ORIGINAL PAPERS
265 One step nucleic acid amplification (OSNA) for detection of lymph node metastasis during robotic radical prostatectomy for prostate cancer : A pilot study Omer Burak Argun, Panagiotis Mourmouris, Yesim Saglican, Tunkut Doganca, Mustafa Bilal Tuna, Cavit Kerem Kayhan, Ozge Yalcinkaya, Ilter Tufek, Halil Kara, Can Obek, Umit Ince, Lazaros Tzelves, Andreas Skolarikos, Ali Rıza Kural
270 Confir mator y transperineal saturation prostate biopsy combined with mpMRI decrease the reclassification rate in men enrolled in Active Sur veillance: Our experience in 100 men submitted to eight years scheduled biopsy Pietro Pepe, Ludovica Pepe, Michele Pennisi, Filippo Fraggetta
274 Targeted prostate biopsy: 68Ga PSMA PET/CT vs. mpMRI in the diagnosis of prostate cancer Pietro Pepe, Ludovica Pepe, Maria Tamburo, Giulia Marletta, Michele Pennisi, Filippo Fraggetta
278 Magnetic resonance imaging target fusion biopsy vs. transrectal ultrasound-guided biopsy - A comparative study of ISUP score upgrading risk in the final radical prostatectomy specimen Thiago Guimarães, Miguel Gil, Mariana Medeiros, Vanessa Andrade, João Guerra, Hugo Pinheiro, Francisco Fernandes, João Pina, João Lopes Dias, Luís Campos Pinheiro
285 Could YouTubeTM encourage men on prostate checks? A contemporar y analysis Simone Morra, Luigi Napolitano, Claudia Collà Ruvolo, Giuseppe Celentano, Roberto La Rocca, Marco Capece, Massimiliano Creta, Francesco Passaro, Francesco Di Bello, Luigi Cirillo, Carmine Turco, Ernesto Di Mauro, Gabriele Pezone, Agostino Fraia, Francesco Mangiapia, Ferdinando Fusco, Vincenzo Mirone, Gianluigi Califano, Nicola Longo

291 Radical cystectomy for bladder urothelial carcinoma with aggressive variant histolog y Vahid Mehrnoush, Logan Brennan, Asmaa Ismail, Ahmed Zakaria, Hazem Elmansy, Walid Shahrour, Owen Prowse, Ahmed Kotb
295 Analysis of benign prostatic obstr uction surger y: A long-ter m evaluation in a real-life context Alberto Costa Silva, Pedro Abreu Mendes, Afonso Morgado, Paulo Dinis, Carlos Martins Silva
300 Hands on wet lab and live surger y training in PCNL: Any impact to surgical skills of attending surgeons? Iason Kyriazis, Panagiotis Kallidonis, Eleni Kyrkopoulou, Theodoros Spinos, Evangelos Liatsikos
305 Management of encr usted ureteral stents: Two center experience Mohanarangam Thangavelu, Mohamed Yehia Abdallah, Olubenga John Isola, Ahmed Kotb
311 Exter nal validation of Resor lu Unsal stone score in predicting outcomes after retrograde intrarenal surger y. Experience from a single institution Antonio Tufano, Marco Frisenda, Antonio Rossi, Pietro Viscuso, Guglielmo Mantica, Pierluigi Bove, Rosario Leonardi, Alessandro Calarco

315 Urodynamic changes following laparoscopic versus vaginal hysterectomy
Tamer Abouelgreed, Doaa Saleh, Mohamed Abdelaal, Adel Elatreisy, Mohamed Elhelaly, El Sayed El Agamy, Ahmed Elgammal, Ashraf Moawad
319 Effects of long ter m sildenafil on the acute phase of Peyronie’s disease in a combination treatment Murat Topcuoglu, Murat Cakan
323 Factors predicting the outcome of percutaneous epididymal sper m aspiration in men with obstr uctive azoosper mia Khaled Mohamed Almekaty, Mohamed Hasan Zahran, Mohamed Lotfy Amer, Ayman Mohamed Hagras, Khaled Abdelaziz Salem, Ayman Sayed Rashed, Ahmed Fayez Ghaith
Vol. 94; n. 3, September 2022
ISSN 1124 3562 continued on page III



Costo di copertina € 180,00 Sconto del 50% valido fino al 31 dicembre 2022 (Indicando il Codice: WINTER22). Prezzo finale: € 90,00* L’opera è acquistabile inviando un’e-mail a: atlantediecografia@gmail.com * IVA e Spese di spedizione comprese 124 autori 592 pagine + di 1500 immagini ecografiche 61 video Hardcover Cofanetto ATLANTE di ECOGRAFIA UROLOGICA, ANDROLOGICA e NEFROLOGICA a cura di PASQUALE MARTINO
EDITOR IN CHIEF Alberto Trinchieri (Milan, Italy)
EDITORIAL BOARD
O f f i c i a l J o u r n a l o f S I E U N , U r O P , S S C U a n d G U N
ASSOCIATE EDITORS
Emanuele Montanari, Department of Urology, IRCCS Foundation Ca’ Granda Ospedale Maggiore Policlinico, University of Milan, Italy Gianpaolo Perletti, Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, Univer sity of Insubria, Varese, Italy; Department of Human Structure and Repair, Ghent University, Ghent, Belgium Angelo Porreca, Robotic Urology and Mini Invasive Uro logic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy
EXECUTIVE EDITORIAL BOARD
Alessandro Antonelli, Department of Urology, Azienda Ospedaliera Universitaria In tegrata (A.O.U.I.), Verona, Italy Antonio Celia, Department of Urology, San Bassiano Hospital, Bassano del Grappa, Italy Luca Cindolo, Department of Urology, Villa Stuart Hospital, Rome, Italy Andrea Minervini, Department of Urology, University of Flo rence, Unit of Oncologic Minimally Invasive Urology and Andrology, Careggi Hospital, Florence, Italy Bernardo Rocco, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy Riccardo Schiavina, Department of Urology, University of Bologna, Bologna, Italy
ADVISORY EDITORIAL BOARD
Pier Francesco Bassi, Urology Unit, A Gemelli Hospital, Catholic University of Rome, Italy Francesca Boccafoschi, Health Sciences Department, University of Piemonte Orientale in Novara, Italy Alberto Bossi, Department of Radiotherapy, Gustave Roussy Institute, Villejuif, France Tommaso Cai, S Chiara Hospital, Trento, Italy
Paolo Caione, Department of Nephrology Urology, Bambino Gesù Pediatric Hospital, Rome, Italy Luca Carmignani, Urology Unit, San Donato Hospital, Milan, Italy Liang Cheng, Department of Urology, Indiana University School of Medicine, India napolis, IN; Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, Indianapolis, IN Giovanni Colpi, Retired Andrologist, Milan, Italy
Giovanni Corona, Department of Urology, University of Florence, Careggi Hospital, Florence, Italy Antonella Giannantoni, Department of Surgical and Biomedical Scien ces, University of Perugia, Italy Paolo Gontero, Department of Surgical Sciences, Mo linette Hospital, Turin, Italy Steven Joniau, Organ Systems, Department of Development and Regeneration, KU Leuven, Belgium Frank Keeley, Bristol Urologi cal Institute, Southmead Hospital, Bristol UK Laurence Klotz, Division of Urology, De partment of Surgery, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Ontario, Canada Börje Ljungberg, Urology and Andrology Unit, Department of Surgical and Perioperative Sciences, Umeå University, Umeå, Sweden Nicola Mondaini, Uro Andrology Unit, Santa Maria Annunziata Hospital, Florence, Italy Gordon Muir, Department of Urology, King's College Hospital, London, UK Giovanni Muto, Urology Unit, Bio Medical Campus University, Turin, Italy Anup Patel, Department of Urology, St Mary's Hospital, Imperial Healthcare NHS Trust, London, UK Glenn Preminger, Division of Urologic Surgery, Duke University Medical Center, Durham, NC, USA David Ralph, St Peter's Andrology Centre and Institute of Urology, London, UK Allen Rodgers, Department of Chemistry, University of Cape Town, Cape Town, South Africa Francisco Sampaio, Urogenital Research Unit, State University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil Kemal Sarica, Department of Urology, Kafkas University Medical School, Kars, Turkey Luigi Schips, Department of Uro logy, San Pio da Pietrelcina Hospital, Vasto, Italy Hartwig Schwaibold, Bristol Uro logical Institute, Southmead Hospital, Bristol, UK Alchiede Simonato, Department of Urology, University of Verona, Azienda Ospedaliera Universitaria Integrata, Verona, Italy Carlo Terrone, Department of Urology, IRCCS S Martino University Hospital, Ge nova, Italy Anthony Timoney, Bristol Urological Institute, Southmead Hospital, Bri stol, UK Andrea Tubaro, Urology Unit, Sant’Andrea Hospital, “La Sapienza” University, Rome, Italy Richard Zigeuner, Department of Urology, Medical University of Graz, Graz, Austria
BOARD OF REVIEWERS
Maida Bada, Department of Urology, S Pio da Pietrelcina Hospital, ASL 2 Abruzzo, Vasto, Italy Lorenzo Bianchi, Department of Urology, University of Bologna, Bologna, Italy Mariangela Cerruto, Department of Urology, Azienda Ospedaliera Universitaria

Integrata (A O U I ), Verona, Italy Francesco Chessa, Department of Urology, Univer sity of Bologna, Bologna, Italy Daniele D’Agostino, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy Fabrizio Di Maida, Department of Urology, University of Florence, Unit of Oncologic Minimally Invasive Urology and Andrology, Careggi Hospital, Florence, Italy Antonio Galfano, Urology Unit, Niguarda Hospital, Milan, Italy Michele Marchioni, Department of Medical, Oral and Biotechnological Sciences, "G. d'Annunzio" University of Chieti, Laboratory of Bio statistics, Chieti, Italy Andrea Mari, Department of Urology, University of Florence, Unit of Oncologic Minimally Invasive Urology and Andrology, Careggi Hospital, Florence, Italy Antonio Porcaro, Department of Urology, Azienda Ospedaliera Universitaria In tegrata (A O U I ), Verona, Italy Stefano Puliatti, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy Daniele Romagnoli, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy Chiara Sighinolf, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy Tommaso Silvestri, Urology Clinic, Department of Medical, Surgical and Health Science, University of Trieste, Trieste, Italy Petros Sountoulides, Aristotle University of Thessaloniki, Department of Urology, Thessaloniki, Greece
SIEUN EDITOR
Pasquale Martino, Department of Emergency and Organ Transplantation Urology I, University Aldo Moro, Bari, Italy
SIEUN EDITORIAL BOARD
Emanuele Belgrano, Department of Urology, Trieste University Hospital, Trieste, Italy
Francesco Micali, Department of Urology, Tor Vergata University Hospital, Rome, Italy Massimo Porena, Urology Unit, Perugia Hospital, Perugia, Italy Francesco Paolo Selvaggi, Department of Urology, University of Bari, Italy Carlo Trombetta, Urology Cli nic, Cattinara Hospital, Trieste, Italy Giuseppe Vespasiani, Department of Urology, Tor Vergata University Hospital, Rome, Italy Guido Virgili, Department of Urology, Tor Ver gata University Hospital, Rome, Italy
UrOP EDITOR



Carmelo Boccafoschi, Department of Urology, Città di Alessandria Clinic, Alessandria, Italy
UrOP EDITORIAL BOARD
Renzo Colombo, Department of Urology, San Raffaele Hospital, Milan, Italy Roberto Giulianelli, Department of Urology, New Villa Claudia, Rome, Italy Massimo Lazzeri, Department of Urology, Humanitas Research Hospital, Rozzano (Milano), Italy Angelo Porreca, Department of Urology, Polyclinic Abano Terme, Abano Terme (Padova), Italy
Marcello Scarcia, Department of Urology, "Francesco Miulli" Regional General Hospital, Acquaviva delle Fonti (Bari), Italy Nazareno Suardi, Department of Urology, San Raf faele Turro, Milano, Italy
GUN EDITOR
Arrigo Francesco Giuseppe Cicero, Medical and Surgical Sciences Department, Sant’Orsola Malpighi University Hospital, Bologna, Italy
GUN EDITORIAL BOARD
Gianmaria Busetto, Department of Urology, Sapienza University of Rome, Italy Tommaso Cai, Department of Urology, Santa Chiara Regional Hospital, Trento, Italy
Elisabetta Costantini, Andrology and Urogynecological Clinic, Santa Maria Hospital of Terni, University of Perugia, Terni, Italy Angelo Antonio Izzo, Department of Pharmacy, University of Naples, Italy Vittorio Magri, ASST Nord Milano, Milano, Italy Salvatore Micali, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy Gianni Paulis, Andrology Center, Villa Benedetta Clinic, Rome, Italy Francesco Saverio Robustelli della Cuna, University of Pavia, Italy
Giorgio Ivan Russo, Urology Department, University of Cata nia, Italy Konstantinos Stamatiou, Urology Department, Tzaneio Hospital, Piraeus, Greece Annabella Vitalone, Department of Physiology and Pharmacology, Sapienza University of Rome, Rome, Italy
NOVITÀ
Un’opera nuova e completa sul microbiota, il complesso consorzio di o malattia. Centinaia di illustrazioni a colori, contenuti multimediali, aggiornati in progress continuo ed accessibili mediante QR code. Un Trattato imprescindibile per chi si occupa di salute interpretando i referti sul microbiota.
Costo di copertina €120,00, IVA e spese di spedizione incluse. Per informazioni ed eventuali ordini, scrivere a: info@edizioniscriptamanent.eu

ORIGINAL PAPERS
328 Premature ejaculation in the era of mobile health application: A cur rent analysis and evaluation of adherence to EAU guidelines Luigi Napolitano, Luigi Cirillo, Giovanni Maria Fusco, Marco Abate, Alfonso Falcone, Vincenzo Morgera, Gianluigi Cacace, Luigi De Luca, Pasquale Reccia, Claudia Mirone, Felice Crocetto, Giuseppe Celentano, Simone Morra, Biagio Barone, Ciro imbimbo, Nicola Longo, Vincenzo Mirone, Roberto La Rocca
334 An original mininvasive corporoplasty technique for penile cur vature without circumcision Antonio Rossi, Giovanni Alei, Pietro Viscuso, Antonio Tufano, Marco Frisenda, Guglielmo Mantica, Pierluigi Bove, Rosario Leonardi, Mauro De Dominicis, Alessandro Calarco
339 Penile lenghthening original technique using a pubo caver nous spacer. Long ter m results from a series of over 200 patients Antonio Rossi, Giovanni Alei, Marco Frisenda, Antonio Tufano, Pietro Viscuso, Guglielmo Mantica, Pierluigi Bove, Rosario Leonardi, Alessandro Calarco
REVIEWS
345 Frailty and benign prostatic hyperplasia: The thrilling under lying impact Themistoklis Ch Bellos, Lazaros I Tzelves, Ioannis S Manolitsis, Stamatios N Katsimperis, Marinos V Berdempes, Andreas Skolarikos, Nikolaos D Karakousis
350 Malakoplakia of the urinar y bladder : A review of the literature Giordano Polisini, Rocco Francesco Delle Fave, Camilla Capretti, Angelo Marronaro, Alessia Mariagrazia Costa, Luigi Quaresima, Daniele Mazzaferro, Andrea Benedetto Galosi
355 Systematic review of urinar y biomarkers of female bladder outlet obstr uction (fBOO) Andreia Bilé Silva, Paulo Jorge Dinis, Luís Abranches Monteiro
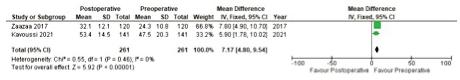
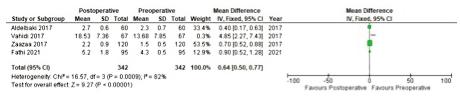
360 Microsurgical varicocelectomy effects on sper m DNA fragmentation and sper m parameters in infer tile male patients:
A systematic review and meta analysis of more recent evidence Alwin Soetandar, Bambang Sasongko Noegroho, Safendra Siregar, Ricky Adriansjah, Akhmad Mustafa
LETTERS TO EDITOR
366 Nocturia due to noctur nal polyuria (NP). A common disorder Anastasios Athanasopoulos
369 How long should we follow patients managed for muscle invasive bladder cancer? Lesson lear ned from a recent clinical practice Aldo Franco De Rose, Francesco Vecco, Francesca Ambrosini, Rafaela Malinaric, Guglielmo Mantica, Carlo Terrone
371 Organ har vesting as a mandator y training step of all PGY1 and PGY2 surgical residents Rafaela Malinaric, Guglielmo Mantica, Carlo Terrone
373 Natural treatments for erectile dysfunction: A focus on mobile health applications Luigi Napolitano, Luigi Cirillo, Giovanni Maria Fusco, Marco Abate, Vincenzo Morgera, Gianluigi Cacace, Giuseppe Celentano, Biagio Barone, Lorenzo Spirito, Vincenzo Mirone, Roberto La Rocca
Edizioni Scripta Manent s.n.c. Via Melchiorre Gioia 41/A 20124 Milano, Italy Tel +39 0270608060 e mail: scriman@tin.it web: www edizioniscriptamanent eu
Registrazione: Tribunale di Milano n 289 del 21/05/2001
GENERAL INFORMATION
AIMS AND SCOPE
Direttore Responsabile: Pietro Cazzola Direzione Marketing e PR: Donatella Tedeschi Comunicazione e Media: Ruben Cazzola Grafica e Impaginazione: Stefania Cacciaglia Affari Legali: Avv Loredana Talia (MI)
41/A 20124
“Archivio Italiano di Urologia e Andrologia” publishes papers dealing with the urological, nephrological and andrological sciences

Original articles on both clinical and research fields, reviews, editorials, case reports, abstracts from papers published elsewhere, book rewiews, congress proceedings can be published
AIII rchivio Italiano di Urologia e Andrologia 2022, 94, 3
Ai sensi della legge 675/96 è possibile in qualsiasi momento opporsi all’invio della rivista comunicando per iscritto la propria decisione a: Edizioni Scripta Manent s n c Via Melchiorre Gioia,
Milano The Publisher is not liable for the opinion expressed by the Authors of the articles and for images used by them
25 Capitoli 64 Autori 480 Pagine a cura di Gianvincenzo Zuccotti Enza D’Auria Elvira Verduci Questo Trattato nasce dall’esigenza di offrire evidenze scientifiche della letteratura in diversi àmbiti clinici, riguardo alla Nutraceutica in Pediatria, in un contesto attuale dove è molto forte da parte della società la propensione a ricorrere a “prodotti naturali”. I temi trattati sono a sostegno di scelte mirate da parte del Pediatra, che possono essere di supporto dal punto di vista preventivo e terapeutico, per la salute di bambini e adolescenti. Prezzo di copertina € 100,00 Per l’acquisto inviare una e-mail a: info@edizioniscriptamanent.eu
Omer Burak Argun 1 , Panagiotis Mourmouris 2 , Yesim Saglican 3 , Tunkut Doganca 4 , Mustafa Bilal Tuna 5 , Cavit Kerem Kayhan 6 , Ozge Yalcinkaya 6 , Ilter Tufek 1 , Halil Kara 7 , Can Obek 1 , Umit Ince 3 , Lazaros Tzelves 2 , Andreas Skolarikos 2 , Ali Rıza Kural 1
1 Acibadem Mehmet Ali Aydinlar University, School of Medicine, Department of Urology, Istanbul, Turkey;
National and Kapodistrian University of Athens, Sismanogleio General Hospital, 2nd Department of Urology, Athens, Greece;
Acibadem Mehmet Ali Aydinlar University, School of Medicine, Department of Pathology, Istanbul, Turkey;
Acibadem Taksim Hospital, Department of Urology, Istanbul, Turkey;
Acibadem Maslak Hospital, Department of Urology, Istanbul, Turkey;
6 Acibadem Maslak Hospital, Department of Pathology, Istanbul, Turkey;
Acibadem Maslak Hospital, Department of General Surgery, Istanbul, Turkey
Summary
Introduction: The OSNA technique is based on reverse transcription loop mediated DNA amplification for the detection of cytokeratin 19 (CK19) messen ger RNA (mRNA) The purpose of our paper, which represents the first study in the literature, is to test the accuracy of this method in the detection of lymph node metastases in patients undergoing robotic radical prostatectomy with lymph node dis section.
Methods: Our cohort consisted of patients that have undergone robotic radical prostatectomy with extended lymph node dissec tion. Lymph nodes were evaluated with imprint technique and then with frozen section examination. The remaining tissue was evaluated by OSNA method. Lymph nodes were defined as ‘neg ative’ or ‘positive’ according to mRNA copy number. Results: 7 patients and 25 lymph nodes were included in our cohort. Two patients were found negative with all pathology methods. In one patient the standard stains revealed a suspi cious outcome but it was positive for micrometastasis with OSNA. In another patient the outcome was positive for standard stains and negative for OSNA. Finally, 2 patients were found positive for OSNA and negative for imprint methods.
Conclusions: One Step Nucleic Acid Amplification (OSNA) method using CK19 seems to fail in detection of lymph node metastases in prostate cancer patients undergoing radical prostatectomy and lymph node dissection
KEY WORDS: Prostate cancer; Metastases; Lymph nodes; One step nucleic acid amplification
Submitted 24 January 2022; Accepted 2 March 2022
INTRODUCTION
Pelvic lymph node metastasis is associated with poor prognosis and upstages prostatic carcinoma Pelvic lymph node dissection (PLND) is currently the most accurate lymph node (LN) staging procedure for prostate cancer (PCa) None of the available radiologic imaging modali ties provides an equivalent sensitivity for the detection of
No conflict
LN involvement The sensitivity of abdominal computed tomography (CT) and multiparametric magnetic resonance imaging (mpMRI) for lymph node metastasis is less than 40% according to a recent study (1)
In addition, nuclear medicine based imaging modalities (11C or 18F choline and 68Ga PSMA), PET CT for ini tial staging of prostate cancer may provide low sensitivity (49 66%) in detection of LN metastases (1, 2)
Today, the gold standard evaluation of lymph node metastasis remains multistep analysis of the lymph nodes via hematoxylin eosin stained sections, combined with i m m u n o h i s t o c h e m i s t r y f o r c y t o k e r a t i n e x p re s s i o n However, there is no standardized assessment method for nodal status in prostate cancer Histopathologic evalua t i o n o f l y m p h n o d e s v a r i e s b e t w e e n l a b o r a t o r i e s Intraoperative frozen section (FS) assessment of pelvic lymph nodes (PLNs) is being used not so often, but for some triage patients Additionally, the role of FS in iden tifying small metastases and influencing the completion of the RP can be queried
The routine FS of PLNs has been questioned by several studies (3, 4) There are studies, which report a wide range of sensitivity for FS of PLNs, between 33% to 77% (5) If the metastasis is small and not visible on macroscopic evaluation, freezing and cryostat section may waste the tis sue, which is very important during permanent embed ding Regarding technical details, fatty lymph nodes are not good candidates for frozen section analysis as micro scopic metastasis can be lost during defatting process All these shortcomings of the pathological evaluation of the lymph nodes brought out different technologies like Polymerase Chain Reaction (PCR) based techniques
PCR based techniques such as one step nucleic acid ampli fication (OSNA) assay are viable alter natives The OSNA technique for pathological evaluation of lymph node is b a s e d o n re v e r s e t r a n s c r i p t i o n l o o p m e d i a t e d D N A amplification for the detection of cytokeratin 19 (CK19)
A265 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
ORIGINAL PAPER
of interest declared
One step nucleic acid amplification (OSNA) for detection of lymph node metastasis during robotic radical prostatectomy for prostate cancer: A pilot study
2
3
4
5
7
DOI: 10 4081/aiua 2022 3 265
O Burak Argun, P Mourmouris, Y Saglican, et al
messenger RNA (mRNA) The idea behind this relatively novel study with micromolecular histopathologic tech nique is detection of CK 19 in lymphatic tissue due to p ro s t a t e c a n c e r m e t a s t a s i s , w h i c h i s n o r m a l l y n o t
expressed Our goal was to evaluate the use of the OSNA method to detect cancer metastasis in entire lymph node in comparison with conventional methods in prostate cancer patients who underwent robotic radical prostatec tomy and lymph node dissection

MATERIAL AND METHODS
Our cohort consisted of patients that have been diag nosed with intermediate and high risk prostate cancer and who have undergone robotic radical prostatectomy w i t h e x t e n d e d l y m p h n o d e d i s s e c t i o n I n s t i t u t i o n a l
Review Board approval was taken from ethical committee
Informed and written consent was obtained from all p a t i e n t s Ly m p h n o d e t e m p l a t e i n c l u d e d c a u d a l l y, femoral canal; medially, the side wall of the bladder; lat erally, up to the genitofemoral nerve; posteriorly, the obturator muscle and floor of the obturator fossa down to the inter nal iliac vessels; cranially, the common iliac region where the ureter crosses the common iliac artery and aortic bifurcation up to the inferior mesenteric artery
Patients with previous and/or additional malignancies and with a history of pelvic radiotherapy were excluded from the study A summary of patient and tumor charac teristics is shown in Table 1
Suspicious lymph node regions were defined pre opera tively with the use of imaging methods such as prostate specific membrane antigen positron emission tomography ( P S M A P E T ) o r M a g n e t i c R e s o n a n c e I m a g i n g ( M R I )
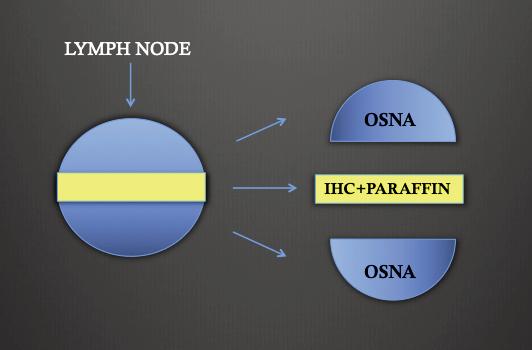
Following the completion of the lymph node dissection, the suspicious lymphatic tissue samples were removed through the assistant port site inside an organ bag Lymphatic tissues were sent to the pathology department immediately and dissected out from the fatty tissue Care has been taken to perform lymph node dissection before the prostatectomy, as this could potentially contaminate the lymph node tissues with CK19 positive tissues Following step was cutting the suspected lymph node through the sagittal plane Each plane (facing each other) was evaluated with imprint technique and then with frozen section examination Touch imprint cytology was carried out by gently touching the fresh tissue on a clean glass slide and fixing immediately imprints in 95% ethyl
Figure
Process of lymph nodes larger than 5 mm.
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
alcohol and staining with hematoxylin and eosin (H&E) stains Frozen section study was performed by processing tissue in cryostat at 10°C to 15°C and cutting thin sec tions of 3 5 μm thickness and staining using H&E If the lymph nodes were large enough (> 5 mm in diameter), a segment of approximately 2 3 mm from the middle of the lymph node was removed and stored for paraffin sam pling and immunohistochemistry (IHC) evaluation as stat ed in the consent form (Figure 1) The remaining tissue was evaluated by OSNA method or stored at minus 18°C if OSNA procedure was not possible at the time of oper ation In case of a small lymph node (< 5 mm), cutting was performed in two pieces and used one piece of it (Figure 2), whereas the second one was examined with H&E staining and paraffin sampling which were golden standard for post operative evaluation The fresh sections stored for OSNA evaluation were trans formed to a homogenized dilution with the use of a 4 ml of lysing buffer (Lynorhag, Sysmex, Kobe, Japan) for 90 sec onds and then the latter was centrifuged for one minute at 10,000 G Next, CK19 and beta actin mRNA were a m p l i f i e d b y R e v e r s e Tr a n s c r i p t i o n L o o p M e d i a t e d A
( RT L A M P )
R D 1 0 0
a m p , Sysmex, Kobe) The use of the dedicated kit provided by the manufacturer (Lynoamp, Sysmex, Kobe) allowed the start of the automated procedure that was performed without the need of RNA purification LNs were defined
Figure
Process
( Ly
266
m p l i f i c a t i o n
i n t h e
i
n o
Table 1 Pre and perioperative characteristics of patients.
1
Patient Age PSA Pre op Clinical Post op Patholog y Surgical GS stage GS stage margins 1 60 7,5 3+4 cT2b 3+4 pT2c Negative 2 68 8 4+5 cT3 4+5 pT3b Negative 3 69 8,5 4+4 cT3 3+4 pT3a Negative 4 64 15 4+4 cT2c 4+4 pT2c Negative 5 73 5,2 4+5 cT3 5+4 pT3b Negative 6 68 20 4+4 cT3 4+4 pT3b Negative 7 68 8 4+3 cT2c 5+4 pT3b Negative PSA: Prostate specif c antigen; GS: G eason Score
2.
of lymph nodes smaller than 5 mm
as ‘negative’ or ‘positive’ according to mRNA copy num ber CK 19 mRNA copies/mL less than 250 were defined as negative ( ), 250 5000 were defined as positive for micrometastases and copies exceeding 5000 were defined as positive for macrometastases, according to manufac turer’s manual
RESULTS
7 patients and 25 lymph nodes were included in our cohort In the first and second patients, 2 and 4 lymph nodes were used for analysis from the harvested lym phatic tissue In all cases OSNA was performed intraop eratively except one that due to device failure was per formed postoperatively They were all negative for imprint analysis, frozen section (H&E) staining and OSNA In third patient 5 lymph nodes from different areas were selected according to the aforementioned criteria and one of them was suspicious in imprint analysis but also it was positive for micrometastatis in OSNA evaluation In fourth patient, there was micrometastasis in imprint analysis and H&E staining but negative for OSNA and frozen section analysis In fifth patient, even though OSNA was positive for micrometastasis, imprint analysis and frozen section +(H&E) staining failed to confirm it In sixth patient, 4 lymph nodes were harvested and in one of them OSNA was positive even though the imprint and frozen section analysis were negative In seventh patient, we harvested 5 lymph nodes and 3 of them were found to be positive for macrometastatis but negative for OSNA (Table 2) In this cohort of lymph nodes, OSNA method was discordant for evaluation of metastatic lymph node status
DISCUSSION
Today, hematoxylin eosin staining and immunohisto chemical methods are used in the detection of lymph node metastases of prostate cancer Because of the techni cal difficulties and also the nature of the sampling method, identification of cancerous cells in the entire lymph node is not feasible and metastasis status is report ed by random sampling of the lymph tissues (1) The sin gle step nucleic acid amplification (OSNA) method, has proven its value in the sentinel lymph node sampling of breast cancer (2) Meanwhile its use in other malignancies (colorectal, head and neck, gynecological, lung, thyroid, gastric) has yielded promising outcomes (5 10) Its use can be expanded to intraoperative identification of posi tive lymph nodes that may potentially alter the course of the procedure in the future (11) As well there are even studies in the literature implying that the OSNA method can potentially gain the first place as a standard for patho logical examination of lymph node infiltration (12)
The presence of lymph node metastasis in patients with prostate cancer can significantly alter the management and the prognosis of the disease Lymph node status remains a significant prognostic factor and an important part of the decision making process regarding adjuvant treatment for prostate cancer patients
Our study represents the first study that tests the poten tial role of the OSNA method in diagnosing lymph node infiltration in patients with prostate cancer
The OSNA system (Sysmex Corporation, Kobe, Japan), combines reverse transcription (RT) with isothermal loop mediated DNA amplification (RT LAMP) for detection of CK19 messenger RNA (mRNA) as a marker of cancerous cells since CK19 mRNA in the glandular epithelial cells should not normally be present in the lymph nodes (13) When compared to other techniques for intraoperative evaluation of sentinel node metastases in breast cancer, outcomes of OSNA technique are relatively controversial
There are studies that report a clear advantage of the more popular imprints cytology (IC) with a calculated accuracy of 96 12% (14), whereas in other studies the OSNA method is found to be equally reliable (detection rates 11 8 vs 12 1%) when compared to other techniques such as cytokeratin immunohistochemistry (CK IHC) (15) When cost is concer ned there is limited data in the literature and mostly achieved from studies for breast cancer
The hypothesis was that with a reliable intra operative diagnostic tool, the patients would be spared from a sec ond procedure in order to excise the remaining lymph nodes that could be potentially infiltrated The data, even though controversial, imply that OSNA method is not cost effective for the intraoperative diagnosis of sentinel lymph node metastases despite its accuracy that reaches almost 91% (16) However, Guillén Paredes MP et al in patients with breast cancer metastases, report reduced hospital stay and operating time with OSNA method resulting in a saving of 439 67 € per patient, but their study is a retrospective with a low number of patients, so their results must be interpreted with caution (17)
Prostate cancer patients can potentially survive for more than 15 years and most of them will be receiving some kind of treatment Hence cost analysis of this method for prostate cancer can potentially yield different outcomes
A267 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
OSNA for lymph node metastasis in prostate cancer
Table 2. Results of lymph nodes analysis of patients Patient Lymph node Imprint+ Frozen+ OSNA location H&E staining H&E staining 1 Right common iliac 000 Negative Right external iliac 000 Negative 2 Right obturator 000 Negative Left obturator 000 Negative Pre sacral 000 Negative Right external iliac 000 Negative 3 Left common iliac 000 Negative Left external i lac 000 Negative Right common iliac S01 1100 copies Left obturator 000 Negative Right external iliac 000 Negative 4 Right obturator 010 Negative 5 Right obturator 001 400 copies Left obturator 000 Negative Right common iliac 000 Negative 6 Right obturator 001 400 copies Left obturator 000 Negative Left external i iac 000 Negative Left common iliac 000 Negative 7 Right obturator+external liac 1S0 Negative Right obturator+external liac 000 Negative Left obturator+external iliac 110 Negative Left obturator+external iliac 110 Negative Left common iliac 000 Negative 0 = Negat ve; 1 = Posit ve; S = Inconc us ve
O Burak Argun, P Mourmouris, Y Saglican, et al
compared to breast cancer No data exist in the literature concer ning the use of OSNA method in detecting possi ble positive lymph nodes in prostate cancer patients The only one available in the literature reports preliminary results of this method in prostatectomy specimens and not in lymph nodes (18) This study implicates CK19 as a potential marker for prostate cancer specimens and presents some promising results Nevertheless, based on our results CK19 doesn’t seem to yield satisfactory results as far as lymph nodes metastasis is concer ned Furthermore, the true clinical impact of this method (if any), lies in positive lymph node detection since the methods for detecting prostate cancer in prostate glands are already completely satisfying something that does not imply for lymph nodes
Our study is a pilot study and so it cannot avoid several limitations First of all the number of patients is very small and the number of lymph nodes tested Nevertheless, this is the first study to test the potential role of OSNA in lymph nodes metastases for prostate can cer and also the number of patients with positive lymph nodes in radical prostatectomy series is relatively small Finally, our study did not test either cost or potential sur vival benefit for patients that were found to be positive with the OSNA method The purpose of our paper was to study the potential role of a novel detection method (OSNA), already used in other malignancies, in prostate cancer Future well designed studies are needed to con firm if these methods can increase the detection rate of lymph node metastases and provide any survival benefit for the patients
CONCLUSIONS
OSNA method using CK19 was not sufficient to demon strate lymph node metastases in prostate cancer patients undergoing radical prostatectomy and lymph node dis section compared to golden standards
REFERENCES
1 Kryvenko ON, Epstein JI Histologic criteria and pitfalls in the diagnosis of lymphovascular invasion in radical prostatectomy speci mens Am J Surg Pathol 2012; 36:1865 73
2 Shi F, Liang Z, Zhang Q, et al The performance of one step nucle ic acid amplification assay for intraoperative detection of sentinel lymph node macrometastasis in breast cancer: An updated meta analysis Breast 2018; 39:39 45
3 Young MP, Kirby RS, O’Donoghue EP, Parkinson MC Accuracy and cost of intraoperative lymph node frozen sections at radical prostatectomy J Clin Pathol 1999; 52: 925 7
4 Kakehi Y, Kamoto T, Okuno H, et al Per operative frozen section examination of pelvic nodes is unnecessary for the majority of clini cally localized prostate cancers in the prostate specific antigen era Int J Urol 2000; 7:281 6
5 Wild JB, Iqbal N, Francombe J, et al Is it time for one step nucle ic acid amplification (OSNA) in colorectal cancer? A systematic review and meta analysis Tech Coloproctol 2017; 21:693 699
6 Zhou M, Wang X, Jiang L, et al The diagnostic value of one step nucleic acid amplification (OSNA) in differentiating lymph node
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
metastasis of tumors: A systematic review and meta analysis Int J Surg 2018; 56:49 56
7 Fanfani F, Monterossi G, Ghizzoni V, et al One Step Nucleic Acid Amplification (OSNA): A fast molecular test based on CK19 mRNA concentration for assessment of lymph nodes metastases in early stage endometrial cancer PLoS One 2018; 13:e0195877
8 Nakagawa K, Asamura H, Tsuta K, et al The novel one step nucle ic acid amplification (OSNA) assay for the diagnosis of lymph node metastasis in patients with non small cell lung cancer (NSCLC): Results of a multicenter prospective study Lung Cancer 2016; 97:1 7
9 González O, Iglesias C, Zafon C, et al Detection of thyroid papil lary carcinoma lymph node metastases using One Step Nucleic Acid Amplification (OSNA): preliminary results J Invest Surg 2015; 28:153 9
10 Nakabayashi K, Uraoka T, Shibuya M, et al Rapid detection of CEA mRNA in peritoneal washes using One Step Nucleic acid Amplification (OSNA) for gastric cancer patients Clin Chim Acta 2015; 439:137 42
11 Yeung TM, Wang LM, Colling R, et al Intraoperative identifica tion and analysis of lymph nodes at laparoscopic colorectal cancer surgery using fluorescence imaging combined with rapid OSNA pathological assessment Surg Endosc 2018; 32:1073 1076
12 Tamaki Y One step nucleic acid amplification (OSNA): where do we go with it? Int J Clin Oncol 2017; 22:3 10
13 Tsujimoto M, Nakabayashi K, Yoshidome K, et al Onestep nucle ic acid amplification (OSNA) for intraoperative detection of lymph node metastasis in breast cancer patients Clin Cancer Res 2007; 13:4808 4816
14 Luna Tomás MA, Solà Suárez M, Mariscal Martínez A, et al Is OSNA better than imprint cytology for intraoperative diagnosis of cancer involvement of axillary sentinel node in breast cancer? Breast 2018; 38:181 187
15 Shigematsu H, Ozaki S, Yasui D, et al Comparison of CK IHC assay on serial frozen sections, the OSNA assay, and in combination for intraoperative evaluation of SLN metastases in breast cancer Breast Cancer 2018; 25:191 197
16 Huxley N, Jones Hughes T, Coelho H, et al A systematic review and economic evaluation of intraoperative tests [RD 100i one step nucleic acid amplification (OSNA) system and Metasin test] for detecting sentinel lymph node metastases in breast cancer Health Technol Assess 2015; 19:v xxv, 1 215
17 Guillén Paredes MP1, Carrasco González L, Cháves Benito A, et al One step nucleic acid amplification (OSNA) assay for sentinel lymph node metastases as an alternative to conventional postopera tive histology in breast cancer: cost benefit analysis Cir Esp 2011; 89:456 62
18 Winter A, Engels S, Goos P, et al Detection of CK19 mRNA
Using One step Nucleic Acid Amplification (OSNA) in Prostate Cancer: Preliminary Results J Cancer 2018; 9:4611 4617
Correspondence
Omer Burak Argun, MD, Associate Professor of Urology drburakargun@gmail com
Ilter Tufek, MD, Professor of Urology iltertuf@gmail com
Ali Rıza Kural, MD, Professor of Urology arkural@gmail com
Acibadem Mehmet Ali Aydinlar University, School of Medicine, Department of Urology Buyukdere Cad 40 Maslak 34457 Istanbul (Turkey)
268
Panagiotis Mourmouris, MD, Urologist (Corresponding Author) thodoros13@yahoo com National and Kapodistrian University of Athens, Sismanogleio General Hospital, 2nd Department of Urology Sismanogliou 37, Marousi 151 26 (Greece)
Yesim Saglican, MD, Associate Professor of Pathology yesim saglican@acibadem com tr Umit Ince, MD, Professor of Pathology umit ince@acibadem com
Acibadem Mehmet Ali Aydinlar University, School of Medicine, Department of Pathology Buyukdere Cad 40 Maslak 34457 Istanbul (Turkey)
Tunkut Doganca, MD, Urologist tunkutdoganca@gmail com
Acibadem Taksim Hospital, Department of Urology Inonu Mahallesi, Nizamiye Cd No:9, 34373 Sisli, Istanbul (Turkey)
Mustafa Bilal Tuna, MD, Urologist mustafabilaltuna@gmail com
Cavit Kerem Kayhan, Biologist cavit kerem kayhan@acibadem com
Acibadem Maslak Hospital, Department of Pathology Buyukdere Cad 40 Maslak 34457 Istanbul (Turkey)
Ozge Yalcinkaya, Pathology Technician ozge yalcinkaya@acibadem com Halil Kara, MD, General Surgeon halil kara@acibadem com
Acibadem Maslak Hospital, Department of General Surgery Buyukdere Cad 40 Maslak 34457 Istanbul (Turkey)
Can Obek, MD, Professor of Urology canobek@yahoo com
Lazaros Tzelves, MD, Urologist lazarostzelves@gmail com
Andreas Skolarikos, MD, PhD, Professor of Urology andskol@yahoo com
2nd Department of Urology, National and Kapodistrian University of Athens, Sismanogleio General Hospital, Sismanogliou 37, Marousi 151 26 (Greece)
A269 rchivio Italiano di Urologia e Andrologia 2022; 94,
3
OSNA for lymph node metastasis in prostate cancer
Urology Unit, Cannizzaro Hospital, Catania, Italy;
Pathology Unit, Cannizzaro Hospital, Catania, Italy
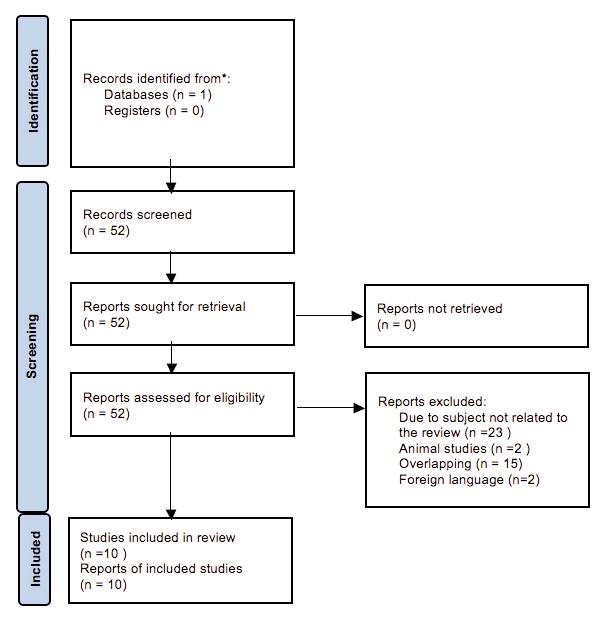
SummaryIntroduction: The reclassification rate for clinically significant prostate cancer (csPCa) in men enrolled in Active Surveillance (AS) as been prospective ly evaluated
Patients and methods: One hundred patients with very low risk PCa underwent after 8 years a scheduled transperineal prostate biopsy (SPBx = 20 cores) combined with additional mpMRI/TRUS fusion biopsies (4 cores) of lesions PI RADS scores ≥ 3 All the patients, after initial diagnosis, previously had mpMRI evaluation combined with transperineal saturation prostate biopsy (confirmatory and 3 year scheduled biopsy). Risk reclassification at repeat biopsy triggering the recommen dation for active treatment was defined as over 3 or more than 10% of positive cores, Gleason score > 6/ISUP Grade Group ≥ 2, greatest percentage of cancer (GPC) > 50%.
Results: Multiparametric MRI was suspicious (PI RADS ≥ 3) in 30 of 100 cases (30.0%); 70 (70.0%) vs. 20 (20.0%) vs. 10 (10.0%) patients had a PI RADS score ≤ 2 vs. 3 vs. 4, respec tively. Two (2.0%) patients with PI RADS score 3 and 4 were upgraded (ISUP Grade Group 2); SPBx and MRI/TRUS fusion biopsy diagnosed 100% and 0% of csPCa, respectively.
Conclusions: Transperineal SPBx combined with mpMRI at ini tial confirmatory biopsy allow to select an high number of men at very low risk of reclassification during the AS follow up (2.0% of the cases at 8 years from diagnosis); these data could be use ful to reduce the number of scheduled repeated prostate biopsy during the AS follow up
KEY WORDS: Saturation biopsy; Active surveillance; Targeted prostate biopsy; Confirmatory prostate biopsy
Submitted 25 June 2022;
INTRODUCTION
3
2022
Active surveillance (AS) is an alter native (1 3) to radical treatment of low risk prostate cancer (PCa) reducing the risk of overtreatment (50% of the cases) (1) and allowing a strict monitoring over time by scheduled clinical evaluations Multiparametric magnetic resonance imaging (mpMRI) and mpMRI/TRUS (transrectal ultrasound) fusion targeted biopsy have improved systematic biopsies in the diagnosis of clinically significant PCa (csPCa) (4, 5), reducing the reclassification rate during the follow up of men in AS Although the timing to perform confirmatory
biopsy has been established within 12 months from ini tial diagnosis, there are no definitive data regarding the number of systematic needle cores (extended or satura tion biopsy) and the best procedure to diagnose all the csPCa reducing the number of scheduled biopsies In our study, the reclassification rate for csPCa at 8 year scheduled transperineal biopsy has been prospectively evaluated in men enrolled in AS protocol
MATERIALS AND METHODS
From May 2013 to September 2017, 160 patients aged between 52 and 73 years (median age 63) with very low risk PCa were enrolled in an AS protocol After institu tional review board and ethical committee approval were granted, informed consents were obtained from all par ticipants included in the study Presence of the following criteria defined eligibility: life expectancy greater than 10 years, clinical stage T1C, PSA below 10 ng/ml, PSA densi ty (PSAD) ≤ 0 20, ≤ 2 unilateral positive biopsy cores, Gleason score 6/International Society of Urologic Pathology (ISUP) Grade Groups (GG) 1 (6), maximum core percent age of cancer (GPC) ≤ 50% (7) All the patients six months after the PCa diagnosis underwent pelvic mpMRI 3 0 Tesla evaluation before confirmatory transperineal saturation prostate biopsy (SPBx; range: 24 32 cores); the procedure was performed with the use of a GE Logiq P6 ecograph (General Electric; Milwaukee, WI) supplied with a bi planar trans rectal probe (5 7 5 MHz) using a tru cut 18 gauge needle (Bard; Covington, GA) under sedation and antibiotic prophylaxis (8, 10) All mpMRI examinations were performed using a 3 0 Tesla scanner, (ACHIEVA 3T; Philips Healthcare Best, the Netherlands) equipped with surface 16 channels phased array coil placed around the pelvic area with the patient in the supine position; multi planar turbo spin echo T2 weighted (T2W), axial diffusion w e i g h t e d i m a g i n g ( D W I ) a n d a x i a l d y n a m i c c o n t r a s t enhanced (DCE) were performed for each patient The mpMRI lesions characterized by Prostate Imaging Reporting and Data System (PI RADS) version 2 scores ≥ 3 were considered suspicious for cancer and submitted to four targeted cores; two radiologists blinded to pre imag ing clinical parameters evaluated the mpMRI data sepa
No conflict of interest declared
Archivio Italiano di Urologia e Andrologia 2022; 94, 23 70 ORIGINAL PAPER
Accepted
July
Confirmatory transperineal saturation prostate biopsy combined with mpMRI decrease the reclassification rate in men enrolled in Active Surveillance: Our experience in 100 men submitted to eight-years scheduled biopsy
Pietro Pepe
1 ,
Ludovica Pepe
1
, Michele Pennisi
1 ,
Filippo Fraggetta
2 1
2
DOI: 10 4081/aiua 2022 3 270
Prostate biopsy and active surveillance
rately and independently;i moreover, one urologist with more than 25 years of experience performed the biopsy procedure The data were collected following the Screening Tool to Alert to Right Treatment (START) criteria (9) At con firmatory biopsy 43/160 (26 8%) were upgraded; con versely, the 117 patients who met clinical criteria to con tinue AS protocol were submitted every six months to PSA, PSAD and clinical evaluation At three years from diagno sis of cancer (range: 24 30 months), also in the presence of stable clinical parameters, the remaining 110/117 men enrolled in AS (7 men abandoned the protocol) underwent scheduled repeated SPBx combined with mpMRI/TRUS fusion guided biopsies of suspicious lesions with PI RADS ≥ 3 (4 targeted fusion cores) (11) and 5 4% of them were upgraded The Clavien Dindo grading system for the clas sification of biopsy complications was used (12)
D u r i n g t h e e n t i re f o l l o w u p 1 1 / 1 6 0 ( 6 8 % ) m e n autonomously decided to leave the AS protocol (other 4 men abandoned the protocol after 3 years follow up); on the contrary, after 8 years from the initial diagnosis the remaining 100 patients who were not upgraded at previ ous follow up visits, again underwent scheduled SPBx (20 cores) combined with mpMRI/TRUS fusion biopsies (4 cores) in the presence of lesions with PI RADS score ≥ 3 Risk reclassification at repeat biopsy, triggering the rec ommendation for active treatment, was defined as over 3 or more than 10% of positive cores, Gleason score > 6/ISUP Grade Group ≥ 2, greatest percentage of cancer (GPC) > 50% Patients being reclassified underwent definitive treatment (radical prostatectomy or exter nal radiotherapy)
RESULTS
Clinical parameters of the 100 patients included in the AS protocol who underwent repeated prostate biopsy are list ed in the Table 1; median PSA value increased 1 3 ng/ml (range: 0 2 2 ng/ml) from time of diagnosis to 8 year s c h e d u l e d re p e a t b i o p s y Tw o ( 2 0 % ) p a t i e n t s h a d unfavourable biopsy histology and were reclassified based on upgrading (2 cases = Gleason score 3 + 4/Grade Group 2), number of positive cores (5 and 6 needle positive cores) and GPC (50% and 80%) In detail, all csPCa were located only in the anterior zone of the gland Of the remaining 98 (98%) patients, 70 (70 0%) were found to have very low risk PCa and in 28 (28 0%) cancer was absent (normal parenchyma); PCa was located in the periphery in 48 (48 0%) cases and in the anterior zone in 22 (22 0%) cases and all the 98 patients continued AS Multiparametric MRI was suspicious (PI RADS ≥ 3) in 30 of 100 cases (30 0%); 70 (70 0%) vs 20 (20 0%) vs 10 (10 0%) patients had a PI RADS score ≤ 2 vs 3 vs 4, respectively In detail, the PIRADS score in the 2 men reclassified was equal to 3 in one case (50%) and 4 in the other case (50%) High level of concordance in the diagnosis of PI RADS score between the two radiologists was found (Cohen’s Kappa 0 85) None of the patients had significant complications (only Clavien Dindo grade I) resulting from the prostate biopsy, requir ing hospital admission; SPBx and MRI/TRUS fusion biop sy diagnosed 100% and 0% of csPCa, respectively Finally, all the men reclassified underwent external hypofraction ated radiotherapy (13)
Table 1.
Clinical parameters of the 100 men enrolled in the Active Surveillance protocol who underwent scheduled eight years prostate biopsy
Median PSA (range) 6 8 ng/ml (2 1 11 3 ng/ml)
Median PSA D (range) 0 12 (0 07 0 18)
DRE negative mpMRI PI RADS score ≤ 2 70 cases; 3 20 cases; 4 10 cases Gleason score 6 (3 + 3)
ISUP Grade Group GG1
GPC (range) 20% (5 50%)
Prostate weight (range) 58 grams (30 110 grams)
PSA: prostate spec fic antigen; PSAD: PSA density; DRE: digita recta examination; mpMRI: mu t parametric magnetic image resonance; PI RADS: Prostate maging Report ng and Data System GPC: greatest percentage of cancer;
ISUP: Internat ona Society of Urologic Patho ogy
DISCUSSION
The estimated treatment free probability at 5, 10 and 15 years from diagnosis of patients enrolled in AS protocol with GG1 PCa has been reported equal to 76, 64 and 58%, respectively (14); on the other hand, more than one third of patients, during follow up, are reclassified (i e , PCa upgrading and/or increase in disease extent or patient preference) and submitted to curative treatment (15) In detail, the confirmatory biopsy within one year from diagnosis upgrade the highest number of patients; in particular, the transperineal template biopsy upgrade about 38 0% of patients (16) A lot of studies reported on criteria of patient selection and follow up policies of men enrolled in AS protocol: type and timing of imaging, fre quency of repeat prostate biopsies, use of PSA density and kinetics, genetics biomarkers, use risk calculators, and frequency of clinical follow up (17 23) Although mpMRI is strongly recommended in patients enrolled in AS pro tocols (24), at present, systematic prostate biopsies should be always combined with targeted fusion biopsy due to the false negative rate of mpMRI (25 27); more over, the number of targeted fusion biopsy (in the pres ence of PI RADS ≥ 3) that should be obtained in addition to systematic prostate biopsy in men enrolled in AS pro tocols (8) has not been established (28) In fact, an accu rate biopsy histology could reduce the risk of reclassifica tion allowing to postpone scheduled prostate biopsies in favour of clinical parameters evaluation reducing, at the same time, the complications rate following repeated biopsies (i e , risk of sepsis and hospitalization) (29) At the same time, an adequate number of needle cores allows to select patients with high volume GG1 PCa at risk of reclassification during follow up (33 4% of the cases) (30) In this respect, the number of systematic and/or targeted biopsy cores is an independent predictor for selection of patients with unfavourable characteristics for AS (31 35) On the other hand, a relevant critical point remain the adherence of patients to scheduled AS follow up; in fact, the estimated drop out to the execution of repeated prostate biopsy at 1 vs 4 vs 7 years from ini tial diagnosis is equal to 11 vs 30 vs 29%, respectively (3); therefore, the European Association of Urology (EAU) guidelines strongly recommend to perform repeat biopsy in the presence of clinical suspicion of PCa progression (i,e , PSAD evaluation, progression on mpMRI) instead to
A271 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
P Pepe, L Pepe, M Pennisi, F Fraggetta
repeat biopsies at scheduled times that, anyway, are sug gested every three years (36, 37) Finally, pathologic parameters play a critical role in identifying appropriate candidates for AS; these findings need to be reproducible and consistently reported by pathologists (38 40)
In our series, 2/100 (2 0%) men were reclassified based on upgrading (Gleason score 7/ ISUP Grade Group 2), num ber of positive cores (5 and 6 positive cores) and GPC (50% and 80%); SPBx and mpMRI/TRUS fusion biopsy detected 100 vs 0% of csPCa In definitive, the execution of SPBx plus mpMRI at initial confirmatory biopsy allowed to select an high number of men at a very low risk of reclassification (from GG1 to GG2) during the AS follow up (5 4% and 2 0% of the cases at respectively 3 and 8 years from diagnosis) (11); these data could be useful to reduce the number of scheduled repeated prostate biopsy during the AS follow up
Regarding our results, some considerations should be made First, in our series there was not a control arm of men submitted to systematic 12 cores prostate biopsy; therefore, the data obtained have been compared with the literature results Second, the results were evaluated on biopsy specimens and not on the entire prostate gland Third, the negative histology of the 9 patients with PI RADS score 4 should be evaluated during the follow up Finally, a large number of men including a longer follow up are needed to confirm our results
CONCLUSIONS
Transperineal SPBx combined with mpMRI at initial con firmatory biopsy allow to select an high number of men at very low risk of reclassification during the AS follow up (2 0% of the cases at 8 years from diagnosis); these data could be useful to suggest reducing the number of sched uled repeated prostate biopsy during the AS follow up
REFERENCES
1 Hugosson J, Roobol MJ, Månsson M, et al A 16 yr follow up of the European Randomized study of Screening for Prostate Cancer Eur Urol 2019; 76:43 51
2 Klotz L Active surveillance for low risk prostate cancer Curr Urol Rep 2015; 16:24
3 Kalapara AA, Verbeek JFM, Nieboer D, Movember Foundation’s Global Action Plan Prostate Cancer Active Surveillance (GAP3) Consortium: adherence to active surveillance protocols for low risk prostate cancer: results of the Movember Foundation's Global Action Plan Prostate Cancer Active Surveillance Initiative Eur Urol Oncol 2020; 3:80 91
4 Pepe P, Garufi A, Priolo G, Pennisi M Can 3 Tesla pelvic phase array MRI avoid unnecessary repeat prostate biopsy in patients with PSA below 10 ng/ml? Clinical Genitourinary Cancer 2015: 13:e27 30
5 Tosoian JI, Mamawala M, Epstein JI, et al Active surveillance of grade group 1 prostate cancer: long term outcomes from a large prospective cohort Eur Urol 2020; 77:675 682
6 Epstein JI, Egevad L, Amin MB, and Grading Committee The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system Am J Surg Pathol 2016; 40:244 252,
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
7 Pepe P, Cimino S, Garufi A, et al Confirmatory biopsy of men under active surveillance: extended versus saturation versus multi parametri c mag n eti c reson an ce i mag i n g /tran srectal u l trasou n d fusion prostate biopsy Scand J Urol 2017; 51:260 263
8 Pepe P, Garufi A, Priolo GD, et al Is it time to perform only MRI targeted biopsy? Our experience in 1032 men submitted to prostate biopsy J Urol 2018: 200:774 778
9 Moore CM, Kasivisvanathan V, Scott ES, START Consortium: Standards of Reporting for MRI targeted Biopsy Studies (START) of the Prostate: Recommendations from an International Working Group Eur Urol 2013; 64:544 552,
10 Pepe P, Garufi A, Priolo G, Pennisi M Transperineal vs transrec tal MRI/TRUS fusion biopsy: detection rate of clinically significant prostate cancer Clin Genitourin Cancer 2017;15:e33 e36
11 Pepe P, Pepe L, Pennisi M, Fraggetta F Which prostate biopsy in men enrolled in active surveillance? Experience in 110 men submit ted to scheduled three years transperineal saturation biopsy com bined with fusion targeted cores Clin Genitourin Cancer 2021; 19:305 308
12 Dindo D, Clavien PA Classification of surgical complications A new proposal with evaluation in a Cohort of 6336 patients and results of survey Ann Surg 2004; 240:205 213
13 Pepe P, Tamburo M, Pennisi M, et al Clinical outcomes of hydro gel spacer injection space OAR in men submitted to hypofractionated radiotherapy for prostate cancer In Vivo 2021; 35:3385 3389
14 Carlsson S, Benfante N, Alvim R, et al Long term outcomes of active surveillance for prostate cancer: the Memorial Sloan Kettering Cancer Center experience J Urol 2020; 203:1122 1127
15 Bruinsma SM, Roobol MJ, Carroll PR, Movember Foundation's Global Action Plan Prostate Cancer Active Surveillance (GAP3) con sortium: Expert consensus document: Semantics in active surveil lance for men with localized prostate cancer results of a modified Delphi consensus procedure Nat Rev Urol 2017; 14:312 322
16 Voss J, Pal R, Ahmed S, et al Utility of early transperineal tem plate guided prostate biopsy for risk stratification in men undergoing active surveillance for prostate cancer BJU Int 2018; 121:863 870
17 Giganti F, Pecoraro M, Stavrinides V,, et al Interobserver repro ducibility of the PRECISE scoring system for prostate MRI on active surveillance: results from a two centre pilot study Eur Radiol 2020; 30:2082 2090
18 Pepe P, Vatrano S, Cannarella R, et al A study of gene expression by RNA seq in patients with prostate cancer and in patients with Parkinson disease: an example of inverse comorbidity Mol Biol Rep 2021; 48:7627 7631
19 Roscigno M, Stabile A, Lughezzani G, et al The use of multi parametric magnetic resonance imaging for follow up of patients included in active surveillance protocol Can PSA density discrimi nate patients at different risk of reclassification? Clin Genitourin Cancer 2020; 18:e698 e704
20 Pepe P, Dibenedetto G, Pepe L, Pennisi M Multiparametric MRI versus SelectMDx accuracy in the diagnosis of clinically significant PCa in men enrolled in active surveillance In Vivo 2020; 34:393 396
21 Lam TBL, MacLennan S, Willemse PM, et al EAU EANM ESTRO ESUR SIOG Prostate Cancer Guideline Panel Consensus statements for deferred treatment with curative intent for localised prostate cancer from an international collaborative study (DETEC TIVE Study) Eur Urol 2019; 76:790 813
22 Cooley LF, Emeka AA, Meyers TJ, et al Factors associated with time to conversion from active surveillance to treatment for prostate
272
cancer in a multi institutional cohort multicenter study J Urol 2021; 206:1147 1156
23 Pepe P, Roscigno M, Pepe L, et al Could 68Ga PSMA PET/CT eval uation reduce the number of scheduled prostate biopsy in men enrolled in Active Sirveillance protocols? J Clin Med 2022; 16; 11:3473
24 Shapiro DD, Gregg JR, Lim AH, et al Comparing confirmatory biopsy outcomes between MRI targeted biopsy and standard system atic biopsy among men being enrolled in prostate cancer active sur veillance BJU Int 2021; 127:340 348
25 Ploussard G, Beauval JB, Lesourd M, et al Impact of MRI and targeted biopsies on eligibility and disease reclassification in MRI positive candidates for active surveillance on systematic biopsies Urology 2020; 137:126 132
26 Pepe P, Garufi A, Priolo G, Pennisi M Can MRI/TRUS fusion tar geted biopsy replace saturation prostate biopsy in the re evaluation of men in active surveillance? World J Urol 2016; 34:1249 1453
27 Pepe P, Pepe L, Cosentino S, et al Detection Rate of 68Ga PSMA PET/CT vs mpMRI targeted biopsy for clinically significant prostate cancer Anticancer Res 2022; 42:3011 3015 15785
28 Pepe P, Pennisi M, Fraggetta F How many cores should be obtained during saturation biopsy in the era of multiparametric mag netic resonance? Experience in 875 patients submitted to repeat prostate biopsy Urology 2020; 137:133 137
29 Pepe P, Aragona F Morbidity following transperineal prostate biopsy in 3,000 patients submitted to 12 vs 18 vs more than 24 nee dle cores Urology 2013; 81:1142 1146
30 Müller G, Bonkat G, Rieken M, et al Potential consequences of low biopsy core number in selection of patients with prostate cancer for current active surveillance protocols Urology 2013; 81:837 842
31 Lu AJ, Syed JS, Ghabili K, et al Role of core number and location in targeted magnetic resonance imaging ultrasound fusion prostate biopsy Eur Urol 2019; 76:14 17
Correspondence
Pietro Pepe, MD (Corresponding Author) piepepe@hotmail com
Ludovica Pepe, MD Michele Pennisi, MD
Urology Unit, Cannizzaro Hospital, Catania (Italy)
Filippo Fraggetta, MD Pathology Unit, Cannizzaro Hospital, Catania (Italy)
Prostate biopsy and active surveillance
32 Villa L, Salonia A, Capitanio U, et al The number of cores at first biopsy may suggest the need for a confirmatory biopsy in patients eli gible for active surveillance implication for clinical decision making in the real life setting Urology 2014; 84:634 41
33 Kaye DR, Qi J, Morgan TM, and Michigan Urological Surgery Improvement Collaborative Pathological upgrading at radical prostatectomy for patients with Grade Group 1 prostate cancer: implications of confirmatory testing for patients considering active surveillance BJU Int 2019; 123:846 853
34 Amin A, Scheltema MJ, Shnier R, et al The Magnetic Resonance Imaging in Active Surveillance "MRIAS" Trial: use of baseline multi parametric magnetic resonance imaging and saturation biopsy to reduce the frequency of surveillance prostate biopsies J Urol 2020; 203:910 917
35 Lacetera V, Antezza A, Papaveri A, et al MRI/US fusion prostate biopsy in men on active surveillance: Our experience Arch Ital Urol Androl 2021; 93:88 91
36 Mottet N, Cornford P, van der bergh RCN, et al EAU Oncology guideline: Prostate Cancer, Amsterdam 2022
37 Ediz C, Akan S, Temel MC, Yilmaz O The importance of PSA Density in active surveillance for prostate cancer Arch Ital Urol Androl 2020; 92:136
38 Rajwa P, Sprenkle PC, Leapman MS When and how should Active Surveillance for prostate cancer be de escalated? Eur Urol Focus 2021; 7:297 300
39 Montironi R, Santoni M, Mazzucchelli R, et al The role of the uro pathologist in this series should be emphasized as shown by Montironi R, Prostate cancer: from Gleason scoring to prognostic grade grouping Expert Rev Anticancer Ther 2016; 16:433 440
40 Fandella A, Scattoni V, Galosi A, et al Italian Prostate Biopsies Group: 2016 updated guidelines insights Anticancer Res 2017; 37:413 424
A273 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Targeted prostate biopsy: 68Ga-PSMA PET/CT vs. mpMRI in the diagnosis of prostate cancer
Ludovica Pepe
Maria Tamburo
Urology Unit, Cannizzaro Hospital, Catania, Italy;
Radiotherapy Unit, Cannizzaro Hospital, Catania, Italy;
Pathology Unit, Cannizzaro Hospital, Catania, Italy
Giulia Marletta
Michele Pennisi
Filippo Fraggetta
Summary
Introduction: To evaluate the diagnostic accuracy of 68Ga prostate specific membrane antigen (PSMA) positron emission tomography/computed tomog raphy (PET/CT) vs. multiparametric magnetic resonance imag ing (mpMRI) targeted biopsy (TPBx) in the diagnosis of clinical ly significant prostate cancer (csPCa: Grade Group ≥ 2).
Materials and methods: From January 2021 to June 2022, 100 patients (median age: 66 years) with negative digital rectal examination underwent transperineal prostate biopsy for abnor mal PSA values (median 7.5 ng/ml). Before prostate biopsy, all patients underwent mpMRI and 68Ga PET/CT examinations and mpMRI (PI RADS version 2 ≥ 3) or 68Ga PET/CT index lesions suspicious for cancer (SUVmax > 5 g/ml) underwent cognitive targeted cores (mpMRI TPBx and PSMA TPBx: four cores) com bined with extended systematic prostate biopsy (eSPBx: median 18 cores) The procedure was performed transperineally using a tru cut 18 gauge needle under sedation and antibiotic prophy laxis
Results: PCa was found in 58/100 (58 0%) men; in detail, 44/58 (75 9%) were csPCa; mpMRI and 68Ga PSMA showed 66/100 (66%) and 62/100 (60%) lesions suspicious for PCa, respective ly 68Ga PSMA TPBx vs mpMRI TPBx vs eSPBx diagnosed 42 (95 4%) vs 36 (81 8%) vs 30 (68 2%) csPCa, respectively; mpMRI TPBx vs 68Ga PSMA TPBx showed a diagnostic accuracy of 76 9% vs 84 9% in diagnosing csPCa
Conclusions: 68GaPSMA PET/CT TPBx demonstrated good accuracy in the diagnosis of csPCa, which was not inferior to mpMRI TPBx (84 9% vs 76 9%) improving the detection rate for cancer of systematic biopsy
KEY WORDS: Prostate cancer; 68Ga PSMA PET/CT; mpMRI; Targeted prostate biopsy
Submitted 21 July 2022; Accepted 6 August 2022
INTRODUCTION
A l t h o u g h m u l t i p a r a m e t r i c m a g n e t i c re s o n a n c e i m a g i n g (mpMRI) has improved diagnostic accuracy of systematic prostate biopsy in the diagnosis of clinically significant prostate cancer (csPCa), about 20 35% of PCa could be missed by mpMRI targeted biopsy (1) Prostate specific membrane antigen (PSMA) is expressed in most primitive and metastatic PCa (2, 3), and PSMA inhibitors conjugat ed with the radionuclides Gallium 68 (68Ga) and fluoride 18 (18F) have been evaluated in clinical practice for the diagnosis of PCa (4 6); morever, tumour uptake, which
represents PSMA expression, is highly correlated with the aggressiveness of the primary prostatic tumour (7, 8) 68Ga PSMA positron emission tomography/computed tomog raphy (PET/CT) demonstrated to be sensitive for the detection of primary prostatic lesions, regional lym phadenopathy (9) and clinical metastases in case of bio chemical recurrence (10, 11)
Our study prospectively compared the diagnostic accura cy of 68Ga PSMA PET/CT vs mpMRI targeted biopsy (TPBx) in the diagnosis of csPCa (grade group ≥ 2) (12)
MATERIALS AND METHODS
From January 2021 to June 2022, 100 patients (median age: 66 years; range: 49 79 years) with negative digital rectal examination under went repeated transperineal prostate biopsy for abnormal PSA values (median 7 5 ng/ml; range: 4 5 83 ng/ml) (13, 14) The study was approved by the Ethics Committee of our Hospital All patients underwent prostate biopsy mpMRI and 68Ga PET/CT imaging examinations; a 1 5 Tesla scanner equipped with surface 16 channels phased array coil placed around the pelvic area with the patient in the supine position, multi planar turbo spin echo T2 weight ed imaging, axial diffusion weighted imaging, and axial dynamic contrast (ADC) enhanced MRI were performed for each patient (15) Two radiologists, blinded to pre imaging clinical parameters, evaluated the MRI data sep arately and independently PET/CT imaging was per formed using a CT integrated PET scanner (Biograph 6; Siemens, Knoxville, TN, USA) 68Ga PSMA was prepared with a fully automated radiopharmaceutical synthesis device based on a modular concept (Eckert & Ziegler Eurotope, Berlin, Germany) 68Ga PSMA 11 was given to patients via an intravenous bolus (mean, 144 ± 12 MBq; range, 122 188 MBq), and the PET acquisition was start ed at a mean of 58 ± 12 min (range, 50 81 min) after ward Scans were acquired in 3 dimensional mode with an acquisition time of 3 min per bed position Emission data were corrected for randoms, dead time, scatter, and attenuation and were reconstructed iteratively using ordered subsets expectation maximization (4 iterations, 8 subsets) followed by a post reconstruction smoothing gaussian filter (5 mm in full width at half maximum) For attenuation correction, a low dose unenhanced CT scan
No conflict of interest declared
Archivio Italiano di Urologia e Andrologia 2022; 94, 23 74 ORIGINAL PAPER
Pietro Pepe
1 ,
1 ,
2 ,
2 ,
1 ,
3 1
2
3
DOI: 10 4081/aiua 2022 3 274
68Ga PSMA PET/CT and PCa diagnosis
was performed from the skull base to the middle of the thigh Images were processed to obtain PET, CT, and PET CT fusion sections in the axial, coronal, and sagittal planes with a thickness of approximately 0 5 cm by two experienced nuclear medicine specialists, who were blinded to the clinical data The location of focal uptake on 68Ga PSMA PET/TC (Figure 1), three dimensional size, and standardised uptake value (SUVmax) values were reported on a per lesion basis with a sexstant scheme (apex, midgland, and base, each split into left and right) (5) All mpMRI (Prostate Imaging Reporting and Data System “PI RADS” version 2 ≥ 3) and 68GaPSMA PET/CT (SUVmax > 5 g/ml) index lesions underwent targeted cores (mpMRI TPBx and PSMA TPBx: four cores) com bined with extended systematic prostate biopsy (eSPBx: median 18 cores) (2, 14) The procedure was performed transperineally using a tru cut 18 gauge needle (Bard, Covington, GA, USA) under sedation and antibiotic pro phylaxis (17) Prostate targeted cores were obtained using a Hitachi 70 Arietta echograph (Chiba, Japan) supplied by a bi planar trans rectal probe (14) by one urologist with 10 years of experience in cognitive targeted biopsy Data were collected following START criteria (18)
RESULTS
PCa was found in 58/100 (58%) men; in detail, 44/100 (44%) were csPCa: 30/44 (75%) and 14 (25%) were located in the peripheral and anterior zones of the gland, respectively Clinical parameters of men with PCa are reported in Table 1; in detail, mpMRI and 68Ga PSMA
Figure 1
68Ga prostate specific membrane antigen (PSMA) PET/CT: presence of high suspicious area fo prostate cancer (SUVmax 20) in both lobe of the prostate (axial evaluation)

showed 66/100 (66%) and 62/100 (60%) lesions suspi cious for PCa, respectively These were submitted to tar geted cores combined with eSPBx The diagnostic accura cy of mpMRI TPBx vs 68Ga PSMA TPBx is shown in Table 2 None of the patients had clinical complications following prostate biopsy (Dindo Clavien grade1) (19) The average intraprostatic SUVmax was 8 5 g/ml (range = 4 49 g/ml) and the average maximal intraprostatic tumor dimension was 12 mm (range = 8 23 mm) 68Ga PSMA TPBx vs mpMRI TPBx vs eSPBx missed 2 (4 5%) vs 8 (18 2%) vs 14 (31 8%) csPCa, respectively
DISCUSSION
To reduce the risk of overdiagnosis following screening protocols for PCa, mpMRI has been recommended to decrease the risk of overtreatment; on the other hand, systematic prostate biopsy should always be combined with mpMRI/TRUS fusion biopsy because of the false negative rate of mpMRI (PCa with low volume and grade group > 2) (20, 21) Recently, 68Ga PSMA PET/CT has been suggested to improve the clinical staging of high risk PCa and disease recurrence (5, 10, 22); similarly, PSMA PET/CT has been proposed for the diagnosis of pri mary intraprostatic cancer The presence of focal uptake on PSMA PET/CT, SUVmax, and the maximal dimensions of PET avid lesions have been correlated with the pres ence of csPCa (23 25) There is a range of proposed cut offs to detect csPCa from SUVmax 3 15 to SUVmax 9 1 (26, 27); in addition, PSMA PET/CT demonstrated high correlation between the ISUP grade group and SUVmax
A275 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Table 1. Clinical parameters of 44 men with clinically significant prostate cancer (csPCa) Clinical and biopsy findings GG2 15 pz GG3 11 pz GG4 10 GG5 8 Initial biopsy 9666 Repeated biopsy 6542 Med an PSA (range: 4 5 83 ng/ml) 6 3 9 5 16 26 Med an GPC 30% 45% 70% 90% Number of pos tive cores overall 69 11 13 mpMRI PI RADS score ≥ 3 9887 68Ga PSMA PET/TC suspicious for PCa 7 11 10 8 GG: Internat ona Soc ety of Urolog cal Pathology Grade Group; mpMRI: mult parametr c magnetic resonance mag ng; PSA: Prostate specif c ant gen; GPC: Greatest percentage of cancer; PSMA: Prostate spec fic membrane antigen; PI RADS: Prostate imaging report ng and data system; PET/TC: Pos tron emission tomography/computed tomography
Table 2 Diagnostic accuracy of mpMRI TPBx vs 68Ga PSMA TPBx in the diagnosis of clinically significant prostate cancer (csPCa). Number of csPCa mpMRI TPBx 68Ga PSMA PET/CT TPBx (44 cases) 36 cases 42 cases Sensitivity 81 8% 95 4% Specific ty 71 8% 80 0% Positive predictive value 54.5% 73.4% Negative predictive value 87 5% 96 5% Diagnostic accuracy 76 9% 84 7% PSMA: Prostate specif c membrane ant gen; mpMRI: mu tiparametric magnetic resonance mag ng; PET/TC: Positron emiss on tomography/computed tomography; TPBx: targeted prostate biopsy
P Pepe, L Pepe, M Tamburo, G Marletta, M Pennisi, F Fraggetta
and maximal dimension of the lesion Zhang et al (28) reported a higher detection rate for csPCa performing a single transgluteal PSMA PET/CT targeted core (SUVmax > 8) in comparison with systematic prostate biopsy (40 vs 25% of the cases) Liu et al (29), found 85 5% of csPCa (47/55 cases) performing PET/CT PSMA targeted cores; Kalapara et al (30) compared the accuracy of 68Ga PSMA PET/CT with mpMRI in 205 men who underwent radical prostatectomy and showed an accuracy of 96% vs 91% for the detection of csPCa Xue et al showed that a SUVmax cut off of 5 4 predicted pathological upgrading at definitive histology, showing 91% specificity and 94% negative predictive value (31) Ferraro et al (32) in 49 men who underwent 68GaPSMA PET/MRI plus template biopsy demonstrated a diagnostic accuracy of PET/MRI targeted cores of 90% with only one false negative result
In definitive, the use of more parameters (i e genetic eval uation, diagnostic imaging, PSA density) (5, 33) included in risk calculator could better select men at risk for csPCa who should underwent prostate biopsy allowing to omit unnecessary procedures also in case of Active Surveillance (34) reducing complications rate (35)
In our series, among the 44/100 (44 0%) men with csPCa, mpMRI TPBx vs 68Ga PSMA TPBx showed a diagnostic accuracy of 76 9% vs 84 9%; 68Ga PSMA TPBx vs mpMRI TPBx vs eSPBx missed 2 (4 5%) vs 8 (18 1%) vs 14 (31 8%) csPCa, respectively Although prospective and randomized studies are awaited, including a greater num ber of patients, 68Ga PSMA PET/CT evaluation could be proposed in men with negative mpMRI or in the presence of claustrophobia, cardiac pacemaker and severe obesity
Our study has some limitations First, the number of patients evaluated was low Second, the results should be evaluated in the entire prostate specimen and not in biop sy histology Finally, a 68Ga PSMA PET/TC fusion platform would increase the accuracy of targeted prostate biopsy
CONCLUSIONS
68GaPSMA PET/CT TPBx demonstrated good accuracy in the diagnosis of csPCa, which was not inferior to mpMRI TPBx (76 9% vs 84 9%) improving the detection rate for cancer of systematic biopsy
AUTHORS’ CONTRIBUTIONS
The Authors contributed equally to all aspects of this study
REFERENCES
1 Panebianco V, Barchetti G, Simone G, et al Negative multipara metric magnetic resonance imaging for prostate cancer: what’s next? Eur Urol 2018; 74: 48 54
2 Pepe P, Pepe L, Cosentino S, et al Detection rate of 68Ga PSMA PET/CT vs mpMRI targeted biopsy for clinically significant prostate cancer Anticancer Research 2022; 42:3011 3015
3 Sheikhbahaei S, Afshar Oromieh A, Eiber M, et al Pearls and pit falls in clinical interpretation of prostate specific membrane antigen (PSMA) targeted PET imaging Eur J Nucl Med Mol Imaging 2017; 44:2117 2136
Archivio Italiano di Urologia e Andrologia 2022;
4 Pepe P, Roscigno M, Pepe L, et al Could 68Ga PSMA PET/CT evaluation reduce the number of scheduled prostate biopsy in men enrolled in active surveillance protocols? J Clin Med 2022; 11:3473
5 Perera M, Papa N, Roberts M, et al Gallium 68 prostate specific membrane antigen positron emission tomography in advanced prostate cancer updated diagnostic utility, sensitivity, specificity, and distribution of prostate specific membrane antigen avid lesions: A systematic review and meta analysis Eur Urol 2020; 77:403 417
6 Privé BM, Israël B, Schilham MGM, et al Evaluating F 18 PSMA 1007 PET in primary prostate cancer and comparing it to multi parametric MRI and histopathology Prostate Cancer Prostatic Dis 2021; 24:423 430
7 Uprimny C, Kroiss AS, Decristoforo C, et al 68Ga PSMA 11 PET/ CT in primary staging of prostate cancer: PSA and Gleason score predict the intensity of tracer accumulation in the primary tumour Eur J Nucl Mol Imaging 2017; 44:941 49
8 Emmett L, Buteau J, Papa N, et al The additive diagnostic value of prostate specific membrane antigen positron emission tomography computed tomography to multiparametric magnetic resonance imag ing triage in the diagnosis of prostate cancer (PRIMARY): a prospec tive multicentre study Eur Urol 2021; 80:682 689
9 Eiber M, Weirich G, Holzapfel K, et al Simultaneous 68GaPSMA HBED CC PET/MRI improves the localization of primary prostate cancer Eur Urol 2016; 70: 829 836
10 Pepe P, Pennisi M: Should 68Ga PSMA PET/CT replace CT and bone scan in clinical staging of high risk prostate cancer? Anticancer Research 2022; 42:1495 1498
11 Carvalho J, Nunes P, Da Silva ET, et al [68Ga] Ga PSMA 11 PET CT: Local preliminary experience in prostate cancer biochemical recurrence patients Arch Ital Urol Androl 2021; 93:21 25
12 Epstein JI, Egevad L, Amin MB, et al Grading Committee: The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system Am J Surg Pathol 2016; 40:244 252
13 Aragona F, Pepe P, Motta M, et al Incidence of prostate cancer in Sicily: results of a multicenter case findings protocol Eur Urol 2005; 47:569 74
14 Pepe P, Panella P, Savoca F, et al Prevalence and clinical signifi cance of prostate cancer among 12,682 men with normal DRE, low PSA (≤ 4 ng/mL) and %fPSA cut off of 15% and 20% Urologia Internationalis 2007; 78:308 312
15 Pepe P, Garufi A, Priolo GD, et al Is it time to perform only MRI targeted biopsy? Our experience in 1032 men submitted to prostate biopsy J Urol 2018; 200:774 778
16 Pepe P, Pennisi M, Fraggetta F How many cores should be obtained during saturation biopsy in the ra of multiparametric mag netic resonance? Experience in 875 patients submitted to repeat prostate biopsy Urology 2020; 137:133 137
17 Pepe P, Pennisi M Prostate cancer diagnosis and management accross twenty years of clinical practice: a songle center experience on 2,500 cases Anticancer Res 2019; 39:1397 1401
18 Moore CM, Kasivisvanathan V, Eggener S, et al , and START con sortium standards of reporting for MRI targeted biopsy studies (START) of the prostate: recommendations from an international working group Eur Urol 2013; 64:544 552
19 Dindo D, Demartines N, Clavien PA Classification of surgical complications A new proposal with evaluation in a cohort of 6336 patients and results of survey Ann Surg 2004; 2:205 213
94, 3
276
20 Pepe P, Garufi A, Priolo G, Pennisi M Can MRI/TRUS fusion targeted biopsy replace saturation prostate biopsy in the re evalua tion of men in active surveillance? World J Urol 2016; 34:1249 1253
21 Rosenkrantz AB, Verma S, Choyke P, et al Prostate magnetic res onance imaging and magnetic resonance imaging targeted biopsy in patients with a prior negative biopsy: a consensus statement by AUA and SAR J Urol 2016; 196:1613 1618
22 Hofman MS, Lawrentschuk N, Francis RJ, et al Prostate specific membrane antigen PET CT in patients with high risk prostate cancer before curative intent surgery or radiotherapy (proPSMA): a prospec tive, randomised, multicentre study Lancet 2020; 395:1208 1216
23 Kwan TN, Spremo S, Teh AYM, et al Performance of Ga 68 PSMA PET/CT for diagnosis and grading of local prostate cancer Prostate International 2021; 9:107 112
24 Franklin A, Yaxley WJ, Raveenthiran S, et al Histological com parison between predictive value of preoperative 3 T multiparamet ric MRI and 68Ga PSMA PET/CT scan for pathological outcomes at radical prostatectomy and pelvic lymph node dissection for prostate cancer BJU Int 2021; 127:71 79
25 Ma L, Wan Chun Zhang WC, Ya Xin Hao YX Current state of prostate specific membrane antigen PET/CT imaging targeted biop sy techniques for detection of clinically significant prostate cancer J Med Imaging Radiat Oncol 2022; 66:776 780
26 Demirci E, Kabasakal L, Sahin OE, et al Can SUVmax values of Ga 68 PSMA PET/CT scan predict the clinically significant prostate cancer? Nucl Med Commun 2019; 40:86 91
27 Rüschoff JH, Ferraro DA, Muehlematter UJ, et al What's behind 6 8 G a P S M A 1 1 u p t a k e i n p r i m a r y p ro s t a t e c a n c e r P E T ? Investigation of histopathological parameters and immunohistochem ical PSMA expression patterns Eur J Nucl Med Mol Imaging 2021; 48:4042 53
Correspondence
Pietro Pepe, MD
piepepe@hotmail com
Michele Pennisi, MD michepennisi2@virgilio it Ludovica Pepe, MD ludopepe97@gmail com
Urology Unit, Cannizzaro Hospital via Messina 829, Catania (Italy)
Maria Tamburo, MD marinellatamburo@virgilio it Giulia Marletta, MD marlettagiulia1@gmail com
Radiotherapy Unit, Cannizzaro Hospital, Catania (Italy)
Filippo Fraggetta, MD filippofra@hotmail com Pathology Unit, Cannizzaro Hospital, Catania (Italy)
68Ga PSMA PET/CT and PCa diagnosis
28 Zhang LL, Li WC, Xu Z, et al 68Ga PSMA PET/CT targeted biopsy for the diagnosis of clinically significant prostate cancer com pared with transrectal ultrasound guided biopsy: a prospective ran domized single centre study Eur J Nucl Med Mol Imaging 2021; 48:483 492
29 Liu Y, Yu H, Liu J, et al A pilot study of 18 F DCFPyL PET/CT or PET/MRI and ultrasound fusion targeted prostate biopsy for intra prostatic PET positive lesions Front Oncol 2021; 11:612157
30 Kalapara AA, Nzenza T, Pan HYC, et al Detection and localisation of primary prostate cancer using 68gallium prostate specific membrane antigen positron emission tomography/computed tomography compared with multiparametric magnetic resonance imaging and radical prosta tectomy specimen pathology BJU Int 2020; 126:83 90
31 Xue AL, Kalapara AA, Ballok ZE, et al 68Ga Prostate Specific Membrane Antigen Positron Emission Tomography maximum stan dardized uptake value as a predictor of Gleason pattern 4 and patho l o g i c a l u p g r a d i n g i n i n t e r m e d i a t e r i s k p ro s t a t e c a n c e r 2 0 2 2 ; 207:341 349
32 Ferraro DA, Becker AS, Kranzbühler B, et al Diagnostic per formance of 68Ga PSMA 11 PET/MRI guided biopsy in patients with suspected prostate cancer: a prospective single center study Eur J Nucl Med Mol Imaging 2021; 48:3315 3324
33 Pepe P, Dibenedetto G, Pepe L, Pennisi M Multiparametric MRI vs Select MDX accuracy in the diagnosis of clinically significant PCa in men enrolled in Active Surveillance In vivo 2020; 34:393 396
34 Roscigno M, Stabile A, Lughezzani G, et al The use of multipara metric resonance imaging for follow up of patients included in active surveillance protocol, can PSA density discriminate patients at different risk of reclassification? Clin Genitourin Cancer 2020; 18:e698 e704
35 Pepe P, Pennisi M Morbidity following transperineal prostate biopsy: our experience in 8,500 men Arch Ital Urol Androl 2022; 94:155 159
A277 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
1 Department of Urology, Centro Hospitalar Universitário de Lisboa Central, Lisbon, Portugal;
Department of Radiology, Centro Hospitalar Universitário de Lisboa Central, Lisbon, Portugal
Summary
Objectives: The aim of this study was to com pare the risk of International Society of Urological Pathology (ISUP) score upgrading between magnetic resonance imaging targeted fusion biopsy (MRI TB) and tran srectal ultrasound guided biopsy (TRUS B) in the final radical prostatectomy (RP) specimen pathological report
Materials and methods: This retrospective single center study included 51 patients with prostate cancer (PCa) diagnosed with MRI TB and 83 patients diagnosed with TRUS B between October/2019 and July/2021 We compared the rates of ISUP score upgrading between both groups after robotic assisted radi cal prostatectomy (RARP) and the specific transition of each ISUP score based on biopsy modality The rate of ISUP score concordance and downgrading were also assessed To define the intra and interobserver concordance for each ISUP score in biopsy and RP specimen for each biopsy modality, the Cohen’s Kappa coefficient was calculated ISUP scores and biopsy modal ity were selected for multivariate analysis and a logistic regres sion model was built to provide independent risk factors of ISUP score upgrading
Results: The difference of the rate of upgrading between MRI TB group and TRUS B group was statistically significant (p = 0 007) with 42 2% of patients of TRUS B group experiencing an upgrade in their ISUP score while only 19 6% in MRI TB group
Concordance and downgrading rates did not statistically differ between the two groups Strength of concordance using Cohen’s Kappa coefficient was fair in both groups but higher in MRI TB group (TRUS B group k = 0 230; p < 0 001; concordance: 47% vs MRI/TB group k = 0 438; p < 0 001; concordance: 62 7%)
Biopsy modality and ISUP 1 on biopsy were independent predic tors of ISUP upgrading after RP
Conclusions: MRI TB is highly accurate with lower risk of PCa upgrading after RP than TRUS B Patients with ISUP 1 on biop sy have greater susceptibility to upgrading their ISUP score
KEY WORDS: Gleason Score; ISUP score; MRI TB; Prostate cancer; TRUS B; Upgrading
Submitted 30 July 2022; Accepted 20 August 2022
INTRODUCTION
According to data from the Global Cancer Observatory, published in March 2021, 6750 new cases of prostate can
cer (PCa) were diagnosed in Portugal in 2020, equivalent to 20% of all malignancy in men (1) In terms of inci dence, PCa ranks first followed by colorectal cancer (19%) and lung cancer (11 6%) (1) PCa is a highly heteroge neous disease and therefore, the European Association of Urology (EAU) has established a risk group classification based on initial serum prostate specific antigen (PSA), biop sy Gleason Score (GS), and clinical stage There are several therapeutic strategies available according to the risk group (2) As a diagnostic assay, PSA clinical utility is ambiguous due to the lack of specificity and sensitivity for PCa, lead ing to many pointless biopsies with possibility of compli cations for the patient and potential overdiagnoses of low risk tumors and its overtreatment (3)
In terms of prognosis, GS has a key role as a predictor of PCa clinical outcome (4) Donald Gleason developed this grading scoring system in 1966 (5) During the evolution and establishment of the GS grading system, multiple refinements were introduced to improve its performance
In 2014, the International Society of Urological Pathology (ISUP) proposed a modified grading system classification (ISUP grading system) based on GS, after reviewing in detail the main limitations of the previous 2005 version
This reviewed version of ISUP grading system was further adopted and disseminated worldwide by World Health Organization in 2016 (6, 7)
In recent years, there has also been a great development in the imaging field The availability of multiparametric magnetic resonance imaging (mpMRI) in current clinical practice has revolutionized PCa diagnosis and staging Magnetic resonance targeted fusion biopsy (MRI TB) tends to be a valuable diagnostic method and more accurate for detecting clinically significant PCa (ISUP > 2 or GS > 7) than conventional strategies (PSA, digital rectal examina tion (DRE), and systematic biopsy) (8 10)
Despite scientific debate, several studies have shown that ISUP score of prostate biopsies is not always in concor dance with the pathological report of RP specimens even when MRI TB is performed (11, 12) The transrectal ultra sound guided biopsy (TRUS B) of the prostate may omit high grade tumors areas because it is not targeted to a specific suspicious lesion but a random biopsy On the
No conflict of interest declared
Archivio Italiano di Urologia e Andrologia 2022; 94, 23 78 ORIGINAL PAPER
Magnetic resonance imaging target fusion biopsy vs. transrectal ultrasound-guided biopsyA comparative study of ISUP score upgrading risk in the final radical prostatectomy specimen
Thiago Guimarães 1 , Miguel Gil 1 , Mariana Medeiros 1 , Vanessa Andrade 1 , João Guerra 1 , Hugo Pinheiro 1 , Francisco Fernandes 1 , João Pina 1 , João Lopes Dias 2 , Luís Campos Pinheiro 1
2
DOI: 10 4081/aiua 2022 3 278
other hand, targeted biopsy may overestimate the pres ence of a high grade tumor (13) The potential for under treatment or overtreatment resulting from the lack of cor relation between the ISUP score of the prostate biopsy and RP specimen may seriously impair the patient’s qual ity of life and prognosis Here we aim to compare ISUP score of prostate biopsy and RP specimen when MRI TB or TRUS B is performed and identify potential predictive factors associated with ISUP score upgrading
MATERIALS AND METHODS
Study design and case selection
We retrospectively analyzed a database of prospectively collected demographics and clinicopathological data from our institution All consecutive patients subjected to robot ic assisted radical prostatectomy (RARP) by four different surgeons, between 10/2019 and 07/2021 were included in the study cohort Those patients were divided into 2 groups according to the biopsy modality used for PCa diag nosis: MRI TB group or TRUS B group Patients under went prostate biopsy due to PSA elevation (> 4 ng/mL), abnormal DRE, or/and at least suspicious abnormalities in ultrasound or mpMRI findings We decided that patients who were submitted to neoadjuvant hormones or chemotherapy and/or radiotherapy before surgery should be excluded because these treatments may influence the histopathology of the RP specimen Patients with PCa diag nosed by transurethral resection of the prostate (TURP) were also discharged Patient’s age at diagnosis, preoperative serum PSA, the time interval between biopsy and surgery, prostate specimen volume, ISUP score of the biopsy and RP specimen, and also other features of the pathological RP specimen including pathological stage, surgical margins, and presence of cribriform pattern were also examined
Imaging acquisition and MRI TB protocol
MRI TB was performed in all patients with mpMRI detect ed abnormalities (PIRADS > 3 5) The imaging acquisition protocol followed the PI RADS v 2 1 criteria according to the European Society of Urogenital Radiology, based on the DWI and T2Wl sequences (14) In our institution, all mpMRI examinations were performed with a 3T MRI scan ner (Magnetom Skyra, Siemens, Erlangen, Germany) All sus pected lesions were evaluated by a genitourinary radiolo gist with expertise in mpMRI, unblinded to clinical infor mation, and further discussed with the urologist for the identification and demarcation of suspicious lesions as well as possible landmarks All outside patients sent to our hos pital with previous mpMRI abnormalities findings were also reviewed by a genitourinary radiologist and urologist
All MRI TB were performed using a mpMRI and transrec tal ultrasound fusion software MIM Symphony BxTM (MIM Software Inc, Ohio, USA) and a cart based ultrasound system (BK PRO Focus ultrasound system, BK Medical, Massachusetts, USA) At our institution, this MRI TB has been used since 2017 by two experienced urologists The patients were placed in lithotomy position, and subjected to general or spinal anesthesia after antibiotic prophylaxis and rectal and perineal disinfection We obtained at least 4 cores of each selected target of the prostate and systematic
biopsies using a transperineal ultrasound guided prostate biopsy approach with the ultrasound probe in the rectum
TRUS B protocol
All TRUS B were performed using a cart based ultra sound system Hitachi EUB 7500A (2013, Hitachi, Ltd, Tokyo, Japan) TRUS B were performed by 6 urologists of our department The patients were placed in the left lat eral decubitus position and subjected to a periprostatic nerve block (10 mL of 1% lidocaine) after rectal povi done iodine disinfection by enema in addition to antimi crobial prophylaxis A double sextant protocol was used with a collection of 2 fragments in the apex, middle and base regions, bilaterally, resulting in a total of 6 regions covered and 12 fragments
Pathological assessment of biopsy and RP specimen
All biopsies and RP specimens were examined and report ed by a selected team of genitourinary pathologists The processing and histopathological reports by the patholo gists of biopsies and RP specimens followed the EAU guidelines recommendations (2) The PCa was classified using the modified ISUP grading system (6, 7): ISUP 1 =
Table 1. Characteristics of study population
MRI TB TRUS B Total P value group group
Total (n) 51 83 134 Age (years; median [IQR]) 69 (7) 64 (11) 67 (9) 0 001*
Preoperative serum PSA (ng/mL; median [IQR]) 6 95 (5 03) 7 81 (5 57) 7 4 (5 60) 0 126
Prostate specimen volume (g; median [IQR]) 48 (22) 41 (13) 42 (16) 0 109
The time interva between biopsy and surgery (days; median [IQR]) 117(125) 126(143) 120 (129) 0 521
Biopsy ISUP score 0 098
ISUP 1 (n %) 7 (13 7%) 8 (9 6%) 15 (11 2%)
ISUP 2 (n %) 17 (33 3%) 49 (59 0%) 66 (49 3%)
ISUP 3 (n %) 20 (39 2%) 18 (21 7%) 38 (28 4%)
ISUP 4 (n %) 5 (9 8%) 5 (6 0%) 10 (7 5%) ISUP 5 (n %) 2 (3 9%) 3 (3 6%) 5 (3 7%)
Pathology specimen ISUP score 0 352 ISUP 1 (n %) 4 (7 8%) 5 (6 0%) 9 (6 7%)
ISUP 2 (n %) 18 (35 3%) 27 (32 5%) 45 (33 4%)
ISUP 3 (n %) 27 (52 9%) 42 (50 6%) 69 (51 5%)
ISUP 4 (n %) 0 (0 0%) 1 (1 2%) 1 (0 8%)
ISUP 5 (n %) 2 (4 0%) 8 (9 6%) 10 (7 5%)
Pathology specimen Cribform pattern 0 031*
Yes (n %) 3 (5 9%) 16 (19 3%) 19 (14 2%)
No (n %) 48 (94 1%) 67 (80 7%) 115 (85 8%)
Pathological stage 0 482 pT2 (n %)
25 (49.0%) 40 (48.2%) 65 (48.5%)
pT3a (n %) 23 (45 1%) 33 (39 8%) 56 (41 8%)
pT3b (n %) 3 (5 9%) 10 (12 0%) 13 (9 7%)
Positive surgical margins 0,035* Yes (n %) 21 (41 2%) 50 (60 2%) 71 (53%) No (n %) 30 58 8%) 33 (39 8%) 63 (47%)
Surgeon 0 082 A (n %) 10 (19 6%) 33(39 8%) 43 (32 1%)
B (n %) 12 (23 5%) 19(22 9%) 31 (23 1%)
C (n %) 19 (37 3%) 20(24 1%) 39 (29 1%) D (n %) 10 (19 6%) 11(13 3%) 21 (15 7%)
IQR:
A279 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Risk of ISUP score upgrading
Interquarti e Range; MRI TB: magnetic resonance mag ng targeted fus on b opsy; PSA: Prostate Spec fic Ant gen; TRUS B: transrectal u trasound guided b opsy
T Guimarães, M Gil, M Medeiros, et al
GS ≤ 6; ISUP 2 = GS 7 (3+4); ISUP 3 = GS 7 (4+3); ISUP 4 = GS 8 (4+4); ISUP 5 = GS 9 or GS10
Statistical analysis
Our primary endpoint in this study was the risk of ISUP score upgrading for each modality of biopsy
The rate of concordance and downgrading were also assessed Descriptive statistics were used for patients’ demographic Approximation to Gaussian distribution for continuous variables was not met on the Shapiro Wilk test Accordingly, a non paramet ric statistic was used Continuous variables were compared using Mann Whitney Test To define the intra and interobserver concordance for each ISUP score in biopsy and RP specimen evaluation for each biopsy modality, the Cohen’s Kappa coefficient was calculated Categorical variables were analyzed by chi square test ISUP scores and biopsy modality were selected for multivariate analysis and a logistic regression model was built The models’ goodness of fit was assessed by the Hosmer Lemeshow test (HL) test Statistical significance was considered for p < 0 05 All Statistical analysis was performed using SPSS v 25 (IBM SPSS Statistics for macOS, Version 25 0 Armonk, NY: IBM Corp )
RESULTS
Groups characteristics
Figure 1.
Distribution of ISUP score after MRI TB and RP specimen pathological examination
MRI TB: Magnetic resonance imaging targeted fusion biopsy; RP: Radical Prostatectomy
Figure 2.
Distribution of ISUP score after TRUS B and RP specimen pathological examination
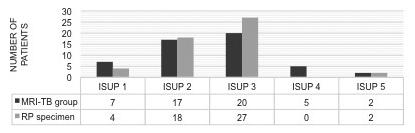
TRUS B: transrectal ultrasound guided biopsy; RP: Radical Prostatectomy
of patients of TRUS B group experiencing an upgrade in their ISUP score while only 19 6% in MRI TB group Concordance and downgrading rates did not statistically differ between the two groups
Group’s baseline characteristics of patients subjected to prostate biopsy between October/2019 and July/2021 are detailed in Table 1 Overall, there were 51 patients in the MRI TB group and 83 patients in TRUS B group There were no statistically significant differences in preoperative serum PSA, prostate specimen volume, the time interval between biopsy and surgery, ISUP score of biopsy and RP specimen, pathological T stage, and surgeons between both groups Patients were statistically different in age (p < 0 001), presence of cribriform pattern (p = 0 031) and pos itive margins (p = 0 035) Figure 1 and 2 show the differ ent distribution of ISUP scores between each biopsy group and the RP specimen pathology The total proportions of ISUP score in MRI TB were: ISUP 1 13 7%, ISUP 2 33 3%, ISUP 3 39 2%, ISUP 4 9 8% and ISUP 5 3 9% In TRUS B group, the proportions were: ISUP 1 9 6%, ISUP 2 59%, ISUP 3 21 7%, ISUP 4 6% and ISUP 5 3 6% (in each group, most PCa in biopsy were ISUP 2 or ISUP 3) At final RP specimen pathology report, the total proportions of ISUP scores in MRI TB group were: ISUP 1 7 8%, ISUP 2 35 3%, ISUP 3 52 9%, ISUP 4 0% and ISUP 5 4% In TRUS B group the proportion were: ISUP 1 6%, ISUP 2 32 5%, ISUP 3 50 6%, ISUP 4 1 2% and ISUP 5 9 6% (in each group, most PCa in RP specimen were ISUP 2 or ISUP3)
ISUP score concordance rates from biopsy and RP specimen in study cohort and in each group
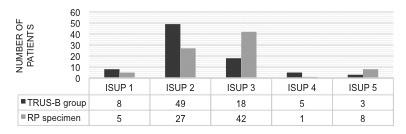
The Table 2 shows the rate of concordance or not (down grading or upgrading) between biopsy and pathological ISUP scores in all study cohort and the two groups The rate of upgrading between MRI TB group and TRUS B group was statistically significant (p = 0 007) with 42 2%
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
Specific ISUP scores transition between biopsy and RP specimen
Specific ISUP scores transition between biopsy and RP specimen when considering all study cohort is depicted in Table 3 The major rates of upgrading were seen in
Table 2.
ISUP score downgrading, concordance and upgrading per groups
ISUP score Study group Downgrading Concordance Upgrading MRI TB group (n %) 9 (17 7%)* 32 (62,7%)** 10 (19 6%)*** TRUS B group (n %) 9 (10 8%)* 39 (47%)** 35 (42 2%)*** Total (n %) 18 (13 4%)* 71 (53%)** 45 (33 6%)***
IMRI TB:
Table 3
ded biopsy;
ISUP score downgrading, concordance and upgrading rates in both groups (MRI TB group plus TRUS B group)
ISUP score RP specimen Total
ISUP score biopsy ISUP 1 ISUP 2 ISUP 3 ISUP 4 ISUP 5 (n%)
ISUP 1 (n %) 6 (40%)** 6 (40%)*** 3 (20%)*** 0 (0%)*** 0 (0%)*** 15 (100%)
ISUP 2 (n %) 3 (4 5%)* 33 (50%)** 27 (41%) 0 (0%)*** 3 (4 5%)*** 66 (100%)
ISUP 3 (n %) 0 (0%)* 5 (13 2%)* 30 (78 9%)** 0 (0%)*** 3 (7 9%)*** 38 (100%)
ISUP 4 (n %) 0 (0%)* 1 (10%)* 5 (50%)* 1 (10%)** 3 (30%)*** 10 (100%)
ISUP 5 (n %) 0 (0%)* 0 (0%)* 4 (80%)* 0 (0%)* 1 (20%)** 5 (100%)
Total (n) 9 45 69 1 10 134
RP:
280
Magnetic resonance mag ng targeted fusion biopsy; TRUS B: Transrecta ultrasound gu
* : Downgrad ng rates; ** : Concordance rates; *** : Upgrad ng rates
Radica prostatectomy; * : Downgrad ng rates; ** : Concordance rates; *** : Upgrad ng rates
Table 4.
ISUP score downgrading, concordance and upgrading rates (MRI/TPB group)
ISUP score RP specimen Total
ISUP score biopsy ISUP 1 ISUP 2 ISUP 3 ISUP 4 ISUP 5 (n%)
ISUP 1 (n %) 3 (42 9%)** 3 (42 9%)*** 1 (14 3%)*** 0 (0%)*** 0 (0%)*** 7 (100%)
ISUP 2 (n %) 1 (5 9%)* 12 (70 6%)** 4 (23 5%)*** 0 (0%)*** 0 (0%)*** 17 (100%)
ISUP 3 (n %) 0 (0%)* 3 (15%)* 17 (85%)** 0 (0%)*** 0 (0%)*** 20 (100%)
ISUP 4 (n %) 0 (0%)* 0 (0%)* 3 (60%)* 0 (0%)** 2 (40%)*** 5 (100%)
ISUP 5 (n %) 0 (0%)* 0 (0%)* 2 (100%)* 0 (0%)* 0 (0%)** 2 (100%)
Tota (n) 4 18 27 02 51
RP: Rad cal prostatectomy; * : Downgrading rates; ** : Concordance rates; *** : Upgrading rates
Table 5
ISUP score downgrading, concordance and upgrading (TRUS B group).
ISUP score RP specimen Total
ISUP score biopsy ISUP 1 ISUP 2 ISUP 3 ISUP 4 ISUP 5 (n%)
ISUP 1 (n %) 3 (37 5%)** 3 (37 5%)*** 2 (25%)*** 0 (0%)*** 0 (0%)*** 8 (100%)
ISUP 2 (n %) 2 (4 1%)* 21 (42 9%)**23 (46 9%)*** 0 (0%)*** 3 (6 1%)*** 49 (100%)
ISUP 3 (n %) 0 (0%)* 2 (11 1%)* 13 (72 2%)** 0 (0%)*** 3 (16 7%)*** 18 (100%)
ISUP 4 (n %) 0 (0%)* 1 (20%)* 2 (40%)* 1 (20%)** 1 (20%)*** 5 (100%)
ISUP 5 (n %) 0 (0%)* 0 (0%)* 2 (66 7%)* 0 (0%)* 1 (33 3%)** 3 (100%)
Total (n) 5 27 42 18 83
RP: Rad cal prostatectomy;
: Downgrad ng rates;
: Concordance rates;
: Upgrading rates
patients with ISUP 1 and 2 in biopsy (60% and 50% of those patients upgraded their initial ISUP score respec tively) In TRUS B group there were a higher upgrading rates in ISUP 1 and 2 (62 5% and 53%) while in MRI TB group, the rates of upgrading were notable higher in ISUP 1 (57 2%) (Table 4 and Table 5, respectively) Strength of concordance using Cohen’s Kappa coefficient was fair in both groups but higher in MRI TB group (TRUS B group k = 0 230; p < 0 001; concordance: 47%/MRI/TB group k = 0 438; p < 0 001; concordance: 62 7%)
Demographics, clinical and pathological features according to upgrade status
Overall, ISUP of 89 patients was upgraded in the final pathological report against 45 whose ISUP was not upgraded On univariate analysis, as displayed in Table 6, there were no statistically significant differences in patients who were upgraded or not in PSA, prostate spec imen volume, time interval between biopsy, presence of surgical positive margins or cribform patterns in PR spec

Upgrading status comparison between
group and
Risk of ISUP score upgrading
imen Upgrading of biopsy ISUP score were associated with the biopsy modality (higher in TRUS B biopsy Figure 3) and ISUP score in biopsy (p = 0 07 and p = 0 001, respectively) In our regression logistic model, biopsy modality and ISUP 1 on biopsy were independent predictors of ISUP upgrading after RP (Table 7)
Table 6.
ISUP upgrading status univariate analysis
Upgrading Non upgrading Upgrading P value status group group
Total (n) 89 45
Age Standard (ng/mL; median [IQR]) 68 (9) 66 (24) 0 245
Preoperative serum PSA (ng/mL; median [IQR]) 7 25 (5 14) 7 7 (6 25) 0 481
Prostate specimen volume (ng/mL; median [IQR]) 44 (19 75) 41 (12) 0 061
The t me interval between biopsy and surgery (standard) (days; med an [IQR]) 122 (129) 112 (125) 0 984
Biopsy ISUP score 0 001*
ISUP 1 (n %) 6 (40%) 9 (60%) 0 022*
ISUP 2 (n %) 36 (54 5$) 30 (45 5%) 0 004*
ISUP 3 (n %) 35 (92 1%) 3 (7 9%) < 0 001*
ISUP 4 (n %) 7 (70%) 3 (30%) 1 000 ISUP 5 (n %) 5 (100%) 0 (0%)
Biopsy modality 0 07*
MRI TB (n %) 41 (80 4%) 10 (19 6%)
TRUS B (n %) 48 (57 8%) 35 (42 2%)
Surgical margins (n (%)) 0.247
Negat ve (n %) 45 (50 6%) 44 (49 4%) Positive (n %) 18 (40%) 27 (60%)
Cribform pattern 0 170 Negat ve (n %) 79(88 8%) 36 (80%)
IQR: Interquarti e Range; MRI TB: magnetic resonance mag ng targeted fus on biopsy; PSA: Prostate Specif c Ant gen; TRUS B: transrectal u trasound guided biopsy
Table 7.
ISUP upgrading status multivariate analysis
ISUP score biopsy Variable P value Odds Ratio CI 95%
ISUP 1 0 028* 6 579 1 230 35 204
ISUP 2 0 134 2 877 0 723 11 451 ISUP 3 0 244 0 353 0 061 2 036
CI: Confidence Interva
DISCUSSION
B group.
The current way to further evaluate the prostate when there is a doubt of a tumor is with a prostate biopsy However, with only a small sample of prostate tissue col lected by a needle, physicians may not have a representa tive knowledge of the main structural features of cancer to predict its aggressiveness GS and consequently ISUP score grading system are an essential prog nostic tool in PCa and are included in many risk predictor normograms (4, 15, 16)
The concordance between the ISUP score of biop sies and the RP specimens is essential to confirm the physicians and patients’ expectations regarding the risk group in which the cancer is assigned, the most appropriate treatment strategy, and the patient’s prognosis Unfortunately, the expected concor dance does not always meet expectations and PCa aggressiveness might be underestimated or overes timated resulting in a delay of treatment in patients i n i t i a l l y q u a l i fi e d f o r a c t i v e s u r v e i l l a n c e ( A S ) ;
A281 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
*
**
***
Figure 3
MRI TB
TRUS
MRI TB: Magnetic resonance imaging targeted fusion biopsy; TRUS B: transrectal ultrasound guided biopsy
T Guimarães, M Gil, M Medeiros, et al
undertreatment in case of high risk PCa that could bene fit not from monotherapy (surgery or radiation) but mul timodal therapy or clinical trial; or overtreatment in patients disqualified to a low risk disease after surgery who would be better candidates for AS (2) Risk normo grams may also be imprecise in terms of whether or not pelvic lymphadenectomy is required Therefore, it’s not s u r p r i s i n g t h a t p r e v i o u s s t u d i e s h a v e r e p o r t e d a n increased risk of biochemical recurrence, distant metasta sis, and death when ISUP score is underestimated (17 20) The vast majority of those studies only assessed the upgrading risk regarding TRUS B, the most widely accept ed method for PCa diagnosing Therefore, this study pro vides further evidence of the clinical utility of MRI TB in daily clinical practice The lower reliability of TRUS B in our study is aligned with the results obtained by Kvale et al and other historical studies that have determined the upgrading risk when a systematic biopsy is performed (21) We demonstrated that 42 2% of patients in the TRUS B group were upgraded In fact, our results are sim ilar to King et al study’ which reported a GS upgrading rate after TRUS B of 35 43% (22) However, it should be noted that those studies used the GS system to classify PCa, rather than ISUP score which ranges from 1 to 5 with Gleason Score 9 and 10 assigned to ISUP 5 Therefore, our study does not assess the risk of upgrading from Gleason Score 9 to 10 Nevertheless, it should be recognized that we use ISUP grading system, a more recent and updated grading system which is based on GS There are a few studies in the literature that specifically assessed the tran sition of ISUP scores between prostate biopsy and RP When both modalities of biopsy are compared, as shown in Table 8, previous studies reported different upgrading rates but lower when magnetic resonance imaging ultra sound guided biopsy is performed (23 25) MRI TB pro vides a lower incidence of ISUP score upgrading, although there is still a non negligible risk of upgrading of 19 6% The major rates of upgrading were detected in patients with ISUP 1 in both groups This has implications mainly for those patients who have postponed RP due to active surveillance On the other hand, 53% (vs 23 5% in MRI TB group) of patients classified as ISUP 2 after TRUS B were upgraded These data are consistent with data from the study by De Lucca et al who demonstrated a lower risk of ISUP 2 upgrading after MRI TB vs systematic biopsy (26) In our study, 6 8% (n = 3) of those patients with ISUP 2 in the TRUS B group upgraded to ISUP 5 (vs 0% in the
MRI TB group) as demonstrated in Table 5 Despite a small number of patients, this is particularly relevant when patients with ISUP 2 in the biopsy are subjected to radio therapy Due to the lack of confirmatory ISUP score of RP specimen, those patients are at risk of undertreatment
In addition to the biopsy modality, to be classified as ISUP 1 in biopsy was identified as a predictive risk for upgrading in multivariate analysis As suggested by Altok et al , when the RP specimen is analyzed, a “regression to the mean GS7” (ISUP 2 3) appears also to occur with our data even with patients who graduated as ISUP 1 in the biopsy, with 100% of patients transiting to ISUP 2 3 (27) In fact, one of the challenges of the pathologist is to dif ferentiate Gleason patterns 3 and 4 due to several reasons based on inherent subjectivity of reporting borderline cases (28) Therefore, it is essential to have a dedicated and experienced team of pathologists to minimize varia tions in interpretations of ISUP score and discrepancy between biopsy and RP specimens
Although our study did not find a relation between prostate specimen volume and upgrading risk, many studies report a higher risk of upgrading in prostate of smaller size (25) We expected that the longer the time interval between biopsy and surgery, the greater the risk of upgrading but we did not find this relation in our study (21) Our study has several limitations concerning its retrospective and non randomized design It was also a single institution study that targeted Portuguese popu lation Other limitations are the small number of patients in each group and heterogeneity between the two groups; the non inclusion of other variables likely to be related to upgrading risk according to previous studies such as the number of cores collected, biopsy core lengths and PSA density (23, 29) Other variables, such as the specific number, extent, location and PIRADS classification of suspicious lesions on mpMRI, and their respective associ ation with the PCa diagnosis in both biopsy cores and surgical specimens were not assessed in our study
However, Lourenço et al suggest that PCa multifocality can be an indicator of ISUP upgrading risk in patients who were discordant in mpMRI location of the suspicious lesions either in the cognitive fusion biopsy cores or PR specimens (30) Nevertheless, we believe that this study reinforces the key role of MRI as a diagnostic and staging tool in PCa Physicians should be aware of potential u p g r a d i n g r i s k f a c t o r s d u r i n g t h e d e c i s i o n m a k i n g process The development of normograms and biomark ers that can predict the risk of upgrading may be essen tial to improve the assertiveness of the clinical decision (31 33) According to Lacetera et al , the incidence of clinically significant PCa in patients under AS protocol is higher in the subgroup of patients who underwent con firmatory and follow up MRI TB vs random biopsy (69% vs 31%) (34) We strongly recommend that patients on AS protocol should be counseled about the risk of ISUP upgrading and informed about the advantage of MRI TB to detect clinically significant PCa
CONCLUSIONS
MRI TB is highly accurate with lower risk of PCa upgrad ing after RP than TRUS B Patients with ISUP 1 on biopsy
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
282
Table 8. Our study and selected previous series that evaluated the risk of upgrading Series citation Groups Patients (n) Upgrading (%) P value Guimarães et al MRI US 51 19 6% TRUS B 83 42 2% 0 07* (25) MRI US 73 16 4% TRUS B 89 31 5% 0 027* (24) MRI US 145 33 5% TRUS B 221 31 7% 0 8 (23) MRI US 92 26 9% TRUS B 137 73 1% 0 027* MR TB: Magnet c resonance imag ng targeted fusion biopsy; TRUS B: tTansrecta ultrasound gu ded biopsy
have greater susceptibility to upgrading and we strongly recommend mpMRI on patients in AS protocol Additional studies are necessary to identify predictive risk factors for ISUP score upgrading to better categorize patients into risk groups and select the best treatment option according to the biological behavior of PCa and prognosis
REFERENCES
1 World Health Organization International Agency for Research on Cancer (IARC) GLOBOCAN 2020: estimated cancer incidence, mortality and prevalence in Portugal in 2020 [Internet] 2021 [cited 2022 Jul 20] Available from: https://gco iarc fr/today/data/fact sheets/populations/620 portugal fact sheets pdf
2 Mottet N, van den Bergh RCN, Briers E, et al EAU EANM ESTRO ESUR SIOG Guidelines on Prostate Cancer 2020 Update Part 1: Screening, diagnosis, and local treatment with curative intent Eur Urol 2021; 79:243 262
3 Adhyam M, Gupta AK A review on the clinical utility of PSA in cancer prostate Indian J Surg Oncol 2012; 3:120 129
4 Sauter G, Steurer S, Clauditz TS, et al Clinical utility of quanti tative Gleason grading in prostate biopsies and prostatectomy speci mens Eur Urol 2016; 69:592 598
5 Gleason DF Classification of prostatic carcinomas Cancer Chemother Rep 1966; 50:125 128
6 Epstein JI, Egevad L, Amin MB, et al The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading pat terns and proposal for a new grading system Am J Surg Pathol 2016; 40:244 252
7 Moch H WHO ISUP Graduierungssystem für Nierenkarzinome [The WHO/ISUP grading system for renal carcinoma] Pathologe 2016; 37:355 360
8 Wallis CJD, Haider MA, Nam RK Role of mpMRI of the prostate in screening for prostate cancer Transl Androl Urol 2017; 6:464 471
9 Abd Alazeez M, Kirkham A, Ahmed HU, et al Performance of multiparametric MRI in men at risk of prostate cancer before the first biopsy: a paired validating cohort study using template prostate map ping biopsies as the reference standard Prostate Cancer Prostatic Dis 2014; 17:40 46
10 Vourganti S, Rastinehad A, Yerram N, et al Multiparametric magnetic resonance imaging and ultrasound fusion biopsy detect prostate cancer in patients with prior negative transrectal ultrasound biopsies J Urol 2012; 188:2152 2157
11 Luzzago S, Petralia G, Maresca D, et al Pathological findings at radical prostatectomy of biopsy naïve men diagnosed with MRI tar geted biopsy alone without concomitant standard systematic sam pling Urol Oncol 2020; 38:929 e11 929 e19
12 Calio BP, Sidana A, Sugano D, et al Risk of upgrading from prostate biopsy to radical prostatectomy pathology Does saturation biopsy of index lesion during multiparametric magnetic resonance imaging transrectal ultrasound fusion biopsy help? J Urol 2018; 199:976 982
13 Bullock N, Simpkin A, Fowler S, Varma M, Kynaston H, Narahari K Pathological upgrading in prostate cancer treated with surgery in the United Kingdom: trends and risk factors from the British Association of Urological Surgeons Radical Prostatectomy Registry BMC Urol 2019; 19:94
14 Weinreb JC, Barentz JO, Choyke PL, et al PI RADS Prostate Imaging Reporting and Data System, v2 1 [Internet] 2019 [cited
Risk of ISUP score upgrading
2022 Jul 18] Available from: https://www acr org/ /media/ACR/ Files/RADS/Pi RADS/PIRADS V2 1 pdf
15 Briganti A, Larcher A, Abdollah F, et al Updated nomogram pre dicting lymph node invasion in patients with prostate cancer undergo ing extended pelvic lymph node dissection: the essential importance of percentage of positive cores Eur Urol 2012; 61:480 487
16 Memorial Sloan Kettering Cancer Center Prostate Cancer N o m o g r a m s [ I n t e r n e t ] [ c i t e d 2 0 2 2 J u l 1 9 ] A v a i l a b l e f r o m : https://www mskcc org/nomograms/prostate
17 Corcoran NM, Hong MK, Casey RG, et al Upgrade in Gleason score between prostate biopsies and pathology following radical prostatectomy significantly impacts upon the risk of biochemical recurrence BJU Int 2011; 108:E202 E210
18 Dogan S, Yıldız KY, Sakaogulları ZS The value of Gleason score upgrade in predicting biochemical recurrence after radical prostate ctomy Bosphorus Med J 2021; 8:88 92
19 Bakavicius A, Drevinskaitc M, Daniunaite K, et al The impact of prostate cancer upgrading and upstaging on biochemical recurrence and cancer specific survival Medicina (Kaunas) 2020; 56:61
20 Kovac E, Vertosick EA, Sjoberg DD, et al Effects of pathological upstaging or upgrading on metastasis and cancer specific mortality in men with clinical low risk prostate cancer BJU Int 2018; 122:1003 1009
21 Kvåle R, Møller B, Wahlqvist R, et al Concordance between Gleason scores of needle biopsies and radical prostatectomy speci mens: a population based study BJU Int 2009; 103:1647 1654
22 King CR, Long JP Prostate biopsy grading errors: a sampling problem? Int J Cancer 2000; 90:326 330
23 Xu N, Wu YP, Li XD, et al Risk of upgrading from prostate biop sy to radical prostatectomy pathology: Is magnetic resonance imag ing guided biopsy more accurate? J Cancer 2018; 9:3634 3639
24 Rührup J , Preisser F , Theißen L, et al MRI fusion targeted vs systematic prostate biopsy How does the biopsy technique affect Gleason grade concordance and upgrading after radical prostatecto my? Front Surg 2019; 6:55
25 Kayano P P , Carneiro A , Castilho T M L , et al Comparison of Gleason upgrading rates in transrectal ultrasound systematic ran dom biopsies versus US MRI fusion biopsies for prostate cancer Int Braz J Urol 2018; 44:1106 1113
26 De Luca S, Fiori C, Bollito E, et al Risk of Gleason Score 3+4=7 prostate cancer upgrading at radical prostatectomy is significantly reduced by targeted versus standard biopsy Minerva Urol Nefrol 2020; 72:360 368
27 Altok M, Troncoso P, Achim MF, Matin SF, et al Prostate can cer upgrading or downgrading of biopsy Gleason scores at radical prostatectomy: prediction of "regression to the mean" using routine clinical features with correlating biochemical relapse rates Asian J Androl 2019; 21:598 604
28 Epstein JI Prostate cancer grading: a decade after the 2005 mod ified system Mod Pathol 2018; 31(S1):S47 S63
29 Corcoran NM, Casey RG, Hong MK, et al The ability of prostate specific antigen (PSA) density to predict an upgrade in Gleason score between initial prostate biopsy and prostatectomy diminishes with increasing tumour grade due to reduced PSA secre tion per unit tumour volume BJU Int 2012; 110:36 42
30 Lourenço M, Pissarra P, Brito DV et al Lesion location agree ment between prostatic multiparametric magnetic resonance, cogni tive fusion biopsy and radical prostatectomy piece Arch Ital Urol Androl 2020; 91:218 223
A283 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
T Guimarães, M Gil, M Medeiros, et al
31 Wang X, Zhang Y, Zhang F, et al Predicting Gleason sum upgrading from biopsy to radical prostatectomy pathology: a new nomogram and its internal validation BMC Urol 2021; 21:3
32 Qin XP, Lu QJ, Yang CH, et al CRMP4 CpG Hypermethylation predicts upgrading to Gleason Score ≥ 8 in prostate cancer Front Oncol 2022; 12:840950
33 Wang T, Dong L, Sun J, et al miR 145 5p: A potential biomark er in predicting Gleason upgrading of prostate biopsy samples scored 3+3=6 Cancer Manag Res 2021; 13:9095 9106
34 Lacetera V, Antezza A, Papaveri A, et al MRI/US fusion prostate biopsy in men on active surveillance: Our experience Arch Ital Urol Androl 2021; 93:88 91
Correspondence
Thiago Guimarães, MD (Corresponding Author) tguimaraesandrade@gmail com
Miguel Gil, MD miguel gil@live com pt
Mariana Medeiros, MD
mmariana medeiros92@gmail com
Vanessa Andrade, MD andrade vanessa2@gmail com
João Guerra, MD
joaoguerra93@gmail com
Hugo Pinheiro, MD
hugopinheiro1985@hotmail com
Francisco Fernandes, MD E mail: franciscof14@hotmail com
João Pina, MD
joaompina@gmail com
João Lopes Dias, MD
joaolopesdias85@gmail com
Luís Campos Pinheiro, MD luiscampospinheiro@gmail com
Rua José António Serrano, 1150 199 Lisbon (Portugal)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
284
Could YouTubeTM encourage men on prostate checks? A contemporary analysis
Simone Morra 1 , Luigi Napolitano 1 , Claudia Collà Ruvolo 1 , Giuseppe Celentano 1 , Roberto La Rocca 1 , Marco Capece 1 , Massimiliano Creta 1 , Francesco Passaro 1 , Francesco Di Bello 1 , Luigi Cirillo 1 , Carmine Turco 1 , Ernesto Di Mauro 1 , Gabriele Pezone 1 , Agostino Fraia 1 , Francesco Mangiapia 1 , Ferdinando Fusco 2 , Vincenzo Mirone 1 , Gianluigi Califano 1 , Nicola Longo 1
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples “Federico II”, Naples, Italy;
2 Urology Unit, Department of Woman, Child and General and Specialized Surgery, University of Campania 'Luigi Vanvitelli', Naples, Italy
Summary
Objectives: To assess YouTube™ videos’ quality on prostate checks, especially on the digital rectal exam (DRE), and to investigate if they can inform patients correctly and eradicate their beliefs and myths
Methods: A search using as keywords “digital rectal exam for prostate cancer” was performed on the YouTubeTM platform
We selected the first 100 videos To assess video quality content, Patient Education Materials Assessment Tool for audio visual content (PEMAT A/V) and Misinformation tool were used
Results: Seventy three videos were suitable for the analyses
The median PEMAT A/V Understandability score and PEMAT A/V Actionability score were 46 2% (interquartile range [IQR]: 30 8 76 9) and 50 0% (IQR: 25 0 75 0), respectively The medi an PEMAT A/V Understandability and Actionability scores were 69 2% (IQR: 46 2 88 5) vs 46 2% (IQR: 30 8 61 5) (p = 0 01) and 100 0% (IQR: 87 5 100 0) vs 25 0% (IQR: 25 0 68 8) (p < 0 001), for healthcare workers vs patients, respectively
According to the Misinformation tool, the median misinforma tion score of the overall videos was 2 2 (IQR:1 7 2 8) According to the target audience, the misinformation score was 2 8 (IQR: 2 4 3 5) vs 2 0 (IQR: 1 5 2 8) (p = 0 02), for healthcare workers vs patients, respectively
Conclusions: Currently, based on our analyses, YouTubeTM videos’ quality on DRE resulted unsatisfactory according to the PEMAT A/V score and the Misinformation tool. Videos targeted to healthcare workers got higher quality scores if compared to videos targeted to patients. Therefore, YouTubeTM videos’ may not be considered a reliable source of information on DRE for patients.
KEY WORDS: Internet; Urology; Misinformation; Prostate cancer; Social media
Submitted 13 June 2022; Accepted 14 July 2022
INTRODUCTION
Prostate cancer (PCa) is the most common malignancy among elderly men, with 1 276 000 new diagnoses and 359 000 deaths in 2018 worldwide (1, 2) Nowadays, PCa burden is expected to grow to almost 2 3 million new cases and 740 000 deaths by 2040 (1, 3) Several studies show as survival is closely related to the stage at
diagnosis: The 5 year survival rate is 100% in patients diagnosed with the earliest stage disease and less than 33% if diagnosed at the latest stage (4 7)
Screening is the best way for PCa early diagnosis and it is recommended to all men with no risk factors over 50 years (8, 9) Digital rectal exam (DRE) in addition to prostate spe cific antigen (PSA) blood test is the most used test to screen for PCa According to American Urology Association (AUA), DRE has considered a useful tool in men referred for an ele vated PSA (10) Moreover, according to European Association of Urology (EAU) guidelines, in 18% of cases PCa is detected by suspect DRE alone, irrespective of PSA level (11, 12) A suspect DRE in patients with a PSA level < 2 ng/mL has a positive predictive value (PPV) of 5 30% (13)
Despite DRE usually is not painful and only takes a short time, fear and shame of patients appear as barriers This is usually due to imagination, beliefs, and fantasies that lead the men to envision the DRE as something much more awkward than it is The lack of knowledge or mis information could be reversed by more comprehensive information (14, 15)
YouTubeTM is the most well known online video sharing site with five billion videos watched daily and has such a large and diverse community of users, it could be a media channel for improving public awareness and understand ing (16, 17) Additionally, over the past 2 years, the severe acute respiratory syndrome coronavirus 2 (SARS COV 2) spread, has made internet consultation a remarkable source of medical information (18 23) Several studies have already evaluated the quality of YouTube™ videos concerning different medical fields To the best of our knowledge, no studies on DRE were found in the literature
Previous studies analyzed YouTube™ videos’ quality on urological (20, 21, 24 30) and non urological topics (31, 32), highlighting a diffuse inaccuracy No previous inves tigators evaluated YouTube™ videos’ quality on DRE as a tool for patients’ information
The current study aimed to assess YouTube™ videos’ quality on prostate checks, especially on DRE, and to investigate if they can inform patients correctly and erad icate their beliefs and myths
A285 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
ORIGINAL PAPER No conflict of interest declared
DOI: 10 4081/aiua 2022 3 ???
S Morra, L Napolitano, C Collà Ruvolo, et
MATERIALS AND METHODS
Search strategy and video selection criteria
On April the 14th 2021, from 5 30 p m to 7 30 p m (CEST), a search using as keywords “digital rectal exam for prostate cancer” was performed on the YouTubeTM plat form The search was limited to the English language To avoid research bias, any personal account was logged out and a proxy located in the United States via Virtual Private Network (VPN) software was set We recorded the first 100 videos displayed by relevance The following exclu sion criteria were applied (Figure 1): non English lan guage videos (n = 5), podcasts (n = 1), commercial pur pose videos (n = 3), animal videos (n = 1), videos over 30 minutes (n = 3), off topic videos (n = 14) If duplicated, only one was considered We recorded, for all the eligible videos, the following variables: length (seconds), views, persistence on YouTubeTM (days), thumbs up (a social media term for like), thumbs down (a social media term for dislike), number of comments, number of videos with disabled comments, channel subscribers (the people or accounts that are subscribed to the channel), video authors (healthcare workers vs patients vs interviewers), target audience (healthcare workers vs patients), Video Power Index (VPI) estimating video popularity (20)
Quality and misinformation assessment tools
Two investigators, a Senior (GS) and a Junior (SM) Urology
Figure 1
PRISMA diagram depicting inclusion and exclusion criteria of YouTubeTM video search.
Resident, analysed the quality of the eligible videos, and when in contrast an additional investigator, an Associate Professor (NL), mediate the disagreement The quality assessment was performed for the overall eligible videos
Patient Education Materials Assessment Tool for audio visual content (PEMAT A/V) 33 and the Misinformation Tool were used to assess videos’ quality (16, 20, 24 26)

First, the PEMAT A/V is developed to evaluate how view ers could process the information displayed in the videos and how viewers could use them It is composed of 17 questions addressing the content Understandability (ques tions 1 13) and Actionability (questions 14 17) Three answers were permitted (agree = 1, disagree = 0, not avail able = NA) The score of all items is added together, divid ed by the number of items on which the material was rated, and multiplied by 100 to give a percentage score for under standability and actionability, respectively There is no set cutoff value for the scores Higher scores detect more understandable and actionable content (31, 33)
Second, the Misinformation tool is a validated tool that explores the grade of video misinformation (16, 20, 24, 26) It consists of 4 questions: “Does the video clearly describe the procedure?” , “Does the video clearly describe the difference between neoplastic disease and other prostate dis eases?” , “Does the video give information on the pain during the examination?” , “Does the video describe the next steps to be per formed after the examination?” It ranges from 1 (extreme misinformation) to 5 (no misinformation)
Statistical analyses
D e s c r i p t i v e s t a t i s t i c s w e r e p r e s e n t e d a s medians and interquartile ranges (IQR) and ranges for continuously coded variables or counts and percentages for categorically coded variables Chi square and Kruskal Wallis tested the statistical significance in p r o p o r t i o n s ’ a n d m e d i a n s ’ d i f f e r e n c e s P o t e n t i a l v a r i a b l e s c o r r e l a t i o n s w e r e assessed with Pearson's test In all statistical analyses, the R software (www rproject org) environment for statistical computing and graphics (R version 4 0 0) was used All tests were two sided with a level of signifi cance set at p < 0 05
RESULTS
Videographic characteristics
Of all 100 videos, 73 were suitable for the analyses (Table 1) The median length was 244 seconds (IQR: 129 0 549 0; range: 38 0 2541 0) The median number of views was 12954 (IQR: 1780 0 199548 0; range: 31 0 17141766 0) and the median persistence on YouTube™ was 985 days (IQR: 237 0 2155 0; range: 1 0 4550 0) Moreover, across the sample, the median number of thumbs up, thumbs down, comments and sub scribers were 41 (IQR: 6 0 256 0 ; range: 0 200000 0), 4 (IQR: 1 0 45 0; range: 0 3673 0), 3 (IQR: 0 35 0; range: 0 12695 0),
Archivio Italiano di Urologia e Andrologia 2022;
94, 3
al 286
YouTubeTM and prostate checks
score was 2 8 (IQR:2 4 3 5) vs 2 0 (IQR:1 5 2 8) (p = 0 02), respectively (Table 3)
Table 1
7120 (IQR: 1350 0 38100 0; range:0 1670000 0), respec tively Disabled comments were recorded in 5 (6 8%) videos Of all videos, 26 0% (n = 19), 13 7% (n = 10), 2 7% (n = 2), 2 7% (n = 2) and 54 8% (n = 40) were produced by med ical doctor, private users, nurse, hospital and other, respectively Finally, 20 5% (n = 15) and 79 5% (n = 58) videos were tar geted to healthcare workers vs patients, respectively
Video quality assessment
The overall median PEMAT A/V U n d e r s t a n d a b i l i t y a n d a c t i o n ability scores were 46 2% (IQR: 3 0 8 7 6 9 ) a n d 5 0 0 % ( I Q R : 25 0 75 0), respectively
According to target audience, the median Understandability score was statistically significant higher for videos targeted to healthcare workers, relative to patients (69 2% [IQR: 46 2 88 5] vs 46 2% [IQR: 30 8 61 5], p = 0 01) Moreover, also the median Actionability score was statistical ly significant higher for videos targeted to healthcare workers, relative to patients (100 0% [IQR: 87 5 100 0] vs 25 0% [IQR: 25 0 68 6], p < 0 001) (Table 2)
The overall median misinforma tion score ranged from 1 0 (IQR: 1 0 4 0) to 2 0 (IQR: 1 0 4 0) A c c o r d i n g t o t a r g e t a u d i e n c e (healthcare workers vs patients) the median Misinformation score ranged from 1 0 (IQR: 1 0 1 5) to 4 0 (IQR: 3 0 5 0) vs 1 0 (IQR: 1 0 3 0) to 2 0 (IQR: 1 0 4 0), r e s p e c t i v e l y S p e c i fi c a l l y , t h e largest median misinformation score differences between videos targeted to healthcare workers vs patients were recorded for ques tion 1 (4 0 [IQR:3 0 5 0] vs 1 0 [IQR:1 0 3 0], p < 0 001) and 2 ( 4 0 [ I Q R : 1 5 4 5 ] v s 2 0 [IQR:1 0 3 0], p = 0 02), defined as “Does the video clearly describe t h e p r o c e d u r e ? ” a n d “ D o e s t h e video clearly describe the difference b e t w e e n n e o p l a s t i c d i s e a s e a n d other prostate diseases?” , respec t i v e l y M o r e o v e r , t h e M e d i a n Total Misinformation score was 2 2 (IQR:1 7 2 8) Specifically, a c c o r d i n g t o t a r g e t a u d i e n c e (healthcare workers vs patients), the median Total Misinformation
Videographic characteristics of overall YouTubeTM videos (n = 73) and according to target audience (healthcare workers vs patients) recorded on April 14th, 2021
V ideos characteristics
Healthcare workers Patients p value 15 (20 5) 58 (79 5)
Length, n (sec) Median (IQR) 244 (129 0 549 0) 586 (412 0 719 0) 219 (120 2 373 2) < 0 05 Range 38 0 2541 0 60 0 1380 0 38 2541
Views Median (IQR) 12954 (1780 0 199548 0) 40905 (5046 5 245701 5) 11412 (1720 131047 8) 0 4 Range 31 17141766 31 0 851104 0 68 17141766
Persistence on YouTubeTM, n (day) Median (IQR) 985 (237 2155) 386 (48 0 1508 5) 1043 (320 2 2604) 0 1 Range 1 4550 1 0 3864 0 2 4550
Thumbs up, n Median (IQR) 41 (6 0 256 0) 97 (27 0 248 0) 21 5 (6 2 255 2) 0 4 Range 0 200000 0 0 6815 0 0 200000 0
Thumbs down, n Median (IQR) 4 (1 0 45 0) 11 (1 0 56 5) 4 (0 2 44 8) 0 7 Range 0 3673 0 0 249 0 0 36730
Number of comments, n Median (IQR) 3 (0 35 0) 11 (1 5 30 0) 2 (0 34 2) 0 3 Range 0 12695.0 0 682.0 0 12695.0
Disab ed comments, n (%) No 68 (93 2) 14 (93 3) 54 (93 1) 0 99 Yes 5 (6 8) 1 (6 7) 4 (6 9)
VPI, n Median (IQR) 23 9(2 1 233 5) 62 8 (12 9 444 6) 14 8 (1 9 206 5) 0 3 Range 0 11972 6 0 11972 6 0 8454 4
Subscribers, n Median (IQR) 7120 (1350 0 38100 0) 4650 (3830 0 31400 0) 9710 (1320 0 159750 0) 0 8 Range 0 1670000 0 60 0 63700 0 0 1670000 0
Author, n (%) Medical Doctor 19 (26) 8 (53 3) 11 (19) 0 02 Private User 10 (13 7) 3 (20) 7 (12 1) Nurse 2 (2 7) 1 (6 7) 1 (1 7) Hospital 2 (2 7) 0 (0) 2 (3 4) Other 40 (54.8) 3 (20) 37 (63.8)
IQR: nterquart le Range; VPI: V deo Power Index
Table 2.
PEMAT A/V scores of overall YouTubeTM videos (n = 73) and according to target audience (healthcare workers vs patients) recorded on April 14th, 2021
Pemat A/V Overall Healthcare workers Patients p value (N = 73) 15 (20 5) 58 (79 5)
Understandability Median (IQR) 46 2 (30 8 76 9) 69 2 (46 2 88 5) 46 2 (30 8 61 5) 0 01 Range 0 100 0 30 8 100 0 0 100 0 Act onabil ty Median (IQR) 50 0 (25 0 75 0) 100 0 (87 5 100 0) 25 0 (25 0 68 8) < 0 001 Range 0 100 0 50 0 100 0 0 100 0
QR: Interquarti e Range
Table 3.
Misinformation scores of overall YouTubeTM videos (n= 73) and according to target audience (healthcare workers vs patients) recorded on April 14th, 2021
Misinfor mation score
Overall Healthcare workers Patients p value (N = 73) 15 (20.5) 58 (79.5)
Does the video clear y describe the procedure? Median (IQR) 2 0 (1 0 4 0) 4 0 (3 0 5 0) 1 0 (1 0 3 0) < 0 001 Range 1 0 5 0 2 0 5 0 1 0 5 0
Does the video clear y describe the difference between Median (IQR) 2 0 (1 0 4 0) 4 0 (1 5 4 5) 2 0 (1 0 3 0) 0 02 neoplastic disease and other prostate diseases? Range 1 0 5 0 1 0 5 0 1 0 5 0
Does the video give information on the pain during Median (IQR) 2 0 (1 0 4 0) 3 0 (2 0 3 0) 2 0 (1 0 4 0) 0 7 the examination? Range 1 0 5 0 1 0 5 0 1 0 5 0
Does the video describe the next steps to be Median (IQR) 1 0 (1 0 3 0) 1 (1 1 5) 1 0 (1 0 3 0) 0 4 performed after the examination? Range 1 0 5 0 1 0 4 0 1 0 5 0
Total Misinformation score Median (IQR) 2 2 (1 7 2 8) 2 8 (2 4 3 5) 2 0 (1 5 2 8) 0 02
Range 1 0 4 75 1 5 4 25 1 0 4 75
IQR: Interquart le Range
A287 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
S Morra, L Napolitano, C Collà Ruvolo, et al
Variable correlations
We recorded a positive statistically significant correlation between video length and PEMAT A/V Actionability (r = 0 26, p = 0 02), video length and Misinformation Question 1 (r = 0 33, p = 0 005), video length and Misinformation Question 2 (r = 0 24, p = 0 05) Conversely, no correlations were recorded between length and PEMAT A/V Understandability (p = 0 06), length and Misinformation Question 3 (p = 0 07), and length and Misinformation Question 4 (p = 0 4) Similarly, no correlations were recorded between all the other Videographic characteristics and quality videos’ assessment tools (all p > 0 05)
DISCUSSION
The current study aimed to assess YouTube™ videos’ quality on prostate checks, especially on DRE, and to investigate if they can correctly inform patients and erad icate their beliefs and myths To the best of our knowl edge, no studies on DRE were found in the literature We addressed this void and identified several noteworthy observations
First, of all 73 videos eligible for the analyses a median of about thirteen thousand views was recorded, conversely less than fifty thumbs up, thumbs down and comments were registered, highlighting a poor interaction between users and YouTubeTM videos currently available on DRE This observation may result from non sufficient high videos quality, in terms of Videographic characteristics or content Moreover, we recorded that out of 73 videos, about 80% were targeted to patients and more than 50% w e r e p r o d u c e d b y p e o p l e o f n o m e d i c a l fi e l d Consequently, most of the videos present on YouTubeTM on DRE aimed to explain DRE to people without a med ical background These observations support further the aim of the present study, which was to investigate if YouTubeTM videos could be used as a reliable tool of cor rect information prostate checks and especially on DRE Second, according to the PEMAT A/V score, the overall median Understandability was 46 2% and the overall median Actionability was 50 0% The Understandability reflects how viewers could process the information dis played in the videos, while the Actionability reflects how viewers could use them According to Shoemaker et al , a PEMAT score < 70% is considered poorly understandable or poorly actionable (34) In consequence, we recorded poorly understandable and actionable content based on our results Specifically, the median Understandability score of videos targeted to healthcare workers was 69 2% and median Actionability score was 100 0% Conversely, the median Understandability score of videos targeted to patients was 46 2% and the median Actionability score was 25 0% Therefore, based on our results, videos tar geted to healthcare workers were actionable and only s l i g h t l y b e l o w t h e l i m i t o f t h e u n d e r s t a n d a b i l i t y Furthermore, based on our results, videos targeted to patients were neither understandable nor actionable U n f o r t u n a t e l y , n o p r e v i o u s i n v e s t i g a t o r s e x a m i n e d
YouTube™ information on DRE However, we compared our results with the ones achieved in other studies deal ing with the fairness of YouTubeTM videos on different medical topics For example, Rubel et al , analyzed 50
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
YouTube™ videos focused on sinusitis, reporting similar Understandability and Actionability scores (57 5% and 33 3, respectively), relative to our results (35)
Conversely, Morra et al , analyzed the quality of 100 YouTubeTM videos on Bladder Pain Syndrome, reporting higher Understandability and Actionability scores (66 7% and 75%, respectively) (20)
Therefore, the Understandability and Actionability scores of videos have a noticeable variation related to the topics addressed It may be useful, for future YouTube™ video authors, to create new tools to guarantee a homogenous level of Understandability and Actionability among all the possible topics
Third, according to the Misinformation tool, we recorded a high rate of misinformation of YouTubeTM videos on DRE Specifically, the lowest overall median score was recorded for Question 4, defined as “Does the video describe the next steps to be performed after the examina tion?” , highlighting the incompleteness of YouTubeTM information on DRE Moreover, we highlight a remark able statistically significant difference between videos tar geted to healthcare workers vs patients in terms of misin formation Specifically, for Question 2, defined as “Does the video clearly describe the difference between neoplastic disease and other prostate diseases?” , we recorded a median of 4 0 (IQR:1 5 4 5) vs 2 0 (IQR:1 0 3 0) (p = 0 02), for healthcare workers vs patient, respectively Indeed, despite PCa is the most common malignancy among eld erly men 1, other non neoplastic diseases can affect the prostate, such as prostatitis or benign prostatic hyperpla sia (36 39) Therefore, YouTubeTM videos on DRE should clearly describe all the different possible diagnostic sce narios, to reduce misinformation F o u r t h , w e t e s t e d P e a r s o n ’ s c o r r e l a t i o n b e t w e e n Videographic characteristics and quality assessment tools scores A mild positive statistically significant correlation between the video length and PEMAT A/V Actionability, Misinformation Question 1, Misinformation Question 2 was recorded These findings, were consistent with Morra et al , highlighting the importance of sufficient time to correctly describe a medical topic, such as DRE, to YouTubeTM users (20) Therefore, video length may not be underestimated during the making video process
Taken together, according to our results the quality of the information provided by YouTubeTM videos on DRE is low Moreover, according to our data a poor interaction between videos and YouTubeTM users, testified by few thumbs up, thumbs down, and comments, was record ed Authors of future videos on DRE should increase the quality of information and improve the appeal of the videos, to increase interaction with the users Given the rising role of multimedia in the various healthcare servic es, a formal standardization of media contents addressed to medical and non medical users would be desirable Indeed, this will potentially decrease the risk of misinfor mation and will provide homogeneous content in the dif ferent paths of the healthcare process useful for the patient and family counseling
Our study is not devoid of limitations First, YouTubeTM search algorithms show videos based on relevance However, to ensure the most unbiased results, the research was conducted after logging out from any per
288
sonal account (incognito status) and changing the loca tion setting a VPN proxy to guarantee that the YouTubeTM videos displayed were not geared toward healthcare pro fessionals or to any previous research Second, we only consider a sample of 100 videos However, this sample is based on general population search strategy (40) Third, It is important to note that this study is limited by the ever changing content of the Internet, which cannot be captured using a cross sectional design In conclusion, based on our analyses, YouTubeTM videos’ quality on DRE resulted unsatisfactory according to the PEMAT A/V score and the Misinformation tool Videos targeted to healthcare workers got higher quality scores if compared to videos targeted to patients Therefore, YouTubeTM videos’ may not be considered a reliable source of information on DRE for patients
REFERENCES
1 Ferlay J, Colombet M, Soerjomataram I, et al Estimating the glob al cancer incidence and mortality in 2018: GLOBOCAN sources and methods Int J Cancer 2019; 144:1941 1953
2 Capece M, Creta M, Calogero A, et al Does physical activity reg ulate prostate carcinogenesis and prostate cancer outcomes? A nar rative review Int J Environ Res Public Health 2020; 17:1441
3 Stolzenbach LF, Rosiello G, Deuker M, et al The impact of race and age on distribution of metastases in patients with prostate can cer J Urol 2020; 204:962 968
4 Jones D, Friend C, Dreher A, et al The diagnostic test accuracy of rectal examination for prostate cancer diagnosis in symptomatic patients: a systematic review BMC Fam Pract 2018; 19:79
5 Wenzel M, Würnschimmel C, Nocera L, et al The effect of lymph node dissection on cancer specific survival in salvage radical prosta tectomy patients The Prostate 2021; 81:339 346
6 Stanzione A, Cuocolo R, Cocozza S, et al Detection of extrapro static extension of cancer on biparametric MRI combining texture analysis and machine learning: preliminary results Acad Radiol 2019; 26:1338 1344
7 Scandurra C, Mangiapia F, La Rocca R,, et al A cross sectional study on demoralization in prostate cancer patients: the role of mas culine self esteem, depression, and resilience Support Care Cancer 2022; 30:7021 7030
8 Mottet N, van den Bergh RCN, Briers E, et al EAU EANM ESTRO ESUR SIOG Guidelines on Prostate Cancer 2020 Update Part 1: Screening, diagnosis, and local treatment with curative intent Eur Urol 2021; 79:243 262
9 Collà Ruvolo C, Stolzenbach LF, Nocera L, et al Comparison of Mexican American vs Caucasian prostate cancer active surveillance candidates Urol Oncol 2021; 39:74 e1 74 e7
10 Carter HB, Albertsen PC, Barry MJ, et al Early detection of prostate cancer: AUA Guideline J Urol 2013; 190:419 426
11 Cornford P, van den Bergh RCN, Briers E, et al EAU EANM ESTRO ESUR SIOG Guidelines on Prostate Cancer Part II 2020 Update: treatment of relapsing and metastatic prostate cancer Eur Urol 2021; 79:263 282
12 Stanzione A, Creta M, Imbriaco M, et al Attitudes and percep tions towards multiparametric magnetic resonance imaging of the prostate: a national survey among Italian urologists Arch Ital Urol Androl 2020; 92:291 296
YouTubeTM and prostate checks
13 Carvalhal GF, Smith DS, Mager DE, et al Digital rectal exami nation for detecting prostate cancer at prostate specific antigen levels of 4 ng /ml or less J Urol 1999; 161:835 839
14 Naccarato AMEP, Reis LO, Matheus WE, et al Barriers to prostate cancer screening: psychological aspects and descriptive vari ables is there a correlation? Aging Male Off J Int Soc Study Aging Male 2011; 14:66 71
15 Scandurra C, Muzii B, La Rocca R, et al Social support mediates the relationship between body image distress and depressive symp toms in prostate cancer patients Int J Environ Res Public Health 2022; 19:4825
16 Loeb S, Sengupta S, Butaney M, et al Dissemination of misinfor mative and biased information about prostate cancer on YouTube Eur Urol 2019; 75:564 567
17 Basch CH, Menafro A, Mongiovi J, et al A Content Analysis of YouTubeTM Videos Related to Prostate Cancer Am J Mens Health 2017; 11:154 157
18 Creta M, Sagnelli C, Celentano G, et al SARS CoV 2 infection affects the lower urinary tract and male genital system: A systemat ic review J Med Virol 2021; 93:3133 3142
19 Teoh JYC, Ong WLK, Gonzalez Padilla D, et al A global survey on the impact of COVID 19 on urological services Eur Urol 2020; 78:265 275
20 Morra S, Collà Ruvolo C, Napolitano L, et al YouTubeTM as a source of information on bladder pain syndrome: A contemporary analysis Neurourol Urodyn 2022; 41:237 245
21 Morra S, Collà Ruvolo C, Napolitano L, et al Reply to a letter to the editor regarding the published article: “YouTubeTM as a source of information on bladder pain syndrome: A contemporary analysis ” Neurourol Urodyn 2022; 41:1194 1196
22 Mirone V, Creta M, Capece M, et al Telementoring for commu nication between residents and faculty physicians: Results from a sur vey on attitudes and perceptions in an Academic Tertiary Urology Referral Department in Italy Arch Ital Urol Androl 2021; 93:450 454
23 Napolitano L, Fusco GM, Cirillo L, et al Erectile dysfunction and mobile phone applications: Quality, content and adherence to European Association guidelines on male sexual dysfunction Arch Ital Urol Androl 2022; 94:211 216
24 Capece M, Di Giovanni A, Cirigliano L, et al YouTube as a source of information on penile prosthesis Andrologia 2022; 54:e14246
25 Melchionna A, Collà Ruvolo C, Capece M, et al Testicular pain and youtubeTM: are uploaded videos a reliable source to get infor mation? Int J Impot Res 2022 Feb 8 doi: 10 1038/s41443 022 00536 w Epub ahead of print
26 Fode M, Nolsøe AB, Jacobsen FM, et al Quality of information in YouTube videos on erectile dysfunction Sex Med 2020; 8:408 413
27 Cilio S, Collà Ruvolo C, Turco C, et al Analysis of quality information provided by “Dr YouTubeTM” on phimosis Int J Impot Res 2022; 24:1 6
28 Turco C, Collà Ruvolo C, Cilio S, et al Looking for cystoscopy on YouTube: Are videos a reliable information tool for internet users? Arch Ital Urol Androl 2022; 94:57 61
29 Di Bello F, Collà Ruvolo C, Cilio S, et al Testicular cancer and YouTube: What do you expect from a social media platform? Int J Urol 2022; 29:685 691
A289 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
S Morra, L Napolitano, C Collà Ruvolo, et al
30 Collà Ruvolo C, Califano G, Tuccillo A, et al YouTubeTM as a source of information on placenta accreta: A quality analysis Eur J Obstet Gynecol Reprod Biol 2022; 272:82 87
31 Rubel KE, Alwani MM, Nwosu OI, et al Understandability and actionability of audiovisual patient education materials on sinusitis Int Forum Allergy Rhinol 2020; 10:564 571
32 Gerundo G, Collà Ruvolo C, Puzone B, et al Personal protective equipment in Covid 19: Evidence based quality and analysis of Y o u T u b e v i d e o s a f t e r o n e y e a r o f p a n d e m i c A m J I n f e c t Control 2022; 50:300 305
33 PEMAT Tool for Audiovisual Materials (PEMAT A/V) Accessed March 7, 2021 http://www ahrq gov/health literacy/patient educa tion/pemat av html
34 Shoemaker SJ, Wolf MS, Brach C Development of the Patient Education Materials Assessment Tool (PEMAT): A new measure of understandability and actionability for print and audiovisual patient information Patient Educ Couns 2014; 96:395 403
35 Rubel KE, Alwani MM, Nwosu OI, et al Understandability and actionability of audiovisual patient education materials on sinusitis Int Forum Allergy Rhinol 2020; 10:564 571
36 Kogan MI, Naboka YL, Ismailov RS, et al Bacterial prostatitis: epidemiology and etiology Urologiia 2018; (6):144 148
37 Califano G, Collà Ruvolo C, Creta M, et al Focus on silodosin: pros and cons of uroselectivity Res Rep Urol 2020; 12:669 672
38 Verze P, Califano G, Sokolakis I, et al The impact of surgery for lower urinary tract symptoms/benign prostatic enlargement on both erectile and ejaculatory function: a systematic review Int J Impot Res 2019; 31:319 327
39 Mirone V, Napolitano L, D’Emmanuele di Villa Bianca R, et al A new original nutraceutical formulation ameliorates the effect of Tadalafil on clinical score and cGMP accumulation Arch Ital Urol Androl 2021; 93:221 226
40 Megaly M, Khalil C, Tadros B, Tawadros M Evaluation of edu cational value of YouTube videos for patients with coeliac disease Int J Celiac Dis 2016; 4:102 104
Correspondence
Simone Morra, MD
Luigi Napolitano, MD
Claudia Collà Ruvolo, MD
Giuseppe Celentano, MD (Corresponding Author)
dr giuseppecelentano@gmail com
Roberto La Rocca, MD
Marco Capece, MD
Massimiliano Creta, MD
Francesco Passaro, MD
Francesco Di Bello, MD
Luigi Cirillo, MD
Carmine Turco, MD
Ernesto Di Mauro, MD
Gabriele Pezone, MD
Agostino Fraia, MD
Francesco Mangiapia, MD
Vincenzo Mirone, MD
Gianluigi Califano, MD
Nicola Longo, MD
Department of Neurosciences, Reproductive Sciences Odontostomatology, Urology Unit, University of Naples “Federico II”, Italy
Via Pansini 5, 80131 Naples (Italy)
Ferdinando Fusco, MD
Urology Unit, Department of Woman, Child and General and Specialized Surgery, University of Campania 'Luigi Vanvitelli', Naples (Italy)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
290
Radical cystectomy for bladder urothelial carcinoma with aggressive variant histology
Urology Department, Northern Ontario School of Medicine, Thunder Bay Regional Health Centre, Ontario, Canada
Summary
Purpose: The aim of this study is to report our experience in managing bladder cancer in patients with variant pathology
Methods: Retrospective data collection for all patients managed by radical cystectomy over the last 3 years for a variant pathol ogy was completed We specifically included micropapillary and nested variants
Results: Ten patients were identified, with eight having micropapillary carcinoma (MPC) and two having nested vari ants Nine patients were male The median age was 75 The two patients with nested variant were 56 and 62 years old, respec tively, whereas all patients with MPC were over the age of 70 Upon cystectomy of all micropapillary cases, three patients (37 5%) had positive lymph node invasion and the final patholo gy was T2 (two patients), T3 (two patients), and T4 (four patients) Barring a grade III complication Clavien Dindo classi fication due to wound dehiscence that necessitated secondary surgical closure, there were no specific perioperative complica tions. Given the urethral invasion, cystourethrectomy was per formed on the female patient. Within a median 13 month fol low up, three patients developed local recurrence, including two urethral and one new lateral pelvic mass.
Conclusions: Considering the muscle invasive nature of micropapillary and nested bladder cancer, aggressive surgical management should not be postponed. Moreover, due to notable prevalence of concurrent and/or recurrent urethral involvement, initial urethrectomy or early and frequent postoperative ure throscopy should be provided. Patients with variant histology bladder cancer may benefit from early radical cystectomy when compared to bladder sparing protocols and prostate sparing cystectomy treatment options.
KEY WORDS: Bladder cancer; Urothelial carcinoma; Variant histology; Radical cystectomy
Submitted 30 July 2022; Accepted 20 August 2022
INTRODUCTION
Bladder cancer varies along a wide spectrum of histologi cal variants with urothelial cancer accounting for the vast majority (1, 2) Variant histology accounts for approxi mately 25% of bladder tumors that can pose distinctive diagnosis and therapy challenges to the overall manage ment of bladder cancer (2) According to the World Health Organization 2016 classification, variant histology of bladder cancer includes urothelial carcinoma with divergent differentiation, such as lymphoepithelioma like
cell variant, sarcomatoid variant, plasmacytoid variant, microcystic variant, micropapillary variant, nested vari ant, and small cell type (2) Histologic variants are classi fied primarily based on morphology that is associated with a distinct biological behavior, such as proclivity for local recurrence and metastasis Moreover there are vari ations in the clinical course including progression pat ter ns and responses to therapy as well as biologic features in molecular subtypes and DNA alterations (3) In the past, it was believed that urothelial tumors with divergent differentiation presented at a later stage of diag nosis, and earlier reports indicated a lower survival rate (4) Recent studies show that patients with squamous or glandular urothelial tumors have survival rates compara ble to those with pure urothelial tumor (3, 5) In a study by Sefik et al patients with variant histology were observed to have proportionally higher T stage compared to nonva riant urothelial carcinoma; however there were no signifi cant differences for overall survival and cancer specific survival (6) A recent study by Pereira et al evidenced that although bladder cancers with histological variants are clearly associated with features of more aggressive behav ior, they had not any significant impact in survival expectancies (7) Therefore, the clinical impact of tumor with variant histology on the treatment options still remains under a cloud of doubt in that whether the pres ence of variant histology justifies an aggressive treatment strategy involving early radical cystectomy (8) The final pathology and prognosis of bladder cancer with variant histology differ from that of pure urothelial bladder cancer, and evidence on the response to systemic therapy in these variant histologies is scarce and divergent (9, 10) Current guidelines place urothelial carcinoma with variant histol ogy in the highest risk category, implying that, despite lacking high level of evidence, early radical cystectomy should be considered (11) It is noteworthy, when it comes to management, evidence in some areas is contradictory and inconclusive therefore necessitating further investiga tion Our study aims to share our institution experience in treating bladder cancer with variant histology
METHODS
A retrospective cohort single center study involving all patients who were treated for bladder cancer with a his tological variant admitted to the Thunder Bay Regional
A291 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
ORIGINAL PAPER No conflict of interest declared
Vahid Mehrnoush, Logan Brennan, Asmaa Ismail, Ahmed Zakaria, Hazem Elmansy, Walid Shahrour, Owen Prowse, Ahmed Kotb
DOI: 10 4081/aiua 2022 3 291
V Mehrnoush, L Brennan, A Ismail, A Zakaria, H Elmansy, W Shahrour, O Prowse, A Kotb
Health Science Centre Our patients were treated with either a radical cystectomy or a transurethral resection of the bladder tumor (TURBT) alone, or a TURBT combined with adjuvant BCG therapy
RESULTS
Ten patients (9 male and 1 female) were identified, with eight having micropapillary cancer and two having nest ed variants The median age was 75 (56 84) The two patients with the nested variant were 56 and 62 years old, respectively, whereas all patients with micropapillary can cer (MPC) were over the age of 70 Of nested variant patients, one patient had a domal T1 tumor and the other had a T2 small trigonal tumor
Localized cancer was confirmed by staging CT scans
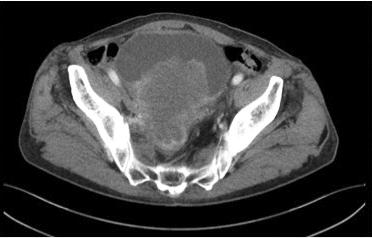
Upon radical cystoprostatectomy, the final pathology for the first patient was pT2N0, while the second patient was pT4aN1 Of the patients with MPC, two were reported to have stage T1 tumors, while six were reported to have stage T2 tumors on TURBT Stage T4b was found on CT scan in two patients Despite the instillation of intravesi cal bacillus Calmette Gue'rin (BCG) induction course, upstaging to T2 was reported in both T1 cases Upon cys tecto my fo r all micro papillar y cases, three patients (37 5%) had positive lymph node invasion and the final p a t h o l o g y c a m e b a c k T 2 ( t w o p a t i e n t s ) , T 3 ( t w o patients), and T4 (four patients)
Barring a grade III complication Clavien Dindo classifica tion due to wound dehiscence that necessitated second ary surgical closure, there were no specific perioperative complications) Given the urethral invasion, the cys tourethrectomy was performed on the female patient
Within a median 13 month follow up, three patients (30%) developed local recurrence, including two urethral and one new lateral pelvic mass

Table 1 illustrates the clinical characteristics and out comes to the patients and Figures 1 and 2 represent two
cases with micropapillary and nested variant urothelial carcinoma respectively
DISCUSSION
The current study is a report on our experience in treating b l a d d e r c a n c e r w i t h a g g re s s i v e v a
g y Micropapillary urothelial carcinoma (MPC) was a male pre dominant variant found in our patients MPC has received the most attention of the variant histologies in recent years and may be more familiar to many pathologists than other variants (8) Clinically, it is an aggressive variant that typi cally manifests at an advanced stage and accounts for 2 5% of urothelial carcinomas (8) which have a poor prog nosis (12) The fast progression of non muscle invasive micropapillary urothelial carcinoma to muscle invasive or metastatic bladder carcinoma is concerning and is a well demonstrated concern in our cases (13)
MPC is tightly linked to lymph vascular invasion and lymph node metastasis, in that pT1 bladder cancer with micropapillary variant is frequently upstaged to more advanced stages during investigation and treatment (12)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
292
r i a n t h i s t o l o
Table 1. Clinical characteristics and outcomes of all cases Median age 75 (56 84) Sex Males 9 Females 1 H stology Micropapillary 8 Nested 2 TURBT stage T1 3 T2 7 Final T pathology (cystectomy) T1 0 T2 3 T3 2 T4 5 Final N stage N0 7 N1 3 Urethral invasion No 7 Present at cystectomy 1 Early (w thin 6 months) 2 Local recurrence (with n 1 year) No 7 Urethra 2 Pelvic side wall 1
Figure 1.
Abdominal axial CT image showing a large cT4 micropapillary cancer
Figure 2.
Abdominal axial CT showing cT1 nested variant.
Radical cystectomy for bladder urothelial carcinoma with aggressive variant histology
As a result, the European Association of Urology European Society of Medical Oncology Guidelines Committees recently agreed that T1 high grade bladder urothelial carcinoma with micropapillary histology should be treated with immediate radical cystectomy and lymphadenectomy (11) Therefore, in such cases, most centers consider early radical cystectomy to be the standard of care; however, there have been reports of reasonable outcomes in series in which bladder preservation therapies were used in highly selected patients with a relatively small micropap illary component (14) Although there is still limited evi dence on the preferred treatment option, reports show no statistically significant differences in overall sur vival between groups that received neoadjuvant chemotherapy plus early radical cystectomy vs radical cystectomy alone in muscle invasive micropapillary urothelial carcinoma (15, 16) On the other hand, evidence is lacking on the added benefit of neoadjuvant chemotherapy to the treat ment of the bladder cancers with variant histology (17)
A study on patients with muscle invasive urothelial carci noma with variant histology comparing neoadjuvant chemotherapy plus radical cystectomy vs early radical cystectomy only showed an improvement in overall sur vival and a lower rate of non organ confined disease at the time of radical cystectomy in patients with neuroen docrine tumor neoadjuvant chemotherapy Neoadjuvant chemotherapy reduced the rate of non organ confined disease but had no effect on overall survival in bladder tumors with micropapillary differentiation, sarcomatoid differentiation, or adenocarcinoma (9) Evidence also rec ommended that muscle invasive bladder urothelial carci noma with micropapillary or plasmacytoid differentia tion, as well as squamous or glandular differentiation, should be treated with neoadjuvant chemotherapy fol lowed by radical cystectomy and concomitant lym phadenectomy (11)
The role of adjuvant radiotherapy for muscle invasive urothelial carcinoma and variant histologies is controver sial Some evidence recommends that adjuvant radiothera py (with or without radiosensitizing chemotherapy) is a standard treatment for patients with muscle invasive urothelial carcinoma with variant histology (11, 18) Other evidence states that it is prudent to consider adjuvant radiotherapy to improve local control This is particularly important in cases with positive margins like patients with urothelial carcinoma with squamous and/or glandular dif ferentiation who are more likely to have pT3 T4 tumors, pelvic lymph node involvement, and local or distant metas tasis related to increased mortality when compared to those with pure urothelial carcinoma (19 21)
It has been reported that the response rate to intravesical BCG administration for micropapillar y variant is poor (11, 22)
In a study of 72 patients with MPC, 40 received primar y intravesical BCG and 26 received early radical cystecto my The BCG group were more inclined to recurrence, progression, and lymph node metastasis at a 75%, 45%, and 35% rate, respectively 22 While certain patients with T1 MPC may respond to intravesical BCG, patients who undergo early radical cystectomy have improved sur vival outcome (22) In our center, we tried a BCG induction course for patients with T1, but due to T2 pro
gression, they eventually under went radical cystectomy Nested variant urothelial carcinoma is more common in men over the age of 60, which is similar to the occurrence of classic urothelial carcinoma; however, it has been reported in patients ranging in age from 42 to 90 years (23) In our findings, the nested variant, in contrast to MPC, were found in younger cases The nested variant, according to the 2016 WHO classification, includes urothelial carcinoma with small tubules and microcysts (24) It is distinguished by disorderly proliferation of con fluent nests with minimal cell atypia (25) which is fre quently mistaken for benign cytology that leads to a delay in the definitive diagnosis Nested urothelial carcinomas typically manifest as advanced disease and may be associ ated with a poor prognosis when compared to pure urothelial carcinoma (26) It has similar characteristics and clinical outcomes to classical urothelial carcinoma, with little to no difference in recurrence or survival rate when treated with radical cystectomy in either non mus cle invasive or muscle invasive bladder cancer (25) Data from two matched cohorts revealed that patients with nested variants had similar oncological outcomes after radical cystectomy compared to pure urothelial carcino ma (27, 28) Although lacking consensus due to a lack of evidence, it is recommended that T1 high grade bladder urothelial carcinoma with nested variants confirmed (after complete TURBT and/or re TURBT) should be treated with immediate radical cystectomy and concomi tant lymph node dissection (11)
The treatment of bladder cancer including transurethral surgery, intravesical chemotherapy and immunotherapy, radical cystectomy, systemic combination chemotherapy, and, in some cases, radiation therapy has evolved over time to the point where clinical risk markers are now employed to make the best decision for patients As a result, variant histology can serve as a risk stratification factor that can contribute to improved clinical decision making (17)
CONCLUSIONS
Aggressive surgical treatment for patients with micropapil lary and nested muscle invasive bladder cancer should not be postponed A large proportion of these patients have urethral involvement
Thus, an initial urethrectomy or early and frequent post operative urethroscopy should be included in the treat ment and management of variant histology bladder can cers For bladder cancer with variant histology, bladder sparing protocols and prostate sparing cystectomy may not be the best treatment options
KEY MESSAGES
1 Urothelial variant bladder cancer is always upstaged on radical cystectomy
2 Radical cystectomy for T1 variant histology should be offered rather than surveillance
3 Urethrectomy may be considered at time of radical cys tectomy
4 Urothelial variant histology was a male predominant finding in our series
3
A293 rchivio Italiano di Urologia e Andrologia 2022;
94,
REFERENCES
1 Chalasani V, Chin JL, Izawa JI Histologic variants of urothelial bladder cancer and nonurothelial histology in bladder cancer Can Urol Assoc J 2009; 3(6 Suppl 4):193 198
2 Humphrey PA, Moch H, Cubilla AL, et al The 2016 WHO Classification of tumours of the urinary system and male genital organs part B: prostate and bladder tumours Eur Urol 2016; 70:106 119
3 Burger M, Kamat AM, McConkey D Does variant histology change management of non muscle invasive bladder cancer? Eur Urol Oncol 2021; 4:510 514
4 Shapur NK, Katz R, Pode D, et al Is radical cystectomy manda tory in every patient with variant histology of bladder cancer Rare Tumors 2011; 3:e22
5 Barata PC, Rini BI Treatment of renal cell carcinoma: Current sta tus and future directions CA Cancer J Clin 2017; 67:507 524
6 Sefik E, Celik S, Basmaci I, et al Effect of variant histology pres ence and squamous differentiation on oncological results and patient's survival after radical cystectomy Arch Ital Urol Androl 2018; 90:172 175
7 Pereira JN, Reis JD, Braga I, et al Variant histologies of urothelial carcinoma: Does it change the survival outcomes in patients managed with radical cystectomy? Arch Ital Urol Androl 2022; 94:138 143
8 Black AJ, Black PC Variant histology in bladder cancer: diagnos tic and clinical implications Transl Cancer Res 2020; 9:6565 6575
9 Vetterlein MW, Wankowicz SAM, Seisen T, et al Neoadjuvant chemotherapy prior to radical cystectomy for muscle invasive blad der cancer with variant histology Cancer 2017; 123:4346 4355
10 Choi W, Porten S, Kim S, et al Identification of distinct basal and luminal subtypes of muscle invasive bladder cancer with different sen sitivities to frontline chemotherapy Cancer Cell 2014; 25:152 165
11 Horwich A, Babjuk M, Bellmunt J, et al EAU ESMO consensus statements on the management of advanced and variant bladder can cer an international collaborative multi stakeholder effort: under the auspices of the EAU and ESMO Guidelines Committees Ann Oncol 2019; 30:1697 1727
12 Compérat E, Roupret M, Yaxley J, et al Micropapillary urothe lial carcinoma of the urinary bladder: a clinicopathological analysis of 72 cases Pathology 2010; 42:650 654
13 Ramos P, Pereira P, Dinis P, Pacheco Figueiredo L Bladder can cer variant histologies: epidemiology, diagnosis, treatment and prog nosis In Ed F Ziglioli Modern approach to diagnosis and treatment of bladder cancer IntechOpen 2021
14 Berg S, D’Andrea D, Vetterlein MW, et al Impact of adjuvant chemotherapy in patients with adverse features and variant histology at radical cystectomy for muscle invasive carcinoma of the bladder: Does histologic subtype matter? Cancer 2019; 125:1449 1458
15 Lobo N, Shariat SF, Guo CC, et al What is the significance of variant histology in urothelial carcinoma? Eur Urol Focus 2020; 6:653 663
16 Sui W, Matulay JT, James MB, et al Micropapillary bladder can cer: insights from the National Cancer Database Bladder Cancer 2016; 2:415 423
17 Black PC, Brown GA, Dinney CPN The impact of variant his tology on the outcome of bladder cancer treated with curative intent Urol Oncol 2009; 27:3 7
18 Chua KLM, Kusumawidjaja G, Murgic J, Chua MLK Adjuvant treatment following radical cystectomy for muscle invasive urothelial
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
carcinoma and variant histologies: Is there a role for radiotherapy? ESMO open 2016; 1:e000123
19 Honma I, Masumori N, Sato E, et al Local recurrence after rad ical cystectomy for invasive bladder cancer: an analysis of predictive factors Urology 2004; 64:744 748
20 Zaghloul MS, Awwad HK, Akoush HH, et al Postoperative radiotherapy of carcinoma in bilharzial bladder: improved disease free survival through improving local control Int J Radiat Oncol Biol Phys 1992; 23:511 517
21 Lewis GD, Haque W, Verma V, et al The role of adjuvant radia tion therapy in locally advanced bladder cancer Bladder Cancer 2018; 4:205 213
22 Willis DL, Fernandez MI, Dickstein RJ, et al Clinical outcomes of cT1 micropapillary bladder cancer J Urol 2015; 193:1129 1134
23 Venyo AK Nested variant of urothelial carcinoma Adv Urol 2014; 2014:192720
24 Warrick JI Clinical significance of histologic variants of bladder cancer J Natl Compr Canc Netw 2017; 15:1268 1274
25 Aron M Variant histology in bladder cancer current understand ing of pathologic subtypes Curr Urol Rep 2019; 20:80
26 Lopez Beltran A, Henriques V, Montironi R, et al Variants and new entities of bladder cancer Histopathology 2019; 74:77 96
27 Beltran AL, Cheng L, Montironi R, et al Clinicopathological characteristics and outcome of nested carcinoma of the urinary blad der Virchows Arch 2014; 465:199 205
28 Linder BJ, Frank I, Cheville JC, et al Outcomes following radical cystectomy for nested variant of urothelial carcinoma: a matched cohort analysis J Urol 2013; 189:1670 1675
Correspondence
Vahid Mehrnoush, MD vahidmehrnoush7@gmail com
Logan Brennan lobrennan@nosm ca
Asmaa Ismail asmaaismail0782@gmail com
Ahmed Zakaria aszakaria81@yahoo com
Hazem Elmansy hazemuro100@yahoo com
Walid Shahrour walid shahrour@gmail com
Owen Prowse owen prowse@tbh net
Ahmed Kotb (Corresponding Author) drahmedfali@gmail com
Urology Department, Northern Ontario School of Medicine, Thunder Bay Regional Health Centre, Ontario, Canada
V Mehrnoush, L Brennan, A Ismail, A Zakaria, H Elmansy, W Shahrour, O Prowse, A Kotb
294
Analysis of benign prostatic obstruction surgery: A long-term evaluation in a real-life context
Alberto Costa Silva 1 , Pedro Abreu Mendes 1, 2, 3 , Afonso Morgado 1 , Paulo Dinis 1, 2 , Carlos Martins Silva 1, 2, 3
Urology Department, Centro Hospitalar Universitário São João, Porto, Portugal;
Faculty of Medicine, University of Porto, Porto, Portugal;
i3S Institute for Research and Innovation in Health, Translational NeuroUrology Group, Porto, Portugal
Summary
Objective: Surgery is the treatment for male lower urinary tract symptoms (LUTS) relat ed to benign prostatic obstruction (BPO) refractory to pharma cological treatment or with complications This study aimed to assess factors associated with the need for surgical reinterven tion and/or continuation of pharmacological treatment
Materials and methods: A retrospective analysis of patients who underwent prostatic surgery for male LUTS associated with BPO between 1 May 2015 and 1 May 2016, with a minimum follow up of five years, in an academic tertiary hospital
The type of surgery, preoperative, postoperative and follow up analysis were collected in a database
Results: A total of 212 patients were included with a mean age of 70 ± 8 66 years at five years follow up At 5 years, a total of 86 9% of patients do not need pharmacological treatment and 12% required surgical reintervention Of the preoperative parameters, it was found a relationship between prior prostatitis and the need for second surgery with an odds ratio of 4 6
Conclusions: Patients should be informed of the potential need for pharmacological treatment following surgery, or even of the need for reintervention History of prostatitis seems to be a risk factor for reintervention
KEY WORDS: Prostatic Hyperplasia; Quality of life; Transurethral resection of prostate; Prostatectomy
Submitted 4 August 2022; Accepted 20 August 2022
INTRODUCTION
Male lower urinary tract symptoms, commonly known as male LUTS, are one of the most frequent reasons for con tact with healthcare, namely with the urologist Presence of LUTS has a negative impact on patients’ quality of life (1) LUTS have historically been linked to bladder outlet obstruction (BOO) and the most frequent cause in males is benign prostatic hyperplasia (BPH) This occurs when BPH advances from benign prostatic enlargement (BPE) to benign prostatic obstruction (BPO) (2)
Currently, the treatment is organized on a therapeutic ladder, starting with lifestyle measures, followed by phar macological treatments Surgical interventions are most often reserved for patients with bothersome LUTS refrac tory to medical therapy Although this ladder is effective for the majority of patients, in real life clinical practice, surgery is not always successful and reintervention or the
need to restart or continue pharmacological treatment may be needed in some patients (3) Risk factors for sur gical reintervention are not well defined but some authors showed that higher prostatic volume and history of uri nary retention with urethral catheterization could be associated with a higher need for reintervention (4) This study aimed to assess factors associated with the need for surgical reintervention and/or continuation of pharmacological treatment
MATERIALS AND METHODS
After ethical committee approval (Protocol number 339/21) and informed consent of the patients, it was per formed a retrospective analysis of all consecutive patients who underwent prostatic surgery for male LUTS associat ed with BPO in an academic tertiary hospital between 1 May 2015 and 1 May 2016, with a minimum follow up of five years
The type of surgery, preoperative, postoperative and fol low up analysis were collected in a database The follow ing preoperative parameters were evaluated: prostate spe cific antigen (PSA), prostate volume, post void residual vol ume (PVR), the pattern of complaints (predominance of storage or emptying), need for previous catheterization, previous episode of acute bacterial prostatitis, duration of pharmacological treatment before surgery and type of drugs used Prostatic volume was measured by transrec tal or suprapubic ultrasound For those taking 5 reduc tase inhibitors (5ARIs) for more than 6 months, tPSA value was adjusted to double Acute bacterial prostatitis was clinically defined as an episode of febrile LUTS with swollen and tender prostate on digital rectal examination and positive urine culture
In terms of surgical procedures, patients were classified as b e i n g s u b m i t t e d t o t r a n s u r e t h r a l r e s e c t i o n ( T U R P ) , open/laparoscopic transvesical prostatectomy (TVP) or open/laparoscopic retropubic prostatectomy (RP) according to the surgical report
Patients with the following conditions were excluded: history of chronic prostatitis or chronic pelvic pain, pre vious surgery in the context of prostatic cancer and patients with post surgical histology of the specimen showing malignancy Prostatic tissue resected was meas ured and a ratio (Percent of Resected Tissue) was calcu
A295 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
ORIGINAL PAPER No conflict of interest declared
1
2
3
DOI: 10 4081/aiua 2022 3 295
A Costa Silva, P Abreu Mendes, A Morgado, P Dinis, C Martins Silva
lated dividing by the preoperative prostate volume
Concerning post surgery parameters, we considered the medication prescribed when the surgery was not effec tive, the need for a reintervention and the type of surgical technique used All medications were verified by access ing the patient's clinical file and by asking the patient himself We grouped the drugs in alpha blockers (AB), 5ARI, anticholinergic (AC) and a3 agonist (B3A) Drugs were prescribed by urologists or primary health care physicians It was confirmed that the medication was not being taken for other purposes (eg, 5ARI for androgenet ic alopecia) Surgical reintervention was verified by the patient’s clinical file and only surgeries performed in the national health service were considered
Overall patients characteristics like age, main comorbidi ties and renal function were also collected
The need for maintenance of pharmacological treatment as well as the need for surgical re intervention at 5 years was assessed and its association with preoperative param eters was explored
Statistical analyses
The data were collected and analysed using SPSS (v 27 IBM, USA) The Shapiro Wilk test was used to test parameter distribution Continuous variables with nor mal distribution were expressed as the mean ± the stan dard deviation, non normally distributed variables were expressed as the median (25th 75th quartiles), and nomi nal variables were expressed in relative frequencies For continuous variables, the differences between the groups were evaluated using the ANOVA test if a normal distri bution was assumed; otherwise, the Kruskal Wallis test was used Categorical variables were compared using the chi square test The p significance was set at < 0 05
RESULTS
A total of 212 patients were included The patient's mean age at five years follow up was 70 ± 8 66 years old Overall patient characteristics and perioperative data are depicted in Tables 1, 2 Regarding the medication taken before surgery, 33 0% were under AB; 13 7% were taking only 5ARI; 34% had a combination of AB and 5ARI; 5 7% took another com bination (mainly AB plus AC) Only 13 7% were not under any medication before surgery Regarding the ini
Table 1.
Demographic characteristics.
1
Table 2.
Perioperative data
PSA 1 2 4 ng/dl (1 20 4 53)
Preoperative prostate volume 1 60 00 cm3 (44 25 85 00)
PVR 2 69 00 ml (± 22 12)
Predominance of symptoms 75% voiding; 25% storage
Presence of nocturia 53 8%
Urethral catheter for urinary retention 30%
Percent of resected tissue 1 22 22% (8 62 35 80) ≤ 30% 68.90% 30 50% 12 76% ≥ 50% 18 34%
1 Median (25th 75th quart le); 2 Mean ± standard error; PSA: Prostate spec fic antigen; PVR: Post vo d res dual volume
Table 3.
Association between preoperative parameters and medication continuation or surgical reintervention; results shown in p values
Variables Medication continuation Surgical reinter vention
Symptoms pattern 1 0 785 0 840
Prostatit s 1 0 073 0 004
Urethral catheter for urinary retention 1 0 611 0 635
Prostatic volume 2 0 262 0 069
PSA 2 0 444 0 903
PVR 2 0 230 0 113
Duration medical treatment 1 0 088 0 022
Percent of Resected Tissue 2 0 643 0 138 1 Chi square test; 2 Kruska Wal is test; PSA: prostate spec fic antigen; PVR: post void residua vo ume
tial surgery performed, 65 6% underwent TURP; 24 1% underwent TVP and 10 4% underwent RP
A total of 86 9% of patients did not need pharmacologi cal treatment 5 years after surgery Of those who required pharmacological treatment after surgery, 24 5% were tak ing AB, 12 2% were taking 5ARI, 20 0% were taking a combination of both, 18 4% were taking AC, 12 2% were taking a combination of AB and AC, and 10% took B3A
Twelve per cent required surgical reintervention and it was performed in the first 2 years in 57 7% men and between the second and third years in the 34% Only 8% underwent surgery after more than 3 years Of the patients who underwent initial TURP, TVP and RP, 84 9%, 98% and 95 5% did not need a surgical reinter vention, respectively
The surgical modality chosen for reintervention was re TURP in 73,1%, internal urethrotomy in 15 4%, bladder neck resection in 7 7% and TVP in 3 8%
disease 1,8% (4)
Hypogonadism 0 4% (1)
There seems to be a statistical association between the presence of a previous episode of prostatitis and the greater need for surgical reintervention (p = 0 004) The relationship between prior prostatitis and the need for a second surgery has an odds ratio of 4 6 (95%, CI 1,71 12,32) Of those with a previous episode of prostatitis, 28 6% required surgical reintervention Of all patients who required a surgical reintervention, 36 4% had previ ous prostatitis The other data were not statistically relat ed to the need for resume pharmacological treatment or of surgical reintervention (Table 3)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
296
Age 1 70 ± 8 66 Serum creatinine 2 0 98 (0 80 1 12) Obesity 34% (74) Hypertension 27% (57) Diabetes 18% (40) Depression 12% (25) Parkinson disease 2 5% (5) Chronic kidney
Mean ± standard error; 2 Med an (25 h 75 h quarti e)
DISCUSSION
Between our patients, 68 9% of them have PSA > 1 4 ng/ml (median PSA of 2 4 ng/dl), corroborating the potential relationship between higher PSA and the need for intervention Previous studies, like the PLESS trial, Olmsted County Study and MTOPS, have shown that patients with this cut off of PSA are at higher risk of need ing surgical treatment (5 7) Thirty percent of our patients were catheterized which is similar to other stud ies (4, 8) We did not find a relationship between the presence of a catheterization (due to urinary retention), higher prostatic volumes, and the need for surgical rein tervention, differently to the findings by other authors (4) Concerning baseline PVR values, it is known that has little prognostic value for the risk of surgery in patients on medical treatment (namely, AB) (9)
Three quarters of patients took medication for less than a year before being submitted for surgery The duration of medical treatment had no impact on the need for reinter vention or the need to return to medication
The predominance of voiding or storage symptoms before first surgery was not associated with the need for post surgery medication This finding diverges from Han et al , w h i c h s h o w e d t h a t s t o r a g e s y m p t o m s a n d u s e o f antimuscarinics were significantly associated with symp tom persistence and the need to continue medical thera py after surgery (10) Moreover, this group also showed that any previous LUTS/BPO medication use was signifi cantly associated with symptom persistency and continu ing medical therapy, a fact that was not corroborated by our sample
The epidemiological relationship between prostatitis and benign prostatic hyperplasia was shown in case control studies and a cohort study (11) However, that associa tion is not broadly accepted In our study, a history of acute prostatitis is significantly associated with the need for a surgical reintervention, resulting in a 4 6 times high er risk of a second procedure, which means a probability of 82% of needing reintervention This data gives strength to the finding of Sauver et al with an odds ratio of 1 69 and a probability of 70% (12) The baseline degree of LUTS, even after surgery, in patients with a history of prostatitis may induce a false sense in the urologist of the need for intervention, lowering the threshold for reinter vention The true benefit and consequences of surgery in these patients remain to be seen, and further studies are needed
In this study, a higher ratio of prostatic tissue resected was not associated with less medical continuation or less surgical reintervention Some studies show that there is a poor correlation between the residual prostate weight and symptoms and these are affected by several other con founding factors (13 18) Some authors even claim that resection of less than 30% of prostatic tissue seems to be sufficient to alleviate lower urinary tract symptoms relat ed to benign prostate hyperplasia (13) A recent study shows that less profound prostate resections may be suf ficient, depending on maximum flow rate (19) In our study, more than two thirds of our patients have less than 30% of prostatic tissue resected and it was not associated with poorer outcomes Despite that, this is a controversial subject, and some authors postulate the opposite
Although nowadays the choice of surgical interventions includes less invasive techniques, our patients were sub mitted to the “classic” techniques of TURP, TVP and RP
In our study, TVP and RP have shown a low rate of need for re intervention, while TURP, although effective, has a higher risk for reintervention
A total of 25 patients (12%) required surgical reinterven tion This number is supported by Rassweiler et al , who showed similar values, between 3 to 14 5% (3) The rein terventions are mainly performed in the first 3 years (92,0%) The follow up of patients after surgical reinter vention is not well defined and should be evaluated in further studies However, given these data, we believe that these patients need to be followed for at least 3 years, although not necessarily by a urologist In the majority of cases, the modality chosen for reintervention was TURP (73% of these 25 patients) In 1 9% and 0 9% of all the 212 patients, the reintervention was an internal urethro tomy for urethral stricture and loop resection of bladder neck for bladder neck contracture (BNC), respectively
Both complications are more common after TURP (20)
All our patients who needed urethrotomy or resection of BNC had previously undergone TURP Our urethrotomy incidence is similar to the study of Sucki et al (21) and is within the lower range of the 1 4 19% referred in litera ture (3, 20) Our BNC is relatively lower than the 1 7 9 7% mentioned in other studies (20, 22, 23)
We only considered surgical reintervention made in our centre or another one of the Portuguese National Health Service, therefore, there is a chance that some patients who have had surgical reintervention in private clinical setting could be missed It would be interesting to com pare the rate of reinterventions and complications of both “classic” and modern techniques being performed nowa days in a real life context as a tertiary hospital where both residents and consultants perform surgeries
Twenty three percent of our patients still needed to use male LUTS medication after surgery and this factor was independent of the type of surgery Some studies show rates of patients needing medication ranging between 15 and 55% A previous study with longer follow up (3 years) showed an estimated rate of use of medication of 22% (24), so data of our cohort is in line with other cen tres Compared with 86 3% of patients who were med icated for BPO before surgery, we have an important decrease in the relative number of patients who need medication after surgery Lifelong medications are cost burden and are associated with consequences given by adverse effects and associated with drug interactions So, medication discontinuation could be an indicator of the success of the procedure, and is important to include it as an effective measure when comparing surgical options, since a large proportion of patients are motivated to undergo surgery in order to discontinuing medication for male LUTS (25) Despite this, we should keep in mind that sometimes the need for medication does not result from a failure in the surgical technique but rather from the LUTS physiopathological pleiotropism, namely the coexistence of other causes for bladder outlet obstruction (as an anatomical abnormality), the presence of underac tive or overactive bladder and of chronic prostatitis (of any type) (10)
A297 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Analysis of benign prostatic obstruction surgery: A long term evaluation in a real life context
A Costa Silva, P Abreu Mendes, A Morgado, P Dinis, C Martins Silva
Only 4 2% and 2 4% of our patients are using AC and B3A, respectively This is lower than 5 7% and 4 7% of the use of AB and its combination with 5ARI
In a study by Campbell et al , it was shown that ABs are used in about 9%, being the most commonly used drug class (25) Because AB’s mechanism of action is mainly on receptors located in the bladder neck and prostatic smooth muscle, AB utility following a thorough surgery should be minimal, these Authors stated that use of AB is a indicator of quality of surgery (25) Given the bladder remodelling and the prevalence of storage symptoms after surgery, they felt that AC and B3A would be commonly used Also, Campbell et al showed that use of AB, 5ARIs, AC/B3A within the first 5 years after surgery is roughly 25%, 20%, and 15%, respectively (26)
A non negligible portion of the patients (13%) was sub mitted to surgery without taking any medication previ ously but our numbers are inferior to those of some liter ature, referring values around 50% (24)
In our series, these were patients referred by primary care physicians with end term BPO (most commonly with a urethral catheter) or with contraindications to male LUTS medication and were quickly scheduled for surgery These data may indicate that primary health care has a more conservative approach to LUTS, namely through watchful waiting These data make us believe that educa tion programs targeted to primary care physicians and medical literacy campaigns for the general population should be encouraged
Our study has some limitations It is a retrospective study with possible selection bias New surgical techniques are the main hot topic nowadays in male LUTS treatment, and most of their benefits are very well expressed (27 30) During the last years, laser enucleation of prostate, namely with Holmium laser (HoLEP), has replaced TURP as the gold standard surgical treatment for BPH (31) On the other hand our study focused on the outcomes of our centre that did not have other newer surgical modalities of BPO treatment Furthermore, the results are from a sin gle tertiary centre where multiple surgeons performed the procedures, including both residents and graduated urol ogists
This is a reality present in most university hospitals and it’s one of the reasons for considering this study a real life based one A limited number of patients were enrolled, although it is quite an elevated number for 1 year in a single centre Medication compliance is an iden tified problem in BPO therapy, and we could not evalu ate it We lack data about the time before the beginning of medical treatment and the first surgery such as IPSS, Qmax and sexual function, which is why we chose not to use data related to these variables collected in the post operative period given the impossibility of a comparison
CONCLUSIONS
Patients should be informed of the potential need for pharmacological treatment following surgery, or even of the need for reintervention
History of prostatitis seems to be a risk factor for reinter vention in patients submitted to prostatic surgery for benign obstruction
Archivio Italiano di Urologia e Andrologia 2022;
REFERENCES
1 Kupelian V, Wei JT, O’Leary MP, et al Prevalence of lower uri nary tract symptoms and effect on quality of life in a racially and eth nically diverse random sample: The Boston Area Community Health (BACH) survey Arch Intern Med 2006; 166:2381 7
2 Gravas S, Cornu JN, Gacci M, et al Management of non neuro genic male lower urinary tract symptoms (LUTS), incl benign pro static obstruction (BPO) Eur Assoc Urol Guidelines [Internet] 2021; A v a i l a b l e f r o m : h t t p s : / / u r o w e b o r g / w p c o n t e n t / u p l o a d s / E A U Guidelines on Non Neurogenic Male LUTS incl BPO 2020 pdf
3 Rassweiler J, Teber D, Kuntz R, Hofmann R Complications of transurethral resection of the prostate (TURP) Incidence, manage ment, and prevention Eur Urol 2006; 50:969 80
4 Reich O, Gratzke C, Bachmann A, et al Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 Patients J Urol 2008; 180:246 9
5 Roehrborn CG The utility of serum prostatic specific antigen in the management of men with benign prostatic hyperplasia Int J Impot Res 2008; 20 (Suppl 3): S19 26
6 Bruskewitz R, Girman CJ, Fowler J, et al Effect of finasteride on bother and other health related quality of life aspects associated with benign prostatic hyperplasia Urology 1999; 54:670 8
7 Jacobsen SJ, Jacobson DJ, Girman CJ, et al Treatment for benign prostatic hyperplasia among community dwelling men: The Olmsted County study of urinary symptoms and health status J Urol 1999;162:1301 6
8 Mebust WK, Holtgrewe HL, Cockett ATK, et al Transurethral p r o s t a t e c t o m y : I m m e d i a t e a n d p o s t o p e r a t i v e c o m p l i c a t i o n s Cooperative study of 13 participating institutions evaluating 3,885 patients J Urol 2002; 167:5 9
9 Mochtar CA, Kiemeney LALM, Van Riemsdijk MM, et al Post void residual urine volume is not a good predictor of the need for invasive therapy among patients with benign prostatic hyperplasia J Urol 2006; 175:213 6
10 Han HH, Ko WJ, Yoo TK, et al Factors associated with continu ing medical therapy after transurethral resection of prostate Urology 2014; 84:675 80
11 Zhang L, Wang Y, Qin Z, et al Correlation between prostatitis, benign prostatic hyperplasia and prostate cancer: A systematic review and meta analysis J Cancer 2020; 11:177 89
12 Sauver JLS, Jacobson DJ, Mcgree ME, et al Longitudinal Association between Prostatitis and Development of Benign Prostatic Hyperplasia Urology 2008; 71:475 9
13 Antunes AA, Srougi M, Coelho RF, et al Transurethral resection of the prostate for the treatment of lower urinary tract symptoms related to benign prostatic hyperplasia: How much should be resect ed? Int Braz J Urol 2009; 35:683 9
14 Park HK, Paick SH, Lho YS, et al Effect of the ratio of resected tissue in comparison with the prostate transitional zone volume on voiding function improvement after transurethral resection of prostate Urology 2012; 79:202 6
15 Melchior J, Valk WL, Foret JD, Mebust WK Transurethral prostatectomy: computerized analysis of 2,223 consecutive cases J Urol 1974; 112:634 42
16 Hahn L, Leiter E The effect of transurethral resection on the weight of resected tissue J Urol 1971;106:405 6
17 Rasmussen F Weight loss of prostatic tissue during electroresec tion Scand J Urol Nephrol 1975; 9:214 5
94, 3
298
Analysis of benign prostatic obstruction surgery: A long term evaluation in a real life context
18 Chen SS, Hong JG, Hsiao YJ, Chang LS The correlation between c l i n i c a l o u t c o m e a n d r e s i d u a l p r o s t a t i c w e i g h t r a t i o a f t e r transurethral resection of the prostate for benign prostatic hyperpla sia BJU Int 2000; 85:79 82
19 Lopes F, Pereira R, Fernandes M, et al Prostate resection weight matters in severely obstructed men undergoing transurethral resec tion of the prostate Arch Ital Urol Androl 2022; 94:169 73
20 Sögütdelen E, Haberal HB, Guliyev F, Akdogan B Urethral stric ture is an unpleasant complication after prostate surgery: a critical review of current literature J Urol Surg 2016; 3:1 6
21 Stucki P, Marini L, Mattei A, et al Bipolar versus monopolar transurethral resection of the prostate: A prospective randomized trial focusing on bleeding complications J Urol 2015; 193:1371 6
22 Chen YZ, Lin WR, Chow YC, et al Analysis of risk factors of bladder neck contracture following transurethral surgery of prostate BMC Urol 2021;21:1 9
23 Lee YH, Chiu AW, Huang JK Comprehensive study of bladder neck contracture after transurethral resection of prostate Urology 2005; 65:498 503
24 Strope SA, Vetter J, Elliott S, et al Use of medical therapy and success of laser surgery and transurethral resection of the prostate for benign prostatic hyperplasia Urology 2015; 86:1115 22
25 Campbell RA, Gill BC Medication discontinuation following
transurethral prostatectomy: an unrecognized effectiveness measure? Curr Urol Rep 2020; 21:61
26 Campbell J, Reid J, Ordon M, Welk B The utilization of benign prostatic hyperplasia and bladder related medications after a transurethral prostatectomy Urology 2019; 130:126 31
27 Pallauf M, Kunit T, Ramesmayer C, et al Endoscopic enucleation of the prostate (EEP) The same but different a systematic review World J Urol 2021; 39:2383 96
28 Cho SY, Park J, Yoo S, et al One year surgical outcomes of com plete or incomplete enucleation of prostate by monopolar electroco agulation, photoselective vapoenucleation of 120 W GreenLight laser, and Holmium laser Urology 2017; 108:142 8
29 Kuntz RM, Lehrich K, Ahyai SA Holmium laser enucleation of the prostate versus open prostatectomy for prostates greater than 100 grams: 5 year follow up results of a randomised clinical trial Eur Urol 2008; 53:160 8
30 Strope SA, Vetter J, Elliott S, et al Use of medical therapy and success of laser surgery and transurethral resection of the prostate for benign prostatic hyperplasia Urology 2015; 86:1115 22
31 Mostafa MM, Patil N, Khalil M, et al Is Holmium laser enucleation of prostate equally effective in management of benign prostatic hyper plasia patients with either voiding or storage lower urinary tract symp toms? A comparative study Arch Ital Urol Androl 2022; 94:174 9
Correspondence
Alberto Costa Silva, MD (Corresonding Author) albertocsilva8@gmail com Urology Department, Centro Hospitalar Universitário São João, Porto, Portugal
ORCID iD: 0000 0001 6753 7206
Pedro Abreu Mendes, MD pamendes@gmail com Author
ORCI iD: 0000 0002 4304 7023
Afonso Morgado, MD amorg@gmail com
ORCID iD: 0000 0002 9647 4360
Paulo Dinis, MD pdinis@gmail com
ORCI iD: 0000 0003 2893 5492
Carlos Martins Silva, MD cmslva@gmail com
ORCI iD: 0000 0003 1739 1039
A299 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Hands on wet lab and live surgery training in PCNL: Any impact to surgical skills of attending surgeons?
Iason Kyriazis 1 , Panagiotis Kallidonis 1 , Eleni Kyrkopoulou 2 , Theodoros Spinos 1 , Evangelos Liatsikos
Department of Urology, University of Patras, Greece;
Department of Economics, Athens University of Economics and Business, Greece
Summary
Objectives: The clinical value and efficiency of hands on training courses in percutaneous nephrolithotomy (PCNL) remains undocumented During the last 9 years, a two day international intensive hands on training course in fluoroscopic guided prone PCNL is taking place in our department on a monthly basis Course includes wet lab training in the porcine model and live surgery training In this work we report the outcomes of a survey send to course participants questioning the impact of the course to their clinical practice
Materials and methods: A survey consisting of 26 questions was distributed online to a total of 91 trainees that had completed the course Comparison of pre and post course surgical practices was performed using the "N 1" Chi squared test
Results: A total of 64 trainees responded to our online survey with 55 6% and 41 3% reporting a modest or major impact to their practice accordingly Notable changes in puncture and dilation technique were evidenced while a uniform reduction in puncture and operative times was documented 79 4% responded that the course increased the safety of their procedure, 73% that it reduced operating times, 39.7% that increased their stone free rates, 23.8% that reduced their complications and 23.8% that induced to change their instrumentation with respect of that they were using in the past. Subgroup analysis including only well experienced surgeons revealed a similar impact to their practice.
Conclusions: In the proper setting, an intensive hands on PCNL course can have a significant impact on attending physicians. Participation to such events even for experienced surgeons should be encouraged.
KEY WORDS: PCNL; Hands on; Wet lab; Training; Surgical skills
Submitted 4 August 2022; Accepted 20 August 2022
INTRODUCTION
Proper training in percutaneous nephrolithotripsy (PCNL) is of outmost importance to ensure high efficacy of PCNL and reduce its potential morbidity (1) Currently, PCNL training is provided by structured residency and fellow ship programs worldwide and is further supported by individual theoretical and hands on training courses Nevertheless, the clinical value and efficiency of the latter short term courses has never been investigated
During the last 9 years, in the University Hospital of Patras in Greece, a two day international intensive hands on training course in fluoroscopic guided prone PCNL is
No conflict of interest declared
taking place on a monthly basis The course is usually supporting 2 3 international trainees per course and includes one day of wet lab training in pigs and one full day of live surgery, where trainees are participating as first and assisting surgeons in the operation of several PCNL cases under the proctoring of a highly skilled sur geon After the training of more than 90 physicians we conducted an online survey examining whether particu lar training course and PCNL intensive hands on training courses in general have any impact in the daily surgical practice of attending trainees
MATERIALS AND METHODS
Survey and training physician characteristics: A survey consisting of 26 questions (2x demographic information, 10x pre and 10x post training experience and surgical preferences, 4x overall impressions from the course) was distributed online to a total of 91 trainees that had com pleted the course All attending physicians were certified urologists with various previous experience in PCNL T h e i r e t h n i c i t y v a r i e d f r o m E u r o p e ( G e r m a n y : 1 5 , F r a n c e : 1 1 , U n i t e d K i n g d o m : 8 , A u s t r i a : 8 , P o l a n d : 8 , R u s s i a : 7 , B u l g a r i a : 5 , S w i t z e r l a n d : 4 , G r e e c e : 4 , Netherlands:4, Cyprus:3, Italy:2, Slovenia:2, Hungary:1, Serbia/Montenegro:1, Spain:1), Africa (South Africa:2, M o r o c c o : 1 ) a n d m i d d l e E a s t ( Q a t a r : 2 , K u w a i t : 1 , Lebanon:1) A total of 64 trainees responded to our online survey leading to a 70 3% response rate Mean age of responding physicians was 44 years (range: 32 68) Self reported experience prior to the course was poor (defined as < 10 cases) in 31 3%, intermediate (defined as > 10 and < 50 cases) in 28 1% and good (defined as > 50 cases) in 40 6% of attending surgeons
Hands on Wet lab training protocol: A female pig weight ing more than 30 Kg was anesthetized and placed in the supine position Under cystoscopic and fluoroscopic guidance a 7 Fr ureteral catheter was advanced to each kidney The animal was then placed in prone position and a retrograde pyelography was performed C arm was then placed at 30 degrees perpendicular to the long axis of the pig and target calyx or renal pelvis was selected
Following a small skin incision an 18G diamond tip nee dle was advanced towards target in a bull’s eye fashion After adequate penetration of the needle, the C arm was rotated to zero degrees and the depth of puncture was
Archivio Italiano di Urologia e Andrologia 2022; 94, 33 00 ORIGINAL PAPER
1 1
2
DOI: 10 4081/aiua 2022 3 300
accessed When needle reached or overpassed the target at zero degree projection, needle introducer was removed and a 20cc syringe was connected to the needle sheath Under constant aspiration needle sheath was retrieved slowly until urine and contrast was aspirated verifying entrance into the system A hydrophilic guidewire was then introduced to the system and directed down the ureter The same process was repeated several times (usu ally 5 6 punctures per kidney) until all trainees had mas tered the technique A track dilation was then performed over each guidewire using a two step (16Fr and 30Fr) Amplatz dilation protocol and a 30Fr percutaneous access sheath was developed over the last 30Fr dilator Each trainee performed at least one track dilation until all attending physicians felt comfortable with the technique Hands on Live surgery training: On the next day, all attending physicians participated on the hands on live surgery course Several cases (mean 7, range 5 10) sched uled to be operated on the regular program of the Department of Urology of the University Hospital of Patras in Greece underwent PCNL by a leading highly experienced surgeon (E L ) All patients had provided an informed consent Under close supervision trainees performed the percutaneous punctures and track dilations of all operat ed cases Each trainee had the chance to assist in 2 3 cases per course
Surgical technique
Our technique has been previously described in details (2, 3) After a retrograde insertion of a ureteral catheter the patient was placed in prone position Puncture target selection and puncture was performed under fluoroscop ic guidance with the C arm at 30 degrees perpendicular to the long axis of the patient According to the demon strated technique in the course, the whole pelvicalyceal system including tip of the calyces, infundibulum and joint of calyces to the pelvis could be safely targeted and dilated according to the given stone scenario Needle was advanced parallel to C arm view in a bull’s eye fashion and its depth of penetration was assessed by rotating C arm at zero degrees Ones entrance into the system was achieved a hydrophilic guidewire was inserted and direct ed down the ureter Special focus on the importance of advancing the wire down the ureter was made Needle was retrieved and an 8Fr, 20 cm polyethylene dilator was i n s e r t e d o v e r t h e w i r e r e a c h i n g t h e u r e t e r T h e hydrophilic guidewire was removed and a super stiff guidewire was introduced inside 8Fr dilator until its end coil into the bladder The short dilator was removed and exchanged over the wire with a 84 cm long polytetrafluo roethylene (PTFE) 8Fr catheter above which a two step Amplatz dilation took place by dilating track sequentially to 16Fr and 30Fr accordingly A 30Fr PTFE sheath was deployed over the last dilator and its proper placement inside the system was verified fluoroscopically The last, 3 0 F r d i l a t o r , w a s r e m o v e d l e a v i n g t h e s t i f f s a f e t y guidewire in place passing through the percutaneous sheath A 26Fr rigid nephroscope was introduced and lithotripsy was performed using an ultrasonic lithotriptor Large stone fragments up to 1cm long were grasped and r e m o v e d i n o n e p i e c e u s i n g g r a s p e r s F l e x i b l e nephroscopy was employed if necessary to reach distant
Wet lab and live surgery training in PCNL
calyces from the initial access and verify stone free status
After the procedure an 18 22Fr Malecot tail stent or a 16Fr nephrostomy was placed in the nephrostomy track
Statistical analysis: Statistical significance of differences between various proportions was tested using the indi cated "N 1" Chi squared test (4, 5)
RESULTS
Effect of the course on the ability of urologist to establish their own access Prior to the course 12 5% (n = 8) of attending physicians were using a radiologist to establish the access of their cases while none employed radiologist assistance after the course (p < 0 01)
Effect of the course on track dilation technique: Prior to the course, 41 9% of surgeons used Alken dilators, 24 2% balloon dilation, 30 6% Amplatz dilation and 3 2% other dilation options (eg mini PCNL instrumentation) After the course, the majority of surgeons are using the Amplatz dilators (54 1%) followed by Alken (26 2%), balloon dilation (16 4%) and others (3 3%)
Effect of course on track establishment time and overall operation time: A significant change in the pre and post course track establishment times and overall operation times was evident In the demonstrated technique, mean access establishment time (from skin puncture to initia tion of lithotripsy) last regularly less than 10 minutes
Prior to the course this was the case for only 15 9% of surgeons while it increased to 47 5% after the course (p < 0 001) In addition, the rate of surgeons requiring more than 20 min to obtain access dropped from 28 6% prior to the course to zero after the course (p<0 001) (Figure 1A) Similarly, mean overall operative time (from skin puncture to nephrostomy tube placement) in our depart ment is regularly less than an hour (2) Prior to the course this was the case for only 12 7% of attending surgeons while rate increased to 36 5% after the course (p < 0 05) and the rate of surgeons reporting more than 1 5 hours for a regular case dropped from 38 1% to 4 8% after the course (p < 0 001) (Figure 1B)
According to the literature on the learning curve of PCNL, operative times reach a plateau after 40 60 cases (6 8) Given that ongoing growing of surgical experience after the course might also contribute to the noted reduc tion in puncture and operational times to attending sur geons, we separately analyzed time reduction in surgeons reporting good experience (defined as > 50 cases) prior to the course (n = 26) Reduction of puncture and operating times in this subgroup of already proficient surgeons was even more prominent than the whole cohort Prior to the course only 30 7% of them could accomplish puncture and dilation in less than 10 min while after the course this rate raised to 65 4% (p < 0 05) Similarly, prior to the course 23% required < 1 hour for a regular PCNL case while this rate raised to 50% after the course and 19 2% reported mean operation lasting more than 1 5 hours prior to the course while none reported such times after our training (p < 0 05 and p < 0 01 accordingly)
Adaptation of tips and tricks: Indirect indications of the educational value of this event can be extracted by the adaptation of several technical aspects that were stressed during our training Our department is one of the few
A301 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
centers worldwide practicing central (non calyceal) punctures in almost all PCNL cases The safety of the approach has been previously documented (2, 3) The adaptation of this policy by the attending physicians after the course was notable Prior to the course only 17 5% of attending surgeons were feel ing free to exercise non calyceal punc tures and 52 4% were performing sole ly calyceal punctures according to the e s t a b l i s h e d g o l d s t a n d a r d p u n c t u r e technique
After the course, 75 8% of attending surgeons are practicing non calyceal punctures either rarely (33 9%) or reg ularly (41 9%) (Figure 2) Another indirect sign of the education al value of our course was that in the demonstrated technique a guidewire should pass down the ureter in almost every case as a safety measure and ori entation tool inside the system Prior to the course 50% of attending physicians had a guidewire down the ureter regu larly (defined as > 75% of their cases) w h i c h i n c r e a s e d t o 7 3 % a f t e r t h e course (p < 0 01) (Figure 3)
Overall impressions on the course: 41 3% of attending surgeons consid ered that the course had a major impact to their daily surgical practice and 55 6% that they gained some tips and tricks to modify their existed tech nique Only 3 2% (n = 2) reported no impact to their practice Examining what parameters did course change in the established surgical practice of each s u r g e o n , 7 9 4 % r e s p o n d e d t h a t i t increased the safety of their procedure, 73% that it reduced operating times, 39 7% that increased their stone free rates, 23 8% that reduced their compli cations and 23 8% that induced to change their instrumentation respect to that they were using in the past (Figure 4) Interestingly, the impact of the course was not only significant for novice or intermediate skilled surgeons but was similar for experienced sur geons with 46 1% of the 26 experi enced surgeons considering that the course had a major impact in their practice

DISCUSSION
Despite the wide applicability of PCNL worldwide, there is a notable lack of data on the evaluation of percutaneous surgery training (9) The vast majority of relevant literature focuses on docu
 Archivio Italiano di Urologia e Andrologia 2022;
Archivio Italiano di Urologia e Andrologia 2022;
94, 3
I Kyriazis, P Kallidonis, E Kyrkopoulou, T Spinos, E Liatsikos
302
Figure 1. Gross estimation of mean access (A) and overall operation times (B) before and after the course h = hours; * = p < 0 001 Figure 2 Puncture site selection preferences before and after the course. Please notice that a subgroup of surgeons in calyceal plus non calyceal puncture group feel free to puncture in every aspect of the kidney based on the given case * = p < 0 01
Figure 3
Percent of cases that a safety guidewire is passed down the ureter before and after the course. * = p < 0.01.
Wet lab and live surgery training in PCNL
in the clinical practice of attending physicians remain completely undocu mented until now This is the first study reporting the effect of a short intensive hands on PCNL course on attending surgeons with 96 8% of par ticipants considering to have a direct impact in their practice

Figure 4
Overall impression (A) and particular effects of the course to clinical practice (B) of participating surgeons.

Basic limitations of the study include the self reporting and retrospective nature of data acquisition and the lack o f s u r r o g a t e m a r k e r s o f o u t c o m e improvement (eg specific operation and fluoroscopy times, blood loss, hos pitalization, stone free status and com p l i c a t i o n s f o r e a c h o f t h e i r c a s e s ) M o r e o v e r , a c c u m u l a t e d e x p e r i e n c e after the course in addition to other e d u c a t i o n a l a c t i v i t i e s t h a t t r a i n e e s potentially followed after this event might have also contributed to their improved outcomes and as a result the examined PCNL course itself cannot be solely responsible for the documented practice changes Another limitation of this current study was, that not all par ticipants responded to our mail It is t h u s p o s s i b l e , t h a t n o n r e s p o n d e r s could not be interested to reply because they were less satisfied of the course Finally, this survey has inherited selec tion bias Some, if not all of participat ing physicians opted to follow a PCNL course aiming to address limitations faced in their previous practice and as a result they might have been prone and ready to change their technique Still, the large number of responders, the uniform nature of responses document ing a positive impact in various aspects of their surgery and improvements in their operational times and the sub group analysis demonstrating similar benefits even for those surgeons that h a d t h e o r e t i c a l l y o v e r p a s s e d P C N L learning curve prior to the course rein force the conclusions of this study
menting the learning curve of individual surgeons, the validation of different PCNL simulators and the descrip tion of particular modular training programs (6 12)
Aslam et al reported global tendencies in endourology training, comparing a significant number of different national systems
They concluded that huge heterogeneity exists in quality of urological training between different countries and continents, underlining the importance of introducing standardization in training worldwide (13)
Procedure specific courses is a very common tool of sur gical training and hands on PCNL courses are widely available in the setting of congresses or expert center ini tiatives Still their effectiveness in inducing real changes
CONCLUSIONS
Literature on the educational value of hands on PCNL training courses is lacking In the proper setting, a 2 day intensive hands on PCNL training course can have a sig nificant impact to attending physicians and participation to such events even for experienced surgeons should be encouraged
REFERENCES
1 Kyriazis I, Panagopoulos V, Kallidonis P, et al Complications in percutaneous nephrolithotomy World J Urol 2015; 33:1069 77
2 Kyriazis I, Kallidonis P, Vasilas M, et al Challenging the wisdom
A303 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
I Kyriazis, P Kallidonis, E Kyrkopoulou, T Spinos, E Liatsikos
of puncture at the calyceal fornix in percutaneous nephrolithotripsy: feasibility and safety study with 137 patients operated via a non calyceal percutaneous track World J Urol 2017; 35:795 801
3 Kallidonis P, Kyriazis I, Kotsiris D, et al Papillary vs nonpapil lary puncture in percutaneous nephrolithotomy: a prospective ran domized trial J Endourol 2017; 31(S1):S4 S9
4 Campbell I Chi squared and Fisher Irwin tests of two by two tables with small sample recommendations Stat Med 2007; 26:3661 75
5 Richardson JT The analysis of 2 × 2 contingency tables yet again Stat Med 2011; 30:890
6 Ziawee SAM, Sichani MM, Kashi AH, Samzadeh M Evaluation of the learning curve for percutaneous nephrolithotomy Urol J 2010; 7:226 231
7 Tanriverdi O, Boylu U, Kendirci M, et al The learning curve in the training of percutaneous nephrolithotomy Eur Urol 2007; 52:206 212
8 Allen D, O’Brien T, Tiptaft R Glass J Defining the learning curve for percutaneous nephrolithotomy J Endourol 2005; 19:279 282
9 de la Rosette JJ, Laguna MP, Rassweiler JJ, Conort P Training in percutaneous nephrolithotomy a critical review Eur Urol 2008; 54:994 1001
10 Schilling D, Gakis G, Walcher U, et al The learning curve in minimally invasive percutaneous nephrolitholapaxy: a 1 year retro spective evaluation of a novice and an expert World J Urol 2011; 29:749 753
11 Stern J, Zeltser IS, Pearle MS Percutaneous renal access simula tors J Endourol 2007; 21:270 3
12 Kallidonis P, Kyriazis I, Vasilas M, et al Modular training for percutaneous nephrolithotripsy: The safe way to go Arab J Urol 2015; 13:270 6
13 Aslam AU, Philipraj J, Jaffrey S, Buchholz N A global snapshot of endourology residency training Arch Ital Urol Androl 2020; 92:219 229
Correspondence
Iason Kyriazis, MD, MSc, PhD, FEBU (Corresponding Author) jkyriazis@gmail com
Theodoros Spinos, MD thspinos@otenet gr
Panagiotis Kallidonis, MD, MSc, PhD, FEBU pkallidonis@yahoo com Evangelos Liatsikos, MD, PhD liatsikos@yahoo com
Department of Urology, University of Patras, Greece Rion, Patras 26504
Eleni Kyrkopoulou kyrkopel@aueb gr Department of Economics, Athens University of Economics and Business, Greece
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
304
Management of encrusted ureteral stents: Two center experience
Mohanarangam Thangavelu
, Mohamed Yehia Abdallah
, Olubenga John Isola
Department of Urology, Ysbyty Gwynedd, Bangor, LL57 2PW, United Kingdom;
Department of Urology, Wrexham Maelor Hospital, Wrexham LL13 7TD, United Kingdom;
Northern Ontario School of Medicine, TBRHSC, 980 Oliver Road, Thunder Bay, Ontario, Canada
, Ahmed Kotb
Summary
Introduction: We present our experience of the endourological management of encrust ed ureteral stents (EUS) and a literature review on forgotten encrusted ureteral stents
Methods: A total of 13 encrusted ureteral stents from 12 patients were removed in two hospitals The medical records were retrospectively analyzed for stent indication, indwelling time, clinical presentation, investigations, type and the number of surgical procedures, operative time, complications, duration of hospital stay, and the follow up
Results: Five ureteral stents (US) inserted before ESWL (extracorporeal shockwave lithotripsy) for renal stones, seven US for ureteric stones with ureteric colic, and one ureteral stent for post ureteroscopy procedure The mean indwelling time was 15 07 ± 7 34 months with a range from 6 to 24 months
The mean Kidney,Ureter and Bladder (KUB) score of encrusta tion grading was 11 84 ± 2 07 with a range from 9 to 15 The encrusted stents were removed by a combination of cystolithotripsy, semi rigid ureteroscopy (URS), retrograde intrarenal surgery (RIRS), percutaneous nephrolithotomy (PCNL), and ESWL The average total number of procedures to remove one EUS was 3 ± 1 08 with a range of 2 to 5 proce dures Six encrusted stents were removed in one, five stents required two, one stent required three and one stent required four hospital admissions The median operative time was 210 minutes with a range of 60 to 660 minutes per EUS removal and the mean hospital stay was 2 69 ± 1 43 days with a range of 1 to 6 days All patients had successful removal of encrusted stent and complete stone clearance with no major complica tions In the follow up, one patient had recurrent ureteric stone, one patient on regular stent exchange due to poor renal function and one patient developed significant ureteric stricture referred for reconstruction Conclusions: Removal of forgotten encrusted impacted ureteral stents is challenging and requires a multimodal surgical approach It adds significant costs to the health care system and in addition it affects patient safety and quality of life
Patient education, avoiding unnecessary ureteral stent place ment and a computerized stent monitoring system reduces the incidence of forgotten ureteral stents and their complications
KEY WORDS: Encrusted ureteral stent; Bioflim; KUB score; Encrustation risk factor; Computerized stent registry
Submitted 9 June 2022; Accepted 23 June 2022
INTRODUCTION
Ureteral stents are commonly used implants in urology practice mainly to relieve the ureteral obstruction due to stones, fibrosis, malignancy, and extrinsic compression It is also used in ureteral reconstructive surgery and iatro genic ureteral injuries to promote ureteral healing (1)
The ureteral stents are intended for temporary use and should be removed or replaced within a specific time frame; otherwise prolonged stent presence beyond the specific time known as forgotten stents can lead to com plications like stent encrustation, fragmentation, obstruc tion, urosepsis, renal failure, and mortality (2)
The incidence of forgotten ureteral stents is approximate ly 12% (2) and in the UK, a study reported that 13 6% of postoperative urology negligence claims are due to forgot ten ureteral stents (3) Divakaruni et al (2) quote that men are 2 8 times more likely to have forgotten stents than females and patients without health insurance are 6 times more likely to have forgotten stents Alnadhari et al (4) in their study of the management of 40 forgotten encrusted ureteral stents found that in 47 5% of forgotten EUS were due to poor patient compliance and either patient ignored or forgot the physician’s advice about the timely removal of the ureteral stents; 30% of the cases failed to attend hos pital for stent removal due to financial reasons, 12 5% of cases were due to delay in the endourological procedure following ESWL, and 10% of cases were due to poor com munication between the doctor and the patient The cost of removal of forgotten encrusted stents is 6 9 times high er than the cost of timely stent removal because of addi tional costs involved in multiple interventions and it affects patient safety and quality of life (5)
METHODS
A retrospective analysis of 13 encrusted impacted ureteral stents in 12 patients treated in two hospitals between 2014 to 2021 was done The inclusion criterion was failed ureteral stent removal by flexible cystoscopy under local anesthetic and clear evidence of stent encrustations on X ray KUB (Kidney, Ureter, and Bladder) or Computed Tomogram Kidney Ureter and Bladder (CT KUB) The pri mary outcome was successful removal of the encrusted impacted stent and the secondary outcome was the num ber and type of surgical procedures, operative time, hospi
Italiano di Urologia e Andrologia 2022;
305Archivio
94, 3 ORIGINAL PAPER No conflict of interest declared
1
2
2
3 1
2
3
DOI: 10 4081/aiua 2022 3 305
M Thangavelu, M Yehia Abdallah, O John Isola, A Kotb
tal stay, perioperative complications, and stone and stent free rates All patients had preoperative renal function tests, urine cultures, X ray KUB, CT KUB and in selective cases a DMSA (Dimercaptosuccinic acid) renal radionuclide scan was done for patients with poor renal parenchyma
The degree of encrustation was graded by the KUB score system based on imaging Treatment was planned based on the degree and location of stent encrustation (KUB Score), renal function, presence of urinary tract infection, and other comorbid conditions Appropriate antibiotics were administered prior to surgical intervention for posi tive urine cultures
Initially, ESWL was given a maximum of 3 sittings for proximal coil encrustations < 15 mm All invasive endourological procedures started with clearing the blad der end encrustation by mechanical cysotolithopaxy by stone punch and some cases with LASER energy through the cystoscope For the ureteral body encrustation, a 7 5 Fr semirigid ureteroscope was passed beside the encrust ed stent from the ureteric orifice to work the way up towards the pelvicalyceal system using Holmium Laser energy for fragmentation After clearing the ureteral body encrustation, a ureteral access sheath was placed and the proximal coil encrustation was cleared by a flexible ureteroscope (Storz Flex X2) and Holmium Laser For denser and larger calcification of the proximal end, PCNL was done as a second sitting Stent fragmentation occurred during the retrograde ureteroscopy and the pieces were left in the pyelocaliceal system which were later retrieved during PCNL or RIRS For non capacious ureter, addi t i o n a l ( T a n d e m ) s t e n t s w e r e i n s e r t e d f o l l o w e d b y ureteroscopy in 2 weeks No undue force was used to pull the encrusted stent during any of the above procedures All patients had postprocedural ureteral stent insertion which was removed in 2 weeks In all our patients we dealt with the bladder and ureteral body encrustation first before dealing with proximal end encrustation with RIRS or PCNL; only in a few patients ESWL was given first for mild to moderate proximal end encrustation
The postoperative complications were graded according to the modified Clavien Dindo classification All patients had postoperative X ray KUB before discharge and follow up non contrast CT KUB and renal function in 4 months
Table 2
Operative and postoperative details.
Variables No of pts. Mean Range
Encrustation grading KUB score 11 84 ± 2 07 9 to 15
Total number of procedures per encrusted stent remova 3 ± 1 08 2 to 5
Total number of hospital Admissions per encrusted stent removal 1 76 ± 0 92 1 to 4
Total number of hospital stay per encrusted stent removal days 2 69 ± 1 43 1 to 6
Total operative time per encrusted stent 249 61 ± 169 19 removal minutes
Post operative complications
Clavien Didno grade 1 6
Clavien Didno grade 2 3
12 months Fo low up Patients
Stone/stent free 8
Recurrent stone 1
Ureteric stricture 1
Lost follow up 2
Combination of procedures per stent removal
Cystolithotripsy/URS/RIRS/ESWL 1 (7 6%)
Cystolithotripsy/URS/ESWL 2 (15 3%)
Cystlithotripsy/URS/PCNL 2 (15 3%)
Cystolithotripsy/URS/RIRS 8 (61 5%)
RESULTS
Demographic details
Variables
Range
13/12
Males/females 11/1
Age years
Side right/left 7/6
Stent indwelling time months
Stent indication
Pre ESWL for renal stones 5
Ureteric stones colic 7
Post ureteroscopy 1
Reasons for delayed stent removal
Forgotten 9 Delay in the secondary procedure 4
EGFR (ml/min)
Urine culture (positive/no growth) patients 5/7
15 ± 13 22 29 to 84
07 ± 7 34 6 to 24
Median 210 min 60 to 660
07 ± 23 28 28 to 90
In our study 13, encrusted stents were removed from 12 patients with one patient with bilateral stents (Table 1)
The average encrustation grading score at the proximal end (K) was 3 15 ± 1 62, at the stent body (U) was 4 3 ± 0 85 and at the distal end (B) was 4 38 ± 0 76 The aver age overall Arenas KUB score was 11 84 ± 2 07 (Table 2)
In our study 3 patients with EUS had ESWL for the prox imal end with poor results, and the majority of the stents were removed by cystolithoripsy, rigid URS, and RIRS, and two stents had PCNL for the proximal end (Figures 1 4)
All the encrusted stents in our study were radio opaque and 5 patients had a course of antibiotics for symptomatic UTIs with positive urine cultures prior to the procedure
The mean total number of procedures carried out was 3 ± 1 08 with a range of 2 to 5 per encrusted stent removal
All patients after the removal of the encrusted stent had post operative ureteral stent which was removed with a flexible cystoscope within 14 days
The median operative time was 210 minutes with a range of 60 to 660 minutes and the mean hospital stay was 2 69 ± 1 43 days
No significant immediate postoperative complications were noted apart from mild haematuria in 6 and fever in 3 patients Three patients had insignificant residual stone fragments (< 3 mm) treated conservatively At 12 months of review, 8 patients were stone free, 2 patients lost fol low up, 1 patient required repeated stenting of a renal unit due to pre existing poor renal function and 1 patient developed significant ureteric stricture referred for recon struction surgery
DISCUSSION
Risk factors and mechanism of encrustation Stent encrustation occurs when minerals from the urine
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
306
Table 1
Total No Mean
Encrusted stents/patients
61
15
61
deposit on the outer and inner surface of the stent in both infected and non infected urine environments Various factors like stent material, bacterial colonization, and patient specific factors influence stent encrustation but the main risk factor is the duration of stent indwelling time El Faquith et al (6) in their study in 1991, reported stent encrustation rates of 9 2 % in 6 weeks, 47 5% between 6 to 12 weeks, and 76 3 % after 12 weeks of indwelling time Kawahara et al (7) reported similar encrustation rates of 27%, 57%, and 76% at equivalent time intervals; 30% of the stents removed before 12 weeks showed luminal encrustation but only 4% of the patients had clinical symptoms of stent obstruction (6) Bacterial colonization and bacterial biofilm play a critical role in stent encrustation but how it exactly triggers the encrustation process is poorly understood Tunney et al reported (8) that 90% of the removed ureteral stents had bacterial colonization and 55% had adherent biofilm Shabeena et al (9) reported 90% colonization rates in 120 d

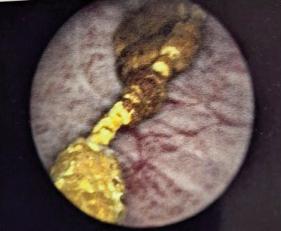

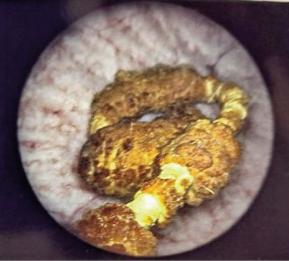
307
Archivio
Italiano di Urologia e Andrologia 2022; 94, 3
Management of encrusted ureteral stents
a y s o f u r e t e r a l s t e n t i n s e r t i o n E s c h e r i c h i a c o l i , Streptococcus spp, and Pseudomonas spp are commonly iso lated but no specific pathogens have been attributed to
Figure
1
Xray KUB Right whole ureteral stent encrustation
Figures
3, 4
Endoscopic picture of lower end ureteral stent encrustation
3 Figure 2
X ray KUB Fine fragmentation and removal of the encrusted stent with ureteric catheter in place
4.
M Thangavelu, M Yehia Abdallah, O John Isola, A Kotb
triggering encrustation Newer studies on the urinary microbiome implicate that commensurate bacteria in urine rather than the pathogenic strains facilitate urolithi asis and stent encrustation (10)
Conditions like recurrent UTI, chronic kidney disease, and diabetes mellitus increase the urinary bacterial load or the presence of urolithiasis risk factors like specific diets, history of stone disease, malabsorption disorders, and cancer chemotherapy facilitate stent encrustation (11) Stent encrustation risk is high in pregnancy due to absorptive hypercalciuria and hyperuricosuria which require frequent stent changes in 4 to 6 weeks to avoid encrustation resulting in blocked stents Urinary infection with urease producing bacteria like Pseudomonas, Proteus, and Klebsiella spp hydrolyze urea into ammonia and car bon dioxide making urine alkaline and resulting in pre cipitation of ammonium, magnesium phosphate (stru vite) on the stent surface
The encrustation rates correlated with stent diameter rather than stent length or patency and a study (7) report ed 6 F stent developed more encrustation than the 7 F stent The mechanism of stent encrustation is complex and all stents after insertion are immediately coated with a conditioning film made of patient specific glycoproteins and materials from the urinary composition Further, the conditioning film may remain stable or could develop a bacterial biofilm that precipitates minerals on the stent surface causing stent encrustation; this provides a nidus for bacterial infection leading to urosepsis, obstruction, or renal failure (1, 12)
Presentation and complications
The clinical presentation of the forgotten encrusted stent is variable Abdelaziz et al (13) reported that predominant symptoms of forgotten stents were storage bladder symp toms, haematuria; other symptoms such as gross haema turia, flank, urethral and suprapubic pain were minimal as these patients tolerated the stent related symptoms for more than 6 months The asymptomatic patients are more prone to neglect or forget the stent and therefore develop serious complications that are time related, such as encrustation, fragmentation, and obstruction In our study 80% of patients with encrusted stents presented with intermittent haematuria, recurrent urinary tract infection (UTIs), storage urinary symptoms, flank pain, and no symptoms in 20%
Challenges in the management of encrusted stents Plain X ray underestimates the stone burden and non contrast computed tomography (CT) is essential for plan ning the treatment The extent and location of encrusta tion, associated stone burden, renal function, and pres e n c e o f u r i n a r y i n f e c t i o n d e t e r m i n e t h e t r e a t m e n t
approach Active urinary infection should be treated appropriately and urosepsis due to obstructed infected kidney may require an initial percutaneous nephrostomy to stabilize the patient before any intervention Nephrectomy may be considered if there is poor renal parenchyma with a split function < 20%
Arenas et al (14) developed a KUB grading system for encrusted ureteral stents This system grades 1 to 5 according to the size of the calcification in or around the stent in the region of the kidney (K), ureter (U), bladder
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
(B), and the total score represented as the KUB score They noted that the K score ≥ 3 was associated with mul tiple surgeries, multimodal surgery, operative time > 180 min, and lower stone free rate, while the U score ≥ 3 was only associated with longer operative time and the B score ≥ 3 was associated with a lower stone free rate Overall KUB score ≥ 9 requires multiple surgeries, longer opera tive time and lower stone free rates Our study results agree with the finding that multiple endourological pro cedures are required for total KUB scores ≥ 9 The proximal stone burden is the main factor that deter mines the requirement of multiple surgeries and associated complications In the presence of normal renal function, ESWL is indicated for mild to moderate encrustation of renal end and proximal ureteral body encrustation The lower encrusted segment in the bladder and in the ureter al part was always released first before dealing with surgi cal removal of the proximal end (15) apart from giving ESWL for the proximal end of the encrusted stent The bladder end and ureteral part of the encrusted stent were removed in pieces after releasing encrustation and cutting the stent with a Holmium LASER during URS, to create space for ureteral access sheath placement and RIRS to deal with the proximal coil encrustation PCNL is reserved for complex proximal end encrustation and for cases of RIRS or ESWL failures Open pyelolithotomy, cystolitotomy, or laparoscopic surgeries are sometimes required following the failure of endourological management
The treatment described is used as a guideline and should be tailored according to the individual patient, clinical assessment, surgeon's experience, and available resources The approach should be in a stepwise multimodal fashion to remove the encrusted stent and achieve stone and stent free status with the preservation of renal function (16) Although majority of the encrusted ureteral stent need multimodal management, Lio et al (17) in their case series described a minimally invasive technique under fluo roscopy of removing and replacing obstructed encrusted ureteral stents in female patients under local anaesthetic, however the obstructed ureteral stents removed with this technique had obstruction mainly caused by intraluminal incrustation
Monga et al (18) reported a series of 22 forgotten ureteral stents left in situ for over 6 months and found that 68% were calcified, 18% fragmented, and 14% fragmented and calcified In their series, which included 22 forgotten and 9 migrated stents, procedures to render stent free were ureteroscopy 52%, PCNL 26%, ESWL 32%, cystolithotrip sy 19%, open cystolithotomy 3%, simple nephrectomy 3% and multiple procedures were necessary in 19% of the patients
In our study of 13 encrusted ureteral stents, 50% had sig nificant proximal encrustation, and all of them had blad der end and ureteral body encrustation; 61 5% of EUS were removed by cystolithotripsy, URS and RIRS, 15 3% by cystolithotripsy, URS and ESWL, 15 3% by cys tolithotripsy, URS and PCNL, 7 6% by cystolithotripsy, URS, RIRS, and ESWL None of the encrusted stents were removed by open surgery in our study
From our results, the average total number of procedures carried out was 3 ± 1 08 with a range of 2 to 5 per EUS removal and the average time of hospital stays was 2 69 ±
308
1 43 days with a range of 1 to 6 days per EUS removal
Alnadhari et al (4) in their study reported a mean of 2 25 urologic procedures needed per EUS removal with a range of 1 to10 procedures performed in a single or multiple anes thetic sessions
Encrustation prevention: stent materials and technology: Stent biomaterials and coating substances could potential ly alter bacterial adhesion thereby reducing bacterial colo nization, bacterial biofilm formation, stent encrustation, and urosepsis Silicone is a highly biocompatible material that resists encrustation and biofilm formation but is not commonly used because of low tensile strength, higher friction co efficiency, and its softness prone to kinking and compression (8, 19) The majority of currently used ureter al stents are made of polyurethane based material with co polymers because of their favorable mechanical properties and low manufacturing cost (20) In vitro study by Tunney et al (8) compared encrustation rates of five different mate rials with an artificial solution similar to the urinary com position for 14 weeks All developed some encrustation but silicone developed the least encrustation by 10 weeks fol lowed by polyurethane, Silitek, Percuflex, and hydrogel coated polyurethane
Stents coated with various materials could alter the stent surface to reduce bacterial adhesion and encrustation
Hydrogel coated polyurethane stent swells on contact with water and retains water to alter the stent surface to reduce bacterial adhesion and encrustation along with reduction of friction coefficiency for easier stent insertion (21) Drug coated stents with silver nitrate, and ofloxacin have not proved to reduce biofilm or encrustation in clin ical trials, moreover antibiotic infused stents have the potential risk of developing antibiotic resistance (22)
Coating with heparin, a naturally occurring glycosamino glycan anticoagulant exhibits antiadhesive properties which could reduce bacterial adhesion and prevent bac terial biofilm formation and encrustation (23) but results from clinical trials are contradictory and heparin coated stents are not regularly used in the clinical practice
Silicone coated polyurethane stents, newer stent coating materials like bacteriolytic enzymes, peptides, oxalate degrading enzymes, and essential oils have been explored (24), and all aimed to alter bacterial adhesion, biofilm for mation, and reduce stent encrustation and urosepsis
Metallic ureteral stents made of alloy are used in malig nant ureteric obstruction has provided superior patency rates at 12 months compared with polyurethane stents requiring less frequent stent changes but still, stent encrustations occurred macroscopically in 22% and microscopically in all after an indwelling time between 8 to 14 months (25)
Biodegradable ureteral stents by constantly altering the stent surface could prevent bacterial adhesion and encrus tation and it also eliminates the need for stent removal
Currently available biodegradable materials made of natu ral or synthetic polymers have excellent biocompatibility with faster degradation which also reduces tissue inflam mation useful in relieving the benign urinary obstruction
Prospective multicenter human trials are required before routine use in clinical practice (26) Similar to the preven tion of urolithiasis, increased fluid intake and citrate sup plements decreased the incidence of stent encrustation
Management of encrusted ureteral stents
Computerized stent registry
Even in current times, ureteral stent logbooks and track ing cards are maintained for monitoring however, human error and negligence are fundamental causes for the fail ure of these manual systems Monga (27) reported that 10% of patients with forgotten stents fail to show up for scheduled stent retrieval despite being educated by physi cians Similarly, 8 66% of patients were aware that they had ureteral stents but did not attend for stent removal (28) Therefore patient education and awareness alone are not sufficient to prevent forgotten stents and related complications
The treating doctor and the hospital are responsible for both the monitoring and removal of ureteral stents and multiple level safety precautions should be implemented for the timely removal or replacement of the stent Computerized applications and electronic reminders appear to be reliable and efficient, and the utilization of automated algorithms has reduced the incidence of for gotten stents (28)
Lin et al (28) retrospectively analyzed the monitoring of 12 440 ureteral stent placements in 10 105 patients reg istered on the Auto registration monitoring system (ARMS) an automated program closely tied with the hospital billing system in Taipei Veterans General Hospital over a period of 8 years They reported 85 07% of patients who had their stents removed before the deadline were auto matically detected In the rest 14 93% of patients whose stents were not registered as removed it was found that 1 2% of patients had stents removed in other hospitals, 4 85% had died, 8 66% patients were aware of ureteral stents but did not come for stent removal and 0 21% of patients were not aware that they have ureteral stent which was placed in the operating room in non urologi cal patients They reported that there were no new for gotten ureteral stents after the introduction of ARMS Development of a universally acceptable automated stent registry interface which could integrate with the existing hospital patient management system but also linked to the regional database would be ideal to monitor the ureteral stents after their insertion till their removal or replacement after the specific time interval
The Healthcare Safety Investigation Branch (HSIB) from the UK published a report on the unplanned delayed removal of ureteric stents in October 2020 (29) The report showed the seriousness of the problem and made four safety recommendations including the development of a stone pathway, the use of a stent registry database, reviewing the B r i t i s h A s s o c i a t i o n o f U r o l o g y s u r g e o n s (BAUS) stent information leaflet, and clear communica tion with the general practitioner following patient dis charge with stents
CONCLUSIONS
Avoidance of unnecessary stent insertion is the key to the prevention of stent related complications Patient educa tion, judicious follow up arrangements, computerized stent registry warning system could help in the timely removal of the stents, avoiding prolonged indwelling time which is the main risk factor for encrustation
Removal of encrusted impacted stents requires a multi
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
309
M Thangavelu, M Yehia Abdallah, O John Isola, A Kotb
modal approach adding significant costs to the health care system and more importantly affecting patient safety and quality of life Ureteral stent technology is continu ously evolving and current research should focus on developing biocompatible materials, newer coating sub stances, surface engineering, and stent design to reduce stent related symptoms and complications
ACKNOWLEDGEMENT
We thank Dr Arundoss Gangadharan, Consultant Paediatrician, who helped in organizing the references in this article
REFERENCES
1 Lange D, Bidnur S, Hoag N, Chew BH Ureteral stent associated complications where we are and where we are going Nat Rev Urol 2015; 12:17 25
2 Divakaruni N, Palmer CJ, Tek P, et al Forgotten ureteral stents: who's at risk? J Endourol 2013; 27:1051 4
3 Osman N, Collins G Urological litigation in the UK National Health Service (NHS): an analysis of 14 years of successful claims BJU international 2011; 108:162 5
4 Alnadhari I, Alwan M, Salah M, Ghilan A Treatment of retained encrusted ureteral Double J stent Arch Ital Urol Androl 2019; 90:265 269
5 Sancaktutar A, H HS, Bozkurt Y, Penbegül N, Atar M Treatment of forgotten ureteral stents: how much does it really cost? A cost effec tiveness study in 27 patients Urol Res 2012; 40:317 25
6 el Faqih SR, Shamsuddin AB, Chakrabarti A, et al Polyurethane internal ureteral stents in treatment of stone patients: morbidity related to indwelling times J Urol 1991; 146:1487 91
7 Kawahara T, Ito H, Terao H, et al Ureteral stent encrustation, incrustation, and coloring: morbidity related to indwelling times J Endourol 2012; 26:178 82
8 Tunney MM, Keane PF, Jones DS, Gorman SP Comparative assessment of ureteral stent biomaterial encrustation Biomaterials 1996; 17:1541 6
9 Shabeena KS, Bhargava R, Manzoor MAP, Mujeeburahiman M Characteristics of bacterial colonization after indwelling double J ureteral stents for different time duration Urol Ann 2018; 10:71 75
10 Zampini A, Nguyen A, Rose E, et al Defining dysbiosis in patients with urolithiasis Sci Rep 2019; 9:5425
11 Beysens M, Tailly TO Ureteral stents in urolithiasis Asian J Urol 2018; 5:274 286
12 Tomer N, Garden E, Small A, Palese M Ureteral stent encrus tation: epidemiology, pathophysiology, management and current technology J Urol 2021; 205:68 77
13 Abdelaziz AY WBF, Mosharafa AA, Abelrasoul MA, et al Forgotten ureteral stents: Risk factors, complications and manage ment African Journal of Urology 2018; 24:28 33
14 Arenas JL, Shen JK, Keheila M, et al Kidney, Ureter, and Bladder (KUB): A novel grading system for encrusted ureteral stents Urology 2016; 97:51 55
15 Lam J, Gupta M Tips and tricks for the management of retained ureteral stents J Endourol 2002; 16:733 41
16 Bultitude MF, Tiptaft RC, Glass JM, Dasgupta P Management of
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
encrusted ureteral stents impacted in upper tract Urology 2003; 62:622 6
17 De Rose AF, Di Grazia E, Magnano San Lio V, et al Complications of endourological procedures and their treatment Arch Ital Urol Androl 2020; 92:321 325
18 Monga M, Klein E, Castañeda Zúñiga W, Thomas R The for gotten indwelling ureteral stent: a urological dilemma J Urol 1995; 153:1817 9
19 Barghouthy Y, Wiseman O, Ventimiglia E, et al Silicone hydro coated ureteral stents encrustation and biofilm formation after 3 week dwell time: results of a prospective randomized multicenter clinical study World J Urol 2021; 39:3623 3629
20 Venkatesan N, Shroff S, Jayachandran K, Doble M Polymers as ureteral stents J Endourol 2010; 24:191 8
21 Ahmed E Hydrogel: Preparation, characterization, and applica tions: A review J Adv Res 2015; 6:105 21
22 Singha P, Locklin J, Handa H A review of the recent advances in antimicrobial coatings for urinary catheters Acta Biomater 2017; 50:20 40
23 Al Aown A, Kyriazis I, Kallidonis P, et al Ureteral stents: new ideas, new designs Ther Adv Urol 2010; 2:85 92
24 Glinel K, Thebault P, Humblot V, Pradier C, TJouenne Antibacterial surfaces developed from bio inspired approaches Acta Biomater 2012; 8:1670 84
25 Kallidonis P, Georgiopoulos I, Kyriazis I, et al The full metallic double pigtail ureteral stent: Review of the clinical outcome and cur rent status Indian J Urol 2015; 31:8 14
26 Janssen P, Tailly T New stent technologies Urol Clin North Am 2022; 49:185 196
27 Monga M The dwell time of indwelling ureteral stents the clock is ticking but when should we set the alarm? J Urol 2011; 185:387
28 Lin K, Chen P, Fan Y, Huang W Preventing forgotten double J ureteral stents in a high volume service medical center: An autoreg istration monitoring system J Chin Med Assoc 2020; 83:382 385
29 Branch HsI Unplanned delayed removal of ureteric stent Healthcare safety Investigation Branch https://www hsib org uk/inves tigations and reports/unplanned delayed removal of ureteric stents/
Correspondence
Mohanarangam Thangavelu, MBBS, FEBU, FRCS (Urology) (Corresponding Author) drtmohan@hotmail com Consultant Urology, Betsi Cadwaladr University Health Board Ysbyty Gwynedd, Bangor, LL57 2PW, United Kingdom
Mohamed Yehia Abdallah, MD, FRCS (Urology) Mohamed yehia@wales nhs uk Olubenga John Isola, MD gbenga isola@yahoo co uk Department of Urology, Wrexham Maelor Hospital, Wrexham, LL13 7TD, United Kingdom
Ahmed Kotb, MD drahmedfali@gmail com Northern Ontario School of Medicine, TBRHSC, 980 Oliver Road, Thunder Bay, Ontario, Canada P7B 6V4
310
: 10 4081/aiua
External validation of Resorlu-Unsal stone score in predicting outcomes after retrograde intrarenal surgery. Experience from a single institution
Antonio Tufano 1 , Marco Frisenda 1 , Antonio Rossi 2 , Pietro Viscuso 1 , Guglielmo Mantica 3 , Pierluigi Bove 4 , Rosario Leonardi 5 , Alessandro Calarco 2
1 Department of Maternal Infant and Urological Sciences, "Sapienza" Rome University, Policlinico Umberto I Hospital, Rome, Italy;
“Cristo Re” Hospital, Rome, Italy;
Policlinico San Martino, Genova, Italy;
San Carlo di Nancy Hospital, Roma, Italy;
Casa di Cura Musumeci Gecas, Gravina di Catania (CT), Italy
Summary
Objective: Pre operative assessment of renal stones is essential in selecting treatment options and achieving high success rates for retrograde intrarenal surgery (RIRS) Several nephrolithometric scoring systems have been developed using pre operative clinical data and stone characteristics Resorlu Unsal stone score (RUSS) is composed of four different parameters, and each of them adds 1 point to the final score One point is added in patients with stone size > 20 mm, lower calyceal stones and infundibulo pelvic angle < 45°, stone number > 1, and abnormal anatomy, respec tively RUSS categorizes patients into four distinct groups and aims to predict stone free rates (SFR) after RIRS We externally validated RUSS and evaluated its predictive accuracy
Materials and Methods: We performed a retrospective analysis of patients who underwent RIRS for renal stones between January 2020 and December 2021 Patient age, pre operative hydronephrosis, stone size, stone density as Hounsfield Unit (HU), operative time and RUSS were investigated as potential preoperative predictive factors for stone free status RUSS was applied to all patients, and the nomogram was externally vali dated Area under the curve (AUC) was used for clinical validity assessment
Results: The present study included a total of 79 patients Mean patient age was 55 1 ± 15 4 years with a mean stone size was 14 2 ± 4 4 mm Overall, 62/79 (78 4%) patients were stone free after the initial treatment After applying RUSS, 36 (45 6%), 29 (36 7%), 10 (12 6%), and 4 (5 1%) patients had a score of 0, 1, 2, and 3, respectively On multivariate logistic regression RUSS (OR = 0 220; 95%CI: 0 086 0 567; p = 0 002) was identified as the only predictor of postoperative stone free status
Conclusions: RUSS is a user friendly scoring system that may predict postoperative stone free rate after RIRS with great effi cacy and accuracy
KEY WORDS: Stone; Kidney; Endoscopic; RIRS; Stone free rate
Submitted 8 September 2022; Accepted 9 September 2022
INTRODUCTION
Urolithiasis is a common and worldwide increasing dis ease in developed countries (1) According to the European Association of Urology (EAU) guidelines, the treatment of kidney stones depends mainly on their size
and location In particular, stones larger than 20 mm should be managed with percutaneous nephrolithotomy (PCNL), while, below this threshold, the retrograde intrarenal surgery (RIRS) and extracorporeal shock wave lithotripsy (ESWL) are the treatments of choice (2 4) However, the continuous technological development and the use of increasingly powerful and safe instruments and techniques broadened the role of RIRS also for stones > 20 mm (5 7)
Stone free rate (SFR) remains one of the primary outcomes after endoscopic surgery for kidney stones Recently, differ ent scores to predict SFR have been formulated for patients undergoing RIRS; such as the R I R S score, the Seoul National University Renal Stone Complexity (S ReSC) and the Resorlu Unsal stone score (RUSS) (8 10) This latter score was conceived in 2012, and takes in consideration the stone size, its presence at the level of the lower calyces, the infundibulum pelvic angle (IPA), the number of stones and anatomical alterations The goal of our study is to external ly validate the applicability of RUSS in a single center cohort of patients undergoing RIRS for kidney stones
MATERIALS AND METHODS
We retrospectively reviewed medical data of 79 patients who under went RIRS between Januar y 2020 and December 2021 at single center institution
Two expert surgeons, highly experienced in RIRS (> 500 procedures) performed the operations in a standardized fashion
All procedures were made with patient in lithotomy posi tion under general anesthesia Preoperative single dose antibiotic prophylaxis was used for all patients A ureter al access sheath (UAS) (Flexor, Cook Medical, Bloomington, USA) was inserted under fluoroscopic control if the ureter was compliant, with its tip always above the ureteral pelvic junction Therefore, the correct irrigating fluid out flow was confirmed and a 7 5 Ch flexible ureteroscope was inserted (Flex X2s, Karl Storz, Tuttlingen, Germany)
Laser lithotripsy was carried out with a 20w Holmium YAG laser (EMS Laser Clast, Electro Medical Systems, Nyon, Switzerland), using a 200 micron fibre Laser setting was
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
311
ORIGINAL PAPER No conflict of interest declared
2
3
4
5
DOI
2022 3 311
A Tufano, M Frisenda, A Rossi, et al
5 12 Hz and 0 6 1 2 J, either long or short pulse width
Gravity irrigation was always used during lithotripsy and an additional intermittent gentle manual irrigation with a 60 ml syringe was added for a short time in case of reduced visibility Irrigating fluid outflow was checked continuously during the whole procedure Residual frag ments were removed using a 2 2 Fr 1 cm Nitinol basket (N Circle, Cook Medical, Bloomington, USA) At the end of the procedure, a final inspection of the upper urinary tract was performed with the aim to detect any residual fragments or ureteral injuries
Our inclusion criteria were: 1) patients > 18 years; 2) pre operative non contrast computed tomography (NCCT) doc umenting a kidney stone > 10 mm
Exclusion criteria were: 1) patients with concurrent ureteral stone or with bilateral renal stones; 2) with prior double J catheter; 3) with ureteral strictures; 4) patients without complete clinical records
Clinical data and stones characteristics were collected for each patient Stone burden was interpreted as the two dimensional area determined by multiplying the longest diameter by the perpendicular diameter of the stone In case of multiple stones, the stone burden was defined as the cumulative size Operation time was intended from the beginning of the cystoscopy to the end of the ureteral placement A score (between 0 and 4) according to RUSS was assigned to each patient This score system is based on four criteria, each having equal weight (1 point); stone size > 20 mm, lower pole stone location with IPA < 45°, num ber of stones in different calyces (> 1) and presence of abnormal renal anatomy (horseshoe kidney or pelvic kid ney) The IPA was measured as the inner angle between the ureteropelvic axis and central axis of the lower pole infundibulum as described by Elbahnasy et al (11)
The stone free status was described as the absence of any residual stone fragment ≥ 5 mm at 1 month after surgery follow up NCCT Complications were recorded according to Clavien Dindo classification
Statistical analysis was carried out using SPSS software version 27 (SPSS Inc, Chicago, USA) Continuous variables a re p re s e n t e d a s m e a n s a n d s t a n d a rd d e v i a t i o n s Categorical variables are described by their absolute num ber and percent frequency A multivariable logistic COX regression analysis was used to identify independent pre dictors of SFR The AUC, calculated by receiver operating characteristics curves (ROC) of RUSS was used to assess predictive accuracy of SFR All p values were two tailed, with statistical significance set at 0 05 and confidence intervals at 95 % level
RESULTS
The patients and stones characteristics are shown in Table 1 Overall, 79 patients were included Of those, 41 (51 9%) were males Mean patient age was 55 1 ± 15 4 years and mean stone size was 14 2 ± 4 4 mm with a mean stone den sity of 1014 4 ± 276 HU Left side was the most interested, n= 49 (69 1%) With regards to the intrarenal location, 23 (29 1%), 29 (36 7%) and 27 stones (34 2%) were located in the upper, middle and lower calyx, respectively A total of 3 patients had ectopic kidney and 1 presented with horseshoe kidney After applying RUSS, 36 (45 6%), 29 (36 7%), 10
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
Table 1.
Patients’ demographic and stone characteristics
Variable
Overall n = 79
Age at surgery (mean, SD) 55 1 (± 15 4)
Gender (n, %)
Male 45 (56 9%)
Female 34 (43 1%)
ASA score (n, %) 1 2 71 (89 9%) 3 4 8 (10 1%)
Hydronephrosis (n,%) 16 (20 3%)
Laterality (n, %)
Left 54 (68 4%)
Rigth 25 (31.6%)
Stone size, mm2 14 2 (4 4)
Stone density, HU 1014 4 (276)
Stones, mean (SD) 1 6 (± 0 9)
Stone location
Upper calyx 23 (29 1%),
Midd e calyx 29 (36 7%)
Lower calyx 27 (34 2%)
Urinary Anomaly (n, %)
Horseshoe kidney 1 (1 3%) Pelvic kidney 3 (3 8%)
Table 2
Perioperative and postoperative outcomes
Variable Overall n = 79
Operative T me, min (mean, SD) 75 3 (± 26 6)
LOS, days (mean, SD) 1 6 (0 9)
Overall complications (n, %) 7 (8 9%)
Clavien Grade (n, %)
I 6 (7 6%) II 1 (1 3%) III IV 1 (1 3%) V-
(12 6%), and 4 (5 1%) patients had a score of 0, 1, 2, and 3, respectively Perioperative and postoperative data are shown in Table 2 Overall, 62/79 (78 4%) patients were stone free after the initial treatment The mean operation time was 75 3 (± 26 6) minutes Mean hospital stay was 1 6 ± 0 9 days A total of 2 urosepsis occurred and were treated with appropriate antibiotic therapy with one of them requir ing intensive care unit admission; 5 postoperative fever and 1 migration of the double J catheter were also recorded
After adjusting logistic multivariate COX regression
Table 3.
Binary logistic Cox regression analysis for predictors for postoperative stone free status
Variable OR Lower Higher P value
Age 1 006 0 956 1 149 0 766
Hydronephrosis 0 724 0 194 2 705 0 331
Stone size, mm 0 955 0 859 1 152 0 448
Stone density, HU 0 992 0 890 1 047 0 806
Operative time 0 982 0 749 1 156 0 499 RUSS 0.220 0.086 0.567 0.002
312
analysis for age, preoperative hydronephrosis, stone size, stone density, RUSS and operative time, only RUSS (OR = 0 220; 95%CI: 0 086 0 567; p = 0 002) was identified as a statistically significant predictor of postoperative stone free status (Table 3) Finally, accuracy of RUSS reached an AUC of 0 76 (Figure 1)
DISCUSSION
According to EAU guidelines, PCNL is the standard of treatment for renal stones > 2 cm Whilst, treatment for renal stones < 2 cm should be performed with either RIRS o r E S W L H o w e v e r, t h e p ro g re s s i v e t e c h n o l o g i c a l improvements in flexible ureterorenoscopy and new per forming lasers have extended the surgical indications for kidney stones reaching a comparable success rate for stones > 2 cm in experienced hands and well selected patients (12, 13)
Notably, several predictive score systems have been recently incorporated in everyday clinical practice in order to predict outcomes following RIRS
Our aim was to externally validate the RUSS score, con ceived by Resorlu et al in 2012, on an Italian cohort of patients
To the best of our knowledge, the present study is the first external validation of RUSS performed in an Italian center Our analysis brought to several noteworthy findings
First, males and left kidney side were the most interested accounting for 56 9% and 68 4%, respectively
Second, when adjusting SFR status on multivariable analysis, neither stone density nor stone size reached sta tistical significance (OR: 0 99; p = 0 80 and OR: 0 95; p= 0 44) Conversely, RUSS was identified as the only pre dictive score for SFR (OR: 0 32; p = 0 002) This is in agreement with Selmi et al who in a pooled comparison of different nephrolithometric scores showed that RUSS was the best predictor of SFR (OR: 0 45) (14)
Third, in the present study overall SFR was 78 4%, this
rate being in line with results reported from other studies on RIRS series (15 17)
Fourth, RUSS registered an AUC of 0 76 Similarly, Sfoungaristos et al RUSS externally validated RUSS esti mating an AUC of 0 70 (18) Interestingly, results from a recent metanalysis comparing the predictive ability of the most used scoring systems for SFR has not revealed any superiority of one scoring tool over another (19)
However, the high heterogeneity between studies and variables between the scoring systems make difficult to statistically generalize these findings
Taken together, RUSS is a simple and reliable score to apply during the preoperative evaluation of kidney stones For sure IPA is the most demanding parameter to calculate for urologists, however after a short learning curve with an expert radiologist we were able to perfect ly assess this angle
We acknowledge that the present study has some limita tions First, should be interpreted in the context of its ret rospective nature Second, the sample size is relatively small and includes fewer cases with high scores for the scoring system Third, RIRS is strongly dependent on operator’s skill and potential risk of bias can occur However, we only selected cases that were performed by expert surgeons in the RIRS field Fourth, the RUSS score has an intrinsic limitation: horseshoe and ectopic kidneys are relatively rare Therefore, only a restricted number of patients scored 3 points For this reason, our results may overestimate the diagnostic accuracy of this technique and potentially undermine their reproducibility in clinical practice Further validation studies with larger cohorts are needed to confirm the diagnostic accuracy of RUSS
CONCLUSIONS
Treatment planning of kidney stones relies on several pre dictive scores RUSS represents a user friendly scoring tool that can be used in the prediction of postoperative SFR after RIRS Further external validations in larger cohorts are needed to confirm these results
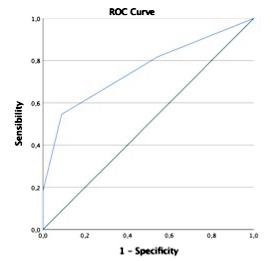
REFERENCES
1 Qian X, Wan J, Xu J, et al Epidemiological trends of urolithiasis at the global, regional, and national levels: a population based study Int J Clin Pract 2022; 2022:6807203
2 Zheng C, Xiong B, Wang H, et al Retrograde intrarenal surgery versus percutaneous nephrolithotomy for treatment of renal stones > 2 cm: a meta analysis Urol Int 2014; 93:417 424
3 Karakoyunlu N, Goktug G, Sener NC, et al A comparison of stan dard PCNL and staged retrograde FURS in pelvis stones over 2 cm in diameter: a prospective randomized study Urolithiasis 2015; 43:283 287
4 Donaldson JF, Lardas M, Scrimgeour D, et al Systematic review and meta analysis of the clinical effectiveness of shock wave lithotrip sy, retrograde intrarenal surgery, and percutaneous nephrolithotomy for lower pole renal stones Eur Urol 2015; 67:612 616
5 Zhao Z, Sun H, Zeng T, et al An easy risk stratification to recom mend the optimal patients with 2 3 cm kidney stones to receive ret rograde intrarenal surgery or mini percutaneous nephrolithotomy Urolithiasis 2020; 48:167 173
313
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
External validation of Resorlu Unsal stone score
Figure 1 Predictive
accuracy of RUSS
A Tufano, M Frisenda, A Rossi, et al
6 Breda A, Angerri O Retrograde intrarenal surgery for kidney stones larger than 2 5 cm Curr Opin Urol 2014; 24:179 183
7 Calarco A, Frisenda M, Molinaro E, Lenci N The active guidewire technique versus standard technique as different way to approach ureteral endoscopic stone treatment Arch Ital Urol Androl 2021; 93:431 435
8 Xiao Y, Li D, Chen L, et al The R I R S scoring system: An inno vative scoring system for predicting stone free rate following retro grade intrarenal surgery BMC Urol 2017; 17:105
9 Jung JW, Lee BK, Park YH, et al Modified Seoul National University Renal Stone Complexity score for retrograde intrarenal surgery Urolithiasis 2014; 42:335 340
10 Resorlu B, Unsal A, Gulec H, Oztuna D A new scoring system for predicting stone free rate after retrograde intrarenal surgery: the "resorlu unsal stone score" Urology 2012;80:512 518
11 Elbahnasy AM, Shalhav AL, Hoenig DM, et al Lower caliceal stone clearance after shock wave lithotripsy or ureteroscopy: the impact of lower pole radiographic anatomy J Urol 1998; 159:676 82
1 2 A b o u m a rz o u k O M , M o n g a M , K a t a S G , e t a l F l e x i b l e ureteroscopy and laser lithotripsy for stones > 2 cm: a systematic review and meta analysis J Endourol 2012; 26:1257 63
13 Hyams ES, Munver R, Bird VG, et al Flexible ureterorenoscopy and holmium laser lithotripsy for the management of renal stone bur
dens that measure 2 to 3 cm: a multi institutional experience J Endourol 2010; 24:1583 8
14 Selmi V, Sari S, Oztekin U, et al External validation and com parison of nephrolithometric scoring systems predicting outcomes of retrograde intrarenal surgery J Endourol 2021; 35:781 788
15 Molina WR, Kim FJ, Spendlove J, et al The S T O N E Score: a new assessment tool to predict stone free rates in ureteroscopy from pre operative radiological features Int Braz J Urol 2014; 40:23 9
16 Park J, Kang M, Jeong CW, et al External validation and evalu ation of reliability and validity of the modified Seoul National University Renal Stone Complexity Scoring System to predict stone free status after retrograde intrarenal surgery J Endourol 2015; 29:888 93
17 Maugeri O, Dalmasso E, Peretti D, et al Stone free rate and clin ical complications in patients submitted to retrograde intrarenal sur gery (RIRS): Our experience in 571 consecutive cases Arch Ital Urol Androl 2021; 93:313 317
18 Sfoungaristos S, Gofrit ON, Mykoniatis I, et al External valida tion of Resorlu Unsal stone score as predictor of outcomes after ret rograde intrarenal surgery Int Urol Nephrol 2016; 48:1247 1252
19 Özman O, Akgül HM, Basataç C, et al RIRSearch Study Group Recent scoring systems predicting stone free status after retrograde intrarenal surgery; a systematic review and meta analysis Cent European J Urol 2022; 75:72 80
Correspondence
Antonio Tufano, MD antonio tufano91@gmail com Marco Frisenda, MD marco frisenda@uniroma1 it Pietro Viscuso, MD pietro viscuso@uniroma1 it Via del Policlinico 155, 00161, Rome, (RM) (Italy)
Antonio Rossi, MD antonio rossicz@gmail com
Department of Urology, “Cristo Re” Hospital, Via delle Calasanziane 25, 00167 Rome (RM) (Italy)
Guglielmo Mantica, MD gugliemo mantica@gmail com Largo Rosanna Benzi, 10, 16132, Genova (Italy)
Pierluigi Bove, MD pierluigi bove@uniroma2 it Via Aurelia, 275,00165, Rome (RM) (Italy)
Rosario Leonardi, MD leonardi r@tiscali it Via Dell’Autonomia 57, Gravina di Catania (CT) (Italy)
Alessandro Calarco, MD alecalarco@gmail com Department of Urology, “Cristo Re” Hospital, Via delle Calasanziane 25, 00167 Rome (RM) (Italy)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
314
Urodynamic changes following laparoscopic versus vaginal hysterectomy
Tamer Abouelgreed 1, 2 , Doaa Saleh 3 , Mohamed Abdelaal 1 , Adel Elatreisy 1 , Mohamed Elhelaly 1 , El Sayed El Agamy 1 , Ahmed Elgammal 1 , Ashraf Moawad 2, 3
Department of Urology, Al Azhar University, Cairo, Egypt;
Al Zahra Private Hospital, NMC Medical group, UAE;
Department of Obstetrics & gynaecology, Al Azhar University, Cairo, Egypt
SummaryObjective: To compare urodynamic changes before and after hysterectomy (laparoscopic vs vaginal approach) for benign gynecological diseases
Patients and methods: A total of 90 women with a mean age of 56 36 years were enrolled in this study between August 2019 and April 2021 They were divided into two equal groups (45 patients each) Group, I had a vaginal hysterectomy, and Group II had a laparoscopic hysterectomy All patients were assessed clinically using ICIQ FLUTS questionnaire and a uro dynamic study before and six months after surgery
Results: Both vaginal and laparoscopic hysterectomy did not significantly change the maximum flow rate, voiding time, and average flow rate The increase in residual urine volume in group I was not significant (p = 0 129), as was in Group II (p = 0 217) All the modifications, however, were within permis sible limits According to the cystometry result, volume at initial sensation rose in both groups after surgery, with no statistically significant difference (p = 0 364) After both forms of hysterecto my, maximum bladder capacity did not vary considerably Preoperatively, all study participants exhibited no overactivity of the detrusor muscle; nevertheless, following surgery, overac tivity was noted in 9 patients after vaginal hysterectomy com pared to three patients after laparoscopic hysterectomy, and all the alterations were within a clinically acceptable range In addition, the ICIQ FLUTS score was not significantly different between the study groups
Conclusions: According to the urodynamic study, hysterectomy for benign uterine conditions, whether vaginal or laparoscopic, did not adversely affect urinary bladder function
KEY WORDS: Hysterectomy; Uroflowmetry; Urodynamic
Submitted 9 June 2022; Accepted 23 June 2022
INTRODUCTION
Hysterectomy is the most common gynecological surgical operation (1) More than 90% of hysterectomies were done for benign conditions The most common indica tion of hysterectomy are leiomyomas and dysfunctional uterine bleeding (2) Hysterectomies are performed with different routes, either vaginally, abdominally, or laparo scopically Laparoscopic and vaginal hysterectomy are minimally invasive approaches with short hospitalization time and fast recovery comparable to open abdominal hysterectomy (3) Vaginal hysterectomy, when feasible, is
associated with good outcomes and is the most cost effec tive approach to hysterectomy (4) The influence of sim ple hysterectomy on the lower urinary tract is still debat ed However, hysterectomy disrupts the local nerve sup ply to the pelvic organs and interrupts the anatomical relationship It has been postulated that the function of the pelvic organs may be adversely affected (5) Thus, the function of the pelvic organs, mainly the urinary func tion, should be considered when deciding the optimum route of hysterectomy (6) Urodynamics is a study that assesses the lower urinary tract function and attempts to reproduce the patients' symptoms to provide a pathophysiological explanation In principle and reality, the clinicians use urodynamic testing results to direct therapy, whether surgical, med ical, or behavioral, alone or in combination Some of the current approaches are water filled, ambulatory, and video urodynamic Urodynamics analyses the functional anatomy of the bladder, urethra, or both, and their reac tion to filling, storing, and voiding, regardless of the method used (7) Urodynamic testing is essential in urog ynecology because it provides objective descriptions of incontinence and voiding dysfunction (8) Therefore, the objectives of this study were to analyze the urodynamic changes before and after laparoscopic and vaginal hys terectomy
PATIENTS AND METHODS
Between August 2019 and April 2021, 90 cases present ing to in patient departments of the Authors’ institute were enrolled in this study The ethics review committee a p p r o v e d t h e s t u d y p r o t o c o l A l l p a t i e n t s s i g n e d informed consent forms detailing the operation and potential risks Patients were divided into two groups of equal size: Group I: with a mean age of 59 16 year old (ranging between 51 66), underwent a vaginal hysterec tomy Group II with a mean age of 54 72 year old (rang ing between 47 59) underwent laparoscopic hysterecto my The route of traditional minimally invasive surgery was chosen by the designated surgeon, with vaginal hys terectomy as the first choice, followed by laparoscopic hysterectomy Our study included all patients undergo ing hysterectomy for benign gynecological diseases We excluded all patients with a history of diabetes mellitus,
A315 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
ORIGINAL PAPER No conflict of interest declared
1
2
3
DOI: 10 4081/aiua 2022 3 315
neurological disorders, previous urological pelvic sur gery, previous caesarian section, and urinary tract infec tion All the procedures were carried out while the patient was sedated A reusable umbilical or 12 mm port (Xcel; Ethicon Endo Surgery, Inc , Somerville, NJ) for the optics and three assistant ports, either three 5 mm or two 5 mm plus one 10 mm port in the lower quadrants, were used for laparoscopic hysterectomy The vaginal hysterectomy was done conventionally All study participants were sub jected to detailed history taking, complete clinical exam ination, routine preoperative investigation ICIQ FLUTS
( I n t e r n a t i o n a l C o n s u l t a t i o n o n I n c o n t i n e n c e M o d u l a r Questionnaire on Female Lower Urinary Tract Symptoms) ( 9 ) , a n d U r o d y n a m i c e v a l u a t i o n ( c y s t o m e t r y a n d uroflowmetry) were obtained before and six months after surgery
Statistical analysis
Data were analyzed using Statistical Program for Social Science (SPSS) version 18 0 Quantitative data were expressed as mean ± stander deviation (SD) Qualitative data were expressed as frequency and percentage The following tests were done: independent samples T test of significance when comparing two continuous means
Paired t test: t = mean's difference between pre and post The chi square (x2) test of significance was applied to compare proportions between two qualitative factors Pearson's correlation coefficient (r) test was employed for data correlation P value (probability): statistical signifi cance was defined as less than 0 05, and high ly significant was defined as less than 0 01
RESULTS
Demographic Data of both groups
T h e c o h o r t s w e r e c o m p a r a b l e r e g a r d i n g patients’ demographics (p > 0 05) (Table 1)
Postoperative evaluation of the urinary symptoms in both studies groups
Post operative frequency was noticed in 18 and 9 patients of groups 1 and 2 respectively (p = 0 32) Urgency occurred in 10 and 6 p a t i e n t s o f g r o u p s 1 a n d 2 r e s p e c t i v e l y (p = 0 39) Urge incontinence occurred in 9 and 6 patients of groups 1 and 2 respectively (p = 0 37) No other symptoms were noticed in both groups In group I, the mean preop erative ICIQ FLUTS score was 0 64 (range between 0 and 2, median 0), and the postop erative mean was 1 5 (range between 0 and 6, median = 0) with a significant p value (p < 0 001) In group II, the mean preoperative ICIQ FLUTS score was 0 33 (range between 0 and 2, median = 0) and the mean postopera tive score was 0 82 (ranged between 0 and 6, median = 0) with a significant p value (p = 0 014) There was no statistically significant difference between groups 1 and 2 regarding preoperative and postoperative ICIQ FLUTS scores (p = 0 1 & 0 11, respectively)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
Changes in Urodynamic parameters in the two studied groups before and after surgery
According to results of cystometry, volume at first sensa tion rose after surgery in both groups, with insignificant p value between pre and postoperative volumes (p = 0 372 and p = 0 364) for groups 1 and 2, respectively (Table 2) After both forms of hysterectomy, maximum bladder capacity did not vary considerably (Table 3)
Preoperatively, no detrusor muscle overactivity was found in either group; however, after surgery, overactivi ty was observed in 9 patients in the vaginal hysterectomy group compared to three patients in the laparoscopic hys terectomy group (Table 4)
Changes in Uroflowmetry parameters in the two groups before and after surgery: According to uroflowmetry measures, vaginal hysterectomy reduced the maximum flow rate and increased voiding time not significantly and laparoscopic hysterectomy did not affect either
Table 1.
Demographic data of both groups
test
Parameters Mean ± SD Mean ± SD Mean difference t P value Age (years) 59 16 3 68 54 72 4 15 2 43 2 402 0 059 Weight (Kg) 70 02 7 86 69 17 6 92 1 68 0 873 0 388 Par ty 2 73 0 79 3 10 0 75 0 07 0 338 0 734 t = ndependent t test
Table 2.
Comparison between group I and group II as regard first sensation
F irst sensation Group I Group II t test Mean (ml) ± SD Mean (ml) ± SD Mean difference t P value Pre 167 78 24 81 169 43 22 26 2 00 4 379 0 364 NS Post 178 00 14 98 179 90 15 19 3 50 0 904 0 372 NS P value 0 6 0 67
Table 3
Comparison between group I and group II as regard cystometric bladder capacity
Cystometric bladder Group I Group II t test capacity (ml) Mean (ml) ± SD Mean (ml) ± SD Mean difference t P value Pre 518 13 25 32 514 00 25 72 3 33 0 505 0 618 Post 477 00 100 19 486 31 65 93 33 33 1 515 0 297 P value 0 1 0 16
Table 4.
Relation between group I and group II as regard post operative presence of detrusor muscle over activity
Post operative Groups Total Presence of detr usor Group I Group II muscle over activity No % No % No % ve 36 80 00 42 93 33 78 86 667 +ve 9 20 00 3 6 67 12 13 333 Total 45 100 00 45 100 00 90 100 000 x2 5 455 P value 0 020
T Abouelgreed, D Saleh, M Abdelaal, A Elatreisy, M Elhelaly, El Sayed El Agamy, A Elgammal, A Moawad
316
Group I n = 45 Group II n = 45 t
The laparoscopic group had a higher average flow rate, while the vaginal group had a lower average flow rate (Table 5) The increase in residual volume after vaginal hysterectomy was modest (p = 0 129), as was the increase in residual urine after laparoscopic hysterectomy (p = 0 217) (Table 6) All the modifications, however, were within permissible limits
Changes in pre and postoperative abdominal detrusor leak point pressure in both groups No detectable changes in pre and postoperative abdomi nal detrusor leak point pressure in group 2 Only six patient of group 1 has decreased their postoperative abdominal detrusor leak point pressure to less than 60 cm H2O
DISCUSSION
To improve life expectancy in women, it is essential to know the long term adverse outcomes of surgical inter ventions (10, 11) We designed this study to analyze the effects of laparoscopic versus vaginal hysterectomy on the lower urinary tract symptoms and functions using urody namic studies and try to detect if the type of operation (whether vaginal or laparoscopic hysterectomy) will affect postoperative lower urinary tract functions or not The relation between the urinary symptoms and the urody namic parameters was evaluated pre and postoperatively
Urodynamic changes post hysterectomy
Many studies compared abdominal and vaginal hysterec tomy Polat et al (2016) (12) underwent a physiological assessment of bladder, urethra, and anorectum on 26 women before hysterectomy, six weeks, and six months afterward They reported that after a hysterectomy for benign disease, some women experience a considerable increase in rectal and bladder sensitivity The alterations lasted for six months, but they weren't linked to any changes in rectal or vesical motor activity being not nec essarily related to the onset of urinary or gastrointestinal problems After a total hysterectomy, they ruled out local damage, infection, and edema as plausible causes of the pelvic organs' increased sensitivity They concluded that the cause of the increase in rectal and vesical sensitivity seen in some women after vaginal and abdominal hys terectomy is unknown; it's possible that removing a major pelvic organ and its related nerve supply changes the gating of sensations from nearby organs Heydari et al (13) reported no noticeable changes in urinary bladder capacity or urethral functions after the operation They f o c u s e d o n u r o d y n a m i c m e a s u r e s b e f o r e a n d a f t e r abdominal and vaginal hysterectomies They discovered a statistically significant decrease in maximum cystometric capacity and a decline in bladder compliance following abdominal extra fascial and vaginal hysterectomies Both findings are linked to a deterioration in the detrusor mus cle's musculoelastic characteristics due to edema and sur gical damage However, they concluded that the decrease in capacity and compliance had little clinical significance They found no evidence that a hysterectomy caused involuntary detrusor contractions or incontinence After the hysterectomy, urethral competence was unaltered, and there was no rise in stress incontinence A second study included 36 women undergoing total hysterecto my; preoperative complaints were observed in 58 3% of patients, although only 38 9% had urodynamically con firmed impairment Seventy five percent of women were symptomatic after hysterectomy, with another 30 6 per cent developing a urodynamic abnormality They con cluded that total hysterectomy is linked to a higher sub jective and objective incidence of vesicourethral dysfunc tion (14) El Toukhy et al did a study that looked at the effects of various hysterectomy procedures, including total abdominal, vaginal, laparoscopic, and subtotal They looked at 187 women between the ages of 29 and 73 who had a hysterectomy for various reasons Urinary symp toms occurred less frequently (p = 0 01) six months following surgery, whereas urodynam ic investigations remained unaltered Furthermore, regardless of the hysterectomy technique employed, the patients reported sig nificantly reduced rates of stress incontinence (p = 0 005) and urgency (p = 0 03) than before the procedure They concluded that subtotal hysterectomy, whether performed abdominal ly, vaginally or laparoscopically, has no nega tive impact on urine function six months fol lowing surgery (15)
In our study, according to pre and postopera tive urodynamic studies in both groups, all changes were within the clinically acceptable range Thus, we can say that urodynamic stud
A317 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Table 5. Uroflowmetry parameters in the two studied groups before and after surgery Group I n = 45 Group II n = 45 Pre Post Pre Post operative operative operative operative Voided volume (ml) 264 5 ± 48 7 274 7 ± 60 8 274 8 ± 58 2 284 5 ± 56 9 P value 0 156 0 157 Maximum flow rate (ml/sec) 26 4 ± 5 3 24 3 ± 5 2 25 7 ± 4 8 27 2 ± 4 6 P value 0 068 0 069 Voiding time (sec) 50 4 ± 11 5 61 1 ± 9 9 48 8 ± 8 6 46 4 ± 9 5 P value 0 059 0 061 Average flow rate (ml/sec) 7 5 ± 2 2 6 7 ± 1 3 6 5 ± 1 7 8 8 ± 2 7 P value 0 063 0 067 Table 6. Residual urine volume in both groups Groups T ime Residual urine Paired Paired sample of testing volume (ml) differences t test Mean (ml) ± SD Mean (ml) ± SD t P value Group I Pre 54 10 7 58 1 29 4 81 0 129 Post 57 32 5 58 3 28 NS Group II Pre 50 73 3 97 1 41 1 03 3 776 0 217 Post 52 13 3 01 NS Residual urine Group I Group II Mean t test volume (ml) Mean (ml) ± SD Mean (ml) ± SD difference t P value Pre 54 10 7 59 50 73 3 97 1 33 0 854 0 396 NS Post 57 32 5 58 52 13 3 01 2 54 3 507 0 082 NS
ies showed no clinically significant effect of vaginal or laparoscopic hysterectomy on bladder function and capacity Some studies suggest a rational and credible anatomical explanation for why a subtotal hysterectomy may not have a negative impact on pelvic organ function
The nerve content of the uterosacral and cardinal liga ments differs along their length, with much more nerve content in the middle two lateral thirds, closer to their origin at the pelvic side wall than in the medial third, closer to their insertion into the uterine body and cervix
The ligaments, and hence the nerves, are split extremely close to the uterus and cervix during a subtotal hysterec tomy As a result, only the nerves that innervate the uterus and cervix are disrupted, whereas those that inner vate the bladder and rectum are unaffected (16)
CONCLUSIONS
Hysterectomy for benign uterine condition, whether vagi nal or laparoscopic, did not adversely affect urinary blad der function According to uroflowmetry and cystometry, hysterectomy for benign uterine conditions, whether vaginal or laparoscopic, did not adversely affect urinary bladder function Thus, we did not recommend depend ing on the effects of hysterectomy on bladder functions as a matter of preference of the vaginal or laparoscopic type of the operation
REFERENCES
1 Dobbas SP, Jackson SR, Wilison AM, et al A prospective random ized trial comparing continuous bladder drainage with catheteriza tion at abdominal hysterectomy, Br J Urol 1997; 80:554
2 Wright ID, Herzog TJ, Ananth CV, et al Nationwide trends in the performance of inpatient hysterectomy in the United States Obstet Gynaecol 2013; 122:233
3 Sculpher M, Manca A, Abbott J, et al Cost effectiveness analysis of laparoscopic hysterectomy compared with standard hysterectomy, results from a randomized trial BMJ 2004; 328:134
4 Lonnerfors C, Reynisson P, Persson I A randomized trial com paring vaginal and laparoscopic hysterectomy vs robot assisted hys terectomy J Mini Invasive Gynaecol 2015; 22:78
5 Thakar R Dispelling the myth does hysterectomy cause pelvic organ dysfunction? BJOG 2004; 111 (Suppl 1):20 3
6 Bohlin K, Ankardal M, Lindkvist H, Milsom I Factors influencing the incidence and remission of urinary incontinence after hysterecto my Am J Obstet Gynecol 2017; 216:53 e1
7 Chen J, Chen C, Li Y, et al Impact of radical hysterectomy on the trans obturator sling pathway: A retrospective three dimensional magnetic resonance imaging study Int Urogynecol J 2017; 2:1359
8 Kupec T, Pecks U, Graf C, et al Size does not make the difference: 3D/4D Trans perineal sonographic measurement of the female ure thra in the assessment of urinary incontinence subtypes Bio Med Res Int 2016:1 6
9 Jackson S, Donovan J, Brookes S, et al The Bristol Female Lower Urinary Tract Symptoms questionnaire: development and psychome tric testing Br J Urol 1996; 77:805
10 Ramdhan RC, Loukas M, Tubbs RS Anatomical complications of hysterectomy: A review Clin Anat 2017; 30:946
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
11 Skorupska K, Miotła P, Kubik Komar A, et al Urinary inconti nence after hysterectomy does type of surgery matter? Ginekol Polska 2016; 87:94
12 Polat M, Kahramanoglu I, Senol T, et al Comparison of the effect of laparoscopic andabdominal hysterectomy on lower urinary tract function, vaginal length, and dyspareunia: A randomized clini cal trial J Laparoendosc Adv Surg Tech 2016; 26:116
13 Heydari F, Motaghed Z, Abbaszadeh S Relationship between hysterectomy and severity of female stress urinary incontinence Electron Physician 2017; 9:4678
14 Pomian A, Majkusiak W, Kociszewski J, et al Demographic fea tures of female urethra length Neurourol Urodynamics 2018; 37:1751
15 El Toukhy T A, Hefini M, Davies A, et al The effect of different types of hysterectomy on urinary and sexual functions: a prospective study J Obstet Gynecol 2004; 24:420
16 Gupta S, Manyonda I Hysterectomy for benign gynecological disease Current Obstet Gynecol 2006; 16:147
Correspondence
Tamer Abouelgreed, MD (Corresponding Author) dr tamer ali@yahoo com tamerali 8@azhar edu eg
Department of Urology, Al Azhar University, Cairo, Egypt & Al Zahra Private Hospital, NMC Medical group, UAE
Doaa Saleh, MD Doaa m saleh@azhar edu eg Department of Obstetrics & Gynaecology, Al Azhar University, Cairo, Egypt
Mohamed Abdelaal, MD maal uro@yahoo com Mohamed Elhelaly, MD elhelalymohammed@yahoo com El Sayed El Agamy, MD abuamr1978@yahoo com Adel Elatreisy, MD Egypt dr adelelatreisy@yahoo com Ahmed Elgammal, MD aelgammal36@gmail com
Department of Urology, Faculty of medicine, Al Azhar University, Cairo, Egypt
Ashraf Moawad, MD ganin1@hotmail com Department of Obstetrics & gynaecology, Al Azhar University, Cairo, Egypt & Al Zahra Private Hospital, NMC Medical group, UAE
T Abouelgreed, D Saleh, M Abdelaal, A Elatreisy, M Elhelaly, El Sayed El Agamy, A Elgammal, A Moawad
318
4081/aiua
PAPER
Murat Topcuoglu 1 , Murat Çakan 2
1
Department of Urology, Alaaddin Keykubat University Alanya Training and Research Hospital, Antalya, Turkey; 2 Department of Urology, Dıs ¸kapı Yıldırım Beyazıt Training and Research Hospital, Ankara, Turkey
SummaryObjectives: The aim of this study was to investigate the impact of the addition of 50 mg daily sildenafil to pentoxifylline colchicine combination ther apy on the Peyronie's plaque features in patients with the acute phase of Peyronie's disease (PD)
Methods: In this retrospective and non randomized clinical study, patients were divided into 2 groups as group 1; (n = 107) who received colchicine and pentoxyfillin plus 50 mg daily oral sildenafil, and as group 2; (n = 79) who received only colchicine and pentoxyfillin. Patients were compared in terms of degree of curvature, pain in erection and erectile function at the baseline and at 6 month follow up. Pain in erection and erectile func tion were evaluated by visual Analogue Scale (EF VAS), and the shortened version of the International Index of Erectile Function (IIEF 5). Improvement in the degree of curvature and change in EF VAS scores were primary endpoints of the study. Change in IIEF 5 score was the secondary endpoint of the study.
Results: The two groups were statistically similar in terms of demographics and baseline features of PD. A statistically signifi cant reduction in degree of curvature and EF VAS scores was shown in group 1 compared to group 2.There was also a signifi cantly higher IIEF 5 score in group 1 compared to group 2. No significant side effects were detected in both groups during treatment period
Conclusions: Adding sildenafil to pentoxifylline colchicine com bination treatment seems to improve PD related symptoms in the acute phase PD PDE5i may contribute to relieve the Peyronie's symptoms in ED patients through their antifibrotic effects
KEY WORDS: Peyronie; Oral treatment; Fibrosis; Antifibrotic treatment
Submitted 29 June 2022; Accepted 2 July 2022
INTRODUCTION
Peyronie’s disease (PD) is a fibrotic disorder of tunica albuginea with the formation of penile plaque PD is a rel atively common disorder, with an estimated prevalence of 1 5% in men between 30 and 40 years old and as high as 6 5% in older men (1) PD is characterized by progressive deformity and unstable plaque with painful erection in the acute phase;stabilization of the penile plaque and penile curvature are the major findings of the chronic phase which may require at least 6 months and up to 18 months (2 3) The exact etiology of plaque formation
conflict
remains unclear The most recognized theory is abnormal wound healing and aberrant fibrosis following minor trauma to the erected penis (4) The association between PD and Dupuytren contraction is a strong proponent of the fibrotic disease theory (5) Although various types of drugs have been used to date in the acute phase of PD, there is currently no satisfactory and approved oral drug therapy Several experimental models in human cell cul tures and rat models have provided new insights into the pathophysiology leading to the investigation of alterna tive approaches, including the phosphodiesterase type 5 inhibitors (PDE5i) as an anti fibrotic modality (6 7) PD is associated with erectile dysfunction (ED) in a percent age of patients ranging from 40 % up to 70% (3, 8) Proven anti fibrotic effect of PDE5i in the experimental studies and high coexistence rate of ED with PD patients suggests that PDE5i may contribute to the treatment of PD However, very limited clinical studies were reported about this subject in the literature
We investigated whether the addition of PDE 5i to com bination therapy with colchicine and pentoxifylline (PTX) has any benefit on PD related symptoms in patients with the acute phase of PD and ED Material and Methods: This study was conducted accord ing to the ethical standard laid down by the 1964 decla ration of Helsinki and its later amendments Medical and sexual history, physical examination, records of penile color Doppler ultrasonography were retrospectively eval uated Patients with PD symptoms for no longer than 12 months and accompanied by ED were included into the study As per our protocol, patients who were receiving any treatment for PD or ED, as well as those with psy chosomatic ED, hypertension, coronary artery disease, diabetes mellitus, hormonal disorders, receiving long term medication for any disease, alcoholism or smoke abuse were excluded To rule out organic sexual dysfunc tions and other underlying diseases, serum fasting blood glucose level, sex hormones and prolactin levels were also evaluated In this retrospective and non randomized clin ical study, 6 year medical records of 636 patients who were treated for the acute phase of PD in our institute were revaluated The review also elucidated that 186 of these patients were included into the study Patients were divided into two groups as group 1, who received PTX (400 mg, twice daily) colchicine (0 5 mg, plus oral daily 50 mg sildenafil (n=107) and as group 2 received PTX
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
319
ORIGINAL
No
of interest declared
Effects of long term sildenafil on the acute phase of Peyronie’s disease in a combination treatment
DOI: 10
2022 3 319
M Topcuoglu, M Çakan
(400 mg, twice daily) colchicine (0 5 mg, twice daily) (n=79) and who were reluctant to use of sildenafil or unable to purchase sildenafil due to financial reasons
Patients with plaque calcification detected on penile ultrasonography were also excluded from the study Plaque calcification has been identified as a sign of chron ic phase and potential poor predictor of response to treat ment (9) Disease duration, erectile pain, erectile func tion, and penile curvature were assessed at the baseline assessment
Penile curvature was measured according to the Kelami’s criteria with a goniometer by the same oper ator following artificial erection stimulated by intracaver nosal vasoactive agent The severity of erectile pain was assessed by erectile function visual Analogue Scale (EF VAS) score on a scale of 0 10, with 0 being no pain and 10 being severe pain Erectile function was evaluated through the shortened version of the International Index of Erectile Function (IIEF 5) questionnaire Each ques tion is scored on a scale of 1 to 5 and 5 is indicating best function The collected database of baseline and out comes at sixth month of treatment in both groups were compared in terms of penile curvature, EF VAS, and IIEF 5 scores The primary endpoints of the study were the improvement in curvature and change in EF VAS scores Change in IIEF 5 score was the secondary end point of the study
Statistical analysis
Mean, standard deviation, median lowest, median high est, frequency and ratio values were used in descriptive statistics of the data The distribution of the variables was measured with the Kolmogorov Smirnov test The Mann Whitney test was used to analyze quantitative independ ent data Chi square test was used for the analysis of qual itative independent data and Fisher test was used when the chi square test conditions were not met SPSS 22 0 program was used in the analysis P value less than 0 05 was considered as statistically significant
RESULTS
Our retrospective review revealed that 636 patients with acute phase of PD were treated at our center during the study period As per our protocol, 186 of 636 patients were enrolled in our study The baseline characteristics of these patients are displayed in Table 1 Mean age was 56 1± 10 2 in group 1 and 53 54 ± 13 4 in group 2 There was no statistical difference between the groups in terms of demographics and PD characteristics at the baseline period The mean duration of PD symptoms was 9 2 ± 2 1
months in group 1 and 8 9 ± 2 0 month in group 2 (no statistically significant difference between the groups) Change in mean degree of curvature angle was 11 02 ± 2 3º and 6 6 ± 1 7º group 1 and group 2, respectively Although a significant difference in mean degree of cur vature was shown in group 1 at the sixth month of the treatment compared to baseline, no significant change in mean degree of curvature was revealed in group 2 after the treatment period EF VAS showed a significant reduc tion in both groups, with a statistically higher reduction in group 1 patients compared to group 2 patients (Table 2) At sixth month treatment follow up, 68 of 107 patients (64%) in group 1 stated completely relief in pain during erection, while completely relief in pain was described by 37 of 79 patients (47%) in group 2 Mean IIEF 5 scores increased from 12 78 ± 6 46 to 17 89 ± 82 in group 1 and from 11 86 ± 6 21 to 13 02 ± 6 78 in group 2 at the postoperative period Compared with the baseline values, the mean IIEF 5 scores in group 1 were significantly different at sixth month treatment follow up, while no significant changes were found in group 2 (Table 2) No clinically significant side effects were observed in any patients in both groups
DISCUSSION
Our study investigated the addition of PDE5i to conven tional combined oral therapy in acute phase PD and found that adding a PDE5i to the conventional treatment of PD patients may be worthwhile, in the improvement of degree of curvature and erectile pain The acute phase is characterized by painful erections, soft plaques, while the chronic phase is characterized by fibrotic/calcified plaque and stable disease Although spontaneous remission is reported in 3 13% of PD cases, the disease stabilizes or worsens in majority of the cases (10) To date, various oral medications have been used in the acute phase, including potassium aminobenzoate, colchicine, PTX, vitamin E, tamoxifen, orgotein, and carnitine acetyl ester
1.
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
320
Table
Mean baseline clinical characteristics of the patients Group 1 (n = 107) Group 2 (n = 79) p Age 56 1 ± 10 2 53 54 ± 13 4 0 456 Duration of symptoms (months) 9 2 ± 2 1 8 9 ± 2 0 0 836 Erect le Function V sual Analog Scale (EF VAS) Score 6 89 ± 3 02 6 14 ± 2 78 0 642 Degree of curvature (º) 35.1 ± 16.3 36.6 ± 17.8 0.696 IIEF 5 score 13 78 ± 6 46 14 10 ± 6 77 0 976 Table 2. Comparison of the groups at pre treatment and post treatment evaluation regarding Peyronie plaque characteristics and IIEF 5 questionnaire Group 1 Group 2 Post treatment comparison (n = 107) (n = 79) between the group 1 and group 2 Pre-treatment Post-treatment p Pre-treatment Post-treatment pp Degree of curvature (º) 35 1 ± 16 3 24 08 ± 11 2 0 045 36 6 ± 17 8 30 0 ± 14 3 0 067 0 022 Erectile Function Visual Analog Scale (EF VAS) score 6 89 ± 3 02 3 89 ± 1 06 0 024 6 14 ± 2 78 4 7 ± 1 78 0 039 0 038 IIEF 5 score 12 78 ± 6 46 17 89 ± 82 0 021 11 86 ± 6 34 13 02 ± 6 78 0 123 0 006
(11) The clinical benefits of oral agents such as potassi um aminobenzoate, PTX, colchicine, and coenzyme Q10 have been reported in different studies and are consid ered as a part of single or multimodal therapy for clinical use, but no single oral pharmacotherapy has been approved for treatment by American Urological Association (AUA) or European Urological Association (EAU) (12, 13) PTX Colchicine combination is a preferred treatment alternative for PD patients in our clinic, which is associ ated with low side effect, low price, and proven success rates from previous studies 10 PTX is an oral drug that works through mechanism that increase collagen metab olism, downregulate TGF beta, and reduce fibrogenesis and has been used clinically in a variety of inflammatory and fibrotic conditions, such as radiation fibrosis, radia tion proctitis, cystic fibrosis, radiation pneumonitis (14, 15) Significant improvements in degree of curvature, plaque volume, pain intensity, and penile rigidity after PTX treatment support the effectiveness of the treatment in PD patients (16, 17) Colchicine, a commonly used oral therapy, can significantly improve pain relief and penile curvature as monotherapy or in combination ther apy (18) Colchicine binds to tubulin, blocks mitosis, reduces inflammation and procollagen formation, and increases collagenase production Colchicine therapy appears to have conflicting results, and most studies show colchicine success in 30% to 50% of PD patients (18 19) Although various oral treatments are effective in PD patients, the lack of consensus on oral treatment increas es the trend towards alternative treatments We assessed the effect of supplementation with 50 mg of sildenafil on the conventional therapy of PD The use of PDE5i in PD patients is supported by the fact that almost all PD patients suffer from ED and the proven effects of PDE5i on both pathologies Several in vitro studies have shown that PDE5i has a potential anti fibrotic effect against Peyronie's like plaque (6 20) NO and cyclic guanosine 3’,5’ monophosphate (cGMP) have anti fibrotic actions with remarkable effects on collagen synthesis and myofi broblast differentiation PDE 5i shows anti fibrotic effects by reducing collagen deposits and oxidative stress, inhibiting myofibroblast proliferation and profibrotic fac tor secretion (3) Transforming growth factor b1 (TGF b1) is a key profibrotic factor, found in many tissues and demonstrated in human PD plaques, that was also shown at high levels in the serum of PD patients (21) Following inhibition of PDE 5, elevated levels of cGMP and cAMP activate protein kinase G, which play important role in the apoptosis and reduced collagen synthesis The men tioned anti fibrotic effects are also mediated by guanylate cyclase inducers by stimulating protein kinase G and inhibiting fibrotic mediators such as angiotensin 2 or acti vating TGF b and Rho activation (22, 23) An experi mental study showed that sildenafil and oral PTX, a major PDE4 inhibitor that increases cAMP synthesis, inhibited the development of PD like plaques (24)
Previous studies have shown a strong relationship between ED and PD, ranging from 20% to 70% (3, 8, 25) Çakan et al indicated that one of the most common (68 5%) pre senting symptom in PD is ED (26) ED may be the result of PD, or the two diseases may share common pathophys iological features The possible mechanisms of develop
Effects of sildenafil on Peyronie’s disease
ment ED in PD include avoiding coitus due to perform ance anxiety, penile pain, difficulty in penetration and vas cular insufficiency Although there are many well designed experimental studies and animal models regarding the anti fibrotic effects of PDE5i, clinical trials investigating the effects PDE5i as monotherapy or in a combination treatment are limited In a retrospective study of patients with isolated septal scarring and no evidence of penile deformity, septal scarring was significantly regressed in the tadalafil group compared with control group (27) Ozturk et al investigated the effect of daily 50 mg of sildenafil on Peyronie's plaque and observed a statistically significant reduction in pain, whereas there was no significant differ ence in penile curvature between the two groups (28) Subjective and objective improvements in the characteris tics of PD receiving daily doses of tadalafil were also reported by Vernet et al (20) It was shown that the addi tion of 25 mg sildenafil to collagenase histolyticum (CCH) was superior to CCH monotherapy in improving penile curvature (10) In contrast, Palmieri et al reported similar outcomes in tadafil ESWT group compared to ESWT group (29)
Our study showed a significant improvement in degree of curvature and significant reduction in EF VAS score in the sildenafil received group, compared to the conventional treatment group Changes in degree of curvature and pain status were considered as the primary endpoints of the study As expected, an improvement in the IIEF 5 score, a secondary endpoint of the study, was found to be more pronounced in the sildenafil treated group At this point, we did not evaluate the change in plaque size as a criteri on for treatment success Some investigators have suggest ed that the evaluation of plaque size using any type of imaging is unnecessary, as these measurements are often inaccurate and changes in plaque size after treatment are not associated with changes in overall deformity and do not directly indicate treatment success (30) Treatment of PD mainly depends on the severity of curvature and the degree of ED (12, 13) In addition Peyronie’s plaque is not well formed in acute phase of the disease and possible spontaneous remission in plaque size can be expected in the acute phase
Our study has some limitations which need to be consid ered while evaluating its findings First, it is a retrospec tive, non randomized study that can be affected by all potential weaknesses stemming from its retrospective design and six months of follow up period of to evaluate the treatment outcomes is relatively short for this chron ic disease
CONCLUSIONS
To our knowledge, this is the first clinical study in the rel evant literature investigating the effect of PDE5i in an oral combination therapy in PD patients We showed that adding daily sildenafil 50 mg to colchicine and PTX com bination treatment improves the PD’s related symptoms of patients in the acute phase of PD Considering the proven antifibrotic efficacy of PDE5i, they may contribute to relieving Peyronie's symptoms in patients with ED Further multicenter prospective studies with larger num ber of cases are needed to obtain more precise results
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
321
Topcuoglu, M Çakan
REFERENCES
1 Tunuguntla HS Management of Peyronie's disease a review World J Urol 2001; 19:244 250
2 Kadioglu A, Tefekli A, Erol B, et al Retrospective review of 307 men with Peyronie’s disease J Urol 2002; 168:1075
3 Schwarzer U, Sommer F, Klotz T, et al The prevalence of Peyronie's disease: results of a large survey BJU Int 2001; 88:727 30
4 Bilgutay AN, Pastuszak AW Peyronıe's disease: a review of etiol ogy, diagnosis, and management Curr Sex Health Rep 2015; 7:117 131
5 Chung E, Ralph D, Kadioglu A, et al Evidence based management guidelines on Peyronie's disease J Sex Med 2016; 13:905 923
6 Ferrini MG, Davila H, Kovanecz I, et al Long term continuous treatment with vardenafil prevents fibrosis and preserves smooth muscle content in the rat corpora cavernosa after bilateral cavernos al nerve transection Urology 2006; 68:429 435
7 Ilg MM, Mateus M, Stebbeds WJ, et al Anti fibrotic synergy between phosphodiesterase type 5 inhibitors and selective oestrogen receptor modulators in Peyronie’s disease models Eur Urol 2019; 75:329 340
8 Kadioglu A, Tefekli A, Erol H, et al Color Doppler ultrasound assessment of penile vascular system in men with Peyronie's disease Int J Impot Res 2000; 12:263 7
9 Vande Berg JS, Devine CJ, Horton CE, et al Mechanisms of calci fication in Peyronie's disease J Urol 1982; 127:52 54
10 Ibrahim A, Gazzard L, Alharbi M, et al Evaluation of oral pen toxifylline, colchicine, and penile traction for the management of Peyronie’s disease Sex Med 2019; 7:459 63
11 Hellstrom WJ, Bivalacqua TJ Peyronie's disease: etiology, med ical, and surgical therapy J Androl 2000; 21:347 354
12 Hatzimouratidis K, Eardley I, Giuliano F, et al EAU Guidelines on penile curvature Eur Urol 2012; 62:543 52
13 Nehra A, Alterowitz R, Culkin DJ, et al Peyronie’s disease: AUA Guideline J Urol 2015; 194:745 753
14 Chiao TB, Lee AJ RoLe of pentoxifylline and vitamin E in atten uation of radiation induced fibrosis Ann Pharmacother 2005; 39:516 522
15 Safarinejad MR, Asgari MA, Hosseini SY, Farid D A double blind placebo controlled study of the efficacy and safety of pentoxifylline in early chronic Peyronie’s disease BJU Int 2009; 106:240 248
16 Alizadeh M, Karimi F, Fallah MR Evaluation of verapamil effi
cacy in Peyronie's disease comparing with pentoxifylline Glob J Health Sci 2014; 6(7 Spec No):23 30
17 Brant WO, Dean RC, Lue TF Treatment of Peyronie's disease with oral pentoxifylline Nat Clin Pract Urol 2006; 3:111 5
18 Prieto Castro RM, Leva Vallejo ME, Regueiro Lopez JC, et al Combined treatment with vitamin E and colchicine in the early stages of Peyronie's disease BJU Int 2003; 91:522 4
19 Akkus E, Breza J, Carrier S, et al Is colchicine effective in Peyronie’s disease? A pilot study Urology 1994; 44:291 295
20 Vernet D, Magee T, Qian A, et al Phosphodiesterase type 5 is not upregulated by tadalafil in cultures of human penile cells J Sex Med 2006; 3:84 94
21 El Sakka AI, Hassoba HM, Pillarisetty RJ, et al Peyronie’s dis ease is associated with an increase in transforming growth factor beta protein expression J Urol 1997; 158:1391 1394
22 Dunkern TR, Feurstein D, Rossi GA, et al Inhibition of TGF b induced lung fibroblast to myofibroblast conversion by phosphodi esterase inhibiting drugs and activators of soluble guanylyl cyclase Eur J Pharmacol 2007; 572:12 22
23 Wang Rosenke Y, Neumayer HH, Peters H NO signaling through cGMP in renal tissue fibrosis and beyond: key pathway and novel therapeutic target Curr Med Chem 2008; 15:1396 1406
24 Valente EG, Vernet D, Ferrini MG, et al L arginine and phos phodiesterase (PDE) inhibitors counteract fibrosis in the Peyronie's fibrotic plaque and related fibroblast cultures Nitric Oxide 2003; 9:229 44
25 Gholami SS, Gonzalez Cadavid NF, Lin CS, et al Peyronie’s dis ease: a review J Urol 2003; 169:1234
26 Cakan M, Akman T, Oktar T, et al The clinical characteristics of Peyronie's patients with notching deformity J Sex Med 2007; 4:1174 1178
27 Chung E, Deyoung L, Brock GB The role of PDE5 inhibitors in penile septal scar modeling: assessment of clinical and radiological outcomes J Sex Med 2011; 8:1472 7
28 Ozturk U, Yesil S, Goktug HN, et al Effects of sildenafil treat ment on patients with Peyronie's disease and erectile dysfunction Ir J Med Sci 2014; 183:449 53
29 Palmieri A, Imbimbo C, Creta M, et al Tadalafil once daily and extracorporeal shock wave therapy in the management of patients with Peyronie’s disease and erectile dysfunction: results from a prospective randomized trial Int J Androl 2012; 35:190 195
30 Levine LA, Greenfield JM Establishing a standardized evaluation of the man with Peyronie’s disease Int J Impot Res 2003; 15:S103 S112
Correspondence
Murat Topcuog lu, MD
muraturo@yahoo com
Assistant Professor, Department of Urology, Alaaddin Keykubat University, Antalya (Turkey)
Murat Çakan, MD muratcakandr@yahoo com
Department of Urology, Dıs kapı Yıldırım Beyazıt Training and Research Hospital, Ankara (Turkey)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
M
322
4081/aiua
Factors predicting the outcome of percutaneous epididymal sperm aspiration in men with obstructive azoospermia
Khaled Mohamed Almekaty
1
Mohamed Hasan Zahran
Tanta University Hospital, Urology Department, Tanta, Egypt;
Mansoura Urology Nephrology Centre, Urology Department, Mansoura, Egypt; 3 October 6 University, Faculty of Medicine, Department of Urology, Cairo, Egypt
Summary
Objectives: To report on the live birth rates (LBRs) following percutaneous epididymal sperm aspiration (PESA) in men with obstructive azoospermia (OA) and factors affecting treatment outcome which is under reported in the literature
Methods: This is a multicenter study that was conducted in Egypt including all couples undergoing intra cytoplasmic sperm injection (ICSI) for OA using PESA derived sperms Men were subdivided according to aetiology into congenital, iatrogenic and idiopathic groups. Fertilization, pregnancy and LBRs were determined and compared in each group. The longitudinal LBR, crude and expected cumulative delivery rates (CCDR, ECDR) were calculated. Multiple logistic regression analysis was used to determine significant associations between maternal, paternal and ICSI factors with successful live births.
Results: Ninety couples were included in the study. Viable sperm for ICSI was retrieved in 89 men (98.9%). A total of 155 ICSI cycles with 17 frozen embryo transfers resulted in 81 pregnan cies and 55 live births. After 5 cycles, the longitudinal LBR, CCDR and ECDR were 30%, 57.3% and 88.6% respectively. Maternal age and number of fertilized eggs were the only fac tors significantly affecting LBRs.
Conclusions: PESA is a minimally invasive procedure for secur ing viable sperm for ICSI in OA men, with high cumulative delivery rates. Maternal age and number of fertilized eggs are the only factors that significantly affecting LBR. The contempo rary longitudinal and cumulative LBRs provide objective out come data to counsel OA patients undergoing fertility treat ments
KEY WORDS: Live birth rates; Obstructive azoospermia; Percutaneous epididymal sperm aspiration
Submitted 1 July 2022; Accepted 17 July 2022
INTRODUCTION
Azoospermia is defined as the complete absence of sperm in the ejaculate and accounts for 10% of all male factor infertility, with an obstructive aetiology constituting up to 40% of azoospermia cases
Obstructive azoospermia (OA) may be congenital, as con genital bilateral absence of vas deferens (CBAVD), or acquired as following genitourinary infection, vasectomy or idiopathic (1) The therapeutic treatment options
include either reconstructive surgery, or sperm retrieval w i t h intracytoplasmic sperm injection ( I C S I ) S u r g i c a l sperm retrieval with ICSI can be used as a primary treat ment modality in patients who do not wish to proceed with surgical reconstruction, or in patients who have failed reconstructive surgery, or in cases of CBAVD Tournaye et al in 1994 reported successful fertilization and pregnancy with spermatozoa retrieved with Microsurgical Epididymal Sperm Aspiration (MESA) in patients with CBAVD Following this; percutaneous epididymal sperm aspiration (PESA) was described as an alternative to MESA for patients with OA (2, 3) Whilst the technique of PESA is well established, the live birth rates (LBRs) and factors affecting outcomes following PESA ICSI are under report ed in the literature (4) In this context, the sperm retrieval, fertilization and pregnancy rates following PESA ICSI vary from 69 to 100%, 58 77 7% and 40 50% respectively, although longitudinal, cumulative LBRs and the impact of male/female and ICSI variables on LBR have not been sys tematically analyzed (3 5) Furthermore, the effect of using fresh versus frozen sperm and embryos on LBRs, remains controversial with very limited contemporary data in the literature
The aim of this study was to analyze fertilization, preg nancy and LBR in couples undergoing PESA ICSI and factors affecting outcomes, including etiology of obstruc tion, the use of fresh versus frozen sperm and fresh ver sus frozen embryo transfer
MATERIALS AND METHODS
This is a multicenter study that was conducted in Egypt in Tanta, 6th of October and Al Mansoura universities The med ical records of patients with OA who underwent PESA ICSI between 2011 and 2021 were analyzed Men were subdi vided according to the aetiology of OA into congenital (eg vasal aplasia), iatrogenic (eg inguinoscrotal surgeries or vasectomy) and idiopathic (epididymal/ejaculatory duct obstruction) The age of the male/female partner, fertiliza tion, pregnancy and LBRs were determined in each group
All men in the vasal aplasia and the idiopathic groups underwent genetic analysis (including karyotyping, Y chro mosome micro deletions and CF gene analysis)
A323 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
ORIGINAL PAPER No conflict of interest declared
1 ,
2 , Mohamed
Lotfy Amer
1 ,
Ayman Mohamed Hagras
1 ,
Khaled Abdelaziz Salem
1 ,
Ayman Sayed Rashed
3 ,
Ahmed Fayez Ghaith
1
2
DOI: 10
2022 3 323
Technique of PESA
PESA was performed under local anaesthetic cord block or general anesthesia on the same day as oocyte retrieval and used immediately for ICSI or cryopreserved for elec tive use After taking written informed consent, the head of the epididymis was grasped between thumb and index finger and a 26 gauge needle attached to 3 ml syringe containing sperm buffer medium was inserted through scrotal skin into the epididymal head Suction with grad ual withdrawal of the needle was performed The aspirate was flushed with sperm buffering medium and immedi ately examined microscopically for presence of viable sperm by an embryologist
ICSI protocol
The unit ICSI protocol including ovarian stimulation, oocyte retrieval and embryo transfer protocol has been previously described (6)
Primary outcome measures
Primary outcome measures were sperm retrieval rate (SRR), fertilization rate (FR), pregnancy rate (PR), longitu dinal LBR and two measures of cumulative delivery rates: Crude cumulative delivery rate (CCDR) is the observed number of live births following a specific, pre deter mined number of ICSI cycles, divided by the total number of participating couples who had ICSI treat ment (7)
Expected cumulative delivery rate (ECDR) is the delivery rate assuming that couples who did not return for treatment had the same chance of a live birth over a specific number of cycles as those who continued their treatment (7)
Longitudinal LBR is the LBR after a single PESA ICSI cycle in all patients undergoing PESA (7)
Miscarriage was defined as the spontaneous loss of a clin ical pregnancy before 12 weeks of gestation
Secondary outcome measures
Secondary outcome measures included potential vari ables affecting LBRs including male/female age, etiology of obstruction; time elapsed since iatrogenic obstruction, the use of fresh versus frozen sperm and fresh versus frozen embryo transfer
Ethics statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integri ty of any part of the work are appropriately investigated and resolved The study was conducted in accordance with the Declaration of Helsinki The study was approved by the Institutional Review Board of Human Fertilization and Embryology Authority (HFEA) and was approved by our institutional review board (IRB approval No 35472/5/22) and individual consent for this retrospective analysis was waived
Statistical analysis
SPSS (IBM, version 22 (13 8 2013) software package was used to analyse data Descriptive statistics were expressed as median (IQR) Differences in outcomes between fresh and frozen sperm were analysed using Chi Square test
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
CCDR and ECDR were calculated using a Kaplan Meier Table & Plot Multiple linear regression was used to determine whether secondary outcome measures were associated with LBR and p values of 0 05 or less were deemed significant
RESULTS
Ninety couples with OA underwent PESA ICSI with a median male and female age of 44 (IQR 38 49) and 36 (IQR 32 39) years respectively In the bilateral vasal apla sia group, 7/18 (38 9%) patients were CFTR gene posi tive All patients had normal karyotype and no Y micro deletions
Sperm retrieval data
Sperm was successfully retrieved in 89 of 90 patients (98 9%) In one patient, PESA was unsuccessful and a conventional TESE was alternatively performed In 2 out of 35 cryopreserved sperm samples (5 7%), sperm was not viable on the day of ICSI and a simultaneous fresh PESA
Table 1. Treatment characteristics and ICSI outcomes Values
Demographics:
Male age, median (IQR) 44 (IQR 38 49)
Female age, median (IQR) 36 (IQR 32 39) Total number of ICSI cycles 155
Total number of frozen ET 27 ICSI cycles/couple, median (IQR) 2 (IQR 1 2)
Fertilization:
Ova retrieved, med an (IQR) 7 (5 11)
Sperm retrieved 89/90 (98 9%)
Cycles using fresh sperm 120 (77 4%) Cycles using Frozen sperm 35 (22 6%) Fertilized ova, median (IQR) 4 (3 8)
Fertilization rate 95 5% (148/155)
Embryo transfer: Per cycle, median (IQR) 2(1 2) Frozen embryo transfer 17 Pregnancy rate: Miscarriage 15/81 (18 5%) Clinical pregnancy 81/155 (52 3%)
Livebirth rate: Longitudinal 30% (27/90) of primary cycle 32 6% CCDR after 5 cycles 57 3% ECDR after 5 cycles 88 6%
Table 2.
CCDR and ECDR following PESA ICSI.
Khaled Mohamed Almekaty, Mohamed Hasan Zahran, Mohamed Lotfy Amer, et al
324
PET: Embryo transfer; ICSI: Intra Cytop asmic Sperm njection; IQR: Interquart le range; CCDR: Crude Cumulat ve Delivery Rates; ECDR: Expected Cumu ative De ivery Rates
Cycle CCDR (%) ECDR (%) 1 32 6 32 6 2 49 4 58 5 3 53 9 69 6 4 55 1 77 2 5 57 3 88 6 CCDR: Crude Cumulat ve Del very Rates; ECDR: Expected Cumu at ve De ivery Rates
Outcomes of percutaneous epididymal sperm aspiration
was performed One patient required a prolonged course of antibiotics to treat epididymitis post operatively
ICSI outcomes
The total number of ICSI cycles was 155, with a further 17 frozen embryo transfers 89 couples underwent a pri mary cycle of ICSI and 39 couples had repeated cycles (a total of 66 repeated cycles), ranging from 1 5 cycles per couple Detailed treatment characteristics and ICSI out comes are shown in Table 1
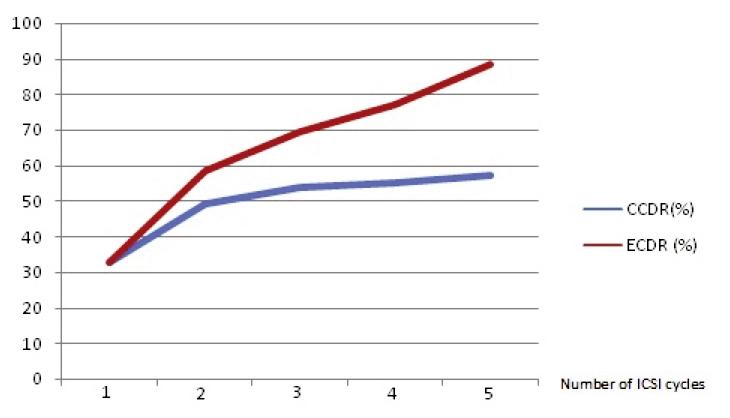
Following 5 cycles of ICSI, the CCDR and ECDR were 57 3% and 88 6% respectively (Table 2, Figure 1), with a longitudinal LBR of 30% (27/90) In total, PESA ICSI resulted in the birth of 6 twins and 49 singletons
Fifty five (61 1%) couples used fresh, while 35 (38 9%) couples used cryopreserved sperm on the day of oocyte retrieval There was no significant difference in pregnan cy (p = 0 731) or live birth rates (p = 0 553) on compar ing the use of fresh and frozen thawed sperm (Table 3)
Multiple logistic regression analysis demonstrated that PR significantly correlated to the number of fertilized ova (p = 0 018), while LBR correlated to the number of fertilized ova and maternal age (p = 0 037 and 0 0067 respectively)
All other factors including male age, aetiology of obstruc tion, time elapsed since iatrogenic obstruction, the use of fresh versus frozen sperm or fresh versus frozen embryos were not significantly associated with PR or LBR (Table 3)
Table 3.
Factors affecting PR and LBR (multiple regression analysis)
Association with pregnancy Association with live bir th (p value) (p value)
Male age 0 672 0 800
Female age 0 146 0 067*
Number of eggs collected 0 400 0
Number of eggs injected 0 129 0
Number of eggs fertilised 0.018* 0.037*
Number of embryo transfers 0 528 0 484
Fresh/frozen sperm 0 972 0
Fresh/frozen embryo transfer 0 166 0 482
Aetiology iatrogenic 0 325 0 542
Aetiology congenital 0 165 0 411
Aetiology iIdiopath c 0.618 0.881
Presence of gene mutation (ma
0 221 0 192
DISCUSSION
In OA patients, microsurgical reconstruction can be done to restore patency of the seminal tract Alternatively, sur gical sperm retrieval combined with ICSI can be utilized as a primary therapeutic option or in men who do not wish to proceed with surgical reconstruction or in whom reconstruction has failed The advancement in the surgical sperm retrieval methods and introduction of ICSI has been a landmark achieve ment in the treatment of OA, although there is very lim ited contemporary data in the literature reporting on LBRs and factors affecting LBRs in this particular cohort of patients (Table 4) (4, 8 12)
In the current study, viable sperm was obtained in almost all men (98 9% SRR) using PESA which proved to be a minimally invasive and effective means of sperm acquisi tion in men with OA Similarly, Kovac et al reported that in men with OA viable sperm was obtained in all 51 patients using PESA (100% retrieval rate) (4) In contrast, Yafiet al reported a much lower retrieval rate in similar patients (75 3%) (13)
Table 4.
Reported PESA and ICSI outcomes in the literature
Study Number of patients Pregnancy rate
attempts (/cycle or/patients)
Pasqualotto et al, 2002 130 patients /cycle: 34 6%/patient: 54
Pasqualotto et al, 2003 23 PESA for 20 patients /cycle: 37 5%
ina, 2003
PESA for 58 patients /cycle: 21/55 (38%)
Naru et al, 2008 53 patients /cycle: 30 (43 5%)
et al, 2014 51 (40 fresh, 11 frozen) /cycle: 17/35 (48.6%)
hanb y et al,
Current study
85 patients /patient: 35 (41 1%)
patients /cycle: 81/155 (52 3%)
Esteve et al 2013 analyzed the outcome of PESA and TESA in various aetiologies of OA and found that sperm retrieval using PESA was higher in men with CBAVD compared to post vasectomy and post infection groups (96 8, 69 5 and 76 4% respectively) and recommended the use of PESA for CBAVD and TESA for other aetiologies (5) These findings were not substantiated in the present study, in which we demonstrate a universally high sperm retrieval rate regard less of the aetiology of obstruction, a finding also observed in other series (4) It could be spec ulated that improvement in surgical and laboratory techniques may explain the improved outcomes in this series of patients More impor tantly, there was no difference in LBRs, irrespective of the aetiology of obstruction
Whilst we have demonstrated no difference in LBR comparing dif ferent aetiologies, an interesting further study would be to deter mine the LBR from ICSI in men with OA comparing epididymal versus testicular sperm in the con text of increased DNA fragmenta
A325 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
443
606
798
e)
* Statistica sign ficance (p < 0 05) CF: Cystic fibrosis
Figure 1 CCDR and ECDR following PESA ICSI
Miscar riage Livebir th rate or PESA
(Number or %)
5% Abortion: 11 1% NA
0 NA G
79
9 9 livebirths
5 NA Kovac
NA NA E
2015
NA 29 livebirths
90
15 Longitudinal 27/90 (30%) CCDR 57 3% ECDR 88 6% NA: not assessed CCDR: Crude Cumulative Del very Rate; ECDR: Expected Cumulative Del very Rates
Khaled Mohamed Almekaty, Mohamed Hasan Zahran, Mohamed Lotfy Amer, et al
tion and examine the potential for improving outcomes using testicular sperm in this cohort of men
An increased association of CFTR mutations has been described in patients with OA “other than CBAVD” and OAT syndrome, and it has been suggested that CFTR mutation screening should be limited to men with vasal aplasia on at least one side or in those with idiopathic epi didymal obstruction (14) Interestingly, we did not find any CFTR mutations, other than those found in the vasal aplasia group
Within the literature, the overall patency and pregnancy rates following vasectomy reversal are 86 and 58% respectively, with pregnancy rates inversely correlated with the duration of obstruction (15) In the present study, iatrogenic obstruction was attributed to bilateral inguinoscrotal surgeries mainly with vasectomy in only 2 patients done abroad Vasectomy as a means of male con traception is not allowed in the Arab and Islamic coun tries However, LBRs were not affected by the duration of obstruction and thus patients can be reassured that the time elapsed since obstruction does not negatively affect LBRs in couples undergoing PESA/ICSI This is in agree ment with a previous study showing no association between the time since vasectomy and clinical pregnancy after PESA (16)
Pregnancy rates following vasectomy reversal have been reported to be between 37 60% with a meantime elapsed since vasectomy of 5 7 10 years (17, 18), Similarly, PESA coupled with ICSI has been reported to result in clinical PR of 40 50 % in OA, although the number of studies report ing on LBRs in the literature is sparse (Table 4) (2 4)
Whilst it is difficult to make direct comparisons, the over all CCDR and ECDR in this study are comparable and consistent with the reported natural PR following vasec tomy reversal However, whilst this study demonstrates that PESA/ICSI patients have high CCDR (57 3%) and ECDR (88 6%), ICSI may not be as cost effective as sur gical reconstruction, as up to 5 cycles of ICSI will be required to achieve comparable paternity rates to surgical reconstruction Nevertheless, this study does provide important and contemporary comparative data on LBRs, which can be utilized when counseling patients prior to intervention for OA and therefore impact upon their deci sion to proceed with ICSI or surgical repair
Some studies have suggested that cryopreservation of sperm can negatively affect the vitality; motility of sperm and their fertilizing capacity (13) However, in this study, there were no differences in miscarriage, pregnancy or LBRs using fresh and frozen thawed epididymal sperm
Similarly, Kovac reported no statistically significant differ ence between fresh and frozen thawed PESA derived sperm in fertilization, overall pregnancy and multiple gestation rates (4) Thus cryopreservation, of sperm does not appear to have any negative impact on LBRs com pared to fresh sperm, although a small number of patients (5 7%) did require a further fresh PESA backup due to non viable sperm found on thawing cryopreserved sperm on the day of oocyte retrieval Similarly, the LBRs from frozen ET were comparable to fresh ET, which may not only improve the cost effectiveness of treatment for cou ples undergoing repeated ICSI cycles, but also reduce repeated interventions in the female partner
In the present study, pregnancy and LBRs were only affect ed by maternal age and number of fertilized ova Similarly, Kumtepe et al have reported that male age did not affect outcome of ICSI, whereas female age did (18) In contrast, Elhanbly et al reported that male age negatively affected the sperm characteristics obtained by PESA, clinical pregnancy and LBRs, yet the age of the female partner did not (12) This study has the limitation of being retrospective and including a relatively small number of patients in each aeti ological subgroup and further well designed prospective studies are needed to consolidate these current findings
PESA is not well adopted in Egypt or Arab countries because vasectomy is rarely done there The population of OA in these countries is different from Europe and US Most cases are congenital or idiopathic while iatrogenic cases are rare However, the outcome of the current study shows that the cumulative LBRs in the form of CCDR and ECDR, in OA patients undergoing PESA ICSI are high (75 3% and 88 6% after 5 ICSI cycles) whilst the longitu dinal LBR of 30% is consistent with the LBR following other assisted reproductive technologies
Based on this study, PESA should be more widely adopt ed in Egypt and Arab countries as a simple noninvasive method of sperm retrieval in OA patients Also, it pro vides contemporary data that should be useful for coun seling patients embarking on PESA/ICSI treatment
CONCLUSIONS
PESA is a simple and effective method of obtaining sperm for ICSI in OA patients, with the opportunity for sperm cryopreservation Only maternal age and number of fer tilized eggs affect pregnancy and LBR There was no dif ference in outcomes using fresh or frozen epididymal sperm or fresh or frozen embryos The longitudinal and cumulative LBRs from PESA/ICSI reported in this study provide contemporary outcome data to counsel patients with OA undergoing fertility interventions
REFERENCES
1 Jarow JP, Espeland MA, Lipshultz LI Evaluation of the azoosper mic patient J Urol 1989; 142:162
2 Tournaye H, Devroey P, Nagy J, et al Microsurgical epididymal sperm aspiration and intracytoplasmic sperm injection: a new effec tive approach to infertility as a result of congenital bilateral absence of the vas deferens Fertil Steril 1994; 61:1045 105
3 Shrivastav P, Nadkarni P, Wensvoort S, Craft I Percutaneous epi didymal sperm aspiration for obstructive azoospermia Hum Reprod 1994; 9:2058 61
4 Kovac JR, Lehmann KJ, Fischer MA A single center study exam ining the outcomes of percutaneous epididymal sperm aspiration in the treatment of obstructive azoospermia Urol Ann 2014; 6:41 45
5 Esteves SC, Lee W, Benjamin DJ, et al Reproductive potential of men with obstructive azoospermia undergoing percutaneous sperm retrieval and intracytoplasmic sperm injection according to the cause of obstruction J Urol 2013; 189:232 7
6 Almekaty K, Abomelha S, Thum Y, et al Reporting on longitudi nal live birth rates and cumulative delivery rates are more realistic outcome measures than sperm retrieval rates in couples undergoing mTESE ICSI Hum Fertil 2018; 22:139 144
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
326
7 Hull M, Eddowes H, Fahy U, et al Expectations of assisted con ception for infertility BMJ 1992; 304:1465 1469
8 Pasqualotto FF, Rossi Ferragut LM, Rocha CC, et al Outcome of in vitro fertilization and intracytoplasmic injection of epididymal and testicular sperm obtained from patients with obstructive and nonob structive azoospermia J Urol 2002; 167:1753 6
9 Pasqualotto F, Rossi Ferragut L, Rocha C, et al The efficacy of repeat percutaneous epididymal sperm aspiration procedures J Urol 2003; 169:1779 81
10 Glina S, Fragoso J, Martins F, et al Percutaneous epididymal sperm aspiration (pesa) in men with obstructive azoospermia Int Braz J Urol 2003; 29:141 146
11 Naru T, Sulaiman MN, Kidwai A, et al Intracytoplasmic sperm injection outcome using ejaculated sperm and retrieved sperm in azoospermic men Urol J 2008; 5:106 10
12 Elhanbly S, El Saied MA, Fawzy M, et al Relationship of pater nal age with outcome of percutaneous epididymal sperm aspiration intracytoplasmic sperm injection, in cases of congenital bilateral absence of the vas deferens Fertil Steril 2015; 104:602 6
Outcomes of percutaneous epididymal sperm aspiration
13 Yafi FA, Zini A Percutaneous epididymal sperm aspiration for men with obstructive azoospermia: predictors of sperm retrieval rates Fertil Steril 2013; 100:S448
14 Krausz C, Chianese C, Swerdloff RS, Wang C Emery and Rimoin's Principles and Practice of Medical Genetics (Sixth Edition), Chapter 33 Genetics of Male Infertility 2013, Pages 1 18
15 Lee R, Li PS, Schlegel PN, Goldstein M Reassessing reconstruc tion in the management of obstructive azoospermia: Reconstruction or sperm acquisition? Urol Clin North Am 2008; 35:289 301
16 Bromage SJ, Douglas J, Falconer DA, et al Factors affecting suc cessful outcome from ICSI in men following previous vasectomy World J Urol 2007; 25:519 24
17 Ozkavukcu S, Erdemli E, Isik A, Oztuna D, et al Effects of cry opreservation on sperm parameters and ultrastructural morphology of human spermatozoa J Assist Reprod Genet 2008; 25:403 11
18 Kumtepe Y, Yakin K, Kahraman S, et al Male age is not an inde pendent factor to affect the outcome of assisted reproductive tech niques Int J Androl 2003; 26:161 5
Correspondence
Khaled Mohamed Almekaty,MD dr khaledhafez@med tanta edu eg Mohamed Lotfy Amer, MD drmlamer@med tanta edu eg
Ayman Mohamed Hagras, MD ahagras80@yahoo com
Khaled Abdelaziz Salem, MD khsalemmd@gmail com
Ahmed Fayez Ghaith, MD (Corresponding Author) dr ahmedfayez@yahoo com
Tanta University Hospital, Urology Department, Tanta (Egypt) El Gharbia Govenorate, Tanta El Gash st Medical Campus, The Faculty of Medicine
Mohamed Hasan Zahran, MD zahranmha@yahoo com
Mansoura Urology Nephrology Centre, Urology Department, Mansoura (Egypt)
Ayman Sayed Rashed,MD aymanrashed@msn com
October 6 University, Faculty of Medicine, Department of Urology, Cairo (Egypt)
A327 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Premature ejaculation in the era of mobile health application: A current analysis and evaluation of adherence to EAU guidelines
Luigi Napolitano 1 , Luigi Cirillo 1 , Giovanni Maria Fusco 1 , Marco Abate 1 , Alfonso Falcone 1 , Vincenzo Morgera 1 , Gianluigi Cacace 1 , Luigi De Luca 1 , Pasquale Reccia 1 , Claudia Mirone 2 , Felice Crocetto 1 , Giuseppe Celentano 1 , Simone Morra 1 , Biagio Barone 1 , Ciro Imbimbo 1 , Nicola Longo 1 , Vincenzo Mirone 1 , Roberto La Rocca 1
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, School of Medicine, University of Naples "Federico II", Naples, Italy;
2 Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania "Luigi Vanvitelli", Naples, Italy
Summary
Introduction: Several mobile health applica tions (MHAs) have been developed to assist and improve the quality of life of patients affected by premature ejaculation, but the scientific quality and adherence to guide lines are not yet addressed
Materials and methods: On 25 May 2022, we conducted a search in the Apple App Store and Google Play Store We reviewed all mobile apps from Apple App Store and Google Play Store for premature ejaculation and evaluated their usage in screening, prevention, management, and adherence to EAU guidelines
Results: In total 9 MHA were reviewed All MHAs are geared towards the patient and provide information about diagnoses and treatment of PE The mean score were 2 87, 3 69, 2 77, 2 55, 2 86 for Engagement, Functionality, Aesthetics, Information, and Subjective quality respectively MHAs reported low and medium adherence to EAU guidelines
Conclusions: MHAs provide different services in many medical fields, including male sexual dysfunction Their development is constantly increasing, but the problems of scientific validation, content, and quality are not yet solved Much future research is necessary to improve the quality of the apps and promote new user designed, and high quality apps
KEY WORDS: App; E health; Mobile phone; Premature ejaculation; Mobile Application Rating Scale (MARS)
Submitted 23 June 2022; Accepted 1 July 2022
INTRODUCTION
Premature Ejaculation (PE) is among the most prevalent male sexual dysfunction worldwide affecting 30 50% of men with a high impact on the quality of life (QoL) of patients and partners (1 6) According to EAU guidelines, PE is defined as ejaculation which always or nearly always occurs prior to or within about one minute of vaginal pen etration, inability to delay ejaculation on all or nearly all vaginal penetrations (7) Several causes of PE like psycho logical issues (depression, stress, anxiety), traumatic sexu al experience, diabetes, hypertension, hyperthyroidism, alcoholism and recreational drugs have been described (8) Nowadays, many treatments are available: systemic
medications (selective serotonin reuptake inhibitors [SSRI], t r i c y c l i c a n t i d e p r e s s a n t s , p h o s p h o d i e s t e r a s e t y p e 5 inhibitors and analgesics), local anesthetics or sprays, and behavioral therapies (sexual therapy) However, men with PE often resort to using self medication for shame reasons (9) Therefore, mobile applications (apps) could represent a valid tool to support health behavior and medical infor mation about PE (10, 11) In the last years, more than 300 000 apps have been developed (12) and their use has increased during SARS Cov 2 pandemic (13 16) Apps can be downloaded from “Play Store” for Android and “App Store” for iOS (17) Several MHAs have been produced in different medical and surgical fields including the urolog ical and andrological fields (18 20) MHAs have been developed to assist patients in several conditions (21, 22) Optale et al reported their experience in a pilot study on 35 patients with PE using a mobile coaching app for ther apeutic exercises (23) Data reported improvement of the 5 question Premature Ejaculation Diagnostic Tool (PEDT) and the 4 question Premature Ejaculation Profile (PEP) in people who used the app compared the non users (23) Despite their number and widely use, quality assessments are still a problem To avoid this, in the last years, several instruments have been developed Among these, the most used tool is Mobile Application Rating Scale (MARS) (24 26) Several MHAs have been developed for assessing and management of PE, representing an important tool for patients However, despite their potential utility, much effort must be made regarding the quality, the validation, and the adherence to guidelines To the best of our knowl edge, there are no studies reporting the quality of apps for PE and their adherence to guidelines The aim of this study is to give an overview of apps for PE, currently free available on the market to evaluate the quality and the adherence to guidelines
MATERIALS AND METHODS
Search strategy
We performed an observational cross sectional descrip
No conflict of interest declared
Archivio Italiano di Urologia e Andrologia 2022; 94, 33 28 ORIGINAL PAPER
DOI: 10 4081/aiua 2022 3 328
tive study of all smartphone apps for patients about PE available on the iOS and Android platforms and evaluated their adherence to EAU guidelines On 25 May 2022, we conducted a search in Google Play Store for Android phones and Apple App Store for iPhones with the key words ‘premature ejaculation’ , ‘premature ejaculation treat ment’ and ‘premature ejaculation diagnosis’ using the search tab We used a wide array of keywords due to the search strategy of Google Play Store and Apple App Store which is based on finding keywords in titles, app descriptions and tags Other searches of information provided in books or other formats were excluded Two authors (GMF, MA) screened separately in App Store and Google Play Store apps during the search by reading the title and description in the app store A third author (LC) resolved any discrepancies At the beginning all apps were report ed in Excel form and, according to the exclusion criteria, were screened All MHAs regarding PE, providing a serv ice to patients, in English, and free to download were included in this analysis Apps not specifically focused on PE, apps not allowing access to all users and those not available in English were excluded Successively, all reviewers downloaded and installed the apps on their personal mobile device They interacted for twenty min utes with each app to explore its features before complet ing the MARS and evaluated their adherence to EAU guidelines To assess apps, they were downloaded to either an Android and an iOS device If apps were avail able in both app stores, the iOS version was assessed A total of 840 apps were found by our search, 816 of them were from the Google Play Store (Android) and 24 of them were from the Apple App Store (iOS) Of the total, 249 apps were screened after removing duplicates and paid apps Of the total screened apps, 196 apps met excluding criteria and were removed In particular 1 app resulted in both stores
The app from the Apple App Store was analyzed In total, 53 apps were eligible for the final evaluation and were down loaded
Finally, 9 apps were included in the final review after removing 44 apps that met exclusion criteria after down load A flow diagram based on the P R I S M A s t a t e m e n t ( F i g u r e 1 ) w a s included for the selected apps (27) Table 1 shows the analyzed apps char acteristics The 9 premature ejaculation apps were evaluated by four members of the research team on a 5 point Likert scale based on MARS characteristics
Data extraction
On 27 May 2022 reviewers discussed methods of recording data to ensure standardized modality and a prede fined Excel form was created to collect data The following data were extracted from MHA: title, language, customers, costs, source (Google Play Store or Apple
Premature ejaculation in the era of mobile health application
App Store), field/disease, rating/feedback from the users and service provided
Assessment of app quality
To assess apps ’ quality, Mobile Application Rating Scale (MARS) was used MARS is a multidimensional instrument of 23 structured questions evaluating engagement, func tionality, esthetics, information, app subjective quality, and app specific, showing a very acceptable reliability and validity MARS is composed of 19 items grouped in four categories of perceived app quality: engagement (five items assessing the extent to which the app engages target users); functionality (four items assessing how easy the app is to navigate and the overall app performance); aesthetics (three items assessing visual appearance and style); information (seven items assessing accuracy, quality, and quantity of the app), and 1 category of subjective quality Each category score is the mean of the different items, rated on a 5 point Likert type scale (from 1 = inadequate to 5 = excellent) within its category The mean of the 4 app quality category scores is used to calculate overall quality score and the final score range from 0 to 5 A score of between 1 and 2/5 is considered as ‘ poor ’ quality, while 3/5 is ‘acceptable’ and at least 4/5 is ‘good’ quality If scores differed by a single point, reviewers use the mean of the two ratings, while if scores differing by more than a single point, reviewers solve the discrepancy through discussion and consensus agreement Mean scores were calculated for each domain and an over all quality score was calculated based on the aggregated mean values for each of the four domains The mean score for subjective quality is calculated
A329 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
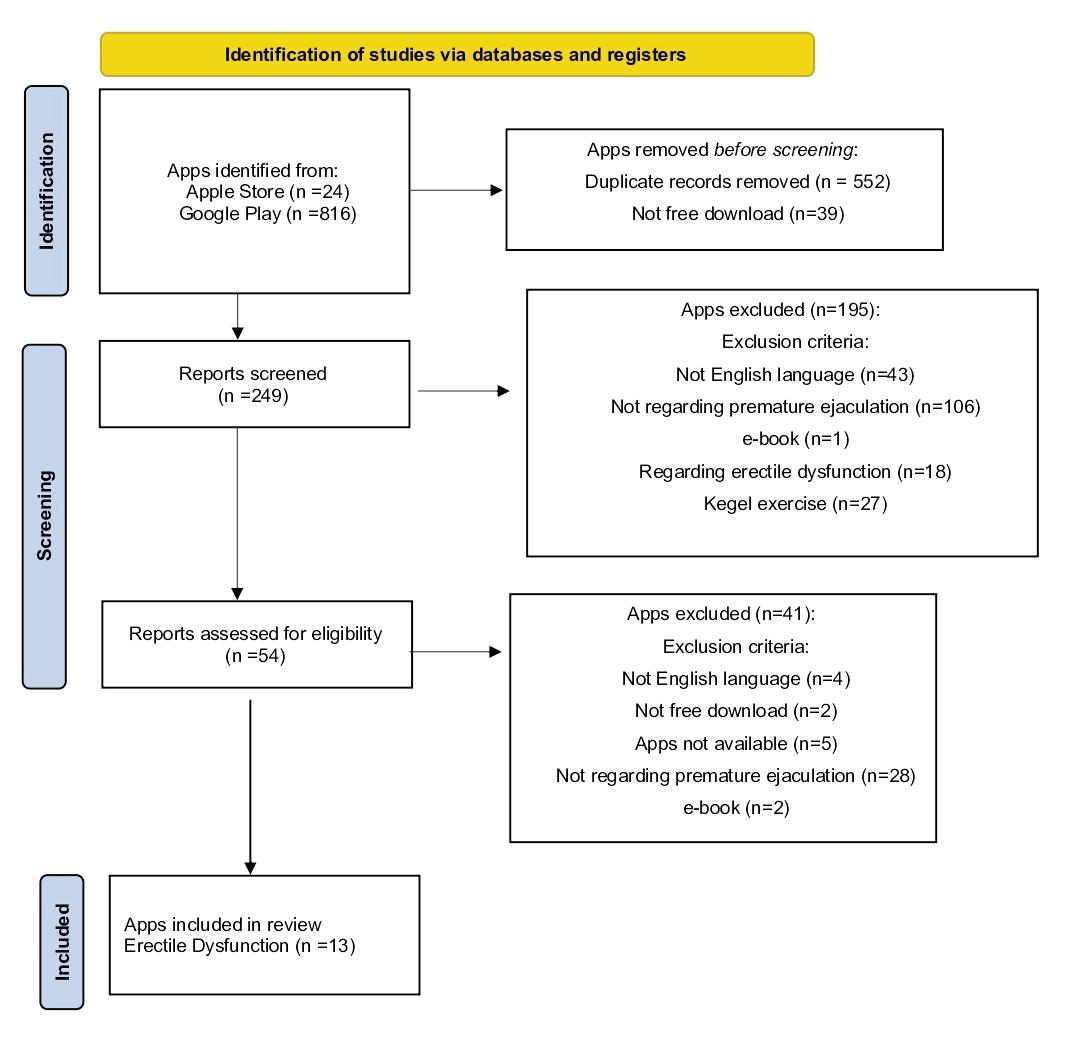 Figure 1 PRISMA
L Napolitano, L Cirillo, G M Fusco, et al
Figure 1 PRISMA
L Napolitano, L Cirillo, G M Fusco, et al
Assessment of app adherence to EAU guidelines
An adherence checklist of five items (definition, phys iopathology, diagnosis, risk factors and treatment) based on section 5 of the EAU guidelines of PE has been created Two independent reviewers (urologist with high experi ence in male sexual dysfunction) analyzed separately apps for their adherence to EAU guidelines According to criteria used in similar studies, raters gave each app a score from 0 to 3 for each of the five items A score of ‘‘0’’ indicated no adherence to guidelines A score of ‘‘1’’ indi cated a weak adherence A score of ‘‘2’’ indicated a partial or moderate adherence A score of ‘‘3’’ indicated strong adherence Where coding scores differed by 1 point, the average of the two ratings was taken If there was a greater than 1 point discrepancy, a third author reviewed apps and resolved the discrepancy The possible score on the checklist ranged from 0 to 15 for each app To facilitate evaluation, adherence to the checklist was arbitrarily con
Table 1.
characteristics
Name
Premature
sidered low with a total score ranging from 0 to 5, medi um (6 10), and high (11 15)
RESULTS
In total 9 apps were included in the final analysis: 4 from the Apple App Store and 5 from the Google Play Store Four apps (44%) provided information about treatment; 2 (22%), 3 (33%) provide information about diagnosis and overall information respectively PE risks factors were men tioned in some MHA Data about downloads were available for 5 apps out of the 9 reviewed Downloads were not available for MHAs presented in the Apple App Store The most downloaded app was Last Longer in Bed & Control Premature Stamina of which more than 100 000 downloads were reported All the apps were planned to be used by patients No information about MHA rating was available MARS scale scores are represented in Table 2
Engagement
Test PEDT
Pea last longer in bed Apple n a Smarter health solution LLC Health and We lness Informative, definition Treatment Exercises
Slow down last longer Apple n.a. Slow down health inc Medicine Exercises
SMART SAA Apple n a PERGALI LTD Health and We lness Informative, definition Test
Last onger in bed & control premature stamina Android 100 000 + MasterpieceApps Lifestyle Treatment My sex Doctor Android 10 000+ MYSD LTD Lifestyle Def nition My sex Doctor lite Android 10 000+ MYSD LTD Lifestyle Def nition
Premature ejaculation Android
Premature ejaculation: Information and treatment
+ Nature Healthy Care Entertrainment Definition D agnos s Treatment
HemiSphere Studio Health
Definition D agnos s Treatment
Table 2.
MARS scale scores
Name
The score in this section was based on a 5 point Likert scale in 5 subscales (Entertainment, Interest, Customization, Interactivity and Target group) The mean score was 2 87 Scores ranged from 2 to 4 out of 5 The “Premature Ejaculation” app (Android) produced by Nature Healthy Care received the highest score for the engagement
This app contains PE definitions, as well as information about diagnosis and treatment
Functionality
The score of the functionality sec tion was based on a 5 point Likert scale in 4 subscales (Performance, Ease of use, Navigation and Gestural design) and the mean score was 3 69 Scores ranged from 2 75 to 4 5 “Last Longer in Bed & Control
Premature Stamina” app (Android) produced by Masterpiece achieved the maximum score
Aesthetics
The aesthetics section was formed by a 5 point Likert scale in 3 sub s c a l e s ( L a y o u t , G r a p h i c s , V i s u a l Appeal) and the average score was 2 77 Scores ranged from 1 33 to 3 3 o u t o f 5 , a n d “ P r e m a t u r e E j a c u l a t
o
p
o d
c
d b
N a t
Healthy Care reached the maximum aesthetics score
Information
The information section was
by a 5 point Likert scale in 7 sub scales and the mean score was 2 55 Score ranged from 1 to 3 6 The “SMART SAA” (Apple) produced by
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
330
i
n ”
r
u
e
y
u r e
formed
App
of application Android/ Download Producer Categor y Focus Apple/Both
ejaculation tools Apple n a Putu angga risky raharja Medicine Informative, definition
5000
Android 1000+
and fitness
of application Engagement Functionality Aesthetics Infor mation Mean App subjective (section A) (section B) (section C) (section D) (A+B+C+D) quality (section E) Premature ejaculation tools 24 1 33 2 2 33 2 Pea last longer in bed 3 8 3 25 3 3 33 3 34 3 25 Slow down last longer 3 4 2 75 3 2 66 2 95 3 SMART SAA 3 6 3 75 3 3 6 3 49 2 75 Last longer in bed & control premature stamina 3 4 5 31 2 88 1 75 My sex Doctor 2432 2 75 3 My sex Doctor lite 2432 2 75 3 Premature ejaculation 44 3 3 3 6 3 72 4 Premature ejaculation: Information and treatment 23 2 3 2 8 2 52 3
Pergali LTD and “Premature Ejaculation” produced by Nature Healthy Care achieved the highest score of 3 6 These two apps respectively offer information and test for PE, and definition, diagnosis, and treatment options for PE
Subjective quality
The subjective quality section consisted of 4 items The mean score was 2 86, with scores ranging from 1 75 to 4 “Premature Ejaculation” app reached the maximum score
EAU adherence checklist
We evaluated the EAU guidelines adherence in 9 apps EAU adherence scores are represented in Table 3 The PE definition was reported in 8 (88 9%) apps, the score ranged from 2 to 3 (mean 2 25); physiopathology was reported in 7 (77 8%) apps, the score ranged from 1 to 2 (mean 1 57); risk factors were reported in 4 (44 4%) apps, the score ranged from 1 to 2 (mean 1 5); diagnosis was reported in 9 (100%), the score range from 1 to 3 (mean 1 67); treatment was reported in 5 (55 6%), the score ranged from 1 to 3 (mean 2 6) The overall score ranged from 2 to 13 (mean 7) The highest score was reported by “Premature Ejaculation” (Android) produced by Nature Healthy Care Only two of the nine evaluated apps reached the maximum definition score of 3 in defi nition, while none of the apps reached 3 in phys iopathology and risk factors Finally, only one app and four apps reached the maximum respectively in diagnosis and treatment
DISCUSSION
The current study aimed to evaluate the overall quality MHAs for PE and their adherence to EAU guidelines To the best of our knowledge, no previous studies examined this topic We addressed this void and identified several note worthy observations First, despite the high number of MHAs no standardized evaluation method has been assessed, but many studies suggest combining the use of different scores In the present study we used MARS to evaluate the apps ’ quality MARS was a tool widely used in several previous published studies In this study, the mean scores of the MARS categories are dramatically low and MHAs are inadequate to assist patients “Information” and
Premature ejaculation in the era of mobile health application
“
Esthetics” show the lowest score, 2 55 and 2 77 respectively
“Functionality” reported the highest score (3 69) As previously showed in our study on MHAs for erectile dysfunction, apps were developed without healthcare support and the most important tool is their usability (28) Jupp et al showed that “Functionality” is the highest score in MHAs for oncology patients (29)
This suggests that MHAs are easy to navigate and efficient and represent an important skill for MHAs geared for the patients The overall low quality of MHAs seems to be related to their commercial tone
Furthermore, our results indicate that healthcare and medical institutions are still missing the potential of reaching patients through this technology, and therefore the MHA were a field of only commercial initia tives In fact, only three (33%) of MHA were considered acceptable The same results were reported in other studies using MARS to evaluate different medical conditions (30) Amor García et al report a score of 2 98 analyzing geni tourinary cancer (17); Kwan et al and Knitza et al report scores of 3 48 and 3 85 in apps for rheumatology condi tions (31, 32) This suggests that overall MHAs regardless of diseases and fields require general improvements, in par ticular, healthcare involvement in MHA development is mandatory Second, most MHAs had low or medium adherence to EAU guidelines The highest adherence is reported in PE definition and treatment “Premature Ejaculation” (Android) produced by Nature Healthy Care shows the highest score (13) and the high adherence to EAU guidelines This is not surprising, because Nature Healthy Care produce several apps in different medical fields MHAs report a wide options of treatment for PE including behavioural and medical options According to the literature, treatment of PE includes pharmacological and non pharmacological treatment as well as psychother apy and behavioral therapies (masturbation before coitus (precoital masturbation) “stop start” and “squeeze” tech niques, use of multiple condoms, and pelvic floor exercise) Pelvic floor exercise/Kegel exercises help strengthen pelvic floor muscles to provide better ejaculation control Ischiocavernous, bulbocavernosus muscles, and sphinc ters, play an important role in sexual function, with high electromyographic activity and rhythmic contractions during the ejaculatory period (8, 33 35) In a prospective quasi randomized controlled trial, Jiang et al reported that penis root masturbation (PRM) and Kegel exercise (KE) have effects on PPE and KE was less effective than PRM EAU guidelines report weak evidence about behavioural and psychotherapy treatments for PE (7) Despite these, our search show 27 MHAs for KE as PE treatment Our study has several strengths: first of all, we examined for the first time the content, the quality, and the adherence to EAU guidelines about PE; we performed a rigorous search, screening, and analysis on Apple and Google stores; reviewer had experience in MARS scale using The main limitation of our study is the number of apps
A331 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
sub Table 3. EAU adherence checklist scores. Name of application Definition Physiopatholog y Risk factors Diagnosis Treatment Total (0 3) (0 3) (0 3) (0 3) (0 3) Premature ejaculation tools n a n a n a 2 n a 2 Pea last longer in bed 31 n a 138 Slow down last longer 21223 10 SMART SAA 2 n a n a 2 n a 4 Last Longer in bed & control premature stamina 211138 My sex Doctor 22 n a 1 n a 5 My sex Doctor lite 22 n a 1 n a 5 Premature ejaculation 32233 13 Premature ejaculation: Information and treatment 221218
jected to the qualitative assessment Furthermore, the reproducibility of the research turns out to be complex due to the working method of the App Store and Google Play Store (the visibility of apps depends on the device and on the country where the search is performed); the exclusion criteria, which led to the exclusion of paid apps; the guidelines developed for healthcare and not for patients and the constant production of new MHA
CONCLUSIONS
The use of MHAs for PE represents an unexplored topic, with much future perspective MHAs have been reported as an integral part of patients’ lives, and although from year to year, their numbers are constantly increasing, the over all quality is still low The problems of scientific validation content and quality in MHA for PE are not yet solved Further several studies are needed to improve the quality, accessibility, user designed, and high quality of apps
REFERENCES
1 Gao J, Zhang X, Su P,, et al Prevalence and impact of premature ejaculation in outpatients complaining of ejaculating prematurely: using the instruments of intravaginal ejaculatory latency time and patient reported outcome measures Int J Impot Res 2014; 26:94 9
2 Sjögren Fugl Meyer K, Fugl Meyer AR Sexual disabilities are not singularities Int J Impot Res 2002; 14:487 93
3 Mirone V, Napolitano L, D’Emmanuele di Villa Bianca R, et al A new original nutraceutical formulation ameliorates the effect of Tadalafil on clinical score and cGMP accumulation Arch Ital Urol Androl 2021; 93:221 6
4 Romano L, Granata L, Fusco F, et al Sexual dysfunction in patients with chronic gastrointestinal and liver diseases: a neglected issue Sex Med Rev 2021; S2050 0521(21)00039 1
5 Barone B, Napolitano L, Abate M, et al The role of testosterone in the elderly: what do we know? Int J Mol Sci 2022; 23:3535
6 Romano L, Pellegrino R, Sciorio C, et al Erectile and sexual dys function in male and female patients with celiac disease: A cross sec tional observational study Andrology 2022; 10:910 918
7 Salonia A, Bettocchi C, Boeri L, et al European Association of Urology guidelines on sexual and reproductive health 2021 update: male sexual dysfunction Eur Urol 2021; 80:333 57
8 Veettil Raveendran A, Agarwal A Premature ejaculation current concepts in the management: A narrative review Int J Reprod Biomed IJRM [Internet] 25 January 2021 [cited 22 June 2022]; A v a i l a b l e f r o m : https://knepublishing com/index php/ijrm/article/view/8176
9 InformedHealth org [Internet] Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006 Premature ejaculation: What can I do on my own? 2019 Sep 12 Available from: https://www ncbi nlm nih gov/books/NBK547551/
10 Iribarren SJ, Akande TO, Kamp KJ, et al Effectiveness of mobile apps to promote health and manage disease: systematic review and meta analysis of randomized controlled trials JMIR MHealth UHealth 2021; 9:e21563
11 Milne Ives M, Lam C, De Cock C, et al Mobile apps for health behavior change in physical activity, diet, drug and alcohol use, and mental health: systematic review JMIR MHealth UHealth 2020; 8:e17046
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
12 Levine DM, Co Z, Newmark LP, Groisser AR, et al Design and testing of a mobile health application rating tool Npj Digit Med 2020; 3:74
13 John Leon Singh H, Couch D, Yap K Mobile health apps that help with COVID 19 management: scoping review JMIR Nurs 2020; 3:e20596
14 Barone B, De Luca L, Napolitano L, et al Lower urinary tract symptoms and mental health during COVID 19 pandemic Arch Ital Urol Androl 2022; 94:46 50
15 Napolitano L, Barone B, Crocetto F, et al The COVID 19 pan demic: is it a wolf consuming fertility? Int J Fertil Steril 2020; 14:159 60
16 Sujarwoto S, Augia T, Dahlan H, et al COVID 19 mobile health apps: an overview of mobile applications in Indonesia Front Public Health 2022; 10:879695
17 Amor García MÁ, Collado Borrell R, Escudero Vilaplana V, et al Assessing apps for patients with genitourinary tumors using the Mobile Application Rating Scale (MARS): systematic search in app stores and content analysis JMIR MHealth UHealth 2020; 8:e17609
18 Rajani NB, Weth D, Mastellos N, Filippidis FT Adherence of popular smoking cessation mobile applications to evidence based guidelines BMC Public Health; 19:743
19 Vaggers S, Puri P, Wagenlehner F, Somani BK A content analy sis of mobile phone applications for the diagnosis, treatment, and pre vention of urinary tract infections, and their compliance with European Association of Urology guidelines on urological infections Eur Urol Focus 2021; 7:198 204
20 Escriche Escuder A, De Torres I, Roldán Jiménez C, et al Assessment of the quality of mobile applications (apps) for manage ment of low back pain using the Mobile App Rating Scale (MARS) Int J Environ Res Public Health 2020; 17:9209
21 Kernebeck S, Busse TS, Böttcher MD, et al Impact of mobile health and medical applications on clinical practice in gastroenterol ogy World J Gastroenterol 2020; 26:4182 97
22 Martínez Pérez B, de la Torre Díez I, López Coronado M Mobile health applications for the most prevalent conditions by the World Health Organization: review and analysis J Med Internet Res 2013; 15(6):e120
23 Optale G, Burigat S, Chittaro L, Riva G Smartphone based ther apeutic exercises for men affected by premature ejaculation: a pilot study Sex Med 2020; 8:461 71
24 Terhorst Y, Philippi P, Sander LB, et al Validation of the Mobile Application Rating Scale (MARS) Moitra E, curatore PLOS ONE 2020; 15:e0241480
25 Dantas LO, Carvalho C, Prando BC, et al Mobile health tech nologies for the management of rheumatic diseases: a systematic review of online stores in Brazil Clin Rheumatol 2021; 40:2601 9
26 Moglia ML, Nguyen HV, Chyjek K, et al Evaluation of smartphone menstrual cycle tracking applications using an adapted APPLICA TIONS Scoring System Obstet Gynecol 2016; 127:1153 60
27 Page MJ, McKenzie JE, Bossuyt PM, et al The PRISMA 2020 statement: an updated guideline for reporting systematic reviews BMJ 2021; 372:n71
28 Luigi Napolitano, Giovanni Maria Fusco, Luigi Cirillo, et al Erectile dysfunction and mobile phone applications: Quality, content and adherence to European Association guidelines on male sexual dysfunction Arch Ital Urol Androl 2022; 94:211 216
29 Jupp JCY, Sultani H, Cooper CA, et al Evaluation of mobile phone
L Napolitano, L Cirillo, G M Fusco, et al
332
applications to support medication adherence and symptom manage ment in oncology patients Pediatr Blood Cancer 2018; 65:e27278
30 Narrillos Moraza Á, Gómez Martínez Sagrera P, Amor García MÁ, et al Mobile apps for hematological conditions: review and con tent analysis using the mobile app rating scale JMIR MHealth UHealth 2022; 10:e32826
31 Kwan YH, Ong WJ, Xiong M, et al Evaluation of mobile apps targeted at patients with spondyloarthritis for disease monitoring: systematic app search JMIR MHealth UHealth 2019; 7:e14753
32 Knitza J, Tascilar K, Messner EM, et al German mobile apps in
Premature ejaculation in the era of mobile health application
rheumatology: review and analysis using the Mobile Application Rating Scale (MARS) JMIR MHealth UHealth 2019; 7:e14991
33 Jiang M, Yan G, Deng H, et al The efficacy of regular penis root masturbation, versus Kegel exercise in the treatment of primary pre mature ejaculation: A quasi randomised controlled trial Andrologia 2020; 52:e13473
34 Pastore AL, Palleschi G, Fuschi A, et al Pelvic floor muscle reha bilitation for patients with lifelong premature ejaculation: a novel therapeutic approach Ther Adv Urol 2014; 6:83 8
35 Pischedda A, Fusco F, Curreli A, et al Pelvic floor and sexual male dysfunction Arch Ital Urol Androl 2013; 85:1 7
Correspondence
Luigi Napolitano luiginap89@gmail com
Luigi Cirillo, MD (Corresponding Author) cirilloluigi22@gmail com
Giovanni Maria Fusco, MD giom fusco@gmail com
Marco Abate, MD marcoabate5@gmail com
Biagio Barone,MD biagio barone@unina it
Alfonso Falcone, MD alfonso falcone01@gmail com
Vincenzo Morgera, MD vincemorgera87@gmail com
Gianluigi Cacace, MD cacace gianlu@gmail com
Felice Crocetto, MD felice crocetto@gmail com
Simone Morra, MD simonemorra@outlook com
Luigi De Luca, MD luigideluca86@gmail com
Pasquale Reccia, MD reccia pasquale1@gmail com
Giuseppe Celentano, MD dr giuseppecelentano@gmail com
Nicola Longo, MD nicolalongo20@yahoo it Ciro Imbimbo,MD ciro imbimbo@unina it Vincenzo Mirone, MD mirone@unina it
Roberto La Rocca, MD robertolarocca87@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples "Federico II", Naples, Italy Via Sergio Pansini n 5, Naples (Italy)
Claudia Mirone, MD claudiamirone@outlook it
Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania "Luigi Vanvitelli", Naples (Italy)
A333 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
4081/aiua
An original mininvasive corporoplasty technique for penile curvature without circumcision
Antonio Rossi 1 , Giovanni Alei 2 , Pietro Viscuso 3 , Antonio Tufano 3 , Marco Frisenda 3 , Guglielmo Mantica 4 , Pierluigi Bove 5 , Rosario Leonardi 6 , Mauro De Dominicis 1 , Alessandro Calarco 1
1 Department of Urology, “Cristo Re” Hospital, Rome, Italy;
2 Department of Plastic and Reconstructive Surgery, "Sapienza" Rome University, Policlinico Umberto I Hospital, Rome, Italy;
Department of Maternal Infant and Urological Sciences, "Sapienza" Rome University, Policlinico Umberto I Hospital, Rome, Italy;
Policlinico San Martino, Genova, Italy;
San Carlo di Nancy Hospital, Roma, Italy;
Casa di Cura Musumeci Gecas, Gravina di Catania (CT), Italy
Summary
Objective: We describe an original minimally invasive penile plication technique with scro tal or infrapubic access, not requiring circumcision, for penile curvature of different severity and types This technique can be used to correct both congenital and acquired curvatures, mono or bidirectional deformities
Materials and methods: Between 2012 and 2018 we treated 134 patients suffering from congenital curvature (33) and acquired curvature from Peyronie's disease (101) The average curvature was 62.2° (± 30.4°). Preoperative evaluation included prostaglandin E1 injection with photographic documentation and measurement of penile angulation, administration of IIEF 15, vasoactive penile Doppler ultrasound, analysis of thermal and vibratory sensitivity with Genito Sensory Analyzer (GSA) and assessment of nocturnal penile stiffness with Rigiscan, per formed twice, for a detailed evaluation of patient’s erectile function.
Scrotal access was performed in patients with dorsal and/or lat eral penile curvature; the infrapubic access was performed in patients with ventral curvature. After preparation and incision of Colles’ fascia, penis was partially degloved and an original plication technique called "binary corporoplasty" was performed at the site or sites established at preoperative assessment, with non resorbable synthetic multifilament (Premicron®) suture.
Results: Complete correction of penile curvature was achieved in 96.8 % of patients. No major complications were reported, and no patients suffered worsening in erectile function or in penile sensitivity The average shortening of convex side was 1 65 cm (± 0 7 cm) and all patients report easy intercourse after correc tion The average time of surgery was 46 minutes (± 11 min) and all procedures were performed as a day hospital or ambula tory settings, with local anesthesia and light sedation Overall satisfaction rate is 96%
Conclusions: This is a simple and rapid technique that perfectly corrects even the most severe and complex penile curvatures In comparison to traditional techniques, such as Nesbit procedure, this technique is associated with low morbidity, a very low recurrence rate and a great aesthetic results Aesthetic and functional patients’ satisfaction was excellent
KEY WORDS: Corporoplasty; Induratio penis plastica; Recurvatum; Peyronie’s disease; Penile disease
Submitted 9 September 2022; Accepted 12 September 2022
INTRODUCTION
Penile curvature (PC) is an increasingly common disorder consisting of an alteration in the shape of the erect penis which instead of being straight appears curved on one or more planes It can be congenital or acquired The curva ture can be ventral, dorsal, lateral or mixed and it can be associated with urethral malformations
Congenital curvature can be caused by disproportionate development of the tunica albuginea of the corporal bod ies (1) Penises with congenital curvature are usually good sized and the young patient notices the anomaly after the onset of puberty The curvature is often ventral, that is the one causing the greatest problems in coital dynamics
Acquired penile curvature can be caused by penile frac tures or traumas or mostly by Peyronie’s disease also called induratio penis plastica (IPP)
In both congenital and acquired curvatures the surgical indication arises when the curvature of the penis does not allow normal sexual intercourse Symptoms are an initial difficulty in penetration with pain for the patient and/or for the partner that can evolve towards the impossibility of penetration when the curvature is severe
Several alternatives and improvements have been pro p o s e d s i n c e t h e fi r s t c o r p o r o p l a s t y t e c h n i q u e w a s described by Nesbit in 1965 (2), although most tech niques require circumcision and total penile degloving
This aggressive approach leads to various problems such as altered sensitivity, unsightly scars and high recurrence rates In order to balance results in term of erectile and a e s t h e t i c f u n c t i o n , e s p e c i a l l y i n t h e p a t i e n t w i t h Peyronie’s disease, it is crucial to seek minimally invasive surgical techniques
We describe a new original plication technique where surgical access is at the base of the penis and the albug inea incision is not performed making the surgery safe, easier and minimally invasive
MATERIALS AND METHODS
Between 2012 and 2018 we treated 134 patients suffering from congenital curvature (33) or curvature acquired from Peyronie's disease (101) (Figure 1)
No conflict of interest declared
Archivio Italiano di Urologia e Andrologia 2022; 94, 33 34 ORIGINAL PAPER
3
4
5
6
DOI: 10
2022 3 334
Figure 1. Some of the clinical cases treated Congenital and acquired curvature
Figure 2. Preoperative identification of the correction point/s.
Original corporoplasty technique
nal incision The technique consists of a dorsal access at the base of the penis in case of ventral bending (Figure 3) or a scrotal access for dorsal and/or lateral bending (Figure 4), with no consequences on penile sheaths or alterations in sensitivity
The procedure can be performed under either local anes thesia with a light sedation To correct a dorsal and/or lat eral curvature we perform a small median longitudinal incision on the scrotal raphe whereas for the ventral cur vatures we perform a small infrapubic incision Both inci sions are about 3 cm in length
We access the Colles space with bevel scissors creating a space to make degloving easier The pre established sites are identified by means of a sterile ruler starting from the meatus while the assistant completely stretches the penis from the glans
With an Allis clamp, the selected site in the Colles space is pressed and a selective degloving is performed at this level to expose the albuginea in order to make the “track” corporoplasty (Figure 5)
Figure 3.
Dorsal incision at the base of the penis


Before the procedure patients were carefully evaluated to assess type and severity of curvature and any associated malformations In particular, initial length of the penis and erectile function were assessed Careful evaluation of all these variables together with the patient is mandatory because this is a functional aesthetic surgical procedure
Accurate measurements were made to plan the site and the number of corporoplasties by simulating the straight ening of the penis Photographs and measures were taken to document the potential result In fact, the patient must be aware of the change in length of his penis which con sists of an adaptation of the length of the convex side to that of the other side (Figure 2)
Accurate preoperative measurements of the site and length of corporoplasties is crucial because the procedure is performed during flaccidity and hydraulic erection is only used intraoperatively to confirm the correction In fact, different from the Nesbit’ s procedure, sites of surgi cal corrections cannot be evaluated intraoperatively because circumcision is not performed
After PGE1 injection, the penis is straightened using a fin ger as a lever and placing the other hand in opposition at the point of greater curvature until the ideal point of cor rection of the curvature is identified According to the radius of the curvature the site and number of corrections is planned
The distance between this identified point of correction and the external urethral meatus is then measured
Photographs are taken to guide the surgeon during the operation and to show the patient the postoperative result in terms of shape and size of the penis The photographs are shown to the patient, so that he could appreciates the change that will occur in his penis Postoperative photo graphs are compared to the preoperative photographs This has great significance from the medico legal point of view
Technique
Our technique does not involve circumcision or subcoro
Figure 4 Median scrotal incision, preparation of the Colles space and penile degloving.

Figure 5
Selective degloving through scrotal access and identification with Allis clamp of the selected site



Figure 6. Schematic drawing of the “binary corporoplasty”
Protecting the urethra with Babcock's forceps, the first corporoplasty is performed medially and the other two laterally to distribute the forces
A335
rchivio Italiano di Urologia e Andrologia 2022;
94, 3
A Rossi, G Alei, P Viscuso, et al
When correcting dorsal curvatures, the site of corporo plasty should be placed as close as possible to the groove of corpus spongioum, whereas for ventral curvature it must be close to the dorsal neurovascular bundle
This maneuver is performed in order to to obtain the maximum correction of the penile curvature with the minimal shortening of the penis

A single 0 non absorbable synthetic multifilament suture is placed in order to perform a special plication on two parallel lines that is therefore called “track” (Figure 6) Laterally to the corporoplasty described, two corporo plasties should be performed along the line that goes from the dorsal neurovascular bundle, or the spongiocav ernosus groove, to the lateral end of the corpus caver nosus at 30° and 60° on the penile sagittal plane The two corporoplasties should measure 50% at 30° and 25% at 60° The suture at 30° is usually performed on a single line going in and out from the tunica albuginea and tying the knot The corporoplasty at 60° is performed with a single suture This asymmetry allows a uniform distribu tion of forces from a mechanical point of view reducing the risk of recurrence with a better aesthetic and palpato ry result When the curvature is only dorsal or ventral same operative steps are performed on the contralateral corpus cavernosus When the curvature is lateral, the described corporoplasty is performed on a single cav ernous body When the curvature is mixed, however, the corporoplastics on the two cavernous bodies will be asymmetrical After having carried out the corporoplas ties at the planned sites, hydraulic erection is obtained to check the achieved correction of the curvature (Figure 7) A photographic documentation of the straightening on different floors is obtained An important advantage of this technique without incision of the albuginea, is that if during the hydraulic erection we have not obtained the
perfect correction, or we have corrected excessively, we can remove the stitches or modify the existing ones Colles’s fascia is rebuilt to ensure that the knots are less palpable and to ensure the correct smoothness of the sub cutaneous planes of the penis The small cutaneous breach is sutured

We used Donati’s silk 0 stitches especially on the scrotum, to be removed on the 6th post operative day (Figures 8, 9) The final dressing is carried out with an elastic bandage of the penis which is maintained for 30 days The func tion of this bandage is initially to avoid swelling and oedema in the immediate post operative and to limit spontaneous and nocturnal erections This expedient reduces the tensions on the corporoplasties and guaran tees an important reduction of the relapse rate It is not necessary to use urethral catheters or drains The patient is asked to avoid sexual activity for 30 days
RESULTS
The average age of the patients was 49 3 years, the aver age length of the penis in erection before surgery was 13 5 cm (± 3 3 cm)
The average curvature was 62 2° (± 30 4°) The most common curvature was dorsal (50), then dorsolateral (40), ventral (30) and ventro lateral (14)
The average duration of surgery was 46 minutes (± 11 min) There were no major complications during the interventions Among the minor complications we report ecchymosis (9%) palpable nodules (18%) and mild hyposensitivity (3%)
After an average 48 months follow up complete correc tion of penile curvature was achieved in 96 8% of patients (Figures 10, 11)
Figure 7 Intraoperative hydraulic erection to evaluate the correction made
The subjective patient report of satisfaction of the results of surgery was 92% The relapse rate, defined as postopera tive curvature of at least 15°, was 3 2% Only two patients (1 5%) were dissatisfied with the final length of the penis, although it was consistent with the measurements taken and photographed before the operation, confirming the importance to establish which are the patient's expecta
Figure 10. Lateral bending, pre and postoperative after 30 days
Figure 8
Aesthetic outcome of scrotal access after 10 days



Figure 11
Dorsal bending, pre and postoperative after 30 daysFigure 9.
Aesthetic outcome of dorsal access after 10 days
Archivio Italiano di Urologia e Andrologia 2022;
94, 3
336
tions before the surgery All patients were satisfied with the aesthetic outcome related to surgical access The mean score of IIEF 15 before surgery was 17 2 and after surgery 18 6
DISCUSSION
Curvature of the penis is an abnormal bend in the penis that occurs during erection It can be congenital or acquired Congenital penile curvature can be caused by disproportionate development of the tunica albuginea of the corporal bodies In the majority of cases the curvature is ventral but it can also be lateral but rarely dorsal Acquired curvature is usually secondary to La Peyronie’s disease It presents with an initial acute inflammatory phase, which may be associated with pain at rest or during erection The following stabilization phase is characterized by the formation of hard palpable plaques, that can be fibrotic or calcified, and by the presence of penile curvature (3) The treatment of the acute phase consists of oral drugs and topical treatments such as ionophoresis (4, 5)
The surgical approach is restricted to the phase of stabi lization In this phase the patient can present penile cur vature, erectile dysfunction, and penile shortening These problems can occur singularly or in combination Surgery is indicated only in patients with stable disease for at least 3 or 6 months, without variations in penile curvature (6) Attesting the stabilization of the disease is very important in order to avoid relapses due to a still active disease rather than to errors or described complications of the technique used Anyway surgery is indicated in patients with penile curvature that does not allow satisfactory intercourse and which is associated with sexual bother
Surgery of congenital curvature is deferred until after puberty and can be performed at any time in adult life However, it is important to solve the problem as soon as possible because the sexual discomfort related to the penile malformation could lead to a loss of self esteem and avoidance of sexual activity Nesbit corporoplasty or plication techniques are currently recommended in order to adapt the long convex side to the shorter contralateral side allowing the patient to easily penetrate and reduce the psychological impact caused by the malformation
In the acquired curvature the surgical strategies are varied in relation to the extent of the curvature, the patient's erec tile function and the size of the penis Possible surgical techniques are: straightening corporoplasties, in case of sufficiently long penis; plaque surgery, which lengthens the penis but can cause erectile dysfunction and with a high risk of recurrence; straightening corporoplasty in association with penile lengthening, in order to compen sate the shortening due to the corporoplasty; penile pros thesis implantation, even in association with fracture of the plaque or plaque surgery in order to lengthen the penis
Corporoplasties can either shorten the longer convex side of the penis (Nesbit’s procedure and its modifications) or lengthen the shorter concave side (plaque surgery) (7)
Several surgical techniques for the correction of penile curvature have been described over the last few years
The first operation to correct penile curvature was described by Nesbit in 1965 (2), consisting of the removal of tunical ellipses on the convex aspect of the penis at the
Original corporoplasty technique
site of major bending of the corpora cavernosa so as to shorten the convexity and correct the curvature
This technique involves circumcision and complete degloving of the penis The number of ellipses to remove, their size and positions are decided intraoperatively, under hydraulically induced erection, by clamping the tunica albuginea with an Allis clamp in order to simulate the effect of the correction
The Nesbit procedure is affected by a 25 30% recurrence rate due to a loss of tension of the suture and causes a considerable penile shortening, especially in patients with dorsal or ventral bending Other reported complications are circumcision outcomes, postoperative haematoma, skin adhesions, unsightly suture tracks and loss of sensa tion in the glans due to neurovascular impairment (8)
On the other hand, the Nesbit technique is extremely simple and easy to perform, as such it is still commonly performed Various modifications to Nesbit procedure were proposed along time, all requiring circumcision to expose the corpora
The occurrence of complications, such as recurrence of c u r v a t u r e ( 1 5 3 3 % ) , e r e c t i l e d y s f u n c t i o n ( 2 0 3 2 % ) , altered local sensation (4 10%), palpable and painful nodules (16 66%), and poor outcomes of circumcision, lead to the development of alternative techniques (9 16)
Plication procedures are based on the same principle as the Nesbit operation but are simpler to perform The use of non absorbable sutures reduced recurrence of the cur vature Results and satisfaction rates are similar to the Nesbit procedure
In the early 90’s, we described a new technique with a different surgical access (at the base of penis rather than distally) and a different type of corporoplasty (double breasted corporoplasty) (17) These minimally invasive surgical accesses allow the rapid resumption of sexual activity, have excellent aesthetic results, and allow to avoid circumcision and total penis degloving
They are minimally invasive because of small incisions but also they minimally affect erectile function of patients In our opinion, when allowed by penis length and function ality conditions, it is important to avoid aggressive proce dures such as the Nesbit technique or plaque surgery
In fact, the straightening corporoplasty does not aim to improve erection, however reducing the section of the corpora cavernosa it slightly increases the pressure inside them This always causes an improvement in erection which is very useful in Peyronie’s patients who may suf fer from a degree of erectile dysfunction
The data on erectile function is very important, the other techniques described can negatively affect the patient's sexual function, although they guarantee an excellent percentage of penile straightening
The patient will never be satisfied if he has a longer penis but a worse functionality than before surgery
CONCLUSIONS
In patients with congenital curvature and in those with acquired curvature and with good size and functionality it is important to perform a minimally invasive surgery
Furthermore, in light of the controversial results of medical procedures, it is correct to propose a resolutive approach to
A337 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
A Rossi, G Alei, P Viscuso, et al
the patients The present technique is easy to perform and overcomes the limitations of other techniques by reducing penile shortening, sensory and aesthetic alterations The rate of straightening is excellent as well as the patient's final satisfaction rate which is 92% This data results from the minimally invasive technique and above all on the absence of worsening of erectile function The possibility of per forming the operation in one day surgery and under local anaesthesia reassures the patients
REFERENCES
1 Makovey I1, Higuchi TT, Montague DK, et al Congenital penile cur vature: update and management Curr Urol Rep 2012; 13:290 7
2 Nesbit RM Congenital curvature of the phallus: report of three cases with description of corrective operation J Urol 1965; 93: 230 2
3 Levine L, Rybak J, Corder C, Farrel MR Peyronie's disease plaque calcification prevalence, time to identification, and development of a new grading classification J Sex Med 2013; 10:3121 8
4 Riedl CR, Plas E, Engelhardt P, et al Iontophoresis for treatment of Peyronie's disease J Urol 2000; 163:95 9
5 Bolgeo T, Di Matteo R, Gardalini M, et al Quality of life of patients with La Peyronie's disease undergoing local iontophoresis therapy: A longitudinal observational study Arch Ital Urol Androl 2022; 94:75 79
6 Carson CC1, Levine LA Outcomes of surgical treatment of Peyronie's disease BJU Int 2014; 113:704 13
Correspondence
Antonio Rossi, MD antonio rossicz@gmail com Mauro De Dominicis, MD dedominicism@alice it Alessandro Calarco, MD (Corresponding Author) alecalarco@gmail com Department of Urology, “Cristo Re” Hospital, Via delle Calasanziane 25, 00167 Rome (Italy)
Giovanni Alei, MD giovanni alei@gmail com Department of General Surgery and Plastic Aesthetic Surgery, Sapienza University of Rome, viale del Policlinico 155, 00161 Rome (Italy)
Pietro Viscuso, MD pietro viscuso@uniroma1 it Antonio Tufano, MD antonio tufano@uniroma1 it Marco Frisenda, MD marco frisenda57hu@gmail com Maternal and Infantile and Urologynaecological Sciences Department Sapienza University of Rome, viale del Policlinico 155, 00161 Rome (Italy)
Guglielmo Mantica, MD gugliemo mantica@gmail com Policlinico San Martino, Largo Rosanna Benzi, 10, 16132, Genova (Italy)
Pierluigi Bove, MD pierluigi bove@uniroma2 it San Carlo di Nancy Hospital Via Aurelia, 275,00165, Rome (RM) (Italy)
Rosario Leonardi, MD leonardi r@tiscali it Casa di Cura Musumeci Gecas, Via dell'Autonomia 57, Gravina di Catania (CT) (Italy)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
7 Hatzimouratidis K, Eardley I, Giuliano F, et al EAU guidelines on penile curvature Eur Urol 2012; 62:543 52
8 Rajmil O, Arrús J, Fernandez M, et al Sensory changes after surgi cal correction of penile curvature Int J Impot Res 2009; 21:366 71
9 Devine CJ Jr, Horton CE Surgical treatment of Peyronie’s disease with a dermal graft J Urol 1974; 111:44 9
10 Ebbehoj J, Metz P New operation for ‘krummerik’(penile curva ture) Urology 1985; 26:76 8
11 Kelâmi A Congenital penile deviation and its treatment with the Nesbit Kelâmi technique Br J Urol 1987; 60:261 3
12 Udall DA Correction of 3 types of congenital curvatures of the penis, including the first reported case of dorsal curvature J Urol 1980; 124:50 2
13 Montague DK Correction of chordee The Nesbit procedure Urol Clin North Am 1986; 13:167 74
14 Yachia D Modified corporoplasty for the treatment of penile cur vature Urol 1990; 143:80 2
15 Garaffa G, Sacca A, Christopher AN, Ralph DJ Circumcision is not mandatory in penile surgery BJU Int 2010; 105:222 4
16 De Rose AF, Ambrosini F, Mantica G, et al Prepuce sparing cor poroplasty as a safe alternative for patients with acquired penile cur vature Arch Ital Urol Androl 2020; 92:182 185
17 Alei G, Letizia P, Alei L, et al New surgical technique for ventral penile curvature without circumcision BJU Int 2014; 113:968 974
338
Antonio Rossi 1 , Giovanni Alei 2 , Marco Frisenda 1 , Antonio Tufano 1 , Pietro Viscuso 1 , Guglielmo Mantica 3 , Pierluigi Bove 4 , Rosario Leonardi
, Alessandro Calarco
Maternal and Infantile and Urologynaecological Sciences Department, Sapienza University of Rome, Rome, Italy;
Department of General Surgery and Plastic Aesthetic Surgery, Sapienza University of Rome, Rome, Italy;
Policlinico San Martino, Genova, Italy;
San Carlo di Nancy Hospital, Rome, Italy;
Casa di Cura Musumeci Gecas, Gravina di Catania (CT), Italy;
Department of Urology, “Cristo Re” Hospital, Rome, Italy
Summary
Introduction: We report our long experience in the surgical treatment of patients request ing penile lengthening by suspensory ligament release and placement of a custom made soft silicone pubo cavernous spac er The aim was to show that with this surgical technique the results obtained are maintained over time It is crucial to achieve postoperative satisfaction of these patients who show fragility and self esteem problems
Methods: From 1999 to 2020, we treated 245 patients with con genital or acquired penile brevity We carefully analysed the preoperative and postoperative (at 6, 12, 24 and 48 months) penile size of the patients to evaluate whether this technique could allow the long term maintenance of aesthetic results We also assessed preoperative erectile function and we focused on the psychological aspects to avoid surgery in patients with dysmorphophobia. This original technique involves the section of the suspensory ligament and the implantation of a silicone spac er between the pubic symphysis and the corpora cavernosa. This spacer is conformed to the patient anatomy and maintains the relationship between the anatomical structures unchanged over time. Sexual self esteem and patient satisfaction were assessed with the APPSSI questionnaire.
Results: The mean increase in penile length was about 2.5 cm in flaccid state and 1.9 cm in stretched state. There were no injuries of the neurovascular bundle or urethra, and no erectile dysfunction was noted. These results persisted at 6, 12, 24 and 48 months without significant differences. Over 80% of patients stated that they were completely satisfied with the results obtained. This satisfaction remained stable along follow up. Conclusion: The section of the suspensory ligament and the implant of the soft silicone spacer provide real penis elongation with satisfactory results that persist over time This technique avoids the frequent complication of short term shortening due to the scar adhesions of the edges of the dissected ligament The high aesthetic satisfaction of patients is stable at controls at 6, 12, 24 and 48 months
KEY WORDS: Penile lenghthening; Penile augmentation; Penile elongation; Pubo cavernous spacer; Small penis; Suspensory ligament release
Submitted 8 September 2022; Accepted 9 September 2022
conflict
INTRODUCTION
Men have always been worried about penis size, which can seriously affect their self esteem They have the tendency to seek their identity in the penis with the belief that ‘‘bigger is better’’ The stigmas of a small penis, as well as the increas ing media influence on sexual issues, have created an increase demand for penile enhancement (1) The term microphallus or micropenis is referred to a penis that is formed normally but is of a small size (less than 7 8 cm during erection or stretched state) and it is probably asso ciated with abnormal production, or a reduced activity, of LH hormone (2) On the other hand, the altered percep tion of the organ size is called “dysmorphophobia” These patients present with a normal sized penis but are dissat isfied both in a flaccid state and during erection (3, 4) It is mandatory for these patients to undergo a psychosexu al counselling and try to avoid surgery
The demand for penile lengthening had a tremendous increase in recent years
According to the published data, majority of men who request penile enhancement surgery usually have a nor mally sized and normally functioning penis (5) In our experience, the most common request for penile length ening comes from patients that suffer from the so called ‘‘locker room syndrome” , i e anxiety and embarrassment arising from changing in front of the others At present, no current consensus guidelines are available for treat ment of patients with a normal sized penis (6) The short penis can be congenital or acquired The con genital small penis is defined as measurements of < 7 8 cm upon erection The acquired disorders are caused by Peyronie’s disease or outcomes of partial penectomy for penile carcinoma Finally, there are cases of relative short penis due to excess pubic fat
The reported normal length of an adult flaccid penis ranges between 7 6 cm and 10 7 cm, and between 11 4 cm and 14 8 cm in erection (7) The increase in length following surgery that is required to satisfy the patient is not well established and is not adequately emphasized in the medical literature
A339 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
ORIGINAL PAPER No
of interest declared
Penile lenghthening original technique using a pubo-cavernous spacer. Long term results from a series of over 200 patients
5
6 1
2
3
4
5
6
DOI: 10 4081/aiua 2022 3 339
A Rossi, G Alei, M Frisenda, et al
The gold standard of penile lengthening technique consists in the dissection of the suspensory ligament followed by cutaneous “V to Y” or “Z” plasties (8 10) In cases where the penile shortening is associated with abundant pubic fat, the dissection of the suspensory ligament is performed along with a suprapubic lipectomy or pubic liposuction (11)
This cosmetic surgery is commonly performed by experi enced plastic surgeons and results in an aesthetic visual lengthening effect In the last years, new surgical techniques for penile lengthening have been developed to improve the aesthetic appearance and functional state of the penis, giv ing rise to much controversy regarding their safety, and effi cacy (12 18)
We report our approach of penile lengthening using a soft silicone pubo cavernous spacer after suspensory ligament release

METHODS
This study is a retrospective analysis of patients who underwent penile lengthening by sectioning of penile suspensory ligament and using a soft silicone custom made spacer made between the 1999 and the 2020 We have used this surgical procedure in 245 patients aging between 18 and 67 (average age 35 years)
The study population included patients with congenital small penis (172); patients with short penis due to fibro sis caused by either Peyronie’s disease or trauma (67); patients with short penis resulting from partial penecto my for penile carcinoma (6)
In order to select patients qualified for surgery, every patient underwent a pre surgical diagnostic screening consisting of: medical history, physical examination, sexual hor mone profiles psychiatric/psychosexual assessment
All patients were interviewed by an andro sexologist This was done especially in order to understand the moti vations, expectations, self esteem, and to discourage from surgery patients with dysmorphic disorder
Preoperative photographs and measurements of the penis were carried out in flaccid state, stretched state and dur ing maximal erection, after intracavernous injection of alprostadil (Prostaglandin E1 PGE1: 1 5 mcg)
The preoperative measures were taken from the base of the penis to the tip of the glans Penile length during erec tion was also evaluated from the pubo penile junction to the tip of the glans in the dorsal surface in order to eval uate the angle between the penis shaft and the pubis This is important to select patients for procedure; in fact patients with laxity of the suspensory ligament or angle > 30° upon erection, were excluded because in these cases we will not obtain significant improvement in length
Average measures were 5 6 cm (from 3 8 to 8 2 cm) in flaccid state (mean initial flaccid length), 10 9 cm (from 6 2 to 13 5 cm) during stretched state (mean initial erect length or SPL) and 11 2 (from 6 5 to 14 cm) during erec tion
Each patient underwent a Doppler penile ultrasound in the flaccid and erect state after PGE1 administration to identify any preexisting condition such as Peyronie’s dis ease and vascular erectile dysfunction
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
The erectile function was also assessed with the adminis tration of the International Index of Erectile Function Questionnaire (IIEF) and with a nocturnal penile tumes cence test (Rigiscan Plus Dacomed Corporation, Minneapolis, MN, USA)
Surgical technique
Skin incision is made with the V Y technique in order to allow simultaneous skin lengthening at the time of sutur ing The incision is performed about 2 3 cm at the mid point of the pubo penile arch (Figure 1)
After the incision of the subcutaneous tissue, the Scarpa fascia is reached This is exposed in order to reveal the
Figure 1
Skin incision with V Y technique. Each branch is about 2 cm
Figure 2.
Exposure of the penis suspensory ligament
Figure 3.
Suspensory ligament release by scissors along the anterior side of the pubic symphysis




Figure 4
Conformation of the spacer and its relations with the anatomical structures
Passage of the points of 0 Prolene

Figure 5.
3D reconstruction of the relationships between the spacer and the surrounding anatomical structures
Figure 6.
Final Y suture in order to stretch the pubic skin
340
Figure 8
Preoperative and postoperative result at 30 days.

Figure 9.
Preoperative and postoperative result at 6 months
Figure 10.
Preoperative and postoperative result at 12 months
fundiform ligament, that is then resected Below it, the suspensory ligament (Figure 2) is dissected by scissors along the anterior side of the pubic symphysis in an area which is usually avascular (Figure 3)
This step is performed while the assistant keeps the patient's penis fully stretch in order to feel the release of the corpora cavernosa
At this point a block of soft silicone (Allied Biomedical carving blocks) is cut to fit the angle created by the cav ernous bodies and the pubic symphysis, taking care to conform with the measurements of the newly formed cav ity; the spacer is shaped to come into contact anteriorly with the surface of the corpora cavernosa which is con vex, while posteriorly with the anterior wall of the pubic symphysis which is concave (Figure 4)
Four 0 Prolene stitches are passed through the spacer, two stiches in the deep part, one on the left and one on the right side, and two stitches in the superficial part
Holding back the spacer, the stitches are passed through the periostium of the pubic symphysis into the deep part
The silicon spacer is inserted into the cavity and the first two stitches, previously placed in the deep part, are tied The other two stitches are secured to the periostium in the uppermost part of the newly formed cavity, taking care not to exert pressure upon the penile structures (Figures 4, 5)
A drain is placed in the deeper part of the formed cavity, which is usually removed 12 to 24 hours after surgery
Penile lenghthening with a pubo cavernous spacer



The subcutaneous part, in the deep tract, is closed with polyglycolic acid, then the Scarpa fascia is sutured using interrupted sutures in polyglycolic acid A Y suture, in polyglycolic acid or silk, is then performed to guarantee lowering of the pubo penile arch (Figure 6)
This latter surgical step is of utmost importance in order to avoid impairment of the lengthening procedure
According to the surgeon ’ s opinion, this can also be inte grated with further cutaneous plasty with Z elongation
Placement of a bladder catheter at the end of surgery depends on the type of anesthesia used In case a catheter is placed, this must be removed within 12 hours
In our case series, the mean operative time was 78 min utes, ranging from 58 to 116 minutes Postoperative antibiotic therapy consists of a combined therapy with rifampicin 300 mg/die, minocycline 50 mg/die and mox ifloxacin 400 mg/die for one week Patients are instruct ed to refrain from sexual intercourses for 30 days after surgery No traction or vacuum device was used postop eratively
Postoperative follow up and statistical analysis
After the post operative checks, the patients were evalu ated at 6, 12, 24 and 48 months
The objective increase in length was calculated by sub tracting the preoperative flaccid length and preoperative SPL from the postoperative flaccid length and postopera tive SPL respectively
The satisfaction of surgical outcome was assessed at 6, 12, 24 and 48 months after surgery by directly asking the patients: “Are you satisfied with the result of surgery?” and with the APPSSI questionnaire at the annual check
The results expressed as mean ± standard deviation (SD) were compared using paired and unpaired Student T test, Fischer exact probability test and Chi squared test
RESULTS
Good aesthetic results were obtained in all cases
The results relating to the aetiology are shown in Table 1
All patients, despite of the aetiology category, showed a significant increase of penile length (Figures 7 9)
The mean increase in flaccid state was 2 54 ± 0 9 cm (p < 0 005), and in stretched state was 1 91 ± 1 1 cm (p < 0 005) Minimal lengthening obtained in flaccid state was 1 6 cm and in stretched state was 0 9 cm The best result was an elongation of 3 5 cm in the flaccid state and of 3 0 cm in stretched state (Figure 10)
The psychosexual impact of the operation was favorable in the majority of cases Sexual self esteem and patient satisfaction were significantly improved, as shown by the results of the Augmentation Phalloplasty Patient Selection and Satisfaction Inventory (APPSSI) completed 12 months postoperatively (Table 2)
Improved self esteem was recorded in all but eleven patients (234 out of 245 patients scored 95 9%)
Two hundred (81 6%) out of 245 patients were com pletely satisfied with the outcomes of surgery to all fol low up checks Sexual activity was encouraged from the fourth postoperative week
At the 6 and 12 month follow up visit, all patients report ed a normal erectile function The 6 month IIEF was com
A341 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Figure 7. Preoperative
and postoperative result at 7 days
A Rossi, G Alei, M Frisenda,
APPSSI results
Suitability assessment (preoperative)
sexual confidence
(total score 10
sturbance and/or weak willingness to
complaints, with surgery appearing as a remote
complaints but skeptical of surgery (total score 4
complaints, with surgery
(total score
(total score 0
(unsuitab
9)
patients
(1
of
(total score 10 12)
excited about postoperative
complaints but satisfied (total score 7 9)
comp aints, with
pleted, and no substantial difference compared to preop erative was found No postoperative nighttime rigidome try was necessary
As far as the complications are concerned, the following minor events have been observed: infection of the wound in 6 patients (2 5%), moderate pain which disappeared after four weeks in 43 patients (17 5%), and pain exceed ing 2 months in 8 patients (3 2%) No alterations in sen sitivity during sexual intercourses were reported
At 12 and 24 months after surgery the penile ultrasound in flaccid state and during erection performed to all patients revealed the correct positioning of space maintainer Only one patient requested removal of the spacer after 13 years This patient had an important weight loss (43 5 kg) and the spacer came slightly to the surface without creat ing problems during intercourse
DISCUSSION
Men with small penis are insecure and question their own sexual value (1)
By cutting the suspensory ligament below the symphysis the penis can be elongated
However, the suspensory ligament resection does not guarantee definitive results due to scarring of the tissue along the edges of the resection of the ligament itself (6, 19)
In order to maintain the distance between the dorsal side of the cavernous bodies and the pubic symphysis, we have made various attempts (considered several possibil ities), at first by using a silicone tip of a penile prosthesis and then a testicular silicone prosthesis as described by other surgeons (10) These materials, both biocompatible and available on the market, were not found to be suit
Archivio Italiano di Urologia e Andrologia 2022;
patients
improvement or indifferent results (tota score 4 6) 10 patients
complaints, condition worse than preoperatively (total score 0 3)
patients
able for this purpose In this case series, a soft type sili cone polymer was used as space maintainer
This material has the following advantages: soft type sili cone is available in many shapes and sizes; all carving blocks are made of solid silicone elastomer designed for permanent implantation; implants may be trimmed with a scalpel or scissors to meet the individual patient’s needs; implants may be adaptable with the shape and dimension of every newly formed cavity
All the above mentioned advantages are not achievable by using a testicular prosthesis or fat flap, because it can not adapt its shape to the cavity
Dermal fat grafts or harvesting fat from remote sites were occasionally used to fill the dead space created by the descent of the corpora off the pubic bone after sectioning the suspensory ligament (20)
The extraction of the fat flap, on the other hand, makes the entire procedure extended in time and more invasive, as it is associated with higher morbidity, and bleeding can occur in the donor site Moreover, it does not avoid the fibrotic retraction that is responsible for the reattachment of the penis to the pubis The adjunctive post operative stretching with vacuum devices or penile extenders is necessary in order to overcome this condition, with an increase in the final cost
Moreover, published data on the resulting change in the penile length, using testicular prosthesis or fat flap, are scarce and controversy (21)
Advancing of the skin is always necessary At this level, particularly in close proximity to the pubo penile junc tion, the skin is thick, with more or less abundant adipose tissue and, in addition, it is hairy, therefore any insuffi cient advancement towards the penile shaft of the penis could cause an unsatisfactory result
94, 3
et al 342
Table 1. Results in relation to etiology Patient Mean initial Mean initial stretched Mean increase Mean increase in stretched Satisfaction n° flaccid length, cm penile length, (SPL ± SD), cm in flaccid state, cm penile lenght (SPL ± SD), cm % Overall 245 5 6 ± 0 8 10 9 ± 1 1 2 54 ± 0 9** 1 91 ± 1 1** 81 6 Congenital small penis 113 6 5 ± 0 9 11 4 ± 1 6 2 7 ± 0 8* 1 2 ± 1 2* 93 Congenital micropenis 69 3 8 ± 1 1 11 5 ± 2 7 2 2 ± 0 7 1 7 ± 1 3 87 Peyronie’s disease 60 4 9 ± 0 9 6 2 ± 1 7 3 ± 0 5 1 8 ± 1 2 80 Penile trauma 7 7 7 9 3 2 8 1 8 93 Penile carcinoma 6 5 6 6 8 2 5 2 75 SPL stretched pen le lenght; SD standard dev at on Student T test * p < 0 005 Student T test ** p < 0 0005 Table 2
n° Outcome evaluation
year postoperative) n° S ight
d
undergo surgery) No complaints
penile inadequacy and
result
12) 0
e candidate)
177 patients Mild
option
7
12
Mild
58
Moderate
6) 68 patients Moderate
no
Severe
inevitabile option
3) 165 patients Severe
0
Patients total (N): 245 pat ents Ch square test w th three degrees of freedom 134 1 P < 0 00001 F sher exact probabi ity test P < 0 00001 APPSSI = Augmentation Pha lop asty Patient Se ection and Satisfact on nventory
Penile lenghthening with a pubo cavernous spacer
M plasty, which became popular in China, is frequently responsible for hypertrophic scars and even necrosis of tissue at the outer edge of the flaps The V Y advancement is the most commonly used technique; however, several concerns have been risen about the site and extent of the incision (22) The advantages of a Y suture, in our opin ion are to guarantee lowering of the pubo penile arch (Figure 5) and to avoid impairment of the lengthening performed
Postoperative penile traction was not used, as per our experience, the positioning of the penile extender or vac uum device caused discomfort for the patients, was com plicated and risky to manage and has given poor results
Our technique on the other hand, which includes insert ing the space maintainer of soft silicone into the new cav ity, showed a very low incidence of penile retraction Finally, it is extremely important that the urologist evalu ates very carefully the patient’s reasons for requesting this kind of treatment, what does the patient expect from it and, in general terms, his psychological situation
We personally insist that our patients have two or more sessions with an andro sexologist and we stress that counselling cannot be conducted either by a “psychologist” or by a “sexologist” who do not have a proven specific competence in andrological problems At the end of the counselling the andro sexologist will prepare a signed report, which in turn will be signed by the patient as his approval
It is also mandatory that the surgeon is particularly care ful in case of patients looking only for cosmetic results, partly because their expectations may be far beyond real ity and partly because the best surgical result involves a “normal” organ Patients with dysmorphic disorder, pro foundly depressed, psychotic patients or patients with not realistic expectations should not be submitted to this surgical procedure (1)
CONCLUSIONS
Suspensor ligament release alone does not guarantee definitive results Moreover, in some cases worsen the clinical situation due to scarring of the tissue along the edges of the resection of the ligament itself The place ment of a silicon spacer between the penis and the pubis seems to give the best results, as it prevents reattachment and a possible reshortening
The definitive separation between the two anatomical structures is simple to carry out thanks to this small device The soft silicone makes it easy to shape the spac er and adapt it to the newly formed anatomical cavity of each patient It is also easy to fix to the pubis and remains stable over time (unlike the fibrosis resulting by use of other materials such as dermal matrix)
In our opinion this technique should finally guarantee excellent long term aesthetic results and high satisfaction rate preventing local recurrence and the loss of the good initial results obtained
FOOTNOTE
Original drawings were made by G Alei
REFERENCES
1 Sharp G, Oates J Sociocultural influences on men's penis size per ceptions and decisions to undergo penile augmentation: a qualitative study Aesthet Surg J 2019; 39:1253 1259
2 Aaronson IA Micropenis: medical and surgical implications J Urol 1994; 152:4 14
3 Woodhouse CR The sexual and reproductive consequences of con genital genitourinary anomalies J Urol 1994; 152:645 51
4 Veale D, Miles S, Read J, et al Relationship between self discrepan cy and worries about penis size in men with body dysmorphic disorder Body Image 2016; 17:48 56
5 Mondaini N, Ponchietti R, Gontero P, et al Penile length is normal in most men seeking penile lengthening procedures Int J Impot Res 2002; 14:283 286
6 Spyropoulos E, Christoforidis C, Borousas D, et al Augmentation phalloplasty surgery for penile dysmorphophobia in young adults: con siderations regarding patient selection, outcome evaluation and tech niques applied Eur Urol 2005; 48:121 128
7 Veale D, Miles S, Bramley S, et al Am I normal? A systematic review and construction of nomograms for flaccid and erect penis length and circumference in up to 15,521 men BJU Int 2015; 115:978 986
8 Campbell J, Gillis J A review of penile elongation surgery Transl Androl Urol 2017; 6:69 78
9 Hoznek A, Rahmouni A, Abbou C, et al The suspensory ligament of the penis: an anatomic and radiologic description Surg Radiol Anat 1998; 20:413 417
10 Li CY, Kayes O, Kell PD, et al Penile suspensory ligament division for penile augmentation: indications and results Eur Urol 2006; 49:729 733
11 Pestana IA, Greenfield JM, Walsh M, et al Management of "buried" penis in adulthood: an overview Plast Reconstr Surg 2009; 124:1186 1195
12 Protogerou V, Anagnostopolou S, Venierates D, et al Penis liga ments: their use in "increasing" the size of the penis in penile augmen tation procedures Anatomical description in human cadavers and clin ical results of a phalloplasty series Ann Ital Chir 2010; 81:199 204
13 Alter GJ, Jordan GH Penile elongation and girth enhancement AUA Update Series 2007; 26:229 237
14 Srinivas BV, Vasan SS, Mohammed S Penile lengthening procedure with V Y advancement flap and an interposing silicone sheath: A novel methodology Indian J Urol 2012; 28:340 342
15 Perovic SV, Djordjevic ML, Kekic ZK, Djakovic NG Penile surgery and reconstruction Curr Opin Urol 2002; 12:191 194
16 Goodwin WE, Scott WW Phalloplasty J Urol 1952; 68:903 908
17 Long DC [Elongation of the penis] Zhonghua Zheng Xing Shao Shang wai ke za zhi = Zhonghua Zheng Xing Shao Shang Waikf [i e Waike] Zazhi = Chinese Journal of Plastic Surgery and Burns 1990; 6:17 9
18 Wessells H, Lue TF, McAninch JW Complications of penile length ening and augmentation seen at 1 referral center J Urol 1996; 155:1617 1620
19 Shaeer O, Shaeer K, el Sebaie A Minimizing the losses in penile lengthening: "V Y half skin half fat advancement flap" and "T closure" combined with severing the suspensory ligament J Sex Med 2006; 3:155 60
20 Vardi Y, Har Shai Y, Gil T, Gruenwald I A critical analysis of penile enhancement procedures for patients with normal penile size:
A343 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
A Rossi, G Alei, M Frisenda, et al
surgical techniques, success, and complications Eur Urol 2008; 54:1042 1050
21 Dillon BE, Chama NB, Honig SC Penile size and penile enlarge ment surgery: a review Int J Impot Res 2008; 20:519 529
22 Mertziotis N, Kozyrakis D, Bogris E Is V Y plasty necessary for penile lengthening? Girth enhancement and increased length solely through circumcision: description of a novel technique Asian J Androl 2013; 15:819 823
Correspondence
Antonio Rossi, MD
antonio rossi@uniroma1 it Marco Frisenda, MD marco frisenda57hu@gmail com Antonio Tufano, MD antonio tufano@uniroma1 it Pietro Viscuso, MD pietro viscuso@uniroma1 it
Maternal and Infantile and Urologynaecological Sciences Department Sapienza University of Rome, viale del Policlinico 155, 00161 Rome (Italy)
Giovanni Alei, MD giovanni alei@gmail com
Department of General Surgery and Plastic Aesthetic Surgery, Sapienza University of Rome, viale del Policlinico 155, 00161 Rome (Italy)
Mantica Guglielmo, MD gugliemo mantica@gmail com Policlinico San Martino, Largo Rosanna Benzi, 10, 16132, Genova (Italy)
Bove Pierluigi, MD San Carlo di Nancy Hospital, Via Aurelia, 275, 00165, Rome (Italy) pierluigi bove@uniroma2 it
Leonardi Rosario, MD leonardi r@tiscali it Casa di Cura Musumeci Gecas, Via dell'Autonomia 57, Gravina di Catania (CT) (Italy)
Alessandro Calarco, MD (Corresponding Author) alecalarco@gmail com Department of Urology, “Cristo Re” Hospital, via delle Calasanziane 25, 00167 Rome (Italy)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
344
REVIEW
Frailty and benign prostatic hyperplasia: The thrilling underlying impact
2nd Department of Urology, Sismanoglio General Hospital of Athens, Athens, Greece;
Primary Healthcare, Internal Medicine Department, Amarousion, Attica, Greece
Summary
Background: World population is aging
The number of individuals aged over 65 are expected to be 71 million only in the US 43% of this population will be men Benign prostatic hyperplasia (BPH), defined as the benign neoplasm of the prostate gland affects 8% of men by their forties, but 90% of men over 90 years old Lower urinary tract symptoms (LUTS) can be caused by an enlarged prostate, and it seems to be associated more with older and frailer indi viduals.
Methods: The purpose of this study is to review the potential interplay between frailty syndrome and benign prostatic hyper plasia. A thorough MEDLINE/PubMed non systematic literature review was conducted from 1990 to March of 2022. The terms used for the search were “frailty and benign prostatic hyperpla sia” and “low muscle mass and benign prostatic hyperplasia”.
Results: It seems that, frailty poses a negative impact on the prognosis of patients with BPH, as it is associated with increased incidence of LUTS. In addition, frailty seems to be a strong predictor concerning surgical procedure failure and mortality following invasive procedures for BPH. Prostatic stent placement on the other hand appears to be the ideal solution for frail patients.
Conclusions: BPH has a strong association with frailty and increasing age.
KEY WORDS: Frailty; Benign prostatic hyperplasia; Transurethral resection of the prostate; Transurethral laser induced prostatecto my; Prostatic stent
Submitted 26 June 2022; Accepted 22 July 2022
INTRODUCTION
Benign prostatic hyperplasia (BPH) is the normal histologi cal process of prostate gland enlargement due to aging and can lead, in many cases, to bladder outlet obstruction (1 3) In that case, BPH in older men can cause lower urinary tract symptoms (LUTS) which can be treated, in the early stages, by medications (1, 2) One third of men older than 75 years old with newly diagnosed LUTS will begin phar macotherapy for BPH (1, 3) BPH is common in older men, as 21% of men aged over 70 years old can experi ence nocturia, 22% can experience the feeling of incom plete bladder emptying and 57% a decrease in urinary stream pressure (4, 5)
Combination therapy with alpha adrenergic receptor
No
antagonists (a blockers) plus 5 alpha reductase inhibitors is the standard medical therapy for BPH, since the trial Medical Therapy for Prostatic Symptoms (MTOPS) exhibited lower rates of BPH clinical progression in individuals who received this pharmacotherapy versus those who received placebo (1, 6)
Pharmacotherapy can be associated with adverse drug events, which can be harmful especially in frail individu als, such as orthostatic hypotension, falls, depression and suicidal ideation (1, 7 11)
Alpha blockers act by decreasing smooth muscle tone in the prostate gland and bladder neck, while 5 alpha reduc tase inhibitors act by decreasing the volume of the prostate (1, 12) Thus, the use of 5 a reductase inhibitors is not indicated in patients with low volume prostate glands, as they will not have any particular benefit (1) Frailty, is a clinical syndrome that can lead to increased side effects of pharmacotherapy and more rapid symptom progression, thus altering the balance of the potential harms and bene fits of each intervention undertaken (1, 2, 13, 14)
LUTS, affecting more than 50% of the male geriatric pop ulation, lead to a reduced quality of life and increased risk of falls, thus contributing to overall mortality (15 18)
LUTS in the elderly population can be multifactorial, hav ing as causality non urologic causes including psychoso matic manifestations (16, 19)
The difficulty of diagnosing and treating this urologic syndrome has been the hallmark of the effort to associate this complex entity with a novel age related risk factor, namely frailty (16)
METHODS
In this non systematic review, PubMed and MEDLINE databases were thoroughly searched from 1990 to March of 2022, using the terms: “benign prostatic hyperplasia”
AND “frailty” OR “decreased muscle mass”
Databases were screened independently by one author and rechecked by other two authors Any disputes were solved by a fourth author (Figure 1)
From the studies screened, the original studies, as shown in Table 1, were used in order to conduct the investiga tion of the potential interplay between the two entities under evaluation Studies concer ning animal models were excluded
A345 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
conflict of interest declared
Themistoklis Ch Bellos 1 , Lazaros I Tzelves 1 , Ioannis S Manolitsis 1 , Stamatios N Katsimperis 1 , Marinos V Berdempes 1 , Andreas Skolarikos 1 , Nikolaos D Karakousis 2
1
2
DOI: 10 4081/aiua 2022 3 345
RESULTS
According to Bauer et al frail patients were more likely to have higher American Urological Association Symptom Index (AUASI) scores (p < 0 001) (both in voiding and storage sub scores), higher maximum flow rate (p = 0 02) and decreased post void residuals (p < 0 01) compared with robust individuals (1) Serum PSA (p = 0 61) and prostate volume (p = 0 15) were comparable between the groups (1) Frail individuals experienced more pronounced adverse events (AEs) from medications, which can stem from their overall worse status (higher body mass index BMI), worse systolic blood pressure, worse physical and mental health, polypharmacy) (p < 0 01) in comparison with robust men of the same chronological age (1) Frailty was not associated with risk for BPH progression ran domized in placebo or finasteride monotherapy (1) However, in the group receiving doxazosin monotherapy, frailty and pre frailty seems to be more associated with clinical BPH progression, as proven by the increased rates o f i n d w e l l i n g c a t h e t e r s o r a c u t e u r i n a r y re t e n t i o n episodes (aHR: 2 64; 95%; CI: 0 86 7 1) (1) In another study of Bauer et al , an association between phenotypic frailty and LUTS severity was demonstrated (3) In this study, the authors exhibited that the prevalence of moderate and severe LUTS was 46% and 13% respec tively in frail men compared to 37% and 5% in robust men (moderate LUTS: HR: 1 4; 95%; CI: 1 1 1 7) (severe LUTS: HR: 2 5; 95%; CI: 1 8 3 6) (3) Those data were independ
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
ent concerning the age, comorbidities or LUTS treatment and persisted among men who did not experience urinary incontinence (3) Compared to mild LUTS, the risk for mobility limitation was increased in people with moderate (HR: 1 35; 95% CI: 1 12 1 63) and severe LUTS (HR: 1 98; 95%; CI: 1 48 2 64) (20)
Patients with severe (HR: 1 62; 95%; CI: 1 07 2 43) and moderate LUTS (HR: 1 32; 95%; CI: 1 05 1 67) expe rienced more restrictions in daily activities (20) LUTS were not associ ated with limitation of cognitive tasks (20) In addition, another study by the same author demonstrated that the prevalence of frailty was higher in severe and moderate LUTS (7%, 11% and 18% for mild, moderate and severe LUTS respectively) (21)
Similarly, in a Korean population study by Jang et al , phenotypic frailty was prevalent in 43% of men with severe LUTS and in 16% and 7% of men with moderate and mild LUTS respectively (22)
According to Bauer et al , frail patients could be diagnosed more frequently with BPH (22% vs 14% in non frail individuals), overactive bladder (OAB) (25% vs 11% in non frail indi viduals) and mixed BPH/OAB (16% vs 12% in non frail individuals) (16)
Moreover, people with BPH were 1 7 times more likely to be assessed as frail (OR: 1 70; 95%; CI: 1 14 2 55) with the TUGT (Timed Up to Go Test) test (16)
According to Soma et al frailty was positively associated with LUTS (HR: 2 13; 95%; CI: 2 48 3 06), OAB (HR: 2 07; 95%; CI: 1 31 3 29) and higher prevalence of noc turia (23)
According to Eredics et al , intraoperative complications, duration of postoperative catheterization and length of hospitalization was identical in frail and non frail patients undergoing transurethral resection of the prostate (TURP) (24) However, success rate of surgery was 80 6% in fit and 75% in frail patients, while 3 month success rates were 95 2% and 83 3% for non rail and frail respectively (24) Post Void Residual (PVR) was less than 50 ml in both cohorts (24)
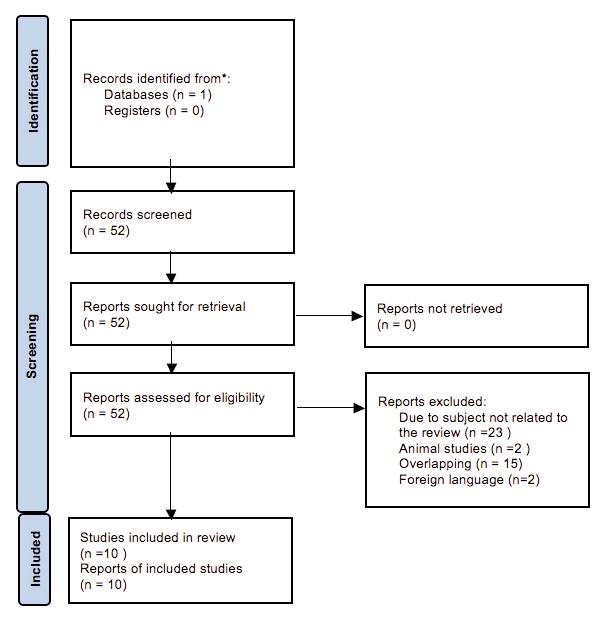
Pichon et al , showed that frail patients had lower success rate at 3 months (55%) compared to non frail patients (95%) (p < 0 05) following TURP (25) The immediate postoperative success rate was 85% vs 41% in non frail and frail cohorts respectively (25) Higher morbidity was also noted in the frail groups compared to the control group (44% vs 15%) (p < 0 05) (25)
Suskind et al , demonstrated that 95% of nursing home patients who underwent de obstructive surgery (TURP or Transurethral Laser Induced Prostatectomy TULIP) were re catheterized at 12 months, whilst 30% of them have passed away (26)
T Ch Bellos, L I Tzelves, I S Manolitsis, S N Katsimperis, M V Berdempes, A Skolarikos, N D Karakousis
346
Figure 1. Flow chart
Table 1.
Studies concerning the potential interplay between BPH and frailty
Authors (ref) Year, study Study population F indings
Bauer (1) Bauer (16)
Bauer (20)
2021, RCT 2021, prospective
3047 men, who were treated with doxazos n monotherapy, finasteride monotherapy, placebo or combination
2026 men over 65 years with BPH, OAB, mixed BPH/OAB
Frailty independently assoc ated with BPH clinica progression and AEs
Frailty and benign prostatic hyperplasia: The thrilling underlying impact
Exclusion criteria
Anticholinergic except g aucoma
Frailty assessed by: BPH/LUTS progression assessed by:
Eredics (24)
Sethi (27)
Bauer (21)
Jang (22)
Soma (23)
Pichon (25)
Suskind (26)
2021, retrospective 2020, retrospective 2017, retrospective 2020, retrospective 2018, cross sectional 2019, retrospective 2017, prospective 2016, retrospective
2716 men ≥ 71 years
Higher inc dence of those diagnosis in frai pat ents
vLUTS severity is associated with mobility and ADL limitations among older men
Cancer, Neurologic Disease, Indwelling Catheter, Cont nuous Incont nence
Baseline self reported functional limitations
FI containing 68 potential deficits TUGT
AUASI scale (LUTS progression, acute urinary retention, urinary incontinence, UTI or sepsis, increase of serum creatinine at least 1 5 mg/dl attributable to BPH)
Based on database diagnosis divided into BPH, OAB, mixed BPH/OAB
54 patients ≥ 75 years who underwent TURP
144 patients with obstructive urinary symptoms or indwelling catheter who had a Memokath stent inserted 5,979 men ≥ 65 years
Fit patients benefit from TURP while frail do not
Prostatic stent is superior to TURP for frail patients
Higher inc dence of phenotypic frailty among elderly with moderate and severe LUTS
Not mentioned
Not mentioned
1 Mobility (2 3 blocks or 10 steps)
2 ADL (any difficulty bathing, showering or transferring)
3 Cognition
7 item CHSA fra lty scale
Not mentioned Physician or anesthesiologist assessment/ not suitable for TURP
AUASI Already diagnosed
Already diagnosed
Not mentioned
Cardiovascular Health Study Index (low mean mass, weakness, exhaustion, slowness and ow physical activity)
492 men ≥ 65 years and were ambulatory 710 people ≥ 60 years 60 patients ≥ 60 years who underwent TURP
The prevalence of frailty and other geriatr c conditions higher in those with severe urologic symptoms
People with LUTS more frail
Patients without urinary catheter, patients with prostate cancer, PSA > 15 ng/m ,patients unfit for anesthesia, patients with prior prostatic surgery
Patients living in a nursing home, hospitalized or bed riden
Not mentioned
Geriatric assessment can pred ct the outcome of TURP in the elderly
Frailty phenotype (exhaustion, inactivity, slowness, weakness and weight loss)
FP, FDS, mFI BGA, CGA
2869 nursing home residents aged ≥ 65 years who underwent TURP or TULIP
Poor baseline functional status and having foley catheter preoperative is associated with higher risk of TURP or TULIP failure
Not mentioned
ADL, survival after surgery, foley catheter status
AUASI score
IPSS questionnaire
IPSS questionnaire Already diagnosed Already diagnosed
According to Sethi et al , prostatic stent placement is more a d v a n t a g e o u s i n f r a i l p a t i e n t s w i t h B l a d d e r O u t l e t Obstruction (BOO); 62 5% of the patients had a significant PVR difference with 550 ml before the procedure and 80 ml postoperatively respectively (p < 0 0001) (27) Two thirds of those patients continued to void without assis tance (27); 37 5% experienced procedure failure with stent migration, occlusion, urinary retention refractory to the procedure and irritative voiding symptoms (27)
DISCUSSION
According to this non systematic narrative review we concluded that it seems to be an increased incidence of frailty in the elderly patients experiencing severe and m o d e r a t e L U T S , a s m e a s u re d b y t h e A U A S I a n d International Prostate Symptom Score (IPSS) scales Frail catheterized patients, undergoing TURP or TULIP, have higher incidence of re catheterization or even death
Prostatic stents seem to have higher success rates in the frail and elderly Most of the studies included in this systematic review have large sample number However, there are certain limitations These studies may include heterogeneous population and use different tools of frailty quantifica tion Most of the studies were observational, retrospec tive, and non randomized, except one Even this study did not randomize patients based on frailty All the afore mentioned factors, necessitate the implementation of a larger multicenter randomized survey that uses a com mon tool for frailty assessment Increased age is one of the most common risk factors for LUTS (16, 28) Although LUTS coexist with frailty, it is unknown which condition preexists, although many theories have been suggested for each temporal direction (16) With increasing age, several genitourinary and neural changes coexist, that can lead to decreased bladder capacity and increased bladder sensation (16, 29) LUTS can interfere with daily routine
A347 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
RCT Randomized Control Trial; BPH: Benign Prostatic Hyperplasia; AEs: Adverse Events F : Fr ed Index; AUASI Amer can Urological Association Symptom ndex UTI: Urinary Tract Infect on OAB: Overactive Bladder; TUGT: T med Up to Go Test ADL: Act vit es of Dai y Liv ng; TURP: Transurethral Resection of the Prostate; CHSA Canadian Study o Hea th And Aging; PSS: Internation Prostate Symptom Score; FP: Frai ty Phenotype; FDS: Frai ty D scrim nant Score; mFI: mod fied Fra lty Index; BGA Brief Geriatric Assessment; CGA: Comprehensive Geriatric Assessment; TULIP: Transurethra Laser Induced Prostatectomy
T Ch Bellos, L I Tzelves, I S Manolitsis, S N Katsimperis, M V Berdempes, A Skolarikos, N D Karakousis
and daily exercise thus increasing the risk of frailty (16, 30, 31) LUTS and frailty can be caused by a common m e c h a n i s m , w h i c h i n c l u d e s i n s u l i n re s i s t a n c e a n d increased inflammatory markers, which are probably associated with LUTS progression (16, 32, 33) Aging is associated with an increase in fat mass and decline of muscle mass and strength (34, 35) Muscle mass decreas es 35% between the age of 20 and 80 years old (34) Loss of strength can subsequently lead to physical function impairment and increased vulnerability (34, 36)
Multimorbidity is a common trait among the geriatric population (37) Frailty can be defined as the accumula tion of health deficits and functional problems which are thought to lead to greater susceptibility to physical stres sors (1) This is caused by the depletion of body physical reserves (1) Frailty can encompass also cognitive and psychosocial changes associated with many conditions (1) According to a recent medical consensus, frailty is defined as “a medical syndrome with multiple causes and contributors that is characterized by diminished strength, endurance and reduced physiologic function that increases an individual’s vulnerability for developing increased dependency and/or death” (1)
Although frailty encompasses chronological age in its def inition, it is a more accurate marker of biological age (1) Associations between chronological age and BPH are well established However, associations between BPH and frailty or even biological age have been scarce till now (1)
The most common clinical characteristics of frailty include weakness and slowness, which are usually associ ated with storage LUTS in older women (16)
Frailty preponderance is 36 88% depending of the meas urement used (4) There are many tools and indexes used to assess frailty One of the most common tools was devel oped by Fried et al (4) This assessment concerns the frailty phenotype and is based on the cardiovascular health study This model assesses muscle mass decline, strength, endurance, balance, walking performance and low physical activity (4) Other indexes and scores of frailty used are the Frailty Index of Accumulative Deficits (FI CD), the Geriatric 8 score (G8 score), the simplified Five item Index (sFI), the American Society of Anesthesiologists (ASA) physical status classification, the Mini Cognitive test (mini COG), the Clinical Frailty Scale (CFS), the Eastern Cooperative Oncology Group (ECOG) performance status, the Cumulative Illness Score Rating Geriatrics (CISR G), the Charlson Comorbidity Index (CCI), the Study of Osteoporotic Fractures (SOF) index, the “Fatigue, Resistance, Ambulation, Illness, Loss of Weight” (FRAIL) index, the Comprehensive Geriatric Assessment (CGA) and the Multidimensional Prognostic Index (MPI) (38 41)
There has been a novel effort in hypogonadal frail patients to reduce the frailty symptoms with the use of testos terone replacement therapy (34, 42, 43) However, testos terone use is not devoid of complications with more strik ing negative effects on cardiovascular system quite possi bly due to polycythemia (34, 42, 43) The hypothesis for increased probability for prostate cancer on testosterone replacement therapy has not yet been proven (34, 42, 43) Novel compounds termed selective androgen receptor modulators (SARMs) that act selectively on androgen receptor could revolutionize testosterone replacement
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
therapy (2) It seems they could provide the anabolic effects without the possible complications (2) However, more studies are needed to validate this
CONCLUSIONS
Older men presenting with non neurogenic LUTS to a urology clinic are more likely to be frail Frailty is a sys temic marker of biological age that can possibly mediate a good association between chronological age and symptoms of BPH Currently, frailty and other markers of increased biological age are not targeted by any intervention meant for BPH, as most of them take into account only the mech anism of prostatic obstruction The only intervention with clinical benefit could be prostatic stent placement Therefore, screening older men with LUTS using simple tests and indexes, would be appropriate when the presence of frailty could change the diagnosis or even the treatment This approach could lead to the development of new ther apeutic strategies incorporating specific measures targeting frailty per se such as physical activity, nutritional interven tion or even individually tailored geriatric models
REFERENCES
1 Bauer SR, Walter LC, Ensrud KE, et al Assessment of frailty and association with progression of benign prostatic hyperplasia symp toms and serious adverse events among men using drug therapy JAMA Netw Open 2021; 4:e2134427
2 Omwancha J, Brown TR Selective androgen receptor modulators: in pursuit of tissue selective androgens Current opinion in investiga tional drugs 2006; 7:873 81
3 Welliver C, Feinstein L, Ward JB, et al Trends in lower urinary tract symptoms associated with benign prostatic hyperplasia, 2004 to 2013: the Urologic Diseases in America Project J Urol 2020; 203:171 8
4 Suskind AM Frailty and lower urinary tract symptoms Curr Urol Rep 2017; 18:67
5 Platz EA, Smit E, Curhan GC, Nyberg LM, Giovannucci E Prevalence of and racial/ethnic variation in lower urinary tract symptoms and noncancer prostate surgery in U S men Urology 2002; 59:877 83
6 McConnell JD, Roehrborn CG, Bautista OM,, et al The long term effect of doxazosin, finasteride, and combination therapy on the clin ical progression of benign prostatic hyperplasia New Engl J Med 2003; 349:2387 98
7 Oelke M, Becher K, Castro Diaz D, et al Appropriateness of oral drugs for long term treatment of lower urinary tract symptoms in older persons: results of a systematic literature review and interna tional consensus validation process (LUTS FORTA 2014) Age Ageing 2015; 44:745 55
8 Welk B, McArthur E, Fraser LA, et al The risk of fall and fracture with the initiation of a prostate selective alpha antagonist: a popula tion based cohort study BMJ 2015; 351:h5398
9 Coupland CAC, Hill T, Dening T, et al Anticholinergic Drug Exposure and the Risk of Dementia: A Nested Case Control Study JAMA Intern Med 2019; 179:1084 93
10 Sarkar RR, Parsons JK, Bryant AK, et al Association of treat ment with 5alpha reductase inhibitors with time to diagnosis and mortality in prostate cancer JAMA Intern Med 2019; 179:812 9
11 Duan Y, Grady JJ, Albertsen PC, Helen Wu Z Tamsulosin and
348
the risk of dementia in older men with benign prostatic hyperplasia Pharmacoepidemiol Drug Saf 2018; 27:340 8
12 Abrams P, Chapple C, Khoury S,, et al Evaluation and treatment of lower urinary tract symptoms in older men J Urol 2013; 189(1 Suppl):S93 S101
13 Walston J, Bandeen Roche K, Buta B, et al Moving frailty toward clinical practice: NIA intramural frailty science symposium summa ry J Am Geriatr Soc 2019; 67:1559 64
14 Platz EA, Joshu CE, Mondul AM, et al Incidence and progression of lower urinary tract symptoms in a large prospective cohort of United States men J Urol 2012; 188:496 501
15 Wei JT, Calhoun E, Jacobsen SJ Urologic diseases in america p ro j e c t : b e n i g n p ro s t a t i c h y p e r p l a s i a J U ro l 2 0 0 8 ; 1 7 9 ( 5 Suppl):S75 80
16 Bauer SR, Jin C, Kamal P, Suskind AM Association between lower urinary tract symptoms and frailty in older men presenting for urologic care Urology 2021; 148:230 4
17 Noguchi N, Chan L, Cumming RG, et al A systematic review of the association between lower urinary tract symptoms and falls, injuries, and fractures in community dwelling older men Aging Male 2016; 19:168 74
18 Akerla J, Pesonen JS, Poyhonen A, et al Impact of lower urinary tract symptoms on mortality: a 21 year follow up among middle aged and elderly Finnish men Prostate Cancer Prostatic Dis 2019; 22:317 23
19 Lepor H Pathophysiology of lower urinary tract symptoms in the aging male population Rev Urol 2005; 7 Suppl 7:S3 S11
20 Bauer SR, Cawthon PM, Ensrud KE, et al Lower urinary tract symptoms and incident functional limitations among older communi ty dwelling men J Am Geriatr Soc 2022; 70:1082 1094
21 Bauer SR, Scherzer R, Suskind AM, et al Co Occurrence of Lower Urinary Tract Symptoms and Frailty among Community Dwelling Older Men Journal of the American Geriatrics Society 2020; 68:2805 13
22 Jang IY, Lee CK, Jung HW, et al Urologic symptoms and burden of frailty and geriatric conditions in older men: the Aging Study of Pyeong Chang Rural Area Clin Interv Aging 2018; 13:297 304
23 Soma O, Hatakeyama S, Imai A, et al Relationship between frailty and lower urinary tract symptoms among community dwelling adults Low Urin Tract Symptoms 2020; 12:128 36
24 Eredics K, Meyer C, Gschliesser T, et al Can a simple geriatric assessment predict the outcome of TURP? Urol Int 2020; 104:367 72
25 Pichon T, Lebdai S, Launay CP,, et al Geriatric assessment can predict outcomes of endoscopic surgery for benign prostatic hyperpla sia in elderly patients J Endourol 2017; 31:1195 202
26 Suskind AM, Walter LC, Zhao S, Finlayson E Functional out comes after transurethral resection of the prostate in nursing home residents J Am Geriatr Soc 2017; 65:699 703
27 Sethi K, Bozin M, Jabane T, et al Thermo expandable prostatic stents for bladder outlet obstruction in the frail and elderly population: An underutilized procedure? Investig Clin Urol 2017; 58:447 52
28 Coyne KS, Wein AJ, Tubaro A, et al The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health related qual ity of life, anxiety and depression: EpiLUTS BJU International 2009; 103 Suppl 3:4 11
29 Suskind AM The aging overactive bladder: a review of aging related changes from the brain to the bladder Curr Bladder Dysfunct Rep 2017; 12:42 7
30 Silva V, Grande AJ, Peccin MS Physical activity for lower uri
Frailty and benign prostatic hyperplasia: The thrilling underlying impact
nary tract symptoms secondary to benign prostatic obstruction Cochrane Database Syst Rev 2019; 4:CD012044
31 Coyne KS, Sexton CC, Kopp Z, et al Assessing patients' descrip tions of lower urinary tract symptoms (LUTS) and perspectives on treatment outcomes: results of qualitative research International journal of clinical practice 2010; 64:1260 78
32 Russo GI, Castelli T, Urzi D, et al Emerging links between non neurogenic lower urinary tract symptoms secondary to benign pro static obstruction, metabolic syndrome and its components: A sys tematic review Int J Urol 2015; 22:982 90
33 Siddiqui NY, Helfand BT, Andreev VP, et al Biomarkers impli cated in lower urinary tract symptoms: systematic review and path way analyses J Urol 2019; 202:880 9
34 Hijazi RA, Cunningham GR Andropause: is androgen replace ment therapy indicated for the aging male? Annu Rev Med 2005; 56:117 37
35 Bhasin S, Buckwalter JG Testosterone supplementation in older men: a rational idea whose time has not yet come J Androl 2001; 22:718 31
36 Roubenoff R, Hughes VA Sarcopenia: current concepts The jour nals of gerontology Series A, Biological sciences and medical sciences 2000; 55:M716 24
37 Dartigues JF, Le Bourdonnec K, Tabue Teguo M, et al Co occur rence of geriatric syndromes and diseases in the general population: assessment of the dimensions of aging J Nutr Health Aging 2022; 26:37 45
38 Pyrgioti EE, Karakousis ND B12 levels and frailty syndrome J Frailty Sarcopenia Falls 2022; 7:32 7
39 Kostakopoulos NA, Karakousis ND Frailty assessment and post operative complications in urologic oncology operations J Frailty Sarcopenia Falls 2020; 5:57 61
40 Pilotto A, Custodero C, Maggi S, et al A multidimensional approach to frailty in older people Ageing Res Rev 2020; 60:101047
41 Dent E, Kowal P, Hoogendijk EO Frailty measurement in research and clinical practice: A review European Journal of Internal Medicine 2016; 31:3 10
42 Hackett GI Testosterone replacement therapy and mortality in older men Drug Saf 2016; 39:117 30
43 Tan RS, Salazar JA Risks of testosterone replacement therapy in ageing men Expert Opin Drug Saf 2004; 3:599 606
Correspondence
Themistoklis Bellos MD (Corresponding Author) bellos themistoklis@gmail com
Lazaros Tzelves, MD lazarostzelves@gmail com
Ioannis Manolitsis, MD giannismanolit@gmail com
Marinos Berdempes, MD marinosberdebes@hotmail com
Andreas Skolarikos, MD andskol@yahoo com
Nikolaos D Karakousis, MD karak2727@gmail com
Sismanogliou 1, 2nd Department of Urology, Sismanoglio General Hospital of Athens, 15126 Athens, Greece
Stamatios Katsimperis, MD stamk1992@gmail com
Primary Healthcare, Internal Medicine Department, Amarousion, Attica, Greece
A349 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
DOI: 10 4081/aiua 2022 3 350
REVIEW
Malakoplakia of the urinary bladder: A review of the literature
Giordano Polisini 1 , Rocco Francesco Delle Fave 1 , Camilla Capretti 2 , Angelo Marronaro 2 , Alessia Mariagrazia Costa 2 , Luigi Quaresima 2 , Daniele Mazzaferro 2 , Andrea Benedetto Galosi 1
1 Division of Urology, University Hospital “Ospedali Riuniti”, School of Medicine, Department of Clinical, Special and Dental Sciences, Marche Polytechnic University, Ancona, Italy; 2 Department of Urology, Civitanova Marche Hospital, Civitanova Marche, Italy
Summary
Objective: The aim of the study is to make a review of the literature about bladder malakoplakia
Material and Methods: We searched articles on the PUBMED web literature database with the following keywords: “vesical malakoplakia” and “bladder malakoplakia” In the literature we found 254 articles At final we have excluded 219 articles, including in our study only 35 articles
Results: The overall average age found was 50 85 years The average age of men was 43 22 years, while that of women was 53 37 years 75% of the patient cases were women and 25% were men Regarding comorbidities, in 5 55% of the cases were missing whereas 47 22% of the patients suffered from recurrent urinary tract infection (UTI) and 19 44% from immune system disorders Urine culture was positive in 69 44% with E coli being isolated in 92% of cases Hydroureteronephrosis was present in 44 44% of the cases: left in 6 25% of cases, right in 18 75% and bilateral in 75% The mean serum creatinine of patients with hydroureteronephrosis was 5 11 (1 21) mg/dl The most fre quent site of the lesion was the vesicoureteral junction (VUJ) (42 31%), followed by the trigone (38 46%) 30 56% of patients were treated with antibiotic and surgery (transurethral resec tion of bladder, partial or radical cystectomy), less frequent options were antibiotics alone and surgery alone The recur rence rate was 15%
Conclusions: Malakoplakia is a disorder usually related to other affections, like UTI and immunodepression, and it seem to be caused by an abnormal macrophage function In almost half of the described cases of isolated bladder malako plakia, hydroureteronephrosis and renal failure were present Treatment is not standardized, but both medical and surgical therapies are effective to avoid recurrence
KEY WORDS: Malakoplakia; Rare disorder; Urinary tract infection
Submitted 9 June 2022; Accepted 23 June 2022
INTRODUCTION
Malakoplakia is a rare disorder which was described for the first time in 1902 by Michaelis and Gutmann It affects both sexes, mostly people over 40 years old, patients with immunosuppression, diabetes mellitus, renal transplanta tion, long term therapy with systemic corticosteroids and patients with a prior infection of E coli (1)
It usually occurs in the genitourinary tract [commonly the bladder (40%), renal parenchyma (16%), prostate and rarely the ureter (11%)], but it can affect all body organs (2, 3)
Bladder malakoplakia can manifest as nodules, plaques, or ulcers with voiding symptoms and it can mimic cysti tis or bladder tumor (4) At cystoscopy it appears as a yel low soft tiny plaque or ulcer (1)
The exact etiology is unknown, but it seems to be caused by a defect of phagocytic or degradative functions of his tiocytes in response to E coli or Proteus infection resulting in a chronic inflammatory process (5) The lesions are characterized by presence of large macrophages; foamy histiocytes (known as von Hansemann cells) containing Michaelis Gutmann bodies (6)
The gold standard for diagnosis and treatment has not yet been decided Only case reports about vesical malako plakia can be found in the literature, hence there is a lack of a review of this disease For this reason the aim of our study was to review all the case reports about bladder malacoplakia in order to compare them
MATERIALS AND METHODS
We searched articles on the PUBMED web literature data base with the following keywords: “vesical malakoplakia” and “bladder malakoplakia” The including criteria for our study were: case report and primary bladder malako plakia as central topic In the literature we found 254 arti cles Of this, we excluded 172 articles because they did not respected the including criteria So we selected 82 case reports Furthermore 47 articles have been dis charged because articles were unavailable or subject of the paper was off topic At final we have included in our study 35 articles
RESULTS
From the 35 articles analyzed, we obtained 36 case reports The major problem was to find all the information considering that many case reports were incomplete or unclear in their writing, in particular regarding follow up The main characteristics of the patients and the patholo gy are shown in Table 1
No conflict of interest declared
Archivio Italiano di Urologia e Andrologia 2022; 94, 33 50
Malakoplakia of the urinary bladder
Table 1.
Characteristics of the patients and the pathology
Ar ticle
Age Sex Comorbility
Hina S et al JCPSP 2019 (5) 55
Serum Urine
Presence of Site of lesion (years) creatinine culture/ ohydro Nephrosis le vels (mg/dl) bacteria at imaging
Female Recurrent UTI, diabetes 1 1 E coli Right Right VUJ
Female Recurrent UTI Normal E coli None Right lateral wall Sir thanaphol W et al JECR 2018 (2) 66
Rabani S et al Urol J 2019 (6) 1 7
Female Pannicul tis, sistem c sc erosis, pulmonar fibrosis Normal Negative None \ Park n CJ et al BJ 2020 (15) 82
Female Recurrent UTI, diabetes, LNH 2 66 E coli
Bilateral Right and left VUJ and the trigone Gao P et al JIMR 2021 (4) 48 Male Diabetes 1 4 E coli Right Right lateral wall involving right VUJ Shah A et a PSI 2005 (8) 11 Male Recurrent UTI, mega o urethra and PUJ Normal E coli None Postero and eft lateral walls
Ristic Petrovic A et al VP 2013 (3) 53 Female Recurrent UTI \ E coli \ Trigone, left VUJ, posterior wall
Nabeshima A et a . J UOEH 2012 (16) 65 Female No significantpasthistory Normal E. coli \ Trigone Bruce R et al UR 1990 (17) 86 Female Recurrent UTI, small cell carcinoma \ E coli none Bladder dome Stamat ou K et al NUM 2014 (1) 72 Male Recurrent UTI, diabetes, CVD 21 Positive Bilateral Trigone, left VUJ, posterior wall Mukha RP et a IUN 2010 (18) 40 Male Recurrent UTI 2 8 \ Bilateral \ Jordaan HF et al Clin Exp Dermatol 1990 (19) 68 Female Recurrent UTI, pemfigo and immunodeficiency \ E coli Normal \ Minor L et al J Uro 2013 (9) 16 Female \3 E coli Bilateral \ Patniak R et al Cases J 2009 (11) 18 Male No significantpasthistory 1 6 Negative Bilateral Trigone, left VUJ, bladder neck Berney DM et al Histopathology 1996 (12) first case 72 Female No significantpasthistory \ Negative \\ Berney DM et al Histopathology 1996 (12) second case 57 Male Acute renal failure \\\\ PozoMengual B et a Actas Urol Esp 2003 (14) 76 Female No urological history Normal Negative None Postero wal and bladder dome Sulman A et a Urology 2002 (20) 40 Female Recurrent UTI \ E coli None Bladder neck and left lateral wall B llis A Nephron 1994 (21) 27 Female CRI/ESDR \ Negative \ Trigone Nukui M et al H nyokika Kiyo, 1997 (22) 63 Female No significant past history 2 9 \ Bilateral Trigone and bilateral VUJ Batchelor JS Br J Urol 1991 (23) 63 Female Recurrent UTI \\\ Posteriorwal Bylund J et a Nat Clin Pract Urol 2008 (24) 51 Female Recurrent UTI, blood hypertension 3 4 E coli Bilateral \ Feldman S et al J Uro 1980 (25) 50 Female Recurrent UTI 3 8 E coli Bilateral Ureteral orifices were not visualized Stanton MJ J Urol 1983 (13) 48 Female Recurrent UTI \ E coli None Right hemitrigone, right latera wal and bladder neck
Fariña Perez LA Actas Uro Esp 1999 (26) 69 Male CVD, TBC \ Corynebacteriumurealyticum
None Postero and bilateralwall Kohda N Hinyokika K et al 1984 (27) 44 Female Recurrent UTI 0 7 Negative None Posterior, left and right wall Zornox DH et a J Urol 1979 (28) 69 Female No significantpasthistory Normal E coli None Right lateralwa l Kato T et al Hinyokika K 2001(29) 70 Female Recent pye onephritis, HCV Normal E coli Right Trigone, bilteral VUJ and neck Stripling JR et al South Med J 1979 (30) 38 Male No significantpasthistory 15 E coli Bilateral Trigoneoblitering the ureteral orifices Cavallone B, et al Urolog a 2018 (31) 65 Female Recurrent UTI, diabetes, obes ty 9 3 E coli Bilateral Anterior and left lateral wall Tsai R et a AJR Am J Roentgenol 2016 (32) 31 Female \\ Negative None Left wall Steele B et a Pediatr Radiol 2003 (33) 16 Female CRI, VUR 2 8 E coli Bilateral \ Tsung SH Urology 1982 (34) 50 Female No significantpasthistory Normal E coli \\ Cowie AG et al Br J Surg 1970 (35) 50 Female Recurrent UTI Normal E coli None Internal meatus Andress MR et al Br J Radiol 1968 (36) 36 Male Dystrophia myotonica \ E coli Bilateral Widely distributed, with bilateral involvment of VUJ Mel cow MM J Urol 1957 (37) 64 Female Cholecystectomy \ E coli Left \
Data considered and collected were: age, sex, comorbidi ty, serum creatinine, presence of bacteria in urine, hydroureteronephrosis, site of injury, treatment and fol low up
The presence or absence of hydronephrosis was derived from imaging examinations: ultrasound, computerized tomography (CT), intravenous pyelography (IVP), etc
As shown in the Table 2, the antibiotics used for the treat ment were quinolones, Trimethoprim sulfamethoxazole and b lactams As not all the articles reported the antibi otic used, we decided to analyze the data by generally referring to the use of antibiotics or not and the same applies to the type of intervention performed
The overall average age found was 50 85 years The aver age age of men was 43 22 years, while that of women was 53 37 75% of the patient cases were women and 25% were men
Regarding comorbidities, in 5 55% of the cases they were missing whereas 47 22% of the patients suffered from recurrent urinary tract infections (UTI) and 19 44% from immune system disorders (such as diabetes) Urine culture was positive in 69 44% The infection was sustained in 92% of cases by E coli Missing or negative c u l t u re a re re p o r t e d i n 3 0 % O n t h e o t h e r h a n d Corynebacterium was occasionally reported Corynebacterium urealyticum is the cause of encrusting cystitis It is usually missed in routine urine cultures since it does not grow after an over night incubation It grows in special media on longer incubation period in special medias Inaccurate search for it could explain the high rate of negative cultures
Of the patients with negative urine culture, 85 71% had no history of recurrent UTI Of the patients with positive urine culture, 60% had a history of recurrent UTI
A351 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Table 2.
Treatment and follow up
Ar ticle Treatment
Hina S et al JCPSP 2019 (5)
Rabani S et al. Urol J 2019 (6)
Sir thanaphol W et al JECR 2018 (2)
Park n CJ et al BJ 2020 (15)
Gao P et al JIMR 2021 (4)
Shah A et al PSI 2005 (8)
Ant biotics, ascrorb c acid, TURB \
Partial cystectomy, trimethoprim sulfamethoxazole
Ciprofloxacin, TURB
Amoxicillin clavulanic acid, TURB
TURB, tazobactam
Ant biotics
Ristic Petrov c A et al VP 2013 (3) TURB \
Nabeshima A et a . J UOEH 2012 (16) TURB \
Bruce R et al UR, 1990 (17)
Stamat ou K et al NUM 2014 (1)
Mukha RP et a IUN, 2010 (18)
Jordaan HF et al Clin Exp Dermatol 1990 (19)
Ant biotics \
Quinolones, TURB
Radical cystectomy \
Follow up
No recurrence after 9 years
No recurrence
No recurrence after 2 months
Bladder recurrence at 6 months w th right idroureteronephrosis
Bladder recurrence 2 and 3 years later
He died 8 months later after a further worsening of renal failure and complications of the cardiovascular system
Trimethoprim sulfamethoxazole, bethanechol, ascorbic acid No recurrence
Minor L et al J Urol 2013 (9) Quinolones, bethanechol
Patniak R et al Cases J 2009 (11)
Ant biotics
Berney DM et al Histopathology 1996 (12) first case Ant biotics, radical cystectomy
Berney DM et al Histopathology 1996 (12) second case Radical cystectomy
PozoMengual B et a Actas Urol Esp 2003 (14) Ciprofloxacin, TURB
Sulman A et a Urology 2002 (20)
Ant biotics, TURB \
B llis A Nephron 1994 (21) \\
Nukui M et al Hinyokika Kiyo 1997 (22)
No recurrence
No recurrence after 10 years
The patient initially improved, but developed renal failure and died 3 months after cystectomy
He died a month after radical cystectomy
At 15 day the pat ent developed a sepsis and she died after 48 hours
TURB, trimethoprim sulfamethoxazole, bethanecol, ascorbic acid No recurrence after 20 months
Batchelor JS. Br J Urol 1991 (23) Follow up
No recurrence after18 months but the patient developed LHN Bylund J et al Nat Clin Pract Urol 2008 (24) Ciprofloxacin, ascorbic acid, bethanechol, TURB
Feldman S et al J Urol 1980 (25) Follow up
No recurrence after 6 9 months
Bladder recurrence after 2 months The pat ent underwent total cystectomy
Trimethoprim sulfamethoxazole, ascorb c acid, bethanechol No recurrence after 18 months Fariña Perez LA Actas Urol Esp 1999 (26) TURB
Stanton MJ J Urol 1983 (13)
Kohda N H nyokika K et al 1984 (27) TURB \
After 30 days, he died for heart failure
Zornox DH et a . J Urol 1979 (28)
trimethoprim sulfamethoxazole, ascorbic acid, TURB
No recurrence after 7 months
No recurrence after 12 month Kato T et al Hinyokika K 2001(29) TURB
Stripling JR et al South Med J 1979 (30) Cephalosporin, TURB No recurrence
Cavallone B et al Urologia 2018 (31) Ciprofloxacin, ascorbic acid, TURB \ Tsai R et a AJR Am J Roentgenol 2016 (32) Bethanechol, rifampicin and trimethoprim sulfamethoxazole
No recurrence after 2 months Steele B et al Pediatr Radiol 2003 (33) Ciprofloxacin
No recurrence, decrease in the number and size of esions Tsung SH. Urology 1982 (34) Ant biotics \ Cowie AG et al Br J Surg 1970 (35) Ant biotics, cystotomy
No recurrence, small residual nodule that was fulgurated No further cystoscopic abnormal ty has developed
Andress MR et al Br J Radiol 1968 (36) TURB, antibiotics \ Mel cow MM J Urol 1957 (37) Cystectomy \
Hydroureteronephrosis was present in 44 44% of the cases, was absent in 36 11%, and was missing in 19 44%
In the patients with hydroureteronephrosis, 6 25% had left, 18 75% right and 75% bilateral hydroureteronephro s i s T h e m e a n s e r u m c re a t i n i n e o f p a t i e n t s w i t h hydroureteronephrosis was 5 11 (1 21) mg/dl
Regarding the site of the lesion, this information was missing in 10 cases (27 78%) In most of the remaining 26 cases the disease occurred in more than one area of the bladder Location, in order of frequency, was vesicoureter al junction (VUJ) in 42 31%, trigone in 38 46%, left later al wall in 30 77%, right lateral wall in 26 92%, posterior wall in 26 92%, bladder neck in 15 38%, bladder floor in 7 69% and anterior wall in 3 85%
With regard to treatment, we excluded from the analy sis nephrostomies, urinary shunts without cystectomy a n d u re t e r a l s t e n t p l a c e m e n t a i m e d a t t re a t i n g h y d ro u re t e ro n e p h ro s i s a n d n o t b l a d d e r p a t h o l o g y
Treatment in 2 78% of cases was not reported 30 56% of p a t i e n t s w e re t re a t e d w i t h a n t i b i o t i c a n d s u rg e r y (transurethral resection of bladder, partial or radical cys
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
tectomy) The remaining were treated as follows: 13 89% with antibiotics alone, 22 22% with surgery alone, 5 56% with antibiotic and bethanechol, 5 56% with antibiotic, bethanechol and ascorbic acid, 5 56% with antibiotic, bethanechol, ascorbic acid and surgery, 8 33% with antibiotic, ascorbic acid and surgery and 5 56% with fol low up only
In total, therefore, the two most frequently used treat ments were antibiotic therapy (69 44%) and surgery (66 67%) Regarding surgery, 75% of operations were transurethral resection of the bladder (TURB), the remaining being partial or radical cystectomy
Regarding recurrences, they were missing in 12 case reports (33 33%) Out of the remaining 24 case reports, we excluded 2 cases because the patient had had a cys tectomy and could not perform bladder follow up and 2 other articles due to sudden death from other causes within about one month after diagnosis In the remaining 20 reports, the recurrence rate was 15% Cases treated with medical therapy alone (without surgical removal) that demonstrated a reduction of the bladder mass on fol
G Polisini, R F Delle Fave, C Capretti, A Marronaro, A M Costa, L Quaresima, D Mazzaferro, A B Galosi
352
low up imaging were not considered as recurrences
The shortest follow up was 2 weeks and the longest was 10 years
The recurrence rate of patients treated with antibiotics alone was 1/3 (33 33%)
The recurrence rate of patients treated with antibiotic and surgery was 1/7 (14 29%)
The recurrence rate of patients treated with follow up was 1/2 (50%)
On the other hand, according to the single treatment, the recurrence rate of antibiotic use was 11 76%, of surgery 9 09% and follow up only 50%
DISCUSSION
Malacoplakia is a rare inflammatory and granulomatous disease It was first identified by Michaelis and Gutmann in 1902 and its histological features were described by Von Hansemann in 1903
T h e t e r m ' m a l a c o p l a k i a ' o r i g i n a t e s f ro m t h e G re e k 'malakos' and 'plakos' and means 'soft plaque' (7)
According to recent literature, the age of onset is over 50 years with a prevalence four times higher in women Malacoplakia mainly affects the urinary tract, particularly the bladder, followed by the kidney, the prostate and rarely the ureter (4, 5, 38) However, it may also affect other parts of the body including the conjunctiva, tonsils, adre nal glands, spleen, pancreas, retroperitoneum, mesenteric lymph node, brain, lung, and skin and potentially any organ In addition, urinary involvement is more frequent in women and extra urinary involvement in men (8)
The exact etiology is still unclear However, a close asso ciation has been seen with recurrent urinary infections (especially from E coli) and immunodepression (diabetes, kidney transplant) (7)
In fact, Malakoplakia is believed to result from defective phagocytosis [due to reduced intracellular levels of cyclic guanosine monophosphate (cGMP)], resulting in inadequate killing of bacteria It results in granulomatous reaction caused by an accumulation of bacterial degradation prod ucts Partially digested bacteria become calcified and accumulate in macrophages, forming the pathognomonic Michaelis Gutmann bodies (9)
In addition, the macrophages involved in malacoplakia contain high immunoreactive a1 antitrypsin levels unlike other inflammatory processes (except for tuberculosis and xanthogranulomatous pyelonephritis) Thus, immunohis tochemical search for a1 antitrypsin can be useful for a dif ferential diagnosis (10)
Clinically, it presents with irritative lower urinary tract symptoms (LUTS) such as dysuria, pollakiuria, urinary urgency and haematuria These symptoms may mimic cystitis and bladder cancer
Diagnosis is histological by biopsy of the visible mass on cystoscopy which as mentioned above, it appears as a yel low soft tiny plaque or ulcer (11)
It is characterized histologically by Von Hansemann oval histiocytes which contain basophilic lysosomal inclusion bodies called Michaelis Gutmann bodies (12)
Imaging examinations (ultrasonography, CT and IVP) may be useful to identify concomitant hydroureteronephrosis and to identify minus defects of the upper urinary tract,
Malakoplakia of the urinary bladder
indicating its involvement Currently there are no validated guidelines regarding its treatment (5) Antibiotics are gener ally administered to treat the underlying infection, such as quinolones, trimethoprim and rifampicin, in combination or not with ascorbic acid and/or bethanechol (4)
Ascorbic acid and bethanechol (cholinergic agent) both seems to increase intracellular cyclic guanine monophos phate levels increasing bactericidal phagocytosis function of macrophages (13)
Surgical intervention is recommended when medical intervention fails (14)
The results listed below are in agreement with the data described in the literature: the average age was found to be around 50 years, the disease is more frequent in women than in men, malacoplakia seems to be associated with recurrent UTI and immune system disorders about 90% of positive urine cultures are sustained by E coli
In our study of the epidemiology, we found a lower mean age of incidence in men than in women by about 10 years, with a women:men frequency ratio of 3:1, instead of 4:1 as reported in the literature
In our review, we decided to look at the site of the disease and found that the most frequently affected sites were the trigone and ureteral meatuses
For the first time in our analysis, we found that about one third of patients had hydronephrosis (mono or bilateral) and that this correlated with involvement of the trigone and/or VUJ In the cases examined, hydronephrosis almost always led to renal failure with mean serum crea tinine values of 5 1 mg/dL (the highest value found in a case of acute renal failure was 21 mg/dL)
CONCLUSIONS
Nowadays, malakoplakia is a disorder not well know, that seems related to other affections, like UTI and immun odepression, and is thought to be the result of abnormal macrophage function
In accordance with the literature, it can present with a very variable spectrum of symptoms although we have shown that in isolated bladder malakoplakia without ureteral involvement, hydroureteronephrosis and renal failure are very common (in almost half of the cases)
Treatment is not standardized, but both medical and sur gical therapies seem to be effective in curing the condition and avoiding recurrence, although we did not collect suf ficient data to perform a statistical analysis
REFERENCES
1 Stamatiou K, Chelioti E, Tsavari A, et al Renal failure caused by malakoplakia lesions of the urinary bladder Nephro Urol Mon 2014; 6:e18522
2 Sirithanaphol W, Sangkhamanon S, Netwijitpan S, Foocharoen C Bladder malakoplakia in systemic sclerosis patient: a case report and review literature J Endourol Case Reports 2018; 4 1:91 93
3 Ristic Petrovi A, Stojnev S, Jankovic Velickovic L, Marjanovic G Malakoplakia mimics urinary bladder cancer: A case report Vojnosanit Pregl 2013; 70:606 8
A353 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
G Polisini, R F Delle Fave, C Capretti, A Marronaro, A M Costa, L Quaresima, D Mazzaferro, A B Galosi
4 Gao P, Hu Z, Du D Malakoplakia of the bladder near the ureter al orifice: a case report, J Intern Med Res 2021; 49:1 5
5 Hina S, Hasan A, Iqbal N, et al Malakoplakia of the urinary bladder and unilateral ureter J Coll Physicians Surg Pak 2019; 29:582 584
6 Rabani S, Rabani S, Bladder Malakoplakia simulating neoplasm in a young girl: report of a case and review of literature Urol J 2019; 16:614 615
7 Cooper KL, Badalato GM, Rutman MP Infection of the urinary tract In: Elsevier (Ed), Campbell Waslsh Wein Urology, 12th ed, 2021; 1129
8 Shah A, Chandran H Malakoplakia of bladder in childhood, Pediatr Surg Int 2005; 21:113 115
9 Minor L, Lindgren BW Malacoplakia of the bladder in a 16 year old girl J Urol 2003; 170:568 9
10 Callea F, Van Damme B, Desmet VJ Alpha 1 antitrypsin in malakoplakia Virchows Arch A Pathol Anat Histol 1982; 395:1 9
11 Patnayak R, Reddy MK, Subramanian S, et al An unusual case of bilateral hydroureteronephrosis caused by uretero vesico malako plakia in a young male: a case report and review of the literature Cases J 2009; 2:7527
12 Berney DM, Thompson I, Baithun SI Alkaline encrusted cystitis associated with malakoplakia Histopathology 1996; 28:253 256
13 Stanton MJ, Lynch JH, Maxted WC, Chun BK Malacoplakia of the bladder: a case report of resolution with bethanechol, trimetho prim sulfamethoxazole and ascorbic acid J Urol 1983; 130:1174 5
14 Pozo Mengual B, Burgos Revilla FJ, Briones Mardones G, et al Malacoplaquia vesical con afectación ganglionar y curso agresivo [Bladder malacoplakia with lymphatic involvement and an aggres sive course] Actas Urol Esp 2003; 27:159 63
15 Parkin CJ, Acland G, Sulaiman B, et al Malakoplakia, a malig nant mimic Bladder 2020; 7:e44
16 Nabeshima A, Yamada S, Xin G, et al A case of malakoplakia of the urinary bladder] J UOEH 2012; 34:265 70
17 Baumgartner BR, Alagappian R Malakoplakia of the ureter and bladder Urol Radiol 1990; 12:157 159
18 Mukha RP, Kumar S, Ramani MK, Kekre NS Isolated mala coplakia of the bladder: a rare case report and review of literature, Int Urol Nephrol 2010; 42:349 350
19 Jordaan HF, Heyns CF, Allen FJ, Schneider J Immunosuppressive therapy for pemphigus vulgaris complicated by malakoplakia of the bladder Clin Exp Dermatol 1990; 15:442 445
20 Sulman A, Goldman H, Malacoplakia presenting as a large blad der mass Urology 2002; 60:163
21 Billis A, Bladder malacoplakia in a patient on chronic hemodial ysis waiting for kidney transplantation Nephron 1994; 67:127 128
22 Nukui M, Nakagawa Y, Uchida M Vesical malacoplakia accom panied with bilateral hydronephrosis: a case report Hinyokika Kiyo 1997; 43:49 52
23 Batchelor JS, Philp NH, Ramsden KL, Scott KWM Primary lym phoma of the bladder arising from an area of malakoplakia Br J Urol 1991; 68:550 1
24 Bylund J, Pais JM Jr A case of acute renal failure caused by bilat eral, multifocal malacoplakia lesions of the bladder and ureters Nat Clin Pract Urol 2008; 5:516 9
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
25 Feldman S, Levy LB, Prinz LM Malacoplakia of the bladder causing bilateral ureteral obstruction J Urol 1980; 123:588 9
26 Fariña Pérez LA, Menéndez P, Astudillo A, et al Cistitis alcalina incrustante y malacoplaquia [Encrusted alkaline cystitis and mala coplakia] Actas Urol Esp 1999; 23:885 7
27 Kohda N, Kamei O, Oda H, A case of vesical malacoplakia, Hinyokika Kiyo 1984; 30:1835 42
28 Sawamura T, Sasagawa I, Kubota Y, et al Malacoplakia of the bladder: efficacy of enoxacine therapy Intern Urol Nephrol 1996; 28:175 179
29 Kato T, Suzuki Y, Sugimura J, et al A case of ureterovesical mala coplakia that manifested hydronephrosis Hinyokika Kiyo 2001; 47:195 7
30 Stripling JR, Tomskey GC, Lanasa JA Jr, Ozog LS Ureteral obstruction caused by malacoplakia of the bladder over the ureteral orifice, South Med J 1979; 72:491 492
3 1 C a v a l l o n e B , S e r a o A , A u d i n o P, e t a l B i l a t e r a l hydroureteronephrosis with renal failure caused by malacoplakia, Urologia 2018; 85:36 37
32 Epstein BM, Patel V, Porteous PH CT appearance of bladder malakoplakia J Comput Assist Tomogr 1983; 7:541 3
33 Steele B, Vade A, Lim Dunham J Sonographic appearance of bladder malacoplakia, Pediatr Radiol 2003; 33:253 255
34 Tsung SH urinary sediment cytology: potential diagnostic tool for malakoplakia, Urology 1932; 10:546 547
35 Cowie AG, Whitaker RH Malakoplakia of the bladder with recurrent passage of pseudo tumour fragments over eight years Br J Surg 1970; 57:883 5
36 Andress MR, Lea Thomas M, Malakoplakia of the bladder demonstrated by double contrast cystography, Br J Radiol 1968; 41:231 232
37 Melicow MM, Malacoplakia Report of case, review of literature J Urol 1957; 78:33 40
38 Scannapieco G, Grasso M, Crippa S, et al Ultrasonographic, serologic, and clinical characteristics of a case of prostatic mala coplakia Arch Ital Urol Androl 2000; 72:254 6
Correspondence
Giordano Polisini, MD gio pol 93@gmail com (Corresponding Author) Rocco Francesco Delle Fave, MD dellefavefrancesco@alice it
Andrea Benedetto Galosi, MD a b galosi@univpm it
Division of Urology, University Hospital “Ospedali Riuniti”, School of Medicine, Department of Clinical, Special and Dental Sciences, Marche Polytechnic University, Ancona, Italy
Camilla Capretti, MD camilla capretti@sanita marche it
Angelo Marronaro, MD angelo marronaro@sanita marche it Alessia Mariagrazia Costa, MD alessia costa@sanita marche it Luigi Quaresima, MD luigi quaresima@sanita marche it
Daniele Mazzaferro, MD daniele mazzaferro@sanita marche it Department of Urology, Civitanova Marche Hospital, Civitanova Marche, Italy
354
REVIEW
Systematic review of urinary biomarkers of female bladder outlet obstruction (fBOO)
Andreia Bilé Silva
, Paulo Jorge Dinis
1 Hospital de Egas Moniz, Lisboa, Portugal;
Hospital Cuf, Lisboa, Portugal
Luís Abranches Monteiro
Summary
Objective: Diagnosis of bladder outlet obstruction (BOO) in females is often chal lenging, not only because of the overlap in storage and voiding symptoms in women with various etiologies of lower urinary tract (LUT) dysfunction but also due to the lack of standardized urodynamic criteria to define the condition There is an unmet need of biologic markers to evaluate BOO in females as an adjunct to other clinical criteria We sought to elucidate the role of urinary biomarkers in female BOO
Material and methods: We performed a systematic review of studies involving urinary biomarkers in female BOO
The search was performed in PubMed A total of 58 papers were retrieved and 2 were included for final analysis
Results: Currently, there are no validated biologic markers for female BOO available Having a biomarker that can be obtained through a urine sample will be an invaluable tool to evaluate and counsel patients with LUT symptoms and possible BOO
The use of NGF as an indicator of BOO in female patients seems to be promising: NGF levels are elevated in women with BOO when compared with normal controls.
Conclusions: We found that NGF levels may be applied as a useful biomarker in the diagnosis and evaluation of female patients with BOO symptoms. It will not completely replace other clinical diagnostic tools such as formal urodynamic testing but play a role as a supplement to it. Nevertheless, further studies should be conducted to establish NGF levels as a female BOO biomarker and a routine testing modality.
KEY WORDS: Urinary biomarkers; Bladder outlet obstruction; Female; Female bladder outlet obstruction
Submitted 12 May 2022; Accepted 6 June 2022
INTRODUCTION
Diagnosis of bladder outlet obstruction (BOO) in females is often challenging, not only because of the overlap in stor age and voiding symptoms in women with various etiolo gies of lower urinary tract dysfunction but also due to the lack of standardized urodynamic criteria to define the condition (1)
The International Continence Society (ICS) defines BOO as “generic term for obstruction during voiding It is a reduced urine flow rate and/or presence of a raised PVR and an increased detrusor pressure It is usually diagnosed by studying the synchronous values of urine flow rate and detrusor pressure and any PVR measurements A urethral stricture or obstruction due to higher degrees of uterovaginal prolapse or obstructed
No conflict of interest declared
voiding after stress incontinence procedures are amongst possi ble causes” (2) Although the prevalence of female BOO has not yet been thoroughly studied, it is estimated to be between 2 7 and 23% (3)
ICS defines dysfunctional voiding as “an intermittent and/or fluctuating flow rate due to involuntary intermittent contractions of the peri urethral striated or levator muscles during voiding in neurologically normal women This type of voiding may also be the result of an acontractile detrusor ( a b d o m i n a l v o i d i n g ) w i t h e l e c t r o m y o g r a p h y ( E M G ) o r video urodynamics required to distinguish between the two entities” (2)
Benign prostatic hyperplasia (BPH) represents the most common cause of BOO in males, being supported by sev eral nomograms that aid in the diagnosis In contrast, the etiology of BOO in women is diverse, being subdivided into anatomical and functional Whereas anatomic causes c o n s i s t m a i n l y o f a n a t o m i c a l c o n d i t i o n s l e a d i n g t o obstruction of the bladder outlet [pelvic organ prolapse ( P O P ) , p o s t a n t i i n c o n t i n e n c e p r o c e d u r e s , s t r i c t u r e s , fibrosis or urethral diverticula], functional BOO results from the inability to achieve a proper relaxation of the ure thral sphincter during bladder emptying [primary bladder neck obstruction, neurogenic detrusor external sphincter, d y s s y n e r g i a , n o n n e u r o g e n i c d y s f u n c t i o n a l v o i d i n g ( a b n o r m a l c o n t r a c t i o n o f p e r i u r e t h r a l m u s c l e ) , a n d Fowler’s syndrome (failure of urethral relaxation)] (4) Most BOO validated questionnaires were developed for prostate pathology and mention prostate specific wording in them Therefore, in addition to a lack of standardized, widely accepted and accurate nomograms, urodynamic criteria and validated questionnaires and quality of life surveys to evaluate female BOO, there is an unmet need of biologic markers to this aim Having an easy to obtain, accurate urine biomarker will be valuable when evaluat ing and counselling patients with lower urinary tract symptoms (5) Accordingly, we conducted a systematic review of studies assessing the role of urinary biomarkers in female BOO
MATERIALS AND METHODS
Systematic literature review
We performed a systematic review of studies utilizing uri nary biomarkers of female bladder outlet obstruction fol
A355 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
1
2 ,
1
2
DOI: 10 4081/aiua 2022 3 355
A Bilé Silva, P J Dinis, L Abranches Monteiro
lowing the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines Comprehensive search strategies were used to identify all relevant studies investigating the use of urinary biomarkers in female blad der outlet obstruction The search was performed in MED LINE using search Medical Subject Headings (MESH) terms “bladder outlet obstruction” , “female” , “ women ” , “urine mark er ” , “urine biomarker” , “biomarker” , “marker” , “urine” , until the end of 2021 using the string [(bladder outlet obstruc tion) AND (women) AND (urine marker)] OR [(bladder outlet obstruction) AND (female) AND (urine biomarker)] OR [(bladder outlet obstruction) AND (female) AND (uri nary marker)] OR [(bladder outlet obstruction) AND (bio marker) AND (female)] OR [(bladder outlet obstruction) AND (marker) AND (female)] Only English language pub lications were considered Studies including BOO in males only were excluded Commentaries were excluded Basic research studies were excluded and only studies in humans were included We did not find multiple reports on the same patient cohort
Study review methodology
Two authors (A B S and L A M ) reviewed and selected studies independently; ; disagreements were resolved by d i s c u s s i o n a n d c o n s e n s u s Titles and abstracts were used t o s c r e e n f o r i n i t i a l s t u d y inclusion Full texts of studies thought to meet or possibly meet the study inclusion were t h e n r e v i e w e d T h e s a m e r e v i e w e r s e x t r a c t e d r e l e v a n t data independently using stan dardized data collection forms Data retrieved from the reports i n c l u d e p u b l i c a t i o n d e t a i l s ( y e a r o f p u b l i c a t i o n a n d authors), methodological com ponents, and trial characteris tics (sample size and outcomes measures)
The association between uri nary biomarkers and BOO in females was recorded
Risk of bias assessment
A formal exclusion of studies due to risk of bias (RoB) assess ment was not carried out as none of the existing RoB scales were felt to be appropriate for this systematic review

Data synthesis
Data synthesis was made after a thorough search through cur rent literature on the diagnosis and management of female BOO, with a specific focus on translational research in the field of urinary biomarker Several potential urine bio
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
markers of female BOO have been studied in a basic research setting, Nerve Growth Factor (NGF) currently rep resenting the most widely accepted one as it represents the only investigated in humans and, specifically, in females Data was stratified by the physiology of voiding and BOO, the basic knowledge on urinary NGF production and role and the relationship between NGF and BOO in female patients
RESULTS
Literature search results
In total, 58 citations were retrieved from the MEDLINE database After removing duplicates and screening of titles and abstracts, 56 citations were excluded from fur ther analysis Figure 1 shows the PRISMA flow diagram of the study
A total of 2 studies were included in the systematic review, one consisting of a nonrandomized comparative study of urinary NGF levels between female patients deemed to have BOO and their asymptomatic counterparts (5) and the other being a narrative review of the literature on eval uation and diagnosis of BOO in women (1)
356
Figure 1. PRISMA flow diagram of the study
Physiology of voiding and BOO
In the setting of BOO, a pathologic increase in outlet resistance is recorded, conducting to a more forceful con traction of the detrusor muscle to generate urine flow across the outlet This dysfunction results in functional and anatomical changes in the detrusor as well as in the neural networks involved in the process (1)
Whereas BOO in males is mainly due to benign prostatic hyperplasia (BPH), the causes are more varied in females, being subdivided into anatomic and functional Among anatomic causes, urethral distortion secondary to pelvic organ prolapse (POP), iatrogenic BOO caused by anti incontinence procedures, intrinsic etiologies (strictures, fibrosis, urethral diverticula), should be considered
Functional BOO results from primary bladder neck obstruction (failure of bladder neck relaxation), neuro genic detrusor external sphincter dyssynergia, non neu rogenic dysfunctional voiding (abnormal contraction of periurethral muscle) and Fowler’ s syndrome (1, 5)
Basic knowledge on NGF production and role
Multiple biomarkers have been studied as potential indi cators of BOO in females NGF is produced by bladder smooth muscle cells, urothelial cells, and sensory afferent neurons The role of NGF in the neurotrophic effects associated with obstruction was first described in 1991 by Steers et al (6)
Under normal conditions, NGF levels in the urine are low Increased urinary NGF levels are associated with bladder inflammation secondary to chemical irritation, detrusor overactivity, and BOO It has been hypothesized that, through mechanical stretching, NGF expression in the bladder wall may increase leading to a reduced sen sory threshold resulting in urgency or a reduced thresh old for mediating detrusor hyperactivity
Liu and Kuo demonstrated that urinary NGF is elevated in male patients with BOO plus overactive bladder (OAB) symptoms compared with normal controls Studies sup port the role of NGF in bladder overactivity, irritative voiding symptoms and afferent pathways plasticity The increased concentration of NGF can reduce the threshold or increase excitability in the afferent fibers leading to increased bladder sensation or overactivity Expression of NGF is modulated by intervention, being reduced after medical or surgical treatment of the obstruction (1, 5)
Relationship between NGF and BOO in female patients
A prospective study conducted in 2015 assessed the uri nary NGF levels in 10 women with anatomic BOO and compared those to 10 asymptomatic female controls All females referred for evaluation and management of BOO f r o m P O P o r p r e v i o u s i n c o n t i n e n c e s u r g e r y w e r e screened for enrollment BOO was caused by POP in 6 patients, post incontinence procedure in 5 patients and both etiologies in 1 patient The urinary ratio between NGF and creatinine (Cr) levels in the patients with BOO (mean 20 8 pg/mg) were significantly higher (p = 0 0001) than the levels in the control group (5 6 pg/mg) A weak positive correlation between urinary NGF level and the symptoms severity (evaluated by the Urinary Distress Inventory 6 symptom score) was reported A significant decrease in mean urinary NGF/Cr to 6 50pg/mg (p =
Urinary biomarkers of fBOO
0 01) was recorded after treatment of the conditions responsible for the anatomic BOO (prolapse repair, sling excision) Furthermore, the decreases in NGF/Cr levels after treatment correlated with subjective improvement in the symptoms of patients as demonstrated by decreased UDI 6 survey scores and objective improvement as demonstrated by increased flow rates Therefore, urinary NGF looks like a promising tool for women with sus pected anatomic BOO as a diagnostic and an objective assessment of the therapeutic effects of surgical and med ical interventions in women with BOO (1, 5)
DISCUSSION
BOO in women is less understood than in men, as symp toms are scarce and misleading Due to anatomical and physiological differences, the boundaries of normality are less well defined, and urodynamic diagnosis is often unsatisfactory and not universally accepted Voiding dys function consists of a combination of BOO and detrusor underactivity (DU) in both sexes BOO, as an increased outlet resistance to flow, cannot be separated from detru sor function: the balance between these two parameters will define a broader concept of voiding dysfunction
Increased urethral resistance in women is not as common as in men, but far from rare In a retrospective study that included 1142 women, 192 (19%) were diagnosed with BOO Functional sphincteric obstruction was diagnosed in 70 women (36%) The most common anatomical cause of BOO was previous anti incontinence surgery, followed by urethral stricture, diagnosed in 21% and 20% of patients, respectively The most common presenting symptoms were storage phase symptoms of daytime and night time urinary frequency Hence, BOO should be suspected in women with refractory LUTS, especially those presenting with urinary frequency (7)
Female voiding dysfunction has often a presentation sim ilar to other conditions, lacking specific symptoms or signs It was found in 23% of patients with OAB BOO is more frequent than DU and should be suspected in patients with higher night time frequency, presence of detrusor overactivity and a high post void residual Instead, DU should be suspected in patients with a small er voided volume (8)
Several combinations of nomograms were tested to increase the accuracy of diagnosing BOO and detrusor u n d e r a c t i v i t y ( D U ) a m o n g w o m e n w i t h L U T S ( 9 )
Evidence on tests used to diagnose female bladder outlet obstruction was recently reviewed The available evidence on diagnostic tests for female bladder outlet obstruction is limited and heterogeneous The most common test used was found to be pressure flow studies with or with out fluoroscopy, which remains the current standard for diagnosing bladder outlet obstruction in women (10) Yet, as these methodologies frequently find blurred boundaries, are expensive, not widely available, and inva sive, alternative or clarifying tests are needed
Currently, no biologic markers for BOO to use as an adjunct to the evaluation and monitoring of lower urinary tract symptoms in women in parallel with nomograms, urodynamics, validated questionnaires, or quality of life surveys are available Having a biomarker that can be eas
A357 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
A Bilé Silva, P J Dinis, L Abranches Monteiro
ily obtained through a urine sample will be an invaluable tool to evaluate and counsel patients with lower urinary tract symptoms and possible BOO (5)
The prospective study included in the review demon strates that the use of NGF as an indicator of BOO in female patients is adequate Women with BOO presented elevated urinary NGF/Cr levels when compared with nor mal controls and these levels significantly decreased with appropriate surgical treatment Nevertheless, the low number of patients included in this study represents its main limitation The results are consistent and significant but further information regarding the diagnostic and appraisal potential of the urine biomarker are still missing (5)
Even though clinical studies in males and basic research studies were not included in the systematic review, sever al other parameters have been the object of investigation in these settings, namely urinary molecules Prior to being studied in females, urinary NGF has been proved to be elevated in men with BOO and to decrease in association with reduction of the prostate volume and relief of BOO making it a potential tool not only to diag nose but also to monitor the improvement of BOO in patients with BPH (5, 11)
Prostaglandin E2
The micturition reflex is stimulated by prostaglandins, which decrease the necessary threshold to trigger detru s o r c o n t r a c t i o n t h r o u g h c a p s a i c i n s e n s i t i v e a f f e r e n t nerves (12) Prostaglandins, such as prostaglandin E2 (PGE2), show increased levels in conditions such as OAB, detrusor overactivity (DO) and BOO (13, 14)
ATP
Urothelial cells release ATP into the urine in response to bladder stretch It may play a major sensory role on pelvic afferent nerve fibers (15) A rat model demonstrated an increase in urothelial ATP release due to partial BOO induction (16) In males with BOO due to BPH, there seems to be a higher release of ATP into the urine The results suggest that urinary ATP may be a high sensitive non invasive biomarker of BOO with additional potential discriminative value of detrusor function when compar i n g B P H p a t i e n t s w i t h l o w u r i n a r y fl o w r a t e s Furthermore, ATP levels may represent a surrogate mark er for the degree of obstruction (17, 18)
mRNA and miRNA
BOO is responsible for significant organ remodeling which conducts to lower urinary tract symptoms and accompanying urodynamic changes in bladder function
BOO patients have mRNA and miRNA expression pro files correlated with urodynamic findings The molecular changes in BOO might indicate an increasing involve ment of miRNAs in the control of bladder function from the overactive to underactive/acontractile states Thus, mRNA and miRNA might represent markers of detrusor competence (19, 20)
Oxidative stress markers
Partial BOO leads to an increase in tissue and systemic oxidative stress markers and cytokines in basic research
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
models A rise in 8 hydroxydeoxyguanosine (8 OHdG) in urine and malondialdehyde (MDA) in plasma of rabbits was documented along with a limited total oxidant capacity in plasma (21); a rise in the number of plasma myeloid derived suppressor cells (MDSCs), interferon gamma, inter leukin 10 and aldosterone was observed in a rat model (22); elevated levels of F2 isoprostane were noted in a chronic injury mouse model of partial BOO (23)
Detrusor muscle biopsy
Although the focus of this review is on urinary biomark ers of female BOO, there is emerging evidence on mus cular hypertrophy as an indicator of this condition, as revealed by pathological analysis of detrusor specimens
Firstly, myohypertrophy was shown to be present in men with BOO (24) Afterwards, Wang et al , proved this phe nomenon to be present in female BOO and to be related to the degree and duration of obstruction with the female controls not displaying this sort of ultrastructural changes (25, 26)
Novel biomarkers
Future developments may involve further studies on NOD , LRR and pyrin domain containing protein 3 (NLRP3) inflammasome, a sensor of cellular damage in the urothelium (27), piezo1, a mechanically activated ion channel present in the detrusor muscle and suburothelial layer implicated in sensation of bladder stretch (28), n i c o t i n i c a c e t y l c h o l i n e r e c e p t o r s i n p a r a s y m p a t h e t i c bladder pelvic ganglion neurons, which expression has been shown to be increased due to its upregulation in BOO (29)
The study is not without limitations It reflects the lack of information on the topic and the unmet need of transla tional studies in the field of urinary biomarkers of BOO in female patients While the evidence on the use of NGF as a biomarker of female BOO grows, many questions on its validity remain including its specificity, sensitivity, cost and time effectiveness
Conclusions
Even though these results indicate that NGF levels may be applied as a useful biomarker in female patients with BOO symptoms, research on biomarkers of BOO is lack ing and further investigation is needed
The use of NGF as a biomarker will not completely replace other clinical diagnostic tools such as formal uro dynamic testing although it will probably be considered as a supplement to it Nevertheless, further studies should be conducted in order to establish NGF levels as a female BOO biomarker and a routine testing modality
F u r t h e r m o r e , t h i s s y s t e m a t i c r e v i e w u n d e r l i n e s t h e unmet need of urinary biomarkers of female BOO
REFERENCES
1 Martinez L, Khavari R New frontiers in molecular and imaging research on evaluation and diagnosis of bladder outlet obstruction in women Curr Bladder Dysfunct Rep 2017; 12:291 297
2 Haylen BT, de Ridder D, Freeman RM, et al An International U r o g y n e c o l o g i c a l A s s o c i a t i o n ( I U G A ) / I n t e r n a t i o n a l C o n t i n e n c e
358
Society (ICS) joint report on the terminology for female pelvic floor dysfunction Neurourol Urodyn 2010; 29:4 20
3 Blaivas JG, Groutz A Bladder outlet obstruction nomogram for w o m e n w i t h l o w e r u r i n a r y t r a c t s y m p t o m a t o l o g y N e u r o u r o l Urodyn 2000; 19:553 64
4 Meier K, Padmanabhan P Female bladder outlet obstruction: an update on diagnosis and management Curr Opin Urol 2016; 26:334 41
5 Chan R, Munoz A, Wenker EP, et al The association of urinary nerve growth factor levels with bladder outlet obstruction in women Female Pelvic Med Reconstr Surg 2015; 21:111 5
6 Steers WD, Kolbeck S, Creedon D, Tuttle JB Nerve growth factor in the urinary bladder of the adult regulates neuronal form and func tion J Clin Invest 1991; 88:1709 15
7 Malde S, Solomon E, Spilotros M, et al Female bladder outlet obstruction: Common symptoms masking an uncommon cause Low Urin Tract Symptoms 2019; 11:72 77
8 Santis Moya F, Calvo CI, Rojas T, et al Urodynamic and clinical features in women with overactive bladder: When to suspect con comitant voiding dysfunction? Neurourol Urodyn 2021; 40:1509 1514
9 Mytilekas KV, Oeconomou A, Sokolakis I, et al Defining voiding dysfunction in women: bladder outflow obstruction versus detrusor underactivity Int Neurourol J 2021; 25:244 251
10 Pang KH, Campi R, Arlandis S, et al Diagnostic tests for female bladder outlet obstruction: a systematic review from the European Association of Urology Non neurogenic Female LUTS Guidelines Panel Eur Urol Focus 2021; S2405 4569(21)00231 5
11 Wada N, Matsumoto S, Kita M, et al Decreased urinary nerve growth factor reflects prostatic volume reduction and relief of outlet obstruction in patients with benign prostatic enlargement treated with dutasteride Int J Urol 2014; 21:1258 62
12 Kim JC, Park EY, Seo SI, et al Nerve growth factor and prostaglandins in the urine of female patients with overactive blad der J Urol 2006; 175:1773 6
13 Kuo HC Potential biomarkers utilized to define and manage overactive bladder syndrome Low Urin Tract Symptoms 2012; 4 Suppl 1:32 41
14 Mikhailidis DP, Jeremy JY, Dandona P Urinary bladder prostanoids their synthesis, function and possible role in the patho genesis and treatment of disease J Urol 1987; 137:577 82
15 Vlaskovska M, Kasakov L, Rong W, et al P2X3 knock out mice reveal a major sensory role for urothelially released ATP J Neurosci 2001; 211:5670 7
16 Shiina K, Hayashida KI, Ishikawa K, Kawatani M ATP release from bladder urothelium and serosa in a rat model of partial bladder outlet obstruction Biomed Res 2016; 37:299 304
17 Chen Z, Liu Y, Zhao M, et al Urinary ATP may be a biomarker for bladder outlet obstruction and its severity in patients with benign prostatic hyperplasia Transl Androl Urol 2020; 9:284 294
18 Silva Ramos M, Silva I, Oliveira JC, Correia de Sá P Increased urinary adenosine triphosphate in patients with bladder outlet obstruction due to benign prostate hyperplasia Prostate 2016; 76:1353 63
19 Gheinani AH, Kiss B, Moltzahn F, et al Characterization of miRNA regulated networks, hubs of signaling, and biomarkers in o b s t r u c t i o n i n d u c e d b l a d d e r d y s f u n c t i o n J C I I n s i g h t 2 0 1 7 ; 2:e89560
Urinary biomarkers of fBOO
20 von Siebenthal M, Besic M, Gheinani AH, et al Urinary miRNA profiles discriminate between obstruction induced bladder dysfunc tion and healthy controls Sci Rep 2021; 11:10204
21 Lin WY, Chen CS, Wu SB, et al Oxidative stress biomarkers in urine and plasma of rabbits with partial bladder outlet obstruction BJU Int 2011; 107:1839 43
22 Lin WY, Hsieh CC, Yang TY, et al Transient increase in circu lating myeloid derived suppressor cells after partial bladder outlet obstruction J Urol 2014; 192:1569 73
23 Clayton DB, Stephany HA, Ching CB, et al F2 isoprostanes as a biomarker of oxidative stress in the mouse bladder J Urol 2014; 191(5 Suppl):1597 601
24 Brierly RD, Hindley RG, McLarty E, et al A prospective evalua tion of detrusor ultrastructural changes in bladder outlet obstruction BJU Int 2003; 91:360 4
25 Wang A, Brammah S, Tse V, Chan L Comparison of ultrastruc tural features in female and male bladder outlet obstruction: a poten tial role for diagnostic detrusor muscle biopsy J Urol 2015; 193 (Suppl 4): E1105
26 Fusco F, Creta M, De Nunzio C, et al Progressive bladder remodeling due to bladder outlet obstruction: a systematic review of morphological and molecular evidences in humans BMC Urol 2018; 18:15
27 Hughes FM Jr, Hill HM, Wood CM, et al The NLRP3 inflam masome mediates inflammation produced by bladder outlet obstruc tion J Urol 2016; 195:1598 1605
28 Michishita M, Yano K, Tomita KI,, et al Piezo1 expression increases in rat bladder after partial bladder outlet obstruction Life Sci 2016; 166:1 7
29 Chung HC, Lee CK, Park KH, Jeong SW Bladder outlet obstruc tion causes up regulation of nicotinic acetylcholine receptors in blad der projecting pelvic ganglion neurons Brain Res 2015; 1602:111 8
Correspondence
Andreia Bilé Silva, MD (Corresponding Author) andreiabile@campus ul pt Luís Abranches Monteiro, MD abranchesmonteiro@gmail com Hospital de Egas Moniz
Paulo Jorge Dinis, MD pj s dinis@gmail com Hospital Cuf
A359 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
REVIEW
Summary
Background: Varicocele is known to have impacts in infertility cases and sperm quality
This review aimed to evaluate the effects of microsurgical varico celectomy on sperm DNA fragmentation index (DFI) and sperm parameters
Methods: Open full English text articles from January 2017 to October 2021 were searched from online database including PubMed, EMBASE, Scopus, Cochrane Library and Google Scholar
Results: Systematic search resulted in 277 potential papers After throughout paper analysis, 5 studies were included in this review From all five analyzed studies, microsurgical varicocelec tomy was statistically proven to reduce DNA fragmentation index by 5 46% (mean difference 5 46; 95% CI: 4 79, 6 13; p< 0 00001) Moreover, the procedure also significantly improved other sperm parameters (sperm concentration +8 23%, sperm motility +7 17%, sperm progressive motility +2 77%, sperm morphology +0 64%)
Conclusion: Microsurgical varicocelectomy significantly improves spermatogenesis as reflected by biomarkers of infertile men including semen parameters and sperm DNA fragmentation (SDF)
KEY WORDS: Microsurgical varicocelectomy; Sperm DNA frag mentation; DNA fragmentation index; Progressive sperm motility; Sperm concentration; Sperm morphology; Total sperm motility
Submitted 23 May 2022; Accepted 14 July 2022
INTRODUCTION
Varicocele is an abnormal dilatation of pampiniform plexus veins in the spermatic cord that commonly corre lates to infertility and bad sperm quality Its incidence reaches up to 15% among normal population while its prevalence varies from 30 80% in primary and secondary infertile patients (1) The etiopathogenesis of varicocele remains unclear The common hypothesis believes the condition is caused by the lack of oxygen in the scrotum, small vessel obstruction and imbalance of reactive oxygen species (ROS) and antioxidant production The imbalance in specific leads to lipid, protein and nucleic acids dam age of the living sperm cells due to high oxidative stress, hence altering their its motility and ability to fuse with oocyte ROS also impair sperm chromatin structure by
breaking DNA strands that negatively affecting develop ment and embryo implantation negatively (2) Sperm integrity, DNA damage and genetic material are reflected by DNA fragmentation index (SDF) parameter that is sug gested as a crucial biomarker for semen quality (3) The sperm DNA fragmentation index (SDF) is a potential parameter for the study of fertility Previous studies hint ed the possibility of using DNA fragmentation with the clinical limit of 25% (4) Men with higher DFI are more susceptible to have reproductive problems A more Recent studies claim surgical repair of varicocele can help improve sperm DNA quality This theory is supported as reviewed by the Schauer et al. (5) meta analysis result, stat ing that regardless of the chosen surgical technique (high ligation, inguinal or subinguinal approach), improve ments can be seen Moreover, microsurgical methods offer adequate simplified anatomic visualization with a lower recurrence and complication rate (6) High SDF coupled with normal sperm parameters has yet to be considered as varicocelectomy indication due to the limited studies regarding the impact of such intervention on SDF (4) Studies have shown that varicocele repair can improve sperm quality and pregnancy rates of people with clinical varicocele Varicocelectomy may also result in the devel opment of testicular regrowth and improve the sperm DNA integrity in up to 80% of cases Considering the impact of untreated varicocele cases, especially on male fertility, it is important to evaluate and provide physicians with the most updated knowledge A recent meta analysis (7) evaluated the effect of varicocelectomy, including microsurgical varicocelectomy, on sperm DNA integrity, but other studies were more recently published targeted on specific populations with infertility associated to varic ocele and with longer follow up Therefore, this paper aims to update the review of current literature regarding the effects of microsurgical varicocelectomy on sperm DNA fragmentation index and sperm parameters
MATERIAL AND METHODS
Eligibility criteria
Inclusion criteria of the chosen studies were: study writ ten in English, available online in full text, published
No conflict of interest declared
Archivio Italiano di Urologia e Andrologia 2022; 94, 33 60
Microsurgical varicocelectomy effects on sperm DNA fragmentation and sperm parameters in infertile male patients: A systematic review and meta-analysis of more recent evidence
Alwin Soetandar, Bambang Sasongko Noegroho, Safendra Siregar, Ricky Adriansjah, Akhmad Mustafa
Department of Urology, Hasan Sadikin Academic Medical Center, Faculty of Medicine, Universitas Padjadjaran Bandung, Indonesia
DOI: 10 4081/aiua 2022 3 360
Microsurgical varicocelectomy effects on sperm DNA fragmentation and sperm parameters in infertile male patients
between January 2017 to October 2021, designed as ran domized controlled trials (RCTs) or cohort prospective studies, reporting DFI and sperm parameters after micro surgical varicocelectomy
Exclusion criteria
Studies were excluded if studies were case reports, reviews and other than microsurgical varicocelectomy therapy was performed
Guidelines
We used the Preferred Reporting Items for Systematic Reviews and Meta Analysis (PRISMA) guidelines in report ing this study (8) (Figure 1)
Search strategy
Literature search was performed on PubMed, EMBASE, Scopus, Cochrane Library, and Google Scholar following P R I S M A g u i d e l i n e s T h e s e a r c h w a s c o n d u c t e d o n September 23rd, 2021 using the search term (“microsurgi cal varicocelectomy” OR “microscopic varicocelectomy” OR “microsurgery of varicocele” OR “varicocele repair”) AND (“sperm parameter” OR “ sperm analysis” OR “SDF"
Data extraction and quality assessment
One reviewer selected literature and inputted data into an Excel database Two independent reviewers screened titles and abstracts to determine their eligibility Then, a full text review was done to obtain detailed information Risk of bias assessment was done based on PRISMA Guidelines
Statistical analysis
Meta analysis compared preoperative vs postoperative sperm parameters and SDF using the Review Manager
5 4 1 software The main outcome was the mean differ ence with 95% CI before and after varicocelectomy If the p value of heterogeneity chi squared test was less than 0 10 or I2 > 50%, the random effect model was used The fixed effect model was then used if p ≥ 0 10 or I2 ≤ 50%
RESULTS
Study selection
Systematic search for studies from all available databases resulted in 277 potential papers After screening and duplicate exclusion, 68 studies were chosen After second evaluation regarding topic relevance, 12 studies were evaluated Finally, after throughout paper analysis, 5 studies were included in this review (Figure 1) Three more studies were retrieved with respect to the previous review of Qiu et al (7) They were specifically targeted on patients with infertility associated to varicocele and one of them reported data at a longer follow up period

Study characteristics
The general characteristics of reviewed prospective stud ies are listed in Table 1 Varicocele repair through micro surgical varicocelectomy was done in 95, 141, 67, 120 and 60 patients, respectively Three out of five studies evaluated SDF after three months from the procedure, whereas the other two did the test after 6 and 12 months of operation The SDF data by varicocele grade was pro vided by two studies
Sperm parameters such as sperm concentration, total and progressive sperm motility and sperm morphology are listed in Table 2 Only one study didn’t measure sperm concentration The rest showed massive improvement in both concentration and morpholo gy after the intervention Other than that, two studies reported total and progressive sperm motili t y , r e s p e c t i v e l y I n g e n e r a l , a l l included studies resulted in the improvement of sperm parameters after the surgery
Pre and post operative SDF
The SDF was evaluated preopera tively, 3 months or 6 months post operatively in all of the included studies The result of meta analysis for 5 studies were presented in Figure 2 The heterogeneity test was statistically significant (chi squared = 108 39, df = 4, p < 00001, I squared = 96%), hence the random effect model was used otherwise On average, SDF percentage among clinical varicocele patients showed 5,61% reduction after the proce dure (mean difference 5 61; 95% CI: 6 28, 4 94; p < 0 00001)
Sperm concentration
Four studies reported sperm con
A361 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
Figure 1. PRISMA
Flow Diagram
centration before and after surgery It was showed an increase of sperm concentration by 8 23% after surgery
Table 1.
Study characteristics and SDF findings
(mean difference: 8 23; 95% CI: 6 62, 9 85; p < 0 00001) (Figure 3)
Reference Design Patients Follow up month SDF assay Surgical technique Main SDF results after surger y
Fathi et al (9) Prospective cohort 95 male patients with a 1 year history 12 months
SCD M crosurgical sub nguinal SDF% decreased from 34 93% ± 5 56% preoperatively of male subfertil ty to 25 75% ± 5 15% postoperatively (p < 0 001)

Kavoussi et al (10) Prospective cohort 141 male patients who underwent 3 months
SCD M crosurgical sub nguinal SDF% decreased from 29 7% ± 5 0% preoperatively varicocele repair for infertility to 22% ± 0% postoperatively (p < 0 38)
Vahidi et al (1) Prospective cohort 67 infertile male patients 3 months TUNEL test M crosurgical sub nguinal SDF& decreased from 15 93 ± 4 96% preoperative with varicocele to 10 86 ± 4 44% postoperat ve (p < 0 001)
Zaazaa et al (11) Prospective cohort 120 male patients associated with 3 months
SCD M crosurgical sub nguinal SDF% decreased from 34 6 ± 4 1% preoperative varicocele grade II and III to 28 3 ± 5 2% postoperative (p < 0 05)
Abdelbaki et al (12) Prospective cohort 60 male patients with varicocele 3 6 months SCSA M crosurgical sub nguinal SDF% decreased from 29 49% preoperative to 18 78% postoperative (p < 0 001)

SDF = sperm DNA fragmentation; SCD = sperm chromatin dispersion; TUNEL = term nal deoxynucleot dy transferase mediated dUTP nick end abe l ng
Table 2
Sperm parameters.
Reference Sper m concentration
Total sper m motility Progressive sper m motility Sper m morpholog y Pregnancy rate
Fathi et al (9) Increased from 26 1 ± 8 5 mil ions/mL N/A Increased from 33 9 ± 1 6% Increased from 4 3 ± 0 5
Higher pregnancy rate of preoperative to 32 5 ± 8 6 millions/mL preoperative to 36 1 ± 6 3% preoperative to 5 2 ± 1 8% varicocelectomy group (31 1%) postoperative (p = 0 002) postoperative (p = 0 82) postoperative (p = 0 09) compared to control group (13 3%) (p = 0 10)
Kavouss et al (10) Increased from 25 5 ± 32 4 millions/mL Increased from 47 5 ± 20 3% Increased from 25 8 ± 3 8% N/A N/A preoperative to 36 0 ± 37 0 mill ons/mL preoperative to 53 4 ± 14 5% preoperative to 30 6 ± 14 3% postoperative (p = 0.25) postoperative (p = 0.25) postoperative (p = 0.38)
Vahid et al (1) N/A N/A N/A
Zaazaa et al (11) Increased from 20 8 ± 18 4 millions/mL Increased from 24 3 ± 10 8% N/A
Increased from 13 86 ± 7 85% N/A preoperative to 18 53 ± 7 36% postoperative (p = 0 016)
Increased from 1 5 ± 0 5% N/A preoperative to 28 0 ± 22 9 mill ons/mL preoperative to 32 1 ± 12 1% preoperative to 2 2 ± 0 9% postoperative (p < 0 05) post operative (p < 0 05) postoperative (p < 0 05)
Abde baki et al (12) Increased from 10 9 ± 2 8 mil ions/mL Increased from 36 4 ± 10 7% Increased from 10 8 ± 4 6% Increased from 2 3 ± 0 7% N/A preoperative to 21 04 ± 8 9 mill ons/mL preoperative to 53 6 ± 18 9% preoperative to 19 1 ± 8 1% preoperative to 2 7 ± 0 6% postoperative (p < 0 001) postoperative (p < 0 001) post operative (p < 0 001) postoperative (p < 0 001)
Figure 2
Forest plot of meta analysis on the efficacy of varicocelectomy for sperm DNA fragmentation improvement (random effect model of 5 studies).
Figure 3.
Forest plot of sperm concentration (fixed effect model)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
A Soetandar, B Sasongko Noegroho, S Siregar, R Adriansjah, A Mustafa
362
Figure
Forest plot
Microsurgical varicocelectomy effects on sperm DNA fragmentation and sperm parameters in infertile male patients
(random
model)
Figure
Forest plot of
(random effect model)
Total sperm motility
Both Kavoussi et al and Zaazaa et al evaluated total sperm motility 3 and 6 months post varicocelectomy There was meaningful increase by 7 17% (mean difference: 7 17; 95% CI: 4 80, 9 54; p < 0 00001) (Figure 4)
Progressive sperm motility
Progressive sperm motility was evaluated in three studies comparing pre and post varicocelectomy results, show ing a significant increase by 3 77% (mean difference: 3 77; 95% CI: 2 73, 4 82; p < 0 00001) (Figure 5)
Sperm morphology
Evaluation of sperm morphology before and after the intervention was done in 4 studies showing an increase of sperm morphology by 0 64% (mean difference: 0 64; 95% CI: 0 50, 0 77; p < 0 00001) (Figure 6)
Table
Risk of Bias Assessment.
Table 4.
Summary of Findings
Patient
population:
Inter vention: Microsurg
varicocelectomy
Comparison: Standard varicocelectomy

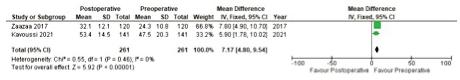
Risk of bias and summary of findings
Results of Risk of Bias assessment and Summary of Findings are reported in Tables 3, 4
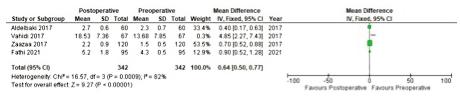
DISCUSSION
Varicocele has long been associated to higher SDF index damage (13) Newer studies has started to include SDF index as a new indicator for varicocelectomy since a prior study had suggested it as a diagnostic tool for clinical varicocele patients (16) The average value of SDF is 15 30% and is regarded as high when detected DFI reaches
A363 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
3.
Author Year Random Allocation Blinding Incomplete Other Overall Sequence Concealment Generation Outcome Data Bias Risk Bias Fathi et al 2021 No No No Yes No High Kavouss et al 2019 No No No Yes No High Vahidi et al 2018 Unclear No No Yes No High Zaazaa et al 2018 Yes Unclear No Yes No Moderate Abde baki et al 2017 No No No No No High
or
Varicocele patients
cal
Outcomes; Sperm DNA Fragmentation Index and other sperm parameters with mean differences (95%CI) SDF 5 61 95% CI 6 28 to 4 94 Sper m concentration 8 23 95% CI 6 62 to 9 85 Total sper m motility 7 17 95% CI 4 8 to 9 54 Progressive sper m motility 3 77 95% CI 2 73 to 4 82 Sper m morpholog y 0 64 95% CI 0 5 to 0 77 Total par ticipants: 483 infertile males [5 studies] Follow up: 3 12 months Figure 4. Forest plot of total sperm motility (fixed effect model)
5
of progressive sperm motility
effect
6
sperm morphology
A Soetandar, B Sasongko Noegroho, S Siregar, R Adriansjah, A Mustafa
more than 30% Majority of men with grade II and III varicocele have SDF level of more than 30% Moreover, a group of scientists has claimed lower embryo implanta tion and pregnancy rate happened if SDF threshold was more than 30% (14) This even more suggests a connec tion between ROS level in spermatozoa and SDF
For more than a century, varicocelectomy has always been the first treatment option for subfertile male with palpable varicocele This procedure is performed through t h r e e s u r g i c a l a p p r o a c h e s s u c h a s r e t r o p e r i t o n e a l , inguinal and subinguinal varicocele repair with or with out magnification (15) In general, sperm DNA integrity in patients improved after the procedure (7) Based on EAU guideline, varicocelectomy in infertility cases has been shown to enhance semen parameters including sperm motility, concentration, and morphology (16) It also significantly decreases testosterone levels, natural and assisted pregnancy rates Varicocelectomy in infertil ity cases with absence of semen parameters abnormality and subclinical varicocele is not recommended (16)
SDF
From meta analysis of all the 5 analyzed studies, varicoc electomy decreased DNA fragmentation index by 5,61% (mean difference 5 61; 95% CI: 6 28, 4 94; p < 0 00001) This result was confirmed in three studies using different methods of assessment (p < 0 001); from 34 93% ± 5 56% preoperatively to 25 75% ± 5 15% post operatively using SDF assay of SCD9, from 15 93 ± 4 96% preoperatively to 10 86 ± 4 44% postoperatively using TUNEL test1, and from 29 49% preoperatively to 18 78% postoperatively using SCSA (12) Moreover, a lower SDF index from 34 6 ± 4 1% preoperatively to 28 3 ± 5 2% postoperatively (p < 0 05) was also seen in 120 grade II and III varicocele patients (11) Similar results of lower DNA fragmentation index from 29 7% ± 5 0% to 22% ± 0% (p < 0 38) after varicocele repair among 141 infertile male patients were also observed (4)
Prior meta analysis by Qiu et al observed a reduction of SDF percentage after varicocelectomy of 6 14 [95% CI, 6 90 to 5 37] 7 Results from Birowo et al and Wang et al also supported this finding (4, 13) Both studies had demonstrated the impact of varicocele repair in decreas ing SDF index, leading to the halt of varicocele progres sion by downregulating systemic oxidative stress (OS) (2) Study by Neto et al added that varicocelectomy improved SDF count in all varicocele condition regardless of its grade without much different in treatment duration (17)
Furthermore, a review of 20 studies reported great reduc tion of SDF after varicocelectomy during 3 12 months follow up time (2) The findings in this study has been constant with previous literatures (4, 13, 17) concluding that varicocelectomy does bring improvement in sperm DNA characteristics in clinical varicocele patients
The DNA damage in varicocele can be one of the causes in lower SDF count after varicocelectomy DNA fragmen tation happens during sperm synthesis and maturation (3) During the sperm maturation, histones are replaced by smaller arginine and cysteine rich protamine (HP)
The replacement hinders sperm DNA ability to repair itself when being exposed to internal and external modi fications The misfolding of DNA supercoil structures in
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
the chromosome due to the tension twist by the double stranded DNA helix that supposed to restore DNA actu ally caused SDF or abnormalities inside the chromatin structure 18 Furthermore, external genital tracts inflam mation, venous statis and reflux increase risk of SDF by promoting hypoxia, inducing and increasing reactive oxy gen species (ROS) within the sperm DNA All those changes lead to worse DNA damage and fragmentation (3, 13, 19) Other than resolving venous stasis and reflux problem, varicocelectomy also reduce ROS synthesis, leading to less DNA damage (4)
Sperm parameters
Schauer et al evaluated semen parameters after proce dures such as high ligation or inguinal or subinguinal were performed Regardless of the methods, meaningful comparable improvements were observed in sperm con centration and motility (5) Furthermore, surgical meth ods (77 5%) had been perceived to give better results in sperm parameter compared to radiological approach (62 5%) (p = 0 032) (20) The measured parameters showed improvement after 3 months of varicocelectomy (21) Sperm DNA fragmentation was not linked to sperm concentration, morphology and progressive motility 3 Result of this review regarding better sperm parameters were similar with prior studies (4, 5, 20)
Sperm concentration
Different results were seen from previous studies Li et al study showed different sperm concentration between control and varicocele group (22) However, Nguyen et al. claimed sperm concentration between two groups were alike (14) Sperm concentration was evaluated before and after surgery An elevation of 8,23% were gained after procedure (mean difference: 8 23; 95% CI: 6 62,9 85; p < 0 00001) Comparison between pre and post interven tion proved there are meaningful rise in sperm concen tration (p = 0 009) (22) Further statistical analysis exhib ited no significant relationship between sperm DNA integrity and sperm concentration (22)
Total sperm motility
Result of this review goes in accordance with previous study that assessed various varicocelectomy methods and sperm motility In that study, sperm motility was higher by 6 80% after suprainguinal approach (95% CI 3 95 to 9 66, p < 0 00001), 9 44% after inguinal approach (95% CI 3 72 to 15 16, p = 0 001) and 12 25% by subinguinal approach (95% CI 4 76 to 19 75, p = 0 001) (5)
Progressive sperm motility
Higher progressive sperm motility was observed in cur rent and prior studies Study by Kadioglu et al had s h o w e d b e t t e r p r o g r e s s i v e s p e r m m o t i l i t y a f t e r s i x months of microsurgical varicocelectomy when com pared to baseline (p < 0 05) (23) This study also had similar result with no association found between progres sive motility and sperm SDF (3)
Sperm morphology
Most of studies showed improvement of sperm morphol ogy after intervention, including result gained in this
364
Microsurgical varicocelectomy effects on sperm DNA fragmentation and sperm parameters in infertile male patients
study Sperm morphology was 2 73% higher after varico celectomy (mean difference: 2 73; 95% CI: 0 65, 4 80; p = 0 01) (4)
Only one study by Li et al that had failed to establish such result (p = 0 028) (22)
CONCLUSIONS
Microsurgical varicocelectomy is not simply the best ther apy approach for varicocele repair It can also benefit in enhancing fertility by lowering SDF as seen in infertility biomarkers including semen parameters and pregnancy rates Among the evaluated studies, only one paper showed better pregnancy rate after surgical procedure Our data supported the hypothesis of spermatogenesis restoration after varicocelectomy in infertile patients However, further studies using more related publications is needed to prevent publication bias In this study, only RCT prospective studies were included
REFERENCES
1 Vahidi S, Moein M, Nabi A, Narimani N Effects of microsurgical varicocelectomy on semen analysis and sperm function tests in patients with different grades of varicocele: Role of sperm functional tests in evaluation of treatments outcome Andrologia 2018; 50:1 6
2 Roque M, Esteves SC Effect of varicocele repair on sperm DNA fragmentation: a review International Urology and Nephrology 2018; 50:583 603
3 Yang H, Li G, Jin H, et al The effect of sperm DNA fragmentation index on assisted reproductive technology outcomes and its relation ship with semen parameters and lifestyle 2019; 8:356 65
4 Birowo P, Rahendra Wijaya J, Atmoko W, Rasyid N The effects of varicocelectomy on the DNA fragmentation index and other sperm parameters: a meta analysis Basic Clin Androl 2020; 30:15
5 Schauer I, Madersbacher S, Jost R, et al The Impact of Varicocelectomy on Sperm Parameters: A Meta Analysis Journal of Urology 2012; 187:1540 7
6 Majzoub A, Cho CL, Agarwal A, Esteves SC Adult Varicocele Diagnosis and Treatment In: Esteves SC, Cho CL, Majzoub A, Agarwal A, editors Varicocele and Male Infertility [Internet] Cham: Springer International Publishing; 2019 [cited 2022 Jul 3] p 581 93 Available from: http://link springer com/10 1007/978 3 319 79102 9 55
7 Qiu D, Shi Q, Pan L Efficacy of varicocelectomy for sperm DNA integrity improvement: A meta analysis Andrologia [Internet] 2021 Feb [cited 2022 Jul 12]; 53(1) Available from: https://onlineli brary wiley com/doi/10 1111/and 13885
8 Moher D, Liberati A, Tetzlaff J, et al Preferred Reporting Items for Systematic Reviews and Meta Analyses: The PRISMA Statement 2009; 6
9 Fathi A, Mohamed O, Mahmoud O, et al The impact of varicoc electomy on sperm DNA fragmentation and pregnancy rate in sub fertile men with normal semen parameters: A pilot study Arab Journal of Urology 2021; 19:186 90
10 Kavoussi PK, Abdullah N, Gilkey MS, et al The impact of ipsi lateral testicular atrophy on semen quality and sperm DNA frag mentation response to varicocele repair Asian Journal of Andrology 2019; 21:1 4
11 Zaazaa A, Adel A, Fahmy I, et al Effect of varicocelectomy
and/or mast cells stabilizer on sperm DNA fragmentation in infertile patients with varicocele Andrology 2018; 6:146 50
12 Abdelbaki SA, Sabry JH, Al Adl AM, Sabry HH The impact of coexisting sperm DNA fragmentation and seminal oxidative stress on the outcome of varicocelectomy in infertile patients: A prospective controlled study Arab Journal of Urology 2017; 15(2):131 9
13 Wang YJ, Zhang RQ, Lin YJ, et al Relationship between varico cele and sperm DNA damage and the effect of varicocele repair: a meta analysis Reproductive biomedicine online 2012; 25:307 14
14 Nguyen TT, Sang T, Thi T, et al Evaluation of sperm DNA frag mentation index, Zinc concentration and seminal parameters from infertile men with varicocele 2018; 1 7
15 Johnson D, Sandlow J Treatment of varicoceles: techniques and outcomes Fertility and sterility 2017; 108:378 84
16 Salonia A, Bettocchi C, Carvalho J, et al EAU Guidelines on Sexual and Reproductive Health 2020
17 Lira Neto FT, Roque M, Esteves SC Effect of varicocelectomy on sperm deoxyribonucleic acid fragmentation rates in infertile men with clinical varicocele: a systematic review and meta analysis Fertility and Sterility 2021; 116:696 712
18 Sakkas D, Alvarez JG Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis Fertility and sterility 2010; 93:1027 36
19 Kimura M, Nagao K Role of varicocele repair for male infertili ty in the era of assisted reproductive technologies 2014; 185 92
20 Çayan S Systematic review of treatment methods for recurrent varicoceles to compare post treatment sperm parameters, pregnancy and complication rates 2019; 1 9
21 Al Bakri A, Lo K, Grober E, et al Time for improvement in semen parameters after varicocelectomy Journal of Urology 2012; 187:227 31
22 Li F, Yamaguchi K, Okada K, et al Significant improvement of sperm DNA quality after microsurgical repair of varicocele Systems Biology in Reproductive Medicine 2012; 58:274 7
23 Kadioglu TC, Aliyev E, Celtik M Microscopic varicocelectomy significantly decreases the sperm DNA fragmentation index in patients with infertility BioMed Research International 2014; 2014
Correspondence
Alwin Soetandar alwin19001@mail unpad ac id
Bambang Sasongko Noegroho Safendra Siregar
Ricky Adriansjah
Akhmad Mustafa
Department of Urology, Hasan Sadikin Academic Medical Center, Faculty of Medicine, Universitas Padjadjaran Bandung, Indonesia
A365 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
LETTER TO EDITOR
Nocturia due to nocturnal polyuria (NP). A common disorder
Anastasios Athanasopoulos
Urology, Medical
Patras, Patra,
To the Editor,
Nocturia is a significantly underestimated medical problem that affects seriously patients' quality of life, work engage ment, productivity, and overall life conditions per se Nocturia is a common condition, proven to be the most bothersome for patients with Lower Urinary Tract Symptoms (LUTS) (1) People with two or more events of micturition per night have a significant increase in mortality rate and an increased risk of fall related fractures if they visit the toilet two or more times per night (1) The pathophysiology behind nocturia falls into five main categories: Noctur nal polyuria (NP), glob al polyuria, reduced bladder capacity, sleep disorders, and circadian clock disorders Urological causes of nocturia are reduced bladder capacity, detrusor overactivity, and other mixed etiologies NP refers to increased urine production during nighttime The International Continence Society defines NP as nocturnal urine production above 20% for young patients and 33% for older patients (> 65 yrs) (2) NP seems to be the most common cause of nocturia According to the current and most used definition of nocturia by the International Continence Society (2), the prevalence of NP, in both genders, is 44% in those under 65 years, and 31 3% in those 65 years or older (3) In a recent study, NP was present in 77% of those with two or more episodes of nocturia per night (4), and in an older study, > 75% of patients with nocturia had NP (5) In a very recent study, 31 5% of men and 38 5% of women had NP (6) Furthermore, it is worth mentioning that in a longitudinal, community based study, the estimated prevalence of NP in men suffering from nocturia was 80% when the classical definition (NP Index > 33%) was used, but it was reduced to just 15% when was used the definition of Noctur nal Urine Production of > 90 ml/h (7) Moreover, using the Noctur nal Urine Production Index, the aforementioned recent study concluded that 23 8% and 18 1% of men and women respectively presented NP (6) Current definitions of NP are critical for estimating the preva lence and diagnosis of this condition It seems that more research and evidence are needed to reach a consensus about the most accurate definition for use in everyday clinical practice (8) NP has a multifactorial pathogenesis Several non urological causes are known to provoke this dysfunction Such causes are untreated diabetes mellitus or insipidus, sleep disorders as obstructive sleep apnea, cardiovascular diseases (hyper tension, heart failure) (9), chronic kidney disease, and primary polydipsia If there is no obvious disorder provoking NP, this is defined as NP Syndrome (10, 11) The interplay among NP and pathological conditions such as hypertension, arte riopathy and arterial stiffness, coronary heart disease, and distribution in the third space of body fluid is thought to be significant and it is a topic of current research (11) This is also the case for the role of brain natriuretic peptide (11) According to a well established point of view, a key factor in the decision to consult a physician is the patient's bother because of this condition The use of the word “disorder” rather than “complaint” would support the medical seriousness of nocturia to the patient's health (12) It is well known that two or more noctur nal voids are considered to be the clin ically meaningful threshold associated with significant adverse consequences to health and well being (13) Furthermore, a strong relationship between NP and nocturia and increased urinary frequency has been demonstrated (14) Commonly associated consequences include increased mortality and morbidity, increased risk of falls and hip fractures, traffic and work accidents, and increased risk of cardiovascular diseases, diabetes mellitus, and depression (13, 15) It also provokes immunological problems and dysfunction of memory and perception, overall deteriorating quality of life, and increase health costs (13, 15) Still, this condition seems to also affect work performance (16) Furthermore, the importance of taking sleep into account should be emphasized when assessing the relationship between nocturia and associated out comes (16) Another critical element to be highlighted is that despite traditionally regarding nocturia as a pronominally male condition, robust data support the evidence that it is just as prevalent in women as in men and especially in post menopausal women (12, 17)
The importance of the 'frequency volume chart, ' a very simple exam, has to be underlined as the main tool to guide diag nosis and identify the appropriate treatment of nocturia Especially for NP, a frequency volume chart is a cor nerstone for the diagnosis of this condition (18)
The treatment rationale for nocturia is that NP, due to inadequate antidiuresis, is a major contributing factor to nocturia
No conflict of interest declared
Italiano
Urologia
Archivio
di
e Andrologia 2022; 94, 33 66
Department of
School, University of
Greece DOI: 10 4081/aiua 2022 3 366 Submitted 12 May 2022; Accepted 23 June 2022
Nocturnal polyuria
Before starting any pharmaceutical treatment, it would be first beneficial to try some lifestyle modifications, as these can offer an improvement of NP For example, less caffeine, alcohol, and generally fluids intake a couple of hours before bed time could be of benefit to the patient (18) Furthermore, desmopressin administration offers a significant reduction in nocturia episodes and noctur nal urine production, translating into improvements in sleep and quality of life (19 22) Newer formulations of desmopressin are well tolerated The risk of hyponatremia is relatively low with appropriate dos ing escalation and taking into consideration that a lower minimum effective dose in females is needed compared to males (22 24) Furthermore, sodium monitoring just before treatment initiation and on the first, third, and seventh day of treat ment is essential Research for the treatment of NP is ongoing and includes highly selective arginine vasopressin 2 recep tor agonists, non steroid anti inflammatory drugs, sex hormone replacement treatment, and short acting diuretics (22) Improved knowledge regarding nocturia, which is a basic symptom of LUTS, provides insight to understanding that noc turia, and especially NP, can be a pathological entity per se Further research in the future will shed light concer ning the pathophysiology of nocturia There is evidence that the burden of this symptom is considerable in many aspects, espe cially for the individual and the society Therefore, NP should be given the attention it deserves in the medical field, espe cially by the urological community
REFERENCES
1 Leslie SW, Sajjad H, Singh S Nocturia In: StatPearls [Internet] Treasure Island (FL): StatPearls Publishing; 2021
2 Van Kerrebroeck P, Abrams P, Chaikin D, et al The standardization of terminology in nocturia: report from the Standardisation Sub commit tee of the International Continence Society Neurourol Urodyn 2002; 21:179 183
3 Zumrutbas AE, Bozkurt AI, Alkis O, et al The Prevalence of nocturia and nocturnal polyuria: can new cutoff values be suggested according to age and sex? Int Neurourol J 2016; 20:304 310
4 Clemens JQ, Wiseman JB, Smith AR, et al LURN Study Group Prevalence, subtypes, and correlates of nocturia in the symptoms of Lower Urinary Tract Dysfunction Research Network cohort Neurourol Urodyn 2020; 39:1098 1107
5 Weiss JP, van Kerrebroeck PE, Klein BM, et al Excessive nocturnal urine production is a major contributing factor to the etiology of nocturia J Urol 2011; 186:1358 1363
6 Weiss JP, Bosch JLHR, Chapple CR et al The prevalence of nocturnal polyuria in the United States: results from the Epidemiology of Nocturnal Polyuria Study Eur Urol Focus 2022; S2405 4569(21)00324 2
7 van Doorn B, Blanker MH, Kok ET, et al Prevalence, incidence, and resolution of nocturnal polyuria in a longitudinal community based study in older men: the Krimpen study Eur Urol 2013; 63:542 547
8 Olesen TK, Denys MA, Walle JV, et al Systematic Review of Proposed Definitions of Nocturnal Polyuria and Population Based Evidence of Their Diagnostic Accuracy Acta Clin Belg 2018; 73:268 274
9 Ohishi M, Kubozono T, Higuchi K, Akasaki Y Hypertension, cardiovascular disease, and nocturia: a systematic review of the pathophysiolog ical mechanisms Hypertens Res 2021; 44:733 739
10 Monaghan TF, Dmochowski RR, Verbalis JG, et al First voided volume: A novel approach to characterize nocturia Neurourol Urodyn 2021; 40:848 54
11 Weiss JP, Monaghan TF,Epstein MR, Lazar JM Future considerations in nocturia and nocturnal polyuria Urology 2019; 133:34 42
12 Van Kerrebroeck P, Andersson KE Terminology, epidemiology, etiology, and pathophysiology of nocturia Neurourol Urodyn 2014; 33(Suppl 1):S2 5
13 Tikkinen KAO, Johnson TM, Tammela TLJ, et al Nocturia frequency, bother, and quality of life: how often is too often? A population based study in Finland Eur Urol 2010; 57:488 498
14 Rubilotta E, Castellani D, Gubbiotti M, et al Nocturnal polyuria in men performing uroflowmetry for lower urinary tract symptoms Arch Ital Urol Androl 2021; 93:445 449
15 Carskadon MA Sleep deprivation: health consequences and societal impact Clin North Am 2004; 88:767 776
16 Torimoto K, Uchimura N, Roitmann E, et al A large survey of nocturia related to sleep quality and daytime quality of life in young Japanese population: NOCTURNE study Neurourol Urodyn 2021; 40:340
17 Pauwaert K, Goessaert AS, Ghijselings L, et al Nocturia through the menopausal transition and beyond: a narrative review Int Urogynecol J 2021; 32:1097 1106
Weiss JP, Everaert K Management of nocturia and nocturnal polyuria Urology 2019; 133:24
Gordon DJ, Emeruwa CJ, Weiss JP Management strategies for nocturia Curr Urol Rep 2019; 20:75
Everaert K, Hervé F, Bosch R, et al International Continence Society consensus on the diagnosis and treatment of nocturia Neurourol Urodyn 2019; 38:478
21 Kim SO, Yu HS, Kwon D Efficacy of desmopressin to treat nocturnal polyuria in elderly men: effects on sleep quality Urol Int 2016; 96:438 442
A367 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
347
18
33 19
20
498
Athanasopoulos
22 Monaghan TF, Weiss JP, Everaert K, Wein AJ Pharmacologic management of nocturnal polyuria: a contemporary assessment of efficacy, safe ty, and progress toward individualized treatment Ther Adv Urol 2021; 13:1756287220988438
23 Juul KV, Klein BM, Sandström R, et al Gender difference in antidiuretic response to desmopressin Am J Physiol Renal Physiol 2011; 300:F1116 1122
24 Juul KV, Malmberg A, van der Meulen E et al Low dose desmopressin combined with serum sodium monitoring can prevent clinically sig nificant hyponatraemia in patients treated for nocturia BJU Int 2017; 119:776 784
Correspondence
Athanasopoulos A MD, PhD tassos athan@hotmail com
Professor of Urology Functional Urology, Head of Urodynamic Urology Unit, University of Patras, Patra (Greece) Papadiamantopoulou 38 str, Patra, Greece, 26225
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
A
368
: 10 4081/aiua 2022 3 369
LETTER TO EDITOR
How long should we follow patients managed for muscle-invasive bladder cancer? Lesson learned from a recent clinical practice
Aldo Franco De Rose 1 , Francesco Vecco 1, 2 , Francesca Ambrosini 1, 2 , Rafaela Malinaric 1, 2 , Guglielmo Mantica 1 , Carlo Terrone 1, 2
1 IRCCS Ospedale Policlinico San Martino, Genova, Italy; 2 Università di Genova, (DISC), Genova, Italy
To the Editor,
The exact time to stop bladder cancer patient’s follow up is not well known and there is not a clear recommendation on if and when stop to follow a patient managed for muscle invasive bladder cancer (MIBC) Major urological guidelines (1, 2) do not provide a precise indication on the timing of follow up, and there is currently no real consensus on optimal time schedule However, MIBC is a disease with a high relapse rate of over 50% of patients at 5 years (considering local, distant and urothelial relapses), and very late recurrences have been detected in several patients after 5 years tumor free periods (3, 4)
Furthermore, patients undergoing radical cystectomy require oncological but also functional follow up, considering that complications related to urinary diversion are detected in 45% of patients during the first five years, reaching 54% after 15 years of follow up (5)
Recently, we detected a very late urethral recurrence in a patient who underwent cystoprostatectomy and Bricker’s ileal conduit urinary diversion in 2002 for MIBC (pT2 G3 N0) The patient, a 73 y/o diabetic man, strong tobacco consumer, had abandoned the follow up 10 years ago, after as many years of surveillance in which he was free from disease In 2021 the patient had urethral bleeding and prepuce edema The urethroscopy found a white, solid mass in the proximal ure thra, that the biopsy confirmed to be a urothelial carcinoma Abdominal penile MRI found a neoplasia likely originated from the urethra and from the corpus spongiosum, invading both corpora caver nosa, and bilateral inguinal lymphade nomegaly After six months of chemotherapy the patient underwent penectomy and lymphadenectomy The definitive his tological diagnosis was urothelial papillary carcinoma, with areas of squamous differentiation (pT3 G3 pN1)
The aim of this letter is not to present in detail the case of this unlucky patient, and therefore many info are voluntarily omitted, but to put the light on the possible need of a life long follow up for patients with MIBC who underwent radical cystectomy
As previously stated, there is currently no clear recommendation on the timing of follow up required in MIBC patients undergoing radical cystectomy Recently a risk adapted schedule (6) has been proposed, based on the interaction between recurrence risk and competing health factors that could lead to individualized follow up recommendations and may increase recurrence detection However, this model has not yet been validated and has several limitations such as not con sidering histological variants (7), which are increasing and that might be responsible of greater rate of recurrences
To offer a patient targeted follow up, could become essential the use of biomarkers (8 10) currently available or in the experimental phase, capable of identifying the risk of recurrence and prognosis of different patients This could lead to specific surveillance schedules, tailoring the patient's characteristics and recurrence risk (TNM, rare variants, urethral preservation, etc ) In this light, It is also essential to help the patient to stop smoking (11), in order to possibly reduce the risk of relapses, a factor that is often not investigated or stressed by the urologists
Ultimately, in our opinion, the patient undergoing cystectomy is a patient who should be followed for life by the urolo gist, both from an oncological, functional and psychological point of view (12, 13)
REFERENCES
1 Muscle invasive and Metastatic Bladder Cancer FOLLOW UP Uroweb Accessed May 29, 2022 https://uroweb org/guidelines/muscle inva sive and metastatic bladder cancer/chapter/followup
2 Treatment of Non Metastatic Muscle Invasive Bladder Cancer: AUA/ASCO/ASTRO/SUO Guideline (Amended 2020) American Urological Association Accessed May 29, 2022 https://www auanet org/guidelines/guidelines/bladder cancer non metastatic muscle invasive guideline
A369 rchivio Italiano di Urologia e Andrologia 2022;
94, 3
No conflict of interest declared Submitted 14 June 2022; Accepted 17 June 2022
DOI
3 Matsumoto K, Kikuchi E, Horiguchi Y, et al Late recurrence and progression in non muscle invasive bladder cancers after 5 year tumor free periods Urology 2010; 75:1385 1390
4 Yoo SH, Kim H, Kwak C, Kim HH, Jung JH, Ku JH Late recurrence of bladder cancer following radical cystectomy: characteristics and out comes Urol Int 2019; 103:291 296
5 Hautmann RE, Volkmer B, Egghart G, et al Functional outcome and complications following Ileal neobladder reconstruction in male patients without tumor recurrence More than 35 years of experience from a single center J Urol 2021; 205:174 182
6 Stewart Merrill SB, Boorjian SA, Thompson RH, et al Evaluation of current surveillance guidelines following radical cystectomy and propos al of a novel risk based approach Urol Oncol Semin Orig Investig 2015; 33:339 e1 339 e8
7 Mantica G, Simonato A, Du Plessis DE, et al The pathologist’s role in the detection of rare variants of bladder cancer and analysis of the impact on incidence and type detection Minerva Urol e Nefrol 2018; 70:594 597
8 Sawazaki H, Arai Y, Ito Y, et al Expression of L type amino acid transporter 1 is a predictive biomarker of intravesical recurrence in patients with non muscle invasive bladder cancer Res Reports Urol 2021; 13:603
9 Saoud R, Sanford TH, Hewitt SM, Apolo AB, Agarwal PK Rapidly progressing urothelial carcinoma due to a rare TP53 (p Arg110Pro) muta tion: a case report and review of the literature Res reports Urol 2021; 13:181 184
10 Singh R, Singh UP, Agrawal V, Garg M Epithelial to mesenchymal transition based diagnostic and prognostic signature markers in non mus cle invasive and muscle invasive bladder cancer patients Mol Biol Rep 2022; 49:7541 7556
11 van Osch FHM, Jochems SHJ, Reulen RC, et al The association between smoking cessation before and after diagnosis and non muscle inva sive bladder cancer recurrence: a prospective cohort study Cancer Causes Control 2018; 29:675
12 Jensen BT, Lauridsen SV, Jensen JB Optimal delivery of follow up care after radical cystectomy for bladder cancer Res Reports Urol 2020; 12:471
13 Borghi C, Manservigi M, Milandri ES, Greco P, Ippolito C, Dell’Atti The impact of orthotopic reconstruction on female sexuality and quali ty of life after radical cystectomy for non malignant bladder conditions Arch Ital di Urol e Androl 2021; 93:255 261
Correspondence
Aldo Franco De Rose, MD aldofrancoderose@gmail com
Francesco Vecco, MD (Corresponding Author) francesco vecco@gmail com
IRCCS Ospedale Policlinico San Martino, Genova
Francesca Ambrosini, MD f ambrosini1@gmail com
Rafaela Malinaric, MD rafaela malinaric@gmail com
Guglielmo Mantica, MD guglielmo mantica@gmail com
Carlo Terrone, MD carlo terrone@med uniupo it
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
A F De Rose, F Vecco, F Ambrosini, R Malinaric, G Mantica, C Terrone
370
LETTER TO EDITOR
Organ harvesting as a mandatory training step of all PGY1 and PGY2 surgical residents
, Guglielmo Mantica
1 Department of Urology, IRCCS Ospedale Policlinico San Martino, Genova, Italy;
Department of Surgical and Diagnostic Integrated Sciences (DISC), University of Genova, Genova, Italy;
European Society of Residents in Urology (ESRU), Arnhem, The Netherlands
Submitted
To the Editor,
Good surgical training is essential for the formation of excellent surgeons, consequently providing the best possible care for our patients in the future Considering the increase in surgeon shortage over the last two decades (1, 2) (estimated between 14,300 and 23,400 by the year 2032 only in the US) (3), it is important for filling the national health system's needs as well Finally, respectable surgical training will allow preservation of residency programs by annually attracting more and more new candidates
Every country has its' own structure of surgical training, and it differs immensely between states, sometimes even with in the same country (4)
In recent years, several issues were raised regarding inadequacy of surgical training in some of the most developed coun tries (5) Resident directed surveys, done primarily in Italy, Spain and Germany, evaluating urological training in partic ular, revealed a lot of training related concer ns such as residents' low exposure to major surgeries and a lack of their active participation during them (4 10) Reasons for this trend might be multiple, starting from the administrative work over load, increasing medico legal assessments and lawsuits, development of the new, high tech devices that do not allow both mentor and trainee working simultaneously (e g single console robotic systems and novel laser techniques) and neo spe cialists still in lear ning curve Although we have training centers with simulators dedicated to resolving these issues, con cer ns such as poor understanding of the skill retention, possibility of the skill decay and scarce evidence about simula tors improving clinical outcomes are often discussed (11, 12)
As if that was not enough, a significant reduction in elective procedures occurred during the COVID 19 pandemic This has had a huge impact on surgical activity and residents, with 50% reduction in procedures with them as primary surgeons (13 15) Furthermore, the reality of many residents is a lack of time they can dedicate to simulators at their disposal (4) So, can this be mediated? What are the questions we are frequently asking our residents and ourselves? What are the most important skills a surgeon should possess before stepping in the OR? A good base of the surgical anatomy, familiarity with dif ferent organ tissues, textures and resistances as well as proficiency in various methods of suturing and knot tying
Although residents have access to a lot of lear ning material (e g recordings of the operations) that might help improving their knowledge about surgical anatomy, it does not provide any practical training nor tactile experience
In some centers, residents have access to simulators or, in other cases where they do not, tutorials on how to build your own, low cost training models1 (6, 17) are available Unfortunately, they often do not reproduce truthfully the real life tissue consistencies
Further, programs that offer training on the cadaveric models are also available (18, 20) The major problems with cadav eric models are firstly, the availability of them, secondly, they are expensive, and lastly, but maybe the most importantly, the ceased circulation, low temperature and electrolytic imbalances alter organs So, in the end, even cadaveric models are not able to faithfully reproduce the real life medical procedures
Now, if we do not teach young surgeons today, we will not have any surgeons, or at least not capable surgeons, tomor row, so these issues need to be addressed as soon as possible
In addition, Italy is facing yet another challenge considering that, a few years back, EPAteam (national association for liver transplant patients) predicted shortage of transplant surgeons (21) and availability to harvest organs at late night hours
All in all, we are in a desperate need of better surgical training and in a serious need of (transplant) surgeons One must wonder, couldn't we simply involve surgical residents in organ harvesting as a mandatory structured program during the first two years of their training? Instead of two transplant surgeons, organs could be harvested (and transplanted for that matter) by one transplant surgeon and one trainee or, even, by two senior supervised trainees Why should we use cadav eric models if we have access to a living body? Could this be a win win solution?
Simply, it seems a nearly perfect answer to all of our problems: surgical anatomy can be mastered very well and quite
No conflict of interest
A371 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
declared
3 July 2022; Accepted 9 July 2022
Rafaela Malinaric 1,
2
1 3
, Carlo Terrone
1, 2
2
3
DOI: 10 4081/aiua 2022 3 371
R Malinaric, G Mantica, C Terrone
quickly, novices could become more acquainted with organ structures, connections and textures as well as lear ning how to manipulate various organs without creating too much damage Moreover, during arterial or venous graft harvesting and abdominal wall closure residents could practice various types of knot tying and improve their knowledge about suture materials, suture size, and the components of the surgical needle
The major pitfall of this proposal is the fact that not all training centers have transplant programs But how many surgi cal residency programs already include rotations in other departments or hospitals? So, couldn't this principle simply be applied to here proposed organ harvesting program? This would provide both, better education for the residents and could help greatly our transplant teams It would mean night hours, and some training programs do not allow or sim ply do not encourage them, but this rotation could have only a three to four months duration
Of course, this is just an idea that needs fur nishing, thought, elaborated and structured plan, but surely worthwhile con sidering, at least for a discussion
REFERENCES
1 Stringer B, et al Trouble on the horizon: an evaluation of the general surgeon shortage in rural and frontier counties Am Surg 2020; 86:76 78
2 Van Way CW Jr Is there a surgeon shortage? Mo Med 2010; 107:309 12
3 https://www aamc org/news insights/press releases/new findings confirm predictions physician shortage
4 Carrion DM et al Current status of urology surgical training in Europe: an ESRU ESU ESUT collaborative study World J Urol 2020; 38:239 246
5 Mattar SG, et al General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors Ann Surg 2013; 258:440 449
6 Borgmann H, Arnold HK, Meyer CP, et al Training, research, and working conditions for urology residents in Germany: a contemporary sur vey Eur Urol Focus 2018; 4:455 460
7 Rodríguez Socarrás ME, et al Medical surgical activity and the current state of training of urology residents in Spain: results of a national survey' Actas Urol Esp 41:391 399
8 Mantica G, Chierigo F, Gallo F; Italian Residents Association of the Italian Urology Association Study Group Patients' perceptions of quality of care delivery by urology residents: A nationwide study BJU Int 2022 doi: 10 1111/bju 15768
9 Almannie R, et al Exposure of Urology residents to the management of urethral strictures in Saudi Arabia: should the program for postgrad uates be customized? Res Rep Urol 2020; 12:367 372
10 Aslam AU, Philipraj J, Jaffrey S, Buchholz N A global snapshot of endourology residency training Arch Ital Urol Androl 2020; 92:219 229
11 Stefanidis D, et al Simulation in surgery what’s needed next?' Ann Surg 2015; 261:846 53
12 Kozan AA, Chan LH, Biyani CS Current status of simulation training in urology: a non systematic review Res Rep Urol 2020; 12:111 128
13 Joint Committee of Surgical Training, Association of Surgeons in Training, British Orthopaedics Trainees’ Association, Confederation of Postgraduate Schools of Surgery Maximising training: making the most of every training opportunity 2021 https://www jcst org/key documents/
14 Coleman JR, Abdelsattar JM, Glocker RJ RAS ACS COVID 19 Task Force COVID 19 pandemic and the lived experience of surgical resi dents, fellows, and early career surgeons in the American College of Surgeons J Am Coll Surg 2021; 232:119 135 e20
15 Mantica G, et al The TOMATO model Urology 2021; 157:280 281;
16 Leonardi R, Bellinzoni P, Broglia L, et al Hospital care in Departments defined as COVID free: A proposal for a safe hospitalization pro tecting healthcare professionals and patients not affected by COVID 19 Arch Ital Urol Androl 2020; 92:67 72
17 Soriero D, et al 'Development and validation of a homemade, low cost laparoscopic simulator for resident surgeons (LABOT)' Int J Environ Res Public Health 2020; 17:323
18 Huri E, et al The novel laparoscopic training 3D model in urology with surgical anatomic remarks: Fresh frozen cadaveric tissue' Turk J Urol 2016; 42:224 229
19 Mantica G, Leonardi R, Diaz R CACTUS group Reporting ChAracteristics of cadaver training and sUrgical studies: The CACTUS guide lines Int J Surg 2022; 101:106619
20 Mantica G, Pini G, De Marchi D, et al Intensive simulation training on urological mini invasive procedures using Thiel embalmed cadav ers: The IAMSurgery experience Arch Ital Urol Androl 2020; 92:93 96
21 https://www repubblica it/salute/medicina e ricerca/2019/02/21/news/15mila trapianti di fegato nei prossimi 10 anni ma mancheran no i chirurghi 219733589/
Correspondence
Rafaela Malinaric, MD (Corresponding Author) rafaela malinaric@gmail com
San Martino Hospital, University of Genoa, Genoa, Italy Guglielmo Mantica, MD guglielmo mantica@gmail com Carlo Terrone, MD carlo terrone@med uniupo it
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
372
: 10 4081/aiua 2022 3 373
LETTER TO EDITOR
Natural treatments for erectile dysfunction: A focus on mobile health applications
Luigi Napolitano, Luigi Cirillo, Giovanni Maria Fusco, Marco Abate, Vincenzo Morgera, Gianluigi Cacace, Giuseppe Celentano, Biagio Barone, Lorenzo Spirito, Vincenzo Mirone, Roberto La Rocca
Department of Neurosciences, Reproductive Sciences and Odontostomatology, School of Medicine, University of Naples "Federico II", Naples, Italy
To the Editor,
Erectile dysfunction (ED) is defined as the persistent inability to achieve or maintain penile erection sufficient for satisfacto ry sexual performance (1) ED represents one of the most important male sexual dysfunctions with a prevalence of 52% and affecting more than 150 million men worldwide (estimated to be 322 million worldwide for 2025) (2 4) In the last years, several dietary supplements and herbal remedies have been introduced alone or in combinations with other treat ments These products have been used in traditional medicine for their aphrodisiac proprieties or as compounds that increase sexual arousal, libido, potency (erection) and/or sexual pleasure Panax ginseng (Korean ginseng), Tribulus terrestris (Tribulus), Epimedium gradiflorum (Horny goat weed), Lepidium meyenii (Maca), Ginkgo biloba (Ginkgo), Eurycoma longifo lia Jack (Tongkat ali), and Pausinystalia johimbe (yohimbine), B complex vitamins, zinc, trace minerals, L arginine, aspar tate and dehydroepiandrosterone (DHEA) have been reported as the most used products on the market (5 6) Despite the increasing use, very low scientific evidence has been described, particularly regarding efficacy, safety, extractions, and dosage Mobile phone applications (MHAs) are mobile software programs, providing information and support to patients in many fields including health Nowadays, more than 325,000 MHAs are available and widely used in the healthcare set ting, to provide information about several medical conditions including sexual dysfunction, but the scientific evidence is very poor (7) In our previous study we analyzed MHAs for ED using the Mobile Application Rating Scale (MARS scale) and reported their adherence to European urology Guidelines MARS is a multidimensional instrument evaluating engagement (items assessing the extent to which the app engages target users), functionality (items assessing how easy the app is to navigate and the overall app performance), esthetics (items assessing visual appearance and style), information (items assessing accuracy, quality, and quantity of the app), app subjective quality, and app specific, showing a very acceptable reliability and validity) (8) We found an overall low quality of MHAs and poor adherence to EAU guidelines Among treatments they suggested there were both herbal interventions and non herbal nutraceuticals, alone or in com binations Over the time several studies suggested herbal interventions in ED management with a high scientific support Balasubramanian et al in a recent meta analysis reported the most popular erectile dysfunction supplements available on online marketplaces: Ginseng is the most popular followed by L arginine, and Tongkat ali (9) Interestingly, none of the analyzed apps reported any of the supplements in this list or the most popular used ones Furthermore, ginseng and L arginine as shown by Borrelli et al are the only two supplements that showed an effective efficacy in ED treatment (10) MHAs suggested using (Table 1): garlic, bryonia laciniosa, butea superba, ginger, ginkgo Biloba, carrots, pomegranate juice, onion, almonds and clove Garlic (Allium sativum) represents one of the oldest plants, recognized for its health benefits in cardiovascular diseases (11) The most important bioactive component is S allyl cysteine (SAC) which possesses antioxi dant property (12) Bryonia laciniosa is characterized by antimicrobial, larvicidal, anti inflammatory, cytotoxic, analgesic, and antipyretic activities and it is very used in India as a tonic and enhancer of sexual behaviors Butea superba increased intracaver nous pressure and caver nous smooth muscle relaxation (13) One MHA suggested using ginger, the only nutraceutical that showed to enhance iNOS activity in vitro Other MHA sug gested products were carrots that improve sexual function and desire through testosterone enhancing; pomegranate juice which is characterized by antioxidant activity (anthocyanins) and involved in endothelial nitric oxide (NO) levels regula tion; in the end, onion which is a source of hydrogen sulfide and quercetin, involved in erection and antioxidant path way respectively (14, 15) Almond is characterized by antistress, antidiabetic, antihypertensive and antioxidant propri eties (16, 17) Many of these home remedies have not reported a great scientific support and few studies have been con ducted on human, with several drawbacks: regarding garlic, Nishimatsu et al reported his experience in 24 men using a preparation containing garlic extract, ginseng, oriental bezoar, velvet antler, cuscuta seed and epimedium herb, with improvement of ED (18) Despite all this, the negative role of oxidative stress and of endothelial dysfunction in ED patho physiology is well established, and all dietary supplements suggested reported antioxidant effects According to the cur rent data no strong scientific evidence supports nutraceutical products suggested by MHAs Therefore, further work, and more involvement of healthcare are necessary to improve the quality of scientific evidences reported by MHAs
A373 rchivio Italiano di Urologia e Andrologia 2022; 94, 3
No conflict of interest declared Submitted 3 July 2022; Accepted 9 July 2022
DOI
Table 1
App characteristics
Name of application
Android/Apple/Both Producer
Categor y
Erectile dysfunction treatment Android Revo xa inc Medicine
Erectile dysfunction remedy 2021 Android Maftal Almafary Education
Nutraceutical product
Asian ginger, Ginkgo biloba
Asian ginger, Ginkgo biloba
Erectile dysfunction remed es Android StatesApps Health and Fitness Gar ic, cloves, fru t nut mix, onion, drumstick, butea superba Home remedies Android Cutepad studio Medicine Ginger, Onion, Pomegranate juice, Almonds, Garlic, Carrots Herbal cure Android NovaRadix Medicine Bryonia
101 Natural Home Android XL Tech Apps Garlic
REFERENCES
1 Pastuszak AW Current diagnosis and management of erectile dysfunction Curr Sex Health Rep 2014; 6:164 76
2 Feldman HA, Goldstein I, Hatzichristou DG, et al Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study J Urol 1994; 151:54 61
3 Romano L, Granata L, Fusco F,, et al Sexual dysfunction in patients with chronic gastrointestinal and liver diseases: a neglected issue Sex Med Rev 2021; S2050 0521(21)00039 1
4 Mirone V, Napolitano L, D’Emmanuele di Villa Bianca R, et al A new original nutraceutical formulation ameliorates the effect of Tadalafil on clinical score and cGMP accumulation Arch Ital Urol Androl 2021; 93:221 6
5 Kuchakulla M, Narasimman M, Soni Y, et al A systematic review and evidence based analysis of ingredients in popular male testosterone and erectile dysfunction supplements Int J Impot Res 2021; 33:311 7
6 Corazza O, Martinotti G, Santacroce R, et al Sexual enhancement products for sale online: raising awareness of the psychoactive effects of yohimbine, maca, horny goat weed, and Ginkgo biloba Biomed Res Int 2014; 2014:841798
7 Napolitano L, Fusco GM, Cirillo L, et al Erectile dysfunction and mobile phone applications: Quality, content and adherence to European Association guidelines on male sexual dysfunction Arch Ital Urol Androl 2022; 94:211 6
8 Stoyanov SR, Hides L, Kavanagh DJ, et al Mobile app rating scale: a new tool for assessing the quality of health mobile apps JMIR MHealth UHealth 2015; 3:e27
9 Balasubramanian A, Thirumavalavan N, Srivatsav A, et al An analysis of popular online erectile dysfunction supplements J Sex Med 2019; 16:843 52
10 Borrelli F, Colalto C, Delfino DV, et al Herbal dietary supplements for erectile dysfunction: a systematic review and meta analysis Drugs 2018; 78:643 73
11 Brace LD Cardiovascular benefits of garlic (Allium sativum L) J Cardiovasc Nurs 2002; 16:33 49
12 Colín González AL, Santana RA, Silva Islas CA, et al The antioxidant mechanisms underlying the aged garlic extract and S allylcysteine induced protection Oxid Med Cell Longev 2012; 2012:907162
13 Tocharus C, Smitasiri Y, Jeenapongsa R Butea superba Roxb enhances penile erection in rats Phytother Res 2006; 20:484 9
14 Gur S, Kadowitz PJ, Sikka SC, et al Overview of potential molecular targets for hydrogen sulfide: A new strategy for treating erectile dys function Nitric Oxide Biol Chem 2015; 50:65 78
15 Zhang W, Wang Y, Yang Z, et al Antioxidant treatment with quercetin ameliorates erectile dysfunction in streptozotocin induced diabetic rats J Biosci Bioeng 2011; 112:215 8
16 Siriwardhana SSKW, Shahidi F Antiradical activity of extracts of almond and its by products J Am Oil Chem Soc 2002; 79:903 8
17 Adefegha SA, Oboh G, Oyeleye SI, Ejakpovi I Erectogenic, antihypertensive, antidiabetic, anti oxidative properties and phenolic composi tions of almond fruit (Terminalia catappa L ) parts (hull and drupe) in vitro J Food Biochem 2017; 41:e12309
18 Nishimatsu H, Kitamura T, Yamada D, et al Improvement of symptoms of aging in males by a preparation LEOPIN ROYAL containing aged garlic extract and other five of natural medicines comparison with traditional herbal medicines (Kampo) Aging Male Off J Int Soc Study Aging Male 2014; 17:112 6
Correspondence
Luigi Napolitano, MD luiginap89@gmail com
Luigi Cirillo, MD (Corresponding Author) cirilloluigi22@gmail com
Giovanni Maria Fusco, MD giom fusco@gmail com
Marco Abate, MD marcoabate5@gmail com
Biagio Barone,MD biagio barone@unina it
Vincenzo Morgera, MD vincemorgera87@gmail com
Gianluigi Cacace, MD cacace gianlu@gmail com
Giuseppe Celentano, MD dr giuseppecelentano@gmail com
Lorenzo Spirito, MD lorenzospirito@msn com
Vincenzo Mirone, MD mirone@unina it
Roberto La Rocca, MD robertolarocca87@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples "Federico II", Naples, (Italy) Via Sergio Pansini n 5, Naples (NA) (Italy)
Archivio Italiano di Urologia e Andrologia 2022; 94, 3
L Napolitano, L Cirillo, G M Fusco, M Abate, et al
374
INSTRUCTIONS TO AUTHORS – ARCHIVIO ITALIANO DI UROLOGIA E ANDROLOGIA
OPEN ACCESS
Open access publishing does have its costs. Information regarding authors’ payment are not made available to editors and reviewers ensuring that they cannot be influenced in their selection of papers for publication by payment conditions or limitations.
The Article Processing Charge for publication in this journal is EUR 300,00 (plus VAT, if applicable).
Our fees cover the costs of peer review, copyediting, publication, different format of publication (HTML, PDF), inclusion in many Open Access databases.
All bank charges shall be borne by the payer.
Please note that our fees do not include taxes (VAT):
- Private or public ITALIAN customers (individuals, universities, hospitals, other organizations) must ALWAYS add VAT (IVA) at standard rate (4%);
- European Union PRIVATE customers must add the standard rate of their own country VAT tax;
- European Union private/public ORGANIZATIONS (universities, hospitals, others with regular VAT number) should not add any taxes at standard rate, provided that they indicate their VAT number;
- Outside the European Union, individuals and organizations should not add any taxes at standard rate.
Important: Authors are NOT required to pay at the moment of submission. If the paper is accepted, the Managing Editor of Open Access Edition will guide the Authors through the payment procedure. No article will be published before waiver or payment.
According to the United Nations list of Least Developed Countries (LCDs) available from: http://www.un.org/en/development/desa/policy/cdp/ldc2/ldc_countries.shtml
Authors coming from those countries are entitled to ask for a discount.
A “Formal Request for discount” has to be forwarded to the Managing Editor of Open Access Edition, after receiving the acceptance letter. The Editorial Committee will then evaluate the merits of each individual case.
Any other informal request (such as comments at the moment of submission, or made in the covering letter of the revised version) will not be taken into consideration.
FAST TRACK PEER REVIEW
All papers published in Archivio Italiano di Urologia e Andrologia (AIUA) are peer reviewed. Fast-track peer review (4 weeks) can be obtained by supplementary fee of € 488 (VAT included).
in Italian language can be published after translation (expenses will be charged to the Authors). Manuscripts should be typed double spaced with wide margins. They must be subdivided into the following sections:
TITLE PAGE
It must contain: a) title; b) a short (no more than 40 characters) running head title; c) first, middle and last name of each Author without abbreviations; d) University or Hospital, and Department of each Author; e) last name, address and e-mail of all the Authors; f) corresponding Author; g) acknowledgement of conflict of interest and financial support.
SUMMARY
Authors must submit a summary (300 words, 2000 characters) divided by subheadings as follows: Objective(s), Material and method(s), Result(s), Conclusion(s). After the summary, three to ten key words must appear, taken from the standard Index Medicus terminology.
TEXT
For original articles concerning experimental or clinical studies, the following standard scheme must be followed: Summary - Key Words - Introduction - Material and Methods - Results - Discussion - Conclusions - References - Tables - Legends - Figures.
Case Report should be divided into: Summary - Introduction (optional) - Case report(s) - Conclusions - References
Supplementary Materials can be added for online publication.
SIZE OF MANUSCRIPTS
Literature reviews, Editorials and Original articles should not exceed 3500 words with 3-5 figures or tables, and no more than 30 references.
Case reports, Notes on surgical technique, and Letters to the editors should not exceed 1000 words (summary included) with only one table or figure, and no more than three references. No more than five authors are permitted.
REFERENCES
References must be sorted in order of quotation and numbered with arabic digits between parentheses. Only the references quoted in the text can be listed. Unpublished studies cannot be quoted, however articles “in press” can be listed with the proper indication of the journal title, year and possibly volume.
Authors can pay their fees by: PayPal is the most recommended and secure payment system. It enables you to pay getting your payment receipt immediately and without sharing your financial information.
METHODS OF PAYMENT
Other methods of payment are:
Bank transfer
BANK NAME: Banca Popolare di Sondrio, Branch #1, Strada Nuova 75, I-27100 Pavia, Italy ACCOUNT HOLDER: PAGEPress Srl BIC/SWIFT: POSOIT22 IBAN: IT85Y0569611301000005086X83
Credit Card The credit card form to be filled and returned either via e-mail or via fax is available for download here.
http://www.pagepress.org/journals/public/credit_card.pdf
Check sent by surface mail Checks must be made payable to PAGEPress Srl and must be sent to our full postal address: PAGEPress Publications, via A. Cavagna Sangiuliani 5, 27100 Pavia, Italy.
Note: In any method of payment you choose, kindly specify: 1. journal name; 2. paper ID number; 3. first author.
IMPORTANT TO KNOW
REGISTERED DRUGS, DIET SUPPLEMENTS, NUTRACEUTICALS, MEDICAL DEVICES
Authors of papers that contain references to registered drugs, diet supplements, nutraceuticals and medical devices are requested to buy a minimum amount of 100 reprints at a cost of € 1.500 (1 to 4 pages) or € 2.000 (5 to 8 pages). Prices for the purchase of number of reprints greater than 100 can be negotiated with Edizioni Scripta Manent
At present, Edizioni Scripta Manent let everyone to read, print and download papers from website, but retains copyright for republishing and distribution rights for commercial purpose.
TRANSLATION
Translation of manuscripts in Italian language is offered on payment.
Translation and reprints can be requested to Edizioni Scripta Manent by e-mail to info@edizioniscriptamanent.eu
AUTHORS’ RESPONSIBILITIES
Manuscripts are accepted with the understanding that they have not been published or submitted for publication in any other journal.
Authors must submit the results of clinical and experimental studies conducted according to the Helsinki Declaration on clinical research and to the Ethical Code on animal research set forth by WHO (WHO Chronicle 1985; 39:51).
The Authors must obtain permission to reproduce figures, tables and text from previously published material. Written permission must be obtained from the original copyright holder (generally the Publisher).
MANUSCRIPT PRESENTATION
Authors must submit their manuscripts (MAC and WINDOWS Microsoft Word are accepted) after registration and login to the link: http://www.aiua.it. Surface or e-mail submission are not accepted.
Manuscripts must be written in English language in accordance with the “Uniform Requirements for Manuscripts submitted to biomedical journals” defined by The International Committee of Medical Journal Editors (http://www.ICMJE.org). Manuscripts
References must be listed as follows.
JOURNAL ARTICLES
All Authors if there are six or fewer, otherwise the first three, followed by “et al.”. Complete names for Work Groups or Committees. Complete title in the original language. Title of the journal following Index Medicus rules. Year of publication; Volume number: First page. Example: Starzl T, Iwatsuki S, Shaw BW, et al. Left hepatic trisegmentectomy Surg Gynecol Obstet. 1982; 155:21.
BOOKS
Authors - Complete title in the original language. Edition number (if later than the first). City of publication: Publisher, Year of publication. Example: Bergel DIA. Cardiovascular dynamics. 2nd ed. London: Aca de mic Press Inc., 1974.
BOOK CHAPTERS
Authors of the chapters - Complete chapter title. In: Book Editor, complete Book Title, Edition number. City of publication: Publisher, Publication year: first page of chapter in the book. Example: Sagawa K. The use of central theory and system analysis. In: Bergel DH (Ed), Cardiovascular dynamics. 2nd ed. London: Aca demic Press Inc., 1964; 115.
TABLES
Tables must be numbered in Arabic digits and referred to in the text by progressive numbers. Every table must be accompanied by a brief title. The meaning of any abbreviations must be explained at the bottom of the table itself.
FIGURES
(Graphics, algorithms, photographs, drawings). Figures must be numbered and quoted in the text by number. The meaning of symbols or abbreviations must be indicated. Histology photograph legends must include the enlargement ratio and the staining method. Legends must be collected in one or more separate pages.
• Do not include any illustrations as part of your text file. • Do not prepare any figures in Word as they are not workable. • Line illustrations must be submitted at 600 DPI.
• Halftones and color photos should be submitted at a minimum of 300 DPI. • Power Point files cannot be uploaded. • If possible please avoid transmitting electronic files in JPEG format or save the JPEG at the highest quality available • PDF files may be uploaded.
MANUSCRIPT REVIEW
Manuscripts are evaluated by the Editorial Board and/or by two referees designated by the Editors. The Authors are informed in a time as short as possible on whether the paper has been accepted, rejected or if a revision is deemed necessary. The Editors reserve the right to make editorial and literary corrections with the goal of making the article clearer or more concise, without altering its contents. Submission of a manuscript implies acceptation of all above rules.
PROOFS
Authors are responsible for ensuring that all manuscripts are accurately typed before final submission. Galley proofs will be sent to the first Author. Proofs should be returned within seven days from receipt.









































www.salutepertutti.it ancheseguiciqui!! Il podcast d ella rIvIsta icisegu a hg nche q i!!qu www lI t di benessercezione non è solo assenza di malattia, ma anche persaluteLa dpod o bene più prnostr menti quotidiani per mantener ovarsu come tr Ogni settimana parliamo di salute, e, sentirsi bene ed occuparsi di cosebenesser ezioso.o e il gie piccoli accorLe voci di Salutepertutti.it sono utili e belle. Alessia Bisini e Ruben Cazzola.













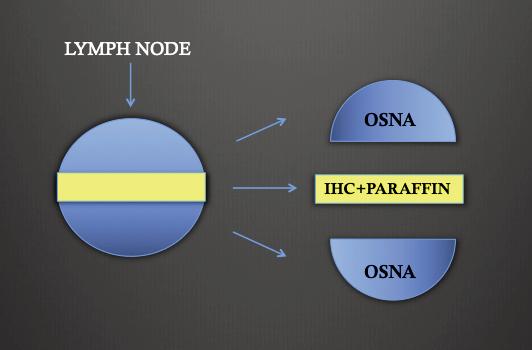

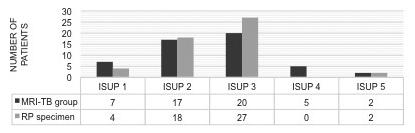
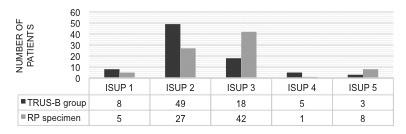


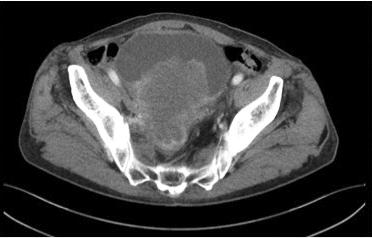


 Archivio Italiano di Urologia e Andrologia 2022;
Archivio Italiano di Urologia e Andrologia 2022;



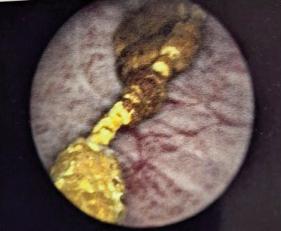

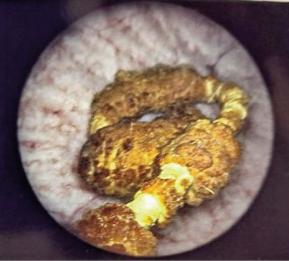
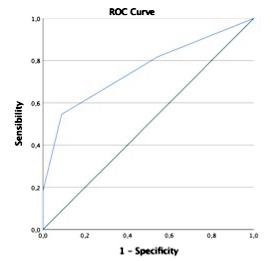
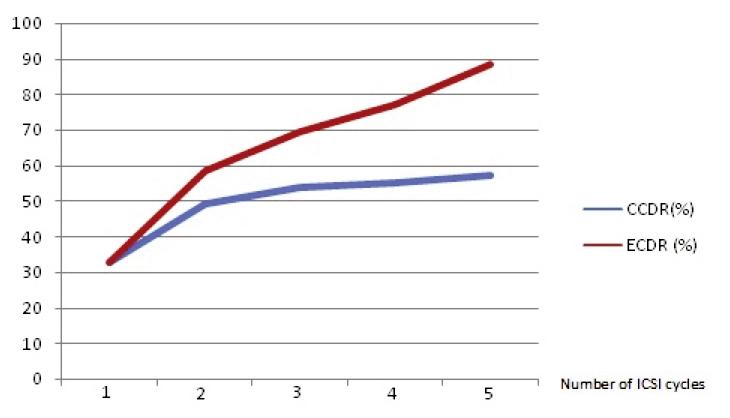
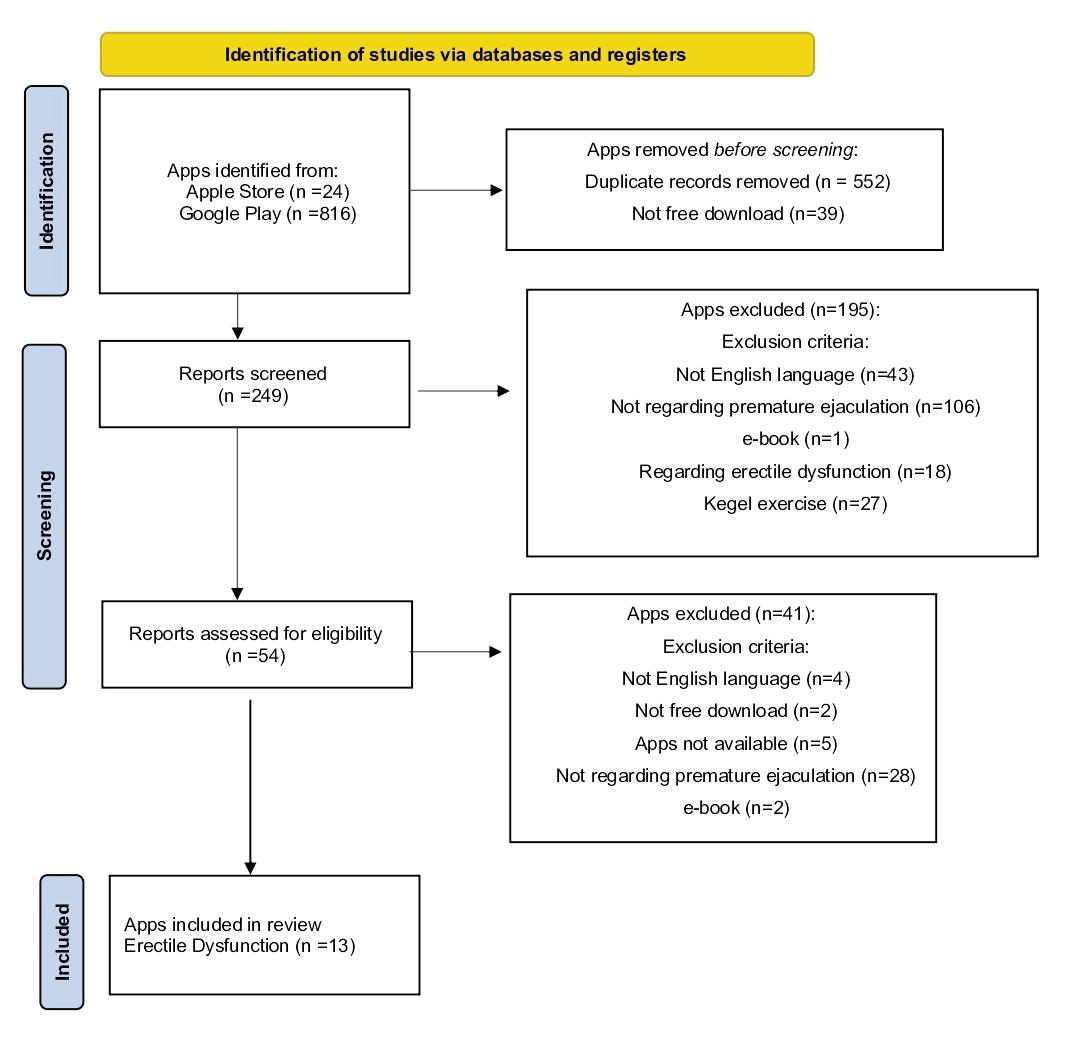 Figure 1 PRISMA
L Napolitano, L Cirillo, G M Fusco, et al
Figure 1 PRISMA
L Napolitano, L Cirillo, G M Fusco, et al