we can proactively plan, communicate, and carry out our loved ones wishes that were designed many years before care was needed.”
California Broker is pleased to have a collaborative relationship with Buddy Insurance, a leading long-term care insurance education, marketing and technology company. CEO Marc Glickman and his specialists will collaborate with health and life insurance professionals to help design LTCi options. Learn more about LTCi and refer clients — or learn how to write your own LTCi policies using Marc’s system.
CONNECT to Buddy Insurance LTCi PORTAL HERE:
Group: www.buddyins.com/program/calbroker/group
Individual: www.buddyins.com/program/calbroker/

Diane Stoddart, CLTC, LTCP, is a BuddyIns LTCi specialist who has been helping families plan for the financial exposure of an extended life since 1992.
Diane and her husband, Paul, bought their long term care policies at age 35. At 40, she was diagnosed with Multiple Sclerosis. By the grace of God, she has no symptoms or troubles with the disease. She is, however, uninsurable and is so grateful that she was led to plan early.
Diane designs customized plans through multiple top-rated insurance carriers. Diane works in all 50 states to help her clients plan today to be able to live at home later, when they need help living.
You can reach Diane at diane@buddyins.com.

By Gretchen Barry
As the demand for long-term care soars, so do anxieties about paying for these essential services. As someone who experienced this recently with a parent, I understand that anxiety. According to a 2023 KFF survey, 43% of respondents don’t feel confident that they’ll be able to afford care as they age. Additionally, only 28% of adults aged 50 to 64 have saved money for future living assistance expenses.1
For this article, I want to focus on how long-term care coverage is and how insurance can help alleviate funding concerns by providing financial support for extended care services. This insurance can give policyholders peace of mind and safeguard their financial futures. By learning about the ins and outs of long-term care insurance, you’ll help your clients effectively plan for their future health needs.
Long-term care insurance — also known as custodial care coverage — covers the costs of extended care services for people who need ongoing support. It pays for expenses not covered by Medicare or traditional insurance, such as assisted living and skilled nursing.2
A long-term care insurance policy can help pay for the cost of care that is needed due to a chronic illness, disability, or injury. Primarily, long term care insurance is designed to cover the costs of custodial and personal care, as opposed to medical care alone.
Coverage may include the cost of staying in a nursing home or assisted living facility, adult day care or in-home care.
So, what does long term care insurance cover? When your policy has been activated you can use it to cover many types of expenses, including:
• Respite care
• Alternative care
• Adult day care
• Nursing home
• Assisted living facilities
• Memory care
• Resident care
• Short term hospice
Ideally, someone would purchase coverage when they are still young and healthy people to cover future medical expenses.
“A long-term care insurance policy can help pay for the cost of care that is needed due to a chronic illness, disability, or injury. Primarily, long term care insurance is designed to cover the costs of custodial and personal care, as opposed to medical care alone.”
Long-term care insurance covers ongoing medical expenses for people with complex health needs that require extended and specialized support. Policyholders must meet specific criteria to begin using their long-term care benefits. Insurers require a physician’s diagnosis for cognitive or physical impairment.
Policy coverage typically includes these essential services:
In-home care coverage allows policyholders to receive healthcare services from the comfort of their homes. These services are available for seniors, people with disabilities, patients recovering from surgery or illness, and others.
In-home care takes many forms, including:
• Companion care: A caretaker provides non-medical services and social support to help patients stay engaged and prevent loneliness. For instance, an aging patient may go on daily strolls with their caretaker and get help with grocery shopping.
• Help with ADLs: An in-home care professional can assist with bathing, caring for dental hygiene, and other daily activities.
• Nursing care: A licensed healthcare provider travels to the patient to deliver healthcare services. For instance, a person recovering from knee replacement surgery may receive wound management and physical therapy.
In-home care allows older adults and others who need ongoing assistance to maintain their independence. Patients who receive these services can remain in their homes and communities instead of moving to an assisted living or skilled nursing facility. However, keep in mind that these services are in high demand. Depending on where one lives, it may be difficult to find a qualified caregiver.
Insurance coverage for long-term care also includes facility care. This type of care allows policyholders to receive healthcare services in residential settings.
Common types of facility care include:
• Assisted living: Residents live in independent units and receive help with ADLs. For instance, staff may provide housekeeping and remind residents to take their medications.
• Nursing home: These facilities provide comprehensive medical care and 24/7 supervision. Nursing homes are a great option for people with limited mobility, cognitive impairment, and other conditions that require around-the-clock support.
• Memory care: Memory units offer specialized support for people with Alzheimer’s disease, dementia, and other cognitive disorders. These facilities typically provide brain-stimulating activities and have security measures to keep residents safe.
Facility care allows residents to build social connections with peers, reducing loneliness. These communities also offer communal dining, recreational facilities, and other amenities that improve residents’ quality of life.
Many people require assistance with everyday activities due to age, disabilities, and illnesses. Long-term care insurance providers typically allow policyholders to receive benefits if they can’t perform two of these six ADLs:3
• Bathing
• Continence
• Dressing
• Eating
• Transferring in and out of a bed or chair
• Toileting
Long-term care insurance enables eligible policyholders to receive daily assistance with these tasks. For instance, a person with a spinal cord injury could have an in-home caretaker who helps them transfer from their bed to their wheelchair. Similarly, someone who experiences a stroke could move into an assisted living facility to receive assistance with bathing and toileting.
Assistance with ADLs improves patients’ quality of life and allows them to maintain their dignity. Coverage for these services also reduces the strain on family members and enables policyholders to receive professional support.
People often assume they can use their long-term care insurance whenever they need it, but that’s not the case. Policyholders must follow their insurance company’s filing process to get reimbursed for claims. At BuddyIns, we recommend that folks reach out to our Community Partner, Amada Senior Care, to get help understanding how to file a claim.
“As healthcare costs continue to rise, insurance coverage for long-term care has become a wise option for many people. This insurance can enable policyholders to receive necessary care without wiping out their savings or going into debt.”
We need to continue to educate more Americans about the importance of planning and communicating a plan to their loved ones. Long-term care services allow individuals to age with dignity and receive essential healthcare. However, these services can cost thousands of dollars a month, especially for people who need specialized care.
As healthcare costs continue to rise, insurance coverage for longterm care has become a wise option for many people. This insurance can enable policyholders to receive necessary care without wiping out their savings or going into debt.
As a reliable advisor, you can help clients understand the benefits of long-term care insurance and make informed decisions about their current and future health.
California Broker is pleased to have a collaborative relationship with Buddy Insurance, a leading long-term care insurance education, marketing and technology company. CEO Marc Glickman and his specialists will collaborate with health and life insurance professionals to help design LTCi options. Learn more about LTCi and refer clients — or learn how to write your own LTCi policies using Marc’s system.
CONNECT to Buddy Insurance LTCi PORTAL HERE:
Group: www.buddyins.com/program/calbroker/group
Individual: www.buddyins.com/program/calbroker/

Gretchen Barry, As Chief Marketing Officer for BuddyIns, Gretchen has been instrumental in shaping the company’s identity as a leading LTCi education, marketing, sales, and technology company. With over 20 years of experience in marketing leadership roles across financial services and tech start-ups, Gretchen brings a wealth of expertise and passion to her work. She oversees a diverse and talented marketing team that delivers innovative and effective solutions for BuddyIns’ clients and partners. Gretchen can be reached at gretchen@buddyins.com
Sources:
www.kff.org/health-costs/poll-finding/the-affordability-of-long-term-care-and-support-services/ www.americanbar.org/groups/law_aging/publications/bifocal/vol45/vol45issue1/ltc-insurancequal/ www.dhcs.ca.gov/services/ltc/Documents/Alert_Glossary.pdf

Recently, I received an important question through my website about what happens if an insurance company is liquidated. As most of you know, I’ve been in this business for decades and I’m pleased to report that the liquidation of insurance companies is an incredibly rare phenomenon.
It’s a fair concern and I’m sure it’s one that many of you have thought about. I’m sharing this information because I want you to be comfortable not only with the long-term care insurance policy that you purchased through my team but also the strength of the carrier who is bearing the risk of and responsibility for that policy.
Comment:
“I have a full paid-up 10-year-pay LTC policy. Per my state’s insurance office, having an active policy like this is not enough -- you need an active claim.”
According to a representative at the state’s Department of Insurance (DOI), “If the carrier were to undergo liquidation AND she did not have an active claim, then her policy would end.”
Signed “K” from Nebraska
My Response:
Thank you for your comment. I will respectfully disagree with the representative at your state DOI. When I have questions about carrier solvency and the laws and regulations around it, I go to the National Organization of Health and Life Insurance Guaranty Associations (NOHLGA) website (1). In this instance, I found specific answers that support my understanding that the guaranty associations will continue coverage and pay claims, not just handle active claims at the time of liquidation.
For instance, part of the response to Frequently Asked Question #2 says, “If a member company is ordered liquidated by a court with a finding of insolvency, the guaranty associations of the states where the company was licensed continue coverage and pay claims under the member company’s covered policies in accordance with state laws.” (2)
Additionally, the response to FAQ #3 repeats the “continue coverage” phrase: “Guaranty associations typically are activated to continue coverage and pay claims when a court issues a liquidation order with a finding of insolvency against a member company.”
Response to FAQ #4: “Depending on the type of contract and other factors, guaranty associations typically continue coverage to the owner of a policy, contract, or group certificate, and to the extent applicable, to the beneficiaries, assignees, and payees of those owners.”
Response to FAQ #10 states there is a specific amount of coverage which is typically $300,000 for long-term care insurance. This is more liberal than the $250,000 FDIC-insurance for bank deposits. What if your claim is more than that? It goes on to say,
“In most states, benefit amounts above the guaranty association levels become a claim against the estate of the insolvent insurer, and policy owners may recover a portion of that claim when the company’s assets are liquidated.”
You can check your specific state’s guaranty association here.
Response to FAQ #7 says the only time the policy is terminated is if the policyowner stops paying premiums that are due. This doesn’t apply to you as your policy is paid up.
You are more likely to see a bank failure than the failure and liquidation of an insurance company. I hope that this policyholder was able to go back to his DOI representative to provide this important information.
“You are more likely to see a bank failure than the failure and liquidation of an insurance company”
California Broker is pleased to have a collaborative relationship with Buddy Insurance, a leading long-term care insurance education, marketing and technology company. CEO Marc Glickman and his specialists will collaborate with health and life insurance professionals to help design LTCi options. Learn more about LTCi and refer clients — or learn how to write your own LTCi policies using Marc’s system.
CONNECT to Buddy Insurance LTCi PORTAL HERE:
Group: www.buddyins.com/program/calbroker/group
Individual: www.buddyins.com/program/calbroker/

Phyllis Shelton, is the President of Got LTCi, part of a long-term care insurance outreach that she founded in 1991. She is widely considered to be the leading long-term care insurance sales trainer in the country. Her book, Protecting Your Family with Long-Term Care Insurance, provides cutting edge information about all phases of financing long-term care. Suze Orman says, “Long-term care insurance for many is the most important insurance you can buy if you can afford it. Phyllis Shelton is the only person I trust to keep me up to date on what I need to know. Read this book.”
Phyllis can be reached through her website at Contact Us | Got LTCi.

By Wendy Boglioli
“It’s time for the collective financial services industry to help more Americans, especially women, take charge of this part of their financial futures and give them more options for long term care planning.”
Each week at BuddyIns, as we strive to inform more American employers and associations about the importance of planning for long-term care, particularly for women, we host educational sessions for employees and association members. These sessions focus on group hybrid long-term care with life insurance, raising awareness about how this dual-benefit option can ease the financial burden on families in times of need.
This educational effort is crucial, as recent industry trends show a growing interest in long-term care benefits. According to a Buck survey, 66% of employers plan to address long-term care benefits in the coming year, recognizing their importance not just for older adults but also for the labor market and younger generations. This is particularly important for women since we are the majority of family caregivers.
As an Olympic gold medalist and a veteran in the long-term care insurance (LTCI) industry for 27 years, I have witnessed the significant impact of long-term care needs for women. Working women face multiple responsibilities, including employment and caregiving challenges, while juggling various responsibilities. This includes being employed outside of their home, caregiving responsibilities for family and loved ones, and being among the 4 in 10 women who are the primary breadwinners in their families. This juggling act is becoming increasingly common, with more than 1 in 6 Americans working full-time or part-time reporting that they assist with the care of an elderly or disabled family member.
I have also personally witnessed the unfortunate circumstances of women passing away during their working years without the benefit of life insurance for their loved ones. It is heartbreaking to see a family scramble during that crisis. The immediate struggles with funeral expenses, mortgage payments, and then, of course, the day-to-day living expenses can be overwhelming. And for my recently deceased friend, who was a single woman and the primary breadwinner, not having life insurance left her dependents with very little financial support.
Enter life insurance with long-term care benefit. When I talk to employees about the importance of insurance options, I have noticed that men seem to hear the value of long-term care insurance, while women genuinely understand its significance. However, it’s puzzling that women are not as focused on the life insurance aspect of the available hybrid plans. In my discussions with women, they tend to perceive life insurance as expensive, although it’s worth noting that women generally pay far less than men for life insurance due to lower risk. Women often view life insurance as a luxury or prioritize other financial responsibilities, such as saving for retirement, ensuring they can support themselves if they are unable to work, and having the means to pay for long-term care without burdening their children.
Additionally, accessibility may also be a factor, which is one of the main reasons why the hybrid life insurance with LTC benefit is so attractive in the workforce as a group policy. This solution addresses and removes all of these concerns. Several group carriers, including Chubb and Trustmark, offer guaranteed issue options along with simplified issue for spouses or higher issue ages, unisex pricing, portability, and age-saving benefits. When it comes to hybrid life insurance with LTC benefit, the savings to women when compared to traditional products can be quite compelling. Plus, life insurance may cover through age 121 - another solid feature. This accessibility is particularly important, as the adoption rate of long-term care insurance by employers remains relatively low.
According to SHRM’s 2023 Employee Benefits Survey, only 20% of employers offer long-term care insurance. However, the trend towards hybrid policies is gaining momentum, attracting a younger and lower-income demographic compared to traditional standalone LTC insurance.
The importance of these hybrid policies extends beyond individual benefits. They’re increasingly seen as part of a broader financial well-being offering for employees. This aligns with data showing that nearly 7 in 10 working adults report they would perform better at work if their employer offered more financial wellness benefits. Moreover, these group policies can help address gender equity in insurance, as women often pay 20-40% more than men for equivalent policies in the individual market.
It’s time for the collective financial services industry to help more Americans, especially women, take charge of this part of their financial futures and give them more options for long term care planning. A hybrid life insurance product with a long-term care benefit can be a game-changer. Let’s empower more companies to offer this valuable dual-benefit insurance product. It’s an opportunity to provide peace of mind for more families.
California Broker is pleased to have a collaborative relationship with Buddy Insurance, a leading long-term care insurance education, marketing and technology company. CEO Marc Glickman and his specialists will collaborate with health and life insurance professionals to help design LTCi options. Learn more about LTCi and refer clients — or learn how to write your own LTCi policies using Marc’s system.
CONNECT to Buddy Insurance LTCi PORTAL HERE:
Group: www.buddyins.com/program/calbroker/group
Individual: www.buddyins.com/program/calbroker/

Wendy Boglioli is a featured speaker, long term care expert, healthy aging advocate, and Olympic gold medalist. Boglioli brings professional versatility and captivating insight to audiences across the country. Her positive message and riveting personal story encourages everyone to take a holistic approach to their physical and financial outlook.
As a BuddyIns partner, Boglioli focuses on educating financial advisors, agents, and consumers about the power of a long-term care plan.
wendy@buddyins.com 425-785-3218
Sources:

As an industry leader in long term care insurance, we understand the complexities of group enrollments Whether you ' re handling large employers, associations, or executive carve-outs, we provide the expertise, resources, and tools to ensure your enrollment is a success.
Access top-tier carrier contracts and powerful quoting platforms that make offering voluntary group benefits easier Exclusive Opportunities
Need help with a group webinar or strategy?
We're here to support you at every step, offering expert advice and guidance when you need it
Gain access to readyto-use strategies, custom collateral, and seamless marketing implementation to enhance your enrollments Strategic Marketing
Our enrollment and billing platforms ensure a smooth experience for your groups, from start to finish Advanced Technology


By Megan Wroe MS, RD, CNE, CLEC
It seems about every decade there are noticeable changes in our bodies and minds. From hormone fluctuations and metabolic shifts to skin and hair color changes, our body’s needs evolve over time so it should come as no surprise that our dietary goals should shift as we get older as well. In this article we will review the main dietary areas of concern for aging and what we can focus on in our meals and snacks to maximize health in our older years.
After age 30, humans lose about 3-8% of muscle mass every decade. After age 50, the body starts breaking down bone faster than it can build it. All this can be exacerbated by lack of movement and inadequate nutrient intake. Emphasize these nutrients to slow muscle degeneration and maximize strong bones:
» Protein: Aim for 0.7-1 gram per pound body weight every single day. Or you can think of this as 30g per meal and 15g per snack.
» Calcium: Yes, dairy is an excellent source but consider other sources that are even more bioavailable such as bony fish, soy and sesame seeds!
» Magnesium: Eat 2 tablespoons daily of nuts and seeds and you’ll be halfway there with your magnesium needs. Other fantastic sources are avocado, poultry, fish and yes dark chocolate!
» Vitamins D3 and K2: While you can get some of these from sunlight and fermented foods, supplementation is often recommended over age 50.
» Hydration: Less talked about in the world of bone and muscle health, but dehydration can lead to muscle wasting and bone leaching. Drink ½ of your body weight in liquids each day and don’t forget the electrolytes! Add ½ teaspoon sea salt + ½ lemon into a glass of water every day.
As we age our gut lining weakens and thins, and our gut bacteria variety tends to diminish. This can lead not only to bowel concerns, but also to nutrient malabsorption which can impact all bodily systems. Keep your gut strong and fighting with the following key nutrients:
◊ Fiber: 5 cups per day of mostly veggies, some fruit will meet most of your fiber needs. Other great sources are legumes, whole grains and even fiber supplements.
◊ Fermented Foods: Kimchi, sauerkraut, kefir and yogurt are all excellent for probiotics. Aim for at least one serving per day.
◊ Minimize Sugar. Sugar will work against all that beautiful probiotic intake you got from fermented foods. Keep added sugar to a maximum of 6 teaspoons (24g) per day.
Our hearts work less effectively as we age but that doesn’t mean a weak heart is inevitable! There are so many things we can do from food to movement to keep a strong beating heart. Dietary areas to focus on here are:
• Eating the Right Number of Calories: Excessive caloric intake can be stressful for our cardiovascular system but so cannot eating enough. Consider working with a dietitian and getting a body composition analysis to find out how your calorie needs may have changed over the years.
• Electrolytes: Sodium, potassium and phosphorus are critical to heart function. Do not eliminate them. Aim for plenty of fruits and veggies and use sea salt when seasoning.
• Healthy Fats: Ditch the industrialized oils that are highly oxidized like canola, sunflower, safflower and vegetable oils. Lean on cold-pressed oils like olive and avocado and even better, eat whole food fats instead of oils like olives, nuts and seeds.
Memory, focus and energy levels are all related to cognitive function which does not need to decline if we pay attention to how we use and what we feed our brains. In addition to quality sleep and challenging your brain often with puzzles, games, hobbies, education and social activities, maintain a brain health diet with the following:
◦ B Vitamins: Our energy powerhouses! Get your B vitamins from animal proteins like egg, fish and dairy, as well as plants like legumes and avocado.
◦ Magnesium: A repeater here! Eat the same foods you do for bone and muscle health to power up your brain too!
◦ Omega3s:Fatty fish is the ultimate source of these healthy fats. Aim for 2-3 servings per week alongside flax and chia seeds. If you can’t reach that goal, then reach for a supplement here.
Minimizing sugar is worth repeating here as well, since Alzheimer’s is often called Type 3 Diabetes.
This is literally just a sampling of ideas to improve your health as you age and minimize disease risk. We didn’t even touch on movement, stress resilience, sleep or social interactions! I hope you feel empowered by all the things you CAN do to be healthy in every decade!

Megan Wroe, manages St. Jude Wellness Center, an integrative wellness department of St. Jude Medical Center. St. Jude Wellness Center is located in Brea, CA and offers a variety of nutrition, fitness and restorative programs and services for prevention and condition management such as PD. Visit their website for more information: www.stjudewellnesscenter.org

By CalBroker Mag
Like the rest of the country, California’s aging population is booming. It is estimated that the number of people aged 60 and over will grow three times as fast as the rest of the population through 2060.1
As the aging population increases, you will likely see an uptick in long-term care needs for your clients. People with chronic illnesses and other disabilities also require long-term care, but older adults are more likely to need it. Knowing the average costs of long-term care can help you prepare your clients and choose the right long-term care insurance coverage for them as they enter their golden years.
Long-term care insurance covers services that help people who have chronic illnesses or disabilities live their lives when they no longer can manage on their own. These services may include in-home health care, in which a caregiver comes and prepares meals, reminds people to take their medications, does chores, and bathes the patient.
As with other medical services, a variety of factors influence the average costs of long-term care.
Population growth is a big factor.2 More people living in an area means that healthcare agencies are treating a higher volume of patients. California’s aging population could put a strain on resources. Older adults use medical services more often than younger people, accounting for over 34% of annual healthcare expenses.3
“Knowing the average costs of long-term care can help you prepare your clients and choose the right long-term care insurance coverage for them as they enter their golden years”
Your clients may also have a loved one in need of specialized care for conditions such as Alzheimer’s disease, dementia, Parkinson’s disease, or multiple sclerosis. Long-term care insurance covers treatments for these diseases and resources for helping patients manage their daily lives.
Other factors affect how much it costs to cover your clients. Their health and lifestyle choices, their commitment to preventive care, and their chronic health conditions can make treating them more expensive.
In California, heart disease is the leading cause of death, and the average life expectancy is 79.4 Other common causes of death in the state that warrant long-term care include cancer, stroke, and complications from COVID-19.
Gone are the days of long-term insurance for life. In reality, about 14% of people will need long-term care for more than two years at the end of their life.5 When recommending policies to your clients, you can help them save money by reducing the benefit period, but you need to factor in their health and their likelihood of needing long-term care.
Some long-term care insurance policies offer added benefits such as inflation protection to help your clients cover their bills even if the cost of care has increased. These benefits add to your clients’ premiums, but they can potentially save on out-of-pocket expenses by adding this option to their policy.6
Your clients can choose from three types of policies, including home care only, nursing home and residential care facility only, and comprehensive. Before recommending a policy to a client, make sure you understand their condition and their needs, so you know they’re getting the right coverage.
On average, the cost of a nursing home with a private room in California is $131,349 a year.7 An assisted living facility costs $72,570, and home care costs $72,846. These costs differ based on where in the state your client lives. For example, a private room in a nursing home in Modesto averages $140,611, while the same room in Santa Cruz averages $126,812.
Premiums vary widely in the state. Policies are available for as low as $300 a year and up to more than $1,000 a year.8
With California hosting three of the 10 most populous cities in the country, it’s not surprising that long-term healthcare costs are higher in the state.9 Less populous states such as Wyoming and Montana have lower healthcare costs, and the lowest averages are in the Southeastern United States.
There are steps you can take to save your clients money on their long-term care insurance premiums. Encourage them to keep up with preventative care and adopt healthy habits. You can also nudge your clients to consider getting insurance coverage earlier. Younger clients pay lower premiums.
You can also encourage your clients to get coverage with financially stable companies with a good reputation. Walk them through ratings from independent agencies to help them find the right coverage.
Seek out insurance policies with longer waiting periods. If your client can wait 90 days for coverage to kick in, they will pay lower premiums than they would for a policy they need in a month.
Considering California’s aging population, you will see an influx of clients in the next decade looking for long-term care insurance. Because the state has more people, it costs more to provide long-term care.
Your clients may pay less if they live in smaller parts of the state rather than the dense urban areas. Whatever their needs, you can help your clients save by encouraging them to stay fit and pay attention to their health. The good news is that technology is improving, allowing physicians to catch chronic illnesses earlier, which makes them easier and less costly to treat.
Health insurance is ever-evolving, too, with new regulations and guidelines developing each election cycle. By staying on top of new developments, you can recommend the best policies for your clients.
Medicare does not provide long-term care coverage or custodial care unless medical care is needed. Learn more about what is covered under your plan.

By CalBroker Mag
As the demand for long-term care soars, so do anxieties about paying for these essential services. According to a 2023 KFF survey, 43% of respondents don’t feel confident that they’ll be able to afford care as they age. Additionally, only 28% of adults aged 50 to 64 have saved money for future living assistance expenses.1
Insurance coverage for long-term care alleviates these concerns by providing financial support for extended care services. This insurance can give policyholders peace of mind and safeguard their financial futures. By learning about the ins and outs of long-term care insurance, you’ll help your clients effectively plan for their future health needs.
Long-term care insurance — also known as custodial care coverage — covers the costs of extended care services for people who need ongoing support. It pays for expenses not covered by Medicare or traditional insurance, such as assisted living and skilled nursing.2
This insurance offers coverage for people with chronic illnesses, disabilities, aging-related conditions, and other long-term health needs. For instance, a person with Alzheimer’s disease could use long-term care insurance to pay for specialized memory care services.
Insurance companies typically sell long-term care policies to young, healthy people to cover future medical expenses.
Eligibility criteria vary by insurer but may include:2
• Ability to climb stairs and walk several blocks
• Ability to perform activities of daily living (ADLs) independently
• Absence of AIDS, HIV, or arthrogryposis renal dysfunction cholestasis syndrome (ARC)
• Absence of symptoms related to Alzheimer’s disease, multiple sclerosis, muscular dystrophy, and other chronic health conditions
Policyholders must also meet specific criteria to begin using their long-term care benefits. Most insurers require a physician’s diagnosis for cognitive impairment. Policyholders can also receive benefits if their physician certifies that they need help with at least two ADLs for 90 days or longer.2
Long-term care insurance covers ongoing medical expenses for people with complex health needs that require extended and specialized support. Policy coverage typically includes these essential services:
In-home care coverage allows policyholders to receive healthcare services from the comfort of their homes. These services are available for seniors, people with disabilities, patients recovering from surgery or illness, and others.
In-home care takes many forms, including:
• Companion care: A caretaker provides non-medical services and social support to help patients stay engaged and prevent loneliness. For instance, an aging patient may go on daily strolls with their caretaker and get help with grocery shopping.
• Help with ADLs: An in-home care professional can assist with bathing, caring for dental hygiene, and other daily activities.
• Nursing care: A licensed healthcare provider travels to the patient to deliver healthcare services. For instance, a person recovering from a knee replacement surgery may receive wound management and physical therapy.
In-home care allows older adults and others who need ongoing assistance to maintain their independence. Patients who receive these services can remain in their homes and communities instead of moving to an assisted living or skilled nursing facility.
Insurance coverage for long-term care also includes facility care. This type of care allows policyholders to receive healthcare services in residential settings.
Common types of facility care include:
• Assisted living: Residents live in independent units and receive help with ADLs. For instance, staff may provide housekeeping and remind residents to take their medications.
• Nursing home: These facilities provide comprehensive medical care and 24/7 supervision. Nursing homes are a great option for people with limited mobility, cognitive impairment, and other conditions that require around-the-clock support.
• Memory care: Memory units offer specialized support for people with Alzheimer’s disease, dementia, and other cognitive disorders. These facilities typically provide brain-stimulating activities and have security measures to keep residents safe.
Facility care allows residents to build social connections with peers, reducing loneliness. These communities also offer communal dining, recreational facilities, and other amenities that improve residents’ quality of life.
Many people require assistance with everyday activities due to age, disabilities, and illnesses. Long-term care insurance providers typically allow policyholders to receive benefits if they can’t perform two of these six ADLs:3
• Bathing
• Continence
• Dressing
• Eating
• Transferring in and out of a bed or chair
• Toileting
Long-term care insurance enables eligible policyholders to receive daily assistance with these tasks. For instance, a person with a spinal cord injury could have an in-home caretaker who helps them transfer from their bed to their wheelchair. Similarly, someone who experiences a stroke could move into an assisted living facility to receive assistance with bathing and toileting.
Assistance with ADLs improves patients’ quality of life and allows them to maintain their dignity. Coverage for these services also reduces the strain on family members and enables policyholders to receive professional support.
People often assume they can use their long-term care insurance whenever they need it, but that’s not the case. Policyholders must follow their insurance company’s filing process to get reimbursed for claims.
First, policyholders should ask their physicians to verify that they need long-term care. This documentation should explain why they need these services and highlight any relevant diagnoses.
Additionally, long-term care insurance companies have a waiting or elimination period before coverage kicks in. Many insurers have a 90-day waiting period, but this window can range from zero days to up to six months. During this time, policyholders must cover all their long-term care expenses themselves.
After the waiting period, policyholders continue paying for their long-term care expenses out of pocket, but they can file claims with the insurance company for reimbursement. The insurer will assess the claims and decide whether to approve them based on its coverage policies.
Long-term care services allow individuals to age with dignity and receive essential healthcare. However, these services can cost thousands of dollars a month, especially for people who need specialized care.
As healthcare costs continue to rise, insurance coverage for long-term care has become a wise investment for many people. This insurance can enable policyholders to receive necessary care without wiping out their savings or going into debt.
As a reliable advisor, you can help clients understand the benefits of long-term care insurance and make informed decisions about their current and future health.
Medicare does not provide long-term care coverage or custodial care unless medical care is needed. Learn more about what is covered under your plan.
Sources: Medicare search.app/m9R7FW8yXmuCNi4d9 www.cahf.org/About/Consumer-Help/Facts-and-Statistics www.canhr.org/overview-of-medi-cal-for-long-term-care/ www.dhcs.ca.gov/services/medi-cal/Pages/DoYouQualifyForMedi-Cal.aspx www.hhs.gov/answers/medicare-and-medicaid/who-is-eligible-for-medicare/index.html

By CalBroker Mag
As California’s population ages, the demand for assisted living and nursing homes has skyrocketed. Currently, over 400,000 Californians stay in licensed long-term care facilities, and this population is projected to grow rapidly in the next decade. Two out of three of these residents depend on Medi-Cal to cover the costs of their extended care.1
Medi-Cal offers many benefits for Californians who need longterm care. However, residents must meet strict eligibility criteria and contribute a portion of their income. By understanding the relationship between Medi-Cal and long-term care expenses, you can help your clients make strategic decisions about their financial and medical futures.
As the name suggests, Medi-Cal refers to California’s state-specific version of federal Medicaid. This program allows qualifying California residents to receive free or low-cost healthcare services.2
Unlike Medicaid, Medi-Cal offers coverage for long-term care expenses. Recipients can get financial support for these services, among others:2
» Assisted living
» Skilled nursing
» Home healthcare
For someone to receive coverage, a physician must deem long-term care services as medically necessary.2
The program also covers many expenses unrelated to long-term care, such as ambulance services, eyeglasses, and X-rays.2
The requirements for qualifying for Medi-Cal have changed as of Jan. 1, 2024. Under the new guidelines, California residents may be eligible for Medi-Cal if they belong to one of the following groups:3
• Children, teenagers, and young adults under 21 years
• Seniors over 65 years
• Pregnant women
• Low-income people with dependent children
• Blind or disabled individuals
• Refugees
• People who have received breast or cervical cancer screenings
• People living in skilled nursing or intermediate care communities
• People who qualify for home- and community-based healthcare services
• Enrollees in CalFresh, Supplemental Security Income (SSI) CalWorks, and foster care
Californians may also be eligible for Medi-Cal if they earn 138% of the poverty level or below. For example, a single adult can qualify if they earn $20,783 annually or less. For a family of four, the income limit is $43,056.3
Historically, Medi-Cal considered assets, but the 2024 guidelines have eliminated this eligibility requirement. Qualifying long-term care residents can get coverage even if they own a home or have other property.3 This change simplifies the administrative process and enables recipients to keep getting support if they receive financial gifts or inheritances.
Medi-Cal doesn’t offer complete coverage for long-term care. Instead, residents in skilled nursing communities must contribute a portion of their income to their monthly care costs. This contribution is known as the monthly resident cost or share of cost.2
Medi-Cal uses a simple formula to calculate the share of cost:2
• Share of cost = Gross monthly income - out-of-pocket medical premiums - $35 for the personal needs allowance
• The personal needs allowance increases to $50 for SSI recipients and $125 for VA Aid and Attendance recipients.2
Say, for instance, a nursing home resident has a gross monthly income of $2,000. They pay $50 monthly for dental coverage and have a $35 personal allowance for clothes and other expenses. Their share of cost would be $2,000 - $50 - $35 = $1,915.
Medi–Cal pays the nursing home for any expenses not covered by the resident’s share of cost. In this scenario, if the monthly expenses total $5,000, the resident would pay $1,915, and Medi-Cal would cover the remaining $3,085.
Medi-Cal may temporarily reduce a long-term care resident’s share of cost if they have old, unpaid medical bills. Residents may also deduct medically necessary equipment, prescriptions, services, and supplies not covered by Medicaid. For example, if a resident pays $80 monthly for a prescription, they may have a lower share of cost.
While many California residents enjoy the benefits of Medi-Cal, it’s not the only way to receive financial support for extended care. Californians may also have coverage through Medicare or longterm care insurance. Here’s a quick comparison:
Medicare is a federal program that provides health insurance for people 65 and older. People with disabilities, end-stage renal disease, or Lou Gehrig’s disease may also qualify for Medicare.4
Medicare and Medi-Cal have different eligibility requirements. Medicare doesn’t have income limits, so anyone over 65 years old or with a qualifying health condition is eligible for this insurance. By contrast, Medi-Cal is only open to people who meet specific income criteria or belong to a covered group.
Additionally, Medicare only covers up to 100 days of short-term nursing care. Members who exceed this cap must pay for extended care expenses with their personal savings or long-term care insurance.
Long-term care insurance bridges the gap between extended care and Medicaid or regular health insurance. These policies offer coverage for many services, such as:
» Assistance with daily living activities like bathing, getting dressed, and getting out of bed
» Adult daycare
» Home healthcare
» Hospice care
» Memory care for people with Alzheimer’s disease and dementia
» Occupational, physical, and rehabilitation therapies
Typically, long-term care insurance companies reimburse members for medical expenses. Some policies have a daily or monthly cap, while others pay for a certain number of years of care.
In some cases, long-term care insurance offers more flexibility than Medi-Cal. Enrollees can receive care at their discretion instead of waiting on a doctor’s order, which Medi-Cal requires. Additionally, policyholders may pay less out-of-pocket than those who pay for Medi-Cal’s share of cost.
However, this insurance has a few limitations. Members must buy a policy before they need extended care and pay costly premiums. Additionally, people who exceed the coverage caps have to pay for additional expenses out of pocket, which can add up quickly.
No one wants to think about getting older or developing a chronic illness. However, many people will eventually need long-term care to support healthy aging and maintain a high quality of life.
Empower your clients to make wise financial decisions by discussing options for long-term care. Some California residents can qualify for Medi-Cal if they meet income requirements and other criteria. Other options include Medicare and long-term care insurance.
As a trusted health insurance professional, you can help your clients understand how each program works. You can also collaborate with them to develop a comprehensive long-term care plan to meet their financial goals and needs.
Medicare does not provide long-term care coverage or custodial care unless medical care is needed. Learn more about what is covered under your plan.
Sources:
www.kff.org/health-costs/poll-finding/the-affordability-of-long-term-care-and-support-services/ www.americanbar.org/groups/law_aging/publications/bifocal/vol45/vol45issue1/ltc-insurance-qual/ www.dhcs.ca.gov/services/ltc/Documents/Alert_Glossary.pdf

By Marcia Israel
Discussing future long-term care health needs and aging with Baby Boomers is tough. Yet, it’s important to have those delicate conversations about future care plans so you, your clients, and the people you love can live life on their own terms. Talking openly about life matters and about how to plan for future personal needs initiates an ACTION PLAN so family members can fulfill a loved one’s wishes--the where, the when, the who, and the how for future care. Deciding ahead about care planning and how pay for care—creates a smooth care transition when needed.
According to 2021 info from the Federal HHS Agency, "about 60% of people eventually need some type of long-term care Even a few years of personal care can be a major financial burden.” (1). Planning for potentially catastrophic healthcare costs at the end of our lives is a vital component of aging and retirement. This video demonstrates ways to begin “The Talk.”
What You May Learn from Your Clients? How You Can Assist Clients in Planning for FUTURE Care Needs
Lifestyle: What is daily life like now? What do their loved ones expect it to look like in the future?
Legal: Is there a will, durable power of attorney, or health care POA in place? Trust? Up to date? Accessible?
Finances: How are the bills currently being paid? Is there income that can be redirected for care if need be?
Medical Care: Are health histories and contact information for medical providers available? Up to date?
Alternate Benefits: Do they qualify for Veteran’s Benefits or Medi-Cal?
The Genworth Financial 2023-24 Cost of Care
Surveys (2) reported that the cost of a home care aide, assistance with the ADL’S, increased by 10% to an annual median cost of $75,500. The national annual median cost of a semi-private room in a skilled nursing facility rose to $104,000, an increase of 4.4%. The cost of a private room in a nursing home increased by 4.9% to $116,800. Assisted living facility rates increased by 1.4% to an annual national median cost of $64,200. With 10,000 baby boomers turning 65 every day until 2030, the demand for skilled personal care workers has increased, affecting future costs.
“Planning today for a future extended health event benefits families financially, emotionally, and/opsychologically.”
“Understanding extended care options and its true costs are critical first steps toward being prepared for whatever you want your aging journey to look like,” Jamala Arland, president/chief executive of Genworth U.S. Life Insurance.
The American Association of Colleges of Nursing reports that “a shortage of RN’s is expected to intensify as Baby Boomers age” ( 3); a recent House Ways and Means Committee hearing also made clear that the U.S. is experiencing a nurse shortage, as Baby Boomers are turning 65 in record numbers.
As trusted Health Insurance and Medicare advisors on the forefront of this “Silver Tsunami,” you are most knowledgeable about your clients’ health care, family, and extended care planning requirements. You can advocate for your clients’ care planning, including LTC Insurance. By proactively addressing these needs, you are helping them navigate complex insurance options and rights, along with comprehensive, sustainable health care plans.
Coverage Gaps: Medicare (ltd coverage for LTC) primarily covers short-term stays in SNF’s. Agents can help clients navigate these gaps.
Financial Planning: Extended care is expensive; costs should be anticipated. Guide clients, perhaps, in exploring payment options: self-funding, buying LTC Insurance.
Personalized Solutions: Advice can be tailored to clients’ health status, financial situation, and family dynamics.
Awareness of Options: Medi-Cal and Veteran’s Benefits eligibility; LTC Insurance choices; alternate funding sources.
Peace of Mind: Discussing care options may alleviate anxiety about future care needs, empowering clients to make better decisions and enhance their quality of life. Advocacy: Advocating for clients helps them navigate complex insurance plans, ensuring that they understand their rights/options.
Typical Objections to LTC Insurance--How
Experienced LTC Insurance Advisors Address These Cost: LTC Insurance premiums are high. Premiums can be individualized so coverage/ payment options fit the financial needs/budget of each family. Premiums may be deductible (check with financial experts). Complexity: Policies can be complex, difficult to understand. Seasoned agents clarify the options, benefits, and exclusions.
Perceived Low Need: Some people are in denial, believing they won't need personal care or assuming that they can rely on family members or other resources. Families differ, as do caregiving options. Fear of Wasting Money: Concerns about paying premiums for years; never using the benefits (or it’s a waste of money). Hybrid policies may mitigate this concern.
Premium Increases: People are wary of future premium increases. Policies sold now in CA are more rate stable.
Health Issues: Those with existing health problems believe it difficult to qualify for coverage (assuming the insurance isn’t available). There is a cost to waiting… Long Sales Cycle: LTCI has an extended underwriting process. Experienced agents explain the financial, caregiving, and psychological/emotional value of the coverage.
“Coming to terms with the fact that, at some point, you may need assistance with basic tasks as you get older isn't easy. Life is unpredictable, and being prepared is smart…LTC Insurance protects savings and assets against the high and ever-increasing cost of care.” (4)

No one can predict when or for how long someone might require extended care. Care costs are increasing. If one doesn’t qualify for government programs (i.e. MediCal) and/or doesn’t have enough assets to cover the costs, an LTC Insurance policy becomes advisable. LTC Insurance eligibility (through age 79) decreases with age; it depends on one’s health at the time of application. Families should decide ahead of the need to fund future care expenses as part of retirement and estate planning to safeguard assets, savings, and legacy.

Marcia Israel, a native of Los Angeles, (Go Bruins!) worked for many years with disadvantaged teens. In 2003, Marcia joined her husband, Stan, opening Stan Israel Insurance Services, Inc., a Life and Disability Insurance brokerage. The team then added Long Term Care Insurance to their portfolio and grew their expertise, offering CE licensing classes, CA Partnership courses, and general LTCI education to agents, financial planners, fiduciaries, and estate planning attorneys. As industry specialists in LTC Insurance, Marcia and Stan collaborate with financial professionals to offer all LTCI coverage options.
Sources:
https://acl.gov/ltc
https://www.genworth.com/aging-and-you/finances/cost-of-care.html
https://www.aacnnursing.org/news-data/fact-sheets/nursing-shortage)
https://money.com/what-is-long-term-care-insurance/

By Jennifer Turner
Medicare provides health coverage for more than 65 million Americans. Medicare, however, will only pay for short-term skilled nursing care. Consider certain medical situations to help your clients.
So, what happens if Mom broke her hip, is recovering in skilled nursing, but her Medicare coverage is running out and she still needs care? Who pays for her continued stay? What if Dad had a stroke, no longer requires skilled nursing care, and cannot live independently? Who pays then? What about when Medicare won’t cover the cost of skilled nursing care because certain criteria, such as a 3-day qualifying hospital stay is not met or one is not expected to recover from their injury or illness? Who pays then?
Adding further concern for many persons who receive Medicare coverage of skilled nursing care is the hefty daily coinsurance (the patient’s share of cost is $204/ day) for most days of skilled nursing care. Is there financial help for this?
When considering who pays for nursing home care, the length of one’s nursing home stay comes into play. Because Medicare varies the amount they will pay based on the length of time, other payers do as well. There are 3 periods of time; 1-20 days, 20-100 days, over 100 days.
Medicaid offers another option for paying for nursing care. In addition to paying for skilled nursing care, Medicaid will pay for non-medical, long-term nursing home care. While Medicaid will pay up to 100% of the cost (indefinitely as long as there is a need), a nursing home resident must contribute nearly all their income towards nursing home care as a Patient Liability. Note that Medicaid coverage is only provided for persons with limited financial means. For some people, the continuum from Medicare coverage of skilled nursing care to Medicaid coverage is fairly straightforward. For people who have income and assets greater than the allowable limits, it is a more complicated process, but not an impossible one.
In addition to discussing Medicare and Medicaid-funded nursing home care, this article will address the benefits of supplement insurance policies and how they are related to paying for nursing care. These plans, which include Medigap, Medicare Advantage plans, and employer-sponsored retiree health plans, can save seniors thousands of dollars. This is because they pick up some of the costs Medicare does not.
Medicare will only pay for short-term skilled nursing care. This is intensive medical care for persons who are in the process of recovering from an illness or injury. Examples include stroke recovery, rehabilitation after breaking a hip, and wound care following an operation.
Medicare Part A (hospital insurance) will cover up to 100 days of skilled nursing facility care per benefit period for persons who meet the eligibility criteria. Medicare will pay 100% of the cost for the first 20 days. In 2024, for days 21 – 100, the Medicare beneficiary must pay a coinsurance of $204 / day. This is their “share of cost”, or in other words, it is an outof-pocket expense for which they are responsible. A benefit period starts the day a Medicare beneficiary is admitted to the hospital or skilled nursing facility. The benefit period ends after 60 consecutive days with no need for hospitalization or skilled nursing care. A Medicare beneficiary is permitted unlimited benefit periods.
Skilled vs Custodial Care
• Days 1-20
Medicare pays 100% of the cost for Short-Term Nursing Facility Care
• Days 21-100
The Medicare Beneficiary Pays $204/Day Days 21+ is Custodial Care
• After 100 Days
The Medicare Beneficiary is Responsible for 100% of the Cost for Custodial Care
For Medicare to pay for skilled nursing care, the following eligibility criteria must be met:
• One must have Medicare Part A (hospital insurance).
• One must have a 3-day qualifying hospital stay (more below in the next section).
• One must be admitted to a skilled nursing facility within 30 days of the 3-day qualifying hospital stay. Care must be required for the same condition that required treatment during the 3-day hospitalization or for another condition that developed while receiving skilled nursing for the original condition treated during hospitalization.
• A physician has determined skilled nursing care is required on a daily basis.
• Skilled nursing care is provided in a Medicare-certified facility.
Medicare Will No Longer Pay, but Nursing Home Care is Still Needed. Now What?
• Private pay is one option. Nursing home care, however, is extremely expensive. Most persons cannot afford to pay privately, or cannot afford to do so for long.
• Long-term care insurance is another option, but again, one that is unavailable to many persons. The cost of such a policy is very high, and if one does not already have long-term care insurance, it is very unlikely an insurance company would sell them one with the current need of nursing home care.
For persons who are “dual eligible” (enrolled in both Medicare and Medicaid), Medicaid will pay for nursing home care for persons who meet all of Medicaid’s criteria for nursing home care.
Persons who are not enrolled in Medicaid, can apply. As long as a Medicaid application is pending, a nursing home resident cannot be forced to leave. It is not recommended that a relative or friend pay for care during this time. If approved for Medicaid coverage, Medicaid will pay for care from the date of one’s application. It may also pay for any days between Medicare coverage ending and one applying for Medicaid. It is possible to have retroactive Medicaid coverage for up to 3 months prior to Medicaid application. This means if one meets all Medicaid’s eligibility criteria during this period, Medicaid may pay for nursing home care during this time.
One does not usually have to switch homes if care becomes Medicaid-funded rather than paid for by Medicare. Most facilities that accept Medicare also accept Medicaid. Furthermore, many facilities offer both short-term skilled nursing facility care and long-term nursing home care.
California Broker is pleased to have a collaborative relationship with Buddy Insurance, a leading long-term care insurance education, marketing and technology company. CEO Marc Glickman and his specialists will collaborate with health and life insurance professionals to help design LTCi options. Learn more about LTCi and refer clients — or learn how to write your own LTCi policies using Marc’s system.
CONNECT to Buddy Insurance LTCi PORTAL HERE:
Group: www.buddyins.com/program/calbroker/group
Individual: www.buddyins.com/program/calbroker/

Jennifer Turner, joined Integrity Advisors in 2020 –a natural move as she became a healthcare advocate after 23 years as a high school teacher with a master’s in education. Jennifer cherishes developing a reliable rapport with each one of her clients. Jennifer loves helping her clients find the coverage that will help them live full, happy, and healthy lives.
By Jon Thomas

Last year I left a role and career in the financial services industry as a financial & insurance wholesaler and joined Amada Senior Care, a senior care agency dedicated to helping seniors age in place at home and find the financial resources to do so. I had come to recognize in my time engaging in the retirement planning conversation, that as retirees aged into the stage of life where they began to need some assistance and support, their best-laid ‘retirement plan’ was inadequate. They had planned, often with the guidance of their financial advisor or planner, for a specific amount of retirement income that was now woefully insufficient with the additional cost of health care, caregiving support services or the transition to a senior community. I met the Amada team at a conference and learned what they,
‘a senior care company’, were doing to help seniors uncover financial resources to fill this income gap. It was one of those ‘aha’ moments for me that led me to this question – does retirement end?
I’m sure you are perceptively saying to yourself now –‘well no, obviously retirement doesn’t end’. Unless of course your thought was, ‘Yes it ends…ahem…when you reach eternal retirement… Haha. That aside, most Americans work through their career years and have a corresponding financial plan that involves saving & investing with the goal of generating enough income to retire well and not have another financial care in the world, right? That is until they age to the point that they need significantly more income to address the costs of their aging. If their goal is to stay home, and they need caregiving support to do so, they could need anywhere from an additional $5K - $15K of additional income monthly. In some cities, a couple could need an additional $30K a month to stay home and receive caregiving support around the clock. Genworth’s annual cost of care study now estimates the median cost of home care in CA at nearly $7K monthly and just over $13K for a private room in a nursing home.
This reality is often an unwelcome surprise to retirees who don’t realize or understand the substantial expense of aging & care options and don’t have a plan to deal with it head on. This then begs the question –if retirement doesn’t end, why aren’t financial professionals addressing ALL of retirement in their clients’ retirement plans?
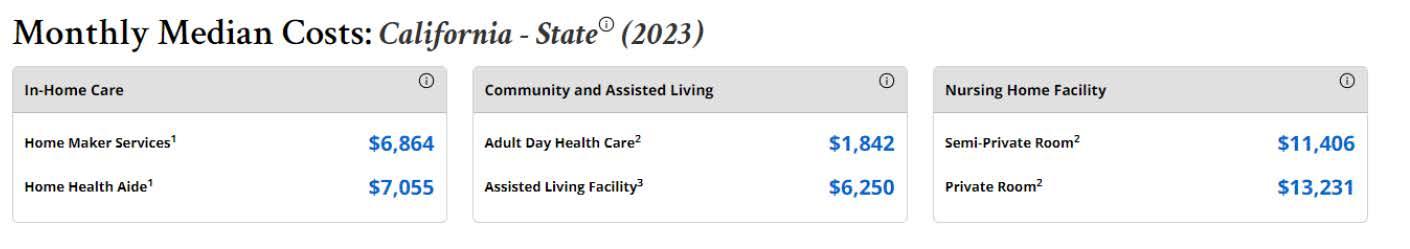
When I have a chance to consult with financial advisors or Medicare planners, I’ve been advancing the idea to use more than a 3-phase model for retirement or wealth planning. This model of Accumulation, Protection & Distribution leads to a retirement income plan that may not account for these increased aging costs. I’ll posit my proposed revision here:
The addition of an Acceleration phase accounts for the reality that the end of the aging continuum often requires an acceleration of assets to provide additional income. This acceleration can be a larger distribution of assets, retirement funds, annuity income or even the acceleration of insurance products.
One of the challenges with planning for this acceleration phase is that unlike retirement expenses which are often fixed, senior care expenses are variable depending on health changes and the degree of care that’s necessary. We cannot know with certainty whether our client will age gracefully, only needing a few thousand a month in income for help around the house and personal care services,

or if they will need substantial care for an Alzheimer’s or Dementia condition. This uncertainty is one of the reasons that I’m a big advocate of LTC insurance. It can create a substantial pool of benefits to cover some or all LTC expenses with the benefit of 1:4 or even 1:6 leverage on an investment. This can be a sort of forced savings for this Acceleration phase of retirement. . Additionally, for clients with life insurance, living benefit or death benefit acceleration riders are a great planning tool for this phase. This allocated resource can protect other assets, investments and keep legacy or inheritance plans in place.
You may now be thinking that this topic is worth some additional exploration, and you might even be open to implementing aging costs into your retirement income modeling. Your reservation is that you don’t have the expertise. Since retirement planning does not include standard aging costs it can be hard to broach this topic without a resource to partner with you in this journey.
This disconnect is why Amada Senior Care has begun partnering with financial professionals across the county and why I encourage you to build partnerships with senior care experts & advocates in your community. Not only can we serve as an aging resource to your clients, but we can also provide you with a real time picture of what the average aging or care story is in your community and what those costs really look like to aid in your client retirement planning. There are key benefits for your practice in this sort of partnership as well. A few reasons I would take this into consideration:
Long-term care expenses can quickly deplete savings and investment portfolios, leading to a drastic reduction in a client’s standard of living. A strategic partnership with your client’s care planning team or agency can allow you to work together to fund care expenses in the most advantageous manner for your client’s portfolio.
As the market evolves, financial advisors who broaden their service offerings to include long-term care planning will differentiate themselves from competitors. Clients are increasingly looking for comprehensive services – an advisor with meaningful senior advisor partnerships can bridge that gap for their clients. It’s astounding how many folks not only don’t have a financial plan for aging, but don’t have a Will in place or a POA, advanced directives or legacy plan. They end up vulnerable and their families scrambling when they inevitably have a health issue or care need.
Planning for long-term care expenses also significantly impacts generational retention. Family dynamics often shape financial decisions, and by proactively involving clients in long-term care discussions, advisors can also engage the next generation. When clients feel secure in their long-term care strategies, they are more likely to involve their children or heirs,fostering a family-oriented approach to wealth management. This multi-generational advisory relationship ensures that clients’ heirs understand their parents’ financial plans, which can lead to a seamless transfer of wealth and continuity in client relationships.
Some estimate that 90% of heirs change advisors promptly upon receiving their inheritance. At Amada, we strategically invite our client’s advisors into a care & financial planning meeting with our clients’ kids or family members, to ensure that connection to the next generation is established.
For an additional resource and more reasons to consider this type of partnership, check out – Amada & Advisor partnership guide
It seems to make great sense that our two industries should seek to partner together. I think of it as a relay race and your client successfully entering retirement. They worked hard, saved & invested. You’ve helped them navigate up to retirement, including Medicare and in many cases financial planning. When it comes time to consider medical and residential care needs, make sure you have subject matter experts to collaborate with to help your clients and their loved ones understand their options and connect them with resources.


Jon Thomas, ChFC, CLTC, Director of National & Strategic Accounts
Jon joined Amada Senior Care in 2023 after spending the last 15+ years working as a financial & insurance professional with companies - Nationwide Insurance and most recently Securian Financial, dedicated to helping grow market awareness of the importance of long-term care (LTC) planning. Jon has firsthand experience caring for aging loved ones and is passionate about the dignity and freedom quality LTC solutions can provide.
jon.t@amadaseniorcare.com 949-994-9690 www.AmadaSeniorCare.com

By Emma Peters
Today, we interviewed Carroll Golden about her most recent book: How Not to Pull Your Life Apart: Caregiving. budget. You’ve dotted every I and crossed every T… or have you?
Carroll S. Golden’s three simple steps kickstart critical conversations. They offer a path of discovery. In the following interview, we ask the author about the best ways to uncover a financially stable plan for you, your family, the people you love, and clients that are more likely than not going to deal with these issues at some point in their lives.
CBM: What was your motivation to write this book and your selection of this title: How Not to Pull Your Family Apart?
Carroll: “Growing up, I witnessed firsthand the importance of financial planning—my mother handled all aspects of long-term care with grace and efficiency. However, when I married into a different family, I experienced the opposite. Disputes over financial matters led to deep divisions, and the conflict between
my husband and his brother persists to this day. This painful experience opened my eyes to the need for a better approach. It inspired me to write my first book, How Not to Tear Your Family Apart, with a focus on equipping financial planners to prevent these situations by guiding families toward more collaborative, informed decisions.”
CBM: Many people will have personal experiences with family and the need for LTCi to address the cost of care. Tell us about the current numbers of people who will need LTC.
Carroll: “In the industry, we refer to this as ‘Peak 65,’ marking the time when a staggering 11,200 people turn 65 every day. This raises an important question: is our government or personal financial systems prepared for this wave of aging baby boomers? Many of them may not have the funds to cover the costs. According to Genworth, the national average for nursing home care in 2023 is $100,000 per year. Between 2021 and 2023, the cost of assisted living increased by nearly 18%, with the average cost of a one-bedroom apartment in assisted living now reaching $64,200 annually.
Many people, however, prefer to age at home, where they feel more in control. Yet, this option also comes with significant costs. Hiring help for daily tasks like cooking and cleaning can run around $30 per hour, with a minimum commitment of 4 to 6 hours a day. Ultimately, regardless of the route one chooses— whether nursing home, assisted living, or aging in place—the reality is that extended or long-term care is expensive."
CBM: In general, what are the options to cover expenses?
Carroll: Many people mistakenly believe that Medicare will cover long-term care, but in reality, generally, it only covers hospice care, which is not considered long-term care. The primary payer for longterm care is Medicaid, but it requires individuals to spend down their assets to qualify, which many people are hesitant to do.
For those who can plan ahead, Health Savings Accounts (HSAs) can be a great tool to pay for long-term care insurance premiums. This allows individuals to set aside money they can rely on to pay premiums during retirement when their income may be lower. While reverse mortgages were once a popular option, rising interest rates have made them less attractive.
I’ve worked with a life settlement company that repositions buy/sell agreements, especially in the context of mergers and acquisitions. Rather than using the entire buy/sell life insurance for one purpose, they divide it up into hybrid care solutions—such as life insurance with long-term care, annuities with long-term care, or a combination of both.
There’s also the option to purchase traditional long-term care insurance while you’re still young, since the cost of purchase becomes more expensive with age. Another approach involves using multi-purpose financial vehicles that combine benefits, which are becoming increasingly popular. There are additional options for multigenerational advanced planning that is best reviewed in the context of health and budget constraints.
The economic effects of family caregiving can result in financial strain with substantial financial consequences. A 2021 AARP study found that 38 million unpaid caregivers provide 36 billion hours of care annually, valued at around $600 billion. This highlights a critical point: caregiving can interfere with your own financial planning for retirement.
CBM: Since care in the home is often a preference over a facility, what advice do you have to work through the in-home process?
Carroll: If you don’t plan ahead, you’ll eventually find yourself in crisis mode, which is much harder to manage. The real challenge is starting the conversation. Approaching a parent or grandparent to discuss how they want to handle aging can feel uncomfortable, and many people may resist or shut down the conversation.
But aging in place isn’t just about finances; it's also about using the right tools to support independence. Today, there’s a wide range of technology available, from wearable healthcare devices to advanced home safety systems, like floors that can detect falls and alert help immediately. These innovations offer valuable solutions for making aging in place more feasible.
The key is to find a way to open the dialogue, emphasizing that it’s a personal and important topic.
CBM: What are your ideas on how to find care givers to help families cover their loved one's daily needs?
Carroll: When it comes to finding caregivers, you have two main options: you can either hire someone directly or go through an agency. In my book, How Not to Tear Your Family Apart, I dedicate pages 72-76 to help families navigate this process.
If you're hiring someone on your own, it’s important to gather the necessary documentation and clearly outline your expectations. For example, what happens if the caregiver gets injured while working in your home? You need to consider liability, insurance, and legal requirements. Be clear about what tasks you want the caregiver to perform.
If you’re using an agency, there are specific questions you need to ask them. For instance, how do they conduct background checks? What are their procedures if a caregiver doesn’t work out? It's crucial to be upfront about your situation. For example, when we hired in-home care for my own mother, she had strong preferences, like not wanting anyone to move her picture frames. These personal details are important for the caregiver to know.
Also, consider who will conduct the interviews—will you, or will the agency? And what happens if the caregiver isn’t a good fit? Does the agency charge for every interview or replacement? These are critical questions to ask before making a decision to ensure the care fits your family’s specific needs.
“Caught in the sandwich generation, slowly morphs from the casual helper to the ‘on-call’ caregiver heading towards ‘full-time’ caregiver.”
CBM: You mention planning is the best way to prepare and your three steps offer a guide to organize. Talk about the key points of each---The Care Guide; Care Squad; and Care Planning Team.
Carroll: Care Guide: Most care guides focus heavily on either medical or financial questions, but there’s so much more to consider when planning for care. For instance, even if you’ve set everything up perfectly, your parents might be using an app to store important medical information, but without access to their passwords, you could be left in the dark. It's crucial to include not just medical information but also practical details like passwords and financial access. A comprehensive care guide goes beyond just medical details—it’s a blueprint for managing all aspects of care.
Care Squad: As an advisor, you often hear clients say, "Don’t worry, my son or daughter will take care of me." But it’s important to dig deeper: How far away do they live? How will they respond in an emergency? Who’s going to contact them? It’s vital to assemble a care squad—a designated group of people responsible for specific tasks during a crisis. For example, one family member may oversee calling 911, another might handle transportation to the hospital, and someone else may take care of notifying the rest of the family. In my book, I’ve included a simple chart to help families organize their care squad, making sure the right people are in place to provide immediate support.
Care Planning Team: The care planning team (CPT) is focused on exploring all available options for extended or long-term care, whether for themselves or their loved ones. This involves researching whether life insurance with long-term care benefits or an annuity might be suitable. The book provides numerous resources and links to help families investigate different solutions. The team’s role is to look at what’s feasible for someone who is insurable, uninsurable, or has budget constraints.
CBM: For a health insurance professional, any last thoughts you want to share?
Carroll: As a health insurance professional, it's important that you can at least guide your clients in the right direction, even if long-term care (LTC) isn’t your specialty. Some advisors may feel uneasy about discussing these issues with clients, but it’s crucial to address them. You can say, 'While this isn't my area of expertise, I care about the work we do together, and I want to ensure you're informed.' You might offer them resources, like a book on the topic, and ask, 'Do you see yourself or a loved one in these scenarios?' This approach helps spark a conversation and distinguishes you from other healthcare brokers who might avoid the subject.
Additionally, there are LTC specialists you can refer your clients to, but first, reflect on your own situation. Are you comfortable discussing these topics with your own family? It's important to be able to handle these conversations before advising clients. Ultimately, as professionals in the healthcare industry, it’s our responsibility to ensure clients understand that while solutions exist, they require proactive planning.
CBM: The book has many resources you explain for covering the LTCi topics. This is a must have resource for both caregiving and how financial stability is connected to this topic. Our subscribers can find the book how?
Carroll: You can find my book, along with the others in the series, at The Caring Conversation. My books are also available for purchase through Amazon via the links on the website. The first book, How Not to Tear Your Family Apart, is a comprehensive resource for financial advisors. The second, How Not to Pull Your Family Apart, is a story-based consumer guide with planning options to discuss with an advisor. The third book, How Not to Pull Your Life Apart Caregiving: Overcome Challenges and Objections to Planning Conversations, focuses on handling difficult client conversations through real-life stories. Each of these books is designed to help advisors and agents provide guidance and planning support for their clients."
CBM: Carroll, thank you so much for your time. We at California Broker Magazine sincerely appreciate your commitment to providing the best advice for caregiving and financial planning.
I first learned the power of care as a financial professional. I worked with men and women who approached their finances with fear. Business owners wanted to do right by their employees, but feared the financial impact. Wives were scared of what would become of them if something happened to their husbands. Daughters, aunts, grandparents, stepchildren, adopted children...I’ve seen it all in planning, but it truly hit home when my own family was ripped apart fighting over financial caregiving of a loved one. My passion to help people unleash the power of care was born.


‘Tis the season for many social events, where you’ll be spending time with friends, close family, distant relatives, neighbors, and –yes – total strangers.
Many of these people might make great clients for you. Many others may never become clients but might have the ability to refer and introduce you to others. And a few might represent products and services to which you can refer others.
By Bill Cates, CSP, CPAE President, Referral Coach International
Let’s say you’re at a holiday party or other social event and someone asks, “What do you do?” How do you respond? Do you whip out your best elevator speech? Do you pretend you don’t want to talk about the great value you bring to your clients and quickly change the subject?
Are you blowing an opportunity by being too promotional or being too modest?
1
Mistake #1 –You smile because you have a chance to use that great networking event elevator speech that you’ve practiced 20 times in front of a mirror. You’re confident, passionate, and irresistible. (or so you think). The other person, looking a little stunned, responds, “That sounds very interesting. Excuse me while I freshen my drink.”
Mistake #2 –Because this is a social event and not a business networking event, you don’t’ want to scare anyone away. You don’t want to make it look like you came to this holiday party to prospect for new clients, so you downplay your value, you get overly modest, and you change the subject.
“So, hot shot Referral Coach, what should I say at social events?”
There is a middle ground. In fact, there are a number of ways to talk about your value at social events, so you don’t come across as salesy or that you’re even trying to turn that old friend into a prospect for your business.
Answer the question. If you’re a financial advisor, you can say, “I’m a financial advisor.” If you’re an executive coach, say, “I’m an executive coach.” But don’t stop there.
Shift to a specific example. You can say something like, “Let me tell you about a client I was working with the other day…” Then tell a little story.
At social events, you don’t want to talk like you’re reading your marketing brochure. Tell a story. The more interesting (or funny) the better. Of course, you leave the names out. And as best you can, tell the story in an interesting way – convey the problem that the client presented to you and then one or more of the solutions you presented in return.
I call this The Miracle VIPS Formula because it allows you to say quite a bit in just a few sentences. I’ve been using and teaching this formula for years. You can use it both in written and oral communication.
By filling in the blanks, you’ll create your ideal message.
1. I/we specialize in 2. I/we work with 3. Who want to 4. For example,
Here’s one example using this formula:
• My firm specializes in employee benefits for businesses.
• We work with owners of business with approximately 5 to 200 employees . . .
• Who want to remain competitive for the best talent and bring great value to their employees.
For example, I just finished transforming the employee benefits package for a company with about 120 employees. The owner hadn’t taken the time to take a close look at her benefits package over the last four years. Now, the employee benefits have been improved while providing substantial savings to the business owner at the same time. She’s ecstatic.
[An expanded explanation of this formula, as well as more examples are available in Bill Cates’s book, Radical Relevance.]
Ask a question that will help put a frame around the work you do and draw the other party into your answer. The question usually takes the form of, “You know how most people (or businesses) . . .”
You know how most people face retirement concerned about running out of money? I work with . . . who want to . . . .
You know how most CEOs wonder if everyone around them is sharing their most pressing concerns and best ideas? I work with . . . who want to
Have you noticed that most business owners seem to complain that their business owns them? I work with . . . who want to . . . .
I think you get the idea.
Play around with this a little. What question might you ask that could draw the listener into the rest of your message?

Bill Cates, is the author of Get More Referrals Now, Beyond Referrals, and Radical Relevance. Bill’s newest book, The Language of Referrals, has just been released and is available as a at Amazon in paperback, Kindle, and Audible. Bill is a highly sought-after coach, consultant, international speaker, and virtual presenter.
CalBroker Readers can get free (and valuable) tools here: www.ReferralCoach.com/resources.
Bill can be reached directly at: BillCates@ReferralCoach.com

2
Petersen International Underwriters piu.org piu@piu.org 800-345-8816
3
Pinnacle Claims Management Inc. www.pinnacletpa.com/excellence
4 Commission Solutions Commission Solutions phil@commission.solutions
31 BuddyIns https://buddyins.com/group Group: www.buddyins.com/program/calbroker/group Individual: www.buddyins.com/program/calbroker/
49
CalCPA Health CalCPAHealth.com/CalBroker 866-954-7406
50
Covered California www.coveredca.com/forsmallbusiness 844-332-8384


































































BONUS PROGRAM - COVERAGE EFFECTIVE: JULY 1, 2024 TO JANUARY 1, 2025




















Earn even more for offering your clients California’s most comprehensive access to doctors and hospitals:
Full Network PPO
• Blue Shield
HMO offerings from
• Blue Shield
• Kaiser Permanente
• Sharp Health Plan
CCSB offers 4-tier selection
Single bill
CCSB offers more Blue Shield Plans
EARN EXTRA WHEN YOU SELL NEW SMALL GROUPS
Contact your local Covered California for Small Business sales representative to learn why we’re growing and how we can help build your business! An increasing number of agents and their clients are glad they did.
CoveredCA.com/ForSmallBusiness 844.332.8384
1. Applies to new to Covered California for Small Business (CCSB) groups with initial effective dates of 07/1/24, 08/1/24, 09/1/24, 10/1/24, 11/1/24, 12/1/24 and 1/1/25
2. Agency must submit minimum of three groups to qualify for bonus program
3. Bonuses will be calculated on number of subscribers (employees) in e ect for the first e ective month of the policy as determined by CCSB.
4. No pro-ration of target values will take place.
5. Business written through partnering General Agencies qualifies.
6. Covered California will issue the second bonus (6+ groups) incentive payment forty-five (45) days following the conclusion of the incentive program so long as qualifying groups satisfy the ninety (90) day requirement outlined in Section (E)(2)(c) of Exhibit F of the Agency Agreement.
For a complete list of the program rules go to: https://www.coveredca.com/pdfs/Exhibit_F_Commission_Schedule_March_2024_Final.pdf
companies vary by region and are subject to change.