

THYROID 101

Chapter 1: The Thyroid
Chapter 2: Diseases of the Thyroid
Chapter 3: Signs and Symptoms of Dysfunction
Chapter 4: Thyroid Testing and Diagnosis
Chapter 5: Treatment Chapter 6: Finding a Thyroid
Introduction
Optimizing your health is the most important factor in achieving a better quality of life
One of the most influential and misunderstood factors involved in maintaining good health is the thyroid. As the primary method of regulating numerous systems involved in weight management, energy regulation, neurological function, hormonal interactions, heart health and many others, the thyroid deserves greater recognition and awareness.
Thyroid 101 aims to educate and inform its readers of the many different roles of the thyroid, how to recognize malfunction, understand quality treatment, and means of gaining the assistance of a well-educated and knowledgeable physician.
Having a greater appreciation and understanding of the thyroid can support your journey towards wellness and greater quality of life.
Chapter 1: The Thyroid
Gaining greater knowledge and appreciation of the thyroid requires that you first know the basics. Thyroid knowledge begins with learning how it interacts with the body, the ways it orchestrates proper hormone balance and metabolism and the other systems associated with its function.
The small gland known as the thyroid is one of the most influential elements in the body. Even though the gland is only about the size of a walnut, weighing between 20-60 grams, it wields incredible power. The thyroid’s influence is far reaching and affects the metabolism of every cell in the body. It is so highly integrated that even minor malfunctions can cause widespread dysfunction throughout the body.
Thyroid Function and Influence
The thyroid produces various hormones that have control over multiple bodily processes, primarily affecting metabolic function. Thyroid hormones influence every cell in the body by regulating the individual metabolic function of each cell. Every cell, gland and organ in the body relies on thyroid hormones to function normally.
Some have likened the thyroid to be the gas pedal that controls the body’s overall speed and functionality. While working correctly, the body maintains a healthy cruising speed that facilitates wellness. When the thyroid is not active enough, however, the throttle is decreased. This causes everything to slow down, and the body feels sluggish, tired and mentally fogged. Alternatively, if the thyroid is overproducing, the throttle is pressed to the floor causing every system in the body to speed up and move at an erratic and potentially dangerous rate, resulting in jitteriness, irregular heart function, anxiety, insomnia and attention disorders.
Perhaps the worst scenario is when the thyroid is functioning inconsistently, which can cause jarring shifts back and forth between sluggishness and hyperactivity, or being "wired but tired".
Suffering from such a condition can cause you to alternate between all the symptoms associated with both hypothyroidism and hyperthyroidism.
Howthe Thyroid Works
The thyroid exercises its control over the body through the secretion of thyroid hormones, T4 and T3. Amazingly, it only takes one teaspoon of thyroid hormone to coordinate and direct the metabolic function of every

For more information on the thyroid, watch this Holtorf Medical Group Health Chat with Dr. Nancy L. Evans.
Thyroxine (T4) – The inactive or storage form of thyroid hormone. A portion of this hormone is converted into T3 by enzymes known as deiodinases. If there is excess T4 in the system (such as from inflammation, chronic infection, or illness), it is likely to be converted into reverse T3. Experts estimate that 40% of T4 is converted to T3 while 20% is converted to reverse T3 in a healthy individual.
Triiodothyronine (T3) – The active form of thyroid hormone that directly influences metabolic function of individual cells. Those with a deficit or low cellular level of T3 will often experience sluggish bodily function with a myriad of symptoms. Whereas an overabundance of T3 causes hyperactivity throughout the body.
Reverse Triiodothyronine (RT3) – As the mirror image of T3, RT3 is responsible for keeping active thyroid hormone levels balanced. This hormone inhibits T3 function to help maintain hormone levels. RT3 is an important part of proper thyroid balance. However, with stress, dieting, inflammation or chronic illness over conversion of T4 to RT3 can result in severe symptoms of hypothyroidism
Thyroid 101 cell in the body. When working properly, thyroid hormones are transported throughout the body at the values needed to maintain healthy bodily function. If any hormonal factors such as production, transport, conversion, receptor activity, etc. are not working as intended, you may experience widespread bodily dysfunction with potentially a wide-range of symptoms.
Diiodothyronine (T2)—T2 is like T3 in that it actively increases metabolic function. However, this hormone appears to focus primarily on mitochondria rather than DNA, has weaker protein binding potential compared to T3, and is likely sourced primarily from tissues rather than the thyroid alone. Interestingly, T2 aids in resolving insulin resistance and inhibiting fat storage, which can be a significant contributor to thyroid disease, specifically hypothyroidism. We have, however, done clinical trials with T2 given to patients. While several patients saw clinical benefits, the numbers have been smaller than we hoped.
The Basic Thyroid Cycle
When thyroid hormone levels of T4 and T3 are low, the hypothalamus should be prompted to produce Thyroptin-Releasing Hormone (TRH). TRH informs the pituitary it needs to release more thyrotropin (also known as Thyroid-Stimulating Hormone or TSH). TSH lets the thyroid know that it needs to produce additional T3 and/or T4 to be released into the bloodstream. If appropriate bodily communications and responses are made, the feedback loop keeps thyroid hormone levels maintained and regulated. However, it is clinically shown that the normal balance is disrupted with stress, depression, dieting, obesity, autoimmune disease, inflammation, diabetes, aging and many more contributing factors.

Production and communication are not the only aspects involved in the thyroid cycle. Once thyroid hormones have entered the bloodstream, they must be transported to the various cells and systems throughout the body to exert their influence over individual metabolic function. Transporting into the cells can be the major issues that impact multiple factors of life including weight control, energy production, temperature regulation, growth, cognitive function, and much more.
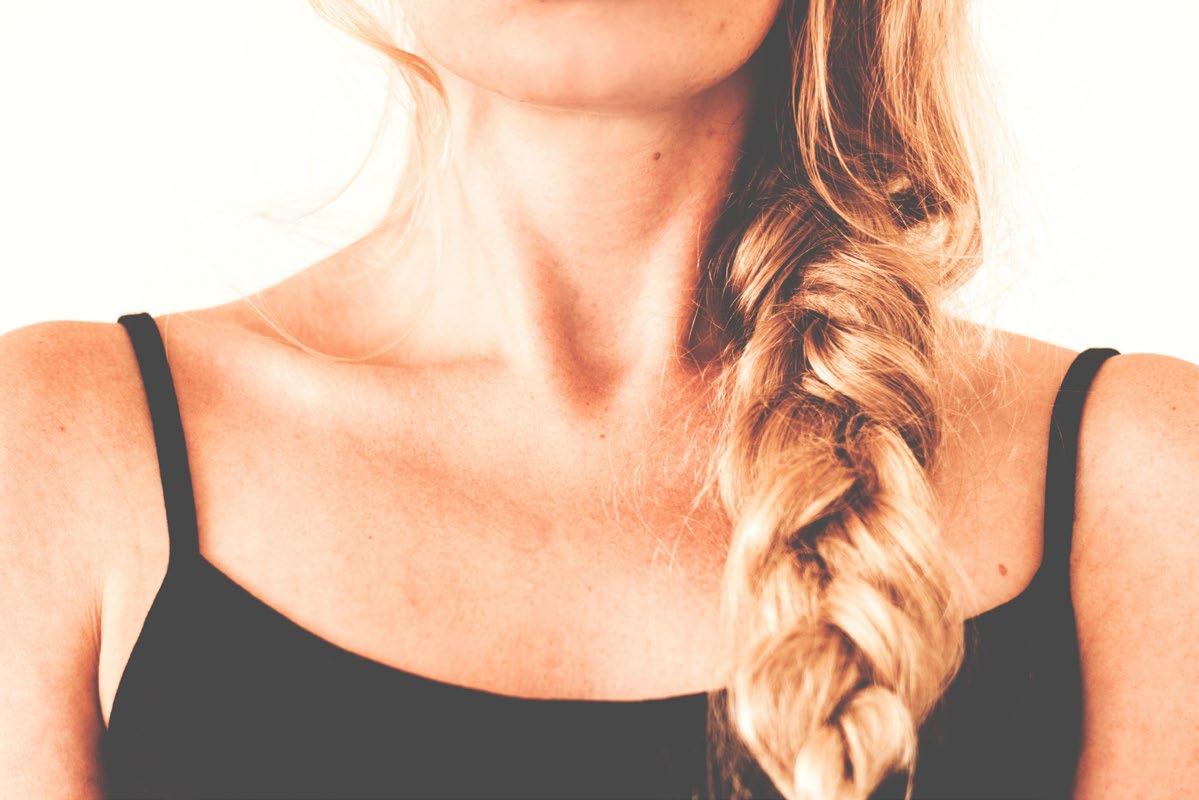
Where the Thyroid Fits
The thyroid is in the neck just below the larynx or voice box. Physiologically, the thyroid gland belongs to the endocrine system. This system includes the hypothalamus, pituitary, adrenals, and thyroid gland. All things hormone-related including production, transport, interaction with other systems, and hormone balance all fall under the jurisdiction of the endocrine system. The endocrine system is highly influenced by the peptide regulatory system.
The endocrine system is involved with the production and regulation of many other important hormones including:
• Cortisol
• DHEA
• Estrogen
• Pregnenolone
• Progesterone
• Testosterone
• Thyroid Hormones (T4, T3, T2, TSH, etc.)
The substances listed above interact with and influence one another. When working in sync, they help control the body’s many functions. If, however, the components of the endocrine system fall out of alignment, serious dysfunction can occur.
The Importance of the Thyroid
High interconnectivity is just one reason it is important to have a deep understanding of not only the thyroid but also the systems associated with it. With greater knowledge of what the thyroid is and how it functions, we can begin discussing the many issues and diseases that inhibit its ability to facilitate wellness.
Chapter 2: Diseases of the Thyroid
As we’ve learned, the thyroid is one of the most important glands in the body. Thyroid hormones affect every cell in the body. Therefore, conditions or diseases that impact the thyroid’s ability to secrete thyroid hormones affect utilization of thyroid hormones, can cause widespread dysfunction and symptoms.
A growing portion of the United States is suffering from a thyroid-related disease, with most of them being women. Females have fewer thyroid receptors than males, meaning that minor fluctuations in thyroid level can dramatically affect their health.
Additionally, women are more likely to have autoimmune conditions which can contribute significantly to thyroid disease. Being aware of the many conditions that affect thyroid function can help individuals protect themselves from thyroid hardships.
Hypothyroidism
Hypothyroidism is the most common type of thyroid disease, most often going undetected by standard blood tests. The condition occurs when there is not enough thyroid hormone present in the cells. This can be caused by poor hormone production, improper conversion of T4 to T3, increased reverse T3
and, most commonly, poor transport of thyroid hormones. Causes of hypothyroidism include the removal of the thyroid gland, exposure to toxins, excess iodide, iodine deficiency, selenium deficiency, aging, chronic illness, obesity and the autoimmune condition known as Hashimoto’s thyroiditis.
There are multiple forms of hypothyroidism that develop from the various forms of dysfunction. The following selection is a sampling of such conditions:
Primary Hypothyroidism—When the thyroid gland cannot produce sufficient amounts of thyroid hormones. This is picked up on a simple blood test with an elevated TSH. Many doctors believe this is the most common cause of low thyroid, but only because they do not know how to detect the other more common causes of low thyroid that do not result in an elevated TSH.
Secondary Hypothyroidism—Resulting from pituitary malfunction leading to poor TSH secretion.
Hypothalamic/Tertiary Hypothyroidism—Caused by a deficiency in thyroid releasing hormone (TRH) stemming from chronic disease or congenital defects.
Abnormal Thyroid Transport/Cellular Hypothyroidism—To have biological activity, the T4 and T3 must cross the cellular membrane from the serum into the target cells. This transport into the cells is energy dependent, and any condition associated with reduced cellular energy—diabetes, obesity, chronic and acute dieting, depression, anxiety, etc.will also be associated with reduced thyroid transport into the cells which results in cellular hypothyroidism. Unfortunately, only primary hypothyroidism is detected with standard thyroid tests.
Thyroid Resistance—Low cellular thyroid levels or function with normal serum testing.

Sub-LaboratoryHypothyroidism
Symptoms of sub-laboratory hypothyroidism and traditional cases of hypothyroidism are similar. The primary difference between the conditions is that sub-laboratory cases return test results that show an increase in TSH and normal T4/T3, even though symptoms are present (we discuss this issue in greater detail in chapter 4). Unfortunately, many doctors are unaware of sub-laboratory hypothyroidism. Therefore, they do not account for it during testing or diagnosis. Those with sub-laboratory hypothyroidism frequently feel fatigued, have trouble thinking clearly, experience muscle and joint pain, and have difficulty losing weight. Patients may experience any of the symptoms associated with hypothyroidism, but likely with lesser intensity.
Hashimoto's Thyroiditis (Autoimmune Hypothyroidism)
Hashimoto’s Thyroiditis is thought to be the most common causes of hypothyroidism, but usually goes undetected. About one out of every thousand people will be diagnosed with this autoimmune condition, but it is much more common. Of this group, women are significantly more likely to have Hashimoto’s, and it is most common between the ages of 45 and 65. Studies show, however, that most cases of Hashimoto’s cannot be detected by blood work—only the worst of the worst test positive.
Hashimoto’s Thyroiditis involves the production of thyroid antibodies that attack thyroid gland proteins resulting in inflammation or the destruction of thyroid cells and reduced hormone production. As the thyroid continues to fall under assault, it releases pockets of thyroid hormone into the bloodstream. This can cause temporary spikes in thyroid levels, resulting in symptoms more commonly associated with hyperthyroidism. Eventually, the thyroid can become too damaged to produce appropriate hormone levels resulting in irreversible hypothyroidism.
Early stage Hashimoto’s may present little to no symptoms. However, as the thyroid continues to be destroyed, symptoms can escalate. It is common for Hashimoto’s patients to alternate between hypothyroid and hyperthyroid states, causing symptoms of both, such as fatigue, anxiety and PMS. Goiters or swelling of the thyroid is also a common symptom. Because of the vague nature of the symptoms, Hashimoto’s is frequently misdiagnosed as depression, bipolar disorder, PMS, chronic fatigue syndrome, fibromyalgia or an anxiety disorder.
Common Diagnoses Typically Caused by Thyroid Disease
Infertility In both excess or deficiency, thyroid hormones can negatively impact fertility, but even slightly low levels that doctors call “normal” can dramatically impair fertility.
Depression Inadequate levels of thyroid hormones, T4 and T3, are commonly the culprit of poor mood and mental wellness. Supplementation with T3 is shown to be a better antidepressant than most antidepressant medications, even with so called “normal” levels.
Obesity—Low thyroid levels that go undetected are often associated with obesity.
Anxiety and Panic Disorders
Besides physical issues, those with hyperthyroidism or hypothyroidism often feel anxious or panicky.
Heart Disease—Hypothyroidism interacts with various substances that can contribute to heart disease.
Hyperthyroidism
Hyperthyroidism is on the opposite end of the spectrum regarding thyroid dysfunction. It is estimated that there are between 3 and 10 million individuals suffering from overactive thyroid or hyperthyroidism. Increased production of T3 and T4 results in accelerated metabolic function, which can cause a wide range of symptoms and the body to burn nutrients faster than it should. Hyperthyroidism frequently causes extreme fatigue, exhaustion, muscle weakness, anxiety and insomnia following states of high energy.
If left untreated hyperthyroidism can cause serious medical conditions including but not limited to congestive heart failure, atrial fibrillation, severe arrhythmia, and stroke. This in no way should be confused with high-dose thyroid supplementation. A suppressed TSH is not the definition of hyperthyroidism.
Graves’ Disease (Autoimmune Hyperthyroidism)
Graves’ Disease is the most common cause of hyperthyroidism. Graves’ Disease is an autoimmune condition involving increased production of thyrotropin receptor antibody (TRAb). This antibody latches on to thyroid receptors known as thyroid stimulating immunoglobulin (TSI). Once bound, the thyroid is stimulated to release additional T4 resulting in a surplus. Thyrotropin receptor antibody (TRAb) can mimic various pituitary hormones that further promote thyroid hormone production.
Thyroid Nodules and Goiter
Growths involving the thyroid can cause fluctuations in thyroid hormone levels resulting in various degrees of
dysfunction. Thyroid nodules are a common occurrence. Some studies show that approximately 30% of people will develop at least one nodule by the time they reach 50 years of age.
Nodules can be small growths, solid masses, or liquid-filled cysts. Fortunately, most nodules do not significantly affect your health. However, it is important to be aware of the various types of nodules and follow their growth.
There are four types of nodules: benign, malignant, suspicious, and inconclusive. Over 90 percent of nodules are benign and do not pose a serious threat. About 5 percent of thyroid nodules are expected to be cancerous or malignant. Such nodules are larger and expand at a faster rate than benign thyroid nodules. You may experience growth or expansion of the thyroid gland because of thyroid nodules, regardless of malignancy. It is important to monitor thyroid related growths. Even though nodules are frequently benign, there is the possibility of malignancy and development of thyroid cancer. It is possible to shrink nodules with proper thyroid replacement and other therapies.
Much like thyroid nodules, a goiter is a growth related to thyroid function. However, goiter specifically pertains to an increase in the thyroid's size. This can be an indicator of serious thyroid dysfunction and is generally associated with hypothyroidism, but can also indicate hyperthyroidism.
Checking for Nodules and Growths
To check for thyroid growths at home follow this simple step-by-step guide. This does not replace an exam by your physician.

Thyroid Cancer
Thyroid cancer involves the development of cancerous tissues of the thyroid gland itself. The most obvious symptom of thyroid cancer is a lump, nodule, growth, or swelling around the neck region. There are different types of thyroid cancer, each has its own unique attributes.
While most doctors recommend that any cancer be immediately removed, centers of excellence, such as Sloan Ketterling, are recommending a more watchful approach.
PapillaryCarcinoma—A slow-growing cancer that accounts for nearly 80% of all thyroid cancer cases. It begins in the follicular cells and can spread to the lymph nodes if left untreated. (Follicular cells create and secrete thyroid hormones and are in the thyroid gland).
FollicularCarcinoma—This strain of thyroid cancer makes up 10-15% of all cases and is less aggressive than papillary carcinoma. Follicular carcinoma is also central to follicular cells but will rarely spread to the lymph nodes. However, it is far more likely to spread to other organs. Those with low iodine intake are at greater risk of developing follicular carcinoma.
Medullary—Making up about 2% of thyroid cancer in the United States, medullary cancer develops from the parafollicular C cells. Unlike follicular cells, C cells produce calcitonin, not thyroid hormone. Medullary cancer can spread to the lymph nodes and other organs.
HurthleCell—A rare form of cancer that is usually classified with follicular thyroid cancer, although it is a distinct type of tumor. It makes up about 3% of all thyroid cancer cases. Unfortunately, people with Hashimoto’s can be wrongly diagnosed with Hurthle Cell cancer.
Anaplastic—The fastest growing form of thyroid cancer. It is also known as undifferentiated thyroid cancer because of the abnormal behavior of the cells involved. Anaplastic thyroid cancer occurs rarely, under 2% of cancer cases, and usually among individuals over the age of 60.
Awareness Leads to Wellness
With an understanding of many common thyroid conditions and how they impact your health, it is easy to see why it is important to protect and support thyroid function. However, it is not enough to simply be aware of the threat of thyroid disease. Recognizing symptoms and dysfunction is imperative to keep the thyroid functioning at its best.
Chapter 3:
Signs and Symptoms of Dysfunction
It is common for patients with a thyroid condition to be misdiagnosed as having generalized anxiety disorder (GAD), a panic disorder, depression, chronic fatigue syndrome (CFS), fibromyalgia, bipolar disease, or a sleep disorder. This can cause doctors to incorrectly diagnose the patient with a mental condition rather than a thyroid problem.
Even though many conditions share symptoms with thyroid disease the treatments are drastically different. Therefore, it is critical that you’re aware of the symptoms associated with thyroid disease and able to differentiate thyroid conditions and other forms of disease.

Signs and Symptoms of Thyroid Dysfunction
Both hypothyroidism and hyperthyroidism can sharesymptoms even though they are caused by imbalances at opposite ends of the spectrum. Furthermore, those with autoimmune disorders such as Graves’ Disease and Hashimoto’s
can present symptoms that fluctuate between overactive and underactive thyroid function.
Because of the many shared symptoms, similarities between diseases, and inconsistency of symptoms, a thyroid condition can be incredibly difficult to identify through symptoms alone. However, recognizing that symptoms are associated with any form of thyroid disease can lead to better response and treatment.
Thyroid disease has over 300 symptoms
associated with it all ranging from mild to severe, and even include other health
conditions like Type 2 Diabetes and Heart disease.
Women are seven times more likely than men to develop a thyroid condition. Therefore, women should be exceptionally attentive and vigilant regarding personal risk of developing a thyroid disorder.
Symptoms may also impact differentareas of the body with varying degrees of intensity. As you get older, the incidence of thyroid disease increases significantly.
The symptoms of aging share a striking similarity to thyroid dysfunction and many believe that poor thyroid function may be a pivotal component of why the body begins to slow down as it ages. Generic symptoms of thyroid dysfunction commonly attributed to aging include:
• Cognitive difficulties
• Depression
• Deteriorating daily ability to function
• Elevated cholesterol
• Heart disease
• Muscle and skeletal abnormalities
• Neuromuscular dysfunction
• Poor memory
• Inability to exercise
Hypothyroidism / Hashimoto's
• Cold hands or feet
• Cold intolerance
• Dry skin
• Muscle pain
• CFS
• Fibromyalgia
• Sluggishness
• Inability to handle stress
Hypothyroidism is caused by a decrease of thyroid hormone resulting in a sluggish metabolism. As the metabolism slows and thyroid hormones become less available the body can experience a wide range of symptoms including:
Thyroid 101
• Weight gain/obesity
• Difficulty losing weight
• Diabetes
• Fibromyalgia/Chronic Fatigue Syndrome
• Brittle Nails
• Chronic yeast infections
• Constipation
• Depression
• Difficulty concentrating
• Dry skin
• Extreme fatigue
• Goiter
• Hypoglycemia or low blood sugar
• Infertility
• Irregular Menstrual Cycles
• Low basal body temperature
• Low libido
• Muscle and joint pain or weakness
• Persistent headaches
• PMS
• Poor digestion
Symptoms of hypothyroidism usually unveil themselves gradually. Starting out, a minor reduction in thyroid levels can cause subtle symptoms that are frequently misconstrued as part of the aging process. However, as hypothyroidism progresses, symptoms begin increasing and becoming more noticeable.
Hyperthyroidism / Graves' Disease
Hyperthyroidism is the result of increased thyroid function. This causes the body to enter a state of acceleration and aggressive metabolization. Those with hyperthyroidism may suffer from the following symptoms:
• Sensitivity to cold Thyroid
• Anxiety and panic attacks
• Blood sugar imbalances
• Changes in vision including vision loss
• Difficulty concentrating
• Difficulty gaining weight or maintaining weight
• Erratic blood sugar levels
• Extreme muscle fatigue
• Great fluctuations in appetite
• Hair loss
• Heart palpitations
• High blood pressure
• Increased perspiration
• Insomnia
• Irregular menstrual periods or absent periods
• Irritability
• Persistent diarrhea
• Protruding eyes
• Shortness of breath
• Sudden weight loss
• Tremors
Those with hyperthyroidism frequently feel jittery and excitable for extended periods throughout the day. Ultimately, the individual crashes and suffers from long-lasting and intense fatigue, muscle pain, and weakness. Because hyperthyroidism accelerates the metabolism to such a significant degree, patients may find it difficult to maintain weight or acquire the nutrients necessary for a healthy diet.
Being Aware and Responsible with Thyroid Symptoms
It is important that individuals be aware of their thyroid function and listen to what their body is telling them. Because thyroid disease is specific to the individual, some may experience more or less symptoms than others and at varying degrees of intensity.
If you’re experiencing symptoms consistent with thyroid disease, even if they fluctuate in severity or occur sporadically it is best to get tested.
Chapter 4:
Thyroid Testing and Diagnosis
As discussed in the previous chapter, an important component of recognizing a thyroid condition is noticing the symptoms and properly attributing them to thyroid dysfunction. However, there is more to diagnosis than thyroid function blood tests. As with all things thyroid, there are multiple factors to consider regarding testing and diagnosis. A combination of symptoms, signs, blood tests, BMR and speed of relaxtion phase
Appropriate analysis of your thyroid health requires examination of multiple elements. Unfortunately, there is a significant lack of thorough diagnostic and examination in the medical community regarding thyroid health. In addition to standard tests, there are other, under-utilized nutrients and non-blood related thyroid tests that can better identify thyroid dysfunction. Being well-informed of the pitfalls of the current approach to diagnosis, the basics of thyroid testing, and the other indicators of thyroid disease can lead to better thyroid treatment.

Baseline of Proper Testing
Thyroid testing is generally composed of taking a sample of your blood and analyzing the prevalence of various thyroid-related hormones.
When ruling out thyroid disease, most doctors only check the TSH. If you are still suffering with thyroid related symptoms, it's best to speak with your doctor.
The Problems with Current Standard of Testing
The following areas are the bare minimum that should be tested when assessing thyroid function:
• TSH
• T4
• T3
• Reverse T3
• Thyroid Antibodies (TPO and TgAb)
• Sex hormone binding globulin (SHBG)
• Leptin Thyroflex BMR
Perhaps one of the greatest difficulties associated with thyroid disease is getting properly diagnosed. It is estimated that maybe up to 10 million cases of thyroid dysfunction go overlooked or undiagnosed every year. A significant contributor to this problem is the reliance on TSH testing.
TSH is only a measure of how well the body is communicating its thyroidal needs. It does not indicate if these needs are being met. TSH is an effective marker of pituitary levels of T3 but does not give good information regarding thyroid hormone levels throughout the rest of the body. Therefore, prominent factors of thyroid conditions such as poor conversion, reduced production, poor transport, and receptor resistance are completely overlooked when using TSH-only tests. Relying on TSH alone misses upwards of 80% of thyroid cases leaving many with poor thyroid function to suffer without an accurate diagnosis.
Another issue with current testing standards are inconsistencies among blood tests and testing facilities. Labs are often not up to date regarding testing ranges and may use different ranges depending on the institution. Therefore, the same patient may be diagnosed as having decreased, nominal, or increased levels simply based on the lab doing the test.
Testing ranges themselves are also a source of inaccuracy. Even if a patient has TSH levels within the established normal range they may experience thyroid-related symptoms such as fatigue, weight fluctuations, infertility, etc. The prescribed normal range in the medical community is a TSH between 0.5 and 4.5, but again, the TSH is a poor measure of the tissue thyroid levels. This suggests that if a patient’s levels shifted from a 4.0

17 Years Ahead: The Truth About Thyroid with Dr. Kent Holtorf
For more information on the inadequacy of thyroid testing, watch this Holtorf Medical Group Health Chat with Dr. Kent Holtorf.
to a 1.0 they would still be considered normal even though their thyroid function shifted significantly. A change of TSH to this degree can result in thyroid-related symptoms. But because the levels are still within “normal” range the patient will likely go without treatment. Additionally, the standard range does not remain constant and continues to grow. Testing ranges are based on population averages among sample groups. As thyroid conditions become more prevalent and extreme the median range continues to spread. The many issues of standard testing allow a multitude of patients to slip past diagnosis and suffer without treatment.
Necessary Nutrients to Test
There are many nutrients essential to proper thyroid function. Unfortunately, these areas are frequently ignored regarding testing and treatment. Without resolving deficiency of the following substances, you may not be able to resolve thyroid dysfunction. Therefore, it is important to test the following factors when assessing thyroid function:
Vitamin D Allows thyroid hormones to enter and interact with cells. Vitamin D deficiency can inhibit thyroid hormone function resulting in dysfunction. Optimal levels of vitamin D should be in the 70-100 ng/ml range.
Magnesium—Needed for the creation of T4. Inadequate magnesium levels can cause many of the enzymes needed for T4 synthesis to malfunction. The result is poor T4 production. Magnesium is also used in the conversion of T4 to T3.
Thyroid 101
Magnesium Needed for the creation of T4. Inadequate magnesium levels can cause many of the enzymes needed for T4 synthesis to malfunction. The result is poor T4 production. Magnesium is also used in the conversion of T4 to T3.
Selenium Critical component of thyroid hormone synthesis and functionality. It is associated with the conversion of T4 to T3, safeguarding against excess iodine, and combats heavy metal toxicity. Adults should acquire approximately 55mg of selenium per day as recommended by the US Office of Dietary Supplements.
Iron A necessary substance, along with selenium, zinc, and iodine, for the synthesis, conversion, and metabolization of thyroid hormones. Iodine, one of the key elements in the creation of thyroid hormones, cannot properly function without adequate iron in the system
Iodine A critical element for multiple systems including the liver, adrenals, and thyroid. If the body has the iodine required, it is converted into iodide, which is eventually used in the creation of hormones. If iodine is excessively high or troublingly low, you may develop hypothyroidism or hyperthyroidism respectively. Testing iodine levels can be done through a simple urine test.
Nutrient Deficiency Symptoms
Thesymptomsofvitaminandnutrientdeficienciescanmimicotherconditions, makingthemhardtodetect.
Makesuretodiscussnutrienttestingwithyourphysicianifyouexperienceanyof thesymptoms!
Non-Blood Thyroid Tests
In some cases, an ultrasound may be recommended or used to assess physical characteristics of your thyroid. A clinical exam may also be administered to test for physical signs of dysfunction such as lumps or enlargement. Additional tests may be run to further assess functionality.
Basal Metabolic Rate – Allows you to accurately assess how well the thyroid is working. Metabolic rate can be gauged by measuring the amount of oxygen used in the metabolic
Thyroid 101
process. An abnormally low BMR is indicative of hypothyroidism whereas a high BMR may suggest hyperthyroidism. This is the gold standard for testing the metabolism and overall thyroid function.
Thyroflex – A non-invasive method of assessing thyroid function. This test is done by measuring the speed of the relaxation phase of a tendon reflex. The thyroid can impact reflexivity and cause delayed or heightened reflexes depending on the prevalence of thyroid hormone. By measuring this relaxation speed, you can acquire an accurate assessment of intracellular T3 as opposed to just serum levels. This method was shown by the prestigious British Medical Journal to be more sensitive than blood work.
Getting all the Data
Acquiring a comprehensive examination of your thyroid including the many important hormones, nutrients, and non-blood related elements discussed in this chapter is the best way of assessing your thyroid health. Reliance on TSH as the sole method for gauging thyroid functionality is a dangerous practice. By examining the many factors that influence the thyroid, you can acquire an accurate assessment of your thyroid wellness. Equipping yourself with this information allows for the creation of a plan to maintain or achieve greater wellness through proper treatment. Thyroid
Chapter 5:
Treatment
Treatment of a thyroid condition requires a deep understanding of how hormones function and interact with the body. Perhaps the most important aspect of thyroid treatment is knowing that each patient has unique needs and will require an individualized approach.
Even though it goes against popular belief, standard treatment for thyroid disease (giving T4 replacement to normalize the TSH) is inadequate for the majority of people If treatment is correct, patients may feel improvement immediately. Others may take longer to feel better as they progress towards effective medication. Understanding the strengths and weaknesses of the many treatment options available allows you to progress further towards optimal thyroid function.

Synthetic T4
Levothyroxine, Synthroid, and Levoxyl are the go-to treatments for hypothyroidism. These synthetic forms of T4 are administered to patients in the hopes that their levels will normalize.
Unfortunately, this is based on an assumption that the body will correctly convert T4 into T3. If T4 remains unconverted or is over-converted into reverse T3, their health will not improve. Most practitioners focus on getting TSH and/or T4 levels to an acceptable range as opposed to ensuring the body is producing the T3 it needs to function correctly. This can result in patients continuing to experience symptoms even though they are being treated. Some patients may garner some benefits from T4-only formulations, but optimizing your thyroid is far more likely with a customized treatment plan.
Troubles with T4-Only Treatments
Even though T4 has become the standard for treating thyroid disease it may not be the best method. Multiple studies have shown that T4-only formulations are not effective for optimizing or resolving thyroid disease. A 1995 study published in the JournalofClinical Investigationfound that reaching optimal levels of TSH and T4 using only T4 formulations did not provide necessary T3 tissue levels. This resulted in the pituitary exemplifying proper TSH and T4 levels but nearly all other tissues were deficient. It was also found that patients who over convert T4 to RT3 experienced worsening of their symptoms with the use of T4 medications. Subverting conversion issues by medicating with T3 may provide better results.
T3 Formulations
T3 formulations such as Cytomel, are underutilized methods of treating thyroid disease. Patients suffering from RT3 issues, causing poor thyroid function even if the patient presents normal levels of T4 and TSH, can benefit greatly from preparations containing T3. Providing the body with appropriate amounts of T3 can reduce the need for additional T4 Thyroid function of those who over convert T4 to RT3 can experience worsening of their condition with T4-only treatments.
Cytomel (liothyronine sodium) is a synthetic formulation of thyroid hormones. This medication acts significantly quicker than Levothyroxine and other T4 medications because the T3 provided by Cytomel does not Thyroid 101
Taking Medication Properly
To ensure you’re taking your thyroid medication properly, follow these 5 simple steps.

need to be converted and can quickly influence metabolic function throughout the body.
Natural Desiccated Thyroid
Unlike synthetic formulations, Natural Desiccated Thyroid (NDT) drugs are a prescription hormone treatment derived from natural sources. These formulations are frequently created from the dried thyroid gland of pigs or cows (NDT is exclusively from pigs in the United States). NDT is also known as natural thyroid, porcine thyroid, or thyroid extract. There are multiple brands of NDT including Nature-throid, Thyroid WP, Armour, and Acella
Unfortunately, there is a common misconception propagated in the medical community that NDT is not a valid method of treatment. However, NDT is regulated by the FDA and undergoes a rigorous quality assurance test making these medications as consistent as other thyroid treatments. Furthermore, many patients benefit greatly by switching from synthetic forms of thyroid hormone to natural formulations.
Part of the reason NDT works better than synthetics for some individuals is that it more closely resembles human thyroid hormones. NDT is also highly customizable allowing for unique formulations of T4, T3, T2, T1 and other thyroid hormones and nutrients to be easily incorporated into the same treatment. As with all thyroid treatments, the efficacy of the approach is reliant on how well it is optimized for the unique needs of the patient.
Compounded Medications
Many patients benefit from a combination of T4 and T3 formulations. Acquiring a quality compound can also eliminate the inclusion of potential thyroid-inhibiting substances such as lactose and gluten, which are common in many medications. Physicians have the ability to customize the levels of T3 and T4 contained in their prescribed medication because it’s being tailor-made by pharmacists. This allows patients to acquire the specific quantities of hormones needed for their unique situation. Patients who have not done well using T4-only formulations or NDT frequently benefit from a specified compound treatment.
Moving Forward into Wellness
The many different brands, formulations, and interactions of thyroid treatments may seem overwhelming. Having a basic introduction to the world of thyroid treatment provides a framework that can be built upon while moving towards better health. Fortunately, there are trained professionals available who are willing to provide guidance through the complex world of thyroid health and treatment
Thyroid 101
Finding a Thyroid Doctor
Finding a doctor who is truly knowledgeable of the thyroid can be challenging. With the prevalence of misinformation and a poor standard of testing and treatment, it is commonplace for patients to receive sub optimal treatment.
Unfortunately, those with thyroid dysfunction or diseases that are harder to diagnose such as Hashimoto’s, Graves’ disease, and sub-laboratory hypothyroidism, will likely receive inadequate treatment unless they are under the care of a thyroid-literate doctor.

Importance of a Knowledgeable Physician
Ideally, you find a specialist who is well acquainted with all things thyroid, hormonal, and metabolic. Generally, those with a thyroid condition are recommended to an endocrinologist to benefit from their expertise in these areas. Unfortunately, endocrinologists are in high demand and even if a patient is able to meet with one regularly, there is a chance that they are underequipped.
Sadly, there is a severe lack of knowledge among medical practitioners regarding the thyroid. Part of the reason for this is that they are unable to stay up to date by reading current medical research. There are multiple reasons why doctors may be unable to maintain current knowledge and practices. Due to the high demand on their time, most physicians rely on their medical school training, which may be out of date depending on how many years they have practiced, and biased pharmaceutical sales representatives This has resulted in many doctors
practicing with outdated, inaccurate or skewed information. Because there is a severe lack of thyroid literacy, identifying a doctor who is well versed in the thyroid has become an important skill.
Finding the Right Doctor
After reading this e-book, you are equipped with much of the information needed to assess a doctor’s proficiency in treating thyroid conditions. Utilizing this information to ask important thyroid-related questions to a prospective practitioner is a good way to gauge ability and see if your specific thyroid needs will be addressed.
The following questions can help you assess a physician’s ability to effectively treat the thyroid:
• What thyroid tests do you typically run? Do you use other, non-blood thyroid tests? (The answer should include more than just TSH. Ideally it will reflect the many tests discussed in chapter 4, including free T3, free T4, reverse T3. SHBG, thyroflex and BMR.)
• What treatments do you use? (Their response should include more than T4 only medications such as Levothyroxine and Synthroid. It is best to hear that they are open to multiple treatment options as noted in chapter 5.)
• Do you gauge health based solely on blood tests or by resolution of symptoms? (If a doctor is not receptive to a patient’s concerns and symptoms while instead relying solely on blood tests, they are likely not equipped to optimally treat thyroid dysfunction.)
• Are you willing to discuss or read research I have acquired from online sources? (Even though not all online material is reliable, there is a wealth of good thyroid information and research available online. If your doctor is unwilling to glance at or discuss research and information you have found online, they may be unwilling to implement the most recent and verified approaches to thyroid health. Also avoid doctors that are unable to justify and defend their treatment recommendations.)
These questions can help identify good thyroid doctors. However, many people have difficulty starting their search.
Holtorf Medical Group Locations
Los Angeles, CA (310) 375-2705
2232 E. Maple Ave. El Segundo, CA 90245
Atlanta, GA (678) 494-7800
3750 Palladian Village Drive Suite
300 Marietta, GA 30066
Telemedicine visits also available.
The Holtorf Approach
It may seem daunting trying to find a new physician while ensuring they incorporate the many practices and information discussed in this e-book. Fortunately, the Holtorf Medical Group specializes in the thyroid and provides numerous resources that can help you achieve greater thyroid wellness, and is able to do worldwide telemedicine consultation. The Holtorf Medical Group prides itself on offering comprehensive testing composed of Free T4, Free T3, Reverse T3, SHGB, Leptin, computer-assisted measuring of your tissue thyroid levels, and BMR assessment. In addition to testing, the doctors at Holtorf Medical Group recognize that patient symptoms are important indicators of wellness and they should not be ignored. They believe that optimization means the patient feels their best, not that their test results remain within vaguely defined ranges.
Treatment through the Holtorf Medical Group provides custom crafted and individualized thyroid hormone formulations. This includes T4, T3, combination T4/T3, time released T3 (of the optimal dose), and an array of nutritional support and supplementation. Their strong understanding of the thyroid allows them to craft a treatment approach that perfectly suits each patient and their unique thyroidal needs. There are two Holtorf locations within the United States that provide high quality and individualized care, as well as telemedicine visits available to those unable to travel to either locations.
If none of these locations are geographically feasible, you can still benefit from the depth of knowledge and expertise found at the Holtorf Medical Group through a virtual appointment. Additionally, the thriving community at Holtorfmed.com and NAHypothyroidism.org offers regular updates on relevant topics, educational material, and opportunities to interact with specialists.
Gaining greater thyroid awareness and comprehension makes it easier to find a knowledgeable thyroid expert. Utilizing the resources provided by Holtorf Medical Group allows you to achieve greater thyroid health by locating the best thyroid practitioner for your unique health goals.
Conclusion
By completing Thyroid 101, you now have the tools needed to support thyroid wellness.
Understanding thyroid function, identifying signs and symptoms of dysfunction, and knowing the methods required for appropriate diagnosis and testing helps support thyroid function and balance. The importance of appropriately treating individual thyroid needs through optimal and customized treatment can be seen in the far-reaching impact of the thyroid. Because this powerful gland supports nearly every aspect of health, finding qualified and knowledgeable support is critical. The many resources provided in Thyroid101and the exceptional services offered by the Holtorf Medical Group gives you the support needed to achieve greater thyroid function and wellness.
Resources
1.Kent Holtorf, MD. "Understanding Local Control of Thyroid Hormones: (Deiodinases Function and Activity)." National Academy of Hypothyroidism and Integrative Sciences.
2.Kent Holtorf, MD. "Thyroid Hormone Transport." National Academy of Hypothyroidism and Integrative Sciences.
3.Kent Holtorf, MD. "Diagnosis of Hypothyroidism: Are we getting what we want from TSH testing?" National Academy of Hypothyroidism and Integrative Sciences.
4.Kent Holtorf, MD. "Why Doesn’t My Endocrinologist Know All of This?" National Academy of Hypothyroidism and Integrative Sciences.
5.Kent Holtorf. "Thyroid Hormone Transport into Cellular Tissue." Journal of Restorative Medicine. 2014; 3: 53-68.
6.Rakel, D. Integrative Medicine, 3rd Ed. Philadelphia, Pa: Elsevier Saunders; 2012: 312-20.
7.Meier C, Trittibach P, Guglielmetti M, Staub JJ, Muller B. "Serum TSH in assessment of severity of tissue hypothyroidism in patients with overt primary thyroid failure: cross sectional survey." The British Medical Journal 326:311-2.
8.Schwartz E, Morelli V, Holtorf K "Hormone Replacement Therapy in the Geriatric Patient: Current State of the Evidence and Questions for the Future— Estrogen, Progesterone, Testosterone, and Thyroid Hormone Augmentation in Geriatric Clinical Practice: Part 2." Clin Geriatr Med 27 (2011) 561–575.
9.Escobar-Morreale HF et al. "Only the combined treatment with thyroxine and triiodothyronine ensures euthyroidism in all tissues of the thyroidectomized rat." Endocrinology, 31 May 1996, 137(6):2490-2502.
10.Escobar-Morreale HF et al. "Replacement therapy for hypothyroidism with thyroxine alone does not ensure euthyroidism in all tissues, as studied in thyroidectomized rats." J Clin Invest. 1995 Dec; 96(6): 2828–2838.
11.Fraser, W D et al. “Are biochemical tests of thyroid function of any value in monitoring patients receiving thyroxine replacement?.” British medical journal (Clinical research ed.) vol. 293,6550 (1986): 808-10.
12.Chopra, I J. “A study of extrathyroidal conversion of thyroxine (T4) to 3,3',5triiodothyronine (T3) in vitro.” Endocrinology vol. 101,2 (1977): 453-63.
13.Kent Holtorf. "Peripheral Thyroid Hormone Conversion and Its Impact on TSH and Metabolic Activity." Journal of Restorative Medicine 2014; 3: page 30.
14.Knudsen, Nils et al. “Small differences in thyroid function may be important for body mass index and the occurrence of obesity in the population.” The Journal of clinical endocrinology and metabolism vol. 90,7 (2005): 4019-24.
15.Kent Holtorf, MD. "Fatigued, depressed, difficulty losing weight?" Holtorf Medical Group.
16.Kent Holtorf, MD. "Endocrinological Assessment and Treatment of Weight Gain & Obesity." Holtorf Medical Group.
17.Kok, Petra et al. “High circulating thyrotropin levels in obese women are reduced after body weight loss induced by caloric restriction.” The Journal of clinical endocrinology and metabolism vol. 90,8 (2005): 4659-63.
18.van den Beld, Annewieke W et al. “Thyroid hormone concentrations, disease, physical function, and mortality in elderly men.” The Journal of clinical endocrinology and metabolism vol. 90,12 (2005): 6403-9.

