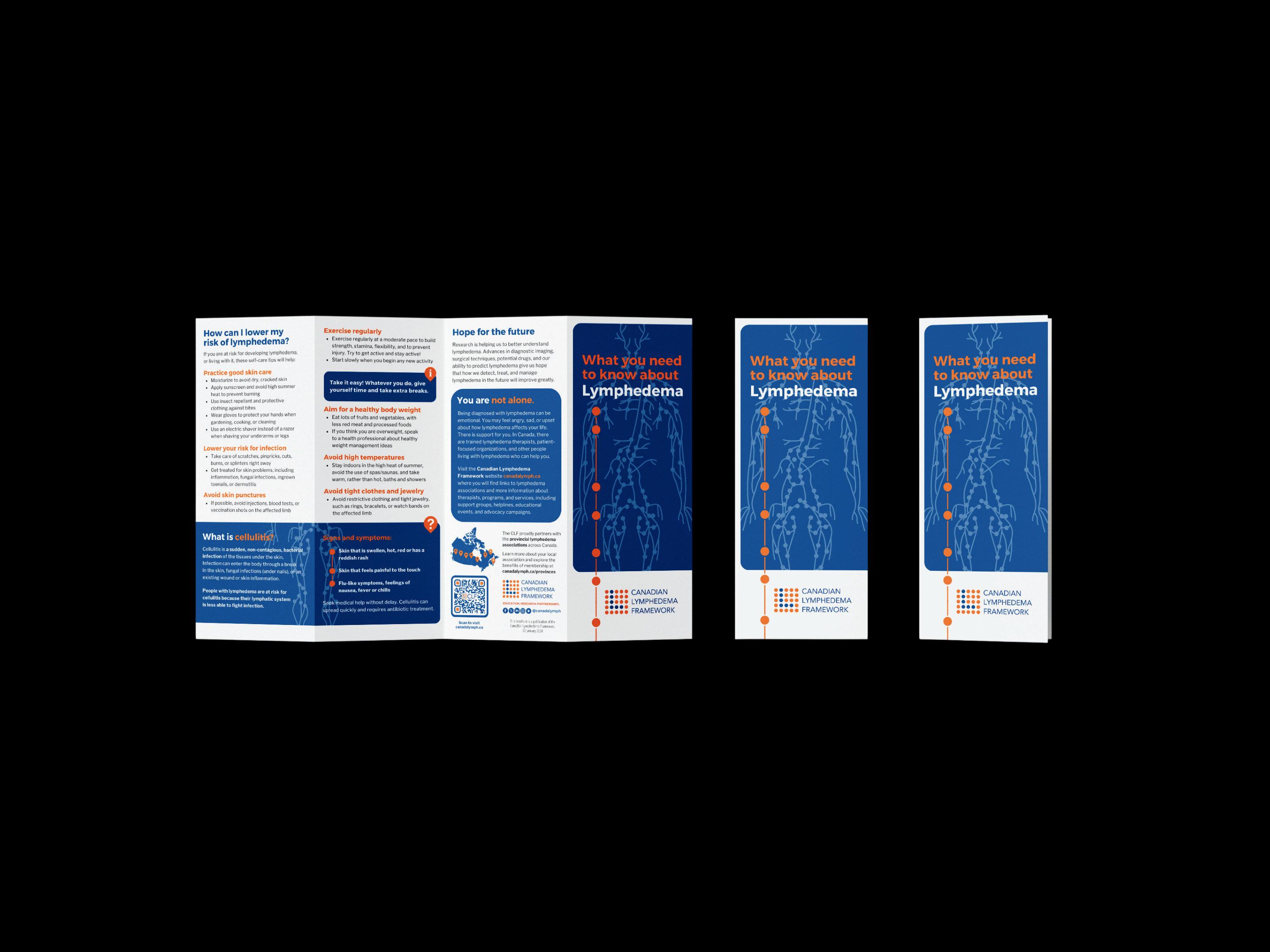
conditions/treating-lymphedema-and-chronic-edema/



conditions/treating-lymphedema-and-chronic-edema/

Patients were the focus of one conference session last fall entitled “What I have learned: patient-to-patient advice.” For many people facing a lymphedema diagnosis, the fear of what lies ahead can be scary. What better way to ease the journey than to hear from other patients who have already been through the challenges before you? Catharine Bowman, Lori Radke and Heather Watt spent a lot of time preparing for the interactive session, leading the discussions and writing the follow-up. They share with our readers the results of the workshop.
In our efforts to reach as many people as possible, this Spring issue of Pathways is complimentary in its digital format to everyone.
We continue our patient perspective series
“Where are they now” by featuring an update from James Lanning. Since his first story as a teenager living with primary lymphedema (Pathways Spring 2017), we feature an update on how James successfully manages his lymphedema as an adult leading an active lifestyle. He also volunteers his accounting services with the Newfoundland and Labrador
Lymphedema Association as Board Treasurer. They are grateful for his CPA professional input. The colourful cover photograph is of James and his partner enjoying a vacation in Italy.
As we were finalizing the production of this issue, we learned of the sad news that the McGill University Health Centre (MUHC) Lymphedema Program will end effective April 1, 2024, due to lack of funding. This funding decision affects us all, so we quickly swapped out an article to make room for this critical announcement and plead for your support. Closing this program will impact multiple advocacy efforts for integrated lymphedema care nationwide. Please download the QR code on page 17 and lend your voice to the important petition.
Yin yoga is a slow-paced style of yoga as exercise, incorporating principles of traditional Chinese medicine, with asanas that are held for longer periods of time than in other styles. Tracy Gardikiotis and Maja Kralovcova introduce us to this style of yoga and its impact on the lymphatics. This exercise could prove to have both physical and mental benefits for those living with lymphedema. You might want to give it a try.
Questions and answers from the closing session at the CLF national lymphedema conference have traditionally been shared with our readers in Pathways issues following the event. Some of the key topics for this issue include lipedema, obesity and prevalence.

We thank the doctors and clinicians who so thoroughly addressed topics of interest from the audience that our readers will benefit from as well.
Dr. Spencer Gibson is working hard to establish a patient registry in Canada. He led a discussion on this topic at the national conference last November. He shares key discussion points, including why this initiative is important and the challenges this project will face. We encourage all to support his efforts so we can learn more specifics about prevalence of lymphedema in Canada and address the gaps in service in order to improve patient care. March is lymphedema awareness month. In our efforts to reach as many people as possible, this Spring issue of Pathways is complimentary in its digital format to everyone. Please get in touch with us to add the email of friends, caregivers, doctors and other healthcare professionals who could benefit from learning more about lymphedema. LP
 Anna Kennedy
Anna Kennedy

Editorial Board
Mei Fu PhD RN FAAN
David Keast MD FCFP
Lori Radke PT CLT
Anna Towers MD FCFP Editor
Anna
Bonnie Baker
Nicole Boulet
Advertising and Submissions
We
The 2023 CLF National Conference featured an inaugural patient-to-patient advice workshop.
Q&A transcribed from the National Conference closing plenary, November 2023.
Identifying lymphedema patients in Canada
Dr. Spencer Gibson discusses the need for databases and the challenges this project will face.

Trying to lead as normal a life as possible.

Advocacy
The struggles of integrating lymphedema care into the healthcare system: An issue of distributive justice.





The 2023 CLF National Lymphedema Conference in Toronto featured an inaugural patient-to-patient advice workshop.
By Catharine Bowman, Lori Radke and Heather Watt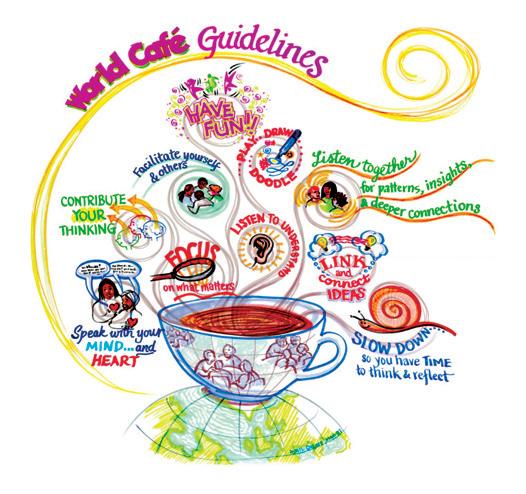
Patients were brought together to share wisdom and lived experiences with each other. The objectives for the session were to provide a safe, inclusive space for patients to collaborate, connect and create: 1) suggestions for newly diagnosed patients to make their lymphedema journey smoother and 2) a list of patient recommendations that reflect a goal of patient centered lymphedema management. Ultimately, the goal was to “elevate the voice of patients”. Workshop participation was restricted to patients (one spouse also participated) to create an open, sharing environment. Demographics of the participants can be seen in Table 1. The workshop structure was adapted from the World Caf é (www. theworldcafe. com) and used their guidelines and etiquette. The room was arranged to promote small, welcoming discussions with 4-5 people per table. All input was kept anonymous, and two disclaimers were stated upfront: 1) recommendations that were potentially harmful or contraindicated for other patients would not be included, and 2) before adopting any recommendations from the session, patients were advised to check with their healthcare provider.



The hosts prepared questions that were vetted and validated by patient representatives prior to the conference. Questions were categorized under four themes: Diagnosis, Initial Treatment, Ongoing Management and Next Steps. The workshop participants had 12 minutes to discuss each question and then post their responses on the wall. Some tables collaborated on their input, while others posted individual responses. The proposed outcomes for the workshop were to present the preliminary results at the conference’s final plenary, produce an article for Pathways and create a patient-to-patient brochure. Here are the results:
Based on your experience, what have you learned about the symptoms that you think a new patient should be aware of?
Contributors discussed the following symptoms.
n Pain n Discomfort n Pressure n Swelling
n Non healing wounds
n Limb heaviness
n Skin changes: hardening or tightness
n Tingling
n Nodular swelling
n Swelling that does not reduce overnight
n “Unexplained” swelling that comes and goes
n Changes in mobility
n Too much or too little movement causing changes in swelling
Catharine Bowman is a PhD Student in the Department of Epidemiology and Population Health at Stanford University and MD Student at the University of Calgary. She has been named one of Forbes Magazine’s 30 under 30.
Lori Radke PT, CLT is a physiotherapist and certified lymphedema therapist who coordinated the Rehabilitation Oncology program at the Tom Baker Cancer Center/Holy Cross from 2009-2021 and continues to work with lymphedema patients, both cancer-related and non-cancer-related, in Calgary.
Heather Watt OT, CLT has been an integral part of the development of an outpatient lymphedema clinic that focuses treatment of primary and secondary lymphedema excluding cancer related lymphedema.
People already have within them the wisdom and creativity to confront even the most difficult of challenges; that the answers we need are available to us; and that we are wiser together than we are alone.
(www.theworldcafe.com)
One contributor who had surgery-related lymphedema mentioned the importance of visually comparing limbs/body regions in a mirror or taking limb measurements to track the size of their limbs. This point was supported by the mention of many cancer survivors feeling that they were not made aware of lymphedema before receiving cancer treatment.
What did you learn about navigating the medical system when you first noticed symptoms? What recommendations would you make to someone trying to get a diagnosis?
Persistence was a major theme for the diagnostic journey:
n Be persistent
n Keep asking questions… don’t quit learning

TABLE 1
Participant demographics
TABLE 2
Theme Advice
Resilience and transformation
Resilience and transformation
Transformation
Just because there is “no cure” doesn’t mean there isn’t something you can do about it
It will get easier and you will manage
Be patient, have an open mind, embrace change and emotions that come with experience
Prioritization Prioritize your treatment needs
Finance
TABLE 3
Financial output for lymphedema management is an investment in your health needs
Category Resource
Online “Lymphie” social media sites
Online, print Websites and books
Online, in person Patient community groups - Be open-minded, but cautious (don’t listen to everything you hear)
Associations and organizations
Provincial organizations, CLF, LE&RN, search international and use all types of forums
n Know your body
n Self-advocate
n Educate yourself
n There is a lack of lymphedema knowledge when navigating the medical system
n Encourage new patients to educate their doctors
n Seek out multiple opinions regarding the diagnosis
n Minimal access to care
n Lack of funding for therapy and treatments
What components of Complex Decongestive Therapy (CDT) did you find the most beneficial and challenging?
Beneficial Challenging components components
n Exercise
n Self-manual lymphatic drainage
n Pool therapy
n Compression (also described as the most challenging)
n Being able to actually see the results of CDT treatments
n Balancing/ juggling the various components
n Encountering a lack of information and self-care information in the medical community
n Finding a CLTtrained therapist (particularly in rural locations)
n Bandaging
n Need for trial and error to find the optimal treatment sequence
Initial treatment
What tips would you give a new patient just starting the initial treatment for their lymphedema?
This question prompted many unique replies:
n Compliance is key
n Be kind and gentle with oneself
n Mindsets help manage life and treatment (see Table 2).
n Consistent compression: “Compression is your best friend!”
n Seek out additional information and a Certified Lymphedema Therapist (CLT)
One contributor suggested that having 1-2 weeks of intensive CDT offered to patients every few years would be beneficial, similar to the treatment model adopted in Germany.
What qualities/attributes would you recommend a new patient look for in their lymphedema therapist or compression garment fitter?
Therapist Fitter
Therapist and fitter
n CLT certification n Uses new techniques n Understanding
n Good listening skills n Are certified to fit n Empathetic
n Detail-oriented various brands
n Compassionate
n Measure accurately n Can work with various vendors n Experienced
n Taking time to connect
n Maintain up-to-date patients with resources product knowledge
When asked for the “best advice for other patients managing chronic lymphedema,” many patients spoke on mental resilience, recognizing there will be good and bad days, and emphasized the need for more self-care on hard days. Being patient with oneself/the process and realizing that acceptance can be a slow process. Socially, patients highlighted the importance of connecting with others in an uplifting way to help maintain a positive mindset, such as asking for help, finding a support group, advocating, and communicating with others (see Table 3 for recommended resources).
Contributors also offered routine and lifestyle advice for management:
n Nutrition and limiting alcohol intake
n Regular/consistent exercises (including pool)
n Elevation and stretching
n Home modifications, such as removing any tripping hazards to reduce potential for injury
n Search online for single shoes when LE increases size of one foot
The session concluded with a discussion on “the most important advice to share with patients recently diagnosed with lymphedema.” Once again, the themes of consistency, routine, and building self-care teams were emphasized.

Advice included “be your own advocate” and “keep being curious and learning”; connect with others and yourself, listen to oneself, do what feels best for the body and be sure to rest. Finally, patients said it is important to “stay positive, never give up and keep your spirits up.” This included being kind and patient and “breathing to know everything is going to be okay.” Ideas for sharing the information from this session included publishing and sharing with provincial lymphedema associations, circulating to general practitioners, therapists, surgeons etc. and sharing on websites and social media.
Powerful energy filled the room throughout the workshop, but it peaked amidst these final discussions. In the words of one workshop contributor: “The energy and enthusiasm was amazing. I had almost given up hope that things would change; this workshop renewed that hope!”
As we all departed the room, one advice caught our eyes: “Have hope. Don’t give up on your passions. Still live your life.” This statement is a powerful and important reminder to all living with chronic lymphedema. As hosts, we thank all the participants for their generous input and support for this endeavour. It certainly would not have happened without you! LP


Q&A transcribed from the closing plenary at National Lymphedema Conference, November 2023.
QRegarding the new ILA recommendation for diagnosis of lipedema. From the presentation, there is a European and US consensus. Can you speak to the difference between the European and US consensus?
Dr. Anna Towers: Yes. There’s an international consensus by the International Lipoedema Association and a US consensus published in 2021 in Phlebology. Dr. Keast and I belong to the International Lipoedema Association, which has a large proportion of Europeans and some non-Europeans. There are some significant differences between the two documents. One critique I have is that in the American document, they don’t have pain as part of the diagnosis, so it’s just a particular body shape. They also state within the document that 6 to 8% of women have lymphedema. They also say that 6.5% of children have lymphedema. There are a lot of things in that document that concern me. They say the treatment is sometimes extensive liposuction and certain medications that are unproven. Now, we have an obesity expert here. I don’t think extensive liposuction, starting with the abdomen, and repeated liposuction, is an accepted treatment for obesity, and it’s not an accepted treatment for lipedema. We’ve seen patients after these surgeries, and they have developed lymphedema and other complications as well. Read both documents and assess for yourself. I have the experience that following the US guidelines may cause harm to women who have obesity.




QHow can we get the medical profession to differentiate between obesity and lymphedema?
Dr. Denise Campbell-Scherer: Have them come to your lymphedema conference!
Dr. Anna Towers: I think the issue that I explained in my session is that once they develop obesity, and 90% of them will develop obesity, it’s hard to say, “This part is obesity, this part is lipedema,” so we need to do research on pure lipedema, which exists, to provide us with more information about how to differentiate between them. At a certain point, it all blends in: obesity, lipedema, lymphedema.
QRegarding Dr. Campbell-Scherer’s presentation on the 5As approach that includes the “warm handoff.” How do we work in a team when most of us usually work independently? What are some tools that we can incorporate?
Dr. Denise Campbell-Scherer: As we move more toward a team of care, we need to figure out creative ways to do that. On our webpage (https://obesitycanada.ca/5as-team/) there are many resources including a link to one of the specific tools for providers (see references). It was created to contain key messages to each other if they were seeing somebody with obesity so they could give them the key information about why they wanted them to see the other colleague. Normally, when people have obesity, they’re not expecting their dietician to be asking about urinary incontinence and things like that. There’s all these key messages that the provider can use with the patient to explain why they’re talking about that, and why they want to have the person see their colleague.

The first part is that therapeutic alliance with the person and shared planning together about what’s the priority for the person and then helping them hand the person to the right team member, and then the person wants to go. Without a warm handoff and the person’s super busy, will they necessarily understand why the provider wanted them to have another visit with another team member?
The second part is that people don’t like to repeat their story each time, so how do we have informational continuity so that everybody on the team knows what’s going on so that there’s a shared expectation?
When the person shows up to the colleague to talk about problem X, they’re expected, the person knows who they are, understand why they’re coming, and perhaps says, “Oh yes, my colleague was saying you’re going to come, so nice to meet you,” and the patient doesn’t have to repeat their whole story. For that, you need some way of having informational continuity. In our context, because I get to work in a primary care network where, in our clinic, we share electronic medical records, we have a way of having that information be shared. If you don’t have that, then what’s the way that you’re going to do that? Do you have some ability to message? Do you have some ability to share that information? What does that look like? As the person develops their care team with the relevant team members who can help them with the challenges they’re facing, they’ll develop relationships, but at the beginning, it needs to be a warm handoff.
QAre there any resources for health professionals interested in learning more about the tools and techniques discussed in your presentation “Motivating patients to make meaningful and sustainable health behaviour changes with relationship-centered care?”
Dr. Denise Campbell-Scherer is a Professor of Family Medicine and the Associate Dean in the Faculty of Medicine and Dentistry at the University of Alberta. Dr. Celine Koryzma is a clinical health psychologist in the Endocrinology and Metabolism Program within Alberta Health Services in Calgary, Alberta. Dr. Anna Towers is Director, Lymphedema Program, Supportive and Palliative Care Services, McGill University Health Centre (Montreal). She sits on the Editorial Board of Pathways magazine. Dr. David Keast is the Medical Director of the Chronic Wound and Lymphedema Consultation Clinic at the Parkwood Institute in London, Canada. He is Co-Chair of the Canadian Lymphedema Framework.




Dr. Celine Koryzma: I have a few resources that could be useful for people who are interested more in self-compassion and mindfulness. One of those I really like is Anxiety Canada (it used to be Anxiety BC). Anxiety is such a common condition that affects us all, including chronic disease patients, with a lot of worries about what the future will bring. There are a lot of fantastic resources and modules on their website (www.anxietycanada.com).
QBased on a report published several years ago, there are at least one million Canadians living with lymphedema. In your opinion, with good cancer treatment, do you think that this prevalence rate will go down?
Dr. Anna Towers: Two colleagues of mine who are here (Marize Ibrahim and Marie-Eve Letellier) are part of a working group mandated by the American Cancer Society and LANA to review the incidence of cancer-related lymphedema. Their work is almost over, and along with the results of the other literature reviews, will be published in a journal in the future. I’ll briefly summarize. The number
of cancer survivors in Canada is increasing because of the aging population and because cancer treatments have become more effective in prolonging life. Also the obesity rate is rising. Therefore the actual prevalence of cancer-related lymphedema is likely at least the same rather than decreasing. Even though surgeons perform fewer node dissections, and radiation oncologists use more conservative techniques, the severity of lymphedema cases may decrease slightly, but the population need will stay about the same. We will be publishing cancer related lymphedema incidence data this year. My colleague, Dr. Keast, is updating the figures for obesity, which is the most common cause of lymphedema in Canada. He will be upgrading those figures so we can publish a new CLF prevalence chart sometime in 2024.
QDo you want to make a few comments about obesity-related lymphedema and prevalence and how that’s going to affect our estimate of the one million Canadians who are affected because of the figures that we will publish in 2024?
Dr. David Keast: The challenges that we’ve got with prevalence data and how we have calculated it, is that one of the things that we depend upon is the census data. Remarkably, statistics counted in the long form of the Canadian census asked people to input their height and weight. So, we can get the percentage of Canadians with class three obesity or greater from that particular data. I have to go and find the last census and update it based on that, but they do have obesity data, bearing in mind that it is probably under-reported because it’s a self-reported height and weight. We all know that we tend to underreport our weight.
Conclusion: Thank you to all our speakers at this closing session for their excellent presentations over the weekend and for addressing questions from the audience. We hope this transcript has enlightened our readers as well. LP
References can be found at https://canadalymph.ca/ pathways-references







Lymphedema is a devastating disease that affects patients’ quality of life. Estimates on how many people suffer from lymphedema range widely. The most often studied incidence is in cancer-related lymphedema, where incidences ranged from 6% to 61%. Of these cancers, breast cancer is the most investigated, with incidences ranging from 11% to 57%1 One limitation of these studies is the reliance on one institution or centre to evaluate the incidence. More extensive studies have been conducted in the United States through the Lymphedema Education and Research Network

(LE&RN), an organization which connects multiple centres. They estimated that 10 million Americans suffer from lymphedema, and two main correlating factors associated with secondary lymphedema are cancer and obesity2. Extending this estimate to Canada, there may be as many as one million Canadians suffering from lymphedema. The Canadian Lymphedema Framework itemized this estimate among those suffering from chronic venous insufficiency, morbid obesity, cancer and other non-cancer related causes3
Using data from the Lymphedema Impact and Prevalence International (LIMPRINT) study, Canadians in an outpatient chronic wound management clinic were assessed. Data showed that most participants had lower extremity edema, and

more males than females were identified. In addition, over half of the participants were morbidly obese, with the most common underlying condition being venous disease4 The limitation of this study is the low number of participants only from one specialized clinic or institution, and the fact that the study is retrospective.
Although the CLF has provided us with an estimate, currently there is no way to accurately determine the number of Canadians suffering from lymphedema. There are few centralized lymphedema clinics, lymphedema is often not recorded in medical records, healthcare systems do not communicate effectively across Canada, and there is no follow-up for many lymphedema patients. The result is that lymphedema patients are left on their own to navigate the healthcare system, and there is limited monitoring of their progress or lack thereof. This leads to lymphedema patients being assessed and treated in various healthcare settings: surgeons, wound care clinics, rehabilitation clinics in cancer centres or hospitals and/or private clinics such as massage therapy clinics. The result is a patchwork of care and limited data to address the issues lymphedema patients face. Thus, there is a significant need to learn more about Canadian lymphedema patients to improve their care.
At the recent National Lymphedema Conference (November 2023), I led a discussion on the need to collect information on Canadian lymphedema patients. Healthcare providers and researchers were in attendance. The discussion focused on developing solutions. We talked about one
Dr. Spencer Gibson Ph.D. is a Professor at the University of Alberta in the Department of Oncology and the first Dianne and Irving Kipnes Endowed Chair in Lymphatic Disorders. At the national level, Dr. Gibson is part of the executive team representing the Prairie provinces for the Terry Fox Research Institute and a member of the Board for the Canadian Lymphedema Framework.
I envision a lymphedema registry/database where differences in the type of treatments lymphedema patients received and differences between male and female patients are discovered.
success story: the creation of cancer registries across Canada. This has allowed healthcare systems to track the incidence of different types of cancer and their outcomes. The annual report from the Canadian Cancer Society on Canadian Cancer Statistics gives important insight into the progress towards treating cancers and the changing incidence of cancers across Canada. In terms of research, these registries provide questions researchers could address, such as factors affecting treatment outcomes, differences between males and females and geographical locations associated with types of cancers.
A lymphedema registry/database could provide information on the prevalence of lymphedema, different types of treatment of lymphedema, differences between males and females, and other factors such as obesity. While living in Manitoba, I established a leukemia clinical database to assist in research. It led to changes in clinical practice in ways we could not predict. For example, we found out that the average age of leukemia patients being seen at the cancer centre was a decade younger than the average age of leukemia patients in the province as determined by the cancer registry. This led to letters sent to family physicians informing them that leukemia patients can be referred to the cancer centre even if they do not need treatment. This increased the age of leukemia patients in the cancer centre close to the provincial average.
I envision a lymphedema registry/database where differences in the type of treatments lymphedema patients received and differences between male and female patients are discovered. However, significant challenges remain. As mentioned, medical records often fail to record a lymphedema diagnosis, which impedes the identification of lymphedema patients.
One solution suggested is identifying healthcare providers that have contact with lymphedema patients and gain their consent for the registry/ database. This will create a network we can build upon. Another challenge is the fragmented provincial healthcare systems. Each province has unique health data systems that cannot be accessed across provinces for privacy concerns. A solution proposed could be creating a network of databases across the country linking information for research purposes. This has been accomplished with different

types of cancers, such as multiple myeloma. The limitations of any registry/database also need to be considered. One limitation often not discussed is patient bias. For lymphedema patients to be part of a database, they must be identified and consent to participate. This gives a bias towards patients actively seeking care, females and patients part of larger healthcare providers such as cancer centres. Another limitation is healthcare information. Many aspects of lymphedema care are not recorded in medical records. We will need to rely on healthcare providers or patient self-reporting to retrieve this information. However, this leads to inconsistent reporting and missing information. Understanding these limitations will provide solutions to overcome or shape research questions in the future.
Finally, funding is a major challenge. Databases and consenting lymphedema patients require money. Many funding agencies
want to fund individual research projects rather than registries/databases. Industry support was suggested for funding, but privacy and conflict of interest concerns must be addressed. Some provincial governments also have funding for this. These solutions will take time and effort, but discussing them now will give us a starting point.
In conclusion, lymphedema patients are underserved in Canada’s healthcare system. Patients are being cared for in different hospitals, wound clinics and rehabilitation centres with little information on their outcomes and rarely is the information shared within the healthcare system. A national registry/ database linking these patients across Canada is needed. This could provide information on the prevalence of lymphedema, types of treatment, and other factors contributing to lymphedema, such as obesity or cancer. The biggest challenge will be how to overcome the institutional and funding barriers. Working together, we can hopefully make patients count. LP
References can be found at https:// canadalymph.ca/pathways-references

mailto:info@klosetraining.com



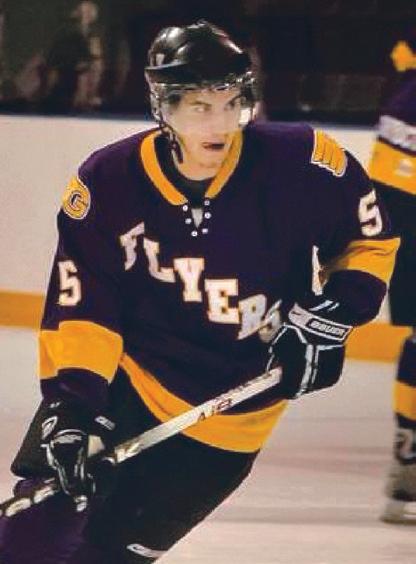
Ihavebeen living with primary lymphedema since I was diagnosed at age 14. The swelling presented in my upper left thigh and was first noticed by my friends in a hockey dressing room. A “growth spurt” that year was felt to be the trigger for my lymphatic system no longer compensating. That started a cascade of repeated infections and life changes that affected my adolescent life. Fast-forward 18 years and I am a 32-year old professional having lived with lymphedema for more than half my life!
Since graduating from University, I have worked with the same group of companies holding various roles in accounting, operations, and finance. Today, I find myself leading a team of passionate business professionals working for a local financial technology start-up whose focus is on helping entrepreneurs and organizations manage and grow their business. This has been a very rewarding career path and one that I am very passionate about.


In 2017, I was featured in Pathways and since then have had the privilege of speaking at national conferences organized by the Canadian Lymphedema Framework and Wounds Canada. I have even had the opportunity to do some modelling of compression garments for Jobst Canada. Where possible, I try to do my part in raising awareness about lymphedema. This has led me to join the board of the Lymphedema Association of Newfoundland and Labrador (LANL) as the treasurer this past year. Some would say this is a good fit given my education and career path. I completed a Bachelor of Commerce Degree from Memorial University in 2014 and then went on to obtain my Chartered Professional Accountant (CPA) designation a few years later.

When I am not helping small businesses manage their finances, I enjoy playing recreational hockey in the winter and golf in the summer. I also enjoy hiking with my Golden Retriever, Sonny along the many trails close to my home. My partner (who is a nurse) and I love to travel, recently visiting Italy, Spain, and France while we cruised the Mediterranean. For those who read the article in the Summer 2017 Pathways, you will know that my mother is also a nurse, who has completed training and certifications in Lymphatic Therapy. While it can be annoying at times to be surrounded by a couple of know-it-alls (just kidding!), I know that I am very fortunate to have health care professionals in my life to help me manage my lymphedema and keep me in check.
While I understand the importance of taking good care of myself to avoid serious illness, I still try to lead as “normal” a life as possible, and try to not let lymphedema define who I am. I have struggled with
James Lanning has been living with lymphedema in his left leg for the past 18 years. He graduated with a Bachelor of Commerce in 2014 and completed his Chartered Professional Accountant (CPA) designation in 2016. James enjoys living an active lifestyle, which includes playing many sports, mainly hockey in the winter and golf in the summer. Melanie Philpott, his partner, is on our cover.

While I understand the importance of taking good care of myself to avoid serious illness, I still try to lead as “normal” a life as possible, and try to not let lymphedema define who I am.
infections/cellulitis in my left leg and spent my share of time in hospital with sepsis! This has led to an increase in my leg swelling, which has progressed over time. Thankfully, I have not had a significant infection in the past two years, but it is always a concern especially when I travel internationally. I typically take a filled prescription of antibiotics with me in case a sudden onset of a skin infection presents.
Wearing compression stockings daily (40-50mmHg) and sometimes nighttime compression has become a way of life for me. I have used custom, readymade, and Velcro forms of compression. Compression garments are often very expensive, with insurance paying limited reimbursement. Unfortunately, the Government of Newfoundland and Labrador does not have an assistive device program for compression that covers everyone. This can cause barriers to effective care for many, including myself.
Newfoundland and Labrador have only a few people with expertise in lymphedema to help with the effective management and proper fitting of compression. There are times when inappropriate treatments are
prescribed, or a garment may not be correctly fitted. If mistakes are made in fitting it is usually the patient that pays the price. A trip to the hospital emergency room is always a marathon of trying to explain what lymphedema is and how infections are generally treated. It can be frustrating when trying to get timely access to care.
I believe that physicians/practitioners need to become better educated on lymphedema. It is important to listen and work with persons with lymphedema, as they are really the only ones who truly understand their condition and how it impacts their life.
While lymphedema is considered a physical illness, it can have just as much impact on your mental health. Living with lymphedema typically means having a limb or limbs that are disproportionately large compared to the rest of your body. This results in difficulties finding
Through living with this condition, I have learned a lot. I have learned perspective, I have learned compassion, and I have learned patience and mental toughness.

clothes that fit and not wanting to wear clothing that expose the affected area from the fear of people noticing. Having to constantly explain to people why I am wearing a garment or in my case, “why my leg is so big?” can at times become frustrating. I battle everyday with negative thoughts around body image and feeling like I am incapable of doing the physical tasks my body once did with ease when I was younger. As someone who is active and spent a large portion of my childhood and adolescence playing competitive sports,
it was certainly a difficult pill to swallow when I learned my lifelong dreams of playing sports at the next level would never be realized. Through living with this condition, I have learned a lot. I have learned perspective, I have learned compassion, and I have learned patience and mental toughness. I have learned that everyone has something they struggle with, many that are much more difficult than mine. So, while my lymphedema certainly does not define me, it has played a significant role in shaping who I am today and the way I choose to live my life. I find it helps to not take myself too seriously, and to find humour in my situation. If I can joke and make light of my condition, then it helps me cope and keep a positive attitude when things might not be going so well. LP

Expertly designed compression bras that feel like a hug


After being charitably funded for 18 years, the Lymphedema Program of the McGill University Health Centre (MUHC) in Montreal is threatened with closure effective April 1, 2024, due to a lack of operating funds. Does this decision impact only lymphedema patients in Quebec?
Absolutely not. The need for standardized quality lymphedema care affects everyone in Canada. But the issue is much more than just
the troubling news that funding has been suddenly and completely withdrawn for the MUHC Lymphedema Program under Dr. Anna Towers. We cannot think of worse news, not only for tens of thousands of lymphedema patients in Québec, but also for the national and international lymphedema care community.
Dr. Towers is internationally regarded as one of the most eminent authorities on lymphedema and its treatment. The MUHC Lymphedema Program is recognized as a Lymphatic Centre of Excellence, and is the only Canadian site to have achieved this distinguished recognition. The interdisciplinary model of care offered by Dr. Towers and her team is highly regarded as a model for other centres. The training and mentoring provided through this Program has yielded a highly skilled team of clinicians and patient advocates. These team members are also now sought for their expertise, for the findings of their continual clinical research, for consultation on challenging cases, and for their contributions to national and international lymphedema education and events.
Dr. Towers is one of the CLF’s founding members and served for many years as our Co-Chair. Though she has now retired from our Board of Directors, she continues to volunteer her time contributing to our mission in multiple ways. She is a member of our Medical Advisory Committee and our Editorial Board, serves on our Scientific Committees and presents at our conferences and educational events. She routinely contributes to our publications and best practice documents. Dr. Towers and her MUHC team have graciously shared their clinical expertise innumerable times over the years in consultation with clinicians and patients alike on complex cases.
Of course, the most distressing aspect of this terrible turn of events is the impact it has on cancer survivors and lymphedema patients in the province of Québec. It is difficult to calculate the ultimate, eventual cost of this misguided decision to withdraw funding. We can confidently assert that the vacuum of care that will result from this decision will have a devastating impact on the health and quality of life for existing and future patients. It will also incur significant costs to the public health system to care for the negative health impacts of not managing lymphedema for thousands of patients. These patients, untreated, are at an elevated risk of developing serious complications, such as cellulitis infections which can lead to sepsis, which can be fatal.
We implore you to seek a swift solution that will ensure the continuity of funding to support the operation of the MUHC Lymphedema Program so that Dr. Towers and her team can continue to care for this too often under-recognized, under-diagnosed and under-treated patient population...
funding. It’s fighting for lymphedema to be recognized as a chronic condition with care that deserves to be covered and integrated into our mainstream healthcare system. The MUHC Lymphedema Program is a model of care that other provinces reference in their advocacy efforts to have lymphedema diagnosis and care covered. Closing this program will impact multiple advocacy efforts across the country. With cancer treatments becoming increasingly high-tech and expensive, we need to increase advocacy for essential support services such as lymphedema care.
Following is an excerpt from the Canadian Lymphedema Framework’s letter of support (Figure 1) directed to MUHC hospital officials by the Executive Director (Bonnie Baker) and their Board of Directors. We encourage all Pathways readers, regardless of where you live in Canada, the United States or abroad, to urgently lend your voice by signing the petition as soon as possible (Figure 2). LP
FIGURE 2 – (Petition: abridged to fit spacing)
Recognition and continuation of the Lymphedema Program of the McGill University Health Centre (MUHC) of Dr. Anna Towers and her specialized interdisciplinary team. My name is Georgina, and I have metastatic breast cancer. In 2012, while undergoing chemotherapy, my left arm started to swell. By the time I found Dr. Towers’ clinic and was diagnosed with lymphedema, my left arm was 40% bigger than my right arm, which really affected my function and quality of life. Had it not been for Dr. Towers and her team, my lymphedema would have probably progressed to a more advanced stage. If the clinic closes in a few weeks, I, along with hundreds of other patients, will no longer receive the best cancer-related lymphedema care. …The Lymphedema Program of the MUHC is an internationally designated LE&RN Network of Excellence, in the same league as the lymphedema programs at the Mayo Clinic and the Memorial Sloan Kettering Cancer Center in the USA. Founded in 1994, this unique interdisciplinary program has served over 20,000 lymphedema patients to date. Comprised of a specialized interdisciplinary team of lymphedema physicians and therapists, this program is recognized provincially, nationally, and internationally for its expertise in the following three areas: Clinical excellence: To provide patients interdisciplinary expertise in the clinical evaluation, diagnosis, and management of lymphedema Education mandate: To educate patients and healthcare professionals in the disciplines of medicine and allied health, and to contribute to the specialized training of the next generation of clinicians Research mission: To act as scientific leaders in the promotion and advancement of best practices in the early identification and management of lymphedema. To supervise university students at all training levels on lymphedema-related research projects.



On behalf of myself and all cancer patients and survivors, I need your help to keep these services! Please sign and share this petition to ensure the sustainability of the MUHC Lymphedema Program, including the integrity of its specialized interdisciplinary team, by securing the operational funding required to pursue its mission.

YinYoga is a slow-paced style of yoga suitable for all levels of fitness and flexibility. Based on ancient Chinese philosophies, yoga postures, also known as asanas, are held longer than most yoga styles. The purpose is to stretch the body’s deep connective tissues, including ligaments, joints, and deep fascia, and to restore healthy flow of energy (Qi) and circulation in our bodies.
The three main principles of Yin Yoga include finding the first edge of intensity (coming into a pose to an appropriate depth), becoming still in each posture (using the breath to resolve to remain still) and holding

the postures for a length of time (one may stay in an asana for up to five minutes or more). Participants are encouraged to utilize props (i.e. bolsters, blocks, blankets, pillows, etc.) to provide additional support in a gentle stretch, such as to increase or decrease intensity, to create length and space, and to make a posture available. During the extended holds of the yoga postures, participants are encouraged to focus on their breathing and staying present with their body’s thoughts and physical sensations. This


focus helps to engage the parasympathetic nervous system and create a more relaxed state.
There are no specific scientific studies of Yin Yoga. However, there are many studies of yoga and meditation in general from which we can reason Yin Yoga would generate similar benefits. A meta-study in 2011 summarized several significant physical and mental health benefits of a regular yoga practice1. These benefits

the thoracic duct and key superficial lymph node areas to facilitate lymphatic drainage through a normal lymphatic system. Adding focused diaphragmatic breathing while in these postures allows for a deeper lengthening of the connective tissue and stimulates deeper lymphatic circulation.
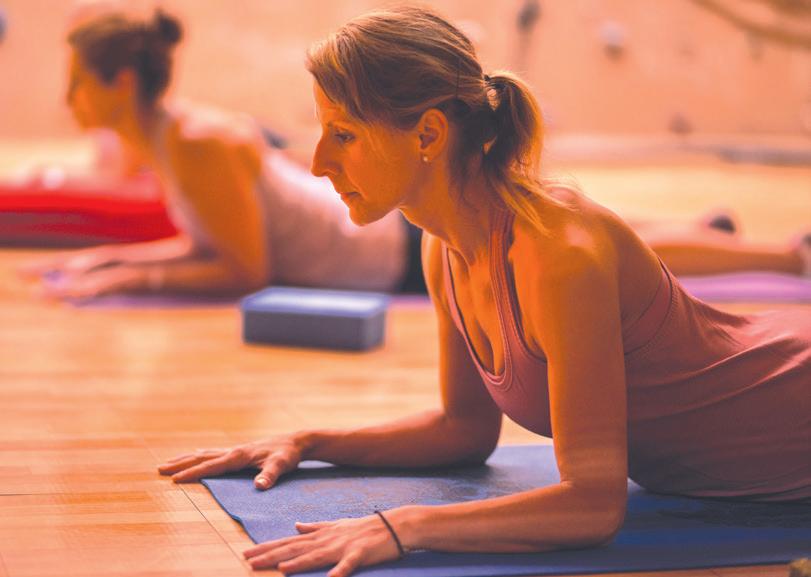
included enhanced muscular strength and body flexibility, promoted and improved respiratory and cardiovascular function, promoted recovery from and treatment of addiction, reduced stress, anxiety, and chronic pain, improved sleep patterns, and enhanced overall well-being and quality of life.
When Yin Yoga is performed to help support the lymphatic system, yoga postures are performed in a specific sequence to release tissues and create joint movement around
Tracy Gardikiotis, BScPT, CLT-LANA, CCES is a senior therapist, lymphedema services at the Pasqua Hospital in Regina, Saskatchewan. She treats all types of lymphedema and specializes in cancer rehabilitation and cancer related lymphedema.
Maja Kralovcova, B.Kin, CSCS, SMSC, RYT is the owner, Premium Performance Coach and certified yin yoga and restorative yoga teacher at Level 10 Fitness in Regina, Saskatchewan. She is a certified strength and conditioning coach with the NSCA.
Yoga has been reported as one of the complementary and alternative approaches used by patients diagnosed with breast cancer-related lymphedema (BRCL). Limited research has shown that yoga positively affects arm range of motion, strength, function, and quality of life amongst women at risk for and with BRCL and no new onset or exacerbation of lymphedema2,3,4. Further application and research are needed to demonstrate its effectiveness fully.
Inpower, a Saskatchewan-based breast cancer support group, has provided a free online yoga program through their Funded Fitness initiative since April 2020 to women with breast cancer across Saskatchewan.


Yin Yoga for The Lymphatic System was initially offered to provide a home-based self-management tool for women at risk for or diagnosed with BCRL during the lockdown phase of COVID-19 when patients had little or no access to in-person lymphedema treatment. This specialized yoga class was developed by Maja Kravlocova, an exercise therapist and certified yoga teacher at Level 10 Fitness, and Tracy Gardikiotis, a local lymphedema and oncology physiotherapist. Through their collaboration, they developed a program utilizing the main principles of yin yoga. They modified the sequence of postures to ensure they follow the principles of manual lymphatic

drainage to use alternate pathways for people with lymphedema or at risk of lymphedema and to help improve mobility in areas affected by cancer treatments. In addition, Maja provides numerous modifications of the different postures during each session, including chair yoga positions, to accommodate the needs of the participants.
Yin Yoga for The Lymphatic System has been offered through Inpower for the past three years. It has become one of the most popular Inpower Funded Fitness initiatives with consistent and high attendance. Many participants have reported positive feedback to Inpower of both physical and mental benefits



and continue to use this program as a selfmanagement tool for their lymphedema and cancer-related impairments.
Maja and Tracy recently presented Yin Yoga for The Lymphatic System sessions for both upper-extremity and lower-extremity lymphedema to patients and healthcare providers at the Canadian Lymphedema Framework 2024 National Conference. They hope to continue to share their experience and help others build programming for their local lymphedema communities. LP
References can be found at https:// canadalymph.ca/pathways-references

https://www.vodderschool.com




Therapists are often asked about the best skincare products for washing and moisturizing. Besides referring them to a pharmacist, is there anything else you could recommend?
Basic principles: Your skin is protected by an acid that is a type of protection layer. Because many soaps are highly alkaline, they strip that acid off the skin, and you lose the protective barrier that’s there to keep foreign objects and organisms from entering your body.
Soaps: Talk to your pharmacist about what soaps are available that have a balanced pH level. You want a pH soap that’s not much more than about seven, which is perfectly neutral to help protect that acid mantle. The key is, particularly for people with lymphedema of the lower extremities, to protect that acid mantle and that barrier





up with a contact allergic dermatitis from using too many “lotions and potions” on their skin.
Summary: It’s a case of simple, good cleansing with a pH-balanced soap and using a topical emollient that doesn’t have a lot of additives, to help protect and preserve that barrier. LP




















function of the skin. That comes from daily cleansing of the skin with pH-balanced soaps and then applying some form of emollient. I use the word “emollient” because we’re not trying to add water to the skin; we’re trying to prevent water loss. Emollients: Normally, at any given time, a great deal of water vapour escapes through the skin. The purpose of an emollient is also to put a barrier there. Simpler is better. Be careful of expensive skincare products that have all kinds of additional ingredients, most of which we have no idea whether they’re helpful or harmful. Unfortunately, people can end




































Source: Dr. David Keast, as presented in the final Q&A of the National Lymphedema Conference.


We would love to hear from you! Please send us your practical hints and tips on managing lymphedema to share
















































https://www.wearease.com/en-ca























Background: Head and neck (H&N) cancer treatments may have significant side effects that could be physically, functionally, and psychologically debilitating. Head and neck lymphedema (HNL) is a commonly neglected side effect that remains underdiagnosed and understudied. HNL could manifest externally, internally, or both, and could affect as much as 97% of the patients and may profoundly impact vital physical functions. Although the use of compression is well documented for the management of cancer-related lymphedema, to date, current data surrounding the use of H&N night compression and its effect on lymphedema management is sparse. Methods: Retrospective analysis of H&N patients seen between January 2016 to May 2023. At each time-point, an inventory questionnaire was used to assess symptoms and functional restrictions. In addition, lymphedema was assessed using neck circumferences, facial composites and tragusto-tragus measurements. Management of HNL using compression garment, along with body weight were recorded and compared over time. Results: A total of 86 patients were reviewed (74% males and 25.6% female), with a mean age of 64.6 years. Total neck circumferences: patients wearing compression, 67% showed a reduction with compression, while 41.5% also showed a reduction, however without the use of compression. Total facial composite: no significant change wearing or not wearing compression. Tragus-to-tragus: 57% showed a reduction with compression, however 54.5% also showed a reduction despite not using compression. Conclusion: Our observations suggest that despite the vital use of compression for upper and lower limb lymphedema, patients with HNL tend to be at their worst initially and significantly improve over time. Our analysis indicated that the majority of patients showed a reduction in their HNL despite not using compression




garments. Future research is warranted to establish if interventions other than compression therapy play a role in favorable HNL outcomes, such as H&N exercises and/ or self-massage.
Source: Management of lymphedema related to head and neck cancer. Presented at the 2023 Canadian National Lymphedema Conference by Marize Ibrahim. Additional authors: M.E.Letellier, A.Yung, M. Asselin, G.Cama, G. Chaput, A. Towers
Background: Lymphovenous anastomosis (LVA) and vascularised lymph nodes transfer (VLNT) are receiving growing attention with an increased number of surgeons being trained in lymphatic surgeries and reporting their own outcomes. We have been independently following patients who have undergone lymphatic surgeries since 2018 with standardized measurements and volume calculation to objectively assess surgical outcomes over time. Methods: Patients who have undergone LVA or VLNT are followed prospectively. Circumference measurements are taken for bilateral extremities pre-surgery and approximately every three months post-operatively for at least two years.

Percentage edema volume is calculated for each limb. Use of compression garments is also recorded at each visit, along with the number of cellulitis episodes. Results: Nine women have been independently followed: 7 with breast cancer-related lymphedema (BCRL), 1 with bilateral primary lower limb lymphedema (LLL) and 1 with bilateral cervical cancer-related LLL. Of the 7 BCRL, 3 had LVA surgery and 4 VLNT. Arm volume measurement increased for 5 women, while a decrease was observed for 2 women. The 2 LLL had LVA procedure: 1 presented with fluctuation in volume over time while the other decreased. Regarding compression, 6 women continued, while 3 stopped, despite volume increase. One episode of cellulitis was recorded post surgery in 3 women. Conclusion: As lymphedema has historically been defined as a chronic condition requiring lifelong care, our results emphasize the benefits and need for longitudinal follow-up
in those who have undergone lymphedema surgeries. It is critical to objectively evaluate post-surgical outcomes of lymphedema, addressing both acute and long-term potential effects. The need for compression garments may also need to be re-evaluated post-surgery as many still require usage, despite the surgical intervention. Longitudinal follow-up with this clientele is essential to better understand the impact of lymphedema surgeries on the lymphatic and venous systems.
Source: Independent prospective follow-up of lymphedema patients who have undergone lymphatic surgeries. Presented at the 2023 Canadian Lymphedema Framework National Conference by Marie-Eve Letellier.
Background: Lymphedema is a common side effect of cancer treatment affecting breast cancer survivors. Patient, cancer, and treatmentrelated factors contribute to the risk of its development. Circulating inflammatory cytokines are not currently used in routine clinical practice for prognostication and their role in predicting lymphedema risk remains unclear. Methods: The study population comprised of a subgroup of breast cancer survivors who participated in a radiotherapy cytokine study from 2010-14. Lymphedema-associated cytokines of interest included IL-4, -6, -17 and TGF-β1. Clinical and integrative risk models were developed to predict the occurrence of lymphedema. The established clinical risk model included age, body mass index, breast density, pathological lymph node burden, and axillary lymph node dissection. Recursive partitioning analysis (RPA) was implemented to develop an integrative model incorporating essential inflammatory cytokine prognostic biomarkers. The discriminative performances of the clinical and integrative risk models were compared using the concordance index (C-index). Results: There were 88 breast cancer survivors who were eligible for the analysis. A total of 10 lymphedema events (11%) occurred within the median follow-up time of 4.9 years [IQR 2.8-8.0]. Using RPA, the change in circulating IL-4 levels post-radiotherapy was a novel prognostic factor for lymphedema risk, which improved the C-index from 0.73 (clinical model) to 0.92 (integrative model, p=0.019). Conclusion: An integrative risk model incorporating circulating cytokine levels resulted in improved prognostication of lymphedema risk and may be useful for triaging patients for earlier management and/or future trials.
March 6, 2024 International World Lymphedema Day (WLD). Worldwide Contact your provincial association to learn about local events.
Mar 12–14, 2024 Power Lymphatics 2024 Lymphedema Education Las Vegas, NV n https://thepowersymposium.com/power-lymphatics/
May 1–5, 2024 Shaping Lymphatic Health. Australian Lymphology Adelaide, Australia Association n https://ala2024conference.com.au/
May 30–Jun 1, 2024 47th Congress of European Society of Lymphology Istanbul, Turkey Connecting the continents with present and future strategies for lymphedema and related disorders. n www.esl2024.org
Summer 2024

The 2024 summer issue of Pathways will mark the 50th issue of this publication. Watch out for this special publication released on June 8, 2024.
October 10-13, 2024 American Vein & Lymphatic Society annual congress. Chicago, IL n www.myavls.org


























Feeling good in your skin is our number one priority! Venotrain® Curaflow compression garments are designed with the individual in mind, because self-confidence is always in style!
Always custom fit
Edema affects everyone differently. Curaflow compression garments are custom-fit to the individual and cater to their specific needs.
Skin-friendly microfiber material
The custom knit is soft and breathable which ensures optimal climate regulation.
Anatomically shaped


Flat knit design allows for a greater freedom of movement, increased wearing comfort, and a reduced pressure sensation.

Feel the Curaflow difference!
#SELFLOVECLUB

Want to learn more?