STORIES BY MEMBERS OF THE MYHEART NETWORK
‘Heart issues don’t mean your life is over’ by Lewis
Nicholson
This is my story and my journey as a person who had a catastrophic birth defect of my heart by chance, and an MRI technician having a good eye, I am still here.
In 2012 I was 18 years old, and despite having an extremely active childhood – including playing Rugby 6 days a week and through all months of the year – I suddenly became symptomatic, having painful and persistent palpitations, spells of dizziness and even episodes of collapse. I was accused of several things, even taking cocaine, when I had to go to hospital.
I went to my GP and got referred to a Cardiologist at Guys & St Thomas’ Hospital. I had multiple ECG’s, stress tests, 24-hour tracing and a functional MRI. When I was 21 in 2015, I was phoned and told to come to St Thomas’ the next day
to see the consultant. I went, and I was told that they had discovered an Anomalous Origin of my Left Coronary Artery and the route the artery was taking from my heart to the rest of my body was being obstructed as it went between my Aorta and Lungs. I was 21 years old and told that I was at risk of collapsing, like I already had done, and my heart stopping and the chance of resuscitating me would be slim to none.
I underwent open heart surgery to correct the issue within a month of being told about the issues and the surgery went well, but I was left with crippling PTSD following the conversation and the surgery itself. I spent 1 week in Hospital – the majority of the time I was alone –and then was finally allowed home with my family.
Fast forward to 2019, I applied to join the Police and, after a much longer process than normal because of the heart Issue, I was successful and have been a Police Officer since; on the frontline, protecting those who are at their most vulnerable and being in extremely stressful situations.
I would like to share my story with those young people who are suffering or at risk and think, like I did in 2015, that their life is over,
because the stereotypes about heart issues are that they will affect you for life.
‘You never think this is going to happen to someone young’ by Megan Turner
Dec 2021 was a scary time for me and my family. I gave birth to my beautiful baby boy on the 11th and on the 17th, I had a sudden cardiac arrest, I got shocked 3-4 times, but my heart just wouldn’t settle. I died for a good 40 minutes but I wasn’t giving up! They put me in a sleep coma until my heart settled down and all my checks came back to normal.
I was in ICU for over a week. Because my body shut down, I had to gain my strength back up, learning to walk again and eating /drinking.
Once they knew my observations were steady, I then got moved to CCU where I spent another 4 weeks with having tests after tests. Having MRI scans, echos, blood tests every other day, I was like a
pin cushion. It was so hard to get blood out of me, they had to go in my feet and other areas, which was painful. I’m now fitted with an ICD.
I have heart failure on the lefthand side of my heart, and I have irregular heartbeats & on medication for life.
It took me a while to leave my mum’s side, after having several panic attacks. I literally just wanted to sleep and not wake up, I was so low and down, panicking over everything. If I felt my heart, I thought I was going again . I went to heart therapy, and it took a few appointments to let the doctor in, but I’m so glad I did because I managed to do a couple of hours in my own house with my partner and baby which, after few weeks, I did longer and even slept over. I managed to move back in, and the panic attacks faded away. I managed to control my emotions and tell myself I’m fine and I’m safe. I’m living everyday as it comes and just enjoying myself.
It’s scary as I was only 28 and you never think this is going to happen to someone so young. I would advise anyone to seek and ask for a MOT no matter what age you are.
I’m so lucky and today I’m forever grateful to be here and watching my little boy grow up.
‘If cardiac screening was available to me, I wouldn’t have had to go through this trauma’ by
Cara Bunn
It was October 2021 – I’d recently just come back off holiday abroad for my 21st birthday and I wasn’t feeling myself at all. I had developed a cough but thinking it was due to me coming back to the colder weather I didn’t think twice about it. One morning before work while getting ready I actually fainted but it wasn’t for long so I carried on as I usually would just thinking I need to eat something sugary.
Fast forward a few days I was at work on a Monday and my cough had got worse, I wasn’t able to catch my breath and I was having palpitations. I rang 111 as I wasn’t able to get a doctor’s appointment and was told a doctor would ring me within a few hours. I then started experiencing
chest pain but was just told it was due to anxiety as I do suffer with anxiety & depression that I take medication for. As the pain didn’t ease, I rang 111 back within the hour and was told to go to A&E as they believed it could’ve been a blood clot on my lung.
In A&E I was given an ECG, chest x-ray and I had my bloods taken. My x-ray was fine, my bloods were all normal, but my ECG had shown up something, but they weren’t sure what. Due to it being nighttime at this point I was told they would need a specialist to look at it the next morning and I would get a phone call. I was then sent home and awaited a call from a specialist in the morning.
Receiving the phone call, I was told to immediately make my way over to the hospital and go onto coronary care unit ward.
I was then admitted and put on a heart monitor. It was so scary! I had no idea what was going on and due to me previously being healthy I had never stayed in hospital before. I had lots of different people come and speak to me and I was then told I would need an operation but at this point I still wasn’t sure what was the problem.
It was during the pandemic, and I was young, alone and so confused in the hospital. It was a horrible time.
I then had a consultant come and
speak to me – it was at this point I was told I had a heart condition called Wolf-Parkinson-white. A condition I had never heard of before.
A couple of days passed. I was on the monitor 24/7. I was not able to leave the hospital room or see anybody but my mom for 1 hour a day which I was eternally grateful for as it was the only normality I had.
It was the Thursday afternoon, and I heard a lot of beeping.
All of a sudden, 4 nurses rushed in, put my bed completely flat and I was rushed into theatre where I was given a catheter ablation.
It was such a scary moment. It was a such a blur. The next couple of hours I had no idea what was happening, but I knew whatever it was, it was what I needed.
I was then kept in hospital for another 24 hours and I was finally told that my heart had started to beat over 200bpm, and I had to have the surgery to keep me alive.
Going from a fit and healthy young girl to a girl that was bed bound for weeks was such a struggle, and since then, my life has never been the same. I have to take aspirin in a morning and carry GTN spray around with me 24/7.
Although my ablation was successful, I still have episodes of fast heart rates, palpitation
and dizziness. I still have to have regular heart monitors because I also have tachycardia and AF (Atrial fibrillation).
I don’t really have any understanding of my condition still, as unfortunately, no face-to-face appointments were available, and I never had a chance to speak to my consultant after my surgery to fully understand what had happened and how it would affect me moving forward.
So for now, I’m just taking every day as it comes but I am getting stronger by the day. I listen to my body, and I can now recognise when an episode is about to happen or is happening.
I truly believe if cardiac screening was available to me, I wouldn’t have had to go through this in the traumatic way I did, and I would’ve been able to help my condition before it got to the point it did.
There are new myheart member stories, as well as our archives, on the myheart website. If you would like to read more, please visit:
www.myheart.org.uk
If you would like to send in your own story to be featured here, please email the myheart coordinator, Kanika at:
myheart@c-r-y.org.uk
CRY RESEARCH
Latest research, medical conferences and interviews with cardiologists and doctors
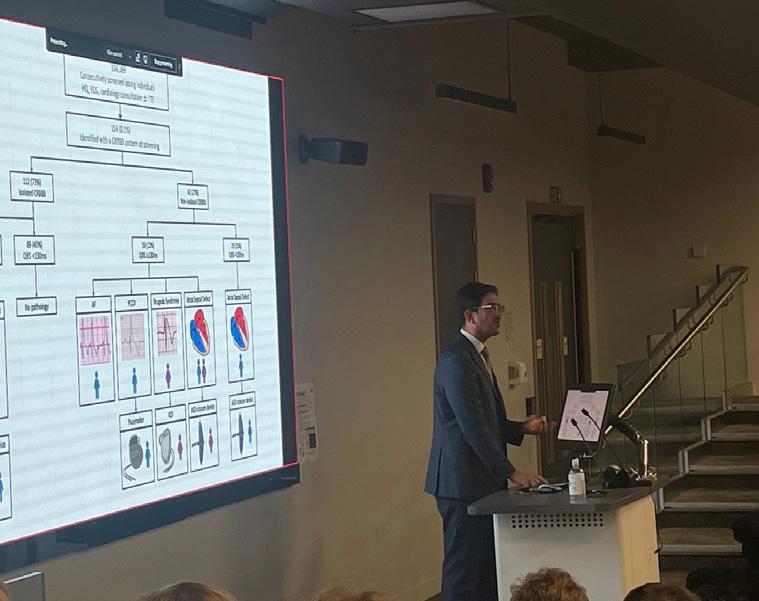
Leading researchers gather at St George’s University of London, to showcase a portfolio of projects funded by Cardiac Risk in the Young
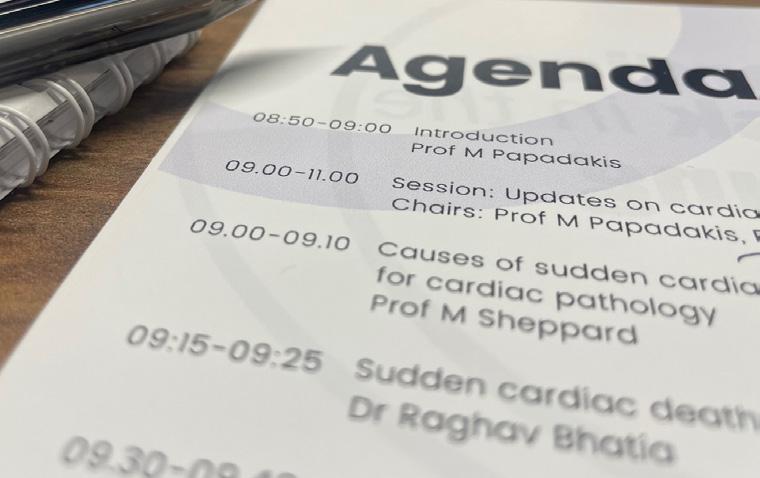
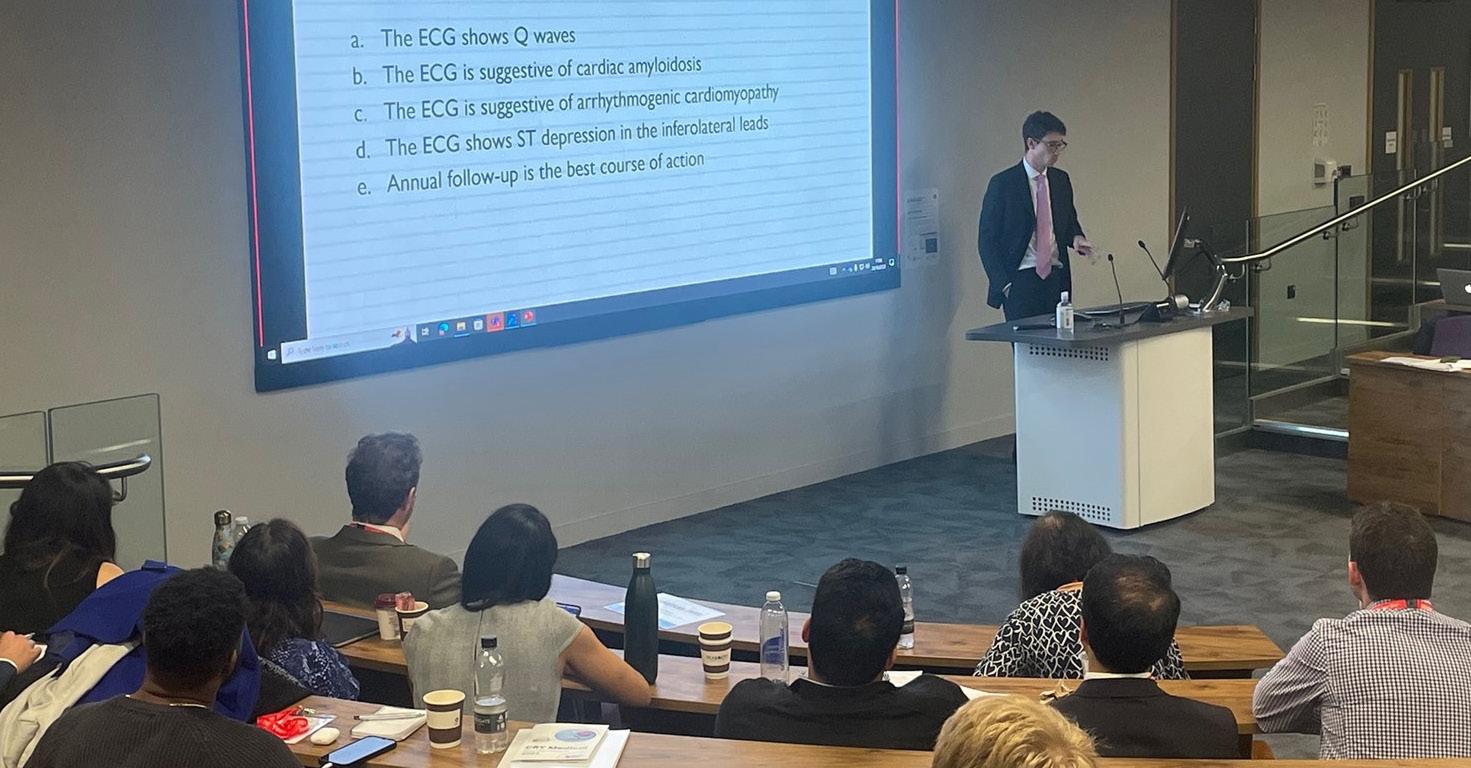
Friday October 20th saw the welcome return of CRY’s Annual Medical Conference to an ‘in person’ event (following three years of remote access) – with a new venue for 2023, The Curve Lecture Theatre at the heart of St George’s University of London, fittingly the home of CRY’s internationally acclaimed research programme and the CRY Centre of Cardiac Pathology (CCCP).
Spearheaded and expertly organised by renowned cardiologist, Professor Michael Papadakis (who has worked closely and committedly with CRY for well over a decade and
is currently also President of the European Association of Preventive Cardiology), the programme included 12 presentations from specially selected speakers on a range of subject areas, profiling exciting and thought-provoking research findings, all with the potential to inform and challenge the way young sudden cardiac death (YSCD) is approached and understood across a global research community.
The day was divided into four sessions with the first two –‘Update on Cardiac Screening’ and ‘Distinguishing physiology from pathology and managing athletes with disease’ –comprising a packed agenda of ‘back-to-back’ presentations, delivered by a truly impressive lineup of leading consultant cardiologists, researchers, registrars and pathologists.
Throughout the morning, subject areas included issues as diverse as ‘safe levels of exercise for people diagnosed with HCM’, to ‘understanding when medics should be concerned about athletes with ventricular arrhythmias’.
The afternoon was then split into two interactive Case Sessions, both delving deep into the
Professor Michael Papadakis
arena of Sports Cardiology, specifically exploring “Catch 22s in Cardiomyopathies and Structural Disease”. Delivered by an esteemed panel of Chairs [Professors Sanjay Sharma, Eljah Behr, Michael Papadakis, Aneil Malhotra, Dr Maite Tome, Dr Gherardo Finocchiaro], the debate and ensuing Q&As were interesting and intense, acknowledging the fact that the very ‘best of the best’ had all come together at CRY’s annual conference to share knowledge and learn from their peers.
Notably, also joining this panel of experts was Professor Domenico Corrado (a revered and familiar face at the event), who is currently Director of Inherited Arrhythmogenic Cardiomyopathies and Sports Cardiology at the University of Padua Medical School, Italy. It was a welcome return to CRY’s Medical Conference and, as in all previous
years, Professor Corrado used his platform and captive audience to reiterate the widely referenced “Italian data” (showing that since mandatory cardiac screening was introduced for all those involved in ‘organised’ sport, the death rates have fallen by a staggering 89%).
Earlier in the day, as part of his own presenting segment, Professor Corrado had talked through this data as part of a discussion exploring the key question of whether ‘one off cardiac screening is ever enough?’.
So, whilst the conference provided
Speakers and delegates on the day
an opportunity to revisit some seminal and well-established research, the event was also a chance to ‘tease’ new and potentially ground-breaking papers.
Speaking after the conference, CRY’s CEO, Dr Steven Cox, commented; “It was so good to be back where it all started, and we’re hugely grateful to all our friends and colleagues at St George’s University of London, for their help in making this happen. It was a brilliant turn out, from both the 100 or so delegates who attended in person and all those who joined us online, and I felt really proud that we were able to gather such a phenomenal panel of experts, bringing together decades of experience from the forefront of research, all with a common goal of improving the prevention of young sudden cardiac death.
“In just one day, we were able
to cover a wealth of important issues from cardiac screening, progress in pathology, improved understanding of ‘safe’ levels of activity for those with a diagnosed condition and important implications and considerations for athletes.”
“The conference also underlined why research will always be at the core of CRY’s work and of our ongoing mission to reduce sudden deaths from cardiac conditions in young people. It also reminds us how important it is to keep our ‘CRY families’, supporters and stakeholders updated with our research outcomes.”
“I’d therefore like to thank each and every one of our speakers who ensured that our programme was original, current, engaging and informative. I’d particularly like to thank the Cleveland Clinic for its generous sponsorship, without which, none of this would have
been possible, as well as ‘loaning’ us its Chair of Cardiology, Prof Bernard Prendergast, who did an excellent job of chairing the first session of the day.”
“I really do encourage our supporters and stakeholders to view the individual video clips of the presentations on our YouTube channel.”
So, following such an inspiring day, full of innovation, insight and above all, hope, it feels appropriate that the final word should go to CRY’s Consultant Cardiologist, Professor Sanjay Sharma, who has championed CRY’s Medical Conference since its inception in 2006.
“What today has shown us, is that CRY is continuing to sow the seeds of the next generation of specially trained cardiologists through its Research Fellow programme. The
If you would like to watch video from the day, please visit our YouTube Channel at:
fact that so many previous Fellows were here, back at St George’s, presenting their incredible research findings (having taken up clinical roles in hospitals across the UK) is testament to the success of this important initiative.”
Thank you to our speakers this year:
Dr Veronika Azidou, Dr Joyee Basu, Professor Elijah Behr, Dr Raghav Bhatia, Dr Mihnea Casian, Professor Domenico Corrado, Dr Harshil Dhutia, Dr Gherardo Finocchiaro, Professor Aneil Malhotra, Dr Sarandeep Marwaha, Professor Michael Papadakis, Professor Bernard Prendergast, Professor Hanne Kruuse Rasmusen, Professor Sanjay Sharma, Professor Mary Sheppard, and Professor Maite Tome.
*Please be aware that whilst videos like the above may be of particular interest to some myheart members, the playlist also includes talks about cardiac pathology and the causes of young sudden cardiac death.
The impact of exercise and physical activity on young people living with a heart condition
The impact of exercise and physical activity on young people living with a heart condition is an issue that often comes up at myheart meetings or is discussed amongst our members. CRY’s cardiology experts are also commonly asked, “is it safe for me to exercise?’ and ‘how far can I push myself when training?’.
As such, CRY has always been committed to supporting a range of research projects, looking at these issues and striving to gain further understanding about the benefits of physical activity for young people with a diagnosed heart condition, as well as ‘safe’ parameters for exercise.
CRY’s Research Fellows have been involved in the publication of a raft of internationally acclaimed research looking into this area and one thing remains unanimous
across all findings; physical activity is almost always beneficial for overall health and well-being and far outweighs the risks associated with a sedentary lifestyle.
Recently, two important research reviews –spearheaded by doctors who both have an association with CRY’s research programme –have been published in Heart (the journal of the British Cardiac Society) to help unpick some of the myths regarding physical activity and inherited heart conditions and to clarify whether exercise really can be the best medicine.
Former CRY Research Fellow, Dr Sabiha Gati, is now Consultant Cardiologist at Royal Brompton and Harefield (RBH) NHS Foundation Trust. Dr Gati has also been a huge supporter of myheart for several years, taking on a supervisory role at many meetings (both virtual and in person).
Here, we look at a published review carried out by Dr Gati, entitled; ‘Exercise prescription in individuals with hypertrophic ardiomyopathy: what clinicians need to know’.
Dr Gati, can you briefly describe the objectives of this literature review and why you felt it was so important to evaluate existing, published research?
In the last few years, we are seeing a favourable outcome in our patients with hypertrophic cardiomyopathy (HCM). There is emerging evidence that most deaths in HCM are occurring at rest rather than with exercise. Previous exercise guidance for patients with HCM was limited to low intensity physical activity only. However, there is new data emerging that supports the idea of moderate exercise being beneficial for these individuals.
In fact, some individuals with the mild form of the disease and with a low risk profile may also take part in vigorous exercise following discussions with their specialists. The current exercise and sports cardiology guidelines from the European Society of Cardiology (ESC), the American Heart Association (AHA) and the American College of Cardiology (ACC) on the management and treatment of HCM have been updated and support a more liberal approach to exercise and sports participation in HCM. This review provided the general physicians and patients with the evidence that is available to support the notion of exercise in HCM and how best to prescribe it.
What were the main findings and recommendations of this review?
In summary, the key conclusions drawn from this research review were as follows:
· Exercise is beneficial for cardiovascular health and light and moderate exercise should be encouraged in all able individuals with hypertrophic cardiomyopathy (HCM)
· A detailed comprehensive risk evaluation of all individuals with HCM is recommended to formulate a safe exercise prescription plan
· The current European Society of Cardiology guidelines and the 2020 AHA/ACC guideline for the diagnosis and treatment of patients with HCM recommend a liberal approach to exercise in HCM. Asymptomatic individuals with a mild phenotype and absence of high-risk features for sudden cardiac death (SCD) may engage in all competitive sports
· Longer term follow-up studies are required in individuals with HCM who exercise vigorously with important considerations to age, sex, ethnicity and sporting disciplines and ESC-risk score
Can you explain to our myheart community how your findings might impact young people who are living with a heart condition and who are keen to take part in exercise and sport?
It is well recognised that a sedentary lifestyle may result in
Dr Sabiha Gati
a detrimental effect in patients with HCM both physically and emotionally. As clinicians we should be encouraging the current minimum physical activity recommendations and also give guidance to those individuals who are limited by symptoms.
We know, based on the evidence in the literature, that moderate exercise is safe. If you are keen to take up exercise, speak to your specialist, ensure that a detailed risk evaluation has been undertaken and discuss a shared exercise plan with realistic goals.
Generally, how can people living with heart conditions know what a ‘safe’ and recommended level of exercise and physical activity is?
The recent ESC guidelines in sports cardiology and the updated AHA/ACC guidelines in management and treatment of HCM support light to moderate exercise in all individuals with HCM. They also provide guidance for other heart conditions too. Most individuals with HCM may engage in recreational sports of low to moderate intensity and competitive sports of low intensity.
Among patients who want to engage in more intensive exercise, a comprehensive assessment is recommended, which considers symptoms, family history, functional capacity, cardiac function, and risk profile. A full complement of cardiac investigations is recommended
including an echocardiogram, exercise stress test, cardiovascular magnetic resonance (CMR) and prolonged ECG monitor.
We recommend that all patients whether with HCM or another heart condition should engage in the minimal physical activity recommendations of 150 minutes of moderate exercise per week divided over 4-5 sessions and preferably 300 minutes per week in able individuals, if symptoms permit, to maximise the benefits of exercise.
They may wish to discuss arranging an exercise stress test with their specialist which can be particularly useful when prescribing exercise because it provides relevant information about functional capacity, exercise induced rhythm abnormalities and your body’s response to exercise.
Apart from walking, patients without symptoms or rhythm abnormalities during moderate levels of exercise may still be able to do gentle cycling, stationary cycling, treadmill, or low intensity weights, at a heart rate below 75% of the maximum predicted for age, but should avoid any exercise that induces symptoms.
We would generally advise avoiding sudden explosive exertion such as sprinting. Exercise programmes are also not recommended, particularly those that involve systematic training with increasing intensities
and workload. We would advise on a gradual warm-up for at least 10 minutes before starting exercise and a cool-down post exercise. We would also advise avoiding exercise during a fever or diarrhoeal symptoms as this may precipitate electrical abnormalities of the heart. Individuals should abstain from exercising in extreme adverse environmental conditions.
If individuals would like to engage in free weights, the general advice is to do six repetitions up to three times followed by 2 minutes of rest to prevent fluctuations in blood pressure. Individuals should not push more than 20% of their body weight with the upper limbs and more than 50% of their body weight with the lower limbs in the initial stages of weight training. This may be increased at a later stage if it does not result in a heart rate exceeding 70% of the maximum predicted for age.
In what cases – if ever – might an individual be advised against exercise?
Individuals considered to be high risk including those who have survived a cardiac arrest, experienced unexplained loss of consciousness, report exercise induced symptoms, or have multiple high-risk features (such as obstruction to the blood flow across the left chamber outflow tract [LVOT]; significant left chamber wall thickness; fatal rhythm abnormalities from the bottom chambers –
NSVT >120bpm) should confine themselves to low intensity only. This equates to <55% of their maximum heart rate.
Can you tell us about any new research (current or upcoming) which you’re involved with?
There is some limited evidence that reduced size electrical complexes/traces of the heart on the electrocardiogram (ECG) may be associated with scarring in the heart muscle, which may predispose to serious life-threatening electrical abnormalities and sudden cardiac death (SCD).
There is no guidance on reduced ECG traces for young individuals and athletes. Their correct interpretation is crucial for identifying athletes with disease and at risk of SCD. Some athletes experience SCD despite normal standard cardiac tests.
We, therefore, propose to study athletes and young people aged 17-35 years old using cardiovascular MRI and genetic analysis to determine the significance of reduced ECG traces. These results should enable informed clinical decisions (at national and international level) following pre-participation screening evaluation and help ultimately to identify young individuals and athletes who are genuinely deemed to be at risk of sudden cardiac death (SCD) whilst providing appropriate
reassurance to those with normal QRS voltages.
This study is being conducted in collaboration between CRY and Royal Brompton and Harefield hospital charity.
And finally Dr Gati, do you have any further insight that you’d like to share with CRY’s ‘community’ about the ongoing positive impact of CRY’s research programme?
I am passionate about research into the athlete’s heart as well as imaging and electrical changes associated with the risk of sudden cardiac death. I have made significant contribution to the CRY screening programme and it’s phenomenal that we have screened over 300,000 young individuals in the UK.
The CRY screening programme has been pivotal in supporting research in young exercising individuals. The results of some of this data collected via CRY’s screening programme have been published and revealed that one in 300 young individuals in the UK harbours a potentially serious cardiac condition. Early detection of affected individuals results in proactive management strategies.
We have to thank all the supporters of CRY who have made this possible and I hope they will continue to generously donate to the charity for this valuable work.
Dr Nikhil Chatrath is one of CRY’s previous Research Fellows.
In the same journal, ‘Heart’, Dr Chatrath published a review looking at; “Physical activity and exercise recommendations for patients with valvular heart disease”.
Can you briefly describe the objectives of this research, and why you decided to focus on valvular heart disease (VHD)?
This is a condition that can actually affect people of all ages – although there is a subset of young individuals who can have congenital defects associated with the heart valves (either the mitral or aortic valve). So, the purpose of looking specifically at valvular defects was to help us analyse the potential impact of exercise.
We know that when we do physical activity, we put additional stress on the heart – which normally is good for us. But strenuous exercise can also cause a widening of the heart muscle or the aorta, and as such, researchers often hypothesise that in some people with an underlying heart condition (such as valvular heart disease) this could be exacerbated by very high levels exercise.
In the first instance, we wanted to review the literature available,
Dr Nikhil Chatrath
looking at various studies amongst both athletes and the general public to assess the effects of both exercise and that of a more sedentary lifestyle. And it’s important to note that, as part of this research review, we looked at European Guidelines, so it was a thorough and comprehensive project.
Generally, how do people who have been diagnosed with VHD living with heart conditions know what a ‘safe’ and recommended level of exercise and physical activity is?
The good news is that, by and large, all individuals with mild to moderate valvular heart disease (whether ‘leaky’ or causing a ‘stiffening’ of the valve’) can still exercise without restrictions. Although, of course, there are caveats if any new symptoms appear, and we would always suggest seeking the advice of your doctor or cardiologist for further assessment. In cases where VHD has been deemed ‘severe’, then it is more than likely that an athlete (or individuals who regularly train at a high level) would be advised to refrain from professional sport and so-called strenuous activity.
If, however, a patient with severe VHD remains symptomless and has undergone an evaluation from their healthcare professional, with ongoing monitoring (e.g. to determine normal heart rhythms, no increase in blood pressure), then low to moderate physical
activity is still encouraged and normally considered safe.
What other conclusions did you draw from this important research review?
Overall, we were reassured by these findings and the fact they aligned with our current understanding and recommendations for ‘safe exercise levels’ in those people living with VHD.
However, what was interesting –and perhaps a cause for some concern – was the fact we also ‘uncovered’ a general lack of data and research looking at VHD in young people and its impact on lifestyle and exercise considerations. So much of the research carried out globally to date (looking at inherited and congenital heart conditions in young people) have focused on arrythmias and cardiomyopathies. VHD affects a small – but significant – amount of younger people and it feels as though the research focus has gone slightly under the radar.
However, thanks to ongoing funding from CRY families, we have recently been working on some important and pioneering new studies looking at heart valve issues, which will further inform our understanding of the impact on risk of sudden cardiac death and how we might improve diagnosis in asymptomatic young people.
“Best of the Best” – CRY Research Fellow reflects on his recent accolade at international cardiac conference
CRY’s Research Fellows – both past and present – spend much of their time writing and submitting manuscripts based on their projects as well as travelling to UK and international conferences to present their key findings and to lead discussions which help to further the understanding of the causes of young sudden cardiac death (YSCD)
And, as another of CRY’s inspiring Research Fellows concludes a 3-year tenure with our team based at St George’s, University of London, we’re delighted to
announce that Dr Raghav Bhatia was recently awarded “Best of the Best” – for the second time running! – at the 2023 British Cardiovascular Society (BSC) held in Manchester at the start of June.
During his time as a CRY Research Fellow, Dr Bhatia (who has now returned to a clinical role in Yorkshire, currently working in the Cardiology Department at Hull University Teaching Hospitals NHS Trust) often went above and beyond in his support for CRY. His involvement included taking part in many media interviews on behalf of the charity, attending numerous screenings across all corners of the UK and being an active member of the “Running for Research” team, who not only trained together during their busy schedule at St George’s, but also helped to raise over £10,000 in sponsorship!
Here, we chat to him to find more
Dr Raghav Bhatia
about this award-winning study and how its findings will help to improve and inform CRY’s nationwide screening programme.
Firstly, congratulations on your recent award at the British Cardiovascular Society (BSC) in the ‘Best of the Best’ category. Can you briefly describe the focus and objectives of this piece of research that you were recognised for?
Thank you very much. It was truly an honour to receive the cardiomyopathy ‘Best of the Best’ award at the BCS for the second consecutive year. The research for which I was recognised forms an integral part of my PhD thesis, which centres around the prevention of young sudden cardiac death.
The specific focus of this project was to gain a deeper understanding of cardiac and sudden death in young individuals, using novel insights from the Office for National Statistics in England and Wales. The background to this topic was rooted in the importance of accurately representing the incidence and underlying causes of cardiac and young sudden cardiac death in individuals under 35 years of age and we analysed ONS data from 2013 to 2021 (focusing on a 9-year period, within an incredible 20-year cohort of unique, CRYdata). Additionally, we aimed to investigate temporal trends in mortality data, which has not been
previously reported. By shedding light on these aspects, our research aimed to make valuable contributions to the understanding and prevention of young sudden cardiac death.
Such an accurate representation is crucial for healthcare policy makers to effectively allocate resources, address issues such as screening for potentially lethal conditions, improvIng post-mortem evaluations and enhancing resuscitation facilities. This topic built upon the existing work published by Professor Papadakis and Professor Sharma in 2009, which has significantly contributed to the CRY screening programme over the past decade.
The main findings of this research have been really quite significant in terms of our current understanding of the incidence of young sudden cardiac death and the most frequent causes of cardiac mortality in young people. Our manuscript will be submitted soon for peer review, and everyone involved in the research looks forward to sharing these findings once published.
What does it mean to you to be recognised for your research at national and international meetings and how do you ensure productivity?
Being recognised for our research at national and international meetings holds immense significance. It demonstrates
that our findings are respected, appreciated, and contribute to the advancement of knowledge in the field. The opportunity to showcase our research conducted at CRY not only highlights the significance of our work but also fosters collaboration, suggestions, and ideas for future work. Most importantly, being recognised at these esteemed gatherings provides hope to the CRY families who have supported my research journey and Fellowship.
My approach to clinical research has always been centred around our patients and addressing key, unanswered questions. The recognition I have received is the result of a lot of hard work, which I would like to emphasise has always been a team effort, facilitated by my incredibly supportive colleagues and mentors in London and East Yorkshire, as well as my family, who
have been a tremendous pillar of support throughout the rigours and challenges of academia.
In addition to the above research award, can you tell us which of your other research outputs have been presented at national and international award categories in the last 24-months?
Over the past 24 months, there have been several research works led by myself and collaborative efforts with my peers at St. George’s. For example, I am honoured to have received recognition and awards for the following research outputs:
•British Cardiovascular Society, Best of the Best cardiomyopathy section, 2023 (Manchester, UK): Understanding Cardiac and Sudden Death in Young Individuals: Novel Insights from the Office for National Statistics (ONS)
in the United Kingdom.
•European Association of Preventative Cardiology, Young Investigator Awards, 2023 (Malaga, Spain): Prevalence and diagnostic significance of de-novo 12-lead electrocardiogram patterns following COVID-19 infection in elite soccer players.
•European Society of Cardiology, Young Investigator Awards (Barcelona, Spain): Sudden cardiac death during exercise in young individuals with hypertrophic cardiomyopathy.
•British Cardiovascular Society, Young Investigator Awards, 2022 (Manchester, UK): Prevalence and diagnostic significance of denovo 12-lead electrocardiogram patterns following COVID-19 infection in elite soccer players.
•British Cardiovascular Society, Best of the Best cardiomyopathy section, 2022 (Manchester, UK): 1) Mitral valve abnormalities in decedents of sudden cardiac death due to hypertrophic cardiomyopathy and idiopathic left ventricular hypertrophy.
2) Prevalence and diagnostic significance of de-novo 12-lead electrocardiogram patterns following COVID-19 infection in elite soccer players.
I have also enjoyed contributing to the annual CRY International Conference from 2020 to date.
What are your next research
topics focussed around?
My future research outputs remain focussed on cardiac screening and the prevention of young sudden cardiac death. For example, I am currently leading two exciting areas of research, which are near completion.
Firstly, I am delving into the field of myocarditis and its association with sudden cardiac death, particularly in the community i.e., non-hospitalised individuals. This project aims to provide valuable clinical and pathological insights, drawing from the expertise and resources available at the CRY Centre for Cardiac Pathology (CRY CCP). Our objective is to contribute to a better understanding of myocarditis-related cardiac events and potentially identify strategies for prevention and improved management.
Secondly, I am in the final stages of a large research project focused on the outcomes of cardiac screening in elite rugby players in the UK. This project aims to shed light on the effectiveness of screening protocols, identify potential risk factors, and explore ways to optimise the cardiac health of these athletes. We aim to contribute to evidence-based recommendations for screening practices in elite sports, ultimately ensuring the well-being and safety of athletes.
If we roll back time, why did you decide to apply for a CRY
Research Fellowship?
From the early years of my medical career as a junior doctor, I had a strong desire to dedicate a specific period of time to research while also developing expertise in a niche and emerging clinical field. It was during this time that I became aware of the CRY Research Fellowship, which offered a unique opportunity to pursue both of these goals simultaneously.
The Fellowship offered the opportunity to work under the mentorship and guidance of renowned experts in the field, Professor Sanjay Sharma and Professor Michael Papadakis. So, in 2019, after speaking to several past and current CRY Fellows at the time, which included Dr Joyee Basu, Dr Rajay Narain, Dr Gemma Parry-Williams and Prof Aneil Malhotra, I made the decision to apply for the highly competitive CRY Research Fellowship. Following a rigorous selection process, I was fortunate enough to be awarded the fellowship, and my tenure as a CRY Fellow began in February 2020, just prior to the onset of the COVID-19 pandemic.
The Fellowship has provided me with an invaluable platform to expand my knowledge base and make meaningful contributions to the field of preventive cardiology. Working alongside esteemed mentors and within the supportive CRY framework has allowed me to not only engage in cutting-edge
research but also develop unique clinical skills and expertise.
Overall, the opportunity to undertake a CRY Research Fellowship has aligned well with my career aspirations and provided the ideal environment to foster my growth as a clinicianscientist.
What have been your main highlights during this time?
There have been so many! I guess the best way would be to contextualise these highlights based on quite a diverse role that I have had with CRY.
Screening: As a CRY Research Fellow, I have had the privilege to travel across the British Isles, personally screening over 15,000 young individuals and working closely with CRY families at each event. Meeting these families and supporters associated with every one of these screenings –and understanding the personal stories behind the fundraising which facilitates CRY’s screening programme – has been a truly humbling and often emotional experience.
Moreover, the welcome I received from CRY families (who were hosting the screenings I attended), was always so warm. There was also a great deal of interest shown in the research I was involved with, and I like to think we developed a positive rapport. And, collaborating with an exceptional group of
volunteers and CRY staff, I really have developed lifelong friendships along the way.
Through my screening experiences, I know that we successfully identified several individuals with ‘dormant’ cardiac conditions associated with young sudden cardiac death and identified individuals with markers requiring onward evaluation.
Assessing risk in the community and communicating this to the individual, their family (and importantly, primary care and secondary care physicians in a timely manner) whilst following up on cases has harnessed the finesse required in the field of inherited cardiac conditions.
Supportive colleagues and team: I would like to acknowledge the incredible nurses, physiologists, doctors and support staff at CRY and St George’s. Some of us recently participated in the
Vitality 10K in London, raising over £10,000 to support the CRY research program. This experience showcased the strong camaraderie and dedication within our team.
Mentorship and exposure to experts in the field: Under the guidance of Professor Papadakis and Professor Sharma, I have had the opportunity to participate in a weekly inherited cardiac clinic and engage in regular local and
regional multidisciplinary team meetings. These experiences have allowed me to develop competencies in managing complex cardiomyopathies, ion channel diseases, and the appraisal of family members following sudden cardiac death.
Additionally, I have gained qualifications in advanced cardiac imaging modalities such as cardiac MRI and worked in the emerging field of sports cardiology, collaborating with prominent organisations like the English Football Association (FA), Rugby Football Union (RFU), England and Wales Cricket Board (ECB), English Institute of Sport (EIS) and British Athletics.
Contributions to Sports Cardiology during the COVID-19 Pandemic: I take particular pride in our contributions to sports cardiology during the novel COVID-19 pandemic. It started with leading a consensus recommendations paper on safe physical activity and exercise during the first wave.
Subsequently, we performed a multi-centre study, which was recently published, involving collaborators from various clubs in the UK, the Netherlands, and Brazil, providing valuable insights in this area.
Lecturer: I have had the opportunity to harness my academic potential as a senior lecturer and module lead in the novel Sports Cardiology MSc at St. George’s, University of London under the guidance of Professor Papadakis, Dr Finocchiaro and Professor Sharma. This has involved working closely with our MSc students, guiding them in their dissertations, delivering lectures and developing comprehensive course materials.
It has been a rewarding experience to contribute to the growth and development of aspiring professionals in the field.
All of these highlights have enriched my journey and I am grateful for the experiences, collaborations, and friendships that have shaped this chapter of my career.
Where are you now in terms of your CRY journey?
While my initial 1-year fellowship evolved into a 3-year tenure at CRY and St. George’s, and I am now at an exciting juncture as I continue to progress in my career. Currently, I am back in Yorkshire,
where I complete the final 12 months of my sub-specialty Cardiology training. This period allows me to enhance my skills and knowledge in a specific area of cardiology while expanding my expertise beyond the scope of my Fellowship.
I am honoured to have recently been appointed as an honorary lecturer at St. George’s, University of London, which allows me to continue my research outputs. Furthermore, I aim to foster close links between my current base hospital, Hull University Teaching Hospitals NHS Trust, and the esteemed team at St. George’s and CRY. Finally, now as a CRY Cardiologist, I am committed to maintaining strong links in the community, as evidenced by facilitating the first in-person CRY myheart support group meeting in London in May 2023 since the COVID-19 pandemic.
The CRY journey certainly continues, and I aspire to continue contributing to this amazing charity.
Do you have any further thoughts and insight you’d like to share with CRY’s ‘community’ or any doctors potentially considering a CRY Research Fellowship?
I have had the privilege of experiencing the positive, diverse and rewarding impact of a CRY Research Fellowship first-hand. The broad exposure facilitates a comprehensive understanding of
inherited cardiac conditions and their impact on young individuals and communities.
The unique setting of the CRY Research Fellowship offers endless potential for impactful clinical research. Above all, the CRY fellowship encourages future generations of Consultant Cardiologists to think differently and adopt a more holistic approach to patient care by engaging with individuals in the community, raising awareness, and embracing the concept of prevention. By working outside the traditional models of care delivered in a hospital setting, CRY Fellows can truly make an impact by addressing the broader needs of patients and their families.
I am grateful for these transformative experiences and insights gained during my CRY journey, and I encourage anyone considering a clinical research fellowship to apply and embrace the opportunities and possibilities on offer.
Focus group for patients with DCM and ARVC
On the 29th of September, a focus group for patients with dilated and arrhythmogenic cardiomyopathy has been organised by CRY and by Dr Gherardo Finocchiaro, Consultant Cardiologist at St George’s Hospital and Honorary Senior Lecturer at St
George’s University of London. Dr Finocchiaro and his team at St George’s Hospital are aiming to organise a randomised clinical trial focused on moderate exercise in patients with arrhythmogenic and dilated cardiomyopathy.
The beneficial effects of regular physical activity are well established both in healthy individuals and in subjects with cardiac disease. A moderate level of exercise has been shown to improve quality of life and to lower the risk of cancer and cardiovascular disease. However, it is unclear whether exercise is safe in patients with dilated and arrhythmogenic cardiomyopathy.
These conditions are predominant causes of sudden cardiac death (SCD) in young individuals and athletes. After a SCD, a thorough examination of the heart is performed by experts and it appears that cardiomyopathies are often diagnosed, raising concerns about the possible risks of sport in these patients.
Fear of SCD during sport is often the predominant feeling not only of patients, but also of doctors that care for them and professionals that should guide their physical training. This attitude results in the adoption of a sedentary lifestyle with increased risk of dying prematurely and of developing serious illnesses.
Approximately 250,000 people suffer from either dilated or
arrhythmogenic cardiomyopathy in the UK. The aim of the focus group was to collect patients’ experiences and perspectives regarding sport and exercise in the context of their condition.
The discussion focused on the barriers to exercise and on how these impact on patients’ lives. The patients who participated in the focus group showed great interest in the study, which would be the first to assess this specific issue. Patients expressed concerns on the lack of robust evidence to support exercise prescription in cardiomyopathies and the lack of rehabilitation programmes offered by the NHS and tailored to patients with inherited cardiac conditions. Following the focus group meeting, participants completed a survey to provide further feedback.
Dr Finocchiaro said after the meeting, “The focus group was a very valuable experience to gain patient’s perspective about an important and understudied subject. Patients were extremely engaged and provided very useful insight into the study methodology. I am very grateful for their participation and for their enthusiasm in helping me to develop the research proposal.”
Dr Finocchiaro and the inherited cardiac condition team at St George’s Hospital are applying for funding to support this study.
NATIONAL MYHEART MEETINGS
myheart holds two meetings a year for young people aged 1835 who have been diagnosed with a heart condition
Anybody between the ages of 18-35 can come along to a myheart meeting if they have been offered or already have an ICD, have suffered a cardiac arrest, or have been diagnosed with an inherited cardiac condition. We hope that members can gain support through meetings by talking to others in a similar situation.
‘In-person’ myheart meeting: May 20, 2023
A myheart members’ meeting was held on Saturday, 20th May 2023.
There was a Q and A session with cardiologist Dr Raghav Bhatia in response to queries and concerns that members had relating to their heart condition and the pandemic.
Online myheart meeting: November 4, 2023
A myheart members’ video meeting was held on Saturday, 4th November 2023. There was a Q and A session with cardiologist, Dr Sabiha Gati. In this session, members asked questions about their condition, the exercise/s they can do, and any other cardiac concerns they had with regards to their current circumstances.