


 Kathleen M Felisca, MD
Kathleen M Felisca, MD

Drowning is the leading cause of unintentional injury-related death in children ages 1-4 years and the 2nd cause of unintentional injury-related death in ages 5-14 years. 2019-2021, 2,786 U.S. children and young adults 0-19 years of age died from drowning. There are certain populations that are at higher risk for drowning such as toddlers and children with long QT and epilepsy. There are also racial disparities; black children have higher rates of drowning compared to white children. There are researchers that surmise that social, cultural, and environmental differences may be at the root of these discrepancies. However, there are few studies that attempt to evaluate why black children have higher rates of drowning compared to children of other racial and ethnic groups.
We hope to highlight factors that contribute to disparities in drowning rates in minority racial and ethnic groups and to guide help guide public policy programs in combatting drowning.

Primary– Assess adolescent perception of their ability to swim and potential factors that impact ability. Assess parental perception of their child’s ability to swim and potential factors that impact this ability. Factors will include history of swim lessons, access to lessons, access to pools or lakes, etc.
Secondary - Assess water safety knowledge of parents and in adolescents presenting to the emergency room.

This is a cross-sectional survey. Target population includes parents of children ages birth-19 years and adolescents ages 13-19 years who present to the Pediatric ED.
Survey is a comprehensive, multiple-part study to assess water competency by assessing for 5 critical water safety skills, water safety knowledge, and factors that potentially influence drowning risk We plan to enroll 500 patients in 6 months. The clinical characteristics of the study groups will be examined using descriptive statistics. T test and chi-square analyses will be used to determine if there are differences in swimming ability by race, ethnicity, other demographic characteristics, and other factors

Our study is still in the process of enrollment. We have collected 367 surveys thus far We are not yet at the point of data analysis.

N/A. Work in Progress.

 Kayla
Kayla
Gonzalez, MD; Samuel Crooks, MD; Jennifer Schwab, MD; Brooke Bohn, MD; Stewart Mackie, MD; Jonah Mandell, DO

"A tenet of pediatric residency is to train the next generation of primary care physicians by creating “experiences that reflect the spectrum of practice in the specialty and emphasize the skills required for practice by a general pediatrician.” However, a standard curriculum does not exist. According to the ACGME guidelines on pediatric residencies: “There must be a longitudinal working experience between each resident and a single or core group of faculty members with expertise in primary care pediatrics and the principles of the medical home.” While all residents have a continuity clinic experience, this alone is insufficient to cover the breadth of primary care. Most residencies use lectures to fill this gap, though there are no standards regarding topic, structure, or implementation."


Using Kern’s 6-step model for curriculum development, the University of Connecticut Pediatric Residency Program developed and implemented a novel pediatric primary care curriculum, measured resident satisfaction, and utilized the curriculum to connect residents to private practice mentors. We developed a case-based curriculum that highlights outpatient cases. A range of key topics were selected and volunteers were solicited from our private practice and ambulatory general pediatricians. The curriculum was built into resident didactic time. The lecture series included discussion of a case with a primary care pediatrician and supplemental reading materials. To assess the effectiveness of the curriculum, residents were surveyed on a 7-point Likert scale in the areas of increasing knowledge of private practice experience, increased awareness of potential outpatient mentors, and overall educational value.

Res: Overall, 41 of 64 pediatric residents responded, and results were analyzed on a 7-point Likert scale In general, the pediatric residents felt the curriculum had not only augmented their education but also given them insight into private practice and potential mentors in the community (see Table 1)




To enhance UConn Pediatric Residents' outpatient primary care experience, we created a novel case-based curriculum run by our outpatient pediatric attendings with a focus on general pediatric topics. Incorporated into our residency didactics, residents felt this curriculum augmented their education. The majority felt it added education that they would otherwise have missed. The case conference also increased exposure to private practice pediatrician mentors and increased their knowledge of the pediatric private practice experience.

 Elisabeth Ekman, DO and Evan Cantor, MD
Elisabeth Ekman, DO and Evan Cantor, MD

Fanconi Anemia (FA) is known to predispose pediatric patients to childhood cancers, most commonly leukemias, some solid tumors, and only rarely CNS tumors. FA is caused by mutations of several known genes, including BRCA2 and PALB2 (alternatively termed FANCN). Patients with biallelic BRCA2 mutations are those most associated with development of pediatric cancers. More recently, patients with biallelic PALB2 mutations have also been suggested to have increased predisposition for childhood cancer Brain tumors in pediatric patients with FA are typically medulloblastomas, and very rarely pediatric high-grade glioma (pHGG), with none identified in prior literature having DMG characteristic H3K27M mutation. DMG is very difficult to treat with very few options for therapy and poor prognosis. EGFR mutations in DMG are associated with a bithalamic location and resistance to Onc201 therapy, but may have response to EGFR-targeting agents.

We report a novel case of H3K27M diffuse midline glioma in a three-year-old patient with FA and two affected copies of the PALB2 gene, one of which was a maternally inherited copy of unknown significance, the other of which was a paternally inherited pathogenic copy.

Case Report

A three-year-old female was noted to have microcephaly, mixed hearing loss, short stature, and café-au-lait macules. Whole exome sequencing was significant for mutations in the PALB2/FANCN gene, a paternally inherited pathogenic variant and a maternally inherited variant of unknown significance. She developed symptoms of tremor and right leg weakness, and on brain MRI was found to have a large bithalamic mass. Sterotactic biopsy was consistent with diffuse midline glioma, including diffusely positive H3K27M mutant protein and loss of H3K27me3. Tumor cytogenetics were significant for overexpression of EGFR missense mutation (likely activating) at the p.A289V site to 59.2% VAF, with overexpression of the EGFR transcript as well. Chromosomal breakage testing was within normal limits Treatment included localized hypofractionated photon radiation to 4005 cGy, with plans for EGFRtargeted therapy with cetuximab, given the known association of EGFR mutation with Onc201 resistance

To our knowledge, this is the first reported case of a pediatric patient with H3K27M diffuse midline glioma with FA While patients with FA and biallelic PALB2 variants are at risk for childhood cancers, this case suggests that high grade gliomas may be one of these cancer types. Annual abdominal ultrasound and brain MRI are recommended for patients with biallelic BRCA2 mutations, however screening in patients with biallelic PALB2 mutations may also be warranted.

 Marissa S. Aaron, MD and Priya Phulwani, MD
Marissa S. Aaron, MD and Priya Phulwani, MD

Transgender and gender diverse (TGD) youth who desire feminine characteristics often pursue pubertal suppression followed by gender-affirming estrogen therapy and anti-androgen medications. Increasingly subcutaneous (SC) estradiol (E2) injections have been offered in TGD feminizing treatment due to the ease of weekly, self-administered dosing despite limited research, especially in adolescent and young adults.

This study aims to demonstrate efficacy and safety of SC E2 injections in our sample population of TGD adolescents and young adults.

Single center retrospective chart review of Connecticut Children’s Gender
Program patients ages 13 – 24 receiving weekly SC E2 cypionate and/or SC E2 valerate was used to determine efficacy in achieving serum E2 levels (100-300 pg/dl) obtained on day 5 post-injection and suppressing testosterone (T) levels (≤50 pg/mL) with simultaneous use of anti-androgens as needed. From these chart reviews, we also assessed adverse effect profile and compared therapeutic doses.

From the total of n=33 transgender female (n=31, 94%) and non-binary (n=2, 6%) individuals, n=23 (70%) participants were able to achieve therapeutic E2 levels on either E2 cypionate, E2 valerate, or both. While therapeutic on SC E2, n=22 (96%) had suppressed T levels with anti-androgen therapy. Most participants switched from patch (n=23) or pill (n=6) E2 to SC preparation, with 79% (n=23) switching due to difficulties with patches or the desire to avoid adverse effects of oral E2. Of the 25 participants who received SC E2 cypionate, 48% (n=12) had therapeutic E2 levels; many of those not reaching therapeutic levels had switched to E2 valerate prior to dose titration (n=11, 44%) due to a national E2 cypionate shortage. On E2 valerate, n=16 (62%) achieved appropriate E2 levels with another n=4 (15%) having supratherapeutic levels requiring further titration. To achieve therapeutic E2 levels, SC E2 valerate required a statistically significant (p<0.01) higher dose (mean 4.1 mg weekly, SD 1 5) as compared to E2 cypionate (mean 2 2 mg weekly, SD 0 5) However, there were associated higher therapeutic serum E2 levels (p=0.02) achieved on E2 valerate (mean 189 pg/dL, SD 57) than E2 cypionate (mean 142 pg/dL, SD 33). When the E2 level range was limited to 100 – 200 pg/mL to match between SC formulations, the difference in dose remained statistically significant (p=0.02). No clinically significant adverse events occurred.

These data suggest efficacy of SC E2 cypionate and valerate, at differing doses, in achieving serum E2 in the range of physiologic post-pubertal females and T suppression (when used with anti-androgens) in TGD adolescents and young adults.

 Katherine Murphy, MD and Natasha Frederick, MD, MPH
Katherine Murphy, MD and Natasha Frederick, MD, MPH

Blastic Plasmaccytoid Dendritic Cell Neoplasm (BPDCN) is an extraordinarily rare and aggressive neoplasm, especially within pediatrics. BPDCN often involves the skin, bone marrow, lymph nodes, and CNS. Given its rarity, there is no standard of care and there are no current clinical trials available for pediatric patients. We present a treatment approach of a 10-year-old with BPDCN.

Review an approach to treatment of a 10-year-old with BPDCN.

Case report obtained by comprehensive chart review.

A 10yo was referred to our clinic for a “hematoma” of the left thigh, which had grown, following minor trauma, over 1.5 years. The physical exam showed a large, round, raised, erythematous, warm, non-tender lesion on the lateral aspect of the left thigh (4.5x5cm), with left inguinal adenopathy. Left thigh MRI showed a heterogeneous mass of the anterolateral left thigh with left femoral/inguinal and external iliac adenopathy concerning for malignancy. Mass biopsy pathology showed a pattern of antigen expression, using flow cytometry, characteristic of BPDCN. Bone marrow biopsy and peripheral flow cytometry were negative for malignancy. PET showed lymphatic spread of disease, to bilateral inguinal and external iliac lymph nodes and paratracheal lymph nodes In collaboration with BPDCN experts, the patient initiated dual therapy with Bcell ALL High-risk induction therapy (per AALL1732), with Venetoclax, a BCL2-antagonist, that targets BPDCN’s BCL-2 antiapoptotic function Following induction therapy, restaging imaging showed complete metabolic resolution of the primary tumor, with a partial response of the patient’s left and right inguinal lymph nodes. To direct the next stage of therapy, an excisional biopsy of the left inguinal lymph node was performed and was negative. Assuming remission at the end of induction, Bcell ALL HighRisk therapy was continued instead of transitioning to Tagraxofusp (targets CD123, expressed in all BPDCNs) with or without Venetoclax, followed by an allogenic stem cell transplant. Post-consolidation MRI showed complete resolution of the previously seen lymph nodes, and therapy was continued per Bcell ALL High-Risk protocol. The patient is currently undergoing delayed intensification and is tolerating treatment well with no evidence of disease recurrence

A 10-year-old diagnosed with BPDCN was treated with high-risk Bcell ALL therapy (per AALL1732) and Venetoclax with a positive metabolic response. This treatment approach serves as an example for future cases of pediatric BPDCN, in which there is currently no standard of care.

 Susana Collazo, MD; Kathryn Schissler, DO; Jessica Serventi-Gleeson, MD; Eric Hoppa, MD
Susana Collazo, MD; Kathryn Schissler, DO; Jessica Serventi-Gleeson, MD; Eric Hoppa, MD

Cervical spine (c-spine) injuries can lead to serious morbidity and mortality. Patients presenting to the emergency department (ED) after blunt trauma are often placed in a cervical collar (c-collar) Medical clearance of the c-spine depends on multiple factors and may involve various subspecialties. Documentation of a thorough evaluation for potential c-spine clearance is imperative to ensure all team members are aware of any necessary precautions and track the patient’s phase of care.

Improve provider documentation of c-spine evaluation in trauma patients by implementing a standardized procedure note embedded into the electronic medical record (EMR). This note serves to improve standardized documentation of c-spine evaluation to facilitate reporting consistencies and track outcomes.

A multidisciplinary group of pediatric emergency medicine (PEM), neurosurgical, and trauma surgery physicians at a tertiary care, urban, level 1 pediatric trauma center developed a templated procedure note for c-spine evaluation and clearance. The elements of the note are based on the Nexus criteria. The note is intended for all trauma patients arriving to the ED in a ccollar or those with concern for a c-spine injury. The note has clickable, mandatory fields and is available in the procedural section of the EMR Questions include: indication for c-spine evaluation, date/time, GCS, neurologic examination, imaging review, if the c-spine can be cleared, among others. Additional notes can be completed if subsequent c-spine evaluations are required. The note was implemented in October 2023 and providers were educated on its use. A retrospective chart review was completed 6 months prior to implementation, and will be completed 6 months post implementation, to evaluate changes in documentation and frequency and quality of c-spine evaluation for trauma patients.

The results are pending final chart reviews.

The conclusion is pending final chart reviews. The project will be completed by April/May 2024 and presentable by research day.

 Christina R. Mallery, Allison Crepeau
Christina R. Mallery, Allison Crepeau

Osteochondritis dissecans (OCD) is a localized disease of the subchondral bone in which there is osteonecrosis with secondary injury to the overlying articular cartilage. Repetitive trauma is theorized to be the primary mechanism. OCD types of lesions can result in pain, swelling, loose body formation, and arthritis. Surgical management is pursued when conservative management fails, with the long-term goal to minimize arthritis Lyme arthritis, a late Lyme disease manifestation, is an inflammatory arthritis.

This case study presents the novel findings of two distinct osteochondritis dissecans lesions in an adolescent male with a history of Lyme arthritis and recurrent knee pain.

A 13-year-old male initially presented to orthopedics with right knee pain and swelling, later developing fever. PCR testing of the synovial fluid was positive for Borrelia species, consistent with Lyme arthritis. He was treated with two courses of amoxicillin due to persistent swelling and concern for treatment resistant Lyme arthritis. At initial presentation, an MRI revealed a small stable OCD lesion to the lateral femoral condyle. He represented 7 months later with recurrent pain Imaging revealed progression of the OCD lesion however it was thought that his pain was likely secondary to post-Lyme inflammatory arthritis and he was treated with oral anti-inflammatories and a steroid injection. His pain returned 12 months later Examination revealed a nonantalgic gait He had a right knee effusion and was tender to palpation over the lateral joint line and lateral femoral condyle. He had FROM though experienced pain with squatting. He had 4/5 strength in the quadriceps and hamstrings however had extreme difficulty with performing a straight leg raise.


X-rays revealed patient’s lateral femoral condyle OCD lesion had notable progression and revealed a new trochlear lesion. MRI confirmed these findings. Patient was treated conservatively with activity modification without improvement in his pain so surgical management was initiated. Pt underwent drilling of both lesions. Post operatively, pt underwent both activity modifications and physical therapy. This case study describes the findings of osteochondritis dessicans in a patient with a history of Lyme arthritis. This is a novel association with no previous description.

 Jacob Kelner, DO; Douglas Moote, MD; Rahul Shah, MD; Amirul Anuar, MS; Annmarie Golioto, MD
Jacob Kelner, DO; Douglas Moote, MD; Rahul Shah, MD; Amirul Anuar, MS; Annmarie Golioto, MD

Respiratory distress syndrome (RDS) is a common cause of respiratory failure in preterm infants admitted to the neonatal intensive care unit (NICU). Guidelines on when to administer rescue exogenous surfactant continues to vary between NICU’s. Preliminary evidence supports bedside lung ultrasound scores (LUS) as a predictive model to identify which infants benefit from exogenous surfactant earlier than current guidelines.


To determine if bedside LUS can predict exogenous surfactant administration in premature infants with respiratory failure. A secondary objective is to determine what LUS cutoff provides the best sensitivity and specificity for surfactant administration Infants born <37 weeks gestational age (GA) with respiratory failure requiring continuous positive airway pressure (CPAP) were included in this study. Infants with lung, cardiac, facial, or airway malformations were excluded. Bedside lung ultrasounds were performed using a LOGIQ E10 ultrasound machine and a L6-24 linear probe within six hours of life prior to an infant being intubated or receiving surfactant. Scores were calculated according to the original Brat et al 2015 methods. Data including demographics, bedside vitals and laboratory values were also collected. Logistic regression models were employed to evaluate the relationship between the LUS and the primary outcome of surfactant administration. Receiver operating characteristic (ROC) analysis was performed using the predicted probabilities from the logistic regression models to assess the models’ predictive performance.

Lung ultrasounds were performed on 30 infants with a median GA of 33 weeks (31-34) and birth weight of 2.0kg (1.5-2.3). A higher LUS was positively correlated with a higher oxygen saturation index (r=0.62) and higher FiO2 needs (r=0.74). LUS’s for predicting surfactant administration had an are under the ROC curve of 0.97. A LUS >9 had 100% sensitivity and 91% specificity for surfactant administration. Lung ultrasounds were obtained at 106 minutes of life (71-164) and infants received surfactant at 324 minutes of life (181-478).




A LUS >9 had high sensitivity and specificity for predicting which infants received surfactant and could decrease time to surfactant administration by as much as several hours. A prospective, randomized control trial using Echography-guided Surfactant THERapy (ESTHER) with a LUS cut-off of >9 is needed.

Shruthishree Sukumar, DO and Donna Boruchov, MD

Hemoglobin (Hb) SE is a hemoglobinopathy resulting from a compound heterozygosity of Hemoglobin S (HBB Glu6Val) and Hemoglobin E (HBB Glu26Lys), the two most common variants in the world. Hb S is commonly found in Africa, Eastern Saudi Arabia and Central India, while Hb E is found in Sri Lanka, Eastern India, Southeast Asia, and Southwest China. Hb SE can be phenotypically similar to Sickle B+ thalassemia presenting commonly with mild anemia, vaso-occlusive crisis, and enlarged spleen. We present two patients with different phenotypes of Hemoglobin SE disease despite similar genotypes.



Review the presentations of two patients with Hemoglobin SE disease. Case report obtained by comprehensive chart review.
Patient 1 is a 6-year-old male with Hb SE found on newborn screen with Hb F 83.4%, Hb S 11.6% and Hb E 36%, and no Hb A. Hemoglobin electrophoresis obtained at nine months of age showed Hb S 53.6%, Hb E 28.2%, Hb A2 3.3%, Hb F 14.9% with a Hb/Hct of 8.6/27.0 and MCV of 53 fL In his first two years of life, he was hospitalized for acute chest syndrome (ACS) requiring treatment with antibiotics, albuterol and steroids. Given his low baseline hemoglobin of 7.8 – 8.3 g/dL and recurrent ACS, he was started on Hydroxyurea (HU) at 20 months of age With continued Hydroxyurea, his hemoglobin significantly improved to hemoglobin of 11 – 12 g/dL with MCV of 78 fL and minimal admissions for ACS. He has maintained a hemoglobin of 11 g/dL on a dose of 300 mg (~14 mg/kg) of HU. Patient 2 is a 5 year old male with Hb SE with mother from Cambodia and Father from St. Lucia. His hemoglobin electrophoresis showed Hb F 84.5%, Hb S 12.3%, Hb E 3% and trace hemoglobin Barts. He has a baseline hemoglobin 10.5 g/dL with no significant symptoms or acute chest. He has had no complications.

Hemoglobin S and Hemoglobin E are the most common variant hemoglobin worldwide Hemoglobin SE commonly presents phenotypically and symptomatically similar to Sickle B+ thalassemia. However, our two patients have portrayed the vast variation in presentation for hemoglobin SE. Longitudinal follow up of these patients are uniquely modeled for patients based on their presentation. We describe 2 disparate cases of hemoglobin SE. Our patient with marked anemia and complications in the first year of life has responded well to Hydroxyurea therapy.

 Shruthishree
Shruthishree
Sukumar, DO and Natasha Frederick, MD, MPH

Hemophagocytic Lymphohistiocytosis (HLH) is a rare life-threatening disease caused by dysregulation with excessive immune activation resulting in hyperinflammation and multi-organ failure. Familial HLH, an autosomal recessive disorder, commonly presents in infancy (80% by two years of age). Despite various symptoms, many manifest fevers, splenomegaly and cytopenias. We present a patient with a unique constellation of symptoms and complicated diagnosis of Familial HLH.



Review a rare presentation of Familial HLH.
Case report obtained by comprehensive chart review.
The patient is a 12-year-old female, with Usher Syndrome in the setting of MYO7A mutation, right sided conductive hearing loss, cerebellar atrophy, retinal vasculitis, growth hormone deficiency resulting in short stature with poor weight gain, hyperlipidemia, and splenomegaly referred to Connecticut Children's Hematology for evaluation of mild pancytopenia. Due to fluctuating then worsening pancytopenia, bone marrow biopsy was performed which revealed marked fibrosis, abnormal T cell population with cytotoxic T cells expressing CD57 consistent with large granular T cells, and mild elevation of double negative T cells at 2.1% in the setting of lymphopenia suggestive of Autoimmune
Lymphoproliferative Syndrome (ALPS). Next Generation Sequencing was positive for 2 variant mutations in the FAS gene associated with Somatic ALPS. ALPS testing showed normal B12 level, elevated IL18 3473 pg/mL, IL10 110 pg/mL and soluble FAS ligand 1102 pg/mL.

Although the patient did not meet all ALPS criteria, she initiated ALPSlike therapy with Mycophenolate and prednisone due to clinical decline with worsening pancytopenia, severe splenomegaly impacting nutrition, and progressive pericardial effusion. The patient demonstrated a good response to MMF and prednisone with normalization of CBC and resolution of pericardial effusion. Given her complex medical history, whole genome sequencing was performed that revealed compound heterozygous variants in UNC13D gene (maternal c 1241G>T p R414L, paternal c.751C>T p.Q251), associated with Familial HLH. HLH testing revealed absent NK function, elevated Soluble IL2R 27,627 U/mL, Soluble IL2R 42,700 pg/mL, CXCL9 94,443 pg/mL, Triglycerides 248 mg/dL, normal Ferritin 319 ug/L, and Fibrinogen 159 mg/dL. Given her underlying UNC13D mutations, a plan was made to transition the patient to HLH therapy that included Ruxolitinib followed by an allogenic stem cell transplant.

Patient exhibited a unique constellation of symptoms and complex presentation with mixed Familial HLH and ALPS based on genetic evaluation Her UNC13D mutation associated with Familial HLH may have predisposed her to develop somatic ALPS secondary to the vulnerability of her immune system

 Caroline Figgie, MD; Rebecca Riba-Wolman, MD
Caroline Figgie, MD; Rebecca Riba-Wolman, MD

Gonadotropin-releasing hormone agonists (GnRHa) are a safe and effective treatment for central precocious puberty (CPP). Histrelin is a GnRHa implant that reversibly suppresses the pituitary-gonadal axis. Transient hypertension (HTN) has rarely been described with GnRHa forms of triptorelin and leuprolide, but has not been described with histrelin.

We present a novel case of a 5-year-old female with CPP and development of treatment-associated HTN with multiple forms of GnRHa, including histrelin.

Thelarche of infancy began at 14 months-of-age, and at 18 months initial endocrine evaluation included Tanner 2 breasts and prepubertal morning gonadotropins. Following 24 months-of-age she had progressive breast growth, estrogenization of vaginal mucosa and uterine peripubertal morphology on ultrasound. Leuprolide stimulation confirmed CPP with stimulated LH 5.15 mIU/mL, FSH 47.71 mIU/mL and estradiol 69 pg/mL.
MRI brain noted a small Rathke’s cleft cyst (stable on repeat). She started treatment with triptorelin (Trip#1) at 26 months, and then placement of histrelin (Hist#1) at 3 years old with replacement (Hist#2) 1 year later.

Within a week of Hist#2 placement daily headaches, abdominal pain and persistent HTN (manual blood pressure (BP) >95th percentile for age/sex/height) occurred. Prior manual BPs were normal. Extensive nephrology/endocrinology evaluation was done, including normal: echo, renal US with doppler, MRI/MRA abdomen, metanephrines/HVA/VMA, complete adrenal metabolite panels, androgens, insulin-like growth factor1, thyroid function, 24hr urine cortisol/cortisone. All testing was normal beyond non-specific low renin with normal aldosterone/potassium. Multiple concurrent antihypertensive medications (amlodipine, hydralazine, and clonidine) were required. Hist#2 implant was removed, without visual abnormalities or defects, and inpatient monitoring demonstrated resolution of hypertension. All antihypertensives were discontinued. Resumption of treatment with leuprolide 7.5mg monthly (Leup#1), lead to re-development of hypertension that persisted with subsequent course of triptorelin (Trip#2), despite previous tolerance.

GnRHa-associated hypertension has not been described with the use of histrelin implant in treating CPP. Furthermore, it has not been described to re-occur in GnRHa preparations, despite prior tolerance. Histrelin-associated hypertension is important knowledge to disseminate for the care and monitoring of patients with CPP.

 Kayla Gonzalez, MD; Allyson McDermott, MD. MAmC; Jonah Mandell, DO; Jane Im, MD
Kayla Gonzalez, MD; Allyson McDermott, MD. MAmC; Jonah Mandell, DO; Jane Im, MD

The ACGME Common Program Requirements require residency programs to monitor work intensity and workload compression that may affect resident wellbeing. The surge in patient volume and acuity in the pandemic and post-pandemic eras unearthed national and local concerns for increasing hospital-based clinician stress and workload, including time spent in the Electronic Health Record (EHR). Though studies have demonstrated the objectively high burden of time spent documenting in ambulatory settings, EHR workload for pediatric residents during inpatient rotations and strategies to decrease its burden have not yet been extensively explored.

To describe and quantify the time spent by pediatric residents at a single, free-standin academic children’s hospital in acute care EHR utilization during inpatient pediatrics rotations before and after workflow optimization.

In this mixed methods study, a focus group of pediatric residents was held to identify areas of strain within the EHR task load of a typical inpatient workday EHR enhancements requested by residents to improve workflow were undertaken (Table). Adjusted for patient volume, mean time spent in the EHR by activity type (writing notes, placing orders, reviewing results) for two cross sectional samples of pediatric residents on inpatient rotations were calculated at baseline and 2-months post-implementation of enhancements. Distribution normality was assessed by Shapiro Wilk testing. EHR metrics over the study period were evaluated using analysis of variance and Kruskall-Wallis nonparametric tests with Bonferroni corrected pairwise comparisons. Statistical analyses were conducted in SPSS version 29.0.1.0. Follow up post-implementation survey was conducted to assess subjective impact.

Overall, time spent in the EHR decreased post-implementation of EHR enhancements. Mean time checking clinical data decreased 2.46 minutes per patient (p=.037) with a reduction in reviewing results by 0.21 minutes per patient (p=.044). Time spent writing notes decreased by 6.87 minutes per patient (p= 013) No significant difference in time spent placing orders was detected. Of survey respondents (n = 14/62, 22.5% response rate), 85.7% reported a subjective time savings ranging from 5-30 minutes per day



At a single, free-standing academic site, implementation of EHR workflow enhancements led to objective and subjective reduction of time pediatric residents spent in the EHR. Continued evaluation needed to account for seasonality and resident experience level.
 Kinga Zgutka, MD, Jennifer Trzaski, MD, James Moore, MD,PhD
Kinga Zgutka, MD, Jennifer Trzaski, MD, James Moore, MD,PhD

NIRS is a non-invasive method of measuring mixed venous tissue oxygenation and is highly sensitive for detecting acute changes in oxygen use and delivery. Infants are at risk for acute kidney injury, or AKI, due to changes in renal perfusion during postnatal transition. Preterm infants are at particular risk due in part to their decreased number of functioning nephrons in comparison to term infants. Antibiotics such as ampicillin and gentamicin are frequently used in the NICU setting as a first line for sepsis rule out and are nephrotoxic. It is unknown whether use of NIRS predicts changes in renal perfusion caused by nephrotoxic agents that may alter normal renal postnatal transition.

Determine whether renal NIRS values are reduced in neonates exposed to ampicillin and gentamicin in the first 6 hours of life.

This was a prospective, case-control study. We included infants ≥30 weeks gestation who received antibiotics within 6 hours of birth as determined by the clinical care team as cases and infants ≥30 weeks gestation who did not receive antibiotics as controls. Exclusion criteria included transfers in, infants <30 weeks gestation, those started on antibiotics after 6 hours of life, those with known congenital anomalies, infants with pulmonary hypertension, infants who were encephalopathic particularly those who had hypoxic ischemic injury and were undergoing cooling, and infants who had skin conditions not allowing for safe attachment of a NIRS probe. A NIRS probe was placed on the flank area for 72 hours from first dose of antibiotic in cases or 72 hours from birth in controls. Probes collected and saved data every seconds We collected renal NIRS values, vital signs, electrolytes, BUN, creatinine and urine output. All labs were part of standard unit protocol and not drawn specifically for this study. Minimums, maximums, means, and standard deviations were calculated and compared for each variable at 1, 3, 12, 24, and 72 hours.

We had 6 cases and 7 controls complete the entire study. The average gestational age and birthweight for cases was 34.0 weeks (range 30.1 - 38.2 weeks) and 2290 grams (range 1585g-2560g). The average gestational age and birthweight for controls was 34.3 weeks (range 32.2 - 38.4 weeks) and 1977 grams (range 1095g-3000g) A comparison of cases and controls at hours of life showed no statistically significant differences. We recognized that as the average time of antibiotic administration in the cases was at 2.8 hours of life, cases who were one hour post antibiotic administration were actually about 3 8 hours old, and at 3 hours post antibiotic administration were about 5.8 hours old, and so on. Therefore, we compared the cases at hours post antibiotic administration to controls at the corresponding hours of life – comparing apples to apples essentially. After this adjustment so that all our subjects were evaluated at a comparable age in hours of life, we did not note any statistically significant differences among the groups. We also looked at the renal NIRS values of the six cases looking at hours of life on the left versus hours after antibiotic administration with their corresponding hours of life noted in the middle. In this analysis, the cases served as their own controls, in essence allowing us to assess pre and post antibiotic administration values. This comparison also showed no significant differences We observed no significant differences in any of the other variables we followed throughout the study at any time points.





The limitations of this study were that it was a single center study, and we had a small sample size, mainly due to difficulties in recruitment due to many infants meeting exclusion criteria or parental concerns regarding participation in a research study. In summary, NIRS is an easy to use and non-invasive tool with minimal complications associated with its use and minimal interference with other aspects of NICU care. In our study population, we did not notice a difference in renal NIRS values following nephrotoxic antibiotic administration within the first 6 hours after birth, during a critical period in postnatal renal transition. There are further studies that need to be done in premature infants under 30 weeks gestation, infants with conditions, such as HIE or those with a PDA, who are receiving nephrotoxic medications, and infants with infection or sepsis who are treated with antibiotics for longer than the 36 hour rule out

Viven Solomon DO, Sydney Kuzoian DO, Genesis Michel DO, Michael Brimacombe PhD, Jeffrey S. Hyams MD

Payer mandates over the past several years have resulted in many children with inflammatory bowel disease (IBD) being switched from originator Remicade® (ORem) to an infliximab biosimilar (B-IFX). Patients and families are often reluctant to switch because disease has been well-controlled on O-Rem and they are fearful of clinical worsening. While there is a large experience of switching from O-Rem to BIFX in adults, pediatric data remain limited. We sought to better understand our experience in a large adolescent and young adult IBD population.

Evaluate the clinical and laboratory course of patients with IBD switching from O-Rem to B-IFX, and compare the switch group to a control group of IBD patients who remained on O-Rem.

Patients 6-26 years of age diagnosed with IBD at Connecticut Children’s who were either in clinical remission or had low disease activity on O-Rem and who were subsequently switched to B-IFX were identified by query of our IBD database. B-IFX was Inflectra® in all cases. Control patients were matched to switch patients by age, gender, IBD type, and time since diagnosis. The minimum duration on O-Rem was 12 months before switch. Demographic, laboratory, drug level monitoring, and clinical information were recorded. A minimum follow-up of 6 months following switch was required. Descriptive analysis was used to describe the patient age, sex, diagnosis, medications, and time since diagnosis. Two-sample t-test was used to estimate the difference between the cases to the controls, while paired t-test was used for comparing cases to cases. Chi-square test was used for equivalent proportions, while Fisher test was used where the sample size was small

Characteristics of the two study groups are shown in Table 1 The two groups (ORem to B-IFX, n=93, O-REM to O-REM n=186) were well-matched. Mean time since diagnosis was >6 years in both groups, and mean duration of anti-TNF use was >5 years. As noted in Table 2, there were no significant changes in key laboratory markers or disease activity in either the switch group or the control group over the 6-month observation period. A small number of patients developed low level antibodies to infliximab (ATI) during the study period, which occurred at similar proportions for both the switch (14%) and control (12%) groups.



In a large number of largely adolescent and young adult patients with IBD, the change from O-REM to B-IFX was not associated with any change in clinical or laboratory evidence of disease activity Clinicians can reliably reassure patients and families that switching is safe. As the cohort is followed longer, we will accrue more data on younger subjects, as well as the frequency of dose intensification if any.
 Jessica Serventi-Gleeson MD, Sravya Gourishetti DO, Megan Kabara DO, Amirul Anuar, Allison S. Cowl MD
Jessica Serventi-Gleeson MD, Sravya Gourishetti DO, Megan Kabara DO, Amirul Anuar, Allison S. Cowl MD

Patients with bronchiolitis and acute respiratory failure (ARF) are admitted to the Pediatric Intensive Care Unit (PICU) requiring differing modes of ventilatory support based on clinical exam, including high flow nasal cannula (HFNC) as well as noninvasive and invasive positive pressure ventilation (PPV). The SpO2/FiO2 (S/F) ratio is used to stratify children into severity of illness and Pediatric Acute Respiratory Distress Syndrome (PARDS) categories.

We aimed to examine the predictive value of S/F ratio in determining escalation from initial to final mode of respiratory support as well as PICU length of stay (LOS).

A retrospective cohort chart review of patients under two years old admitted with ARF secondary to bronchiolitis was performed. S/F ratio, LOS, and mode of respiratory support were recorded throughout PICU admission.

99 children were included. No correlation was found between S/F ratio on admission and PICU LOS (r=0.092; p =0.364). Patients requiring escalation from HFNC to PPV had significantly longer PICU LOS than those without escalation (p = 0.008). However, S/F ratio on admission was not a predictor of need for escalation of respiratory support (p = 0.092). S/F ratio at the first escalation of respiratory support was a predictor

S/F ratio at admission was not predictive of a patient’s LOS nor need for an increase in respiratory support. However, as hypothesized, those without an escalation in respiratory support had a significantly shorter PICU LOS than those requiring PPV.
 Corey Baker, Courtney Stark, Sophia Izhar, Dhiren Patel, Lina Elmansy, Eric Gershon, Leonel Rodriguez
Corey Baker, Courtney Stark, Sophia Izhar, Dhiren Patel, Lina Elmansy, Eric Gershon, Leonel Rodriguez

Globus sensation is defined by the Rome IV criteria in adults, no definition or information of natural history is available in children.

Our aim is to describe this condition in children.

This is a multicenter retrospective study. Patients were identified by searching electronic medical record system for ICD 10 codes R13.13 (pharyngeal dysphagia) and/or R09 89 (feeling of foreign body stuck in throat) from January 1st, 2018 to December 31st, 2022. Each case was reviewed by a research team member to confirm the diagnosis of globus sensation according to Rome IV criteria given by the clinical provider Data collected included clinical presentation, diagnostic workup, therapeutic interventions, and clinical outcomes. Response to therapy was defined as resolution of symptoms or improvement that did not require any further intervention. SPSS software version 29 was used for statistical analysis.

A total of 36 patients were included, median age at presentation was 13.6 y (818y), 59% (n=21) were female and 53% (n=19) were Caucasian. A total of 39% (n=14) had an identified event (infection, traumatic experience with swallowing, or social trauma) preceding the onset of symptoms while 25% (n=9) had a history of anxiety before symptoms started Diagnosis was established after 1 clinical visit in 64% (n=23) and 72% (n=26) had symptoms for less <6 months. Diagnostic work up included: 55% (n=20) upper endoscopy, 44% (n=16) upper GI study, 19% (n=7) flexible laryngoscopy, and 11% (n=4) esophageal manometry, all studies were normal. Outcome information was available in 28 (78%) patients and 8 (22%) were lost to follow. Acid suppression was the most common initial recommendation (16 or 44%) resulting in improved symptoms in 10. Pain neuromodulation (cyproheptadine or gabapentin or SSRI) was recommended in 7 (19%) and resulted in improvement in 4 patients. A total of 3/5 patients responded to behavioral interventions. Lastly, treatment with inhaled steroids and cetirizine in 3 (8%) of patients resulted in the resolution of symptoms. Spontaneous resolution was reported by 3 patients. At last visit, 28 patients with outcome information reported improvement (including 3 with spontaneous resolution) while 18 (50%) reported complete symptom resolution and therapy discontinuation with a median time to resolution of 9 months (1 month to 3 7 years). We found no association between resolution of symptoms and age, gender, ethnicity or presence of preceding factors (p=0.62, p=0.41, p=0.59 and p=0 58, respectively)

This is the first comprehensive description of globus sensation in children. Our findings highlight the current variability in the diagnostic and therapeutic approach among clinicians with this diagnosis in children and further stresses the need for more prospective studies.
 Mariyam
Mariyam
Hashmi, MBBS; Courtney Stark, DO; Leena Kader; Jasmeet Mokha, MD; Jeffrey Hyams, MD; Erin Young; Corey Baker, MD

While functional dyspepsia (FD) is a chronic condition in adults with waxing and waning of symptoms over time, the natural history of FD in children has not been well described.


The aims of the present study were to characterize symptoms and overall healthcare burden in a previous inception cohort of children who had been diagnosed with FD at least 5 years previously Following IRB approval, we attempted to contact study participants who had been part of a previously described inception cohort of children diagnosed with FD including FD subtypes using Rome IV criteria and who participated in a study of duodenal eosinophilia by Mokha et al. If they agreed to participate, they were given a standardized set of questions to assess current F symptoms Patients who reported being symptomatic were also asked to complete the pain frequency-severity-duration scale (PFSDS) and pain burden questionnaires. These follow-up scores were compared to the initial scores at the time of FD diagnosis to determine if the patient's PFSDS and pain burden had improved over a five-year time period. We then completed a retrospective chart review to further clinically characterize this group of patients.

A total of 74 patients were contacted via telephone. 41 (55%) patients agreed to participate in the follow-up study. After reviewing these patients' records, 11 patients were excluded as these patients developed additional diagnoses including eosinophilic esophagitis (EoE), H. pylori infection, celiac disease, and inflammatory bowel disease Of the 30 patients remaining 63 3% (n=19) were female and 36.7% (n=11) were male. The average age of this group at the time of their initial enrollment into the FD study in 2017 was 12.8 years old with 53 3% of them having FD post-prandial distress syndrome (PPDS) subtype, 10% with epigastric pain syndrome (EPS) subtype, and 36.7% had both PPDS and EPS. At enrollment all of the patients reported the symptom of epigastric abdominal pain, 90% reported nausea, 90% reported bloating, 90% had early satiety, and 66.7% reported epigastric burning. The average age of the 30 patients contacted at 5-year follow-up was 18.5 years. 40% (n=12) of patients reported still experiencing at least one persistent symptom of FD. Of the 60% (n=18) of patients that were asymptomatic at follow-up, they reported that their symptoms resolved on average, 15.5 months after the initial diagnosis of FD with 55.6% reporting that a medication improved their symptoms, 16.7% from dietary restrictions, and 5.6% from stress reduction. 27 8% of patients report that their symptoms self-resolved The initial PFSDS of these 30 patients in 2017 was 34 (range 0-140) and a pain burden score of 9 (range 0-28). There was no difference in the average of the initial pain severity scores between the patients that had persistent pain at follow-up (41.8, n=12) and those without pain at follow-up (29.9, n=17, p=0.3942) nor was there a difference between these two groups for the average initial pain burden scores, (10.25, n=12 vs. 8.2, n=17, p=0.4574). As expected, the average PFSDS and pain burden scores at follow-up for patients without pain were lower than those with pain at follow-up, (p=0.0004 (PFSDS) and p=0.0002 (pain burden scores)). Of the 12 FD patients who reported persistent dyspeptic symptoms at 5 years follow-up, there were decreased average PSDS and pain burden scores when compared to the initial scores, (Follow up PFSDS average: 17.4, (p=0.07); Follow up pain burden average: 6.58 (p=0.21)).





This study describes the natural history of pain symptoms in children with FD. We report that 60% of patients had complete resolution of their symptoms on average 15 5 months after initial diagnosis Roughly half of these patients reported that their symptoms resolved due to medication (i.e., acid suppression therapy, neuromodulator, or probiotics). Of the 40% of patients that reported still having symptoms of FD roughly five years after their initial diagnosis, their pain severity and pain burden had decreased when compared to their initial scores. Future studies with a larger sample size are needed to better characterize these findings.
 Sravya Gourishetti DO, Megan Kabara DO, Michael Brimacombe PhD, Allison S. Cowl MD
Sravya Gourishetti DO, Megan Kabara DO, Michael Brimacombe PhD, Allison S. Cowl MD

Social Determinants of Health (SDOH) have been shown to significantly impact patient outcomes, but this relationship has been inadequately studied in the PICU. The Childhood Opportunity Index (COI) is a composite measure to estimate a child’s cumulative SDOH and are grouped into categories called Childhood Opportunity Levels (COL). In this study, we aimed to delineate the impact of SDOH on severity of bronchiolitis and illness course.

To delineate the impact of SDOH, using COI as a marker, on the severity illness in patients with bronchiolitis who are admitted to the PICU.

A retrospective cohort chart review of patients under two years old admitted to the PICU with Acute Respiratory Failure due to bronchiolitis was performed. The patients’ COI and COL were identified using their home zip code and the COI 2.0 index data set.

99 children were included. The incidence of patients in the very low, low, moderate, high, and very high COL categories was 21.21%, 8.08%, 17.17%, 23.23%, and 30.30%, respectively. Patients were grouped into 3 groups: those with low COL (patients with low and very low COL), moderate COL, and high COL (patients with high and very high COL) Those with moderate COL had significantly lower S/F ratio than their low and high COL counterparts (p=0.034). Most patients were on High Flow Nasal Cannula (HFNC) at PICU admission. Of those patients, there were more patients in the nationally normed high COL group than low or moderate COL group (p=0.001). When using metro-normed COL however, there were more patients in the low COL group on HFNC at admission than the moderate or high COL groups (p < 0.001). There were more patients with high nationally normed COL that required HFNC as their highest level of respiratory support than other groups (p=0.001). However, based on metro-normed COL, there were more patients with low COL than their moderate or high COL counterparts (p < 0.001). Lastly, more patients with a lower COI (040) were on HFNC at admission compared to higher COI (p=0.001).

Amongst patients admitted to the PICU with bronchiolitis, the nationally normed and metro-normed COL categories had inconsistent results. As metro-normed COL captures more inequalities within a metro region, our patients with low COL may be inadequately represented if using different normed COL categories. Further research is required to explore the impact of these differences on illness severity and course.
 Megan Kabara DO, Sravya Gourishetti DO, Michael Brimacombe PhD, Allison S. Cowl MD
Megan Kabara DO, Sravya Gourishetti DO, Michael Brimacombe PhD, Allison S. Cowl MD

Children at our center admitted to the Pediatric Intensive Care Unit (PICU) with bronchiolitis are often cared for with High Flow Nasal Cannula (HFNC) and do not require Non-invasive Positive Pressure Ventilation (NIV) and intubation, but the illness severity of our population was unknown. Utilizing the SpO2/FiO2 (S/F) ratio definition of Pediatric Acute Respiratory Distress Syndrome (PARDS), we were able to stratify children into PARDS categories to evaluate those successfully managed with HFNC and those requiring intubation or NIV.

To evaluate the association between S/F ratio and modes of ventilation, including non invasive and invasive ventilatory modes, in patients admitted to the PICU with bronchiolitis.

Retrospective cohort chart review of patients under two years old admitted to the PICU with Acute Respiratory Failure (ARF) secondary to bronchiolitis. S/F ratio was collected on admission to the PICU.

99 children were included. 88 were supported initially on HFNC with 38% categorized as ARF, 29% at risk, 27% mild/moderate, and 4% severe PARDS. There was no difference in need for positive pressure amongst those with ARF, at-risk, nor with mild/moderate PARDS (p=0.917). 14 patients failed HFNC needing higher levels of support, 35% were in ARF, 35% at risk, 21%, mild/moderate, 7% severe PARDS. There was a similar percent failure in each of the S/F categories showing no significant difference (p=0.917). There was no significant difference of S/F ratio (p=0 63) between the cohort that failed HFNC, mean S/F ratio 266.4, as compared to the cohort that succeeded on HFNC, mean S/F ratio 257.5. 11 patients were admitted on positive pressure support, either NIV or intubation, having a categorical distribution of none with 27% at risk, 27% mild/moderate, and 45% severe PARDS. Looking at the cohorts of HFNC versus NIV/intubation at initial PICU admission, the only significant difference was in those with severe PARDS in which 50% of the population needed NIV/intubation (p<0.001).

Patients at risk for and with mild to moderate PARDS can be successfully managed with HFNC. No S/F ratio category was found to predict need for positive pressure as rates of NIV and intubation were essentially equivalent in all categories. However, not surprisingly, the sickest patients, having the lowest S/F ratios and in the severe PARDS category, had a significant difference (p<0.001) from the other categories in the need for positive pressure ventilation To evaluate the association between S/F ratio and modes of ventilation, including non-invasive and invasive ventilatory modes, in patients admitted to the PICU with bronchiolitis.

 Erin Pastor, DO Maddie Walker & Natalie Bezler, MD
Erin Pastor, DO Maddie Walker & Natalie Bezler, MD

The prevalence of elevated blood pressure (BP) and hypertension in the general pediatric population is an increasing concern, with risk factors such as family history and obesity playing a significant role. Among survivors of pediatric childhood cancer, the estimated prevalence of hypertension is 37%, a 2.5-fold increase compared to the general population Pediatric cancer survivors face a unique set of risk factors that amplify their susceptibility to hypertension, including cytotoxic drugs, corticosteroids, radiation, and acute kidney injury. The ramifications of hypertension in these patients include accelerated vascular aging, damage to vital organs and an elevated risk of heart failure.

Obtain baseline data to establish intuitional prevalence of abnormal BP in oncology patients.

Baseline data obtained with retrospective chart review. Using SlicerDicer we captured a population of oncology patients actively receiving chemotherapy Using this patient population, we assessed outpatient clinic visits. We reviewed patient demographics, oncology diagnosis, vitals, documentation of abnormal BP, inclusion of abnormal BP on problem list as well as historic mention of abnormal BP Vitals entered in the electronic health record (EHR) were compared with standard norms as established by American Academy of Pediatrics (AAP) Clinical Practice Guidelines (CPG).

Baseline data revealed 36% of patients met AAP CPG criteria for abnormal blood pressure. Of this population, only 9% had abnormal blood pressure documented on the problem list in the EHR. Of the abnormal population, only 4% had clinical documentation during clinic note in the assessment and plan. Chart review and audit also revealed inconsistency between EHR identification of abnormal BPs as compared to AAP CPG, exposing that the cutoffs to flag BPs as out-of-range in the EHR are not specific to patients’ age, gender or height. Current EHR ranges under identify abnormal BPs and therefore lead to decreased provider recognition, assessment and treatment.

Despite the prevalence and notable consequences associated with hypertension in oncology patients, it is an under-recognized and therefore undertreated condition in many patients. We believe by adjusting EHR alerts we will be able to better capture abnormal BPs which are specific to patients age, gender and height (using AAP CPG standards). In addition to better capture of abnormal values, we expect that establishing a standardized workflow for the recognition, documentation, follow up and management of elevated BP and HTN will help patients receive appropriate therapy.

 Erin Pastor, DO & Natalie Bezler, MD
Erin Pastor, DO & Natalie Bezler, MD

Acute lymphoblastic leukemia (ALL) is the most common pediatric malignancy and typically progresses rapidly. ALL is fatal without timely diagnosis and initiation of treatment.



Review an unusual presentation of ALL
Case report
A 15-year-old healthy male presented for evaluation of leukopenia. Review of systems revealed a 28kg weight loss, fatigue, nausea, and vomiting. Initial studies revealed WBC 2.6 and ANC 1070, other cell lines intact. During weight loss evaluation, patient was admitted with prolonged fevers (>8 days). During admission, he was found to have new pancytopenia with profound inflammatory response (ferritin >30,000 ug/L), raising concern for hemophagocytic lymphohistiocytosis. He did not meet other criteria for diagnosis. Patient improved clinically despite continued lab abnormalities and was discharged to continue work up as an outpatient. Patient had normal CT of the abdomen and pelvis, endoscopy and colposcopy. Serial labs, over the next 4 months revealed improvement in cytopenias and inflammatory markers. Two months later, about 6 after initial presentation patient presented with altered mental status requiring intubation. While admitted, pancytopenia returned LDH and uric acid remained normal CSF analysis was unremarkable. Peripheral flow cytometry was unremarkable. Bone marrow revealed preservation of trilineage hematopoiesis and an abnormal immature B cell population comprising up to 6% by flow cytometry; abnormal cells were noted in an unusually clustered distribution in the core biopsy.

This population displayed features that differ from the usual benign B cell precursors (weaker CD45 and over-expression for CD10, CD58 and CD86). PET revealed patchy heterogeneous hypermetabolism throughout entire skeleton. During the subsequent 4 weeks, immature B cell population persisted <10% on peripheral flow cytometry Repeat bone marrow obtained one month after initial biopsy revealed 3% abnormal lymphoid blasts by flow. Core biopsy showed a significant increase in CD34+/TdT+/PAX5+ B-lymphoid blasts ranging from 1040%, focally present in small sheets and clusters, and overall approaching 25%
This marrow was diagnostic for B-Cell ALL.

This case highlights the importance of close follow up in the setting of clinical uncertainty. Both the timeline and the marrow findings were atypical for ALL. ALL is commonly not an insidious process. Normally, diagnosis is proceeded by only a few weeks of symptoms. In this case, diagnosis was made nearly 8 months from initial presentation. The marrow findings were also atypical for ALL with the flow cytometry not being representative of marrow findings due to the clustering of blasts noted only on review of core biopsy.
 Nickolas Mancini, MD, MBA; Sharon Smith, MD; James Rudloff, MD; Marvin Harper, MD; Amir Kimia, MD
Nickolas Mancini, MD, MBA; Sharon Smith, MD; James Rudloff, MD; Marvin Harper, MD; Amir Kimia, MD

Elevated inflammatory markers have long been associated with Osteoarthritic infections (OAI) and the assessment of inflammatory markers is integral to both diagnostic and management decision-making. For patients diagnosed with OAI, elevated inflammatory markers, like fever, are not present in 100% of cases, yet the actual prevalence is unknown. Understanding the prevalence of low/normal levels of inflammatory markers among OAI cases and evaluating differences in the clinical presentations associated with this subset of the population may better inform clinicians on how to best incorporate inflammatory results in their diagnostic workflow.

Assess the prevalence of low inflammatory markers in children with OAI and identify clinical elements that may be associated with a higher prevalence of OAI with low inflammatory markers.

IRB-approved retrospective cross-sectional study across three hospital EDs (Connecticut Children’s Hospital, St. Louis Children’s Hospital and Boston Children’s Hospital) involving otherwise healthy children ultimately diagnosed with OAI during their hospital stay Included are children 0-18 years of age, evaluated between October 2015 and December 2023. Cases identified with corresponding ICD10 diagnoses. Excluded are immunocompromised patients, those with chronic OAI, and co-diagnoses that may interfere with results (i.e. rheumatologic diseases) and those treated with systemic antibiotics >24 hours prior to presentation. Data collected includes demographic, history, examination, laboratory, imaging, and management variables. Natural language processing will be used for data abstraction.

Statistical plan: descriptive statistics (prevalence, 95% confidence interval) to assess prevalence; and a multivariable logistic regression model with low inflammatory marker OAI cases as dependent variable and fever, bone involved, and duration as independent variables, controlling for demographics, additional laboratory studies, with robust standard errors. Final data collection and complete analytics expected by February 1, 2024.

Pending; currently performing data acquisition (initial AI-assisted chart review completed, performing variable extraction the week of 2/4/24). Will update submission prior to March 8th deadline.

Pending; currently performing data acquisition (initial AI-assisted chart review completed, performing variable extraction the week of 2/4/24). Will update submission prior to March 8th deadline.
 Meghan Wilson, MD, MPH; Amy A. Hunter, MPH, PhD; Susan DiVietro, PhD; Sharon Smith, MD
Meghan Wilson, MD, MPH; Amy A. Hunter, MPH, PhD; Susan DiVietro, PhD; Sharon Smith, MD

In the United States pediatric firearm mortality has been one of the leading causes of death for decades. Since 2020 childhood deaths from firearms has sharply risen and surpassed motor vehicle collisions as the primary cause of death for the pediatric population. Previous studies have shown there is an inverse relationship between child firearm deaths and the presence of stricter state firearm laws; however, there is limited examination of this relationship since the marked increase of children dying from firearms since 2020.

The purpose of this study is to examine state firearm legislation and pediatric firearm mortality in children using data from the National Violent Death Reporting System (NVDRS) and Giffords Law Center Scorecard Data from 2018-2021 Our primary aim is to investigate the relationship between state firearm legislation and pediatric firearm mortality in children aged 0-17 years. For consistency in exposures pediatric firearm deaths among 41 states that annually reported to NVDRS from 2018-2021 will be used along with respective Giffords Law Center Gun Scorecard Data. For each state, Giffords assigns a numeric scoring system to compare the strength of firearm laws and policies based on their respective strength or weaknesses. Our secondary aim is to examine potential differences between individual state firearm legislation and pediatric firearm deaths by high-risk subgroups whom are known to have higher firearm mortality risk either by suicide or homicide. This includes children who identify as Lesbian, Gay, Bisexual, Transgender, Queer, Intersex, and Asexual (LGBTQIA+) and those who have mental health conditions and previous suicidal thoughts or attempts. Our third aim is to investigate firearm specific variables and narratives to determine if there are relationships between state firearm policies and firearm storage and access resulting in pediatric firearm deaths.

The CDC NVDRS has a restricted access database (RAD) that contains deidentified, multi-state, case-level data with hundreds of unique variables. The CDC has accepted and approved us to receive access to the RAD. IRB review is pending with anticipated exempt status. An agreement with Giffords Law Center with complete access to gun scorecard data has been secured. Statistical analyses include: standard descriptive statistics and univariate and bivariate analysis (as appropriate) to summarize study population characteristics and pediatric firearm mortality; Poisson regression to measure pediatric firearm death rate among states with varying firearm law scores. In addition, to better understand the complexities and circumstances of pediatric firearm deaths we will use qualitative content analysis to review all law enforcement and medical examiner/coroner narratives, noting patterns regarding weapon characteristics and gun access themes that appear frequently, and instances where circumstances diverge.

This is a works in progress submission with data analysis currently pending and will be presented at PAS 2024 in Toronto, Canada.

This is a works in progress submission with conclusions currently pending and will be presented at PAS 2024 in Toronto, Canada.

Antoinette Farrell, MD; Eric Hoppa, MD; Sharon Smith, MD; Rebecca RibaWolman, MD

• Obtaining critical laboratory studies at the time of hypoglycemia is essential • Aids in identifying underlying etiology • Delayed work up increases burden and costs • Emergency department (ED) presentation • Opportunity to efficiently obtain laboratory studies
• Priority labs include: plasma glucose (PG), beta-hydroxybutyrate (BOHB), lactate, bicarbonate (HCO3), and free fatty acids (FFA)1,2
• 8-10% have underlying pathologic disorders3,4 • The opportunity for obtaining a critical sample is frequently missed in the ED • Published rates for ED critical lab obtainment are 38-59%5-7 • In 2022, <20% of these children received any workup outside of PG in our ED

SMART Aim: Increase the frequency of priority labs obtained in our ED from 19% to 75% by December 2023

• 6 months pre-intervention data (February 2023-July 2023)
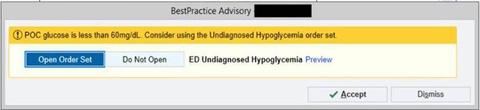
• 4 monthly PDSA Cycles utilizing education and electronic health record (EHR) tools 1. Pediatric resident education 2. Electronic health record (EHR) undiagnosed hypoglycemia order set edits (Fig. 2) Preselected priority labs (PG, HCO3 and lactate via venous blood gas [VBG], BOHB, FFA) 3. ED provider education 4. Creation of an EHR Best Practice Advisory (BPA) EHR automatically launches alert to clinical staff when POCT glucose < 60 mg/dL and links to order set
• 8 months of data since first intervention (August 2023-March 2024)
• Single center quality improvement initiative • Inclusion criteria:
• Age birth - 21 years old

• ED diagnosis of Hypoglycemia OR POCT glucose <60mg/dL during an ED visit
• Exclusion criteria:
• History of diabetes (any type)
• History of metabolic disorder impacting glucose metabolism

a. EHR order set with pre-selected highest priority critical labs.
b. BPA alerts clinical user if POCT glucose < 60 mg/dL and provides link to order set

• 52,949 patients seen in ED during study period
• 22,676 pre-intervention period
• 30, 273 intervention period
• 424 patients (0 8%) met inclusion/exclusion criteria
• 191 [0.84%] pre-intervention period
• 233 [0.77%] intervention period
• Average monthly frequencies
• PG: 36.5% (SD 8.6) pre-intervention, 56.6% (SD 7.2) after intervention (p = 0.0004) (fig 2a)

• BOHB: 15.4% (SD 2.1) pre-intervention, 28.5% (SD 7.7) after intervention (p = 0.0017) (fig 2b)
• Complete set: 2.3% (SD 2.9) pre-intervention, 12% (SD 7) after intervention (p = 0.008) (fig 2c)
• VBG HCO3: 19.1% (SD 4.6) pre-intervention, 28.4% (SD 12.9) after intervention (p = 0.12)
• Lactate: 13 1% (SD 6 2) pre-intervention,18 5% (SD 6 0) after intervention (p = 0.13)
• FFA: 7.2% (SD 3.7) pre-intervention, 18.2% (SD 8.8) after intervention (p = 0 0144)
• The greatest increase in complete priority lab draw was seen following BPA release, delta +9.7%



Run charts showing percent of patients meeting inclusion/exclusion criteria each month who had obtained a. plasma glucose, b. beta-hydroxybutyrate, and c. all 5 priority labs.

• Education and EHR tools significantly increased the rate of the highest priority critical labs obtained in ED
• Largest increase in rate was after BPA creation
• We demonstrate a novel use of educational curriculum and EHR tools to increase adherence to guideline driven assessment in undiagnosed hypoglycemia patients
Next steps:
• nurse education
• ongoing provider education
• assessing BPA firing and fatigue
• assess further burdens to obtaining labs
• Point of care (POC) ketone meter
