ORIGINAL PAPERS
11533 Primar y Bladder Sarcoma: A multi-institutional experience from the Rare Cancer Network

Piero Bettoli, ZhihuiAmy Liu, Natalia Jara, Federico Bakal, William Wong, Mario Terlizzi, Paul Sargos, Thomas Zilli, Juliette Thariat, Sebastian Sole, Guillaume Ploussard, Sharad Goyal, Peter Chung, Alejandro Berlin, Claudio V Sole
11610 Are elevated mitochondrial DNA fragments in prostatic inflammation a potential biomarker for prostate cancer?
Ugur Aferin, Nurten Bahtiyar, Ilhan Onaran, Hamdi Ozkara
11242 C reactive protein/Albumin ratio as predictor of prognosis in castration resistant metastatic prostate cancer
João Lorigo, Edgar Tavares Silva, João Pedroso Lima, Vasco Quaresma, Rui Pedrosa, Arnaldo Figueiredo
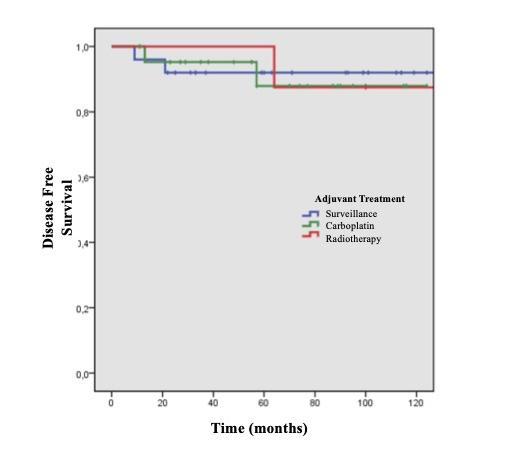
11513 Sur veillance as a safe and effective option for treatment of stage I seminoma
Vasco Quaresma, Diogo Henriques, Lorenzo Marconi, João Lorigo, Ana-Marta Ferreira, Roberto Jarimba, Pedro Nunes, Arnaldo Figueiredo, Belmiro Parada
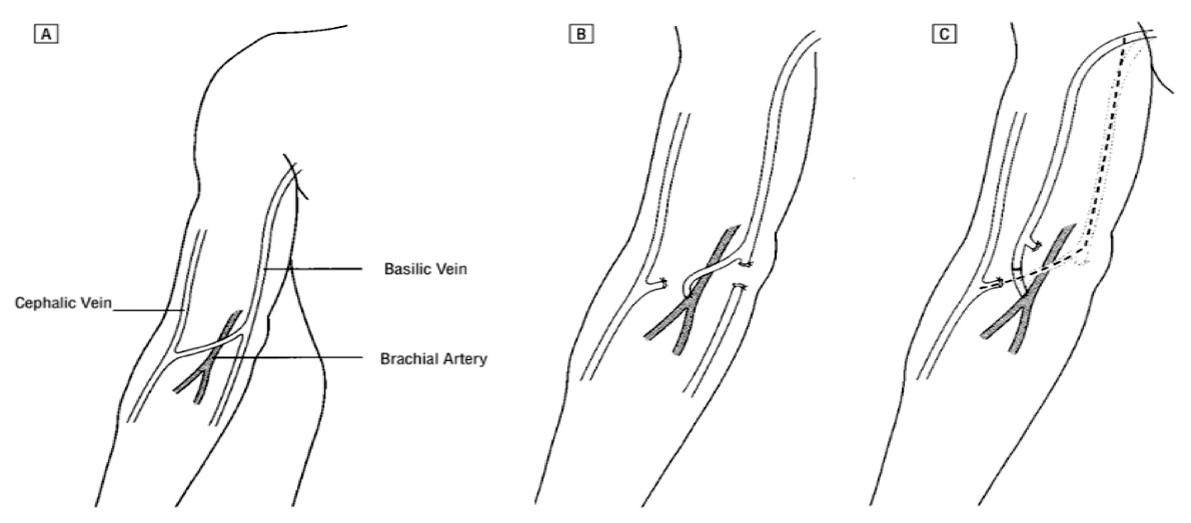
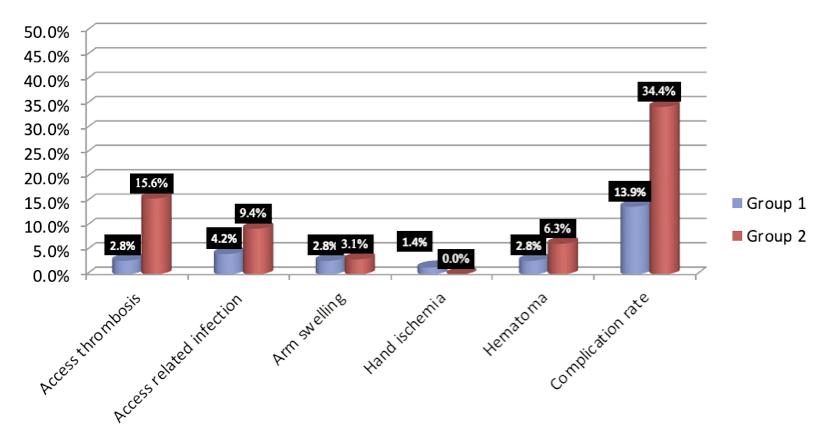
11455 Use of Basilic vein in ar teriovenous fistulas constr uction for hemodialysis access. Is it a good option alter native to prosthetic ar teriovenous grafts?
Ehab M Abdo, Tamer A Abouelgreed, Waleed E Elshinawy, Nehal Farouk, Mohamed A Abdelaal, Hassan Ismail, Amal H Ibrahim, Samar A Kasem, Ahmed A Aboomar
11588 The outcome of ultrasound-guided inser tion of central hemodialysis catheter
Ehab M Abdo, Tamer A Abouelgreed, Waleed E Elshinawy, Nehal Farouk, Hassan Ismail, Amal H Ibrahim, Samar A Kasem, Lobna Kh Sakr, Naglaa M Aboelsoud, Nermeen M Abdelmonem, Salma F Abdelkader, Ahmed A Abdelwahed, Anas A Qasem, Mosab F Alassal, Ahmed A Aboomar
11361 Evaluation of risk factors for recur rent renal stone for mation among Saudi Arabian patients: Comparison with first renal stone episode
Mohammed Alshehri, Hind Alsaeed, Malath Alrowili, Faisal Alhoshan, Ali Abdel Raheem, Ayman Hagras
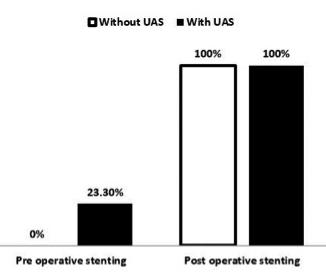
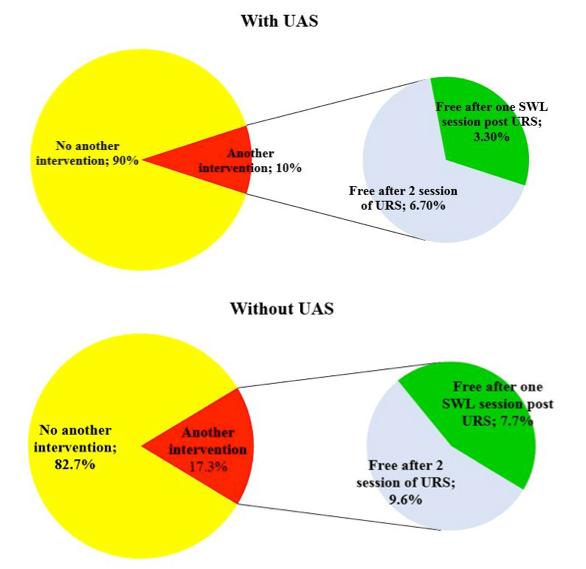
11524 The outcomes of flexible ureteroscopy for renal calculi of 2 cm or more with and without the use of ureteral access sheath: A retrospective study
Basem A Fathi, Ahmed A Elgammal, Tamer A Abouelgreed, Osama M Ghoneimy, Ahmed Y Aboelsaad, Mohamed A Alhefnawy
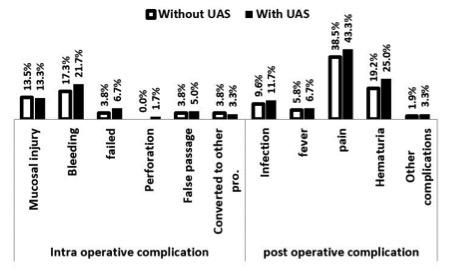
11581 Safety and efficacy of percutaneous nephrolithotripsy in comorbid patients: A 3 years prospective obser vational study
Tamer A Abouelgreed, Hassan Ismail, Sameh S Ali, Ayman K Koritenah, Yasser Badran, Mahmoud Ali, Rasha Ahmed, Mohamed Algammal, Ahmed Alrefaey, Aly Gomaa, Mohamed F Elebiary, Hany A Eldamanhory, Abdelhamid A Khattab, Nermeen M Abdelmonem, Mohammad Thabet Alnajem, Tamer G Abdlhamid, Ahmed A Abdelwahed, Salma F Abdelkader
11584 Is quadratus lumbor um block combined with low dose-spinal anesthesia an effective alter native to general anesthesia in patients undergoing percutaneous nephrolithotomy?
Tamer A Abouelgreed, Ahmed M Elgarhy, Adel Elatreisy, Tamer M Ewieda, Wael M Ibrahim, Othman Saadeldien Yahia, Ahmed M Elnaggar, Mohamed A Elbadawy, Ali A Alkumity, Yasser Badran, Mahmoud Ali, Aly Gomaa, Mohamed F Elebiary & Mahmoud Aboelnasr
11605 Supine mini percutaneous nephrolithotomy in horseshoe kidney
Orazio Maugeri, Eugenio Di Grazia, Letterio D’Arrigo, Roberta Agliozzo, Gianluca Calvano, Federica Trovato, Christian Di Gaetano, Giuseppe Trefiletti, Salvatore Privitera, Giorgio Ivan Russo, Sebastiano Cimino
11662 Are voiding volumes and frequencies different in the three-day voiding diar y in children with lower urinar y tract dysfunction?
Raziye Ergun, Cagri Akin Sekerci, Mehmet Cetin, Mohammad Yasir Sahak, Selcuk Yucel, Tufan Tarcan
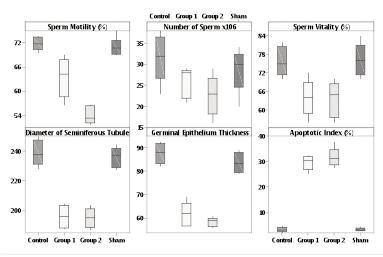
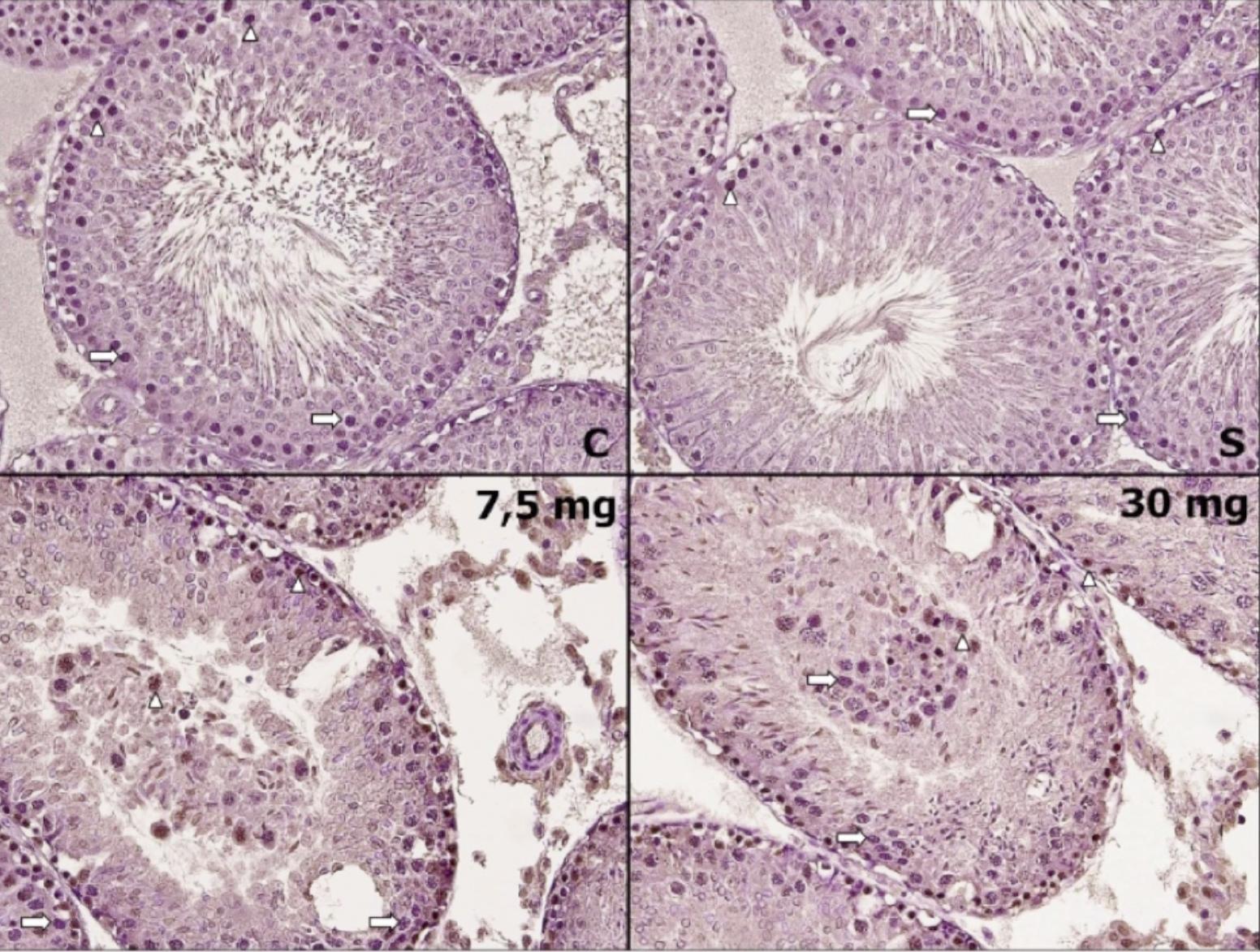
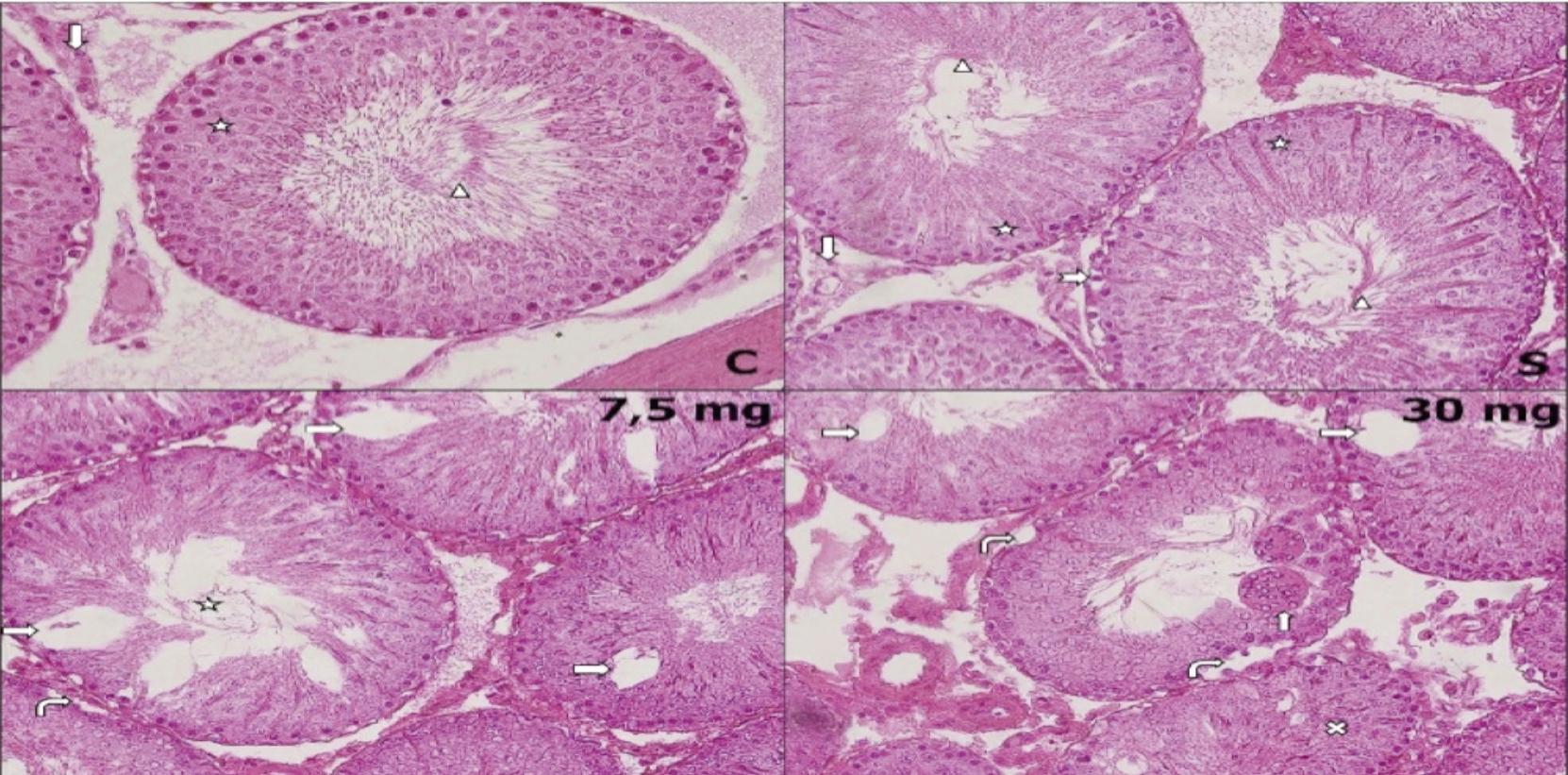
11502 Does isotretinoin affect sper matogenesis in the long ter m? A rat model
Abdullah Cirakoglu, Sevda Onder, Hatice Hancı, Erdal Benli, Ahmet Yüce, Yeliz Kasko Arici, Orhan Bas, Ismail Nalbant
11462 Galectin-1 (Gal-1) and Galectin-3 (Gal-3) levels in seminal plasma and ser um in azoosper mic patients versus fer tile men: A cross-sectional study
Sameh Fayek GamalEl Din, Olfat Gamil Shaker, Ahmad Fawzy Megawer, Mohamed Ahmed Abdel Salam, Abdelhalim Nabil Abdelhalim, Ahmed Adel
11450 Prognostic deter minants and treatment outcomes of Four nier’s Gangrene treatment in a resource-limited setting: A retrospective study
Saif Ghabisha, Faisal Ahmed, Saleh Al-wageeh, Mohamed Badheeb, Qasem Alyhari, Abdulfattah Altam, Afaf Alsharif
continued on page III
Vol. 95; n. 3, September
2023
ISSN 1124-3562
ATLANTE di ECOGRAFIA UROLOGICA, ANDROLOGICA e NEFROLOGICA
124 autori
592 pagine + di 1500 immagini ecografiche
61 video


Hardcover Cofanetto
Costo di copertina € 180,00 Sconto del 50%



Indicando il Codice: AIUA2023
Prezzo finale: € 90,00*

L’opera è acquisabile inviando un’e-mail a: atlantediecografia@gmail.com * Spese di spedizione escluse

PRESENTANO
PASQUALE MARTINO
EDITORIAL BOARD
ASSOCIATE EDITORS
EDITOR IN CHIEF
Alberto Trinchieri (Milan, Italy)
Emanuele Montanari, Department of Urology, IRCCS Foundation Ca’ Granda Ospedale Maggiore Policlinico, University of Milan, Italy – Gianpaolo Perletti, Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy; Department of Human Structure and Repair, Ghent University, Ghent, Belgium - Angelo Porreca, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy
EXECUTIVE EDITORIAL BOARD
Alessandro Antonelli, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Antonio Celia, Department of Urology, San Bassiano Hospital, Bassano del Grappa, Italy - Luca Cindolo, Department of Urology, Villa Stuart Hospital, Rome, Italy - Andrea Minervini, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Bernardo Rocco, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Riccardo Schiavina, Department of Urology, University of Bologna, Bologna, Italy
ADVISORY EDITORIAL BOARD
vasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy - Fabrizio Di Maida, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Antonio Galfano, Urology Unit, Niguarda Hospital, Milan, Italy - Michele Marchioni, Department of Medical, Oral and Biotechnological Sciences, "G. d'Annunzio" University of Chieti, Laboratory of Biostatistics, Chieti, Italy - Andrea Mari, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Luigi Napolitano, Unit of Urology, Department of Neurosciences, Reproductive Sciences, and Odontostomatology University of Naples “Federico II”, Naples, Italy - Antonio Porcaro, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Stefano Puliatti, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Daniele Romagnoli, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy - Chiara Sighinolf, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Tommaso Silvestri, Urology Clinic, Department of Medical, Surgical and Health Science, University of Trieste, Trieste, Italy - Petros Sountoulides, Aristotle University of Thessaloniki, Department of Urology, Thessaloniki, Greece - Alessandro Tafuri, Department of Urology, Vito Fazzi Hospital, Lecce, Italy
SIEUN EDITOR
Pasquale Martino, Department of Emergency and Organ Transplantation-Urology I, University Aldo Moro, Bari, Italy
SIEUN EDITORIAL BOARD
Giovanni Colpi, Retired Andrologist, Milan, Italy
Pier Francesco Bassi, Urology Unit, A Gemelli Hospital, Catholic University of Rome, Italy – Francesca Boccafoschi, Health Sciences Department, University of Piemonte Orientale in Novara, Italy – Alberto Bossi, Department of Radiotherapy, Gustave Roussy Institute, Villejuif, France –Tommaso Cai, S Chiara Hospital, Trento, Italy –Paolo Caione, Department of Nephrology-Urology, Bambino Gesù Pediatric Hospital, Rome, Italy – Luca Carmignani, Urology Unit, San Donato Hospital, Milan, Italy –Liang Cheng, Department of Urology, Indiana University School of Medicine, Indianapolis, IN; Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, Indianapolis, IN
– Giovanni Corona, Department of Urology, University of Florence, Careggi Hospital, Florence, Italy – Antonella Giannantoni, Department of Surgical and Biomedical Sciences, University of Perugia, Italy – Paolo Gontero, Department of Surgical Sciences, Molinette Hospital, Turin, Italy – Steven Joniau, Organ Systems, Department of Development and Regeneration, KU Leuven, Belgium – Frank Keeley, Bristol Urological Institute, Southmead Hospital, Bristol UK – Laurence Klotz, Division of Urology, Department of Surgery, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Ontario, Canada – Börje Ljungberg, Urology and Andrology Unit, Department of Surgical and Perioperative Sciences, Umeå University, Umeå, Sweden –Nicola Mondaini, Uro-Andrology Unit, Santa Maria Annunziata Hospital, Florence, Italy – Gordon Muir, Department of Urology, King's College Hospital, London, UK –Giovanni Muto, Urology Unit, Bio-Medical Campus University, Turin, Italy – Anup Patel, Department of Urology, St Mary's Hospital, Imperial Healthcare NHS Trust, London, UK – Glenn Preminger, Division of Urologic Surgery, Duke University Medical Center, Durham, NC, USA – David Ralph, St. Peter's Andrology Centre and Institute of Urology, London, UK – Allen Rodgers, Department of Chemistry, University of Cape Town, Cape Town, South Africa – Francisco Sampaio, Urogenital Research Unit, State University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil – Kemal Sarica, Department of Urology, Kafkas University Medical School, Kars, Turkey – Luigi Schips, Department of Urology, San Pio da Pietrelcina Hospital, Vasto, Italy – Hartwig Schwaibold, Bristol Urological Institute, Southmead Hospital, Bristol, UK – Alchiede Simonato, Department of Urology, University of Verona, Azienda Ospedaliera Universitaria Integrata, Verona, Italy – Carlo Terrone, Department of Urology, IRCCS S Martino University Hospital, Genova, Italy – Anthony Timoney, Bristol Urological Institute, Southmead Hospital, Bristol, UK – Andrea Tubaro, Urology Unit, Sant’Andrea Hospital, “La Sapienza” University, Rome, Italy – Richard Zigeuner, Department of Urology, Medical University of Graz, Graz, Austria
BOARD OF REVIEWERS
Maida Bada, Department of Urology, S Pio da Pietrelcina Hospital, ASL 2 Abruzzo, Vasto, Italy - Lorenzo Bianchi, Department of Urology, University of Bologna, Bologna, Italy - Mariangela Cerruto, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Francesco Chessa, Department of Urology, University of Bologna, Bologna, Italy - Daniele D’Agostino, Robotic Urology and Mini In-
Emanuele Belgrano, Department of Urology, Trieste University Hospital, Trieste, ItalyFrancesco Micali, Department of Urology, Tor Vergata University Hospital, Rome, ItalyMassimo Porena, Urology Unit, Perugia Hospital, Perugia, Italy – Francesco Paolo Selvaggi, Department of Urology, University of Bari, Italy – Carlo Trombetta, Urology Clinic, Cattinara Hospital, Trieste, Italy – Giuseppe Vespasiani, Department of Urology, Tor Vergata University Hospital, Rome, Italy – Guido Virgili, Department of Urology, Tor Vergata University Hospital, Rome, Italy
UrOP EDITOR
Carmelo Boccafoschi, Department of Urology, Città di Alessandria Clinic, Alessandria, Italy
UrOP EDITORIAL BOARD
Renzo Colombo, Department of Urology, San Raffaele Hospital, Milan, Italy – Roberto Giulianelli, Department of Urology, New Villa Claudia, Rome, Italy – Massimo Lazzeri, Department of Urology, Humanitas Research Hospital, Rozzano (Milano), Italy – Angelo Porreca, Department of Urology, Polyclinic Abano Terme, Abano Terme (Padova), Italy –Marcello Scarcia, Department of Urology, "Francesco Miulli" Regional General Hospital, Acquaviva delle Fonti (Bari), Italy – Nazareno Suardi, Department of Urology, San Raffaele Turro, Milano, Italy
GUN EDITOR
Arrigo Francesco Giuseppe Cicero, Medical and Surgical Sciences Department, Sant’Orsola-Malpighi University Hospital, Bologna, Italy
GUN EDITORIAL BOARD
Gianmaria Busetto, Department of Urology, Sapienza University of Rome, Italy –Tommaso Cai, Department of Urology, Santa Chiara Regional Hospital, Trento, Italy –Elisabetta Costantini, Andrology and Urogynecological Clinic, Santa Maria Hospital of Terni, University of Perugia, Terni, Italy – Angelo Antonio Izzo, Department of Pharmacy, University of Naples, Italy – Vittorio Magri, ASST Nord Milano, Milano, Italy – Salvatore
Micali, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy –




Gianni Paulis, Andrology Center, Villa Benedetta Clinic, Rome, Italy – Francesco Saverio Robustelli della Cuna, University of Pavia, Italy – Giorgio Ivan Russo, Urology
Department, University of Catania, Italy – Konstantinos
Stamatiou, Urology Department, Tzaneio Hospital, Piraeus, Greece – Annabella Vitalone, Department of Physiology and Pharmacology, Sapienza University of Rome, Rome, Italy
O f f i c i a l J o u r n a l o f S I E U N , U r O P , S S C U a n d G U N
–
NOVITÀ
Un’opera nuova e completa sul microbiota, il complesso consorzio di omalattia. Centinaia di illustrazioni a colori, contenuti multimediali, aggiornati in progress continuo ed accessibili mediante QR code. Un Trattato imprescindibile per chi si occupa di salute interpretando i referti sul microbiota.
Costo di copertina €120,00, spese di spedizione escluse. Per informazioni ed eventuali ordini, scrivere a: info@edizioniscriptamanent.eu

ORIGINAL PAPERS
11494 Complications of non-medical assisted circumcision in Burkina Faso. Clinical presentation, management, and outcomes - about 23 cases and literature review
Adama Ouattara, Abdoul-Karim Paré, Delphine Yé, Ali Sherazi, Mohamed Simporé, Mickael Rouamba, Aristide F Kaboré, Timothée Kambou
11549 Calcification in Peyronie's disease:
Its role and clinical influence on the various symptoms and signs of the disease, including psychological impact. Our study of 551 patients
Gianni Paulis, Andrea Paulis
11567 Predictive factors for successful testicular biopsy
Duarte Vieira Brito, Manuel Lopes, Jose Pereira, Ana Maria Ferreira, Luis Sousa, Belmiro Parada, Arnaldo Figueiredo
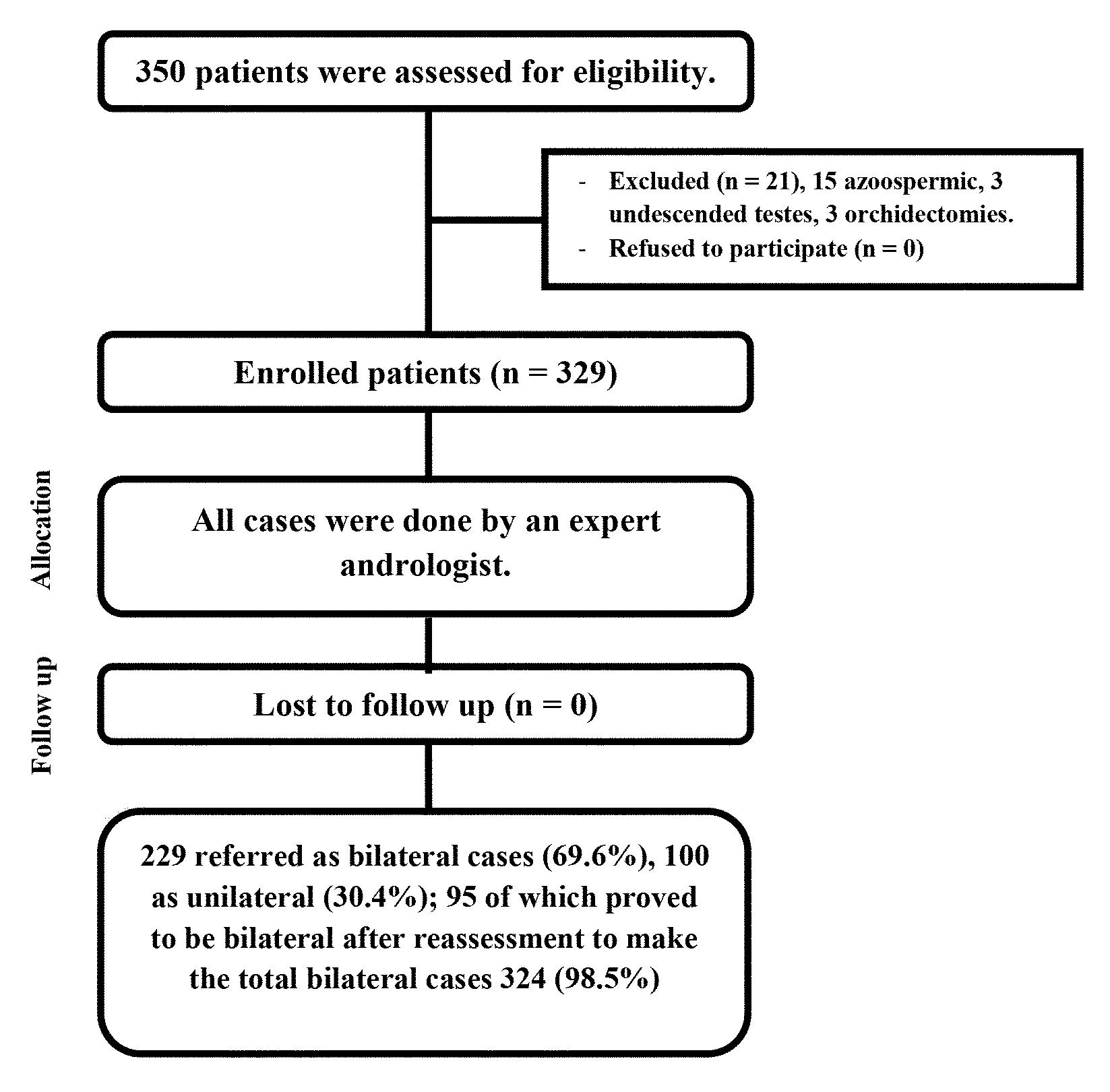
11580 Bilaterality of varicocele: The over looked culprit in male infer tility. Case series study
Khaled Mohamed Almekaty, Ahmed Mostafa Elsharkawy, Mohamed Hasan Zahran, Maged Mostafa Ragab, Ayman Sayed Rashed, Mahmoud Mohamed Soliman, Khaled Abdelaziz Salem, Ahmed Fayez Ghaith
11528 Reference value of testicular temperature measured by finite element analysis after first staged inguinal orchidopexy in children with abdominal testis and shor t sper matic cord
Mehdi Shirazi, Ali Eslahi, Mohsen Ostovari, Faisal Ahmed, Ahmed Zaid, Mohammad Reza Askarpour, Hossein-Ali Nikbakht, Zeinab Gholami, Sania Shirazi
SYSTEMATIC REVIEWS
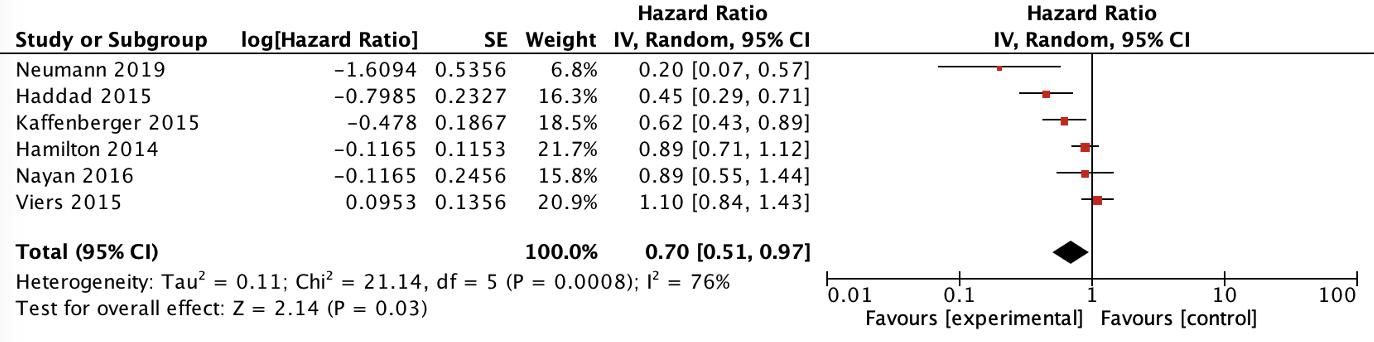
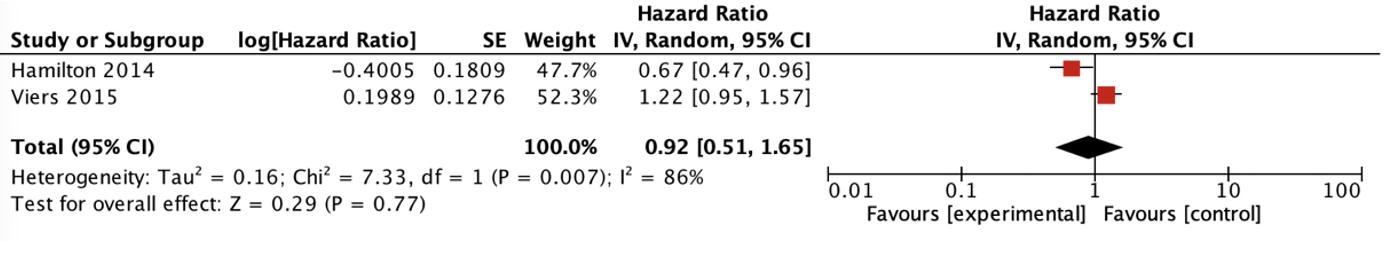
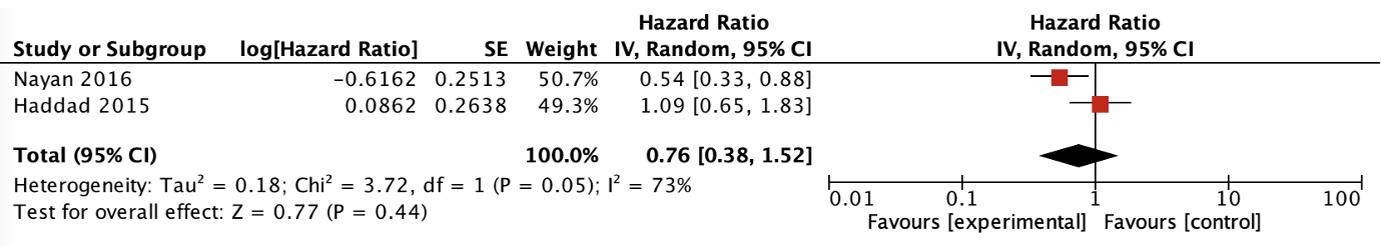
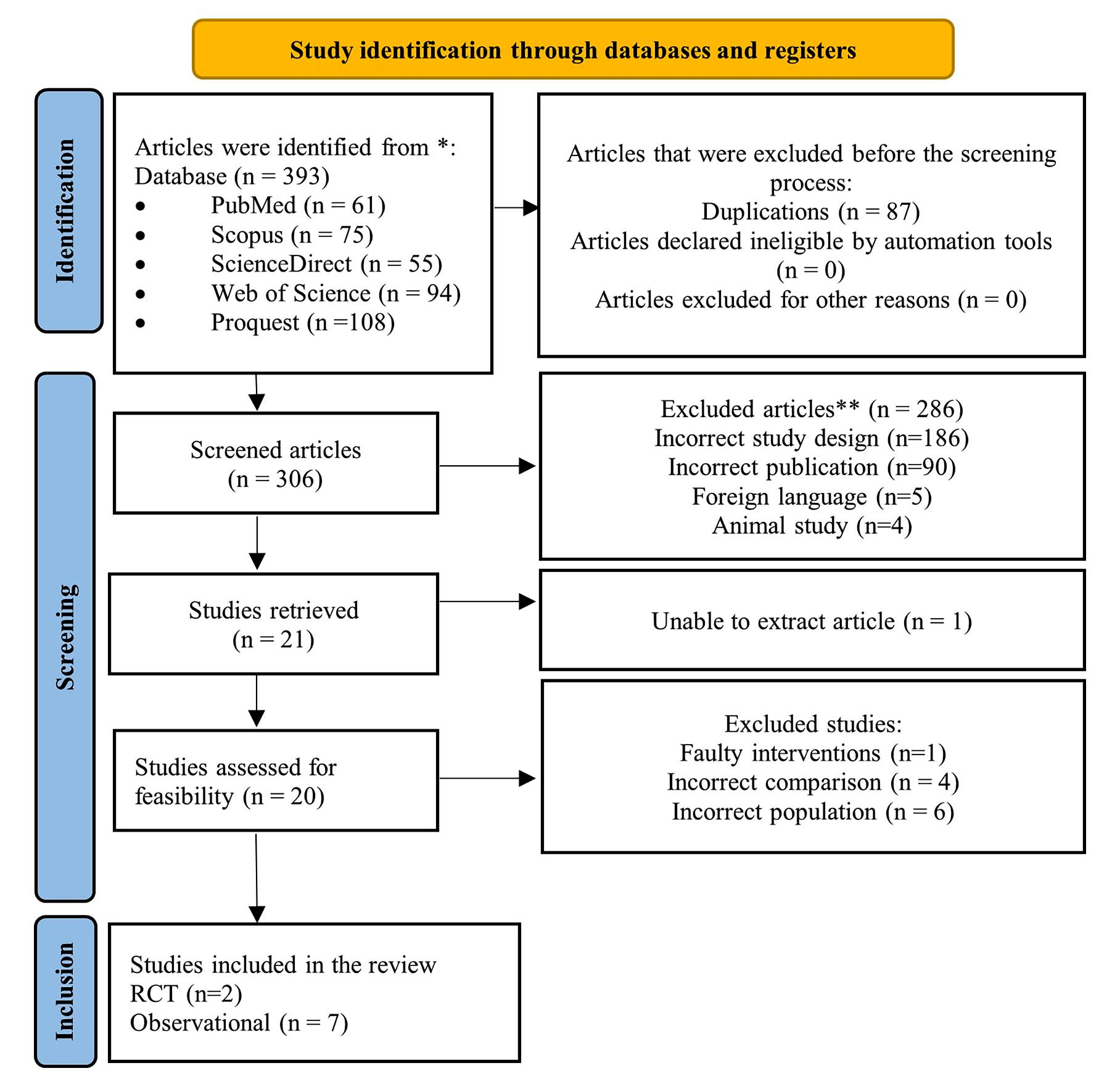
11672 Impact of statin on renal cell carcinoma patients undergoing nephrectomy Does it affect cancer progression and improves sur vival?
A Systematic Review and Meta-Analysis
Ghazian Adli, Niwanda Yogiswara, Ida Bagus Gde Tirta Yoga Yatindra, Rheza Maulana Putra, Wahjoe Djatisoesanto
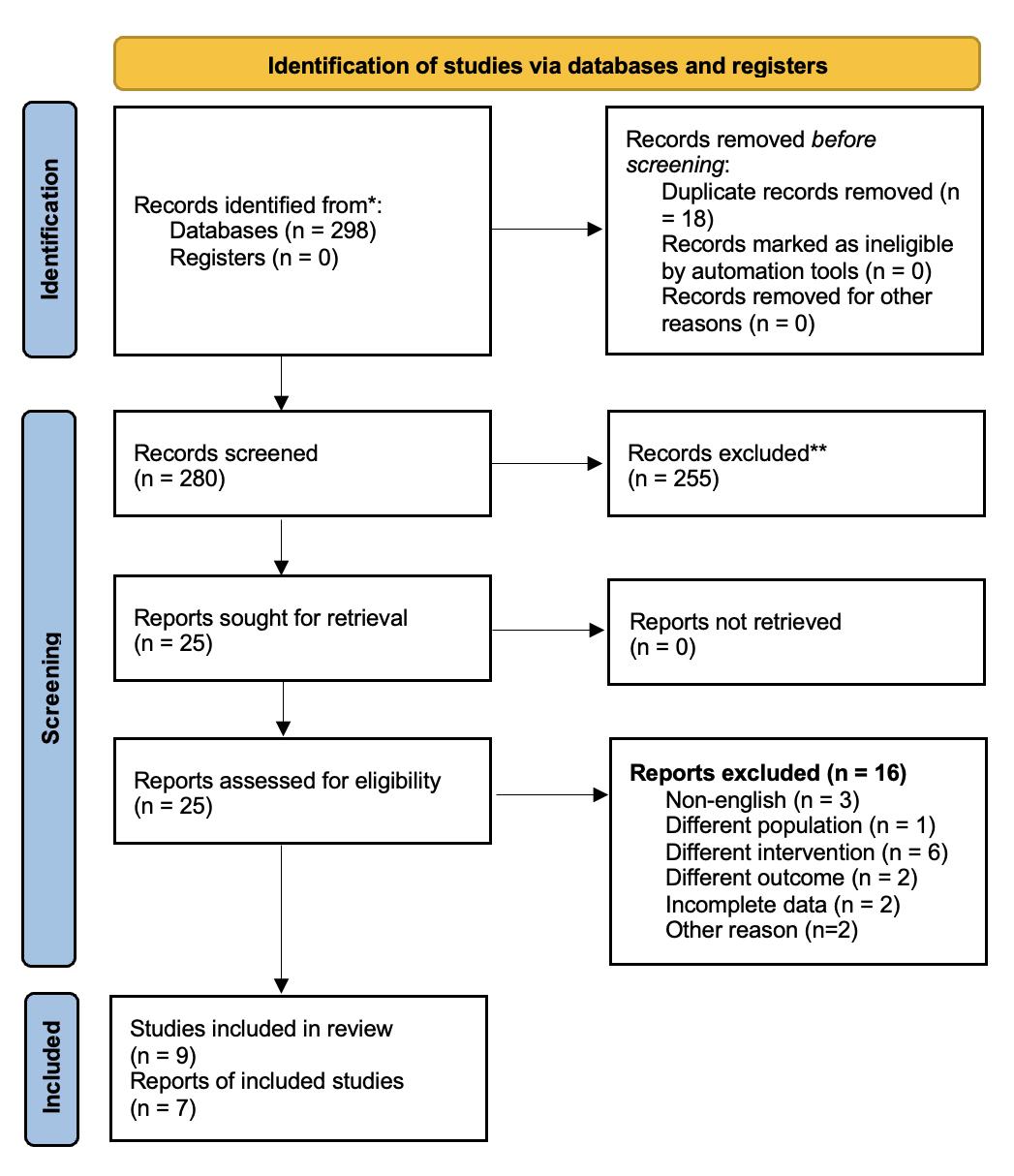
11627 A systematic review and meta-analysis on the efficacy of inter nal sper matic ar ter y ligation during laparoscopic varicocelectomy in children and adolescents: Is it safe?
Ahmad Nurfakhri Syarief, Ilham Akbar Rahman, Agung Ravi Saputra Sangadji, Tarmono Djojodimedjo, Fikri Rizaldi
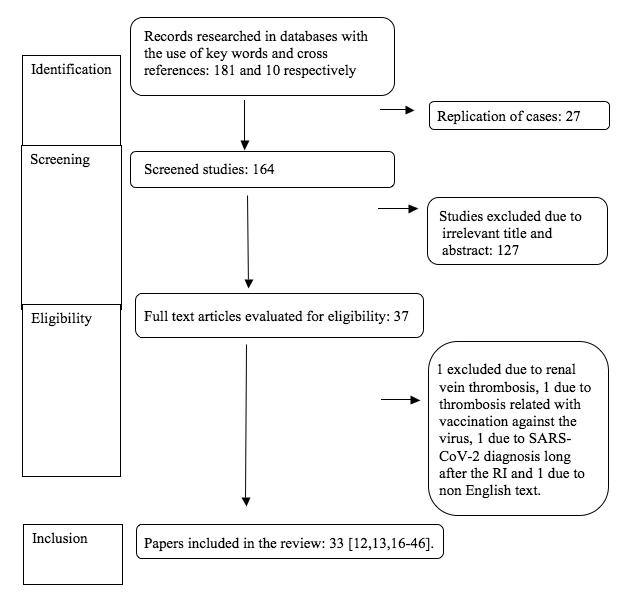
11625 Renal ar ter y infarction in the SARS-Cov-2 era: A systematic review of case repor ts Diomidis Kozyrakis, Georgios Kallinikas, Anastasios Zarkadas, Dimitrios Bozios, Vasileios Konstantinopoulos, Georgios Charonis, Konstantinos Safioleas, Athanasios Filios, Evangelos Rodinos, Despoina Mytiliniou, Gerasimos Vlassopoulos, Ioannis Gkerzelis, Panagiotis Filios
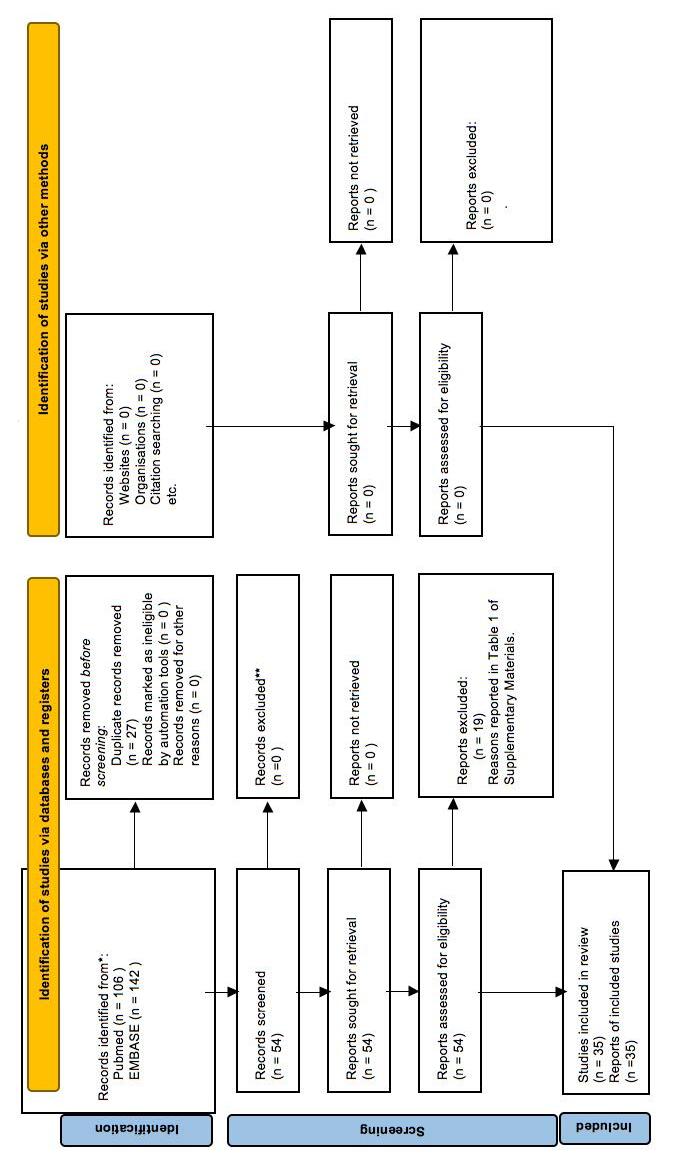
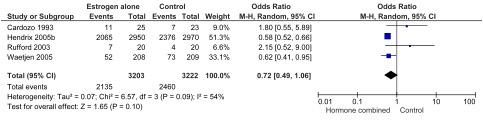
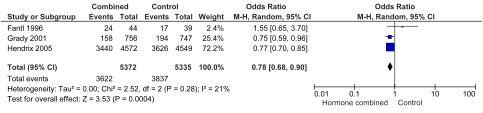
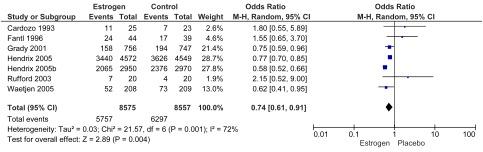
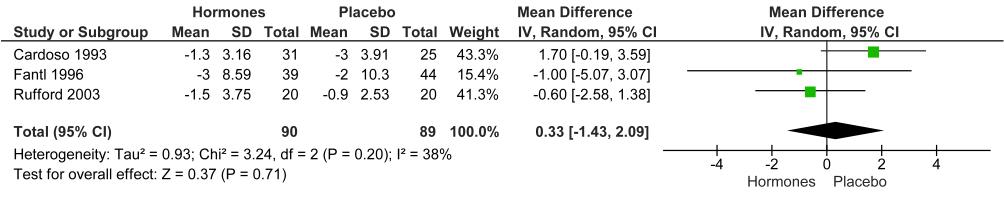
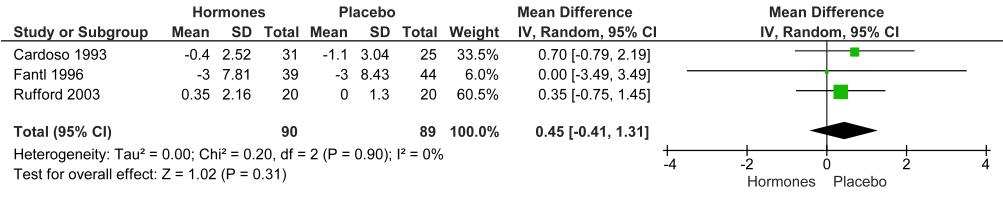
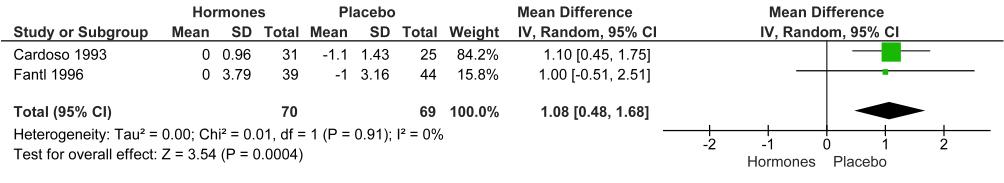
11718 Treatment of urge incontinence in postmenopausal women: A systematic review
Rawa Bapir, Kamran Hassan Bhatti, Ahmed Eliwa, Herney Andrés García-Perdomo, Nazim Gherabi, Derek Hennessey, Vittorio Magri, Panagiotis Mourmouris, Adama Ouattara, Gianpaolo Perletti, Joseph Philipraj, Konstantinos Stamatiou, Musliu Adetola Tolani, Lazaros Tzelves, Alberto Trinchieri, Noor Buchholz
LETTER TO EDITOR
11481 Benign prostatic obstr uction (BPO) as a possible risk factor for Peyronie's disease (PD)
The influence of BPO and PD on mental health
Gianni Paulis, Andrea Paulis
Edizioni Scripta Manent s.n.c.
Via Melchiorre Gioia 41/A - 20124 Milano, Italy
Tel +39 0270608060
e-mail: scriman@tin.it
web: www edizioniscriptamanent eu
Registrazione: Tribunale di Milano n 289 del 21/05/2001
Ai
Direttore Responsabile: Pietro Cazzola
Direzione Marketing e PR: Donatella Tedeschi
Comunicazione e Media: Ruben Cazzola
Grafica e Impaginazione: Stefania Cacciaglia
Affari Legali: Avv Loredana Talia (MI)
Edizioni Scripta Manent s n c - Via Melchiorre Gioia, 41/A - 20124 Milano
The Publisher is not liable for the opinion expressed by the Authors of the articles and for images used by them
GENERAL INFORMATION
AIMS AND SCOPE
“Archivio Italiano di Urologia e Andrologia” publishes papers dealing with the urological, nephrological and andrological sciences
Original articles on both clinical and research fields, reviews, editorials, case reports, abstracts from papers published elsewhere, book rewiews, congress proceedings can be published
III Archivio Italiano di Urologia e Andrologia 2023, 95, 3
sensi della legge 675/96 è possibile in qualsiasi momento opporsi all’invio della rivista comunicando per iscritto la propria decisione a:
Questo Trattato nasce dall’esigenza di offrire evidenze scientifiche della letteratura in diversi àmbiti clinici, riguardo alla Nutraceutica in Pediatria, in un contesto attuale dove è molto forte da parte della società la propensione a ricorrere a “prodotti naturali”.
I temi trattati sono a sostegno di scelte mirate da parte del Pediatra, che possono essere di supporto dal punto di vista preventivo e terapeutico, per la salute di bambini e adolescenti.
25 Capitoli
64 Autori
480 Pagine a cura di
Gianvincenzo Zuccotti
Enza D’Auria
Elvira Verduci
Prezzo di copertina € 100,00 (spese di spedizione escluse)
Per l’acquisto inviare una e-mail a: info@edizioniscriptamanent.eu
ORIGINAL PAPER
Primary Bladder Sarcoma: A multi-institutional experience from the Rare Cancer Network
Piero Bettoli 1, 2 , ZhihuiAmy
3 , Natalia Jara 4 , Federico
Mario Terlizzi 6 , Paul Sargos 6 , Thomas Zilli 7 , Juliette Thariat 8 , Sebastian Sole 4, 9 , Guillaume Ploussard 10 , Sharad Goyal 11 , Peter Chung 3 , Alejandro Berlin 3 , Claudio V. Sole 4, 9
1 Department of Radiation Oncology, Fundación Arturo López Pérez, Santiago, Chile;
2 Facultad de Medicina, Universidad de Los Andes, Santiago, Chile;
3 Radiation Medicine Program, Princess Margaret Cancer Centre, University Health Network, University of Toronto, Toronto, ON, Canada;
4 Department of Radiation Oncology, Instituto de Radiomedicina, Santiago, Chile;
5 Department of Radiation Oncology, Mayo Clinic Arizona, Phoenix, USA;
6 Department of Radiation Oncology, Institute Bergonie, Bordeaux, France;
7 Department of Radiation Oncology, Geneva University Hospital, Geneva, Switzerland;
8 Department of Radiation Therapy, Centre Francoise Baclese, Caen, France;
9 Facultad de Medicina, Universidad Diego Portales, Santiago, Chile;
10 Department of Urology, La Croix du Sud Hospital, Toulouse, France;
11 Department of Radiation Oncology, George Washington University Hospital, Washington DC, USA
Summary
Purpose or Objective: Primary sarcoma of the urinary bladder (SUB) is a rare but aggressive form of bladder cancer (BCa) Available evidence on SUB is limited to case reports and small series The aim of the present multi-institutional study was to assess the clinical features, treatments, and outcomes of patients with SUB
Materials and methods: Using a standardized database, 7 institutions retrospectively collected the demographics, risk factors, clinical presentation, treatment modalities and follow-up data on patients with SUB between January 1994 and September 2021. The main inclusion criteria included BCa with soft tissue tumor histology and sarcomatoid differentiation.
Results: Fifty-three patients (38 men and 15 women) were iden-
tified Median follow-up was 18 months (range 1-263 months)
Median age at presentation was 69 years (range 16-89 years)
Twenty-six percent of patients had a prior history of pelvic radiotherapy (RT), and 37% were previous smokers The main presenting symptoms at diagnosis were hematuria (52%), pelvic pain (27%), and both hematuria and pelvic pain (10%).
American Joint Committee on Cancer (AJCC) 8 th edition stage II, III and IV at diagnosis were 21%, 63% and 16%, respectively. Treatment modalities included surgery alone (45%), surgery plus neo- or adjuvant-chemotherapy (17%), surgery plus neo- or adjuvant-RT (11%), RT with concurrent chemotherapy (4%), neo-adjuvant chemotherapy plus surgery plus adjuvant RT (2%) and palliative treatment (21%) Rates of local and distant recurrences were 49% and 37%, respectively Five-year overall survival and progression-free survival (PFS) were 66 5% and 37.6%, respectively. No statistically significant differences in PFS between the treatment modalities were observed.
Conclusions: Primary SUB is a heterogeneous disease group, commonly presenting at advanced stages and exhibiting aggressive disease evolution In contrast to urothelial carcinoma, the primary pattern of recurrence of SUB is local, suggesting the need for multimodal approaches Continuous international collaborative efforts seem warranted to provide guidance on how to best tailor treatments based on SUB-specific indices
KEY WORDS: Primary sarcoma of the urinary bladder (SUB); Bladder cancer
Submitted 19 June 2023; Accepted 1 July 2023
INTRODUCTION
Although uncommon, primary sarcoma of the urinary bladder (SUB) is an aggressive type of bladder cancer (BCa), accounting for less than 1% of all BCa The most common risk factors for the development of this disease is smoking and previous exposure to radiotherapy (RT) and cyclophosphamide (1, 2)
Based on mesenchymal and epithelial components, SUB can be classified as Sarcomatoid carcinoma (SC) and Carcinosarcoma (CS), both considered malignant biphasic tumors (MBT) by the World Health Organization having malignant epithelial and mesenchymal elements (3) More recently researchers have cast doubts on the significance of distinguishing between these two entities in both bladder and other solid malignancy as they consider these two histological subtypes as separate moments between epithelial (Sarcomatoid carcinoma) and mesenchymal differentiation (Carcinosarcoma) (4) Usually, the epithelial element contains high-grade transitional-cell carcinoma with some epidermoid and/or glandular differentiation, while the heterologous element contains chondrosarcoma, malignant fibrous histiocytoma, osteosarcoma, leiomyosarcoma, fibrosarcoma, or rhabdomyosarcoma Both SC and CS cases are most common among older men, manifesting as fastgrowing, advanced-stage polypoid tumors (1-4) When the mesenchymal element lacks epithelial components, SUB can be considered a true heterologous sarcoma (TS) Usually, treatment of SUB has been deduced from the management of urothelial carcinoma (UC) of the bladder Muscle-invasive UC of the bladder often results in distant metastasis after radical cystectomy, and therefore, neoadjuvant or adjuvant chemotherapy has been recommended as a part of a multimodal approach (5, 6)
However, because of to the rarity of SUB and the absence of randomized controlled trial in this setting, definitive conclusions about the optimal treatment option cannot be made Poor outcomes have been reported in patients with SUB, whatever the treatment used Even after adjust-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11533 1
Liu
Bakal 1 , William Wong 5 ,
DOI: 10 4081/aiua 2023 11533
ing for tumor stage, overall survival (OS) rates for SUB vs high-grade, pure UC are 54% vs 77% at 1 year and 37% vs 47% at 5 years, respectively (4, 7)
Published data on SUB only consist of case reports and limited case series Not much is understood of SUB biology and behavior and its rarity does not permit to design specific treatment guidelines Thus, we intend to summarize the current multi-institutional knowledge of SUB and present an overview of the epidemiology, clinical features, and management of this uncommon type of BCa that can help clinicians to better tailor clinical decisions on this rare disease
METHODS
Data on SUB from January 1994 to September 2021 from 7 institutions were retrospectively collected International Review Board (IRB) approval based on each country/institution was obtained for retrospective review of data
We only collected data from localized primary bladder tumors with soft tissue tumor histology, including SC, CS and TS The data obtained included age, gender, country and institution, symptoms at the time of diagnosis, risk factors (smoking and RT exposure), tumor size, tumor location, margins and nodal status Sarcoma subtype, grade and specific immuno-histochemical markers of these tumors were noted Staging at the time of pathological diagnosis was based on the TNM (tumor, lymph node, metastasis) classification for genitourinary tumors
Treatment modalities analyzed included cystectomy (radical, partial, other), RT (definitive, adjuvant, neo-adjuvant or palliative) and chemotherapy (neo-adjuvant, adjuvant, radio-sensitizer or palliative)
Overall survival (OS), cancer-specific survival (CSS), disease-free survival (DFS), distant metastases (DM) and local control (LC) were calculated from diagnosis to the date of any specific event or the date of last follow-up in case an event did not occur
Probabilities for OS, CSS and DFS were determined by Kaplan-Meier estimates Local recurrence (LR) and DM were estimated using cumulative incidence function considering death as a competing risk Selective comparisons of survival curves were calculated by the log-rank test Multivariate models were not used because of the small number of patients and events For statistical analyses the software program STATA (version 13; College Station, Texas, USA) was used
RESULTS
Fifty-three patients were evaluated, 38 men (72%) and 15 women (28%), who had a median age at presentation of 69 years (range 16-89 years) Twenty-six percent of patients had a prior history of pelvic RT; contrary to patients with transitional cell carcinoma, only 37% of patients had a history of tobacco use Symptoms at diagnosis were mainly hematuria (52%), pelvic pain (27%), and both hematuria and pelvic pain (10%)
Median tumor size was 4 5 cm (range 1 5-9 5 cm) Extravesical spread (T3/T4) was the most common presentation of the primary tumor in 59% of cases Nodal metastases were identified in 35% of patients AJCC 8th edition
Table 1. Patient and tumor characteristics
stage II, III and IV at diagnosis were 21%, 63% and 16%, respectively The majority of tumors presented with high grade histology (88%) Distribution of TS and MBT were 43% and 57%, respectively Leiomyosarcoma was the most common histology in the TS group (63%), followed by angiosarcoma (13%), pleomorphic undifferentiated sarcoma (10%), rhabdomyosarcoma (7%), chondrosarcoma of soft tissue (3%) and leiomyoma (3%) Table 1 presents patient and tumor characteristics
Seventy-three percent of patients underwent radical or partial cystectomy Specifically, treatment modalities included surgery alone (45%), surgery preceded or followed by either chemotherapy (17%) or radiotherapy (11%), definitive radiotherapy with concurrent chemotherapy (4%), neo-adjuvant chemotherapy plus surgery plus adjuvant radiotherapy (2%) and palliative treatment (21%)
Treatment
in Table 2
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11533 P Bettoli, Z Liu, N Jara, et al 2
modalities are outlined
Patients characteristics N (%) Age mean 69 Gender Male 38 (72) Female 15 (28) Prior history of RT 14 (26) Tobacco exposure 20 (37) Symptoms Hematuria 28 (52) Pelvic pain 14 (27) Both 5 (10) Other 6 (11) Tumor size (median) 4 5 cm (1 5 -9 5) T stage T1/T2 22 (41) T3/T4 31 (59) Nodal metastases 19 (35) AJCC II 11 (21) III 33 (63) IV 9 (16) Malignant Biphasic Tumors (MBT) 23 (43) True Sarcoma (TS) 31 (57) Leiomyosarcoma 19 (61) Angiosarcoma 7 (22) Pleomorphic undifferentiated sarcoma 2 (7) Rhabdomyosarcoma 2 (7) Chondrosarcoma 1 (3) Table
Treatment modalities. Treatment modalities N (%) Surgery alone 24 (45) Surgery plus neo-adjuvant or adjuvant chemotherapy 9 (17) Surgery plus neo-adjuvant or adjuvant radiotherapy 6 (11) Definitive radiotherapy with concurrent chemotherapy 2 (4) Neo-adjuvant chemotherapy plus surgery plus adjuvant radiotherapy 1 (2) Palliative 11 (21)
2.
Median follow-up was 18 months (range 1-263 months)
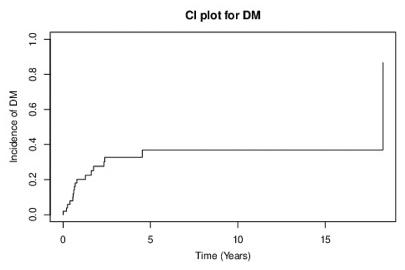
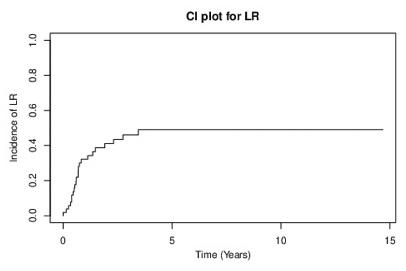
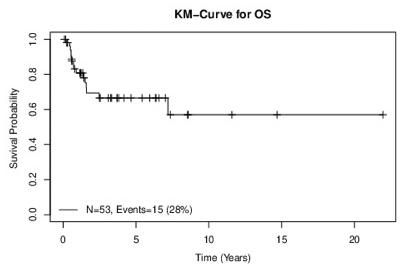
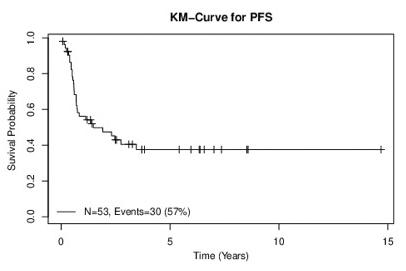
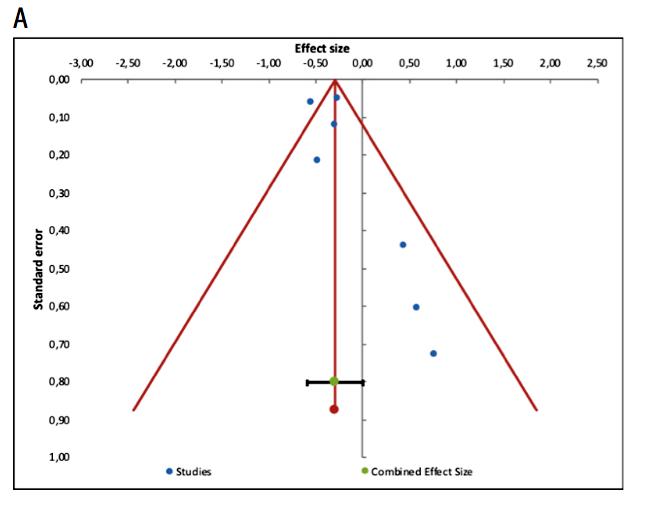
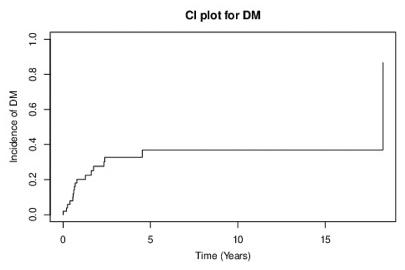
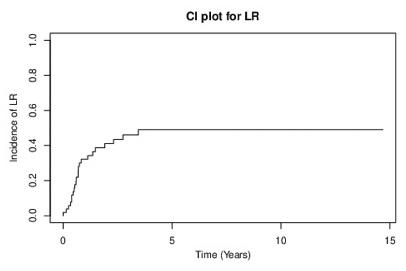
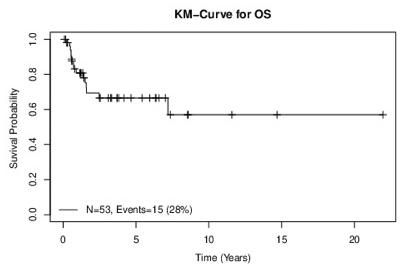
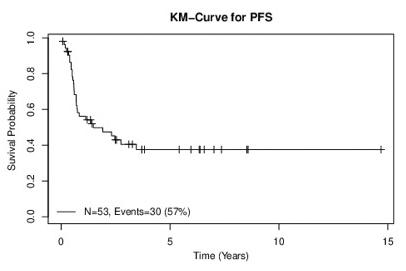
Local recurrence (LR) occurred in 49% of patients and distant metastases (DM) were present in 37% Five-year OS and PFS were 66 5% and 37 6%, respectively KaplanMeier curves for OS and PFS and the cumulative incidence for LR and DM are shown in Figures 1, 2, 3 and 4 respectively
When outcomes in subgroups were examined, a more advanced tumor stage (T2 vs T3/T4) correlated to shorter PFS (median PFS for T2-category was not reached and for T3/T4 was 8 4 months; p = 0 059) Prior history of pelvic radiotherapy also related to lower PFS (7 vs 31 months, p = 0 0018) and OS (9 vs 43 months, p = 0 0007) We found no statistically significant differences in PFS between treatment modalities or between the presence vs absence of epithelial components (TS and MBT)
DISCUSSION
Although the occurrence of rare cancers in the general public is a serious health issue as a whole, acquiring statistically-reliable clinical trial data is difficult due to the low number of patients with an individual rare cancer type within specific areas (8)
Since most available literature on rare cancers is published as single-institution case reports, it is arduous to
draw prognostic implications from these data; furthermore the impact of local practices on treatment outcomes is amplified when dealing with rare diseases Patients with rare neoplasm show significantly poorer results than patients with more common malignancies; mean 5-year survival for the former is up to 20% lower than for the latter (9) This is the case with primary SUB, a disease comprising less than 1% of all BCa, which poses a challenge in the treatment of this uncommon histological variant Poor outcomes have been reported in patients with SUB, whatever the treatment used The five-year overall survival (OS) rate of the present cohort is 66 5%, which exceeds the findings of previous studies where survival rates at five years were consistently below 50% (4, 10, 11) This difference in outcomes can be attributed, at least partially, to two key factors within the study Firstly, this cohort predominantly consisted of a younger population, with a median age at presentation of 69 years, which is lower than other reports (4) Younger patients have generally been associated with better treatment tolerance, higher overall fitness levels, and potentially more favorable disease characteristics, all of which could contribute to improved survival rates Secondly, the analysis encompassed both malignant biphasic tumors (CS and SC) and true heterologous sarcomas (TS) By including both types of tumors, we accounted for the inherent biological diver-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11533 3 Primary bladder sarcoma
Figure 1
OS 5-year rate 66 5% (53 3-83)
Figure 2. PFS 5-year rate: 37.6% (25.8-54.7).
Figure 3
LR 5-year rate: 49% (34-64)
Figure 4 DM 5-year rate: 36 9% (21 4-52 4)
sity, variable clinical behavior of both entities and perhaps different outcomes.
Twenty-six percent of the patients of the cohort have a previous history of pelvic radiation therapy (RT), observing inferior outcomes in this subgroup compared to those without prior RT (median OS of 9 vs. 43 months, p = 0.0007).
Is well known that Radiation-induced sarcomas pose treatment challenges as they arise in areas with complications from previous treatments, making surgical removal difficult. Retrospective analyses have shown poor prognosis in these patients compared to sporadic soft-tissue sarcomas, with 5-year OS rates ranging between 32% and 45% (12) which are in line with the findings of this study.
Continuing with subgroup analyses, patients with extravesical spread (T3/T4) exhibit notable decreases in progression-free survival (PFS) compare to those with less advanced tumors (median PFS for T2-category was not reached and for T3/T4 was 8.4 months). The reduced PFS observed in this particular subgroup of patients (T3/T4) can be attributed to the higher likelihood of developing distant metastases, but also because of the complex relationship between advanced tumor stage and critical anatomical structures, resulting in a potentially decreased effectiveness of local treatment. Data from pelvic sarcomas exemplify this last phenomenon, with successful attainment of a microscopically margin-negative resection (R0) surgery achieved only in 70% of cases (13).
Contrary to UC, where distant recurrence is the primary pattern, this study reveals that rates of local and distant recurrences observed were 49% and 37%, respectively. These findings hold significant implications, particularly considering that approximately 60% of patients in this cohort exhibit extra-vesical spread (T3/T4). The high rates of local failures observed emphasize the critical need for optimizing local therapies, particularly within the latter sub-group.
Typically, the treatment approach for SUB has been extrapolated from the management of UC of the bladder, where cystectomy and chemotherapy are considered fundamental in a multimodality approach (5, 6).
Retroperitoneal sarcomas (RPS) exhibit a behavioral pattern that aligns more closely with the presents findings, showing a higher incidence of local recurrence, which remains the primary cause of mortality (14). Within this context, local recurrence and metastatic disease occur in approximately 50-60% and 20% of cases, respectively (15), mirroring the failure pattern observed in this study. The importance of local control drives management of RPS, with surgery been the mainstay of curative intent therapy (16). Complete gross resection (R0 or R1) has been associated with improved disease-free survival (17). However, even with a histologically negative margin (R0), local recurrence can still occur (18). Considering the high incidence of local recurrences following surgery, neoadjuvant radiotherapy has emerged as an attractive yet controversial option for RPS (19, 20).
Despite the retrospective nature of this study, and therefore hampered by its intrinsic biases, the high local failure rates seen in this cohort prompts the hypothesis that neoadjuvant radiotherapy as part of a multi-disciplinary approach for SUB may play an important role in reducing loco-regional failure rate and improving, at least to some
extent, the survival of this patients, especially in higher tumor stages (T3/T4) where R0 surgery with wide margins is more difficult to obtain and were poorer outcomes we have observed.
Although the existing evidence is limited, our retrospective data can provide valuable insights into this uncommon neoplasm, enabling clinicians to make more informed clinical decisions tailored to this rare disease.
CONCLUSIONS
Primary SUB is a heterogeneous disease group, commonly presenting at advanced stages and exhibiting aggressive disease evolution. In contrast to UC, the primary pattern of recurrence of SUB is local, suggesting the need for multimodal approaches. Continuous international collaborative efforts seem warranted to provide guidance on how to best tailor treatments based on SUB-specific indices.
REFERENCES
1.Lopez-Beltran A, Pacelli A, Rothenberg HJ. Carcinosarcoma and sarcomatoid carcinoma of the bladder: clinicopathological study of 41 cases. J Urol. 1998; 159:1497-1503.
2. Mukhopadhyay S, Shrimpton AE, Jones LA. Carcinosarcoma of the urinary bladder following cyclophosphamide therapy: evidence for monoclonal origin and chromosome 9p allelic loss. Arch Pathol Lab Med. 2004; 128:e8-e11.
3.Wick MR, Swanson PE. Carcinosarcomas: current perspectives and an historical review of nosological concepts. Semin Diagn Pathol. 1993; 10:118.
4.Wright JL, Black PC, Brown GA, et al. Differences in survival among patients with sarcomatoid carcinoma, carcinosarcoma, and urothelial carcinoma of the bladder. J Urol. 2007; 178:2302-2307.
5.EAU (European Association of Urology). Guidelines on Muscleinvasive and Metastatic Bladder Cancer. 2021 Edition. Available at: https://uroweb.org/guideline/bladder-cancer-muscle-invasive-andmetastatic/.
6.NCCN (National Comprehensive Cancer Network). Bladder Cancer. NCCN Clinical Practice Guidelines in Oncology. Available at: https://www.nccn.org/professionals/physician_gls/default.aspx#bladder.
7.Lobo N, et al. What Is the Significance of Variant Histology in Urothelial Carcinoma? Eur Urol Focus. 2020 Jul 15; 6:653-663.
8.Blay JY, Coindre JM, Ducimetière F, Ray-Coquard I. Rare cancers: the value of research collaborations and consortia in rare cancers. Lancet Oncol. 2016; 17:e62.
9.DeSantis CE, Kramer JL, Jemal A. The burden of rare cancers in the United States. CA Cancer J Clin. 2017; 67:261-72.
10.Zieschang H, Koch R, Wirth M, Froehner M. Leiomyosarcoma of the urinary bladder in adult patients: a systematic review of the literature and meta-analysis. UrolInt. 2019; 102:96-101.
11.Li S. Development and validation of a prognostic nomogram for predicting overall survival in patients with primary bladder sarcoma: a SEER-based retrospective study. BMC Urol. 2021; 21:162.
12.Callesen LB, et al. Radiation-induced sarcoma: a retrospective population-based study over 34 years in a single institution. Clin Oncol. 2021; 33:e232-e238.
13.Lee JS. Management of pelvic sarcoma. Eur J Surg Oncol. 2022; 48:2299-2307.
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11533 P. Bettoli, Z. Liu, N. Jara, et al. 4
14. Brennan MF, Antonescu CR, Moraco N, Singer S. Lessons learned from the study of 10,000 patients with soft tissue sarcoma. Ann Surg. 2014; 260:416-21.
15.Chouliaras K, Senehi R, Ethun CG, et al. Recurrence patterns after resection of retroperitoneal sarcomas: an eight-institution study from the US Sarcoma Collaborative. J Surg Oncol. 2019; 120:340-7.
16.Trans-Atlantic RPSWG. Management of primary retroperitoneal sarcoma (RPS) in the adult: a consensus approach from the TransAtlantic RPS Working Group. Ann Surg Oncol. 2015; 22:256-63.
17.Singer S, Antonescu CR, Riedel E, Brennan MF. Histologic subtype and margin of resection predict pattern of recurrence and survival for retroperitoneal liposarcoma. Ann Surg. 2003; 238:358-70, discussion 370-351.
18.Stojadinovic A, Leung DH, Hoos A, Jaques DP, Lewis JJ, Brennan MF. Analysis of the prognostic significance of microscopic margins in 2,084 localized primary adult soft tissue sarcomas. Ann Surg. 2002; 235:424-34.
Correspondence
Piero Bettoli, MD (Corresponding Author) piero.bettoli@falp.org postal address 7591067
Federico Bakal, MD federico.bakal@falp.org
Fundación Arturo López Pérez, Santiago, Chile
ZhihuiAmy Liu, MD ZhihuiAmy.liu@uhn.ca
Peter Chung, MD Peter.Chung@rmp.uhn.ca
Alejandro Berlin, MD Alejandro.Berlin@rmp.uhn.ca
Princess Margaret Hospital, Radiation Oncology, Toronto, Canada
Natalia Jara, MD njarao@gmail.com
Sebastian Sole, MD sebasole@gmail.com
Claudio Sole, MD claudio.solep@iram.cl
Clinica Instituto de Radiomedicina (IRAM), Santiago, Chile
Facultad de Medicina, Universidad Diego Portales, Santiago, Chile
William Wong, MD wong.william@mayo.edu
Mayo Clinic Arizona, Radiation Oncology, Phoenix, USA
Mario Terlizzi, MD terlizzimario@yahoo.fr
Paul Sargos, MD P.Sargos@bordeaux.unicancer.fr
Institute Bergonie, Radiation Oncology, Bordeaux, France
Thomas Zilli, MD Thomas.Zilli@hcuge.ch
Hospitaux Universiaires de Geneve, Radiation Oncology, Geneve, Switzerland
Juliette Thariat, MD jthariat@gmail.com
Centre Francoise Baclese, Radiation Oncology, Caen, France
Guilaume Ploussard, MD g.ploussard@gmail.com
La Croix du Sud Hospital, Urology Department, Quint Fonsergrives, France
Sharad Goyal, MD shgoyal@mfa.gwu.edu
George Washington University Hospital, Radiation Oncology, Washington DC, USA
Conflict of interest: The authors declare no potential conflict of interest.
19.Molina G, Hull MA, Chen YL, et al. Preoperative radiation therapy combined with radical surgical resection is associated with a lower rate of local recurrence when treating unifocal, primary retroperitoneal liposarcoma. J Surg Oncol. 2016; 114:814-20.
20.Bonvalot S, Gronchi A, Le Pechoux C, et al. Preoperative radiotherapy plus surgery versus surgery alone for patients with primary retroperitoneal sarcoma (EORTC-62092: STRASS): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol 2020; 21:1366-77.
CONFERENCEPRESENTATION
Bettoli P, Liu ZA, Jara N, et al. Primary Bladder Sarcoma: a multi-institutional experience from the Rare Cancer Network Presentation Number: PO-1219: European Society for Radiotherapy and Oncology (ESTRO) congress; July 319Facultad de Medicina, Universidad Diego Portales, Santiago, Chile. August 04, 2020; Vienna, Austria
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11533 5 Primary bladder sarcoma
ORIGINALPAPER
Ugur Aferin 1, Nurten Bahtiyar 2, Ilhan Onaran 3, Hamdi Ozkara 4
1 Department of Urology, Medical Faculty, Demiroglu Bilim University, Istanbul, Turkey;
2 Department of Biophysics, Cerrahpasa Medical Faculty, Istanbul University-Cerrahpasa, Istanbul, Turkey;
3 Department of Medical Biology, Cerrahpasa Medical Faculty, Istanbul University-Cerrahpasa, Istanbul, Turkey;
4 Department of Urology, Cerrahpasa Medical Faculty, Istanbul University-Cerrahpasa, Istanbul, Turkey.
Summary
Background: We sought to determine whether two soluble forms with different size of mtDNA are linked to prostatic inflammation, and whether they discriminate prostate cancer (PCa) from inflammatory prostatic conditions.
Methods: Histopathologically diagnosed prostatitis, PCa and benign prostatic hyperplasia patients (n = 93) were enrolled in this study and they were categorized as with and without prostate inflammation. Quantitative RT-PCR was used to analyze the levels of 79-bp and 230-bp fragments in urine and blood samples collected following prostate massage.
Results: The urine mtDNA-79 and mtDNA-230 were significantly increased in patients with prostate inflammation compared with those in without inflammation. Here, 79-bp fragment of apoptotic origin was significantly higher level than 230-bp fragment of necrotic origin. Although mtDNA-79 copy number in serum samples was also increased in patients with prostate inflammation, mtDNA-230 was similar in the two groups. Furthermore, mtDNA-79 and mtDNA-230 copy numbers in postprostate massage urine were higher (about 16-fold and 22-fold, respectively) than those from serum samples. ROC analysis showed that, although post-prostate massage urine have relatively higher performance than blood, ability to discriminate cases of both fragments was not better than that of serum total PSA.
Conclusions: Our results demonstrate that shorter cf-mtDNA fragment size in particular, increase in the presence of prostate inflammation in post-prostatic massage urine but both fragments could never improve serum total PSA performance.
KEYWORDS: Prostate; Inflammation; Cancer; Mitochondrial DNA; Post-prostatic massage.
Submitted 26 July 2023; Accepted 2 September 2023
INTRODUCTION
A possible link between inflammation and prostate cancer (PCa) has been suggested, but not yet confirmed. Several cross-sectional studies indicate that prostatic inflammation is more common in patients without cancer (1, 2). The factors contributing to prostate inflammation are largely unknown, and inflammation could play a role in false positive prostate-specific antigen (PSA) results in cancer screening (1, 3).
Inflammatory lesions contain dead cells, including apoptosis and necrosis, and evidence shows a bidirectional relationship between cell death forms and inflammation.
Both genomic DNA (gDNA) and mitochondrial DNA (mtDNA) are released from dying cells, and circulating mtDNA fragments may trigger pro-inflammatory responses (4-12). Elevated levels of circulating cell-free mtDNA (cf-mtDNA) have been found in patients with various diseases, including urological malignancies, but the association with cancer is still debated (13-16). Different diseases have been associated with specific mtDNA fragmentation patterns related to cell death type (17-19). There may be a link between mtDNA fragments and prostate inflammation, but it remains unclear, and the studies have mainly focused on blood samples. Evaluating the fragmentation pattern of cf-mtDNA in urine might provide insights into mtDNA-mediated inflammation and improve PCa biomarkers. Therefore, this study aimed to determine if the apoptosis- and necrosis-derived mtDNA fragments (79 bp and 230 bp, respectively) in postprostate massage urine are related to prostate inflammation and can discriminate between PCa and inflammatory conditions, using serum PSA levels for comparison.
MATERIALSANDMETHODS
Case selection
This study was conducted with 93 male patients, who applied the Istanbul University-Cerrahpasa, Department of Urology. Patients aged 40 and older, PSA value > 2.5 ng/mL, and suspicious findings on rectal examination were included in the study (Table 1). Transrectal ultrasound (TRUS) guided biopsies (12-28 cores) were performed for evaluation. The patients were divided into 3 groups according to the histopathological evaluations of TRUS biopsies: prostate cancer (PCa), prostatitis (Inflammation), and benign prostatic hyperplasia (BPH) groups. The results of biopsy showing adenocarcinoma and BPH were included in the PCa group. Similarly, the results showing prostatitis and BPH were included in the Inflammation group, whereas the results containing alone BPH were included in the BPH group. Additionally, according to the inflammation status in the results of TRUS biopsies, cases without inflammation (including cases of PCa and BPH groups) were defined as the Noninflammation group. Patients with other malignant disease, distant metastases, infectious or inflammatory dis-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11610 1
Are elevated mitochondrial DNA fragments in prostatic inflammation a potential biomarker for prostate cancer?
DOI: 10.4081/aiua.2023.11610
Table 1.
Demographic data of all groups
TAAAGGTTCG-3’ The sequence of the reverse primer specific for mtDNA-79 was 5’-CCTGGATTACTCCGGTCTGA-3’, of the reverse primer specific for mtDNA230 was 5’-GGGCTCTGCCATCTTAACAA-3’
The qPCR was performed in duplicate on a Real Time PCR Detection system (Bio Rad Laboratories, Inc , Hercules, CA, USA) Each 20 µL reaction consisted of 2 mL DNA, 10 µl EvaGreen 2X qPCR MasterMix (abm, Canada) and 0 40 µL (10mM) forward/reverse primer PCR conditions were 95 ºC for 10 min, followed by 40 cycles at 95 ºC for 15 s, 60 ºC for 60 s, and 72 ºC for 30 s Each run included water blanks as a negative control The specificity of the PCR products was confirmed by melting curve analysis The quantity of each target gene in the samples was subsequently calculated according to the corresponding standard curve The formula published by the Genomics and Sequencing Center of the University of Rhode Island (Kingston, RI, USA; cels uri edu/gsc/cndna html) was used to calculate the mtDNA copy number (20)
Statistical analysis
eases, histologically defined with both inflammation and cancer findings were excluded from the study All patients provided written informed consent This study was approved by the Istanbul University-Cerrahpasa Ethics Committee (approval no 83045809; Istanbul, Turkey), and was performed according to the criteria set out by the Declaration of Helsinki
Sample collection
Before TRUS biopsy, following a digital rectal examination of 3 strokes per prostate lobe, each subject provided 2030 ml urine in a first catch specimen All urine specimens were centrifuged at 2500 x g for 10 min at 4°C, followed by storage of the urine and pellet at -80°C Five milliliter venous blood samples were collected into anticoagulantfree tubes after prostatic massage and centrifugation was performed at 2500×g for 10 min at 4°C Then obtained supernatants were stored at -80°C until analyses
DNA isolation, and Determination of mtDNA-79 and mtDNA-230 Copies
The Plasma/Serum Cell-Free Circulating DNA Purification Kit (Norgen Biotek, Canada) and Urine Cell-Free Circulating DNA Purification Kit (Norgen Biotek, Canada) were used to isolate circulating DNA from serum and urine Cell-free DNA was isolated according to the kit manufacturers' protocols Quantitative analysis of mtDNA fragments in serum and urine was performed by quantitative real-time PCR (qPCR) In this study, two primer sets specific for the mitochondrial ribosomal 16S RNA were used The first primer pair amplified a 79-bp fragment (mtDNA-79), and the second primer pair amplified a 230-bp fragment (mtDNA-230) The sequence of the forward primer specific for both mtDNA fragments was 5’-CAGCCGCTAT-
Continuous variables were presented as means ± SD or medians, and categorical variables were presented as frequencies with percentages Differences between groups were compared with Mann Whitney-U, and KruskalWallis tests Receiver operating characteristic (ROC) analysis, and area under the ROC curve (AUC) were used for determination of diagnostic performance of mtDNA levels Point-biserial correlation was used for correlation between categorical variables and mtDNA levels All stat
(GraphPad Software, San Diego, CA) A value of p < 0 05 was considered statistically significant
RESULTS
Assessment of mtDNA levels in urine and serum according to inflammation status
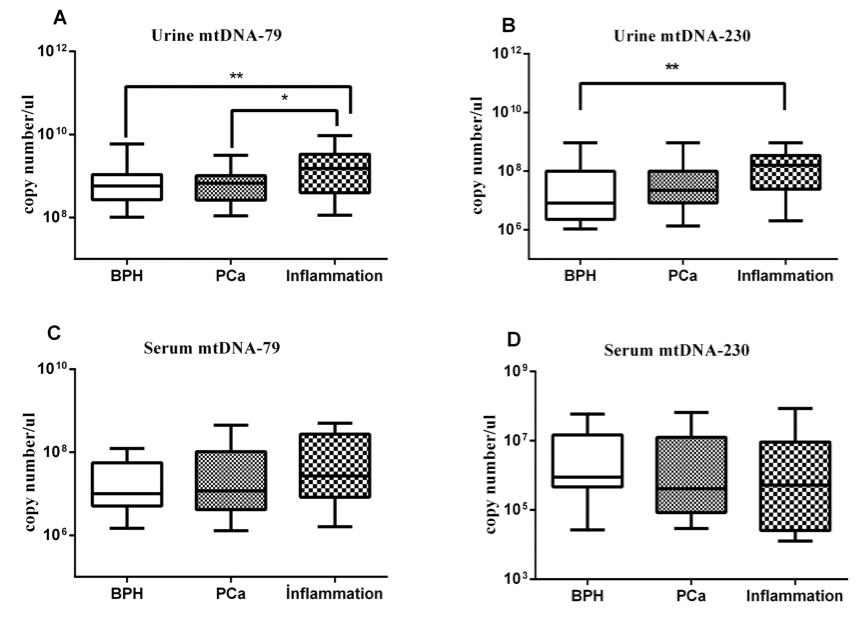
Urine mtDNA-79 (median: 1 52 x 109 vs. 0 66 x 109 copies/ml) and mtDNA-230 (1 59 x 108 vs 1 71 x 107 copies/ml) levels were increased in the Inflammation group compared to the Non-inflammation group (p < 0 001 and p < 0 01, respectively) (Figure 1 A-B)
Serum mtDNA-79 (median: 2 45 x 107 vs 1 05 x 107 copies/ml) levels were higher in the Inflammation group compared with the Non-inflammation group (p < 0 05), but the differences were not significant in serum mtDNA230 levels (median: 0 87 x 106 vs 0 51 x 106 copies/ml) between these groups (p > 0 05) (Figure 1 C-D)
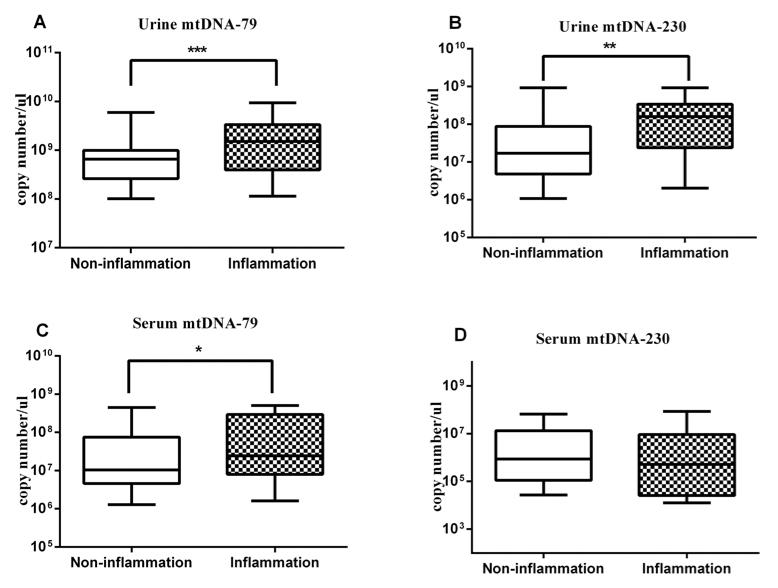
Assessment of urine and serum mtDNA levels in Inflammation, PCa, and BPH groups
Urine mtDNA-79 (median: 1 52 x 109 vs 0 58 x 109 copies/ml) and mtDNA-230 (1 59 x 108 vs 0 81 x 107 copies/ml) levels were increased in the Inflammation group compared to the BPH group (p < 0 01, for both) (Figure 2 A-B) whereas the differences were not significant in serum mtDNA-79 (median: 2 69 x 107 vs 1 01 x 107 copies/ml) and mtDNA-230 levels (median: 0 51 x 106 vs 0 88 x 106 copies/ml) between these groups (p > 0 05) (Figure 2 C-D) There were statistically significant differences in urine
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11610 U
2
Aferin, N Bahtiyar, I Onaran, H Ozkara
i s t i c a l a n a l y s e s w e r e p e r f o r m e d u s i n g P r i s m 5
0
Non-inflammation Inflammation Variable BPH PCa Prostatitis (n: 29) (n: 34) (n: 30) Age (years) 65 51 ± 6 85 65 09 ± 9 18 63 32 ± 6 71 PSA (ng/ml) 5 72 ± 2 80 18 24 ± 21 04 a*** 11 36 ± 9 81 b *** Histology Adenocarcinoma, n (%) NA 34 (100%) NA Pathological tumour stage pT1, n (%) NA 15 (44 12%) NA pT2, n (%) NA 19 (55.88%) NA Gleason Grading Gleason Score < 7, n (%) NA 12 (35 29%) NA Gleason Score = 7, n (%) NA 15 (44 12%) NA Gleason Score > 7, n (%) NA 7 (20 59%) NA Histology Biopsy core with cancer Median, n NA 4 5 NA Range, n NA 1-12 NA Histology Biopsy core with inflammation Median, n NA NA 6 Range, n NA NA 3-15 Values were presented as Mean ± standard dev ation; BPH: ben gn prostat c hyperplas a; PCa: prostate cancer; NA: not appl cable; a PCa vs BPH; b Inflammat on vs BPH; *** p < 0 001
Figure 1. Comparison of the A.urine mtDNA-79, B.urine mtDNA-230, C.serum mtDNA-79, and D. serum mtDNA230 between the Inflammation and Noninflammation groups, *p < 0.05, **p < 0.01, ***p < 0.001. The bold line in the box plots represents the median value.
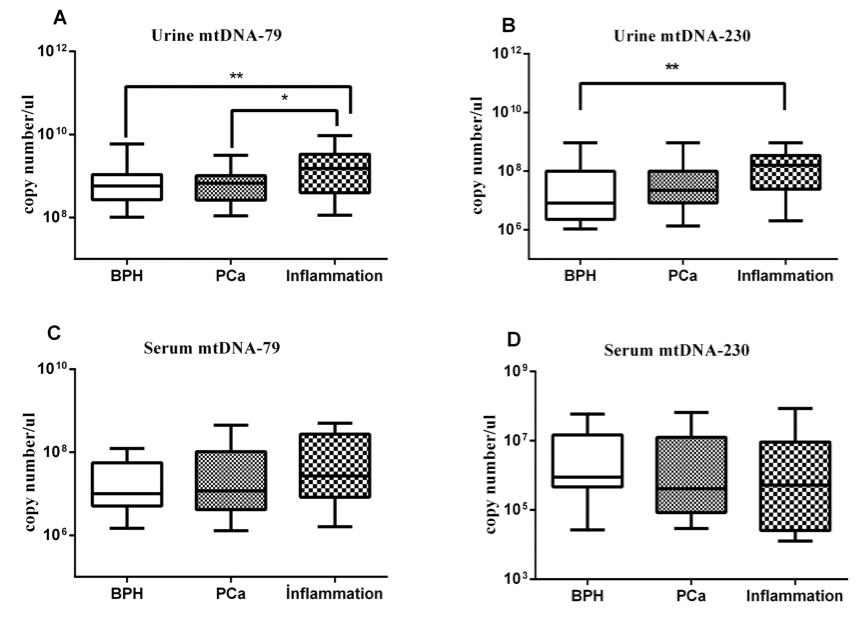
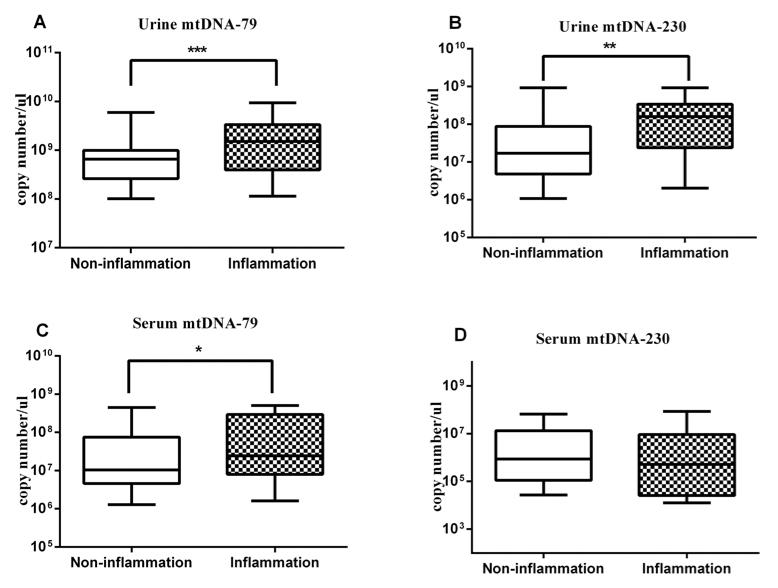
Figure 2. Pairwise comparisons of the A. urine mtDNA-79, B.urine mtDNA-230, C.serum mtDNA-79, and D. serum mtDNA230 among the Inflammation, PCa, and BPH groups; *p<0.05, **p < 0.01, The bold line in the box plots represents the median value.
mtDNA-79 (median: 1.52 x 109 vs. 0.67 x 109 copies/ml) (p < 0.05), but not in urine mtDNA-230 (median: 1.59 x 108 vs. 2.23 x 107 copies/ml), serum mtDNA-79 (median: 2.69 x 107 vs. 1.18 x 107 copies/ml), and mtDNA-230 (median: 0.51 x 106 vs. 0.41 x 106 copies/ml) levels between the Inflammation and the PCa groups (p > 0.05, for all).
Additionally, there were no significant changes in urine mtDNA-79 (median: 0.67 x 109 vs. 0.57 x 109 copies/ml), urine mtDNA-230 (median: 2.23 x 107 vs. 0.81 x 107 copies/ml), serum mtDNA-79 (median: 1.18 x 107 vs. 1.01 x 107 copies/ml) and serum mtDNA-230 (median: 0.41 x 106 vs. 0.88 x 106 copies/ml) levels between the comparison of the PCa and BPH groups (Figure 2 A-D).
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11610 3 DNA
in prostatic inflammation
fragments
Table 2.
Diagnostic performance of serum PSA, serum and post-prostatic massage urine specimens mtDNA
Urine mtDNA-79
Inflammation vs. Non-Inflammation
Inflammation vs BPH
Inflammation vs PCa
PCa vs BPH
Urine mtDNA-230
Inflammation vs Non-Inflammation
Inflammation vs BPH
Inflammation vs PCa
PCa vs BPH
Serum mtDNA-79
Inflammation vs Non-Inflammation
Inflammation vs BPH
Inflammation vs PCa
PCa vs BPH
Serum mtDNA-230
Inflammation vs Non-Inflammation
Inflammation vs BPH
Inflammation vs. PCa
PCa vs BPH
Serum PSA
Inflammation vs. Non-Inflammation
Inflammation vs BPH Inflammation vs PCa
an ROC curve; BPH: benign prostat c hyperp asia; PCa: prostate cancer; NS: not signif cant
Diagnostic performances of mtDNA combinations in serum and post-prostatic massage urine specimens.
ROC curve analysis of serum and urine
mtDNA and serum PSA in Inflammation, PCa, and BPH groups
AUC values of ROC curve analysis were determined for urine and serum mtDNA, and serum PSA in the Inflammation, PCa, and BPH groups Mostly the results in Inflammation vs BPH, and Inflammation vs PCa groups had moderate diagnostic performance (Figure 4) Urine mtDNA-79 and mtDNA-230 had better diagnostic performance (AUC range 0 7250 691) than serum mtDNA-79, and mtDNA230 (AUC range 0 682-0 572) AUC values of serum PSA were higher than urine mtDNA-79, and mtDNA-230 The combination of urine mtDNA-79 and mtDNA-230 results had moderate AUC values similarly as urine mtDNA-79 and mtDNA-230
ROC curve analysis between the PCa and the BPH groups indicated that except for serum PSA (AUC:0 793) , all other parameters had mild AUC values (range 0 534-0 594) Urine mtDNA-79 and mtDNA-230 values were higher than serum, but all of them were in mild AUC levels (Tables 2, 3)
Correlation analyzes of urine and serum mtDNA
The correlation analysis showed that the presence of prostatic inflammation was positively c o r r e l a t e d w i t h u r i n e m t D N A - 7 9 , u r i n e mtDNA-230, and serum mtDNA-79 levels Also, urine mtDNA-79 levels were positive correlated with urine mtDNA-230 results Similarly, serum mtDNA-79 levels were posit i v e l y a s s o c i a t e d w i t h s e r u m m t D N A - 2 3 0 (Table 4)
DISCUSSION
To date, a few studies have quantified cfmtDNA levels and mtDNA fragmentation pattern in urologic cancer patients Some studies found elevated cf-mtDNA content in PCa (15, 21, 22), but another study on cf-mtDNA could-
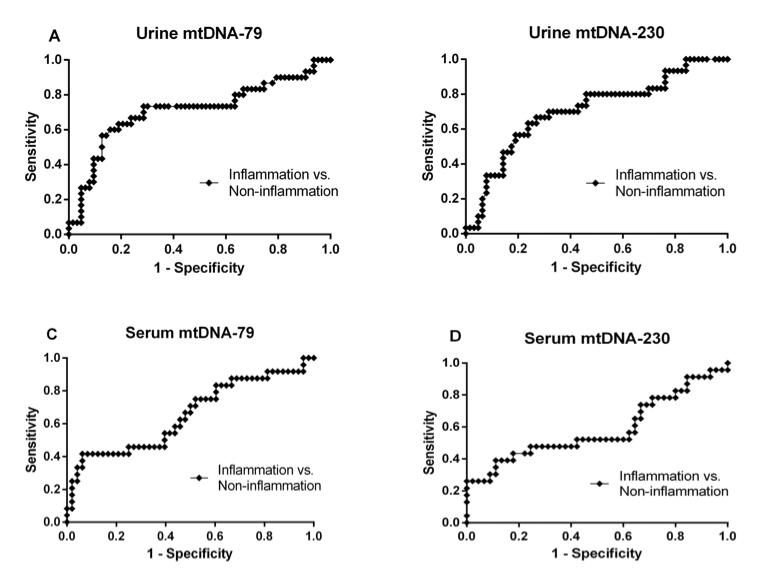
ROC curve analysis of serum and urine mtDNA, and serum PSA according to inflammation status
Generally, AUC values demonstrated moderate discriminatory power, and urine AUC results (mtDNA-79, and mtDNA-230, 0 712, and 0 707, respectively) were higher than serum (mtDNA-79, and mtDNA-230, 0 653, and 0 585, respectively) in the Inflammation group compared to the Non-inflammation group Similarly, urine mtDNA79 and mtDNA-230 AUC values were higher than serum
PSA AUC values (0 712, 0 707, and 0 585, respectively)
Urine mtDNA-79 and mtDNA-230 levels showed similar diagnostic performance with urine combined mtDNA-79 and mtDNA-230 results (Figure 3) Sensitivity and specificity values for all testing were given in Tables 2, 3
Correlation analyzes of urine and serum mtDNA according to inflammation status
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11610 U Aferin, N Bahtiyar, I Onaran, H Ozkara 4
Sensitivity Specificity AUC (95%Cl) P
BPH
under
%73 3 %73 4 %73.2 %41 2 %70 1 %63 3 %66 7 %58 8 %54 2 %56 1 %48 1 %42 3 %47 8 %52 2 %47 8 %56 1 70 0% 70 1% 56 7% 64 7% 0 001 0 006 0 003 NS 0 001 0 002 0 008 NS 0 04 0 03 NS NS NS NS NS NS NS < 0 001 NS < 0 001 %71 4 %72 4 %70.6 %68 9 %66 7 %72 4 %73 5 %58 6 %60 4 %63 6 %65 4 %63 6 %75 6 %75 0 %68 1 %75 0 60 3% 89 7% 61 8% 89 6% 0 712 (0 588-0 836) 0 709 (0 570-0 847) 0.714 (0.580-0.849) 0 534 (0 388-0 679) 0 707 (0 591-0 823) 0 725 (0 594-0 857) 0 691 (0,557-0 825) 0 595 (0 449-0 741) 0 653 (0 511-0 794) 0 682 (0 528-0 836) 0 651 (0 498-0 803) 0 542 (0 377-0 707) 0 585 (0 427-0 744) 0 602 (0 429-0 776) 0 572 (0 403-0 741) 0 580 (0 408-0 752) 0 609 (0 495-0 725) 0 823 (0 711-0 935) 0 572 (0 429-0 716) 0 793 (0 679-0 907)
PCa vs
AUC: area
Table
3
Sensitivity Specificity AUC (95%Cl) P Combination of urine mtDNA-79 and mtDNA-230 Inflammation vs Non-Inflammation Inflammation vs BPH Inflammation vs PCa PCa vs BPH Combination of serum mtDNA-79 and mtDNA-230 Inflammation vs Non-Inflammation Inflammation vs BPH Inflammation vs PCa PCa vs BPH AUC: area under an ROC curve; BPH: ben gn prostat c hyperplas a; PCa: prostate cancer; NS: not significant 66 67% 80 02% 72 72% 51.51% 47 6% 50.02% 54 17% 50 20% 0 001 < 0 001 < 0 001 NS NS NS NS NS 85 36% 76 67% 73 33% 53 57% 60 97% 63 16% 68 18% 55 56% 0 715 (0 592-0 837) 0 810 (0 694-0 926) 0 756 (0 634-0 877) 0 488 (0 342-0 634) 0 647 (0 494-0 800) 0 651 (0 481-0 821) 0 671 (0 489-0 811) 0 542 (0 364-0 719
Table 4
Parameter Correlation Coefficient Sig. (2-tailed) Inflammation status vs urine mtDNA-79 r = 0 343 p = 0 001 Inflammation status vs urine mtDNA-230 r = 0 335 p = 0 001 Inflammation status vs serum mtDNA-79 r = 0 250 p = 0 035 Urine mtDNA-79 vs urine mtDNA-230 r 0 601 p < 0 001 Serum mtDNA-79 vs. serum mtDNA-230 r = 0.262 p = 0 035
Receiver operating characteristic (ROC) curves of the A.urine mtDNA-79, B.urine mtDNA-230, C.serum mtDNA-79, and D.serum mtDNA230 between the Inflammation and Non-inflammation groups.
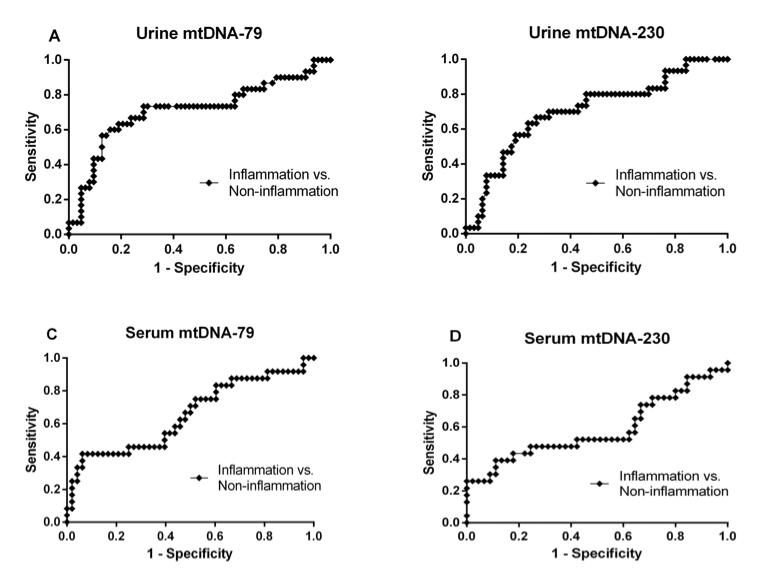
Pairwise comparisons of the receiver operating characteristic (ROC) curves of the A.urine mtDNA-79, B.urine mtDNA-230, C.serum mtDNA-79, and D.serum mtDNA230 among the Inflammation, PCa, and BPH groups.
n't distinguish between PCa and BPH (15). In addition to previous publications on blood samples (23), this study found higher levels of mtDNA fragments in post-prostate

massage urine in cases with prostate inflammation than those without inflammation.
Different studies revealed a positive link between elevat-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11610 5 DNA
in
inflammation
fragments
prostatic
Figure 3.
Figure 4.
ed systemic mtDNA levels and inflammation-associated diseases (9, 24, 25) and inflammatory cell death is often necrotic (7). We expected that a possible increase in the long mtDNA fragments (> 200 bp) derived from nonapoptotic types of cell death (i.e. necrosis) may be associated with prostate inflammation according to the histopathological examination. Surprisingly, we found that 230 bp fragment was significantly lower than 79 bp fragment (an implication of an active apoptotic phenomenon) in prostate inflammation. Additionally, our results show no correlation between urine and serum mtDNA230 fragment in patients with inflammation, implying different factors contribute to elevated cf-mtDNA levels in each compartment.
Prostate massage can stimulate the release of tissue’s viable cells as well dying/dead cells and increase the distribution concentration of circulating cf-mtDNA in urine. The influence of exfoliated inflammatory or endothelial cells on mtDNA fragments cannot be excluded, complicating our results. The cause of changes in cf-mtDNA fragment levels due to prostate inflammation remains unclear with our experimental design and existing literature. Although the origin of cf-mtDNA and cf-DNA lacks consensus (26), excessive release by apoptotic or necrotic cells and reduced clearance by inflammatory cells may alter mtDNA content. The mtDNA-79 fragment might be more resistant to DNAse activity than long fragments. Furthermore, whether the higher levels of cf-mtDNA fragments is a cause or a consequence for prostate inflammation in the context of mitochondrial damage, is the chicken or the egg causality dilemma.
Although cf-mtDNA is found in blood, urine, or saliva samples, data for prostate diseases associated with malignancy were mostly based on blood samples. Urine samples collected after prostate massage may provide more evidence for prostate-associated conditions due to fewer confounding factors. Therefore, we expected urine mtDNA fragments to reflect prostate inflammation magnitude better than blood ones. As anticipated, postprostate massage urine from patients with prostate inflammation showed higher mean mtDNA-79 and mtDNA-230 copy numbers (approximately 16-fold and 22-fold, respectively) compared to serum samples. Serum mtDNA-79 was significantly increased in patients with inflammation (p < 0.05), while serum mtDNA-230 remained similar between inflamed and non-inflamed patients (p > 0.05). Post-prostate massage urine mtDNA79 and mtDNA-230 copy numbers showed slightly higher AUC values for discriminating prostate inflammation than serum. The differences in fragment levels between urine and serum could be due to urine's enrichment in prostate-derived cf-mtDNA and the rapid clearance of nucleic acids from blood. Furthermore, urinary cfmtDNA concentrations have lower coefficient of variations (CV)than serum, but further investigation is needed as their CVs still exceed 100%.
In this work, we also performed ROC curve analysis for urine cf-mtDNA fragments to differentiate PCa from inflammatory prostatic conditions, and compared it with the diagnostic performance of serum PSA levels.
Considering the AUC, sensitivity and specificity, the levels of post-prostate massage urine mtDNA-79 and
mtDNA-230 had slightly higher performance in distinguishing prostate inflammation than their serum levels. Here, the discrimination performance of single parameter for prostate inflammation is moderate with an AUC of about 0.7. Nevertheless, each fragment yielded performance similar to than serum PSA levels. Furthermore, when we tested the ability of these fragments in urine to discriminate PCa from BPH, PCa from prostate inflammation, and prostate inflammation from BPH, the AUC values of both fragment were within the range of 0.530.73, which were close to those (0.58-0.82) for the serum PSA. Moreover, combining of two fragment copy numbers did not significantly improve performance over using a single fragment alone. Therefore, mtDNA fragments alone does not seem to be a reliable predictor of differentiating PCa or BPH from inflammatory prostatic conditions.
This study had several limitations, including focusing only on histologically measurable inflammation, being a singlecenter trial, and lacking adjustment for prostate volumerelated variables and other potential confounding factors due to small sample sizes. Additionally, although this study was conducted on the samples from PCa patients without prostatitis, it is essential to keep in mind that presence of prostatitis in PCa is not an infrequent event. In conclusion, the present data demonstrate that cfmtDNA fragments in post-prostatic massage urine increase in the presence of prostate inflammation; shorter cf-mtDNA fragment size in particular, may be a result of mostly an active apoptotic phenomenon associated with prostate inflammation. Even though both mtDNA fragments in the urine samples show relatively higher performance than blood, they do not seem to help identify patients with PCa from non-PCa patients more than the conventional PSA test. Further research is required to elucidate the sources of inter-individual variability observed in mtDNA copy numbers.
REFERENCES
1.Gui-Zhong L, Libo M, Guanglin H, Jianwei W. The correlation of extent and grade of inflammation with serum PSA levels in patients with IV prostatitis. Int Urol Nephrol. 2011; 43:295-301.
2.MacLennan GT, Eisenberg R, Fleshman RL, et al. The influence of chronic inflammation in prostatic carcinogenesis: a 5-year followup study. J Urol. 2006; 176:1012-1016.
3.Bergamini S, Bellei E, Bonetti LR, et al. Inflammation: an important parameter in the search of prostate cancer biomarkers. Proteome Sci. 2014; 12:1-12.
4.Shu Y, Wu X, Tong X, et al. Circulating tumor DNA mutation profiling by targeted next generation sequencing provides guidance for personalized treatments in multiple cancer types. Sci Rep. 2017; 7:1-11.
5. Man SM, Kanneganti T-D. Converging roles of caspases in inflammasome activation, cell death and innate immunity. Nat Rev Immunol. 2016; 16:7.
6.McCully JD, Cowan DB, Pacak CA, et al. Injection of isolated mitochondria during early reperfusion for cardioprotection. Am J Physiol Heart Circ Physiol. 2009; 296:H94-H105.
7. Zhang Q, Raoof M, Chen Y, et al. Circulating mitochondrial DAMPs cause inflammatory responses to injury. Nature. 2010; 464:104-107.
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11610
6
U. Aferin, N. Bahtiyar, I. Onaran, H. Ozkara
8.Klinman DM, Barnhart KM, Conover J. CpG motifs as immune adjuvants. Vaccine. 1999; 17:19-25.
9.Caielli S, Athale S, Domic B, et al. Oxidized mitochondrial nucleoids released by neutrophils drive type I interferon production in human lupus. J Exp Med. 2016; 213:697-713.
10.Collins LV, Hajizadeh S, Holme E, et al. Endogenously oxidized mitochondrial DNA induces in vivo and in vitro inflammatory responses. J Leukoc Biol. 2004; 75:995-1000.
11.Barbalat R, Ewald SE, Mouchess ML, Barton GM. Nucleic acid recognition by the innate immune system. Annu Rev Immunol. 2011; 29:185-214.
12.Zhang Q, Itagaki K, Hauser CJ. Mitochondrial DNA is released by shock and activates neutrophils via p38 map kinase. Shock. 2010; 34:55-59.
13.Yu M. Circulating cell-free mitochondrial DNA as a novel cancer biomarker: opportunities and challenges. Mitochondrial DNA. 2012; 23:329-332.
14.Ellinger J, Wittkamp V, Albers P, et al. Cell-free circulating DNA: diagnostic value in patients with testicular germ cell cancer. J Urol. 2009; 181:363-371.
15.Ellinger J, Müller DC, Müller SC, et al. Circulating mitochondrial DNA in serum: a universal diagnostic biomarker for patients with urological malignancies. Urol Oncol. 2012; 30:509-515.
16.Herranz R, Oto J, Plana E, et al. Circulating Cell-Free DNA in Liquid Biopsies as Potential Biomarker for Bladder Cancer: A Systematic Review. Cancers. 2021; 13:1448.
17.Budnik LT, Kloth S, Baur X, et al. Circulating mitochondrial DNA as biomarker linking environmental chemical exposure to early preclinical lesions elevation of mtDNA in human serum after expo-
sure to carcinogenic halo-alkane-based pesticides. PloS one. 2013; 8:e64413.
18.Pisetsky DS. The origin and properties of extracellular DNA: from PAMP to DAMP. Clin Immunol. 2012; 144:32-40.
19.Jahr S, Hentze H, Englisch S, et al. DNA fragments in the blood plasma of cancer patients: quantitations and evidence for their origin from apoptotic and necrotic cells. Cancer Res. 2001; 61:1659-1665.
20.Nakahira K, Kyung S-Y, Rogers AJ, et al. Circulating mitochondrial DNA in patients in the ICU as a marker of mortality: derivation and validation. PLoS Med. 2013; 10:e1001577.
21.Mehra N, Penning M, Maas J, et al. Circulating mitochondrial nucleic acids have prognostic value for survival in patients with advanced prostate cancer. Clin Cancer Res. 2007; 13:421-426.
22.Zhou W, Zhu M, Gui M, et al. Peripheral blood mitochondrial DNA copy number is associated with prostate cancer risk and tumor burden. PloS one. 2014; 9:e109470.
23.Ellinger J, Müller SC, Wernert N, et al. Mitochondrial DNA in serum of patients with prostate cancer: a predictor of biochemical recurrence after prostatectomy. BJU Int. 2008; 102:628-632.
24.Deus CM, Tavares H, Beatriz M, et al. Mitochondrial DamageAssociated Molecular Patterns Content in Extracellular Vesicles Promotes Early Inflammation in Neurodegenerative Disorders. Cells. 2022; 11:2364.
25.Liu R, Xu F, Bi S, et al. Mitochondrial DNA-induced inflammatory responses and lung injury in thermal injury murine model: protective effect of cyclosporine-A. J Burn Care Res. 2019; 40:355-360.
26.Aucamp J, Bronkhorst AJ, Badenhorst CP, Pretorius PJ. The diverse origins of circulating cell-free DNA in the human body: a critical re-evaluation of the literature. Biol. Rev. 2018;93:1649-1683.
Correspondence
Ugur Aferin, MD ugur.aferin@demiroglu.bilim.edu.tr
Department of Urology, Medical Faculty, Demiroglu Bilim University, Istanbul, Turkey
Nurten Bahtiyar, PhD (Corresponding Author) nurten.bahtiyar@iuc.edu.tr
Department of Biophysics, Cerrahpasa Medical Faculty, Istanbul University-Cerrahpasa, Istanbul, Turkey
Ilhan Onaran, PhD ilonaran@iuc.edu.tr
Department of Medical Biology, Cerrahpasa Medical Faculty, Istanbul University-Cerrahpasa, Istanbul, Turkey
Hamdi Ozkara, MD hozkara@iuc.edu.tr
Department of Urology, Cerrahpasa Medical Faculty, Istanbul UniversityCerrahpasa, Istanbul, Turkey
Conflict of interest: The authors declare no potential conflict of interest. The present study was supported by the Research Fund of the Istanbul University-Cerrahpasa (Grant no. 30381).
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11610 7 DNA
in prostatic inflammation
fragments
ORIGINAL PAPER
C reactive protein/Albumin ratio as predictor of prognosis in castration resistant metastatic prostate cancer
Summary
Objective: To assess the association of C reactive protein/Albumin ratio (CAR) with progression free survival (PFS) and overall survival (OS) in castration resistant metastatic prostate cancer (mCRPC) patients
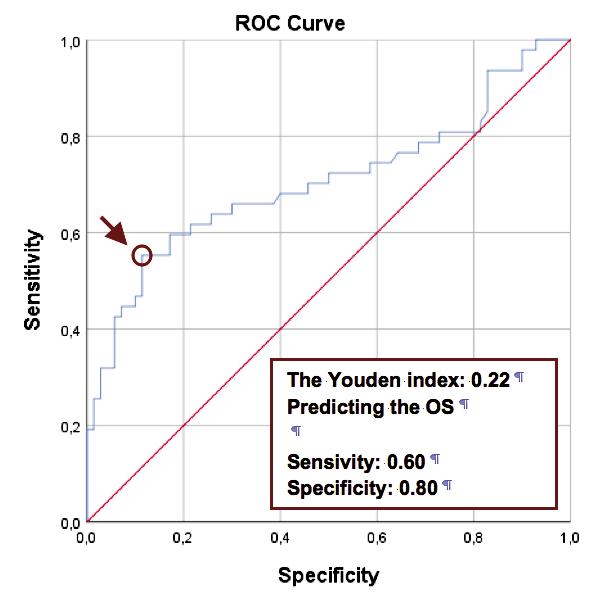
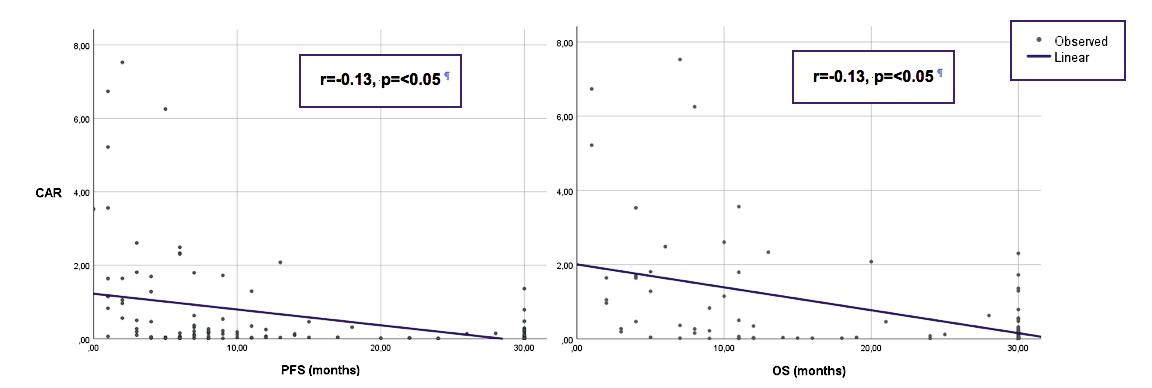
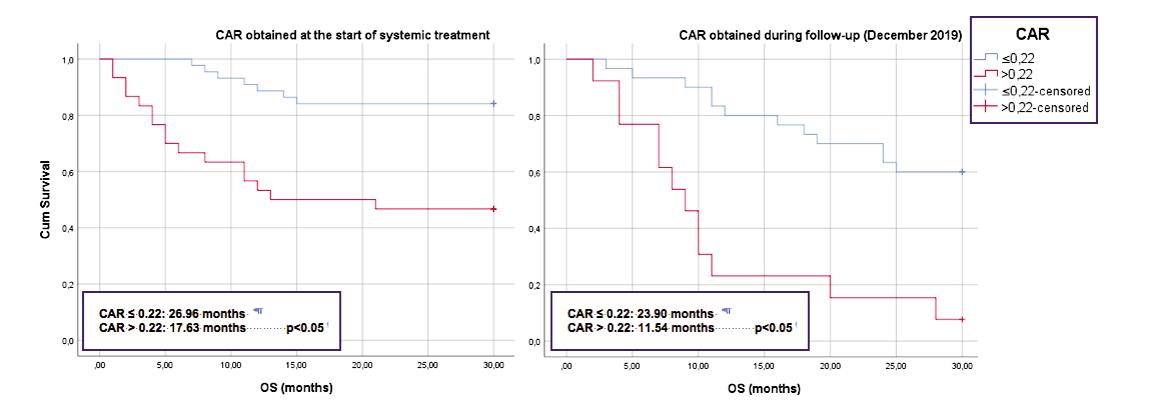
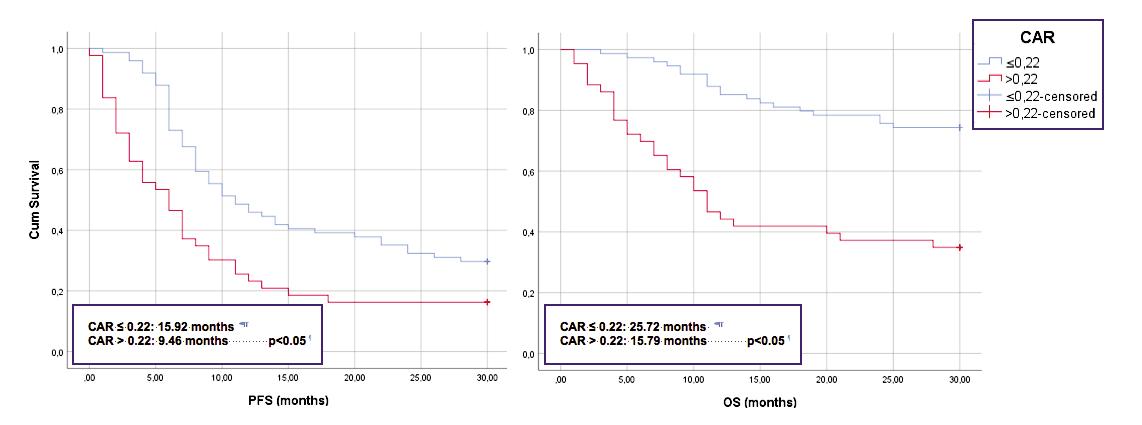
Materials and methods: A transversal study was conducted, including all patients diagnosed with mCRPC within a Central Hospital Urological Oncology consultation between December 2019 and December 2021 (n = 178) and that were submitted to systemic therapy. CRP and albumin results were collected at the beginning of the systemic treatment for mCRPC in 103 patients and, in 75 patients already under treatment at the start of the study, on that occasion (December 2019) All patients were then followed. CAR was correlated with PFS and OS. OS and PFS were measured from the day the CRP and Alb were collected until the event of interest or the final date of follow-up. The sample was divided in two groups according to an optimal cutoff point found in a ROC curve.
Results: The sample showed a median age of 75 76 ± 9 17 years old. Using a cut-off point of 0.22, patients with a CAR ≤ 0.22 (63 2%) showed, compared to CAR > 0 22, longer PFS (15 92 vs 9.46 months, r = -0.13, p < 0.05) and OS (p = < 0.05, 25,72 vs. 15 79 months, r = -0,24, p < 0 05) Better OS in patients with CAR ≤ 0.22 vs > 0.22 was detected on both the group evaluated at the beginning of systemic treatment (26 96 vs 17 63 months, p < 0 05) and the group of patients already under treatment (23 90 vs 11 54 months, p < 0 05) Dividing the sample according to the first line treatment chosen, we found OS of 26 25 vs 5 9 months (p < 0 05), 27 71 vs 22 57 months (p < 0 05) and 27 36 vs 23 75 months (p = 0 12), for docetaxel, abiraterone and enzalutamide, respectively
Conclusions: According to this study, higher values of CAR are associated with lower PFS and OS in mCRPC patients We found a cut-off value of 0 22 providing the best discrimination for prognosis. CAR is a good prognosis biomarker, irrespective of the moment of evaluation and chosen treatment option
KEY WORDS: Prostatic cancer; C-reactive protein; Albumin; Biomarker; Prognosis
Submitted 6 February 2023; Accepteed 25 February 2023
INTRODUCTION
Prostate cancer (PCa) is the most common non cutaneous malignancy among men (1), and the second leading cause of death from cancer in this population (2) It is estimated that approximately 1 in 8 men (12 9%) will be diagnosed with prostate cancer, and 1 in 40 (2 5%) will die from this
disease (3) Despite a substantial shift to a more favourable stage at presentation of newly diagnosed disease, average age of death from prostate cancer is 77 years of age and has remained stable over the past three decades (3, 4) Since Huggins reported that surgical castration is an effective treatment for advanced prostate cancer (5), hormonal manipulation with the suppression of gonadal testosterone is a cornerstone for systemic treatment of metastatic prostate cancer (3) However, the disease eventually evolves into mCRPC and death (3)
In recent years, the addition of several newly approved combination therapies to androgen deprivation therapy (ADT) for treatment in metastatic hormone-sensitive prostate cancer (mHSPC), such as abiraterone, docetaxel, apalutamide, enzalutamide or darolutamide, have shown improvements in OS and PFS (6-11) Despite being extremely effective initially, almost all patients under ADT for mHSPC eventually develop biochemical and/or clinical evidence of treatment resistance Median OS after mCRPC diagnosis is estimated to be between 13 2 to 23 2 months depending on the burden of metastasis at presentation (12) mCRPC is a very heterogeneous disease, representing a vast group of patients with a wide range of characteristics and prognosis Many factors have been pointed out to stratify these patients, such as PSA, metastatic burden, age, Gleason score and time to castration resistance (13) However, new methods or biomarkers to help clinicians sub-classify and manage these patients are still needed Some inflammation-based and/or nutritional markers have been studied with this goal, such as neutrophil/lymphocyte ratio (14), platelet/lymphocyte ratio (PLR) (15), prognostic nutritional index (PNI) (16), among others (17-22) Serum C-reactive protein (CRP), and acute phase reactant, has been used as a surrogate marker of systemic inflammation (17-19) Systemic inflammatory response has been shown to be associated with carcinogenesis, tumour progression and metastasis (20) Serum albumin (Alb) is accepted as a marker of the nutritional status of the body (18) The lower the serum albumin, the more frail the patients tend to be Several recent studies have reported the utility of the CAR as a prognosis factor in cancer patients (20-22) A higher CAR corresponds to a status of elevated systemic inflammation and lower nutritional status, suggesting that the patient’s overall condition is poor (18) CAR value as a prognostic marker has been previously reported in some cancers, such as hepa-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11242 1
João Lorigo 1 , Edgar Tavares Silva 1, 2 , João Pedroso Lima 1, 2 , Vasco Quaresma 1 , Rui Pedrosa 1 , Arnaldo Figueiredo 1, 2
DOI: 10 4081/aiua 2023 11242
1 Department of Urology, Centro Hospitalar e Universitário de Coimbra, Coimbra, Portugal; 2 University, Coimbra, Portugal
tocellular, colorectal, esophageal, pancreatic, small cell lung and cervical neoplasia (14-16, 20-22)
However, there is only limited data in prostate cancer patients
The objective of this study was to assess the association of CAR with PFS and OS in a group of mCRPC patients
MATERIALS AND METHODS
A transversal study was conducted, including all patients diagnosed with mCRPC with a follow-up in a urological oncology consultation at a Central Hospital in Portugal, between December 2019 and December 2021 (n = 178) and that were submitted to systemic therapy (74 abiraterone, 56 enzalutamide and 48 docetaxel) Twenty-two patients had received docetaxel before for metastatic hormone-sensitive prostate cancer (mHSPC)
Table 1.
Patients’ characteristics and comparison between studied groups.
Seventy-five patients were already under treatment and follow-up in December 2019 and this group had the CRP and albumin data collected at that date The remaining 103 patients had the biochemical data collected in the beginning of the systemic treatment (between December 2019 and December 2021)
The participants’ characteristics were gathered from the medical records including age, histological grade, disease risk and volume, treatment modality, CRP, Alb, progression free survival and overall survival The follow up data were collected until August of 2022
A taxane-based chemotherapy was chosen in the presence of clinical criteria of poor prognosis (short period of response under ADT, high metastatic burden, visceral metastasis or poor prognostic genetic mutations) or in patients progressing after novel hormonal agents (NHA; abiraterone or enzalutamide) NHA were preferred in patients with less aggressive features (asymptomatic, durable response under previous ADT, low metastatic burden and no visceral metastases), and as second line therapy in patients that progressed under taxane-based chemotherapy In the absence of contraindication for either pharmaceutical drugs, patients were sequentially assigned to either enzalutamide or abiraterone group
Castration resistance was defined using the European Association of Urology criteria: 1) three consecutives rises in PSA at least one week apart resulting in two 50% increases over the nadir, and a PSA > 2 ng/mL, or 2) appearance of new lesions (either two or more new bone lesions or a soft lesion using Response Evaluation Criteria in Solid Tumours [RECIST)), or 3) clinical deterioration OS was measured from the day the CRP and Alb were collected to death from any cause or the final date of followup PFS was also measured from the day the CRP and Alb were collected until one of the above-mentioned criteria were met or the final date of follow-up Comparisons between groups were performed using the chi-square test CAR was correlated with PFS and OS For that, samples were divided in two groups according to the optimal cutoff point found in a ROC curve OS and PFS curves were generated using the Kaplan-Meier method, and differences between groups were compared using the log-rank test All data were analysed using a linear regression
model and Kaplan-Meier survival curves The statistical hypothesis tests with p-value < 0 05 were considered significant Statistical analyses were performed using SPSS software ver 25 0 (IBM, Armonk, NY, USA)
RESULTS
A total of 200 patients diagnosed with mCRPC were included, median age at inclusion being 75 76 ± 9 17 years old After a median follow-up of 23 months, 72 patients (36 1%) had died The most prescribed treatment was abiraterone Table 1 resumes the baseline characteristics of the population
Mean CRP was 2 30 mg/dL (range from 0 02 to 24 08 mg/dL), mean Alb was 3 99 g/dL (range from 1 7 to 5 5 g/dL) and mean CAR was 0 64
In the present study, the value of 0 22 for CAR was used as the cut-off value It provided the maximal Youden index values, with an area under the curve (AUC) of 0 71 (Figure 1) CAR showed an inverse and significant correlation with
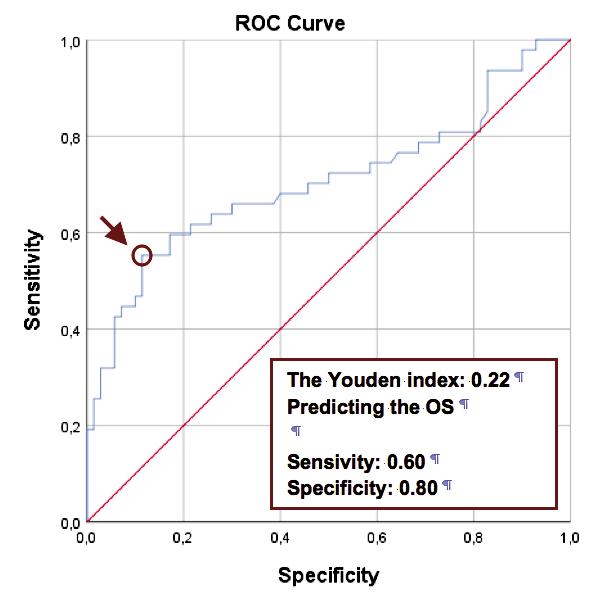
Archivio Italiano di Urologia e
2023;
Andrologia
95(3):11242
2
J Lorigo, E Tavares Silva, J Pedroso Lima, V Quaresma, R Pedrosa, A Figueiredo
Variables Total CAR ≤ 0.22 CAR > 0.22 p value n % n % n % ISUP Score ISUP1 6 0% 5 6% 6 7% n s ISUP2 20 2% 24 1% 13 3% n s ISUP3 34 5% 33 3% 36 7% n s ISUP4 17 9% 18 5% 16 7% n s ISUP5 21 4% 18 5% 26 7% n s Disease burden Low volume 49.4% 52.5% 43.3% n.s. High volume 50 6% 47 5% 56 7% n s Disease risk Low risk 64 1% 74 6% 45 5% 0 005 High risk 35 9% 25 4% 54 5% 0 005 Local treatment (LT) With LT 67 0% 61 7% 75 7% n s Without LT 33 0% 38 3% 24 3% n s First-line treatment for mCRPC Docetaxel 23 5% 15 6% 36 8% 0.015 Abiraterone 46.1% 51.6% 36.8% n.s. Enzalutamide 30 4% 32 8% 26 3% n s
Figure 1. ROC curve
both PFS and OS (r = -0 13 and r = -0 24, p = < 0 05, respectively) Correlations shown in Figure 2
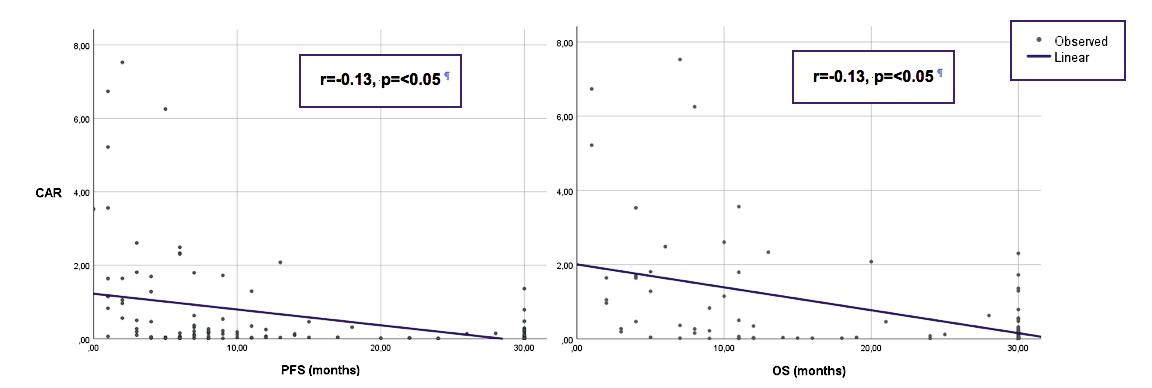
Using a cut-off value of 0 22, patients with a CAR ≤ 0 22 (63 2%) showed longer PFS (15 92 vs 9 46 months, p = < 0 05) and OS (25 72 vs 15 79 months, p = < 0 05)
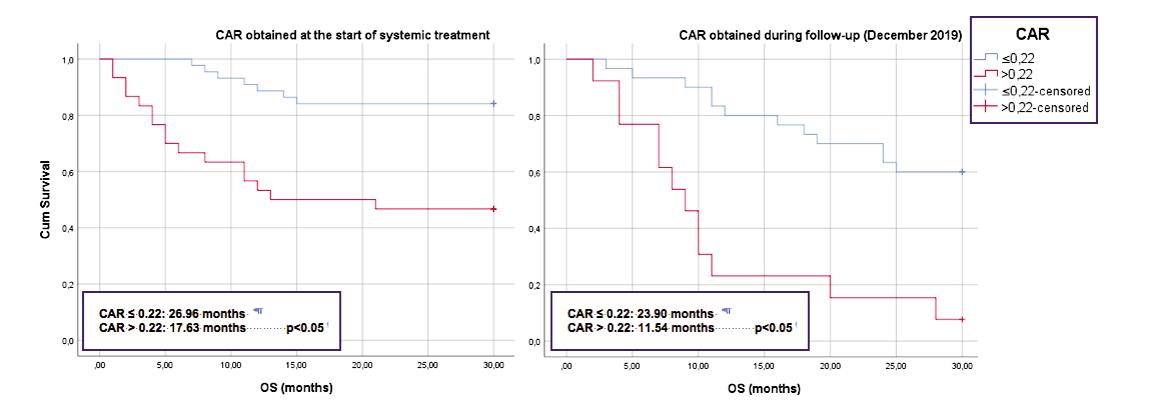
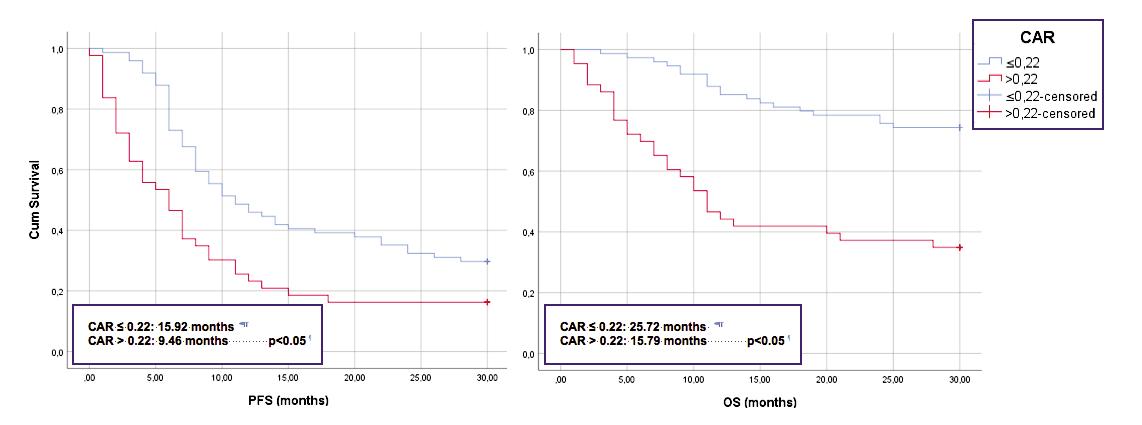
Survival curves shown in Figure 3
When dividing the sample according to when the biochemical parameters were collected, the OS of the group evaluated at the beginning of systemic treatment was 26 96
vs 17 63 months, for a CAR ≤ 0 22 vs > 0 22, respectively (p < 0 05) In the group evaluated during follow-up, the OS using the same cut-off point was 23 90 vs 11 54 months, respectively (p < 0 05) Survival curves below Dividing the sample according to the first line treatment chosen for mCRPC, it was observed an OS of 26 25 vs 5 9 months (p < 0 05), 27 71 vs 22 57 months (p < 0 05) and 27 36 vs 23 75 months (p = n s ), for docetaxel, abiraterone and enzalutamide, respectively
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11242 3 CAR as a prognosis biomarker in mCRPC
Figure 3. Comparing progression free survival (PFS) and overall survival (OS) between groups according to CAR.
Figure 2,. Correlations between CAR and clinical outcomes
Figure 4. Comparing overall survival (OS) between groups at the start of systemic treatment and during follow-up
DISCUSSION
In this study, we analysed the prognostic value of CAR in 178 mCRPC patients. We found CAR to be an independent prognostic factor for patients with mCRPC, either at diagnosis and start of systemic treatment and at any point during follow-up.
CRP production in the liver is up-regulated by proinflammatory cytokines (e.g. interleukin-6 [IL-6]) (25). Increased CRP levels have been reported in many types of malignancies (23). Cancer cell proliferation, necrosis, invasion, and hypoxia trigger immune responses in the tumour microenvironment that leads to the generation of various proinflammatory factors (25, 26). Two metaanalyses evaluated the role of CRP in kidney, bladder and prostate cancers and found a potential prognostic value in all three malignancies (24, 26).
Despite not being a perfect marker of nutritional status, because of its long half-life and susceptibility to other systemic factors, albumin is well correlated with nutrition status (25). Low serum albumin levels are caused by low nutrient intakes and tumour overconsumption (26). Protein malnutrition can lead to oedema, impaired organ function and immunosuppression. Moreover, hypoalbuminemia is associated with higher mortality in cancer patients (23, 25, 26).
Recently, several studies have reported the relation between high CAR and poor prognosis in cancer patients (20-22). Accordingly, we found a mean CRP and Alb, respectively, above (2.30 mg/dL) and below (3.99 g/dL) normal range values. In this study, we used the ROC analysis to yield a CAR 0.22 cut-off value for predicting PFS and OS in mCRPC and we were able to find a significant difference between patients with a CAR ≤ 0.22 or > 0.22. Taking advantage of the study design, we tried to find if the ratio was useful at the start of systemic treatment and during follow-up. We found a significant correlation irrespectively of the analysis timing. These findings are in line with previous studies (23, 25, 26). However, all those studies have only evaluated patients in the beginning of systemic treatment. Although not surprising, this study proves the usefulness of CAR predicting outcomes during the oncological follow-up.
The number of drugs approved for treatment of mCRPC is vast (27-30). In our study, 27% of the patients received docetaxel, 41.6% abiraterone and 31.5% enzalutamide. We observed a significantly higher proportion of patients with CAR > 0.22 receiving docetaxel vs NHA. This can be due to the higher disease stress associated with the poor risk factors present in these sub-group. Because docetaxel was prescribed in patients with more aggressive disease, their OS were also lower. However, CAR was still able to differentiate patients receiving docetaxel according to their prognosis. The groups receiving abiraterone and enzalutamide were more homogenous. When grouping the sample by treatment type, we found longer OS for patients with CAR ≤ 0.22 taking abiraterone, however, patients on enzalutamide didn´t showed a significant difference in OS, CAR (p = 0.12), with patients showing an OS of 27.36 and 23.75 months, for a CAR ≤ 0.22 vs > 0.22, respectively. We attribute this lack of significance to the small sample size.
It should be noted that the current study has limitations,
including its retrospective nature and a relatively small sample size, which might have caused selection bias. Large-scale and prospective studies are further warranted to confirm our preliminary findings.
CONCLUSIONS
In conclusion, according to this study, higher values of CAR are associated with lower PFS and OS in mCRPC patients. These results suggest that CAR is a good prognosis biomarker, irrespective of the moment of evaluation and chosen treatment option.
REFERENCES
1.Prostate Cancer - Statistics [Internet]. Cancer.net. 2012 [cited 2022 Nov 12]. Available from: https://www.cancer.net/cancertypes/prostate-cancer/statistics.
2.Key Statistics for Prostate Cancer | Prostate Cancer Facts [Internet]. Cancer.org. 2022 [cited 2022 Nov 12]. Available from: https://www. cancer.org/cancer/prostate-cancer/about/key-statistics.html
3.Wein AJ, Kavoussi LR, Partin AW, Peters CA. Campbell-Walsh urology. Philadelphia, Pa: Elsevier; 2016.
4.Epstein MM, Edgren G, Rider JR, et al. Temporal trends in cause of death among Swedish and US men with prostate cancer. J Natl Cancer Inst. 2012; 104:1335-42.
5.Huggins C, Hodges CV. Studies on Prostatic Cancer: I. The Effect of Castration, of Estrogen and of Androgen Injection on Serum Phosphatases in Metastatic Carcinoma of the Prostate. J Urol. 2002; 168:9-12.
6.Teo MY, Scher HI. CHAARTED/GETUG 12—docetaxel in noncastrate prostate cancers. Nat Rev Clin Oncol. 2015; 12:687-8.
7.James N, Woods B, Sideris E, et al. Addition of docetaxel to firstline long-term hormone therapy in prostate cancer (STAMPEDE): Long-term survival, quality-adjusted survival, and cost-effectiveness analysis. J Clin Oncol. 2018; 36(6 suppl):162-2.
8.Sharma A. A game changing LATITUDE: Role of abiraterone plus prednisolone in metastatic hormone-sensitive prostate cancer. Indian J Urol. 2017; 33:333.
9.Davis ID, Stockler MR, Martin A, et al. Randomised Phase 3 Trial of Enzalutamide in First Line Androgen Deprivation Therapy for Metastatic Prostate Cancer: Enzamet (Anzup 1304). Annal Oncol. 2014; 25:iv278.
10.Chi KN, Chowdhury S, Radziszewski P, et al. TITAN: A randomized, double-blind, placebo-controlled, phase 3 trial of apalutamide (ARN-509) plus androgen deprivation therapy (ADT) in metastatic hormone-sensitive prostate cancer (mHSPC). Annal Oncol. 2016; 27:vi265.
11.Tombal B, Saad F, Hussain M, et al. ARASENS: A phase 3 trial of darolutamide in males with metastatic hormone-sensitive prostate cancer (mHSPC). Annal Oncol. 2017; 28:v291-2.
12.Aly M, Leval A, Schain F, et al. Survival in patients diagnosed with castration-resistant prostate cancer: a population-based observational study in Sweden. Scand J Urol. 2020; 54:115-21.
13.Capoun O, Mikulová V, Jancíková M, et al. Prognosis of Castration-resistant Prostate Cancer Patients - Use of the AdnaTest® System for Detection of Circulating Tumor Cells. Anticancer Research. 2016; 36:2019-26.
14.Kasymjanova G, MacDonald N, Agulnik JS, et al. The predictive
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11242 J.
4
Lorigo, E. Tavares Silva, J. Pedroso Lima, V. Quaresma, R. Pedrosa, A. Figueiredo
value of pre-treatment inflammatory markers in advanced nonsmall-cell lung cancer. Cur Oncol 2010; 17:52-8.
15.Wang D, Luo H, Qiu M, et al. Comparison of the prognostic values of various inflammation based factors in patients with pancreatic cancer. Med Oncol. 2012; 29:3092-100.
16.Buzby GP, Mullen JL, Matthews DC, et al. Prognostic nutritional index in gastrointestinal surgery. Am J Surg 1980; 139:160-7.
17.Sugimoto A, Toyokawa T, Miki Y, et al. Preoperative C-reactive protein to albumin ratio predicts anastomotic leakage after esophagectomy for thoracic esophageal cancer: a single-center retrospective cohort study. BMC Surg. 2021; 21:348
18.Liu Z, Shi H, Chen L. Prognostic role of pre-treatment C-reactive protein/albumin ratio in esophageal cancer: a meta-analysis. BMC Cancer. 2019; 19:1161.
19.Bodner-Adler B, Kimberger O, Schneidinger C, et al. Prognostic Significance of Pre-treatment Serum C-Reactive Protein Level in Patients with Adenocarcinoma of the Uterine Cervix. Anticancer Res. 2016; 36:4691-6.
20.He X, Li J-P, Liu X-H, et al. Prognostic value of C-reactive protein/albumin ratio in predicting overall survival of Chinese cervical cancer patients overall survival: comparison among various inflammation based factors. J Cancer. 2018; 9:1877-84.
21.Haruki K, Shiba H, Horiuchi T, et al. Impact of the C-reactive protein to albumin ratio on long-term outcomes after hepatic resection for colorectal liver metastases. Am J Surg. 2017; 214:752-6.
22.Wu M, Guo J, Guo L, Zuo Q. The C-reactive protein/albumin ratio predicts overall survival of patients with advanced pancreatic cancer. Tumour Biol 2016; 37:12525-33.
23.Uchimoto T, Komura K, Fujiwara Y, et al. Prognostic impact of C-reactive protein-albumin ratio for the lethality in castration-resistant prostate cancer. Med Oncol. 2019; 37:9.
24.O’Brian D, Prunty M, Hill A, et al. The Role of C-Reactive Protein in Kidney, Bladder, and Prostate Cancers. Front Immunol. 2021; 12:721989.
25.Guo S, He X, Chen Q, et al. The C-reactive protein/albumin ratio, a validated prognostic score, predicts outcome of surgical renal cell carcinoma patients. BMC Cancer. 2017; 17:171.
26.Wu M, Zhou Y, Chen Q, et al. Prognostic Role of Pretreatment CReactive Protein to Albumin Ratio in Urological Cancers: A Systematic Review and Meta-Analysis. Front Oncol. 2022; 12:879803.
27.Berthold DR, Pond GR, Soban F, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer: updated survival in the TAX 327 study. J Clin Oncol. 2008; 26:242-5.
28.Beer TM, Armstrong AJ, Rathkopf D, et al. Enzalutamide in Men with Chemotherapy-naïve Metastatic Castration-resistant Prostate Cancer: Extended Analysis of the Phase 3 PREVAIL Study. Eur Urol. 2017; 71:151-4.
29.Ryan CJ, Smith MR, Fizazi K, et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2015; 16:152-60.
30.Jarimba RS, Eliseu MN, Pedroso Lima J, et al. Novel hormonal agents for metastatic Castration-Resistant Prostate Cancer: comparing outcomes. A single-center retrospective study. Arch Ital Urol Androl. 2021; 93:393-8.
Correspondence
João Diogo Abreu Lorigo, MD (Corresponding Author) joaolorigo@gmail.com
Department Urology-Centro Hospitalar e Universitário de Coimbra Praceta Professor Mota Pinto, 3004-561 Coimbra, Portugal
Edgar Tavares Silva, MD edsilvaelv@gmail.com
João Pedroso Lima, MD joaopedrosolima@gmail.com
Vasco Quaresma, MD vpdquaresma@gmail.com
Rui Pedrosa, MD ruimdp93@gmail.com
Arnaldo Figueiredo, MD ajcfigueiredo@gmail.com
Praceta Professor Mota Pinto, 3004-561 Coimbra
Conflict of interest: The authors declare no potential conflict of interest.
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11242 5 CAR as a prognosis biomarker in mCRPC
Surveillance as a safe and effective option for treatment of stage I seminoma
Summary
Introduction: Stage I seminoma has a very good prognosis, yet approximately 15% have subclinical metastatic disease and will relapse after orchidectomy alone. Several management approaches have been investigated. We aimed to evaluate the clinical outcomes of real-world patients with stage I seminoma, analysing prognostic factors influencing treatment choice and oncological outcomes.
Methods: Retrospective, single institution study, with 55 patients diagnosed with clinical stage I seminoma between 2007 and 2020. Selected patients were analysed regarding three management approaches - surveillance, adjuvant radiotherapy and adjuvant carboplatin AUC7. Overall survival and progressionfree survival outcomes were analysed. Predictors of treatment choice were determined, and predictors of recurrence were analysed in patients on active surveillance.
Results: The median follow-up time was 91 months (13-165). Overall survival at 10 years was 98.2%. Stage I seminoma patients had a 1-, 3- and 10-year progression free survival of 98%, 94% and 89%, respectively. Three-year progression free survival was 92.0% for those on active surveillance (IC95%, 91.5-92.5%), 95.2% for carboplatin (IC95%, 94.8-95.6%) and 100% for those on adjuvant radiotherapy (p > 0.05). All relapses on active surveillance protocols occurred during the first 24 months. Overall, 43% of patients who underwent adjuvant treatment reported adverse effects of therapy, with higher incidence on radiotherapy group (63%).
Conclusions: Stage I seminoma have excellent prognosis, high cure rates, and low treatment-associated morbidity. Active surveillance is a safe modality when applied to selected patients. Adjuvant radiotherapy and adjuvant chemotherapy with carboplatin show similar results, with fewer adverse effects on chemotherapy arm.
KEYWORDS: Seminoma; Surveillance; Radiotherapy; Adjuvant chemotherapy; Recurrence.
Submitted 8 June 2023; Accepted 14 July 2023
INTRODUCTION
The incidence of Testicular Germ Cell Tumours (TGCT) has increased during recent decades and continues to rise (1). Stage I seminoma is the most common presentation of TGCT and accounts for approximately 40% of all occurrences (2). Patients presenting with clinical stage I
(CS I) have very good prognosis with an overall survival rate of 98% (3). Even metastatic patients have a good prognosis with a 5-year survival rate of 72-86% (3). Despite modern staging procedures, approximately 15% of clinical stage I seminoma patients have subclinical metastatic disease (in the retroperitoneum) and will relapse after orchidectomy alone (4). Unselected CS I patients managed by active surveillance (AS) have shown an overall risk of relapse of 12-20% at five years (5). Identification of CS I seminoma patients who are at a high risk of recurrence has largely been based on two prognostic factors: primary testicular tumour size, and the presence or absence of rete testis invasion (3, 6). Patients with and without both risk factors have a 32% and 6% risk of relapse, respectively (7). Patients with one risk factors had 12% risk of relapse (8).
Three management approaches have been investigated: surveillance, adjuvant radiotherapy and carboplatin (6, 914). The adjuvant treatment results were compared in large clinical trials and showed that a single injection of carboplatin at seven times the area under the curve dose (AUC) was noninferior to RT in preventing metastatic relapse and, in addition, may reduce the risk of subsequent contralateral testicular cancer (10). Furthermore, radiotherapy is associated with increased morbidity and late effects, in particular the risk of secondary cancers (15). The priority for those patients with low stage disease is limiting the burden of therapy and treatment-related toxicity without compromising cancer control. The optimal management strategy for stage I seminoma seems to be a matter of debate and controversy. The aim of this study was to evaluate the clinical outcomes of real-world patients with CSI seminoma treated in a national referral centre. Furthermore, we aimed to analyse prognostic factor influencing treatment choice and oncological outcomes.
PATIENTSANDMETHODS
The present study was approved by Coimbra’s University Hospital (CHUC) and Faculty of Medicine (FMUC) ethical boards - CE-026/2022. Using the institutional prospective TGCT database, we selected patients with histologically proven pure seminoma after inguinal orchiectomy. Routine staging at diagnosis consisted in computed tomography (CT)
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11513 1 ORIGINALPAPER
Vasco Quaresma 1, 2, *, Diogo Henriques 2, *, Lorenzo Marconi 1, 2, João Lorigo 1, Ana-Marta Ferreira 1 , Roberto Jarimba 1, 2, Pedro Nunes 1, 2, Arnaldo Figueiredo 1, 2, Belmiro Parada 1, 2
1 Urology Department, Centro Hospitalar e Universitário de Coimbra, Portugal; 2 Faculty of Medicine of the University of Coimbra, Portugal;
DOI: 10.4081/aiua.2023.11513
* Both authors equally contributed as first co-authors.
of thorax, abdomen, and pelvis, with additional clinical history and physical examination. All included patients had serum tumour markers before and after orchiectomyα-fetoprotein (AFP) and β-human chorionic gonadotropin (BHCG).
The selected patients were retrospectively analysed and assigned to three management approaches - surveillance, adjuvant radiotherapy and carboplatin.
Therapeutic modality was assigned after multidisciplinary uro-oncology discussion and informed discussion with patients. Treatment decision was influenced by pathological characteristics and risk factors, serum tumour markers and patient option.
Patients undergoing adjuvant carboplatin had a single dose of intravenous carboplatin on an outpatient basis, calculated according to Calvert equation - dose of carboplatin (mg) = area below curve 7 mg/ml/min x (GFR + 25). 16 Patients treated with radiotherapy had a total of 20-24 Gray (Gy) directed to the para-aortic and ipsilateral iliac fields.
Most of included patients were followed with clinical assessment and serum tumour markers every 3 months in the first year, every 6 months until third year, and then yearly. CT of thorax, abdomen and pelvis was performed biannually in the first two year and then yearly.
Co-Primary endpoints were the overall survival (OS) and disease-free survival (DFS).
Overall survival was defined as the time from orchiectomy to death from any cause. Progression-free survival was defined as the time from orchiectomy to imagological disease progression. Increased serum tumour markers were not considered as recurrence. Secondary endpoints were the evaluation of risk factor at the time of diagnosis and safety assessment according to National Cancer Institute Common Terminology Criteria for Adverse Events version 4.0
Statistical analysis
Descriptive analyses were performed using standard summary statistics. Overall survival, progression-free survival, and duration of response were estimated with the use of the Kaplan-Meier method. Predictors of adjuvant treatment decision were determined by Qui-square test of independency (with Yates correction). In the analysis of overall survival, patients who were alive had their data censored at the time of last contact. In the analysis of progression-free survival, patients who were alive and without disease progression had their data censored at the time of last tumour assessment. Cox multivariate analysis were performed to adjust survival for risk factors (rete testis invasion and dimensions) and adjuvant treatment. Medians are reported with corresponding 95% confidence intervals (CIs).
RESULTS
From 157 patients with TCGT followed between 2007 and 2020, 55 patients had clinical stage I seminoma at diagnosis. The selected patients were retrospectively analysed and assigned to three management approachessurveillance, adjuvant radiotherapy and carboplatin. Diagram is show in Figure 1. We included a total of 55 patients of testicular seminoma

with no evidence of metastatic disease at the time of diagnosis (CS I Seminoma). Median patient age was 35 years (range: 24 to 66). Pre-operatively, 7 patients (13%) showed elevated serum BHCG (> 5 mU/mL), and an additional 19 patients (35%) had high serum LDH levels (> 248 U/L). All patients were pre- and postorchiectomy AFP negative, and BHCG levels normalized after orchiectomy. Median tumour dimension was 40 mm (range: 7 to 120 mm). Most specimens (57%) showed tumour confined to testis, with no lymphovascular invasion (pT1). Demographic characteristics of patients and disease at the diagnosis according to treatment modality are summarized on Table 1.
Of the included patients, 25 underwent an active surveillance protocol and 30 were submitted to adjuvant therapy - 8 radiotherapy and 22 carboplatin AUC 7.
Most patients on active surveillance (60%) had no risk factors of recurrence on initial management (rete testis invasion or size > 4 cm). Only 16% had lymphovascular invasion and 4% showed positive pre-operative tumour markers. Conversely, risk factors (rete testis invasion or size > 4 cm) were present on 83% of the patients in adju-
Demographic and disease characteristics.
Characteristic Surveillance CarboplatinRadiotherapyP value (n = 25)(n = 22)(n = 8)
Age-yrs.
Median333536T-Test
Range26-6624-5425-41p>0.05
Pre-operativeSerumTumorMarkers
Positive7(28%)11(50%)3(37%)X2 Negative18(72%)11(50%)5(63%)p>0.05
Stage IA3(12%)14(64%)3(37%)X2 IB22(88%)8(36%)5(63%)p<0.05
ReteTestisInvasion
Yes5(20%)12(55%)5(37%)X2 No20(80%)10(45%)3(63%)p>0.05
Tumourdimension(cm)
Median354T-Test
Range1.2-121-122.2-8p>0.05
BHCG: β-humanchorionicgonadotropin;LDH:lactatedehydrogenase.
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11513
2
V. Quaresma, D. Henriques, L. Marconi, et al.
Table 1.
Figure 1. Assignment of selected patients to three management approaches - surveillance, adjuvant radiotherapy and carboplatin.
Risk factor and treatment groups.
PFS analysis Three-year PFS was 92 0% for those on active surveillance (95% CI, 91 5 to 92 5%), 95 2% for carboplatin (95% CI, 94.8 to 95.6%) and 100% for those on adjuvant radiotherapy, with no statistically difference between groups of treatment (p > 0 05)
vant treatment groups Therefore, we conducted a comparative analysis on baseline characteristics, which verified that only pT stage was statistically different between treatment groups
Considering subgroups of adjuvant treatment, 86% patients on Carboplatin group and 75% on radiotherapy had one or two risk factors Comparative analysis is summarized on Table 2 Tumour maximal dimensions (p < 0 05) and limphovascular invasion (p < 0 05) were predictors of adjuvant treatment decision in this setting
Median time from orchiectomy to adjuvant treatment was 37 days (range 24-92)
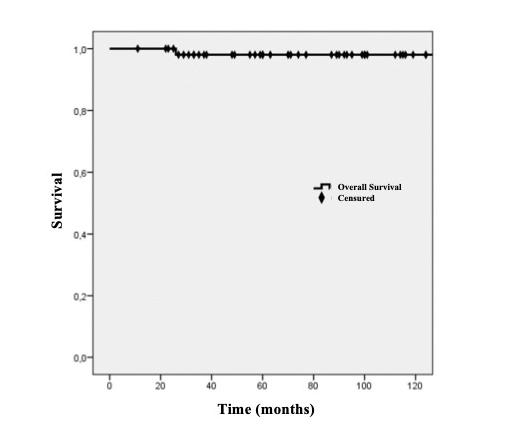
Overall survival. Ten-year overall survival (OS) was 98.2%, with an average overall survival of 162 months (95% CI, 157 to 167 months) - median not reached
with no statistically difference between groups of treatment (p > 0 05) PFS analysis is illustrated on Figure 3
Median time to relapse for patients with tumour recurrence was 21 months (range: 9-64) All relapses on active surveillance protocols occurred during the first 24 months (9 and 21 months) Adjuvant treatment groups showed later relapses - Carboplatin at 13 and 57 months and radiotherapy at 64 months All relapses were retroperitoneal and detected on follow up CT scan No patient had symptoms on relapse These patients were treated with second line therapy with 4 cycles of BEP (Bleomycin, Etoposide, and Cisplatin) Of those, 4 patients were free of disease at last follow up One patient on surveillance group died of the disease, as mentioned before, after relapse and second line treatment One patient on radiotherapy group showed seminoma on contralateral testis and was submitted to orchiectomy
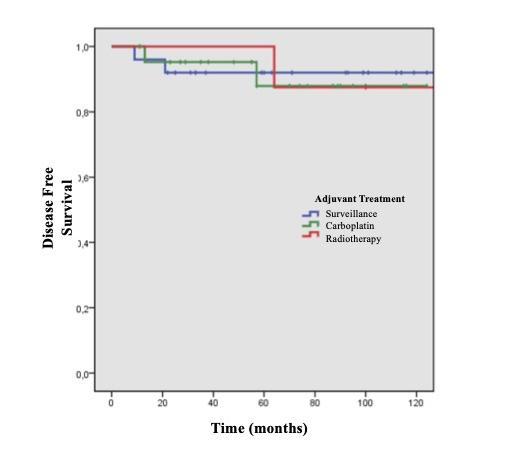
Safety
Survival analysis
Median follow-up time was 91 months (range 13 - 165 months), with 98% of patients being followed for more than 2 years No patient was lost to follow-up Ten-year overall survival (OS) was 98 2%, with an average overall survival of 162 months (95% CI, 157 to 167 months)median not reached (Figure 2) One patient died due to febrile neutropenia following second line chemotherapy
At the time of present analysis, relapses were observed in 5 patients Stage I seminoma patients had a 1-, 3- and 10year PFS of 98%, 94% and 89%, respectively Three-year PFS was 92 0% for those on active surveillance (95% CI, 91 5 to 92 5%), 95 2% for carboplatin (95% CI, 94 8 to 95 6%) and 100% for those on adjuvant radiotherapy,
Safety analysis was performed with retrospective analysis of clinical records in the adjuvant treatment groups Treatment-related adverse events of any grade were reported in 43% of the patients Patients on Carboplatin group reported 27% grade 1-2 events, with no grade 3-5 events Most common adverse effect of chemotherapy was nausea and vomitus Radiotherapy group had 63% reported adverse events, with 13% grade ≥ 3 One patient had secondary neoplasia after radiation treatment
Predictors of recurrence
We analysed the potential predictors of recurrence in patients with no adjuvant treatment Elevated preoperative β-hCG (> 5 mU/mL), pT > 1, rete testis invasion, and tumour size > 4 cm were not predictors of recurrence in patients on active surveillance (Pearson X2; p > 0 05) Two patients with no risk factors for relapse (rete testis
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11513 3 Surveillance for stage I seminoma
Figure 2.
Figure 3.
Table 2.
Active sur veillance Adjuvant therapy (n = 25) (n = 30) ReteTestisinvasionand/orsize>4cm15(40%)25(83%) >pT14(16%)20(66%) SerumTumorMarkers1(4%)6(20%)
3
Predictors of recurrence
invasion or > 4 cm) recurred on follow up, both in AS group Three patients who recurred after adjuvant treatment, had both risk factors Table 3 shows the recurrence rates despite treatment modality To eliminate the effect of adjuvant treatment, we conducted a Cox Regression with the following predictors: adjuvant treatment, rete testis invasion and dichotomous dimensions There were no differences in PFS in the model (X2 = 0 95; p > 0 05) Adjusted hazard ratio (HR) for adjuvant treatment was 0 6 (95% CI, 0 1 to 4 0, p = 0 5) Adjusted HR of 1 3 for rete testis invasion (95% CI, 0 1 to 15 2, p = 0 8) and HR of 2 2 for dimensions (95% CI, 0 2 to 17 3, p = 0 4)
DISCUSSION
Approximately 76% of patients with testicular seminoma in a Portuguese referral centre present with stage I disease at diagnosis, results that are comparable to recent epidemiologic studies and a previous Portuguese referral centre study (1, 17) These patients have excellent prognosis, with high cure rates (3) Therefore, the treatment of stage I seminoma mostly addresses the principles of fast diagnosis and staging, short time between diagnosis and orchiectomy, and precise and fast decision of adjuvant treatment, aiming to avoid deaths without increasing the morbidity of treatment Adjuvant treatment recommendation mostly relies on a risk adapted strategy and last decision must be made by the individual patient In stage I seminoma, primary testicular tumour size and invasion of the rete testis have been identified as predictors for relapse (7, 9) Although, two recent systematic reviews have questioned the prognostic value of these risk factors, and so far, there is no ideal prognostic factor for relapse in patients with stage I seminoma (3, 18) Both systematic reviews highlighted the low quality of the studies included and that the level of evidence is too low to recommend the use of these pathological risk factors to drive adjuvant treatment decisions (3, 18) Nevertheless, absence of rete testis invasion together with a tumour diameter < 4 cm is associated with a very low risk of recurrence (6%) (19) Therefore, these are the most suitable patients for AS
In our centre experience, both tumour maximal dimensions (continuous) and lymphovascular invasion influenced the choice of adjuvant treatment Using dimensions as a continuous variable may help counseling patients about their expected tumor recurrence risk (12)
Risk factors of relapse were analysed on AS patients to eliminate the bias of adjuvant treatment
Pre-operative β-hCG; rete testis invasion; dimensions; > pT1 were not significant predictors of relapse In the evaluation of recurrence without considering treatment modality, only 4% patients relapsed with no risk factors
Patients with risk factors recurred in 6% Although the
global model was not significant, patients with rete testis invasion (HR of 1 3) and higher dimensions (HR of 2 2) were associated with worse PFS
Overall survival in the CSI Seminoma in our centre was 98 2% OS was comparable to most studies, and confirms excellent prognosis and high cure rates, even in the longer follow up of our design Nine percent of patients had recurrence of disease At 3-year PFS no treatment modality showed to be superior, although more patients were free of disease in adjuvant treatment group at this time cut-off Patients on AS showed earlier relapses (first 24 months) which justifies an intense follow up with CT scan in the first two years
Growing experience with active surveillance has demonstrated that nearly 80% of CSI Seminoma can expect to be cured without adjuvant treatment, and almost all recurrences can be successfully rescued (14) Possible disadvantages of clinical surveillance are incremental costs, need of patient compliance to the follow-up protocol, psychological distress, and the chance of early relapses (20) Low number of relapses in our study support active surveillance as a safe option with comparable results to adjuvant treatment Both patients who relapse in AS are alive and free of disease AS allows to mitigate the morbidity of adjuvant therapies, complying with the principles of treatment of testicular neoplasms when good selection criteria are applied
Patients on adjuvant treatment groups presented more aggressive characteristics at orchidectomy (size, vascular invasion and pT), as well as a higher percentage of positive markers preoperatively As discussed earlier, PFS was similar, even with more aggressive disease at diagnosis Radiotherapy, once the treatment of choice, is being abandoned as adjuvant treatment Despite long term PFS of 96% and OS of 98%, significantly morbidity is associated with this modality, especially a two to three-fold increased risk of second malignancies (21) Our experience also shows a low number of patients who underwent radiotherapy, confirming the tendency to abandon this modality in stage I seminoma, which confirms the change in pattern of care indicated by previous studies (22) Carboplatin generally has excellent tolerability and is not associated with grade 3 or 4 adverse effects On the other hand, RT presented more frequent adverse effects and the risk of secondary neoplasia Given the low age at diagnosis of patients with testicular neoplasia, one of the main objectives in treatment must be decreased morbidity Study limitations where its low number of participants, retrospective design, and the lack of inclusion criteria in the different modalities
CONCLUSIONS
Patients with stage I seminoma have excellent prognosis, high cure rates, and low treatment-associated morbidity Active surveillance is a safe modality, with results comparable to other modalities, when applied to selected patients Intense follow up on the first 2 years after orchiectomy is mandatory Adjuvant radiotherapy and adjuvant chemotherapy with carboplatin show similar results, with fewer adverse effects in patients who underwent chemotherapy
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11513 V Quaresma, D Henriques, L Marconi, et al 4
Table
CS I (n = 55) Rete Testis invasion and/or size > 4 cm (n = 34) No Risk Factors (n = 21) RecurrenceDiseasefreeRecurrenceDiseasefree 3(55%)32(582%)2(36%)18(327%)
REFERENCES
1 Park JS, Kim J, Elghiaty A, Ham WS Recent global trends in testicular cancer incidence and mortality Medicine 2018; 97:e12390
2 Powles TB, Bhardwa J, Shamash J, et al The changing presentation of germ cell tumours of the testis between 1983 and 2002 BJU Int 2005; 95:1197-1200
3 Boormans JL, Mayor de Castro J, Marconi L, et al Testicular Tumour Size and Rete Testis Invasion as Prognostic Factors for the Risk of Relapse of Clinical Stage I Seminoma Testis Patients Under S u r v e i l l a n c e : a S y s t e m a t i c R e v i e w b y t h e T e s t i c u l a r C a n c e r Guidelines Panel Eur Urol 2018; 73:394-405
4 Kollmannsberger C, Tandstad T, Bedard PL, et al Patterns of relapse in patients with clinical stage I testicular cancer managed with active surveillance J Clin Oncol 2015; 33:51-57
5 Groll RJ, Warde P, Jewett MAS A comprehensive systematic review of testicular germ cell tumor surveillance Crit Rev Oncol Hematol 2007; 64:182-197
6 Warde PR, Gospodarowicz MK, Goodman PJ, et al Results of a policy of surveillance in stage I testicular seminoma Int J Radiat Oncol Biol Phys 1993; 27:11-15
7 Aparicio J, Maroto P, García del Muro X, et al Prognostic factors for relapse in stage I seminoma: a new nomogram derived from three consecutive, risk-adapted studies from the Spanish Germ Cell Cancer Group (SGCCG) Ann Oncol 2014; 25:2173-2178
8 Aparicio J, Maroto P, García del Muro X, et al Prognostic factors for relapse in stage I seminoma: A new nomogram derived from three consecutive, risk-adapted studies from the Spanish Germ Cell Cancer Group (SGCCG) Annals of Oncology 2014; 25:2173-2178
9 Tandstad T, Ståhl O, Dahl O, et al Treatment of stage I seminoma, with one course of adjuvant carboplatin or surveillance, riskadapted recommendations implementing patient autonomy: a report f r o m t h e S w e d i s h a n d N o r w e g i a n T e s t i c u l a r C a n c e r G r o u p (SWENOTECA) Ann Oncol 2016; 27:1299-1304
10 Oliver RTD, Mason MD, Mead GM, et al Radiotherapy versus single-dose carboplatin in adjuvant treatment of stage I seminoma: a randomised trial Lancet 2005; 366:293-300
11 Oliver RTD, Mead GM, Rustin GJS, et al Randomized trial of carboplatin versus radiotherapy for stage I seminoma: mature results on relapse and contralateral testis cancer rates in MRC TE19/EORTC 30982 study (ISRCTN27163214) J Clin Oncol 2011; 29:957-962
Correspondence
Vasco Pedro Duarte Quaresma, MD (Corresponding Author)
vpdquaresma@gmail com
Rua António Manso Cunhavaz, Lote 2, 5ºB, 3030-779, Coimbra, Portugal
Lorenzo Marconi, MD
João Lorigo, MD
Ana-Marta Ferreira, MD
Roberto Jarimba, MD
Pedro Nunes, MD
Arnaldo Figueiredo, MD
Belmiro Parada, MD
Urology Department, Centro Hospitalar e Universitário de Coimbra, Portugal
Diogo Henriques, MD
Faculty of Medicine of the University of Coimbra, Portugal
Conflict of interest: The authors declare no potential conflict of interest
12 Chung P, Mayhew LA, Warde P, et al Management of stage I seminomatous testicular cancer: a systematic review Clin Oncol 2010; 22:6-16
13 Fischer S, Tandstad T, Wheater M, et al Outcome of Men With Relapse After Adjuvant Carboplatin for Clinical Stage I Seminoma J Clin Oncol 2017; 35:194-200
14 Aparicio J, García del Muro X, Maroto P, et al Multicenter study evaluating a dual policy of postorchiectomy surveillance and selective adjuvant single-agent carboplatin for patients with clinical stage I seminoma Ann Oncol 2003; 14:867-872
15 Fosså SD, Horwich A, Russell JM, et al Optimal planning target volume for stage I testicular seminoma: A Medical Research Council randomized trial Medical Research Council Testicular Tumor Working Group J Clin Oncol 1999; 17:1146-1154
16 Calvert AH, Newell DR, Gumbrell LA, et al Carboplatin dosage: prospective evaluation of a simple formula based on renal function J Clin Oncol 1989; 7:1748-1756
17 Marques-Pinto A, Gomes AI, Febra J, et al Specialist management of testicular cancer: Report of the last 10 years at a Portuguese tertiary referral academic centre Arch Ital Urol Androl 2021; 93:153-157
18 Zengerling F, Kunath F, Jensen K, et al Prognostic factors for tumor recurrence in patients with clinical stage I seminoma undergoing surveillance A systematic review Urologic Oncology: Seminars and Original Investigations 2018; 36:448-458
19 Aparicio J, Maroto P, Muro XG del, et al Risk-Adapted Treatment in Clinical Stage I Testicular Seminoma: The Third Spanish Germ Cell Cancer Group Study J Clin Oncol 2011; 29:4677-4681
20 Sharda NN, Kinsella TJ, Ritter MA Adjuvant radiation versus observation: a cost analysis of alternate management schemes in early-stage testicular seminoma J Clin Oncol 1996; 14:2933-2939
21 Zagars GK, Babaian RJ Stage I testicular seminoma: rationale for postorchiectomy radiation therapy Int J Radiat Oncol Biol Phys 1987; 13:155-162
22 Mahmoud Sayed M, Nasr AM, Saad Eldin IM, Abdelazim YA Stage I seminoma: outcome of different treatment modalities and changes in patterns of care: A single institution experience Arch Ital Urol Androl 2023; 95:11057
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11513 5 Surveillance for stage I seminoma
1 Department of Vascular Surgery, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
2 Department of Urology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
3 Department of Internal Medicine, Nephrology Unit, Faculty Medicine, Al-Azhar University, Cairo, Egypt;
4 Department of Internal Medicine, Nephrology Unit, Faculty Medicine, Tanta University, Tanta, Egypt
Summary
Purpose: For patients with a failed forearm autogenous fistula (AF) and an exhausted cephalic vein, there is controversy about whether a brachial basilic AF with transposition or an arteriovenous prosthetic bridging graft (BG) must be the second vascular access option This work measured and compared these two modalities according to patency rates, complications, and revisions
Patients and methods: A retrospective study of 104 cases that had either a brachial basilic AF (72) or an Arteriovenous BG (32). Technical success, operative complications, procedurerelated mortality, maturation time, functional primary, secondary, and overall patency rates were all assessed.
Results: Technical success was obtained in all participants
No procedure-linked mortality. Maturation time for BGs was significantly shorter than AFs The complication rate was significantly higher in BGs than in AFs. The most prevalent complication was access thrombosis The functional primary patency rate was significantly higher in AF than in BG at 12-month followup: 77 7% vs 53 1% (𝑝 < 0 012) secondary patency rate was higher in AF than in BG at 1-year follow-up 62.5% vs 42.8% (𝑝 = 0 063), respectively In addition, BGs required more interventions to preserve patency
Conclusions: AF had higher primary, secondary and overall functional patency rates and needed fewer procedures to keep patency than BGs Cases that need early vascular access as a result of central venous catheter complications or who have a reduced life expectancy may benefit from BGs
KEY WORDS: Hemodialysis; Basilic vein superficialization; Arteriovenous fistula
Submitted 6 May 2023; Accepted 8 June 2023
INTRODUCTION
End-stage renal disease (ESRD) impacts over 1500 people per million populations in high-prevalence countries like Taiwan, Japan, and the United States Nearly two-thirds of ESRD patients receive hemodialysis (HD), one-quarter receive kidney transplants, and one-tenth require peritoneal dialysis (1) Three types of procedures are commonly performed for HD, an indwelling central venous catheter, an AF, and prosthetic BGs The ideal access
should deliver a flow rate sufficient for performing effective dialysis, durable, easily punctured, and has a low complication rate (2) AF comes closest to fulfilling these criteria, but AF use depends on the identification of a suitable artery and vein (3) Autogenous arteriovenous radial cephalic or brachial cephalic fistulas were recommended as 1st-line choices for vascular access by the Kidney Disease Outcome Quality Initiative (KDOQI) (4) However, not all HD patients can have a distal forearm fistula due to the small size of the vessel, diseased or exhausted peripheral veins, and arteries Additionally, around 30% of the fistulas fail within 3 years and need alternative vascular access Alternative access options are brachiocephalic AF in the forearm or brachial basilic AF in the arm or forearm or an arteriovenous BG in the arm Brachiocephalic AF is the second option if a radial cephalic or forearm AF fails or is unsuitable (5, 6) However, when the cephalic vein in the arm cannot be utilized, a brachial basilic AF could be constructed This study highlights our clinical surgical results for all types of basilic vein-based fistulas comparable to the results of prosthetic BG-based fistulas performed in the same period
PATIENTS AND METHODS
Between March 2018 and February 2020, 72 patients were included in this retrospective study whose basilic vein was used for brachial-basilic AF at our hospital, and their surgical results were compared to the results of arm prosthetic BG constructed for hemodialysis Patients included in this study had either previously failed radial-cephalic and brachial-cephalic AF operations or the diameter or quality of the arteries and cephalic veins are not suitable for AF construction The most frequently linked diseases were recorded and analyzed Additionally, the patient’s demographics including age and gender were collected and analyzed All cases were preoperatively examined using Doppler ultrasonography (USG) for assessment of basilic and cephalic veins Furthermore, central veins (jugular and subclavian veins) were examined for occlusion and stenosis Because the procedures necessitated long incisions and basilic vein dissection, they were carried out under region-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11455 1
ORIGINAL PAPER
Use of Basilic vein in arteriovenous fistulas construction for hemodialysis access. Is it a good option alternative to prosthetic arteriovenous grafts?
Ehab M. Abdo 1 , Tamer A. Abouelgreed 2 , Waleed E. Elshinawy 1 , Nehal Farouk 1 , Mohamed A. Abdelaal 2 , Hassan Ismail 2 , Amal H. Ibrahim 3 , Samar A. Kasem 3 , Ahmed A. Aboomar 4
DOI: 10 4081/aiua 2023 11455
al or general anesthesia The basilic vein arises from the dorsal venous network of the hand and travels the medial aspect of the upper limb The vein travels deep into the arm towards the teres major boundary It joins the brachial veins of the deep venous system creating the axillary vein Different techniques were used to construct brachial basilic AF: two stages of basilic vein elevation and transposition without anastomosis, two stages of arm basilic vein transposition and re-anastomosis, and forearm basilic vein loop transposition The first stage consists of creating an end-to-
side basilic vein to the brachial artery fistula at the elbow level with 6/0 polypropylene sutures The second stage is scheduled to begin in 6-8 weeks First, a small incision was made in the antecubital region to locate both the basilic vein and brachial artery Then the incision was extended proximally to expose the proximal portion of the basilic vein To prevent injury, the median antebrachial cutaneous nerve waa carefully separated from the vein After isolating the basilic vein, a subcutaneous flap was performed, and the vein was transposed without being transacted (Figure 1) The subcutaneous flap was then sutured in place between the nerve and the transposed vein on the ventral surface of the arm If the nerve had crossed the basilic vein and could not be spared without causing injury, or if the vein length was sufficient, the basilic vein was transacted at the level of the antecubital fossa and transported through a tunnel created over the deep fascia beneath the skin Then, the vein was gently augmented with heparinized saline and anastomosed to the basilic vein stump (Figure 2)
If the basilic vein diameter in the forearm is appropriate but the forearm arteries are not, the vein was exposed along its course in the forearm and its tributaries were tied before the vein was transected distally and mobilized through a subcutaneous forearm tunnel to be anastomosed to the brachial artery (end-to-side technique with 6/0 polypropylene sutures) (Figure 3)
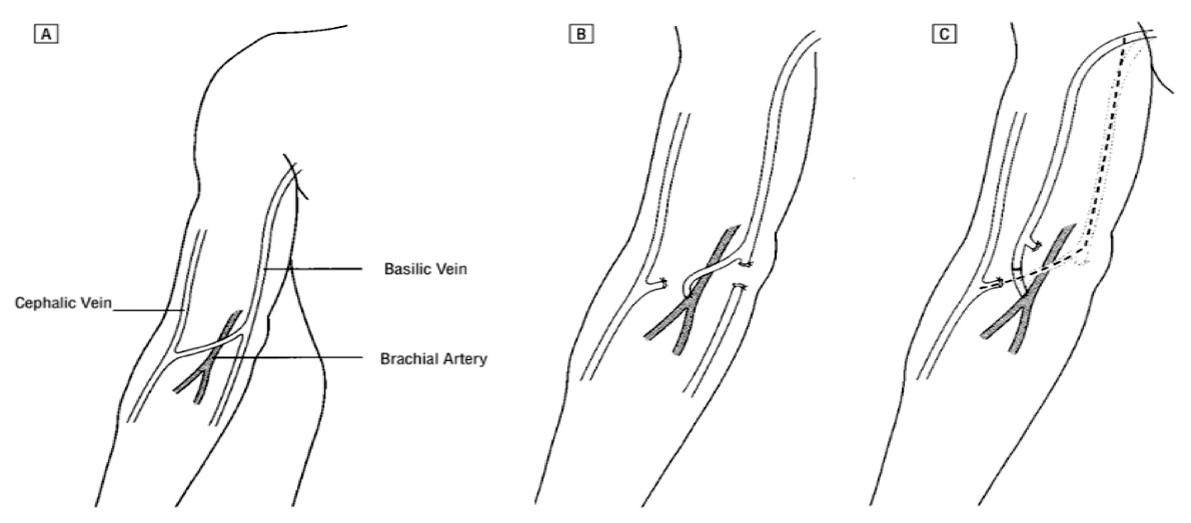
Thirty-two patients had prosthetic BG fistulas during the same study period All grafts are made of Polytetrafluoroethylene (PTFE) material The cases were discharged the day after the surgery Postoperatively, the cases were followed up for twelve months and any procedure-linked complication or mortality was recorded If not related to the p r o c e d u r e , d e a t h w i t h a p r o p e r l y working fistula was regarded as a failure to follow-up For short segment t h r o m b o s e d b r a c h i a l b a s i l i c A F , thrombectomy was performed with or without balloon angioplasty (PTA) But for long segment thrombosis, the fistula was abandoned Technical success was described as the occurrence of a bruit or thrill on the arteriovenous fistula Primary patency was described as the time at which the fistulas were functioning for hemodialysis until the time when an intervention was perf o r m e d t o r e e s t a b l i s h o r m a i n t a i n access patency Secondary patency was described as the time from successful access cannulation until access aban-
(A) Ultrasound-guided marking of basilic vein
(B) Augmentation of a mobilized basilic vein after ligation of its branches


(C) The looped basilic vein was anastomosed to the brachial artery.
(D) Two weeks postoperative
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11455 E M Abdo, T A Abouelgreed, W E Elshinawy, et al 2
Figure 1.
Mobilization of the matured basilic vein (retracted with red vessel loop)
Figure 2.
Schematic diagram showing the normal anatomy (A) and the procedure The basilic vein is anastomosed to the brachial artery (B) The arterialized basilic vein is superficialized and re-anastomosed (C).
Figure 3.
donment, or the patient has demised regardless of how often interventions are required to maintain patency
Overall patency was described as the patency of all HD accesses involved in this project
Statistical analysis
Statistical analysis was performed with the SPSS for Windows version 23 0 (SPSS Inc , Chicago, IL, USA) Data were explored for normality utilizing KolmogorovSmirnov and Shapiro-Wilk tests The following tests were done: independent-samples t-test of significance was utilized when comparing between two means A chi-square (𝝌2) test was also used to compare qualitative parameters' proportions The influence of the different variables on the specific access type was analyzed using the log-rank test
P-value < 0 05 was regarded as statistically significant
Ethical approval and consent for participation
All procedures performed in this study complied with institutional and/or national research council ethical standards as well as the 1964 Declaration of Helsinki and its subsequent amendments or similar ethical standards
Protocols and written informed consent for all participants were approved by the Research Ethics Committee of the Faculty of Medicine for Girls, Al-Azhar University (FMGIRB) (approval Number: 1403/22)
RESULTS
Seventy-two patients were offered 72 AFs (47 males, 25 females), while another 32 cases (22 males, 10 females) received upper arm prosthetic BG during the same period
The mean age of the cases who received AF and upper arm AV grafts was 55 (37 to 74) and 54 (37 to 75) years, respectively Table I displays demographic information for patients Nondominant left upper extremities were preferred in 55 patients who received AFs (76 3%) and 22 patients who received prosthetic BG (68 7%) Different techniques were used to construct brachial cephalic AF: two-stages basilic vein elevation and transposition without re-anastomosis (22 patients), two-stages arm basilic vein
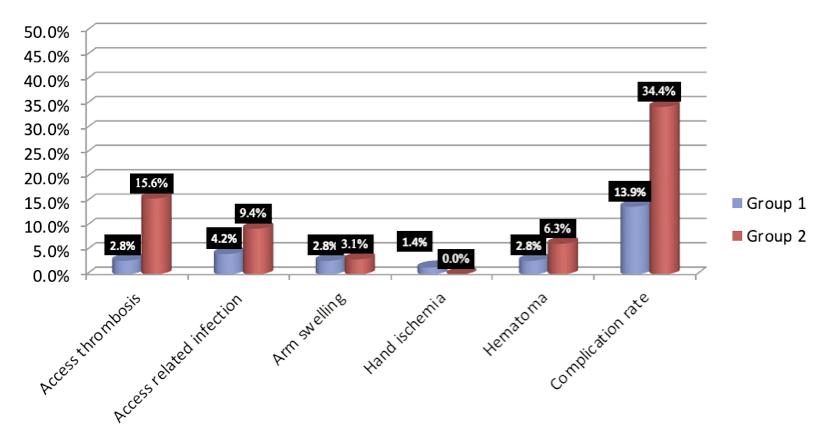
1. Patient’s characteristics
transposition with re-anastomosis (28 patients), and forearm basilic vein loop transposition (22 patients) No procedure-linked mortality Technical success was obtained in all cases (100%) (Table 1) The complication rate for AFs was (13 9%) while the complication rate for the BGbased fistulas was (34 4%) Complications of AFs requiring additional procedures to maintain patency developed in 6 patients (8 3%), including 2 patients who revealed prolonged arm swelling because of subclavian vein occlusion for which balloon angioplasty was successful to dilate one lesion and failed to treat the other because of failure of the guidewire to cross the lesion and 2 fistulas necessitating surgical thrombectomy for acute short segment thrombosis In addition, the brachial basilic fistula was banded in 1 case with hand ischemia, and 1 case required reexploration for postoperative bleeding Complications of prosthetic BG-based fistulas requiring additional procedures developed in 8 cases (25%), involving 5 patients that were treated by surgical thrombectomy for acute graft thrombosis PTA was used to dilate proximal subclavian vein stenosis in 1 patient who revealed arm swelling Two patients who presented with postoperative bleeding were explored for control of bleeding Access-related complications are described in Figure 4
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11455 3 Use
in arteriovenous
for hemodialysis access
of Basilic vein
fistulas construction
Age (years) Mean ± SD 55 15 ± 10 96 54 19 ± 10 98 t = 0 414 0 680 Range 37-74 37-75 Gender Female 25 (34 7%) 10 (31 3%) 𝝌2 = 0 120 0 729 Male 47 (65 3%) 22 (68 8%) Comorbidities IHD 25 (34 7%) 12 (37 5%) 0 075 0 785 DM 50 (69 4%) 20 (62 5%) 0 486 0 486 HTN 43 (59.7%) 16 (50.0%) 0.853 0.356 HD: schem c heart d sease; DM: diabetes m l ets; HTN: hypertension
Table
Patient’s AF group Prosthetic BG fistulas Test value p-value characteristics (n = 72) (n = 32)
Figure
4.
Access-related complications
Group 1 represents AF patients and group 2 represents Prosthetic BG patients
Cannulation of AF started at an average of 59 (range, 40 to 85) days after the first surgery While cannulation of prosthetic bridging grafts started at an average of 15 (range, 14 to 20) days post-surgery A statistically significantly higher primary patency rate was noticed for the AF in comparison to the BG-based fistulas, with a 12-months primary patency rate of 77 7% and 53 1% for AF and BGbased fistulas groups, respectively (p < 0 012) A similar pattern was noticed for secondary patency rates as well, with a 12-months secondary patency rate of 62 5% and 42 8% for AF and BG-based fistulas, respectively (p = 0 063) The AF group had a superior overall patency rate in comparison to the BG-based fistulas (84 7% and 59 3% respectively)
All patients completed 1-year follow-up
DISCUSSION
The Kidney Disease Outcome Quality Initiative (KDOQI) guidelines recommended native fistulas over graft fistulas
(7) The radial-cephalic fistula at the wrist was first described in 1966 and is still considered the procedure of choice because it is easy to construct, has good long-term results, and low blood flow rate so distal steal is uncommon, and nearly never results in high output cardiac failure It also preserves the upper arm vessels for future use
(8) Proximal accesses are required in some situations like patients with prior forearm AF dysfunction, and patients with a sclerosed vascular system, furthermore, if the distal veins have been subjected to repeated trauma from punctures and indwelling catheters, the radial artery, and forearm veins are deemed inappropriate for AF Proximal accesses are easier to cannulate, have a longer vein or graft length for cannulation, have a higher blood flow with an increased chance for steal syndrome, and may result in high output cardiac failure (9) After the cephalic vein-based AF has exhausted as primary vascular access choice, the available options are a brachial basilic AF or a forearm or arm prosthetic BG-based fistula Upperextremity access with PTFE has been found effective, but complication rates are higher and patency rates are lower than with autologous fistulas (10) Several studies have recommended AFs over prosthetic BG-based techniques based on improved patency rates and fewer interventions (11) Furthermore, clinical practice guidelines from the USA, Australia, Canada, and the UK all recommend an AF over a prosthetic graft for chronic HD access (12) The majority of participants in this review were of working age (37-75 years old) (65%) Diabetic nephropathy was the most frequent cause of ESRD in both groups Males are more affected by ESRD than females These previous results are echoic to the results of other studies performed in KSA to study the prevalence of ESRD and related risk factors (13) In regards to patient demographic variables, no significant differences were detected between the two groups Technical success was achieved in all cases In our study, the procedure-related complication rate after AF (13 9%) was statistically significantly lower than for the upper arm prosthetic BG (34 4%) Reported results of AF showed a complication rate lower than BG because a native vein fistula is more resistant to infection than a prosthetic graft, the large-caliber basilic vein offers a high
flow rate because AF only needs one anastomosis and venous outlet stenosis can be reduced, limiting the most common problem encountered with PTFE (14, 15) The most prevalent complication in this review was access thrombosis, which was significantly more common in BG (15 6%) than in AF (2 8%) (p = 0 062) Early graft thrombosis was caused by a technical error, but late graft thrombosis was caused by anastomotic stenosis caused by intimal hyperplasia More procedures were required to keep the patency of the BG-based fistulas compared to AF e c h o i n g p r e v i o u s r e s u l t s f r o m o t h e r r e p o r t s ( 1 6 ) Wound-related infection was not statistically significant for both groups but some studies reported an increased incidence of infection with AF as it requires longer incisions Minimally invasive approaches like video-assisted basilic vein transposition have been used to minimize wound complications (17) Cannulation of the AF began on average 59 days after the first surgery, while cannulation of the BG began on average at 15 days, which was consistent with the Dialysis Outcomes Quality Initiative (DOQI) guidelines for access maturation, which state that a dialysis AV graft should not be used until 14 days after it has been placed (19) When deciding on AF, the anticipated time for maturation and cannulation should be balanced against the elevated risk of complications associated with prolonged central venous catheterization and the reduced quality of life linked with the tunneled catheter Prosthetic BG was considered for cases with a short life expectancy and those who could not tolerate tunneled central venous catheters in place The tunneled forearm basilic vein loop technique has the advantages of earlier cannulation, being easily accessible, and preserving the proximal portion of the basilic vein for future use When compared to BG, AF procedures had higher primary, secondary, and overall patency rates Previous studies reported higher primary patency rates of AF, ranging from 65 to 70% at one year and 49 to 51% at two years (19) A limitation of the article is the small sample size and also a smaller representation of the forearm BB AVG group
CONCLUSIONS
Brachial basilic AF is a technically successful procedure with higher patency rates and lower operative complication rates than prosthetic BG Furthermore, if the AF fails and the venous outflow is open, there is a chance that BG could be used in the future at the same site We suggested that for patients with failed forearm dialysis fistulas and no adequate cephalic vein, a brachial basilic fistula be regarded as an alternative to prosthetic graft insertion Patients with a short life expectancy or those who are unable to tolerate tunneled central venous catheters should consider prosthetic BG
REFERENCES
1 Maaz Abbasi, Glenn M Chertow, and Yoshio N Hall End-stage renal disease BMJ 2010; 7:1-16
2 Michael B Silva, JR and Brajesh K LAL Decision making in vascular surgery by Jack L Cronenwett, and Robert B Rutherford Copyright 2001 Chapter 72:354-359
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11455 E M Abdo, T A Abouelgreed, W E Elshinawy, et al 4
3 Kherlakian GM, Roedersheimer LR, Arbaugh JJ, et al Comparison of autogenous fistula versus expanded polytetrafluoroethylene graft fistula for angioaccess in hemodialysis Am J Surg 1986; 152:238243
4 Vascular Access Work Group, “Clinical practice guidelines for vascular access, ” Am J Kidney Dis 2006; 48:248-273
5 Oliver MJ, McCann RL, Indridason OS, Butterly DW Comparison of transposed brachiobasilic fistulas to upper arm grafts and brachiocephalic fistulas Kidney Int 2001; 60:1532-1539
6 Hakaim AG, Nalbandian M, Scott T Superior maturation and patency of primary brachiocephalic and transposed basilic vein arteriovenous fistulae in patients with diabetes J Vasc Surg 1998; 27:154-157
7 Oliver MJ, McCann RL, Indridason OS, et al Comparison of a transposed brachiobasilic fistula to upper arm grafts and brachiocephalic fistulas Kidney Int 2001; 60:1532-1539
8 Brescia MJ, Cimino JE, Apple K, Hurwich BJ Chronic hemodialysis using venipuncture and a surgically created arteriovenous fistula N Engl J Med 1966; 275:1089-1092
9 Bender MHM, Bruyninckx CMA, Gerlag PGG The brachiocephalic elbow fistula: a useful alternative angioaccess for permanent hemodialysis J Vasc Surg 1994; 20:808-813
1 0 K h e r l a k i a n G M , R o e d e r s h e i m e r L R , A r b a u g h J J , e t a l Comparison of autogenous fistula versus expanded polytetrafluoroethylene graft fistula for angioaccess in hemodialysis Am J Surg 1986; 152:238-2343
11 Benedetto BJ, Madden RL, Kurbanov A, Lipkowitz GS Transposed
Correspondence
Ehab M Abdo, MD ehababdo48@yahoo com
Waleed E Elshinawy, MD waleed elshinay82@gmail com
Nehal Farouk, MD dr nehalfarouk@yahoo com
Department of Vascular Surgery, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Tamer A Abouelgreed, MD (Corresponding Author) dr tamer ali@yahoo com
tamerali 8@azhar edu eg
Mohamed A Abdelaal, MD maal uro@yahoo com
Hassan Ismail, MD drhassan ismail@yahoo com
Department of Urology, Faculty of medicine, Al-Azhar University, Cairo, Egypt
Amal H Ibrahim, MD mkellany@yahoo com
Samar A Kasem, MD summerahmed1983@yahoo com
Department of Internal Medicine, Nephrology Unit, Faculty Medicine, Al-Azhar University, Cairo, Egypt
Ahmed A Aboomar, MD ahmed abo omar12@yahoo com
Department of Internal Medicine, Nephrology Unit, Faculty Medicine, Tanta University, Tanta, Egypt
basilic vein fistula: a superior alternative to prosthetic grafts? Curr Surg 2000; 57:503-504
12 M A Frances D, Yufan LU, Amanda J Robertson, Robert J Millar and Jayne Amy Two-stage brachiobasilic arteriovenous fistula for chronic hemodialysis access ANZ J Surg 2007; 77:150-151
13 Hussain Gadelkarim Ahmed, Tahani Altamimi Survey for potential risk factors for susceptibility to chronic kidney disease in Hail region, in KSA Management in health XVII/122013; pp 31-36
14 Kumar A, Sinha S, Sharma AK Long-term results of arteriovenous fistulas using transposed autologous basilic vein Br J Surg 2000; 87:1735-1736
15 Taghizadeh A, Dasgupta P, Khan MS, et al Long-term outcomes of brachiobasilic transposition fistula for hemodialysis Eur J Vasc Endovasc Surg 2003; 26:670-672
16 Sgroi MD, Patel MS, Wilson SE, et al The optimal initial choice for permanent arteriovenous hemodialysis access J Vasc Surg 2013; 58:539-548
17 Hayakawa K, Tsuha M, Aoyagi T, et al New method to create a vascular arteriovenous fistula in the arm with an endoscopic technique J Vasc Surg 2002; 36:635-638
18 Chieh-Hung Lee, Po-Jen Ko, Yun-Hen Liu, et al Brachiobasilic Fistula as a Secondary Access Procedure: An Alternative to a Dialysis Prosthetic Graft Chang Gung Med J 2004; 27:816-23
19 Murphy GJ, White SA, Knight AJ, et al Long-term results of arteriovenous fistulas using transposed autologous basilic vein Br J Surg 2000; 87:819-23
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11455 5 Use
in arteriovenous
construction for hemodialysis access
of Basilic vein
fistulas
ORIGINAL PAPER
The outcome of ultrasound-guided insertion of central hemodialysis catheter
Ehab M. Abdo 1 , Tamer A. Abouelgreed 2 , Waleed E. Elshinawy 1 , Nehal Farouk 1 , Hassan Ismail 2 , Amal H Ibrahim 3 , Samar A Kasem 3 , Lobna Kh Sakr 4 , Naglaa M Aboelsoud 4 , Nermeen M Abdelmonem 5 , Salma F Abdelkader 6 , Ahmed A Abdelwahed 6 , Anas A Qasem 7 , Mosab F Alassal 8 , Ahmed A Aboomar 9
1 Department of Vascular Surgery, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
2 Department of Urology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
3 Department of Internal Medicine, Nephrology Unit, Faculty Medicine, Al-Azhar University, Cairo, Egypt;
4 Department of Radiology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
5 Department of Radiology, Thumbay University Hospital, Ajman, UAE;
6 Department of Radiology, Faculty of Medicine Ain Shams University, Cairo, Egypt;
7 Department of Internal Medicine, Faculty Medicine, Zagazig University, Zagazig, Egypt;
8 Department of Vascular Surgery, Saudi German Hospital, Ajman, UAE;
9 Department of Internal Medicine, Nephrology Unit, Faculty of Medicine, Tanta University, Tanta, Egypt
Summary
Objective: To point out our experience and assess the efficacy and safety of real-time ultrasound-guided central internal jugular vein (IJV) catheterization in the treatment of hemodialysis patients
Methods: This retrospective study comprised 150 patients with end-stage renal disease (ESRD) who had real-time ultrasonography (US)-guided IJV HD catheters placed in our hospital between March 2019 and March 2021 Patients were examined for their demographic data, etiology, site of catheter insertion, type (acute or chronic) of renal failure, technical success, operative time, number of needle punctures, and procedure-related complications Patients who have had multiple catheter insertions, prior catheterization challenges, poor compliance, obesity, bony deformity, and coagulation disorders were considered at high-operative risk.
Results: All patients experienced technical success In terms of patient clinical features, an insignificant difference was observed between the normal and high-risk groups (p-value > 0 05) Of the 150 catheters, 62 (41.3%) were placed in high-risk patients. The first-attempt success rate was 89 8% for the normal group and 72.5% for the high-risk group (p = 0.006). IJV cannulation took less time in the normal-risk group compared to the highrisk group (21.2 ± 0.09) minutes vs (35.4 ± 0.11) minutes, (p < 0 001) There were no serious complications During the placing of the catheter in the internal jugular vein, four patients (6 4%) experienced arterial puncture in the high-risk group Two participants in each group got a small neck hematoma One patient developed a pneumothorax in the high-risk group, which was managed with an intercostal chest tube insertion
Conclusions: Even in the high-risk group, the real-time US-guided placement of a central catheter into the IJV is associated with a low complication rate and a high success rate Even under US guidance, experience lowers complication rates Real-time USguided is recommended to be used routinely during central venous catheter insertion
KEY WORDS: Central HD catheters; Hemodialysis; Central HD catheters; Real-time ultrasound
Submitted 17 July 2023; Accepted 30 July 2023
INTRODUCTION
Two-thirds of end-stage renal disease (ESRD) patients undergo hemodialysis (HD), one-quarter have kidney transplants, and one-tenth require peritoneal dialysis (1) For HD, three access procedures are commonly used: an autogenous arteriovenous fistula (AVF), a prosthetic bridging graft (BG), and an indwelling central venous catheter The ideal access should be durable, easily punctured, provide a sufficient flow rate for efficient dialysis, and have a low complication rate (2) The autogenous AVF was approved by the Kidney Disease Outcome Quality Initiative (KDOQI) recommendations as to the first-line technique for vascular access since it tends to get closer and closer to meeting these standards (3) Although AVF is the first option for permanent vascular access, it is required at least 6-8 weeks pass after its construction before using it (4, 5) Furthermore, persistent respiratory failure, ischemia steal syndrome, and patients with severe cardiac failure may not be suitable for AVF (6, 7) The BGs should not be punctured before 14 days and are not recommended as primary vascular access As a result, both permanent and temporary cuffed tunneled catheters are used in these cases and in those with acute HD (8, 9) If the patient needs access for longer than a month, tunneled catheters should be used (10) According to a recent report, approximately 80% of those with ESRD will require a hemodialysis catheter during their long-term treatment (11) Anatomical landmarks are used in traditional hemodialysis catheter insertion methods The absence of a pulsatile flow pattern and the dark color of venous blood indicate successful cannulation Based on landmarks, success rates range from 60% to more than 90%, with the reported risk of complications ranging from 5% to 20% (12) Anatomical landmark methods have a higher failure rate, require more attempts, and have a higher complication rate (13) Long-term problems such as thrombosis, infections, and central venous stricture, as well as early complications like pneumothorax, arterial puncture, and puncture site hematoma, have been attributed to HD catheters (14) In 1973, the first description of catheter
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11588 1
DOI: 10 4081/aiua 2023 11588
implantation into the IJVs using US guidance was published (15) To lower the arterial puncture risk, US guidance has been followed (16) As a result, the National Kidney Foundation suggested using real-time ultrasound to guide the central venous catheters’ insertion, to improve insertion success and reduce placement-related complications as well as fluoroscopic screening for proper catheter tip localization after tunneled catheter insertion (5) In the real-time US, the US probe can be positioned longitudinally, leading to a long-axis view on the screen, or transversely relative to the vessel, resulting in a cross-sectional image of the vessel on the screen The cross-sectional image offers the advantage of enhanced vein imaging in association with the artery and other anatomic structures, which may help prevent accidental arterial puncture (17) The needle, on the other hand, is only visible as a hyperechoic point in the cross-sectional picture, which may or may not be the needle's tip The entire needle, as well as the needle tip depth, are visible on the US image when utilizing the long-axis view, decreasing posterior venous wall puncture (18) The current research aimed to assess the complication rate and technical success and provide our center's experience with real-time US-guided IJV central cannulation for HD patients

MATERIALS AND METHODS
This retrospective study included all patients who had USguided internal jugular vein (IJV) central HD catheters placed at our facility between March 2019 and March 2021 All procedures performed in this study complied with institutional and/or national research council ethical standards as well as the 1964 Declaration of Helsinki and its subsequent amendments or similar ethical standards Protocols and written informed consent for all participants were approved by the Research Ethics Committee of the Faculty of medicine, Al-Azhar University (FMG-IRB)
The medical records of 150 participants with ESRD were examined Demographic data like age and gender were collected and analyzed Other Information like the etiology and type (acute or chronic) of renal failure, operative time, number of needle punctures, technical success, site of catheter insertion, and procedure-related complications were also collected and analyzed Patients were considered high risk if they had multiple catheter insertions, had prior catheter difficulties, had poor compliance, were obese, had disturbed conscious levels, had a bony deformity, or had a blood coagulation disorder Prior and post-insertion chest X-ray findings were reviewed Prior to catheter implantation, all participants underwent full blood count, and coagulation profiles were examined Fresh frozen plasma was used when necessary For the procedure, all patients signed a written informed consent form Permanent tunneled catheters were silicon-based and featured two lumens with a diameter of 14-15 F Depending on the body size of the participant, the length was optimized (19, 23, or 28 cm) The catheters' Dacron cuffs were around 5 cm away from the exit point, providing a barrier to infections and stability by forming fibrous tissue around them All procedures were carried out in the main operating room, which has a portable US machine (Esaote MyLab One, MeCan Medical, China) and a portable C-arm machine available all the time
Vascular surgery consultants or senior specialists carried out all procedures The skin overlying the intended insertion location was prepared, cleaned, and draped while the patient was supine IJVs were used for permanent catheters first on the right and then on the left (in case of thrombosis or stenosis of the right one) If both veins are obstructed, the subclavian vein was utilized Using a 7 MHz linear probe, the internal jugular vein was visualized horizontally After monitoring the carotid artery on the medial side and the internal jugular vein on the lateral side, the vein's compressibility and the artery's pulsatility were investigated (Figure 1) Cannulation of the IJV was attempted The operator noticed the needle's pathway while centering a large-bore needle (16 G, 10 cm) under the middle of the probe at a 45° slope to the skin (Figure 2)


Archivio Italiano di Urologia e Andrologia 2023; 95(3):11588 E M Abdo, T A Abouelgreed, W E Elshinawy, et al 2
Figure 1.
Visualizing the carotid artery and the IJV using real-time US.
Figure 2 A needle is directed towards the middle of the probe at a 45° slope to the skin to cannulate the IJV.
Figure 3. Detection of a flush of blood coming out of the IJV
The needle path shows up as a spot in the horizontal view and a hyperechoic line in the longitudinal view, with ringdown artifacts When a flush of blood was detected, the US probe was taken down and the conventional Seldinger method was performed under fluoroscopic guidance (Figure 3) and (Figure 4)
Statistical analysis was carried out by SPSS for Windows version 13 0 The mean ± and standard deviation of numerical variables were calculated
The paired Student, t-test, or Mann-Whitney U test was utilized for intergroup comparisons P values less than 0 05 was significant statistically
RESULTS
150 HD patients were categorized into two groups: normal (88) and high-risk (62) Female patients represent (64 7%, and 35 4%) respectively, while male patients represent (65 3% and 64 5%) respectively The patients' mean ages were 55 (37 to 74) for the normal group and 54 (37 to 75) for the high-risk group Table 1 presents the clinical characteristics of the study patients The nephrology clinics referred 126 patients (84%), while other clinics referred the remaining (16%)
Diabetes mellitus was ESRD’s most common etiology, accounting for 54 individuals (36%), and hypertension in 22 (14 6%) Other causes like chronic glomerulonephritis, polycystic kidney disease, obstructive uropathy, and unknown accounted for 49 4% of patients In the normal group, 79 (89 7%) catheters were inserted through the right IJV, while 9 (10 2%) catheters were inserted through the left IJV Thirty-two catheters (51 6 percent) were inserted through the right IJV in the high-risk group, while 30 (48 3 percent) were inserted through the left IJV 70 (79 5%) participants within the normal group and 23 (37 1%) participants within the high-risk group had their first dialysis session after catheterization; the remaining patients were already on regular HD therapy and required new vascular access because of the failed previous one 21 (33 8%) of the high-risk group referred to us due to catheter malfunction For the high-risk group, fresh frozen plasma was given to 5 patients prior to the procedures due to abnormalities in the coagulation profile IJV cannulation was performed on all patients
The normal group's first-attempt success rate was 89 8%, while the high-risk group was 72 5% (p = 0 006)
The high-risk group took longer to cannulate IJV than the normal-risk group (35 4 ± 0 11) minutes versus (21 2 ± 0 09) minutes (p < 0 001) Table 2
During the study, no serious complications took place Arterial puncture did not occur in either of the patients in the normal group, but it did occur in four patients (6 4%) within the high-risk group during catheter insertion in the IJV (p = 0 017) Two patients in each group got a small neck hematoma After placing a left IJV tunneled



Archivio Italiano di Urologia e Andrologia 2023; 95(3):11588 3 The
outcome of ultrasound-guided insertion of central hemodialysis catheter
Table 1 Patient’s clinical characteristics Patient’s Normal group High-risk group P-value characteristics (n = 88) (n = 62) Age (years) # Mean ± SD 55 15 ± 10 96 54 19 ± 10 98 0 598 Range 37-74 37-75 Gender ▲ 0 888 Female 31 (64 7%) 22 (35 4%) Male 57 (65 3%) 40 (64 5%) Comorbidities ▲ IHD 23 (26 1%) 15 (24 1%) 0 782 DM 48 (54.5%) 38 (61.2%) 0.416 HTN 51 (57 9%) 39 (62 9%) 0 540 # Independent Sample t-test; ▲: Ch -square test; P-value > 0 05 NS
2. The number of venous cannulation attempts and average procedure time Normal group High-risk group P-value (n = 88) (n = 62) Number of attempts ▲ 1 79 (89 8%) 45 (72 5%) 0 006* 2 9 (10 2%) 14 (22 6%) 0 039* > 2 Non 3 (4 9%) 0 037* Average procedure time (35.4 ± 0.11) minutes (21.2 ± 0.09) minutes < 0.001** # Independent Samp e t-test; ▲ Chi-square test; P-va ue > 0 05 NS; * p-value < 0 05 S; ** P-va ue < 0 001 Figure 4A Progression of the catheter inside a subcutaneous tunnel Figure 4B. Peeling the peel-away sheath Figure 4C. Testing the catheter for smooth blood flow (right)
Table
permanent catheter, one patient in the high-risk group developed a pneumothorax, which was managed by inserting an intercostal chest tube
DISCUSSION
Traditionally, anatomical feature sites have been used for central venous access placement Despite this, the landmark procedure was associated with a statistically significant risk of complications and failure rate due to the p a t i e n t s ' a b n o r m a l a n a t o m y a n d p ro b a b l e v a s c u l a r pathology, as well as depending on the individual operators' proficiency (19) Prior studies conducted reported a 35% failure rate for central vein catheterization using anatomic landmarks alone, with published complication rates ranging from 5% to 40% (20) The US access guidance has lately become commonly utilized as a quality indicator to prevent procedure-related sequelae Realtime ultrasonography has been utilized for directing interventional procedures in a variety of situations for many years and has become a clinical practice standard Because of technological advancements and enhanced image quality, real-time ultrasound allowed for the location of the appropriate target vessel and optimized puncture site Anatomical variation is easily identified, and venous thrombosis is excluded (21) There is strong evidence that using real-time ultrasound guidance for vascular access increases the procedure's safety and efficacy when compared to anatomical landmarks Numerous studies have found that using ultrasonography during central venous catheterization improves clinical and technical success and reduces technical difficulties (22)
In a study comparing the US Guided central venous catheterization to the anatomical landmark technique, the total rate of success was estimated to be higher in the US-guided technique (98% vs 90%), and the first attempt success rate was higher in the US-guided technique (80 vs 60 %) With US-guided catheterization, the complication rate was also significantly smaller (arterial puncture, 1% vs 8% pneumothorax, 0 vs 4% and neck hematoma, 4% vs 10%) (23) US guidance was found to significantly minimize the probability of arterial puncture (p = 0 002) in a randomized study (9) The blind technique was not preferred in our study, even in emergencies, because the portable US machine was available in the operating room around the clock Furthermore, only the real-time method was used, rather than the static technique, as European Best Practice Guidelines strongly suggested that real-time ultrasound guidance, rather than ultrasound assistance, be used routinely for both long- and short-term central venous access (Strong consensus) (100%) (19) In our research, we found an insignificant difference between the normal and highrisk groups regarding the patient’s clinical characteristics (p-value > 0 05) The most common cause of ESRD was diabetic nephropathy In this current study, the total success rate was (100%) and the first attempt's success rate was 82 6% (89 8 % for the normal group and 72 5 % for the high-risk group) Nine cases (10 2%) in the normal group required more than one attempt, while 17 cases (27 5%) in the high-risk group needed further attempts In the high-risk group, three cases needed 3 attempts
(one case was due to obesity, another patient had previous catheter difficulties, and the third was due to poor compliance) During this research, there were no recorded major complications The overall rate of arterial puncture was (2 6%) During catheter insertion in the IJV, only individuals in the high-risk group had an inadvertent arterial puncture Two patients in each group got a minor neck hematoma In the high-risk group, one patient developed pneumothorax after placing a left IJV tunneled permanent catheter which was managed with an intercostal chest tube insertion Our results regarding higher success rate and low complication rate were comparable to the results of the above-mentioned studies (9, 22) The current study's high success rate and low complication rate could be attributed to the use of US guidance, the procedures being performed by competent physicians, and the preferential use of IJVs as access sites Even under US guidance, the physician's experience, according to Tordoir et al , is an important determinant of the complication rate (4) No difference was found by Geddes et al between experienced and inexperienced physicians when US advice was utilized (24) In our report, we exclusively utilized subclavian veins in patients with IJV occlusions because they are no longer used routinely due to the risk of central venous stenosis
CONCLUSIONS
Real-time ultrasound has been indicated as a means to improve success rates, shorten operation time, and lower the number of complications associated with HD catheter implantation in IJVs Even when using US guidance, prior catheter placement experience reduces complication rates Ultrasound guidance is becoming a standard technique that should be recommend in all cases
REFERENCES
1 Maaz Abbasi, Glenn M Chertow, and Yoshio N Hall End-stage renal disease BMJ 2010; 7:1-16
2 Michael B Silva, JR and Brajesh K LAL Decision making in vascular surgery by Jack L Cronenwett, and Robert B Rutherford Copyright 2001 Chapter 72:354-359
3 Vascular Access 2006 Work Group Clinical practice guidelines for vascular access Am J Kidney Dis 2006; 48 (Suppl 1):S176-247
4 Tordoir J, Canaud B, Haage P, et al , European best practice guidelines on hemodialysis (EBPG) on vascular access, Nephrology Dialysis Transplantation 2007; 22(suppl 2): 88-117
5 National Kidney Foundation K/DOQI Clinical Practice Guidelines for vascular access Am J Kidney Dise 2000; 37(suppl 1): S137-S180
6 Ori Y, Korzets S, Katz M, et al The contribution of an arteriovenous access for hemodialysis to left ventricular hypertrophy, Am J Kidney Dis 2002; 40:745-752
7 Bay WH, Van Cleef S, Owens M The hemodialysis access: preferences and concerns of patients, dialysis nurses and technicians, and physicians Am J Nephrol 1998; 18:379-383
8 Rayner HC, Pisoni RL, Gillespie BW, et al Creation, cannulation, and survival of arteriovenous fistulae: data from the Dialysis Outcomes and Practice Patterns Study Kidney Int 2003; 63:323-330
9 Rayner HC, Besarab A, Brown WW, et al Vascular access results
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11588 E M Abdo, T A Abouelgreed, W E Elshinawy, et al 4
The outcome of ultrasound-guided insertion of central hemodialysis catheter
from the Dialysis Outcomes and Practice Patterns Study (DOPPS): performance against Kidney Disease Outcomes Quality Initiative (K/DOQI) Clinical Practice Guidelines Am J Kidney Dis 2004; 44:S22-S26
10 Weijmer MC, Vervloet MG, ter Wee PM Compared to tunnelled cuffed haemodialysis catheters, temporary untunnelled catheters are associated with more complications already within 2 weeks of use Nephrol Dial Transplant 2004; 19:670-7
11 Saran R, Li Y, Robinson B, et al US Renal Data System 2015 annual data report: epidemiology of kidney disease in the United States Am J Kidney Dis 2016; 67:A7-A8
12 Gupta PC, Burli P Ultrasound-guided vascular access J Indian Coll Cardiol 2016; 6S:92-94
13 Tammam TF, El-Shafey EM, Tammam HF Ultrasound-guided internal jugular vein access: comparison between short axis and long axis techniques Saudi J Kidney Dis Transplant 2013; 24:707-713
14 Zeki A, Meltem G, Sami U, et al Placement of hemodialysis catheters with a technical, functional, and anatomical viewpoint Int J Nephrol 2012; 302826:5
15 Ozersky DJ, Olson RM, Coons HG, et al Doppler controlled needle director: a useful adjunct to angiography Radiology 1973; 109:221-2
16 Oguzkurt L, Tercan F, Kara G, et al US-guided placement of temporary internal jugular vein catheters: immediate technical success and complications in normal and high-risk patients Eur J Radiol 2005; 55:125-9
17 Troianos CA, Hartman GS, Glas KE, et al Special articles: guide-
lines for performing ultrasound-guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists Anesth Analg 2012; 114:46-72
18 Stone MB, Moon C, Sutijono D, Blaivas M Needle tip visualization during ultrasound-guided vascular access: short-axis vs longaxis approach Am J Emerg Med 2010; 28:343-347
19 Jenssen C, Brkljacic B, Hocke M, et al EFSUMB Guidelines on Interventional Ultrasound (INVUS) Part VI ultrasound-guided vascular interventions Ultraschall Med 2016; 37:473-476
20 Denys BG, Uretsky BF, Reddy PS Ultrasound-assisted cannulation of the internal jugular vein A prospective comparison to the external landmark guided technique Circulation 1993; 87:1557-1562
21 Lorentzen T, Nolsoe CP, Ewertsen C, et al , EFSUMB Guidelines on Interventional Ultrasound (INVUS), Part I General Aspects (long Version) Ultraschall Med 2015; 36:E1-14
22 Christoph F Dietrich, et al , Ultrasound-guided central vascular interventions, comments on the European Federation of Societies for Ultrasound in Medicine and Biology guidelines on interventional ultrasound J Thorac Dis 2016; 8:E851-E868
23 Srceva MJ, Sazdov D, Todorova ZN Comparative analysis of ultrasound-guided central venous catheterization compared to blind catheterization Pril (Makedon Akad Nauk Umet Odd Med Nauki) 2017; 38:107-114
24 Geddes CC, Walbaum D, Fox JG, Mactier RA Insertion of internal jugular temporary hemodialysis cannulae by direct ultrasound guidance--a prospective comparison of experienced and inexperienced operators Clin Nephrol 1998; 50:320-5
Correspondence
Ehab M Abdo, MD ehababdo48@yahoo com
Waleed E Elshinawy, MD waleed elshinay82@gmail com
Nehal Farouk, MD dr nehalfarouk@yahoo com
Department of Vascular Surgery, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Tamer A Abouelgreed, MD (Corresèonding Author) dr tamer ali@yahoo com; tamerali 8@azhar edu eg
Hassan Ismail, MD drhassan ismail@yahoo com
Department of Urology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Amal H Ibrahim, MD mkellany@yahoo com
Samar A Kasem, MD summerahmed1983@yahoo
Department of Internal Medicine, Nephrology Unit, Faculty Medicine, Al-Azhar University, Cairo, Egypt
Lobna Kh Sakr, MD lobnakhaled910@hotmail com
Naglaa M Aboelsoud, MD nglaa mahmoud@gmail com
Nermeen M Abdelmonem, MD neeermeeenmohamed@gmail com
Department of Radiology, Thumbay University Hospital, Ajman, UAE
Salma F Abdelkader, MD salmafathy4@gmail com
Ahmed A Abdelwahed, MD
Department of Radiology, Faculty of Medicine Ain Shams University, Cairo, Egypt
Anas A Qasem, MD
Department of Internal Medicine, Faculty Medicine, Zagazig University, Zagazig, Egypt
Mosab F Alassal, MD
Department of Vascular Surgery, Saudi German Hospital, Ajman, UAE
Ahmed A Aboomar, MD ahmed abo omar12@yahoo com
Department of Internal Medicine, Nephrology Unit, Faculty Medicine, Tanta University, Tanta, Egypt
Department of Radiology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11588 5
ORIGINAL PAPER
Evaluation of risk factors for recurrent renal stone formation among Saudi Arabian patients:
Comparison with first renal stone episode
1 Department of Urology, King Abdullah bin Abdulaziz University Hospital, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia;
2 Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia;
3 Prince Sultan Military Hospital, Taif, Saudi Arabia;
4 Department of Urology, King Saud Medical City, Riyadh, Saudi Arabia;
5 Department of Urology, Tanta University Hospital, Tanta, Egypt;
6 Division of Urology, Surgery Department, Sharurah Armed Forces Hospital,
Summary
Objectives: We evaluated the baseline characteristics, and risk factors of renal stone recurrence among Saudi Arabian patients after successful primary stone treatment
Materials and methods: In this cross-sectional comparative study, we reviewed the medical records of patients who presented consecutively with a first renal stone episode from 2015 to 2021 and were followed-up by mail questionnaire, telephone interviews, and/or outpatient clinic visit We included patients who achieved stone-free status after primary treatment Patients were divided into two groups: group I (patients with first episode renal stone) and group Ⅱ (patients who developed renal stone recurrence) The study outcomes were to compare the demographics of both groups and to evaluate the risk factors of renal stone recurrence after successful primary treatment We used Student’s t-test, Mann Whitney test or chi-square (𝝌2) to compare variables between groups. Cox regression analyses were used to examine the predictors
Results: We investigated 1260 participants (820 males and 440 females) Of this number, 877 (69 6%) didn’t develop renal stone recurrence and 383 (30 4%) had recurrence Primary treatments were percutaneous nephrolithotomy (PCNL), retrograde intrarenal surgery (RIRS), extracorporeal shock wave lithotripsy (ESWL), surgery and medical treatment in 22 5%, 34 7%, 26.5%, 10.3%, and 6%, respectively. After primary treatment, 970 (77%) and 1011 (80 2%) of patients didn’t have either stone chemical analysis or metabolic work-up, respectively
Multivariate logistic regression analysis revealed that male gender (OR: 1 686; 95% CI, 1 216-2 337), hypertension
(OR: 2 342; 95% CI, 1 439-3 812), primary hyperparathyroidism (OR: 2.806; 95% CI, 1.510-5.215), low fluid intake (OR: 28 398; 95% CI, 18 158-44 403) and high daily protein intake (OR: 10 058; 95% CI, 6 400-15 807) were predictors of renal stone recurrence.
Conclusions: Male gender, hypertension, primary hyperparathyroidism, low fluid intake and high daily protein intake increase the risk of renal stone recurrence among Saudi Arabian patients
KEY WORDS: Renal stone; Risk factors; Recurrence; Saudi Arabia
Submitted 5 April 2023; Accepted 28 May 2023
INTRODUCTION
Worldwide, nephrolithiasis is one of the commonest urologic diseases In the last decades, the prevalence of nephrolithiasis has changed, with prevalence ranges from 7% to 13%, 5% to 9%, and 1% to 5% in North America, Europe, and Asia, respectively (1) The wide prevalence ranges among countries reflect several multifactorial conditions including age, sex, race, climate, occupation, dietary habits, fluid intake, genetic and metabolic diseases (2) In Asia, the prevalence and incidence of urolithiasis have increased in most of the countries specifically more in the south Asian countries than in the north Asian countries (5 5% to 11 6% compared to 2 6% to 7 2%, respectively) (3) This is because of the higher temperature and excessive sunshine exposure in the south countries than that in the north countries Saudi Arabia is located in the west Asian region and due to its high temperature and semiarid climate the prevalence of urinary tract stones was documented to be rising During the period from 1989 through 2008, the prevalence rate of urolithiasis has been increased from 6 8% (4) to 19 1% (5)
Renal stone recurrence is a devastating health problem, which affects the patients’ health-related quality of life (6), as well as represents an extra economic burden for its management (7) In a prospective study, Trinchieri et al studied the stone recurrence rate and risk after a first stone episode and found that 27% of patients developed symptomatic stone recurrence at mean follow-up of 7 5 years In addition, age at onset of the disease was significantly lower for patients with ≥ 2 recurrence than those who had only 1 or no recurrence (8) Among Asian countries, the reported recurrence rate of urolithiasis in the first year was about 6% to 17%, and at 5 years reaching up to 53%, while the lifetime risk of urinary stones recurrence is estimated to be 60% to 80% (9) In Saudi Arabia, Abdel-Halim et al reported a recurrence rate of renal stone ranging from 38 6% to 53 2% (4)
Studies evaluating the risk factors of renal stone recurrence are not common Our study aimed to explore the demographic characteristics of primary renal stones for-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11361 1
Mohammed Alshehri 1 , Hind Alsaeed 2 , Malath Alrowili 2 , Faisal Alhoshan 3 , Ali Abdel Raheem 4, 5 , Ayman Hagras 5, 6
DOI: 10 4081/aiua 2023 11361
Sharurah, Saudi Arabia
mer, as well as the risk factors of renal stone recurrence after successful primary treatment in Saudi Arabia We believe that the results of this study may provide an insight into ways that can help us to prevent the recurrence of renal stones
MATERIALS AND METHODS
Study design and ethical statement
A prospective cross-sectional comparative study was carried out at four Saudi Arabia's tertiary centers in Riyadh, Taif and Sharurah cities The study was approved by the institutional review boards and ethical committee of Princess Nourah bint Abdulrahman University and was performed in accordance with the ethical standards and the Helsinki declaration (Institutional review board “IRB” registration number: H-01-R-059) All patients included in our study signed a written informed consent
We reviewed the medical records of patients who presented consecutively with a first renal stone episode from 2015 to 2021 at urology departments of the participating centers From March 2020 through March 2021, patients were interviewed either during their follow-up visits in the clinic or by telephone interviews to fill out a questionnaire A total of 1260 patients completed the questionnaires successfully Patients were divided into two groups: group I (patients with first episode renal stone) and group II (patients who developed renal stone recurrence)
Inclusion and exclusion criteria
Patients aged ≥ 18 years old with history of successful primary renal stone treatments (i e , medical or surgical) were included in the current study We excluded patients with remaining stones after the initial stone episode, patient who had urinary tract malformation, urinary tract obstructive disease, history of pyeloplasty or ureteric reimplantation surgery, renal failure, chronic gastric diseases, and incomplete questionnaire data
Patients' characteristics
Demographic and baseline patients' characteristics were retrieved from our database including age, gender, body mass index (BMI), medical comorbidities such as diabetes mellitus (DM), hypertension (HTN), cardiac diseases etc, city of residency, nationality, family history of urolithiasis, and history of recurrent urinary tract infection (UTI)
Moreover, data regarding renal stone were gathered such as primary or recurrent renal stone, time to first recurrence, frequency of recurrence, previous treatment methods (either surgical or medical), chemical analysis of the stone, and routine metabolic work-up after successful primary treatment
Follow-up
All patients were followed-up after treatment at 6 weeks, 3 months then yearly until the last visit Routine postoperative imaging study included Kidney-Ureter-Bladder (KUB) X-ray, urinary ultrasound (UUS), or computed tomography (CT) scan that were performed according to the surgeon preference and/or stone radiopacity Stonefree status was defined as non-obstructing residual stone
fragments of ≤ 2 mm in size detected at 3 months posto
Recurrent renal stone was defined as new stone formation and/or stone growth during routine follow-up that was diagnosed radiologically (11)
Patients' lifestyle information regarding the level of physical activity per week and dietary habits were obtained through asking the patients to complete a previously p u b l i s h e d ( 1 2 , 1 3 )
e d questionnaire including selected items (1 question for physical activity and 5 questions for dietary habit) Questionnaires were disseminated among patients either in the clinic during follow up visits and/or through telephone calls The commonest dietary habits that are associated with increased risk of stone formation and recurrence include; low fluid intake (< 1 liter/day), high salt diet (> 10 g/day), high protein intake (> 100 g/day), lowcalcium diet (≤ 400 mg/day), and high intake of oxalate containing foods (14)
Outcome measurement
The primary outcome was to compare groups in order to evaluate the predictors of renal stone recurrence after successful primary treatment The secondary outcome was to assess demographic characteristics of stone formers in Saudi Arabia
Statistical analysis
Continuous variables were illustrated as mean ± standard deviation (SD) or median and interquartile range (IQR), whereas categorical variables were illustrated as frequency and percentages (%) To compare variables of group I and group II, we used the Student’s t-test, Mann Whitney test or chi-square (𝝌2) test to examine the statistical significance of normally distributed data, nonparametric data, or categorical data, respectively A univariable and multivariable Cox regression analyses were used to examine the predictors of renal stone recurrence All tests were twosided and P value of less than 0 05 was considered statistically significant
All tests used the SPSS version 23 software (IBM SPSS Statistics, IBM Corp , Armonk, NY, USA)
RESULTS
A total of 1260 participants (820 males and 440 females) with history of successful renal stone primary treatment completed the questionnaire and were included in our study Baseline patients’ clinical and demographic data are summarized in (Table I) Median patients’ age was 29 years (IQR: 23-41), and median BMI was 25 3 kg/m2 (IQR: 21 8-29) The incidence of HTN was 10 2% and PHPT was 5 8% Most of patients 811 (64 4%) are living in the central region of the country
Previous primary treatments were PCNL, RIRS, ESWL, surgery and medical treatment in 283 patients (22 5%), 437 patients (34 7%), 334 patients (26 5%), 130 patients (10 3%), and 76 patients (6%), respectively Among the participants, 383 patients (30 4%) had recurrent renal stone and 877 patients (69 6%) didn’t develop recurrence after primary stone treatment The median follow-up period from the onset of primary stone treatment was 32
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11361
2
M Alshehri, H Alsaeed, M Alrowili, F Alhoshan, A Abdel Raheem, A Hagras
p e r a t i v e l y o n p o s t o p e r a t i v e i m a g i n g s t u d i e s ( 1 0 )
n o n
v a l i d a t e d s e l f - a d m i n i s t e r
-
Table 1
Baseline characteristic of patients with renal stone in Saudi Arabia (n = 1260)
Predictors of renal stone recurrence
months (IQR: 24-41) The median time to first recurrence of renal stone was 29 months (IQR: 14-35) After successful primary treatment, 970 (77%) and 1011 (80 2%) of patients didn’t have either stone chemical analysis or metabolic work-up, respectively The comparison of patients with primary and recurrent renal stones is showed in (Table 2) No significant differ-
Table 2
Comparing characteristic of patients with first time and recurrent renal stones.
Calcium oxalate 49 (5 6%) 71 (18 5%) 0 000 Calcium phosphate 20 (2 3%) 24 (6 3%)
Cystine 24 (2 7%) 30 (7 8%) Struvite 36 (4 1%) 36 (9 4%)
Previous treatment, n (%)
UUS: ultrasound scan, CTU; computed tompgraphy; HTN: hypertension; DM: d abetes me litus; BMI: body mass ndex; PHPT: primary hyperparathyro dism; UTI: urinary tract infect on; PCNL: percutaneous nephrostomy; RIRS: retrograde ntrarenal surgery; ESWL: extracorporea shockwave ithotripsy
748 (85 3%) 222 (58%)
PCNL 203 (23.1%) 80 (20.9%) 0.654
RIRS 307 (35%) 130 (33 9%)
ESWL 232 (26 5%) 102 (26 6%) Surgery 84 (9.6%) 46 (12%)
Controlled diet + medical ttt 51 (5 8%) 25 (6 5%)
UUS: u trasound scan, CTU; computed tompgraphy; HTN: hypertens on; DM: diabetes mel itus; BMI: body mass index; PHPT: primary hyperparathyroidism; UTI: urinary tract nfection; PCNL: percutaneous nephrostomy; RIRS: retrograde intrarenal surgery; ESWL: extracorporea shockwave l thotripsy
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11361 3
Age (yr): mean ± SD 32 5 ± 12 4 median (IQR) 29 (23-41) BMI (kg/m2): mean ± SD 25 9 ± 6 1 median (IQR) 25 3 (21 8-29) BMI classification, n (%) Underweight (< 18 5) 82 (6 5%) Normal (18 5-24 9) 525 (41 7%) Overweight and obese (> 25) 653 (51 8%) Gender, n (%) Female 440 (34 9%) Male 820 (65 1%) Chronic diseases, n (%) HTN 129 (10 2%) DM 98 (7 8%) Asthma 106 (8 1%) Hypercholesterolemia 101 (8%) PHPT 73 (5.8%) Gout 27 (2 1%) Residency, n (%) Central region 811 (64 4%) Eastern region 225 (17.9%) Western region 125 (9 9%) Southern region 55 (4 4%) Northern region 44 (3 5%) Nationality, n (%) Saudi 1191 (94 5%) Other 69 (5 5%) Physical activity, n (%) Low (≤ 1 day/week) 504 (40%) Moderate (2-4 days/week) 548 (43 5%) High (≥ 5 days/week) 208 (16 5%) Recurrence of kidney stones, n (%) First time 877 (69 6%) Recurrent ≥ 2 times 383 (30 4%) Family history of renal stone, n (%) No 854 (67 8%) Yes 406 (32 2%) History of UTI, n (%) No 721 (57 2%) Yes 539 (42 8%) Dietary habits, n (%) High salt diet (> 2 gm/day) 256 (20 3%) Low fluid intake (< 1 L/day) 459 (36 4%) High protein intake (≥ 3 times/week) 763 (60 6%) Low calcium intake (≤ 400 mg/day) 205 (16 3%) High oxalate containing foods 158 (12 5%) Stone chemical analysis, n (%) Yes 290 (23%) No 251 (19 9%) Nobody asked 719 (57 1%) Stone type, n (%) Calcium oxalate 120 (9 5%) Calcium phosphate 44 (3 5%) Cystine 54 (4 3%) Struvite 72 (5 7%) Unknown 970 (77%) Metabolic workup, n (%) Yes 249 (19 8%) No 294 (23 3%) Nobody asked 717 (56.9%) Previous treatment, n (%) PCNL 283 (22 5%) RIRS 437 (34 7%) ESWL 334 (26.5%) Surgery 130 (10 3%) Controlled diet + medical ttt 76 (6%)
Primar y stone Recurrent stone P-value Variables (Group I, n = 877) (Group II, n = 383) Age (yr), mean ± SD 31 3 ± 12 1 35 1 ± 12 6 0.000 BMI (kg/m2), mean ± SD 25 9 ± 6 1 26 2 ± 6 3 0 421 BMI classification, n (%) Underweight 56 (6 4%) 26 (6 8%) 0 492 Normal 375 (42 8%) 150 (39 2%) Overweight and obese 446 (50 9%) 207 (54%) Gender, n (%) Female 340 (38 8%) 100 (26 1%) 0.000 Male 607 (61 2%) 283 (73 9%) Hypertension (HTN), n (%) 73 (8 3%) 56 (14 6%) 0 001 Diabetes (DM), n (%) 63 (7 2%) 35 (9 1%) 0 253 Asthma, n (%) 71 (8 1%) 35 (9 1%) 0 581 Hypercholesterolemia, n (%) 62 (7.1%) 39 (10.2%) 0.071 Hyperparathyroidism, n (%) 41 (4 7%) 32 (8 4%) 0.013 Gout, n (%) 15 (1 7%) 12 (3 1%) 0 137 Residency, n (%) Central region 580 (66 1%) 231 (60 3%) 0 133 Eastern region 156 (17 8%) 69 (18%) Western region 82 (9 4%) 43 (11 2%) Southern region 33 (3 8%) 22 (5 7%) Northern region 26 (3%) 18 (4 7%) Nationality, n (%) Saudi 835 (95 2%) 356 (93%) 0 105 Other 42 (4 8%) 27 (7%) Physical activity, n (%) Low 363 (41 4%) 141 (36 8%) 0 300 Moderate 371 (42 3%) 177 (46 2%) High 143 (16 3%) 65 (17%) History of UTI, n (%) No 479 (54 6%) 242 (63 2%) 0 005 Yes 398 (45 4%) 141 (36 8%) Family history, n (%) No 607 (69 2%) 247 (64 5%) 0 101 Yes 270 (30 8%) 136 (35 5%) Dietary habits, n (%) High salt diet (yes) 180 (20 5%) 76 (19 8%) 0 782 Low fluid intake (yes) 191 (21 8%) 268 (70%) 0.000 High protein intake (yes) 507 (57 8%) 256 (66
Low
High
8%) 003
calcium intake (yes) 151 (17 2%) 54 (14 1%) 0 168
oxalate intake (yes) 105 (12%) 53 (13 8%) 0 358 Stone type, n (%)
Unknown
ence was found in most variables (p > 0 05) Mean patients’ age was 35 1 ± 12 6 yr in group I compared to 31 3 ± 12 1 yr in group II (p = 0 000) More male patients were present in group II compared to group I (73 9% vs 61 2%, p = 0 000, respectively) The rates of HTN, PHPT, low fluid intake, and high daily protein diet were significantly higher in group II (14 6% vs 8 3% in group I, p = 0 001), (8 4% vs 4 7% in group I, p = 0 013), (70% vs 21 8 % in group I, p = 0 000) and (66 8% vs 57 8% in group I, p = 0 003), respectively
Univariate logistic regression analysis showed that age, male patients, HTN, PHPT, history of UTI, low fluid intake, and high daily protein intake were associated with increased risk of renal stones recurrence (p < 0 05)
Multivariate logistic regression analysis revealed that male patients (OR: 1 686; 95% CI, 1 216-2 337), HTN (OR: 2 342; 95% CI, 1 439-3 812), PHPT (OR: 2 806; 95% CI,
1 510-5 215), low fluid intake (OR: 28 398; 95% CI, 18 158-44 403) and high daily protein intake (OR: 10 058; 95% CI, 6 400-15 807) were predictors of renal stone recurrence
DISCUSSION
In this prospective study, the risk factors and baseline characteristics of renal stone formers, as well as the predictors of recurrent renal stone formations were investigated in Saudi Arabian A total of 1260 patients (820 males and 440 females) were included in the analysis
The rate of kidney stone recurrence after successful primary stone treatment was 30 4% among the participants
The results demonstrated that male gender, HTN, PHPT, low oral fluid intake and high daily protein intake were potential risk factors for recurrent kidney stone formation We believe that the result of our study may provide better insight into the prevention of kidney stones recurrence through proper control and management of its risk factors
Renal stone recurrence is a common disease Patients with renal stones have an increase chance of forming another stone in the future Stones can recur as long as 10 years after the first episode (8) In our cohort, the overall renal stone recurrence rate was 30 4% Among them, 11 3% of patients had two-time recurrences, 9 8% had three-time recurrences, and 9 4% had four-time recurrences Our results are in accordance with previous study reporting the recurrence rate of nephrolithiasis recurrence of 38 6% to 53 2% in Saudi Arabia (4) In the present study, the median time of renal stone recurrence was 29 months (IQR: 14-35) Generally, following the initial episode, nephrolithiasis carries a high recurrence rate of 3 4 per 100 person-years, 7 1 after the second episode, 12 1 after the third episode, and 17 6 after the fourth episode or higher (15) Moreover, the natural cumulative recurrence stone rate was estimated to be 6 to 17%, 35%, and 52% at one year, five years, and ten years, respectively (15)
0 000
High protein intake 1.471 (1.144-1.892) 0.003 10.058 (6.400-15.807) 0.000
Low calcium intake 0 789 (0 563-1 105) 0 168
High oxalate intake 1 181 (0 828-1 683) 0 358
Previous treatment:
PCNL Ref
RIRS 1 075 (0 772-1 495) 0 670
ESWL 1 116 (0 788-1 580) 0 538
Surgery 1 390 (0 892-2 164) 0 145
Diet + medical ttt 1 244 (0 722-2 143) 0 432
UUS: ultrasound scan, CTU; computed tompgraphy; HTN: hypertension; DM: d abetes me litus; BMI: body mass ndex; PHPT: primary hyperparathyro dism; UTI: urinary tract infect on; PCNL: percutaneous nephrostomy; RIRS: retrograde ntrarenal surgery; ESWL: extracorporea shockwave l thotripsy
Our study showed that the recurrent kidney stone rate was found to be significantly higher in men (56 6%) than in women (44 4%) In addition, male gender was identified as a predictor for nephrolithiasis recurrence This may be attributed to the hormonal differences between men and women In women, estrogen stimulates the secretion of citric acid in urine and regulates the synthesis of 1,25-dihydroxy-vitamin D which are considered protective factors against nephrolithiasis On the other hand, men ’ s androgen induces the urinary accumulation of uric acid, calcium, and oxalate which increase the risk of kidney stone formation (16, 17)
Of note, 10 2% of the cases in our study had HTN and the odds of recurrent renal stone in HTN cases was 2 34 compared with non-HTN cases Sahng et al found that the risk of renal stone formation was directly associated with the incidence of HTN (18) Interestingly, in a recent study 29 7% of patients with nephrolithiasis had HTN (19) In a recent systematic review and meta-analysis, HTN was found to be one of the risk factors for renal stone recurrence (20) It worth note that, the exact mechanism of renal stone formation in patients with HTN remains unclear, and only few studies have examined it
Archivio Italiano di Urologia e Andrologia 2023;
95(3):11361
4
M Alshehri, H Alsaeed, M Alrowili, F Alhoshan, A Abdel Raheem, A Hagras
Table 3. Univariate and multivariate analysis of predictors of recurrent renal stone ≥ 2 times in Saudi patients Univariable analysis Multivariable analysis Variable OR (95% CI) P-value OR (95% CI) P-value Age 1 025 (1 015-1 035) 0.000 BMI 1 008 (0 989-1 028) 0 421 BMI classification: Underweight Ref Normal 0 862 (0 521-1 424) 0 561 Overweight and obese 1 000 (0 610-1 637) 0 999 Male patient 1 794 (1 401-2 298) 0 000 1 686 (1 216-2 337) 0 002 HTN 1 886 (1 301-2 734) 0 001 2 342 (1 439-3 812) 0 001 DM 1 299 (0 844-2 001) 0 234 Asthma 0 142 (0 747-1744) 0 540 Hypercholesterolemia 1 490 (0 979-2 268) 0 063 PHPT 1 859 (1 152-3 001) 0.011 2 806 (1 510-5 215) 0.001 Gout 1 859 (0 862-4 010) 0 114 Residency: Central region Ref Eastern region 1 111 (0 805-1 532) 0 523 Western region 1.738 (0.935-3.231) 0.081 Southern region 1 647 (0 956-2 932) 0 072 Northern region 1 317 (0 883-1 963) 0 177 Saudi patient 0 663 (0 403-1 092) 0 107 Physical activity: Low Ref Moderate 1.228 (0.943-1.600) 0.127 High 1 170 (0 823-1 664) 0 381 History of UTI 1 426 (1 114-1 825) 0.005 Renal stone Family history 1 238 (0 960-1 595) 0 099 Dietary habits: High salt diet 0 959 (0 710-1 294) 0 782 Low fluid intake 8 370 (6 383-10 976) 0 000 28 398 (18 158-44 403)
Frequent changes in the levels of blood pressure have a direct effect on the urinary microbiomes, which may stimulate nephrolithiasis (21)
Dietary habits play an important role in the renal stone formation Excessive meat consumption and low fluid i n t a k e w e r e c o n s i d e r e d a s m a i n r i s k f a c t o r s f o r nephrolithiasis Our study showed that in patients with recurrent kidney stones high protein intake rate was significantly higher (66 8%) than in primary stone formers (57 8%), similarly low fluid intake was significantly higher (70% vs 21 8%) High protein intake leads to acidification of urine, which stimulate the formation of calcium
oxalate stone (22) Xu et al found that each 500 mL increase in water intake was significantly associated with a reduced risk of kidney stone formation (RR = 0 93; 95% CI: 0 87, 0 98; p < 0 01) Additionally, daily water intake
> 2000 mL decreases the risk of first kidney stone formation by at least 8% compared to 1500 mL (23)
PHPT is one of the listed risk factors for renal stone formation It has been estimated that 20% of patients with PHPT have nephrolithiasis, and approximately 5% of patients who presented with renal stones have PHPT (24) Our results are in agreement with the aforementioned results Notably, 73 patients (5 8%) have PHPT in our cohort analysis Moreover, the rate of patients with recurrent renal stone and PHPT was significantly higher (8 4%) than those without PHPT (4 7%), in addition, the odds of recurrent renal stone in PHPT patients was 2 8 compared with non-PHTP patients
The current study has limitations and strengths The strength points of our study are the following: a prospective study, large sample size (n = 1260), and extensive data gathering for the factors of interest related to stone formation and recurrence (e g , age, sex, BMI, medical comorbidities, dietary habits, area of residency etc ) However, our study does not devoid of limitations, and the results have to be interpreted with caution For instance, the short median follow-up period (32 months) may be not enough to estimate the actual rate of renal stone recurrence Non-recurrent stone formers in this study are “patients who formed a first stone” although they may develop stone recurrence after longer follow-up period Also, stone composition and metabolic work-up results are unknown in 77% and 80 2% of patients, respectively Excluding those patients was not possible to complete the analysis
On the other hand, these findings raise an important concern regarding urologists practice in Saudi Arabia where best clinical practice guidelines regarding metabolic work-up and stone chemical analysis are underutilized and need to be applied by our urologists extensively among stone former patients
CONCLUSIONS
Our study revealed that male gender, hypertension, primary hyperparathyroidism, low fluid intake and high daily protein intake are factors potentially increasing the risk of renal stone recurrence among Saudi Arabian patients Being aware of these risk factors can provide proper guidance for the prevention of nephrolithiasis recurrence and its management
REFERENCES
1 Sorokin I, Mamoulakis C, Miyazawa K, et al Epidemiology of stone disease across the world World J Urol 2017; 35:1301-1320
2 Romero V, Akpinar H, Assimos DG Kidney stones: a global picture of prevalence, incidence, and associated risk factors Rev Urol 2010; 12: 86-96
3 Zeng G, Mai Z, Xia S, et al Prevalence of kidney stones in China: an ultrasonography based cross-sectional study BJU Int 2017; 120:109-116
4 Abdel-Halim RE, Al-Hadramy MS, Hussein M, et al The prevalence of urolithiasis in the western region of Saudi Arabia: a population study In: Walker VR, Sutton RAL, Cameron ECB, Pak CYC, Robertson WG, editors Urolithiasis Boston, MA: Springer; p 1989; 711-712
5 Ahmad F, Nada MO, Farid AB, et al Epidemiology of urolithiasis with emphasis on ultrasound detection: a retrospective analysis of 5371 cases in Saudi Arabia Saudi J Kidney Dis Transpl 2015; 26:386-391
6 Raja A, Hekmati Z, Joshi HB How Do Urinary Calculi Influence Health-Related Quality of Life and Patient Treatment Preference: A Systematic Review J Endourol 2016; 30:727-43
7 Lotan Y Economics and Cost of Care of Stone Disease Advances in Chronic Kidney Disease 2009; 16:5-10
8 Trinchieri A, Ostini F, Nespoli R, et al A prospective study of recurrence rate and risk factors for recurrence after a first renal stone J Urol 1999; 162:27-30
9 Liu Y, Chen Y, Liao B, et al Epidemiology of urolithiasis in Asia Asian Journal of Urology 2018; 5, 205-214
10 Ho HC, Hughes T, Pietropaolo A, et al Apnoea is not necessary for flexible ureteroscopy and lasertripsy of renal stones: A prospective study over 6 years Cent European J Urol 2020; 73:193-198
11 Matthew D’Costa, Vernon M Pais, and Andrew D Rule Leave No Stone Unturned: Defining Recurrence in Kidney Stone Formers Curr Opin Nephrol Hypertens 2019; 28: 148-153
12 Khalili P, Jamali Z, Sadeghi T, et al Risk factors of kidney stone disease: a cross-sectional study in the southeast of Iran BMC Urol 2021; 21:141
13 Dai M, Zhao A, Liu A, et al Dietary Factors and Risk of Kidney Stone: A Case-Control Study in Southern China J Ren Nutr 2013;23:e21-8
14 Ferraro PM, Bargagli M, Trinchieri A, et al Risk of Kidney S t o n e s : I n fl u e n c e o f D i e t a r y F a c t o r s , D i e t a r y P a t t e r n s , a n d Vegetarian-Vegan Diets Nutrients 2020; 12:779
15 Vaughan LE, Enders FT, Lieske JC, et al Predictors of symptomatic kidney stone recurrence after the first and subsequent episodes Mayo Clin Proc 2019; 94:202-10
16 Heller HJ, Sakhaee K, Moe OW, et al Etiological role of estrogen status in renal stone formation J Urol 2002; 168:1923-7 23
17 Liang L, Li L, Tian J, et al Androgen receptor enhances kidney stone-CaOx crystal formation via modulation of oxalate biosynthesis & oxidative stress Mol Endocrinol 2014; 28:1291-303
18 Shang W, Li Y, Ren Y, et al Nephrolithiasis and risk of hypertension: a meta-analysis of observational studies BMC Nephrol 2017; 18:1-6
19 Kalani L, Rashidi N, Mehranfard S, et al Epidemiology of the
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11361 5 Predictors
of renal stone recurrence
urinary stones: a 6-year retrospective study at Dezful-Iran Int J Pharm Phytopharmacol Res 2020; 10:79-85
20 Wang K, Ge1 J, Han W, et al Risk factors for kidney stone disease recurrence: a comprehensive meta-analysis BMC Urology 2022; 22:62
21 Liu F, Zhang N, Jiang P, et al Characteristics of the urinary microbiome in kidney stone patients with hypertension J Transl Med 2020; 18:130
22 Nasir SJ The mineralogy and chemistry of urinary stones from the United Arab Emirates Qatar Univ Sci J 1999; 18:189-202
23 Xu C, Zhang C, Wang XL, et al Self-Fluid Management in Prevention of Kidney Stones: A PRISMA-Compliant Systematic Review and Dose-Response Meta-Analysis of Observational Studies Medicine (Baltimore) 2015; 94:1042
24 Parks J, Coe F, Favus M Hyperparathyroidism in nephrolithiasis Arch Intern Med 1980; 140:1479-81
Correspondence
Mohammed Alshehri, MD mohammedalshehri95@yahoo com
Department of Urology, King Abdullah bin Abdulaziz University Hospital, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Hind Alsaeed, MD alsaeedhindx@gmail com
Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Malath Alrowili, MD pc435000386@gmail com
Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Faisal Alhoshan, MD fmialhoshan@gmail com
Prince Sultan Military Hospital, Taif, Saudi Arabia
Ali Abdel Raheem, MD, PhD (Corresponding Author) aliraheem82@yahoo com a-hassan@ksmc med sa
Urology Consultant, Urology Department, King Saud Medical City, Riyadh, Saudi Arabia
Lecturer of Urology, Urology Department, Tanta University Hospital, Tanta, Egypt
Ayman Hagras, MD ahagras80@yahoo com
Department of Urology, Faculty of Medicine, Tanta University, Tanta, Egypt
Division of Urology, Surgery Department, Sharurah Armed Forces Hospital, Sharurah, Saudi Arabia
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia
e Andrologia 2023; 95(3):11361
6
M Alshehri, H Alsaeed, M Alrowili, F Alhoshan, A Abdel Raheem, A Hagras
1 Department of Urology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
2 Department of Urology, Faculty of Medicine, Al-Azhar University, Damietta, Egypt;
3 Department of Urology, Faculty of Medicine, Benha University, Egypt.
Summary
Introduction: The rate of success of retrograde intrarenal surgery (RIRS) for treating urinary tract stones is high, and the procedure is growing in popularity. The routine use of ureteral access sheath (UAS) remains somewhat controversial. The aim of this study was to assess the efficacy and safety of employing UAS during flexible ureteroscopy for treating renal stones ≥ 2 cm.
Methods: This retrospective study was accomplished from January 2021 to February 2023. From 495 consecutives flexible ureteroscopies, 112 patients had renal stones ≥ 2 cm (60 patients with the use of UAS and 52 patients without). The stone-free status was verified after 8 weeks of operation.
Results: The average diameter of the renal stones in non-UAS or UAS treated groups was 22.5 mm and 22.6, respectively. None of the groups differed significantly in terms of stone side, stone size, stone position, or Hounsfield unite but there was significant difference (p < 0.001) among two groups as regard pre-operative stenting (cases with UAS had 23.3% pre-operative stenting).
Conclusions: It is not always necessary to use UAS in conjunction with flexible ureteroscopy and laser lithotripsy to treat renal calculi bigger than or equal two cm. Without the assistance of UAS, the surgery may be carried out successfully and safely.
KEYWORDS: Retrograde intrarenal surgery; Laser lithotripsy; Ureteral access sheath; Kidney calculi.
Submitted 15 june 2023; Accepted 14 July 2023
INTRODUCTION
The rate of success of retrograde intrarenal surgery (RIRS) for treating urinary tract calculi is high, and the procedure is growing in popularity (1, 2). The first reported introduction of a guide tube (with a polytetrafluoroethylene coating, a length of 38 cm and a diameter of 3 mm) through the ureteral orifice to pass a completely passive flexible ureteroscope was by Takayasu and Aso in 1974 (3). Its initial use was accompanied by a high rate of complications; 12 of 43 cases had ureter perforation (eight of them due to ureteral sheath and four cases to other causes) (4). In spite of those bad results, the use of ureteral access sheath (UAS) did not stop, and technological development made it more easy and safe to use UAS during the
routine practice of the endourologists, especially after the introduction of the hydrophilic coated UASs with the hub-locking mechanisms and in a study that compared the commonly used UASs they concluded that there were no differences between them as regard safety and efficacy. Also, less resistance during the insertion of UAS was noted in the pre-stented and dilated ureters (5, 6). UAS can allow repeated access to the renal pelvis without trauma to the ureter, improve visibility, protect the ureteroscope, improve drainage and allow rapid extraction of stone fragments (7, 8). Also, UAS will lower intra-renal pressures, which may reduce pyelovenous backflow, leading to a decrease in the risk of infectious complications (9). The routine use of UAS for standard URS remains somewhat controversial (10). UASs can directly damage the ureteral wall and compromise ureteral blood flow transiently (11, 12). The major aim of this study was to assess the efficacy, safety, and feasibility of employing UAS during flexible ureteroscopy for the removal of renal stones 2 cm in size or larger.
MATERIALANDMETHODS
This retrospective study compared the effectiveness of flexible ureteroscopy with and without UAS in the treatment of renal stones 2 cm or larger at “Al-Azhar” and “Benha University Hospitals”. 495 consecutives flexible ureteroscopies were accomplished from January 2021 to February 2023 for kidney and ureter calculi. From them, 112 patients had renal stones 2 cm or more (60 patients with the use of UAS and 52 patients without). Inclusion criteria included patients with renal stones ≥ 2 cm, while exclusion criteria were patients with ureteric stones or combined renal and ureteric stones, patients with kidney calculi < 2 cm, patients with related congenital renal abnormalities and cases with incomplete records of postoperative data (Figure 1). The “Faculty of Medicine for Girls at Al-Azhar University in Cairo (FMG-IRB)” in Nasr City, Cairo, Egypt, had accepted the study's protocol with “approval number: 1657”. All procedures were performed under the Helsinki Declaration. As this was a retrospective study, the necessity for obtaining informed permission was waived. We retrieved the following data for all patients of the study:
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11524 1 ORIGINALPAPER
The outcomes of flexible ureteroscopy for renal calculi of 2 cm or more with and without the use of ureteral access sheath: A retrospective study
Basem A. Fathi 1, Ahmed A. Elgammal 1, Tamer A. Abouelgreed 1, Osama M. Ghoneimy 1 , Ahmed Y. Aboelsaad 2, Mohamed A. Alhefnawy 3
DOI: 10.4081/aiua.2023.11524
age, sex, main presentation, previous surgeries, associated comorbidities, renal function, location and density of the stones, intra and after surgery details, surgery duration, stenting duration, stone-free rates (SFR) and any auxiliary procedures A semi-rigid ureteroscope was used to check the ureter up to the level of the pelvis for any abnormalities and to widen the ureter while the patient was under general anaesthesia and in the lithotomy position Another safety guide wire was utilized throughout The decision for using UAS or not was strictly based on surgeon's preference and not on patient and stone characteristics The UAS is inserted into the patient at the beginning of the surgery under fluoroscopic guidance, with the sheath's tip resting at the ureteropelvic junction The Flexor® UAS (Cook Medical) was used; it is a hydrophilic, soft, twopiece device consisting of an inner tapered obturator that is detachable and an outside functioning sheath that may be any of three lengths (20, 28, or 35) It is offered in a choice of two sizes “10/12F and 12/14F”
The dimension of the sheath is determined by the anatomy of the case and the endoscope being utilized The flexible ureteroscope was positioned over a wire under fluoroscopic guidance on direct vision in circumstances where the UAS was not

employed All stones were fragmented to a very small sizes by means of holmium laser (30 W Litho Quantasystem, Lumenis Pulse™ 120H Boston Scientific) using a 365 -µm holmium laser fiber with power settings of 0 8-1 5 J at 10-15 Hz, except in lower calyceal stones where a 200-µm fiber was used Two kinds of flexible ureteroscopes were used for all surgeries: “OTU-100SR WiScope® Single-Use Digital Flexible Ureteroscope and LithoVue™ Single-Use Digital Flexible Ureteroscope Boston Scientific” After laser lithotripsy, stones were repositioned in the collecting system, and pieces were removed using a nitinol basket if needed Patients underwent either plain abdominal X-rays with ultrasonography or a non-contrast-enhanced spiral computed tomography (CT) scan for radiolucent stones to verify stone-free status after 8 weeks from operation Success was considered when there was no residual stone or if the residual stone was less than 5 mm
Table 1.
Comparison of baseline parameters between studied groups
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11524 B A Fathi, A A Elgammal, T A Abouelgreed, O M
A
A
2
Ghoneimy,
Y Aboelsaad, M
Alhefnawy
Without UAS With UAS P N = 52 N = 60 Demographics Age (years) Mean ± SD 42 1 11 6 40 7 10 5 0 505 Range 23 73 20 67 Sex Males N, % 30 57 7% 38 63 3% 0 542 Females N, % 22 42 3% 22 36 7% Histor y Medical Absent N, % 46 88 5% 52 86 7% 0 987 HTN N, % 3 5 8% 4 6 7% NIDDM N, % 2 3 8% 3 5 0% HTN&DM N, % 1 1 9% 1 1 7% Surgical Absent N, % 32 61 5% 37 61 7% 1 PNL N, % 2 3 8% 2 3 3% SWL N, % 9 17 3% 11 18 3% URS N, % 6 11 5% 7 11 7% Pyelolithotomy N, % 2 3 8% 2 3 3% URS and SWL N, % 1 1 9% 1 1 7% Main presentation Loin pain Present N, % 52 100 0% 60 100 0%Hematuria Absent N, % 42 80 8% 48 80 0% 0 919 Present N, % 10 19 2% 12 20 0% Laborator y data Pus cell Mean ± SD 9 3 17 9 10 3 17 6 0 755 Range 0 100 0 100 Urine culture Absent N, % 40 76 9% 48 80 0% 0 285 E-coli N, % 9 17.3% 8 13.3% Klebsiella N, % 3 5 8% 1 1 7% Staphyloccocus areus N, % 0 0 0% 3 5 0% Blood urea (mg/dL) Mean ± SD 32 0 7 6 32 1 7 4 0 964 Range 18 46 18 46 Serum creatinine (mg/dL) Mean ± SD 1 0 0 2 1 0 0 3 0 324 Range 0 10 1 50 0 50 1 90
Figure 1.
A schematic representation of the study.
Statistical analyses
Revisions, coding, tabulation, and introduction of the acquired data to a computer were made utilizing Statistical Package for Social Science (IBM Corp Released 2017 IBM SPSS Statistics for Windows, Version 25 0 Armonk, NY: IBM Corp) In order to assess the statistical significance difference between two study groups means, Student T test was used When compari n g t w o n o n - p a r a m e t r i c g r o u p s , t h e Mann-Whitney test was utilized for analysis 𝝌2 test was utilized to analyse the correlation among two categorial quantities A probability (P) is regarded as statistically significant if less than 0 05 at CI (confidence interval) 95%
RESULTS
The existing research was performed on 52 patients without UAS (first group) and 60 cases with UAS (second group) The indications of ureteroscopy were the failure of other therapies, comorbidities, skeleto-muscular deformity, body habitus and patient preference No significant differences were found among both groups c o n c e r n i n g d e m o g r a p h i c d a t a , h i s t o r y (medical and surgical), presentation and laboratory data (Table 1) Additionally, there were no notable variations among the groups concerning the calculi side, dimension, position and Hounsfield unit, as shown in Table 2 The average dimension of the renal calculi in non-UAS or UAS treated groups was 22 5 mm and 22 6, respectively The mean hardness was 953 6 HU in the first group and 953 1 HU in the second group Another finding is that there was significant difference (p < 0 001) among both groups as regard preoperative stenting (cases with UAS had 23 3% pre-operative stenting) (Figure 2) Additionally, as demonstrated in Table 3 and Figure 3, there were no discernible differences among the study groups in terms of intra- or post-intervention complications Two cases were intra-operatively converted to standard percutaneous nephrolithotomy (PCNL) in each group based on the surgeon's decision We also found that cases without UAS required another intervention in 17 3% (5 cases required a 2nd session of URS, and 4 cases required a session of SWL), while those with UAS required another intervention in 10% (4 cases required 2nd session of URS and 2 cases required a session of SWL), with no observable variations among the two groups In addition, no obvious alterations were found between groups con-
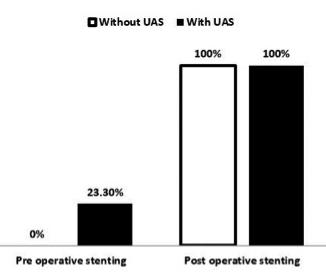
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11524 3 The
of 2
and without the use of ureteral access sheath
outcomes of flexible ureteroscopy for renal calculi
cm or more with
Figure 2
Pre and postoperative stenting among studied groups
Table 2.
Stone characteristics Without UAS With UAS P N = 52 N = 60 Side Left N, % 25 48 1% 29 48 3% 0 978 Right N, % 27 51 9% 31 51 7% Stone size (mm) Mean ± SD 22 5 2 0 22 6 2 5 0 839 Range 15 26 14 27 Stone location Pelvis N, % 29 55 8% 34 56 7% 0 987 Upper calyx N, % 7 13 5% 9 15 0% Middle calyx and pelvis N, % 8 15.4% 9 15.0% Pelvis &lower calyx N, % 8 15 4% 8 13 3% Hounsfield units Mean ± SD 953 6 341 8 953 1 337 2 0 994 Range 250 1700 250 1700
Comparison of Stone characteristics between studied groups
Without UAS With UAS P N = 52 N = 60 Intraoperative complication Mucosal injury Absent N, % 45 86 5% 52 86 7% 0 984 Present N, % 7 13 5% 8 13 3% Bleeding Absent N, % 43 82 7% 47 78 3% 0 563 Present N, % 9 17 3% 13 21 7% Failed Absent N, % 50 96 2% 56 93 3% 0 684 Present N, % 2 3 8% 4 6 7% Perforation Absent N, % 52 100% 59 98 3% 0 350 Present N, % 0 0 0% 1 1 7% False passage Absent N, % 50 96 2% 57 95 0% 0 768 Present N, % 2 3 8% 3 5 0% Converted to other procedure Absent N, % 50 96 2% 58 96 7% 0 884 Present N, % 2 3 8% 2 3 3% Post-operative complication Infection Absent N, % 47 90 4% 53 88 3% 0 726 Present N, % 5 9 6% 7 11 7% Fever Absent N, % 49 94 2% 56 93 3% 0 845 Present N, % 3 5 8% 4 6 7% Pain (loin or suprapubic) Absent N, % 32 61 5% 34 56 7% 0 601 Present N, % 20 38 5% 26 43 3% Hematuria Absent N, % 42 80 8% 45 75 0% 0 465 Present N, % 10 19 2% 15 25 0% Other complications Absent N, % 51 98.1% 58 96.7% 0.645 Present N, % 1 1 9% 2 3 3%
Table 3. Comparison of complications between studied groups.
Comparison of operative time and outcome between studied groups
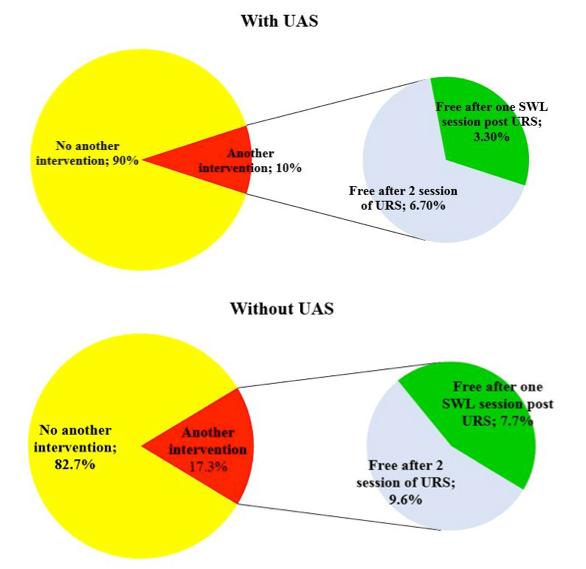
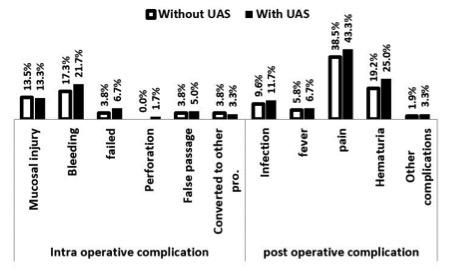
cerning operative time, stent duration and r e a d m i s s i o n ( T a b l e 4 a n d F i g u r e 4 ) Hospital readmissions were due to fever and persistent pain
DISCUSSION
Though PCNL was the first-line treatment of renal calculi greater than 2 cm, many studies demonstrated that RIRS can be a safer and effective alternative in managing r e n a l s t o n e s 2 c m o r m o r e ( 1 3 - 1 5 ) According to a recent comprehensive study by De Coninck et al , UAS installation is not something that should be done routinely during RIRS It may be used only in cases when gaining access to the ureter is challenging, when treating patients with stones who have an elevated risk of infection complications, or in cases where visibility is poor owing to insufficient irrigation fluid outflow The authors also draw the conclusion that, in the near future, the reasons for using a UAS might become less due to the advancement of smaller size single-use flexible digital ureteroscope (improved outflow by allowing more space between the ureteral wall and flexible ureteroscope), thulium fiber laser, and pressurem e a s u r i n g i n s t r u m e n t s a n d i n t e g r a t e d aspiration technology (16) In our study, we compared the utilization or not of UAS in treating renal stones 2 cm Except for the fact that pre-stenting the ureter was much more common in the group that employed UAS, we found no statistically differences in the examined parameters between the two groups Aboumarzouk et al performed a meta-analysis and a comprehensive review of studies using flexible ureteroscopy and laser lithotripsy to treat renal calculi more than 2 cm Nine studies involving 445 patients reported an average SFR of around 93 7 percent The mean number of operations per patient was 1 6 The average time of operations was 82 5 minutes SFR for stones between 2 and 3 cm was considerably higher than those for stones > 3 cm (95 7 % vs 84 6 %; p = 0 01) The researchers concluded that laser l i t h o t r i p s y p e r f o r m e d u s i n g a fl e x i b l e ureteroscope could be an alternative to PCNL for individuals with calculi ≥ 2 cm
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11524 B A
A A
T A
O
4
Fathi,
Elgammal,
Abouelgreed,
M Ghoneimy, A Y Aboelsaad, M A Alhefnawy
Table 4
Without UAS With UAS P N = 52 N = 60 Operative time (min) Operative time (min) Mean ± SD 81 4 4 5 82 8 13 6 0 469 Range 75 90 43 100 Outcome Stone free rate After the first procedure N, % 43 82.7% 54 90.0% 0.257 Another intervention 9 17 3% 6 10 0% Free after 2 sessions of URS N, % 5 55 6% 4 66 7% 0 667 Free after one SWL session Post-URS N, % 4 44 4% 2 33 3% 0 667 Stent duration (days) Mean ± SD 24 6 7 1 24 0 6 0 0 650 Range 15 45 15 45 Readmission Absent N, % 47 90.4% 56 93.3% 0.731 Present N, % 5 9 6% 4 6 7%
Figure 3 Complications among studied groups
Figure 4. The stone-free rate among (A) with UAS and (B) without UAS.
(15) Scotland et al , in their study for treating large renal calculi (average dimension 2 75 cm) in 167 patients achieved a SFR in the first session of 57 1%, 90 2% in the second session and 94 0% in the third session In their study, significant complications occurred in patients who had received UASs, which were utilized in 47% of cases It was determined that either one or many sessions of retrograde ureteroscopic lithotripsy could be used to successfully treat large kidney calculi (17) In the present study, we found that intra and post-operative complications were less in the group treated without UAS, although there was no significant difference Also, the SFR after the first procedure was 82 7% in the group treated without UAS and 90 0% in the other group, although again the difference was not significant Nine cases in the group treated without UAS (17 3%) and six cases in the other group (10 0%) required a second intervention Meier et al , in their study on 5316 patients who underwent primary flexible ureteroscopy used the UAS in 1969 patients (37 7%) and found that those in whom a UAS was used had increased visits to the emergency department and hospitalization (p < 0 05) compared to those without UAS use They concluded that using UAS is not without risk and UAS should be judiciously employed (18) Grasso et al did not use a UAS in their study on managing 2 cm or more stones in the upper urinary tract The study included 51 patients with 66 large upper urinary tract stones The rate of success was 76% next to the initial procedure, 91% after a second session of flexible ureteroscopy and laser lithotripsy, and 93% after a third endoscopic session In conclusion, they found that large upper urinary tract stones could be treated appropriately and efficiently with flexible ureteroscopy and laser lithotripsy (19) El-Anany et al performed a study that included thirty patients with a renal stone of more than 2 cm managed with either a semi-rigid ureteroscope or flexible ureteroscopy and laser lithotripsy without using the UAS The success rate was 77% (23 of the 30 patients), with a negligible incidence of complications Of the other seven patients, three of them converted to PCNL and four to extracorporeal shock wave lithotripsy (ESWL) If there was a lot of debris remaining after fragmentation, they employed two ureteric catheters with “a 5 F catheter in the most dependent calyx and a 6 F catheter in the upper calyx” for constant irrigation (100 mL/h of saline with 80 mg/L of gentamicin) They determined that a retrograde endoscopic approach employing laser lithotripsy was a secure and successful means of treating big renal calculi (20) Palmero et al performed a retrospective review of 106 patients with renal calculi 2 cm or more who underwent RIRS with UAS in all cases The average calculi size was 2 46 cm The success rates was 73 6% (for a single procedure) and 93 4% for retreatment with a 6 7% postoperative minor complication rate They concluded that for renal stones 2 cm or more, RIRS is a valid alternative to PCNL with few complications and a high success rate (21) Similarly, in a separate study by Al-Qahtani et al , on 120 patients with renal stones more than 2 cm, they achieved stone-free status in 58 5% after the first session, 87% after the second session, and 96 7% after the third session They concluded that flexible ureteroscopy using a holmium laser is a successful and
safe treatment with little morbidity It could be an alternative to PCNL, especially for stone burdens from 2 to 3 cm (22) Another recent study was performed by Huang et al to treat renal stones 2 cm or greater In 279 patients with a mean stone diameter of 26 5 mm SFR was 61 9% at the first, 82 9% at the second, and 89 5% at the third procedure Fever was the most common complication, with a 15 1% overall complication rate
The conclusion was that RIRS could be utilized to treat large kidney stones (2 to 4 cm) with an acceptable complication rate and efficacy (23) This study has some limitations; the first is being retrospective in nature with selection bias Second, the follow-up time is short, so long-term complications couldn’t be assessed The third, there were three surgeons and not only one who performed the operations in both groups Last, stone-free rate was not assessed by the same modality in all cases, with plain abdominal radiography with ultrasonography being done in most of the cases CT scan was only done in patients with radiolucent stones
CONCLUSIONS
It is not always necessary to use UAS in conjunction with flexible ureteroscopy and laser lithotripsy to treat renal stones of 2 cm or more in diameter Without the assistance of UAS, the surgery may be carried out successfully and safely More studies are needed to corroborate this finding; ideally, they would be prospective and randomized and include long-term follow-up
REFERENCES
1 Kılıç Ö, Akand M, Van Cleynenbreugel B Retrograde intrarenal surgery for renal stones - Part 2 Turk J Urol 2017; 43:252-260
2 Heers H, Turney BW Trends in urological stone disease: a 5-year update of hospital episode statistics BJU International 2016; 118:785789
3 Takayasu H, Aso Y Recent development for pyeloureteroscopy: guide tube method for its introduction into the ureter J Urol 1974; 112:176-178
4 Newman RC, Hunter PT, Hawkins IF, Finlayson B The ureteral access system: a review of the immediate results in 43 cases J Urol 1987; 137:380-383
5 Monga M, Bhayani S, Landman J, et al Ureteral access for upper urinary tract disease: the access sheath J Endourol 2001; 15:831-834
6 Elsaqa M, Hyder Z, Thai K, et al Comparison of commonly utilized ureteral access sheaths: A prospective randomized trial Arch Ital Urol Androl 2023; 95:11149
7 Vanlangendonck R, Landman J Ureteral access strategies: proaccess sheath Urol Clin North Am 2004; 31:71-81
8 Abrahams HM, Stoller ML The argument against the routine use of ureteral access sheaths Urol Clin North Am 2004; 31:83-87
9 Auge BK, Pietrow PK, Lallas CD, et al Ureteral access sheath provides protection against elevated renal pressures during routine flexible ureteroscopic stone manipulation J Endourol 2004; 18:33-36
10 Loftus CJ, Ganesan V, Traxer O, et al Ureteral Wall Injury with Ureteral Access Sheaths: A Randomized Prospective Trial J Endourol 2020; 34:932-936
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11524 5 The
outcomes of flexible ureteroscopy for renal calculi of 2 cm or more with and without the use of ureteral access sheath
11 Lallas CD, Auge BK, Raj GV, et al Laser Doppler flowmetric determination of ureteral blood flow after ureteral access sheath placement J Endourol 2002; 16:583-590
12 Traxer O, Thomas A Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery J Urol 2013; 189:580-584
13 Tiselius HG, Ackermann D, Alken P, et al Guidelines on urolithiasis Eur Urol 2001; 40:362-371
14 Ben Saddik MA, Al-Qahtani Sejiny S, Ndoye M, et al Flexible ureteroscopy in the treatment of kidney stone between 2 and 3 cm Progr Urol 2011; 21:327-332
15 Aboumarzouk OM, Monga M, Kata SG, et al Flexible ureteroscopy and laser lithotripsy for stones >2 cm: a systematic review and meta-analysis J Endourol 2012; 26:1257-1263
16 De Coninck V, Somani B, Sener ET, et al Ureteral Access Sheaths and Its Use in the Future: A Comprehensive Update Based on a Literature Review J Clin Med 2022; 11:5128
17 Scotland KB, Rudnick B, Healy KA, et al Retrograde Ureteroscopic
Management of Large Renal Calculi: A Single Institutional Experience and Concise Literature Review J Endourol 2018; 32:603-607
18 Meier K, Hiller S, Dauw C, et al Understanding Ureteral Access Sheath Use Within a Statewide Collaborative and Its Effect on Surgical and Clinical Outcomes J Endourol 2021; 35:1340-1347
19 Grasso M, Conlin M, Bagley D Retrograde ureteropyeloscopic treatment of 2 cm or greater upper urinary tract and minor Staghorn calculi J Urol 1998; 160:346-351
20 El-Anany FG, Hammouda HM, Maghraby HA, Elakkad MA Retrograde ureteropyeloscopic holmium laser lithotripsy for large renal calculi BJU International 2001; 88:850-853
21 Palmero JL, Castelló A, Miralles J, et al Results of retrograde intrarenal surgery in the treatment of renal stones greater than 2 cm Actas Urol Esp 2014; 38:257-262
22 Al-Qahtani SM, Gil-Deiz-de-Medina S, Traxer O Predictors of clinical outcomes of flexible ureterorenoscopy with holmium laser for renal stone greater than 2 cm Adv Urol 2012; 2012:543537
23 Huang JS, Xie J, Huang XJ, Yuan Q, et al Flexible ureteroscopy and laser lithotripsy for renal stones 2 cm or greater: A single institutional experience Medicine 2020; 99:e22704
Correspondence
Basem A Fathi, MD (Corresponding Author) basemhara@gmail com; basemabdalla 8@azhar edu eg
Ahmed A Elgammal, MD aelgammal36@gmail com
Tamer A Abouelgreed, MD dr tamer ali@yahoo com; tamerali 8@azhar edu eg
Osama M Ghoneimy, MD elgendyosama787@gmail com
Department of Urology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Ahmed Y Aboelsaad, MD aboelsaadurology@hotmail com
Department of Urology, Faculty of Medicine, Al-Azhar University, Damietta, Egypt
Mohamed A Alhefnawy, MD dr mohamedalhefnawy@gmail com
Department of Urology, Faculty of Medicine, Benha University, Egypt
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11524 B A
A
6
Fathi,
A Elgammal, T A Abouelgreed, O M Ghoneimy, A Y Aboelsaad, M A Alhefnawy
Safety and efficacy of percutaneous nephrolithotripsy in comorbid patients: A 3 years prospective observational study
Tamer A Abouelgreed 1 , Hassan Ismail 1 , Sameh S Ali 2 , Ayman K Koritenah 1 , Yasser Badran 1 , Mahmoud Ali 1 , Rasha Ahmed 1 , Mohamed Algammal 1 , Ahmed Alrefaey 1 , Aly Gomaa 1 , Mohamed F. Elebiary 1 , Hany A. Eldamanhory 1 , Abdelhamid A. Khattab 3 , Nermeen M. Abdelmonem 4 , Mohammad Thabet Alnajem 5 , Tamer G. Abdlhamid 6 , Ahmed A. Abdelwahed 7 , Salma F. Abdelkader 7
1 Department of Urology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
2 Department of Radiology, Sheikh Khalifa general Hospital, UAQ, UAE;
3 Department of Urology, Damanhur Teaching Hospital, Albuheira Government, Egypt;
4 Department of Radiology, Thumbay University Hospital, Ajman, UAE;
5 Department of Radiology, Tawam Hospital, Alain, UAE;
6 Department of Anesthesia, Emirates specialty Hospital, Dubai, UAE;
7 Department of Radiology, Faculty of Medicine, Ain shams University, Cairo, Egypt
Summary
Purpose: To report the result of percutaneous nephrolithotripsy (PCNL) via standard nephrostomy tract in a single training institution The perioperative complications in relation to the comorbid state are particularly assessed
Patients and methods: A prospective interventional study between January 2019 to November 2022, included 210 patients scheduled for PCNL The average age was 40 3 ± 11 8 years (range 18- 67 years) Patients were categorized into two groups The first group comprised 146 cases (69 .5%) with no associated co-morbidities while the second group 64 (30 5%) had co-morbidities such as obesity in 4 cases (1.9%), hypertension (HTN) in 24 cases (11 4%) cases, diabetes mellitus (DM) in 17 (8 1%) cases, history of recurrent stone surgery in 11 (5.2%) cases and more than one in 8 cases (3 8%) Co-morbidities, stone burden, location of stone, time of surgery, stay in the hospital, further operations, and negative events were among the reported data Complications and the stone-free rate were the main outcome indicators
Results: Intraoperative complications were reported in 40 (18 8%) patients (18 group 1 and 22 group 2) during PCNL Bleeding occurred in 22 (10.5%) patients (9 group 1 and 13 group 2), blood transfusions were needed in 4 (1 9%) (2 group 1 and 2 group 2), extravasation was observed in 11 patients (5 2%) (6 group 1 and 5 group 2) and cardiac arrhythmia in 3 (1.4%) (1 group 1 and 2 group 2) patients. Postoperative complications occurred in 61 patients (29%) (24 group 1 and 37 group 2) in the form of fever in 10 patients (4 8 %) (3 group 1 and 7 group 2) and prolonged leakage in 50 patients (23 8%) (21 group 1 and 29 group 2) One patient of group 2 died from postoperative sepsis Extravasation and postoperative leakage were higher in diabetic patients than in non-diabetics Stonefree rate was 60 5% (127 of 210) Clinically significant residual fragments (CSRFs) found in 70 cases (33 3%) (33 group 1 and 37 group 2) In 13 cases (6 2%) (5 group 1 and 8 group 2), clinically insignificant residual fragments (CIRFs) were found In 8 (3 group 1 and 5 group 2) of the 13 cases, spontaneous stone
passage was observed within 4-6 weeks of surgery Residual stones in three cases (1 group 1 and 2 group 2) were asymptomatic and 4 mm or less, whereas stones increased in two cases of group 2. Among all factors studied, stone burden was significantly correlated to both intraoperative and postoperative complications. The occurrence of postoperative fever increased with large stone burden
Conclusions: PCNL is a therapeutic modality that is effective, feasible, and safe for a wide range of patients with concurrent medical issues. A steep curve is required to reduce intraoperative and postoperative complications
KEY WORDS: Percutaneous nephrolithotripsy; Nephrostomy; Renal stones
Submitted 10 July 2023; Accepted 1 August 2023
INTRODUCTION
Percutaneous nephrolithotomy (PCNL), which completely outperformed open surgical methods for kidney stone treatment, is now the standard therapy method for large stones (1) Complete stone elimination with the fewest complications is the main objective of therapy Despite recent advancements, complications are still frequent (2) The clinical research office of the endourological society (CROES) recorded complications in approximately onefifth of the subjects in the PCNL global study (3) In spite of the benefits of smaller incisions, less blood loss, and a quicker time to recover than with open surgery, complications after PCNL are still a serious problem It has been reported that complications happen in 10 3% to more than 50% of PCNLs (4) Usually, patients with comorbidities and a lower functional level are at a higher risk for surgical complications (5) As per the modified Clavien classification system, perioperative (intraoperative and early postoperative) complications have been divided into
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11581 1
ORIGINAL PAPER
DOI: 10 4081/aiua 2023 11581
five grades Grade 1 represents all occurrences that, if left untreated, might resolve spontaneously or require a simple bedside intervention, Grade 2 is assigned when specific medications, such as antibiotics and blood transfusions, were necessary; Grade 3 if endoscopic, surgical, or radiologic intervention was required; Grade 4 in case of organ failures and damage to nearby organs; Grade 5 in case of death (6) To lessen the complications related to PCNL, it’s crucial to carefully choose and prepare patients Renal bleeding is the most concerning PCNL complication, which may be so severe to require a blood transfusion Early complications of PCNL also include renal vein rupture, ureteral or renal pelvic perforations, duodenal or colonic perforations, injuries to the spleen and liver, sepsis, and retained stones (7) This study aimed to report the outcome of PCNL via standard nephrostomy tract in one training institution The perioperative complications in relation to the comorbid state are particularly assessed
PATIENTS AND METHODS
Between January 2019 to January 2022, 210 patients from inpatient department of the author’s institute who scheduled for PCNL, were enrolled into this prospective observational study On average, they were 40 3 ± 11 8 years old (range 18-67 years) They were categorized into two groups The first group included 146 (69 5%) cases with no associated co-morbidities while patients of the second group 64 cases (30 5%) had co-morbidities such as obesity in 4 cases (1 9%), hypertension (HTN) in 24 cases (11 4%), diabetes mellitus (DM) in 17 cases (8 1%), history of recurrent stone surgery in 11 cases (5 2%) Eight cases (3 8%) had more than one complication
All procedures performed in the study complied with institutional and/or national research council ethical standards as well as the 1964 Declaration of Helsinki and its subsequent amendments or similar ethical standards
Protocols and written informed consent for all participants were approved by the Research Ethics Committee of Al-Azhar University, Faculty of medicine (Urosurg 2023/0001) All the patients provided their informed consent that explained nature of procedure, its complications and possible clearance of his stones
Preoperative workups included a full blood count, platelet count, serum creatinine, hemorrhage and coagulation profiles, and urine culture for all patients Intravenous urography (IVU), urinary tract ultrasonography, and non-contrast computed tomography (NCCT) were all used in the radiologic assessment of patients Stone burden has been determined using radiographic examinations, and stones were classified as simple (isolated calyceal stones or isolated renal pelvis stonees) or complex (complete or partial staghorn stones, kidney pelvic stones accompanied by calyceal stones), irrespective of size
Every subject underwent PCNL, which started with a cystoscopy and ureteral catheter insertion, all of the patients under study were placed in the prone position to acquire percutaneous access; then through a Chiba needle, pelvicalyceal system was accessed under fluoroscopy After a correct calyceal puncture, a 30F Amplatz sheath has been inserted after the tract had been dilated with Alken metal
telescopic dilators Using a rigid 26-Fr nephroscope, nephroscopy was carried out When necessary, further tracts were made during the same session to gain access to all stones A pneumatic Swiss Lithoclast was used to fragment the stone burden By using antegrade nephrostography and fluoroscopy intraoperatively, the collecting system's integrity and stone removal were verified At the conclusion of PCNL, a 22-Fr nephrostomy tube has been inserted into the renal pelvis or the affected calyx If the urine was clear or light pink on the first postsurgical day, the Foley and ureteral catheters have been eliminated The kidneys, ureters, and bladder were examined with a plain film The nephrostomy tube was removed on the second postsurgical day after antegrade nephrostography showing that patients had clinically insignificant residual fragments (CIRFs) < 4 mm or no residual stones and drainage of the ureter down to the bladder If urinary leakage from the tract persisted for more than 24 to 48 hours after the nephrostomy tube was removed, a Double-J catheter was deemed necessary If a second PCNL session was planned due to remaining stones, the nephrostomy tube was left in place The PCNL technique was deemed successful when the patient was either stone-free or had CIRFs, which were defined as <4 mm, non-obstructive, non-infectious, and asymptomatic residual fragments
Statistical analysis: SPSS was used to analyze the data, (version 13 0, SPSS Inc , Chicago, Ill, USA) We compared the two groups using the Student t test, Mann-Whitney U test, and chi-square test The mean standard deviation was reported for quantitative variables P values < 05 were deemed significant
RESULTS
The study comprised 210 patients treated by PCNL There were 132 men (group I 84 and group II 48) and 78 women (group I 62 and group II 16) The age was 40 3 mean ± SD ± 12 8 years; 40 2 ± 11 6 years in group I and 41 13 ± 13 2 years in group II (p = 0 77) The average body weight index in groups I and II was 29 5 ± 7 1 and 30 0 ± 8 2 kg/m2, respectively (p = 0 53) (Table 1) Mean stone burden was 7 5 ± 5 6 cm2 (range: 2 5-30 cm2); 7 3 ± 3 4 cm2 and 8 1 ± 4 8 cm2 in groups I and II, respectively (p = 0 47) Mean follow up was 41 2 ± 32 3 months in group I and 45 3 ± 24 3 months in groups II (p = 0 79) (Table 2)
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11581 Tamer A
et al 2
Abouelgreed, Hassan Ismail, Sameh S Ali,
Table
1
Characteristics No. (210 cases) Group I (n = 146) Group II (n = 64) Age (mean ± SD) 40 3 ± 12 8 yrs 40 2 ± 11 6 41 13 ± 13 2 Sex Males 132/210 (62 9%) 84 48 Females 78/210 (37 1%) 62 16 Complaint Pain 201/210 (95 7%) 141 60 Hematuria 9/210 (4 3%) 5 4 Mean body weight index (kg/m2) 29 5 ± 7 2 29 5 ± 7 1 30 0 ± 8 2
Clinical c of treated patients
Table 2
Stones characteristics and PCNL access in the two groups
Table 4. Overall complications in relation
successfully managed with intravenous broad-spectrum antibiotics, but one patient who died from postoperative sepsis (Table 3) No pleural injury neither hydrothorax nor hemothorax and no colonic injury developed in any of our cases
One-access subcostal PCNL was performed in 189 (90%) cases (group I 136 and group II 53), while 21 (10%) cases underwent multi-tract PCNL (group I 10 and group II 11) Supracostal approach was indicated in four cases (1 9%) in group I The average surgical time was 75 15 ± 32 75 mins (range 40 to 140) Nephrostomy tube removal took an average of 2 86 ± 0 83 days (ranging from 3 to 8), and the mean hospital stay was 3 93 ± 3 17 days No complications occurred intraoperatively in 82 9% (174/210) of the patients, while one or more complications have been noticed in 36 (17 1%) cases during PCNL Bleeding occurred in 22 (10 5%) patients; transfusions of blood were needed in 4 out of the 22 patients (Table 3) whereas the remaining patients were successfully treated with conservative measures Postoperative complications occurred in 61 cases (29%) Prolonged leakage following nephrostomy tube removal occurred in 50 (23 8%) patients Stenting was required in 8 patients (3 8%) because of persistent urine leakage Fifteen out of the 17 patients with diabetes mellitus developed prolonged leakage after PCNL In 10 patients (4 8%), there was a transient fever that required antipyretics Nine out of the ten patients with fever had urosepsis, which was
3 Intraoperative and postoperative
Complications in relation to stone burden were observed in 49 (72%),77(60 6%) and 6 (40%) patients with stone size ≤ 3 cm2, 3 1-5 cm2 and > 5 cm2 respectively Conversely, no complications were reported in 19 (27 9%, 50 (39 %) and 9 (60%) patients with stone size ≤ 3 cm2, 3 1-5 cm2 and > 5 cm2 respectively (Table 4) At three months after surgery, the total stone-free rate reached 60 5% (127 of 210) Clinically significant residual fragments were found in 70 cases (33 3%) (33 group 1 and 37 group 2) whereas in 13 cases (6 2%) (5 group 1 and 8 group 2), clinically insignificant residual fragments were found In 8 (3 group 1 and 5 group 2) of the 13 cases with clinically insignificant fragments, spontaneous stone passage was observed within 4-6 weeks of surgery Residual stones were asymptomatic and 4 mm or less in three cases (1 group 1 and 2 group 2), whereas stones increased in two cases of group 2
DISCUSSION
Despite the high rate of success of PCNL, major risks associated with percutaneous renal surgery involve blood loss requiring transfusion, fever, urinary tract infections, and injury to nearby organs (8, 9) According to Olbert et al (10), there are links between the result of PCNL and patient- and stone-related parameters, including age of the patient, BMI, metabolic syndrome, and type and burden of stone The PCNL morbidity is significantly influenced by the burden of stones (11)
The most frequent complication in a study by Lee et al (12) on 500 patients who had undergone PCNL was hemorrhage, with a 12% rate of transfusion
The nephrostomy tract itself is a frequent source of hemorrhage during PCNL (8) The number of serious hemorrhages was recorded as < 8% (13) In the majority of such cases, conservative therapy is successful; in the study of Tefekli et al (6) no blood transfusion was required whereas Mousavi-Bahar et al (14) reported a transfusion rate of 0 6% In our study, the transfusion rate was 1 9% in agreement with Vorrakitpokatorn et al (9), who reported a 1 4% transfusion rate
Transfusions rates were reported to be 25% in early investigations, but they were significantly reduced due to advances in percutaneous stone removal techniques, and more recent studies have found that they are now between 1% and 2% (15)
Earlier investigations have proposed that diabetes, the
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11581 3 PCNL in comorbid patients
Stone and access criteria Group I Group II Mean stone burden: 7 5 ± 5 6 cm2 (range: 2 5–30 cm2) 7 3 ± 3 4 cm2 8 1 ± 4 8 cm2 Classification of stones: Simple: 49% (n = 103) 68 35 Complex: 51% (n = 107) 78 29 Mean operation time: 75 ± 32 minutes (range 40 to 140) 70 ± 20 72 ± 22 Mean number of percutaneous access no : 1 1 ± 0 5 (range: 1–5) Single access: 90% (n 189) 136 53 Multi-tract accesses: 10% (n = 21) 10 11 Percutaneous access location Subcostal access: 98 1% (n = 206) 145 61 Supracostal access: 1 9% (n 4) 13 Overall postsurgical result: Mean duration of urethral catheterization: 1.08 ± 0.2 d (range: 2–4 d) 1.3 ± 0.1 d 1. 4 ± 0.8 d Mean time with nephrostomy tube: 2 86 ± 0 83 d (range: 3–8 d) 2 53 ± 0 71 d 2 74 ± 0 22 d Mean hospital stay was 3 93 ± 3 17 days (range: 3–15 d) AKE 3 88 ± 2 07 d 4 03 ± 3 66 d
Intraoperative complications No. of cases (%) Group I (n = 146) Group II (n = 64) Bleeding 22 (10 5%) 9 (6 2%) 13 (20 3%) Transfusion 4 (1 9%) 2 (1 4%) 2 (3 1%) Extravasation 11 (5 2%) 6 (4 1%) 5 (7 8%) Cardiac arrhythmia 3 (1 4%) 1 (0 7%) 2 (3 1%) No complications 174 (82 9%) 130 (89%) 44 (68 7%) Postoperative complications Fever 10 (4 8%) 3 (2%) 7 (10 9%) Leakage 50 (23.8%) 21 (14.4%) 29 (45.3%) Death 1 (0 4%) (0 0%) 1 (1 6%) No complications 149 (71%) 122 (83 6%) 27 (42 2%) (Either colonic or pleural)
Table
complications
to
Stone burden Complications occurred No complications ≤ 3 cm2 49 (72 1%) 19 (27 9%) 3 1- 5 cm2 77 (60 6%) 50 (39 4%) > 5 cm2 6 (40%) 9 (60%)
stone burden.
type of stone, and the size of the stone can all predict blood loss in PCNL (16)
The incidence of bleeding complications was found to be 7 0% (109/1555) after telescopic dilatation of the track using large sheaths (27F, 28F, 30F) with 5 9% (208 /3533) requiring blood transfusion (17) Obesity is thought to make PCNL more technically challenging, which could increase the chance of complications However, impact of obesity on PCNL results and complications is not well defined A negative effect of obesity on complication rate was found in Bagrodia et al (18) In a large recent series, 234 patients were divided into 4 groups based on their BMIs as ideal body weight (< 25 kg/m2), overweight (25 to 29 9 kg/m2), obese (≥ 30 to 34 9 kg/m2), and severely obese (≥ 35 kg/m2) After stratification with regard to BMI, no statistically significant difference was observed in length of hospital stay, stone-free rate, rate of complications, or change in hematocrit This was supported by a more recent study (19), which concluded that BMI was not related to a higher risk of hemorrhage and transfusions
In our study, the procedures were performed on obliquely prone that we found more suitable for proper puncture of the collecting system PCNL is most effective when the patient is in the prone position although patient may be placed in any of the following positions: flat prone on a fluoroscopic table, deflected prone on a cushion, oblique prone on a fluoroscopic table, or oblique supine on a fluoroscopic table The oblique supine position is favored by some urologists because they believe it makes it simpler to access the succeeding PCNL It must be highlighted that the kidney's axis differs when the patient is lying in an oblique supine position versus a flat prone position (7) The number and type of access is influenced by the treatment approach and by the stone size and location Some surgeons favor a standard access via the lower calyx with subsequent ESWL therapy for stones not reachable through this access (20) Others recommend using many tracts (such as the upper pole) in a single session to clear the collecting system (21) Upper pole access offers the best manipulation in cases with stone burdens in the upper and lower calices but involves a slight increase in the rate of complications (i e , pleural injury) A subcostal technique is usually used, though a supracostal technique is preferred in some cases, like those of proximal ureter stones, superior calyx stones, or staghorn stones When selecting the supracostal technique, significant chest complication rates of roughly 5% must be taken into account (22) Our policy was to use the subcostal approach However, supracostal approach was needed in four patients (1 9%) due to stones extending into the upper calyx We had no complications related to supracostal approach in the four cases One-access subcostal PCNL was performed in 189 (90%) cases (group I had 136 and group II had 53), while 21 (10%) underwent multi-tract PCNL (group I has 10 and group II has 11) The average surgical time ranged from 55 to 90 minutes (10) although most studies overlook the variables that influence PCNL’s surgical time In the current study, the average surgical time was 75 15 ± 32 75 minutes (range 40 to 140), which lies in the range described Takeuchi et al (23) reviewed the clinical records of 1897 patients who underwent PCNL for renal calculi splitting them into
2 groups depending on their median surgical time (group 1: ≤ 60 min; group 2: > 60 min) The average operation time was 64 9 ± 27 6 minutes (with a range of 10-220 minutes)
In the present study intraoperative extravasation occurred in 5 2% (11 cases) and was managed conservatively The overall incidence of postoperative prolonged leakage was 23 8% although it was significantly higher in group II compared to group I (45 3% versus 14 4%, p < 0 045)
Fifteen out of the 17 cases with diabetes mellitus developed prolonged leakage after PCNL
Septicemia can occur as a result of an infection introduced through the renal access tract or because the stones are infected Individuals with infected urinary stones experience fever more frequently following PCNL than patients with sterile stones (24) Prior to undergoing PCNL, a pyonephrotic kidney must be drained and prophylactic antibiotics must be taken In the instance of sterile urine, antibiotics could be administered using single-dose or short-course prophylactic procedures without any significant differences between them There are significant risk factors for postsurgical fever, including the length of the operation and the amount of irrigation fluid used Additionally, it is critical to avoid an increase in collecting system pressure, and operating times should be kept to a minimum (i e , < 90 minutes)
The literature reports sepsis rates up to 0 97% (25) although other series (26), reported lower incidence of such complication (0 3%)
In our series, despite proper antibiotic therapy, a diabetic patient with staghorn stone died of urosepsis He received prophylactic antibiotic, and his preoperative urine culture was negative The surgical time was 120 minutes
The total stone-free rate in this study at three months was 60 5% (127 of 210), which was lower than previously reported Altunrende F et al (27) reported total stone-free rate as 74 5%
The impact of case volumes on PCNL's efficacy and safety results was recently analyzed in a large database including data from 3933 patients (28) In high-volume centers, stone-free rates were higher (82 5% versus 75 1%; p < 0 001) High-volume centers had also a lower rate of complications (15 9% versus 21 7%; p = 0 002) and a shorter mean length of stay (3 4 versus 4 9 days) After controlling for stone burden, urine culture status, and the presence of staghorn stones, the stone free rate increased with case volume, while the complication rate and length of stay decreased Centers that undertook a large number of PCNLs annually had better outcomes and the highest stone free rates have been found in centers with more than 120 cases annually (28)
A study evaluated the natural history of CIRFs (27) in 38 patients who had CIRFs three months following PCNL (22% of the total) and were followed for a minimum of 24 months During follow-up, 10 (26 3%) patients experienced a symptomatic episode that required medical treatment, whereas the other patients were asymptomatic According to the radiologic evaluation, the size of the fragments increased in 8 (21 1%) cases while remaining stable or decreasing in 27 (71 1%) cases A spontaneous stone passage occurred in three (7 9%) of the patients
In our study, CIRFs were found in 13 cases (6 2%) Eight
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11581 Tamer
4
A Abouelgreed, Hassan Ismail, Sameh S Ali, et al
of those 13 cases had spontaneous stone passage, whereas the size of the stones increased in two cases, and three had asymptomatic residual stones measuring 4 mm or less Clinical significant residual fragments (CSRFs) were found in 70 cases (33 3%) and were managed by auxiliary SWL treatment
According to Margel et al (29), PCNL is time-consuming and may necessitate auxiliary operations in patients who had previous open stone surgery due to scar tissue and anatomic changes in the operated kidney In contrast, our research found no difference in the rate of complications between patients who had open stone surgery and those who did not, which is consistent with other studies (30)
Limitation of study
We have relatively high complications rate because our institution is a training center for junior staff and young residents
CONCLUSIONS
PCNL represents an efficacious, feasible, and safe treatment modality that can be used in a wide range of patients with concomitant illnesses who need a steep curve for decreasing intraoperative and postoperative complications
REFERENCES
1 Karakoyunlu N, Goktug G, Sener NC, et al A comparison of standard PCNL and staged retrograde FURS in pelvis stones over 2 cm in diameter: A prospective randomized study Urolithiasis 2015; 43:283e7
2 Jessen JP, Honeck P, Knoll T, Wendt-Nordahl G Percutaneous nephrolithotomy under combined sonographic/radiologic guided puncture: Results of a learning curve using the modified Clavien grading system World J Urol 2013; 31:1599e603
3 Taylor E, Miller J, Chi T, Stoller ML Complications associated with percutaneous nephrolithotomy Transl Androl Urol 2012; 1:223e8
4 Tseng J-S, Lin W-R, Sun F-J, et al Predicting Percutaneous Nephrolithotomy Outcomes and Complications in Elderly Patients Using Guy's Scoring System and Charlson Comorbidity Index, International Journal of Gerontology 2018; 12:239-243
5 Rizvi SAH, Hussain M, Askari SH, et al Surgical outcomes of percutaneous nephrolithotomy in 3402 patients and results of stone analysis in 1559 patients BJU Int 2017; 120:702e709
6 Tefekli A, Karadag MA, Tepeler K, et al Classification of Percutaneous Nephrolithotomy Complications Using the Modified Clavien Grading System: Looking for a Standard Eur Urol 2008; 53:184-190
7 Michel MS, Trojan L, Rassweiler JJ Complications in percutaneous nephrolithotomy Eur Urol 2007; 51:899-906
8 Karakoyunlu N, Goktug G, Sener NC, et al A comparison of standard PCNL and staged retrograde FURS in pelvis stones over 2 cm in diameter: A prospective randomized study Urolithiasis 2015; 43:283e7
Phettongkam A Perioperative complications and risk factors of percutaneous nephrolithotomy J Med Assoc Thai 2006; 89:826-833
10 Olbert PJ, Hegele A, Schrader AJ Pre and perioperative predic-
tors of short-term clinical outcomes in patients undergoing percutaneous nephrolitholapaxy Urol Res 2007; 35:225
11 Juan YS, Huang CH, Chuang SM Colon perforation: a rare complication during percutaneous nephrolithotomy Kaohsiung J Med Sci 2006; 22:99-102
12 Lee WJ, Smith AD, Cubelli V, Vernace FM Percutaneous nephrolithotomy: analysis of 500 consecutive cases Urol Radiol 1986; 8:61-66
13 Srivastava A, Singh KJ, Suri A Vascular complications after perc u t a n e o u s n e p h r o l i t h o t o m y : a r e t h e r e a n y p r e d i c t i v e f a c t o r s ? Urology 2005; 66:38-40
14 Mousavi-Bahar SH, Mehrabi S, Moslemi MK Percutaneous Nephrolithotomy Complications in 671 Consecutive Patients: A Single-Center Experience Urol J 2011; 8:271-276
15 Al-Bareeq R, and Denstedt, JD Percutaneous nephrolithotomy for the treatment of lower pole renal calculi CUAJ 2008; 2:628-630
16 Turna B, Nazli O, Demiryoguran S, et al Percutaneous nephrolithotomy: Variables that influence hemorrhage Urology 2007; 69:603-607
17 Yamaguchi A, Skolarikos A, Buchholz NN, et al Operating Times and Bleeding Complications in Percutaneous Nephrolithotomy: A Comparison of Tract Dilation Methods in 5537 Patients in the Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study J Endourol 2011; 25:933-939
18 Bagrodia A, Gupta A, Raman JD, et al Impact of body mass index on cost and clinical outcomes after percutaneous nephrostolithotomy Urology 2008; 72:756-760
19 Tomaszewski JJ, Smaldone MC, Schuster T, et al Outcomes of Percutaneous Nephrolithotomy Stratified by Body Mass Index J Endourol 2010; 24:547-550
20 Rassweiler JJ, Renner C, Eisenberger F Management of complex renal stones BJU Int 2000; 86:919-928
21 Liatsikos EN, Kapoor R, Lee B, et al Angular percutaneous renal access Multiple tracts through a single incision for staghorn calculous treatment in a single session Eur Urol 2005; 48:832-837
22 Gupta R, Kumar A, Kapoor R, et al Prospective evaluation of safety and efficacy of the supracostal approach for percutaneous nephrolithotomy BJU Int 2002; 90:809-813
23 Takeuchi H, Ueda M, Nonomura M Fever attack in percutan e o u s n e p h r o l i t h o t o m y a n d t r a n s u r e t h r a l u r e t e r o l i t h o t r i p s y Hinyokika Kiyo 1987; 32:1357-1363
24 Dogan HS, Sahin A, Cetinkaya Y, et al Antibiotic prophylaxis in percutaneous nephrolithotomy: prospective study in 81 patients J Endourol 2002; 16:649-53
25 Aron M, Yadav R, Goel R Multi-tract percutaneous nephrolithotomy for large complete staghorn calculi Urol Int 2005; 75:327332
26 Osman M, Wendt-Nordahl G, Heger K, et al Percutaneous nephrolithotomy with ultrasonography-guided renal access: experience from over 300 cases BJU Int 2005; 96:875-878
27 Altunrende F, Tefekli A, Stein RJ, et al Clinically insignificant residual fragments after percutaneous nephrolithotomy: mediumterm follow-up J Endourol 2011; 25:941-945
28 Opondo D, Tefekli A, Esen T, et al ; CROES PCNL study group Impact of case volumes on the outcomes of percutaneous nephrolithotomy Eur Urol 2012; 62:1181-7
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11581 5
PCNL in comorbid patients
V o r r a k i t p o k a t o r n P , P e r m t o n g c h u c h a i K , R a k s a m a n i E O ,
9
29 Margel D, Lifshitz DA, Kugel V, et al Percutaneous nephrolithotomy in patients who previously underwent open nephrolithotomy J Endourol 2005; 19:1161-1164
30 Sofikerim M, Demirci D, Gulmez I, Karacagil M Does previous o
Correspondence
Tamer A Abouelgreed, MD (Corresponding Author) dr tamer ali@yahoo com; tamerali 8@azhar edu eg
Hassan Ismail, MD drhassan ismail@yahoo com
Ayman K Koritenah, MD dr ayman kotb@gmail com
Yasser Badran, MD dryasserbadran@gmail com
Mahmoud Ali, MD dr mahmoud72@hotmail com
Rasha Ahmed, MD rashaahmed1511@gmail com
Mohamed Algammal, MD gemykarter2020@gmail com
Ahmed Alrefaey, MD a7medrefa3y ash@gmail com
Aly Gomaa, MD alygomaa68@yahoo com
Mohamed F Elebiary, MD dr elebiary@yahoo com
Hany A Eldamanhory, MD drhanyeldamanhory@gmail com
Department of Urology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Sameh S Ali, MD drsamehsaied@yahoo com
Department of Radiology, Sheikh Khalifa General Hospital, UAQ, UAE
Abdelhamid A Khattab, MD abdelhamed1123ufw@gmail com
Department of Urology, Damanhur Teaching Hospital, Albuheira Government, Egypt
Nermeen M Abdelmonem, MD neermeeenmohamed@gmail com
Department of Radiology, Thumbay University Hospital, Ajman, UAE
Mohammad Thabet Alnajem, MD mtnajem@gmail com
Department of Radiology, Tawam Hospital, Alain, UAE
Tamer G Abdlhamid, MD dr tamer gamal@yahoo com
Department of Anesthesia, Emirates Specialty Hospital, Dubai, UAE
Ahmed A Abdelwahed, MD ahmed abdelwahed@yahoo com
Salma F Abdelkader, MD Cairo, Egypt salmafathy4@gmail com
Department of Radiology, Faculty of Medicine, Ain Shams University, Cairo, Egypt
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11581
6
Tamer A Abouelgreed, Hassan Ismail, Sameh S Ali, et al
p e n n e p h r o l i t h o t o m y a f f e c t t h e o u t c o m e o f p e r c u t a n e o u s nephrolithotomy? J Endourol
21:401-403
2007;
ORIGINAL PAPER
1
2
Summary
Background: General anesthesia in high-risk patients has many complications and needs long preoperative preparations and postoperative intensive care unit (ICU). Therefore the present study aimed to evaluate the efficacy of combined low-dose spinal anesthesia with quadratus lumborum block (QLB) as an alternative to general anesthesia for patients undergoing percutaneous nephrolithotomy
Patients and methods: A prospective study was conducted at the urology department of Al-Azhar University Hospitals in Cairo, Egypt, from January 2021 to January 2022. The study included 60 patients of ASA ll-lll scheduled for percutaneous nephrolithotomy. All patients received low-dose spinal anesthesia (5 mg bupivacaine) and QLB (QL1-QL2-QL3) approaches The primary observation parameter was the efficacy of this technique as an alternative to general anesthesia The secondary parameters measured were evaluation of need for intraoperative narcotics, postoperative pain score (VAS), and patients satisfaction as assessed using a 5-point Likert Scale
Results: None of the patients was given general anesthesia, and intraoperative sedation was given to nineteen patients (32 2%) No hemodynamic changes were observed in all patients
There was a significant correlation between the use of intraoperative sedation and stone site, intraoperative blood loss, and hospital stay Pain intensity on VAS at rest and movement was low until the 24th postoperative hour. Patient satisfaction score was 3, 4, and 5 in 1 (1 7%), 4 (6 7%), and 55 (91 6%) patients, respectively.
Conclusions: Combined low-dose spinal anesthesia with quadratus lumborum block is an effective alternative to general anesthesia in patients undergoing PCNL procedures with good postoperative analgesia. Patients with lower calyceal punctures have a lower incidence of intraoperative sedation requirements
KEY WORDS: Quadratus lumborum block; Low dose spinal anesthesia; Percutaneous nephrolithotomy
Submitted 12 July 2023; Accepted 1 August 2023
INTRODUCTION
Percutaneous nephrolithotomy (PCNL) is considered the standard method for managing large or complex renal calculi (1) Although opioids are effective in controlling
intra and postoperative pain, they are associated with significant side effects (2) Recently, a new regional analgesic technique, known as Quadratus Lumborum Block (QLB), has been introduced for pain relief following abdominal surgery This technique has been used successfully to provide postoperative analgesia for patients undergoing various types of abdominal surgeries, including renal surgeries (3-7) The QLB technique functions by blocking somatic nerve fibers that supply the abdominal wall, and it may potentially block the sympathetic nerve supply of the abdomen, inhibiting visceral pain (8) Several modifications to the technique have been introduced, including injection into the posterior segment of the quadratus lumborum muscle (QLM) (QLB2), injection into QLM and the fascia of the psoas muscle using the trans-muscular approach (QLB3), and injection into the QLM itself (QLB4) It is apparent that this block is highly effective in providing analgesia from T7 to L1 dermatomes, and it affords analgesia to the anterior abdominal wall while reducing visceral pain (9) The current study presents a novel technique for providing anesthesia by fascial peripheral block with low-dose spinal anesthesia The fascial block serves as the primary element of anesthesia for PCNL, and we are optimistic that it can be used as a standalone anesthesia We utilized l o w - d o s e s p i n a l a n e s t h e s i a f o r c y s t o s c o p y , u r e t e r i c catheter insertion, and the long-term onset of QLB This technique will serve as the foundation for further research aimed at reducing the requirement for general anesthesia, with its attendant complications, among high-risk patients The present study aimed to evaluate the efficacy of combined low dose spinal anesthesia with quadratus lumborum block as an alternative to general anesthesia for patients undergoing PCNL
PATIENTS AND METHODS
A prospective study was conducted at the urology department of Al-Azhar University Hospitals in Cairo, Egypt, from January 2021 to January 2022
The study included 60 patients who were deemed suitable
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11584 1
Is quadratus lumborum block combined with low dose-spinal anesthesia an effective alternative to general anesthesia in patients undergoing percutaneous nephrolithotomy?
Tamer A. Abouelgreed 1 , Ahmed M. Elgarhy 2 , Adel Elatreisy 1 , Tamer M. Ewieda 2 , Wael M. Ibrahim 2 , Othman Saadeldien Yahia 2 , Ahmed M. Elnaggar 2 , Mohamed A. Elbadawy 2 , Ali A. Alkumity 2 , Yasser Badran 1 , Mahmoud Ali 1 , Aly Gomaa 1 , Mohamed F. Elebiary 1 & Mahmoud Aboelnasr 1
Department of Urology, Faculty of medicine, Al-Azhar University, Cairo, Egypt;
DOI: 10 4081/aiua 2023 11584
Department Anesthesia, Al-Azhar University, Cairo, Egypt
candidates for PCNL The local ethics committee approved the research (registration number of: ClinicalTrial gov ID NCT04852874 ), and all patients provided informed written consent to participate The study adhered to ethical guidelines and regulations, ensuring the safety and confidentiality of all participants
We excluded patients with coagulopathy, mental retardation, airway problem, sleep apnea syndrome, pregnancy, and ASA (IV) Upon induction of anesthesia, an intravenous line was established for all patients and oxygen was administered at a rate of 3 liters per minute through a nasal cannula while vital signs were continuously monitored Spinal anesthesia was then administered using a 25-gauge (BD Quincke spinal needle), which was inserted and directed towards the midline in order to access the intrathecal space between the L3 and L4 intervertebral space following successful dural puncture A combination of 5 milligrams of bupivacaine (1 milliliter) and 25 micrograms of fentanyl (0 5 milliliters) were then administered via the intrathecal space Low-frequency ultrasound with a curved probe (6:15 MHs) (Sonosite M Turbo, Fujifilm, Bothel Washington USA) was utilized in all patients, and a 22-gauge spinal needle (BD Quink spinal needle) was used to administer the local anesthetic injection The injection was performed with the patient in the lateral position The needle tip was carefully positioned at the anterolateral border of the quadratus lumborum muscle (QLM) at its junction with the transversalis fascia (QL1) Subsequently, the needle was placed between QLM and the erector spinae muscle (QL2) and between QLM and the psoas muscle (QL3) After ensuring the correct position of the needle, an injection of 0 25 ml/kg of 0 25% bupivacaine, along with 1 5 mg dexamethasone and 100 mg magnesium sulfate, was administered at each site of the quadratus lumborum muscle under ultrasound guidance After performing the block, each patient was evaluated for effectiveness of the technique (accomplishing of the procedure with no need to general anesthesia with surgeon and patient satisfaction) Intraoperative hemodynamics (BP, Pulse, SPO2) were measured at beginning then every 10 /min Intraoperative pain was assessed utilizing a 10 cm visual analog scale (VAS), in case of VAS > 4, narcotic was given in the form of 50 mcg fentanyl The evaluation of postoperative analgesia was conducted at the conclusion of surgery, followed by assessments at 1, 2, 4, 8, 12, 16, 20, and 24 hours, utilizing the Visual Analogue Scale (VAS) both at rest and during movement In cases where patients reported pain intensity exceeding a VAS score of 4, intravenous infusion of paracetamol at a dose of 15 mg per kg was administered, limited to a maximum of 1000 mg per dose for analgesia purposes, with a maximum cumulative dose of 4000 mg over 24 hours Nonsteroidal medication was prescribed as a secondary option if the pain remained unresolved following the administration of paracetamol Adverse effects were monitored and documented, including but not limited to direct needle trauma to abdominal viscera, bleeding, prolonged muscle weakness, and hemodynamic instability On the second postoperative day, perioperative patient satisfaction was assessed using a 5-point Likert Scale ranging from very dissatisfied (1) to completely satisfied (5)
Table 1. General descriptive data
Age, S ze of stones, HFU of stones, HB pre and post, Creatinine, Operat on t me, Blood loss, Hosp stay, Pu se and VAS parameters were represented as Min- Max and Mean ± SD, whi e Sex, S te of stones, Urine analysis, Previous surgery, Morb d ty, B ood transfus on, KUB, US, Success rate and Intraoperat ve narcot cs were represented as frequency and percent F (%)
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11584 TA
et al 2
Abouelgreed, AM Elgarhy, TM Ewieda,
Min-max Mean ± SD or F (%) Age 34-65 50 5 ± 8 4 Sex Female 19 (31 7%) Male 41 (68 3%) Site of stones Lower calyx 6 (10%) Pelvis 11 (18 3%) Pelvis, Lower calix 28 (46 7%) Pelvis, Upper calyx 15 (25%) Size of stones/cm 2-4 3 0 ± 0 5 HFU of stones 650-1500 1010 2 ± 162 0 Urine analysis Pus negative 53 (88.3%) Pus positive 7 (11 7%) Hb Pre 12-16 13 4 ± 0 8 Creatinine 0 7-1 5 1 1 ± 0 2 Previous surgery NO 44 (73 3%) YES 16 (26 7%) Morbidity ASA2 39 (65%) ASA3 21 (35%) Operative time/min 50-150 80 5 ± 16 7 Blood loss/ml 80-700 248 0 ± 112 1 Hospital stay/days 1-3 2.7 ± 0.5 Ambulation After 2 hrs 40 (66 7%) After 3 hrs 20 (33 3%) MAP base 64-95 77 6 ± 6 4 MAP 10 m 62-91 76 8 ± 6 2 MAP 20 m 60-90 75 1 ± 6 9 MAP 30 m 66-95 79 6 ± 6 3 MAP 1 hour 68-95 80 9 ± 6 5 MAP 2 h 68-91 79 3 ± 5 4 MAP 4 h 68-91 81 4 ± 5 4 Pulse base 66-785 92 4 ± 9 1 Pulse 10 m 64-90 76 6 ± 6 0 Pulse 20 m 75-99 84 2 ± 5 9 Pulse 30 m 74-99 84 7 ± 5 9 Pulse 1 h 75-96 84 2 ± 5 3 Pulse 2 h 72-95 81 5 ± 4 7 Pulse 4 h 73-93 83 2 ± 5 0 VAS 10 2-4 2 9 ± 0 8 VAS 30 2-5 3.0 ± 0.8 VAS 1 h 2-5 3 2 ± 1 0 VAS 2 h 2-5 2 9 ± 1 0 VAS 2 h 2-5 3 2 ± 0 9 VAS 4 h 2-5 3 2 ± 0 9 VAS 8 h 2-5 2 8 ± 0 7 VAS 16 h 2-5 3 1 ± 0 9 VAS 24 h 2-5 3.2 ± 1.0 Hb post 10 5-13 11 5 ± 0 6 Blood transfusion No 60 (100%) Yes 0 (0%) KUB Free 57 (95%) Positive 3 (5%) US Free 60 (100%) Positive 0 (0%) Success rate No 0 (0%) Yes 60 (100%) Intraoperative narcotics No 41 (67 8%) Yes 19 (32 2%)
Statistical analysis
The Statistical Package for Social Science (SPSS) software, version 29 ( S P S S I n c , Chicago, IL, USA), was utilized for data analysis Categorical variables were presented as frequency and percentage, while numeric variables were presented as a mean and standard deviation The paired-sample t-test was employed to determine the significance level between different data within the same group
A P value less than 0 05 was considered statistically significant
RESULTS
Sixty patients were included in the study Table 1 illustrates the patients' demographics, renal stone criteria, operative time, blood loss, and hospital stay None of the patients was given general anesthesia, and intraoperative sedation was given to nineteen patients (32 2%)
Univariate analysis revealed a significant correlation between the use of intraoperative sedation and stone site, intraoperative blood loss, and hospital stay Specifically, patients with lower calyceal and combined pelvic and lower calyceal stones exhibited a statistically significant infrequent utilization of intraoperative sedation, 100% of patients with lower calyceal stones had no intraoperative sedation, while 71 4% of patients with combined pelvic and lower calyceal stones had no sedation (p = 0 02) (Table 2)
The mean intraoperative blood loss was significantly higher in patients requiring intraoperative sedation; it was 260 5 ml compared to 242 2 ml in patients who did not require intraoperative sedation (p = 0 03) Similarly, the mean hospital stay was longer in patients receiveing intraoperative sedation (p = 0 05) (Table 2) Regarding patients who required narcotics, there were no significant differences in mean arterial pressure (MAP) or pulse rate at any point in time when compared to patients who did not require them (P-value > 0 05) Similarly, there were no statistically significant differences in the stone-free rate between patients who required narcotics (94 7%) and those who did not (95 1%) (p-value > 0 05)
(Table 2) Pain intensity on VAS at rest and on the movement was low till the 24th postoperative hour (Table 1) Patient satisfaction score was 3, 4, and 5 in 1 (1 7%), 4 (6 7%), and 55 (91 6%) patients, respectively
DISCUSSION
The QLB, originally described by Blanco et al , is a variant of the transversus abdominis
Table 2.
The associations of studied in relation of use of intraoperative narcotics
Age, Age, S ze of stones, HFU of stones, HB pre and post, Creatinine, Operation t me, Blood loss, Hosp stay, Pulse and VAS parameters were represented as Min- Max and Mean ± SD, the data were analyzed by t test Whi e Sex, S te of stones, Urine analysis, Previous surgery, Morbidity, Blood transfusion, KUB, US, Success rate and Intraoperat ve narcot cs were represented as frequency and percent F(%); the data were analyzed by X2 test
OR: Odd Ratio; C I: Conf dence Interval; p va ue calcu ated depend on log l near regression ana ysis
* p value < 0 05 is signif cant, ** p value < 0 01 is high y sign ficant
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11584 3
Combined low-dose spinal anesthesia with quadratus lumborum block for PCNL
Intraoperative narcotics Risk assessment No n = 41 Yes n = 19 P-value OR (95% C I) P-value Age 50 6 ± 8 4 50 2 ± 8 5 0 9 1 0 (0 9- 1 1) 0 8 Sex Female 13 (31 7%) 6 (31 6%) 0 9 1 0 (0 3- 3 2) 0 9 Male 28 (68 3%) 13 (68 4%) Site of stones Lower calyx 6 (14.6%) 0 (0.0%) 0.02 * Pelvis 5 (12 2%) 6 (31 6%) 0 7 1 2 (0 4- 3 9) 0 8 Pelvis, Lower calix 20 (48 8%) 8 (42 1%) 0 02 * 0 4 (0 2- 0 9) 0 03 * Pelvis, Upper calyx 10 (24 4%) 5 (26 3%) 0 1 0 5 (0 2- 1 5) 0 2 Size of stones/cm 3 0 ± 0 5 3 0 ± 0 5 0 7 1 1 (0 3- 3 5) 0 9 HFU of stones 1024 2 ± 157 9 0 9 1 0 (1 0- 1 0) 0 6 Urine analysis Pus negative 38 (92 7%) 15 (78 9%) 0 1 3 4 (0 7-16 9) 0 2 Pus positive 3 (7.3%) 4 (21.1%) HB pre 13 5 ± 0 8 13 0 ± 0 8 0 8 0 4 (0 2- 1 0) 0 8 Creatinine 1 1 ± 0 2 1 1 ± 0 2 0 7 1 0 (0 1- 2 6) 0 9 Previous surgery NO 28 (68 3%) 16 (84 2%) 0 2 0 4 (0 1- 1 6) 0 3 YES 13 (31 7%) 3 (15 8%) Morbidity ASA2 25 (61.0%) 14 (73.7%) 0.3 0.6 (0.2- 1.9) 0.4 ASA3 16 (39 0%) 5 (26 3%) Op time/min 80 6 ± 12 8 80 3 ± 23 4 0 08 1 0 (1 0 - 1 0) 0 9 Blood loss/ml 242 2 ± 88 1 260 5 ± 154 0 0 02 * 1 0 (1 0- 1 0) 0 6 Hosp st /days 2 7 ± 0 5 2 8 ± 0 4 0 05 * 1 8 (0 5- 6 1) 0 3 Ambulation After 2 hrs 28 (68 3%) 12 (63 2%) 0 7 1 3 (0 4- 3 9) 0 8 After 3 hrs 13 (31 7%) 7 (36 8%) MAP base 77 7 ± 6 8 77 3 ± 5 5 0 4 1 02 (0 4- 1 34) 0 3 MAP 10 m 76 6 ± 6 1 77 3 ± 6 7 0 6 1 0 (0 9- 1 2) 0 6 MAP 20 m 75 0 ± 6 9 75 2 ± 7 0 0 9 1 0 (0 9- 1 1) 0 9 MAP 30 m 79 5 ± 6 4 79 8 ± 6 4 0 8 1 0 (0 9- 1 2) 0 8 MAP 1 hour 80 8 ± 6 6 80 9 ± 6 7 0 7 1 0 (0 9- 1 1) 0 8 MAP 2 h 78.9 ± 5.4 80.1 ± 5.4 0.8 1.1 (0.9- 1.2) 0.4 MAP 4 h 81 1 ± 5 5 81 8 ± 5 2 0 96 1 0 (0 9- 1 2) 0 5 Pulse base 98 6 ± 110 1 79 1 ± 4 7 0 2 1 1 (0 7- 1 21) 0 3 Pulse 10 m 76 8 ± 6 1 76 3 ± 6 0 0 8 1 0 (0 9- 1 1) 1 0 Pulse 20 m 84 0 ± 6 1 84 6 ± 5 6 0 9 1 1 (1 0- 1 3) 0 2 Pulse 30 m 85 2 ± 6 2 83 5 ± 4 9 0 4 0 9 (0 8- 1 1) 0 4 Pulse 1 h 84 0 ± 5 4 84 5 ± 5 2 0 6 1 0 (0 8- 1 2) 0 9 Pulse 2 h 81.5 ± 4.8 81.5 ± 4.6 0.7 1.0 (0.9- 1.1) 0.7 Pulse 4 h 83 9 ± 4 8 81 9 ± 5 2 0 4 0 9 (0 8- 1 0) 0 1 VAS 10 3 0 ± 0 8 2 6 ± 0 7 0 7 1 15 (0 8- 1 31) 0 3 VAS 30 2 9 ± 0 9 3 1 ± 0 8 0 7 1 0 (0 4- 1 1) 0 3 VAS 1 h 3 2 ± 0 9 3 2 ± 1 1 0 1 1 3 (0 6- 3 0) 0 5 VAS 2 h 3 0 ± 1 0 2 6 ± 0 9 0 8 0 9 (0 5- 1 8) 0 8 VAS 2 h 3 3 ± 0 9 2 8 ± 0 8 0 3 0 7 (0 3- 1 4) 0 3 VAS4 h 3.2 ± 1.0 3.1 ± 0.8 0.09 0.5 (0.2- 1.1) 0.07 VAS 8 h 2 7 ± 0 7 2 8 ± 0 8 0 3 1 2 (0 5- 2 5) 0 7 VAS 16 h 3 1 ± 0 9 3 0 ± 0 9 0 4 1 1 (0 4- 2 7) 0 9 VAS 24 h 3 2 ± 0 9 3 2 ± 1 1 0 4 0 6 (0 3- 1 5) 0 3 Hb Post 11 4 ± 0 6 11 6 ± 0 6 0 6 0 9 (0 5- 1 7) 0 7 Blood transfusion No 41 (100 0%) 19 (100 0%) N A Yes 0 (0 0%) 0 (0 0%) KUB Free 39 (95 1%) 18 (94 7%) 0 9 1 1 (0 1- 12 7) 0 9 Positive 2 (4 9%) 1 (5 3%) US Free 41 (100 0%) 19 (100 0%) N A Positive 0 (0 0%) 0 (0 0%) Success rate No 0 (0 0%) 0 (0 0%) N A Yes 41 (100 0%) 19 (100 0%)
plane (TAP) block that has four subtypes named on the location of the local anesthetic delivery in relation to the quadratus lumborum muscle
These subtypes include the lateral QLB, posterior QLB, anterior QLB, and intramuscular QLB Lateral QLB, also known as QLB Type 1, was initially proposed The posterior QLB is administered by depositing the local anesthetic between the posterior surface of the quadratus lumborum muscle and the medial lamina of the thoracolumbar fascia (TLF) Like other interfascial blocks, the posterior QLB has a variable spread of the drug solution However, it consistently spreads to the TAP, around the quadratus lumborum muscle, and along the middle lamina of the TLF The TLF contains a dense network of sympathetic nerve fibers of the abdomen Blocking these nerve fibers provides relief from sympathetic-mediated
pain
Furthermore, the injected drug may spread cranially to the lumbar paravertebral space along the TLF and endothoracic fascia, which may be responsible for the additional visceral and somatic block with wider width of analgesia (T7 to L4 dermatome) observed in posterior QLB compared to the more traditional TAP block (1011) In this trial, we studied the efficacy of combined low dose spinal anesthesia with quadratus lumborum block as an alternative to general anesthesia for patients undergoing PCNL We observed that this anesthesia technique is safe and feasible specifically in high-risk patient for general anesthesia
The results of previous studies are consistent with our own findings, which indicate that QLB provides effective postoperative analgesia with low VAS scores and minimal need for additional analgesia Chen et al observed that QLB reduced intraoperative sufentanil consumption and provided effective postoperative pain relief within 24 hours for patients undergoing PCNL procedures (12) Kılıç and Bulut reported that QLB effectively managed pain levels and reduced morphine consumption for up to 48 hours post-surgery in PCNL patients (13) In a randomized, double-blind, controlled, prospective study, Raman and Prabha found that QLB provided significantly longer analgesia duration compared to placebo in patients undergoing PCNL They concluded that QLB is a viable option for prolonged postoperative pain control (11) Similarly, Peksoz et al reported that QLB significantly reduced postoperative opioid consumption and VAS scores compared to a control group for PCNL patients Opioid consumption was significantly lower in the QLB group compared to the control group at all times (14) In the current study, there was a significant correlation between the use of intraoperative sedation and stone site, intraoperative blood loss, and hospital stay
The mean intraoperative blood loss was significantly higher in patients requiring intraoperative sedation; similarly, the mean hospital stay was longer in patients receiving intraoperative sedation
Interestingly, patients with lower calyceal stones, and patients with combined pelvic and lower calyceal stones had a statistically significant lower intraoperative sedation utilization; this can be explained with lower calyceal puncture in such patients accompanied with lower pain compared to middle and upper calyceal punctures
Limitations of the study
Although our study was conducted prospectively focusing on a single anesthesia technique used to manage patients undergoing PCNL, it is not a comparative or randomized trial Additionally, we did not record the dermatomal distribution of analgesia in our patients It is highly recommended that a prospective randomized study be conducted to evaluate the effectiveness of this technique This approach will provide a more comprehensive understanding of the technique's potential benefits and limitations
CONCLUSIONS
Combined low-dose spinal anesthesia with quadratus lumborum block is effective for patients undergoing PCNL procedures with good postoperative analgesia Patients with lower calyceal punctures have a lower incidence of intraoperative sedation requirements
REFERENCES
1 Ghani KR, Andonian S, Bultitude M, et al Percutaneous Nephrolithotomy: Update, Trends, and Future Directions Eur Urol 2016; 70:382-396
2 Sauter AR, Ullensvang K, Niemi G, et al The Shamrock lumbar plexus block: A dose-finding study Eur J Anaesthesiol 2015; 32:764-70
3 Jin Z, Liu J, Li R, et al Single injection Quadratus Lumborum block for postoperative analgesia in adult surgical population: A systematic review and meta-analysis J Clin Anesth 2020; 62:109715
4 Verma K, Malawat A, Jethava D, Jethava DD Comparison of transversus abdominis plane block and quadratus lumborum block for post-caesarean section analgesia: A randomised clinical trial Indian J Anaesth 2019; 63:820-826
5 Baytar Ç, Yılmaz C, Karasu D, Topal S Comparison of Ultrasound-Guided Subcostal Transversus Abdominis Plane Block and Quadratus Lumborum Block in Laparoscopic Cholecystectomy: A Prospective, Randomized, Controlled Clinical Study Pain Res Manag 2019; 2019:2815301
6 Cardoso JM, Sá M, Reis H, et al Bloqueio do quadrado lombar tipo II para uma gastrectomia subtotal em um paciente séptico [Type II Quadratus Lumborum block for a sub-total gastrectomy in a septic patient] Braz J Anesthesiol 2018; 68:186-189
7 Li X, Xu ZZ, Li YT, et al Analgesic efficacy of two approaches of ultrasound-guided quadratus lumborum block for laparoscopic renal surgery: A randomised controlled trial Eur J Anaesthesiol 2021; 38:265-274
8 Akerman M, Pejcic N, Velickovic I A review of the quadratus lumborum block and ERAS Front Med 2018; 5:44-49
9 Blanco R 271 Tap block under ultrasound guidance: the description of a “ no pops ” technique Regional Anesthesia and Pain Medicine 2007; 32:130-130
10 Blanco R, Ansari T, Girgis E Quadratus lumborum block for postoperative pain after caesarean section: A randomised controlled trial Eur J Anaesthesiol 2015; 32:812-8
11 Raman R, Prabha R Quadratus Lumborum Block for Patients
Controlled Study Anesth Essays Res 2021; 15:174-178
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11584
4
TA Abouelgreed, AM Elgarhy, TM Ewieda, et al
U n d e r g o i n g P e r c u t a n e o u s N e p h r o l i t h o t o m y : A R a n d o m i z e d
Combined low-dose spinal anesthesia with quadratus lumborum block for PCNL
12 Chen L, Ji J, Tian Sun Q, et al Retrospective study of quadratus lumborum block for postoperative analgesia in patients undergoing percutaneous nephrolithotomy BMC Anesthesiology 2020; 20:1-9
13 Kılıç E, Bulut E Quadratus Lumborum Block III for Postoperative
Pain After Percutaneous Nephrolithotomy Turk J Anaesthesiol Reanim 2018; 46:272-275
14 Peksoz U, Celik M, Alici HA, et al The Effect of Transmuscular Quadratus Lumborum Block on Postoperative Opioid Consumption i n P a t i e n t s U n d e r g o i n g P e r c u t a n e o u s N e p h r o l i t h o t o m y : A Randomized Controlled Study Cureus 2021; 13:e18344
Correspondence
Tamer A Abouelgreed, MD (Corresponding Author) dr tamer ali@yahoo com; tamerali 8@azhar edu eg
Adel Elatreisy, MD dr adelelatreisy@yahoo com
Yasser Badran, MD dryasserbadran@gmail com
Mahmoud Ali, MD dr mahmoud72@hotmail com
Aly Gomaa, MD alygomaa68@yahoo com
Mohamed F Elebiary, MD dr elebiary@yahoo com
Mahmoud Aboelnasr, MD mdaboelnasr@gmail com
Department of Urology, Faculty of Medicine, Al-Azhar University, Cairo, Egypt
Ahmed M Elgarhy, MD elgarhy 79@yahoo com
Tamer M Ewieda, MD tamerewieda@yahoo com
Wael M Ibrahim, MD waelelmahdy@gmail com
Othman Saadeldien Yahia, MD yahiadrothmansaadeldien@gmail com
Ahmed M Elnaggar, MD ahmed elnaggar@azhar edu eg
Mohamed A Elbadawy, MD dr m albadawy@gmail com
Ali A Alkumity, MD alkumityali74@gmail com
Department Anesthesia, Al-Azhar University, Cairo, Egypt
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e
2023;
5
Andrologia
95(3):11584
Supine mini percutaneous nephrolithotomy in horseshoe kidney
Orazio Maugeri 1 , Eugenio Di Grazia 2, 3 , Letterio D’Arrigo 4 , Roberta Agliozzo 1 , Gianluca Calvano 1 , Federica Trovato 1 , Christian Di Gaetano 1 , Giuseppe Trefiletti 1 , Salvatore Privitera 1 , Giorgio Ivan Russo¹, Sebastiano Cimino 1
1 Urology Section, Department of Surgery, University of Catania,Catania, Italy;
2 Endourology Unit, Casa di Cura Villa Azzurra, Siracusa, Italy;
3 Endourology Unit, Casa di Cura Mater Dei, Catania, Italy;
4 Urology Unit, Cannizzaro Hospital, Catania, Italy
Summary described technique for PCNL in HSK should be an option. Nevertheless these results must be confirmed by further studies.
Objective: The percutaneous nephrolithotomy (PCNL) in Horseshoe kidneys (HSK) is usually performed in the prone position, allowing entry through the upper pole and providing good access to the collecting system However, in patients with normal kidney anatomy, the supine position is reliable and safe in most cases, but it is unknown whether the supine position is adequate in patients with HSK. The purpose of this study was to describe the results of PCNL in HSK in three different surgical institutions and to evaluate the impact of supine position during surgery, comparing pre-operative and post-operative data, complications, and stone status after surgery.
Material and Methods: Between 2017 and 2022, a total of 10 patients underwent percutaneous renal surgery for stone disease in HSK All patients were evaluated pre- and post- operatively with non-contrast CT We evaluated patients (age and gender), stones characteristics (size, number, side, site and density ), and outcomes The change in haemoglobin, hematocrit, creatinine and eGFR were assessed between the most recent preoperative period and the first postoperative day Procedure success was defined as stone-free or presence of ≤4 mm fragments (Clinically Insignificant Residual Fragments – CIRF) Complications were registered and classified according to Clavien-Dindo Grading System, during the 30 - day postoperative period and Clavien scores ≥ 3 were considered as major complications Statistical analysis was performed using “R 4.2.1” software, with a 5% significance level. We also compared pre-operative and post-operative data using “Wilcoxon signedrank test”.
Results: No statistical difference was observed between preoperative and post-operative renal function data. At one post operative day CT scan, an overall success rate of 100% was registered. 9/10 patients were completely free from urolithiasis (stone-free rate: 90%), while 1/10 patients had ≤4 mm residual stone fragments (CIRF rate: 10%). No cases of intraoperative complications were registered Post-operative complications were reported in 1/10 patients. A patient developed urosepsis (defined as SIRS with clinical signs of bacterial infections involving urogenital organs - Clavien-Dindo Grade II) after procedure, and was treated with intravenous antibiotic therapy successfully
Conclusions: This study shows that in patients with HSK miniPCNL in supine position allows to achieve good stone free rate with a very low morbidity According to our series, the
KEY WORDS: Galdakao modified supine Valdivia; Horseshoe kidney; Percutaneous nephrolithotomy
Submitted 23 July 2023; Accepted 31 August 2023
INTRODUCTION
The guidelines of the American and European Urological Associations advise to treat stones larger than 2 cm the percutaneous nephrolithotomy (PCNL) including the patients with Horseshoe kidneys (HSK) (1) This in HSK is usually performed in the prone position, allowing entry through the upper pole and providing good access to the collecting system Several case series have investigated prone PCNL in patients with HSK However, in patients with normal kidney anatomy, the supine position is reliable and safe in most cases, but it is unknown whether the supine position is adequate in patients with HSK (2) The purpose of this study was to describe the results of PCNL in HSK in three different surgical institutions and to evaluate the impact of supine position during surgery, comparing pre-operative and post-operative data, complications, and stone status after surgery
Setting, patients and outcomes
We conducted a retrospective analysis of procedures performed between 2017 and 2022 that studied supine miniPCNL in patients with horseshoe kidney All patients were evaluated with non-contrast CT as the preferred pre- and post-operative imaging method We evaluated 10 miniPCNLs performed in three medical centres including S Croce and Carle Cuneo Hospital (4 cases), Cannizzaro Hospital (3 cases) and Mater Dei Clinic of Catania (3 cases) The following pre-operative data were collected in all patients: gender, age, side, mean stone size and density (using Hounsfield classification derived from CT scan), number of stones for single patient, stone position frequencies, mean pre-intervention values of Creatinine and eGFR The change in haemoglobin, hematocrit, creatinine and eGFR were assessed between the most recent preop-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11605 1
ORIGINAL PAPER
DOI: 10 4081/aiua 2023 11605
erative period and the first postoperative day Procedure success was defined as stone-free or presence of ≤ 4 mm fragments Clinically Insignificant Residual Fragments (CIRF) (3) Complications were registered and classified according to Clavien-Dindo Grading System, during the 30 - day postoperative period and Clavien scores ≥ 3 were considered as major complications (4)
Preparation and operative technique
All procedures were performed by three experienced endourologists Placement was chosen based on surgeon preference All surgeons are trained and experienced with PCNL in supine position The positions used for PCNL were the complete supine or supine modified GaldakaoValdivia (GMSV) After positioning the patient, it is important to mark the inferior edge of the 12th rib, the iliac crest and the posterior axillary line on the patients ‘skin in order for the surgeon to maintain his or her orientation after the patients are draped For the Valdivia modified by Galdakao the patient’s legs are placed in a modified lithotomy position with both legs in stirrups in order to facilitate simultaneous percutaneous antegrade access and ureteroscopic retrograde to the urinary system All procedures started with retrograde pyelography After these propaedeutic steps, a ureteral access sheath (UAS) was positioned (9 5, 10/12 or 12/14 Ch) in 6/10 cases depending on the ureteral diameter and compliance and position used In some patients, and precisely in 6/10, it was decided to place an ureteral sheath with the aim to perform a flexible ureteroscopy to obtain stone clearance Nevertheless, horseshoe kidney unfavourable anatomy made retrograde approach unfeasible, then switching to real-time PCNL was carried out
In all patients the puncture was performed with ultrasound/radiological guidance followed by a “single-step dilation” A 12 Fr Mini nephroscope MIP M (Karl Storz, Berlin GmbH, Germany) was used for stone fragmentation and removal Lithotripsy was performed in 9 cases with Holmium YAG laser (550 µ fiber laser) and Lithoclast EMS in 1 case An intraoperative stone-free status was verified with fluoroscopy and flexible nephroscope A 8 Fr nephrostomy tube and 6 Fr x 26 cm ureteral stent was placed in all cases at the end of surgery
Statistical analysis
Statistical analysis was performed using “R 4 2 1” software, with a 5% significance level Qualitative variables were reported as numbers and percentages Quantitative discrete variables were described as median interquartile range (IQR) values, while Quantitative continuous variables were reported as mean standard deviation (DS) values We also compared pre-operative and post-operative data using “Wilcoxon signed-rank test”
RESULTS
Patient characteristics
Demographics and stones characteristics are reported in Table 1 Mean age was 54 7 (SD: 10,18) Male sex percentage was 90% (9 patients) and female sex percentage was 10%, (1 patient) 2 (20%) vs 8 (80%) stones were located in the right and left kidney; in detail, 3 (30%)
Table
Patient’s demographic data and baseline characteristics.
(80%)
Right: 2 (20%)
Past kidney stone interventions, n (%) Yes: 0 No: 10 (100%)
Number of stones/single patient 1 (IQR: 1-1 25)
Stone size (mm) 23 3 (SD: 6)
Stone density HU 1233 (SD: 54)
Stone site - n° of patients (%) Upper calyx: 0 Middle calyx: 0
Inferior calyx: 3 (30%)
Renal pelvis: 7 (70%)
Mean Pre-intervention Creatinine (mg/dl) 0 85 (SD: 0 22)
Mean Pre-intervention eGFR (ml/min/1 73 m2) 95 50 (SD: 15 48)
stones were located in the lower pole and 7 stones (70%) in the renal pelvis, respectively The median stone size was 23 3 mm (SD: 6), in 1/10 (10%) case the stones were multiple; CT stone density was 1233 (HU) (SD: 54)
Peri-operative data and outcomes
Mean operative time was 110 (SD: 11 17) minutes (Table 2) Mean post-operative Serum Creatinine and eGFR at day 1 after surgery were 0 86 (SD: 0 2) mg/dl and 93 10 (SD: 12 55) ml/min/1 73m2, while preoperative values were 0 8 (SD: 0 22) mg/dl and 95 50 (SD: 15 48) ml/min/1 73m2 Nevertheless, any statistical difference was observed between pre-operative and post-operative renal function data (p = 1 and p = 0 294 respectively), as listed in Table 3
Diameter Access, mean (SD) 16,16 (SD: 6 69)
Calyx of puncture Upper: 5 (50%)
Middle: 5 (50%)
Lower: 0
Dilation technique Balloon: 3 (30%)
Energy, n (%)
Serial: 7 (70%)
Laser: 9 (90%)
Ultrasonic: 1 (10%)
Pneumatic: 0
Combined: 0
Surgical time (minutes) 110 (SD: 11, 17)
Amplatz-sheath Yes: 10 (100%)
No: 0
Post-operative Stent Yes: 10 (100%) No: 0
Table 3
Pre-operative and post-operative data
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11605 O
2
Maugeri, E Di Grazia, L D’Arrigo, et al
Pre-operative mean Post-operative mean p-value Creatinine (mg/dl) 0 85 (SD: 0 22) 0 86 (SD: 0 20) 1 eGFR (ml/min/1 73 m2) 95 50 (SD: 15 48) 93 10 (SD: 12 55) 0 294 Hemoglobin (g/dl) 14.62 (SD: 2.05) 13.61 (SD: 1.89) 0.012 Hematocrit (%) 43 73 (SD: 6 63) 40 23 (SD: 6 40) 0 009
Age, years mean (SD) 54 7 (SD: 10 18) Gender, n (%) Male: 9 (90%) Female: 1 (10%) Side, n (%) Left: 8
1.
Table 2. Surgical outcomes and features.
Stone
At one day CT scan, an overall success rate of 100% (10/10) was registered 9/10 patients were completely free from urolithiasis (stone-free rate: 90%), while 1/10 patients had ≤ 4 mm stone fragments in the same renal localization of previously treated lithiasis (CIRF rate: 10%) At stone analyses, 5 (50%) patients were found to have Calcium oxalate monohydrate stones (COM), 1 (10%) patient had Calcium oxalate dihydrate stones (COD), and 4 (40%) patients had mixed Calcium-Uric acid stones (Mixed Ca-UA) Table 4
Complications
No cases of intraoperative complications were registered Post-operative complications were reported in 1/10 patients (10%) The patient developed urosepsis (defined as SIRS with clinical signs of bacterial infections involving urogenital organs - Clavien-Dindo Grade II) after procedure Septic complication was treated with intravenous antibiotic therapy successfully, without necessity of transfer to Intensive Care Unit None “late” post-operative complication emerged during the follow-up until the visit at third month after surgery All complications are reported in Table 5 There were no hollow visceral injuries, which indicates that supine operations have a lower risk of any abdominal or thoracic injuries There were no IRA complication and renal function was normal in all the patients A non-contrast CT scan was performed in all cases during the first post-operative day and for the first follow up after 30 days
DISCUSSION
Horseshoe kidney (HSK) is the most common fusion defect of the kidneys, although it amounts to only about 0 25% of the population (5) There is no clear genetic cause for, but the incidence is higher in those with chromosomal disorders such as Edward syndrome (67%), Turner syndrome (from 14% to 20%) and Down syndrome (1%) (68) In 1522, Carpi described HSK during autopsies for the first time (9) He identified functioning renal masses present on both sides of the vertebral column fused together
with ureters that remain uncrossed from the renal hilum to the urinary bladder (10) In most cases the fusion occurs at the lower pole, but it may occur at the upper pole (11) Due to fusion, malrotation and anatomical defects, HSK shows high insertion and lateralization of the ureter which causes urine stasis with a consequent greater risk of hydronephrosis, infection and stone formation (9) Although ureteropelvic junction obstruction is the most common complication associated with HSK, Pawar et al estimated that that 36% of patients with a horseshoe kidney will develop nephrolithiasis throughout their life (12) About treatment of renal stones, all surgical techniques can be used in patients with HSK, but success rates are usually lower than in kidneys with regular anatomy, especially with external shockwave lithotripsy (ESWL) (13, 14) The guidelines of the American and European Urological Associations recommend the use of PCNL to treat renal stones larger than 2 cm 1 In patients with normal kidney anatomy, this procedure is performed in the supine position, but in patients with HSK many surgeons prefer to use the prone position because it allows access through the upper pole and provides good access to the collecting system 2 However, it is unknown whether the prone position is more adequate than supine approach to treat renal stones in patients with HSK Most urologists believe that PCNL should be performed in the prone position in patients with HSK and that access should be obtained through the upper pole, which is usually subcostal and offers a straight way to most calyces The results are good, and the technique is well-established However, the supine position for PCNL is gaining popularity worldwide, even in the US, where it was less used (15) Using this position, it is not necessary to turn the patient prone and therefore, the total operative time can be reduced 2 This position has also been used for complex cases, showing similar effectiveness (16) A group used to perform PCNL in the supine position, facing HSK, would probably tend to use that position However, until now, little information was available to support this choice Therefore, this study shows that supine mini-PCNL in the horseshoe kidney, as performed in several centres, can achieve optimal results Vicentini et al in a multicentric comparison study retrospectively analyzed 106 PCNLs performed for complex stones in HSK in the prone and supine positions (17) The analysis of their large cohort of patients confirmed that supine PCNL is also suitable in HSK because it is characterized by a lower complication rate and shorter operating time In our study, we aimed to answer the question of whether supine PCNL is an option as good as prone PCNL for complex kidney stones in case of HSK Our date show that the supine PCNL seems to be suitable for complex stones in the horseshoe kidney, as the immediate success, complications, transfusion rates and operative times were like those found in the literature in the prone position Furthermore, sepsis and visceral injury rates were significantly low or absent, showing a possible safer profile for the supine position Our hypothesis is that during the supine position there is less chance of pyelovenous urinary reflux due to the lower intrarenal pressure compared to prone cases, as the better irrigation flow through the Amplatz sheath is intuitive This could explain the lower
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11605 3 Supine PCNL in HSK
Table 4.
Stone composition. no. (%) Value Calcium oxalate monohydrate 5/10 (50%) Calcium oxalate dihydrate 1/10 (10%) Mixed 4/10 (40%)
composition to spectrophotometric analysis
Table 5.
Number Description Treatment Grade System of patients Grade I 1/10 1: Nausea and Vomiting Anti-emetics and supportive care Grade II 1/10 1: Urosepsis Antibiotic therapy Grade III a Grade III b Grade IV a
Clinical complications following mini-PCNL classified according to Clavien-Dindo Grading System
Clavien-Dindo
sepsis rate observed in our cases Our study included patients from three different centres, the demographics were similar in all groups, and we used a comprehensive prospective database which reduced the possibility of bias in the similarity of results regarding position The surgeries were performed by different expert endourologists, not just one surgeon Another positive point of our study was that all patients underwent a pre- and postoperative non-contrast CT scan, making outcome evaluations more accurate
CONCLUSIONS
This study shows that mini-PCNL in supine position allows to achieve good stone free rate with a very low morbidity in patients with HSK According to our series, the described technique for supine PCNL in HSK should be an option Nevertheless, these results must be confirmed by further studies
REFERENCES
1 C Türk, A Neisius, A Petrík, et al European Association of Urology 2021, EAU Guidelines on Urolithiasi, 2021
2 Li J, Gao L, Li Q, et al Supine versus prone position for percutaneous nephrolithotripsy: A meta-analysis of randomized controlled trials Int J Surg 2019; 66:62-71
3 Osman Y, Harraz AM, El-Nahas AR, et al Clinically insignificant residual fragments: an acceptable term in the computed tomography era? Urology 2013; 81:723-726
4 Tefekli A, Ali Karadag M, Tepeler K, et al Classification of percutaneous nephrolithotomy complications using the modified Clavien grading system: looking for a standard Eur Urol 2008; 53:184-190
5 Schiappacasse G, Aguirre J, Soffia P, et al CT findings of the main pathological conditions associated with horseshoe kidneys Brit J Radiol 2015; 88:20140456
6 Cereda A and Carey JC The Trisomy 18 Syndrome Orphanet Journal of Rare Diseases 2012; 7:81
7 Ranke, Michael B, Saenger P Turner's Syndrome Lancet 2001; 358:309-314
8 Bhattarai B, Kulkarni AH, Rao ST, Mairpadi A Anesthetic consideration in downs syndrome--a review Nepal Med Coll J 2008; 10:199-203
9 Natsis K, Piagkou M, Skotsimara A, et al Horseshoe kidney: a review of anatomy and pathology Surg Radiol Anat 2014; 36:517-26
10 Cook WA, Stephens FD Fused kidneys: morphologic study and theory of embryogenesis Birth Defects Orig Artic Ser 1977; 13:327-40
11 Glodny B, Petersen J, Hofmann KJ, et al Kidney fusion anomalies revisited: clinical and radiological analysis of 209 cases of crossed fused ectopia and horseshoe kidney BJU Int 2009; 103:224-35
12 Pawar AS, Thongprayoon C, Cheungpasitporn W, et al Incidence and characteristics of kidney stones in patients with horseshoe kidney: A systematic review and meta-analysis Urol Ann 2018; 10:87-93
13 Kartal I, Çakıcı MÇ, Selmi V, et al Retrograde intrarenal surgery and percutaneous nephrolithotomy for the treatment of stones in horseshoe kidney; what are the advantages and disadvantages compared to each other? Cent European J Urol 2019; 72:156-162
14 Gokce MI, Tokatli Z, Suer E, et al Comparison of shock wave lithotripsy (SWL) and retrograde intrarenal surgery (RIRS) for treatment of stone disease in horseshoe kidney patients Int Braz J Urol 2016; 42:96-100
15 Tzou DT, Metzler IS, Usawachintachit M, et al Ultrasound-guided Access and Dilation for Percutaneous Nephrolithotomy in the Supine Position: A Stepby-Step Approach Urology 2019; 133:245-246
16 Vicentini FC, Perrella R, Souza VMG, et al Impact of patient position on the outcomes of percutaneous neprolithotomy for complex kidney stones Int Braz J Urol 2018; 44: 965-971
17 Vicentini FC, Mazzucchi E Gökçe, et al Percutaneous nephrolithotomy in horseshoe kidneys: Results of a multicentric study J Endourol 2021; 35:979-984
Correspondence
Orazio Maugeri, MD (Corresponding Author) omaugeri@gmail com
Urology Section, Department of Surgery, University of Catania Via S Sofia, 78 - 95123 Catania
Eugenio Di Grazia, MD eugeniodigrazia@hotmail com
Endourology Unit, Casa di Cura Villa Azzurra, Siracusa, Italy
Endourology Unit, Casa di Cura Mater Dei, Catania, Italy
Letterio D'Arrigo, MD eliodarrigo@gmail com
Urology Unit, Cannizzaro Hospital, Catania, Italy
Roberta Agliozzo, MD roberta agliozzo@outlook it
Gianluca Calvano, MD gianluca calvano10@gmail com
Federica Trovato, MD fede-tr@hotmail it
Christian Di Gaetano, MD christian digaetano@gmail com
Giuseppe Trefiletti, MD peppetrefiletti@gmail com
Salvatore Privitera, MD salvoprivi82@gmail com
Giorgio Ivan Russo, MD giorgioivan1987@gmail com
Sebastiano Cimino, MD ciminonello@hotmail com
Urology Section, Department of Surgery, University of Catania, Catania, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11605 O Maugeri, E Di Grazia, L D’Arrigo, et al 4
ORIGINAL PAPER
1 Pediatric Urology, Kocaeli Derince Training and Research Hospital, Kocaeli, Turkey;
2 Department of Urology, Division of Pediatric Urology, School of Medicine, Marmara University, Istanbul, Turkey;
3 Department of Urology, School of Medicine, Marmara University, Istanbul, Turkey;
4 Department of Urology, School of Medicine, Koç University, Istanbul, Turkey
Summary
Aim: The voiding diary (VD) yields crucial insights into voiding volumes (VV), voiding frequency (VF), and management habits in children with lower urinary tract (LUT) dysfunction. It is recommended to be conducted for a minimum of 2 days. Nevertheless, certain studies have indicated similarities in voided volumes between days in a three-day VD This study aims to compare VV and VF values across days based on bladder capacity and symptom scores Materials and Methods: Children who applied to the pediatric urology clinic due to LUT symptoms between 2022 and 2023 were included in the study. Retrospective evaluation was conducted on the records. Children with neurological deficits and incomplete data were excluded from the study All children were assessed following the guidelines of ICCS and EUA and underwent a 3-day voiding diary Mean VV and VF values of the whole group for each day were compared and subgroup analyzes were performed in terms of gender, Voiding Dysfunction Symptom Score (VDSS), bladder capacity (BC), and diagnoses. Results: A total of 109 (53 girls (48.6%), 56 boys (51.4%)) children with a median age of 8 (3-17) were included in the study 77 (70 6%) children were diagnosed with overactive bladder, 8 (7 4%) with dysfunctional voiding, and 24 (22%) with monosymptomatic enuresis nocturne The mean VVs between days were similar in the whole group (p = 0 759) Moreover, the mean VV of the first day was similar to the average of both the first two days and the three days (p = 0.021, p = 0.490). Also, the maximum and minimum VVs were similar between days (p = 0 942, p = 0 160, respectively) In subgroup analyses based on gender, bladder capacity, and symptom score, mean VV was also found to be similar VF values were found to be significantly different between days There was also a difference between VF values in children with VDSS > 8.5 (p = 0.012) and BC/EBC (%) > 65 (p = 0.030). In subgroup analysis for diagnoses, mean and maximum VV and VF were similar between the groups, except for VF (p = 0 026) in OAB
Conclusion: While the voided volumes of children with non-neurogenic LUT dysfunctions appear to be consistent across the days of the VD, variations in VF might arise, especially among children with a VDSS of > 8.5 and normal bladder capacity. As a result, we believe that using a VD spanning at least two days could enhance diagnostic accuracy and help prevent unnecessary treatment
KEY WORDS: Voiding diary; Lower urinary tract dysfunction; Bladder; Incontinence; Children
Submitted 15 August 2023; Accepted 2 September 2023
INTRODUCTION
The presence of lower urinary tract (LUT) symptoms in children without congenital anatomical or neurological abnormalities indicates functional bladder disorders, and the International Children's Continence Society (ICCS) recommends using the term "daytime LUT conditions" for these cases (1) Initial evaluation of children presenting with LUT symptoms includes physical examination, urinalysis, symptom scores, voiding diary (VD), uroflowmetry, and residual urine measurement VD is a highly useful tool that allows to show voiding habits, features of bladder function and is characterized by being an easy, non-invasive, no cost method A properly completed VD provides information about maximum voiding volumes (MVV), mean voiding volumes (MVV), nocturnal urine volumes, voiding frequency (VF), presence and type of incontinence, enuresis, and fluid intake habits (2) It is recommended to be applied for at least 2 days in ICCS and European Urology Association (EAU) guidelines (1-3) However, some studies have reported similarities in VV between days at three-day VD (4, 5) Franck et al reported that one-day VD was correlated with three-day VD and emphasized that one-day VD could be sufficient to evaluate LUT functions in children (5) However, a symptom score that gives information about the severity of symptoms was not evaluated together with VD parameters in these studies We hypothesized that the VV and VF between days may vary depending on the severity of the symptoms Therefore, in this study, it was aimed to compare VV and VF values between days according to bladder capacity and symptom score
MATERIALS AND METHODS
Children who applied to the pediatric urology clinic due to LUT symptoms between 2022 and 2023 were includ-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11662 1
Are voiding volumes and frequencies different in the three-day voiding diary in children with lower urinary tract dysfunction?
Raziye Ergun 1 , Cagri Akin Sekerci 2 , Mehmet Cetin 3 , Mohammad Yasir Sahak 3 , Selcuk Yucel 2 , Tufan Tarcan 3, 4
DOI: 10 4081/aiua 2023 11662
ed in the study The records were evaluated retrospectively Ethical approval was obtained from the local ethics committee before the study (09 2023 674)
Children with congenital genitourinary system anomalies such as ectopic ureter, duplicated collecting system, posterior urethral valve, bladder diverticula, epispadias, exstrophy vesica, etc , and congenital or acquired neurological deficits such as myelodysplasia, cerebral palsy, sacral agenesis, spinal cord injury, central and peripheral neural system malignancy, and children with missing data were excluded from the study All children were evaluated in accordance with ICCS and EUA recommendations and underwent VD for 3 days (2) Mean VV and VF values of the whole group for each day were compared and subgroup analyzes were performed
The first subgroup analysis was made by gender The second subgroup was created according to V o i d i n g D y s f u n c t i o n Symptom Score (VDSS) (6) VDSS by Akbal et al was filled in by all parents
Table 1.
Comparison of voiding volume in voiding diary
Comparison of voiding frequencies in voiding diary
Children were divided into two groups as below and above the cut-off value of 8 5 showing LUT dysfunctions The third subgroup was formed according to bladder capacity (BC) Bladder capacity is calculated as: uroflowmetry voided volume + residual urine volume The Koff formula was used to calculate the expected bladder capacity (EBC) by age (7) BC/EBC of less than 65% was considered a low-capacity bladder (8) The last subgroup was formed according to diagnoses overactive bladder (OAB), dysfunctional voiding, monosymptomatic nocturnal enuresis (MNE) Decreased VF was accepted as < 4 per day, normal VF 4-7 per day, and increased VF > 7 per day
Statistical analysis
Data were analyzed using the IBM Statistical Package for the Social Sciences version 22 (IBM SPSS Statistics for Windows, Chicago, IL, USA) The normality of the distribution of the variables was evaluated using the ShapiroWilk test As the distribution of continuous variables did not show a normal distribution, comparison of independent and dependent groups were done with MannWhitney U test and Wilcoxon Signed Ranks Test, respectively Mc-Nemar test was used for binary categorical dependent data and Fisher's Exact test was used for independent data The p value < 0 05 was accepted as statistically significant
RESULTS
A total of 109 (53 girls (48 6%), 56 boys (51 4%)) children with a median age of 8 (3-17) were included in the study 77 (70 6%) children were diagnosed with OAB, 8 (7 4%) with dysfunctional voiding, and 24 (22%) with MNE The mean VVs between days were similar in the whole group (p = 0 759) (Table 1) Moreover, the mean
VV of the first day was similar to the average of both the first two days and the three days (p = 0 021, p = 0 490) Also, the maximum and minimum VVs were similar between days (1st day = 215 29+/-116 10 and 70 51+/54 56 ml, 2nd day = 222 09+/-249 86 and 71 75+/-56 82 ml, 3rd day = 205 99+/-110 98 and 69 15+/-44 83 ml, p = 0 942, p = 0 160) In subgroup analyses based on gender, bladder capacity, and symptom score, mean VV was also found to be similar (Table 1) VF values were found to be significantly different between days There was also a difference between VF values in children with VDSS > 8 5 (p = 0 012) and BC/EBC (%) > 65 (p = 0 030) (Table 2) In addition, 72 (66 1%) normal VF, 5 (4 6%) decreased VF, 32 (29 4%) increased VF were detected in first day; 75 (68 8%) normal VF, 10 (9 2%) decreased, 24 (22%) increased VF in second day; 77 (70 6%) normal VF, 6 (5 5%) decreased VF, 26 (23 9%) increased VF in third day (Table 3) When subgroup analysis was performed
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11662
2
R Ergun, C Akin Sekerci, M Cetin, M Yasir Sahak, S Yucel, T Tarcan
Table 3.
1st Day 2nd Day 3rd Day Decreased VF 5 (4 6%) 10 (9 2%) 6 (5 5%) Normal VF 72 (66.1%) 75 (68.8%) 77 (70.6%) Increased VF 32 (29 4%) 24 (22%) 26 (23 9%) Total 109 109 109 P 1st & 2nd = 0 016, p 1s & 3 d = 0 237, p 2nd & 3 d = 0 289 Decreased VF < 4x per day, norma VF = 4-7x per day, increased VF > 7x per day
Comparison of number of decreased, normal and increased VF between days
Table 2.
1st Day VF 2nd Day VF 3rd Day VF P value (Mean+/-SD) (Mean+/-SD) (Mean+/-SD) All patients (n = 109) 6 67+/-2 53 6 15+/-2 59 6 23+/-2 74 0 011 Boys (n = 56) 7 03+/-2 78 6 35+/-2 66 6 38+/-2 51 0 054 Girls (n 53) 6 25+/-2 24 5 88+/-2 47 5 54+/-2 99 0 138 VDSS < 8 5 (n 33) 6 06+/-2 13 5 37+/-1 84 5 75+/-1 90 0 663 VDSS > 8 5 (n = 76) 6 93+/-2 66 6 43+/-2 79 6 43+/-3 02 0 012 BC/EBC (%) < 65 (n = 51) 6.74+/-2.67 6.39+/-2.64 6.21+/-2.41 0.162 BC/EBC (%) > 65 (n = 58) 6 61+/-2 43 5 94+/-2 55 6 24+/-3 03 0 030 VF: vo ding frequency, VDSS: Vo d ng Dysfunct on Symptom Score, BC: b adder capac ty, EBC: expected bladder capacity
1st Day Mean VV (ml) 2nd Day Mean VV (ml) 3rd Day Mean VV (ml) P value (Mean+/-SD) (Mean+/-SD) (Mean+/-SD) All patients (n = 109) 134 11+/-69 83 127 30+/-69 43 131 10+/-64 69 0 759 Boys (n = 56) 125 51+/-60 47 121 37+/-69 47 127 22+/-61 21 0 099 Girls (n = 53) 144 62+/-78 03 134 28+/-70 30 136 62+/-68 74 0 488 VDSS < 8 5 (n = 33) 172 54+/-84 19 166 15+/-89 36 165 33+/-73 02 0 636 VDSS > 8 5 (n = 76) 117 42+/-55 36 110 43+/-50 82 116 23+/-54 87 0 334 BC/EBC (%) < 65 (n = 51) 122 72+/-70 52 108 66+/-57 64 115 11+/-58 53 0 345 BC/EBC (%) > 65 (n 58) 144 12+/-68 25 143 68+/-75 07 145 15+/-67 03 VV: vo d ng volume, VDSS: Void ng Dysfunct on Symptom Score, BC: b adder capac ty, EBC: expected bladder capacity
Table 4
Comparison of mean and maximum voiding volumes and voiding frequencies
according to diagnoses
according to diagnoses, mean and maximum VV and VF were similar between the groups, except for VF (p = 0 026) in OAB (Table 4)
DISCUSSION
VD is a highly useful tool that allows to show voiding habits, features of bladder function and is characterized by being an easy, non-invasive, no cost method A properly completed VD provides information about VV, VF, presence and type of incontinence, enuresis, and fluid intake habits Although at least two or three days of VD is recommended, it is known that this form is difficult for p a r e n t s t o fi l l o u t , e s p e c i a l l y d u r i n g s c h o o l d a y s Therefore, in the present study, we compared the parameters of one-, two-, and three-day VDs and evaluated the consistency of the one-day VD Although we found similar mean VV between days in subgroup analysis according to gender, IBSS and ratio to EBC, we observed statistically differences in VF Interestingly, even if there was a change in mean VFs between days, they were found to be remained within the normal daily voiding frequency Hence, we believe that the clinical significance of this statistical difference between VFs should be considered with suspicion However, since there can be a transition between normal and pathological voiding frequencies, as shown in Table 3, we think that children with IBSS > 8 5 or with bladder capacity below 65% according to EBC should be evaluated more carefully in terms of VF There are a limited number of studies in the literature comparing VD between days in children In the study of Franck et al , in which they evaluated the voiding diaries of 89 children (59 MNE, 30 OAB), it was reported that the VF, mean VV, and nocturnal volume were similar between the three days, but the maximum voiding volumes gradually decreased (5) They found that first day had 96% sensitivity, 71% specificity, and 75% overall accuracy in estimating bladder capacity One of the interesting findings of the study is that the maximum VVs were lower than EBC in both the OAB (1st day: 69%, 2nd day: 67%, 3rd day: 53%) and MNE (1st day: 67%, 2nd day: 61%, 3rd day: 58%) groups The authors stated that one day's VD may be sufficient to evaluate LUT dysfunctions and shows good correlation with the three-day chart Unlike these results, present study showed that VVs are
similar in all group and sub-group a n a l y s e s b u t t h e r e a r e d i f f
between VFs Although the ages were similar between the two studies (8 years), only 45 7% of patients in this study had mean VV below 65% of EBC Also, Franck et al study, unlike ours (OAB %70 6), had an MNE (66 2%) dominant study group Despite these differences, mean VVs were consistent between days in both studies
In another study evaluating 92 children with LUT symptoms, mean VV, maximum VV, and fluid intake were shown to be similar between 2- and 3-day VD (4) In addition, high number of voids numbers and low bladder capacities were found to be close to each other Moreover, 2- and 3day VFs (7 05+/-3 83 & 6 87+/-3 85, p = 0 007) were reported to be different, similar to present study It has been emphasized once again that a two-day VD may be sufficient for the evaluation of children with LUT dysfunctions The prominent feature of the current study is the evaluation of VV and VF by creating subgroups according to symptom score and bladder volumes
On the other hand, while VVs are similar between VD days, there are studies recommending longer VDs before moving on to invasive testing and other treatment modalities Elmer et al examined the impact of 1-day and 3-day voiding diaries on the test and treatment preferences of urogynecologists (9) In this study involving 186 women with urinary incontinence and other lower urinary tract symptoms, they found that a 1-day voiding diary led to a higher utilization of urine culture, urodynamics, cystoscopy, and other imaging techniques compared to a 3day voiding diary Likewise, they mentioned that shorter voiding diaries increased the probability of suggesting treatment methods like clean intermittent catheterization, pelvic floor rehabilitation, and surgical interventions Nevertheless, they found a best agreement between the two voiding diaries for conservative approaches such as fluid restriction and scheduled voiding and medical treatments (kappa: 0 64, 0 61, 0 51, respectively) Thus, the authors recommend a three-day VD prior to invasive tests and treatments However, to the best of our knowledge, we did not find any studies that investigated the impact of voiding diary duration on invasive tests and treatment preferences in children
Completely and accurately filling out the three-day VD seems to be another challenge for patients In a study conducted by The Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN), a three-day VD was requested from 1064 (510 men, 545 women) volunteer participants with a mean age of 58 8 years (10) However, 84 8% (n = 902) of the participants returned a baseline voiding diary, and only 49 7% (n = 448) of them were completely filled out in terms of fluid intake and voiding records While 57 patients filled less than three days, 306 patients were missing VVs, and 62 patients were lacking in fluid intake Younger age and lower education levels were found to be associated with a higher probability of not submitting a diary or submitting an
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11662 3 Are voiding volumes and frequencies similar in the voiding diary?
e r e n c e
s
Diagnosis 1st Day 2nd Day 3rd Day P value (Mean+/-SD) (Mean+/-SD) (Mean+/-SD) OAB (n 77) Mean VV (ml) 130 11+/-73 25 126 81+/-74 18 127 71+/-67 75 0 798 Maximum VV (ml) 209 63+/-121 05 228 48+/-292 29 199 77+/-112 28 0 743 VF 6 93+/-2 62 6 30+/-2 80 6 46+/-2 96 0 026 DV (n 8) Mean VV (ml) 164 87+/-71 14 152 12+/-45 67 171 87+/-63 33 0 792 Maximum VV (ml) 293 75+/-129 27 255 00+/-85 52 303 75+/-149 87 0 565 VF 5 87+/-1 55 5 75+/-1 16 5 62+/-2 13 0 183 MNE (n 24) Mean VV (ml) 136 66+/-56 87 120 58+/-59 61 128 37+/-51 34 0 376 Maximum VV (ml) 207 29+/-86 48 190 62+/-84 18 193 33+/-75 66 0 831 VF 6 12+/-2 45 5 83+/-2 25 5 70+/-2 11 0 602 OAB: overact ve bladder, DV: dysfunct ona voiding, MNE:
monosymptomatic enuresis nocturne, VV: vo d ng vo ume, VF: vo d ng frequency
unusable diary Additionally, female gender was linked to a higher likelihood of submitting an unusable diary or a usable but incomplete diary To the best of our knowledge, we believe that this process is more challenging for parents, even though there is no available data regarding appropriately filled voiding diary returns in children We are aware that parents often express difficulties in completing voiding diaries, particularly when children are at school and engaged in play, or when the parents themselves are at work In our own practice, we suggest completing the voiding diaries during weekends and holidays to facilitate this process
The present has some limitations We did not include fluid intakes of VDs in this study We did not compare patients' control VDs after appropriate treatment We did not perform subgroup analysis according to age groups, but we tried to compensate for this deficiency by proportioning the expected bladder capacity We didn't investigate whether one-day and three-day VDs go on preference of treatment modalities
CONCLUSIONS
Although the voiding volumes of children with non-neurogenic LUT dysfunctions are similar between the days of the VD, there may be differences in the voiding frequencies particularly in children with IBSS > 8 5 and normal bladder capacity Therefore, we think that at least two daily voiding diary will contribute to strengthen the diagnosis and avoid overtreatment
REFERENCES
1 Austin PF, Bauer SB, Bower W, et al The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the standardization committee of the International Children's Continence Society Neurourol Urodyn 2016; 35:471-81
2 Bauer SB, Nijman RJ, Drzewiecki BA, et al International Children's Continence Society standardization report on urodynamic studies of the lower urinary tract in children Neurourol Urodyn 2015; 34:640-7
3 Radmayr C, Bogaert G, Burgu B, et al Day-time lower urinary tract conditions EAU Guidelines On Paediatric Urology 2023:44-8
4 Lopes I, Veiga ML, Braga AA, et al A two-day bladder diary for children: Is it enough? J Pediatr Urol 2015; 11:348 e1-4
5 Franck HHM, Guedes ACS, Alvim YFS, et al One-day voiding diary in the evaluation of Lower Urinary Tract Symptoms in children Int Braz J Urol 2023; 49:89-96
6 Akbal C, Genc Y, Burgu B, et al Dysfunctional voiding and incontinence scoring system: quantitative evaluation of incontinence symptoms in pediatric population J Urol 2005; 173:969-73
7 Koff SA Estimating bladder capacity in children Urology 1983; 21:248
8 Nevéus T, von Gontard A, Hoebeke P, et al The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children's Continence Society J Urol 2006; 176:314-24
9 Elmer C, Murphy A, Elliott JO, Book NM Twenty-Four-Hour
Comparison Female Pelvic Med Reconstr Surg 2017; 23:429-32
10 Cameron AP, Wiseman JB, Smith AR, et al Are three-day voiding diaries feasible and reliable? Results from the Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN) cohort Neurourol Urodyn 2019; 38:2185-93
Correspondence
Raziye Ergun, MD raziye ergun@hotmail com
Pediatric Urology, Kocaeli Derince Training and Research Hospital, Kocaeli, Turkey
Mehmet Cetin, MD m cetin 47@hotmail com
Mohammad Yasir Sahak, MD m yasirsahak@gmail com
Department of Urology, School of Medicine, Marmara University, Istanbul, Turkey
Selcuk Yucel, MD drsyucel@yahoo com
Department of Urology, Division of Pediatric Urology, School of Medicine, Marmara University, Istanbul, Turkey
Tufan Tarcan, MD tufan@marmara edu tr
Department of Urology, School of Medicine, Marmara University, Istanbul, Turkey
Department of Urology, School of Medicine, Koç University, Istanbul, Turkey
Cagri Akin Sekerci, MD (Corresponding Author) cagri sekerci@hotmail com
Assoc Professor of Urology
Department of Urology, Division of Pediatric Urology, School of Medicine, Marmara University, Istanbul, Turkey
Fevzi Çakmak Mah , Muhsin Yazicioglu Cad No:10 Ust Kaynarca/ Pendik/ Istanbul, Turkey
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11662 R
C
T
4
Ergun,
Akin Sekerci, M Cetin, M Yasir Sahak, S Yucel,
Tarcan
V o i d i n g D i a r i e s V e r s u s 3 - D a y V o i d i n g D i a r i e s : A C l i n i c a l
Does isotretinoin affect spermatogenesis in the long term? A rat model
1 Ordu University, Faculty of Medicine, Urology Department, Ordu, Turkey;
2 Ordu University, Faculty of Medicine, Dermatology Department, Ordu, Turkey;
3 Ordu University, Faculty of Medicine, Histology and Embriyology, Ordu, Turkey;
4 Ordu University, Faculty of Medicine, Biostatistics Department, Ordu, Turkey;
5 Samsun University, Faculty of Medicine, Anatomy Department, Samsun, Turkey;
6 Lokman Hekim University, Faculty of Medicine, Urology Department Ankara, Turkey
Summary
Objectives: Spermatogenesis, in which cell regeneration continues, can be affected by environmental, chemical, psychological factors or various diseases. There is conflicting information in the literature about the effect of isotretinoin, which is widely used in acne treatment, on testes and spermatogenesis. Therefore, we planned a rat study to evaluate the long-term efficacy of oral isotretinoin on testicular tissues and spermatogenesis.
Materials and methods: The Group 1 (n = 6) 7 5 mg/kg/day and the Group 2 (n = 6) received isotretinoin at a dose of 30 mg/kg/day dissolved in sunflower oil, the Sham Group (n = 6) received only sunflower oil by gavage, and the control group (n = 6) received standard feed and water for four weeks After the 4th week, all animals were fed with standard feed and water and followed for the next four weeks At the end of the 8th week, all animals were sacrificed under deep anesthesia. Seminiferous tubule diameters, epithelial thickness, apoptotic index, sperm number and motility recorded
Results: Sperm count, motility, vitality, diameter of seminiferous tubule and germinal epithelium thickness were decreased and apoptotic index increased in the groups received isotretinoin There was no significant difference between the groups in terms of testosterone levels
Conclusions: We consider that further comprehensive studies, including human clinical trials, should be conducted to examine the negative effects of isotretinoin on spermatogenesis in the long term especially when there is a need using isotretinoin in men for various reasons and to eliminate the contradictions in the literature in this regard
KEY WORDS: Isotretinoin; Rat; Spermatogenesis; Testis
Submitted 31 May 2023; Accepted 1 June 2023
INTRODUCTION
Spermatogenesis is a complex process in which mature sperm cells are formed from spermatogonial stem cells as a result of mitosis, meiosis, and cell differentiation In this active process, the cell cycle continues in seminiferous tubules, which can make the spermatogenetic process sensitive to various factors such as environmental, chemical, toxic and pharmacological agents One of them is
isotretinoin, which is widely used in the treatment of acne, one of the most common and disturbing diseases among young people Isotretinoin is the only drug effective on all pathogenic mechanisms of acne, such as inflammation, increased sebum secretion, overgrowth of bacteria such as Propionibacterium acnes, and ductal hypercornification (1) Although oral isotretinoin is a very effective treatment, it has a teratogenic effect in pregnant women (2) However, there is controversial information on the effect of isotretinoin in men While there are several studies on spermatogenesis, we have limited information on the long-term effectiveness of isotretinoin use on testicles and spermatogenesis In addition, it may not be ethically appropriate to conduct studies for evaluating its histological effects in humans As there is no clear information about the effects of isotretinoin on spermatogenesis, this situation can be a matter of concern and curiosity in male patients using the drug and physicians recommending this drug Therefore, we planned a rat study to evaluate the long-term efficacy of oral isotretinoin on testicular tissues and spermatogenesis
MATERIALS AND METHODS
Animals
The animals were procured from the Samsun Experimental Animals Research and Ethical Application Center (EARAC) after obtaining an ethics committee approval from the Animal Studies Ethical Committee at Ordu University This study was performed in accordance to the Guiding Principles for the Care and Use of Laboratory Animals
In our study, we used a total of 24 male Wistar-albino rats, 4-8 weeks old, with an initial weight of 250-300 g
The rats were housed in rooms at 22 ± 1°C and 45-55% humidity, ensuring 12-hour light and dark cycles and including a maximum of 3 rats in each cage The temperature and humidity were measured by thermometer and hygrometer, respectively The ventilation was provided by a room aspirator The rats had free access to feed and water All rats were fed with normal rat chow (Nucleon, Ankara, Turkey)
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11502 1
ORIGINAL PAPER
Abdullah Cirakoglu 1 , Sevda Onder 2 , Hatice Hancı 3 , Erdal Benli 1 , Ahmet Yüce 1 , Yeliz Kasko Arici 4 , Orhan Bas 5 , Ismail Nalbant 6
DOI: 10 4081/aiua 2023 11502
Formation of the groups and experimental design
A total of 24 male Wistar-albino rats, 4-8 weeks old, were used and randomly divided into 4 groups, including 6 in each group The Group 1 (n = 6) received isotretinoin ( R o a c c u t a n e , R o c h e , B a s e l , S w i s s ) a t a d o s e o f 7 5 mg/kg/day dissolved in sunflower oil, the Group 2 (n = 6) received isotretinoin at a dose of 30 mg/kg/day dissolved in sunflower oil, the Sham Group (n = 6) 6) received only sunflower oil by gavage, and the control group (n = 6) received standard feed and water for four weeks After the 4th week, all animals were fed with standard feed and water and followed for the next four weeks At the end of the 8th week, all animals were sacrificed by cervical dislocation under deep anesthesia with intraperitoneal of ketamine 90 mg/kg (Ketalar; Eczacıbaşı, Istanbul, Türkiye) and xylazine hydrochloride 3 mg/kg (Rompun; Bayer, Leverkusen, Germany) Their testicles were excised bilaterally and their epididymis and testicular tissues were separated from each other for analysis
Biochemical analyses in serum
After being kept at room temperature for 30 minutes, the blood specimens placed into gel-containing tubes were centrifuged at 3000 g for 15 minutes The serum samples separated from the centrifuged blood were stored at -80°C until analysis Their testosterone, FSH and LH levels were measured after the serums were dissolved (Cobas 8000 e 602, Hitachi, Roche autoanalyzer)
Histological procedure
At the end of the experiment, while the animals were under deep anesthesia, a midline incision was made, and their testicular and epididymis tissues were meticulously separated from the surrounding tissues Then their epididymis and testicular tissues were separated from each other for analysis The epididymis tissues were placed in Tris phosphate buffer solutions and the testicular tissues in Bouin solutions for fixation after they were divided vertically into two pieces After the tests were fixed in Bouin solution, the entire half tests were kept for 3 days in a dry environment protected from light The tissues were then subjected to routine histological tissue follow-up procedures on the Thermo Scientific Excelsior™ AS (Thermo Fisher Scientific, Waltham, MA USA), an automatic tissue tracking device
After the follow-up process, the tissues were blocked by embedding in paraffin in HistoCore Arcadia H and HistoCore Arcadia C (Leica Biosystems Nussloch GmbH, Nussloch, Germany)
Then, 5-μm thick sections were taken with a fully automatic microtome (Leica RM 2255, Tokyo, Japan) The sections were mounted on slides and stained with hematoxylin and eosin (H & E, Leica autostainer XL, Minnesota, USA) for histopathological examination and measurements of seminiferous tubule diameter and epithelial thickness The seminiferous tubule diameter and epithelial thickness were measured using the Olympus DP 71 camera-mounted microscope (Olympus, Tokyo, Japan)
The Analysis 5 Research (Olympus Soft Imaging Solution GmbH, Münster, Germany) program was used for this purpose and the properties of the interstitial space We used the same microscope to take photographs
Epididymal sperm count, and sperm motility and vitality
The right epididymis was used to evaluate epididymal sperm count, sperm motility and viability The epididymis was placed in a Petri dish with 2 ml of Tris buffer solution and divided into 4 parts It was incubated at 37°C for 30 min to permit sperm release Sperm count and motility were evaluated using the Makler sperm counting chamber (Sefi -Medical Instrument, Haifa, Israel) Five milliliters of sperm fluid were dropped from the homogenate into the center of the chamber, and the glass lid was closed Thus, the sperms were allowed to swim in the area with a depth of 10 μm The sperm count was performed by a light microscope at x 100 magnification
Percentages of the motile sperm were calculated among at least 100 spermatozoa Then, to evaluate sperm viability, 5 μl of sperm sample was placed on slides, a drop of 1% eosin Y was added and closed with a coverslip It was evaluated by counting 100 motile and immotile sperms in different areas at x 200 magnification Orange colored sperms were considered dead, and the unstained ones were considered alive The percentage of viable sperms was calculated (3)
TUNEL staining and apoptosis
Apoptosis was examined using TUNEL staining to detect DNA fragmentation in the seminiferous tubule epithelium TUNEL staining was performed using the In Situ Cell
D i a g n o s t i c s , M a n n h e i m , Germany) Evaluation of the TUNEL stained sections was performed using the light microscope at x 400 by an experienced histologist blinded to the identity of the specimens TUNEL-positive cells with no necrotic areas and a brown nucleus were considered apoptotic TUNELpositive cell numbers in 10 seminiferous epithelium regions and the total number of cells were used to calculate AI (TUNEL-positive cells/total cells x 100) (4)
Statistical analysis
The data were tested for normality using the ShapiroWilk test and for homogeneity of variance using the Levene's test prior to the analyses One-way ANOVA followed by Tukey as post-test was used to compare the g r o u p s D e s c r i p t i v e s t a t i s t i c s o f t h e d a t a s e t w e r e expressed as means, standard deviations, and minimum and maximum values A p-value less than 0 05 (twosided) was considered statistically significant All statistical analyses were performed using the SPSS v25 (IBM Inc , Chicago, IL, USA) statistical software
RESULTS
As a result of the analysis of variance for sperm motility, the difference between the groups was found to be statistically significant (p < 0 001) As a result of the Tukey test performed to determine different averages, the sperm motility rate in Group 1 and Group 2 was significantly lower than the control and Sham groups, but there was no significant difference between the control and Sham groups (p > 0 05) (p < 0 05) In addition, the decrease in sperm motility was higher in the Group 2 than in the Group 1
As a result of the analysis of variance for sperm count, the
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11502 A
S Onder, H
et al 2
Cirakoglu,
Hancı,
D e a t h D e t e c t i o n K i t ( R o c h e
difference between the groups was found to be statistically significant (p < 0 0) As a result of the Tukey test, the sperm count was significantly lower in the Group 2 than in the control group (p < 0 05), but the differences between the other groups were not statistically significant (p > 0 05)
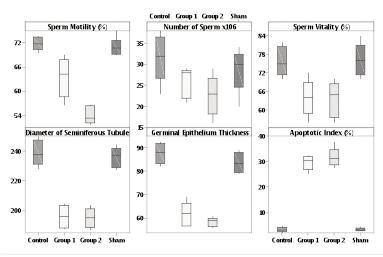
As a result of the analysis of variance for sperm vitality, diameter of seminiferous tubule, germinal epithelium thickness, and apoptotic index, the differences between the groups were found to be statistically significant (p < 0 001)
(Table 1) As a result of the Tukey test performed to determine different averages; while there was no significant difference between the control and Sham groups (p > 0 05), the Groups 1 and 2 had significantly lower sperm vitality, diameter of seminiferous tubule (p < 0 05) and germinal epithelial thickness (p < 0 05) and higher apoptotic index value than the control and sham groups (p < 0 05) (Figure 1)
As a result of the variance analysis performed to compare the testosterone amounts of the groups, the difference between the group averages was not found to be statistically significant (p > 0 05)
For all groups, FSH and LH values were below 0 10 mIU/ml, therefore it was not possible to compare their FSH and LH values There was no statistically significant difference between the groups in terms of testosterone levels
DISCUSSION
Isotretinoin is a synthetic retinoid used in the treatment of severe nodulocystic acne where other treatments have failed (5) Retinoids are also used to manage other dermatological conditions, such as rosacea, folliculitis, sarcoidosis, granuloma annulare, seborrheic dermatitis, and a variety of keratinization disorders (6) Although isotretinoin has been used for many years, hesitations about its side effects still exist Both human and animal studies have reported that it has serious teratogenic effects, decreasing ovarian reserves after 6 months of use of isotretinoin in women (2, 7, 8) Given the wide clinical usage of retinoids, clarification of whether retinoids affect the reproductive system in male patients of childbearing age is urgently needed In addition, there are conflicting results regarding its side effects on male reproductive system Studies have argued that both deficiency and high levels of vitamin A suppress spermatogenesis (9) Some other studies have suggested that vitamin A is necessary for spermatogenesis and its deficiency may cause defects in germ cell and testosterone production (10)
Some human studies argue that isotretinoin has a positive effect on sperm parameters, however we have reached the opposite results in our study For example, Cinar et al administered a cumulative dose of isotretinoin to 81 male patients to investigate the effects of systemic
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11502 3
Effects of isotretinoin on spermatogenesis
Figure 1. Box-plot of the study variables in the groups
Table 1.
Variables Group N Mean Std. Dev. Min-Max P-value Sperm Motility (%) Control 6 71 80a 1 59 69 56-73 68 < 0 001 (F = 51 24) Sham 6 71 10a 2 20 68 96-75 00 Group 1 5 63 43b 4 92 56 52-68 96 Group 2 6 53 85c 2 09 51 72-56 52 Number of Sperm x106 Control 6 31 50a 5 58 23 00-38 00 < 0 05 (F = 3 67) Sham 6 28 67ab 5 05 20 00-34 00 Group 1 5 25.80ab 3.56 21.00-29.00 Group 2 6 22 67b 4 68 16 00-29 00 Sperm Vitality (%) Control 6 75 67a 4 63 70 00-82 00 < 0 001 (F = 10 20) Sham 6 76 33a 5 13 70 00-84 00 Group 1 5 64 00b 5 83 56 00-72 00 Group 2 6 63 67b 5 57 56 00-70 00 Diameter of Seminiferous Tubule Control 6 239 31a 9 02 228 42-252 81 < 0 001 (F = 60 75) Sham 6 236 32a 6 58 227 63-244 35 Group 1 5 196 27b 7 59 187 96-204 48 Group 2 6 195 34b 6 44 187 20-203 68 Germinal Epithelium Thickness Control 6 87 69a 4 43 82 14-92 64 < 0 001 (F = 75 92) Sham 6 83 74a 4 41 78 96-88 93 Group 1 5 61.73b 5.20 56.66-69.10 Group 2 6 58 58b 1 93 55 87-60 80 Apoptotic Index (%) Control 6 3 41b 0 93 2 25-4 84 < 0 001 (F = 263 47) Sham 6 3.49b 0.65 2.91-4.56 Group 1 5 29 78a 2 80 25 53-32 45 Group 2 6 31 94a 3 66 27 87-37 84 F, one-way ANOVA According to Tukey's test, means that do not share a letter are signif cantly different (p < 0 05)
Descriptive statistics and the results of statistical analysis for the study variables
isotretinoin on male fertility They examined spermiogram parameters (sperm concentration, total progressive motility, total progressively motile sperm, normal morphology and viability) and total testosterone, FSH and LH levels before and after the treatment They observed no significant change in the hormone profile after the treatment, but found significant positive changes in the spermiogram parameters (11) Amory et al administered isotretinoin to patients between the ages of 21 and 60 years with impaired sperm parameters, and found no significant change in their sperm motility, but observed an increase in their sperm concentrations (12) On the other hand, some other human studies reported that isotretinoin treatment did not affect spermatogenesis and hypothalamicpituitary-gonadal axis (13-15)
The reason for the different results in our study and those mentioned above may be due to the difference in molecular doses, various uncontrollable non-standard subjective factors that affect the sperm parameters of people with different physical factors such as environment and diet The wide age range of participants or the investigation of people with damaged spermatogenesis may be the reason for this difference alone In addition, due to the nature of the research and ethical restrictions in these human studies, it was tried to have an idea by looking at very limited sperm parameters Apart from this, most of these studies in humans do not have a placebo and control groups Our study is valuable as it provides objective histopathological data with peers raised in controlled environments together with standard environment and environmental factors
So much so that at the end of our study, we found that isotretinoin reduced sperm motility, viability and numbers, decreased germinal epithelial thickness and seminiferous tubule diameters, and impaired spermatogenesis by stimulating apoptotic index in testicles Also, interestingly, despite studies claiming that synthetic retinoids may have beneficial effects on semen parameters, isotretinoin has never been offered as a treatment option in patients with impaired spermiogram parameters (16)
Sengör et al examined the effects of another synthetic retinoid, acitretin, on spermatogenesis, reported no significant change in the spermatogenesis evaluation and mean tubular diameter between the acitretin-treated and control groups, and found that acitretin had no effect on spermatogenesis (17) We found the opposite results in our study and reached objective histopathological data showing that retinoids stimulate the apoptotic index This difference may be due to dose-dependence or because Sengör et al could not control some valuable parameters, including the apoptotic index
Apoptosis is a complex event regulated by the balance of inducer and repressor factors It has a critical role in the elimination of damaged spermatogonial cells to prevent the production of abnormal sperm cells (18)
Spermatocytes that cannot complete their mitotic division are eliminated by apoptosis (19) Apoptosis in germ cells increases in infertile men (20, 21) Our study found significantly higher apoptotic index in both the groups 1 and 2 than in the control group This increase in the apoptotic index may be a natural regulation to protect against possible teratogenicity In addition, although the exact mechanism of action of retinoids is not known, they
stimulate apoptosis in sebaceous glands and disrupt cell cycle arrest (22, 23)
Spermatogenesis is an active process in testis, including continuous cell cycle It is a natural result that systemic isotretinoin acts on the seminiferous tubules, where cell division continues, along with the sebaceous glands We consider that this may be the reason for the deterioration in sperm quality and the increase in apoptotic index in our study Like our study, a study examined the apoptotic index and suggested that isotretinoin had damaging effects on spermatogenesis (24) Studies about the relationship between different molecules and spermatogenesis have shown an inverse relationship between apoptotic index and spermatogenesis, and this result is in line with those in our study (25, 26) The apoptotic index has not been examined in any of the studies suggesting that isotretinonin has a positive effect on spermatogenesis If isotretinoin had a spermatogenesis stimulating effect as claimed, it should have decreased in the apoptosis index However, such information is not mentioned in the presented studies
In particular, the germinal epithelium in the seminiferous tubules is the testicular component directly related to spermatogenic activity (27) Therefore, germinal epithelial thickness is a useful parameter in evaluating sperm production (28) It decreases due to decreased cell division (29) Isotretinoin-induced cell cycle arrest may also be responsible for the decrease in germinal epithelial thickness, which is one of the results of our study, and therefore the decrease in sperm counts In our study, isotretinoin decreased germinal epithelial thickness and seminiferous tubule diameters and sperm concentration in testis These results suggest that isotretinoin has serious damaging effects on spermatogenesis, which is in line with the histopathological results in the literature indicating impaired spermatogenesis
Sperm motility is an absolutely necessary function for male fertility Although it has not been fully explained how the sperm gain this ability while passing through the epididymis, it is known that various signaling pathways are effective in developing this ability (30, 31) To be motile, human sperm need a morphologically complete flagellum, be able to produce energy to power flagellar movement and functional signaling pathways Although our study did not reveal precisely which part of this system isotretinoin affects, it has clearly shown that isotretinoin decreases sperm motility in both groups using drugs
The effect of environmental factors on spermatogenesis is well known Several factors such as environmental toxins, diet, stress, drugs, frequency of ejaculation can affect sperm parameters (32, 33) In human studies, it is practically not possible to ensure that all subjects live under the same conditions This may be the reason for contradictory results in studies We consider that our results are more reliable since the feeding and environmental conditions of all animals were standard We also think that our study is more objective, as it revealed the drug’s negative effects on testicular tissue histologically (Figures 2, 3)
There are also conflicting results regarding the effects of isotretinoin on pituitary hormones In their study with 47 patients, Karadag˘ et al (22) reported that isotretinoin may have an effect on pituitary hormones Cinar et al , on
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11502 A Cirakoglu, S Onder, H Hancı, et al 4
Histological sections in rat testis stained with hematoxylin and eosin (H‐E, ×400) Control group (C), sham group (S), 7 5 mg/kg isotretinoin and 30 mg/kg isotretinoin
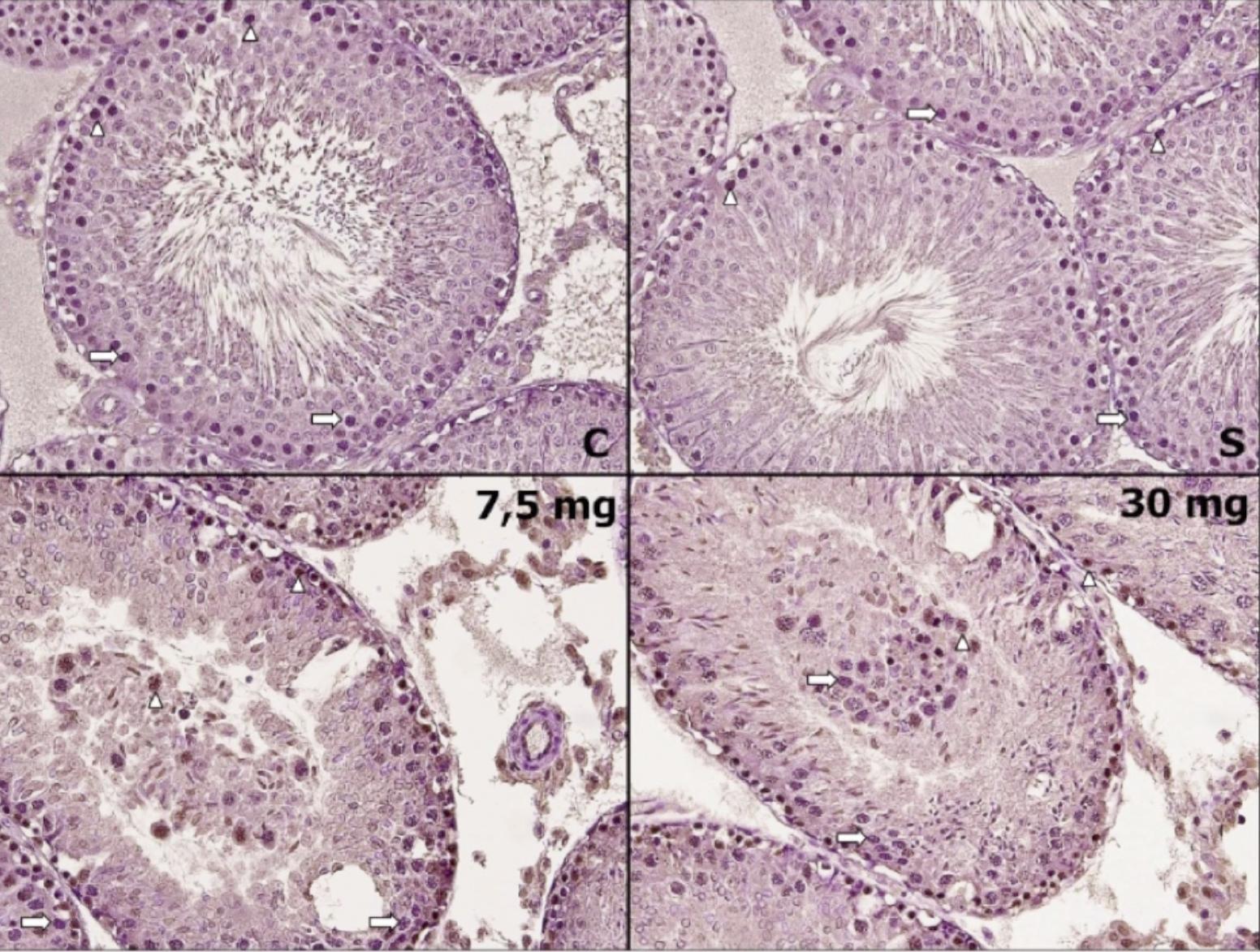
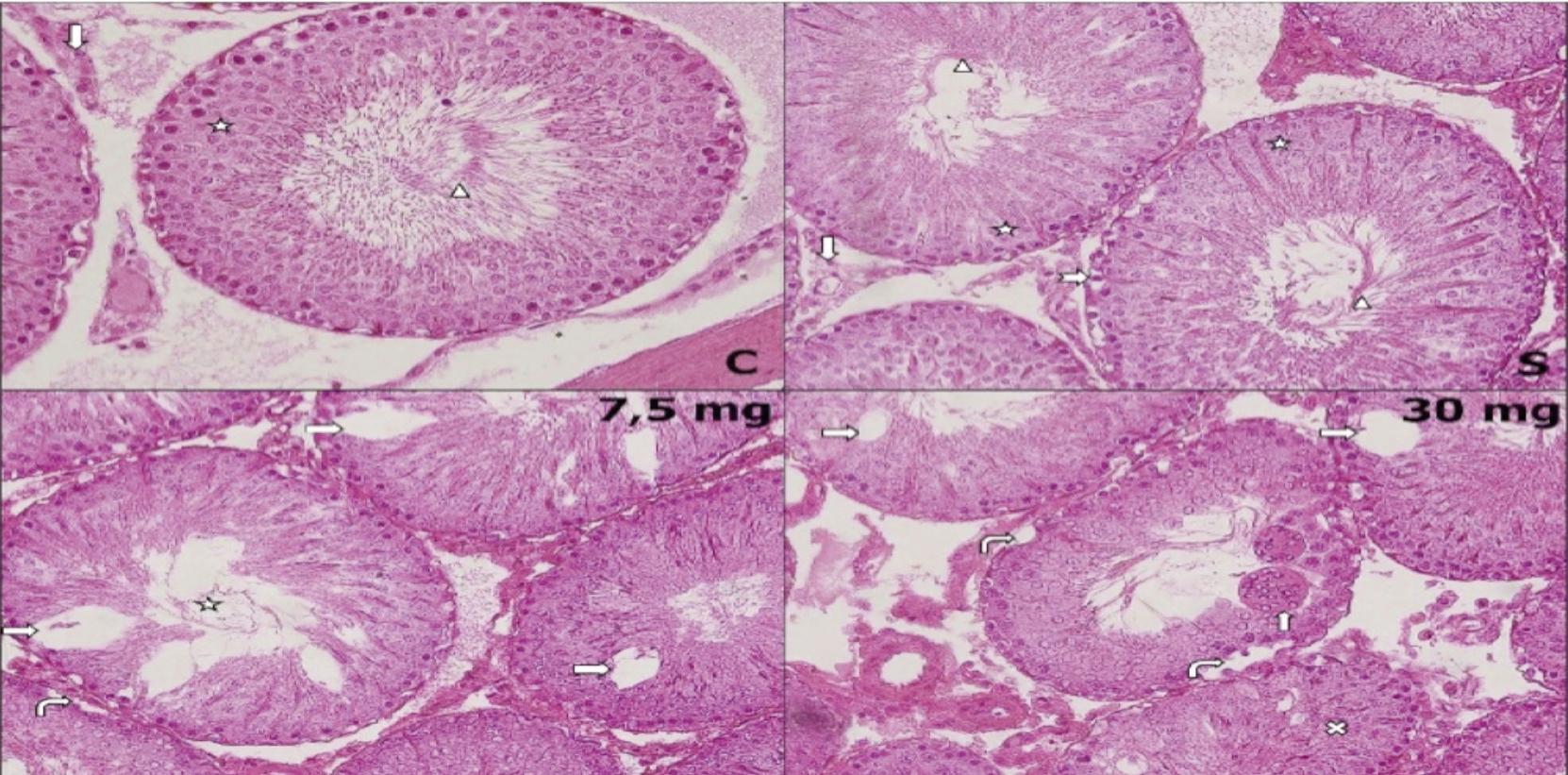
no significant difference between their testosterone levels in the long term, but the FSH and LH levels were below measurable values in all groups Therefore, it was not possible to compare the FSH and LH values However, our results suggest that the effect of isotretinoin on testicles is due to its direct effect on the tissue rather than hormonal changes
Histological sections in rat testis stained with TUNEL (×400). Control group (C), sham group (S), 7,5 mg/kg isotretinoin and 30 mg/kg isotretinoin
Normal cells (right arrow) and apoptotic cells (arrowhead)
C: Seminiferous tubule (star) with regular germinal epithelium and normal structure observed, spermatozoa in the seminiferous tubule lumen (arrowhead), interstitial area with normal structure and Leydig cell (lower arrow);
S: Seminiferous tubule (star) with regular germinal epithelium and normal structure observed, spermatozoa in the seminiferous tubule lumen (arrowhead), occasional vacuolization around spermatogonium (dashed right arrow)
7 5 mg/kg: Loss or reduction of spermatozoa (star), vacuolar degeneration (right arrow), opening between seminiferous tubule basal membrane and germinal epithelium (right bent arrow)
30 mg/kg: Opening between seminiferous tubule basal membrane and germinal epithelium (right bent arrow), vacuolar degeneration (right arrow), giant cells with multiple nuclei (upper arrow), disorganization and degenerations of germinal epithelium in the seminiferous tubule (multiplication sign)
As a result, rat studies about the long-term effect of isotretinoin are limited and include contradictory results Therefore, the inability to reach sufficient studies to be a benchmark for our study may be one of the limitations in our study However, considering that the results obtained from rats subjected to the same environmental factors and feeding are supported by apoptotic index, parallel objective histopathological results and biochemical values, our study makes a valuable contribution to the literature
CONCLUSIONS
Our study concludes that the negative effects of isotretinoin on spermatogenesis may be due to its direct damage to testicular tissues In addition to the necessity of conducting human studies to evaluate the long-term effects of isotretinoin on testicles, we consider that further comprehensive studies, including human clinical trials, should be conducted to examine the negative effects of isotretinoin on spermatogenesis in the long term especially when there is a need using isotretinoin in men for various reasons, and to eliminate the contradictions in the literature in this regard
REFERENCES
1 Zouboulis CC, Bettoli V Management of severe acne Br J Dermatol 2015; 172:27-36
2 Henry D, Dormuth C, Winquist B, et al Occurrence o f p r e g n a n c y a n d p r e g n a n c y o u t c o m e s d u r i n g isotretinoin therapy CMAJ 2016; 188:723-730
3 Sankako MK, Garcia PC, Piffer RC, et al Possible mechanism by which zinc protects the testicular function of rats exposed to cigarette smoke Pharmacol Rep 2012; 64:1537-1546
4 Hancı H, Odacı E, Kaya H, et al The effect of prenatal exposure to 900-MHz electromagnetic field on the 21-old-day rat testicle Reprod Toxicol 2013; 42:203209
5 Shahada OO, Kurdi AS, Aljawi AF, et al Synovitis, Acne, Pustulosis, Hyperostosis, and Osteitis Syndrome Diagnosis in Adolescent and Isotretinoin as a Possible Serious Exacerbating Factor Cureus 2022; 14:e22776
the other hand, reported no significant change in FSH, LH, and testosterone levels after the use of isotretinoin (12) Comparing the control group with the groups using 7 5 mg/kg and 30 mg/kg of isotretinoin, our study found
6 Motamedi M, Chehade A, Sanghera R, Grewal P A Clinician's Guide to Topical Retinoids J Cutan Med Surg 2022; 26:71-78
7 Mehra T, Borelli C, Burgdorf W, et al Treatment of severe acne with low-dose isotretinoin Acta Derm Venereol 2012; 92:247-248
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11502 5 Effects of isotretinoin on spermatogenesis
Figure 2.
Figure 3.
8 Aksoy H, Cinar L, Acmaz G, et al The effect of isotretinoin on ovarian reserve based on hormonal parameters, ovarian volume, and antral follicle count in women with acne Gynecol Obstet Invest 2015; 79:78-82
9 Sadek IA, Abdul-Mohsen MH Long-term administration of vitamin A and the process of spermatogenesis East Mediterr Health J 1999; 5:123-129
10 Livera G, Rouiller-Fabre V, Pairault C, et al Regulation and perturbation of testicular functions by vitamin A Reproduction 2002; 124:173-180
11 Çinar L, Kartal D, Ergin C, et al The effect of systemic isotretinoin on male fertility Cutan Ocul Toxicol 2016; 35:296-299
12 Amory JK, Ostrowski KA, Gannon JR, et al Isotretinoin administration improves sperm production in men with infertility from oligoasthenozoospermia: a pilot study Andrology 2017; 5:1115-1123
13 Parsch EM, Ruzicka T, Przybilla B, Schill WB Andrological investigations in men treated with acitretin (Ro 10-1670) Andrologia 1990; 22:479-482
14 Török L, Kádár L, Kása M Spermatological investigations in patients treated with etretinate and isotretinoin Andrologia 1987; 19:629-633
15 Hui Liu, Jie Li, Li Yu Effects of acitretin on semen quality and reproductive hormone levels in patients with psoriasis vulgaris Dermatologica Sinica 2017; 35:55-58
16 Onder S, Çırakog˘lu A, Nalbant I, et al Does isotretinoin affect spermatogenesis? a rat study Egypt J Dermatol Venerol 2021; 41:75-82
17 Sengör B, Bayramgürler D, Müezzinoglu B, et al Effects of acitretin on spermatogenesis of rats J Eur Acad Dermatol Venereol 2006; 20:689-692
18 Cai L, Hales BF, Robaire B Induction of apoptosis in the germ cells of adult male rats after exposure to cyclophosphamide Biol Reprod 1997; 56:1490-1497
19 Print CG, Loveland KL Germ cell suicide: new insights into apoptosis during spermatogenesis Bioessays 2000; 22:423-430
20 Lin WW, Lamb DJ, Wheeler TM, et al In situ end-labeling of human testicular tissue demonstrates increased apoptosis in conditions of abnormal spermatogenesis Fertil Steril 1997; 68:1065-1069
21 Høst E, Lindenberg S, Ernst E, Christensen F DNA strand breaks in human spermatozoa: a possible factor, to be considered in couples suffering from unexplained infertility Acta Obstet Gynecol Scand 1999; 78:622-625
22 Karadag AS, Ertugrul DT, Tutal E, Akin KO Isotretinoin influences pituitary hormone levels in acne patients Acta Derm Venereol 2011; 91:31-34
23 Altucci L, Gronemeyer H The promise of retinoids to fight against cancer Nat Rev Cancer 2001; 1:181-193
24 Gencoglan G, Tosun M Effects of isotretinoin on spermatogenesis of rats Cutan Ocul Toxicol 2011; 30:55-60
25 Ghasemnezhad R, Mohammadghasemi F, Faghani M, Bahadori MH Oxytocin can decrease germ cells apoptotic index in testis under acute ischemia reperfusion in a rat model Iran J Reprod Med 2015; 13:283-290
26 Kandirali E, Cayan S, Armagan A, et al Does the testicular apoptotic index vary with serum gonadotropins and testicular histopathology in infertile men? Urol Int 2009; 83:349-353
27 Wing TY, Christensen AK Morphometric studies on rat seminiferous tubules Am J Anat 1982; 165:13-25
28 Udoumoh AF, Igwebuike UM, Okoye CN, et al Assessment of age-related morphological changes in the testes of post-hatch light ecotype Nigerian indigenous chicken Anat Histol Embryol 2021; 50:459-466
29 Mohammadnejad D, Abedelahi A, Soleimani-Rad J, et al Degenerative effect of Cisplatin on testicular germinal epithelium Adv Pharm Bull 2012; 2:173-177
30 Abou-haila A, Tulsiani DR Signal transduction pathways that regulate sperm capacitation and the acrosome reaction Arch Biochem Biophys 2009; 485:72-81
31 Visconti PE, Westbrook VA, Chertihin O, et al Novel signaling pathways involved in sperm acquisition of fertilizing capacity J Reprod Immunol 2002; 53:133-150
32 Pelit ES, Katı B, Akın Y, Yeni E The impact of environmental stress factors on sperm Androl Bul 2017; 19:61-64
33 Nasr M, Abd-Allah H, Ahmed-Farid OAH, et al A comparative study between curcumin and curcumin nanoemulsion on high-fat, high-fructose diet-induced impaired spermatogenesis in rats J Pharm Pharmacol 2022; 74:268-281
Correspondence
Abdullah Cirakoglu, MD
Ahmet Yüce, MD (Corresponding Author) ahmetyuce7@gmail com
Erdal Benli, MD
Ordu University, Faculty of Medicine, Urology Department, Ordu, Turkey
Sevda Onder, MD
Ordu University, Faculty of Medicine, Dermatology Department, Ordu, Turkey
Hatice Hancı, MD
Ordu University, Faculty of Medicine, Histology and Embriyology, Ordu, Turkey
Yeliz Kasko Arici, MD
Ordu University, Faculty of Medicine, Biostatistics Department, Ordu, Turkey
Orhan Bas, MD
Samsun University, Faculty of Medicine, Anatomy Department, Samsun, Turkey
Ismail Nalbant, MD
Lokman Hekim University, Faculty of Medicine, Urology Department, Ankara, Turkey
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11502 A Cirakoglu, S Onder, H Hancı, et al 6
Galectin-1 (Gal-1) and Galectin-3 (Gal-3) levels in seminal plasma and serum in azoospermic patients versus fertile men: A cross-sectional study
1 Department of Andrology, Sexology and STDs, Kasr AlAiny Faculty of Medicine, Cairo University, Egypt;
2 Department of Medical Biochemistry and Molecular Biology, Kasr AlAiny Faculty of Medicine, Cairo University, Egypt;
Summary
Introduction: Galectin-1 (Gal-1) and galectin-3 (Gal-3) are expressed by many immune cells and receive considerable attention in the context of immunity. We aimed to compare between seminal plasma and serum levels of Gal-1 and Gal-3 in azoospermic patients and fertile men.
Materials and methods: This cross-sectional study was conducted at the andrology outpatient clinic from January (2022) to September (2022). A total of 90 participants were enrolled and divided into two equal groups: azoospermic and normal group. Semen analysis was done for all participants. Hormonal profile including FSH, LH, serum prolactin, total testosterone and estradiol was performed as well as assessment of serum and seminal levels of Gal-1 and Gal-3 by ELISA commercial kits. Finally, scrotal Duplex was done in standing and supine position.
Results: Serum and seminal levels of Gal-1 and Gal-3 were statistically significant higher in azoospermic patients compared with normal individuals (p < 0.001 for all). In addition, in healthy individuals there were statistically significant positive correlations between serum levels of Gal-1 and age, FSH, LH levels (r = 0.296, p = 0.005; r = 0.333, p = < 0.001; r = 0.312, p= 0.003, respectively) and serum levels of Gal-2 and FSH and LH (r = 0.436, p < 0.001; r = 0.350, p < 0.001, respectively), whereas serum Gal-3 showed a borderline positive correlation with age (r = 0.2, p = 0.059). Additionally, statistically significant positive correlations between seminal levels of Gal-1 and Gal-3 and free testosterone in healthy individuals were reported (r = 0.205, p = 0.053; r = 0.219, p = 0.038, respectively).
On the other hand, there were negative correlations between serum and seminal levels of Gal-1 and Gal-3, total and progressive sperm motility, sperm count and abnormal sperm forms in healthy individuals (r = -0.382, p < 0.001; r = -0.405, p < 0.001; r= -0.376, p < 0.001; r = -0.364, p < 0.001) (r = -0.394, p < 0.001; r = -0.467, p < 0.001; r = -0.413, p < 0.001; r = -0.433, p< 0.001); (r = -0.372, p < 0.001; r = -0.377, p < 0.001; r = -0.317, p = 0.002; r = -0.311, p = 0.003)(r = -0.445, p< 0.001; r = -0.498, p < 0.001; r = -0.453, p < 0.001; r = -0.463, p < 0.001, respectively).
Furthermore, statistically significant positive correlations between serum levels of Gal-1 and Gal-3 and age in azoospermic patients were reported (r = 0.511, p < 0.001; r = 0.390, p= 0.008, respectively). On the other hand, there were negative correlations between seminal Gal-1 and estradiol (E2) and seminal Gal-3 and FSH and LH in azoospermic patients
(r=-0.318, p=0.033; r=-0.322, p = 0.031; r = -0.477, p < 0.001, respectively). Also, negative correlations between serum Gal-3 and total and free testosterone in azoospermic patients were detected (r = -0.396, p = 0.007; r = -0.375, p = 0.011, respectively).
Conclusions: Elevated serum and seminal levels of Gal-1 and Gal-3 have detrimental effects on spermatogenesis. Furthermore, the current study demonstrated potential regulatory effects of reproductive hormones on Gal-1 and Gal-3. Thus, future studies are needed to confirm such findings.
KEYWORDS: Gal-1; Gal-3; Azoospermia; Normal spermatogenesis.
Submitted 11 May 2023; Accepted 20 June 2023
INTRODUCTION
Non-obstructive azoospermia (NOA) is one of the most important causes of male infertility. It characterized by the absence of sperm in semen repeatedly (1). At present, its pathogenesis is complex and can be categorized into primary and secondary testicular failure (1). About 10-15% of people of childbearing age are infertile in the world, of which male infertility accounts for about 50% (2). NOA is a type of male infertility caused by spermatogenic dysfunction of testicular tissue. Patients with NOA cannot produce sperm or can only produce a very small amount of sperm. In patients with NOA, the structure of the seminiferous tubules in the testis is disordered, while the maturation of spermatogenic cells is blocked, and the meiosis of spermatogenic cells is arrested (3). Galectins are a family of soluble carbohydrate-binding proteins that regulate cell phenotype and function in development and disease (4). Galectin-1 (Gal-1) and Galectin-3 (Gal-3) are expressed by many immune cells and receive considerable attention in the context of immunity (5, 6). Gal-1 was the first member of the lectin family, reported more than 3 decades before, as a +15 kDa protein existing in a noncovalent homodimer form that was previously known as electrolectin, b-galactosidebinding lectin, galaptin or L-14 (4). Different organs and tissues secrete it including thymus (7), spleen (8), smooth muscle (9), colon (10), ovary (11)and also the nervous system (12). It is an endogenous
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11462 1 ORIGINALPAPER
Sameh Fayek GamalEl Din 1, Olfat Gamil Shaker 2, Ahmad Fawzy Megawer 1, Mohamed Ahmed Abdel Salam 1, Abdelhalim Nabil Abdelhalim 1, Ahmed Adel 1
DOI: 10.4081/aiua.2023.11462
protein that might play a key role in Leydig cell biology as well as potential control of the development of normal Leydig cells through autocrine and paracrine mechanisms (13) However, cells such as Sertoli or peritubular cells might be responsible for Gal-1 regulation in Leydig cell functions (13) In contrast, Gal-3 is the most commonly reported type (14) Gal-3 is approximately 30kDa protein that acts several roles in cell to cell interaction, cancer progression, pathogenesis of infections, and immunomodulation (15) In male reproductive tract, Gal-3 is present in testes, epididymis, vas deferens, prostate, seminal vesicles and in semen (15)
Early reports demonstrated that extracellular Gal-3 signals apoptosis via cytochrome c-release and caspase-3 activation independent of caspase-8 activation (16), with more recent data suggesting that Gal-3 activates caspase9 upstream of caspase-3 through phosphorylation of extracellular signal-regulated kinase (ERK) (17)
Differences in the pro-apoptotic signaling pathways activated by extracellular Gal-1 and Gal-3 may arise because they recognize different cell surface glycoproteins by way of their selectivity for different oligosaccharide ligands
(18) Gal-3 expression has been identified in human Sertoli cells where it is under follicle stimulating hormone (FSH) control (19, 20) A potential role of Gal-3 in germ cell survival/regeneration is suggested based on its increased expression one month after a transient germ cell death process (20) Although luteinizing hormone (LH)/testosterone and FSH potentially exert their control on spermatogenesis via identified components, there are still other hormonally regulated Sertoli cell factors which remain unknown (20) We aimed in the current study to compare between seminal plasma and serum levels of Gal-1 and Gal-3 in azoospermic patients and fertile men Also, we aimed to find out the potential relationships between reproductive hormones and Gal-1 and Gal-3
METHODS
This cross-sectional study was conducted at the andrology outpatient clinic from January 2022 to September 2022 A total of 90 participants were enrolled and divided into two equal groups as follows: azoospermic and normal group All participants signed an informed consent The ethical committee approved the study that conforms to Helsinki declaration (2013) (21) (MS-197-2022)
Inclusion criteria
Any azoospermic patient or fertile individual aged 20-50 years old was included
Exclusion criteria
Any azoospermic patient with abnormal karyotyping was excluded Also, any participant with chronic medical condition was excluded
All participants were evaluated by history taking as well as general and local examinations Testicular volume (V) was calculated from measurements of length (L) and width (W) according to the formula, (V = pi/6 X L X W2) using a plastic ruler or caliper Two semen analyses with an interval of 1 month were obtained Hormonal profiles including: FSH, LH, serum prolactin, total testosterone,
and estradiol were performed Scrotal Duplex in standing and supine position was done Gal-1 and Gal-3 were assessed in seminal plasma and serum Serum and semen were used for determination of Gal-1 using ELISA kit provided by Bioassay Technology Laboratory with Cat No E2989Hu (Zhejiang China) Serum and semen were used for determination of Gal-3 using ELISA kit provided by Bioassay Technology Laboratory with Cat No E3449Hu (Zhejiang China) Serum separator tubes (SST) were used, and samples were allowed to clot for 30 min at room temperature before centrifugation for 15 min at 1000 x g Serum was removed and assayed immediately or divided into aliquot and stored at ≤ -20°C Repeated freeze-thaw cycles were avoided The ejaculates were obtained after 4 days of sexual abstinence into sterile containers for immediate analysis Semen was examined according to 5th guidelines WHO guidelines (2010) (22) Seminal plasma was centrifuged for 15 min at 1000 x g within 30 min of collection Next, it was assayed immediately or divided into aliquot and stored at ≤ -20°C Repeated freeze-thaw cycles were avoided
Statistical analysis
Recorded data were analyzed using the statistical package for social sciences, version 23 0 (SPSS Inc , Chicago, Illinois, USA) The quantitative data were presented as mean± standard deviation and ranges Qualitative variables were presented as number and percentages Data were explored for normality using Kolmogorov-Smirnov and Shapiro-Wilk Test Independent-samples t-test of significance was used when comparing between two means Mann Whitney U test was used for two-group comparisons in non-parametric data Chi-square (x2) test of significance was used in order to compare proportions between qualitative parameters Spearman's rank correlation coefficient (rs) was used to assess the degree of association between two sets of variables if one or both of them was skewed Values of two variables are plotted along two axes as scatter plots showing the presence of correlations The confidence interval was set to 95% and the margin of error accepted was set to 5%
RESULTS
The current study did not reveal any statistically significant difference among participants regarding age There were statistically significant higher means of Gal-1 and Gal-3 in azoospermic patients compared to healthy individuals (p < 0 001 for all) (Table 1)
In addition, in healthy individuals there were statistically significant positive correlations between serum levels of Gal-1 and age, FSH, LH levels (r = 0 296, p = 0 005; r = 0 333, p = < 0 001; r = 0 312, p = 0 003, respectively) and serum levels of Gal-2 and FSH and LH (r = 0 436, p < 0 001; r = 0 350, p < 0 001, respectively), whereas serum Gal-3 showed a borderline positive correlation with age (r = 0 2, p = 0 059) (Table 2)
Additionally, statistically significant positive correlations between seminal levels of Gal-1 and Gal-3 and free testosterone in healthy individuals were observed (r = 0 205, p = 0 053; r = 0 219, p = 0 038, respectively) (Table 2) On the other hand, there were negative correlations
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11462 GamalEl Din S F , Shaker O G , Fawzy Megawer A , et al 2
Gal-1 and Gal-3 and spermatogenesis and reproductive hormones
between serum and seminal levels of Gal-1 and Gal-3, total and progressive sperm motility, sperm count and abnormal sperm forms in healthy individuals (r = -0 382, p < 0 001; r = -0 405, p < 0 001; r = -0 376, p < 0 001; r = -0 364, p < 0 001=) (r = -0 394, p<0 001; r = -0 467, p < 0 001; r = -0 413, p < 0 001; r = -0 433, p < 0 001) (r = -0 372, p < 0 001; r = -0 377, p < 0 001; r = -0 317, p = 0 002; r = -0 311, p = 0 003)(r = -0 445, p < 0 001; r = -0 498, p < 0 001; r = -0 453, p < 0 001; r = -0 463, p < 0 001, respectively) (Table 2) Furthermore, statistically significant positive correlations between serum levels of Gal-1 and Gal-3 and age in azoospermic patients were reported (r = 0 511, p < 0 001; r = 0 390, p = 0 008, respectively) (Table 3) On the other hand, there were negative correlations between seminal Gal-1 and estradiol (E2) and seminal Gal-3 and FSH and LH in azoospermic patients (r = -0 318, p = 0 033; r = -0 322, p = 0 031; r = -0 477, p < 0 001, respectively) (Table 3) Also, negative correlations between serum Gal-3 and total and free testosterone in azoospermic patients were detected (r = -0 396, p = 0 007; r = -0 375, p = 0 011, respectively) (Table 3)
DISCUSSION
The current cross-sectional study was conducted at andrology outpatient clinic The current study had shown that serum and seminal levels of Gal-1 and Gal-3 were statistically significant higher in azoospermic cases compared to fertile individuals This finding is attributed to the fact that Gal-3 expression and/or its subcellular localization could be modified in the human infertile testes as Gal-3 immunostaining appears more intense in the infertile testes with an absence of germ cells (Sertoli cell-only syndrome) (20) Furthermore, animal studies on rat testes had revealed that Gal3 levels are increased in severely damaged spermatogenesis (20)
These findings could be seen in agreement with GamalEl Din et al who evaluated seminal plasma and serum levels of Gal-1 in NOA patients (23) The aforementioned casecontrol study that included in total 48 NOA patients and 50 age matched healthy controls demonstrated that seminal plasma levels of Gal-1 were higher in NOA men versus healthy controls (23) Consistently, Gal-3 levels are increased in oligozoospermic cases (24) In addition, there
Table
Shows levels of seminal plasma and serum Gal-1 and Gal-3 in azoospermic cases and healthy individuals
Table 2. Shows correlation between Gal-1 (ng/ml) and Gal-3 (pg/ml) with age and different sperm parameters and reproductive hormones.
Shows correlation between Gal-1 (ng/ml) and Gal-3 (pg/ml) with age and reproductive hormones among azoospermic patients
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11462 3
Azoospermic cases (n = 45) Healthy individuals (n = 45) Mean SD range Mean SD range p-value Serum Galectin 1 (ng/ml) 13 79 ± 10 14 6 7-56 7 35 ± 1 12 5 2-9 3 < 0 001 Seminal plasma Gal-1 (ng/ml) 12.11 ± 6.24 3.6-27.4 7.25 ± 0.90 5.7-8.7 < 0.001 Serum Gal-3 (pg/ml) 402 56 ± 295 59 153 8-1300 230 11 ± 59 33 120-312 3 < 0 001 Seminal plasma Gal-3 (pg/ml) 404 15 ± 300 11 114 6-1230 152 77 ± 22 50 120 6-198 2 < 0 001 P value was ca culated using Mann-Whitney test
1.
Parameters Gal-1 (ng/ml) Gal-3 (pg/ml) Serum Seminal plasma Serum Seminal plasma r p-value r p-value r p-value r p-value Age (years) 0 296 0 005 0 013 0 904 0 200 0 059 -0 092 0 387 Sperm count -0 382 < 0 001 -0 394 < 0 001 -0 372 < 0 001 -0 445 < 0 001 Total sperm motility -0 405 < 0 001 -0 467 < 0 001 -0 377 < 0 001 -0 498 < 0 001 Progressive sperm motility -0 376 < 0 001 -0 413 < 0 001 -0 317 0 002 -0 453 < 0 001 Abnormal sperm forms -0 364 < 0 001 -0 433 < 0 001 -0 311 0 003 -0 463 < 0 001 FSH 0 333 < 0 001 0 319 0 002 0 436 < 0 001 0 151 0 155 LH 0 312 0 003 0 337 < 0 001 0 350 < 0 001 0 007 0 951 Total testosterone -0 139 0 191 0 046 0 666 -0 184 0 082 0 054 0 614 Free testosterone -0 111 0 298 0 205 0 053 -0 197 0 063 0 219 0 038 PRL 0 033 0 757 0 120 0 260 0 032 0 765 0 008 0 940 E2 0 053 0 622 -0 151 0 155 0 079 0 460 -0 049 0 645 P va ue calcu ated using Spearman's rank corre ation coefficient
Table 3
Parameters Serum Gal-1 Seminal plasma Gal-1 Serum Gal-3 Seminal plasma Gal-3 (ng/ml) (ng/ml) (pg/ml) (pg/ml) r p-value r p-value r p-value r p-value Age (years) 0.511 < 0.001 0.064 0.674 0.390 0.008 -0.102 0.505 FSH 0 077 0 615 -0 024 0 874 0 265 0 078 -0 322 0 031 LH 0 093 0 546 0 053 0 731 0 152 0 320 -0 477 < 0 001 Total testosterone -0 236 0 118 0 045 0 769 -0 396 0 007 0 127 0 405 Free testosterone -0 207 0 173 0 224 0 138 -0 375 0 011 0 293 0 051 PRL 0 077 0 613 0 279 0 064 0 032 0 834 0 046 0 765 E2 -0 011 0 945 -0 318 0 033 0 004 0 980 -0 173 0 256 P va ue calcu ated us ng Spearman's rank corre ation coefficient
were statistically significant positive correlations between serum and seminal levels of Gal-1 and Gal-3, age, FSH, LH and abnormal sperm forms Similarly, it should be noted that FSH enhances Gal-3 expression probably through the classical cAMP/PKA/CREB transducing pathway (20) Furthermore, CAMP responsive element (CRE) and activator protein complex (AP1) have been detected in gal-3 promoter, a finding which agrees with the potential direct stimulatory actions of FSH and EGF, respectively On the contrary, Gal-1 has been detected in interstitial cells in mouse testis (25) where it might modulate Leydig cell growth through its multivalent binding and crosslinking properties as well as its ability to interact with extra cellular matrix causing changes in cell adhesivity (26) In the same context, the same study had reported that Gal-1 induces changes in Leydig cell morphology and reduces cell viability and testosterone production (26) Furthermore, this is the first time that an endogenous protein, Gal-1, is shown to possess apoptosis-inducing activity on Leydig cells Also, there were negative correlations between Gal-1, Gal-3, total and progressive sperm motility and sperm count We agreed with Mentes¸og˘lu and colleagues (2021) who assessed the correlation between semen parameters and galectin-3 levels of infertile men (24) Moreover, the possible role of Gal-3 and sperm motility in the current study is also supported by the negative correlation between Gal-3 levels and total progressive motile sperm
Consistently, Gal-3 levels were found to be negatively correlated with total progressive sperm count in oligozoospermic patients (24) Furthermore, there was a highly statistically significant positive correlation between serum Gal-1 and Gal-3 and age in azoospermic patients that could be seen contradictory to the study conducted by GamalEl Din et al who failed to demonstrate any correlation between serum Gal-1 and age in NOA patients (23) Furthermore, there was a statistically significant negative correlation between seminal plasma Gal-1 and estradiol (E2) in azoospermic patients Similarly, Perzelova et al demonstrated an inverse relation between Gal-1 and estrogen as they showed that the pharmacological activation of estrogen receptor-b led to a significant alteration in the pattern of differentiation and the proliferation activity of keratinocytes including Gal-1 (27) Interestingly, there were statistically significant negative correlations between serum Gal-3, total testosterone and free testosterone in azoospermic patients These findings could be seen contradictory to a recent study that was conducted on rats and revealed the favorable effect of testosterone administration to halt the progression of cavernosal fibrosis by decreasing Gal-1 through enhancing the expression of miR-22-3p (28) Furthermore, there were statistically significant negative correlations between seminal plasma Gal-3, FSH and LH in azoospermic patients
Remarkably, there are several points of strength of the current study that can be summarized as follows It clearly demonstrates the detrimental effects of Gal-1 and Gal3 on spermatogenesis Also, it highlights the horizons for a potential regulatory effect of reproductive hormones on these proteins Admittedly, lack of immunohistochemistry can be seen as the major limitation of the current study Also, small sample size can be added as another
limitation Finally, five cases of the healthy individuals suffering from hypothyroidism and diabetes mellitus and hypertension and disc prolapsed were included
CONCLUSIONS
Elevated serum and seminal levels of Gal-1 and Gal-3 have detrimental effects on spermatogenesis Furthermore, the current study demonstrated potential regulatory effects of reproductive hormones on Gal-1 and Gal-3 Thus, future studies are needed to confirm such findings
REFERENCES
1 Wu X, Lin D, Sun F, Cheng CY Male Infertility in Humans: An Update on Non-obstructive Azoospermia (NOA) and Obstructive Azoospermia (OA) Adv Exp Med Biol 2021; 1288:161-173
2 Gifford JA The role of WNT signaling in adult ovarian folliculogenesis Reproduction 2015; 150:R137-R148
3 Kohn TP, Pastuszak AW Non-obstructive azoospermia and shortened leukocyte telomere length: further evidence linking poor health and infertility Fertil Steril 2018; 110:629-630
4 Cummings RD, Liu FT Galectins In: Varki AC, Cummings RD, Esko JD, et al, editors Essentials of glycobiology cold spring harbor New York: Cold spring harbor laboratory press 2009; Chapter 33
5 Rabinovich GA, Toscano MA Turning ‘sweet' on immunity: galectin-glycan interactions in immune tolerance and inflammation Nat Rev Immunol 2009; 9:338-352
6 Thiemann S, Baum LG Galectins and immune responses-just how do they do those things they do? Annu Rev Immunol 2016; 34:243264
7 Baum LG, Pang M, Perillo NL, et al Human thymic epithelial cells express an endogenous lectin, galectin1, which binds to core 2 O-glycans on thymocytes and T lymphoblastoid cells J Exp Med 1995; 181:877-87
8 Ahmed H, Fink NE, Pohl J, Vasta GR Galectin-1 from bovine spleen: biochemical characterization, carbohydrate specificity and tissue-specific isoform profiles J Biochem 1996; 120:1007-19
9 Moiseeva EP, Javed Q, Spring EL, de Bono DP Galectin 1 is involved in vascular smooth muscle cell proliferation Cardiovasc Res 2000; 45:493- 502
10 Hittelet A, Legendre H, Nagy N, et al Upregulation of galectins1 and -3 in human colon cancer and their role in regulating cell migration Int J Cancer 2003; 103:370-9
11 Van den Brule F, Califice S, Garnier F, et al Galectin-1 accumulation in the ovary carcinoma peritumoralstroma is induced by ovary carcinoma cells and affects both cancer cell proliferation and adhesion to laminin-1 and fibronectin Lab Invest 2003; 83:377-86
12 Akazawa C, Nakamura Y, Sango K, et al Distribution of the galectin-1 mRNA in the rat nervous system: its transient up regulation in rat facial motor neurons after facial nerve axotomy Neuroscience 2004; 125:171-8
13 Biron VA, Iglesias MM, Troncoso MF, et al Galectin-1: biphasic growth regulation of Leydig tumor cells Glycobiology 2006; 16:81021
14 Dumic J, Dabelic S, Flögel M Galectin-3: an open-ended story Biochim Biophys Acta 2006; 1760:616-35
15 Jones JL, Saraswati S, Block AS, et al Galectin-3 is associated with prostasomes in human semen Glycoconj J 2010; 27:227-36
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11462 GamalEl Din S F , Shaker O G , Fawzy Megawer A , et al 4
Gal-1 and Gal-3 and spermatogenesis and reproductive hormones
16 Fukumori T, Takenaka Y, Yoshii T, et al CD29 and CD7 mediate galectin-3-induced type II T-cell apoptosis Cancer Res 2003; 63:8302-8311
17 Xue H, Liu L, Zhao Z, et al The N-terminal tail coordinates with carbohydrate recognition domain to mediate galectin-3 induced apoptosis in T cells Oncotarget 2017; 8:49824
18 Stowell SR, Arthur CM, Mehta P, et al Galectin-1, -2, and -3 exhibit differential recognition of sialylated glycans and blood group antigens J Biol Chem 2008a; 283:10109-10123
19 Wollina U, Schreiber G, Görnig M, et al Sertoli cell expression of galectin-1 and -3 and accessible binding sites in normal human testis and Sertoli cell only-syndrome Histol Histopathol 1999; 14:779-84
20 Deschildre C, Ji JW, Chater S, et al Expression of galectin-3 and its regulation in the testes Int J Androl 2007; 30:28-40
21 World medical association World medical association declaration of Helsinki: ethical principles for medical research involving human subjects JAMA 2013; 310:2191-4
22 World Health Organization (WHO) WHO laboratory manual for the examination and processing of human semen 5th ed Geneva: WHO: 2010
23 GamalEl Din SF, Abougabal Kh, Saad HM, et al Estimation of Serum and Seminal Plasma Levels of Glactin-1 in NonObstructive Azoospermia Cases and Their Correlations with the Rate of Sperm Retrieval: A Comparative Prospective Study J Reprod Infertil 2022; 23:257-263
24 Mentesoglu P, Tangal S, Yigman M, et al The Correlation Between Semen Parameters and Galectin-3 Levels of Infertile Men
TJRMS 2021; 5:1-5
25 Timmons PM, Rigby PWJ, Poirier F The murine seminiferous ephitelial cycle is pre-figured in the Sertoli cells of the embryonic testis Development 2002; 129:635-647
26 Martinez VG, Pellizzari EH, Díaz ES, et al Galectin-1, a cell adhesion modulator, induces apoptosis of rat Leydig cells in vitro Glycobiology 2004; 14:127-37
27 Perželová V, Sabol F, Vasilenko T, et al Pharmacological activation of estrogen receptors-α and -b differentially modulates keratinocyte differentiation with functional impact on wound healing Int J Mol Med 2016; 37:21-8
28 Hu Z, Zhang Y, Chen J, et al Testosterone attenuates senile cavernous fibrosis by regulating TGFbR1 and galectin-1 signaling pathways through miR-22-3p Mol Cell Biochem c2023; 478:1791-1802
Correspondence
Sameh Fayek GamalEl Din, MD (Corresponding Author)
samehfayek@kasralainy edu eg
Department of Andrology and STDs Kasr Al-Ainy, Faculty of Medicine
Cairo University, Al-Saray Street, El Manial, Cairo, 11956, Egypt
Ahmad Fawzy Megawer, MD
Mohamed Ahmed Abdel Salam, MD
Abdelhalim Nabil Abdelhalim, MBBCH
Ahmed Adel, MD
Department of Andrology, Sexology and STDs, Kasr AlAiny Faculty of Medicine, Cairo University, Cairo, Egypt
Olfat Gamil Shaker, MD
Department of Medical Biochemistry and Molecular Biology, Kasr AlAiny Faculty of Medicine, Cairo University, cairo, Egypt
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11462 5
Prognostic determinants and treatment outcomes of Fournier’s Gangrene treatment in a resource-limited setting: A retrospective study
1 Department of General Surgery, School of Medicine, Ibb University of Medical Sciences, Ibb, Yemen;
2 Department of Urology, School of Medicine, Ibb University of Medical Sciences, Ibb, Yemen;
3 Department of Internal Medicine, Yale New Haven Health, Bridgeport Hospital, Bridgeport, USA;
4 Department of General Surgery, School of Medicine, 21 September University, Sana'a, Yemen;
5 Department of Gynaecology, School of Medicine, Jeblah University for Medical and Health Sciences, Ibb, Yemen.
Summary
Background: Fournier’s gangrene (FG) is a destructive necrotizing infection with a generally poor prognosis. This study aims to share our experience in handling FG patients in a resource-limited setting and identify prognostic factors for FG mortality.
Methods: A retrospective study of thirty-six patients diagnosed with FG and treated at our teaching hospital between Jun 2010 to Oct 2022 was conducted. Laboratory and nonlaboratory data and patients' outcomes were gathered. A univariate analysis was computed for identifying prognostic factors for FG mortality.
Result: The main age was 68.30 ± 5.61years and most (69.4%) were older than 65 years. The overall survival was 63.9% and the mortality rate was 36.1%. Univariate analysis showed that advanced age (p = 0.02), delayed in hospital presentation (p = 0.024), involvement of larger area (p = 0.001), a history of diabetes mellitus (p < 0.006), end-stage renal disease (p = 0.018), heart failure (p = 0.005), cerebrovascular accident (p = 0.003), liver cirrhosis (p = 0.001), presence of multiple comorbidities (p = 0.001), septic conditions at admission (p = 0.048), need for mechanical ventilation (p = 0.001), hypoalbuminemia (p < 0.001), and elevated blood urea nitrogen (p = 0.002) were found to be risk factors for mortality in patients with FG.
Conclusions: Fournier’s gangrene is a fulminant condition with a high mortality rate, especially in resource-limited settings. In this study, the mortality rate was 36.1%. Advanced age, delayed in hospital presentation, involvement of larger area, a history of diabetes mellitus, end-stage renal disease, heart failure, cerebrovascular accident, liver cirrhosis, presence of multiple comorbidities, septic conditions at admission, need for mechanical ventilation, hypoalbuminemia, and elevated blood urea nitrogen were associated with FG mortality.
KEYWORDS: Fournier's gangrene; Mortality; Prognostic factors; Outcome.
Submitted 5 May 2023; Accepted 8 June 2023
INTRODUCTION
Fournier's gangrene (FG) is a poly-microbial necrotizing infection that spread drastically to involve the genital, perianal area, or perineal deep tissue causing rapid tissue
and is usually caused by an aerobic bacterial invasion (1). The bacterial species' combined invasive and toxic activities produce endarteritis obliterans, cutaneous and subcutaneous artery thrombosis, local tissue necrosis and gangrene, and subsequently life-threatening adverse events such as multiple organ system failures, septic shock, and death if left untreated (1, 2).
Despite the advancement of medical knowledge towards FG’s pathobiology, diagnosis, and management, the mortality rate remains high, with some reported rates of approximately 50% (3). FG is a predominantly male illness and is commonly observed in men aged 40 to 50, with a reported annual incidence of 1.6 cases per 100.000 men. Diabetes mellitus (DM), older age, liver cirrhosis, vascular disease, cancer, chronic alcoholism, overweight, paraplegia, and renal impairment are all thought to be associated with higher mortality rates; however, up to 30% to 50% of FG cases present with no identifiable risk fact (4). There are numerous scoring methods for predicting FG mortality, such as the Acute Physiology and Chronic Health Evaluation (APACHE) II scoring system, which is an extensively used tool for predicting mortality outcomes, Charlson Comorbidity Index (CCI), and Fournier's Gangrene Severity Index (FGSI) which are well-defined disease-specific metric (5, 6). However, those scorings still had limitations and some factors are not included such as length of hospital stay, which is related to hospitalization costs and treatment approaches (4).
In low-income countries, such as Yemen, there is limited information available about the extent of FG mortality rate, and its predisposing factors (7). Here, we studied the characteristics and clinical course of patients diagnosed with FG at our institution over a period of 12 years. Our primary objective was to discern the prognostic factors intricately linked to this debilitating disease. By furnishing essential data, we aspire to enhance the foundation for future investigations and therapeutic interventions. Such endeavors hold immense potential to empower healthcare practitioners in promptly identifying FG and initiating timely and efficacious care for afflicted individuals.
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11450 1 ORIGINALPAPER
Saif Ghabisha 1, Faisal Ahmed 2*, Saleh Al-wageeh 1, Mohamed Badheeb 3, Qasem Alyhari 1 , Abdulfattah Altam 4, Afaf Alsharif 5
DOI: 10.4081/aiua.2023.11450
MATERIALSANDMETHODS
Study design
Between Jun 2010 to Oct 2022, this retrospective study was conducted at Ibb University-affiliated Hospitals and included 36 consecutive patients diagnosed with FGand treated by the same surgeon (Professor S. Ghabisha). The Ethics Research Committees of Ibb University provided their approval for the study (ID: IBBUNI.AC.YEM.2023.55, on 03.03.2023), which adhered to the ethical principles outlined in the Declaration of Helsinki.
Inclusion criteria
Patients diagnosed with FG and treated at Ibb Universityaffiliated hospitals (Al-Nasar Hospital) were included in the study. The presence of fever (> 38°C), erythema and swelling in the perianal or scrotal region, purulent-malodorous discharge, and the detection of fluctuation or crepitation at the wound site were used to make the diagnosis of FG (8).
Exclusion criteria
Patients treated at other hospitals and those with scrotal, periurethral, or perianal abscesses with no fascial or soft tissue extension were excluded.
Surgical procedure and postoperative care
All participants received immediate aggressive debridement under general or spinal anesthesia to remove necrotic tissue until healthy tissue was observed. In addition, cystostomy catheters were placed, limiting the contact of the urethra with urine. Empiric intravenous antibiotic therapy, including crystalline penicillin (4miu IV every 6 hours), ceftriaxone (1 g every 12 hours), and metronidazole (500 mg every 12 hours), was administered until culture results were obtained and in cases of sepsis, imipenem and vancomycin were used. Dressings were changed three times daily with sterile gauze soaked in a solution of povidone-iodine, 0.2% nitrofurazone ointment, and 250 mg rifampicin ampoule and hyperbaric oxygen was done in cases needing multiple debridements (9). A fecal diversion (colostomy) was performed in cases where the perirectal and anal regions were affect-
ed, while an orchiectomy was performed in testicular involvement cases (5). Patients were transferred to the Plastic and Reconstructive Surgery Clinic once their general health status and wound cleanliness had improved.

Data collection
Patient demographic characteristics, including age, time to hospital admission, comorbidities, albumin level, number of surgical debridements, need for mechanical ventilation, need for colostomy diversion or orchiectomy, length of hospital stay, and mortality were extracted from the patient's medical records. Mortality refers to all-cause mortality and any cause of FG-related death during the initial admission or follow-up. To assess the FG extension, we used a modified body surface area nomogram commonly used for estimating the extension of burn injuries. This involved assigning a value of 1% for penile, scrotal, and perineal involvement, and 2.5% for ischiorectal fossa involvement (5, 8).
The comorbidities were heart failure, end-stage renal disease (ESRD), liver cirrhosis, history of anorectal surgery, and old cerebrovascular accident (CVA), which were also evaluated as several comorbidities (presence of one versus more than one of comorbidities) (10). The number of surgical debridements was defined as the number of times a patient entered the operating room (10). The albumin level was dived into two categories (equal or more than 3 g/dL and less than 3 g/dL).
Variables and measures
The outcome variable was FG mortality expressed as a binary variable: alive and dead. Independent variables included age (≤ 65 years and more than 65 years), CVA (yes and no), heart disease (yes and no), liver cirrhosis (yes and no), ESRD (yes and no), the number of debridement (≤ 2 times and ≥ times), comorbidity number (one and more than one), need for a colostomy (yes and no), need for orchiectomy (yes and no), mean hospital stays, etiological subtypes (genitourinary infection versus nongenitourinary infections), septic condition (yes and no), comorbidity number (< two comorbidities and ≥ two comorbidities), mean total affected body surface area (≤ than 3% and more than 3%), blood urea nitrogen
Archivio Italiano di Urologia e
Andrologia 2023; 95(3):11450
2
Saif Ghabisha, Faisal Ahmed, Saleh Al-wageeh, Mohamed Badheeb, Qasem Alyhari, Abdulfattah Altam, Afaf Alsharif
Figure 1.
A.Fournier’s gangrene involved the scrotum.
B.Fournier’s gangrene involved the penis, scrotum, and ischiorectal fossa.
C.Fournier’s gangrene involved both the penis and scrotum with a purulent discharger.
(BUN) (more than 50 mg/dl and less), Albumin level (≤ 3 g/dL and more than 3 g/dL), need for mechanical ventilation (yes and no), time to hospital presentation (≤ 7 days and more than 7 days), and DM (yes and no)
Study outcome
The mortality rate and the independent predictors of FG mortality
Statistical analysis
The study utilized both quantitative and qualitative, for which means and standard deviations were used to present quantitative data, while frequencies and percentages were reported for qualitative variables The normality of the data was confirmed using the Smirnov-Kolmogorov test To determine the independent risk variables related to FG mortality, univariate analysis was done Effect sizes in the model were expressed using odds ratios and confidence intervals at 59%
The statistical significance level was set at p < 0 05 The IBM SPSS version 22 software (IBM Corp , Armonk, New York) was used for statistical analysis
RESULT
Baseline clinical characteristics
The mean age was 68 30 ± 5 61 years and most of patients (69 4%) were aged more than 65 years The main time to hospital presentations was 7 47 ± 4 10 days and 15 (41 7%) patients presented after 7 days from starting symptoms
Most of them (25, 69 4%) were in septic conditions
Table 1
Demographic characteristics of patients
History of DM, heart failure, ESRD, CVA, anorectal surgery, and liver cirrhosis was present in 20 (55 6%), 11(30 6%), 8 (22 2%), 5(13 9%), 6 (16 7%), 6 (16 7%), respectively Additionally, 14 (38 9%) had more than one comorbid number The source of infection was a genitourinary infection in 15 (41 7%) patients, perianal infection in 6 (16 7%) patients, and an unknown source in 15 (41 7%) patients The mean calculated total affected body surface area was 3 59 ± 1 47 (%) and was more than 3% in (19, 52 8%) patients The serum albumin level was less than 3 g/dL in 14 (38 9%) patients Most of the patients (72 2%) more than one surgical debridement Colostomy and orchiectomy were done on 6 (16 7%) and 3 (8 3%) patients respectively The mean hospital stay was 57 00 ± 4 01 days and 15 (41 7%) patients need mechanical ventilation Within a median follow-up time of 14 0 months (range 2-30 months), 23(63 9%) of patients survived and the total mortality rate was 36 1%
Table 1 summarizes the baseline c l i
t h e research cohort
Mortality predictors in patients with Fournier’s gangrene
The association of independent variables with the dependent variable was investigated using univariate, analysis Univariate analy-
Table 2.
sis showed that advanced age (p = 0 02), delayed in hospital presentation (p = 0 024), involvement of larger area (p = 0 001) (Table 2), a history of DM (p < 0 006), ESRD (p = 0 018), heart failure (p = 0 005), CVA (p = 0 003), liver cirrhosis (p = 0 001), presence of multiple comorbidities (p = 0 001), septic conditions at admission (p = 0 048), (p = 0 018), need for mechanical ventilation (p = 0 001), hypoalbuminemia (p < 0 001), and elevated blood urea nitrogen (p = 0 002) were found to be risk factors for mor-
Comparison between survivors and survivors for quantitative variables
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11450 3 Fournier's Gangrene outcome
c
a r a c t e r i s t i c s o
n i c a l
h
f
Variable Subgroup N (%) Age (year) Mean ± SD 68 30 ± 5 61 < 65 years 11 (30 6) ≥ 65 years 25 (69 4) Time to hospital admission (days) Mean ± SD 7 47 ± 4 10 (2-20) ≤ 7 days 21 (58 3) > 7 days 15 (41.7) Source of infection Urinary tract infection 15 (41 7) Perianal or perirectal infection 6 (16 7) Unknown 15 (41 7) Septic condition - 25 (69 4) Predisposing factors Diabetes mellitus 20 (55 6) Heart failure 11 (30 6) Renal failure 8 (22 2) Cerebrovascular accident 5 (13 9) Liver cirrhosis 6 (16.7) Anorectal surgery 6 (16 7) Comorbid number One 22 (61 1) ≥ Two 14 (38 9) Total affected body surface area (%) Mean ± SD 3 59 ± 1 47 ≤ 3% 17 (47.2) > 3% 19 (52 8) Number of debridement Mean ± SD 2 27 ± 1 13 (1-5) One 10 (27 8) ≥ Two 26 (72 2) Needs for colostomy - 6 (16.7) Needs for orchiectomy - 3 (8 3) Need for mechanical ventilation - 15 (41 7) Blood urea nitrogen (mg/dl) ≥ 50 18 (50) Albumin level (mg/dl) < 3 14 (38 9) Hospital stay (day) Mean ± SD 7 00 ± 4 01 Outcome Survivors 23 (63 9) Non-survivors 13 (36 1)
Variable Outcome Mean difference (95 % CI) t & z P-value * Sur vivors N = 23 Died N = 13 Mean (SD) Mean (SD) Age (year) 66.69 (5.19) 71.15 (5.35) -4.45(-8.15 to -0.75) -2.44 0.020 Number of debridements 2 21(1 12) 2 38(1 19) -0 16(-0 97 to 0 64) -0 42 0 678 Time to hospital presentation (days) 6 91 (4 83) 8 46(2 14) -1 54(-4 43 to 1 33) -1 09 0 024 Total BSA (%) 3 00(1 47) 4 65(0 65) -1 65(-2 53 to -0 77) -3 81 0 001 Hospital stay (days) 7 08 (3 42) 6 84(5 04) 0 24(-2 63 to 3 11) 0 170 0 361 BSA: Body surface area * P-values of < 0 05 were considered s gn ficant
Table 3. Comparison between survivors and non-survivors for categorical variables
The mortality associated with the disease is high and has been reported from 6% to as high as 76% (12) In this study, the total mortality rate was 36 1% This is in agreement with other studies in most developing countries For example, Sabzi et al study in Iran reported a mortality rate of 37 5% (12)
tality in patients with FG (Table 3) The relative risk of SSI occurrence was also higher among patients with genitourinary infection; however, it was not statistically significant in univariate analysis (p = 0 075)
DISCUSSION
In this study, we evaluated the predictive factor for mortality in FG patients who were treated in resource-limited settings The survival rate was 63 9% and the mortality rate was 36 1% Univariate analysis showed that advanced age, delayed in hospital presentation, involvement of larger area, a history of DM, ESRD, heart failure, CVA, liver cirrhosis, presence of multiple comorbidities, septic conditions at admission, need for mechanical ventilation, hypoalbuminemia, and elevated blood urea nitrogen were found to be risk factors for mortality in patients with FG FG is a polymicrobial illness that resulted typically from facultative aerobic and anaerobic bacterial growth The rapid proliferation is linked to decreased cellular immunity of FG’s patients and the synergistic release of toxins (11)
In our study, genitourinary infection was the most common cause of FG and one-third of cases had an unknown etiology Our result was similar to Tahmaz et al 's study, which reported that 33% of FG cases were due to genitourinary infections (13) Nevertheless, no identifiable cause was observed in one-quarter of the patients in the El-Qushayri et al study (14) The factors that predict FG mortality are, for the most part, debatable Because many studies are retrospective and included a small number of patients For that, solid criteria are still missing and statistical analysis is still limited There is a discrepancy in the literature r e g a r d i n g s e v e r a l i n d e p e n d e n t prognostic factors in patients with FG For example, some studies have shown that younger age was associated with improved survival (8, 15, 16) While other studies have not found a significant difference in disease onset between various age groups (17, 18) In our study group, advanced age was noticed among non-surviving patients and was a risk factor for FG mortality in univariate analysis
In line with earlier research, the majority of our patient population had DM as the most common comorbidity This pathology in our study was a predictive factor for mortality in univariate analysis (19, 20) According to previous researchers, the incidence of DM was found in between 50% and 70% of FG patients (19, 21) DM has been identified as a risk factor for FG and has been linked to a more progressive and poorer outcome due to reduced phagocytic and intracellular bactericidal activity and neutrophil dysfunction (19)
Certain conditions such as alcohol consumption, immunocompromised status, malignancy, heart failure, hepatic disease, and ESRD were reported to be associated with FG mortality (8, 13, 22) Similarly, in our study, those factors were associated with FG mortality and were statistically significant in univariate analysis
Additionally, 38 9% of our patients had at least one of the following conditions: ESRD, cardiac insufficiency, CVA, and liver cirrhosis; these conditions were highly represented among nonsurvivors patients In Roghmann et al
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11450
4
Saif Ghabisha, Faisal Ahmed, Saleh Al-wageeh, Mohamed Badheeb, Qasem Alyhari, Abdulfattah Altam, Afaf Alsharif
Variable Sub Total (n = 36) Outcome Univariate analysis variable N (%) Sur vivors N (%) Died N (%) OR (95 % CI) P-value * Age (year) < 65 11 (30 6) 9 (81 8) 2 (18 2) 0 28 (0 05 to 1 58) 0 151 ≥ 65 25 (69 4) 14 (56 0) 11 (44 0) Reference group Diabetes mellitus Yes 20 (55 6) 8 (40 0) 12 (60 0) 22 50 (2 46 to 205 7) 0 006 No 16 (44 4) 15 (93 8) 1 (6 3) Reference group Number of debridements ≤ 1 10 (27 8) 6 (60 0) 4 (40 0) 1 25 (0 28 to 5 65) 0 763 > 2 26 (72 2) 17 (65 4) 9 (34 6) Reference group Time to the presentation (day) ≤ 7 21 (58 3) 16 (76 2) 5 (23 8) 0 27 (0 06 to 1 14) 0 075 > 7 15 (41 7) 7 (46 7) 8 (53 3) Reference group Comorbidity number ≤ 1 22 (61.1) 19 (86.4) 3 (13.6) 0.06 (0.01 to 0.33) 0.001 > 1 14 (38 9) 4 (28 6) 10 (71 4) Reference group Need colostomy Yes 6 (16 7) 4 (66 7) 2 (33 3) 0 86 (0 13 to 5 50) 0 877 No 30 (83.3) 19 (63.3) 11 (36.7) Reference group Need orchiectomy Yes 8 (8 3) 2 (66 7) 1 (33 3) 0 87 (0 07 to 10 69) 0 917 No 33 (91 7) 21 (63 6) 12 (36 4) Reference group Septic condition Yes 25 (69 4) 13 (52 0) 10 (90 9) 9 23 (1 02 to 83 33) 0 048 No 11 (30 6) 1 (9 1) Reference group CVA Yes 0 (0 0) 0 (0 0) 5 (100 0) - 0 003 No 0 (0 0) 23 (74 2) 8 (25 8) Reference group Liver cirrhosis Yes 0 (0 0) 6 (100 0) - 0 001 No 23 (76 7) 7 (23 3) Reference group History of heart failure Yes 11 (30 6) 3 (27 3) 8 (72 7) 10 66 (2 04 to 55 51) 0 005 No 25 (69 4) 20 (80 0) 5 (20 0) Reference group ESRD Yes 8 (22 2) 2 (25 0) 6 (75 0) 9 00 (1 46 to 55 24) 0 018 No 28 (77 8) 21 (75 0) 7 (25 0) Reference group History of anal surgery Yes 6 (16 7) 4 (66 7) 2 (33 3) 0 86 (0 13 to 5 50) 0 877 No 30 (83 3) 19 (63 3) 11 (36 7) Reference group Mechanical ventilation Yes 15 (41 7) 4 (26 7) 11 (73 3) 26 12 (4 09 to 166 0) 0 001 No 21 (58 3) 19 (90 5) 2 (9 5) Reference group Etiology Non-GU 21 (58 3) 16 (76 2) 5 (23 8) 0 27 (0 06 to 1 14) 0 075 GU 15 (41 7) 7 (46 7) 8 (53 3) Reference group BUN (mg/dl) < 50 18 (50.0) 17 (94.4) 1 (5.6) 0.03 (0.003 to 0.27) 0.002 ≥ 50 18 (50 0) 6 (33 3) 12 (66 7) Reference group Albumin (g/dL) < 3 22 (61 1) 2 (14 3) 12 (85 7) 126 0 (10 31 to 1539) < 0 001 ≥ 3 14 (38 9) 21 (95 5) 1 (4 5) Reference group BSA: body surface area; BUN: B ood urea n trogen; CI: confidence nterval; CVA: cerebrovascu ar acc dent; ESRD End-Stage Renal D sease; GU: Genitourinary; OR: odds rat o * P-values of < 0 05 were considered sign f cant
study, history of DM, ESRD, cardiac insufficiency, CVA, liver cirrhosis, and comorbidity were outcome predictors and Authors suggested that the presence of multiple comorbidities might predict poorer outcomes (23) In our study, the presence of multiple comorbidities was associated with FG mortality in univariate analysis
The duration between symptom onset and treatment initiation has been reported as a significant predictor of outcomes for patients with FG (19, 24) However, these findings are not universally agreed upon For instance, a study by Sallami et al reported no significant difference in time to admission between survivors and non-survivors (20) In our study, we found that a longer time to hospital admission was significantly associated with FG mortality (p = 0 024) Other reports mentioned higher mortality among FG patients with delayed hospital admission (19, 24) These inconsistencies may be attributed to variations in study settings, patient demographics, hospital accessibility, income, and educational levels In our study, the delayed patient presentation may be attributed to the limited access to healthcare facilities Specifically, the residence of our cohort was located at a considerably far distance from the specalized health centers, from the study area, which likely contributed to the delay in seeking medical attention
Various laboratory abnormalities have been evaluated to predict FG mortality, including white blood cell (WBC) count, blood urea nitrogen (BUN), serum creatinine, albumin, calcium, and sodium (12, 23) However, there is a discrepancy in the literature regarding several independent laboratory prognostic factors in patients with FG Sabzi Sarvestani et al. reported a significant correlation between those factors and FG mortality (12) These findings were also endorsed by Yeniyol et al , who showed elevated WBC, BUN, creatinine, alkaline phosphatase (ALP), and lactate dehydrogenase levels, and lower hematocrit, metabolic acidosis, hyponatremia, hypokalemia, in addition to decreased total protein, and albumin levels in non survivors compared to survivors (17) Reduced sodium levels, along with lower serum albumin and total protein levels, can signify both a catabolic state and a poor response to therapy, which were seen among these patients with a worse prognosis and higher mortality rates These factors are directly correlated with poor outcomes (20) Laor et al found a higher level of calcium, albumin, and cholesterol, and lower levels of BUN and ALP at admission of surviving patients compared to nonsurvivors (25) Another retrospective study, reported that BUN > 50 mg/dL was significantly associated with a higher mortality (26) It should be noted that various confounding factors or effect modifiers (e g , severe dehydration, sepsis, and shock) that were not controlled in the study may have influenced these findings Our univariate analysis showed that albumin levels lower than 3 g/dL and BUN > 50 mg/dL were associated with overall increased mortality Nevertheless, the generalizability of these findings is limited by the small and heterogeneous nature of our cohort
The reported indications for orchidectomy in FG patients were preexisting epididymorchitis, gangrenous testis damage, or scrotal abscess (21) Although testicular involvement appears to be uncommon in FG, a modest incidence
rate was reported by Sallami et al as seven patients, of 40 included, underwent orchidectomy for gangrenous testis damage; in addition to four patients needed subcutaneous testicular repositioning (20) In our study, three patients underwent orchidectomy as a sequala of testicular gangrenous necrosis A colostomy is sometimes needed to decrease fecal contamination, especially in the presence of infective sphincteric destruction or rectal perforation (20, 27) In our study, six patients underwent colostomy diversion due to the extensively involved perianal area
This study found a significant difference in the average extent of body surface area affected by necrotizing tissue between patients who survived and those who did not (3 0 ± 1 5 vs 4 7 ± 0 7 respectively) The number of surgical debridements, on the other hand, did not have a significant impact on patient outcomes, which is in line with the findings of Yeniyol et al (17) However, the result reported by Spirnak et al differs from these findings, as they showed a higher mortality rate among patients who underwent more frequent debridements due to more extensive disease (28)
Generally, prompt surgical intervention (aggressive and often repeat debridement), broad-spectrum antibiotics, and appropriate resuscitation are crucial in these patients (29) As expected, patients with large involved body surface areas usually died during the hospital course, and the chance of undergoing multiple debridements subsequently decreased in this group A similar report has been mentioned by Sabzi Sarvestani et al (12)
Postoperative mechanical ventilation has been demonstrated as a powerful factor in FG mortality In Benjelloun et al. and Yanar et al. studies, the need for mechanical ventilation is a predictive factor for FG mortality (30, 31) Our findings are consistent with those previously reported in the literature and the need for mechanical ventilation was an independent predictor of mortality (30, 31) This study has several limitations Firstly, the retrospective design and the small sample size were potential sources of bias that might limit the generalizability of our findings Secondly, due to the nature of the study, some relevant factors, such as blood gas analysis data, APACHE II scoring system, CCI, and FGSI, were not included in our analysis Future studies with more sample sizes and prospective designs are recommended to strengthen the validity and generalizability of our findings
CONCLUSIONS
FG represents a critical medical condition with notable morbidity and mortality rates In this study, Advanced age, delayed in hospital presentation, involvement of larger area, a history of DM, ESRD, heart failure, CVA, liver cirrhosis, presence of multiple comorbidities, septic conditions at admission, need for mechanical ventilation, hypoalbuminemia, and elevated blood urea nitrogen were associated with FG mortality
ACKNOWLEDGMENTS
The authors would like to thank the general manager of Al-Thora General Hospital and Al-Nassar Hospital, Ibb, Yemen, Dr Abdulghani Ghabisha, for editorial assistance
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11450 5 Fournier's Gangrene outcome
REFERENCES
1 Boughanmi F, Ennaceur F, Korbi I, et al Fournier's gangrene: its management remains a challenge Pan Afr Med J 2021; 38:23
2 Thwaini A, Khan A, Malik A, et al Fournier's gangrene and its emergency management Postgrad Med J 2006; 82:516-519
3 Tuncel A, Aydin O, Tekdogan U, et al Fournier's gangrene: Three years of experience with 20 patients and validity of the Fournier's Gangrene Severity Index Score Eur Urol 2006; 50:838-843
4 Zhang KF, Shi CX, Chen SY, et al Progress in Multidisciplinary Treatment of Fournier's Gangrene Infect Drug Resist 2022; 15:6869-6880
5 Hong KS, Yi HJ, Lee RA, et al Prognostic factors and treatment outcomes for patients with Fournier's gangrene: a retrospective study Int Wound J 2017; 14:1352-1358
6 Noegroho BS, Adi K, Mustafa A, et al The role of quick Sepsisrelated Organ Failure Assessment score as simple scoring system to predict Fournier gangrene mortality and the correlation with Fournier's Gangrene Severity Index: Analysis of 69 patients Asian J Urol 2023; 10:201-207
7 Al-Kohlany K, Baker K, Ahmed F, et al Treatment outcome of Fournier's gangrene and its associated factors: A retrospective study Arch Ital Urol Androl 2023:11318
8 Doluoglu Ö G, Karagöz MA, Kılınç MF, et al Overview of different scoring systems in Fournier's Gangrene and assessment of prognostic factors Turk J Urol 2016; 42:190-196
9 Feres O, Feitosa MR, Ribeiro da Rocha JJ, et al Hyperbaric oxygen therapy decreases mortality due to Fournier's gangrene: a retrospective comparative study Med Gas Res 2021; 11:18-23
10 Griebling TL Re: Prognostic Factors of Fournier's Gangrene in the Elderly: Experiences of a Medical Center in Southern Taiwan J Urol 2017; 197:709
11 Huang CS Fournier's Gangrene N Engl J Med 2017; 376:1158
12 Sabzi Sarvestani A, Zamiri M, Sabouri M Prognostic Factors for Fournier's Gangrene; A 10-year Experience in Southeastern Iran Bull Emerg Trauma 2013; 1:116-122
13 Tahmaz L, Erdemir F, Kibar Y, et al Fournier's gangrene: report of thirty-three cases and a review of the literature Int J Urol 2006; 13:960-967
14 El-Qushayri AE, Khalaf KM, Dahy A, et al Fournier's gangrene mortality: A 17-year systematic review and meta-analysis Int J Infect Dis 2020; 92:218-225
15 Tuncel A, Keten T, Aslan Y, et al Comparison of different scoring systems for outcome prediction in patients with Fournier's gangrene: experience with 50 patients Scand J Urol 2014; 48:393-399
16 Martinschek A, Evers B, Lampl L, et al Prognostic aspects, survival rate, and predisposing risk factors in patients with Fournier's gangrene and necrotizing soft tissue infections: evaluation of clinical outcome of 55 patients Urol Int 2012; 89:173-179
17 Yeniyol CO, Suelozgen T, Arslan M, et al Fournier's gangrene: experience with 25 patients and use of Fournier's gangrene severity index score Urology 2004; 64:218-222
18 Wetterauer C, Ebbing J, Halla A, et al A contemporary case series of Fournier's gangrene at a Swiss tertiary care center-can scoring systems accurately predict mortality and morbidity? World J Emerg Surg 2018; 13:25
19 Chalya PL, Igenge JZ, Mabula JB, et al Fournier's gangrene at a tertiary health facility in northwestern Tanzania: a single centre experiences with 84 patients BMC Res Notes 2015; 8:481
20 Sallami S, Maalla R, Gammoudi A, et al Fournier's gangrene :
what are the prognostic factors? Our experience with 40 patients Tunis Med 2012; 90:708-714
21 Dahm P, Roland FH, Vaslef SN, et al Outcome analysis in patients with primary necrotizing fasciitis of the male genitalia Urology 2000; 56:31-35
22 Lewis GD, Majeed M, Olang CA, et al Fournier's Gangrene
Diagnosis and Treatment: A Systematic Review Cureus 2021; 13:e18948
23 Roghmann F, von Bodman C, Löppenberg B, et al Is there a need for the Fournier's gangrene severity index? Comparison of scoring systems for outcome prediction in patients with Fournier's gangrene
BJU Int 2012; 110:1359-1365
24 Villanueva-Sáenz E, Martínez Hernández-Magro P, Valdés Ovalle M, et al Experience in management of Fournier's gangrene Tech Coloproctol 2002; 6:5-10
25 Laor E, Palmer LS, Tolia BM, et al Outcome prediction in patients with Fournier's gangrene J Urol 1995; 154:89-92
26 Clayton MD, Fowler JE, Jr , Sharifi R, et al Causes, presentation and survival of fifty-seven patients with necrotizing fasciitis of the male genitalia Surg Gynecol Obstet 1990; 170:49-55
27 Sarofim M, Di Re A, Descallar J, et al Relationship between diversional stoma and mortality rate in Fournier's gangrene: a systematic review and meta-analysis Langenbecks Arch Surg 2021; 406:2581-2590
28 Spirnak JP, Resnick MI, Hampel N, et al Fournier's gangrene: report of 20 patients J Urol 1984; 131:289-291
29 Auerbach J, Bornstein K, Ramzy M, et al Fournier Gangrene in the Emergency Department: Diagnostic Dilemmas, Treatments and Current Perspectives Open Access Emerg Med 2020; 12:353-364
30 Benjelloun el B, Souiki T, Yakla N, et al Fournier's gangrene: our experience with 50 patients and analysis of factors affecting mortality World J Emerg Surg 2013; 8:13
31 Yanar H, Taviloglu K, Ertekin C, et al Fournier's gangrene: risk factors and strategies for management World J Surg 2006; 30:1750-1754
Correspondence
Saif Ghabisha, MD - saifalighabisha@yahoo com
Saleh Al-wageeh, MD - alwajihsa78@gmail com
Department of General Surgery, School of Medicine, Ibb University of Medical Sciences, Ibb, Yemen
Faisal Ahmed, MD (Corresponding Author) fmaaa2006@yahoo com
Urology Research Center, Al-Thora General Hospital, Department of Urology, School of Medicine, Ibb University of Medical Sciences, Ibb, Yemen
Mohamed Badheeb, MD - badheeb2009@gmail com
Internal Medicine Office, Yale New Haven/Bridgeport Hospital, CT (USA)
Qasem Alyhari, MD - qalyhary@hotmail com
Department of General Surgery, School of Medicine, Ibb University of Medical Sciences, Ibb, Yemen Urology Office, Althora General Hospital, Alodine Street, Ibb (Yemen)
Abdulfattah Altam, MD - dral tam@yahoo com
Urology Office, School of Medicine, 21 September University, Sana'a (Yemen)
Afaf Alsharif, MD - afafmussa2018@gmail com
Department of Gynaecology, School of Medicine, Jeblah University for Medical and Health Sciences, Ibb, Yemen
Gynaecology Office, Jeblah Hospital, Jeblah, Ibb (Yemen)
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11450
6
Saif Ghabisha, Faisal Ahmed, Saleh Al-wageeh, Mohamed Badheeb, Qasem Alyhari, Abdulfattah Altam, Afaf Alsharif
Complications of non-medical assisted circumcision in Burkina Faso.
outcomes - about 23 cases and literature review
Summary
Objective: To report the clinical presentation of circumcision complications encountered at our center and evaluate their management and outcomes.
Patients and methods: A retrospective and descriptive study was conducted at Souro Sanou University Hospital between January 1, 2014, and December 31, 2018. All patients presenting with circumcision complications were included. Parameters related to clinical aspects of circumcision complication, their management and outcomes were studied.
Results: During the study period, 23 cases of circumcision complications were reported. The average age of patients with circumcision complications was 8.3 years ± 3.5 years, with ages ranging from 18 months to 65 years old. Circumcision was performed by nurses in 12 cases and traditional practitioners in 11 cases. Observed complications included post-circumcision bleeding and hematoma (n = 8), leading to surgical exploration and hemostasis; total or partial amputation of the glans (n = 4), requiring regularization and meatoplasty; infectious complications (n = 3), managed with combined resuscitation, antibiotic administration, and penile debridement; penile urethra-cutaneous fistulas (n = 2), which were repaired; and stenosis of the external urethral meatus (n = 2), treated by meatoplasty. No deaths were reported.
Conclusions: Circumcision complications presented various clinical manifestations, including hemorrhagic complications, glans amputation, infection, penile fistulas, and meatal stenosis. These complications were effectively managed from a functional perspective; however, aesthetic issues may persist. Emphasis should be placed on preventing these complications by ensuring circumcisions are performed by appropriately trained medical professionals.
KEYWORDS: Circumcision; Complications; Hemorrhage; Amputation; Prevention.
Submitted 30 May 2023; Accepted 18 June 2023
INTRODUCTION
Circumcision involves the partial or complete removal of the foreskin. It is not only a religious requirement for Israelites, a custom for Muslims, and a rite of passage into adulthood for many Africans, but also a common surgical procedure used to treat various balanopreputial diseases
(1). In Africa, circumcisions are often not carried out in hospital settings and are typically performed by lesstrained nurses and traditional practitioners. Circumcision complications can range from minor to major, impacting patients' vital or functional prognosis. This study aimed to review clinical presentations and evaluate the management and outcomes of circumcision at Souro Sanou University Teaching Hospital in Burkina Faso
PATIENTSANDMETHODS
This retrospective descriptive study examined all circumcision complications collected between January 1, 2014 and December 31, 2018, at the Urology Division in Souro Sanou University Hospital. All patients admitted to the Urology Division with circumcision complications were included. Variables considered included age, reason for visit, reason for circumcision, place of residence, admission delay, qualification of the practitioner who performed the circumcision, clinical presentation upon admission, medication, surgical revision technique, voiding quality, and aesthetic appearance of the penis for each subject included in this study. All patients or their parents or legal guardian when they are minor consent for the publication of chosen images to illustrate our clinical presentation. The study obtain the approval of the local ethical committee of the department of surgery of Souro Sanou University Hospital registered under the number N°007/2018.
RESULTS
We documented a total of 23 circumcision complications, averaging 4.6 cases per year. The patients' mean age was 8.33 years ± 3.5 years, with a range spanning from 18 months to 65 years. Among the 23 patients, 22 underwent circumcision without medical indication, while one case involved circumcision for medical reasons due to phimosis. We identified three cases of hemophilia and one case of HIV infection.
Most patients (60.87%) lived in rural areas and worked in agriculture, compared to 39.13% who resided in urban areas. Nurses performed 52% of the circumcisions, while
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11494 1
ORIGINALPAPER
Clinical presentation, management, and
Adama Ouattara 1, Abdoul-Karim Paré 1, Delphine Yé 1, Ali Sherazi 2, Mohamed Simporé 1 , Mickael Rouamba 1, Aristide F. Kaboré 3, Timothée Kambou 1
1 Urology Division, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso;
2 Department of Medicine, Dalhousie Medicine New Brunswick, Saint John, New Brunswick, Canada;
DOI: 10.4081/aiua.2023.11494
3 Urology Division, Yalgado Ouedraogo University Teaching Hospital, Ouagadougou, Burkina Faso.
traditional practitioners conducted 48% The average consultation delay was 12 ± 8 5 hours, with a range between 2 hours and 15 days According to patients or their relatives, all circumcisions took place without anesthesia However, we could not determine if the general rules of asepsis were adhered to when nurses performed the circumcision
Consultation reasons included urine leakage through a urethrocutaneous fistula for two patients (n = 2), local hemorrhage with blood loss for patients with partial or complete glandular section or hematoma (n = 8), dysuria with urine retention for patients with external urethral stenosis or incomplete circumcision, and local signs of suppuration for patients Table 1 lists the main consultation reasons that prompted patients to seek emergency care
Nurses employed the classic guillotine method for foreskin removal, a technique commonly used by various professionals This method involves removing the fore-

skin by placing forceps over the glans and cutting it flat
Techniques performed by traditional practitioners are not described
The study reported various types of complications, including hemorrhages (n = 8), penile amputations (n = 4), incomplete circumcisions (n = 3), external urethral stenosis (n = 3), urethrocutaneous fistulas (n = 2), and infections (n = 3) These complications are detailed in Table 2

Figures 1 through 7 illustrate the different complications observed in this study All patients admitted due to complications underwent both medical and surgical management This comprehensive approach included medical resuscitation, antibiotic administration, tetanus prevention and serotherapy, as well as surgical treatments tailored to the specific complication
Among patients with bleeding complications (n = 8), seven required an isogroup isorhesus blood transfusion to address anemia with signs of hypovolemic shock and hemoglobin levels below 7 g/dL Additionally, three patients (n = 3) with hemorrhagic complications related to hemophilia necessitated collaborative management with hematologists The various surgical management methods for circumcision complications are outlined in Table 3
external genitalia

Archivio Italiano di Urologia e Andrologia 2023; 95(3):11494 A Ouattara, A -K Paré, D Yé, et al 2
Reasons of consultation Frequency (n) Percentage (%) Local bleeding 10 26 08 Amputation of glans 4 17 39 Dysuria 3 13 04 Urinary leakage from fistula 3 13 04 Tumefaction of the penis 3 13 04 Local infection 2 8 69 Acute urinary retention 2 8 69
Table 1.
Main reasons of consultation.
Figure 1.
Total amputation of the glans
Figure 2
Post-circumcision infection
Circumcision complications reported Type of complication Frequency (n) Percentage (%) Post-circumcision bleeding 6 26 08 Total amputation of the glans 3 13 04 Incomplete circumcision 3 13 04 External urethral stenosis 3 13 04 Urethro-cutaneous fistula 2 8.69 Gangrene of external genitalia 2 8 69 Post-circumcision hematoma 2 8 69 Necrosis of the glans 1 4 34 Partial amputation of the glans 1 4 34 Total 23 100
Figure 3. Gangrene of
Table 2
of
Type of surger y Frequency (n) Percentage (%) Revision of circumcision with hemostasis 6 26 08 Regularisation of the glans stump 4 13 04 Revision of circumcision/posthectomy 3 13 04 Meatoplasty 3 13 04 Cure of penile fistula 2 8 69 Gangrene of external genitalia 2 8 69 Evacuation of penile hematoma 2 8 69 Glanduloplasty 1 4 34 Total 23 100
Table 3.
Distribution
patients by type of surgery
In general, the management of circumcision complications led to delayed healing for the three patients (n = 3) experiencing infectious complications The four patients (n = 4) who underwent glans amputations exhibited functional sequelae and an unaesthetic appearance of the glans, although they maintained good voiding quality



Psychological trauma was not assessed in this study, and no deaths were reported Figure 8 and Figure 9 provide an example of re-circumcision following an incomplete procedure and the final appearance after the procedure's revision
DISCUSSION

In 1997, Bankolé et al (1) reported 22 cases of traditional circumcision and excision sequelae in Abidjan Sylla et al (2) documented 63 cases of circumcision complications in Dakar in 2003, while Dieth et al. (3) recorded 35 cases of circumcision accidents in Abidjan in 2008 Kimassoum et al (4) reported 28 cases of circumcision complications in Chad in 2016 In the West, Gross et al (5) studied ritual circumcision complications in Paris in 1986


Many authors argue that circumcision reduces the risk of urinary tract infections in children, helps prevent penile cancer in adults, and plays a significant role in preventing sexually transmitted infections, including HIV (6, 7, 9, 11) In Muslim and Jewish communities, circumcision is practiced as a religious rite, while in others (particularly traditional ones), it is performed for sociocultural or initiation reasons, with fewer than 10% having a medical indication (6, 7, 3, 9)
In our series, the mean age of patients was 8 33 years, with a range between 1 month and 65 years Sylla et al (2) reported a mean age of 10 5 ± 6 7 years in their Dakar
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11494 3 Complications of non-medical
in
management, and outcomes
assisted circumcision
Burkina Faso Clinical presentation,
Figure 4 Huge penile hematoma extended to perineum
Figure 5. Incomplete circumcision
Figure 6. Urethro-cutaneous fistula with glans penis buria
Figure 7. Incomplete circumcision with phimosis
Figure 8 Revision of circumcision
Figure 9 Final appearance of glans after revision
series, while Gross et al (5) in Paris published a mean age of under 16 months This age variability can be attributed to the fact that in African countries, the age at which circumcision is performed depends on the sociocultural and ritual practices of the populations In our work environment, circumcision is practiced in early childhood and represents a sacred act that confirms a child's male identity and anticipates flawless sexuality in adulthood
However, with the increasing influence of Muslim culture, neonatal circumcision is becoming more popular
In our study, only complications requiring surgical management were referred to hospitals This was the case for the 23 circumcision complications we collected over five years In Côte d'Ivoire, Dieth et al (3) reported 35 circumcision complications over 14 years, while in Senegal, Sylla et al (2) had already reported 63 complications over 11 years Numerous factors contribute to these complications, and they largely depend on the operator
In our cases, 47 82% of patients were circumcised by traditional practitioners This can be attributed to the influence of tradition, poverty, insufficient and inaccessible healthcare structures, and low education levels
Circumcision is primarily a surgical procedure performed by a doctor, requiring knowledge of contraindications, adherence to rigorous asepsis during the procedure, understanding of anatomy, and expertise in circumcision techniques Failing to meet these requirements can result in complications and does not guarantee safety in terms of infectious risks and iatrogenic injuries In our study, 52 17% of patients had their circumcision performed by a nurse This highlights the need for improved training, especially since studies (11) have shown that the prevalence of circumcision complications increases when the procedure is performed by untrained individuals
In Burkina Faso and many other sub-Saharan African countries, there is a shortage of urologists Considering these observations, it may be worthwhile to explore proposals from authors like Dieth et al (2) and Okeke et al (12), which suggest integrating circumcision into medical student curricula and training nurses to perform the procedure with minimal risk In Africa, nurses are often the only healthcare workers available in remote rural areas
The average consultation time in our department was 11 89 days Kimassoum et al (4) in Chad reported an average consultation time of 896 days This difference in average consultation time can be attributed to the higher representation of late complications in their series
In our series, hemorrhage was due to a hemostasis defect (n = 3) or a hemostasis disorder, specifically hemophilia (n = 3) Hemorrhage is a common complication in countries where ritual circumcision is performed by nurses or traditional practitioners and often leads to early consultation due to parental concern Three of our patients were hemophiliacs, emphasizing the importance of performing a coagulation test before any circumcision Glans amputation, one of the most horrifying aspects of circumcision accidents, occurred in 13 04% (n = 3) of our patients
Diabaté et al (10) in Senegal found similar results in 2016
In contrast, Kimassoum et al (4) in Chad reported a significant number of amputation cases in their series (n = 10) This reflects the incompetence of the practitioner and is sometimes a direct consequence of poor child
immobilization during foreskin removal, lack of general anesthesia, and inadequate knowledge of the procedure
In the cases we collected, patients were seen late (more than 12 hours after the accident), making reimplantation impossible due to microvascular anastomosis challenges and insufficient technical resources In our series, treatment consisted of a meatoplasty with satisfactory results in terms of urination but poor aesthetic outcomes, leading to an unfavorable social prognosis in a context where respecting the body's integrity is sacred We report one case of penile denudation in our study, with similar results found in the literature (4, 10) This injury occurs after excessive removal of penile skin due to exaggerated traction of the skin covering the glans Retraction of the proximal part leaves a completely exposed penile area Treatment involved debridement and a wet oily dressing for healing, although other authors opt for a skin graft Some studies rank infectious complications as the second most common issue after hemorrhage (2, 10) These complications result from inadequate asepsis and the presence of skin flora (8) Locally, at the circumcision wound site, they cause delayed healing Although rare, we observed two cases of necrotizing cellulitis of the external genitalia a n d p e r i n e u m Tre a t m e n t f o r t h e s e c a s e s re q u i re d debridement, resuscitation with antibiotic therapy, and local care Urethrocutaneous penile fistulas were the most frequent complication in Kimassoum et al (4) series; however, in our study, we only recorded two cases These fistulas are located in the balanopreputial groove where the urethra is more superficial, and adhesions increase its vulnerability Inadequate hemostasis of the frenulum artery can also lead to urethral injury and subsequent fistula formation Clinically, urine passes through the fistula during urination, negatively affecting body image The urethrocutaneous splitting technique with separate suturing of the two planes was most commonly used in our series, yielding good results
Stenosis of the external urethral meatus has a traumatic and/or infectious origin, with ligation of the frenulum artery implicated as well (8) The main symptom is dysuria, and rarely, urinary retention It occurs at varying times after the healing process A meatotomy is usually sufficient to remove the stenosis, but recurrences are frequent Unsightly, incomplete circumcision was noted in one of our patients Kimassoum et al (4) reported six cases in their series This issue highlights the importance of anatomical knowledge and mastery of the learning curve before performing circumcisions In our series, this patient underwent laborious adhesion lysis to expose the glans up to the balanopreputial groove before proceeding with the circumcision
CONCLUSIONS
Accidents resulting from ill-timed and imprudent circumcision practices can sometimes be serious enough that this surgical procedure should either be reserved for expert hands or, at the very least, supervised The challenge now lies in raising public awareness and providing appropriate training for everyone involved in circumcision practice, from medical students to doctors and even nurses, who remain the most widely distributed healthcare personnel in remote areas of the country
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11494 A Ouattara, A -K Paré, D Yé, et al 4
Complications of non-medical assisted circumcision in Burkina Faso Clinical presentation, management, and outcomes
REFERENCES
1 Bankole Sanni R, Coulibaly B, Nandiolo R, et al Sequelae of traditional circumcision and excision Med Afr Noire 1997; 44:239-41
2 Sylla C, Diao B, Diallo AB, et al Complications of circumcision About 63 cases Prog Urol 2003; 13:266-72
3 Dieth AG, Moh-Elloh N, Fiogbe M, et al Circumcision accidents in children in Abidjan, Ivory Coast Bull Soc Path Exo 2008; 101:314-5
4 K i m a s s o u m R , F r a n k l i n D S , A r y a Z AT, M i g n a g n a l K Epidemiological, anatomoclinical and therapeutic characteristics of circumcision complications Uro'Andro 2016; 1:218-224
5 Gross PH, Pages R, Bourdelat D Complications of ritual circumcision Chir Pediatr 1986; 27:224-5
6 Ceylan K, Burhan K, Yılmaz Y, et al Severe complications of circumcision: an analysis of 48 cases J Pediatr Urol 2007; 3:32-5
7 Chaim JB, Livne PM, Binyamini J, et al Complications of circumcision in Israel: a one-year multicentre survey Isr Med Assoc J 2005; 7:368-70
8 Krill AJ, Palmer LS, Palmer JS Complications of circumcision SciWorld J 2011; 11:2458-68
9 Moses S, Bailey RC, Ronald AR Male circumcision: assessment ofhealth benefits and risks Sex Transm Infect 1998; 74:368-73
10 Diabaté I, et al Management of complications of circumcision Sexologies 2017; 3:169-175
11 Muula AS, Prozesky HW, Mataya RH, Ikechebelu JI Prevalence of complications of male circumcision in Anglophone Africa: a systematic review BMC Urol 2007; 7:4
12 Okeke LI, Asinobi AA, Ikuerowo OS Epidemiology of complications of male circumcision in Ibadan, Nigeria BMC Urol 2006; 6:21
Correspondence
Adama Ouattara, MD (Corresponding Auhor) adamsouat1@hotmail com
Urologist, Associate Professor of Urology Division of Urology, Souro Sanou University Teaching Hospital BP: 676 Bobo-Dioulasso, Burkina Faso Abdoul-Karim Paré boupare@yahoo fr
Delphine Yé delphineye73@gmail com
Mohamed Simporé mohamedsimpore25@hotmail com
Mickael Rouamba rouambami@yahoo com
Timothée Kambou tkambou@hotmail com
Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso
Ali Sherazi, BMsc ali sherazi@dal ca
Department of Medicine, Dalhousie Medicine New Brunswick, Saint John, New Brunswick, Canada
Aristide F Kaboré
Urology Division, Yalgado Ouedraogo University Teaching Hospital, Ouagadougou kaborefamd@icloud com
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11494 5
Gianni Paulis 1 , Andrea Paulis 2
1 Peyronie’s Care Center, Department of Uro-Andrology, Castelfidardo Clinical Analysis Center, Rome, Italy;
2 Neurosystem Center for applied Psychology and Neuroscience, Janet Clinical Centre, Rome, Italy
Summary
Background: The aim of study was to evaluate the impact of plaque calcification on symptoms of patients with Peyronie’s disease (PD) and to evaluate mental health in PD patients with or without calcification. Methods: We performed a retrospective analysis of the clinical database of a single andrology clinic. We extracted 551 PD patients, and we sorted them into two groups: the first group included 201 PD patients with plaque calcification; the second group included 350 PD patients without plaque calcification The inclusion criteria for both groups were as follows: aged between 21 and 81 years; thorough and available data on clinical history; baseline levels of blood glucose, glycosylated hemoglobin, cholesterol, and triglycerides; photographic documentation of the penile curvature; dynamic penile eco-color Doppler ultrasound with plaque measurements and volume calculation; and completion of the generalized anxiety disorder 7 questionnaire, patient health questionnaire 9 (for depression), visual analog scale for penile pain measurements, and the International Index of Erectile Function (IIEF) questionnaire Results: Plaque calcification was present in 36.4% of cases. The presence of calcification affects the presence and severity of penile curvature Calcification is associated with the presence of hypertension In PD patients, the prevalence of significant anxiety and significant depression was 89 1% and 57 3%, respectively Calcification is associated with the presence of anxiety and depression but does not lead to an increase in their prevalence Conclusions: In PD patients, the calcification was present in more than one third of cases The size of the plaque calcification was < 15 mm in most cases Calcification influences the presence of the curve and influences its severity There was a prominent prevalence of anxiety and depression in PD patients.
KEY WORDS: Peyronie’s disease; Plaque calcification; Depression; Anxiety
Submitted 27 June 2023; Accepted 14 July 2023
INTRODUCTION
Peyronies’s disease (PD) is a chronic inflammatory disease that affects the tunica albuginea of the corpora cavernosa of the penis PD has a genetic origin; however, it requires the concomitance of some risk factors Among these are
penile trauma, diabetes mellitus, hypertension, congenital penile curvature, radical pelvic surgery, erectile dysfunction, obesity, smoking, hypertension, autoimmune diseases (rheumatoid arthritis, psoriatic arthritis, psoriasis), alcohol consumption, and dyslipidemia (1-11) The prevalence of PD ranges from 3 2 to 13 1% in Western countries (12-17) However, PD prevalence is influenced by the geographic location of patients; prevalence in the Asian region seems to be lower, with 5 0% in Japan and 0 6% in China (18, 19)
PD takes place in two phases, the first of which represents the active phase of the disease; the second phase represents the phase of stabilization In the first phase, which has a duration of about 12-18 months, inflammation causes an overproduction of collagen with the relative formation of a fibrotic plaque which causes penile deformation (curvature, shortening, dip, indentation, hourglass, etc ) (20-22)
The fibroblasts and myofibroblasts present in the disease area (plaque) can transform into osteoblasts with a relative production of calcified areas (22, 23) Vernet et al (2005) demonstrated that progenitor cells are present in the fibrotic plaque tissue of PD and in the normal tunica albuginea of the penis, which, in culture, can differentiate into other cell lines (23) During PD, the differentiation of these progenitor cells into osteoblasts and myofibroblasts is stimulated by the profibrotic cytokine transforming growth factor beta-1 (TGF-β1) This cell differentiation can also be activated during chronic inflammation, oxidative stress, and fibrosis, where TGF-β1 is upregulated (23) This cell differentiation into osteoblasts and the related plaque calcification in PD occurs in about 20-43% of cases (22-26) The stabilization phase represents the end of the progression of the disease; in this phase, there is no more penile pain and penile deformation has ceased to progress The diagnosis of plaque calcification necessarily requires a penile ultrasound or other imaging methods (MRI, CT) as the simple penile palpation is not able to recognize the calcification for sure (27-32)
The aim of our study is to evaluate the impact of plaque calcification on the clinical symptoms of patients with PD
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11549 1
ORIGINAL PAPER
Calcification in Peyronie's disease: Its role and clinical influence on the various symptoms and signs of the disease, including psychological impact. Our study of 551 patients
DOI: 10 4081/aiua 2023 11549
MATERIALS AND METHODS
Study design
We performed a retrospective analysis of the clinical database of a single andrology clinic From the database, we extracted 551 PD patients who were examined in our urology/andrology clinic between January 2013 and April 2023 We divided all PD patients into two groups: the fi r s t g r o u p i n c l u d e d 2 0 1 p a t i e n t s d i a g n o s e d w i t h Peyronie's disease (PD) and with plaque calcification; the second group included 350 PD patients without plaque calcification All data were obtained from the available patient records The diagnosis of penile calcification was made in all cases with a penile ultrasound examination performed by the same andrologist operator with a highresolution ultrasound device, Philips HD 15 until the year of 2018, and thereafter with Philips Affinity 70 G (Philips, Washington, United States) The diagnosis of penile calcification was made when the hyperechoic area presented characteristic acoustic shadowing (33)
This retrospective observational study was conducted in c o m p l i a n c e w i t h t h e p r i n c i p l e s c o n t a i n e d i n t h e
Declaration of Helsinki: all study subjects were contacted to provide their informed consent to participate in the study Sensitive data were anonymized to respect privacy according to Legislative Decree, 10 August 2018, n 101, adapted to the GDPR (Official Gazette of the Italian Republic, General Series n 205, dated 04-09-2018)
Inclusion criteria
The inclusion criteria for both groups were as follows: aged between 21 and 81 years and available data of thorough clinical history examination (comprising all diseases) and the availability of the following blood tests: baseline blood glucose, glycosylated hemoglobin, cholesterol, and triglycerides
The diagnosis of Peyronie's disease was made as follows: performing penile palpation for all PD patients and availability of a (i) photographic documentation of the penile deformation (according to Kelâmi) with a goniometric measurement of the angulation and evaluation of the possible presence of the multiplanarity of the curvature (34) and a (ii) dynamic penile eco-color Doppler ultrasound with plaque measurements and volume calculation (mm3, in three dimensions in mm) using an ellipsoid formula (volume = 0 524 x width x length x thickness) (35, 36)
Exclusion criteria
The exclusion criteria were as follows:
For both groups, PD patients and non-PD patients aged under 21 years or over 81 years;
All patients who had not undergone the tests listed above
Clinical data
All clinical data (including the presence of concomitant diseases) were obtained from the clinical records of the 551 PD patients In the clinical records of the 551 PD patients, the results of the following blood tests were searched: baseline blood glucose, glycosylated hemoglobin (hemoglobin A1c), cholesterolemia, and triglyceridemia All PD patients were asked to complete the following questionnaires: visu-
al analog scale (VAS) questionnaire for pain measurement (37, 38); International Index of Erectile Function (IIEF) for erectile function measurement (39); and two validated psychometric tests: the generalized anxiety disorder 7 questionnaire (GAD-7, concerning anxiety) and the patient health questionnaire 9 (PHQ-9, concerning depression)
(40, 41) The VAS questionnaire consists of a 10 cm line drawn on paper, and each 1 cm point corresponds to a degree of pain intensity; the patient indicates their perceived pain point on this line Scores range from 0 (no pain) to 10 (most intolerable pain) (37) We considered the following interpretation VAS: 1-5, mild/moderate pain; 67, severe pain; and 8-10, very severe pain (38)
The IIEF erectile function questionnaire (for measuring possible erectile dysfunction) consists of 15 questions with 5 answers, and the final score varies from a minimum of 0 to 30 The interpretation of the score is: severe ED, from 0 to 10; moderate ED, 11 to 16; mild to moderate ED, 17 to 21; mild ED, 22 to 25; and no erectile dysfunction, 26 to 30 (39) We considered ED as present when the score was < 26
The GAD-7 anxiety questionnaire consists of seven questions with four answers, and the final score ranges from 0 to 21 We interpreted this score as follows: least anxiety, 0-4; mild anxiety, 5-9; moderate anxiety, 10-14; and severe anxiety, 15-21 (40) In this study, we considered the presence of "significant" anxiety when the GAD-7 score was > 9
The PHQ-9 questionnaire (patient health questionnaire 9) includes 9 questions with 4 answers, and the final score ranges from 0 to 27 We interpreted this score as follows: minimal depression, 0-4; mild depression, 5-9; moderate depression, 10-14; moderately severe depression, 15-19; and severe depression, 20-27 (41) We considered the presence of "significant" depression when the PHQ-9 score was > 9 (moderate to severe depression) In accordance with the classification of Levine et al (24), the size of the calcification (measured in mm) was stratified into three groups according to the maximum size of the calcified zone: grade 1= punctiform or ≤ 3 mm; grade 2= > 3 mm and < 15 mm; and grade 3 = ≥ 15 mm or ≥ 2 plaques > 10 mm
Study endpoints
The primary endpoints of the study were the impact of calcification in PD patients on presence and severity of penile curvature, penile curve multiplanarity, presence and severity of ED, presence and severity of penile pain, presence and severity of anxiety, and presence and severity of depression
The secondary endpoints of the study were the impact on the presence of calcification of diabetes mellitus, hypertension (high blood pressure), dyslipidemia (hypercholesterolemia and/or hypertriglyceridemia), cardiovascular diseases, and obesity and the prevalence of anxiety an depression in Peyronie’s disease patients
Statistical analysis
We used MedCalc statistical software (Version 16 4 3, 2016) for the following statistical studies: Chi-square two tailed test, relative risk (RR) test, odds ratio (OR) test, and two-tailed t-test For the statistical study of logistic regres-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11549 G Paulis, A Paulis 2
–
–
sion, we used AgriMetSoft's software (2019) For the statistical study of the Mann-Whitney-Wilcoxon test, we used Statistics Kingdom software (2017) For the statistical study of standard deviation, median, and interquartile range calculation (IQR), we used CalculatorSoup® software (2006-2023)
The impact of calcification on penile curvature severity in PD patients was investigated via a relative risk (RR) test after stratification of PD patients with calcification into two groups (Group A, ≤ 45 degrees; Group B, > 45 degrees)
The impact of multiple calcifications on the multiplanarity of the penile curvature (when present) in PD patients was investigated using the odds ratio (OR) test
The effect of calcification on the presence of ED in PD patients was investigated by comparing the median IIEF scores of patients with and without calcification To calculate this comparison, we employed the two-tailed MannWhitney-Wilcoxon test as well as the calculation of the median IIEF scores and the interquartile range (IQR) Furthermore, to investigate the impact of calcification on ED presence in PD patients, we employed a logistic regression study
The impact of calcification on penile pain in PD patients, was investigated by comparing the median VAS scores of patients with and without calcification To calculate this comparison, we employed the two-tailed Mann-WhitneyWilcoxon test as well as the calculation of the median VAS scores and the IQR
Furthermore, to investigate the impact of calcification on penile pain in PD patients, we employed a logistic regression study
The impact of calcification on the presence of anxiety in PD patients was investigated by comparing the mean and standard deviation (SD) of the GAD-7 scores (of significantly anxious patients both with and without a calcification) To calculate this comparison using the GAD-7 scores, we used the two-tailed Mann-Whitney-Wilcoxon test as well as the calculation of the median scores and the IQR Furthermore, to investigate the impact of calcification on anxiety in PD patients, we employed a logistic regression study
The impact of calcification on the presence of depression in PD patients was investigated by comparing the mean and SD of the scores (PHQ-9) of significantly depressed patients with and without a calcification To calculate this comparison using the PHQ-9 scores, we employed the two-tailed Mann-Whitney-Wilcoxon test as well as the calculation of the median scores and IQR
Furthermore, to investigate the impact of calcification on depression in PD patients, we employed a logistic regression study
The influence of diabetes mellitus, hypertension, hypercholesterolemia, cardiovascular diseases, and obesity on the presence of calcification in PD patients was investigated using the OR test
In all statistical analyses, a 5% threshold for an alpha error was used to define statistical significance (significant p-value < 0 05)
RESULTS
In total, 551 patients with PD met the inclusion criteria for this study The mean age was 49 55 years ± 12 17 years, range 21-81 We found that in the 551 patients
affected by Peyronie's disease, calcification was present in 36 4% of cases (201 cases) After dividing all PD patients into two groups according to the presence of plaque calcification, the first group included 201 PD patients with plaque calcification (mean age 49 57 years ± 12 19 years, range 21-81) and the second group included 350 patients diagnosed as PD patients without plaque calcification (mean age 49 54 years ± 12 18 years, range 21-73)
In 107 cases, the penile calcifications were multiple (53 2% out of 201 cases, and 19 4% of all PD patients) Having stratified the calcifications of 201 PD patients according to the classification proposed by Levine et al (23), we found the following results: grade 1 calcifications, 23 cases (11 4%); grade 2 calcifications, 130 cases (64 6%); and grade 3 calcifications, 48 cases (23 8%) The plaque calcification was < 15 mm (grade 1 and grade 2) in 76 1% of cases
Out of a total of 551 PD patients, 499 had penile curvature (90 05% of cases), and the bend angle ranged from 5 to 100 degrees (mean 35 6 degrees ± 17 67) In the 201 PD patients with plaque calcification (group 1) the angle of curvature ranged from 5 to 100 degrees (mean 38 37 degrees ± 17 72); in the 350 patients with PD and without plaque calcification (group 2) the angle of curvature ranged from 5 to 100 degrees (mean 34 09 degrees ± 17 48)
Out of a total of 551 PD patients, 169 cases had a complex curve (multiplanarity) (30 67%), 217 erectile dysfunction (39 38% of cases), 296 penile pain (53 72% of cases), 491 significant anxiety (89 1% of cases), 317 significant depression (57 3% of cases), 32 diabetes mellitus (5 8% of cases), 103 hypertension (18 69% of cases), 56 dyslipidemia (10 16% of cases), 41 cardiovascular diseases (7 44%), and 31 were obese (5 6%)
The clinical characteristics of the 551 PD patients, as a whole and divided by group 1 and group 2 are shown in Table 1
The impact of plaque calcification on the presence and severity of penile curvature in PD patients
The mean penile curvature degree of group 1 and group 2 were significantly dufferent (p = 0 009) (Table 1)
Using the two-tailed Mann-Whitney-Wilcoxon test, the medians of penile angulation degrees in patients with or without calcification were statistically different (with calcification = 39, IQR = 15; no calcification = 30, IQR = 25, p = 0 004) (p < 0 05)
Using the logistic regression test and considering the penile angulation degrees of all PD patients with or without calcification, the results we obtained are as follows:
Odds ratio = 1 013, (95% CI, 1 003 to 1 024), deviance 643 5, and p-value = 0 009 (p < 0 05)
All statistical studies indicate that calcification has an influence on the presence and severity of penile curvature
The influence of calcification on penile curvature severity in PD
PD patients with calcification were stratified into two groups (Group A, ≤ 45 degrees; Group B, > 45 degrees)
There were 161 patients with calcification with a curve ≤ 45 degrees (80 09%), 40 with a curve > 45 degrees (19 90%); 309 patients without calcification had a curve ≤ 45 degrees (88 28%), and there were 41 patients with a curve > 45 degrees (11 71%) The resulting relative risk
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11549 3 Calcification in Peyronie's disease
Table 1.
Clinical characteristics and results of the 551 PD patients, and the two subdivided groups (PD patients with and without calcifications)
= standard deviat on
* S gn ficant anx ety s present when Genera ized Anx ety Disorder-7 (GAD-7) questionnaire score > 9 Severe anx ety is present when GAD-7 score ≥ 15 (40)
** Sign f cant depress on is present when Pat ent Hea th Questionnaire-9 (PHQ-9) quest onnaire score > 9 Severe depression is present when PHQ-9 score ≥ 20 (41)
*** A though the P-value was found to be s gn ficant, this must be interpreted in favor of cases w thout calcification; in fact, n the 201 cases with calcif cat on, dys ip demia was present in 11 cases (5 47% of cases), wh le n the 350 cases w thout calcification, dys ipidem a was present in 45 cases (12 8% of cases)
of calcification on penile curvature severity was 0 22 (95% CI, 0 17 to 0 29, p < 0 0001) The Z statistic was 10 4 (p < 0 0001) It was found that calcification has an influence on penile curvature severity
The impact of multiple calcifications on the multiplanarity of penile curvature in PD patients There were 35 patients with multiple calcifications and multiplanarity of the curve, and 72 without multiplanarity; there were 134 patients without multiple calcifications and with multiplanarity of the curve, and there were 310 without multiplanarity
The resulting odds ratio (OR) was 1 12 (95% CI, 0 71 to 1 76, p = 0 610) The Z-statistic was 0 509 (p > 0 05) These results indicate that calcification has no impact on the multiplanarity of curvature
The impact of calcification on the presence of erectile dysfunction (ED) in PD patients
Using the two-tailed Mann-Whitney-Wilcoxon test the medians of the IIEF scores in patients with or without calcification were not statistically different (with calcification = 26, IQR = 2; no calcification = 26, IQR = 3, p = 0 1123) (p > 0 05)
Using the logistic regression test and considering the IIEF scores of all PD patients with or without calcification, odds ratio was 1 034, (95% CI, 0 971 to 1 102), deviance = 721 9, and p-value = 0 284 (p > 0 05)
We found no correlation between the presence of calcification and IIEF score
The impact of calcification on the presence of penile pain in PD patients
Using the two-tailed Mann-Whitney-Wilcoxon test the medians of the VAS scores in patients with or without calcification were not statistically different (with calcification = 1, IQR = 4; no calcification = 1, IQR = 4, p = 0 536) (p > 0 05) Using the logistic regression test and considering the VAS scores of all PD patients with or without calcification, odds ratio was 1 019, (95% CI, 0 952 to 1 091), deviance = 722 7, and p-value = 0 572 (p > 0 05)
We found no correlation between the presence of calcification and VAS score
The impact of calcification on the presence of anxiety in PD patients
Using the two-tailed Mann-Whitney-Wilcoxon test the medians of the GAD-7 scores in patients with or without calcification were not statistically different (with calcification = 14, IQR = 7; no calcification = 14, IQR = 7, p = 0 764) (p > 0 05)
Using the logistic regression test and considering the GAD-7 scores of all PD patients with or without calcification, odds ratio was 1 015 (95% CI, 0 976 to 1 056), deviance = 720 6, and p-value = 0 438 (p > 0 05)
We found no correlation between the presence of calcification and GAD-7 score
The impact of calcification
on the presence of depression in
PD patients
Using the two-tailed Mann-Whitney-Wilcoxon test the
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11549 G Paulis, A Paulis 4
All n 551 Group 1 Group 2 Statistical analysis PD patients n. 201 PD patients n. 350 PD patients Group-1 ver sus Group-2 with calcified plaque without calcified plaque P-value (t-test) Mean age (SD) 49 55 years 49 57 years 49 54 years 0 977 (± 12 17) (± 12 19) (± 12 18) Means of the degrees of penile curvature (SD) 35 6 degrees 38 37 degrees 34 09 degrees 0 009 (± 17.67) (± 17.72) (± 17.48) Variable All n. 551 Group 1 Group 2 P-value (𝝌2-test) PD patients n 201 PD patients n 350 PD patients with calcified plaque without calcified plaque n. cases (%) n. cases (%) Plaque calcification 201 (36 4) 201 (100 0) 0 (0) / Penile curvature 499 (90 05) 178 (88 5) 321 (91 7) 0 285 Curvature multiplanarity 169 (30 67) 69 (34 3) 132 (37 7) 0 482 Erectile dysfunction (ED) 217 (39 38) 77 (38 3) 140 (40 0) 0 763 Penile pain 296 (53 7) 113 (56 2) 183 (52 2) 0 422 Significant anxiety * 491 (89 1) 183 (91 04) 308 (88 0) 0 335 Severe anxiety * 216 (39 2) 82 (40 79) 134 (38 28) 0 623 Significant depression ** 317 (57 3) 125 (62 18) 192 (54 8) 0 112 Severe depression ** 25 (4 5) 7 (3 48) 18 (5 1) 0 491 Diabetes mellitus 32 (5 8) 11 (5 4) 21 (6 0) 0 947 Hypertension 103 (18 69) 47 (23 38) 56 (16 0) 0 042 Dyslipidemia 56 (10 16) 11 (5 4) 45 (12 8) 0 008 *** Cardio-vascular diseases 41 (7 4) 13 (6 4) 28 (8 0) 0 623 Obesity 31 (5 6) 14 (6 9) 17 (4 8) 0 400 SD
Table 2
Results for primary and secondary endpoints of the study
The resu ts regarding the preva ence of anxiety and depress on in PD patients (secondary endpo nts) are shown n Table 1
* Although the P-va ue was found to be signif cant, this must be nterpreted in favor of cases without ca c fication; n fact, in the 201 cases with calcification, dyslipidem a was present in
medians of the PHQ-9 scores in patients with or without calcification were not statistically different (with calcification = 12, IQR = 7; no calcification= 10, IQR = 8, p = 0 308) (p > 0 05) Furthermore, using the logistic regression test and considering the PHQ-9 scores of all PD patients with or without calcification, odds ratio was 1 015, (95% CI, 0 979 to 1 052), deviance = 719 4, and pvalue = 0 404 (p > 0 05)
We found no correlation between the presence of calcification and PHQ-9 score
ca
fication, dysl p demia was present n 45 cases (12 8% of cases)
eases (7 44%) The resulting OR was 0 79 (95% CI, 0 402 to 1 572, p = 0 510) and Z-statistic was 0 659 (p > 0 05)
These results indicate that cardiovascular diseases have no impact on calcification
In our study 31 PD patients were obese (5 6%) The resulting OR was 1 46 (95% CI, 0 706 to 3 042, p = 0 303) and Z-statistic was 1 028 (p > 0 05) These results indicate that obesity has no impact on calcification
The impact of PD on anxiety and depression
Anxiety
Diabetes,
hypertension, dyslipidemia, cardiovascular disease, obesity in PD patients with plaque calcification
In our study 32 PD patients had diabetes mellitus (5 8%); 26 were affected by type-2 diabetes; and 6 were affected by type-1 diabetes The resulting OR was 0 90 (95% CI, 0 428 to 1 922, p = 0 799) and Z-statistic was 0 255 (p > 0 05) After separately studying the impact of type-1 and type-2 diabetes on the presence of calcification, the result of the pvalue was always > 0 05 (0 494 and 0 536, respectively)
These results indicate that diabetes mellitus has no impact on calcification
Among the 551 PD patients, 103 had hypertension (18 69%) In the 201 cases with calcification, hypertension was present in 47 cases (23 38% of cases), while in the 350 cases without calcification, hypertension was present in 56 cases (16 0% of cases) The resulting OR was 1 6 (95% CI, 1 038 to 2 473, p = 0 03) and the Z-statistic was 2 129 (p < 0 05) These results indicate that calcification is associated with the presence of hypertension
In our study 56 PD patients had dyslipidemia (high cholesterol and/or hypertriglyceridemia) (10 16%)
The resulting OR was 0 39 (95% CI, 0 191 to 0 777, p = 0 007) and Z-statistic was 2 68 (p < 0 05) P-value was significant, but odds was lower in cases with calcification; in fact, in the 201 cases with calcification, dyslipidemia was present in 11 cases (5 47% of cases), while in the 350 cases without calcification, dyslipidemia was present in 45 cases (12 8% of cases)
These results indicate that dyslipidemia has no positive impact on calcification
Among the 551 PD patients, 41 had cardiovascular dis-
• 4 out of 551 patients (0 7%) had minimal anxiety (GAD-7 scores ranging from 0 to 4)
• 54 out of 551 patients (9 8%) had mild anxiety (GAD7 scores ranging from 5 to 9)
• 275 out of 551 patients (49 9%) had moderate anxiety (GAD-7 scores ranging from 10 to 14)
• 216 out of 551 patients (39 2%) had severe anxiety (GAD-7 scores ranging from 15 to 21)
The prevalence of “significant anxiety” was 89 1% (491 out of 551 patients) (40)
Depression
• 63 out of 551 patients (11 4%) had minimal depression (PHQ-9 scores ranging from 0 to 4)
• 171 out of 551 patients (31 0%) had mild depression (PHQ-9 scores ranging from 5 to 9)
• 201 out of 551 patients (36 4%) had moderate depression (PHQ-9 scores ranging from 10 to 14)
• 91 out of 551 patients (16 5%) had moderately severe depression (PHQ-9 scores ranging from 15 to 19)
• 25 out of 551 patients (4 5%) had severe depression (PHQ-9 scores ranging from 20 to 27)
The prevalence of “significant depression” was 57 3% (317 out of 551 patients) (41)
The prevalence of severe anxiety and severe depression in PD patients with or without plaque calcification are shown in Table 1
Results for the primary and secondary endpoints of the study are shown in Table 2
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11549 5 Calcification in Peyronie's disease
PRIMARY ENDPOINTS IMPACT Statistical analysis Yes or No P-value The impact of plaque calcification on the presence and severity of penile curvature Yes < 0 05 presence and severity of erectile dysfunction No > 0 05 presence and severity of penile pain No > 0 05 presence and severity of anxiety No > 0 05 presence and severity of depression No > 0 05 The impact of multiple calcifications on penile curvature multiplanarity No > 0 05 SECONDARY ENDPOINTS The impact of diabetes mellitus on the presence of calcification No > 0 05 The impact of hypertension on the presence of calcification Yes < 0 05 The impact of dyslipidemia on the presence of calcification No < 0 05 * The impact of cardio-vascular diseases on the presence of calcification No > 0 05 The impact of obesity
of calcification No > 0 05
on the presence
11
(5 47% of
e in the 350 cases
cases
cases), whi
without
c
DISCUSSION
In our study, in 551 patients affected by Peyronie's disease, plaque calcification was present in 36 4% of cases Our results do not differ much from the percentage detected by Levine et al (34 1%) (24) Unfortunately, the literature lacks studies focusing on the prevalence of calcification in Peyronie's disease
Two other classifications of penile calcifications in PD patients have been proposed The classification proposed by Bekos et al categorizes patients according to the severity of calcification and echogenicity This classification divides patients into three groups: A, B, and C Group A: a solitary hyperechoic zone without acoustic shadow; group B: multiple scattered moderately hyperechoic calcifications with acoustic shadow; and group C: densely calcified hyperechoic plaques with acoustic shadow (42) Pawlowska and Bianek-Bodzak proposed the following classification of PD plaques: type 1 = thickening of the tunica albuginea without acoustic shadow; type 2 = moderately calcified plaque with a typical acoustic shadow; and type 3 = severely calcified plaques with complete shadowing (43)
However, we believe that the classification proposed by Levine et al is more precise because it mainly considers the size of the calcifications Having stratified the calcifications of 201 PD patients according to the classification proposed by Levine et al (24), we found the following results: grade 1 calcifications, 23 cases (11 4%); grade 2 calcifications, 130 cases (64 6%); and grade 3 calcifications, 48 cases (23 8%) The calcification was < 15 mm (grade 1 and grade 2) in 76 1% of cases
Our results differ markedly from those reported in Levine's study that reported grade 1 calcifications in 40 8%, grade 2 calcifications in 27 6%, and grade 3 calcifications in 31 6% We believe that the difference in the results of the two studies is due to the numerical difference in the two samples (201 versus 98 cases of Levine’s study) (24) However, when examining the two studies, we noticed that grade 3 calcifications are less frequent (our study 23 8%; Levine’s study 31 6%) than the total sum of grade 1 and grade 2 calcifications
In our study, it was found that calcification has an influence on the presence and severity of penile curvature (p < 0 05); this correlation is also present in the study conducted by Levine et al (24)
Our study found that the presence of calcifications in PD patients has no influence on the presence of erectile dysfunction and its severity, penile pain and its severity, and anxiety and depression and their severity Our study also found that the presence of multiple calcifications in PD patients has no influence on the presence of multiplanarity of penile curvature
In Levine's study, the correlation between plaque calcification and multiplanar penile curvature or erectile dysfunction was not investigated Also in Levine's study, no correlation was found between plaque calcification and penile pain (24), as well as no correlation was found between plaque calcification and emotional distress/anxiety (24)
Our study found that the presence of calcification in PD patients is not influenced by the presence of diabetes mellitus, dyslipidemia, cardiovascular diseases, and obesity
Our results differ from those of the study by Levine et al
where diabetes mellitus was found to influence the presence of plaque calcification (Levine study, p = 0 012 versus our study, p = 0 799) (24)
However, our study found that calcification in PD patients is associated with the presence of hypertension (p = 0 03); in contrast, in Levine’s study, hypertension did not appear to influence the presence of plaque calcification (p = 0 865) (24)
The prevalence of “significant anxiety” that we have found in PD patients (89 1% of cases) appears higher than the results of some studies which more generically refer to "distress" and "emotional" difficulties (80-81% of cases) (44, 45) In Levine's study, the presence of "emotional distress" was found in 83% of cases of PD patients (24)
In our study, we found the presence of "significant depression" in 57 3% of PD patients; this percentage is higher than that documented in Nelson's studies (48%) (46, 47)
It is most likely that the greater number of cases in our study (551 cases) compared to the 92 cases in Nelson's study caused the disparity in the two results
CONCLUSIONS
Our results indicate that in patients with Peyronie's disease, plaque calcification is present in more than 1/3 of cases (36 4% of cases); this does not differ much from the data in the literature We found that the size of the plaque calcification was < 15 mm in the majority of cases In our study, it was found that plaque calcification has an influence on the presence and severity of penile curvature We also found that calcification in PD patients is associated with the presence of hypertension
Our results indicate that anxiety and depression have an important prevalence in PD patients; moreover, we are especially alarmed by the high percentages of "severe" anxiety (39 2%)
We therefore believe that psychotherapy should be associated with the treatment of these patients in order to improve their quality of life and to avoid dropping out of ongoing medical therapies
REFERENCES
1 Bias WB, Nyberg Jr LM, Hochberg MC, et al Peyronie's disease: a newly recognized autosomal-dominant trait Am J Med Genet 1982; 12:227-235
2 Devine CJJ, Somers KD, Jordan GH, et al Proposal: trauma as the cause of the Peyronie's lesion J Urol 1997; 157:285-290
3 Jarow JP, Lowe FC Penile trauma: an etiologic factor in Peyronie's disease and erectile dysfunction J Urol 1997; 158:1388-1390
4 La Pera G, Pescatori ES, Calabrese M, et al SIMONA Study Group Peyronie's disease: prevalence and association with cigarette smoking A multicenter population-based study in men aged 50-69 years Eur Urol 2001; 40:525-530
5 El-Sakka AI Prevalence of Peyronie's disease among patients with erectile dysfunction Eur Urol 2006; 49:564-569
6 Bjekic MD, Vlajinac HD, Sipetic SB, et al Risk factors for Peyronie's disease: a case-control study BJU Int 2006; 97:570-574
7 Carrieri MP, Serraino D, Palmiotto F, et al A case-control study on risk factors for Peyronie's disease J Clin Epidemiol 1998; 51:511-515
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11549 G Paulis, A Paulis 6
8 Ventimiglia E, Capogrosso P, Colicchia M, et al Peyronie's disease and autoimmunity a real-life clinical study and comprehensive review J Sex Med 2015; 12:1062-1069
9 Tal R, Heck M, Teloken P, et al Peyronie's disease following radical prostatectomy: incidence and predictors J Sex Med 2010; 7:1254-1261
10 Paulis G, Paulis A, Perletti G Congenital penile curvature as a possible risk factor for the onset of Peyronie's disease, and psychological consequences of penile curvature Arch Ital Urol Androl 2023; 95:11238
11 Segundo A, Glina S Prevalence, Risk Factors, and Erectile Dysfunction Associated With Peyronie's Disease Among Men Seeking Urological Care Sex Med 2020; 8:230-236
12 Stuntz M, Perlaky A, des Vignes F, et al The Prevalence of Peyronie's Disease in the United States: A Population-Based Study PLoS One 2016; 11:e0150157
13 Bella AJ, Lee JC, Grober ED, et al 2018 Canadian Urological Association guideline for Peyronie's disease and congenital penile curvature Can Urol Assoc J 2018; 12:E197-E209
14 Johnson HM, Weerakoon P, Stricker PD The incidence, aetiology, and presentation of Peyronie’s disease in Sydney, Australia J Sex Disability 2002; 20:109-116
15 La Pera G, Pescatori ES, Calabrese M, et al Peyronie's disease: prevalence and association with cigarette smoking A multicenter population-based study in men aged 50-69 years Eur Urol 2001; 40:525-530
16 Schwarzer U, Sommer F, Klotz T, Braun M, Reifenrath B, Engelmann U The prevalence of Peyronie's disease: results of a large survey BJU Int 2001; 88:727-30
17 Rhoden EL, Teloken C, Ting HY, et al Prevalence of Peyronie's disease in men over 50-y-old from Southern Brazil Int J Impot Res 2001; 13:291-293
18 Shiraishi K, Shimabukuro T, Matsuyama H The prevalence of Peyronie's disease in Japan: a study in men undergoing maintenance hemodialysis and routine health checks J Sex Med 2012; 9:27162723
19 Wong A, Tsang SSl, O RYM, et al MP33-12 Prevalence of Peyronie,e disease and its psychosexual impact in the Chinese population: a large cohort population-based cross-sectional study J Urol 2020; 203(Supplement 4):e499-e499
20 Garaffa G, Trost LW, Serefoglu EC, et al Understanding the course of Peyronie's disease Int J Clin Pract 2013; 67:781-788
21 Levine LA, Larsen, S Diagnosis and Management of Peyronie Disease In: Campbell-Walsh Urology 11th Ed , Wein AJ, Kavoussi LR, Partin AW, Peters CA, Eds ; Elsevier Saunders: Philadelphia (PA), 2015 Volume 1 (Chapter 31); 722–748
22 Paulis G, De Giorgio G, Paulis L Role of Oxidative Stress in Peyronie's Disease: Biochemical Evidence and Experiences of Treatment with Antioxidants Int J Mol Sci 2022; 23:15969
23 Vernet D, Nolazco G, Cantini L, et al Evidence that osteogenic progenitor cells in the human tunica albuginea may originate from stem cells: implications for peyronie disease Biol Reprod 2005; 73:1199-1210
24 Levine L, Rybak J, Corder C, et al Peyronie's disease plaque calcification Prevalence, time to identification, and development of a new grading classification J Sex Med 2013; 10:3121-3128
25 Gelbard MK Dystrophic penile calcification in Peyronie's disease J Urol 1988; 139:738-740
26 Rainer QC, Rodriguez AA, Bajic P, et al Implications of Calcification in Peyronie's Disease, A Review of the Literature Urology 2021; 152:52-59
27 Andresen R, Wegner HEH, Miller K, et al Imaging modalities in Peyronie's disease - an intrapersonal comparison of ultrasound sonography, X- ray in mammography technique, computerized tomography, and nuclear magnetic resonance in 20 patients Eur Urol 1998; 34:128-134
28 Hauck EW, Hackstein N, Vosshenrich R, et al Diagnostic value of magnetic resonance imaging in Peyronie's disease a comparison both with palpation and ultrasound in the evaluation of plaque formation Eur Urol 2003; 43:293-299
29 Pawlowska E, Bianek-Bodzak A Imaging modalities and clinical assesment in men affected with Peyronie's disease Pol J Radiol 2011; 76:33-37
30 McCauley JF, Dean C Diagnostic utility of penile ultrasound in Peyronie’s disease World J Urol 2020; 38:263-268
31 Hatzimouratidis K, Eardley I, Giuliano F, et al EAU guidelines on penile curvature Eur Urol 2012; 62:543-552
32 Parmar M, Masterson JM, Masterson 3rd TA The role of imaging in the diagnosis and management of Peyronie's disease Curr Opin Urol 2020; 30:283-289
33 Chou YH, Tiu CM, Pan HB, et al High-resolution real-time ultrasound in Peyronie's disease J Ultrasound Med 1987; 6:67-70
34 Kelâmi A Autophotography in evaluation of functional penile disorders Urology 1983; 21:628-629
35 Eri LM, Thomassen H, Brennhovd B, Håheim LL Accuracy and repeatability of prostate volume measurements by transrectal ultrasound Prostate Cancer Prostatic Dis 2002; 5:273-278
36 Lee JS, Chung BH Transrectal ultrasound versus magnetic resonance imaging in the estimation of prostate volume as compared with radical prostatectomy specimens Urol Int 2007; 78:323-327
37 Kahl C, Cleland JA Visual analogue scale, numeric pain rating scale and the McGill pain Questionnaire: an overview of psychometric properties Phys Ther Rev 2005; 10:123-128
38 Cepeda MS, Africano JM, Polo R, et al What decline in pain intensity is meaningful to patients with acute pain? Pain 2003; 105:151-157
39 Rosen RC, Riley A, Wagner G, et al The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction Urology 1997; 49:822-830
40 Spitzer RL, Kroenke K, Williams JB, Löwe B A brief measure for assessing generalized anxiety disorder: the GAD-7 Arch Intern Med 2006; 166:1092-1097
41 Kroenke K, Spitzer RL, Williams JB The PHQ-9: validity of a brief depression severity measure J Gen Intern Med 2001; 16:606613
42 Bekos A, Arvaniti M, Hatzimouratidis K, et al The natural history of Peyronie's disease: an ultrasonography-based study Eur Urol 2008; 53:644-650
43 Pawłowska E, Bianek-Bodzak A Imaging modalities and clinical assesment in men affected with Peyronie's disease Pol J Radiol 2011; 76:33-37
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11549 7 Calcification in Peyronie's disease
44 Terrier JE, Nelson CJ Psychological aspects of Peyronie's disease Transl Androl Urol 2016; 5:290-295
45 Smith JF, Walsh TJ, Conti SL, et al Risk factors for emotional and relationship problems in Peyronie’s disease J Sex Med 2008; 5:2179-2184
46 Nelson CJ, Diblasio C, Kendirci M, et al The chronology of depression and distress in men with Peyronie's disease J Sex Med 2008; 5:1985-1990
47 Nelson CJ, Mulhall JP Psychological impact of Peyronie's disease: a review J Sex Med 2013; 10:653-660
Correspondence
Gianni Paulis, MD (Corresponding Author)
paulisg@libero it
Peyronie’s Care Center, Department of Uro-Andrology, Castelfidardo Clinical Analysis Center, Rome, Italy
Andrea Paulis
andrea fx 94@gmail com
Neurosystem Center for applied Psychology and Neuroscience, Janet Clinical Centre, Rome, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11549 G
8
Paulis, A Paulis
ORIGINALPAPER
Predictive factors for successful testicular biopsy
Urology and Renal Transplantation Department, Coimbra University Hospital Centre, Coimbra, Portugal;
Introduction: Infertility, the inability to conceive, constitutes a major problem in modern societies. It affects 10 to 15 percent of couples in the United States. Evaluation of infertile men is usually complex and often demands a testicular biopsy.
Materials and methods: We reviewed all azoospermic men submitted to testicular biopsy, in our center, during infertility investigation between January 2015 and December 2021.
Results: A total of 117 patients with a mean age of 36.5 was considered. Biopsy was positive, as defined by the presence of viable spermatozoids by microscopy, in 48.7% of patients (n = 57). Patients were divided in two separate groups based on positive (PB) or negative biopsy (NB) and compared. PB-group had normal serum total testosterone levels and higher than NB-group (3.7 ng/mL vs. 2.85 ng/mL, p = 0.021), and normal serum FSH levels and lower than NB-group (6.0 mIU/mL vs. 16.0 mIU/mL, p < 0.001). The groups were similar concerning serum LH levels (3.9 mIU/mL vs. 6.3 mIU/mL, p = 0.343.
Conclusions: Predicting outcomes of testicular biopsy is a difficult task. Our study found that men with normal testicular volume, normal levels of testosterone and FSH and those with type 1 diabetes mellitus had a higher probability of positive testicular biopsy.
KEYWORDS: Male infertility; Azoospermia; Testicular biopsy; Predictive factors.
Submitted 5 July 2023; Accepted 30 July 2023
INTRODUCTION
Infertility, the inability to conceive after one year of regular unprotected intercourse, constitutes a major problem in modern societies. It affects 10 to 15 percent of couples in the United States, with male component being the isolated cause in about 20% of cases and representing part of the aetiology in another 30% (1-3). Multiple factors contribute for male infertility, from anatomic obstruction and genetic alterations to hormonal disturbances, among many others. Evaluation of infertile men is usually complex and requires a careful clinical history, physical exam, semen analysis, hormonal profile and imaging and genetic testing (4).
Azoospermia, the complete absence of spermatozoa in the ejaculate, is present in 10-20% of all infertile men and can be classified as obstructive or non-obstructive (5). The evaluation of these men often demands a testicular biopsy, with associated morbidity. A non-invasive diagnostic technique predicting the presence of spermatozoa in the testis would be useful to avoid surgical intervention
in cases of absence of spermatozoa. This would decrease surgical risks, patient discomfort and likely the costs of infertility workup and treatment.
In men with non-obstructive azoospermia, spermatozoa may be found in testicular tissue, but their complete absence in testicular biopsy makes the couple unable to conceive (6, 7). Although several testicular biopsy techniques are described, the most currently used are testicular sperm aspiration (TESA), open testicular sperm extraction (TESE) and microscopic testicular sperm extraction with similar outcomes being reported (4, 6-8).
Previous studies correlated FSH levels with the rate of success in testicular biopsy but other factors remain to be established of important predictive value, as spermatozoa can still be found in patients with high FSH levels and patients with low volume testicles (7-9).
Besides, in cases of non-obstructive azoospermia, pregnancies are achieved in 30-50% of couples when spermatozoa are found after sperm harvesting (10).
Infertile couples usually go through a hard psychological pathway during pregnancy process and predictive factors for positive testicular biopsy may help identifying patients with higher probabilities of successful pregnancy and help to manage expectations (4, 7, 8).
Therefore, our aim was to identify possible predictive factors for a successful testicular biopsy in men with azoospermia after a diagnostic sperm analysis during infertility evaluation.
MATERIALANDMETHODS
Patient selection, surgical technique and variables definition
All man submitted to testicular biopsy during infertility investigation between January 2015 and December 2021 in Centro Hospitalar e Universitário de Coimbra, Portugal, were evaluated. A complete medical history and physical examination was performed. Testicular volume was evaluated and classified as normal or decreased by physical exam and further confirmed by testicular ultrasonography. Serum FSH, LH, total testosterone, free testosterone, and prolactin morning levels for endocrinologic evaluation were assessed and patients had at least two semen analysis confirming azoospermia, according to World Health Organization Guidelines (11). All patients were testicular biopsy naïve. Patients with microdelitions and cariotype alterations were excluded.
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11567 1
Duarte Vieira Brito, Manuel Lopes, Jose Pereira, Ana Maria Ferreira, Luis Sousa, Belmiro Parada, Arnaldo Figueiredo
DOI: 10.4081/aiua.2023.11567
Summary
Patients were submitted to testicular biopsy under local anaesthesia after spermatic cord blockage as an outpatient procedure A step-by-step approach is done in our institution, as forward described Percutaneous epididymal sperm aspiration (PESA) is performed as a first procedure in one testicle and then in the contralateral in the case of no spermatozoa retrieval) If no spermatozoa are obtained after PESA, open TESE is done A small scrotal incision is performed without exteriorization of the testicle and testicular parenchyma is excised from at least two different sites If no spermatozoa are identified the same approach is performed in the contralateral testicle
The extracted tissue is then preserved in sperm preparation substrate and samples are analysed by an experienced biologist Sperm retrieved by PESA or TESE was classified as of good quality (sperm concentration > 1/HPF; with mobility in situ > 10%; Progressive motility), medium quality (sperm concentration < 1/HPF; with mobility in situ < 10%) or bad quality (rare sperm or spermatid; without mobility) Biopsy was considered positive when sperm of good or medium quality sperm was obtained
When no sperm is found a sample is sent for histological confirmation and diagnosis
Statistical analysis
A demographic analysis of the entire cohort was performed Patients were divided into two groups for comparative analysis: patients who had a positive biopsy (PBgroup) and patients who had a negative biopsy (NBgroup) Pearson chi-square and Mann-Whitney tests were used to compare quantitative and categorical variables across groups Unconditional binary logistic regression was used to evaluate the independent association between possible predictors and detection of spermatozoa in the biopsy Statistical significance in this study was set as p< 0 05 Statistical analysis was performed using IBM SPSS®, version 27 0 for Windows
RESULTS
We had a total of 117 patients with a mean age of 36 5 ± 6 0 years Study sample features are described in Table 1
Concerning the main conditions that may affect testicular function 22 2% patients (n = 26) presented reduced testicular volume and 20 5% (n = 24) presented with left varicocele Twenty patients (17 1%) had previous history of inguinal or scrotal surgery: four had inguinal hernia correction, eight had radical orchiectomy, four had orchiopexy and four the excision of hydrocele or epididymal cysts Six patients (5%) had been previously treated with systemic chemotherapy Regarding metabolic factors, 32% of patients (n = 37) had overweight or obesity (body mass index > 25 kg/m2), 14 5% (n = 17) had type 1 diabetes mellitus and 36 8% (n = 43) were active smokers
Testicular biopsy was positive in 48 7% of patients (n = 57) and these form the PB-group The remaining 60 patients with negative biopsy constitute NB-group Groups were similar regarding demographic and clinical features, with no difference in age, history of smoking, presence of varicocele and history of inguinal and scrotal surgery (data not shown) On the other hand, the study groups were statistically different in testicular volume
Table 1. Patients characteristics
(p < 0 001) history of cryptorchidy (p = 0 047) and history of type 1 diabetes mellitus (p = 0 015) with normal testicular volume, no history of cryptorchidy and type 1 diabetes mellitus being predictive factors for successful testicular biopsy From the 24 patients with imaging diagnosis of varicocele only 8 had a clinical varicocele and these were the patients submitted to repair (varicocele embolization) From those who received varicocele correction, 7 patients (88%) had a positive testicular biopsy (p = 0 059) (Table 2)
In terms of endocrine evaluation (Table 3) PB-group had normal serum total testosterone levels and higher than NB-group (3 7 ng/mL vs. 2 85 ng/mL, p = 0 021), and normal serum FSH levels and lower than NB-group (6 0 mIU/mL vs 16 0 mIU/mL, p < 0 001) The groups were similar concerning serum LH levels (3 9 mIU/mL vs 6 3 mIU/mL, p = 0 343) and serum prolactin levels (1 5
Potential
Hormonal
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11567 D
2
Vieira Brito, M Lopes, J Pereira, A M Ferreira, L Sousa, B Parada, A Figueiredo
Variable Frequency (%) Decreased testicular volume 26 (22 2) Varicocele 24 (20 5) Cryptorchidism 4 (3 4) Previous systemic chemotherapy 6 (5 1) Type 1 diabetes mellitus 17 (14 5) Body mass index > 25 kg/m2 37 (31 6) Active smoker 43 (36 8) Inguinal or scrotal procedures 20 (17 1) Radical orchiectomy 8 Orchiopexy 4 Hydrocele or epididymal cyst correction 4 Inguinal hernioplasty 4 Positive testicular biopsy 57 (48.7)
Table 2.
Variable PB-group a NB-group a p value Testicular volume – normal 52 39 < 0 001 Cryptorchidism 04 0 047 Previous systemic chemotherapy 24 0 439 Type 1 diabetes mellitus 13 4 0 015 Body mass index > 25 kg/m2 21 16 0 237 Active smoker 19 24 0.455 Varicocele embolization 71 0 059 a frequency, in abso ute number PB: positive biopsy; NB: negat ve biopsy
predictive factors for positive testicular biopsy
Table 3.
Hormone PB-group NB-group p value Total testosterone (ng/mL) 3 7 2 85 0 021 FSH (mIU/mL) 6 0 16 0 < 0 001 LH (mIU/mL) 3 9 6 3 0 343 Prolactin (ng/mL) 1 5 1 2 0 274 FSH: fo l c e-st mu ating hormone; LH: luteiniz ng hormone
differences between positive biopsy (PB) and negative biopsy (NB) groups
ng/mL vs 1 2 ng/mL, p = 0 274) Normal FSH serum levels and normal total testosterone levels are predictive factors for positive testicular biopsy
DISCUSSION
Infertility diagnostic work-up and treatment is associated with elevated costs for health systems and has a major impact in individual well-being and couples relationship (2) The development and dissemination of new fertilisation techniques allowed men who were previously defined as infertile to father children, in great part due to testicular biopsy (12, 13) About half of all infertile patients has no identified cause for infertility and determining which men will benefit from a testicular biopsy is still controversial (5) Some of the predictive factors for a positive testicular biopsy shown in our analysis are already described in literature but are not strongly established Our cohort is similar to other populations in literature regarding age (minimum 24 years old and maximum 54 years old) and number of positive biopsies (14, 15) An interesting point we found is age: the oldest patient in our population is 54 years old but that was not necessarily associated with lower number of positive biopsies (data no shown) indicating the ability of men to preserve fertility even into older age (16)
A total of 8 patients had clinically evident varicocele and were submitted to endovascular embolization All these patients presented with azoospermia in the spermogram after correction and, despite this, 7 out of 8 had positive biopsy (after correction) Some authors advocate the correction of varicocele as beneficial in all patients with infertility, in particular men with semen parameters alterations, even when fertility is still not a concern but as a way to achieve normal testosterone production (16-19) A comparison to patients with untreated varicocele was not done, so a conclusion regarding formal recommendation for varicocele correction in all azoospermic men cannot be made Notwithstanding, the results of successful biopsy after varicocele correction highlights the potential role of the procedure, mainly because in most cases it is a low-risk technique
Hormones play a major role in spermatogenesis and so the idea that hormonal levels could predict the success of biopsy has been postulated In our analysis, patients with a positive biopsy comparing to the ones with negative biopsy had lower (in normal range) FSH levels (6 0 mIU/mL vs 16 0 mIU/mL), in line with other studies (9) Some studies define a cut-off of 9 9 mIU/mL as a predictor for a positive biopsy with > 90% sensitivity, but other levels have been proposed Although it is known that even patients with very high FSH levels can have a positive testicular biopsy, a recent meta-analysis evaluating men with non-obstructive azoospermia reaffirmed FSH levels as a poor predictor for evaluating the success of sperm retrieval (20, 21) This lack of consensus may be due to the fact that FSH levels reflect the amount of testicular germ cells and not mature cells, which does not exclude the presence of mature sperm cells foci (20, 22, 23) In concordance to other studies, our results suggest that normal levels of FSH increase the probability of a positive biopsy but men with increased levels should not be excluded, as sperm may still be found
Another testicular function hormone, LH, has been investigated as a possible marker: in our cohort, as in most studies, there was no correlation between serum LH levels and the success of biopsy (20, 24) Testosterone, the main hormone produced by the testicular tissue, is hypothesized as a valuable marker of testicular health and fertile capacity (9, 24) Our data found that men with negative biopsies had significant lower mean baseline levels of serum testosterone than patients with a positive biopsy (3 7 ng/mL vs 2 85 ng/mL) Most literature did not find a relationship between serum total testosterone level and positive biopsy as our data shows (9, 16)
Patients with normal testicular volume in our population presented with a higher likelihood of positive biopsy as it is shown by data from other authors (1, 8) The analysis of metabolic factors shows that patients with type 1 diabetes mellitus had higher probability of positive biopsy, while smoking and overweight or obesity did not influence these outcomes High blood glucose levels are toxic to cellular viability, particularly in testis (25) Patients with diabetes in most cases have altered sperm parameters and are more likely to have retrograde ejaculation and atonia of seminal vesicles among other complications (26, 27) Data on sperm alterations in diabetic patients is variable: some studies showed spermatozoa with lower motility, altered morphology or decreased sperm production, while others stated that no pathological alterations were found The prevalence of infertility may also be increased in cases of pre-diabetes (26, 28, 29) Men with diabetes mellitus have higher probability of azoospermia and need for fertilization techniques as the disease progresses, and most of them present with normal serum levels of FSH, LH and testosterone (29) Our data suggests that type 1 diabetic men benefit from performing testicular biopsy in the presence of azoospermia A limitation of our analysis was not considering the current drugs used for diabetes treatment as they could affect fertility Overweight and obesity alter fertility, since excessive fatty tissue interferes with hormonal balance and induces sperm parameters alterations: lower sperm motility and total sperm counts and higher risk of azoospermia However, few studies evaluate the impact of these factors in sperm retrieval from testicular biopsy (30, 31) In general, the higher the body mass index the greater the risk of infertility worsening (30-34) Our data found no difference in biopsy success concerning body mass index Besides the potential bias and limitations previously mentioned, sample size is a limitation of our study Strong points are the homogeneity of our sample and the steady team of urologist and biologist performing biopsies and sperm analysis, respectively, ensuring a similar technique
CONCLUSIONS
Investigating infertile men and predicting biopsy outcomes is a difficult task Our study found that men with normal testicular volume, normal levels of testosterone and FSH and those with type 1 diabetes mellitus had a higher probability of positive testicular biopsy More research with larger samples is still needed to ensure more robust data and conclusions
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11567 3 Prediction
of success of testicular biopsy
REFERENCES
1 Cerilli LA, Kuang W, Rogers D A practical approach to testicular biopsy interpretation for male infertility Arch Pathol Lab Med 2010; 134:1197-204
2 Meng MV, Greene KL,Turek PJ Surgery or assisted reproduction? A decision analysis of treatment costs in male infertility J Urol 2005; 174:1926-31
3 Kim MJ et al , Molecular and cytogenetic studies of 101 infertile men with microdeletions of Y chromosome in 1,306 infertile Korean men J Assist Reprod Genet 2012; 29:539-46
4 Gudeloglu A and Parekattil SJ Update in the evaluation of the azoospermic male Clinics (Sao Paulo) 2013; 68 (Suppl 1):27-34
5 Iammarrone E et al Male infertility Best Pract Res Clin Obstet Gynaecol 2003; 17:211-29
6 Hauser R, et al Comparison of efficacy of two techniques for testicular sperm retrieval in nonobstructive azoospermia: multifocal testicular sperm extraction versus multifocal testicular sperm aspiration J Androl 2006; 27:28-33
7 Ishikawa T Surgical recovery of sperm in non-obstructive azoospermia Asian J Androl 2012; 14:109-15
8 Botelho F, et al Predictive factors of a successful testicular biopsy and subsequent clinical pregnancy Andrologia 2012; 44:237-42
9 Zarezadeh R, et al Hormonal markers as noninvasive predictors of sperm retrieval in non-obstructive azoospermia J Assist Reprod Genet 2021; 38:2049-2059
10 Minhas S, et al European Association of Urology Guidelines on Male Sexual and Reproductive Health: 2021 Update on Male Infertility Eur Urol 2021; 80:603-620
11 Björndahl L, Kirkman Brown J; other Editorial Board Members of the WHO Laboratory Manual for the Examination and Processing of Human Semen The sixth edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen: ensuring quality and standardization in basic examination of human ejaculates Fertil Steril 2022; 117:246-251
12 Schoor RA, et al The role of testicular biopsy in the modern management of male infertility J Urol 2002; 167:197-200
13 Pesce CM The testicular biopsy in the evaluation of male infertility Semin Diagn Pathol 1987; 4:264-74
14 Jashnani K, et al Fine-Needle Aspiration Cytology of the Testes for the Classification of Azoospermia and Its Value in the Assessment of Male Infertility Acta Cytol 2020; 64:216-223
15 Chan PT and Schlegel PN Diagnostic and therapeutic testis biopsy Curr Urol Rep 2000; 1:266-72
16 Kavoussi PK, et al A comprehensive assessment of predictors of fertility outcomes in men with non-obstructive azoospermia undergoi n g m i c r o d i s s e c t i o n t e s t i c u l a r s p e r m e x t r a c t i o n R e p r o d B i o l Endocrinol 2020; 18:90
17 Ficarra V, et al Varicocele repair for infertility: what is the evidence? Curr Opin Urol 2012; 22:489-94
18 Cho CL, Esteves SC, Agarwal A Indications and outcomes of varicocele repair Panminerva Med 2019; 61:152-163
19 Abdel-Meguid TA Predictors of sperm recovery and azoospermia relapse in men with nonobstructive azoospermia after varicocele repair J Urol 2012; 187:222-6
20 Ziaee SA, et al Prediction of successful sperm retrieval in patients with nonobstructive azoospermia Urol J 2006; 3:92-6
21 Li H, et al Predictive value of FSH, testicular volume, and histopathological findings for the sperm retrieval rate of microdissection TESE in nonobstructive azoospermia: a meta-analysis Asian J Androl 2018; 20:30-36
22 Silber SJ, et al Normal pregnancies resulting from testicular sperm extraction and intracytoplasmic sperm injection for azoospermia due to maturation arrest Fertil Steril 1996; 66:110-7
23 Ramasamy R, et al High serum FSH levels in men with nonobstructive azoospermia does not affect success of microdissection testicular sperm extraction Fertil Steril 2009; 92:590-3
24 Tsujimura A, et al Prediction of successful outcome of microdissection testicular sperm extraction in men with idiopathic nonobstructive azoospermia J Urol 2004; 172:1944-7
25 O'Neill J, et al Differences in mouse models of diabetes mellitus in studies of male reproduction Int J Androl 2010; 33:709-16
26 La Vignera S, et al Diabetes mellitus and sperm parameters J Androl 2012; 33:145-53
27 Mallidis C, et al The influence of diabetes mellitus on male reproductive function: a poorly investigated aspect of male infertility Urologe A 2011; 50:33-7
28 Boeri L, et al Undiagnosed prediabetes is highly prevalent in primary infertile men - results from a cross-sectional study BJU Int 2019; 123:1070-1077
29 Liu X, et al Effects of testicular sperm aspiration upon first cycle ICSI-ET for type 2 diabetic male patients Syst Biol Reprod Med 2020; 66:355-363
30 Craig JR, et al Obesity, male infertility, and the sperm epigenome Fertil Steril 2017; 107:848-859
31 Leisegang K, et al Obesity and male infertility: Mechanisms and management Andrologia 2021; 53:e13617
32 Leisegang K, Henkel R, Agarwal A Obesity and metabolic syndrome associated with systemic inflammation and the impact on the male reproductive system Am J Reprod Immunol 2019; 82:e13178
33 Reis LO and Dias FG Male fertility, obesity, and bariatric surgery Reprod Sci 2012; 19:778-85
34 Hammoud AO, et al Impact of male obesity on infertility: a critical review of the current literature Fertil Steril 2008; 90:897-904
Correspondence
Duarte Vieira Brito, MD (Corresponding Author) duartevbrito@hotmail com
Manuel Lopes, MD manuel11070@gmail com
Jose Pereira, MD joseaclpereira@gmail com
Ana Maria Ferreira, MD anaferreira6842@gmail com
Luis Sousa, MD luismtbsousa@gmail com
Belmiro Parada, MD parada belmiro@gmail com
Arnaldo Figueiredo, MD ajcfigueiredo@gmail com
Urology and Renal Transplantation Department, Coimbra University Hospital Centre, Coimbra
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11567 D Vieira Brito, M Lopes, J Pereira, A M Ferreira, L Sousa, B Parada, A Figueiredo 4
Bilaterality of varicocele: The overlooked culprit in male infertility. Case series study
Khaled Mohamed Almekaty 1 , Ahmed Mostafa Elsharkawy 2 , Mohamed Hasan Zahran 3 , Maged Mostafa Ragab 1 , Ayman Sayed Rashed 4 , Mahmoud Mohamed Soliman 5 , Khaled Abdelaziz Salem 1 , Ahmed Fayez Ghaith 1
1 Urology Department, Tanta University, Tanta, Egypt;
2 Radiology Department, Tanta University, Tanta, Egypt;
3 Mansoura Urology and nephrology centre, Mansoura University, Mansoura, Egypt;
4 Urology Department, 6th of October University, Cairo, Egypt;
5 Obstetrics and Gynecology Department, Cairo University, Cairo, Egypt
Summary
Objectives: Varicocele is the most common correctable cause of male infertility that always has been a debatable subject as regards how it affects fertility and the best way to treat it. Proper assessment of the disease bilaterality is crucial not to miss one side and not to jeopardize treatment outcome. This study aimed to objectively assess varicocele bilaterality in infertile men aiming to improve treatment outcome in this cohort of patients
Methods: This prospective study was conducted between January 2019 and January 2022 including infertile males with varicoceles Assessment of missed concomitant contralateral varicocele done pre-operatively by Color Doppler Ultrasound and intraoperatively by intraoperative Doppler device and measurement of maximal vein diameter of contralateral side
Results: A total of 329 cases completed the study A hundred cases (30 4%) were initially referred as unilateral varicoceles and 229 (69.6%) as bilateral varicoceles. After reassessment of the study population, bilaterality of varicocele was found to be as high as 98.5% (324/329). Repeat CDUS strongly correlated with the intraoperative measured varicocele diameter (r = 0 9, p < 0.001). Moreover, sperm parameters showed significant improvement 3 and 6 months post varicocelectomy Normal pregnancy after 1 year of surgery occurred in 118 cases (35 9%)
Conclusions: Varicocele bilaterality in infertile men is underreported Thorough assessment by expert radiologists and andrologists is of paramount importance not to miss significant pathology or hazard treatment outcome
KEY WORDS: Male infertility; Varicocele bilaterality; Varicocelectomy; Semen parameters
Submitted 9 July 2023; Accepted 28 July 2023
INTRODUCTION
Varicocele is the commonest surgical cause of male infertility and is found in 40% of patients with primary and 8 0 % o f t h o s e w i t h s e c o n d a r y i n f e r t i l i t y ( 1 ) T h e etiopathogenesis of varicocele-induced infertility and the effect of surgical repair on the fertility potentials has always been a matter of debate (2)
As reported in the literature, varicocele is found in 78% -
93% of cases on the left side, while bilateral varicoceles are only found in about 25% of patients (3) Majority of the left sided varicocele is related to the anatomic factors of the left testicular vein (4)
In 1952, Tulloch for the first time reported an azoospermic case which responded very well to bilateral varicocelectomy with not only sperm development in the ejaculate, but also normal pregnancy of the wife (5) Since then, many studies reported significant improvement in the sperm parameters of patients following bilateral varicocelectomy (6, 7) One theory that claims varicocele to be a disease of bilaterality is the reflux theory It depends on the presence of either incompetent or absent gonadal vein valves that allow blood to shunt back into the pampiniform plexus of veins Obviously, this is an anatomical deficit that should theoretically exist on both sides (8) This explains why left varicocele can also affect spermatogenesis of the right side as well
Previously, the incidence of coexisting right varicocele in the presence of palpable left varicocele was 21-60% as reported by venographic studies Recently, the incidence of bilateral varicoceles is increasing due to the use of modern diagnostic means besides the physical examination, such as Color Doppler Ultrasound (CDUS) which has a sensitivity of 97% and specificity of 94% (9) As CDUS is operator dependent, its reliability to diagnose and grade varicocele is still controversial (10)
Thus, assessment of varicocele bilaterality in infertile men seems to be deficient in the literature On this basis, this study tried to objectively assess varicocele bilaterality in infertile men aiming to improve treatment outcome in this cohort of patients
PATIENTS AND METHODS
This is a case series study that was conducted in Tanta Urology Department in Egypt between January 2019 and January 2022 The study was conducted in accordance with the Declaration of Helsinki and it was approved by Tanta University, Faculty of Medicine review board (IRB number is 35903/10/22) Informed consent was obtained by all subjects when they were enrolled
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11580 1
ORIGINAL PAPER
DOI: 10 4081/aiua 2023 11580
Infertile men (either primary or secondary infertility) initially assessed or referred as unilateral or bilateral varicocele patients were enrolled Patients with history of orchidectomy, cryptorchidism, azoospermia or concomitant female partner infertility were excluded
All patients were subjected to physical examination including local scrotal examination to evaluate the degree and laterality of varicocele and semen analysis before the operation A repeat scrotal Doppler ultrasonography was done for all patients to confirm diagnosis of varicocele and reassess bilaterality of the disease This repeat CDUS was performed by the same expert uroradiologist who was blinded to the findings of physical examination
All patients underwent microsurgical subinguinal varicocelectomy by expert uroandrologists after taking a written informed consent with explanation of the potential complications of the procedure
Patients who were diagnosed with bilateral varicoceles underwent bilateral subinguinal ligation straight away Those who were referred with unilateral varicocele had a repeat CDUS for reassessment of missed concomitant contralateral varicocele Their palpable sides were operated on first; then the contralateral side was explored as follows; the spermatic cord was delivered and opened at the level of the external inguinal ring Then, the maximal dilated internal spermatic vein diameter was measured using a micrometer fixed to the surgical microscope Also, the veins of the contralateral side were examined for reflux using an intraoperative Doppler device (VTI intraoperative Doppler system 20 MHz) The sound of venous reflux confirmed varicocele
diagnosis
Patients were followed up for at least 6 months after surgery to evaluate any complications and assess improvement in semen parameters
The primary outcome measure was to assess disease bilaterality and the secondary outcome measure was to report on improvement in semen 3 and 6 months post varicocelectomy and normal pregnancy rate after 1 year
Female partners were evaluated by full history taking and thorough examination to exclude female factor infertility Good ovulation was suggested if the female showed menstrual regularity, premenstrual syndrome (PMS), mid cyclic pain or discharge, confirmed by normal Follicle-stim-
ulating hormone (FSH), Luteinizing hormone (LH), Thyroid stimulating hormone (TSH), Prolactin, Estradiol (E2), and Anti-mullerian hormone (AMH) Transvaginal ultrasound was done to exclude any uterine pathology or mullerian anomalies that may interfere with the occurrence of pregnancy Furthermore, folliculometry was done and the presence of good ovulation was declared and confirmed by mid-luteal phase progesterone After varicocelectomy, the female partners were followed up for 1 year to assess normal pregnancy rate
Statistical analysis
Statistical analysis was performed using SPSS 16 0 for Windows software (SPSS, Inc , Chicago, IL) Chi-Square test is used to determine the significant association between the observed frequencies and the expected frequencies Wilcoxon sign test and simple Student t-test were used for continuous variables The difference was considered statistically significant at < 0 05
RESULTS
In this study 350 patients were initially enrolled and after exclusion, a total of 329 cases completed the study Figure 1 shows the flowchart of cases A hundred cases (30 4%) were initially referred as unilateral and 229 (69 6%) as bilateral varicoceles Table 1 shows the baseline data of the study population
Bilaterality of the disease was reassessed preoperatively by
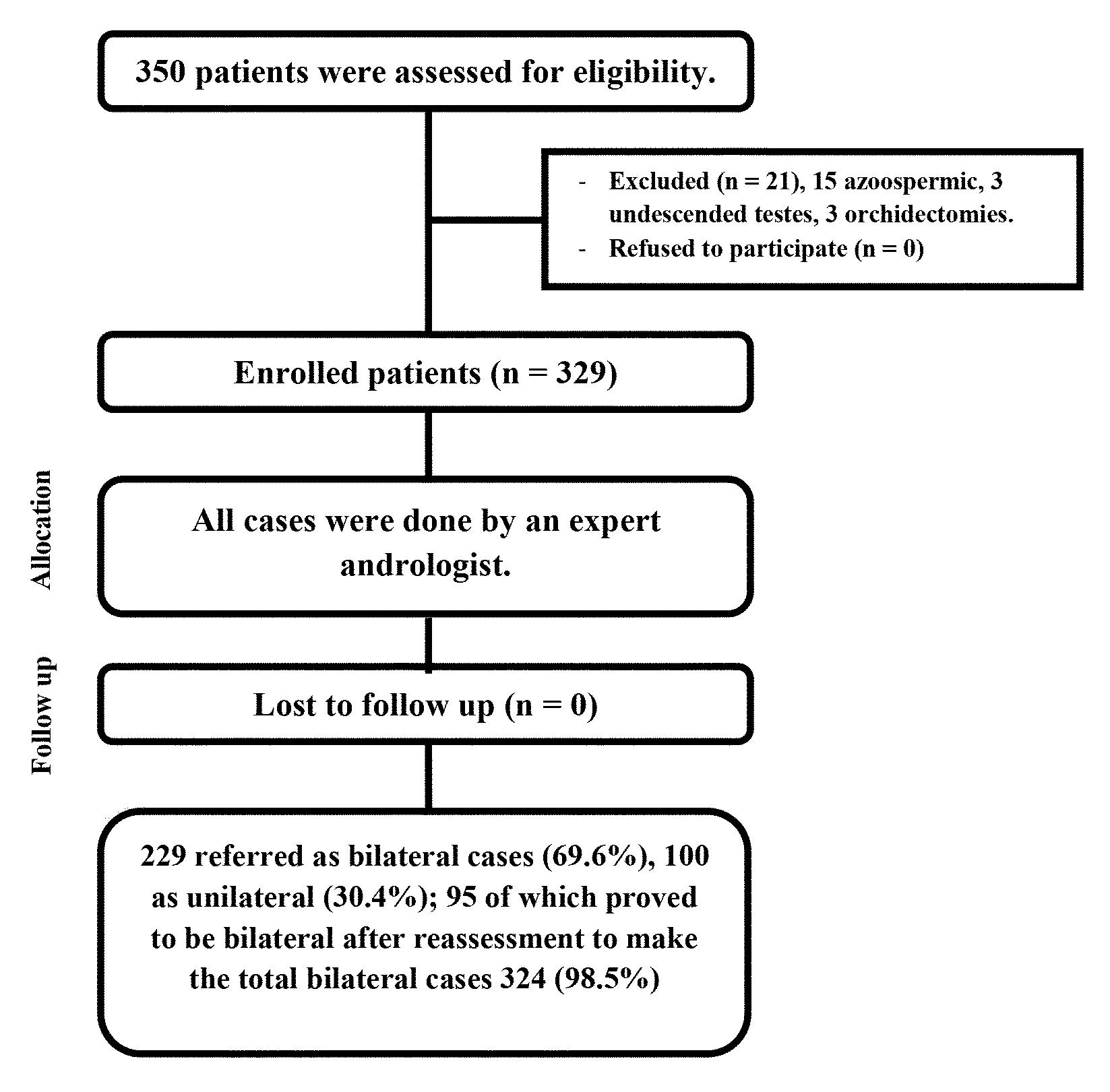
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11580
2
K Mohamed Almekaty, A Mostafa Elsharkawy, M Hasan Zahran, et al
Figure 1
Flowchart of study population
Table 1
Patients’ demographics.
a repeat CDUS and intraoperatively by measuring the maximal diameter of the largest vein and detecting venous reflux using operative Doppler as mentioned in the methodology section
After reassessment of the study population, bilaterality of varicocele was found to be as high as 98 5% (324/329) This is statistically significantly higher than initial CDUS (p < 0 001)
Repeat CDUS showed bilaterality in 95 out of the 100 cases (95%) and all had grade 2 varicoceles with median (range, IQR) diameter of 3 2 (2 5-4 1, 2 8-3 5) mm
The CDUS diameter strongly correlated with the intraoperative measured diameter 3 4 (1 5-4, 3-3 6) mm, (r = 0 9, p < 0 001)
Moreover, seminal parameters showed significant improvement at 3 and 6 months post varicocelectomy as shown in Table 2 Normal pregnancy after 1 year of surgery occurred in 118 cases (35 9%)
DISCUSSION
The exact relationship between bilateral varicocele and infertility is not fully understood, but since Tulloch noticed the positive effect of varicocelectomy on improving male fertility, many studies have been conducted to investigate this Interestingly, the degree of varicocele seems to be unrelated to the degree of testicular function affection or even the improvement after varicocelectomy as even a subclinical varicocele can result in male subfertility (11)
The only study that tried to clearly address whether or not varicocele in infertile males is a disease of bilaterality
is that of Gat et al (12) They used venography and contact thermography to detect “clinically missed” varicoceles
Using these 2 modalities, they detected varicocele in 255 out of 286 infertile males (89 1%); bilaterality was confirmed in 206 (80 8%) In the current study, reassessment of varicocele was done by repeat CDUS by an expert uroradiologist and intraoperatively by measuring the diameter of the largest vein at the level of the external inguinal ring and by detecting venous reflux using intraoperative Doppler device Out of a total of 329 patients, 229 were referred as bilateral (69 6%) but rate of bilaterality reached 98 5% (324 cases) after the “second look” evaluation
Most of the studies in the literature reporting the prevalence of varicocele in infertile men rely on physical examination and scrotal ultrasound Gonda et al. (13) reported 95% sensitivity with a 2-mm cutoff for vein diameters for diagnosis of varicocele
Both are subjective, operator dependent with significant interpersonal variability In the current study, 30 4% of patients were referred as unilateral varicocele cases and after reassessment bilaterality was proven in 98 5% (28 9% was misdiagnosed)
Reports in the literature looking at the prevalence of varicocele bilaterality are scarce In 1986, McClure and Hricak used CDUS to detect subclinical varicocele and detected bilaterality in 70% of their study population (14)
Chatel et al , Gonzalez et al , Cockett et al and Gat Y et al detected bilaterality in 60%, 61%, 57% and 89 1% respectively (15-17, 12) The higher prevalence of the disease bilaterality in the Gat et al and the current study as compared to others can be attributed to the use of
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11580 3 Bilaterality of varicocele: Examining its disease status
Total number Referred as bilateral varicocele Referred as unilateral varicocele P-value (No = 329) (No = 229) (No = 100; 4 right and 96 left) Age (years) Mean ± SD 29 1 ± 3 7 29 1 ± 3 6 29 3 ± 4 5 0 8 Age of the partner (years) Mean ± SD 27 1 ± 4 1 26 7 ± 3 6 28 6 ± 5 7 0 7 Duration of infertility (years) Median (IQR) 3 5 (2-5) 3 5 (2-5) 3 5 (2-4) 0 9 Right testicular size (ml) Mean ± SD 14 9 ± 2 1 14 9 ± 1 9 15 1 ± 3 2 0 4 Left testicular size (ml) Mean ± SD 14 ± 1 5 14 ± 1 4 14 3 ± 1 6 0 1 Sperm density (million/ml) Mean ± SD 4 2 ± 1 5 4 2 ± 1 5 4 1 ± 1 2 0 5 Sperm motility (A+B) Mean ± SD 18 2 ± 5 7 18 3 ± 5 8 17 5 ± 4 6 0 3 Grade of varicoceles G1:109 G1: 25 G2:211 G2: 60 G3:138 G3: 15
Outcomes
varicocelectomy. Baseline 3 months after surger y 6 months after surger y P1 P2 Sperm density (million/ml) Median (range, IQR) 5 (0 15-13, 4-5) 7 5 (0-80, 7-10) 11 (0-60, 10-13) < 0 001 < 0 001 Sperm motility (A+B) Median (range, IQR) 20 (0-60, 15-20) 25 (0-70, 20-30) 40 (0-60, 35-45) < 0 001 < 0 001 P1: compar son between baseline and 3 months P2: compar son between baseline and 6 months
Table 2
of
objective methods of assessment; venography in the former and intraoperative Doppler and measurement of the diameter of largest vein in the latter and to the improvement in the accuracy of the modern CDUS devices available nowadays
In the current study, both radiologists and surgeons have extensive experience in this field; so repeat CDUS strongly correlated to intraoperative assessment of the disease; (r = 0 9, p < 0 001; Pearson correlation coefficient) This means that the experience of the ultrasonographer and the surgeon should play a vital role to avoid misdiagnosed varicoceles
The exact mechanism by which varicocele might lead to infertility is still unclear The pathogenesis is thought to be multifactorial and complex, with several factors mostly acting together In this complex etiopathogenesis, oxidative stress seems to have a crucial role, among others Oxidative stress results from increased hydrostatic pressure in the pampiniform plexus of veins which leads to stagnation of toxic metabolites, hypoxia together with increased temperature (18)
One of the theories that can explain varicocele bilaterality is that there are venous anastomotic channels between the right and left gonadal veins that were detected in venography studies Another theory is the reflux theory which supposes that damage or absence of valves in the gonadal veins is the etiology behind varicocele development which most probably is a bilateral disease (8) This explains why a unilateral palpable varicocele can affect the global testicular function (right and left) and why unilateral varicocelectomy may fail to improve sperm parameters in some cases The current study supports these theories as varicocele bilaterality was found in 98 5% of patients This finding shows that varicocele bilaterality is clearly underestimated in practice and in the literature Our technique of artery preservation varicocelectomy using intraoperative Doppler was previously described Preserving testicular arteries during varicocelectomy provide significantly better sperm improvement especially in patients with severe oligozoospermia (19)
Regarding the indication of varicocelectomy, current evidence suggests a positive effect of varicocelectomy on sperm parameters and pregnancy rates only in couples with male factor infertility with a clinically palpable varicocele and abnormal semen parameters (18)
Randomized controlled trials looking at the effect of varicocelectomy on sperm parameters and pregnancy outcomes are lacking Consequently, available metaanalyses are negatively affected by wide heterogeneity of available studies However, the randomized controlled trial by Abdel-Meguid et al supports the findings of metaanalyses which suggest a beneficial effect of varicocelectomy on sperm parameters Abdel-Meguid et al in 2011 randomized the patients into subinguinal varicocelectomy (treatment group) and observation (control group)
After 1 year of follow up all sperm parameters significantly improved in the treatment group (32 2 ± 10 6 vs 18 1 ± 5 8× 106 sperm/ml, 41 0 ± 10 vs 25 3 ± 12 8%, and 39 0 ± 4 5 vs 31 2 ± 4 1% for sperm concentration, motility and morphology, respectively); while no significant difference found in the control group (20)
In the current study sperm density and motility signifi-
cantly improved after 3 and 6 months and 35 9% of the couples achieved normal pregnancy after 1 year from varicocelectomy (Table 2)
The points of strength of this study among others is the good sample size, prospective design and using objective tools for varicocele reassessment, while the limitation is the lack of sperm morphology data To the best of our knowledge, this is one of a very few reports addressing possible underestimation of varicocele bilaterality which must be taken into account during management of male factor infertility
CONCLUSIONS
Varicocele bilaterality in infertile patients seems to be underestimated in the literature and in clinical practice In our experience, varicocele bilaterality exists in 98 5% of infertile men Thorough assessment of varicocele bilaterality in infertile men by expert uroradiologist and andrologists is of utmost importance to avoid disease recurrence and optimize treatment outcomes
REFERENCES
1 Sigman M, Jarow JP Male infertility In: Walsh PC, Retik AB, Vaughn ED, Wein AJ (eds ), Campbell’s Urology 8th ed Philadelphia: Saunders 2002; 1475-1532
2 Yamaguchi M, Sakatoku J, Takihara H the application of intrascrotal deep body temperature measurement for the non-invasive diagnosis of varicoceles Fertil Steril 1989; 52:295-301
3 Masson P, Brannigan RE The varicocele Urol Clin North Am 2014; 41:129-144
4 Sabanegh E, Agarwal A Male infertility, in Campbell-Walsh Urology, A J Wein, L R Kavoussi, A C Novick, and A W Partin, Eds , pp 636-637, Saunders, Philadelphia, Pa, USA, 10th edition, 2012
5 Tulloch WS A consideration of sterility factors in the light of subsequent pregnancies Edinburgh Med J 1952; 59:29-34
6 Fujisawa M, Ishikawa T, Takenaka A The efficacy of bilateral varicocelectomy in patients with palpable bilateral varicoceles: comparative study with unilateral varicocele Urol Res 2003; 31:407-9
7 Libman J, Jarvi K, Lo K, Zini A Beneficial effect of microsurgical varicocelectomy is superior for men with bilateral versus unilateral repair J Urol 2006; 176:2602-5
8 Gat Y, Bachar GN, Zukerman Z, et al Varicocele: a bilateral disease Fertil Steril 2004; 81:424-9
9 Trum J, Gubler F, Laan R, Van der Veen F The value of palpation, varicoscreen contact thermography and colour Doppler ultrasound in the diagnosis of varicocele Hum Rep 1996; 11:1232-1235
10 Hussein AF The role of color Doppler ultrasound in prediction of the outcome of microsurgical subinguinal varicocelectomy J Urol 2006; 176:2141-2145
11 Paduch D, Niedzielski J Repair versus observation in adolescent varicocele: a prospective study J Urol 1997; 158:1128-32
12 Gat Y, Bachar GN, Zukerman Z, et al Varicocele: a bilateral disease Fertil Steril 2004; 81:424-9
13 Gonda RL Jr, Karo JJ, Forte RA, O'Donnell KT Diagnosis of subclinical varicocele in infertility AJR Am J Roentgenol 1987; 148:7175
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11580
4
K Mohamed Almekaty, A Mostafa Elsharkawy, M Hasan Zahran, et al
Bilaterality
of varicocele: Examining its disease status
14 McClure RD, Hricak H Scrotal ultrasound of infertile man: detection of subclinical unilateral and bilateral varicoceles J Urol 1986; 135:711-15
15 Chatel A, Bigot JM, Helenon C, et al Interet de la phlebographie spermatique dans le diagnostic des sterilites d'origine circulatoire (varicocele) Comparaison avec les donnees cliniques, thermographiques et anatomiques Ann Rad 1978, 21:565
16 Gonzalez R, Reddy P, Kaye KW, Narayan P Comparison of Doppler examination and retrograde spermatic venography in the diagnosis of varicocele Fertil Steril 1983; 40:96-9
17 Cockett ATK, Harrison RM, Comhaire F, Dubin L The varicocele and its effect on fertility Contemp Surg 1984; 24:111-14
18 Jensen CFS, Østergren P, Dupree JM, et al Varicocele and male infertility Nat Rev Urol 2017; 14:523-533
19 Almekaty K, Zahran MH, Zoeir A, et al The role of artery-preserving varicocelectomy in subfertile men with severe oligozoospermia: a randomized controlled study Andrology 2019; 7:193-198
20 Abdel-Meguid TA, Al-Sayyad A, Tayib A, Farsi HM Does varicocele repair improve male infertility? An evidence-based perspective from a randomized, controlled trial Eur Urol 2011; 59:455-461
Correspondence
Khaled Mohamed Almekaty, MD dr khaledhafez@med tanta edu eg
Maged Mostafa Ragab, MD mmregy@yahoo com
Khaled Abdelaziz Salem, MD khsalemmd@gmail com
Ahmed Fayez Ghaith, MD (Corresponding Author) dr ahmedfayez@yahoo com
Urology Department, Tanta University, Tanta, Egypt El-Gharbia Govenorate, Tanta El-Gash st Medical Campus, The Faculty of Medicine
Ahmed Mostafa Elsharkawy, MD ahmed elsharkawy84@gmail com
Radiology Department, Tanta University, Tanta, Egypt
Mohamed Hasan Zahran, MD ahmed elsharkawy84@gmail com
Mansoura Urology and Nephrology Centre, Mansoura University, Mansoura, Egypt
Ayman Sayed Rashed, MD aymanrashed@msn com
Urology Department, 6th of October University, Cairo, Egypt
Mahmoud Mohamed Soliman, MD dr mahmoudsoliman@yahoo com
Obstetrics and Gynecology Department, Cairo University, Cairo, Egypt
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11580 5
Reference value of testicular temperature measured by finite element analysis after first staged inguinal
Mehdi Shirazi 1, 2, Ali Eslahi 1, 3, Mohsen Ostovari 4, Faisal Ahmed 5, Ahmed Zaid 1, Mohammad Reza
7, Sania Shirazi 8
1 Department of Urology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran;
2 Histomorphomettery and Stereology Research Center, Shiraz University of Medical Sciences, Shiraz, Iran;
3 Shiraz Geriatric Research Center, Shiraz University of Medical Sciences, Shiraz, Iran;
4 Department of Medical Physics and Biomedical Engineering, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran;
5 Department of Urology, School of Medicine, Ibb University, Ibb, Yemen;
6 Social Determinants of Health Research Center, Department of Biostatics and Epidemiology, Faculty of Medicine, Babol University of Medical Sciences, Babol, Iran;
7 Department of Radiology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran;
8 Student Research Committee, Shiraz University of Medical Sciences, Shiraz, Iran.
Summary
Purpose: In this study, we aimed to build a 3D reconstruction computed simulation model and to establish a regression equation for detecting the testis's temperature by its location after first staged open orchidopexy in children with abdominal undescended testis (UDT) and short spermatic cords.
Methods: In this cross-sectional study, we enrolled 31 children with abdominal UDT and short spermatic cords who underwent first staged orchiopexy between 2017 and 2020. Using ultrasonography to obtain the testis's location distance from the skin surface (X1), external iliac vessel (X2), and internal inguinal ring (X3), we input the data into a 3D reconstruction computed simulation along with COMSOL to calculate the testicular temperature. We also used multivariate regression to establish the testicular temperature regression equation from the gathered data.
Result: The mean age of the participants was 4.47 ± 1.21 years. The mean size of the operated testis was 0.39 ± 0.13 cc. The mean distance of the testis from X1, X2, and X3 was 3.27 ± 1.25 mm, 21.06 ± 6.42 mm, and 27.19 ± 10.09 mm, respectively. The testicular temperature regression equation derived from testis location was calculated by the formula: 34.57 + 0.0236 X12 - 0.0105 X2 - 0.0018 X3. The concordance for testis temperature calculated via the computational method and regression equation was 83%.
Conclusions: The current study provided a reference value for the testicular temperature of children with abdominal UDT and short spermatic cords after the first stage of orchiopexy. A testicular temperature regression equation can be established based on the testis location, which will provide relevant information for the testicular development assessment, disease diagnosis, and follow-up, and possibly determination of the time of the second stage of orchiopexy.
KEYWORDS: Abdominal testis; Temperature; Short spermatic cord; Finite element; Referential values; Simulation method.
Submitted 1 July 2023; Accepted 27 July 2023
INTRODUCTION
One of the most common birth anomalies in children is undescended testis (UDT), with estimates ranging from 1 to 4.6% of full-term newborn males affected by one or both testes failing to descend (1). Congenital UDT is caused by the failure of the first or second stage of testicular descent. Some theories about the causes of UDT include primary testicular hormonal dysfunction, secondary hormonal dysfunction (hypothalamic-pituitary axis deficiency or placental failure to produce chorionic gonadotropin), and anatomical defects in the mechanism of descent (2). Testicular maldevelopment in children with UDT is characterized by disturbed tubular structure, mainly by decreased germ cells and quantitative and qualitative changes in the Leydig cells. These tubular alterations are detectable from the UDT's first or second year of life (3). The histologic disturbances in the UDT might be related to the increased testicular exposure to elevated extra scrotal temperature (4).
Intra-abdominal testis with a short spermatic cord that does not allow the surgeons to place it in the scrotum represents approximately 30% of all UDT cases (5). There is no consensus regarding the best operation because of the testicular artery and vein length, which limits the distal placement of the testis into the scrotum. For these particular cases, the surgical solution proposed is first-stage superficial inguinal orchiopexy, then scrotal orchiopexy, tow-stage laparoscopic Fowler-Stephens orchiopexy, and/or autotransplantation (6).
The testis's temperature is 2 to 4°C below the core body (6). Scrotal thermoregulation serves to liberate the large amount of heat produced during spermatogenesis. Several supporting mechanisms like thin skin with abundant vascularization, numerous sweat glands, and the absence of subcutaneous fat facilitate heat exchange and maintain the testicular temperature below body temperature (7).
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11528 1
ORIGINALPAPER
orchidopexy in children with abdominal testis and short spermatic cord
Askarpour 1, Hossein-Ali Nikbakht 6, Zeinab Gholami
DOI: 10.4081/aiua.2023.11528
In UDT patients, monitoring the testis's temperature can provide valuable information for assessing disease progression and therapeutic efficacy and might help choose optimal surgery timing However, it is impossible to measure temperature distribution directly inside the human body to validate simulation because of ethical considerations
Alternative approaches have been proposed to model scrotal cutaneous thermoregulation based on the automatic control theory, such as the computed tomographybased finite element model (CT-FEM) (8, 9) Pham et al used COMSOL FEM for the thermal simulation of testis to understand the dynamics of temperature change with time and location throughout the testicle after heat was applied to the surface of the testicle (10)
Few detailed studies on the testis's temperature have been performed in the superficial inguinal region after the first stage of open orchiopexy The anatomical heterogeneity and the diverse geometry of the testis in the superficial inguinal area make it impossible to accurately predict the testis's temperature in this location with the usual methods (11)
The present study aimed to build a 3D reconstruction computed simulation model and to establish a regression equation for detecting the testis's temperature by its location after first staged open orchidopexy in children with abdominal (UDT) and short spermatic cords
MATERIALS AND METHODS
The Ethics Committee of Shiraz University of Medical Sciences approved the study protocol (IR SUMS MED REC 1397 598) which was in accordance with the Declaration of Helsinki Additionally, each participant’s family provides written informed consent
Study design
In this retrospective cross-sectional study, from June 2017 to June 2020, we enrolled 31 patients with previous abdominal UDT and short spermatic cord that underwent the first stage of superficial inguinal orchiopexy at least six months prior to selection in Shiraz University Hospital (Shaheed Faghihi Hospital, Ali Asghar Hospital, and Namazi Hospital)
Exclusion criteria
Patients with congenital anomalies, scrotal orchidopexy, previous orchiectomy, prior hernia surgery, or other pathological conditions affecting the development of the external genitalia were excluded
A computational model for calculating the testis temperature
It is impossible to directly measure temperature distribution inside the human body to validate simulation due to ethical considerations In this study, we used a computed tomography-based finite element model to estimate the temperature inside the body This method consisted of several steps, which can be described as follows:
1 Measuring essential and influential parameters of the testis using ultrasonography (US) imaging: Before performing an inguinal testis ultrasound examination, adequate reassur-
ance was given The patients were placed in a supine position and covered with a towel Palpation was performed to assess the testis in the superficial inguinal area
A US system with high-frequency broadband linear transducer (10 MHz) and high resolution (Ws850; Samsung, Seoul, South Korea) was used to determine the structure and volume of the testis Testis's volume was calculated using the ellipsoid formula: (volume = 0 523 × length × thickness × width) The testis's structure was assessed in grayscale with the same gain, focus, and depth settings Measurements of the distance were taken by the testis's distance from the skin surface (X1), external iliac vessel (X2), and internal inguinal ring (X3) to the testis Table 1 shows these measurement results
2 Building a computational phantom: To build the model, we used a computed tomography (CT) scan of a patient, and using image segmentation and image processing methods, different organs in the abdominal and inguinal areas were segmented from CT images The entire image set consisted of 250 CT image slices, each 3 mm in slice thickness and of a matrix size of 512 × 512 pixels (12, 13) Then, the segmented anatomical regions were used to create a 3D model (Able Software, Lexington, MA) using Mimics Innovation Suite software toolbox After that, the 3D model was transformed into 3-Matics software to generate a computational volumetric model
3 Examining the equations and heat transfer in the computer model using COMSOL software: To solve the heat transfer equations and calculate the temperature of different parts, we converted the computational model created by 3-Matics software into executable formats in the COMSOL software (12, 14) Then, the initial processing of these models was performed to solve the heat transfer equations (15) The final model consisted of the skin surface (X1), external iliac vessel (X2), internal inguinal ring (X3), and testis, and the area between them was filled with soft tissue with specific thermodynamic properties to better represent the testis environment in the patient’s body (16) Also, the outside ambient temperature, abdominal cavity temperature, iliac artery temperature, and skin surface temperature in the upper scrotal region were considered based on previous studies to be 27°C, 37°C, 36 5°C, and 32°C, respectively (17) Using these constant temperature regions and solving the bio-heat equation with the finite element method in COMSOL software, the temperature of other parts inside the abdomen, testis, and soft tissue around it were calculated For each patient, the parameters of the testis distance from the skin surface (X1), external iliac vessel (X2), internal inguinal ring (X3), and testis volume were applied in a computational model (Figure 1)
4 Establish a regression equation: In order to establish an equation between the parameters measured in the US imaging and the temperature calculated for the testis in a computer simulation, we sought consultation with a statistician We were advised to use a multivariate regression statistical model (Table 1)
5 Statistical analysis: Statistical analysis was performed
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11528
2
M Shirazi, A Eslahi, M Ostovari, et al
using SPSS (IBM SPSS, version 22, Armonk, New York: IBM Corp) Descriptive statistics for variables were calculated as mean and standard deviation Multivariate linear regression was used to estimate the relationship between the measured variables with US (distance from skin surface, iliac vessels, and internal inguinal ring) and testis temperature calculated with computer simulation Then, mathematical formula was represented by an equation This analysis presented standard and non-standard regression coefficients and their 95% confidence interval
Finally, Bland-Altman plots and Pitman’s tests were applied to compare and agree for two temperatures checked by simulation and mathematical formula assessment methods P-values less than 0 05 were considered significant

RESULTS
The mean age of the participants was 4 47 ± 1 21 years (range 2 5-7 years) 11 (35 5%) children had left UDT, while 20 (64 5%) children had right UDT The mean size Table
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11528 3 Finite element analysis for testicular temperature
testis
distance from variable
1. Data of the
volumes, temperatures, and the
locations in all the patients
No Distance from exter nal Iliac Distance from inter nal inguinal Distance from the skin Testis temperature by Computer TestisVolume Testis temperature by fitting vessels (mm) ring (mm) surface (mm) Simulation (°C) (ml) for mula* (°C) 1 22 11 7 35 44 0 24 35 48185411 2983 34 73 0 23 34 67952861 3 24 35 2 34 51 0 56 34 35409452 4 16 29 5 35 02 0 34 34 94528678 5 13 17 2 34.5 0.29 34.50285529 6 32 21 2 3 34 32 0 64 34 32592489 7 21 30 4 5 34 82 0 28 34 77862047 858 2 2 34 65 0 55 34 62340101 9 12 17 4 34 85 0 37 34 79679894 10 19 18 5 35 04 0 62 34 93381565 11 23 18 2 3 34 43 0 49 34 4261874 12 25 39 5.6 35.06 0.67 34.98242921 13 19 41 1 8 34 29 0 42 34 377823 14 24 19 3 34 52 0 45 34 50144957 15 17 28 3 5 34 64 0 37 34 63545896 16 22 31 2 5 34 4 0 36 34 43561217 17 25 30 2 3 34 35 0 22 34 38317657 18 18 12 4 5 34 88 0 37 34 84313672 19 16 23 3.5 34.81 0.27 34.65513524 20 30 37 2 34 33 0 42 34 28725284 21 18 28 3 34 54 0 29 34 54817069 22 25 39 1 9 34 25 0 38 34 32703646 23 19 23 4 34 35 0 34 34 71211013 24 27 35 2 3 34 3 0 73 34 35296973 25 24 28 3 8 34 43 0 39 34 61346789 26 34 39 2 34.25 0.25 34.2414723 27 18 30 3 34 53 0 31 34 5445124 28 25 34 2 9 34 42 0 35 34 4495474 29 22 39 3 34 68 0 45 34 48592786 30 30 41 3 5 34 64 0 24 34 47478277 31 19 35 4 34 41 0 25 34 69016043 * The formula is: T(°C) = 34 57 + 0 0236 X12 - 0 0105 X2 - 0 0018 X3
Figure 1. (A and B): A computer model created in COMSOL software.
Characteristics of the patients
and testis (N = 31)
of the operated testis was 0 39 ± 0 13 ml (ranging from 0 22-0 73 ml) The mean distances of the testis from the skin surface, external iliac vessel, and internal inguinal ring were 3 27 ± 1 25 mm, 21 06 ± 6 42 mm, and 27 19 ± 10 09 mm, respectively The mean testis temperature was 34 59 ± 0 28°C (ranged 34 25-35 44°C) Table 2 demonstrates the patient and testis characteristics (Table 2)
Table 3
Prediction of the simulation method using linear regression
The results showed that the three measured variables (distance from skin, iliac vessels, and internal inguinal ring) together predicted 83% of the testis's temperature changes, which was statistically significant (Table 3) Also, the results showed that the distance from the skin surface variable had a robust and positive correlation with the simulated temperature of the testes Also, the iliac vessels had a low inverse correlation with the simulated temperature, which was statistically significant However, the internal inguinal ring had a weak inverse correlation, which was insignificant and had a minor role in prediction
The Bland-Altman plot from Standard and Formula limits of agreement for temperatures were between -0 229 to 0 240, with a mean difference of 95% CI: 0 005 (-0 038 to 0 048) and a range of 34 24 to 35 45 The spread around the mean for temperatures shows consistent variations across all levels, and only a few participants fell
The relationship between simulated testis temperature and three measurement indicators

Figure 2.
A: Scatter plots for temperatures between the simulation method and mathematical fitting formula; Pearson's correlation (r = 0 912, p =< 0 001),
B: Bland-Altman plot for agreement of temperatures checked by the simulation method and mathematical fitting formula
Establish a regression equation
Using multivariate regression, the testicular temperature regression equation derived from its location was calculated by the formula:
T = 34 57 + 0 0236 X12 - 0 0105 X2 - 0 0018 X3 (Equation 1) while X1 = Distance from Skin (mm), X2 = Distance from Iliac Vessels (mm), X3 = Distance from the internal inguinal ring (mm), T = Temperature of testes center (°C)
outside the limit of the agreement The mean difference was not associated with the means of the two methods, confirming an acceptable level of agreement (Pitman's test of difference invariance: r = 0 223, n = 31, p = 0 229) (Figure 2)
DISCUSSION
To our knowledge, this is the first series of pediatric orchiopexies reported from a single institution, and the
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11528 M Shirazi, A Eslahi, M Ostovari, et al 4
Table 2
Variables Mean ± SD (Range) Mean age (years) 4 47 ± 1 21 (2 5-7) Mean testis size (ml) 0 39 ± 0 13 (0 22-0 73) Mean testis temperature (°C) * 34 59 ± 0 28 (34 25-35 44) Mean distance from the skin surface (mm) 3 27 ± 1 25 (1 8-7) Mean distance from iliac vessels (mm) 21 06 ± 6 42 (5-34) Mean distance from internal inguinal ring (mm) 27 19 ± 10 09 (8-41)
Variable Coefficients (B) Standard er ror Beta 95% Confidence Inter val P-value lower upper Distance from the skin (mm) 2 0.024 0.002 0.823 0.019 0.028 0.000 Distance from iliac vessels (mm) -0 011 0 004 -0 237 -0 020 -0 001 0 026 Distance from the internal inguinal ring (mm) -0 002 0 003 -0 065 -0 008 0 004 0 538 Multiple R = 0
R
0
912;
Square = 0 832; Adjusted R Square =
813
first to be accompanied by a finite element model for assessing the testicular temperature and establishing a regression equation by its location after open first staged superficial inguinal orchiopexy in children with abdominal UDT and short spermatic cords Our model provides great value for the testicular development assessment, and it may be possible to decide on the time of the second stage of orchiopexy
The thermal modeling of human tissue is important as a tool to investigate the effect of external heat sources and to predict abnormalities in the tissue The modeling of heat transport in human tissue was first introduced by Pennes based on the heat diffusion equation (18) The equation is normally called Pennes’ bioheat equation and is frequently used for the analysis of heat transfer in human tissues The topic of temperature increase in human tissue after exposure to electromagnetic waves has been of interest for several years There are some experimental studies in animals such as rats, cows, and pigs (9) However, the results may not represent the practical behavior of human tissues
Finite element image evaluation of the scrotal surfaces is an easy and quick solution, shown to be a practical, noninvasive, and risk-free technique, as was previously shown for other species (9, 19) Wessapan et al developed a 3D model of the human head to investigate the specific absorption rate and temperature distributions in the human head and testis during exposure to mobile phone radiation (9, 19) Keangin et al carried out a numerical simulation of liver cancer treated using a complete mathematical model that considered the coupled model of electromagnetic wave propagation and heat transfer (20) Although many advanced transport models of biological tissue have been proposed, the minimum data requirement and easy implantation of Pennes’ bioheat model, still make it a good approximation and a widely used model of heat transfer in biological tissues
In this study, a case of simulated results was validated against the results with the model studied by Kang et al. (11) We used the computer simulation method to evaluate the testis parameters of UDT patients and the relationships of these variables with testis temperatures
According to this method, it has been reported that the counter-current heat-exchange mechanism involving the spermatic artery and the pampiniform plexus represents the primary system that controls the testis' temperature to preserve normal spermatogenesis (21) A computerassisted model of the counter-current heat-exchange mechanism at the testicular vascular pedicle simulates the normalization of the upset heat-exchange gradient mechanism through the correction of the physical parameters and, consequently, the rheology of the blood flow in the pampiniform plexus, considering the testis as a reservoir for space-variable, time-constant heat dissipation (22)
In our study, the testis temperature was not correlated with age and testis volume In the same manner, Mieusset et al reported that the testis temperature was not associated with age, empty intra-scrotal cavity, and the simultaneous rectal temperature (3) Kenneth et al measured the intratesticular and scrotal skin temperatures in 34 men who had undergone scrotal or inguinal surgical procedures Scrotal temperatures were measured before and
after a dry scrotal shave The intratesticular temperature was measured under direct vision with a needle thermistor, revealing a strong correlation between the intratesticular and scrotal skin temperatures These observations suggest that scrotal skin temperature measurements might help detect elevations of intratesticular temperature (23) Similarly, our result showed that the distance from the external iliac vessel and skin surface had a more significant effect on the testis temperature (p = 0 0012, 0 0037), respectively The positive correlation between the testis temperature and distance from the skin surface and the external iliac vessel reveals the interdependence between the scrotum areas in the testis thermoregulation, which was in line with the result of Ruediger et al study (24)
In our study, the correlation between the temperatures of the testis and the distance from the internal inguinal ring was less significant in comparison to other parameters that affect the testis temperature (p = 0 1943) This poor correlation can be explained by a lesser heat exchange area According to Kastelic et al , the ambient temperature had a significant effect on the temperature of the lower region of the scrotum, a negligible impact on the temperature of the upper region, and an intermediate effect on the temperature of the middle region of the scrotum (25) The dominant process in the heat energy transfer between the testis and their surroundings is the heat conduction process The following equation expresses the rate of heat transfer:
K is the conductivity coefficient, A is the contact crosssection, and is the temperature gradient The negative sign in this formula indicates that heat transfers from the higher temperature region to the lower temperature region The temperature gradient (𝛻T) is defined as the temperature ratio of two environmental points to their spatial distance (26, 27) Since, in UDT patients, heat transfer through the testis and temperature reduction is disrupted, we aim to find the location that provides better heat emission to cool down the testis
In the abdomen, heat sources are the main arteries and the body's core region in the thermoregulation system that have a temperature higher than that of the testicles, and the heat sink area is the skin surface through which heat energy is transferred out of the body
During UDT surgery, it is impossible to change such parameters as thermal conductivity (k) and the cross-sectional area of the testis and the surrounding tissues (A), whereas the location of the testis is the only parameter that the surgeon can adjust The surgeon can control the temperature gradient by changing the distance between the testicles and the heat sources or the heat sinks There is a temperature gradient between the testis and the three areas of the internal inguinal ring, external iliac vessel, and skin surface The temperature of the external iliac vessel and the internal inguinal ring are equal to the core body temperature and higher than the temperature of the testis, but the temperature of the skin surface is close to the ambient temperature and is lower than that of the testis (6)
The results of this study show that among the three
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11528 5 Finite
for testicular temperature
element analysis
∆𝑄 = -𝑘𝐴𝛻𝑻 (Equation
∆𝑡
2)
parameters of distance from the skin surface (X1), distance from the iliac vessel (X2), and distance from the internal inguinal ring (X3), the X1 parameter has more influence on the testicular temperature than others In equation 1, the coefficient of X1 is positive, so when the distance from the skin decreases, the central temperature of the testis decreases Therefore, the most suitable position to place the testicles is the closest distance from the skin Equation 1 also shows that between X2 and X3, the influence of the X2 on the testis temperature is more dominant than X3 The coefficients of X2 and X3 are negative
Therefore, the proper position is the one that is farthest from the iliac arteries and internal inguinal ring
This study had several limitations, such as its retrospective nature, the lack of a control group, and the small sample size Also, the testis size before surgery and contralateral intra-scrotal testis temperatures in children were not checked We detected the heterogenicity of the testis size and age among the patients The period between surgery and temperature checking was six months at least
Therefore, this is just an observational report requiring validation with a large sample size and randomized criteria Because the thermal factors involved in the heat exchange of children’s environment are not all determinable, these models are valuable only when the children's thermal conditions and environment are both known or may be controlled
CONCLUSIONS
The current study provided a reference value for the testicular temperature of boys with abdominal UDT and short spermatic cords after the first stage of orchiopexy A testicular temperature regression equation derived from its location can be established, which will provide relevant information for the testicular development assessment, disease diagnosis, and follow-up, and possibly for deciding on the time of the second stage of orchiopexy
ACKNOWLEDGMENTS
The authors would like to thank Shiraz University of Medical Sciences, Shiraz, Iran, the Center for Development of Clinical Research of Nemazee Hospital, and Dr Nasrin Shokrpour for editorial assistance
REFERENCES
1 Kurz D Current Management of Undescended Testes Curr Treat Options Pediatr 2016; 2:43-51
2 Hutson JM, Li R, Southwell BR, et al Germ cell development in the postnatal testis: the key to prevent malignancy in cryptorchidism? Front Endocrinol (Lausanne) 2012; 3:176
3 Mieusset R, Fouda PJ, Vaysse P, et al Increase in testicular temperature in case of cryptorchidism in boys Fertil Steril 1993; 59:1319-21
4 Humphrey G, Najmaldin A, Thomas D Laparoscopy in the management of the impalpable undescended testis Br J Surg 1998; 85:983-5
5 Wang CY, Wang Y, Chen XH, et al Efficacy of single-stage and two-stage Fowler-Stephens laparoscopic orchidopexy in the treatment of intraabdominal high testis Asian J Surg 2017; 40:490-4
6 Shiraishi K, Takihara H, Matsuyama H Testicular Temperature and the Effects of Orchiopexy in Infants with Cryptorchidism J Urol 2021; 206:1031-7
7 Ismail E, Orlando G, Pompa P, et al Time-domain analysis of scrotal thermoregulatory impairment in varicocele Front Physiol 2014; 5:342
8 Imai K Computed tomography-based finite element analysis to assess fracture risk and osteoporosis treatment World J Exp Med 2015; 5:182-7
9 Wessapan T, Rattanadecho P Temperature induced in the testicular and related tissues due to electromagnetic fields exposure at 900 MHz and 1800 MHz Int J Heat Mass Transf 2016; 102:1130-40
10 Pham S, Schultz JS Testicular thermoregulation with respect to spermatogenesis and contraception J Therm Biol 2021; 99:102954
11 Kang Z, Wang F, Udayraj An advanced three-dimensional thermoregulation model of the human body: Development and validation Int Commun Heat Mass Transf 2019; 107:34-43
12 Gür Y Additive Manufacturing of Anatomical Models from Computed Tomography Scan Data Mol Cell Biomech 2014; 11:249-58
13 Zukowska M, Rad MA, Górski F Additive Manufacturing of 3D Anatomical Models-Review of Processes, Materials and Applications Materials (Basel) 2023; 16:880
14 Sander IM, McGoldrick MT, Helms MN, et al Three-dimensional printing of X-ray computed tomography datasets with multiple materials using open-source data processing Anat Sci Educ 2017; 10:383-91
15 Steinberger A Effects of Temperature on the Biochemistry of the Testis In: Zorgniotti AW, editor Temperature and Environmental Effects on the Testis Boston, MA: Springer US; 1991 p 33-47
16 Popovic M, Pantovic Pavlovic M, Pavlovic M Ghosts of the past: Elemental composition, biosynthesis reactions and thermodynamic properties of Zeta P 2, Eta B 1 525, Theta P 3, Kappa B 1 617 1, Iota B 1 526, Lambda C 37 and Mu B 1 621 variants of SARS-CoV2 Microb Risk Anal 2023; 24:100263
17 Taylor NA, Tipton MJ, Kenny GP Considerations for the measurement of core, skin and mean body temperatures J Therm Biol 2014; 46:72-101
18 Pennes HH Analysis of tissue and arterial blood temperatures in the resting human forearm 1948 J Appl Physiol (1985) 1998; 85:5-34
19 Siriwitpreecha A, Rattanadecho P, Wessapan T The influence of wave propagation mode on specific absorption rate and heat transfer in human body exposed to electromagnetic wave Int J Heat Mass Transf 2013; 65:423-34
20 Keangin P, Rattanadecho P, Wessapan T An analysis of heat transfer in liver tissue during microwave ablation using single and double slot antenna Int J Heat Mass Transf 2011; 38:757-66
21 Sheehan MM, Ramasamy R, Lamb DJ Molecular mechanisms involved in varicocele-associated infertility J Assist Reprod Genet 2014; 31:521-6
22 Tritto G Computer-assisted simulation model of the counter-current heat-exchange mechanism at the testicular vascular pedicle Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 1988 4-7 Nov 1988
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11528
6
M Shirazi, A Eslahi, M Ostovari, et al
Finite element analysis for testicular temperature
23 Kurz KR, Goldstein M Scrotal temperature reflects intratesticular temperature and is lowered by shaving J Urol 1986; 135:290-2
24 De Ruediger FR, Chacur MGM, Alves FCPE, et al Digital infrared thermography of the scrotum, semen quality, serum testosterone levels in Nellore bulls (Bos taurus indicus) and their correlation with climatic factors J Semina: Ciências Agrárias 2016; 37:221-32
25 Kastelic J, Cook R, Coulter G, et al Environmental factors affecting measurement of bovine scrotal surface temperature with infrared thermography Anim Reprod Sci 1996; 41:153-9
26 Kaviany M Heat Transfer Physics 2 ed Cambridge: Cambridge University Press; 2014
27 Lienhard JH, Lienhard JH A Heat Transfer Textbook 4th edition ed Newburyport: Dover Publications; 2013
Correspondence
Mehdi Shirazi shirazim@sums ac ir
Ali Eslahi alieslahi@yahoo com
Dpt of Urology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran
Faisal Ahmed fmaaa2006@yahoo com
Mohsen Ostovari Mohsen Ostovari@gmail com
Ahmed Zaid ahmadzaid333@gmail com
Mohammad Reza Askarpour askarvip2@gmail com
Hossein-Ali Nikbakht Ep nikbakht@gmail com
Zeinab Gholami Gholamii zb@gmail com
Sania Shirazi saniashirazi046@gmail com
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11528 7
Impact of statin on renal cell carcinoma patients undergoing nephrectomy.
Does it affect cancer progression and improves survival? A Systematic Review and Meta-Analysis
Summary
Introduction: Renal cell carcinoma (RCC) is regarded as one of the most common malignant tumors. Various concomitant medications in RCC patients undergoing surgery are investigated to explore the potential for improving survival and preventing disease recurrence, including statin. It has been observed that these drugs induce apoptosis, thereby inhibiting tumor growth and angiogenesis. We aimed to perform a systematic review and meta-analysis to enhance the level of evidence for statin in RCC.
Methods: A systematic literature search was conducted in several online databases, including PubMed, Scopus, and Sciencedirect, using terms relevant to the use of statins in RCC patients undergoing nephrectomy for publications published up to July 2023, according to a registered review procedure (CRD42023452318). The Newcastle-Ottawa Scale (NOS) was used to assess the risk of bias of the included study. Review Manager 5.4 was used for all analyses.
Results: Seven articles was eligible for our study. The analysis revealed that patients receiving statin had a better overall survival compared to patients who does not receive statin (HR 0.71, 95% CI 0.51-0.97, p = 0.03, I2 = 76%). However, there was insignificant difference in terms of CSS, DFS, and PFS between RCC patients receiving statin and without statin.
Conclusions: Statin has substantial benefits for improving OS. Even though the outcomes for CSS, DFS, and PFS were insignificant, the potential role of statins as a supplementary therapy in surgically treated RCC still requires further investigation.
KEYWORDS: Statin; Renal cell carcinoma; Nephrectomy; Survival rate; Outcome.
Submitted 24 August 2023; Accepted 31 August 2023
INTRODUCTION
Renal cell carcinoma (RCC) is regarded as one of the most common malignant tumors, accounting for approximately 2% of all tumors and 90% of all kidney malignancies. Renal cancer is expected to remain a major threat to global health as the global incidence of this disease has been steadily growing in recent decades (1). In order to manage the disease, surgical resection of the tumor is the cornerstone treatment. As a curative or palliative treatment, surgical therapy is performed using either partial or radical
nephrectomy techniques according to the staging of the disease (2, 3). Despite the fact that surgical resection of tumors in localized disease can be curative, disease progression and mortality could be up to 20% of patients after primary treatment, and therefore any intervention to improve the oncological outcomes would be considered a significant benefit (4). Several variables including age, race, gender, stage, grade, tumor size, performance status, and blood type, have been found as independent predictors of mortality after nephrectomy for locoregional RCC. Although these risk variables may provide useful prognostic information, they typically offer limited opportunity for intervention to modify the disease's trajectory (5, 6).Unlike in metastatic RCC, targeted therapy and immunotherapy such as Vascular Endothelial Growth Factor (VEGF) or mammalian-target of rapamycin (mTOR) inhibitor are shown to have minimal benefits in an adjuvant treatment scenario for localized RCC after surgery and a high-risk profile for disease recurrence (7-9). Given the high costs and limited availability of pharmacological development and clinical implementation of targeted therapies, the technique of drug repositioning (DR) of selected non-anticancer drugs is being investigated (10). Various concomitant medications in RCC patients undergoing surgery are investigated to explore the potential for improving survival and preventing disease recurrence, including insulin, beta-blockers, metformin, statins, and other therapies (11). Statins are the most widely used drugs for the treatment of hypercholesterolemia, and several authors discovered the anti-tumor activities in this medication. These drugs have been observed to induce apoptosis, thereby inhibiting tumor growth and angiogenesis (12). Even though the exact mechanism is still unclear, clinical trials have been conducted to explore the potential benefits of statin in several cancers such as lung cancer, liver cancer, and colorectal cancer (13-15). Several cohorts are also currently being conducted to evaluate the impact of statins on the oncological outcomes of RCC patients having surgery (5, 1619). The results are encouraging but often conflicting, and there are currently no strong recommendations regarding the use of statins as either neo-adjuvant or adjuvant therapy in RCC. Therefore, we aimed to perform a systematic
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11672 1
SYSTEMATICREVIEW
Ghazian Adli 1, 2, Niwanda Yogiswara 1, 2, Ida Bagus Gde Tirta Yoga Yatindra 1, 2 , Rheza Maulana Putra 1, 2, Wahjoe Djatisoesanto 1, 2
1 Department of Urology, Faculty of Medicine, Universitas Airlangga, Indonesia.
DOI: 10.4081/aiua.2023.11672
2 Dr. Soetomo General-Academic Hospital, Surabaya, East Java, Indonesia.
review and meta-analysis to enhance the level of evidence for statin in RCC
METHODS
Review protocol and search strategy
This study evaluates the impact of statin on RCC patients who underwent nephrectomy on the oncological outcomes through systematic review and meta-analysis design (20), following the latest Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement in PubMed, Science-direct, and Scopus The literature search followed Medical Subject Headings (MeSH®) Terms related to the use of statin in RCC patients who underwent nephrectomy for articles published up to July 2023
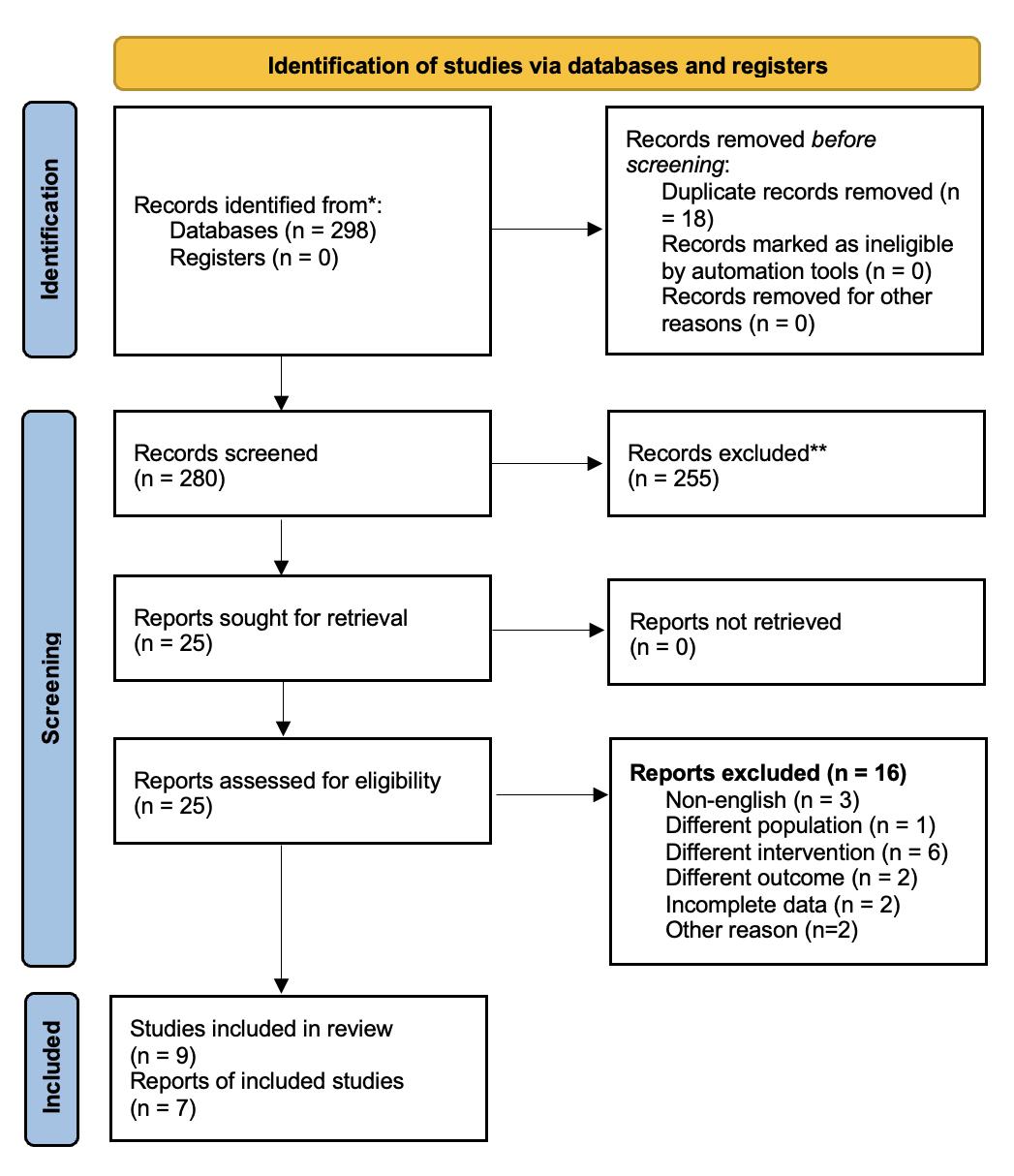
cally significant using the software Review Manager 5 4 (Cochrane Collaboration)
Heterogeneity between studies was evaluated using I2, where an I2 value above 50% indicated high heterogeneity and a random-effects model was applied for pooled analysis
RESULTS
Study search
T h e p r o t o c o l h a s b e e n r e g i s t e r e d i n
O (CRD42023452318)
Eligibility criteria for review
The inclusion criteria are (1) observational studies (2) evaluation of RCC patients who underwent open or laparoscopic nephrectomy diagnosed with histopathological examination, (3) compare patients who receive statin and without statin (4) and reporting the outcome
The outcomes analysed in this study were overall survival (OS), cancerspecific survival (CSS), disease-free survival (DFS), and progression-free survival (PFS) We excluded nonEnglish studies, studies without full text, and duplicate studies
Data extraction and risk of bias assessment
Baseline characteristics of the study were extracted by two independent authors, while the third author resolved all disagreements through a discussion The extracted data consisting of publication details as first author name and year of publication, study design, sample size, and sample characteristics such as age, RCC grade, cell type, stage of RCC, and surgical methods were collected in spreadsheet software Microsoft Excel® 2021 The risk of bias was assessed with the Newcastle-Ottawa Scale (NOS), which has the domain of selection, comparison, and exposure
Data analysis and presentation
The analysis effect size was estimated in a Forest plot with a hazard ratio (HR) with a 95% confidence interval (95% CI) and a p-value below 0 05 was considered statisti-
Our preliminary search found 298 results Twenty-five full articles were retrieved for eligibility Following the assessment of the full-text articles, sixteen were eliminated for several reasons, including differences in intervention, population, and incomplete data The remaining seven publications were investigated further, as shown in Figure 1 The clinical characteristics of the included participants are described in Table 1
Baseline characteristics and quality assessment
All of the included studies were retrospective cohorts The majority of the populations of the included studies were American, ranging from 55-66 years The type of statins that were used in the study comprised Atorvastatin,
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11672 G
2
Adli, N Yogiswara, I Bagus Gde Tirta Yoga Yatindra, R Maulana Putra, W Djatisoesanto
P R O S P E R
Figure 1. Identification of included studies
Table 1.
Baseline
of the included study.
Table 2. Quality assessment using Newcastle-ottawa scale
Simvastatin, Lovastatin, Pravastatin, Rosuvastatin, Fluvastatin, and Cerivastatin The techniques used for surgical resection were varied such as open, laparoscopic, and robotic approach The follow-up of the studies ranged from 25 to 93 months The risk of bias assessed using NOS revealed a moderate score ranging from 5 to 9, with a median of 7 as presented in Table 2
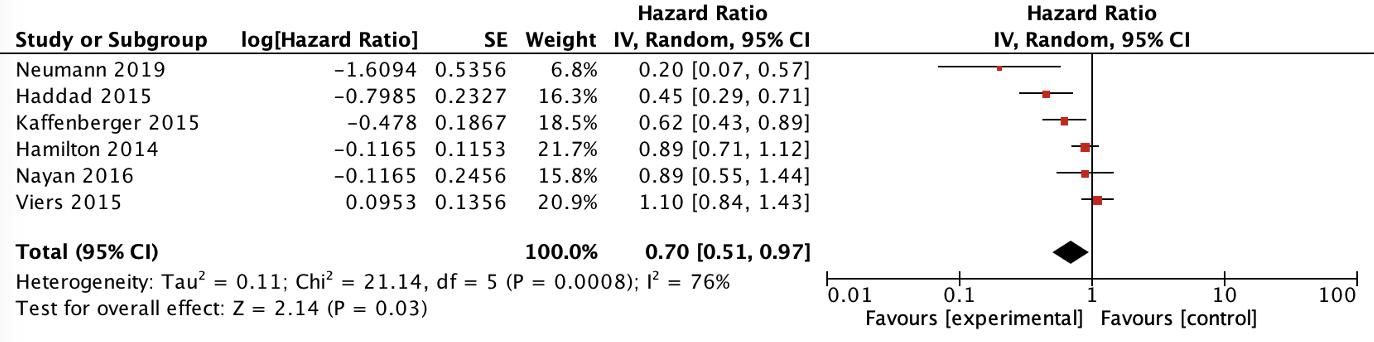
Impact of statin on overall survival
Six articles were included in the analysis of overall survival using the random-effect model, as presented in Figure 2
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11672 3 Statin affecting survival in surgically treated RCC
Author Selection Comparability Exposure Score Berquist, 2017 *** ** *** 8 Haddad, 2015 **** ** ** 8 Choi, 2012 *** **5 Hamilton, 2013 **** ** ** 8 Kaffenberger, 2014 *** ** *** 8 Nayan, 2016 **** ** **** 9 Neumann, 2019 *** ** *** 8 Viers, 2015 *** ** *** 8 Haide, 2019 *** ** *** 8
Author Countr y Study Sample Inter vention N Age Follow Up Nephrectomy Cancer Outcome Adjusted variable Type size (n) (years) (month) (n) histology analyzed in multivariate Median (IQR) analysis Choi, 2012 Korea Retrospective 115 Statin 21 58 95 ± 12 33 40 Radical and Clear Cell, Papillary, PFS, RFS Age, gender, BMI cohort Non Statin 94 65 24 ± 6 82 Partial (115) Chromophobe, Collecting Duct, Sarcomatoid Hamilton, 2013 America Retrospective 2608 Statin 708 66 (59-72) 36 Radical (1580) Clear Cell, Papillary, Progression, Age, gender, race, cohort Non Statin 1900 59 (50-68) Partial (1028) Chromophobe, overall mortality type of surgery, commorbidity, Unclassified renal function, tumor stage, year of surgery, local and systemic symptoms Kaffenberg, 2014 America Retrospective 916 Statin 270 60 8 (51 3–69 3) 42 5 (19 1–67 1) Radical (584) Clear Cell, DSS, OS Age, ASA score, staging, nodes, cohort Non Statin 646 Partial (332) Non-Clear Cell metastatic status, blood group, corrected hypercalcemia Viers, 2015 America Retrospective 2357 Statin 630 66 (59–73) 93 6 (63 6-134 4) Radical (1727) Clear Cell, Papillary, PFS, CSS, OS Age, gender, type of surgery, cohort Non Statin 1727 61 (52–70) Partial (630) Chromophobe, Clear Cell, smoking status, tumor stage, Mucinous-Spindle Cell tumor grade, sarcomatoid Translocation-Associated differentiation Collecting Duct, NOS Haddad, 2015 America Retrospective 850 Statin 342 62 (19-92) 25 (7.8-52.3) Radical (384) Clear cell, Non-Clear Cell RFS,OS Tumor stage, tumor grade, cohort Non Statin 508 55 (20-87) Partial (466) lymphovascular invasion, LDL, TG Nayan, 2016 Canada Retrospective 839 Statin 259 66 ± 16 47 (20-80) Radical (477) Clear Cell, Papillary, DFS, CSS, OS Age, gender, type of surgery, cohort Non Statin 634 57 ± 18 Partial (259) Chromophobe, tumor stage Unclassified Berquist, 2017 America Retrospective 283 Statin 180 57 5 ± 15 68 (50-90) Radical (204) Clear Cell, Papillary, DFS Tumor stage and grade cohort Non Statin 103 Partial (77) Chromophobe RCC, Other histology Neumann, 2019 Germany Retrospective 388 Statin 207 64 26 (17 12–90 32) 57 93 (0–237 18) Radical Clear Cell OS Commedication, tumor stage, cohort Non Statin 39 Partial Haide, 2019 Germany Retrospective 104 Statin 41 62 (53-70 35 4 (12 3-73 3) Radical Clear Cell, Non-Clear Cell CSS Tumor stage, hypertension cohort Non Statin 63 Partial
characteristics
Figure 2. Impact of statin on Overall Survival
The meta-analysis revealed that RCC patients receiving statin had better overall survival compared to patients who did not receive statin (HR 0 71, 95% CI 0 51-0 97, p = 0 03, I2 = 76%)
Impact of statin on cancer-specific survival, disease-free survival, and progression-free survival
Four studies were included in the analysis of CSS
The meta-analysis using the random-effects model in Figure 3 revealed that there was an insignificant difference in terms of CSS between RCC patients receiving statin and those without statin (HR: 0 85 95% CI 0 541 33, p = 0 47, I2 = 55%) Analysis of DFS was performed using two studies

The meta-analysis result using the random-effects model in Figure 4 showed that there was an insignificant difference in terms of DFS between RCC patients receiving statin and without statin (HR: 0 76 95% CI 0 38-1 52; p = 0 44, I2 = 73%) Based on the result from the Forest plot shown in the Figure 5, there was an insignificant difference in PFS between RCC patients receiving statin and those without statin (HR: 0 92 95% CI 0 51-1 65; p = 0 77, I2 = 86%)
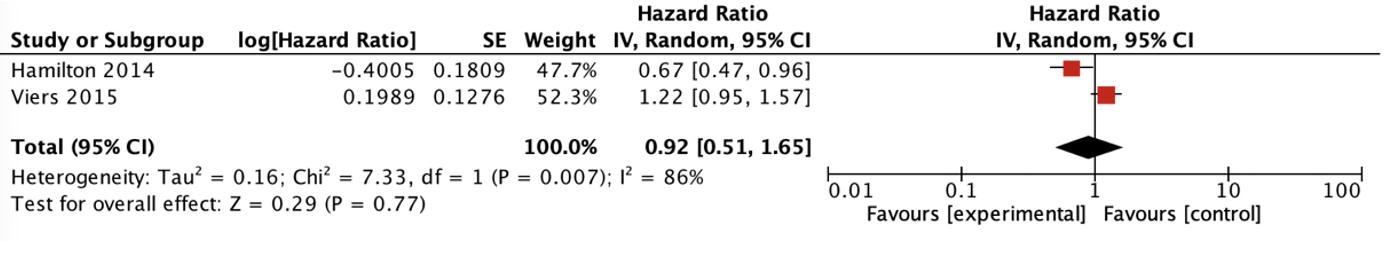
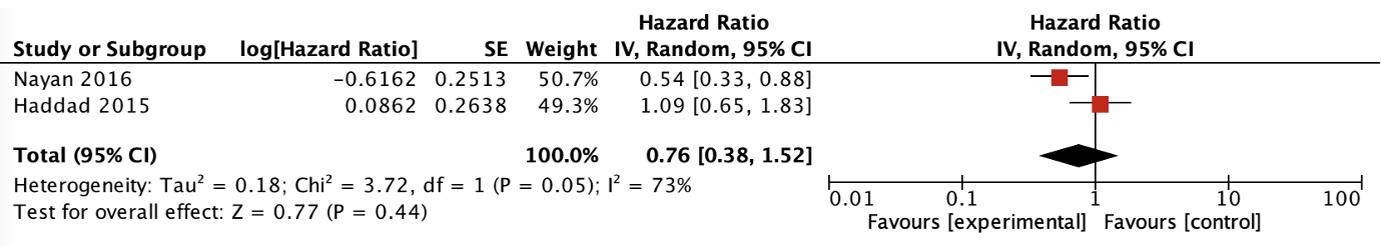
DISCUSSION
This meta-analysis includes seven retrospective cohorts investigating oncological outcomes in the form of OS, DFS, CSS, and PFS in statin administration in surgically treated RCC patients (5, 11, 16-19, 21) The pooled analysis revealed that RCC patients receiving statin had a better OS compared to patients who did not receive statin, while there are no differences in DFS, CSS, and PFS Overall survival is a critical parameter for evaluating the efficacy, safety, and clinical benefits of a cancer intervention The effect of statins on improving OS has been explored in many tumors in urology, including patients with RCC, although investigations in RCC patients having nephrectomy were limited to a retrospective cohort and the results were contradictory Based on the results of combined observational studies, we discovered higher overall survival in RCC patients who received statin therapy compared to those without statins The results of this meta-analysis are consistent with the previous metaanalysis by Nayan et al which reported that statins were significantly associated with an improvement in OS in all patients kidney cancer patients with HR of 0 74 (22) Our finding also aligns with a recent meta-analysis conducted
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11672 G Adli, N Yogiswara, I Bagus Gde Tirta Yoga Yatindra, R Maulana Putra, W Djatisoesanto 4
Figure 3. Impact of statin on cancer-specific survival
Figure 4. Impact of statin on disease-free survival
Figure 5. Impact of statin on progression-free survival
by Luo et al (23), who incorporated 35 studies to evaluate on the beneficial effects of statins in various urological cancers and discovered a significant improvement in OS in patients with RCC and bladder cancer However, Wu et al (24) observed no significant difference in OS in RCC patients, but their analysis only included American cohorts, which can be biased if generalized in the global population The strength of the current analysis is that this review mainly focused on RCC patients undergoing surgical treatment, whereas prior meta-analyses included all RCC patients, surgical or non-surgical (22) Statin improves the OS of RCC patients undergoing surgery by several mechanisms One possible mechanism of statins in improving the OS of cancer patients is by inhibiting the proliferation and progression of RCC and inducing apoptosis of cancer cells thereby directly improving OS (11) Another possible mechanism is lowering cholesterol levels by blocking the active site of the HMG-CoA reductase enzyme, reducing the risk of coronary artery blockage and deadly cardiovascular events such as myocardial infarction or stroke which indirectly improves OS (17) Tumor cells can activate the coagulation process by releasing procoagulants, tissue factors, and fibrinolytic proteins, or by invading the vessel wall In cancer patients including RCC, increased blood hypercoagulation can occur which causes an increased risk of arterial thrombosis and thromboembolic events, whereas one of the ways statins reduce death is by preventing thrombosis (17) Furthermore, our study tried to evaluate comprehensively the synergistic effect of statin in RCC patients receiving targeted therapy McKay et al (25) discovered that patients who had targeted therapies and concomitant statins had improved OS compared to non-statin patients (25 6 versus 18 9 months, respectively) with insignificant differences in drug-related toxicity Although statin has been proven to improve the OS, this parameter has a weakness because it can be affected by bias from external factors and confounding factors
There is currently no high level of evidence demonstrating the advantage of adjuvant radiation therapy, VEGFR, or mTOR inhibitors for improving survival, and these treatments are not recommended in adjunctive contexts due to unfavorable tolerability Given that a third of RCC patients will develop recurrence or advancement after nephrectomy, any adjunctive therapies to reduce the progression and improve cancer-related survival were considered a substantial benefit
In this study, we assessed the effects of statin as adjunctive therapy on several other oncology outcomes including PFS, DFS, and CSS Based on the results of the combined analysis, we found that statins had an insignificant effect on CSS in RCC patients undergoing nephrectomy procedures (p = 0 47) These results differ from a metaanalysis study by Nayan et al , which found that statins were significantly associated with improved cancer-specific survival (HR 0 67) (26) The discrepancy could be attributed to several factors, including the inclusion of n o n - s u r g i c a l l y t r e a t e d R C C i n t h e e a r l i e r r e v i e w
According to the literature, the outcome of CSS in patients with surgically treated and non-surgically treated RCC differs, therefore combining the populations may have resulted in bias After performing a combined analy-
sis using Forest plots, we found that statins had no significant effect on DFS and PFS in RCC patients undergoing nephrectomy These results are in accordance with a meta-analysis by Nayan et al which included 2 studies, with the result that there was no relationship between statin administration in PFS and DFS in RCC patients in general (22)
Various statin mechanisms for reducing cancer progression and death in RCC patients have been discussed in the literature Statins have previously been proven in vitro and in vivo to reduce proliferation, angiogenesis, and tumor invasion, thereby reducing cancer growth (27) Data suggests that in general statin reduces cancer growth by two possible mechanisms, including cholesterol-dependent and cholesterol-independent pathways Statins limit mevalonate production and the generation of downstream lipid isoprenoid intermediates in the HMGCoA pathway The latter chemical regulates angiogenesis, apoptosis, and inflammation In the cholesterol-independent process, interactions with proteasomes and lymphocyte-function antigen 1 agents have impacts on invasion, cell adhesion, inflammation, and proliferation The latest evidence suggests that statins can decrease RCC cell growth by prompting cell cycle arrest and apoptosis in a dose and time-dependent manner Furthermore, statins suppress the phosphorylation of AKT, mTOR, and ERK, resulting in decreased RCC cell motility (28)
Although there are various mechanisms through which statins have been shown to prevent cancer progression, in this meta-analysis, we discovered that statins did not provide substantial benefits in preventing cancer progression The insignificant results in this study could be attributed to lower statin bioavailability due to liver metabolism and variations in lipid metabolism in RCC (29) Statins are selectively absorbed by the liver, with less than 5% of the provided dose reaching the systemic circulation, resulting in limited statin penetrating RCC cells (28)
Furthermore, lipid metabolism in RCC differs from that of other cancers RCC has much lower expression of cholesterol synthase proteins including HMG-CoA reductase (HMGCR) than adjacent normal tissues (30) In fact, the major mechanism of statins is HMGCR downregulation
This might explain the reason that statins have a lower impact on RCC than on other forms of cancer Statin plasma levels depend on dose, statin type, and liver function
The higher the dose the higher level of statin in the plasma Lipophilic statin (atorvastatin, simvastatin, lovastatin, fluvastatin, and pitavastatin) tends to have higher uptake in the liver than hydrophilic statin (pravastatin and rosuvastatin) which can affect the liver function and rising the creatinine kinase level (28) Statin plasma levels are higher in altered liver function patients due to reduced statin metabolism and transport activities (31)
In general, this review provided evidence of the beneficial effect of statin on improving the OS of surgically treated RCC patients Despite the insignificant result of CSS, DFS, and PFS, the potential role of statins as adjunctive therapy in surgically treated RCC still needs to be explored This meta-analysis provides support for future prospective and randomized controlled studies to evaluate the potential benefit of statins in extending the survival of surgically treated RCC patients, especially when
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11672 5
Statin affecting survival in surgically treated RCC
considering
the limited efficacy and toxicity of targeted therapies in adjunctive settings
There are several limitations to this review This review was confined only to retrospective cohort studies, which cannot establish causality Furthermore, there was significant heterogeneity among the studies due to variation of histological subgroups, surgical technique, intervention protocol, and RCC stage, which we could not further analyze using subgroups analysis due to the lack of data Moreover, the several included studies were conducted o n s m a l l s a m p l e s i z e a n d i n a s i n g l e i n s t i t u t i o n Therefore, larger cohorts, and multi-institutional or population-based research are necessary
CONCLUSIONS
In the context of limited recommendations for adjunctive immunotherapy or targeted therapy for improving OS of surgically treated RCC patients, the present review highlights the substantial benefits of statin for improving OS in this population Even though the outcomes for CSS, DFS, and PFS were insignificant, the potential role of statins as a supplementary therapy in surgically treated RCC still requires further investigation To confirm the beneficial effects of statin on surgically treated RCC more evidence from prospective and clinical studies may be required
REFERENCES
1 Bray F, Ferlay J, Soerjomataram I, Siegel RL, et al Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries CA Cancer J Clin 2018; 68:394-424
2 Hanna N, Sun M, Meyer CP, et al Survival Analyses of Patients With Metastatic Renal Cancer Treated With Targeted Therapy With or Without Cytoreductive Nephrectomy: A National Cancer Data Base Study J Clin Oncol 2016; 34:3267-75
3 Krabbe LM, Bagrodia A, Margulis V, Wood CG Surgical Management of Renal Cell Carcinoma Semin Intervent Radiol 2014; 31:27
4 Teloken PE, Thompson RH, Tickoo SK, et al Prognostic Impact of Histological Subtype on Surgically Treated Localized Renal Cell Carcinoma J Urol 2009; 182:2132-6
5 Heide J, Ribback S, Klatte T, et al Evaluation of the prognostic role of co-morbidities on disease outcome in renal cell carcinoma patients World J Urol 2020; 38:1525-33
6 B r i e r l e y J , G o s p o d a r o w i c z M D , W i t t e k i n d C T T N M Classification of Malignant Tumors International Union Against Cancer 8th Oxford, England: Wiley; 2017 Wiley 2017
7 Larkin JMG, Eisen T Kinase inhibitors in the treatment of renal cell carcinoma Crit Rev Oncol Hematol 2006; 60:216-26
8 Rini BI, Escudier B, Tomczak P, et al Comparative effectiveness of axitinib versus sorafenib in advanced renal cell carcinoma (AXIS): a randomised phase 3 trial Lancet 2011; 378:1931-9
9 Sternberg CN, Davis ID, Mardiak J, et al Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial J Clin Oncol 2010; 28:1061-8
10 Li X, Shong K, Kim W, et al Prediction of drug candidates for
clear cell renal cell carcinoma using a systems biology-based drug repositioning approach EBioMedicine 2022; 78:1039633
11 Neumann E, Klaiber P, Freitag K, et al Assessment of concomitant non-oncologic medication in patients with surgically treated renal cell carcinoma: impact on prognosis, cell-cycle progression and proliferation J Cancer Res Clin Oncol 2019; 145:1835-43
12 Santoni M, Monteiro FSM, Massari F, et al Statins and renal cell carcinoma: Antitumor activity and influence on cancer risk and survival Crit Rev Oncol Hematol 2022; 176:103731
13 Seckl MJ, Ottensmeier CH, Cullen M, et al Multicenter, Phase I
Pravastatin Added to First-Line Standard Chemotherapy in SmallCell Lung Cancer (LUNGSTAR) J Clin Oncol 2017; 35:1506-14
14 Kawata S, Yamasaki E, Nagase T, et al Effect of pravastatin on survival in patients with advanced hepatocellular carcinoma A randomized controlled trial Br J Cancer 2001; 84:886-91
15 Alarfi H, Youssef LA, Salamoon M A Prospective, Randomized, Placebo-Controlled Study of a Combination of Simvastatin and C h e m o t h e r a p y i n M e t a
2020:4174395
16 Nayan M, Finelli A, Jewett MAS, et al Statin use and kidney cancer outcomes: A propensity score analysis Urol Oncol 2016; 34:487 e1-487 e6
17 Viers BR, Houston Thompson R, Psutka SP, et al The association of statin therapy with clinicopathologic outcomes and survival among patients with localized renal cell carcinoma undergoing nephrectomy Urol Oncol 2015; 33:388 e11-8
18 Kaffenberger SD, Lin-Tsai O, Stratton KL, et al Statin use is associated with improved survival in patients undergoing surgery for renal cell carcinoma Urol Oncol 2015; 33:21 e11-21 e17
19 Hamilton RJ, Morilla D, Cabrera F, et al The association between statin medication and progression after surgery for localized renal cell carcinoma J Urol 2014; 191:914-9
20 Higgins JP, Green S Cochrane Handbook for Systematic Reviews of Interventions®
21 Haddad AQ, Jiang L, Cadeddu JA, et al Statin Use and Serum Lipid Levels Are Associated With Survival Outcomes After Surgery for Renal Cell Carcinoma Urology 2015; 86:1146-52
22 Nayan M, Punjani N, Juurlink DN, et al Statin use and kidney cancer survival outcomes: A systematic review and meta-analysis Cancer Treat Rev 2017; 52:105-16
23 Luo Y, She DL, Xiong H, et al The Prognostic Effect of Statin Use on Urologic Cancers: An Updated Meta-Analysis of 35 Observational Studies Medicine (Baltimore) 2015; 94:e1523
24 Wu P, Xiang T, Wang J, et al Statin use and the overall survival of renal cell carcinoma: A meta-analysis Clin Invest Med 2020; 43:E17-23
25 McKay RR, Lin X, Albiges L, et al Statins and survival outcomes in patients with metastatic renal cell carcinoma Eur J Cancer 2016; 52:155-62
26 Nayan M, Hamilton RJ, Finelli A, et al The value of complementing administrative data with abstracted information on smoking and obesity: A study in kidney cancer Can Urol Assoc J 2017; 11:167-71
27 Di Bello E, Zwergel C, Mai A, Valente S The Innovative Potential of Statins in Cancer: New Targets for New Therapies Front Chem 2020; 8:516
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11672 G
6
Adli, N Yogiswara, I Bagus Gde Tirta Yoga Yatindra, R Maulana Putra, W Djatisoesanto
I I , R a n d o m i z e d , D o u b l e - B l i n d , P l a c e b o - C o n t r o l l e d T r i a l o f
s t a t i c B r e a s t C a n c e r J O n c o l 2 0 2 0 ;
Statin affecting survival in surgically treated RCC
28 Petyaev IM Improvement of hepatic bioavailability as a new step for the future of statin Arch Med Sci 2015; 11:406-10
29 Petyaev IM Improvement of hepatic bioavailability as a new step for the future of statin Arch Med Sci 2015; 11:406
30 Stepanovska Tanturovska B, Manaila R, Fabbro D, Huwiler A
Lipids as Targets for Renal Cell Carcinoma Therapy Int J Mol Sci 2023; 24:3272
31 Calderon RM, Cubeddu LX, Goldberg RB, Schiff ER Statins in the Treatment of Dyslipidemia in the Presence of Elevated Liver Aminotransferase Levels: A Therapeutic Dilemma Mayo Clin Proc 2010; 85:349
Correspondence
Ghazian Adli ghazianadli@gmail com
Niwanda Yogiswara niwandayogiswara@gmail com
Ida Bagus Gde Tirta Yoga Yatindra tirtayogastudi@gmail com
Rheza Maulana Putra putrarhe@gmail com
Wahjoe Djatisoesanto (Corresponding Author) djatisoe@gmail com
Department of Urology, Faculty of Medicine, Universitas Airlangga Dr Soetomo General-Academic Hospital, Surabaya, East Java, Indonesia
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11672 7
Summary
Introduction: Challenges in identifying small testicular arteries and lack of microscopic experience have led to a rising trend in the use of laparoscopic technique for pediatric and adolescent varicocele. The controversy over artery ligation (AL) and artery preservation (AP) during laparoscopic varicocelectomy (LV) is still debatable. This study investigates the effectiveness of AL and AP during LV in pediatric and adolescent varicocele cases.
Methods: The systematic searches based on PRISMA guideline were conducted in PubMed, Scopus, ScienceDirect, Web of Science and ProQuest databases with pre-defined keywords. Both quantitative and qualitative analyses were performed to assess catch-up growth, persistence, recurrence, hydrocele, operative time, post-operative testicular volume, and sperm analysis. Results: A total of 1512 patients from 9 eligible studies were included. There were no significant differences in catch up growth (OR 0.89; 95%CI 0.53, 1.51; p = 0.68) or hydrocele incidence (OR 0.59; 95%CI 0.28, 1.24; p = 0.16). The recurrence rate and persistence rate in AP group is significantly higher compared to AL group (OR 2.95; 95%CI 1.53, 5.68; p = 0.001 and OR 5.13; 95% CI 2.04, 12.88; p = 0.0005, respectively).
The mean operative time during laparoscopic varicocelectomy is significantly longer when arteries are preserved as opposed to when they are ligated (OR 5.33; 95%CI 2.05, 8.60; p = 0.001). AL and AP both improved testicular volume and post-operative sperm analysis.
Conclusions: AL showed higher efficacy and comparable safety to AP. We recommend using AL with lymphatic sparing to minimize hydrocele complications.
KEYWORDS: Adolescent; Pediatric andrology; Varicocele; Undescended; Testes; Laparoscopic; Ligation; Testicular artery.
Submitted 31 July 2023; Accepted 3 August 2023
INTRODUCTION
Varicocele is a medical condition characterized by the enlargement of the pampiniform plexus veins within the spermatic cord and is known to be a leading cause of male infertility (1, 2). The incidence in boys until puberty ranges from 2% to 11% and increases up to 16% in postpubertal adolescents (3, 4). Inadequate management of varicocele in adolescents can lead to impairment of testicular growth, which can result in spermatogenesis dysfunc-
tion and infertility. Discomfort due to varicocele, testicular size asymmetry exceeding 20% or testicular atrophy, bilateral varicocele, and high-grade varicocele are indications of varicocelectomy in adolescents (5, 6). Previous studies have shown that testicular hypotrophy can improve in 40100% of cases after varicocelectomy, significantly enhancing parameters such as sperm concentration, total and progressive motility, and morphology (7, 8).
Microsurgical varicocelectomy is still rarely used in the pediatric population due to several factors (9). Lack of experience with microscopic techniques, smaller testicular arteries, and lower blood pressure from systemic arteries in pediatric patients are difficulties that make arterial identification more difficult in the subinguinal or inguinal approach. Consequently, there has been a growing adoption of laparoscopic techniques by pediatric urologists over the past decade. This is primarily attributed to the numerous advantages these techniques offer, including faster operating and recovery times as well as visualization capabilities comparable to microsurgery (10, 11).
Laparoscopic varicocelectomy (LV) using Palomo's method, which involves the simultaneous ligation of the internal spermatic vein (ISV) and internal spermatic artery (ISA), has demonstrated a favorable success rate without any significant increase in the risk of testicular atrophy (12). However, there is debate among pediatric urologists regarding the importance of artery preservation during varicocelectomy. The controversy surrounding the need for artery preservation (AP) during LV has also been reported in several studies. Some studies suggest that the AP procedure is more appropriate as it prevents iatrogenic testicular trauma and reduces the incidence of postoperative hydrocele, while others report that artery ligation (AL) has a low recurrence and hydrocele rate but may disrupt testicular growth and future fertility. Conversely, the AP procedure has been associated with higher rates of persistence and recurrence compared to AL during LV (3, 4, 13). Currently, there is a lack of well-established evidencebased medicine (EBM) studies comparing AL and AP during LV. In order to determine the impact of arterial ligation following LV, this systematic review and meta-analysis aims to assess the efficacy and safety of laparoscopic varicocelectomy, comparing procedures with or without artery preservation in pediatric and adolescent population.
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11627 1
SYSTEMATICREVIEW
A systematic review and meta-analysis on the efficacy of internal spermatic artery ligation during laparoscopic varicocelectomy in children and adolescents: Is it safe?
AhmadNurfakhri Syarief, Ilham Akbar Rahman, Agung Ravi Saputra Sangadji, Tarmono Djojodimedjo, Fikri Rizaldi
DOI: 10.4081/aiua.2023.11627
Department of Urology, Faculty of Medicine, Universitas Airlangga and Dr. Soetomo General-Academic Hospital, Surabaya, East Java, Indonesia.
MATERIALS AND METHODS
This study followed a predetermined protocol according to the guidelines outlined by the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) (14) Initial searches were conducted to ensure that the specific characteristics outlined in the PICO (Population, Intervention, Comparison, Outcome) framework had not been previously investigated, thereby avoiding duplication of existing metaanalyses The literature searches were conducted using several databases, including PubMed, Scopus, ScienceDirect, Web of Science, and ProQuest The selected keywords used for the search were described as “varicocele” , “varicocelectomy ” , “laparoscopic varicocelectomy” , “laparoscopic Palomo” , “ligated artery” , “artery ligation” , “spared artery” , “artery sparing” , “preserved artery” , and “artery preservation” The study's protocol was registered with PROSPERO (CRD42023445437)
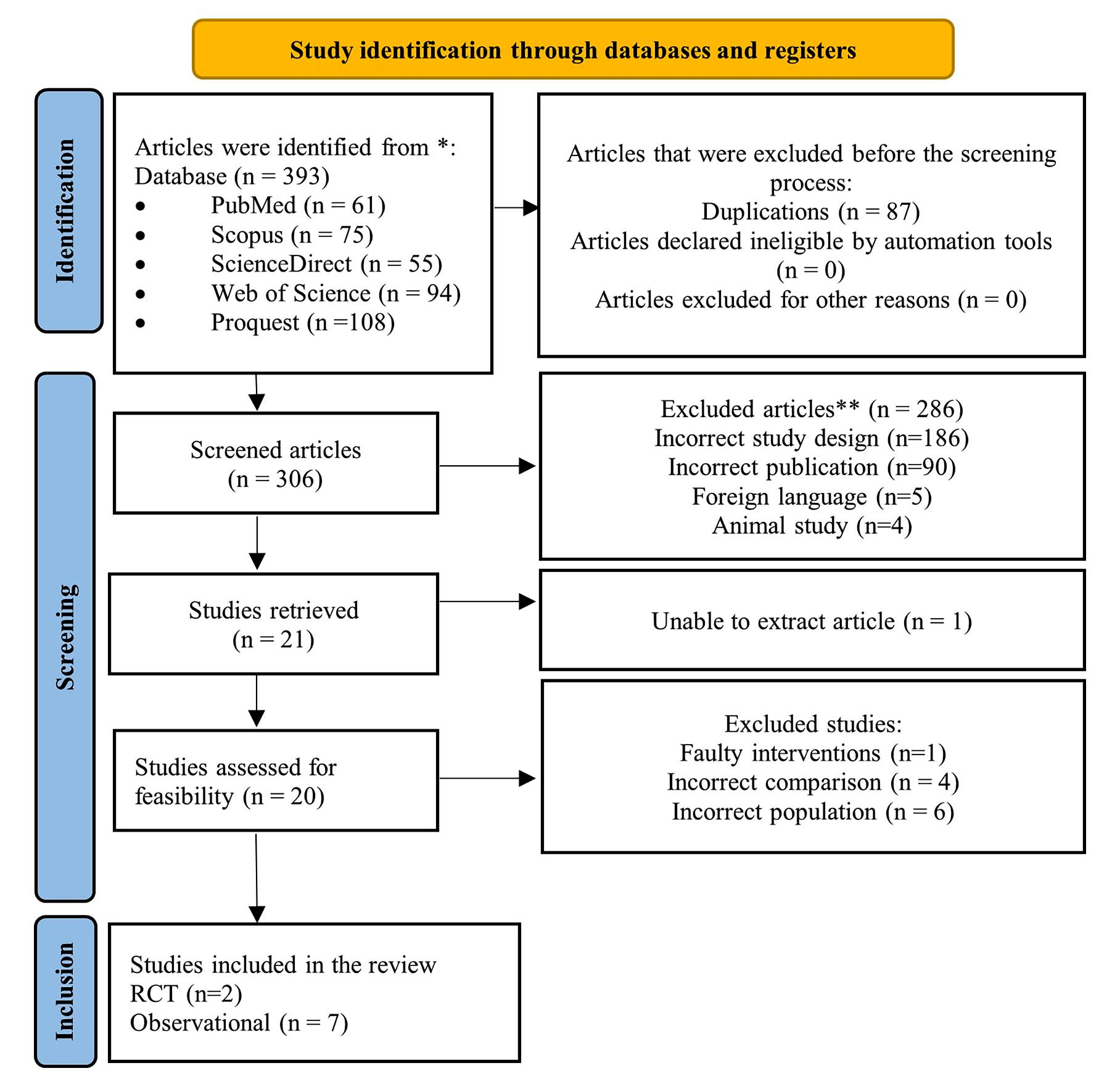
Criteria for inclusion and exclusion
To be considered for inclusion, eligible articles need to meet specific criteria These criteria included comparative studies, written in English, having at least two comparison groups, and reporting data on catch-up growth, persistence, recurrence, hydrocele, and operation time in laparoscopic varicocelectomy with or without artery preservation
During the selection process, studies that fell under the following categories were excluded: animal experimental studies, publication types other than original research, unpublished articles, and abstract-only findings
Data extraction
Two separate researchers collected the data using a predefined extraction template In cases of discrepancies or disagreements during data extraction, a third investigator would be involved to discuss and make the final decision
The extracted information encompassed various aspects, including study details (such as authors, publication date, study design, sample size, inclusion and exclusion criteria, and follow-up duration), subject characteristics at baseline (such as age, intervention types, and study location), also qualitative and quantitative outcomes (such as catchup growth, persistence, recurrence, hydrocele, operation time, testicular volume, and sperm analysis)
Quality assessment
The assessment of potential research bias in non-randomized studies was conducted using the NewcastleOttawa Scale (NOS), which evaluates parameters related to selection, comparability, and exposure The results obtained from the NOS assessment are categorized into three groups A score ranging from 0 to 3 implicates a low-quality study, a score from 4 to 6 implicates a medium-quality study, and a score from 7 to 9 implicates a high-quality study For randomized controlled trial (RCT) studies, the assessment of potential research bias was conducted using the Cochrane RoB tools V2, which evaluates four domains, such as randomization process, deviations from intended intervention, missing outcome data, measurement, and selection of reported outcome (15)
Statistical analysis
The measured endpoints included catch-up growth, persistence, recurrence, hydrocele incidence, and mean operative time For the dichotomous variable analysis, Odds Ratio (OR) with a 95% Confidence Interval (CI) was used, and a p-value below 0 05 was considered statistically significant The continuous variable was assessed using Mean Difference (MD) Heterogeneity between studies was evaluated using I2, where an I2 value above 50% indicated high heterogeneity and a random-effects model was applied for pooled analysis If I2 was less than 50%, a fixed-effects model was used The statistical analysis
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11627
2
A
Nurfakhri Syarief, I Akbar Rahman, A Ravi Saputra Sangadji, T Djojodimedjo, F Rizaldi
Figure 1. identification of studies
Table 1.
Characteristics data of included studies
was conducted using RevMan 5 4 for Windows software, and the results were presented through Forest plots and descriptive narratives
RESULTS
Systematic search results
An initial 393 articles were found according to the used keywords Complete eligibility assessment resulted in nine matched articles for further qualitative and quantitative analysis (Figure 1) Seven included studies were retrospective cohorts in design, while the other two were RCTs
Baseline characteristics of the included studies
This research included a total of 1512 patients with a mean age of 13 7 years, ranging from 6 to 20 years old These participants comprised various articles published between 1999 and 2020
This study represented a total of 1409 patients with unilateral left-side varicocele and 103 patients with bilateral varicocele Most of the participants presented with varicocele grade II-III The detailed characteristics and outcomes data of the included studies are shown in Table 1 and Table 2
Risk of bias assessment
Regarding the selection aspect, all included studies demonstrated a robust selection process, ensuring the populations were fairly representative of young men with varicocele Moreover, the comparative and exposure aspects were well addressed, with adequate follow-up duration and relatively low dropout rates Based on the final assessment, three studies achieved a NOS score of eight, while the other four studies received a NOS score of seven, indicating a low risk of bias (Table 3) However, the RCT studies assessed using the Cochrane RoB tool V2 (Figure 2) raised some concerns due to insufficient clarity regarding the randomization process described in the article
Risk of bias assessment
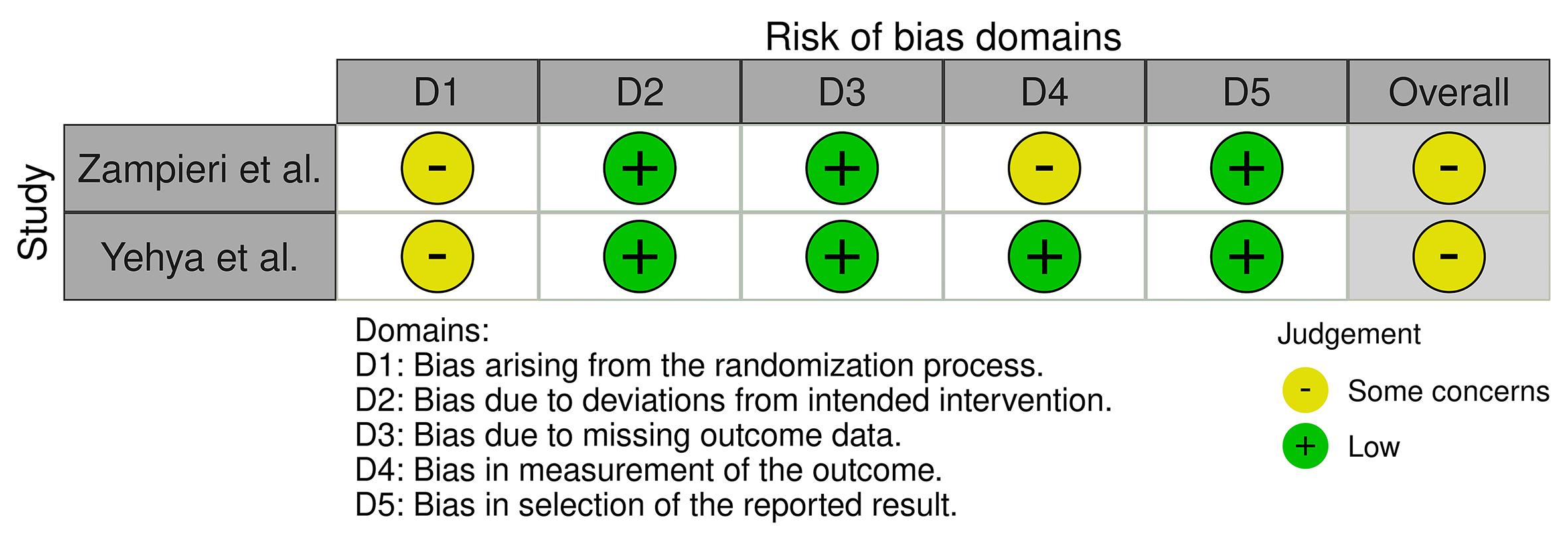
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11627 3 Safety of artery ligation in pediatric laparoscopic varicocelectomy
Study Design Age (years) Inter vention Sample Varicocele type Degree Outcome Follow up size of varicocele (month) Lund, 1999 (17) Observational 12 9 (8-15) Laparoscopy varicocelectomy AP 13 6 (left), NR Recurrency, catch up growth 6-48 AL 7 7 (bilateral) NR F Var et, 2000 (16) Observational 12 15 (7-16) Laparoscopy varicocelectomy AP 28 84 (left), NR Persistency, testicular hypotrophy/ 11 1 (2-36) AL 59 3 (bilateral) NR atrophy, catch up growth Ciro Espos to, 2001 (6) Observational 11 5 (6-17) Laparoscopy varicocelectomy AP 30 209 (left), I: 26, II :98, 7 Hydrocele, Recurrency 26 (12-72) AL 181 2 (bilateral) III: 8 Nicola Zampieri, RCT 14 3 (12-16) Laparoscopy varicocelectomy AP 59 59 (left) II: 82, III: 40 Recurrency/persistency, Hydrocele, 18 2007 (20) AL 63 63 (left) Operative time, Sperm quality parameters A M Fast, 2013 (13) Observational 15 5 (9 3-20 6) Laparoscopy varicocelectomy AP 41 28 (left), 13 (bilateral) NR Recurrency, catch up growth 30 5 or lymph node sparing AL 312 241 (left), 71 (bilateral) NR 33 3 laparoscopy varicocelectomy K S Kim, 2013 (19) Observational 13 2 ± 2 1 Laparoscopy varicocelectomy AP 50 50 (left) II: 10, III: 40 Recurrency/persistency, Catch up growth, 21 ± 12 3 AL 42 42 (left) II: 9, III: 33 Operative time Weimin Yu, 2015 (4) Observational 17 3 ± 2 4 Laparoscopy varicocelectomy AP 57 122 (left) II: 36, III: 21 Recurrency, Hydrocele, Catch up growth, 17 1 ± 7 4 AL 65 II: 41, III: 24 Sperm quality parameters 17 8 ± 7 0 Ciro Espos to, 2017 (8) Observational 12 5 (8-17) Laparoscopy varicocelectomy AP 10 345 (left) III: 10 Recurrency, operative time, testis volume, 28 8 ± 8 3 or lymph node sparing AL 335 II: 66, III: 269 hydrocele laparoscopy varicocelectomy Abdelaziz Yehya, RCT 14 25 ± 1 6 Lymph node sparing AP 80 160 (left) II: 28, III: 52 Persistency, Catch up growth, operative time, 42 2020 (18) laparoscopy varicocelectomy AL 80 II: 32, III: 48 testicular volume NR: Not Reported; AP: Artery Preservat on; AL: Artery Ligation
Figure 2
Table 2. Outcomes data of included studies
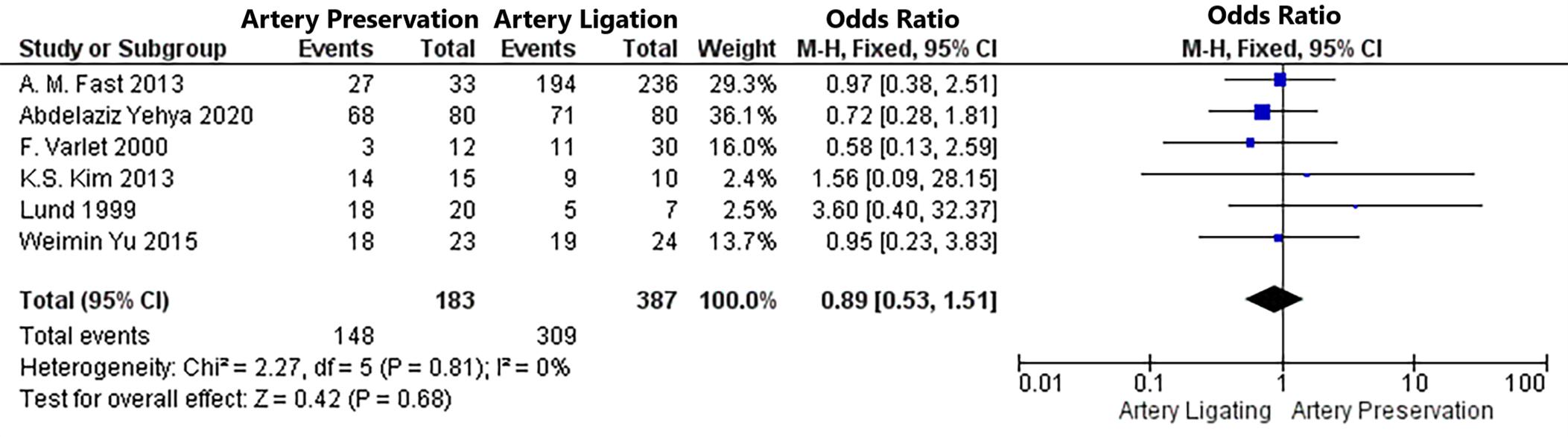
Table 3. Risk of bias assessmment using Newcastle Ottawa Scale
in the amount of catch-up growth between AL and AP during laparoscopic varicocelectomy (OR 0 89; 95%CI 0 53, 1 51; p = 0 68) (Figure 3) The fixed-effects model was used due to low heterogeneity between studies (p = 0 81; I2 = 0%) Of the six studies, Fast et al and Yehya et al represented higher statistical weight compared to other studies due to a larger sample size (13, 18)
Meta-analysis result on persistence rate
Meta-analysis result on catch-up growth
Based on a meta-analysis of the six papers included (4, 13, 16-19), there is no statistically significant difference
Four studies were analyzed in this meta-analysis (16, 1820), the persistence rate revealed a significant difference in which the AP group provided the higher persistence compared to the AL group (OR 5 13; 95%CI 2 04, 12 88; p = 0 0005) (Figure 4) Because of the low heterogeneity observed between studies, the fixed-effects model was employed (p = 0 88; I2 = 0%)
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11627
4
A
Nurfakhri Syarief, I Akbar Rahman, A Ravi Saputra Sangadji, T Djojodimedjo, F Rizaldi
Authors Selection Comparatibility Exposure Total Score Lund, 1999 *** ** *** 8 Varlet et al 2000 *** ** *** 8 Esposito et al 2001 *** ** *** 8 Kim et a 2013 *** ** ** 7 Fast et al 2013 *** ** ** 7 Weimin Yu et al 2015 *** ** ** 7 Esposito et al 2018 *** ** ** 7
Study Intervention Recurrence Persistence Hydrocele Catch-up growth Post-op Operative time Post-op Sperm Analysis Volume testis 12 24 F inal Hypotrophy/ (minutes) Sperm count Motility Morphology Pre op Post op months months visit Testicular Atrophy (miillion/ml) (%) (%) Lund, 1999 AP 2/20 NR 3/20 NR NR 18/20 NR NR NR NR NR NR NR AL 2/7 NR 0/7 NR NR 5/7 NR NR NR NR NR NR NR F Var et, 2000 AP NR 9/28 11 NR NR 3/12 1/12 NR NR NR NR NR NR AL NR 5/60 NR NR 11/30 3/30 NR NR NR NR NR NR Ciro Espos to, 2001 AP 2/30 NR 0/30 NR NR NR 0/30 30 (20-70) NR NR NR NR NR AL 3/181 NR 14/181 NR NR NR 0/181 NR NR NR NR NR Nicola Zampieri, 2007 AP 5/59 1/59 1/59 NR NR NR NR 35-60 73 81 45 73 45 13 NR NR (0 2-250) (0-75) (9-89) AL 0/63 0/63 8/63 NR NR NR NR 20-40 58 85 39 04 38 NR NR (3 5-182) (11-68) (6-85) A M Fast, 2013 AP 5/41 NR NR 12/33 22/33 27/33 0/41 NR NR NR NR NR NR AL 17/312 NR NR 81/236 147/236 194/236 0/312 NR NR NR NR NR NR K S Kim, 2013 AP 8/50 3/50 0/50 14/15 NR NR 0/50 83 1 ± 31 8 NR NR NR NR NR AL 1/42 1/42 2/42 9/10 NR NR 0/42 72 5 ± 33 4 NR NR NR NR NR Weimin Yu, 2015 AP 3/57 NR 4/57 14/23 18/23 NR NR 41.3 ± 8.8 62.5 ± 39.2 52.2 ± 16.6 11.5 ± 1.5 NR NR AL 2/65 NR 4/65 10/24 19/24 NR NR 39 5 ± 7 1 60 4 ± 38 2 49 1 ± 19 9 10 7 ± 1 5 NR NR Ciro Espos to, 2017 AP 1/10 NR 2/10 NR NR NR 0/10 26 (18-50) NR NR NR 12 4 ± 4 9 NR 29 3 ± 10 3 AL 4/335 NR 23/335 NR NR NR 0/335 17 (14-45) NR NR NR 12 0 ± 5 2 15 4 ± 4 8 17 6 ± 5 3 Abdelaziz Yehya, 2020 AP NR 8/80 0/80 NR 68/80 NR 0/80 40 ± 2 6 NR NR NR 12 2 ± 3 1 16 3 ± 4 AL NR 1/80 0/80 NR 71/80 NR 0/80 35 ± 2.8 NR NR NR 14.1 ± 4.6 17.1 ± 5.1 NR: Not Reported; AP: Artery Preservat on; AL: Artery Ligation
Figure 3. Meta-analysis result on catch-up growth
Meta-analysis result on recurrence rate
Seven studies were analyzed for this outcome (8, 13, 1721) On pooling analysis of the data, the recurrence rate in AP group is higher compared to AL group (OR 2 95; 95%CI 1 53, 5 68; p = 0 001) (Figure 5) Most of the studies demonstrated a higher recurrence rate in artery preservation group, except for one study (17) The fixed-effects model was applied because there was minimal heterogeneity observed between studies (p = 0 25; I2 = 23%)
Meta-analysis result on hydrocele incidence
The analysis of six included studies reveals that there is no significant statistical difference in hydrocele incidence between AL and AP during laparoscopic varicocelectomy (OR 0 59; 95%CI 0 28, 1 24; p = 0 16) (Figure 6) (4, 8,
17, 19-21) The choice of the fixed-effects model was based on the minimal heterogeneity observed among the studies (p = 0 08; I2 = 50%) Varlet et al reported 11 patients with postoperative hydrocele, but the number of patients in each group was unknown (16)
Meta-analysis result on mean operative time
According to a meta-analysis of the four papers included (8, 18-20), the mean operative time during laparoscopic varicocelectomy is significantly longer when arteries are preserved as opposed to when they are ligated (OR 5 33; 95%CI 2 05, 8 60; p = 0 001) (Figure 7) The mean operative time was expressed in minutes Due to significant heterogeneity observed between studies, the randomeffects model was employed (p = 0 02; I2 = 69%) Esposito
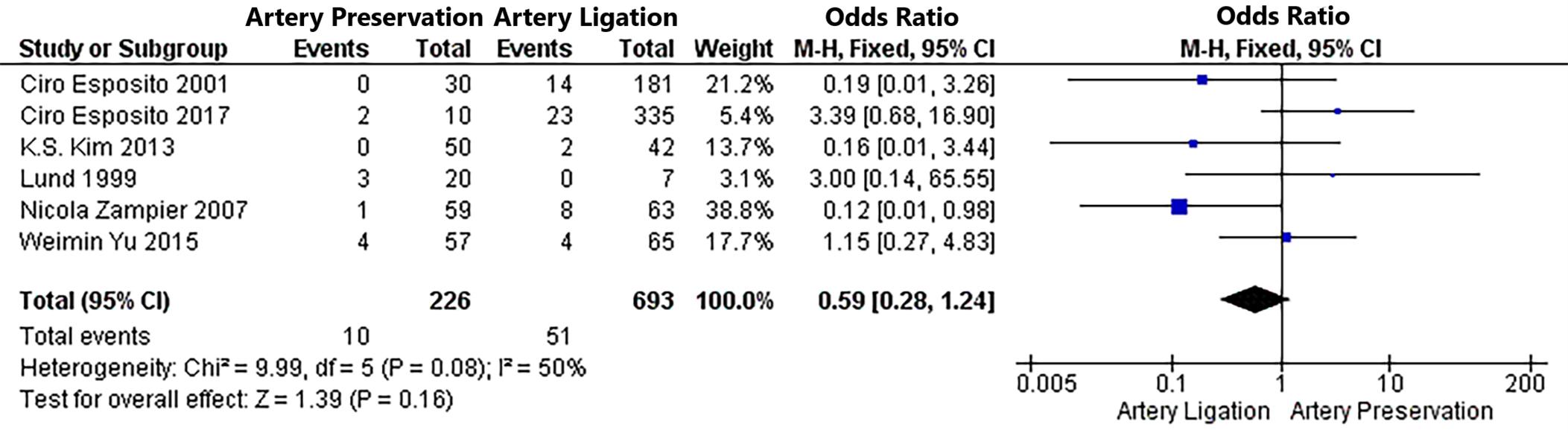


Archivio Italiano di Urologia e Andrologia 2023; 95(3):11627 5 Safety of artery ligation in pediatric laparoscopic varicocelectomy
Figure 4. Meta-analysis result on persistence rate
Figure 5. Meta-analysis result on recurrence rate
Figure 6 Meta-analysis result on hydrocele incidence
et al reported an average operating time of 30 minutes However, it was unclear for each group (6)
Qualitative synthesis of testicular volume
In this study, two separate studies reported the change in testicular volume before and after surgery (8, 18) There was an increase in testicular volume observed in both AL and AP groups during laparoscopic varicocelectomy However, the significance of the difference could not be analyzed due to the absence of one data point in the postsurgery testicular volume in the study conducted by Esposito et al (8)
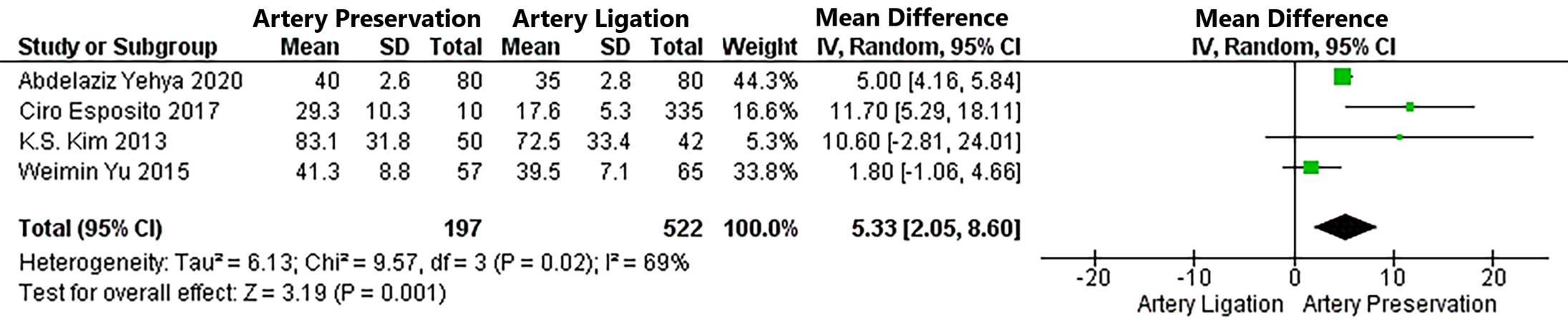
Qualitative synthesis of postoperative sperm analysis
Two included studies provided information regarding post-surgery sperm analysis in the AL and AP groups (4, 20) The results reported that AL and AP laparoscopic varicocelectomy both resulted in normal sperm parameters following the surgery, with slightly higher values observed in the AP group However, due to the lack of studies reporting sperm analysis after the surgery, it was not possible to analyze and provide the quantitative data comprehensively However, the initial result of this qualitative analysis may provide an idea that there is no difference in postoperative sperm outcome between AP and AL during laparoscopic varicocelectomy
DISCUSSIONS
This is the first systematic review and meta-analysis that compares the efficacy and safety of AL and AP during LV in pediatric and adolescent population In our research, we have prioritized catch-up growth as the main focus due to its significant potential for enhancing testicular function and positively influencing fertility outcomes in individuals with varicocele Both AL and AP groups demonstrated an increase of 63 to 86% testicular catchup growth within 12 to 24 months after surgery (22-25)
Weimin Yu et al in their study, reported that a lower rate of catch-up growth was observed in the AL group during the first year of follow-up They suggested that the remodeling of neovascularization in testicular drainage after the AL procedure, which is important for maintaining normal testicular metabolism, may require a relatively longer time (4) The findings of similar outcome in catch-up growth between AL and AP procedures in this study may be due to the fact that both techniques demonstrated identical effects on testicular blood flow (26) As
observed in a recent meta-analysis, surgical correction of varicocele may result in superior catch-up growth of the affected testis It can be inferred that the acceleration of growth in the affected testes is attributed to the removal of the detrimental effects of varicocele on testicular development (19)
One of the concerns in this study was the incidence of postoperative hypotrophic testes From the analysis of nine included studies, only study conducted by Varlet et al reported the incident (4, 8, 13, 16-21) Contrast with Yehya et al , whose study reported a significant increase in testicular volume even though the ISA were ligated during LV (18) Ligation above the level of the internal inguinal ring is considered safe because there are collateral arteries below the internal ring that play a role in providing an adequate blood supply to the testicle, preventing a significant decrease in oxygen and nutrient delivery (27, 28) Those collateral arteries become more favorable for maintaining blood supply to the testicles as a result of reduced blood flow from the main artery after ligation (8) Previous surgery on the inguinal area like hernia repair, may result in significant injury to the collateral testicular arteries, such as the cremasteric and differentialis arteries These injuries may provide an impact on postoperative hypotrophy events in case AL procedure is performed (16) Although no studies have specifically observed the role of collateral arteries in testicular volume growth in the ligation artery group, an increase in volume s u g g e s t s t h e o c c u r r e n c e o f v a s c u l a r a d a p t a t i o n s However, it is important to note that an increase in testicular volume after arterial ligation is not always accompanied by an increase in testicular function or sperm quality Spermatogenesis may still be impaired due to loss of primary blood supply (20)
Sperm analysis after varicocelectomy in adolescents is not routinely examined because of the barriers of parental consent, even though it is an important parameter after varicocelectomy (29) This is maybe the reason that only two of our nine included studies reported the sperm analysis parameters post-operation (4, 20) According to the findings of Zampieri et al , the AP group demonstrated superior semen quality compared to the AL group, even though there is no statistically significant difference between the two groups In terms of mean sperm concentration outcome, the AP group demonstrated a higher value compared to the AL group (73 81 x 106 and 58 85 x 106, respectively) Furthermore, the AP group exhibited higher sperm motility (45 73%) compared to the AL
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11627 A
6
Nurfakhri Syarief, I Akbar Rahman, A Ravi Saputra Sangadji, T Djojodimedjo, F Rizaldi
Figure 7
Meta-analysis result on mean operative time
group (39 04%), with a greater proportion of normal morphology sperm cells (45 13% vs 38%) They believe that AP is necessary since preserving the normal blood supply of the arteries seems more appropriate to prevent testicular damage and dysfunction (20) Therefore, it is important to consider further studies with long-term follow-up to assess the parameters of sperm function and quality in the postoperative evaluation of the AL group before determining whether the AL method adversely affects testicular function and spermatogenesis
Our study reveals a notable contrast in the recurrence and persistence rates between AP and AL groups Specifically, the group that underwent arterial preservation showed a higher recurrence and persistence rate This finding aligns with Kattan et al 's findings, which reported that AP exhibited a higher recurrence rate compared to AL This was mainly due to the presence of blood flow in nonfunctional collateral veins as a result of venous pressure increases following ISV ligation or failing to ligate the small veins along the anterior wall of ISA due to fear of injuring the artery Mass ligation of the gonadal vessels allows for complete obliteration, thus preventing missed collateral veins (30) Another possible reason for persistency could be the existence of collateral veins that originate from the internal spermatic vein below the occlusion site and directly drain into the internal iliac vein or the inferior cava (31) However, there have been several studies reporting a low recurrent rate (0 6-3%), even though the testicular artery and lymphatic vessels are preserved
A study by Chung et al declares that the possibility of missing small periarterial veins can be minimized They can be easily divided and dissected using 3 mm mini laparoscopic instruments (32) However, future research needs to be done on a larger scale to prove this statement
Our investigation showed no significant difference in the incidence of hydroceles between artery preservation and ligation, in contrast to the findings of a study by Zampieri et al , which found a correlation between AL and the development of hydroceles They suggest that the complete ligation of spermatic and lymphatic vessels can cause blood stasis within the scrotum (20) The risk of developing hydrocele may be increased if lymphatic preservation is not performed However, there was no association between artery preservation or ligation and hydrocele incidence, as reported in a study by Weimin Yu et al (4) Liang et al.'s meta-analysis indicated that selecting a lymphatic preservation method is advisable to decrease the occurrence of hydroceles This is because the standard Palomo procedure does not involve the preservation of lymphatic glands, leading to the accumulation of lymphatic fluid in the scrotum, which contributes to a higher risk of hydrocele formation (33) Mathias et al found that there was no significant difference between arterial sparring and ligation regarding the incidence of postoperative hydrocele in lymphatic sparing varicocelectomy Yehya et al also confirmed this by reporting no incidence of hydrocele in both the AP and AL groups during lymphatic sparring LV (18) While we found that the AP group significantly had a longer mean operative time than the AL group, Weimin Yu et al found no statistically significant difference between the two groups (4) The operating time may vary depending on the surgeon's experience (24) This is probably the
reason that this outcome in this study possessed a higher heterogeneity compared to another outcome This meticulous process involves carefully locating and preserving the arterial blood supply while removing or ligating the dilated veins causing the varicocele The surgeon must exercise caution and take the necessary time to ensure the arteries are properly identified and spared from damage Consequently, this longer time requirement is attributed to the surgeon's focus on accuracy and the intricate nature of preserving the arterial blood flow during the procedure (34) Together with practical experience, it appears that there is a learning curve that enables surgeons to perform this technique more efficiently, resulting in shorter operative times as their expertise grows (24)
One of several limitations of this meta-analysis is the lack of RCT studies in contrast with more observational studies RCTs are considered the gold standard for establishing causal relationships due to their rigorous design and randomization process On the other hand, observational studies rely on naturally occurring data and a lack of random assignment of participants, making them more susceptible to confounding factors and biases Moreover, the long-term assessment regarding catch-up growth and testicular function following varicocelectomy in this age group could be feasibly obtained by performing prospective cohort studies and retrospective analyses Several variations such as interventions in LV procedures where some were accompanied by lymphatic sparring and subsequently testicular development which were assessed by different standards became another limitation in this study Therefore, outcome measures such as hydrocele and catch-up growth can be biased We expect that future research will include longterm follow-up and a uniform examination of sperm parameters while adhering to strict ethical approval protocols
CONCLUSIONS
This study highlights the superior efficacy of the AL technique, which maintains similar safety to the AP technique We recommend adopting the AL technique with lymphatic sparing routinely to enhance efficacy and minimize hydrocele complications Additionally, the evaluation of sperm parameters is essential to fully establish the efficacy profile of laparoscopic varicocelectomy in the pediatric and adolescent population
REFERENCES
1 Vanlangenhove P, Everaert K, Van Maele G, Defreyne L Tolerance of glue embolization under local anesthesia in varicoceles: a comparative study of two different cyanoacrylates Eur J Radiol 2014; 83:559-63
2 Elbardisi H, Agarwal A, Majzoub A, Al Said S, Alnawasra H, Khalafalla K, Al Rumaihi K, Al Ansari A, et al Does the number of veins ligated during microsurgical subinguinal varicocelectomy impact improvement in pain post-surgery? Transl Androl Urol 2017; 6:264-270
3 Park S, Kim KS, Lee C, et al Impact of internal spermatic artery preservation during laparoscopic varicocelectomy on recurrence and the catch-up growth rate in adolescents J Pediatr Urol 2014; 10:435-40
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11627 7 Safety of artery ligation in pediatric laparoscopic varicocelectomy
4 Yu W, Rao T, Ruan Y, et al Laparoscopic Varicocelectomy in Adolescents: Artery Ligation and Artery Preservation Urology 2015; 89:150-4
5 Chrouser K, Vandersteen D, Crocker J, Reinberg Y Nerve injury after laparoscopic varicocelectomy J Urol 2004; 172:691-3
6 Esposito C, Monguzzi G, Gonzalez-Sabin MA, et al Results and complications of laparoscopic surgery for pediatric varicocele Int J Ped Surg 2001; 36:767-9
7 Youssef T, Abdalla E Single incision transumbilical laparoscopic varicocelectomy versus the conventional laparoscopic technique: A randomized clinical study Int J Surg 2015; 18:178-83
8 Esposito C, Escolino M, Castagnetti M, et al Two decades of experience with laparoscopic varicocele repair in children: Standardizing the technique J Pediatr Urol 2017; 14:10 e1-10 e7
9 Parrilli A, Roberti A, Escolino M, Esposito C Surgical approaches for varicocele in pediatric patient Transl Pediatr 2016; 5:227-32
10 Hassan JM, Adams MC, Pope JC, et al Hydrocele Formation Following Laparoscopic Varicocelectomy J Urol 2006; 175:1076-9
11 Méndez-Gallart R, García-Palacios M, Rodríguez-Barca P, et al 15 years' experience in the single-port laparoscopic treatment of pediatric varicocele with Ligasure® technology Cir Pediatr 2023; 36:33-9
12 Tong Q, Zheng L, Tang S, et al Lymphatic sparing laparoscopic Palomo varicocelectomy for varicoceles in children: intermediate results J Pediatr Surg [Internet] 2009; 44:1509-13
13 Fast AM, Deibert CM, Van Batavia JP, et al Adolescent varicocelectomy: does artery sparing influence recurrence rate and/or catch-up growth? Androl 2013; 2:159-64
14 Page MJ, McKenzie JE, Bossuyt PM, et al The PRISMA 2020 statement: an updated guideline for reporting systematic reviews BMJ 2021; 29; 372:n71-n71
15 Sterne JAC, Savovic J, Page MJ, et al RoB 2: a revised tool for assessing risk of bias in randomised trials BMJ 2019; 366:l4898
16 Varlet F, Becmeur F, Thieme G, et al Laparoscopic Treatment of Varicoceles in Children Multicentric Prospective Study of 90 Cases Eur J Pediatr Surg 2001; 11:399-403
17 Lund L, Tang YC, Roebuck D, et al Testicular catch-up growth after varicocele correction in adolescents Pediatr Surg Int 1999; 15:234-7
18 Yehya A, Abdalrazek M, Gamaan I, et al Lymphatic sparing laparoscopic varicocelectomy with or without testicular artery preservation: is there a difference? Ann Pediatr Surg 2020; 16:16
19 Kim KS, Lee C, Song SH, et al Impact of internal spermatic artery preservation during laparoscopic varicocelectomy on recurrence and the catch-up growth rate in adolescents J Pediatr Urol 2013; 10:435-40
20 Zampieri N, Zuin V, Corroppolo M, et al Varicocele and A d o l e s c e n t s : S e m e n Q u a l i t y A f t e r 2 D i f f e r e n t L a p a r o s c o p i c
Procedures J Androl 2007; 28:727-33
21 Esposito C, Monguzzi GL, Gonzalez-Sabin MA, et al Laparoscopic treatment of pediatric varicocele: a multicenter study of the italian society of video surgery in infancy J Urol 2000; 163:1944-6
22 Poon SA, Kozakowski KA, DeCastro GJ, et al Adolescent varicocelectomy: Postoperative catch-up growth is not secondary to lymphatic ligation J Pediatr Urol 2009; 5:37-41
23 Yaman O, Soygur T, Zumrutbas AE, Resorlu B Results of microsurgical subinguinal varicocelectomy in children and adolescents Urol 2006; 68:410-2
24 Koyle MA, Oottamasathien S, Barqawi A, et al Laparoscopic palomo varicocele ligation in children and adolescents: Results of 103 cases J Urol 2004; 172:1749-52
25 Riccabona M, Oswald J, Koen M, et al Optimizing the operative treatment of boys with varicocele: sequential comparison of 4 techniques J Urol 2003; 169:666-8
26 Poddoubnyi I V, Dronov AF, Kovarskyi SL, et al Laparoscopic ligation of testicular veins for varicocele in children: A report of 180 cases Surg Endosc 2000; 14:1107-9
27 Islam S, Islam M, Sarkar S, Paran S Outcome of laparoscopic varicocelectomy with mass ligation technique for symptomatic varicocele Arch Surg Clin Res 2019; 3:065-9
28 Mirilas P, Mentessidou A Microsurgical subinguinal varicocelectomy in children, adolescents, and adults: Surgical anatomy and anatomically justified technique J Androl 2012; 33:338-49
29 Fine RG, Gitlin J, Reda EF, Palmer LS Barriers to use of semen analysis in the adolescent with a varicocele: Survey of patient, parental, and practitioner attitudes J Pediatr Urol 2016; 12:41 e141 e6
30 Kattan S The Impact of Internal Spermatic Artery Ligation during Laparoscopic Varicocelectomy on Recurrence Rate and Short Post Operative Outcome Scand J Urol Nephrol 2001; 35:218-21
31 Fallara G, Tang S, Pang KH, et al Treatment of Persistent or Recurrent Varicoceles: A Systematic Review Eur Urol Focus; 2023; 9:531-40
32 Chung SD, Wu CC, Lin VCH, et al Minilaparoscopic varicocelectomy with preservation of testicular artery and lymphatic vessels by using intracorporeal knot-tying technique: Five-year experience World J Surg 2011; 35:1785-90
33 Liang Z, Guo J, Zhang H, et al Lymphatic sparing versus lymphatic non-sparing laparoscopic varicocelectomy in children and adolescents: A systematic review and meta-analysis Vol 21, European J Pediatr Surg 2011; 21:147-53
3
Varicocelectomy by Artery Preserving and Mass Ligation TechniqueA Comparative Study J Biomed Eng Med Imaging 2022; 11:87-95
Correspondence
Ahmad Nurfakhri Syarief afkurologi@gmail com
Ilham Akbar Rahman ilhamakbaarr@gmail com
Agung Ravi Saputra Sangadji agung ravi saputra-2022@fk unair ac id
Tarmono Djojodimedjo tar urology@yahoo com
Fikri Rizaldi, MD (Corresponding Author) fikririz@gmail com
Department of Urology, Faculty of Medicine, Universitas Airlangga and Universitas Airlangga Teaching Hospital, Surabaya, East Java, Indonesia
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11627 A
8
Nurfakhri Syarief, I Akbar Rahman, A Ravi Saputra Sangadji, T Djojodimedjo, F Rizaldi
4 I s l a m S R , P a u l D , S a r k a r S A , e t a l L a p a r o s c o p i c
SYSTEMATIC REVIEW
Renal artery infarction in the SARS-Cov-2 era: A systematic review of case reports
Diomidis Kozyrakis, Georgios Kallinikas, Anastasios Zarkadas, Dimitrios Bozios, Vasileios Konstantinopoulos, Georgios Charonis, Konstantinos Safioleas, Athanasios Filios, Evangelos Rodinos, Despoina Mytiliniou, Gerasimos Vlassopoulos, Ioannis Gkerzelis, Panagiotis Filios
Konstantopouleio General Hospital of Nea Ionia, Department of Urology, Nea Ionia, Attiki, Greece
Summary
Aim: Renal artery infarction (RI) is the presence of blood clot in the main renal artery or its branches causing complete or partial obstruction of the blood supply Its etiology is either related with disorders of the renal vasculature or with cardiovascular diseases Recently, the SARSCoV-2 virus is an emerging cause of thromboembolic events and the incidence of RI is anticipated to increase after the pandemic. Methods: A systematic review based on COVID-19 associated RI was conducted Protocol: A systematic review of the Medline/Pubmed and Scopus databases was conducted in accordance to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (the PRISMA statement). Search strategy and information sources: A hand-search was performed using the terms “SARS-Cov-2” OR “COVID-19” AND “renal thrombosis” OR “renal infarction” OR “renal “thromboembolism”
Eligibility criteria: all types of publications (case reports, case series, letters to the editor, short communications) were evaluated for relevance Inclusion criteria were: confirmed SARS-Cov-2 infection irrespectively of the age, diagnosis of RI during or after the onset of viral infection, and exclusion of other potential causes of thromboembolic event except of SARS-Cov-2. Patients with renal transplantation were also considered Study criteria selection: after checking for relevance based on the title and the abstract, the full texts of the selected papers were retrieved and were further evaluated. Duplicated and irrelevant cases were excluded Any disagreement was resolved by consensus with the involvement of a third reviewer Quality of studies: The assessment of the quality case reports was based on four different domains: selection, ascertainment, casualty and reporting. Each paper was classified as “Good”, “Moderate” and “Poor” for any of the four domains Data extractions: Crucial data for the conduct of the study were extracted including: age, sex, time from SARS-Cov-2 infection till RI development, medical history, previous or current antithrombotic protection or treatment, laterality and degree of obstruction, other sites of thromboembolism, treatment for thromboembolism and SARS-Cov-2 and final outcome Data analysis: methods of descriptive statistics were implicated for analysis and presentation of the data.
Results: The systematic review retrieved 35 cases in 33 reports
In most cases, RI was diagnosed within a month from the SARSCov-2 infection albeit 17 out of 35 patients were receiving or had recently received thromboprophylaxis. Right, left, bilateral and allograft obstruction was diagnosed in 7, 15, 8 and 5 patients respectively 17 cases experienced additional extrarenal thromboembolism primarily in aorta, spleen, brain and lower limbs. Low molecular weight heparins (LMWH) (usually 60-80 mg enoxaparine bid) was the primary treatment, followed by combinations of unfractionated heparin and salicylic acid, apix-
aban and rivaraxaban, warfarin, acenocoumarol or clopidogrel. Kidney replacement therapy was offered to five patients while invasive therapies with thrombus aspiration or catheter directed thrombolysis were performed in two Regarding the outcomes, five of the patients died. The total renal function was preserved in 17 cases and renal impairment with or without hemodialysis was recorded in 5 patients, two of them having lost their kidney allografts Limitations: The majority of included studies are of moderate quality The results and the conclusions are based on case-reports only and crucial data are dissimilarly presented or missing through the relevant publications
Conclusions: Thromboprophylaxis may not offer adequate protection against SARS-Cov-2 induced thrombosis Most patients could be effectively treated with conservative measures, while in more severe cases aggressive treatment could be recommended Implications of key findings: Therapeutic doses of LMWH could be considered for protection against RI in SARS-Cov-2 cases Interventional treatment could be offered in a minority of more severe cases after carful balancing the risks and benefits.
KEY WORDS: Keywords: Renal; Artery infarction; Thromboembolism; SARS-Cov-2; COVID-19
Submitted 30 July 2023; Accepted 3 September 2023
INTRODUCTION
Renal artery infarction (RI) describes the presence of blood clot in the main renal artery or its branches causing complete or partial obstruction of the blood supply Its etiology is either related with intrinsic disorders of the renal vasculature or with cardiovascular disorders outside the kidney (1-2) The blood perfusion impairment results in renal injury and failure, partial or total, permanent or not, though the final outcome is primarily related with the prompt diagnosis and treatment (3-5)
The correct diagnosis of RI is a challenge for the physician The disease may mimic the renal colic or other conditions such as urinary tract infection, acute abdomen, cardiac and pulmonary diseases, necessitating a multidisciplinary diagnostic work up (1-2, 6-8) Several case series are referred to RI management, mainly reflecting the experience and preferences of each group, but highquality comparative series investigating the prognostic factors, the optimal diagnostic algorithm, the best treatment strategy and the role of prompt management in disease outcome are lacking A number of different pharma-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11625 1
DOI: 10 4081/aiua 2023 11625
ceutical regimens and interventional therapies have been tested in RI patients but with inconclusive results in terms of preservation of renal function (1-3, 6-10)
The new SARS-Cov-2 infection, the etiology of the COVID-19 pandemic outbreak may cause significant infection of the respiratory system and at the same time may affect multiple other organs through a prothrombotic and inflammatory effect involving the immune and vascular system albeit the mechanism of activation of the cascade of events leading to clot formation is still under investigation (11-13)
The incidence of RI is anticipated to increase after the SARS-CoV-2 pandemic At present, the management of post COVID-19 RI is based on the experience accumulated before the pandemic onset and therefore contemporary clinical research might be beneficial Attempting to add on the existing body of evidence we conducted a review of the literature exclusively with patients who developed RI during or after the infection with SARSCov-2 Emphasis is given in the history, the diagnostic workup, the laboratory findings and the treatment options A discussion regarding the role of the new virus in the development of the thrombosis is also attempted
The optimal treatment of respiratory infection due to SARS-Cov-2 is beyond the scope of this review
MATERIALS AND METHODS
Protocol
A systematic review of the Medline/ Pubmed and Scopus databases was conducted in accordance to the Preferred Reporting Items for Systematic R e v i e w s a n d M e t a - A n a l y s e s (the PRISMA statement) (14)
Search strategy and information sources
The aforementioned databases were hand-searched until mid
D e c e m b e r 2 0 2 2 u s i n g t h e t e r m s “ S A R S - C o v - 2 ” O R “ C O V I D - 1 9 ” A N D “ r e n a l thrombosis” OR “renal infarction” OR “renal “thromboembolism”
Eligibility criteria
Based on the title and the abstract’s content all types of publications (case reports, case series, letters to the editor, short communications) were independently evaluated for relevance by two of the authors of this manuscript (DK and GK) Inclusion criteria were: 1 confirmed SARS-Cov-2 infection irrespectively of the age, 2 diagnosis of RI during or after
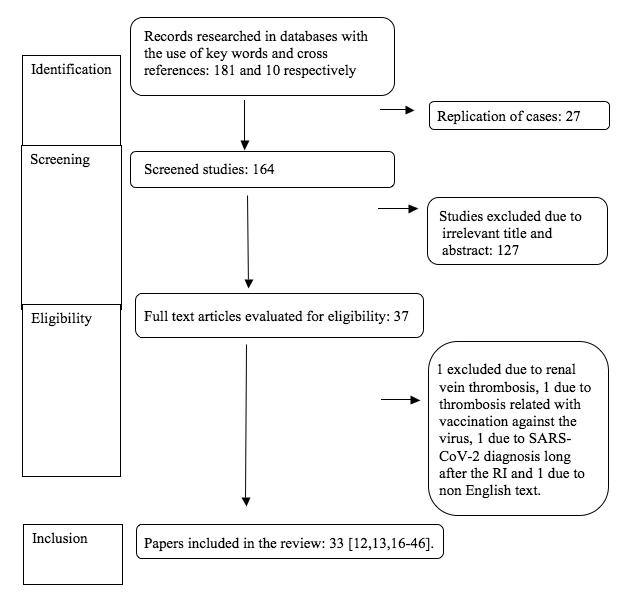
the onset of viral infection, and 3 exclusion of other potential causes of thromboembolic event except of SARS-Cov2 Patients with renal transplantation or/and the co-existence of thromboembolic events outside the renal vascular system were also considered Exclusion criteria were the absence of SARS-Cov-2 infection or of RI, the inadequate/poor presentation of the case, included the abstractonly cases and the non-English articles
Study selection
After checking for relevance based on the title and the abstract, the full texts of the selected papers were retrieved and were further evaluated Duplicated and irrelevant cases were excluded Any disagreements were resolved by consensus with the involvement of a third reviewer (PF)
Data extraction
Three of the authors (DK, VK, PF) determined and extracted the crucial data for the conduct of the study: Age, sex, time from SARS-Cov-2 infection till RI development, medical history, previous or current antithrombotic protection or treatment, laterality and degree of obstruction, other sites of thromboembolism, treatment for thromboembolism and SARS-Cov-2 and final outcome
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11625
2
D Kozyrakis, G Kallinikas, A Zarkadas, et al
Figure 1. Prisma Flow diagram of selected cases
Table 1
Assessment of risk of bias for each one of the included case reports for the domains of Selection, Ascertainment, Causality and Report For each one of the four domains a classification in low (L), moderate (M) and high (H) risk is provided.
Author Selection Ascer tainment Causality Repor t
Xu (16) HMML
Acharya (17) HMHM
Mocerino (18) HLML
Mukher ee (19) HLLL
Deshmukh (20) HHHM
Ramanathan (21) HMLM
Post (12) MMML MMLL
Añazco (22) HMLM
Lushina (23) HMHM
Kundal (13) HMHM
Besutti (24) MLMH MMHH
Imoto (25) HMMM
Ammous (26) HLML
Kenizou (27) HLMM
Webb (28) HHML
P ouffe (29) MHHM
S ngh (30) HHHM
Tantisattamo (31) MMHL
Belfort (32) MLML
Topel (33) HMHM
Sethi (34) HMLM
Jentzsch (35) HMLL
Farias (36) HMLM
Al-Mashdali (37) HMML
Mavraganis (38) HLLL
Jain (39) HLMM
Rigual (40) HMML
Huang (41) HLML
Mancini (42) HLLL
Gjonbalaj (43) HMML
Brem (44) HLLM
Kourien (45) HMHM
Veterano (46) HMHL
Table 2. Overview of retrieved papers.
Quality of studies
Two of the authors independently assessed the quality of each paper included in the study Murad et al (15) published a guide of assessment tools of a case report quality based on four different domains: Selection, Ascertainment, Causalty and Reporting Considering that all the included papers were case report the studies were rated accordingly Each paper was classified as “Good” , “Moderate” and “Poor” for any of the four domains Any disagreement in quality assessment was resolved with third part involvement (GV or IG)
Data analysis
Methods of descriptive statistics were applied for analysis and presentation of the demographics and clinical characteristics of the included population
RESULTS
A checklist of the included items in PRISMA systematic review is presented in supplementary Table 1 33 papers with 35 RI cases were retrieved after the search of the databases (Figure 1) An overview of the quality of the papers is provided in Table 1 (12, 13, 16-46) Most of the case reports were assessed with moderate risk of bias The overview of the retrieved papers is provided in Table 2 The demographics and clinical characteristics with the relevant rates are provided in Table 3 All the patients except one were adults, the majority of whom were males in their sixth or seventh decade of their lives usually with a history of obesity, diabetes mellitus (DM) and/or smoking Noteworthy, 17 6% of the patients had unremarkable medical history In most of the cases the RI event was diagnosed within a month from the SARS-Cov-2 infection (mean 15 3 days) It is of interest that almost half of the cases (17/35) were receiving or had recently received thromboprophylaxis
The most frequently used thromboprophylaxis was low
Author Age Sex Days after Antithrombotic/ Laterality, Other sites of Tx for Tx for Outcome (y) COVID-19 anti-PLT Tx & degree thromboembolism SARS-Cov-2 thromboembolism diagnosis/histor y before RI of obstr uction
Xu 2020 (16)
kidney–pancreas transplant ND/hypothyreoidism, CAD, COPD, smoking, lung cancer, aortic aneurysm and bilateral renal stenting, recent embolization for leak ND/DM, AH, CAD
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11625 3 Renal artery infarction as a sequela of SARS-Cov-2 infection
Acharya 2020 (17) Mocerino 2020 (18) Mukherjee 2020 (19) Deshmukh 2020 (20) 46 77 69 71 55 M F F M F 27/DM,
9/unremarkable 3/recent appendicitis Intermittent enoxaparin 40
bid ASA ASA, Clopidogrel Enoxaparin No Segmental artery, incomplete Bilateral incomplete Left main incomplete Left superior Bilateral left incomplete, right complete No No No Ascending aorta Abdominal aorta Suppl O2, azithromycin, prednisone, lopinavir/ritonavir, HCLQ cefuroxime ND ND Suppl O2, methylprednisolone, lopinavir/ritonavir, HCLQ ND Alive, RF ND Alive, RF ND Preservation RF Preservation RF Multiorgan dysfunction, sepsis Enoxaparin 80 mg bid, at discharge apixaban 5 mg bid ASA IV heparine then apixaban Stop enoxaparin, Heparine IV, Clopidogrel then apixaban + clopidogrel ND
mg
Rigual 2022 (40)
Huang 2022 (41)
Mancini 2022 (42)
Gjonbalaj 2022 (43)
10/cerebral infarction Tx with IV thrombolysis + thrombectomy
19/DM
Enoxaparin 1 mg/kg, ASA 100 mg
Bilateral segmental
Left main & posterior complete
Suppl O2, methylprednisolone
Suppl O2, methylprednisolone, ceftriaxone, antiviral
1 mg enoxaparin/kg, ASA 100 mg, then ASA 300 mg
Clopidogrel 75 mg, nadroparin 3800U/q12h then rivaroxaban
Rehab center
Preservation RF
Brem 2022 (44)
Kourien 2022 (45)
Veterano 2022 (46)
3/mild stenosis of aortic valve, adrenal adenoma (non functioning)
60/unremarkable 14/DM
30/unremarkable
30/Idiopathic CKD, kidney transplant, allograft dysfunction, obesity, heart failure, DM, AH, popliteal vein thrombosis
LMWH prophylaxis
Enoxaparin prophylaxis
ASA, enoxaparin 20 mg, prophylaxis
Left upper, middle segmental
Left mid/distal segmental
Piperacillin/ tazobactam ND
Enoxaparin 7000 UI bid, recur of thrombosis, then enoxaparin 8000 UI bid + ASA 100 mg ASA 100 mg/d + heparin 25,000 UI/d
thrombus aspiration + tirofiban 5 ml, stent, then ASA 100 mg+ Clopidogrel 75 mg
DMSA 28% relative renal function
Left
Bilateral segmental Allograft main, quasi-complete
Azithromycin, ceftriaxone, HCLQ
Remdesivir, methylprednisolone, tocilizumab, positive pressure O2 DXM, O2 with nasal cannula
LMWH 60 mg bid, limb embolectomy
Bilateral nephrectomy, combined antfungal agents
Catheter directed thrombolysis (alteplase, 5cc bolus, then 0 8 mg/h + IV heparine 500U/h) for 2 days + endoprosthesis, ASA 100 mg + enoxaparin 60 mg bid, then apixaban 5 mg bid
Full recovery Limb amputation, RF preservation
Permanent hemodialysis
Allograft preservation, RF improved
AH: arter al hypertension, ICU: intensive care unit, GI: gastrointest na ,
AKI: acute k dney njury CK : chron c kidney njury, SC: subcutaneous, ASA: acety salicyl c acid, ESKD: end stage k dney disease, LMWH: low molecular we ght heparin, CKD: chronic kidney disease, HCLQ: Hydroxych oroquine, Suppl O2: Supplementary oxygen,
DXM: dexamethasone, ECMO: extracorporea membrane oxygenation, V ntravenous
dose low molecular weight heparins (LMWH), usually enoxaparin, followed by amino-salicylic acid (ASA), either as monotherapy or combined with heparin
Of the 35 patients, five experienced allograft thrombosis In the rest 30 patients, right, left and bilateral obstruction was diagnosed in 7, 15 and 8 patients respectively In 17 cases, one or more organs outside the urinary tract were affected by the thromboembolic event with the aorta being most frequently involved (10 cases), followed by the spleen (8 cases), brain (3 cases), lower limb (3 cases), lung (3 cases) and elsewhere (2 cases)
All the patients were reported to complain about pain of sudden onset in the upper lateral abdominal quadrant and/or in the costovertebral angle ipsilateral to the affected kidney The abdomen was tender in the affected side but the guarding reflex was rarely elicited The WBC level is frequently elevated with the reported values being mostly above 15000 WBC/μL Serum LDH and D-Dimers are almost uniformly above the normal range Kidney injury is described in 12 cases while for 7 others reliable information were lacking
The mainstay of the diagnosis was the contrast-enhanced CT (CECT) scan or preferably CT angiography (CTA) and in only one case digital subtractive angiography (DSA) as an adjuvant diagnostic modality to the CT scans In two other cases the diagnosis of ischemia was established with renal biopsy Massive or complete thromboembolism was
revealed in eight patients The rest of the patients had incomplete infarction of either the main artery or the segmental branches
As it is shown in Table 3, the treatment for SARS-Cov-2 is reported for 29 patients and different combinations of drugs have been used Steroids were most frequently delivered (51 4% of patients), followed by antibiotics (37 1%) and by antiviral treatment (31 4%) Hydroxychloroquine was delivered in 5 patients and monoclonal antibodies in 3 LMWH, mainly high dose enoxaparin (60-80 mg bid), was the primary treatment against thromboembolism in 19 cases, followed by therapeutic combinations containing unfractionated heparin (9 patients) and salicylic acid in dosages ranging from 81 to 300 mg/day Upfront apixaban or other antithrombotic and anti-platelet agents (rivaraxaban, warfarin, acenocoumarol or clopidogrel) have also been delivered in RI patients
Kidney replacement therapy was urgently offered to only five of the cases Invasive therapies were performed in two patients In one of them, with mid-distal segmental occlusion, aspiration and stent placement was performed and tirofiban was delivered to the thrombus site while the patient was under treatment with unfractionated heparin plus ASA The patient experienced full recovery (43) In another 56-year female with massive allograft thrombosis, history of chronic kidney disease, obesity, heart failure, diabetes type 2, arterial hypertention and lower limb
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11625 5 Renal artery infarction as a sequela of SARS-Cov-2 infection
NV: normal va ues, DM: diabetes mell tus, CAD: coronary artery disease, COPD: chronic obstruct ve pulmonary disease, RF: rena funct on, ND: not defined, AF: atria f bril ation,
53 62 43 5th decade 59 32 56 M M M M M M F
No No No
Spleen No No No Spleen, lung, femoral
thoracic aorta No No
artery
Overview of primary Tx Therapeutic agent in primary Tx Long term Tx or Tx after for RI (%) for RI (no of pts) Discharge (no of pts)
Single medical Tx 22 pts (62 9) LMWH (19) Apixaban (5)
Combined medical Tx 7 pts (20) ASA (7) ASA (5)
Surgical Tx 2 pts (5 7) Heparin IV (9)
ND 4 pts (11 4) Clopidogrel (2)
(2)
(1)
Apixaban (2) Oral anticoagulant (1)
ND Heparin (1) Warfarine (2)
Nephrectomy (2) Rivaroxaban (2)
Interventional/endovascular treatment (2) Fondaparinux (1)
ND (4) Dabigatran (1)
Outcomes: no of pts Dead: 5, Alive: 30
RF preservation: 8
Full recovery: 2
Improved /improving: 6
Multiorgan dysfunction/sepsis: 1
ICU: 2
Discharged home (no further info): 3
Discharged to rehabilitation center: 2
Renal dysfunction: 5
Loss of renal unit: 1
Cardiac arrest, AF: 1
GI bleeding: 2
* n one case RI was d agnosed 4 days before the defin te SARS-Cov-2 d agnosis
** Irrelevant to history of transplantat on
*** Rates are not d splayed due to missing data
thrombosis, the treatment consisted of catheter directed thrombolysis with alteplase combined with IV heparin, endoprothesis placement, ASA and enoxaparin resulting in preservation of the transplant and improvement of renal function (46) Nephrectomy was necessitated in three other cases, one bilateral one unilateral and one for allograft removal
Regarding the outcomes, five of the patients died The total renal function was preserved or improving in 16 cases, while in another one the relative function was diminished to 28% in DMSA scans without affecting though the overall renal function Renal impairment with or without hemodialysis was recorded in 5 patients, two of them having lost their kidney allografts For 7 cases data regarding renal function outcome are inconclusive
DISCUSSION
The most frequent etiologic factor for RI of any cause is
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11625 D
6
Kozyrakis, G Kallinikas, A Zarkadas, et al
demographics and clinical characteristics Epidemiology Age (range) years 52 1 (6-84) Male/female ratio 3 4/1 Male %, Female % 77%, 23% Days for RI after COVID-19 diagnosis 15 3 d (0-63)* Histor y (for 34 pts) Unremarkable (%) 6 (17 6) Transplantation (%) 6 (17 6) Heart diseases CAD (%) 2 (6) Chronic heart diseases (%) 4 (11 7) AF (%) 1 (3) AH (%) 8 (23 5) DM (%) 7 (20 5) Obesity/overweight (%) 7 (20 5) Smoking (%) 4 (11 7) Pulmonary diseases Asthma (%) 3 (8.8) COPD (%) 1 (3) Sleep apnea (%) 1 (3) Lung cancer (%) 1 (3) Vascular diseases Vasculitis/thromboembolism (%) 6 (17 7) Aorta aneurysm/dissection (%) 2 (6) Renal dysfunction (%) ** 4 (11 7) Gastrointestinal diseases (%) 2 (6) Others Appendicitis (%) 1 (3) Migraines (%) 1 (3) Dyslipidemia (%) 1 (3) Deafness (%) 1 (3) Adrenal adenoma (%) 1 (3) Hypothyroidism (%) 1 (3) Contraceptive drug consumption (%) 1 (3) Antithrombotic/anti-PLT Tx before RI (17 cases) LMWH (%) 11 (31 4) IV Heparin (%) 1 (2 8) ASA (%) 5 (14 3) Clopidogrel (%) 2 (5 7) Laterality Right side (%) 7 (20) Left side (%) 15 (42 9) Bilateral (%) 8 (22 8) Allograft (%) 5 (14 3) Degree of obstr uction Segmental artery (%) 25 (58) Main artery (%) 9 (21) The arterial site is not defined (%) 9 (21) Incomplete *** 9 Complete *** 6 Massive/quasi-complete *** 2 Other sites of thromboembolism Aorta (%) 10 (28 6) Spleen (%) 8 (22 8) Lower limb (%) 3 (8.6) Lung (%) 3 (8 6) Brain (%) 3 (8 6) Upper limb (%) 1 (2 9) Bowel (%) 1 (2 9) No (%) 18 (51 4) Tx for SARS-Cov-2 Antibiotics (some pts received Azithromycin 6 combinations) 13 pts (37 1%) Cefuroxime 1 Ceftriaxone/Cefotaxime 7 Ceftaroline 1 Levofloxacin 1 Piperacillin/tazobactam 1 Meropenem/carbapenem 2 Teicoplanin 1 ND antibiotics 1 Steroid agents (51 4%) Prednisone/methylprednisolone/DXM 18 Antiviral 11 pts (31 4%) Remdesivir 3 Opinavir/ritonavir 5 Favipiravir 2 ND antiviral 1 HCLQ (14 3%) HCLQ 5 Inhaler (5 7%) Albuterol 1 Ciclesonide 1 Mechanical ventilation/ Mechanical ventilation/intubation 4 intubation (11 4%) Ivermectin 1 Others Tocilizumab 3 ECMO 1 Norepinephrine 1 O2 treatment (45 7%) Positive pressure 1 ND (Supplementary) 10 High flow 4 Non-rebreathing 1 ND (20%) ND 7
Table 3 Patients’
Clopidogrel
Acenocoumarol
atrial fibrillation (AF) encountered 25% to 75% of the patients (2, 8, 47) However, amongst patients with COVID-19-induced RI, AF is a rare occasion The cytokine storm has been described in these patients predisposing to pro-inflammatory, prothrombotic and profibrotic effects induced by activated neutrophils and monocytes, as well as in causing damage to the endothelium (endothelitis) through the activation of angiotensin-converting enzyme-2 receptor This cascade of events leads to activation and aggregation of factor VII, von Willebrand factor and fibrinogen and consequently to thrombin activation and fibrin clot formation and also in aggregation of platelets resulting in multiple thrombotic events (28, 32)
Several other factors predispose to the onset of the RI such as diabetes mellitus, arterial hypertension, hyperlipidemia, congestive heart failure, coronary artery disease, myocardial infarction, mitral valve disease and cerebrovascular disease (10, 47, 48) A relevant history has also been recorded in many patients of this review
Occasionally, in situ thrombosis may be iatrogenic in origin or traumatic (4, 49) History of a previous embolic event or thrombophilia with potential resistance of activated protein C and deficiency of protein S should also be examined (4, 5, 9)
Almost half of the COVID-19 related RI cases were receiving or had recently received thromboprophylaxis It seems that low dose of LMWH or ASA do not offer adequate protection against RI so as to overcome the cytokine storm effect The use of intermediate-dose enoxaparin in COVID19-induced-hypoxia and before the onset of RI could be proposed as a measure to overcome the failure of throboprophylaxis attributed to high levels of factor VII, von Willebrand factor and fibrinogen (28) Therefore based on the results of a randomized clinical trial Spyropoulos et al recommended the administration of 1mg/kg bid of LMWH and 0 5 mg/kg bid for patients with clearance creatinine ≥ 30 and < 30 mL/min/1 73 m2 respectively for hospitalized patients The beneficial effect of the proposed dosages was evident in non ICU patients though (50)
The prompt diagnosis and treatment is the cornerstone of a favorable outcome for RI of any case 90 minutes of normothermic ischemia can lead to irreversible damage of the renal parenchyma (3, 4), albeit this threshold is not always confirmed in clinical practice Several groups have reported the preservation of renal function after many hours or even days after the onset of infarction (6, 51) In COVID19-associated RI the delay in seeking for medical help cannot be evaluated because this piece of information is not reported in many of the included case reports but it seems that the degree of obstruction is more crucial than the delay in diagnosis Three out of the five deaths of the review were recorded in the 8 patients with complete or massive infarction, indicating that the high degree of obstruction might be life threatening compared with the lower degree of RI
The most frequently affected renal unit by COVID-19 was the left-sided, representing a finding that is poorly understood In most case series with RI of any etiology both sides were almost equally infracted (2, 6, 9, 51) Three case series of the pre-COVID-19 era demonstrated a predominance of left RI which is a finding similar to that of the present review (47, 48, 52) Another paper from
Korea though reported a higher incidence of right-sided RI (1) Domanovits et al favor the hypothesis that the right renal artery has an acute angle of divergence with the aorta (48) In a more recent report it was revealed that the degrees of angulation were similar for both sides but the left orifice is larger than the right one and this fact may have influenced the laterality of RI (52) Apart from the dimensions of the orifice, it could be speculated that the length of renal arteries as well as the distance of the branching from the orifice may also play a role in the predominance of the left side
Noteworthy pulmonary embolism (PE) among SARS-Cov-2 patients is a usual finding with an overall incidence of 16 5% (53) In the present review however PE was a rare finding among RI patients with the aorta and spleen being most frequently affected If pulmonary infection was the triggering event of thromboembolism through the dissemination of infection and inflammation to the adjacent lung vessels it is anticipated that the incidence of PE would be much higher However, the figure of three PE events of this review is too low to support this assumption It has been shown that the virus may directly attack the respiratory system causing pneumonia, while the cardio-vascular system is affected either directly from the virus or indirectly through the blood stream with activation of cytokine storm and pro-inflammatory pathways It seems that some vessels are more vulnerable than others perhaps due to endothelitis or to increased permeability of the endothelium enhancing the clot formation and platelet aggregation (54) This might explain the higher incidence of aortic and splenic infarctions compared to pulmonary or brain embolism Moreover, in some patients the synchronous diagnosis of viral pneumonia and visceral infarction is indicative of the direct attack against the vascular system, while in others the long time interval (up to 63 days) between the COVID-19 pneumonia till the onset of infarction could be associated with an indirect assault (54) In most of the cases the WHO definition of long post-COVID-19 syndrome is met should the duration of RI symptoms lasts at least 2 months (55)
In the pre-SARS-CoV-2 era some authors advocate the DSA as the diagnostic gold standard The sensitivity rates are as high as 100% but at a cost of increased invasiveness (3, 4) This modality has now been broadly replaced by contrast enhanced CT (CECT) imaging and CT angiography (CTA) showing single or multiple wedge-shaped filling defects of the renal parenchyma or global hypo-attenuation of the affected renal unit (compared with the healthy one) The blood clots may be also revealed in the vascular system Infarcts involving greater than 50% of the renal parenchyma are considered global Smaller single or multiples lesions (less than 50% of the renal unit) are classified as focal or multifocal respectively (56) The CECT/CTA sensitivity ranges from 80 to 97 3%, representing a rapid, non invasive, comprehensive and informative method for the diagnosis of RI and it should be performed as early as possible should renal infarction is suspected (2, 8, 48)
Nephrotoxicity due to radiopaque agents is well described and acute kidney injury may occur in the grounds of an already impaired renal function (57) However, the correct diagnosis cannot be established with other means and the
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11625 7 Renal
a
infection
artery infarction as
sequela of SARS-Cov-2
benefits from the administration of the contrast agent should be balanced against the potential risks Therefore many authors proceeded to IVC administration in patients with renal impairment even at the risk of subsequent hemodialysis (12, 16, 20, 22, 27, 34, 37, 44, 46) The treatment options against SARS-Cov-2 show a significant variability among the different medical centers The combinations of regimens comprise mainly steroids plus broad spectrum antibiotics and usually antiviral treatment Due to this variability the impact of anti-SARSCov-2 treatment on the natural history of thrombosis cannot not be reliably evaluated Large scale studies with meticulous designed statistical analysis models might address the question whether some medications or combinations might play a preventive role against infarction
Revascularization of RI is rarely attempted (1, 6, 8) In one of the biggest series comprising 438 RI of any cause the rate of thrombolysis with urokinase and embolectomy was as low as 4 5% and 0% respectively (2) However, it could be assumed that following a prompt diagnosis and perhaps in the settings of a massive or bilateral RI, endovascular surgery or thrombolytic management may be applied despite the risks of complications (3-5, 46, 48) In the present review, revascularization techniques were applied in one case with almost complete allograft obstruction and in another with a lesser degree of occlusion both with favorable results (43, 46)
Mortality rate after RI of any cause ranges from 0% to 23 4% (1-3, 7-9) The total number of 5 deaths in 35 patients with post COVID-19 RI corresponds to a rate of 14 3% which is reasonable for a severe disease burdened by the unfavorable prognosis of SARS-Cov-2 Perhaps the prompt diagnosis with modern CT-scanners, the close monitoring of the patients and the availability of new generation anti-coagulative agents may all have contributed to acceptable survival rates Nevertheless, the broader use of higher dosages of thromboprophylaxis might further enhance the outcomes in post-COVID-19 renal infarction (28, 50)
This review has several limitations As it is shown in table 2 the majority of included studies are of moderate quality
The results and the conclusions are based only on casereports and data are missing through the relevant publications Any treatment of RI is based upon the preferences of the responsible physicians since therapeutic and follow up protocols differ among the medical centers The outcomes are dissimilarly presented increasing the likelihood of bias Therefore, a direct comparison of the studies or classification of the patients from different reports should be made with caution Moreover, papers published in non English language and presentations in scientific meetings were not included in this review increasing the likelihood of missing data
CONCLUSIONS
Thromboprophylaxis may not offer adequate protection against SARS-Cov-2 induced thrombosis If RI is suspected the correct diagnosis is based on CECT/CTA scan and it should be performed as soon as possible, even in patients with renal impairment after careful balancing the risks and benefits Most patients could be effectively treated with
conservative measures, particularly with therapeutic-dose LMWH, while in more severe cases with massive and complete occlusion perhaps more aggressive treatment could be recommended Large scale multicenter studies might address the role o SARS-Cov-2 treatment on infarction, as well as the optimal treatment option against thromboembolism
REFERENCES
1 Yun WS Long-term follow-up results of acute renal embolism after anticoagulation therapy Ann Vasc Surg 2015; 29:491-5
2 Oh YK, Yang CW, Kim Y-L, et al Clinical Characteristics and Outcomes of Renal Infarction Am J Kidney Dis 2016; 67:243-250
3 Piffaretti G, Riva F, Tozzi M, et al Catheter-directed thrombolysis for acute renal artery thrombosis: report of 4 cases Vasc Endovascular Surg 2008; 42:375-9
4 Blum U, Billmann P, Krause T, et al Effect of local low-dose thrombolysis on clinical outcome in acute embolic renal artery occlusion Radiology 1993; 189:549-54
5 Gasparini M, Hofmann R, Stoller M Renal artery embolism: clinical features and therapeutic options J Urol 1992; 147:567-72
6 Bourgault M, Grimbert P, Verret C, et al Acute renal infarction: a case series Clin J Am Soc Nephrol 2013; 8:392-8
7 Bolderman R , Oyen R, Verrijcken A, et al Idiopathic Renal Infarction Am J Med 2006; 119:356 e9-12
8 Hazanov N, Somin M, Attali M, et al Acute renal embolism Forty-four cases of renal infarction in patients with atrial fibrillation Medicine (Baltimore) 2004; 83:292-299
9 Korzets Z, Plotkin E, Bernheim J, et al The clinical spectrum of acute renal infarction Isr Med Assoc J 2002; 4:781-4
10 Lessman RK, Johnson SF, Coburn JW, et al Renal artery embolism: clinical features and long-term follow-up of 17 cases Ann Intern Med 1978; 89:477-82
11 Kappel C, Piticaru J, Jones G, et al A case of possible Fournier's gangrene associated with proning in COVID-19 ARDS Can J Anaesth 2020; 67:1697-1698
12 Post A, den Deurwaarder ESG, Bakker SJL, et al Kidney Infarction in Patients With COVID-19 Am J Kidney Dis 2020; 76:431-435
13 Kundal SV, Emeasoba EU, Harris C, et al Aortic thrombosis and renal infarction in a young female with patent foramen ovale and COVID-19 antibody Clin Case Rep 2020 2; 9:345-349
14 Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for Systematic Reviews and MetaAnalyses: The PRISMA Statement PLoS Med 2009; 6:e1000097
15 Murad MH, Sultan S, Haffar S, et al BMJ Evidence-Based Medicine 2018; 23:60-63
16 Xu JJ, Samaha D, Mondhe S, et al Renal infarct in a COVID-19positive kidney-pancreas transplant recipient Am J Transplant 2020; 20:3221-3224
17 Acharya S, Anwar S, Siddiqui FS, et al Renal artery thrombosis in COVID-19 IDCases 2020; 22:e00968
18 Mocerino R, Kumar N Acute Abdominal Pain in a COVID-19 Patient Kidney360 2020 25; 1:584-585
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11625 D
8
Kozyrakis, G Kallinikas, A Zarkadas, et al
19 Mukherjee A, Ghosh R, Furment MM Case Report: COVID-19 Associated Renal Infarction and Ascending Aortic Thrombosis Am J Trop Med Hyg 2020; 103:1989-1992
20 Deshmukh SB, Upadhyay KM, Kulkarni A, et al Renal Artery Thrombosis: A Post COVID-19 Sequel J Adv Res Med 2020; 7:2224
21 Ramanathan M, Chueng T, Fernandez E, et al Concomitant renal and splenic infarction as a complication of COVID-19: a case report and literature review Infez Med 2020; 28:611-615
22 Añazco PH, Balta FM, Córdova-Cueva L Bilateral renal infarction in a patient with severe COVID-19 infection J Bras Nefrol 2021; 43:127-131
23 Lushina N, Kuo JS, Shaikh HA Pulmonary, Cerebral, and Renal Thromboembolic Disease in a Patient with COVID-19 Radiology 2020; 296:E181-E183
24 Besutti G, Bonacini R, Iotti V, et al Abdominal Visceral Infarction in 3 Patients with COVID-19 Emerg Infect Dis 2020; 26:1926-1928
25 Imoto W, Kaga S, Noda T, et al Coronavirus disease with multiple infarctions QJM 2020 1; 113:907-908
26 Ammous A, Ghaffar MA, El-Charabaty E, et al Renal infarction in COVID-19 patient J Nephrol 2021; 34:267-268
27 Kenizou D, Perrin C, Harzallah I, et al Multiple Arterial Thrombosis in a 78-Year-Old Patient: Catastrophic Thrombotic Syndrome in COVID-19 CJC Open 2021; 3:198-200
28 Webb C, Davidson B, Jones ESW, et al COVID-19-Associated Graft Loss From Renal Infarction in a Kidney Transplant Recipient Kidney Int Rep 2021; 6:1166-1169
29 Plouffe B, Van Hooren T, Barton M, et al Renal Infarcts-A Perplexing Case in the Middle of the COVID-19 Pandemic Front Pediatr 2021 14; 9:669453
30 Singh T, Chaudhari R, Gupta A Renal artery thrombosis and mucormycosis in a COVID-19 patient Indian J Urol 2021; 37:267269
31 Tantisattamo E, Dafoe DC, Ferrey AJ, et al Kidney allograft infarction associated with transplant renal artery stenosis in a COVID-19 kidney transplant recipient Clin Nephrol Case Stud 2021 26; 9:93-104
32 Belfort DSP, Marcondes-Braga FG, Mangini S, et al Aortic and Renal Artery Thrombosis as the First Clinical Manifestation of COVID-19 in a Heart Transplant Recipient Arq Bras Cardiol 2021; 117:1045-7
33 Topel C, Yıldırım C, Yavas MA, et al Aortic floating thrombi with lower limb ischemia and renal infarct in COVID-19: A remote thromboembolic complication Turk Kardiyol Dern Ars 2021; 49:233-236
34 Sethi S, Mehta S, Mahajan R Coronavirus Disease 2019
Infection Presenting with Renal Infarction: A Rare Case Report Saudi J Kidney Dis Transpl 2021; 32:865-868
35 Jentzsch MS, Hsueh L, Pallapati KJ, et al Abdominal Pain Due to Renal Infarction: An Unexpected Presentation of COVID-19 R I Med J (2013) 2021; 104:16-19
36 Farias LABG, Cruz EA, Silva AMHPD, et al Renal infarction in a patient with Coronavirus Disease 2019: another rare thrombotic event Rev Soc Bras Med Trop 2021; 54:e0038-2021
37 Al-Mashdali AF, Alwarqi AF, Elawad SM Simultaneous renal
infarction and splenic infarction as a possible initial manifestation of COVID-19: A case report Clin Case Rep 2021; 9:e04819
38 Mavraganis G, Ioannou S, Kallianos A, et al A COVID-19 Patient with Simultaneous Renal Infarct, Splenic Infarct and Aortic Thrombosis during the Severe Disease Healthcare (Basel) 2022; 10:150
39 Jain A, Bector G, Jain D, et al Renal Artery Thrombosis with R e n a l I n f a r c t i o n S e c o n d a r y t o C O V I D - 1 9 I n f e c t i o n : A R a r e Presentation Indian J Nephrol 2022; 32:191-2
40 Rigual R, Ruiz-Ares G, Rodriguez-Pardo J, et al Concurrent Cerebral, Splenic, and Renal Infarction in a Patient With COVID-19 Infection Neurologist 2022; 27:143-6
41 Huang H, Lin C, Chen Y, et al Renal artery thrombosis in SARSCoV-2 infection: a case report BMC Nephrol 2022; 23:175
42 Mancini M, Randazzo G, Piazza G, et al Arterial Thrombotic C o m p l i c a t i o n s i n C O V I D - 1 9 : A C a s e o f R e n a l I n f a r c t i o n Biomedicines 2022; 10:2354
43 Gjonbalaj N, Uka S, Olluri E, et al Renal artery thrombosis as a long-term complication of COVID-19 Radiol Case Rep 2022; 18:260-5
44 Brem FL, Tayef TAA, Rasras H, et al Concomitant renal and splenic infarctions in a COVID-19-patient with a catastrophic thrombotic syndrome Radiol Case Rep 2022; 17:4030-3
45 Kurien AA, Srinivasaprasad ND, Valavan KT Renal infarction due to COVID-19-associated renal mucormycosis Kidney Int 2022; 101:655
46 Veterano C, Antunes I, Coelho A, et al Endovascular Treatment of Renal Artery Thrombosis in Living-Donor Kidney Transplant Recipient With Severe COVID-19 Disease J Endovasc Ther 2022; 29:966-970
47 Rhee H, Song SH, Won Lee D, et al The significance of clinical features in the prognosis of acute renal infarction: single center experience Clin Exp Nephrol 2012; 16:611-6
48 Domanovits H, Paulis M, Nikfardjam M, et al Acute renal i n f a r c t i o n C l i n i c a l c h a r a c t e r i s t i c s o f 1 7 p a t i e n t s M e d i c i n e (Baltimore) 1999; 78:386-394
49 Singh O, Gupta SS, Sharma D, et al Isolated renal artery thrombosis because of blunt trauma abdomen: report of a case with review of the literature Urol Int 2011; 86:233-8
50 Spyropoulos AC, Goldin M, Giannis D, et al HEP-COVID Investigators Efficacy and Safety of Therapeutic-Dose Heparin vs S t a n d a r d P r o p h y l a c t i c o r I n t e r m e d i a t e - D o s e H e p a r i n s f o r T h r o m b o p r o p h y l a x i s i n H i g h - r i s k H o s p i t a l i z e d P a t i e n t s W i t h COVID-19: The HEP-COVID Randomized Clinical Trial JAMA Intern Med 2021; 181:1612-20
51 C-W Huang, M-J Lee, C-Y Hsu, et al Clinical outcomes associated with anti-coagulant therapy in patients with renal infarction QJM 2018; 111:867-73
52 Kagaya S, Ojima Y, Aoki S, et al The size of the renal artery orifice contributes to laterality of acute renal infarction Clin Exp Nephrol 2018; 22:1128-32
53 Suh YJ, Hong H, Ohana M, et al Pulmonary Embolism and Deep Vein Thrombosis in COVID-19: A Systematic Review and MetaAnalysis Radiology 2021; 298:E70-E80
54 Evans PC, Rainger GE, Mason JC, et al Endothelial dysfunction in COVID-19: a position paper of the ESC Working Group for
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11625 9 Renal artery infarction as a sequela of SARS-Cov-2 infection
Kozyrakis, G Kallinikas, A Zarkadas, et al
Atherosclerosis and Vascular Biology, and the ESC Council of Basic Cardiovascular Science Cardiovasc Res 2020; 116:2177-84
55 Soriano JB, Murthy S, Marshall JC, et al WHO Clinical Case Definition Working Group on Post-COVID-19 Condition A clinical case definition of post-COVID-19 condition by a Delphi consensus Lancet Infect Dis 2022; 22:e102-7
56 Suzer O, Shirkhoda A, Jafri SZ, et al CT features of renal infarction Eur J Radiol 2002; 44:59-64
57 Obed M, Gabriel MM, Dumann E, et al Risk of acute kidney injury after contrast-enhanced computerized tomography: a systematic review and meta-analysis of 21 propensity score-matched cohort studies Eur Radiol 2022; 32:8432-42
Correspondence
Diomidis Kozyrakis, MD (Corresponding Author) dkozirakis@yahoo gr; urology@konstatnopouleio gr
Konstantopouleio General Hospital of Nea Ionia, Department of Urology Th Konstantopoulou 3-5 Str , Nea Ionia, 14233, Attiki, Greece
Georgios Kallinikas, MD georgioskallinikas@gmail com
Anastasios Zarkadas, MD azark13@hotmail com
Dimitris Bozios, MD dbozios@gmail com
Vasileios Konstantinopoulos, MD vkonstantinopoulos@yahoo com
Georgios Charonis, MD george xarwnhs@gmail com
Konstantinos Safioleas, MD konstantinossafioleas@yahoo gr
Athanasios Filios, MD athanfilios@gmail com
Evangelos Rodinos, MD vag international@hotmail com
Despoina Mytiliniou, MD dmitiliniou@yahoo gr
Gerasimos Vlassopoulos, MD vlassger@gmail com
Ioannis Gkerzelis, MD ioannisgkerzelis@gmail com
Panagiotis Filios, MD panosfilios@yahoo gr
Konstantopouleio General Hospital of Nea Ionia, Department of Urology, Nea Ionia, Attiki, Greece
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11625
10
D
SYSTEMATIC REVIEW
Treatment of urge incontinence in postmenopausal women: A systematic review
Rawa Bapir 1, 15 , Kamran Hassan Bhatti 2, 15 , Ahmed Eliwa 3, 15 , Herney Andrés García-Perdomo 4, 15 , Nazim Gherabi 5, 15 , Derek Hennessey 6, 15 , Vittorio Magri 7, 15 , Panagiotis Mourmouris 8, 15 , Adama Ouattara 9, 15 , Gianpaolo Perletti 10, 15 , Joseph Philipraj 11, 15 , Konstantinos Stamatiou 12, 15 , Musliu Adetola Tolani 13, 15 , Lazaros Tzelves 8, 15 , Alberto Trinchieri 14, 15 , Noor Buchholz 15
1 Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq;
2 Urology Department, HMC, Hamad Medical Corporation, Qatar;
3 Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt;
4 Universidad del Valle, Cali, Colombia;
5 Faculty of Medicine Algiers 1, Algiers, Algeria;
6 Department of Urology, Mercy University Hospital, Cork, Ireland;
7 Urology Unit, ASST Fatebenefratelli Sacco, Milan, Italy;
8 2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece;
9 Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso;
10 Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy;
11 Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India;
12 Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece;
13 Division of Urology, Department of Surgery,Ahmadu Bello University/Ahmadu Bello University Teaching Hospital, Zaria, Kaduna State, Nigeria;
14 Urology School, University of Milan, Milan, Italy;
15 U-merge Ltd (Urology for emerging countries), London-Athens-Dubai *
Authors 1-14 have equally contributed to the paper and share first authorship
* U-merge Ltd (Urology for Emerging Countries) is an academic urological platform dedicated to facilitate knowledge transfer in urology on all levels from developed to emerging countries U-merge Ltd is registered with the Companies House in London/UK www U-merge com
Summary
Background: Urinary incontinence and other urinary symptoms tend to be frequent at menopause because of hormonal modifications and aging
Urinary symptoms are associated with the genitourinary syndrome of menopause which is characterized by physical changes of the vulva, vagina and lower urinary tract. The treatment strategies for postmenopausal urinary incontinence are various and may include estrogens, anticholinergics, and pelvic floor muscle training A comparison of these treatments is difficult due to the heterogeneity of adopted protocols. We systematically reviewed the evidence from randomized controlled trials (RCTs) focusing on treatment of postmenopausal women with urge incontinence
Methods: We conducted a systematic review and meta-analysis by searching PubMed and EMBASE databases for randomized controlled trials (RCTs) reporting results of treatments for postmenopausal urinary urge incontinence Odds ratios for improvement of urinary incontinence were calculated using random effect Mantel-Haenszel statistics.
Results: Out of 248 records retrieved, 35 eligible RCTs were assessed for risk of bias and included in the meta-analysis
Compared with placebo, systemic estrogens were associated with decreased odds of improving urinary incontinence in postmenopausal women (OR = 0 74, 95% CI: 0 61-0 91, 7 series, 17132 participants, Z = 2 89, P = 0 004, I2 = 72%) In most studies, no significant improvement in urinary symptoms was observed in patients treated with local estrogens, although they showed to be helpful in improving vaginal symptoms Vitamin D, phytoestrogens and estrogen modulators were not effective in
improving symptoms of incontinence and other symptoms of genitourinary menopause syndrome or yielded contradictory results A randomized controlled trial demonstrated that oxybutynin was significantly better than placebo at improving postmenopausal urgency and urge incontinence. The combination of anticholinergics with local estrogens has not been shown to be more effective than anticholinergics alone in improving urinary incontinence symptoms in postmenopausal women. Physical therapy showed an overall positive outcome on postmenopausal urinary incontinence symptoms, although such evidence should be further validated in the frame of quality RCTs
Conclusions: The evidence for effective treatment of postmenopausal urinary incontinence is still lacking. Welldesigned large studies having subjective and objective improvement primary endpoints in postmenopausal urinary incontinence are needed. At present, a combination of different treatments tailored to the characteristics of the individual patient can be suggested
KEY WORDS: Urinary incontinence; Urgency; Menopause; Estrogens; Anticholinergics; Vitamin D; Soy
Submitted 3 September 2023; Accepted 7 September 2023
INTRODUCTION
Urinary incontinence affects 15-35% of communitydwelling postmenopausal women (1, 2) Urge inconti-
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 1
DOI: 10 4081/aiua 2023 11718
nence is the more common form of incontinence after menopause It presents in association with a combination of urinary symptoms, including frequency, nocturia, urgency, and dysuria Urge syndrome disorders are often misunderstood to be symptoms of urinary tract infection and, consequently, are not treated appropriately Estrogen deficiency is thought to play an important role in the etiology of the “ urge syndrome” , that tends to rise in prevalence and to enhance in intensity as the years of estrogen deficiency increase In fact, estrogens affect the urethral mucosa, the smooth muscle, and the alpha-adrenergic tone in the urinary tract (3) Both oral and vaginal estrogens have been used in the management of urinary incontinence in postmenopausal women, although the effectiveness of hormonal therapy on urinary incontinence is controversial Alternative treatments include anticholinergic medication, pelvic floor muscle exercise and bladder training
Combinations of anticholinergics and topical vaginal estrogen are also used for treatment of urge incontinence and female sexual dysfunction In addition, posterior tibial nerve stimulation and acupuncture were used in the conservative treatment of these syndromes, in order to tackle the functional physiological changes associated with urge incontinence Moreover, fractional CO2 laser and low intensity shock wave treatment (LiSWT) have emerged as new treatment modalities, as these approaches may improve the atrophy of the urethral and bladder mucosa
Evaluation of the efficacy of the treatment of urge incontinence is difficult due to heterogeneity of the protocols adopted, and to the paucity of randomized controlled studies Our research was aimed to systematically review the available evidence resulting from randomized controlled trials (RCTs) aiming to treat postmenopausal women with urge incontinence
METHODS
Protocol and registration
This review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (5) The review protocol was registered on the PROSPERO platform (registration code: CRD42023405369)
Types of studies
We considered articles written in English, reporting the results of randomized controlled trials (RCTs) evaluating the efficacy of treatment of urge incontinence in postmenopausal women
Types of patients
We included postmenopausal women of any ethnicity or age
Types of interventions
We included studies focusing on any treatment aimed at addressing the signs and symptoms of urge incontinence
Outcomes
The outcomes considered for this review were the rate and/or severity of symptoms and signs (urge incontinence,
urgency, nocturia, pelvic floor muscle strength) evaluated by specific interview questions, or by administering questionnaires to patients (e g , the Revised Urinary incontinence Scale, the Overactive Bladder Questionnaire, the International Consultation on Incontinence Questionnaire) or by recording the reports of structured bladder diaries Microbiologic, cytologic and urodynamic findings were also evaluated The outcomes were compared in patients receiving treatment compared to placebo or to no treatment
Search strategy
Two electronic databases (PubMed and EMBASE) were searched for records reporting RCTs published up to 31 January 2023 The search was performed using strings b a s e d o n b r o a d M e S H t e r m s ( e g , f e m a l e A N D menopause AND (dysuria OR urination disorders OR incontinence) AND treatment) Relevant data were also searched by browsing the reference lists of reviews and clinical trial reports, or through other sources (e g , clinicaltrials gov; https://www clinicaltrialsregister eu/)
Data collection and analysis (selection of studies and data extraction)
Title and abstract screening to exclude records that did not meet the inclusion criteria were performed independently by 4 authors (2 authors for PubMed and 2 for EMBASE) Duplicate references were deleted Full texts were downloaded for a second round of screening and to extract relevant information Controversies were resolved by the research coordinator (AT)
A PRISMA flow diagram was drawn to illustrate the results of the study selection process (Figure 1) (6)
Data extraction was conducted by 4 authors using a standardized form The following data were obtained from each study: author(s), publication year, study design, population, intervention(s), results In case of missing or insufficient information, we performed sensitivity analysis, in order to consider the impact of missing data on the meta-analysis results
Quality evaluation on methodology
Three authors independently performed the quality assessment by identifying potential biases using the Cochrane risk of bias tool (9) The following potential sources of bias were considered: randomization process (D1), deviations from the intended interventions (D2), missing outcome data (D3), measurement of the outcome ( D 4 ) a n d s e l e c t i o n o f t h e r e p o r t e d r e s u l t ( D 5 ) Disagreements were resolved by discussion Risk of bias was not used to exclude studies
Statistical analysis
Statistical analysis was performed using the RevMan5 software Dichotomous data and number of subjects were extracted to calculate odds ratios (OR), confidence intervals (CI) to OR, and Z statistics (Random-effects model, Mantel-Haenszel method)
Assessment of heterogeneity
The heterogeneity of pooled results was assessed by the I2 statistic, reported with 95% CIs, and interpreted as of lesser importance (I2 ≤ 40%), moderate (I2 = 30%-60%),
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R
et
2
Bapir, K Hassan Bhatti, A Eliwa,
al
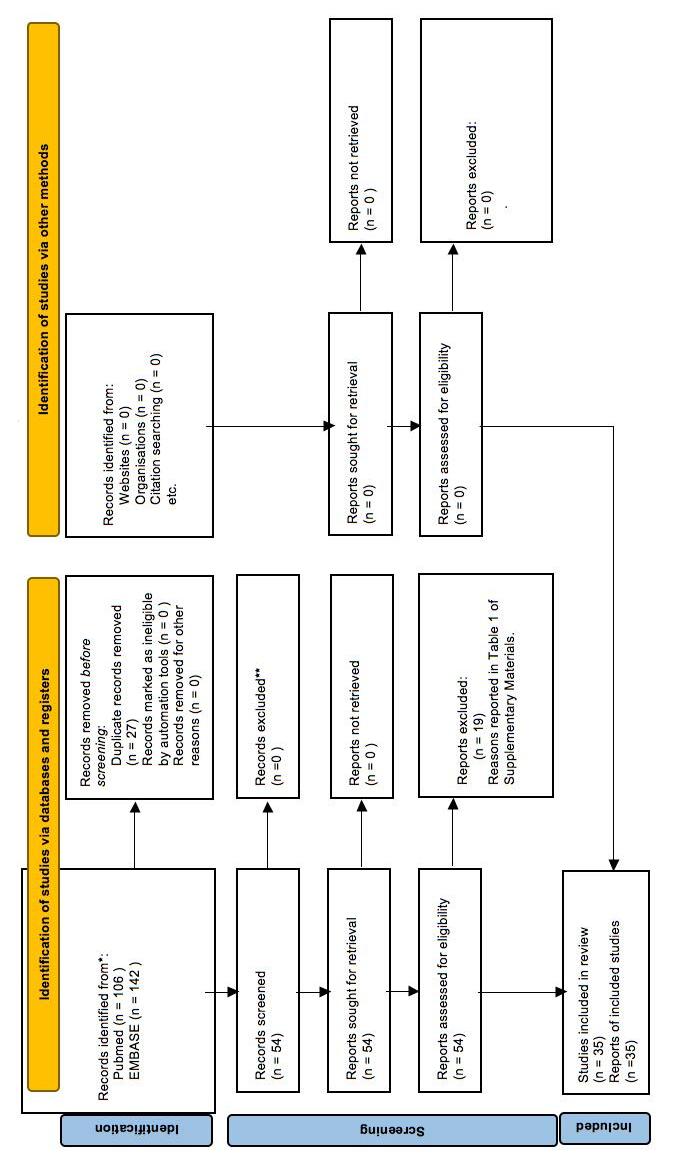
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 3 Postmenopausal urge incontinence F i g u r e 1 . P R I S M A 2 0 2 0 fl o w d i a g r a m f o r n e w s y s t e m a t i c r e v i e w s w h i c h i n c l u d e d s e a r c h e s o f d a t a b a s e s , r e ig s t e r s a n d o t h e r s o u r c e s .
substantial (I2 = 50%-90%) or considerable (I2 ≥ 75%), according to Cochrane criteria Sensitivity analysis was planned if considerable heterogeneity of pooled analyses including at least 4 studies was detected
Assessment of publication bias
Publication bias was assessed by generating funnel plots if meta-analyses included at least 4 trials The Begg’s and Egger’s tests were used to test funnel plot (a)symmetry and to confirm or exclude the presence of publication bias or small study effect Data on funnel plots were presented as the natural logarithm of odds ratios
T h e M e t a E s s e n t i a l 2 s o f t w a r e ( R o t t e r d a m S c h o o l o f Management, Erasmus University, The Netherlands) was used for funnel plot analysis
RESULTS
From 248 retrieved records ((Pubmed = 106, EMBASE = 142), and after removal of 27 duplicates, we selected 54 reports which were examined by full-text reading After full-text examination, 19 reports were excluded for various reasons (Supplementary Materials - Table 1) The remaining 35 reports were classified according to different types of treatment, namely estrogen treatment, including systemic (N = 9) and local (N = 6) administration, anticholinergics (N = 5), other treatments (N = 6), and physical treatment (N = 9)
Risk of bias
Of the 35 reports, only 8 were rated as having a low risk of bias, whereas 5 reports presented slight concerns and 23 high concerns of bias The randomization process was associated to risk of bias in most reports (n = 24) and to unclear risk in 10 Only one study presented high concerns of bias with respect to the randomization process Risk of deviations from the intended intervention (blinding) was rated as low in 18 reports, unclear in 4 and high in 13 The risk for missing outcome data was judged low in 20 reports, unclear in 4 and high in 11 The risk of bias in measurement of outcome was considered low in 27 reports, unclear in 1 and high in 7 The risk of bias in selection of the reported results was judged low in 34 and unclear in 1 (Supplementary Materials - Figure 1)
Systemic estrogens
The effect of estrogen administration on urinary incontinence in postmenopausal women was compared to placebo or no treatment in 9 studies Most studies date back to the 1990s or early 2000s, and some relate to programs that had women's general health after menopause as their main outcome, namely the Women's Health Initiative, the Heart and Estrogen/Progestin Replacement Study (HERS), the Estrogen Replacement and Atherosclerosis (ERA) trial, the Danish Osteoporosis Prevention Study (DOPS)
In a study, estriol produced not significant subjective and objective changes of the lower urinary tract function compared with placebo (8)
In three studies (9-11), administration of combined estrogen and progestogen therapy (0 625 mg/day conjugated equine estrogen plus 10 mg/day medroxyprogesterone acetate) was compared with placebo
Fantl et al observed no significant changes in the number of incontinence episodes, weight of fluid losses and number of diurnal or nocturnal voids (9)
Conversely, Grady et al showed that oral estrogen plus progestin treatment was associated with a worsening of urinary incontinence in postmenopausal women of the HERS (10)
An article by Steinauer et al , reporting about some results of HERS, confirmed a higher rate of weekly incontinence in patients on hormone treatment compared to a placebo group (64% vs 49%) (11) In two other studies (12, 13), both estrogens alone and a combination of estrogen and progestinics were compared with placebo Oral estrogen plus progestinic treatment had no significant effects on the de novo development of urge urinary incontinence in patients who were asymptomatic at baseline (RR 1 15) but increased the frequency of urinary incontinence (RR 1 38) and worsened the amount of urinary incontinence episodes (RR 1 20) in patients who reported urinary incontinence at baseline compared to placebo Oral estrogens alone increased the risk of the de novo development of urinary incontinence (RR 1 32), worsened the urinary frequency (RR 1 47) and increased the amount of urinary incontinence episodes in patients with incontinence at baseline (RR 1 59) (12) A similar study showed significantly higher rates of urinary incontinence in the estrogen-only group compared to the placebo group (13) In two studies, the effect of an estrogen implant, or of transdermal estrogen, was compared with placebo (14, 15) After two years of treatment with ultralow-dose transdermal estriol (0 014 mg/d), the prevalence of incontinence symptoms did not differ in treated women compared to placebo The odds ratio for incontinence worsening in women with incontinence at baseline was 1 35 in the estradiol treated compared with placebo group, and the odds of developing at least one weekly incontinence episode in women without incontinence at baseline was 1 20 (14) In neither case were odds ratios statistically significant Rufford et al evaluated the effect of systemic estrogen replacement by a 25 mg 17bestradiol implant compared to placebo implant No significant differences between the groups were observed by videocystourethrography, frequency volume chart, visual analogue score of symptoms, and King’s Health Care Quality of life Questionnaire (15) Finally, an open label study had a more complex design, as it included a group that was randomized to receive hormonal treatment versus no treatment and a second group in which patients chose whether to receive hormonal treatment or no treatment (16) Firstline hormonal treatments were: (a) sequential oral estrogen and progestogen (2 mg estradiol for the first 12 days, 2 mg estradiol plus 1 mg norethisterone acetate for 10 days, and 1 mg estradiol for 6 days) in women with intact uterus and (b) oral continuous estradiol, 2 mg per day, in hysterectomized women Hormonal treatment did not seem to influence the degree of voiding frequency, or the severity of incontinence (16)
The effect of hormone therapy both as combination of estrogens with progestogens or estrogens alone was quantitatively evaluated In 7 studies
Meta-analysis
Treatment of incontinence was considered successful
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718
4
R Bapir, K Hassan Bhatti, A Eliwa, et al
when the Authors defined the patients as cured (absence of the symptom(s) present at baseline) (8, 15) or improved (9, 10, 14) or without worsening of the degree of bother or disturbance attributed to urinary incontinence (12)
The odds of successful treatment were significantly lower in the hormone treatment group compared to the placebo or control groups (OR = 0 74, 95% CI: 0 61-0 91, 7 series, 17132 participants, Z = 2 89, P = 0 004, I2 = 72%, Figure 2) Funnel plot analysis for detection of publication bias produced uncertain results (Supplementary Materials Figure 2) Visual analysis of the plot suggest a significant degree of asymmetry, which was confirmed by
the Egger regression test (p = 0 016), but not to the Begg’s test (p = 0 88)
When women treated with a combined hormonal protocol were analyzed separately, the odds of success of incontinence treatment were confirmed to be significantly lower than the control group (OR = 0 78, 95% CI: 0 68-0 90, 3 series, 10707 participants, Z = 3 53, p = 0 0004, I2 = 21%, Figure 3), while the odds ratios of success of treatment with estrogen alone were not significantly different from controls (OR = 0 72, 95% CI: 0 49-1 06, 4 series, 6425 participants, Z = 1 65, p = 0 10, I2 = 54%, Figure 4, panel A) Visual analysis of the funnel plot suggested the presence of asymmetry, which was not confirmed by the Egger
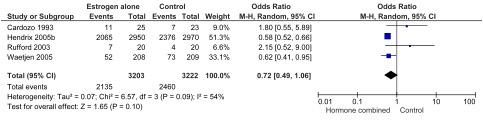
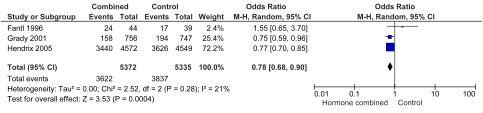
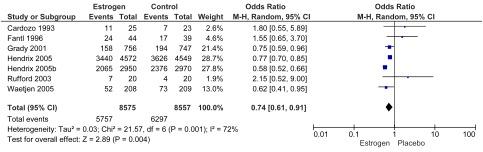
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 5 Postmenopausal urge incontinence
Figure 2.
Odds for success of systemic hormone treatment of urinary postmenopausal incontinence.
Figure 3. Odds for success of combined systemic hormone treatment of urinary postmenopausal incontinence
Figure 4
Odds for success of treatment for urinary postmenopausal incontinence with systemic estrogens alone
Figure 5.
Odds for urgency, nocturia and urinary incontinence in patients on systemic hormone treatment
a) diurnal voids
b) nocturia
c) urinary incontinence
regression test (p = 0 078) or by the Begg’s test (p = 0 17) (Supplementary materials Figure 2)
On the other hand, meta-analyses of three studies demonstrated that the odds for diurnal voids and urinary incontinence in women on systemic hormone treatment were not different from those in women treated with placebo, while in two studies the odds for nocturia worsened for women on hormonal treatment compared to controls (Figure 5)

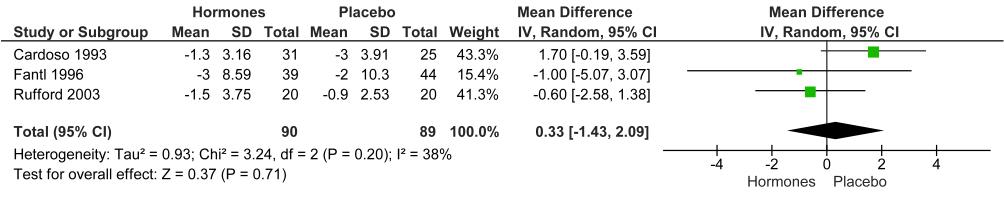
Similarly, in two studies, the odds of improvement in urodynamic parameters (volume at first desire to void, cystometric capacity, and detrusor pressure) were not sig-
Figure 6.
nificantly different in patients receiving hormone treatment compared to controls (Figure 6)
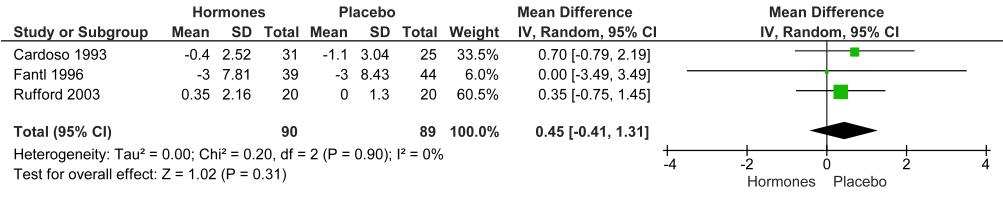
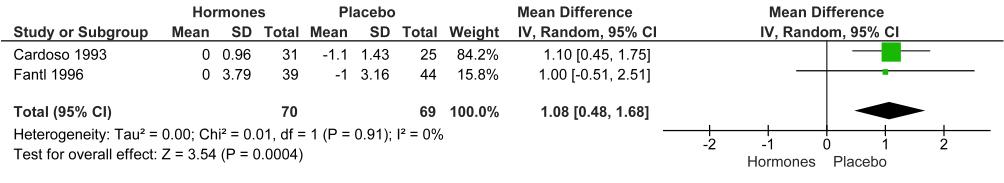
Local estrogens
Three studies compared the use of local estrogens with placebo (17-19) One study compared local estrogens alone with local estrogens combined with benzydamine (20) Another study compared estrogen delivery via a vaginal ring with an estriol pessary (21) Finally, a study compared ultralow-dose estradiol vaginal ring with oral oxybutynin (22)
Odds for improvement of urodynamic parameters in patients on systemic hormone treatment compared to controls
a) volume at first desire to void
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R Bapir, K Hassan Bhatti, A Eliwa, et al 6
b) cystometric capacity
c) detrusor pressure
Cardozo et al evaluated the effect of 17-beta estradiol 25 mg vaginal tablets or placebo daily for 12 weeks (17) No significant improvement was observed in urinary frequency and urgency following treatment with intravaginal 17-beta estradiol The only statistically significant difference was a greater reduction in urinary urgency in women with a urodynamic diagnosis of sensory urgency In this subgroup, urgency was related to urogenital atrophy secondary to estrogen deficiency
In a study by Dessole et al , the treatment cohort received intravaginal estriol ovules (1 mg ovule once-daily for 2 weeks and subsequently 2 ovules once-weekly for a 6 months), and the control group received inert placebo vaginal suppositories in a similar regimen A subjective improvement of incontinence was observed in 68% of the treated participants in comparison to 16% of the controls Speroff et al assessed the efficacy of a vaginal ring, delivering the equivalent of 50 or 100 mcg per day of estradiol compared with placebo (19) There was a general trend towards the improvement of urogenital symptoms in patient with active rings, although a significant improvement compared with placebo was observed only for certain vaginal symptoms (vaginal dryness, pain during intercourse)
Melis et al compared vaginal administration of a low dose of estriol (0 5 mg daily for 14 days, followed by 0 5 mg every two days for 3 months) with the same regimen plus an anti-inflammatory and antibacterial compound (benzidamine) (20) The efficacy on urinary symptoms (nocturia, incontinence, urge incontinence) was not different between the two groups, although the combination of estriol with benzidamine was more effective in reducing vaginal symptoms (itching, burning, leucorrhea, dryness)
Lose et al compared the efficacy of an estradiol-releasing vaginal ring with an estriol pessary, showing that these strategies were equally efficacious in reducing urinary urgency, urge incontinence, stress incontinence and nocturia (21) The vaginal ring showed higher patient acceptability compared to estriol pessaries
Nelken et al evaluated women who were randomized to
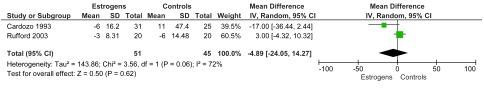
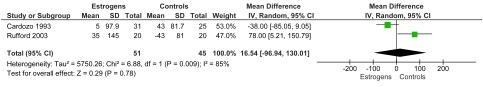
receive either a vaginal ring releasing ultralow-dose estradiol (2 mg of 17beta-estradiol released at a rate of 7 5 Kg microgr daily) or oral oxybutynin (5 mg twice daily) for 12 weeks (22) Both treatments achieved a reduction in the number of voids per day, with no significant difference between the groups
Anticholinergics
Only one study compared anticholinergics with placebo (23) In four studies (24-27) the efficacy of anticholinergics alone was compared with anticholinergics in combination with local estrogens
Tapp et al performed a placebo controlled cross over study of oxybutynin chloride in postmenopausal women suffering from detrusor instability (23) Oxybutynin therapy significantly reduced the symptoms of urgency, urge incontinence, and nocturia Oxybutynin therapy was significantly better than placebo at improving urgency and urge incontinence
Chughtai et al compared fesoterodine with topical vaginal estrogen once daily with fesoterodine once daily alone for 12 weeks (24) Both treatments were associated with a significant improvement in urinary symptom severity and quality of life Compared to fesoterodine alone, the combination treatment showed a reduced symptom severity (OAB score) and higher quality of life (HRQL and SQOLF score) Urinary frequency was significantly reduced from baseline in the combination group alone
Jiang et al randomized patients to receive solifenacin 5 mg plus promestriene vaginal capsules, or solifenacin 5 mg alone for 12 weeks (25) There were no significant intergroup differences in the number of daily voids, urgency episodes, urge incontinence episodes and nocturia
Martin et al randomized patients to treatment with fesoterodine in combination with either a conjugated estrogen vaginal cream or a placebo vaginal cream (26) Both treatments decreased the severity of urinary symptoms (OAB and USIQ scores) and increased the quality of life (HRQL score) No significant intergroup differences were
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 7 Postmenopausal urge incontinence
observed In addition, there was no significant improvement in data recorded in bladder diaries
Tseng et al randomized patients to treatment with 2 mg tolterodine twice daily compared to 2 mg tolterodine twice daily associated to vaginal conjugated equine estrogen 0 625 mg twice a week for 12 weeks (27) The comparison between groups showed a significantly greater improvement in daytime frequency and voided volume after combination treatment Other symptoms, including nocturia, urgency and urge incontinence were improved with both treatments, though intergroup differences were n o t r e p o r t e d T h e q u a l i t y o f l i f e w a s s i g n i fi c a n t l y improved after combination treatment compared to the single-agent protocol
Other treatments
Two reports presented the results of treatment with soy extracts (28, 29)
Bumbu et al compared the effect of long-term administration of soy extracts (40% isoflavones) with the results of continuous combined hormonal treatment based on 1 mg estradiol and 0 5 mg noretisterone acetate daily, with a control no-treatment group (28) After 12 months, s y m p t o m s c o r e s , a c c o r d i n g t o t h e R e v i s e d U r i n a r y Incontinence Scale (RUIS), and the incidence of urinary incontinence, were influenced neither by soy nor by hormone treatment compared to placebo
Manorai et al compared the effect of a soy-rich diet (25 g soy protein in various forms of soy food, containing more than 50 mg/day of isoflavones) with an isocaloric control diet (soy-free diet) (29) The symptoms of urge incontinence and vaginal dryness significantly increased after 12-weeks of soy-free diet
Two studies evaluated the effect of vitamin D supplementation on urinary incontinence symptoms (30, 31) Markland et al conducted a randomized trial in women with serum 25-hydroxyvitamin D (25[OH]D) of 30 ng/mL or less, comparing treatment with weekly oral 50 000 IU vitamin D3 or placebo for 12 weeks (30) Vitamin D treatment demonstrated a greater than 40% decrease in urinary incontinence episodes, which however did not reach statistical significance compared to placebo
Oberg at al (31) allocated patients to 20 000 IU of vitamin D3 twice a week, or to a similarly looking placebo
After 12 months, a statistically significant reduction in the severity of urine incontinence in the high dose vitamin D group was observed, compared to placebo
Other pharmacological treatments were evaluated in two studies (32, 33)
Waetjen et al assigned patients to raloxifene or placebo (32) After 3 years of treatment, there was no significant difference between raloxifene and placebo groups in terms of urinary incontinence severity (OR 1 02) In addition, the odds of worsening urinary incontinence severity were 1 05 and the odds of developing new onset incontinence were 0 95
Green et al assigned women to treatment with aprepitant at a daily dose of 160 mg versus placebo for 8 weeks (33)
Aprepitant is a neurokinin-1 receptor antagonist that may be efficacious in the treatment of urge urinary incontinence, since preclinical evidence suggested that incontin e n c e m a y b e a s s o c i a t e d t o u p - r e g u l a t i o n o f t h e
tachykinin mediated bladder/spinal reflex signaling
Treatment significantly decreased the number of daily voids and urgency episodes compared with placebo at 8 weeks, although the daily number of urge urinary incontinence and the total urinary incontinence episodes were not significantly reduced
Physical treatment
Three studies compared postmenopausal women treated with pelvic floor muscle training (PFTM) with a control group (34-36) An increase of pelvic floor muscle contractility after PFMT, as evaluated by surface electromyography (sEMG) and digital palpation, was observed in two reports (34,35) Alves et al demonstrated an improvement of incontinence symptom scores (ICIQ-OAB, ICIQ UI-SF, MESA), as well as of the anterior pelvic organ prolapse score (POP-Q System) after PFTM, compared to controls (34) Sran et al reported an improvement of symptoms as measured by Urogenital Distress Inventory (UDI) after PFTM (p = 0 026), whereas changes of Incontinence Impact Questionnaire (IIQ) and Geriatric SelfPerceived Efficacy scores were not significantly improved (36)
Results of bladder diaries showed a reduction of nocturia and frequency together with an increase of intervoid intervals (35), and a reduction of weekly leakage episodes (36) Finally, the same group demonstrated that physical treatment significantly reduced the amount of leakage on the 24-hour pad test
A study compared PFMT alone with PFMT combined with postural instructions and demonstrated that addition of the latter improved pelvic muscle strength as evaluated by Oxford Grading Scale However, incontinence symptoms were not improved (37)
Another study compared two formats of unsupervised PFMT programs (2-hr Class or 20 min Video instruction), showing no difference in terms of nocturia and urinary urgency episodes reduction and inter-void interval extension (38)
Other studies evaluated the effectiveness of other physical treatments (vaginal electrostimulation, radiofrequency, fractional CO2 laser, LiESWT) in reducing urinary incontinence in post-menopausal women
The effect of vaginal electrostimulation was compared with the outcome of PFMT; no significant improvement in subjective and objective outcome variables were reported in the population treated with electrostimulation compared with the population treated with PFMT
The rates of women reporting improvements in urinary leakage were 29 2% vs 27 3% (39)
A study compared radiofrequency treatment and fractional CO2 laser treatment (4 weeks apart, about 1-2 minute(s) per session) with a control group It was demonstrated that mixed urinary incontinence decreased after the intervention including radiofrequency and laser compared to the control group However, the changes in the laser group were not statistically significant (40) Borges Aguiar et al compared the efficacy of CO2 laser treatment with local estrogen treatment and a control treatment (vaginal lubricant) (41) The laser group showed a more significant reduction in the total ICIQ-UI SF score and nocturia compared to controls
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R
et al 8
Bapir, K Hassan Bhatti, A Eliwa,
Finally, a study investigated the therapeutic efficacy of low intensity extracorporeal shock wave treatment (LiESWT) on urinary incontinence of postmenopausal women in comparison to sham treatment (42) LiESWT decreased urinary frequency, nocturia, urgency, urgency incontinence, and post-voided residual urine volume and increased voided urine volume and maximal flow rate compared to the sham control
Summary of findings
A Summary of Findings (SOF) table prepared according to GRADE criteria is shown in the Supplementary materials (Table 2) The quality of the evidence ranged between moderate (presence of Risk of Bias) and very low (publication bias, risk of bias and inconsistency due to substantial heterogeneity)
DISCUSSION
The prevalence of bladder symptoms, such as frequency, urgency and incontinence, tends to increase around the menopause, although it is still debated whether these disorders are due to menopause, or aging, or a combination of the two
Urinary symptoms are associated with the genitourinary syndrome of menopause (GSM) which is characterized by physical changes of the vulva, of the vagina and of the lower urinary tract, including the presence of pallor or erythema of the genital mucosa, loss of vaginal wrinkles, introital retraction, vaginal dryness and the prolapse of the urethral mucosa
These genital alterations have been all correlated with local estrogen deficiency, and were shown to benefit from local estrogen administration However, the effects of local estrogens on urinary symptoms such as urgency, frequency and urinary incontinence are still unclear (43-45)
For these reasons, the treatment of postmenopausal incontinence remains not well defined by therapeutic guidelines, which sometimes do not consider postmenopausal incontinence as an independent and specific condition, but as a subtype of other clinical disorders (overactive bladder, lower urinary tract symptoms, urge and urinary incontinence)
Our search and literature review retrieved the results of studies focusing on various forms of treatment or combinations of different treatments
Estrogens
High affinity estrogen receptors are present in the female urinary tract and in the structures of the pelvic floor Clinical and urodynamic modifications are observed during pregnancy, the menstrual cycle and following the onset of the menopause In animal studies, pretreatment with estrogens enhanced detrusor contractility in response to alpha-adrenoceptor agonists, cholinomimetics and prostaglandins, and contractile response to alpha-agonists in the ureter and urethra, conversely, progesterone decreases the muscle tone in the ureter, bladder and urethra by enhancing beta-adrenergic responses (46) In postmenopausal women, atrophic mucosal changes respond well to low-dose estrogen replacement therapy (43) Two meta-analyses by Cody et al extensively evaluated
the role of estrogen therapy for urinary incontinence in post-menopausal women (44, 45) The authors concluded that systemic treatment with conjugated equine estrogen may worsen urinary incontinence However, too few data were retrieved to extensively evaluate the effects of estrogen type, different dosage, and route of administration Furthermore, the authors highlighted the potential risk of endometrial and breast cancer onset associated with long-term high-dose estrogen treatment and suggested cautious and limited in time use of estrogen, especially in non-hysterectomized women
Estriol has less uterotrophic effect compared to other estrogens; conversely, the addition of a progestogen to long-term estrogen therapy to reduce the risk of endometrial cancer may increase the risk of incontinence due to a decrease in urethral pressure induced by the latter
Local treatment with estrogen was considered safer and was deemed to improve urinary incontinence, though the optimal duration of treatment and long-term effects have been poorly studied (44, 45)
EAU guidelines suggest offering vaginal estrogen therapy to women with lower urinary tract symptoms (LUTS) and associated symptoms of genitourinary syndrome of menopause (47) Our analysis showed that no significant improvements in urinary symptoms were observed in patients treated with local estrogens, except for a reduction in urgency severity in a subgroup of patients presenting with sensory urgency Similarly, no significant changes in urodynamic parameters were observed Local estrogens do not seem to give a substantial benefit of urinary symptoms in postmenopausal patients, although they may be helpful in improving vaginal irritation symptoms
Vitamin D, phytoestrogens and estrogens modulators
An alternative to estrogen treatment is the use of other drugs acting on estrogen receptors or on other receptors present in the genitourinary organs
Phytoestrogens, such as the isoflavones of soy, show structural similarities to natural and synthetic estrogens and antiestrogens, acting as estrogen agonists and producing estrogen-like effects Consumption of a phytoes t r o g e n - r i c h d i e t h a s b e e n s u g g e s t e d t o a l l e v i a t e menopausal symptoms without increasing the risk of cancer (48) Conversely, studies retrieved by our review showed that a soy-rich diet was not effective in improving the symptoms of incontinence and other symptoms of t h e g e n i t o u r i n a r y m e n o p a u s e s y n d r o m e ( 2 8 , 2 9 )
Raloxifene is a second-generation selective estrogen receptor modulator that is used for the prevention and treatment of osteoporosis in postmenopausal women because of its estrogenic effect on the bone, associated to an antiestrogenic effect on breast, and a neutral effect on the endometrium and the vaginal mucosa In the RCT included in this review, raloxifene had no significant effect on urinary incontinence in postmenopausal women after 3 years of treatment (32)
The use of vitamin D for the treatment of urinary incontinence in postmenopausal women is supported by the finding of vitamin D receptors on the bladder detrusor and striated muscle (48) Vitamin D could act on stromal and smooth muscle cells by improving the muscle response to bladder filling in women with low vitamin D intake (50)
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 9 Postmenopausal urge incontinence
In our review, two studies (30, 31) evaluated the effects of vitamin D administration on urinary incontinence in menopausal women, but the results appear to be contradictory, and no conclusive statement can be made on this matter
Anticholinergics
Anticholinergics are successfully used in the treatment of neurogenic or idiopathic overactive bladder symptoms, although their use is limited by side effects such as dry mouth and constipation (51) In addition, a specific limitation of the use of anticholinergics in the treatment of postmenopausal urinary incontinence could be the potential risk of cognitive impairment in older women In fact, treatment with anticholinergics in elderly people could be associated with cognitive impairment, as has been demonstrated in recent longitudinal cohort studies (52, 53) Cognitive impairment could be a consequence of central nervous system metabolism alterations and brain atrophy
EAU guidelines (47) confirm the efficacy of anticholinergic drugs in elderly patients with overactive bladder and urinary incontinence but warn of the risk of a cognitive impact with a cumulative effect related to the length of treatment
Worsening of cognitive function has been observed in patients taking oxybutynin (52, 54), but not in short-term studies with darifenacin, fesoterodine, solifenacin and trospium Although a previous meta-analysis (55) found inconclusive evidence of the impact of anticholinergics on cognition, a cautious use of long-term anticholinergics has been recommended, especially in patients at risk or with pre-existing cognitive dysfunction or on treatment with other drugs with anticholinergic effects (54)
Mirabegron
A possible alternative to anticholinergics could be b3adrenoceptor agonists, which have demonstrated efficacy and safety in elderly patients In patients aged ≥ 65 years, d r y m o u t h o c c u r re d m u c h l e s s f re q u e n t l y w i t h mirabegron than with tolterodine Mirabegron also had a low incidence of central nervous system effects, and a systematic review of the cardiovascular safety profile has shown no clinically significant effects on blood pressure or pulse rate amongst patients aged ≥ 65 years (56, 57)
Our literature review found no RCT comparing mirabegron or other b3-adrenoceptor agonists with placebo for the treatment of postmenopausal incontinence Further studies are warranted in this respect A recent study (58), published after the conclusion of our literature search, compared two b 3-adrenoceptor agonists, mirabegron and vibegron, in postmenopausal women with treatment naive overactive bladder After 12 weeks of treatment, both drugs significantly improved symptom scores, micturition frequency, urgency and incontinence episodes, as well as the voided volume per 24 hours, compared with baseline, without significant difference in postvoid residual urine volume Severe side effects requiring the discontinuation of treatment were observed in 6 2% of patients in the mirabegron group and in 6 8% in the vibegron group
Physical therapy
The studies included in our review demonstrated an overall positive outcome of pelvic floor muscle training (PFMT)
on postmenopausal urinary incontinence symptoms, although in most studies no effort was made to distinguish between the different types of incontinence Similarly, a recent systematic review demonstrated that PFMT in combination with physical training was effective in reducing urinary incontinence and improving quality of life in elderly patients (> 65 years) (59) Moreover, an ICI consensus paper stated that age and frailty alone did not represent a contraindication for PFMT in selected patients with sufficient cognition to comply with treatment (60)
Other forms of physical treatment for urinary incontinence need to be validated by quality, adequately powered RCTs EAU guidelines report slight, short-term improvement of overactive bladder symptom after vaginal laser therapy, but data about long-term efficacy and safety are missing
Vaginal laser therapy is not recommended outside the frame of well-designed controlled clinical trials (61)
CONCLUSIONS
In conclusion, the results of our review demonstrate that there is no robust evidence of an effective treatment for postmenopausal urinary incontinence There is still a need of large, adequately powered and well-designed studies, focusing on subjective and objective improvements in urinary incontinence as their primary outcome Currently, no treatment by itself has been shown to be fully effective and superior to another From the limited evidence available, a combined approach, including different forms of treatment tailored to the characteristics of the individual patient can be suggested
REFERENCES
1 Diokno A, Brock B, Brown M, Herzog A Prevalence of urinary incontinence and other urological symptoms in the noninstitutionalized elderly J Urol 1986; 136:1022-5
2 Brown JS, Seeley D, Fong J, et al Urinary incontinence in older women: Who is at risk? Obstet Gynecol 1996; 87:715-21
3 Iosif C, Batra S, Ek A, Astedt B Estrogen receptors in the human female lower urinary tract Am J Obstet Gynecol 1981; 141:817-20
4 Chen YC, Chen GD, Hu SW, et al Is the occurrence of storage and voiding dysfunction affected by menopausal transition or associated with the normal aging process? Menopause 2003; 10:203-208
5 Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and MetaAnalyses: The PRISMA Statement PLoS Med 2009; 6:e1000097
6 Page MJ, McKenzie JE, Bossuyt PM, et al The PRISMA 2020 statement: an updated guideline for reporting systematic reviews BMJ 2021; 372:n71
7 Sterne JAC, Savovic J, Page MJ, et al RoB 2: a revised tool for assessing risk of bias in randomised trials BMJ 2019; 366:l4898
8 Cardozo L, Rekers H, Tapp A, et al Oestriol in the treatment of postmenopausal urgency: a multicentre study Maturitas 1993; 18:47-53
9 Fantl JA, Bump RC, Robinson D, et al Efficacy of estrogen supp
Continence Program for Women Research Group Obstet Gynecol 1996; 88:745-9
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R
et al 10
Bapir, K Hassan Bhatti, A Eliwa,
l e m e n t a t i o n i n t h e t r e a t m e n t o f u r i n a r y i n c o n t i n e n c e T h e
10 Grady D, Brown JS, Vittinghoff E, et al ; HERS Research Group
Estrogen/Progestin Replacement Study Obstet Gynecol 2001; 97:116-20
11 Steinauer JE, Waetjen LE, Vittinghoff E, et al Postmenopausal hormone therapy: does it cause incontinence? Obstet Gynecol 2005; 106:940-5
12 Hendrix SL, Cochrane BB, Nygaard IE, et al Effects of estrogen with and without progestin on urinary incontinence JAMA 2005; 293:935-48
13 Sherman AM, Shumaker SA, Sharp P, et al No effect of HRT on health-related quality of life in postmenopausal women with heart disease Minerva Ginecol 2003; 55:511-7
14 Waetjen LE, Brown JS, Vittinghoff E, et al The effect of ultralowd o s e t r a n s d e r m a l e s t r a d i o l o n u r i n a r y i n c o n t i n e n c e i n p o s tmenopausal women Obstet Gynecol 2005; 106:946-52
15 Rufford J, Hextall A, Cardozo L, Khullar V A double-blind placebo-controlled trial on the effects of 25 mg estradiol implants on the urge syndrome in postmenopausal women Int Urogynecol J Pelvic Floor Dysfunct 2003; 14:78-83
16 Vestergaard P, Hermann AP, Stilgren L, et al Effects of 5 years of hormonal replacement therapy on menopausal symptoms and blood pressure-a randomised controlled study Maturitas 2003; 46:123-32
17 Cardozo LD, Wise BG, Benness CJ Vaginal oestradiol for the treatment of lower urinary tract symptoms in postmenopausal women--a double-blind placebo- controlled study J Obstet Gynaecol 2001; 21:383-5
18 Dessole S, Rubattu G, Ambrosini G, et al Efficacy of low-dose intravaginal estriol on urogenital aging inm postmenopausal women
Menopause 2004; 11:49-56
19 Speroff L Efficacy and tolerability of a novel estradiol vaginal ring for relief of menopausal symptoms Obstet Gynecol 2003; 102:823-34
20 Melis GB, Paoletti AM, Murgia C, et al Vaginal estriol and benzidamine in the treatment of urogenital disorders during the postmenopause Giornale Italiano di Ostetricia e Ginecologia 1997; 19:303-312
21 Lose G, Englev E Oestradiol-releasing vaginal ring versus oestriol vaginal pessaries in the treatment of bothersome lower urinary tract symptoms BJOG 2000; 107:1029-34
22 Nelken RS, Ozel BZ, Leegant AR, et al Randomized trial of estradiol vaginal ring versus oral oxybutynin for the treatment of overactive bladder Menopause 2011; 18:962-6
23 Tapp AJ, Cardozo LD, Versi E, Cooper D The treatment of detrusor instability in post-menopausal women with oxybutynin chloride: a double blind placebo controlled study Br J Obstet Gynaecol 1990; 97:521-6
24 Chughtai B, Forde JC, Buck J, et al The concomitant use of fesoterodine and topical vaginal estrogen in the management of overactive bladder and sexual dysfunction in postmenopausal women Post Reprod Health 2016; 22:34-40
25 Jiang F, Zhu L, Xu T, et al Efficacy and safety of solifenacin succinate tablets versus solifenacin succinate tablets with local estrogen for the treatment of overactive bladder in postmenopausal women--a multicenter, randomized, open-label, controlled comparison study Menopause 2016; 23:451-7
26 Martin L, Hidalgo R, Schachar J, et al Anticholinergic medication and local estrogen for overactive bladder: A randomized placebo controlled trial International Urogynecology Journal 2018; 29 (Supplement 1): S112
27 Tseng LH, Wang AC, Chang YL, et al Randomized comparison of tolterodine with vaginal estrogen cream versus tolterodine alone for the treatment of postmenopausal women with overactive bladder syndrome Neurourol Urodyn 2009; 28:47-51
28 Bumbu A, Bianca P, Tit DM, et al The effects of soy isoflavones and hormonal replacing therapy on the incidence and evolution of postmenopausal female urinary incontinence Farmacia 2016; 64:419-422
29 Manonai J, Songchitsomboon S, Chanda K, et al The effect of a soy-rich diet on urogenital atrophy: a randomized, cross-over trial Maturitas 2006; 54:135-40
30 Markland AD, Tangpricha V, Mark Beasley T, et al Comparing Vitamin D Supplementation Versus Placebo for Urgency Urinary Incontinence: A Pilot Study J Am Geriatr Soc 2019; 67:570-575
31 Oberg J, Verelst M, Jorde R, et al High dose vitamin D may improve lower urinary tract symptoms in postmenopausal women J Steroid Biochem Mol Biol 2017; 173:28-32
32 Waetjen LE, Brown JS, Modelska K, et al MORE Study Group
Effect of raloxifene on urinary incontinence: a randomized controlled trial Obstet Gynecol 2004; 103:261-6
33 Green SA, Alon A, Ianus J, et al Efficacy and safety of a neurokinin-1 receptor antagonist in postmenopausal women with overactive bladder with urge urinary incontinence J Urol 2006; 176:2535-40
34 Alves FK, Riccetto C, Adami DB, et al A pelvic floor muscle training program in postmenopausal women: A randomized controlled trial Maturitas 2015; 81:300-5
35 Diokno AC, Sampselle CM, Herzog AR, et al Prevention of urinary incontinence by behavioral modification program: a randomized, controlled trial among older women in the community J Urol 2004; 171:1165-71
36 Sran M, Mercier J, Wilson P, et al Physical therapy for urinary incontinence in postmenopausal women with osteoporosis or low bone density: a randomized controlled trial Menopause 2016; 23:286-93
37 Fuentes-Aparicio L, Rejano-Campo M, López-Bueno L, et al The effect of an abdominopelvic exercise program alone VS in addition to postural instructions on pelvic floor muscle function in climacteric women with stress urinary incontinence A randomized controlled trial Physiother Theory Pract 2023; 39:738-749
38 Wu C, Newman D, Schwartz TA, et al Effects of unsupervised behavioral and pelvic floor muscle training programs on nocturia, urinary urgency, and urinary frequency in postmenopausal women: Secondary analysis of a randomized, two-arm, parallel design, superiority trial (TULIP study) Maturitas 2021; 146:42-48
39 Spruijt J, Vierhout M, Verstraeten R, et al Vaginal electrical stimulation of the pelvic floor: a randomized feasibility study in urinary incontinent elderly women Acta Obstet Gynecol Scand 2003; 82:1043-8
40 Eftekhar T, Ghorbani L, Ghanbari Z, et al Comparison of the Effect of Radiofrequency and Laser Treatment on Mixed Urinary Incontinence and Vulvovaginal Atrophy in Iranian Menopausal Women: A Randomized Controlled Trial International Journal of Women’s Health and Reproduction Sciences 2021; 9:61-68
41 Aguiar LB, Politano CA, Costa-Paiva L, Juliato CRT Efficacy of Fractional CO2 Laser, Promestriene, and Vaginal Lubricant in the Treatment of Urinary Symptoms in Postmenopausal Women: A Randomized Clinical Trial Lasers Surg Med 2020; 52:713-720
42 Lin KL, Lu JH, Chueh KS, et al Low-Intensity Extracorporeal Shock Wave Therapy Promotes Bladder Regeneration and Improves Overactive Bladder Induced by Ovarian Hormone Deficiency from Rat Animal Model to Human Clinical Trial Int J Mol Sci 2021; 22:9296
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 11 Postmenopausal urge incontinence
P o s t m e n o p a u s a l h o r m o n e s a n d i n c o n t i n e n c e : t h e H e a r t a n d
43 Biehl C, Plotsker O, Mirkin S A systematic review of the efficacy and safety of vaginal estrogen products for the treatment of genitourinary syndrome of menopause Menopause 2019; 26:431-453
44 Cody JD, Richardson K, Moehrer B, et al Oestrogen therapy for u r i n a r y i n c o n t i n e n c e i n p o s t - m e n o p a u s a l w o m e n C o c h r a n e Database Syst Rev 2009; (4):CD001405
45 Cody JD, Jacobs ML, Richardson K, et al Oestrogen therapy for u r i n a r y i n c o n t i n e n c e i n p o s t - m e n o p a u s a l w o m e n C o c h r a n e Database Syst Rev 2012; 10:CD001405
46 Miodrag A, Castleden CM, Vallance TR Sex hormones and the female urinary tract Drugs 1988; 36:491-504
47 Harding CK, Lapitan MC, Arlandis S, et al EAU Guidelines on Management of Non-Neurogenic Female Lower Urinary Tract Symptoms EAU Guidelines Edn presented at the EAU Annual Congress Milan March 2023 EAU Guidelines Office, Arnhem, The Netherlands http://uroweb org/guidelines/compilations-of-all-guidelines/
48 Glazier MG, Bowman MA A review of the evidence for the use of phytoestrogens as a replacement for traditional estrogen replacement therapy Arch Intern Med 2001; 161:1161-72
49 Crescioli C, Morelli A, Adorini L, et al Human bladder as a novel target for vitamin D receptor ligands J Clin Endocrinol Metab 2005; 90:962-972
50 Dallosso HM, McGrother CW, Matthews RJ, et al Incontinence Study Group Nutrient composition of the diet and the development of overactive bladder: a longitudinal study in women NeurourolUrodyn 2004; 23:204-210
51 Bapir R, Bhatti KH, Eliwa A, et al Efficacy of overactive neurogenic bladder treatment: A systematic review of randomized controlled trials Arch Ital Urol Androl 2022; 94:492-506
52 Gray SL, Anderson ML, Dublin S, et al Cumulative use of strong
anticholinergics and incident dementia: a prospective cohort study JAMA Intern Med 2015; 175:401-7
53 Risacher SL, McDonald BC, Tallman EF, et al ; Alzheimer’s Disease Neuroimaging Initiative Association Between Anticholinergic Medication Use and Cognition, Brain Metabolism, and Brain Atrophy in Cognitively Normal Older Adults JAMA Neurol 2016; 73:721-32
54 Sink KM, Thomas J 3rd, Xu H, et al Dual use of bladder anticholinergics and cholinesterase inhibitors: long-term functional and cognitive outcomes J Am Geriatr Soc 2008; 56:847-53
55 Tannenbaum C, Paquette A, Hilmer S, et al A systematic review of amnestic and non-amnestic mild cognitive impairment induced by anticholinergic, antihistamine, GABAergic and opioid drugs Drugs Aging 2012; 29:639-58
56 Wagg A, Nitti VW, Kelleher C, et al Oral pharmacotherapy for overactive bladder in older patients: mirabegron as a potential alternative to antimuscarinics Curr Med Res Opin 2016; 32:621-38
57 Kennelly MJ, Rhodes T, Girman CJ, et al Efficacy of Vibegron and Mirabegron for Overactive Bladder: A Systematic Literature Review and Indirect Treatment Comparison Adv Ther 2021; 38:5452-5464
58 Kinjo M, Masuda K, Nakamura Y, et al Comparison of Mirabegron and Vibegron in Women With Treatment-Naive Overactive Bladder: A Randomized Controlled Study Urology 2023; 175:67-73
59 Stenzelius K, et al The effect of conservative treatment of urinary incontinence among older and frail older people: a systematic review
Age Ageing 2015; 44:736
60 Wagg A, Chen LK, Johnson T, et al Committee 11, Incontinence in frail older persons, in Incontinence, P Abrams, et al , Editor 2017
61 Alsulihem A, Corcos J The use of vaginal lasers in the treatment of urinary incontinence and overactive bladder, systematic review
Int Urogynecol J 2021; 32:553-572
Correspondence
Rawa Bapir, MD
Dr rawa@yahoo com
Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq
Kamran Hassan Bhatti, MD
kamibhatti92@gmail com
Urology Department, HMC, Hamad Medical Corporation, Qatar
Ahmed Eliwa, MD ahmedeliwafarag@gmail com
Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt
Herney Andrés García-Perdomo, MD
herney garcia@correounivalle edu co
Universidad del Valle, Cali, Colombia
Nazim Gherabi, MD ngherabi@gmail com
Faculty of Medicine Algiers 1, Algiers, Algeria
Derek Hennessey, MD
derek hennessey@gmail com
Department of Urology, Mercy University Hospital, Cork, Ireland
Vittorio Magri, MD
vittorio magri@asst-fbf-sacco it
Urology Unit, ASST Fatebenefratelli Sacco, Milan, Italy
Panagiotis Mourmouris, MD
thodoros13@yahoo com
Lazaros Tzelves, MD
lazarostzelves@gmail com
2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece
Adama Ouattara, MD adamsouat1@hotmail com
Division of Urology, Souro Sanou University Teaching Hospital, BoboDioulasso, Burkina Faso
Gianpaolo Perletti, Dr Biol Sci M Clin Pharmacol Gianpaolo Perletti@uninsubria it
Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy
Joseph Philipraj, MD josephphilipraj@gmail com
Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India
Konstantinos Stamatiou, MD stamatiouk@gmail com
Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece
Musliu Adetola Tolani, MD adetolatolani@yahoo com
Division of Urology, Department of Surgery, Ahmadu Bello University/ Ahmadu Bello University Teaching Hospital, Zaria, Kaduna State, Nigeria
Alberto Trinchieri, MD alberto trinchieri@gmail com Urology School, University of Milan, Milan (Italy)
Noor Buchholz,MD noor buchholz@gmail com
Sobeh's Vascular and Medical Center, Dubai Health Care City, Dubai, United Arab Emirates
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718
12
R Bapir, K Hassan Bhatti, A Eliwa, et al
The influence of BPO and PD on mental health
Gianni Paulis 1 , Andrea Paulis 2
1 Peyronie’s Care Center, Department of Uro-Andrology, Castelfidardo Clinical Analysis Center, Rome, Italy;
2 Neurosystem Center for applied Psychology and Neuroscience, Janet Clinical Centre, Rome, Italy
KEY WORDS: Benign prostatic obstruction; Peyronie’s disease; Mental health
Submitted 27 June 2023; Accepted 14 July 2023
To the Editor,
Our study aimed to investigate a possible relationship between benign prostatic obstruction (BPO) and Peyronie's disease (PD) and to characterize the psychological profile of patients affected by Peyronie's disease, with or without concomitant BPO In this study, we have investigated whether there is a relationship between the two diseases The typical symptoms of PD are as follows: penile deformation, local pain, erectile dysfunction (ED), and anxious-depressive state Benign prostatic hyperplasia (BPH) causes symptoms only in the case of urinary obstruction (benign prostatic obstruction/BPO) BPO is an emotionally stressful condition, but any type of treatment, such as surgery, by significantly decreasing LUTS, can significantly improve the general well-being of the affected patient (1)
We performed a retrospective analysis of the clinical database of a single uro-andrology clinic From the database, we considered two separate cohorts of patients observed between January 2013 and February 2023 The first cohort included 539 patients diagnosed with Peyronie's disease As a comparator population, we considered a cohort of 2208 outpatients referred to our clinic for any disease, but not Peyronie's disease
In the two cohorts, we identified patients with a diagnosis of long-standing BPO
All data were obtained from patient records This retrospective observational study was conducted in compliance with the principles contained in the Declaration of Helsinki (Fortaleza, 2013); all study subjects were contacted and provided informed consent for study inclusion Sensitive data were anonymized to warrant patients’ privacy according to Legislative Decree 10 August 2018, n 101, published in the Official Gazette of the Italian Republic, General Series, issue 205, 09/04/2018
All 539 PD patients underwent photographic documentation of the penile deformation and dynamic penile eco-color Doppler with plaque and volume measurements and answered the following questionnaires: the Generalized Anxiety Disorder-7, the Patient Health Questionnaire-9, the Visual Analog Scale for penile pain measurements, the International Index of Erectile Function (IIEF), and the International Prostate Symptom Score (IPSS) In the cohort of 539 PD patients and in a cohort of 2208 outpatients (comparator population), BPO was diagnosed in patients with urinary symptoms according to the following examinations: clinical history, thorough physical examination, including a digital rectal exam, prostate ultrasound, and microbiological assessment (pre- and post-massage urine and sperm cultures) to exclude concomitant chronic bacterial prostatitis, and the compilation of the International Prostate Symptom Score (IPSS)
The primary endpoint of the study was the association between a diagnosis of BPO and the occurrence of PD in a single outpatient center patient population The secondary endpoints were as follows: the impact of PD on the psychological status of patients with or without BPO; the impact of BPO in PD patients on the severity of penile curvature, on the multiplanarity of penile curvature, on plaque volume, on plaque multifocality, on plaque calcification, on the presence and severity of ED, and on presence and severity of penile pain To investigate an association between PD and a history of BPO, we calculated the odds ratio (OR) test We completed a post hoc analysis of the statistical power obtained by calculating the crude odds ratio
Our findings show that cases (PD patients) and controls (comparator population) did not differ in age and most associated pathologies However, for some associated diseases such as diabetes mellitus, erectile dysfunction, hypertension, BPO, and chronic prostatitis (CP), there was a statistically significant difference between the two groups Clinical features and basic demographics of the patients in the two groups, as well as the results for the primary and secondary endpoints of the study, are shown in Table 1
Although many studies indicate some risk factors that influence the appearance of Peyronie’s disease (penile trauma, diabetes mellitus, Dupuytren’s disease, erectile dysfunction, congenital penile curvature, hypertension, obesity, smoking,
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11481 1 LETTER TO EDITOR
Benign prostatic obstruction (BPO) as a possible risk factor for Peyronie's disease (PD).
DOI: 10 4081/aiua 2023 11481
Table 1.
Clinical features and basic demographics of patients in the two groups, and results for the primary and secondary endpoints of the study
* Although the P-value was found to be sign ficant, th s must be interpreted in favor of cases w thout BPO
Note that median anxiety and depress on scores were found to be higher in PD patients without BPO Consequently, no posit ve impact of BPO on presence of anxiety or depress on n patients with PD was found
** Although the P-value was found to be signif cant, th s must be nterpreted in favor of cases without BPO, n fact, the sever ty of tota BPO symptom scores assessed with the IPSS test corre ated sign f cantly and nverse y with IIEF scores These results nd cate that, in PD pat ents, no positive impact of BPO on presence and severity of erectile dysfunction was found
*** Although the P-value was found to be signif cant, the trend line of the og st c regress on test indicated that the VAS score is higher in PD patients without BPO than the VAS score n BPO patients These resu ts nd cate that, in PD patients, no pos t ve impact of BPO on pain sever ty was found
hypertension, rheumatoid arthritis, psoriatic arthritis, psoriasis, dyslipidemia, and alcohol consumption), studies on BPO as a risk factor for PD are unfortunately lacking
Our results show that the overall prevalence of benign prostatic obstruction in patients with Peyronie’s disease is significantly higher (22 07%) than the prevalence in a non-PD control population (13 49%) The resulting significant crude odds ratio for BPO was 1 81 (p < 0 0001) Our data suggest that BPO and PD are frequently associated
We have also ascertained that in PD patients, there is no impact of BPO on the psychological status of patients, on the severity of penile curvature, on the multiplanarity of penile curvature, on plaque volume, on plaque multifocality, on plaque calcification, on the presence and severity of ED, or on the presence and severity of penile pain Nevertheless, the severity of BPO symptom scores (IPSS) correlated significantly with the severity of erectile dysfunction (p < 0 0001) Furthermore, in Peyronie's disease patients, we ascertained the presence of significant depressive symptoms in 57 1% of cases in contrast to the lower percentages documented in Nelson's studies (48%) (2, 3) Additionally, the prevalence of significant anxiety symptoms that we found in Peyronie's disease patients (89 2%) appears to be higher when compared to the findings of other studies that generically refer to “distress” and “emotional” difficulties (80-81%) (4, 5)
Our findings indicate that BPO and PD are often associated Although our study has the limitations of being a retrospective analysis based on patient medical records, the the size of the odds ratio (OR = 1 81) and its statistical significance (p < 0 0001) support our conclusions sufficiently Nevertheless, we believe that more studies are needed to confirm BPO as a risk factor for PD Our study confirms that BPO affects the severity of ED in patients with Peyronie's disease, and this suggests that BPO should be treated early and efficiently to hinder the onset and progression of ED in these patients
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11481 G Paulis, A Paulis 2
Clinical features and basic demographics of patients in the two groups (PD patients and non-PD patients) Variable PD patients Non-PD control population Statistical analysis (539 cases) (2208 cases) P-value (t-test) Mean age 49 6 (± 12 16 SD) 50 5 (± 12 04 SD) 0 120 Variable PD patients Non-PD control population Statistical analysis n. cases (%) n. cases (%) P-value (𝝌2-test) Varicocele 13 (2 4) 62 (2 8) 0 720 Hydrocele 6 (1 1) 23 (1 04) 0 884 Hypercholesterolemia 48 (8 9) 151 (6 8) 0 117 Thyroid disease 27 (5 00) 111 (5 02) 0 986 History of myocardial infarction 13 (2 4) 50 (2 2) 0 964 History of malignant urological neoplasm 43 (7 97) 176 (7 97) 0 995 History of non-urological malignancy 11 (2 04) 48 (2 17) 0 979 History of urinary stones 52 (9 6) 207 (9 37) 0 910 Urogenital infections 19 (3 5) 120 (5 4) 0 088 Diabetes mellitus 32 (5 9) 77 (3 48) 0 0128 Hypertension 101 (18 7) 299 (13 5) 0 0027 Erectile dysfunction (ED) 216 (40 07) 529 (23 95) < 0 0001 Chronic prostatitis (CP) 200 (37 1) 384 (17 39) < 0 0001 Benign prostatic obstruction (BPO) 119 (22 07) 298 (13 49) < 0 0001 PRIMARY ENDPOINTS Cohort of patients with Non-PD control Statistical analysis Peyronie's disease (PD) population odds ratio (OR) - P-value Benign prostatic obstruction (BPO) 119 298No Benign prostatic obstruction (BPO) 420 1910TOTAL 622 2208Prevalence of BPO (%) 22 07 13 49 OR = 1 81 - P < 0 0001 SECONDARY ENDPOINTS IMPACT Statistical analysis Yes or no P-value The impact of benign prostatic obstr uction on the presence and severity of anxiety No < 0 05 * presence and severity of depression No < 0.05 * presence and severity of penile curvature No > 0 05 penile curvature multiplanarity No > 0 05 plaque volume No > 0.05 plaque multifocality No > 0 05 plaque calcification No > 0 05 presence and severity of erectile dysfunction No < 0.05 ** presence and severity of penile pain No < 0 05 ***
Bemign prostatic obstruction and Peyronie’s disease
Our results also revealed an important prevalence of anxiety and depression in PD patients; furthermore, we are especially concerned about the high percentages of “ severe ” anxiety (39 3%) present in the course of PD
Consequently, we believe that simultaneous psychological therapy is highly desirable in these patients, both to improve their quality of life and to avoid a drop-out of medical treatments
REFERENCES
1 Anderson D, Kumar D, Divya D, et al Mental Health in Non-Oncologic Urology Patients Health Psychol Res 2022; 10:38352
2 Nelson CJ, Diblasio C, Kendirci M, et al The chronology of depression and distress in men with Peyronie's disease J Sex Med 2008; 5:19851990
3 Nelson CJ, Mulhall JP Psychological impact of Peyronie's disease: a review J Sex Med 2013; 10:653-660
4 Terrier JE, Nelson CJ Psychological aspects of Peyronie's disease Transl Androl Urol 2016; 5:290-295
5 Smith JF, Walsh TJ, Conti SL, et al Risk factors for emotional and relationship problems in Peyronie’s disease J Sex Med 2008; 5:2179-2184
Correspondence
Gianni Paulis, MD (Corresponding Author)
paulisg@libero it
Peyronie’s Care Center, Department of Uro-Andrology, Castelfidardo Clinical Analysis Center, Rome, Italy
Andrea Paulis andrea fx 94@gmail com
Neurosystem Center for applied Psychology and Neuroscience, Janet Clinical Centre, Rome, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11481 3
SYSTEMATICREVIEW - SUPPLEMENTARYMATERIAL
Treatment of urge incontinence in postmenopausal women: A systematic review
Rawa Bapir 1, 15, Kamran Hassan Bhatti 2, 15, Ahmed Eliwa 3, 15, Herney Andrés García-Perdomo 4, 15 , Nazim Gherabi 5, 15, Derek Hennessey 6, 15, Vittorio Magri 7, 15, Panagiotis Mourmouris 8, 15 , Adama Ouattara 9, 15, Gianpaolo Perletti 10, 15, Joseph Philipraj 11, 15, Konstantinos Stamatiou 12, 15 , Musliu Adetola Tolani 13, 15, Lazaros Tzelves 8, 15, Alberto Trinchieri 14, 15, Noor Buchholz 15
1 Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq;
2 Urology Department, HMC, Hamad Medical Corporation, Qatar;
3 Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt;
4 Universidad del Valle, Cali, Colombia;
5 Faculty of Medicine Algiers 1, Algiers, Algeria;
6 Department of Urology, Mercy University Hospital, Cork, Ireland;
7 Urology Unit, ASST Fatebenefratelli Sacco, Milan, Italy;
8 2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece;
9 Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso;
10 Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy;
11 Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India;
12 Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece;
13 Division of Urology, Department of Surgery,Ahmadu Bello University/Ahmadu Bello University Teaching Hospital, Zaria, Kaduna State, Nigeria;
14 Urology School, University of Milan, Milan, Italy;
15 U-merge Ltd. (Urology for emerging countries), London-Athens-Dubai *.
Authors 1-14 have equally contributed to the paper and share first authorship.
* U-merge Ltd. (Urology for Emerging Countries) is an academic urological platform dedicated to facilitate knowledge transfer in urology on all levels from developed to emerging countries. U-merge Ltd. is registered with the Companies House in London/UK. www.U-merge.com
SUPPLEMENTARY MATERIALS TABLE 1. REASONSFORDISCARDINGPAPERSAFTERFULLTEXTLECTURE
–a study dealing with patients with genitourinary syndrome (Archer 2018)
–evaluation of patients at enrollment (Brown 1999)
–a study dealing with postmenopausal patients with UTI (Brown 2001)
–a study dealing with patients with stress incontinence (Capobianco 2012)
–a study dealing with patients with stress incontinence (Capobianco 2014)
–meta-analysis (Cody 2009)
–comment about a paper (Easton 2001)
–a feasibility study without clinical data about urinary incontinence (Felsted 2019)
–a study of survivors from breast cancer (Ganz 2000)
–letter reporting about a series included in the review (Holroyd-Leduc 2005)
–a study not restricted to postmenopausal women (Ignacio Antonio 2022)
–a feasibility single-arm study (Mercier 2019)
–a study of self-efficacy as predictor to adherence to treatment (Messer 2007.
–duplicate study published by other Authors (Moore 2009)
–a study dealing with patients with stress incontinence (Pereira 2012)
–a study dealing with patients with stress incontinence (Pereira 2013)
–a study dealing with genitourinary syndrome (Ribeiro 2018)
–a study dealing with patients with stress incontinence (Wang 2019)
–a single-arm study without controls (Yaksi 2013)
1.Archer DF, Kimble TD, Lin FDY, et al. A Randomized, Multicenter, Double-Blind, Study to Evaluate the Safety and Efficacy of Estradiol Vaginal Cream 0.003% in Postmenopausal Women with Vaginal Dryness as the Most Bothersome Symptom. J Womens Health (Larchmt). 2018; 27:231-237.
2.Brown JS, Grady D, Ouslander JG, et al. Prevalence of urinary incontinence and associated risk factors in postmenopausal women. Heart & Estrogen/Progestin Replacement Study (HERS) Research Group. Obstet Gynecol. 1999; 94:66-70.
3. Brown JS, Vittinghoff E, Kanaya AM, et al. Heart and Estrogen/Progestin Replacement Study Research Group. Urinary tract infections in postmenopausal women: effect of hormone therapy and risk factors. Obstet Gynecol. 2001; 98:1045-52.
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 1
DOI: 10.4081/aiua.2023.11718
4 Capobianco G, Donolo E, Borghero G, et al Effects of intravaginal estriol and pelvic floor rehabilitation on urogenital aging in postmenopausal women Arch Gynecol Obstet 2012; 285:397-403
5 Capobianco G, Wenger JM, Meloni GB, et al Triple therapy with Lactobacilli acidophili, estriol plus pelvic floor rehabilitation for symptoms of urogenital aging in postmenopausal women Arch Gynecol Obstet 2014; 289:601-8
6 Cody JD, Jacobs ML, Richardson K, et al Oestrogen therapy for urinary incontinence in post-menopausal women Cochrane Database Syst Rev 2012;10:CD001405
7 Easton BT Is hormone replacement therapy (estrogen plus progestin) effective for the treatment of urinary incontinence in postmenopausal women? J Fam Pract 2001; 50:470
8 Felsted KF, Supiano KP Mindfulness-Based Stress Reduction Versus a Health Enhancement Program in the Treatment of Urge Urinary Incontinence in Older Adult Women: A Randomized Controlled Feasibility Study Res Gerontol Nurs 2019;12:285-297
9 Ganz PA, Greendale GA, Petersen L, et al Managing menopausal symptoms in breast cancer survivors: results of a randomized controlled trial J Natl Cancer Inst 2000; 92:1054-64
10 Holroyd-Leduc JM, Straus SE In the Literature: Is there a role for estrogen in the prevention and treatment of urinary incontinence? I CMAJ 2005; 172:1003-4
11 Ignácio Antônio F, Bø K, Pena CC, et al Intravaginal electrical stimulation increases voluntarily pelvic floor muscle contractions in women who are unable to voluntarily contract their pelvic floor muscles: a randomised trial J Physiother 2022; 68:37-42
12 Mercier J, Morin M, Zaki D, et al Pelvic floor muscle training as a treatment for genitourinary syndrome of menopause: A single-arm feasibility study Maturitas 2019; 125:57-62
13 Messer KL, Hines SH, Raghunathan TE, et al Self- efficacy as a predictor to PFMT adherence in a prevention of urinary incontinence clinical trial Health Educ Behav 2007; 34:942-52
14 Moore KH, Goldstein M, Hay D The treatment of detrusor instability in postmenopausal women with oxybutynin chloride: a double blind placebo controlled study Br J Obstet Gynaecol 1990; 97:1063-4
15 Pereira VS, de Melo MV, Correia GN, Driusso P Long-term effects of pelvic floor muscle training with vaginal cone in post-menopausal women with urinary incontinence: a randomized controlled trial Neurourol Urodyn 2013; 32:48-52
16 Pereira VS, de Melo MV, Correia GN, Driusso P Vaginal cone for postmenopausal women with stress urinary incontinence: randomized, controlled trial Climacteric 2012; 15:45-51
17 Ribeiro AE, Monteiro NES, Moraes AVG, et al Can the use of probiotics in association with isoflavone improve the symptoms of genitourinary syndrome of menopause? Results from a randomized controlled trial Menopause 2018; 26:643-652
18 Wang W, Liu Y, Sun S, et al Electroacupuncture for postmenopausal women with stress urinary incontinence: secondary analysis of a randomized controlled trial World J Urol 2019; 37:1421-1427
19 Yaksi E, Çapan N, Akalin E, et al Role of neuromodulation in physical therapy-resistant urge urinary incontinence Turkiye Fiziksel Tip ve Rehabilitasyon Dergisi 2013; 59(Suppl 1):300
Archivio Italiano di Urologia
2023; 95(3):11718 R
2
e Andrologia
Bapir, K Hassan Bhatti, A Eliwa, et al
SUPPLEMENTARY MATERIALS TABLE 2. PICO TABLES SYSTEMIC ESTROGENS
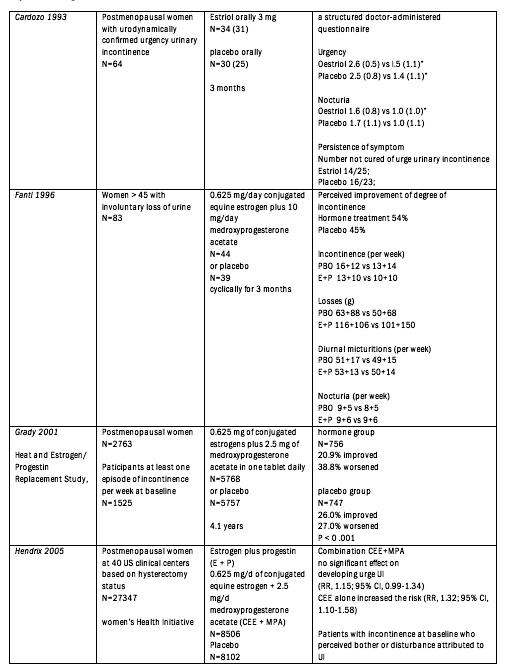
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 3 Postmenopausal urge incontinence
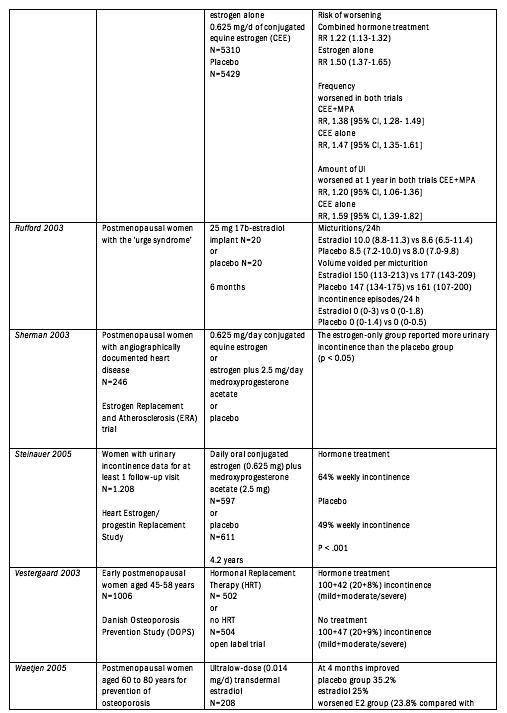
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R Bapir, K
Bhatti, A Eliwa, et al 4
Hassan
LOCAL ESTROGENS

Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 5 Postmenopausal urge incontinence
ANTICHOLINERGICS
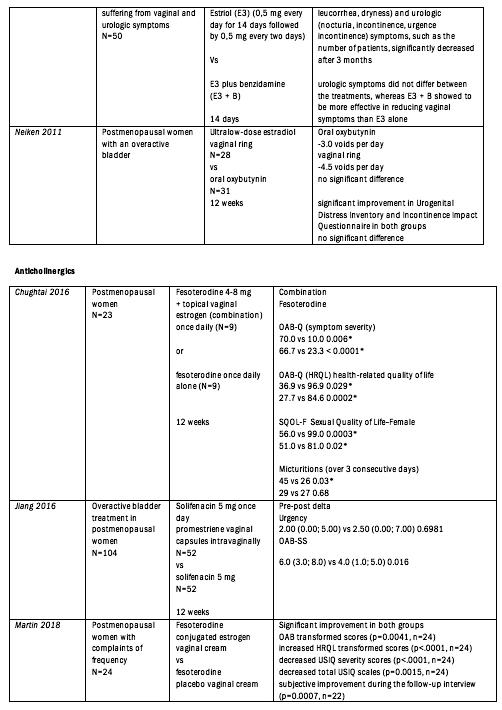
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R
K
A
et
6
Bapir,
Hassan Bhatti,
Eliwa,
al
OTHER DRUGS
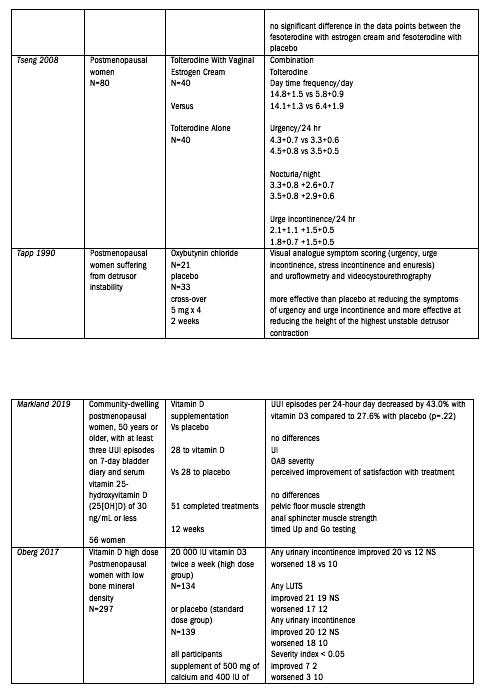
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 7 Postmenopausal urge incontinence
PELVIC FLOOR MUSCLE TRAINING & PHYSICAL TREATMENT
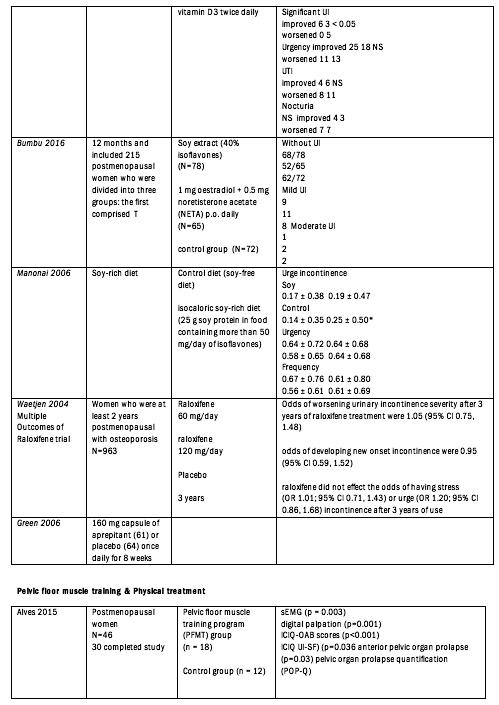
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R Bapir, K Hassan Bhatti, A Eliwa, et al 8
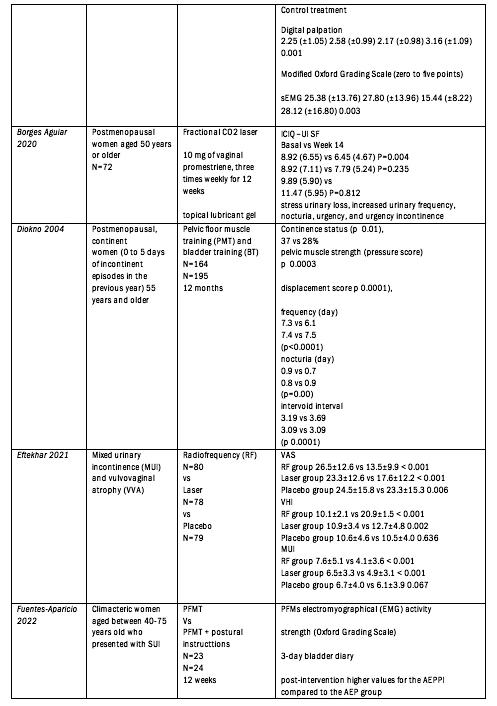
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 9 Postmenopausal urge incontinence
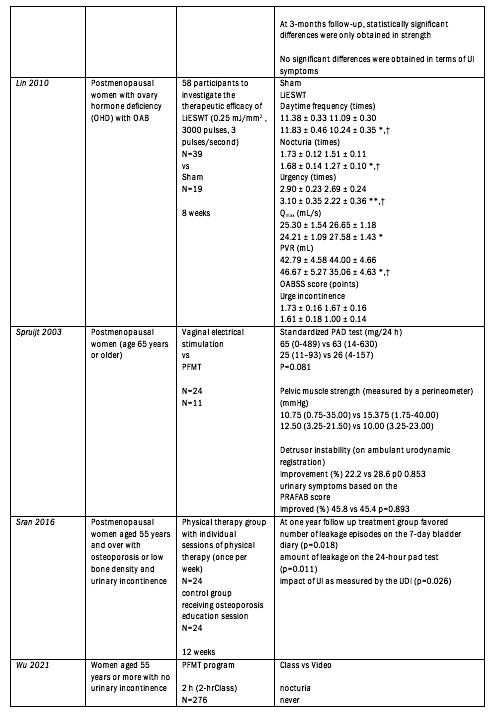
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R Bapir, K
Bhatti, A Eliwa, et al 10
Hassan
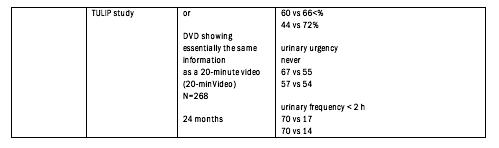
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 11 Postmenopausal urge incontinence
SUPPLEMENTARY MATERIALS TABLE 3. SUMMARY OF FINDINGS
Effect of hormone treatment versus placebo or no treatment on post-menopausal incontinence
Patient or population: post-menopausal women
Settings: outpatient
Intervention: various hormone therapy protocols
Comparison: placebo or no treatment
Outcome: urinary incontinence
Comparison
risks
-
The corresponding intervention risk (and ts 95% conf dence interva ) s based on the assumed control r sk n the compar son group and the relative effect of the intervent on (and its 95% CI)
It is calcu ated from the odds ratio us ng the formu a: OR x ACR/[1-ACR + (OR x ACR)]
CI: Conf dence Interval; OR: Odds Ratio; ACR: Assumed Control Risk
GRADE Work ng Group grades of ev dence
H gh qua ity: Further research is very unl ke y to change our conf dence in the estimate of effect
Moderate qual ty: Further research is l ke y to have an mportant impact on our confidence in the estimate of effect and may change the estimate
Low qual ty: Further research is very likely to have an important impact on our confidence in the estimate of effect and s likely to change the estimate
Very low quality: We are very uncertain about the estimate
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R
12
Bapir, K Hassan Bhatti, A Eliwa, et al
Corresponding intervention risk Comparison Intervention Hormone treatment 735 88 per 1000 673 40 per 1000 OR 0 74 17132 ⊕⊝⊝⊝ Reasons for downgrading: vs placebo (629 57 to 717 15) (0 61 to 0 91) (7) Very low none
for downgrading:
probable publication bias
risk of bias
Illustrative comparative
Relative effect No of Par ticipants Quality of the e vidence Comments (condition) (95% CI) (95% CI) (studies or comparisons) (GRADE) Assumed control risk
Reasons
-
-
inconsistency
to substantial heterogeneity Systemic estrogen treatment 719.21 per 1000 666.43 per 1000 OR 0 78 10707 ⊕⊕⊕⊝ Reasons for upgrading: vs. placebo (635.27 to 697.45) (0.68 to 0.90) (3) Moderate none Reasons for downgrading:
risk of bias Combined systemic hormone treatment 763.50 per 1000 699.19 per 1000 OR 0 72 6425 ⊕⊕⊕⊝ Reasons for downgrading: vs placebo (612 68 to 773 86) (0 49 to 1 06) (4) Moderate none
for downgrading:
risk of bias
due
-
Reasons
-
SUPPLEMENTARY MATERIALS FIGURE 1. RISKOF BIAS (ROB) 2 ASSESSMENT
1.Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366:l4898.
2.Lundh A, Gotzsche PC. Recommendations by Cochrane Review Groups for assessment of the risk of bias in studies. BMC Med Res Methodol 2008; 8:22.

SYSTEMICESTROGENS
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 13 Postmenopausal urge incontinence
1.Cardozo 1993: randomization was held centrally and there was code; double blinded; 50 patients per arm were needed though recruitment was 64 and 8 of them were lost during follow-up (> 10%).
2.Fantl 1996: randomization ok, double blinded, lost during follow-up < 10%.
3.Grady 2001: randomization ok, double blinded, although not all patients were followed-up to 3 years the majority of them had at least one follow-up visit and they were counted in follow-up so it was rated as low risk.
4.Hendrix 2005: randomization ok, double blinded, not quite sure about the follow-up but most patients had at least one follow-up visit so rated as low risk.
5.Rufford 2003: randomization ok, double blinded, none lost at follow up at 3 months.
6.Sherman 2003: randomized unclear, double blinded, follow-up not shown.
7.Steinauer 2005: randomization ok, double blinded, lost during follow-up < 10%.
8.Vestergaard 2003: partial randomization, no blinding, change of hormone type during trial; limited reporting on voiding disturbances; followup < 10%.
9.Waetjen 2005: randomization ok, double blinded, 90% completed the study.
LOCALESTROGENS
1.Cardozo 2001: randomization not described in detail, double blinded, < 10% lost during follow-up.
2.Dessole 2004: randomization ok, blinding ok, > 10% lost at follow up (4/44 treatment, 7/44 control).
3.Lose 2000: randomization ok, no blinding, different number of participants in the two groups.
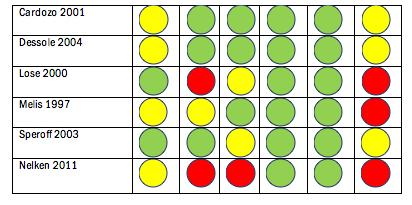
4.Melis 1997: randomization not described in detail, blinding not described, < 10% lost during follow-up.
5.Speroff 2003: randomization ok, blinding ok, lost at follow-up 12.4% and 9.8% in the treatment groups and 26.9% in the placebo.
6.Nelken 2011: randomization not described in detail, no blinding, loss to follow-up > 10% (oxybutinin group).
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718
14
R. Bapir, K. Hassan Bhatti, A. Eliwa, et al.
ANTICHOLINERGICS
1.Chughtai, et al. 2016: randomization described, unblinded study, significant number of patients stopped treatment but due to side effects and not lost during follow-up, therefore rated as low risk.
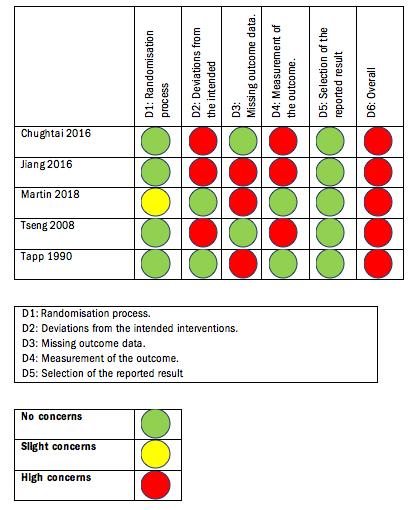
2.Jiang et al 2016: randomization described, open label study, very large number of patients dropped out in both groups.
3.Martin, et al. 2018: randomization not described in detail: unblinded study, increased number of dropouts mentioned (63 enrolled, 24 completed the study).
4.Tseng et al. 2008: randomization described, unblinded study, all patients completed the study.
5.Tapp et al. 1990: randomization described (cross-over design), double blinded study, increased number of patients lost during follow-up (>10%).
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 15 Postmenopausal urge incontinence
OTHERS
1.Markland 2019: randomization ok, double blinded study, high number of patients who did not complete bladder diary in both groups.
2.Oberg 2017: randomization described in detail in other study, double blinded study, lost during follow-up < 10% in both groups.
3.Bumbu 2016: mentions randomization but no details, no mentioning of patients lost during follow-up and blinding, therefore rated them as moderate risk.
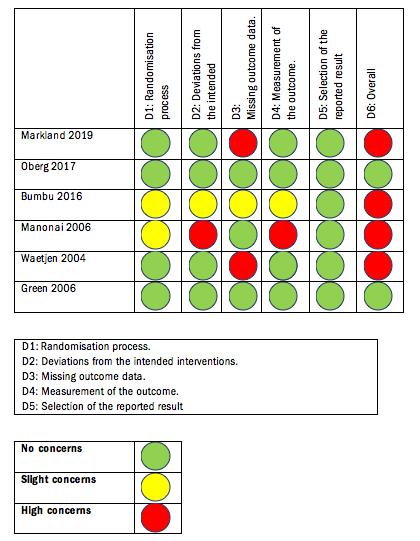
4.Manonai 2006: mentions randomization but no details, I think not blinded since not mentioned and also is a diet study, lost during follow-up 1 due to loss of contact but some more who discontinued Tx (marked it as low risk though).
5.Waetien 2004: randomization ok, double blinded, 21% lost from baseline to 3 years of final questionnaire completion.
6.Green 2006: randomization ok, double blinded, 7% lost during follow-up.
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R. Bapir, K.
16
Hassan Bhatti, A. Eliwa, et al.
PELVIC FLOOR MUSCLE TRAINING & PHYSICAL TREATMENT
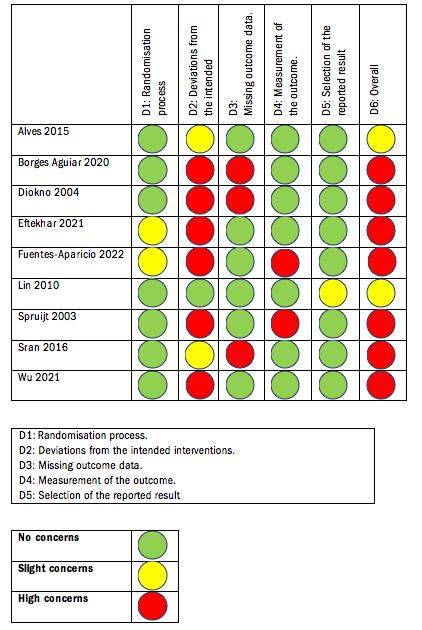
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 17 Postmenopausal urge incontinence
REASONS
D2: in most studies patients, carers and people delivering the interventions were aware of the group assignment, but the study of Lin et al which submitted controls to sham treatment In some studies assessors were blinded to treatment (Alves et al, Sran et al ) (scored as “ some concerns”)
Alves et al: no double blinding-only assessor, 12 missing patients (> 10%), otherwise well designed
Borges Aguiar et al: no blinding, 14 patients lost during follow-up (> 10%) although ITT analysis was performed
Diokno et al: single blinding (although not entirely clear in the text), 41 missing patients (> 10%)
Eftekhar et al: no information on randomization (only refer to it as a RCT), no blinding mentioned thus assumed it was an open trial
Fuentes-Aparicio et al: no blinding thus marked as high-risk in the relevant domains
Lin et al: single blinded (I understand patients were blinded since there was a sham procedure), adequately described randomization process
It’s a rather confusing paper It’s hard to see if all the results are reported
Spruijt et al: no blinding is mentioned thus assumed that this is an open-label study, patients lost to follow-up 2 (< 10%) and randomization done with blocks
patients knew which group that they were being allocated to A large number of patients rejected the trial because of this I think this is a major bias that affects the outcome
Sran et al: single-blinded for researchers, 5 patients lost to follow-up (> 10%)
Wu et al: patients lost during follow-up but < 10%, single blinded for researchers, randomization adequately described
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 R
18
Bapir, K Hassan Bhatti, A Eliwa, et al
Postmenopausal urge incontinence
SUPPLEMENTARY MATERIALS FIGURE 2 – FUNNELPLOTSFORPUBLICATIONBIASANALYSIS

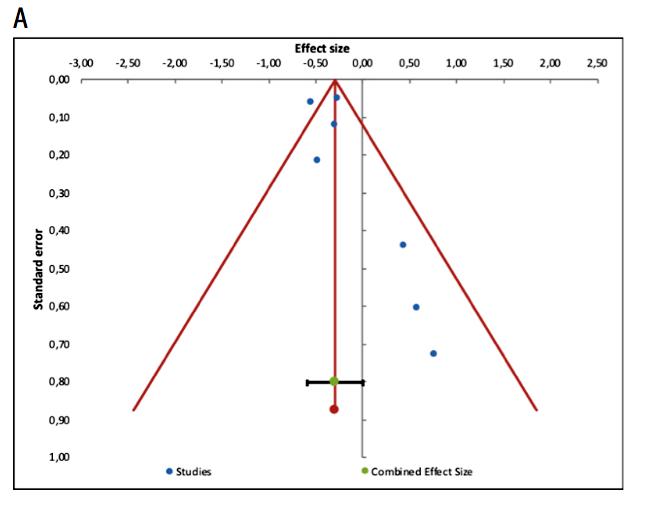
A)success of systemic hormone treatment of urinary postmenopausal incontinence
B)success of systemic estrogens alone
Archivio Italiano di Urologia e Andrologia 2023; 95(3):11718 19
INSTRUCTIONS TO AUTHORS – ARCHIVIO ITALIANO DI UROLOGIA E ANDROLOGIA
OPEN ACCESS
Open access publishing does have its costs. Information regarding authors’ payment are not made available to editors and reviewers ensuring that they cannot be influenced in their selection of papers for publication by payment conditions or limitations.
The Article Processing Charge for publication in this journal is EUR 300,00 (plus VAT, if applicable).
Our fees cover the costs of peer review, copyediting, publication, different format of publication (HTML, PDF), inclusion in many Open Access databases.
All bank charges shall be borne by the payer.
Please note that our fees do not include taxes (VAT):
-Private or public ITALIAN customers (individuals, universities, hospitals, other organizations) must ALWAYS add VAT (IVA) at standard rate (4%);
-European Union PRIVATE customers must add the standard rate of their own country VAT tax;
-European Union private/public ORGANIZATIONS (universities, hospitals, others with regular VAT number) should not add any taxes at standard rate, provided that they indicate their VAT number;
- Outside the European Union, individuals and organizations should not add any taxes at standard rate.
Important: Authors are NOT required to pay at the moment of submission. If the paper is accepted, the Managing Editor of Open Access Edition will guide the Authors through the payment procedure. No article will be published before waiver or payment.
According to the United Nations list of Least Developed Countries (LCDs) available from: http://www.un.org/en/development/desa/policy/cdp/ldc2/ldc_countries.shtml
Authors coming from those countries are entitled to ask for a discount.
A “Formal Request for discount” has to be forwarded to the Managing Editor of Open Access Edition, after receiving the acceptance letter. The Editorial Committee will then evaluate the merits of each individual case. Any other informal request (such as comments at the moment of submission, or made in the covering letter of the revised version) will not be taken into consideration.
FAST-TRACK
PEER REVIEW
All papers published in Archivio Italiano di Urologia e Andrologia (AIUA) are peer reviewed. Fast-track peer review (4 weeks) can be obtained by supplementary fee of € 488 (VAT included).
in Italian language can be published after translation (expenses will be charged to the Authors). Manuscripts should be typed double spaced with wide margins. They must be subdivided into the following sections:
TITLE PAGE
It must contain: a) title; b) a short (no more than 40 characters) running head title; c) first, middle and last name of each Author without abbreviations; d) University or Hospital, and Department of each Author; e) last name, address and e-mail of all the Authors; f) corresponding Author; g) acknowledgement of conflict of interest and financial support.
SUMMARY
Authors must submit a summary (300 words, 2000 characters) divided by subheadings as follows: Objective(s), Material and method(s), Result(s), Conclusion(s). After the summary, three to ten key words must appear, taken from the standard Index Medicus terminology.
TEXT
For original articles concerning experimental or clinical studies, the following standard scheme must be followed: Summary - Key Words - Introduction - Material and Methods - Results - Discussion - Conclusions - References - Tables - Legends - Figures.
Case Report should be divided into: Summary - Introduction (optional) - Case report(s) - Conclusions - References
Supplementary Materials can be added for online publication.
SIZE OF MANUSCRIPTS
Literature reviews, Editorials and Original articles should not exceed 3500 words with 3-5 figures or tables, and no more than 30 references.
Case reports, Notes on surgical technique, and Letters to the editors should not exceed 1000 words (summary included) with only one table or figure, and no more than three references. No more than five authors are permitted.
REFERENCES
Authors can pay their fees by: PayPal is the most recommended and secure payment system. It enables you to pay getting your payment receipt immediately and without sharing your financial information. Other methods of payment are:
METHODS OF PAYMENT
Bank transfer
BANK NAME: Banca Popolare di Sondrio, Branch #1, Strada Nuova 75, I-27100 Pavia, Italy
ACCOUNT HOLDER: PAGEPress Srl
BIC/SWIFT: POSOIT22
IBAN: IT85Y0569611301000005086X83
Credit Card The credit card form to be filled and returned either via e-mail or via fax is available for download here. http://www.pagepress.org/journals/public/credit_card.pdf
Check sent by surface mail Checks must be made payable to PAGEPress Srl and must be sent to our full postal address: PAGEPress Publications, via A. Cavagna Sangiuliani 5, 27100 Pavia, Italy.
Note: In any method of payment you choose, kindly specify: 1. journal name; 2. paper ID number; 3. first author.
IMPORTANT TO KNOW
REGISTERED DRUGS, DIET SUPPLEMENTS, NUTRACEUTICALS, MEDICAL DEVICES
Authors of papers that contain references to registered drugs, diet supplements, nutraceuticals and medical devices are requested to buy a minimum amount of 100 reprints at a cost of € 1.500 (1 to 4 pages) or € 2.000 (5 to 8 pages). Prices for the purchase of number of reprints greater than 100 can be negotiated with Edizioni Scripta Manent At present, Edizioni Scripta Manent let everyone to read, print and download papers from website, but retains copyright for republishing and distribution rights for commercial purpose.
TRANSLATION
Translation of manuscripts in Italian language is offered on payment.
Translation and reprints can be requested to Edizioni Scripta Manent by e-mail to info@edizioniscriptamanent.eu
AUTHORS’ RESPONSIBILITIES
Manuscripts are accepted with the understanding that they have not been published or submitted for publication in any other journal.
Authors must submit the results of clinical and experimental studies conducted according to the Helsinki Declaration on clinical research and to the Ethical Code on animal research set forth by WHO (WHO Chronicle 1985; 39:51).
The Authors must obtain permission to reproduce figures, tables and text from previously published material. Written permission must be obtained from the original copyright holder (generally the Publisher).
MANUSCRIPT PRESENTATION
Authors must submit their manuscripts (MAC and WINDOWS Microsoft Word are accepted) after registration and login to the link: http://www.aiua.it. Surface or e-mail submission are not accepted.
Manuscripts must be written in English language in accordance with the “Uniform Requirements for Manuscripts submitted to biomedical journals” defined by The International Committee of Medical Journal Editors (http://www.ICMJE.org). Manuscripts
References must be sorted in order of quotation and numbered with arabic digits between parentheses. Only the references quoted in the text can be listed. Unpublished studies cannot be quoted, however articles “in press” can be listed with the proper indication of the journal title, year and possibly volume. References must be listed as follows.
JOURNAL ARTICLES
All Authors if there are six or fewer, otherwise the first three, followed by “et al.”. Complete names for Work Groups or Committees. Complete title in the original language. Title of the journal following Index Medicus rules. Year of publication; Volume number: First page. Example: Starzl T, Iwatsuki S, Shaw BW, et al. Left hepatic trisegmentectomy Surg Gynecol Obstet. 1982; 155:21.
BOOKS
Authors - Complete title in the original language. Edition number (if later than the first). City of publication: Publisher, Year of publication. Example: Bergel DIA. Cardiovascular dynamics. 2nd ed. London: Aca de mic Press Inc., 1974.
BOOK CHAPTERS
Authors of the chapters - Complete chapter title. In: Book Editor, complete Book Title, Edition number. City of publication: Publisher, Publication year: first page of chapter in the book. Example: Sagawa K. The use of central theory and system analysis. In: Bergel DH (Ed), Cardiovascular dynamics. 2nd ed. London: Aca demic Press Inc., 1964; 115.
TABLES
Tables must be numbered in Arabic digits and referred to in the text by progressive numbers. Every table must be accompanied by a brief title. The meaning of any abbreviations must be explained at the bottom of the table itself.
FIGURES
(Graphics, algorithms, photographs, drawings). Figures must be numbered and quoted in the text by number. The meaning of symbols or abbreviations must be indicated. Histology photograph legends must include the enlargement ratio and the staining method. Legends must be collected in one or more separate pages.
• Do not include any illustrations as part of your text file. • Do not prepare any figures in Word as they are not workable. • Line illustrations must be submitted at 600 DPI. • Halftones and color photos should be submitted at a minimum of 300 DPI. • Power Point files cannot be uploaded. • If possible please avoid transmitting electronic files in JPEG format or save the JPEG at the highest quality available • PDF files may be uploaded.
MANUSCRIPT REVIEW
Manuscripts are evaluated by the Editorial Board and/or by two referees designated by the Editors. The Authors are informed in a time as short as possible on whether the paper has been accepted, rejected or if a revision is deemed necessary. The Editors reserve the right to make editorial and literary corrections with the goal of making the article clearer or more concise, without altering its contents. Submission of a manuscript implies acceptation of all above rules.
PROOFS
Authors are responsible for ensuring that all manuscripts are accurately typed before final submission. Galley proofs will be sent to the first Author. Proofs should be returned within seven days from receipt.
Salutepertutti.it è un progetto indipendente. Abbonati per i tuoi pazienti in sala d’aspetto. 10,00€/anno per 3 numeri


SEGUICI SUI NOSTRI CANALI SOCIAL @salutepertutti.it
Per info inquadra il QR Code