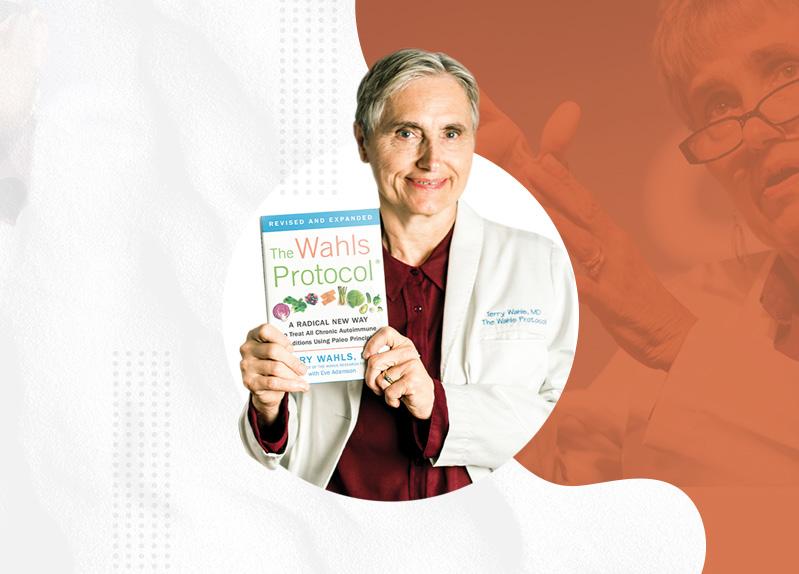
Top Targeted Supplements For Autoimmune and Neuroimmune Patients On The
Wahls Protocol®
A COLLECTION OF ESSAYS

 By Dr. Terry Wahls
Best-selling Author, Physician, and Founder of the Wahls Research Fund
By Dr. Terry Wahls
Best-selling Author, Physician, and Founder of the Wahls Research Fund




These are the top ten problems that are associated with a higher risk of developing a systemic autoimmune diagnosis.
• Migraine or chronic headache
• Endometriosis
• Migratory muscle and joint pain
• Infertility
• Constipation and/or diarrhea
• Fatigue
• Abdominal pain
• Anxiety
• Pelvic pain
• Depression
Rheumatoid arthritis, systemic lupus, inflammatory bowel disease, multiple sclerosis (MS), and other systemic autoimmune diseases have a long prodromal period--years, sometimes decades, of migraines, chronic headache, migratory muscle and joint pain, bloating and belly pain.1-4
Endometriosis and pelvic pain are associated with increased risk of infertility and development of an autoimmune condition, including MS.5 Fatigue, anxiety, and depression are part of the multiple sclerosis prodrome, often occurring 5 to 10 years before the MS diagnosis is made.3,6,7 If your patients have any of these issues, they likely have autoimmune processes creating tissue damage. Investigate their other risk factors more thoroughly, including smoking and air pollution exposure, solvent exposure, blood glucose, and insulin levels, which increase the risk of a more severe disease course. Many people have unrecognized diabetes, pre-diabetes, and metabolic syndrome, which, if present, shorten the time to disability.8-11 In addition, a history of high blood pressure and/or obesity will also increase the severity of the autoimmune disease process.12,13 Having more of these disease states and/or symptoms increases the risk of a more aggressive systemic autoimmune disease course.
The presence of these symptoms or diagnoses is an opportunity for clinicians to support patients as they address their modifiable lifestyle factors. The goal is to create a healthy micro-environment for their immune cells, restore healthy physiology, and regress tissue damage. If the patient has autoantibodies present, an elevated autoantibody test result that will often decline back to nondetectable, symptoms will diminish, and vitality improve as patients address and improve their diet, stress, exercise, sleep, relationships, and connectedness.

Barratt SM, Leeds JS, Robinson K, Lobo AJ, McAlindon ME, Sanders DS. Prodromal irritable bowel syndrome may be responsible for delays in diagnosis in patients presenting with unrecognized Crohn’s disease and celiac disease, but not ulcerative colitis.


1. Dig Dis Sci. 2011;56(11):3270-3275.
2. Edmeads J. Migraine--disease or syndrome? Pathol Biol (Paris). 1992;40(4):279-283.
3. Wijnands JM, Zhu F, Kingwell E, et al. Five years before multiple sclerosis onset: Phenotyping the prodrome. Mult Scler. 2019;25(8):1092-1101.
4. Zhao H, Zhao L, Shi W, et al. Is it bowel-associated dermatosis-arthritis syndrome induced by small intestinal bacteria overgrowth? Springerplus. 2016;5(1):1551.
5. Shigesi N, Kvaskoff M, Kirtley S, et al. The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis. Hum Reprod Update. 2019;25(4):486-503.
6. Makhani N, Tremlett H. The multiple sclerosis prodrome. Nat Rev Neurol. 2021;17(8):515-521.
7. Wijnands JMA, Zhu F, Kingwell E, et al. Prodrome in relapsing-remitting and primary progressive multiple sclerosis. Eur J Neurol. 2019;26(7):1032-1036.
8. Bagher OM, Golbarg M, Hossein S. Pattern of rheumatic diseases in two outpatient clinics in Iran: similarities with some different features. Indian J Med Sci. 2011;65(1):7-17.
9. Guenther L, Gulliver W. Psoriasis comorbidities. J Cutan Med Surg. 2009;13 Suppl 2:S77-87.
10. Horreau C, Pouplard C, Brenaut E, et al. Cardiovascular morbidity and mortality in psoriasis and psoriatic arthritis: a systematic literature review. J Eur Acad Dermatol Venereol. 2013;27 Suppl 3:12-29.
11. Pinhas-Hamiel O, Livne M, Harari G, Achiron A. Prevalence of overweight, obesity and metabolic syndrome components in multiple sclerosis patients with significant disability. Eur J Neurol. 2015;22(9):1275-1279.
12. Sternberg Z, Leung C, Sternberg D, et al. The prevalence of the classical and non-classical cardiovascular risk factors in multiple sclerosis patients. CNS Neurol Disord Drug Targets. 2013;12(1):104-111.
13. Wens I, Dalgas U, Stenager E, Eijnde BO. Risk factors related to cardiovascular diseases and the metabolic syndrome in multiple sclerosis - a systematic review. Mult Scler. 2013;19(12):1556-1564.
Diet How Times Are Changing
The world is changing. Neurology and MS care are changing. It’s been a long journey to this point, and not an easy one. Let me tell you how we got here.
New ideas never take hold easily. When I began speaking about diet and MS 15 years ago, many scientists and physicians condemned me. I tell my students and post-doctoral fellows that it typically takes 30 years to change the standard of clinical care. I am halfway there.
In that time, I have gone from being banned as a speaker, my ideas perceived as dangerous, to being recognized as a leading dietary intervention researcher in the setting of multiple sclerosis (MS). I am not so crazy anymore.
More neurologists agree with me that diet matters. It is much less hard these days to get our papers accepted by top tier scientific journals. A very exciting thing recently happened at the


journal Neurology, one of the highest impact journals covering MS clinical care and research. They published an editorial stating that there is sufficient evidence that diet matters a great deal for people with MS. I have been saying this for years and am heartened that one of the leading journals finally agrees with me.
For me, this is personal. After experiencing my own personal healing journey, I felt morally compelled to share my story and give hope to others with severe disability caused by chronic health problem(s).
But new ideas like mine are usually met enormous resistance and I was no exception. I was labeled as dangerous, accused of faking MS. Some claimed I sat in wheelchair for 4 years while at work but worked out at home every day, which is why I was able to recover. Others said the MS specialists who treated me must have been incompetent, misdiagnosing my disease.
I gave lots of interviews. Mostly people wanted to introduce their audience to my story of healing and thoughts on what is possible for people with complex chronic disease. Sometimes the interviews were quite hostile. When that happened, I reminded the host I was simply sharing my experience, theories, and the research I believed needed to happen.
In 2010, I published my first book Minding Your Mitochondria. In 2009 and 20101,2 , I published care reports and case studies of people with multiple sclerosis who experienced significant improvement in function using diet, exercise, and electrical stimulation of muscles as part of their MS treatments. Our first clinical trial (NCT01381354) tested the same interventions I had used in my clinical recovery in others with progressive multiple sclerosis. It took us several tries, but in 2014, we published our first paper on the study results, which showed that people with progressive MS could implement my program and experience remarkable reductions in fatigue and improvement in quality of life.3
I gave talks wherever I was invited, including a TEDx talk I gave in 2011 that would eventually be seen by nearly 4 million people.
My next book, The Wahls Protocol®, was published in 2014. The National MS Society (NMSS) monitors social media to know what their constituents are saying about MS treatments. After my book came out, there was a sudden and dramatic uptick in the conversation about diet, exercise, and the Wahls Protocol® that exceeded the mentions about all the disease-modifying drug treatments combined. 4 The NMSS then decided to have a Wellness Conference, inviting researchers, patient advocates, and me. At that conference I saw the dramatic graphs depicting


the social media mentions,4 explaining why the NMSS held the conference, and why I was there. NMSS made Wellness Research a priority for 2015. I helped them find researchers who conducted dietary intervention studies, which are very different from drug development studies.
In 2016, the NMSS society began funding pilot Dietary Intervention studies. I submitted a research proposal to conduct a study comparing the effect of the Swank and Wahls diets on fatigue and quality of life. Our project was funded by the National Multiple Sclerosis Society, allowing us to launch our 4th clinical trial. The results demonstrated that adopting both the Swank and Wahls diets was associated with significant reductions in fatigue and improvements in quality of life. We have 3 more studies whose data we are analyzing and will present at the spring meeting of the Consortium of MS Centers.
We now have several meta-analyses of these dietary intervention studies. A meta-analysis, which combines several studies, provides the strongest evidence that an intervention is helpful (or harmful). A network meta-analysis combines the studies and compares them to identify which treatments are the most effective. To be included in a meta-analysis, a study must be randomized and conducted on humans with MS.
Meta-analyses drive change in the standard of care, but they take time. Most studies take 3 to 5 years to complete, and a meta-analysis needs multiple studies that show the benefit of the intervention, which is why it takes 20 to 30 years for practice patterns to change. Research is an endurance sport. You must be in it for the long haul.
The first meta-analysis examined the role of fish in the diet5 and included six studies. The analysis found that including fish in the diet decreased the odds ratio or risk of developing MS (P=0.004). Having at least ½ serving of fish per day during adolescence may reduce the risk of developing MS later in life. According to the analysis, the consumption of fish decreases the risk of MS [OR (95% CIs): 0.77 (0.64, 0.92); p-value = 0.004; I2 = 54.7%] compared with controls. Eating at least a half serving of fish per week during adolescence and as an adult may reduce the risk MS.
The next paper was a meta-analysis of the health benefits of green leafy vegetables and multiple health outcomes6. They found 24 meta-analyses and 29 health outcomes to include in the review. Researchers found that per 100 grams/day of green leafy vegetables was associated with 25% decreased risk of cancer, heart disease, stroke, all cause death, macular degeneration, metabolic syndrome, and ALS. Green leafy vegetables are rich sources of vitamin K, lutein, zeaxanthin and other carotenoids that protect the retina from the harmful effects of ultraviolet light and are associated with lower risk of cognitive decline.


The next paper was a meta-analysis of dietary intervention studies in the setting of MS.7 They found 8 studies with 515 patients. They combined all dietary interventions into one intervention labeled “diet.” Five studies analyzed the effect on disability as measured by the expanded disability status scale (EDSS), 3 examined fatigue severity as measured by the modified fatigue impact scale (MFIS), and 2 examined quality of life (QoL). They found evidence of a trend in reduction in fatigue (308 patients). The difference between the means of the control group and diet intervention group was -2,033, 95%-IC (-3,195, -0,152), a p-value of 0.0341)-. There was an increase in QoL (77 patients studied), but no significant effect on EDSS (337 patients studied) and no severe adverse events. The authors concluded that diet improvement is beneficial and should be recommended based on the patient’s and family’s preferences, according to what they can adopt and sustain as a family. That is remarkably close to my message.
The last paper was published on January 24, 2023 in Neurology, the most widely read journal among practicing neurologists. Dr. Linda Snetselaar conducted a network meta-analysis of randomized dietary intervention studies in MS that lasted at least 12 weeks and had either fatigue or quality of life as an outcome.8 A network meta-analysis allows the researcher to compare the various interventions with each other through comparisons to control arms, which is how researchers can compare the efficacy of various drug treatments for MS. The study team found 12 dietary intervention studies and 8 dietary interventions. Dr. Snetselaar used the study team’s classification to assign studies to 8 different dietary interventions: Mediterranean, Paleolithic, ketogenic, anti-inflammatory, low-fat, fasting, calorie restriction, and control diet, which was the participant’s usual diet. A total of 608 participants were enrolled in the 12 studies. When comparing each dietary intervention to the control diet, three diets were associated with significant reduction in fatigue. The other 5 dietary patterns had smaller effect sizes that were not significantly better than the control diets. The magnitude of change for reducing fatigue severity in descending order was: Paleolithic (SMD: -1.27; 95% CI: -1.81, -0.74), low-fat diet (SMD: -0.90; 95% CI: -1.39, -0.42), and Mediterranean (SMD: -0.89; 95% CI: -1.15, -0.64). When comparing each diet to usual diet for improving quality of life, there were two diets associated with significant improvement in quality of life: Paleolithic (SMD: 1.01; 95% CI 0.40, 1.63) and Mediterranean (SMD: 0.47; 95% CI 0.08, 0.86).
I am not surprised that the diet with the largest effect size is the Paleolithic diet since that diet removes the three most common food antigens (gluten, casein, and egg albumin) that cause excessive activation of the immune system.
The Paleolithic Diet and Mediterranean diets have many common features: less added sugar,


less ultra-processed foods, and more non-starchy vegetables. The authors acknowledge that the studies were small pilot studies of relatively brief duration (a year or less) and that larger, longer (ideally 2 years or longer) studies are needed to develop stronger evidence of the benefits of improving diet.
The same issue of Neurology included an editorial entitled The Role of Diet in Multiple Sclerosis: Food for Thought. The authors discussed the network meta-analysis and found that there is sufficient evidence to recommend a healthy diet as an adjunct to treating MS. They discussed the common features of the Paleolithic and Mediterranean diets and said that neurologists should talk to their MS patients about the importance of a healthy diet but not feel compelled to say there is one best diet for MS. Rather, they encourage neurologists to have their patients choose the most appealing diet based on their individual tastes, culture, and background. They also suggest neurologists consider referring patients to registered dietitians for guidance and support on diet improvement, referrals that would likely be covered by many health insurance plans. Finally, they called for more research that includes MRI findings and follows people for two years. I agree that larger, longer studies are needed.
We are currently conducting our 8th clinical trial, a two-year study comparing modified Paleolithic elimination diet and time-restricted ketogenic diet to usual diet control (NCT05007483). We are also recruiting participants for future trials as well as our MS disease registry. Complete the screening here to see if you are eligible to participate in our study, Efficacy of Diet on Quality of Life in Multiple Sclerosis. If you have optic neuritis, radiologically isolated syndrome, clinically isolated syndrome or multiple, I encourage you to complete this short survey and join our patient registry.
We have made so much progress. This year we are presenting our research at the Consortium of MS Centers’ annual meeting, the largest meeting of medical teams who care for MS patients and conduct research on MS. This year, for the first time, the meeting will include a full track on nutrition. My team is scheduled to give six presentations about nutrition and nutrition-related research. In addition, we have submitted four research abstracts about our current studies.
The world is changing. We will continue to do research and learn more about the impact of diet on disease states. And we will continue to tell our patients and the world what we already we know: that improving your diet improves your health. The low fat, Paleolithic, and Mediterranean diets all encourage more vegetables and fruits, fiber, nuts, and seeds as well as a reduction in added sugars, fast food, and ultra-processed foods. For most people, these dietary choices result in better health. If you want to improve your health, consider adopting one of these diets. Keep in mind that the modified Paleo diet has the largest effect size for reducing fatigue and improving quality of life.

Citations:
1. Reese D, Shivapour ET, Wahls TL, Dudley-Javoroski SD, Shields R. Neuromuscular electrical stimulation and dietary interventions to reduce oxidative stress in a secondary progressive multiple sclerosis patient leads to marked gains in function: a case report. Cases J. 2009;2:7601.
2. Wahls TL, Reese D, Kaplan D, Darling WG. Rehabilitation with neuromuscular electrical stimulation leads to functional gains in ambulation in patients with secondary progressive and primary progressive multiple sclerosis: a case series report. J Altern Complement Med. 2010;16(12):1343-1349.
3. Bisht B, Darling WG, Grossmann RE, et al. A multimodal intervention for patients with secondary progressive multiple sclerosis: feasibility and effect on fatigue. J Altern Complement Med. 2014;20(5):347-355.
4. Dunn M BP, Kalb R. Your Patients with Multiple Sclerosis have Set Wellness as a High Priority— And the National Multiple Sclerosis Society is Responding. US Neurology. 2015;11(1):6.
5. Rezaeizadeh H, Mohammadpour Z, Bitarafan S, Harirchian MH, Ghadimi M, Homayon IA. Dietary fish intake and the risk of multiple sclerosis: a systematic review and meta-analysis of observational studies. Nutr Neurosci. 2022;25(4):681-689.
6. Li N, Wu X, Zhuang W, et al. Green leafy vegetable and lutein intake and multiple health outcomes. Food Chem. 2021;360:130145.
7. Guerrero Aznar MD, Villanueva Guerrero MD, Cordero Ramos J, et al. Efficacy of diet on fatigue, quality of life and disability status in multiple sclerosis patients: rapid review and meta-analysis of randomized controlled trials. BMC Neurol. 2022;22(1):388.
8.Snetselaar LG, Cheek JJ, Fox SS, et al. Efficacy of Diet on Fatigue and Quality of Life in Multiple Sclerosis: A Systematic Review and Network Meta-analysis of Randomized Trials. Neurology. 2023;100(4):e357-e366.
Are You Overcomplicating Your Health Priorities?
See what happens when you shift your focus to monitoring your metabolic health. I have a family history of illness. My grandparents had diabetes. My father was severely obese, and on my mother’s side, I have multiple aunts and uncles with heart disease. Even though I am quite lean, I have risk factors for metabolic syndrome, including very low HDL cholesterol and higher triglycerides.
I want to live to 120 and thrive. Healthspan matters more to me than life span. I don’t want to develop diabetes or heart disease so I take care of my metabolic health. If you take care of your metabolic health, you give yourself a better chance of healthy aging, of surviving and thriving well into old age.
To improve my health span, I make sure my blood sugars and blood pressure are under good

control. For those reasons, I wear a continuous glucose monitor and take targeted supplements to support better glucose metabolism. Excellent metabolic health means fasting blood sugar under 100 and fasting insulin under 7. Do you know what your blood sugar control looks like?
We know that having diabetes, pre-diabetes, and metabolic syndrome all increase the risk of heart disease and stroke. And we know that all of those conditions also increase the risk of more aggressive disease course in the setting of multiple sclerosis and other autoimmune diseases.1-4
Unfortunately, elevated blood sugar, pre-diabetes, and metabolic syndromes are silent. There are no symptoms alerting you that something is amiss. The definition for metabolic syndrome is met if three of the following five criteria are met:
• Waist > 40 (101 Cm) Inches (Men) Or > 35 (89 Cm) Inches (Women)
• Blood Pressure Over 130/85
• Fasting Triglyceride > 150 Mg/Dl
• Fasting HDL Cholesterol < 40 Mg/Dl (Men) Or < 50 Mg/Dl (Women)
• Fasting Blood Sugar Over 100 Mg/Dl.5
• While metabolic syndrome is more of a risk for those who are overweight, it can occur in thin people too.6
Do you know your risk factors for metabolic syndrome?
Do you know your fasting blood sugar, blood lipids, blood pressure, and waist circumference? It’s important to assess your risk factors. Speak with your primary care team about your metabolic health and have your lipids and blood sugar measured.
You can also get your blood lipids tested through YourLabWork, they offer accessible and affordable testing.
You can also monitor your blood sugar for two weeks to assess metabolic health. I use LEVELS to monitor my blood sugar and how it responds to my diet, sleep, stress, and activity levels.
Because metabolic syndrome, pre-diabetes, and diabetes have zero physical symptoms, are so prevalent across the world, and increase the risk of so many health problems, I urge everyone to check on their metabolic health.
It’s also important to monitor insulin resistance. In my clinical practice, I recommend a target of fasting insulin under 7. You can ask your primary care team for a fasting insulin and glucose level

test. You can also wear a continuous glucose monitor for two weeks, which I also urge my patients to do.
If you have one or more risk factors for metabolic syndrome, you would likely benefit from wearing a continuous glucose monitor and getting feedback on your how your diet, sleep, stress management, and exercise are all impacting your blood sugar levels. Again, people who have elevated blood sugars, metabolic syndrome, or diabetes have a more rapid worsening of autoimmune complications and shorter time to disability.7-9
You may also benefit from targeted supplements to support better blood sugar metabolism. Alpha lipoic acid (ALA),10,11 berberine12,13, and biotin14,15 have been observed to support insulin activity and glucose metabolism. Berberine supports achieving improved hemoglobin A1C levels.16

I have multiple risk factors for metabolic syndrome and work hard to make sure my metabolism and blood sugar are ideal. To improve my health, I wear a glucose monitor, take targeted supplements, follow a ketogenic diet, and pay attention to my sleep. All of that has improved my metabolism, which protects my brain, my heart, and my future.
Had I never checked, I might’ve been on my way to developing diabetes and earlier cognitive decline and frailty. None of those are in my plans for my future. I imagine they aren’t in yours either.
The Wahls Protocol® collection carries blood sugar synergy, designed to help support cardiometabolic health.
It delivers alpha-lipoic acid (ALA), the plant alkaloid berberine, and biotin in one convenient formula. These ingredients have been observed to support insulin activity and glucose metabolism. Research also suggests a role for berberine in supporting normal A1C levels.
References:
1. Marck CH, Aitken Z, Simpson S, Weiland TJ, Jelinek GA. Does a modifiable risk factor score predict disability worsening in people with multiple sclerosis? Mult Scler J Exp Transl Clin. 2019;5(4):2055217319881769.
2. Marck CH, Neate SL, Taylor KL, Weiland TJ, Jelinek GA. Prevalence of Comorbidities, Overweight and Obesity in an International Sample of People with Multiple Sclerosis and Associations with Modifiable Lifestyle Factors. PLoS One. 2016;11(2):e0148573.

3. Marrie RA. Comorbidity in multiple sclerosis: Past, present and future. Clin Invest Med. 2019;42(1):E5-E12.
4. Marrie RA, Garland A, Schaffer SA, et al. Traditional risk factors may not explain increased incidence of myocardial infarction in MS. Neurology. 2019;92(14):e1624-e1633.
5. Huang PL. A comprehensive definition for metabolic syndrome. Dis Model Mech. 2009;2(5-6):231-237.
6. Sanyal D. Lean Metabolic Syndrome: An Emerging Concept. Indian J Endocrinol Metab. 2018;22(3):301-302.
7. Pinhas-Hamiel O, Livne M, Harari G, Achiron A. Prevalence of overweight, obesity and metabolic syndrome components in multiple sclerosis patients with significant disability. Eur J Neurol. 2015;22(9):1275-1279.
8. Smith AE, Molton IR, Jensen MP. Self-reported incidence and age of onset of chronic comorbid medical conditions in adults aging with long-term physical disability. Disabil Health J. 2016;9(3):533-538.
9. Dao HH, Do QT, Sakamoto J. Increased frequency of metabolic syndrome among Vietnamese women with early rheumatoid arthritis: a cross-sectional study. Arthritis Res Ther. 2010;12(6):R218.
10. Aslfalah H, Jamilian M, Rafiei F, Khosrowbeygi A. Reduction in maternal serum values of glucose and gammaglutamyltransferase after supplementation with alpha-lipoic acid in women with gestational diabetes mellitus. J Obstet Gynaecol Res. 2019;45(2):313-317.
11. Rahimlou M, Asadi M, Banaei Jahromi N, Mansoori A. Alpha-lipoic acid (ALA) supplementation effect on glycemic and inflammatory biomarkers: A Systematic Review and meta- analysis. Clin Nutr ESPEN. 2019;32:16-28.
12. Han Y, Xiang Y, Shi Y, et al. Pharmacokinetics and Pharmacological Activities of Berberine in Diabetes Mellitus Treatment. Evid Based Complement Alternat Med. 2021;2021:9987097.
13. Li C, He JZ, Zhou XD, Xu X. [Berberine regulates type 2 diabetes mellitus related with insulin resistance]. Zhongguo Zhong Yao Za Zhi. 2017;42(12):2254-2260.
14. Dakshinamurti K. Vitamins and their derivatives in the prevention and treatment of metabolic syndrome diseases (diabetes). Can J Physiol Pharmacol. 2015;93(5):355-362.
15. Kouzi SA, Yang S, Nuzum DS, Dirks-Naylor AJ. Natural supplements for improving insulin sensitivity and glucose uptake in skeletal muscle. Front Biosci (Elite Ed). 2015;7(1):94-106.
16. Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57(5):712-717.

Supplments vs Food
Adopting and sustaining change is hard. Learning new diet and lifestyle behaviors can be a challenge, and many people would rather just take a supplement or a pill instead of taking the time to put together nourishing, home-cooked meals or take the time to implement important self-care strategies. While I pormote a food-first approach to health and wellness, supplements have a purpose and a place for many people on their healing journey. I put together the webinar below to share my experience with supplements and to educate on how they can be a supportive part of your own personal wellness protocol.



Managing Homocysteine
DO YOU NEED ACTIVATED B VITAMINS OR MTHFR COMPLETE?
Fatigue is one of top reasons people with multiple sclerosis (MS) leave employment. Cognitive decline is the next most common reason. I had years of relentlessly worsening fatigue. My neurologist gave me Provigil to treat the fatigue, which provided a slight improvement. I was still exhausted by 10 in the morning, but I definitely was more exhausted without it.
When I found myself in a tilt/recline wheelchair, I asked myself if I was doing everything I could to support my body and health. That was when I began reading the basic science to look for things that might help.
I would eventually decide that mitochondrial strain was the cause of disability in the setting of secondary and primary progressive MS. So I created a cocktail of supplements to support my mitochondria, which included lipoic acid, carnitine, coenzyme Q, and B vitamins. The cocktail did not recover my energy, strength, or stamina. After six months, I stopped them.
After 36 hours, I couldn’t get out of bed and go to work. Three days after I stopped taking my cocktail of supplements, Jackie suggested I start taking it again. The next morning I was back to my usual level of energy and was able to go back to work.
I was super excited. Two weeks later, I retested the experiment, stopping the supplements again. After 36 hours, I could not get out of bed. Again, I resumed my supplements 3 days after stopping them, and was able to go back to work the following morning. The success of this second experiment inspired me. I read more research papers and continued tinkering with my supplement cocktail to support my mitochondria.
That was 2008. In the intervening 14 years, I have learned a lot more about B vitamin pathways, genetic variants, and homocysteine metabolism.
In my clinical practice I ask my patients about their family history. Do they have relatives with macular degeneration, a leading cause of blindness? Do they have a family history of anxiety, depression, bipolar, or schizophrenia? Do they have a family history of memory problems, dementia, Parkinson’s, seizures, neuropathies, or restless legs? Do they have a family history of cardiovascular disease? Do they have a personal history of any of those same issues?


I have multiple aunts with macular degeneration and multiple uncles with early heart disease. I have family members with schizophrenia, bipolar, seizures, restless legs, and neuropathies. All this means I likely have multiple genetic variants that influence how my cells manage methylation pathways.
Methylation pathways are the B vitamin pathways for folate (vitamin B9), cobalamin (vitamin B12), pyridoxine (vitamin B6), riboflavin (B2), and thiamin (vitamin B1). I have checked my genetics and those of my family members and confirmed we have multiple genetic variants of the methylation pathways involving one or more of the following pathways: folate (vitamin B9), cobalamin (vitamin B12), pyridoxine (vitamin B6), and riboflavin (vitamin B2). These genetic variants are single nucleotide pathways where a single nucleotide is swapped with a different nucleotide (called SNPs) in the DNA. This change can produce good or bad outcomes. Sometimes SNPs make changes that are fatal. Sometimes SNPs improve the vitality of the organism and are beneficial. In other cases, SNPs create inefficiencies in our chemistry and increase the probability of chronic symptoms.
I’ve also checked my homocysteine, a marker for the efficiency of B vitamin utilization by our cells. Mine is elevated, which further indicates I do not have efficient methylation. My enzymes have a difficult time activating the B vitamins in the foods I eat into the active forms that methylate the B vitamins and cycle methionine to homocysteine. This explains why my homocysteine was moderately to severely elevated, placing me at risk of cognitive decline and early heart disease. To address these problems, I added activated B vitamins to my supplement cocktail.
The activated Bs were helpful, but I needed an even higher dose of the activated folate and cobalamin. I kept checking my homocysteine every 6 months until it was optimal, 5 to 7.5 mmol/L. (The conventional cutoff for elevated homocysteine is 15 mmol/L, though some labs place the upper level at 10 mmol/L.) I did not want to overcorrect, as that can be a problem too. Elevated homocysteine is toxic to brain cells3,4 and retinal cells5,6 and is a marker of insufficient B vitamin levels, which can contribute to the development of cardiovascular, neurological, and psychiatric disorders.4,7

In my clinical practice, I check my patients’ basic primary care labs (complete blood count, kidney function, liver function, and metabolic health). I also monitor folate, vitamin B12, homocysteine, and methylmalonic acid levels to understand their B vitamin status. I review the folate, B12, CLICK HERE TO SHOP


methylmalonic, and homocysteine levels and begin replacing the missing B vitamins.
A mild elevation of homocysteine is 7.6 mmol/L to 15 mmol/L, moderate elevation is 16 to 30 mmol/L, severe elevation is 31 to 60 mmol/L, and very severe elevation is > 60 mmol/ L. People with mild homocysteine elevation are often able to correct their homocysteine with 1-2 daily capsules of Activated B vitamins. People with moderate elevations are sometimes able to correct their homocysteine with 2 capsules of Activated Bs each day. People with severe and very severe elevations of homocysteine are more likely to need higher doses of activated folate, activated cobalamin, and other activated B vitamins as well as closer follow up of their homocysteine. They are more likely to benefit from MTHFR Complete.

I test my patients’ homocysteine every 3 months and make adjustments to supplements based on the results, until the patient reaches an optimal homocysteine level between 5-7.5 mmol/L. I do not want people to go below 5. If it falls below 5, I lower the B vitamin dose. You can ask your medical team to monitor your B vitamins and homocysteine. If you are unable to obtain these labs through your medical team, you may be able to obtain them through Your Lab Work. I also follow the homocysteine every 3 months to ensure my patients’
The foods that we eat have a variety of vitamins and minerals that are critical to healthy cells and bodies. Most commercially available vitamin supplements are made with synthetic vitamins, which share many of the properties of naturally occurring vitamins but are not quite as effective. For example, folic acid is a synthetic B vitamin that is used to fortify white flours to reduce the risk of neural tube defects but has been associated with increased risk of cancer (likely because it can suppress some of the activity of natural form of folate).1,2
I recommend that my patients avoid synthetic vitamin preparations and instead take a B vitamin complex that utilizes the activated forms of the vitamins, which bypass problem SNPs. The activated form of vitamin B12 (methylcobalamin), B9 (methylfolate), and B6 (pyridoxal-5phosphate) reduces homocysteine to more optimal levels. I also recommend activated vitamin B1 (benfotiamine), which supports brain,8 retinal9,10 and heart health11, and activated vitamin B2 (riboflavin 5 phosphate) for those with migraine and chronic headache.12,13 Other activated B vitamins that may be useful include niacin and niacinamide, which have been helpful in migraine


and chronic headache14; choline, an important nutrient for cognition and mental health15,16; and biotin, which is involved the production of myelin.17
All B vitamins work together synergistically to support the physiology of our cells.18,19 Thus I urge my patients to take a B complex to reduce the risk of insufficiency of these key vitamins and the symptoms that may cause or worsen. Activated Bs contain the entire spectrum of B vitamins to support cardiovascular, neurological, and retinal health, including vitamins B2, B6, and B12; benfotiamine, a fat soluble, more physiologically active form of thiamine; and folate as Quatrefolic®, which is proven to have greater stability, solubility, and bioavailability than calcium salt forms of 5-MTHF.
Activated Bs are an excellent way to ensure that you do not have an insufficiency of these key vitamins, even if you have an SNP that increases your vulnerability to retinal, cardiovascular, neurological, or psychiatric issues because of mild to moderate elevation of homocysteine. If you have severe or very severe elevation of homocysteine, you will likely benefit from higher doses of methylfolate, methylcobalamin, pyridoxal-5-phosphate, riboflavin 5’-phosphate, and trimethylglycine (betaine), which are found in MTHFR Complete.
My fatigue was resolved years ago, and I have been successful with helping thousands of people resolve their fatigue using diet, lifestyle, and targeted supplements. I take a careful history, asking about family history, personal history, and request relevant labs. Then I provide specific recommendations to address problems with B vitamin metabolism that contribute to fatigue and increased risk of neurodegeneration, early heart disease, and macular degeneration.
References:
1. Wien TN, Pike E, Wisloff T, Staff A, Smeland S, Klemp M. Cancer risk with folic acid supplements: a systematic review and meta-analysis. BMJ Open. 2012;2(1):e000653.
2. Baggott JE, Oster RA, Tamura T. Meta-analysis of cancer risk in folic acid supplementation trials. Cancer Epidemiol. 2012;36(1):78-81.
3. Ansari R, Mahta A, Mallack E, Luo JJ. Hyperhomocysteinemia and neurologic disorders: a review. J Clin Neurol. 2014;10(4):281-288.
4. Obeid R, McCaddon A, Herrmann W. The role of hyperhomocysteinemia and B-vitamin deficiency in neurological and psychiatric diseases. Clin Chem Lab Med. 2007;45(12):1590-1606.
5. Ola MS, Nawaz MI, Khan HA, Alhomida AS. Neurodegeneration and neuroprotection in diabetic retinopathy. Int J Mol Sci. 2013;14(2):2559-2572.
6. Elsherbiny NM, Sharma I, Kira D, et al. Homocysteine Induces Inflammation in Retina and Brain. Biomolecules. 2020;10(3).


7. Dardiotis E, Arseniou S, Sokratous M, et al. Vitamin B12, folate, and homocysteine levels and multiple sclerosis: A metaanalysis. Mult Scler Relat Disord. 2017;17:190-197.
8. Dhir S, Tarasenko M, Napoli E, Giulivi C. Neurological, Psychiatric, and Biochemical Aspects of Thiamine Deficiency in Children and Adults. Front Psychiatry. 2019;10:207.
9. Chakrabarti R, Chen M, Liu W, Chen S. Preventive effects of benfotiamine in chronic diabetic complications. J Diabetes Investig. 2011;2(2):123-131.
10. Cinici E, Mammadov R, Findik H, et al. The Protective Effect of Thiamine Pryophosphate Against Sugar-Induced Retinal Neovascularisation in Rats. Int J Vitam Nutr Res. 2018;88(3-4):137-143.
11. Wong EKC, Lee JY, Chow J, et al. High-Dose Thiamine Supplementation in Older Patients With Heart Failure: A Pilot Randomized Controlled Crossover Trial (THIAMINE-HF). CJC Open. 2022;4(6):532-539.
12. Grech O, Mollan SP, Wakerley BR, Fulton D, Lavery GG, Sinclair AJ. The Role of Metabolism in Migraine Pathophysiology and Susceptibility. Life (Basel). 2021;11(5).
13. Lisicki M, Schoenen J. Metabolic treatments of migraine. Expert Rev Neurother. 2020;20(3):295-302.
14. Fila M, Chojnacki C, Chojnacki J, Blasiak J. Nutrients to Improve Mitochondrial Function to Reduce Brain Energy Deficit and Oxidative Stress in Migraine. Nutrients. 2021;13(12).
15. Freedman R, Hunter SK, Law AJ, Clark AM, Roberts A, Hoffman MC. Choline, folic acid, Vitamin D, and fetal brain development in the psychosis spectrum. Schizophr Res. 2021.
16. Gonzalez HF, Visentin S. Micronutrients and neurodevelopment: An update. Arch Argent Pediatr. 2016;114(6):570-575.
17. Sedel F, Papeix C, Bellanger A, et al. High doses of biotin in chronic progressive multiple sclerosis: a pilot study. Mult Scler Relat Disord. 2015;4(2):159-169.
18. Borges-Vieira JG, Cardoso CKS. Efficacy of B-vitamins and vitamin D therapy in improving depressive and anxiety disorders: a systematic review of randomized controlled trials. Nutr Neurosci. 2022:1-21.
19. Kennedy DO. B Vitamins and the Brain: Mechanisms, Dose and Efficacy–A Review. Nutrients. 2016;8(2):68.
Not Getting Sufficient Sulfur In Your Diet? You Could Be Missing This Nutrient Powerhouse.
Sulfur is an important part of a health-promoting diet, which is why I stress cabbage and onion family vegetables. The body needs sulfur to manufacture glutathione, which is the master antioxidant in our cells. The body also needs sulfur to manufacture L-cysteine, an amino acid. Amino acids are the building blocks for structural and functional proteins and peptides (very short amino acid sequences) that are essential to human health. There are 20 essential amino acids and 10 conditionally essential amino acids. Essential means that we cannot make that particular amino acid. Conditionally essential means that if we have all the ingredients needed to make that amino acid, we can. L-Cysteine is a conditional amino acid, meaning that our body can make L-cysteine if there is enough sulfur in the diet to do so.


Many people do not have sufficient sulfur in their diet, which means they cannot manufacture enough L-cysteine. Our body uses L-Cysteine in many essential functions, and a deficiency may compromise cellular health. The addition of N-acetyl-L-cysteine (NAC) often provides a wellness boost for those with complex chronic disease as well as those who simply want to enjoy healthier aging. It is generally a very welltolerated way to improve cellular health.
NAC is often used as an add-on supplement to support detoxification, neurological function, and immune function.1-3 NAC has been used as an adjuvant to the treatment of many chronic neurological diseases, including Parkinson’s disease, multiple sclerosis, peripheral neuropathies, diabetes neuropathies, Alzheimer’s, tardive dyskinesia, and stroke.1,2 It has also been used as an add-on therapy for people with depression, anxiety, bipolar, attention deficit disorder, obsessivecompulsive disorder, and schizophrenia.4,5 In addition, NAC has been used as an adjuvant for a wide variety of chronic health issues that are not related to the brain, including polycystic ovary disease, male infertility, sleep apnea, acquired immune deficiency, influenza, inflammatory bowel disease, and as a chelator for metal detoxification.2 NAC has been used as an add-on therapy when treating heavy metal (mercury, lead, arsenic, cadmium) exposure.6 It is also used as an add-on therapy to reduce the risk of pulmonary fibrosis in patients who have persisting respiratory symptoms after COVID.7

My professors taught us to be suspicious of compounds used for many disease states. However, the same professors used FDA-approved drugs for off-label indications when the science supported that use. NAC does have many disease states that have published favorable outcomes. When a natural compound has been found to be helpful for many conditions, that compound is likely providing a molecule key to healthy human physiology.
In my clinical experience, many patients benefit from the addition of NAC to their supplement regimen. I stress the need to support cellular health, brain health, immune health, and detoxification by eating more cabbage and onion family vegetables. I also use NAC as an add-on wellness plan for my patients with neurological, psychiatric, or autoimmune disease.
References:
1. Bavarsad Shahripour R, Harrigan MR, Alexandrov AV. N-acetylcysteine (NAC) in neurological disorders: mechanisms of action and therapeutic opportunities. Brain Behav. 2014;4(2):108-122.

2. Schwalfenberg GK. N-Acetylcysteine: A Review of Clinical Usefulness (an Old Drug with New Tricks). J Nutr Metab. 2021;2021:9949453.
3. Zafarullah M, Li WQ, Sylvester J, Ahmad M. Molecular mechanisms of N-acetylcysteine actions. Cell Mol Life Sci. 2003;60(1):6-20.
4. Deepmala, Slattery J, Kumar N, et al. Clinical trials of N-acetylcysteine in psychiatry and neurology: A systematic review. Neurosci Biobehav Rev. 2015;55:294-321.
5. Minarini A, Ferrari S, Galletti M, et al. N-acetylcysteine in the treatment of psychiatric disorders: current status and future prospects. Expert Opin Drug Metab Toxicol. 2017;13(3):279-292.
6. Blanusa M, Varnai VM, Piasek M, Kostial K. Chelators as antidotes of metal toxicity: therapeutic and experimental aspects. Curr Med Chem. 2005;12(23):2771-2794.
7. De Flora S, Balansky R, La Maestra S. Rationale for the use of N-acetylcysteine in both prevention and adjuvant therapy of COVID-19. FASEB J. 2020;34(10):13185-13193.
The Endless Benefits Of Sulfur-Rich Vegetables: Cancer
Prevention, Detoxification, Gene Expression And More…
How often are you getting three cups of sulfur-rich vegetables in your diet?
There is ample evidence of the health benefits of eating broccoli and other cabbage family vegetables. These foods contain glucoraphanin, which, in the right circumstances, is metabolized to sulforaphane, which is associated with many health benefits.
To create sulforaphane, broccoli and other cabbage family vegetables must be chewed, which mixes the glucoraphanin with the enzyme myrosinase.1 Again, we can’t get sulforaphane directly from the cabbage family vegetables. We need to have the glucoraphanin acted upon by the myrosinase enzymes, which produce sulforaphane.
Both sulforaphane and glucoraphanin have been associated with many health benefits. Sulforaphane and glucoraphanin favorably modulate inflammation through the NFKappaB, Nrf2, and Keap1 pathways.2-4 They also improve biotransformation and the ability to excrete toxins by favorably modulating phase 1 and phase detoxification pathways that are used by the liver and kidneys process and eliminate toxins from the body.4 This means that glucoraphanin has antiinflammatory, anti-apoptotic, and antioxidant properties, meaning it may help prevent and treat many types of cancer as well as neurologic and psychiatric disorders.5,6

One study found that glucoraphanin boosted the expression of detoxification-related genes and attenuated acute liver injury in a rat model of liver injury.7; Glucoraphanin stimulates Nrf2-related genes, which improves mitochondrial function and stem cell function in tissue culture and animal studies.8 In studies of Chinese smokers, glucoraphanin improved detoxification and elimination of air pollutants benzene and acreolein, which are found in tobacco smoke.9 Sulforaphane inhibits breast cancer growth in animal models and human tissue cultures of cancer. Other studies have indicated benefit to treat or preventing breast cancer,10 colon cancer,11 prostate cancer,12 oral cancer,13 stomach cancer,14 and lung cancer.14 Thus eating more cabbage family vegetables and increasing glucoraphanin is a useful strategy for cancer prevention and as part of the wellness plan for anyone undergoing cancer treatment.1
The NFKappaB, Nrf2, and Keap1 pathways are also involved in mood disorders and neurologic disorders. Excessive stimulation of NFKappaB will lead to overactivation of the innate immune system and increased autoimmune activity. It will also lead to increased mitochondrial strain and more oxidative stress. The result is more anxiety and lower mood, more autoimmune disease flares, and greater risk for cognitive decline and worsening memory.
That is why glucoraphanin and sulforaphane are being investigated in animal models of psychiatric and neurological diseases. In animal models of depression and memory, the addition of glucoraphanin with myrosinase was associated with better memory and less depression.15,16 In animal models of stress, glucoraphanin was associated with improved stress resilience.17 It also improved memory18 and reduced the onset of psychoses19 in animal models of psychiatric disease. It improved neuronal production of nerve growth factors in mice and genes related to nerve growth factor production.20 Glucoraphanin reduced disability accumulation in an animal model of multiple sclerosis.21 It has reduced leakiness of the blood-brain barrier,22 reduced microglial reactivity,21,23 and improved memory18,23,24 in animal models of neurologic disease. In human trials, glucoraphanin and myrosinase have been helpful in reducing irritability and hyperactivity in children with autism spectrum disorder.25 The two compounds have also been helpful in improving working memory and mood in older adults.26
For all these reasons I encourage everyone to include cabbage family vegetables in their diets.
These foods include compounds associated with favorable changes in the Nrf2, NFKappaB, and Keap1 pathways, leading to reduced inflammation and reduced oxidative stress. These foods are also excellent for reducing the risk of developing cancers and improving the clearance of toxins from the body. Given the large number of chemicals that we all encounter in our daily lives,


cabbage family vegetables and glucoraphanin are a helpful part of everyone’s wellness plan.
The Wahls Protocol® Collection carries Brocco Detox. Brocco Detox features broccoli seed extract enhanced with myrosinase, the enzyme that promotes the conversion of naturally occurring glucoraphanin in broccoli to sulforaphane (SFN).
A potent activator of antioxidant activity, healthy cell-life cycles, and the production of detoxification enzymes, SFN is linked to the many health benefits associated with cruciferous vegetables.
References:
1. Kaiser AE, Baniasadi M, Giansiracusa D, et al. Sulforaphane: A Broccoli Bioactive Phytocompound with Cancer Preventive Potential. Cancers (Basel). 2021;13(19).
2. Naoi M, Maruyama W, Shamoto-Nagai M. Disease-modifying treatment of Parkinson’s disease by phytochemicals: targeting multiple pathogenic factors. J Neural Transm (Vienna).2022;129(5-6):737-753.
3. Mozaffarian D, Wu JHY. Flavonoids, Dairy Foods, and Cardiovascular and Metabolic Health: A Review of Emerging Biologic Pathways.Circ Res.2018;122(2):369-384.
4. G WW, L MB, D EW, R HD, Ho E. Phytochemicals from cruciferous vegetables, epigenetics, and prostate cancer prevention. AAPS J.2013;15(4):951-961.
5. Schepici G, Bramanti P, Mazzon E. Efficacy of Sulforaphane in Neurodegenerative Diseases. Int J Mol Sci. 2020;21(22).
6. Tarozzi A, Angeloni C, Malaguti M, Morroni F, Hrelia S, Hrelia P. Sulforaphane as a potential protective phytochemical against neurodegenerative diseases. Oxid Med Cell Longev. 2013;2013:415078.
7. Yoshida K, Ushida Y, Ishijima T, et al. Broccoli sprout extract induces detoxification-related gene expression and attenuates acute liver injury. World J Gastroenterol. 2015;21(35):10091-10103.
8. Holmstrom KM, Kostov RV, Dinkova-Kostova AT. The multifaceted role of Nrf2 in mitochondrial function. Curr Opin Toxicol. 2016;1:80-91.
9. Bauman JE, Hsu CH, Centuori S, et al. Randomized Crossover Trial Evaluating Detoxification of Tobacco Carcinogens by Broccoli Seed and Sprout Extract in Current Smokers. Cancers (Basel). 2022;14(9).
10. Jackson SJ, Singletary KW. Sulforaphane inhibits human MCF-7 mammary cancer cell mitotic progression and tubulin polymerization. J Nutr. 2004;134(9):2229-2236.
11. Bessler H, Djaldetti M. Broccoli and human health: immunomodulatory effect of sulforaphane in a model of colon cancer. Int J Food Sci Nutr. 2018;69(8):946-953.
12. Livingstone TL, Saha S, Bernuzzi F, et al. Accumulation of Sulforaphane and Alliin in Human Prostate Tissue. Nutrients. 2022;14(16).
13. Bauman JE, Zang Y, Sen M, et al. Prevention of Carcinogen-Induced Oral Cancer by Sulforaphane. Cancer Prev Res (Phila).

2016;9(7):547-557.
14. Ullah MF. Sulforaphane (SFN): An Isothiocyanate in a Cancer Chemoprevention Paradigm. Medicines (Basel). 2015;2(3):141-156.
15. Hashimoto K. Essential Role of Keap1-Nrf2 Signaling in Mood Disorders: Overview and Future Perspective. Front Pharmacol. 2018;9:1182.
16. Zhang JC, Yao W, Dong C, et al. Prophylactic effects of sulforaphane on depression-like behavior and dendritic changes in mice after inflammation. J Nutr Biochem. 2017;39:134-144.
17. Yao W, Zhang JC, Ishima T, et al. Role of Keap1-Nrf2 signaling in depression and dietary intake of glucoraphanin confers stress resilience in mice. Sci Rep. 2016;6:30659.
18. Park HS, Hwang ES, Choi GY, et al. Sulforaphane enhances long-term potentiation and ameliorate scopolamine-induced memory impairment. Physiol Behav. 2021;238:113467.
19. Shirai Y, Fujita Y, Hashimoto R, et al. Dietary Intake of Sulforaphane-Rich Broccoli Sprout Extracts during Juvenile and Adolescence Can Prevent Phencyclidine-Induced Cognitive Deficits at Adulthood. PLoS One. 2015;10(6):e0127244.
20. Kim J, Lee S, Choi BR, et al. Sulforaphane epigenetically enhances neuronal BDNF expression and TrkB signaling pathways. Mol Nutr Food Res. 2017;61(2).
21. Giacoppo S, Galuppo M, Iori R, et al. Protective role of (RS )-glucoraphanin bioactivated with myrosinase in an experimental model of multiple sclerosis. CNS Neurosci Ther. 2013;19(8):577-584.
22. Giacoppo S, Galuppo M, Iori R, De Nicola GR, Bramanti P, Mazzon E. The protective effects of bioactive (RS)-glucoraphanin on the permeability of the mice blood-brain barrier following experimental autoimmune encephalomyelitis. Eur Rev Med Pharmacol Sci. 2014;18(2):194-204.
23. Subedi L, Cho K, Park YU, Choi HJ, Kim SY. Sulforaphane-Enriched Broccoli Sprouts Pretreated by Pulsed Electric Fields Reduces Neuroinflammation and Ameliorates Scopolamine-Induced Amnesia in Mouse Brain through Its Antioxidant Ability via Nrf2-HO-1 Activation. Oxid Med Cell Longev. 2019;2019:3549274.
24. Shimizu S, Kasai S, Yamazaki H, et al. Sulforaphane Increase Mitochondrial Biogenesis-Related Gene Expression in the Hippocampus and Suppresses Age-Related Cognitive Decline in Mice. Int J Mol Sci.2022;23(15).
25. Momtazmanesh S, Amirimoghaddam-Yazdi Z, Moghaddam HS, Mohammadi MR, Akhondzadeh S. Sulforaphane as an adjunctive treatment for irritability in children with autism spectrum disorder: A randomized, double-blind, placebocontrolled clinical trial.Psychiatry Clin Neurosci. 2020;74(7):398-405.
26. Nouchi R, Hu Q, Ushida Y, Suganuma H, Kawashima R. Effects of sulforaphane intake on processing speed and negative moods in healthy older adults: Evidence from a randomized controlled trial.Front Aging Neurosci.2022;14:929628. Are

Are You Making This Common Vitamin D Mistake?
Many clinicians and patients now know that vitamin D plays an important role in immune health, bone health and brain health.
However, most physicians and patients are unaware that vitamin D can create some problems.
…or that menatetrenone (K2mk4) is a key partner in bone, cardiovascular health, and brain health.
That ignorance is putting people’s hearts, brains, blood vessels and bones at risk. Are yours at risk?

Vitamin D is a vitamin with hormone-like properties. When ultraviolet light hits the cholesterol molecules in our skin, the light on our skin will begin the initial step in making vitamin D3 (cholecalciferol).
Mushrooms that are exposed to ultraviolet light make ergocalciferol. (Vitamin D2). Both Vitamin D3 and Vitamin D3 are biologically inactive until they are activated, first by the liver, and then by the kidneys to make 1,25 dihydroxycholecalciferol or calcitriol.
This is the biologically active form of vitamin D. Calcitriol has a major role in regulating calcium and phosphate and the mineralization of teeth and bones. Vitamin D receptors are found throughout the body and the central nervous system. Low vitamin D blood levels are associated with an increased risk of a cardiovascular event, autoimmune diagnoses, and multiple sclerosis diagnosis.1-6
Because most people work indoors, away from sun exposure, and are covering their skin with clothing or sunscreen to reduce the risk of skin cancer, many are no longer having sufficient sun exposure to generate enough vitamin D3 by their skin. Physicians are often measuring vitamin D levels and advising their patients to take vitamin D supplements or get blood levels to reach the top half of the reference range.
That is helpful, but there are still major health risks that are not being sufficiently addressed.

Nutrition and physiology are complex with multiple interacting pathways. Calcitriol, the active form of vitamin D, increases the absorption of calcium from the gut into the bloodstream. Calcium supplementation may be beneficial for bone, however calcium supplementation may increase the risk of ectopic calcification in blood vessels.7 The increased absorption of calcium from the gut into the bloodstream increases the risk of calcification of blood vessels which can increase the risk of atherosclerosis, cardiovascular, and or cerebrovascular disease.7 Vitamin K2 is a key contributor to calcium and phosphate metabolism and is involved in the uptake of calcium and phosphate into teeth and bones and out of blood vessel walls.8-12 Vitamin K2mk7 is the bacterial form and vitamin K2mk4 is the mammalian form of vitamin K and is highest in the brain. Vitamin K2 is increasingly recognized as important in cardiovascular,10,12 bone,10,12 tooth,13 and healthy aging.8,14,15
There is relatively little vitamin K2 in the modern Western diet. This is due to the radical change in the current farming practices for raising meat and dairy livestock in the United States. To increase the efficiency of livestock production, meat animals and dairy cattle are typically grown in concentrated animal feeding operations (CAFOs). Although cattle have a digestive system that evolved from eating grasses and green plants and hogs and chickens evolved from eating plants and insects and are actually omnivores. Now, cattle, hogs, and chicken are fed corn, kept indoors and no longer consume green plants. The result is that the meat and milk from these animals has very little vitamin K2 with a significant decline in vitamin K2 intake in the typical Western diet.12 Vitamin K2 is present in fermented soybean Natto and fermented cheeses from animals that consumed grass.16-18 Taking the combination of vitamin D and vitamin K2 is associated with improved bone mineral density compared to taking only vitamin D.19
In addition to the benefits of vitamin K on mineralization of teeth and bone and prevention of calcification of blood vessels, vitamin K is involved in the maturation of oligodendrocyte precursor cells (brain stem cells) into oligodendrocytes (the cells that build and repair myelin, the insulation on the wiring between brain cells.20,21 Vitamin K2 levels are significantly lower in multiple sclerosis patients compared to controls.22
In my clinical practice, I advise my patients to protect their bone and tooth health by monitoring their vitamin D blood levels with the goal of having their vitamin D level in the top half of the laboratory reference range for vitamin D.
I recommend strength training and vibration plate training for bone health and chewing food thoroughly and avoiding added sugars and flour-based foods for tooth health.

In addition, for tooth health, bone health, blood vessel health and brain health I recommend regular intake of vitamin K2. Include fermented soybean or fermented black bean natto in the diet. Include clarified butter in the diet.
For my patients who take vitamin D supplements to achieve the targeted vitamin D levels, I have them take a vitamin D supplement that also includes vitamin K2 in the product.
This is the vitamin D and K2 supplement I recommend from The Wahls Protocol® Supplement line.
That way they have both vitamin K and vitamin D. For those who get their vitamin D through sunshine, I have the patient either consume natto daily or take a vitamin K2 supplement.
References
1. Barnard K, Colon-Emeric C. Extraskeletal effects of vitamin D in older adults: cardiovascular disease, mortality, mood, and cognition. Am J Geriatr Pharmacother. 2010;8(1):4-33.
2. Duan S, Lv Z, Fan X, et al. Vitamin D status and the risk of multiple sclerosis: a systematic review and meta-analysis. Neurosci Lett. 2014;570:108-113.
3. Norman PE, Powell JT. Vitamin D and cardiovascular disease. Circ Res. 2014;114(2):379-393.
4. Lin J, Liu J, Davies ML, Chen W. Serum Vitamin D Level and Rheumatoid Arthritis Disease Activity: Review and MetaAnalysis. PLoS One. 2016;11(1):e0146351.
5. Makrani AH, Afshari M, Ghajar M, Forooghi Z, Moosazadeh M. Vitamin D and fibromyalgia: a meta-analysis. Korean J Pain. 2017;30(4):250-257.
6. Lee YH, Song GG. Association between circulating 25-hydroxyvitamin D levels and psoriasis, and correlation with disease severity: a meta-analysis. Clin Exp Dermatol. 2018;43(5):529-535.
7. Wang J, Zhou JJ, Robertson GR, Lee VW. Vitamin D in Vascular Calcification: A Double-Edged Sword? Nutrients. 2018;10(5).
8. Schwalfenberg GK. Vitamins K1 and K2: The Emerging Group of Vitamins Required for Human Health. J Nutr Metab. 2017;2017:6254836.
9. Arnold A, Dennison E, Kovacs CS, et al. Hormonal regulation of biomineralization. Nat Rev Endocrinol. 2021;17(5):261275.
10. Hariri E, Kassis N, Iskandar JP, et al. Vitamin K2-a neglected player in cardiovascular health: a narrative review. Open Heart. 2021;8(2).
11. Hartley L, Clar C, Ghannam O, Flowers N, Stranges S, Rees K. Vitamin K for the primary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2015(9):CD011148.
12. Maresz K. Proper Calcium Use: Vitamin K2 as a Promoter of Bone and Cardiovascular Health. Integr Med (Encinitas). 2015;14(1):34-39.

13. Southward K. A hypothetical role for vitamin K2 in the endocrine and exocrine aspects of dental caries. Med Hypotheses. 2015;84(3):276-280.
14. Grober U, Reichrath J, Holick MF, Kisters K. Vitamin K: an old vitamin in a new perspective. Dermatoendocrinol. 2014;6(1):e968490.
15. Simes DC, Viegas CSB, Araujo N, Marreiros C. Vitamin K as a Diet Supplement with Impact in Human Health: Current Evidence in Age-Related Diseases. Nutrients. 2020;12(1).
16. Gille D, Schmid A, Walther B, Vergeres G. Fermented Food and Non-Communicable Chronic Diseases: A Review. Nutrients. 2018;10(4).
17. Katsuyama H, Ideguchi S, Fukunaga M, Fukunaga T, Saijoh K, Sunami S. Promotion of bone formation by fermented soybean (Natto) intake in premenopausal women. J Nutr Sci Vitaminol (Tokyo). 2004;50(2):114-120.
18. Yamaguchi M, Kakuda H, Gao YH, Tsukamoto Y. Prolonged intake of fermented soybean (natto) diets containing vitamin K2 (menaquinone-7) prevents bone loss in ovariectomized rats. J Bone Miner Metab. 2000;18(2):71-76.
19. Kuang X, Liu C, Guo X, Li K, Deng Q, Li D. The combination effect of vitamin K and vitamin D on human bone quality: a meta-analysis of randomized controlled trials. Food Funct. 2020;11(4):3280-3297.
20. Goudarzi S, Rivera A, Butt AM, Hafizi S. Gas6 Promotes Oligodendrogenesis and Myelination in the Adult Central Nervous System and After Lysolecithin-Induced Demyelination. ASN Neuro. 2016;8(5).
21. Popescu DC, Huang H, Singhal NK, et al. Vitamin K enhances the production of brain sulfatides during remyelination. PLoS One. 2018;13(8):e0203057.
22. Lasemi R, Kundi M, Moghadam NB, Moshammer H, Hainfellner JA. Vitamin K2 in multiple sclerosis patients. Wien Klin Wochenschr. 2018;130(9-10):307-313.
Cytokine Modulator
I have an autoimmune disorder, which means my immune cells have been overly active, damaging my brain and spinal cord for many years, and earlier in my life, I struggled with depression. Inflammation is linked to both of these health issues.
With anxiety and depression, there is often excessive inflammation in the brain. The same is true for schizophrenia. In those conditions, the immune system is making too many cytokines like Il-1b, IL-6, and TNF-alpha. Those molecules induce more immune cell activation and more inflammation, which can negatively impact health.
It’s likely that there was excessive inflammation in my body for years, explaining my problems with mild exercise–induced asthma, depression, chronic migraines, and endometriosis. All these conditions were tied to excessive cytokines and an overly active innate immune system. So how can we dial back the innate immune system?


In leaky gut, bacterial fragments get into the bloodstream and increase cytokine production. My approach is to work on diet, to reduce the issue of leaky gut by addressing food sensitivity issues and consuming more bone broths and soups.
Next, I look to stimulate the Nrf2 pathway to calm the innate immune system. Dietary strategies to stimulate the Nrf2 pathway include eating more garlic, onions, turmeric, sulforaphane, and green tea and eliminating added sugars and processed foods. The Wahls™ diet plans support the Nrf2 pathways. How’s your diet? Have you reduced or eliminated added sugars and processed foods? Do you still show signs of too much inflammation, like fatigue, brain fog, pain, or persisting autoimmune-related symptoms? Do you need to do more to turn off the inflammation?
Notably, some of the disease-modifying drug treatments for autoimmune conditions work by modulating the Nrf2 pathway. This is the mechanism by which dimethyl fumarate (Tecfidera®) works in treating autoimmune diseases such as optic neuritis, multiple sclerosis, and inflammatory bowel disease.1 This pathway regulates the production of important molecules that impart antioxidant activity, such as glutathione and superoxide dismutase (SOD). It also regulates the production of detoxification enzymes, including glutathione S-transferase, and downregulates signalling factors such as NFβB. These pathways have been shown to mitigate pathological mechanisms in multiple sclerosis, psoriasis, and optic neuritis.2-4
Taking a nutraceutical that stimulates the Nrf2 pathway is an excellent way to optimize your physiology if you have an autoimmune condition such as optic neuritis, multiple sclerosis, or psoriasis. Or you could take a prescription medicine such as Tecfidera®. I prefer that my patients optimize their diet and consider using targeted nutraceuticals to optimize the Nrf2 pathway and reduce inflammation. Some people will need to take a disease-modifying drug treatment in addition to targeted supplements, diet, and lifestyle modification.
Whatever path you take, it is important to get the inflammation turned off. Once the inflammation is stabilized, it is often possible to manage the symptoms with diet, lifestyle, and targeted nutraceuticals. It takes time to repair all the damage that has likely accumulated over decades, but it is possible.

References
1. Yadav SK, Soin D, Ito K, Dhib-Jalbut S. Insight into the mechanism of action of dimethyl fumarate in multiple sclerosis. J Mol Med (Berl). 2019;97(4):463-472.
2.Carvalho AN, Lim JL, Nijland PG, Witte ME, Van Horssen J. Glutathione in multiple sclerosis: more than just an antioxidant? Mult Scler. 2014;20(11):1425-1431.
3. Rosito M, Testi C, Parisi G, Cortese B, Baiocco P, Di Angelantonio S. Exploring the Use of Dimethyl Fumarate as Microglia Modulator for Neurodegenerative Diseases Treatment. Antioxidants (Basel). 2020;9(8).
4. Gesser B, Rasmussen MK, Iversen L. Dimethyl Fumarate Targets MSK1, RSK1, 2 and IKKalpha/beta Kinases and Regulates NF-kappaB /p65 Activation in Psoriasis: A Demonstration of the Effect on Peripheral Blood Mononuclear Cells, Drawn from Two Patients with Severe Psoriasis Before and After Treatment with Dimethyl Fumarate. Psoriasis (Auckl). 2020;10:1-11.
Mitigating The Risks Of Gluten Contamination
People with Celiac disease follow a lifelong gluten-free diet to manage their condition. I too follow a strict gluten-free diet. When I travel, I am always concerned about being exposed to gluten–20-40% of restaurant foods that are labeled gluten-free and 20% of grocery items that are labeled gluten-free actually have detectable gluten in them.1,2
Protein is supposed to be fully digested in the gut, broken down into amino acids which then pass from the gut into the bloodstream. If a person has incompletely digested proteins in their gut and increased permeability of the gut lining (leaky gut), gluten from the meal they ate may get into the bloodstream. If that person was meticulously eating gluten-free but ate food cross-contaminated with gluten, they may have just been “glutened” without being aware of the exposure.
If you are severely gluten sensitive as I am, you may have anxiety about eating food you did not prepare. It has happened to me–I have had adverse reactions to a restaurant meal labeled glutenfree that was probably contaminated with gluten.
When eating a meal someone else is going to prepare, I always offer to bring food. Unless people are gluten-sensitive themselves, they are unlikely to be aware of the perils of cross-contamination that can easily occur in the kitchen. They may not be aware that gluten is often a hidden ingredient in sauces and packaged foods. For the gluten-sensitive person, even a tiny amount of gluten in the bloodstream will activate the immune system, causing a flare of autoimmune disease processes. The older we are, the more likely we are to have an increased leakiness of the gut as well as decreased production of enzymes needed to digest protein and carbohydrates. This combination increases the risk of developing food sensitivities and having a flare if we are exposed to even small amounts of gluten. If you are noticeably bloated, particularly after eating protein, you are more likely to have poor protein digestion. This increases the risk of muscle wasting as we age.

Patients with multiple food sensitivities who have difficulty finding foods they can safely consume may benefit from adding digestive enzymes and betaine to increase stomach acid.
There has been considerable interest in finding a digestive enzyme formulation that would make it possible for someone with Celiac disease to consume gluten regularly. Thus far those efforts have been unsuccessful. However, there is an interesting report on gluten-digesting enzymes improving symptoms for people with Non-Celiac Gluten Sensitivity. In a randomized trial, patients took active enzymes or a placebo prior to a gluten challenge. Then they scored their symptoms and had blood markers of T-cell activation and inflammation measured (interleukin 8, tumor necrosis factor (TNF)). The enzyme preparation protected participants from symptoms and prevented activation of the immune system when exposed to gluten.3
I would not consider using digestive enzymes and betaine to provide sufficient protection to eat gluten-containing breads and pastas. However, I do think they are useful in decreasing the risk of symptoms that may arise from eating foods labeled gluten-free that actually have low level crosscontamination.
I now travel with digestive enzymes and begin taking them as soon as I start eating away from home. For me, gluten exposure brings a devastating level of face pain. Because so many foods are contaminated with gluten, I take enzymes to help guard against possible painful reactions to supposedly gluten-free food.
I still am meticulous about what I eat away from home.
I order foods that are naturally gluten-free and avoid gluten-free versions of bread, pasta, and other traditionally gluten-containing foods. I avoid sauces and salad dressing. If I order a salad, I ask for olive oil on the side. I opt for a grilled source of protein and always take digestive enzymes.
For patients who have multiple food sensitivities and are having difficulty finding foods they can safely consume, adding digestive enzymes and a betaine supplement to increase stomach acid can facilitate the digestion of the small amount of gluten that the “gluten-free” meal may be contaminated with. It also helps to break down other food proteins that may be the source of multiple food sensitivity issues. These supplements are not enough to allow for consumption of regular bread, but they can prevent the severe side effects some get from being “glutened” by cross-contamination.


I know I feel safer when I travel by taking digestive enzymes and betaine.
Adding digestive enzymes to their supplement program has also been very helpful for those with multiple food sensitivities, allowing them to eat a less restrictive diet.
The Wahls Protocol® Collection carries Gluten Shield MD, the digestive enzymes I use when I travel, or before I eat when at a restaurant or with friends and family who may not eat a gluten free diet.
Learn more or click here to shop.
References:
1. Lerner BA, Phan Vo LT, Yates S, Rundle AG, Green PHR, Lebwohl B. Detection of Gluten in Gluten-Free Labeled Restaurant Food: Analysis of Crowd-Sourced Data. Am J Gastroenterol. 2019;114(5):792-797.
2. Falcomer AL, Santos Araujo L, Farage P, Santos Monteiro J, Yoshio Nakano E, Puppin Zandonadi R. Gluten contamination in food services and industry: A systematic review. Crit Rev Food Sci Nutr. 2020;60(3):479-493.
3. Ido H, Matsubara H, Kuroda M, et al. Combination of Gluten-Digesting Enzymes Improved Symptoms of Non-Celiac Gluten Sensitivity: A Randomized Single-blind, Placebo-controlled Crossover Study. Clin Transl Gastroenterol. 2018;9(9):181.
Histamine Intolerance And Mast Cell Activation
Some people are troubled by histamine intolerance. Histamine is produced and released by immune cells (mast cells and basophils). Gut microbes also make histamine. In addition, some foods also contain histamine.
Histamine induces the contraction of smooth muscles (bronchioles in the lungs and small intestine) and dilates blood vessels, increasing their leakiness. Histamine release can cause heart rhythm disturbance, change in blood pressure, increased mucus secretion (runny nose), and pain.
Symptoms that may arise from excessive activation of mast cells and release of histamine include:
• bloating
• skin rashes (flushing, hives, or eczema)
• itching
• runny nose
• increased tearing
• headaches
• diarrhea
• severe menstrual cramps
• and low blood pressure.1-3

Some may also experience:
• anxiety
• depression
• panic disorders
• sleep disturbance
• and severe fatigue.
Clinical diagnosis of mast cell activation and histamine sensitivity remains a challenge. There are hundreds of different mediators in mast cells, not just histamine. And the mediators that are released when mast cells are activated are quickly metabolized. That is why it is difficult to have a single blood test that can confirm mast cell activation or histamine sensitivity issues. Standardized testing is simply not available.
At present, other causes of the symptoms must be ruled out. Diagnosis requires at least two clinical symptoms that occur in less than four hours after eating high-histamine foods, and improvement in symptoms after adopting a low-histamine diet. A good response is a significant reduction in symptoms after 2 months of a low histamine diet.1,3
Foods high in histamine may trigger histamine-related symptoms.
High histamine foods include:
• citrus fruits
• strawberries
• bananas
• pineapple
• eggplant
• avocado
• tomatoes
• olives
• beans,
• canned meats
• smoked meats
• dried meats or fish
• yogurt
• cheese
• vinegar
• soy sauce
• fermented foods
• kimchi
• sauerkraut
• kombucha
• vinegar
• soy sauce
• beer,
• wine
• coffee
• and black tea
In my clinical practice, I discuss the possibility that symptoms may be related to unrecognized gluten and casein sensitivity and direct patients to start with level one of the Wahls™ diet.
If they are still symptomatic after 3 months of the Wahls™ diet, I have the patient implement a low FODMAPS version of the Wahls™ diet. FODMAP (fermentable oligo-, di-, monosaccharides, and polyol) sensitivity may be the true cause of the symptoms.

Again the Wahls™ diet (level one) is often very helpful in reducing these types of symptoms, as is a low FODMAP version of the Wahls™ diet.
Eliminating legumes and reducing or eliminating onions, garlic, and fruit for six months can be very revealing.
The main dietary sources for the FODMAPS are:
• Oligosaccharides: wheat, rye, legumes, garlic, onions
• Disaccharides: milk, yogurt, cheese (lactose)
• Monosaccharides: honey, agave nectar, and fructose (fruit sugars)
• Polyols: blackberries, lychee
If symptoms persist, a trial of a low-histamine diet is in order. The first step is freezing leftover foods; prolonged food storage increases histamine content. Slow cooking also increases histamine levels in food, as does frying and grilling.
Boiling and steaming decrease histamine content.
Pressure cooking for a shorter time at high pressure does not increase histamine content.
Another strategy for managing histamine intolerance is to use Diamine Oxidase (DAO) to facilitate the breakdown of histamine in the gut.
Adding Diamine Oxidase has improved dietary tolerance of histamine and increased the ability of many patients to consume more histamine-rich foods. In a research study, adding supplemental DAO reduced histamine-related symptoms (rashes, headaches, blood pressure, abdominal complaints) and improved dietary tolerance of histamine-rich foods.1 Adding a DAO supplement has been helpful to my patients with histamine sensitivity, allowing them to follow a less restrictive diet.
If you believe you have histamine intolerance, I suggest you begin by adopting level one of the Wahls™ diet. If that is insufficient, reduce the FODMAP foods–onions, garlic, berries, and fruit sugars.
Consider a trial of a low histamine diet coupled with a DAO supplement.
After 6 months, you may slowly try adding back some higher histamine foods to assess if you can now tolerate a more moderate intake of histamine. Make dietary changes slowly to assess the

impact of higher histamine foods. Often people are able to have a less restrictive diet when they also include DAO in their supplement routine.
The Wahls Protocol® Histamine Shield is a patented enzyme formula containing diamine oxidase (DAO)—the main enzyme responsible for the degradation of ingested histamine. This enzyme has been clinically tested and found to break down food-derived histamine in the digestive tract. DAO is not absorbed and does not have systemic activity.
Click here to shop.
References:
1. Comas-Baste O,Sanchez-Perez S, Veciana-Nogues MT, Latorre-Moratalla M, Vidal-Carou MDC. Histamine Intolerance: The Current State of the Art. Biomolecules.>2020;10(8).
2. Fogel WA, Lewinski A, Jochem J. Histamine in food: is there anything to worry about? Biochem Soc Trans. 2007;35(Pt 2):349-352.

CLICK HERE TO SHOP
3. Smolinska S, Winiarska E, Globinska A, Jutel M. Histamine: A Mediator of Intestinal Disorders-A Review. Metabolites.2022;12(10).
Is Candida Taking Over Your Gut?
Increasingly scientists recognize the importance of our microbiome to health. The microbiome is a unique fingerprint—each individual has a slightly different microbiome that is stable and unique to them and influenced by major events in their early life. By the time we are three years old, our microbiome community has established itself. Unfortunately, I, like many with autoimmune disease, had a sub-optimal start to my microbiome, which faced several challenges that reduced its quality.
I was born vaginally at term, which is a great start for a microbiome. In vaginal births, the baby travels through the mother’s vagina, which inoculates them with all the bacteria that live there. Babies born via C-section are seeded with different bacterial species at birth and have a higher risk than babies born vaginally of developing a variety of chronic health problems, including autoimmune, metabolic, and mental health issues.

As I passed through my mother’s vagina, I was seeded with bifidobacterial species that thrive on the oligosaccharides in breast milk. Unfortunately, I was born in an era when it was not fashionable to breastfeed and the health benefits of breast milk were not as well known. I was formula fed, which meant I missed out on the boost my bifidobacterial species would have gotten breast milk.
As a toddler, I had several episodes of streptococcal infections of the throat and tonsils and was given multiple rounds of penicillin before the age of three. I had my tonsils removed when I was four because of recurrent tonsillitis. Penicillin prevented the development of rheumatic fever and valvular heart disease, which I am grateful for. But each time I took penicillin, the bacteria in my bowels died and the yeast candida albicans grew more dominant. Because all of this happened before the age of three, my microbiome was established with an overgrowth of candida species in my bowels that will stay with me forever.
I have since learned that having an excessive amount of candida in the bowels leads to increased risk of anxiety and other mental health issues as well as autoimmunity.1-3 Candida infections are increased in patients with MS as compared to healthy controls.4,5 In addition, candida can create a biofilm with multiple other bacterial and fungal organisms that is resistant to antibiotic and antifungal treatment.6
Signs of candida overgrowth that I look for in my patients are:
• thickened toenails or fingernails,
• redness under the breasts, in the groin, around the testicles or anus,
• and a history of recurrent vaginal yeast infections.
• I tell patients whose history suggests they have increased yeasts in the gut due to early or chronic antibiotic use that issues with mood, fatigue, and brain fog may also be associated with candida overgrowth.
Controlling yeasts is a lifelong commitment. Gut microbes will always revert to what the person had at age three. In addition, over the age of 50 the diversity of the gut microbiome tends to decline, more so with each decade. As the diversity declines, the risk of cognitive decline and frailty increases.
My approach for myself and my patients with autoimmune or mental health issues is to assess the first three years of life to better understand how their individual microbiome was established. Was the person born vaginally? Did they receive antibiotics in the first 3 years of life? Did they have

a diet high in sugar and processed foods? Did they have multiple rounds of antibiotics? The more questions a patient answers yes to, the more likely they are to have excessive candida and other yeasts in their bowels and not enough bifidobacterial and lactobacillus species.
For these individuals, I recommend a lower carbohydrate diet (to starve the yeast), an ongoing herbal suppression of yeast, and a probiotic that has multiple strains of lactobacillus and bifidobacterial species that have been shown to improve metabolic health and mood. I also explain that this will be a lifelong intervention because the microbiome is mostly set by the age of 3 and that over the age of 60, microbiome diversity tends to decline, increasing the risk of frailty and cognitive decline.
I feel much better following a low carbohydrate diet and taking an herbal candida suppression product and a probiotic. I also rely on herbs and essential oils that have demonstrated effectiveness at controlling candida and restoring a healthier microbial community in the gut, including oregano oil 7, ginger oil 8, olive leaf 9, and turmeric 10 .
In addition, I take a probiotic with a blend of over 10 strains of Bidifobacterium lactis and Lactobacillus rhamnosus. These species have demonstrated efficacy for rebalancing the gut immune balance 11,12 and increasing production of butyrate in the bowels.13 These probiotic bacteria blends have also been shown to improve the health of the gut-immune-brain axis.14 Butyrate-producing probiotics have been shown to be beneficial to mood, general health, and disease progression in the setting of multiple sclerosis.15

I now recognize that my microbiome will always drift back towards what it was when I was 3 years old. I will always need to tend the microbial garden living in my bowels. If I eat more carbohydrates or stop the candida suppression herbs or probiotics, I do not feel as well. I also tend my microbial garden by eating sauerkraut and kimchi and plenty of greens.
How do you tend your microbial garden? Given that our microbiome gravitates to what it was when we were 3 and begins to deteriorate further over age 60, it’s important to take care of it. There is a lot you can do to support your microbiome and increase your chances of thriving as you age. CLICK HERE TO SHOP

The Wahls Protocol® Supplements carry two helpful items: Candida Clear capsules or the more comprehensive Candida Clear Support Kit... If you suspect you have a candida overgrowth, assess which option is best for you!
References:
1. Aaron L, Torsten M. Candida albicans in celiac disease: A wolf in sheep’s clothing. Autoimmun Rev. 2020;19(9):102621
2. Palma-Carlos AG, Palma-Carlos ML. Candida and human disease. Eur Ann Allergy Clin Immunol.2004;36(8):291-296.

3. Gerard R, Sendid B, Colombel JF, Poulain D, Jouault T. An immunological link between Candida albicans colonization and Crohn’s disease.Crit Rev Microbiol.2015;41(2):135-139.
4. Benito-Leon J, Pisa D, Alonso R, Calleja P, Diaz-Sanchez M, Carrasco L. Association between multiple sclerosis and Candida species: evidence from a case-control study.Eur J Clin Microbiol Infect Dis. 2010;29(9):1139-1145.
5. Saroukolaei SA, Ghabaee M, Shokri H, Badiei A, Ghourchian S. The role of Candida albicans in the severity of multiple sclerosis.Mycoses.2016;59(11):697-704.
6. Ponde NO, Lortal L, Ramage G, Naglik JR, Richardson JP. Candida albicans biofilms and polymicrobial interactions. Crit Rev Microbiol.2021;47(1):91-111.
7. Hacioglu M, Oyardi O, Kirinti A. Oregano essential oil inhibits Candida spp. biofilms.Z Naturforsch C J Biosci. 2021;76(1112):443-450.
8. Huong LT, Chung NT, Huong TT, et al. Essential Oils of Zingiber Species from Vietnam: Chemical Compositions and Biological Activities.Plants (Basel). 2020;9(10).
9. Nasrollahi Z, Abolhasannezhad M. Evaluation of the antifungal activity of olive leaf aqueous extracts against Candida albicans PTCC-5027.Curr Med Mycol.2015;1(4):37-39.
10. Samadi FM, Suhail S, Sonam M, et al. Antifungal efficacy of herbs.J Oral Biol Craniofac Res. 2019;9(1):28-32.
11. Ashraf R, Shah NP. Immune system stimulation by probiotic microorganisms.Crit Rev Food Sci Nutr. 2014;54(7):938-956.
12. Sichetti M, De Marco S, Pagiotti R, Traina G, Pietrella D. Anti-inflammatory effect of multistrain probiotic formulation (L. rhamnosus, B. lactis, and B. longum). Nutrition.2018;53:95-102.
13. Srivastav S, Neupane S, Bhurtel S, et al. Probiotics mixture increases butyrate, and subsequently rescues the nigral dopaminergic neurons from MPTP and rotenone-induced neurotoxicity.J Nutr Biochem.2019;69:73-86.
14. Michels M, Jesus GFA, Abatti MR, et al. Effects of different probiotic strains B. lactis, L. rhamnosus and L. reuteri on brainintestinal axis immunomodulation in an endotoxin-induced inflammation.Mol Neurobiol.2022;59(8):5168-5178.
15. Mirashrafi S, Hejazi Taghanaki SZ, Sarlak F, Moravejolahkami AR, Hojjati Kermani MA, Haratian M. Effect of probiotics supplementation on disease progression, depression, general health, and anthropometric measurements in relapsing-remitting multiple sclerosis patients: A systematic review and meta-analysis of clinical trials.>Int J Clin Pract. 2021;75(11):e14724. CLICK HERE TO SHOP

The Strategies I Use For Getting Great Sleep
Sleep has always been difficult for me. For years it was difficult to fall asleep and stay asleep. Often I would wake up at 2 in the morning, unable to fall back asleep again. Earlier in my life, I was fine with sleeping only 4 or 5 hours at night. I was ambitious. I had a lot to do. I thought that sleeping was a waste of my time. I did that in college, medical school, during my residency, and when I began working as a physician. When I had Zach and Zebby, I thought it was an advantage that I slept so little. Now I know better.
Sleep is an essential part of life1. Important functions occur in our brains as we sleep, including the consolidation of memory4 and the removal of beta-amyloid and other toxins5 in the brain. Unfortunately, too many of us do not get enough sleep.
There are many varieties of sleep problems. Some people have trouble falling asleep, while others have trouble staying asleep. Restless legs–involuntary twitchiness, movement, or jerking of the legs at night–is also a common complaint, as is sleep apnea. Poor sleep increases the risk of weight gain,7 metabolic syndrome,8 diabetes,9 and mental health issues.10
Sleep disruptions are incredibly common among people with multiple sclerosis and other neuroimmune conditions2 as well as those with Parkinson’s disease, Alzheimer’s disease, or other neurodegenerative problems.3 Sleep problems are an early sign of trouble brewing in the nervous system and often develop before a diagnosis of multiple sclerosis, Parkinson’s, or other neuroimmune or neurodegenerative disease.
Scientists don’t know if sleep problems are part of the cause of many nervous system disorders, or if they are simply part of the prodrome that often precedes nervous system disorders,6 but all those years of poor sleep likely accelerated my decline. I routinely ask my patients about their sleep and educate them about why sleep is critical to our health. Then we work to improve both sleep quality and quantity.
So, how is your sleep? Do you wake up refreshed most mornings? Do you fall asleep easily and stay asleep through the night? If you wake up during the night, can you easily fall back asleep again? If sleep is a problem for you, I have a few suggestions for you to consider.
• Spend 20 minutes outside in daylight. This will help you get ultraviolet light to the retina in your eyes, signaling the biological clock in your brain and helping your brain make more melatonin at the right time.

• Turn off the television, computer, and smartphones an hour before you want to sleep. At a minimum, activate the applications that remove the blue light in the evening. Blue light disrupts the brain’s ability to make melatonin and get your body to sleep at the right time.
• Develop a calming, evening ritual that helps you set the stage for falling asleep. I do a gratitude meditation as I fall asleep. I visualize someone who has been helpful in my life, replay how that person helped me, and thank them for their help. It is a lovely way for me to gently slow down, give thanks, and drift into sleep.
• Keep a notepad by the bed. If you have something that you want to remember, write it on the notepad. It will be easier to let go of the thought and drift off to sleep.
• Take a melatonin supplement 2 hours before you want to fall asleep. Over the age of 60, the brain makes less melatonin, which contributes to problems falling asleep and staying asleep that occur as we age. I take melatonin and have found it useful.
• Take magnesium threonate. Most people with sleep problems also have a relative deficiency of magnesium, which contributes to poor sleep. Magnesium is vital to healthy cognition, which includes long- and short-term memory, learning, stress management, and sleep.11 Magnesium threonate is the only form of magnesium that crosses the blood-brain barrier and gets into the central nervous system.11 Magnesium improves sleep quality and quantity. I have found taking magnesium threonate in the evening to be very helpful for improving my sleep and reducing problems with restless legs. It has made a significant difference in my ability to fall asleep and stay asleep.
Now that I understand the critical role of sleep for the health of my brain, I prioritize getting 7 to 8 hours of sleep each night. I pay attention to what disrupts my sleep and what supports getting a great night’s sleep. These changes have made a huge difference in my overall health and well-being.
In summary, getting good sleep is essential for our health and healthy aging. Pay attention to your sleep. Note when you sleep well and when you sleep poorly. What factors contribute to having better sleep and what factors likely contribute to having poor sleep? Once you know what affects your sleep, you can slowly make changes and hopefully consistently sleep 7 to 8 hours each night, waking up in the morning fully refreshed.
References
1. Grandner MA. Sleep, Health, and Society. Sleep Med Clin. 2017;12(1):1-22.


2. Besedovsky L, Lange T, Haack M. The Sleep-Immune Crosstalk in Health and Disease.Physiol Rev. 2019;99(3):1325-1380.
3. Kokosova V, Filip P, Kec D, Balaz M. Bidirectional Association Between Sleep and Brain Atrophy in Aging. Front Aging Neurosci. 2021;13:726662.
4. Girardeau G, Lopes-Dos-Santos V. Brain neural patterns and the memory function of sleep.Science. 2021;374(6567):560564.
5. Wang C, Holtzman DM. Bidirectional relationship between sleep and Alzheimer’s disease: role of amyloid, tau, and other factors. Neuropsychopharmacology. 2020;45(1):104-120.
6. Bohnen NI, Hu MTM. Sleep Disturbance as Potential Risk and Progression Factor for Parkinson’s Disease. J Parkinsons Dis.2019;9(3):603-614.
7. Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring). 2008;16(3):643-653.
8. Smiley A, King D, Bidulescu A. The Association between Sleep Duration and Metabolic Syndrome: The NHANES 2013/2014. Nutrients.<2019;11(11).
9. Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care.2010;33(2):414-420.
10. Sampasa-Kanyinga H, Colman I, Goldfield GS, et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: a systematic review.Int J Behav Nutr Phys Act. 2020;17(1):72.
11. Vink R. Magnesium in the CNS: recent advances and developments. Magnes Res. 2016;29(3):95-101.