




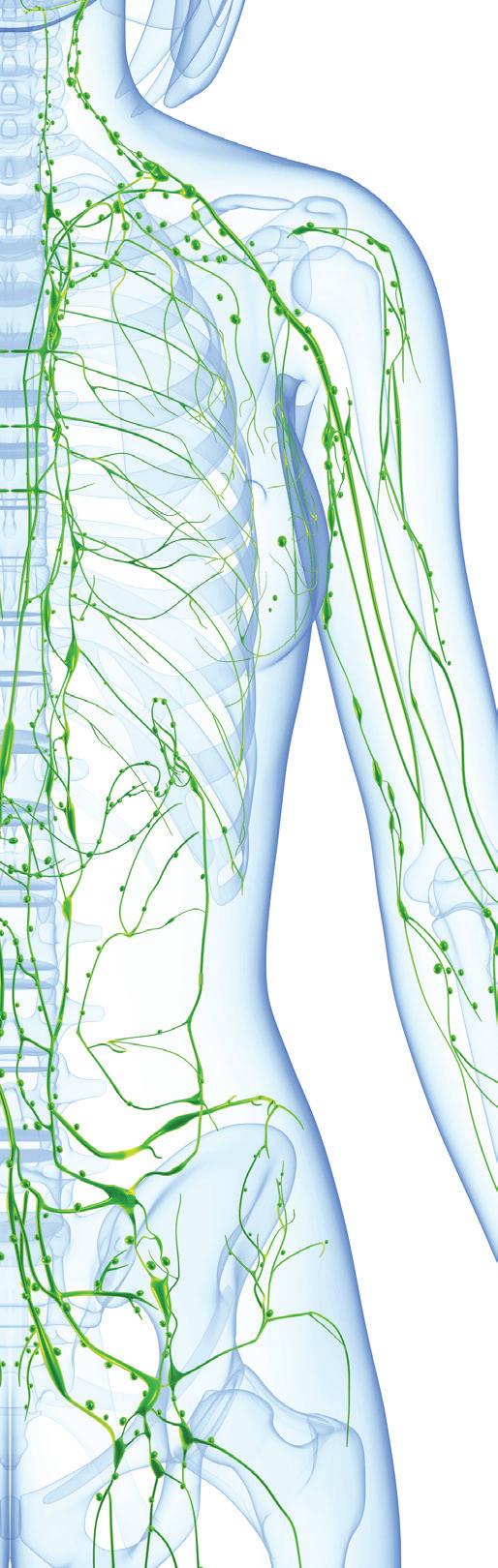
In Canada, lymphedema awareness is still in its infancy, and provincial associations are still fighting for recognition of the condition.
Aslymphedema treatment is under provincial legislation, every province has their own policies for compression garments and/or related therapies, leading to inequity in terms of care and coverage1. Nevertheless, people living with lymphedema share a few things in common: 1) lymphedema impacts their quality of life (QOL), 2) it has a financial impact (e.g. cost of compression devices and/or therapy), and 3) most are in search of a solution to reduce its burden2,3
It is recognized that lymphedema is a chronic and lifelong condition. Conservative approaches such as decongestive lymphatic therapy (DLT) and compression garments

The following points represent essential information for patients when considering surgery as a treatment option for lymphedema.
1 Surgical options that attempt to prevent or treat lymphedema, such as lymphaticovenous anastomoses, lymph node transplants, specialized liposuction and combination procedures are becoming increasingly available in Canada, with many subtypes and variations being offered. Availability and funding of surgical treatment may vary from province to province.
2 Not everyone is a suitable candidate. For example: in those with active malignant disease, obesity with BMI over 35 or 40, and severe venous insufficiency in the case of lower limb edema, surgery would likely not be appropriate.
3 You should be knowledgeable and consistent regarding conservative treatments (compression bandaging, devices and garments; other elements of decongestive therapy), and be well managed, prior to being considered for surgery.
4 Surgery is not a cure. You will have to live with a “new” lymphedema after surgery, hopefully requiring less onerous conservative treatment.
are key elements, but are not always easy to maintain, because the person is frustrated with ongoing lymphedema management (e.g. compression) and/or is impacted by financial limitations, as examples. Today, DLT is still considered the gold standard for therapy4 However, the last decade has seen lymphatic surgeries steadily increase in availability across the country. Procedures that had been offered for over thirty years in Europe and Asia and were only available if one was willing to travel and incur significant expense are now more accessible. As lymphatic surgeries are now in the picture, how are these changing overall lymphedema management? Time will tell! Through the
Marie-Eve Letellier, PhD, is a kinesiologist, a lymphedema therapist (Vodder) and an aqualymphatic therapy instructor (Tidhar). She is a clinician-researcher working in a hospital setting and she also has a private practice. She is a theory lymphedema instructor for the Vodder School International.
5 Imagery (such as CGI lymphography) will be necessary to determine if you are a candidate. Be wary if assessment of lymphatics via imagery is not offered.
6 Surgery should be provided within the context of a multidisciplinary team that includes lymphedema professionals who can assess, offer supportive therapies, and provide appropriate pre and post-operative care plus long-term follow-up to evaluate the results of surgery.
7 Do your research, speak with your therapist.
Produced by CLF Medical Advisors, Dr. Anna Towers and Dr. David Keast, and endorsed by CLF Board September 2021



lens of a brief, summary scoping review that the author conducted on lymphatic surgeries, the following is an overview of what these surgeries are, and their potential implications.
Lymphatic surgeries are broadly divided into two categories4-6:
1 Microsurgical procedures (physiologic therapy)
This type of procedure requires a thorough evaluation of the person, including at least a physical examination and a lymphography using indocyanine green (ICG). For best results, body mass index (BMI) should be less than 30 kg/m2 and not over 35 kg/m2
a. Lympho-venous anastomosis (LVA) or lympho-venous bypass (LVB)
This is the least invasive lymphatic surgery as it involves superficial vessels and is performed under local anesthesia. The aim of this procedure is to improve lymphatic function in the affected limb by redirecting lymphatic flow from a healthy lymphatic vessel into a nearby venule. The number of anastomoses varies depending on the limb (e.g., arm vs. leg) and based on the person’s patent lymphatic vessels.
b. Vascularized lymph node transfer (VLNT)
This procedure involves a donor site (e.g., omental, inguinal, mesenteric, lateral thoracic, axillary, gastroepiploic or submental nodes) unaffected by lymphedema, from which lymph nodes are taken, along with their vascular supply, and transferred to the limb impacted by lymph node dissection or where lymph flow is otherwise impaired.
therapy)
This type of therapy is proposed in advanced stages of lymphedema, where extensive interstitial tissue fibrosis and abnormal fat deposition have occurred. This does not address the etiology of lymphedema, but it is used to improve aesthetic outcome in a disproportionate limb.
a. Excisional procedures (Charles procedure)
The aim of this intervention is to perform a radical circumferential excision of subcutaneous tissue followed by skin grafting. This is rarely performed nowadays as it has a poor aesthetic outcome and many possible consequences, such as lymphedema recurrence.
b. Power assisted liposuction
This type of liposuction uses smaller cannulas that are possibly less damaging to lymphatic vessels. To be a candidate for this type of liposuction, the person must have no visible sign of pitting, indicating that edema as been replaced by fatty deposits.
As our understanding of lymphedema has progressed, techniques and technologies have evolved as well. In the last decade, improvements have been made in microsurgical procedures. For example, in different cancer centers anastomoses are now offered prophylactically at the time of axillary node dissection for breast cancer, reducing the risk of lymphedema development7. In addition, combination procedures are also seen (e.g., liposuction followed by LVA or VNLT) in order to provide the best outcome possible to the
person severely affected by lymphedema5
Suitable lymphatic surgery options depend on the person’s lymphatic mapping and pitting status. However, no matter the type of lymphatic surgery performed, the person must have already undergone conservative therapy and have either failed or plateaued. Furthermore, the person needs to accept that they will very likely still need to wear compression garments after the procedure, as well as continuing to perform daily management (e.g. exercise, skin care).
Like all procedures, lymphatic surgeries are not immune to complications. The risks associated with them are surgeryand patient-dependent.
Like all procedures, lymphatic surgeries are not immune to complications. The risks associated with them are surgery- and patient-dependent. These include, but are not limited to, bleeding, infection, poor healing of incision, anesthesia risk, donor site complication (e.g. seroma or lymphocoele, lymphedema), poor esthetic outcome, loss of sensation, partial or complete loss of the flap (VLNT)5,8-11. In the end, after having the confirmation of being a good candidate and being well informed, it is up to the patient to decide if the benefits will achieve their goals and if the potential complications are acceptable.
What does the literature say about these surgeries? Many reviews have been conducted in the last five years5,8-11. Their common conclusion: all lymphatic surgeries seem to provide the lymphedema patient with potentially improved lymphatic function and quality of life, with the affected limb(s) being reduced in volume, and with a possible decrease in the frequency of cellulitis and in pain. They also stipulate that long term follow-up and larger sample sizes are required to determine who the best candidates for each particular procedure are.
are acceptable.
In the end, after having the confirmation of being a good candidate and being well informed, it is the patient’s decision to choose if the benefits will achieve their goals and if the potential complications
Most studies will publish up to two years of follow-up data, and the literature reports that it could take from 12 to 24 months before the person obtains or sees results from the surgery. Long-term follow-up is also important to determine if the surgeries performed remain successful in the long run. Are the vascularized lymph nodes transferred still working or only the surrounding vasculature? Are the anastomoses still functioning? What is the limb lymphedema state after liposuction?
From a scientific rehabilitation perspective, a difference observed is the way that results are disseminated in the surgical literature. Often the “big picture” is missing in the reported data. For example, “from 2010 to 2021, 521 patients were operated on with (xxx type of lymphatic surgery), reporting on 457 as 64 were lost in follow-up (providing indications on the reason of the loss—ex. death, living out of the country, discharge from clinic, etc.) “
Another example: in the case of retrospective analysis, in some reports, it appeared that patients were excluded from the reported results if they were not compliant with the therapy or they had less than 3 volume measurements12. In order to know if the surgery is effective or not, this is valuable information that should be reported. The ideal process, to obtain the most accurate data on which to base effectiveness evaluations, would be for all patients who have had lymphedema surgery to be followed long-term by an independent resource, with no lost data (or at least reporting on the reason for the loss), but this is a dream and is unlikely to happen!
As with most published papers, this summary scoping review has its limitations. There is a plethora of literature available on lymphatic surgeries and it is mostly systematic reviews reported here, limited to English literature. This paper provides an overview of available lymphatic surgeries and does not provide a detailed analysis of each technique and sub-technique, nor are pre and postoperative care addressed.
To conclude, lymphatic surgeries are not a cure and should not be seen as a “quick fix”. They are a “no go” if the person is not a good candidate. Finally, they may potentially help patients who are already compliant with conventional therapies, have plateaued, have recurrent episodes of cellulitis, and/or want to obtain further improvement through lymphatic surgery. A full multidisciplinary team should be involved to work hand-in-hand, in a patientcentered approach. LP
A full set of references can be found at www.lymphedemapathways.ca
In summary, a few considerations if lymphatic surgery is even an option
Come visit us during the conference !
Friday, Dec. 3rd
Don‘t miss our Session on the Future of Lymph- and Lipedema Treatment !

• New products
• New technology
• Prizes
• And more ...




4 A thorough evaluation should be performed, ideally by a multidisciplinary team, including at least the surgeon and a lymphedema therapist.
4 The outcome of the surgery may depend on good lymphatic imaging, the surgeon’s experience, and the person’s adherence with pre and post-operative care. While aftercare is well defined after liposuction, protocols after LVA and VLNT will vary. Different recommendations are described and often these are surgeon-dependent.
4 Be informed and search for credible evidence: sites like PubMed or Google Scholar.
4 Viewpoints may differ among patients who have had lymphatic surgery, with some being positive as their lymphedema was reduced and less compression was required. Others might have had a negative experience in that there was a worsening of their lymphatic condition or no change occurred at all.
The content of this article has been reviewed by Dr. Joshua Vorstenbosch, MD PhD FRCSC, Plastic and reconstructive surgeon, McGill University Health Centre and Assistant Professor of Surgery, McGill University.