Vol. 96; n. 1, March 2024
ORIGINAL PAPERS
12132 Ductal prostate cancer staging: Role of PSMA PET/CT
Pietro Pepe, Ludovica Pepe, Mara Curduman, Michele Pennisi, Filippo Fraggetta 12104 Revolutionizing localized prostate cancer treatment: Stereotactic radiotherapy “Moroccan experience”
Asmâ a Naim, Zineb Lahlou, Othmane Kaanouch, Abdelajalil Heddat, Safae Mansouri
12244 Patter ns of treatment of high-risk BCG-unresponsive non-muscle invasive bladder cancer (NMIBC) patients among Arab urologists
Mohamad Moussa, Mohamad Abou Chakra, Neal D Shore, Athanasios Papatsoris, Yasser Farahat, Michael A O’Donnell
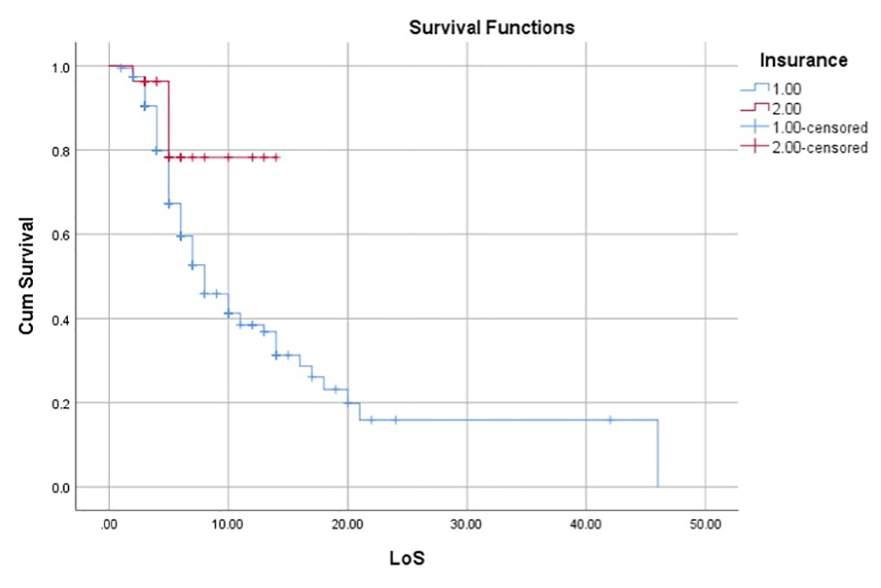
12305 The relationship between income, health insurance, and employment status as prognostic indicators of bladder cancer : A sur vival analysis
Wahjoe Djatisoesanto, Yufi Aulia Azmi, Ida Bagus Gde Tirta Yoga Yatindra
12179 Quality of bladder cancer treatment infor mation on YouTube: May the user’s profile affect the quality of results?
Pier Paolo Prontera, Francesca Romana Prusciano, Marco Lattarulo, Emanuele Utano, Francesco Schiralli, Carmine Sciorio, Lorenzo Romano, Francesco Saverio Grossi
12228 Endoscopic enucleation of the prostate with Thulium F iber Laser (ThuFLEP). A retrospective single-center study
Angelis Peteinaris, Vasileios Tatanis, Paraskevi Katsakiori, Theodoros Spinos, Solon Faitatziadis, Kristiana Gkeka, Anastasios Natsos, Theofanis Vrettos, Evangelos Liatsikos, Panagiotis Kallidonis
12181 Clinical characteristics of adult cases with urolithiasis from Turkey: A regional epidemiological study
Mehmet Ezer, Rasim Guzel, Mehmet Uslu, Selc ̧ uk Guven, Kemal Sarica
12022 Occupational hazard in urolithiasis patients in Qatar : A single-center cross-sectional study
Kamran Hassan Bhatti, Rawa Bapir, Nadeem Sohail, Faaz Salah Gomha, Ahmed H A Shaat, Aftab Ahmed Channa, Khalid Mohammed Abdelrahman, Bryar Othman Muhammed, Nali H Hama, Fahmi H Kakamad, Berun A Abdalla, Jihad Ibrahim Hama, Hiwa O Abdullah
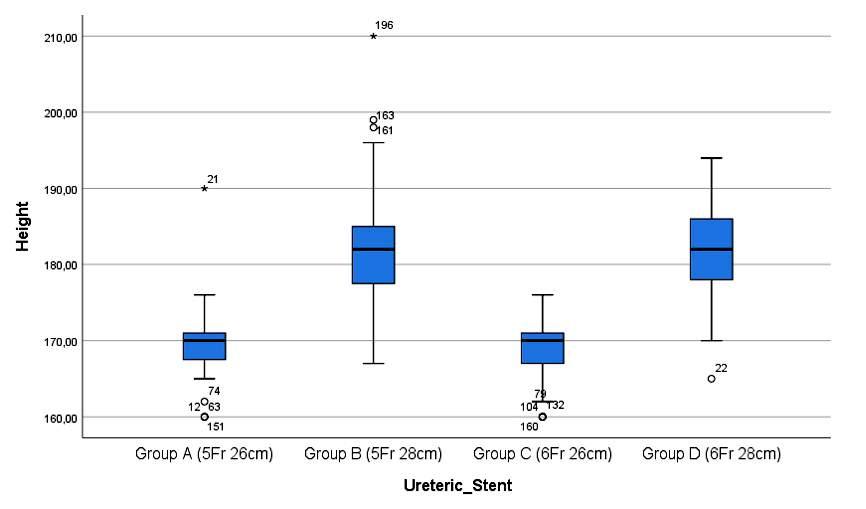
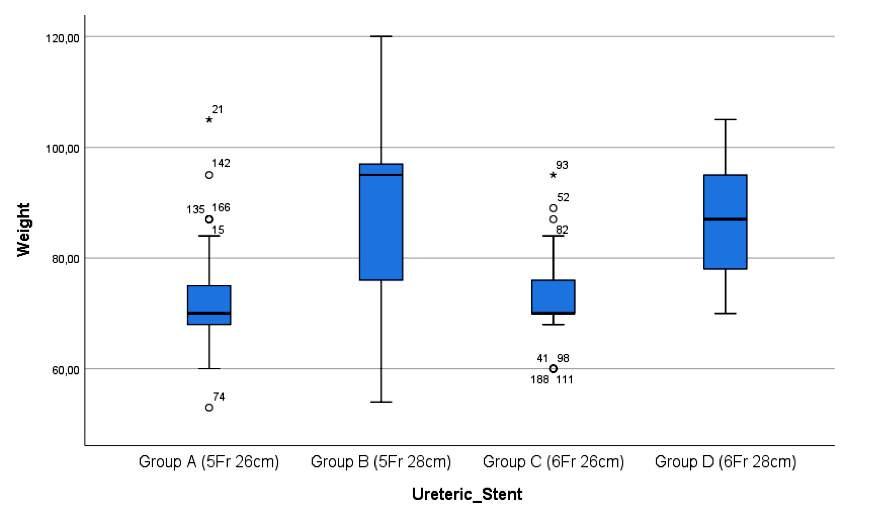
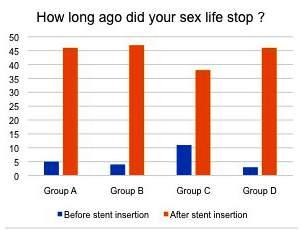
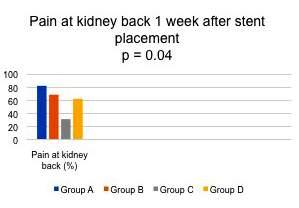
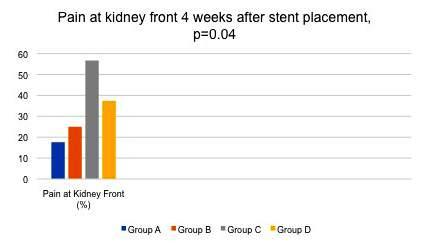
12231 Ureteral stent related symptoms: A comparative study
Themistoklis Ch Bellos, Ioannis S Manolitsis, Stamatios N Katsimperis, Panagiotis A Angelopoulos, Sotirios G Kapsalos-Dedes, Panagiotis K Deligiannis, Lazaros I Tzelves, Nikolaos A Kostakopoulos, Iraklis C Mitsogiannis, Ioannis M Varkarakis, Athanasios G Papatsoris, Andreas A Skolarikos, Charalampos N Deliveliotis
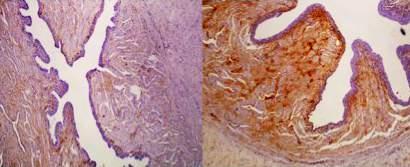
12248 Minimal invasive treatment of urethral strictures: An experimental study of the effect of Paclitaxel coated balloons in the wall of strictured rabbit’s urethra Konstantinos Pagonis, Angelis Peteinaris, Constantinos Adamou, Vasileios Tatanis, Athanasios Vagionis, Anastasios Natsos, Mohammed Obaidat, Solon Faitatziadis, Evangelos Liatsikos, Panagiotis Kallidonis
12214 Eighteen years of experience in laparoscopic implantation of ar tificial urinar y sphincter in women with intrinsic sphincter deficiency
Débora Araújo, Pierre-Emmanuel Bryckaert, Miguel Miranda, Vasco Rodrigues, Nicolas de Saint Aubert, Johann Menard, Eric Mandron
12082 Microsurgical varicocelectomy efficacy in treatment of men with primar y and secondar y infer tility (retrospective study)
Shomarufov Azizbek
12186 Examination of ejaculate fr uctose levels on male infer tility patients at various times and centrifugation using semiautomatic method
Hermansyah Hermansyah, Muhammad Fadhli Abdullah, Cennikon Pakpahan, Reny I’tishom, Supardi Supardi, Ilhamsyah Ilhamsyah
12285 Evaluation of human bone mar row mesenchymal stem cells in the treatment of non obstr uctive azoosper mia
Mohamed A Alhefnawy, Gamal Elmorsy, Sayed Bakry, Hesham El-amrosy, Ibrahim Mearaj, Ebrahim A Sabra, Osama M Badr, Dalia Ibraheem, Taymour Khalifa
12246 Cellular senescence in testicular cancer Is there a cor relation with the preoperative markers and the extent of the tumor? An experimental study
Vasileios Tatanis, Dimitris Veroutis, Pavlos Pantelis, George Theocharous, Helen Sarlanis, Alexandros Georgiou, Angelis Peteinaris, Anastasios Natsos, Napoleon Moulavasilis, Nikolaos Kavantzas, Athanassios Kotsinas, Ioannis Adamakis


continued on page III
ISSN 1124-3562
Lauretana: l’acqua più leggera d’Europa

Il 60% del peso corporeo di un individuo adulto è rappresentato dall’acqua. Il fabbisogno idrico di un soggetto sano è di circa 2000-2500 ml/die. L’equilibrio del contenuto in acqua, necessario per il corretto svolgimento delle funzioni metaboliche, viene raggiunto grazie agli apporti e le perdite.
Le acque minerali, in base al contenuto totale di Sali in milligrammi dopo l’evaporazione di 1 litro di acqua minerale essiccata a 180°C (residui secchi), possono essere classificate come (1,2):
• Acque minimamente mineralizzate: il residuo fisso è inferiore a 50 mg/l.
• Acque oligominerali (o leggermente mineralizzate): il residuo fisso è compreso tra 50 e 500 mg/l.
• Acque minerali: il residuo fisso è compreso tra 500 e 1500 mg/l.
• Acque ricche di sali minerali: il residuo fisso è superiore a 1500 mg/l.
Quanto più un’acqua ha valori di durezza bassi, tanto più viene definita “dolce” ed è da preferire alle acque “dure” che sono controindicate in parecchie patologie mediche (es. calcolosi renale ed epatica).
Le analisi chimico-fisiche condotte presso il Dipartimento di Biotecnologie Molecolari e Scienze per la Salute (Università di Torino) hanno evidenziato che l’acqua minerale Lauretana delle Prealpi Biellesi è leggerissima, con poco sodio e un pH leggermente acido, quindi ideale per la depurazione dalle tossine e la digeribilità.
Autorevoli testimonianze indicano che l’acqua minerale Lauretana è clinicamente utilizzata nelle seguenti indicazioni:
• Diete per calo ponderale (3);
• Stimolo della diuresi (3);
• Diete per atleti (3)
• Panniculopatia edemato fibro sclerotica (cellulite) (3);
• Depurazione dai residui azotati (urea, ammonio, acido urico) (4);
• Omeostasi metabolica nell’atleta di endurance (5);
• Prevrenzione della calcolosi urinaria e delle sue recidive (6);
• Diete povere di sodio (7);
• Idratazione tessuti e termoregolazione (8)
Letture
1. Petraccia L, Liberati G, Masciullo SG, Grassi M, Fraioli A. Water, mineral waters and health. Clin Nutr. 2006 Jun;25(3):377-85.
2. Decreto Legislativo numero 105 del 25 gennaio 1992.
3. Prof. Dott. Antonio Paoli. Docente corso di Laurea in Scienze Motorie Facoltà di Medicina e Chirurgia - Università di Padova
4. Prof. Dott.Franco Fraschini Rettore Dipartimento di Farmacologia Università degli Studi di Milano Prof. Dott. Roberto Dall’Aglio Dipartimento di Farmacologia Università degli Studi di Milano
5. Dott. Luigi Simonetto Presidente Commissione Tutela della Salute Federazione Ciclistica Italiana
6. Dott. Marco Laudi Direttore U.O. di Urologia Ospedale Mauriziano Umberto I Torino
7. Prof. Dott. Giancarlo Levra Scuola di specializzazione in Idrologia Medica -Università degli Studi di Pisa
8. Dott. Marco Neri
Nutrizionista, Comitato Scientifico FIF
INFORMAZIONE SCIENTIFICA


EDITORIALBOARD
EDITORINCHIEF
Alberto Trinchieri (Milan, Italy)
ASSOCIATEEDITORS Emanuele Montanari, Department of Urology, IRCCS Foundation Ca’ Granda Ospedale Maggiore Policlinico, University of Milan, Italy – Gianpaolo Perletti, Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy; Department of Human Structure and Repair, Ghent University, Ghent, Belgium - Angelo Porreca, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy
EXECUTIVEEDITORIALBOARD
Alessandro Antonelli, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Antonio Celia, Department of Urology, San Bassiano Hospital, Bassano del Grappa, Italy - Luca Cindolo, Department of Urology, Villa Stuart Hospital, Rome, Italy - Andrea Minervini, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Bernardo Rocco, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Riccardo Schiavina, Department of Urology, University of Bologna, Bologna, Italy
ADVISORYEDITORIALBOARD Pier Francesco Bassi, Urology Unit, A Gemelli Hospital, Catholic University of Rome, Italy – Francesca Boccafoschi, Health Sciences Department, University of Piemonte Orientale in Novara, Italy – Alberto Bossi, Department of Radiotherapy, Gustave Roussy Institute, Villejuif, France –Tommaso Cai, S Chiara Hospital, Trento, Italy –Paolo Caione, Department of Nephrology-Urology, Bambino Gesù Pediatric Hospital, Rome, Italy – Luca Carmignani, Urology Unit, San Donato Hospital, Milan, Italy –Liang Cheng, Department of Urology, Indiana University School of Medicine, Indianapolis, IN; Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, Indianapolis, IN – Giovanni Colpi, Retired Andrologist, Milan, Italy – Giovanni Corona, Department of Urology, University of Florence, Careggi Hospital, Florence, Italy – Antonella Giannantoni, Department of Surgical and Biomedical Sciences, University of Perugia, Italy – Paolo Gontero, Department of Surgical Sciences, Molinette Hospital, Turin, Italy – Steven Joniau, Organ Systems, Department of Development and Regeneration, KU Leuven, Belgium – Frank Keeley, Bristol Urological Institute, Southmead Hospital, Bristol UK – Laurence Klotz, Division of Urology, Department of Surgery, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Ontario, Canada – Börje Ljungberg, Urology and Andrology Unit, Department of Surgical and Perioperative Sciences, Umeå University, Umeå, Sweden –Nicola Mondaini, Uro-Andrology Unit, Santa Maria Annunziata Hospital, Florence, Italy – Gordon Muir, Department of Urology, King's College Hospital, London, UK –Giovanni Muto, Urology Unit, Bio-Medical Campus University, Turin, Italy – Anup Patel, Department of Urology, St Mary's Hospital, Imperial Healthcare NHS Trust, London, UK – Glenn Preminger, Division of Urologic Surgery, Duke University Medical Center, Durham, NC, USA – David Ralph, St. Peter's Andrology Centre and Institute of Urology, London, UK – Allen Rodgers, Department of Chemistry, University of Cape Town, Cape Town, South Africa – Francisco Sampaio, Urogenital Research Unit, State University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil – Kemal Sarica, Department of Urology, Kafkas University Medical School, Kars, Turkey – Luigi Schips, Department of Urology, San Pio da Pietrelcina Hospital, Vasto, Italy – Hartwig Schwaibold, Bristol Urological Institute, Southmead Hospital, Bristol, UK – Alchiede Simonato, Department of Urology, University of Verona, Azienda Ospedaliera Universitaria Integrata, Verona, Italy – Carlo Terrone, Department of Urology, IRCCS S Martino University Hospital, Genova, Italy – Anthony Timoney, Bristol Urological Institute, Southmead Hospital, Bristol, UK – Andrea Tubaro, Urology Unit, Sant’Andrea Hospital, “La Sapienza” University, Rome, Italy – Richard Zigeuner, Department of Urology, Medical University of Graz, Graz, Austria
BOARDOFREVIEWERS Maida Bada, Department of Urology, S Pio da Pietrelcina Hospital, ASL 2 Abruzzo, Vasto, Italy - Lorenzo Bianchi, Department of Urology, University of Bologna, Bologna, Italy - Mariangela Cerruto, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Francesco Chessa, Department of Urology, University of Bologna, Bologna, Italy - Daniele D’Agostino, Robotic Urology and Mini In-
vasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy - Fabrizio Di Maida, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Antonio Galfano, Urology Unit, Niguarda Hospital, Milan, Italy - Michele Marchioni, Department of Medical, Oral and Biotechnological Sciences, "G. d'Annunzio" University of Chieti, Laboratory of Biostatistics, Chieti, Italy - Andrea Mari, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Luigi Napolitano, Unit of Urology, Department of Neurosciences, Reproductive Sciences, and Odontostomatology University of Naples “Federico II”, Naples, Italy - Antonio Porcaro, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Stefano Puliatti, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Daniele Romagnoli, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy - Chiara Sighinolf, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Tommaso Silvestri, Urology Clinic, Department of Medical, Surgical and Health Science, University of Trieste, Trieste, Italy - Petros Sountoulides, Aristotle University of Thessaloniki, Department of Urology, Thessaloniki, Greece - Alessandro Tafuri, Department of Urology, Vito Fazzi Hospital, Lecce, Italy
SIEUNEDITOR
Pasquale Martino, Department of Emergency and Organ Transplantation-Urology I, University Aldo Moro, Bari, Italy
SIEUNEDITORIALBOARD
Emanuele Belgrano, Department of Urology, Trieste University Hospital, Trieste, ItalyFrancesco Micali, Department of Urology, Tor Vergata University Hospital, Rome, ItalyMassimo Porena, Urology Unit, Perugia Hospital, Perugia, Italy – Francesco Paolo Selvaggi, Department of Urology, University of Bari, Italy – Carlo Trombetta, Urology Clinic, Cattinara Hospital, Trieste, Italy – Giuseppe Vespasiani, Department of Urology, Tor Vergata University Hospital, Rome, Italy – Guido Virgili, Department of Urology, Tor Vergata University Hospital, Rome, Italy
UrOPEDITOR
Carmelo Boccafoschi, Department of Urology, Città di Alessandria Clinic, Alessandria, Italy
UrOPEDITORIALBOARD
Renzo Colombo, Department of Urology, San Raffaele Hospital, Milan, Italy – Roberto Giulianelli, Department of Urology, New Villa Claudia, Rome, Italy – Massimo Lazzeri, Department of Urology, Humanitas Research Hospital, Rozzano (Milano), Italy – Angelo Porreca, Department of Urology, Polyclinic Abano Terme, Abano Terme (Padova), Italy –Marcello Scarcia, Department of Urology, "Francesco Miulli" Regional General Hospital, Acquaviva delle Fonti (Bari), Italy – Nazareno Suardi, Department of Urology, San Raffaele Turro, Milano, Italy
GUNEDITOR
Arrigo Francesco Giuseppe Cicero, Medical and Surgical Sciences Department, Sant’Orsola-Malpighi University Hospital, Bologna, Italy
GUNEDITORIALBOARD
Gianmaria Busetto, Department of Urology, Sapienza University of Rome, Italy –Tommaso Cai, Department of Urology, Santa Chiara Regional Hospital, Trento, Italy –Elisabetta Costantini, Andrology and Urogynecological Clinic, Santa Maria Hospital of Terni, University of Perugia, Terni, Italy – Angelo Antonio Izzo, Department of Pharmacy, University of Naples, Italy – Vittorio Magri, ASST Nord Milano, Milano, Italy – Salvatore Micali, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy – Gianni Paulis, Andrology Center, Villa Benedetta Clinic, Rome, Italy – Francesco Saverio Robustelli della Cuna, University of Pavia, Italy – Giorgio Ivan Russo, Urology Department, University of Catania, Italy – Konstantinos Stamatiou, Urology Department, Tzaneio Hospital, Piraeus, Greece – Annabella Vitalone, Department of Physiology and Pharmacology, Sapienza University of Rome, Rome, Italy
O f f i c i a lJ o u r n a lo f S I E U N ,U r O P ,S S C Ua n dG U N
Un’opera completa sul microbiota, il complesso consorzio di omalattia. Centinaia di illustrazioni a colori, contenuti multimediali, aggiornati in progress continuo ed accessibili mediante QR code. Un Trattato imprescindibile per chi si occupa di salute interpretando i referti sul microbiota.
Costo di copertina €120,00, IVA e spese di spedizione incluse. Per informazioni ed eventuali ordini, scrivere a: info@edizioniscriptamanent.eu
ORIGINAL PAPERS
12452 Psychological and sexological assessment of patients with chronic prostatitis
Konstantinos Stamatiou, Vittorio Magri, Margherita Trinchieri, Alberto Trinchieri, Gianpaolo Perletti on behalf of Mediterranean study group for prostatitis and prostatic diseases
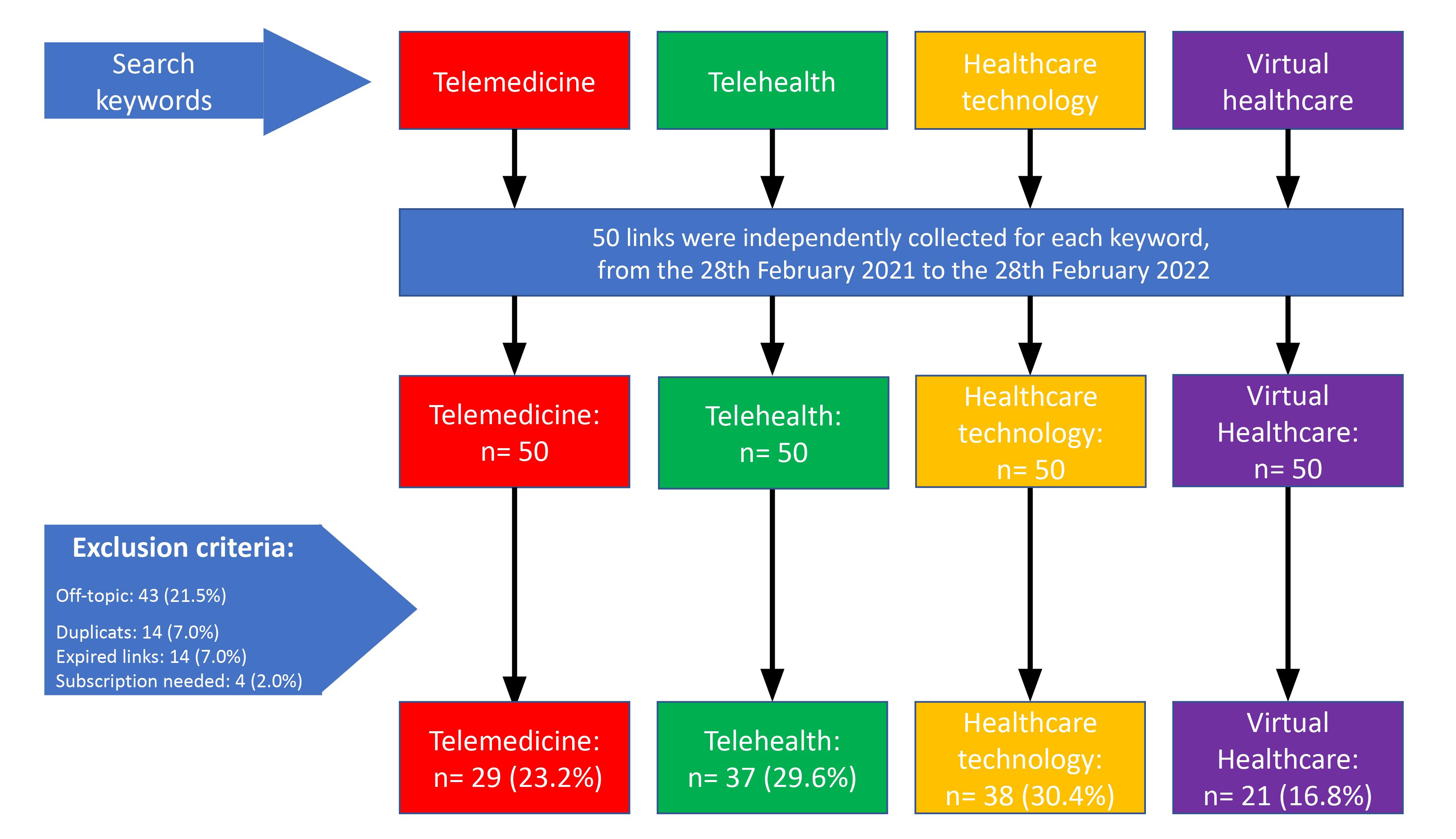
11206 Telemedicine and social media: A contemporar y analysis of the most shared content by inter net users
Vincenzo Mirone, Francesco Di Bello, Simone Morra, Gianluigi Califano, Luigi Cirillo, Marco Abate, Giovanni Maria Fusco, Stefano Luzzago, Claudia Mirone, Luigi Napolitano, Roberto La Rocca, Massimiliano Creta, Giuseppe Celentano, Marco Capece, Gennaro Musi, Francesco Mangiapia, Nicola Longo, Claudia Collà Ruvolo
12437 Retraction: Effect of preoperative ureteral stenting on the surgical outcomes of patients with 1-2 cm renal stones managed 12102 by retrograde intrarenal surger y using a ureteral access sheath
Tamer A Abouelgreed, Mohamed A Elhelaly, El-Sayed I El-Agamy, Rasha Ahmed, Yasser M Haggag, M Abdelwadood, Salma F Abdelkader, Sameh S Ali, Naglaa M Aboelsoud, Mosab F Alassal, Gehad A Bashir, Tarek Gharib
SYSTEMATIC REVIEWS
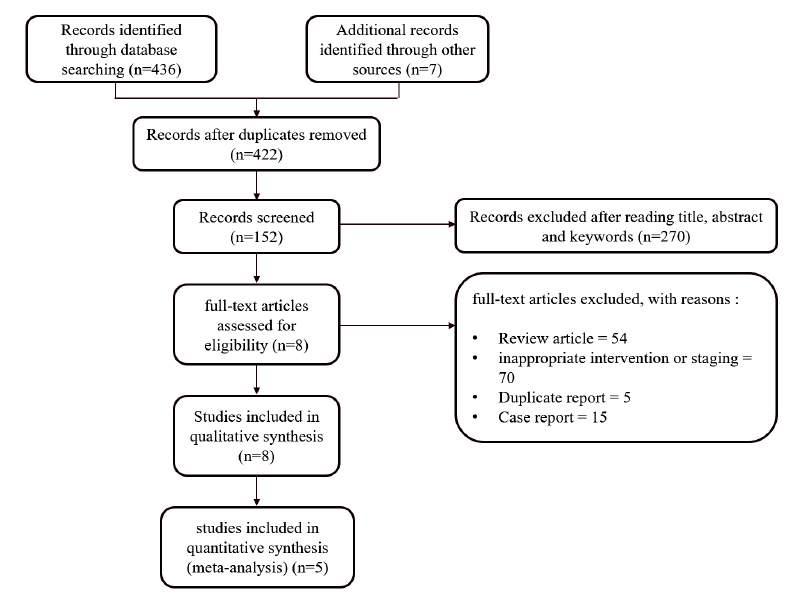
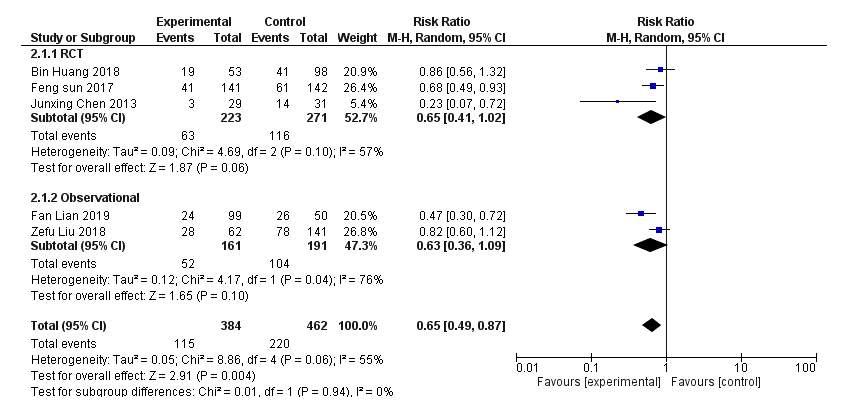
12154 A systematic review and meta-analysis of intraar terial chemotherapy for non muscle invasive bladder cancer :
Promising alter native therapy in high tuberculosis burden countries
Zakaria Aulia Rahman, Furqan Hidayatullah, Jasmine Lim, Lukman Hakim
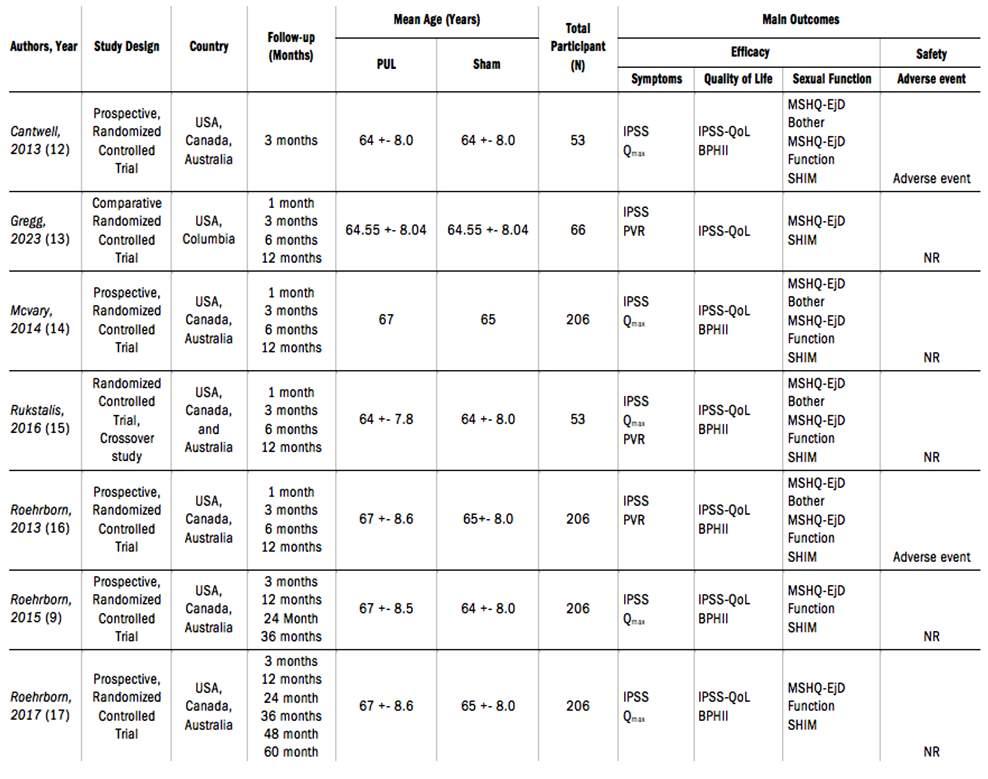
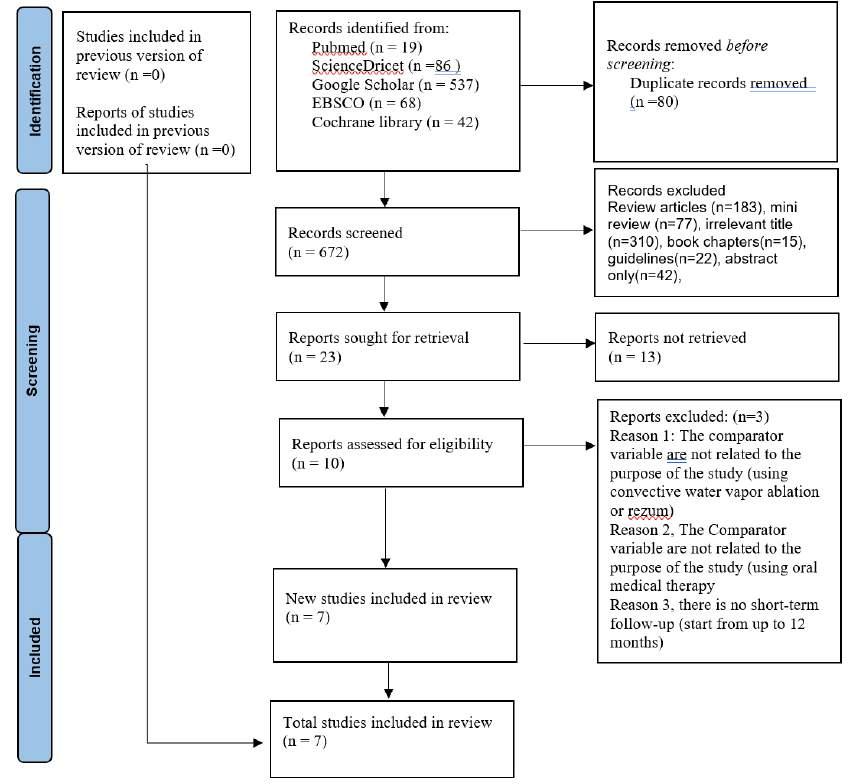
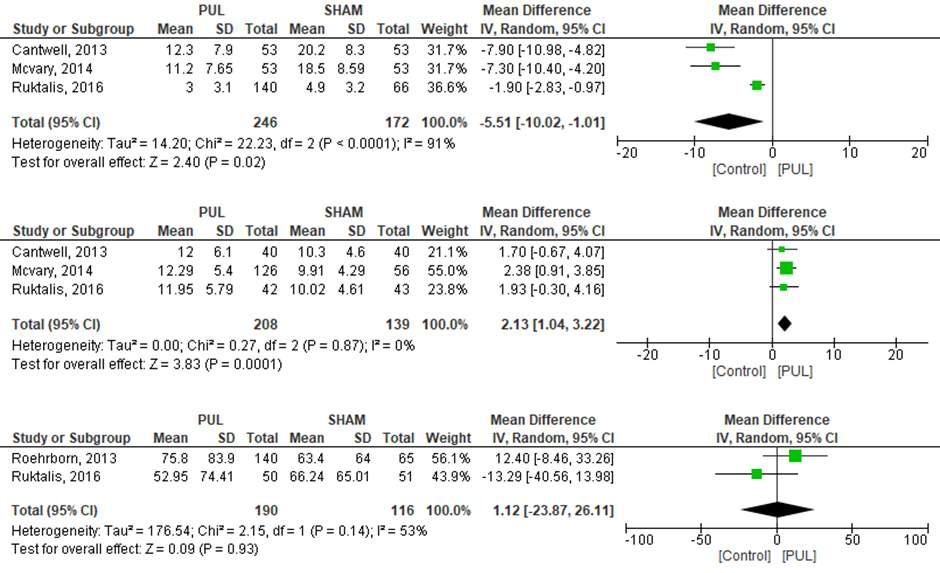
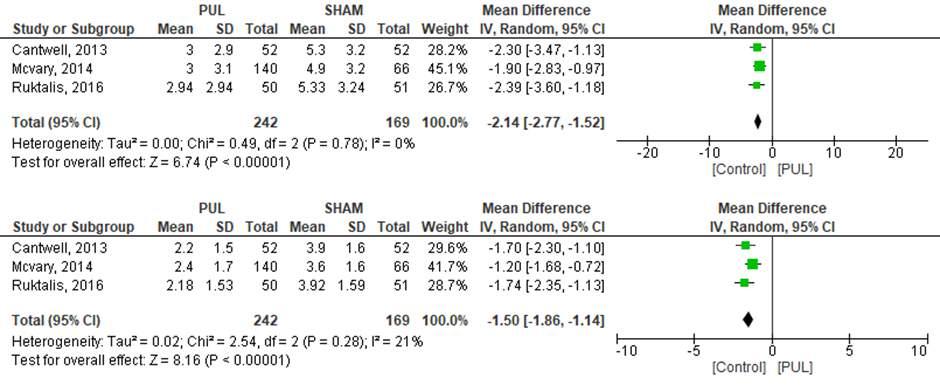
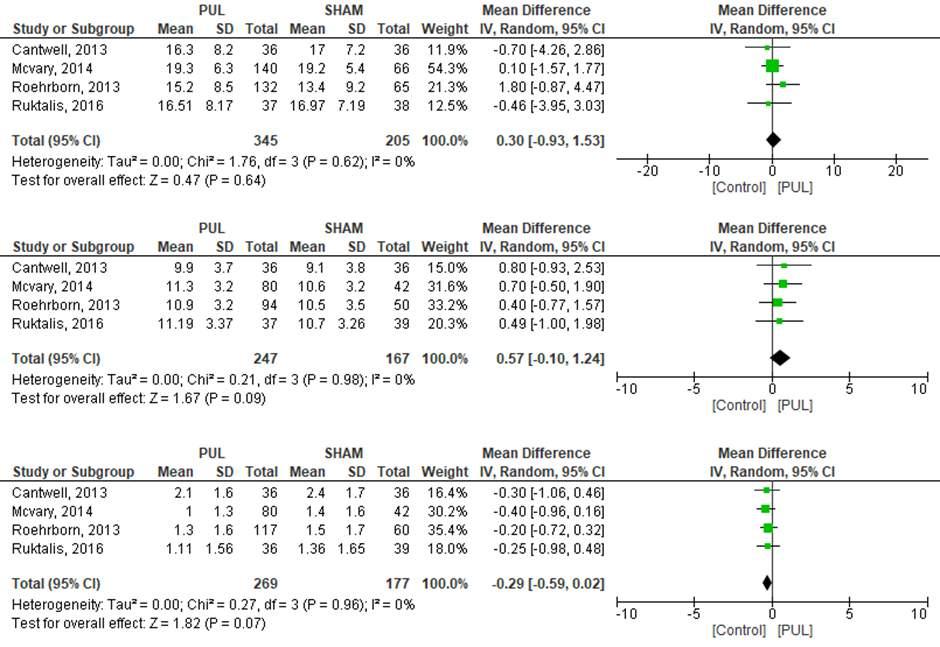
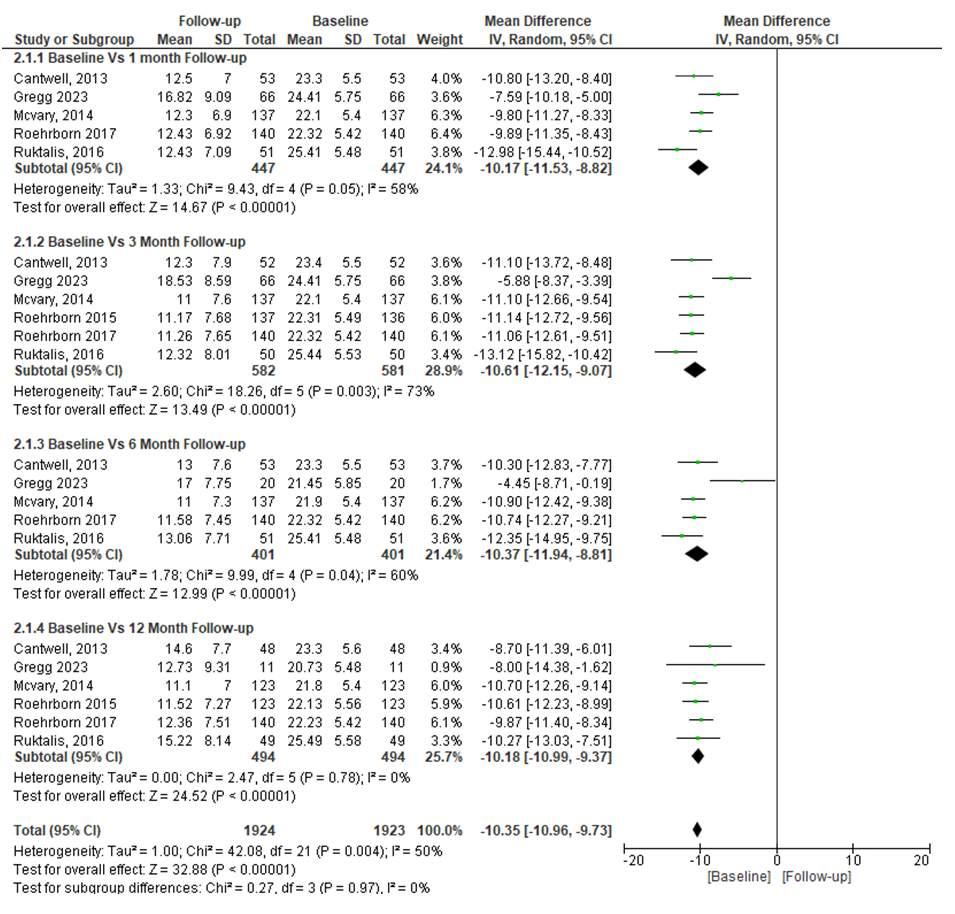
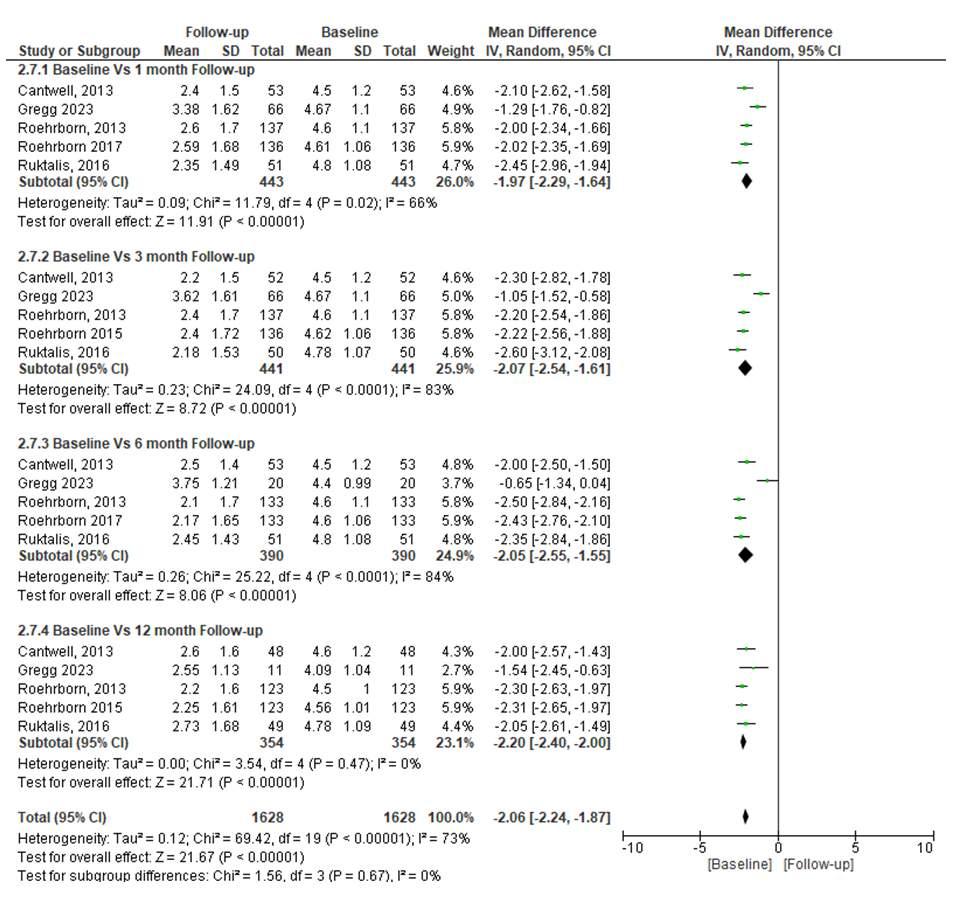
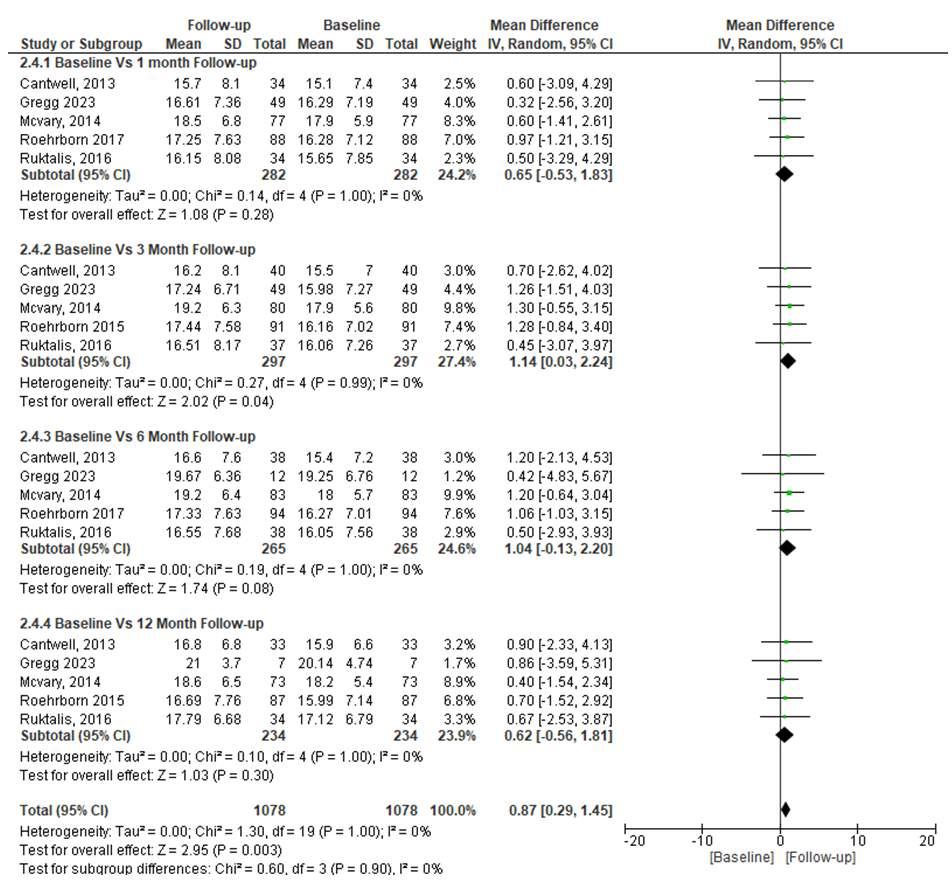
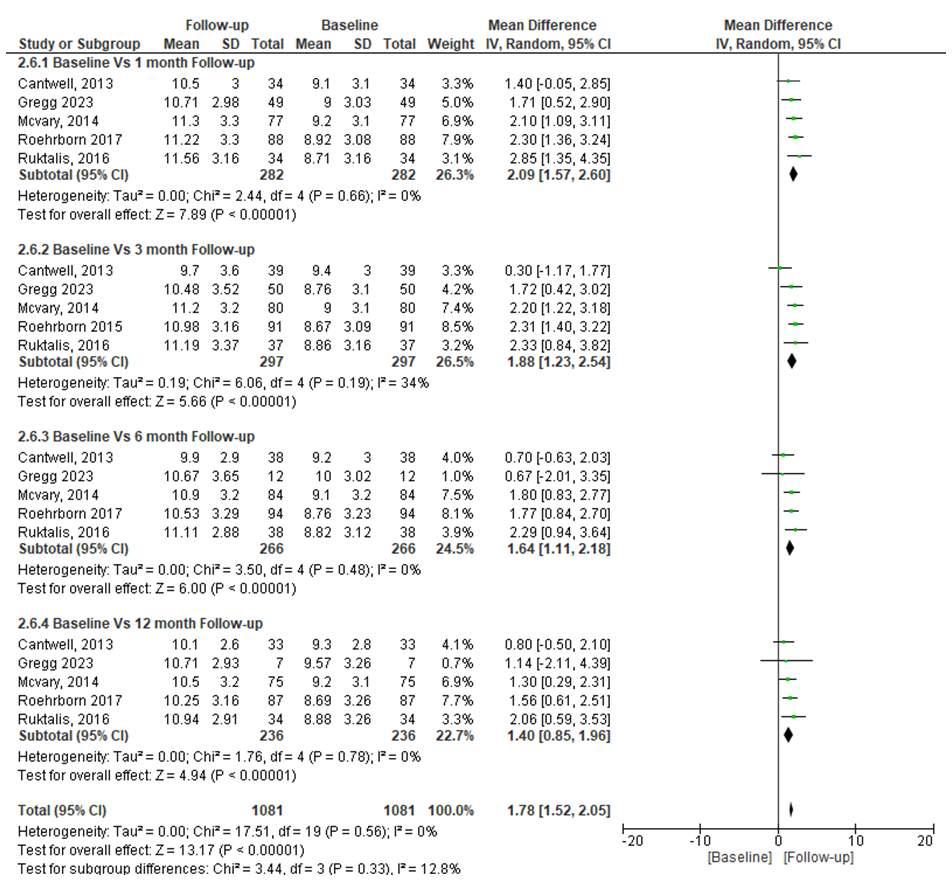
12066 The efficacy and safety of prostatic urethral lift as a minimally invasive therapeutic modality to treat lower urinar y tract symptoms while maintaining sexual function in patients with benign prostatic hyperplasia: A systematic review and meta-analysis of randomized controlled trials
Syah Mirsya Warli, Muhammad Fahmi Ikram, Raja Gerald Sarumpaet, Zaimah Zulkarnaini Tala, Ignatius Ivan Putrantyo
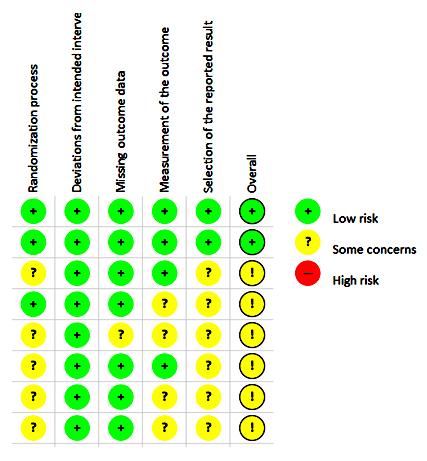
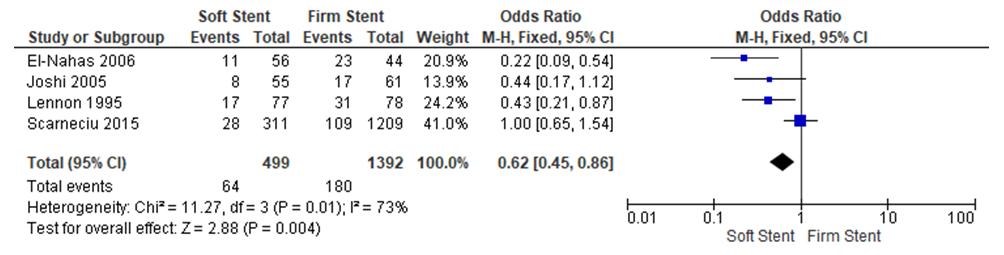
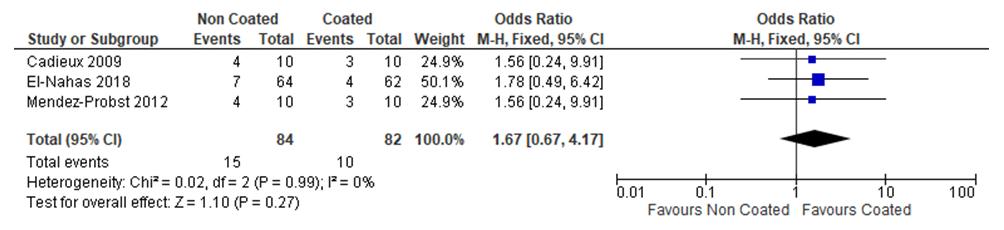
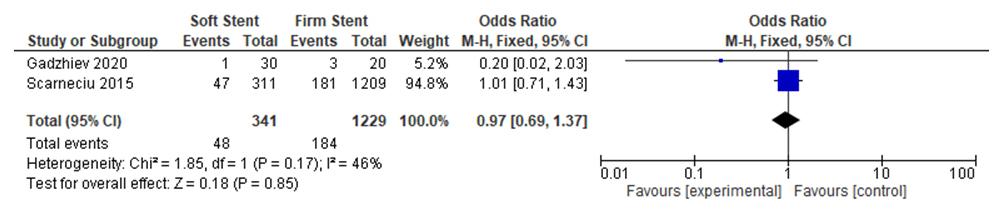
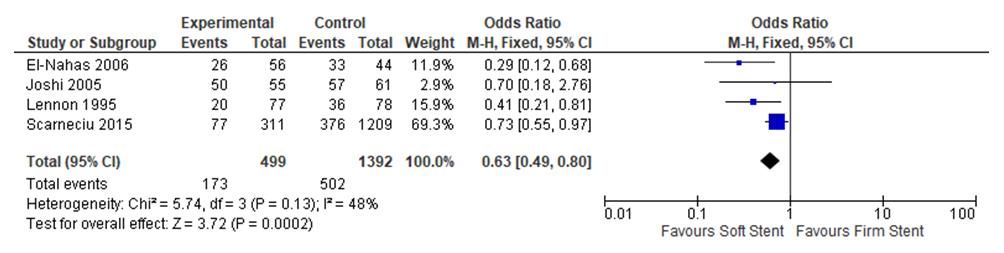
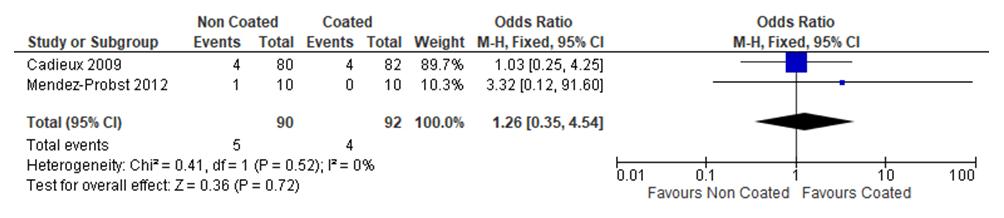
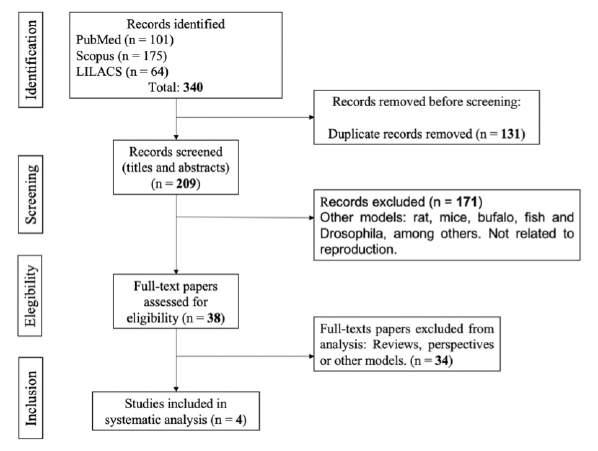
12067 Role of ureteral stent material and coating to prevent ureteral stent related issue: A systematic review and meta analysis
Ignatius Ivan Putrantyo, Syah Mirsya Warli, Ginanda Putra Siregar, Fauriski Febrian Prapiska, Dhirajaya Dharma Kadar, Bungaran Sihombing
12192 Effects of nanotubes on semen quality and fer tility in humans: A systematic review of literature
William Felipe Fernández Zapata, Yamile Cardona Maya, Cesar Isaza Merino, Walter D Cardona Maya
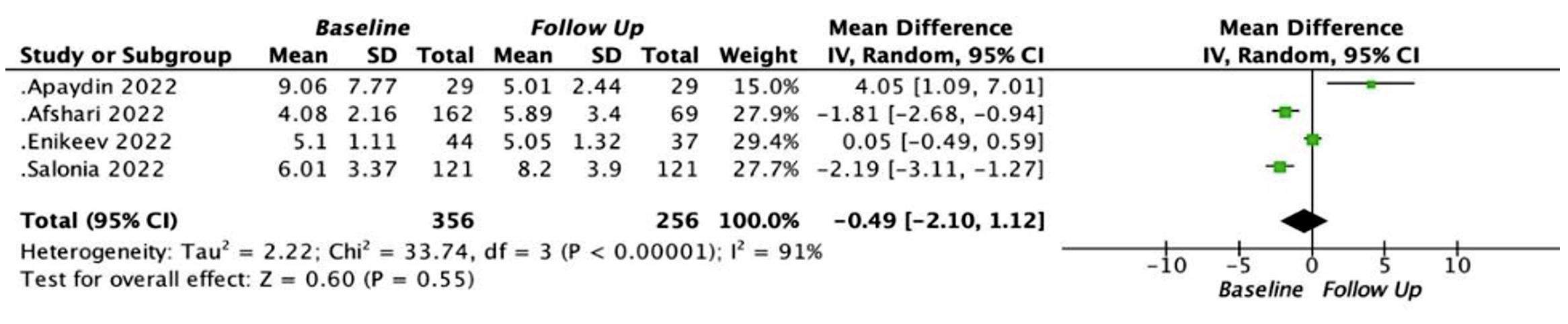
12113 Effect of SARS-CoV-2 viral infection on male sexual hor mones levels post COVID-19 exposure: A systematic review and meta-analysis
Anak Agung Patriana Puspaningrat, Lukman Hakim, Johan Renaldo
LETTERS TO EDITOR
12404 Office-based management of Non-Muscle Invasive Bladder Cancer (NMIBC): A position paper on cur rent state of the ar t and future perspectives
Rosario Leonardi, Francesca Ambrosini, Angelo Cafarelli, Alessandro Calarco, Renzo Colombo, Domenico Tuzzolo, Ferdinando De Marco, Giovanni Ferrari, Giuseppe Ludovico, Stefano Pecoraro, Ottavio De Cobelli, Carlo Terrone, Guglielmo Mantica
12245 Iron homeostasis alterations and erectile dysfunction: A new issue in erectile disfunction treatment?
Claudio Marino, Salvatore Iaconis, Francesco Di Bello, Gianluigi Cacace, Giovanni Fusco, Lorenzo Romano, Ernesto Di Mauro, Luigi Cirillo, Vincenzo Maria Altieri, Francesco Mastrangelo, Luigi Napolitano, Alessandro Palmieri
12263 Robotic pyeloplasty: Technological global panacea or geo-surgical nightmare?
Panagiotis Nikolinakos, Nikolaos Chatzikrachtis, Ivo Donkov, Elisavet Kotsi, Georgios Antonoglou, Ioannis Alexandrou, Nikolaos Zavras, Joseph M Norris
Edizioni Scripta Manent s.n.c.
Via Melchiorre Gioia 41/A - 20124 Milano, Italy
Tel +39 0270608060
e-mail: scriman@tin.it
web: www edizioniscriptamanent eu
Registrazione: Tribunale di Milano n 289 del 21/05/2001
Direttore Responsabile: Pietro Cazzola
Direzione Marketing e PR: Donatella Tedeschi
Comunicazione e Media: Ruben Cazzola
Grafica e Impaginazione: Stefania Cacciaglia
Affari Legali: Avv Loredana Talia (MI)
Ai sensi della legge 675/96 è possibile in qualsiasi momento opporsi all’invio della rivista comunicando per iscritto la propria decisione a: Edizioni Scripta Manent s n c - Via Melchiorre Gioia, 41/A - 20124 Milano
The Publisher is not liable for the opinion expressed by the Authors of the articles and for images used by them
GENERAL INFORMATION
AIMS AND SCOPE
“Archivio Italiano di Urologia e Andrologia” publishes papers dealing with the urological, nephrological and andrological sciences
Original articles on both clinical and research fields, reviews, editorials, case reports, abstracts from papers published elsewhere, book rewiews, congress proceedings can be published
III Archivio Italiano di Urologia e Andrologia 2024, 96, 1

PARTNER CELEBRATING WITH US

EDITORIAL
Dear Authors and Readers,
This year marks the centenary of the foundation of th Archivio Italiano di Urologia e Andrologia
In fact, the journal was founded in 1924 by three of the most prominent urologists at that time: Ulisse Gardini from Bologna, Giovanni Battista Lasio from Milan and Giorgio Nicolich senior from Trieste These urologists were among the founders of the Italian Society of Urology in 1921 and all of them were Presidents of the Society at different times: Nicolich from 1923 to 1924, Lasio from 1928 to 1930 and Gardini from 1932 to 1934 The journal was originally published as Archivio Italiano Urologia and then as Archivio Italiano di Urologia e Nefrologi the publisher Editore Cappelli in Bologna In the 80s, the was taken over by Masson Italia which changed the journal s name into Archivio Italiano di Urologia e Andrologia The journal was initially written in Italian and hosted for many years the official reports of the Society of Lombard Urologists In 2001 Archivio Italiano di Urologia e Andrologia was given by Prof Enrico Pisani, Editor in charge, to the publisher Edizioni Scripta Manent At that time numerous international experts were co-opted into the Editorial Board

Before his retirement, Professor Enrico Pisani entrusted me with the prestigious task of directing the journal in times that proved to be very difficult due to the changes underway in scientific publishing In Italy, scientific publishing had until then been limited to a restricted audience of clinicians and scientists with a horizon mainly limited to the national borders The publications were mainly written in Italian and often were the transcription of reports presented at regional conferences Starting from the 80s of the last century, participation in European and International conferences intensified thanks to the progressive reduction in air transport costs and the improved knowledge of foreign languages The increasing membership of Italian urologists in international urology societies such as the European Association of Urology, the American Urological Association, the Société Internationale d'Urologie, and the Endourological Society contributed to this internationalization process
For this reason, in 2003, with some fear and concern, I decided together with the owners of the Edizioni Scripta Manent, Pietro Cazzola and Armando Mazzù, to stop publishing in Italian and to switch exclusively to English
The choice proved to be a winning one because the magazine began to attract the interest of foreign authors who began to publish in our magazine
Currently over 80% of the articles published on Archivio are written by international authors
A second step that proved crucial was the online publication of the magazine on a web platform To do this, Edizioni Scripta Manent allied with PagePress publishing which already had extensive experience in the online publication of numerous journals It was decided to publish with the Open Access model which leaves ownership of the text to the Authors and allows the texts to be downloaded for free from the website At the time, this innovative model of publication was adopted by a few publishers, but time demonstrated the adequacy of this model to the needs of modern scientific publishing, and today it has been adopted by most journals
Thanks to these choices, the journal found itself ready for the great challenges of recent years which have seen the appearance of new fearsome competitors from numerous countries experiencing recent economic development as Arabia, Turkey, India, Brazil, and Iran
Archivio Italiano di Urologia e Andrologia 2024; 96(1)
The journal had long since been reviewed by Medline/Index Medicus, EMBASE/Excerpta Medica, Medbase/Current Opinion, SIIC Data Base, Scopus and by the bibliographic database (PubMed) of the National Institute of Health (NIH) and in 2023 it received its first Impact Factor from Clarivate
As we reflect on the achievements of the last years, we are reminded of the tireless efforts and dedication of the editorial board, reviewers, authors, and contributors who have upheld the highest standards of academic rigor and integrity Their commitment to excellence has been instrumental in elevating the journal to its esteemed position and ensuring its continued relevance and impact in the years to come
Thanks are also due to the scientific societies that have supported us for many years such as SIUrO, SIA, SIEUN and UrOP
As we celebrate this event, let us not only pay tribute to the legacy of the Archivio Italiano di Urologia e Andrologia but also reaffirm our commitment to advancing the frontiers of urological and andrological research and practice
Alberto Trinchieri Editor in Chief
Archivio Italiano di Urologia e Andrologia 2024; 96(1)
ORIGINAL PAPER
Pietro Pepe 1 , Ludovica Pepe 1 , Mara Curduman 2 , Michele Pennisi 1 , Filippo Fraggetta 3
1 Urology Unit, Cannizzaro Hospital, Catania, Italy;
2 Pathology Unit, Cannizzaro Hospital, Catania, Italy;
3 Pathology Unit, Gravina and S Pietro Hospital, Caltagirone (CT), Italy
Summary
Introduction: To evaluate the accuracy of PSMA PET/CT in the diagnosis and clinical staging of prostatic ductal adenocarcinoma (DAC).
Materials and methods: Two Caucasian men 58 and 62 years old were admitted to our Department for dysuria: the patients had not familiarity for prostate cancer (PCa), PSA values were 5.6 and 2.8 ng/ml, digital rectal examination was positive, multiparametric magnetic resonance image (mpMRI) showed for both the presence of an index lesion PIRADS score 5. The patients underwent extended transperineal prostate biopsy combined with four mpMRI/TRUS fusion biopsy under sedation and antibiotic prophylaxis; biopsy histology demonstrated the presence of a mixed PCa characterized by DAC and acinar PCa (Grade Group 4/Gleason score 8) The patients underwent clinical staging performing lung and abdominal CT, bone scan and fluoride 18 (18F) PSMA PET/CT
Results: Conventional imaging was negative for distant metastases; 18F-PSMA PET/CT showed in both patients an intraprostatic lesion characterized by a standardized uptake value (SUVmax) equal to 4 6 and 4 9 in the absence of distant lesions suspicious for metastases Following multidisciplinary evaluation, the patients underwent radical prostatectomy plus extended pelvic lymphadenectomy Definitive specimen showed the presence in both cases of a mixed pT3bN1 PCa (ductal plus acinar pattern Grade Group 4) with positive surgical margins, neuronal invasion, and nodes metastases (5/20 and 6/24, respectively) Post-operative PSA in the two patients was 0 8 and 0 3 ng/ml, therefore patients underwent adjuvant therapy.
Conclusions: Conventional imaging and PSMA PET/CT could result inadequate in clinical staging of DAC, the use of more imaging data (i e mpMRI and/or F-18 FDG) could improve overall accuracy.
KEY WORDS: PSMA PET/CT; Prostate cancer; Ductal PCa; Ductal PCa staging
Submitted 25 November 2023; Accepted 30 November 2023
Prostate cancer (PCa) is the most commonly diagnosed malignancy in men; although, conventional imaging with computed tomography (CT) and technetium-based bone scan are widely used for staging, recently, cumulative evidence indicates that prostate-specific membrane antigen (PSMA) positron-emission tomography (PET/CT) should be a centerpiece of diagnosis and staging for intermediate/high risk patients (1-5) Although, PSMA PET/CT seems about 27% more accurate than conventional imaging (6), 5-10%
of primary PCa tumours have low PSMA activity which evade detection by PSMA PET, mostly in high-grade and variant tumour types (7-10)
Prostatic ductal adenocarcinoma (DAC) is an uncommon variant of prostatic carcinoma with aggressive behavior and worse prognosis and, still today, the of role PSMA PET/CT in its diagnosis and staging has not been clearly established (11)
We evaluated the accuracy of fluoride 18 (18-F) PSMA PET/CT in the diagnosis and clinical staging in two patients with DAC
CASEREPORT
Two Caucasian men 58 and 62 years old were admitted to our Department for dysuria: the patients had not familiarity for PCa and assumed antihypertensive drugs PSA values were equal to 5 6 and 2 8 ng/ml, digital rectal examination was highly suspicious for PCa and magnetic resonance image (mpMRI) showed for both the presence of a index lesion Prostate Imaging Reporting and Data System (PIRADS) score 5 The patients underwent extended transperineal prostate biopsy (18 cores) combined with four mpMRI/TRUS fusion biopsy using a 18 gauge needle under sedation and antibiotic prophylaxis (12, 13) The biopsy histology demonstrated the presence of a mixed PCa characterized by ductal and acinar PCa (Grade Group 4/Gleason score 8) with a Greatest Percentage of Cancer equal to 100%, a mean number of positive cores of 15 (3 targeted cores and 12 systematic biopsies)) and a mean total percentage of cancer equal to 45% (35-55%) The clinical staging performing lung and abdominal CT plus technetium-based bone scan did not demonstrate distant metastases and/or others primitive tumors; in addition, the 18-F PSMA PET/CT (5) showed in both patients an intraprostatic lesion provided of a standardized uptake value (SUVmax) equal to 4 6 and 4 9 in the absence of distant lesions suspicious for metastases (Figure 1) Following multidisciplinary evaluation, the patients underwent open radical prostatectomy (RP) plus extended pelvic lymphadenectomy Definitive specimen showed the presence in both cases of a mixed pT3bN1 PCa (ductal plus acinar Grade Group 4/Gleason score 8) with positive surgical margins, perineuronal invasion and nodes metastases (5/20 and 6/24, respectively) Postoperative PSA (one month from surgery) in the two patients was 0 8 and 0 3 ng/ml, therefore patients under-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12132 1
ODUC
INTR
TION
Ductalprostatecancerstaging:RoleofPSMAPET/CT
DOI: 10 4081/aiua 2024 12132
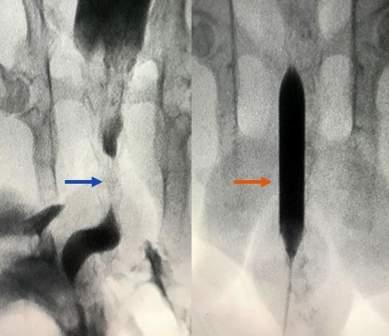
Figure 1.
18-F PSMA PET/CT in man with mixed prostate cancer (ductal plus acinar PCa Grade Group 4/Gleason score 8): intraprostatic standardized uptake value (SUVmax) was equal to 4 9 (a) in the absence of distant metastases (b)

went adjuvant radiotherapy of prostatic fossa and androgen deprivation therapy (ADT)
DISCUSSION
DAC is rare, aggressive, and characterized by cancer involving ducts and/or acini usually associated with a high-grade Gleason score/Grade Group, large tumor volume, and adverse prognostic parameters, including extraprostatic extension and seminal vesicle invasion (14, 15) In the WHO Classification fifth edition the term ‘ductal adenocarcinoma’ is now reserved for those radical prostatectomy cases with more than 50% ductal morphology, while in needle biopsy cases the term ‘adenocarcinoma with ductal features’ is recommended for both pure ductal and mixed ductal and acinar features (16) Although DAC is treated with conventional therapies, it demonstrated worse outcomes in comparison with highgrade acinar PCa, regardless of the treatment modality Ranasinghe et al. (17) in 228 men with DAC submitted to RP vs radiotherapy demonstrated a 5-yrs overall survival (OS) and metastases free survival (MFS) equal to 75 vs 62% and 88 vs 82%, respectively; in addition, 76 men who received adjuvant/salvage ADT after RP, DAC also had worse MFS and OS and was characterized in 91% of them by intrinsic upregulation of androgen-resistant pathways Although mpMRI and PSMA PET/CT are provided of superimposable accuracy in the diagnosis of high risk PCa (12, 18) showing direct correlation between PIRADS score and SUVmax values (19), in the presence of DAC only mpMRI (20) allows to perform diagnosis because PSMA PET/CT demonstrated a very limited diagnostic accuracy (21) In this respect, PSMA uptake has sometimes been poor compared with prominent 18-flourodeoxyglucose (F-18 FDG) avidity, which would suggest that FDG PET/CT scans are important in staging of ductal pattern (22, 23) The diagnostic utility of dual-tracer FDG/PSMA PET/CT for PCa may assist in characterizing high-risk disease during primary staging and restaging especially with concurrently negative PSMA PET When applied to highrisk or variant histology (i e , DAC), detection of the FDGpositive phenotype may signal a poorer prognosis to prompt more aggressive intervention earlier in the disease

course and dual PSMA/FDG PET/CT may improve oncological outcomes (24); in definitive, the use of PSMA and FDG PET imaging in PCa should be examined individually and the potential diagnostic impact for individual patients to undergo dual-tracer PET imaging could be reserved in case of inconclusive conventional imaging and/or negative PSMA PET (25)
In our series, both the patients had a negative conventional imaging (CT and technetium-based bone scan) and 18F PSMA PET/CT despite a locally advanced disease with the presence of metastatic nodes (pT3bN1) underlining the lower accuracy of imaging in local and distant staging in case of DAC
In conclusion, conventional imaging and PSMA PET/CT could result inadequate in clinical staging of DAC, the use of more imaging data including mpMRI and F-18 FDG could improve overall accuracy
ACKNOWLEDGEMENTS
The Authors thank Nuclear Medicine Unit of Cannizzaro Hospital (Catania, Italy) for the images
REFERENCES
1 Kawada T, Yanagisawa T, Rajwa P, et al Diagnostic Performance
P
Tomography-targeted biopsy for Detection of Clinically Significant Prostate Cancer: A Systematic Review and Meta-analysis Eur Urol Oncol 2022; 5:390-400
2 Combes AD, Palma CA, Calopedos R PSMA PET-CT in the diagnosis and staging of prostate cancer Diagnostics 2022; 12:2594
3 Pepe P, Pennisi M Targeted Biopsy in Men High Risk for Prostate Cancer: 68Ga-PSMA PET/CT Versus mpMRI Clin Genitourin Cancer 2023; 21:639-642
4 Pepe P, Pepe L, Tamburo M, et al Targeted prostate biopsy: 68GaPSMA PET/CT vs mpMRI in the diagnosis of prostate cancer Arch Ital Urol Androl 2022; 94:274-277
5 Pepe P, Pennisi M Should 68Ga-PSMA PET/CT replace CT and bone scan in clinical staging of high-risk prostate cancer? Anticancer Res 2022; 42:1495-1498
6 Hofman MS, Lawrentschuk N, Francis RJ, et al proPSMA Study
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12132
2
P Pepe, L Pepe, M Curduman, M Pennisi, F Fraggetta
t e - s
e m b r a n e
t i g e n P o s i t ro n E m i s s i o n
o f
ro s t a
p e c i f i c M
A n
a b
Group Collaborators: Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study Lancet 2020; 395:1208-1216
7 Zhao Q, Dong A, Bai Y, Zuo C Prostate-Specific Membrane Antigen Uptake Heterogeneity in Mixed Ductal-Acinar Adenocarcinoma of the Prostate Clin Nucl Med 2023; 48:750-752
8 Qiu S, Dong A, Zhu Y, Zuo C 68 Ga-PSMA-11 and 18 F-FDG PET/CT in a Case of Ductal Adenocarcinoma of the Prostate Clin Nucl Med 2022; 47:836-838
9 Alabed YZ Ductal Variant of Prostate Cancer: Serial Imaging With 18F-PSMA PET/CT Clin Nucl Med 2021; 46:e551-e552
10 Salemi M, Pettinato A, Fraggetta F, et al Expression of miR-132 and miR-212 in prostate cancer and metastatic lymph node: Case report and revision of the literature Arch Ital Urol Androl 2020; 92:209-210
11 Guner LA, Unal K, Beylergil V, et al Enhancing PSMA PET/CT imaging of prostate cancer: investigating the impact of multiple time point evaluation, diuretic administration, cribriform pattern, and intraductal carcinoma Ann Nucl Med 2023; 37: 618-628
12 Pepe P, Pepe L, Cosentino S, et al Detection Rate of 68Ga-PSMA PET/CT vs mpMRI Targeted Biopsy for Clinically Significant Prostate Cancer Anticancer Res 2022; 42:3011-3015
13 Pepe P, Pennisi M Morbidity following transperineal prostate biopsy: Our experience in 8 500 men Arch Ital Urol Androl 2022; 94:155-159
14 Divatia MK, Ro JY: Intraductal Carcinoma of the Prostate Gland: Recent Advances Yonsei Med J 2016; 57:1054-62
15 Kench JG, Amin MB, Berney DM WHO Classification of Tumours fifth edition: evolving issues in the classification, diagnosis, and prognostication of prostate cancer Histopathology 2022; 81:447-58
16 Kench JG, Amin MB, Berney DM, et al WHO Classification of Tumours fifth edition: evolving issues in the classification, diagnosis, and prognostication of prostate cancer Histopathology 2022; 81:447-458
17 Ranasinghe W, Shapiro DD, Hwang H, et al Ductal Prostate Cancers Demonstrate Poor Outcomes with Conventional Therapies Eur Urol 2021; 79:298-306
18 Pepe P, Garufi A, Priolo GD, et al Is it Time to Perform Only Magnetic Resonance Imaging Targeted Cores? Our Experience with 1,032 Men Who Underwent Prostate Biopsy J Urol 2018; 200:774778
19 Pepe P, Pepe L, Tamburo M, et al 68Ga-PSMA PET/CT and Prostate Cancer Diagnosis: Which SUVmax Value? In Vivo 2023; 37:1318-1322
20 Pahouja G, Patel HD, Desai S, et al The rising incidence of ductal adenocarcinoma and intraductal carcinoma of the prostate: Diagnostic accuracy of biopsy, MRI-visibility, and outcomes Urol Oncol 2023; 41:48 e11-48 e18
21 Zhao Q, Dong A, Bai Y, Zuo C Prostate-Specific Membrane A
Adenocarcinoma of the Prostate Clin Nucl Med 2023; 48:750-752
22 McEwan LM, Wong D, Yaxley J Flourodeoxyglucose positron emission tomography scan may be helpful in the case of ductal variant prostate cancer when prostate specific membrane antigen ligand positron emission tomography scan is negative J Med Imaging Radiat Oncol 2017; 61:503-505
23 Qiu S, Dong A, Zhu Y, Zuo C 68 Ga-PSMA-11 and 18 F-FDG PET/CT in a Case of Ductal Adenocarcinoma of the Prostate Clin Nucl Med 2022; 47:836-838
24 McGeorge S, Kwok M, Jiang A, et al Dual-Tracer PositronEmission Tomography Using Prostate-Specific Membrane Antigen and Fluorodeoxyglucose for Staging of Prostate Cancer: A Systematic Review Adv Urol 202; 2021:1544208
25 McEwan LM, Wong D, Yaxley J Flourodeoxyglucose positron emission tomography scan may be helpful in the case of ductal variant prostate cancer when prostate specific membrane antigen ligand positron emission tomography scan is negative J Med Imaging Radiat Oncol 2017; 61:503-505
Correspondence
Pietro Pepe, MD (Corresponding Author) piepepe@hotmail com
Ludovica Pepe, MD ludopepe97@gmail com
Michele Pennisi, MD michepennisi2@virgilio it
Unità Operativa di Urologia, Azienda Ospedaliera Cannizzaro, Catania, Italy
Mara Curduman, MD
mara curduman@aoec it
Unità Operativa di Anatomia Patologica, Azienda Ospedaliera Cannizzaro, Catania, Italy
Filippo Fraggetta, MD filippofra@hotmail com
Unità Operativa Anatomia Patologica, Presidio Ospedaliero Gravina e San Pietro, Caltagirone, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12132 3 PSMA PET/CT and ductal PCa
n t i g e n U p t a k e H e t e ro g e n e i t y i n M i x e d D u c t a l - A c i n a r
ORIGINAL PAPER
Asmâa Naim 1, 2, 3 , Zineb Lahlou 1, 2 , Othmane Kaanouch 3, 4 , Abdelajalil Heddat 1, 2, 5 , Safae Mansouri 6
1 Faculty of Medicine, Mohammed VI University of Sciences and Health, Casablanca, Morocco;
2 Research Unit, Mohammed VI Center for Research and Innovation, Rabat, Morocco;
3 Radiotherapy Department of Casablanca Cancer Center, University International Hospital Cheikh Khalifa, Casablanca, Morocco;
4 Hassan First University of Settat, High Institute of Health Sciences, Laboratory of Sciences and Health Technologies, BP 555, 26000, Settat, Morocco;
5 Urology Department, University International Hospital Cheikh Khalifa, Casablanca, Morocco;
6 Faculty of Medicine, University Hassan II, Casablanca, Morocco
Summary
Introduction: Prostate cancer is the most common urological cancer, and its incidence is increasing Radical prostatectomy and radiotherapy are the primary treatments for localized forms. Stereotactic Body RadioTherapy (SBRT), a new and innovative therapy, has been validated for some cancer localizations but not yet for localized prostate cancer Our study aims to report the efficacy and tolerance results of SBRT for localized prostate cancer.
Materials and methods: This is a retrospective study of 27 patients with localized prostate cancer (CaP) who were treated with SBRT in our department from 2017 to 2021 using transponders for tumor tracking. The dose was 36.25 Gy delivered in five fractions of 7 25 Gy The delineation and doses of organs at risk were determined based on the recommendations of the SFRO and the TG101 report of medical physics All patients were treated using a latest-generation linear accelerator (True Beam STXÒ)
Results: Acute toxicities were observed in 33 3% of cases, with 22 2% grade 1 or 2 genitourinary (GU) and no grade 3 while 11 1% gastrointestinal (GI) toxicities were reported as grade 1-2 (7 4%) and one case grade 3 (3 7%) Late grade 1 or 2 GU toxicity was observed in 14 84% of cases, with no reports of late GI toxicity After a 26-month follow-up period, the biochemical failure-free survival rate was 92 6%
Conclusions: The results of our study are consistent with the existing literature and support the safety and effectiveness of SBRT as a treatment option for localized prostate cancer (CaP). In the United States, both ASTRO and the NCCN recognize SBRT as a valid treatment option for localized CaP. Ongoing phase III trials are being conducted to further substantiate these long-term results and to establish SBRT as the future standard of care for localized CaP
KEY WORDS: Localized prostate cancer; Stereotactic radiotherapy; Toxicity; Efficacy
Submitted 17 November 2023; Accepted 23 December 2023
INTRODUCTION
Prostate cancer (CaP) is a common cancer, with approximately 1 4 million new cases reported globally in 2020 (1) It accounts for 14 1% of all human cancers and is the fifth leading cause of cancer-related deaths, responsible for 375 000 deaths each year In the United States, about
80% of CaP cases are localized, and the survival rate for localized cases is over 99% (2) The treatment of localized CaP involves a combination of modalities, and radiation therapy is a standard treatment option recognized as an alternative to radical prostatectomy
Conventional normo-fractionated radiation therapy is the most commonly used treatment option for localized CaP, but it has a major drawback: it requires a long treatment duration and repetitive patient’s displacement, which can cause fatigue and adding financial burden Short-term therapies with similar efficacy and toxicity to other radiation therapy techniques are needed Hypofractionated radiation therapy (2 4 to 3 Gy) in CaP is recommended by several scientific studies (3) Advances in imaging and radiation therapy have led to the development of ultra-fractionated radiation therapy techniques, such as Stereotactic Body Radiation Therapy (SBRT) However, there is a lack of scientific evidence for SBRT in the treatment of localized CaP
This study aims to present the clinical and biological results in terms of efficacy and tolerance of SBRT in localized CaP, according to the experience of Radiotherapy Department of the Casablanca Cancer Center (CCC) of the International University Hospital Cheikh Khalifa
MATERIALSANDMETHODS
Study and patient characteristics
This is a retrospective, descriptive, observational study conducted at a single center, which included 27 patients with localized prostate adenocarcinoma treated with curative intent using SBRT at the CCC Radiotherapy Department between 2017 and 2021 The median age of patients was 66 years, and the three quarters of the patients had a PSA level less than 10 ng/ml The Gleason score was 6 in 59 3% of patients, 7 in 40 7% Regarding the tumor stage 14 8% were classified as T1 and 85,2% as T2 According to the D’Amico classification, 33 3% of patients were low-risk, 51 9% were intermediate-risk, and 14 8% were high-risk (Table 1)
Protocols and techniques
The decision to treat with SBRT was made during multi-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12104 1
Revolutionizinglocalizedprostatecancertreatment: Stereotacticradiotherapy“Moroccanexperience”
DOI: 10 4081/aiua 2024 12104
A Naim, Z Lahlou, O Kaanouch, A Heddat, S Mansouri
Table 1.
PPLA score system for renal papillae (16)
Median age 66 years (53-76)
Initial PSA data
Medium
8 9 ng (5-17)
= 5 ng/ml 2 (7 4%)
5-10 ng/ml 18 (66 7%)
10 1- 15 ng/ml 5 (18 5%)
> 15 ng/ml 2 (7 4%)
ISUP Classification
Group 1 (3+3) 16 (59 3%)
Group 2 (3+4) 6 (22 2%)
Group 3 (4+3) 5 (18 5%)
Group 4 (4+4) 0
Group 5 (4+5 ou 5+4) 0
TNM Classification
T1cN0M0 4 (14 8%)
T2aN0M0 11(40 8%)
T2bN0M0 8 (29 6%)
T2cN0M0 4 (14 8%)
D’Amico Classification
Low risk 9 (33 3%)
Intermediate risk 14 (51 9%)
High risk 4 (14 8%)
Androgen deprivation therapy (ADT)
Yes 12 (44 5%)
Non 15 (55.5%)
d i s c i p l i n a r y c o n s u l t a t i o n m e e t i n g s ( R C P s ) f o r a l l patients
The first step in the SBRT treatment process involved the placement of three electromagnetic transponders, by an urologist under general anesthesia, by ultrasound guidance In fact the urologist sets up two transponders at the base and one at the apex
These transponders were used to track the tumor during prostate irradiation with the Calypso® repositioning system
Patients were positioned in a supine position with their hands crossed on their chest and immobilized using restraints such as footrests, headrests, and logs under their knees A simulation scan was then performed 6 to 15 days after transponder placement with average of 11 days, with sub-millimeter sections
The target volumes for treatment were determined based on the ICRU 91 report, which involved a systematic fusion of dosimetric scanner images and previously obtained prostate MRI images The gross tumor volume (GTV) corresponded to the clinical target volume (CTV) GTV=CTV (4), whereas the planning target volume (PTV) was defined by adding a 3 mm posterior safety margin and a 5 mm margin in other directions to the GTV/CTV Organs at risk (OARs), including the bladder, rectum, urethra, penile bulb, anal canal, and right and left femoral heads, were delineated following the recommendations of the French Society of Oncological Radiotherapy (SFRO) (5)
All patients received the dose of 36 25 Gy in five fractions and were treated using a True Beam STX linear accelera-
tor with real-time automatic correction for target translational and rotational motion thanks to Calypso® system
O u t c o m es
Patients were monitored for treatment tolerance and effectiveness following each irradiation session
Evaluations were done 1 month after treatment, every three months for the first year, every 6 months for the next 3 years, and annually thereafter Physicians reported any toxicities, which were classified as acute if they occurred within 90 days of treatment and late if they developed after 90 days, using CTCAE v5 (6) The study's primary endpoint was the incidence of biochemical or clinical failure Biochemical recurrence was defined according to the Phoenix criteria (7) Overall survival was defined as death from any cause
RESULTS
The entire tumor volume (CTV) received 100% of the prescribed dose, while the planning target volume (PTV) received 95% coverage The dose constraints for the organs at risk (OARs) were met for all patients (Table 2) and the principals parameters of irradiation are summarized in Table 3
Table 2.
Dose constraints for the Organs at risk (OAR) in our series.
Table 3
Irradiation parameters of our patients
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12104
2
Mean Maximum Minimum Prostate dose (Gy) 36 25 36 25 36 25 Fractionation (Gy) 7 25 7 25 7 25 Number of fractions 5 5 5 Total Duration of radiotherapy (days) 10 14 9 Maximum Dose (Gy) 43 41 45 3 38 94 Maximum Dose (%) 119 9 125 111 3 Minimum Dose (Gy) 34 47 37 3 30 39 Minimum Dose (%) 95 1% 102% 84%
Reference Patients OAR contraints constraints Mean Min Max Bladder V 18 3 Gy < 15 cc 13 54 2 14 34 V 37 Gy < 10 cc 0,7 0 2 16 V 35 5 Gy < 5 cc 1 0 3 45 Rectum V 25 Gy < 20 cc 4 7 0 31 14 V 36 25 Gy < 1 cc 0 43 0 1 77 V 36 25 Gy < 5% 1 0 10 V 33 625 Gy < 10% 3 0 11 74 V 29 Gy < 20% 5 0.061 17 V 18 125 Gy < 50% 17 69 3 48 44 D max = 38 Gy 38 32 39 66 Femoral heads V 30 Gy < 10 cc 0 0 2 Urethra V 47 Gy < 20% 0 0 0 Penile bulb V 30 Gy < 3 cc 0 0 0 77 V 50 Gy < 0.5 cc 0 0 0 V 29 5 Gy < 50% < 0% 0 56
Table 4.
Acute toxicity
During and after the 90 days of radiotherapy, we observed 29 6% grade 1-2 genitourinary (GU) and gastrointestinal (GI) toxicity, and one patient (3 7%) presented grade 3 acute GI toxicity exacerbated by an abscess treated surgically (Table 4)
Late toxicity
We observed 14 8% (n = 4) grade 2 late urinary toxicity, including urethral stricture resolved by drilling in 11 1% of patients and haematuria related to bladder cancer in one patient No late GI toxicity was detected (Table 4)
Biological control
At 26 months, the biochemical relapse-free survival rate was 92 5% (n = 25), and two patients had a biological recurrence All patients were alive when we performed o u r a n a l y s i s e x c e p t o n e w h o d i e d b y p u l m o n a r y embolism caused by associated lung cancer
DISCUSSION
Biological rationale
The Biologically Equivalent Dose (BED) formula is used to explain cell sensitivity to larger fraction sizes The formula is BED = nd [1 + d/(α/β)], where n is the number of radiation fractions, and d is the dose size per fraction The BED formula shows that increasing the dose per fraction, or hypofractionation, has a greater impact on tissues with a low α/β ratio compared to those with a high ratio If the tumor's α/β ratio is lower than the surrounding tis-
Table 5
Results of trials on the efficacy of SBRT in localized prostate cancer
sues' α/β ratio (assumed to be between 3 and 5 for bladder and rectum), then increasing the dose per fraction will increase the BED for the tumor more than for the normal tissues, improving the therapeutic ratio Many publications suggest that the α/β ratio for CaP is around 1 5 Gy (8-11), indicating that hypofractionated radiotherapy may improve the efficacy of treatment This differential sensitivity to fractionation between the tumor and normal tissue favors the use of hypofractionated radiotherapy for CaP (12-13) Furthermore, higher BED is associated with improved local control (14)
Benefits of SBRT in CaP
The radiobiological data indicate that SBRT is a more effective treatment for localized CaP than conventional radiotherapy Moreover, SBRT provides several other benefits, including a reduction in treatment duration and better quality of life for patients due to fewer treatment sessions (15) SBRT is also more logistically cost-effective for radiation therapy departments and may have financial b e
Studies have shown that 5-fraction prostate SBRT is a cost-effective and non-invasive treatment with equivalent results to conventional radiotherapy or surgery without compromising patient safety (16)
Acute toxicity
Several trials have studied the acute toxicity of SBRT in patients with localized CaP Our study found that nearly a quarter of patients had grade 1-2 GU acute toxicity and none had grade 3 or higher toxicity Two patients had grade 1-2 GI toxicity (bleeding, discomfort, or mucosal discharge), and one patient developed grade 3 acute GI toxicity (abscess) probably due to receiving a D100 on 10% of the rectal volume, which was higher than the group average Our results found the same conclusions reported in the literature (Table 5)
Late toxicity
Several studies have examined the toxicity profiles of different radiotherapy treatments for CaP, with a focus on SBRT One study found that while SBRT and intensity-modulated radiation therapy (IMRT) had similar rates of geni-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12104 3 Stereotactic radiotherapy for prostate cancer
n e fi t s i n s y s t e m s w i t h f r a c t i o n a l r e i m b u r s e m e n t
acute and late toxicities Acute toxicity Acute toxicity Late toxicity Late toxicity Grade 1-2 Grade ≥ 3 Grade 1-2 Grade ≥ 3 GU Cystitis 22.2% (6) 0% (0) 0% (0) 0% (0) Hemorrhage 0% (0) 0% (0) 3 7% (1) 0% (0) Urethral stricture 0% (0) 0% (0) 11 1% (3) 0% (0) GI Proctitis 7 4% (2) 3,7 (1) 0% (0) 0% (0)
Results of
Studies Number Endpoints Dose PTV Number α/β Ratio Allocated Median bRFS (%) of patients (Gy) (Gy) of fractions (Gy) time (days) follow-up (month) SBRT Conv Pace B (2012-2018) 874 Toxicity 36 25 40 5 *7 25 7 à 14 60 On Going SSRB HYPO-RT-PT (2005-2015) 1200 Toxicity SSRB 47 7 7 * 6 8 3 16 (15-17) 60 84% 84% QOL Sharp 2017 40 Toxicity SSRB 33 5 5 *6 7 1 5 41 90% NC R M Meier 309 Toxicity SSRB 40 36,25 5 * 8 5 à 11 61 97 1% NC King and al 2013 67 Toxicity SSRB 32 94% NC Katz and al 2006-2009 67 Toxicity SSRB QOL 35 - 5*7 25 -5 96 94 4% NC 36 25 93 4% Jackson and a 2013-2018 6000 Toxicity SSRB 36 25 - 5*7 25 2 5 - 30 95 3% NC Our study 27 Toxicity SSRB 36 25 40 5*7 25 1 5 9 26 92 6% NC Conv : Conventiona ; NC: Not comparat ve; bRFS: Biologica re apse-free survival; QoL: Qua ity of life
Table 6.
Study results of acute SBRT toxicity in localized CaP
Studies
tourinary (GU) and gastrointestinal (GI) toxicities, SBRT patients had a higher risk of urinary fistula (17) Another meta-analysis estimated rates of late grade 3 GU and GI toxicities over 5 years of follow-up (18) The Hypo-RT-PC and PACE B trials found no significant differences in late GU and GI toxicities between treatment groups, although the ultra-hypofractionation group in the former had an increase in GU toxicity at 1-year follow-up (19, 20)
Another study found that SBRT was associated with a higher rate of GU toxicity, potentially due to the lower α/β ratio in urinary tract tissue compared to GI tissue Ongoing trials are investigating the long-term toxicity and efficacy of SBRT in low and intermediate-risk CaP patients (23)
Effectiveness of SBRT
Studies have indicated that ultra-hypofractionated radiotherapy, also known as SBRT, is a secure and efficient treatment option for patients with intermediate and highrisk localized CaP (21-22) The randomized phase III HYPO-RT-PC trial and PACE B trial have reported comparable recurrence-free survival rates with SBRT and conventional radiotherapy, indicating that SBRT may be a viable alternative for these patients (19-20) Katz et al 's research has also revealed outstanding long-term control with low toxicity, demonstrating SBRT's potential as a promising treatment option for localized CaP (23)
Additionally, the multicenter study by Meier et al. has shown higher rates of overall survival and biological control with SBRT when compared to IMRT, reinforcing the demonstration of the efficacy of SBRT for CaP treatment (17) Although the addition of androgen deprivation therapy (ADT) is recommended for unfavorable intermediaterisk patients, further research is needed to determine if SBRT alone can suffice (24)
Our findings exhibit a high degree of similarity to the results of the main trials, specifically in terms of Biological Relapse-Free Survival (bRFS), as indicated in Table 6
CONCL
USIONS
Stereotactic radiotherapy (SBRT) has emerged as a recent treatment option for managing localized CaP and offers a multitude of benefits, including radiobiological, logisti-
cal, and financial advantages Numerous studies have demonstrated that SBRT is comparable to conventionally fractionated radiotherapy for intermediate to high-risk CaP patients This treatment has the potential to achieve satisfactory levels of acute and late genitourinary and gastrointestinal toxicity, consistent with radiobiological principles Our findings indicate that ultra-hypofractionation should be regarded as a safe and effective treatment for localized CaP At present, several phase III trials are ongoing to validate SBRT as the best standard treatment for all localized CaP, such as the SPARC trial and PACE C However, the potential advantages of combining androgen deprivation therapy with SBRT remain unclear
ACKNOWLEDGMENTS
We thank all the staff of Department of Radiotherapy and Urology Hospital International Cheikh Khalifa, Casablanca, Morocco
We thank all the staff of Medical Physics of Cheikh Khalifa International Hospital, Casablanca, Morocco: Kamal Saidi, Hanae Elgouach
REFERENCES
1 Sung H, Ferlay J, Siegel RL, et al Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries CA Cancer J Clin 2021; 71:209-49
2 Siegel RL, Miller KD, Jemal A Cancer statistics, 2017 CA Cancer J Clin 2017; 67:7-30
3 Langrand-Escure J, de Crevoisier R, Llagostera C, et al Dose constraints for moderate hypofractionated radiotherapy for prostate cancer: The French genito-urinary group (GETUG) recommendations Cancer/Radiothérapie 2018; 22:193 8
4 Wilke L, Andratschke N, Blanck O, et al ICRU report 91 on prescribing, recording, and reporting of stereotactic treatments with small photon beams Strahlenther Onkol 2019; 195:193-8
5 Noël G, Antoni D, Barillot I, Chauvet B Délinéation des organes à risque et contraintes dosimétriques Cancer/Radiothérapie 2016; 20:S36-60
6 Freites-Martinez A, Santana N, Arias-Santiago S, Viera A Using the Common Terminology Criteria for Adverse Events (CTCAE -
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12104
4
A Naim, Z Lahlou, O Kaanouch, A Heddat, S Mansouri
Number Endpoints Dose PTV Number α/β Ratio Allocated Acute GU toxicity Acute GI toxicity of patients (Gy) (Gy) of fractions (Gy) time (days) SBRT Conv SBRT Conv Pace B (2012-2018) 874 Toxicity 36 25 40 5 * 7 25 7 à 14 G2: 23 2% G2: 27 2% G2: 10 1% G2: 12 1% SSRB HYPO-RT-PT (2005-2015) 1200 Toxicity 47 7 7 * 6 8 3 16 (15-17) G2: 28% G2: 23% G2: 10% G2: 7% SSRB QOL Sharp 2017 40 Toxicity 33 5 5 * 6 7 1 5 G2: 20 5% NC G2: 13% NC SSRB R M Meier (20) 309 Toxicity 40 36 25 5 * 8 5 à 11 G2: 26% NC G2: 8% NC SSRB Our study 27 Toxicity 36 25 40 5 * 7 25 1 5 9 G1-2: 22 2 NC G1-2: 7 4% NC SSRB G3: 3 7% Conv : Conventiona ; NC: Not comparative; SSRB: biolog ca re apse-free surv val; QoL: Quality of l fe
Version 5 0) to Evaluate the Severity of Adverse Events of Anticancer Therapies Actas Dermosifiliogr (Engl Ed) 2021; 112:90-2
7 Roach M, Hanks G, Thames H, et al Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: Recommendations of the RTOG-ASTRO Phoenix Consensus Conference Int J Radiat Oncol Biol Phys 2006; 65:965-74
8 Fowler J, Chappell R, Ritter M Is alpha/beta for prostate tumors really low? Int J Radiat Oncol Biol Phys 2001; 50:1021-31
9 Leborgne F, Fowler J, Leborgne JH, Mezzera J Later outcomes and alpha/beta estimate from hypofractionated conformal three-dimensional radiotherapy versus standard fractionation for localized prostate cancer Int J Radiat Oncol Biol Phys 2012; 82:1200-7
10 Brenner DJ, Martinez AA, Edmundson GK, et al Direct evidence that prostate tumors show high sensitivity to fractionation (low α/βratio), similar to late-responding normal tissue Int J Radiat Oncol Biol Phys 2002; 52:6-13
11 Miralbell R, Roberts SA, Zubizarreta E, Hendry JH Dose-fractionation sensitivity of prostate cancer deduced from radiotherapy outcomes of 5,969 patients in seven international institutional datasets: α/β = 1 4 (0 9-2 2) Gy Int J Radiat Oncol Biol Phys 2012; 82:e17-24
12 Avkshtol V, Dong Y, Hayes SB, et al A comparison of robotic arm versus gantry linear accelerator stereotactic body radiation therapy for prostate cancer Res Rep Urol 2016; 8:145-58
13 Zaorsky NG, Palmer JD, Hurwitz MD, et al What is the ideal radiotherapy dose to treat prostate cancer? A meta-analysis of biologically equivalent dose escalation Radiother Oncol 2015; 115:295-300
14 Boustani J, Grapin M, Laurent PA, et al The 6th R of Radiobiology: Reactivation of Anti-Tumor Immune Response Cancers 2019; 11:860
15 Dee EC, Muralidhar V, Arega MA, et al Factors Influencing Noncompletion of Radiation Therapy Among Men With Localized Prostate Cancer Int J Radiat Oncol Biol Phys 2021; 109:1279-85
16 Lischalk JW, Kaplan ID, Collins SP Stereotactic Body Radiation Therapy for Localized Prostate Cancer Cancer J 2016; 22:307-13
17 Meier RM, Bloch DA, Cotrutz C, et al Multicenter Trial of Stereotactic Body Radiation Therapy for Low- and Intermediate-Risk Prostate Cancer: Survival and Toxicity Endpoints Int J Radiat Oncol Biol Phys 2018; 102:296-303
18 Pan HY, Jiang J, Hoffman KE, et al Comparative Toxicities and Cost of Intensity-Modulated Radiotherapy, Proton Radiation, and Stereotactic Body Radiotherapy Among Younger Men With Prostate Cancer J Clin Oncol 2018; 36:1823-1830
19 Brand DH, Tree AC, Ostler P, et al PACE Trial Investigators Intensity-modulated fractionated radiotherapy versus stereotactic body radiotherapy for prostate cancer (PACE-B): acute toxicity findings from an international, randomised, open-label, phase 3, noninferiority trial Lancet Oncol 2019; 20:1531-1543
20 Widmark A, Gunnlaugsson A, Beckman L, et al Ultra-hypofractionated versus conventionally fractionated radiotherapy for prostate cancer: 5-year outcomes of the HYPO-RT-PC randomised, non-inferiority, phase 3 trial Lancet 2019; 394:385 95
21 Madsen BL, Hsi RA, Pham HT, et al Stereotactic hypofractionated accurate radiotherapy of the prostate (SHARP), 33 5 Gy in five fractions for localized disease: first clinical trial results Int J Radiat Oncol Biol Phys 2007; 67:1099-105
22 Jackson WC, Silva J, Hartman HE, et al Stereotactic Body Radiation Therapy for Localized Prostate Cancer: A Systematic Review and Meta-Analysis of Over 6,000 Patients Treated On Prospective Studies Int J Radiat Oncol Biol Phys 2019; 104:778-789
23 Katz A Stereotactic Body Radiotherapy for Low-Risk Prostate Cancer: A Ten-Year Analysis Cureus 2017; 9:e1668
24 Bian SX, Kuban DA, Levy LB, et al Addition of short-term androgen deprivation therapy to dose-escalated radiation therapy improves failure-free survival for select men with intermediate-risk prostate cancer Ann Oncol 2012; 23:2346 52
Correspondence
Asmaa Naim, MD doc a naim@gmail com
Zineb Lahlou, MD lahlouzineb@outlook fr Faculty of Medicine, Mohammed VI University of Sciences and Health, Casablanca, Morocco
Othmane Kaanouch, MD
othmane kaanouch@gmail com
Radiotherapy Department of Casablanca Cancer Center, University International Hospital Cheikh Khalifa, Casablanca, Morocco
Hassan First University of Settat, High Institute of Health Sciences, Laboratory of Sciences and Health Technologies, BP 555, 26000, Settat, Morocco
Abdeljalil Heddat, MD abdeljalilheddat@yahoo fr
Faculty of Medicine, Mohammed VI University of Sciences and Health, Casablanca, Morocco
Safae Mansouri, MD
m-safae@hotmail fr Faculty of Medicine, University Hassan II, Casablanca, Morocco
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12104 5 Stereotactic radiotherapy for prostate cancer
ORIGINAL PAPER
Mohamad Moussa 1, 2* , Mohamad Abou Chakra 1, 3* , Neal D Shore 4 , Athanasios Papatsoris 1, 5 , Yasser Farahat 6, 7 , Michael A. O’Donnell 3
1 Department of Urology, Lebanese University, Beirut, Lebanon;
2 President of the Arab Association of Urology (AAU);
3 Department of Urology, University of Iowa, Iowa City, Iowa, USA;
4 Carolina Urologic Research Center, Myrtle Beach, South Carolina, USA;
5 2nd Department of Urology, School of Medicine, Sismanoglio Hospital, National and Kapodistrian University of Athens, Athens;
6 Urology Department, Sheikh Khalifa General Hospital, Umm Al Quwain, United Arab Emirates;
7 Secretary General of the Arab Association of Urology (AAU);
* Both authors contributed equally to this work
Summary
Purpose: To understand the treatment plans suggested for BCG-unresponsive non-muscle invasive disease (NMIBC) patients in the Arab countries and therapeutic decisions applied for BCG-naive patients during BCG shortage time
Methods: A 10-minute online survey was distributed through the Arab Association of Urology (AAU) office to urologists in the Arab countries who treat patients with NMIBC
Results: One hundred six urologists responded to the survey. The majority of urologists had treated, in the past 6 months, > 10 patients with NMIBC who were considered BCG-unresponsive (55% of respondents). Radical cystectomy (RC) was the most popular treatment option (recommended by 50%) for these patients This was followed by intravesical chemotherapy (30%), repeat BCG therapy (12%), resection with ongoing surveillance (8%) Clinical trials and intravenous checkpoint inhibitors were never selected The most preferred intravesical chemotherapy was by ranking: 60% gemcitabine, 19% mitomycin C, 8% docetaxel, 8% gemcitabine/docetaxel, 4% sequential gemcitabine/mitomycin C, and 1% valrubicin The use of intravesical chemotherapy appears limited by Arab urologists due to concerns regarding clinical efficacy (fear of progression) and the lack of clear recommendations by urology societies Given the BCG shortage, which may vary per Arab country, Arab urologists have adjusted by prioritizing BCG for T1 and carcinoma in situ (CIS) patients over Ta, adapting intravesical chemotherapy, and reducing the dose/strength of BCG administered Most physicians report an eagerness to utilize novel therapies to address the BCG deficit, especially to try intravesical chemotherapy
Conclusions: Even though Arab urologists are in the majority of cases selecting RC for BCG-unresponsive cases, one-third of them are most recently initiating intravesical chemotherapy as an alternative option To further assist Arab urologists in the appropriate selection of BCG unresponsive high risk NMIBC patient treatments, enhanced education and pathway protocols are needed
KEY WORDS: Non-muscle invasive bladder cancer; BCG unresponsive; Practice pattern; Arab urologists; BCG shortage
Submitted 30 December 2023; Accepted 17 January 2024
(NMIBC) is an aggressive disease with significant risks of both recurrence and progression Intravesical Bacillus Calmette-Guérin (BCG) has been the standard of therapy for NMIBC for decades (1) Unfortunately, despite frontline BCG therapy, progression to muscle-invasive cancer can occur in up to 20% of cases, especially during the first 2 years of the disease (2) Thus, a proper definition of the BCG disease state is crucial for the appropriate management of NMIBC This includes BCG-naïve patients and BCG-unresponsive patients Most recently, a new category has emerged between the two groups called BCG exposed patients (aka, less than adequate) which includes patients in whom BCG has failed but does not include the guidelines mandated criteria necessary for defining BCGunresponsive (3, 4) The current standard of care for BCG-unresponsive cases does not include repeat BCG therapy or rechallenge with BCG (5)
The management of NMIBC cases has been challenged by BCG shortages that started in 2012 This may increase the number of patients in the BCG-exposed group and, subsequently, BCG-failed cases (6) Urological societies have recommended radical cystectomy (RC) as the best choice for patients in whom BCG has failed (4, 7) However, many patients are assuredly reluctant to undergoing this major life altering operation Thus, numerous intravesical chemotherapy regimens such as gemcitabine (Gem), mitomycin C (MMC) valrubicin, and a combination of gemcitabine and docetaxel (Gem/Doce) and gemcitabine and mitomycin (Gem/MMC) have emerged despite a lack of formal regulatory approvals These therapies may offer promising results with less toxicity than BCG for some patients (8) Interestingly, only three treatment options have been approved by the US Food and Drug Administration (FDA) for BCG unresponsive carcinoma in situ (CIS) tumors: intravesical valrubicin (1998), systematic pembrolizumb (2020), and Nadofaragene firadenovec, a non-replicating adenovirus that produces human interferon alpha-2b
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12244 1
NTRODUCTION
i s k
n o n - m u s c l e - i n v a s i v e b l a d d e r c a n c e r
I
H i g h - R
( H R )
Patternsoftreatmentofhigh-riskBCG-unresponsive non-muscleinvasivebladdercancer(NMIBC)patients amongAraburologists
DOI: 10 4081/aiua 2024 12244
(2022) (9) The application of these therapies is limited by their narrow indication for only CIS-containing tumors, their cost, and their limited worldwide availability
Our survey suggests a paucity of knowledge about the treatment plans utilized for BCG-unresponsive NMIBC patients in Arab countries The purpose of this survey was to learn more about the therapies and options provided to N M
Additional goals included determining which intravesical agents are currently preferred as second-line therapy while understanding the obstacles to offering and implementing new therapeutic alternatives In addition, we aimed to assess the practice pattern of urologists during the BCG shortage The results of the survey will be utilized to establish best practices for the better management of BCG-unresponsive NMIBC cases in the Arab Region
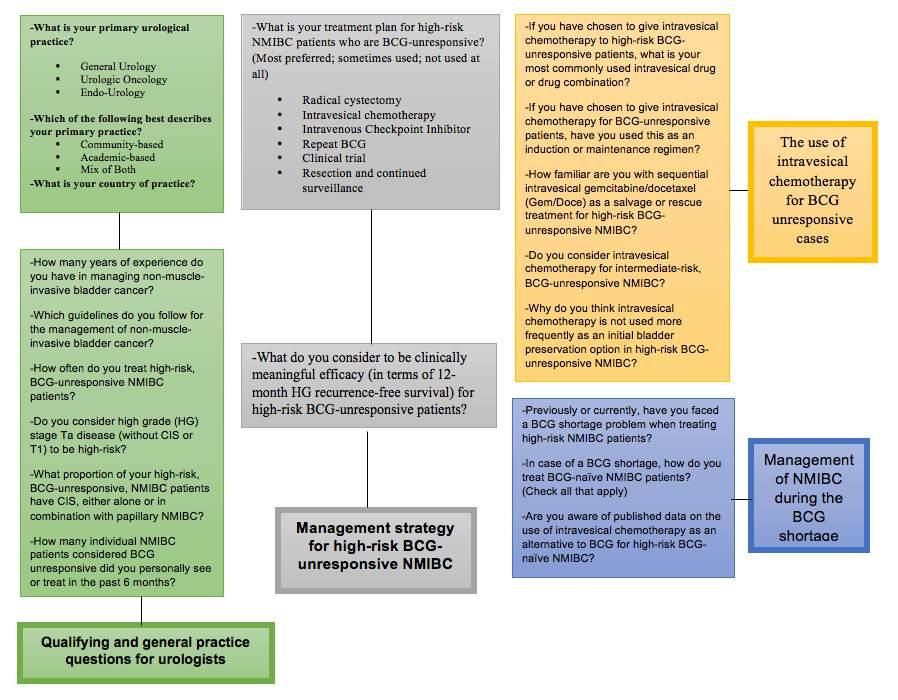
Questionnaire design
The survey included questions on eligibility, treatment preferences, and regimens used for NMIBC patients who are BCG unresponsive, as well as the views of urologists regarding the use of intravesical chemotherapy in those patients and the challenges are encountered Choosing the next course of treatment and managing BCG-unresponsive patients other than by radical cystectomy was queried Additional inquiries were made concerning BCG shortages and the course of action taken to manage BCGnaive cases during shortages
Statistical analysis
Descriptive statistics were used to analyze the data for all combined countries To adequately portray the data, frequencies and percentages were employed for categorical variables There was no missing data because respondents had to complete each question before moving on to the next, and a ‘don’t know’ answer was not allowed
Survey method
Arab urologists received by email a web-based survey with a 10-minute time expectation to complete This survey was sent through the Arab Association of Urology office to urologists recorded in their database More than ten thousand urologists in the Arab world are members of the AAU Data were collected from 22 Arab countries between October 17 and November 17, 2023 (Table 1) Participation in the survey was completely voluntary and anonymous for all respondents No patient records have been collected Responses were kept confidential at all stages of data analysis
RESULTS
Survey respondent demographics and general practice outlines
A survey was sent to the AAU members (more than thousand members), and one hundred and six urologists responded to the survey Among the respondents, 46% were in academic-based practice, 19% in communitybased practice, and the other 35% were in a mix of academic and community-based practice 46% of urologists were subspecialized in urologic oncology and 8% in endourology, while the other 46% were general urologists The majority of urologists had experience managing NMIBC for 10 to 20 years (25%) and > 20 years (49%) Concerning guidelines followed in the management of NMIBC, 31% chose American Urological Association (AUA) guidelines, 36% chose European Association of Urology (EAU) guidelines, 28% chose National Comprehensive Cancer Network (NCCN) guidelines, and 5% chose other guidelines (Society of Urologic Oncology (SUO) and local guidelines)
Management strategy for high-risk BCG-unresponsive NMIBC
The majority of urologists had treated > 10 patients in the past 6 months with NMIBC who were considered BCG unresponsive (55% of respondents), while 45% reported treating < 10 of these patients in the last 6 months When asked about the number of high-risk (HR) BCG unresponsive patients treated per month, 66% of urologists reported treating more than 5 patients per month
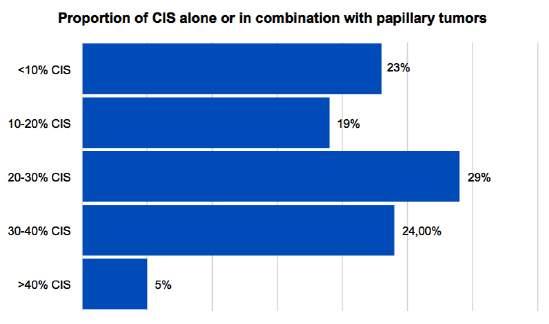
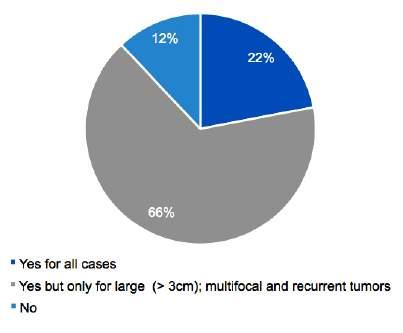
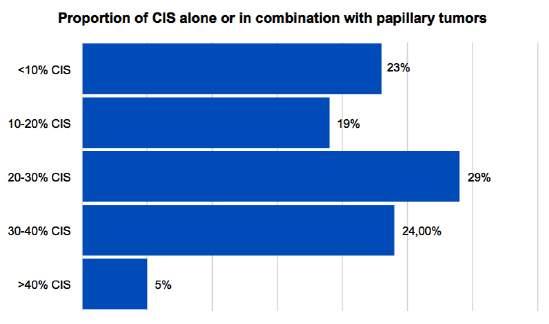
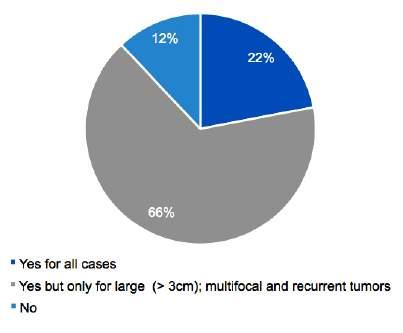
In terms of the proportion of CIS tumors in HR disease, 58% reported treating a proportion > 20% 22% of urologists consider high-grade (HG) Ta disease (without CIS or T1) as an HR tumor; 66% of respondents only consider this type of tumor as HR if the tumor is large (> 3 cm), multifocal, or multi-recurrent (> 1 recurrence per year); and 12% do not consider this type of disease as HR regardless of additional clinical factors A detailed response on tumor characteristics is summarized in Figures 2a, b When questioned on the management strategy for highTable 1.
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12244
2
M Moussa, M Abou Chakra, N D Shore, et al
B C p a t i e n t s w h o f a i l a d e q u a t e B C G t h e r
I
a p y
ATERIALSANDMETHODS
M
Number of respondents according to country of practice in the Arab region Countr y Number of respondents Algeria 5 Bahrain 14 Comoros 0 Djibouti 0 Egypt 12 Iraq 10 Jordan 4 Kuwait 5 Lebanon 16 Libya 0 Mauritania 0 Morocco 4 Oman 9 Palestine 0 Qatar 6 Saudi Arabia 5 Somalia 0 Sudan 0 Syria 0 Tunisia 4 United Arab Emirates 7 Yemen 5
High-risk BCG-unresponsive non-muscle invasive bladder cancer
Figure 1.
Survey-relevant questions delivered to urologists
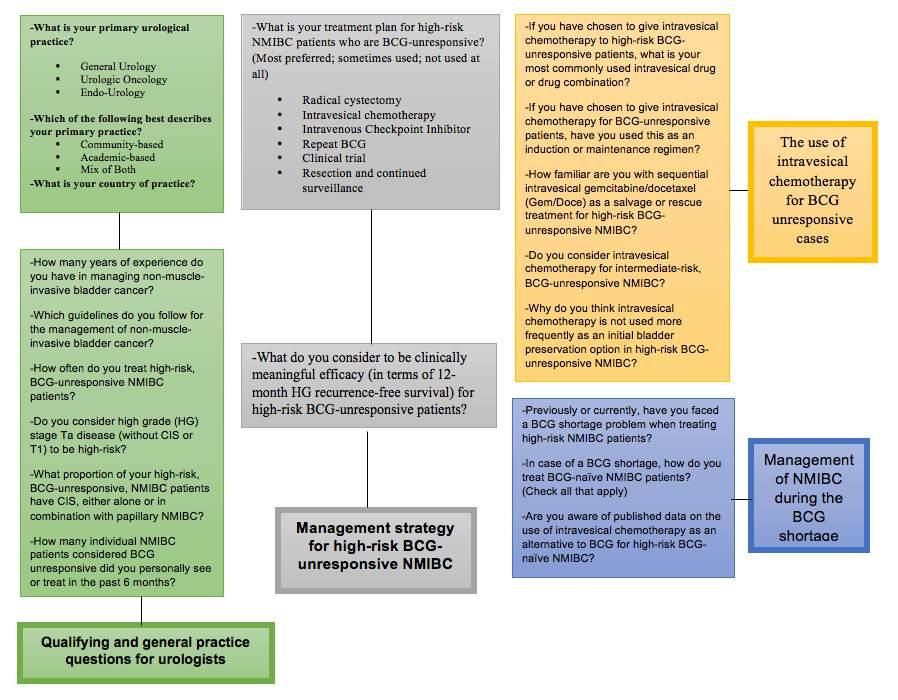
Figure 2.
A Proportion of CIS tumors found in high-risk, BCG-unresponsive, NMIBC patients
B. Percentage of urologists considering HG-stage Ta disease (without CIS or T1) to be high-risk tumors
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12244 3
CIS: carcinoma in situ; BCG: bacille Calmette-Guerin; NMIBC: non-muscle invasive bladder cancer
CIS: carcinoma in situ
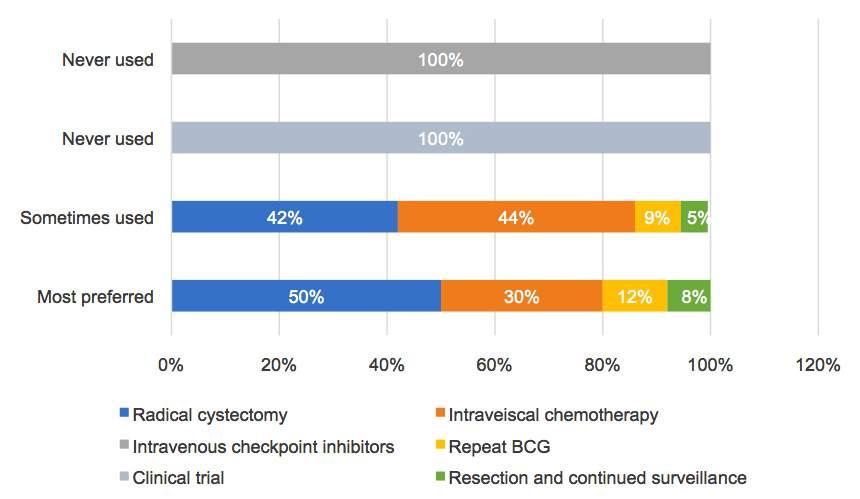
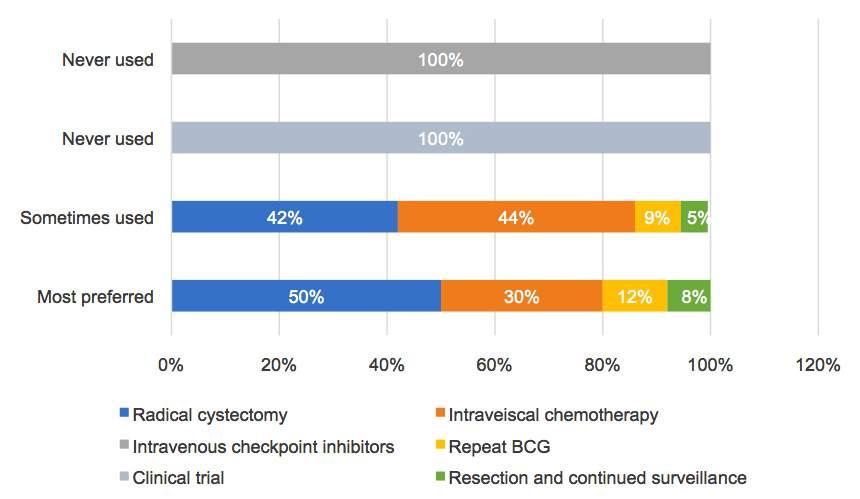
Figure 3. Management strategy for high-risk NMIBC patients who are BCG-unresponsive.
NMIBC: non-muscle-invasive bladder cancer
risk NMIBC patients who are BCG-unresponsive, most preferred RC (50%) followed by intravesical chemotherapy (30%), repeat BCG therapy (12%), and resection with
continued surveillance (8%) Intravenous checkpoint inhibitors and clinical trials were never selected The treatment strategy used by urologists is listed in Figure 3
Figure 4. The most commonly used intravesical drug or drug combination for high-risk BCG-unresponsive patients.

Archivio Italiano di Urologia e Andrologia 2024; 96(1):12244
4
M Moussa, M Abou Chakra, N D Shore, et al
Figure 5. Clinically meaningful efficacy (in terms of 12-month high-grade recurrence-free survival) for BCG-unresponsive patients treated with intravesical chemotherapy
When RC was chosen, 66% of urologists personally performed the cystectomy, while 34% referred patients to another center for cystectomy
The use of intravesical chemotherapy for BCG unresponsive cases
With regard to the most commonly used intravesical drug or combination of drugs, 60% reported gemcitabine, 19% MMC, 8% docetaxel, 8% Gem/Doce, 4% sequential Gem/MMC, and 1% valrubicin The sometimes-used regimen varied with a rank order of 37% MMC, 13% sequential Gem/MMC, 11% docetaxel, 7% gemcitabine, 7% Valrubicin/Docetaxel, 6% Gem/Doce, 6% valrubicin, 3% epirubicin, and 10% other agents The detailed drugs used for intravesical chemotherapy are summarized in Figure 4 60% of urologists used intravesical chemotherapy for induction and maintenance, while the other 40% used it for induction only
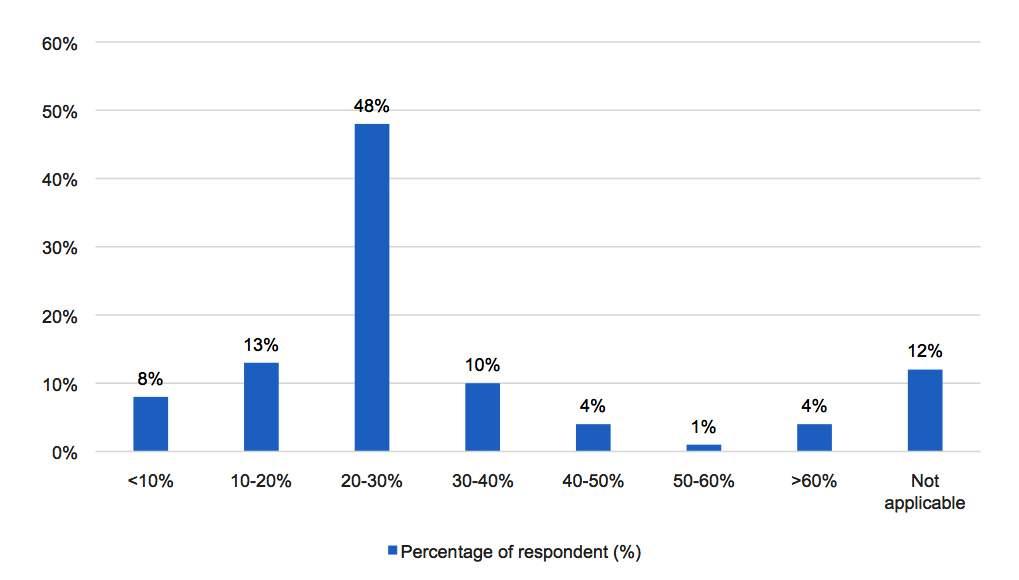
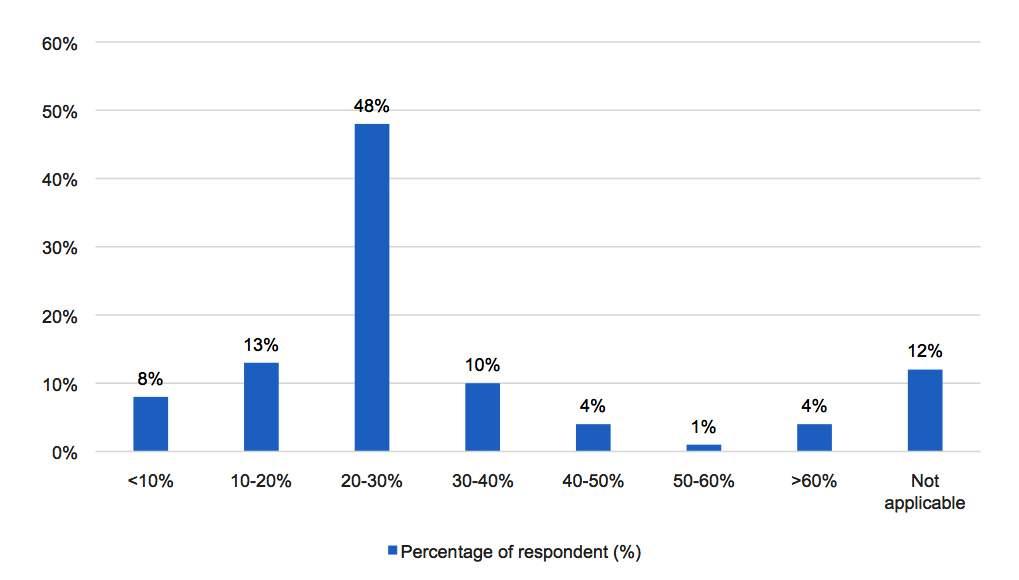
Urologists were also specifically asked what level of clinical response would be a sufficient at 1 year to be clinically meaningful for high-risk BCG-unresponsive patients
Almost 50% of urologists define a 12-month HG RFS of at least 20-30% (Figure 5)
Reporting on the use intravesical chemotherapy for intermediate-risk disease among BCG-failures, 21% of urologists mentioned that they would use further intravesical chemotherapy as a preferred therapy, 27% would use it as a second line treatment, and 52% would never use it in such a situation
A separate question inquired about the familiarity of urologists with sequential intravesical Gem/Doce as salvage therapy for BCG-unresponsive HR-NMIBC patients Only
14% of urologists currently use this therapy but are still evaluating its efficacy; 33% were familiar with this therapy but considered it outside their current practice; and the majority (53% of respondents) were not familiar enough with treatment to consider using it in their daily practice
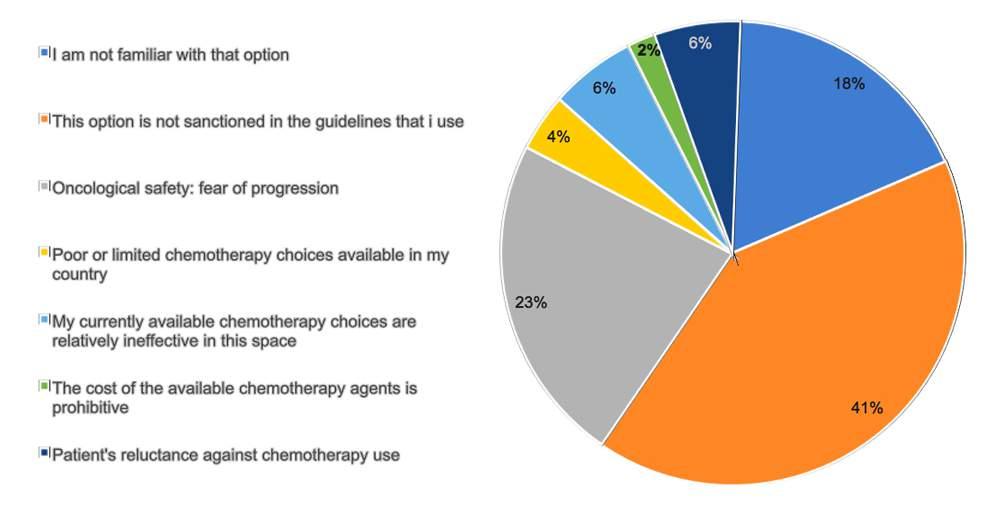
The predominant reasons for not frequently using intravesical chemotherapy as a bladder preservation option in HR BCG-unresponsive NMIBC were investigated 18% of urologists were not familiar with many of the intravesical chemotherapy regimens; 41% stated that bladder sparing options were not sanctioned in the guidelines that they use; while 23% were reluctant due to concern for progression of tumor after usage of those drugs Other reasons cited included patients' refusal of chemotherapy use, limited availability, or cost of treatment (18%) (Figure 6)
Management
of
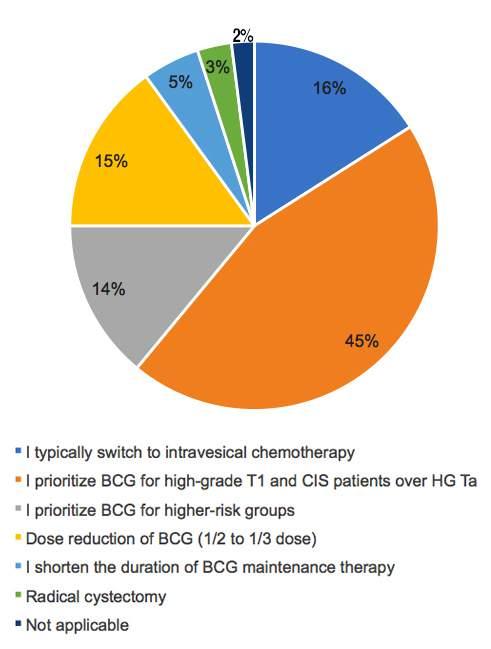
NMIBC during the BCG shortage
In a question inquiring about the current BCG shortage issue faced by urologists when treating HR NMIBC, 68% of respondents confirmed the ongoing shortage, 21% mentioned that they had some shortage problems but not in the past 6 months, and 11% had no shortage at all (Table 2) To treat BCG-naïve patients in cases of BCG shortage, 45% of urologists prioritize BCG for T1 and CIS patients over Ta, 16% switch to intravesical chemotherapy, 15% use dose reduction of BCG (1/2 to 1/3 dose), 14% prioritize BCG for the higher-risk groups, 5% shorten the duration of maintenance therapy, 3% perform radical cystectomy, and 2% just wait to get BCG (Figure 7) Additional questions were asked enquiring about the published data on the use of intravesical chemotherapy as an alternative to BCG for HR BCG-naïve NMIBC Only
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12244 5 High-risk BCG-unresponsive non-muscle invasive bladder cancer
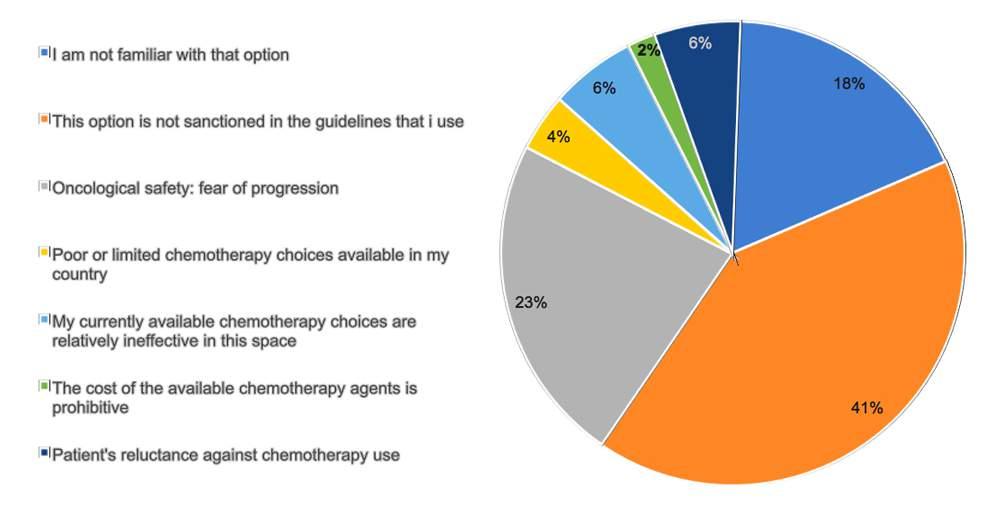
Table 2
BCG supplements according to country of practice in the Arab region.
Countr y Number Ongoing Some shor tage No shor tage of respondents shor tage but not in the past at all 6 months
Algeria 55--
Bahrain 14 842
Comoros 0---
Djibouti 0---
Egypt 12 543
Iraq 10 73-
Jordan 4211
Kuwait 5131
Lebanon 16 15 1-
Libya 0---
Mauritania 0---
Morocco 422-
Oman 97-2
Palestine 0---
Qatar 63-3
Saudi Arabia 523-
Somalia 0---
Sudan 0---
Syria 0---
Tunisia 44--
United Arab Emirates 761-
Yemen 55-72 (68%) 22 (21%) 12 (11%)
21% were not aware of the data published on the topic, and 27% had limited familiarity with the data 34% of urologists would use intravesical chemotherapy if BCG were unavailable, and 18% think the current published data is sufficient to consider certain chemotherapy regimens (Gem/Doce) as a first-line alternative to BCG
DISCUSSION
The management of BCG-unresponsive disease is challenging While new therapies have emerged and addi-
Figure 6.
The most common reasons for not using intravesical chemotherapy as an initial bladder preservation option in high-risk BCG-unresponsive NMIBC
7.
Frequency of options used by urologists to treat BCG-naïve NMIBC patients during the BCG shortage
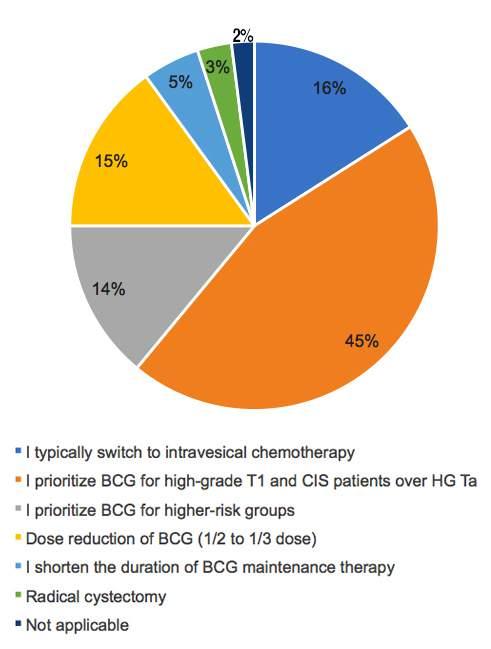
tional novel therapies may soon receive approvals, intravesical chemotherapy remains a real-world, practical and efficacious alternative Several points are notable from this survey of Arab Country Urologists First, RC was chosen as the most preferred initial therapy for BCG-unresponsive cases by half of the Arab urologists This is not consistent with previous surveys from
Urologia
Archivio Italiano di
e Andrologia 2024; 96(1):12244
6
M Moussa, M Abou Chakra, N D Shore, et al
Figure
other regions worldwide, where RC was not selected in the majority of cases Whereas urological societies recommend in their guidelines to do radical surgery for BCGunresponsive cases (4, 7) In a survey in the US evaluating the practice pattern of unresponsive BCG among 259 urologists, only 24% of urologists routinely performed RC for those patients (10) Patients from the UK, France, Germany, and Canada who have received RC within the previous year, were on BCG, or had BCG unresponsiveness were invited to participate in a cross-country study by completing an online choice poll Of the 107 participants, the majority (89%) never chose RC as their preferred form of initial treatment (11) In a US survey on therapy for NMIBC, more than 80% of urologists were reluctant to use RC right away for patients in whom BCG therapy had failed twice (12)
Second, intravesical chemotherapy has been used more and more in real-world practice to manage HR NMIBC cases who failed on BCG 30% of Arab urologists mentioned this therapy as a preferred option, and up to 44% sometimes used it While systemic checkpoint inhibitors or clinical trials have not been used, those results are quite different from those in other countries Recently, according to US data, 55% of urologists have used intravesical chemotherapy and 14% have used intravenous checkpoint inhibitors to manage HR-BCG-unresponsive NMIBC patients Additionally, clinical trials were proposed in less than 10% of cases from the same survey (10) In another multi-country analysis of urologic practice managing BCG unresponsive cases, data were collected in eight countries: France, Germany, Spain, Italy, the UK, the US, China, and Japan 508 physicians were included in the study 48 6% of physicians may use intravesical chemotherapy, and up to 64% may use intravenous checkpoint inhibitors as options for BCG failure disease (13) In additional real-world analysis of the management of BCG-unresponsive patients from three continents, initial intravesical chemotherapy was used in up to 64% of cases in China, but as low as 11% in Japan, and 12% in France While repeat BCG therapy has been rarely used in the UK (9%), Germany (6%), and Italy (10%), it has been frequently used in China and Japan (data not shown) (14) In our survey, only 12% reported repeating BCG as their preferred option, which is in line with other countries results
Third, the most commonly used intravesical chemotherapy in our survey was Gem and MMC, not unlike that reported elsewhere (10) While intravesical Gem has been widely used for BCG unresponsive cases, RFS rates at 24 months are about 40% for high-grade papillary-only cases but only about 20% for CIS-containing NMIBC (15) In contrast, sequential therapy of Gem/Doce and Gem/MMC has also been explored in this area Gem/Doce and Gem/MMC therapy provide 24-month RFS’s of over 40% in BCG failure cases, including those with CIS (8) In our survey, Gem/Doce and Gem/MMC were used by 14% and 17% of urologists, respectively The use of these drugs is also quite different across regions worldwide In a recent US survey, the rank order of intravesical chemotherapy used to treat HR BCG unresponsive NMIBC patients was: Gem 49%, MMC 23%, Gem/Doce 15%, Valubicin 11%, and other 2% (10) In China, the most often administered
drugs are epirubicin (37%), followed by doxorubicin (34%), and Gem (26%) In European countries like France, the UK, and Italy, intravesical MMC is the most common drug used in this setting (13) Fourth, in our survey, almost 50% of urologists determined that the clinically meaningful efficacy (in terms of 12-month HG RFS) for BCG-unresponsive patients treated with intravesical chemotherapy should range from 2030% According to FDA guidelines, an experimental drug should have a 30% RFS rate for papillary tumors in BCGrefractory patients at 18–24 months (16) The fastest
required to process a simulation model with several input parameters, such as survival probability and event timings This was used to conduct a simulated analysis to determine which efficacy in BCG-unresponsive tumors may compete with early RC Following model validation, it was determined that in order to provide clinically relevant efficacy, the FDA/AUA recommendation on efficacy (RFS) should be raised by at least 5% at 18-24 months (17) We note that urologists in our survey expected a lower efficacy of intravesical chemotherapy (less than 30% RFS), thus perhaps the urgent need for an alternate treatment for BCG-unresponsive disease, previous experiences with new drugs, or lack of knowledge of FDA guidelines about the effectiveness of novel therapies impacted such expectations A proper understanding of efficacy outcomes is important in practice when interpreting emerging data from clinical trials and suggesting this treatment in shared decisions with patients Fifth, it was observed that BCG shortages are an ongoing problem in Arab countries, as 68% of urologists encountered shortages of BCG during their practice This parallels other regions globally Options offered to urologists to adapt to the shortage included: dose reduction of BCG, prioritizing BCG for certain tumor stages (T1 or CIS), and using second-line alternatives such as chemotherapy (18) In our survey, Arab urologists have used these strategies Interestingly, only 21% of urologists were not aware of data published on the efficacy of intravesical chemotherapy in HR BCG-naïve NMIBC cases, and only 18% were convinced enough by the data to use the combination of Gem/Doce in this setting Recently, a 2-year RFS of 80% was reported for Gem/Doce used as the first line treatment of HR NMIBC cases, comparable to BCG, making this combination a good choice to substitute for BCG, especially if BCG’s availability is limited (19) The Arab region consists of 22 countries that are situated in North Africa and the Middle East The gross national income of these nations varies greatly from one another leading to significant differences in health care expenditures (20) The cost of therapy for NMIBC includes direct medical costs paid by the patient or its insurance company and indirect costs including home care costs, on-leave costs, and the loss of work productivity Direct costs can be assessed using gross domestic product (GDP) per capita, based on purchasing power parity (PPP), according to World Bank income data (21) With Qatar's GDP per capita PPP of USD $114,049 2 and Somalia's of USD $1,711, there is widespread economic disparity (Table 3) The economic status of the country clearly affected the choice of therapy for BCG-unresponsive NMIBC In high-income countries, the
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12244 7 High-risk BCG-unresponsive non-muscle invasive bladder cancer
s u p e r c o m p u t e r ( u n i f o r m 6 0 , 0 0 0 - c o r e c l u s t e r ) w a s
Algeria 5 13,226 8 53020
Bahrain * * 14 61,248 2 89500
Comoros 0 3,833 7
Djibouti 0 5,893 2
Egypt 12 15,096 584--
Iraq 10 10,865 4 76202
Jordan 4 11,209 9 22200
Kuwait * * 5 58,349 2 11400
Lebanon 16 14,330 5 15 7261
Libya 0 23,382 7
Mauritania 0 6,295 8
Morocco 4 9,547 7 22-2-
Oman * * 9 41,738 2 7630
Palestine * 0------
Qatar * * 6 114,049 2 333--
Saudi Arabia * * 5 59,279 9 23200
Somalia 0 1,711 0
Sudan 0 4,217 4
Syria * 0------
Tunisia 4 12,483.6 41111
United Arab Emirates * * 7 88,489 0 624-1
Yemen 5 3,437 4 5--23 106 72 (68%) * Missing GDP per capita PPP data; ** H gh ncome country; PPP: Purchasing power parity; GDP: gross domestic product; IVC: ntravesical chemotherapy; RC: radical cystectomy; USD: Un ted States do lar
most preferred treatment chosen by urologists was RC or intravesical chemotherapy, whereas options like repeat BCG therapy or resection and surveillance (considered less effective) were more often chosen by urologists from low- or low-middle income countries However, more than 20% of urologists in low-income countries are starting to use intravesical chemotherapy with only 2% of urologists reporting that the cost of drugs was the main reason for not using it (Figure 6) Making these alternatives affordable remains an important goal Interestingly, the BCG shortage was an ongoing problem in all countries, and the prevalence of shortages was not related to income (Table 3) This is likely due to source limitations in the production of BCG It’s possible the strain of BCG used may also vary according to economic factors, but this was not assessed in our survey Intra-arterial chemotherapy (IAC) has been reported for HR-NMIBC by some groups, but in our survey, urologists did not use IAC for BCG-naïve or unresponsive disease Intravesical chemotherapy (IVC) with IAC therapy prevented tumor recurrence and progression more effectively than IVC alone, with only mild to moderate side effects (22) A recent study compared the efficacy of a combination of IAC+IVC (cisplatin and epirubicin + epirubicin or pirarubicin) (n = 43) vs BCG (n = 53) for HR-NMIBC patients Despite having almost the same pathological stage and grade in two groups, there was no significant difference between the recurrence and progression rates 83 1% of patients experienced adverse events linked to BCG, while 46 5% of patients experienced adverse events related to IAC (23) The combination IAC+IVC is effective in both IR and HR cases For HR disease, the 5-year' recurrence rate was reported as 56 3% vs 26 1% in the IVC vs IAC+IVC groups, respectively (p = 0 007) For IR disease, 5 years ’ recurrence rate was reported as 44 4% vs
Table 3
Therapy options for BCG-unresponsive disease and BCG shortage status according to country of practice in the Arab region and their GDP per capita PPP
22 2% in the IVC vs IVC+IAC groups, respectively (p = 0 030) (24) When BCG is unavailable or patients cannot tolerate BCG, IAC may be a viable option to add to IVC for increased efficacy Prospective randomized trials are needed to validate IAC use for NMIBC patients
This survey has several strengths It is the first survey that assesses the practice patterns of urologists treating BCGunresponsive NMIBC in Arab countries It also sheds light on strategies used by urologists and their knowledge about alternative therapies to BCG during the ongoing BCG shortage This survey has several limitations
First, the small sample size may indicate that the results may not be representative of all Arab countries due to the low response rate to the survey
Second, by asking urologists about their patients seen during the last 6 months, a recall bias may exist
Third, the survey was sent only to urologists It is unclear whether medical oncologists have a role in the selection of second-line therapy for BCG-unresponsive NMIBC patients Fourth, selection bias based on prior experience in non-BCG-unresponsive cases might be inappropriately applied by urologists when asked about their preferred therapy
CONCLUSIONS
The present survey found that in Arab countries, RC is still highly used for HR BCG-unresponsive NMIBC patients, while there is an emerging role for intravesical chemotherapy The most preferred chemotherapies used are gemcitabine and MMC Oncological safety (fear of progression) and the lack of inclusion of specific chemotherapy drugs in their guidelines mostly limit their usage by Arab urologists
While the BCG shortage is still an ongoing problem, Arab
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12244
8
M Moussa, M Abou Chakra, N D Shore, et al
Countr y Number GDP per capita PPP Ongoing BCG RC IVC Repeat BCG Resection and of respondents (cur rent inter national USD) shor tage sur veillance
urologists are aware of new evidence emerging on intravesical chemotherapy, especially Gem/Doce, and are willing to utilize those new therapies to cope with the shortage Novel drugs, which include intravesical and intravenous immunotherapy as well as bacterial and viral intravesical therapies, have shown promising results as alternatives to RC in BCG-unresponsive disease It is crucial to raise awareness among urologists about these emerging therapies There is also a need to develop clinical trials for NMIBC in Arab countries and facilitate patient access to these trials to further advance this field
REFERENCES
1 Taylor J, Becher E, Steinberg GD Update on the guideline of guidelines: non-muscle-invasive bladder cancer BJU Int 2020; 125:197-205
2 van den Bosch S, Alfred Witjes J Long-term cancer-specific survival in patients with high-risk, non-muscle-invasive bladder cancer and tumour progression: a systematic review Eur Urol 2011; 60:493-500
3 Roumiguié M, Kamat AM, Bivalacqua TJ, et al International Bladder Cancer Group Consensus Statement on Clinical Trial Design for Patients with Bacillus Calmette-Guérin-exposed High-risk Nonmuscle-invasive Bladder Cancer Eur Urol 2022; 82:34-46
4 Babjuk M, Burger M, Compérat EM, et al European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer (TaT1 and Carcinoma In Situ) - 2019 Update Eur Urol 2019; 76:639-657
5 Yassaie O, Chehroudi C, Black PC Novel and emerging approaches in the management of non-muscle invasive urothelial carcinoma Ther Adv Med Oncol 2021; 13:17588359211039052
6 Bandari J, Maganty A, MacLeod LC, et al Manufacturing and the Market: Rationalizing the Shortage of Bacillus Calmette-Guérin Eur Urol Focus 2018; 4:481-484
7 Chang SS, Boorjian SA, Chou R, et al Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Guideline J Urol 2016; 196:1021-1029
8 Nazmifar M, Williams C, Naser-Tavakolian A, et al Clinical and P r e c l i n i c a l T h e r a p i e s f o r B l a d d e r C a n c e r F o l l o w i n g B a c i l l u s Calmette-Guérin Failure J Urol 2023; 209:32-48
9 Goldberg IP, Lichtbroun B, Singer EA, et al Pharmacologic Therapies for Non-Muscle Invasive Bladder Cancer: Current and Future Treatments Arch Pharmacol Ther 2022; 4:13-22
10 Abou Chakra M, Shore ND, Dillon R, et al US Clinical Practice Patterns of Intravesical Chemotherapy for Bacillus Calmette-GuérinUnresponsive and Bacillus Calmette-Guérin-Exposed NonmuscleInvasive Bladder Cancer Urol Pract 2024; 11:97-107 1
11 Collacott H, Krucien N, Heidenreich S, et al Patient Preferences for Treatment of Bacillus Calmette-Guérin-unresponsive Non-muscle-invasive Bladder Cancer: A Cross-country Choice Experiment Eur Urol Open Sci 2023; 49:92-99
12 Joudi FN, Smith BJ, O'Donnell MA, et al Contemporary management of superficial bladder cancer in the United States: a pattern of care analysis Urology 2003; 62:1083-8
13 Broughton EI, Gooden KM, Mycock KL, et al Multi-country clinical practice patterns, including use of biomarkers, among physicians' treatment of BCG-unresponsive non-muscle invasive bladder cancer (NMIBC) BMC Urol 2022; 22:27
14 Broughton EI, Chun DS, Gooden KM, et al Treatment and dis-
ease management patterns for bacillus Calmette-Guérin unresponsive nonmuscle invasive bladder cancer in North America, Europe and Asia: A real-world data analysis Curr Urol 2022; 16:147-153
15 Abou Chakra M, Packiam VT, O'Donnell MA Real-world efficacy of adjuvant single-agent intravesical gemcitabine for non-muscle invasive bladder cancer (published online ahead of print, 2023 Oct 16) Expert Opin Pharmacother 2023; 1-11
16 Jarow JP, Lerner SP, Kluetz PG, et al Clinical trial design for the development of new therapies for nonmuscle-invasive bladder cancer: report of a Food and Drug Administration and American Urological Association public workshop Urology 2014; 83:262-4
17 Wettstein MS, Naimark D, Hermanns T, et al Required efficacy for novel therapies in BCG-unresponsive non-muscle invasive bladder cancer: Do current recommendations really reflect clinically meaningful outcomes? Cancer Med 2020; 9:3287-3296
18 Bandari J, Maganty A, MacLeod LC, et al Manufacturing and the Market: Rationalizing the Shortage of Bacillus Calmette-Guérin Eur Urol Focus 2018; 4(4):481-484
19 McElree IM, Steinberg RL, Mott SL, et al Comparison of Sequential Intravesical Gemcitabine and Docetaxel vs Bacillus Calmette-Guérin for the Treatment of Patients With High-Risk Non-Muscle-Invasive Bladder Cancer JAMA Netw Open 2023; 6:e230849
20 Katoue MG, Cerda AA, García LY, Jakovljevic M Healthcare system development in the Middle East and North Africa region: Challenges, endeavors and prospective opportunities Front Public Health 2022; 10:1045739
21 World Bank GDP Per Capita, PPP (Current International $) World Development Indicators Database World Bank, 2023 (https://data worldbank org/indicator/NY GDP PCAP PP CD)
22 Chen J, Yao Z, Qiu S, et al Comparing intra-arterial chemotherapy combined with intravesical chemotherapy versus intravesical chemotherapy alone: a randomised prospective pilot study for T1G3 bladder transitional cell carcinoma after bladder-preserving surgery Cardiovasc Intervent Radiol 2013; 36:1521-1526
23 Huang B, Huang G, Li W, et al Intra-arterial chemotherapy combined with intravesical chemotherapy compared with intravesical BCG immunotherapy retrospectively in high-risk non-muscle-invasive bladder cancer after transurethral resection of the bladder tumor J Cancer Res Clin Oncol 2021; 147:1781-1788
24 Lian F, Chen W, Liu Y, et al Intra-arterial chemotherapy combined with intravesical chemotherapy is effective in preventing recurrence in non-muscle invasive bladder cancer J Cancer Res Clin Oncol 2019; 145:1625-1633
Correspondence
Mohamad Moussa, MD mohamadamoussa@hotmail com Mohamad Abou Chakra, MD (Corresponding Author) mabouchakra@uiowa edu University of Iowa, IA, US
Neal D Shore, MD nshore@auclinics com Athanasios Papatsoris, MD agpapatsoris@yahoo gr Yasser Farahat, MD yasserafarhat@gmail com Michael A O'Donnell, MD michael-odonnell@uiowa edu
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12244 9 High-risk BCG-unresponsive non-muscle invasive bladder cancer
ORIGINAL PAPER
Wahjoe Djatisoesanto 1, 2 , Yufi Aulia Azmi 1, 2, 3 , Ida Bagus Gde Tirta Yoga Yatindra 1, 2
1 Department of Urology, Faculty of Medicine, Universitas Airlangga;
2 Dr Soetomo General-Academic Hospital, Surabaya, East Java, Indonesia;
3 Department of Health Sciences, University of Groningen, University Medical Center Groningen, Groningen, The Netherlands
Summary
Background: Bladder Cancer (BC) is one of the health problems. Socioeconomic status (SES) may correlate with patient treatment, possibly impacting patient prognosis. This study aimed to determine the relationship between income, health insurance, and employment status as prognostic indicators of BC.
Methods: A retrospective observational study for patients diagnosed with BC in a hospital during the 5-year period between January 2019 and December 2023 Kaplan-Meier test analysis was used to generate overall survival curves stratified by income, employment status, and health insurance Multivariate Cox proportional-hazards regression was used to identify factors associated with worse overall survival
Results: The results of the analysis on 219 patients showed no difference in patient survival based on income (p > 0 05), while employment status and health insurance showed significant difference in patient survival (p < 0.05). Moreover, there were 99 (45 2%) patients died, with the average patient being 58 years old and dominant in male patients.
Conclusions: Prevention of poor outcomes in patients needs to pay attention to certain characteristics, particularly for the loweconomic patients without appropriate national health insurance coverage.
KEY WORDS: Bladder cancer; Insurance; Outcomes; Income; Employment
Submitted 23 January 2024; Accepted 3 February 2024
Bladder cancer (BC) is a neoplasm that arises from the bladder and is the most common type of urinary tract neoplasm (1) This cancer is included in one of the 10 most common cancers worldwide and has a high mortality rate (2) BC accounts for 3% of global cancer diagnoses and is particularly common in developed countries This case is mainly found in people aged 55 years, who are found in as many as 90% of diagnoses, and the disease is four times more common in men than women (3) The incidence rate is twice as high in developing countries than in developed countries (1)
Treatment of bladder cancer tends to be significant and expensive (4) Diagnosis relies mainly on cystoscopy, an invasive and costly procedure Most BCs are diagnosed at an
early stage when they can be treated However, about 25% of BCs are diagnosed at an advanced stage (2) The prognosis depends on many factors (1) SM survival varies significantly according to stage, in both non-invasive and invasive cases The percentage of non-invasive cancers is relatively high Stage, age, and histology associated with survival (5) The probability of accumulated survival at the end of 1, 3, 5, and 10 years in patients with BC is 0 8989, 0 7132, 0 5752, and 0 2459, respectively There are significant differences in survival rates between age groups and types of treatment (6) The stage and extent of the cancer are important factors in determining the best treatment for BC (7) Continuity Cancer survival is generally lower for residents of more socio-economically disadvantaged areas Socio-economic inequality decreases survival due to certain factors (8) In addition, health insurance is the determinant of patient treatment The burden of cancer survival also affects healthcare systems and society (9) Inhospital mortality can occur in patients with BC The objective of this study was to determine the relationship between income, health insurance, and employment status as prognostic indicators of bladder cancer
Study design
Indonesia, Dr Soetomo General Academic Hospital, carried out a retrospective observational study for patients with bladder cancer Hospitalized BC patients were the subject of the research, which ran for five years, from January 2019 to December 2023 Adult BC patients were included, and patients with missing data met the exclusion criteria The Dr Soetomo General Academic Hospital's ethical review board granted approval for the research, which was carried out under the Declaration of Helsinki (approval number: 1527/ LOE/ 301 4 2/ XI/ 2023)
Data collection
The following socioeconomic data were extracted for analysis: income, employment status, and health insurance Patients were divided by income below 4 million Rupiah or more than 4 million Rupiah, according to the basic salary in
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12305 1
MATERIALSANDMETHODS
T h e l a r g e s t t e r t i a r y r e f e r r a l h o s p i t a l i n E a s t J a v a ,
INTRODUCTION
Therelationshipbetweenincome,healthinsurance, andemploymentstatusasprognosticindicators ofbladdercancer:Asurvivalanalysis
DOI: 10 4081/aiua 2024 12305
Indonesia They were divided by type of health insurance as patients with National Health Insurance (Jaminan Kesehatan Nasional/JKN) or private insurance Mortality in this insurance system was defined as death during the hospital stay
Statistical analysis
Survival analysis was done for patients whose income, work status, and health insurance were known Time in months from diagnosis to death from any cause was the primary outcome For every variable, descriptive epidemiological and survival statistics were computed The overall survival curves were stratified by income, job status, and health insurance using Kaplan-Meier test analysis Log-rank tests were used to analyze survival differences To find the variables linked to a lower overall survival rate, multivariate Cox proportional-hazards regression was used Hazard ratios (HR) and accompanying 95% confidence intervals (CI) were utilized We also analyzed the regression to predict sepsis and metastases as strata The criterion for statistical significance was fixed at P < 0 05 The statistical studies were conducted using IBM Corp 's SPSS 25 program in Armonk, NY
RESULTS
There were 99 (45 2%) patients who died Results show that the average patient is 58 years old with prevalence of male patients Our analysis shows that the characteristics of income below 4 million rupiah and education level have significant impact in mortality rates
Sociodemographic characteristics are shown in Table 1
The results of the socio-economic status (SES) data assessment show that most patients have an income of more than 4 million rupiahs every month More than half of the
Table 1. Socioeconomic Status
respondents were employed Most have health coverage SES data are shown in Table 2 Based on the results of survival analysis using Kaplan Meier (Log-rank), there was no difference in patient survival based on income (p > 0 05) (Figure 1), while there was a difference in patient survival based on employment status and health insurance (p < 0 05) (Figures 2, 3)

1. Survival analysis of bladder cancer patients with different income
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12305
2
W Djatisoesanto, Y Aulia Azmi, I Bagus
Gde
Tirta Yoga Yatindra
Component N%P Race Javanese 164 74 9 0 253 Madurese 50 22 8 Chinese 5 2.3 Income ≥ 4 million rupiah 192 87 7 < 0 001 < 4 million rupiah 27 12 3 Employment Status Yes 113 51 6 0 013 No 106 48 4 Farmer Yes 21 10 6 0 002 No 198 89.4 Location Urban 52 23 7 0 812 Rural 167 76 3 Health Insurance National Insurance 174 79.5 0.827 Private Insurance 45 20 5 Education Educated 177 80 8 < 0 001 Non-Educated 42 19 2
Figure

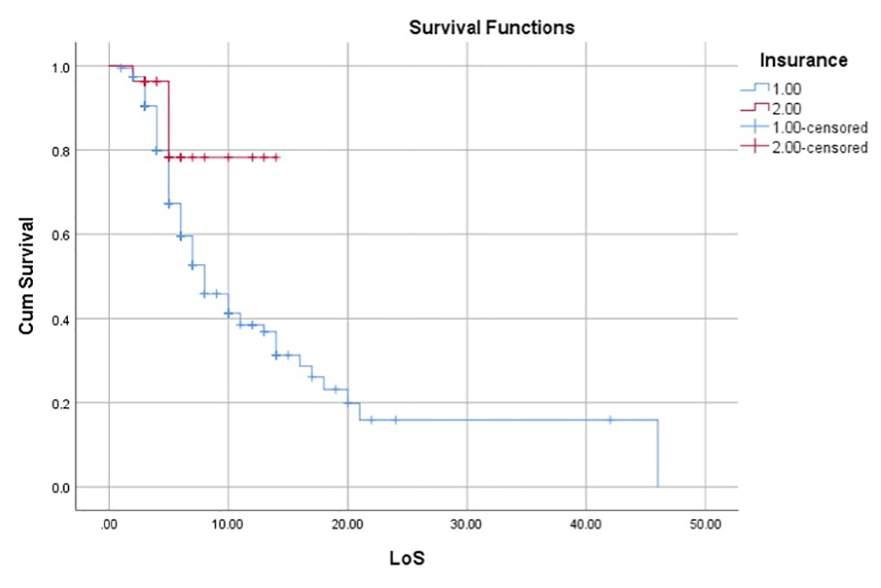
DISCUSSION
The results showed that there was no difference in patient survival based on income, while, there were differences in patient survival based on employment status and health insurance Previous research has found relationship between socioeconomic status and survival, although socioeconomic assessments were carried out with different standards (10) Other studies have found that cancer
Figure 2. Survival analysis of bladder cancer patients with different employment status
Figure 3 Survival analysis of bladder cancer patients within different health insurance
survival is often poorer among people from more socioeconomically disadvantaged areas For tumors of connective/soft tissue, bladder, and unknown primary origin, socioeconomic differences in survival decrease with increasing age at diagnosis (8) In addition, health insurance is the determinant of patient treatment Finally, the burden of cancer survival also affects healthcare systems and society (9)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12305 3 Prognostic indicators of bladder cancer
Taylor et al discovered that characteristics related with a greater chance of bladder cancer presenting at an advanced stage compared to early stages were race, ethnicity, gender, insurance status, one or more comorbidities, and a median household income of less than $63,000 (11) Other researchs have found that lower SES, Medicaid insurance, and no insurance all resulted in a higher tumor stage Regardless of the stage of the tumor, poorer SES, having Medicaid insurance, and no insurance linked to worse overall survival (OS) and disease specific survival (DSS) (12)
Worse overall survival is related to male gender and significant prognostic factors of overall survival include gender (13) Other studies found that women's risk levels were significantly higher than men's for up to two years after a bladder cancer diagnosis, especially for muscleinvasive cancers The common belief that the prognosis for bladder cancer is poorer in women compared to men must be reconsidered (14)
In Indonesia, National Health Insurance (NHI) significantly enhances public health and offers low-income households access to care Nonetheless, NHI coverage below the federal minimum or the government's guidelines may affect health at all phases and developments The growth and development of stunted children, immunization rates, and the quality of life for those with non-communicable illnesses may all be negatively impacted by low NHI coverage Moreover, health insurance is less common among rural homes The main criterion for eligibility for Indonesia's subsidized and contributory programs is that participants must be employed and live in Java or Bali Low coverage may also be due to the cost of traveling to the health insurance office (15)
This burden should be evenly distributed across stakeholders considered in the evaluation of the cost-effectiveness of new anti-cancer drugs (9) Patient survival rates can be enhanced through strategic planning for early detection and screening, as well as proper access to appropriate diagnostic and treatment services, particularly in men, considering the significant influence on disease stage at diagnosis (16)
CONCLUSIONS
There is no difference in patient survival based on income, while there are differences in patient survival based on employment status and health insurance Health insurance and employment status, specifically being a farmer, might affect the mortality outcomes significantly
3 Saginala K, Barsouk A, Aluru JS, et al Epidemiology of Bladder Cancer Med Sci 2020; 8:15
4 Cumberbatch MGK, Noon AP EAU on behalf of the Young Academic Urologists- Urothelial Cancer Working party Epidemiology, aetiology and screening of bladder cancer Transl Androl Urol 2019; 8:5-11
5 Ripoll J, Ramos M, Montaño J, et al Cancer-specific survival by stage of bladder cancer and factors collected by Mallorca Cancer Registry associated to survival BMC Cancer 2021; 21:676
6 Rezaianzadeh A, Mohammadbeigi A, Mobaleghi J, Mohammadsalehi N Survival analysis of patients with bladder cancer, life table approach J Midlife Health 2012; 3:88-92
7 Bethesda (MD): National Cancer Institute (US) PDQ Cancer
books/NBK66044/
8 Afshar N, English DR, Blakely T, et al Differences in cancer survival by area-level socio-economic disadvantage: A population-based study using cancer registry data PLoS One 2020; 15:e0228551
9 Michaeli JC, Boch T, Albers S, et al Socio-economic burden of disease: Survivorship costs for bladder cancer J Cancer Policy 2022; 32:100326
10 Russell B, Häggström C, Holmberg L, et al Systematic review of the association between socioeconomic status and bladder cancer survival with hospital type, comorbidities, and treatment delay as mediators BJUI Compass 2021; 2:140-58
11 Taylor A, Gallegos JM, Verplancke K, et al Socioeconomic factors associated with stages of bladder cancer at diagnosis: Analysis of the National Cancer Database J Clin Oncol 2022; 40(16 suppl):e16531e16531
12 Nazemi A, Ghodoussipour S, Pearce S, et al Socioeconomic and insurance status are independent prognostic indicators of higher disease stage and worse prognosis in bladder cancer Urol Oncol Semin Orig Investig 2019; 37:784-90
13 Fang W, Yang ZY, Chen TY, et al Ethnicity and survival in bladder cancer: a population-based study based on the SEER database J Transl Med 2020; 18:145
14 Andreassen BK, Grimsrud TK, Haug ES Bladder cancer survival: Women better off in the long run Eur J Cancer 2018; 95:52-8
15 Sukartini T, Arifin H, Kurniawati Y, et al Factors Associated with National Health Insurance Coverage in Indonesia F1000Res 2021; 10:563
16 Amiri M, Heshmatollah S, Esmaeilnasab N, et al Survival rate of patients with bladder cancer and its related factors in Kurdistan Province (2013-2018): a population-based study BMC Urol 2020; 20:1-9
ETHICALAPPROVAL
The Dr Soetomo General Academic Hospital’s ethical review board grants approval for this research carried out under the Declaration of Helsinki (approval number: 1527/LOE/301 4 2/XI/ 2023)
REFERENCES
1 Kaseb H, NR A Bladder Cancer In: StatPearls [Internet] Treasure Island (FL): StatPearls Publishing 2023
2 IARC Bladder cancer 2023; Available from: https://www iarc who int/cancer-type/bladder-cancer/
Correspondence
Wahjoe Djatisoesanto wahjoe djatisoesanto@fk unair ac id
Yufi Aulia Azmi y aulia azmi@umcg nl, yufiazmi@gmail com
Ida Bagus Gde Tirta Yoga Yatindra tirtayogastudi@gmail com
Department of Urology, Faculty of Medicine, Airlangga University, Soetomo General Academic Hospital
Jl Mayjen Prof Dr Moestopo No 6-8, Surabaya, East Java, Indonesia, 60286
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12305
4
W Djatisoesanto, Y Aulia Azmi, I Bagus
Gde
Tirta Yoga Yatindra
I n f o r m a t i o n S u m m a r i e s : B l a d d e r C a n c e r T r e a t m e n t : P a t i e n t V e r s i o n 2 0 2 3 ; A v a i l a b l e f r o m : h t t p s : / / w w w n c b i n l m n i h g o v /
ORIGINAL PAPER
ofresults?
Pier Paolo Prontera 1 , Francesca Romana Prusciano 2 , Marco Lattarulo 1 , Emanuele Utano 1 , Francesco Schiralli 1 , Carmine Sciorio 3 , Lorenzo Romano 4 , Francesco Saverio Grossi 1
1 Department of Urology, “S S Annunziata” Hospital, Taranto, Italy;
2 Department of Emergency and Organ Transplantation-Urology, Andrology and Kidney Transplatation Unit, University of Bari, Bari, Italy;
3 Department of Urology, “Alessandro Manzoni” Hospital of Lecco, Lecco, Italy;
4 Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples “Federico II”, Naples, Italy
Summary
Background: Social media are widely used information tools, including the medical/health field Unfortunately, the levels of misinformation on these platforms seem to be high, with a medium-low quality of the proposed content, as evidenced by previous studies You Tube is one of the most important platforms for audio/video content It shows content to users through a recommendation algorithm system
Materials and methods: We have classified in two cohorts the first results obtained by researching "bladder tumor treatment" on You Tube through two different user profiles: "Cohort A" with a not logged-in session in incognito mode (46 videos enrolled) and "Cohort B" with a logged-in session with a physician profile (50 videos enrolled) The videos were evaluated using validated instruments such as DISCERN and PEMAT-AV Furthermore, we used a Likert’s scale for the evaluation of levels of misinformation.
Results: Overall quality of information was moderate to poor (DISCERN 3) in 54% of cohort A and 24% of cohort B. Moreover, a high degree of misinformation (Likert score 3) was found in 52% of cohort A cases and 32% of cohort B.
Conclusions: Levels of misinformation in both cohorts are positively correlated to the number of views per month. Globally, the levels of information quality, understandability and actionability are lower for the results obtained from searches performed with anonymous user profile (Cohort A)
KEY WORDS: Bladder cancer; YouTube; Misinformation; Social media; Bladder
Submitted 11 December 2023; Accepted 24 December 2023
Since YouTube platform was established, on February 14th 2005, the world of information and communication has been revolutionized This social media is a widely used tool, with more than 1 5 billion users (1), allowing to find information on many areas of interest
The quality of information available on YouTube is evoking considerable interest in scientific literature in recent years Several authors have already assessed the reliability of the
information on YouTube about some urological pathologies
In particular, the quality of information about neoplastic bladder disease has been evaluated (2, 3)
Bladder cancer is the 10th most frequent cancer in the world (4) A high number of patients with this disease use social media for information and support (5)
The quality of information available on YouTube about this disease appears mostly moderate or poor (2) and this leads to a high risk of disinformation for users Other social media, such as Twitter, also collect information about this disease (6)
The therapeutic opportunities and the possible surgical indication determine a strong emotional impact for these patients, for instance, the possible urinary diversion after radical cystectomy
The possibility of obtaining reliable information about these aspects, using social tools such as YouTube, therefore, appears an important factor in the path of understanding and acceptance of the pathology by these patients
YouTube platform is very dynamic with thousands of hours of contents up-loaded per second
Deep learning has recently had a huge impact on the Yo u Tu b e v i
, YouTube’ s algorithm selects output based on different factors like user ’ s history and context (7, 8)
Nowadays, the absence of information about the characteristics of YouTube users has not allowed authors who investigated this field to evaluate the impact of these videos on patient’s decision making (2), furthermore we have no data about the quality of information related to YouTube user ’ s profile
The primary end point of this paper is to evaluate quality of informations available on the YouTube platform in 2023, with focus on informations about the bladder cancer treatment, evaluating the relation between numbers of views and other point of interest, such as age of the videos, level of misinformation, DISCERN score and PEMAT-AV score
Authors also wanted to explore a secondary endpoint in order to evaluate the differences in term of quality of information and level of disinformation of contents
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12179 1
e o re c o m m e n d a t i o n s s y s t e m
t h e re f o re
d
,
INTRODUCTION
Qualityofbladdercancertreatmentinformation onYouTube:Maytheuser’sprofileaffectthequality
DOI: 10 4081/aiua 2024 12179
emerged from researches made by different user ’ s profile (in particular comparing the results obtained using a logged-in session with a physician profile (Urologist) with those obtained using a not logged-in session (in incognito mode)
MATERIALSANDMETHODS
YouTube algorithm was queried independently of the two different authors, on November 19th, 2023, at 10 o'clock
The keywords used were: "bladder tumor treatment"
Authors used two different user setting: a logged-in session with a physician profile (Urologist) and a not loggedin session in incognito mode
We decided to exclude from the analysis advertising video and ten "very short videos" , which by definition can be a maximum of 60 seconds long and should be a minimum of 15 seconds long, without any information about number of views and comments
We received first 60 videos for both cohorts so we enrolled 50 videos in the first cohort (logged-in session with physician profile) and 46 videos in the second cohort (not logged-in session in incognito mode) Were excluded ten and fourteen videos respectively in the two groups, given the exclusion criteria
All contents enrolled were analysed using validate instruments: the Patient Education Materials Assessment Tool for Audio-Video (PEMAT-AV) and DISCERN quality criteria for consumer health information (9, 10) The Patient Education Materials Assessment Tool (PEMAT) is a systematic method to evaluate and compare the understandability and actionability of patient education materials It is designed as a guide to help determine whether patients will be able to understand and act on information Separate tools are available for use with print and audiovisual materials (11)
DISCERN is a brief questionnaire which provides users with a valid and reliable way of assessing the quality of written information on treatment choices for a health problem DISCERN can also be used by authors and publishers of information on treatment choices as a guide to the standard which users are entitled to expect (12) Moreover, we rated the level of misinformation using a Likert scale (13) We also evaluated other parameters according to other authors (2): Length of video (less than 4 minutes, 4 to 20 minutes, or more than 20 minutes), presence of advertising during viewing, age of video, number of views, type of publisher (academic journal/company, commercial/industrial, consumer/patient, physician, foundation, health/wellness channel, hospital/clinic, medical education, news, source/media outlet, professional society, university, other), number of thumbs-up and thumbs-down, audience (anyone/public, medical education), audience (any/general public, patients, healthcare providers, caregivers), characters in the video (animation/drawing, celebrity/public figure, doctor/healthcare professional, patient, other)
We also assessed the relation between numbers of views (globally and per months) and other variables using Pearson correlation coefficients
We also evaluated the total number of comments per video Analysis for both cohorts lasted twelve days
RESULTS
From now on the group of videos searched using the user profile not logged-in and with session in incognito mode will be called "Cohort A" , and the group of videos obtained using logged-in physician user profile will called "Cohort B" (Table 1)
The total length of videos was 271 31 minutes (median length of 5 51 minutes) for the cohort A and 268 45 minutes (with a median length of 5 35 minutes) for cohort B
The majority of the videos was less than 4 minutes in both cohorts (43 5% and 56% respectively)
The median numbers of views for both groups were respectively 19 6k and 57 5k for Cohort A and Cohort B, with a median age of each videos calculated of 5 21 and 3 66 years respectively
A median of 111 65k thumbs up were found in the Cohort A and 545 24k in Cohort B While no thumbs down were funded in both Cohorts
Most of the contents in Cohort A was aimed at anyone (83%) and to Healthcare providers (15%) Only 1% of contents of the Cohort A was specifically for patients
Table 1.
Property of the analysed YouTube® videos.
Value
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12179
2
P Paolo Prontera, F Romana Prusciano, M Lattarulo, et al
Cohor t A Cohor t B Lenght of video Total lenght 271 31 268 45 Median lenght (h:min:sec) (range) 5 51 (0 49-51 04) 5 36 (48 3-0 52) Less than 4 min (n°) 20 (43 5%) 28 (56%) 4-20 min (n°) 19 18 More than 20 min , n° (%) 64 Views, median (range) 19 6k (26-247k) 57 5K (0-362k) Thumbs up, median (range) (tot) 111 65 (0-2 39k) (4801k) 545,24 (0-3 58k) (27 26k) Thumbs down, median (range) 0 (0) 0 (0) Comment, median (range) (tot) 35 3 (0-196) (1658) 43 4 (0-242) (2040) Intended audience, n° (%) Anyone 38 (83%) 37 (74%) Specifically for patients 1 (2%) 12 (24%) Healtcare providers 7 (15%) 1 (2%) Caregivers 0 0 (0) Others 0 0 (0) Publisher type, n° (%) Academic journal/company 6 (13%) 0 (0) Commercial/industry 1 (2%) 4 (8%) Consumer/patient 0 (0) 0 (0) Doctor 11 (24%) 4 (8%) Foundation 2 (4%) 9 (18%) Healt/wellness channel 15 (33%) 11 (22%) Hospital/clinic 5 (11%) 6 (12%) Medical/education 0 (0) 8 (16%) News source/media 1 (2%) 2 (4%) Professional society 4 (9%) 3 (6%) University 0 (0) 2 (4%) Others 1 (2%) 1 (2%) Who is in?,
(%) Doctor/healthcare professional 40 (87%) 34 (68%) Others 6 (13%) 16 (32%) Presence of advertising, n° (%) 18 (39%) 13 (26%) Presence of “very short videos” 4 (9%) 3 (6%) Median age of the videos (years) 5 21 3 66
n°
Table 2.
Results of analysis with validated tools (DISCERN, PEMAT-AV) Value
DISCERN overall rating, n° (%)
1 6 (13%) 0 (0)
2 8 (17%) 2 (4%) 3 11 (24%) 10 (20%)
4 13 (29%) 32 (64%)
5 8 (17%)
MISINFORMATION score (Likert Scale) no (%)
1 3 (6%) 14 (28%) 2 15 (32%) 20 (40%) 3 10 (22%) 10 (20%)
4 6 (13%) 6 (12%)
5 12 (27%) 0 (0%)
Similar results emerged from the analysis of Cohort B with the 74% of contents directed to anyone, but with an inversion of proportion regarding Healthcare providers and patients (2% and 24% respectively)
Doctors or health care professional were the most frequent characters in the contents in both Cohorts (87% for Cohort A and 68% for Cohort B)
The presence of advertisements that interrupted the viewing of the video was found in 39% of cases in cohort A and in 26% of cases in Cohort B
According to the DISCERN score, the quality of information was moderate to poor for the Cohort A (median range 42 4) and moderate to high for the cohort B (median range 59 56), and the score 1 appears in 13% of the cohort A while it was never present in the Cohort B
Moreover, in both groups the DISCERN most representative score was 4 with a prevalence of 64% for the cohort B instead of the 29% for the Cohort A
In the cohort A the understandability score and the actionability score, calculated using PEMAT-AV tool, were median to poor (respectively 49% and 44%), whereas the same parameters were evaluated moderate to high for the cohort B (respectively 76% and 77 7%)
The application of a Likert scale revealed a low level of misinformation in cohort B if compared with cohort A In particular, we found 28% vs 6% of score 5 and 0% vs 27% of score 1, in cohort B and A respectively (Table 2)
Application of Pearson correlation coefficients highlighted a moderate positive correlation between overall views and the level of misinformation, considering cohort B, and a weak negative correlation considering cohort A for the same factors
The relation between overall views and PEMAT-AV score (understandability and actionability both) was weakly positive for both groups, while we discovered a weak negative correlation between overall views and DISCERN score for the cohort B versus a weak positive correlation found for the cohort A (Table 3)
Investigating relationships of DISCERN score, PEMAT-AV score and misinformation levels to the views per months,
Table 3
Correlation between the number of total views and the variables examined.
Tot view Variables Pearson
(r) (n°)
* Age of the video 0 144 (weak) 0 25 (weak)
* Misinformation (Likert scale) -0 028 (weak) 0 400 (moderate)
* DISCERN score 0 166 (weak) -0 252 (weak)
* PEMAT-AV understandability 0 009 (weak) 0 150 (weak)
* PEMAT-AV actionability 0 031 (weak) 0 170 (weak)
* Rounded to the three decimal places
Table 4.
Correlation between the number of views/month and the variables examined
V iew per Variables Pearson Index (r) month (n°) Cohor t A Cohor t B
* Age of the video -0 26 (weak) 0 25 (weak)
* Misinformation (Likert scale) 0 012 (weak) 0 007 (weak)
* DISCERN score 0 153 (weak) -0 75 (strong)
* PEMAT-AV understandability -0 004 (very weak) -0 550 (moderate)
* PEMAT-AV actionability 0 073 (weak) 0 097 (weak)
* Rounded to the three dec ma places
we found a strong negative correlation between DISCERN score and views per months in Cohort B and a weak positive correlation in cohort A (Table 4) These findings are in line with the results of other authors (2, 3)
DISCUSSION
Social media today represent a mass information tool also regarding the demand for information in the healthcare sector The same health professionals (healthcare professionals) use social media for scientific dissemination Unfortunately, the massive presence of disinformation on the Web is a serious social problem (2, 14), which, in our opinion, can have an impact both on the psychological sphere of the patient undergoing medical treatment, especially if it is invasive, and on the ability of the professional to convey the appropriate information in the most correct way In recent years several authors have investigated the quality and levels of misinformation present in content published on various social media, through the use of validated tools (9, 10, 13], showing a high percentage of erroneous content in the publications (2, 3, 14) YouTube is one of the leading platforms for visual audio content and uses a search algorithm that, thanks to deep learning, offers results selected according to the characteristics of the user and his activity on the site (8) Therefore, we decided to evaluate the results obtained from the research of "bladder tumor treatment" performed through two different user accounts: Cohort A and Cohort B
Overall, the quality of the contents obtained in cohort B was higher (96% of medium-high quality compared to 69% obtained in cohort A) On average the contents of cohort B have higher levels of understandability and
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12179 3 Bladder cancer treatment information on YouTube
Cohor t A Cohor t B
6 (12%) DISCERN sum (median range) 42 4 (19-78) 59 56 (22-76)
Understandability 49% (0-100) 76% (0-100%) Actionability 44% (0-100) 77 7% (0-100%)
PEMAT-AV, median (range)
Cohor t A Cohor t B
Index
Table 5. Spread of contents about treatment of bladder tumor on
Cohor t A Cohor t B
Moderate to poor quality (DISCERN ≤ 3)
High Misinformation (Likert score ≥ 3)
High Understandability (> 50%)
Actionability (> 50%)
actionability (76% and 77 7% respectively compared to 49% and 44% observed in cohort A) (Table 5)
This data seems to confirm that the same search performed by a user profile closely related to the field of interest of the search, returns results of higher quality and with higher level of understandability and actionability However, this could be a contradiction because if on the one hand it is logical for the algorithm to propose higher quality videos based on the level of affinity of the user profile to the search, on the other hand it seems controversial to show videos with a lower level of understandability and actionability to an average user not associated with a health profile and therefore potentially with a lower ability to understand the content
As for the level of misinformation, obtained through the use of a Likert scale, our data are almost in line with previous published studies
In fact, the calculation of the linear correlation coefficient shows a positive correlation between the number of views of the videos and their degree of misinformation; this is particularly evident and relevant if we look at the results obtained by relating the number of total views and the degree of misinformation in cohort B, which is associated with the average health profile This correlation becomes weakly negative if we consider the results obtained with the same variables in cohort A This might seem like a paradox since from this data we could deduce that the videos with more views proposed by the YouTube algorithm to a health profile are at the same time those with a higher degree of misinformation If instead we consider as variable the visualizations for month this correlation becomes weakly positive in both cohorts It is also interesting to note that there is a strong negative correlation between the number of views per month and the DISCERN score in cohort B, unlike a weak positive correlation present in cohort A From this, we could then deduce that the videos proposed to the user with health profile with a higher number of views per month are actually those with lower quality
On average, enlisted videos have a medium-low quality level of 30% and 4% in cohorts A and B respectively This figure is apparently not in line with the findings of other authors (2, 3) who report a low average quality level of about 67% (2) and 66,7% (3) This discrepancy, however, could be linked to different research criteria: in the study of García Cano Fernández et al videos were enlisted exclusively in Spanish and with a duration of less than four minutes, which instead represent 43,5% and 56% of cohorts A and B respectively in our paper In the paper by Loeb at al videos with a range of duration from 21 seconds to 76 minutes were enlisted However, in both
papers, the type of user profile from which the search was made has not been specified and this, in our opinion, represents an important limitation
The limitations of this study are linked to the exclusive use of YouTube, and not of other social media, although this platform represents the mainly used Another limit, as probably for all the studies presented on this issue to date, is intrinsically related to the huge number of variables that affect the results offered by YouTube’ s algorithm
The evaluation of the results obtained by two profiles with deeply different characteristics (medical profile and anonymous profile) is a first step in the understanding and interpretation of the health information offered to users on social media, and the consequent impact on the clinical practice of these instruments
CONCLUSIONS
According to our study, in accordance with the literature data available today, the level of misinformation of the YouTube’ s contents about bladder cancer treatment is positively related to the number of views per month
The same search performed by a user profile related to the field of interest of the search itself offers higher quality results
The quality of information provided by YouTube regarding bladder cancer therapy, as well as levels of understandability and actionability, is, in general, medium-low if the research is performed with anonymous profile (Cohort A), while such results are reversed if the research is performed by a profile with high level of affinity with the field of interest of the research
This could be an important step in better understanding the correlation between the results suggested by YouTube's video recommendation algorithm and the characteristics of the user profile from which the search is performed
We also hope that future studies will investigate the positive correlation that appears to exist between higher levels of misinformation and more views
REFERENCES
1 Borgmann H, Cooperberg M, Murphy D, et al Online professionalism 2018 update of european association of urology (@uroweb) recommendations on the appropriate use of social media Eur Urol 2018; 74: 644-50
2 Loeb S, Reines K, Abu-Salha Y, et al Quality of Bladder Cancer Information on YouTube Eur Urol 2021; 79:56-59
3 García-Cano-Fernández AM, Szczesniewski-Dudzik JJ, GarcíaTello A, et al Quality of bladder cancer information on YouTube Cent European J Urol 2022; 75:248-251
4 International Agency for Research on Cancer Bladder cancer G L O B O C A N I n : h t t p s : / /
cers/30-Bladder-fact-sheet pdf2018
5 Kamat AM, Agarwal P, Bivalacqua T, et al Collaborating to move research for-ward: proceedings of the 10th annual bladder cancer think tank Bladder Cancer 2016; 2:203-13
6 Tariq A, Khan SR, Vela I, Williams ED Assessment of the use of the internet and social media among people with bladder cancer and their carers, and the quality of available patient-centric online BJU Int 2019; 123(Suppl 5):10-18
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12179
4
P Paolo Prontera, F Romana Prusciano, M Lattarulo, et al
g c o i a rc f r / t o d a y / d a t a / f a c t s h e e t s / c a n -
YouTube®
54%
24%
52% 32%
49% 76%
44% 77 7%
High
7 Covington C, Adams J, Sargin E Deep neural networks for youtube recommen-dations RecSys '16: Proceedings of the 10th ACM Conference on Recom-mender Systems 2016; pp 191-198
8 Davidson J, Liebald B, Liu J, et al The youtube video recommendation system In Proceedings of the Fourth ACM Conference on Recommender Sys-tems, RecSys’10, pages 293-296, New York, NY, USA, 2010 ACM
9 AHRQ The patient education materials assessment tool (pemat) and user ’ s guide https://www ahrq gov/professionals/preventionchronic-care/improve/self-mgmt/pemat/pemat-av html
10 Charnock D, Shepperd S, Needham G, Gann R DISCERN: an instrument for judging the quality of written consumer health infor-
mation on treatment choices J Epidemiol Commun Health 1999; 53:105-11
11 Available from: http://www ahrg gov/healt-literacy/patient-education/pemat html
12 Available from: http://www discern org uk
13 Herbert AS, Nemirovsky A, Hess DS, et al Pelvic organ prolapse on YouTube: evaluation of consumer information BJU Int 2020; 125:759-760
14 Fode M, Jensen CFS, Østergren PB How Should the Medical Community Respond to the Low Quality of Medical Information on Social Media? Eur Urol 2021; 79:60-61
Correspondence
Pier Paolo Prontera, MD (Corresponding Author) pierpaolo prontera@asl taranto it
Marco Lattarulo, MD
marco lattarulo@asl taranto it Emanuele Utano, MD emanuele utano@asl taranto it Francesco Schiralli, MD Francesco Saverio Grossi, MD, PhD grossifs@libero it
Department of Urology, “S S Annunziata” Hospital, Taranto (Italy) Via Bruno Francesco 1 - 74010 Taranto (Italy)
Francesca Romana Prusciano, MD
Department of Emergency and Organ Transplantation, Urology, Andrology and Kidney Transplantation Unit, University of Bari, 70124 Bari (Italy)
Carmine Sciorio, MD carminesciorio@gmail com
Department of Urology, “Alessandro Manzoni” Hospital of Lecco, Lecco (Italy)
Lorenzo Romano, MD loryromano@hotmail it
Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples “Federico II”, 80131 - Naples (Italy)
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12179 5 Bladder cancer treatment information on YouTube
ORIGINAL PAPER
Angelis Peteinaris 1* , Vasileios Tatanis 1* , Paraskevi Katsakiori 1 , Theodoros Spinos 1 , Solon Faitatziadis 1 , Kristiana Gkeka 1 , Anastasios Natsos 1 , Theofanis Vrettos 2 , Evangelos Liatsikos 1, 3 , Panagiotis Kallidonis 1
1 Department of Urology, University of Patras, Patras, Greece;
2 Department of Anesthesiology and ICU, University of Patras, Patras, Greece;
3 Department of Urology, Medical University of Vienna, Vienna, Austria
* The authors contributed equally to the study
Summary
Purpose: The aim of the present, retrospective study was to describe our initial experience and early outcomes of Thulium Fiber Laser enucleation of the prostate (ThuFLEP) with the use of the FiberDust™ (Quanta System, Samarate, Italy) in patients with benign prostate hyperplasia
Methods: From June 2022 to April 2023, all patients who underwent endoscopic enucleation of the prostate at Urology Department of the University Hospital of Patras were included A single surgeon utilizing the same standardized operative technique performed all the surgeries The primary endpoints included the uneventful completion of the operation, the surgical time and any minor or major complication observed intra- or post-operatively
Results: Twenty patients with benign prostate hyperplasia were treated with ThuFLEP All the surgeries were completed successfully and uneventfully The enucleation phase of the operation was completed in a mean time of 45 ± 9.1 min, while the average time needed for the morcellation was 17 65 ± 3 42 min No significant complications were observed intra- or post-operatively The average hemoglobin drop was calculated to be 0 94 ± 0.71 g/dL.
Conclusions: All the operations were successfully and efficiently completed with the use of the FiberDust™ (Quanta System, Samarate, Italy) in ThuFLEP Significant blood loss or major complications were not observed.
KEY WORDS: Benign Prostatic Hyperplasia; Enucleation; Prostate; ThuFLEP; Thulium
Submitted 23 December 2023; Accepted 27 December 2023
INTRODUCTION
Lower urinary tract symptoms (LUTS) constitute a major concern for many men over 50 years old The symptoms may usually be caused by the presence of enlarged prostatic adenomas, a condition known as Benign Prostatic Hyperplasia (BPH) BPH constitutes a major healthcare burden, affecting almost one out of four men in their lifetime (1) The treatment options include both conservative and surgical approaches Treatment decision-making process is based on the grade of the symptoms, the renal function, the
prostate volume and the post-voiding residual urine (1) Transurethral resection of the prostate (TURP) has been the milestone surgical option for BPH for many years despite the relatively high complication rates observed in patients with enormous prostatic volume (2) In the last decades, however, endoscopic enucleation of the prostate (EEP) techniques have been rapidly developed and implemented into the urological armamentarium The main idea was to adjust the open procedure to the endoscopic approach In addition, EEP techniques have been associated with improved outcomes in terms of the removed percentage of prostatic volume as well as minimized surgical intervention (3) Although EEP techniques evolved as a promising alternative to conventional TURP, they seem to show a steeper learning curve According to current literature, the completion of the learning curve needs the performance of 40 to 60 cases (4)
Apart from the development of endoscopic surgical techniques, the simultaneous evolution of laser technology and laser devices has also played an important role in the expansion of EEP (5) The rapid development of the established holmium: Yttrium-Aluminum-Garnet (Ho: YAG) laser was followed by the integration of the Thulium Fiber Laser (TFL) TFL produces a wavelength of 1940 nm, while the penetration depth is 0 077 mm The pulse energy ranges from 0 025 to 6 J, and the frequency may reach up to 2400 Hz (6) These technical aspects show a laser with a precise cutting function, which is convenient for the handling of soft tissues This fact is also confirmed by experimental studies showing that TFL is associated with higher efficiency and safer profile in tissue application compared to Ho: YAG (7) Consequently, TFL has recently been widely integrated into EEP techniques (ThuFLEP)
The aim of the current study is to present our initial experience and early outcomes of ThuFLEP with the use of theFiberDust™ (Quanta System, Samarate, Italy) in patients with BPH
The current study is a retrospective single-center study conducted at the Urology Department of the University
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12228 1
MATERIALSANDMETHODS
EndoscopicenucleationoftheprostatewithThulium
etrospectivesingle-centerstudy
FiberLaser(ThuFLEP).Ar
DOI: 10 4081/aiua 2024 12228
Hospital of Patras The study was approved by the Institutional Ethics Committee Informed consent was obtained from all the participants
Study design
From June 2022 to April 2023, all patients with BPH treated at our department with ThuFLEP using the FiberDust™ (Quanta System, Samarate, Italy) were included in the study A single expert surgeon with experience in EEP techniques conducted all the surgeries and the follow-up management of the participants Patients with prostatic volume under 80 cm3, serious coagulation disorders, neurogenic bladder, concomitant bladder stones, or a history of urethral strictures were excluded from the study
Data collection
The preoperative patients’ data included age, height, weight, and Body Mass Index (BMI)
The preoperative use of alpha-1 adrenoreceptor antagonists (a-blocker) and 5-alpha reductase inhibitors (5-ARI) was recorded as well as the history of acute urinary retention (AUR) or permanent catheterization All patients underwent abdominal ultrasound for the estimation of the prostate volume, uroflowmetry for the evaluation of the maximum flowrate (Qmax) and blood exams for the investigation of hemoglobin (Hgb) level The International Prostate Symptom Score (IPSS) was used for the evaluation of symptoms’ severity The perioperative data included the record of enucleation and morcellation time as well as the presence of intra- and postoperative complications
The volume of enucleated prostatic adenoma was estimated based on the histopathological report
Postoperatively, all patients underwent blood exams on the first post-operative day and afterwards in case any complication occurred The catheter removal was scheduled on the first postoperative day if no hematuria was present and a trial without catheter (TWOC) was performed
Surgical technique
The surgical approach used was based on the description of the en bloc enucleation of the prostate by Saitta et al (8) The patient was placed in lithotomy position under general or epidural anesthesia The irrigation bags were placed 1 m above the surgical table Cefuroxime was administered intravenously 1-hour preoperatively and afterward, twice a day during hospitalization
Urethrocystoscopy with the use of a resectoscope (Karl Storz SE & Co KG, Tuttlingen, Germany) was conducted for the observation of the anatomical landmarks, the sphincter limits, the ureteral orifices and their distance from the adenoma and the possibility of any pathological finding in the urethral lumen and the bladder The power settings used were 60 W (2Jx30Hz) Minor differentiations were used in a few cases with harder tissue and/or persistent hemorrhage The diameter of the laser fiber used was 550 μm
The initial incision was a marking of the external sphincter connecting 11 and 1 o ’clock A second incision between the fifth and seventh hour was conducted alongside the verumontanum The next step was the connec-
tion of these initial incisions, aiming at the demarcation of the sphincter from the prostate apex The importance of minimization of mechanical stress and the activation of the laser for the gentle tissue dissection after the early apical release of the prostate should be underlined as it is believed to contribute to the postoperative continence maintenance The gradual deepening of the incisions until the prostate capsule was crucial After the capsule was observed, the dissection became circumferential respecting the plane of enucleation starting from 6 o ’clock with direction to 12 o'clock (Figure 1)
The resectoscope was rotated for better placement of the laser fiber and avoidance of mechanical pressure for dissection The same movements were followed for the gradual detachment of the adenoma The proximal detachment of the prostate for the bladder entry was conducted through the anterior enucleation plane, followed by careful circumferential release of the adenoma The ureteral orifices were reobserved before the final dissection of the prostate from the capsule near the bladder neck The detached adenoma was then freely pushed into the bladder Meticulous hemostasis was conducted exclusively with the use of the laser with no need for additional electrocautery use The importance of this step should be underlined as clear view is crucial for the uneventful morcellation process The final step of the procedure was the replacement of the resectoscope with a 26 Fr nephroscope (Karl Storz SE & Co KG, Tuttlingen, Germany) For maximal irrigation conditions and prevention of bladder collapse during morcellation, the inflow of irrigation fluid was facilitated simultaneously through the inflow and outflow lumens of the nephroscope The morcellator (Quanta Blade, Quanta System, Samarate, Italy) was placed into the bladder through the working channel of the nephroscope A 22 Fr 3-way urethral catheter was placed into the bladder, and bladder irrigation was used at least until the patient returned to the department
Figure 1
Start of the prostate enucleation from 6 o’clock and circumferential development towards 12 o’clock.

Archivio Italiano di Urologia e Andrologia 2024; 96(1):12228
2
A Peteinaris, V Tatanis, P Katsakiori, et al
Follow-up
Post-operative evaluation was performed 1, 3, 6 and 12 months after the surgery The follow-up examination included the record of incontinence or additional symptoms, ultrasonography of the urinary tract as well as Qmax and IPSS measurement The presence of incontinence was defined as the use of at least one pad per day
Endpoints
The successful completion of the surgeries, the duration of the procedures (divided into enucleation and morcellation time), the volume of enucleated prostate and the documentation of complications based on the ClavienDindo classification were the primary endpoints of the study (9) Enucleation and morcellation time were defined as the time between the first and the last activation of the laser and the time between the first and the last activation of the morcellator, respectively The secondary endpoints of the study were the hemoglobin decrease (the difference between the pre-operative and the last postoperative sample) and the differentiation of the Qmax and IPSS pre- and post-operatively (as postoperative Qmax and I P S S d e fi
Additionally, the catheterization and hospitalization duration as well as the presence of postoperative incontinence were also evaluated
Statistical analysis
All the quantitative data are presented as mean values and standard deviations, while the qualitative variables are presented as numbers and rates
RESULTS
In total, 20 patients were included in the study The mean follow-up was 10 2 ± 2 04 months The participants had a mean age of 72 5 ± 6 4 years The mean BMI was calculated to be 27 59 ± 3 53 kgr/m2 More specifically, the average height was 1 72 ± 0 08 m, while the mean weight was 81 1 ± 10 05 kg In addition, the mean preoperative prostate volume as measured in the abdominal ultrasound was 112 75 ± 28 9 ml Preoperatively, nine (45%) and eleven (55%) patients used 5-ARI and a-blocker, respectively Additionally, six (30%) patients had a prior history of AUR, while seven (35%) patients were catheterized (Table 1)
The completion of all the procedures was successful without any intraoperative event The mean time of enucleation was 45 ± 9 1 min The average morcellation duration was calculated to be 17 65 ± 3 42 min The mean hemoglobin decrease was 0 94 ± 0 71 g/dL (Table 2) The average catheterization and hospitalization duration were 1 15 ± 0 37 and 1 7 ± 1 38 days, respectively Two patients presented persistent hematuria after the discontinuance of irrigation; thus, the catheterization was prolonged until the second postoperative day (ClavienDindo I) One patient presented postoperative AUR without hematuria The catheter was placed again, and TWOC was successful during the second postoperative day (Clavien-Dindo I) Finally, two patients presented with fever 12 hours postoperatively The antibiotic regimen was not modified, and the TWOC was not post-
Table 1.
Demographic and preoperative data
Variable Outcomes
Age (mean ± SD)
Height (mean ± SD)
Weight (mean ± SD)
(mean ± SD)
Prostate Volume (mean ± SD)
5-ARI (n, %)
a-blocker (n, %)
(45%)
(55%)
AUR (n, %) 6 (30%)
Permanent Catheterization (n, %) 7 (35%)
Qmax (mean ± SD)
(mean ± SD)
SD: Standard Dev ation; BMI: Body Mass Index; 5-ARI: 5-alpha reductase inhibitor; a-b ocker: A pha-1 adrenoreceptor antagonist; AUR: Acute Urinary Retention; Qmax: Max mum Flow rate; IPSS: Internat ona Prostate Symptom Score
Table 2.
Intra- and perioperative outcomes
Variable Outcomes
Enucleation time (mean ± SD) 45 ± 9 1 min
Morcellation time (mean ± SD) 17 65 ± 3 42 min
Hemoglobin drop (mean ± SD) 0 94 ± 0 71 g/dL
Catheterization duration (mean ± SD) 1 15 ± 0 37 days
Hospitalization duration (mean ± SD) 1 7 ± 1 38 days
Complications (n, %) 5 (25%)
Clavien-Dindo I 5 (25%)
Clavien-Dindo II 0 (0%)
Clavien-Dindo > II
SD: Standard Dev at on
Table 3
Postoperative and functional outcomes
0 (0%)
Variable Outcomes
Enucleated Prostatic Volume (mean ± SD)
Mean Enucleation Rate (mean ± SD)
Qmax Increase (mean ± SD)
85 ± 20 87 ml
34 ± 11 43%
15 ± 4 43 ml/s
IPSS Decrease (mean ± SD) 13 55 ± 3 9
Incontinence (n, %) 1 (5%)
SD: Standard Deviation; Qmax: Max mum F ow rate; IPSS: nternationa Prostate Symptom Score
poned and was performed successfully in both of them Nevertheless, the hospitalization was prolonged until they were fit for discharge (Clavien-Dindo I) (Table 2) The mean volume of enucleated prostate was 76 85 ± 20 87 ml, while an average rate of 68 34 ± 11 43% of the prostate was enucleated The mean pre- and post-operative Qmax were 7 6 ± 3 35 ml/s and 21 75 ± 3 30 ml/s, respectively The average increase of Qmax was estimated to be 14 15 ± 4 43 ml/s Concerning IPSS, the pre- and post-operative mean values were calculated to be 22 75 ± 2 22 and 9 2 ± 3 04, respectively The average IPSS decrease was 13 55 ± 3 9 One (5%) patient presented with incontinence (use of one pad daily) (Table 3)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12228 3
enucleation
the
Endoscopic
of
prostate with Thulium Fiber Laser (ThuFLEP)
e d t h e v a l u e s o f t h e l a s t f o l l o w - u
n
p )
72 5
6 4 years
±
1 72
0 08 m
81
BMI
27
±
1 ± 10 05 kg
59 ± 3 53 kg/m2
112
75 ± 28 9 ml
9
11
7 6 ± 3 35 ml/s
22 75 ± 2 22
IPSS
76
68
14
DISCUSSION
The wide adoption of lasers in the urological field is partially due to their great hemostatic properties (10) Various laser devices and a plethora of surgical techniques’ modifications have gradually been developed and enriched the enucleation process, making it an appealing and efficient treatment option for BPH In this clinical retrospective study, we aimed to present our operative and functional outcomes Twenty ThuFLEP procedures in patients with enlarged prostate glands (> 80 cm3) were performed A sphincter preservation technique with a high-power laser device was adopted and modified The surgeries were completed successfully The enucleation and morcellation times were 45 ± 9 1 min and 17 65 ± 3 42 min, respectively Postoperatively no significant hemoglobin drop was detected Despite the reported complication rate of 25%, all of them were Clavien-Dindo I and consequently, the mean catheterization and hospitalization durations were not influenced Additionally, on average 68 34 ± 11 43% of the total prostatic volumes were enucleated while the postoperative functional outcomes were encouraging Fraundonfer and Gilling described the first EEP using laser, followed by morcellation in 1998, developing the enucleation technique described by Hiraoka et al (11, 12) The initial description of laser enucleation of the prostate was the 3-lobe detachment including 14 patients Lasers’ adaptation and rapid evolution played a major role in the implementation of multiple techniques and the gradual evolution of the original one (13) The early recognition and preservation of the sphincter and the easier development and safe dissection of the surgical plane have led to increased popularity of the en bloc technique The enrichment of the technique with several modifications has also minimized the residual prostatic volume (8, 14) The latest addition and adjustment of TFL devices have significantly contributed to the wider EEP implementation One of the main advantages of TFL is the greater efficiency regarding the management of hemorrhage This is partially because of the shallow tissue penetration and the pulsed wavelength delivery (15) Nevertheless, Holmium lasers have been widely used and investigated in terms of safety and efficiency for EEP The comparison between the two lasers has been the ground for many studies and discussions between surgeons and researchers According to Hartung et al , recent bibliography on EEP suggests that both laser types are associated with great and comparable outcomes in terms of the LUTS improvement and the pattern of voiding characteristics after the surgery (16) In compliance with the structural function of TFL, Hartung et al noticed that Holmium laser enucleation of the prostate (HoLEP) was found to be partially inferior to ThuFLEP regarding the postoperative incontinence rates and hemostasis In their randomized controlled trial, Enikeev et al compared TFL and TURP in terms of efficiency (17) The superiority of ThuFLEP in terms of resection percentage, grade and frequency of complications and duration of hospital stay was demonstrated The experience and convenience of the urologist as well as the availability of surgical means in each setting are the factors that determine the surgical treatment of BPH
In the present clinical study, we presented our retrospectively collected data of 20 patients regarding the out-
comes of ThuFLEP using FiberDust™ A comparative study including 234 participants was published by Pirola et al (18) The researchers conducted a retrospective match-pair analysis, dividing the 234 patients’ sample into 117 participants who underwent HoLEP and 117 who were treated with Thulep for BPH The authors reported that the median enucleation time was 70 min (58 0-87 3 IQR) and 70 5 min (58-104 IQR) for the ThuLEP and the HoLEP group, respectively In addition, they observed that the median morcellation time was 12 12 min (9 5-14 5 IQR) and 11 5 min (8-16 IQR) in the same groups The current study revealed that the mean enucleation time was 45 ± 9 1 min, and the average morcellation duration was 17 65 ± 3 42 min In addition, the HoLEP group demonstrated an intraoperative complication rate of 5 7% and the ThuLEP group 7% The hemoglobin decrease was 0 9 g/dl (range: 0 3-1 67) and 0 5 g/dl (range: 0 3-1 1) for the holmium and the thulium groups, respectively In the current study, no intraoperative complication was observed and the average hemoglobin decrease was 0 94 ± 0 71 g/dL The followup evaluation (IPSS, Qmax and incontinence rates) presented similar results in the two studies In addition, in the current one, it was calculated that 68 34 ± 11 43% of the adenoma was removed A retrospective clinical study including 125 patients with prostate volume larger than 80 ml was conducted by Chang et al (19) The patients were treated with ThuLEP by a single experienced surgeon The authors reported that the mean prostate volume before surgery was 106 80 ± 45 77ml and it was reduced by about 74 17 ± 11 27% after the treatment Additionally, the authors demonstrated that IPSS postoperatively was 7 35 ± 5 89 and Qmax at the three-month follow-up was 23 20 ± 6 87ml/s In the current study, the mean postoperative IPSS and Qmax were 9 2 ± 3 04 and 21 75 ± 3 30 ml/s, respectively Enikeef et al demonstrated the efficiency of ThuFLEP by conducting a retrospective study including 130 patients with prostate volume over 80 ml and comparing EEP to open prostatectomy (20) Similar operation duration but significantly less hospitalization in favor of EEP were described In addition, the incontinence rate was 1 1% for the ThuFLEP group which is in agreement with our results Besides, a mean hemoglobin drop of 1 g/dl was d e m o n s t r a t e d , w h i l e t h e c a t h e t e r w a s s u c c e s s f u l l y removed during the first 24 hours after the operation in 79% of the patients
The present study included 20 cases with BPH treated with ThuFLEP Nevertheless, the current study is not without limitations Firstly, the urologist who conducted all the procedures was an experienced surgeon, who specializes in EEP and has conducted more than 100 cases before the initiation of the study Therefore, the learning curve could not be evaluated Additionally, the sample size was relatively small and further prospective studies with larger cohorts and longer follow-up are deemed necessary to confirm our findings However, the objective of the study was to present our initial experience and patients’ outcomes with the ThuFLEP in BPH The advantages of the enucleation technique have been thoroughly analyzed and a promising trend in outcomes has been revealed
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12228
4
A Peteinaris, V Tatanis, P Katsakiori, et al
CONCLUSIONS
We presented the surgical and early functional outcomes of ThuFLEP with the use of FiberDust™ (Quanta System, Samarate, Italy) in patients with BPH All the cases were successfully completed without intraoperative complications, major postoperative complications, or significant blood loss The functional outcomes reported are in agreement with the current literature
REFERENCES
1 Lee SWH, Chan EMC, Lai YK The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: A systematic review and meta-analysis Sci Rep 2017; 7:7984
2 Cornu JN, Ahyai S, Bachmann A, et al A Systematic Review and Meta-analysis of Functional Outcomes and Complications Following Transurethral Procedures for Lower Urinary Tract Symptoms Resulting from Benign Prostatic Obstruction: An Update Eur Urol 2015; 67:1066-96
3 Elzayat EA, Elhilali MM Holmium laser enucleation of the prostate (HoLEP): long-term results, reoperation rate, and possible impact of the learning curve Eur Urol 2007; 52:1465-71
4 Brunckhorst O, Ahmed K, Nehikhare O, et al Evaluation of the Learning Curve for Holmium Laser Enucleation of the Prostate Using Multiple Outcome Measures Urology 2015; 86:824-9
5 Nair SM, Pimentel MA, Gilling PJ A Review of Laser Treatment for Symptomatic BPH (Benign Prostatic Hyperplasia) Curr Urol Rep 2016; 17:45
6 Denstedt J, Gabrigna Berto FC Thulium fiber laser lithotripsy: Is it living up to the hype? Asian J Urol 2023; 10:289-97
7 D o i z i S , G e r m a i n T , P a n t h i e r F ,
Holmium:YAG and Thulium Fiber Lasers on Soft Tissue: An Ex Vivo Study J Endourol 2022; 36:251-8
8 Saitta G, Becerra JEA, Del Álamo JF, et al 'En Bloc' HoLEP with early apical release in men with benign prostatic hyperplasia World J Urol 2019; 37:2451-8
9 Pan TT, Li SQ, Dai Y, Qi JX Observation of complications assessed by Clavien-Dindo classification in different endoscopic procedures of benign prostatic hyperplasia: An observational study Medicine 2023; 102:e32691
10 Katta N, Santos D, McElroy AB, et al Laser coagulation and hemostasis of large diameter blood vessels: effect of shear stress and flow velocity Sci Rep 2022; 12:8375
11 Fraundorfer MR, Gilling PJ Holmium:YAG laser enucleation of the prostate combined with mechanical morcellation: preliminary results Eur Urol 1998; 33:69-72
12 Hiraoka Y A new method of prostatectomy, transurethral detachment and resection of benign prostatic hyperplasia Nihon Ika Daigaku zasshi 1983; 50:896-8
13 Oh SJ Current surgical techniques of enucleation in holmium laser enucleation of the prostate Invest Clinl Urol 2019; 60:333-42
14 Scoffone CM, Cracco CM The en-bloc no-touch holmium laser enucleation of the prostate (HoLEP) technique World J Urol 2016; 34:1175-81
15 Schembri M, Sahu J, Aboumarzouk O, et al Thulium fiber laser: The new kid on the block Turk J Urol 2020; 46:S1-s10
16 Hartung FO, Kowalewski KF, von Hardenberg J, et al Holmium Versus Thulium Laser Enucleation of the Prostate: A Systematic
Review and Meta-analysis of Randomized Controlled Trials Eur Urol Focus 2022; 8:545-54
17 Enikeev D, Netsch C, Rapoport L, et al Novel thulium fiber laser for endoscopic enucleation of the prostate: A prospective comparison with conventional transurethral resection of the prostate IJU 2019; 26:1138-43
18 Pirola GM, Saredi G, Codas Duarte R, et al Holmium laser versus thulium laser enucleation of the prostate: a matched-pair analysis from two centers Ther Adv Urol 2018; 10:223-33
19 Chang C-H, Lin T-P, Huang J-Y Safety and effectiveness of highpower thulium laser enucleation of the prostate in patients with glands larger than 80 mL BMC Urol 2019; 19:8
20 Enikeev D, Okhunov Z, Rapoport L, et al Novel Thulium Fiber Laser for Enucleation of Prostate: A Retrospective Comparison with Open Simple Prostatectomy J Endourol 2019; 33:16-21
Correspondence
Angelis Peteinaris, MD peteinarisaggelis@gmail com
Vasileios Tatanis, MD (Corresponding Author) tatanisbas@gmail com
Department of Urology, University of Patras Medical School, Rio, Patras, 26500, Greece
Paraskevi Katsakiori, MD vkatsak@upatras gr
Theodoros Spinos, MD thspinos@otenet gr
Solon Faitatziadis, MD solonasfait@gmail com
Kristiana Gkeka, MD kristianagkeka@gmail com
Anastasios Natsos, MD a natsos@gmail com
Panagiotis Kallidonis, MD pkallidonis@yahoo com
Theofanis Vrettos, MD teovret@gmail com
Department of Anesthesiology and ICU, University of Patras, Patras, Greece
Evangelos Liatsikos, MD liatsikos@yahoo com
Department of Urology, Medical University of Vienna, Vienna, Austria
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12228 5
Endoscopic enucleation of the prostate with Thulium Fiber Laser (ThuFLEP)
e t a l C o m p a r i s o n o f
ORIGINAL PAPER
Mehmet Ezer 1 , Rasim Güzel 2 , Mehmet Uslu 1 , Selçuk Güven 3 , Kemal Sarica 4, 5
1 Department of Urology, Kafkas University, Kars, Turkey;
2 Department of Urology, Medistate Kavacık Hospital, Istanbul, Turkey;
3 Department of Urology, Necmettin Erbakan University, Konya, Turkey;
4 Department of Urology, Sancaktepe Sehit Prof Dr Ilhan Varank Training and Research Hospital, Istanbul, Turkey;
5 Department of Urology, Biruni University Medical School, Istanbul, Turkey
Summary
Objective: To evaluate the metabolic and clinical characteristics of adult cases with stone disease from a regional part of Turkey.
Methods: The study included 2348 adult patients with sonography and/or computed tomography-proven urinary stones. All cases were given a questionnaire about the epidemiological features of urolithiasis. Aside from the type and severity of stoneforming risk factors, both patient (age, gender, BMI, associated comorbidities, first onset of stone disease, positive family history, educational level) and stone-related (size, number, location, chemical composition, previous stone attacks) factors have been thoroughly assessed The data were evaluated in multiple aspects to outline the epidemiological features.
Results: The overall mean age value of the cases was 43 3 years, and the M/F ratio was 1.34. The first onset of the disease was found to vary between 15-57 years, with a mean value of 32 4 years While most of the stones were located in kidney and ureter, calcium-containing stones constituted the most common type (CaOx 69%, CaOxPO4 7%) More than 42% of the cases suffered from multiple stone attacks; positive family history waspresent in 31 6% Among the associated comorbidities, hypertension was the most common pathology (45 8%), and the BMI index value was > 30 in 31 3% of the cases 57 7% of the patients had just one stone attack, and 42 2% had recurrent stone formation
Conclusions: Our findings clearly show that important implications may be extracted from epidemiologic data acquired from local scale research to implement an effective preventative program and closely monitor the patients
KEY WORDS: Urinary stones; Epidemiology; Kidney stones
Submitted 11 December 2023; Accepted 25 December 2023
INTRODUCTION
As an endemic problem in certain parts of the world, urolithiasis constitutes an evident risk to the healthcare system and a certain burden on the economy The etiology of the disease is multifactorial, and an increase in incidence and prevalence ranging from 7% to 13% in North America, 5-8 % in Europe, and 1-5% in Asia has been reported (1) Environmental and dietary factors, lifestyle, and some individual personal factors, such as age, gender, body mass index (BMI), and familial anamnesis, seem to play a critical role in the course of the disease (2)
Considering the urolithiasis-related epidemiological factors as an important parameter, gender-based prevalence has been subjected to several studies where the male-tofemale ratio ranged from 1 3 to 3 (3) On the other hand, as a precious predictive factor, positive family history is a significant risk factor for stone formation in individuals with family members suffering from urolithiasis (4) Geographic conditions are also important, and factors i n c l u d
comorbidities may further affect the prevalence of stone formation (2, 5) Components of metabolic syndrome like diabetes mellitus, hypertension, or obesity have also been implicated in constituting an additional risk for urinary stone formation (6) Related to metabolic problems, in addition to less fluid intake, hypercalciuria, hyperoxaluria, hyperuricosuria, and hypocitraturia are the most common urinary stone-forming risk factors identified, particularly in recurrent cases (7, 8) The dietary habits of the community, both in developing countries and in developed ones, are essential in stone formation by altering urine composition and increasing relevant risk status (9, 10) Lastly, despite some contradictory reports, education might play a role in urolithiasis Some studies show that a lower education level may be a possible reason for stone formation (11, 12)
In this present study, we aimed to assess certain clinical and metabolic factors to update epidemiological risk factors in the Turkish population in a regional evaluationbased manner
METHODS
Ethics committee approval was obtained for the study from the Local Ethics Committee with the number 2023/4203 on 17 February 2023 While conducting this study, the Declaration of Helsinki and inter national ethical standards were taken into consideration at every stage
A total of 2348 adult patients referring to the urology departments of different hospitals in the same region with sonography and/or computed tomography-proven stones were included in the study program Following close collaborative work with epidemiologists, our team designed a simple questionnaire and conducted a face-to-face survey Staff nurses and resident doctors in urology wards
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12181 1
i n g c l i m a t e , s o c i o e c o n o m i c s t a t u s , d i e t , a n d
Clinicalcharacteristicsofadultcaseswithurolithiasis fromTurkey:Aregionalepidemiologicalstudy
DOI: 10 4081/aiua 2024 12181
completed each form after interviewing study participants prior to medical or surgical management of stones
Regarding the questions with respect to the established epidemiological features of urinary calculi, in addition to the type and severity of stone-forming risk factors, both patient-related factors (such as age, gender, BMI, associated comorbidities, the first onset of stone disease, positive family history, educational level) and stone related factors (such as size, number, location, chemical composition, previous stone attacks) have all been evaluated and recorded
Obtained data were assessed from multiple aspects to outline the epidemiological features in our patients
RESULTS
Evaluation of our data revealed the following findings
The mean age value of the 2348 adult cases was 43 3 years (15-69), and the gender distribution was 1346 males and 1002 females with an M/F ratio of 1 34
The first onset of the disease was found to vary between 15-57 years, with a mean value of 32 4 years (Table 1)
Table 1. Evaluation of the patient characteristics and stone-related factors by gender
The majority of the stones were located in the kidney (62 3%) and ureter (35 2%), and calcium-containing stones constituted the most common type (CaOx 69%, CaOxPO4 7%) (Table 2)
On referral, 57 7% of the cases had the first stone attack; 42 2% had recurrent stone formation Regarding the previous interventions for stone removal, pyelolithotomy was present in 12 patients (0,5%), cystolithotomy in 14 (0,6%), PCNL in 108 (4,6%), ureterorenoscopy in 213 (9%), and lastly SWL in 284 cases (12 %) (Table 2) A positive family history was present in 743 patients (31 6%) (Table 2)
Positive family history was strongly associated with the mean age of the cases at first presentation and the disease's number of stone attacks (recurrence)
Stones are formed at younger ages in these cases, with more recurrent stone formation than those with no family history
Of the clinical presentation symptoms noted, while the majority of the cases referred with colic pain (n:1902, 81%), 50 3% (n:1181) of the patients had microscopic hematuria, and 7 2% (n:169) presented with macroscopic hematuria High-grade hydronephrosis (Grade 3-4) was present at first presentation in 14 2% of the cases, and 53 3% had no dilatation (Table 3)
Among the associated comorbidities evaluated, while
Table 2.
Urolithiasis characteristics of the patients at first presentation
Table 3.
Clinical characteristics of the patients at first presentation.
hypertension was present in 45 8% of the cases, diabetes was present in 2 8%, hypercholesterolemia in 27 6%, and obesity in 31 3% (in 735 cases, BMI index value was 3035) While the mean BMI was 25 7 ± 8 8 in male patients, this value was 26 8±9 2 in female cases (Table 3)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12181
2
M Ezer, R Güzel, M Uslu, S Güven, K Sarica
Male Female Total number of cases (n) 1346 1002 Mean age of the cases (years) 42 6 ± 9 8 44 3 ± 11 3 First onset of the disease (years) 31 7 ± 10 2 33 5 ± 12 8 Stone size (mm) 1 3 ± 0 8 1 1 ± 0 6 Height (cm) 170 1 ± 9 7 165 7 ± 10 2 Body weight (kg) 75 0 ± 9 4 79 2 ± 10 2 Body mass index (BMI) (kg/m2) 25 7 ± 8 8 26 8 ± 9 2
Total Male Female n%n%n% Stone analysis data 1945 82 8 981 72 9 964 96 2 Calcium oxalate 1342 69 703 71 7 639 66 3 Calcium phosphate 136 7 74 7 5 62 6 4 Infection stones 233 12 86 8 8 147 15 2 Uric acid 156 8 83 8 5 73 7 6 Cystine 78 4 35 3 5 43 4 5 Number of stone episodes One episode 1355 57 7 731 54 3 624 62 3 2-4 episodes 647 27 6 388 28 8 259 25 8 5 and more 346 14 7 227 16 9 119 11 9 Stone localization at the first presentation Kidney 1463 62 3 786 58 4 677 67 5 Single 696 29 6 372 27 6 324 32 3 Multiple 767 32 7 414 30 8 353 35 2 Ureter 826 35 2 437 32 5 389 38 8 Bladder 59 2 5 59 4 4 00 Previous interventions Pyelolithotomy 12 0 5 7 0 5 5 0 5 Uretrorenoscopy 213 9 134 10 79 7 9 PCNL 108 4 6 53 3 9 55 5 5 Cystolithotomy 14 0 6 14 100 SWL 284 12 123 9.1 161 16.1 Family history Positive 743 31 6 331 24 5 412 41 1
Total Male Female n%n%n% Total number of cases 2348 100 1346 57 9 1002 42 1 Associated morbidities Hypertension 1075 45 8 623 46 3 452 45 1 Diabetes Mellitus 66 2 8 29 2 2 37 3 7 Hypercholesterolemia 648 27 6 403 29 9 245 24 5 Obesity (BMI of > 30) 735 31 3 347 25 8 388 38 7 Presence of urinary tract infection (UTI) 802 34 2 114 8 5 688 68 6
of obstruction
findings) None 1252 53 3 883 65 6 369 36 8 Grade I 356 15 2 124 9 2 232 23 2 Grade II 406 17 3 226 16 8 180 18 Grade III 187 8 52 3 9 135 13 5 Grade IV 147 6 2 61 4 5 86 8 5
of hematuria Microscopic 1181 50 3 671 49 9 510 50 9 Macroscopic 169 7 2 87 6 5 82 8 2 Presence of pain * No 446 18 9 253 18 8 193 19,3 Mild (VAS 1-3) 680 29 408 30 3 272 27,1 Moderate (VAS 4-6) 483 20 6 267 19 8 216 21,6 Severe (VAS ≥ 7) 739 31 5 418 31 1 321 32
0-10
Presence
(sonographic
Presence
* Eva uation accord ng to v sual Analogus sc ala
When the education level of the cases was evaluated, 36 4% (n = 856) were primary school graduates, 14 3% (n = 335) were secondary school graduates, 34 5% (n = 810) were high school graduates, and 14 8% (n = 347) were college graduates
DISCUSSION
Urinary system stone disease is an endemic pathology in many parts of the world, which poses an evident risk to the healthcare system with a significant burden on the economy The etiology of the disease is multifactorial, consisting of several risk factors evaluated in detail so far Regarding the evident differences among several regions and countries of the world, variations in specific etiologic parameters like age, gender, dietary preferences, fluid consumption, the climate they live in, their occupation, level of education, socioeconomic status, and genetic and metabolic factors have been considered to be responsible (2, 9)
On the other hand, the formation of new stones based on the present metabolic and other risk factors is commonly observed, particularly in recurrent stone-forming cases Studies on this aspect have revealed that after the initial stone passage, the rate of stone recurrence in patients with previous urolithiasis was reported to be 40% at five years and 75% at 20 years, respectively (13)
Considering all these facts, it is clear that data from regional epidemiological studies will help us assess the prevalence and underlying etiological factors, which will support developing policies for effective metaphylaxis and treatment of the disease appropriately In other words, in light of reported evident geographic differences i n t h e p re v a l e n c e o f u ro l
local/regional studies may provide a detailed understanding of the disease nationwide
When we look at the studies examining the effect of gender on kidney stone formation, several gender-based studies have shown that although infection stones were more commonly reported in women, the general incidence of urinary calculi tends to be more frequent in men (14, 15) Statistics show that males tend to indulge in higher amounts of alcohol and coffee as well as meat consumption compared to females Moreover, it has been observed that testosterone can increase the likelihood of stone formation, whereas estrogen plays a role in inhibiting stone formation by regulating the synthesis of 1 25dihydroxy-vitamin D (5) Stone formation is often linked to anatomical factors, with infravesical obstruction being a common risk factor This obstruction is usually caused by benign prostatic hyperplasia or urethral stricture (16) In many countries, it has been observed that the ratio in favor of females is increasing while the ratio in favor of males is decreasing Changes observed in the living standards resulting in the differences in diet, lifestyle, and occupations of the female population could be responsible for the decreased ratio (17)
As another important factor affecting the prevalence of stone disease, geographic conditions may also affect the occurrence of urolithiasis (2, 5) Differences in factors such as climate, socioeconomic status, race, genetics, dietary habits, and the presence of other medical condi-
tions may contribute to significant variations in the prevalence of kidney stone formation in a particular geographic or regional area This scenario has the potential to mirror the urolithiasis problem at a national and even global level Apart from commonly diagnosed urinary tract infections, patients with urolithiasis frequently present with the component pathologies of metabolic syndrome like diabetes mellitus, hypertension, or obesity, which could potentially be another factor that increases the risk for urinary stone formation (2, 18) The involved patients' associated comorbidities and metabolic factors play a specific role in the presence and severity of urinary stoneforming risk factors Related to this important subject, in addition to reduced fluid intake, decreased urine output, h y p e rc
hypocitraturia are the most commonly reported risk factors for stone formation in adults and children (7, 8) Based on this fact, a comprehensive metabolic evaluation seems mandatory in risk group cases prone to form recurrent stones requiring interventional procedures for a stone-free status
Considering the formation of metabolic risk factors in these cases, apart from the lifestyle playing a significant role in the formation of stones, the dietary habits of the community have a more critical role While cereals and vegetables contain high levels of oxalate and its precursors are widely consumed in developing countries, in the western part of the world, a Westernized diet containing excessive protein, lipid, calcium, and sodium is also important in stone formation, changing the urine composition and increasing the associated risk status (9, 19)
Among the dietary risk factors evaluated so far, in addition to excessive calcium and oxalate-rich food consumption, a high sodium intake may increase calcium absorption into the blood or decrease absorption from urine into renal tubular cells, resulting in hypercalciuria On the other hand, higher consumption of animal protein can also lead to urine acidification (10)
Last but not least, education might play a role in urolithiasis In support of this, Data from studies in Iran and Turkey suggest that lower education levels may contribute to kidney stone formation (11, 20) However, some studies also show a negative relationship between the incidence of stone disease and the education level or occupation (12, 21)
Taking all the above facts, we believe that significant implications could be derived from the epidemiologic data obtained from local scale studies With this aim to update urolithiasis epidemiological data by examining certain epidemiological risk factors in the Turkish population, we conducted this study
Our findings revealed valuable data showing useful clinical implications that could be derived from our trial The majority of the stones were located in the upper tract and were calcium-containing stones The number of stone attack episodes was an important issue, and most cases did present with the first attack (57 7%), where a limited percentage had high recurrence rates with more than five attacks (14 7%) Men were affected by the disease at relatively younger ages than women Hypertension was the most common co-morbidity Additionally, as another important component of metabolic syndrome, BMI values
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12181 3 Clinical characteristics of adult cases with urolithiasis from Turkey
i t h i a s i s , w e l l - c o n d u c t e d
a l c i u r i a
e ro x a l u r i a , h y p e r u r i c o s u r i a , a n d
, h y p
were well evaluated, and 31 3% of the cases had severe obesity with BMI values of > 30 On the first presentation, most cases presented with persistent microscopic hematuria (50 3%), and recurrent infection, colic pain were the other presenting symptoms 26 8% of the patients have a previous stone-related intervention A considerable percentage of the cases have severe (Grade III-IV) obstruction at first evaluation Last but not least, positive family history was a critical and predictive parameter noted where 1/3 of all cases did have this history, and men were more likely to have this anamnesis This parameter affected the course of the disease, and mean age at first onset was less in these cases Also, stone attacks were higher in these cases than in patients without family history Our study is not free of limitations The number of patients evaluated may be limited, and the need for a control group may constitute another critical drawback However, taking limited information regarding the epidemiological data on stone disease, particularly in a regional evaluation-based manner, we believe our findings will be contributive to a greater extent Additionally, taking the endemic nature of the stone disease in our country, these values coming from a regional part of the country will give further insights into the epidemiologic features of the disease
In light of the data published so far and our findings obtained in adult cases with urinary stones, we may say that local and regional epidemiological studies focusing on personal, environmental, and metabolic risk factors could be critical These data can be used to derive practical, predictive clinical implications from limiting the risk of stone recurrence, lowering the economic burden of the disease, and outlining the most rational treatment alternative
REFERENCES
1 Sorokin I, Mamoulakis C, Miyazawa K, et al Epidemiology of stone disease across the world World J Urol 2017; 35:1301-20
2 Stamatelou K, Goldfarb DS Epidemiology of Kidney Stones Healthcare 2023; 11:424
3 Worcester EM, Coe FL Clinical practice Calcium kidney stones N Engl J Med 2010; 363:954-63
4 Huang WY, Chen YF, Carter S, et al Epidemiology of upper urinary tract stone disease in a Taiwanese population: a nationwide, population based study J Urol 2013; 189:2158-63
5 Marya RK, Dadoo RC, Sharma NK Genetic predisposition to renal stone disease in the first-degree relatives of stone-formers Urol Int 1981; 36:245-7
6 Trinchieri A Epidemiological trends in urolithiasis: impact on our health care systems Urol Res 2006; 34:151-6
7 Soligo M, Morlacco A, Zattoni F, et al Metabolic syndrome and stone disease Panminerva Med 2022; 64:344-58
8 Chandrajith R, Wijewardana G, Dissanayake CB, Abeygunasekara A Biomineralogy of human urinary calculi (kidney stones) from some geographic regions of Sri Lanka Environ Geochem Health 2006; 28:393-9
9 Yasui T, Iguchi M, Suzuki S, Kohri K Prevalence and epidemiological characteristics of urolithiasis in Japan: national trends between 1965 and 2005 Urology 2008; 71:209-13
10 Trinchieri A Diet and renal stone formation Minerva Med 2013; 104:41-54
11 Nasir SJ The mineralogy and chemistry of urinary stones from the United Arab Emirates Qatar Univ Sci J 1999; 18:189-202
12 Muslumanoglu AY, Binbay M, Yuruk E, et al Updated epidemiologic study of urolithiasis in Turkey I: Changing characteristics of urolithiasis Urol Res 2011; 39:309-14
13 Lee YH, Huang WC, Tsai JY, et al Epidemiological studies on the prevalence of upper urinary calculi in Taiwan Urol Int 2002; 68:172-7
14 Scales Jr CD, Curtis LH, Norris RD, et al Changing gender prevalence of stone disease J Urol 2007; 177:979-82
15 Strope SA, Wolf Jr JS, Hollenbeck BK Changes in gender distribution of urinary stone disease Urology 2010; 75:543-6, 546 e1
16 Sierakowski R, Finlayson B, Landes RR, et al The frequency of urolithiasis in hospital discharge diagnoses in the United States Invest Urol 1978; 15:438-41
17 Silva GR, Maciel LC Epidemiology of urolithiasis consultations in the Paraíba Valley Rev Col Bras Cir 2016; 43:410-5
18 Shastri S, Patel J, Sambandam KK, Lederer ED Kidney Stone Pathophysiology, Evaluation and Management: Core Curriculum 2023 Am J Kidney Dis 2023; 82:617-634
19 Yitgin Y, Asrak H, Tefik T Role, importance and assessment of dietary habits in urolithiasis patient World J Urol 2023; 41:1229-33
20 Basiri A, Shakhssalim N, Khoshdel AR, et al The demographic profile of urolithiasis in Iran: a nationwide epidemiologic study Int Urol Nephrol 2010; 42:119-26
21 Abomelha MS, al-Khader AA, Arnold J Urolithiasis in Saudi Arabia Urology 1990; 35:31-4
Correspondence
Mehmet Ezer, MD (Corresponding Author) mehmetezer@gmail com Department of Urology, Kafkas University, Kars, Turkey, 36100
Mehmet Uslu, MD dr mhmtuslu@gmail com Department of Urology, Kafkas University, Kars, Turkey
Rasim Güzel, MD rasimguzel@hotmail com Department of Urology, Medistate Kavacık Hospital, Istanbul, Turkey
Selçuk Güven, MD selcukguven@hotmail com Department of Urology, Necmettin Erbakan University, Konya, Turkey
Kemal Sarıca, MD saricakemal@gmail com Department of Urology, Sancaktepe S ¸ ehit Prof Dr Ilhan Varank Training and Research Hospital, Istanbul, Turkey Department of Urology, Biruni University Medical School, Istanbul, Turkey
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12181
4
M Ezer, R Güzel, M Uslu, S Güven, K Sarica
CONCLUSIONS
ORIGINAL PAPER
Kamran Hassan Bhatti 1 , Rawa Bapir 2-4 , Nadeem Sohail 1 , Faaz Salah Gomha 1 , Ahmed H.A. Shaat 1 , Aftab Ahmed Channa 5 , Khalid Mohammed Abdelrahman 1 , Bryar Othman Muhammed 6 , Nali H. Hama 2, 7 , Fahmi H. Kakamad 2, 3, 7 , Berun A. Abdalla 2, 3 , Jihad Ibrahim Hama 8 , Hiwa O. Abdullah 2, 3
1 Urology Department, Hamad Medical Corporation, Alkhor, Qatar;
2 Smart Health Tower, Madam Mitterrand Street, Sulaimani, Kurdistan, Iraq;
3 Kscien Organization for Scientific Research (Middle East Office), Hamid Str, Azadi Mall, Sulaimani, Kurdistan, Iraq;
4 Department of Urology, Surgical Teaching Hospital, Sulaimani, Kurdistan, Iraq;
5 Urology Unit, Islam Medical College, Sialkot, Pakistan;
6 Smart Health Tower (Raparin Branch), Karux Street, Rania, Sulaimani, Kurdistan, Iraq;
7 College of Medicine, University of Sulaimani, Madam Mitterrand Street, Sulaimani, Kurdistan, Iraq;
8 Research Center, University of Halabja, Halabja, Kurdistan, Iraq
Summary
Background: Urolithiasis is one of the most prevalent urological diseases and is associated with a substantial economic burden Its prevalence varies according to geographical location Qatar is a Middle Eastern country located in the Afro-Asian Stone Belt It has a dry and hot climate, which may predispose individuals working in these environments to form kidney stones (KSs) Methods: A population sample of 4204 patients was categorized into five occupational classes. The frequencies and correlations of these occupations with KS formation were calculated Results: Among the total cases, 2000 presented with KSs, with the majority being of Asian descent (49%), followed by individuals of Middle Eastern descent (35.1%). Technicians accounted for 35 15% of KS cases followed by clerks (29 2%) and executives (14.6%). Among KS cases, 44% had a single stone, 30% had multiple stones, and 26% had two stones In comparing both KS and non-KS groups, age, gender, occupation, and race were significantly associated with KS formation (p-value < 0.05), while BMI did not show any significant correlation (p-value > 0 05) Asian males aged 31-40, working as technicians, were significantly more prone to urolithiasis. In comparing age, BMI, and gender with stone characteristics, only age was found significantly associated with stone size (p-value < 0 05) Occupation showed an impact on all studied stone characteristics Clerks and technicians presented more frequently with stones within the 11-15 mm range, while executives more frequently presented with smaller stones (p-value < 0 001) Stone density was more frequently < 500 HU in workers, technicians and housewives and > 500 HU in executives and clerks (p-value < 0 001)
Conclusions: Our findings revealed an elevated risk of urolithiasis among certain occupational groups, particularly technicians, who frequently work outdoors in high-temperature environments. Alternatively, the sedentary nature of clerical and executive positions can also contribute to the risk of urolithiasis
KEY WORDS: Urolithiasis; Occupational risk; Environmental factors; Geographic prevalence; Qatar
Submitted 24 October 2023; Accepted 9 January 2024
INTRODUCTION
Urolithiasis is the presence of stones inside the urinary tract It is one of the most prevalent urological diseases, preceded only by urinary tract infections and prostate diseases (1)
Urolithiasis is a multifaceted condition and doesn’t have a specific etiology Risk factors for the development of kidney stones (KSs) are divided into intrinsic and extrinsic factors Intrinsic factors are age, gender, ethnicity, and genetics Extrinsic factors are climatic and environmental conditions, dietary habits, and occupation (2-4)
The prevalence of KSs increases with age in both men and women Men are more susceptible to developing KSs than females, while in children, both sexes have the same probability of KS formation (2, 5) The prevalence of this condition differs across various geographical areas, with an estimated prevalence ranging from 1% to 5% in Asia, 5% to 9% in Europe, and a significantly higher at 13% in North America
Additionally, it is important to highlight that the likelihood of recurrence for this condition is on the rise, exceeding 50% within a 5- to 10-year timeframe (6)
Occupations that involve dehydration, prolonged exposure to the sun and high temperatures, perspiration, prolonged sitting, and infrequent urination increase the likelihood of KS formation (7-11) The economic burden of KSs is substantial The USA spent 1 83 billion dollars and 2 1 billion dollars in the years 1995 and 2000, respectively The estimated cost of stone-related problems could reach 4 1 billion dollars by the year 2030 (12)
Qatar is a Middle Eastern country that is characterized by its dry and subtropical desert climate It is situated within the Afro-Asian-Stone Belt region, and the workforce composition is marked by the presence of diverse nationalities (13, 14)
This study aims to investigate the role of occupation in urolithiasis in the Qatar population Additionally, it seeks to examine the correlation of occupation and several intrinsic factors with KS characteristics
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12022 1
OccupationalhazardinurolithiasispatientsinQatar: Asingle-centercross-sectionalstudy
DOI: 10 4081/aiua 2024 12022
METHODS
Study design
This was a retrospective cross-sectional study of 4204 patients who visited Al-Khor Hospital over the past eight years Specific information such as age, gender, BMI, occupation, race, smoking status, comorbidities, medical history, having KS or not, stone characteristics (in patients with KS), and any previous history of renal surgery (in cases with KS) were collected The review of the data presented no risks to the subjects involved, as it entailed a comprehensive review of historical medical records without the implementation of any new or invasive measures
Study population and setting
The study sample comprised medical records of 4204 patients, sourced from pre-existing data within the registry of Al-Khor Hospital, encompassing individuals who have either presented with renal or ureteric stones or visited the hospital for general check-ups over the preceding 8 years The study population encompassed a diverse spectrum of occupational categories, including clerks, executives, technicians, workers, and housewives Within this classification, technicians were engineers and skilled laborers who were engaged in tasks related to machinery and technology Workers represented a broader category encompassing individuals involved in manual labor or strenuous physical activities, spanning various industries including construction, agriculture, and manufacturing Clerks denoted employees fulfilling various roles within an office setting, while executives were supervisors primarily engaged in meetings and responsible for decisionmaking processes The frequencies of these occupations were calculated in both groups of patients with or without KSs and compared against each other
Inclusion and exclusion criteria
The study included adult patients who were admitted to Al-Khor Hospital with renal or ureteric colic or visited it for routine check-ups between January 1, 2014, and December 31, 2022 Individuals within the pediatric age group were excluded from this study
Statistical analysis
The acquired data were inputted into the Statistical Package for the Social Sciences (SPSS, v.25; IBM Corp.), with optimization of variables for subsequent analysis Descriptive statistics were then generated, followed by correlation testing, where the Chi-squared (𝝌²) test was employed to identify associations among diverse parameters The significance level was predetermined at p ≤ 0 05
RESULTS
Among the total number of individuals included, 2000 presented with KS, with the majority being of Asian descent (49%), followed by individuals of Middle Eastern descent (35 1%) In both KS and non-KS cases, a higher proportion of subjects were male (84 1% and 80 6%, respectively), with male-to-female ratios of 5 3:1 and 4 1:1, respectively The mean age of KS cases was 36 9 ± 9 1, concentrated in their thirties to forties, while non-KS
cases were commonly distributed over thirty years with a mean age of 41 6 ± 13 4 The BMI of KS cases was 28 9 ± 3 6, compared to 29 ± 3 71 in non-KS cases
Table 1.
The baseline characteristics of the patients
Patients with KS (No , %) Patients with no KS (No , %) Overall (No , %)
Race
Asian (979, 49 0%)
Middle Eastern (701, 35 1%)
Unknown (184, 9 0%)
African (132, 6 6%)
American (3, 0 2%)
European (1, 0 1%)
Sex
Male (1682, 84 1%)
Female (318, 15.9%)
Age (yrs )
18-23 (0, 0 0%)
Asian (1081, 49 1%)
Middle Eastern (843, 38 2%)
Unknown (0, 0 0%)
African (245, 11 1%)
American (12, 0 5%)
European (23, 1 0%)
Male (1776, 80 6%)
Female (428, 19.4%)
18-23 (155, 7 0%)
Asian (2060, 49 0%)
Middle Eastern (1544, 36 7%)
Unknown (184, 4 4%)
African (377, 8 9%)
American (15, 0 4%)
European (24, 0 6%)
Male (3458, 82 3%)
Female (746, 17.7%)
18-23 (155, 3 7%)
24-30 (488, 24.4%) 24-30 (347, 15.7%) 24-30 (835, 19.9%)
31-40 (851, 42 55%) 31-40 (621, 28 2%)
31-40 (1472, 35 0%)
41-50 (330, 16 5%) 41-50 (557, 25 3%) 41-50 (887, 21 1%)
> 50 (331, 16 55%) > 50 (524, 23 8%) > 50 (855, 20 3%)
(39 3
11 8) BMI (kg/m2) * Normal (209, 10 45%) Normal (242, 11 0%) Normal (451, 10 7%) Overweight (1048, 52 4%) Overweight (1109, 50 3%) Overweight (2157, 51 3%) Obese (743, 37 15%) Obese (853, 38 7%) Obese (1596, 38 0%)
Smoking Yes (504, 25 0%) Yes (327, 14 8%) Yes (831, 19 8%) No (1496, 75 0%) No (1877, 85 2%) No (3373, 80 2%)
Comorbidity
None (1952, 97 6%) None (1752, 79 5%) None (3704, 88 1%)
Diabetes mellitus (26, 1 3%) Diabetes mellitus (220, 10%)
Diabetes mellitus (246, 5 9%)
Hypertension (22, 1 1%) Hypertension (232, 10 5%) Hypertension (254, 6 0%)
Occupation
Clerk (584, 29 2%)
Executive (292, 14 6%)
Housewife (87, 4 35%)
Technicians (703, 35 15%)
Worker (334, 16 7%)
Previous renal surgery
Yes (1154, 57 7%)
No (846, 42 3%)
Number of stones
One (879, 44 0%)
Two (522, 26 0%)
Multiple (599, 30.0%)
Location of stones
Ureter (330, 16 5%)
Renal pelvis (512, 25.6%)
Upper Calyx (303, 15 15%)
Middle Calyx (411, 20 55%)
Lower Calyx (444, 22 2%)
Size of stones
5-10 mm (551, 27 55%)
11-15 mm (935, 46 75%)
16-20 mm (514, 25 7%)
Laterality
Right (958, 47 9%)
Left (1042, 52 1%)
Density of stones
< 500 HU (1093, 54.65%)
> 500 HU (907, 45 35%)
Clerk (342, 15 5%)
Executive (302, 13 7%)
Housewife (392, 17 8%)
Technicians (416, 18 9%)
Worker (752, 34 1%)
Clerk (926, 22 0%)
Executive (594, 14 1%)
Housewife (479, 11 4%)
Technicians (1119, 26 6%)
Worker (1086, 25 8%)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12022
2
K Hassan Bhatti, R Bapir, N Sohail, et al
Mean
Mean age ± SD
Mean age ± SD
Mean BMI
SD
Mean BMI
SD
age ± SD (36 9 ± 9 1)
(41 6 ± 13 4)
±
Mean BMI ± SD (28 9 ± 3 6)
±
(29 ± 3 71)
±
(29 ± 3 67)
Regarding occupations, technicians comprised the largest group (26 6%), accounting for 35 15% of KS cases and 18 9% of non-KS cases They were followed by workers (25 8%), representing 16 7% of KS cases and 34 1% of non-KS cases, and clerks (22%), comprising 29 2% of KS cases and 15 5% of non-KS individuals (Table 1)
More than half of the KS cases (57 7%) had a history of previous renal surgery Among KS cases, 44% had a single stone, 30% had multiple stones, and 26% had two stones, which were almost evenly distributed in terms of laterality The most common locations were the renal pelvis (25 6%), lower calyx (22 2%), and middle calyx ( 2 0 5 5 % ) S t o n e s
d between 11-15 mm (46 75%) with a density smaller than 500 HU in 54 65% (Table 1)
In comparing the two groups, age, gender, occupation, and race were significantly distributed in subjects with and without KS (p-value < 0 05), while BMI was not significantly different (p-value > 0 05)
The correlation of age, BMI, gender, and occupation with having KS
Par t 1
Par t. 2
Table 3.
Par t 2
Asian males aged 31-40, working as technicians, were the group significantly more prone to urolithiasis (Table 2)
In comparing age, BMI, and gender with stone characteristics (number, size, density), only stone size was differently distributed by age (p-value < 0 05) The 11-15 mm stone size was the most frequent in all age groups, although in patients between ages 31-40 years, the rate of 11-15 mm stones was higher (49%) than in the other age groups
All three stone characteristics were significantly correlated with occupation; stones were mostly single in clerks, housewives, technicians, and workers, while in executives, stones were mostly multiple (p-value < 0 001)
The most common stone size among clerks and technicians was within the 11-15 mm range, while executives more frequently presented with smaller stone sizes in comparison to other occupations (p-value < 0 001)
Stone density was more frequently < 500 HU in workers, technicians and housewives and > 500 in executives and clerks (p-value < 0 001)
* Ch -square test BMI:
ndex Yrs: years, HU: Hounsfie d units
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12022 3 Occupational hazard in urolithiasis patients
z e s w e r e
o
m o n l y d i s t r
b u t e
i
c
m
i
Table 2.
Variables Age (yrs ) BMI Total 18-23 24-30 31-40 41-50 > 51 P-value * Normal Overweight Obese P-value * Having stone Yes 2000 0 488 851 330 331 < 0 001 209 1048 743 0 401 No 2204 155 347 621 557 524 242 1109 853
Variables Gender Occupation Race Total Male Female P-value* Clerk Executive Housewife Technician Worker P-value * Total African American Asian European Middle eastern P-value * Having stone Yes 2000 1682 318 0 003 584 292 87 703 334 < 0 001 1816 132 3 979 1 701 < 0 001 No 2204 1776 428 342 302 392 416 752 2204 245 12 1081 23 843 * Chi-square test BMI: body mass index KS: kidney ston
Variables Age (yrs.) BMI Total 24-30 31-40 41-50 > 50 P-value* Normal Overweight Obese P-value * Stone number One 879 215 366 147 151 0 867 90 471 318 0 474 Two 522 124 232 89 77 59 278 185 Multiple 599 149 253 94 103 60 299 240 Stone size 5-10 mm 551 109 249 102 91 0 027 58 304 189 0 55 11-15 mm 935 250 401 139 145 97 476 362 16-20 mm 514 129 201 89 95 54 268 192 Stone density < 500 HU 1093 271 466 181 175 0 9 105 588 400 0 255 > 500 HU 907 217 385 149 156 104 460 343
The correlation of age, BMI, gender, and occupation with stone characteristics Par t. 1
Variables Gender Occupation Total Male Female P-value * Clerk Executive Housewife Technician Worker P-value * Stone number One 879 732 147 0 612 363 38 39 310 129 < 0 001 Two 522 445 77 107 106 16 199 94 Multiple 599 505 94 114 148 32 194 111 Stone size 5-10 mm 551 459 92 0 642 29 142 36 205 139 < 0 001 11-15 mm 935 794 141 551 35 21 284 44 16-20 mm 514 429 85 4 115 30 214 151 Stone density < 500 HU 1093 920 173 0.923 266 56 62 465 244 <0.001 > 500 HU 907 762 145 318 236 25 238 90
body mass
DISCUSSION
In the course of this study, we conducted an assessment of the role of occupation in urolithiasis and examined the correlation of occupation and other several intrinsic factors with KS characteristics in the population of Qatar In this study, only validated studies were used for discussion (15)
Factors estimated to contribute to the pathogenesis of nephrolithiasis include genetic predisposition, gender, geographic location, dietary habits, insufficient fluid intake, and socioeconomic status (16)
It has been well established that males are more susceptible to nephrolithiasis than females due to exposure to risk factors (16-18)
A review study indicated an elevated prevalence of exposure to occupational hazards among men These hazards include engaging in repetitive tasks, extended periods of sitting or standing at work, physically demanding labor involving lifting and manual material handling and exposure to occupational ultraviolet radiation from sunlight
The review found no evidence in any study suggesting that women had a higher susceptibility than men to these specific occupational hazards, most of which are recognized as risk factors for the development of KS (18)
Another study indicated that the increased occurrence and prevalence of KS in men could be attributed to higher rates of obesity and alcohol consumption in men compared to women, leading to heightened production of oxalic acid in men (17)
Urolithiasis predominantly impacts adults in the third to fourth decade of life, with a generally observed male-tofemale ratio ranging from 1 5:1 to 2 5:1 (19) Some studies, particularly in the United States, suggested a potential decline in this ratio to below 1 5:1 (20-22) Another study conducted in Morocco reported a male-to-female ratio of 2 03:1, while Hossain et al documented a ratio of 2 68:1 in Japan (19, 23)
In Bouatia's study, the age group most susceptible to KS was between 31 and 60 years old, with a peak incidence observed at the age of 53 (19)
In addition to the intrinsic factors, some studies also mentioned high BMI or obesity as a factor for KS formation (17, 19, 24, 25)
In line with the literature, the findings of our study revealed that males were significantly more affected by nephrolithiasis This association was attributed to the nature of the patients' work, which often involved exposure to sunlight, high temperatures, or a sedentary work style in the workplace The male-to-female ratio among our KS cases was 5 3:1, significantly higher than the ratios reported in previous studies
The mean age of KS cases was 36 9 ± 9 1, consistent with the literature
While some authors have reported an association between BMI and KS formation, our findings, to the contrary, indicate no significant role of BMI in nephrolithiasis
In our study, the races most significantly affected by KS were Asian, followed by Middle Eastern and African populations, underscoring the correlation between KS formation and geographical location, as indicated in the literature (16)
In terms of stone composition, most studies reported similar findings In a renal stone clinic in Southampton, in a
population of 2800 patients, the predominant stone composition was calcium oxalate (89%), with a ratio of 1:4 for calcium oxalate to mixed calcium oxalate phosphate stones Pure calcium phosphate stones were infrequent, accounting for only 2% of cases In Sweden, approximately 85% of urinary tract stones were classified as calcium stones, encompassing both calcium oxalate and calcium phosphate varieties (26, 27) In another study involving 888 cases, calcium oxalate and calcium phosphate were identified as the most common primary components of the stones (28) In a series of 802 patients with 828 KS, Bouatia et al identified calcium oxalate as the main component, followed by uric acid and calcium phosphate (19)
Unfortunately, due to the nature of the study design, we could not represent any data regarding stone composition in our cases However, the stone density in 54 65% of our cases was < 500 HU, and according to the literature, stones with < 500 HU were usually uric acid stones
Therefore, we estimate that stones in more than half of our cases were uric acid type (29)
Our findings revealed that the majority of patients at risk of KS formation were the technicians and the clerks The technicians with KS accounted for 35 15% of our dataset
They may spend a significant amount of time outdoors, often exposed to adverse weather conditions, including high temperatures and direct sunlight These environmental factors, notably high-temperature environments and prolonged sun exposure, are recognized as significant risk factors in the etiology of urinary stone formation, especially uric acid stones (30) Nevertheless, workers, akin to technicians, are exposed to elevated temperatures and sunlight However, in this study, their association with KS formation did not reach the same level of significance as observed with technicians
In 1945, Pierce et al studied the effects of high-temperature exposure as a risk factor for the formation of urolithiasis in American troops in desert areas (31) Later on, multiple studies indicated the association between the incidence of stone and working in ambient temperatures, under the sun, and perspiration (10, 30, 31)
Better et al studied the increased incidence of nephrolithiasis in lifeguards who are exposed to the sun more than the normal population (10) Lu et al reported an increase in the prevalence of radiolucent stones among workers in a steel factory who were exposed to heat (11) The correlation between urolithiasis and ambient temperature, as well as heat exposure, can be attributed to several factors, including low urine volume with saturation of stone-forming salts in urine due to perspiration (32)
Perspiration also leads to acidic urine with a reduction of uric acid solubility, which also contributes to stone formation (31)
The incidence of urolithiasis peaks in the summer, which further supports the impact of ambient temperatures on stone formation (8)
This assumption aligns perfectly with our region, characterized by a dry and subtropical desert climate
Another hypothesis for the development of stone in warmer climates is that sunlight leads to higher levels of Vitamin D (32), although it is not concretely supported (33-35)
A substantial portion of our dataset (43 8%) in the KS
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12022
4
K Hassan Bhatti, R Bapir, N Sohail, et al
group consisted of individuals employed in clerical and executive positions This notable prevalence can be attributed to a myriad of factors Executive professionals occupied pivotal roles within our dataset, characterized by their accountability for formulating high-level decisions and overseeing the management of organizations or departments Their responsibilities encompassed strategic planning, leadership, and frequent engagement in meetings and office-based activities Clerical personnel within our dataset primarily performed administrative functions such as data entry, record-keeping, and meticulous management of paperwork They often worked indoors with executives Staying indoors and the sedentary features of these occupations have the potential to place individuals in a vulnerable position regarding the development of metabolic syndrome, elevated BMI, and infrequent urination Consequently, it is plausible to assert that such occupational pursuits may indirectly elevate the susceptibility of individuals to urolithiasis (8) Infrequent urination due to prolonged working hours and low urine volume are other occupational risks for the development of urolithiasis Individuals in various professions such as taxi drivers, aviation personnel, teachers, and healthcare workers are at risk due to these factors (7, 8, 36)
On the other hand, the potential for urolithiasis development in factory workers is exacerbated by occupational exposure to metallic substances Jarup et al documented an increased prevalence of KSs in individuals exposed to Cadmium (37) Additionally, Liu and colleagues identified an association between KSs and the presence of heavy metals such as Arsenic and Cadmium, while Chromium, Mercury, and Lead did not manifest discernible associations with this condition (4)
In the present study, we were unable to explore any relationships between metallic substances and KS formation due to the absence of data regarding the extent of exposure among cases or workers
Finally, there is insufficient knowledge on the correlation of stone characteristics with intrinsic and extrinsic factors for stone formation
A study by Krambeck et al reported no significant difference in stone size and location in relation to age Nonetheless, older individuals were more likely to have stones with a larger diameter or staghorn calculi (28) A meta-analysis of 15 studies involving 13 233 patients found no significant correlation between BMI and stone size (25)
In the present study, all stone characteristics, including number, size, and density, were found to be significantly correlated only with occupation, whereas stone size showed a correlation with age In contrast to the study by Krambeck et al , the stone size of 11-15 mm was the most frequent in all age groups, particularly in patients aged 31-40 years; no evidence suggested that older patients had larger stone sizes Furthermore, consistent with the meta-analysis by Wang et al , BMI did not exhibit a significant impact on stone size
Our study had several limitations The primary constraints included the retrospective nature of the work, which may have omitted certain data that could directly or indirectly influence the results Specifically, information about alcohol consumption status, urination volume,
daily water intake, and the presence of kidney diseases or other diseases that could enhance KS formation may not have been adequately captured
CONCLUSIONS
This study has provided insights into different working activities that may increase the risk of urinary stone formation in the Qatari population Our findings suggested an elevated risk of urolithiasis among certain occupational groups, particularly technicians, who frequently work outdoors in high-temperature environments Similarly, the sedentary nature of clerical and executive positions, characterized by prolonged indoor working hours can also indirectly contribute to the risk of urolithiasis Implementing proactive measures and awareness plans targeted at these at-risk groups may significantly contribute to reducing the incidence of urolithiasis among the workforce
DECLARATIONS
• Ethical approval: This study does not involve any human or animal testing
• Availability of data and material: All data and materials are kept by the first and corresponding authors
• Competing interests: None
• Funding: No source to be stated
• Authors' contributions: Kamran Hassan Bhatti, Rawa Bapir, and Nadeem Sohail were major contributors to the study Hiwa O Abdullah, Faaz Salah Gomha, Ahmed H A S h a a t , A f t a b A h m e d C h a n n a , N a l i H H a m a , K h a l i d Mohammed Abdelrahman, and Bryar Othman Muhammed were involved in the literature review, the writing of the manuscript, and data analysis and interpretation Fahmi H Kakamad, Berun A Abdalla, and Jihad Ibrahim Hama were involved in the design of the study, and the critical revision of the manuscript All authors have read and approved the final manuscript
• Acknowledgments: None to be declared
REFERENCES
1 Wigner P, Grebowski R, Bijak M, et al The molecular aspect of nephrolithiasis development Cells 2021; 10:1926
2 Z i e m b a J B , M a t l a g a B R E p i d e m i o l o g y a n d e c o n o m i c s o f nephrolithiasis Investigative and clinical urology 2017; 58:299-306
3 Najeeb Q, Masood I, Bhaskar N, et al Effect of BMI and urinary pH on urolithiasis and its composition Saudi journal of kidney diseases and transplantation 2013; 24:60-6
4 Liu Y, Zhang C, Qin Z, et al Analysis of threshold effect of urinary heavy metal elements on the high prevalence of nephrolithiasis in men Biological Trace Element Research 2022:1-1
5 Worcester EM, Coe FL Nephrolithiasis Primary Care: Clinics in Office Practice 2008; 35:369-91
6 Bouatia M, Benramdane L, Idrissi MO, Draoui M An epidemiological study on the composition of urinary stones in Morocco in relation to age and sex African journal of urology 2015; 21:194-7
7 Linder BJ, Rangel LJ, Krambeck AE The effect of work location on urolithiasis in health care professionals Urolithiasis 2013; 41:327-31
8 Malieckal DA, Goldfarb DS Occupational kidney stones Current opinion in nephrology and hypertension 2020; 29:232-6
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12022 5 Occupational hazard in urolithiasis patients
9 Bird VY, Chastain-Gross R, Sutkowski R, et al Pseudomonas aeruginosa as an etiologic agent of nephrolithiasis in deep water divers Journal of Endourology Case Reports 2017; 3:4-6
10 Better OS, Shabtai M, Kedar S, et al Increased incidence of nephrolithiasis (N) in lifeguards (LG) in Israel Phosphate and minerals in health and disease 1980:467-72
11 Lu IC, Yang CC, Huang CH, et al The Risk Factors for Radiolucent Nephrolithiasis among Workers in High-Temperature W o r k p l a c e s i n t h e S t e e l I n d u s t r y I n t e r n a t i o n a l J o u r n a l o f Environmental Research and Public Health 2022; 19:15720
12 Roberson D, Sperling C, Shah A, et al Economic considerations in the management of nephrolithiasis Current urology reports 2020; 21:1-9
13 Pathan SA, Mitra B, Bhutta ZA, et al A comparative, epidemiological study of acute renal colic presentations to emergency departments in Doha, Qatar, and Melbourne, Australia International Journal of Emergency Medicine 2018; 11:1-6
14 Jure Snoj Population of Qatar by Nationality in 2019 Priya D’Souza, 15 August 2019, https://priyadsouza com/population-ofqatar-by-nationality-in-2017/
15 Aso S Muhialdeen, Jaafar Omer Ahmed, Hiwa O Baba, et al Kscien’s List; A New Strategy to Discourage Predatory Journals and Publishers (Second Version) Barw Medical Journal 2023; 1
16 Hara A, Yang WY, Petit T, et al Incidence of nephrolithiasis in relation to environmental exposure to lead and cadmium in a population study Environmental research 2016; 145:1-8
17 Heo J, Son J, Lee W Epidemiology of urolithiasis with sex and working status stratification based on the national representative cohort in republic of Korea Safety and health at work 2022; 13:482-6
18 Biswas A, Harbin S, Irvin E, et al Sex and Gender Differences in Occupational Hazard Exposures: a Scoping Review of the Recent Literature Curr Environ Health Rep 2021; 8:267-280
19 Bouatia M, Benramdane L, Idrissi MO, et al An epidemiological study on the composition of urinary stones in Morocco in relation to age and sex African journal of urology 2015; 21:194-7
20 Daudon M, Traxer O, Lechevallier E, et al Épidémiologie des lithiases urinaires Prog Urol 2008; 18:802-14
21 Michelle L, Bernd H History, epidemiology and regional diversities of urolithiasis Pediatr Nephrol 2010; 25(1):49-59
22 Denstedt JD, Fuller A (2012) Epidemiology of Stone Disease in North America In: Talati, J , Tiselius, HG , Albala, D , YE, Z (eds) Urolithiasis Springer, London
23 Hossain RZ, Ogawa Y, Hokama S, et al Urolithiasis in Okinawa, Japan: a relatively high prevalence of uric acid stones International Journal of Urology 2003; 10(8):411-5
24 Chang MA, Goldfarb DS Occupational risk for nephrolithiasis and bladder dysfunction in a chauffeur Urological research 2004; 32:41-3
25 Wang D, Tan J, Geng E, et al Impact of body mass index on size and composition of urinary stones: a systematic review and metaanalysis International braz j urol 2023; 49:281-98
26 Walker V, Stansbridge EM, Griffin DG Demography and biochemistry of 2800 patients from a renal stones clinic Annals of clinical biochemistry 2013; 50:127-39
27 Tiselius HG Who forms stones and why? European Urology Supplements 2011; 10:408-14
28 Krambeck AE, Lieske JC, Li X, et al Effect of age on the clinical
presentation of incident symptomatic urolithiasis in the general population The Journal of urology 2013; 189:158-64
29 Kim JC, Cho KS, Kim DK, et al Predictors of Uric Acid Stones: Mean Stone Density, Stone Heterogeneity Index, and Variation C o e f fi c i e n
Computed Tomography and Urinary pH J Clin Med 2019; 8:243
30 Li Z, Li Y, Wang X, et al Extreme temperature exposure and urolithiasis: A time series analysis in Ganzhou, China Frontiers in Public Health 2022; 10:1075428
31 Pierce LW, Bloom B Observations on urolithiasis among American troops in a desert area The Journal of urology 1945; 54:466-70
32 Fakheri RJ, Goldfarb DS Association of nephrolithiasis prevalence rates with ambient temperature in the United States: a reanalysis Kidney international 2009; 76:798
33 Ferraro PM, Taylor EN, Gambaro G, et al Vitamin D intake and the risk of incident kidney stones The Journal of urology 2017; 197:405-10
34 Letavernier E, Daudon M Vitamin D, hypercalciuria and kidney stones Nutrients 2018; 10:366
35 Bargagli M, Ferraro PM, Vittori M, et al Calcium and vitamin D supplementation and their association with kidney stone disease: a narrative review Nutrients 2021; 13:4363
36 Hari SB, Morrow MS Rethinking nephrolithiasis in military aviation Aviation, Space, and Environmental Medicine 2012; 83:445-8
37 Jarup L, Elinder CG Incidence of renal stones among cadmium exposed battery workers Br J Ind Med 1993; 50:598-602
Correspondence
Kamran Hassan Bhatti, MD kamran bhatti@gmail com
Nadeem Sohail, MD
Faaz Salah Gomha, MD
Ahmed H A Shaat, MD
Khalid Mohammed Abdelrahman, MD Urology Department, Hamad Medical Corporation, Alkhor, Qatar
Rawa Bapir, MD
Nali H Hama, MD
Berun A Abdalla, MD
Hiwa O Abdulla, MD hiwaabdullah588@gmail com
Smart Health Tower, Madam Mitterrand Street, Sulaimani, Kurdistan, Iraq
Aftab Ahmed Channa, MD Urology Unit, Islam Medical College, Sialkot, Pakistan
Bryar Othman Muhammed, MD
Smart Health Tower (Raparin Branch), Karux Street, Rania, Sulaimani, Kurdistan, Iraq
Fahmi H Kakamad, MD (Corresponding Author) fahmi hussein@univsul edu iq
Doctors City, Building 11, Apartment 50, Sulaimani, Iraq
Road Number: GFG6+M6F Sulaymaniyah, Iraq
Jihad Ibrahim Hama, MD
Research Center, University of Halabja, Halabja, Kurdistan, Iraq
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12022
6
K Hassan Bhatti, R Bapir, N Sohail, et al
e - E n e r g y N o n - C o n t r a s t
t o f S t o n e D e n s i t y b y S i n g l
ORIGINAL PAPER
Themistoklis Ch Bellos 1 , Ioannis S Manolitsis 1 , Stamatios N Katsimperis 1 , Panagiotis A Angelopoulos 1 , Sotirios G Kapsalos-Dedes 1 , Panagiotis K Deligiannis 1 , Lazaros I Tzelves 2 , Nikolaos A Kostakopoulos 2 , Iraklis C Mitsogiannis 1 , Ioannis M Varkarakis 1 , Athanasios G. Papatsoris 1 , Andreas A. Skolarikos 1 , Charalampos N. Deliveliotis 1
1 2nd Department of Urology, Sismanoglio General Hospital of Athens, Athens, Greece; 2 1st Department of Urology, Metropolitan General, Cholargos, Greece
Summary
Background: In urology, ureteral stents are used to treat obstructive diseases Hematuria (54%), fever, discomfort, and lower urinary system symptoms are the predominant symptoms related to ureteral stent
Aim: This article links stent symptoms to double-j width and length, as well as patient’s height, weight, and body mass index (BMI). Ureteric Stent Symptoms Questionnaire (USSQ) was used to measure ureteral stent symptoms at 1st and 4th week of stent in situ as well as the 4th week after pigtail removal.
Methods: A 200-patient prospective study, where patients were allocated into four groups following ureteral stent insertion depending on the stent characteristics Those groups were: 4 8 Fr./26 cm (Group A), 4.8 Fr./28 cm (Group B), 6 Fr/26 cm (Group C), and 6 Fr/28 cm (Group D)
Results: Men comprised 53.5% of 200 patients. Participants had an average age of 49 ± 15 5 years, height of 175 ± 8 94 cm, and BMI of 23 8 ± 7 6 cm The laboratory results were identical between groups At the first and fourth week, groups had similar urine symptoms, pain severity, health status and occupational activities The difference in pain location was statistically significant Group A had 82 4% renal back pain in the first week, whereas Group B had 68 8%, Group C 31 3% and Group D 62 5 (p = 0 04) At the fourth week, 64 7% of Group A patients reported kidney front pain, compared to 100% of Group B, 93 3% of Group C, and 100% of Group D (p = 0 04) There was statistical significance in the sexual activity of the patients. 24 4% of Group C patients stopped sexual activity before stent installation, compared to 10.6%, 8.3%, and 6.4% of the other groups (p = 0 03) A moderate percentage of patients had active sexual activity at week 4 (Group A: 7.8%, Group B: 5.8%, Group C: 8 2%, Group D: 4 1%), p = 0 83 In multivariate analysis, urinary catheter group, age, weight, height, and BMI did not significantly affect urine index score (UIS), pain index score (PIS), general health (GH), quality of work (QW), and quality of sex (QS)
Conclusions: Despite various attempts to establish the best ureteral stent, the effect of double-j stent physical features on stent-related symptoms remained unknown. No verdict is conceivable without adequate empirical data
KEY WORDS: Ureteral stents; Pigtails; Urinary symptoms; Hematuria; Pain; USSQ; Pigtail characteristics; Pigtail diameter; Pigtail length; Double-j stent; Ureteral stent
Submitted 25 December 2023; Accepted 29 December 2023
INTRODUCTION
The single-pigtail stent, was first introduced to the medical community by Hepperlen and Mardis This innovative stent design revolutionized the field by providing a reliable and effective solution for various urological conditions (1-3) On the other hand, the double-J® stent, manufactured by American Cystoscope Makers located in Southborough, MA, was initially described by Finney (1-3) This particular stent design has gained significant recognition and widespread use Over the years, significant advancements have been made in the field of catheter technology, leading to notable improvements in both the location and design of these medical devices (4-6) These advancements have played a crucial role in enhancing patient care and overall medical outcomes One area that has witnessed remarkable progress is the location of catheters In the past, catheters were often placed using conventional techniques that relied heavily on the expertise of healthcare professionals In a comprehensive study conducted by Joshi et al , it was observed that a staggering 80% of individuals who had double-j stent insertion experienced the manifestation of at least one undesirable symptom related to the urinary tract (7) This finding sheds light on the significant impact that double-j stents can have on the overall health and quality of life of affected patients In recent years, there has been a growing interest in the field of medicine regarding the potential benefits of various pharmaceutical treatments to prevent or minimize the stent related symptoms
The primary objective of this investigation is to establish a correlation between the symptoms associated with stents and the physical attributes of the ureteral stent, namely its width and length Additionally, we aim to examine the potential relationship between these symptoms and the patient's biometric measurements, including height, weight, and body mass index (BMI)
MATERIALSANDMETHODS
Design of the study
This is a prospective, single center study The collection of data was performed in patients, where ureteral stents (pigtails) were inserted in a tertiary urology hospital from September 2021 to September 2023 The study was
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231 1
Ureteralstentrelatedsymptoms:Acomparativestudy
DOI: 10 4081/aiua 2024 12231
approved by the Institutional Review Board of the hospital (Protocol Number:6014/22 3 22) The study is registered to clinicaltrials gov with ID:14778, clinical trials ID: NCT05598710
Each double-j stent size that was inserted to each patient depended on the material availability and the surgeon ’ s preference at the time of surgery Intraoperatively the double-j stent was inserted by the standard way with the use of fluoroscopy Postoperatively the correct position inside the kidney and the bladder was assessed by KUB X-ray Correct position was considered the pelvis of the kidney and the lower end of the double-j stent inside the bladder not crossing to the contralateral side
For each patient the following data were recorded:
I Demographic and anthropometric data: age (in years), sex (male, female), height (in cm), weight (in kg), body mass index (BMI, in kg/m2) The patients according to BMI were categorized according to Centers for Disease Control (CDC) in: normal weight (BMI 18 5-24 9 kg/m2), overweight (BMI 25-29 kg/m2) and obese patients (BMI ≥ 30 kg/m2) (8)
II Clinical characteristics: reason for stent insertion (urolithiasis or pelviureteral junction stenosis), stone size, stone location, length of hospital stay (Length of Stay, LOS) in days, temperature measurement (appearance of fever postoperatively and the duration of fever), bloodwork pre-operatively, immediately postoperatively and during exiting the hospital (urea-U, creatinine-Cr, White Blood Cells-WBC, C-Reactive Protein) The change of those values was calculated as 1) the difference between the post-operative and pre-operative values 2) the difference between the values at hospital exit and the pre-operative values
III Ureteral Stent Characteristics: length (cm) (26 or 28) and width (Fr) (4 8, sometimes referred to as 5 in the text, and 6) In this particular study, there were four groups of patients with different ureteral stents: Group A: 4 8Fr, 26 cm, Group B: 4 8Fr, 28 cm, Group C: 6 Fr, 26 cm, Group D: 6 Fr, 28 cm
IV Ureteric Stent Symptoms Questionnaire (USSQ) (7) was completed at the first week (t1: end of the first week) and at four weeks (t2: end of fourth week) after stent placement but also at 4 weeks after removing the ureteral stent (t3: end of fourth week after double-j stent removal)
USSQ is a questionnaire with 6 groups of questions: – 1st group of questions: 11 questions in Likert scale about urinary symptoms By adding the results of those questions, we get the Urinary Index Score (UIS) which ranges from 11 to 56 Higher values of UIS, suggest higher severity of urinary symptoms UIS is presented – 2nd group of questions: questions regarding the body pain that the patient perceives The P1 question is about if the patient experiences pain (yes/no), P2 question is about the body sites where the patient perceives pain (I: Kidney Front, II: Groin Area, III: Bladder Area, IV: Kidney Back) Consequently by adding the results of the questions P3-P9, we get the Pain Index Score (PIS) The proportion of the patients that report pain in a particular body region as well as the PIS are reported – 3rd group of questions: They are 6 questions with answers in Likert scale, about the general health and physical activity By adding the results from those questions, we get the General Health Index Score (GHIS), which ranges from 4 to 28 Higher GHIS val-
ues, suggest higher general health burden due to the placement of ureteral stent GHIS is presented – 4th group of questions: 7 questions about professional life The first (question W1) is about professional status, the second (question W2) and third (question W3) is about the days that the patient was bed-ridden (W2) and did not perform his usual daily activities (W3), after the placement or removal of ureteral stent (depending on when the questionnaire was filled) The fourth question is about the kind of professional occupation, and the rest of the questions were answered only by those that were currently working and are about the quality of their work with questions in Likert scale From adding the answers in questions W5-W7, we get the Quality of Work Score (QWS), which ranges from 3 to 15 By adding the QWS and the answers to the questions W2, W3, we get the Work Performance Score (WPS) The days of being bedridden, the half days of loss of activity, the QWS and WPS are presented – 5th group of questions: it is about 3 questions (S1, S2i and S2ii or S3 and S4, the patients were asked to answer the questions S2i and S2ii or S3 and S4 depending on the answer they gave on the question S1 about sexual life) The percentage of patients that did not have active sexual life (S1), either due to stent placement or due to lack of effort on their behalf (S2i, S2ii) is presented Additionally, by adding the values from the answered questions S3, S4, we get the Œ (QSS) – 6th group of questions: it is about questions regarding additional problems that emerge while the ureteral stent is in place (in situ) The results from the answered questions A1-A4 are presented as the percentage of patients that mention each particular problem and/or the frequency of the particular problem occurrence – 7th question: it is the “Global Quality of Life” for the time period that the stent was in situ The answer to the question GQ is presented
Inclusion criteria
In this particular prospective observational study, only patients aged over 18 years old who had double-j stent placement were included The material of the double-j stent was Percuflex This particular material was selected due to its availability in our hospital
The double-j stents placed were of the following sizes: 4 8Fr26cm, 4 8Fr28cm, 6Fr26cm and 6Fr28cm
The choice of the size for each particular case depended on the double-j stent availability at the time of the operation as well as on the surgeon ’ s preference All the participants signed an informed consent form
The patients should have an adequate knowledge of the English language so they would be able to fill the USSQ
Exclusion criteria
Patients with hydronephrosis due to malignant diseases were excluded from this trial
Outcome of interest
The purpose of this trial is to investigate the relationship between the double-j stent’s characteristics and the appearance of complications from double-j stent use, as defined by «Ureteric Stent Symptoms Questionnaire»
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231
2
T Ch Bellos, I S Manolitsis, S N Katsimperis, et al
Statistical analysis
The statistical analysis was performed according to protocol (per protocol analysis), for all the patients that were included in the prospective observational study The level of statistical importance was set to 0 05 and all p- values were two-tailed The description of the results of the quantitative variables was performed with the presentation of mean values and standard deviations The description of the results of the qualitative variables was performed with the use of frequency and percentages Because the sample was 200 patients (N > 50), the test used for normality was the Kolmogorov-Smirnov test Pearson Chi-Square test was used to compare qualitative variables, and ANOVA was used to compare continuous quantitative variables SPSS software was used for statistical analysis
RESULTS
In total, during the period 01 09 2021-01 09 2023, BSPercuflex double-j stents were placed in 500 patients at our tertiary Urology Clinic Of these, 300 were excluded and were not included in the statistical analysis because the double-j stents were placed in those patients in order to relieve obstruction due to oncological causes The statistical analysis according to the protocol was performed on the data of 200 patients who met all the inclusion criteria
Basal patients’ characteristics
The baseline characteristics of the patients are presented in Table 1 A total of 200 patients were enrolled in the study of which 53 5% were male Their mean age was 49 ± 15 5 years and mean height and BMI, 175 ± 8 94 cm and 23 8 ± 7 6 cm respectively In the majority (97%) the reason for ureteral stent placement was the presence of a
stone in the ureter, either left (57 5%) or right (42 5%) with a mean size of 12 5 ± 3 7 mm
Table 2 shows the baseline characteristics of the patients and data on urological interventions in the 4 study groups
Regarding anthropometric characteristics, there were statistically significant differences between the 4 groups in terms of weight (p < 0 001) and height (p < 0 001)
Group B and D were composed of patients of greater weight and height, compared to the other two groups (Figure 1)
The sample was homogeneous in terms of the presence of comorbidities, the characteristics (diameter, material) of the Foley urinary catheter used and the reason for ureteral stent placement In all groups, ureteral stents were placed mainly due to the presence of a stone (96 1-100%) with no statistically significant differences in size, stone location and duration of the procedure between the 4 groups
Regarding the laboratory findings of the patients in the 4
Table 1
Basal patient characteristics
Table 2. Basic characteristics of patients and interventions by group
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231 3
stent related symptoms
Ureteral
Mean (SD) N (%) Sex Male - 107 (53 5) Female - 93 (46.5) Age (years) 49 (15 5)Weight (kg) 79 84 (12 5)Height (cm) 175 (8 94)BMI (kg/m2) 23 8 (7 6)Reason for stent insertion Stone - 194 (97) Stenosis - 6 (3) Stone Size (mm) 12 5 (3 7)Stone or Stenosis Location Left - 115 (57 5) Right - 85 (42.5) BMI:
Body Mass Index; SD: Standard Deviat on
Group A Group B Group C Group D P (N = 51, 25 5%) (N = 51, 25 5%) (N = 49, 24 5%) (N = 49, 24 5%) (95% CI) Mean ± SD Mean ± SD Mean ± SD Mean ± SD Sex, N (%) Male 31 25 24 27 0.58 ++ Female 20 26 25 22 Age (years) 51 7 ± 14 47 4 ± 15 8 49 5 ± 15 7 47 4 ± 16 5 0 14 + Weight (kg) 72.3 ± 9.6 88.6 ± 13 73.1 ± 8.1 85.4 ± 9.6 < 0.001 + Height (cm) 169 ± 4 6 183 ± 8 4 168 7 ± 4 181 4 ± 6 < 0 001 + BMI (kg/m2) 22 3 ± 9 24 6 ± 7 6 23 6 ± 7 9 25 ± 5 7 0 19 + Hypertension 9 (17 6) 3 (5 8) 8 (16 3) 9 (18 4) 0 24 ++ Diabetes Mellitus 2 (3 9) 1 (1 9) 1 (2) 0 (0) 0 58 ++ Coronary Heart Disease 5 (9 8) 2 (3 9) 4 (8 2) 0 (0) 0 13 ++ Prostate Hyperplasia 5 (9 8) 1 (1 9) 2 (4 1) 5 (10 2) 0 24 ++ Foley Diameter (Fr ) 14 2 (3 9) 0 (0) 0 (0) 1 (2) 0 450 ++ 16 36 (70 6) 34 (66 6) 29 (59 2) 32 (65 3) 18 13 (25 5) 17 (33 3) 20 (40 8) 16 (32 7) Latex 32 (62 7) 28 (54 9) 38 (77 5) 35 (71 4) 0 08 ++ Silicone 19 (37 3) 23 (45 1) 11 (22 4) 14 (28 6) Reason for stent insertion (N %) Stone 49 (96 1) 50 (98) 49 (100) 47 (96) 0 14 ++ Stenosis 2 (3 9) 1 (2) 0 (0) 2 (4) Procedure Duration 38 2 ± 31 4 38 5 ± 19 1 39 ± 14 7 43 4 ± 28 8 0 69 + Stone Size (mm) 12 5 ± 3 4 12 9 ± 4 12 2 ± 3 7 12 3 ± 4 0 86 + Stone or Stenosis Location (N %) Left 29 (56 9) 30 (58 9) 32 (65 3) 24 (49) 0 43 ++ Right 22 (43 1) 21 (41 1) 17 (34 7) 25 (51) + One
Anova (ANOVA); ++
Way
Pearson Chi Square
T Ch Bellos, I S Manolitsis, S N Katsimperis, et al
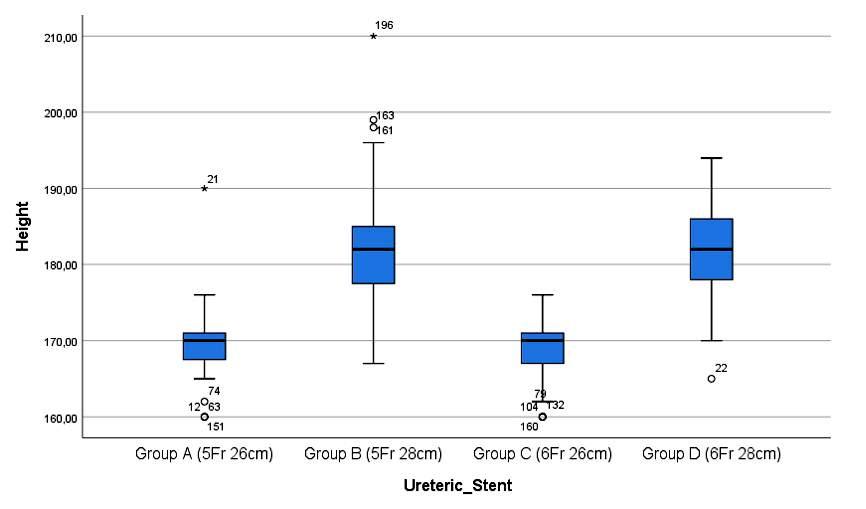
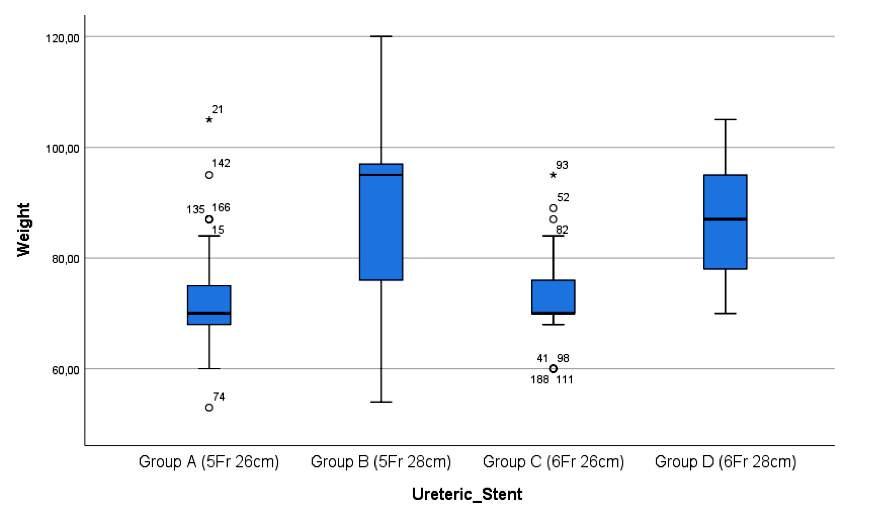
groups, no statistically significant differences were observed in urea, creatinine, white blood cells, C reactive protein (CRP), urine and blood culture There was no difference in any of the measured time-points (preoperative, postoperative, values at discharge) The same was true for the observed change in the values of the aforementioned variables, between postoperative and preoperative period, and between discharge and preoperative period However, in terms of clinical characteristics, febrile episodes after ureteral stent placement occurred only in patients in groups A and D, but there was no difference between these two in terms of the mean duration of febrile episodes and temperature values
Responses to the Ureteric Stent Symptoms
Questionnaire at 1 week after placement of the ureteric stent (stent in situ)
The results regarding the patients' responses during the first week after ureteral stent placement are presented in Table 4 In general, no statistically significant differences
Figure 1.
Box-Plot presenting the height (up) and weight (down) of the patients in the 4 groups
Y axis: Height (cm), Weight (kg)
X axis: Patient Group (A, B, C, D)
were observed between the 4 groups in terms of urinary symptoms, pain severity, general health status, occupational activity, and additional problems that may be related to the ureteral stent However, a statistically significant difference was observed in the location of pain In particular, 82 4% of patients in Group A reported pain in the Kidney Back region which was higher compared to the percentages of patients in the other groups (Group B: 68 8%, Group D: 62 5) and with Group C reporting the lowest percentage i e 31 3% (p = 0 04) (Figure 2)
In addition, differences were also present regarding the sexual life of the patients Although no one had an active sex life in the 1st week after stent placement, Group C patients had stopped being sexually active before stent placement, at 22 4% which is three times higher than the rates in the other groups (Group A: 9 8%, Group B: 7 8%, Group D: 6 1%, p = 0 04) The same proportions of patients, as expected, stated that the reason for sexual inactivity was not related to the symptoms caused by the stent (p = 0 04) (Figure 3)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231
4
Table 3
Clinical laboratory findings of patients by group
+ One Way ANOVA, ++ Independent Samples t-test, *Pearson Ch -Square test, **Fever Postoperatively Post-pre: Difference between postoperat ve and preoperative va ues; D scharge-Pre: Difference between discharge and preoperat ve values; BMI: Body Mass Index; SD: Standard Dev ation; 95% CI: 95% Confidence Interva Discharge-pre: Difference between values at hospita discharge and preoperative values; WBCs: White Blood Cells; CRP: C-react ve prote n
Figure 2.
Bar chart presenting the pain in the kidney back region, one week after ureteral stent placement
X axis: Groups of patients.
Y axis: Percentage of patients who reported pain in the kidney back area
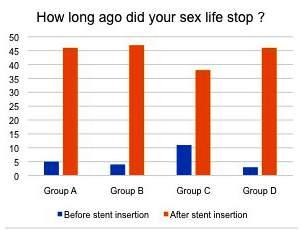
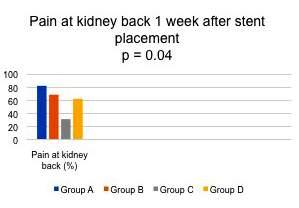
Figure 3
Bar chart which shows the percentage of patients who reported that they stopped having an active sex life before (blue) and after (orange) ureteral stenting
X axis: Groups of patients.
Y axis: Percentage of patients who reported that they stopped having an active sex life before (blue) and after (orange) ureteral stent placement.
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231 5 Ureteral stent related symptoms
Group A Group B Group C Group D P (N = 51, 25.5%) (N = 51, 25.5%) (N = 49, 24.5%) (N = 49, 24.5%) (95% CI) Mean ± SD Mean ± SD Mean ± SD Mean ± SD Urea (mg/dl) Preoperative 54 2 ± 85 6 38 9 ± 9 3 44 3 ± 13 4 62 6 ± 134 0 47+ Postoperative 43 4 ± 13 4 42 ± 9 2 46 1 ± 11 8 44 7 ± 13 8 0 37 + Discharge 33 2 ± 10 6 32 9 ± 10 2 35 ± 10 2 57 1 ± 165 3 0 44 + Post-pre -10 9 ± 80 3 1 ± 11 8 1 6 ± 11 6 -17 8 ± 126 0 44 + Discharge-Pre -21 ± 79 2 -3 12 ± 15 -9 4 ± 17 2 -5 4 ± 33 9 0 20 + Creatinine
Preoperative 1 17 ± 0 7 1 05 ± 0 3 1 15 ± 0 45 0 98 ± 0 54 0 64 + Postoperative 1 07 ± 0 67 1 02 ± 0 24 1 01 ± 0 31 1 1 ± 0 6 0 82 + Discharge 0 99 ± 0 57 0 96 ± 0 15 0 91 ± 0 14 0 99 ± 0 28 0 66 + Post-pre -0 1 ± 0 27 -0 02 ± 0 21 -0 14 ± 0 2 -0 04 ± 0 33 0 12 + Discharge-Pre -0 2 ± 0 37 -0 09 ± 0 26 -0 24 ± 0 4 -0 15 ± 0 38 0 17 + WBCs
mg/dl) Preoperative 7 9 ± 3 4 7 12 ± 1 8 5 85 ± 4 5 6 17 ± 3 5 0 56 + Postoperative 11,4 ± 5.5 9.92. ± 5.1 8.95 ± 6.1 8.57 ± 5.8 0.85 + Discharge 4 93 ± 5 4 4 17 ± 5 2 5 1 ± 5 4 5 42 ± 5 5 0 69 + Post-pre 2 6 ± 5 4 2 3 ± 3 9 3 5 ± 4 4 2 4 ± 5 1 0 59 + Discharge-Pre -3.53 ± 2.1 -2.8 ± 3.3 -3.1 ± 1.6 -2.48 ± 2.3 0.86 + CRP (mg/L) Preoperative 85 ± 51 75 ± 64 88 ± 49 76 ± 80 0 34 + Postoperative 50 ± 29 46 ± 45 58 ± 81 47 ± 75 0 34 + Discharge 39 ± 28 33 ± 32 37 ± 23 31 ± 38 0 81 + Post-pre -35 ± 22 -29 ± 19 -30 ± 32 -29 ± 5 0 65 + Discharge-Pre -46 ± 22 -42 ± 32 -51 ± 26 -45 ± 42 0 33 + Fever** N (%) 6 (11 8) 0 (0) 0 (0) 3 (6 1) 0 01 * Temperature (°C) 39 3 ± 0 3 39 3 ± 0 32 0 79 ++ (-0 32, 0 4) Duration (days) 3 ± 0 6 2 4 ± 0 8 0 2 ++ (-0 35,1 46) Blood Culture Positive 0 (0) 0 (0) 0 (0) 0 (0) Urine Culture
Preoperative 4 (7 8) 2 (3 9) 6 (12 2) 2 (4 1) 0 32 * Postoperative 0 (0) 0 (0) 3 (6 1) 0 (0) 0 15 *
(mg/dl)
(x10}
(positive)
T Ch Bellos, I S Manolitsis, S N Katsimperis, et al
Table 4.
Responses to the ureteric stent symptoms Questionnaire 1, one week after placement of the ureteric stent (stent in situ).
U1-U11 Urinary Index Score (UIS) (Mean ± SD)
P1 Do you experience body pain or discomfort in association with the stent? (N
P2 Site(s) where you experience pain or discomfort in association Kidney Front
with the stent typically (N %) Groin
P3 Sum of the VAS scores for all sites of pain (Mean ± SD)
P3-P9 Pain Index Score (Mean ± SD)
G1-G6 General Health Index Score (Mean ± SD)
W1 Status of
(N %)
W2 How many days did the symptoms associated with the stent keep you
(Mean ± SD)
W3. How many half days or more did you cut down your routine activities because
W5-W7 Quality of work for those who are in active paid jobs (Mean ± SD)
S1 Do you have an active sex life?
S2 i) If no sex life, how long ago did this stop? (N %)
ii) Why did this stop? (N %)
S3-S4 Quality of sex (Mean ± SD)
Because of the problems
associated with the stent
Some other reason – not to do
with the symptoms of the stent
A1 How many times have you felt you may be suffering from a urinary tract infection Never
(e.g. running temperature, feeling unwell and pain while passing urine)? (N
A2 Have you needed to take antibiotics as a result of insertion of the stent? (N
A3 Have you needed to seek help of a health professional (such as GP, nurse)
due to any problem associated with the stent? (N %)
A4 Have you needed to visit the hospital due to any problem associated
with the stent? (N
GQ Global Quality of life with the stent in situ:
In the future, if you were advised to have another stent inserted, Pleased
how would you feel about it? (N %)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231
6
Group A Group B Group C Group D P (N = 51, 25 5%) (N = 51, 25 5%) (N = 49, 24 5%) (N = 49, 24 5%) (95% CI) Mean ± SD Mean ± SD Mean ± SD Mean ± SD
23 06 ± 2 6 23 02 ± 2 8 23 4 ± 2 6 23 6 ± 2 5 0 61 +
%) No 34 (66 6) 35 (68 6) 33 (67 3) 33 (67 3) 0 99 ++ Yes 17 (33 4) 16 (31 4) 16 (32 7) 16 (32 7)
17/17 (100) 16/16 (100) 16/16 (100) 16/16 (100) N/A
Area 16/17 (94.1) 15/16 (93.8) 15/16 (93.8) 14/16 (87.5) 0.88 ++ Bladder Area 1/17 1/16 2/16 0 0 51 ++ Kidney Back 14/17 (82 4) 11/16 (68 8) 5/16 (31 3) 10/16 (62 5) 0 04 ++
7 2 ± 0 4 7 3 ± 0 6 7 4 ± 0 8 6 9 ± 0 8 0 2 +
20 47 ± 1 5 20 25 ± 2 3 19 3 ± 2 4 19 8 ± 2 6 0 45 +
10 5 ± 3 1 10 4 ± 2 9 10 8 ± 3 1 9 6 ± 2 1 0 17 +
Full time 16 (31 4) 18 (35 25) 14 (28 6) 15 (30 6) 0 53 ++ Part time 19 (37 2) 16 (31 4) 16 (32 7) 15 (30 6) 0 42 ++ Retired on health ground 000 0 (2) 0 67 ++ Retired for other reason 2 (3 9) 1 (1 95) 01 0 8 ++ Student 0000 N/A Unemployed, looking for work 14 (27 5) 16 (31 4) 19 (38 7) 18 (36 8) 0 67 ++
employment
2 45 ± 1 7 2 29 ± 1 5 2 18 ± 1 8 2 36 ± 1 4 0 85 +
day
in bed all or most of the
2.56 ± 1.7 2.73 ± 1.1 2.49 ± 1.5 2.61 ± 1.8 0.37 +
SD)
Type of employment (N %) Employee 15 (29 4) 17 (33 3) 18 (36 7) 15 (30 6) 0 6 ++ Employer 9 (17 6) 12 (23 6) 9 (18 3) 10 (20 4) Self Employed 27 (53) 22 (43 1) 22 (45) 24 (49)
of the symptoms associated with the stent (Mean ±
W4
6 8
1 6 6 9 ± 1 7 6 7 ± 1 4 6 4 ± 1 5 0 6 +
±
No 51 (100) 51 (100) 49 (100) 49 (100) N/A
46 (90 2) 47 (92 2) 38 (77 6) 46 (93 9) 0 04 ++
5 (9 8) 4 (7 8) 11 (22 4) 3 (6 1)
0000
After insertion of the stent
Before insertion of the stent
activity 46/51 (90 2) 47/51 (92 2) 38/49 (77 6) 46/49 (93 9) 0 04 ++
5/51 (9 8) 4/51 (7 8) 11/49 (22 4) 3/49 (6 1)
Did not attempt any sexual
N/A N/A N/A N/A N/A
49 (96 1) 43 (84 3) 46 (93 4) 43 (87 8) 0 16 ++
%) Occasionally 2 (3.9) 8 (15.7) 3 (6.6) 6 (12.2) Sometimes 0000 Most of the time 0000 All of the time 0000
Not at all 51 (100) 51 (100) 49 (100) 49 (100) N/A One course 0000 Two Courses 0000 Three or more courses 0000
%)
51 51 49 49 N/A
Once 0000 Twice 0000 Three
more times 0000
Never
or
51 (100) 49 (96 1) 48 (97 9) 49 (100) 0 44 ++
%) Once 0 1 (1 95) 00 Twice 00 1 (2 1) 0 Three or more times 0 1 (1.95) 00
Never
Delighted 0111 0 37 ++
21 16 19 19
Mostly satisfied 9 20 15 20 Mixed feelings 18 12 13 8 Mostly dissatisfied 3101 Unhappy 0110 Terrible 0000
cable; SD:
Deviation;
+ One Way ANOVA test; ++ Pearson Chi Square test; N/A: Not Appl
Standard
VAS: Visua Ana ogue
Table 5.
Responses to the ureteric stent symptoms
Questionnaire 1, four (4) weeks after ureteric stent placement
Urinary Index Score (UIS) (Mean ±
P1 Do you experience body pain or discomfort in association with the stent? (N %) No
P2. Site(s) where you experience pain or discomfort in association Kidney Front
with the stent typically (N %) Groin
P3 Sum of the VAS scores for all sites of pain (Mean ± SD)
P3-P9 Pain Index Score (Mean ± SD)
G1-G6 General Health Index Score (Mean ± SD)
W1 Status of employment (N %)
W2 How many days did the symptoms associated with the stent keep you
in bed all or most of the day (Mean ± SD)
W3 How many half days or more did you cut down your routine activities because
of the symptoms associated with the stent (Mean ± SD) W4
W5-W7 Quality of work for those who are in active paid jobs (Mean ± SD)
S2 i) If no sex life, how long ago did this stop? (N %)
ii) Why did this stop? (N %)
S3-S4 Quality of sex (Mean ± SD)
insertion of the stent
Some other reason – not to do
with the symptoms of the stent
A1 How many times have you felt you may be suffering from a urinary tract infection Never
(e g running temperature, feeling unwell and pain while passing urine)? (N %) Occasionally
A2 Have you needed to take antibiotics as a result of insertion of the stent? (N %) One course
A3. Have you needed to seek help of a health professional (such as GP, nurse) Never
due to any problem associated with the stent? (N %) Once
A4 Have you needed to visit the hospital due to any problem associated
with the stent? (N %)
GQ Global Quality of life with the stent in situ: Delighted
In the future, if you were advised to have another stent inserted, Pleased
how would you feel about it? (N %)
Way
Responses to the Ureteric Stent Symptoms
Questionnaire at week 4 after placement of the ureteric stent (stent in situ)
The results regarding the patients' responses at the fourth week after ureteral stent placement are presented in Table 5 In general, no statistically significant differences were observed between the 4 groups in terms of urinary symptoms, pain severity, general health status, occupational
activity, and additional problems that may be related to the ureteral stent However, a statistically significant difference was observed in the location of pain Specifically, 64 7% of Group A patients reported pain in the kidney front area which was lower compared to the percentages of patients in the other groups (Group B: 100%, Group C: 93 3%, Group D: 100%, p = 0 04) (Figure 4) In addition, differences were also present regarding the patients' sex life As
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231 7 Ureteral stent related symptoms
Group
51, 25
51, 25 5%) (N = 49, 24 5%) (N = 49, 24 5%) (95% CI) Mean ± SD Mean ± SD Mean ± SD Mean ± SD U1-U11
SD) 18 5 ± 2 3 18 6 ± 2 3 18 7 ± 2 5 18 4 ± 2 7 0 87 +
A Group B Group C Group D P (N =
5%) (N =
34 (66 7) 35 (68 6) 34 (69 4) 33 (67 3) 0 99 ++ Yes 17 (33 3) 16 (31 4) 15 (30 6) 16 (32 7)
11/17 (64.7) 16/16 (100) 14/15 (93.3) 16/16 (100) 0.04++
12/17 (70 6) 6/16 (37 5) 4/15 (26 7) 7/16 (43 8) 0 1 ++
1/17 (5 9) 1/16 (6 3) 1/15 (6 7) 0 (0) 0 8 ++ Kidney Back 12/17 (70 6) 6/17 (35 3) 4/15 (26 7) 7/16 (43 8) 0 1 ++
Area
Bladder Area
5 7 ± 0 8 5 5 ± 0 9 5 6 ± 0 9 5 8 ± 0 8 0 78 +
15 5 ± 2 1 14 8 ± 1 8 14 7 ± 2 3 15 1 ± 2 1 0 7 +
8 7 ± 1 9 8 6 ± 1 7 8 9 ± 2 3 8 ± 1 1 0 07 +
Full time 16 (31 4) 18 (35 25) 14 (28 6) 15 (30 6) 0 53 ++ Part time 19 (37 2) 16 (31 4) 16 (32 7) 15 (30 6) 0 42 ++ Retired on health ground 000 0 (2) 0 67 ++ Retired for other reason 2 (3.9) 1 (1.95) 01 0.8 ++ Student 0000 N/A Unemployed, looking for work 14 (27 5) 16 (31 4) 19 (38 7) 18 (36 8) 0 67 ++
1 75 ± 1 2 1 73 ± 1 2 1 76 ± 1 4 1 65 ± 1 01 0 98 +
1 47 ± 1 2 1 58 ± 1 19 1 81 ± 1 24 1 71 ± 1 0 48 +
of employment
%) Employee 15 (29 4) 17 (33 3) 18 (36 7) 15 (30 6) 0 6 ++ Employer 9 (17 6) 12 (23 6) 9 (18 3) 10 (20 4) Self Employed 27 (53) 22 (43 1) 22 (45) 24 (49)
Type
(N
6 8 ± 1 6 6 9 ± 1 7 6 7 ± 1 4 6 4 ± 1 5 0 6 +
sex life? No 47 (92 2) 48 (94 2) 45 (91 8) 47 (95 9) N/A Yes 4 (7 8) 3 (5 8) 4 (8 2) 2 (4 1)
S1 Do you have an active
42/47 (89 4) 44/48 (91 7) 34/45 (75 6) 44/47 (93 6) 0 03 ++
5/47 (10 6) 4/48 (8 3) 11/45 (24 4) 3/47 (6 4)
42/47 (89 4) 44/48 (91 7) 35/45 (77 8) 43/47 (91 5) 0 04 ++
5/47 (10 6) 5/48 (8 3) 10/45 (22 2) 4/47 (8 5)
After
Before insertion of the stent
Did not attempt any sexual activity
4 3 ± 0 9 4 ± 1 2 7 ± 0 9 3 3 ± 0 6 0 16 +
49/51 (96 1) 44/51 (86 3) 46/49 (93 9) 44/49 (89 8) 0 29 ++
2/51 (3 9) 7/51 (13 7) 3/49 (6 1) 5/49 (10 2)
51 (100) 51 (100) 49 (100) 49 (100) N/A
51 51 49 49 N/A
0 (0) 1 (2) 0 (0) (0)
Never 51 (100) 49 (96 1) 48 (97 8) 49 (100) 0 44 ++
Once 0 (0) 2 (3.9) 1 (2.2) (0)
0 (0) 1 (2) 1 (2 1) 1 (2 1) 0 06 ++
21 (41,2) 16 (31 4) 19 (38 8) 19 (38 8)
Mostly satisfied 9 (17 6) 20 (39 2) 19 (38 8) 23 (46 9) Mixed feelings 19 (37 3) 14 (27 4) 9 (18 2) 6 (12 2) Mostly dissatisfied 2 (3 9) 000
00 1 (2 1) 0
Unhappy
Terrible + One
ANOVA test; ++ Pearson Ch Square test; N/A: Not Applicab e; SD: Standard Dev ation; VAS: V sual Analogue
T Ch Bellos, I S Manolitsis, S N Katsimperis, et
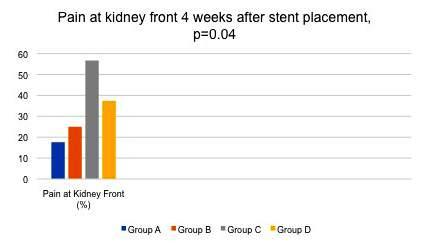
Table 6
U1-U11 Urinary Index Score (UIS) (Mean ± SD)
P2 Site(s) where you experience pain or discomfort in association
P3 Sum of the VAS scores for all sites of pain (Mean ± SD)
W2 Following removal of the stent, how many days did the symptoms associated
with the kidney problem keep you in bed all or most of the day (Mean ± SD)
W3 Following removal of the stent, how many half days or more did you cut down
your routine activities because of the symptoms associated with the kidney problem (Mean ± SD) W4
W5-W7 Quality of work for those who are in active paid jobs (Mean ± SD)
S2 i) If no sex life, how long ago did this stop? (N %)
insertion of the stent
Before insertion of the
S3-S4 Quality of sex (Mean ± SD)
GQ Global Quality of life with the stent in situ:
In the future, if you were advised to have another stent inserted,
how would you feel about it? (N
Figure 4.
Bar chart where pain is present in the kidney front area four weeks after placement of the ureteral stent.
X axis: Groups of patients
Y axis: Percentage of patients who reported pain in the kidney front area
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231
8
al
Group A Group B Group C Group D P-value (N = 51, 25.5%) (N = 51, 25.5%) (N = 49, 24.5%) (N = 49, 24.5%) Mean ± SD Mean ± SD Mean ± SD Mean ± SD
14 4 ± 1 7 14 4 ± 1 8 14 1 ± 1 6 14 5 ± 1 8 0 68 +
you experience body pain or discomfort in association with the stent? (N %) No 38 (74) 39 (76 5) 36 (73 5) 36 (73 5) 0 98 ++ Yes 13 (26) 12 (23 5) 13 (26 5) 13 (26 5)
P1 Do
11 (84 6) 7 (58 3) 11 (84 6) 10 (76 9) 0 57++ with the stent typically (N %) Groin Area 7 (53 8) 9 (75) 10 (76 9) 9 (69 2) 0 85 ++ Bladder Area 1 (7 6) 1 (8 3) 1 (7 6) 0 (0) 0 81 ++ Kidney Back 12 (92 3) 6 (50) 5 (38 5) 7 (53 8) 0 25 ++
Kidney Front
5 6 ± 0 7 5 6 ± 1 1 5 6 ± 0 9 5 7 ± 0 8 0 96 + P3-P9 Pain Index Score (Mean ± SD) 3 8 ± 6 7 3 4 ± 6 3 3 8 ± 6 4 4 1 ± 6 9 0 97 + G1-G6.
Health Index Score (Mean ± SD) 7.1. ± 1.2 7.1 ± 1.1 7.1 ± 1.2 6.8 ± 0.8 0.57 + W1 Status of employment (N %) Full time 16 (31 4) 18 (35 25) 14 (28 6) 15 (30 6) 0 53 ++ Part time 19 (37 2) 16 (31 4) 16 (32 7) 15 (30 6) 0 42 ++ Retired on health ground 000 0 (2) 0 67 ++ Retired for other reason 2 (3 9) 1 (1 95) 01 0 8 ++ Student 0000 N/A Unemployed, looking for work 14 (27 5) 16 (31 4) 19 (38 7) 18 (36 8) 0 67 ++
General
0 (0) 0 (0) 0 (0) 0 (0) N/A
0 (0) 0 (0) 0 (0) 0 (0) N/A
Type of employment (N %) Employee 15 (29 4) 17 (33 3) 18 (36 7) 15 (30 6) 0 6 ++ Employer 9 (17 6) 12 (23 6) 9 (18 3) 10 (20 4) Self Employed 27 (53) 22 (43.1) 22 (45) 24 (49)
3 5 ± 0 5 3 6 ± 0 5 3 5 ± 0 6 3 5 ± 0 5 0 86 +
sex life? No 5 (9 8) 4 (7 8) 7 (14 3) 3 (5 9) 0 55 ++ Yes 46 (90 2) 47 (92 2) 42 (85 7) 46 (93 8)
S1 Do you have an active
After
0 (0) 0 (0) 0 (0) 0 (0) N/A
stent 5/5 (100) 4/4 (100) 7/7 (100) 3/3 (100) ii) Why did this stop? (N %) Did not attempt any sexual activity 0 (0) 0 (0) 0 (0) 0 (0) N/A Some other reason – not to do 5/5 (100) 4/4 (100) 7/7 (100) 3/3 (100)
the symptoms
the stent
with
of
2 52 ± 0 5 2 51 ± 0 5 2 4 ± 0 5 2 3 ± 0 6 0 29 +
Delighted 3 (5 8) 0 3 (6 1) 0 0 12 ++
Pleased 9 (17 6) 20 (39 3) 15 (30 6) 21 (42 8)
Mostly satisfied 35 (68 6) 30 (58 8) 26 (53 1) 26 (53 1) Mixed feelings 4 (8) 1 (1 9) 3 (6 1) 2 (4 1) Mostly dissatisfied 00 1 (2 05) 0 Unhappy 00 1 (2 05) 0 Terrible 0000 +
ANOVA test; ++ Pearson Chi Square test; N/A: Not Appl cable; SD: Standard Deviation; VAS: Visua Ana ogue
%)
One Way
Table 7a
Dependent variables
Table 7b.
Independent variables
Ureteric Stent Group -0 14, p 0 3 -0
* Mu t p e L near regress on analysis P-values are shown
Qual
of
in the questionnaire completed at week 1 after stent placement, Group C patients reported that they had stopped being sexually active before stent placement, at a higher rate of 24 4% compared to the rates of the other groups (Group A: 10 6%, Group B: 8 3%, Group D: 6 4%, p = 0 03) The difference in rates with those of the first week is due to the fact that a small number of patients achieved active sexual activity at week 4 (Group A: 7 8%, Group B: 5 8%, Group C: 8 2%, Group D: 4 1%, p = 0 83)
Responses to the Ureteric Stent Symptoms
Questionnaire at week 4 after removal of the ureteric stent (post stent)
At 4 weeks after ureteral stent removal, no statistically significant difference was observed between ureteral catheter groups Almost all domains have returned to normal in all patients groups
In multivariate analysis, no statistically significant differences were found between the effects of ureteral catheter group, age, weight, height and BMI variables on urinary index score (UIS), pain index score (PIS), general health (GH), quality of work (QW) and quality of sex (QS) scores (Tables 7a, b)
Discussion
Aside from other purposes not covered in this text, the use of ureteral stenting acts as a preventive strategy against renal obstruction caused by leftover stone pieces, edema, hematoma, and the potential leakage of urine (9) Potential factors that may contribute to the development o f s t e n t - r e l a t e d s y m p t o m s ( S R S ) e n c o m p a s s v a r i o u s aspects, such as the irritation in the trigonal and renal regions due to the presence of the ureteral stent, vesicorenal reflux facilitated by the stent, as well as considerations regarding stent size, length, and position within the bladder or kidney Furthermore, the choice of materials utilized for the stent can also exert an influence
on its performance and efficacy The source of patient discomfort primarily stems from various factors, including the extended ureteral stent intravesical s e g m e n
drainage, ureteral stent displacement or migration, and the rigidity of the ureteral stent (10)
Urinary reflux, characterized by the retrograde flow of urine up the stent, is a p r e v a l e n t p h e n o m e n o n o b s e r v e d i n cases where intravesical pressures are elevated during voiding This particular condition has been identified as the underlying cause in approximately 25% of instances involving moderate colic-like flank pain that was closely associated with stents Elevated intravesical pressure exerts its impact on the renal system by inducing an elevation in intrarenal pressure This rise in pressure within the kidney subsequently results in kidney distension, a condition characterized by the expansion or enlargement of the renal organ Additionally, individuals e x p e r i e n c i n g e l e v a t e d i n t r a r e n a l p r
encounter flank pain, a discomfort localized in the region between the lower ribcage and the pelvis The phenomenon was commonly referred to as "water hammer" , that is a prevalent term in the medical field Persistent irritation of the mucosal lining of the bladder may result in enduring discomfort despite the removal of the stent
The alterations in the bladder mucosa are frequently encountered during cystoscopic examinations, particularly when indwelling catheters are retained for prolonged periods (11)
The presence of microscopic hematuria is commonly observed throughout the duration of ureteral stent placement, while macroscopic hematuria is frequently noted but typically self-resolves following stent insertion (11)
Stent migration, encrustation, stone formation, and fragmentation are recognized as potential complications that may arise subsequent to the implantation of a stent Stent occlusion, a commonly encountered occurrence, necessitates expeditious replacement of the double-j stent for resolution (12) Moreover, it has been observed that a considerable proportion of individuals who have been implanted with indwelling stents, reaching up to 86% according to existing literature (13), experience suboptimal occupational functioning and diminished sexual gratification as additional complications Females exhibit a higher propensity to present with the perception of an alien entity within the urinary bladder, primarily attributable to the distressing sensations it elicits (11)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231 9 Ureteral stent related symptoms
t , s u b o p
a l d o u b l e - j s t e n t
t i m
e s s u r e m a y a l s o
Independent variables UIS t1 UIS t2 UIS t3 PIS t1 PIS t2 PIS t3 GH t1 GH t2 GH t3 Ureteric Stent Group 0.170, p = 0.8 -0.035, p = 0.8 -0.004, p = 0.9 -0.336, p = 0.2 0.047, p = 0.8 -0.177, p = 0.7 -0.131, p = 0.5 -0.091, p = 0.5 -0.068, p = 0.4 Age -0 003, p = 0 8 -0 007, p = 0 6 -0 002, p = 0 8 0,001, p = 0 9 0 011, p = 0 5 -0 038, p = 0 2 0 018, p = 0 2 0 01, p = 0 3 0 004, p = 0 4 Weight -0 014, p = 0 6 -0 047, p = 0 06 -0 015, p = 0 4 0 021, p = 0 6 0 011, p = 0 7 -0 012, p = 0 8 0 027, p = 0 4 0 01, p = 0 6 -0 001, p = 0 9 Height -0 004, p 0 9 0 023, p 0 47 0 002, p 0 9 0 047, p 0 3 0 015, p 0 7 0 047, p 0 56 -0 049, p 0 2 -0 035, p 0 1 -0 004, p 0 7
0
= 0 8 0 004, p = 0 15 0 002, p = 0 4 0 003, p = 0 6 0 001, p = 0 9 0 007, p = 0 4 -0 005, p = 0 1 -0 002, p = 0 3 -0 001, p = 0 6 * Mu tip
regress on analysis
are shown
Index Score; PIS: Pa n Index Score; GH: Genera Health; t1: one week after stent p acement;
BMI
001, p
e L near
P-values
UIS: Urinary
t2: four weeks after stent placement; t3: four week after stent removal
QW t1 QW t2 QW t3 QS t2 QS t3
076, p 0 4 -0 011, p 0 8 -0 521, p 0 09 -0 069, p 0 07 Age -0 002, p = 0 8 -0 004, p = 0 6 0 001, p = 0 7 -0 182, p = 0 1 0 001, p = 0 7 Weight 0 021, p = 0 2 0 009, p = 0 5 0 003, p = 0 7 -0 06, p = 0 2 -0 002, p = 0 7 Height -0 007, p = 0 7 -0 008, p = 0 6 0 005, p = 0 5 0 096, p = 0 1 0 007, p = 0 4 BMI -0 001, p = 0 5 -0 001, p = 0 4 0 001, p = 0 7 0 007, p = 0 2 -0 001, p = 0 4
week
QW:
ty
Work; QS: Qual ty of sex; t1: one week after stent placement; t2: four weeks after stent p acement; t3: four
after stent removal
The potential influence of stent diameter on ureteral stent symptoms remains inconclusive The available evidence does not support the notion that employing a stent of larger diameter is associated with elevated levels of discomfort, hematuria, or symptoms pertaining to lower urinary tract obstruction The propensity for proximal stent migration is heightened in the context of smaller diameter stents (4 8 Fr) when juxtaposed with their 6 Fr counterparts, thereby establishing them as a notable risk factor The risk of complications in stent placement is influenced by various factors, including the duration of indwelling, the length of the stent, and the specific site of stent implantation (11)
According to our study, there was only statistical difference in the pain characteristics among the different ureteral stents, specifically during the first week a significant proportion of patients belonging to Group A, specifically 82 4%, experienced discomfort in the Kidney Back region This percentage was notably higher when compared to the corresponding figures for patients in the other groups, with Group B reporting 68 8% and Group D reporting 62 5% and with Group C exhibiting the lowest percentage, with only 31 3% of patients reporting pain in the Kidney Back region This disparity in percentages was found to be statistically significant, as indicated by a p-value of 0 04 During the fourth week of stent in situ, there were no statistically significant variations observed among the four groups with regards to urinary symptoms, severity of pain, overall health status, occupational activity, and other potential complications associated with the ureteral stent A notable disparity was observed in the spatial distribution of pain, which yielded statistical significance A significant proportion of patients belonging to Group A, namely 64 7%, experienced discomfort in the anterior region of the kidney Remarkably, this percentage was found to be considerably lower when compared to the corresponding figures in the other groups, with Group B reporting 100%, Group C reporting 93 3%, and Group D reporting 100% pain occurrence The statistical analysis revealed a noteworthy p-value of 0 04, indicating a significant difference among the groups However, during the fourth week after stent removal there were no significant differences between the groups since all the preoperative parameters returned to normal
Based on the studies conducted by Bolat et al. and Sighinolfi et al , it has been observed that the introduction of a double-j stent is closely linked to the occurrence of sexual dysfunction in nearly all individuals, irrespective of their gender (14, 15) In our prospective observational study, Group C patients reported that they had stopped being sexually active before stent placement, at a higher rate of 24 4% compared to the rates of the other groups (Group A: 10 6%, Group B: 8 3%, Group D: 6 4%, p = 0 03) In the fourth week of stent in situ some patients managed active sexual activity (Group A: 7 8%, Group B: 5 8%, Group C: 8 2%, Group D: 4 1%, p = 0 83) The fourth week after stent removal the sexual activity returned back to normal
Despite the optimal positioning and appropriate sizing of the stent, patients may still encounter urinary symptoms and pain that are correlated with the existence of the stent
(11) In a recent study conducted by Al-Kandari et al , the investigation focused on evaluating the potential influence of upper coil placement on the manifestation of stent-related complaints The study findings revealed that the positioning of the upper coil did not yield any discernible impact on the occurrence of such complaints
However, it has been postulated that the translocation of the bladder coil across the body's midline elicits augmented sensations of urgency and discomfort during micturition (16) Several investigations carried out by Inn et al , Ho et al , and Taguchi et al have yielded compelling findings suggesting a significant association between the insertion of a double-j stent coil into the urinary bladder, particularly on the contralateral side of the body, and the exacerbation of urinary symptoms and heightened pain levels (17-19) In a recent investigation carried out by Abt et al , it was determined that the precise positioning of the stent within the bladder does not yield any discernible effects on the symptoms induced by a ureteral stent (19)
In our cohort, all the double-j stents were positioned so they will not cross the midline
The present study is subject to certain limitations, primarily stemming from its non-randomized trial design
CONCLUSIONS
The potential influence of ureteral stent physical properties on stent-related symptoms remains inconclusive, despite numerous trials dedicated to identifying the optimal ureteral stent In light of the limited availability of robust empirical data, a definitive conclusion cannot be ascertained at this time The prioritization of establishing a benchmark for the quantification and documentation of the physical characteristics of stents is of utmost importance as the preliminary stage of forthcoming investigations
REFERENCES
1 Finney RP Experience with new double J ureteral catheter stent J Urol 1978; 120:678-81
2 Hepperlen TK, Mardis HK Pigtail stent termed means of lessening ureteral surgery Trends Clin Urol 1978; 1:405
3 Beiko DT, Knudsen BE, Denstedt JD Advances in ureteral stent design J Endourol 2003; 17:195-9
4 Marmar JL The management of ureteral obstruction with silicone rubber splint catheters J Urol 1970; 104:386-9
5 Orikasa S, Tsuji I, Siba T, Oashi N A new technique for transurethral insertion of a silicone rubber tube into an obstructed ureter J Urol 1973; 110:184-7
6 McCullough JL Shepards Crook self-retaining ureteral catheter Urol Lett Club 1974; 32:54-5
7 Joshi HB, Newns N, Stainthorpe A, et al Ureteral stent symptom questionnaire: development and validation of a multidimensional quality of life measure J Urol 2003; 169:1060-4
8 https://www cdc gov/healthyweight/assessing/bmi/index html
9 Dellis A, Joshi HB, Timoney AG, Keeley FX Jr Relief of stent related symptoms: Review of engineering and pharmacological solutions J Urol 2010; 184:1267-72
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231
10
T Ch Bellos, I S Manolitsis, S N Katsimperis, et al
10 Raju T Indwelling ureteral stents: Impact of material and shape in patient comfort J Endourol 2009; 7:2
11 Vogt B, Desgrippes A, Desfemmes FN Changing the double-pigtail stent by a new suture stent to improve patient's quality of life: A prospective study World J Urol 2015; 33:1061-8
12 Ahallal Y, Khallouk A, El Fassi MJ, Farih MH Risk factor analysis and management of ureteral double-j stent complications Rev Urol 2010; 12:e147-51
13 Giannarini G, Keeley FX Jr, Valent F, et al Predictors of morbidity in patients with indwelling ureteric stents: Results of a prospective study using the validated ureteric stent symptoms questionnaire BJU Int 2011; 107:648-54
14 Bolat MS, Akdeniz E, Asci R, et al Ureterorenoscopy with stenting and its effect on male sexual function: A controlled randomised prospective study Andrologia 2017; 49: e12746
15 Sighinolfi MC, Micali S, De Stefani S, et al Indwelling ureteral stents and sexual health: A prospective, multivariate analysis J Urol 2007; 178:229-31
16 Al-Kandari AM, Al-Shaiji TF, Shaaban H, et al Effects of proximal and distal ends of double-J ureteral stent position on postprocedural symptoms and quality of life: A randomized clinical trial J Endourol 2007; 21:698-702
17 Inn FX, Ahmed N, Hou LG, et al Intravesical stent position as a predictor of quality of life in patients with indwelling ureteral stent Int Urol Nephrol 2019; 51:1949-53
18 Ho CH, Tai HC, Chang HC, et al Predictive factors for ureteral double-J-stent-related symptoms: A prospective, multivariate analysis J Formos Med Assoc 2010; 109:848-56
19 Abt D, Mordasini L, Warzinek E, et al Is intravesical stent position a predictor of associated morbidity? Korean J Urol 2015; 56:370-8
Correspondence
Themistoklis Bellos, MD (Corresponding Author) bellos themistoklis@gmail com
2nd Department of Urology, Sismanoglio General Hospital of Athens, Athens Kassandras 8, Marathon, Attica, Greece 19007
Ioannis Manolitsis, MD giannismanolit@gmail com
Stamatios Katsimperis, MD stamk1992@gmail com
Panagiotis Angelopoulos, MD angelopoulospanag@gmail com
Sotirios Kapsalos Dedes, MD kapsalos13@gmail com
Panagiotis Deligiannis, MD panosdlg@gmail com
Iraklis Mitsogiannis, MD imitsog@med uoa gr
Ioannis Varkarakis, MD, Professor medvark3@yahoo com
Athanasios Papatsoris, MD, Professor agpapatsoris@yahoo gr
Andreas Skolarikos, MD, Professor andskol@yahoo com
Charalampos Deliveliotis, MD, Professor chdeliveli@gmail com
2nd Department of Urology, Sismanoglio General Hospital of Athens, Athens
Lazaros Tzelves, MD lazarostzelves@gmail com
Nikolaos Kostakopoulos, MD nikostakop@gmail com
1st Department of Urology, Metropolitan General, Cholargos, Greece
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12231 11 Ureteral stent related symptoms
ORIGINAL PAPER
Konstantinos Pagonis 1 , Angelis Peteinaris 1 , Constantinos Adamou 1 , Vasileios Tatanis 1 , Athanasios Vagionis 1 , Anastasios Natsos 1 , Mohammed Obaidat 1 , Solon Faitatziadis 1 , Evangelos Liatsikos 1, 2 , Panagiotis Kallidonis 1
1 Department of Urology, University Hospital of Rion, Patras, Greece;
2 Medical University of Vienna, Vienna, Austria
Summary
Purpose: The aim of this study is the evaluation of the distribution of Paclitaxel (PTX) released by a coated balloon in the layers of rabbit’s urethra
Methods: 18 rabbits were included. A Laser Device was used for the stricture formation After two weeks, dilation of the strictured urethra was performed by using Advance 35LP PTA balloons and Advance 18 PTX PTA balloons The experimental models were divided into 3 groups The group Α included two rabbits without any intervention except for the stenosis procedure Group B compromised six rabbits that underwent dilation with Advance 35LP PTA balloons Group C consisted of 10 rabbits to which dilation with both Advance 35LP PTA balloons and Advance 18 PTX PTA balloons was applied Histological evaluation and Immunohistochemistry were performed on all specimens
Results: Inflammation, fibrosis and ruptures were detected in the specimens of the study. In specimens of Group C the decrease of inflammation and fibrosis rate was greater Anti-PTX antibody was detected in the epithelium, lamina propria and smooth muscle layer of all specimens of urethras that have been harvested immediately and 1 day after the dilation with Advance 18 PTX PTA balloon and it was not observed in any layer of the urethral wall of the rest of the examined specimens of Group C.
Conclusions: PTX’s enrichment was detected in the smooth muscle layer of all specimens that have been harvested immediately and 24h after the dilation with Advance 18 PTX PTA balloons. PTX may play an inhibitive role in the recurrence of the stenosis
KEY WORDS: Urethra; Stricture; Balloon; Dilation; Paclitaxel
Submitted 31 December 2023; Accepted 17 January 2024
INTRODUCTION
Urethral strictures constitute a significant urological disease that presents a high incidence in the male population (1) The available minimally invasive approaches are associated with high recurrence rates (2) Drug Coated Balloons (DCBs) that release cytostatic substances have been used for the prevention of vascular stenosis (3) In the same concept, these balloons can be used for the reduction of the recurrence rates after the management of
the urethral strictures with balloon dilation (4) The successful effect of the drug requires its distribution to the muscle layer of the urethra where the smooth muscle cells are present (5) These cells are responsible for restenosis through their proliferation and production of inappropriate collagen (6) Paclitaxel has been proven to inhibit the proliferation of these cells and reduce the production of collagen (7, 8) Thus, the use of paclitaxel-coated balloons for the prevention of restenosis after balloon dilation seems to be a promising approach The distribution of paclitaxel in the normal rabbit urethra has already been evaluated (9) The aim of this experimental study is to provide evidence about the benefits of the application of DCBs in urethral strictures The current protocol aims to provide evidence on the distribution of paclitaxel (PTX) in the wall of the strictured urethra of rabbits The drug should be distributed to the muscle layer of the urethra in order to achieve maximal efficiency Moreover, data regarding the efficacy of this approach on the recurrence of the urethral strictures treated by the paclitaxel-coated balloons will be presented
Materials and Methods
Ethical standards
The current experimental trial was pre-approved by the Veterinary Administration of the Prefecture of Western Greece and the animals were treated according to the current veterinary protocols
Experimental models
Eighteen domestic male rabbits weighing between 3-4 kg were included in the conduction of the current experimental study
Sedation
The rabbits were sedated by intramuscular injection with a combination of ketamine and xylazine
Intervention
The experimental models were placed in the supine posi-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12248 1
Minimalinvasivetreatmentofurethralstrictures: AnexperimentalstudyoftheeffectofPaclitaxel coatedballoonsinthewallofstricturedrabbit’surethra
DOI: 10 4081/aiua 2024 12248
tion A urethroscopy was conducted on each rabbit by using a 7FR pediatric nephroscope (Storz 27095AA Pediatric Nephroscope Set, Karl Storz SE & Co KG, Tuttlingen, Germany) Stricture formation took place by using the Thulium fiber laser device (Quanta Fiber Dust, Samarate, Italy) with a 200-μm fiber and power settings 8W (0 5J x 16Hz) Strictures were formed in the penile urethra approximately 1-2 cm before the sphincter (Figure 1) After 2 weeks, an urethrography and an urethroscopy of each model were held The presence of a urethral stricture of approximately 1 cm in length in all experimental models was confirmed by these procedures Dilation of the stricture with Advance 35LP- high pressure balloon (HPB) (Cook Medical, Cook Ireland Ltd , Limerick, Ireland - 16, diameter 6 mm/ length 40 mm) and Advance 18PTX- DCB (Cook Medical, Cook Ireland Ltd , Limerick, Ireland – 16, diameter 6 mm/ length 40 mm) depending on the study group was conducted in the same session (Figure 2) A 0 035’’ inch hydrophilic guidewire was inserted into each urethral lumen under fluoroscopic guidance A stiff guidewire exchanged the hydrophilic wire over a 7 Fr ureteral catheter (Cook Medical, Cook Ireland Ltd , Limerick, Ireland) The balloon dilator was placed over the stiff guidewire and inflated to its maximum pressure of 8 atm for at least 5 minutes and then was emptied and removed Follow-up to 6 weeks with urethrography every 2 weeks depending on the study group took place
Study groups
The experimental models were divided into 3 main groups (groups A, B, and C) The rabbits were sacrificed on specific time periods and the whole length their urethra was obtained Group A: The control group included 2 experimental models where stricture formation was performed without any other intervention These specimens were obtained two weeks after the stricture formation
Group B: 6 rabbits were included in this group Two weeks after the stricture formation, dilation with HPB took place The subgroups were divided based on the postoperative duration until the harvesting of the urethras to provide information on the stricture condition after conventional balloon dilation All subgroups included 2 rabbit’s urethras and were defined as:
Group B 1: Harvested urethras 2 weeks after the dilation procedure
Group B 2: Harvested urethras 4 weeks after the dilation procedure
Group B 3: Harvested urethras 6 weeks after the dilation procedure
Group C: 10 experimental models were included in this study group Two weeks after the stenosis formation, dilation with HPB, at first, and then with DCB took place at the same time The subgroups were divided in the same way as in Group B 2 rabbit’s urethras were included in each subgroup The subgroups of group C were defined as:

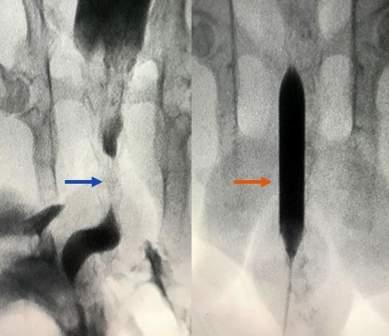
Figure 1.
Endoscopic images before and after the stricture formation
a The laser fiber inside the urethral lumen during urethoscopy.
b The initiation of stricture formation
c. Urethral stricture 2 weeks after the initial intervention.
Group C 1: Harvested urethras immediately after the dilation procedure with both HPB and DCB
Group C 2: Harvested urethras 1 day after the dilation procedure with both HPB and DCB
Group C 3: Harvested urethras 2 weeks after the dilation procedure with both HPB and DCB
Group C 4: Harvested urethras 4 weeks after the dilation procedure with both HPB and DCB
Group C 5: Harvested urethras 6 weeks after the dilation procedure with both HPB and DCB
Figure 2
Fluoroscopic images
a. Antegrade urothrography. Recognition of the stricture (blue arrow)
b. Dilation with Advance 18 PTX PTA balloon on the previously depicted stricture (orange arrow)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12248
2
K Pagonis, A Peteinaris, C Adamou, et al
ab ab c
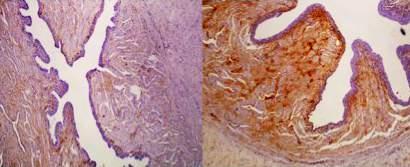
Pathology process
The specimens of urethras were embedded in formalin and standard fixing process with paraffin was performed 4μmthick sections were enriched with hematoxylin/eosin and were placed on gelatin-eluting glass slides
Histological evaluation of the specimens
All glass slides were tested by the same expert uropathologist This procedure is conducted by using a standard l i g h t m i c r o s c o p e w i t h a n a t t a c h e d c a m e r a ( N i k o n ECLIPSE 50i and Nikon HD color camera head DS-Fi2, Nikon GmbH, Dusseldorf, Germany) Slides were received from each urethral specimen for the conduction of histology and immunohistochemistry
Morphological alterations (stricture, connective tissue formation) and inflammation were microscopically evaluated The inflammation rate of the urethral layers was estimated according to Nakada classification (10) Normal appearance of the urethra after microscopic examination was graded as 0 and severe inflammation was graded as 3
Immunohistochemistry (IHC)
IHC was performed by using the monoclonal anti-body for IHC (Anti-Taxol antibody from Abcam) This process aimed into elucidating the enrichment of PTX in different layers of urethral wall The PTX’s presence and the loca-
Table 1
Figure 3.
Histolpathological Images from the urethral wall of the experimental models a. Specimen from Group C 4 b. Specimen from Group C.1
tion of the agent in the examined slides was evaluated with IHC (Figure 3)
Histology
Ruptures across the urethral wall and inflammation were observed in all specimens In Group A the inflammation grade was 3 (according to Nakada classification), fibrosis was observed in all layers (squamous epithelium, submucosa, smooth muscle layer) of the urethra In Groups B 1 and B 2 the inflammation grade was 2 and fibrosis was observed in all layers of the urethral tissue In Group B 3 fibrosis in all layers of the urethral wall and inflammation (Grade 1) were observed As for the Group C 1 and C 2, the inflammation Grade was 3 in both groups and fibrosis was observed in the epithelium tissue, submucosa and smooth muscle layer Blood clots were found in both groups In Group C 3 and C 4 the inflammation grade of the urethral wall was 2 and 1, respectively Fibrosis was observed only in the squamous epithelium and submucosal layer in both groups In Group C 5 the inflammation grade was 1 and fibrosis was observed only in the epithelium tissue of the urethral wall These results are presented in Table 1
Histological findings of the harvested urethral specimens regarding the Inflammation Grade, Fibrotic Formation, and the integrity of the urethral lumen.
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12248 3 Paclitaxel coated balloon for urethral stricture
RESULTS
Experimental Study Group Inflammation Grade F ibrosis Model (Nakada Classification) 1 A (stricture formation-no intervention) 3 Squamous epithelium Submucosa Smooth Muscle Layer 2 A (stricture formation-no intervention) 3 Squamous epithelium Submucosa Smooth Muscle Layer 3 B 1 (stricture formation-dilation 35LP PTA balloon-2 weeks) 2 Squamous epithelium
Smooth Muscle Layer 4 B.1 (stricture formation-dilation 35LP PTA balloon-2 weeks) 2 Squamous epithelium
Smooth Muscle Layer ab
Submucosa
Submucosa
Submucosa Smooth
Submucosa
Submucosa
Submucosa
Submucosa
Submucosa
IHC
The specimens of Group C were examined for the presence of the antibody of PTX In all specimens examined of Group C 1 and C 2, the anti-PTX antibody was found in the squamous epithelium, submucosa and smooth muscle layer of rabbit’s urethra In one specimen of
group C 1, the anti-PTX antibody was observed, also, in the corpus cavernosum and the connective tissue of the rabbit’s penis In the rest examined specimens of Group C the antibody wasn’t detected in any layer of the urethral wall The results of the IHC are summarized in Table 2
Paclitaxel (PTX) distribution in the layers of the examined specimens of the urethral wall based on the Immunohistochemical report Experimental Study Group
9 C.1 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-immediately)
10 C 1 (stricture formation-dilation 35LP PTA balloon+18
13 C 3 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-2 weeks)
14 C 3 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-2 weeks)
15 C 4 (stricture
DISCUSSION
DCBs contribute to the treatment of atherosclerosis, instent recurrence of stenosis and the reduction of the risk o f t h r o m b o s i s w i t h o u t t h e placement of a permanent foreign object (11-14) DCB is a standard angioplasty balloon coated with a drug, which is embedded in the matrix coating by using a hydrophilic spacer in order to allow the drug to be released after the expansion of the balloon into the vessel lumen Then, the drug is absorbed in the layers
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12248
et al 4
K Pagonis, A Peteinaris, C Adamou,
Table 2.
Squamous
Submucosal Smooth Muscle Model Epithelium T issue Layer
+++
PTX PTA balloon-immediately) +++
2
formation-dilation 35LP PTA balloon+18 PTX PTA balloon -24h) +++
35LP PTA balloon+18 PTX PTA balloon -24h)
11 C
(stricture
12 C 2 (stricture formation-dilation
+++
formation-dilation 35LP PTA balloon+18 PTX PTA balloon-4 weeks) 16 C 4 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-4 weeks) 17 C 5 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-6 weeks) 18 C.5 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-6 weeks)
B 2 (stricture formation-dilation 35LP PTA balloon-4 weeks) 2 Squamous epithelium
5
Muscle Layer 6 B 2 (stricture formation-dilation 35LP PTA balloon-4 weeks) 2 Squamous epithelium
Layer 7 B 3 (stricture formation-dilation 35LP PTA balloon-6 weeks) 1 Squamous epithelium
Smooth Muscle
Muscle Layer 8 B 3 (stricture formation-dilation 35LP PTA balloon-6 weeks) 1 Squamous epithelium
Smooth
9 C 1 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-immediately) 3 Squamous epithelium
Smooth Muscle Layer
Muscle Layer 10 C 1 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-immediately) 3 Squamous epithelium
Smooth
Muscle Layer 11 C.2 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon -24h) 3 Squamous epithelium Submucosa Smooth Muscle Layer 12 C 2 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-24h) 3 Squamous epithelium
Smooth Muscle Layer 13 C 3 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-2 weeks) 2 Squamous epithelium Submucosa 14 C 3 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-2 weeks) 2 Squamous epithelium
15 C 4 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-4 weeks) 1 Squamous epithelium
Submucosa Smooth
Submucosa
Submucosa
16 C 4 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-4 weeks) 1 Squamous epithelium
17 C 5 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-6 weeks) 1 Squamous epithelium 18 C 5 (stricture formation-dilation 35LP PTA balloon+18 PTX PTA balloon-6 weeks) 1 Squamous epithelium
Submucosa
of the vessel wall and reduces the tissue formation which is the normal effect in cases of either balloon expansion or stent placement in the lumen of a vessel (15) The effect of DCBs is attributed to the cytostatic drugs which are coated onto the balloons (16) The currently drug of choice is PTX PTX constitutes the most tested anti-proliferative drug for the urinary tract (17) The aim of our study is the distribution of PTX in the different layers of the urethral strictured wall Barbalias et al evaluated the distribution of PTX in the normal rabbit urethral wall (9) The researchers investigated the distribution of PTX in the layers of normal rabbit’s urethra after the inflation of a PTX-coated balloon They proved that PTX was detected to the epithelium, submucosal, and muscle layers of the normal rabbit’s urethra immediately after the dilatation procedure by using DCB Also, PTX was found 24 and 48 hours after the dilatation process Nonetheless, there is no evidence in this study if the substance is adequately distributed in the case of strictured urethra or the effectiveness of the approach Another difference between the two studies was the timeline In our study the experiment was conducted in 8 weeks and the follow up of the experimental models lasted up to 6 weeks However, both studies proved that the smooth muscle layer was enriched by PTX in both normal and strictured urethras, even 6 weeks after the dilatation with DCBs Fu et al investigated the impact of docetaxel (PTX’s synthetic analogue) in management of urethral strictures (18) They randomly separated forty rabbits in 2 equal groups of 16 rabbits which received high and low dose of docetaxel respectively and a control group of 8 rabbits Retrograde urethral irrigation was used for the administration of docetaxel, once per day for 28 days Normal saline was administrated in the control group The urethral diameters and the histological findings were evaluated The diameter of the urethral lumen was significantly lower and the fibrosis and collagen concentration rate was greater in the control group compared to the other groups These results are similar to the results of our study Nevertheless, the researchers didn’t use any antibody for testing the exact distribution of docetaxel in the different layers of rabbits’ urethras Wikan et al tested the role of docetaxel and captopril in RNA expression of TGF-β1, MMP-1, CTGF, PAI-1 These genes play an important role in the formation of fibrotic tissue They tested four groups of rabbit’s urethra: a control group, a docetaxel group, a combined docetaxel/captopril group and a captopril group They proved that, only, single docetaxel could decrease the expression of the 3 out of 4 prereferred genes Consequently, this PTX’s synthetic analogue could, also, contribute to the inhibition of fibrotic formation Ji Hoon et al evaluated the effect of PTX-coated stents in dog’s canine urethra (19) They placed two stents (one PTX-coated stent and one polyurethane-coated stent) in each urethral model, one in the proximal and one in the distal urethra They separated the dogs in 2 equal groups of 10 individuals First group ’ s models were sacrificed 4 weeks after the stent’s placement and second group ’ s models were sacrificed 8 weeks after the stent’s placement In the first group, they placed the drug-coated stent and the polyurethane-coated stent in the proximal urethra and the distal urethra respectively in 5 dogs
and, also, placed the same stents reversely in the remaining five dogs of the group Retrograde urethrography was performed in each model just before the sacrifice of the models and proved that tissue hyperplasia was significantly less in PTX-coated stenting part of the urethra in both groups The histological evaluation of their experimental study showed that the granulation formation, the papillary projection and the submucosal inflammatory were significantly less in PTX-stenting specimens in both the 4-week and the 8-week group Even if they tested different parameters in different experimental models, their outcomes strengthen theoretically the results of our study and provide evidence about the efficacy of PTX in the urethral tissue
Other experimental studies were, also, conducted in the past for the efficacy of PTX in other parts of the urinary tract Liourdi et al conducted an experimental study in porcine ureteral wall by using DCBs (20) The aim of this study was the elucidation of the possibility of the clinical use of DCBs in ureteral strictures As for the results, we concluded that PTX was distributed in the urothelium, submucosal, and smooth muscle layers of porcine ureter
Also, the inflammation rate was lower in the PTX groups of the study This result comes to agreement with the results of our study and proves the efficacy of PTX
Nevertheless, it is worth mentioning that the experimental models and the anatomical structures of the urinary tract were different In addition, in our experimental study the urethral wall was already strictured, in contrast with the normal tissue of the ureter of porcine models in the previous mentioned experiment Liatsikos et al presented an experimental study for the comparison of the efficacy of standard bare metal stents and PTX-coated metal stents in the ureteral wall of porcine models (21) Ten standard stents were placed randomly in the right or left ureter of 10 female pigs and ten PTX-coated stents placed in the other ureter of the same porcine models After a follow-up period of 21 days all experimental models were sacrificed After the histological evaluation, they concluded that PTX-coated stents contributed to less inflammation and hyperplasia of the ureteral wall compared to standard stents Another important study about the effect of PTX-coated stents in the ureteral tissue’s hyperplasia was presented by Kram et al (22) They compared the efficacy of uncoated polyurethane stents and PTX-coated stents in a rat ureteral model after the conduction of ureteroureterostomy Their outcomes indicated that PTX contributed to decreasing hyperplastic proliferation and postoperative restenosis rate
Consequently, PTX-coated balloons or stents may be a promising approach for the management of strictures even in the upper or in the lower urinary tract
A plethora of drugs has been tested regarding the efficacy in the restenosis formation of the urothelial lumen, such as poly-DL-lactic acid, zotarolimus, captopril, halofuginone, protein nanofilm-controlled drugs, rapamycin, insulin-like growth factors, Clostiridium histolyticum and others (23-26) However, only PTX proved its feasibility both in experimental and clinical aspects Virasoro et al presented a prospective, multi-center, clinical study about the usage of Optilume® PTX-coated balloon (Laborie Medical Technologies, Mississauga, Ontario, Canada) for the
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12248 5
coated balloon for urethral stricture
Paclitaxel
management of patients with urethral stricture (27) The follow-up of the patients lasted 3 years and included the measurement of IPSS score, maximum flow rate, post-void residual urine volume and the evaluation of erectile function All parameters of the study were improved after the intervention with PTX-coated balloons in most of the participants and there was no influence in the sexual function of the patients Elliott and colleagues prepared a randomized controlled trial where 127 patients separated in 2 groups (28) First group included patients treated by Optilume® PTX-coated balloon and second group patients treated by urethral dilation or optical internal urethrotomy After 6 months they evaluated the anatomic success by a simple passage of a flexible cystoscope 1 year after the primal intervention they measured the IPSS score and the maximum flow rate in all participants They, also, investigated in which of the participants a repeated intervention was necessary All results of the study were in favor of Optilume® PTX-coated balloon group except of minor complications, such as minor hematuria and dysuria which were observed more frequently in patients treated by PTX-coated balloons
There are some limitations related to our experimental trial which should be mentioned First of all, human anatomy and tissue differs from the experimental rabbit’s model that was used in the current experimental study Moreover, the follow up period of the models lasted until only six weeks Longer-term outcomes are needed for the evaluation of the distribution of PTX in different layers of the urethral wall In the current study, we have some clues about the efficacy of DCBs in the treatment of strictured urethral lumen as we evaluated the inflammation and fibrosis of the strictured rabbit‘s urethras
Nonetheless, it is not possible to do flow studies to the rabbits to obtain more information on the efficacy of the approach
CONCLUSIONS
PTX-coated balloons seem to be an effective approach for the treatment of urethral stenosis When PTX was released in the strictured rabbit’s urethra, its distribution included all layers of the urethral wall and most importantly the smooth muscle layer, which related to the fibrosis and the restenosis of the lumen The results showed reduced inflammation and fibrosis Consequently, DCBs may play an important inhibitive role in the restenosis formation
REFERENCES
1 Jacobs ME, de Kemp VF, Albersen M, et al The use of local therapy in preventing urethral strictures: A systematic review PloS one 2021; 16:e0258256
2 Pang KH, Chapple CR, Chatters R, et al A Systematic Review and Meta-analysis of Adjuncts to Minimally Invasive Treatment of Urethral Stricture in Men Eurn Urol 2021; 80:467-479
3 Tepe G, Brodmann M, Micari A, et al 5-Year Outcomes of DrugCoated Balloons for Peripheral Artery In-Stent Restenosis, Long Lesions, and CTOs JACC: Cardiovas Interv 2023; 16:1065-1078
4 Will TA, Polcari AJ, Garcia JG, et al Paclitaxel inhibits ureteral
smooth muscle cell proliferation and collagen production in the absence of cell toxicity
J Urol 2011; 185:335-340
5 Lee C-H, Hsieh M-J, Liu S-C, et al Novel bifurcation stents coated with bioabsorbable nanofibers with extended and controlled release of rosuvastatin and paclitaxel Mater Sci Eng C Mater Biol Appl 2018; 88:61-69
6 Liu L, Lan X, Chen X, et al Multi-functional plant flavonoids regulate pathological microenvironments for vascular stent surface engineering Acta Biomater 2023; 157:655-669
7 Chen N, Guo D, Guo Y, et al Paclitaxel inhibits cell proliferation and collagen lattice contraction via TGF-β signaling pathway in human tenon's fibroblasts in vitro Eur J Pharmacol 2016; 777:3340
8 Choritz L, Grub J, Wegner M, et al Paclitaxel inhibits growth, migration and collagen production of human Tenon's fibroblasts potential use in drug-eluting glaucoma drainage devices Graefes Arch Clin Exp Ophthalmol 2010; 248:197-206
9 Barbalias D, Lappas G, Ravazoula P, et al Evaluation of the Distribution of Paclitaxel After Application of a Paclitaxel-Coated Balloon in the Rabbit Urethra J Endourol 2018; 32:381-386
10 Nakada SY, Soble JJ, Gardner SM, et al Comparison of acucise endopyelotomy and endoballoon rupture for management of secondary proximal ureteral stricture in the porcine model J Endourol 1996; 10:311-318
11 Parwani D, Ahmed MA, Mahawar A, et al Peripheral Arterial Disease: A Narrative Review Cureus 2023; 15:e40267
12 Sharma N, Finn MT, Parikh SA, et al The Ranger drug-coated balloon: advances in drug-coated technology for treatment of femoropopliteal segment arterial disease Future Cardiol 2023; 19:127-135
13 Kulyassa P, Engh MA, Vámosi P, et al Drug-coated balloon therapy is more effective in treating late drug-eluting stent in-stent restenosis than the early occurring one-a systematic review and meta-analysis Front Cardiovasc Med 2023; 10:1062130
14 Byrne RA, Joner M, Alfonso F, et al Drug-coated balloon therapy in coronary and peripheral artery disease Nat Rev Cardiol 2014; 11:13-23
15 Kar S Outcomes of New-Generation Drug-Eluting Stents in Women with Acute Myocardial Infarction Cur Cardiol Rep 2019; 21:2
16 Woolford S, Tran M, Yoda C, et al Studying the effect of drugto-excipient ratio on drug release profile for drug coated balloons Int J Pharm 2022; 620:121749
17 Kallidonis P, Adamou C, Castillo SV, et al Drug-delivering devices in the urinary tract: A systematic review Arab J Urol 2021; 19:191-204
18 Fu D, Chong T, Li H, et al Docetaxel inhibits urethral stricture formation, an initial study in rabbit model PloS one 2014; 9:e112097
19 Shin JH, Song HY, Choi CG, et al Tissue hyperplasia: influence of a paclitaxel-eluting covered stent--preliminary study in a canine urethral model Radiology 2005; 234:438-444
20 Liourdi D, Kallidonis P, Kyriazis I, et al Evaluation of the distribution of Paclitaxel by immunohistochemistry and nuclear magnetic resonance spectroscopy after the application of a drug-eluting balloon in the porcine ureter J Endourol 2015; 29:580-589
21 Liatsikos EN, Karnabatidis D, Kagadis GC, et al Application of
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12248
6
K Pagonis, A Peteinaris, C Adamou, et al
paclitaxel-eluting metal mesh stents within the pig ureter: an experimental study Eur Urol 2007; 51: 217-223
22 Kram W, Rebl H, Wyrwa R, et al Paclitaxel-coated stents to prevent hyperplastic proliferation of ureteral tissue: from in vitro to in vivo Urolithiasis 2020; 48:47-56
23 Han K, Park JH, Yang SG, et al EW-7197 eluting nano-fiber covered self-expandable metallic stent to prevent granulation tissue formation in a canine urethral model PloS one 2018; 13:e0192430
24 Kotsar A, Nieminen R, Isotalo T, et al Biocompatibility of new drug-eluting biodegradable urethral stent materials Urology 2010; 75:229-234
25 Sangkum P, Yafi FA, Kim H, et al Collagenase Clostridium his-
tolyticum (Xiaflex) for the Treatment of Urethral Stricture Disease in a Rat Model of Urethral Fibrosis Urology 2015; 86:647 e641-646
26 Kallidonis P, Kitrou P, Karnabatidis D, et al Evaluation of zotarolimus-eluting metal stent in animal ureters J Endourol 2011; 25:1661-1667
27 Virasoro R, DeLong JM, Estrella RE, et al A Drug-Coated Balloon Treatment for Urethral Stricture Disease: Three-Year Results from the ROBUST I Study Res Rep Urol 2022; 14:177-183
28 Elliott SP, Coutinho K, Robertson KJ, et al One-Year Results for the ROBUST III Randomized Controlled Trial Evaluating the Optilume(®) Drug-Coated Balloon for Anterior Urethral Strictures J Urol 2022; 207:866-875
Correspondence
Konstantinos Pagonis, MD (Corresponding Author) pagonisk7@gmail com
Angelis Peteinaris, MD peteinarisaggelis@gmail com
Constantinos Adamou, MD constantinos adamou@live com
Vasileios Tatanis, MD tatanisbas@gmail com
Athanasios Vagionis, MD thanos vagionis@hotmail gr
Anastasios Natsos, MD a natsos@gmail com
Mohammed Obaidat, MD kasious klay@gmail com
Solon Faitatziadis, MD solonasfait@gmail com
Panagiotis Kallidonis, MD pkallidonis@yahoo com
Department of Urology, University Hospital of Rion, Patras, Greece
Evangelos Liatsikos, MD liatsikos@yahoo com
Department of Urology, University Hospital of Rion, Patras, Greece
Medical University of Vienna, Vienna, Austria
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12248 7
Paclitaxel coated balloon for urethral stricture
ORIGINAL PAPER
Débora Araújo 1 , Pierre-Emmanuel Bryckaert 2 , Miguel Miranda 3 , Vasco Rodrigues 4 , Nicolas de Saint Aubert 2 , Johann Menard 2 , Eric Mandron 2
1 Urology Department, Centro Hospitalar Vila Nova de Gaia/Espinho EPE, Vila Nova de Gaia, Portugal;
2 Urology Department, Clinique du Pré, Technopôle Université, Le Mans, France;
3 Urology Department, Centro Hospitalar Universitário Lisboa Norte EPE, Lisboa, Portugal;
4 Urology Department, Centro Hospitalar Universitário de São João EPE, Porto, Portugal
Summary
Introduction and objectives: Artificial urinary sphincter (AUS) is a treatment option for women with stress urinary incontinence (SUI) after failure of previous surgery or as a primary procedure in severe intrinsic sphincter deficiency (ISD) The aim of the study was to assess the long-term efficacy and risk factors for surgical revision and definitive explantation of AUS laparoscopic implantation in female patients
Methods: A retrospective review of all women submitted to AUS implantation between April 2005 and March 2023 was conducted The AUS was implanted via transperitoneal laparoscopic approach, by two experienced surgeons. The primary endpoint was postoperative continence Continence was defined as no leakage and no pad usage or leakage and/or pad usage with no impact on social life and failure as leakage and/or pad usage impacting social life. As secondary outcomes, clinical predictive factors for AUS revision and definitive explantation were evaluated.
Results: In the last 18 years, females with a mean age of 68 ± 12 years-old were submitted to laparoscopic implantation of AUS. Early overall complication rate was 16%, but only one case was Clavien-Dindo ≥ 3. After a median follow-up of 67 months, 22 2% of the patients needed a device revision, the majority due to mechanical device dysfunction. AUS definitive explantation was performed in 16%, mainly due to urethral/vaginal erosion (9.9%) and infection (6.2%). Patients with age ≥ 70 years and follow-up ≥ 10 years significantly predisposed for device revision At the time of the last follow-up, 72% of the patients were keeping the urinary continency
Conclusions: Laparoscopic AUS implantation in females is an effective treatment for SUI due to ISD Meanwhile, adequate patient selection, multidisciplinary evaluation and careful expectation management are essential to achieving good results, concerning their significant complication rate
KEY WORDS: Artificial urinary sphincter; Female urinary incontinence; Intrinsic sphincter deficiency; Laparoscopy
Submitted 20 December 2023; Accepted 23 December 2023
INTRODUCTION
Stress urinary incontinence (SUI) in women is a prevalent and bothersome condition with significant impact on quality of life (1) It is mainly attributed to two patho-
physiological mechanisms: urethral hypermobility and intrinsic sphincter deficiency (ISD) (2) While in the former case there is a more consensual treatment strategy, the latter has a less unanimous management approach Artificial urinary sphincter (AUS) is a treatment option for women with severe SUI after failure of previous urinary incontinence surgeries and/or as a primary procedure in severe ISD (3, 4) However, since it is a challenging technique with high risk morbidity and due to the paucity of longterm follow-up, its current role in the surgical treatment of SUI is still lacking evidence According to the European Association of Urology guidelines, AUS should be implanted only as a last resort procedure and only in expert centers The panel recommends synthetic sling, colposuspension and autologous sling as first options in these patients When proposing AUS, it is important to inform the patients of the high risk of complications, mechanical failure, or need for explantation (level of evidence 3, grade of recommendations: weak) (3) We report 18-year experience of AUS laparoscopic implantation in Clinique du Pré, assessing the long-term efficacy and risk factors for surgical revision and definitive explantation of AUS laparoscopic implantation in female patients
MATERIALSANDMETHODS
A retrospective and descriptive review of all female patients submitted to AUS implantation between April 2005 and March 2023 was conducted Eighty-one females with SUI as a result of ISD were treated with laparoscopic implantation of the AMS 800 Urinary Control System (Boston Scientific, Marborough, MA, USA) All patients were diagnosed with ISD based on clinical history, physical examination and urodynamics, namely maximum urethral closure pressures (MUCP) and Valsalva leak point (VLPP) Manual dexterity was determined as no evidence of cognit i v e i m p a i r m e n t , e x t re m i t y w e a k e
o r t re m o r Inclusion criteria included: motived women with type III incontinence, with proper dexterity and with no cervical urethral hypermobility; negative Marshall/Bonney or Ulmsten test (urine leakage on straining or coughing not corrected by urethral support); MUCP under 20 cmH2O and a VLPP under 60 cmH2O; and normal detrusor func-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12214 1
n i n g
Eighteenyearsofexperienceinlaparoscopicimplantation ofartificialurinarysphincterinwomenwithintrinsic
sphincterdeficiency
DOI: 10 4081/aiua 2024 12214
tion and bladder compliance Previous anti-incontinence procedures or the presence of genital prolapse were not a contraindication for AUS implantation Patients with urge incontinence alone or previously submitted to pelvic radiotherapy were excluded The AUS was implanted via transperitoneal laparoscopic approach, by two experienced surgeons, according to a previous described technique (5, 6) In cases of 132 concomitant genitourinary prolapse, laparoscopic anterior and posterior mesh sacrocolpopexy was carried out before inserting the AUS components, according to a previous described technique (7, 8) Informed consent was obtained from all patients Patients were assessed at 6 weeks (sphincter activation), on periodical follow-up visits at 3-, 6- and 12-months post-operative and yearly subsequently Data collected included demographic and baseline characteristics; surgical procedure details; post operative results and complications; revision for partial or total component replacement, deactivation and definitive explantation rates, as well as their causes; and current continence The primary endpoint was postoperative continence Continence was defined as no leakage and no pad usage or leakage and/or pad usage with no impact on social life and failure as leakage and/or pad usage impacting social life The results were evaluated short term (1 year after implantation) and long term (at last follow-up), based on clinical interviews
As secondary outcomes, clinical predictive factors of AUS revision and definitive explantation were assessed Statistical analyses were performed using IBM SPSS Statistics software version 25 Categorical variables are presented as frequencies and percentages, and continuous variables as means and standard deviations, or medians and interquartile ranges for variables with skewed distributions Pearson's chi-squared or Fisher's Exact test were used to test for associations in categorical variables Simple and multiple logistic regression were performed to determine clinical predictive factors of need of revision and definitive explantation AUS surgery A p-value ≤ 0 05 was considered statistically significant
RESULTS
In the last 18 years, 81 females with a mean age of 68 ± 12 years-old were submitted to laparoscopic implantation of AUS All patients reported continual use of pads (> 3 pads/day) The median body index mass (BMI) was 29 kg/m2 (IQR 25-35) The patients' medical history included hypertension (49 4%), anxiety/depression (17 3%), diabetes (17 3%), smoking (14 8%) and asthma or others pulmonary diseases (16 0%) In 4 patients (5 1%), ISD resulted from an underlying neurological condition (three myelomeningocele and one spinal cord injury) Most of the patients had previous pregnancies (64 5%) and the mean number of deliveries per patient was 2 ± 1 A total of 12 patients underwent to a primary AUS implantation without previous urogynecological surgeries as a result of severe ISD Regarding previous surgeries, 38 3% underwent a hysterectomy, 84% incontinence surgery (mainly midurethral slings) and 27 1% prolapse surgery (mainly laparoscopic sacropromontofixation) A history of other abdominal or pelvic surgeries was present in 49 4% of patients, for example appendicectomy or cholecystecto-
Table 1
Patient characteristics
(Kg/m2 ) [Median (IQR)]
birth number, [Mean ± SD]
of pelvic urogynecological surgery, n (%)
previous laparoscopic surgeries, n (%)
urethral closure pressure (cmH2O) [Median (IQR)]
TOT: transobturador tape; TVT: Transvag nal tape
my On urodynamics, median MUCP was 16 cmH2O (IQR 12-20) Patients’ characteristics are summarized in Table 1 Mean operative time was 115 ± 40 minutes (range to 50-190 min) No case of laparotomy conversion was reported In 6 cases, simultaneous laparoscopic anterior and posterior sacrocolpopexy was carried out Intraoperative blood loss was negligible with no need of blood transfusion The most frequently chosen cuff length was 7 cm (48 6%) and all patients had balloon pressure of 61-70 cmH2O in the reservoir The average length of hospital stay was 2 days (with a range of 1 to 8 days) There were no intraoperative complications, except for one small vaginal perforation (less than 1 cm) It was immediately repaired in two layers with resorbable sutures and without any comorbidity involved Early overall complication rate was 16% (n = 13) Most were Clavien-Dindo as acute pelvic pain, urinary tract infections and acute urinary retention Just one case of Clavien-Dindo ≥ 3 was observed: a sepsis due to sphincter infection with necessity of AUS removal; the follow-up of this patient was lost Considering the functional outcomes in the first 12 months, 77 patients were continent (96 3%) and 3 (3 8%) had unchanged incontinence After a median follow-up of 67 months (IQR 14-110), 48 of the patients were continent (72%) The follow-up was lost in 14 cases Eighteen patients needed a device revision (22 2%) All revision surgeries were performed laparo-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12214
2
D Araújo, P -E Bryckaert, M Miranda, et al
Value No, patients included
81 Age (years)
± SD] 68 ± 12 Body mass index
29 (25-35) Diabetes,
(%) 14 (17 3) Hypertension, n (%) 40 (49 4) Smoking, n (%) 12 (14 8) Anxiety or depression, n (%) 14 (17.3) Asthma
others pulmonary diseases,
(%) 13 (16 0) Previous
2 ± 1 History
Hysterectomy 31 (38 3) Vaginal 7 (9 3) Suprapubic 19 (25 3) Laparoscopy 1 (1 3) Missing data 4 (4 9) Anti-incontinence surgery 69 (85 2) TOT procedure 48 (59 3) TVT procedure 7 (8 6) Burch procedure 9 (11 1) Marshall-Marchetti procedure 3 (3 7) Artificial urinary
2 (2 5) Surgical prolapse repair 14 (17 3) Laparoscopic sacrocolpopexy 8 (9 9) Abdominal sacrocolpopexy 2 (2 5) Vaginal prolapse repair 3 (3 7) Missing data 1 (1.2) Others
40 (49 4)
Variables
(n)
[Mean
n
or
n
sphincter (vaginal approach)
Maximum
16 (12-20)
scopically Most of them were needed to mechanical device dysfunction (n = 12, 14 8%) such as perforation of the cuff/balloon/tubing or depressurization of the system Failure in achieving continence, need for pump reposition and periurethral atrophy with cuff dislodgement (loss of weight in obese patients) were additional reasons for device revisions (n = 6, 7 4%) The mean time between implantation and device 197 exchange due to mechanical problems was 76 ± 49 months Patients with age ≥ 70 years and follow-up ≥ 10 years significantly predisposed for device revision (OR = 0 27, 95% CI [0 08, 0 93], p = 0 04 and OR = 5 5, 95% CI [1 67, 18 1], p = 0 01, respectively) Nine patients (11 1%) required AUS deactivation The main reasons were decreased manual dexterity or cognitive ability due to diseases such as rheumatism, dementia and bedridden patients These pathologies resulting in poor bladder emptying with high postvoiding residues, frequent urinary tract infections and incontinence were the main reasons to AUS deactivation Two of these patients had permanent catheterization and the others used adsorbent pads AUS definitive explantation was performed in thirteen patients (16%), mainly due to urethral/vaginal erosion (n = 8, 9 9%) and infection (n = 5, 6 2%) The median time between implantation and definite explantation was 38 months (IQR 2-75) Diabetes, history of previous prolapse surgery or history of other previous abdominal or pelvic surgeries are significantly associated with definitive explantation rate on univariate analyses but not in multivariate analyses
DISCUSSION
AUS implantation in females is an effective long-term treatment for SUI due to ISD with a good postoperative success rate With a median follow-up of 6-years, 72% of the patients were continent The excellent functional outcomes of AUS in female patients with SIU due to ISD have been reported for decades (9) The definition of ISD is controversial, however, most authors advocate the use of a
Table 2.
Simple and Multiple logistic regression analyses of clinical parameters in predicting device revision (n = 18) and AUS definitive explantation (n = 13).
combination of clinical and urodynamic criteria The combined presence of a negative urodynamic evaluation and negative Marshall-Bonney and Ulmsten tests is the most favoured scenario to AUS implantation in women with non-neurogenic SUI (10) Peyronnet et al performed a systematic review and showed the complete continence rates and improved incontinence ranged from 61 1% to 100% and 81% to 100%, respectively, regardless of the surgical approach (11) Reus et al demonstrated that the outcome “ zero to one pad” varied between 58% and 100% in the female AUS implantation (12) Comparing to other SIU surgeries, as transobturador tape outcomes, the cure rate was lower in females with ISD combined with fixed urethra (67%) (13) Women with low urethral closure pressure, isolated or combined with a lack of urethral mobilit y, h a v e a n i n c re a s e d
midurethral slings, as high as 75% (14) The main theorical advantage of AUS over other surgical options for female SUI due to ISD is that it is the only anti-incontinence procedure that can mimic the physiological function of the sphincter with the ability to restore both normal storage and voiding function by increasing the outlet resistance at rest when the cuff is closed but maintaining low resistance during the voiding phase with the cuff being opened (11) Despite its efficacy there is a non-negligible associated morbidity The revision rate (22 2%), including mechanical failure (14 8%) and explantation rate (16%), is comparable to those in the current literature A recent systematic review reported revision rates ranging between 6 to 45%, with mechanical failure between 2% to 41% The explantation rate due to infection and/or erosion varied between 2% to 31% (12) Peyronnet et al also reported explantation rates up to 45% (11) During the last decades, the retropubic open approach was the most popular, but the rise of minimally invasive surgical approaches reduced the inherent morbidity (9) The main advantage of laparoscopic and robotic-assisted approach is the easier access to the pelvis and better dissection of the bladder neck with better visualization, especially in obese patients (15) Mandron and col-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12214 3 Laparoscopic implantation of artificial urinary sphincter
r i s k o f
f r a c t o r y S U
f
re
I a
t e r
Device Revision AUS definitive explantation Variables Simple logistic Multiple logistic Simple logistic Multiple logistic regression regression regression regression P value 95% CI OR P value P value 95% CI OR P value Age ≥ 70 years 0 03 0 08- 0 93 0 27 0 04 0 46 Obesity 0 23 0 08 Diabetes 0 50 0 04 0 36 Hypertension 0 31 0 73 Smoking 0 06 0 40 Asthma or others pulmonary diseases 0 72 1 00 Obstetric history 0 98 0 76 History of previous hysterectomy 0 95 0 55 History of previous anti-incontinence surgeries 1 00 1 00 History of previous prolapse surgeries 0 37 0 04 0 13 History of other abdominal or pelvic surgeries 0 06 0 08 0 03 0 06 MUCP ≤ 16 0 71 1 00 AUS surgery time > 10 years 0 01 1 67- 18 1 5 5 0 01 0 28 Surgery time ≥ 120 minutes 0 81 0 13 0 337
AUS: art ficia ur nary sphincter; MUCP: max mum urethral closure pressure
leagues were the first teams to publish their preliminary experience in laparoscopic AUS implantation in the late 2000s Some of these patients were included in this cohort They reported good results, as 82 6% of the patients were continent at a mean follow-up of 26 1 months (6) In the last years, several series with a roboticassisted approach were published, including “anterior” robotic technique and more recently a “posterior” technique (16-18) Considering the laparoscopic or robotic approaches, the continence rate reported as zero pads ranged from 63% to 83% in female patients, similar to what demonstrated in open technique (42 to 86%) (12)
To our knowledge, there was only one study comparing robotic to open approach and reported a significantly decrease in intra- and postoperative complications rate with similar continence results (17) Robotic approach allows lower technical complexity, enhanced dexterity, better mobility of the instruments and physiological tremor filtering relatively to the laparoscopic route (9, 19) Given the limited information available in literature, it is still early to compare the performance and safety of the different surgical techniques and further prospective studies are required We believe that the differences in complication and explantation rates between centers can be explained by distinct levels of experience There was low level of evidence-based data, with significant clinical and methodological heterogeneity across studies Most of the studies had a limited number of patients, had mainly short-term follow-up and were single-center retrospective in nature The VENUS study is a prospective cohort study in recruitment with the purpose to evaluate the outcomes of female AUS surgery involving 25 European centers, including robotic assisted, laparoscopic and open patients When compared to other works, our results are similar with the ones from larger series which may reflect that surgical experience and high volume could favour successful outcomes As the AUS implantation is more demanding than sling procedures, specialized centers with a proper training are required to perform this surger y (10) Therefore, we believe that AUS implantation must be restrict to a limited number of hospitals/centers worldwide It was advocated that the specialized centers are trained in making the correct diagnosis, had experience to perform other surgical interventions for SUI (not limiting the patients’ choice) and, more importantly, had experience in managing the complications of AUS implantation (10) The optimal time to AUS implantation was unknown and AUS was rarely used as a first surgical intervention Some authors support performing the procedure after failure of at least one and a maximum of two previous interventions The number of previous anti-incontinence procedures decreases the success rate of AUS and increases the risk of erosion (10, 12, 16) In our study the number of previous surgeries did not correlate with the success rate However, we demonstrate that advanced age and long-term AUS (more than 10 years) significantly predisposed for device change The median time until mechanical failure was 76 months, which corresponds to approximately 6 years of device survival Device failure was managed by either exchange of the damaged component or by total replacement, without the need of definitive explantation Chung et al advised that all patients need to be
informed that the risk for potential revision surgery increases with time; in his cohort the median time of AUS revision surgery was 88 months and he demonstrated that women with more than 35 years had more revision or removal surgery for cuff erosion and infection (20) Other study reported that a presence of higher BMI (more than 30 kg/m2) and multiple surgeries were associated with higher revision rates (21) In the literature, the major risk factors for explantation are pelvic irradiation, age > 70 years, neurological pathology and history of pelvic surgery, including the Burch procedure and sacral colpopexy (16, 22, 23) In our cohort, history of diabetes, previous prolapse surgery or other previous abdomino-pelvic surgeries may predispose for definitive explantation, although these association were not statistically significant Our study had several limitations First, the single-center, retrospective design of the study and the fact that the procedures were performed by two surgeons with extensive experience in the implantation of AUS, limit the generalization of the results to centers with a low volume of procedures Second, the absence of a validated incontinence questionnaire, since our surgeries started 18 years ago, to evaluate patient satisfaction Thirdly, larger studies, prospective and randomized, are required to properly evaluate the value of laparoscopic female AUS implantation compared with the open or robotic approaches and other therapeutic options (eg, pubovaginal sling) Regarding the risk factors of surgical revision and definitive AUS explantation, more studies are needed
CONCLUSIONS
Laparoscopic AUS implantation in females is an effective treatment for SUI due to ISD Meanwhile, adequate patient selection, multidisciplinary evaluation and careful expectation management are essential to achieving good results, concerning their significant complication rate The patients should be informed about the high risk of complications, need to surgical revision, mechanical failure or need for explantation More studies are needed to identify the best approach and best candidates for the surgical intervention
REFERENCES
1 Hampel C, Artibani W, Espuña Pons M, et al Understanding the Burden of Stress Urinary Incontinence in Europe: A Qualitative Review of the Literature Eur Urol 2004; 46:15-27
2 Osman NI, Li Marzi V, Cornu JN, Drake MJ Evaluation and Classification of Stress Urinary Incontinence: Current Concepts and Future Directions Eur Urol Focus 2016; 2:238-44
3 EAU Guidelines Edn presented at the EAU Annual Congress Milan 2023 ISBN 978-94-92671-19-6
4 Abrams P, Andersson KE, Apostolidis A, et al 6th International Consultation on Incontinence Recommendations of the International Scientific Committee: Evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence Neurourol Urodyn 2018; 37:2271-2
5 Ferreira C, Brychaert PE, Menard J, Mandron E Laparoscopic implantation of artificial urinary sphincter in women with intrinsic sphincter deficiency: Mid-term outcomes Int J Urol 2017; 24:308-13
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12214
4
D Araújo, P -E Bryckaert, M Miranda, et al
Laparoscopic implantation of artificial urinary sphincter
6 Mandron E, Bryckaert PE, Papatsoris AG Laparoscopic artificial urinary sphincter implantation for female genuine stress urinary incontinence: technique and 4-year experience in 25 patients BJU Int 2010; 106:1194-8 350
7 Rozet F, Mandron E, Arroyo C, et al Laparoscopic Sacral Colpopexy Approach for Genito-Urinary Prolapse: Experience with Cases Eur Urol 2005; 47:230-6
8 Mandron E, Bryckaert PE Prolapsus et colpocèle antérieure D o u b l e p ro m o n t o f i x a t i o n c œ l i o s c o p i q u e Te c h n i q u e A n n U ro l (Paris) 2005; 39:247-56
9 Peyronnet B, Greenwell T, Gray G, et al Current Use of the Artificial Urinary Sphincter in Adult Females Curr Urol Rep 2020; 21:53
10 Chartier-Kastler E, Van Kerrebroeck P, Olianas R, et al Artificial urinary sphincter (AMS 800) implantation for women with intrinsic sphincter deficiency: a technique for insiders? BJU Int 2011; 107:1618-26
11 Peyronnet B, O’Connor E, Khavari R, et al AMS‐ 364 800 Artificial urinary sphincter in female patients with stress urinary incontinence: A systematic review Neurourol Urodyn 2019; 38(S4)
12 Reus CR, Phé V, Dechartres A, Grilo NR, et al Performance and Safety of the Artificial Urinary Sphincter (AMS 800) for Non neurogenic Women with Urinary Incontinence Secondary to Intrinsic Sphincter Deficiency: A Systematic Review Eur Urol Focus 2020; 6:327-38
13 Haliloglu B, Karateke A, Coksuer H, et al The role of urethral hypermobility and intrinsic sphincteric deficiency on the outcome of transobturator tape procedure: a prospective study with 2-year follow-up Int Urogynecol J 2010; 21:173-8
14 Lo TS, Pue LB, Tan YL, Wu PY Risk factors for failure of repeat
midurethral sling surgery for recurrent or persistent stress urinary incontinence Int Urogynecol J 2016; 27:923-31
15 Leal Ghezzi T, Campos Corleta O 30 Years of Robotic Surgery World J Surg 2016; 40:2550-7
16 Costa P, Poinas G, Ben Naoum K, et al Long-Term Results of Artificial Urinary Sphincter for Women with Type III Stress Urinary Incontinence Eur Urol 2013; 63:753-8
17 Peyronnet B, Vincendeau S, Tondut L, et al Artificial urinary sphincter implantation in women with stress urinary incontinence: preliminary comparison of robot-assisted and open approaches Int Urogynecol J 2016; 27:475-81
18 Gondran-Tellier B, Boissier R, Baboudjian M, et al Robot-assisted implantation of an artificial urinary sphincter, the AMS-800, via a posterior approach to the bladder neck in women with intrinsic sphincter deficiency BJU Int 2019; 124:1077-80
19 Peyronnet B, Capon G, Belas O, et al Robot assisted AMS-800 Artificial Urinary Sphincter Bladder Neck Implantation in Female Patients with Stress Urinary Incontinence Eur Urol 2019; 75:169-75
20 Chung E, Cartmill RA 25-year experience in the outcome of artificial urinary sphincter in the treatment of female urinary incontinence BJU Int 2010; 106:1664-7
21 Chung E, Navaratnam A, Cartmill RA Can artificial urinary sphincter be an effective salvage option in women following failed anti-incontinence surgery? Int Urogynecol J 2011; 22:363-6
22 Thomas K, Venn SN, Mundy AR Outcome of the artificial urinary sphincter in female patients J Urol 2002; 167:1720-2
23 Vayleux B, Rigaud J, Luyckx F, et al Female urinary incontinence and artificial urinary sphincter: study of efficacy and risk factors for failure and complications Eur Urol 2011; 59:1048-53
Correspondence
Débora Araújo, MD deboracerqueiraaraujo@gmail com
Urology Department, Centro Hospitalar Vila Nova de Gaia/Espinho EPE
Conceição Fernandes st , 4434-502, Vila Nova de Gaia, Portugal Pierre-Emmanuel Bryckaert, MD bryckaert@wanadoo fr Nicolas de Saint Aubert, MD nicolas desaintaubert@gmail com Johann Menard, MD johann menard@orange fr Eric Mandron, MD dr mandron@wanadoo fr
Urology Department, Clinique du Pré, Technopôle Université
René Laennec 13 Avenue, 72000 Le Mans, France
Miguel Miranda, MD msmmmiranda@gmail com
Urology Department, Centro Hospitalar Universitário Lisboa Norte EPE
Professor Egas Moniz Avenue, 1649-028 Lisbon, Portugal
Vasco Rodrigues, MD ocsav 1992@gmail com
Urology Department, Centro Hospitalar Universitário de São João EPE
Professor Hernâni Monteiro Avenue, 4200-319 Porto, Portugal
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12214 5
ORIGINAL PAPER
Microsurgical varicocelectomy efficacy in treatment of men with primary and secondary infertility (retrospective study)
Shomarufov Azizbek 1, 2
1 Urology Department of Tashkent Medical Academy, Uzbekistan;
2 Republican Specialized Scientific-Practical Medical Center of Urology, Tashkent City, Uzbekistan
Summary
Introduction and objectives: Varicocele is the most common treatable cause of male infertility The study aimed to compare varicocelectomy efficacy in men with primary (PI) and secondary infertility (SI)
Patients and methods: Medical records of 100 men suffering from PI and SI and having varicocelectomy at the Republican Specialized Scientific-Practical Medical Center of Urology were retrospectively selected and analyzed. Patients were divided into 2 groups Group I included 58 men with PI and Group II 42 men with SI. Preoperative clinical characteristics and semen parameters before and after varicocelectomy were analyzed and compared between groups.
Results: Analysis revealed that the mean age of patients of group I was significantly lower (p < 0.001) and the duration of infertility was accurately shorter (p < 0 01) than those of group II. Main semen parameters increased significantly in group I (e g , sperm concentration increased by 50%, from 62 2 ± 8 7 to 93.5 ± 10.0 M/ml, and total motile sperm count increased by 113%, from 76 7 ± 17 1 to 163 4 ± 27 8 M p < 0 05), while in group II only rate of progressive motile sperm increased significantly (by 107%, from 13 5 ± 2 6 to 28 0 ± 5 2% p < 0 05)
We identified a significant difference in varicocelectomy efficacy between group I and group II in change of total motile sperm count (by 113% vs 74% respectively, p < 0 01) We also revealed a discrepancy between groups in correlation ratio (r) between initial and post-surgical percent of progressive motile sperm
Conclusions: Patients with SI were older and had longer infertility period Varicocelectomy resulted in significant semen parameters improvement in patients with PI In patients with SI, only percent of progressively motile sperm improved significantly. It indicates that advanced male age and long infertility duration may have a negative impact on varicocelectomy success.
KEY WORDS: Varicocele; Varicocelectomy; Primary infertility; Secondary infertility
Submitted 23 December 2023; Accepted 27 December 2023
INTRODUCTION
Currently, research are conducted actively on possible causes of male infertility Varicocele is the most common cause of primary and secondary infertility in men In this regard, varicocele repair remains the most frequently per-
formed surgery to correct male factor infertility (1, 2)
Analysis of the literature demonstrated that among men with primary infertility, the proportion of patients with varicocele is 33-40%, and among those who suffer from secondary infertility it is up to 81% (1)
According to data from many authors, in varicocele, the testis suffers from venous overflow and it is supplied with blood poor in oxygen and nutrients, leading to atrophy of its tissue (1, 6) Another pathogenetic factor is the increase of testicular temperature to + 37°C due to the overflow of venous blood Most men with varicocele are fertile, but the prevalence of infertility in this group is i n c r e a s e d c o m p
However, more than 40% of patients with varicocele have reduced sperm quality (1) The relationship between varicocele and semen parameters may be different Microcirculation disorders evolving with varicocele leads to an increase in the testis cells' concentration of reactive oxygen species and oxidative stress The latter is nowadays considered a leading pathophysiological mechanism of pathozoospermia with varicocele (6)
Recent randomized controlled trials (RCTs) have demonstrated that varicocele repair (varicocelectomy) in patients with clinical varicocele and pathologies of semen analysis leads to a significant increase in pregnancy rates (3) and improvement of semen quality in relation to observation group (control) (4) Other authors in RCTs revealed low efficiency of varicocelectomy in cases of subclinical varicocele and normal semen parameters (5)
Persad et al and Cayan et al referring to a large number of studies indicated that microsurgical (inguinal and subinguinal) ligation of spermatic cord veins is the most appropriate surgery for the treatment of clinical varicocele with infertility (6, 7)
Fukuda et al conducted a study of 71 infertile men who underwent microsurgical varicocelectomy The subjects had their semen analysis taken 3 times (before and after the intervention, at 3 and 12 months) The results showed that the quality of semen analysis at 3 months after surgery was significantly better than that before surgery No statistically significant differences were detected between semen parameters taken at 3 and 12 months after surgery (8) Walsh et al in their study came to the conclusion that
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12082 1
r e
i t
t h e g e n e r a l p o p u l a t i o n
a
d w
h
DOI: 10 4081/aiua 2024 12082
Azizbek
men with primary and secondary infertility with varicocele may have different clinical characteristics including semen parameters, i e males with secondary infertility had significantly better parameters of the semen (sperm concentration) (9)
In this regard, we aimed to assess initial semen parameters and varicocelectomy efficacy in men with primary and secondary infertility dividing them into two separate groups
PATIENTS AND METHODS
During the study, we evaluated the main semen parameters: semen volume (ml), sperm concentration (million/ml) and total sperm count (million), % of sperm with progressive motility, total sperm motility (%), and total motile sperm count (TMC) according to WHO 2010 Manual (10)
The presence of varicocele was determined by visual and palpation methods, as well as using Doppler ultrasound of the testis according to the 2000 WHO classification of varicocele (subclinical varicocele, I, II, III) (11)
Patient selection
We used the following inclusion and exclusion criteria for recruiting appropriate patients for our study
Inclusion criteria
- patients had their semen analysis taken before and after varicocelectomy (at 3 - 12 months);
- patients with a pathological deviation of at least one of the studied parameters of semen analysis;
- patients with clinical varicocele (grade I-III);
- patients with complaints of pregnancy absence in their partners for 12 months and longer period
Exclusion criteria
- p a t i e n t s
(according to WHO 2010 Manual);
- patients with other infertility causes
Patients
According to those criteria we selected for the study and carefully explored the medical cards of 100 men aged from 21 to 46 years, who suffered from infertility and varicocele
Patients were divided into 2 groups: 58 men with pri-
mary infertility (aged from 21 to 38 years) were included in group I and 42 ones with secondary infertility (aged from 24 to 46 years) were recruited into group II
Ethical approval
The collection and the analysis of these data were approved by the Republican Specialized Scientific-Practical Medical Center of Urology local ethics committee
Surgical procedure
A l l p a t i e n t s u n d e r w e n t m i
o s u r g i c a l
b i n g u i n a l / inguinal varicocelectomy Procedures were performed by three experienced surgeons following the techniques described below A 4-5 cm incision was made inferior to the external inguinal ring in the subinguinal technique and over the inguinal canal in the inguinal technique
The spermatic cord was isolated, and the veins were dissected away from the arteries, lymphatics, vas deferens, and ligated under special surgical loupes or microscope
Statistical analysis
Statistical data were analyzed by MS Excel 2019 and IBM SPSS© Statistics 21 0 statistical packages The significance of differences between groups was calculated using Student's t test for means; differences were considered significant at p < 0 05
RESULTS
Analysis revealed that the mean age of patients in group I was significantly lower (p < 0 001) and the mean duration of infertility was significantly shorter (p < 0 01) than those of patients of group II (Table 1) Most patients had left-sided varicocele (76 patients, 76%) (Table 1)
BMI of 36 (36%) patients was slightly higher than normal (25 0-30 0), which was evaluated as pre-obese, BMI of 18 (18%) was significantly higher than normal (> 30 0), which was assessed as obesity, and BMI of 46 (46%) patients was within normal range (18 5-25 0) (12)
Following Table 2 shows the main semen parameters of patients of both groups before surgery for statistical comparison
As it is seen from Table 2, no statistically significant differences in the initial semen parameters were revealed between groups
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12082 S
2
w i t h a z o o s p e r m i a a n d n o r m o z o o s p e r m i a
c r
s u
Groups Age Anthropometric Varicocele * Duration of infer tility M ± G data (in months) M ± G Side Grade Height Weight BMI ** Left Right Bilater lal I II III Group I 27 4 ± 0 6 1 7 81 2 26 8 40 -2 8 (29) 19 (68) 1 (3) 28 7 ± 4 6 Group II 31 0 ± 0 6 1 7 79 9 26 5 36 24 5 (23) 15 (68) 2 (9) 51 8 ± 5 6 Р < 0 001 < 0 01 TOTAL 76 (76) 2 (2) 6 (12) 8 (20) 34 (68) 3 (6)* Data are given n absolute numbers in relation to the group ** Body mass index
Table 1. Key features of group of patients.
Table 2.
Main parameters of semen analysis in both groups in preoperative period for their comparative estimation
Table 3.
Comparative assessment of main semen parameters of both groups in pre- and post-surgical period
1 Preoperative period; 2 Postoperative period; 3 Statistically significant changes; 4 Statistically significant differences between groups
Preoperative and postoperative semen parameters of patients of both groups are given in Table 3 for comparison of varicocelectomy efficacy before and after repair, as well as between groups
In the postoperative period, the following changes were observed in average counts of studied semen parameters in both groups:
- semen volume in both groups remained unchanged (p > 0 05);
- sperm concentration increased significantly in group I (by 50% p < 0 05), while in group II it increased not significantly (by 39% p > 0 05);
- total sperm count increased by 60% (p < 0 05) in group I, whereas in the second one this parameter increased by 44% (p > 0 05);
- percent of sperm with progressive motility increased more in group II (by 107% p < 0 05) than in group I (by 75% p < 0 05) and the difference between groups was significant (p < 0 01);
- total sperm motility also increased significantly (by 50% p < 0 05) in group I, while in group II this parameter also increased, but not significantly (by 31% p > 0 05);
- total motile sperm count in group I increased more significantly (p < 0 01) than in group II (113% p < 0 05 vs 74% p > 0 05 respectively)
As it was shown above, statistically significant differences were revealed between groups in changes in some postoperative semen parameters In patients of group I varicocelectomy resulted in significant improvements in all semen parameters In contrast to group I in group II, statistically accurate improvement occurred for only percent of sperm with progressive motility, which increased more significantly than in group I
We also revealed a significant discrepancy between groups in correlation ratio (r) between the initial and post-operative % of sperm with progressive motility In patients of group I there was no correlation (r = -0 02), whereas in patients of group II correlation was direct and strong (r = 0 71) In general, differences between groups in mean correlation ratios between initial and postsurgical semen parameters were not significant (r = 0 4 for group I and r = 0 5 for group II)
DISCUSSIONS
Currently, a varicocele is the most common surgically curable cause of male infertility Although the vast majority of research supports the opinion of the beneficial effect of surgical treatment of varicocele on sperm parameters (3, 4, 13), the question of the true effect of surgery on testicular function remains unresolved (1) Although the exact relationship between improvements in indicators of semen analysis and surgical treatment of varicocele has not been finally determined, a meta-analysis of RCTs conducted by Agarwal et al showed significant improvement in semen parameters after varicocelectomy (13), which corresponds to the results of our research However, interesting is the fact that greater significant changes occurred in patients with primary infertility and varicocele than those in patients with secondary infertility and varicocele, although in patients with secondary infertility a positive effect of intervention was also determined
There are a number of reports on the association between initial semen parameters and the efficacy of the varicocele repair These studies assumed that men with higher preoperative semen parameters are more likely to see an improvement in their semen parameters after varicocelec-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12082 3 Microsurgical varicocelectomy for infertility
Groups Semen volume ml Sper m concentration Total sper m count Sper m with progressive Total sper m motility Total motile sper m count M±m (M/ml) M±m (M) M±m motility (%) M±m (%) M±m (M) M±m First 3 4 ± 0 3 62 2 ± 8 7 213 6 ± 35 9 11 4 ± 2 3 30 8 ± 3 6 76 7 ± 17 1 Second 3 7 ± 0 3 47 2 ± 8 6 171 9 ± 33 5 13 5 ± 2 6 35 1 ± 4 6 76 3 ± 19 2 P > 0 05 > 0 05 > 0 05 > 0 05 > 0 05 > 0 05
Semen volume ml Sper m concentration Total sper m count Sper m with progressive Total sper m motility Total motile sper m count M±m (M/ml) M±m (M) M±m motility (%) M±m (%) M±m (M) M±m Group I 1 3 4 ± 0 3 62 2 ± 8 7 213 6 ± 35 9 11 4 ± 2 3 30 8 ± 3 6 76 7 ± 17 1 Group I 2 3 4 ± 0 2 93 5 ± 10 0 341 8 ± 46 6 20 0 ± 3 1 46 1 ± 4 5 163 4 ± 27 8 P 3 > 0 05 < 0 05 < 0 05 < 0 05 < 0 05 < 0 05 Group II 1 3 7 ± 0 3 47 2 ± 8 6 171 9 ± 33 5 13 5 ± 2 6 35 1 ± 4 6 76 3 ± 19 2 Group II 2 3.9 ± 0.3 65.7 ± 10.2 246.9 ± 40.8 28.0 ± 5.2 46.0 ± 6.0 132.7 ± 31.3 P > 0 05 > 0 05 > 0 05 < 0.05 > 0 05 > 0 05
Groups
05 > 0 05 > 0 05 < 0.01 > 0 05 < 0.01
P 4 > 0
tomy (14, 15) Our study partially confirmed this statement because the association between initial and postsurgical semen parameters was moderate
According to some authors, varicocele is more common in men with SI than in men with PI, but the difference is not so high (+3 5%, p < 0 05) (16) They also noted that patients with PI and SI were almost of the same age which finding does not agree with our results
It is also worth noting that according to some authors, the average age of men with secondary infertility is older, which corresponds to our data However, they also state that there is no significant difference in the duration of infertility, whereas our study revealed a significant difference in this parameter between primarily and secondarily infertile men (9, 17) In addition, the above-mentioned authors claim the presence of differences in initial semen p a r a
y , although to our knowledge no statistically significant differences were revealed between baseline semen parameters of men with primary and secondary infertility
The main limitation of our study was the small sample size that in turn resulted in the differences between groups in mean patient’s age and infertility duration
CONCLUSIONS
The mean age and duration of infertility in patients with S I w e r e h i g h e r t h a n t h o s e i n p a t i e n t s w i t h P I Varicocelectomy resulted in significant improvement of main semen parameters in patients with PI In patients with SI varicocelectomy resulted in significant improvement of only a percent of progressively motile sperm It indicates that advanced male age and long infertility duration may have a negative impact on varicocelectomy success Further large-scale clinical trials are needed to confirm this statement
ACKNOWLEDGMENTS
The authors want to express their gratitude to the head of the Urology Department of Tashkent Medical Academy, DSc , Prof Akilov F A , and to the Director of Republican Specialized Scientific-Practical Medical Center of Urology, DSc , Prof Mukhtarov Sh T for their assistance in the arrangement of this study
REFERENCES
1 Salonia A, Bettocchi C, Capogrosso P, et al European Association o f U r o l o g y S e x u a l a n d r e p r o d u c t i v e h e a l t h A r n h e m , T h e Netherlands; EAU, 2023 Available at: uroweb org/guidelines/sexual-and-reproductive-health
2 Wein AJ, Kavoussi LR, Novick AC, et al (Eds ) Campbell-Walsh Urology 11th ed Saunders, Elsevier, Philadelphia 2016, pp 636637
3 Abdel-Meguid TA, Al-Sayyad A, et al Does varicocele repair improve male infertility? An evidence-based perspective from a randomized, controlled trial Eur Urol 2011; 59:455-61
4 Baazeem A, Belzile E, Ciampi A, et al Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair Eur Urol 2011; 60:796-808
5 Ficarra V, Cerruto MA, Liguori G, et al Treatment of varicocele in subfertile men: the Cochrane review a contrary opinion Eur Urol 2006; 49:258-263
6 Persad E, O'Loughlin CA, Kaur S, et al Surgical or radiological treatment for varicoceles in subfertile men Cochrane Database Syst Rev 2021; 23;4:CD000479
7 Çayan S, Shavakhabov S, Kadioglu A Treatment of palpable varicocele review in infertile men: a meta-analysis to define the best technique J Androl 2009; 30:33-40
8 Fukuda T, Miyake H, Enatsu N, et al Assessment of Timedependent Changes in Semen Parameters in Infertile Men After Microsurgical Varicocelectomy Urology 2015; 86:48-51
9 Walsh TJ, Wu AK, Croughan MS, Turek PJ Differences in the clinical characteristics of primarily and secondarily infertile men with varicocele Fertil Steril 2009; 91:826-830
10 World Health Organization WHO Laboratory Manual for the Examination and processing of human semen 5th edition Geneva: WHO Press, 2010
11 Jungwirth A, Giwercman A, Tournaye H, et al European Association of Urology Guidelines on Male Infertility: The 2012 Update Eur Urol 2012; 62:324-332
12 BMI Classification Global Database on Body Mass Index World Health Organization 2006
13 Argawal A, Deepinder F, Cocuzza M, et al Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach Urology 2007; 70:532-538
14 Samplaski MK, Yu C, Kattan MW, et al Nomograms for predicting changes in semen parameters in infertile men after varicocele repair Fertil Steril 2014; 102:68-74
15 Bozhedomov VA, Shomarufov AB, Bozhedomova GE, et al Varicocele and reproductive function: pathozoospermia treatment (a prospective comparative study) Urologiia 2021; 5:62-8
16 Bozhedomov VA, Shomarufov AB, Bozhedomova GE, et al Varicocele and reproductive function: epidemiology and infertility risk (the examination of 3632 patients) Urologiia 2021; 3:122-8
17 Gowri V, Venkiteswaran KP, Al-Zakwani I, et al Comparison of the Demographics, Semen Parameters and Hormone Profiles in Men with Primary and Secondary Infertility Sultan Qaboos Univ Med J 2010; 10:350-353
Correspondence
Dr Azizbek B Shomarufov, PhD (Corresponding Author) doctor shomarufov@gmail com 2, Farabi, 100109, Tashkent, Uzbekistan
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12082 S Azizbek 4
e t e r s o f p a t i e n t s w i t h s e c o n d a r y i n f e r t i l i t
m
ORIGINAL PAPER
Hermansyah Hermansyah 1, 3* , Muhammad Fadhli Abdullah 1, 3* , Cennikon Pakpahan 1, 2, 3* , Reny I’tishom 1, 2 , Supardi Supardi 1, 3 , Ilhamsyah Ilhamsyah 1, 3
1 Andrology Study Program, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia;
2 Department of Biomedical Sciences, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia;
3 Andrology Outpatient Clinic, General Academic Dr Soetomo Hospital, Surabaya, Indonesia
* These authors contributed equally to this paper
Summary
Objective: Various factors, such as obstructive azoospermia, cause infertility in men
Biochemical examination of ejaculate, especially measurement of fructose, can be an additional investigation that can be used for this diagnosis in reproductive health Examination of fructose is carried out after routine ejaculate analysis, resulting in prolonging the examination time so that it will affect the measurement of fructose level in the ejaculate and the accuracy of the diagnosis This study aims to determine the best timing and procedure for measurement of fructose using a semiautomatic method
Methods: This research is an analytic observational study conducted at Dr Soetomo General Hospital, Surabaya A total of 13 ejaculate samples from infertile male patients who met the inclusion criteria were evaluated Each ejaculate was divided into eight aliquots that were examined for fructose using a semiautomated method after different intervals of time and centrifugation modalities.
Results: This study showed a significant difference in fructose levels when aliquots were centrifuged and examined immediately or after different interval of time (p = 0 036) In addition, aliquots left standing for more than 60 minutes (p = 0 012) and 120 minutes (p < 0 001) before centrifugation, showed significantly lower levels compared to aliquots that were centrifuged and then immediately examined
Conclusions: We suggest that measuring fructose immediately after centrifugation is more reliable than measuring fructose left standing before or after centrifugation Leaving the ejaculate standing will reduce the fructose level so that it does not resemble its real level
KEY WORDS: Infertile; Fructose; Semiautomatic; Time; Centrifugation; Reproductive health
Submitted 13 December 2023; Accepted 4 January 2024
INTRODUCTION
The fructose examination is one of the biochemical tests used to diagnose the cause of male infertility (1) It is not a routine test, but it is a useful supplemental test to provide information on specific clinical conditions, that is done after routine testing ejaculate analysis (2) According to
World Health Organization (WHO) ejaculate analysis laboratory guidelines 2021, each standard ejaculate analysis test takes about 60 minutes, so the timing to test fructose is extended, which may affect the measurement of the level of fructose in ejaculate (3) In fact, when fructose is tested in this way, the fructose level obtained will differ from the real fructose level because the fructose in the ejaculate will undergo fructolysis Nonspecific and sensitive test results will inevitably influence the diagnosis
There are several methods to test for fructose, including colorimetric, enzymatic, and chromatographic methods (4) WHO used Karvonen and Malm's modified methods to test the amount of fructose in ejaculation (3) The manual fructose testing method has disadvantages, such as a complicated procedure with a long waiting time Since 1981, the use of semiautomatic or automatic machines for testing fructose began to develop (5) The semiautomatic machine can shorten the time to test the fructose level The advantages of the semiautomatic fructose m e t h o d i n c l u d e e a s y r e a g e n t p r e
m a l reagent use, minimal error, reduced human resources, and easy calibration and quality control processes (6)
There is no standardized time and method for semi-automated fructose testing, so the researchers felt it was necessary to research to find the best timing for testing fructose in order to obtain results close to real fructose levels In this study, we carried out the process using a BTS-350 semiautomatic machine The method used was an enzymatic method using hexokinase and phosphoglucoisomerase enzymes and then switching to a colorimetric method The method used in BTS-350 semiautomatic machines makes the processing time much faster
METHODS
This was an observational analytic study using the ejaculates of infertile men who visited the Policlinic Andrology Outpatient General Hospital, Dr Soetomo Surabaya
The study was approved by the ethics committee of RSUD Dr Soetomo with no 0669/KEPK/V/2023
Based on the sample calculation, 13 ejaculates from different men were included in this study
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12186 1
p a r a t i o
n , m i n i
Examinationofejaculatefructoselevelsonmaleinfertility patientsatvarioustimesandcentrifugationusing semiautomaticmethod
DOI: 10 4081/aiua 2024 12186
Inclusion criteria were samples from men aged 18-50 years old, with ejaculate volume > 2 ml, and willing to participate in the study by signing informed consent; we exclude men with anejaculation, haematospermia, hyperviscosity, and men with reproductive infection
Each man who meets the criteria was explained about the procedures and objectives of the study and signed an informed consent if he was willing to participate to the research with his sample Then, the participant was asked to masturbate and collect ejaculate into a non-toxic container
After that, each ejaculate was divided into eight aliquots which were managed in different ways after ejaculate liquefaction K1: the aliquot was immediately examined for fructose content; K2: the aliquot was centrifuged, then the supernatant was taken, and fructose content was examined; K3: the aliquot was centrifuged and allowed to stand for 30 minutes, then the supernatant was taken and examined for fructose; K4: the aliquot was centrifuged, then was left standing for 60 minutes and examined for fructose; K5: the aliquot was centrifuged, left for 120 minutes and then the supernatant was taken and examined for fructose; K6: the aliquot was allowed to stand for 30 minutes, then centrifuged, and the supernatant was examined for fructose content; K7: the aliquot was allowed to stand for 60 minutes, then centrifuged, and supernatant examined for fructose content; K8: the aliquot after standing for 120 minutes was centrifuged and supernatant examined for fructose content Fructose was examined using a Semi-Automated Method
The procedure of Fructose Test with Semi-Automated Method
Using the BTS-350 semiautomatic machine, a colorimetric procedure followed an enzymatic process involving phosphoglucoisomerase and hexokinase enzymes
A spectrophotometer was used to detect NADPH To measure fructose with the BTS 350 semiautomatic device, the reagent mixture Reagent A (PIPES 70 mmol/l, NADP+ 1 2 mmol/l, hexokinase > 15 U/ml, phosphoglucose isomerase > 10 U/ml, preservative, pH 7), Reagent B (ATP > 15 mmol/l, glucose-6-phosphate dehydrogenase > 10 U/ml, preservative, pH 9), and fructose standard (D-fructose 75 mg/dL equivalent to 375 mg/dL or 28 mmol/l fructose according to the sample dilution factor) were used Samples were added to reagents and put in a unique tube made of Teflon to be sucked automatically by the machine until, within a few minutes, the value of fructose content will appear After that, the fructose concentration needs to be calculated manually
Statistical analysis
The data obtained were analyzed statistically with the Graph Pad Prism 10 software package Data normality test was conducted with the Shapiro Wilk test, and comparative analysis between variables was tested with the Wilcoxon Sign Rank Test for non-normally distributed data, and paired t-test for normally distributed data
RESULTS
The results of this study were obtained from samples of
13 subjects divided into eight aliquots The general characteristics of the study participants and observational data of macroscopic analysis of ejaculate are shown in Table 1 In this study, the results of ejaculate ejaculate of infertile men with azoospermia criteria were 8%, severe oligozoospermia 23%, oligoteratozoospermia 23%, asthnezoospermia 31%, and teratozoospermia 15%
Table 2 shows no significant difference between fructose levels measured in the aliquot that was immediately examined after centrifugation compared to fructose levels measured in aliquots that were left standing after centrifugation for 30 (p = 0 100) and 60 (p = 0 133) minutes However, there was a significant difference between the level measured immediately after centrifugation compared to the level measured in the aliquot left for 120 minutes (p = 0 036) These results suggest that 60 minutes may be the recommended most extended time limit for measurement of fructose after centrifugation, as after that time, fructose levels may drop not resembling real levels
Table 1.
The general characteristics of the study participants and observational data of macroscopic analysis of ejaculate
General characteristics of par ticipants Mean ± SD Median and results of macroscopic ejaculate analysis (min-max)
(years old)
Table 2
Comparison of fructose concentrations (Mean ± SD) in seminal plasma standing for 0, 30, 60, or 120 minutes after centrifugation of ejaculate
Aliquot
In the comparison between fructose levels that are left standing before centrifugation, there was a significant difference between immediate measurement and measurements aliquots that are left standing for 60 minutes (p = 0 012) and 120 minutes (p < 0 001) before centrifugation The decrease in fructose levels between direct examination and 120 minutes was highly significant This finding indicates that leaving samples for more than 60 minutes before centrifugation significantly decreases the measurement of the level of fructose content (Table 3) The results of the measurements of fructose in the different eight aliquots were plotted on a graph, showing that aliquots that were left standing for a period of time and
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12186
2
H Hermansyah, M Fadhli Abdullah, C Pakpahan, et al
Age
32 69 ± 4 76Abstinence
- 4 (2-7) Volume (ml) 3 39 ± 1 31Liquefaction
pH - 7 5 (7-8,1) Viscosity
- < 2
(day)
(minute)
(cm)
N Fr uctose (mmol/L) 0 minutes 13 15 77 ± 4 81 30 minutes 13 15 18 ± 5 34 a 60 minutes 13 14 87 ± 5 47 b 120 minutes 13 14.23 ± 5.76 c a p 0 100; b p 0 133; c p 0
036
Table 3.
Comparison of fructose concentrations (Mean ± SD) in seminal plasma obtained from centrifuged ejaculate after standing for 0, 30, 60, or 120 minutes.
due to different centrifugation speeds and the number of samples measured The present study used a centrifugation speed of 4000 rpm for 30 minutes, while the research conducted by Lu et al used a centrifugation speed of 3000 x g for 15 minutes Although research conducted by Lu et al showed that different centrifugation speeds have little effect on fructose levels, remaining spermatozoa or non-cellular components (7, 8), including zinc, alpha-glucosidase, citric acid may mildly affect the fructose level (9)
The difference may also be due to differences in sample size being the sample size in the present study was 13
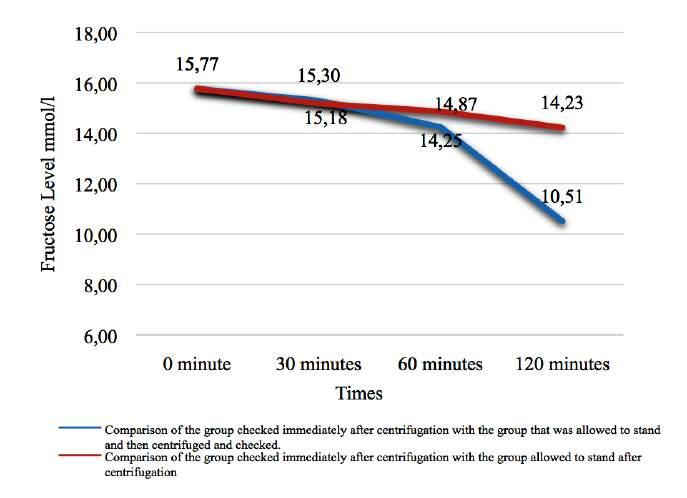
then centrifuged showed a more significant decrease in fructose levels than measurement in aliquots that were centrifuged and then left standing for a period of time Our findings suggest that the best procedure for fructose examination is immediate centrifugation with measurement within 60 minutes Levels of fructose in samples left standing before centrifugation tend to be lower than real levels (Figure 1)
DISCUSSION
The results showed that there was a significant difference in fructose levels in the aliquots that were immediately centrifuged after liquefaction and then immediately checked compared to the aliquots that, after centrifugation, were allowed to stand for 120 minutes before measurement (p = 0 036) There is a significant difference in fructose levels in the aliquots immediately checked compared to those allowed to stand 60 minutes and 120 minutes after liquefaction, then centrifuged and checked (p = 0 012 and p < 0 001)
The difference in results in the present study for the aliquots that were allowed to stand 120 minutes after centrifugation compared to the results of Lu et al may be
Figure 1
Comparison of mean fructose levels measured in aliquots immediately centrifugated and then allowed to stand compared to levels measured in aliquots allowed to stand before centrifugation
people, while the study research by Lu et al included 20 subjects
The data from the aliquots examined directly after centrifugation compared to those examined after a standing period before centrifugation showed no significant difference after a 30-minute standing (15 78 mmol/L and 15 30 mmol/L), but after 60- and 120-minute standing the fructose levels decreased significantly (14 25 mmol/L and 10 51 mmol/L) The finding of no difference of fructose level after 30 minutes standing align with the research of Elzanaty and Malm although they found no significant difference between ejaculate fructose levels examined also 60 minutes, and 90 minutes after ejaculation (10)
The fructose levels of the aliquots that were allowed to stand for 60 and 120 minutes before centrifugation were significantly lower than those allowed to stand for only 30 minutes This is in line with research conducted by Lu et al , although the method used is different Lu et al used the resorcinol method, while this study used the enzymatic method They reported a difference in the fructose content of ejaculate that was allowed to stand for 2 hours compared to those directly examined, and fructose levels significantly lower after 4 hours with
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12186 3 Semen fructose levels and semiautomatic method
Aliquot N Fr uctose (mmol/L) 0 minutes 13 15 77 ± 4 81 30 minutes 13 15 30 ± 5 64 a 60 minutes 13 14 25 ± 5 84 b 120 minutes 13 10 51 ± 7 21 c a p = 0 294; b p = 0 012; c p = < 0 001
respect to 0 or 2 hours In other words, the fructose concentration decreased with the length of standing time (7) The results in this study are also in line with the research conducted by Andrade-Rocha, in which fructose concentration was significantly lower in the samples examined after 120 minutes of liquefaction (11) The process of fructolysis causes a decrease in fructose levels in ejaculate This process is influenced by many factors such as concentration, motility and metabolism of spermatozoa, temperature, pH, and other substances in the ejaculate (9) An increase in spermatozoa concentration requires more fructose, which decreases fructose levels in ejaculate and vice versa (12) Increased fructose levels due to decreased fructose utilization can be caused by reduced spermatozoa, abnormal spermatozoa morphology, and decreased spermatozoa activity Low fructose levels can be caused by good spermatozoa motility (13) There is a positive correlation between the motility rate of spermatozoa and the fructolysis rate in human ejaculation (9) Very low temperatures can stop all spermatozoa metabolic activity, affecting fructose utilization and resulting in a slow decline in fructose levels (14)
REFERENCES
1 Trang NT Seminal Fructose Concentration in Man Infertility and the Fructose Test’s Meaning In Diagnosis Reason of Azoospermia Man Biomed J Sci Tech Res 2018; 8:11-3
2 Baskaran S, Finelli R, Agarwal A, Henkel R Diagnostic value of routine ejaculate analysis in clinical andrology Andrologia 2021; 53:1-12
3 World Health Organization WHO laboratory manual for examining and processing human ejaculate Sixth Edition [Internet] Vol
Edition, V, World Health Organization 2021 286 p Available from: http://whqlibdoc who int/publications/2010/9789241547789 eng pdf
4 Tanga BM, Qamar AY, Raza S, et al Ejaculate evaluation: Methodological advancements in sperm quality-specific fertility assessment - A review Anim Biosci 2021; 34:1253-70
5 S S V Male infertility: A clinical approach In: Male Infertility: A Clinical Approach 2016, p 55-83
6 Aucky Hinting, Agustinus A Technology Updates in Male Infertility Management Indones Androl Biomed J 2021; 2:63-7
7 Lu JC, Chen F, Xu HR, et al Standardization and quality control for determination of fructose in seminal plasma J Androl 2007; 28:207-13
8 Feng RX, Lu JC, Zhang HY, Lü NQ A Pilot Comparative Study of 26 Biochemical Markers in Seminal Plasma and Serum in Infertile Men Biomed Res Int 2015; 2015
9 A GS and K Basics of Human Andrology In: Basics of Human Andrology New Delhi: Springer Nature Singapore Pte Ltd; 2017, p 163-70
10 Elzanaty S, Malm J Effects of ejaculation-to-analysis delay on levels of markers of epididymal and accessory sex gland functions and sperm motility J Androl 2007; 28:847-52
11 Andrade-Rocha FT Physical analysis of ejaculate to evaluate the secretory activity of the seminal vesicles and prostate Clin Chem Lab Med 2005; 43:1203-10
12 Kataria J, Gill GK, Cojandaeaj L Relationship of Seminal Fructose and Serum Prolactin Levels in Infertile Men Asian J Pharm Clin Res 2021; 14:85-7
13 Toragall MM, Satapathy SK, Kadadevaru GG, Hiremath MB Evaluation of seminal fructose and citric acid levels in men with fertility problem J Hum Reprod Sci 2019; 12:199-203
14 Srivastava N, Pande M Protocols in semen biology (comparing assays) Springer, Singapore, 2017; p 1-288
Correspondence
Hermansyah Hermansyah drherman09@gmail com
Muhammad Fadhli Abdullah muhammad fadhli abdullah-2021@fk unair ac id
Cennikon Pakpahan cennikon pakpahan@fk unair ac id
Reny I’tishom (Corresponding Author) ritishom@fk unair ac id
Department of Biomedical Sciences, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia
Supardi Supardi
supardi unair@gmail com
Ilhamsyah Ilhamsyah ilhamsyah-2021@fk unair ac id
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12186
4
H Hermansyah, M Fadhli Abdullah, C Pakpahan, et al
ORIGINAL PAPER
Evaluation of human bone marrow mesenchymal stem cells in the treatment of non obstructive azoospermia
Mohamed A Alhefnawy 1 , Gamal Elmorsy 2 , Sayed Bakry 3 , Hesham El-amrosy 4 , Ibrahim Mearaj 5 , Ebrahim A Sabra 6 , Osama M Badr 6 , Dalia Ibraheem 7 , Taymour Khalifa 5
1 Urology, Benha University, Benha, Egypt;
2 Clinical Pathology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
3 Genetic Engineering, Faculty of Science for Boys in Cairo, Al-Azhar University, Egypt;
4 Clinical Pathology, Egypt Ministry of Health and Population, Cairo, Egypt;
5 Dermatology and Andrology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
6 Animal cell and tissue culture, Genetic engineering and Biotechnology Institute, Sadat University, Sadat City, Egypt;
7 Department of Tissue engineering, Faculty of Science, Al-Azhar University, Cairo, Egypt
Summary
Background: Non-obstructive azoospermia (NOA) represents an infertility problem that is usually difficult to treat. Such patients usually have testicular biopsy of germ cell aplasia or spermatogenic arrest In recent decades, Mesenchymal Stem Cells (MSCs) had been studied thoroughly and proved safe and effective regarding their capability for trans-differentiation into different cell types. The aim of this study was to evaluate the effect of MSCs local intratesticular injection in induction of spermatogenesis
Patients and method: The current study included 87 infertile non-obstructive azoospermic patients Clinical assessment and repeated semen analysis with centrifugation were done to confirm azoospermia Karyotyping and AZF study were done Some of the patients had previous testicular biopsy proving a lack of sperm in the testes Single intratesticular injection of purified MSCs suspension was done
Results: 20 7% of patients showed sperm in their semen after variable period of time. Hormonal profile among treated patients showed significant improvement regardless success of treatment. Also most of the treated patients appreciated the improvement of their sexual function and libido
Conclusions: Bone marrow derived MSCs could be a new hope and therapeutic modality for treatment of refractory cases of NOA.
KEY WORDS: Stem cells; Non-obstructive azoospermia (NOA); Spermatogenesis; Semen analysis
Submitted 14 January 2024; Accepted 22 January 2024
INTRODUCTION
About 1% of males and up to 10-15% of infertile men have azoospermia, which is defined as the absence of sperm in the ejaculate upon evaluation of the centrifuged semen In two thirds of instances, severe spermatogenic dysfunction, also known as non-obstructive azoospermia (NOA), is the primary cause (1) Azoospermia can be categorized as either obstructive (OA) or NOA (2) Many medications like antihypertensive medications and antidepressants might cause NOA; all of them have the potential to disrupt spermatogenesis and even cause nonobstructive azoospermia (3)
The majority of occurrences of azoospermia are due to irreversible testicular illnesses that affect spermatogenesis These conditions are frequently related to inflammatory, genetic, and endocrine issues If no obvious causes are found, NOA will be considered idiopathic The affected testes are tiny and swollen (4, 5)
Male infertility can be brought on by a number of chromosomal or genetic disorders, including Klinefelter syndrome, 47(XXY) syndrome, XX male syndrome, and Ychromosome microdeletions (6)
The foundation for spermatogenesis and male fertility in males is provided by spermatogonial stem cells (SSCs) Throughout the male reproductive life, SSCs can maintain the self-renewal process, differentiate into spermatozoa, and pass on genetic material to the following generation (7)
Stem cell transplantation is one method of treatment for male infertility related to a problem with spermatogenesis The reason for this is that stem cells are unspecialized cells being capable of self-renewal, regeneration, and cell differentiation When existing spermatogonial cells are lost or injured, spermatogenesis can be restored by spermatogonial cells (SSCs) Therefore, stem cell transplantation represents an effective method for restoring spermatogenesis in individuals with cancer and other spermatogenic disorders (8)
The Mesenchymal Stem Cells (MSC) multi-linear differentiation capacity, moderate immunogenicity, and active involvement in tissue repair and regeneration following migration to injured locations account for their widespread use For clinical usage in cell-based therapeutics, MSCs generally have an advantage over other types of stem cells (9)
One of the primary sources of MSCs is the bone marrow, and although aspirating the bone marrow is the most painful way to isolate MSCs, it is also the most used method for cell therapy (10)
The differentiation of MSCs into the male or female germ cell epithelium can be induced using a specific combination of growth factors, chemicals and genetic modifications Distinct methods of differentiation induction have been devised to differentiate distinct types of MSCs into male germ cells Retinoic acid, growth factors, minerals,
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12285 1
DOI: 10 4081/aiua 2024 12285
co-culture, conditioned medium, magnetic fields, and gene over-expression are a few examples of these (11) Mild symptoms such as transitory fever, insomnia, nausea, vomiting, or mild changes at the administration site may occur as a side effect of MSCs treatment, necessitating medical supervision and follow-up (12)
As evidenced by improved expression of germ cell markers, a decrease in apoptosis-induced sterility, a reduction in oxidative stress, and an increase in testosterone production, MSCs transplanted into the testes of NOA demonstrated both activation of spermatogenesis and differentiation into germ cells The inhibition of antisperm antibodies (ASA) may also be a function of MSCs (13)
The implanted MSCs produce a variety of growth factors, including the male germ cell potential factors transforming growth factor beta (TGF-) and bone morphogenetic proteins (BMPs), which stimulate and restore the recipient's cellular function (14)
The grey area about the effect of MSCs local intratesticular injection to induce spermatogenesis has motivated the authors to conduct this study
SUBJECTS AND METHODS
Study design
The current study was conducted following the ethical p e r s p e c t
approval was obtained from the ethical and research committees of both Benha and Al Azhar Universities The current study was conducted at the Urology Department, B e n h a
International Islamic Institute for Population Studies and Research, Al-Azhar University The study was conducted throughout the period from January 2020 till January 2022 The study included 87 subjects with primary infertility, with non-obstructive azoospermia for at least 2 years durations All cases were volunteers and informed by explaining complete details of the procedure (expected benefits and possible complications) A written consent was obtained from each patient
Clinical trial registry at: clinicaltrials gov/study/NCT02025270
Every patient underwent a thorough history-taking process, paying particular attention to the marital history (including age of the couple, length of marriage, and previous marriage
Clinical examination, paid particular attention to gigantism, dwarfism, myxedema, Klinefelter syndrome, mongolism etc Local examination was performed to check testicular volume, consistency, varicocele, cord anomalies, and vas alterations in order to rule out obstruction or scrotal enlargements, absence as well as congenital malformations of the testis
Following a 2-7-day period of abstinence, the semen analysis was performed three times in a row in accordance with WHO guidelines to confirm azoospermia
Follicle stimulating hormone (FSH), luteinizing hormone (LH), and testosterone measurements and testicular biopsy were used to estimate hormonal profiles and to discover histological patterns underlying azoospermia (such as SCOS and phases of spermatogenic arrest)
Karyotyping was done to display chromosomal abnormal-
ities, such as the XX male syndrome and the Klinefelter syndrome 47XXY Assessing Y-chromosome microdeletions (AZF) was done to identify the loci of spermatogenesis that were affected (A, B, or C)
Instrumentation
• Laminar Air flow Cabinet (Biological Safety Cabinet) Class 11 type A/B3
• Octomax: for magnetic cell selection (Miltenyi Biotec, Germany) MACS Multistand
• Inverted phase – Contrast microscope: for cell examination and counting
• Light Microscope: for cell counting (Leitz)
• Water bath: for sampling preparations and manipulation
• Humidified CO2 Incubator with air Jacket: for Cell Stem Cell cultivation, Model MJPX- C 50
• Refrigerator to keep the media
• Centrifuge (Eppendorf): to centrifuge the sampling for separation, sedimentation
• Sterile Pasteur pipettes
• Automatic pipettes (10-200 UL, Scororex)
• Sterile tissue culture tubes & dishes
• Hemocytometer: Improved Neuber
• Vortex Mixer: for sample mix & resuspending
Media
• MACS Buffer; Auto MACS Rinsing Solution (EDTA, Phosphate Buffered Saline)
• D u l b e c c o ’ s P h o s
Calcium and Magnesium)
• HiSep LSM 1077: Phicoll for cell separation (buffy coat layer)
• Alcohol 70% for sterilization
METHODS
Under complete aseptic condition, about 60 ml of bone marrow blood were aspirated from iliac bones This volume is diluted with phosphate buffer saline (PBS) The diluted blood sample was gently layered to Ficoll hypaque Centrifugation was done to separate the buffy coat layer and aspirate this layer that present at the interphase between the plasma and Ficoll carefully This separated layer is also subjected to magnetic labeling and separation by CD105 microbeads and FCR blocking antibodies by OctaMACS apparatus to get finally pure Mesenchaymal Stem Cells (MSC) These cells are finally re-suspended in 1 ml of PBS A 30 micr of this volume are subjected to viability testing using trypan blue and counting by improved Neuber hemocytometer Cell counting for cases ranged (3 7-5 2 mil/cm), viability around 98 4-99 2% The extracted cells were injected into cortex of both testes of patients under local anesthesia The patents were followed after 4 months from injection, by semen analysis, hormonal profile (FSH, LH and testosterone) and testicular volume The follow up was every 2 months for at least one year
RESULTS
This current study included 87 infertile male patients with a mean age of 35 87 ± 4 22 years in whom the
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12285
2
M A Alhefnawy, G Elmorsy, S Bakry, et al
v e s o f
e l s i
i D e c l a r a t i o n w h e r e e t h i c a l
n i v e r s i t y a n d A n d r o l o g y o u t p a t i e n t c l i n i c o f
i
H
n k
U
p h a t e B u f f e r s S a l i n e ( P h e n o l r e d ,
repeated spermiogram revealed azoospermia After MSCs injection, 69 (79 3%) patients did not show sperm in their semen while the remaining 18 (20 7%) patients showed different numbers of sperm in their semen
The mean age of the non-responding group 36 9 ± 7 35 years Other clinical data and testicular biopsy results were illustrated in Table 1
In the successful group, the surprising finding is the rate of responders with Sertoli Cell only Syndrome (SCOS) (61 1%)
The most prominent parameters among responding cases is normal karyotyping and absence of chromosome Y AZF micro deletion (Table 1)
Table 1 demonstrated that there was a statistically significant decrease in the FSH and LH hormone levels as well as significant increase in the testosterone level after MSCs therapy in the responding group more than the nonresponding group
Karyotyping was the only variable showing statistically sig-
Table 1.
Comparison between successful vs. non responding cases (clinical, testicular biopsy before, genetic background and hormonal level before and after MSCs therapy)
Table 2.
Comparison
No of patients, n (%)
Age (Mean ± SD)
Testicular Size before MSCs therapy
Normal, n (%) 30
Small, n (%) 25 4
Testicular Examination before MSCs therapy 0 245 Normal, n (%) 48 10 Varicocele, n (%) 60 Cryptorchidism, n (%) 11
Karyotyping before MSCs therapy
Microdeletion before MSCs therapy
(Mean ± SD)
changes
LH (Mean ± SD)
Testicular Examination before MSCs therapy
n (%) 61 17
Varicocele, n (%) 70
Cryptorchidism, n (%) 11
Testicular biopsy before MSCs therapy
Primary spermatocyte, n (%) 92
Secondary spermatocyte, n (%) 34
Spermatid, n (%) 21
SCOS, n (%) 55 11
Karyotyping before MSCs therapy
Microdeletion before MSCs therapy
18 AZF a 10 AZF b 20 AZF c 1 F S H (Mean ± SD)
003* P < 0 001*
% of changes 18 6 26 11 < 0 001*
Testosterone (Mean ± SD)
MSCs therapy
MSCs
P = 0 041 P = 0 04* 0 001*
% of changes
004*
nificant differences between successful and non-responding patients with SCOS (Table 2)
Regarding patients with SCOS, FSH level after treatment showed significant differences between responding and non-responding Also FSH percentage of level changes after treatment showed statistically significant differences between both responding and non-responding patients On the other hand, LH levels showed significant differences between SCOS responders and nonresponders either before or after treatment Also, the hormonal level change percentage was significantly different Moreover, testosterone showed significant differences between both groups regarding level before, after as well as change s percentage All successful cases of SCOS have normal karyotyping and absence of AZF microdeletions (Table 2)
Table 3 Showed that FSH level and percentage of changes after treatment showed significant differences between successful vs failed cases There was no statistically significant differences among successful vs failed cases with different levels of spermatogenic arrest as regards the Testesterone and LH hormones although significant difference was noticed within each group before and after MSC injection
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12285 3 Mesenchymal stem cells in the treatment of azoospermia
(%) 69
3%) 1 (20 7%) Age
SD) 36 9 ± 7 35 34 83 ± 5 85 0 269
therapy 0 227 Normal,
Small,
Failed Success P value No of patients, n
(79
(Mean ±
Testicular Size before MSCs
n (%) 35 12
n (%) 34 6
0
231 Normal,
0 084
0
58
070 Normal
18
Klinefelter 11 0
0
Normal 65
therapy 24 70 ± 10 2 22 07 ± 5 5 0 301 After MSCs therapy 19.68 ± 8.617 11.96 ± 2.97 < 0.001* P = 0 016 P < 0 001*
20 32 45 81 < 0 001* LH
Before MSCs therapy 10 18 ± 4 75 7 03 ± 2 07 0 008* After MSCs therapy 8 27 ± 3 679 5 143 ± 1 014 < 0 001* P = 0 023* P < 0 001*
changes 18.76 26.84 0.01*
Before MSCs therapy 2 367 ± 1 041 3 44 ± 0 66 < 0 001* After MSCs therapy 3 52 ± 1 30 5 29 ± 0 77 < 0 001* P = 0 041 P < 0 001*
of changes 32.76 34.97 0.01*
779
Before MSCs
% of changes
(Mean ± SD)
% of
Testosterone (Mean ± SD)
%
Failed Success P value
55 11
between successful vs non responding cases of SCOS (clinical & genetic background) and hormonal levels
36 93 ± 7 45 35 09 ± 7 012 0 752
0
579
7
< 0 001* Normal 44 11 Klinefelter 11 0
0
19.67 ± 8.5 22.2 ± 5.87 0.093
15 2 ± 13 3 12 29 ± 2 25 < 0 007*
<
22.7 44.6 < 0.001*
Before
10 18 ± 4 7 6 7 ± 1 6 0 008* After
8 28 ± 3 65 4 96 ± 0 96 < 0
P
214 Normal 52 11 AZF a 00 AZF b 20 AZF c 10 F S H
Before MSCs therapy
After MSCs therapy
P = 0 012* P
0 001* % of
MSCs therapy
MSCs therapy
001*
= 0
Before
2.35 ± 1.045 3.4 ± 0.818 < 0.003* After
therapy 3 5 ± 1 30 5 13 ± 0 8 < 0 001*
32 9 33 7 < 0
Table 3.
Comparing hormonal levels among successful vs failed cases with different levels of spermatogenic arrest
No of patients, n (%) 14 7 Age (Mean ± SD) 36 9 ± 7 12 34 43 ± 3 2 0 3946
F S H (Mean ± SD)
Before MSCs therapy 19 45 ± 6 5 21 87 ± 4 94 0 403
After MSCs therapy 16 1 ± 4 98 11 37 ± 2 06 0 30 P 0 007* P < 0 001*
% of changes 17 2 48 < 0 001*
LH (Mean ± SD)
Before MSCs therapy 7 53 ± 2 86 7 57 ± 2 6 0 098
After MSCs therapy 6 1 ± 1 96 5 5 ± 1 02 0 46 P = 0 082 P < 0 073
% of changes 19 31 3 0 0085*
Testosterone (Mean ± SD)
Before MSCs therapy 3 19 ± 1 13 3 51 ± 0 272 0 38
After MSCs therapy 4 34 ± 1 18 5 26 ± 0 75 0 078 P 0 041 P 0 002* 0 001*
% of changes 36 1 49 8 0 755
DISCUSSION
Aside from the extremely rare occurrences of patients with hypogonadotropic hypogonadism, Caroppo E & Colpi G (15) came to the conclusion that azoospermia caused by spermatogenic malfunction is an incurable illness MSCs, also referred to as fibroblast precursor cells, are non-hematopoietic cells found in the bone marrow
A c c o r d i n g t o s t a n d a r d c r i t e r i a e s t a b l i s h e d b y t h e
International Society for Cellular Therapy (ISCT), MSCs must be plastic adhering and capable of differentiating into the osteoblast, adipocyte, and chondroblast lineages Frequently, they have low immunogenicity (16) MSCs use paracrine and immunomodulatory pathways to provide their beneficial effects (17, 18)
In their meta-analysis investigation, Wang et al (12) found no direct evidence that MSC injection had the potential to cause tumours Additionally, no major safety incidents were noted Some research (19) have demonstrated that MSCs can trans-differentiate into spermatogenetic cells in the right milieu BM (Bone Marrow)-MSCtransplanted mice produced germ cells in vivo, according to several research (20, 21)
BM-MSCs have the ability to fuse with the local cells in the damaged area or to differentiate or trans-differentiate into multi-lineage cells, produce paracrine substances to entice the local stem cells to take part in tissue regeneration (22)
Pittenger et al 2019 (23) concluded that MSC infusion treatments had a very good safety profile during the previous 25 years, which was backed up by more than 950 registered MSC clinical trials that were filed with the FDA
In the present study, a single intratesticular injection of pure MSCs was used to treat patients Out of 87 patients, 18 (or 20 7%) showed sperm in their semen at various times In contrast to the successful case report of Cassim & Mohamed (24), using local injection with three sessions of intravenous MSC infusion, our investigation used a single intratesticular injection
Treatment with MSCs had a favourable impact on hor-
mone levels, decreasing FSH and LH levels and raising blood testosterone levels Improvements in sexual function and libido were reported alongside elevated testosterone levels in the treated subjects from the patient history On the other hand, there were notable hormone level disparities between responding and non-responder patients, particularly following treatment Based on the observation of successful cases when the FSH level was double or more than the usual level, the baseline FSH level appeared to be of little use as a predictor of success
All the successful cases had normal karyotyping and no chromosomal abnormalities in the AZF region This might be seen as a reliable indicator of a successful outcome
All SCOS cases that are successful have normal karyotyping and no AZF microdeletions, which was true for all cases that were successful despite having differing testicular biopsy results
The success rate for cases of SCOS was comparable to other non-obstructive azoospermic cases This is also a strong indicator of MSCs' capacity for homing and transdifferentiation To summarize, the complete lack of spermatogonia is not a contraindication to MSC therapy
Although the hormonal profile significantly improved in the case of the classic Klinefelter syndrome, no sperm were found in the seminal fluid despite decreased FSH, LH, and higher testosterone levels This study's findings align with those of Baghae et al (25)
No problems were noted during aspiration from the BM or during intra testicular injection in any of the instances that were monitored both during and after the MSCs injection
Based on Neri's (26) findings, we avoided using in vitro numerous replications in this study because they could raise the danger of accumulating genetic and epigenetic modifications and having a negative impact on the cell biology and therapeutic characteristics, safety, and efficacy According to an experimental investigation in the ram by Fedder et al (27), pathological testicular abnormalities such scar tissue and micro-calcifications were discovered r e g a r d l e s s o f t h e s p e r m r e t r i e v a
s e d Additionally, blood supply impairment was linked to it Furthermore, Eliveld et al (28) concluded that transient hypogonadism, which can persist up to 26 months, is demonstrated by testosterone levels that are below normal He also noted that some patients' testicular volume had decreased, but only a small number of patients had erectile dysfunction (ED) Because melancholy and anxiety may be the root of ED rather than hypogonadism, it was particularly prevalent in the group of men who had negative sperm retrieval results
CONCLUSIONS
Regardless of baseline hormonal levels, local intratesticular injection therapy using human MSCs may offer some hope for patients with refractory NOA
ACKNOWLEDGMENTS
Thanks and gratitude must be extended to the late Dr B a h g a t A b d e l g h a f a r E l fi k y , F o r m e r h e a d o f A n i m a l Biotechnology Department, Al-Azhar University for his participation and great effort of this work
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12285
4
M A Alhefnawy, G Elmorsy, S Bakry, et al
l m e t h o d
u
value
Failed Success P
REFERENCES
1 Caroppo E and Colpi GM Update on the Management of NonObstructive Azoospermia: Current Evidence and Unmet Needs J Clin Med 2021; 11:62
2 W o s n i t z e r M , G o l d s t e i n M a n d H a r d y M P R e v i e w o f
Azoospermia Spermatogenesis 2014; 4:e28218
3 Boivin J, Bunting L, Collins JA, Nygren KG International estimates of infertility prevalence and treatment-seeking: potential need and demand for infertility medical care Hum Reprod 2007; 22:1506-12
4 Oud MS, Ramos L, O'Bryan MK, et al Validation and application of a novel integrated genetic screening method to a cohort of 1,112 men with idiopathic azoospermia or severe oligozoospermia Hum Mutat 2017; 38:1592-1605
5 Kanatsu-Shinohara M, Toyokuni S, Morimoto T, et al Functional assessment of self-renewal activity of male germline stem cells following cytotoxic damage and serial transplantation Biol Reprod 2003; 68:1801-7
6 Ferlin A, Raicu F, Gatta V, et al Male infertility: role of genetic background Reprod Biomed Online 2007; 14:734-45
7 Caroppo E, Colpi EM, Gazzano G, et al The seminiferous tubule caliber pattern as evaluated at high magnification during microdissection testicular sperm extraction predicts sperm retrieval in patients with non-obstructive azoospermia Andrology 2019; 7:8-14
8 Valli H, Gassei K, Orwig KE Stem cell therapies for male infertility: where are we now and where are we going? In DT Carrell, PN Schlegel, C Racowsky, & L Gianaroli (Eds ), Biennial Review of Infertility 2015 (Vol 4) Switzerland: Springer International Publishing, pp 17-39
9 Kim HJ, Park JS Usage of Human Mesenchymal Stem Cells in Cell-based Therapy: Advantages and Disadvantages Dev Reprod 2017; 21:1-10
10 Chikhovskaya JV, Jonker MJ, Meissner A, et al Human testisderived embryonic stem cell-like cells are not pluripotent, but possess potential of mesenchymal progenitors Hum Reprod 2012; 27:210-21
11 Wei Y, Fang J, Cai S, et al Primordial germ cell-like cells derived from canine adipose mesenchymal stem cells Cell Prolif 2016; 49:503-11
12 Wang Y, Yi H, Song Y The safety of MSC therapy over the past 15 years: a meta-analysis Stem Cell Res Ther 2021; 12:545
13 Ghasemzadeh-Hasankolaei M, Batavani R, Eslaminejad MB, S a y a h p o u r F T r a n s p l a n t a t i o n o f A u t o l o g o u s B o n e M a r r o w Mesenchymal Stem Cells into the Testes of Infertile Male Rats and New Germ Cell Formation Int J Stem Cells 2016; 9:250-263
14 Wang F, Liu C, Zhang S, et al Transplantation of goat bone marrow mesenchymal stem cells (MScs) help restore spermatogenesis in endogenous germ cells-depleted mouse models J Integr Agric 2013; 12:483-494
15 Caroppo E, Colpi GM Hormonal treatment of men with nonobstructive azoospermia: What does the evidence suggest? J Clin Med 2021; 10:387
16 Chen C From mesenchymal stem cell therapy to discovery of d r u g t h e r a p y f o r s y s t e m i c s c l e r o s
n California, ProQuest Dissertations Publishing, 2014; 3628-36
17 Liu F, Qiu H, Xue M, Zhang S, Zhang X, Xu J, Chen J, Yang Y, Xie J MSC-secreted TGF-b regulates lipopolysaccharide-stimulated macrophage M2-like polarization via the Akt/FoxO1 pathway Stem Cell Res Ther 2019; 10:345
18 Zhang S, Teo KYW, Chuah SJ, et al MSC exosomes alleviate temporomandibular joint osteoarthritis by attenuating inflammation and restoring matrix homeostasis Biomaterials 2019; 200:35-47
19 Cakici C, Buyrukcu B, Duruksu G, et al Recovery of fertility in azoospermia rats after injection of adipose-tissue-derived mesenchymal stem cells: the sperm generation Biomed Res Int 2013; 2013:529589
20 Lue Y, Erkkila K, Liu PY, et al Fate of bone marrow stem cells transplanted into the testis: potential implication for men with testicular failure Am J Pathol 2007; 170:899-908
21 Yang S, Bo J, Hu H, et al Derivation of male germ cells from induced pluripotent stem cells in vitro and in reconstituted seminiferous tubules Cell Prolif 2012; 45:91-100
22 Zhang D, Liu X, Peng J, et al Potential spermatogenesis recovery with bone marrow mesenchymal stem cells in an azoospermic rat model Int J Mol Sci 2014; 15:13151-65
23 Pittenger MF, Discher DE, Péault BM, et al Mesenchymal stem cell perspective: cell biology to clinical progress NPJ Regen Med 2019; 4:22
24 Cassim MI, Mohamed T Novel Therapy for the Treatment of Male factor Infertility Due to Non-obstructive Azoospermia: A Case Report Crescent Journal of Medical and Biological Sciences 2019; 6:129-131
25 Baghaei K, Hashemi SM, Tokhanbigli S, et al Isolation, differentiation, and characterization of mesenchymal stem cells from human bone marrow Gastroenterol Hepatol Bed Bench 2017; 10:208-213
26 Neri S Genetic Stability of Mesenchymal Stromal Cells for Regenerative Medicine Applications: A Fundamental Biosafety Aspect Int J Mol Sci 2019; 20:2406
27 Fedder J, Marcussen N, Fedder MDK, Engvad B Testicular Damage following Testicular Sperm Retrieval: A Ram Model Study Biomed Res Int 2017; 2017:2472805
28 Eliveld J, van Wely M, Meißner A, et al The risk of TESEinduced hypogonadism: a systematic review and meta-analysis Hum Reprod Update 2018; 24:442-454
Correspondence
Mohamed Abdelrahman Alhefnawy, MD - dr mohamedalhefnawy@gmail com
Assistant Professor of Urology, Benha UniversityFareed Nada Street 13518, Banha, Egypt
Gamal Elmorsy, MD - gamalz7070@gmail com
Assistant Professor of Clinical Pathology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Sayed Bakry, MD - sbakry@azhar edu eg
Professor of Genetic Engineering, Faculty of Science for Boys in Cairo, Al-Azhar University, Cairo, Egypt
Hesham El-amrosy, MD - egypttala889@gmail com
Consultant of Clinical Pathology, Egypt Ministry of Health and Population, Cairo, Egypt
Ibrahim Mearaj, MD - mearaj@hotmail com
Taymour Khalifa, MD - Taymour khalifa@gmail com
Professor of Dermatology and Andrology, Al-Azhar University Faculty of Medicine, Cairo, Egypt
Ebrahim Sabra, MD - ebrahim sabra@gebri usc edu eg
Osama Badr, MD - osama badr@gebri usc edu eg
Assistant Professor of Animal cell and tissue culture, genetic engineering and Biotechnology Institute, Sadat University, Sadat City, Egypt
Dalia Ibraheem, MD - daliaibraheem23@gmail com
Department of Tissue engineering, Faculty of Science, Al-Azhar University, Cairo, Egypt
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12285 5 Mesenchymal stem cells in the treatment of azoospermia
i s U n i v e r s i t y o f S o u t h e r
ORIGINAL PAPER
Vasileios Tatanis 1 , Dimitris Veroutis 2 , Pavlos Pantelis 2 , George Theocharous 2 , Helen Sarlanis 3 , Alexandros Georgiou 3 , Angelis Peteinaris 1 , Anastasios Natsos 1 , Napoleon Moulavasilis 4 , Nikolaos Kavantzas 3 , Athanassios Kotsinas 2 , Ioannis Adamakis 4
1 Department of Urology, University of Patras, Patras, Greece;
2 Molecular Carcinogenesis Group, Department of Histology and Embryology, Medical School, National Kapodistrian University of Athens (NKUA), Athens, Greece;
3 Department of Pathology, Medical School, National and Kapodistrian University, Athens, Greece;
4 1st Department of Urology, National and Kapodistrian University of Athens, Athens, Greece
Summary
Purpose: The aim of this experimental study is to investigate the correlation between the presence of senescent cells and the tumor size, the lymphovascular invasion (LVI), the invasion of rete testis (RTI), the preoperative tumor markers or pathological stage in patients who underwent orchiectomy for malignant purposes
Methods: This experimental study included patients with a history of radical orchiectomy performed from January 2011 to January 2019. The testicular tissue specimens underwent an immunohistopathological process for the detection of the presence of cellular senescence. Besides, the tumor size, the histopathological type, the pathological stage of the tumor and the presence of Lymphovascular (LVI) or rete testis (RTI) invasions were also recorded Additionally, the preoperative serum levels of alpha-fetoprotein, beta-human chorionic gonadotropin and lactate dehydrogenase were recorded After the completion of immunohistochemical analysis, the rate of senescent cells in each specimen was also recorded
Results: The mean senescent cell rate was estimated to be 14.11 ± 11 32% and 15 46 ± 10 58% in patients with presence of LVI or absence of LVI, respectively (p = 0.46). The mean senescent cell rate was calculated at 18 13±12 26% and 12 56 ± 9.38% (p = 0.096) in patients with presence of RTI or absence of RTI, respectively The mean senescent cell rate in the pT1 group was calculated at 14 58 ± 9 82%, while in T2 and T3 groups the mean senescent cell rate was estimated to be 15 22 ± 12 03% and 15 35 ± 14 21%, respectively (p = 0 98) A statistically significant correlation was detected between the senescence rate and the tumor size (Pearson score 0 40, p = 0 027) and between the rate of senescent cells and the preoperative level of lactate dehydrogenase (LDH) (Pearson score -0 53, p = 0 002)
Conclusions: The presence of cellular senescence was correlated with the extent of the testicular tumor in terms of tumor size as well as the preoperative level of the LDH serum marker
KEY WORDS: Testicular cancer; Cellular senescence; Preoperative tumor markers; GL13; Senescent cells
Submitted 31 December 2023; Accepted 12 January 2024
INTRODUCTION
Testicular cancer is associated with a survival rate of over 95% in 5 years, constituting a solid malignancy with a good prognosis There are many factors leading to this fact including the young age of the patients, the complete surgical excision of the tumor as well as the effective use of chemotherapeutic agents (1) The staging of testicular cancer plays a crucial role in the successful management of the disease including the use of preoperative tumor markers (2) In clinical practice, Alpha-fetoprotein (a-FP), beta-human chorionic gonadotropin (b-hCG) and lactate dehydrogenase (LDH) constitute the most common serum markers used in staging stratification
A-FP is a 70kD serum-binding protein that is mainly produced by the yolk sac, liver and intestines The a-FP levels are peaked between 12-14 weeks of gestation, while they are decreased under 15 ng/ml after the first year of life (3) It has a serum half-life of 5-7 days, while it is considered the most commonly elevated tumor marker in testicular cancer patients (4)
HCG is a 38kD protein that is produced by the placental syncytiotrophoblasts and consists of two subunits (a and b) In contrast to subunit a which resembles the pituitary hormones, b-hCG resembles only 70% of Luteinizing Hormone (LH) and thus is easier to be detected
The b-hCG is characterized by a serum half-life time of 24-36 hours (3, 5)
LDH is a 134kD catalytic agent for the interconversion of lactate and pyruvate LDH is not associated with high specificity for testicular cancer, nevertheless, it may highlight intense enzymatic processes (3) High levels of LDH over 2 000 U/L seem to be associated with an extremely elevated risk for recurrence (6)
In recent years, the integration of cellular senescence was r e m a r k e d a s
r
i
g y Interestingly senescence plays a crucial role in tumorigenesis and is considered as hallmark of cancer It is determined as a special condition of cells and it includes their irreversible growth arrest, metabolism deregulation,
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12246 1
a
e v o l u t
o n i n t h e fi e l d o f b i o l o
Cellularsenescenceintesticularcancer. Isthereacorrelationwiththepreoperativemarkers andtheextentofthetumor?Anexperimentalstudy
DOI: 10 4081/aiua 2024 12246
macromolecular damage and a specific secretory phenotype termed Senescence Associated Secretory Phenotype (SASP) (7) The cellular senescence could be classified into two types depending on its triggering factors The first type is widely known as replicative senescence in which the arrest of cellular proliferation is caused by telomere attrition The second type is stress-induced premature senescence in which stressful stimuli constitute the triggering factors The role of cellular senescence in the aged skin, in diseases that are determined as age-related and in the procedure of the formation of premalignant lesions is widely studied and presented in the literature The action of senescence in terms of oncological diseases remains controversial, as it is proven to present both oncosuppressive and oncogenetic characteristics (8) On the one hand, the senescent cells act as tumor-barrier, whereas the accumulation of cells that are vulnerable due to the semi-active metabolic condition may enhance the oncogenesis or the tumor relapses (9)
The association of cellular senescence with visceral tumors o r m a
although the available literature is restricted The role of senescent cells has been described in the frame of a plethora of cancer types such as colorectal, pancreatic and Hodgkin lymphoma (10) Concerning the urogenital region, the presence of cellular senescence in seminomas was detected by Savelyeva et al , while Majumder et al evalu a t e d t h
Intraepithelial Neoplasia (PIN) and in prostatic cancer (11, 12) To our knowledge, the impact of cellular senescence in different histopathological types and its correlation with the tumor characteristics was not investigated The aim of this experimental study is to evaluate the correlation of cellular senescence with the extent of the testicular tumor and with the level of preoperative serum markers
MATERIALSANDMETHODS
Statement of human rights
The ethical committee of the University of Athens has approved the conduction of this study in the “Laiko” General Hospital of Athens Informed consent was obtained from all the participants, while the experiments were performed based on the principles of the Helsinki Declaration
Study design
This experimental study was conducted retrospectively The study population included patients with a history of r a d i c a l o r c h i e c t o m y p e r f o r m e d a t t h e 1 s t U r o l o g y
Department of Athens Medical School from January 2011 to January 2019 The radical orchiectomy was performed due to testicular cancer in all the patients Patients with secondary testicular tumors, incomplete pre- and postoperative data, younger than 18 years old, a history of chemotherapy or patients who were lost during the follow-up were excluded The investigated samples consisted of formalin-fixed paraffin-embedded (FFPE) testicular tissue including tumor, cancerous and premalignant (if available) structures concomitantly and were obtained from the histopathological laboratory Moreover, the samples were sliced into specimens of 4mm thickness
and were stained immunohistochemically against lipofuscin with GL13 (SenTraGor™), p21WAF1/CIP1 and Ki67, to confirm the presence of senescent cells according to the proposed algorithm (13) GL13 is a biotinylated Sudan Black-B analogue that recognized lipofuscin as a hallmark of senescent cells (8, 14) The p21WAF1/CIP1 constitutes a protein that is hardly associated with non-cancerous testicular tissue or Germ Cell Neoplasia In Situ (GCNIS) (14, 15) Finally, Ki67 is strongly associated with the growth fraction cells, as it identifies their proliferative activity 16
Data collection
The preoperative variables included the age of the patient and the date of the operation The testicular dimensions were recorded based on the report of the pathological examination as it is proven to be the most rigorous measurement (17) Besides the testicular and tumor sizes, the histopathological type and the pathological stage were recorded The presence of Lymphovascular Invasion (LVI) and Rete testis Invasion (RTI) presence was also recorded, based on the pathological report
In the case of mixed tumors, despite the documentation of all the included types and the corresponding rates, the primary histological diagnosis was utilized as the milestone for the patient’s subgrouping Additionally, the preoperative serum levels of a-FP, b-hCG and LDH were recorded After the completion of immunohistochemical analysis, the total rate of senescent cells in each specimen was also recorded
Immunohistochemistry for anti-biotin, p21Waf1/Cip1 and Ki-67 staining
The samples were deparaffinized and hydrated while the antigen retrieval was heated mediated using 10 mM of citric acid (pH 6 0) for 15 minutes in a steamer (in the case of SenTraGor™ staining) In the case of incubation with p21WAF1/Cip1 and Ki67 antibodies, antigen retrieval was completed similarly, but a 25-minute microwave was applied for the heating mediation Normal goat serum was applied for 1 hour at room temperature (dilution 1:40, Abcam, ab138478) to achieve the blocking of nonspecific binding of the aforementioned antibodies The applied primary antibodies included: anti-biotin antibody (dilution 1:300, Hyb-8, ab201341, Abcam) or antip21WAF1/Cip1 (dilution 1:200, 12D1, Cell Signaling) or anti-Ki67 (dilution 1:250, Sp-6, Abcam) and the tissues were incubated overnight at 4°C The use of the Dako REAL EnVision Detection System kit, (Cat no: K5007) according to the manufacturer’s instructions using DAB (brown color), led to the progression of the signal The specimens were counterstained with Hematoxylin to encounter the positive cells
Finally, the sections were observed using ZEISS Axiolab5 optical microscope on the 20x objective (200x magnification, 25μM scale bar) (13)
SenTraGor™ (GL13) staining for senescence detection
The SenTraGor™ staining was performed following the step of blocking non-specific binding sites of primary antibody The specimens were incubated in 50% ethanol for 5 minutes and then in 70% ethanol for 5 minutes more SenTraGor™ was applied in tissues and the speci-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12246
2
V Tatanis, D Veroutis, P Pantelis, et al
j o r p r e m a l i g n a n t s t r u c t u r e s w a s i n v e s t i g a t e d ,
e p r e s e n c e o f s e n e s c e n t c e l l s i n P r o s t a t i c
mens were covered with glass coverslips, followed by 10minutes incubation at 37°C Afterward, coverslips were gently removed and sections were washed with 50% Ethanol for 30 seconds An extra wash step was performed (3-5 minutes) using Triton-X 0 3%/TBS
Afterward, the sections were washed with TBS, followed by an overnight application of the anti-biotin antibody (dilution: 1/300, Cat no: K5007) at 4°C (13)
Statistical analysis
Continuous variables were presented using the mean value and standard deviation Categorical variables were described as absolute numbers and rates The comparison of continuous variables was investigated using the two-way t-test, while the correlation between variables was investigated using the Pearson Correlation Coefficient The differences between multiple groups were evaluated using the one-way ANOVA test Statistical analysis was conducted utilizing the Statistical Package for the Social Sciences (SPSS) software package version 25 0 (IBM Corp , Armonk, NY)
RESULTS
In this scientific work in order to evaluate the correlation of senescent cells with the pathological tumor stage, preoperative serum tumor markers, LVI and RTI in different histological types, specimens from 30 patients were utilized The mean age of the patients was estimated to be 30 97 ± 8 68 years, while the mean maximum diameter of the testis was recorded to be 6 ± 2 80 cm
Tumor size and cellular senescence
The mean size of tumors in all groups was estimated to be 4 16 ± 3 25 cm Based on the stratification into groups based on the primary histopathological diagnosis, the larger tumors were identified in the yolk sac groups with a mean maximum diameter of 9 27 ± 4 97 cm, followed by the teratoma group where the mean maximum diameter of the tumor was calculated at 3 83 ± 0 97 cm The seminomas and embryonal carcinomas were associated with shorter maximum mean diameters (2 9 ± 1 15 cm and 3 46 ± 2 67 cm, respectively) The difference between the groups was statistically significant (p = 0 002) The correlation between cellular senescence and the tumor size overall was statistically significant (Pearson Score: 0 40, p = 0 027) Nevertheless, the correlation in the subgroups did not reach the statistically significant level More precisely, the Pearson score in the seminoma group was estimated at -0 45 (p = 0 13), while in the embryonal tumor group was calculated at 0 05 (p = 0 89) Additionally, the Pearson scores in the teratomas and yolk sac tumors groups were 0 18 (p = 0 97) and 0 22 (p = 0 86), respectively (Table 1)
LVI and cellular senescence
The LVI was presented in 15/30 (50%) cases, while no LVI was noticed in the remaining 50% of the cases (15/30) More precisely, in 5/13 (38 5%) patients of the seminoma group LVI was detected, while 6/9 (66 7%) patients of the embryonal groups presented with similar pathological characteristics The LVI was detected in 2/4 (50%) and 2/3 (66 7%) patients in the teratomas and yolk
Table 1.
Evaluation of the senescent cells in relationship to the tumor size
Tumor’s maximum Senescent cells Pearson p-value dameter (mean ± SD) rate (mean ± SD) score Overall
SD: Standard Deviation
Table 2.
Evaluation of the senescent cells in the presence or absence of LVI
Overall
Patients (%) 15 (50%) 15 (50%)
Seminoma
Patients (%) 5 (38 5%) 8 (61 5%)
Senescent cells rate (mean ± SD) 25 98 ± 8 41% 23 96 ± 6 64% 0 66
Embryonal
Patients (%) 6 (66 7%) 3 (33 3%) Senescent cells rate (mean ± SD) 8 92 ± 7 94% 4 53 ± 0 93% 0 30
LVI: Lymphovascular Invasion; SD: Standard Deviat on
sac tumors, respectively, whereas no LVI was mentioned in the patients with chondrosarcoma The mean senescent cell rate was estimated to be 14 11 ± 11 32% and 15 46 ± 10 58% in patients with present LVI and absent LVI, respectively
The difference was not statistically significant (p = 0 46) Moreover, a statistically significant association between the senescent cell rate and LVI was not observed in seminoma (25 98 ± 8 41% vs 23 96 ± 6 64%, p = 0 66) or embryonal groups (8 92 ± 7 94% vs 4 53 ± 0 93%, p = 0 30) (Table 2)
RTI and cellular senescence
The RTI was presented in 12/30 (40%) cases, while no RTI was noticed in the remaining 60% of the cases (18/30) More precisely, in 6/13 (46 2%) patients of the seminoma group RTI was detected, while 4/9 (44 4%) patients of the embryonal groups presented with similar pathological characteristics The RTI was detected in 1/4 (25%) and 1/3 (33 3%) patients in the teratomas and yolk sac tumors, respectively, whereas no RTI was mentioned in the patients with chondrosarcoma The mean senescent cell rate was estimated to be 18 13 ± 12 26% and 12 56 ± 9 38% in patients with present RTI or absent RTI, respectively
The difference was not statistically significant (p = 0 096) Moreover, a statistically significant association between the senescent cell rate and RTI was not observed in seminoma (27 58 ± 5 16% vs 22 3 ± 7 97%, p = 0 18) or embryonal groups (9 78 ± 8 16% vs 5 6 ± 1 64%, p = 0 54) (Table 3)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12246 3 Cellular senescence in testicular cancer
4 16 ± 3 25 cm 14 79 ± 10 79% 0 40 0 027* Seminoma 2 9 ± 1 15 cm 24 74 ± 7 1% -0 45 0 13 Embryonal 3 46 ± 2 67 cm 7 46 ± 6 82% 0 05 0 89 Teratoma 3 83 ± 0 97 cm 6 9 ± 1 8% 0 18 0 97 Yolk Sac 9 27 ± 4 97 cm 6 06 ± 1 79% 0 22 0 86
LVI positive LVI negative p-value
Senescent cells rate (mean ± SD) 14 11 ± 11 32% 15 46 ± 10 58% 0 46
Table 3.
Evaluation of the senescent cells in the presence or absence of RTI RTI positive RTI negative p-value
Overall Patients (%) 12 (40%) 18 (60%)
Senescent cells rate (mean ± SD) 18 13 ± 12 26% 12 56 ± 9 38% 0 096
Seminoma
Patients (%) 6 (46 2%) 7 (53 8%)
Senescent cells rate (mean ± SD) 27 58 ± 5 16% 22 3 ± 7 97% 0 18
Embryonal
Patients (%) 4 (44 4%) 5 (55 6%)
Senescent cells rate (mean ± SD) 9 78 ± 8 16% 5 6 ± 1 64% 0 54
RTI: Rete Testis Invasion; SD: Standard Deviat on
Pathological stage and cellular senescence
The association between senescent cell rate and pathological stage of the tumor was also evaluated In eleven (36 7%), seventeen (56 7%) and two (6 6%) patients the pathological stage was T1, T2 and T3, respectively The mean senescent cell rate in the T1 group was calculated at 14 58 ± 9 82%, while in the T2 and T3 groups, the mean senescent cell rates were estimated to be 15 22 ± 12 03% and 15 35 ± 14 21%, respectively The difference did not reach the statistical significance level, as p = 0 98 (Table 4)
Table 4.
Evaluation of the senescent cell rate based on the pathological stage
SD: Standard Deviat on
Preoperative tumor markers and cellular senescence
The correlation between the cellular senescence rate and the preoperative tumor markers constituted another endpoint of the study In total samples, the correlation between LDH and cellular senescence reached a statistically significant level, as the Pearson score was calculated at -0 53 (p = 0 002) On the other hand, no statistically significant correlation between the rate of senescent cells and the a-FP (Pearson score: -0 24, p = 0 20) or the bhCG (Pearson score: -0 23, p = 0 23) was detected After the stratification based on the primary histopathological type, LDH was statistically correlated with cellular senescence only in the seminoma subgroup The Pearson scores for LDH were estimated to be 0 56 (p = 0 045),0 04 (p = 0 92), 0 091 (p = 0 90) and -0 06 (p = 0 96) in seminoma, embryonal, teratoma and yolk sac groups, respectively The outcomes concerning the Pearson scores of a-FP were -0 13, p = 0 66 in the seminoma group; 0 30, p = 0 43 in the embryonal group; 0 39, p = 0 61 in the teratoma group; 0 06, p = 0 96 in the yolk sac group The correlation between senescent cell rate and the b-hCG did not reach a statistically significant level in
Table 5.
The correlation scores between cellular senescence and the preoperative serum tumor markers
Overall
Teratoma
Yolk Sac
LDH: Lactate Dehydrogenase; a-FP: Alpha-fetoprotein; b-hCG: beta-human chor on c gonadotrop n
any subgroup (Pearson score 0 11, p = 0 72 in the seminoma group; Pearson score 0 56, p = 0 11 in the embryonal group; Pearson score 0 37, p = 0 63 in the teratoma group; Pearson score -0 2, p = 0 87 in the yolk sac group) (Table 5)
DISCUSSION
The aim of this scientific study was to evaluate the association of the senescent cell detection rate with the tumor size, the preoperative tumor markers, the pathological stage and the presence of LVI and RTI In order to investigate the aforementioned correlation, stains with specific biomarkers showing the state of the examined tissues (proliferation or cellular senescence) were applied The lipofuscin, which constitutes an established biomarker of senescence, was detected by the GL13 staining (8) The staining pattern in these cells seems to be both perinuclear and cytoplasmic Besides GL13, p2121WAF1/CIP1 and Ki67 stains were utilized to perform a more robust disclosure of the cellular senescence in situ and to elucidate additional elements of the molecular behaviour of the evaluated tissues (18) The outcomes of the study proved that there is a statistical correlation between cellular senescence and the tumor size in overall the sample size, although this correlation was not confirmed in the subgroup analysis Despite being significantly associated with tumor size, cellular senescence does not seem to be strongly correlated with the pathological stage of the tumors Additionally, the presence of LVI or RTI does not seem to have a specific association with the senescent cell detection rates Concerning the preoperative tumor markers, no significant association between cellular senescence and the a-FP or b-hCG was detected in either the overall sample size or subgroups On the other hand, LDH was statistically sig-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12246
4
V Tatanis, D Veroutis, P Pantelis, et al
pT1 Stage pT2 Stage pT3 Stage p-value Sample size (%) 11 (36 7%) 17 (56 7%) 2 (6 6%) Senescent cells rate (mean ± SD) 14 58 ± 9 82% 15 22 ± 12 03% 15 35 ± 14 21% 0 98
Pearson Score p-value
LDH -0 53 0 002* aFP -0 24 0 20 b-HCG -0 23 0 23
LDH 0 56 0 045* a-FP -0 13 0 66 b-hCG 0 11 0 72 Embryonal LDH -0 04 0 92 a-FP 0 30 0 43 b-hCG 0.56 0.11
Seminoma
LDH 0 091 0 90 a-FP 0 39 0 61 b-hCG 0 37 0 63
LDH -0 06 0 96 a-FP 0 06 0 96 b-hCG 0 2 0 87
nificantly correlated with the senescent cell detection rates in the overall sample size and seminoma group, whereas no significant correlation with the embryonal, teratoma and yolk sac groups To our knowledge, this is the first study that investigated the correlation of cellular senescence with the extent of the tumor and the preoperative serum tumor markers
The impact of cellular senescence in the carcinogenesis of the genitourinary system was documented in both testicular and prostate cancer The presence of senescent cells in testicular cancer was described by Savelyeva et al (11) The authors investigated the microenvironment of pure seminomas and they identified that it compromises senescent cells (11) Concerning prostate cancer, the role of cellular senescence was investigated by Majumder et al and Mourkioti et al Majumder et al evaluated the presence of senescent cells in both premalignant conditions of PIN and prostatic cancer tissues Based on their outcomes, senescent cells were detected in cases of PIN or PIN and prostatic cancer structures concomitantly, whereas no cellular senescence was identified in prostate cancer-only tissues In our study, cellular senescence was investigated in terms of correlation to the extent of the disease and to the preoperative tumor serum markers in various histopathological types of testicular cancer (12) Moreover, Mourkioti et al proved that the downregulation of CDC6 gene expression may enhance androgen receptor blockadeinduced senescence in metastatic prostate cancer cells highlighting the therapeutic impact of cellular senescence even in advanced cancer stages (19) Based on our outcomes, a significant correlation of cellular senescence with the tumor size (Pearson Score: 0 40, p = 0 027) and LDH (Pearson Score: -0 53, p = 0 045) was identified Thus, we can confirm the presence of senescent cells in various histological types of testicular cancer, even if the correlation was not statistically significant, as was described by Savelyeva et al (11) Additionally, contrary to Majumder et al , cellular senescence was detected in all histological types of testicular tissue A possible explanation for that phenomenon could be the different methodology of senescence detection, as GL13 seems to be the most accurate marker for senescence detection since it detects lipofuscin accumulation as a result of the deregulated metabolism, macromolecular damage and cell cycle arrest, the three out of four hallmarks of senescence (14) Moreover, the application of additional senescence markers contributed to an improved evaluation of the tissue structures
The controversial impact of cellular senescence in oncogenesis was widely evaluated in the literature Cellular senescence seems to be a barrier to the triggered oncogenes showing its important tumor-suppressive role (18) The cycle arrest condition that characterizes cellular senescence seems to improve the efficacy of the apoptosis or DNA-damage repair processes On the contrary, senescent cells may accumulate in different types of tissue due to the disturbance of the induction/elimination balance
The aforementioned disturbance leads to the accumulation of senescent cells that are vulnerable to modifications of their genome or SASP These modifications result in either endothelial-to-mesenchymal transition (EMT) or selfrenewal which are characterized by invasive/metastatic or stemness potential, respectively (20) Besides the cycle
arrest, they seem to escape and re-enter the cell cycle, a phenomenon termed “Escape from Senescence” The latter are associated with a different phenotype compared to the primary senescent cells and thus they may be characterized as more aggressive and potentially oncogenetic SASP has a paracrine function that promotes cellular senescence and its tumor-suppressive role in low-grade preneoplastic cells increasing the interleukin, chemokine, growth factors and regulator, receptor and ligand levels, and altering the function of collagens, laminin and reactive oxygen species (bright side) (21) On the contrary, it encourages the escape from senescence and relapse to the cell cycle in the malignant cells (dark side) (7) The modifications of the SASP profile are considered the cause of the bimodal role of cellular senescence Normally, SASP includes interleukins, chemokines, growth factors and additional soluble factors in equilibrium that enhance its tumor-suppressive role On the other hand, under the impact of p53 loss or oncogenic RAS gain, the SASP is modified compromising abnormally elevated interleukins, chemokines and other inflammatory factors that induce the escape phenomenon More precisely, in prostate cancer, the secretion of SDF-1α factor in the frame of SASP of senescent fibroblasts seems to enhance the prostate cancer progress, while the hypersecretion of inflammatory factors of senescent cells’ SASP may be associated with higher risk for relapse after chemotherapy (21) The latter proves the negative aspect of cellular senescence that is related to the oncological diseases (9, 22) This phenomenon may explain the negative correlation between cellular senescence and the LDH, which has been proved in our study Senescent cells are normally accumulated in premalignant lesions, as described in prostatic and pancreatic cancer, whereas LDH is elevated in some cases of testicular neoplasia as accompanied by intense enzymatic processes (3, 10, 12) In our study, the negative correlation (Pearson score: -0 53) may indicate the decrease of senescent cell detection rate during the transformation of the premalignant to malignant conditions (which are characterized by elevated LDH) highlighting the escape phenomenon as described by Zampetidis et al (9)
Besides the significant negative correlation between LDH and cellular senescence in overall the sample size, another positive correlation was identified in the seminoma subgroup (Pearson score: 0 56, p = 0 045) Thus, we can consider that the senescent cell detection rate remains at relatively high levels in the seminoma group, while it is decreased in the other histopathological subgroups This observation may be explained by the sequence of testicular cancer as proposed by von Eyben et al (23) The authors supported that the seminoma constitutes the first step of the transformation of the premalignant conditions (GCNIS) to testicular cancer Afterward, the seminoma may be transformed into embryonal carcinoma, followed by the parallel development of teratoma or yolk sac tumor Consequently, we can consider that a significant rate of senescent cells remains in the seminoma, which may escape from senescence in the latter steps (9)
There is detailed documentation in the literature regarding the association between senescent cells and colorectal cancer, lung adenocarcinoma, or classical Hodgkin lymphoma (10, 24, 25) Moreover, the role of cellular senes-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12246 5 Cellular senescence in testicular cancer
cence is also important in the failure of chemotherapy and the disease relapses The presence of senescent Hodgkin and Reed-Sternberg cells in high proportions (over 10-15%) seems to be a risk factor for poor prognosis in patients suffering from Hodgkin lymphoma, as described by Broeckelman et al (26) In our study, the positive correlation of cellular senescence with LDH in the seminoma groups may indicate the presence of a relatively high proportion of senescent cells in the seminomas Taking into consideration the example of Hodgkin lymphoma, we may consider the management of both the tumor and the senescent cells in specific cases The combination of chemotherapeutic agents with senolytics may improve the efficacy of the treatment, prevent tumor relapses and ameliorate the prognosis and the quality of life of the patients
Consequently, novel combined chemotherapeutic strategies aiming at both cancerous and senescent cells may be developed and evaluated
There are limitations in our study The sample size is relatively small, as it includes tissue specimens of 30 patients Besides the reduced sample size, this is the first study to our knowledge that evaluated the correlation between cellular senescence and the extent of testicular cancer or the preoperative tumor markers Moreover, the outcomes of the immunohistochemical staining are not associated with the clinical presentation and the prognosis of the patients
Further studies should be conducted for the correlation of immunohistochemical and clinical outcomes
The presence of cellular senescence was correlated with the extent of the testicular tumor in terms of tumor maximum diameter, whereas the association was insignificant regarding the pathological stage and the lymphovascular or rete testis invasions
The levels of LDH preoperatively seem to be negatively correlated to the presence of cellular senescence, while an additional positive correlation was detected in patients suffering from seminoma
REFERENCES
1 Biggs ML SS Cancer of the testis In: Ries LAG YJ, Keel GE, Eisner MP, Lin YD, Horner M-J, editor SEER survival monograph: cancer survival among adults: US SEER Program, 1988-2001, patient and tumor characteristics: National Cancer Institute 2007; p 165-70
2 Urology EA EAU Guidelines Edn presented at the EAU Annual Congress Milan 2023 ed
3 Milose JC, Filson CP, Weizer AZ, Hafez KS, Montgomery JS Role of biochemical markers in testicular cancer: diagnosis, staging, and surveillance Open Access J Urol 2011; 4:1-8
4 Germa-Lluch JR, Garcia del Muro X, Maroto P, et al Clinical pattern and therapeutic results achieved in 1490 patients with germ-cell tumours of the testis: the experience of the Spanish Germ-Cell Cancer Group (GG) Eur Urol 2002; 42:553-62
5 Lempiainen A, Stenman UH, Blomqvist C, Hotakainen K Free beta-subunit of human chorionic gonadotropin in serum is a diagnos-
tically sensitive marker of seminomatous testicular cancer Clin Chem 2008; 54:1840-3
6 Carl J, Christensen TB, von der Maase H Cisplatinum dose dependent response in germ cell cancer evaluated by tumour marker modelling Acta Oncol 1992; 31:749-53
7 Gorgoulis VG, Halazonetis TD Oncogene-induced senescence: the bright and dark side of the response Curr Opin Cell Biol 2010; 22:816-27
8 Georgakopoulou EA, Tsimaratou K, Evangelou K, et al Specific lipofuscin staining as a novel biomarker to detect replicative and stress-induced senescence A method applicable in cryo-preserved and archival tissues Aging (Albany NY) 2013; 5:37-50
9 Zampetidis CP, Galanos P, Angelopoulou A, et al A recurrent chromosomal inversion suffices for driving escape from oncogeneinduced senescence via subTAD reorganization Mol Cell 2021; 81:4907-23 e8
1 0 M y r i a n t h o p o u l o s V , E v a n g e l o u K , V a s i l e i o u P V S , e t a l Senescence and senotherapeutics: a new field in cancer therapy Pharmacol Ther 2019; 193:31-49
11 Savelyeva AV, Medvedev KE Seminoma subtypes differ in the organization and functional state of the immune microenvironment
3 Biotech 2023; 13:110
12 Majumder PK, Grisanzio C, O'Connell F, et al A prostatic intraepithelial neoplasia-dependent p27 Kip1 checkpoint induces senescence and inhibits cell proliferation and cancer progression Cancer Cell 2008; 14:146-55
13 Kohli J, Wang B, Brandenburg SM, et al Algorithmic assessment of cellular senescence in experimental and clinical specimens Nat Protoc 2021; 16:2471-98
14 Evangelou K, Lougiakis N, Rizou SV, et al Robust, universal biomarker assay to detect senescent cells in biological specimens Aging Cell 2017; 16:192-7
15 Bartkova J, Thullberg M, Rajpert-De Meyts E, et al Cell cycle regulators in testicular cancer: loss of p18INK4C marks progression from carcinoma in situ to invasive germ cell tumours Int J Cancer 2000; 85:370-5
16 Hilbold E, Bergmann M, Fietz D, et al Immunolocalization of DMRTB1 in human testis with normal and impaired spermatogenesis Andrology 2019; 7:428-40
17 Paltiel HJ, Diamond DA, Di Canzio J, et al Testicular volume: c
Radiology 2002; 222:114-9
18 Gorgoulis V, Adams PD, Alimonti A, et al Cellular Senescence: Defining a Path Forward Cell 2019; 179:813-27
19 Mourkioti I, Polyzou A, Veroutis D, et al A GATA2-CDC6 axis m o d u l a t e s a n
prostate cancer J Exp Clin Cancer Res 2023; 42:187
20 Evangelou K, Belogiannis K, Papaspyropoulos A, et al Escape from senescence: molecular basis and therapeutic ramifications J Pathol 2023; 260:649-65
21 Coppe JP, Desprez PY, Krtolica A, Campisi J The senescenceassociated secretory phenotype: the dark side of tumor suppression Annu Rev Pathol 2010; 5:99-118
22 Galanos P, Pappas G, Polyzos A, et al Mutational signatures reveal the role of RAD52 in p53-independent p21-driven genomic instability Genome Biol 2018; 19:37
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12246
6
V Tatanis, D Veroutis, P Pantelis, et al
CONCLUSIONS
o m p a r i s o n o f o r c h i d o m e t e r a n d U S m e a s u r e m e n t s i n d o g s
r e c e p t o r b l o c k a d e - i n d u c e d s e n e s c e n c e i n
d r o g e n
23 von Eyben FE, Parraga-Alava J Meta-Analysis of Gene Expressions in Testicular Germ Cell Tumor Histologies Int J Mol Sci 2020; 21
24 Haugstetter AM, Loddenkemper C, Lenze D, et al Cellular senescence predicts treatment outcome in metastasised colorectal cancer Br J Cancer 2010; 103:505-9
25 Collado M, Gil J, Efeyan A, et al Tumour biology: senescence in premalignant tumours Nature 2005; 436:642
2 6 B r o c k e l m a n n P J , A n g e l o p o u l o u M K , V a s s i l a k o p o u l o s T P Prognostic factors in Hodgkin lymphoma Semin Hematol 2016; 53:155-64
Correspondence
Vasileios Tatanis, MD (Corresponding Author) tatanisbas@gmail com
Department of Urology, University of Patras, Patras, Greece University of Patras, Rio, Patras, 26500, Greece
Angelis Peteinaris, MD peteinarisaggelis@gmail com
Anastasios Natsos, MD anatsos@gmail com
Dimitris Veroutis, MD dimitrisveroutis1@gmail com
Pavlos Pantelis, MD pavlospantelis7@gmail com
George Theocharous, MD theocharousgiorgos@gmail com
Athanassios Kotsinas, MD akotsin@gmail com
Molecular Carcinogenesis Group, Department of Histology and Embryology, Medical School, National Kapodistrian University of Athens (NKUA), Athens, Greece
Helen Sarlanis, MD elenisarlani@gmail com
Alexandros Georgiou, MD alexandrosge11@gmail com
Nikolaos Kavantzas,MD nkavantz@med uoa gr
Department of Pathology, Medical School, National and Kapodistrian University, Athens, Greece
Napoleon Moulavasilis, MD napomoul@hotmail com
Ioannis Adamakis, MD yianton@hotmail com
1st Department of Urology, National and Kapodistrian University of Athens, Athens, Greece
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12246 7 Cellular senescence in testicular cancer
ORIGINAL PAPER
Gonçalo Mendes 1 , Bernardo Teixeira 1 , Mariana Madanelo 1 , Alexandra Rocha 1 , Sofia Mesquita 1 , João Vital 2 , Miguel Monteiro 1 , Avelino Fraga 1 , Nuno Louro 1
1 Department of Urology, Santo António University Hospital Center, Porto, Portugal;
2 Department of Urology, Hospital of Funchal, Funchal, Portugal
Summary
Purpose: To evaluate the influence of testicular cancer histology and stage on sperm parameters in cryopreserved samples collected prior to orchiectomy
Materials and methods: We conducted a retrospective analysis of tumor histology, stage and sperm parameters of patients who underwent pre-orchiectomy sperm cryopreservation for testicular cancer between March 2010 and March 2023. The World Health Organization (WHO) 2010 sperm reference values were used to identify patients with subnormal semen parameters and to further categorize patients by sperm alteration Localized disease was classified as Stage I, while metastatic disease encompassed Stages II and III Continuous variables were compared using t-test or Mann Whitney U test, and categorical variables using Chi-square and Fisher s exact test
Results: A total of 64 patients was identified, 48 (75%) classified as stage I and 16 (25%) classified as stage II/III No difference was found in semen parameters between patients with seminoma and patients with non-seminoma germ cell tumor (NSGCT)
Patients with stage II/III disease had significantly lower percentages of progressive motility (36% vs 53%, p = 0 021) and total motility (60% vs 69%, p = 0 015) than stage I patients
When categorizing by sperm alterations according to WHO 2010 reference values, patients with stage II/III disease had significantly higher proportions of asthenozoospermia (38% vs 15%, p = 0 048) and teratozoospermia (63% vs 31%, p = 0 027) than stage I patients Elevated tumor markers were not associated with sperm abnormalities
Conclusions: Patients with metastatic testicular cancer present with worse sperm quality than patients with localized disease
Sperm cryopreservation should be offered to all patients with testicular cancer, and especially emphasized in patients with metastatic disease.
KEY WORDS: Testicular cancer; Male infertility; Cryopreservation; Sperm parameters; Orchiectomy
Submitted 28 December 2023; Accepted 29 December 2023 INTRODUCTION
Testicular cancer (TCa) is the most common malignant tumor in young adult men aged 15-40 years, and accounts for about 1% of all neoplasms in men (1) The incidence of TCa has been steadily increasing in recent years, predominantly in developed countries (2, 3) Despite having
high cure and long-term survival rates, the fertility burden on survivors is still a major concern Studies have demonstrated a reduction in semen parameters, notably preorchiectomy sperm concentration and total sperm count, as well as a decrease in fertility among patients with TCa compared to their healthy counterparts (4)
Moreover, patients with TCa often need additional treatments which further impair spermatogenesis and fertility
Despite advancements in these treatments, the gonadotoxic effects of chemotherapy and radiation, coupled with the potential for impaired ejaculation and subsequent infertility following retroperitoneal lymph node dissection (RPLND), contribute to a consistent decrease in fertility
a m o n g m a l e s u n d e r g o i n g a d d i t i o n a l t h e r a p y p o s torchiectomy (5)
In that regard, there is a need for literature investigating the potential role of TCa stage in the fertility potential of these patients The aim of our study was to evaluate the impact of TCa stage and histology on preorchiectomy semen parameters, as a surrogate for fertility We also analyzed the role of elevated tumor markers on sperm abnormalities
MATERIALSANDMETHODS
Patient selection
We retrospectively collected data on all patients who consecutively received radical orchiectomy for presumed TCa and who underwent semen cryopreservation before orchiectomy, between March 2010 and March 2023 We excluded patients with bilateral tumors, patients without germ cell tumor (GCT) on final pathology, patients who did not undergo semen cryopreservation and patients who underwent cryopreservation after orchiectomy
The study was approved by the Ethical Committee of our center
Variables
Our database included data regarding age at diagnosis, body mass index (BMI), tumor size, tumor histology, clinical stage, serum tumor markers, namely alpha-fetoprotein (a-FP), beta subunit of human chorionic gonadotropin (b-hCG) and lactate dehydrogenase (LDH), and semen
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12238 1
Semenparametersintesticulartumorpatients beforeorchiectomy:Whatistheimpactoftesticular tumorstageandhistology?
DOI: 10 4081/aiua 2024 12238
parameters Serum tumor markers were considered elevated if they were above the upper normal limit provided by the laboratory (a-FP 0-7 µg/L, b-hCG 0-2 U/L, LDH 135-225 U/L) Semen parameters reviewed included patient s semen volume, sperm concentration, progressive motility, total motility and morphology The World Health Organization (WHO) 2010 sperm reference values (6) were used to identify patients with subnormal semen parameters and to further categorize patients by sperm alteration (oligozoospermia was defined as < 15 million spermatozoa/mL, asthenozoospermia as < 32% progressive motile spermatozoa and teratozoospermia as < 4% normal forms) Stage I disease was considered localized disease, whereas Stage II/III disease was considered metastatic disease
Statistical analysis
Continuous variables with normal distribution are presented as mean ± standard deviation and compared by Student s t-test, while continuous variables with non-normal distribution are presented as medians accompanied by interquartile ranges (IQRs) and compared by the MannWhitney-U test Categorical variables are presented as proportions, and comparisons of two categorical variables are performed with the Pearson’s Chi-square test and Fisher exact test A multivariate regression analysis was performed Statistical analyses were conducted using SPSS Statistics version 27 All tests were two-sided, and statistical significance was set at p < 0 05
RESULTS
A total of 123 patients were diagnosed with TCa at our institution in the studied timeframe A total of 64 patients (52%) were included (patients who underwent semen cryopreservation before orchiectomy) Of these, 48 patients (75%) classified as stage I and 16 patients (25%) classified as stage II/III According to histology, 33 patients (52%) were seminoma and 31 patients (48%) were non-seminoma GCT (NSGCT) Baseline characteristics are presented in Table 1 Age, BMI and tumor size were similar between groups There was a significantly bigger proportion of NSGCT in stage II/III patients as compared to patients in the stage I group (75% vs 40%, p = 0 014)
A comparison of sperm parameters between both groups according to histology (seminoma vs NSGCT) is presented in Table 2 All semen parameters were similar between groups, and therefore no difference was observed between patients with seminoma and patients with NSGCT
A comparison of sperm parameters between both groups according to stage (stage I vs stage II/III) is presented in Table 3 In general, all sperm parameters where lower in the stage II/III patients Stage II/III patients had significantly lower percentage of progressive motility (35 51% in stage II/III vs
Table 1.
Baseline characteristics of the patients
Table 2.
53 00% in stage I, p = 0 021) and significantly lower percentage of total motility (59 95% in stage II/III vs 69 10% in stage I, p = 0 015) Additionally, there was a trend towards lower progressive motility and lower total motility (as absolute numbers) in stage II/III patients, as well as a tendency to a lesser percentage of morphologically normal spermatozoids in this group
Sperm parameters were further categorized according to the WHO 2010 sperm reference values, and the groups according to stage (I vs II/III) were compared The results are presented in Table 3 Stage II/III patients had a significantly higher proportion of asthenozoospermia (38% in stage II/III vs 15% in stage I, p = 0 048) and a significantly higher proportion of teratozoospermia (63% in stage II/III vs 31% in stage I, p = 0 027) Despite not reaching statistical significance, patients in stage II/III
Table 3.
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12238
2
G Mendes, B Teixeira, M Madanelo, et al
Stage I Stage II/III P (n = 48) (n = 16) Age 31 00 ± 5 88 30 69 ± 12 34 0 923 BMI 24 84 ± 4 33 26 67 ± 4 03 0 506 Tumor size 38 85 ± 21 59 42 88 ± 23 07 0 528 Histology Seminoma 29 (60%) 4 (25%) 0 014 NSCGT 19 (40%) 12 (75%) BMI: body mass index; NSGCT: non-sem noma germ ce l tumor
of preorchiectomy sperm parameters according to tumor histology Total Seminoma NSGCT p (n = 64) (n = 33) (n = 31) Semen volume (mL) 2 95 ± 1 60 3 09 ± 1 56 2 79 ± 1 66 0 468 Sperm concentration (millions/mL) 31 50 (10 48-70 00) 37 00 (15 50-84 50) 28 00 (9 00-66 00) 0 330 Progressive motility (millions/mL) 19 21 (3 98-39 31) 22 08 (4 11-42 88) 11 50 (3 38-33 53) 0 295 Progressive motility (%) 48 63 ± 22 20 50 61 ± 23 36 46 52 ± 21 07 0 465 Total motility (millions/mL) 21 83 (6 35-51 32) 26 91 (7 00-54 20) 16 40 (5 75-43 20) 0 347 Total motility (%) 65 55 (52 45-77 75) 67 00 (52 95-79 80) 64 50 (52 30-74 50) 0 444 Normal morphology (millions/mL) 1 56 (0 29-4 83) 1 70 (0 52-5 51) 1 55 (0 26-4 20) 0 493 Normal morphology (%) 4.00 (2.25-7.00) 5.00 (3.00-7.00) 4.00 (2.00-8.00) 0.866 NSGCT: non-sem noma germ cell tumor
Comparison
of preorchiectomy sperm parameters according to tumor stage Total Stage I Stage II/III p (n = 64) (n = 48) (n = 16) Semen volume (mL) 2 95 ± 1 60 3 01 ± 1 71 2 75 ± 1 28 0 578 Sperm concentration (millions/mL) 31 50 (10 48-70 00) 33 50 (15 25-73 00) 23 00 (0 03-47 00) 0 129 Progressive motility (millions/mL) 19 21 (3 98-39 31) 20 79 (5 33-42 48) 9 65 (0 01-30 84) 0 077 Progressive motility (%) 48 63 ± 22 20 53 00 ± 19 29 35 51 ± 25 67 0 021 Total motility (millions/mL) 21 83 (6 35-51 32) 24 43 (8 37-54 06) 12 45 (0 01-36 32) 0 088 Total motility (%) 65 55 (52 45-77 75) 69 10 (55 43-79 25) 59 95 (5 00-66 68) 0 015 Normal morphology (millions/mL) 1 56 (0 29-4 83) 1 63 (0 50-5 40) 0 80 (0 01-4 15) 0 195 Normal morphology (%) 4 00 (2 25-7 00) 5 00 (3 00-7 00) 3 00 (0 00-7 50) 0 102
Comparison
Table 4.
Comparison of categories of preorchiectomy sperm alterations according to the WHO 2010 sperm reference values and to tumor stage
Stage I Stage II/III P (n = 48) (n = 16)
Oligozoospermia
(< 15 millions/mL) n (%) 11 (23%) 7 (44%) 0 108
Asthenozoospermia
(< 32% progressive motility) n (%) 7 (15%) 6 (38%) 0 048
Teratozoospermia (< 4% normal forms) n (%) 15 (31%) 10 (63%) 0 027
Azoospermia (complete absence of spermatozoa) 2 (4%) 1 (6%) 1 000 Any abnormality n (%) 21 (44%) 10 (63%) 0 194
Table 5.
Multivariate regression analysis for the role of elevated tumor markers as predictors of any abnormality in sperm parameters in patients with testicular cancer
Covariate OR 95% CI P
Elevated a-FP 2 859 0 693, 11 787 0 146
Elevated β-hCG 0 486 0 125, 1 890 0 297
Elevated LDH 2 748 0 895, 8 436 0 097
CI: conf dence nterva ; OR: odds ratio
group also had higher percentage of oligozoospermia (44% in stage II/III vs 23% in stage I, p = 0 108) The proportion of patients with azoospermia was similar between groups
On multivariate regression analysis, elevated tumor markers (AFP, b-hCG and LDH) were not associated with abnormalities in sperm parameters (Table 5)
Three patients (5%) used their cryopreserved semen for assisted reproduction techniques (ART); two patients had a seminoma and one patient had a NSGCT Two patients had stage I disease and one patient had stage II/III disease Non-cryopreserved paternity data was unavailable
DISCUSSION
Testicular cancer can play a major role in infertility
Analysis of cryopreservation data demonstrates that normal sperm quality is observed in less than half of men with TCa before treatment, and 10-35% suffer from infertility Fertility may be impacted by TCa through a multitude of axis, including intrinsic infertility associated with the testicular dysgenesis syndrome, the testicular tumor local effect, and systemic effects of hormones secreted by the tumor (7) There is a paucity of literature on the impact of tumor stage and histology in sperm outcomes of patients with TCa, with a previous study failing to demonstrate any relation between these factors (8) To the best of our knowledge, this is the largest series on the impact of tumor stage and histology on sperm quality In our study, we demonstrated that patients with metastatic disease (stage II/III) have worse sperm parameters than patients with localized disease (stage I), namely lower
progressive and total motility and a higher proportion of asthenozoospermia and teratozoospermia Tumor histology showed no influence on sperm parameters in individuals with TCa and elevated tumor markers were not associated with sperm abnormalities
TCa can have local adverse effects on spermatogenesis through local growth of the testicular tumor The occurrence of spermatogenesis defects is most prominent in the vicinity of malignant tumors (9), a trend not observed in benign tumors (10) Larger tumor size is correlated with lower levels of spermatogenesis in the ipsilateral testis (11) In fact, testicular tumors > 4 cm exhibit a significant decrease in spermatogenesis compared to tumors < 4 cm (12) TCa can also exert deleterious effects on sperm quality through secreted hormones Elevated serum levels of a-FP or b-hCG can disrupt the physiologic feedback mechanism of the hypothalamic-pituitary-gonadal (HPG) axis, which directly regulates testicular function, and hence spermatogenesis (13) Disruptions in the levels of luteinizing hormone (LH), follicle-stimulating hormone (FSH), and testosterone are associated with spermatogenesis and a reduction in sperm concentration (5) It has also been demonstrated that any kind of cancer, including TCa, may lead to worse sperm quality, with sperm parameters below the WHO reference values; causative factors have been hypothesized to be a rise in pro-inflammatory circulating cytokines and interleukins (14) Moreover, testicular cancer is associated with elevated oxidative stress and DNA fragmentation, both potentially contributing to decreased fertility (15, 16) Despite these detrimental effects of testicular tumor on sperm quality, orchiectomy does not result in improvement of spermatogenesis; instead, it further deteriorates sperm quality Petersen et al (17) demonstrated a reduction in sperm concentration, total sperm count and serum inhibin B levels in patients who underwent radical orchiectomy for TCa, as well as de novo azoospermia in 9% of patients
A more recent multicenter study evaluating pre and post orchiectomy semen samples concluded that sperm concentration significantly decreased after orchiectomy (18)
These studies highlight the importance of cryopreservation, which should ideally be done before orchiectomy, since there is currently no evidence that expedited radical orchiectomy translates into oncological benefit (19) Furthermore, in this setting we might find patients who are amenable to surgical testicular sperm extraction (TESE) at the time of orchiectomy (onco-TESE) (7)
Patients with TCa may be subject to additional treatments other than radical orchiectomy, and these treatments may further impair the fertility of these patients
Chemotherapy in TCa is dependent on platinum-based agents (cisplatin and carboplatin), which may be combined with other agents, such as bleomycin and etoposide (7) By penetrating the testis blood barrier and targeting a c t i v e l y d i v i d i n g c e l l s , c h e m o t h e r a p y s i g n i fi c a n t l y impairs spermatogenesis, resulting in oligozoospermia and azoospermia There is a well-established correlation between the failure to conceive and the cumulative dose of chemotherapy (20, 21) In a study of 1191 TCa survivors, higher doses of chemotherapy translated into a significant impairment of spermatogenesis, resulting in only 29% of patients being normozoospermic after 11
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12238 3 Semen parameters in testicular tumor
years of follow-up (22) There is potential for recovery of spermatogenesis, in a time-dependent manner, with 48% and 80% of patients with normal pretreatment sperm concentrations recovering spermatogenesis by 2 and 5 years, respectively (23) Radiation therapy is another modality for treatment of TCa It may be applied to retroperitoneal metastases, in which case the testes are exposed to scatter radiation only, generally at low doses which protect fertility, or directly to the testes, in case of germ cell neoplasia in situ; in the latter case, with radiation doses of 16-20 Gy frequently used, there are high rates of irreversible azoospermia (5) Finally, RPLND is another modality of additional treatment in TCa RPLND might cause retrograde ejaculation or anejaculation due to damage of lumbar plexus and splenic nerves, which renders the patients infertile Despite the very high rates of ejaculatory function preservation with modern nerve sparing techniques, fibrosis might still make this technique difficult, resulting in substantial rates of anejaculation (7) Our study concluded that patients with metastatic disease (stage II/III) have significantly worse semen parameters than patients with localized disease (stage I); these findings underscore the need for cryopreservation especially in metastatic patients, and a greater emphasis should be placed on cryopreservation in this subset of patients, given that treatment of these patients with one or more of these modalities of adjuvant treatment is generally the rule
Only a few studies have evaluated the potential role of histology and stage on sperm quality (8, 24, 25) Fraietta et al (24) reviewed the data of 100 patients with TCa and analyzed the patients’ sperm quality according to histologic type (seminoma vs NSGCT) and concluded that patients with seminoma had a higher number of motile and morphologically normal spermatozoids than those with NSGCT A more recent study by Badia et al (8) concluded that histology did not influence semen parameters, as these were similar between patients with seminoma and NSGCT This aligns with the results of our study, where we showcased that patients with distinct histology exhibited comparable semen parameters As for the role of stage, Halstuch et al (25) demonstrated that severe oligozoospermia (< 5 million/mL) was more common in metastatic than non-metastatic NSGCT The same conclusion could not be drawn for patients with seminoma Badia et al. (8) also evaluated the role of stage on semen parameters, and again concluded that semen parameters were similar in TCa patients with localized and metastatic disease These results are conflicting with the results of our study We did demonstrate differences between different stages, with metastatic disease showing less progressive and total motility and a higher proportion of asthenozoospermia and teratozoospermia, and this was demonstrated for patients with stage II/III irrespective of histology Rates of oligozoospermia were, however, similar between groups, despite a tendency towards less oligozoospermia in localized disease Moreover, despite the previously noted effect of secreted hormones, we did not demonstrate and association between elevated tumor markers and sperm abnormalities We hypothesize that it is the systemic inflammatory process of metastatic testicular cancer, rather than the hormonal burden of elevated
tumor markers, that might be responsible for a detrimental effect on spermatogenesis
Semen cryopreservation should be discussed and offered to all patients with TCa, ideally before orchiectomy to maximize chances of fertility, and if not done before orchiectomy should be pursued prior to chemotherapy or radiation therapy (26) Despite these recommendations, only 24-30% of TCa patients undergo sperm cryopreservation (24, 27-29) In our study, 64 patients (52%) out of 123 patients diagnosed with TCa underwent semen cryopreservation before orchiectomy, with an additional 12 (10%) patients undergoing semen cryopreservation after orchiectomy and before adjuvant treatments, which translated into a total sperm cryopreservation rate of 62% The timing of cryopreservation is of importance, as noted by the work of Rives et al (18), in which they demonstrated that mean sperm concentration before orchiectomy was significantly higher than after surgery (32x106/mL vs 24x106/mL) Moreover, as previously noted, semen cryopreservation before orchiectomy has the potential for selection of patients for onco-TESE, which is another advantage (7) It is also worth noting that despite advancements in ART in the last years, sperm cryopreservation remains the most cost-effective strategy for fertility preservation (30) Therefore, it is the authors’ opinion that semen cryopreservation should be offered in every patient with TCa, if possible before orchiectomy, and in light of the results of our study a heightened emphasis should be placed on patients with metastatic disease, as these display overall worse sperm quality and will most probably be subject to additional treatments
Our study has several limitations that deserve acknowledgment The main shortcomings come from its retrospective nature We could only analyze the information on the medical records, and as a consequence the success rate of pregnancies from cryopreserved sperm samples could not be evaluated Furthermore, we used decreased semen parameters as a surrogate for decreased fertility, even though a direct relationship between the two hasn’t been established Additionally, despite our institution being a high-volume referral center for TCa, the relatively short sample size of 64 patients may limit statistical power In that sense, further studies, preferably prospective and multicenter, are needed in the future to support our findings
CONCLUSIONS
Testicular cancer has the potential for infertility Patients with metastatic testicular cancer (stage II/III) have worse sperm quality, namely less progressive and total motility of spermatozoids and a bigger proportion of asthenozoospermia and teratozoospermia than patients with localized testicular cancer (stage I) Histology appears to play no major role in sperm quality and elevated tumor markers were not shown to be associated with sperm abnormalities Sperm cryopreservation should be offered to all patients with testicular cancer, ideally before orchiectomy, and this should be further emphasized in patients with metastatic disease Further studies are recommended to validate these findings
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12238
4
G Mendes, B Teixeira, M Madanelo, et al
REFERENCES
1 Park JS, Kim J, Elghiaty A, Ham WS Recent global trends in testicular cancer incidence and mortality Medicine 2018; 97:e12390
2 Nigam M, Aschebrook-Kilfoy B, Shikanov S, Eggener S Increasing incidence of testicular cancer in the United States and Europe between 1992 and 2009 World J Urol 2015; 33:623-31
3 Gurney JK, Florio AA, Znaor A, et al International Trends in the Incidence of Testicular Cancer: Lessons from 35 Years and 41 Countries Eur Urol 2019; 76:615-23
4 Djaladat H, Burner E, Parikh PM, et al The Association Between Testis Cancer and Semen Abnormalities Before Orchiectomy: A Systematic Review J Adolesc Young Adult Oncol 2014; 3:153-9
5 Parekh N V, Lundy SD, Vij SC Fertility considerations in men with testicular cancer Transl Androl Urol 2020; 9(Suppl 1):S14-23
6 Cooper TG, Noonan E, von Eckardstein S, et al World Health Organization reference values for human semen characteristics Hum Reprod Update 2010; 16:231-45
7 Moody JA, Ahmed K, Yap T, et al Fertility managment in testicular cancer: the need to establish a standardized and evidence-based patient-centric pathway BJU Int 2019; 123:160-72
8 Badia RR, Patel A, Chertack N, et al Impact of testicular cancer stage on semen parameters in patients before orchiectomy Urol Oncol 2023; 41:151 e11-151 e15
9 Ho GT, Gardner H, DeWolf WC, et al Influence of testicular carcinoma on ipsilateral spermatogenesis J Urol 1992; 148:821-5
10 Ho GT, Gardner H, Mostofi K, et al The effect of testicular nongerm cell tumors on local spermatogenesis Fertil Steril 1994; 62:162-6
11 Choy JT, Wiser HJ, Bell SW, et al Predictors of spermatogenesis in orchiectomy specimens Urology 2013; 81:288-92
12 Shoshany O, Shtabholtz Y, Schreter E, et al Predictors of spermatogenesis in radical orchiectomy specimen and potential implications for patients with testicular cancer Fertil Steril 2016; 106:70-4
13 Coward RM, Kovac JR, Smith RP, Lipshultz LI Fertility Preservation in Young Men Treated for Malignancies: Options for Precancer Treatment Sex Med Rev 2013; 1:123-34
14 Peluso G, Tisato V, Singh AV, et al Semen Cryopreservation to Expand Male Fertility in Cancer Patients: Intracase Evaluation of Semen Quality J Pers Med 2023; 13:1654
15 Said TM, Tellez S, Evenson DP, Del Valle AP Assessment of sperm quality, DNA integrity and cryopreservation protocols in men diagnosed with testicular and systemic malignancies Andrologia 2009; 41:377-82
16 Kumar K, Lewis S, Vinci S, et al Evaluation of sperm DNA quality in men presenting with testicular cancer and lymphoma using alkaline and neutral Comet assays Andrology 2018; 6:230-5
17 Petersen PM, Skakkebaek NE, Rørth M, Giwercman A Semen quality and reproductive hormones before and after orchiectomy in men with testicular cancer J Urol 1999; 161:822-6
18 Rives N, Perdrix A, Hennebicq S, et al The semen quality of 1158 men with testicular cancer at the time of cryopreservation: results of the French National CECOS Network J Androl 2012; 33:1394-401
19 Emmanuel A, Kanthabalan A, Alexander C, et al Expedited Radical Orchidectomy for Testicular Cancer: Compromising Fertility Outcomes Without Oncological Benefit? Eur Urol 2021; 80:766-7
20 Puscheck E, Philip PA, Jeyendran RS Male fertility preservation and cancer treatment Cancer Treat Rev 2004; 30:173-80
21 Brydøy M, Fosså SD, Klepp O, et al Paternity following treatment for testicular cancer J Natl Cancer Inst 2005; 97:1580-8
22 Brydøy M, Fosså SD, Klepp O, et al Sperm counts and endocrinological markers of spermatogenesis in long-term survivors of testicular cancer Br J Cancer 2012; 107:1833-9
23 Lampe H, Horwich A, Norman A, et al Fertility after chemotherapy for testicular germ cell cancers J Clin Oncol 1997; 15:239-45
24 Fraietta R, Spaine DM, Bertolla RP, et al Individual and seminal characteristics of patients with testicular germ cell tumors Fertil Steril 2010; 94:2107-12
25 Halstuch D, Shtabholtz Y, Neufeld S, et al The absence of spermatogenesis in radical orchiectomy specimen is associated with advanced-stage nonseminomatous testicular cancer Urol Oncol 2021; 39:838 e15-838 e20
26 Patrikidou A, Cazzaniga W, Berney D, et al European Association of Urology Guidelines on Testicular Cancer: 2023 Update Eur Urol 2023; 84:289-301
27 Ping P, Gu BH, Li P, et al Fertility outcome of patients with testicular tumor: before and after treatment Asian J Androl 2014; 16:107-11
28 Sonnenburg DW, Brames MJ, Case-Eads S, Einhorn LH Utilization of sperm banking and barriers to its use in testicular cancer patients Support Care Cancer 2015; 23:2763-8
29 Magelssen H, Haugen TB, von Düring V, et al Twenty years experience with semen cryopreservation in testicular cancer patients: who needs it? Eur Urol 2005; 48:779-85
30 Gilbert K, Nangia AK, Dupree JM, et al Fertility preservation for men with testicular cancer: Is sperm cryopreservation cost effective in the era of assisted reproductive technology? Urol Oncol 2018; 36:92 e1-92 e9
Correspondence
Gonçalo Mendes, MD (Corresponding Author) goncalo grilomendes@gmail com Bernardo Teixeira, MD bernardolat@gmail com
Mariana Madanelo, MD marianacmadanelo@gmail com
Alexandra Rocha, MD marialexandrarocha@gmail com
Sofia Mesquita, MD sofiaoplmesquita@gmail com Miguel Monteiro, MD mmonteiro iam@gmail com
Avelino Fraga, MD avfraga@gmail com
Nuno Louro, MD nunorlouro@gmail com
Department of Urology, Santo António University Hospital Center, Porto, Portugal
João Vital, MD joaopvital@gmail com
Department of Urology, Hospital of Funchal, Funchal, Portugal
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12238 5 Semen parameters in testicular tumor
ORIGINAL PAPER
Psychological and sexological assessment of patients with chronic prostatitis
Konstantinos Stamatiou 1 , Vittorio Magri 2 , Margherita Trinchieri 3 , Alberto Trinchieri 4 , Gianpaolo Perletti 5 on behalf of Mediterranean study group for prostatitis and prostatic diseases
1 Department of Urology, Tzaneio Hospital, Pireus, Greece;
2 Urology Unit, ASST Fatebenefratelli Sacco, Milan, Italy;
3 Psichiatry Unit, ASST Rhodense, G Salvini Hospital, Garbagnate (Milan), Italy;
4 School of Urology, University of Milan, Milan, Italy;
5 Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy
Summary
Purpose: Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is characterized by a multiform clinical presentation requiring a differentiated treatment based on different phenotypes including the psychosocial and sexual domains The aim of this study was assessing the complex correlations between somatic, psychological, and sexual symptoms of CP/CPPS patients
Materials and methods: We performed a cross-sectional study on patients attending a Prostatitis Clinic Patients were administered the following questionnaires: National Institutes of HealthChronic Prostatitis Symptom Index (NIH-CPSI), International Prostate Symptom Score (IPSS), International Index of Erectile Function (IIEF), Premature Ejaculation Diagnostic Tool (PEDT), Patient Health Questionnaire-9 (PHQ-9), Generalized Anxiety Disorder 7-item (GAD-7), Oxford Happiness Questionnaire (OHQ), and Temperament Evaluation of Memphis, Pisa, Paris and San Diego Autoquestionnaire (TEMPS-A)
Results: Linear regression analyses show highly significant correlations between scores of the NIH-CPSI and the scores of the GAD-7, PHQ-9 and OHQ psychometric questionnaires IPSS scores correlate significantly with the psychometric scores only when a non-parametric analysis is performed IIEF and PEDT sexual function scores did not correlate with any of the psychometric tests NIH-CPSI scores correlate positively with most of the TEMPS-A profiles but the hyperthymic profile correlated negatively with the total and QoL NIH-CPSI and with PEDT scores.
Conclusions: Scores measuring anxiety, depression, and psychological well-being in patients with CP/CPPS are strictly correlated with prostatitis-like symptoms although they are poorly correlated with symptoms of prostatism, as measured by IPSS, and not correlated with scores of sexual dysfunctions, as measured by IIEF and PEDT. A hyperthymic temperament may temperament may increase resilience against the disease
KEY WORDS: Chronic prostatitis; chronic pelvic pain syndrome; Depression; Anxiety; Affective temperaments
Submitted 3 March 2024; Accepted 7 march 2024
INTRODUCTION
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is a common clinical condition presenting with a variety of signs and symptoms including chronic pain, voiding
symptoms, sexual and psychosocial disturbances (1)
The importance of recognizing the psychological impact of CP/CPPS has been taken into primary consideration by the UPOINT phenotyping and therapeutic algorithm (2), which rates a specific “Psychosocial” domain in the frame of the work-up of chronic prostatitis (CP) patients It is suggested to use self-administered questionnaires to assess depression and anxiety and to measure negative thoughts associated with pain
The implementation of the UPOINT system with the evaluation of a sexual domain (“S”) has further extended the evaluation of patients with CP/CPPS who frequently present with significant rates of erectile and orgasmic dysfunction (3)
The aim of this study was an in-depth assessment of the complex correlations between somatic, psychological, and sexual disorders in CP/CPPS patients
METHODS
Study design and endpoints
We performed a cross-sectional study on a cohort of patients with CP-CP/CPPS, consecutively enrolled among patients attending two outpatient clinics The study was ethically approved by the local Ethics Committee of Tzaneio Hospital (protocol 8295/05-05-2022) and complied with the requirements of the Helsinki declaration
The primary endpoint of the study was the association between the total and subdomain scores (pain, voiding symptoms, quality of life) of the National Institute of Health-Chronic Prostatitis Symptom Index (NIH-CPSI) (4), and the total score of the Patient Health Questionnaire-9 (PHQ-9), a self-administered tool focusing on the presence and severity of depression (5)
Secondary endpoints of the study included the assessment of an association between the scores (i) of the NIH-CPSI questionnaire, (ii) of the International Prostate Symptom Score (IPSS) (6), (iii) of the erectile function domain of the International Index of Erectile Function (IIEF) (7), and (iv) of the Premature Ejaculation Diagnostic Tool (PEDT) (8) (independent variables), and the scores of the following psychosocial tests: (i) the PHQ-9 questionnaire (5), (ii) the
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12452 1
DOI: 10 4081/aiua 2024 12452
Generalized Anxiety Disorder 7-item questionnaire (GAD-7) (9), (iii) the Oxford Happiness Questionnaire (OHQ) (10), and (iv) the Temperament Evaluation of Memphis, Pisa, Paris and San Diego Autoquestionnaire (TEMPS-A, 39-item short version), which includes 5 domains, focusing on the presence of cyclotimic, depressive, irritable, hyperactive and anxious personalities (11)
Patient selection criteria
We included adult patients (>/= 18 years) who agreed to participate in the study, referring for long-standing (at least 18 months) documented signs and symptoms of category II CP or category III CP/CPPS assessed according to NIH criteria (12) after a thorough work up including clinical and laboratory assessments
Exclusion criteria were: signs and symptoms present for a period shorter than 6 months; recent (< 8 weeks) category I acute bacterial prostatitis; neoplasia, indwelling catheters; nephrostomy; any chronic and/or painful and/or disabling illness significantly affecting the quality of life, potentially generating anxiety or depression; recent events (< 3 months) that may have had a considerable impact on the psychological profile of patients, possibly acting as confounders in this study (e g , the loss of a child or spouse, divorce, loss of a job, other traumatic events)
Data collection
At referral, patients were informed about the aim of the study and reassured about the anonymous handling of their data After signing an informed consent, patients underwent a thorough urological examination after being interviewed about their clinical history Patients were also asked to fill the questionnaires listed above
Questionnaires were collected by the consulting urologist and uploaded in a study database Personal data were rendered anonymous in such a manner that patients were no longer identifiable in the database Data were analyzed by a member of the research group (GP) in a blinded fashion
Statistical analysis
Median and interquartile range (IQR) or mean and standard deviation were used as measures of the central tendency and data dispersion of non-continuous and continuous variables, respectively
Simple linear regression
Simple linear regression was performed to analyze the significance of associations between baseline scores of the NIH-CPSI, IPSS, IIEF (short version) and PEDT questionnaires (independent variables), and the scores of the PHQ9, GAD-7, OHQ and TEMPS-A (39-item short version) questionnaires (dependent variables in the present prediction model)
Both nonparametric (Kendall’s rank coefficient ‘tau’) and parametric (Pearson’s product-moment ‘rho’) correlation coefficients were calculated, to take into account the existence of non-linear relationships between the bivariates
Sample size calculation
To estimate the effect size for sample size calculation, we referred to the Koh et al (13) trial, reporting a significant correlation between the NIH-CPSI and PHQ-9 scores (p
= 0 009), resulting in a Spearman’s coefficient (r) equal to 0 307 Sample size calculations was performed using the G*Power 3 1 3 software (14) We computed that a sample of 127 patients was required to analyze by simple linear regression (one predictor) the primary endpoint of the study, namely, the correlation between the NIH-CPSI total score and the PHQ-9 depression score, with 95% power, a 5% alpha error probability, a f^2 effect size of 0 104 and a f^2 coefficient equal to 0 0942
Logistic regression analysis
Simple binary logistic regression analysis was performed to ascertain the goodness of fit of models whereby the increasing symptom scores of tests (e g , the NIH-CPSI) showing significant linear correlation with psychometric scores, would be significant predictor of dichotomized psychometric outcomes (e g , no depression vs moderate-to-severe depression)
The null hypothesis for the logistic regression was the absence of an association between the symptom score predictor and the psychologic condition dichotomic outcome
The coefficients of the logistic functions, the intercepts, the odds ratios, and the confidence intervals related to the odds ratios (95%CI) were calculated The statistical significance of the model was evaluated by means of the Wald test and the likelihood ratio test
The Hosmer/Lemeshow test was performed to evaluate the goodness-of-fit of the models, and the NagelkerkeR^2 value was be calculated For the Hosmer and Lemeshow test, the null hypothesis was that the number of expected dichotomic psychological disturbances –when the entire patient cohort is divided into 10 groups of approximately similar size – is not significantly different from the same outcomes observed in the overall logistic model Values > 0 05 of the probability associated with the zero hypothesis indicated an acceptable goodness-of-fit
For statistical analysis only two-tailed tests were performed, 95% confidence intervals were calculated, and the conditional probability of a type I error, in the presence of a true null hypothesis, was set at < 0 05
Statistical softwares
Statistical analysis of linear and logistic regressions was carried out in the “R” software environment for statistical computing and graphics (https://www r-project org/) Logistic regression analysis was performed using the car and lmtest packages
The Hosmer and Lemeshow goodness-of-fit test was performed with the Resource Selection package, whereas the Nagelkerke pseudo (y)-R2 was calculated using the rcompanion package Odds ratios and 95% CIs for the model were calculated using the epiDisplay package Intergroup differences between questionnaire scores were analyzed with the two-tailed Mann-Whitney-Wilcoxon test, using the R platform
RESULTS
One hundred and forty-one consecutive patients were prospectively enrolled for the study between January 1st and November 30th, 2022 The median age of patients
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12452
2
K Stamatiou, V Magri , M Trinchieri, et al
Table 1.
Test
NIH-CPSI (total)
NIH-CPSI (pain domain) 99 NIH-CPSI (voiding domain) 34
(QoL impact domain) 65
Anxious
NIH-CPSI: Nat onal Inst tutes of Health Chron c Prostat tis Symptom Score (QoL, impact of the d sease on the qual ty of l fe)
IPSS: Internat onal Prostate Symptom Score
IIEF (1-5,15), Short Internationa Index of Erecti e Function (sum of questions 1, 2, 3, 4, 5, 15)
PEDT: Premature E aculation D agnostic Tool
GAD-7: Genera Anxiety Disorder-7
PHQ-9, Pat ent Health Questionnaire-9
TEMPS-A: Temperament Eva uation of Memphis, Pisa, Par s and San D ego - Auto-quest onnaire version
was 48 (IQR, 18) The median year of first diagnosis of CP was 2018
Baseline clinical and psychological symptoms are shown in Table 1
Linear regression
Table 2 shows the results of linear regression analyses comparing the scores of the NIH-CPSI, IPSS, IIEF and PEDT questionnaires with the GAD-7, PHQ-9 and Oxford questionnaires
The results show highly significant correlations between all domains (pain, voiding, quality of life impact and total
Table 2
scores) of the NIH-CPSI test and the scores of the GAD7, PHQ-9 and Oxford psychometric questionnaires
Conversely, the IPSS, IIEF and PEDT tests correlate poorly and, in most cases, not significantly with any of the psychometric tests, except for IPSS, whose scores correlate significantly with the scores of the GAD-7, PHQ-9 and Oxford tests only when a non-parametric analysis is performed (The Kendall’s Tau)
Temperament profiling
Table 3 shows the results of linear regression analyses comparing the scores of the NIH-CPSI, IPSS, IIEF and PEDT questionnaires with the scores of basic patient temperament profile, measured with the TEMPS-A test
Highly significant correlations were found between NIHCPSI scores (total score and pain, voiding and QoL subscores) with most of the TEMPS-A profiles An exception was the hyperthymic profile, which correlated significantly and negatively with the total and QoL NIH-CPSI scores In other words, a less severe impact of prostatitis on total and QoL NIH-CPSI correlated with higher hyperthymic scores
Conversely, the IPSS, IIEF and PEDT tests correlate poorly and in almost all cases not significantly with any of the TEMPS-A profile scores Exceptions were the significant correlation of the IPSS scores with the TEMPS-A depressive profile and the significant negative correlation of PEDT scores with the hyperthymic TEMPS-A profile
Logistic regression models
We tested the NIH-CPSI and the IPSS interval scores as predictors versus dichotomized outcomes of the GAD-7, PHQ-9 and Oxford happiness scores
Dichotomization was as follows: for the GAD-7 test, a score equal or higher than 5 predicted mild to severe anxiety according to Spitzer et al (2006) (9); for the PHQ-9 test a score equal or higher than 10 predicted moderate to severe depression according to Kroenke et al (2001) (5), and for the Oxford happiness test a score equal to 3 5 was the cutoff to discriminate between happy or unhappy responses (Hills & Argyle, 2002)(15)
Psychological profiling of chronic prostatitis patients included in our study according to the GAD-7, PHQ-9 and Oxford Happiness questionnaires. Scores are analyzed by linear regression against the total or subdomain scores of the NIH CPSI, IPSS, IIEF and PEDT tests Correlation coefficients are shown Statistically significant differences are shown in bold
NIH-CPSI: Nat onal Inst tutes of Health Chron c Prostatitis Symptom Score
IPSS: International Prostate Symptom Score
I EF (1-5,15): Short Internationa Index of Erecti e Function (sum of questions 1, 2, 3, 4, 5, 15)
PEDT: Premature E aculation D agnostic Too
GAD-7: Genera Anxiety Disorder-7
PHQ-9, Pat ent Hea th Questionnaire-9
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12452 3 Psychosexologic assessment in prostatitis
Baseline scores of clinical symptom tests and psychological questionnaires
Median score Interquar tile range
16
18
IPSS
IIEF 26 8 5 PEDT 4 5 5 GAD-7 7 7 25 PHQ-9 65 Mean score Standard deviation TEMPS-A Cyclothymic 0 38 0 29 TEMPS-A Depressive 0 32 0 30 TEMPS-A Irritable 0 21 0 24 TEMPS-A Hyperthymi 0
0 28
NIH-CPSI
79
53
TEMPS-A
0 33 0 38 Oxford Happiness 3 68 0 54
NIH-CPSI, Total Score NIH-CPSI, Pain domain NIH-CPSI, Voiding domain NIH-CPSI, QoL domain Kendall’s Tau (P) Pearson's r (P) Kendall’s Tau (P) Pearson's r (P) Kendal ’s Tau (P) Pearson's r (P) Kendall’s Tau (P) Pearson's r (P) GAD-7 0 285 (< 0 0001) 0 413 (< 0 0001) 0 316 (< 0 0001) 0 439 (< 0 0001) 0 188 (0 0023) 0 271 (0 0011) 0 283 (< 0 0001) 0 407 (< 0 0001) PHQ-9 0.365 (< 0.0001) 0.464 (< 0.0001) 0.392 (< 0.0001) 0.475 (< 0.0001) 0.218 (0.0004) 0.290 (0.0004) 0.375 (< 0.0001) 0.469 (< 0.0001) Oxford Happiness Score -0.230 (0.002) -0.335 (0.001) -0.229 (0.002) -0.335 (0.001) -0 1 (0 20) -0.21 (0.043) -0.21 (0.005) -0.288 (0.006) IPSS IIEF (1-5,15) PEDT GAD-7 0 170 (0 026) 0 191 (0 075) -0 129 (0 094) -0 119 (0 27) 0 09 (0 25) 0 179 (0 096) PHQ-9 0 198 (0 009) 0 267 (0 012) -0 077 (0 32) -0 052 (0 63) 0 085 (0 27) 0 114 (0 29) Oxford Happiness Score -0 168 (0 024) -0 17 (0 102) 0 138 (0 067) 0 189 (0 078) -0 097 (0 20) -0 131 (0 22)
Table 3.
Temperament profiling of chronic prostatitis patients included in our study according to the Temperament Evaluation of Memphis, Pisa, Paris and San Diego auto-questionnaire (TEMPS-A) TEMPS-A scores are analyzed by linear regression against the total or subdomain scores of the NIH CPSI, IPSS, IIEF and PEDT tests Statistically significant differences are shown in bold
NIH-CPSI,
N H-CPSI: Nationa Institutes of Hea th Chronic Prostatit s Symptom Score
IPSS: Internationa Prostate Symptom Score
IIEF (1-5,15): Short Internat onal Index of Erectile Funct on (sum of quest ons 1, 2, 3, 4, 5, 15)
PEDT: Premature Ejacu ation Diagnost c Tool
TEMPS-A: Temperament Evaluat on of Memph s, P sa, Paris and San Diego - Auto-questionnaire version
Bivariate analysis comparing all NIH-CPSI scores (pain, micturition, impact on QoL and total scores) with GAD-7 PHQ-9 and Oxford Happiness resulted in significant prediction models (Table 4) The only exception was the model comparing the voiding NIH-CPSI domain with the Oxford test of happiness
Analysis of the predictor significance and goodness-of-fit of all models showed statistical significance in all cases, apart from the comparison of the voiding NIH-CPSI domain with the Oxford test of happiness (Table 5)
Conversely, logistic regression models comparing IPSS
Table 4.
predictor scores against dichotomized anxiety (GAD-7), depression (PHQ-9) or happiness (Oxford) outcomes were found to be not statistically significant (Table 4) This was confirmed by the predictor significance and goodness-of-fit parameters shown in Table 5
Severity of CP symptoms in patients showing various degrees of happiness, depression and anxiety
We investigated whether any significant difference could be observed by dichotomizing our population into two cohorts Cohorts included patients with moderate/severe
Logistic regression models for Generalized Anxiety Disorder (GAD-7 test), depression (PHQ-9 test), or degree of happiness (Oxford test) as function of the score of the NIH-CPSI test (total score and pain, voiding symptoms and impact on the quality of life subdomains) and of the IPSS test Significant results are shown in bold
Psychometric test
(outcome)
Model
NIH-CPSI: National Institutes of Health Chronic Prostatit s Symptom Score (QoL, impact of the disease on the quality of ife of patients)
IPSS: Internationa Prostate Symptom Score
IIEF (1-5,15): Short International Index of Erectile Funct on (sum of questions 1, 2, 3, 4, 5, 15)
GAD-7: General Anx ety D sorder-7
PHQ-9: Patient Health Questionna re-9
SE: Standard Error
96% CI: 95% Confidence Interva
EL50: median effective eve , e , symptom score associated w th 50% probab lity of the psychometric test outcome
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12452
4
K Stamatiou, V Magri , M Trinchieri, et al
Total NIH-CPSI, Pain domain NIH-CPSI, Voiding domain NIH-CPSI, QoL domain Kendall’s Tau (P) Pearson's r (P) Kenda l’s Tau (P) Pearson's r (P) Kendall’s Tau (P) Pearson's r (P) Kendall’s Tau (P) Pearson's r (P) TEMPS-A Cyclothymic 0 411 (< 0 0001) 0 590 (< 0 0001) 0 433 (< 0 0001) 0 612 (< 0 0001) 0 206 (0 0009) 0 344 (< 0 0001) 0 369 (< 0 0001) 0 512 (< 0 0001) Depressive 0.367 (< 0.0001) 0.503 (< 0.0001) 0.362 (< 0.0001) 0.479 (< 0.0001) 0.257 (< 0.0001) 0.361 (< 0.0001) 0.355 (< 0.0001) 0.468 (< 0.0001) Irritable 0.366 (< 0.0001) 0.485 (< 0.0001) 0.402 (< 0.0001) 0.512 (< 0.0001) 0.216 (0.001) 0.296 (0.0003) 0.310 (< 0.0001) 0.390 (< 0.0001) Hyperthymic -0 115 (0 058) -0.172 (0.042) -0 944 (0 127) -0 132 (0 12) -0 051 (0 42) -0 075 (0 37) -0.132 (0.03) -0.186 (0.02) Anxious 0 288 (< 0 0001) 0 393 (< 0 0001) 0 326 (< 0 0001) 0 421 (< 0 0001) 0 184 (0 006) 0 237 (0 004) 0 222 (0 0008) 0 302 (0 0002) IPSS IIEF (1-5,15) PEDT Cyclothymic 0 126 (0 11) 0 147 (0 17) -0 10 (0 20) -0 166 (0 12) -0 026 (0 74) 0 044 (0 68) Depressive 0 233 (0 004) 0 294 (0 005) -0 06 (0 45) -0 006 (0 94) 0 076 (0 36) 0 126 (0 24) Irritable 0 11 (0 24) 0 049 (0 65) 0 116 (0 18) 0 123 (0 25) -0 032 (0 71) -0 06 (0 55) Hyperthymic -0 051 (0 51) -0 84 (0 44) 0 143 (0 071) 0 20 (0 059) -0.199 (0.012) -0.263 (0.013) Anxious 0 067 (0 43) 0 11 (0 31) -0 15 (0 078) -0,138 (0 19) -0 0042 (0 96) -0 0065 (0 95)
Logistic
Prostatitis/Prostate Symptom Scores (predictor)
Parameters NIH-CPSI, Total Score NIH-CPSI, Pain domain NIH-CPSI, Voiding domain NIH-CPSI, QoL domain IPSS GAD-7 Intercept ± SE -0 356 ± 0 37 -0 435 ± 0 31 0 285 ± 0 29 -0 56 ± 0 39 0 101 ± 0 37 Corfficient ± SE (P) 0 073 ± 0 020 (0 0003) 0 142 ± 0 034 (< 0 0001) 0 141 ± 0 07 (0 05) 0 220 ± 0 059 (0 0002) 0 045 ± 0 033 (0 183) Odds Ratio (96% CI) 1.08 (1.03-1.12) 1.15 (1.08-1.23) 1.15 (1-1.33) 1.25 (1.11-1.4) 1 05 (0 98-1 12) EL50 4 88 3 07 2 03 2 58 2 23 PHQ-9 Intercept ± SE -2 93 ± 0 54 -2 717 ± 0 49 -1 96 ± 0 36 -2 79 ± 0 57 -1 131 ± 0 39 Corfficient ± SE (P) 0 093 ± 0 021 (< 0 0001) 0 159 ± 0 030 (< 0 0001) 0 218 ± 0 072 (0 002) 0 227 ± 0 067 (0 0007) 0 014 ± 0 033 (0 668) Odds Ratio (96% CI) 1 1 (1 05-1 15) 1 17 (1 09-1 27) 1 24 (1 08-1 43) 1 26 (1 1-1 43) 1 01 (0 95 to 1 08) EL50 31 65 17 06 8 99 12 31 78 21 Oxford Happiness Score Intercept ± SE 2 09 ± 0 52 2 29 ± 0 51 1 51 ± 0 42 1 92 ± 0 52 1 741 ± 0 51 Corfficient ± SE (P) -0.075 ± 0.026 (0.0038) -0.155 ± 0.05 (0.0023) -0 201 ± 0 11 (0 072) -0.177 ± 0.074 (0.014) -0 999 ± 0 051 (0 051) Odds Ratio (96% CI) 0.93 (0.88-0.98) 0.86 (0.77-0.95) 0 82 (0 66-1 02) 0.84 (0.73-0.97) 0 9 (0 82-1) EL50 27 76 14 74 7 51 10 85 17 42
Table 5
Predictor significance and goodness-of-fit parameters of the logistic regression models shown in Table 3
Psychometric test Test
Symptom Scores (predictor) (outcome)
NIH-CPSI: Nat onal Inst tutes of Health Chron c Prostat tis Symptom Score (QoL, impact of the d sease on the qual ty of l fe of patients)
IPSS: Internat onal Prostate Symptom Score
IIEF (1-5,15): Short Internationa Index of Erecti e Function (sum of questions 1, 2, 3, 4, 5, 15)
GAD-7: Genera Anxiety Disorder-7
PHQ-9: Pat ent Health Questionnaire-9
SE: Standard Error
96% CI: 95% Confidence Interval
P: stat st cal probabi ity of an alpha error
EL50: med an effective evel, i e , symptom score assoc ated with 50% probabil ty of the psychometr c test outcome n a : not avai able
versus absent or very mild anxiety or depression The Oxford score was also used to distinguish patients showing a happiness versus little or no happiness Dichotomization thresholds are indicated in the previous paragraph Table 6 shows that the pain, quality of life impact, and total scores of the NIH-CPSI test are significantly higher in patients with moderate to severe depression or anxiety and in patients with a poor Oxford happiness score A significantly higher NIH-CPSI voiding score was related to moderate to severe depression, but no difference was observed between patients with or without symptoms of anxiety and between patients reporting or not psychological well-being
Table 6.
The IPSS score was significantly higher in patients showing a poor Oxford happiness score
DISCUSSION
The bidirectional relationship between psychological disturbances and prostatitis is complex, with several factors interacting or interfering with each other (16) Our findings can be divided into two sections, the first evaluating correlations between measures of anxiety, depression, and psychological well-being and the scores of symptoms associated with CP/CPPS as measured with NIH-CPSI and questionnaires evaluating sexual function (IIEF or
Severity of CP symptoms in patients showing various degrees of happiness, depression and anxiety Statistically significant differences are shown in bold
PEDT: Premature Ejaculat on Diagnostic Too
GAD-7: General Anx ety Disorder-7
PHQ-9, Patient Hea th Quest onnaire-9
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12452 5 Psychosexologic assessment in prostatitis
NIH-CPSI, Total Score NIH-CPSI, Pain domain NIH-CPSI, Voiding domain NIH-CPSI, QoL domain IPSS GAD-7 Wald c2 = 12 86, P = 0 00035 c2 = 17 11, P < 0 0001 c2 = 3 75, P = 0 05 c2 = 13 63, P = 0 00022 ��2 = 1 77, P = 0 18 Likelihood Ratio c2 = 14 91, P = 0 0001 c2 = 20 16, P < 0 0001 c2 = 4 06, P = 0 043 c2 = 15 50, P < 0 0001 ��2 = 1 87, P = 0 17 Hosmer & Lemeshow ��2 = 19 24, P = 0 013 ��2 = 4 22, P = 0 83 ��2 = n a ��2 = 1 62, P = 0 99 ��2 = 35 93, P < 0 0001 Nagelkerke ��R2 = 0 364 ��R2 = 0 652 ��R2 = 0 318 ��R2 = 0 701 ��R2 = 0 078 PHQ-9 Wald c2 = 17.76, P < 0.0001 c2 = 16,49, P < 0.0001 c2 = 9.20, P = 0.0024 c2 = 11.38, P = 0.00074 ��2 0 18, P 0 67 Likelihood Ratio c2 = 21.93, P < 0.0001 c2 = 20.02, P < 0.0001 c2 = 9.54, P = 0.002 c2 = 13.20, P = 0.00027 ��2 0 18, P 0 67 Hosmer & Lemeshow ��2 = 5 87, P = 0 661 ��2 = 1 66, P = 0 98 ��2 = 0 85, P = 0 99 ��2 = 1 87, P = 0 98 ��2 = 5 01, P = 0 75 Nagelkerke ��R2 = 0 469 ��R2 = 0 648 ��R2 = 0 591 ��R2 = 0 645 ��R2 = 0 0081 Oxford Happiness Score Wald c2 = 8 36, P = 0 038 c2 = 9 27, P = 0 023 ��2 = 3 21, P = 0 072 c2 = 5 99, P = 0 014 ��2 = 3 80, P = 0 051 Likelihood Ratio c2 = 9 34, P = 0 022 c2 = 10 73, P = 0 0011 ��2 = 3 28, P = 0 069 c2 = 6 50, P = 0 011 c2 = 3 91, P = 0 047 Hosmer & Lemeshow ��2 = 6 83, P = 0 55 ��2 = 6 94, P = 0 54 ��2 = 3 22, P = 0 919 ��2 = 0 83, P = 0 999 ��2 = 7 77, P = 0 45 Nagelkerke ��R2 0 293 ��R2 0 485 ��R2 0 315 ��R2 0 412 ��R2 0 201
Prostatitis/Prostate
GAD-7 0-4 GAD-7 5-21 P PHQ-9 1-9 PHQ-9 10-27 P Oxford Oxford P median (IQR) median (IQR) (Mann-Whitney) median (IQR) median (IQR) (Mann-Whitney) happiness >3 5 happiness </=3 5 (Mann-Whitney) median (IQR) median (IQR) NIH-CPSI Total score 15 (14) 21 (19) 0.0003 18 (14) 28 (15) 0.0002 12 (15) 19 (9) 0.0074 NIH-CPSI Pain score 7 (9) 11(9) 0.0002 8 (8) 13 (9 5) < 0.0001 4 5 (10) 10 (5) 0.0083 NIH-CPSI Voiding score 2 (3) 3 (3 5) 0 073 2 (4) 4 (5) 0 0024 2 (3) 3 (3) 0 21 NIH-CPSI Quality of life impact score 5 (5) 7 (6) 0 0003 6 (4) 10 (5) 0 0005 5 (6) 7 (3) 0 025 IPSS score 6 (10) 8 (8) 0 27 7 (8 75) 8 (10) 0 15 6 (9) 8 (10) 0.048 IIEF score 27 (4 5) 25 (10) 0 123 25 5 (9) 26 (8) 0 88 26 (6 75 27 (14) 0 41 PEDT score 4 (4 75) 5 (6) 0 37 4 (5 5) 2 5 (6 25) 0 34 4 (5) 4 (5) 0 63
IIEF
ons 1, 2, 3, 4, 5, 15)
NIH-CPSI: Nationa nstitutes of Hea th Chronic Prostatitis Symptom Score IPSS: International Prostate Symptom Score
(1-5,15): Short Internat onal Index of Erect le Function (sum of quest
K Stamatiou, V Magri , M Trinchieri, et al
PDT), the second studying the correlation of CP/CPPS symptom intensity and different personality traits
Among patients with CP/CPPS, a higher rate of psychiatric disorders as diagnosed by a psychiatrist using a semi-structured interview was previously observed (17)
The higher rate of patients with CP/CPPS on psychiatric drugs can also be considered a reliable measure of the association between an existing substrate of psychiatric conditions and the subsequent onset of chronic prostatitis (18, 19)
A recent metanalysis (20) found several case-control studies showing higher scores of psychological disturbances in CP/CPPS using a variety of diagnostic tools
Some of those series showed a correlation of symptoms measured with NIH-CPSI and the severity of psychological dysfunctions
The results of our study confirm a good correlation between NIH-CPSI scores (total, pain, voiding symptoms and, QoL) and measures of depression, anxiety, and psychological well-being although median values of these measures are indicative of mild disturbances
However, the question whether chronic prostate inflammation is the cause of anxiety or depression, or, on the contrary, a chronic depressive or anxious condition can generate or enhance the symptoms of chronic prostatitis remains still unsolved
In our series, logistic regression analysis of increasing NIH-CPSI score as predictor of the dichotomized GAD-7 test outcome (absent versus mild-to-severe anxiety) showed that anxiety in at least 50% of cases (EL50) is predicted by very low levels of the NIH-CPSI total score (4 88), pain score (3 07), voiding score (2 03) and QoL score (2 58) This finding could suggest that an anxious profile may be a “background” feature independent from the prostatitis syndrome In other words, it may be hypothesized that traits of preexisting anxiety may be part of the general psychological profile of an individual, and that this may precede the manifestation of chronic prostatitis and, when the syndrome presents, lead to an exaggerated perception of its symptoms
On the contrary, poor correlation of IPSS scores with GAD-7, PHQ-9 and Oxford scores may be explained by the structure of the IPSS questionnaire that is designed to assess symptoms of prostatism including voiding symptoms related to bladder neck obstruction rather than filling or irritative symptoms that are typical of prostatitis
When our CP/CPPS patients with and without psychological disorders were separately assessed, the total NIHCPSI scores and the sub scores for pain and QoL were higher in patients with psychological dysfunction compared to those without Conversely, voiding sub scores were different in patients with depression but not in those with anxiety or psychological distress This finding suggests that pain symptoms are crucial in the comorbidity of CP/CPPS and depression or anxiety
Although the prevalence of erectile dysfunction was high in our series (52% of patients showed an IIEF score ≤ 26), we did not find significant correlations between anxiety, depression and psychological well-being scores and the IIEF-5 and PEDT scores This observation contrasts with the common knowledge that psychological disorders negatively impact sexual function (21-23) On the contrary,
the lack of a relationship between psychological dysfunctions and sexual functioning in a CP/CPPS population could be explained by a prevalent impact of other factors in the pathogenesis of sexual dysfunction in CP/CPPS subjects (inflammatory cytokines, vascular dysfunction) (24)
Information on the impact of personality traits in CP/CPPS patients is scarce In the present study, we administered TEMPS-A, which is an instrument suitable for measuring traits which could make subjects vulnerable to affective episodes Affective temperaments (depressive, anxious, irritable, hyperthymic, and cyclothymic) are regarded as subclinical manifestations and high-risk states for various affective disorders and some somatic diseases (25)
In our series, scores for depressive, anxious, irritable, and cyclothymic characters were significantly and positively correlated with NIH-CPSI scores, showing that all these tracts may increase the clinical expression of the disease
On the contrary, a hyperthymic character was negatively correlated with the severity of total NIH-CPSI scores and NIH-CPSI QoL sub score
Temperaments affected the International Prostate Symptom Score (IPSS) with a similar trend, although correlation was statistically significant only for depressive temperament In fact, as above discussed, both IPSS and NIHCPSI (voiding domain) score voiding dysfunctions, but IPSS focuses more on voiding symptoms related to bladder neck obstruction (incomplete emptying, intermittency, weak stream and straining) rather than to storage symptoms, that are mainly related to prostatitis
Affective temperaments showed a limited influence on scores of sexual functions in our series, although PEDT scores were negatively correlated with hyperthymic scores The negative correlation of PEDT scores with hyperthymic temperament scores confirms that this personality trait could be present in subjects who are able to better manage symptoms associated with prostatitis
A limitation of this study was the lack of a cohort of healthy controls, that would have been useful to better define the clinical relevance of the levels of psychological dysfunction observed in our patients with CP/CPPS In addition, the study design did not include measures of catastrophism and perceived stress for a more complete assessment of the psychological profile of patients
Previous studies confirmed an association between catastrophizing and pain intensity and quality of life whereas data on the influence of stress are less consistent (16)
Another aspect that would have deserved more attention is the interrelationship between patients and their spouses, that could have an impact on painful symptoms (26)
All these aspects will be the goal of future studies
CONCLUSIONS
Our results confirm the strict correlation between scores measuring anxiety, depression and well-being and scores of prostatitis-like symptoms In particular, the presence on anxiety disorders is predicted at very low NIH-CPSI values IPSS, an assessment tool for measuring symptoms of patients with prostatism is more focused on bladder neck obstruction symptoms and correlated poorly with measures of anxiety, depression and well-being No correlations were observed between scores measuring
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12452
6
psychological conditions and those measuring erectile and ejaculatory dysfunction. Information on temperamental profiling of patients with prostatitis-like symptoms is limited, although depressive, anxious, irritable, and cyclothymic temperaments are associated to more severe prostatitis symptoms whereas hyperthymic temperament seems to be protective against symptoms of prostatitis and ejaculatory dysfunction.
REFERENCES
1.Propert KJ, McNaughton-Collins M, Leiby BE, et al. Chronic Prostatitis Collaborative Research Network. A prospective study of symptoms and quality of life in men with chronic prostatitis/chronic pelvic pain syndrome: the National Institutes of Health Chronic Prostatitis Cohort study. J Urol. 2006; 175:619-23.
2.Shoskes DA, Nickel JC, Dolinga R, Prots D. Clinical phenotyping of patients with chronic prostatitis/chronic pelvic pain syndrome and correlation with symptom severity. Urology. 2009; 73:538-42.
3.Magri V, Wagenlehner F, Perletti G, et al. Use of the UPOINT chronic prostatitis/chronic pelvic pain syndrome classification in European patient cohorts: sexual function domain improves correlations. J Urol. 2010; 184:2339-45.
4.Propert KJ, Litwin MS, Wang Y, et al. Responsiveness of the National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI). Qual Life Res. 2006; 15:299-305.
5. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16:606-13.
6.Gyasi-Sarpong CK, Acheampong E, Yeboah FA, et al. Predictors of the international prostate symptoms scores for patients with lower urinary tract symptoms: A descriptive cross-sectional study. Urol Ann. 2018; 10:317-323.
7.Cappelleri JC, Rosen RC, Smith MD, et al. Diagnostic evaluation of the erectile function domain of the International Index of Erectile Function. Urology. 1999; 54:346-51.
8.Symonds T, Perelman MA, Althof S, et al. Development and validation of a premature ejaculation diagnostic tool. Eur Urol. 2007; 52:565-73.
9.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006; 166:1092-7.
10.Meleddu M, Guicciardi M, Scalas LF, Fadda D. Validation of an Italian version of the Oxford happiness inventory in adolescence. J Pers Assess. 2012; 94:175-85.
11. Akiskal HS, Mendlowicz MV, Jean-Louis G, et al. TEMPS-A: validation of a short version of a self-rated instrument designed to measure variations in temperament. J Affect Disord. 2005; 85:45-52.
12. Krieger JN, Nyberg L Jr, Nickel JC. NIH consensus definition and classification of prostatitis. JAMA. 1999; 282:236-7.
13.Koh JS, Ko HJ, Wang SM, et al. The impact of depression and somatic symptoms on treatment outcomes in patients with chronic prostatitis/chronic pelvic pain syndrome: a preliminary study in a naturalistic treatment setting. Int J Clin Pract. 2014; 68:478-85.
14.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009; 41:1149-60.
15.Hills P, Argyle M. The Oxford Happiness Questionnaire: A Compact Scale for the Measurement of Psychological Well-Being, Pers. Individ. Diff. 2002; 33:1073-1082
16.Riegel B, Bruenahl CA, Ahyai S, et al. Assessing psychological factors, social aspects and psychiatric co-morbidity associated with Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) in men -- a systematic review. J Psychosom Res. 2014; 77:333-50.
17.Chung SD, Lin HC. Association between chronic prostatitis/chronic pelvic pain syndrome and anxiety disorder: a population-based study. PLoS One. 2013; 8:e64630.
18.Clemens JQ, Brown SO, Calhoun EA. Mental health diagnoses in patients with interstitial cystitis/painful bladder syndrome and chronic prostatitis/chronic pelvic pain syndrome: a case/control study. J Urol. 2008; 180:1378-82.
19.Mändar R, Korrovits P, Rahu K, et al. Dramatically deteriorated quality of life in men with prostatitis-like symptoms. Andrology 2020; 8:101-109.
20.Stamatiou K, Trinchieri M, Trinchieri M, et al. Chronic prostatitis and related psychological problems. Which came first: The chicken or the egg? A systematic review. Arch Ital Urol Androl. 2023; 95:11300.
21.Liu Q, Zhang Y, Wang J, et al. Erectile Dysfunction and Depression: A Systematic Review and Meta-Analysis. J Sex Med. 2018; 15:1073-1082.
22.Velurajah R, Brunckhorst O, Waqar M, et al. Erectile dysfunction in patients with anxiety disorders: a systematic review. Int J Impot Res. 2022; 34:177-186.
23.Xia Y, Li J, Shan G, et al. Relationship between premature ejaculation and depression: A PRISMA-compliant systematic review and meta-analysis. Medicine (Baltimore). 2016; 95:e4620.
24.Chen X, Zhou Z, Qiu X, et al. The Effect of Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) on Erectile Function: A Systematic Review and Meta-Analysis. PLoS One. 2015; 10:e0141447.
25.Eory A, Gonda X, Lang Z, et al. Personality and cardiovascular risk: association between hypertension and affective temperaments-a cross-sectional observational study in primary care settings. Eur J Gen Pract. 2014; 20:247-52.
26.Tripp DA, Nickel JC, Shoskes D, Koljuskov A. A 2-year followup of quality of life, pain, and psychosocial factors in patients with chronic prostatitis/chronic pelvic pain syndrome and their spouses. World J Urol. 2013; 31:733-9.
Correspondence
Konstantinos Stamatiou, MD stamatiouk@gmail.com
Department of Urology, Tzaneio Hospital, Pireus, Greece
Vittorio Magri, MD vittorio.magri@asst-fbf-sacco.it Urology Unit, ASST Fatebenefratelli Sacco, Milan, Italy
Margherita Trinchieri, MD margherita.trinchieri@gmail.com Psichiatry Unit, ASST Rhodense, G. Salvini Hospital, Garbagnate (Milan), Italy.
Alberto Trinchieri, MD alberto.trinchieri@gmail.com School of Urology, University of Milan, Milan, Italy
Gianpaolo Perletti, Dr. Biol. Sci. M. Clin. Pharmacol. (Corresponding Author) gianpaolo.perletti@uninsubria.it
Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy
Conflict of interest: The authors declare no potential conflict of interest.
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12452 7
in prostatitis
Psychosexologic assessment
ORIGINAL PAPER
Telemedicine and social media: A contemporary analysis of the most shared content by internet users
Vincenzo Mirone 1 , Francesco Di Bello 1 , Simone Morra 1 , Gianluigi Califano 1 , Luigi Cirillo 1 , Marco Abate 1 , Giovanni Maria Fusco 1 , Stefano Luzzago 2 , Claudia Mirone 3 , Luigi Napolitano 1 , Roberto La Rocca 1 , Massimiliano Creta 1 , Giuseppe Celentano 1 , Marco Capece 1 , Gennaro Musi 2 , Francesco Mangiapia 1 , Nicola Longo 1 , Claudia Collà Ruvolo 1
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples “Federico II”, Naples, Italy;
2 Urology Department, Istituto Europeo di Oncologia (I E O ), Milan, Italy;
3 Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania "Luigi Vanvitelli", Naples, Italy
Summary
Objective: To evaluate the telemedicine information published on the most popular social media platforms, during the second year of the COVID-19 pandemic
Methods: We queried the BuzzSumo tool to identify relatedtelemedicine article links that were shared most on social media, from February 2021 to February 2022. The PEMAT-P was used for the quality assessment of the most shared links
Results: 125 links were eligible for the analysis Facebook was the most used social media platform for sharing articles (median engagement: 1000) Most of the articles were published by magazines (n = 82, 65 6%) and the main topic addressed was general information (n = 49, 39 2%) In the subgroup analyses of the 34 most shared articles, Facebook was the most used social media platform (median engagement:1950), most of the articles were published by magazines (n = 24, 70 6%), whereas the main topic addressed was the prescription of the abortion pill (n = 9, 26.5%). According to the PEMAT-P tool, the median understandability and actionability score was 63 8 and 20%, respectively.
Conclusions: The interest in telemedicine has increased all over the world, as evidenced by the high engagement in social media articles, recorded during the last year However, the access to digital health services is still limited, the information provided is often not verified by an official entity and unable to fill the digital divide exacerbated by COVID 19 pandemic crisis. Hence, health policy should be developed or modified to ensure a more egalitarian Internet access for all citizens. Official medical institutions should standardize telemedicine regulation and online content to reduce the widespread of misleading information.
KEY WORDS: Telehealth; Virtual healthcare; Healthcare technology; COVID-19
Submitted 27 March 2023; Accepted 6 April 2023
INTRODUCTION
Telehealth represents a fast-developing area of contemporary medicine during the last decades The word “telehealth” is defined by “the use of information technology and telecommunications to provide access to health assessment, consultation, diagnosis, intervention, supervision, and infor-
mation across distance” (1) Telemedicine specifically refers to remote clinical services and was first adopted in the 1950’s when a closed-circuit television connected to a prison was employed by an American psychiatrist to provide mental health services (2-4)
Due to the COVID-19 pandemic outbreak, the request for information on telemedicine activity increased exponentially (5) This phenomenon emerged in an attempt to reduce the chance of infection without compromising patients’ care (6, 7) Additionally, the COVID-19 pandemic has stressed the digital divide, especially in remote and rural areas (8) Hence, the advantages of remote care include both a reduction of the overcrowding in health centers and solving the inequalities in health care access due to sociodemographic and economic characteristics Recently new telemedicine platforms and schedules, such as Amazon care or Telehealth apps, were created and more and more used by the public (7, 9-11) Despite this scenario, health policymakers had to work smarter, promoting more realistic planning and interventions to standardize the information and communication technology (ICT)
Nowadays, social media (SoMe), are important tools for professional networking, medical education, research recruitment, and patient information (12-19) Among internet sources, YouTube is the second most used website and over 2 6 billion people worldwide use it once a month (17) Facebook is the third most used website and counts around 2 9 billion monthly active users in the world (https://www semrush com/website/top/) Finally, Twitter is at eleventh place in the top 500 sites on the web and counts 206 million daily active users worldwide (https://www semrush com/website/top/) However, the material available on these platforms differs from studies published within the scientific literature community, which underwent a peer review process, whereas information on the Internet is not always checked and verified Consequently, low quality information may be available on the Internet and the users may acquire misleading information
The current study aims to evaluate the content type and quality of information on telemedicine available on the most clicked SoMe platforms during the second year following the COVID-19 pandemic outbreak
Archivio Italiano di Urologia e Andrologia 2024; 96(1):11206 1
DOI: 10 4081/aiua 2024 11206
MATERIALS AND METHODS
Search strategy and links selection criteria
On February 28th, 2022, from 9:00 a m To 6:00 p m UTC-4, the BuzzSumo online analytic tool (http://buzzsumo com) was used in order to gather the most shared i n t e r n
, BuzzSumo is an online analytic tool working as a data controller application that searches for articles based on keywords and provides data about the number of shares on t h e m o s t p o p
s Facebook, Twitter, Reddit, and Pinterest reporting the article’s engagement Engagement is defined as the total number of interactions (meaning likes, comments, or sharing) that users have with a particular article link This tool has already been used in previous research papers, in order to collect links regarding a specific topic, also in the medical and public health field (18-21) Conversely, other studies evaluated the medical content uploaded in only one of social media platforms (22, 23) For example, Loeb et al evaluated the quality of bladder cancer information on YouTube™, without considering other important sharing websites (22) Moreover, Alex J Xu et al examined the quality of prostate cancer content only on the Instagram social media platform (23) Thus, in the current study, thanks to the BuzzSumo tool, it was possible to explore internet content simultaneously on several and independent social media platforms According to the BuzzSumo 30-day free trial rules, only links published during the year preceding the search date (from the 28th February 2021 to the 28th February 2022) were available for consultation Only “English language” and “all country” settings were applied before searching The BuzzSumo systematic research was performed using the following four keywords: “Telemedicine” , “Telehealth” , “Healthcare technology” and “Virtual healthcare” , selected among ten keywords obtained by BuzzSumo suggestions (Supplementary Table 1) Only the keyword which pro-
vides at least 1000 results and with at least 50% of links related to the telemedicine topic were included Thus, four different searches were performed For each keyword, the first 50 links were collected, obtaining a total of 200 links The threshold of 50 links was since BuzzSumo allowed to open only the first 100 links and that approximately over the 50th link most of those were with low engagement value and were almost off-topic
The following exclusion criteria were applied (Figure 1): i) off-topic (n = 43, 21 5%), ii) duplicates (n = 14, 7 0%), iii) expired links (n = 14, 7 0%) and links with a subscription needed (n = 4, 2 0%) Thus, 29, 37, 38 and 21 l i n k s (
“Telemedicine” , “Telehealth” , “Healthcare technology” and “Virtual healthcare” keywords, respectively For each link, the following characteristics were collected: Facebook, Twitter, Pinterest, and Reddit engagement, evergreen score (measuring the number of social engagements and back-
Supplementary Table 1.
Search keywords obtained by BuzzSumo analytic tool suggestions Only the keyword which provides at least 1000 results and with at least 50% of links related to the telemedicine topic were included Number of links Percentage of on-topic links
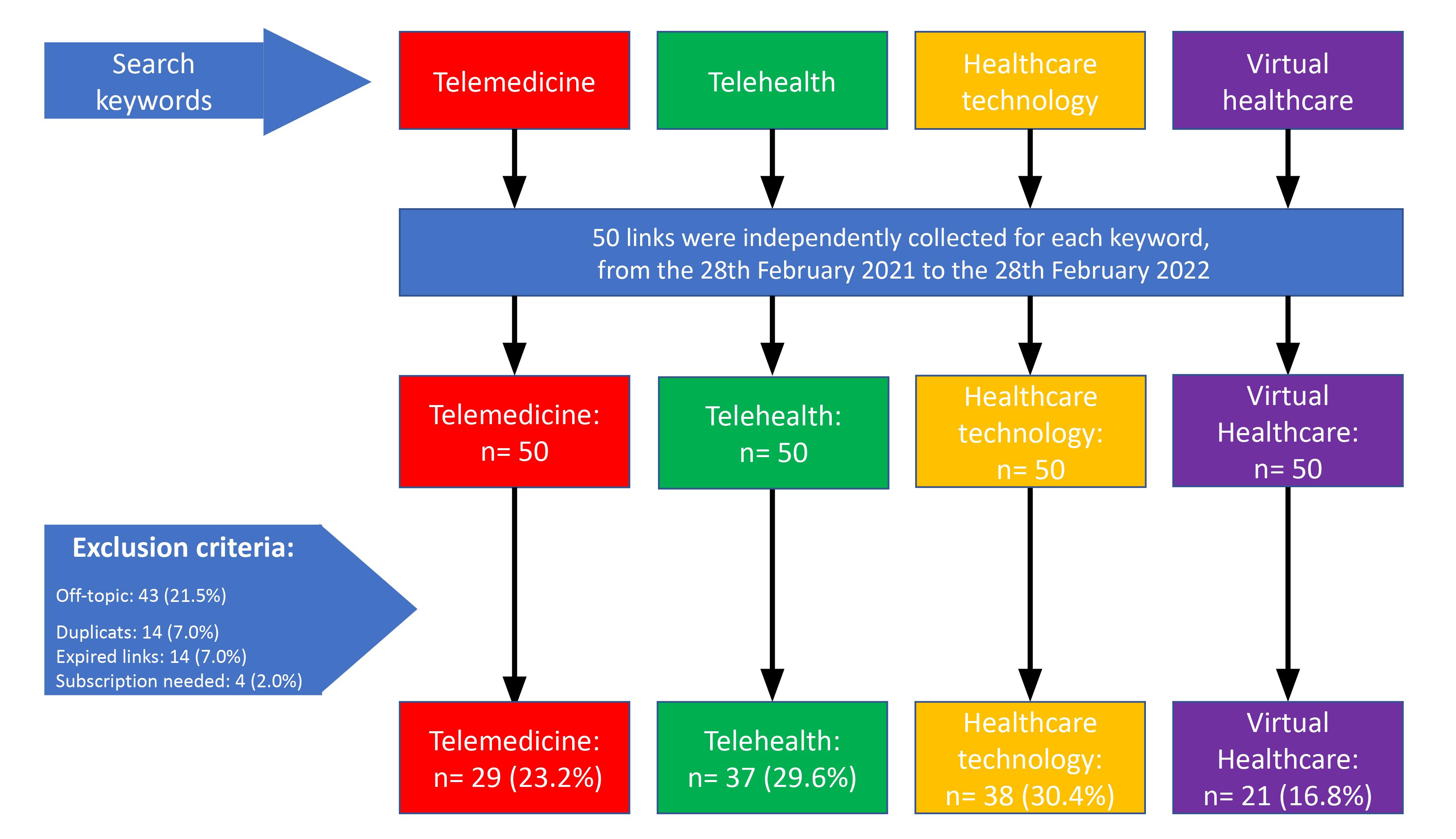
Figure 1 BuzzSumo links identification and selection, from the 28th February 2021 to the 28th February 2022
Archivio Italiano di Urologia e Andrologia 2024; 96(1):11206
2
V Mirone, F Di Bello, S Morra, et al
t l i n k s r e g a r d i n g t e l e m e d i c i n e S p e c i fi c a l l y
l a r s o c i a l m e d i a p l a t f o r m s , s u c h a
e
u
f o r a t o t a l o f 1 2 5 ) w e r e i n c l u d e d u s i n g
Included ke ywords Telemedicine 12709 80% Telehealth 22908 76% Virtual healthcare 5915 64% Healthcare Technology 1679 76% Included ke ywords Videoconsultation 9147 34% Telemedicine and Healthcare 920Teleconsultation 469Telemonitoring 269Healthcare on demand 205Televisit 18 -
links an article receives 30 days after beginning publication, if an article is considered “Evergreen” it has maintained it is relevance to an audience for longer) and total engagement Additionally, links’ source (defined as nonmedical informative site [such as magazines], communication channel, alternative media [such as blogs]), medical centers, hospitals or universities, YouTube or official national website), topic (defined as information on the role of telemedicine through the years, obstetrics and gynecology [defined as prescription of abortion pill, contraception or pregnancy), telehealth platform, new technologies, health policy, telehealth human relationship, mental health) and country (defined as United States, Asia, Australia, Canada, and Europe) data was also collected In the links’ quality assessment, the following tools, in their language, were used: the Jama benchmark score and t h e P
Printable Materials (PEMAT-P) The JAMA benchmark tool scores website quality based on four criteria: disclosure of authorship, attribution of sources, disclosure of commercial interest and website ownership, and currency (date of update) (24) The PEMAT-P is a systematic method to evaluate and compare the understandability (17 items) and actionability (7 items) of patient education materials Higher the score and more understandable or actionable is the material (25-28)
The links’ content was independently assessed by two investigators (a junior and a senior resident doctor) A third investigator (an Associate Professor) adjudicated any differences, and a consensus was achieved among all reviewers
Statistical analyses
Descriptive statistics were presented as means with the standard deviation (SD) and medians with the interquartile ranges (IQR) for continuously coded variables or counts and percentages for categorically coded variables All data were collected for each link included in the analyses Subsequently, subgroup analysis was performed on the most shared links defined as links characterized by Facebook, Twitter engagement and evergreens score values above the respective overall median score In all statistical analyses, the R software (www rproject org) environment for statistical computing and graphics (R version 4 0 0) was used
RESULTS
Link’s engagement
Of all 200 links examined, 125 were selected for the analyses (Table 1) Facebook was the most used SoMe platform to share articles on telemedicine (mean: 3195 5 [SD:967 5], median: 1000 [IQR:130-220]), followed by Twitter (mean: 114 8 [SD:20 5], median: 48 [IQR:6-124]), Reddit (mean: 41 3 [SD: 29 3], median: 0 [IQR:0-1]) and Pinterest (mean:0 4 [SD:0 1], median: 0 [IQR:0]) The mean and median evergreen score was 2 2 (SD:0 3) and 1 (IQR:0-4), respectively Finally, the mean and median total score was 3353 9 (SD:971 4) and 1200 (IQR:211-2500), respectively
Link’s characteristics
According to the source of the link, most of the articles
Table 1
Social media engagements of 125 links on telemedicine collected with BuzzSumo analytic tool, from the 28th February 2021 to the 28th February 2022 Engagement is defined as the total number of interactions (meaning likes, comments, or sharing) that users have with a particular article link
Overall
Facebook Mean (SD) 3195 5 (967 5)
Median (IQR) 1000 (130-2200)
Twitter Mean (SD) 114 8 (20 5)
Median (IQR) 48 (6-124)
Pinterest Mean (SD) 0 4 (0 1)
Median (IQR) 0 (0-0)
Reddit Mean (SD) 41.3 (29.1) Median (IQR) 0 (0-1)
Evergreen
(0 3)
(IQR) 1(0-4)
Total Mean (SD) 3353 9 (971 4) Median (IQR) 1200 (211-2500)
IQR: Interquart le range; SD: Standard Dev ation
were published by Magazines (n = 82, 65 6%), followed by news organizations (n = 20, 16%), alternative media (n = 10, 8%), YouTube (n = 6, 4 8%), medical centers, hospitals or universities (n = 4, 3 2%) and official national website (n = 3, 2 4%) The main topic addressed was information on the role of telemedicine through the years (n = 49, 39 2%), followed by obstetrics and gynecological field (n = 22, 17 6%; specifically the prescription of abortion pill [n = 20, 90 9%]), platform proposal (n = 20, 16%), new technology (n = 15, 12%), health policy (n = 9, 7 2%), mental health (n = 5, 4 0%) and human relationship (n = 4, 3 2%) Finally, most of the links were published in the United States (n = 106, 84 8%) (Table 2)
Table 2.
Content characteristics of 125 links on telemedicine collected with BuzzSumo analytic tool from the 28th February 2021 to the 28th February 2022.
Source
Archivio Italiano di Urologia e Andrologia 2024; 96(1):11206 3 Telemedicine and social media
t i e n t E d u c a t i o n M a t e r i a l s A s s e s s m e n t T o o l f o r
a
Median
score Mean (SD) 2 2
Overall
(n = 125)
Number of articles (%) Non-medical informative sites 82 (65 6) Communication channel 20 (16 0) Alternative media 10 (8 0) Medical center, Hospital or University 4 (3 2) YouTube 6 (4 8) Official national website 3 (2 4) Topic Number of articles (%) Obstetric and gynecology 22 (17 6) Prescription of abortion pill 20 (90.9) Contraception 2 (9 0) Pregnancy 1 (4 5) Information on the role of Telemedicine through the years 49 (39.2) Telehealth platform 20 (16 0) New technologies 15 (12 0) Health policy 9 (7.2) Telehealth human relationship 4 (3 2) Mental health 5 (4 0) Country Number of articles (%) United States 106 (84 8) Asia 11 (8 8) Australia 4 (3 2) Canada 3 (2 4) Europe 1 (0 8)
Table 3.
Social media engagements, content charavteristics quality assessment of 34 most shared links on telemedicine collected with BuzzSumo analytic tool from the 28th February 2021 to the 28th February 2022 Those links were characterized by a Facebook and Twitter engagements and evergreens score values above the respectively median score recorded in the overall analysis.
Overall (n = 34)
Facebook Mean (SD)
3 (2970 6)
(1425-3950)
(22.225)
score recorded in the overall analyses Of all 125 links examined, 34 were selected for the analyses As well as in the overall analyses, Facebook was the most used SoMe p l a t f o r m
(mean:6385 3 [SD:2970 6], median:1950 [IQR:14253950]), most of the articles were published by Magazines (n = 24, 70 6%) and were published in the United States (n = 31, 91 2%) Differently from the overall analyses, the main topic addressed was the obstetrics and gynecological field (n = 10, 29 4%), specifically the prescription of abortion pill [n = 9, 90%]) (Table 3)
According to the JAMA benchmark score, all links respected the four criteria defined as disclosure of authorship, attribution of sources, disclosure of commercial interest and website ownership, and currency (date of update) According to the PEMAT-P tool, the median understandability score was 63 8% (IQR:50 7-81 2), and the median actionability score was 20% (IQR:0-50 0)
9 (2981 643)
(1550-4400)
(70 6)
(17 6)
(5 9)
center, Hospital or
JAMA Benchmark scoring Number Percentage of links (1 point for each criteria, max= 4 points) of links adhering to criteria
Authorship Authors and contributors, 34 100 affiliations, and relevant credentials
Attribution References and sources used 34 100 for the content and relevant copyright information
Disclosures Ownership, sponsorship, advertising, 34 100 underwriting, commercial funding, and potential conflicts of interests
Currency Dates of posted 34 100 and updated information
Subgroup analysis
We performed a subgroup quality assessment analysis on the link characterized by the highest engagement, defined as links with a Facebook and Twitter engagement and evergreens score values above the respective median
DISCUSSION
After the COVID-19 pandemic outbreak in March 2020, the need and interest for telemedicine development increased all over the world (4, 6, 7) The current study aims to evaluate the articles and videos’ content type and quality on telemedicine uploaded on the most clicked SoMe platforms Our analyses identified several noteworthy observations
First, from the overall analyses, it emerged that the social media platform used most to share information on telemedicine was Facebook, followed by Twitter While Facebook has the greatest number of active user accounts worldwide, Twitter appears to be a good platform for the dissemination of scientific information and knowledge transfer These observations may be explained by a Facebook audience of a wide age group Moreover, Facebook’s users are allowed to share videos and articles and fix them to posts over a long period (21) Conversely, social media platforms such as Pinterest or Reddit have poorly used for this aim Similar observations were recorded in other studies (13, 19, 21) For example, Alsyouf et al used the BuzzSumo analytic tool to gather the most shared articles on genitourinary malignancies and Facebook resulted in the most used SoMe platform (13) Altogether, SoMe had revolutionized the health information spread, communication and monitoring in health care (29) For instance, Petruzzi et al measured telemedicine impressions via WhatsApp and clinical assessments that were consistent in 82% of the cases examined (30) Additionally, this new form of knowledge could solve the digital divide of our society, enlightened by the COVID-19 pandemic (8) Indeed, it should be noted that for people who live in remote and rural areas or COVID-19 infected, the access to digital technologies for diagnosis, follow-up and treatment has been a significant resource (8) Moreover, telehealth and digital health had decreased the COVID-19 exposure, reducing the likelihood of contamination and infection during the pandemic (31) A great contribution was also given by the physicians that started to use the Internet to book an appointment, to send and receive examinations and laboratory results through a web-based portal (29) For
Archivio Italiano di Urologia e Andrologia 2024; 96(1):11206
4
V Mirone, F Di Bello, S Morra, et al
n g a r t i c l
o n t e l e m e d i c i n
f o r s h a r i
e s
e
6385
Median
1950
Twitter Mean (SD) 194.9
Median
145
Mean
Median (IQR) 1
Mean (SD) 137 3
Median (IQR) 1.5
score Mean (SD) 5 4
Median
4
Total Mean
6705
Median
2400
(IQR)
(IQR)
5 (103 2-258 2) Pinterest
(SD) 1 1 (0 222)
(0-2) Reddit
(106 052)
(0-5.8) Evergreen
(0 593)
(IQR)
(3-6 8)
(SD)
(IQR)
Non-informative
24
Communication
6
Alternative
2
Medical
University 2 (5 9) YouTube 0 (0) Official national website 0 (0) Topic, n (%) Obstetrics and Gynecology 10
4) Prescription of abortion pill 9 (90 0) Contraception 1
0) Pregnancy 0
Information
9
Health policy 5
Telehealth human relationship 4
Mental health 3
8) Telehealth platform 3
8) New technologies 0 (0) Country
(%) United States 31 (91 2) Asia 1 (2 9) Australia 2 (5 9) Canada 0 (0) Europe 0 (0)
Median
63 4
Actionability Median
20
Source, n (%)
channel
channel
media
(29
(10
(0)
on the role of Telemedicine through the years
(26 5)
(14 7)
(11 8)
(8
(8
, n
PEMAT-P Understandability
(IQR)
(50 7-81 2)
(IQR)
(0-50 0)
i n s t a n c e , t h e Georgia Health Sciences University h a s enabled the communication between patients and their physicians through a web-based platform for asking questions or requesting prescription refills (32) As a result, both physicians and patients were willing to embrace digital tools to maintain and continue the highquality care delivery (33) In conclusion, the SoMe should be considered as an unprecedented tool that could make evidence-based information accessible to the public and promote positive health behaviors (29) In this regard, the governments must consider telemedicine as an opportunity to facilitate access to the Internet and ICT for their citizens (33) Thus, health policymakers and health care managers must learn about the digital divide and must plan and promote more realistic interventions to improve the access to telehealth (33)
Second, we recorded that most of the links (65 5%) were published on non-official websites, such as Magazines Conversely, only 5% of articles were published by the official national website or medical entities, which should be considered a reliable source In consequence, the quality content of telemedicine information on the Internet is not guaranteed by medical organizations and misleading information may be widespread In addition, more than 80% of the articles were uploaded in the United States, highlighting a higher interest in them, with respect to the rest of the world Finally, most of the articles wrote about Information on the role of telemedicine through the years For example, Alena Kharlamenko wrote an article on the platejoy blog describing in detail telemedicine’s definition and the different approaches providing several televisits examples From our results, it emerged that a non-negligible part of the viewed links focused on telehealth human relationships and mental health One of the main concerns regarding telemedicine use is the absence of physical contact between patients and physicians, which may impair the clinical evaluation and the correct patient management The in-person visit is particularly crucial for some kind of specialty, such as psychiatry, where a simple check of laboratory blood exams or a pill prescription is not possible However, in specific conditions, such as during a COVID-19 pandemic, the application of the telemedicine is noteworthy Thus, the category of psychologists and psychiatrists could benefit from telemedicine implementation For instance, in Ireland, 92% of the psychiatrists surveyed reported a reduction in diagnostic confidence due to the absence of a visual comparison with the patients (34) The transitioning from telephone consultations to video consultations would improve to allow a better acceptance of the service and a better receptivity from the specialist physicians (34) In addition to these aspects, several other links focused the attention on the development of new technologies Specifically, mobile health applications (MHAs) represent a potential educational instrument of telemedicine The use of MHAs is constantly increasing year to year, but the main concern was the lack of scientific validation (1, 911) This lack is highly restricted Indeed, the MHAs could be used both to educate patients about their conditions and to promote high-quality health information Moreover, apps could become a library service accessible to everyone, from health care workers to patients
Scientific Society should create and validate their own MHAs and then promote their use through the general population and to the patients affected by specific diseases Moreover, policymakers should have learnt from COVID-19 pandemic crisis that more equal Internet access should be guaranteed for the public also in normal times (8) Hence, health policy should be developed or modified to ensure a more egalitarian Internet access for all citizens In addition to increasing and widening access to the Internet and the health knowledge services, ICTs should be employed to lead towards digitization of health care (1, 8) In conclusion, several relevant topics were addressed by the link shared on the SoMe However, few articles better explained the traps hidden with telemedicine, such as an increased level of distrust with doctors and a higher risk of defrauding patients resulting from an absence of appropriate regulation (3)
Third, in the subgroup analysis, we quantified internet users ’ engagement across a variety of social media platforms on the 34 most shared links on telemedicine Subsequently, we evaluated the quality of information shared on these platforms We recorded that as well for the overall analyses, Facebook resulted in the most used platform, whereas the main topic addressed was the prescription of the abortion pill through telemedicine In December 2021, the Food and Drug Administration permanently removed the in-person requirement for picking up abortion medication (https://www fda gov/drugs/postmark e t - d r u g - s a f e t y - i n f o r m a t i o n - p a t i e n t
/ mifeprex-mifepristone-information) and in 2022 the World Health Organization recommend the use of telemedicine for abortion pill prescriptions in its abortion care guidelines (World Health Organization 2022) However, multiple governments place limits on telehealth access to abortion care as evidenced by several articles available on the web This topic has aroused great interest in the United States, as revealed by our analyses It may represent a starting point to interpret telemedicine as a powerful instrument to use in several circumstances, from chronic disease management for medical advice Finally, according to the PEMAT-P results, we recorded a higher understandability than actionability score (median 63 8 vs 20 0%) The understandability score reflects how viewers could process and assimilate articles’ key messages, despite their cultural and medical backgrounds The actionability score reflects how viewers could apply the information achieved These observations confirmed what we expected since most of the articles were informative rather than instructive Taken together, telemedicine has become a hot topic during the last years, especially after the need emerged from the COVID-19 outbreak, which did not allow patients to get in person visits and healthcare in general These interests resulted in higher investments from governments all over the world (7) From our analyses emerged that the telemedicine advantages (such as lower costs, access to health care from rural areas, or fastest interaction between patients and physicians or between physicians of different specialties) and the disadvantages (such as lower control of privacy and security, lower patient engagement and the evolving patient-physician relationship, limited and fragmented insurance coverage of telemedicine) were not
Archivio Italiano di Urologia e Andrologia 2024; 96(1):11206 5 Telemedicine and social media
s - a n d - p r o v i d e r s
well discussed on the internet (35) In the future, a standard regulation should be promoted to increase telemedicine knowledge allowing people to properly use this essential service today Moreover, the use of MHAs should be promoted both for their educational role as a telemedicine instrument and for spreading high-quality health information
Our study is not devoid of limitations First, BuzzSumo tool only collected data from Facebook, Twitter, Pinterest, Reddit, and YouTube In consequence, information available on other social media platforms such as Instagram and TikTok may be missed Second, Facebook was the most used platform to share articles However, we were not able to discriminate if a person sharing an article actually promoted it or warned against it Third, some reliable or unreliable articles may be missed, due to our search terms choose and to the number of links included for each term However, we used four different keywords with the highest number and on-topic links Fourth, quality assessment videos were subjectively evaluated However, to reduce this confounder, three investigators were involved to independently analyze video contents Finally, according to the 30-day free trial BuzzSumo version, we were only able to collect the links uploaded during the last year In consequence, our study observations represent a frame on what was mostly shared during the second year following the COVID-19 outbreak Future studies should update our observations in order to confirm or reject them Regardless of these limitations, the present study can be considered as a snapshot of the latest and most shared information on telemedicine available on the Internet
CONCLUSIONS
The interest in telemedicine has increased all over the world, as evidenced by the high engagement in social media articles, recorded during the last year However, the access to digital health services is still limited, the information provided is often not verified by an official entity and unable to fill the digital divide exacerbated by COVID 19 pandemic crisis Hence, health policy should be developed or modified to ensure a more egalitarian Internet access for all citizens In addition to increasing and widening access to the Internet and the health knowledge services, ICTs should be employed to lead towards digitization of health care In the future, official medical institutions should standardize telemedicine regulation, creating their own MHAs and online content to reduce the widespread of misleading information
REFERENCES
1 Mirone V, Celentano G, Collà Ruvolo C, et al Perceptions and attitudes toward the use of telemedicine for the postoperative outpatient urological care during the COVID-19 pandemic in an Academic Hospital in Southern Italy Arch Ital Urol Androl 2022; 94:375-9
2 Chaet D, Clearfield R, Sabin JE, Skimming K, on behalf of the C o u n c i l o n E t h i c a l a n d J u d
Association Ethical practice in Telehealth and Telemedicine J Gen Intern Med 2017; 32:1136-40
3 Dorsey ER, Topol EJ State of Telehealth Campion EW, editor N Engl J Med 2016; 375:154-61
4 Mirone V, Creta M, Capece M, et al Telementoring for communication between residents and faculty physicians: Results from a survey on attitudes and perceptions in an Academic Tertiary Urology Referral Department in Italy Arch Ital Urol Androl 2021; 93:450-4
5 Creta M, Sagnelli C, Celentano G, et al SARS-CoV-2 infection affects the lower urinary tract and male genital system: A systematic review J Med Virol 2021; 93:3133-42
6 Hollander JE, Carr BG Virtually Perfect? Telemedicine for Covid19 N Engl J Med 2020; 382:1679-81
7 Lukas H, Xu C, Yu Y, Gao W Emerging Telemedicine Tools for Remote COVID-19 Diagnosis, Monitoring, and Management ACS Nano 2020; 14:16180-93
8 Samadbeik M, Bastani P, Fatehi F Bibliometric analysis of COVID-19 publications shows the importance of telemedicine and equitable access to the internet during the pandemic and beyond Health Info Libr J 2023; 40:390-399
9 Fusco GM, Cirillo L, Abate M, et al Male infertility, what Mobile Health Applications ‘know’: quality analysis and adherence to European Association of Urology Guidelines Arch Ital Urol Androl 2022; 94:470-5
10 Napolitano L, Fusco GM, Cirillo L, et al Erectile dysfunction and mobile phone applications: Quality, content and adherence to European Association guidelines on male sexual dysfunction Arch Ital Urol Androl 2022; 94:211-6
11 Napolitano L, Cirillo L, Fusco GM, et al Premature ejaculation in the era of mobile health application: A current analysis and evaluation of adherence to EAU guidelines Arch Ital Urol Androl 2022; 94:328-33
12 Melchionna A, Collà Ruvolo C, Capece M, et al Testicular pain and youtube™: are uploaded videos a reliable source to get information? Int J Impot Res 2023; 35:140-146
13 Alsyouf M, Stokes P, Hur D, et al ‘Fake News’ in urology: evaluating the accuracy of articles shared on social media in genitourinary malignancies BJU Int 2019; 124:701-6
14 Capece M, Di Giovanni A, Cirigliano L, et al YouTube as a source of information on penile prosthesis Andrologia 2022; 54:e14246
15 Cilio S, Collà Ruvolo C, Turco C, et al Analysis of quality information provided by "Dr YouTubeTM" on Phimosis Int J Impot Res 2023; 35:398-403
16 Gerundo G, Collà Ruvolo C, Puzone B, et al Personal protective equipment in Covid-19: Evidence-based quality and analysis of YouTube videos after one year of pandemic Am J Infect Control 2022; 50:300-305
17 Morra S, Collà Ruvolo C, Napolitano L, et al YouTube™ as a source of information on bladder pain syndrome: A contemporary analysis Neurourol Urodyn 2022; 41:237-245
18 Moscadelli A, Albora G, Biamonte MA, et al Fake News and Covid-19 in Italy: Results of a Quantitative Observational Study IJERPH 2020; 17:5850
19 Obiała J, Obiała K, Manczak M, et al COVID-19 misinformation: Accuracy of articles about coronavirus prevention mostly shared on social media Health Policy Technol 2021; 10:182-186
20 Diaz P, Takele RA, Thaker S, et al Kidney Stone Surgery: Assessing Public Interest and Evaluating Social Media Content J Endourol 2022; 36:954-960
Archivio Italiano di Urologia e Andrologia 2024; 96(1):11206
6
V Mirone, F Di Bello, S Morra, et al
i r s A m e r i c
n
e d i c a l
i c i a l A f f a
a
M
21 Zaila KE, Osadchiy V, Shahinyan RH, et al Social Media Sensationalism in the Male Infertility Space: A Mixed Methodology Analysis World J Mens Health 2020; 38:591
22 Loeb S, Folkvaljon Y, Makarov DV, et al Five-year Nationwide Follow-up Study of Active Surveillance for Prostate Cancer Eur Urol 2015; 67:233-8
23 Xu AJ, Myrie A, Taylor JI, et al Instagram and prostate cancer: using validated instruments to assess the quality of information on social media Prostate Cancer Prostatic Dis 2022; 25:791-3
24 Silberg WM, Lundberg GD, Musacchio RA Assessing, controlling, and assuring the quality of medical information on the Internet: Caveant lector et viewor--Let the reader and viewer beware JAMA 1997; 277:1244-5
25 Collà Ruvolo C, Califano G, Tuccillo A, et al "YouTube™ as a source of information on placenta accreta: A quality analysis" Eur J Obstet Gynecol Reprod Biol 2022; 272:82-87
26 Di Bello F, Collà Ruvolo C, Cilio S, et al Testicular cancer and YouTube: What do you expect from a social media platform? Int J Urol 2022; 29:685-691
27 The Patient Education Materials Assessment Tool (PEMAT) and User’s Guide https://www ahrq gov/health-literacy/patient-education/pemat html
28 Turco C, Collà Ruvolo C, Cilio S, et al Looking for cystoscopy on
YouTube: Are videos a reliable information tool for internet users? Arch Ital Urol Androl 2022; 94:57-61
29 Farsi D, Martinez-Menchaca HR, Ahmed M, Farsi N Social Media and Health Care (Part II): Narrative Review of Social Media Use by Patients J Med Internet Res 2022; 24:e30379
30 Petruzzi M, De Benedittis M WhatsApp: a telemedicine platform for facilitating remote oral medicine consultation and improving clinical examinations Oral Surg Oral Med Oral Pathol Oral Radiol 2016; 121:248-54
31 Sageena G, Sharma M, Kapur A Evolution of Smart Healthcare: Telemedicine During COVID-19 Pandemic J Inst Eng India Ser B 2021; 102:1319-24
32 Chauhan B, George R, Coffin J Social media and you: what every physician needs to know J Med Pract Manage 2012; 28:206-9
33 Burbury K, Wong ZW, Yip D, et al Telehealth in cancer care: during and beyond the COVID-19 pandemic Intern Med J 2021; 51:125-33
34 Hincapié MA, Gallego JC, Gempeler A, et al Implementation and Usefulness of Telemedicine During the COVID-19 Pandemic: A S c o p i n g R e v i e w
11:2150132720980612
35 Wootton R, Geissbuhler A, Jethwani K, et al Long-running telemedicine networks delivering humanitarian services: experience, performance and scientific output Bulletin of the World Health Organization 2012; 90:341-347D
Correspondence
Vincenzo Mirone, MD mirone@unina it
Francesco Di Bello, MD fran dibello12@gmail com
Simone Morra, MD simonemorra93@gmail com Luigi Cirillo, MD cirilloluigi22@gmail com
Marco Abate, MD marcoabate5@gmail com
Giovanni M Fusco, MD giom fusco@gmail com
Luigi Napolitano, MD luiginap89@gmail com
Roberto La Rocca, MD robertolarocca87@gmail com
Massimiliano Creta, MD max creta@gmail com
Giuseppe Celentano, MD dr giuseppecelentano@gmail com
Conflict of interest: The authors declare no potential conflict of interest
Marco Capece, MD
drmarcocapece@gmail com Francesco Mangiapia, MD mangiapiaf@gmail com
Nicola Longo, MD nicola longo@unina it
Claudia Collà Ruvolo, MD c collaruvolo@gmail com
Gianluigi Califano, MD (Corresponding Author) gianl califano2@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples “Federico II”
Via Sergio Pansini n°5, 80138 Naples
Gennaro Musi, MD
Stefano Luzzago, MD
Urology Department, Istituto Europeo di Oncologia (I E O ), Milan, Italy
Claudia Mirone, MD
claudia mirone@unina it
Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania "Luigi Vanvitelli", Naples, Italy
Archivio Italiano di Urologia e Andrologia 2024; 96(1):11206 7 Telemedicine and social media
r i m C a r e C o m m u n i t y H e a l t h 2 0 2 0 ;
J P
Tamer A. Abouelgreed 1, 2 , Mohamed A. Elhelaly 1 , El-Sayed I. El-Agamy 1 , Rasha Ahmed 1 , Yasser M. Haggag 3 , M. Abdelwadood 4 , Salma F. Abdelkader 5 , Sameh S. Ali 6 , Naglaa M. Aboelsoud 7 , Mosab F. Alassal 8 , Gehad A. Bashir 9 , Tarek Gharib 10
1 Department of Urology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
2 Gulf medical university, Ajman;
3 Department of Urology, Faculty of Medicine, Al-Azhar University, Asyut , Egypt;
4 Department of Urology, Faculty of Medicine, Ain Shams University, Cairo, Egypt;
5 Department of Radiology, Faculty of Medicine Ain Shams University, Cairo, Egypt;
6 Department of Radiology, Sheikh Khalifa general Hospital, UAQ, UAE;
7 Department of Radiology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
8 Department of Vascular Surgery, Saudi German Hospital, Ajman, UAE;
9 Department of Urology, Sheikh Khalifa Medical City, Abu Dhabi, UAE;
10 Department of Urology, Faculty of medicine, Benha University, Benha, Egypt
This retracts the article “Effect of preoperative ureteral stenting on the surgical outcomes of patients with 1-2 cm renal stones managed by retrograde intrarenal surgery using a ureteral access sheath” (https://doi org/10 4081/aiua 2023 12102) published on December 28, 2023
––––––––––––––––––––––––––
The undersigned Tamer Abouelgreed, as corresponding author and on behalf of the co-authors, requests the retraction of the above article because he has found that the wording used to present his original data has excessive similarities with the wording of a previously published article
Tamer A Abouelgreed
https://doi org/10 4081/aiua 2024 12437
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12437 1
PAPER
ORIGINAL
Retraction:Effectofpreoperativeureteralstenting onthesurgicaloutcomesofpatientswith1-2cm renalstonesmanagedbyretrogradeintrarenalsurgery usingaureteralaccesssheath
DOI: 10 4081/aiua 2024 12437
SYSTEMATIC REVIEW
burdencountries
Zakaria Aulia Rahman 1, 2 , Furqan Hidayatullah 1, 2 , Jasmine Lim 3 , Lukman Hakim 1, 4
1 Department of Urology, Faculty of Medicine, Universitas Airlangga;
2 Dr Soetomo General-Academic Hospital, Surabaya, East Java, Indonesia;
3 Department of Surgery, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia;
4 Universitas Airlangga Teaching Hospital, Surabaya, East Java, Indonesia
Summary and progression These findings highlight the importance of further multi institutional randomized controlled trials with bigger sample size using a standardized IAC protocol to validate the current results
Introduction: Local therapies for high risk non-muscle-invasive bladder cancer (NMIBC) such as intravesical chemotherapy (IVC) have shown a high rate of progression and recurrence (1) Intravesical Bacillus Calmette-Guérin (BCG) for local therapies has been shown to reduce progression and recurrence in patient with NMIBC However, its potential role is limited in high burden countries for tuberculosis (TB) due to its low specificity that can cause wrong diagnosis or false positive in patients with clinically diagnosed tuberculosis BCG vaccine that has to be given for most people in tuberculosis endemic countries will induce trained immunity that could reduce the effectivity of intravesical BCG for NMIBC Moreover, intravesical BCG is contraindicated in patient with or previous tuberculosis The potential clinical benefit of intraarterial chemotherapy (IAC) in delaying the recurrence and progression of high-risk NMIBC have been investigated with promising results (2, 3). We aimed to conduct a meta-analysis to evaluate the potential anti-tumor effect of IAC in NMIBC.
Methods: We conducted a comprehensive search of published articles in Cochrane Library, Pubmed, and Science-Direct to identify relevant randomized controlled trials (RCTs) and observational studies comparing IAC alone or combined with IVC versus IVC/BCG alone in NMIBC The protocol of preferred reporting items for systematic review and meta-analysis (PRISMA) was applied to this study
Results: Four RCTs and 4 cohort observational studies were eligible in this study and 5 studies were included in meta-analysis The risk ratio of tumor recurrence was reduced by 35% (RR = 0 65; 95% CI 0 49-0 87; p = 0 004) in IAC plus IVC, while recurrence-free survival (RFS) was prolonged by 45% (HR: 0 55; 95% CI, 0 44-0 69; p < 0 001) The risk of tumor progression was reduced by 45% (RR = 0 55; 95% CI 0 41-0 75; p = 0 002) and tumor progression-free survival (PFS) was also prolonged by 53% (HR: 0 47; 95% CI, 0 34-0 65; p < 0 001) Some RCT’s had high or unclear risk of bias, meanwhile 4 included cohort studies had overall low risk of bias, therefore the pooled results need to be interpreted cautiously. Subgroup analysis revealed that the heterogeneity outcome of tumour recurrence might be attributed to the difference in NMIBC stages and grades. Conclusions: The IAC alone or combined with IVC following bladder tumor resection may lower the risk of tumor recurrence
KEY WORDS: Intraarterial chemotherapy; Bladder cancer; NMIBC; Tumor recurrence; Tumor progression
Submitted 4 December 2023; Accepted 3 January 2024
INTRODUCTION
Urothelial bladder cancer is one of the most common cancer by incidence in men and women (4) It occurs four times more frequently in men than in women worldwide with an average age of 70 years at diagnosis (5) The WHO classifies primary tumor of bladder as non-muscle invasive bladder cancer (NMIBC) and muscle invasive bladder cancer (MIBC) (6) The NMIBC accounts for 75% of all bladder cancer incidence and 20-25% of NMIBC cases presented with T1 stages (7, 8) The 5-year progression and recurrence rates in patients with T1 stage of NMIBC are 20 7% and 41 8%, respectively Cancer specific death for highrisk NMIBC progressing to MIBC is 65 0% (8, 9) The disease management for NMIBC should be stratified into low risk, intermediate risk, high risk and very high risk group Transurethral bladder tumor resection (TURBT) followed by single instillation of intravesical chemotherapy ( I V C ) i s r e c o m m e n d e d f o r l o w r i s k g r o u p M o r e advanced therapy is needed for intermediate, high risk and very high risk group Intermediate risk group need to add intravesical BCG for 1 year or IVC for up to 1 year For high risk group, only intravesical BCG for 1-3 years after TURBT is an alternative to radical cystectomy IVC is not recommended by some guidelines for high risk group Radical cystectomy is the therapy of choice for very high risk group Intravesical therapy is one strategy for bladder preservation, although the efficacy of IVC in reducing recurrence and progression is arguable On the other hand, early cystectomy might result in excessive t r e a t m e n t f
h decreasing patient’s quality of life (QoL) (4, 10)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154 1
o c i a t e d w
o r s o m e p a t i e n t s b e i n g a s s
i t
Asystematicreviewandmeta-analysisofintraarterial chemotherapyfornonmuscleinvasivebladdercancer: Promisingalternativetherapyinhightuberculosis
DOI: 10 4081/aiua 2024 12154
Nowadays, transurethral tumor resection followed with Bacillus Calmette-Guérin (BCG) instillation has been considered the gold standard of bladder preservation treatment (7, 11) Nonetheless, 37-45% patients with NMIBC suffer recurrence within 2 years (12) A systematic review of 1 476 patients concluded that adjuvant IVC after TURBT may help to prevent recurrence but not progression (13) Furthermore, the use of BCG for IVC in tuberculosis-burden/endemic countries can be challenging, since the primary diagnostic tests for tuberculosis (acidfast bacillus smear or culture) could not differentiate between mycobacterium bovis as the cause of BCG disease and mycobacterium tuberculosis, leading to false positive/wrong diagnosis BCG vaccine that has to be given for most people in tuberculosis endemic countries will induce trained immunity that could reduce the effectivity of intravesical BCG for NMIBC Some clinicians are afraid of giving this treatment due to the evidence of disseminated BCG, urinary tract tuberculosis and miliary tuberculosis, moreover, intravesical BCG is contraindicated in patient with or previous tuberculosis (14-16) Looking to these drawbacks, a novel strategy to enhance the efficacy of IVC following TURBT in delaying the recurrence and progression of high-risk NMIBC is currently emerging Intra-arterial chemotherapy (IAC), which was initially introduced by Kubota et al (1986), could reduce disease recurrence and progression to MIBC The injection of chemotherapeutic agents into the artery that lead to the tumor, may increase its efficacy and reduce the systemic toxicity (17, 18) Administration of chemotherapy using the IAC method increases the local peak of plasma concentration of the drug, resulting in higher tumor concentrations of the chemotherapy agent (17-19) The IAC has been shown to be an effective treatment for NMIBC patients and even MIBC Three- and five-years overall survival in patients with MIBC that received IAC for bladder preservation therapy were 70-75% and 60-65%, respectively, whilst their five year rates of recurrence and progression were 62 2% and 76 9%, respectively The potential toxicity of IAC is less when compared to systemic chemotherapy in patient with MIBC (17-20) To date, systematic reviews and meta-analysis supporting the use of IAC for NMIBC are scarce The objective of this meta-analysis was to critically review and evaluate the quality of the evidence supporting the use of IAC for high-risk NMIBC
Table 1
Search strategy including search terms and databases
Database Search Ter ms
This meta-analysis followed The Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) protocol for conducting and reporting meta-analyses (21)
This systematic review and meta-analysis was registered through the international prospective register of systematic reviews (PROSPERO) as CRD42020165004
Systematic search
A systematic search was carried out in August 2022 Cochrane Library, PubMed and Science-Direct were used to identify the relevant studies The detailed search strategy was performed using advanced search of each database (Table 1) The reference list of trials, review and clinical practice guidelines were also searched to find other relevant literatures
Inclusion and exclusion criteria
Randomized controlled trials (RCT) and observational studies were included in this study Only English-language publications that meet the inclusion criteria were included The included studies must contain intra-arterial chemotherapy, and a control group that only receive intravesical chemotherapy (IVC) or another treatment
The IAC group could receive instillation of intravesical chemotherapy for both induction and maintenance with subsequent intra-arterial chemotherapy or receive only IAC using Seldinger technique Meanwhile the control group only received intravesical chemotherapy instillations for induction and maintenance or received another treatment such as intravesical BCG There was no restriction of any type and dose of chemotherapy for this systematic review and meta-analysis
The 1973 or 2004 World Health Organization (WHO) system of TNM classification and tumor grade was used in this study for bladder cancer staging and grading (22, 23) Patients with Ta, T1 and carcinoma in situ (CIS) transitional cell carcinoma of the bladder that was histologically confirmed with all tumor grades (G1, G2, G3 or LG and HG) are considered appropriate as long as meet the criteria of high risk group Any method of bladder tumor resection was considered acceptable
Studies without control were included in the systematic review Review articles, editorials, commentaries, letters, animal studies, abstract only and case series or case con-
Pubmed ((((("intraarterial"[All Fields] OR "intraarterially"[All Fields]) AND (((((("chemotherapy s"[All Fields] OR "drug therapy"[MeSH Terms]) OR ("drug"[All Fields] AND "therapy"[All Fields])) OR "drug therapy"[All Fields]) OR "chemotherapies"[All Fields]) OR "drug therapy"[MeSH Subheading]) OR "chemotherapy"[All Fields])) OR ("intra-arterial"[All Fields] AND (((((("chemotherapy s"[All Fields] OR "drug therapy"[MeSH Terms]) OR ("drug"[All Fields] AND "therapy"[All Fields])) OR "drug therapy"[All Fields]) OR "chemotherapies"[All Fields]) OR "drug therapy"[MeSH Subheading]) OR "chemotherapy"[All Fields]))) AND ("nmibc"[All Fields] OR "nmibcs"[All Fields])) OR ("non"[All Fields] AND ((("muscle s"[All Fields] OR "muscles"[MeSH Terms]) OR "muscles"[All Fields]) OR "muscle"[All Fields]) AND (((((((("invasibility"[All Fields] OR "invasible"[All Fields]) OR "invasion"[All Fields]) OR "invasions"[All Fields]) OR "invasive"[All Fields]) OR "invasively"[All Fields]) OR "invasiveness"[All Fields]) OR "invasives"[All Fields]) OR "invasivity"[All Fields]))) AND (((("urinary bladder neoplasms"[MeSH Terms] OR (("urinary"[All Fields] AND "bladder"[All Fields]) AND "neoplasms"[All Fields])) OR "urinary bladder neoplasms"[All Fields]) OR ("bladder"[All Fields] AND "cancer"[All Fields])) OR "bladder cancer"[All Fields])
Additional Filter: Randomized controlled trial, Clinical Study, Clinical Trial, Controlled Clinical Trial, Comparative Study, Multicenter Study and Observational Study Science-Direct Intraarterial bladder cancer: title, abstract, keywords; Intraarterial chemotherapy bladder cancer: title, abstract, keywords Cochrane (intraarterial chemotherapy): ti,ab,kw AND (bladder cancer): ti,ab,kw
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154
2
Z Aulia Rahman, F Hidayatullah, J Lim, L Hakim,
MATERIALSANDMETHODS
trol were excluded Studies that did not measure the tumor progression or recurrence rates in IAC and control group were also excluded
Study selection and data extraction
The first (ZRA) and second (LHA) investigator independently performed both the study selection and data extraction Should problems or disagreements occur, they were resolved by discussion The information retrieved from each study included: author name, year, country and type of the study, clinical follow-up protocol, intraarterial chemotherapy protocol, numbers of intervention and control group outcomes (tumor recurrence, tumor progression, toxicity, withdrawal), Risk Ratio (RR), Hazard Ratio (HR) and confidence interval (95% CI) of each outcome results
Statistical analysis
The primary outcomes of this meta-analysis were tumor recurrence and tumor progression RR with a 95% CI was used to measure the primary outcomes Recurrence-free survival (RFS) and progression-free survival (PFS) were measured using HR with a 95% CI In a study without published HR, we measured the HR and 95% CI using a method for estimating HR by Tierney (24)
Statistical heterogeneity
The Cochrane Q test and I2 statistics were used to evaluate the heterogeneity of studies This method would have quantified inconsistency among studies Heterogeneity was considered significant if the I2 was greater than 50% and P value less than 0 05 (25) Random-effects model was used should a significant heterogeneity occur; otherwise, a fixed-effects model was used (26, 27) Data analysis and
synthesis were performed using Review Manager software (version 5 3 5, The Cochrane Collaboration, Oxford, UK)
Risk of Bias
The risk of bias for each RCT study that meet the inclusion criteria was assessed by the Cochrane tool using review manager software, which included selection bias, performance bias, detection bias, attrition bias, and reporting bias (28) We used CLARITY system tool to assess the risk of bias for cohort studies (29) In addition, the quality of the included observational studies was evaluated according to the Newcastle Ottawa quality assessment scale (30)
Sensitivity analysis
A sensitivity analysis was performed by excluding a study one by one, to validate the results consistency of this meta-analysis (31) Subgroup analyses were also performed considering the highest risk of NMIBC to analyse the sources of potential heterogeneity (32)
RESULTS
Search results and study characteristics
We identified 436 references in our systematic literature search Following a full text review of 152 articles, eight relevant studies consisting of 4 RCTs and 4 cohort studies were synthesized and analysed Three studies were included only in the systematic review because of difference in the control group The excluded studies were listed in this meta-analysis protocol (Figure 1)
A total of 846 patients were pooled from 5 eligible stud-
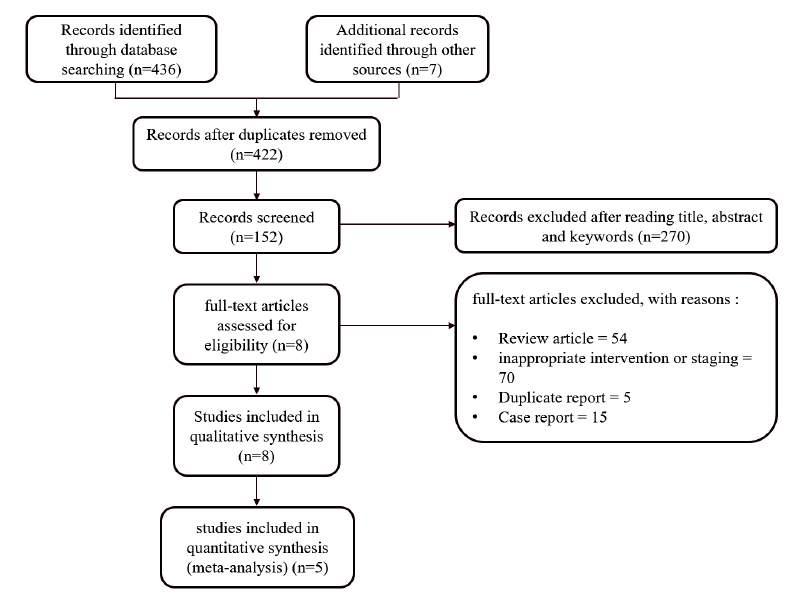
Figure 1. PRISMA Flowchart for Systematic Search Strategy.
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154 3 A systematic review and meta-analysis of intraarterial chemotherapy for non muscle invasive bladder cancer
Z Aulia Rahman, F Hidayatullah, J Lim, L Hakim,
Table 2.
Studies included in this meta-analysis comparing intra-arterial only or combined with intravesical chemotherapy with control groups
Study
B n Huang et a . 2018 (2)
Feng Sun et al 2019 (3)
Junxing Chen et al 2013 (36)
Zefu Liu et al 2018 (35)
Fan L an et al 2019 (34)
B n Huang et a 2021 (37)
Eapen L et al 2004 (20)
Chen M K et a 2009 (40)
Table 3
Characteristics of all studies Study
Bin Huang et al 2018 (2)
Feng Sun et al 2019 (3)
Junxing Chen et al 2013 (36)
Zefu Liu et al 2018 (35)
Fan Lian et a 2019 (34)
Bin Huang et al 2021 (37)
L et al 2004 (20)
Chen M K et al 2009 (40)
Primary, High grade T1 NMIBC
Primary or recurrence NMIBC, T1G3 tumor, CIS, multiple and recurrent and large (> 3 cm) Ta, and G1 and G2 tumors (High risk NMIBC)
Primary or recurrence NMIBC, T1G3 tumor
Primary or recurrence NMIBC, T1 G1-G3 tumor
Primary tumor, NMIBC, Histopathological diagnosis transitional cell carcinoma
Primary or recurrence tumor, NMIBC, High risk features
Primary or recurrence tumor, all stage and grade tumor
Primary tumor, G3 superficial without any other concomitant types of tumor, no less than three tumors, T1, no less than 3 cm in diameter
Cisplatin; Pirarubicin
Cisplatin; Epirtubicin
4 cycles with 1 month interval between each injection
3 cycles with 4 weeks interval between each injection
Cisplatin; Epirtubicin
Cisplatin; Gemcitabine
Cisplatin; Epirubicin
50
4-6 weeks interval between each injection
28 days interval between cycles
4-6 weeks interval between each injection
month (4 cycles)
months (3 cycles) No data
Cystoscopy, urine cytology and blood test every 3 months for 2 years and yearly thereafter
Cystoscopy, urine cytology, routine blood examination, serum biochemistry every 3 months, chest X ray, CTU, enhanced pelvic MRI every 6 months in the first 2 years, and then cystoscopy every 6 months between 3 and 5 years and annually thereafter
Cystoscopy and urine cytology every 3 months for the first 2 years and then cystoscopy every 6 months between 3 to 5 years and annually thereafter
(2 cycles)
months (3 cycles)
Cisplatin; Epirubicin
Cisplatin (with adjuvant radiotherapy to bladder 40 gy)
Gemcitabine; Cisplatin
1 month interval between each injection
3 weeks interval between each injection
4 weeks interval
months (4 cycles)
months (3 cycles) 3 months (3 cycles)
Cystoscopy every 3 months for the first 2 years and then every 6 months for 5 year and then every year thereafter
Cystoscopy every 3 months for the first 2 years and then every 6 months thereafter, CT urogram at 3 months postoperatively and then 6-12 months thereafter
Cystoscopy every 3 months for a period of 2 years and then every 6 months for the next 3 years
Bladder biopsy if there was suspicious of tumor during follow up
Cystoscopy, bladder biopsies and urinary cytology 6-8 weeks after last cycles CT scan imaging
Cystoscopy every 3 months in first 2 years then every 6 months for 2-5 years
Chest X ray annually
ies Inclusion criteria, number of patients, tumor recurrence, tumor progression, chemotherapy protocol and follow-up protocol were recorded (Tables 2, 3) One study included all the stages of bladder cancer, therefore we only included the data of NMIBC patients from that study (33) Cisplatin chemotherapy (25-120 mg) for IAC
was used in all of the studies It was combined with epirubicin (30-50 mg) in 3 studies, with pirarubicin (50 mg) in one study and with gemcitabine (800 mg) in another study The IAC protocols varied from one instillation every 2-3 weeks to one every 4 weeks (Tables 2, 3) (2, 3, 33-38)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154
4
Countr
No of patient Follow up (mo) Recur rence Progression IAC IVC IAC IVC IAC IVC IAC IVC
y
China 53 98 79 (7-131) 59 (7-127) 19 (35 8%) 41 (41 8%) 11 (20 7%) 23 (23 5%)
China 141 142 47 3 (16-78) 46 8 (13-76) 41 (29 1%) 61 (42 9%) 22 (15 6%) 36 (25 3%)
China 29 31 22 (5-58) 23 (11-58) 3 (10 3%) 14 (45 2%) 0 (0%) 7 (22 6%)
China 62 141 51 (21-83) 35 (23-60) 28 (45 2%) 78 (55 3%) 10 (16 1 %) 48 (34 0%)
China 99 50 24 25 (5-50) 22 30 (10-42) 24 (24 2%) 26 (52 0%) 2 (2 0%) 4 (8 0%)
China 43 53 28 (10-58) 25 (11-56) 12 (27 9%) 14 (26 4%) 4 (9 3%) 5 (9 4%) BCG (BCG) (BCG) (BCG)
America 21 - 34 (2-180) - 5 (23%) - n a -
China 25 27 40 (6-67) 40 (6-67) 3 (12%) 14 (51 8) 0 (0%) 7 (25 9%)
Inclusion criteria IAC protocol Follow up protocol Dr ugs Dose frequency T ime
Eapen
60;
50;
60;
25;
60;
60 ; 50 60-120 900; 30
50
30
50
800
4
4
3
2 months
3-4
2
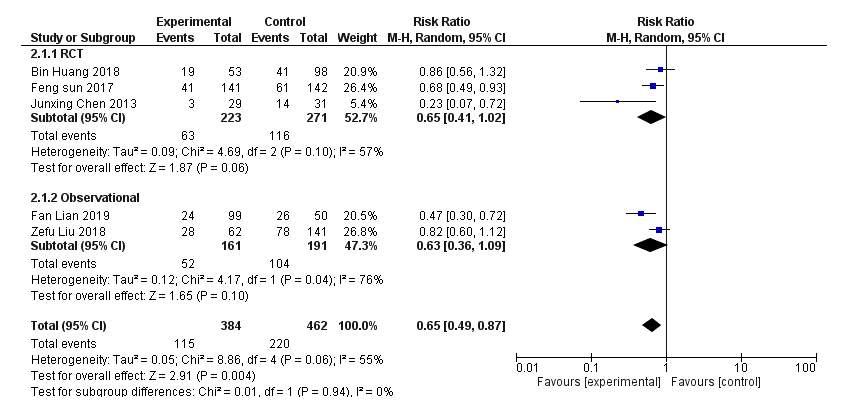
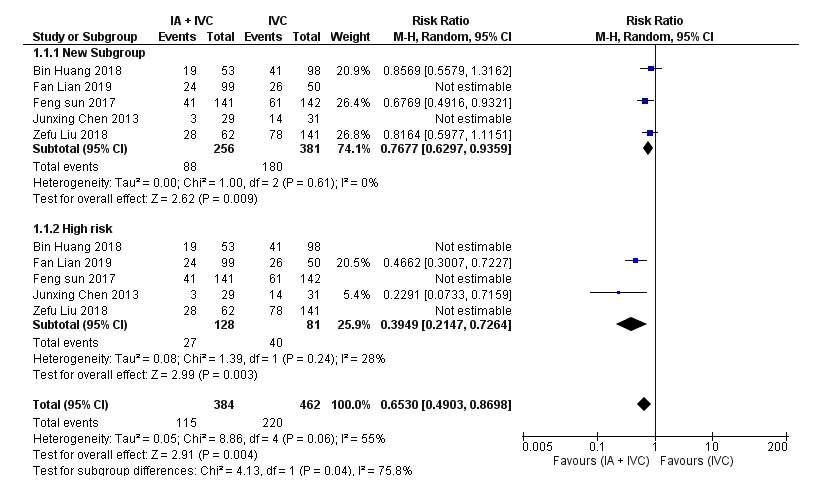
Tumor recurrence
All five studies showed that the IAC group had lower tumor recurrence rate; however, 2 studies did not show a statistical significance for this outcome The overall I2 was 55 5% and p-value for heterogeneity was 0 06, therefore random effects model was used for this outcome About 115 (29 94%) patients on IAC group and 220 (47 61%) on IVC group, had tumor recurrence during the follow up of each study We observed a reduction of 35% in the recurrence ’ s risk ratio on IAC group (RR = 0 65; 95% CI 0 49-0 87;
p= 0 004), as shown in Figure 2 Pooled-effects of RCTs were similar to those of cohort studies for all outcome measurements We further performed a subgroup analysis for this outcome that included the highest risk NMIBC Tumor recurrence reduction in the IAC group was different for these two subgroups, suggesting that the different stage and grade of tumors might increase the heterogenity of this outcome (Figure 3) IAC only showed less recurrence if compared with IVC only and had comparable result with BCG instillation only (Table 2) (37, 38)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154 5 A systematic review and meta-analysis of intraarterial chemotherapy for non muscle invasive bladder cancer
Figure 2 Forrest plot of Recurrence Rates
Figure 3. Forrest plot of Recurrence Rates with subgroup of difference risk stratification of NMIBC


Tumor progression
All five included studies favoured IAC group, although 3 studies did not reach statistical significance We used fixed-effects model for this outcome since there was low heterogeneity between all included studies (I2 = 26%, p = 0 25) We found that 11 71% (45/384) of patients in the IAC group experienced tumor progression compared to 25 54% (118/462) in patients who received IVC only There was 45% reduction in the RR of tumor progression on patients receiving IAC When stratified by study design, cohort observational studies showed a lower risk of tumor progression in the IAC group compared to the IVC group (RR = 0,44; 95% CI = 0 25-0,78; p < 0,005;
I2 = 0%) (Figure 4) Moreover, in qualitative measure, IAC only showed less progression if compared with IVC only and had comparable result with BCG instillation only (Table 2) (37, 38)
Recurrence free survival and progression free survival
In this meta-analysis, we observed that the IAC group had longer RFS compared to the IVC group (HR: 0 55; 95% CI, 0 44-0 69; p < 0 001) (Figure 5)
There was a slight increase of heterogenity in all pooledstudies (I2 =32%, p = 0 21) We used fixed effects model despite of the moderate heterogenity for this outcome
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154
6
Z Aulia Rahman, F Hidayatullah, J Lim, L Hakim,
Figure 4. Forrest plot of Progression Rates
Figure 5. Forrest plot of Reccurence Free Survival.
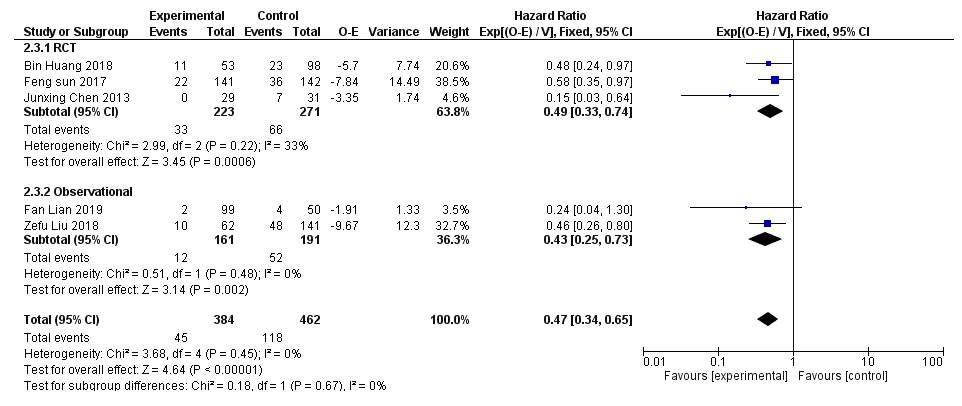
Table 4
Side effects in maintenance group of included studies
and
Bin Huang et al 2018 (2) Cisplatin 60; 4 months
Pirarubicin; 50
Feng Sun et al 2019 (3) Cisplatin 50;
Epirubicin 30
Junxing Chen et al 2013 (36) Cisplatin 60; n a 29 15
Epirubicin 50
Zefu L u et al. 2018 (35) Cisplatin 25;
Gemcitabine 800
Fan Lian et al 2019 (34) Cisplatin 60; 3-4 months
Epirubicin 50
Bin Huang et al 2020 (37) Cisplatin 60; 4 months 43 12
Epirubicin 50
Chen M K et al 2009 (40) Gemcitabine 900; 3 months 25 3 n a n a 2521 cisplatin 30 n a, data was not ava lab e
Similarly, PFS was significantly increased in the IAC group (HR: 0 47; 95% CI, 0 34-0 65; p < 0 001) (Figure 6) Fortunately, the measured heterogeneity between all pooled- studies was very low (I2 = 0%, p = 0 45) When stratified by study design, both RCT and cohort observational studies subgroups of RFS and PFS showed a similar and significant pooled effect
Side effects of treatment
Seven studies reported the number of patients suffered from chemotherapy side effects in group receiving IAC (Table 4) One study couldn’t be extracted for side effect data because they added pelvic radiotherapy to IAC (33) The common toxicities were nausea/ vomiting, neutropenia, anemia, low leukocyte count, increased liver enzyme, increased serum
creatinine and thrombocytopenia Table 4 showed the number of patients withdrew from the intraarterial chemotherapy and their main reasons We measured that 75% of all patients in 5-pooled studies could stand and completed the whole IAC protocol (Table 5)
Table 5. Withdrawal in maintenance group of included studies
Bin Huang et a 2018 (2)
Zefu Liu et a . 2018 (35) 62
caused by progressed bladder cancer (3), Tumor reccurence (16)
caused by bladder tumor (9), Died caused by pneumonia (1), tumor recurrence (41)
caused by non-oncologic factor (1), Tumor recurrence (3)
caused by bladder tumor (8), Recurrence and progression (9), severe hematological toxicity (2), Personal reasons (1) Fan L an et al 2019 (34)
(2)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154 7 A systematic review and meta-analysis of intraarterial chemotherapy for non muscle invasive bladder cancer
Figure 6.
Study No. of No. of W ithdrawal reasons (n) Patients W ithdrawal
Forrest plot of Progression Free Survival
53 19 Died
141 51 Died
Feng Sun et al. 2019 (3)
29 4 Died
Junxing Chen et al 2013 (36)
Died
99 2
20
Tumor progression
Study IAC type T ime No. of total Nausea/ Neutropenia Increased Liver Increased Low Leukocytes Anemia Thrombocytopenia
dose Patients vomiting Enzyme Creatinine Count
53 35 9 12 37 n a n a
141 53 14 n a n a n a 21 9
3 months
a n a
3523 n
62 24 21 99 23 24 16
2 months
n a n a n a n a 22
99 8
a n a
5417 n
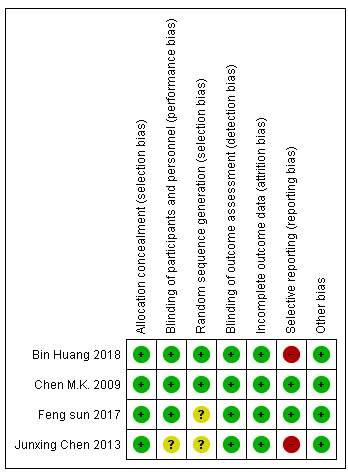
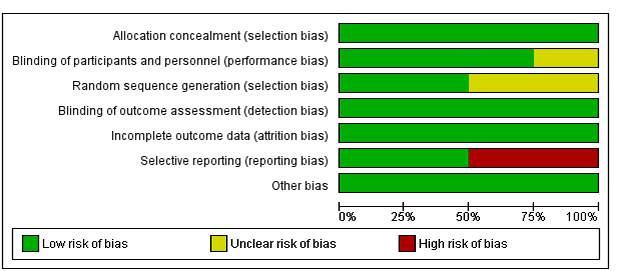
The causes of withdrawal were toxicity, tumor recurrence and progression Quantitative analyses were not performed as all 5 pooled studies did not report the side effects and withdrawal patients in their control group
Sensitivity analysis
Sensitivity analysis was performed to validate the results consistency by excluding studies one by one We did not find any significant variation in the combined-RR for the primary outcomes (tumor recurrence and tumor progression), thus the results may be considered relatively stable and consistent among studies However, the IAC did not significantly reduce the risk of recurrence (RR = 0 70; 95% CI 0 49-1 00; p = 0 05) after excluding Sun et al and Chen et al studies
The tumor progression showed similar trend, where IAC did not significantly prevent patients from progression if we excluded Lian et al , Sun et al and Liu et al studies (RR = 0 63; 95% CI 0 35-1 15; p = 0 13)
Risk of Bias
Cochrane tools was used to evaluate the risk of bias of randomized controlled trial study (Figure 7)
For all included RCT’s study, patients were assigned randomly into IAC or control (IVC or BCG) with adequate technical description However, there are two studies that did not describe the process of randomization (3, 36) All RCT studies have low risk of bias in allocation concealment Only one study did not describe how the physicians were blinded to the study participants Figure 7 shows that 50% of the studies had high risk of bias in selective reporting due to the unreported
HR of progression and recurrence free survival in two of the studies (2, 36) Therefore, we had to use an indirect method of estimating HR (24) All studies had low risk of bias in attrition bias and other bias In conclusion 2 studies has high risk of bias, 1 study has unclear risk bias and another one has low risk of bias
For non-randomised studies, the risk of bias was assessed using CLARITY tools for cohort studies Fortunately, all included cohort studies had low risk of bias in all 7 points of CLARITY tools (Table 6)
In Addition, the quality of included observational studies was evaluated according to the Newcastle Ottawa quality assessment scale (30)
Table 7 summarized the total score acquired for each quality domain Based on the selection domain, three studies scored four out of four points In the comparability domain, 2 studies scored one over two points and another 2 studies scored a full point of two In the exposure domain, all four cohort studies scored three out of four quality score points
Four cohort studies were considered to have good quality of study design (20, 34, 35, 37)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154
8
Z Aulia Rahman, F Hidayatullah, J Lim, L Hakim,
Study Study year CLARITY tools 1234567 Zefu Liu et al 2018 Low risk Low risk Low risk Low risk Low risk Low risk Low risk Fan Lian et al 2019 Low risk Low risk Low risk Low risk Low risk Low risk Low risk Bin Huang et al 2021 Low risk Low risk Low risk Low risk Low risk Low risk Low risk Eapen L et al 2004 Low risk Low risk Low risk Low risk Low risk Low risk Low risk
Table 6. CLARITY tool for assessing quality of observational studies.
Figure 7. Risk of Bias of RCT Studies
Table 7
Newcastle Ottawa Scale (NOS) tool for assessing quality of observational studies.
Study Study year Quality Score Point
Selection Comparability Exposure Total
Zefu Liu et al 2018 4138
Fan Lian et al. 2019 4239
Bin Huang et al 2021 4239
Eapen L et al 2004 3137
Select on: maximum 4 po nts
Comparabi ity: maximum 2 po nts
Exposure: maximum 3 po nts
≥ 7 points were considered as “good”, 2 to 6 points were cons dered as “fa r”, and ≤ 1 point was considered as “poor” qua ity
DISCUSSION
The present study was based on RCTs and cohort observational study that explored the effect of IAC on the risk of recurrence, progression, RFS and PFS when treating NMIBC This study was restricted to the trials comparing intraarterial only or combined with intravesical chemotherapy (IAC) versus intravesical chemotherapy (IVC) or BCG directly, to avoid trials with major differences in treatment regimens (28) Low heterogeneity between included studies was detected by the Cochrane Q test and I2 statistics and RR was used to compare the treatment effect in groups of patients categorized by several confounders However, our study was not without limitations We have included 4 non RCTs which may involve eliminating selection, recall, and confounder biases Moreover, we have also included one pilot RCT which only enrolled few subjects for its trial Potential clinical heterogeneity might results by inclusion of studies, in which patients with NMIBC of different tumor stages,grades and risk were considered and treatment protocols were performed with different chemotherapy agents, doses and schedules However, previous studies suggested that the optimal number of induction instillations and optimal frequency and duration of IAC was not fully known, and there was no large differences in efficacy between various drugs and different dose of intraarterial chemotherapy (13, 35, 39)
Interestingly, with the exception of tumor recurrence, low heterogeneity between included studies was detected by the Cochrane Q test and I2 statistics in our study So the potential clinical heterogeneity of included studies might not significantly interfere with the pooled results of our study and we considered it appropriate to perform a metaanalysis Different follow-up protocols among the included studies could also affect the outcomes as patients less frequently monitored would appear to have a recurrence at later time frames compared to those that were more closely monitored Our study could not perform quantitative analyses of side effects and withdrawal since they were not reported in the control groups (IVC only)
Several weaknesses affected the quality of the data provided Four of 8 studies included in this meta-analysis were cohort studies It is undeniable that these cohort studies had good study designs and robust data collection and each study had appropriate sample size and clear comparison However, the evidence from cohort studies have to be considered as level 2, thus they had lower hier-
archy of evidence than RCTs To evaluate the efficacy of IAC in NMIBC more accurately, more RCTs with good study design and large sample sizes are necessary
Additionally, we also observed some drawbacks in the RCTs that were included in this review Despite the importance for assessing quality of a study, we found that most of the included RCTs did not describe the details of allocation concealment and blinding, therefore the potential biases-involved were unclear (Figure 7) If bias existed, it would have a great impact on the interpretation of the meta-analysis
The pooled results in our study showed that for intermediate or high-risk NMIBC, induction IVC followed by IAC instillation after bladder tumor resection, compared with IVC only, could reduce the risk ratios of tumor recurrence and tumor progression, and prolong RFS by 45% and PFS by 63% All studies demonstrated prolonged-PFS with IAC, but progression was defined as a broad, composite end point: worsening-free survival, which was created by the authors Studies that couldn’t be measured in meta-analysis also showed that IAC only is superior than IVC and has comparable result with BCG only in terms of reducing recurrence and progression
There was some confusion in treating patients with NMIBC in high tuberculosis burden country Most guidelines suggested BCG instillation in intermediate, high and very high risk of NMIBC, although there is a risk of tuberculosis seeding, mislead diagnosis and reduced treatment efficacy in tuberculosis endemic area, where IAC could be a promising therapy
To explore the sources of potential clinical heterogeneity of included studies, a subgroup analysis for tumor recurrence was performed by different risk criteria of NMIBC in our study (21) The reduction in tumor recurrence with IAC differed from those with highest risk NMIBC and those who are not This result implied that the stage, grade and risk of NMIBC might be one of the sources of potential clinical heterogeneity of included studies However, since the subgroup analysis might be underpowered, the conclusions should be drawn cautiously The optimal duration and schedule of IAC protocol is not fully defined yet Previous studies recommended at least 3-4 cycles (with 2-4 weeks interval between each instillation) of IAC that are required in order to obtain superiority of IAC over IVC for prevention of recurrence or progression The IAC is associated with more systemic side effects compared to control group, but all of these were minor Finally, the benefit of IAC should be weighed against its added cost, side effects and inconvenience
CONCLUSIONS
It may be concluded from this meta-analysis that IAC injections only or combined with IVC instillation preceded by bladder tumor resection could reduce the risk of tumor recurrence and progression, and extend the recurrence free survival and progression free survival in intermediate, high-risk or even the highest risk of NMIBC, compared to the IVC or BCG instillation only IAC could be a promising treatment option for NMIBC in high tuberculosis burden country However, a standardized-IAC protocol has not been definitely determined, therefore further RCTs with
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154 9 A systematic review and meta-analysis of intraarterial chemotherapy for non muscle invasive bladder cancer
larger number of NMIBC patients in a multi-institutional scheme are emerging to reach this aim
REFERENCES
1 Abern MR, Owusu RA, Anderson MR, et al Perioperative intravesical chemotherapy in non-muscle-invasive bladder cancer: A systematic review and meta-analysis J Natl Compr Canc Netw 2013; 11:477-84
2 Huang B, Wang H, Lin H, et al Evaluation of the effects of intraarterial chemotherapy combined with intravesical chemotherapy against intravesical chemotherapy alone after transurethral resection of bladder tumor in T1-staged Grade 3 bladder cancer J Cancer Res Clin Oncol 2019; 145:487-94
3 Sun F, Zhao R, Zhu Y, et al A prospective comparison of intraarterial chemotherapy combined with intravesical chemotherapy and intravesical chemotherapy alone after transurethral resection with a thulium laser in high-risk non-muscle invasive bladder cancer Cancer Chemother Pharmacol 2017; 79:1099-107
4 European Association of Urology 2023 “Non-Muscle-Invasive Bladder Cancer (TaT1 and CIS) EAU Guidelines ” European Urology 31: 1-48 https://uroweb org/guideline/non-muscle-invasive-bladdercancer/%0Ahttp://uroweb org/wp-content/uploads/EAU-GuidelinesN o n - m u s c l e - i n v a s i v e - B l a d d e r - C a n c e r - T a T 1 - C I S - 2 0 1 8 p d f EAU Guidelines on Non-muscle-invasive Bladder Cancer (TaT1 and CIS)
5 Katafigiotis I, Sfoungaristos S, Martini A, et al Bladder cancer to patients younger than 30 years: a retrospective study and review of the literature Urologia 2017; 84:231-5
6 Burger M, Catto JWF, Dalbagni G, et al Epidemiology and risk factors of urothelial bladder cancer Eur Urol 2013;63:234-41
7 Van Den Bosch S, Witjes JA Long-term cancer-specific survival in patients with high-risk, non-muscle-invasive bladder cancer and tumour progression: A systematic review Eur Urol 2011; 60:493-500
8 Martin-Doyle W, Leow JJ, Orsola A, et al Improving selection criteria for early cystectomy in high-grade T1 bladder cancer: A metaanalysis of 15,215 patients J Clin Oncol 2015; 33:643-50
9 Sylvester RJ, Brausi MA, Kirkels WJ, et al Long-Term Efficacy Results of EORTC Genito-Urinary Group Randomized Phase 3 Study 30911 Comparing Intravesical Instillations of Epirubicin, B a c i l l u s C a l m e t t e - G u é r i n , a n d B a c i l l u s C a l m e t t e - G u é r i n p l u s Isoniazid in Patients with Intermediate- and High-Risk Eur Urol 2010; 57:766-73
10 Shen PL, Lin ME, Hong YK, He XJ Bladder preservation approach versus radical cystectomy for high-grade non-muscle-invasive bladder cancer: A meta-analysis of cohort studies 11 Medical and Health Sciences 1103 Clinical Sciences 11 Medical and Health Sciences 1112 Oncology and Carcinogene World J Surg Oncol 2018; 16:1-15
11 Chang SS, Cookson MS Non-muscle-invasive bladder cancer: The role of radical cystectomy Urology 2005; 66:917-22
12 Alhunaidi O, Zlotta AR The use of intravesical BCG in urothelial carcinoma of the bladder Ecancermedicalscience 2019; 13:1-9
13 Sylvester RJ, Oosterlinck W, Van Der Meijden APM A single immediate postoperative instillation of chemotherapy decreases the risk of recurrence in patients with stage Ta T1 bladder cancer: A meta-analysis of published results of randomized clinical trials J Urol 2004; 171:2186-90
14 Wansaula Z, Wortham JM, Mindra G, et al Bacillus calmetteguérin cases reported to the national tuberculosis surveillance system, United States, 2004-2015 Emerg Infect Dis 2019; 25:451-6
15 To U, Kim J, Chia D Disseminated BCG: Complications of Intravesical Bladder Cancer Treatment Case Rep Med 2014: 362845
16 Buffen, Kathrin et al 2014 “Autophagy Controls BCG-Induced Trained Immunity and the Response to Intravesical BCG Therapy for Bladder Cancer ” PLoS Pathogens 10(10)
17 Stewart DJ, Benjamin RS, Zimmerman S, et al Clinical pharmacology of intraarterial cis-diamminedichloroplatinum(II) Cancer Res 1983; 43:917-20
18 Mokarim A, Uetani M, Hayashi N, et al Combined intraarterial chemotherapy and radiotherapy in the treatment of bladder carcinoma Cancer 1997; 80:1776-85
19 Tester W, Caplan R, Heaney J, et al Neoadjuvant combined modality program with selective organ preservation for invasive bladder cancer: Results of Radiation Therapy Oncology Group phase II trial 8802 J Clin Oncol 1996; 14:119-26
20 Eapen L, Stewart D, Collins J, Peterson R Effective bladder sparing therapy with intra-arterial cisplatin and radiotherapy for localized bladder cancer J Urol 2004; 172:1276-80
21 Shamseer L, Moher D, Clarke M, et al PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation BMJ 2015; 350:g7647
22 MacLennan GT, Kirkali Z, Cheng L Histologic Grading of Noninvasive Papillary Urothelial Neoplasms Eur Urol 2007; 51:889-98
23 Sobin LH, Fleming ID TNM classification of malignant tumors, Fifth edition (1997) Cancer 1997; 80:1803-4
24 Tierney JF, Stewart LA, Ghersi D, et al Practical methods for incorporating summary time-to-event data into meta-analysis Trials 2007; 8:1-16
25 Grant J, Hunter A Measuring inconsistency in knowledgebases J Intell Inf Syst 2006; 27:159-184
26 Schmidt FL, Oh IS, Hayes TL Fixed- versus random-effects models in meta-analysis: Model properties and an empirical comparison of differences in results Br J Math Stat Psychol 2009; 62:97-128
27 Borenstein M, Hedges LV , Higgins JPT, Rothstein HR A basic introduction to fixed-effect and random-effects models for metaanalysis Res Synth Methods 2010; 1:97-111
28 Higgins JPT, Altman DG, Gøtzsche PC, et al The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials BMJ (Online) 2011; 343:1-9
29 Evidence Partners Tools to Assess Risk of Bias in Cohort Studies 2019;CLARITY Working Group; McMaster University
30 GA Wells D O’Connell, J Peterson, et al Newcastle-Ottawa quality assessment scale Ottawa Hospital Research Institute, (OHRI) 2014; 3:2-4
31 Copas J Meta-analysis, funnel plots and sensitivity analysis Biostatistics 2000; 1:247-62
32 Richardson M, Garner P, Donegan S Interpretation of subgroup analyses in systematic reviews: A tutorial Clin Epidemiol Glob Health 2019; 7:192-8
33 Eapen L, Stewart D, Collins J, Peterson R Effective bladder sparing therapy with intra-arterial cisplatin and radiotherapy for localized bladder cancer J Urol 2004; 172:1276-80
34 Lian F, Chen W, Liu Y, et al Intra-arterial chemotherapy com-
Archivio Italiano di Urologia
Andrologia
96(1):12154
e
2024;
10
Z Aulia Rahman, F Hidayatullah, J Lim, L Hakim,
A systematic review and meta-analysis of intraarterial chemotherapy for non muscle invasive bladder cancer
bined with intravesical chemotherapy is effective in preventing recurrence in non-muscle invasive bladder cancer J Cancer Res Clin Oncol 2019; 145:1625-1633
35 Liu Z, Ye Y, Li X, et al The effects of intra-arterial chemotherapy on bladder preservation in patients with T1 stage bladder cancer
World J Urol 2018; 36:1191-200
36 Chen J, Yao Z, Qiu S, et al Comparing intra-arterial chemotherapy combined with intravesical chemotherapy versus intravesical chemotherapy alone: A randomised prospective pilot study for T1G3 bladder transitional cell carcinoma after bladder-preserving surgery
Cardiovasc Intervent Radiol 2013; 36:1521-6
Correspondence
Zakaria Aulia Rahman zakariaaulia04@gmail com Furqan Hidayatullah furqanhidayatullah26@gmail com Department of Urology, Faculty of Medicine, Universitas Airlangga
Jasmine Lim jasmine lim@um edu my Department of Surgery, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia
Lukman Hakim (Corresponding Author) lukman-h@fk unair ac id
Department of Urology, Faculty of Medicine, Universitas Airlangga Jl Mayjen Prof Dr Moestopo No 6-8, Surabaya, East Java, Indonesia, 60286
Conflict of interest: The authors declare no potential conflict of interest
37 Huang B, Huang G, Li W, et al Intra-arterial chemotherapy combined with intravesical chemotherapy compared with intravesical BCG immunotherapy retrospectively in high-risk non-muscle-invasive bladder cancer after transurethral resection of the bladder tumor J Cancer Res Clin Oncol 2021; 147:1781-8
38 Chen MK, Qin ZK, Zhou FJ, et al Intra-arterial chemotherapy is reliable in preventing high-risk superficial bladder cancer from recurrence and progression J Chemother 2009; 21:681-6
39 International SRI, Avenue R, Park M Cancer chemotherapy and pharmacology© Growth (Lakeland) 1985; 127:160-4
11
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12154
SYSTEMATIC REVIEW
Syah Mirsya Warli 1, 2 , Muhammad Fahmi Ikram 3 , Raja Gerald Sarumpaet 3 , Zaimah Zulkarnaini Tala 4 , Ignatius Ivan Putrantyo 5
1 Department of Urology, Universitas Sumatera Utara Hospital, Universitas Sumatera Utara, Medan, Indonesia;
2 Division of Urology, Department of Surgery, Faculty of Medicine, Universitas Sumatera Utara-Haji Adam Malik General Hospital, Medan, Indonesia;
3 Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia;
4 Department of Nutrition, Faculty of Medicine, Universitas Sumatera Utara;
5 Department of Urology, Faculty of Medicine, Universitas Indonesia - Haji Adam Malik General Hospital, Medan, Indonesia
Summary
Background: Benign Prostatic Hyperplasia (BPH) is prevalent among elderly men, necessitating focused attention The Prostatic Urethral Lift (PUL) procedure, a minimally invasive intervention, has emerged as a promising option for BPH management It has shown remarkable results in ameliorating Lower Urinary Tract Symptoms (LUTS), enhancing quality of life, and preserving sexual function This study aims to evaluate the effectiveness and safety of PUL in BPH patients.
Methods: Key databases (MEDLINE, Cochrane CENTRAL, ScienceDirect, EBSCO, Google Scholar) were systematically searched using pertinent terms related to PUL and BPH Following the PRISMA checklist, we considered only Randomized Controlled Trials studies (RCTs) from 2013 to 2023. The assessment focused on LUTS, Quality of Life, sexual function, and Adverse Events, within three months Follow-up post-treatment mean values compared with controls (Sham) and the improvement from baseline to post-treatment follow-up duration were considered. Statistical analysis and risk of bias evaluation were conducted using Review Manager 5 4 1, presenting results as difference of mean values (MD) and Risk Ratios (RR)
Results: A meta-analysis with a Random Effects Model of 7 RCTs involving 378 confirmed BPH patients demonstrated significant improvements in the PUL arm including International Prostate Symptom Score (IPSS) (MD 5 51, p < 0 0001), maximum urinary flow rate (Qmax) (MD 2 13, p = 0 0001), BPH Impact Index (BPHII) (MD 2 14, p = 0 0001), and IPSS-QoL (MD 1 50, p < 0 0001), without significant increase of Adverse Events (RR 1 51; p = 0 50) Positive outcomes were observed in sexual function variables and post-void residual measurements when post-treatment values were compared to baseline
Conclusions: PUL holds advantages over control interventions, providing encouraging prospects for BPH management
This study underscores the need for further exploration of PUL's efficacy and safety in BPH patients
KEY WORDS: Benign prostatic hyperplasia; Lower urinary tract symptoms; Prostathic urethral lift; Quality of life; Sexual function
Submitted 9 November 2023; Accepted 14 November 2023
INTRODUCTION
Benign prostatic hyperplasia (BPH), an affliction prevalent among aging men, is characterized by the proliferation of prostate cellular components Its prevalence reaches up to 80% among those aged over 80 (1) BPH gives rise to lower urinary tract symptoms (LUTS), significantly impacting patients' lives As a consequence of its considerable impact, increased research focus and awareness are imperative The American Urological Association (AUA) defines BPH based on increased smooth muscle and epithelial cell growth in the prostate transition zone (2) Symptomatic BPH manifests as LUTS, including urgency, nocturia, and weak urine flow, occasionally associated with erectile dysfunction Traditional treatments involve oral medication and surgeries like Transurethral Resection of the Prostate (TURP), which can lead to long-term complications (3) Recently, the PUL procedure has gained interest for its minimally invasive approach PUL addresses LUTS by gently dilating the prostatic urethra using trans-prostatic UroLift implants (4) Encouragingly, PUL has demonstrated swift LUTS relief, improved urinary flow, and preserved sexual function Although multiple trials have established its effectiveness, a systematic review and meta-analysis are essential to comprehensively assess PUL's efficacy and safety (5) This study aims to consolidate available data on PUL through system-
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066 1
Theefficacyandsafetyofprostaticurethrallift asaminimallyinvasivetherapeuticmodalitytotreat lowerurinarytractsymptomswhilemaintainingsexual functioninpatientswithbenignprostatichyperplasia: Asystematicreviewandmeta-analysisofrandomized controlledtrials
DOI: 10 4081/aiua 2024 12066
S Mirsya Warli, M Fahmi Ikram, R Gerald Sarumpaet, Z Zulkarnaini Tala, I Ivan Putrantyo
atic search strategies and meta-analysis of RCT, providing a comprehensive evaluation of PUL's potential as a viable BPH treatment
METHODS
Protocol registration
The Protocol of this review was registered in PROSPERO: International Prospective Register of Systematic Reviews under issued ID of CRD42023410982
Elegibility criteria
In this review, we utilized the PICO (Population, Intervention, Comparison, Outcome) framework to evaluate the effectiveness and safety of PUL procedure in enhancing the condition of individuals diagnosed with BPH Consequently, we formulated the PICO strategies for this meta-analysis, which are presented in Table 1 The data results were presented in numerical format, including means and Standard Deviation (SD) We specifically focused on RCT studies, preferably those conducted on a small to large scale with explicit protocols and published in English-based literature During the literature identification process, studies were excluded if they had incompatible trial designs (e g , trials involving oral therapy intervention, intervention versus standard surgical therapy such as TURP, or intervention versus any other surgical procedure for BPH or if they had incomplete data reporting
Table 1. PICO strategies.
Aspects Criteria
Population - All patients with Benign Prostatic Hyperplasia, regardless of their race or ethnicity
- Men at least aged 50 years
- Had no prior surgical treatment for BPH
Intervention - Prostatic Urethral Lift (PUL)
Compatison - Sham or placebo surgery as rigid cystoscopy
Outcome LUTS Symptoms:
1. International Prostate Symptom Score (IPSS)
2 Qmax
3 Post Volume Residual (PVR) Quality of Life (QoL):
1 International Prostate Symptom Score-Quality of Life (IPSS-QoL)
2 Benign Prostatic Hyperplasia Index (BPHII)
Sexual Function:
1 Male Sexual Health Qustionnaire-Ejaculatory Dysfunction Bother (MSHQ-EjD Bother)
2 Male Sexual Health Qustionnaire-Ejaculatory Dysfunction Function (MSHQ-EjD Function)
3 Sexual Health Inventory for Men (SHIM) Adverse Event
Database searching and systematic literature screening
Two authors, M F I and R G S, conducted a comprehensive literature search using three medical electronic databases: MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL), and Cumulated Index to Nursing and Allied Health Literature (CINAHL) Additionally, we utilized five search engines, namely PubMed, ScienceDirect, Google Scholar, EBSCO, and the Cochrane Library, for
study screening This search was performed from January to February 2023 To facilitate study tracing and identify suitable studies, we employed the PICO strategy We identified relevant literature using strategic keywords specific to each search engine We also manually screen the article references list the previous systematic-reviews and meta-analysis studies related to our objective to secure every possible litrerature and include them as "studies from other source or review source ”
Study
selection
Our systematic review is based on Prefered Reporting Items for Sytematic Review and Meta-analysis (PRISMA) statements as shown in Figure 1 The inclusion criteria for this study are RCT studies in accordance to PICO, full-text article, published in the last 10 years and written in English (6) The study excluded systematic reviews, meta-analyses, case reports, animal studies, guidelines, and more Identified studies were gathered, duplicates removed, and those meeting format requirements were further assessed Full-text articles were evaluated by both authors independently based on titles and abstracts For selected articles, complete manuscripts were examined, and any differences in assessment were discussed and resolved
Risk of bias and data extraction
This systematic review and meta-analysis study exclusively includes RCTs The quality assessment of the RCTs was conducted using the revised Cochrane Risk of Bias for Randomized Controlled Trials (RoB) tool, which was performed using Microsoft Excel software This tool consists
Outcome Data, Measurement of Outcome Data, and Selection of the Reported Result Each domain was interpreted as low, some concern, or high The data were extracted from baseline mean and SD values, as well as from follow-up reports, using Microsoft E
Manager (RevMan) 5 4
Statistical design and analysis
In this study, we employed diverse methods for mathematical and structured analysis, focusing on comparing post-treatment values of variables in treated subjects versus controls and on changes of values of variables from baseline to follow-up evaluations Results were presented as differences of mean values (MD) between groups Notably, the comparison with controls was conducted at 3-month post-treatment follow-up, employing rigid cystoscopy as control procedure (sham surgery) (7) All analyses were carried out using Review Manager (RevMan) 5 4 software Continuous data models were applied for most outcomes, while the dichotomous model was used for Adverse Event (AE) rates Depending on heterogeneity levels, the fixed effect or random effects model was chosen for pooled effect size calculations When I2 is less than 25%, it indicates low heterogeneity A value of 50% suggests moderate heterogeneity, and 75% suggests high heterogeneity Depending on the level of heterogeneity, either the fixed effect model or the random effects model
Archivio
Italiano di Urologia e Andrologia 2024; 96(1):12066
2
o f fi v e d o m a i n s , n a m e l y R a n d o m i z a t i o n P r o c e s s , D e v i a t i o n s f r o m I n t e n d e d I n t e r v e n t i o n s , M i s s i n g
e l s o f t w a r e a n d t h e s t a t i s t i c a l s o f t w a r e R e v i e w
x c
The efficacy and safety of prostatic urethral lift as a minimally invasive therapeutic modality to treat lower urinary tract symptoms
was used to calculate the pooled effect size The fixed effect model was used when there was low heterogeneity, while the random effects model was used when there was significant heterogeneity (8)
Characteristic of included study
ical therapy) and short-term follow-up This screening yielded seven eligible studies aligning with our PICO criteria, all RCTs, published within the past decade, and available in full-text format No additional studies meeting inclusion criteria were sourced from prior reviews The review encompassed a total of 378 patients
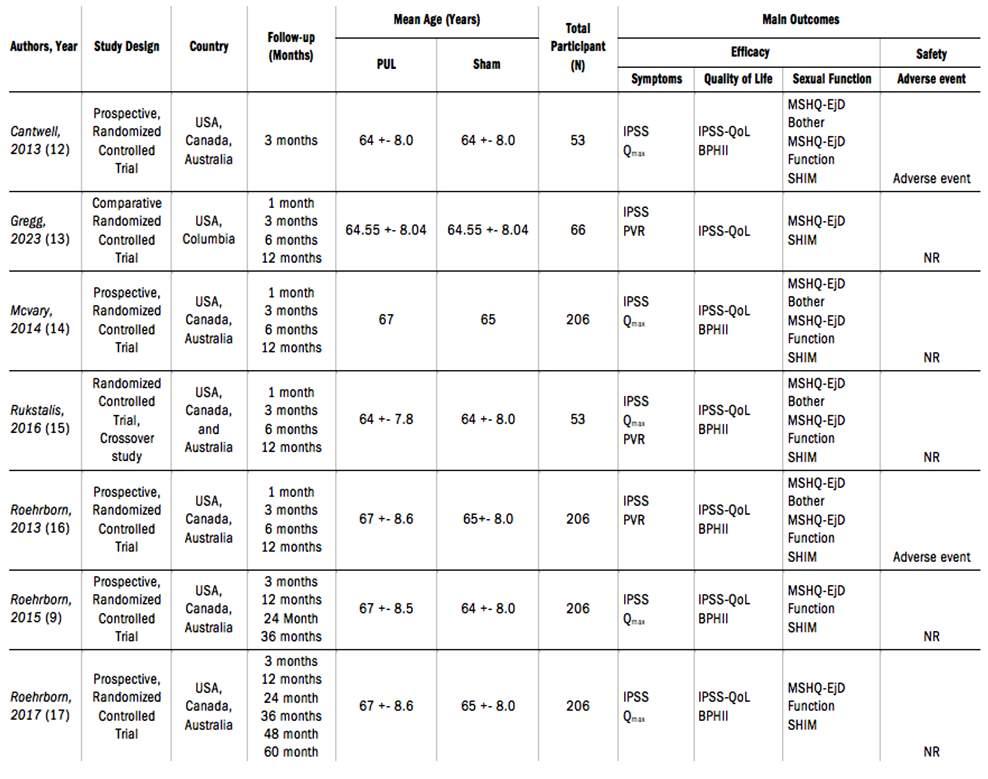
RESULTS
Literature search
According to the standard PRISMA protocol as the foundation of this study, our initial search yielded 753 articles After removing 80 duplicated articles, we were left with 672 articles for title and abstract screening Out of these 672 articles, 649 did not meet the required form of the article and were subsequently excluded Consequently, we sought retrieval for the remaining 23 articles Among them, we were able to access the full text of ten studies for further analysis From an initial pool of ten studies, three were excluded for reasons such as unrelated comparator variables (e g , vapor therapy, oral med-
Additionally, a thorough manual search of reference lists from various sources was conducted to ensure comprehensive coverage
Risk of bias from included studies
All studies incorporated were prospective, randomized controlled trials The Revised Cochrane Risk of Bias (RoB) tool, tailored for such trials, was used to evaluate risk of bias One study had a moderate bias risk due to questionnaire measurement and outcome reporting issues Similarly, another study displayed suboptimal outcome reporting The remaining studies showed uncertainties regarding questionnaire measurement
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066 3
Table 2
Characteristics of the studies
Internat onal prostate symptom score (IPSS); Post Vo ume Residual (PVR); Internat onal prostate symptom score – Qua ity of L fe (IPSS-QOL); Benign Prostatic Hyperplas a Impact Index (BPHII); Ma e Sexual Health Questionna re - Ejaculatory Dysfunct on Bother (MSHQ-EjD Bother); Male Sexua Health Questionna re - E aculatory Dysfunction Funct on (MSHQ-EjD Function); Sexua Health Inventory for Men (SHIM)
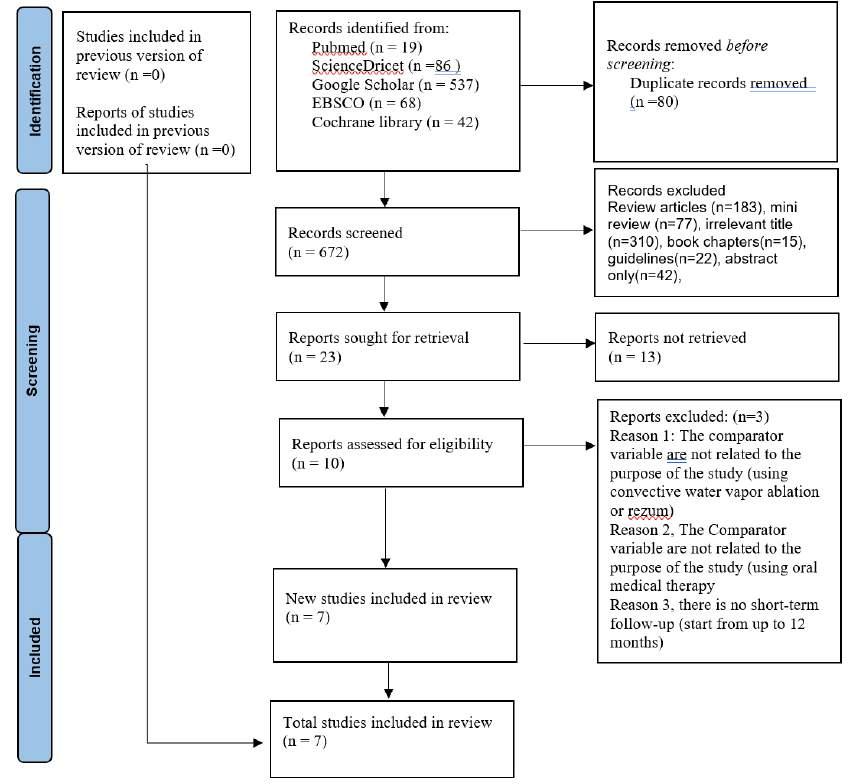
LUTS
Based on the analysis of three studies, the average IPSS score after 3 months of PUL action was significantly lower by 5 51 (95% CI 1 01-10 02) compared to the Sham group In other words, the Sham group had an average post-treatment IPSS score 5 51 points higher than the PUL group A higher IPSS score indicates a greater severity of symptoms (p = 0 02) Based on the results of Egger's test of IPSS findings an asymmetrical funnel plot was found indicating publication bias (p = 0 0382) Based on the analysis involving three studies, it was found that Qmax value after 3 months of PUL action was significantly higher by 2 13 (CI 95% 1 04-3 22) compared to Sham (p-value = 0 0001) Based on the Egger’s test of Qmax results, there was no funnel plot asymmetry which indicates that there is no publication bias (p = 0 1003) Based on the forest plot results, there was no significant difference between the PUL and Sham groups for the PVR value (P = 0 93) (Figure 2)
Quality of Life
Based on the analysis of three studies, the average BPHII score after 3 months of PUL action was significantly lower by 2 14 (95% CI 1 52-2 77) compared to the Sham group (p < 0 0001) In other words, the Sham group had an
Figure 1 PRISMA 2020 flow diagram used to identify the analyzed study in this review
average BPHII score 2 14 points higher than the PUL group, indicating a significantly worse severity of symptoms Based on the results of Egger's test for BPHII, it was found an asymmetrical funnel plot indicating publication bias (p = 0 0371)
Based on the analysis of three studies, the average quality of life (QoL) score after 3 months of PUL action was significantly lower by 1 50 (95% CI 1 14-1 86) compared to the Sham group (p < 0 00001)
This indicates that the PUL group had a significantly better QoL score compared to the Sham group
Based on the results of Egger's test of IPSS-Qo, t was found an asymmetrical funnel plot indicating publication bias (p = 0 0108) (Figure 3)
Sexual function
Based on the forest plot results, there was no significant difference between the PUL and Sham groups for SHIM scores (p = 0 64), MSHQ- EjD Function (p = 0 09), and MSHQ- EjD Bother (p = 0 07) Based on the egger ’ s test results for SHIM, MSHQ-Ejd Function, and MSHQ-EjD Bothers, there is no funnel plot asymmetry which indicates that there was no publication bias (p = 0 8806; p = 0 5414; p = 0 9147) (Figure 4)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066
4
S Mirsya Warli, M Fahmi Ikram, R Gerald Sarumpaet, Z Zulkarnaini Tala, I Ivan Putrantyo
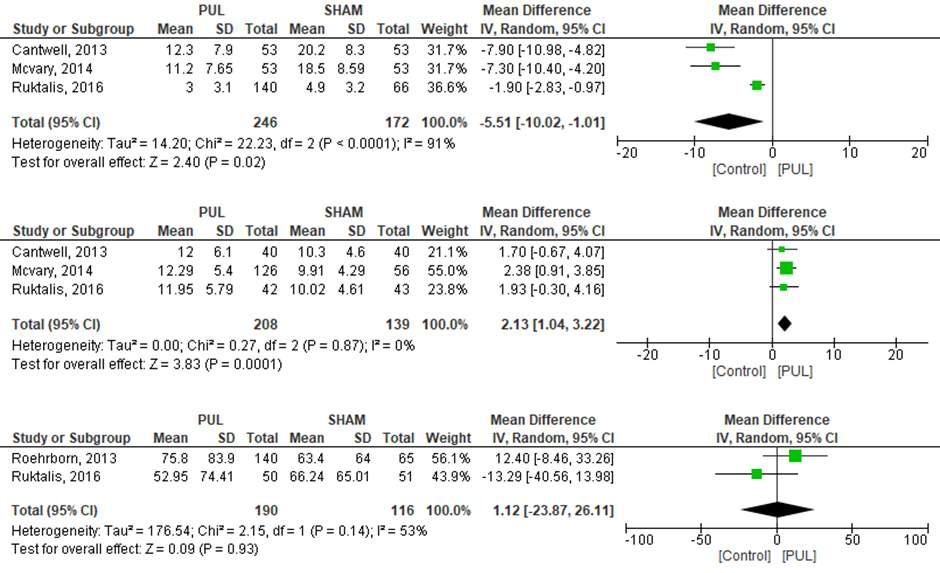
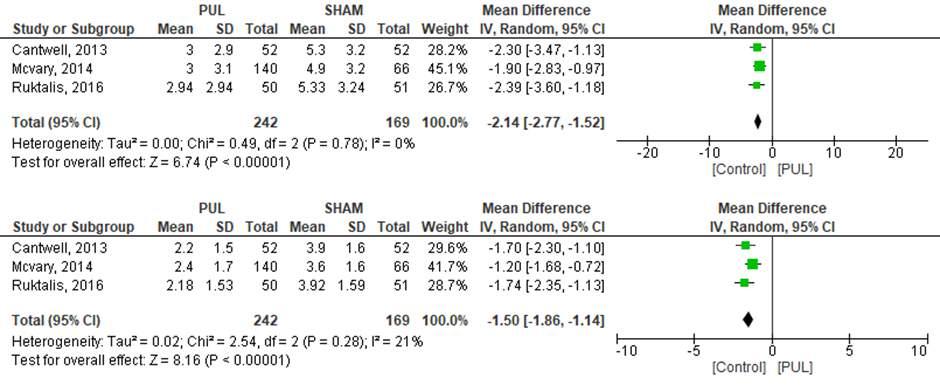
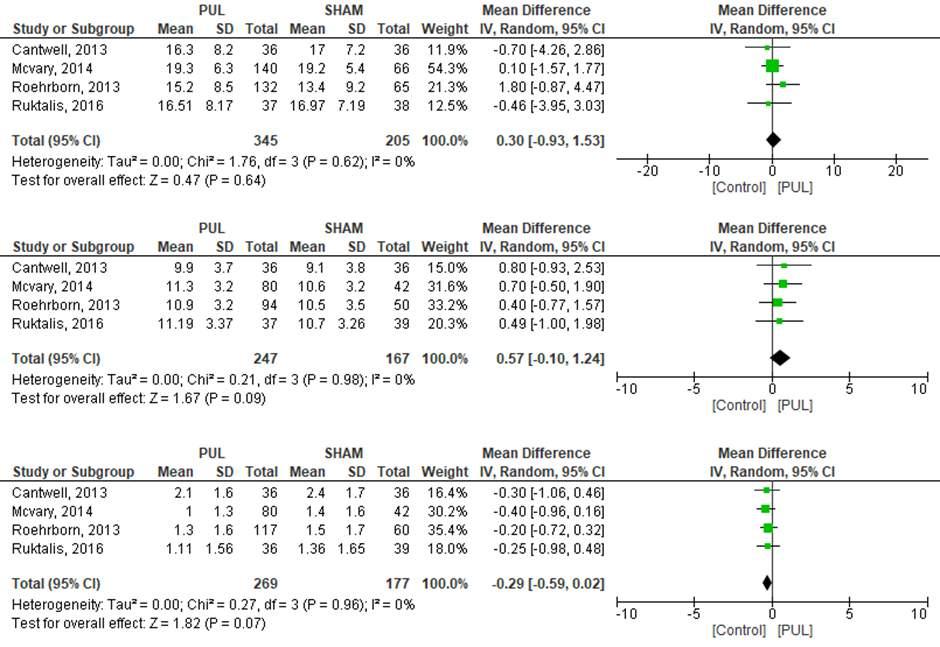
Figure 2. (A) Meta-analysis of comparison of IPSS between PUL and control group (Rigid Cystoscopy) after 3 months follow-up (B) Qmax value between PUL and control group (Rigid Cystoscopy) after 3 months follow-up (C) PVR value between PUL and control group (Rigid Cystoscopy) after 3 months follow-up
Figure 3 (A) Meta-analysis of comparison of BPHII between PUL and control group (Rigid Cystoscopy) after 3 months follow-up (B) IPSS-QoL score between PUL and control group (Rigid Cystoscopy) after 3 months follow-up.
Figure 4. (A) Meta-analysis of comparison of SHIM score between PUL and control group (Rigid Cystoscopy) after 3 months follow-up (B) MSHQ-EjD Function score between PUL and control group (Rigid Cystoscopy) after 3 months follow-up (C) MSHQ-EjD Bother score between PUL and control group (Rigid Cystoscopy) after 3 months follow-up
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066 5 The efficacy and safety of prostatic urethral lift as a minimally invasive therapeutic modality to treat lower urinary tract
symptoms
A B. C. A B. C. A B.
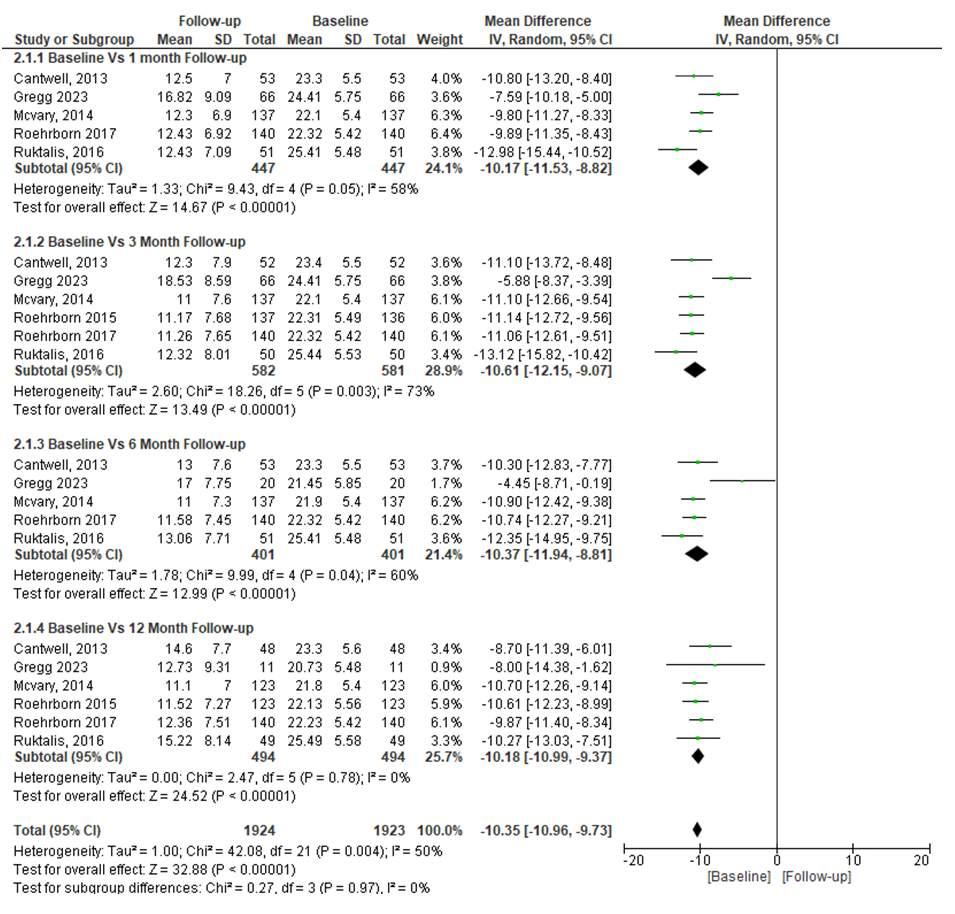
Subgroup analysis
LUTS
Subgroup analysis was performed based on IPSS score along follow-up The analysis demonstrated that IPSS scores at 1, 3, 6, and 12 months post-PUL were significantly lower by 10 17, 10 61, 10 37, and 10 18, respectively, compared to baseline (p < 0 0001 for all) Lower IPSS scores indicate higher symptom improvement No significant difference in average IPSS value across different follow-up durations was observed (p = 0 97) Egger's test results for IPSS indicated no funnel plot asymmetry, suggesting no publication bias for each follow-up duration (p = 0 7614; p = 0 6467; p = 0 2887; p = 0 1703) (Figure 5)
Quality of Life
The analysis revealed that QoL scores at 1, 3, 6, and 12 months post-PUL were significantly lower by 1 97, 2 07, 2 05, and 2 20, respectively, compared to baseline (p < 0 0001 for all) Lower QoL scores indicate higher symptom improvement No significant difference in average QoL value across different follow-up durations was
Figure 5
Subgroup Meta-analysis of comparison of IPSS between baseline and 1, 3, 6, and 12 months follow-up after PUL treatment
observed (p = 0 67) However, Egger's test for IPSS-QoL indicated asymmetrical funnel plots at 6 and 12 months follow-up, suggesting publication bias, although not at 1 and 3 months follow-up (p = 0 9806; p = 0 838; p = 0 0483; p = 0 0002) (Figure 6)
Sexual function
Subgroup analysis based on SHIM score during follow-up was conducted The analysis showed no significant SHIM score difference between baseline and follow-up at 1 month (p = 0 28), 3 months (p = 0 04), 6 months (p = 0 08), and 12 months (p = 0 34) Likewise, there was no significant difference in average SHIM values across different follow-up durations (p = 0 90) Egger's test for SHIM indicated asymmetrical funnel plots at 3 months follow-up, suggesting publication bias, but not at other follow-up durations (p = 0 5326; p = 0 0487; p = 0 1436; p = 0 1360) (Figure 7)
The analysis revealed that MSHQ-EjD Function scores at 1, 3, 6, and 12 months post-PUL were significantly higher by 2 09, 1 88, 1 64, and 1 40, respectively, compared to baseline (p < 0 00001 for all) Higher MSHQ-EjD Function scores indicate greater symptom improvement
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066
6
S Mirsya Warli, M Fahmi Ikram, R Gerald Sarumpaet, Z Zulkarnaini Tala, I Ivan Putrantyo
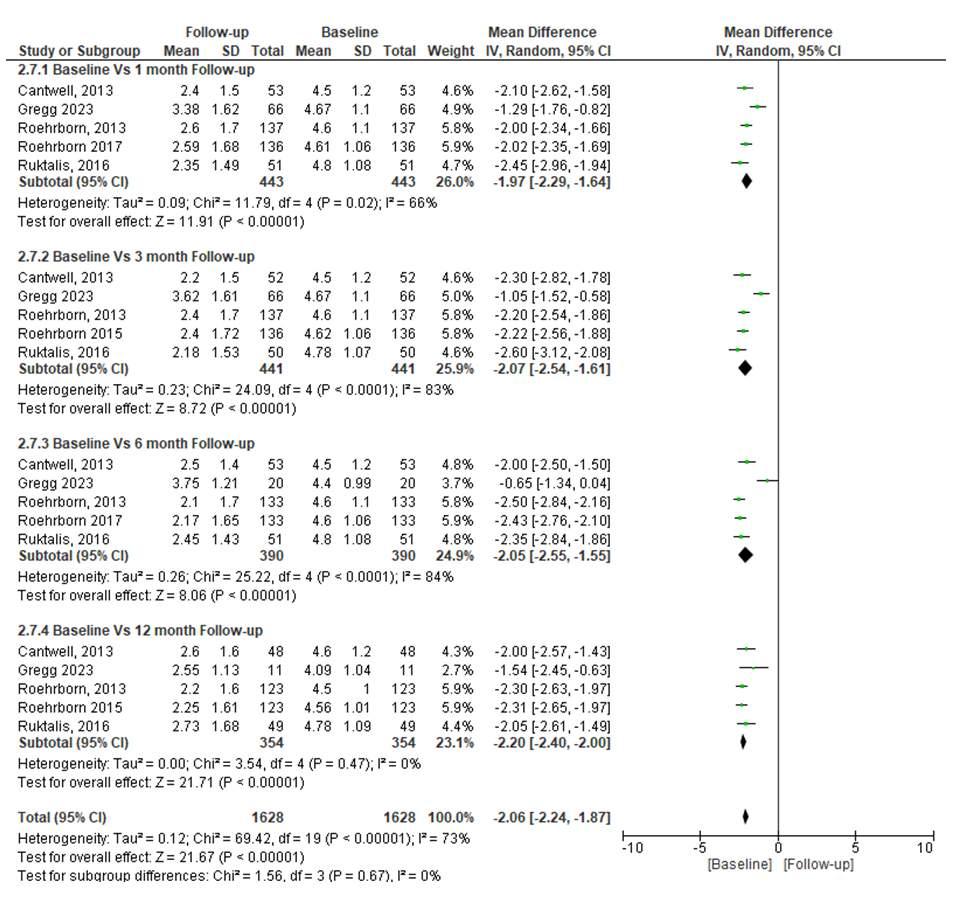
No significant difference in average MSHQ-EjD value across different follow-up durations was observed (p = 0 33) Egger's test for MSHQ-EjD Function showed no funnel plot asymmetry, suggesting no publication bias for each follow-up duration (p = 0 8395; p = 0 2660; p = 0 8406; p = 0 9254) (Figure 8)
Adverse events
Two studies, Roehrborn (16) and Cantwell (12), reported adverse events in the analysis In the study of Roehrborn et al , the PUL group had 113 events out of 140, while the Sham group had 20 events out of 66 In the study of Cantwell et al , the PUL group had 12 events out of 53, and the Sham group had 15 events out of 53
The PUL group showed a nonsignificant 1 51 higher risk for adverse events (OR 1 51; 95% CI 0 46-4 89; p = < 0 50), with high heterogeneity in the analysis (I2 = 90%) (Figure 9)
Publication bias
The funnel plots based on the outcomes are shown in Figure 10 Because all studies laid inside the 95% CI limits, no evidence of publication bias was noted Egger test
Figure 6 Subgroup Meta-analysis of comparison of QoL score between baseline and 1,3,6 and 12 months follow-up after PUL treatment
was performed to provide statistical evidence regarding funnel plot symmetry Results still did not reveal any evidence of publication bias for Qmax (p = 0 1003), MSHQEjD Function (p = 0 5414), SHIM (p = 0 8806), and MSHQ-Ejd Bother (p = 0 9147) of PUL vs Sham in 3 months follow-up duration (Figure 10)
DISCUSSION
Benign Prostatic Hyperplasia (BPH) is a common condition in aging men, with a significant global rise In 2019, 612 7 million men were affected, up by 41% since 1990 Incidence can be high, reaching 80% to 90% in men aged 70 and above
This worries urologists due to BPH's impact on quality of life Enlarged prostate disrupts urinary function, causing LUTS that affect bladder, urethra, and sexual health Tools like IPSS, PVR, and Qmax quantify symptoms TURP is the standard treatment, but lasers are emerging as alternatives (9) A new minimally invasive method, PUL, is promising for managing BPH-related LUTS PUL involves repositioning the prostate with small implants, swiftly relieving symptoms and causing minimal side effects
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066 7 The efficacy and safety of prostatic urethral lift as a minimally invasive therapeutic modality to treat lower urinary tract symptoms
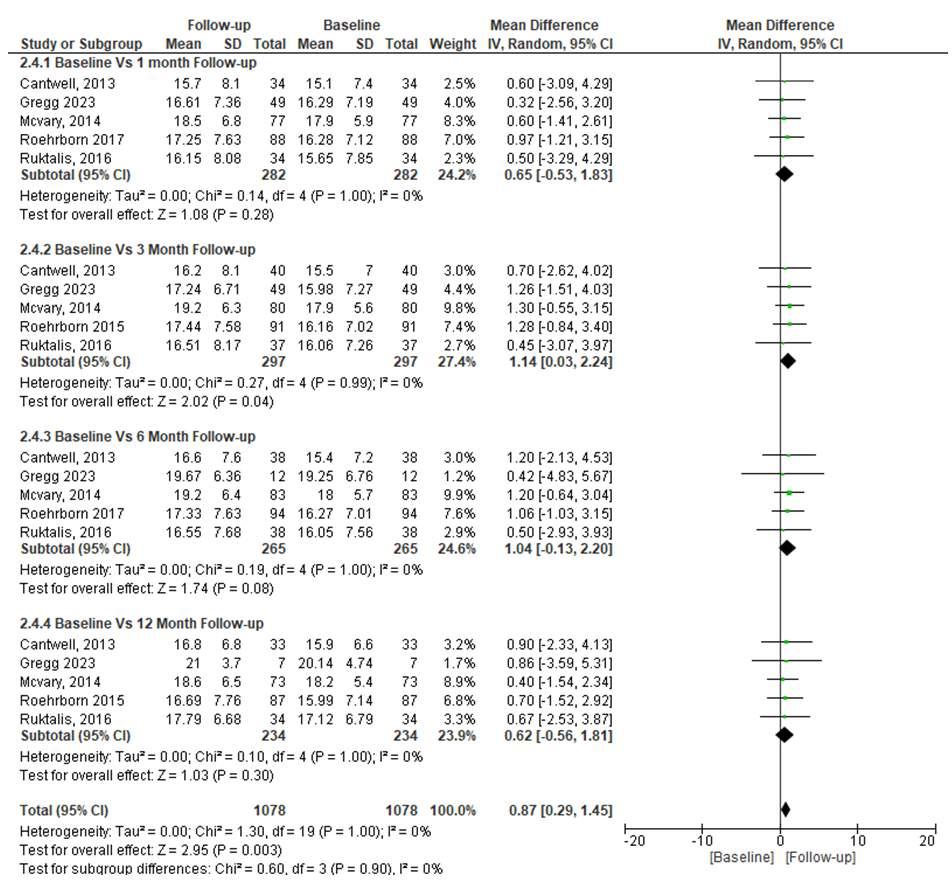
This approach aims to balance symptom relief, better quality of life, and maintained sexual function, offering a valuable alternative to existing treatments This review focused on assessing PUL's effectiveness in improving LUTS symptoms, quality of life, and sexual function in BPH patients, using internationally validated scores and comparing them with control variables and baseline measurements post-PUL therapy (10) In this review, the Sham procedure served as a control, mimicking a placebo surgery for comparison This could be done under various forms of anesthesia It involves placing implants to gently retract obstructive prostate lobes, distinguishing it from other BPH treatments (11) In contrast to TURP, the PUL procedure provides measurable functional improvements and quality of life enhancements without major adverse events It preserves erectile and ejaculatory function, albeit with mild to moderate, short-term side effects (12)
As per the European Association of Urology (EAU), PUL effectively treats BPH with fewer side effects than TURP, especially regarding recovery time and sexual function However, more research is needed to confirm these findings (13) Short- and medium-term studies highlight
Figure 7 Subgroup Meta-analysis of comparison of SHIM score between baseline and 1, 3, 6 and 12 months follow-up after PUL treatment
PUL's significant improvement in urination ability and overall quality of life after the procedure (14) An advantage of PUL is its lack of negative effects on erectile and ejaculatory function No instances of worsened function have been reported following PUL, thanks to its tissuesparing approach that maintains bladder neck integrity and avoids thermal damage, minimizing the risk of ED (15) In relation to enhancing LUTS in BPH patients with PUL, this review observed a significant 3-month reduction in mean IPSS score, 5 51 times lower than Sham Similar results were found in Cantwell's study, where PUL showed a 122% greater mean IPSS improvement, with a change of 11 1 points (7 2) versus 5 points (7 5) in 53 patients (16) Subgroup analysis revealed the most notable mean IPSS improvement at 3 months, decreasing significantly by 10 61 times from baseline, followed by 10 37 times at 6 months Improvement persisted at 12 months, albeit with a slight reduction However, no significant differences in IPSS score change were noted between follow-up periods
The IPSS score, a globally standardized tool with 8 questions, quantitatively evaluates LUTS symptoms post-diagnosis or in treated patients, categorizing scores of 0, 8-19,
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066
8
S Mirsya Warli, M Fahmi Ikram, R Gerald Sarumpaet, Z Zulkarnaini Tala, I Ivan Putrantyo
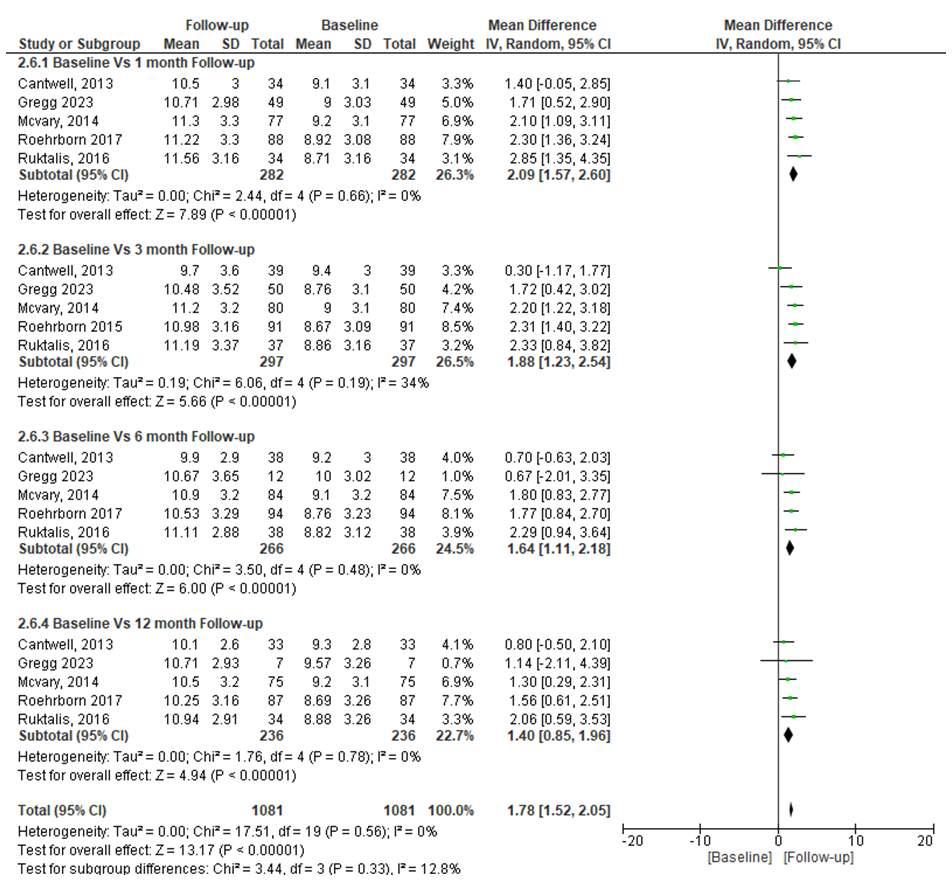

and 20-35 as no/mild, moderate, and severe symptoms, respectively (17)
Other findings highlighted PUL's efficacy in addressing LUTS symptoms through uro-flowmeter-assessed max imum flow rate (Qmax), a non-invasive urodynamic test for BPH-related bladder detrusor muscle function (18) From this review's analysis of 3 studies, PUL significantly outperformed Sham in mean Qmax improvement at 3 months post-procedure Notably, the greatest Qmax enhancement was at 3 months post-PUL, a 4 03 times increase from baseline
This aligns with Rukstalis et al 's study, reporting a substan-
Figure 8. Subgroup Meta-analysis of comparison of MSHQ-EjD Function score between baseline and 1, 3, 6 and 12 months follow-up after PUL treatment
Figure 9. Meta-analysis of all related adverse events of PUL treatment.
tial Qmax increase from 7 95 mL/sec to 11 95 mL/sec at 3 months post-PUL (19) While the 12-month post-PUL Qmax change showed a decrease, significant improvement remained evident Results showed no significant Qmax change between follow-ups Normal Qmax in men is > 15 mL/second, potentially declining with age (20) Post residual volume (PVR) assessment reveals leftover urine after urination, often using a catheter Elderly normal PVR values range from 50-100 mL; > 200 mL or < 50 mL suggests bladder or prostate issues (20-22) Compared to baseline, PVR significantly improved, especially at 3 months postPUL At 12 months, improvement remained PUL exhibit-
Italiano di Urologia e Andrologia 2024; 96(1):12066 9 The efficacy
safety of prostatic urethral lift
invasive therapeutic
to treat lower urinary tract
Archivio
and
as a minimally
modality
symptoms
Figure 10.
Based on the Egger’s test results for Qmax, SHIM, MSHQ-Ejd Function, and MSHQ-EjD Bothers, there is no funnel plot asymmetry which indicates that there is no publication bias (p = 0 1003; p = 0 8806; p = 0 5414; p = 0 9147)

ed swift, significant LUTS symptom improvement within 3 months, supporting its potential for treating BPH patients' symptoms Its minimally invasive nature makes widespread use likely (22)
The analysis of 3 studies in this review found that BPHII scores at 3-month after PUL were less worse compared to Sham (22) Another subgroup analysis comparing change in mean BPHII scores between baseline and post-PUL follow-up showed significant improvement across different intervals, with the best enhancement at 6 months (4 11 times lower) (22) The BPHII questionnaire includes 4 domains assessing micturition problems' impact on physical discomfort, health concerns, symptom bother, and interference with activities Scores range from 0 (no symptoms) to 13 (severe symptoms) (22, 23)
Similarly, the IPSS-QoL score assesses a patient's outlook on his current micturition condition, with scores ranging from 0 (happy) to 6 (very bad) (23) This review revealed that IPSS-QoL scores at 3 months after PUL were significantly better when compared to Sham Another subgroup analysis found the best IPSS-QoL score improvement at 12 months post-PUL (24) However, IPSS score change showed no significant difference between follow-up durations Given PUL's significant impact on improving the quality of life by rapidly addressing LUTS complaints linked to BPH and its high effectiveness, its steady use in various health centers is anticipated to reduce morbidity and mortality rates in BPH patients
Impaired sexual function is common in BPH patients due to the impact of LUTS symptoms and prostate enlargement This review indicated that PUL therapy's effective-
ness in improving sexual function wasn't significantly better than Sham at the 3-month follow-up for such patients (24) However, McArvy et al 's study intriguingly found that mean SHIM scores increased at each follow-up interval without worsening Similar findings were supported by Rukstalis et al , showing stable improvement in SHIM scores at 1, 3, 6, and 12 months post-PUL from baseline (25) Conversely, the mean MSHQ-EjD Function score significantly improved, with scores increasing at each follow-up interval compared to baseline, notably at 1-month post-PUL These results suggest that PUL doesn't negatively impact urogenital anatomy, allowing sexual function to naturally progress while also improving LUTS symptoms Notably, PUL's positive effect on sexual function contrasts with other therapies like TURP, often causing significant sexual function disorders such as erectile dysfunction and ejaculation issues (25) The adverse effects of PUL therapy vary A review of two studies revealed that the common adverse events after PUL were dysuria, hematuria, pelvic pain, and urgency, all resolving within two weeks No severe events leading to mortality occurred Hematuria improved within 3 days without needing blood transfusion Pelvic pain was measured using VAS during follow-up (26) Notably, there were no reports of adverse events impacting sexual function, like impaired ejaculation or erectile function, highlighting a clear advantage of the PUL procedure Its bladder neck integrity preservation and absence of thermal tissue damage allow for controlled antegrade ejaculation and reduced risk of erectile dysfunction (27) This review has limitations due to the limited number of
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066
10
S Mirsya Warli, M Fahmi Ikram, R Gerald Sarumpaet, Z Zulkarnaini Tala, I Ivan Putrantyo
The efficacy and safety of prostatic urethral lift as a minimally invasive therapeutic modality to treat lower urinary tract symptoms
studies, resulting in some analyses having high heterogeneity However, subgroup analysis and random effects models helped minimize this issue Most studies didn't categorize score results according to international guidelines, preventing risk analysis using RR or OR Additional studies are needed for a comprehensive analysis More studies comparing PUL with common BPH therapies like TURP are expected PUL is recommended for high BPH risk populations like the elderly in densely populated areas where qualified therapy modalities are advised
CONCLUSIONS
PUL plays a vital role in rapidly and significantly improving BPH-related LUTS and urinary flow, making it a viable operative option for BPH patients Beyond swift symptom relief, PUL preserves sexual function, enhancing it as symptoms resolve Additionally, its minimally invasive nature results in minimal side effects and low morbidity compared to other therapies With these significant outcomes, PUL holds promise to replace established procedures like TURP or enucleation in BPH management However, broader clinical studies are recommended to comprehensively assess its efficacy, especially given its current limited use
AUTHOR’SCONTRIBUTIONS
Syah Mirsya Warli contributed to the conception, editing, and supervision for this work
Zaimah Zulkarnaini Tala contributed to the design, supervision, and providing resources and funding for this work
Muhammad Fahmi Ikram, Raja Gerald Sarumpaet, and Ignatius Ivan Putrantyo contributed equally to drafting, data curation and analysis, data interpretation and writing original draft for this work
ACKNOWLEDGEMENTS
W e t h a n k D e a n o f F a c u l t y o f M e d i c i n e , U n i v e r s i t a s Sumatera Utara for their continuous support
REFERENCES
1 Madersbacher S, Sampson N, Culig Z Pathophysiology of Benign Prostatic Hyperplasia and Benign Prostatic Enlargement: A MiniReview Gerontol 2019; 65:458-464
2 Egan KB The Epidemiology of Benign Prostatic Hyperplasia Associated with Lower Urinary Tract Symptoms: Prevalence and Incident Rates Urol Clin North Am 2016; 43:289-97
3 Lokeshwar SD, Harper BT, Webb E, et al Epidemiology and treatment modalities for the management of benign prostatic hyperplasia Transl Androl Urol 2019; 8:529-539
4 De Nunzio C, Roehrborn CG, Andersson KE, McVary KT Erectile Dysfunction and Lower Urinary Tract Symptoms Eur Urol Focus 2017; 3:352-63
5 Sønksen J, Barber NJ, Speakman MJ, et al Prospective, randomized, multinational study of PUL versus transurethral resection of the prostate: 12-month results from the BPH6 study Eur Urol 2015; 68:643-652
6 Moher D, Liberati A, Tetzlaff J, et al Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement PLoS Med 2009; 6:e1000097
7 Higgins J, Thompson S, Deeks J, Altman D Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice J Heal Serv Res Policy 2002; 7:51-61
8 Higgins JPT, Green S Cochrane handbook for systematic reviews of interventions version 5 1 0 [updated March 2011] In: The Cochrane collaboration, vol 2, p 126
9 Roehrborn CG, Rukstalis DB, Barkin J, et al Three-year results of the prostatic urethral L I F T study CJU 2015; 22:7772-82
10 Bozkurt A, Karabakan M, Keskin E, et al Prostatic Urethral Lift: A New Minimally Invasive Treatment for Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia Urol Int 2016; 96:202-206
11 Perera M, Roberts MJ, Doi SAR, Bolton D Prostatic Urethral Lift improves urinary symptoms and flow while preserving sexual function for men with benign Eur Urol 2015; 67:704-13
12 Cantwell AL, Bogache WK, Richardson SF, et al Prostatic Urethral Lift for the treatment of LUTS BJU Int 2014; 113:615-622
13 Eure G, Rukstalis D, Roehrborn C Prostatic Urethral Lift for Obstructive Median Lobes: Consistent Results Across Controlled Trial and Real-World Settings J Endourol 2023; 37:50-59
14 McVary KT, Gange SN, Shore ND, et al Prostatic Urethral Lift for BPH Preserves Sexual Function J Sex Med 2014; 11:279-287
15 Rukstalis D, Rashid P, Bogache WK, et al 24-month durability after crossover to the prostatic urethral lift from randomised, blinded Sham BJU Int 2016; 118:14-22
16 Roehrborn CG, Gange SN, Shore ND, et al The prostatic urethral lift for the treatment of lower urinary tract symptoms associated with prostate enlargement due to benign prostatic hyperplasia: the L I F T Study J Urol 2013; 190:2161-7
17 Roehrborn CG, Barkin J, Gange SN, et al Five-year results of the prospective randomized controlled prostatic urethral L I F T study Can J Urol 2017; 24:8802-8813
18 Dawu AE, Tosepu R, Effendy DS Benign Prostate Hyperplasia (BPH) in Inpatient Rooms at Aliyah II General Hospital Kendari, Southeast Sulawesi, Indonesia KnE Life Sciences 2022; 78-81
19 Chughtai B, Forde IC, Thomas DDM, et al Benign prostatic hyperplasia Nat Rev Dis Primers 2016; 2:16031
20 Wang YB, Yang L, Deng YQ, et al Causal relationship between obesity, lifestyle factors and risk of benign prostatic hyperplasia: a univariable and multivariable Mendelian randomization study 2022; 20:495
21 Engström G, Henningsohn L, Engström MLW, Leppert J Impact on quality of life of different lower urinary tract symptoms in men measured by means of the SF 36 questionnaire Scand J Urol 2006; 40:485-494
22 Burke N, Whelan JP, Goeree L, et al Systematic review and metaanalysis of transurethral resection of the prostate versus minimally invasive procedures for the treatment of benign prostatic obstruction Urology 2010; 75:1015-22
23 Sun F, Sun X, Shi Q, Zhai Y Transurethral procedures in the treatment of benign prostatic hyperplasia: A systematic review and m e t a - a n a l y s i s o f e ff e c t i v e n e s s a n d c o m p l i c a t i o n s M e d i c i n e (Baltimore) 2018; 97:e13360
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066 11
S Mirsya Warli, M Fahmi Ikram, R Gerald Sarumpaet, Z Zulkarnaini Tala, I Ivan Putrantyo
24 Shore N, Freedman S, Gange S, et al Prospective multi-center study elucidating patient experience after prostatic urethral lift Can J Urol 2014; 21:7094-7101
25 Pessoa R, Kim FJ Urodynamics and Voiding Dysfunction In Abernathy’s Surgical Secrets: Seventh Edition Elsevier Inc 2018; 103:452-452
26 Johnson TV, Abbasi A, Ehrlich SS, et al IPSS quality of life question: a possible indicator of depression among patients with lower urinary tract symptoms Can J Urol 2012; 19:6100-6104
27 Favilla V, Cimino S, Salamone C, et al Risk factors of sexual dysfunction after transurethral resection of the prostate (TURP): a 12 months follow-up J Endocrinol Invest 2013; 36:1094-1098
Correspondence
Syah Mirsya Warli, MD, PhD warli@usu ac id
Division of Urology, Department of Surgery, Faculty of Medicine, Universitas Sumatera Utara-Haji Adam Malik General Hospital, Medan, Indonesia; Address: Jl Bunga Lau No 17, Medan, Indonesia
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12066
12
SYSTEMATIC REVIEW
Role of ureteral stent material and coating to prevent ureteral stent related issue: A systematic review and meta analysis
Ignatius Ivan Putrantyo 1 , Syah Mirsya Warli 2, 3 , Ginanda Putra Siregar 2 , Fauriski Febrian Prapiska 2 , Dhirajaya Dharma Kadar 2 , Bungaran Sihombing 2
1 Department of Urology, Faculty of Medicine, Universitas Indonesia, Depok; Haji Adam Malik General Hospital, Medan, Indonesia;
2 Division of Urology, Department of Surgery, Faculty of Medicine, Universitas Sumatera Utara, Haji Adam Malik General Hospital, Medan, Indonesia;
3 Department of Urology, Universitas Sumatera Utara Hospital, Universitas Sumatera Utara, Medan, Indonesia
Summary
Introduction: Ureteral stents require materials that balance bulk and surface properties. Achieving both can be challenging, as ideal bulk properties may not align with optimal surface properties. Thus, researching coatings and biomanufacturing methods for ideal materials is essential.
Methods: A systematic review and meta-analysis, following PRISMA Guidelines, involved literature searches across five databases: PubMed, Scopus, Embase, ClinicalKey, and Cochrane From 417 screened articles, eight studies were deemed eligible for qualitative and quantitative analysis The selected articles underwent bias assessment using ROB Tools 2
Results: The systematic review analyzed 1 356 participants Findings revealed that firm ureteral stents significantly increased risk of infection, hematuria, and lower body pain On the contrary, soft stents reduced infection (OR: 0 62; p = 0 004), hematuria (OR: 0.60; p = < 0.001), and lower body pain (OR: 0 63; p = 0 0002) However, infection reduction effect was uncertain due to heterogeneity. Coated vs. non-coated material analysis found no difference in encrustation (OR: 1 26; p = 0 52) or infection (OR: 1.67; p = 0.99). Stent firmness didn't affect encrustation on double J stent (OR: 0 97; p = 0 17)
Conclusions: Softer materials like silicone are preferred for ureteral stents to reduce symptoms like hematuria and lower body pain. Coatings like silver nanoparticles and triclosan, while enhancing antimicrobial properties, didn't effectively lower infection risk.
KEY WORDS: Double J (DJ) stent; Bulk properties; Surface properties; Material coating; Polymers
Submitted 9 November 2023; Accepted 14 November 2023
INTRODUCTION
Ureteral stent is one of the medical implants more often used by urologists after urinary catheter Double J stent (DJ stent) insertion procedure could be categorized as a routine and simple urology procedure Despite various materials researched to fulfill the demand for ideal ureteral stent, there are still numerous issues to be solved Based on research conducted by Geavlete et al in 2021, there were 41 369 complications from 50 000 procedures (82 7%),
which was considered an high rate The most common complication from DJ stent insertion is irritative bladder symptoms with 16 326 occurrences (32 7%), followed by hematuria with 7 436 cases (14 8%) (1) These ureteral stent-related problems are often considered a problem arising from the stent materials A material that is too firm could cause discomfort which lower the patient’s quality of life On the other hand, soft material could reduce its drainage ability Hydronephrosis, which is caused by external forces such as tumors, could easily beat the resistance force of the stent Firmness is not the only bulk property that could affect stent-related issues Other properties such as wear resistance, Young’s modulus, and tensile strength are also fundamental for DJ Stent material
Problems that arise from DJ Stent could come from mucosal friction during stent placement, infection due to retained microbes in the stent, and encrustation Nowadays, there are various materials used for DJ Stents although the use of metal is uncommon Metal is very firm, rigid, and has low brittleness The inflexibility and rigidity of metal stents are highly likely to cause ureteral injury during their placement Furthermore, metal DJ Stent replacement could be very challenging and risky Thus, polymer is still considered the best option for DJ Stent
Recently, the technology in additive manufacturing has grown rapidly Therefore, the idea to use coating in DJ stent to reduce friction, encrustation occurrences, and infection rate has been researched intensively The research was not limited only to improve bulk properties, but also the surface properties Silver nanoparticle, as one of the most well-researched nanoparticles, has a very potent antimicrobial properties since its positive ion charge could damage the bacterial cell membrane and bind to bacterial DNA, preventing the bacteria to perform their basic function (2) Therefore, coating material with silver nanoparticles is quite promising to reduce the infection rate Other than silver nanoparticles, triclosan's ability to prevent biosynthesis of bacterial fatty acid allows it to be one of the surging coating materials (3) In summary, both bulk and surface properties are important to determine the characteristics of a material There are several criteria for the ideal material for DJ stent, which are
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12067 1
DOI: 10 4081/aiua 2024 12067
high Poisson ratio, high Young’s modulus, and high tensile properties and tear resistance with low brittleness and hardness Furthermore, a material with surface properties such as high wettability and hydrophilicity is preferred for ureteral stents since it will lower the risk of infection and risk of ureteral injury during ureteral stent placement (4) However, a material that has good bulk properties mostly does not have ideal surface properties Therefore, further research to seek an ideal material through coating and biomanufacturing is paramount to solve this issue
METHODS
Study objective
The study was done to determine the material for DJ stent with the least side effects and whether it has a significant role in reducing ureteral stent-related issues This study also aimed to determine whether the coating material has a role in reducing ureteral stent-related problem
Eligibility criteria
Type of studies
This study only included controlled trials which focus on ureteral stentrelated symptoms and comparing stents based on their material and coating We used the PICO (Patient, Intervention, Comparison, Outcome) model to answer the clinical question of this study Patient: Adults requiring DJ stent procedure; Intervention: DJ stent; Comparison: DJ stent with various materials, coating, and firmness; Outcome: Infection (primary), hematuria, encrustation, and pain after DJ stent placement
Type of participant
All participants were adult aged 18 years or above who underwent DJ stent procedure Participants who consume immunosuppressant or have autoimmune disease, hematological abnormalities, HIV/AIDS, malignancy, Systemic Lupus Erythematosus were excluded
Study screening and selection
The authors made a robust search strategy based on the PICO concept recommended by Cochrane Handbook for Systematic Reviews of Intervention version 5 1 0
Statistical analysis
Statistical analysis was performed with Review Manager 5 The authors performed six different subgroup analysis Heterogeneity
was assessed using the I2 statistics The significance of the pooled effects was evaluated by a Z test, and p < 0 05 was defined as significant The author prespecified a sensitivity analysis to investigate the effect of excluding studies with a high risk of bias to investigate the robustness of this review The author also repeated primary meta-analysis in case the range of values for decisions was uncertain by using alternative measures of effect size and statistical model Funnel plot was not performed since there were less than ten included studies
Results
Search results
Initially, the systematic search yielded 2696 articles The authors then removed 1133 studies due to duplication and other reasons The rest 1459 were then screened for its relevance based on title and abstract This process yielded 38 potentially eligible studies Following the fulltext reading, 30 studies were excluded for various reasons and only eight were eligible and included in this study (512) (Figure 1)

Archivio Italiano di Urologia e Andrologia 2024; 96(1):12067
2
I Ivan Putrantyo, S Mirsya Warli, G Putra Siregar, et al
Figure 1. PRISMA Chart Flow
Included studies
Eight controlled trials were included and no cluster trial and cross-over trial were included in this review
Settings
The studies were conducted in Canada, USA, Egypt, UK, Ireland, and Romania
All studies were performed in a hospital setting.
Patients
There was a total of 2249 patients which comprised 529 participants from soft DJ stent group, 1412 participants from the firm DJ stent group, 154 participants from the coated group, and 154 participants from the non-coated group
Risk of Bias in included studies
Figure 2 illustrated a summary of the authors’ assessment on eight included controlled trials in this study In summary, there were two studies which regarded to have a low risk of bias by the other, while the rest had moderate risk Since there was no high-risk bias from the studies included, no study was excluded from the meta-analysis
Bulk properties
In this review, the authors conducted six subgroup analysis, and half of them tried to find out whether firmness has a significant ureteral stent-related side effect Based on Figure 3A, it could be concluded that softer DJ Stent would lower the risk of urinary infection significantly (OR: 0 62; 95% CI: 0 45-0 86; p = 0 004) However, this result should be further investigated since it has high heterogeneity (> 50%) Therefore, more studies should be conducted in the future to obtain a better understanding of soft stent effect in reducing urinary tract infection (UTI) Softness also played a key role in reducing hematuria as
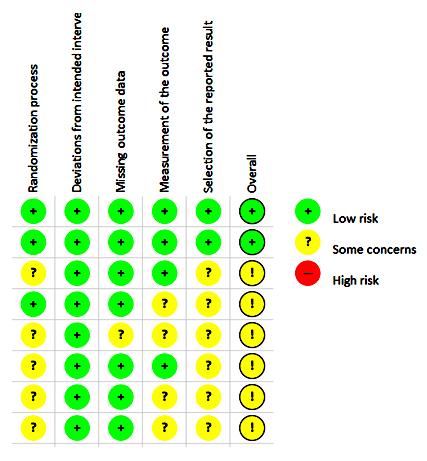
illustrated in Figure 3C, with the odds of people who had soft DJ stent will be 0 6 times compared to their counterparts (OR: 0 60; 95% CI: 0 48-0 75; p = < 0 001) Besides reducing risk of UTI and hematuria, soft DJ Stent could also lower the risk of experiencing lower body pain as depicted in Figure 3E Patient who received a relatively softer DJ stent experienced a significantly rate of lower body pain (OR: 0 63; 95% CI: 0 49-0 80; p = 0 0002) However, softness has no impact in reducing encrustation occurrences, as illustrated in Figure 3D (OR: 0 97; 95% CI: 0 69-1 37; p = 0 17)
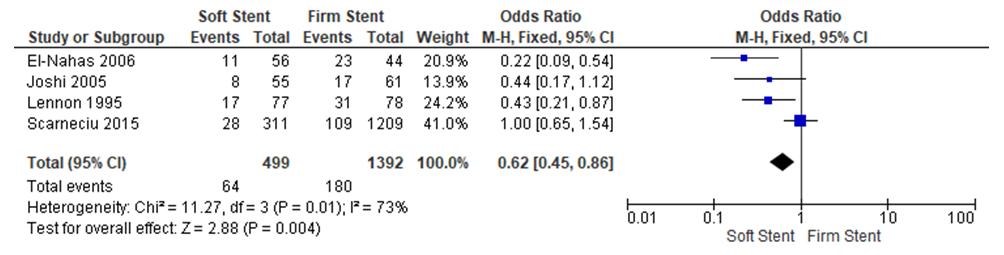
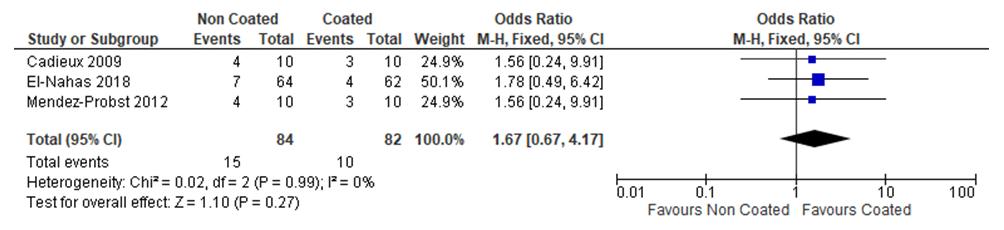
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12067 3 Ureteral stent material and coating
Figure 3. Generated Forest Plot
Figure 2
A. B.
Assessment of Risk of Bias

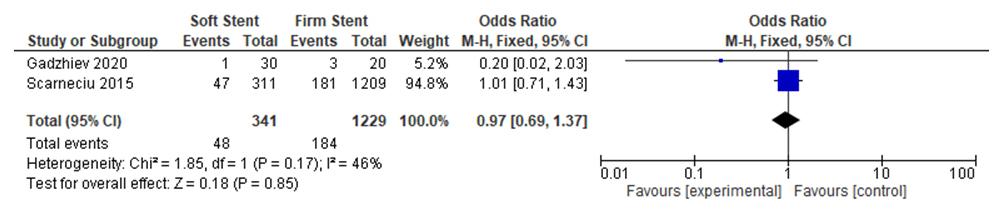
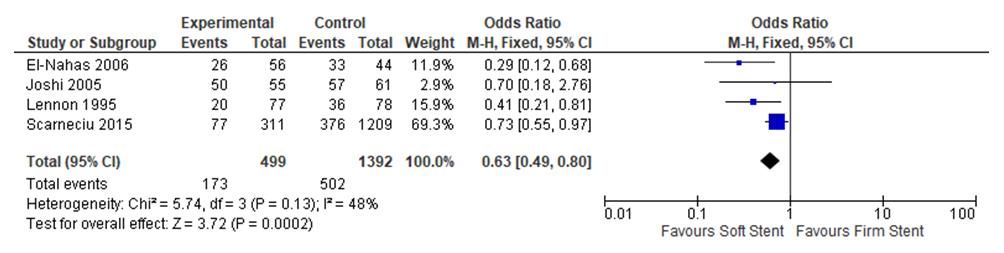
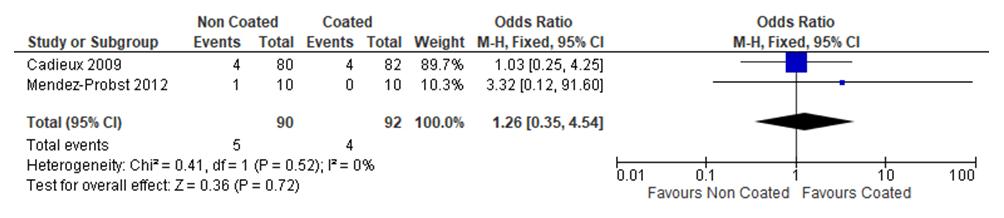
Surface properties
In this review, the authors also observed the role of surface properties in reducing ureteral stent-related issue The authors conducted a subgroup analysis on coated and non-coated DJ Stent As illustrated in Figure 3F, there were two studies included where Triclosan-Eluted Stent was used as coating material However, it was not effective to reduce encrustation (OR: 1 26; 95% CI: 0 354 54; p = 0 52) In another subgroup analysis, three studies were included One of them used silver as coating material, while the rest used triclosan The authors found that there is no significant effect of coated materials to reduce the occurrences of UTI, as shown in Figure 3B (OR: 1 67; 95% CI: 0 67-4 17; p = 0 99)
Heterogeneity
In this review, there were three reported imprecision and inconsistency in the results where the heterogeneity of subgroup analysis conducted in Figure 3A is higher than 40%,
and both the p-values given for Chi-square in Figure 3B and 3F were less than 0 1
DISCUSSION
There are numerous ways to categorize DJ stent materials In this review, the authors chose the easiest way, which is based on bulk and surface properties In terms of bulk properties, the authors would like to observe closely on several items such as firmness, Young’s modulus, elasticity, tensile strength, wear resistance, and biocompatibility However, there were very limited research which focus on those areas and the authors only managed to compare based on firmness alone
Firmness and softness are often defined ambiguously Thus, a certain parameter to make a clear line between them is of paramount importance Material with value of 40-64 A is categorized as soft while above 65 A is categorized as firm when measured using durometer (9)
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12067
4
I Ivan Putrantyo, S Mirsya Warli, G Putra Siregar, et al
C.
D.
E.
F.
In this study, we can conclude that softer stents will yield less hematuria and lower body pain Even though softness and elasticity could not be used interchangeably, they are closely related Firm DJ stent is predicted to increase difficulty in DJ stent placement
This means the force needed to insert DJ stent would be higher and ureteral mucosal injury would be unavoidable Therefore, it is expected that occurrences of hematuria will be higher Firm DJ stent is also considered to cause a higher rate of lower abdominal pain since it will stretch the ureter and sphincter in the ureter with stronger force compared to its counterparts As mentioned above, firmness is closely related to inflexibility The inability of firm DJ stent to adapt in various body position would cause discomfort in patients (13) Nevertheless, firm DJ stent has its advantage since it has stronger coil strength and better shaped memory When placed successfully, it would be a better option to maintain ureteral shape or return to its original shape Therefore, in some cases such as ureter kinking or malignancy-related hydronephrosis, firm DJ stent should be considered as an option
Bulk properties of material are indeed important to determine DJ stent characteristics Advancement in additive manufacturing pushed researchers to further develop DJ stent in an untouched area before, which is to improve its surface properties Most of the polymers are hydrophobic while it is known that DJ stent placement would be much easier and less in friction if the material is hydrophilic (4, 14) There are several research which focus on hydrophilic coating material However, the authors could not provide the analysis in this review since some of those manuscripts were made unavailable Thus, this review only focused on triclosan eluted stent and silver nanoparticle stent Based on the studies included in this review, silver nanoparticles and triclosan have insignificant impact in lowering the occurrences of UTI and encrustation Silver nanoparticles coating is considered to have a strong antimicrobial activity due to its ability to punch a hole in bacteria cell membrane due to its positive ion charge on the surface (2, 15) Similarly, triclosan is also considered to have a potent antimicrobial property due to the ability to prevent biosynthesis of essential DNA of the bacteria (3, 16)
The authors hypothesized that the inability of these two materials to reduce UTI and encrustation could be due to the hydrophobic nature Hydrophobicity is one of the surface properties that is not very essential for DJ stent material as it would increase friction between DJ stent and ureteral mucosa which later caused ureteral injury Ureteral injury could make the ureter prone to retainment of bacteria and infection
On the other hand, hydrophilic material could make bacteria adhering to DJ stent to be flushed easier Even though hydrophilic surface could preserve the original protein conformation and retain its bioactivity, hydrophilic surface resist protein adsorption stronger compared to its counterpart Therefore, it is hypothesized that hydrophilic characteristics are beneficial in reducing infection and encrustation rate
There are also other surface properties which could play a key role in reducing infection and encrustation rate such as
nanopattern on the surface material (17) Different nanopattern could yield a different cell behavior However, it is still yet to be further determined which nanopattern surface is optimal to reduce UTI and hematuria
CONCLUSIONS
In conclusion, softness played an important role to reduce ureteral stent-related symptoms such as hematuria, and lower body pain Softer polymers such as silicone is more preferrable as ureteral stent material
Additional coating material such as silver nanoparticles and triclosan are not effective to reduce risk of infection even though it could enhance its antimicrobial properties through its positive net ion charge and ability to prevent biosynthesis of bacterial fatty acid
ACKNOWLEDGEMENTS
We thank Medical Faculty of Universitas Indonesia, Medical Faculty of Universitas Sumatera Utara and Adam Malik General Hospital for their consistent support for the author during this research
REFERENCES
1 Geavlete P, Georgescu D, Multescu R, et al Ureteral stent complications - experience on 50,000 procedures J Med Life 2021; 14:769-775
2 Yin IX, Zhang J, Zhao IS, et al The Antibacterial Mechanism of S i l v e r N a n o p a r t i c l e
Nanomedicine 2020; 15:2555-2562
3 Nudera WJ, Fayad MI, Johnson BR, et al Antimicrobial effect of triclosan and triclosan with Gantrez on five common endodontic pathogens J Endod 2007; 33:1239-42
4 Yang L, Whiteside S, Cadieux PA, Denstedt JD Ureteral stent technology: Drug-eluting stents and stent coatings Asian J Urol 2015; 2:194-201
5 El-Nahas AR, El-Assmy AM, Shoma AM, et al Self-retaining ureteral stents: analysis of factors responsible for patients' discomfort J Endourol 2006; 20:33-7
6 Cadieux PA, Chew BH, Nott L, et al Use of triclosan-eluting ureteral stents in patients with long-term stents J Endourol 2009; 23:1187-94
7 El-Nahas AR, Lachine M, Elsawy E, et al A randomized controlled trial comparing antimicrobial (silver sulfadiazine)-coated ureteral stents with non-coated stents Scand J Urol 2018; 52:76-80
8 Gadzhiev N, Gorelov D, Malkhasyan V, et al Comparison of silicone versus polyurethane ureteral stents: a prospective controlled study BMC Urol 2020; 20:10
9 Joshi HB, Chitale SV, Nagarajan M, et al A prospective randomized single-blind comparison of ureteral stents composed of firm and soft polymer J Urol 2005; 174:2303-6
10 Lennon GM, Thornhill JA, Sweeney PA, et al 'Firm' versus 'soft' double pigtail ureteric stents: a randomised blind comparative trial Eur Urol 1995; 28:1-5
11 Mendez-Probst CE, Goneau LW, MacDonald KW, et al The use of triclosan eluting stents effectively reduces ureteral stent symptoms: a prospective randomized trial BJU Int 2012; 110:749-54
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12067 5
stent material and coating
Ureteral
a n d
l i c a t i o n i n D e n t i s t r y I n t J
s
I t s A p p
12 Scarneciu I, Lupu S, Pricop C, Scarneciu C Morbidity and impact on quality of life in patients with indwelling ureteral stents: A 10-year clinical experience Pak J Med Sci 2015; 31:522-6
13 Boeykens M, Keller EX, Bosio A, et al Impact of Ureteral Stent Material on Stent-related Symptoms: A Systematic Review of the Literature Eur Urol Open Sci 2022; 45:108-117
14 Al-Aown A, Kyriazis I, Kallidonis P, et al Ureteral stents: new ideas, new designs Ther Adv Urol 2010; 2:85-92
Nanoparticles and Their Antibacterial Applications Int J Mol Sci 2021; 22:7202
16 Alfhili MA, Lee MH Triclosan: An Update on Biochemical a
2019:1607304
17 Modaresifar K, Azizian S, Ganjian M, et al Bactericidal effects of nanopatterns: A systematic review Acta Biomater 2019; 83:29-36
Correspondence
Ignatius Ivan Putrantyo ivan putrantyo@gmail com
Department of Urology, Faculty of Medicine, Universitas Indonesia Haji Adam Malik General Hospital, Indonesia
Syah Mirsya Warli (Corresponding Author) warli@usu ac id
Department of Urology, Universitas Sumatera Utara Hospital Universitas Sumatera Utara, Medan 20154, Indonesia
Ginanda Putra Siregar ginandaputras@gmail com
Fauriski Febrian Prapiska fauriskifprapiska@gmail com
Dhirajaya Dharma Kadar dhirajayadharmakadar@gmail com
Bungaran Sihombing bungaranhombing@gmail com
Division of Urology, Department of Surgery, Faculty of Medicine, Universitas Sumatera Utara – Haji Adam Malik General Hospital, Indonesia
Conflict of interest: The authors declare no potential conflict of interest
Archivio
di
Italiano
Urologia e Andrologia 2024; 96(1):12067
6
I Ivan Putrantyo, S Mirsya Warli, G Putra Siregar, et al
1 5 B r u n a T , M a l d o n a d o - B r a v o F , J a r a P , C a r o N S i l v e r
u l a r M e c h a n i s m s O x i d M e d C e l l L o n g e v 2 0 1 9 ;
n d M o l e c
SYSTEMATIC REVIEW
William Felipe Fernández Zapata 1, 2 , Yamile Cardona Maya 3 , Cesar Isaza Merino 4 , Walter D. Cardona Maya 2
1 “SYMBIOSIS” Research Hotbed in Human Reproduction and Gestation, Faculty of Medicine, University of Antioquia, UdeA, Medellín, Colombia;
2 Reproduction Group, Department of Microbiology and Parasitology, Faculty of Medicine, University of Antioquia, UdeA, Medellín, Colombia;
3 Department of Basic Foundation, Pascual Bravo University Institution, Medellín, Colombia;
4 Department of Mechanical Engineering, Faculty of Engineering, University of Antioquia, UdeA, Medellín, Colombia
Summary
Background: In the medical field, it is increasingly common to observe the use of nanotubes, for example, in the administration of drugs
However, nanotubes raise concerns for male fertility due to potential effects on hormone levels and sperm quality observed in animal studies. In addition, animal exposure to multi-walled carbon nanotube models found alterations in hormone levels, sperm motility, and sperm count Limited evidence in humans suggests no adverse effects, but further research is needed This study aimed to perform a systematic review to assess the in vitro effects of nanotubes on semen and fertility in humans
Methods: We included all published in vitro studies about semen or sperm or male fertility and nanotubes in humans A search was conducted in LILACS, PubMed, and SCOPUS as of May 2023 The risk of bias was assessed using the QUIN tool
Results: Four studies using nanotubes on human sperm were included, nanotubes exposure appears not to affect sperm viability; however, some alterations to motility, velocity and production of reactive oxygen species were reported. Limited evidence is provided because of the small quantity of publications
Conclusions: Nanotubes appear to have no adverse effects on human sperm
KEY WORDS: Nanotubes; Semen; Fertility; Human; Nanoparticles; Reproduction
Submitted 14 December 2023; Accepted 23 December 2023
INT
RODUCTION
Carbon nanotubes (CNTs) are nanomaterials that have garnered attention due to their unique properties and potent i a l a c r o s s v a r i o u s fi e l d
Composed of carbon atoms arranged in a hexagonal lattice, CNTs form cylindrical structures, akin to rolled-up graphene sheets This structural arrangement imparts CNTs with remarkable mechanical strength, electrical conductivity, and chemical reactivity (2)
CNTs exhibit a wide range of dimensions, with typical diameters ranging from a few nanometers to tens of nanometers, and lengths varying from a few micrometers to millimeters Based on their structural characteristics, CNTs can be categorized into two types: single-walled nan-
otubes (SWNTs) and multi-walled nanotubes (MWNTs) SWNTs consist of a single cylindrical graphene sheet, whereas MWNTs comprise multiple concentric layers of graphene sheets (3)
The remarkable physical properties of CNTs result from their nanoscale architecture CNTs possess a high aspect ratio and extraordinary tensile strength, granting them unmatched mechanical resilience that exceeds traditional materials like steel and diamond in the strength-toweight ratio (4) Additionally, CNTs exhibit excellent thermal conductivity, facilitating efficient dissipation of heat These desirable characteristics, along with their electrical conductivity, make CNTs highly attractive for diverse applications, including electronics, energy storage, and biomedical devices (5)
In the field of medicine, integrating CNTs offers significant potential for revolutionary advancements in healthcare (6) The considerable surface area-to-volume ratio of CNTs, coupled with their molecular transport capabilities, positions them as promising candidates for drug delivery systems (7) Through the functionalization and loading of therapeutic agents onto CNTs, controlled and targeted release of drugs to specific tissues or cells becomes achievable (8) Additionally, the electrical properties of CNTs enable the development of biosensors and implantable devices for precise diagnostic and therapeutic applications, facilitating real-time monitoring and precise control
However, as the utilization of CNTs in medical applications continues to expand, thorough evaluation of their impact on human health becomes paramount (9) The interactions between CNTs and biological systems necessitate meticulous examination to ensure the safety and efficacy of these nanomaterials Particularly, investigating the potential effects of CNTs on reproductive health assumes significance, as reproduction represents a fundamental process for the survival and perpetuation of the human species
CNTs interaction with the male reproductive system raises concerns regarding health and fertility Studies of exposure in animals to multi-walled carbon nanotubes models found alterations on hormone levels, sperm motility, sperm count (10) In humans, some studies found no adverse effects on
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12192 1
s , i n c l u d i n g m e d i c i n e
( 1 )
Effectsofnanotubesonsemenqualityandfertility inhumans:Asystematicreviewofliterature
DOI: 10 4081/aiua 2024 12192
sperm quality (11, 12) Further research is needed
Therefore, the objective of this study was to perform a systematic review to assess the in vitro effects of the nanotubes on semen and fertility in humans
MATERIALSANDMETHODS
The systematic review was performed following the Preferred Items for Systematic R e v i e w s a n d M e t a - a n a l y s i s ( P R I S M A ) reporting guidelines (13)
Eligibility criteria
All publication original investigation peerreviewed articles in English and Spanish languages related to In vitro studies on human sperm in humans until may 2023 were included
Exclusion criteria
All publications related to animal models investigation were excluded
Search methods
Flow diagram of the study selection process
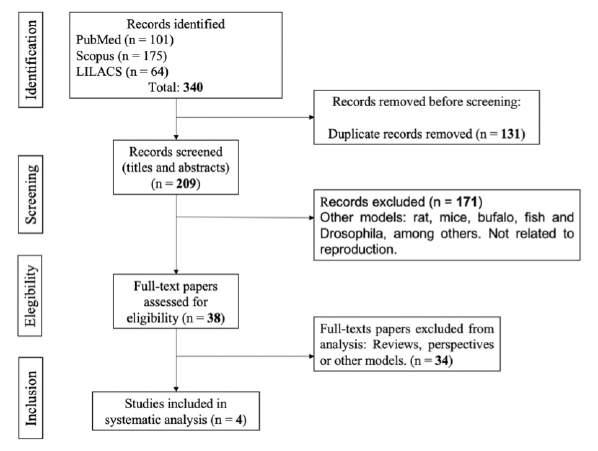
The following search strategy was used in PubMed (Fertility OR infertility OR semen OR Sperm*) AND Nanotubes); in Scopus (TITLE-ABS-KEY (nanotubes AND "male infertility") OR TITLE-ABS-KEY (nanotubes AND s p e r m a t o z o a ) O R T I T L E - A B S - K E Y ( n a n o t u b e s A N D semen)), and in LILACS ((Fertility) OR (Infertility) OR (Semen) OR (Sperm)) AND (Nanotubes)
Study records
The search results from electronic databases were imported into EndNote X8 software, and then duplicates were i d e n t i fi e d T w o i n d e p e n d e n t a u t h o r s ( W F F Z a n d WDCM) screened the titles and abstracts of the identified studies to assess their eligibility based on predefined inclusion and exclusion criteria Full-text articles of potentially relevant studies were retrieved for further evaluation Any disagreements between the reviewers were resolved through discussion or consultation with a third reviewer to ensure a consensus-based selection process The study protocol was registered with the Prospero International Prospective Register of Systematic Reviews (CRD42023435569)
During the data collection process, two independent authors (WFFZ and WDCM) extracted relevant information from the selected studies using a standardized data extraction form This form captured the main characteristics of the study, the title of the study, the characteristics of the nanotubes, the details of the nanotubes, the outcome measures, and the main characteristics of the study The data extraction process was conducted meticulously for accurate and consistent data collection Any discrepancies or uncertainties were resolved by consensus or with a third reviewer's opinion (Figure 1)
Risk of bias in studies
The risk of bias was assessed using the QUIN tool (14)
The present study conducted a risk of bias assessment, examining potential biases in twelve item criteria which wiere scored, and the scores were used to grade the in vitro study as high, medium or low risk of bias A traffic light plot summarizing the risk of bias was generated using Robvis (15)
RESULTS
Literature searches identified 340 documents, and 4 articles (11, 12, 16, 17) were finally included after excluding duplicate studies, irrelevant literature, and review articles adhering strictly to the inclusion and exclusion criteria (Figure 1)
Three of the studies used sperm from healthy male volunteers: Aminzadeh et al (17) obtained samples from 30 nonsmoking males, Cardona-Maya et al (12) obtained 12 samples from 24,6 ± 5,7 aged males; Jha et al (16) used sperm from fertile males aged 25 to 40 Ashgar et al (11) used semen vials from a cryobank (as in Table 1)
These studies (11, 12, 16, 17) were conducted in the US, India, Iran and Colombia; all of them agreed that sperm viability was not affected by nanotubes, NO was not significantly produced compared to control in any of the two studies evaluating it (11, 17) Aminzadeh et al (17) found a correlation between nanotubes concentrations added to sperm and ROS production similar to Ashgar et al (11), which found an increase of ROS generation sperm Jha et al (16) proved MWNTs can interact with and infiltrate sperm cells without causing cell damage Their r e s e a r c h r e v e a l s t h a t M W N T s , c o m p a r e d t o o t h e r nanoparticles, has markedly lower interaction rates with nucleic acids Making it less likely to disrupt the cellular functions associated with these biological macromolecules They also demonstrate the ability of CNTs to penetrate cell nuclei This characteristic, combined with their
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12192
2
W F Fernández Zapata, Y Cardona Maya, C Isaza Merino, W D Cardona Maya
Figure 1
Table 1.
Summary of the studies included.
Study Used nanotubes Variables
Methodolog y
Conclusion
Ashgar et al 2016 (11) SWCNT Viability, straight linear and curvilinear A solution of SWCNT was added to Exposing sperm to MWCNT did not lead to notable impacts on sperm velocity, ROS generation, NO generation human sperm viability, NO was not significantly produced Nonetheless, there were observable alterations in sperm velocity and oxidative stress caused by ROS
Jha et a 2016 (14) MWCNT Suitability of drug delivery carrier MWCNT type 5 was added to human sperm MWCNT covers and enters sperm cells and produces no cell damage, produces less interaction with nucleic acids compared to other nanoparticles, CNT can penetrate nuclei and can be used as a marker, thus can be a candidate for drug delivery to the nucleus
Aminzadeh et al 2016 (15) SWCNT-COOH Viability, motility ROS generation, Different concentrations (0, 1-100 µg) of a Viability was not altered, motility visible altered after 30 min exposure and MWCNT-COOH NO generation solution of acid-oxidized SWCNT and MWCNT and decreased with CNT concentration, concentrations upper to 100 were added to human sperm μg/ml at any time and exposures longer to 3 hours of SWCNT-COOH and MWCNT COOH could induce ROS production and NO production similar to control
Cardona-Maya et al 2020 (12) MWCNT Sperm motility A solution of 1% MWCNT was added MWCNT does not affect sperm motility to human sperm
MWCNT: Mu t -wal erd carmbon nanotubes; ROS: Reactive oxigen spec es; NO: N tr c ox de
Figure 2.
Risk of bias assessment with corresponding biases (D1 to D2) and risk indicators
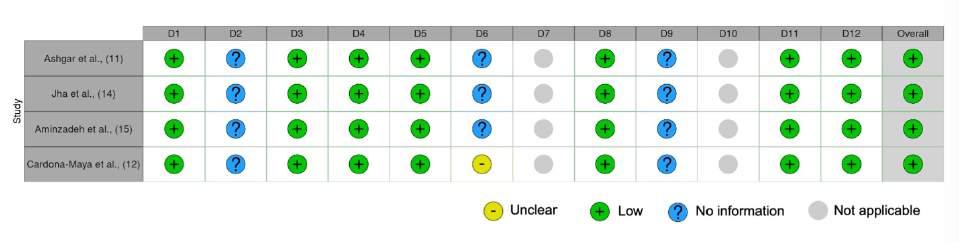
reduced interaction with nucleic acids, makes them an excellent candidate for use as intracellular markers Furthermore, these attributes suggest that MWNTs could be a promising tool for targeted drug delivery to the nucleus, opening up an exciting new avenue in nanoparticle-based therapeutics
In conducting our review, we made the decision to exclude the works of Fan et al (18) and Eyni et al (19) Although Fan et al (18) provides essential insights into the utilization of nanotubes as part of an immunosensor for the follicle-stimulating hormone, their research unfortunately lacks any direct experimentation with human sperm This absence limits the relevancy of their findings to our review, primarily focused on direct interactions and impacts of nanotubes on human sperm Similarly, the study of Eyni et al (19) while notable for its use of nanotubes in crafting a scaffold to induce differentiation of human stem cells into spermatogonial sperm cells, falls outside of our current review parameters This study concentrates more on cellular differentiation and less on the i n t e r a c t i o n b e t w e e n n a n o t u b e s a n d h u m a n s p e r m
Therefore, despite their in the respective fields, these studies did not fit closely enough with the purpose of inclusion in our review
None of the included studies specified the sample size calculation nor outcome assessor details; only one study
specified operator details However, it did not provide valuable details of the operator s training, and overall, we conclude that the risk of bias in the included studies is low (Figure 2) There is no risk of bias standardized tool for in vitro studies in medicine, therefore, we used QUIN tool for reviewing risk of bias in the selected studies (14) (Figure 2)
DISCUSSION
Our review aimed to assess the in vitro effects of nanotubes on human semen and fertility; four articles matched the requirements and were analyzed demonstrating that exposure of human sperm to CNT does not significantly affect its viability
We did not find another systematic review addressing the research question The absence of a previous systematic review in this field may be attributed to various factors, including the emerging nature of the research topic, limited research interest, or the absence of a consolidated body of evidence
Our study represents a pioneering effort in systematically reviewing the impact of nanotubes on human sperm and male fertility This is because most research has identified the effect of carbonaceous materials on other species such as rats and mice (20) Additionally, some research has
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12192 3 Nanotubules and semen quality
found that carbonaceous structures such as graphene, graphene oxide, and reduced graphene oxide have no significant effect on sperm viability However, there were some significant changes in sperm velocity and oxidative stress due to reactive oxygen species (21) These changes were attributed to the exposure times Likewise, some studies have investigated the viability of human sperm exposed to functionalized carbon nanotubes and have not found a significant effect However, these studies reported that sperm motility decreased and oxidative stress increased, possibly associated with mitochondrial and DNA damage (17)
One limitation of our systematic review was omitting grey literature and unpublished works, potentially excluding relevant information
CONCLUSIONS
In conclusion, we recommend that the scientific community advance studies employing human in vitro models to comprehend this phenomenon further Such models can be used to comprehend the phenomenon better, resulting in more precise and valuable conclusions
REFERENCES
1 He H, Pham-Huy LA, Dramou P, et al Carbon nanotubes: Applications in pharmacy and medicine Biomed Res Int 2013; 2013:578290
2 Popov VN Carbon nanotubes: Properties and application Materials Science and Engineering: R: Reports 2004; 43:61-102
3 Anzar N, Hasan R, Tyagi M, et al Carbon nanotube-a review on synthesis, properties and plethora of applications in the field of biomedical science Sensors International 2020; 1:100003
4 Isaza M CA, Rudas JS, Cardona-Maya Y, et al Interfacial phenomena in multiwalled carbon nanotube-reinforced magnesium n a n o c o m
Metallography, Microstructure, and Analysis 2023:1-9
5 Atiq Ur Rehman M, Chen Q, Braem A, et al Electrophoretic deposition of carbon nanotubes: Recent progress and remaining challenges International Materials Reviews 2021; 66:533-562
6 Sharifi M, Pothu R, Boddula R, Bardajee GR Trends of biofuel cells for smart biomedical devices International Journal of Hydrogen Energy 2021; 46:3220-3229
7 Zare H, Ahmadi S, Ghasemi A, et al Carbon nanotubes: Smart drug/gene delivery carriers Int J Nanomedicine 2021:1681-1706
8 Saleemi MA, Kong YL, Yong PVC, Wong EH An overview of recent development in therapeutic drug carrier system using carbon nanotubes Journal of Drug Delivery Science and Technology 2020; 59:101855
9 Barbarino M, Giordano A Assessment of the carcinogenicity of carbon nanotubes in the respiratory system Cancers 2021; 13:1318
10 Farombi EO, Adedara IA, Forcados GE, et al Responses of testis, epididymis, and sperm of pubertal rats exposed to functionalized multiwalled carbon nanotubes Environ Toxicol 2016; 31:543-551
11 Asghar W, Shafiee H, Velasco V, et al Toxicology study of single-walled carbon nanotubes and reduced graphene oxide in human sperm Sci Rep 2016; 6:1-11
12 Cardona Maya Y, Isaza Merino CA, Cardona Maya WD [expo-
sure of multi-walled carbon nanotubes to human sperm] Revista Cubana de Obstetricia y Ginecología 2020; 46:1-11
13 Page MJ, McKenzie JE, Bossuyt PM, et al The prisma 2020 statement: An updated guideline for reporting systematic reviews Int J Surg 2021; 88:105906
14 Sheth VH, Shah NP, Jain R, Bhanushali N, Bhatnagar V Development and validation of a risk-of-bias tool for assessing in vitro studies conducted in dentistry: The QUIN J Prosthet Dent 2022; S0022-3913(22)00345-6
15 McGuinness LA, Higgins JPT Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments Res Synth Methods 2021; 12:55-61
16 Jha R, Jha PK, Gupta S, et al Probing suitable therapeutic nanoparticles for controlled drug delivery and diagnostic reproductive health biomarker development Mater Sci Eng C Mater Biol Appl 2016; 61:235-245
17 Aminzadeh Z, Jamalan M, Chupani L, et al In vitro reprotoxicity of carboxyl-functionalised single- and multi-walled carbon nanotubes on human spermatozoa Andrologia 2017; 49:e12741
18 Fan Y, Guo Y, Shi S, Ma J An electrochemical immunosensor based on reduced graphene oxide/multiwalled carbon nanotubes/ thionine/gold nanoparticle nanocomposites for the sensitive testing of follicle-stimulating hormone Anal Methods 2021; 13:3821-3828
19 Eyni H, Ghorbani S, Shirazi R, et al Three-dimensional wetelectrospun poly (lactic acid)/multi-wall carbon nanotubes scaffold induces differentiation of human menstrual blood-derived stem cells into germ-like cells J Biomater Appl 2017; 32:373-383
20 Francis AP, Devasena T Toxicity of carbon nanotubes: A review Toxicol Ind Health 2018; 34:200-210
21 Hadizadeh N, Zeidi S, Khodabakhsh H, et al An overview on the reproductive toxicity of graphene derivatives: Highlighting the importance Nanotechnology Reviews 2022; 11:1076-1100
Correspondence
William Felipe Fernández Zapata, MD
william fernandezz@udea edu co
Walter D Cardona Maya, PhD (Corresponding Author) wdario cardona@udea edu co
“SYMBIOSIS” Research Hotbed in Human Reproduction and Gestation; Reproduction Group, Department of Microbiology and Parasitology, Faculty of Medicine, University of Antioquia, UdeA, Medellín, Colombia
Yamile Cardona Maya, PhD y cardona5837@pascualbravo edu co
Department of Basic Foundation, Pascual Bravo University Institution, AA 6564, Medellín, Colombia
Cesar Isaza Merino, PhD
cesar isaza@udea edu co
Department of Mechanical Engineering, Faculty of Engineering, University of Antioquia, AA 6564, Medellín, Colombia
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12192
4
W F Fernández Zapata, Y Cardona Maya, C Isaza Merino, W D Cardona Maya
o s i t e s y n t h e s i z e d b y t h e s a n d w i c h t e c h n i q u e
p
SYSTEMATIC REVIEW
Effect of SARS-CoV-2 viral infection on male sexual hormones levels post COVID-19 exposure: A systematic review and meta-analysis
Anak Agung Patriana Puspaningrat 1, 2 , Lukman Hakim 1, 3 , Johan Renaldo 1, 3
1 Department of Urology, Faculty of Medicine, Universitas Airlangga, Surabaya, Indonesia;
2 Dr Soetomo General-Academic Hospital, Surabaya, East Java, Indonesia;
3 Universitas Airlangga Teaching Hospital, Surabaya, East Java, Indonesia
Summary
Introduction: The COVID-19 can affect human testicles, thus will interfere the production of important male sexual hormone such as testosterone
Our study provides scientific evidence through systematic reviews and meta-analyses that focus on the effects of SARSCoV-2 virus infection on male sexual hormonal disorders in patients post-exposure to COVID-19
Methods: This meta-analysis was made in accordance with the PRISMA guidelines The outcomes of this study were the level of total testosterone, free testosterone, LH and FSH. Chi-square and I2 tests were used to evaluate heterogeneity between studies. The standardized mean deviation (SMD) with 95% CI were used and analysis was performed using the Review Manager 5 4 software.
Results: The four included studies reported a total of 256 patients with COVID-19 with time of follow-up time post COVID-19 varying from one month to 7 months The mean age distribution in the study was 34-57 years old. Total testosterone level (SMD = -158 71; 95% CI= -205 30 – -112 12; p < 0 00001) was significantly higher at follow-up post COVID-19, while LH (SMD = 0 40; 95% CI = 0 15-0 65; p = 0 002) was lower The free testosterone level and FSH level showed no significant difference between baseline and after following up post COVID-19
Conclusions: At follow up, the total testosterone level in patients with SARS-CoV-2 infection appeared to be elevated while LH was lower compared to the baseline
KEY WORDS: COVID-19; Male sexual hormones; Total testosterone; Free testosterone; Luteinizing hormone; Follicle stimulating hormone
Submitted 21 November 2023; Accepted 5 December 2023
INTRODUCTION
Coronavirus disease, known as COVID-19, is an acute respiratory syndrome caused by coronavirus type-2 or SARS-CoV-2 As of 2021, there have been approximately 200 million COVID-19 infections worldwide, resulting in more than 4 million deaths (1) Although many people with COVID-19 infection are asymptomatic or have very mild symptoms, a small number of patients develop s e v e r e s y m p t o m s a n d p o t e n t i a l l y l o n g - t e r m c o n s equences COVID-19 has been linked to more than 50
long-term side effects, such as impact to the blood vessels, heart, lungs, kidneys, and brain Also it was just discovered to have an effect on human testes, interfering with the production of vital male hormones such as testosterone (2)
As a result of SARS-CoV-2 virus infection, systemic or local cytokine synthesis has the potential to inhibit Leydig cell differentiation, thereby compromising testicular cells by affecting testosterone production and the process of spermatogenesis (3) This inflammatory process was further identified in the testicles of six males who died from SARSCoV-2 (4) This study focused on total testosterone since it is one of the easiest and basic male sexual hormone parameters to measure with acceptable precision in most hospital laboratories Furthermore, the impact of lower testosterone is becoming an issue when there is concern regarding the long-term impact of the SARS-CoV-2 virus on decreased sexual desire and impaired male fertility Other characteristics, such as free testosterone, Luteinizing Hormone (LH), and Follicle Stimulating Hormone (FSH), were included in the study as supporting data to better understand the pattern of male sexual hormone alterations
There is still no consensus or global agreement regarding the management of sexual and hormonal disorders after COVID-19 infection Therefore, researchers are interested in providing scientific evidence through a systematic review and meta-analysis focusing on the effects of SARSCoV-2 virus infection on male sexual hormonal abnormalities in patients after exposure to COVID-19
MATERIALS AND METHODS
Protocol registration
The protocol of this systematic review and meta-analysis is registered at PROSPERO (CRD42023445406)
Search strategy and study selection
This meta-analysis was made in accordance with the Preferred Reporting Items for Systematic Reviews and Metaanalyses (PRISMA) guidelines (5) The review topic was determined based on Population, Intervention, Comparison, Outcome (PICO) methods The population was male over 18 years old without country or race restrictions The
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12113 1
DOI: 10 4081/aiua 2024 12113
i n t e r v e n t i o n w a s c o n d i t i o n o n w h e n a d m i t t e d f o r
COVID-19 (baseline) The comparison was condition on follow up after COVID The outcomes were total testosterone levels, free testosterone, LH and FSH The inclusion criteria for studies were: (1) Observational study, (2) Studies that report the level of total testosterone and at least one of free testosterone, LH, and FSH level at baseline and follow up in patients with SARS CoV-2 Studies that were case reports, conference abstracts, reviews, editorials letters, not available in full text as well as non-English studies were omitted The systematic s e a r c h w a s c a r r i e d o u t a c r o s s P u b M e d , S c o p u s , ScienceDirect, Web of Science, and grey literature The keywords used to search are “ C O V I D ” , “ S A R S - C o V - 2”, “ C O V I D - 1 9 ” , “ C o r o n a v
” , “Androgen” , “FSH” , “Follicle Stimulating Hormone” , “LH” , “Luteinizing hormone” , “Free Testosterone”
Quality assessment and data extraction
Two authors worked independently to extract data by filling out tabulation templates that had been produced in advance of time When there are disputes during data extraction, the ultimate choice will be discussed with the senior author The data obtained comprises study characteristics (first author's name, year of publication, sample size, study design, range data collection), and basic characteristics of the research sample (age, severity of covid, follow-up range, laboratory outcome, and sexual function outcome) The risk of bias was determined using the Newcastle Ottawa Scale (NOS), with a score of 7-9 indicating a low risk of bias, 4-6 suggesting a high risk of bias, and 0-3 indicating a very high risk of bias
Statistical analysis
Data analysis was performed using the Review Manager 5 4 software
The outcomes of this study were the level of total testosterone, free testosterone, LH and FSH Chisquare and I2 tests were used to evaluate heterogeneity between studies The random-effects model analysis was applied if the heterogeneity test was high (I2 test > 50% and chi-square p < 0 05) If the heterogeneity test was low (I2 < 50%, chi-square p > 0 05), the fixed-effect model analysis was used The pooled standardized mean and deviation (SMD) with 95% CI were used to perform the analysis on continuous data i e , testosterone level, free testosterone, LH and FSH If there is Median (IQR) or Median (Range) data, it will be converted to Mean ± SD with Median (Range) using
scenario 1 and Median (IQR) using scenario 2 from the following online calculator https://www math hkbu edu hk/ ~tongt/papers/median2mean html Studies featuring Mean ± SD data that have been stratified by COVID-19 severity will be combined with the following online calculator https://www statstodo com/ CombineMeansSDs php The results are significant when the P value < 0 05
RESULTS
The results of a systematic search for studies using predetermined keywords identified a total of 606 studies in fi
p u s , ScienceDirect, Web of science, and grey literature The number of studies found in each database can be seen in Figure 1 All these studies were then checked for duplication, resulting in 287 duplicate studies Selection was then carried out on 319 studies by reading titles and abstracts, as many as 15 articles that met the criteria and selection continued by reading the full text The result obtained four studies that met the inclusion criteria and were included in the systematic review of meta-analysis The four cohort studies revealed a total of 356 COVID-19 patients (6-9) These studies are carried out in a variety of nations, including Italy, Turkey, Russia, and Iran The first study was conducted in February 2020 At the time of the study,
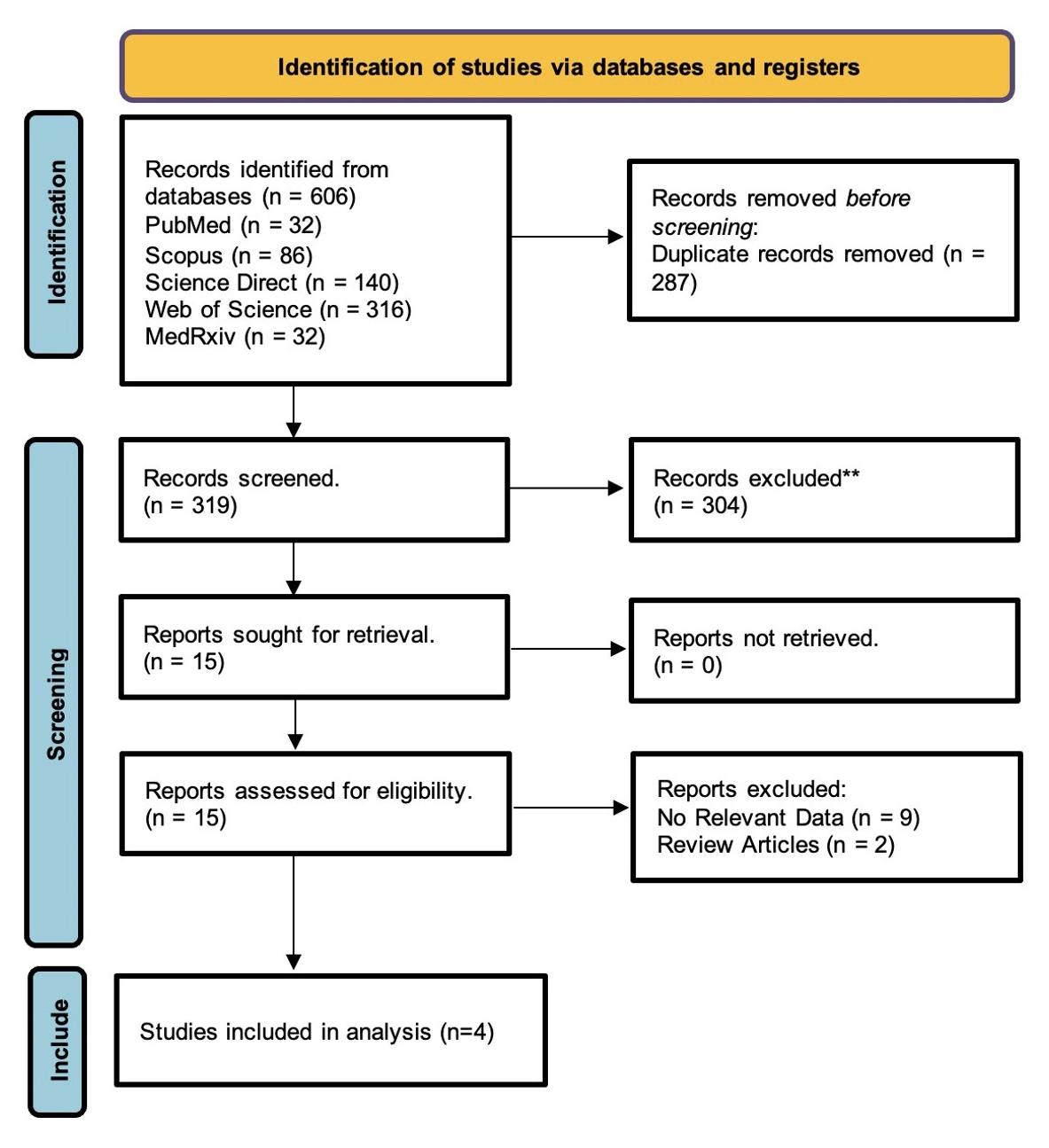
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12113
2
A Agung Patriana Puspaningrat, L Hakim, J Renaldo
r u s
t o s t e r o
e
i
” , “ T e s
n
l e v e l
v e d a t a b a s e s , n a m e l y P u b M e d
D
I N E
c o
/ M E
L
, S
Figure 1.
PRISMA diagram of the study search and selection process
Table 1
Basic characteristics of the study
No. Author (year) Data Countr y Design N Covid
1 Salonia et al (2022) (6) February 29 - May 2, 2020 Italy Cohort 121
2 Apaydin et al (2022) (7) April - October 2020 Turkey Cohort
3 Enikeev et al (2022) (8) NR Russia
4 Afshar et a (2022) (9) July 2020 - February 2021 Iran
NR: Not reported; tT: Total testosterone; fT:
Table 2.
Characteristic of study Outcomes.
1 Salonia et al (2022) (6) February 29 - May 2, 2020
2 Apaydin et al (2022) (7) April - October 2020
3 Enikeev et al (2022) (8) NR
4 Afshari et al (2022) (9) July 2020 - February 2021
NR: Not reported
Table 3.
Quality assessment of the study New Ottawa-Scale (NOS).
Author (year)
Sa onia et al., 2022
Enikeev et al , 2022 Cohort
Apaydin et al , 2022
Afshari et a , 2022
participants ranged in age from 34 to 57 years old The reported follow-up time spans from one month to seven months Tables 1 and 2 indicate the features of the studies Newcastle Ottawa Scale was used to measure the quality of the studies Table 3 shows the quality assessment results, which found three studies with a total score of 8
Figure 2
Forest plot of mean total testosterone level
± 12 WBC, neutrophils, lymphocytes, NLR, NR creatinine, CRP, IL-6, FSH, LH, tT
FSH, LH, tT, fT, Bioavailable testosterone, NR SHBG, lymphocyte, thrombocyte, creatinine, ALT, KDH, ferritin, D-dimer
prolactin, LH, FSH IIEF-5
and one studies with a total score of 7 that were considered to have low risk of bias
Mean total testosterone level
Analysis of four studies reporting testosterone level on COVID-19 showed a significant difference between total testosterone level on baseline and after following up (pooled SMD = -158 71; 95% CI = -205 30-112 12; p < 0 00001) (6-9) The total testosterone level appears to be lower at baseline
The forest plot for total testosterone level is provided in Figure 2
Mean free testosterone level
Analysis of two studies reporting free testosterone level on
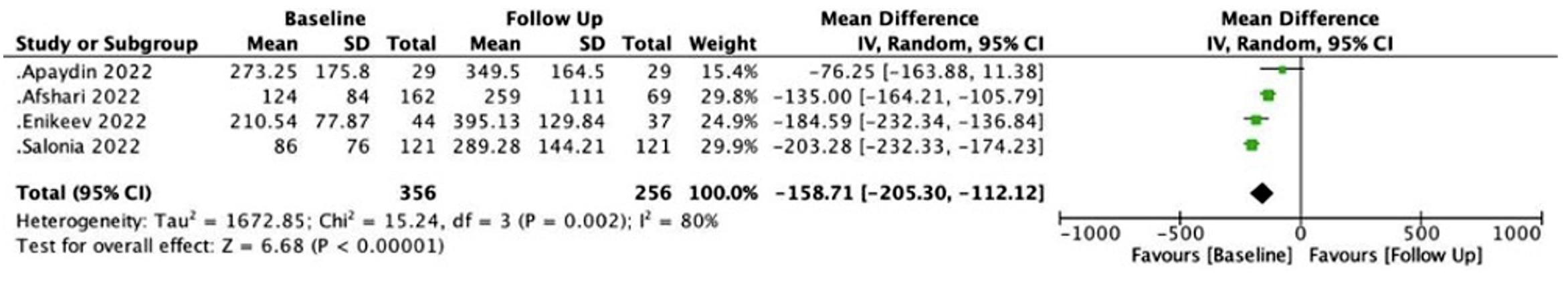
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12113 3 SARS-CoV-2 on male sexual hormones
Study design Selection Comparability Outcome Total
*** ** *** 8
Cohort
** ***
***
8
Cohort *** ** *** 8
Cohort *** ** ** 7
Follow-up Age
severity Mean ± SD
(years) Laborator y Sexual Function collection
Outcome Outcome
NR 7 months 57
NR 6 months 43
29
3 ± 28 6
Prospective 44 NR 3 months 46
9
7±9
Testosterone,
162 Severe, moderate 1 month 39 88 ± 7 04 LH, FSH,
Total sample size 356
testosterone;
White Blood Cel
NLR: Neutroph l
Rat o; SHBG: Sex Hormone Binding
obul n; ALT: Alanine
LDH:
IL-6: Inter euk n-6;
Internat
5.
Prospective
tT, fT NR
Free
WBC:
;
Lymphocyte
G
Aminotransferase;
Lactate Dehydrogenase;
CRP: C-reactive prote n; IEF-5: The
onal Index of Erect le Function
No Author
Data Group N Total testosterone Free testosterone LH FSH IIEF collection (ng/dL) (ng/dL) (mIU/L) (mIU/L)
(year)
Baseline 121 86 ± 76 NR 5 ± 2 1 6 01 ± 3 37 NR Follow-up 7 months 121 289.28 ± 144.21 NR 4.3 ± 2.25 8.2 ± 3.9 NR
Baseline 29 273 25 ± 175 8 7 74 ± 5 32 9 06 ± 7 77 9 06 ± 7 77 NR Follow-up 6 months 29 349 5 ± 164 5 7 18 ± 2 8 11 1 ± 14 6 5 01 ± 2 44 NR
Baseline 44 210 54 ± 77 87 NR 3 3 ± 0 5 5 1 ± 1 11 20 7 ± 5 3 Follow-up 3 months 37 395 13 ± 129 84 NR 2 975 ± 0 76 5 05 ± 1 32 23 1 ± 4 3
Baseline 162 124 ± 84 5 14 ± 2 94 7 02 ± 4 83 4 08 ± 2 16 NR Follow-up 1 month 69 259 ± 111 4 76 ± 2 19 6 55 ± 5 48 5 89 ± 3 4 NR Total
Baseline 356 Follow-up 256
Sample Size

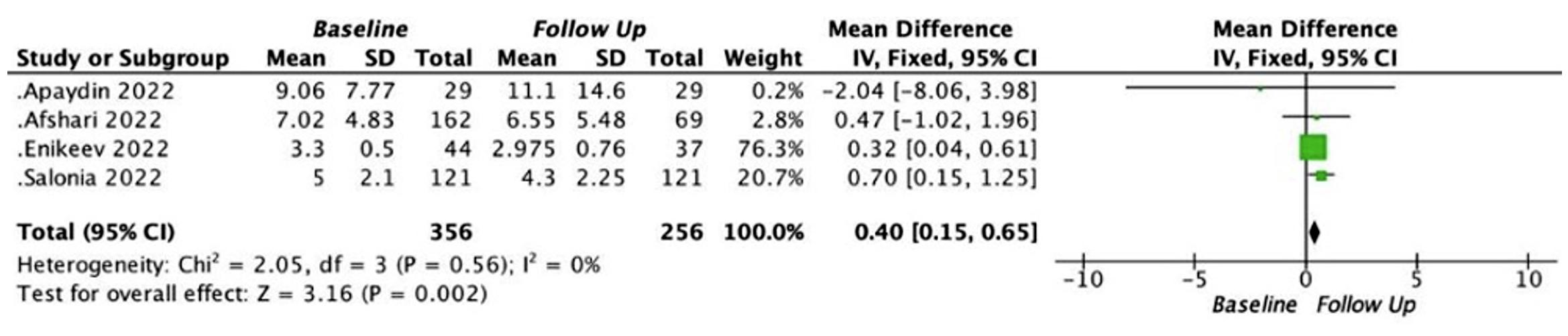
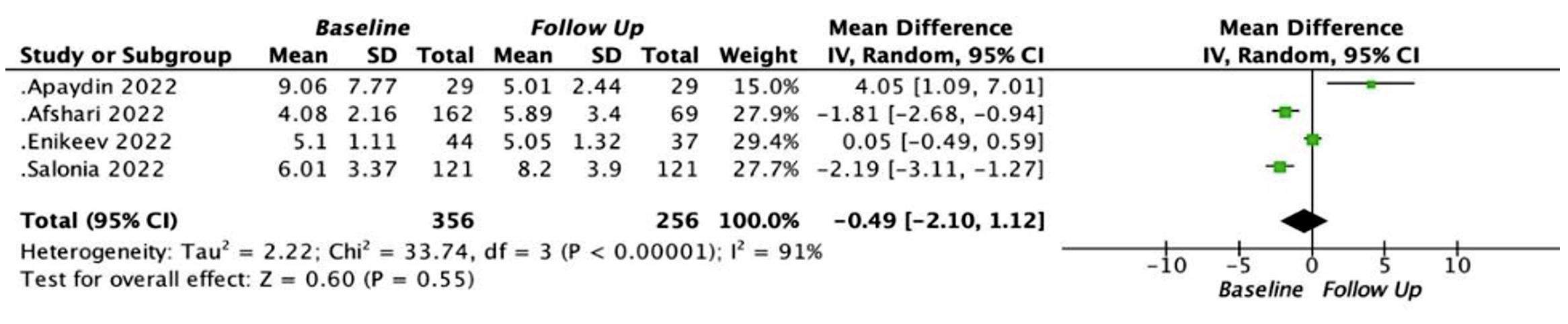
COVID-19 showed no significant difference between free testosterone level on baseline and after following up (pooled SMD = 0 40; 95% CI = -0 26-1 05; p = 0 24) (7, 9) The forest plot for testosterone level is provided in Figure 3
Mean luteinizing hormone level
Analysis of four studies reporting LH level on COVID-19 showed a significant difference between LH level on baseline and after following up (pooled SMD = 0 40; 95% CI = 0 15-0 65; p = 0 002) (6-9) The forest plot for LH level is provided in Figure 4
Mean follicle stimulating hormone level
Analysis of four studies reporting FSH level on COVID19 showed no significant difference between FSH level on baseline and after following up (pooled SMD: -0 49; 95% CI = -2 10-1 12; p = 0 55) (6-9) The forest plot for LH level is provided in Figure 5
DISCUSSION
This study is the first systematic review and meta-analysis to compare male sexual hormone levels in patients with COVID-19 when the SARS-CoV-19 virus was first
detected and at follow-up after a negative COVID-19 PCR swab Four studies were meta-analyzed with a total baseline sample of 356 patients and 256 patients at follow-up with reported follow-up times ranged from 1 month to 7 months The parameters studied were total testosterone, free testosterone, Luteinizing Hormone (LH), and Follicle
Stimulating Hormone (FSH) levels as Mean ± SD ACE-2 receptors are abundant in testicular tissue As a result, it is hypothesized that SARS-CoV-2 infection may cause testicular tissue injury, which may lead to impaired sexual function and fertility in men The primary endpoint of this study is the change in total testosterone because it is one of the easiest and simplest male sexual hormone parameter measured with good accuracy in most hospital laboratories Furthermore, the impact of lower testosterone is concerning given the long-term impact of the SARS-CoV-2 virus on decreased libido levels and impaired male fertility Changes in free testosterone levels, Luteinizing Hormone (LH) levels, and Follicle Stimulating Hormone (FSH) levels were secondary outcomes of this study The resulting decrease in testosterone levels may lead to dysregulation of GnRH production in the hypothalamus followed by abnormal secretion of LH and FSH from the pituitary These results indicate
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12113
4
A Agung Patriana Puspaningrat, L Hakim, J Renaldo
Figure 3. Forest plot of mean free testosterone level
Figure 4. Forest plot of mean luteinizing hormone level.
Figure 5. Forest plot of mean follicle stimulating hormone level
a decrease in peripheral organ function and a compensatory increase in central function (29)
Total testosterone
The four studies meta-analyzed in this study showed significant differences in total testosterone levels between baseline and follow-up At follow up, total testosterone levels in individuals with SARS-CoV-2 infection appeared to be higher in relation to the baseline
This study also found that the testosterone levels of patients who served as baseline data in this study were below the normal range Most (95%) testosterone is produced in the Leydig cells of the testes depending on stimulation by LH Only a small amount (5%) is produced in the adrenal glands Low testosterone levels can originate from the testes (primary hypogonadism), hypothalamuspituitary (secondary hypogonadism), or a combination of both, which is mostly found in the aging male population as late onset hypogonadism (30) In patients with COVID19, the increase in gonadotropin concentration as a form of central function compensation may be insufficient because SARS-CoV-2 virus infection may also disrupt homeostatic and cause HPG axis feedback failure (29)
The influence of testosterone levels in men on COVID-19 prognosis is currently the focus of attention in several research literatures Suppressive effects on the gonadal axis through inflammatory mediators, decreased testicular response to gonadotropins, and increased metabolic clearance rate of testosterone have been described as potential causes of lower testosterone concentrations during acute illness due to the SARS-CoV-2 virus (31)
Total testosterone levels can be a prognostic factor of disease severity as low testosterone levels are associated with a high risk of intensive care unit admission and death (10) When there is a decrease in total testosterone levels, the probability of death increases significantly (11) The more severe the comorbidities at the time of treatment, the less likely testosterone levels are to improve over time In general, testosterone has immunosuppressive effects
Testosterone activates CD8 cells and increases T-helper 1 responses while decreasing natural killer cell responses by decreasing TNF-α and increasing anti-inflammatory IL-10 production (13) Therefore, a poor prognosis in COVID19 patients with low testosterone is predictable However, the Salar et al study found no significant difference between testosterone levels before the disease in the mild and moderate COVID-19 groups Possible reasons for this are that severe symptomatic cases were previously excluded and the low number of patients in the study (12)
The gradual recovery of total testosterone levels also indicated progressive recovery from the severe multisystemic symptoms associated with COVID-19 (10) The study by Xu H et al also found improvements in testosterone levels that can even reach the normal range during recovery from COVID-19 (14) The recovery of physiological testosterone levels can occur as lymphocyte and neutrophil homeostasis returns, this is also related to old age factors, with or without comorbidities that may affect the ability of some COVID-19 patients to restore testosterone production (13) Thus, the discovery of an upward trend in testosterone levels at follow-up suggests the effect of this decrease in testosterone levels is reversible
Free testosterone
The meta-analysis of the two studies in this study did not find any significant changes in baseline and follow-up free testosterone levels This could be due to the number of studies that could be meta-analyzed only 2 studies with a small sample size and did not include all degrees of COVID-19
Free testosterone levels are decreased in COVID-19 patients Some studies found a significant association between free testosterone levels and the risk of ICU care or death Together with total testosterone, free testosterone levels were significantly associated with higher serum levels of LDH, ferritin, procalcitonin, as well as increased neutrophil levels and decreased lymphocyte counts Such inflammatory biomarkers are poor prognostic factors for SARS-CoV-2 infection (15) In the Van Zeggeren et al study, free testosterone levels were significantly lower in patients with severe COVID-19 and in patients who died from severe COVID-19 compared to those who survived SHBG levels were also associated with the outcome of patients treated with COVID-19 (16) Like total circulating testosterone, free testosterone levels were significantly decreased in severe patients compared to the mild-moderate group (13)
SHBG levels are also associated with the outcome of p a t i e n t s t r e a t e d w i t h C O V I D - 1 9 H y p o a l b u m i n e m i a occurs due to increased vascular permeability and capillary leakage is common in critically ill patients and similar mechanisms can lead to low albumin, or CBG concentrations (16) In addition, serum levels of SHBG, the most widely circulated testosterone-binding protein, showed a significant association with older age in mildmoderate patients, but not in severe patients (13) With age, SHBG levels also increase, causing a decrease in bioavailable testosterone and free testosterone, which affects androgenic activity (20) In COVID-19 patients, SHBG levels were also found to be elevated (30) Thus, in some cases, a decrease in testosterone levels can be caused by an increase in SHBG levels It takes a decrease in bioavailable testosterone levels or a significant increase in SHBG levels to produce a significant decrease in free testosterone levels (30)
Luteinizing Hormone and Follicle Stimulating Hormone
This meta-analysis study conducted on 4 studies found significant changes in LH levels between baseline and follow-up There was a decrease in LH levels at follow-up A possible mechanism is that the SARS-CoV-2 virus enters cells through the ACE-2 receptor which is found in many testicular Leydig cells that regulate testosterone through the conversion of Angiotensin II to Angiotensin 1-7 increasing LH levels (7) Elevated serum LH levels indicate primary hypogonadism and testicular failure, rather than secondary causes so this condition is more likely to be influenced by a severe inflammatory state (32) When the inflammatory condition improves characterized by the return of lymphocyte and neutrophil homeostasis, accompanied by the restoration of physiological testosterone levels, according to the negative feedback mechanism of the HPG axis, there will be a decrease in LH and FSH levels (13) However, FSH levels were found to be insignificant These inconsistent results may be due to the small number of samples, the follow-up time of each
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12113 5
on male sexual hormones
SARS-CoV-2
study and the varying age ranges of research subjects and the varying degrees of severity of COVID-19 In their study, Salar et al also found no significant difference between FSH or LH hormone levels before and after exposure to COVID-19 in mild or moderate degree groups (12) This could be due to previous exclusion of cases with severe symptoms and the low number of patients in the study (12)
The elevated levels of circulating LH and FSH reported in COVID-19 cases may indicate transient activation of GnRH due to the initial inflammatory response (3) This compensatory process by LH against decreased testosterone levels is also significantly higher in COVID-19 patients compared to healthy men (21) High luteinizing hormone indicates loss of peripheral organ function and compensatory increase in central function (19) SARSCoV-2 virus has been shown to alter the hypothalamicpituitary-testis axis, increasing LH and FSH levels in men by suppressing the HPG axis According to Cayan et al 's study, blood concentrations of LH and FSH increased with the severity of COVID-19 FSH levels were found to be significantly higher in the ICU group compared to the asymptomatic group (11)
In addition to direct damage to the testes by the virus, other factors such as fever, inflammation, and dysregulation of the HPG axis may also play a role in testosterone secretion or sperm production (19) Hypothalamic and pituitary tissues also express ACE-2 receptors and therefore could be targets of the SARS-CoV-2 virus Low testosterone with normal or low gonadotropins may be caused by the combined effects of COVID-19 on the hypothalamus-pituitary-testis axis and on the testes 7, (13) In addition, emotional, physical, or psychological stress and pain associated with infection may affect the hypothalamic-pituitary axis causing abnormalities in the rhythm of LH secretion (19)
COVID-19 treatment
Medications given to COVID-19 patients in the general ward or ICU can alter sexual hormone levels such as corticosteroids, anticoagulant drugs, and antiviral drugs such as Remdesivir (26) Animal studies have found that antiviral drugs such as ribavirin (the treatment of choice for COVID-19) can induce oxidative stress, lower testosterone levels, and severely impair spermatogenesis (4) A considerable decrease in sperm count was observed upon ribavirin treatment In addition, sperm DNA fragmentation was found up to 8 months even after discontinuation of such treatment
Glucocorticoid treatment is also given to patients who must be admitted to the ICU, potentially affecting testosterone levels (7) Corticosteroid use and stress-induced hypercortisolism may have a suppressive impact on the hypothalamic-pituitary-Forest plot of mean follicle stimulating hormone levelgonadal axis Corticosteroids can suppress gonadotropin-releasing hormone in the hypot h a l a m u s a n d m a y a f f e c t t h e a c t i o n o f p i t u i t a r y gonadotropin on the testes (27)
Post COVID-19 hypogonadism
The results of the Paoli et al study show that overall andrological health does not appear to be compromised
at 3 months after COVID-19 recovery After a full spermatogenetic cycle of 3 months there was recovery of semen parameters and sperm DNA fragmentation This suggests no significant long-term impairment and no sperm autoimmune response Likewise, the hormone profiles of total testosterone, FSH, and LH showed no relevant changes Ultrasound examination also showed no damage to the testicular parenchyma These findings reinforce the hypothesis that once clinical recovery occurs, the SARS-CoV-2 virus does not appear to cause direct damage to testicular function, while the impact of indirect damage appears to be transient (28) In the study of Xu et al using more than 50 days as the cutoff for defining long-term positive cases, Authors found no significant relationship between testosterone levels and the severity of COVID-19 This means that although the disease course of these patients is longer, the tissues and organs, especially the testes, can still maintain normal conditions or can return to normal This may be due to the low virulence, achieved immunity, and adequate compensatory capacity to cope with the long-term impact of the virus (14) Circulating testosterone levels were also found to continue to increase over time in men recovering from COVID-19 However, nearly 30% of men still showed low testosterone levels even after 12 months during the recovery period (10)
Based on observations, this study is the first systematic review and meta-analysis to compare male sexual hormone levels in COVID-19 survivors when the SARS-CoV19 virus was first detected and at follow-up This study can also be the basis for rationalizing the provision of testosterone replacement therapy in cases of acute hypogonadism which has the possibility of being reversible in male COVID-19 survivors Currently, there is no direct evidence to confirm that SARS-CoV-2 causes testicular injury leading to hypogonadism and infertility, but the potential risk cannot be ignored This study has several limitations Most of the studies had varying follow-up times, many patients were lost to follow-up, most studies did not include the severity of COVID-19, as well as other presence of factors that may affect hormone levels, such as age, comorbidities, psychological conditions, use of medications such as antivirals, corticosteroids, and glucocorticoids
CONCLUSIONS
There was a significant differentiation in total testosterone levels between the initial COVID-19 and the follow-up Total testosterone levels in individuals with SARS-CoV-2 infection appeared to be higher relative to the baseline, i m p l y i n g t h a t t e s t o s t e r o n e w o u l d r e t u r n o n c e t h e COVID-19 infection is resolved, while LH was lower during follow-up period There was no statistically significant difference in free testosterone and FSH levels between baseline and follow-up
ACKNOWLEDGEMENTS
Thank you to Ida Bagus Gde Tirta Yoga Yatindra and Niwanda Yogiswara for the valuable corrections and suggestions for this research
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12113
6
A Agung Patriana Puspaningrat, L Hakim, J Renaldo
REFERENCES
1 Joshee S, Vatti N, Chang C Long-Term Effects of COVID-19 Mayo Clin Proc 2022; 97:579-99
2 Khan R, Naseem T, Hussain MJ, et al Possible Potential Outcomes from COVID-19 Complications on Testes: Lesson from SARS Infection J Coll Physicians Surg Pak 2020; 30:118-20
3 Selvaraj K, Ravichandran S, Krishnan S, et al Testicular atrophy and hypothalamic pathology in COVID-19: possibility of the incidence of male infertility and HPG axis abnormalities Reproductive Sciences 2021; 28:2735-42
4 Sabz FTK, Amjadi F, Zandieh Z, Ashrafi M SARS-CoV-2 and its Implications for the Human Reproductive System: A Review Article Nephrourol Mon 2022; 14
5 Page MJ, McKenzie JE, Bossuyt PM, et al The PRISMA 2020 statement: An updated guideline for reporting systematic reviews Int J Surg 2021; 88:105906
6 Salonia A, Pontillo M, Capogrosso P, et al Testosterone in males with COVID-19: A 7-month cohort study Andrology 2022; 10:34-41
7 Apaydin T, Sahin B, Dashdamirova S, et al The association of free testosterone levels with coronavirus disease 2019 Andrology 2022; 10:1038-46
8 Enikeev D, Taratkin M, Morozov A, et al Prospective two-arm study of the testicular function in patients with COVID-19 Andrology 2022; 10:1047-56
9 Afshari P, Zakerkish M, Abedi P, et al Effect of COVID-19 infection on sex hormone levels in hospitalized patients: A prospective longitudinal study in Iran Health Sci Rep 2022; 6:e1011
10 Salonia A, Pontillo M, Capogrosso P, et al Testosterone in males with COVID-19: a 12-month cohort study Andrology 2023; 11:1723
11 Çayan S, Uguz M, Saylam B, Akbay E Effect of serum total testosterone and its relationship with other laboratory parameters on the prognosis of coronavirus disease 2019 (COVID-19) in SARSCoV-2 infected male patients: a cohort study Aging Male 2020; 23:1493-503
12 Salar R, Erbay G, Sanlı A, et al Effect of COVID-19 infection on the erectile function Andrology 2023; 11:10-6
13 Toscano-Guerra E, Martínez-Gallo M, Arrese-Muñoz I, et al Recovery of serum testosterone levels is an accurate predictor of survival from COVID-19 in male patients BMC Med 2022; 20:1-18
14 Xu H, Wang Z, Feng C, et al Effects of SARS-CoV-2 infection on male sex-related hormones in recovering patients Andrology 2021; 9:107-14
15 Rastrelli G, Di Stasi V, Inglese F, et al Low testosterone levels predict clinical adverse outcomes in SARS-CoV-2 pneumonia patients Andrology 2021; 9:88-98
16 van Zeggeren IE, Boelen A, van de Beek D, et al Sex steroid hormones are associated with mortality in COVID-19 patients: Level of sex hormones in severe COVID-19 Medicine 2021; 100:e27072
17 Anifandis G, Tempest HG, Oliva R, et al COVID-19 and human reproduction: A pandemic that packs a serious punch Syst Biol Reprod Med 2021; 67:3-23
18 Giagulli VA, Guastamacchia E, Magrone T, et al Worse progression of COVID-19 in men: Is testosterone a key factor? Andrology 2021; 9:53-64
19 Cai Z, Zhong J, Jiang Y, Zhang J Associations between COVID19 infection and sex steroid hormones Front Endocrinol 2022; 13:940675
20 Krakowsky Y, Grober ED Testosterone deficiency-establishing a biochemical diagnosis EJIFCC 2015; 26:105
21 Ma L, Xie W, Li D, et al Evaluation of sex-related hormones and semen characteristics in reproductive-aged male COVID-19 patients
J Med Virol 2021; 93:456-62
22 Bechmann N, Maccio U, Kotb R, et al COVID-19 Infections in Gonads: Consequences on Fertility? Horm Metab Res 2022; 54:54955
23 Li X, Chen Z, Geng J, et al COVID-19 and Male Reproduction: A Thorny Problem Am J Mens Health 2022; 16:155798832210748
24 Selvaraj K, Ravichandran S, Krishnan S, et al Testicular atrophy and hypothalamic pathology in COVID-19: possibility of the i n c i d e n c e
Reproductive Sciences 2021; 28:2735-42
25 Oduwole OO, Huhtaniemi IT, Misrahi M The Roles of L u t
Testosterone in Spermatogenesis and Folliculogenesis Revisited IJMS 2021; 22:12735
26 Afshari P, Zakerkish M, Abedi P, et al Effect of COVID-19 infection on sex hormone levels in hospitalized patients: A prospective longitudinal study in Iran Health Sci Rep 2023; 6:e1011
27 Aboelnaga MM, Abdelrazek A, Abdullah N, El Shaer M Late impact of COVID-19 pneumonia on testosterone levels in recovered, post-hospitalized male patients J Endocrinol Metab 2021; 11:76-82
28 Paoli D, Pallotti F, Anzuini A Male reproductive health after 3 m o n t h s f r o m S A R S - C o V - 2 i n f e c t
t u d y J Endocrinol Invest 2023; 46:89-101
29 Hackett G, Kirby M, Rees RW, et al The British Society for Sexual Medicine Guidelines on Male Adult Testosterone Deficiency, with Statements for Practice World J Mens Health 2023; 41:508537
30 Schroeder M, Schaumburg B, Mueller Z, et al High estradiol and low testosterone levels are associated with critical illness in male but not in female COVID-19 patients: a retrospective cohort study Emerg Microbes Infect 2021; 10:1807-18
31 Dhindsa S, Zhang N, and McPhaul MJ Association of Circulating Sex Hormones with Inflammation and Disease Severity in Patients With COVID-19 JAMA Netw Open 2021; 4:e2111398
32 Nassau DE, Best JC, Kresch E, et al Impact of the SARS-CoV-2 virus on male reproductive health BJU Int 2022; 129:143-150
Correspondence
Anak Agung Patriana Puspaningrat patriana ptty@yahoo com
Department of Urology, Faculty of Medicine, Universitas Airlangga, Dr Soetomo General-Academic Hospital, Surabaya, East Java, Indonesia
Lukman Hakim lukman-h@fk unair ac id
Department of Urology, Faculty of Medicine, Universitas Airlangga, Universitas Airlangga Teaching Hospital, Surabaya, East Java, Indonesia
Johan Renaldo (Corresponding Author) joeurologi@gmail com
Department of Urology, Faculty of Medicine, Airlangga University, Soetomo General Academic Hospital
Jl Mayjen Prof Dr Moestopo No 6-8, Surabaya, East Java, Indonesia, 60286
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12113 7 SARS-CoV-2 on male sexual hormones
a l e
i l i t y a n d H P G a x i s a b n o r m a l i t i e s
o f m
i n f e r t
e i n i z i n g H o r m o n e , F o l l i c l e - S t i m u l a t i n g H o r m o n e a n d
i
i o n : a m u l t i c e n t r
c s
LETTER TO EDITOR
Rosario Leonardi 1, 2 , Francesca Ambrosini 3 , Angelo Cafarelli 4, 2 , Alessandro Calarco 5, 2 , Renzo Colombo 6, 2 , Domenico Tuzzolo 2 , Ferdinando De Marco 7, 2 , Giovanni Ferrari 8, 2 , Giuseppe Ludovico 9, 2 , Stefano Pecoraro 10, 2 , Ottavio De Cobelli 11, 2 , Carlo Terrone 12 , Guglielmo Mantica 12
1 Casa di Cura Musumeci GECAS, Gravina di Catania, Italy;
2 Urologi Ospedalità Gestione Privata (UrOP), Italy;
3 IRCCS Policlinico San Martino, Genova, Italy;
4 Urology Unit, Villa Igea, Ancona, Italy;
5 Villa Pia Hospital, Rome, Italy;
6 Department of Urology, Vita e Salute San Raffaele University, Milan, Italy;
7 I N I Grottaferrata, Rome, Italy;
8 Hesperia Hospital, Modena, Italy;
9 Ospedale Miulli, Acquaviva delle Fonti, Bari, Italy;
10 NEUROMED, Avellino, Italy;
11 Department of Urology, IEO European Institute of Oncology, IRCCS, Milan, Italy;
12 Department of Surgical and Diagnostic Integrated Sciences (DISC), University of Genova, Genova, Italy
KEY WORDS: Bladder cancer; Office fulguration; Office laser; Local bladder treatment; NMIBC
Submitted 20 February 2024; Accepted 23 February 2024
To the Editor,
Bladder cancer is one of the most common cancers in humans, representing the 7th and 17th type of neoplasm in both genders (1) Its incidence and mortality are quite heterogeneous in different countries and are due to different risk factors, quality and prevalence of healthcare and the possibility of early diagnosis and treatment of the tumor and its potential recurrences (2-3) Bladder cancer can be divided into muscle-invasive (MIBC) and non-muscle invasive (NMIBC) Early detection of the primary tumors and the recurrences is of paramount importance to enable a better prognosis (3) While MIBC is known to be treated very aggressively, i e with surgery, radiotherapy, and chemotherapy (4-8), NMIBC has a better prognosis but still has a high recurrence rate despite measures such as the use of local drugs Although most of these recurrences in low-grade tumors guarantee a good prognosis if treated promptly with TURB, they still pose a management problem for both the patient and the healthcare system
Indeed, the patient is often forced to undergo multiple anesthesia, surgical and psychophysical stress related to hospitalization and the anxiety of the operation itself Furthermore, performing a transurethral resection of the bladder (TURB) may lead to transport management issues and organization problems for the patient's family From a healthcare perspective, hospitalization for TURB requires an economic cost of several thousand euros, considering the cost of the surgical staff, the materials used during the operation and the hospital stay (9, 10) Furthermore, this contributes to longer waiting lists, which also has a negative impact on other patients This problem is highly relevant, given the organizational problems of healthcare systems and surgical waiting lists in the post-COVID era (11)
Last but not least, there is the "green" problem considering that further hospitalization requires more surgical and hospital supplies, an increase in travel for patients and relatives, and thus an impact on the carbon footprint
The EAU guidelines also include office-based fulguration and laser vaporization among the possible treatment options for NMIBC (3) Specifically, it states that that patients with a history of small Ta LG/G1 lesions can undergo fulguration or laser vaporization on an outpatient basis for small papillary recurrences
Outpatient treatment can be performed either by fulguration or using laser, generally under local anesthesia with instillation of intravesical lidocaine prior to the procedure and may warrant histologic examination by pre-fulguration biopsy
If HG is found, the patient can then be scheduled for TURB in the following weeks
The literature now presents numerous reports on the efficacy and safety of performing office-based procedures for the treatment of NMIBC (12-19) Recently, Vitug et al evaluated the outcomes of fulguration in 270 patients with recurrent TaLG NMIBC in an outpatient setting (20) The 10-year incidence of cancer-specific mortality (CSM) and progression were
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12404 1
Office-basedmanagementofNon-MuscleInvasiveBladder Cancer(NMIBC):Apositionpaperoncurrentstate oftheartandfutureperspectives
DOI: 10 4081/aiua 2024 12404
R Leonardi, F Ambrosini, A Cafarelli, et al
0% and 3 1%, respectively They estimated a savings of nearly 7,000 Canadian dollars per patient The savings in economic terms have also been demonstrated by other authors in other contexts (15, 21-23)
Pedersen et al in a prospective randomized controlled trial proved that laser photocoagulation in an outpatient setting is non-inferior to standard TURB for the 4-month recurrence rate (24)
Halstuch et al introduced an additional step, namely the use of a single dose of mitomycin (MMC), after performing office-based procedures such as fulguration (25) They found that a single dose of MMC instilled after fulguration was associated with longer recurrence free survival (RFS) compared to patients who did not receive MMC after the procedure, with no high-grade complications
One of the potential limitations of office-based procedures is the pain experienced by the patient However, Strock et al evaluated the pain perceived by patients during the procedure and obtained satisfactory results in this respect The VAS scores after diagnostic cystoscopy report no or only mild pain in the totality of their case series
Despite the current evidence, we are still far from knowing which patients are safe candidates for these procedures (number of lesions, size of lesions, number of previous TURB with histologic pTa LG/G1, age, etc ) and to consider these procedures the "standard of care" in selected patients
We believe that outpatient treatment of NMIBC should be implemented for reasons of economic and environmental sustainability as well as for reasons of benefit to the patient, as illustrated previously A stronger stance in national and international guidelines in favor of these procedures in selected patients could be of fundamental importance However, for the committees to move further in this direction, the scientific community must bring results from further randomized trials, perhaps multicenter, which can make the scientific evidence stronger
Furthermore, the definition of the ideal candidate for these procedures is un unmet need Since it is now clear that that the patients for whom the treatments are indicated are patients with relapses of a previous pTa LG/G1 in the absence of rare variants of bladder cancer, some inclusion criteria need to be defined more precisely such as age, number of recurrences/papillary lesions, time since the last TURB, etc
In this sense, the application of new biomarkers could become useful to define the patients with the highest risk and therefore not subject them to office-based treatment
Furthermore, the definition of the patient eligible for these procedures is also fundamental It has now been established that the patients for whom the treatments are indicated are patients with relapses of previous pTa LG/G1 in the absence of rare variants of bladder cancer, some inclusion criteria must be defined in more detail such as age, the number of relapses/papillary lesions, time since last TURB, etc
In this sense, the application of new biomarkers could become useful to define the patients most at risk and therefore not candidate to office-based treatment (26)
In conclusion, we believe that the office-based management of NMIBC should be much more under the spotlight of the scientific community It is essential to properly define either the ideal candidates and the optimal settings
R
EFERE
NCES
1 Siregar GP, Parwati I, Noegroho BS, et al The association between serum hypoxia inducible factor-1α level and urothelial bladder cancer: A preliminary study Arch Ital Urol Androl 2023; 95:11292
2 MacDonald A, Mehrnoush V, Ismail A, et al History of infantile BCG immunization did not predict lamina propria invasion and/or high-grade in patients with non-muscle invasive bladder cancer Arch Ital Urol Androl 2023; 95:11380
3 EAU Guidelines Edn presented at the EAU Annual Congress Milan 2023 ISBN 978-94-92671-19-6
4 Mantica G, Smelzo S, Ambrosini F, et al Port-site metastasis and atypical recurrences after robotic-assisted radical cystectomy (RARC): an updated comprehensive and systematic review of current evidences J Robot Surg 2020; 14:805-812
5 Maffezzini M, Fontana V, Pacchetti A, et al Age above 70 years and Charlson Comorbidity Index higher than 3 are associated with reduced survival probabilities after radical cystectomy for bladder cancer Data from a contemporary series of 334 consecutive patients Arch Ital Urol Androl 2021; 93:15-20
6 Malinaric R, Mantica G, Balzarini F, et al Extraperitoneal cystectomy with ureterocutaneostomy derivation in fragile patients - should it be performed more often? Arch Ital Urol Androl 2022; 94:144-149
7 Slovacek H, Zhuo J, Taylor JM Approaches to Non-Muscle-Invasive Bladder Cancer Curr Oncol Rep 2021; 23:105
8 Alvarez-Maestro M, Chierigo F, Mantica G, et al The effect of neoadjuvant chemotherapy among patients undergoing radical cystectomy for variant histology bladder cancer: A systematic review Arab J Urol 2021; 20:1-13
9 Joyce DD, Sharma V, Williams SB Cost-Effectiveness and Economic Impact of Bladder Cancer Management: An Updated Review of the Literature Pharmacoeconomics 2023; 41:751-769
10 Richters A, Aben KKH, Kiemeney LALM The global burden of urinary bladder cancer: an update World J Urol 2020; 38:1895-1904
11 Leonardi R, Bellinzoni P, Broglia L, et al Hospital care in Departments defined as COVID-free: A proposal for a safe hospitalization protecting healthcare professionals and patients not affected by COVID-19 Arch Ital Urol Androl 2020; 92:67
12 Soloway MS Active Surveillance or Office Fulguration for Low Grade Ta Bladder Tumors: A Win-Win for Patients and Urologists J Urol 2018; 199:1120-1122
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12404
2
13 Xu Y, Guan W, Chen W, et al Comparing the treatment outcomes of potassium-titanyl-phosphate laser vaporization and transurethral electroresection for primary nonmuscle-invasive bladder cancer: A prospective, randomized study Lasers Surg Med 2015; 47:306-11
14 Planelles Gómez J, Olmos Sánchez L, Cardosa Benet JJ, et al Holmium YAG Photocoagulation: Safe and Economical Alternative to Transurethral Resection in Small Nonmuscle-Invasive Bladder Tumors J Endourol 2017; 31:674-678
15 Green DA, Rink M, Cha EK, et al Cost-effective treatment of low-risk carcinoma not invading bladder muscle BJU Int 2013; 111:E78-84
16 Leonardi R, Vecco F, Iacona G, et al TULA DUAL: Trans Urethral Laser Ablation of recurrent bladder tumors in outpatient setting Arch Ital Urol Androl 2023; 95:11171
17 Ströck V, Holmäng S Is bladder tumour fulguration under local anaesthesia more painful than cystoscopy only? Scand J Urol 2020; 54:277280
18 Meeks JJ, Herr HW Office-based management of nonmuscle invasive bladder cancer Urol Clin North Am 2013; 40:473-9
19 O'Neil BB, Lowrance WT Office-based Bladder Tumor Fulguration and Surveillance: Indications and Techniques Urol Clin North Am 2013; 40:175-82
20 Vitug C, Lajkosz K, Chavarriaga J, et al Long-term outcomes and cost savings of office fulguration of papillary Ta low-grade bladder cancer BJU Int 2024; 133:289-296
21 Al Hussein Al Awamlh B, Lee R, Chughtai B, Donat SM, et al A cost-effectiveness analysis of management of low-risk non-muscle-invasive bladder cancer using office-based fulguration Urology 2015; 85:381-6
22 Wong KA, Zisengwe G, Athanasiou T, et al Outpatient laser ablation of non-muscle-invasive bladder cancer: is it safe, tolerable and costeffective? BJU Int 2013; 112:561-7
23 Svatek RS, Hollenbeck BK, Holmäng S, et al The economics of bladder cancer: costs and considerations of caring for this disease Eur Urol 2014; 66:253-62
24 Pedersen GL, Erikson MS, Mogensen K, et al Outpatient Photodynamic Diagnosis-guided Laser Destruction of Bladder Tumors Is as Good as Conventional Inpatient Photodynamic Diagnosis-guided Transurethral Tumor Resection in Patients with Recurrent Intermediate-risk Lowgrade Ta Bladder Tumors A Prospective Randomized Noninferiority Clinical Trial Eur Urol 2023; 83:125-130
25 Halstuch D, Lotan P, Karchever I, et al Single-Dose Post-Office Fulguration Mitomycin C Instillation Appears to Improve Recurrence-Free Survival in Patients With Low-Grade Noninvasive Bladder Cancer Clin Genitourin Cancer 2023; 21:e320-e325
26 Malinaric R, Mantica G, Lo Monaco L, et al The Role of Novel Bladder Cancer Diagnostic and Surveillance Biomarkers-What Should a Urologist Really Know? Int J Environ Res Public Health 2022; 19:9648
Correspondence
Rosario Leonardi, MD - leonardi r@tiscali it
Casa di Cura Musumeci GECAS, Gravina di Catania (CT), Italy
Francesca Ambrosini, MD - f ambrosini1@gmail com
Guglielmo Mantica, MD - guglielmo mantica@gmail com
Carlo Terrone, MD - carlo terrone@hsanmartino it Department of Surgical and Diagnostic Integrated Sciences (DISC), University of Genova, Largo Rosanna Benzi 10, 16132, Genova, Italy
Angelo Caffarell, MD - info@angelocafarelli it Urology Unit, Villa Igea, Ancona, Italy
Alessandro Calarco, MD - info@alessandrocalarco com Villa Pia Hospital, Via Folco Portinari 5, Rome, Italy
Renzo Colombo, MD - colombo renzo@hsr it Department of Urology, Vita e Salute San Raffaele University, Milan, Italy
Domenico Tuzzolo, MD - info@casadelsole it Urologi Ospedalità Gestione Privata (UrOP), Italy
Ferdinando De Marco, MD - info@clinicavillamargherita it I N I Grottaferrata, Rome
Giovanni Ferrari, MD - visite@giovanniferrariurologo it Hesperia Hospital, Modena
Giuseppe Ludovico, MD - g ludovico@miulli it Ospedale Miulli, Acquaviva delle Fonti, Bari, Italy
Stefano Pecoraro, MD - cup@diagnosticamedica org NEUROMED, Avellino, Italy
Ottavio De Cobelli, MD - Ottavio DeCobelli@unimi it Department of Urology, IEO European Institute of Oncology, IRCCS, Milan, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio
Andrologia 2024; 96(1):12404 3 Office-based management of Non-Muscle Invasive Bladder Cancer (NMIBC)
Italiano di Urologia e
LETTER TO EDITOR
Claudio Marino 1 , Salvatore Iaconis 1 , Francesco Di Bello 1,Gianluigi Cacace 1 , Giovanni Fusco 1 , Lorenzo Romano 1 , Ernesto Di Mauro 1 , Luigi Cirillo 1 , Vincenzo Maria Altieri 2, 3 , Francesco Mastrangelo 1 , Luigi Napolitano 1 , Alessandro Palmieri 1
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples Federico II, Naples, Italy;
2 Department of Medicine and Health Sciences "V Tiberio", University of Molise, Campobasso, Italy;
3 Department of Urology, Humanitas Gavazzeni, Bergamo, Italy
KEY WORDS: Erectile dysfunction; Nitric oxide; Iron
Submission 31 December 2023; Accepted 17 January 2024
To the Editor,
Erectile dysfunction (ED) is one of the most prevalent conditions affecting men globally, with significant psychological and social consequences (1-2)
The prevalence varies across different populations, and it is estimated around 50% in men aged between 40 to 70 (3) The etiology of ED is multifactorial, involving a complex crosstalk between psychological, hormonal, neurogenic, vascular, and structural factors (2, 4, 5) Recently, the role of iron homeostasis (IH) is emerging Indeed, it is known that in hereditary hemochromatosis patients, the iron overload accumulated in the penis tissue, resulting in oxidative stress, tissue damages and consequently ED To date, IH is an essential aspect of human health, and its dysregulation has been historically implicated in neurodegenerative disorders, anemia, or cardiovascular diseases (6) Albeit the novel evidence on iron overload consequences on penis tissues, the underlying mechanisms of iron-related-ED remains unknown (7) Several hypotheses have been postulated, such as endothelial dysfunction related either to iron overload and deficiency, the anemia, oxidative stress overproduction, and neurogenic dysfunction First, in hemochromatosis patients the ED could occur due to the storage of iron in penis tissue, endocrine dysfunction as well as decreased serum testosterone level (8) Furthermore, also the iron deficiency has been associated with ED The mechanism underlying the above observations is due to the reduced nitric oxide (NO) bioavailability (9) Reactive oxygen species (ROS) may be involved in the ironrelated-ED Indeed, ROS disrupt the oxidative balance, affecting the hypothalamic-pituitary-gonadal axis (HPG) functionality (10) Moreover, the reaction of superoxide (O2•-) with NO, resulting in acute impairment of cavernosal relaxation and in long-term penile vasculopathy due to a cellular damage Additionally, iron deficiency can also increase the oxidative stress, compromising antioxidant defense mechanisms (11) Indeed, super-Oxide dismutase, one of the most antioxidants enzymes, is increased in patients with iron deficiency anemia, due to a compensatory reaction to the oxidative stress Moreover, Iron accumulation in the central nervous system can lead to neurodegeneration, and potentially affecting the neural pathways involved in erectile function with reduction of dopamine synthesis (12) In conclusion, IH represents a key role in endothelial and cavernous nerves function Both iron overload and deficiency could impair endothelial function, reducing NO bioavailability and vasodilation in the penile vasculature (13) Furthermore, the iron storage in the nervous plex could determine nerve injury, leading to ED The relationship between IH alterations and ED represent a promising research area, with potential implications for the diagnosis and treatment of ED Further research is needed to determine the effective mechanism of neurogenic dysfunction which contributes to ED in the context of IH alterations and whether targeting this mechanism could lead to novel therapeutic interventions
REFERENCES
1 Mirone V, Napolitano L, D'Emmanuele di Villa Bianca R, et al A new original nutraceutical formulation ameliorates the effect of Tadalafil on clinical score and cGMP accumulation Arch Ital Urol Androl 2021; 93:221-226
2 Napolitano L, Fusco GM, Cirillo L, et al Erectile dysfunction and mobile phone applications: Quality, content and adherence to European Association guidelines on male sexual dysfunction Arch Ital Urol Androl 2022; 94:211-216
3 Feldman HA, Goldstein I, Hatzichristou DG, et al Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study J Urol 1994; 151:54-61
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12245 1
Ironhomeostasisalterationsanderectiledysfunction: Anewissueinerectiledisfunctiontreatment?
DOI: 10 4081/aiua 2024 12245
4 Cirillo L, Fusco GM, Di Bello F, et al Sexual dysfunction: Time for a multidisciplinary approach? Arch Ital Urol Androl 2023; 95:11236
5 Shamloul R, Ghanem H Erectile dysfunction Lancet 2013; 381:153-65
6 Camaschella C Iron-deficiency anemia N Engl J Med 2015; 372:1832-43
7 Brissot P, Ropert M, Le Lan C, Loréal O Non-transferrin bound iron: a key role in iron overload and iron toxicity Biochim Biophys Acta 2012; 1820:403-10
8 Barton JC, McDonnell SM, Adams PC, et al Management of hemochromatosis Hemochromatosis Management Working Group Ann Intern Med 1998; 129:932-9
9 Choi JW, Pai SH, Kim SK, et al Iron deficiency anemia increases nitric oxide production in healthy adolescents Ann Hematol 2002; 81:1-6
10 Darbandi M, Darbandi S, Agarwal A, et al Reactive oxygen species and male reproductive hormones Reprod Biol Endocrinol 2018; 16:87
11, et al Atli G, Canli M Response of antioxidant system of freshwater fish Oreochromis niloticus to acute and chronic metal (Cd, Cu, Cr, Zn, Fe) exposures Ecotoxicol Environ Saf 2010; 73:1884-9
12 Simonsen U, Rodriguez-Rodriguez R, Dalsgaard T, et al Novel approaches to improving endothelium-dependent nitric oxide-mediated vasodilatation Pharmacol Rep 2009; 61:105-15
13 He H, Qiao Y, Zhou Q, et al Iron Overload Damages the Endothelial Mitochondria via the ROS/ADMA/DDAHII/eNOS/NO Pathway Oxid Med Cell Longev 2019; 2019:2340392
Correspondence
Claudio Marino, MD marinoclaudio88@outlook it
Salvatore Iaconis, MD salvatore iaconis@gmail com
Francesco Di Bello, MD fran dibello12@gmail com
Gianluigi Cacace, MD cacace gianlu@gmail com
Giovanni Maria Fusco, MD giom fusco@gmail com
Lorenzo Romano, MD
lorenzo romano@unina it
Ernesto Di Mauro, MD ernesto dimauro@unina it Luigi Cirillo, MD cirilloluigi22@gmail com
Francesco Mastrangelo, MD fmastrangelo91@gmail com
Alessandro Palmieri, MD info@alessandropalmieri it
Luigi Napolitano, MD (Corresponding Author) dr luiginapolitano@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples Federico II, Naples, 80100, Italy
Vincenzo Maria Altieri, MD vincenzomaria altieri@gmail com
Department of Medicine and Health Sciences "V Tiberio", University of Molise, 86100 Campobasso, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12245
2
C Marino, S Iaconis, F Di Bello, et al
LETTER TO EDITOR
Panagiotis Nikolinakos 1, 5 , Nikolaos Chatzikrachtis 1 , Ivo Donkov 1 , Elisavet Kotsi 2 , Georgios Antonoglou 3 , Ioannis Alexandrou 4 , Nikolaos Zavras 5 , Joseph M Norris 6
1 Department of Urology, West Middlesex University Hospital, Chelsea & Westminster Hospital NHS Foundation Trust, London, UK;
2 Department of Pediatrics, Penteli Children’s Hospital, 8 Ippokratous STR, 15236 Athens, Greece;
3 Department of Urology, Royal Surrey County Hospital, Royal Surrey NHS Foundation Trust, Guildford, Surrey, UK;
4 Department of Pediatric Surgery, Pendeli Children’s Hospital, 8 Ippokratous STR, 15236 Athens, Greece;
5 Department of Pediatric Surgery, School of Medicine, Attikon University Hospital, National and Kapodistrian University of Athens, 12462 Athens, Greece;
6 UCL Division of Surgery & Interventional Science, University College London, London, UK
KEY WORDS: Pyeloplasty; Robotic surgery; Urology; Minimally invasive
Submitted 7 January 2024; Accepted 22 January 2024
To the Editor
Pelvi-ureteric junction obstruction (PUJO) is a well-recognised clinical entity characterised by functionally significant impairment of drainage of urine at the level of the pelvi-ureteric junction due to extrinsic or intrinsic obstruction and is encountered both by adult and paediatric urologists alike Management of PUJO has been surgical historically, and the gold standard has been an open Anderson-Hynes dismembered pyeloplasty (1) This remains the gold standard with a success rate greater than 90% (2) Minimally invasive surgery to correct PUJO was introduced in 1984 by Arthur Smith using an endopyelotomy technique Since its introduction the technique has evolved and performed in multiple ways using electricity, laser and cold knife to cut the PUJ The routine use of endopyelotomy became questionable however due to lower success rates than open pyeloplasty (3) In the United Kingdom and many other affluent nations there has been a paradigm shift in the last 20 years towards minimally invasive techniques and the standard of care now is a robotassisted laparoscopic pyeloplasty (RALP), due to shorter hospital stay, quicker recovery and improved cosmetic results (2) However, robotic surgery is associated with increased costs, often beyond what is affordable for many countries This poses a challenging question – do the benefits of robotic pyeloplasty outweigh the increased cost? And if so, is it justifiable to deny patients this benefit, purely based on their geographical location?
Moretto et al , recently sought to address this challenge by correlating perioperative and functional outcomes of open and robotic pyeloplasty with their cost effectiveness (2) In their trial 91 patients were included, 48 underwent an open pyeloplasty and 43 a RALP and the authors found similar success rates and operating times but statistically significant lower intraoperative blood loss and early postoperative complication rate and better cosmetic results with RALP Predictably, the authors found a budget gap between surgical methods related to the cost of the robotic equipment They found that the total cost of a RALP was € 8 700 90 ± € 1 274 70 and the open pyeloplasty group had a total cost of € 6 327 10 ± € 2 404 40 In parallel, similar trends and outcomes have been demonstrated in the treatment of the paediatric population with pelvi-ureteric junction obstruction
Table 1 summarises different trials and the costs associated with RALP, laparoscopic and open pyeloplasties (2-5)
Others have taken this exploration further Mjaess et al ran a cost analysis of robot assisted radical cystectomy in Europe (6) They have found that costs varied significantly across European countries and were mainly attributed to the length of stay and operating time, rather than robotic instrumentation
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12263 1
Roboticpyeloplasty: Technologicalglobalpanaceaorgeo-surgicalnightmare?
DOI: 10 4081/aiua 2024 12263
1. Literature summary of cost of RALP, laparoscopic and open pyeloplasty Authors Countr y Source Cur rency Cost of RALP Cost of LP Cost of OP Sun (4) China Asian J Surg (2022) € (CN¥) 7985 ± 364 2880 ± 447(61464 75 ± 2800 53) (22169 52 ± 3442 15) Moretto (2) Italy J Clin Med (2023) € 8700 9 ± 1274 7 - 6327 1 ± 2404 4 Casella (5) USA J Urol (2013) € 14192 14867 ($) (15337) (16067)
Table
Panagiotis Nikolinakos, Nikolaos Chatzikrachtis, Ivo Donkov, Elisavet Kotsi, et al
They concluded that reducing these might decrease the cost of robot-assisted radical cystectomy and make it more widely accessible It is plausible that these conclusions can also be translatable to RALP
Lam et al have analyzed the uptake and accessibility of surgical robots in England and revealed their cost to be exceeding £1 million per unit (7) This financial burden poses challenges for many hospitals, in particular those in less economically affluent countries Consequently, these hospitals, may be unable to provide robotic procedures to patients, limiting access to the improved outcomes associated with them Perhaps one solution to aid in solving this discrepancy could be to increase the competition in the market and to centralise further the robotic centres, aiming for economies of scale to make the robot more cost-effective
It appears that the majority of extant evidence suggests that RALP for PUJO would be mostly advantageous compared to an open pyeloplasty (2) However, given the increased associated costs, it appears likely that the advantages of robotic surgery are not available to all patients, with big discrepancies even inside Europe Key changes are now needed to reduce the healthcare disparities highlighted here, including, increasing uptake with increasing market competition (such as with the Versius robot, and others) with the hope that it would drive down costs The Royal College of Surgeons of England has a yearly Global Appeal, and in 2023 this aimed to support global access to paediatric surgery, and perhaps as an extension from this, an appeal for access to robotic surgery could follow Accessible surgical robots will help usher in a new era for patients and surgeons alike in both adult and paediatric urology, and would help us to meet the common goal of delivering the highest quality of surgical care, regardless of global location
FU
NDING
J M Norris has received funding from the MRC (UK) and RCSEng
REFERENCES
1 González ST, Rosito TE, Bujons A, et al Multicenter comparative study of open, laparoscopic, and robotic pyeloplasty in the pediatric population for the treatment of ureteropelvic junction obstruction (UPJO) International Braz J Urol (Internet) 2022; 48:961-8
2 Moretto S, Gandi C, Bientinesi R, et al Robotic versus Open Pyeloplasty: Perioperative and Functional Outcomes Journal of Clinical Medicine (Internet) 2023; 12:2538
3 Nadu A, Mottrie A, Geavlete P Ureteropelvic Junction Obstruction: Which Surgical Approach? European Urology Open Science 2009; 8:778-81
4 Sun L, Zhao D, Shen Y, et al Laparoscopic versus robot-assisted pyeloplasty in infants and young children Asian J Surg 2022; 46:868-73
5 Casella DP, Fox J, Schneck FX, et al Cost analysis of pediatric Robot-Assisted and laparoscopic pyeloplasty J Urol 2013; 189:1083-6
6 Mjaess G, Diamand R, Aoun F, et al Cost-analysis of robot-assisted radical cystectomy in Europe: A cross-country comparison Eur J Surg Oncol 2023; 49:1511-8
7 Lam K, Clarke J, Purkayastha S, Kinross J Uptake and accessibility of surgical robotics in England Int J Med Robot 2021; 17:1-7
Correspondence
Panagiotis Nikolinakos, MD, MSc (Corresponding Author) pnikolinakos@yahoo gr
Nikolaos Chatzikrachtis, MD nikolaos chatzikrachtis@nhs net Ivo Donkov, MD i donkov@nhs net
Department of Urology, West Middlesex University Hospital, Chelsea & Westminster Hospital NHS Foundation Trust, Twickenham Road, Isleworth, London, TW7 6AF, UK
Elisavet Kotsi, MD elisabethkotsi@gmail com
Department of Pediatrics, Penteli Children’s Hospital, 8 Ippokratous STR, 15236 Athens, Greece
Georgios Antonoglou, MD georgios antonoglou@nhs net
Department of Urology, Royal Surrey County Hospital, Royal Surrey NHS Foundation Trust, Guildford, Surrey, UK
Ioannis Alexandrou, MD inalexandrou@hotmail com
Department of Pediatric Surgery, Pendeli Children’s Hospital, 8 Ippokratous STR, 15236 Athens, Greece
Nikolaos Zavras, MD nzavras@med uoa gr
Department of Pediatric Surgery, School of Medicine, Attikon University Hospital, National and Kapodistrian University of Athens, 12462 Athens, Greece
Joseph Norris, MD josephnorris@nhs net
UCL Division of Surgery & Interventional Science, University College London, London, UK
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2024; 96(1):12263
2
INSTRUCTIONSTOAUTHORS–A
OPEN ACCESS
Open access publishing does have its costs. Information regarding authors’ payment are not made available to editors and reviewers ensuring that they cannot be influenced in their selection of papers for publication by payment conditions or limitations. The Article Processing Charge for publication in this journal is EUR 300,00 (plus VAT, if applicable).
Our fees cover the costs of peer review, copyediting, publication, different format of publication (HTML, PDF), inclusion in many Open Access databases.
All bank charges shall be borne by the payer. Please note that our fees do not include taxes (VAT):
-Private or public ITALIAN customers (individuals, universities, hospitals, other organizations) must ALWAYS add VAT (IVA) at standard rate (4%); -European Union PRIVATE customers must add the standard rate of their own country VAT tax;
-European Union private/public ORGANIZATIONS (universities, hospitals, others with regular VAT number) should not add any taxes at standard rate, provided that they indicate their VAT number; - Outside the European Union, individuals and organizations should not add any taxes at standard rate.
Important: Authors are NOT required to pay at the moment of submission. If the paper is accepted, the Managing Editor of Open Access Edition will guide the Authors through the payment procedure. No article will be published before waiver or payment.
According to the United Nations list of Least Developed Countries (LCDs) available from: http://www.un.org/en/development/desa/policy/cdp/ldc2/ldc_countries.shtml Authors coming from those countries are entitled to ask for a discount.
A “Formal Request for discount” has to be forwarded to the Managing Editor of Open Access Edition, after receiving the acceptance letter. The Editorial Committee will then evaluate the merits of each individual case. Any other informal request (such as comments at the moment of submission, or made in the covering letter of the revised version) will not be taken into consideration.
FAST-TRACK PEER REVIEW
All papers published in Archivio Italiano di Urologia e Andrologia (AIUA) are peer reviewed. Fast-track peer review (4 weeks) can be obtained by supplementary fee of € 488 (VAT included).
METHODS OF PAYMENT Authors can pay their fees by: PayPal is the most recommended and secure payment system. It enables you to pay getting your payment receipt immediately and without sharing your financial information. Other methods of payment are:
Bank transfer
BANK NAME: Banca Popolare di Sondrio, Branch #1, Strada Nuova 75, I-27100 Pavia, Italy
ACCOUNT HOLDER: PAGEPress Srl
BIC/SWIFT: POSOIT22
IBAN: IT85Y0569611301000005086X83
Credit Card The credit card form to be filled and returned either via e-mail or via fax is available for download here.
http://www.pagepress.org/journals/public/credit_card.pdf
Check sent by surface mail Checks must be made payable to PAGEPress Srl and must be sent to our full postal address: PAGEPress Publications, via A. Cavagna Sangiuliani 5, 27100 Pavia, Italy.
Note: In any method of payment you choose, kindly specify: 1. journal name; 2. paper ID number; 3. first author.
IMPORTANT TO KNOW
REGISTERED DRUGS, DIET SUPPLEMENTS, NUTRACEUTICALS, MEDICAL DEVICES
Authors of papers that contain references to registered drugs, diet supplements, nutraceuticals and medical devices are requested to buy a minimum amount of 100 reprints at a cost of € 1.500 (1 to 4 pages) or € 2.000 (5 to 8 pages). Prices for the purchase of number of reprints greater than 100 can be negotiated with Edizioni Scripta Manent At present, Edizioni Scripta Manent let everyone to read, print and download papers from website, but retains copyright for republishing and distribution rights for commercial purpose.
TRANSLATION
Translation of manuscripts in Italian language is offered on payment.
Translation and reprints can be requested to Edizioni Scripta Manent by e-mail to info@edizioniscriptamanent.eu
AUTHORS’ RESPONSIBILITIES
Manuscripts are accepted with the understanding that they have not been published or submitted for publication in any other journal.
Authors must submit the results of clinical and experimental studies conducted according to the Helsinki Declaration on clinical research and to the Ethical Code on animal research set forth by WHO (WHO Chronicle 1985; 39:51). The Authors must obtain permission to reproduce figures, tables and text from previously published material. Written permission must be obtained from the original copyright holder (generally the Publisher).
MANUSCRIPT PRESENTATION
Authors must submit their manuscripts (MAC and WINDOWS Microsoft Word are accepted) after registration and login to the link: http://www.aiua.it. Surface or e-mail submission are not accepted.
Manuscripts must be written in English language in accordance with the “Uniform Requirements for Manuscripts submitted to biomedical journals” defined by The International Committee of Medical Journal Editors (http://www.ICMJE.org). Manuscripts
in Italian language can be published after translation (expenses will be charged to the Authors). Manuscripts should be typed double spaced with wide margins. They must be subdivided into the following sections:
TITLE PAGE
It must contain: a) title; b) a short (no more than 40 characters) running head title; c) first, middle and last name of each Author without abbreviations; d) University or Hospital, and Department of each Author; e) last name, address and e-mail of all the Authors; f) corresponding Author; g) acknowledgement of conflict of interest and financial support.
SUMMARY
Authors must submit a summary (300 words, 2000 characters) divided by subheadings as follows: Objective(s), Material and method(s), Result(s), Conclusion(s). After the summary, three to ten key words must appear, taken from the standard Index Medicus terminology.
TEXT
For original articles concerning experimental or clinical studies, the following standard scheme must be followed: Summary - Key Words - Introduction - Material and Methods - Results - Discussion - Conclusions - References - Tables - Legends - Figures.
Case Report should be divided into: Summary - Introduction (optional) - Case report(s) - Conclusions - References
Supplementary Materials can be added for online publication.
SIZE OF MANUSCRIPTS
Literature reviews, Editorials and Original articles should not exceed 3500 words with 3-5 figures or tables, and no more than 30 references.
Case reports, Notes on surgical technique, and Letters to the editors should not exceed 1000 words (summary included) with only one table or figure, and no more than three references. No more than five authors are permitted.
REFERENCES
References must be sorted in order of quotation and numbered with arabic digits between parentheses. Only the references quoted in the text can be listed. Unpublished studies cannot be quoted, however articles “in press” can be listed with the proper indication of the journal title, year and possibly volume. References must be listed as follows.
JOURNAL ARTICLES
All Authors if there are six or fewer, otherwise the first three, followed by “et al.”. Complete names for Work Groups or Committees. Complete title in the original language. Title of the journal following Index Medicus rules. Year of publication; Volume number: First page. Example: Starzl T, Iwatsuki S, Shaw BW, et al. Left hepatic trisegmentectomy Surg Gynecol Obstet. 1982; 155:21.
BOOKS
Authors - Complete title in the original language. Edition number (if later than the first). City of publication: Publisher, Year of publication. Example: Bergel DIA. Cardiovascular dynamics. 2nd ed. London: Aca de mic Press Inc., 1974.
BOOK CHAPTERS
Authors of the chapters - Complete chapter title. In: Book Editor, complete Book Title, Edition number. City of publication: Publisher, Publication year: first page of chapter in the book. Example: Sagawa K. The use of central theory and system analysis. In: Bergel DH (Ed), Cardiovascular dynamics. 2nd ed. London: Aca demic Press Inc., 1964; 115.
TABLES
Tables must be numbered in Arabic digits and referred to in the text by progressive numbers. Every table must be accompanied by a brief title. The meaning of any abbreviations must be explained at the bottom of the table itself.
FIGURES
(Graphics, algorithms, photographs, drawings). Figures must be numbered and quoted in the text by number. The meaning of symbols or abbreviations must be indicated. Histology photograph legends must include the enlargement ratio and the staining method. Legends must be collected in one or more separate pages.
• Do not include any illustrations as part of your text file. • Do not prepare any figures in Word as they are not workable. • Line illustrations must be submitted at 600 DPI.
• Halftones and color photos should be submitted at a minimum of 300 DPI. • Power Point files cannot be uploaded. • If possible please avoid transmitting electronic files in JPEG format or save the JPEG at the highest quality available • PDF files may be uploaded.
MANUSCRIPT REVIEW
Manuscripts are evaluated by the Editorial Board and/or by two referees designated by the Editors. The Authors are informed in a time as short as possible on whether the paper has been accepted, rejected or if a revision is deemed necessary. The Editors reserve the right to make editorial and literary corrections with the goal of making the article clearer or more concise, without altering its contents. Submission of a manuscript implies acceptation of all above rules.
PROOFS
Authors are responsible for ensuring that all manuscripts are accurately typed before final submission. Galley proofs will be sent to the first Author. Proofs should be returned within seven days from receipt.
RCHIVIOITALIANODIUROLOGIAEANDROLOGIA







PASQUALE MARTINO
124 autori
592 pagine +di 1500 immagini ecografiche 61 video Hardcover Cofanetto
Costo di copertina € 180,00 Sconto del 50% Indicando il Codice: AIUA2024
Prezzo finale: € 90,00*
L’opera è acquisabile inviando un’e-mail a: atlantediecografia@gmail.com
*IVA e Spese di spedizione comprese
PRESENTANO
ATLANTE di
ANDROLOGICA e NEFROLOGICA
ECOGRAFIA UROLOGICA,
Questo Trattato nasce dall’esigenza di offrire evidenze scientifiche della letteratura in diversi àmbiti clinici, riguardo alla Nutraceutica in Pediatria, in un contesto attuale dove è molto forte da parte della società la propensione a ricorrere a “prodotti naturali”.
I temi trattati sono a sostegno di scelte mirate da parte del Pediatra, che possono essere di supporto dal punto di vista preventivo e terapeutico, per la salute di bambini e adolescenti.
25 Capitoli
64 Autori
480 Pagine
a cura di
Gianvincenzo Zuccotti
Enza D’Auria
Elvira Verduci
Prezzo di copertina € 100,00
Per l’acquisto inviare una e-mail a: info@edizioniscriptamanent.eu















è u nst’ada que tt tt p nè u ti per i p bbona ogepr

no n e o int enizati per i p p tti.iit t tti.itu e. ten per a tualelti sa /a p t’aspe pe d 10,00 i sa vof fo er in o.tt tt no per 3 nu n
da quest’anno salutepertutti.it è un progetto ind ipendente. abbonati per i pazienti della tua sala d’aspetto. 10,00€/anno per 3 numeri




















www.salutepertutti.it I l podcast d ella rIvIsta que
wui s tuepertulaw.s ttiiit t tti.itu p w.s www w wui s epertulaw.s Una raccolta
foto e curiosità, sul mondo della Salute e dello stare bene. e pol Salutepertutti.it
rella
www.salutepertutti.it
per info vai su
tula
di
non è più solo la rivista della sala d’aspetto. In questo podcast parliamo sì di salute, ma lo facciamo legandola ta
anche alla cultura pop, al cinema, ai social e all'attualità. Le voci di Salutepertutti.it sono Ruben Cazzola e Alessia Bisini.