

THE 7 ROOT CAUSES OF AUTOIMMUNITY AND
CHRONIC INFLAMMATION
One in every 10 people is affected by an autoimmune condition. You may be one of them. You may be at risk. And you most likely know people with an autoimmune condition. There are currently over 80 different kinds of known autoimmune diseases, but there are likely more that we don’t have a name for yet. Many with an autoimmune disease are at risk of developing one. It’s clear that autoimmune diseases are a serious health issue in our society. But what are the major factors that can cause or increase your risk of autoimmunity? Without understanding the root cause issues and risk factors, we can’t reduce your risks and improve your health.
In this book, I will explain what autoimmunity is. I will go over the most common autoimmune conditions. I will discuss the connection between autoimmunity and the cell danger response (CDR). I will go over the 7 major factors causing autoimmune conditions. You will understand the role of the allostatic load and the cell danger response. Throughout the article, I will share resources on how to reduce your risk for certain risk factors and improve your health.


WHAT IS AUTOIMMUNITY?
The job of a healthy immune system is to protect you from infections and diseases. Your immune system does this by attacking viruses, bacteria, and other pathogens that are trying to enter and harm your body. A normally functioning immune system is able to tell apart pathogens from cells that are part of your body. They don’t harm your cells, tissues, and organs, but only pathogens. However, if you have an autoimmune condition, your immune system has trouble differentiating between foreign pathogens and parts of your body. It will end up attacking your cells, organs, and tissues instead of pathogens by mistake because it confuses them with foreign invaders.
Autoimmune diseases affect about 1 in every 10 people (1). Considering that many people go undiagnosed, and we haven’t identified every autoimmune disease yet, these numbers may be higher. Certain autoimmune conditions only affect one organ or one area of your body. For example, autoimmune hepatitis affects your liver, and alopecia areata causes hair loss. Other types of autoimmune conditions may affect various areas and multiple organs. Rheumatoid arthritis may affect multiple joints across your body but may also affect your eyes and lungs. Systemic lupus erythematosus (SLE or lupus) can cause widespread problems from joint pain, rashes, hair loss, kidney issues, mouth sores, and more (2).


MOST COMMON AUTOIMMUNE CONDITIONS
There are over 80 different kinds of known autoimmune conditions out there (2). There may be more that researchers haven’t identified or named yet.
The most common autoimmune conditions include:
• Celiac disease
• Hashimoto’s thyroiditis
• Graves’ disease
• Inflammatory bowel diseases (IBDs), including ulcerative colitis and Crohn’s disease.
• Rheumatoid arthritis
• Reactive arthritis
• Systemic lupus erythematosus
• Addison disease
• Sjögren syndrome
• Type I diabetes
• Psoriasis
• Multiple sclerosis
• Pernicious anemia
• Myasthenia gravis


AUTOIMMUNITY AS PART OF THE CELL DANGER RESPONSE
The cell danger response (CDR) is a hot topic in the functional medicine field. There is a good reason for it.
The CDR may play a role in all kinds of health issues, including autoimmunity, metabolic disease, hypothyroidism, neurological issues, chronic fatigue syndrome, and more. But what is the CDR?

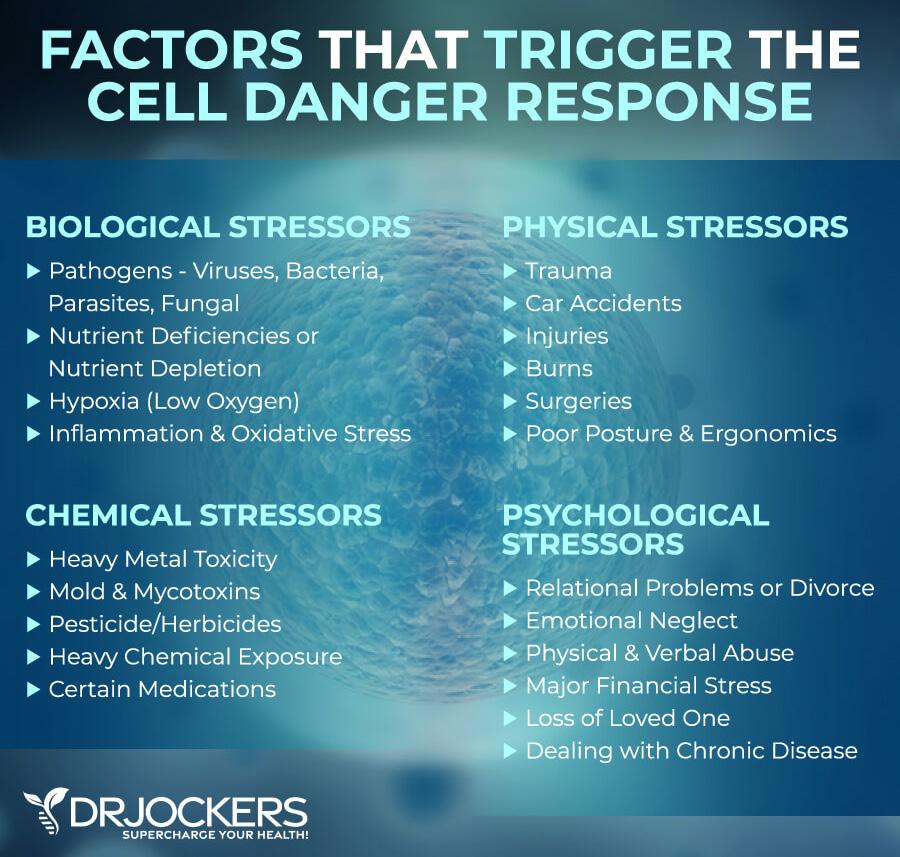
According to a 2013 review published in Mitochondrion, the CDR as a critical evolutionarily conserved metabolic response that is part of your body’s innate defense system (3). The role of the CDR is to protect your individual cells from cellular threat, danger, and harm. The threat may be physical, biological, or chemical. It doesn’t matter, but if it goes beyond your cell’s natural capacity to ensure homeostasis, it can trigger a CDR.
If you think about your body, it is a complex system of individual cells that work together to form tissues, organs, and other systems in your body. Together, these cells, tissues, organs, and systems form a complex organism that you know as the human body. Within this system, all of your cells work relentlessly to keep your body healthy. Each of your cells has several components, including the most important one, the mitochondria. The mitochondria are well-known as the powerhouse of your cells. It’s responsible for creating energy from the food you eat to fuel and energize your cells, tissues, and organs It is critical for energy, function, and health.


The mitochondria also serve as energy sensors within your cells, as well as cellular defense agents. The goal of each cell and each mitochondrion within these cells is to maintain cellular homeostasis. Your mitochondria’s job is to create and provide enough energy needed for this cellular balance. When there is a significant drop in energy, and there isn’t enough to upkeep homeostasis, your mitochondria will note this as a threat to your health and balance. This perceived threat will prompt your mitochondria to change their primary function and move from energy production and optimal cell metabolism to cellular defense. This is a major shift in cellular physiology called the CDR.
Now, in the short term, the CDR is an evolutionarily conserved multi-system response that helps your body to fight off a threat and to recover from injury or illness. However, if the threats are ongoing from chronic emotional or mental stress, ongoing physical stress, a poor diet on a daily basis, ongoing stressors from environmental toxins, or other ongoing issues, it can lead to an ongoing CDR. An ongoing CDR may lead to a hypometabolic state, which may lead to a fight, flight, or freeze stress response. This state, when ongoing, may increase the risk of disease, including autoimmunity. This ongoing state of threat can become overwhelming to the body, leading to a chronic inflammatory response that may trigger autoimmune conditions.


7 FACTORS CAUSING AUTOIMMUNE CONDITIONS
We don’t know the exact cause of autoimmune conditions. It seems that rather than one cause, multiple factors may play a role. Some autoimmune conditions tend to run in the family, so genetics may play a role.
Besides genetics, though, there are a number of dietary, lifestyle, and health factors that may increase your risk of developing an autoimmune condition. Let’s look at the main 7 factors that may cause autoimmune and chronic inflammatory conditions.


LEAKY GUT AND LOW STOMACH ACID LEVELS
Your gut affects your entire body, including your immune system. Poor microbiome balance or gut dysbiosis may increase digestive issues, chronic inflammation, and the risk of autoimmune conditions. It causes poor nutrient absorption, increases toxin build-up, and reduces detoxification (4).
This also increases the risk of leaky gut syndrome and low stomach acid levels, which then increases the risk of autoimmune conditions.


IMPORTANCE OF STOMACH ACID
Stomach acid is a digestive fluid created in your gut to help the digestion of food. Its main component is hydrochloric acid (HCL), along with potassium chloride and sodium chloride (5, 6). With the help of HCL, your stomach is able to transform a large solid meal into a semi-liquid soupy substance called chyme that can move through the rest of the digestion process without a problem.
If your body doesn’t produce enough HCL and stomach acid, it won’t be able to provide a healthy gut environment. This means that your body won’t be able to break down and digest food properly. Low stomach acid levels, make it very challenging for the body to fight pathogens properly, either. It may increase digestive issues and gut microbiome imbalance, increasing the risk of leaky gut syndrome.


LEAKY GUT CREATES FOOD SENSITIVITIES
Leaky gut syndrome is one of the major root cause factors behind immune dysfunction. Under normal circumstances, your gut lining is semi-permanent. It’s able to allow micronutrients to pass through into your bloodstream, but stop bigger food particles, toxins, and pathogens.
However, if you are following a poor diet, exposed to too many environmental toxins, experiencing high stress, dealing with low stomach acid levels disrupting healthy digestion, and dealing with poor microbiome balance, it may cause the small semi-permeable holes to become bigger. When your gut lining has a bigger hole that allows toxins, microbes, and large food particles to pass into your bloodstream, we call this leaky gut.
According to 2020 research published in the International Journal of Molecular Sciences, damage to the intestinal wall and leaky gut may increase the risk of autoimmunity (7). When toxins, microbes, and food particles enter your bloodstream due to leaky gut, your immune system will recognize them as harmful invaders.
It will attack them to protect you. However, unless you do something about it, with leaky gut, these particles will keep on flooding your bloodstream. And your immune system will keep on attacking them, causing one wave of inflammation after another, leading to chronic inflammation.


AUTOIMMUNE CONDITIONS AND LEAKY GUT
Over time, your immune system will become overwhelmed and confused. Eventually, it won’t be able to differentiate between unwanted substances and your body, leading to autoimmune issues.
According to a 2022 review published in Frontiers in Immunology, gut microbiome imbalance and leaky gut may increase the risk of autoimmune diseases, including type 1 diabetes, multiple sclerosis, and systemic lupus erythematosus (8).
Moreover, leaky gut syndrome may increase food sensitivities. Consuming foods that you are sensitive to will increase inflammation. Unfortunately, some of the top food sensitivities, namely gluten and dairy, look very similar to your own body’s cells.
We call this mistaken identity molecular mimicry. Molecular mimicry will only increase confusion within the body and increase autoimmune reactions.


HIGH TOXIC LOAD
We all wish we lived in a clean and safe world. Unfortunately, this is not the case. Our world is full of environmental toxins, including exhaust fumes, air pollution, cigarette smoke, chemicals in cleaning, personal hygiene, body, and beauty products, plastics, toxins in tap water, pesticides, and so on. According to the Environmental Working Group, there are over 80,000 toxic chemicals used regularly in the United States (9).
The body has a built-in metabolic detoxification system to address this problem by converting fat-soluble toxins into inactive water-soluble metabolites. This process is carried out by a series of enzymes that transform, conjugate (attach), and transport the toxins out of the body. Unfortunately, with so many toxins and chemicals around, our bodies get overwhelmed. In many, genetic polymorphisms may affect their ability to detoxify.
High exposure to environmental toxins and poor detoxification may increase chronic inflammation and oxidative stress. It may also impact your gut health and increase your risk of gut issues, leaky gut syndrome, and gut microbiome imbalance. Chronic inflammation and gut issues due to high toxicity may increase the risk of autoimmune disorders too.


PESTICIDES & HERBICIDES
Pesticides and herbicides such as glyphostate are some of the major environmental toxins that may affect you and increase your risk of autoimmunity if you are exposed to non-organic food and food products. Pesticides are chemicals used in farming to kill, prevent, reduce, destroy or repel a pest. And herbicides are used to manipulate or control undesirable vegetation.
Pesticides and herbicides not only interfere with natural biodiversity on our farmlands but also get into your body when eaten in produce. When animals raised for meat are fed with nonorganic feed, you may be impacted by pesticides or herbicides when consuming their meat.
Unfortunately, pesticides and herbicides both increase the risk of chronic inflammation, gut imbalance, chronic health issues, and autoimmune disorders. According to 2019 research published in Frontiers in Immunology, long-term pesticide use may increase the risk of systemic autoimmunity in farmers (10). According to a 2022 study published in Environmental Research, pesticides may increase the risk of autoimmunity, including SLE and a related disease, Sjögren’s syndrome (SS) (11).


MOLD AND MYCOTOXINS
Mold toxicity occurs when mycotoxins are produced by micro-fungi, such as mold, that can affect your body’s system leading to chronic symptoms.
Toxins produced by mold will start to accumulate inside the body and trigger inflammatory reactions that cause a wide variety of symptoms, from allergies, sinus congestion, and breathing issues to fatigue, brain fog and mood disorders such as depression and anxiety.
It may also increase the risk of autoimmunity. According to a 2021 study published in the International Journal of Molecular Science, mold and mycotoxins may lead to a dysregulated immune system and related autoimmunity (12).


HEAVY METALS
A heavy metal is a metal that has a density of at least 5 g/cm3. It is generally understood that heavy metals have adverse effects on living organisms and the environment when present in large amounts. Heavy metals that may harm your body include lead, cadmium, arsenic, aluminum, nickel, copper, and tin.
When present in the human body, heavy metals have no beneficial role. On the contrary, they usually interfere with normal biological processes instead (13).
They do this partly by binding to proteins in the body that would otherwise be activated by normally occurring minerals like magnesium and zinc.
This causes massive cellular interference, oxidative stress, and chronic inflammation. According to a 2022 review published in the European Journal of Inflammation, heavy metals may disrupt your immune system and cause an inappropriate immune response, increasing the risk of chronic inflammation and autoimmunity (14).


PHTHALATES
Phthalates are a group of chemicals that are incredibly toxic and weaken immunity. They are the most commonly found in plastics (BPA) and cosmetics but may be found elsewhere.
According to the US Food and Drug Administration (FDA), they are “used in hundreds of products, such as toys, vinyl flooring and wall covering, detergents, lubricating oils, food packaging, pharmaceuticals, blood bags and tubing, and personal care products, such as nail polish, hair sprays, aftershave lotions, soaps, shampoos, perfumes, and other fragrance preparations” (15).
Phthalates may increase the risk of gut health issues, chronic inflammation, and autoimmunity. According to a 2021 study published in Frontiers in Pharmacology, phthalates are endocrine disruptors that may increase immune dysfunction and the risk of autoimmune and chronic health issues (16).


OTHER MAJOR TOXINS
Exotoxins is another word for environmental toxins. They include endocrine-disrupting and carcinogenic (cancer-causing) chemicals. Exotoxins include chemicals, toxic heavy metals, and biotoxins.
Besides pesticides, herbicides, and phthalates, other chemical toxins include insecticides, plastics, industrial solvents, radon, formaldehyde, and electromagnetic fields.
Besides mold, other biotoxins include viruses, parasites, and bacteria. These other major toxins may also increase your risk of chronic inflammation, gut imbalances, and autoimmune disorders.


BLOOD SUGAR IMBALANCE AND INSULIN RESISTANCE
Blood sugar balance and insulin sensitivity are incredibly important for your health. Insulin helps your cells to absorb and use glucose for energy. Insulin resistance happens if your body is unable to respond to and use the insulin produced by your body. Insulin resistance may increase the risk of prediabetes, diabetes, and an array of other health issues. Type 1 diabetes is one of the most common autoimmune disorders (17). However, blood sugar imbalance and insulin resistance may increase the risk of other autoimmune disorders as well.
According to a 2020 study published in Circulation Research, insulin resistance may increase inflammation (18). According to a 2021 study published in the World Journal of Diabetes, there is a link between gut health and insulin resistance (19). As you know, chronic inflammation and gut imbalances both may trigger autoimmunity. Moreover, consuming refined and processed sugars, refined oils and other unhealthy fats, and following an overall high-carb inflammatory diet may increase the risk of blood sugar imbalances, insulin resistance, gut health issues, and chronic inflammation. This is a recipe for chronic health issues and the risk of developing an autoimmune disorder.


CHRONIC STRESS & MENTAL/EMOTIONAL OR PHYSICAL TRAUMA
Chronic stress is a major underlying issue and the development of chronic health issues. The Adverse Childhood Events (ACE) score was developed to score people on their early childhood trauma. High ACE scores and lots of childhood trauma have been linked to the increased risk of developing chronic health issues, including autoimmune diseases. According to a 2009 study published in Psychosomatic Medicine, cumulative childhood stress may increase the risk of developing an autoimmune disorder as an adult (21).
However, adulthood trauma and chronic stress may also increase your risk. For example, according to a 2020 study published in BMC Psychiatry, posttraumatic stress disorder (PTSD) in military members may increase the risk of autoimmune disorders (22). Even if you don’t have major (big “T”) trauma, more minor (small “T”) trauma and daily chronic stress and a high mental and emotional stress load may increase chronic inflammation, poor sleep, gut health issues, and other factors that may contribute to the increased risk of autoimmune disorders. Chronic physical stress from bad posture or a poor diet may also increase chronic inflammation and the risk of autoimmunity.


CIRCADIAN RHYTHM DYSFUNCTION
Sleep is critical for your health. Chronically poor sleep may increase chronic inflammation and related health issues. According to a 2015 study published in Sleep, sleep disorders may increase the risk of autoimmunity (23). To improve your sleep, paying attention to your circadian rhythm is critical. Your circadian rhythm is your body’s natural sleep cycle. Under natural circumstances, when it gets dark, your body gets tired, and you sleep overnight, then your body naturally should wake up with the sun and brightness.
The problem is, in order modern world, we have indoor lighting interfering with this natural cycle and our schedule, causing circadian rhythm dysfunction. Mal illumination is something some refer to as an indoor epidemic, caused by indoor light.
Bright light after dark can suppress melatonin production and increase cortisol and dopamine levels at night. On the other hand, most people don’t get enough natural light and sun exposure during the day to stimulate mitochondrial melatonin levels during the day to set the proper sleep cycle.


MELATONIN AND AUTOIMMUNE CONDITIONS
This may also affect your mitochondrial health. Melatonin is a natural hormone. It is mainly made by your pineal gland. It aids your sleep, but it’s also essential for mitochondrial function.
Melatonin plays an important role in your mitochondrial health. According to a 2020 review published in Physiology, melatonin production in the mitochondria may help to reduce oxidative stress and other health dangers (24).
Optimal mitochondrial function is critical for cell survival and overall health. Mitochondrial dysfunction may increase the risk of chronic disease. But simply poor melatonin levels are enough for an increased risk of autoimmunity.
According to a 2019 review published in Cytokine Growth Factor Review, poor melatonin levels may play a role in autoimmune disorders (25).


CHRONIC INFECTIONS
Chronic infections, including oral infections, gut infections, and infections affecting your blood or organs, may increase chronic inflammation, immune dysfunction, gut microbiome imbalance, leaky gut syndrome, and multiple organ damage. As a result, they may also increase your risk of autoimmunity. According to a 2019 study published in the Journal of Immunology Research, there is a link between gut dysbiosis and the risk of autoimmune diseases (26). According to a 2018 study published in Science, small intestinal bacterial overgrowth (SIBO) may trigger bacteria to travel to other organs and cause an autoimmune response (27).

According to a 2022 study published in Frontiers in Immunologfy, H. pylori bacterial overgrowth may increase the risk of gastric autoimmunity (28).
According to a 2021 study published in Cureus, Lyme borreliosis may increase the risk of developing an autoimmune disease (29). According to a 2020 review published in Frontiers in Immunology, chronic Epstein Barr Virus infections may increase the risk of systemic autoimmune diseases (30).
According to a 2023 review published in Rheumatology International, long COVID may increase the risk of latent autoimmunity and rheumatic autoimmune diseases due to immune imbalance and multiple organ damage (31).


NUTRIENT DEFICIENCIES
Nutrient deficiencies may also increase the risk of chronic inflammation, immune health disturbances, gut health issues, and autoimmune health issues. Some of the specific nutrient deficiencies that may increase your risk of autoimmune disorders include vitamin D, zinc, B vitamins, selenium, and omega-3 fatty acids.

Vitamin D
Vitamin D is a fat-soluble vitamin essential for bone, muscle, immune, brain, and mental health. According to a 2013 review published in Clinical Reviews in Allergies and Immunology, vitamin D is essential for regulating immune responses (32). Deficiencies may increase the risk of autoimmune diseases. A 2018 study published in The BMJ looked at the effects of vitamin D and omega-3 fatty acids on autoimmunity (33). Researchers found that supplementing with vitamin D with or without marine omega-3 fatty acids may decrease the risk of autoimmune disease by 22 percent.


Zinc
Zinc is a critical mineral for immune health. It plays an important role in cell communication, proliferation, differentiation, and survival.
According to a 2018 systematic review and meta-analysis published in Nutrients, low zinc levels are commonly seen in autoimmunity (34).
According to a 2020 review published in the Journal of Nutritional Biochemistry, supplementing with zinc and vitamin D may play a therapeutic role in autoimmune diseases (35).


B Vitamins
B vitamins are a group of vitamins that are important for cellular function, nutrient transport, and brain health.
According to a 2022 study published in Nutrients, B vitamins play a role in gut microbiome balance, and deficiencies along with gut dysbiosis may play a role in autoimmunity (36).


Selenium
Selenium is a powerful antioxidant that plays a role in immune, thyroid, heart, and mental health. According to a 2019 review published in Current Rheumatology Reviews, there may be a link between low selenium and autoimmunity (39). According to 2017 research published in Current Opinions in Endocrinology, Diabetes, and Obesity, supplementing with selenium may be beneficial in autoimmune thyroid diseases in case of a severe deficiency (40).
Omega-3 Fatty Acids
Omega-3 fatty acids are healthy fatty acids with anti-inflammatory properties that may be beneficial for brain, metabolic, heart, mental, bone, and joint health, may help to reduce chronic inflammation and pain, and may be helpful for those with autoimmune diseases. According to a 2011 study published in California Agriculture (Berkeley), using omega-3 fatty acids may be beneficial for autoimmune disorders, inflammatory diseases, metabolic diseases, and heart disease (42).
A 2018 study published in The BMJ looked at the effects of vitamin D and omega-3 fatty acids on autoimmunity (33). Research found that supplementing with omega-3 fatty acids with or without vitamin D may decrease the risk of autoimmune disease by 15 percent.


ALLOSTATIC LOAD AND THE CELL DANGER RESPONSE
An allostatic load is the cumulative effect of chronic stress on your physical and mental health. It basically refers to what we call the ‘wear and tear’ of the body due to environmental stressors, life events, and health stressors.
All of us have a certain capacity to cope with a certain level of allostatic load. When your body is experiencing more stressors than it can bear and the cumulative toll leads to cumulative overload, this can lead to a constant fight-or-flight response and the release of various hormones, including cortisol, catecholamines, and glucocorticoids. Under healthy circumstances, these hormones help your body to deal with threats, adapt, and maintain homeostasis.
But when there is constant stress, and these hormones are constantly released, they can have damaging effects on your body and increase the risk of illness and disease and an accelerated progression of disease. These negative effects may cause high blood pressure, blood sugar imbalance, chronic inflammation, metabolic problems, immune dysfunction, and autoimmunity.
This state of allostatic load can also trigger the CDR and a constant CDR state. According to a 2023 research published in Mitochondrion, an “abnormal persistence of any phase of the CDR inhibits the healing cycle, creates dysfunctional cellular mosaics, causes the symptoms of chronic disease, and accelerates the process of aging” (43).
Among many issues, a constant CDR due to the cumulative load of all these factors listed in this guide may increase the risk of the development of autoimmune disorders.

WHAT TO DO ABOUT IT:
To learn more about the CDR and its role in chronic illness, I recommend reading our specific Ebook on the Cell Danger Response.
Since we are talking about the cumulative role of many issues, it is important that you consider all the factors listed this summary Ebook and in the infographic below, including following an anti-inflammatory, nutrient-dense diet for normal blood sugar levels, low inflammation levels, gut health, and healthy nutrient levels.

You also need to reduce environmental toxin exposure and supporting your detoxification pathways, supporting your gut health, supporting your circadian rhythms and getting daily restorative sleep, addressing underlying chronic infections, moving your body, reducing your stress levels, addressing emotional and mental health issues, and supplementation based on your body’s need.


Sources For This Guide:
1. Conrad N. Incidence, prevalence, and co-occurrence of autoimmune disorders over time and by age, sex, and socioeconomic status: a population-based cohort study of 22 million individuals in the UK. The Lancet. Link Here
2. Autoimmune diseases. NIH. Link Here
3. Naviaux RK. Metabolic features of the cell danger response. Mitochondrion. 2014 May;16:7-17. doi: 10.1016/j. mito.2013.08.006. Epub 2013 Aug 24. PMID: 23981537
4. Vighi G, Marcucci F, Sensi L, Di Cara G, Frati F. Allergy and the gastrointestinal system. Clin Exp Immunol. 2008 Sep;153 Suppl 1(Suppl 1):3-6. doi: 10.1111/j.1365-2249.2008.03713.x. PMID: 18721321
5. Smith JL. The role of gastric acid in preventing foodborne disease and how bacteria overcome acid conditions. J Food Prot. 2003 Jul;66(7):1292-303. PMID: 12870767
6. Kelly GS. Hydrochloric acid: Physiological functions and clinical implications. Link Here
7. Paray BA, Albeshr MF, Jan AT, Rather IA. Leaky Gut and Autoimmunity: An Intricate Balance in Individuals Health and the Diseased State. Int J Mol Sci. 2020 Dec 21;21(24):9770. doi: 10.3390/ijms21249770. PMID: 33371435
8. Gut Microbiota, Leaky Gut, and Autoimmune Diseases. 2022. Frontiers in Immunology. Link Here
9. Toxic Chemicals Found in Minority Cord Blood EWG Link Here
10. Lifetime Pesticide Use and Antinuclear Antibodies in Male Farmers From the Agricultural Health Study. 2019. Front. Immunol., 11 July 2019 Link Here
11. Parks CG, Costenbader KH, Long S, Hofmann JN, Beane FLE, Sandler DP. Pesticide use and risk of systemic autoimmune diseases in the Agricultural Health Study. Environ Res. 2022 Jun;209:112862. doi: 10.1016/j.envres.2022.112862. Epub 2022 Feb 4. PMID: 35123967
12. Kraft S, Buchenauer L, Polte T. Mold, Mycotoxins and a Dysregulated Immune System: A Combination of Concern? Int J Mol Sci. 2021 Nov 12;22(22):12269. doi: 10.3390/ijms222212269. PMID: 34830149
13. Jaishankar M, Tseten T, Anbalagan N, Mathew BB, Beeregowda KN. Toxicity, mechanism and health effects of some heavy metals. Interdiscip Toxicol. 2014 Jun;7(2):60-72. doi: 10.2478/intox-2014-0009. Epub 2014 Nov 15. PMID: 26109881
14. Potential mechanisms of some selected heavy metals in the induction of inflammation and autoimmunity. European Journal of inflammation. 2022. Link Here
15. Phthalates. FDA. Link Here
16. Popescu M, Feldman TB, Chitnis T. Interplay Between Endocrine Disruptors and Immunity: Implications for Diseases of Autoreactive Etiology. Front Pharmacol. 2021 Mar 23;12:626107. doi: 10.3389/fphar.2021.626107. PMID: 33833678
17. Petrelli A, Giovenzana A, Insalaco V, Phillips BE, Pietropaolo M, Giannoukakis N. Autoimmune Inflammation and Insulin Resistance: Hallmarks So Far and Yet So Close to Explain Diabetes Endotypes. Curr Diab Rep. 2021 Dec 13;21(12):54. doi: 10.1007/s11892-021-01430-3. PMID: 34902055
18. Metabolic Inflammation and Insulin Resistance in Obesity Link Here
19 Jang HR, Lee HY. Mechanisms linking gut microbial metabolites to insulin resistance. World J Diabetes. 2021 Jun 15;12(6):730-744. doi: 10.4239/wjd.v12.i6.730. PMID: 34168724
20. Adverse Childhood Experiences Increase Risk for Chronic Diseases – It’s Not Psychological Lnk here

21. Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, Croft JB. Cumulative childhood stress and autoimmune diseases in adults. Psychosom Med. 2009 Feb;71(2):243-50. doi: 10.1097/PSY.0b013e3181907888. Epub 2009 Feb 2. PMID: 19188532
22. Bookwalter DB, Roenfeldt KA, LeardMann CA, Kong SY, Riddle MS, Rull RP. Posttraumatic stress disorder and risk of selected autoimmune diseases among US military personnel. BMC Psychiatry. 2020 Jan 15;20(1):23. doi: 10.1186/s12888020-2432-9. PMID: 31941473
23. Hsiao YH, Chen YT, Tseng CM, Wu LA, Lin WC, Su VY, Perng DW, Chang SC, Chen YM, Chen TJ, Lee YC, Chou KT. Sleep disorders and increased risk of autoimmune diseases in individuals without sleep apnea. Sleep. 2015 Apr 1;38(4):581-6. doi: 10.5665/sleep.4574. PMID: 25669189
24. Reiter RJ. Melatonin in Mitochondria: Mitigating Clear and Present Dangers. Link Here
25. Zhao CN, Wang P, Mao YM, Dan YL, Wu Q, Li XM, Wang DG, Davis C, Hu W, Pan HF. Potential role of melatonin in autoimmune diseases. Cytokine Growth Factor Rev. 2019 Aug;48:1-10. doi: 10.1016/j.cytogfr.2019.07.002. Epub 2019 Jul 16. PMID: 31345729
26. Xu H, Liu M, Cao J, Li X, Fan D, Xia Y, Lu X, Li J, Ju D, Zhao H. The Dynamic Interplay between the Gut Microbiota and Autoimmune Diseases. J Immunol Res. 2019 Oct 27;2019:7546047. doi: 10.1155/2019/7546047. PMID: 31772949
27. Translocation of a gut pathobiont drives autoimmunity in mice and humans Science. 2018. Lnk Here
28. Wang L, Cao ZM, Zhang LL, Dai XC, Liu ZJ, Zeng YX, Li XY, Wu QJ, Lv WL. Helicobacter Pylori and Autoimmune Diseases: Involving Multiple Systems. Front Immunol. 2022 Feb 10;13:833424. doi: 10.3389/fimmu.2022.833424. PMID: 3522242
29. Yehudina Y, Trypilka S. Lyme Borreliosis as a Trigger for Autoimmune Disease. Cureus. 2021 Oct 10;13(10):e18648. doi: 10.7759/cureus.18648. PMID: 34786243
30. Houen G, Trier NH. Epstein-Barr Virus and Systemic Autoimmune Diseases. Front Immunol. 2021 Jan 7;11:587380. doi: 10.3389/fimmu.2020.587380. PMID: 33488588
31. Fedorchenko Y, Zimba O. Long COVID in autoimmune rheumatic diseases. Rheumatol Int. 2023 Jul;43(7):1197-1207. doi: 10.1007/s00296-023-05319-0. Epub 2023 Mar 30. PMID: 3699543
32. Yang CY, Leung PS, Adamopoulos IE, Gershwin ME. The implication of vitamin D and autoimmunity: a comprehensive review. Clin Rev Allergy Immunol. 2013 Oct;45(2):217-26. doi: 10.1007/s12016-013-8361-3. PMID: 23359064
33. Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial
34. Sanna A, Firinu D, Zavattari P, Valera P. Zinc Status and Autoimmunity: A Systematic Review and Meta-Analysis. Nutrients. 2018 Jan 11;10(1):68. doi: 10.3390/nu10010068. PMID: 29324654
35. Wessels I, Rink L. Micronutrients in autoimmune diseases: possible therapeutic benefits of zinc and vitamin D. J Nutr Biochem. 2020 Mar;77:108240. doi: 10.1016/j.jnutbio.2019.108240. Epub 2019 Oct 30. PMID: 31841960
36. Mandić M, Mitić K, Nedeljković P, Perić M, Božić B, Lunić T, Bačić A, Rajilić-Stojanović M, Peković S, Božić Nedeljković B. Vitamin B Complex and Experimental Autoimmune Encephalomyelitis -Attenuation of the Clinical Signs and Gut Microbiota Dysbiosis. Nutrients. 2022 Mar 17;14(6):1273. doi: 10.3390/nu14061273. PMID: 35334928
37. Yang H, Song J, Li A, Lv L, Sun X, Mao Y, Ye D. Genetically predicted levels of folate, vitamin B12, and risk of autoimmune diseases: A Mendelian randomization study. Front Immunol. 2023 Mar 10;14:1139799. doi: 10.3389/ fimmu.2023.1139799. PMID: 36969181
38. Sahebari M, Rezaieyazdi Z, Khodashahi M. Selenium and Autoimmune Diseases: A Review Article. Curr Rheumatol Rev. 2019;15(2):123-134. doi: 10.2174/1573397114666181016112342. PMID: 30324883

40. Winther KH, Bonnema SJ, Hegedüs L. Is selenium supplementation in autoimmune thyroid diseases justified? Curr Opin Endocrinol Diabetes Obes. 2017 Oct;24(5):348-355. doi: 10.1097/MED.0000000000000356. PMID: 28639965
41. Zivkovic AM, Telis N, German JB, Hammock BD. Dietary omega-3 fatty acids aid in the modulation of inflammation and metabolic health. Calif Agric (Berkeley). 2011 Jul;65(3):106-111. doi: 10.3733/ca.v065n03p106. PMID: 24860193
43. Naviaux RK. Mitochondrial and metabolic features of salugenesis and the healing cycle. Mitochondrion. 2023 May;70:131-163. doi: 10.1016/j.mito.2023.04.003. Epub 2023 Apr 27. PMID: 37120082
about dr. david jockers dnm, dc, ms
Dr. David Jockers is a doctor of natural medicine and author and podcaster. He runs one of the most popular natural health websites in DrJockers.com which has gotten over 1 million monthly visitors and his work has been seen on popular media such as the Dr Oz show and Hallmark Home and Family.
Dr Jockers is the author of the best-selling book “The Keto Metabolic Breakthrough” by Victory Belt publishing and “TheFasting Transformation.” He is a world-renowned expert in the area of ketosis, fasting and functional nutrition. He is also the host of the popular Dr Jockers Functional Nutrition podcast.

Dr Jockers lives in Canton, Georgia with his wife Angel and his twin boys David & Joshua and his daughters Joyful and Shine.


