ORIGINAL PAPERS
375 Perceptions and attitudes toward the use of telemedicine for the postoperative outpatient urological care during the COVID-19 pandemic in an Academic Hospital in Souther n Italy

Vincenzo Mirone, Giuseppe Celentano, Claudia Collà Ruvolo, Luigi Cirillo, Giovanni Maria Fusco, Marco Abate, Simone Morra, Francesco Di Bello, Gianluigi Califano, Claudia Mirone, Gianluigi Cacace, Vincenzo Morgera, Roberto La Rocca, Marco Capece, Nicola Longo, Luigi Napolitano, Massimiliano Creta
380 Goldfinger bypassing and en bloc stapling without dissection of renal vessels during laparoscopic nephrectomy
Murad Asali, Muhammad Asali
384 Outcomes of continent and incontinent exter nal urinar y diversion in management of patients with refractor y non-malignant lower urinar y tract dysfunction
Mostafa M Mostafa, Ashraf Khallaf, Mohamed Kamel, Nilesh Patil, Ayman Mahdy
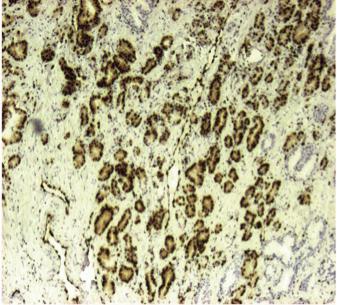
390 Clinical impact of ERG and PTEN status in prostate cancer patients underwent radical prostatectomy
Charalampos Fragkoulis, Ioannis Glykas, Lazaros Tzelves, Panagiotis Velissarios Stamatakos, Georgios Papadopoulos, Georgios Stathouros, Athanasios Dellis, Konstantinos Ntoumas, Akrivi Kostopoulou, Charalampos Deliveliotis, Athanasios Papatsoris
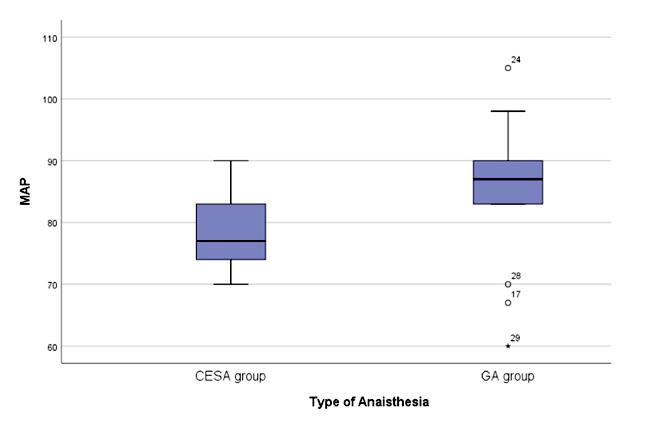
396 The effects of method of anaesthesia on the safety and effectiveness of Radical Retropubic Prostatectomy
Konstantinos Pikramenos, Maria Zachou, Eleftheria Apostolatou, Dimitrios Papadopoulos, Maria Mitsogianni, Athanasios Papatsoris, Ioannis Varkarakis, Iraklis Mitsogiannis
401 Accuracy of PET-choline in nodal staging of localized ver y high-risk prostate cancer
Nuno Dias, Gianmarco Colandrea, Francisco Botelho, Lara Rodriguez-Sanchez, Yann Barbé, Petr Macek, Xavier Cathelineau
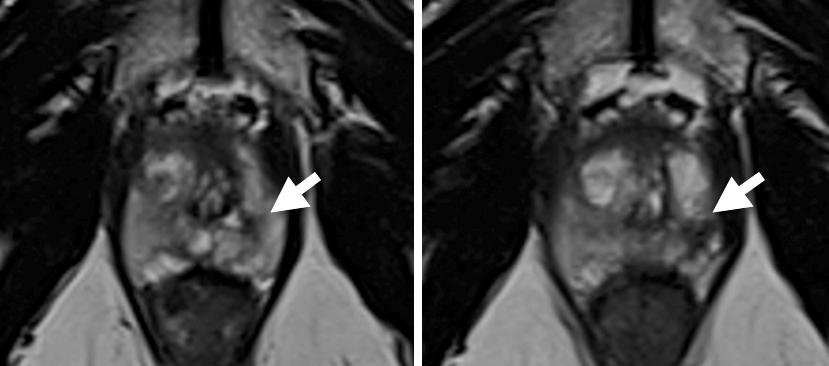
406 A single-operator experience using EchoLaser SoracteLiteTM for focal laser ablation of prostate cancer : One more ar row in the quiver for the conser vative management of the disease
Iacopo Meneghetti, Demostene Giardino, Riccardo Morganti, Vincenzo Marino, Filippo Menchini Fabris, Riccardo Bartoletti, Novello Pinzi
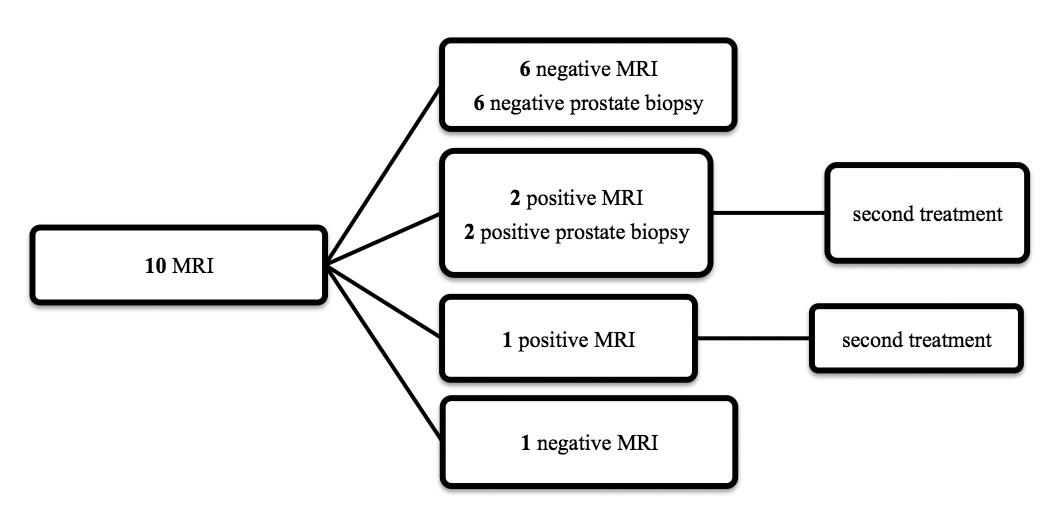
413 Medium-ter m oncological outcomes of inter mediate-risk prostate cancer treated with HIFU or cr yotherapy. A single center 10-year experience
Nuno Dias, Lara Rodriguez-Sanchez, Gianmarco Colandrea, Petr Macek, Xavier Cathelineau
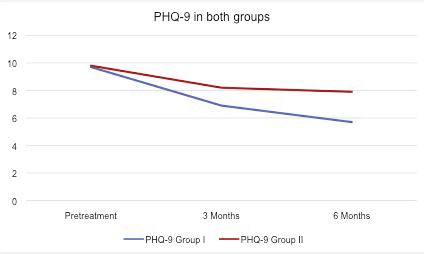
420 The impact of prostate biopsy on erectile and ejaculator y function: A prospective study
Michele Morelli, Gianluca Sampogna, Samuele Molteni, Carmine Sciorio, Vito Lorusso, Lorenzo Romano, Roberto La Rocca, Marco Capece, Assunta Zimarra, Luigi Napolitano, Paolo Verze, Lorenzo Spirito
424 Could we safely omit a Repeat Transurethral Resection of the Bladder (re-TURB) after Hexaminolevulinate Photodynamic Diagnostics (PDD)-TURB?
Vito Lorusso, Laure Doisy, Antonio Maria Granata, Andrea Gregori, Celeste Manfredi, Lorenzo Spirito, Carmine Sciorio, Luca Giuseppe Maria Ciancimino, Samuele Molteni, Michele Morelli, Luigi Cirillo, Luigi Napolitano, Jochen Walz, Geraldine Pignot
428 AB0 blood groups and oncological and functional outcomes in bladder cancer patients treated with radical cystectomy
Alessandro Tafuri, Andrea Panunzio, Antonio Soldano, Giovanni Mazzucato, Paola Irene Ornaghi, Giacomo Di Filippo, Alessandra Gozzo, Nicola De Maria, Francesco Cianflone, Aliasger Shakir, Zhe Tian, Matteo Brunelli, Antonio Benito Porcaro, Vincenzo Pagliarulo, Walter Artibani, Pierre I Karakiewicz, Alessandro Antonelli, Maria Angela Cerruto
434 Does the placement of a collagen-fibrin sealant reduce complications of radical inguinal lymph node dissection –Comparative study in patients with penile cancer
Andreia Bilé Silva, João Nuno Pereira, Rui Freitas, Isaac Braga, João Carvalho, José Sanches Magalhães, Vítor Silva, Francisco Lobo, António Morais
439 Can we predict the ancillar y treatments after extracorporeal shockwave lithotripsy for renal and upper ureteral stones?

Ahmed Ibrahim, Adel Elatreisy, Abdulghani Khogeer, Abdulsalam Ahmadi, Shashikant Mishra, Mahmoud Faisal, Ravindra Sabnis, Mélanie Aubé-Peterkin, Serge Carrier, Arvind Ganpule, Mahesh Desai
443 Urinar y epider mal growth factor and monocyte chemotactic protein-1 as biomarkers of renal injur y in patients with obstr ucted nephropathy
Eman M El-Dydamony, Mohamed Ahmad Abdelaal, Sammar Ahmad Kasim, Doaa Refaat Ameen, Doaa Aly Abd El-Fattah
continued on page III
Vol.
94; n. 4, December 2022
ISSN 1124-3562
ATLANTE di ECOGRAFIA UROLOGICA, ANDROLOGICA e NEFROLOGICA
PASQUALE MARTINO
124 autori
592 pagine + di 1500 immagini ecografiche 61 video
Sconto speciale -50% Natale 2022
















Per averne diritto, scrivere a info@edizioniscriptamanent.eu indicando il codice "NATALE_2022"

Costo di copertina


































* IVA e Spese di spedizione comprese


EDITOR IN CHIEF
Alberto Trinchieri (Milan, Italy)
EDITORIAL BOARD
ASSOCIATE EDITORS
Emanuele Montanari, Department of Urology, IRCCS Foundation Ca’ Granda Ospedale Maggiore Policlinico, University of Milan, Italy – Gianpaolo Perletti, Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy; Department of Human Structure and Repair, Ghent University, Ghent, Belgium - Angelo Porreca, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy
EXECUTIVE EDITORIAL BOARD
Alessandro Antonelli, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A.O.U.I.), Verona, Italy - Antonio Celia, Department of Urology, San Bassiano Hospital, Bassano del Grappa, Italy - Luca Cindolo, Department of Urology, Villa Stuart Hospital, Rome, Italy - Andrea Minervini, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Bernardo Rocco, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Riccardo Schiavina, Department of Urology, University of Bologna, Bologna, Italy
ADVISORY EDITORIAL BOARD
Pier Francesco Bassi, Urology Unit, A Gemelli Hospital, Catholic University of Rome, Italy – Francesca Boccafoschi, Health Sciences Department, University of Piemonte Orientale in Novara, Italy – Alberto Bossi, Department of Radiotherapy, Gustave Roussy Institute, Villejuif, France –Tommaso Cai, S Chiara Hospital, Trento, Italy –Paolo Caione, Department of Nephrology-Urology, Bambino Gesù Pediatric Hospital, Rome, Italy – Luca Carmignani, Urology Unit, San Donato Hospital, Milan, Italy –Liang Cheng, Department of Urology, Indiana University School of Medicine, Indianapolis, IN; Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, Indianapolis, IN – Giovanni Colpi, Retired Andrologist, Milan, Italy – Giovanni Corona, Department of Urology, University of Florence, Careggi Hospital, Florence, Italy – Antonella Giannantoni, Department of Surgical and Biomedical Sciences, University of Perugia, Italy – Paolo Gontero, Department of Surgical Sciences, Molinette Hospital, Turin, Italy – Steven Joniau, Organ Systems, Department of Development and Regeneration, KU Leuven, Belgium – Frank Keeley, Bristol Urological Institute, Southmead Hospital, Bristol UK – Laurence Klotz, Division of Urology, Department of Surgery, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Ontario, Canada – Börje Ljungberg, Urology and Andrology Unit, Department of Surgical and Perioperative Sciences, Umeå University, Umeå, Sweden –Nicola Mondaini, Uro-Andrology Unit, Santa Maria Annunziata Hospital, Florence, Italy
Gordon Muir, Department of Urology, King's College Hospital, London, UK –Giovanni Muto, Urology Unit, Bio-Medical Campus University, Turin, Italy – Anup Patel, Department of Urology, St Mary's Hospital, Imperial Healthcare NHS Trust, London, UK – Glenn Preminger, Division of Urologic Surgery, Duke University Medical Center, Durham, NC, USA – David Ralph, St Peter's Andrology Centre and Institute of Urology, London, UK – Allen Rodgers, Department of Chemistry, University of Cape Town, Cape Town, South Africa – Francisco Sampaio, Urogenital Research Unit, State University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil – Kemal Sarica, Department of Urology, Kafkas University Medical School, Kars, Turkey – Luigi Schips, Department of Urology, San Pio da Pietrelcina Hospital, Vasto, Italy – Hartwig Schwaibold, Bristol Urological Institute, Southmead Hospital, Bristol, UK – Alchiede Simonato, Department of Urology, University of Verona, Azienda Ospedaliera Universitaria Integrata, Verona, Italy – Carlo Terrone, Department of Urology, IRCCS S Martino University Hospital, Genova, Italy – Anthony Timoney, Bristol Urological Institute, Southmead Hospital, Bristol, UK – Andrea Tubaro, Urology Unit, Sant’Andrea Hospital, “La Sapienza” University, Rome, Italy – Richard Zigeuner, Department of Urology, Medical University of Graz, Graz, Austria
BOARD OF REVIEWERS
Maida Bada, Department of Urology, S Pio da Pietrelcina Hospital, ASL 2 Abruzzo, Vasto, Italy - Lorenzo Bianchi, Department of Urology, University of Bologna, Bologna, Italy - Mariangela Cerruto, Department of Urology, Azienda Ospedaliera Universitaria

Integrata (A O U I ), Verona, Italy - Francesco Chessa, Department of Urology, University of Bologna, Bologna, Italy - Daniele D’Agostino, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy - Fabrizio Di Maida, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Antonio Galfano, Urology Unit, Niguarda Hospital, Milan, Italy - Michele Marchioni, Department of Medical, Oral and Biotechnological Sciences, "G. d'Annunzio" University of Chieti, Laboratory of Biostatistics, Chieti, Italy - Andrea Mari, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Antonio Porcaro, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Stefano Puliatti, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Daniele Romagnoli, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy - Chiara Sighinolf, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Tommaso Silvestri, Urology Clinic, Department of Medical, Surgical and Health Science, University of Trieste, Trieste, Italy - Petros Sountoulides, Aristotle University of Thessaloniki, Department of Urology, Thessaloniki, Greece
SIEUN EDITOR
Pasquale Martino, Department of Emergency and Organ Transplantation-Urology I, University Aldo Moro, Bari, Italy
SIEUN EDITORIAL BOARD
Emanuele Belgrano, Department of Urology, Trieste University Hospital, Trieste, ItalyFrancesco Micali, Department of Urology, Tor Vergata University Hospital, Rome, ItalyMassimo Porena, Urology Unit, Perugia Hospital, Perugia, Italy – Francesco Paolo Selvaggi, Department of Urology, University of Bari, Italy – Carlo Trombetta, Urology Clinic, Cattinara Hospital, Trieste, Italy – Giuseppe Vespasiani, Department of Urology, Tor Vergata University Hospital, Rome, Italy – Guido Virgili, Department of Urology, Tor Vergata University Hospital, Rome, Italy
UrOP EDITOR

Carmelo Boccafoschi, Department of Urology, Città di Alessandria Clinic, Alessandria, Italy
UrOP EDITORIAL BOARD
Renzo Colombo, Department of Urology, San Raffaele Hospital, Milan, Italy – Roberto Giulianelli, Department of Urology, New Villa Claudia, Rome, Italy – Massimo Lazzeri, Department of Urology, Humanitas Research Hospital, Rozzano (Milano), Italy – Angelo Porreca, Department of Urology, Polyclinic Abano Terme, Abano Terme (Padova), Italy –Marcello Scarcia, Department of Urology, "Francesco Miulli" Regional General Hospital, Acquaviva delle Fonti (Bari), Italy – Nazareno Suardi, Department of Urology, San Raffaele Turro, Milano, Italy
GUN EDITOR
Arrigo Francesco Giuseppe Cicero, Medical and Surgical Sciences Department, Sant’Orsola-Malpighi University Hospital, Bologna, Italy
GUN EDITORIAL BOARD
Gianmaria Busetto, Department of Urology, Sapienza University of Rome, Italy –Tommaso Cai, Department of Urology, Santa Chiara Regional Hospital, Trento, Italy –Elisabetta Costantini, Andrology and Urogynecological Clinic, Santa Maria Hospital of Terni, University of Perugia, Terni, Italy – Angelo Antonio Izzo, Department of Pharmacy, University of Naples, Italy – Vittorio Magri, ASST Nord Milano, Milano, Italy – Salvatore Micali, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy
– Gianni Paulis, Andrology Center, Villa Benedetta Clinic, Rome, Italy – Francesco Saverio Robustelli della Cuna, University of Pavia, Italy –
Giorgio Ivan Russo, Urology Department, University of Catania, Italy – Konstantinos Stamatiou, Urology Department, Tzaneio Hospital, Piraeus, Greece – Annabella Vitalone, Department of Physiology and Pharmacology, Sapienza University of Rome, Rome, Italy

O f f i c i a l J o u r n a l o f S I E U N , U r O P , S S C U a n d G U N
–
NOVITÀ
Un’opera nuova e completa sul microbiota, il complesso consorzio di o malattia. Centinaia di illustrazioni a colori, contenuti multimediali, aggiornati in progress continuo ed accessibili mediante QR code. Un Trattato imprescindibile per chi si occupa di salute interpretando i referti sul microbiota.
Costo di copertina €120,00, IVA e spese di spedizione incluse. Per informazioni ed eventuali ordini, scrivere a: info@edizioniscriptamanent.eu

ORIGINAL PAPERS
447 Evaluation of pain and quality of life after hyaluronic acid instillation in addition to botulinum toxin-A injection in women with refractor y Interstitial Cystitis/Painful Bladder Syndrome: A pilot study
Ahmed Fayez Ghaith, Mohamed Hasan Radwan, Mohamed Rasheed Taha, Mohamed Ahmed Elbendary, Mahmoud Elsayed Al Damhogy, Ayman Mohamed Hagras
451 The choice of therapeutic agent in female overactive bladder patients in real-wor ld practice
Hiroshi Masuda, Kosuke Mikami, Kotaro Otsuka, Kyokusin Hou, Takahito Suyama, Kazuhiro Araki, Satoko Kojima, Yukio Naya
455 Is there a difference in fecal microbiota of children with and without voiding dysfunction?
Ilker Akarken, Huseyin Tarhan, Gamze Sener, Hasan Deliktas, Nurcan Cengiz, Hayrettin Sahin
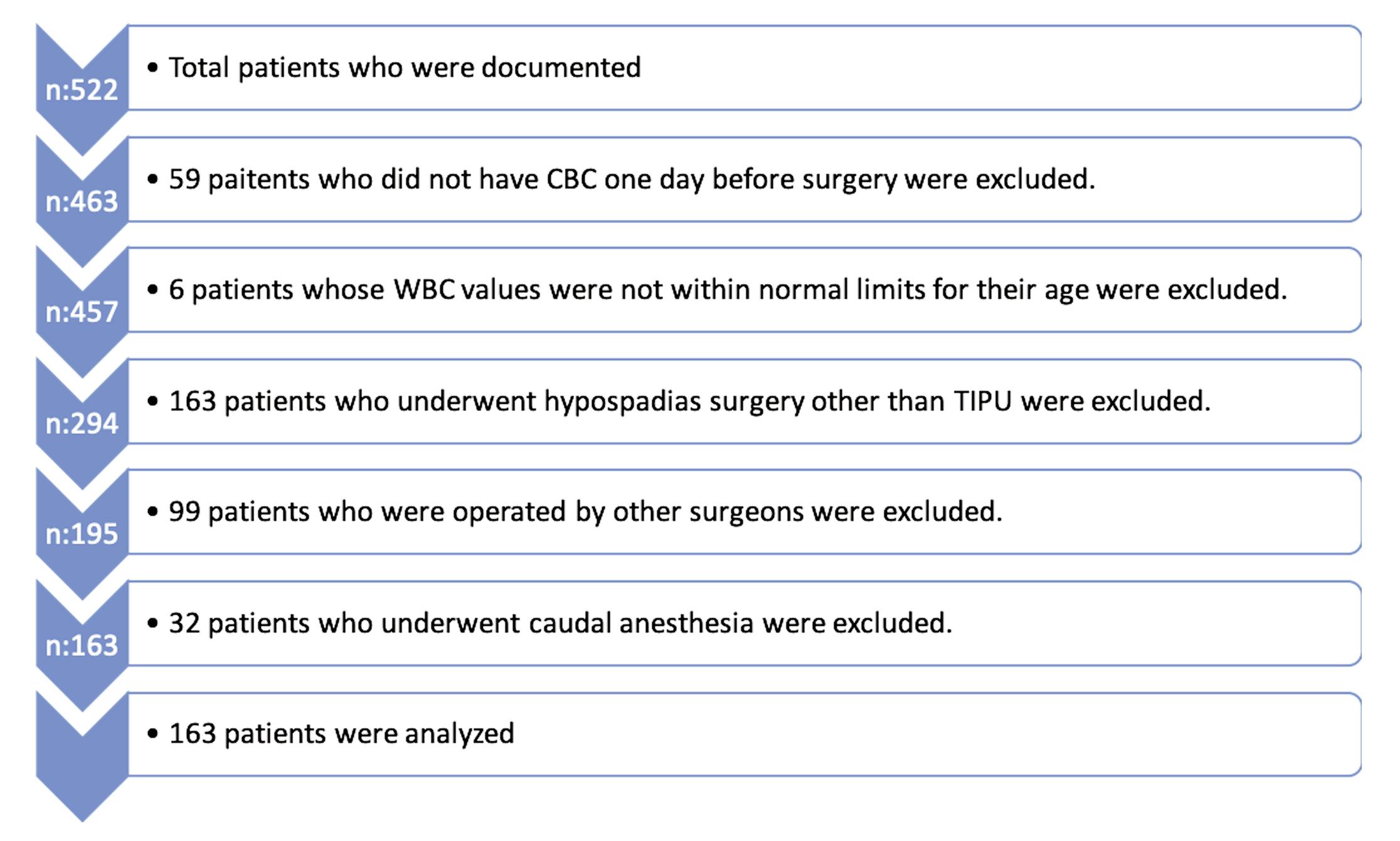
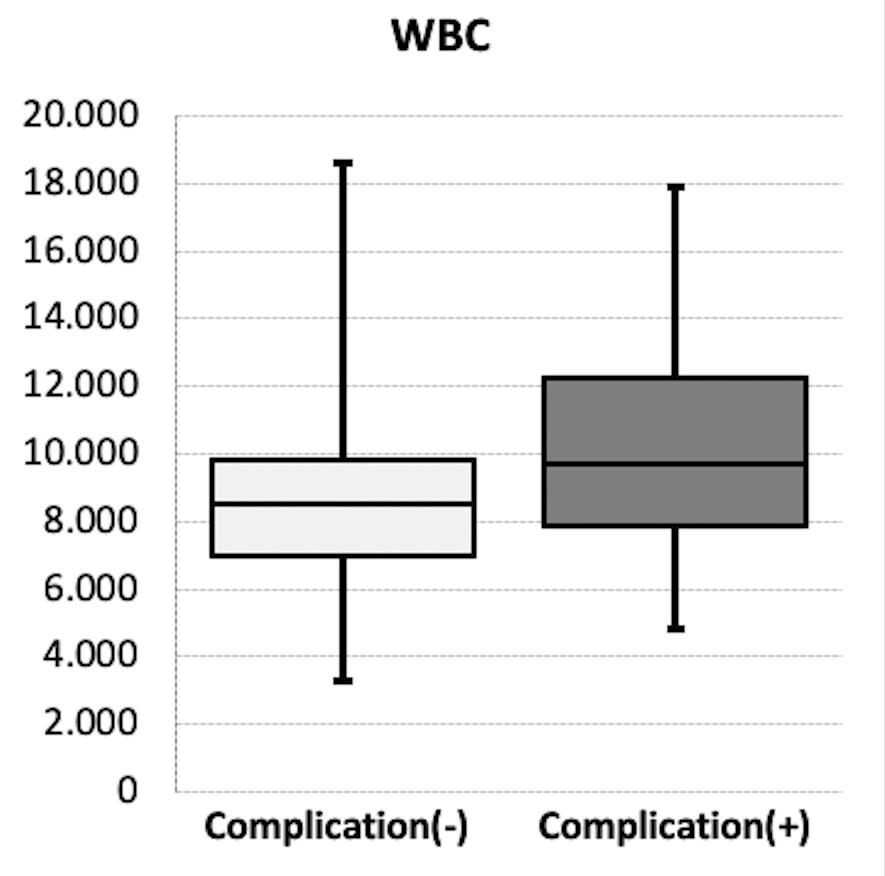
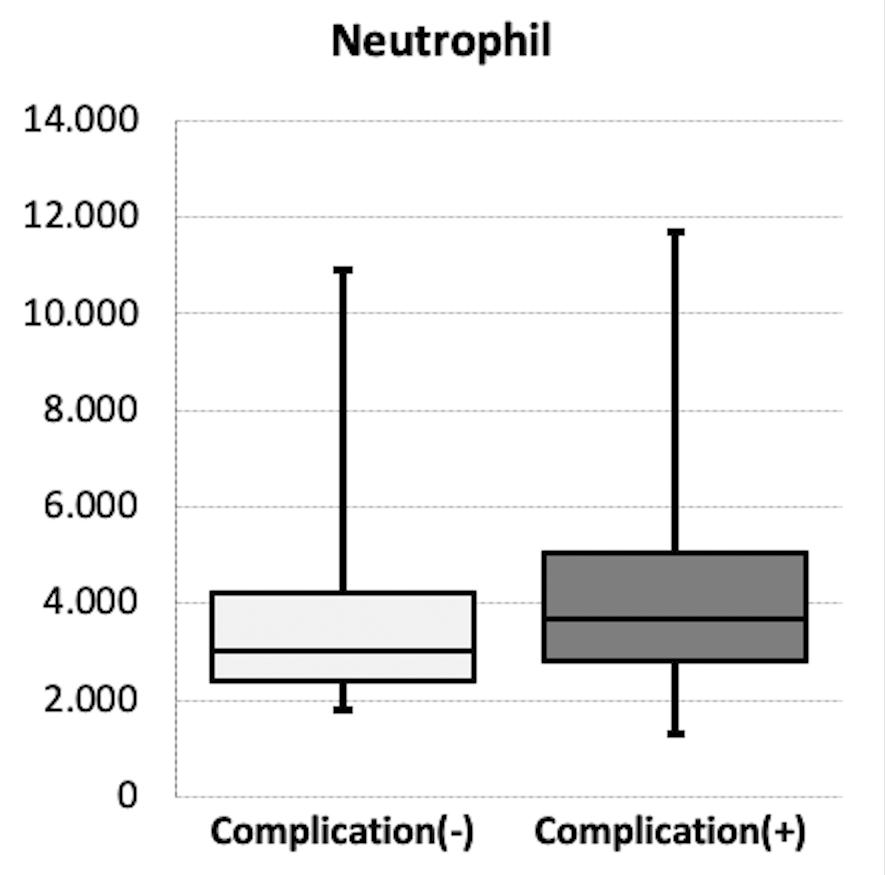
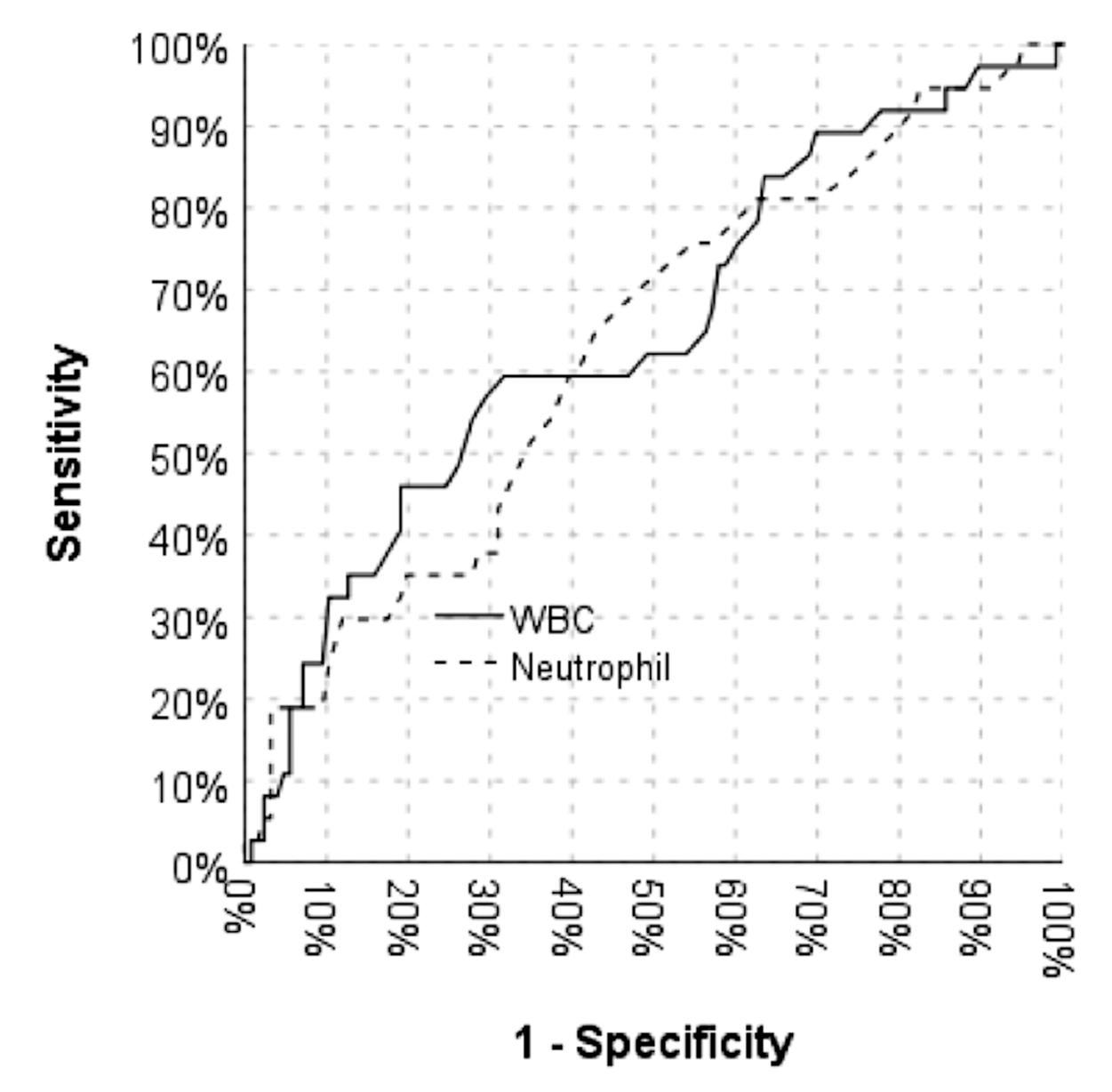
459 Do preoperative leukocyte and neutrophil levels have a predictive value on the complications of hypospadias repair in children?
Ahsen Karago ̈zlu ̈ Akgu ̈l, Sadık Abidog˘lu, Ayten Ceren Bakır, Embiye Adalı, Gu ̈ rsu Kıyan, Halil Tuğ tupe
464 Testosterone deficiency in non-obese type 2 diabetic male patients
Sherihan I Gouda, Mohamed M Aboelnaga, Ahmed M G Elbeltagy, Amro Elbaz
470 Male infer tility, what Mobile Health Applications “know”: quality analysis and adherence to European Association of Urolog y Guidelines
Giovanni Maria Fusco, Luigi Cirillo, Marco Abate, Simone Morra, Vincenzo Morgera, Biagio Barone, Felice Crocetto, Gianluigi Cacace, Francesco Di Bello, Lorenzo Spirito, Celeste Manfredi, Davide Arcaniolo, Alessandro Palmieri, Ciro Imbimbo, Vincenzo Mirone, Luigi Napolitano
REVIEWS
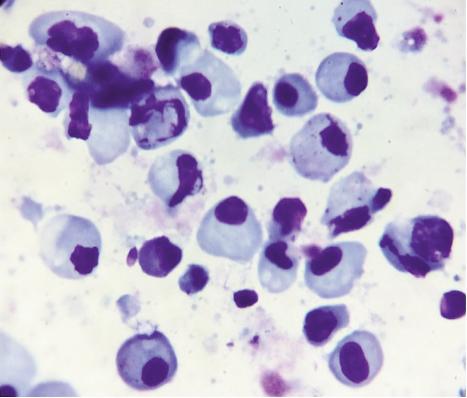
476 Cytoreductive nephrectomy for synchronous metastatic renal cell carcinoma. Is there enough evidence?
Stamatios Katsimperis, Lazaros Tzelves, Themistoklis Bellos, Konstantinos Pikramenos, Ioannis Manolitsis, Ioannis Tsikopoulos, Iraklis Mitsogiannis
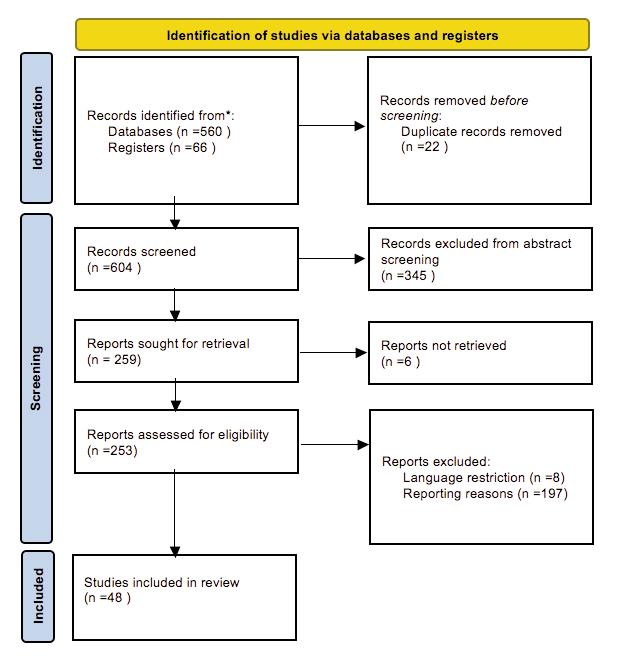
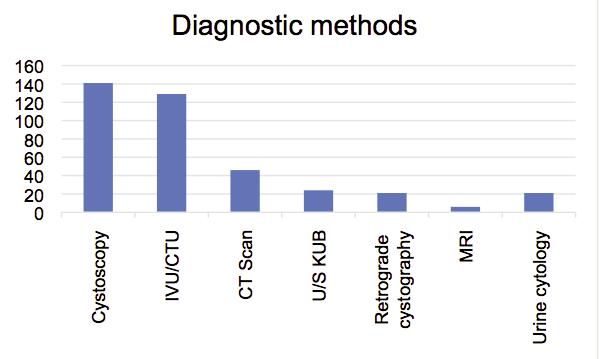
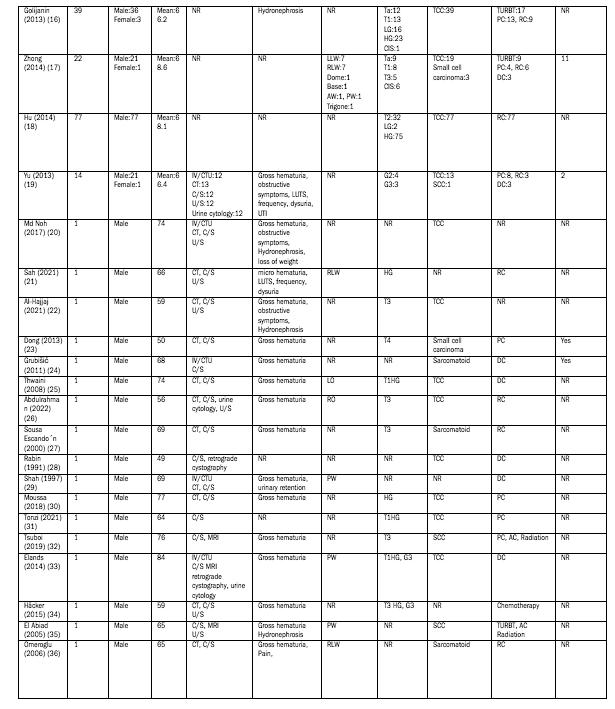
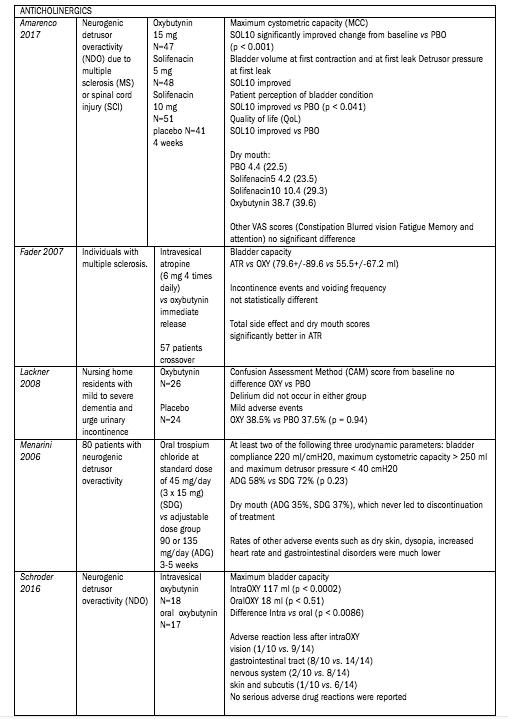
486 Diagnosis and management of intradiver ticular bladder tumours: A pooled analysis of 498 cases
Stamatios Katsimperis, Lazaros Tzelves, Themistoklis Bellos, Panagiotis Angelopoulos, Ioannis Tsikopoulos, Iraklis Mitsogiannis, Athanasios Papatsoris
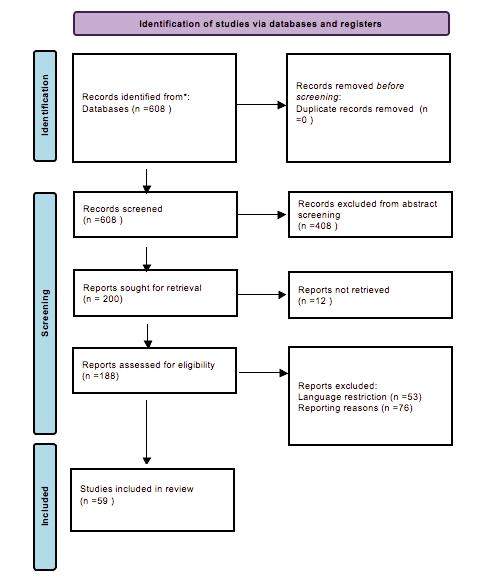
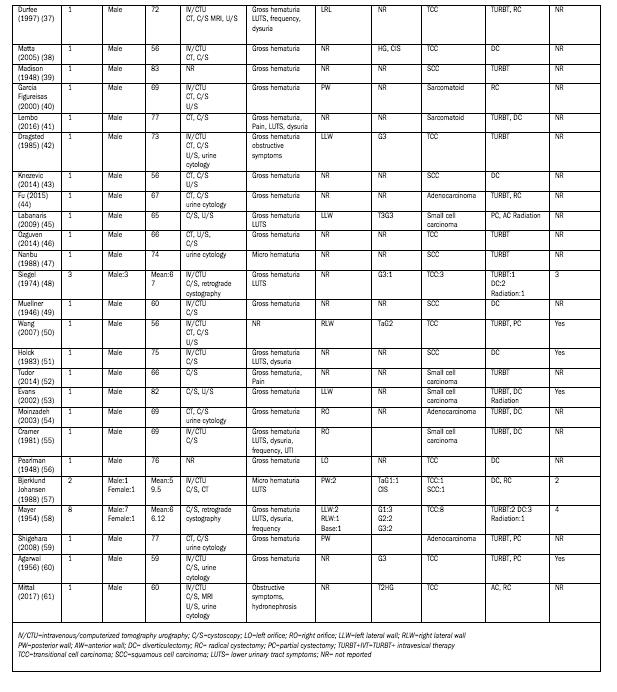
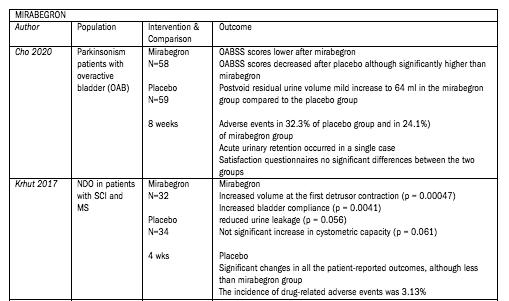
492 Efficacy of overactive neurogenic bladder treatment: A systematic review of randomized controlled trials
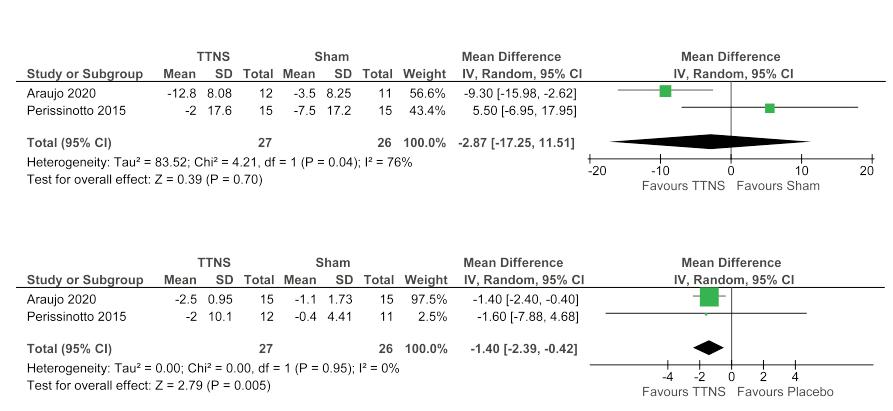
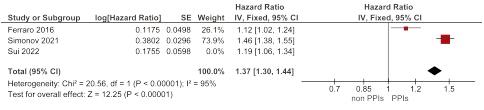
Rawa Bapir, Kamran Hassan Bhatti, Ahmed Eliwa, Herney Andrés García-Perdomo, Nazim Gherabi, Derek Hennessey, Vittorio Magri, Panagiotis Mourmouris, Adama Ouattara, Gianpaolo Perletti, Joseph Philipraj, Konstantinos Stamatiou, Alberto Trinchieri, Noor Buchholz
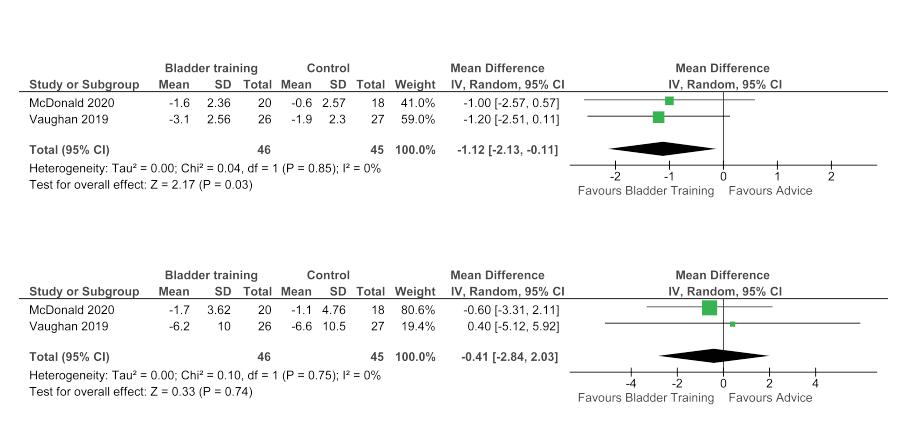
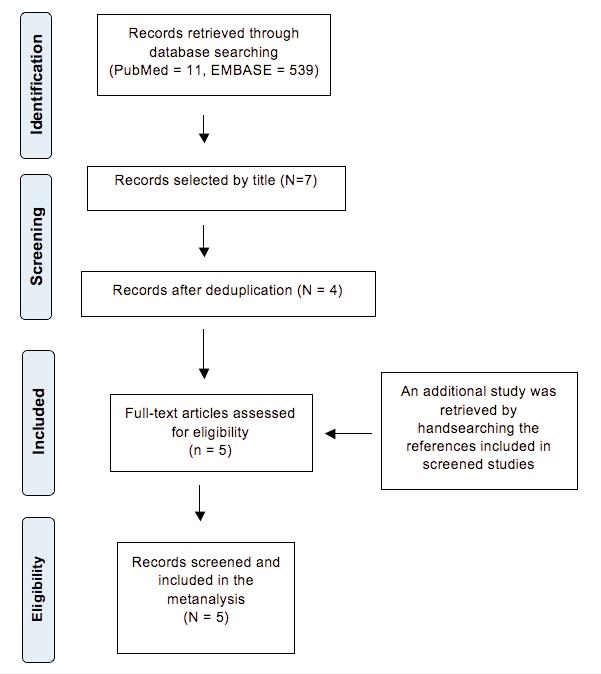
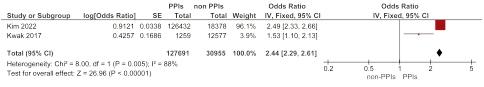
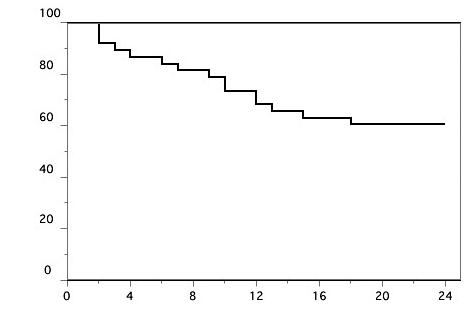
507 Risk of urinar y stone for mation associated to proton pump inhibitors: A systematic review and metanalysis
Rawa Bapir, Kamran Hassan Bhatti, Ahmed Eliwa, Herney Andrés García-Perdomo, Nazim Gherabi, Derek Hennessey, Vittorio Magri, Panagiotis Mourmouris, Adama Ouattara, Gianpaolo Perletti, Joseph Philipraj, Konstantinos Stamatiou, Musliu Adetola Tolani, Lazaros Tzelves, Alberto Trinchieri, Noor Buchholz
LETTERS TO EDITOR
515 The Discipline of Pediatric Urolog y: Prerogatives and Necessities
Walter Artibani, Luca Carmignani, Giuseppe Carrieri, Marco Castagnetti, Giuseppe Cretì, Mario De Gennaro, Gianantonio Manzoni, Lorenzo Masieri, Francesco Porpiglia, Roberto M Scarpa
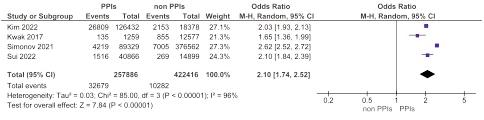
519 Increased exfoliation of immature ger m cells detected in semen analysis routine and its clinical significance
Fernando Tadeu Andrade-Rocha, Walter D Cardona Maya
521 Outcomes of dutasteride discontinuation in patients with benign prostatic hyper trophy
Hiroshi Masuda, Kosuke Mikami, Kotaro Otsuka, Kyokusin Hou, Takahito Suyama, Kazuhiro Araki, Satoko Kojima, Yukio Naya
Edizioni Scripta Manent s.n.c.
Via Melchiorre Gioia 41/A - 20124 Milano, Italy
Tel +39 0270608060
e-mail: scriman@tin.it
web: www edizioniscriptamanent eu
Registrazione: Tribunale di Milano n 289 del 21/05/2001
Direttore Responsabile: Pietro Cazzola
Direzione Marketing e PR: Donatella Tedeschi
Comunicazione e Media: Ruben Cazzola
Grafica e Impaginazione: Stefania Cacciaglia
Affari Legali: Avv Loredana Talia (MI)
Ai sensi della legge 675/96 è possibile in qualsiasi momento opporsi all’invio della rivista comunicando per iscritto la propria decisione a: Edizioni Scripta Manent s n c - Via Melchiorre Gioia, 41/A - 20124 Milano
The Publisher is not liable for the opinion expressed by the Authors of the articles and for images used by them
GENERAL INFORMATION
AIMS AND SCOPE
“Archivio Italiano di Urologia e Andrologia” publishes papers dealing with the urological, nephrological and andrological sciences
Original articles on both clinical and research fields, reviews, editorials, case reports, abstracts from papers published elsewhere, book rewiews, congress proceedings can be published

III Archivio Italiano di Urologia e Andrologia 2022, 94, 4
Questo Trattato nasce dall’esigenza di offrire evidenze scientifiche della letteratura in diversi àmbiti clinici, riguardo alla Nutraceutica in Pediatria, in un contesto attuale dove è molto forte da parte della società la propensione a ricorrere a “prodotti naturali”.

I temi trattati sono a sostegno di scelte mirate da parte del Pediatra, che possono essere di supporto dal punto di vista preventivo e terapeutico, per la salute di bambini e adolescenti.
25 Capitoli
64 Autori
480 Pagine a cura di Gianvincenzo Zuccotti
Enza D’Auria
Elvira Verduci
Prezzo di copertina € 100,00
Per l’acquisto inviare una e-mail a: info@edizioniscriptamanent.eu
Perceptions and attitudes toward the use of telemedicine for the postoperative outpatient urological care during the COVID-19 pandemic in an Academic Hospital in
Southern Italy
Vincenzo Mirone 1 , Giuseppe Celentano 1 , Claudia Collà Ruvolo 1 , Luigi Cirillo 1 , Giovanni Maria Fusco 1 , Marco Abate 1 , Simone Morra 1 , Francesco Di Bello 1 , Gianluigi Califano 1 , Claudia Mirone 2 , Gianluigi Cacace 1 , Vincenzo Morgera 1 , Roberto La Rocca 1 , Marco Capece 1 , Nicola Longo 1 , Luigi Napolitano 1 , Massimiliano Creta 1
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, School of Medicine, University of Naples "Federico II", Naples, Italy;
2 Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania "Luigi Vanvitelli", Naples, Italy
Summary
Introduction: Telemedicine is a most used tools in various medical and surgical scenarios
The aim of the present study was to explore attitudes and perceptions by urologic patients toward the use of telemedicine in the context of patient-physicians communication during the post-operative follow-up in a large academic tertiary urology referral department in Italy.
Materials and methods: An anonymous questionnaire consisting of 15 multiple choice questions was designed including three sections: respondents’ demographics, attitudes, and perceptions towards the use of telemedicine Invitations to participate to this anonymous questionnaire was given to outpatients attended at Urology Department, University of Naples Federico II
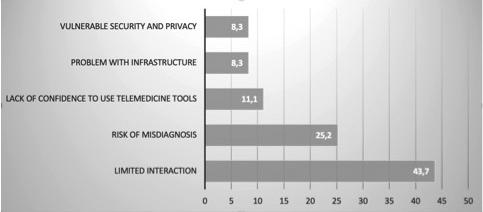
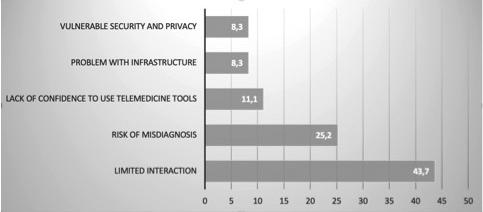
Results: In total 697 responses were received (participation rate 73%) The frequency of telemedicine use was described as frequently, occasional, rarely, and never by 41 6%, 30 4%, 15 1%, and 12 6% of respondents, respectively WhatsApp messenger used by 59 5% of respondents and telephone call (34 3%) were the most common type of tools Satisfaction in using telemedicine was reported as very satisfied, satisfied, neutral, dissatisfied, and very dissatisfied by 39 6%,41 4%,10%,7% and 2% of respondents respectively. Overall, 43.7%% of participants individuated limited interaction and risk of misdiagnosis as the major limit of telemedicine.
Conclusions: Telemedicine represents the future of medical practice due to several benefits as well as convenience, increased access to care and decreased healthcare costs
KEY WORDS: Telemedicine; Telehealth; Healthcare; Virtual Healthcare; Urology
Submitted 28 July 2022; Accepted 2 August 2022
INTRODUCTION
Telehealth represents a rapidly evolving field of medicine
It is defined as the use of information technology and telecommunications to provide access to health assessment, consultation, diagnosis, intervention, super-vision, and information across distance (1, 2) Telemedicine refers
specifically to remote clinical services and was first adopted in the 1950’s when an American psychiatrist connected to a prison through a closed-circuit television to provide mental health services (3)
In recent years, with the advancement of mobile technologies, the adoption and accessibility of telemedicine has significantly increased, after COVID-19 pandemic declaration in several clinical and surgical fields including urology (410) Advantages of remote care include reduction of the use of resources in health centers, improving access to care (3) Moreover, telemedicine has the potential to reduce the risk of direct transmission of infectious agents (11) Approximately 15 million Americans receive remote medical assistance yearly (2) The urological literature on telehealth is sparse The telemedicine experience in urology spans from new patient consultations to telesurgery to post-operative rounds and even virtual house calls (12) In details, telemedicine has been described in patients with hematuria, prostate cancer, urinary stones, pelvic organ prolapse, urinary infections, and urinary incontinence (2) The aim of the present study was to explore attitudes and perceptions by urologic patients toward the use of telemedicine in the context of patient-physicians communication during the post-operative follow-up in a large academic tertiary urology referral department in Italy
MATERIALS AND METHODS
Questionnaire
An anonymous 15 multiple choice questions (formulated in Italian with the aim of increasing the response rate) questionnaire was administered to a total of 955 patients who had visited the outpatient Department of Urology at University Federico II, Naples, from September 2020 to April 2021 The questionnaire was composed of three sections: a first one to assess respondents’ demographics (age, sex, urologic disease) a second one to evaluate their attitudes using telemedicine, and a third to evaluate per-
375 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 ORIGINAL PAPER No conflict of interest declared
DOI: 10 4081/aiua 2022 4 375
ceptions towards telemedicine Questions about attitudes toward use of telemedicine included:
t o o l s a d o p t e d ( t e l e p h o n e c a l l , e - m a i l s , WhatsApp, others), context in which telemedicine was used, content of multimedia data shared
Questions about perceptions investigated the perceived usefulness of telemedicine and the potential developments
Respondents were invited to "strongly agree" , "moderately agree" , "slightly agree" , "strongly disagree" , "moderately disagree" , "slightly disagree" with a series of statements about perceptions Some questions required a single answer while others gave the respondents the choice to select as many answers as they felt appropriate
Data analysis
Data were expressed as mean (Standard Deviation) and raw numbers and percentages of survey answers Statistical analyses were two-sided using a significance level of 0 05
All statistical analyses were performed with SPSS version 17 0 (SPSS, Inc , Chicago, IL) software
RESULTS
In total 697 responses were received (participation rate 73 %) All patients were Caucasian
Of them, 572 patients (82%) were male and 125 (18%) were female Mean (SD) patients’ age was 67 5 (5 3) years In details the number of patients aged between 18-34, 35-54, 55-74, and those aged > 75 were 12 (1 7%), 16 (2 3%), 466 (66 8%), and 203 (29 1%), respectively
Concerning educational level, the number of patients with elementary school or no title, middle school diploma, high school diploma, and university degree were 104 (15%), 139 (20%), 175 (25%), and 279 (40%), respectively
As regards the occupational status of respondents, the number of them working, retired and unemployed were 367 (52 6%), 265 (38 1%), and 65 (9 3%), respectively
The disease for which patients received outpatient post-operative care were bladder cancer (n = 209, 30%), prostate cancer (n = 160, 23%), kidney cancer (n = 69, 10%), testis cancer (n = 4, 0 5%), penis cancer (n = 2, 0 3%), obstructive uropathy (n = 105, 15%), urolithiasis (n = 69, 10%), urinary tract infections (n = 4, 0 5%) and others (n = 75, 10 7%) Overall, 267 patients (38 3%) were in the early post-operative follow-up (within 30 days from surgery) and 430 (61 7%) in the late post-operative follow-up (> 30 days from surgery)
Table 1 describes attitudes toward the use of telemedicine
Figure 1 describes the frequency of telemedicine use according to patients’ age Perceptions about the usefulness and limits of telemedicine in the context of outpatient post-

Table 1
Attitudes of patients toward telemedicine
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 V
376
Mirone, G Celentano, C Collà Ruvolo, et al
N (%) Frequency of telemedicine use Frequently 290 (41 6) Occasionally 212 (30 4) Rarely 109 (15 7) Never 86 (12 3) Use of telemedicine during the COVID-19 pandemic compared
pre-pandemic period Increased 387 (63 4) Remained stable 159 (25 9) Decreased 65 (10 7) Purpose of availing telemedicine facility Booking and appointment 246 (40 2) Consultation 322 (52 7) Treatment 43 (7 1) Tools adopted Telephone call 209 (34 3) WhatsApp messages 364 (59 5) Video-call 24 (3.9) e-mail 2 (0 3) Other 12 (1) Media-contents shared Video 3 (0 8) Audio 129 (32 1) Text 220 (54.7) Photo 50 (12 4) Reason for not using telemedicine I don’t know the existence of this type of medical service 42 (48 9) I don’t know how to use this type of medical service 19 (22 5) I don’t trust telemedicine 13 (14 7) My technical conditions do not allow me to use telemedicine 8 (9 3) Other reasons 4 (4 6) W illingness to continue using telemedicine after COVID-19 pandemic Yes 416 (68 1) Not 195 (31 9) Satisfaction with telemedicine use Very satisfied 242 (39 6) Satisfied 253 (41 4) Neutral 61 (10) Dissatisfied 43 (7) Very dissatisfied 12 (2)
to the
telemedicine use according to
age.
Figure 1. Percentage of
patients’
operative follow-up are reported in Table 2 Figure 2 describes the percentage of patients reporting specific challenges in availing telemedicine
DISCUSSION
In the last years, several surgeons have incorporated telemedicine into pre- and post-operative visits and specialty consultations (13) The use of telemedicine modalities for perioperative care has been reported to represent a cost-effective strategy and has been associated with a relatively high rate of patient satisfaction (13)
Urologists described the successful use of telemedicine in several settings: shared decision-making counseling for prostate cancer treatment, administration of behavioral therapies for urinary incontinence, and post-operative follow-up care (13) More recently, The COVID-19 pandemic has radically changed the landscape of health care and has further stimulated the use of telemedicine (13-14) Attitudes and perceptions toward the use of telemedicine by patients varies significantly across the word and accord-
ing to the setting of adoption To our knowledge this represents the first time a survey investigating the attitudes and perceptions about telemedicine by urology patients referring to an outpatient department in Southern Italy
Interestingly, 72% of respondents declared to having freq u e n t l y o r o c c a s i o n a l l y u s e d telemedicine during the COVID19 pandemic
Not surprisingly, the percentage o f p a t i e n t s d e c l a r i n g t o u s e t e l e m e d i c i n e r a r e l y o r n e v e r increased with increasing age with most patients never using medicine being aged > 75 years Of note, about half of patients declaring to have never used telemedicine did not know the existence of this type of medical service
These findings point out the current limits of telemedicine, mainly il old people, for which lack of knowledge and confidence with telemedicine may represent a significant barrier
Whatsapp messenger was the most frequently adopted tool by respondents during remote communication
Accordingly, a comprehensive systematic review presented compelling evidence that WhatsApp Messenger is a promising system when used as a communication tool between health care professionals and the general public (15)
Limited patient-physician interaction and risk of misdiagnosis were perceived as limitations of telemedicine by most respondents Accordingly, many criticize that telehealth may adversely affect continuity of care Online interactions are perceived as impersonal and dangerous because the virtual provider does not offer the benefit of a complete medical history and physical examination
377 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Perceptions and attitudes toward the use of telemedicine for the postoperative outpatient urological care during the COVID-19 pandemic
(15-18) Therefore, telehealth should be considered as
Agree strongly Agree moderately Agree slightly Disagree slightly Disagree moderately Disagree strongly N (%) N (%) N (%) N (%) N (%) N (%) Telemedicine, in combination with in-person appointments, is useful in improving patient- physician communication in the post-operative period 229 (32 9) 264 (38) 75 (10 8) 87 (12 5) 26 (3 7) 16 (2 1) Telemedicine, in combination with in-person appointments, is useful in improving the quality of assistance in the post-operative period 248 (35 6) 196 (28,1) 111 (15,9) 86 (12 3) 35 (5 1) 21(3) Telemedicine, in combination with in-person appointments,
the interpretation of findings from laboratory and radiological investigations 222 (31 7) 175 (25 1) 139 (20) 139 (20) 15 (2 2) 7 (1) Telemedicine, in combination with in-person appointments, is useful in improving the interpretation of clinical findings 211 (30 3) 158 (22 6) 189 (27 1) 114 (16 4) 18 (2 6) 7 (1) Telemedicine, in combination with in-person appointments, is helpful in reducing unnecessary visits to hospitals 306 (43 9) 175 (25 1) 111 (16) 70 (10) 35 (5) 0 (0) Telemedicine, in combination with in-person appointments, is helpful in reducing costs of post-operative follow-up 258 (37) 141 (20 2) 203 (29 1) 63 (9) 32 (4 7) 0 (0) Telemedicine, in combination with in-person appointments, is helpful in improving patients’ adherence to prescriptions 315 (45 3) 227 (32 6) 72 (10 3) 57 (8 2) 26 (3 6) 0 (0) Telemedicine, in combination with in-person appointments, is helpful in helps in the prompt recognition of complications and side effects 256 (36 8) 154 (22 1) 104 (14 9) 111 (15 9) 72 (10 3) 0 (0)
Table 2. Perceptions about the usefulness and limits of telemedicine in the context of outpatient post-operative follow-up of urological patients (n = 697)
is useful in improving
Figure 2.
Percentage of patients reporting specific limitations in availing telemedicine (n = 611)
an adjunct and best used to supplement in-person visits
(15) Although vulnerable security and privacy was perceived as a limit of telemedicine by only 8 3% of patients, this issue deserve careful attention According to Morris et al , despite the widespread use of WhatsApp, clinicians are either failing in their ethical, legal, regulatory, and clinical responsibility to keep records of WhatsApp consults, or are not reporting how they do so or that they do so (19) Unfortunately, the literature does not report any clear “best practices” for recordkeeping, or the secure storage of patient information obtained and there is a need to raise awareness on this issue and to urgently provide viable guidance (19) Interesting is patient satisfaction with use of telemedicine We reported an overall good satisfaction using this technology: 39 6% and 41 4% of respondents reported satisfaction and very satisfaction respectively Our data corroborated results of previous published studies Holzman et al reported high grade of satisfaction with telemedicine compared to in person visits in pediatric urology outpatient patients (20) A high satisfaction of patients in telehealth experience compared to in person visit were also reported by Polinski et al and by Ambrosini et al (21-22) Despite advantages using telemedicine, some disadvantages and barriers as well as performing physical examinations, possibilities for technical difficulties, security breaches, and regulatory barriers have been reported (23) Limited interaction and misdiagnosis were the most reported barriers in our survey, 43 7% and 25 2% respectively The topic is very important with several legal and economic aspects
Our data corroborated findings reported in previous studies: Chandhanayingyong reported an overall misdiagnosis rate of 40%, with over-diagnosis of 12% and under-diagnosis of 27% using teleconsultation using the mobile phone multimedia messaging service (MMS) in emergency orthopedic patients (24) Spear at al in a survey on 781 patients that experienced telemedicine, reported as main disadvantages the lack of hands-on care, the lack of intimacy, and technical difficulties (25) Our study has some limitations: first of all, the simple size represents a small group of the providers in the academic setting, and it is limited to academic urology experience Telemedicine represents the future of medical practice including several benefits as well as convenience, increased access to care and decreased healthcare costs Further studies are necessary to improve clinical, administrative, and research aspects to expand the use of telemedicine among patients
REFERENCES
1 Ayoub CH, El-Asmar JM, Abdulfattah S, El-Hajj A Telemedicine and Telementoring in Urology: A Glimpse of the Past and a Leap Into the Future Front Surg 2022; 9:811749
2 Novara G, Checcucci E, Crestani A, et al Telehealth in Urology: a systematic review of the literature How much can telemedicine be useful during and after the COVID-19 pandemic? Eur Urol 2020; 78:786-811
3 Mirone V, Creta M, Capece M, et al Telementoring for communication between residents and faculty physicians: Results from a sur-
vey on attitudes and perceptions in an Academic Tertiary Urology Referral Department in Italy Arch Ital Urol Androl 2021; 93:450454
4 Melchionna A, Collà Ruvolo C, Capece M, et al Testicular pain and youtube™: are uploaded videos a reliable source to get information? Int J Impot Res 2022 Feb 8 doi: 10 1038/s41443-022-00536w Epub ahead of print
5 Capece M, Di Giovanni A, Cirigliano L, et al YouTube as a source of information on penile prosthesis Andrologia 2022; 54:e14246
6 Morra S, Collà Ruvolo C, Napolitano L, et al YouTubeTM as a source of information on bladder pain syndrome: A contemporary analysis Neurourol Urodyn 2022; 41:237-245
7 Napolitano L, Fusco GM, Cirillo L, et al Erectile dysfunction and mobile phone applications: Quality, content and adherence to European Association guidelines on male sexual dysfunction Arch Ital Urol Androl 2022; 94:211-216
8 Creta M, Sagnelli C, Celentano G, et al SARS-CoV-2 infection affects the lower urinary tract and male genital system: A systematic review J Med Virol 2021; 93:3133-3142
9 Barone B, De Luca L, Napolitano L, et al Lower urinary tract symptoms and mental health during COVID-19 pandemic Arch Ital Urol Androl 2022; 94:46-50
10 Sen V, Aydogdu O, Yonguc T, et al Telerounding & telementoring for urological procedures Arch Ital Urol Androl 2016; 88:206207
11 Gerundo G, Collà Ruvolo C, Puzone B, et al Personal protective equipment in Covid-19: Evidence-based quality and analysis of YouTube videos after one year of pandemic Am J Infect Control 2022; 50:300-305
12 Castaneda P, Ellimoottil C Current use of telehealth in urology: a review World J Urol 2020; 38:2377-2384
13 Connor J, Zheng Y, Houle K, Cox L Adopting Telehealth During The COVID-19 Era: The Urologist's Perspective Urology 2021; 156:289-295
14 Di Bello F, Collà Ruvolo C, Cilio S, et al Testicular cancer and YouTube: What do you expect from a social media platform? Int J Urol 2022; 29:685-691
15 Giordano V, Koch H, Godoy-Santos A, et al WhatsApp Messenger as an Adjunctive Tool for Telemedicine: An Overview Interact J Med Res 2017; 6:e11
16 Boehm K, Ziewers S, Brandt MP, et al Telemedicine Online Visits in Urology During the COVID-19 Pandemic-Potential, Risk Factors, and Patients' Perspective Eur Urol 2020; 78:16-20
17 Ellison LM, Nguyen M, Fabrizio MD, et al Postoperative robotic telerounding: a multicenter randomized assessment of patient outcomes and satisfaction Arch Surg 2007; 142:1177-81
18 Pinar U, Anract J, Perrot O, et al Preliminary assessment of patient and physician satisfaction with the use of teleconsultation in urology during the COVID-19 pandemic World J Urol 2021; 39:1991-1996
19 Morris C, Scott RE, Mars M WhatsApp in Clinical Practice-The Challenges of Record Keeping and Storage A Scoping Review Int J Environ Res Public Health 2021; 18:13426
20 Holzman SA, Davis-Dao CA, Khoury AE, et al Telemedicine and patient satisfaction during the COVID-19 pandemic: A case-con-
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
378
V Mirone, G Celentano, C Collà Ruvolo, et al
Perceptions and attitudes toward the use of telemedicine for the postoperative outpatient urological care during the COVID-19 pandemic
trol study of outpatient pediatric urology patients J Child Health Care 2021:13674935211058272
21 Polinski JM, Barker T, Gagliano N, et al Patients' Satisfaction with and Preference for Telehealth Visits J Gen Intern Med 2016; 31:269-75
22 Ambrosini F, Di Stasio A, Mantica G, et al COVID-19 pandemic and uro-oncology follow-up: A "virtual" multidisciplinary team strategy and patients' satisfaction assessment Arch Ital Urol Androl 2020; 92:78-79
23 Gajarawala SN, Pelkowski JN Telehealth Benefits and Barriers J Nurse Pract 2021; 17:218-221
24 Chandhanayingyong C, Tangtrakulwanich B, Kiriratnikom T Teleconsultation for emergency orthopaedic patients using the multimedia messaging service via mobile phones J Telemed Telecare 2007; 13:193-6
25 Spear KL, Auinger P, Simone R, et al Patient Views on Telemedicine for Parkinson Disease J Parkinsons Dis 2019; 9:401-404
Correspondence
Vincenzo Mirone, MD mirone@unina it
Department of Neurosciences, Reproductive Sciences and Odontostomatology, School of Medicine, University of Naples "Federico II", Naples (Italy)
Giuseppe Celentano, MD dr giuseppecelentano@gmail com
Claudia Collà Ruvolo, MD c collaruvolo@gmail com
Luigi Cirillo, MD cirilloluigi22@gmail com
Giovanni Maria Fusco, MD giom fusco@gmail com
Marco Abate, MD marcoabate5@gmail com
Simone Morra, MD simonemorra@outlook com
Francesco Di Bello, MD fran dibello12@gmail com
Gianluigi Califano, MD gianl califano2@gmail com
Gianluigi Cacace, MD cacace gianlu@gmail com
Vincenzo Morgera, MD vincemorgera87@gmail com
Roberto La Rocca, MD robertolarocca87@gmail com
Marco Capece, MD drmarcocapece@gmail com
Nicola Longo, MD
nicola longo@unina it
Massimiliano Creta, MD max creta@gmail com
Luigi Napolitano, MD (Corresponding Author) dr luiginapolitano@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples "Federico II"
Via Sergio Pansini n 5, Naples (NA), Campania (Italy)
Claudia Mirone, MD
claudiamirone@outlook it
Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania "Luigi Vanvitelli", Naples (Italy)
379 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Goldfinger bypassing and en bloc stapling without dissection of renal vessels during laparoscopic nephrectomy
1 Urology Department, Barzilai Medical Center, Ben Gurion University of the Negev, Beer Sheva, Israel;
2 Assuta Medical Center, Beer Sheva, Ramat Hyal, Ben Gurion University of the Negev, Beer Sheva, Israel;
3 International School of Economics, Tbilisi, Georgia;
4 IZA, Bonn, Germany;
5 School of International and Public Affairs, Columbia University, New York
Summary
Objective: To test the employment of the Goldfinger Dissector (GD) to bypass and en bloc stapling of renal hilus without vascular dissection Thus far no study has experimented the use of this integrated technique. Patients and methods: From July 2002 to October 2020, clinical data were collected from 288 patients who underwent transperitoneal laparoscopic nephrectomies They were divided into two groups: using GD with en bloc stapling (n = 174, group I) or the separation and ligation method (n = 114, group II) using the same Endo GIA Universal (Vascular) Stapler. Comparative analysis was carried out between the two groups, examining blood loss, operative time, intra and postoperative complications and hospital stay
Results: The mean age was 58.3 and 55.1 years in group I and II, respectively Ratio of 90/84 and 55/59 males/females was found in group I and II, respectively.Blood loss was 65.5 ml and 188 9 ml, operative time was 156 5 and 189 2 minutes, wound infection occurred in three patients in each group (1.7% and 2 6%), ileus in 4 (2 3%) and 1 (0 87%), atrial fibrillation in 1 (0.57%) and 0%, incisional hernia in 0 (0%) and 2 (1.75%), deep vein thrombosis (DVT) in 0 (0%) and 1 (0 87%), conversion to open surgery in 2 (1 15%) and 5 (4 39%), mean hospital stay 3 5 days and 4 days in group I and II, respectively
Conclusions: Routine use of the GD and en bloc stapling of the renal pedicle in laparoscopic nephrectomy is safe and useful This technique can decrease blood loss, operative time, and have some benefit in conversion to open surgery
KEY WORDS: Goldfinger dissector; Laparoscopic nephrectomy; En bloc; GIA vascular stapler; Hilum dissection
Submitted 25 November 2022; Accepted 2 December 2022
INTRODUCTION
Since the original report of a successful laparoscopic nephrectomy by Clayman et al in 1991, laparoscopic nephrectomy has become an alternative to traditional open surgery (1) This procedure is considered technically difficult because of the vessel injury risk, leading to massive hemorrhage during renal pedicle management (2) There is no doubt that the main and dangerous part of laparoscopic nephrectomy is the dissection of the kidney blood vessels, as minimal trauma of the large blood ves-
sels can be disastrous, resulting in massive bleeding that requires blood transfusions and opening the abdomen in the most hustle way to save lives So hilar dissection and control of renal vessels are the most critical steps in laparoscopic nephrectomy Multiple techniques have been utilized for these steps and several studies have reported their experience with renal pedicle control (2-9) Rapp et al used the technique of en bloc hilar ligation They deployed a stapler across the renal hilum without individual dissection of the renal artery and vein (9) Resorlu et al found that en bloc ligation of both the renal artery and vein using a stapler is an easy and reliable technique that allows safe and fast control of the renal pedicle during laparoscopic nephrectomy (2) This technique is successful also in laparoscopic nephroureterectomy, without the need for separation between the renal vessels (8) The hilar dissection is even more difficult in laparoscopic nephrectomy after past surgeries (10-11), or in cases with an inflammatory process such as xanthogranulomatous pyelonephritis (XGP) (12)
To the best of our knowledge, GD had not been used for t h i s p u r p o s e ( w e e x p l o re d re s e a rc h p u b l i s h e d i n PUBMED and MEDLINE) Articles were published using the GD in laparoscopic sacrocolpopexy (13) and during liver surgery (14-15) Since there have been previous reports of GIA malfunction, there has been an attempt to safely and inexpensively use both wires and Hem-O-Loc clips simultaneously for renal vein control (6)
PATIENTS AND METHODS
From July 2002 to October 2020, all patients that underwent laparoscopic nephrectomy by the same surgeon were examined Out of 525 cases undergoing laparoscopic nephrectomy, there were 288 consecutive cases, which had a transperitoneal approach and had all the necessary information according to the working protocol
The cases were divided into two groups In the first group (I), a flexible Goldfinger dissector (Goldfinger DissectorEthicon Endo Surgery, Johnson and Johnson, New Brunswick, NJ, USA) was used for the dissection of the renal hilum and a vascular stapler (Endo GIA Universal Vascular Stapler,
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 380
PAPER No conflict of
ORIGINAL
interest declared
Murad Asali 1, 2 , Muhammad Asali 3, 4, 5
DOI: 10 4081/aiua 2022 4 380
Medtronic Parkway Minneapolis, MN, USA) was used to close and cut the kidney hilus without separating the renal vessels
In the second group (II) a dissection of the blood vessels was carried out, and the closure of the renal artery and renal vein separately was done with the same previously cited stapler

There were various causes for nephrectomy including cancers, benign tumours or dysfunctional kidneys
All cases were operated by one surgeon (MA), and in all cases there was a transperitoneal surgical approach
The surgical technique is the same in both groups up until access to the kidney hilum Five trocars were used on the right side (two 5 mm, two 12 mm and one 11 mm) and four were used on the left (5 mm, 11 mm, and two of 12 mm)
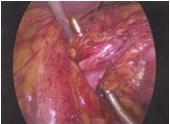
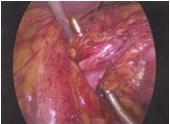
The patient was laying on the flank, with the operated side upwards, in the position of lateral decubitus The abdominal cavity was entered with medialization of the colon and dissection of duodenum when operating the right side The ureter was identified and cut between clips and dissected towards the kidney hilum The kidney was dissected outside the boundaries of Gerota's fascia From this step the surgical approach was different between the two groups In the first group, the GD device was inserted caudal and posterior to the renal hilus tissue creating a small window above the hilum of the kidney and under the adrenal to have the feeling of controlling the whole hilum (Figure 1) At this moment, the GD is removed, and with all devices kept in place without movement, a 60 mm Vascular GIA stapler is inserted for ligation and dividing (Figure 2)
In contrast, in the second group the dissection was continued between the renal artery and renal vein in the renal hilum until they were completely separated, and then the stapler was used on the renal artery and later on the renal vein individually
The tip of the stapler was visualized beyond the hilum
and free from any adjacent tissue before engaging the stapler mechanism
The first group (I) consisted of 174 cases in which the entire hilum was closed together (en bloc stapling) by using GD The second group (II) consisted of 114 cases in which a dissection was performed between the artery and renal vein and the closure of each blood vessel was done separately with GIA from the same company
We evaluated the following clinical and perioperative data: age at surgery; sex; laterality; history of ureteroscopy, percutaneous nephrolithotomy (PCNL), peritoneal or retroperitoneal operations, pyonephrosis, nephrostomy insertion; complications, estimated blood loss (EBL), operation time, and length of stay (LOS)
Operation time was defined as the time from the beginning (incision) to the end of procedure (closure of the skin)
RESULTS
The mean age was 58 3 and 55 1 years in group I and II respectively Ratio of 90/84 and 55/59 males/ females were observed in group I and II respectively (Table 1)
Blood loss was 65 5 ml and 188 9 ml, operative time was 156 5 and 189 2 minutes, wound infection occurred in three patients in each group (1 7% and 2 6%), ileus in 4 (2 3%) and 1 (0 87%), atrial fibrillation in 1 (0 57%) and 0%, incisional hernia in 0 (0%) and 2 (1 75%), deep vein thrombosis (DVT) in 0 (0%) and 1 (0 87%), in group I and II respectively (Table 2) Conversion to open surgery occurred in 2 (1 15%) and 5 (4 39%), mean hospital stay was 3 45 days and 3 9 days in group I and II, respectively
Post-operative
381 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Stapling of renal vessel during laparascopic nephrectomy
Table 1
GD and en bloc-I Hilum Dissection-II Difference (Std. dev.) (Std. dev.) [P-value] Age mean (years) 58.3 55.1 3.2 (16 77) (20 41) [0 155] Male 90 (51 7%) 55 (48 2%) 3 5% (0 50) (0 50) [0 565] Stricture side Right 80 (46%) 54 (47%) -1% (0 50) (0 50) [0 818] Left 94 (54%) 60 (53%) 1% (0 50) (0 50) [0 818] Observations (N) 174 114 Standard dev ations n parentheses P-values n square brackets
Patient demographics
renal
Figure
1
Goldfinger bypassing the
hilus
Figure 2 GIA vascular stapler- en bloc stapling of renal hilus.
Table 2
GD and en bloc-I Hilum Dissection-II (%) (% Wound Infection Ileus 3 (1 7%) 3 (2 6%) 4 (2.3%) 1 (0.87%) Atrial Fibrillation 1 (0 57%) 0 (0%) Incisional Hernia 0 (0%) 2 (1 75%) DVT 0 (0%) 1 (0 87%) Observations (N) 87 Total (%) 4 6% 6 1% DVT: Deep Ve n Thrombosis
complications
DISCUSSION
Laparoscopic nephrectomy has become a standard surgery since the description of the surgery by Clayman et al in 1991 (1) The difficulty arises when dissecting the kidney hilum, separating the renal blood vessels, as an injury and bleeding from the blood vessels vastly increases the chances of a conversion to open surgery, rendering the patients losing all the advantages of the laparoscopic surgery over the open one Early on, Chan et al described the technique of rapid ligation of the renal hilum, and in their technique, they proposed a dissection of the renal vein, which is anterior, and tying all the posterior tissue (posterior packet) containing the renal artery, and subsequently closing the renal vein separately, thus providing a safe and quick approach to closing the hilum (17) In several studies there was a discussion regarding dissection of blood vessels, and cases where blood vessel were ligated en bloc due to the fear to separate blood vessels when there was no progress with the surgery or for other reasons in the attempt to control the blood vessels (2, 4, 67, 9, 16) The efficacy of en bloc method has also been observed during laparoscopic nephroureterectomy in the first part of the surgery, before the completion of the ureteral dissection from the bladder (7-9)
Table 3 shows the list of peritoneal and retroperitoneal surgeries that were done before laparoscopic nephrectomy in the same kidney unit A difference was shown only in the number of ureteroscopies between the two groups (p < 0 05) This difference in ureteroscopies should not be relevant because these procedures have not much effect on the tissues around the kidney hilus and should not affect the results History of PCNL, peritoneal and retroperitoneal operations, pyonephrosis and percutaneous nephrostomy, were not different when comparing the two groups (Table 3)
In the current study we compared group I and II, and we found a significant difference in the average surgery time and in bleeding in favor of the group that used GD with closing and cutting the kidney hilum en bloc at the same time The values of our study were not higher when compared to other series where even longer times and higher
Table 4.
Transperitoneal Laparoscopic Nephrectomy series dealing with renal vessels
Vascu ar dissect on; E: En bloc stapl ng; HS: Hosp tal stay; GIA: Endo Vascular GIA: Medtron c, H: Hem-o- ock; OT: Operating t me; BL: Blood loss; M n : M nute Device used in a l studies s GIA, except for D Zhang et al which s H/GIA Ad difference refers to the statistical d fference n the respective variable between the two groups when controll ng for the demographic variables of age, gender, and r ght or left kidney
< 0 05
Kidney pathology.
RCC: Rena Cell Carc noma; UCC: Urothel al Ce l Carcinoma; Pyelo: Pyelonephr tis; Hydro: Hydronephrosis; NF: Nonfunct on ng Kidney; AML: Angiomyo ipoma; Onco: Oncocytoma; XGP: Xanthogranulomatous Pye onephr tis; AS: Angiosarcoma
volumes were observed (Table 4) One of the reasons for this difference is that some cases were at the beginning of the learning curve, whereas years later duration of surgeries became shorter, yet the significant advantage of group I over group II is apparent The differences in conversion rate from laparoscopic surgery to open surgery and complications also were in favor of the first group (Table 4), but the difference is not statistically significant The average bleeding is much lower in the first group compared to the second, and relatively lower than other world series (Table 4) We observed a statistically difference in hospital stay, although most patients were discharged three days post-surgery
We have no information about the use of the GD device in laparoscopic nephrectomy in other world series, although whoever is trying this device can feel full confidence when bypassing the entire renal hilum from all directions The use of the device allows to evaluate the entire thickness of the tissue before employment the GIA- stapler If tissue appears to be too bulky, it can be divided by the same GD to identify another surgical plane in order to safely employ the GIA- stapler twice without seeing the blood vessels In both groups, the nephrectomy was performed for various reasons as detailed in Table 5 including cancerous renal
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 M Asali, M Asali 382
peritoneal
retroperitoneal
invasive
GD and en bloc-I Hilum Dissection-II Difference (Std. dev.) (Std. dev.) [P-value] URS 0 376 0 254 0 121*** (0 49) (0 44) [0 029] PCNL 0 046 0 079 -0 033 (0 21) (0 27) [0 277] RP Operation 0 238 0 227 0 011 (0 43) (0 42) [0 830] Pyonephrosis 0 231 0 234 -0 003 (0 42) (0 43) [0 963] PCN 0 150 0 216 -0 066 (0 36) (0 41) [0 169] Peritoneal 0 438 0 456 -0 018 operation (0 50) (0 50) [0 763] Observations (N) 174 114 URS: Ureteroscopy, PCNL: Percutaneous nephrolithotomy, RP: Retroperitoneal, PCN: Percutaneous nephrostomy *** P-va ue < 0 05
Table 3. Prior
or
operations and
procedures
Reference D/E N BL OT Conversion Complications HSML Min %% Days Resorlu et al (2) E 27 225 98 0 3 7 5 1 Conradie et al (7) E 93 32 56 2 1 2 2 2 9 Ma et al (4) E 33 75 2 99 6 3 12 1 4 8 Zhang et al (5) D 191 94 8 171 5 0 52 4 2 5 6 Sherer et al. (16) E 433 155 169 1 4 1 4This study: Asali et al E 174 65 5 156 5 1 15 4 6 3 45 (68 81) (45 21) (0 11) (0 21) (0 87) D 114 188 9 189 2 4 39 6 1 3 90 (306 44) (53 64) (0 21) (0 24) (1 98) Difference E-D -123 50 -32 75 -3 2 -1 5 -0 45 [P-value] [0 000] [0 000] [0 124] [0 577] [0 023] P-value < 0 05 *** *** *** Adj difference -128 64 -31 79 -3 49 -2 07 -0 49 [P-value] [0 000] [0 000] [0 115] [0 468] [0 019] P-value
*** *** ***
P-value
< 0 05
D:
***
Table
5.
Group No RCC UCC Pyelo./Hydro./NF. AML Onco. XGP AS. En bloc- I 174 74 26 74 4201
II 114 30 20 65 0241
Dissection-
tumors (renal cell carcinoma, urothelial cell carcinoma, angiosarcoma), some benign tumors (oncocytoma, angiomyolipoma), and chronic renal inflammatory processes related to history of recurrent urinary tract infections or stone disease Although the causes of nephrectomy are different, the surgery performed in all the cases was the same, and the kidney was always dissected on a plane outside the Gerota's fascia even when it was affected by an inflammatory non-tumor process, because this surgical plane is less involved in the inflammatory process as shown by Ma et al (4) Laparoscopic nephrectomy outside Gerota's fascia of the kidney could reduce the difficulty of procedure (4)
The strength of this article is related to several factors
First, it was introduced the use of an endoscopic device for the purpose of bypassing the renal blood vessels, that was never used elsewhere in the world for this purpose
Secondly, the larger number of cases in which ligation of renal blood vessels was carried out simultaneously (en bloc) in relation to other most known series in the world
Thirdly, all cases were operated by a single surgeon
Finally, in all cases GD and vascular GIA-stapler from the same companies were used The major limitation of our study is that data were acquired in a retrospective manner
CONCLUSIONS
Routine use of the GD and en bloc stapling of the renal pedicle in laparoscopic nephrectomy is safe and useful This technique can decrease blood loss, operative time and have some benefit in conversion to open surgery
REFERENCES
1 Clayman RV, Kavoussi LR, Soper NJ, et al Laparoscopic nephrectomy: initial case report J Urol 1991; 146:278-82
2 Resorlu B, Oguz U, Polat F, et al Comparative analysis of pedicular vascular control techniques during laparoscopic nephrectomy: en bloc stapling or separate ligation? Urol Int 2015; 94:79-82
3 Yang F, Zhou Q, Li X, Xing N The methods and techniques of identifying renal pedicle vessels during retroperitoneal laparoscopic radical and partial nephrectomy World J Surg Oncol 2019;17:38
4 Ma L, Yu Y, Ge G, Li G Laparoscopic nephrectomy outside gerota fascia and En bloc ligation of the renal hilum for management of inflammatory renal diseases Int Braz J Urol 2018; 44:280-287
5 Zhang L, Yao L, Li XS, et al Technique of renal pedicle control in transperitoneal laparoscopic nephrectomy: experience of 191 cases by a single surgeon Beijing Da Xue Xue Bao Yi Xue Ban 2014; 18;46:537-40
6 Janetschek G, Bagheri F, Abdelmaksoud A, et al Ligation of the renal vein during laparoscopic nephrectomy: an effective and reliable method to replace vascular staplers J Urol 2003; 170:1295-7
7 Conradie MC, Urry RJ, Naidoo D, et al Advantages of en bloc hilar ligation during laparoscopic extirpative renal surgery J Endourol 2009; 23:1503-7
8 Ou CH, Yang WH, Tzai TS En bloc stapling of renal hilum during hand-assisted retroperitoneoscopic nephroureterectomy in dialysis patients Urology 2008; 72:589-92
9 Rapp DE, Orvieto MA, Gerber GS, et al En bloc stapling of renal hilum during laparoscopic nephrectomy and nephroureterectomy Urology 2004; 64:655-9
10 Aminsharifi A, Goshtasbi B Laparoscopic simple nephrectomy after previous ipsilateral open versus percutaneous renal surgery JSLS 2012; 16:592-6
11 Aminsharifi A, Taddayun A, Niroomand R, et al Laparoscopic nephrectomy for nonfunctioning kidneys is feasible after previous ipsilateral renal surgery: a prospective cohort trial J Urol 2011; 185:930-4
12 Asali M, Tsivian A Laparoscopic nephrectomy in xanthogranulomatous pyelonephritis Cent European J Urol 2019; 72:319-323
13 Talla P, Ekotomati M, O'Leary T, Ben Ali N The Use of the Goldfinger Dissector (GD) in Laparoscopic Sacrocolpopexy Front Med (Lausanne) 2018; 31;5:155
14 Cai LX, Wei FQ, Yu YC, Cai XJ Can retrohepatic tunnel be quickly and easily established for laparoscopic liver hanging maneuver by Goldfinger dissector in laparoscopic right hepatectomy? J Zhejiang Univ Sci B 2016; 17:712-21
15 Troisi RI, Montalti R Modified hanging maneuver using the goldfinger dissector in laparoscopic right and left hepatectomy Dig Surg 2012; 29:463-7
16 Sherer BA, Chow AK, Newsome MJ, et al En Bloc Stapling of the Renal Hilum During Laparoscopic Nephrectomy: A Double-institutional Analysis of Safety and Efficacy Urology 2017; 105:69-75
17 Chan DY, Su LM, Kavoussi LR Rapid ligation of renal hilum dur-
Correspondence
Muhammad Asali, MD, Professor ma90002611@gmail com
School of International and Public Affairs, Columbia University, New York
Murad Asali, MD (Corresponding Author) dr muradasali@gmail com
Department of Urology, Barzilai Medical Center Ben Gurion University, Beer Sheva, Sokolov 26/99, 8430905
383 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Stapling of renal vessel during laparascopic nephrectomy
i n g t r a n s p e r i t o n e a l l a p a ro s c o p i c n e p h re c t o m y U ro l o g y 2 0 0 1 ; 57:360-2
Outcomes of continent and incontinent external urinary diversion in management of patients with refractory non-malignant lower urinary tract dysfunction
Summary
Objective: To evaluate the early and late outcomes of continent and incontinent external urinary diversion in management of patients with refractory non-malignant lower urinary tract dysfunction (LUTD)
Materials and methods: The charts of patients with refractory non-malignant LUTD who underwent continent or incontinent external urinary diversion at University of Cincinnati hospitals in the period between March 2012 and December 2019 were retrospectively reviewed. The demographic and baseline characteristics, surgery indications, operative data, early and late outcomes were collected, analyzed, and compared
Results: A total of 78 patients including 55 patients with neurogenic bladder (NGB) and 23 patients with non-neurogenic bladder (non-NGB) refractory non-malignant LUTD were included Fifty-three patients underwent incontinent urinary diversions (IUD), while 25 patients underwent continent urinary diversions (CUD). During the first 4 postoperative weeks, 53.85% (n=42) of patients developed complications, and the incidence was nonsignificantly higher in patients with NGB than those with nonNGB (56 36% vs 47 83%, p-value=0 490) Fever was exclusively encountered in patients with NGB earlier, while stomal retraction occurred only in patients with non-NGB later. More nonNGB patients had early wound infection. There was an overall improvement of urological symptoms in 52 patients (66.67%), and the rate was non-significantly higher in non-NGB patients than NGB patients (78 26% vs 61 82%, p-value=0 160) Late complications were reported in 47 patients and were more encountered in those with non-NGB than those with NGB (65 22% vs 58 18%) Stomal leakage and stenosis occurred more with CUD than with IUD (52% vs 0% and 28% vs 3.77%, respectively).
Conclusions: External urinary diversion can achieve a reasonable level of urological symptoms control in patients with refractory non-malignant LUTD, but with associated adverse outcomes Although non-significantly, these complications tend to be higher in patients with IUD and/or NGB during the early postoperative period and higher with CUD and/or non-NGB on the long-term.
KEY WORDS: Continent Urinary Diversion (CUD); Incontinent Urinary Diversion (IUD); Neurogenic bladder (NGB); Non-neurogenic bladder (non-NGB); lower urinary tract dysfunction (LUTD)
Submitted 12 November 2022; Accepted 25 November 2022
INTRODUCTION
The lower urinary tract can be affected by multiple benign conditions that can eventually lead to significant lower urinary tract dysfunction (LUTD) These benign conditions can generally be classified into two main categories; neurogenic bladder (NGB) that results from the permanent loss of neuronal control over the bladder due to a neurological disorder such as spinal cord injuries (SCI), multiple sclerosis (MS), Parkinson’s disease (PD) or spina bifida (SB) and non-neurogenic bladder (non-NGB) that results from structural or functional bladder damage rather than loss of neuronal control of the bladder and that can occur with urinary tract fistulas, radiation-induced lower urinary tract damage, refractory urinary incontinence or bladder pain syndrome (BPS) (1-4) Based on the underlying disorder, the presenting symptoms of these benign conditions can vary widely from continuous urinary leakage to urinary retention, recurrent urolithiasis, bladder pain, and recurrent urinary tract infections (UTIs) These disorders can ultimately lead to a significant quality of life deterioration and have a detrimental effect on the upper urinary tract (3-5)
The main goal of management of these benign lower urinary tract conditions is to protect the upper urinary tract, keep the patients socially dry, eliminate the recurrent urosepsis episodes, and maintain the act of urination whenever possible This is mainly achieved by conservative and/or minimally invasive measures (5, 6)
A well-established procedure in the management of bladder cancer, urinary diversion is usually considered the last resort for treating these non-malignant lower urinary tract conditions (7-9) External urinary diversions are generally classified into incontinent diversions such as ileal conduit and colonic conduit and continent diversions such as Indiana Pouch and continent urinary diversion using the ileum (10-13)
The primary aim of this study is to report the early and late outcomes of external urinary diversion in patients with refractory non-malignant LUTD The secondary aim is to evaluate these outcomes independently based on both the underlying condition and the type of external urinary diversion
MATERIALS AND METHODS
After approval by University of Cincinnati Institutional Review
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 384 ORIGINAL PAPER No conflict of interest declared
Mostafa M. Mostafa 1, 2 , Ashraf Khallaf 1 , Mohamed Kamel 1 , Nilesh Patil 1 , Ayman Mahdy 1
DOI: 10 4081/aiua 2022 4 384
1 Division of Urology, Department of Surgery, University of Cincinnati College of Medicine, Cincinnati, OH, United States; 2 Asiut University Hospitals, Asiut, Egypt
Board, we started reviewing the charts of all patients who underwent continent and incontinent external urinary diversion procedures for refractory non-malignant LUTD at University of Cincinnati Hospitals in the period between March 2012 and December 2019 All surgeries were performed via open surgery by one surgeon (AM) who is welltrained in genitourinary reconstructive surgeries Inclusion criteria included all patients with refractory non-malignant LUTD who underwent external urinary diversion Exclusion criteria included patients who were diagnosed with lower urinary tract malignancies and those who did not complete a minimum follow-up of 6 months We collected the demographic and baseline characteristics, surgery indications and operative data Furthermore, we reported early postoperative outcomes that occurred within the first 4 postoperative weeks including fever, pelvic infection or abscess, wound infection, pneumonia, UTI, paralytic ileus (defined by abdominal pain other than incisional, abdominal distension, failure to pass stool and/or flatus in addition to radiological findings suggestive of obstruction), sepsis, blood loss (defined by hemoglobin drop that required blood transfusion), cardiac complications, and re-operation rate Late postoperative outcomes that manifested more than 6 months after surgery including urological symptom control, stomal complications, anastomotic ureteric strictures, stone formation, wound complications, hydronephrosis with renal function impairment, and need for re-operation were also reported Urological symptom control was assessed based on the successful resolution of the specific urological symptoms related to patients’ preoperative urological conditions that were the main drive for intervention Resolution of these symptoms in terms of resolution of hydronephrosis, reduction in urosepsis episodes, alleviation of bladder pain, reduction in urolithiasis, social dryness, and independence was confirmed based on both history taking and clinical examination after a minimum follow-up of 6 months postoperatively
1
Statistical analysis
All statistical analyses were conducted using the SPSS software (SPSS, Inc , Chicago, IL, USA; version 26) Quantitative variables are presented as means ± standard deviation, and qualitative variables are expressed as frequencies with percentages Results were compared between two groups using Student’s t-test and MannWhitney U test for quantitative variables and chi-square test and McNemar’s test for qualitative variables A p-value of < 0 05 was considered significant
RESULTS
After fulfilling the inclusion and exclusion criteria, 78 patients were included in the study Fifty-five patients (70 51%) had NGB while 23 patients (29 49%) suffered from
non-NGB Most non-NGB patients had radiation-induced urinary tract damage (39 13%, n = 9), followed by refractory overactive bladder (OAB) (21 74%, n = 5), stress urinary incontinence (SUI) (17 39%, n = 4), BPS (17 39%, n = 4), and finally traumatic urethral rupture (4 35%, n = 1) Fifty-three patients (67 95%) underwent IUD, while CUD was performed for 25 patients (32 05%) CUD procedures included cutaneous catheterizable ileocystoplasty (19 patients), CUD using ileal catheterizable stoma via Yang-Monte technique (4 patients), and Indiana pouch (2 patients) On the other hand, IUD procedures included cystectomy with ileal conduit (22 patients), ileovesicostomy (21 patients), and cystectomy with colon conduit (10 patients) The cystectomy was done via a simple supratrigonal approach without concomitant prostatectomy in males to avoid the associated increased morbidity in those patients with benign conditions Although ileum is the most commonly used bowel segment for IUD, 10 patients needed a colon conduit in our study to avoid the use of the irradiated devitalized small bowel in those with prior pelvic irradiation and to avoid the need for bowel re-anastmosis in those with a colostomy
Most of the study population were overweight with BMI of 27 77 ± 7 06 and 29 44 ± 7 29 for IUD and CUD groups respectively, female (62 82%) and white (79 49%) with no significant differences between the IUD and CUD groups regarding the demographic and baseline characteristics (Table 1)
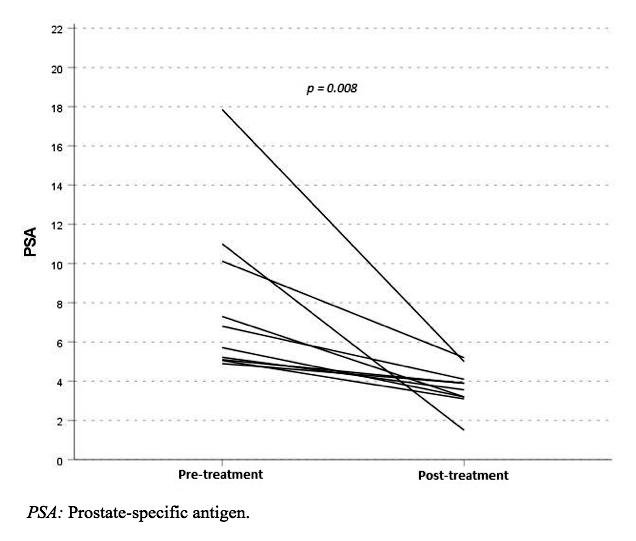
Based on the underlying condition, there was no significant difference in early and late postoperative complications and urological symptoms control between NGB and non-NGB patients with p-values of 0 490, 0 563, and 0 160, respectively Noticeably, fever was exclusively encountered in patients with NGB with p-value of 0 011, while more non-NGB patients had early wound infection (p-value = 0 007) The only significant difference in the late outcomes between the two groups was the incidence
Demographic and baseline characteristics of the two groups
385 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Continent vs incontinent urinary diversion for non-malignant lower urinary tract dysfunction
Table
Variables Incontinent Urinar y Continent Urinar y P-value Diversion Diversion (IUD) (n = 53) (CUD) (n = 25) • Age in years (mean ± SD) 51 45 ± 15 44 52 04 ± 16 52 0 996 • Follow-up duration in months (mean ± SD) 25 ± 18 26 ± 17 0 951 • Gender 1) Female n (%) 30 (56 60%) 19 (76%) 0 098 2) Male n (%) 23 (43 40%) 6 (24%) • Race 1) White n (%) 39 (73 58%) 23 (92%) 2) Black n (%) 12 (22 64%) 2 (8%) 0 296 3) Hispanic n (%) 1 (1 89%) 0 (0%) 4) Native American n (%) 1 (1 89%) 0 (0%) • BMI (mean ± SD) 27 77 ± 7 06 29 44 ± 7 29 0 370 • Smoking n (%) 11 (20 75%) 3 (12%) 0 347 • Concomitant Comorbidities 1) DM n (%) 11 (20 75%) 4 (16%) 0 619 2) HTN n (%) 25 (47 17%) 9 (36%) 0 353 • Hospital stay (days) 9 89 ± 6 32 8 04 ± 2 62 0 825 • Indications for surgery I) Neurogenic bladder (NGB) n (%) 40 (75 47%) 15 (60%) 0 162 II) Non-neurogenic bladder (non-NGB) n (%) 13 (24.53%) 10 (40%)
of stomal retraction which occurred only in patients with non-NGB (p-value = 0 027) (Table 2)
The mean times to stomal complications, anastomotic ureteric strictures, renal and ureteric urolithiasis, wound complications, and hydronephrosis or renal impairment were 23 34 ± 9 54, 14 32 ± 2 13, 13 45 ± 6 74, 12 67 ± 5 64, and 14 56 ± 5 78 months, respectively The average number of complications per patient was 0 83 for early complications, and 1 03 for late complications
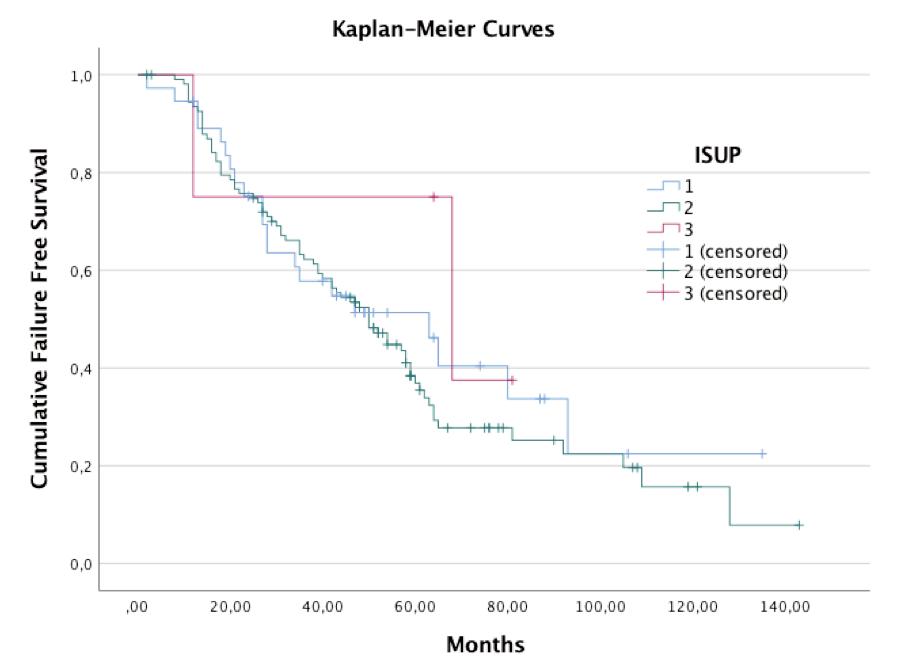
Based on the type of urinary diversion, no significant difference was observed between patients who underwent IUD and those who underwent CUD in terms of early and late postoperative complications and urological symptoms control with p-values of 0 822, 0 146, and 0 732, respectively
The incidence of stomal leakage and stenosis was significantly higher in the CUD group than in the IUD group (52% vs 0%, p-value = < 0 001 and 28% vs 3 77%, pvalue = 0 002, respectively) (Table 3)
Interestingly, none of the patients experienced grade V complications based on modified Clavien-Dindo classification system
The majority of patients with early complications had grade I and II complications (29 49% and 14 10% of patients, respectively), while most patients with late complications suffered from grade IIIa and II complications (21 79% and 15 38%, respectively) (Table 4)
DISCUSSION
A well-established treatment of bladder cancer, external urinary diversion can also be used for management of benign urinary conditions that cause significant LUTD The management of such conditions is primarily achieved by conservative and/or minimally invasive measures If these measures fail, surgical interventions are indicated (7, 8, 14, 15) These surgical interventions, however, have a significant impact on patients’ quality of life In an interesting study by Borghi et al 2021 (16), they discussed orthotopic urinary diversion as a feasible surgical intervention in refractory non-malignant LUTD and its impact on quality of life and sexual function particularly in females They reported that although orthotopic neobladder improves physical and mental health in patients with refractory non-malignant LUTD, urinary symptoms were frequently encountered affecting general health and sexual function in females as compared to males (16) The optimal surgery prevents recurrent episodes of symptomatic UTIs or urosepsis, prevents urinary stone formation, provides satisfactory continence between voids, and prevents upper urinary tract damage (9, 12, 13) In this study, we analyzed the outcomes of external urinary diversion in refractory non-malignant lower urinary tract conditions aiming to evaluate their effectiveness and complications
Although complications were higher in NGB patients in
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 M M Mostafa, A Khallaf, M Kamel, N Patil, A Mahdy 386
Table 2.
Variables Total (n = 78) Neurogenic bladder Non-neurogenic bladder P-value (n (%) (NGB) (n = 55) (non-NGB) (n = 23) (n (%) (n (%) Early outcomes within the first 4 postoperative weeks Patients with early complications 42 (53 85%) 31 (56 36%) 11 (47 83%) 0 490 Fever 13 (16 67%) 13 (23 63%) 0 (0%) 0 011 Pelvic infection/abscess 4 (5 13%) 4 (7 27%) 0 (0%) 0 184 Wound infection 11 (14 10%) 4 (7 27%) 7 (30 43%) 0 007 Pneumonia 2 (2 56%) 2 (3 64%) 0 (0%) 0 354 Urinary tract infection (UTI) 4 (5 13%) 4 (7 27%) 0 (0%) 0 184 Ileus 21 (26 92%) 18 (32 73%) 3 (13 04%) 0 074 Sepsis 1 (1 28%) 1 (1 82%) 0 (0%) 0 515 Blood Loss+ Transfusion 4 (5 13%) 4 (7 27%) 0 (0%) 0 184 Cardiac Complications (Arrythmias/NSTEMI) 3 (3 85%) 1 (1 82%) 2 (8 70%) 0 150 Reoperation (Acute Surgical Complications) 2 (2 56%) 2 (3 64%) 0 (0%) 0 354 Late Outcomes after 6-month follow-up Urological symptoms control 52 (66.67%) 34 (61.82%) 18 (78.26%) 0.160 Resolution of hydronephrosis, social dryness, and independence/patients with voiding dysfunction and/or hydronephrosis 40/57 (70 18%) 32/44 (72 73%) 8/13 (61 54%) 0 438 Reduction in urosepsis episodes/patients with recurrent urosepsis episodes 38/55 (69 09%) 25/34 (73 53%) 13/21 (61 90%) 0 365 Alleviation of bladder pain and reduction in urolithiasis/patients with recurrent urolithiasis and bladder pain 28/45 (62.22%) 20/30 (66.67%) 8/15 (53.33%) 0.384 Patients with late complications 47 (60 26%) 32 (58 18%) 15 (65 22%) 0 563 Stomal complications 1) Stomal leakage 13 (16 67%) 7 (12 73%) 6 (26 09%) 0 149 2) Stomal stenosis 9 (11 54%) 6 (10 91%) 3 (13 04%) 0 788 3) Stomal hernia 10 (12.82%) 6 (10.91%) 4 (17.39%) 0.435 4) Stomal site pain/Bleeding 1 (1 1) 1 (1 82%) 0 (0%) 0 515 5) Stomal retraction 2 (2 56%) 0 (0%) 2 (8 70%) 0 027 Anastomotic Ureteric Stricture 2 (2.56%) 2 (3.64%) 0 (0%) 0.354 Stones (Ureters, Kidneys) 15 (19 23%) 12 (21 82%) 3 (13 04%) 0 370 Wound complications 1) Wound separation/Incisional hernia 7 (8.97%) 3 (5.45%) 4 (17.39%) 0.093 2) Sinus/Fistula formation 3 (3 85%) 2 (3 64%) 1 (4 35%) 0 882 3) Recurrent wound infection/Abscess 2 (2 56%) 1 (1 82%) 1 (4 35%) 0 519 Hydronephrosis/Renal impairment 6 (7 69%) 3 (5 45%) 3 (13 04%) 0 251 Reoperation (Persistent Symptoms) 10 (12 82%) 7 (12 73%) 3 (13 04%) 0 970
Demographic and baseline characteristics of the two groups
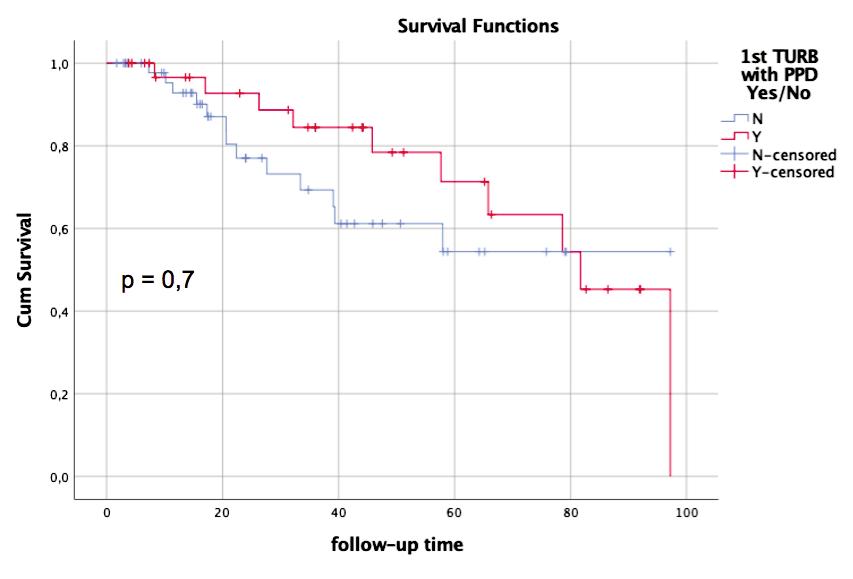
Table 3
Early and late outcomes based on the type of urinary diversion
the early postoperative period and higher in non-NGB patients on the long-term, the differences were generally non-significant and can possibly be attributed to the difference in numbers of patients between the two groups (55 patients with NGB versus 23 patients with nonNGB) In contrast to our study, Cohn et al , 2014 (7) reported fewer overall complications in patients with
NGB than with other non-neurogenic conditions During the early postoperative period, we reported paralytic ileus as the most common complication, with an overall incidence of 26 92%, and the rate was non-significantly higher in patients with NGB than those with nonNGB which can be attributed to the fact that NGB patients usually have a baseline neurogenic bowel making them vulnerable to paralytic ileus Fever, pelvic infections with or without abscesses, pneumonia, and UTI were reported only in p a t i e n t s w i t h N G B , a fi n d i n g explained by higher rates of UTIs, stone formation and lung complications in NGB population in general However, the overall long term c o m p l i c a t i o n r a t e ( 6 0 2 6 % ) w a s comparable to that reported by Erfan et al , 2015 in patients who underwent urinary diversion after radical cystectomy for bladder cancer (60%) (17) Surprisingly, although considered major procedure, urinary diversion is not usually associated with major blood loss with proper handling of the bowel and its mesentery The overall rate of postoperative blood loss that required transfusion
387 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Continent vs incontinent urinary diversion for non-malignant lower urinary tract dysfunction
Table 4
Variables Total (n = 78) Incontinent Urinar y Continent Urinar y P-value (n (%) Diversion (IUD) Diversion (CUD) (n = 53) (n = 25) Early outcomes within the first 4 postoperative weeks Procedures with early complications, n (%) 42 (53 85%) 29 (54 72%) 13 (52%) 0 822 I, n (%) 23 (29 49%) 17 (32 08%) 6 (24%) 0 465 II, n (%) 11 (14 10%) 5 (9 43%) 6 (24%) 0 084 IIIa, n (%) 2 (2 56%) 2 (3 77%) 0 (0%) 0 325 IIIb, n (%) 2 (2 56%) 2 (3 77%) 0 (0%) 0 325 IV, n (%) 4 (5 13%) 3 (5 66%) 1 (4%) 0 756 V, n (%) 0 (0%) 0 (0%) 0 (0%) --Complications after 6-month follow-up Procedures with late complications, n (%) 47 (60 26%) 29 (54 72%) 18 (72%) 0 146 I, n (%) 8 (10 26%) 5 (9 43%) 3 (12%) 0 727 II, n (%) 12 (15 38%) 6 (11 32%) 6 (24%) 0 147 IIIa, n (%) 17 (21 79%) 10 (18 87%) 7 (28%) 0 362 IIIb, n (%) 10 (12 82%) 8 (15 09%) 2 (8%) 0 382 IV, n (%) 0 (0%) 0 (0%) 0 (0%) --V, n (%) 0 (0%) 0 (0%) 0 (0%) ---
Modified Clavien-Dindo classification of complications
Variables Total (n = 78) Incontinent Urinar y Continent Urinar y P-value (n (%) Diversion (IUD) Diversion (CUD) (n = 53) (n = 25) Early outcomes within the first 4 postoperative weeks Patients with early complications 42 (53 85%) 29 (54 72%) 13 (52%) 0 822 Fever 13 (16 67%) 10 (18 87%) 3 (12%) 0 448 Pelvic infection/abscess 4 (5 13%) 4 (7 55%) 0 (0%) 0 158 Wound infection 11 (14 10%) 6 (11 32%) 5 (20%) 0 304 Pneumonia 2 (2 56%) 1 (1 89%) 1 (4%) 0 582 Urinary tract infection (UTI) 4 (5 13%) 3 (5 66%) 1 (4%) 0 756 Paralytic ileus 21 (26 92%) 16 (30 19%) 5 (20%) 0 344 Sepsis 1 (1 28%) 1 (1 89%) 0 (0%) 0 489 Blood Loss+ Transfusion 4 (5 13%) 4 (7 55%) 0 (0%) 0 158 Cardiac Complications (Arrythmias/NSTEMI) 3 (3 85%) 2 (3 77%) 1 (4%) 0 961 Reoperation (Acute Surgical Complications) 2 (2 56%) 2 (3 77%) 0 (0%) 0 325 Late Outcomes after 6-month follow-up Urological symptoms control 52 (66 67%) 36 (67 92%) 16 (64%) 0 732 Resolution of hydronephrosis, social dryness, and independence/patients with voiding dysfunction and hydronephrosis 40/57 (70.18%) 25/40 (62.5%) 15/17 (88.24%) 0.052 Reduction in urosepsis episodes/patients with recurrent urosepsis episodes 38/55 (69 09%) 24/34 (70 59%) 14/21 (66 67%) 0 760 Alleviation of bladder pain and reduction in urolithiasis/patients with recurrent urolithiasis and bladder pain 28/45 (62 22%) 16/26 (61 53%) 12/19 (63 16%) 0 912 Patients with late complications 47 (60 26%) 29 (54 72%) 18 (72%) 0 146 Stomal complications 1) Stomal leakage 13 (16 67%) 0 (0%) 13 (52%) <0 001 2) Stomal stenosis 9 (11 54%) 2 (3 77%) 7 (28%) 0 002 3) Stomal hernia 10 (12 82%) 6 (11 32%) 4 (16%) 0 564 4) Stomal site pain/ Bleeding 1 (1.28%) 0 (0%) 1 (4%) 0.143 5) Stomal retraction 2 (2 56%) 1 (1 89%) 1 (4%) 0 582 Anastomotic ureteric stricture 2 (2 56%) 2 (3 77%) 0 (0%) 0 325 Stones (Ureters, Kidneys) 15 (19.23%) 13 (24.53%) 2 (8%) 0.084 Wound complications 1) Wound separation/ Incisional hernia 7 (8 97%) 6 (11 32%) 1 (4%) 0 291 2) Sinus/Fistula formation 3 (3.85%) 3 (5.66%) 0 (0%) 0.225 3) Recurrent wound infection/Abscess 2 (2 56%) 1 (1 89%) 1 (4%) 0 582 Hydronephrosis/Renal impairment 6 (7 69%) 6 (11 32%) 0 (0%) 0 080 Reoperation (Persistent Symptoms) 10 (12.82%) 8 (15.09%) 2 (8%) 0.382
M Mostafa, A Khallaf, M Kamel, N Patil, A Mahdy
in our study was low (5 13%) and only reported in patients with NGB unlike the higher rate of perioperative blood transfusion (28%) reported by Osborn et al , 2014 (18) following cystectomy with urinary diversion for benign conditions and Schiavina et al , 2013 (19) who reported 6 5% transfusion rate after radical cystectomy with urinary diversion for bladder cancer
Although adequately studied following malignancies, the outcomes of external urinary diversions following benign urinary conditions have not been sufficiently addressed
Compared to our study, Osborn et al , 2014 (18) reported a slightly lower rate of postoperative ileus, pneumonia, blood loss requiring transfusion, and stoma complications in patients who underwent cystectomy with urinary diversion for benign conditions Cohn et al , 2014 (7) reported a higher rate of urinary symptom resolution (73%) in 26 patients who underwent cystectomy with u r i n a r y d i v e r s i o n f o r r e f r a c t o r y b e n i g n c o n d i t i o n s
However, they reported a higher rate of infections and wound complications (35% and 23% respectively) than in our study In contrast to our study results, Andersen AV et al , 2012 (20) reported a moderate rate of complications after bladder augmentation and/or cystectomy with urinary diversion for 41 patients with BPS while attributing this rate mainly to stomal and intestinal issues
Another study done by Al Hussein Al Awamlh B et al , 2015 (21) investigated the quality of life in 29 patients with refractory benign conditions who underwent cystectomy with urinary diversion, and reported a significant rate of early postoperative complications of 65 5% which they attributed to pelvic pain, infections, and gut disturbances Additionally, the cumulative physical health domain and cumulative mental health domain used to assess the quality-of-life revealed worsening in 26% and 21% of patients respectively
There was considerable resolution of urological symptoms in 66 67% of patients, and the rate of improvement was non-significantly higher in non-NGB patients than in NGB patients These findings were supported by several studies such as Cohn et al , 2014 (7) and E Brown et al , 2015 (6) who reported that cystectomy and urinary d i v e r s i o n p r o c e d u r e s w e r e s u c c e s s f u l m a n a g e m e n t options for benign lower urinary conditions Relevant to that, the re-operation rate for uncontrolled symptoms and/or acute surgical complications including wound complications and stomal complications such as stomal retraction, recurrent stomal stenosis, and stomal leakage was 12 82% and 2 56%, respectively with non-significant difference between NGB and non-NGB groups
Generally, incontinent diversions were associated with higher rates of early postoperative complications, while continent diversions were associated with more late postoperative complications, although the differences were non-significant Many studies previously investigated the outcomes of bladder reconstruction and urinary diversion surgeries (12, 22, 23) One of the most well-structured studies was conducted by Cody et al , 2012 (12) who concluded that, based on a pool of five studies, there was no significant difference in the outcomes among continent diversion, incontinent diversion, and bladder augmentation On the other hand, Clark et al , 2005 (22) demonstrated higher rate of complications in patients with con-
tinent diversion than in patients who underwent ileal conduit
Study strengths
We investigated the outcomes of external urinary diversion exclusively in patients with refractory non-malignant LUTD Additionally, we highlighted the distinctive outcomes based on both the underlying condition and the type of external urinary diversion
The included cases in our study were performed by one surgeon who is well trained in urinary reconstructive surgeries eliminating bias related to technical issues
Study limitations
Besides being a single-center single-surgeon experience, this is a retrospective study that represented a heterogeneous group of population including NGB and non-NGB Additionally, the underlying pathology usually determines the type of surgery; therefore, the urinary diversions are indicated for more complicated cases which can skew the patient population in our study
A standardized questionnaire was not used in the followup to report patient’s satisfaction regarding the urological symptoms; However, this was related to the multiple social and demographic factors that could limit those patients’ ability to return accurately filled questionnaires
CONCLUSIONS
External continent and incontinent urinary diversion can be utilized as the last resort for patient with refractory non-malignant LUTD These procedures can achieve a reasonable level of urological symptoms control, but with a s s o c i a t e d a d v e r s e o u t c o m e s T h e m o s t c o m m o n l y reported complication during the early postoperative period is paralytic ileus, while stomal complications and recurrent urolithiasis are the most frequently encountered complications on the long-term Fever is more likely to be encountered in patients with NGB, while early wound infection and late stomal retraction are more associated with non-NGB Stomal leakage and stenosis are more encountered with CUD Although the differences were non-significant, complications tend to be higher with IUD and in NGB patients during the early postoperative period and higher with CUD and in non-NGB patients on the long-term
REFERENCES
1 Pozza G, Iafrate M, Mancini M, et al Outcome and quality of life of patients with augmented bladder or urinary diversion after kidney transplantation Arch Ital Urol Androl 2020; 92:286-290
2 Ginsberg D The epidemiology and pathophysiology of neurogenic bladder Am J Manag Care 2013; 19(10 Suppl):s191-6
3 Shingleton WB, Bodner DR The development of urologic complications in relationship to bladder pressure in spinal cord injured patients J Am Paraplegia Soc 1993; 16:14-7
4 Taweel WA, Seyam R Neurogenic bladder in spinal cord injury patients Res Rep Urol 2015; 7:85-99
5 Thuroff JW, Abrams P, Andersson KE, et al EAU Guidelines on Urinary Incontinence Actas Urol Esp 2011; 35:373-88
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
388
M
6 Brown ET, Osborn D, Mock S, et al Temporal Trends in Conduit U
Indications: A Population-based Analysis Urology 2016; 98:70-4
7 Cohn JA, Large MC, Richards KA, et al Cystectomy and urinary diversion as management of treatment-refractory benign disease: the impact of preoperative urological conditions on perioperative outcomes Int J Urol 2014; 21:382-6
8 Stein R, Schroder A, Thuroff JW Bladder augmentation and urinary diversion in patients with neurogenic bladder: surgical considerations J Pediatr Urol 2012; 8:153-61
9 Shreck E, Gioia K, Lucioni A Indications for Augmentation
Cystoplasty in the Era of OnabotulinumtoxinA Curr Urol Rep 2016; 17:27
10 Cicala C Classifications of urinary diversions Urologia 2012; 79(Suppl 19):20-3
11 Davis I Urinary Diversions: Reviewing the most common types of diversion Can Fam Physician 1991; 37:1485-90
12 Cody JD, Nabi G, Dublin N, et al Urinary diversion and bladd e r r e c o n s t r u c t i o n / r e p l a c e m e n t u s i n g i n t e s t i n a l s e g m e n t s f o r intractable incontinence or following cystectomy Cochrane Database Syst Rev 2012:CD003306
13 Stein R, Hohenfellner M, Pahernik S, et al Urinary diversion-approaches and consequences Dtsch Arztebl Int 2012; 109:617-22
14 Brown ET, Osborn D, Mock S, et al Perioperative complications of conduit urinary diversion with concomitant cystectomy for benign indications: A population-based analysis Neurourol Urodyn 2017; 36:1411-6
15 Jeong SJ, Oh SJ The Current Positioning of Augmentation
Correspondence
Mostafa M Mostafa, MD (Corresponding Author) mostafaabdelaziz91@gmail com
Research Fellow of Urology, Division of Urology, Department of Surgery, University of Cincinnati College of Medicine, 231 Albert Sabin Way,Cincinnati, OH 45267
Assistant Lecturer of Urology, Asiut University Hospitals, Asiut, Egypt,
Ashraf Khallaf, MD
ashraf m khallaf2@gmail com
Visiting Scholar of Urology, Department of Surgery, University of Cincinnati College of Medicine, 231 Albert Sabin Way, Cincinnati, OH 45267
Mohamed Kamel, MD
kamelme@ucmail uc edu
Professor of Urology, Department of Surgery, University of Cincinnati College of Medicine, 231 Albert Sabin Way,Cincinnati, OH 45267
Nilesh Patil, MD
patilnh@ucmail uc edu
Associate Professor of Urology, Department of Surgery, University of Cincinnati College of Medicine, 231 Albert Sabin Way, Cincinnati, OH 45267
Ayman Mahdy, MD, PhD, MBA
mahdyan@uc edu
Chief of Urology, Professor of Urology, R Bruce and Barbara Bracken Endowed Chair in Surgical Urology, Director of Voiding Dysfunction and Female Urology, Medical Director of Urology, the West Chester Hospital, Department of Surgery, University of Cincinnati College of Medicine, 231 Albert Sabin Way, ML 0589, Cincinnati, OH 45267
Enterocystoplasty in the Treatment for Neurogenic Bladder Int Neurourol J 2020; 24:200-10
16 Borghi C, Manservigi M, Milandri ES, et al The impact of orthotopic reconstruction on female sexuality and quality of life after radical cystectomy for non-malignant bladder conditions Arch Ital Urol Androl 2021; 93:255-61
17 Amini E, Djaladat H Long-term complications of urinary diversion Curr Opin Urol 2015; 25:570-7
18 Osborn DJ, Dmochowski RR, Kaufman MR, et al Cystectomy with urinary diversion for benign disease: indications and outcomes Urology 2014; 83:1433-7
19 Schiavina R, Borghesi M, Guidi M, et al Perioperative complications and mortality after radical cystectomy when using a standardized reporting methodology Clin Genitourin Cancer 2013; 11:18997
20 Andersen AV, Granlund P, Schultz A, et al Long-term experience with surgical treatment of selected patients with bladder pain syndrome/interstitial cystitis Scand J Urol Nephrol 2012; 46:284-9
21 Al Hussein Al Awamlh B, Lee DJ, et al Assessment of the quality-of-life and functional outcomes in patients undergoing cystectomy and urinary diversion for the management of radiation-induced refractory benign disease Urology 2015; 85:394-400
22 Clark PE, Stein JP, Groshen SG, et al Radical cystectomy in the elderly: comparison of clincal outcomes between younger and older patients Cancer 2005; 104:36-43
23 Boyd SD, Feinberg SM, Skinner DG, et al Quality of life survey of urinary diversion patients: comparison of ileal conduits versus continent Kock ileal reservoirs J Urol 1987; 138:1386-9
389 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Continent vs incontinent urinary diversion for non-malignant lower urinary tract dysfunction
r i n a r y D i v e r s i o n W i t h C o n c o m i t a n t C y s t e c t o m y f o r B e n i g n
Clinical impact of ERG and PTEN status in prostate cancer patients underwent radical prostatectomy
Charalampos
, Lazaros Tzelves 2 , Panagiotis Velissarios Stamatakos 1 , Georgios Papadopoulos 1 , Georgios Stathouros 1 , Athanasios Dellis 3 , Konstantinos Ntoumas 1 , Akrivi Kostopoulou 4 , Charalampos Deliveliotis 2 , Athanasios Papatsoris 2
1 Department of Urology, General Hospital of Athens “G Gennimatas”, Athens, Greece;
2 2nd Department of Urology, School of Medicine, Sismanoglio Hospital, National and Kapodistrian University of Athens, Athens, Greece;
3 1st Department of Urology, School of Medicine, Laiko Hospital, National and Kapodistrian University of Athens, Athens, Greece;
4 Department of Pathology, General Hospital of Athens “G Gennimatas”, Athens, Greece
Summary
Objectives: Phosphate and tensin homolog gene (PTEN) acts as a regulator of PI3-KAkt molecular pathway ETS Related gene (ERG), an oncogene located in chromosome 21q22.2, is involved in prostate cancer (PCa) by serine 2 (TMPRSS2), a protein encoded by TMPRSS2 gene. The aim of this study is to evaluate the clinical impact of PTEN loss and ERG rearrangement in terms of oncologic results in patients diagnosed with localized PCa who underwent radical prostatectomy
Materials and methods: Prospective data were collected from a total of 74 patients who underwent open radical retropubic prostatectomy for localized PCa and immunohistochemical study was performed in tissue samples The primary antibodies for anti-ERG antibody as well as anti-PTEN antibody were obtained from DAKO ERG was considered positive if at least 20% of the evaluated cells were stained at least with medium intensity PTEN protein loss was considered when the intensity of cytoplasmic and nuclear staining was mild or entirely negative across > 10% of tumor cells
Results: Homogenous loss of PTEN was associated with higher clinical International Society of Urological Pathology (ISUP) grade (p = 0 018) while no statistical significant association was present regarding the presence of ERG rearrangement with either ISUPc or ISUPp After a median follow up of 34 months, 24 patients developed biochemical recurrence. No statistical significant correlation of ERG status with biochemical recurrence was noted while PTEN was associated with biochemical recurrence development in a statistical significant way Lastly the combination of PTEN loss with ERG rearrangement presence was detected more often in higher ISUPc and ISUPp as well as biochemical recurrence development, although in a non statistical significant way
Conclusions: Homogenous and heterogenous PTEN loss was associated with biochemical recurrence No association of ERG and biochemical recurrence was noted. The combination of PTEN loss and ERG rearrangement presented a trend for higher ISUPc and ISUPp as well as biochemical recurrence but not in a statistical significant way
KEY WORDS: ERG; PTEN; Prostate cancer; Radical prostatectomy
Submitted 18 July 2022; Accepted 24 July 2022
INTRODUCTION
Prostate cancer (PCa) represents a major health problem as it is the second most commonly diagnosed malignancy among males leading to severe morbidity and mortality (1) PCa presents a wide variety of clinical behavior ranging from tumors of low metastatic potential to highly aggressive tumors characterized by a high risk of biochemical failure and metastasis development after initial treatment (2)
As several molecular pathways and oncogenes are involved in PCa progression to lethal disease, understanding the genetic and molecular differences separating indolent from highly aggressive tumors is the cornerstone of risk stratification and selection of best treatment available
The PI3-K-Akt molecular pathway, found to be upregulated in 30-50% of PCa patients, regulates a variety of cellular function including cell survival and proliferation, cell growth and differentiation and cell cycle progression and metabolism (3) The phosphate and tensin homolog gene (PTEN), a tumor suppressor gene located on chromosome 10q23 3, is quite frequently mutated in PCa patients and acts as a regulator of PI3-K-Akt molecular pathway (4) ERG oncogene (ETS Related gene) is a member of the ETS gene family located in chromosome 21q22 2 (5) In 50% of PCa patients ERG is involved as a fusion protein with transmembrane protease, serine 2 (TMPRSS2), a protein encoded by TMPRSS2 gene located in 21q22 3 (6) Although ETS fusion is encountered early in the carcinogenesis process, the presence of the fusion protein is also associated with poorly differentiated tumors, higher stage disease as well as lymph node involvement (7) As far as it concerns the clinical impact of PTEN loss combined with the presence of ETS fusion protein, both preclinical and clinical studies suggest that the co-existence of these aberrations may be indicative of poor prognosis (8)
The aim of this study is to evaluate the clinical impact of PTEN loss and ERG rearrangement in terms of oncologic results in patients diagnosed with localized PCa who underwent radical prostatectomy
MATERIALS AND METHODS
Data were collected in a prospective way from a total of 74 patients who underwent open radical retropubic
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 390 ORIGINAL PAPER No conflict of interest declared
Fragkoulis 1 , Ioannis Glykas 1
DOI: 10 4081/aiua 2022 4 390
prostatectomy for localized PCa during the years 2017 and 2018 Demographic information, PSA levels at diagnosis and clinical TNM stage were recorded All patients underwent bone scan and CT scan prior to surgery for staging purpose Patients with PSA levels above 20 ng/dl were excluded from the study Histopathological examination of radical prostatectomy specimens defined the pathological stage, histopathological type as well as the Gleason score Patients were followed up by PSA testing every three months until biochemical recurrence defined as PSA levels above 0 2 ng/dl
Immunohistochemical study was performed in paraffinembedded formalin-fixed tissue samples Sections of 4mm were mounted on TOMO slides and fixated in oven at 70-80°C, de-waxed in xylene and then underwent through decreasing concentrations of alcohol For antiERG antibody, the primary antibody was obtained from DAKO (FLEX Monoclonal Rabbit Rabbit Anti-Human ERG, Clone EP111, Ready-to-Use) After heat-induced epitope retrieval and a PH9 buffer, the sections were incubated for 1h with the antibody and counterstained in hematoxylin For anti-PTEN antibody, the primar y antibody was obtained from DAKO [Monoclonal Mouse Anti-Human PTEN (Concenctrate) Clone 6H2 1] After heat-induced epitope retrieval and PH9 buffer, the sections were incubated for 1h in 1:100 of the primary antibody, followed by 15min in Linker Counterstain was performed with hematoxylin ERG was considered positive if at least 20% of the evaluated cells (neoplastic or with HGPIN) were stained at least with medium intensity (Figure 1) Endothelial cells were used as positive control A tissue sample was considered to have PTEN protein loss if the intensity of cytoplasmic and nuclear staining was mild or entirely negative across > 10% of tumor cells, compared with surrounding benign glands and/or stroma, used as positive controls for PTEN protein expression If the neoplastic cells showed PTEN loss in 10-90% of neoplastic cells, it was considered heterogeneous PTEN protein loss If neoplastic cells showed PTEN protein loss in > 90%, it was considered homogeneous PTEN loss
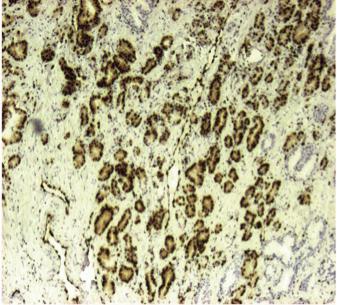
Regarding statistical methodology, continuous variables were expressed using medians, minimum-maximum values and interquartile range, while categorical variables using numbers and proportions Fisher’s exact test or Chi square test and Kruskal-Wallis test were used to analyze data, since after testing for distributions non-normality was detected When a statistical significance was noted, pairwise comparisons were used to detect which exact groups differ Pairwise comparisons were performed whenever a statistical significance was detected, using the Dunn’s procedure Statistical significance was set at p = 0 05 All analyses were done with IBM SPSS Statistics 25 0 software (SPSS Inc , Chicago, IL )
RESULTS
Median age was 70 years and median PSA was 7 3 ng/dl Demographics as well as clinical and pathological ISUP grade and TNM stage are presented in Table 1
PTEN status was defined as homologous loss in 15 patients, heterologous loss in 43 patients and as intact in 16 patients ERG rearrangement was present in 29 patients and absent in 45
In terms of correlation of PTEN status with ISUP grade, homogenous loss was associated with higher clinical ISUP grade (p = 0 018) while the medians of intact-homogeneous groups differed significantly for median ISUP pathology grade (p = 0 022) (Table 2)
On the other hand, no statistical significant association
**
391 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 ERG and PTEN status in prostate cancer
Patients’ demographics Number of patients 74 Age (median) 70 PSA 7 3 ng/dl Clinical ISUP (number of patients) 1 23 2 17 3 20 47 57 Pathology ISUP (number of patients) 1 10 2 25 3 24 47 58 Pathology TNM pT2 50 pT3a 14 pT3b 10
Table 1.
Table 2
Median ISUPc Median ISUPp Homogeneous loss 33 Heterogeneous loss 23 Intact 12 p-value 0 018 * 0 022 **
PTEN status correlation with ISUPc and ISUPp
* Using Kruskall-Wal is H test, the medians of intact-homogeneous groups d ffered s gnificantly or med an ISUPc grade
Using Kruskal -Wa lis H test, the medians of intact-homogeneous groups differed significant y for median ISUPp grade
Figure 1
Positive ERG staining using anti-human ERG antibody
was present regarding the presence of ERG rearrangement with either ISUPc or ISUPp (Table3)
After a median follow up of 34 months, 24 patients developed biochemical recurrence defined as PSA levels above 0 2 ng/dl No statistical significant correlation of ERG status with biochemical recurrence was noted (Table 4) On the other hand, both homogenous and heterogenous loss was associated with biochemical recurrence development in a statistically significant way (Table 5) As far as it concer ns the combination of PTEN loss with ERG rearrangement presence, a trend in higher ISUPc and ISUPp as well as biochemical recurrence development was detected, although in a non-statistical significant way Among patients who presented with combined PTEN homogenous loss and ERG rearrangement, 56% presented with biochemical recurrence during follow up The combination of PTEN homogenous loss combined with no ERG rearrangement also presented high rates of biochemical failure (66%) Nevertheless, this group consisted only of 6 patients, thus no strong evidence could be extracted regarding this combination
DISCUSSION
It is nowadays well established that PCa is a disease presented with a wide clinical heterogeneity Spectrum includes from indolent tumors of low clinical significance to highly aggressive tumors of high probability of biochemical recurrence after local treatment as well as severe metastatic potential Currently, risk stratification for biochemical recurrence development after radical prostatectomy for patients with localized disease stratifies patients into three groups based on PSA, Gleason score and TNM status (9) To further stratify patients according to molecular and genetic profile, it is of great interest to develop
novel markers based in the genomic instability characterized by activation of oncogenes or deactivation of tumor suppressor genes
PTEN is a tumor suppressor gene located in chromosome 12q23 3 acting as a regulator of the PI3-K-Akt molecular pathway (4) The PI3-K-Akt pathway, frequently upregulated in PCa patients, is an important intracellular molecular pathway regulating crucial cellular functions including cell proliferation, growth, differentiation, cell cycle progression, metabolism and survival (3) Several growth factors including epidermal growth factor (EGF), platelet derived growth factor (PDGF) and insulin like growth factor (IGF) initiate the activation of the PI3-K-Akt pathway by activating tyrosine kinase receptors promoting the phosp h o r y l a t i o n o f P I 3 K a t t h e c e l l m e m b r a n e l e v e l Phosphorylated PI3K becomes active and promotes the conversion of PIP2 to PIP3 This event leads to the phosphorylation of Akt mediated by PDK1 (10) Akt plays an important role in carcinogenesis and tumor progression mainly by interfering with antiapoptotic pathways (11) Moreover, it may influence the activity of tumor suppressor gene p53 (12) Akt also interacts with the androgen receptor promoting nuclear translocation in an androgen independent manner (13) Activated Akt has also a profound role in carcinogenesis by promoting cell growth and protein synthesis through the regulation of the mammalian target of rapamycin (mTOR) pathway (14) PTEN suppressor gene protein product is a dual lipid phosphatase which acts as a negative regulator of the PI3-KAkt pathway PTEN protein removes the 3-phosphatase from PIP3 converting it back to PIP2 thus inhibiting the phosphorylation of Akt (4, 10) In addition, genomic stability is also influenced by PTEN protein through involvement with the MAPK signaling network which affects both directly and indirectly the androgen receptor activity (14)
Since PTEN is the most commonly tumor suppressor gene mutated in PCA, PTEN loss may act as a prognostic marker associated with poor oncological outcomes and may facilitate the selection of patients who are more likely to benefit from intensive definite treatment modalities (15) PTEN mutations are more frequently encountered in metastasis providing further evidence that PTEN loss is associated with the disease progression (16) More specifically, PTEN deletion is associated with higher disease stage among patients with Gleason score 7 (17) A metaanalysis involving 26 published studies with a total of 8097 patients presented that intact PTEN status results in less aggressive disease and lower Gleason score (18) Results from a multicenter analysis support that PTEN deletion is strongly associated with seminal vesicle involvement as well as extracapsular extension (19) Furthermore, homologous, and heterologous PTEN loss is associated with greater risk of biochemical recurrence compared with no PTEN loss (20, 21) In a meta-analysis including 2,154 cases with positive expression of PTEN and 1 006 PTEN deletion cases, PTEN positive expression was associated with prolonged biochemical free survival (22) Nevertheless, patients with homologous PTEN loss present worst prognosis in terms of biochemical free survival (23) Lotan et al , presented data supporting that only homologous PTEN loss is associated with worst bio-
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 C Fragkoulis, I Glykas, L Tzelves, et al 392
Table 3. ERG status and correlation with ISUPc and ISUPp Median ISUPc Median ISUPp ERG (+) 23 ERG (-) 23 p-value 0 836 0 993 Table 4. Biochemical recurrence and ERG status (chi-square test) No biochemical recur rence Biochemical recur rence p-value (%) (%) Negative ERG 29 (64 4) 16 (35 6) 0 475 Positive ERG 21 (72 4) 8 (27 6) Table 5. Biochemical recurrence and PTEN status (chi-square test) No biochemical recur rence Biochemical recur rence p-value (%) (%) Heterogeneous loss 31 (72 1) 12(27 9) 0 031 Homogeneous loss 6 (40) 9 (60) Intact 13 (81 3) 3 (18 7)
chemical free survival, while heterogenous loss has the same impact as PTEN intact status (24) As far as it concer ns lymph node involvement, it is more frequently encountered in patients with PTEN deletion (25)
ETS Related gene (ERG) is an oncogene member of the ETS gene family located in chromosome 21q22 5 It encodes ERG protein which is involved in PCa carcinogenesis and progression as a fusion protein with transmembrane protease, serine 2 (TMPRSS2), a protein encoded by TMPRSS2 gene located in 21q22 3 (5, 6) TMPRSS2:ERG fusion is the most common ETS family rearrangement and is detected in 50% of PCa patients (26) Such rearrangement leads to neoplastic phenotype by overexpressing transcription factors which are important from the first step of carcinogenesis (27) ERG rearrangement is encountered rarely in indolent PCa tumors and it is usually associated with more advanced stage with either extracapsular extension or seminal vesicles involvement (28, 29) Furthermore, it presents an independent prognostic value regarding both biochemical and clinical recurrence, especially among grade group 4 or 5 patients (30) Among patients with localized PCa treated with radical prostatectomy, TMPRSS2-ERG fusion was associated with higher tumor stage but not with other oncological parameters (31) On the other hand, Lee et al demonstrated that positive ERG status is frequently present among patients with perineural invasion or positive apical margins (32) Quite interesting is the fact that ERG status among PCa patients is characterized by racial disparities Highest frequencies of ERG rearrangements are encountered among Caucasian descents, lower frequencies among African Americans and even lower prevalence among Asian men In Asian cohorts, ERG positive status was more frequent in low Gleason score and low stage patients in contrast with wester n cohorts (33) As TMPRSS2-ERG fusion is not a frequent genomic alteration among Asian PCa patients it has limited significance in clinical practices in Asian populations (34) In a metaanalysis including 6744 patients, Liu et al. conclude that ERG status is not correlated with biochemical free survival or recurrence free survival (35) In non-surgical cohorts, ERG expression is associated with advanced stage, higher probability of metastasis as well as increased mortality (36)
As far as it concer ns immunohistochemistry as a method of PTEN and ERG status evaluation, the technique presents 100% sensitivity and 97 8% specificity for detecting PTEN genomic alterations (37) Although most studies use FISH in order to detect PTEN alterations, immunohistochemistry using commercially available antibodies is a validated method with similar results as high concordance is present between the two methods (38, 39) Characterization of ERG status by immunohistochemistry in prostate tissue has also an excellent correlation with FISH and is validated method to be used in clinical practice (40)
ERG fusion protein is often accompanied by PTEN loss, a condition which further up regulates the Akt pathway leading to more aggressive cancer progression (41) Early in the carcinogenesis process, PTEN loss and subsequent low PTEN protein results in genomic instability Such instability may provoke ERG fusion and thus a synergis-
tic action in Akt pathway leading to poor prognosis (10, 41) Regarding the relationship between PTEN and ERG status in terms of oncological results, Brady et al presented that combined loss of PTEN with negative ERG expression leads to a trend over immediate recurrence after surgery but not in a statistically significant way (42) On the other hand, Mehra et al concluded that patients who exhibited ERG rearrangement and loss of PTEN had no significant difference in time to recurrence compared to patients with wild-type ERG and loss of PTEN (21) A proposed method for risk stratification in a non-surgical cohort including patients treated with androgen deprivation therapy suggests that worst clinical outcome is among patients with decreased PTEN intensity without ERG positivity Patients with positive ERG expression presented intermediate risk for lethal disease regardless PTEN status (43) In an analysis of 80 PCa patients no p a t i e n t w i t h l o w g r a d e d i s e a s e b a re d c o n c u r re n t TMPRSS2-ERG fusion and PTEN loss (44) In a large radical prostatectomy cohort including 815 patients, loss of PTEN in ERG negative patients was predictive of secondary therapies as well as shorter disease specific survival (45) It is quite clear that although great interest exists in determining the role of combined PTEN status with ERG fusion no solid conclusions can be made as data remain conflicting (46, 47)
To our knowledge this is the first study evaluating the role of individual PTEN and ERG status and their possible combination regarding oncological results in men who underwent radical prostatectomy Disadvantages of the present study include the relatively low sample which underpowered statistical analysis and the fact that PTEN and ERG status was examined only by immunohistochemistry and not by FISH
CONCLUSIONS
Homogenous and heterogenous PTEN loss was associated with biochemical recurrence in PCa patients treated with radical prostatectomy No association of ERG status and biochemical recurrence was noted The combination of PTEN loss and ERG rearrangement presented a trend for higher ISUPc and ISUPp as well as biochemical recurrence but not in a statistically significant way
REFERENCES
1 Culp MB, Soerjomataram I, Efstathiou JA, et al Recent Global Patterns in Prostate Cancer Incidence and Mortality Rates Eur Urol 2020; 77:38-52
2 Hoag J, Barbieri C Clinical variability and molecular heterogeneity in prostate cancer Asian J Androl 2016; 18:543-548
3 De Velasco MA, Uemura H Preclinical Remodeling of Human Prostate Cancer through the PTEN/AKT Pathway Adv Urol 2012; 2012:419348
4 Hopkins BD, Parsons RE Molecular pathways: intercellular PTEN and the potential of PTEN restoration therapy Clin Cancer Res 2014; 20:5379-83
5 Park K, Tomlins SA, Mudaliar KM, et al Antibody-based detection of ERG rearrangement-positive prostate cancer Neoplasia 2010; 12:590-8
393 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 ERG and PTEN status in prostate cancer
6 van Leenders GJ, Boormans JL, Vissers CJ, et al Antibody EPR3864 is specific for ERG genomic fusions in prostate cancer: implications for pathological practice Mod Pathol 2011; 24:1128-38
7 Demichelis F, Rubin M TMPRSS2: ERG gene fusion associated with lethal prostate cancer in a watchful waiting cohort Oncogene 2007; 26:4596-4599
8 Yo s h i m o t o M , J o s h u a A M , C u n h a I W, e t a l A b s e n c e o f TMPRSS2:ERG fusions and PTEN losses in prostate cancer is associated with a favorable outcome Mod Pathol 2008; 21:1451-60
9 Cooperberg MR, Pasta DJ, Elkin EP, et al The University of California, San Francisco Cancer of the Prostate Risk Assessment score: a straightforward and reliable preoperative predictor of disease recurrence after radical prostatectomy J Urol 2005; 173:1938-42
10 Phin S, Moore MW, Cotter PD Genomic Rearrangements of PTEN in Prostate Cancer Front Oncol 2013; 3:240
11 Brunet A, Bonni A, Zigmond MJ, et al Akt promotes cell survival by phosphorylating and inhibiting a Forkhead transcription factor Cell 1999; 96:857-68
12 Mayo LD, Donner DB A phosphatidylinositol 3-kinase/Akt pathway promotes translocation of Mdm2 from the cytoplasm to the nucleus Proc Natl Acad Sci U S A 2001; 98:11598-603
13 Navarro D, Luzardo OP, Fernández L, et al Transition to androgen-independence in prostate cancer J Steroid Biochem Mol Biol 2002; 81:191-201
14 Papatsoris AG, Karamouzis MV, Papavassiliou AG The power and promise of "rewiring" the mitogen-activated protein kinase network in prostate cancer therapeutics Mol Cancer Ther 2007; 6:811-9
15 Jamaspishvili T, Berman DM, Ross AE, et al Clinical implications of PTEN loss in prostate cancer Nature Reviews Urology 2018; 15:222-234
16 Dong JT, Li CL, Sipe TW, Frierson HF Jr Mutations of PTEN/MMAC1 in primary prostate cancers from Chinese patients Clin Cancer Res 2001; 7:304-8
17 Patel DM, Varma PK, Kazi MM, et al Assessment of PTEN Gene Loss as a Possible Prognostic Marker for Prostate Cancer J Assoc Genet Technol 2022; 48:63-67
18 Gao T, Mei Y, Sun H, et al The association of Phosphatase and tensin homolog (PTEN) deletion and prostate cancer risk: A metaanalysis Biomed Pharmacother 2016; 83:114-121
19 Troyer DA, Jamaspishvili T, Wei W, et al A multicenter study shows PTEN deletion is strongly associated with seminal vesicle involvement and extracapsular extension in localized prostate cancer Prostate 2015; 75:1206-15
20 Jamaspishvili T, Patel PG, Niu Y, et al Risk Stratification of Prostate Cancer Through Quantitative Assessment of PTEN Loss (qPTEN) J Natl Cancer Inst 2020; 112:1098-1104
21 Mehra R, Salami SS, Lonigro R, et al Association of ERG/PTEN status with biochemical recurrence after radical prostatectomy for clinically localized prostate cancer Med Oncol 2018; 35:152
22 Xie H, Xie B, Liu C, Wang J, Xu Y Association of PTEN expression with biochemical recurrence in prostate cancer: results based on previous reports Onco Targets Ther 2017; 10:5089-5097
23 Geybels MS, Fang M, Wright JL, et al PTEN loss is associated with prostate cancer recurrence and alterations in tumor DNA methylation profiles Oncotarget 2017; 8:84338-84348
24 Lotan TL, Wei W, Morais CL, et al PTEN Loss as Determined by Clinical-grade Immunohistochemistry Assay Is Associated with
Worse Recurrence-free Survival in Prostate Cancer Eur Urol Focus 2016; 2:180-188
25 Switlyk MD, Salberg UB, Geier OM, et al PTEN Expression in Prostate Cancer: Relationship With Clinicopathologic Features and Multiparametric MRI Findings AJR Am J Roentgenol 2019; 19:1-9
26 Pettersson A, Graff RE, Bauer SR, et al The TMPRSS2:ERG rearrangement, ERG expression, and prostate cancer outcomes: a cohort study and meta-analysis Cancer Epidemiol Biomarkers Prev 2012; 21:1497-509
27 Park K, Tomlins SA, Mudaliar KM, et al Antibody-based detection of ERG rearrangement-positive prostate cancer Neoplasia 2010; 12:590-8
28 Krstanoski Z, Vokac NK, Zagorac A, et al TMPRSS2:ERG gene aberrations may provide insight into pT stage in prostate cancer BMC Urol 2016; 16:35
29 Fisher KW, Zhang S, Wang M, et al TMPRSS2-ERG gene fusion is rare compared to PTEN deletions in stage T1a prostate cancer Mol Carcinog 2017; 56:814-820
30 Kidd SG, Bogaard M, Carm KT, et al In situ expression of ERG protein in the context of tumor heterogeneity identifies prostate cancer patients with inferior prognosis Mol Oncol 2022; 16:2810-2822
31 Yılmaz Ö, Berber U, Okçelik S, et al TMPRSS2-ERG gene fusion in Turkish patients with localized prostate cancer: results of radical prostatectomy specimens Turk J Urol 2016; 42:60-3
32 Lee SR, Choi YD, Cho NH Association between pathologic factors and ERG expression in prostate cancer: finding pivotal networking J Cancer Res Clin Oncol 2018; 144:1665-1683
33 Baohong J, Sedarsky J, Srivastava S, et al ERG Tumor Type is Less Frequent in High Grade and High Stage Prostate Cancers of Chinese Men J Cancer 2019; 10:1991-1996
34 Kong DP, Chen R, Zhang CL, et al Prevalence and clinical application of TMPRSS2-ERG fusion in Asian prostate cancer patients: a large-sample study in Chinese people and a systematic review Asian J Androl 2020; 22:200-207
35 Liu R, Zhou J, Xia S, Li T The impact of PTEN deletion and ERG rearrangement on recurrence after treatment for prostate cancer: a systematic review and meta-analysis Clin Transl Oncol 2020; 22:694702
36 Khosh Kish E, Choudhry M, Gamallat Y, et al The Expression of Proto-Oncogene ETS-Related Gene (ERG) Plays a Central Role in t h e O n c o g e n i c M e c h a n i s m I n v o l v e d i n t h e D e v e l o p m e n t a n d Progression of Prostate Cancer Int J Mol Sci 2022; 23:4772
37 Lotan TL, Gurel B, Sutcliffe S, et al PTEN protein loss by immunostaining: analytic validation and prognostic indicator for a high risk surgical cohort of prostate cancer patients Clin Cancer Res 2011; 17:6563-73
38 Lotan TL, Heumann A, Rico SD, et al PTEN loss detection in prostate cancer: comparison of PTEN immunohistochemistry and P T E N F I S H i n a l a rg e re t ro s p e c t i v e p ro s t a t e c t o m y c o h o r t Oncotarget 2017; 8:65566-65576
39 Lotan TL, Wei W, Ludkovski O, et al Analytic validation of a clinical-grade PTEN immunohistochemistry assay in prostate cancer by comparison with PTEN FISH Mod Pathol 2016; 29:904-14
40 Navaei AH, Walter BA, Moreno V, et al Correlation between E R G F u s i o n
y Immunohistochemistry in Prostate, Possible Role in Diagnosis and Therapy J Cancer 2017; 8:2604-2613
41 Squire JA TMPRSS2-ERG and PTEN loss in prostate cancer Nat Genet 2009; 41:509-10
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
394
C Fragkoulis, I Glykas, L Tzelves, et al
e
a n d A n d ro g e n R e c e p t o r E x p re s s
P ro t
i n
i o n b
42 Brady L, Carlsson J, Baird AM, et al Correlation of integrated ERG/PTEN assessment with biochemical recurrence in prostate cancer Cancer Treat Res Commun 2021; 29:100451
43 Bismar TA, Hegazy S, Feng Z, et al Clinical utility of assessing PTEN and ERG protein expression in prostate cancer patients: a proposed method for risk stratification J Cancer Res Clin Oncol 2018; 144:2117-2125
44 Hernández S, Font-Tello A, Juanpere N, et al Concurrent TMPRSS2-ERG and SLC45A3-ERG rearrangements plus PTEN loss are not found in low grade prostate cancer and define an aggressive tumor subset Prostate 2016; 76:854-65
45 Lahdensuo K, Erickson A, Saarinen I, et al Loss of PTEN expression in ERG-negative prostate cancer predicts secondary therapies and leads to shorter disease-specific survival time after radical prostatectomy Mod Pathol 2016; 29:1565-1574
46 Ullman D, Dorn D, Rais-Bahrami S, Gordetsky J Clinical Utility and Biologic Implications of Phosphatase and Tensin Homolog (PTEN) and ETS-related Gene (ERG) in Prostate Cancer Urology 2018; 113:59-70
47 Fragkoulis C, Glykas I, Dellis A, et al Clinical impact of combined PTEN and ERG rearrangements in localized prostate cancer Arch Ital Urol Androl 2021; 93:84-85
Correspondence
Charalampos Fragkoulis, MD harisfrag@yahoo gr
Ioannis Glykas, MD giannis glykas@gmail com
Panagiotis Velissarios Stamatakos, MD (Corresponding Author) pvstamatakos@gmail com
Georgios Papadopoulos, MD gipapadopoulos@yahoo gr
Georgios Stathouros, MD gstathouros@yahoo gr
Konstantinos Ntoumas, MD ntoumask@yahoo com
Department of Urology, General Hospital of Athens “G Gennimatas”, Athens (Greece)
Lazaros Tzelves, MD lazarostzelves@gmail com
Charalampos Deliveliotis, MD chdeliveli@gmail com
Athanasios Papatsoris, MD agpapatsoris@yahoo gr
2nd Department of Urology, School of Medicine, Sismanoglio Hospital, National and Kapodistrian University of Athens, Athens (Greece)
Athanasios Dellis, MD aedellis@gmail com
1st Department of Urology, School of Medicine, Laiko Hospital, National and Kapodistrian University of Athens, Athens (Greece)
Akrivi Kostopoulou, MD akrivikostopoulou@hotmail com
Department of Pathology, General Hospital of Athens “G Gennimatas”, Athens (Greece)
395 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 ERG and PTEN status in prostate cancer
The effects of method of anaesthesia on the safety and effectiveness of Radical Retropubic Prostatectomy
1 2nd Urology Department, Sismanoglio Hospital, National and Kapodistrian University of Athens, Greece;
2 Gastroenterology Department, Sismanoglio Hospital, Athens Greece;
3 Anaesthesiology Department, Evgenidio Hospital, National and Kapodistrian University of Athens, Greece;
4 4th Department of Medical Oncology, Hygeia Hospital, Athens, Greece
Summary
Objective: The aim of this study is to determine if patients undergoing radical retropubic prostatectomy with localized prostate cancer under combined (epidural-spinal) anaesthesia have any benefit over patients undergoing the procedure under general anaesthesia. Material and Methods: Patients with clinically localised prostate cancer, scheduled for radical retropubic prostatectomy, were allocated to undergo the operation under either general anaesthesia (GA) or under combined (epidural-spinal) (CESA) anaesthesia Several parameters were recorded both preoperatively (medical history, biometric data, PSA, biopsy Gleason score) and postoperatively (blood pressure, heart rate, haemoglobin levels, operation time and total hospital stay). In addition, mean arterial pressure, change in heart rate, total blood loss, blood transfusions, SAS score, intravenous fluid administration and operation time were also noted down intraoperatively Patient pain levels and total satisfaction were evaluated using appropriate questionnaires At the 12-month follow-up, biochemical recurrence using PSA levels and urinary continence status were evaluated.
Results: A total of 60 patients were included (30 in each group). Intraoperatively, mean MAP and heart rate change was higher in the GA group (MAP+7,46, HR+27) and mean SAS was higher in the CESA group (+0 93) The time needed for patients’ recovery was faster (-3 5 min) and hospitalization was shorter for patients in the CESA group (-0 6 days) Intraoperative blood loss, time for induction and duration of operation were not significantly different. Mean postoperative drop of haemoglobin was greater in the GA group (+0 56) while blood transfusions, VAS pain scores and amount of intravenous fluids did not differ significantly between the two groups No complications were reported Patient satisfaction and urinary continence were comparable between the groups and there were no cases of biochemical recurrence.
Conclusions: Radical retropubic prostatectomy can safely be performed under combined (spinal epidural anaesthesia, with possible benefits of lower blood loss, less post-operative complications and earlier discharge Both procedures have equal oncological and functional outcomes at the 12-month follow-up
KEY WORDS: Prostatic neoplasm; Radical prostatectomy; Complications; Combined anaesthesia
Submitted 12 October 2022; Accepted 31 October 2022
INTRODUCTION
Prostate cancer (PCa) is the most common neoplasm in men and accounts for 27% of all cancers diagnosed (1) In developed countries, population awareness and wide Prostatic Specific Antigen (PSA) screening has resulted in an early on-set detection, with most cases being discovered as localized disease and therefore being eligible for definitive therapy, including radical prostatectomy or radiotherapy (2) Surgical excision of the prostate may be carried out either with a retropubic open approach or with the laparoscopic or robot-assisted technique (2)
The goal of radical prostatectomy, is eradication of the disease with preservation of continence and erectile functions (3) Due to high-costs of acquiring and maintaining robotic equipment, the retropubic open approach is still being practiced alongside newer methods worldwide, providing excellent results in patient survival rates and quality of life (4)
In this study we aimed to evaluate two methods of anaesthesia (general and combined epidural-spinal) in patients undergoing open retropubic radical prostatectomy and define whether these may have an impact on the oncological outcome and safety of the procedure
MATERIALS AND METHODS
The study was conducted at the 2nd Urology University Department of Sismanoglio Hospital in Athens Greece, from August 2020 to July 2022, after being approved by the Institutional Review Board of the Hospital
Patients with clinically localized PCa and eligible for Radical Retropubic Prostatectomy (RRP), were preoperatively allocated to receive either Combined Epidural and Spinal Anaesthesia (CESA) or General Anaesthesia (GA)
All patients were preoperatively informed about both methods of anaesthesia and signed a consent form Patients with a medical history of severe heart disease, haemostasis disorders, previous pelvic surgery and lung disease were excluded from the study
A Body Mass Index (BMI) value was calculated for all patients, preoperatively, as weight in kg divided by squared height in meters (kg/m2) There are 4 BMI categories Underweight (< 18 5), Normal weight (18 5-24 9), Overweight (25-29 9) and Obesity (> 30)
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 396
PAPER No conflict of interest declared
ORIGINAL
Konstantinos Pikramenos 1 , Maria Zachou 2 , Eleftheria Apostolatou 1 , Dimitrios Papadopoulos 3 , Maria Mitsogianni 4 , Athanasios Papatsoris 1 , Ioannis Varkarakis 1 , Iraklis Mitsogiannis 1
DOI: 10 4081/aiua 2022 4 396
Patients in the GA group were premedicated with intravenously administered (IV) midazolam (2 mg) and fentanyl (100 mcg) A simple oxygen mask was applied Induction was performed using IV propofol (2 5-3 mg/kg) and lidocaine (40 mg); at that time dexamethasone 8 mg, metoclopramide 10 mg and omeprazole 40 mg were also administered After successful tracheal intubation, Total Intravenous Anaesthesia (TIVA) was maintained by administering propofol (0 05 mg/kg/sec IV) and remifentanil (0 2 mcg/kg/sec iv) Pain management was achieved by administering paracetamol (1g IV) and ramadol (100 mg iv) whereas muscle relaxation was obtained by vecuronium (0 6 mg/kg IV)
CESA group was performed using an epidural 18G needle and a spinal 27G needle, which were inserted in the L2-L3 or L3-L4 interspace Induction was carried out by spinal intrathecal administration of levobupivacaine (2 63ml of 0 5%) whereas mild sedation was achieved by midazolam (5 mg IV in bolus) All patients were administered dexamethasone 8 mg, metoclopramide 10 mg and omeprazole 40 mg IV, at that time Maintenance was performed 75 minutes after induction and obtained using an epidural administration of levobupivacaine (4-5 ml of 0 5%) An epidural catheter was maintained until successful completion of the procedure and removed in the recovery room The medications used for both types of anaesthesia are presented in Table 1
All patients in both groups received a standard postoperative regimen of intravenous paracetamol (1 g x 4 for the first 2 days) and cefoxitin (1 g x 3 until discharge); a prophylactic dose of enoxaparin was also given subcutaneously for 2 weeks, starting from postoperative day 2 If a patient was experiencing pain that could not be alleviated using the standard analgesic regimen, extra tramadol was administered on demand and recorded by the reviewer Several parameters were recorded intra- and postoperatively The time (minutes) required for induction of anaesthesia, the operation time and the total postoperative time (defined as that required for patients’ recovery, i e , from completion of the operation to patient transfer to the recovery room) were noted down Intraoperative haemodynamic status was constantly being monitored by measuring systolic pressure (SP) and diastolic arterial pressure (DP) and heart rate every 15 minutes; the Mean Arterial Pressure (MAP) was also being calculated using the formula MAP=DP+1/3(SP-DP) Haemoglobin levels, both preoperative and at specific times postoperatively (at the 12th, 24th and 48th postoperative hours) were also measured In addition, total blood loss (litres of fluid collected by suction during surgery which were categorised in < 100 ml, 100-600 ml and > 1000 ml), fluids administered intravenously during surgery (in litres) and the Surgical Apgar Score (SAS) (5) were calculated Postoperatively, total hospitalization days, patient pain intensity using the Visual Analogue Scale (VAS) and any need for extra analgesics were recorded VAS is based on a linear “ zero ” (No pain) to “ten” (Worst Pain Possible) scale Patients were asked to quantify their pain on that scale, at three different postoperative time points (after 6, 24, and 48 hours) Complications from the cardiovascular and respiratory systems as well as those related to the anaesthetic techniques were recorded; in addition, postoperative headache, nausea and vomiting and any signs of
potential nerve damage (manifested as inability to gain leg motility) were also assessed and recorded before hospital discharge (6, 7) All patients upon discharge filled in a Short Assessment of Patient Satisfaction (SAPS) Questionnaire (8) measuring their overall satisfaction for the care they received In SAPS, satisfaction is measured in a scale of 0 to 28, with 0 to 10 equals to “Very Dissatisfied” , 11-18 equals to “Dissatisfied” , 19-26 equals to “Satisfied” and 27-28 equals to “Very Satisfied”
Patients were followed for up to 12 months postoperatively PSA levels were measured at the 6th and 12th month to record a potential biochemical recurrence At the same time, patients were asked to assess their urinary continence by completing the International Consultation on Incontinence Questionnaire (9) - Urinary Incontinence Short Form
Statistical analysis was carried out using SPSS 24 0 Mean values, standard deviations, median values, Interquartile Range (IQR) and histograms were used to describe quantitative variables whether the data followed the normal distribution Collected data for systolic blood pressure, diastolic blood pressure, heart rate and haemoglobin were used with new quantitative variables being created by calculating the differences between the aforementioned timepoints for each one of these variables The KolmogorovSmirnov test was run to check the normality of the distributions The Student's t-test or the non-parametric MannWhitney U test were used to compare quantitative variables between the two groups, depending on whether the data followed the normal distribution A Kruskal-Wallis test (nonparametric equivalent of the one-way ANOVA) was used to make comparisons among the BMI-categories in CESA and GA group Moreover, linear or logarithmic models were used to check for differences between the studied groups, taking into account other factors (e g , demographic and clinical characteristics) In case of asymmetrical distribution, logarithmic transformations of the variables were used Significance levels were bilateral and the statistical significance were set at p < 0 05
RESULTS
Overall, 60 patients were included in the Study (30 in each group) Both groups were demographically compa-
Table 1
Anaesthetic techniques in the study groups
Anaesthesia stage Combined epidural - Spinal anaesthesia General anaesthesia
Premedication None
Midazolam 2 mg bolus IV
Fentanyl 100 mcg bolus IV
Induction Levobupivacaine 0 5% 2 6-3cc Spinal intrathecal Lidocaine 40 mg bolus IV
Midazolam 5 mg IV
Dexamethasone 8 mg IV
Metoclopramide 10 mg IV
Omeprazole 40 mg IV
Propofol 2,5-3 mg/kg bolus IV
Dexamethasone 8 mg IV
Metoclopramide 10 mg IV
Omeprazole 40 mg IV
Maintenance Levobupivacaine 0 5% 4-5cc epidural Propofol 0 05 mg/kg/sec IV
Remifentanil 0 2 mcg/kg/sec IV
Paracetamol 1 g IV
Tramadol 100 mg IV
Vecuronium 0 6 mg/kg IV
Recovery room Paracetamol 1g IV
IV Intravenous; mg Mi l gram; g Grams; kg Kilograms; mcg Microgram
Paracetamol 1g IV
397 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Anesthesia effects on Radical Prostatectomy
Demographic and oncological characteristics of patients
SAS scores in the CESA and GA groups.
= Comb ned Epidural and Spinal Anaesthesia; GA = Genera Anaesthesia; ASA = American Society of Anaesthesiologists; PSA = prostate-specif c ant gen; NS = non-signif cant
** Pearson Chi-square test
rable and homogeneous with regard to age, height, weight, smoking habit, alcohol use, history of diabetes mellitus, biopsy Gleason Score and preoperative PSA
Preoperative characteristics are presented in Table 2 Intraoperative MAP was found to be significantly higher in the GA group [85 13 ± 11 84] vs CESA group [77 67 ± 5 66] (p = 0 036) (Figure 1) Furthermore, patients in the GA group exhibited higher heart rate intraoperatively when compared to the preoperative measurement, as opposed to those in the CESA group who exhibited lower heart rate than the preoperative measurement (GA: +25 (17), CESA: -2 (7), (p < 0 01) Intraoperative blood loss, as collected by the suction, did not differ significantly between the two groups Time for anaesthesia induction was identical in both groups (13 6 ± 3 5 min in the CESA group vs 13 6 ± 2 9 min in the GA group, p > 0 05)
Duration of the operation in the CESA and GA groups was 127 ± 17 29 min and 126 33 ± 10 93 min, respectively (p > 0 05) However, the time needed for patients’ recovery and transfer to the recovery room was significantly shorter in the CESA group (16 13 ± 4 9 min) as compared to that in the GA group (19 6 ± 3 5) (p = 0 03)
CESA Combined Ep dura and Spinal Anaesthes a; GA General Anaesthes a; SAS Surgica APGAR score; MAP Mean Arter al Pressure
Statistically significant difference was also noticed in the mean intraoperative SAS (8 13 ± 0 63 in the CESA group vs 7 2 ± 1 37 in the GA group, p < 0 03) A SAS score ≤ 6 was recorded in 6 patients (20%) in the GA group in comparison to none in the CESA Group (Figure 2) Hospitalisation was significantly shorter for patients in the CESA group compared to those of the GA group (2 6 ± 0 5 vs 3 2 ± 0 41, respectively, p = 0 003)

Postoperative mean drop of haemoglobin was 1 5 ± 0 81 in the CESA group vs 2 06 ± 1 1 in the GA group (p = 0 029), indicating a statistically significant difference in blood loss in favour of the combined anaesthesia Blood transfusion was required in 1 patient in the CESA group and 2 patients in the GA group (p = 0 54) VAS score was found to be equal between the two groups and all patients reported only mild pain 48 hours after the surgery, contrary to moderate and severe pain reported on the day of surgery and 24 hours after Data regarding haemoglobin changes and VAS score are listed in Tables 3, 4
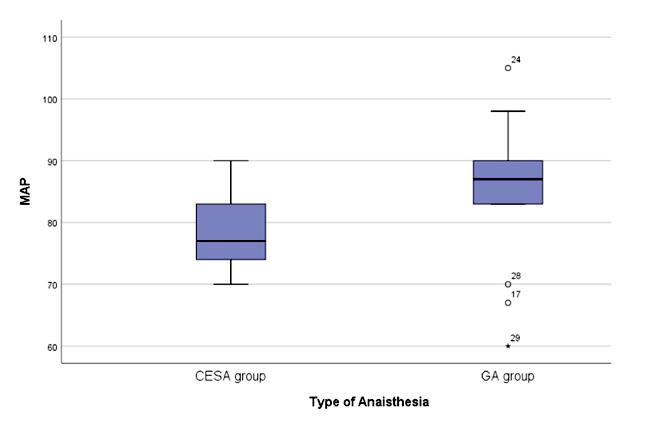
Table 3.
Haemoglobin change within the first 48 hours
Table 4.
VAS Score within the first 48 hours.
CESA = Combined Epidural and Spina Anaesthesia; GA = Genera Anaesthesia; SAS = Surgical APGAR score;
= Mean Arteria Pressure
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 K Pikramenos, M Zachou, E Apostolatou, et al 398
Figure 1
MAP values in the CESA and GA groups
Table 2.
Demographics CESA (n = 30) GA (n = 30) 95% CI, p-value Mean ± SD Mean ± SD Age (years) 66 93 ± 5 66 66 40 ± 4 89 (-3 42, 4 49), 0 78 * Height (m) 1 72 ± 0 078 1 75 ± 0 044 (-0 08, 0 01), 0 140 * Weight (kg) 78 8 ± 10 57 81 87 ± 14 96 (-12 75, 6 62), 0 52 * ASA physical status (II/III) 23/7 20/10 NS ** Preoperative PSA (ng/ml) 6 81 ± 3 06 8 01 ± 2 78 (-3 38, 0 99), 0 27 * Gleason Score NS ** 6 6/30 4/30 3+4 10/30 8/30 4+3 8/30 10/30 8 6/30 7/30 9 0/30 1/30 CESA
t-test
* Independent samples
Hb change CESA group GA group p-value * Mean ± SD Mean ± SD Pre-op/Post-op -2 06 ± 1 1 -1 5 ± 0 81 0 029 24h – after surgery -0.9 ± 0.59 -1.18 ± 0.84 0.305 48h – 24h -0 28 ± 0 73 -0 48 ± 0 71 0 439 48h – after surgery -1 18 ± 0 66 -1 67 ± 0 93 0 113 48h – before surgery -3 24 ± 1 19 -3 18 ± 1 19 0 771 Pre-op: Pre operative y; Post-op: Post operatively * Independent samp es t-test
VAS CESA group GA group p-value * Day of surgery 6 47 ± 0 51 6 53 ± 0 51 0 720 24h after surgery 5 13 ± 0 51 5 ± 0 53 0 487 48h after surgery 3 2 ± 0 41 3 33 ± 0 48 0 417 SD: standard
CESA: comb ned ep dural spinal anaesthes a; GA: genera anaesthesia; VAS:
Ana og Scale * Independent samp es t-test
dev ation;
Visua
MAP
Figure 2.
No complications were reported across any group and none of the patients in the CESA group reported either post-subarachnoid puncture headache or any nerve damage or difficulty in regaining leg motility In the CESA group, there was no case with a need for the anaesthesia to be dynamically converted to GA during surgery
Additional postoperative analgesic requirements as well as the daily amount of intravenous fluids did not differ significantly between the two groups, (CESA: 2933 ± 703 7 ml daily vs GA: 3000 ± 845 15 ml, p = 0 945) All patients in both groups reported to be satisfied with the care they received (p > 0 05); also regain of urinary continence was comparable between the two groups after 12 months Lastly, there were no cases of biochemical recurrence in either group at the 6th and 12th postoperative months
When participants were sub-analysed according to BMI categories, there were no underweight patients, 24 of normal weight (CESA: 10, GA: 14), 26 overweight (CESA: 16, GA: 10) and 10 obese patients (CESA: 4, GA: 6) A higher heart range change was observed in obese patients in the GA group when compared to overweight and normal patients (32 vs 25 and 23, respectively; p = 0 002) There was no difference of statistical importance between any other factors, when comparing each BMI group of GA In the CESA BMI groups, there were no statistical differences for any of the factors
DISCUSSION
In this comparative study, all patients undergoing RRP for organ-confined PCa under either general or combined (epidural and spinal) anaesthesia were safely treated and discharged without any major complications Time for induction of anaesthesia and surgical time were the same in both groups In addition, no post-subarachnoid puncture headaches, nerve damages or difficulty in regaining leg motility were recorded in the CESA group whereas no cases of vomiting and/or postoperative delirium were found in the GA group
In the GA group, intraoperative heart rate was recorded higher and there was a greater drop in the post-operative mean haemoglobin value, when compared to the CESA group, potentially indicating a greater blood loss in patients under GA Nonetheless the amount of fluids retrieved by the suction was similar in both groups, hence one has to assume that a greater amount of blood was held within the gauzes during surgery This parameter however was not measured in our study Shir Y et al (10) also demonstrated mean intraoperative blood loss to be significantly higher in patients undergoing surgery under GA compared to those receiving epidural anaesthesia (respective mean values 1940 and 1490 litres) and similar in those receiving combined general/epidural anaesthesia (mean 1810 litres); they concluded that epidural anaesthesia did not reduce bleeding, it was rather the administration of GA that increased intraoperative haemorrhage (10) The authors recognised positive pressure ventilation to be a potential contributing factor, due to the increase in intrathoracic pressure and decrease in venous retur n to the heart that causes (11), which in tur n results in increased peripheral venous pressure (12) and conse-
quent increased bleeding during surgery (13) However, contrary to the results of Shir Y et al , we found no differe
epidural/GA, compared to general alone, was also reported by others (14, 15)
SAS was statistically different between the groups, with patients in the CESA group having an overall higher mean score, indicating a potentially reduced risk for postoperative complications It is noteworthy that a SAS score < 6, which is deemed a threshold for increased risk for major complications, was reported in 20% of patients in the GA group, compared to none in the CESA group This potentially implies a greater risk for postoperative complications in those receiving GA Postoperative complications may delay not only patients’ recovery and discharge from hospital but also retur n to their normal activities with an o v e r a l l re d u c t i o n i n t h e i r q u a l i t y o f l i f e ( 1 6 ) Nevertheless, the potential safety benefits of CESA over GA, need to be further investigated in larger-scale studies Both groups reported equal VAS scores, with higher pain levels reported immediately after surgery and a constant reduction thereafter In the literature, there have been reports indicating lower pain levels in patients receiving CESA Dunet F et al (15) demonstrated an improvement in required postoperative analgesics, within the first 48 hours, in patients undergoing RRP under combined general/epidural anaesthesia over patients receiving GA alone This observation however, was not confirmed in the present study
Patients receiving CESA remained in the operating theatre for a shorter period of time (average -3 5 minutes), compared to those receiving GA, and furthermore their hospitalisation was significantly shorter (-0 6 days) A shorter operating theatre and hospital stay is beneficial for both patients and Health Services alike, because it reduces patients’ exposure to specific pathogens, reduces anxiety and, at the same time, reduces costs (15, 17) By streamlining the CESA technique for RRP, the duration of surgery will further decrease, leaving time for more operations, thereby increasing hospital incomes (18) Medical economics are equally important to other aspects of Medicine and treatment options, apart from being personalized, should be cost-effective (19) In general, application of techniques which enable provision of the best health care possible, while reducing risks of hospitalacquired infections and at the same time, requiring less funds, is of great importance
Overall satisfaction at the time of discharge was similar in both groups and after a one-year of follow-up, no biochemical recurrences and no difference in the incidence of urinary incontinence, were reported These results, which are in line with other reports (20), indicating that both methods of anaesthesia are safe to perform with equal oncological and functional results
BMI is another important factor that may potentially influence various parameters during the operation We have noticed a higher intraoperative HR change in obese patients receiving GA, compared to those in the CESA group This finding, combined with the higher drop in the mean postoperative haemoglobin level, may indicate a greater blood loss in obese patients However, due to the
399 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Anesthesia effects on Radical Prostatectomy
n c e i n b l o o d t r a n s f u s i o n s b e t w e e n t h e 2 g ro u p s S i g n i f i c a n t l y l o w e r b l o o d l o s s w i t h c o m b i n e d
small number of obese patients (10) included in the study, no clear inference can be drawn on this issue Cai T et al (21), in their study of 78 patients undergoing radical prostatectomy, reported an increased blood loss in obese patients compared to patients with normal weight; nonetheless the differences were not statistically significant In contrast to our results, Cai et al also found that obese patients were significantly more likely to have urinary incontinence postoperatively compared to nonobese patients, a finding not observed in our study Lastly, it should be noted that the data presented in this study apply only to patients undergoing open radical prostatectomy and not to those undergoing laparoscopic or robotic procedures A potential advantage of either form of anaesthesia in these procedures should be investigated in separate studies
CONCLUSIONS
Open RRP carried out under combined spinal/epidural anaesthesia is a safe procedure to perform and is associated with less intraoperative blood loss and potentially reduced risks of postoperative complications It may lead to a shorter total operation time and reduced hospitalization, while providing similar oncological and functional outcomes Further studies are needed to reliably confirm the substantial role of combined anaesthesia in this major oncological operation
REFERENCES
1 Siegel RL, Miller KD, Fuchs HE, Jemal A Cancer statistics, 2022 CA Cancer J Clin 2022; 72:7-33
2 Sebesta EM, Anderson CB The Surgical Management of Prostate Cancer Semin Oncol 2017; 44:347-357
3 Lepor H A review of surgical techniques for radical prostatectomy Rev Urol 2005; 7(Suppl 2):S11-7
4 Kim SP, Shah ND, Karnes RJ, et al Hospitalization costs for radical prostatectomy attributable to robotic surgery Eur Urol 2013; 64:11-6
5 Gawande AA, Kwaan MR, Regenbogen SE, et al An Apgar score for surgery J Am Coll Surg 2007; 204:201-8
6 Hinkelbein J, Lamperti M, Akeson J, et al European Society of Anaesthesiology and European Board of Anaesthesiology guidelines for procedural sedation and analgesia in adults Eur J Anaesthesiol 2018; 35:6-24
7 Horlocker TT Complications of spinal and epidural anesthesia Anesthesiol Clin North Am 2000; 18:461-85
8 Hawthorne G, Sansoni J, Hayes L, et al Measuring patient satisfaction with health care treatment using the Short Assessment of Patient Satisfaction measure delivered superior and robust satisfaction estimates J Clin Epidemiol 2014; 67:527-37
9 Avery K, Donovan J, Peters TJ, et al ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence Neurourol Urodyn 2004; 23:322-30
10 Shir Y, Raja SN, Frank SM, Brendler CB Intraoperative blood loss during radical retropubic prostatectomy: epidural versus general anesthesia Urology 1995; 45:993-9
11 Nanas S, Magder S Adaptations of the peripheral circulation to PEEP Am Rev Respir Dis 1992; 146:688-93
12 Morgan BC, Martin WE, Hornbein TF, et al Hemodynamic effects of intermittent positive pressure respiration Anesthesiology 1966; 27:584-90
13 DiStefano VJ, Klein KS, Nixon JE, Andrews ET Intra-operative analysis of the effects of position and body habitus on surgery of the low back A preliminary report Clin Orthop Relat Res 1974(99):51-6
14 Tikuisis R, Miliauskas P, Samalavicius NE, et al Epidural and general anesthesia versus general anesthesia in radical prostatectomy Medicina (Kaunas) 2009; 45:772-7
15 Dunet F, Pfister C, Deghmani M, et al Clinical results of combined epidural and general anesthesia procedure in radical prostatectomy management Can J Urol 2004; 11:2200-4
16 Archer S, Pinto A, Vuik S, et al Surgery, Complications, and Quality of Life: A Longitudinal Cohort Study Exploring the Role of Psychosocial Factors Ann Surg 2019; 270:95-101
17 Kofler O, Prueckner S, Weninger E, et al Anesthesia for Open Radical Retropubic Prostatectomy: A Comparison between Combined S p i n a l E p i d u r a l A n e s t h e s i a a n d C o m b i n e d G e n e r a l E p i d u r a l Anesthesia Prostate Cancer 2019; 2019:4921620
18 Gardner TA, Bissonette EA, Petroni GR, et al Surgical and postoperative factors affecting length of hospital stay after radical prostatectomy Cancer 2000; 89:424-30
19 Salonia A, Crescenti A, Suardi N, et al General versus spinal anesthesia in patients undergoing radical retropubic prostatectomy: results of a prospective, randomized study Urology 2004; 64:95-100
20 Tsui BC, Rashiq S, Schopflocher D, et al Epidural anesthesia and cancer recurrence rates after radical prostatectomy Can J Anaesth 2010; 57:107-12
21 Cai T, Cocci A, Di Maida F, et al Visceral adiposity is associated with worse urinary and sexual function recovery after radical prostatectomy: Results from a longitudinal cohort study Arch Ital Urol Androl 2021; 93:285-290
Correspondence
Konstantinos Pikramenos, MD (Corresponding Author) kpikramenos@gmail com
Eleftheria Apostolatou, MD apostolatoy1989@gmail com
Athanasios Papatsoris, MD agpapatsoris@yahoo gr
Ioannis Varkarakis, MD medvark3@yahoo com
Iraklis Mitsogiannis, MD imitsog@med uoa gr
2nd Urology Department, Sismanoglio Hospital, National and Kapodistrian University of Athens, Greece
Maria Zachou, MD zachou maria@yahoo com
Gastroenterology Department, Sismanoglio Hospital, Athens Greece
Dimitrios Papadopoulos, MD dimitris76papadopoulos@yahoo gr
Anaesthesiology Department, Evgenidio Hospital, National and Kapodistrian University of Athens, Greece
Maria Mitsogianni, MD mitsogiannimaria@gmail com
4th Department of Medical Oncology, Hygeia Hospital, Athens, Greece
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 K
et al 400
Pikramenos, M Zachou, E Apostolatou,
Accuracy of PET-choline in nodal staging of localized very high-risk prostate cancer
Nuno Dias
1 Urology Department, Institut Mutualiste Montsouris, Paris, France;
2 Urology Department, São João Hospitalar and University Center, Porto, Portugal;
3 Unit of Urology, Division of Experimental Oncology, URI Urological Research Institute, IRCCS San Raffaele Scientific Institute, Vita-Salute San Raffaele University, Milan, Italy;
4 Institute for Life and Health Sciences Investigation, School of Medicine, Minho University, Braga, Portugal
Summary
Objectives: Localized very high-risk prostate cancer (VHR PCa) has long suffered from the inex-istence of good lymph node staging methods other than invasive surgery, as computed tomogra-phy has low sensitivity for nodal disease With the rising use of positron emission tomography (PET), it is clinically meaningful to know its value for these patients Our goal was to evaluate the real-life diagnostic accuracy of PET Choline in nodal staging, comparing it with the gold standard of extended pelvic lymph node dissection (ePLND).
Materials and methods: We reviewed data from a high-volume center, including patients with VHR PCa according to current NCCN guidelines who underwent community 18F-fluorocholine
PET/CT; followed by ro-botic assisted laparoscopic prostatectomy (RALP) and ePLND between 2010 and 2021
Results: We included 44 patients and 88 lymph node regions
Among those, 14/44 (31 8%) patients and 20/88 (22 7%) regions had nodal disease present on definitive pathology
In comparison with ePLND, we found a sensitivity of 64 3% (95% CI, 39 2-89 4%), specificity of 83 3% (95% CI, 70 096 7%), PPV of 64 3% (95% CI, 39 2-89 4%), and NPV of 83 3% (95% CI, 70 0-96 7%) for nodal disease on a patient-based analysis; and sensitivity of 35 0% (95% CI, 14 1-60 0%), specificity of 88 2% (95% CI, 80 6-95 9%), PPV of 46 7% (95% CI, 21.4-71.9%), and NPV of 82.2% (95% CI, 73.4-91.0%) on a region-based analysis
Conclusions: In our view 18F-fluorocholine PET/CT doesn’t meet the criteria to be a standard exam for pre-operative staging for patients with VHR PCa, mostly due to its low sensitivity. However, other radiotracers should continue to be investigated in this setting.
KEY WORDS: Positron-emission tomography; Prostatic neoplasms; Neoplasm staging
Submitted 23 October 2022; Accepted 30 October 2022
INTRODUCTION
Adequately staging of very high-risk (VHR) localized prostate cancer (PCa) is of utmost importance, as staging may alter treatment choice Even when patients are well selected for radical treatment, their biochemical recurrence, metastasis, cancer specific mortality and all-cause mortality at 5 years can be as high as 69%, 20%, 5% and
7%, respectively (1, 2) After the diagnosis, a better staging would allow both clinician and patient a betterinformed choice and a better tailored treatment approach Current recommendations from European Association of Urology (EAU) (3) and National Comprehensive Cancer Network (NCCN) (4) are for high-risk and VHR localized PCa patients to undergo computed tomography (CT) of abdomen and pelvis and whole-body bone scan (BSc) However, it is commonly known that CT and alternatives such as Magnetic Resonance Imaging (MRI) have a modest performance for nodal staging (5)
More recent nuclear imaging such as Positron Emission T o m o g r a p h y ( P E T ) w i t h C h o l i n e o r P r o s t a t e - S p e c i fi c Membrane Antigen (PSMA) isotopes have been explored, but their utilization in staging localized PCa is not standard (6, 7) PET-PSMA is currently regarded as the most promising radiotracer, but in most of the world it is more expensive and of more limited availability than PETCholine (8) As such, in France, it is frequent that we find patients being staged with PET-Choline, exam considered in guidelines as having a role in biochemical recurrence It has the advantage of being cheaper, easily available and reproducible (8) However, its role in staging of localized PCa is disputed, with some papers reporting interesting results in the subset of high risk and VHR patients (9, 10) In this work we explore the role of PET Choline realized in community non-centralized centers in node staging, when compared with CT findings and with the gold standard of bilateral extended pelvic lymphadenectomy, in patients with VHR PCa
METHODS
Our center is a high-ranking hospital in PCa care, receiving patients mainly from Paris, but also from all France and the rest of the World We maintain a prospectively updated database with all patients who undergo a radical prostatectomy in our center, including our study population We explored this database for patients with VHR localized PCa who underwent PET Choline as a method of pre-operative staging, who were treated with Robotic Assisted Laparoscopic Prostatectomy (RALP) and Extended Pelvic Lymph Node Dissection (ePLND), between 2010 and
401 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
PAPER No conflict of interest declared
ORIGINAL
1, 2 , Gianmarco Colandrea 1, 3 , Francisco Botelho 2, 4 , Lara Rodriguez-Sanchez 1 , Yann Barbé 1 , Petr Macek 1 , Xavier Cathelineau 1
DOI: 10 4081/aiua 2022 4 401
2021 Patients who had a previous malignancy or history of prior hormonal therapy were excluded
Data collection
Data was collected from our continuously updated database and patient records We recorded age at time of surgery, pre-operative total PSA, clinical T staging, biopsy results, PET Choline results, anatomopathological study of prostatectomy and lymph node dissection specimens
The study has received approval by the institutional Ethics’ Committee All research was conducted respecting the latest version of Helsinki’s declaration
Risk groups
Patients were included if they fulfilled current NCCN guidelines (4) criteria for VHR patients: a) at least 1 of: cT3b-cT4, primary Gleason pattern 5, > 4 cores with Gleason Group 4 or 5; and/or b) at least 2 of: cT3a, Gleason Group 4 or 5, PSA > 20 ng/mL
PET Choline
PET/CT exams were performed in various local centers in France, with images acquired using 18F-fluorocholine tracer being obtained according to institutional protocols, with images being reported by several different community radiologists PET Choline imaging were acquired alongside a tho-raco-abdominal-pelvic CT scan Images were not centrally reviewed
The diagnosis of pathological lymph nodes was based on the presence of increased uptake on PET images of the radiotracer, with exams being considered as positive if reported by the radiologist as positive or suspicious, irrespective of standardized uptake value (SUV) CT adjunctive imaging was used only to locate the anomalies and not as a staging method by itself
Surgery
RALP + ePLND was performed in our institution by seven different assistants, with long experience in robotic surgery and RALP, with frequent participation of fellows under their direct supervi-sion RALP was performed transperitoneally, and ePLND was performed as per guidelines standard (including node packets from common iliac distal to the ureteric crossing, external iliac, internal iliac, and obturator origins), with nodes from each side being sent and analyzed separately (3) Other nodal regions such as presacral and retroperitoneal would only be removed in select cases where imaging was suspicious of lymph node metastasis in those locations, with no cases present in our population
Histology
Biopsy cores were analyzed in the institution where the biopsy was performed and not reviewed, except in doubtful cases Prostatectomy and lymph node dissection products were fixed in formalin and examined in our center by specialized uropathologists, in accordance with ISUP guidelines, with left and right templates being observed separately (11)
Statistics
Statistical analysis was performed with IBM® SPSS® v27
software Median and interquartile range are presented for continuous variables; frequencies are reported for categorical variables Characteristics of patients were compared using Chi-squared analysis for categorical variables and non-parametric Mann-Whitney U tests for continuous variables (age) Statistically significance in this study was set as p < 0 05 All reported p values are two-sided Test characteristics (sensitivity, specificity, VPP, VPN) were calculated for both patient and region based analysis, with 95% confidence intervals
RESULTS
We identified 2104 consecutive patients submitted to RALP, with 104 being VHR patients and 45 who had had PET Choline as part of their disease staging One patient meeting the inclusion criteria was excluded for not having all information regarding PET Choline examen available Forty-four patients and eighty-eight lymph node regions were included in our analysis
Patient characteristics
Patient characteristics are shown in Table 1 Median patient age was of 63 years old (IQR 59-68) and median total PSA of 15 (IQR 9 8-22 2) ng/mL, with 23 patients having a PSA > 15 ng/mL All 44 patients had VHR PCa,
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
402
N
Dias, G Colandrea, F Botelho, L Rodriguez-Sanchez, Y Barbé, P Macek, X Cathelineau
Table 1 Patient characteristics Total n = 44 Age, median (P25-P75) 63 (59-68) Total PSA, ng/mL, median (P25-75) 15 (9 8-22 2) Clinical T stage, n (%) T1c 4 (9) T2a 6 (14) T2b 4 (9) T2c 8 (18) T3a 17 (39) T3b 5 (11) Biopsy at our institution 15 (34) Biopsy ISUP, n (%) 1 5 (11) 2 6 (14) 3 8 (18) 4 16 (36) 5 9 (21) Number positive cores, median (P25-75) 6 (4-7) > 4 cores with ISUP ≥ 4, n (%) 17 (39) Pathological T stage, n (%) T2b 1 (2) T2c 7 (16) T3a 21 (48) T3b 15 (34) Prostatectomy ISUP, n (%) 2 8 (18) 3 22 (50) 4 4 (9) 5 10 (23) Nodal disease, n (%) 14 (32) Number of positive lymph-nodes, n (%) 0 30 (68) 1 4 (9) 2 1 (2) ≥ 3 9 (20) Number removed nodes, median (P25-75) 19 (11-26)
Table 2.
Two-by-two tables presenting cross-results for nodal disease of ePLND and 18F PET-Choline, on patient and region-based analysis.
we performed the same analysis for patients with PSA > 15ng/mL and on a region basis; sensitivity was 50% (95% CI, 24-76%), with specificity of 84% (95% CI, 72-97%), PPV of 58% (95% CI, 30-86%) and NPV of 79% (95% CI, 66-93%)
Sub-group with ≥ 3 positive lymph nodes
Nine (20%) patients had at least 3 positive lymph nodes at final pathology, with 6 of them having a positive 18Ffluorocholine PET/CT For this subgroup, on a patientbased analysis (n=9); sensitivity was 66 7% (95% CI, 35 9-97 5%), specificity 77 1% (95% CI, 63 2-91 1%), PPV 42 9% (95% CI, 16 9-68 8%), and NPV 90 0% (95% CI, 79 3-100 0%)
with 17 (39%) and 5 (11%) having cT3a and cT3b disease, respectively Overall, 9 (21%) patients had ISUP of 5, and 17 (39%) had more than 4 biopsy cores with ISUP ≥ 4 Histological results after RALP + ePLND showed most patients locally advanced disease, with 48% presenting with pT3a and 34% with pT3b disease; and 23% of patients had a Gleason Grade Group of 5 With a median 19 (IQR 11-26) nodes removed per patient, 14 out of 44 (32%) of patients had nodal metastasis Four (9%) patients had 1 positive lymph node, 1 (2%) had 2 positive lymph nodes and 9 (20%) had ≥ 3 positive lymph nodes identified
18F-fluorocholine PET/CT and ePLND
Table 2 presents the cross results between 18F-fluorocholine PET/CT and anatomopathological findings, in a patient and region base analysis When compared with ePLND, 18F-fluorocholine PET/CT had a false negative rate of 17% and 18% for patient and region-based analysis, respectively; and a false positive rate of 50% and 53%, respectively
Table 3 shows the performance of 18F-fluorocholine
PET/CT as a test for nodal staging On a patient-based analysis (n=44); sensitivity was 64 3% (95% CI, 39 289 4%), specificity 83 3% (95% CI, 70 0-96 7%), PPV 64 3% (95% CI, 39 2-89 4%), and NPV 83 3% (95% CI, 70 0-96 7%) On a region-based analysis (n=88); sensitivity was 35 0% (95% CI, 14 1-56 0%), specificity 88 2% (95% CI, 80 6-95 9%), PPV 46 7% (95% CI, 21 471 9%), and NPV 82 2% (95% CI, 73 4-91 0%) Knowing the correlation between biomarkers uptake and PSA,
DISCUSSION
The importance of a good nodal staging in VHR PCa patients is three ways First, patients with node positive disease should be well identified, since these patients may benefit from adjuvant hormonal therapy and/or radiotherapy after surgery, and because they have worse outcomes in biochemical free survival, metastasis free survival and overall survival (2) Second, when discussing treatment options with a patient before deciding on a radical treatment, we should be able to provide him with the best information possible, in order to allow the best individual decision In VHR patients in particular, the rate of node positive disease has been estimated to be as high as 37% (2) Third, when surgery for VHR patients is performed, it entails not only radical prostatectomy but also an ePLND, which increases surgical time and risk of perioperative complications, and has not been shown to lead to better patient outcomes (12)
As such, if an accurate enough non-invasive staging method were easily available, it could lead to better identifications of node positive patients before intervention, best individualized information before treatment decisions and eventual nonrealization of a procedure with significant comorbidities but no increased benefit to patients (12)
Current recommended staging of localized VHR PCa is CT and whole-body bone scan (3, 4) CT scan relies mainly on size criteria, location and contrast enhancement to classify lymph nodes as suspicious or not However, CT scan has been extensively reported as having a poor performance for nodal staging, with sensitivity depending on the prostate cancer risk, but remaining low even for high-risk patients (13) Knowing this, previous studies have searched for adequate methods for non-invasive PCa staging Those alternatives should be sensitive, specific, clinically useful, easily accessible and reproducible (14) Previous studies have explored the role of PET Choline and PET PSMA as staging imaging for localized PCa, mostly in a trial setting
Van den Bergh et al (9) performed a prospective study with 75 patients with negative CT scans and lymph node extension risk assessed to be between 10-35% with Partin tables and compared the performance of pre-operative staging with 11C-Choline PET and pelvic MRI with super-extended pelvic lymphadenectomy results They reported a low performance of both PET and MRI, main-
403 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 PET-choline in nodal staging of prostate cancer
18F PET-Choline Values Patient-based analysis Patients with positive LN 14/44 (31.8%) Sensitivity 64 3% [39 2-89 4%] Specificity 83 3% [70 0-96 7%] PPV 64.3% [39.2-89.4%] NPV 83 3% [70 0-96 7%] Region-based analysis Regions with positive LN 20/88 (22 7%) Sensitivity 35 0% [14 1-56 0%] Specificity 88.2% [80.6-95.9%] PPV 46 7% [21 4-71 9%] NPV 82 2% [73 4-91 0%]
Table 3. Test performance on patient and region-based analysis
18F PET-Choline Positive ePLND Negative ePLND Patient-based analysis Total, n 14 30 Positive/suspicious, n (%) 9 (64) 5 (17) Negative, n (%) 5 (36) 25 (83) Region-based analysis Total, n 20 68 Positive/suspicious, n (%) 7 (35) 8 (12) Negative, n (%) 13 (65) 60 (88)
ly at the expenses of a low sensitivity (PET: 19% and 8% on patient and region-based analysis; MRI: 36% and 10% on patient and region-based analysis), which lead them to suggest the absence of benefit in this patient cohort Schiavina et al (10) reported their retrospective experience with 11C-Choline PET in a cohort of intermediate, high and VHR patients They report low sensitivities for the detection of nodal disease both on medium and highrisk patients, with 17% and 40% in a region-based analysis, respectively However, in a subgroup of 28 VHR patients where 50% harbored nodal disease, the test performance was better, with sensitivity, specificity, positive predictive value and negative predictive value of 71%, 93%, 91% and 76%, respectively
In our sub-analysis of 9 patients with ≥ 3 positive lymph nodes on high-quality ePLND, 18F-fluorocholine PET/CT on a patient-based analysis had sensitivity, specificity, PPV and NPV of 66 7%, 77 1, 42 9, and 90 0%, respectively This was similar to our results in the overall VHR PCa population, with a high NPV pointing to a potential role as means of excluding ≥ 3 positive lymph nodes disease As the number of patients in this group was low (n=9) it would be interesting to see multicenter results in this subgroup, as the presence of ≥ 3 positive lymph nodes has been suggested as an independent risk factor for both biochemical recurrence and metastatic progression, with these patients benefiting from adjuvant treatment after surgery (15)
More recently, some studies have shown promise of good results with PSMA PET/CT staging in the treatment-naïve high-risk patients Hope et al (16) performed a trial which enrolled 764 patients with intermediate and high-risk PCa being considered for prostatectomy at a single institution, who performed 68Ga-PSMA-11 PET/CT prior to intervention 277 patients ended up receiving radical prostatectomy with extended lymph node dissection, in which the PET sensitivity, specificity, positive predictive value and negative predictive value were of 40% (95% CI, 34-46%), 95% (95% CI, 92-97%), 75% (95% CI, 7080%) and 81% (95% CI, 76-85%), respectively Hofman et al (17) published the results of probably the most important study so far, the proPSMA trial This was a m u l t i c e n t e r r a n d o m i z e d c o n t r o l l e d t r i a l i n 1 0 Australian hospitals 302 patients with high-risk PCa were randomly selected for either usual imaging or 68GaPSMA-11 PET/CT PSMA PET performed better than CT scan, and very well, with an 85% (95% CI, 74-96%) sensitivity and 91% (95% CI, 85-97%) specificity for nodal disease Also, although patients who underwent PSMA PET as staging method didn’t undergo classical staging previously, the exam results are reported to have changed the clinical preferred options in 28% of patients, with 14% being directed from curative to palliative treatment, 7% with a change in radiotherapy technique and 7% with a change in surgical technique
Our work analyzed a real-life experience of a region and country where availability of 68Ga-PSMA-11 PET/CT is scarce and 18F-fluorocholine is widespread As such, many of our patients don’t have the option for the newest but less accessible radiotracer For that reason, it was important for us to understand the value caretakers are providing VHR PCa patients regarding staging imaging
It comes with the limitations of being a retrospective study, which includes patients operated in a single center, with imaging being performed in many centers The inclusion of only patients who underwent RALP + ePLND may have selected patients with less advanced localized disease stages, more amenable for radical prostatectomy as a treatment choice; and also excluded metastatic patients and radiotherapy patients who didn’t have surgery
The analysis of 18F-fluorocholine PET/CT accuracy was also only made by patient and side, and using every lymph node region separately, as our current technique of ePLND retrieves all nodes of a side all together in a single packet
Reviewing our data is important to understand what real life results we get when using 18F-fluorocholine PET/CT in VHR patients, and we found that even though the exam specificity and NPV were > 80%, its low sensitivity both on patient (64 3%) and side (35 0%) based analysis are not enough to consider the exam as a “game changer” , even in the VHR PCa group
After the first data on new imaging modalities emerged, some studies started suggesting the wide-spread study of new tracers, such as 177Lu-PSMA (18) and government approval of PET/CT for staging (19), which should facilitate the increasing the availability and decreasing the costs of those exams
As such, efforts to advance the knowledge in the field and maintain low-cost accessibility to exams considered clinically useful should be pursued continuously
CONCLUSIONS
We conclude that 18F-fluorocholine PET/CT as staging for patients with VHR localized PCa doesn’t meet the criteria to be a standard exam for pre-operative staging We therefore believe new radiotracers such as the 68Ga-PSMA-11 s h o u l d c o n t i n u e t o b e a s s e s s e d i n t h i s s e t t i n g Governments and health services should also make efforts to ensure that new meth-ods of imaging with clinical utility have a reasonable financial cost and availability
REFERENCES
1 Sundi D, Wang VM, Pierorazio PM, et al Very-high-risk localized prostate cancer: definition and outcomes Prostate Cancer Prostatic Dis 2013; 17:57-63
2 Sundi D, Tosoian JJ, Nyame YA, et al Outcomes of Very HighRisk Prostate Cancer After Radical Prostatectomy: Validation Study From 3 Centers Cancer 2019; 125:391-397
3 Mottet N, Cornford P, van den Bergh RCN, et al EAU, EANM, ESTRO, ESUR, ISUP, SIOG: Guidelines on prostate cancer 2022
4 NCCN Clinical practice guidelines in oncology: prostate cancer V e r s i o n 3 2 0 2 2 , c o n s u l t e d 2 3 r d A p r i l 2 0 2 2 A v a i l a b l e f r o m : https://www nccn org/professionals/physician gls/pdf/prostate pdf
5 Hövels AM, Heesakkers RAM, Adang EM, et al The diagnostic accuracy of CT and MRI in the staging of pelvic lymph nodes in patients with prostate cancer: a meta-analysis Clin Radiol 2008; 63:387-95
6 Umbehr MH, Muntener M, Hany T, et al The role of 11C- choline and 18F-fluorocholine positron emission tomography (PET) and
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
404
N Dias, G Colandrea, F Botelho, L Rodriguez-Sanchez, Y Barbé, P Macek, X Cathelineau
PET/CT in prostate cancer: a systematic review and meta-analysis Eur Urol 2013; 64:106-17
7 Evangelista L, Guttilla A, Zattoni F, et al Utility of choline positron emission tomography/computed tomography for lymph node involvement identification in intermediate- to high-risk prostate cancer: a systematic literature review and meta-analysis Eur Urol 2013; 63:1040-8
8 Alberts I, Mingels C, Zacho HD, et al Comparing the clinical performance and cost efficacy of 68Ga-PSMA-11 and 18F-PSMA-1007 in the diagnosis of recurrent prostate cancer: a Markov chain decision analysis Eur J Nucl Med Mol Imaging 2022; 49:4252-4261
9 van den Bergh L, Lerute E, Haustermans K, et al Final analysis of a prospective trial on functional imaging for nodal staging in patients with prostate cancer at high risk for lymph node involvement Urol Oncol 2015; 33:109 e23-31
10 Schiavina R, Bianchi L, Bianchi FM, et al Preoperative staging with 11C-Choline PET/CT is adequately accurate in patients with very high-risk prostate cancer Clin Genitourin Cancer 2018; 16:305-312 e1
11 Saramatunga H, Montironi R, True L, et al International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens Working group 1: specimen handling Mod Pathol 2011; 24:6-15
12 Bianchi L, Gandaglia G, Fossati N, et al Pelvic lymph node dissection in prostate cancer: indications, extent and tailored approaches Urologia 2017; 84:9-19
13 Briganti A, Abdollah F, Nini A, et al Performance characteristics of computed tomography in detecting lymph node metastasis in contemporary patients with prostate cancer treated with extended pelvic lymph node dissection Eur Urol 2012; 61:1132-8
14 Balboaca SD Medical diagnostic tests: a review of test anatomy, phases and statistical treatment of data Comput Math Methods Med 2019; 2019:1891569
15 Stolzenbach LF, Knipper S, Mandel P, et al Oncological outcomes of pathologically organ-confined, lymph node-positive prostate cancer after radical prostatectomy Urol Oncol 2021; 39:234 e1234 e7
16 Hope T, Eiber M, Armstrong W, et al Diagnostic accuracy of 68Ga-PSMA-11 PET for pelvic nodal metastasis detection prior to radical prostatectomy and pelvic lymph node dissection JAMA Oncol 2021; 7:1635-1642
17 Hofman M, Lawrentschuk N, Francis RJ, et al Prostate specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a p
395:1208-1216
18 Farolfi A, Calderoni L, Mattana F, et al Current and emerging clinical applications of PSMA PET diagnostic imaging for prostate cancer J Nucl Med 2021; 62:596-604
19 Afaq A, Ell PJ, Bomanji JB Is it time to fund routine NHS usage of PSMA PET CT? Nucl Med Commun 2019; 40:975-979
Correspondence
Nuno Dias, MD (Corresponding Author) nunodiasds@gmail com
Gianmarco Colandrea,MD
colandrea gianmarco@hsr it
Lara Rodriguez-Sanchez rodriguezsanchezlara@gmail com
Yann Barbé
yann barbe@imm fr
Petr Macek, MD
petr macek@imm fr
Xavier Cathelineau, MD, PhD
xavier cathelineau@imm fr
Urology Department, Institut Mutualiste Montsouris, Paris (France)
42 Bd Jourdan; 75014 Paris (France)
Francisco Botelho, MD, MSCE
francisco botelho@gmail com
Urology Department, São João Hospitalar and University Center, Porto (Portugal)
405 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 PET-choline in
of prostate cancer
nodal staging
r o s p e c t i v e , r a n d o m i z e d , m u l t i - c e n t r e s t u d y L a n c e t 2 0 2 0 ;
Iacopo Meneghetti 1 , Demostene Giardino 2 , Riccardo Morganti 3 , Vincenzo Marino 2 , Filippo Menchini Fabris 2 , Riccardo Bartoletti 4 , Novello Pinzi 2
1 Urology Department, Ospedale Apuane, Massa, Italy;
2 Surgery Unit, Casa di Cura San Rossore, Pisa, Italy;
3 Section of Statistics, University of Pisa, Pisa, Italy;
4 Urology Department, University of Pisa, Pisa, Italy
Summary
Background: The aim of this study was to evaluate the outcomes of patients suffering prostate cancer (PCa) treated conservatively using 1064 nm laser energy for focal laser ablation (FLA) The patients included in the study were unsuitable for surgery or unwilling to receive external beam radiotherapy because they were afraid of the possible side effects of whole-gland therapies
Methods: This study included patients with a diagnosis of nonmetastatic PCa who underwent FLA using SoracteLiteTM system. Tissue ablation was performed at a fixed power of 5 W by the diode multichannel laser system EchoLaser X4 that uses laser light transmitted through optical fibres causing the target tissue to undergo irreversible thermal damage. Functional outcomes were evaluated with the International Prostatic Symptoms Score (IPSS) and 5-item version of the International Index of Erectile Function (IIEF-5) before the treatment and one year later
Results: Ten patients suffering non-metastatic PCa were included Four decided upon a conservative treatment because of reduced performance status and for six patients the procedure was chosen electively All patients underwent multiparametric magnetic resonance imaging at 3 and 12 months and eight out of ten patients underwent prostate biopsy at 6 months
Persistent disease was detected in 3 patients who underwent a second ablation In these patients at the biopsy following the second ablation none harbored residual disease. At follow-up, no patient suffered urinary incontinence requiring the use of pads No significant worsening in sexual potency measured with IIEF-5 (p = 0 356) or prostatic symptoms measured at IPSS (p = 0 462) were recorded comparing pre-treatment condition vs one-year follow-up Compared with baseline, prostate-specific antigen was significantly reduced at one-year follow-up (3 7 ± 1 1 vs 7 9 ± 4 1 ng/mL; p = 0 008)
Conclusions: Although whole gland therapies remain the gold standard treatment for PCa, our results indicate that the SoracteLiteTM system for focal laser ablation, as a very preliminary step, appears to offer a short-term oncologic control of PCa with negligible side effects
KEY WORDS: Focal laser ablation; Focal therapy; Prostate cancer; Prostate magnetic resonance imaging; Transperineal treatment
Submitted 10 September 2022; Accepted 23 October 2022
INTRODUCTION
Currently whole-gland therapy such as radical prostatectomy (RP) and external beam radiotherapy (EBRT) still represent the gold standard treatments for localized prostate cancer (PCa) Both treatments are effective but they can be burdened with procedure-related side effects such as urinary incontinence and erectile dysfunction (1, 2)
Nowadays there are well-established studies in support of prostate-sparing procedures in low-risk cancer, but the treatment indications have also expanded to small intermediate-risk and high-risk tumours, which are considered life-threatening (3-5)
Concerns have arisen about the focal treatment of a disease that has been found to be multifocal in 50-76% of patients (6) A high degree of genomic heterogeneity and a 13-26% Gleason Score heterogeneity have also been reported, even within the positive cores of prostate biopsy (7, 8)
In a therapeutic approach for PCa the concept of index lesion is therefore decisive Despite the multifocality and heterogeneous disease pattern inside the same gland, the index lesion represents the largest prostatic tumour with the highest histologic grade within the prostate This is likely to drive the biology of the patient’s disease In fact, the same genomic sequence has been found in metastatic lesions and in the index lesion within the prostate (9) Interestingly, despite being limited to one case, Haffner et al used the whole-genome sequencing and molecular analyses to characterize the lethal clone in a patient who died of PCa Surprisingly, the lethal clone arose from a small, relatively low-grade cancer focus in the primary tumour These findings highlighted le potential importance of investigate molecular prognostic and/or predictive markers to optimize the pathological evaluation and delineate clonal heterogeneity (10)
Laser interstitial thermotherapy performed by the diode multichannel laser system EchoLaser X4 is a transperineal percutaneous procedure named SoracteLiteTM that uses laser light transmitted through optical fibres to produce irreversible thermal damage of target tissue
The EchoLaser X4 system allows multifibre ablation management and provides planning software for optimization
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 406 ORIGINAL PAPER No conflict of interest declared
A single-operator experience using EchoLaser SoracteLiteTM for focal laser ablation of prostate cancer: One more arrow in the quiver for the conservative management of the disease
DOI: 10 4081/aiua 2022 4 406
of the ablation strategy It also supports the surgeon with planning for effective and safe needle positioning with respect to the tumour and critical structures to be spared Here, we present the results obtained from our updated single-surgeon prospective cohort of 10 patients with at least one-year follow-up after the use of 1064 nm laser energy for focal laser ablation (FLA) of PCa In this cohort we treated patients with only one lesion so as not to have to decide whether to treat the index lesion or also the other/s considered less aggressive/s
MATERIALS AND METHODS
Population characteristics
Between October 2019 and October 2020, 10 patients candidate to organ-sparing treatment for PCa were selected to undergo FLA using the SoracteLiteTM procedure
SoracteLiteTM for FLA treatment was offered to patients with no metastatic PCa, Gleason score ≤ 8, TNM stage T1c-T2cN0M0, prostate-specific antigen (PSA) ≤ 20 ng/mL, a single lesion with a concordant multiparametric magnetic resonance imaging (mpMRI), a tumour volume ≤ 20 mL and a good life expectancy All patients included in this study had a prostate volume smaller than 65 mL
The patients included in the study were unsuitable for surgery or unwilling to receive EBRT
It was fully explained to the patients that different focal therapies validated were available, but the patients, due to the trust acquired with our working group, choose the aforementioned approach that was presented as experimental Each case had been previously discussed in a m
l y w i t h t h e patient, who received written information on the benefits and risks of the procedure
Prior to the start of patient recruitment, the surgeon (NP) followed a training program, visiting centres with expertise in FLA with SoracteLiteTM technology to achieve proficiency in the main aspects of FLA (fibre positioning, energy dose, ablation strategy and ablation margin) Finally, a representative from the manufacturer of the device trained the surgeon and operating theatre staff on the use of SoracteLiteTM, and assisted the operator for the first 3 cases
Protocol and assessment of data
The study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments The confidentiality of patient data was guaranteed as the patients were entered into a database in the form of a number Following Institutional Review Board Commitee approval and registration of the protocol (0014161/2019), patients with localized PCa were prospectively recruited The informed consent was obtained from all patients for the use of their data
Pre-operative assessment
All the patients we followed had undergone mpMRI and transperineal prostate biopsy with systematic sampling of the prostate with 12 samples per side for a total minimum of 24 samples Six out of 10 patients underwent biopsy before the mpMRI, in the other 4 mpMRI was done before the biopsy In those patients in whom a mpMRI
was performed before the biopsy, two more samples were taken, targeted, as cognitive biopsy, in the area identified on mpMRI The inclusion of random samples was fundamental for us to exclude the presence of disease in areas not frankly suspicious on mpMRI We classified these patients as carriers of single lesion disease inasmuch the positive biopsy samples were found only in the area highlighted as suspicious on mpMRI All patients had undergone systematic PSA testing prior to diagnostic biopsy
In addition, a questionnaire for the evaluation of urinary symptoms and sexual function were administered to the patients before undertaking the therapeutic treatment
Technique
SoracteLiteTM for FLA consists of ultrasound-guided positioning of up to 4 applicators (depending on the tumour volume and shape) consisting of a 21-gauge Chiba needle (INTRODUCER, Elesta SpA, Calenzano, Italy) in whose lumen is inserted a 272-μm quartz optic fibre (Fiber Optic for PLA, Elesta SpA, Calenzano, Italy) The fibre tip protrudes 10 mm from the introducer tip The optic fibres are connected to a multisource laser system operating at 1064 nm (EchoLaser X4, ELESTA SpA, Calenzano, Italy) Each treatment is performed at a fixed power of 5 W, with the single illumination dose determined on a caseby-case basis according to the tumour size Additional laser fibres can be placed within the tumour volume at a mutual distance ranging from 5 to 10 mm in order to amplify the volume of necrosis obtained by simultaneous tissue irradiation and summative volumetric necrosis
Depending on the tumour size in the longitudinal direction, one or more consecutive illuminations are performed with a ‘pull-back’ technique (retraction of the needle-fibre kit by 5-10 mm) during the same treatment session For the same duration of illumination and dose of energy administered, the thermoablated area is always reproducible regardless of tissue properties and vascularity The anatomopathological study of a thermoablated tissue area showed that the necrotic area assumes an ellipsoid shape
The treatment ends when the total planned dose is delivered A single illumination dose ranges from 1200 J to 1800 J, which corresponds to an illumination time of 4 to 6 minutes In cases where a ‘pull-back’ maneuver is used, the illumination time doubles
A touch panel device (ESI, EchoLaser Smart Interface, Elesta SpA, Calenzano, Italy) can be connected to the auxiliary video output of a general ultrasound scanner and used for treatment planning ESI has a dedicated planning software that allows the visualization of needles insertion trajectories of the needle guide mounted on the US biplanar probe of the connected ultrasound This facilitates the insertion of regularly spaced multiple parallel needles simultaneously The treatment planning is crucial for the outcome of the treatment The ESI superimposes on the ultrasound image a graphical representation, consisting of guidelines for the needle trajectories and the depiction of two concentric closed perimeters, an external one for the size of safety distances and an internal one for the size of the ablation area
The size and position of both of these perimeters depend on the treatment parameters (dose, number of fibres, ‘pullback’) and the surgeon can simulate the best treatment strategy before needle insertion The planning ends when the
407 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 EchoLaser SoracteLiteTM for focal laser ablation of prostate cancer
u l t i d i s c i p l i n a r y m e e t i n g a n d e x t e n s
i v e
tumour is visualized within the internal closed perimeter and all critical structures (urethra, vascular bundle, sphincters, bladder wall and rectum) are located outside the external perimeter If required, it is possible to increase the distance from the rectum by injecting a 33% (w/v) glucose solution between the prostate and the rectum The goal of the planning phase of the procedure is to identify the point where the tip of the needle will be located, with respect to the area that will be ablated The ultrasound software associated with a directional template for guidance allows the placement of the laser fiber(s) in the index lesion with millimeter precision (Figure 1)
After an observation period of about one hour, a transrectal contrast enhanced ultrasonography to evaluate the extent of the coagulation zone is performed Patients are discharged the day of the procedure without a catheter

Follow-up, functional and oncological outcomes
All patients were advised to undergo a 6-monthly biopsy sampling, and mpMRI at 3 and 12 months
Complete response was defined on the basis of negative imaging study results and negative prostate biopsy at 6 months Persistent disease was defined as the presence of suspected or positive imaging study results and/or positive prostate biopsy performed at 6 months In case of persistent disease, a second ablation was planned
The International Prostatic Symptoms Score (IPSS) and 5-item
Patient characteristics.
On the left: EchoLaser Smart Interface settings during the planning phase The ablation area (dotted magenta line) is simulated in order to define the best approach in terms of number of fibres, mutual tip position, ‘pullback’ and energy dose The external circle (dotted cyan line) represents the safety distance to be assured with respect to critical structures (nerves, rectum)
On the right: two introducer needles are positioned in a parallel orientation according to the planning
version of the International Index of Erectile Function (IIEF-5) were completed by each patient prior to the procedure and at 1-year follow-up without changing the intake of any type of drug PSA was also confronted before treatment and at one-year follow-up
Intraoperative and postoperative complications were recorded according to Satava (11) and Clavien-Dindo (12), respectively
Statistical analysis
Categorical data were described by frequency; continuous data were expressed as mean and standard deviation
To compare data (IPSS, IIEF-5 and PSA) measured at baseline and after 12 months of follow-up, t-tests for paired data were applied Statistical significance was set at p < 0 05 and all analyses were carried out with SPSS Statistics version 27 0 (IBM Corp , Armonk, NY)
RESULTS
Patient characteristics are summarised in Table 1 A total of 10 patients suffering non-metastatic PCa were included in the present study FLA for PCa was selected as the initial treatment for the following reasons: reduced performance status (4 patients) and patient’s own choice (6 patients) At the diagnostic biopsy four patients suffered PCa Gleason 6 (3+3), two patients had Gleason 7 (3+4)
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
408
I Meneghetti, D Giardino, R Morganti, V Marino, F Menchini Fabris, R Bartoletti, N Pinzi
Table 1.
Patient number Age (years) Indication for FLA DRE PSA (ng/mL) GS Laterality Diameter of tumour at mpMRI (mm) PSA (ng/mL) (12 mo) 1 65 Elective + 7 3 6 Right 5 3 2 2 73 Elective - 5 1 6 Left 14 3 1 3 60 Elective - 5 1 6 Left 7 3 9 4 67 Unfit for surgery + 11 7 (4+3) Right 20 1.5 5 75 Elective - 5 2 8 (4+4) Left 9 3 6 6 69 Elective + 5 7 7 (3+4) Left 10 3 2 7 74 Unfit for surgery + 17 8 7 (4+3) Right 15 5 8 78 Elective + 10 1 7 (3+4) Right 15 5 2 9 73 Unfit for surgery - 6 8 7 (4+3) Left 11 4 1 10 70 Unfit for surgery + 4 9 6 Left 7 3 9 +: Suspicious -: Non-suspicious DRE: D g ta recta exam nation FLA: Focal laser ab ation GS: Gleason Score mpMRI: Mu tiparametr c magnetic resonance maging PSA: Prostate-spec fic antigen
1.
Figure
On the left: mpMRI T2-weighted sequences on the axial view showing a 7 mm carcinoma located in the left apical portion (arrowhead) in a 53-year-old patient before treatment
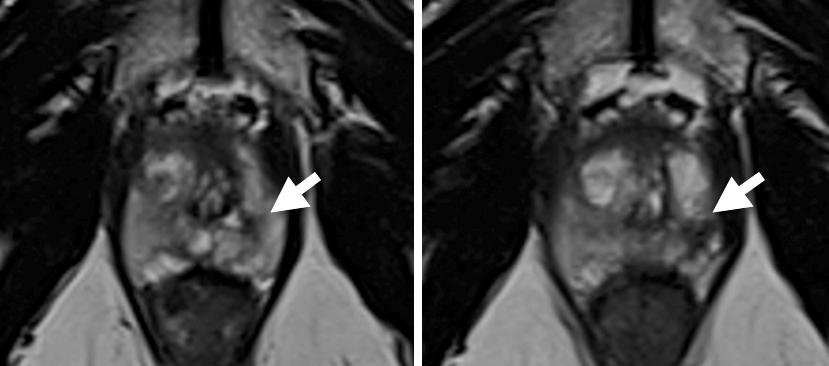
On the right: the same patient at 3-month follow-up after transperineal FLA
A hypointense area compatible with necrotic-coagulative necrosis (arrowhead) matching the previous tumoural area is visible on the mpMRI T2weighted image
and three Gleason 7 (4+3) Only one patient presented a Gleason 8 (4+4) disease
All patients underwent mpMRI at 3 and 12 months (Figure 2) Eight out of ten patients underwent prostate biopsy at 6 months Six patients in which the mpMRI did not highlight suspected lesions (PI-RADS category < 3) had negative biopsy results according to the scheme (12 samples per side with the addition of sampling in the area previously subjected to FLA) These patients were considered to have a complete response to treatment Three patients had a persistent disease according to positive (PIRADS category ≥ 3) mpRMI at 3 months Two of them underwent a prostate biopsy according to the scheme with additional samplings in the suspected area
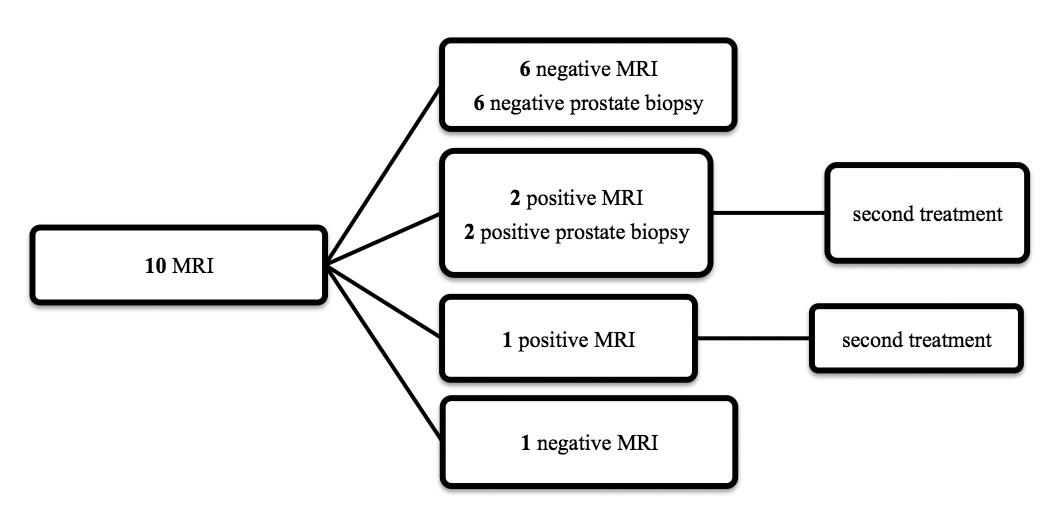
The pathology report revealed that those two patients still harbored PCa One of them refused to undergo prostate biopsy and agreed to directly receive a second treatment in the area of persistence of disease identified on mpMRI (PIRADS category 5)
The diagram in Figure 3 summarizes the diagnostic-therapeutic process of the entire cohort of patients in our study
The three aforementioned patients with persistent disease underwent a second ablation and at 12 months, mpMRI revealed no lesions with PI-RADS category > 3 All three patients underwent a transperineal prostate biopsy at 12 months that was negative for PCa
All the patients who required a second ablation had a disease > 10 mm at the first mpMRI
Two patients were unwilling to repeat the biopsy at 6 months One of them was the aforementioned patient who received directly a second treatment, the other one underwent a mpMRI at 6 and 12 months In the latter patient, a PI-RADS category 2 was found in the ablated area at mpMRI, compatible with a necrotic area
No complications related to diagnostic prostate biopsies were reported No patient developed extracapsular invasion (> cT3) or appearance of bone lesions or lymph node
swellings (> 1 cm) in the fields of inclusion on any mpMRI pelvic scan performed for primary diagnosis or follow-up at 6 months or 1 year No intraoperative complications were recorded according to the Satava classification system (11) Postoperatively four patients required analgesic drugs (Clavien-Dindo grade I)
At 1-year follow-up, no patient suffered urinary incontinence that required the use of pads Compared with baseline, no significant worsening in functional outcomes at 1 year was observed as measured with the IIEF-5 (p = 0 356) and IPSS (p = 0 462) (Table 2)
Table 2.
PSA (ng/ml), IPSS and IIEF-5 levels at baseline and after 12 months
IIEF: Internat onal Index of Erectile Funct on
Internat onal Prostate Symptoms Score
Prostate-specif c ant gen
409 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 EchoLaser SoracteLiteTM for focal laser ablation of prostate cancer
Factor Mean (SD) p-value PSA pre-treatment 7 9 (4 1) 0 008 PSA at 1 year follow-up 3 7 (1 1) IPSS pre-treatment 6 9 (3 1) 0 462 IPSS at 1 year follow-up 7 3 (4 1) IIEF-5 pre-treatment 11 1 (5 1) 0 356 IIEF-5 at 1 year follow-up 10 2 (6 7)
IPSS:
PSA:
Figure 2.
Figure 3.
Diagnostic-therapeutic process of the entire cohort of the 10 patients included in our study at follow-up
At 1 year follow-up, mean ± SD PSA was significantly reduced relative to baseline (3 7 ± 1 1 vs 7 9 ± 4 1 ng/mL; p = 0 008) (Table 1, Table 2 and Figure 4)
DISCUSSION
Conservative treatments aim to control the disease while minimizing the risk of developing side effects, primarily sexual impotence, urinary incontinence and bowel toxicity In fact, the possibility to treat only a targeted part of the gland reduces the risk of damage to the neurovascular bundles, external urethral sphincter, bladder neck or rectum
Our results regarding lower urinary tract symptoms (LUTS) and sexual function measured with IPSS and IIEF-5 did not demonstrate a statistically significant change one year after the treatment (p = 0 462 and p = 0 356 vs baseline, respectively) Our results are in agreement with Eggener et al , who found no worsening of IPSS symptoms in FLA-treated
patients Interestingly, however, these investigators found a worsening of sexual function at 1 month (p = 0 03) and 3 months (p = 0 05), although the difference vs baseline was not significant at 12 months (p = 0 38) (13) Also van Riel et al found a worsening of sexual function at 1 week after the procedure, although the difference vs baseline was not significant at 1 month (14) Moreover, Chao et al in their experience using FLA for localized PCa found no adverse impact on LUTS or sexual function at 1 year (15) The presence of an expert technician for the device alongside the surgeon during the first cases is essential to reduce the initial learning curve and thus to improve safety of the procedure (16) Regarding the learning curve in using SoracteLiteTM, we believe that it is comparable to the training required for transperineal prostate biopsy, so that in the hands of an expert urologist, the use of the SoracteLiteTM procedure is quite simple
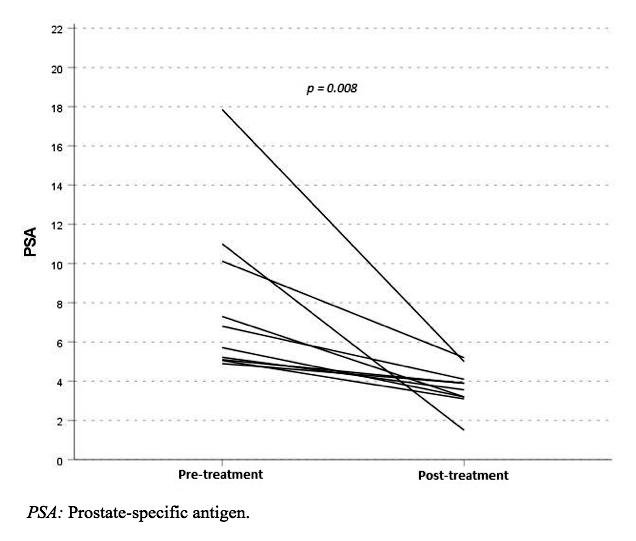
Another strength of our study is the fact that all the procedures were performed by a single operator with extensive experience of the transperineal approach, and without the potential confounder of inter-operator differences
The urologist (NP) who performed all the procedures in
g transperineal prostate biopsies To date, it is far more common to perform prostate biopsies via the transrectal access (17), so for the urologist who approaches the use of SoracteLiteTM for FLA it would be advisable to first acquire some biopsy experience with a transperineal access before engaging in ablative treatment We believe that for the urologist experienced in transperineal access, three procedures are sufficient to complete the learning process and carry out adequate treatments
Although our results and the overall literature are too preliminary to determine with adequate accuracy any possible advantage or disadvantage regarding the use of SoracteLiteTM for the treatment of PCa, we believe that an extraordinary advantage of the method is the ability to evaluate one hour later the effect on the tissue and to be able, in the same session, to expand the ablation in the desired area if this is not satisfactory (Figure 5)
On the left: transverse ultrasound image during ablation
On the right: longitudinal ultrasound image of the same tumour during ablation phase Coagulated tissue appears as a hypoechoic area overlapped by gas artefacts (arrowhead)

Archivio Italiano di Urologia e Andrologia 2022; 94, 4
410
I Meneghetti, D Giardino, R Morganti, V Marino, F Menchini Fabris, R Bartoletti, N Pinzi
o u r s t u d y h a d e x t e n s i v e e x p e r i e n c e i n p e r f o r m i n
Figure 4. Ladder plot illustrating individual changes in PSA from pre-treatment (at baseline) to post-treatment (12 months)
Figure 5
Similar to other authors who have approached PCa with focal therapy for PCa, no patient in our cohort needed pads or complained of urinary incontinence after the treatment (18) This represents an outstanding success, as incontinence is statistically the most bothersome side effect of RP with an incidence that in some series reaches 65% (19) Even approaches such as EBRT or brachytherapy, which are considered less invasive, are burdened with considerable rates of worsening of urinary obstruction, irritation and worsened bowel symptoms (2) One year after the procedure, a statistically significant reduction in PSA was observed compared with baseline (p = 0 008) Although three of the patients who had residual disease at 6 months prostate biopsy underwent a second ablation before 12 months, a reduction in PSA was evident for each patient in our cohort (Figure 4) In contrast to our results, Chao et al , reporting oncological and functional outcomes for 34 men who had undergone FLA for PCa, found that PSA was a poor discriminator of disease recurrence in the ablated zone at two-year follow-up (15) None of our patients had a PSA > 20 ng/mL at diagnosis, which, as a single factor for D'Amico's criteria, would place the case into a high-risk category While there is no clear indication on the use of both PSA and PSA-density as eligibility criteria for FLA (20), it is often suggested to consider PSA ≤ 15 ng/mL as a limit for a patient's suitability for focal therapy (21) The only patient who presented with Gleason Score 8 disease was a patient who wished to undergo some kind of treatment but was con-
because of age and comorbidities
In three patients, disease was persistent after the first FLA procedure and in all three cases the disease was present in the same area at follow-up This is likely related to inaccuracy in pinpointing the entire lesion during the first procedure Our results suggest that the treatment of lesions > 10 mm could be less accurate and require a second-look The disadvantage of not achieving complete disease ablation at the first attempt, especially in more aggressive diseases, could potentially give the disease the chance to progress
In a study of ultrasound-guided laser ablation in the thyroid gland of a porcine model, Ridouani et al concluded that 3 W/1800 J was the optimal setting to obtain a coagulated necrotic zone of 10 mm with 2 mm margin when utilizing a single needle (22) In our cohort of patients, the energies used were greater and for a single treatment were not lower than 5 W/3600 J
Other clinicians who used the SoracteLiteTM system for benign prostatic hyperplasia used a power of 3W for tissue ablation (23) We chose to use greater ablation power for tumour tissue with the aim of greater certainty in disease ablation In fact, higher powers reduce the duration of the initial phase of heating which can be affected by local tissue properties, and therefore trigger the ablation phase very quickly This leads to lower interpatient variability of treatment outcomes In the case of larger lesions, depending on the tumour shape with respect to the needle insertion direction, a ‘pull-back’ maneuver was carried out (needle retraction and second energy dose delivery) or a second fibre was placed in a parallel way with respect to the first one and simultaneous energy delivery was performed
There are some limitations to our study Firstly, the small number of patients limits the robustness of our results, especially those concerning cancer control Secondly, follow-up in this study was limited to one year Therefore, while our data on functional outcome are interesting, the oncological results still need to be validated with a longer follow-up
Finally, our data are not sufficient by themselves to formulate an indication for SoracteLite FLA in PCa, especially since this is a non-randomized series without a strict exclusion criterion for class of risk
Our study highlights important opportunities for future work It would be interesting to carry out a comparative study for functional and oncological results, standardizing it with patients in the same class of risk, comparing different conservative approaches for the treatment of PCa Furthermore, to evaluate the possibility of adopting this technique on a large scale it would be useful to involve both experienced and novice operators to evaluate the feasibility of this technique in therapeutic practice
CONCLUSIONS
Our results confirm that SoracteLiteTM for FLA treatment is an interesting emerging technology for the treatment of PCa As is the case for other conservative approaches, it must find its place in the landscape of treated patients Safety profiles and functional and oncological results are promising; however, long-term follow-up results are not yet available Additional prospective, multicenter studies are awaited to confirm our results
REFERENCES
1 Boorjian SA, Eastham JA, Graefen M, et al A critical analysis of the long-term impact of radical prostatectomy on cancer control and function outcomes Eur Urol 2012; 61:664-75
2 Chen RC, Basak R, Meyer AM, et al Association Between Choice o f R a d i c a l P r o s t a t e c t o m y , E x t e r n a l B e a m R a d i o t h e r a p y , Brachytherapy, or Active Surveillance and Patient-Reported Quality of Life Among Men With Localized Prostate Cancer JAMA 2017; 317:1141-1150
3 Prepelica KL, Okeke Z, Murphy A, et al Cryosurgical ablation of the prostate: high risk patient outcomes Cancer 2005; 103:1625-30
4 Bass R, Fleshner N, Finelli A, et al Oncologic and Functional Outcomes of Partial Gland Ablation with High Intensity Focused Ultrasound for Localized Prostate Cancer J Urol 2019; 201:113-119
5 Guenther E, Klein N, Zapf S, et al Prostate cancer treatment with Irreversible Electroporation (IRE): Safety, efficacy and clinical experience in 471 treatments PLoS One 2019; 14:e0215093
6 Djavan B, Susani M, Bursa B, et al Predictability and significance of multifocal prostate cancer in the radical prostatectomy specimen Tech Urol 1999; 5:139-42
7 Løvf M, Zhao S, Axcrona U, et al Multifocal Primary Prostate Cancer Exhibits High Degree of Genomic Heterogeneity Eur Urol 2019; 75:498-505
8 Porpiglia F, De Luca S, Passera R, et al Multiparametric Magnetic Resonance/Ultrasound Fusion Prostate Biopsy: Number and Spatial Distribution of Cores for Better Index Tumor Detection and Characterization J Urol 2017; 198:58-64
411 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 EchoLaser SoracteLiteTM for focal laser ablation of prostate cancer
s i d e r e d u n s u i t a b l e f o r o t h e r t h e r a p e u t i c t r e a t m e n t s
I Meneghetti, D Giardino, R Morganti, V Marino, F Menchini Fabris, R Bartoletti, N Pinzi
9 Liu W, Laitinen S, Khan S, et al Copy number analysis indicates monoclonal origin of lethal metastatic prostate cancer Nat Med 2009; 15:559-65
10 Haffner MC, Mosbruger T, Esopi DM, et al Tracking the clonal origin of lethal prostate cancer J Clin Invest 2013; 123:4918-22
11 Satava RM Identification and reduction of surgical error using simulation Minim Invasive Ther Allied Technol 2005; 14:257-61
12 Dindo D, Demartines N, Clavien PA Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey Ann Surg 2004; 240:205-13
13 Eggener SE, Yousuf A, Watson S, et al Phase II Evaluation of Magnetic Resonance Imaging Guided Focal Laser Ablation of Prostate Cancer J Urol 2016; 196:1670-1675
14 van Riel LAMJG, van Kollenburg RAA, Vis AN, et al Safety and Feasibility of Soractelite Transperineal Focal Laser Ablation for Prostate Cancer and Short-term Quality of Life Analysis from a Multicenter Pilot Study Eur Urol Open Sci 2022; 39:48-54
15 Chao B, Llukani E, Lepor H Two-year Outcomes Following Focal Laser Ablation of Localized Prostate Cancer Eur Urol Oncol 2018; 1:129-133
16 Brunckhorst O, Volpe A, van der Poel H, et al Training, Simulation, the Learning Curve, and How to Reduce Complications in Urology Eur Urol Focus 2016; 2:10-18
17 Tamhankar AS, El-Taji O, Vasdev N, et al The clinical and financial implications of a decade of prostate biopsies in the NHS: analysis of Hospital Episode Statistics data 2008-2019 BJU Int 2020; 126:133-141
18 Lepor H, Llukani E, Sperling D, et al Complications, Recovery, and Early Functional Outcomes and Oncologic Control Following In-bore Focal Laser Ablation of Prostate Cancer Eur Urol 2015; 68:924-6
19 Alivizatos G, Skolarikos A Incontinence and erectile dysfunction following radical prostatectomy: a review ScientificWorldJournal 2005; 5:747-58
20 van Luijtelaar A, Greenwood BM, Ahmed HU, et al Focal laser ablation as clinical treatment of prostate cancer: report from a Delphi consensus project World J Urol 2019; 37:2147-2153
21 Wenger H, Yousuf A, Oto A, et al Laser ablation as focal therapy for prostate cancer Curr Opin Urol 2014; 24:236-40
22 Ridouani F, Tuttle RM, Ghosn M, et al Ultrasound-Guided Percutaneous Laser Ablation of the Thyroid Gland in a Swine Model: Comparison of Ablation Parameters and Ablation Zone Dimensions Cardiovasc Intervent Radiol 2021; 44:1798-1806
23 Pacella CM, Patelli G, Iapicca G, et al Transperineal laser ablation for percutaneous treatment of benign prostatic hyperplasia: a feasibility study Results at 6 and 12 months from a retrospective multi-centric study Prostate Cancer Prostatic Dis 2020; 23:356-363
Correspondence
Iacopo Meneghetti, MD (Corresponding Author) iacopo meneghetti@tiscali it
Urology Department, Ospedale Apuane, Massa (Italy)
Demostene Giardino, MD demosteneg@libero it
Vincenzo Marino, MD
vincenzo mar@tiscali it
Filippo Menchini Fabris, MD menchinifabris@andrologia it
Novello Pinzi, MD pinzinovello@gmail com
Surgery Unit, Casa di Cura San Rossore, Pisa (Italy)
Riccardo Morganti, MD
r morganti@ao-pisa toscana it
Section of Statistics, University of Pisa, Pisa (Italy)
Riccardo Bartoletti, MD riccardo bartoletti@unipi it
Urology Department, University of Pisa, Pisa (Italy)
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
412
A single center 10-year experience
1 Urology Department, Institut Mutualiste Montsouris, Paris, France;
2 Urology Department, São João Hospitalar and University Center, Porto, Portugal;
3 Unit of Urology, Division of Experimental Oncology, URI Urological Research Institute, IRCCS San Raffaele Scientific Institute, Vita-Salute San Raffaele University, Milan, Italy
Summary
Objectives: Focal therapies (FTs) are promising techniques for the treatment of localized prostate cancer We assessed the medium-term oncological outcomes of intermediate-risk prostate cancer (PCa) treated with HIFU or cryotherapy
Materials and methods: One-hundred and fifty consecutive patients with intermediate-risk PCa, treated between 2009 and 2018 at a single center were included. Primary study outcome was failure-free survival (FFS), defined as absence of additional treatment, systemic progression or prostate cancer related death
Results: Thirty-seven (25%) patients underwent cryotherapy and 113 (75%) HIFU Median age was 69 (IQR 62-72) years, with 36 (24%) presenting palpable disease on rectal examination, and median total PSA of 7 85 (IQR 5 75-10 62) ng/mL
Patients were followed for a median of 61 (IQR 48-82) months FFS at 2 and 4 years was of 75 6% and 53 6%, respectively
Survival from whole gland or systematic treatment at 2 and 4 years was of 78 9% and 53 9%, respectively
Patients with FFS presented lower total PSA nadir (1 89 vs 3 25 ng/mL, p < 0 001), higher % PSA reduction at 3 months (66 1% vs 49 3%, p < 0 001), and at nadir (75 5% vs 55 8%, p < 0 001) Other characteristics such has the treatment modality, age, prostate size, initial total PSA, cT stage, International Society of Urological Pathology (ISUP), tumor location and biopsy results by region did not differ between patients failing and not failing FT. Complications were uncommon (13%), with only onr (1%) patient having Clavien-Dindo grade > II No deaths due to treatment were registered.
Conclusions: At medium-term, FTs for intermediate-risk PCa presented good oncological results, with an excellent safety profile
KEY WORDS: Prostatic neoplasms; Cryotherapy; Focal therapy; Ablation
Submitted 21 October 2022; Accepted 30 October 2022
INTRODUCTION
Current standard treatment options for localized prostate cancer (PCa) include active surveillance and radical treatment (surgery or radiotherapy) (1), which has been known to have negative impacts on quality of life (2) ProtecT trial results (3), first published in 2014, have
shown that active monitoring of PCa would achieve a similar overall survival as radical treatment, while enduring less treatment related side-effects (2) However, in this same cohort, Active Surveillance (AS) had a higher risk of disease progression and of metastatic disease (3)
If for low-risk PCa, AS is looked at as the mostly consensual choice, for intermediate-risk PCa, focal therapies (FTs) are being studied in an attempt to allow a treatment that assures less morbidity while allowing acceptable oncological outcomes The improvement in imaging modalities, mainly the MRI, has allowed to improve diagnostic accuracy and localization of regions of interest for directed treatment, which allows FT to be considered in selected patients (4)
Despite being considered experimental treatments, FTs are viewed by some as a potential treatment choice for intermediate-risk PCa with a favorable safety profile (5) Our goal was to describe medium-term oncological outcomes for patients with intermediate-risk localized PCa treated primarily with High-Intensity Focused Ultrasound (HIFU) or Cryotherapy
METHODS
We conducted an observational, single-center, cohort study, evaluating data on all consecutive patients undergoing FT (HIFU or cryotherapy) for intermediate-risk localized PCa
Patients were included if they fulfilled the following criteria: > 18 years, treatment naïve for PCa at the moment of FT, multi-parametric Magnetic Resonance (mpMRI) and subsequent biopsy, diagnosis of intermediate-risk localized PCa having primary FT (either HIFU or Cryotherapy) between the years 2009 and 2018 Patients were excluded if: no mpMRI was performed by any reason or if they had hormonal therapy as a bridge for FT Using these criteria, we identified 150 patients after querying our continuously maintained institutional database
Definitions
We defined intermediate-risk PCa as per the current NCCN Prostate Cancer Guidelines (6): at least one of the intermediate-risk factors – cT2b-cT2c, Gleason Grade
413 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
No conflict of interest declared
ORIGINAL PAPER
Medium-term oncological outcomes of intermediate-risk prostate cancer treated with HIFU or cryotherapy.
Nuno Dias 1, 2 , Lara Rodriguez-Sanchez 1 , Gianmarco Colandrea 1, 3 , Petr Macek 1 , Xavier Cathelineau 1
DOI: 10 4081/aiua 2022 4 413
Group 2-3, total PSA 10-20 ng/mL; without having high or very high-risk factors – any of cT3+, Gleason Grade Group 4-5, PSA ≥ 20 ng/mL or >4 cores with Gleason Grade Group 4 or 5 We further stratified patients between the categories of favorable intermediate (all of the following: having 1 intermediate-risk factor, Gleason Grade Group 1 or 2, and < 50% of biopsy cores positive) and unfavorable intermediate-risk (at least one of the following criteria: having 2 or 3 intermediate-risk factors, Gleason Grade Group 3, and ≥ 50% of biopsy cores positive) prostate cancer
Clinically significant prostate cancer (csPCa) was defined as Gleason Grade Group [or International Society of Urological Pathology (ISUP) Grade] ≥ 2
Data collection
Data was collected from our continuously updated database and patient records We recorded age at time of treament, pre-operative total PSA, clinical T staging, prostate volume, initial mpMRI results, initial biopsy results, date of FT and type of FT performed We obtained follow-up data including total PSA values, MRI and biopsies results We registered if patients developed disease biochemical, imagiological and histological recurrences; if there was a need for subsequent treatment and its indication, overall survival, prostate cancer specific survival and last followup date
Procedures
Multi-parametric MRI was performed at community centers If there was a disagreement between radiologist and urologist interpretation, it was reviewed with an in-house urologist specialized in uro-oncological imaging, and repeated if advised
Prostate biopsies were performed in our center, transrectally, with a 12-core systematic biopsy and 2-4 targeted samples being obtained from suspicious lesions, defined as score Prostate Imaging Reporting & Data System (PIRADS) ≥ 3
Among patients with suspicious lesions on imaging, 3 regions of interest were considered Target zone cancer was considered when PCa was identified on the targeted samples obtained from suspicious MRI lesions Near target zone cancer was considered when PCa was identified on randomized samples obtained from a region adjacent to the suspicious lesion location Away from target zone cancer was considered when PCa was identified on randomized samples obtained from a region not adjacent to the suspicious lesion location
Cryotherapy (n = 37) was performed using the various devices, using a previously described standard technique (7), for all cases
HIFU was performed using Ablatherm® Fusion (EDAP) (n = 29) and Focal One® (EDAP) (n = 84), through an evolving technique (8), until arriving at what we use today
After an initial learning period, the energy to use was typically chosen based on lesion location, with cryotherapy being preferred for anterior tumors and HIFU for peripheral tumors
In patients with well delimited lesions on MRI and no extra-lesion csPCa disease we performed uniquely a targeted FT Patients with MRI lesions and ipsilateral peri-
lesion csPCa disease on systematic biopsy, we performed targeted FT with a widened field Patients with MRI lesions and ipsilateral csPCa disease on systematic biopsy cores non-adjacent to the lesion site, we performed hemiablation
Patients with bothering emptying symptoms underwent TUR-P in the 2 weeks prior to the FT procedure
Study outcomes
Primary study outcome was Failure Free Survival (FFS), defined as absence of additional gland-directed (being focal or radical) or systemic treatment, metastatic disease or PCa related death
Other study outcomes included biochemical recurrence free survival, metastasis free survival, overall survival, adverse events and complications classified by the Clavien-Dindo system
Follow-up
The recommended follow-up strategy consisted in performing PSA measurements every 3 months during the 1st year after treatment and every 6 months thereafter, performing mpMRI 1 month and 1, 2 and 3 years after treatment and performing control biopsies 1, 2 and 3 years after FT Additional repeat MRI and biopsies were performed if clinically judged indicated, based on various criteria If patients declined to perform imaging and/or biopsies, they would remain in surveillance based on total PSA measurement alone, on a 3-6 months basis
Treatment failure was considered when a patient was submitted to any additional PCa directed treatment, apart from complementary FT during the first 3 months after initial treatment Patients were classified as having biochemical recurrence using the PHOENIX criteria (4)measurement of total PSA higher than nadir total PSA + 2 ng/mL In patients with recurrent or persistent disease, treatment was decided on a case-by-case basis
Statistics
Statistical analysis was performed with IBM® SPSS® v27 software Categorical variables are presented as frequencies and percentages, and were compared using Chisquared analysis or Fisher’s Exact Test, as appropriate C o n t i n u o u s v a r i a b l e s a r e p r e s e n t e d a s m e a n s a n d interquartile ranges (IQR), and were compared using nonparametric Mann-Whitney U tests Statistically significance was set as p < 0 05 All reported p values are twosided Kaplan-Meier survival curves were calculated for failure-free survival according to described variables Logrank test was used to calculate for difference between groups Patients with peri-treatment transurethral prostate resection (TUR-P) were excluded from total PSA reduction analysis
The study has received approval from the local Ethics Committee, and all research was conducted respecting the latest version of Helsinki’s declaration Patients were provided information on their PCa disease and available standard treatment modalities (active surveillance, radical prostatectomy, radiotherapy), that FTs were not standard of care and have chosen FT as their desired treatment choice They provided consent agreeing to participate in this research on FT oncological results
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
414
N Dias, L Rodriguez-Sanchez, G Colandrea, P Macek, X Cathelineau
RESULTS
Pre-treatment patient characteristics
Among 150 patients with intermediate-risk PCa, 37 (25%) underwent cryotherapy and 113 (75%) HIFU (Table 1)
The median age was 69 (IQR 62-72) years, with 114 (76%) patients having no palpable disease on digital rectal examination Median total PSA was of 7 85 (IQR 5 75-10 62) ng/mL, with 46 (31%) of patients having an initial total PSA between 10-20 ng/mL and none higher than 20 ng/mL The mean prostate volume was 40 (IQR 35-48) mL
Regarding NCCN risk groups, 117 (78%) patients had intermediate favorable PCa and 33 (22%) intermediate
unfavorable PCa; 37 (25%) presented with ISUP 1, 109 (73%) with ISUP 2 and 4 (3%) with ISUP 3 PCa A total of 115 (77%) patients had suspicious lesions present on mpMRI
When analyzing biopsy results by region among the 126 (84%) patients with suspicious lesions on MRI: 93 (74%) had csPCa - 46 (37%) had csPCa only on suspicious lesions; 31 (25%) had csPCa on suspicious lesions and lesion-adjacent systematic biopsy cores; 8 (6%) had csPCa only on lesion-adjacent systematic biopsy cores; 4 (3%) had csPCa only on non-lesion-adjacent systematic biopsy cores; 3 (2%) had csPCa on suspicious lesions, lesion-adjacent and non-lesion-adjacent systematic biopsy cores; 1 (1%) had csPCa on lesion-adjacent and nonlesion-adjacent systematic biopsy cores but not on suspicious lesions; 0 (0%) had csPCa on suspicious lesions and non-lesion-adjacent systematic biopsy cores
Primary outcome - Failure free survival
Patients were followed for a median time of 61 (IQR 48-82) months Over all treated patients, the FFS at 2, 4, 5 and 7 years was of 75 6%, 53 6%, 42 1% and 27 3%, respectively Survival from whole gland or systematic treatment at 2 and 4 years was of 78 9% and 53 9%, respectively
Table 2 lists studied factors and their association with the need of additional treatment
Table 2.
Patients’ characteristics according to necessity of salvage treatment and univariate analysis
* Exams performed before PI-RADS classification v1 was pub ished
** Results tak ng into consideration 126 patients with MRI susp c ous for prostate cancer
415 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Intermediate-risk prostate cancer treated with HIFU or cryotherapy
Characteristics Value (n = 150) Treatment, n (%) Cryotherapy 37 (25) HIFU 113 (75) Treatment year, n (%) 2009-2012 22 (15) 2013-2015 65 (43) 2016-2018 63 (42) Age, Median (IQR) 69 (62-72) Prostate volume (mL), Median (IQR) 40 (35-48) Total PSA (ng/mL), Median (IQR) 7 85 (5 75-10 62) Initial total PSA < 10 ng/mL, n (%) 104 (69) Initial total PSA 10-20 ng/mL, n (%) 46 (31) cT stage, n (%) cT1c 114 (76) cT2a 18 (12) cT2b 13 (9) cT2c 5 (3) Biopsy overall ISUP Grade, n (%) 1 37 (25) 2 109 (73) 3 4 (3) NCCN risk group, n (%) Intermediate favorable 117 (78) Intermediate unfavorable 33 (22) PI-RADS score 1-2 24 (16) Suspicious MRI, with no PI-RADS score * 11 (7) 3 27 (18) 4 65 (43) 5 23 (15) Biopsy results by region, n (%) ** csPCa @ suspicious lesion(s) 80 (63) csPCa @ lesion-adjacent systematic biopsy cores 43 (34) csPCa @ non-lesion-adjacent systematic biopsy cores 8 (6) Tumor per specific locations, n (%) Anterior zone 16 (11) Apex 23 (15) Base 51 (34) Bilateral 11 (7) If peri-treatment TUR-P, n (%) 21 (14) Total PSA nadir (ng/mL), Median (IQR) 2 52 (1 59-4 51) Time to PSA nadir (months), Median (IQR) 3 0 (3 0-9 8) PSA % reduction, Median (IQR) @ 3 months 55 (39-72) @ nadir 62 (45-78)
Table 1. Patient clinical characteristics.
Characteristics Failure free Non-Failure free Univariate (n = 53) (n = 97) P-value Treatment, n (%) 0.553 Cryotherapy 15 (28) 22 (23) HIFU 38 (72) 75 (77) Age, Median (IQR) 66 (61-2) 69 (63-74) 0 245 Prostate volume (mL), Median (IQR) 41 0 (35 0-47 0) 40 0 (34 0-50 0) 0 835 Total PSA (ng/mL) 0 580 Initial tPSA < 10 ng/mL, n (%) 35 (66) 69 (71) Initial tPSA 10-20 ng/mL, n (%) 18 (34) 28 (29) cT stage, n (%) 1 000 cT1c 40 (75) 74 (76) cT2a-c 13 (25) 23 (24) Biopsy overall ISUP Grade, n (%) 0 436 1 16 (30) 21 (22) 2 35 (66) 74 (76) 3 2 (4) 2 (2) NCCN risk group, n (%) 0 542 Intermediate favorable 43 (81) 74 (76) Intermediate unfavorable 10 (19) 23 (24) Tumor per specific locations, n (%) Anterior zone 8 (15) 8 (8) 0 268 Apex 11 (21) 12 (12) 0 235 Base 15 (28) 36 (37) 0 287 Bilateral 5 (9) 6 (6) 0.520 Total PSA nadir (ng/mL), Median (IQR) 1 89 (0 96-2 81) 3 25 (1 93-5 68) < 0 001 Time to PSA nadir (months), Median (IQR) 6 (3-12) 3 (3-6) < 0 001 PSA % reduction, Median (IQR) @ 3 months 66 1 (53 1-78 3) 49 3 (26 9-63 4) < 0 001 @ nadir 75.5 (61.6-84.7) 55.8 (36.6-68.0) < 0.001 If PSA % reduction @ 3 months, n (%) > 30% 38 (97) 55 (72) 0 002 > 50% 31 (79) 36 (47) < 0 001 > 70% 18 (34) 13 (17) < 0 00
N Dias, L Rodriguez-Sanchez, G Colandrea, P Macek, X Cathelineau
Patients who needed additional treatment were more likely to have higher total PSA nadir (3 25 vs 1 89 ng/mL, p < 0 001), lower time to PSA nadir (3 vs 6 months, p < 0 001), lower total PSA reduction at 3 months (49 3% vs 66 1%, p < 0 001), lower total PSA reduction at nadir (55 8% vs 75 5%, p < 0 001) Other characteristics such has the treatment modality, age, prostate size, initial total PSA, cT stage, ISUP, NCCN risk group, tumor location and biopsy results by region did not differ between patients failing and not failing FT
Kaplan Meier-analysis showed a significant difference for PSA reduction > 70% (log-rank test p = 0 002) (Figure 1a), but not for initial total PSA (log-rank test = 0 915) (Figure 1b), ISUP grade (log-rank test = 0 560) (Figure 1c) or NCCN sub-risk group (log-rank test = 0 676) (Figure 1d) Other variables not presented also haven’t shown differences on the Kaplan-Meier analysis (treatment energy, age, prostate volume, clinical stage, csPCa locations and tumor location)
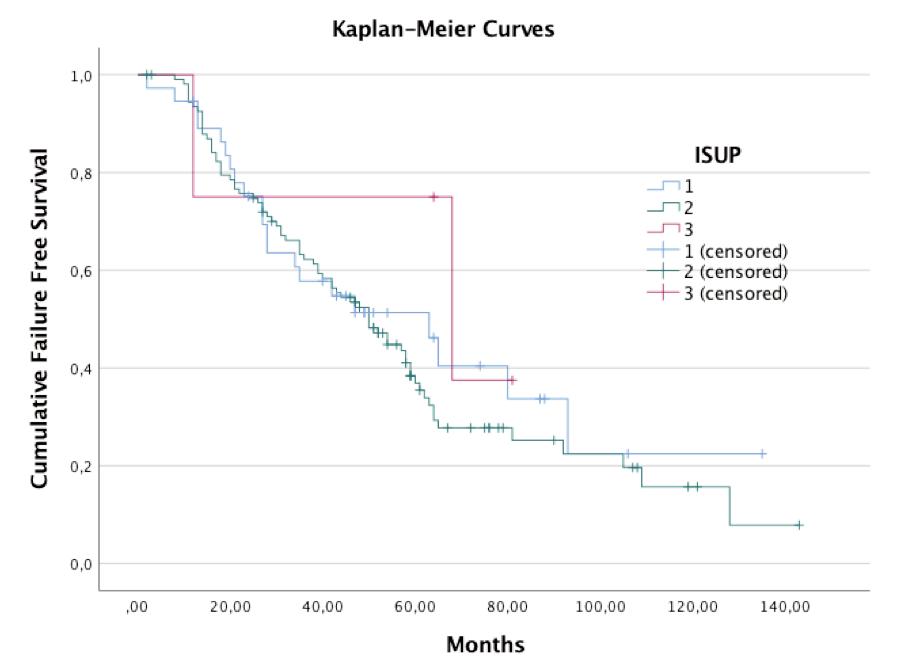

The additional selected treatment for the 97 (65%) patients who failed FT was radiotherapy + hormonal therapy in 37 (25%), radiotherapy in 6 (4%), radical prostatectomy in 16 (11%), hormonal therapy in 12 (8%),
Table 3.
Reasons for first additional treatment being performed
HIFU in 12 (8%), brachytherapy in 10 (7%) and cryotherapy in 4 (3%) Median time to additional treatment was of 45 5 (IQR 21 8-61 0) months Reasons for further treatment are presented on Table 3
Treatment complications
Nineteen (13%) patients presented treatment related complications One (1%) patient had a Clavien-Dindo
showing Failure Free Survival according to (a) PSA reduction > 70% at 3 months (log-rank test p = 0 002), (b) initial total PSA categories (log-rank test = 0 915), (c) ISUP grade (log-rank test = 0 560), and (d) NCCN sub-risk group (log-rank test = 0 676)

Kaplan-Meier

Archivio Italiano di Urologia e Andrologia 2022; 94, 4
416
for treatment Value (n = 150) ISUP 1 infield persistence + PSA and/or image progression 6 (4 0%) ISUP 2 infield persistence 3 (2 0%) New ISUP 1 outfield 5 (3 3%) New ISUP ≥ 2 outfield 20 (13 3%) Infield progression to ISUP 2 1 (0 7%) Infield progression to ISUP ≥ 3 13 (8 7%) ISUP 2 infield recurrence 14 (9 3%) In & Outfield ISUP ≥ 2 27 (18 0%) Biochemical recurrence +/- image progression 6 (4 0%)
Reason
a. b. c. d.
Figure 1.
analysis
grade I complication: hematuria needing hospitalization for continuous bladder irrigation Twelve (8%) patients had Clavien-Dindo grade II complications: 11 (7%) urinary retentions, 6 (4%) acute bacterial prostatitis, 3 (2%) acute orchitis, 1 (1%) intense perineal pain One (1%) patient had a Clavien-Dindo grade IIIb complication, a recto-cutaneous fistula needing colostomy No deaths due to treatment were registered
Biochemical recurrence after treatment
A total of 88 (59%) patients presented biochemical recurrence according to the Phoenix criteria, with median time to PSA failure of 24 0 months Patients with biochemical recurrence were younger than patients without biochemical recurrence (66 vs 70 years, p = 0 035) Other studied factors were not statistically different between patients with and without biochemical recurrence (Table 4)
Other follow-up data
Nadir total PSA was reached at a median time of 3 0 (IQR 3 0-9 8) months
MRI was performed at least once for 125 (83%) patients during the first 3 years; in 68 patients at 1 month and 79 at 1 year, being positive in 10 (15%) and 44 (56%) patients, respectively Control biopsies were performed at least once for 122 (81%) patients during the first 3 years; in 96 cases during the first year Presence of csPCa on
biopsy after treatment was detected in 79 (53%) patients; in 31 (21%) cases with csPCa only on previous treated area and/or its borders, 20 (13%) with only outfield csPCa and 28 (19%) in both infield and outfield areas Systemic progression was found in 10 (7%) patients, with 4 (3%) presenting with pelvic lymph node disease and 6 (4%) with other metastatic progression
Patients who developed metastatic disease were in 1 case a patient with initial total PSA of 12 1 ng/mL and highvolume ISUP 1 PCa, with total PSA of 16 4 ng/mL 3 months after HIFU, who had retroperitoneal metastasis on re-staging; and 5 cases of patients with initial total PSA > 10 ng/mL and csPCa, who had biochemical recurrence, underwent additional treatment, but had disease progression with metastasis detected 30-72 months after Three (2%) patients died during follow-up, both due to reasons unrelated to PCa
DISCUSSION
This study represents our experience as one of the first centers treating patients with intermediate-risk PCa with FTs, and shows our experience since the beginning of this practice As such, during this time period treatment instruments have evolved, patient selection criteria have been refined, and knowledge has improved
We report the oncological outcomes of 150 consecutive patients with intermediate-risk localized PCa treated with either cryotherapy (25%) or HIFU (75%) 144 patients were followed longer than 24 months, with a median follow-up time of 61 (IQR 48-82) months Although a big proportion of patients (65%) were submitted to additional treatments (with 71 in 97 of those cases being treated with whole-gland or systemic treatment), the median time of FFS was of 45 5 (IQR 21 8-61 0) months, which means that FT resulted in a substantial delay to radical treatment for a big proportion of patients The safety profile of the treatment was good, with only 1 patient having a complication Clavien-Dindo ≥ 3 Only 10 (7%) of patients presented disease progression, with 6 (4%) as metastatic disease, and there were no deaths related to PCa
It has the limitations of being a single center retrospective study, capturing patients during a long timeframe, in which treatment instruments, diagnostic methods, and disease comprehension has evolved We also note that the first cases included account to 2009 when FT treatments were undergoing their first discovery period In addition, since some patients referred to us for treatments come from other big distances their follow-up is sometimes changed to a local physician after an initial time of stable disease, leading to some early censoring of patients who have good outcomes These 2 factors may tilt our results to seem worse than current
practice
With the debate on FT for intermediate-risk disease still ongoing (9, 10), we believe gathering to be important in counseling patients who search for non radical treatment options; or wish to change from active surveillance to active treatment due to desire to act and fear of progression, which are reasons as common as common as disease progression (11, 12)
Regarding oncological safety, groups as the Imperial College London have reported on their experience On a propensi-
417 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Intermediate-risk prostate cancer treated with HIFU or cryotherapy
Table 4.
Characteristics Biochemical Biochemical Univariate recur rence free recur rence P-value (n = 62) (n = 88) Treatment, n (%) 0.702 Cryotherapy 14 (23) 23 (26) HIFU 48 (77) 65 (74) Age, Median (IQR) 70 (64-73) 66 (61-71) 0 035 Prostate volume (mL), Median (IQR) 40 5 (32 75-48 25) 40 (35-49 25) 0 782 Total PSA (ng/mL) 1.000 Initial tPSA < 10 ng/mL, n (%) 43 (69) 61 (69) Initial tPSA 10-20 ng/mL, n (%) 19 (31) 27 (31) cT stage, n (%) 0 442 cT1c 45 (73) 69 (78) cT2a-c 17 (27) 19 (22) Biopsy overall ISUP Grade, n (%) 0 699 1 17 (27) 20 (23) 2 44 (71) 65 (74) 3 1 (2) 3 (3) NCCN risk group, n (%) 0 165 Intermediate favorable 52 (84) 65 (74) Intermediate unfavorable 10 (16) 23 (26) Tumor per specific locations, n (%) Anterior zone 8 (13) 8 (9) 0 592 Apex 9 (15) 14 (16) 0 824 Base 16 (26) 35 (40) 0 083 Bilateral 3 (5) 8 (9) 0 365 Total PSA nadir (ng/mL), Median (IQR) 2 28 (1 02-4 19) 2 73 (1 80-4 65) 0 085 Time to PSA nadir (months), Median (IQR) 5 (3-11) 3 (3-8) 0 580 PSA % reduction, Median (IQR) @ 3 months 57 14 (43 24-76 28) 55 43 (37 56-68 70) 0 517 @ nadir 64.16 (46.97-79.06) 62.16 (42.58-77.13) 0.522
Patients’ characteristics according to biochemical recurrence free survival and univariate analysis
ty-score matched study (13) comparing oncological outcomes between patients who underwent FT or radical prostatectomy at their center, they report a FFS (95% CI) at 3, 5 and 8 years of 86% (81-91%), 82% (77-88%) and 79% (73-86%) for radical prostatectomy and of 91% (8795%), 86% (81-92%) and 83% (76-90%) after FT (p = 0 12) Their report shows similar oncological outcomes between both modalities However, this was a retrospective study and the groups compared after matching included 38 2% and 37 0% patients with ISUP 1 PCa
Recently, Reddy et al (14) published the largest reported cohort on FT: a multi-center study including 1379 men undergoing HIFU for localized PCa treatment, with 66% in the intermediate-risk group They reported an overall FFS rate of 69% at 7 years Of note is that in their protocol, a second HIFU treatment regardless of timing is allowed and was performed in 252 patients, placing the re-treatment free survival at 7 years at 43% For intermediate-risk patients, they report a FFS of 83% at 5 years, and 68% at 7 years In this study, no patients developed metastasis or died due to PCa, and 7 (0 5%) patients had complications with Clavien-Dindo score > 2 (14) Their nominal FFS was higher than in our current report since the 2 year time-frame However, we note that the authors allowed for a second FT without considering a treatment failure, and their retreatment-free survival at 7 years was of 49% and the whole-gland or systemic treatment survival at 7 years was of 78%, which is also above our reported values Complications were in line with our current study, with serious events being rare In a multi-center study including 703 men with low or intermediate-risk PCa receiving FT, % PSA reduction was found to be an independent predictor of any additional treatment, with FFS at 5 years of approximately 70%, 50% and 20%, for % PSA reductions of 0%, 50%, and close to 100%, respectively (15) The same association was found in our study, with this factor seeming a possible measure that can help setting up an adequate follow-up strategy and counseling patients on risk of disease recurrence
Although here we do not report on functional outcomes, many groups have reported good results with FT, with 94-100% pad-free rate regarding urinary incontinence and 47-86% erectile function (16)
With FT on the rise in both recognition and availability (17, 18), our current and other’s reports (19) show that clinicians have been treating patients with higher risks both on and off trial, as some patients express a desire to undergo FT outside of those criteria, searching for a chance of benefit (avoiding or delaying complications) when treatment is advised but there is no immediate threat to life, as is the case of localized intermediate-risk PCa
While urological guidelines (1, 6) still consider FT as experimental treatments, the German Society of Urology (20) has published in 2022 a list of recommendations considering FT an option for patients with unilateral low-risk PCa who decline “standard therapies” and active surveillance, but reminding of the available data being insufficient to access FT oncological effectiveness Other publication has reported on a Delphi-method consensus meetings of 47 FT experts recommending allowing treatment of low and intermediate-risk PCa with volume up to 3 mL in 1 hemi-gland, if total PSA lower than 10 ng/mL (21)
The oncological and functional reported outcomes for FT in PCa have also been reported in at least 72 studies, with 8 different energy modalities and including 5827 patients (19) However, those are mostly from single-arm stage 2 studies To add to the current data, we would like next years to bring us results on randomized controlled trials for FT versus radical treatment and active surveillance, w i t h p o p u l a t i o n s o f m a i n l y i n t e r m e d i a t e - r i s k P C a patients Those trials will need to prove both efficacy and safety of FT
CONCLUSIONS
This series adds information on the outcomes of FT in the treatment of localized intermediate-risk PCa The oncological control and survival without whole-gland or systemic treatment were satisfactory In those who needed additional treatment, FT delayed its need in a reasonable amount of time, with a very good side-effect profile
With a low percentage of metastatic disease and no PCa related deaths, this study advocates for allowing FT as a treatment option in selected cases of intermediate-risk disease
Randomized controlled trials comparing FT with active surveillance and radical treatments are needed to further establish the role of those treatments
REFERENCES
1 Mottet N CP, vand den Bergh RCN, Briers E, et al EAU EANM ESTRO ESUR ISUP SIOG Guidelines on Prostate Cancer European Association of Urology 2022
2 Lane JA, Donovan JL, Young GJ, et al Functional and quality of life outcomes of localised prostate cancer treatments (Prostate Testing for Cancer and Treatment [ProtecT] study) BJU Int 2022; 130:370-380
3 Lane JA, Donovan JL, Davis M, et al Active monitoring, radical prostatectomy, or radiotherapy for localised prostate cancer: study design and diagnostic and baseline results of the ProtecT randomised phase 3 trial Lancet Oncol 2014; 15:1109-18
4 Lomas DJ, Ahmed HU All change in the prostate cancer diagnostic pathway Nat Rev Clin Oncol 2020; 17:372-81
5 Kasivisvanathan V, Emberton M, Ahmed HU Focal therapy for prostate cancer: rationale and treatment opportunities Clin Oncol (R Coll Radiol) 2013; 25:461-73
6 Network NCC NCCN Clinical Practice Guidelines in OncologyProstate Cancer Version 1 2023
7 Redondo C, Srougi V, da Costa JB, et al Focal cryotherapy: step by step technique description Int Braz J Urol 2017; 43:995-6
8 Claros OR, Tourinho-Barbosa RR, Carneiro A, et al HIFU focal therapy for prostate cancer using intraoperatory contrast enhanced ultrasound Arch Esp Urol 2019; 72:825-30
9 Gontero P, Marra G, Teber D, et al Making a case "against" focal therapy for intermediate-risk prostate cancer World J Urol 2021; 39:719-28
10 Wang AZ, Lebastchi AH, O'Connor LP, et al Making a case "for" focal therapy of the prostate in intermediate risk prostate cancer: current perspective and ongoing trials World J Urol 2021; 39:729-39
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
418
N Dias, L Rodriguez-Sanchez, G Colandrea, P Macek, X Cathelineau
11 McIntosh M, Opozda MJ, O'Callaghan M, et al Why do men with prostate cancer discontinue active surveillance for definitive treatment? A mixed methods investigation Psychooncology 2022; 31:1420-30
12 Bokhorst LP, Valdagni R, Rannikko A, et al A Decade of Active Surveillance in the PRIAS Study: An Update and Evaluation of the Criteria Used to Recommend a Switch to Active Treatment Eur Urol 2016; 70:954-60
13 Shah TT, Reddy D, Peters M, et al Focal therapy compared to radical prostatectomy for non-metastatic prostate cancer: a propensity score-matched study Prostate Cancer Prostatic Dis 2021; 24:567-74
14 Reddy D, Peters M, Shah TT, et al Cancer Control Outcomes Following Focal Therapy Using High-intensity Focused Ultrasound in 1379 Men with Nonmetastatic Prostate Cancer: A Multi-institute 15-year Experience Eur Urol 2022; 81:407-13
15 Stabile A, Orczyk C, Giganti F, et al The Role of Percentage of Prostate-specific Antigen Reduction After Focal Therapy Using Highintensity Focused Ultrasound for Primary Localised Prostate Cancer Results from a Large Multi-institutional Series Eur Urol 2020; 78:155-60
16 Fujihara A, Ukimura O Focal therapy of localized prostate cancer Int J Urol 2022; 29:1254-1263
17 Jain AL, Sidana A, Maruf M, et al Analyzing the current practice patterns and views among urologists regarding focal therapy for prostate cancer Urol Oncol 2019; 37:182 e1-e8
18 Marra G, Ploussard G, Ost P, et al Focal therapy in localised prostate cancer: Real-world urological perspective explored in a cross-sectional European survey Urol Oncol 2018; 36:529 e11-e22
19 Hopstaken JS, Bomers JGR, Sedelaar MJP, et al An Updated Systematic Review on Focal Therapy in Localized Prostate Cancer: What Has Changed over the Past 5 Years? Eur Urol 2022; 81:5-33
20 Borkowetz A, Blana A, Bohmer D, et al German S3 EvidenceBased Guidelines on Focal Therapy in Localized Prostate Cancer: The First Evidence-Based Guidelines on Focal Therapy Urol Int 2022; 106:431-9
21 Tay KJ, Scheltema MJ, Ahmed HU, et al Patient selection for p r o s t a t e f o c a l t h e r a p y i n t h e e r a o f a c t i v e s u r v e i l l a n c e : a n International Delphi Consensus Project Prostate Cancer Prostatic Dis 2017; 20:294-9
Correspondence
Nuno Dias, MD (Corresponding Author) nunodiasds@gmail com
Gianmarco Colandrea, MD colandrea gianmarco@hsr it
Lara Rodriguez-Sanchez, MD rodriguezsanchezlara@gmail com
Petr Macek, MD
petr macek@imm fr
Xavier Cathelineau, MD
xavier cathelineau@imm fr
Urology Department, Institut Mutualiste Montsouris; 42 Bd Jourdan; 75014 Paris (France)
419 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Intermediate-risk prostate cancer treated with HIFU or cryotherapy
The impact of prostate biopsy on erectile and ejaculatory function: A prospective study
Michele Morelli 1, 2 , Gianluca Sampogna 2, 3 , Samuele Molteni 1, 2 , Carmine Sciorio 1 , Vito Lorusso 2 , Lorenzo Romano 4 , Roberto La Rocca 4 , Marco Capece 4 , Assunta Zimarra 4 , Luigi Napolitano 4* , Paolo Verze 5 , Lorenzo Spirito 6
1 Urology Unit, ASST Ospedale Manzoni, Lecco, Italy;
2 University of Milan, Milan, Italy;
3 Urology Unit, Niguarda Hospital, Milan, Italy;
4 Unit of Urology, Department of Neurosciences, Reproductive Sciences, and Odontostomatology University of Naples “Federico II”, Naples, Italy;
5 Department of Medicine and Surgery "Scuola Medica Salernitana", University of Salerno, Fisciano, Campania, Italy
6 Unit of Urology, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli,", Naples, Italy
Summary
Objective: To evaluate the impact on erectile and ejaculatory function following transrectal ultrasound-guided biopsies of the prostate (TRUS-Bx) in sexually active men
Methods: Monocentric prospective study from May 2021 to January 2022 of consecutive patients with suspected prostate cancer [elevated prostate specific antigen (PSA) level and/or abnormal digital rectal examination] undergoing TRUS-Bx The 15-item version of the International Index of Erectile Function (IIEF-15), Premature Ejaculation Diagnostic Tool (PDET) and short form of Male Sexual Health Questionnaire (MSHQ-EjD Short Form) were assessed before, one and three months after TRUS-Bx. The primary endpoint was to evaluate the risk of temporary post-biopsy erectile and/or ejaculatory dysfunctions
The statistical significance was set as p value < 0.05.
Results: A total of 276 consecutive patients were included in the study. The median age, PSA and biopsy cores were 65 years (IQR 59-69), 7 ng/ml (IQR 5-9 7) and 16 (IQR 12-16), respectively We compared the IIEF subdomains before TRUS-Bx vs one or three months: the erectile function (EF) decreased after one month (p<0 001) but recovered after three months (p=0 833); the Orgasmic Function (OF), the Sexual Desire (SD), the Intercourse Satisfaction (IS), the Overall Satisfaction (OS), and Total IIEF decreased significantly after both one and three months compared to pre-biopsy values (p < 0 05) As for ejaculatory function (EjF), PDET, MSHQ-EjD Short Form 1, 2, 3 and MSHQ-EjD Short Form 4 scores decreased significantly after one month (p < 0.001), but they returned to pre-biopsy values after 3 months: p = 0 538, p = 0 071 and p = 0 098, respectively
Conclusions: Our study proved that EF, assessed through IIEF15, and ejaculatory function, assessed through PDET and MSHQ-EjD Short Form, were negatively affected by TRUS-Bx one month after the procedure and recovered after three months. Interestingly, the other IIEF-15 subdomains (OF, SD, IS, OS and Total) resulted as significantly reduced also after 3 months: this issue highlights the importance of carefully considering the indication to TRUS-Bx
KEY WORDS: Prostate cancer; Prostate needle biopsy; Erectile dysfunction; Ejaculatory dysfunction
Submitted 6 September 2022; Accepted 14 October 2022
INTRODUCTION
Prostate cancer (PCa) is the second most common cause of cancer death among men (1) Transrectal ultrasound-guided biopsies of the prostate (TRUS-Bx), is a well-known d
million/procedures per year in Europe and North America combined (2)
Despite recent evidence that suggests reduced infection risk with the transperineal route (3), TRUS-Bx is still routinely performed all over the world and is considered a relatively safe procedure with low risk of serious adverse events Nevertheless, minor complication such as transient erectile dysfunction (ED) or ejaculatory dysfunctions (EjD) are rare though possible complication after TRUSBx with complete recovery after 1-3 mos (4) Notably, data on ED following TRUS-Bx are heterogeneous as a consequence of varied patient populations and ED classifications Moreover, Mehta et al (5) showed the lack of outcome measurement through validated questionnaires, with only three studies that included the International Index of Erectile Function-15 (IIEF-15) and just one the Male Sexual Health Questionnaire (MSHQ-EjD)
Thus, the aim of our study was to prospectively evaluate, through validated questionnaires, the likelihood of a short-term post-TRUS-Bx erectile and/or ejaculatory dysfunctions in sexually active men
MATERIALS AND METHODS
Study population and data collection
Declaration of Helsinki We prospectively included all male patients, suspected of prostate cancer, undergoing TRUS-BX in the department of Urology, Federico II University, Naples, Italy, between May 2021 and January 2022 The indications for biopsy were the following: elevated prostate specific antigen (PSA) level, PSA between 410 ng/mL with PSA density ≥ 0 15 ng/mL/cm3 , PSA > 10 ng/mL and/or abnormal digital rectal examination (DRE)
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 420 ORIGINAL PAPER No conflict of interest declared
i a g n o s t i c t o o l f o r p r o s t a t e c a n c e r , w i t h o v e r 2
T h e s t u d y w a s c o n d u c t e d i n a c c o r d a n c e w i t h t h e
DOI: 10 4081/aiua 2022 4 420
The validated questionnaires were administered by the urologist who conducted the study via e-mail Baseline parameters were recorded and included: Patients age, B o d y M a s s I n d e x (
s c o r e , D i a b e t e s , Hypertension, Anticoagulant therapy, Antiaggregant therapy, Angiotensin receptor blockers therapy, 5-alpha reductase inhibitors therapy, PSA values and number of biopsy cores
Sexual function questionnaires
The participants were asked to answer the validated questionnaires (translated in Italian) via e-mail: 15- items
IIEF-15 (6), Premature Ejaculation Diagnostic Tool (PDET) (7) and a short form of Male Sexual Health Questionnaire (MSHQ-EjD Short Form) (8) Patients were followed with IIEF-15, PDET and MSHQ-EjD Short Form during the study period divided in before (T1) and at 1 (T2) and 3 (T3) months after TRUS-Bx Only the complete questionnaires were recorded in the analysis
The IIEF-15 score included 5 categories: erectile function (EF), orgasmic function (OF), sexual desire (SD), intercourse satisfaction (IS) and overall satisfaction (OS) Response options ranged from 0 (no sexual intercourse) to 5 (normal sexual activity) A Total IIEF-15 score ranging from 5 to 25 was then calculated
The PDET score was categorized from 0 (no problem at all) to 4 (always), with higher scores indicating difficulty with premature ejaculation
The MSHQ-EjD Short Form, comprised the four-item ejaculatory function domain assessing frequency of ejaculation, strength of ejaculation, volume of ejaculation and satisfaction
Biopsy procedure
Antibioprophylaxis was started 1 day before the procedure with Ciprofloxacin 500 mg (2 tablets per day)
TRUS-Bx was performed by senior urologists (> 100 procedures) under local anesthesia (10 mL of 2% lidocaine), with automated tru-cut 18-gauge needle (Bard; Covington, GA) We performed sextant biopsies (with six cores each lobe) and additional cores from suspected areas
The primary endpoint was to determine early post TRUSBx erectile and/or ejaculatory dysfunctions through validated questionnaires in men suspected for PCa
Data analysis
Descriptive statistics included frequencies and proport i o n s f o r c a t e g o r i c a l v a r i a b l e s M e a n , m e d i a n s a n d interquartile ranges (IQR) were reported for continuously coded variables The categorical variables between the groups were analyzed using the chi-squared and Fisher's exact tests, while the continuous variables between groups were analyzed using the Mann-Whitney U test Wilcoxon sign rank test for paired sample was used to compare continuous non-parametric variables In all statistical analyses, Statistical Package for Social Science (SPSS), Version 20 (IBM Corporation, Armonk, NY, USA) was used All tests were two-sided with a level of significance set at p < 0 05
RESULTS
Study population
A total of 276 male patients that underwent TRUS-Bx between May 2021 and January 2022 met the inclusion criteria: elevated prostate specific antigen (PSA) level, PSA between 4-10 ng/mL with PSA density ≥ 0 15 ng/mL/cm3, PSA > 10 ng/mL and/or abnormal digital rectal examination (DRE)
The baseline characteristics are summarized in Table 1 In the overall cohort, the median age, BMI and Charlson Comorbidity score were 65 (IQR 59-69) years, 26 (IQR 24-29) and 4 (IQR 2-6), respectively The median PSA was 7 (IQR 5-9 7) and a median of 16 (IQR 12-16) biopsy cores were taken during the TRUS-Bx procedure
IIIEF-15 Questionnaire
From T1 to T2, the IIEF-EF score decreased significantly (21 (IQR 3 0-25 0) vs 19 (IQR 2 0-22 5), p < 0 001) and from T1 to T3, no statistically significant difference was recorded (p = 0 833) (Table 2)
Finally, in the other subdomains (OF, SD, IS, OS) and Total, from T1 to both T2 and T3, the IIEF score decreased significantly (p < 0 05), the changes of specific domains are shown in Table 2
Table 2.
International Index of Erectile Function (IIEF) Questionnaire administrated to 276 patients before prostate biopsy (Time 1), 1 month after (Time 2) and 3 mos after (Time 3)
421 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Prostate biopsy and sexual dysfunction
M I
C
a r l s o
B
) ,
h
n
Baseline
Overall cohor t (n = 276) Median (IQR) age, years 65 (59-69) Median (IQR) Body Mass Index 26 (24-29) Median (IQR) Charlson score 4 (2-6) Diabetes, n (%) 37(14 4) Hypertension, n (%) 29 (10 5) Anticoagulant therapy, n (%) 8 (2 9) Antiaggregant therapy, n (%) 39 (14 1) Angiotensin receptor blockers therapy, n (%) 72 (26) 5-alpha reductase inhibitors therapy, n (%) 42 (15 2) Median (IQR) PSA antigen 7 (5 -9 7) Median (IQR) biopsy cores 16 (12 -16) IQR: Interquart le range; PSA: Prostate-specific antigen
Table 1.
and patients characteristics
ilcoxon sign rank test p-value T ime 1 T ime 2 T ime 3 T ime 1 vs time 2 T ime 1 vs time 3 IIEF-EF Median 21 19 21 < 0 001 0 833 IQR 3 0-25 0 2 0-22 5 3 0-25 0 IIEF-OF Median 7 5 6 5 7 < 0 015 < 0 001 IQR 0-9 8 0-7 5 0-8 0 IIEF-SD Median 6 5 6 < 0 02 < 0 023 IQR 5 0-7 0 4 5-6 5 0-7 0 IIEF-IS Median 10 9 9 5 < 0 015 < 0 001 IQR 0-12.0 0-11.0 0-12.0 IIEF-OS Median 7 6 7 < 0 001 < 0 001 IQR 4 0-8 0 2 0-8 0 4 0-8 0 IIEF-TOT Median 53 49 51 < 0 001 < 0 001 IQR 12 0-61 0 7 0-58 12 0-60 0 EF: Erectile Funct on; IS: Intercourse Satisfact on; OF: Orgasmic Function: OS: Overa l Satisfact on; SD: Sexua Desire
W
Table 3
Ejaculatory function questionnaires administrated to 276 patients before prostate biopsy (Time 1), 1 month after (Time 2) and 3 mos after (Time 3)
PDET Questionnaire
From T1 to T2, the PDET score decreased significantly (2 (IQR 0-4 0) vs 2 (IQR 0-4 0), p < 0 001) and from T1 to T3, no statistically significant difference was observed (p = 0 098) (Table 3)
MSHQ-EjD Short Form Questionnaire
From T1 to T2, the MSHQ-EjD Short Form score (1,2,3) decreased significantly (12 (IQR 5 0-14 0) vs 11 (IQR 6 3-14 0), p < 0 001) and from T1 to T3, no statistically significant difference was observed (p = 0 538) (Table 3)
Similarly, From T1 to T2, the MSHQ-EjD Short Form score (4) decreased significantly (5 (IQR 3 0-5 0) vs 4 (IQR 4 0-5 0), p < 0 001) and from T1 to T3, no statistically significant difference was observed (p = 0 071) (Table 3)
A univariate analysis failed to identify the independent predictive factors of erectile and sexual disfunction (results not shown)
DISCUSSION
The study showed a rapid decrease in erectile and ejaculatory function at one month but a promising return to pre TRUS-Bx values was observed Aetiology of ED after TRUS-Bx is likely multifactorial As suggested by Zisman et al (9), trauma caused by compression associated with haematoma or oedema in the neurovascular bundle are considered the main reasons Moreover, Tuncel et al. (10) described multiple radiological changes in prostate parenchyma and bundle in post biopsy men with ED, indeed this could be explained by the fact that the most common form of analgesia used for this procedure is periprostatic nerve block (PPNB) and it is likely to be responsible for damage in neurovascular bundle area, leading to a possible cause of transient ED (11) Despite many studies have been correlating ED and prostate biopsy, only limited and controversial results are shown in literature, ranging from no meaningful effect to significant linking with ED in short- and long-term post TRUS-Bx Chrisofos et al (12), prospectively evaluated 46 men after TRUS-Bx; post biopsy ED were reported in just 6 5% and 4 3% of patients at one and three months, meaning that TRUS-Bx did not induce ED in a statistically significant manner On the other hand, Kamali et al (13) showed that TRUS-Bx was linked to ED,
and by the passage of time (6 months later); the degree of dysfunction significantly worsened (IIEF-5 mean scores 1 month after biopsy: 18 (6-25); 3 months after: 17 (5-25); 6 months after: 14 5 (5-25)) Herein, we assessed the decrease in EF through IIEF-EF in sexually active men one month after TRUS-Bx and recovering after three months Notably, the other IIEF subdomains (OF, SD, IS, OS and Total) resulted significantly reduced also after 3 months There are several explanations to this discrepancy of results First, despite the use of validated questionnaires, the patients may not have sufficient cognition to understand the different subdomains of IIEF-15 Second, in the multifactorial nature of ED, a prevalent issue on psychological condition in our study was observed (IS, OF, OS, SD) Deep effect on increased anxiety in patients who undergo TRUS-Bx may be related to the acute healing phase after the procedure and presence of a potentially lethal cancer specific disease (9, 12, 14) Moreover, an important aspect of our study, comparable to the current literature (15, 16) was that Ejaculation function, assessed through PDET and MSHQ-EjD short form, didn’t show any change between pre and post TRUS-Bx values
The limitations of the present study should also be acknowledged First, the absence of a complete psychologic and mental health assessment in our study population considering that the main statistic differences at 3 months were IS, OF, OS and SD Another limitation was the lack of a control group; we were unable to determine the relative short term erectile and ejaculatory disfunction of TRUS-Bx compared to the transperineal approach
However, our study also has several strengths which lies on his methodology This study is a longitudinal study in which participants were evaluated before, 1 month after and 3 months after TRUS-Bx to avoid possible memory bias Additionally, all subdomains of the international validated scales for examining sexual functions, such as IIEF, PDET and MSHQ-EjD short form, were evaluated
CONCLUSIONS
The discrepancy of results existing in literature and the issue in our study highlights the importance of carefully considering the indication to TRUS-Bx Magnetic resonance imaging and other tools (e g , PSA-density/velocity, biomarkers) are warranted to determine the real need for T R U S - B x , w h i c h m a y n e g a t i v e l y a f f e c t i m p o r t a n t domains of male sexual life
REFERENCES
1 Culp MB et al Recent global patterns in prostate cancer incidence and mortality rates Eur Urol 2020; 77:38
2 Loeb S, Vellekoop A, Ahmed HU, et al Systematic review of complications of prostate biopsy Eur Urol 2013; 64:876-92
3 Pepe P, Pennisi M Morbidity following transperineal prostate biopsy: Our experience in 8 500 men Arch Ital Urol Androl 2022; 94:155-159
4 Fujita K, Landis P, McNeil BK, Pavlovich CP Serial prostate biopsies are associated with an increased risk of erectile dysfunction in men with prostate cancer on active surveillance J Urol 2009; 182:2664-2669
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 M Morelli, G Sampogna, S Molteni 422
W ilcoxon sign rank test p-value T ime 1 T ime 2 T ime 3 T ime 1 vs time 2 T ime 1 vs time 3 MSHQ-EjD Median 12 11 12 < 0.001 0.538 1, 2, 3 IQR 5 0-14 0 6 3-14 0 5-14 5 MSHQ-EjD Median 5 4 5 < 0 001 0 071 4 IQR 3 0-5 0 4 0-5 0 3 0-5 0 PDET Median 222 < 0 001 0 098 IQR 0-4 0 0-4 0 0-4 0 PEDT:
Premature E aculation D agnostic Tool; MSHQ-E D: Male Sexual Hea th-Ejacu atory Dysfunct on Questionnaire-
Ejacu atory Dysfunct on
5 Mehta A, Kim WC, Aswad KG, et al Erectile function post prostate biopsy: a systematic review and meta-analysis Urology 2021; 155:1-8
6 Rosen RC, Riley A, Wagner G, et al The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction Urology 1997; 49:822-830
7 Symonds T, Perelman MA, Althof S, et al Development and validation of a premature ejaculation diagnostic tool Eur Urol 2007; 52:565-573
8 Rosen RC, Catania JA, Althof SE, et al Development and validation of four-item version of Male Sexual Health Questionnaire to assess ejaculatory dysfunction Urology 2007; 69:805-9
9 Zisman A, Leibovici D, Kleinmann J, et al The impact of prostate biopsy on patient well-being: a prospective study of pain, anxiety and erectile dysfunction J Urol 2001; 165:445-54
10 Tuncel A et al Impact of transrectal prostate needle biopsy on erectile function: results of power Doppler ultrasonography of the prostate Kaohsiung J Med Sci 2014; 30:194-9
11 Glaser AP, Novakovic K and Helfand BT The impact of prostate biopsy on urinary symptoms, erectile function, and anxiety Curr Urol Rep 2012; 13:447-54
12 Chrisofos M, Papatsoris AG, Dellis A, et al Can prostate biopsies affect erectile function? Andrologia 2006; 38:79-83
13 Kamali K, Nabizadeh M, Ameli M, et al Impact of prostate needle biopsy on erectile function: A prospective study Urologia 2019; 86:145-147
14 Korfage IJ, Essink-Bot ML, Janssens AC, et al Anxiety and depression after prostate cancer diagnosis and treatment: 5-year follow-up Br J Cancer 2006; 94:1093-8
15 Song PH, Lee KS, Choi JY, et al 1012 When does ejaculatory dysfunction recover after transrectal ultrasound guided prostate biopsy? Eur Urol Suppl 2016; 15:e1012
16 Verze P, La Rocca R, Spirito L, et al Premature Ejaculation patients and their partners: arriving at a clinical profile for a real optimization of the treatment Arch Ital Urol Androl 2021; 93:42-47
Correspondence
Michele Morelli
Samuele Molteni
Carmine Sciorio
Urology Unit, ASST Ospedale Manzoni, Lecco, Italy
Gianluca Sampogna
Urology Unit, Niguarda Hospital, Milan, Italy
Vito Lorusso
University of Milan, Milan, Italy
Lorenzo Romano
Roberto La Rocca
Marco Capece
Assunta Zimarra
Luigi Napolitano (Corresponding Author)
dr luiginapolitano@gmail com
Unit of Urology, Department of Neurosciences, Reproductive Sciences, and Odontostomatology - University of Naples “Federico II”
Via Sergio Pansini 5, 80131 Naples, Italy
Paolo Verze
Department of Medicine and Surgery "Scuola Medica Salernitana", University of Salerno, Fisciano, Campania, Italy
Lorenzo Spirito
Unit of Urology, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli,", Naples, Italy
423 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Prostate biopsy and sexual dysfunction
Could we safely omit a Repeat Transurethral Resection of the Bladder (re-TURB) after Hexaminolevulinate Photodynamic Diagnostics (PDD)-TURB?
Lorusso 1,
3 , Laure Doisy 1 , Antonio Maria Granata 2 , Andrea Gregori 2 , Celeste Manfredi 4 , Lorenzo Spirito 4 , Carmine Sciorio 5 , Luca Giuseppe Maria Ciancimino 5 , Samuele Molteni 5 , Michele Morelli 6 , Luigi Cirillo 7 , Luigi Napolitano 7 , Jochen Walz 1 , Geraldine Pignot 1
1 Department of Urology, Institut Paoli-Calmettes Cancer Center, Marseille, France;
2 Department of Urology, ASST Fatebenefratelli-Sacco Hospital, Milan, Italy;
3 University of Milan, Milan, Italy;
4 Urology Unit, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli", Naples, Italy;
5 Department of Urology, ASST Lecco, Ospedale Alessandro Manzoni, Lecco, Italy;
6 Department of Urology, Foundation IRCCS Ca' Granda Ospedale Maggiore Policlinico, Milan, Italy;
7 Department of Neurosciences, Science of Reproduction and Odontostomatology, University of Naples Federico II, Naples, Italy
Summary
Objective: Bladder cancer (BC) is considered one of the malignancies with moderate-high incidence, high rate of recurrence and costly management
Diagnosis and staging are thus important for therapeutic purposes Considering the risk of residual tumour and understaging, in specific cases, international guidelines recommend performing a second transurethral resection of the bladder (reTURB) Our study aimed to evaluate the impact of hexaminolevulinate
Photodynamic Diagnostics (PDD) at first TURB on the rate of residual tumour
Materials and Methods: We retrospectively analysed patients undergoing TURB in our centre between 2012 and 2020. Eightytwo patients had a re-TURB after a first complete TURB with a delay < 3 months Patients who had an incomplete first resection were excluded. We compared patients who underwent standard white light cystoscopy/TURB and then hexaminolevulinate PDDguided reTURB (group A, n = 49) and patients with PDD-cystoscopy/TURB at the first procedure then white light cystoscopy/reTURB (group B, n = 33) The residual tumour rate at reTURB as well as median recurrence-free survival (RFS) were compared between the two groups
Results: Residual tumour at reTURB was detected in 48 8% of cases in our cohort, with a significant difference between the two groups (71 4% in group A versus 12 5% in group B, p < 0 001) After a median follow-up of 22 months, the median RFS was 15 months in Group A and 32 months in Group B, but this difference was not significant (p = 0 7)
Conclusions: Using PDD at the time of the initial TURB had a statistically significant impact on the rate of residual tumour at the reTURB Nevertheless, the percentage of residual tumour even with the use of PDD does not allow for safely omitting second resection. Performing a reTURB with PDD for patients who did not have it initially, provides the same benefit in terms of recurrence-free survival
KEY WORDS: Bladder cancer; Hexvix; TURB; Second resection; Residual tumor
Submitted 9 October 2022; Accepted 19 November 2022
INTRODUCTION
Bladder cancer (BC) represents the seventh most diagnosed cancer in men worldwide, and the tenth one considering both genders Moreover, Europe is considered one of the countries with the highest incidence with an age-standardized rate of 20 per 100,000 person/years for men (compared to 9 5 worldwide) and 4 6 for women (compared to 2 4 worldwide) (1) Furthermore, it is one of the malignancies with a high economic burden due to its treatments and follow-up (2)
Hence, a correct diagnosis and staging are of utmost importance for correct treatment Transurethral resection of the bladder (TURB) is considered the gold standard to ascertain BC diagnosis, and plan further treatments and can be a curative procedure for early-stage disease (pTa/T1 tumours) (3-5) Nonetheless, guidelines also recommend performing a second TURB in specific clinical scenarios, mainly: after an incomplete first TURB, when there are doubts about the completeness of the first resection, in case of the absence of detrusor muscle in the specimen (except for Ta LG/G1 tumours and primary CIS) and when there is the presence of T1 tumours (6, 7)
Second TURB (reTURB) has the intent to eradicate all the tumour burden since there is a consistent risk of leaving residual tumours and consequently of recurrence (1, 8, 9) To improve the correct tumour identification and
Photodynamic Diagnostics (PDD)-guided TURB has been proposed and demonstrated to be more sensitive than conventional procedures (10-13) For these reasons, European guidelines propose to use methods to improve tumor visualization including PDD (1) The aim of our study was to evaluate the advantage of using PDD at first TURB on the rate of residual and evaluate if using this technology, we could safely omit a reTURB, without compromising oncological outcomes
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 424 ORIGINAL PAPER No conflict of interest declared
i m p ro v e s t a g i n g a n d t re a t m e n t , H e x a m i n o l e v u l i n a t e
Vito
2,
DOI: 10 4081/aiua 2022 4 424
MATERIALS AND METHODS
We retrospectively analysed patients undergoing TURB in our centre between 2012 and 2020 Eighty-two patients had a reTURB after a first complete TURB with a delay < 3 months Patients who had an incomplete first resection were excluded We compared patients who underwent standard white light cystoscopy/TURB and then hexaminolévulinate PDD-guided reTURB (Group A, n = 49) and patients with PDD-cystoscopy/TURB at the first procedure then white light cystoscopy/reTURB (Group B, n = 33) The residual tumour rate at reTURB as well as median recurrence-free survival were compared Comparisons of the proportions were done by the 𝛘² test Kaplan-Meier
curves were used to analyze time to recurrence and to compare the two groups The statistical analysis was done with SPSS version 25 (SPSS Inc , Chicago, IL, USA)
RESULTS
No statistically significant differences were obser ved between the two groups in terms of age, sex, history of bladder cancer, stage, grade, presence of CIS, presence of muscle and multifocality (Table 1) Residual tumour at reTURB was detected in 48 8% of cases in our cohort, with a significant difference between the two groups (71 4% in group A versus 12 5% in group B, p < 0 001) After a median follow-up of 22 months, the median recurrence-free survival (RFS) was 15 months in group A and 32 months in group B (Figure 1), but this difference was not significant (p = 0 7)
DISCUSSION
In this retrospective study, we compared patients who underwent standard white light cystoscopy/TURB then P D D - g u i d e d re T U R B a n d p a t i e n t s w i t h P D D - c y stoscopy/TURB at the first procedure then white light cystoscopy/reTURB After the first resection, there was a risk of disease recurrence due to a regrowth of undetected lesions We found that PDD cystoscopy at the time of the initial TURB had a statistically significant impact on the rate of residual tumor at the reTURB In fact, we found that residual tumor rates at reTURB were 71 4% and 12 5% in Group A and B respectively Our result corroborated data from previously published studies Since its first use in 1994, the benefits of fluorescent light cystoscopy with hexaminolevulinate (HAL) in non-muscleinvasive bladder cancer (NMIBC) have been reported in many trials Nowadays PDD is widely used for the diagnosis and treatment of superficial bladder cancer In NMIBC the possible benefits of using PDD- guided TURB were higher detection rates, a higher rate of complete resection, and fewer residual tumors (14) Several s t u d i e s re p o r t e d a n i n c re a s e d tumor detection rate by HAL-PDD with a most pronounced benefit for CIS lesions (15)
Riedel et al. found lower residual tumor rates for Ta and T1 tumors using PDD, while Filbeck et al f o u n d a s t a t i s t i c a l l y s i g n i f i c a n t reduction of residual tumors only in Ta tumors (16, 17) Albarghouth et al showed that the use of PDD significantly reduces the risk of re s i d u a l t u m o r s c o m p a re d w i t h conventional TURB In the same study, they have also shown that PDD can significantly improve 3 and 12-month recurrence-free survival especially in low and intermediate-risk tumors, and 1-year progression-free survival in high-risk tumors (18) Burger et al conduct-
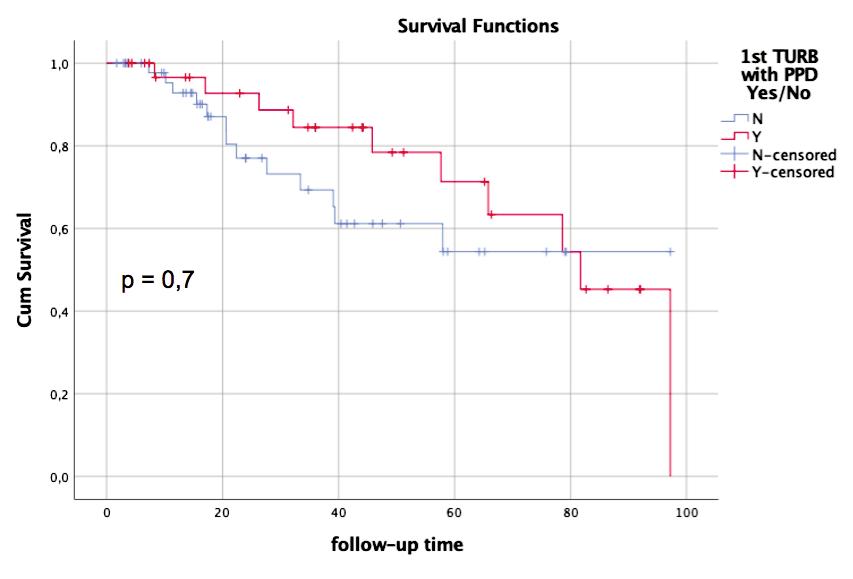
425 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Re-TURB after PDD-TURB
Table 1
Blue Light Cystoscopy at F irst TURB P value No-Group A (n = 49) Yes-Group B (n = 33) N%N% Age (years), median (SD) 69 (9) - 71 (9) - 0 7 a Sex F8 47 9 52 0.23 b M 41 63 24 36 Stage Ta 11 73 4 26 0 23 b T1 38 56 29 43 Presence of CIS Yes 32 64 18 36 0 32 b No 17 53 15 46 Presence of muscle Yes 9 69 4 30 0 44 b No 40 58 29 42 Multifocality Yes 29 60 19 39 0 8 b No 20 58 14 41 R+ Yes 14 33 28 66.7 < 0.001 b No 35 87 5 12 5 Recidive Yes 36 61 23 39 0 7 b No 13 56 10 43 RFS 15 32 0 7 c F: Fema e; M: Ma e; CIS: Carcinoma in s tu; R+: Residual tumor; RFS: Recurrence free survival; a Student t Test; b Ch Test; c Log-rank Test
Baseline characteristic and postoperative variable statistics of patient (n = 82).
Figure 1. Kaplan-Meier curves for recurrence-free
survival time
ed a meta-analysis confirming that HAL-PDD cystoscopy significantly improves the detection of bladder tumours leading to a reduction of recurrence at 9-12 month (19) Mariappan et al found that HAL-PDD-assisted TURB was associated with a significantly lower risk of early recurrence compared to white light TURB Moreover, recurrence rate at the first follow-up cystoscopy in the study cohort was 13 6% and 30 9% in the two settings respectively (20) Gakis et al systematically reviewed literature reporting a significantly lower rate of progression in patients treated with PDD compared to white light TURB (21) In a recent meta-analysis Sun et al reported that cystoscopy with aminolevulinic acid (ALA) or HAL was associated to a reduced residual tumor rate compared with standard cystoscopy in NMIBC and RFS was higher in the first case at the 12- to 24-month follow-up (22)
Even if we confirmed that the use of PDD allows reducing residual tumour rate, we did not find a statistically significant difference in terms of RFS This can be explained by the design of our study which establishes the use of PDD in both groups but at different times
Probably the difference in terms of RFS favouring the group who perform PDD initially, which is also marked at the beginning of follow-up, tends to be mitigated later by the delayed use of PDD in the other group as shown by the Kaplan-Meier curves
We also conceived this study to question if the use of PDD at the initial TURB would allow for the omission of a reresection that, meaning a second surgical procedure, can have an impact not only for the patient (psychological, surgical or medical-related complications) but also for the healthcare systems in terms of costs However, despite the advantages of the PDD technique, considering the biological characteristic of bladder cancer and the percentage of the residual tumour even after PDD cystoscopy we do not consider it safe to spare a second resection
Our study is not devoid of limitations: mainly its retrospective nature and the small sample size
Concluding, reTURB even with the aid of PDD technology seems to be necessary Even if all studies showed a reduced risk of residual tumour, none of them suggested to avoid a reTURB
CONCLUSIONS
The quality of the initial TURB, when performed by using PDD, had a statistically significant impact on the rate of residual tumour at the reTURB Nevertheless, the percentage of residual tumour even after PDD cystoscopy is not negligible and cannot allow to safely avoid a second resection Performing a reTURB with PDD for patients who did not have it initially, provides the same benefit in terms of recurrence free survival
REFERENCES
1 Babjuk M, Burger M, Capoun O, et al European Association of Urology Guidelines on Non-muscle-invasive Bladder Cancer (Ta, T1, and Carcinoma in Situ) Eur Urol 2022; 81:75-94
2 Sievert KD, Amend B, Nagele U, et al Economic aspects of bladder cancer: what are the benefits and costs? World J Urol 2009; 27:295-300
3 Napolitano L, Barone B, Reccia P, et al Preoperative monocyte-tolymphocyte ratio as a potential predictor of bladder cancer J Basic Clin Physiol Pharmacol 2022; 33:751-757
4 Creta M, Celentano G, Napolitano L, et al Inhibition of Androgen Signalling Improves the Outcomes of Therapies for Bladder Cancer: Results from a Systematic Review of Preclinical and Clinical Evidence and Meta-Analysis of Clinical Studies Diagn Basel Switz 2021; 11:351
5 Manfredi C, Spirito L, Calace FP, et al Oral Preparation of Hyaluronic Acid, Chondroitin Sulfate, Curcumin, and Quercetin (Ialuril® Soft Gels) for the Prevention of LUTS after Intravesical Chemotherapy Pathophysiol Off J Int Soc Pathophysiol 2022; 29:365-73
6 Longo N, Celentano G, Napolitano L, et al Metastasis-Directed Radiation Therapy with Consolidative Intent for Oligometastatic Urothelial Carcinoma: A Systematic Review and Meta-Analysis Cancers 2022; 14:2373
7 Ferro M, Del Giudice F, Carrieri G, et al The Impact of SARSCoV-2 Pandemic on Time to Primary, Secondary Resection and Adjuvant Intravesical Therapy in Patients with High-Risk NonMuscle Invasive Bladder Cancer: A Retrospective Multi-Institutional Cohort Analysis Cancers 202; 13:5276
8 Imperatore V, Creta M, Di Meo S, et al Intravesical administration of combined hyaluronic acid and chondroitin sulfate can improve symptoms in patients with refractory bacillus Calmette-Guerininduced chemical cystitis: Preliminary experience with one-year follow-up Arch Ital Urol Androl 2018; 90:11-4
9 Morelli M, Baboudjian M, Vanacore D, et al Early Photodynamic D
Significantly Increased the Detection of BCG Refractory Tumors J Endourol 2021; 35:1824-8
10 Kausch I, Sommerauer M, Montorsi F, et al Photodynamic diagnosis in non-muscle-invasive bladder cancer: a systematic review and cumulative analysis of prospective studies Eur Urol 2010; 57:595606
11 Mowatt G, N’Dow J, Vale L, et al Photodynamic diagnosis of bladder cancer compared with white light cystoscopy: Systematic review and meta-analysis Int J Technol Assess Health Care 2011; 27:3-10
12 Turco C, Collà Ruvolo C, Cilio S, et al Looking for cystoscopy on YouTube: Are videos a reliable information tool for internet users? Arch Ital Urol Androl 2022; 94:57-61
13 Capece M, Spirito L, La Rocca R, et al Hexaminolevulinate blue light cystoscopy (Hal) assisted transurethral resection of the bladder tumour vs white light transurethral resection of the bladder tumour in non-muscle invasive bladder cancer (NMIBC): a retrospective analysis Arch Ital Urol Androl 2020; 92:17-20
14 Konecki T, Kutwin P, Łowicki R, et al Hexaminolevulinate in the Management of Nonmuscle Invasive Bladder Cancer: A MetaAnalysis Photobiomodulation Photomed Laser Surg 2019; 37:551-8
15 Witjes JA, Babjuk M, Gontero P, et al Clinical and cost effectiveness of hexaminolevulinate-guided blue-light cystoscopy: evidence review and updated expert recommendations Eur Urol 2014; 66:863-71
16 Riedl CR, Daniltchenko D, Koenig F, et al Fluorescence endoscopy with 5-aminolevulinic acid reduces early recurrence rate in superficial bladder cancer J Urol 2001; 165:1121-3
17 Filbeck T, Pichlmeier U, Knuechel R, et al Clinically relevant improvement of recurrence-free survival with 5-aminolevulinic acid
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 V Lorusso, L Doisy, A M
et al 426
Granata,
i a g n o s i s C y s t o s c o p y A f t e r B a c i l l u s C a l m e t t e - G u é r i n ( B C G ) I n d u c t i o n f o r H i g h - R i s k N o n m u s c l e I n v a s i v e B l a d d e r C a n c e r
induced fluorescence diagnosis in patients with superficial bladder tumors J Urol 2002; 168:67-71
18 Albarghouth MH, Hamza A The impact of using intraoperative photodynamic diagnosis on the prognosis of bladder cancer Aktuelle Urol 2022; 53:552-558
19 Burger M, Grossman HB, Droller M, et al Photodynamic diagnosis of non-muscle-invasive bladder cancer with hexaminolevulinate cystoscopy: a meta-analysis of detection and recurrence based on raw data Eur Urol 2013; 64:846-54
20 Mariappan P, Rai B, El-Mokadem I, et al Real-life Experience: Early Recurrence With Hexvix Photodynamic Diagnosis-assisted
Transurethral Resection of Bladder Tumour vs Good-quality White Light TURBT in New Non-muscle-invasive Bladder Cancer Urology 2015; 86:327-31
21 Gakis G, Fahmy O Systematic Review and Meta-Analysis on the
Transurethral Bladder Tumor Resection on Progression in NonMuscle Invasive Bladder Cancer Bladder Cancer Amst Neth 2016; 2:293-300
22 Sun J, Ma X, Shen H, Liu B Effects of fluorescent light cystoscopy in non-muscle-invasive bladder cancer: A systematic review and meta-analysis Photodiagnosis Photodyn Ther 2021; 34:102248
Correspondence
Vito Lorusso, MD vito lorusso@unimi it
Laure Doisy, MD doisyl@ipc unicancer fr
Antonio Maria Granata, MD antonio granata@asst-fbf-sacco it
Andrea Gregori, MD andrea gregori@asst-fbf-sacco it
Celeste Manfredi, MD manfredi celeste@gmail com
Lorenzo Spirito, MD
lorenzo spirito@unicampania it
Carmine Sciorio, MD carminesciorio@gmail com
Samuele Molteni, MD sa molteni@asst-lecco it
Luca Giuseppe Maria Ciancimino, MD lucaciancimino91@gmail com
Michele Morelli, MD michelemorelli4@gmail com
Luigi Cirillo, MD cirilloluigi22@gmail com
Luigi Napolitano, MD (Corresponding Author) luiginap89@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples "Federico II", Naples, Italy
Via Sergio Pansini n 5, Naples (NA), Campania (Italy)
Jochen Walz, MD
walzj@ipc unicancer fr
Geraldine Pignot, MD
pignotg@ipc unicancer fr
427 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Re-TURB after PDD-TURB
I m p a c t o f H e x a m i n o l e v u l i n a t e - Ve r s u s W h i t e - L i g h t G u i d e d
AB0 blood groups and oncological and functional outcomes in bladder cancer patients treated with radical cystectomy
Alessandro Tafuri 1, 2*
Andrea Panunzio 1,3*
Soldano 1*
Giovanni Mazzucato 1
Irene Ornaghi 1 , Giacomo Di Filippo 4 , Alessandra Gozzo 1 , Nicola De Maria 1 , Francesco Cianflone 1 , Aliasger Shakir 5 , Zhe Tian 3 , Matteo Brunelli 6 , Antonio Benito Porcaro 1 , Vincenzo Pagliarulo 2 , Walter Artibani 1 , Pierre I. Karakiewicz 3 , Alessandro Antonelli 1 , Maria Angela Cerruto 1
1 Department of Urology, University of Verona, Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Italy;
2 Department of Urology, “Vito Fazzi” Hospital, Lecce, Italy;
3 Cancer and Prognostics Health Outcomes Unit, Division of Urology, University of Montreal Health Center, Montreal, Quebec, Canada;
4 Department of General and Hepatobiliary Surgery, University of Verona, Azienda Ospedaliera Universitaria Integrata Verona, Verona, Italy;
5 USC Institute of Urology, Catherine and Joseph Aresty Department of Urology, Keck School of Medicine, University of Southern California (USC), Los Angeles, CA;
6 Department of Pathology, University of Verona, Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Italy
* These Authors contributed equally to the manuscript
Summary
Objectives: We investigated AB0 blood groups prevalence according to preoperative and pathological tumor characteristics, and their association with oncological outcomes, and renal function decline in a contemporary large cohort of bladder cancer (BCa) patients, who underwent radical cystectomy (RC) at a tertiary referral center Materials and Methods: We retrospectively evaluated data of patients with histologically confirmed and clinically non metastatic BCa, who underwent RC between 2014 and 2021 at our Institution Kaplan-Meier (KM) plots and Cox regression (CR) models tested the relationship between AB0 blood groups and local recurrence-, metastasis-, cancer specific mortality-, and overall mortality-free survival. Logistic regression (LR) models tested the association between AB0 blood groups and renal function decline, defined as an estimated Glomerular Filtration Rate (eGFR) < 60 mL/min, at post-operative day 1, discharge and 6months of follow-up
Results: Of 301 included patients, 128 (42.5%) had group A, 126 (41 9%) had group 0, 28 (9 3%) had group B, and 19 (6 3%) had group AB Patients with group 0 developed higher rates of muscle-invasive BCa (p = 0 028) with high-grade features (p = 0 005) at last bladder resection, and less frequently received preoperative immunotherapy with Bacillus of Calmette-Guerin (p = 0 044), than their non-0 counterparts Additionally, these patients harbored more advanced pathologic tumor stage at RC (p = 0.024). KM plots showed no differences among all tested cancer control outcomes between AB0 blood groups (p > 0.05 in all cases) Patients with group AB presented the lowest median eGFR at each time point In multivariable LR analyses addressing renal function decline, group AB was independently associated with eGFR< 60 mL/min at discharge (Odds Ratio: 4.28, p = 0.047).
Conclusions: Among AB0 blood groups, patients with group 0 exhibited the most aggressive tumor profile However, no differences were recorded in recurrence or survival rates Group AB independently predicted renal function decline at discharge.
KEY WORDS: AB0 blood groups; Bladder cancer; Radical cystectomy; Outcomes
Submitted 21 September 2022; Accepted 2 October 2022
INTRODUCTION
Bladder cancer (BCa) is the tenth most common cancer among men and women and its mortality varies according to sex, geographic location, race/ethnicity, risk factor exposure, and availability of diagnostic and treatment modalities (1) Currently, BCa is the eighth cause of cancer specific mortality (CSM) in the United States, among both sexes (1) Radical cystectomy (RC) with bilateral pelvic lymph node dissection and urinary diversion after chemotherapy is the gold-standard treatment for non-metastatic muscle-invasive bladder cancer (MIBC) or recurrent high-risk non-muscleinvasive bladder cancer (NMIBC) refractory to previous intravesical therapies (2) BCa remains affected by a high rate of local and distant recurrences, which are usually up to 50%, especially in patients with advanced stage and lymph node involvement (3) Several markers and nomograms have been proposed for BCa survival and recurrence prediction (4-6) However, no tool is strongly recommended by international guidelines in disease assessment (2), and pathological tumor features remain the main predictors of oncological outcomes and actually guide decision making regarding use of secondary treatment or follow up schedule (2) Among clinical factors, renal function seems to impact oncological outcomes in NMIBC, MIBC, as well as upper tract urothelial carcinoma Renal function has a pivotal role in patients’ eligibility to chemotherapy (7-9) or different post-operative approaches choice, and in a more adequate follow-up schedule (10, 11)
AB0 blood group is commonly assessed in every patient before RC due to the risk of blood transfusion during and after surgery The role of AB0 blood group system as a predictor of oncological outcomes has been previously investigated among other malignancies due its implication in cellular dynamics (12) Specifically, many authors have already shown the association between AB0 blood groups and survival in pancreatic (13), breast (14), and gastro-intestinal tumors (15) Few studies investigated the role of AB0 blood group as a predictor of outcome in
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 428 ORIGINAL PAPER No conflict of interest declared
,
, Antonio
,
, Paola
DOI: 10 4081/aiua 2022 4 428
BCa, revealing controversial results (16-19) The aim of this study is to investigate the prevalence of AB0 blood groups and their distribution according to patients’ characteristics and pathological tumor features, in addition to determining the association between AB0 blood groups and renal function decline and oncological outcomes in a contemporary cohort of BCa patients, who underwent RC at a high-volume tertiary center
MATERIALS AND METHODS
Population, data collection and evaluation of parameters
Data collected from patients with histologically confirmed and clinically non metastatic BCa, who were treated with RC at the Department of Urology at the University of Verona between September 2014 and February 2021, were retrospectively evaluated Informed consent was obtained for all subjects The indication for surgery was given in presence of MIBC or history of high-risk NMIBC refractory to previous intravesical treatment, according to international guidelines (2)
For each patient the AB0 genotype blood group system was assessed preoperatively by the Department of Transfusion Medicine Blood groups were routinely determined on microplates using LIFE reagent and instrumentation (AstraFormedic, De Mori Group) Additional personal information such as age, Body Mass Index (BMI; kg/m2), smoking history and Charlson Comorbidity Index (CCI) were collected Preoperative pathological features as NMIBC history, tumor grading and staging after last trans-urethral bladder resection (TURB), as well as local immunotherapy administration were reported Tumor staging was assessed according to the tumor, node, metastasis (TNM) classification by the Union International Contre le Cancer (UICC, 8th edition) (20), whereas tumor grading was assessed according to the World Health Organization (WHO) 20042016 classification system (21) Additionally, estimated glomerular filtration rate (eGFR) according to Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation (22), was assessed preoperatively, at post-operative day 1 (POD-1), at discharge and at 6 months of follow up Renal function decline was defined as an eGFR < 60 mL/min at each evaluated timepoint After RC surgical specimens were evaluated for tumor stage, grade, concomitant presence of carcinoma in situ (CIS), lymph vascular invasion (LVI), positive surgical margins (PSM), number of lymph nodes removed,
and number of metastatic lymph nodes, by dedicated uropathologists Pelvic lymph node dissection was performed according to international recommendations and the template used included the external iliac, obturator, Cloquet and Marcille lymph nodes sites (2) All surgical procedures were performed by five experienced and dedicated surgeons, two of whom were classified as high-volume
Statistical analyses
Descriptive statistics included frequencies and proportions for categorical variables Median and interquartile ranges (IQR) were reported for continuously coded variables Kruskal-Wallis rank sum test, Fisher’s exact test and Pearson’s Chi-squared test were used to examine the statistical significance of differences in medians and proportions, respectively Kaplan-Meier (KM) plots were utilized to depict local recurrence-free survival (LRFS), metastasisfree survival (MFS), CSM-free survival (CSMFS) and overall mortality-free survival (OMFS), according to AB0 blood groups Univariable and multivariable Cox proportional hazards regression models tested the relationship between AB0 blood groups and oncological outcomes Covariates consisted of age, sex, pT stage, pN stage, presence of CIS, PSM and LVI Univariable and multivariable logistic regression models were used to test the association between AB0 blood groups and renal function decline at POD-1, discharge and 6-months follow up All tests were two-sided with a level of significance set at p < 0 05
Kruskal-Wall s rank sum test; Fisher's exact test; Pearson's Chi-square test * p-va ue not estimable
Bacillus Calmette Guer n; TURB, trans urethral b adder resection; NMIBC, non-muscle- nvas ve bladder cancer; MIBC, muscle-invasive bladder cancer; CIS, carcinoma in
429 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 AB0 blood groups and bladder cancer
Table 1
Variable Overall 0AB AB p-value 2 301 (100) 1 126 (41 9) 1 128 (42 5) 1 28 (9 3) 1 19 (6 3%) 1 Age at surgery (years) 70 (62, 77) 70 (63, 77) 70 (60, 77) 69 (60, 74) 72 (68, 77) 0 4 Sex 0 1 Female 62 (20 6) 31 (24 6) 22 (17 2) 8 (28 6) 1 (5 3) Male 239 (79.4) 95 (75.4) 106 (82.8) 20 (71.4) 18 (94.7) Body Mass Index (Kg/m2) 25 9 (23 8, 28 6) 25 8 (23 4, 28 6) 25 6 (23 8, 28 1) 26 5 (23 9, 29 0) 26 9 (25 6, 29 5) 0 4 Smoking history 226 (75 8) 91 (72 8) 94 (74 6) 24 (85 7) 17 (89 5) 0 3 Diabetes Mellitus 56 (18 6) 20 (15 9) 25 (19 5) 3 (10 7) 8 (42 1) 0 049 Charlson Comorbidity Index 0 1 ≤ 2 172 (57 1) 76 (60 3) 70 (54 7) 18 (64 3) 8 (42 1) > 2 129 (42 9) 50 (39 7) 58 (45 3) 10 (25 7) 11 (57 9) Preoperative BCG administration 88 (29 2) 29 (23) 45 (35 1) 9 (33 1) 5 (26 3) 0 2 Clinical tumor stage (TURB) 0 1 NMIBC 137 (45 5) 48 (38 1) 64 (50) 13 (46 4) 12 (63 1) MIBC 164 (54 5) 78 (61 9) 64 (50) 15 (53 6) 7 (36 9) Grading (TURB) 0.002 Low grade 15 (5 2) 1 (0 8) 11 (8 9) 0 (0) 3 (15 8) High grade 273 (94 8) 119 (99 2) 113 (91 1) 25 (100) 16 (84 2) Pathologic tumor stage NR* pT0-T1 119 (39 7) 45 (36) 55 (43) 10 (35 7) 9 (47 4) pT2 44 (14 7) 14 (11 2) 20 (15 6) 5 (17 8) 5 (26 3) pT3 83 (27 6) 46 (36 8) 28 (21 9) 6 (21 5) 3 (15 8) pT4 54 (18) 20 (16) 25 (19 5) 7 (25) 2 (10 5) Presence of CIS at final pathology 84 (28) 35 (28) 37 (28 9) 6 (21 4) 6 (31 6) 0 9 Pathologic lymph node involvement 96 (32 2) 45 (36) 36 (28 3) 13 (46 4) 2 (11 1) 0.047 Number of lymph nodes removed 22 (15, 30) 22 (15, 28) 21 (14, 30) 26 (20, 30) 21 (14, 30) 0 4 Lymph vascular invasion 149 (56) 68 (60 2) 63 (55 3) 12 (46 1) 6 (46 1) 0 5 Positive surgical margins 34 (11 3) 15 (11 9) 11 (8 6) 5 (17 8) 3 (15 8) 0 4 1
2
BCG,
s tu
Descriptive statistics of 301 bladder cancer patients, who underwent radical cystectomy, according to the AB0-blood group system.
Median (IQR); n (%)
R software environment for statistical computing and graphics (version 4 1 2) was used for all analyses (R: the R Project for Statistical Computing https://www r-project org)
RESULTS
Study population
Overall, 301 patients were included of which 128 (42 5%) had group A, 126 (41 9%) had group 0, 28 (9 3%) had group B, and 19 (6 3%) had group AB (Table 1)
The AB0 blood group antigens were only associated with the presence of diabetes mellitus (p = 0 049), tumor grade at last endoscopic procedure (p = 0 002) and pathologic lymph node involvement (p = 0 047) No other statistically significant differences were recorded among demographic and preoperative patients’ characteristics or pathological tumor stage distribution S u b g r o u p a n a l y s i s showed that patients with group 0 developed higher rates of MIBC (p = 0 028) with concomitant high-grade features (p = 0 005) at last bladder resection, and in c o n s e q u e n c e r e c e i v e d l e s s f r e q u e n t l y p r e o p e r a t i v e immunotherapy with Bacillus of Calmette-Guerin (BCG, p = 0 044), compared with their non-0 counterparts Moreover, these patients harbored more advanced pathological tumor stage (T2-4) at RC compared with non-0 patients (p = 0 024, Table 2)
Impact of AB0 blood groups on oncological outcomes
Median follow up was 22 months (IQR 9-48) Of 248 patients with available follow up data, 43 (17 3%) developed local disease recurrence, 63 (25 4%) experienced metastatic progression, 74 (29 8%) died due to any causes, and 52 (21 0%) died due to BCa KM plots illustrated the relationship between AB0 blood groups and LRFS, MFS, CSMFS and OMFS, respectively (Figure 1) No statistically significative difference was recorded between the four groups for all tested cancer control outcomes (p > 0 05)
Univariable and multivariable Cox proportional hazards regression models confirmed that AB0 blood group system was not an independent predictor for all tested oncological outcomes, even after adjustment for all covariates (Table 3)
Table 2.
Descriptive statistics of 301 bladder cancer patients, who underwent radical cystectomy, according to AB0-blood group system: 0 vs non-0
1 Median (IQR); n (%) 2 Wi coxon rank sum test; Pearson's Chi-square test
BCG, Bac llus Ca mette Guerin; TURB, trans urethra bladder resect on; NMIBC, non-musc e-invas ve b adder cancer; M BC, muscle- nvasive bladder cancer; CIS, carcinoma n s tu
Table 3. Multivariable Cox proportional hazards regression models predicting local recurrence, metastatic progression, cancer specific mortality and overall mortality, in 248 bladder cancer patients, who underwent radical cystectomy, with available follow-up data
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 A Tafuri, A Panunzio, A Soldano, et al 430
Variable 0 non-0 (A, B, AB) p-value 2 126 (41 9) 1 175 (58 1) 1 Age at surgery (years) 70 (63, 77) 70 (60, 77) 0 4 Sex 0 1 Female 31 (24 6) 31 (17 7) Male 95 (75 4) 144 (82 3) Body Mass Index (Kg/m2) 25 8 (23 4, 28 6) 26 1 (23 9, 28 6) 0 4 Smoking history 91 (73) 135 (78) 0 3 Diabetes Mellitus 20 (15 9) 36 (20 6) 0 4 Charlson Comorbidity Index 0 3 ≤ 2 76 (60 3) 96 (54 9) > 2 50 (39 7) 79 (45 1) Preoperative BCG administration 29 (23) 59 (34) 0.044 Clinical tumor stage (TURB) 0 028 NMIBC 48 (38 1) 89 (50 9) MIBC 78 (61 9) 86 (49 1) Grading (TURB) 0 005 Low grade 1 (0 8) 14 (8 3) High grade 119 (99 2) 154 (91 7) Pathologic tumor stage 0.024 pT0-1 45 (36) 74 (42 3) pT2 14 (11 2) 30 (17 1) pT3 46 (36.8) 37 (21.1) pT4 20 (16) 34 (19 5) Presence of CIS at final pathology 35 (28) 49 (28) 0 9 Pathologic lymph node involvement 45 (36) 51 (29) 0 2 Number of lymph nodes removed 22 (15, 30) 22 (15, 28) 0 9 Lymph vascular invasion 68 (60) 81 (53) 0.2 Positive surgical margins 15 (12) 19 (11) 0 8
Variable Local Recur rence Metastatic progression Cancer Specific Mor tality Overall Mor tality HR (95% CI) 1 p-value HR (95% CI) 1 p-value HR (95% CI) 1 p-value HR (95% CI) 1 p-value AB0 Blood group A vs 0 0 9 (0 45, 1 79) 0 8 1 15 (0 66, 2) 0 6 1 05 (0 57, 1 95) 0 9 1 41 (0 83, 2 39) 0 2 B vs. 0 0.38 (0.08, 1.75) 0.2 0.70 (0.23, 2.11) 0.5 0.8 (0.23, 2.78) 0.7 1.19 (0.47, 3) 0.7 AB vs 0 3 68 (0 98, 13 84) 0 054 0 56 (0 07, 4 21) 0 6 1 13 (0 26, 4 99) 0 9 1 14 (0 34, 3 85) 0 8 Age at surgery (years) 0 97 (0 94, 1) 0 08 1 05 (1 02, 1 08) 0.003 1 05 (1 01, 1 08) 0.005 1 06 (1 03, 1 09) < 0.001 Sex Male vs Female 1 02 (0 45, 2 35) 0 9 0 86 (0 44, 1 66) 0 7 1 06 (0 52, 2 15) 0 9 0 9 (0 5, 1 62) 0 7 Pathologic tumor stage pT2 vs pT0-T1 2 70 (0 61, 12 01) 0 2 0 85 (0 25, 2 9) 0 8 1 24 (0 26, 5 84) 0 8 0 91 (0 3, 2 74) 0 9 pT3 vs. pT0-T1 3.89 (0.89, 17.07) 0.07 1.45 (0.49, 4.3) 0.5 1.74 (0.43, 6.98) 0.4 1.46 (0.56, 3.78) 0.4 pT4 vs pT0-T1 5 64 (1 15, 27 54) 0.033 2 62 (0 83, 7 25) 0 1 4 04 (0 97, 16 78) 0 055 3 06 (1 12, 8 35) 0.029 Presence of CIS at final pathology Yes vs No 1 94 (0 99, 3 78) 0 053 0 98 (0 54, 1 77) 0 9 1 55 (0 83, 2 86) 0 2 1 52 (0 91, 2 53) 0 1 Pathologic lymph node status pN1-2-3 vs pN0 2 30 (1 13, 4 71) 0 022 2 16 (1 2, 3 88) 0 010 2 31 (1 22, 4 35) 0 010 1 72 (1 01, 2 94) 0 046 Surgical margins status Positive vs Negative 0 64 (0 22, 1 84) 0 4 1 3 (0 61, 2 76) 0 5 1 05 (0 48, 2 27) 0 9 1 05 (0 53, 2 08) 0 9 Lymph vascular invasion Yes vs No 1 69 (0 54, 5 31) 0 4 1 59 (0 66, 3 85) 0 3 2 5 (0 82, 7 67) 0 1 1 41 (0 65, 3 06) 0 4 1 1HR Hazard Rat o, CI Conf dence Interval
Figure 1
Kaplan-Meier plots illustrating (a) local recurrence free survival, (b) metastasis free survival, (c) cancer specific mortality free survival, (d) overall mortality free survival, in 248 bladder cancer patients, who underwent radical cystectomy with available follow up data, stratified according to the AB0-blood group system
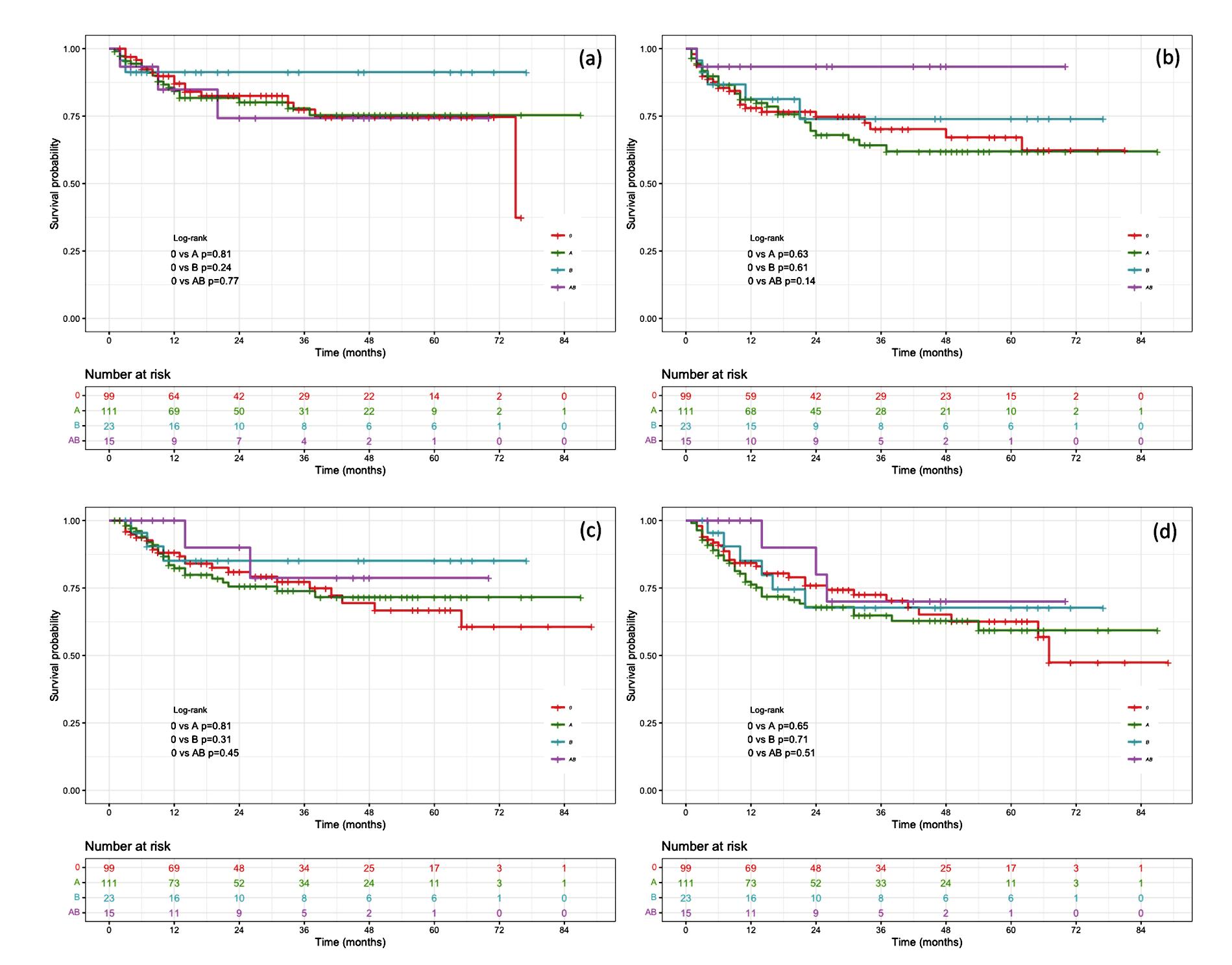
Association between AB0 blood groups and renal function decline
Patients with group AB exhibited the lowest median eGFR at each specified time point compared to their non-AB counterparts (66 4 vs 47 8 vs. 57 9 vs 52 8 mL/min at preoperative evaluation, POD-1, discharge, and 6-months follow up, respectively) Conversely, patients with group B exhibited the highest median eGFR at the preoperative evaluation (78 6 mL/min), as well as at POD-1 (70 6 mL/min) and at discharge (70 4 mL/min)
Finally, patients with group 0 exhibited the highest median eGFR 6 months after RC (71 2 mL/min) However, a statistically significative difference among median eGFR within AB0 blood groups was recorded only at discharge (p = 0 030), as shown in Supplementary Figure 1
In univariable logistic regression models addressing renal function decline at each specified time point, AB group strongly predicted eGFR < 60 mL/min at discharge (Odds Ratio [OR]: 3 27, p = 0 025 Supplementary Table 1) In
decline at discharge even after adjustment for age, preoperative eGFR, CCI, urinary derivation type and postoperative complications (OR: 4 28, p = 0 047)
DISCUSSION
i o
m o d e l s A B g r o u p remained an independent predictor of renal function
The role of AB0 blood group system as a predictor of oncological outcomes in BCa is not well established The AB0 gene is located in the long arm of chromosome 9 (9q34) (23), and encodes a specific glycosyl transferase, which catalyzes the addition of a monosaccharide to the H antigen, thereby generating surface antigens A and B (23) AB0 blood group antigens are involved in various biological mechanisms They are expressed on the erythrocytes’ surface, as well as on the surface of many types of epithelial cells, including urothelial cells (23) Interestingly, AB0 antigens are mutated or absent in tumor cells in BCa (24) Loss of blood group antigens on the cell surface can affect cell adhesion, cell signaling, and immune surveillance, crucial factors in the development and progression of cancer (25) The main evidence for this effect has been stud-
431 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 AB0 blood groups and bladder cancer
m u l t i v a r i a b l e l o g i s t i c r e g r e s
s
n
ied in stomach and pancreatic tumors (13, 15) Two large independent prospective studies showed that compared to patients with group 0, the risk of pancreatic cancer is 1 3 to 1 7-fold higher for patients with non-0 blood type (13) Among urological malignancies, more than 40 years ago, Cazzola et al showed in a small population that AB0 antigens were present on urothelial cells’ surface and that their concentration decreased in less differenced urothelial tumors (26) Joh et al reported an increased risk of developing renal cell carcinoma (RCC) among female patients with non-0 blood groups However, no survival differences were recorded between RCC patients according to blood groups (27) In prostate cancer, Porcaro et al found in 1114 patients, who underwent robot-assisted radical prostatectomy that the risk of PSM was increased in group 0-patients independent of other standard preoperative factors as an expression of more aggressive disease (28)
The association between AB0 blood groups and oncological outcomes in BCa was previously studied by other investigators with controversial results In the current study, we observed that group 0 was associated with a worse pathological tumor stage (p = 0 028) and a higher tumor grade (p = 0 05) at the time of last TURB before RC, as well as with more advanced pathological tumor stage at the definitive histological examination after RC (p = 0 024) However, these findings did not affect prognosis and survival, due to no statistically significative differences noted among LRFS, MFS, CSMFS and OMFS according to AB0 blood groups A historical report by Orihuela et al showed that AB0 blood group system was not associated with stage at presentation in 494 newly diagnosed BCa patients However, among patients with NMIBC, those who had group 0 more frequently harbored higher-grade tumors and experienced progression to advanced disease than their non-0 counterparts (29) Similarly, Klatte et al in a retrospective cohort including 931 BCa patients, found that individuals with blood group 0 had higher recurrence and progression rates than those with group A or B (all p < 0 05) (30) Engel et al. examined a case series of 511 BCa patients, who underwent RC between 1996 and 2011 and found no differences in survival between the four AB0 blood groups (17) Similarly, in a recent single-institution study, D'Andrea et al analyzed data of 463 BCa patients, who underwent RC between 1988 and 2003 These authors observed that AB0 blood group system was not associated with oncological outcomes Rather, Rhesus-positive patients had an increased risk of relapse-free survival, as well as of CSM and OM, when compared to Resus-negative patients However, these associations were not confirmed after multivariable adjustment (19) Finally, a large multicenter study involving 7906 BCa patients, demonstrated that blood group B was associated with higher mortality when compared with other blood groups (p = 0 026) However, even in this case, statistical significance disappeared in multivariable analysis (16) In contrast, Gershman et al retrospectively evaluated data of 2086 BCa patients, who underwent RC between 1980 and 2008, and observed that non-0 groups, and in particular group A, was associated with higher CSM (HR: 1 23; p = 0 007) (18)
In the current study we also tested the association between AB0 blood group system and renal function decline after surgery Interestingly, we observed that patients with
group AB exhibited the lowest median eGFR values at POD-1, discharge and after 6 months follow up, compared to A, B, and 0 blood group patients However, a statistically significant difference was recorded only at discharge (p = 0 030) Similarly, in multivariable logistic regression models, where group 0 was the referent, AB was associated with a 4-fold higher risk of renal function decline at discharge (p = 0 047) These results could be partially attributable to a more guarded pre-operative clinical conditions of AB patients Additionally, most AB patients were diabetic (p = 0 049) This study might be in line with studies demonstrated an higher thrombotic risk in ABpatients with non-valvular atrial fibrillation (31), as well as a higher incidence of cardiovascular diseases in non-0 patients (32), which may induces renal failure
The present study is not devoid of limitations First, the current investigation is retrospective and suffers of the bias related to these types of studies Second, despite our data being sourced from a high-volume center for BCa treatment, the overall sample size is limited In consequence, our observations required interpretations that account for marginal sample sizes and comparisons of small subgroups In this context, the observed number of BCa patients with group B and AB was very small However, the prevalence of AB0 blood groups recorded in the current study corresponded to the general AB0 frequency and distribution reported in previous larger historical analyses Additionally, various surgeons as well as pathologists were involved, and AB0 blood group antigen expression within the tumor as well as Rhesus factor were not assessed In the future, a combined evaluation of the patient's blood group and the degree of AB0 antigen expression within the tumor is needed in higher level studies
CONCLUSIONS
Among AB0 blood groups, patients with group 0 exhibited the most aggressive tumor profile However, no differences were recorded in recurrence or survival rates Patients with group AB presented the lowest median eGFR at each specified time point Group AB was independently associated with eGFR < 60 mL/min at discharge
REFERENCES
1 Siegel RL, Miller KD, Fuchs HE, Jemal A Cancer statistics, 2021 CA: a cancer journal for clinicians 2021; 71:7-33
2 Powles T, Bellmunt J, Comperat E, et al Bladder cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up Ann Oncol 2022; 33:244-258
3 van Hauen MB, Maibom SL, Thind PO, et al Risk of recurrence and long-term mortality following radical cystectomy for bladder cancer Scand J Urol 2022; 56:149-154
4 Zhan X, Jiang M, Deng W, et al Development and Validation of a Prognostic Nomogram for Predicting Cancer-Specific Survival in Patients With Lymph Node Positive Bladder Cancer: A Study Based on SEER Database Front Oncol 2022; 12:789028
5 Mir MC, Marchioni M, Zargar H, et al Nomogram predicting bladder cancer–specific mortality after neoadjuvant chemotherapy and radical cystectomy for muscle-invasive bladder cancer: results of an international consortium Eur Urol Focus 2021; 7:1347-1354
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
432
A Tafuri, A Panunzio, A Soldano, et al
6 Bratu O, Marcu D, Anghel R, et al Tumoral markers in bladder cancer Exp Ther Med 2021; 22:1-8
7 Fujita N, Hatakeyama S, Okita K, et al Impact of chronic kidney disease on oncological outcomes in patients with high-risk non-musc l e - i n v a s i v e b l a d d e r c a n c e r w h o u n d e r w e n t a d j u v a n t b a c i l l u s Calmette-Guérin therapy Urol Oncol 2021; 39:191 e9-191 e16
8 Jiang DM, Gupta S, Kitchlu A, et al Defining cisplatin eligibility in patients with muscle-invasive bladder cancer Nat Rev Urol 2021; 18:104-114
9 Tafuri A, Odorizzi K, Di Filippo G, et al Acute kidney injury strongly influences renal function after radical nephroureterectomy for upper tract urothelial carcinoma: A single-centre experience Arch Ital Urol Androl 2021; 93:9-14
10 Leow JJ, Chong YL, Chang SL, et al Neoadjuvant and Adjuvant Chemotherapy for Upper Tract Urothelial Carcinoma: A 2020 Systematic Review and Meta-analysis, and Future Perspectives on Systemic Therapy Eur Urol 2021; 79:635-654
11 Tafuri A, Smith DD, Cacciamani GE, et al Programmed Death 1 and Programmed Death Ligand 1 Inhibitors in Advanced and Recurrent Urothelial Carcinoma: Meta-analysis of Single-Agent Studies Clin Genitourin Cancer 2020; 18:351-360 e353
12 Idris E, Tahir R, Amhamed A, Aboualkasem S A Study on the Relationship between Blood Group and Type of Cancer Scientific Journal for the Faculty of Science-Sirte University 2022; 2:23-27
13 Wolpin BM, Chan AT, Hartge P, et al ABO blood group and the risk of pancreatic cancer J Natl Cancer Inst 2009; 101:424-431
14 Gates MA, Xu M, Chen WY, et al ABO blood group and breast cancer incidence and survival Int J Cancer 2012; 130:2129-2137
15 Wang Z, Liu L, Ji J, et al ABO blood group system and gastric cancer: a case-control study and meta-analysis Int J Mol Sci 2012; 13:13308-13321
16 Klatte T, Xylinas E, Rieken M, et al Effect of ABO blood type on mortality in patients with urothelial carcinoma of the bladder treated with radical cystectomy Urol Oncol 2014; 32:625-630
17 Engel O, Soave A, Peine S, et al The impact of the AB0 and the Rhesus blood group system on outcomes in bladder cancer patients treated with radical cystectomy World J Urol 2015; 33:1769-1776
18 Gershman B, Moreira DM, Tollefson MK, et al The association of ABO blood type with disease recurrence and mortality among patients with urothelial carcinoma of the bladder undergoing radical cystectomy Urol Oncol 2016; 34:4 e1-9
19 D'Andrea D, Moschini M, Soria F, et al ABO Blood Group and Rhesus Factor Are Not Associated with Outcomes After Radical Cystectomy for Non-metastatic Urothelial Carcinoma of the Bladder Anticancer Res 2017; 37:5747-5753
20 Würdemann N, Wagner S, Sharma SJ, et al Prognostic impact of AJCC/UICC 8th edition new staging rules in oropharyngeal squamous cell carcinoma Front Oncol 2017; 7:129
21 Humphrey PA, Moch H, Cubilla AL, et al The 2016 WHO classification of tumours of the urinary system and male genital organs part B: prostate and bladder tumours Eur Urol 2016; 70:106-119
22 Levey AS, Stevens LA, Schmid CH, et al A new equation to estimate glomerular filtration rate Ann Int Med 2009; 150:604-612
23 Franchini M, Liumbruno GM ABO blood group: old dogma, new perspectives Clin Chem Lab Med 2013; 51:1545-1553
24 Orntoft TF, Meldgaard P, Pedersen B, Wolf H The blood group ABO gene transcript is down-regulated in human bladder tumors and growthstimulated urothelial cell lines Cancer Res 1996; 56:1031-1036
25 Hakomori S Antigen structure and genetic basis of histo-blood groups A, B and O: their changes associated with human cancer Biochim Biophys Acta 1999; 1473:247-266
26 Cazzola P, Matturri L, Trinchieri A, et al Impiego di una metodica di immunofluorescenza indiretta nella ricerca degli antigeni di superficie AB0 (H) sulle cellule dell'epitelio di transizione Arch It Urol Nefrol 1981; 53:297
27 Joh HK, Cho E, Choueiri TK ABO blood group and risk of renal cell cancer Cancer Epidemiol 2012; 36:528-532
28 Porcaro AB, Amigoni N, Migliorini F, et al ABO blood group system and risk of positive surgical margins in patients treated with robot-assisted radical prostatectomy: results in 1114 consecutive patients J Robot Surg 2021; 16:507-516
29 Orihuela E, Shahon RS Influence of blood group type on the natural history of superficial bladder cancer J Urol 1987; 138:758-759
30 Klatte T, Xylinas E, Rieken M, et al Impact of ABO blood type on outcomes in patients with primary nonmuscle invasive bladder cancer J Urol 2014; 191:1238-1243
31 Jang AY, Seo J, Park YM, et al ABO Blood Type Is Associated w i t h T h r o m b o t i c R i s k i n P a t i e n t s w i t h N o n v a l v u l a r A t r i a l Fibrillation J Clin Med 2022; 11:3064
32 Neshat S, Rezaei A, Farid A, et al Cardiovascular Diseases Risk Predictors: ABO Blood Groups in a Different Role Cardiol Rev 2022 doi: 10 1097/CRD 0000000000000463
Correspondence
Alessandro Tafuri, MD (Corresponding Author) tafuri alessandro@gmail com
Vincenzo Pagliarulo, MD - enzopagliarulo@yahoo com
Department of Urology, “Vito Fazzi” Hospital, Lecce Piazza Filippo Muratore, 1, 73100 Lecce (Italy)
Andrea Panunzio, MD - panunzioandrea@virgilio it
Antonio Soldano, MD - soldanoantonio@libero it
Giovanni Mazzucato, MD - gio mazzucato@gmail com
Paola Irene Ornaghi, MD - paolairene ornaghi@gmail com
Alessandra Gozzo, MD - la ale gozzo@gmail com
Nicola De Maria, MD - nicola demaria02@gmail com
Francesco Cianflone, MD - fra1178@gmail com
Antonio Benito Porcaro, MD - drporcaro@yahoo com
Walter Artibani, MD - prof artibani@gmail com
Alessandro Antonelli, MD - alessandro antonelli@me com
Maria Angela Cerruto, MD - mariaangela cerruto@univr it
Department of Urology, University of Verona, Azienda Ospedaliera
Universitaria Integrata di Verona, Verona (Italy)
Matteo Brunelli, MD - matteo brunelli@univr it
Department of Pathology, University of Verona, Azienda Ospedaliera
Universitaria Integrata di Verona, Verona (Italy)
Giacomo Di Filippo, MD - giacomo difilippo90@gmail com
Department of General and Hepatobiliary Surgery, University of Verona, Azienda Ospedaliera Universitaria Integrata Verona, Verona (Italy)
Aliasger Shakir, MD USC - aliasgershakir@gmail com
Institute of Urology, Catherine and Joseph Aresty Department of Urology, Keck School of Medicine, University of Southern California (USC), Los Angeles, CA, US
Zhe Tian, MSc - zhe tian24@gmail com
Pierre I Karakiewicz, MD - pierrekarakiewicz@gmail com
Cancer and Prognostics Health Outcomes Unit, Division of Urology, University of Montreal Health Center, Montreal, Quebec, Canada
433 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 AB0 blood groups and bladder cancer
lymph node dissection
Comparative study in patients with penile cancer
1 Hospital de Egas Moniz - Centro Hospitalar de Lisboa Ocidental, Lisboa, Portugal;
2 Instituto Português de Oncologia Francisco Gentil do Porto, Porto, Portugal
Summary
Objective: Management of patients with penile cancer (PeC) with palpable inguinal lymph nodes (ILNs) relies on radical ILN dissection (RILND). Low burden of nodal metastatic disease may lead to long-lasting survival with surgical management. Nevertheless, RILND involves significant postoperative morbidity We compared the complications of patients undergoing RILND with (RILND-T) and without (RILND-0T) placement of a collagen-fibrin sealant patch on the resection bed.
Materials and methods: We conducted an observational retrospective study. Data from men submitted to RILND-T and RILND-0T from Jan/2001 to Feb/2022, in a tertiary care centre were compared. The primary endpoint was the overall incidence of complications until 1 month after the procedure and their respective severity in both cohorts (Clavien-Dindo classification system) Secondarily, length of hospital stay (LOHS) was analysed The placement of a collagen-fibrin sealant patch was left at the surgeon’s discretion
Results: Seven patients underwent RILND-T and 20 underwent RILND-0T, respectively There were no differences in pathologic TNM stage nor in the total number of ILNs removed (17 ± 4 vs 20 ± 8, p = 0 37) Overall, 23 (85 2%) patients had complications The complication rate was similar in both cohorts (85 7% vs 85%, p = 0 73) Surgical wound infection (3/7 vs 11/20) and lymphocele (4/7 vs 11/20) were the most reported complications. Patients undergoing RILND-T were discharged faster (mean length of hospital stay 9 ± 3 vs 19 ± 20 days, p = 0 22)
Conclusions: The application of a collagen-fibrin sealant patch on the resection bed does not seem to reduce the postoperative complication rate in patients undergoing RILND. Nevertheless, a trend towards a shorter LOHS in patients with RILND-T cannot be excluded and should be validated by further studies with a higher number of patients
KEY WORDS: Penile Cancer; Radical Inguinal Lymph Node Disssection; Radical Inguinal Lymphadenectomy; Complications of Radical Inguinal Lymph Node Dissection
Submitted 3 August 2022; Accepted 21 August 2022
INTRODUCTION
Penile cancer (PeC) is a rare neoplasm representing the 32nd most common cancer worldwide (1) It displays an overall incidence of around 1/100 000 males in Europe
and the USA (2) In 2020, 36 068 new cases were diagnosed, and 13 211 men died due to PeC (1) The incidence increases with age with a peak in the sixth decade (3)
In Portugal, PeC represents the 30th most common cancer with 119 new cases diagnosed in 2020 (4)
PeC metastatic spread complies with the route of anatomical drainage, beginning with the inguinal lymph nodes (superior medial zone of the inguinal region and, afterwards, central inguinal nodes) followed by the pelvic lymph nodes Whenever inguinal lymph nodes are palpab l y e n l a r
approach (2) Other diagnostic tools have already been evaluated Positron-Emission Tomography (PET) computed tomography (CT) using 18-F-fluorodeoxyglucose (18FFDG-PET-CT) has shown good accuracy confirming inguinal metastasis and detecting systemic disease (8299% sensitivity for ILN metastasis in patients with clinically evident disease) whereas magnetic resonance imaging (MRI) with lymphotrophic nanoparticles (ferumoxtran10, ferucarbotran, ultrasmall superparamagnetic iron oxides) might be an adequate choice for the evaluation patients with a limited physical and/or clinical exam (100% sensitivity and 97% specificity) Even though ultrasound-guided biopsy may allow for the pathological diagnosis of disease in clinically positive patients, they will ultimately require radical inguinal lymph node dissection as for local staging The risk of distant metastasis whenever inguinal lymph nodes are palpable is high deeming radiographical evaluation with CT or MRI necessary (5)
The involvement of locoregional lymph nodes represents the most clinically significant prognostic factor for patients with PeC (6) The recurrence free and overall survival are largely dependent on ILN disease burden with a significant decrease in the 5-year survival in patients with positive deep pelvic lymph nodes (0-12%) versus patients with a single involved inguinal node (80%) (7)
The surgical excision of clinically positive lymph nodes is decisive for patient survival as it may result in cure Nevertheless, RILND might be delayed by physicians and patients due to its anticipated postoperative morbidity leading to worsened overall survival (8) The complica-
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 434 ORIGINAL PAPER No conflict of interest declared
d i c a l i n g u i n a l l y m p h n o d e d i s s e c t i
n
R I L N D ) s h o u l d b e t h e d i a g n o s t i c a n d t h e r a p e u t i c
g e d , r a
o
(
Does the placement of a collagen-fibrin sealant reduce complications of radical inguinal
–
Andreia Bilé Silva 1* , João Nuno Pereira 2* , Rui Freitas 2 , Isaac Braga 2 , João Carvalho 2 , José Sanches Magalhães 2 , Vítor Silva 2 , Francisco Lobo 2 , António Morais 2
DOI: 10 4081/aiua 2022 4 434
* Andreia Bilé Silva and João Nuno Pereira contributed equally
tions of RILND can be as high as 50% (9), ranging from seroma and hematoma formation to wound infection and even more severe complications such as difficulty in ambulating, deep venous thrombosis (DVT) and chronic lymphoedema More recent studies have reported a lower morbidity in about 25% of cases (10)
Meticulous surgical technique with careful tissue handling along with avoidance of electrocauterization, modified incision lines, suction drainage devices, videoendoscopic surgery, omentoplasty and placement of a collagen-fibrin sealant patch have already demonstrated efficacy in achieving hemostasis after liver and kidney surgery (11), in preventing leakage after lung surgery (12), and in reducing lymphatic fluid production after mediastinal (13) and axillary (14) lymph-node dissection and, therefore, minimise postoperative morbidity (15)
Additionally, there is evidence that the placement of a fibrin glue sealant is beneficial towards reducing the complication rates in RILND, namely seroma (16)
On the other hand, evidence of benefit due to vacuum suction in RILND for PeC (17), sealants in RILND for melanoma (18), or collagen-fibrin sealant patch in ILND in vulvar cancer (19) is still lacking
To our knowledge, this is the first observational study reporting the efficacy of placing a collagen-fibrin sealant patch (TachoSil®) in the resection bed of patients with PeC submitted to RILND
MATERIALS AND METHODS
Our study complies with the STROBE (Strengthening the Reporting of Observational studies in Epidemiology) guidelines for observational original research studies
A retrospective observational study was conducted at a tertiary oncological care centre Consecutive patients with PeC who underwent any kind of inguinal lymph node dissection (ILND) between January of 2000 and February of 2022 were identified From the 214 patients with PeC initially retrieved, 110 did not undergo ILND and were excluded from the study Patients who underwent ILND other than RILND, namely modified ILND (n = 54) or dynamic sentinel ILND (n = 23) were excluded
RILND technique was the same in all patients included It involved an incision parallel and 1-2 cm inferior to the inguinal ligament Skin flaps were created preserving the Scarpa’s fascia to avoid necrosis RILND comprised the traditional boundaries margin of the external inguinal ring until the anterior superior iliac spine (ASIS), superiorly, the ASIS and a line drawn 20cm inferiorly, laterally, the pubic tubercle and a line drawn 15 cm inferiorly from it, medially, and a line connecting both lateral and medial limits A long saphenous vein ligation was usually performed at the apex of the femoral triangle Sartorius muscle transposition might be done to cover the femoral vessels Placement of TachoSil® on the resection bed was left at the surgeon ’ s discretion Cohorts were compared based on the placement of TachoSil® during the RILND A single patch of TachoSil® was applied, with the yellow active side onto the resection bed, after blood and other fluids were cleaned The patch had to extend around the inguinal lymphadenectomy area and maintained in place for at least 3 min Data was obtained through the available consultation
records Data concerning clinical history (including risk factors for PeC), physical examination and pathological results were collected Patients’ comorbidities were documented and assessed with Charlson Comorbidity Score (CCI) Pertaining to the surgical procedure, surgical reports were examined and data on the surgical technique and amount of blood loss were gathered
Postoperative complications after RILND were defined as those that occurred immediately after surgery, whether during the initial hospital stay or within 30 days of RILND RILND postoperative complications were quantified using the Clavien-Dindo classification system for surgical complications (20)
H o s p i t a l i z a t i o n r e c o r d s w e r e a v a i l a b l e A m o u n t o f drainage volume, duration of drain placement and deambulation start were assessed
All complications were followed until resolution and hospital discharge and, when applicable, surgical interventions of major complications were recorded by their specific date and type of procedure required Readmissions during the first 30 postoperative days were determined as well as the hospitalization reason and duration
Statistical analysis
The primary outcome was the overall complication rate in both cohorts Secondary endpoint measures were the incidence of each complication in RILND-T and RILND0T groups
To determine whether the data had a Gaussian distribution, Gaussian curve and Kolmogorov-Smirnov test were used Comparisons of the continuous variables between groups were made using the Student’s T-test for normally distributed and Mann-Whitney U for not normally distributed variables The chi-squared and Fisher’s exact t e s t s w
s Statistical analyses were performed using SPSS 25 0 (IBM Software division, Somers, NY, USA) All reported p values are two-sided, and p values < 0 05 were considered to indicate statistical significance
RESULTS
A total of 27 patients with PeC submitted to RILND were collected for the present study While 7 patients underwent RILND-T, 20 patients underwent RILND-0T Table 1 displays patient demographics, surgical outcomes and lymph node counts
The mean age (70 ± 7 vs 64 ± 14 years, p = 0 32), CCI (6 ± 2 vs 5 ± 2, p = 0 35) and body mass index (BMI - 25 ± 4 vs 27 ± 4 kg/m2, p = 0 27) were comparable in both cohorts
The majority of patients (n = 26) had confirmed conventional squamous cell carcinoma of the penis (SCCP), with only one patient having a mixed warty-basaloid subtype
The primary penile tumour grade (Table 2) was similar in both cohorts (p = 0 42) as well as lymphovascular invasion (14 8% vs 29 6%, p = 0 85)
Patients had a mean 17 ± 4 and 20 ± 8 lymph nodes harvested in the RILND-T and in the RILND-0T group (p = 0 37), respectively The median largest diameter lymph node with tumour present was 2 7 (range 0 5-5-3) and 3 7 (range 0 4-6 5) cm (p = 0 65)
435 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Does the placement of a collagen-fibrin sealant reduce complications of radical inguinal lymph node dissection
r e u s e d t o c o m p a r e c a t e g o r i c a l v a r i a b l e
e
The mean length of hospital stay after RILND was longer in the cohort without placement of collagen-fibrin sealant patch (9 ± 3 vs 19 ± 20 days, p = 0 22) The mean time to ambulation was 2 ± 1 in both cohorts (p = 0 16) Inguinal suction drains were kept in place for a mean of 5 ± 3 and 5 ± 1 days (p = 0 55)
A detailed summary of clinical nodal staging and pathological staging can be found in Tables 3 and 4, respectively
Overall, of the 27 patients with PeC included in the present study, 23 (85 2%) had at least one postoperative complication and 20 patients having more than a single complication (88 instances of complications overall) The complication rate was similar in both cohorts (85 7% vs 85%, p = 0 73) and when analysing the complications on a per patient basis, there was a comparable mean number of 3 complications per patient in both groups (p = 0 88)
The most commonly encountered complications were lymphocele (57 1% vs 55%, p = 0 4) and wound infection (42 9% vs 55%, p = 1) Vascular and neural injuries were
Pathological staging, PeC and nodes
RILND-T: Radica nguinal lymph node dissect on with TachoSi ® p acement; R LND-0T: Rad cal ingu nal lymph node dissect on without TachoSil® placement; CIS: Carcinoma n situ
Table 5.
Complication incidence rates according to Clavien-Dindo classification
RILND-T: Rad ca nguinal lymph node dissect on with TachoSi ® placement; RILND-0T: Rad cal ingu nal ymph node dissect on without TachoSil® p acement
not noted All of the complications recorded were Clavien-Dindo II grade or less
A total of 3 patients were readmitted due to complications, 1 from the RILND-T (1/7) and 2 (2/20) from the RILND-0T cohort The hospital readmission time was similar in both groups (11 and 10 days, respectively) None of the patients were submitted to surgical exploration nor surgical management of major complications
Table 5 shows complication rates and type as categorised by the Clavien-Dindo classification
T
Portuguese high-volume oncological care centre It details the postoperative complication rates from RILND, as categorised by the Clavien-Dindo classification system, from January of 2001 until February of 2022 with and without placement of collagen-fibrin sealant patch on the resec-
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
436
A
Bilé Silva, J Nuno Pereira, R Freitas, I Braga, J Carvalho, J Sanches Magalhães, V Silva, F Lobo, A Morais
DISCUSSION
h e p r e s e n t s t u d y r e p o r t s t h e e x p e r i e n c e f r o m a
Table
Patient demographic characteristics, surgical outcomes
counts Characteristics RILND-T RILND-0T p Age, in years (mean ± standard deviation) 70 ± 7 64 ± 14 0 32 BMI, in kg/m2 (mean ± standard deviation) 25 ± 4 27 ± 4 0 27 Length of hospital stay, in days (median, range) 9 ± 3 19 ± 20 0 20 Post-surgical walk day (mean ± standard deviation) 2 ± 1 2 ± 1 0 16 Post-surgical drain removal (mean ± standard deviation) 5 ± 3 5 ± 1 0 55 Total number of lymph nodes taken (mean ± standard deviation) 17 ± 4 20 ± 8 0 37 Total number of positive lymph nodes (mean ± standard deviation) 1 ± 1 4 ± 4 0.13 Largest lymph node size, in cm (median, range) 2 7, 0 5-5 3 3 7, 0 4-6 5 0 65 RILND-T: Rad ca inguinal lymph node dissection with TachoS l® placement; RILND-0T: Radical ingu na ymph node dissection without TachoSi ® p acement; BMI: Body mass ndex
1.
and lymph node
grade. Characteristics RILND-T RILND-0T p Tumour grade, in percentage 0 42 – Well-differentiated (G1) 26 7 0 – Moderately differentiated (G2) 40 80 – Poorly differentiated (G3) 33 3 20 – Undifferentiated (G4) 00
Table 2. Penile tumour
Table 4
Characteristics RILND-T RILND-0T p Tumour stage, in percentage 0 81 – CIS 00 – pT1 21.1 14.3 – pT2 42 1 42 9 – pT3 36 8 42 9 – pT4 00 Nodal stage, in percentage 0 35 – pN0 20 42 9 – pN1 5 14 3 – pN2 20 0 – pN3 55 42 9
Characteristics RILND-T RILND-0T p Chronic lymphoedema, n (percentage) 1 (14 3) 1 (5) 0 46 – Clavien-Dindo grade I, in percentage 14 3 5 Deep venous thrombosis, n (percentage) 1 (5) 0 (0)– Clavien-Dindo grade II, in percentage 50 Lymphocele, n (percentage) 4 (57 1) 11 (55) 0 4 – Clavien-Dindo grade I, in percentage 42 9 55 – Clavien-Dindo grade II, in percentage 14 3 0 Lymphorrhea, n (percentage) 3 (42 9) 9 (45)– Clavien-Dindo grade I, in percentage 42 9 45 Neural injury, n (percentage) 0 (0) 0 (0)Skin necrosis, n (percentage) 2 (28 6) 6 (30) 0 75 – Clavien-Dindo grade I, in percentage 2 20 – Clavien-Dindo grade II, in percentage 0 10 Vascular injury, n (percentage) 0 (0) 0 (0)Wound dehiscence, n (percentage) 3 (42 9) 4 (20) 0 48 – Clavien-Dindo grade I, in percentage 15 42 9 – Clavien-Dindo grade II, in percentage 50 Wound infection, n (percentage) 3 (42 9) 11 (55)– Clavien-Dindo grade II, in percentage 42 9 55
Table 3
Characteristics RILND-T RILND-0T p Nodal stage, in percentage 0 21 – cN0 57 1 15 – cN1 0 15 – cN2 28 6 35 – cN3 14 3 35 RILND-T:
Clinical node staging
Radical inguina ymph node d ssection w th TachoSil® placement; RILND-0T: Radica nguinal lymph node d ssection w thout TachoS l® placement
tion bed To our knowledge, this is the first observational study reporting the efficacy of placing a collagen-fibrin sealant patch in the resection bed of patients with PeC submitted to RILND
Previous series on complication rates state results averaging 40-70% (21) Although we report a higher overall complication rate, all of the patients had minor complications (Clavien-Dindo I and II) which translated into a regular postoperative management in most cases
Lymphocele and wound infection were the most common complications (57 1% vs 55% and 42 9% vs 55%, respectively)
A high rate of complications was seen in both groups (more than 85% of the patients had some sort of complication) Nevertheless, none of the complications were graded higher than II, as assessed by the Clavien-Dindo classification
Measures to avoid complications during RILND
Several studies have been conducted in order to find validated measures to reduce morbidity Careful tissue handling and avoiding electrocautery as well as preserving the saphenous vein and postoperative measures to improve drainage (stocking, bandaging, inguinal pressure dressings or vacuum suction) minimise postoperative morbidity (10, 22, 23) A systematic review and meta-analysis (24) on surgical techniques to reduce postoperative lymphoedema reported that sparing the long saphenous vein, fascia preserving dissection, pedicled omental flap and microsurgery are efficient When available, minimallyinvasive surgical approaches (laparoscopic, robot-assisted) for inguinal lymphadenectomy, in small series, have been reported to significantly reduce post-operative morbidity except for the rate of lymphoceles (10, 17, 25-27)
Collagen-fibrin sealant patch as an adjuvant to reduce RILND complications
As previously stated, collagen-fibrin sealant patch and other similar fibrin-based sealants have already been studied in different fields as surgical adjuvants to reduce lymphadenectomy-related morbidity, namely, lymphorrhea, lymphoceles, and lymphoedema
The reported results are conflicting In breast cancer patients undergoing axillary lymph node dissection, the fi b r i n - b a s e d s e a l a n t r e d u c e d t h e o v e r a l l l y m p h a t i c drainage amount, which allowed an earlier removal of closed suction drains; on the other hand, other studies noted no significant differences regarding the incidence and severity of the above-mentioned complications (28, 29) It was also investigated in patients with endometrial cancer: even though the placement of TachoSil® in laparoscopic pelvic lymphadenectomy translated into a significantly lower prevalence of lymphocele, there was no significant difference regarding the symptomatic forms of lymphocele (30) The outcomes after collagen-fibrin sealant patch placement on the resection bed are inconsistent Accordingly, a meta-analysis from 2014 (25) concluded that the available evidence is not robust enough to recommend the use of fibrin-based sealants in inguinofemoral lymphadenectomy for malignant conditions, especially considering the additional cost for these products
Overall, our results suggest that collagen-fibrin sealant patch did not seem to be effective in improving postoperative complications both in quantity and in severity as assessed by the Clavien-Dindo classification
Additionally, in our study, the inguinal drains were not removed earlier in the cohort submitted to RILND-T (on average, on the fifth postoperative day in both groups) Nevertheless, there is a trend towards a shorter length of hospital stay in patients who underwent placement of the collagen-fibrin sealant agent
Pitfalls
Because of the relative rarity of penile cancer, there was a paucity of patients undergoing RILND with and without placement of collagen-fibrin sealant patch on the resection bed Future studies, grouping together multiple patient series from different centres, might help overcome this by providing a greater database of patients, which is required to achieve statistical significance Furthermore, by combining patient data from multiple centres, variability of patient demographics and surgical technique could be unbiased and therefore externally validated for the general patient experience
Furthermore, because of the retrospective nature of the present study, data collection was limited to what was reported initially at the time of patient care and during the follow-up This is largely the reason why complication reporting was limited to 30 days postoperatively; there were difficulties in collecting long-term follow-up data
Accordingly, the small dimension of the study does not allow to exclude completely a potential effect of collagenfibrin sealant patch for all complications, although results of our study refute its utility and data previously gathered in other studies suggest that it is improbable
CONCLUSIONS
The significant morbidity associated with RILND for penile cancer treatment highlights the relevance of adopting techniques that minimise and avoid complications With better understanding of the possible complications after RILND and its rate, attitudes towards diminishing their incidence may be implemented By tailoring peri- and postoperative care accordingly, outcomes may be improved
There seems to exist a clear trend towards a lower length of hospital stay in patients in whom the collagen-fibrin sealant patch was placed surgically on the resection bed
Even though we did not prove collagen-fibrin sealant patch placement on the resection bed of patients undergoing RILND to improve the outcomes, we cannot comp l e t e l y e x c l u d e a p o t e n t i a l b e n e fi c i a l e f f e c t o f t h i s approach without having conducted a prospective randomised trial
REFERENCES
1 Sung H, Ferlay J, Siegel RL, et al Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries CA Cancer J Clin 2021; 71:209-249
2 Hakenberg OW, Minhas ES, Necchi A, et al EAU Guidelines on Penile Cancer 2020 Eur Assoc Urol Guidel 2020 Ed [Internet] 2020; 1-38 Available from: http://uroweb org/guideline/penile-can-
437 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Does the placement of a collagen-fibrin sealant reduce complications of radical inguinal lymph node dissection
cer/ LK - Penile Cancer Uroweb%7Chttp://uroweb org/guideline/ penile-cancer/%7C FG - 0
3 Barnholtz-Sloan JS, Maldonado JL, Pow-sang J, Guiliano AR Incidence trends in primary malignant penile cancer Urol Oncol 2007; 25:361-7
4 W o r l d H e a l t h O r g a n i z a t i o n P o r t u g a l - G l o b a l C a n c e r Observatory Globocan 2020 [Internet] 2020; 501:1-2 Available from: https://gco iarc fr/today/data/factsheets/populations/620-portugal-fact-sheets pdf
5 Leone A, Diorio GJ, Pettaway C, et al Contemporary management of patients with penile cancer and lymph node metastasis Nat Rev Urol 2017; 14:335-47
6 Pow-Sang MR, Ferreira U, Pow-Sang JM, et al Epidemiology and natural history of penile cancer Urology 2010; 76(2 Suppl 1):S2
7 Leijte JAP, Kerst JM, Bais E, et al Neoadjuvant chemotherapy in advanced penile carcinoma Eur Urol 2007; 52:488-94
8 Gopman JM, Djajadiningrat RS, Baumgarten AS, et al Predicting postoperative complications of inguinal lymph node dissection for penile cancer in an international multicentre cohort BJU Int 2015; 116:196-201
9 Stuiver MM, Djajadiningrat RS, Graafland NM, et al Early wound complications after inguinal lymphadenectomy in penile cancer: a historical cohort study and risk-factor analysis Eur Urol 2013; 64:486-92
10 Koifman L, Hampl D, Koifman N, et al Radical open inguinal lymphadenectomy for penile carcinoma: Surgical technique, early complications and late outcomes J Urol 2013; 190:2086-92
11 Siemer S, Lahme S, Altziebler S, et al Efficacy and Safety of TachoSil® as Haemostatic Treatment versus Standard Suturing in Kidney Tumour Resection: A Randomised Prospective Study Eur Urol 2007; 52:1156-63
12 Anegg U, Lindenmann J, Matzi V, et al Efficiency of fleece-bound sealing (TachoSil®) of air leaks in lung surgery: a prospective randomised trial Eur J Cardio-thoracic Surg 2007; 31:198-202
13 Czerny M, Fleck T, Salat A, et al Sealing of the mediastinum with a local hemostyptic agent reduces chest tube duration after complete mediastinal lymph node dissection for stage I and II non-small cell lung carcinoma Ann Thorac Surg 2004; 77:1028-32
14 Moore M, Burak WE, Nelson E, et al Fibrin sealant reduces the duration and amount of fluid drainage after axillary dissection: a randomized prospective clinical trial J Am Coll Surg 2001; 192:591-9
15 Baggio S, Laganà AS, Garzon S, et al Efficacy of a collagen-fibrin sealant patch (TachoSil®) as adjuvant treatment in the inguinofemoral lymphadenectomy for vulvar cancer: A double-blind randomized-controlled trial Arch Gynecol Obstet 2019; 299:1467-74
16 Fawzy A, Balbaa MA, Gaber A Role for fibrin glue (sealant) in seroma reduction after inguinal lymphadenectomy; a randomized controlled trial Int J Surg 2021; 89:105950
17 Tauber R, Schmid S, Horn T, et al Inguinal lymph node dissection: epidermal vacuum therapy for prevention of wound complications J Plast Reconstr Aesthet Surg 2013; 66(3):390-6
18 Gerken ALH, Dobroschke J, Reißfelder C, et al Tissue sealants for the prevention of lymphoceles after radical inguinal lymph node dissection in patients with melanoma: A systematic review and individual patient data meta-analysis J Surg Oncol 2019; 119:728-36
19 Saner FA, Schötzau A, Mackay G, et al Fibrin-thrombin sealant does not reduce lymphocele formation in patients with inguinofemoral lymphadenectomy for vulvar cancer Cancer Manag Res 2019; 11:3575-3582
20 Dindo D, Demartines N, Clavien PA Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey Ann Surg 2004; 240:205-13
21 Spiess PE, Hernandez MS, Pettaway CA Contemporary inguinal lymph node dissection: minimizing complications World J Urol 2009; 27:205-12
22 Thuret R, Sun M, Lughezzani G, et al A contemporary population-based assessment of the rate of lymph node dissection for penile carcinoma Ann Surg Oncol 2011; 18:439-46
23 Protzel C, Alcaraz A, Horenblas S, et al Lymphadenectomy in the surgical management of penile cancer Eur Urol 2009; 55:107588
24 Abbas S, Seitz M Systematic review and meta-analysis of the used surgical techniques to reduce leg lymphedema following radical inguinal nodes dissection Surg Oncol 2011; 20:88-96
25 Weldrick C, Bashar K, O’Sullivan TA, et al A comparison of fibrin sealant versus standard closure in the reduction of postoperative morbidity after groin dissection: A systematic review and metaanalysis Eur J Surg Oncol 2014 2022; 40:1391-8
26 Cui Y, Chen H, Liu L, et al Saphenous vein sparing during laparoscopic bilateral inguinal lymphadenectomy for penile carcinoma patients Int Urol Nephrol 2016; 48(3):363-6
27 Kumar V, Sethia KK Prospective study comparing video-endoscopic radical inguinal lymph node dissection (VEILND) with open radical ILND (OILND) for penile cancer over an 8-year period BJU Int 2017; 119:530-4
28 Vinchant M, Bonneau C, Lesavre M, et al Interest of a thrombin and fibrinogen combipatch in preventing breast cancer seroma after lymph node dissection Gynecol Obstet Fertil 2013; 41:583-7
29 Lacoste C, Ouldamer L, Body G, Marret H Does the use of TachoSil allow to reduce the morbidity of axillary dissection? Gynecol Obstet Fertil 2013; 41:141-3
30 Grimm C, Polterauer S, Helmy S, et al A collagen-fibrin patch (Tachosil®) for the prevention of symptomatic lymphoceles after pelvic lymphadenectomy in women with gynecologic malignancies: a randomized clinical trial BMC Cancer 2014; 14:365
Correspondence
Andreia Bilé Silva, MD andreiabile@campus ul pt
Hospital de Egas Moniz - Centro Hospitalar de Lisboa Ocidental, Lisboa, Portugal
João Pereira, MD jnp urologia@gmail com
Rui Freitas, MD rui azevedo freitas@gmail com
Isaac Braga, MD isaac braga@gmail com
João Carvalho, MD
joao andre mendes carvalho@gmail com
José Sanches Magalhães, MD sanmagalh@gmail com
Vítor Silva, MD
vitormoreira silva@gmail com
Francisco Lobo, MD lobfrancisco@gmail com
António Morais, MD morais aj@gmail com
Instituto Português de Oncologia Francisco Gentil do Porto, Porto, Portugal
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 A
438
Bilé Silva, J Nuno Pereira, R Freitas, I Braga, J Carvalho, J Sanches Magalhães, V Silva, F Lobo, A Morais
ancillary treatments after extracorporeal shockwave lithotripsy for renal and upper ureteral stones?
predict
1 Department of Surgery, Division of Urology, McGill University Health Center, Montreal QC, Canada;
2 Urology Department, Al-Azhar University, Cairo, Egypt;
3 Department of Surgery, Faculty of Medicine, Rabigh, King Abdulaziz University, Jeddah, Saudi Arabia;
4 Muljhibhai Patel Urological Hospital, Nadiad, India
* Co-First Author
Summary
Objective: To quantify the predictors for the ancillary treatments after extracorporeal shock wave lithotripsy (SWL) for renal and upper ureteral stones
Materials and methods: From January 2014 to January 2017, patients undergoing SWL using an electromagnetic lithotripter machine (Compact Delta; Dornier MedTech GmbH, Wessling, Germany) for renal and upper ureteral stones ≤ 20 mm were retrospectively reviewed All patients underwent CT urography prior to SWL. The cohort was subdivided into three groups according to stone attenuation values in Hounsfield Units (HU) Group I; HU < 500 (n = 20), group II; HU 500-1000 (n = 51) and group III; HU ≥ 1000 (n = 180) The parameters included for multivariate analysis were stone size, location, multiplicity, stone attenuation value, number of shocks and stone clearance rate by 3 months The ancillary treatments were ureteroscopy (URS), ureteral stenting and hospital readmission for pain or fever Results: A total of 251 patients were included in the study. The overall SWL success rate was 92.4%. Mean stone size was 10 9 ± 2 1, 11 6 ± 3 and 11 4 ± 3 6 mm and mean stone attenuation values were 364 ± 125, 811 ± 154 and 1285 ± 171 HU for groups I, II and III respectively The stone clearance rates by 3 months were 96%, 92% and 88.4% for groups I, II and III respectively On subgroup analysis, group III required ancillary treatments in 70% of patients whereas group I, II, did not require any ancillary treatments On multivariate analysis, stone multiplicity, stone location (lower calyceal stones) and HU were independent significant predictors for the need for ancillary treatments after SWL (p values < 0 05)
Conclusions: Patients with stone attenuation value (HU) > 1000, multiple stones and/or lower calyceal stones have higher risk to necessitate ancillary treatments after SWL. These patients would likely benefit from upfront endoscopic lithotripsy for treating symptomatic renal or upper ureteral stones
KEY WORDS: SWL; Urolithiasis; Fragmentation; Ancillary treatment; Lower calyceal stone
Submitted 19 November 2022; Accepted 5 December 2022
INTRODUCTION
The outcome of extracorporeal shockwave lithotripsy (SWL) relies on several factors, including stone factors such as
stone composition, size, and location, as well as the mechanism and parameters of the shockwave generator (1) Several studies have proved that stone attenuation values –measured in Hounsfield Units (HU) on computed tomography (CT) – can predict the outcome of SWL Although the threshold values differ in various studies it has generally been accepted that higher CT attenuation values have poor outcomes in terms of success rates (2-5) However, most of these studies address only the role of CT attenuation values from the success rate standpoint and there is a paucity of literature investigating the association between preoperative stone characteristics and the need for postoperative ancillary procedures We believe that the challenge is not only to fragment the stone, but also to reduce the risk of subsequent ancillary treatments Ancillary treatments such as ureteroscopy (URS) and hospital readmission for pain or fever are frequently encountered after SWL These ancillary treatments have put an undue burden on urological treatment waiting lists
For small ureteral or renal calculi, SWL has a comparable efficacy when compared with retrograde intra-renal surgery (RIRS) (6) According to the latest guidelines, SWL should be considered as the first treatment option in patients with renal stones less than 20 mm and without unfavorable factors for SWL success (1) However, the predictors for ancillary procedures after SWL are still under investigated and eagerly awaited Therefore, the aim of the present study was to investigate the predictors for the ancillary treatments after (SWL) for renal and upper ureteral stones
MATERIALS AND METHODS
From January 2014 to January 2017, patients undergoing SWL using an electromagnetic lithotripter machine ( C o m p a c t D e l t a ; D o r n i e r M e d T e c h G m b H , W e s s l i n g , Germany) for renal and upper ureteral stones ≤ 20 mm were retrospectively reviewed All patients included in the analysis underwent CT urography prior to SWL The cohort was subdivided into three groups according to stone attenuation values (HU) Group I; HU < 500, group II; HU 500-1000 and group III; HU ≥ 1000 The param-
439 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
PAPER No conflict of interest declared
ORIGINAL
Can we
the
Ahmed Ibrahim 1 , Adel Elatreisy 2 , Abdulghani Khogeer 3 , Abdulsalam Ahmadi 4 , Shashikant Mishra 4 , Mahmoud Faisal 2 , Ravindra Sabnis 4 , Mélanie Aubé-Peterkin 1 , Serge Carrier 1 , Arvind Ganpule 4 , Mahesh Desai 4
DOI: 10 4081/aiua 2022 4 439
A Ibrahim, A Elatreisy, A Khogeer, et al
eters included in the multivariate analysis were stone size, location, multiplicity, stone attenuation value, number of shocks and stone clearance rate by 3 months Ureteroscopy (URS), ureteral stenting and hospital readmission for pain or fever were considered post-SWL ancillary procedures For each stone, the mean attenuation value was calculated from a small, non-overlapping region of interest
The SWL procedures were all performed as previously described (3) The treatments were performed under conscious sedation using intravenous fentanyl as the primary anesthetic agent The stones were located under fluoroscopic and/or ultrasonographic guidance, and the shock impulses were given at a frequency of 60 shocks per minutes in all patients (1 Hz) Shock impulse energy was started at level 1 (10 kv) and ramped up to 6 level (16 kv) The total number of shocks did not exceed 3000 Plain X-ray kidney-ureter-bladder (KUB) and ultrasound were performed 6 weeks post SWL Success rate was defined as inability to detect stone on ultrasound and KUB or a residual fragment measuring less than 4 mm
Review of literature
A PubMed-MEDLINE search was conducted for SWL contemporary literature and relevant data regarding SWL auxiliary procedures and predictors of failure Several articles based on the same patient cohort and success rate measures were included
Statistical analysis
Statistical analyses were performed using SPSS (SPSS Inc , Chicago, IL, USA) version 22 Comparison of quantitative variables was done using the paired t test (if normally distributed) or the Wilcoxon signed rank test (if not normally distributed) or Fisher’s exact test for categorical variable A multivariate logistic regression analysis was used to assess predictors of postoperative ancillary treatments Two-tailed p-values of less than 0 05 were set for statistical significance
RESULTS
A total of 251 patients were included in this study, including 20 patients in group I, 51 patients in group 2 and 180 patients in group 3 The overall SWL success rate at 3 months was 92 4% including 14 patients (5 5%) who developed post SWL steinstrasse The mean stone size was 10 9 ± 2 1, 11 6 ± 3 and 11 4 ± 3 6 mm and the mean stone attenuation values were 364 ± 125, 811 ± 154 and 1285 ± 171 HU for groups I, II and III respectively Stone clearance rates were 96%, 92%, 88 4% for groups I, II and III respectively SWL failure was encountered in 26 patients (10 4%), 24 patients of them (6 8%) were stone-free after second session of SWL and 2 patients (0 8%) necessitated URS The three groups were comparable in terms of body mass index, stone size and stone location (Table 1)
On subgroup analysis, group III patients required URS and ureteral stenting in 10 cases (5 6%), and hospital readmission for persistent renal colic in 4 cases (2 2%) whereas no patients in groups I and II required ancillary treatments
Table 1
Patients and stone demographic data
Table 2
Predictors for ancillary treatments using univariable and multivariate regression analysis
Univariate analysis revealed that there was a significant correlation between age, stone location, stone multiplicity, HU and the need for ancillary procedures (p < 0 05) whereas no significant correlation could be detected for stone size, and gender (Table 2) On multivariate analysis, it was found that stone multiplicity, stone location and HU were independent significant predictors for the treatments after SWL (p values < 0 05) (Table 2)
Table 3 summarizes SWL contemporary series tracking the required auxiliary procedures after SWL and predictors of SWL failure (7-20)
DISCUSSION
According to the latest guidelines, SWL remains the procedure of choice for most upper urinary tract stones ≤ 20 mm in size because of its minimally invasive nature, shorter operative time, established success rates, and minimal complications with long-term safety (1) However, SWL monotherapy is not successful in 9 4% to 26 3% of renal and upper ureteric stones (6, 21) Several studies have shown that SWL efficacy is significantly lower for stones with higher attenuation values (5-8) Nevertheless, there is
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
440
Parameter Value Mean age ± SD (years) 37 79 ± 17 7 Gender Male 181 Female 70 Mean BMI (Kg/M2) 23 97 ± 3 8 Stone side, n (%) Right 125 Left 126 Mean stone size ± SD (mm) 11 46 ± 2 74 Multiple stones, n (%) 19 (7 57%) Stone location, n (%) Upper calyx 21 (8 37%) Middle calyx 44 (17 53%) Lower calyx 50 (19 92%) Renal pelvis 82 (32 67%) Upper ureter 54 (21 51%) Associated hydronephrosis, n (%) Mild 51 (20 32%) Moderate 25 (9 96%) Mean Stone attenuation value (HU) 1115 ± 329 79 Overall SWL success rate 92 4% SWL onset, n (%) Primary treatment 243 (96 8%) Residual stone post PCNL and RIRS 16 (6 4%)
Variable Univariable Multivariable OR 95%CI p OR 95%CI p Age, years 1 04 (1 01, 1 07) 0 027 0 97 (0 89-1 71) 0 09 Stone size (mm) 0 81 (0 78-1 11) 0 082 Stone location 1 18 (0 88-1 01) 0 01 1 1 (0 99–1 78) 0 02 Stone multiplicity 2 81(1 26-3 54) < 0 001 1 45 (1 16–2 11) 0 01 Number of shocks per session 0.91 (0.54–1.02) 0.306 HU (< 1000 vs ≥ 1000) 2 75 (1 40-4 99) 0 001 3 01 (1 61-6 71) 0 01 Gender, Male/Female 0 81 (0 51–1 00) 0 351 OR = Odds rat o; C = Conf dence interva ; HU = Hounsfield unit
a paucity of literature investigating the association between preoperative stone characteristics and the need of postoperative ancillary procedures Therefore, the aim of the present study was to investigate the predictors for the ancillary treatments after (SWL) for renal and upper ureteral stones
It was found that overall SWL success rate at 3 months was 92 4% After 3 months follow-up, the stone-free rates were 96%, 92%, and 88 4% for groups I, II, and III respectively On subgroup analysis, group III (HU > 1000) required URS and ureteral stenting in 5 6% of patients, and hospital readmission for persistent renal colic in 2 2% whereas groups I and II did not require any ancillary treatments These results are consistent with current medical literature, indicating that SWL is associated with significantly higher retreatment rates compared with RIRS and PCNL (21) On multivariate analysis, it was found that stone multiplicity, stone location and HU > 1000 were independent significant predictors for the treatments after SWL (p values < 0 05; Table 2) Interestingly, when we analyzed stone location cases, we found that most of the lower calyceal stone were associated with SWL failure and required ancillary treatments It was reported that several factors such as obesity, stone density, stone composition and unfavorable lower pole anatomy would also affect stone clearance rates (22)
These results may change our clinical practice in the following manner; for those patients with multiple stones, a 1-2 cm lower calcyeal stone or stone attenuation value > 1000 HU and who are anxious about the increased com-
plication rates of RIRS and PCNL and do not mind retreatment or multiple procedures, SWL could be considered an acceptable first management option Favorable lower pole anatomy [infundibular-pelvic angle (> 30°), short calyx (< 10 mm), and wide infundibulum (> 5 mm)] should also be considered in the treatment algorithm (22) Most patients, who fail primary SWL treatment, are best suited to be treated with endoscopic treatments (RIRS or PCNL) due to its high stone-free rate, significantly lower operative and fluoroscopy time
However, patients with challenging lower pole calyceal anatomy, PCNL would be the first option
Our study had some limitations including, first the retrospective nature resulting in some missing data such as stone to skin distance, infundibulo-pelvic angle
However, these variables are sufficiently reported in medical literature Secondly, there exists a selection bias which explains the high heterogeneity between groups Finally, the interpretation of our findings may be affected by these confounders Nevertheless, this is one of the rare studies investigating the predictors for the ancillary treatments after SWL
CONCLUSIONS
Our study suggests that patients with stone attenuation value (HU) > 1000, multiple stones and/or lower calyceal stones have higher risk to necessitate ancillary treatments after SWL Those patients could be offered an
441 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Ancillary treatments after SWL
endoscopTable 3. Contemporary published SWL series Series Study design N Ancillar y treatment Success rate Predictors of failure Garrido-abad et al (7) Retrospective 270 N/A 68 8% - Stone size > 9 3 mm - Stone volume > 237 - SAV > 951, SSD 133 mm - BMI > 26 9 Nakasato et al (8) Retrospective 260 N/A 76 5% - HU > 815 - Stone location Massoud et al (9) Prospective 305 - Stienstrusse in 3 6% - BMI > 30 - Conservative in 2 6% - Lower calyceal stone - URS in 10 8% 83% - SAV > 956 5 Abdelaz z et al (10) Retrospective 89 N/A 68 5% - HU > 800 - SSD > 11 2 ± 2 6 cm Quzaid et al (11) Prospective 50 N/A 52% - HU > 970 Park et al (12) Retrospective 43 N/A 69 7% - SSD > 92 03 ± 14 51 mm O ive et al (13) Retrospective 98 - Cystoscopy + ureteric stents in 40 6% 56 3% - Obesity - BMI > 35 Bandi et al (14) Retrospective 94 N/A 62% - Stone volume > 500 microL Talas et a (15) Retrospective 198 N/A 61% - In lower calyceal stones - IP angle and infundibular width A -ansari et al (16) Retrospective 427 - Post-ESWL 78% - Stone size, location and number - Auxiliary procedures were required in 8 4% - Radiological renal features and congenital renal anomalies Ghoneim et al (17) Retrospective 205 N/A 68 8% - IP Angle more than 70 degrees - Infundibular length of > 50 mm Wang et al (18) Prospective 89 N/A 52 5% - Stone burden > 700 mm3 - Stone density of > 900 HU Abdel-khalek et a (19) Retrospective 2954 - Static steinstrassae in 4 9% 86 7% - Patient age, stone size, location and number - Auxiliary - Radiological renal features and congenital renal anomalies - Procedures in 4% Sumino et al (20) Retrospective 63 N/A 54% - Higher infundibular Length-to-diameter ratio - Diameter and number of minor calices
A Ibrahim, A Elatreisy, A Khogeer, et al
ic lithotripsy as a first line therapy for treating symptomatic renal or upper ureteral stones Future prospective studies are definitely warranted
REFERENCES
1 Türk C, Knoll T, Petrik A, et al EAU guidelines on urolithiasis Eur Urol 2014; 258-89
2 Jeong US, Lee S, Kang J, Han DH, et al Factors affecting the outcome of extracorporeal shock wave lithotripsy for unilateral urinary stones in children: a 17-year single-institute experience Korean J Urol 2013; 54:460-466
3 Hevia M, García Á, Ancizu FJ, et al Predicting the effectiveness of extracorporeal shock wave lithotripsy on urinary stones, risk groups for accurate retreatment Actas Urol Esp 2017; 41:451-457
4 El-Nahas AR, EI-Assmy AM, Madbouly K, et al Predictors of clinical significance of residual fragments after extracorporeal shockwave lithotripsy for renal stones J Endourol 2006; 20:870-4
5 Weld KJ, Montiglio C, Morris MS, et al Shock wave lithotripsy success for renal stones based on patient and stone computed tomography characteristics Urology 2007; 70:1043-1046
6 Garrido-Abad P, Rodríguez-Cabello MÁ, Platas-Sancho A Analysis of success predictive factors in the treatment of urinary lithiasis by extracorporeal shock wave lithotripsy patient optimization: ESWL score Arch Esp Urol 2017; 70:715-724
7 Nakasato T, Morita J, Ogawa Y Evaluation of Hounsfield Units as a predictive factor for the outcome of extracorporeal shock wave lithotripsy and stone composition Urolithiasis 2015; 43:69-75
8 Massoud AM, Abdelbary AM, Al-Dessoukey AA, et al The success of extracorporeal shock-wave lithotripsy based on the stone-attenuation value from non-contrast computed tomography Arab J Urol 2014; 12:155-61
9 Abdelaziz H, Elabiad Y, Aderrouj I, et al The usefulness of stone density and patient stoutness in predicting extracorporeal shock wave efficiency: Results in a North African ethnic group Can Urol Assoc J 2014; 8: E567-9
10 Ouzaid I, Al-qahtani S, Dominique S, et al A 970 Hounsfield units (HU) threshold of kidney stone density on non-contrast computed tomography (NCCT) improves patients' selection for extracorporeal shockwave lithotripsy (ESWL): evidence from a prospective study BJU Int 2012; 110:E438-42
11 Byung-Hun Park, Hoon Choi, Jin-Bum Kim, and Young-Seop Chang Analyzing the Effect of Distance from Skin to Stone by Computed Tomography Scan on the Extracorporeal Shock Wave Lithotripsy StoneFree Rate of Renal Stones Korean J Urol 2012; 53:40-43
12 Olivi B1, Védrine N, Costilles T, et al Extra corporeal shock wave lithotripsy in patients with body mass index over 35 Kg/m2 Prog Urol 2011; 21:254-9
13 Bandi G, Meiners RJ, Pickhardt PJ, Nakada SY Stone measurement by volumetric three-dimensional computed tomography for predicting the outcome after extracorporeal shock wave lithotripsy BJU Int 2009; 103:524-8
14 Talas H, Kilic O, Tangal S, Safak M Does lower-pole caliceal anatomy predict stone clearance after shock wave lithotripsy for primary lower-pole nephrolithiasis? Urol Int 2007; 79:129-32
15 Al-Ansari A1, As-Sadiq K, Al-Said S, et al Prognostic factors of success of extracorporeal shock wave lithotripsy (ESWL) in the treatment of renal stones Int Urol Nephrol 2006; 38:63-7
16 Ghoneim IA, Ziada AM, Elkatib SE Predictive factors of lower
calyceal stone clearance after Extracorporeal Shockwave Lithotripsy (ESWL): a focus on the infundibulopelvic anatomy Eur Urol 2005; 48:296-302
17 Wang LJ1, Wong YC, Chuang CK Predictions of outcomes of renal stones after extracorporeal shock wave lithotripsy from stone characteristics determined by unenhanced helical computed tomography: a multivariate analysis Eur Radiol 2005; 15:2238-43
18 Abdel-Khalek M, Sheir KZ, Mokhtar AA, et al Prediction of success rate after extracorporeal shock-wave lithotripsy of renal stones--a multivariate analysis model Scand J Urol Nephrol 2004; 38:161-7
19 Sumino Y, Mimata H, Tasaki Y, et al Predictors of lower pole renal stone clearance after extracorporeal shock wave lithotripsy J Urol 2002; 168:1344-7
20 Zhang W, Zhou T, Wu T, et al Retrograde Intrarenal Surgery v
Shockwave Lithotripsy for Treatment of Lower Pole Renal Stones: A Meta-Analysis and Systematic Review J Endourol 2015; 29:745-59
21 Junbo L, Yugen L, Guo J, et al Retrograde Intrarenal Surgery vs Percutaneous Nephrolithotomy vs Extracorporeal Shock Wave Lithotripsy for Lower Pole Renal Stones 10-20 mm: A Meta-analysis and Systematic Review Urol J 2019; 16:97-106
22 Bozzini G, Verze P, Arcaniolo D, et al A prospective randomized comparison among SWL, PCNL and RIRS for lower calyceal stones less than 2 cm: a multicenter experience: A better understanding on the treatment options for lower pole stones World J Urol 2017; 35:1967-75
Correspondence
Ahmed Ibrahim, MD ahmed eldemerdash@muhc mcgill ca
Adel Elatreisy, MD (Corresponding Author) dr adelelatreisy@yahoo com
Al-Azhar University, Faculty of Medicine Cairo, Egypt
Abdulghani Khogeer, MD dr-abdulghani@hotmail com
Abdulsalam Ahmadi, MD abdulsalamahmadi@hotmail com
Shashikant Mishra, MD mishra@mpuh org
Mahmoud Faisal, MD drfaysl2012e@yahoo com
Ravindra Sabnis, MD rbsabnis@gmail com
Mélanie Aubé-Peterkin, MD melanie aube-peterkin@mcgill ca
Serge Carrier, MD serge carrier@mcgill ca
Arvind Ganpule, MD doctorarvind1@gmail com
Mahesh Desai, MD mrdesai@mpuh org
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
442
e r s u s P e r c u t a n e o u s N e p h r o l i t h o t o m y v e r s u s E x t r a c o r p o r e a l
1 Department of Urology, Faculty of Medicine (for Girls), Al-Azhar University, Cairo, Egypt;
2 Department of Internal medicine, Faculty of Medicine (for Girls), Al-Azhar University, Cairo, Egypt;
3 Department of Biochemistry, Faculty of Medicine (for Girls), Al-Azhar University, Cairo,Egypt;
4 Department of Clinical Pathology, Faculty of Medicine (for Girls), Al-Azhar University, Cairo, Egypt
Summary
Objective: To evaluate the role of urinary Monocyte Chemotactic Protein-1 (MCP1) and urinary epidermal growth factor (EGF) in diagnosing of upper urinary tract obstruction (UUTO)
Patient and methods: Over a period of 6 months (January 2022 to June 2022) this prospective case control comparative study was conducted on 120 participants, 60 of them with UUTO and 60 healthy controls A morning urine sample of all participants was tested for EGF and MCP-1. after taking a detailed history taking and laboratory and radiological evaluation
Results: Urinary MCP-1(uMCP-1) was significantly (p-value = 0 000) increased in UUTO group showing a mean ± SD of 518.10 ± 51.19 ng/L compared to a mean ± SD of 143.32 ± 58 03 ng/L in the controls, whereas a significantly (p-value = 0.000) decrease of urinary EGF (uEGF) was observed in patients with UUTO compared to control group A significant difference of uEGF level and uEGF/uMCP1 ratio was observed between mild compared to moderate/severe UUTO
Conclusions: Utilization of the urinary biomarker MCP1, EGF and uEGF/uMCP1 ratio in patients with UUTO can adequately be used as a simple, efficacious and noninvasive way in diagnosis of UUTO
KEY WORDS: Upper urinary tract obstruction; Urinary monocyte chemotactic protein-1 (uMCP-1); Urinary epidermal growth factor (uEGF)
Submitted 27 October 2022; Accepted 12 November 2022
INTRODUCTION
Obstructed nephropathy is a frequent and demanding urological condition caused by a variety of diseases, such as pelviureteric junction obstruction (PUJO), ureteric stone, ureteric stricture, and malignant ureteral obstruction either intra or extra luminal The disease may occur in patients of any age Surgical intervention is necessary for moderate to severe cases, according to the degree and cause of the obstruction Hydronephrosis may be occur either unilateral or bilateral due to incomplete emptying However, the extent of hydronephrosis does not prominently reflect the severity of UUTO Obstruction may be
minimal despite moderate to severe hydronephrosis, or it may be severe without marked hydronephrosis Renal scans together with determination of the glomerular filtration rate constitute the standard method of evaluating the presence and severity of UUTO (1) These investigations can be time-consuming and distressing for the patients, and are not sensitive or specific enough to identify all the cases requiring treatment Also, renal scans are expensive and not always available Therefore, there is a great need for the development of new methods to stratify and monitor patients, and the biomarker research field is a promising approach for this purpose Urinary as well as serum proteins provide information of the physiological condition in the kidney and have the potential to be used as prognostic tools for early disease detection and the choice of the optimal treatment and monitoring (1) The etiopathogenesis of renal damage and the progression of renal insufficiency in obstructive nephropathy consist of several processes at the cellular and molecular level These include the hemodynamic response of the kidneys (i e decrease in blood flow mainly in the renal cortex, decrease in capillary wall permeability, infiltration of the interstitium by macrophages, reflux of filtrate through the damaged tubule wall into the interstitium, dilatation of renal tubules and apoptosis and accumulation of peeled tubular cells in the lumen of the renal tubules) This process proceeds under the influence of various enzymes, cytokines, chemokines, growth factors, signaling molecules, and genes In recent years, several molecules have been identified that could potentially be used as biomarkers with promising results in both diagnosis and treatment, as well as a prognostic factors in children with UUTO (2)
A biomarker is defined as a parameter that can be measured objectively and is evaluated as an indicator of both normal physiological and pathogenic processes and/or pharmacological responses to a therapeutic intervention (3)
Epidermal growth factor (EGF) is one of the well-known polypeptide growth factors which plays a fundamental role in the regulation of cell proliferation and differentiation (4) The kidney is one of the major sites of its production thick ascending limb of Henle’s loop and the dis-
443 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
No conflict of interest declared
ORIGINAL PAPER
Urinary epidermal growth factor and monocyte chemotactic protein-1 as biomarkers of renal injury in patients with obstructed nephropathy
Eman M El-Dydamony 1 , Mohamed Ahmad Abdelaal 1 , Sammar Ahmad Kasim 2 , Doaa Refaat Ameen 3 , Doaa Aly Abd El-Fattah 4
DOI: 10 4081/aiua 2022 4 443
tal convoluted tubule being the main sites of EGF production It is considered as a mitogen for variant renal c e l l s a n d h a s e s s e n t i a l f u n c t i o n a l e ff e c t s o n i n t a c t glomeruli, proximal tubules and collecting ducts Also, it is a powerful trophic factor for tubular epithelial cells; so, its concentration in the urine may reflect the number of functional nephrons and it may be a good marker for assessment of renal function (5, 6)
MCP-1is one of the most promising biomarkers of kidney injury, it is a chemokine protein that mediates monocyte chemotaxis (7) In the case of obstruction, its expression at the level of the renal tubules appears to be directly associated with the accumulation of these inflammatory cells within the interstitial space Thus, urinary excretion of MCP1 may be associated with the rate of monocyte infiltration and subsequent progression of interstitial renal fibrosis (8, 9)
All studies have shown a high correlation between MCP1 levels in urine and the extent of tubular atrophy and interstitial fibrosis MCP-1 mRNA is undetectable in the normal kidney, but MCP-1 gene expression is markedly increased at the tubulointerstitial level in UPJO biopsy samples and correlates with the extent of monocyte infiltration (10, 11)
Recently, urinary EGF/MCP-1 ratio was suggested as an useful early biomarker of progressive renal damage for obstructive nephropathy It can have a potential role in predicting the long term renal function outcome (12)
PATIENTS AND METHODS
A prospective case control comparative study was conducted in the Urology Department on 120 participants, male and female , aged between 18-60 years who were selected from Urology out-patient’s clinic of Al-Zahra'a Hospital, Al-Azhar University from January 2022 to July 2022
The study was approved from the Institutional Ethics Committee and all study participants provided written consent for inclusion in the study
Participants were divided in to two groups as:
Group I: 60 patients with varying degrees of upper urinary tract obstruction (UUTO) either unilateral or bilateral (obstruction was caused by ureteral stone, PUJO or ureteral stricture)
Group II: 60 healthy controls with no chronic illnesses including hypertension or kidney diseases
All participants were tested by Urinary Epidermal Growth Factor and Urinary Monocyte Chemotactic Protein Patients with end stage renal disease, malignant disease, aged below 18 or or more than 60 years, with thyroid disorders, acute or chronic inflammatory disease, autoimmune diseases as lupus nephritis, diabetic nephropathy, kidney transplants and pregnant female were excluded from the study
All subjects included in the study were subjected to history taking (onset and duration of the disease, medical and surgical history); full general and systemic examination; blood pressure measurement; complete blood count and serum urea, creatinine, and proteins measurement; liver function tests; glomerular filtration rate measurement (GFR); urine analysis
Morning urine samples were collected in sterile containers from all subjects Samples were centrifuged at 2000-3000 RPM for 20 minutes then the supernatants were collected and were stored at -20°C until measurement The concentration of urinary MCP1 and urinary EGF were quantified using quantitative double-antibody sandwich ELISA kits (Bioassay Technology Laboratory, China, Cat No E0124Hu and E0144Hu respectively) Concentrations were expressed as ng/L Urine MCP-1 and EGF were normalized to urine creatinine excretion (ng/mg urine creatinine) Also participants underwent kidney/ureter/bladder (KUB) X-ray, pelvic-abdominal ultrasound, and computed tomography (CT)
The comparison between groups for qualitative data was done by using Chi-square test The comparison between groups for quantitative data and parametric distribution were done by using independent t-test The comparison between more than two groups with quantitative data and parametric distribution were done by using one way ANOVA test followed by post hoc analysis using LSD test when significant Spearman correlation coefficients were used to assess the correlation between two quantitative parameters in the same group Receiver operating characteristic curve (ROC) was used in the quantitative form to determine sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), area under curve (AUC) and best cut off point for the studied markers between groups The confidence interval was set to 95% and the margin of error accepted was set to 5% So, the pvalue was considered significant at the level of < 0 05
RESULTS
The present study was conducted on 120 participants, including 60 patients with varying degrees of UUTO (48 of them with ureteral stone, 4 with ureteral stricture and 8 with PUJO) and 60 healthy controls All of them were tested by Urinary Epidermal Growth Factor and Urinary Monocyte Chemotactic Protein to assess their role in diagnosis of UUTO cases
In Table 1 there is a statistically significant (p-value = 0 000) decrease of urinary EGF (uEGF) in patients with UUTO with respect to control group Mean ± SD was (70 91 ± 17 90 ng/L) in control group, while it was 26 85 ± 10 82 ng/L) in the UUTO group Urinary MCP-1 (uMCP-1) values showed a statistically significant (pvalue = 0 000) increase in UUTO group UUTO patients showed Mean ± SD of 518 10 ± 51 19 ng/L compared to controls showing 143 32 ± 58 03ng/L
Receiver operating characteristic (ROC) curve analysis was used to determine the diagnostic profiles of uEGF and uMCP-1 in distinguishing patients with UUTO from control healthy participants (Table 2)
Using roc curve, it was shown that:
• uMCP1 can be used to discriminate between cases and control at a cutoff level of > 345 8, with 100% sensitivity, 100% specificity, 100% PPV and 100% NPV (AUC = 1 0 & p-value < 0 001)
• uMCP1/u Creatinine can be used to discriminate between cases and control at a cutoff level of > 0 57, with 98 3% sensitivity, 96 7% specificity, 96 8% PPV and 98 3% NPV (AUC = 0 99 & p-value < 0 001)
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 E
444
M
El-Dydamony, M Ahmad Abdelaal, S Ahmad Kasim, D Refaat Ameen, D Aly Abd El-Fattah
Table 1
DISCUSSION
Currently, there is no gold standard for the assessment of renal obstruction in individual cases The diagnosis in most cases is only possible by repeated investigations and comparisons of changes of the parameters during a longer follow up
Frequently used investigations are grey-scale renal ultrasound, Doppler ultrasound, radioisotope renography, excretory urography, contrast enhanced computed tomography and magnetic resonance urography Each of these modalities has its own merits and disadvantages, but none of them is ideal (13)
Receiver operating characteristic curve (ROC) for the studied markers to differentiate between cases group and control group
A biochemical marker in the urine that could provide information to the obstructive nature of hydronephrosis would reduce the degree of invasiveness, subjectivity and operator dependent proficiency required of the currently available radiological modalities (14) Consequently, the clinical usefulness of a bladder urine biomarker for aiding in the diagnosis of upper urinary tract obstruction is obviously appealing
• uEGF can be used to discriminate between cases and control at a cutoff level of < 0 56 4, with 98 3% sensitivity, 96 7% specificity, 96 8% PPV and 98 3% NPV (AUC = 0 99 & p-value < 0 001)
• uEGF/u Creatinine can be used to discriminate between cases and control at a cutoff level of < 0 075, with 100% sensitivity, 100% specificity, 100% PPV and 100% NPV (AUC = 1 0 & p-value < 0 001)
• uEGF/uMCP1 can be used to discriminate between cases and control at a cutoff level of < 0 142, with 100% sensitivity, 100% specificity, 100% PPV and 100% NPV (AUC = 1 0 & p-value < 0 001)
Table 3 shows a significant difference between uEGF level and uEGF/u MCP1 ratio in mild vs moderate/severe UUTO
Relation of grade of hydronephrosis with the studied markers
The study done by Madsen et al demonstrated significantly increased uEGF and uMCP-1 levels in children with UPJO, which normalized postoperatively This indicates that EGF and MCP-1 are regulated as a response to the obstruction, suggesting that they may be potential urinary biomarkers in hydronephrosis (15) In the present study there is a statistically significant (p-value = 0 000) decreased urinary EGF (uEGF) in patients with UUTO with respect to control group Mean ± SD was 70 91 ± 17 90 ng/L in the control group, while it was 26 85 ± 10 82 ng/L in the UUTO group, whereas urinary MCP-1 (uMCP-1) values were significantly (p-value = 0 000) increased in UUTO group In UUTO the mean ± SD was 518 10 ± 51 19 ng/L compared to 143 32 ± 58 03 ng/L in the controls
The maturation and proliferation of kidney cells occurs through the potential role of the EGF receptor (EGFR) and its ligand (EGF) in cell division Lin et al (16) stated that EGFR and its ligand might function together as a trans activation complex that can bind to specific DNA sequences to a c t i v a t e t h e g e n e e x p re s s i o n required for highly proliferative activities Thus reductions in EGF levels might reflect reduced EGFR signalling
Grandaliano et al (11) reported significantly less urinary EGF in a group with PUJO than in controls in accordance with the finding of the present study
Taranta-Janusz et al (17) showed increased levels of urinary MCP1 in patients developing kidney obstruction before undergoing surgical intervention Surgically
445 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Urinary
epidermal growth factor and monocyte chemotactic protein-1 as biomarkers of renal injury in patients with obstructed nephropathy
Control group Cases group Test value + P-value Sig. No = 60 No = 60 uMCP-1 (ng/L) Mean ± SD 143 32 ± 58 03 518 10 ± 51 19 -37 516 0 000 HS Range 58 2 - 268 5 423 - 598 8 uMCP1/urinary creatinine (ng/mg creatinine) Mean ± SD 42 41 ± 8 88 74 78 ± 7 89 -21 103 0 000 HS Range 27 13 - 64 51 50 47 - 92 22 uEGF (ng/L) Mean ± SD 70 91 ± 17 90 26 85 ± 10 82 16 315 0 000 HS Range 50 3 - 125 9 14 - 58 6 uEGF/urinary creatinine(ng/mg creatinine) Mean ± SD 10 22 ± 2 35 3 77 ± 1 27 18 700 0 000 HS Range 7 85 - 16 76 1 94 - 7 19 uEGF/uMCP1 ratio (ng/ng) Mean ± SD 0 25 ± 0 06 0 05 ± 0 02 25 358 0 000 HS Range 0 162 - 0 385 0 022 - 0 122 P-va ue > 0 05: Non s gnificant; P-value < 0 05: Sign ficant; P-va ue < 0 01: H gh y s gn ficant; * : Independent t-test
Comparison between control group and case group regarding the studied markers
Table 2.
Cut off AUC Sensitivity Specificity PPV NPV P-value uMCP-1 (ng/L) > 345.8 1.0 100% 100% 100% 100% < 0.001 uMCP1/urinary creatinine > 0 57 0 99 98 3% 96 7% 96 8 98 3 < 0 001 uEGF (ng/L) < 56 4 0 99 98 3% 96 7% 96 8 98 3 < 0 001 uEGF/urinary creatinine < 0 075 1 0 100% 100% 100% 100% < 0 001 uEGF/uMCP1 Ratio (ng/ng) < 0 142 1 0 100% 100% 100% 100% < 0 001 AUC: Area under curve; PPV: Posit ve pred ct ve value; NPV: Negat ve pred ct ve value
Table 3
Mild Mod/Severe Test value + P-value Sig. No = 18 No = 42 uMCP-1 (ng/L) Mean ± SD 531 9 ± 60 8 512 2 ± 45 9 287 0 1452 NS Range 429 9 - 598 8 423 - 591 uMCP1/urinary creatinine (ng/mg creatinine) Mean ± SD 0 74 ± 0 08 0 74 ± 0 07 376 0 974 N Range 0 58 - 0 86 0 5 - 0 92 uEGF (ng/L) Mean ± SD 32 2 ± 12 1 24 5 ± 9 4 212 5 0 008 S Range 14 - 58 6 15 3 - 51 7 uEGF/urinary creatinine (ng/mg creatinine) Mean ± SD 0 04 ± 0 01 0 03 ± 0 01 221 0 001 S Range 0 02 - 0 07 0 02 - 0 06 uEGF/uMCP1 ratio (ng/ng) Mean ± SD 0 06 ± 0 02 0 04 ± 0 01 230 0 017 S Range 0 03 - 0 1 0 02 - 0 12 P-value > 0 05: Non signif cant; P-va ue < 0 05: Significant; P-value < 0 01: Highly signif cant; * : Independent t-test
managed cases revealed a significant difference in urinary MCP-1 levels in comparison with cases managed conservatively and control groups (p < 0 05) Grandaliano and al analyzed both MCP-1 expression on renal biopsies and urinary MCP-1 concentrations in severe PUJO and found a four fold higher urinary MCP-1 concentration in studied children than in healthy controls (11)
Several studies have shown that children with UPJO have a marked reduction of renal EGF gene expression compared with controls but the role of urinary EGF concentration in UPJO is still not fully understood Grandaliano et al demonstrated decreased mean EGF urine excretion decreased EGF mRNA expression in the stenotic tissue after clinical ureteropelvic junction obstruction (18) At our study, ROC curve analysis reveal that uMCP1 can be used to discriminate between cases and control at a cutoff level of > 345 8, with 100% sensitivity, 100% specificity, 100% PPV and 100% NPV (AUC = 1 0 & p-value < 0 001) uMCP1/u Creatinine can be used to discriminate between cases and control at a cutoff level of > 0 57, with 98 3% sensitivity, 96 7% specificity, 96 8% PPV and 98 3% NPV (AUC = 0 99 & p-value < 0 001) uEGF can be used to discriminate between cases and control at a cutoff level of < 0 56 4, with 98 3% sensitivity, 96 7% specificity, 96 8% PPV and 98 3% NPV (AUC = 0 99 & p-value < 0 001) uEGF/u Creatinine can be used to discriminate between cases and control at a cutoff level of < 0 075, with 100% sensitivity, 100% specificity, 100% PPV and 100% NPV (AUC = 1 0 & p-value < 0 001) F
between cases and control at a cutoff level of < 0 142, with 100% sensitivity, 100% specificity, 100% PPV and 100% NPV (AUC = 1 0 & p-value < 0 001)
CONCLUSIONS
Utilization of urinary biomarker MCP1, EGF and uEGF/ uMCP1 ratio in patients with UUTO can adequately be used as a simple, efficacious and noninvasive tool in diagnosis of UUTO
Also, there is a significant difference of uEGF level and uEGF/u MCP1 ratio between mild and moderate/severe UUTO cases
REFERENCES
1 Mesrobian H-GO, Mitchell ME, See WA, et al Candidate Urinary Biomarker Discovery in Ureteropelvic Junction Obstr uction: A Proteomic Approach J Urol 2010; 184:709-714
2 Seifriedova Z, Flogelova H, Sarapatka J, et al The use of biomarkers in the diagnosis and treatment of obstruction of the upper urinary tract in children Biomedical Papers of the Medical Faculty of the University Palacky, Olomouc, Czechoslovakia, 2022
3 Downing G Biomarkers definitions working group Biomarkers and surrogate endpoints Clin Pharmacol Ther 2001; 69:89-95
4 Boonstra J Growth factor-induced signal transduction in adherent mammalian cells is sensitive to gravity FASEB J 1999; 13:S35-42
5 Breyer JA, Cohen S The epidermal growth factor precursor isolated from murine kidney membranes (chemical characterization and biological properties) J Biol Chem 1990; 265:16564-70
6 Harris RC Potential physiologic roles for epidermal growth factor in the kidney Am J Kidney Dis 1991; 17:627-30
7 Moledina DG, Isguven S, McArthur E, et al Plasma Monocyte Chemotactic Protein-1 Is Associated With Acute Kidney Injury and Death After Cardiac Operations Ann Thorac Surg 2017; 104:613620
8 Yu L, Zhou L, Li Q, et al J Elevated urinary lipocalin-2, interleukin-6 and monocyte chemoattractant protein-1 levels in children with congenital ureteropelvic junction obstruction Pediatr Urol 2019; 15:44 e1-7
9 Karakus S, Oktar T, Kucukgergin C, et al Urinary IP- 10, MCP1, NGAL, cystatin-C, and KIM-1 levels in prenatally diagnosed unilateral hydronephrosis: the search for an ideal biomarker Urology 2016; 87:185-92
10 Grandaliano G, Gesualdo L, Ranieri E, et al Monocyte chemotactic peptide-1 expression in acute and chronic human nephritides: A pathogenetic role in interstitial monocytes recruitment J Am Soc Nephrol 1996; 7:906-913
11 Grandaliano G, Gesualdo L, Bartoli F, et al MCP-1 and EGF renal expression and urine excretion in human congenital obstructive nephropathy Kidney Int 2000; 58: 182-192
12 Lucarelli G, Mancini V, Galleggiante V, et al Emerging urinary markers of renal injury in obstructive nephropathy Biomed Res Int 2014; 2014:303298
13 Shokeir AA The diagnosis of upper urinary tract obstruction Br J Urol 1999; 83:893-901
14 Palmer LS, Maizels M, Kaplan WE, et al Urine levels of transforming growth factor-beta-l in children with ureteropelvic junction obstruction Urology 1997; 50:769-73
15 Madsen MG, Nørregaard R, Palmfeldt J, et al Epidermal growth factor and monocyte chemotactic peptide-1: potential biomarkers of urinary tract obstruction in children with hydronephrosis Journal of Pediatric Urology 2013; 9:838-45
16 Lin SY, Makino K, Xia W, et al Nuclear localization of EGF receptor and its potential new role as a transcription factor Nat Cell Biol 2001; 3:802-8
17 Taranta-Janusz K, Wasilewska A, Debek W, Waszkiewicz-Stojda M Urinary cytokine profiles in unilateral congenital hydronephrosis Pediatr Nephrol 2012; 27:2107-2113
18 Yi Yang , Xin Zhou, Hong Gao, et al The expression of epidermal growth factor and transforming growth factor-beta1 in the stenotic tissue of congenital pelvi-ureteric junction obstruction in children J Pediatr Surg 2003; 38:1656-60
Correspondence
Eman M El-Dydamony, MD (Corresponding Author)
emanmohamed 8@azhar edu eg Mohamed Ahmad Abdelaal, MD maal uro@yahoo com
Department of Urology, Faculty of Medicine (for Girls), Al-Azhar University, Cairo, Egypt
377J+VHW, Greek Hospital St, As Sarayat, El Weili, Cairo Governorate 4391050
Sammar Ahmad Kasim, MD
Department of Internal medicine, Faculty of Medicine (for Girls), Al-Azhar University, Cairo, Egypt
Doaa Refaat Ameen, MD
Department of Biochemistry, Faculty of Medicine, (for Girls), Al-Azhar University, Cairo, Egypt
Doaa Aly Abd El-Fattah, MD
Department of Clinical Pathology, Faculty of Medicine(for Girls), Al-Azhar University, Cairo, Egypt
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 E
446
M El-Dydamony, M Ahmad Abdelaal, S Ahmad Kasim, D Refaat Ameen, D Aly Abd El-Fattah
a l l y,
E G F / u M C P 1 c a n b e u s e d t o d i s c r i m i n a t e
i n
u
Evaluation of pain and quality of life after hyaluronic
acid instillation in addition to botulinum toxin-A injection in women with refractory Interstitial Cystitis/Painful Bladder Syndrome: A pilot study
Summary
Objectives: The aim of this study was to assess changes in quality of life and pain alleviation in women with refractory Interstitial Cystitis/Painful Bladder syndrome following a combined intravesical injection of Botulinum Toxin-A and Hyaluronic Acid instillation versus Hyaluronic acid instillation alone
Methods: Two groups of women with painful bladder syndrome/interstitial cystitis were randomly divided (one to one randomization). Intravesical injections of botulinum toxin-A and intravesical Hyaluronic acid were given to Group (I) Only Hyaluronic acid was instilled intravesically in Group II. Patients were given voiding diaries, a visual analogue scale for pelvic pain, the International Cystitis Symptom Index and Problem Index, the Pelvic Pain Urgency/Frequency Patient Symptom Scale, and the Patient Health Questionnaire-9 to assess the candidates' quality of life The Student t-test and mean and standard deviation were used in statistical analysis, with p 0.05 considered as significant (IBM SPSS statistics)
Results: Thirty-four women were included in this study. The pain severity (VAS) of group (I) cases dropped dramatically from 8 5 ± 1.5 at the start to 3.9 ± 2.4 after three months and 2.9 ± 2.1 after six months Among group (II) cases, the pain score reduced dramatically from 8.6 ± 1.3 to 5.8 ± 1.4 to 4.3 ± 2.6.
Conclusions: In patients with refractory Interstitial Cystitis/Bladder Discomfort Syndrome, Botulinum Toxin-A injection combined with Hyaluronic Acid instillation improves pelvic pain and improves quality of life
KEY WORDS: Painful Bladder Syndrome; Botulin toxin; Hyaluronic acid
Submitted 5 November 2022; Accepted 19 November 2022
INTRODUCTION
Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS) is a condition presenting pelvic pain and urinary storage symptoms like as urgency and frequency that has no recognized cause (1)
The injury or dysfunction of the urothelium's glycosaminoglycan (GAG) layer caused by urine diffusion hypothetically leads to sensory nerve activation, mast cell stimulation, and bladder inflammation (2) Hyaluronic
acid (HA) instillation intravesically in patients with IC/BPS may help to regenerate the GAG layer
Furthermore, it appears that HA inhibits mast cell degranulation (3) After several weeks of weekly HA administration in the bladder, a significant reduction in symptoms was noted (1) Botulinum toxin-A, on the other hand, is an effective, well-tolerated, and safe therapy option for patients with ICS/PBS It aids in the relief of pain and the treatment of bladder ulcers (3) The duration of botulinum toxin-A treatment is less than nine months, and 88 percent of cases require repeating injection (2) IC/BPS has a significant impact on patients' psychological well-being, including sleep disturbances, sadness, anxiety, and a poor quality of life (4) The goal of this study was to assess the improvement criteria and the improvements in quality of life for women with refractory IC/BPS who received a combined intravesical injection of Botulinum toxin-A with HA instillation
MATERIALS AND METHODS
Thirty-four adult women with refractory IC/BPS were prospectively considered in this pilot trial between January 2017 and January 2020
Inclusion criteria
Inclusion criteria were bothering urinary nocturia, frequency, urgency and pelvic pain not responding to oral medications for a period of 6 months or more
Exclusion criteria
Exclusion conditions were: pregnancy, malignancy, radiation cystitis, other urogenital diseases (e g , congenital anomalies, infection, or stones) and bleeding disorders
Gynecologic examination was done to exclude vaginal infection, prolapse, menopausal changes and endometriosis
Randomization
The cases were evenly randomized (one to one randomization) into two groups, each with 17 women BTX-A
447 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
No conflict of interest declared
ORIGINAL PAPER
Ahmed Fayez Ghaith 1 , Mohamed Hasan Radwan 1 , Mohamed Rasheed Taha 1 , Mohamed Ahmed Elbendary 1 , Mahmoud Elsayed Al Damhogy 2 , Ayman Mohamed Hagras 1
DOI: 10 4081/aiua 2022 4 447
1 Urology Department, Faculty of Medicine, Tanta University, Tanta, Egypt; 2 Urology Department, Almogammaa Altebby Insurance Hospital, Tanta, Egypt
was given to group (I) in addition to HA, while group (II) received only HA
Procedures
Table 1.
Reported data of the candidates of both groups: pre-treatment, at 3 months visit and 6 months post-treatment
Routine laboratory testing and an abdominalpelvic ultrasonography were performed on all women To rule out any pathology, a cystoscopy with hydrodistension (using semirigid cystoscopy at a pressure of 80 to 100 cm H2O for 1 to 2 minutes and up to 2 times) was performed at least one month prior to enrolment Bladder biopsies for suspected bladder granulations were performed in 11 instances Group (I) received a sub mucosal intravesical injection of 200 units of botulinum toxin-A (BTX-A) in 20 locations of the superficial bladder muscles, including the trigone under spinal anesthesia Intravesical instillation of 40 mg/50 ml of Hyaluronic acid was done every two weeks in all patients (groups I&II) for a total of twelve sessions The HA was administered to group (I) two weeks following the BTX-A injection After two weeks of HA implantation, patients were examined for any negative effects Before and after 3 and 6 months of treatment, all patients completed voiding diaries for four days, the International Cystitis Symptom Index and Problem Index (ICSI & ICPI), the Pelvic Pain Urgency/Frequency Patient Symptom Scale (PUF), pelvic pain on a visual analogue scale (0-10 VAS), and the candidates' quality of life (PHQ-9)
Ethical approval
Ethical approval was obtained from our local university ethical committee before enrollment (187/12/2016) Informed consent was obtained from the patients before enrollment with full knowledge of risks and benefits of the study
Statistics
The Student t-test and mean and standard deviation were used in statistical analysis, with p 0 05 considered significant (IBM SPSS statistics)
RESULTS
T h e s u r v e y w a s c o m p l e t e d b y 3 4 women, ranging in age from 37 to 63
Inflammatory and mast cell infiltration were seen in bladder samples of 11 patients All patients completed the questionnaires before therapy, three m o n t h s a f t e r t r e a t m e n t , a n d s i x months later Treatment resulted in s i g n i fi c a n t i m p r o v e m e n t s i n b o t h groups as compared to pretreatment values (Table 1) The improvement in g r o u p ( I ) w a s g r e a t e r t h a n t h e improvement in group (II) (Table 1)
The pain severity (VAS) of group (I) patients dropped dramatically from

8 5 ± 1 5 (pretreatment) to 3 9 ± 2 4 after 3 months and to 2 9 ± 2 1 after 6 months Also, in group (II) patients, pain score (VAS) improved from 8 6 ± 1 9 (pretreatment) to 5 8 ± 1 4 at 3 months and to 4 3 ± 2 6 at 6 months Furthermore, at 3 months (p = 0 041) and 6 months (p = 0 022), there was a substantial pain improvement (VAS) in group (I) cases (BTX-A+ HA) compared to group (II) women (Figure 1)
In group (I) women, their quality of life changed dramatically from 9 7 ± 2 3 (before treatment) to 6 9 ± 1 9 (3 months) and to 5 7 ± 1 5 after 6 months PHQ-9 scores for group (II) patients changed from 9 8 ± 2 06 to 8 2 ± 1 8 and 7 9 ± 1 9 at 3 months and 6 months respectively Patients in group (I) had a much higher quality of life than patients in group (II) (Figure 2)
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
448
A Fayez Ghaith, M Hasan Radwan, M Rasheed Taha, M Ahmed Elbendary, M Elsayed Al Damhogy, A Mohamed Hagras
Pre-treatment 3 months 6 months P-value P-value post-treatment post-treatment pre/6-months Gp I/II 6 months post-treatment post-treatment VAS (Gp I) 8 5 ± 1 5 3 9 ± 2 4 2 9 ± 2 1 0 009 0 022 VAS (Gp II) 8 6 ± 1 3 5 8 ± 1 4 4 2 ± 2 6 0 032 VV (Gp I) 150 9 ± 26 4 185 6 ± 27 1 188 1 ± 39 9 0 002 0 019 VV (Gp II) 149 9 ± 27 9 162 8 ± 24 04 177 8 ± 26 5 0 033 Freq (Gp I) 16 05 ± 2 4 11 7 ± 2 2 10 4 ± 1 3 0 0002 0 001 Freq (Gp II) 15 4 ± 2 5 12 9 ± 2 1 12 3 ± 2 02 0 010 ICSI (Gp I) 15 4 ± 3 4 10 5 ± 2 6 7 41 ± 2 2 0 0007 0 0008 ICSI (Gp II) 15 7 ± 3 3 12 5 ± 2 9 11 1 ± 2 9 0 012 ICPI (Gp I) 13 1 ± 2 7 7 8 ± 2 01 6 2 ± 2 03 0 007 0 009 ICPI (Gp II) 13 5 ± 2 5 9 5 ± 2 06 8 6 ± 1 8 0 036 PUF (Gp I) 20 4 ± 3 1 13 8 ± 3 00 11 9 ± 2 6 0 0004 0 001 PUF (Gp II) 20 1 ± 3 4 16 8 ± 2 6 15 7 ± 3 06 0 001 PHQ (Gp I) 9.7 ± 2.8 6.9 ± 1.9 5.7 ± 1.5 0.0007 0.0005 PHQ (GP II) 9 8 ± 2 06 8 2 ± 1 8 7 9 ± 1 9 0 020 ICSI: Interstitia cyst tis symptom ndex; ICPI: Interstitia cystitis prob em ndex; PHQ-9: Pat ent health questionna re-9; PUF: Urgency/frequency patient symptom scale; VAS: V sual analogue sca e; VV: Vo ding vo ume
Figure 1.
Visual analogue scale in both groups
DISCUSSION
PBS/IC (painful bladder syndrome/interstitial cystitis) is a disorder characterized by supra-pubic and/or bladder pain associated with bladder filling, as well as urine frequency and urgency, which has a significant impact on quality of life (2, 5) Women are nine times more affected than men Because the actual etiology is complex and multifactorial, no consistent treatment method exists (6) Infection, autoimmunity, defective urothelium, mast cell activation, neural inflammation, and other causes have all been suggested (7) The disruption of the glycosaminoglycan (GAG) layer, which covers the bladder epithelium and acts as an impermeable barrier to solutes, may play a key role in PBS/IC pathogenesis (8) Hydrated hyaluronic acid, heparin sulphate, dermatan sulphate, chondroitin sulphate, and keratin sulphate make up the GAG layer (9) Interstitial cystitis/bladder pain syndrome is linked to unfavorable cognitive, behavioral, and sexual outcomes, as well as bothersome urine symptoms (2) To address lower urinary tract symptoms, a variety of oral medications have been tried, including pentosan polysulfate sodium (PPS), tricyclic antidepressants, and anti-muscarinics Intravesical therapy is commonly utilized as a second-line treatment for individuals who do not react to oral medication (3) Many studies looked at the effectiveness of HA or BTX-A alone, in conjunction with other medicines, or in combination with other techniques such hydrodistension The results of adding BTX-A to HA versus HA alone were compared in this study In patients with refractory IC/PBS, we got a better response when we combined the two medicines BTX-A has been used to treat persistent pelvic pain, and preliminary results indicate that it is a safe therapeutic option with no severe side effects (10) Intravesical HA was examined in women with refractory interstitial cystitis by Hung et al (1) in a prospective, multicenter study After treatment, pain ICSI, VAS, and ICPI scores improved significantly in 103 individuals However, patients' bladder discomfort and storage symptoms improved at various speeds (74 percent vs 48 percent; respectively) Lower pain score and
decreased bladder capacity were the characteristics that adversely affected treatment results, according to repeated statistical studies In their randomized trial, Kuo et al (11) enrolled 67 patients with refractory IC/PBS In patients with r e f r a c t o r y I C / P B S , t h e y f o u n d t h a t intravesical injections of BTX-A followed by HD had superior clinical results than HD alone Later, Kuo et al (12) In patients with IC/BPS, intravesical injections of BTX-A improved bladder pain symptoms Gao and Liao (10) studied the efficacy of an intravesical injection of 100 U Chinese BTX-A followed by cystoscopic hydrodistension under general anesthesia in 124 women w i t h I C / B P S T h e y c o n c l u d e d t h a t intravesical injections of Chinese BTX-A were a safe and effective treatment for IC/BPS patients Furthermore, Smith et al (13) found that BTX-A had an anti-nociceptive impact on the bladder, improving both symptoms and urodynamics Akiyama et al (14) randomized 34 patients with refractory IC/BPS into two groups: group A received immediate BTX-A injections and group B received BTX-A injections one month later They concluded that BTX-A injection could be an alternate treatment for refractory IC/BPS patients
Furthermore, Shim et al (15) demonstrated that BTX-A injection is more effective for IC/BPS pain control than placebo, with no differences in adverse effects Pinto et al. (16) also concluded that trigonal BTX-A injection is a safe treatment for refractory BPS/IC According to Kim et al (17), the VAS score, mean changes in the PUF, ICSI, and ICPI all decreased significantly after 4 weeks of intravesical HA instillation Furthermore, Akbay et al (18) found that intravesical hyaluronic acid instillation alleviated symptoms in IC/BPS patients on a short-term follow-up Lai et al (4) compared four weekly 40 mg hyaluronic acid intravesical instillations followed by five monthly instillations to 12 intravesical instillations every two weeks There was no significant difference between the two groups in terms of symptom scores or the Quality-of-Life Index Furthermore, according to the findings of Peng et al. (19), enhanced first desire to void and maximum cystometric capacity are linked to improved urinary symptoms after HA treatment Cervigni et al (20) also looked at the efficacy of HA and chondroitin sulphate (CS) intravesical instillations in individuals with refractory PBS/IC Pain and urine symptoms such as urgency (p = 0 005), frequency (p = 0 045), and pain (p = 0 001) improved significantly In their meta-analysis, Pyo and Cho (21) found that intravesical HA and HA/CS instillation improved pain symptoms and quality of life in patients with IC/BPS In individuals with IC/BPS, Liang et al (22) found that pain and urine symptoms may improve after 6 months of intravesical HA therapy There were no significant changes in the psychological and sexual functioning ratings at the time Lv and colleagues (23), in women with refractory severe PBS/IC, demonstrated that intravenous instillation of HA and AL resulted in immediate and long-term allevi-
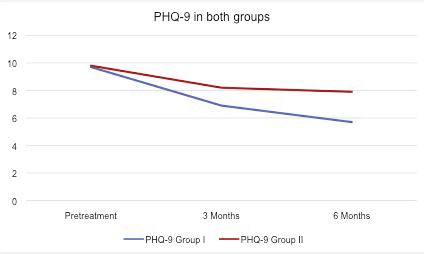
449 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Hyaluronic acid in addition to botulinum toxin-A injection in refractory interstitial cystitis
Figure 2
Health related quality of life in both groups
ation of symptoms Hyaluronic acid intravesical instillation was successful in reducing the degree of pain in women with refractory PBS/IC in the current pilot trial Botulinum Toxin-A added to Hyaluronic acid resulted in much higher quality of life and pain reduction than Hyaluronic acid alone This is the only publication that we are aware of that discussing the advantages of combining HA with BTX-A injection for the treatment of IC/BPS
Limitations to the study
A longer follow-up and larger number of patients should be considered in the upcoming studies
CONCLUSIONS
In patients with refractory Interstitial Cystitis/Bladder Discomfort Syndrome, Botulinum Toxin-A injection combined with Hyaluronic Acid instillation improves pelvic pain and improves quality of life
REFERENCES
1 Hung MJ, Tsai CP, Lin YH, et al Hyaluronic acid improves pain symptoms more than bladder storage symptoms in women with interstitial cystitis Taiwan J Obstet Gynecol 2019; 58:417-422
2 Hanno P, Lin A, Nordling J, et al Bladder pain syndrome committee of the international consultation on incontinence Neurourol Urodyn 2010; 29:191-198
3 Garzon S, Laganà AS, Casarin J, et al An update on treatment options for interstitial cystitis Prz Menopauzalny 2020; 19:35-43
4 Lai MC, Kuo YC, Kuo HC Intravesical hyaluronic acid for interstitial cystitis/painful bladder syndrome: A comparative randomized assessment of different regimens International Journal of Urology 2013; 20:203-207
5 Wein AJ, Hanno PM Targets for therapy of the painful bladder Urology 2002; 59:68-73
6 Jhang JF, Kuo HC Novel Treatment of Chronic Bladder Pain Syndrome and Other Pelvic Pain Disorders by OnabotulinumtoxinA injection Toxins (Basel) 2015; 7:2232-50
7 Grover S, Srivastava A, Lee R, et al Role of inflammation in bladder function and interstitial cystitis Ther Adv Urol 2011; 3:19-33
8 Parsons CL The role of the urinary epithelium in the pathogenesis of interstitial cystitis/prostatitis/urethritis Urology 2007; 69:9-16
9 Teichman JM, Moldwin R The role of the bladder surface in interstitial cystitis/painful bladder syndrome Can J Urol 2007; 14:3599607
10 Gao Y, Liao L Intravesical injection of botulinum toxin A for treatment of interstitial cystitis/bladder pain syndrome: 10 years of experience at a single center in China Int Urogynecol J 2015; 26:1021-1026
11 Kuo HC, Chancellor MB Comparison of intravesical BTX-A injections plus HD with HD alone for the treatment of refractory i n t e r s t i t i a l c y s t i t i s / p a i n f u l b l a d d e r s y n d r o m e B J U I n t 2 0 0 9 ; 104:657-61
12 Kuo HC, Jiang YH, Tsai YC, Kuo Y Intravesical botulinum toxinA injections reduce bladder pain of interstitial cystitis/bladder pain syndrome refractory to conventional treatment - A prospective, multicenter, randomized, double-blind, placebo-controlled clinical trial Neurourol Urodyn 2016; 35:609-6014
13 Smith CP, Radziszewski P, Borkowski A, et al Botulinum toxin
A has antinociceptive effects in treating interstitial cystitis Urology 2004; 64:871-875
14 Akiyama Y, Nomiya A, Niimi A, et al Botulinum toxin type A injection for refractory interstitial cystitis: A randomized comparative study and predictors of treatment response Int J Urol 2015; 22:835-41
15 Shim SR, Cho YJ, Shin IS, Kim J Efficacy and safety of botulinum toxin injection for interstitial cystitis/bladder pain syndrome: a systematic review and meta-analysis Int Urol Nephrol 2016; 48:12151227
16 Pinto R, Lopes T, Frias B, et al Trigonal Injection of Botulinum Toxin A in Patients with Refractory Bladder Pain Syndrome/Interstitial Cystitis European Urology 2010; 58:360-365
17 Kim A, Lim B, Song M, Choo M Pretreatment Features to Influence Effectiveness of Intravesical Hyaluronic Acid Instillation in R
J 2014; 18:163-167
18 Akbay E, Çayan S, Kılınç C, et al The short-term efficacy of intravesical instillation of hyaluronic acid treatment for bladder pain syndrome/interstitial cystitis Turk J Urol 2019; 45:129-34
19 Peng YC, Chiu SY, Feng M, Liang C The effect of intravesical hyaluronic acid therapy on urodynamic and clinical outcomes among women with interstitial cystitis/bladder pain syndrome Taiwan J Obstet Gynecol 2020; 59:922-926
20 Cervigni M, Natale F, Nasta L, et al A combined intravesical therapy with hyaluronic acid and chondroitin for refractory painful bladder syndrome/interstitial cystitis Int Urogynecol J 2008; 19:943-947
21 Pyo JS, Cho WJ Systematic Review and Meta-Analysis of Intravesical Hyaluronic Acid and Hyaluronic Acid/Chondroitin Sulfate Instillation for Interstitial Cystitis/Painful Bladder Syndrome Cell Physiol Biochem 2016; 39:1618-1625
22 Liang CC, Lin YH, Hsieh WC, Huang L Urinary and psychological outcomes in women with interstitial cystitis/bladder pain syndrome following hyaluronic acid treatment Taiwanese Journal of Obstetrics & Gynecology 2018; 57:360-363
23 Lv Y, Zhou H, Mao H, et al Intravesical hyaluronic acid and alkalinized lidocaine for the treatment of severe painful bladder syndrome/interstitial cystitis Int Urogynecol J 2012; 23:1715-1720
Correspondence
Ahmed Fayez Ghaith, MD (Corresponding Author) dr ahmedfayez@yahoo com
Mohamed Hasan Radwan, MD drradwanm@yahoo com
Mohamed Rasheed Taha, MD dr-rasheed@hotmail com
Mohamed Ahmed Elbendary, MD mbendary@hotmail com
Ayman Mohamed Hagras, MD ahagras80@yahoo com
Urology Department, Faculty of Medicine, Tanta University, Tanta (Egypt) El-Gharbia Govenorate, Tanta El-Gash st Medical Campus, The Faculty of Medicine
Mahmoud Elsayed Al Damhogy, MD moodseg@gmail com
Urology Department, Almogammaa Altebby Insurance Hospital, Tanta (Egypt)
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
450
A Fayez Ghaith, M Hasan Radwan, M Rasheed Taha, M Ahmed Elbendary, M Elsayed Al Damhogy, A Mohamed Hagras
e f r a c t o r y I n t e r s t i t i a l C y s t i t i s / P a i n f u l B l a d d e r S y n d r o m e I n t Neurourol
The choice of therapeutic agent in female overactive bladder patients in real-world practice
Department of Urology, Teikyo University Chiba Medical Center, 3426-3 Anesaki, Ichihara, Chiba 299-0111, Japan
Summary
Objective: The reasons why anticholinergic drugs or β3 adrenergic agonists are selected as treatments for overactive bladder (OAB) are unclear The aim of this study was to investigate the background data of female OAB patients that were prescribed anticholinergic drugs or β3 adrenergic agonists in a real-world setting
Materials and methods: Between January 2013 and December 2014, 75 patients who had been diagnosed with OAB were included in this study. Administered medications, age, the persistence on treatment rate at one-year, medical history, pretreatment total Overactive Bladder Symptom Score (OABSS), pretreatment score for each OABSS factor, body mass index (BMI), and various comorbidities were evaluated retrospectively Since there were many types of anticholinergic drugs and few patients, we grouped the patients into those that were prescribed anticholinergic drugs (group A) and those that were prescribed β3 adrenergic agonists (group B).
Results: 75 patients (29 in group A and 46 in group B) were included in this study. There were no significant differences in age, BMI, obesity, medical history, pretreatment total OABSS, or pretreatment score for each OABSS factor. There was a significant difference in the post-voiding residual urine volume (PVR) between the groups (group A: 22 ml, group B: 9 ml; p= 0 0252) The 1-year persistence on treatment rate was 28% in both groups
Conclusions: There were no significant differences in clinical characteristics of patients who were prescribed anticholinergics and β3 adrenergic agonists for OAB treatment, but a marginal difference of PVR value before treatment
The 1-year persistence rates of anticholinergic drugs and β3 adrenergic agonists were considered to be almost equivalent
KEY WORDS: Overactive bladder; Anti-cholinergic drugs; β3 adrenergic agonists; Post-voiding residual urine volume
Submitted 28 October 2022; Accepted 10 November 2022
INTRODUCTION
Overactive bladder (OAB) is a condition with characteristic symptoms of urinary urgency, usually accompanied by increased urinary frequency and nocturia, with or without urge incontinence, in the absence of a urinary tract infection (UTI) or any other obvious pathology (1) It was observed that the prevalence of OAB among Japanese adults aged ≥ 40 years is 12 4%, and the estimated number of patients with OAB is 8 1 million (2) OAB affects
11 8-24 7% of adults in North America and Europe, and its prevalence increases with age (3) In addition to age, the risk factors for OAB include diabetes, UTI, and obesity (4, 5) Pharmacotherapy is the main treatment for OAB in Japan, and anticholinergic drugs are considered to be first-line drugs (6) Recently, β3 adrenergic agonists, which have completely different mechanism of action from anticholinergic drugs, have become available and have been shown to be effective β3 adrenergic agonists were awarded a grade-A recommendation in the Japanese OAB treatment guidelines However, no study on the criteria for choosing between anticholinergics and β3 adrenergic agonists has been published When treating patients with OAB, how do clinicians choose among these medications, which both have grade-A recommendations and exhibit comparable therapeutic efficacy? Are there any factors that influence the selection of these medications?
In the present study, we investigated the factors that influence the selection of anticholinergic drugs or β3 adrenergic agonists for OAB in the real world practice
MATERIALS AND METHODS
This was a retrospective study, which used data extracted from electronic records Seventy-five who were diagnosed with OAB at the Department of Urology, Teikyo University Chiba Medical Center (Ichihara, Japan), between January 2013 and December 2014 were included in this study
The Overactive Bladder Symptoms Score (OABSS) was calculated for each patient, and all of the patients met the diagnostic criteria for OAB OAB was diagnosed based on the OABSS or the presence of urinary urgency (6)
The OABSS is a validated self-assessed questionnaire created by the Japanese Continence Society and consists of four questions about OAB symptoms (Q1: daytime frequency, Q2: nighttime frequency, Q3: urgency, and Q4: urge incontinence) (6)
We retrospectively evaluated various factors, including age, administered treatments, body mass index (BMI), pretreatment total OABSS, pretreatment score for each OABSS factor, post-voiding residual volume (PVR), smoking habits, presence or absence of hypertension, diabetes mellitus, and dyslipidemia
The post-voiding residual (PVR) urine was measured on a transabdominal ultrasonic echogram in all cases
451 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
No conflict of interest declared
ORIGINAL PAPER
Hiroshi Masuda, Kosuke Mikami, Kotaro Otsuka, Kyokusin Hou, Takahito Suyama, Kazuhiro Araki, Satoko Kojima, Yukio Naya
DOI: 10 4081/aiua 2022 4 451
Masuda, K Mikami, K Otsuka, K Hou, T Suyama, K Araki, S Kojima, Y Naya
Regarding the administered medications, since many kinds of anticholinergic drugs were administered in small groups of patients, patients were categorized into two groups as those treated with anticholinergic drugs (group A) and those treated with β3 adrenergic agonists (group B) The patients were allowed to discontinue their medication during the follow-up period, according to their desires and the judgement of the attending physician We investigated the continuation/discontinuation of anticholinergic drug and β3 adrenergic agonist treatment although we could not examine the reasons for discontinuation
Statistical analysis
Statistical analyses were carried out to identify clinical parameters that differed significantly between groups A and B The results are shown as mean ± SE or percentage
The Mann-Whitney U test and Chi-squared test were used for the statistical analyses All analyses were performed with JMP version 10 (SAS Institute Inc , Cary, NC, USA) A probability value of < 0 05 was considered statistically significant
Ethical approval The institutional review board of Teikyo University approved this study (TUIC-COI 21-1218)
RESULTS
Table 1 shows the patients’ background characteristics
We evaluated 75 patients (29 in group A and 46 in group B) that were prescribed anticholinergic drugs or β3 adrenergic agonists by our department There were no significant differences in age, BMI, obesi-
Table 2
Comparisons between the groups
ty, medical history, the pretreatment total OABSS, or the pretreatment scores for individual OABSS factors The mean pretreatment PVR was significantly greater in group A than in group B (22 ml vs 9 ml, respectively; P = 0 0252) (Table 2)
A younger age, a lower pretreatment total OABSS score,
Table 3
Assessment of the factors affecting the continuation of medical treatment.
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
452
H
Table 1. Patient characteristics. No. of patients N = 75 Age (years, mean ± SE) 70 ± 1 4 Medication Anticholinergics N( 29 Propiverine 3 Imidafenacin 9 Fesoterodine 6 Solifenacin 11 β3 adrenergic agonists 46 Body mass index (kg/m2, mean ± SE) 28 2 ± 0 3 OABSS Daytime frequency 1 0 ± 0 1 Nighttime frequency 2 4 ± 0 1 Urgency 2 9 ± 0 2 Urge incontinence 1 7 ± 0 2 Total score 8.1 ± 0.5 PVR (ml, mean ± SE) 14 ± 2 6 Smoking Positive/Negative 7/68 Alcohol consumption Positive/Negative 7/68 Hypertension Positive/Negative 38/37 Diabetes mellitus Positive/Negative 10/65 Dyslipidemia Positive/Negative 24/51 OABSS: Overactive Bladder Symptom Score; PVR: Post-vo ding residual urine vo ume
Variable Group A (n = 29) Group B (n = 46) P-value Age (years, mean ± SE) 69 ± 1 4 71 ± 1 7 0 5029 Body mass index (kg/m2, mean ± SE) 28 2 ± 0 5 28 3 ± 0 3 0 6414 OABSS Daytime frequency 1 1 ± 0 1 1 0 ± 0 1 0 2736 Nighttime frequency 2 5 ± 0 1 2 4 ± 0 1 0 7708 Urgency 3 1 ± 0 2 2 8 ± 0 3 0 5017 Urge incontinence 2 1 ± 0 2 1 5 ± 0 3 0 1298 Total score 8 8 ± 0 7 7 7 ± 0 6 0 1639 PVR (ml, mean ± SE) 22 ± 5 8 9 2 ± 2 2 0 0247 0-50 ml/51-100 ml/100 ml< 26/3/0 45/1/0 0 1251 Smoking Positive/Negative 4/25 3/43 0 151 Alcohol consumption Positive/Negative 2/27 5/14 0 3061 Hypertension Positive/Negative 13/16 25/21 0 4219 Diabetes mellitus Positive/Negative 3/26 7/39 0 5455 Dyslipidemia Positive/Negative 7/22 17/29 0 2465 OABSS: Overact ve Bladder Symptom Score; PVR: Post-voiding res dual urine volume
Variable Continuation Discontinuation P-value group (n = 21) group (n = 54) Age (years, mean ± SE) 74 ± 1 4 68 ± 1 7 0 2328 Medication 0 9495 Anticholinergics 8 21 Mirabegron 13 33 Body mass index (kg/m2, mean ± SE) 28 0 ± 0 5 28 3 ± 0 3 0 5236 OABSS Daytime frequency 1 2 ± 0 1 1 0 ± 0 1 0 201 Nighttime frequency 2 6 ± 0 3 2 4 ± 0 1 0 2912 Urgency 2 8 ± 0 4 3 0 ± 0 3 0 5301 Urge incontinence 1 9 ± 0 4 1 7 ± 0 3 0 614 Total score 8 6 ± 0 9 8 1 ± 0 5 0 8093 PVR (ml, mean ± SE) 18 ± 5 6 12 ± 3 0 0 3325 Smoking Positive/Negative 0/21 7/47 0 151 Alcohol consumption Positive/Negative 2/19 5/49 0 3061 Hypertension Positive/Negative 9/12 29/25 0 3989 Diabetes mellitus Positive/Negative 4/17 6/48 0 364 Dyslipidemia Positive/Negative 6/15 18/36 0 6914 OABSS: Overact ve B adder Symptom Score; PVR: Post-voiding res dual urine volume
and a lower PVR were associated with a tendency towards medication discontinuation However, no potential predictors of discontinuation differed significantly between the groups (Table 3) The one-year persistence rate of prescriptions from our department was 28% in both groups
DISCUSSION
In the Japanese guidelines for OAB, anticholinergic drugs and β3 adrenergic agonists are given grade-A recommendations as treatments for OAB (6) However, while there has been some debate about the usage of different anticholinergic drugs, there was insufficient discussion and there are no clear indicators or guidelines regarding the usage of anticholinergic drugs versus β3 adrenergic agonists Therefore, individual medications are being administered for OAB without any particular reason in real-world practice, and it seems that choices between anticholinergic drugs and β3 adrenergic agonists are based on the treating doctor’s preferences and experience In the present study, we investigated the factors that influence the selection of anticholinergic drugs and β3 adrenergic agonists in the real-world To the best of our knowledge, this is the first study to investigate this among OAB patients
Safety
Safety is the first consideration when selecting a drug, and avoiding adverse events should be prioritized over efficacy β3 adrenergic agonists cause side effects, such as dry mouth and constipation, less frequently than anticholinergic drugs This should favor the selection of β3 adrenergic agonists Regarding dry mouth, it has been reported that β3 adrenergic agonists cause this symptom in 33% fewer cases than tolterodine (7) In another study, it was reported that the incidence of dry mouth during β3 adrenergic agonist treatment was similar to that produced by a placebo, and that it was associated in one-fifth of cases with anticholinergic drugs (8) It has been observed that dry mouth is an important factor influencing oral medication discontinuation (9) Therefore, there is an advantage in choosing β3 adrenergic agonists over anticholinergic drugs It has also been reported that β3 adrenergic agonists have higher persistence rates than anticholinergics drugs and should be considered for firstline pharmacological treatment for OAB (10) Furthermore, it should be considered that elderly patients would be more likely to be prescribed β3 adrenergic agonists than anticholinergics because of their high frequency of abnormal bowel movements
Finally, it is likely that medications that involve fewer oral doses should be selected for elderly patients because they may already be taking a large number of medications
Post-voiding residual urine
In a comparative study of anticholinergic drugs and β3 adrenergic agonists, it was reported that there was no significant difference in the increase in the PVR seen during the study period (0 86 ml for the placebo, 0 80 ml for β3 adrenergic agonists, and 0 44 ml for tolterodine) (11)
Moreover, Stöhrer et al reported that the PVR increased significantly from 50 ml to 87 ml in patients treated with propiverine (12) Also, Khullar et al reported that a PVR
exceeding 300 ml was seen in 0 2% of patients treated with β3 adrenergic agonists (7)
These studies suggest that the PVR is not a determining criterion during the selection of anticholinergic drugs or β3 adrenergic agonists
Regarding the frequency of urinary retention, it has been reported that it was < 1% in patients treated with anticholinergic drugs, while it was almost negligible in patients treated with β3 adrenergic agonists (13)
In the present study the pretreatment PVR was significantly higher in patients who were prescribed anticholinergics compared to those who were treated with β3 adrenergic agonists, but this finding seemed to be of limited clinical significance because it was related to only three patients with high PVR taking anticholinergics
Compliance to treatment
It has been reported that the 1-year persistence rates of anticholinergic drugs and mirabegron ranged from 17% to 35% (14) and 19-38% (9, 15, 16), respectively
The 1-year persistence rates of anticholinergic drugs and β3 adrenergic agonists at our institution were similar It has been reported that treatment discontinuation is also seen in younger age groups, and our study showed a similar trend (17)
We suggest that this could be explained by the fact that the drugs were administered at hospital, and an appointment was required to visit the hospital
However, a recent study suggested that β3 adrenergic agonists have very high 1-year persistence rates of 63% in females and 67% in males (18) It was considered that this was probably because β3 adrenergic agonists are safe and well tolerated
Non-medical factors
Recently, a study reported that when physicians received complimentary meals and hospitality by a pharmaceutical company they increased their prescriptions of drugs marketed by that company (19) Although this may have affected our prescription patterns, we do not have any information about this in the present study This could be an important subject for further study, including other oral medications
Limitations
Our study presented some limitations:
1) It was a retrospective cohort study, which involved the extraction of electronically stored clinical data, and it had a small sample size Thus, it will be necessary to validate the findings of this retrospective analysis in prospective studies, including a randomized study, with larger populations in future We expect that such studies will provide new perspectives on how decisions regarding the selection of anticholinergic drugs and β3 adrenergic agonists are made
2) Since this study only involved females, the factors influencing the selection of anticholinergic drugs or β3 adrenergic agonists in male OAB patients were not evaluated
3) The patients’ complications and the other types of medications they were taking were not investigated, and hence, more detailed patient background information is needed
4) The two-year observation period was relatively short,
453 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment in female OAB
and hence, it may not have been long enough to allow appropriate evaluations to be performed
5) Patients assuming anticholinergics were analyzed collectively because the small number of patients taking different anticholinergics did not allow to analyze them separately Collection of larger populations taking different anticholinergics could give information about difference of outcomes between them
6) Untreated patients were not investigated
7) We did not investigate refractory OAB separately
CONCLUSIONS
There were no significant differences in clinical characteristics of patients who were prescribed anticholinergics and β3 adrenergic agonists for OAB treatment, but a marginal difference of PVR value before treatment
The 1-year persistence rates of anticholinergic drugs and β3 adrenergic agonists were considered to be almost equivalent
REFERENCES
1 Abrams P, Cardozo L, Fall M Paul Abrams, et al The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society Neurourol Urody 2002; 21:167-178
2 Homma Y, Yamaguchi O, Hayashi K Neurogenic bladder society committee An epidemiological survey of overactive bladder symptoms in Japan BJU Int 2005; 96:1314-1318
3 Eapen RS, Radomski SB Review of the epidemiology of overactive bladder Res Rep Urol 2016; 8:71-76
4 Brown JS, McGhan WF, Chokroverty S Comorbidities associated with overactive bladder Am J Manag Care 2000; 6:S574-579
5 Subak LL, Richter HE, Hunskaar S Obesity and urinary incontinence: epidemiology and clinical research update J Urol 2009; 182:S2-7
6 Yamaguchi O, Nishizawa O, Takeda M, et al Clinical guidelines for overactive bladder Int J Urol 2009; 16:126-142
7 Khullar V, Amarenco G, Angulo J, et al Efficacy and tolerability of mirabegron, a β (3)-adrenoceptor agonist, in patients with overactive bladder: results from a randomised European-Australian phase 3 trial Eur Urol 2013; 63:283-295
8 Yamaguchi O, Marui E, Kakizaki H, et al Phase III, randomised, double-blind, placebo-controlled study of the β3-adrenoceptor ago-
nist mirabegron, 50 mg once daily, in Japanese patients with overactive bladder BJU Int 2014; 113:951-960
9 Chapple CR, Nazir J, Hakimi Z, et al Persistence and adherence with mirabegron versus antimuscarinic agents in patients with overactive bladder: a retrospective observational study in UK clinical practice Eur Urol 2017; 72:389-399
10 Yeowell G, Smith P, Nazir J et al Real-world persistence and adherence to oral antimuscarinics and mirabegron in patients with overactive bladder (OAB): a systemic literature review BMJ open 2018; 8:e021889
11 Yamaguchi O, Ikeda Y, Ohkawa S Phase III study to assess longterm (52-week) safety and efficacy of mirabegron, a β3-adrenoceptor agonist, in Japanese patients with overactive bladder LUTS 2017; 9:38-45
12 Stöhrer M, Madersbacher H, Richter R, et al Efficacy and safety of propiverine in SCI-patients suffering from detrusor hyperreflexia-a double-blind, placebo-controlled clinical trial Spinal Cord 1999; 37:196-200
13 Nitti VW, Khullar V, van Kerrebroeck P, et al Mirabegron for the treatment of overactive bladder: a prespecified pooled efficacy analysis and pooled safety analysis of three randomised, doubleblind, placebo-controlled, phase III studies Int J Clin Pract 2013; 67:619-632
14 Wagg A, Compion G, Fahey A, Siddiqui E Persistence with prescribed antimusucarinic therapy for overactive bladder: a UK experience BUJ Int 2012; 110:1767-1774
15 Wagg A, Franks B, Ramos B, Berner T Persistence and adherence with the new beta-3 receptor agonist, mirabegron, versus antimuscarinics in overactive bladder: Early experience in Canada Can Urol Asso J 2015; 9:343-350
16 Sussman D, Yehoshua A, Kowalski J, et al Adherence and persistence of mirabegron and anticholinergic therapies in patients with overactive bladder: a real-world claims data analysis Int J Clin Prac 2017; 71:e12824
17 Kalder M, Pantazis K, Dinas K, et al Discontinuation of treatment using anticholinergic medications in patients with urinary incontinence Obstet Gynecol 2014; 124:794-800
18 Wada N, Watanabe M, Banjo H, et al Long-term persistence with mirabegron in a real-world clinical setting Int J Urol 2018; 25:501-506
19 DeJong C, Aguilar T, Tseng CW, et al Pharmaceutical Industry–Sponsored Meals and Physician Prescribing Patterns for Medicare Beneficiaries JAMA Intern Med 2016; 176:1114-1122
Correspondence
Hiroshi Masuda, MD, PhD (Corresponding Author)
hrsmasuda@yahoo co jp
Kosuke Mikami, MD
Kotaro Otsuka, MD
Kyokusin Hou, MD
Takahito Suyama, MD
Kazuhiro Araki, MD
Satoko Kojima, MD
Yukio Naya, MD
Department of Urology, Teikyo University Chiba Medical Center, 3426-3
Anesaki, Ichihara, Chiba, 299-0111, Japan
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
454
H Masuda, K Mikami, K Otsuka, K Hou, T Suyama, K Araki, S Kojima, Y Naya
ORIGINAL PAPER
Summary
Objective: Voiding dysfunction (VD), which encompasses many urinary symptoms that are not caused by neurological or anatomical anomalies, is a frequently encountered functional urinary bladder disorder in children. It was reported that there was an association between lower urinary tract symptoms and fecal microbiota in adult patients. Therefore, we aimed to investigate the differences in fecal microbiota between children with or without VD
Methods: Two patient groups, including 30 patients, were compared Group 1 included patients with VD, while Group 2 consisted of healthy children All study participants were asked to fill lower urinary tract and voiding dysfunction symptom score forms with the assistance of their parents Subsequently, uroflowmetry tests and postvoiding residual urine measurements were performed Fresh stool samples were collected from all children and analyzed by polymerase chain reaction General bacterial load and presence of Roseburia intestinalis, Clostridium difficile, Fusobacterium nucleatum, and Bacteroides clarus were tested
Results: The two groups were significantly different regarding general bacterial load; the presence of Fusobacterium nucleatum. Clostridium difficile and Bacteroides clarus was not detected in the fresh stool samples of the patients in Group 2; the counts of Roseburia intestinalis were less in Group 1 than in Group 2, although there was no statistically significant difference. There was a negative correlation between symptom scores, general bacterial load, and the presence of Fusobacterium nucleatum. However, there was no correlation between the presence of Roseburia intestinalis and symptom scores
Conclusions: There is a potential relationship between VD and a deviation in the fecal microbiota in the pediatric population
KEY WORDS: Voiding dysfunction; Fecal microbiota; Fecal microbiota change
Submitted 28 October 2022; Accepted 6 November 2022
INTRODUCTION
Voiding dysfunction (VD) is also named bladder dysfunction in children It is a general term encompassing both voiding and storage dysfunctions It is a functional bladder anomaly encountered in children who do not have any neurological and anatomical abnormalities It is not rare in children; approximately 40% of children presenting to pediatric urology clinics are affected by VD (1, 2) The human body is a complex system hosting various microorganisms, including bacteria, fungi, and parasites The assemblage of
these commensal, symbiotic or pathogenic microorganisms is called human microbiota The human microbiota is mainly located at four anatomical regions: Skin, genitourinary system, respiratory system, and gastrointestinal system (3) The full array of these microorganisms that live on and in humans and, more specifically, the collection of microbial genomes that contribute to the genetic portrait is called the human microbiome The specific changes in the microbiome are named dysbiosis (3) The gut microbiome plays a major role in the regulation, maturation, and function of the host immune system from the birth The immune system has co-evolved a mutualistic relationship with the gut microbiome residing our bodies while mounting efficient responses to fight invading pathogens Distortion of the balance between the useful and harmful intestinal microorganisms in favor of the harmful ones was associated with acute or chronic disease processes such as irritable bowel syndrome, inflammatory bowel disease, allergic diseases, obesity, depression, atherosclerosis, and colon cancer (4)
It was reported that urinary dysbiosis was associated with lower urinary tract symptoms (5) However, while the relevant studies were conducted with adult patients, none included the pediatric population Therefore, we investigated the differences between children with and without VD regarding intestinal (fecal) microbiota
MATERIALS AND METHODS
This study was approved by the Ethical Review Committee of the Sitki Kocman University (180172) Informed consent was obtained by parents or caregivers of all participants who signed the relevant forms before assignment to the study
The subjects were selected among children aged between 5 and 16 who presented to the pediatric urology and nephrology outpatient clinics Patients with congenital genitourinary (GU) or gastrointestinal (GI) anomalies, GI diseases, acute infections, neurological anomalies, and chronic constipation were excluded Also, patients with a history of GU surgery, GI surgery, or monosymptomatic enuresis, those treated for VD or given antibiotics, antiviral or antifungal medications during the last six months were omitted
Any functional disturbance in voiding after the completion of toilet training was defined as VD This occurs due to over activity or inadequate relaxation of the pelvic floor muscles, which are striated muscles under voluntary control The
455 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
No conflict of interest declared
Ilker
1
S
2
1
3
S
ahin 1
Is there a difference in fecal microbiota of children with and without voiding dysfunction?
Akarken 1 , Hüseyin Tarhan
, Gamze
¸ ener
, Hasan Deliktas
, Nurcan Cengiz
, Hayrettin
¸
1 Mugla Sıtkı Kocman University, School of Medicine, Department of Urology, Turkey;
2 Izmir Katip Celebi University, School of Medicine, Department of Microbiology, Turkey;
DOI: 10 4081/aiua 2022 4 455
3 Mugla Sıtkı Kocman University, School of Medicine, Department of Pediatric Nephrology, Turkey
patients presented to outpatient clinics with lower urinary tract symptoms (LUTS) and diagnosed with VD were included in Group 1 Group 2 consisted of healthy pediatric patients who presented to the same outpatient clinic for check-up purposes
All study participants were evaluated regarding LUTS with the assistance of their caregivers First, voiding dysfunction symptom score (VDSS) forms were filled for each subject (6) Subsequently, a uroflowmetry test was performed Next, the voiding patterns (i e , normal, parabolic, tower, plateau, staccato, interrupted) and voided volumes were recorded for each patient Following this, post-voiding residual urine volumes were measured and recorded
A 3-gram fresh stool sample was collected from all patients, and the samples were stored at -80°C
Analysis of the stool samples
DNA isolation
Roche Magna Pure Compact robotic DNA isolation system (Roche, Germany) protocol was used to isolate DNA at room temperature
DNA quantification
The DNA was quantified using a Nanodrop 2000 (Thermo Scientific, USA) The absorbance ratios 260/280 and 260/230 were used to assess the purity of DNA
Real-time PCR (qPCR)
Bacteroides clarus (BacC), Roseburia intestinalis (RosIn) and general intestinal bacteria (16SInt) were detected in the samples
Primers and the Taqman probe (Hydrolysis probe) were designed for five targets (Figure 1)
The ready-to-use lyophilized primers (5 nmol) and probes (3 nmol) were wettened on synthesis paper (TIB Molbiol, Germany) and diluted to 10 pmol/ul stocks
LightCycler480 Probes Master (Roche Diagnostics, Germany) served as Enzyme&master mix The processes were implemented in LightCycler480 II (Roche Diagnostics, Germany) The results were analyzed in the Abs Quant/2nd derivative analysis module Samples creating sigmoidal curves were considered positive, while others were considered negative General bacterial load was measured, and the presence of Roseburia intestinalis, Clostridium difficile, Fusobacterium nucleatum, and Bacteroides clarus was assessed
Statistical analysis
The Kolmogorov-Smirnov test was used for assessing the distribution of data Student’s t-test was used to compare the groups regarding continuous variables and the chisquare test was used to compare categorical variables The Pearson correlation coefficients (r) were used for correlation analysis The data were displayed as means, standard deviations (SD), and ranges (minimum-maximum)
The p value was considered statistically significant when it was less than 0,05 All statistical analyses were performed using the Statistical Package for Social Sciences software (SPSS v24, IBM Corporation, New York, US)
Table 1
Demographic and clinical data and results of the comparative analysis.
Gene Sequencee
FusN-F TTCAATAAAAgTggCAggTCAAg
FusN-R TAACAACACATgCAggTCAATgg
FusN-Pr 6FAM-ACTCgAACCCCCAACCCTCggTTT--TMR
CloD-F gCAAgTTgAgCgATTTACTTCggT
CloD-R gTACTggCTCACCTTTgATATTYAAgAg
CloD-Pr 6FAM-TgCCTCTCAAATATATTATCCCgTATTAg--TMR
BacC-F TCCATCCgCAAgCCTTTACT
BacC-R gCTTCCggTgCCATTgACTA
BacC-Pr 6FAM-TTCATCATCACAgCCgACAACgCA--TMR
RosIn-F CggATTTgCAgTggCAAgTT
RosIn-R TgATTgCAgACgCCAATgTC
RosIn-Pr 6FAM-CgTgAAAAATCCgCgCATCTggC--TMR
16S-IntC-F CgTCAgCTCgTgYCgTgAg
16S-IntC-R CgTCRTCCCCRCCTTCC
16S-IntC-Pr HEX-TTAAgTCCCRYAACgAgCgCAACCC--BBQ
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
456
I Akarken, H Tarhan, G Sener, H Deliktas, N Cengiz, H Sahin
F u s o b a c t e r i u m n u c l e a t u m ( F u s N ) , C l o s t r i d i u m d i f fi c i l e
(CloD),
Groups Group 1 Group 2 p value Age- year 8 26 ± 1 9 8 00 ± 1 6 0 574 Gender 0.902 Female n (%) 15 (60 0) 14 (58 3) Male n (%) 10 (40 0) 10 (41 7) Frequency (8 >) 0 001 Present n (%) 21 (84 0) 4 (16 7) Absent n (%) 4 (16 0) 20 (83 3) Urgency 0 001 Present n (%) 19 (76 0) 6 (25 0) Absent n (%) 6 (24 0) 18 (75 0) Hesitancy 0 015 Present n (%) 11 (44 0) 3 (12 5) Absent n (%) 14 (56 0) 21 (87 5) Terminal dribbling 0 001 Present n (%) 18 (72 0) 4 (16 7) Absent n (%) 7 (28 0) 20 (83 3) Low urine flow rate 0 001 Present n (%) 13 (52 0) 1 (4 2) Absent n (%) 12 (48.0) 23 (95.8) Maneuvers to hold urine 0 001 Present n (%) 19 (76.0) 2 (8.3) Absent n (%) 6 (24 0) 22 (91 7) Interrupted voiding 0 001 Var n (%) 16 (64 0) 4 (16 7) Yok n (%) 9 (36 0) 20 (83 3) Straining to void 0 001 Present n (%) 15 (60 0) 0 (0 0) Absent n (%) 10 (40 0) 24 (100) Voiding pattern 0 001 Normal n (%) 8 (32 0) 21 (87 5) Staccato n (%) 6 (24 0) 0 (0) Tower n (%) 11 (44 0) 3 (12 5) Plateau n (%) 0 (0) 0 (0) Interrupted n (%) 0 (0) 0 (0) Voided volume 0 001 Lower than expected bladder capacity (%) 17 (68 0) 1 (4 2) Consistent with the expected bladder capacity (%) 8 (32 0) 23 (95 8) Post-voiding residual urine volume (ml) 44 4 ± 21 6 19 4 ± 6 4 0 574 Voiding dysfunction symptom scores 21 9 ± 6 9 6 3 ± 1 3 0 001
Figure 1. Primer sequences.
RESULTS
The mean patient age was 8 1 ± 0 25 (6-13) Although we planned to include 30 patients in each group, 5 patients were excluded from Group 1, and 6 patients were excluded from Group 2 due to the failure in the DNA isolation process Thus, there were 25 patients in Group 1 and 24 patients in Group 2 Demographic data and clinical features of the study patients, including lower urinary tract symptoms, uroflowmetry, PVR measurement results, and voiding dysfunction symptom scores, are displayed in Table 1 The comparative analysis revealed that general bacterial load and the rate of Fusobacterium nucleatum presence were significantly lower in patients with VD than in healthy patients (p = 0 043 and p = 0 009, respectively) Although Roseburia intestinalis was present in fresh stool samples of both patient groups, its rate was relatively lower in the patient group with VD Clostridium difficile and Bacteroides clarus were not detected in the fresh stool samples of the healthy patient group (Table 2) In fresh stool samples, the correlation between voiding dysfunction symptom score (VDSS) and general bacterial load, Roseburia intestinalis, Clostridium difficile, Fusobacterium nucleatum, and Bacteroides clarus counts were analyzed There was a negative correlation between VDSS and general bacterial load and Fusobacterium nucleatum counts (p = 0 033 and p = 0 004, respectively) Although there was also a negative correlation with Roseburia intestinalis, it was statistically insignificant (p = 0 25) (Table 3)
Since Clostridium difficile was not detected in the fresh stool samples of the patients in Group 2, a correlation analysis could not be performed
DISCUSSION
Since bowels have a 250 m2 absorptive surface area and a nutrient-rich content, they have the most extensive flora bearing various microorganisms Therefore, it is difficult to determine all types of bacteria and their counts included in the intestinal flora However, investigations utilizing
current methods elucidated more than 100 trillion bacteria and more than 1000 bacteria types in the bowel (7)
T h e m i c r o b i o t a , w h i c h i n c l u d e s v a r i o u s a n d m a n y microorganisms, starts to develop after birth Its initial content depends on genetic and geographical factors, route of labor, age at labor, and diet (8) continues to develop and modulate in species abundance for about 3 years, until the microbiota becomes adult-like
Until age 1, bowel microbiota shows significantly less variation than microbiota in toddlers, adolescents, or adults
Remarkable changes occur in the content of intestinal microbiota until age 3 The primary microbiota evolves to adult microbiota after age 3 regarding the variability of bacteria types (9, 10) Anaerobic, facultative anaerobic, and aerobic bacteria are present in the gastrointestinal microbiota Approximately 90% of this flora consists of Bacteroides and Firmicutes species Other microbial phyla are Actinobacteria, Proteobacteria, Verrucomicrobia, and Fusobacteria The bacteria investigated in our study were selected as per the variability in microbiota
The association between LUTS and urinary microbiome was previously reported using 16S rRNA gene sequence (5) However, only a few studies investigated the association between intestinal microbiota and LUTS Holland et al studied 30 male patients with LUTS and suggested a significant relationship between the symptom scores and the presence of specific bacteria types in the intestinal microbiota Of note, this study did not include a comparative analysis between patients with and without LUTS (11) Braundmeier-Fleming et al compared the stool samples of the patients who had interstitial cystitis with those of healthy subjects (12) In line with our study, these researchers performed polymerase chain reaction (PCR) on stool samples They reported that the counts of E sinensis, C aerofecaciens, F prausnitzii, and O splanchnicus were significantly lower in the fecal microbiota of the patients with interstitial cystitis than in healthy subjects In a fecal microbiota study including patients with chronic prostatitis/ chronic pelvic pain syndrome (another functional lower urinary tract disorder such as interstitial cystitis) the alpha diversity analysis revealed that the diversity of fecal microbiota was significantly lower in the patient group than in healthy subjects (13) Okamoto et al studied 1113 patients comparing patients with high overactive bladder symptom scores and urgency with those who had low symptom scores without urgency They found that the former group had a significantly lower bacterial load in the fecal microbiota (14) They suggested that the natural bacterial load reduction might be correlated with the disease process Our study determined a significant difference between patients with normal and abnormal voiding dysfunction symptom scores concerning general bacterial load and a negative correlation between VDSS and the general bacterial load Of note, reduction in the bacterial load infers reduction of the microorganisms beneficial for health
Some bacteria such as Bifidobacterium species in microbiota have beneficial critical roles, and they can be used as probiotics These bacteria were low in patients with overactive bladder (14) On the other hand, the counts of Faecalibacterium species were higher in patients with overactive bladder than in the control group patients (14) Detection of high numbers of these bacteria in overactive
457 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Microbiota of children with urinary dysfunction
Table 2
Groups Group 1 Group 2 p value General bacterial load 16 5 ± 3 2 18 3 ± 2 9 0 043 Fusobacterium nucleatum 34.8 ± 2.6 37.2 ± 2.9 0.009 Clostridium difficile 33 8 ± 0 Bacteroides clarus 27 3 ± 4 4 Roseburia intestinalis 27 3 ± 4 9 28 4 ± 2 5 0 486
The comparison of the groups regarding bacteria in the fresh stool samples.
Table 3.
Cor relation coefficient p value General bacterial load -0 305 0 033 Fusobacterium nucleatum -0 435 0 004 Roseburia intestinalis -0 225 0 250 Bacteroides clarus 0 919 0 258 Clostridium difficile** *
Results of the correlation analysis between voiding dysfunction symptom scores, general bacterial load and counts of specific bacteria.
Since C ostr d um D ffici e was not detected in the fresh stool samples of the pat ents in Group 2, a corre at on analys s cou d not be performed
Akarken, H Tarhan, G Sener, H Deliktas, N Cengiz, H Sahin
bladder patients is an unfavorable sign indicating the deviation in the intestinal microbiota
In our study, Fusobacterium nucleatum counts were significantly lower in patients with VD than in controls (p = 0 009) The counts of Roseburia intestinalis were relatively lower in the former group than in the latter although the difference was not statistically significant (p = 0 486)
Clostridium difficile and Bacteroides clarus were not detected in the healthy patient group Detection of these bacteria in the patient group with VD can be considered an indicator of dysbiosis It is widely accepted that deviations in the intestinal microbiota led to an increase in the levels of toxic metabolites and a reduction in the number of useful metabolites, thus contributing to disease processes (15) The intestine-brain axis is a two-way communication network This network consists of the central nervous system (CNS), which includes the brain and the spinal cord, autonomic nervous system, enteric nervous system, and the hypothalamic-pituitary-adrenal axis (16) Thus, the intestinal microbiota can affect the enteric neurons and the CNS via metabolites secretion A potential dysfunction affects both sides since this is a two-way interaction (17) The effects of the intestinal microbiota on brain development and the emergence of neurodegenerative diseases were also reported (18) Also, it was noted that there was a relationship between the reduction of intestinal microbial diversity and cognitive dysfunction In addition, it was suggested that a healthy microbiota was associated with learning skills and memory development (19) Our study showed a significant reduction in the general bacterial load in the patient group with VD Therefore, we suggest that dysbiosis could negatively affect autonomic nervous system maturation or the coordination between the CNS and the lower urinary tract
Our study has some limitations First, it was conducted with a limited number of patients because of Coronavirus disease-2019 (COVID-19) pandemic during the study period Second, the total bacterial diversity could not be analyzed since DNA sequence sampling could not be performed in fresh stool samples due to financial reasons
CONCLUSIONS
We conclude that there is a potential relationship between VD and a deviation of the fecal microbiota However, we further studies, including more extensive patient series, are needed in to confirm this finding
ACKNOWLEDGEMENTS
The authors would like to thank “Mugla Sitki Kocman University Scientific Research Project Department” for their support
REFERENCES
1 Farhat W, Bägli Dj, Capolicchio G, et al The dysfunctional voiding scoring system: quantitative standardization of dysfunctional voiding symptoms in children J Urol 2000; 164:1011-5
2 Austin PF, Bauer SB, Bower W, et al The standardization of terminology of lower urinary tract function in children and adolescents: Update report from the standardization committee of the International Children's Continence Society Neurourol Urodyn 2016; 35:471-81
3 Gill SR, Pop M, DeBoy RT, et al Metagenomic analysis of the human distal gut microbiome Science 2006; 312:1355-9
4 Duvallet C, Gibbons SM, Gurry T, et al Meta-analysis of gut microbiome studies identifies disease-specific and shared responses Nat Commun 2017; 8:1-10
5 Antunes-Lopes T, Vale L, Coelho AM, et al The role of urinary microbiota in lower urinary tract dysfunction: a systematic review Eur Urol Focus 2020; 6:361-9
6 Akbal C, Genc Y, Burgu B, et al Dysfunctional voiding and incontinence scoring system: quantitative evaluation of incontinence symptoms in pediatric population J Urol 2005; 173:969-73
7 Qin J, Li R, Raes J, Arumugam M, et al A human gut microbial gene catalogue established by metagenomic sequencing Nature 2010; 464:59-65
8 Pelzer E, Gomez-Arango LF, Barrett HL, Nitert MD Maternal health and the placental microbiome Placenta 2017; 54:30-7
9 Arrieta M-C, Stiemsma LT, Amenyogbe N, et al The intestinal microbiome in early life: health and disease Front Immunol 2014; 5:427
10 Yatsunenko T, Rey FE, Manary MJ, et al Human gut microbiome viewed across age and geography Nature 2012; 486:222-7
11 Holland B, Karr M, Delfino K, et al The effect of the urinary and faecal microbiota on lower urinary tract symptoms measured by the International Prostate Symptom Score: analysis utilising next-generation sequencing BJU Int 2020; 125:905-10
12 Braundmeier-Fleming A, Russell NT, Yang W, et al Stool-based biomarkers of interstitial cystitis/bladder pain syndrome Sci Rep 2016; 6:1-10
13 Shoskes DA, Wang H, Polackwich AS, et al Analysis of gut microbiome reveals significant differences between men with chronic prostatitis/chronic pelvic pain syndrome and controls J Urol 2016; 196:435-41
14 Okamoto T, Hatakeyama S, Imai A, et al Altered gut microbiome associated with overactive bladder and daily urinary urgency World J Urol 2021; 39:847-53
15 Yin J, Liao SX, He Y, et al Dysbiosis of gut microbiota with reduced trimethylamine-N-oxide level in patients with large-artery atherosclerotic stroke or transient ischemic attack J Am Heart Assoc2015; 4:e002699
16 Carabotti M, Scirocco A, Maselli MA, Severi C Erratum: The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems Ann Gastroenterol 2015; 28:203-209
17 Yang NJ, Chiu IM Bacterial signaling to the nervous system through toxins and metabolites J Mol Biol 2017; 429:587-605
18 Martin CR, Osadchiy V, Kalani A, Mayer EA The brain-gutmicrobiome axis Cell Mol Gastroenterol Hepatol 2018; 6:133-48
19 Davidson GL, Cooke AC, Johnson CN, Quinn JL The gut microbiome as a driver of individual variation in cognition and functional behaviour Philos Trans R Soc Lond B Biol Sci 2018; 373:20170286
Correspondence
Ilker Akarken, MD - ilkerakarken@gmail com
Hüseyin Tarhan, MD (Corresponding Author) drhuseyintarhan@gmail com
Hasan Deliktas, MD - drhasand@gmail com
Hayrettin S ¸ ahin, MD - hsahin63@gmail com
Mugla Sıtkı Kocman University, School of Medicine, Department of Urology, Turkey
Gamze S ¸ ener, MD - asligamze seher@saglik gov tr
Izmir Katip Celebi University, School of Medicine, Department of Microbiology, Turkey
Nurcan Cengiz, MD - nurcandinler@mu edu tr
Mugla Sıtkı Kocman University, School of Medicine, Department of Pediatric Nephrology, Turkey
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
458
I
1 Marmara University Faculty of Medicine, Department of Pediatric Surgery, Division of Pediatric Urology, Istanbul, Turkey;
2 Ministry of Health, Marmara University Pendik Education and Research Hospital, Department of Pediatric Surgery, Istanbul, Turkey;
3 St Helens and Knowsley Teaching Hospitals, Department of Pediatric Accident and Emergency Medicine;
4 Marmara University Faculty of Medicine, Department of Pediatric Surgery, Istanbul, Turkey;
5 Tug tepe Center of Pediatric Urology and Pediatric Surgery, Istanbul, Turkey
Summary
Objective: Surgeons observed that the outcomes after the same repair technique in the same type of hypospadias performed by the same surgeon may be different. There may be some indeterminate factors that influence the results such as subclinical inflammation Our study evaluated the predictor values of inflammatory hematologic parameters on the complications after hypospadias repair
Materials and methods: We retrospectively reviewed the data of patients who underwent hypospadias repair between January 2016 and January 2019 in our clinic. Age at surgery, hypospadias type, repair technique, complications were recorded
Patients who underwent Snodgrass repair by a single surgeon were included in the study while patients who underwent different techniques or procedures that were performed by other surgeons were excluded The levels of white blood cell, neutrophil, lymphocyte, platelet and monocyte, the mean platelet volumes were recorded from blood test that were performed one day before surgery Neutrophil-lymphocyte ratio (NLR), plateletlymphocyte ratio (PLR), and other parameters were analyzed to determine their relationship with complications after hypospadias surgery
Results: WBC and neutrophil levels were statistically higher in patients with complications (p = 0.006 and 0.017 respectively). Other hematological parameters were not different between patients with or without complications. To predict the complications, the WBC cutoff was 9500/mm3, the neutrophil cutoff was 3000/mm3.
Conclusions: WBC and neutrophil values were statistically significant in predicting the complications after Snodgrass repair in patients with hypospadias Our result determined no relation between complications and NLR, PLR.
KEY WORDS: Hypospadias; Leukocyte; Neutrophil; NLR; Complication
Submitted 11 September 2022; Accepted 24 September 2022
INTRODUCTION
Hypospadias repair is one of the most common surgery in pediatric urology More than 100 different procedures were described to obtain better results, but complication rates are still a challenge for the surgeons However bet-
ter techniques and thinner suture materials reduce the rate of complications (1) Better wound dress materials and surgery with or without stent were also discussed to i m p r o v e t h e r e s u l t s S e n i o r s h a d e x p e r i e n c e d t h a t patients with same characteristics, operated with the same technique and material by the same surgeon had different results The difference may be depending on subclinical inflammation that may be a predictor about these unexpected complications
The neutrophils and the lymphocytes are the main cellular components of the immune system of human being During an infection the level of white blood cells may vary depending on the stage of the disease, the patient’s immunologic features and the etiology of the infection Increment in the level of neutrophils and reduction in the level of lymphocytes shows a possible infection (2) All these parameters can be measured in complete blood count (CBC)
Physiological immune response of circulating white blood to various stressful events such as tissue injury, severe trauma characterized by major surgery, burns, sepsis syndrome consists in elevation of neutrophils and d e c r e a s e o f l y m p h o c y t e c o u n t s T h i s i n fl a m m a t o r y response sometimes causes fibrosis and poor neovascularization which are the main factors for poor wound healing (3) It is shown that spongiofibrosis with urethral stricture was related with inflammation (4, 5) Several medications with anti-inflammatory effect have been used to treat urethral strictures either systematically or locally (6-10) In adult’s series, it was reported that neutrophillymphocyte ratio (NLR) revealed the inflammatory status of the urethral tissue predicting urethral stricture after non-hypospadias surgery (11) Also, NLR was shown as a marker to predict for systemic inflammatory response syndrome after flexible ureteroscopic lithotripsy (12) Subclinical systemic inflammation may have impact on the outcomes of hypospadias repair in children
Preoperatively the number of white blood cell (WBC) and neutrophils, NLR, platelet-lymphocyte ratio (PLR) or mean platelet volume (MPV) may predict complications after hypospadias surgery, but this was not studied yet The
459 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
No conflict of interest declared
ORIGINAL PAPER
Do preoperative leukocyte and neutrophil levels have a predictive value on the complications of hypospadias repair in children?
Ahsen Karagözlü Akgül 1 , Sadık Abidog ˘ lu 1 , Ayten Ceren Bakır 2 , Embiye Adalı 3 , Gürsu Kıyan 4 , Halil Tug ˘ tupe 5
DOI: 10 4081/aiua 2022 4 459
aim of the present study is to investigate the relationship between the h e m a t o l o g i c p a r a m e t e r s a n d t h e c o m p l i c a t i o n s a f t e r h y p o s p a d i a s repair in children
MATERIALS AND METHODS
Institutional Review Board approval was obtained before chart review and data analysis with the reference number of 09 2020 1155 Informed consent was approved by the parents of all patients Records of the children who underwent hypospadias repair between January 2015 and January 2019 in our clinic were reviewed Data collected included age of the patients, types of hypospadias, repair t e c h n i q u e s , s u t u r e m a t e r i a l s , s u rgeons who performed the hypospadias repair, follow-up time, complications, and hematological parameters Hematological parameters including white blood count (WBC), neutrophil, lymphocyte, monocytes, platelet counts, and mean platelet volume were recorded from the complete blood count (CBC) which was performed the day before surgery Patients with hypospadias who underwent tubularized incised plate urethroplasty (TIPU) repair by a single surgeon (HT) were included Patients with abnormal WBC values for their age in the complete blood count the day before the operation were excluded Patients with follow up time shorter than 12 months and incomplete data were not recorded
In the study period 522 patients who underwent hypospadias repair were recorded 59 patients whose complete blood count was not performed the day before the surgery, 6 patients whose WBC values were not within the normal range for their age, 163 patients who underwent two-session hypospadias repair or who underwent hypospadias repair with another technique, 99 patients who were operated by other surgeons, and 32 patients who underwent caudal anesthesia, whose effect on the outcomes after hypospadias repair is controversial, were excluded from the study (Figure 1)
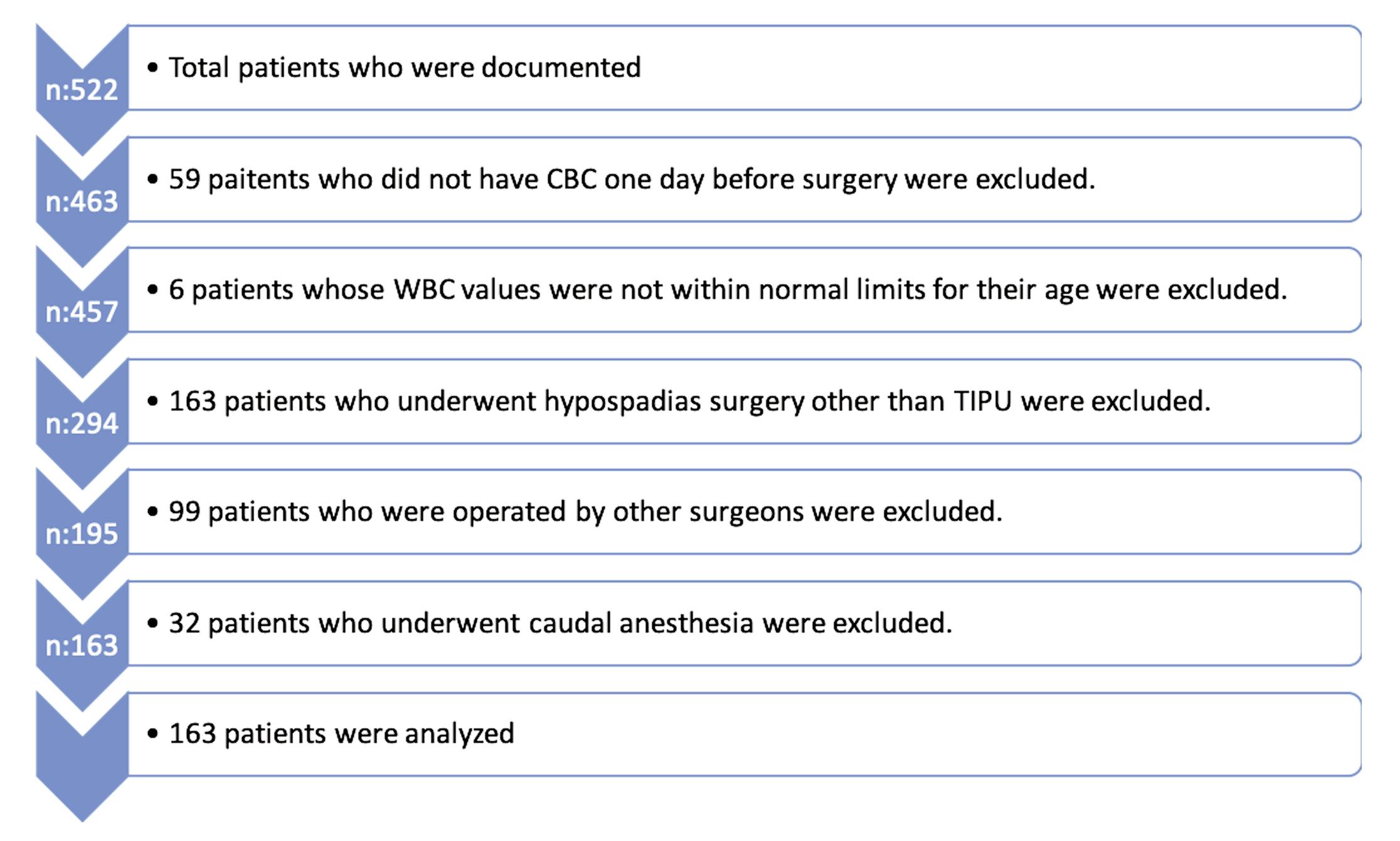
P a t i e n t s w e r e d i v i d e d i n t o t w o groups depending on the presence of complication Hematological parameters detected from CBC were statistically analyzed whether if they are related with complications or not
Operative technique
All procedures were performed under general anesthesia and penile block was performed at the beginning of the procedure Sterile urine was controlled with urine culture 3-7 days before the surgery Antibiotic prophylaxis was applied one-hour prior the
surgery All patients underwent TIPU technique by the same surgeon (HT) The urethral plate was tabularized over a 6 Fr urethral catheter in two layers, the first layer with continuous subcuticular 7/0 coated polyglactin sutures and the second layer with interrupted 7/0 coated polyglactin sutures Tourniquet for less than 15 minutes was used while the dissection of glandular wings A pedicle flap from dartos fascia was prepared and placed on the neourethra Glanduloplasty was done with 6/0 polydioxanone sutures Subcutaneous epinephrine was not used during surgery The 6 Fr urethral catheter was left in place for seven days postoperatively The patients were followed up in the second week, first month and third month postoperatively Follow-up continues with outpatient visits every 3 months in the first year and once a year thereafter Patients were evaluated for penile cosmetics, meatal and urethral steno-
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
460
A Karagözlü Akgül, S Abidoglu, A Ceren Bakır, E Adalı, G Kıyan, H Tugtupe
Table 1.
Complication (-) Complications (+) Mean ± sd/n-% Median Mean ± sd/n-% Median P Age at surgery (months) 43 5 ± 32 9 33 5 45 5 ± 38 4 29 0 0 874 m Type of the hypospadias Distal 101 80 2% 21 56 8% 0 008 X2 Midpenile 22 17 5% 12 32 4% 0 082 X2 Proximal 3 2 4% 4 10 8% 0 078 X2 WBC (x103) 8 8 ± 2 5 8 5 10 2 ± 3 0 9 7 0 006 m Neutrophil 3356 ± 1563 3000 4176 ± 2054 3700 0 017 m Lymphocyte 4302 ± 1726 4100 4630 ± 2372 4300 0 529 m Monocyte 808 ± 462 700 803 ± 246 700 0 303 m HB 12 0 ± 1 1 11 9 12 0 ± 1 1 11 9 0 810 m PLT (x103) 316.0 ± 83.4 313.5 325.5 ± 86.1 313.0 0.563 m NLR 0 9 ± 0 5 0 8 1 4 ± 1 6 0 9 0 240 m PLR 83 6 ± 34 7 80 2 102 7 ± 116 9 85 9 0 876 m MLR 0 2 ± 0 2 0 2 0 2 ± 0 2 0 2 0 768 m MPV 7 7 ± 0 8 7 6 7 8 ± 0 8 7 7 0 504 m mMann-Whitney U test X2 Chi-square test WBC: White blood cel ; HB: Hemoglobin; PLT: Platelet; NLR: Neutroph l-Lymphocyte Rat o; PLR: Plate et-Lymphocyte Rat o; MLR: Monocyte-Lymphocyte Ratio; MPV: Mean P atelet Volume
Demographic features and hematological parameters of patients in the groups
Figure 1. Flowchart.
sis, urethrocutaneous fistula and for other complications with physical examination, calibration of the neourethra with 6-8 Fr catheter and voiding video
Statistical analysis
In the descriptive statistics of the data, mean, standard deviation, median, minimum, maximum, frequency and ratio values were used The distribution of variables was measured with the Kolmogorov-Smirnov test The Mann-Whitney U test was used in the analysis of quantitative independent data Chi-square test was used in the analysis of qualitative independent data, and Fisher-Exact test was used when the Chi-square test conditions were not met ROC curve was performed to analyze the capacity of hematological parameters in predicting the complication of hypospadias repair Probability chart was performed to determine the possibility of complications after surgery Cut off values were determined according to Youden index SPSS 27 0 program was used in the analysis
All p-values less than 0 05 were considered statistically significant
RESULTS
One hundred sixty-three patients were analyzed retrospectively The median age of the patients was 32 months (Table 1) Of the patients, 122 had distal hypospadias, 34 had midpenile hypospadias, and 7 had proximal hypospadias There were 126 patients without complication and 37 with complications The complications were urethral fistula in 19 patients, urethral stricture requiring reoperation in 3 patients, urethral diverticula in 3 patients, dehiscence (partial or complete) in 4 patients and mild meatal stenosis that solved with dilatation in 8 patients Patients were divided into two groups according to the presence of complications and there was no difference between groups in case of age at operation (p > 0 05) (Table 1) The ratio of complications in patients with distal hypospadias was lower than the ratio of complications in patients with mid-penile and proximal hypospadias (p = 0 008)
WBC and neutrophil levels were statistically higher in patients with complications (p < 0 05) (Table 1, Figure 2) NLR, PLR and other hematological parameters were not different between patients with or without complications (Table 1) Although area under curve (AUC) was not so high, significant effectiveness of WBC value was observed in predicting patients with and without complications (Table 2) WBC value was found to be a significant variable in the occurrence of complications The cut off value of WBC to predict the complications was 9500 m/mm3, the sensitivity was 56 8%, specificity was 70 6%, (Figure 3), positive prediction was 36 2%, and negative prediction was 84 8%
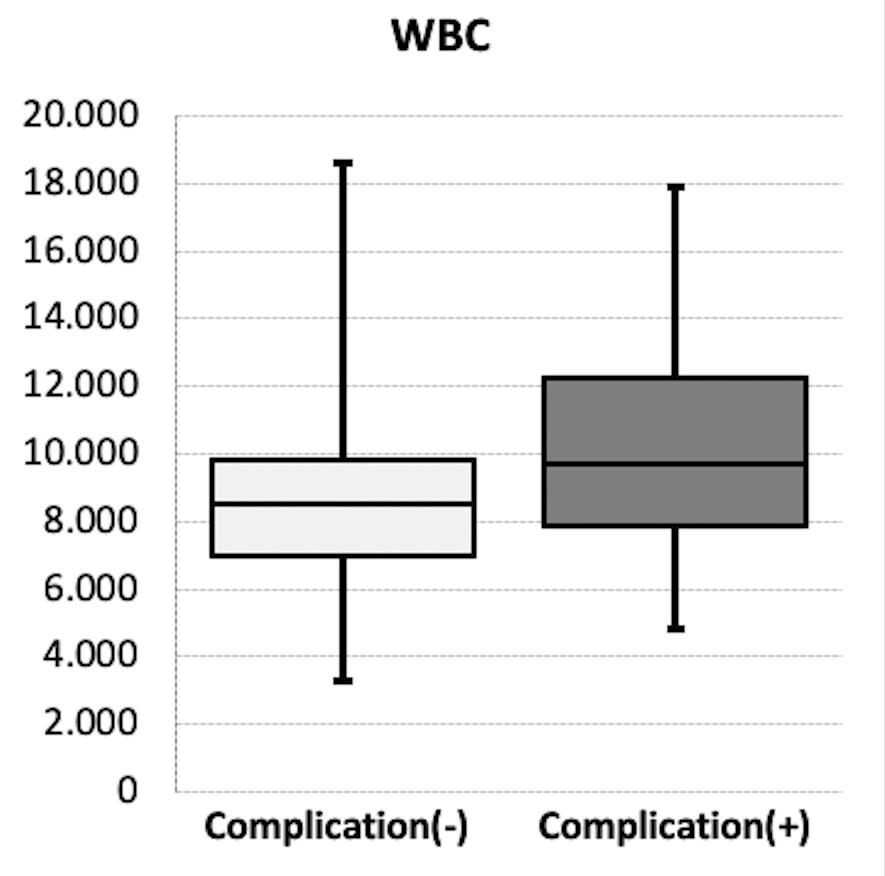
In predicting the patients with and without complications, the neutrophil count was also statistically significant (Table 2) The neutrophils cut off value to predict the complications was 3000 m/mm3, the sensitivity was 70 3%, specificity was 51 6% (Figure 3), positive prediction was 29 9%, and negative prediction was 85 5% There was no statistically significant difference in NLR, PLR, MPV and also WBC and neutrophils between patients with or without urethral fistula (p > 0 05)
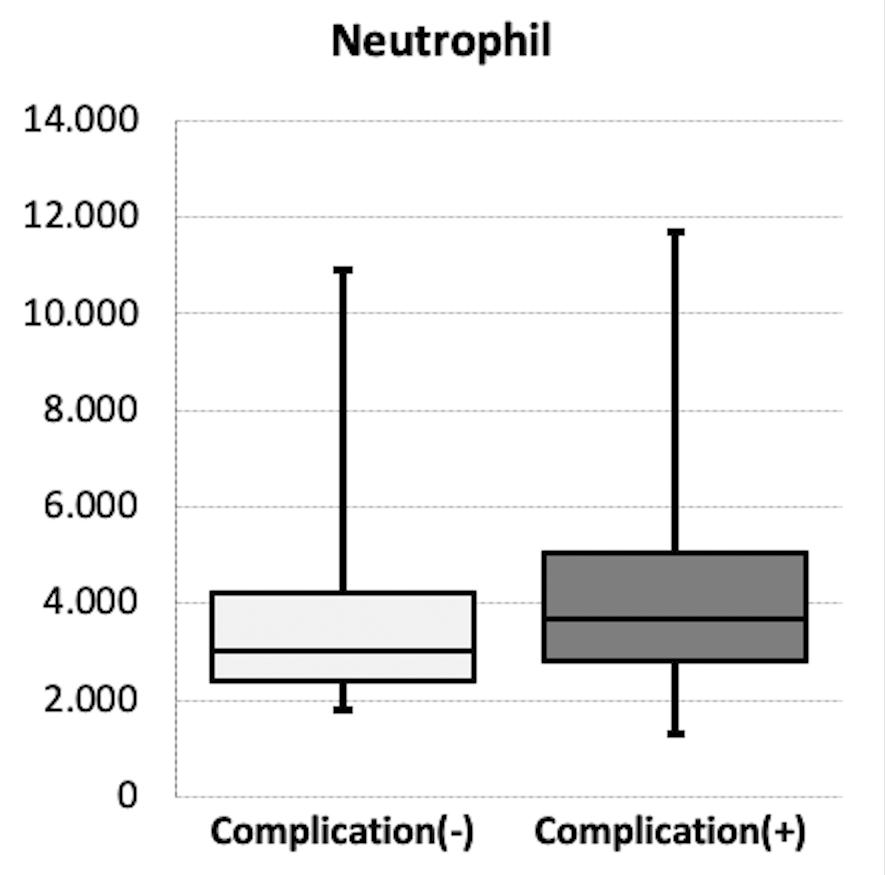
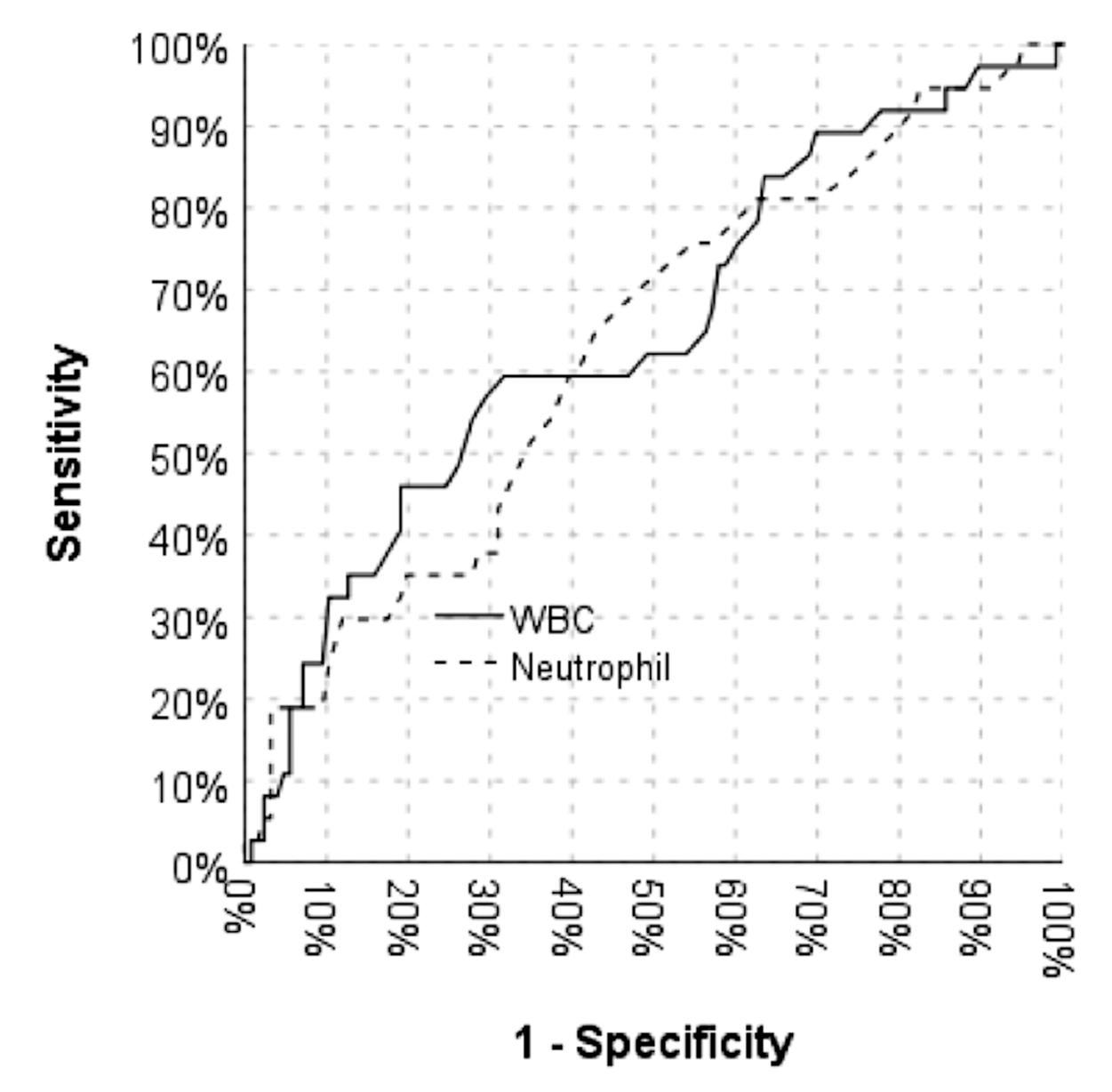
461 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 WBC/NLR predicting outcome of hypospadias
Table 2
AUC 95% Cl p WBC 0 647 0 544 - 0 751 0 006 Neutrophil 0 629 0 527 - 0 731 0 017 WBC:
Area under curve for WBC and neutrophil values
Wh te blood ce l; AUC: Area under curve
Figure 2. WBC: White blood cell
Figure 3. Graphics of sensitivity and specificity of WBC and neutrophil values
DISCUSSION
Complications of hypospadias repair are reported frequently in the previous literature (1, 13) Especially the complications of the TIPU which is a commonly used technique are well known by pediatric urologists The main complications of this technique are urethral stricture, meatal stricture, urethral fistula, and dehiscence (14) To reduce the complication rate, surgeons used better suture materials, preferred waterproof and tension free suture lines, using dartos flap on the neourethra, etc (15) But it is observed that results were different in patients with the same hypospadias type who underwent exactly same repair technique with using high-quality suture materials by same experienced surgeon The reasons of this difference are not clear yet Subclinical inflammation may be a factor for complications of hypospadias surgery and our study revealed that WBC or neutrophil value could be predictors for these complications
WBC differs in the systemic inflammation This inflammatory response sometimes causes fibrosis and poor neovascularization which are the main factors for poor wound healing (3) Hampson et al reported subepithelial inflammation results with spongiofibrosis (5) Mundy reported a review article in 2011 and determined that 40% of urethral strictures were related with inflammation (4) Sciarra et al (6) used anti-inflammatory drugs to reduce urethral complications after TURP Based on the same mechanism, several medications including colchicine (16), mitomycin-c (7), triamcinolone (8), and corticosteroids (9), which all have anti-inflammatory effects, have been used to treat urethral strictures either systematically or locally Therefore, subclinical systemic inflammation may have impact on the outcomes of hypospadias repair Level of leukocyte and neutrophils, Neutrophil-to-Lymphocyte Ratio (NLR), Plateletto-Lymphocyte Ratio (PLR) and Mean Platelet Volume (MPV) are simple markers that can reflect the inflammation which can easily be obtained from CBC (18-21)
This study evaluated the predictive values of the WBC, neutrophils, NLR, PLR and MPV on the results of hypospadias repair The best of our knowledge, this study is the first study that evaluate the value or capacity of hematological parameters in predicting the complications
of hypospadias repair in children There are three studies t h a t e v a l u a t e d t h e i m p a c t o f these parameters in recurrence of urethral stricture after surgical treatment in adults (10, 11, 22) Topaktas et al (22) had reported 117 adult cases with urethral stricture who underwent urethroplasty and assessed the correlation between the systemic inflammation markers and recurrence rate of urethral stricture after surgery They determined that neutrophil, lymphocyte counts, or their ratio are not t h e p r e d i c t o r s f o r r e c u r r e n c e urethral stricture after urethroplasty
Urkmez et al (11) reported a study to determine the impact of these parameters in predicting the course of the urethral stricture and its recurrence in adults and they emphasized that by using NLR, inflammatory status of the urethral tissue can be revealed, and possible urethral stricture recurrence can be predicted


Gül et al (10) reported the value of hematologic parameters in predicting urethral stricture after transurethral resection of prostate and determined that PLR can be used to predict the urethral stricture Our results revealed that WBC value and neutrophil counts are related with complications after hypospadias repair (Figure 4) However, other parameters such as NLR, PLR, MLR, and MPV were not indicative of postoperative complications
Urkmez et al (11) reported that the cut-off value of NLR in detecting the recurrence after internal urethrotomy was 2 25 with a sensitivity of 70% and specificity of 67 7% Our study revealed that the cut off value of WBC to predict the complications was 9500 m/mm3 (AUC: 0 647, p = 0 006), the sensitivity was 56 8%, positive prediction was 36 2%, specificity was 70 6%, and negative prediction was 84 8% The neutrophil’s cut off value to predict the complications was 3000 m/mm3 (AUC: 0 629, p = 0 017), the sensitivity was 70 3%, positive prediction was 29 9%, specificity was 51 6%, and negative prediction was 85 5% The major limitation of our study is its retrospective design We did not analyze the penile lengths of the patients such as glans diameter, width of the plate and depth of the groove Although some studies suggested that these measurements have impact on the outcomes of the hypospadias repair (23-25), Bush and Snodgrass argue that there is no effect of these factors on postoperative complications (26) Single surgeon and single operative technique with exactly the same details such as penile block and tourniquet use, also not using caudal block and local epinephrine are the superiority of our study The considerable number of patients of this study is another superiority
CONCLUSIONS
WBC and neutrophil values were higher in pediatric patients with complications who underwent TIPU repair by single surgeon Other hematological parameters such
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 A Karagözlü Akgül, S Abidoglu, A Ceren Bakır, E Adalı, G Kıyan, H Tugtupe 462
Figure 4. Possibility graphics for WBC and neutrophil values
as NLR, PLR, MLR were not related with complications after hypospadias repair Our results revealed that postponing the hypospadias surgery may be more appropriate in patients with high blood WBC and neutrophil values
REFERENCES
1 Retik AB, Atala A Complications of hypospadias repair Urol Clin North Am 2002; 29:329-339
2 Dursun A, Ozsoylu S, Akyildiz BN Neutrophil-to-lymphocyte ratio and mean platelet volume can be useful markers to predict sepsis in children Pak J Med Sci 2018; 34:918-922
3 Chapman D, Kinnaird A, Rourke K Independent Predictors of Stricture Recurrence Following Urethroplasty for Isolated Bulbar Urethral Strictures J Urol 2017; 198:1107-1112
4 Mundy AR, Andrich DE Urethral strictures BJU International 2011; 107:6-26
5 Hampson LA, McAninch JW, Breyer BN Male urethral strictures and their management Nat Rev Urol 2014; 11:43-50
6 Sciarra A, Salciccia S, Albanesi L, et al Use of cyclooxygenase-2 inhibitor for prevention of urethral strictures secondary to transurethral resection of the prostate Urology 2005; 66:1218-1222
7 Mazdak H, Meshki I, Ghassami F Effect of Mitomycin C on Anterior Urethral Stricture Recurrence after Internal Urethrotomy Eur Urol 2007; 51:1089-1092
8 Tabassi KT, Yarmohamadi A, Mohammadi S Triamcinolone injection following internal urethrotomy for treatment of urethral stricture Urol J 2011; 8:132-136
9 Zhang K, Qi E, Zhang Y, et al Efficacy and safety of local steroids for urethra strictures: A systematic review and meta-analysis J Endourol 2014; 28:962-968
10 Gül M, Altıntas E, Kaynar M, et al The predictive value of platelet to lymphocyte and neutrophil to lymphocyte ratio in determining urethral stricture after transurethral resection of prostate Turk J Urol 2017; 43:325-329
11 Urkmez A, Topaktas R, Ozsoy E, et al Is neutrophil to lymphocyte ratio a predictive factor for recurrence of urethral stricture? Rev Assoc Med Bras 2019; 65:1448-1453
12 Bai R, Gao L, Jiang L, et al The Validity of Neutrophil/lymphocyte Ratio as A Predictive Factor for Systemic Inflammatory Response Syndrome after Flexible Ureteroscopy Lithotripsy Urol J 2022; 19:17-21
13 Faasse MA, Liu DB Early vs late-presenting urethroplasty complications after hypospadias repair: A retrospective analysis of patient follow-up J Pediatr Urol 2017; 13:354 e1-354 e5
14 Snodgrass W, Villanueva C, Bush NC Duration of follow-up to diagnose hypospadias urethroplasty complications J Pediatr Urol 2014; 10:208-211
15 Hadidi AT History of hypospadias: Lost in translation J Pediatr Surg 2017; 52:211-217
16 Urkmez A, Topaktas R, Ozsoy E, et al Is neutrophil to lymphocyte ratio a predictive factor for recurrence of urethral stricture? Rev Assoc Med Bras 2019; 65:1448-1453
17 Carney KJ, House J, Tillett J 38: Effects of Dviu and Colchicine Combination Therapy on Recurrent Anterior Urethral Strictures J Urol 2007; 177:14-14
18 Polat N, Yildiz A, Yuksel M, et al Association of neutrophil-lym-
phocyte ratio with the presence and severity of rheumatic mitral valve stenosis Clin Appl Thromb Hemost 2014; 20:793-8
19 Alkhouri N, Morris-stiff G, Campbell C, et al Neutrophil to lymphocyte ratio: a new marker for predicting steatohepatitis and fibrosis in patients with nonalcoholic fatty liver disease Liver Int 2012; 32:297-302
20 Raungkaewmanee S, Tangjitgamol S, Manusirivithaya S, et al Platelet to lymphocyte ratio as a prognostic factor for epithelial ovarian cancer J Gynecol Oncol 2012; 23:265-273
21 Kim EY, Lee JW, Yoo HM, et al The Platelet-to-Lymphocyte Ratio Versus Neutrophil-to-Lymphocyte Ratio: Which is Better as a Prognostic Factor in Gastric Cancer? Ann Surg Oncol 2015; 22:4363-4370
22 Topaktas R Hematologic parameters and Neutrophil/Lymphocyte ratio in the prediction of urethroplasty success Int Braz J Urol 2019; 45:369-375
23 Holland AJA, Smith GHH Effect of the depth and width of the urethral plate on tubularized incised plate urethroplasty J Urol 2000; 164:489-491
24 Tugtepe H, Thomas DT, Calikli Z, et al A new objective scoring system for the prediction of complications after hypospadias surgery In: 29th Congress of ESPU Abstract Book; 2018:96
25 Sarhan O, Saad M, Helmy T, et al Effect of Suturing Technique and Urethral Plate Characteristics on Complication Rate Following Hypospadias Repair: A Prospective Randomized Study J Urol 2009; 182:682-686
26 Bush NC, Snodgrass W Pre-incision urethral plate width does not impact short-term Tubularized Incised Plate urethroplasty outcomes J Pediatr Urol 2017; 13:625 e1-625 e6
Correspondence
Ahsen Karagözlü Akgül, MD (Corresponding Author) ahsenkaragozlu@yahoo com
Sadık Abidog˘ lu, MD s abidoglu@yahoo com
Marmara University, Pendik Education and Research Hospital, Department of Pediatric Surgery, Division of Pediatric Urology
Fevzi Çakmak, Muhsin Yazıcıog lu Cd No:10, 34899 Pendik, Istanbul (Turkey)
Ayten Ceren Bakır, MD aytenceren@gmail com
Fevzi Çakmak, Muhsin Yazıcıog lu Cd No:10, 34899 Pendik, Istanbul (Turkey)
Embiye Adalı, MD embiye mba@gmail com
Apartment 503, West Africa House, 25 Water Street, Liverpool, L2 0RG (United Kingdom)
Gürsu Kıyan, MD gursukiyan@gmail com
Fevzi Çakmak, Muhsin Yazıcıog lu Cd No:10, 34899 Pendik, Istanbul (Turkey)
Halil Tug tupe, MD htugtepe@yahoo com
Küçükbakkalköy Mah Is ¸ ıklar Cad, S¸enlik Sokag ı No:14/A, 34750 Atas ¸ehir/Istanbul (Turkey)
463 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 WBC/NLR predicting outcome of hypospadias
Testosterone deficiency in non-obese type 2 diabetic male patients
Summary
Background and aims: it is unclear whether male hypogonadism is ascribable to the diabetic state per se, or because of other factors, such as obesity or age. We aimed to investigate the prevalence and identify the predictors for testosterone deficiency among non-obese type 2 diabetic males.
Methods: This cross-sectional study was conducted on 95 nonobese type 2 diabetic males with BMI below 30. We evaluated the total testosterone (TT) levels to determine prevalence and risk factors of testosterone deficiency. Serum TT ≤ 300 ng/dl defined testosterone deficiency
Results: The prevalence of testosterone deficiency was 29 1% Testosterone deficient patients had statistically significantly higher visceral adiposity index (VAI), waist, and triglyceride in comparison with normal testosterone patients TT level correlated with VAI, waist, BMI, LH, and age VAI was the only significant predictor of TT levels even after adjustment for age and BMI in regression analysis Furthermore, VAI was a statistically significant risk factor for testosterone deficiency in binary logistic analysis
Conclusions: testosterone deficient non-obese type 2 diabetic male patients had elevated VAI, waist, and triglyceride
Moreover, elevated VAI was a risk factor for testosterone deficiency VAI could be an easily applicable and reliable index for the evaluation and prediction in type 2 non-obese diabetic males
KEY WORDS: Non-obese; T2DM; Visceral obesity; Testosterone; VAI; Males
Submitted 5 March 2022; Accepted 2 April 2022
INTRODUCTION
Diabetes mellitus (DM) is a major cause of health concern due to its increasing prevalence rate worldwide By the turn of the last decade, the International Diabetes Federation (IDF) estimated that 404 7 million people worldwide had type 2 diabetes mellitus (T2DM), with the total number of diabetic patients expected to rise to 679 7 million by 2045 (1) One complication of type 2 diabetes (T2DM) is hypothalamic-pituitary-testicular axis (HPT axis) dysfunction
The hallmark of HPT axis dysfunction is characterized by subnormal testosterone levels in association with non-elevated luteinizing hormone concentrations These abnormalities were not affected by the duration or severity of diabetes (2) Testosterone deficiency is associated with many
comorbidities such as chronic fatigue, loss of libido, erectile dysfunction, low haematocrit level, cardiovascular events, and decreased bone density (3)
Several studies consistently show significant relationships between serum testosterone and T2DM (4) Many studies reported that 25% to 50% of type 2 diabetic males have lowered testosterone levels (5) Hence, testosterone deficiency in T2DM has high clinical importance Although male hypogonadism (MHG) in T2DM has been investigated in many researches, the mechanism underlying the pathogenesis of testosterone deficiency in diabetes is still not fully understood yet (6) The majority of previous studies have assessed testosterone levels in elderly, obese males with T2DM (7)
On other hand, it is well established that obesity is a major risk factor for type 2 diabetes and cardiovascular disease (8) Several studies have linked male hypogonadism with being overweight or obese (9) Large population-based studies have confirmed that obesity is the single most important factor associated with low testosterone, overriding the effects of age and comorbidities (10) Therefore, it is unclear whether this is ascribable to the diabetic state per se, or because of other factors, such as obesity or age Hence, the role of the diabetic state in relation to the effects of obesity and comorbidities on testosterone levels in diabetic men is debatable (11) In this study, we tried to limit the confounding factor that affects the testosterone levels in diabetic males such as obesity Therefore, we aimed to investigate the prevalence and identify the predictors for testosterone deficiency among non-obese type 2 male diabetic patients
PATIENTS AND METHODS
Study population
This cross-sectional study was conducted at Mansoura University's Endocrinology, Diabetes, and Metabolism Unit, Specialized Medical Hospital, between March 2021 and A u g u s t 2 0 2 1 T h e M a n s o u r a
Institutional Research Board approved the study design All study participants provided written informed consent
We enrolled 95 patients aged 25 to 65 who had been diagnosed with T2DM using the American Diabetes Association's diabetes diagnosis criteria Inclusion criteria were set as follows: males with type 2
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 464
PAPER No conflict of interest declared
ORIGINAL
F a c u l t y o f M e d i c i n e ' s
Sherihan I. Gouda 1 , Mohamed M. Aboelnaga 1 , Ahmed M.G. Elbeltagy 2 , Amro Elbaz 1
1 Endocrinology and Diabetes Unit, Faculty of Medicine, Mansoura University, Mansoura, Egypt;
DOI: 10 4081/aiua 2022 4 464
2 Clinical Pathology Department, Faculty of Medicine, Mansoura University, Mansoura, Egypt
diabetes; body mass index below 30; history of normal pubertal development; a normal sense of smell for exclusion of Kallman syndrome; age between 18 and 65 In contrast, patients were excluded from this study in case of: female sex; abnormal renal function; abnormal albumin levels; diabetes with macro albuminuria; liver disorders; heart failure; usea of drugs that may affect testosterone levels, such as replacement therapy and anabolic steroids; patients with known causes of hypogonadism; history of malignancy; autoimmune diseases; diseases of the endocrine system other than Type 2 DM, including Type 1 DM, pituitary disorders, and abnormal thyroid functions All patients were divided into either a low testosterone group (TT ≤ 300 ng/dl) or a normal testosterone group (TT > 300 ng/dl)
Clinical assessment and anthropometric measurements
All subjects underwent a comprehensive medical evaluation including medical history with special emphasis on diabetes duration, medication, smoking history, and diabetic complications history; physical examination and measurement of anthropometric parameters The patient's height and weight were measured while they were dressed casually and were not wearing shoes BMI was calculated by dividing weight (kg) by height square (m2) Waist circumference (WC) was measured halfway between the inferior border of the last rib and the crest of the ilium at the end of expiration Following standard procedure, blood pressure was measured with a sphygmomanometer VAI was calculated for all participants using the following formula for males (12):
VAI: WC / [39:68 + (1 88 × BMI)] × TG/1:03 × 1:31/HDL
Biochemical parameters
After a 12-hour overnight fast, venous blood samples were collected from all patients between 8 A M and 10 A M including: complete blood count (CBC), fasting lipid profile that included triglycerides (TG), total cholesterol ( T C ) , l o w - d e n s i t y l i p o p r o t e i n ( L D L ) , a n d h i g h - d e n s i t y lipoprotein (HDL); serum creatinine; glycosylated haemoglobin (HbA1C); fasting blood sugar; albumin; luteinizing hormone (LH); serum total testosterone LDL-cholesterol was estimated according to the Friedewald formula (TC minus HDL-cholesterol minus TGs/5 in mg/dl) Visceral adiposity index (VAI) was calculated for women and men according to the formulas
Definition
Diabetes was defined as a fasting plasma glucose of 100 mg/dl or higher, HbA1c of 6 5% or higher, or a previous diagnosis of type 2 diabetes Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, current use of the antihypertensive drug Overweight was defined by a body mass index of at least 25 kg/m2 Testosterone deficiency was defined as serum TT less than 300 ng/dl that is the lower limit of the normal range according to the American urological association guidelines (13)
L H l e v e l a b o v e 9 4 I U / L w a s d e fi n e d a s h y p e r gonadotropic hypogonadism, while LH levels below 9 4 IU/L were defined as hypogonadotropic hypogonadism (14)
Statistical analysis
The Statistical Package for the Social Sciences (SPSS), Version 23 was used to analyze the statistical data Continuous variables were presented as the mean ±standard deviation, and categorical variables were expressed as a proportion (%) whereas non-normally distributed data are expressed as the median (interquartile range) Differences between groups of patients were compared by the Mann-Whitney U or Student T-test for continuous variables and the Chi-square test for categorical variables The relationship between testosterone (the dependent variable) and other statistically significant correlated parameters in Pearson correlation (the independent variables) was investigated using linear regression The risk factors associated with Testosterone deficiency were assessed using binary logistic regression, and the odds ratio (OR) and 95 per cent confidence interval (CI) were calculated P values less than 0 05 were considered statistically significant
RESULTS
We enrolled ninety-six non-obese patients with type 2 DM in this cross-sectional study Among those diabetic patients, 27 (28 4%) were of normal weight, while 68 (71 6%) were overweight Their age ranged between 34 and 65 years We observed that the prevalence of testosterone deficiency was 29 1% (28 patients) We observed high abnormal level of LH in 14 patients with low testosterone levels The prevalence of hypergonadotropic hypogonadism was 50% of testosterone deficient patients Other clinical, anthropometric, and laboratory details of the patient were presented in Table 1
Data expressed as mean ( nterquarti e range) according norma ity of distribut on, Data expressed as mean ± standard deviation or Data expressed in parenthes s are percentage BM: Body mass ndex; WC: Waist circumference; SBP: Systol c b ood pressure; DBP: Diastolic blood pressure;
Low-dens ty ipoprote n; HDL: H gh-dens ty l poprote n; uACR: Urinary album n creat nine rat o;
Glycated hemog ob n; LH: ute nizing hormone; VA : V scera adiposity index
465 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Testosterone
deficiency in non-obese type 2 diabetic male patients
Table 1 General characteristics of the study population N = 96 Age (year) 51 41 ± 7 17 Diabetic duration(year) 9 59 ± 4 18 Smoker ratio 66 (47 1% ) Insulin therapy 52 (37 1% ) Body weight (kg) 86 69 ± 7 96 Height (m) 1 78 ± 058 BMI (Kg/m2) 28 245 (3 05) Waist circumference(cm) 99 48 ± 9 68 Systolic BP (mmHg) 135 00 (15) Diastolic BP (mmHg) 85 00 (15) Total cholesterol mg/dl 248 54 ± 43 29 LDL-C mg/dl 155 88 ± 47 98 HDL-C mg/dl 43 83 ± 6 85 Triglycerides mg/dl 244 14±74
UACR mg/gm 28 (62) Retinopathy 29 (30 2% ) Hba1c % 8 5 ± 1 613 Total testosterone ng/dl 405 71 ± 133 78 Testosterone deficiency 28 (29 1%) LH mIU/L 7 44 ± 2 67 VAI 3 25 (1 58)
48
LDL:
Hba1c:
Data are presented as the mean ± SD median (IQ range) or the number of patients in each group with percentages BM: Body mass ndex; WC: Wa st circumference; SBP: Systol c b ood pressure; DBP: Diasto ic blood pressure;
LDL: Low-dens ty l poprote n; HDL: H gh-density l poprotein; TG: Tr g ycer de;; Hba1c: Glycated hemog obin;
LH: Lutein zing hormone; uACR: Ur nary albumin creatinine rat o; VAI: Visceral ad pos ty ndex
In the comparison between 28 patients in the low testosterone group (TT ≤ 300 ng/dl) and 68 patients in the normal testosterone group (TT > 300 ng/dl), we found that the low testosterone group had a statistically significant higher mean or median of VAI, WC, and triglyceride in comparison with normal testosterone group Moreover, a higher percentage of patients complicated with retinopathy was observed in low testosterone groups Other differences between the two groups were shown in Table 2 According to Pearson correlations, TT was negatively correlated with VAI (log), WC, BMI (log), and LH On the other hand, TT was positively correlated to age However, TT was not correlated with duration of diabetes, Hba1c, or lipid parameters We conducted a regression analysis to determine predictors of total testosterone levels as the dependent variable and age, BMI (log), LH, and VAI (log) as the independent variables in our study patients We observed that VAI was the only significant predictor of TT
Table 3.
Pearson correlation and stepwise multiple regression analysis between total testosterone levels with other statistically significant correlated independent factor
levels (p-value = 0 41) Furthermore, VAI was a statistically significant predictor of TT levels even after adjustment for age and BMI as shown in Tables 3, 4
Table
Association between total testosterone levels and other statistically significant correlated independent factors in regression analysis after adjustment for BMI and age
Model 1 adjusted for age and mode 2 ad usted for BMI and age BM: Body mass index; WC: Waist c rcumference; LH: Luteiniz ng hormone;
Visceral adiposity ndex
The binary logistic regression was performed with hypogonadism as the dependent variable and age, overweight (defined by BMI more than 30), WC, LH, retinopathy, and VAI (log) as the independent variables We observed that the Visceral adiposity index was a statistically significant risk factor for testosterone deficiency among nonobese type 2 diabetic males (p-value = 0 46) More data are available in Table 5
DISCUSSION
Despite the high prevalence of male hypogonadism in type 2 diabetic, regardless of diabetic control status, the underlying mechanisms of hypogonadism pathogenesis in type 2 diabetes mellitus have not been fully clarified yet (15) In the same consent, the contribution of the diabetic status or hyperglycaemia on androgen levels in males is still debated The strong association between type 2 diabetes with obesity, insulin resistance status, and aging may be the significant contributory factor in testosterone deficiency in type 2 DM patients rather than diabetes itself (16)
The main result in this cross-sectional study is that visceral adiposity functional activity evaluated by VAI is the main risk factor in type 2 diabetic males with BMI below 30 Moreover, VAI was the only predictor for testosterone levels in non-obese type 2 diabetic males even after adjustment for age and BMI,
levels
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 S I Gouda, M M Aboelnaga, A M G Elbeltagy, A Elbaz 466
although testosterone
Table 2. Comparison of clinical and laboratory characteristics of male type 2 DM patients with TT > 300 VS ng/dl those with TT ≤ 300 ng/dl TT > 300 ng/dl (n = 68) TT ≤ 300 ng/dl (n = 28) P value Age (year) 52 1 ± 7 29 49 71 ± 6 69 0 139 DM duration (year) 9 34 ± 4 27 10 21 ± 3 98 0 354 Smoker ratio 30 (44 1%) 11 (39 2%) 0 821 Height (m) 1 78 ± 06 1 7675 ± 05 0 290 Body weight (kg) 86 54 ± 8 39 87 04 ± 6 96 0 785 BMI (Kg/m2) 27 75 (3 44) 28 73 (2 13) 0 197 WC (cm) 98 24 ± 9 35 102 50 ± 9 95 0 049 Systolic BP (mmHg) 135 00 (15) 137 50 (14) 0 218 Diastolic BP (mmHg) 85 (15) 85 (13) 0 09 microalbumiric 24 (35 5%) 12 (42 8%) 0 497 Retinopathy ratio 16 (23 5%) 13 (46 4%) 0 049 TV mg/dl 249 96 ± 41 94 245 11 ± 47 02 0 620 LDL-c mg/dl 158 51 ± 45 48 149 49 ± 53 93 0 405 HDL-c mg/dl 44 56 ± 7 53 42 07 ± 4 44 0106 TG mg/dl 234 43 ± 76 267 71 ± 66 14 0 046 Hba1c % 8 36 ± 1 53 8 93 ± 1 7 0 111 LH mIU/L 7 2 ± 1 85 8 02 ± 4 01 0 173 UACR mg/gm 28 (62 53) 28 (74) 0 812 VAI 3 03 (1 54) 3 86 (1 77) 0 006
r P value B β P value Age 218 033 2 723 146 145 Log BMI 213 037 25 488 040 760 WC -.255 .012 -1.723 -.125 .352 LH - 222 030 -8 630 - 172 082 Log VAI - 278 006 -164 284 - 208 041 BM: Body mass index; WC: Waist circumference; LH: Luteinizing hormone; VAI: Visceral ad pos ty ndex
4
Model 1 Model 2 B β P value B β P value Age 2 723 146 145 2 721 146 147 WC -1 723 - 125 352 -1 638 118 397 BMI (log) 25 488 - 208 760 4 984 008 974 LH -8 630 - 172 082 -8 654 - 173 083 VAI (log) -164 284 040 041 -165 076 - 209 041
VAI:
Table 5
C.I.
Lower Upper Age - 046 037 1 563 218 956 891 1 027 Overweight - 802 878 834 367 2 373 363 15 536 Waist 045 033 1 891 207 344 066 1 806 Log VAI 3 629 1 629 4 965 046 1 436 1 007 2 048 Retinopathy -1 138 514 4 901 060 382 140 1 043 LH .049 0.84 .308 .579 1.050 .883 1.249 B:
interval; WC, waist circumference; VAI:
LH:
hormone
Logistic regression analysis for risk factor of testosterone deficiency.
B S.E Wald P value OR 95%
for Odds ratio
Estimated coefficient; S E: Standard error; CI: Confidence
Visceral adiposity ndex;
Lute nizing
in our study correlated with anthropometric parameters such as BMI and waist circumference VAI as a index for visceral fat dysfunction is more reliable than other obesity parameters in predicting testosterone deficiency Low TT levels were strongly associated with increased VAI in our cross-sectional study regardless of age, or diabetes status control
Although many studies evaluated hypogonadism in diabetic patients, only a few studies evaluated obesity by VAI A recent population-based study among diabetic and nondiabetic observed that VAI was the best predictor of male hypogonadism among different obesity indices (17, 18)
Likewise, VAI is more reliable than other metabolic or anthropometric parameters in the evaluation of visceral adiposity effect on erectile dysfunction (19, 20)
In this cross-sectional study, the prevalence of testosterone deficiency was 29 1 per cent This prevalence of testosterone deficiency in type 2 diabetic males was lower than that reported in previous studies in Egypt (21) and the Middle East region (22) The difference is expected by t h e s e l e c t i o n o f o u r p a t i e n t s w i t h B M I b e l o w 3 0 Surprisingly, we have a high prevalence of hypergonadotropic hypogonadism We observed high abnormal level of LH in 14 patients (50%) with low testosterone levels In our study, we observed that other obesity parameters such as BMI or waist diameters correlated with testosterone levels in Pearson correlation However, BMI and WC were not a significant predictor for testosterone levels in regression analysis Several studies consistently reported a negative impact for obesity on testosterone levels (18, 19, 23) These results in non-obese type 2 diabetic male patients could point to the role of abdominal obesity in the pathogenesis of male hypogonadism in T2DM The results in this study may indicate that adipose fat function may be important than fat mass In this study, age correlated with testosterone levels This result was in concordance with many previous studies that observed decreased levels of testosterone with aging in diabetic patients (11, 24, 25) and the general population (26) However few studies did not observe this link in type 2 diabetic patients (27, 28)
In this study, we observed significantly higher triglyceride levels in testosterone deficient diabetics However, HDLc levels were insignificantly different between the two groups This may be attributed to the effect of patients’ selection and lifestyle such as exercise and diet that could affect HDL levels Many studies linked hypogonadism and dyslipidaemia (21, 22, 27) Moreover, cont r o l l e d t r i a l s o n t e s t o s t e r o n e r e p l a c e m e n t o b s e r v e d favourable effects for testosterone on lipid profile in diabetics (29) However, the effect of dyslipidaemias on testosterone levels is still unexplored VAI includes anthropometric and metabolic parameters as TG or HDLc Hence, the correlation between testosterone and TG or HDL-c cannot be excluded
Surprisingly, testosterone deficiency was not related to diabetic status Testosterone deficiency in this study did not correlate with glycated haemoglobin or the duration of diabetes These results are in agreement with many studies in diabetics in general (28) However, our findings contradict another large study which correlated testosterone levels with diabetic status control (30)
In this study, we found that non-obese diabetics with testosterone deficiency had higher significant retinopathy prevalence However, we found non-significant different urinary albumin excretion between both groups The effect of nephropathy was not assessed in this study as we excluded macro-albuminuria patients Micro-vascular complications were reported in many studies to correlate with low testosterone levels in males (21, 22, 31)
Although the pathophysiological mechanism of testosterone deficiency in Type 2 DM is still not fully revealed, few mechanisms have been hypothesized The role of inflammatory mediators such as tumour necrosis factoralpha and Interleukin-1 beta was postulated Obesity is considered as a state of chronic inflammation (33) These mediators have been reported to suppress hypothalamic gonadotropin-releasing hormone (GnRH) at the hypothalamic level (34) Insulin resistance is another mechanism that could be involved in hypogonadism pathogenesis Insulin resistance and brain insulin resistance, which was defined as impaired insulin action in the neuron (34) Normal insulin response is required for the HPG axis's functional integrity to be maintained (35) According to one study, hyperinsulinemia caused by neuronal insulin receptor knockout can result in a 60-90% decrease in LH concentrations (33) Another mechanism could be related to adipokines such as leptin and adiponectin which have been reported to have a permissive role in the regulation of the hypothalamic-pituitary-gonadal (HPG) axis
Leptin resistance in the hypothalamus or other neurons may play a role in the pathogenesis of hypogonadism seen in obesity, insulin resistance, and T2DM (29) Furthermore, leptin directly suppresses the stimulatory action of gonadotropins on the testicular Leydig cells, r e d u c i n g t e s t o s t e r o n e f o r m a t i o n ( 2 8 ) F u r t h e r m o r e , testosterone has a direct correlation with circulating adiponectin (36) Finally, the aromatase enzyme converts testosterone to oestrogen in adipose tissue, resulting in hypothalamic-pituitary-gonadal axis inhibition and subsequent hypogonadism (37)
In the light of those postulated mechanisms for male hypogonadism in diabetic patients, VAI could be a valuable index for predicting male hypogonadism and is linked with these postulated mechanisms VAI by involvi n g t h e m e t a b o l i c p a r a m e t e r s c o u l d r e fl e c t c h r o n i c i n fl a m m a t o r y s t a t u s D e c r e a s e s i n s e r u m H D L a n d increases in triglycerides were reported to be linked with inflammatory status and mediators (38) Likewise, VAI was reported to be strongly correlated with insulin resistance estimated by HOMA-IR and metabolic syndrome (39, 40) Furthermore, among the most commonly used adiposity assessment indices, VAI has the strongest correlation with the most well-known adipocytokines in diabetic patients (41) and non-diabetic (42) Finally, a population-based study observed that VAI correlates with estradiol levels in males which reflect aromatase enzyme activity (43) Hence, the VAI value could better reveal the effects of WC, BMI, HDL, and TG on testosterone levels
This cross-sectional study cannot inform whether low testosterone is the cause or the result of visceral obesity Current evidence, however, suggests that this relations h i p i s b i d i r e c t i o n a l ( 1 1 ) A t w o - w a y r e l a t i o n s h i p between low testosterone levels and abdominal obesity
467 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Testosterone deficiency in non-obese type 2 diabetic male patients
was reported (44) Weight loss could increase testosterone levels, indicating that testosterone deficiency is functional (45) Weight loss bariatric surgery-induced resulted in a significant increase in Testosterone levels (46) In contrast, lower testosterone level after androgen deprivation therapy is associated with weight gain (45)
In our study, a higher prevalence of hypergonadtropic hypogonadism could point to an increased risk of T2DM with testosterone deficiency
This study is not devoid of some limitations, firstly the cross-sectional design The second limitation was the relatively small case number that might limit the power to detect a difference Thirdly, because free testosterone levels can reflect the extent of testosterone's biological activities, free testosterone concentration should be used to assess hypogonadism However, free testosterone determination is difficult, so free testosterone is frequently calculated with a formula in practical activity Finally, this study is a single-centre study in a tertiary hospital
Therefore, patient selection bias might exist
This research highlights the value of an easily applicable tool such as the visceral adiposity index in predicting testosterone deficiency in non-obese diabetics VAI could be more reliable than other parameters in predicting testosterone deficiency in diabetics
In conclusion, the elevated VAI index is associated with higher risks of testosterone deficiency in non-obese diabetic males VAI is an easily applicable reliable index for the prediction of male hypogonadism in non-obese type 2 diabetic male patients
REFERENCES
1 Hassan M, Hatata EZ, Al-Arman M, Aboelnaga MM Urinary cystatin C as a biomarker of early renal dysfunction in type 2 diabetic patients Diabetes Metab Syndr 2021; 15:102152
2 Gianatti EJ, Grossmann M Testosterone deficiency in men with Type 2 diabetes: pathophysiology and treatment Diabet Med 2020; 37:174-186
3 Anupam B, Shivaprasad C, Vijaya S, et al Prevalence of hypogonadism in patients with type 2 diabetes mellitus among the Indian population Diabetes Metab Syndr 2020; 14:1299-1304
4 Gianatti EJ, Grossmann M Testosterone deficiency in men with Type 2 diabetes: pathophysiology and treatment Diabet Med 2020; 37:174-186
5 Castellano-Castillo D, Royo JL, Martínez-Escribano A, et al Effects of SHBG rs1799941 polymorphism on free testosterone levels and hypogonadism risk in young non-diabetic obese males J Clin Med 2019; 8:1136
6 Gianatti EJ, Grossmann M Testosterone deficiency in men with Type 2 diabetes: pathophysiology and treatment Diabet Med 2020; 37:174-186
7 Grossmann M Low testosterone in men with type 2 diabetes: significance and treatment J Clin Endocrinol Metab 2011; 96:23412353
8 Mozafar Saadati H, Sabour S, Mansournia MA, et al Effect modification of general and central obesity by sex and age on cardiovascular outcomes: Targeted maximum likelihood estimation in the atherosclerosis risk in communities study Diabetes Metab Syndr 2021; 15:479-485
9 Fernandez CJ, Chacko EC, Pappachan JM Male obesity-related secondary hypogonadism - Pathophysiology, clinical implications and management Eur Endocrinol 2019; 15:83-90
10 Lee DM, O'Neill TW, Pye SR, et al The European Male Ageing Study (EMAS): design, methods and recruitment Int J Androl 2009; 32:11-24
11 Ng Tang Fui M, Hoermann R, et al Obesity and age as dominant correlates of low testosterone in men irrespective of diabetes status Andrology 2013; 1:906-912
12 Amato MC, Giordano C, Galia M, et al Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk Diabetes Care 2010; 33:920-922
13 Bhasin S, Cunningham GR, Hayes FJ, et al Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline J Clin Endocrinol Metab 2010; 95:25362559 (erratum in J Clin Endocrinol Metab 2021; 106:e2848)
14 Tajar A, Forti G, O'Neill TW, et al Characteristics of secondary, primary, and compensated hypogonadism in aging men: evidence from the European Male Ageing Study J Clin Endocrinol Metab 2010; 95:1810-8
15 Ganesh HK, Vijaya Sarathi HA, George J, et al Prevalence of hypogonadism in patients with type 2 diabetes mellitus in an Asian Indian study group Endocr Pract 2009; 15:513-520
16 Al-Goblan AS, Al-Alfi MA, Khan MZ Mechanism linking diabetes mellitus and obesity Diabetes Metab Syndr Obes 2014; 7:587-591
17 Turan E, Öztekin Ü Relationship between visceral adiposity index and male infertility Andrologia 2020; 52:e13548
18 Haymana C, Sonmez A, Aydogdu A, et al Visceral adiposity index and triglyceride/high-density lipoprotein cholesterol ratio in hypogonadism Arch Endocrinol Metab 2017; 61:282-287
19 Akdemir AO, Karabakan M, Aktas BK, et al Visceral adiposity index is useful for evaluating obesity effect on erectile dysfunction Andrologia 2019; 51:e13282
20 Dursun M, Besiroglu H, Cakir SS, et al Increased visceral adiposity index associated with sexual dysfunction in men Aging Male 2018; 21:187-192
21 Ghazi S, Zohdy W, Elkhiat Y, Shamloul R Serum testosterone levels in diabetic men with and without erectile dysfunction Andrologia 2012; 44:373-380
22 Al Hayek AA, Khader YS, Jafal S, et al Prevalence of low testosterone levels in men with type 2 diabetes mellitus: a cross-sectional study J Family Community Med 2013; 20:179-186
23 Fui MN, Dupuis P, Grossmann M Lowered testosterone in male obesity: mechanisms, morbidity and management Asian J Androl 2014; 16:223-231
24 Anupam B, Shivaprasad C, Vijaya S, et al Prevalence of hypogonadism in patients with type 2 diabetes mellitus among the Indian population Diabetes Metab Syndr 2020; 14:1299-1304
25 Tajar A, Forti G, O'Neill TW, et al Characteristics of secondary, primary, and compensated hypogonadism in aging men: evidence from the European Male Ageing Study J Clin Endocrinol Metab 2010; 95:1810-1818
26 Zheng R, Cao L, Cao W, et al Risk factors for hypogonadism in
2016:5162167
27 Zheng R, Cao L, Cao W, et al Risk factors for hypogonadism in
2016:5162167
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 S I Gouda, M M Aboelnaga, A M
A
468
G Elbeltagy,
Elbaz
m a l e p a t i e n t s w i t h t y p e 2 d i a b e t e s J D i a b e t e s R e s 2 0 1 6 ;
a l e p a t i e n t s w i t h t y p e 2 d i a b e t e s J D i a b e t e s R e s 2 0 1 6 ;
m
28 Cai X, Tian Y, Wu T, et al Metabolic effects of testosterone replacement therapy on hypogonadal men with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials Asian J Androl 2014; 16:146-152
29 Fukui M, Tanaka M, Hasegawa G, et al Association between serum bioavailable testosterone concentration and the ratio of glycated albumin to glycated hemoglobin in men with type 2 diabetes Diabetes Care 2008; 31:397-401
30 Šimoniene D, Platukiene A, Prakapiene E, et al Insulin resistance in type 1 diabetes mellitus and its association with patient's micro- and macrovascular complications, sex hormones, and other clinical data Diabetes Ther 2020; 11:161-174
31 Blaya R, Blaya P, Rhoden L, Rhoden EL Low testosterone levels and metabolic syndrome in aging male Curr Pharm Des 2017; 23:4470-4474
32 Dandona P, Dhindsa S Update: Hypogonadotropic hypogonadism in type 2 diabetes and obesity J Clin Endocrinol Metab 2011; 96:2643-2651
33 Watanobe H, Hayakawa Y Hypothalamic interleukin-1 beta and tumor necrosis factor-alpha, but not interleukin-6, mediate the endot o x i n - i n d u c e d s u p p r e s s i o n o f t h e r e p r o d u c t i v e a x i s i n r a t s Endocrinology 2003; 144:4868-4875
34 Brüning JC, Gautam D, Burks DJ, et al Role of brain insulin receptor in control of body weight and reproduction Science 2000; 289:2122-2125
35 Elsaied MA, Masallat D, Abdel-Hamid IA Correlation of adiponectin with testosterone in patients with and without type 2 diab e t e s a n d e r e c t i l e d y s f u n c t i o n A m J M e n s H e a l t h 2 0 1 9 ; 13:1557988318807049
36 C Langer, B Gansz, C Goepfert et al Testosterone up-regulates s c a v e n g e r r e c e p t o r B I a n d s t i m u l a t e s c h o l e s t e r o l e f fl u x f r o m m a c r o p h a g e s B i o c h e m i c a l a n d B i o p h y s i c a l R e s e a r c h
Communications 2002; 296:1051-1057
37 Feingold KR, Grunfeld C The effect of inflammation and infec-
tion on lipids and lipoproteins In: Feingold KR, Anawalt B, Boyce A, et al , eds Endotext South Dartmouth (MA): MDText com, Inc ; January 8, 2019
38 Ji B, Qu H, Wang H, et al Association between the visceral adiposity index and homeostatic model assessment of insulin resistance in participants with normal waist circumference Angiology 2017; 68:716-721
39 Štepánek L, Horáková D, Cibicková L, et al Can visceral adiposity index serve as a simple tool for identifying individuals with insulin resistance in daily clinical practice? Medicina (Kaunas) 2019; 55:545
40 Amato MC, Pizzolanti G, Torregrossa V, et al Visceral adiposity index (VAI) is predictive of an altered adipokine profile in patients with type 2 diabetes PLoS One 2014; 9:e91969
41 Al-Daghri NM, Al-Attas OS, Alokail MS, et al Visceral adiposity index is highly associated with adiponectin values and glycaemic disturbances Eur J Clin Invest 2013; 43:183-189
42 Wang N, Zhai H, Han B, et al Visceral fat dysfunction is positively associated with hypogonadism in Chinese men Sci Rep 2016; 6:19844
43 Blaya R, Blaya P, Rhoden L, Rhoden EL Low testosterone levels and metabolic syndrome in aging male Curr Pharm Des 2017; 23:4470-4474
44 Grossmann M, Hamilton EJ, Gilfillan C, et al Bone and metabolic health in patients with non-metastatic prostate cancer who are receiving androgen deprivation therapy Med J Aust 2011; 194:301306
45 Pekgor S, Duran C, Berberoglu U, Eryilmaz MA The role of visceral adiposity index levels in predicting the presence of metabolic syndrome and insulin resistance in overweight and obese patients Metab Syndr Relat Disord 2019; 17:296-302
46 Aboelnaga EM, Aboelnaga MM, Elkalla HM Metformin addition to androgen deprivation therapy effect on cancer prostate patients with type 2 diabetes Diabetes Metab Syndr 2021; 15:102251
Correspondence
Sherihan I Gouda, MD
Endocrinology and Diabetes Unit, Faculty of Medicine, Mansoura University, Mansoura (Egypt)
Mohamed Mosaad Aboelnaga, MD (Corresponding Author) dr mhd endocrine@gmail com
Endocrinology and Diabetes Unit, Faculty of Medicine, Mansoura University, 2 El Gomhouria Street, Zip code: 35516, Mansoura (Egypt)
Ahmed MG Elbeltagy, MD
Clinical Pathology Department, Faculty of Medicine, Mansoura University, Mansoura (Egypt)
Amro Elbaz, MD
Endocrinology and Diabetes Unit, Faculty of Medicine, Mansoura University, Mansoura (Egypt)
469 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Testosterone
deficiency in non-obese type 2 diabetic male patients
Male infertility, what Mobile Health Applications “know”: quality analysis and adherence to European Association of Urology Guidelines
Giovanni Maria Fusco 1 , Luigi Cirillo 1 , Marco Abate 1 , Simone Morra 1 , Vincenzo Morgera 1 , Biagio Barone 1 , Felice Crocetto 1 , Gianluigi Cacace 1 , Francesco Di Bello 1 , Lorenzo Spirito 2 , Celeste Manfredi 2 , Davide Arcaniolo 2 , Alessandro Palmieri 1 , Ciro Imbimbo 1 , Vincenzo Mirone 1 , Luigi Napolitano 1
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples "Federico II", Naples, Italy;
2 Urology Unit, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli", Naples, Italy
Summary
Introduction: Male infertility (MI) is one of the most important worrying topics for the fertile age population. Nowadays, several mobile health applications (MHAs) have been developed to help and assist patients suffering from male infertility (MI), but their quality and adherence to the guidelines is not solved issue yet
Materials and methods: On 2nd July 2022, an observational cross-sectional descriptive study of all MHAs on male infertility was conducted: a search on both the iTunes App Store and Google Play Store was performed Our group reviewed all MHAs, evaluating the quality, using Mobile Application Rating Scale (MARS), and the adherence to European Association of Urology guidelines, with a special tool created for this manuscript
Results: In the final analysis we included 10 MHAs: 20% (n = 2) from the iTunes App Store and 80% (n = 8) from the Google Play Store. Across the sample, 80% (n = 8) of the apps provided general information on MI, 60% (n = 6) focused on diagnosis and 50% (n = 5) focused on treatment options, respectively
According to MARS tool, the mean score was 2 18 (0 78), 3 78 (0 36), 3 0 (0 53), 3 19 (0 45), 2 18 (0 54) for Engagement, Functionality, Aesthetic, Information and Subjective quality, respectively According to EAU Adherence Score, the highest score was reported by “Infertilità” with 12/15 points while the lowest score was reported by “Fertility Diet Guide”, 0/15 points
Conclusions: Nowadays, MHAs present in the market are not a reliable source of information on MI An ideal MHAs should be based on scientific evidence, user friendly, respecting privacy and security laws, making patients feel capable and confident to change personal behavior or attitudes.
KEY WORDS: Keywords: App; Male infertility; E-health; Mobile phone; MARS
Submitted 6 September 2022; Accepted 24 September 2022
INTRODUCTION
In recent years new technologies, such as Internet, social media telemedicine, and mobile health (mHealth) have rapidly grown, particularly during SARS COV 2 pandemic outbreak (1-7), supporting patients in several medical
and surgical fields and increasing medication adherence and self-management of diseases
The World Health Organization has defined mHealth as “a medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants, and other wireless devices” (8) Nowadays, the global usage of smartphones stands at 3 5 billion (9) An increasing number of mobile health applications (MHAs) are available for download through the iTunes App Store and Google Play Store (10)
Male infertility (MI) is defined as the inability of a male to make a fertile female pregnant, also for a minimum of at least one year of unprotected intercourse Male factor contributes about 50% of all cases of infertility (11, 12) Contemporary data suggests that there has been a decline in global fertility rates from 4 7 to 2 4 live births between 1950 and 2017 (13, 14) Several reasons were recognized as causes of impaired sperm parameters, among the main ones, varicoceles (15), hypogonadism (16), and genetic disorders (17) Treatment can be divided in medical and surgical treatment (Lifestyle modifications (18), antioxidant therapy (19, 20), hormone stimulation therapy (21, 22) TESE and other surgical approaches (23)
MHAs development has not regulated, and several apps, currently available (10) in several fields, including andrological, are characterized by poor-quality The most important evaluation criteria are the number of downloads and the user ratings (24) Due to this searching for high-quality information is still more difficult Mobile Application Rating Scale (MARS), represents the most widely used and recommended tool providing quantitative, and validated evaluation of MHAs (25, 26) Several studies reported data about MHAs evaluation and adherence to guidelines in different medical and surgical setting (27-30)
To the best of our knowledge, no previous studies analyzed the quality of MHAs for MI and their adherence to guidelines Our current project aims to provide an overview of MHAs, available on the market, developed for MI analyzing quality through the MARS and their adherence to European Association of Urology (EAU) guidelines
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 470 ORIGINAL PAPER No conflict of interest declared
DOI: 10 4081/aiua 2022 4 470
MATERIALS AND METHODS
Search strategy
On 2nd July 2022, an observational cross-sectional descriptive study of all MHAs on MI was conducted A search on both the iTunes App Store and Google Play Store was performed using an IPhone 13 and a Samsung s10, respectively “Male infertility” AND/OR “diagnosis” , AND/OR “treatment” were the keywords used for search tab These keywords were used according to the search strategy of Google Play Store and iTunes App Store, which is based on finding keywords in titles, app descriptions and tags We excluded information available in books, and in other formats
Two authors (GC, VM) screened separately in iTunes App Store and Google Play Store apps during the search by reading the title and description in the app store One reviewer conducted a search in the iTunes App Store, and the other in the Google Play Store
Reviewers created an Excel form to report all MHAs and in the second time they were screened according to the exclusion criteria They included in the present studies all MHAs regarding MI, providing a service to patients, in English, and free to download MHAs not specifically focused on MI, not allowing access to all users and those not available in English were excluded

On 4th July 2022 reviewers downloaded and installed the
apps on their personal mobile devices They interacted for thirty minutes with each app to explore its features before completing the MARS and then they evaluated adherence to EAU guidelines In case of MHAs present in both stores, only the iTunes App Store version was analyzed A total of 35 apps were found by our search, 30 (85 7%) of them were from the Google Play Store (Android) and 5 (14 3%) of them were from the iTunes App Store Of all the MHAs, 17 were excluded: present in both stores (n=1), not in English (n = 3) and off-topic (n = 13) Only 18 MHAs were eligible for the final evaluation and were downloaded Finally, 10 MHAs were included in the final review after removing 8 MHAs that met exclusion criteria after download The search strategy was performed according to PRISMA statement (Figure 1) MHAs characteristics were reported in the Table 1
Assessment of app quality
Mobile Application Rating Scale (MARS) was used to assess the quality of MHAs MARS is a multidimensional instrument of 23 structured questions evaluating different domains: engagement, functionality, esthetics, information, app subjective quality, and app-specific, showing a very acceptable reliability and validity Engagement (interest, customizability, interactivity), Functionality (performance, ease of use, navigation), Aesthetics (layout, graphics, visual appeal) and Information (accuracy of a p p , c r e d i b i l i t y , e v i d e n c e b a s e ) S u b j e c t i v e ( r e c o mm e n d a b l e , w o r t h b u y i n g ) and 1 category of subjective quality Each category score is the mean of the different items, rated on a 5-point Likert-type scale (from 1 = inadequate to 5 = excellent) w i t h i n i t s c a t e g o r y T h e mean of the 4 app quality category scores is used to c a l c u l a t e o v e r a l l q u a l i t y s c o r e a n d t h e fi n a l s c o r e range from 0 to 5 A score of between 1 and 2/5 is considered as ‘ poor ’ quality, while 3/5 is ‘acceptable’ and at least 4/5 is ‘good’ quality If scores differed by a single point, reviewers use the mean of t h e t w o r a t i n g s , w h i l e i f scores differed by more than a s i n g l e p o i n t , r e v i e w e r s s o l v e t h e d i s c r e p a n c y through discussion and cons e n s u s a g r e e m e n t M e a n scores were calculated for each domain and an overall quality score was calculated b a s e d o n t h e a g g r e g a t e d mean values for each of the f o u r d o m a i n s T h e m e a n score for subjective quality is calculated
471 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Male infertility and mobile health applications
Figure 1.
Table 1.
General characteristics of applications
Assessment of app adherence to EAU guidelines
Based on the EAU guidelines 2022 on Sexual and Reproductive Health, an adherence checklist of five items (definition, physiopathology, diagnosis, risk factors and treatment) according to the sections (9) Two independent reviewers (VM, and CF, urologists with high experience in MI) analyzed separately apps for their adherence to EAU guidelines According to criteria used in similar studies, raters gave each app a score from 0 to 3 for each of the five items A score of ‘‘0’’ indicated no adherence to guidelines A score of ‘‘1’’ indicated a weak adherence A score of ‘‘2’’ indicated a partial or moderate adherence A score of ‘‘3’’ indicated strong adherence Where coding scores differed by 1 point, the average of the two ratings was taken If there was a greater than 1-point discrepancy, a third author reviewed apps and resolved the discrepancy
The possible score on the checklist ranged from 0 to 15 for each app To facilitate evaluation, adherence to the checklist was arbitrarily considered low with a total score ranging from 0 to 5, medium (6-10), and high (11-15)
Statistical analysis
Google Play Store Across the sample, 80% (n = 8) of the apps provided general information on MI, 60% (n = 6) focused on diagnosis and 50% (n = 5) focused on treatment options, respectively Risks factors were reported in 50% (n = 5) MHAs Information of downloads were available for 80% (n = 8) MHAs out of the 10 reviewed Downloads were not reported in MHAs downloaded by iTunes Apple Store All the apps were planned to be used by patients No information about MHAs rating was available MARS scores are represented in Table 2
Engagement
The score in this section was based on a 5-point Likert scale in 5 subscales (Entertainment, Interest, Customization, Interactivity and Target-group) The mean score was 2 18 (0 78) The “YO Sperm Test Wi-Fi” app produced by “Medical Electronic System, LLC” received the highest score for the engagement
Functionality
The score of the Functionality section was based on a 5point Likert scale in 4 subscales (Performance, Ease of use, Navigation and Gestural design) The mean score was 3 78 (0 36)
Aesthetics
The aesthetics section was formed by a 5-point Likert scale in 3 subscales (Layout, Graphics, Visual Appeal) and the mean score was 3 0 (0 53) “Fertility Diet Guide” pro-
Table 2
MARS evaluation
Means, standard deviations and range values for each MARS domain, as well as the overall quality scores and subjective quality scores, were calculated Means and standard deviations were reported for continuous variables while frequencies and percentages were reported for categorical variables Pearson’s correlations were used to analyze correlations between app downloads and MARS ratings Microsoft excel was used for data segregation and a n a l y s i s S t a t i s t i c a l a n a l y s i s w a s c o n d u c t e d u s i n g I B M SPSS software (version 25, IBM Corp, Armonk, NY, USA), considering p < 0 05 as statistically significant
RESULTS
I n t h e fi n a l a n a l y s i s w e included 10 MHAs: 20% (n = 2) from the iTunes App Store and 80% (n = 8) from the
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 G M Fusco, L Cirillo, M Abate, et al 472
Name of application Android/Apple/Both Download Producer Categor y Focus Infertility solutions Android 500 Dagana Apps Instruction Definition, Causes, Diagnosis, Treatment Fertility treatment Android 10000 Di natale Health & fitness Definition, Diagnosis, Treatment Sperm count advice Android 10000 moreFlow Health & fitness Diet , Workouts, Lifestyle Infertility and its management Android 100 FUMO Medicine Definition, Causes and Risk factors, Diagnosis Fertility diet guide Android 10000 Prestige Worldwide Apps, Inc Health & fitness Diet, Lifestyle (male/female) Infertility Android 1000 Nature Healthy Care Entertainment Definition, Causes, Risk factors, Diagnosis, Treatment How to get pregnant fast Android 10000 Saleha Group Entertainment Causes, Diagnosis, Treatment How to get pregnant fast Android 5000 Dvapps-bsl Social Causes, Diagnosis YO Sperm Test Wi-Fi Apple n a Medical Electronic System, LLC Medicine Informative, Practital (marketing) VaricoHealth Apple n a Varicocele Healing Ltd Health & fitness Risk factors, Causes, Lifestyle
Apps Name Engagement Functionality Aesthetic Infor mation Overall mean App subjective (section A) (section B) (section C) (section D) score (SD) quality (section E) YO Sperm Test Wi-Fi 4 2 4 3 67 4 17 4 01 (0 24) 3 5 VaricoHealth 1 8 3 25 2 2 8 2 46 (0 68) 2 5 Infertility solutions 2 6 4 2 7 3 7 3 25 (0 70) 2 Fertility treatment 2 2 4 3 3 3 25 3 18 (0 74) 1 75 Sperm count advice 1.6 4 3.3 3.25 3.04 (1.01) 2.5 Infertility and its management 1 6 3 25 2 7 3 25 2 7 (0 78) 1 75 Fertility diet guide 2 2 4 3 7 3 3 23 (0 80) 2 Infertility 1 6 3 25 2 7 3 2 64 (0 73) 1,75 How to get pregnant fast 24 2 7 2 75 2 86 (0 83) 2 How to get pregnant fast 24 3.3 2.75 3.01 (0.84) 2 Mean (SD) 2 18 (0 78) 3 78 (0 36) 3 0 (0 53) 3 19 (0 45) 3 04 (0 43) 2 18 (0 54) SD = standard deviat on
Table 3
EAU guidelines adherence
duced by “Prestige Worldwide Apps, Inc” reached the highest aesthetics score
Information
The information section was formed by a 5-point Likert scale in 7 subscales The mean score was 3 19 (0 45) The “YO Sperm Test Wi-Fi” app produced by “Medical Electronic System, LLC” received the highest score of Information
Overall mean score
The App quality mean score correspond to the mean of the sum of Engagement, Functionality, Aesthetic and Information scores The mean score was 3 04 (0 43) The “YO Sperm Test Wi-Fi” app produced by “Medical Electronic System, LLC” received the highest mean score of 4 01 (0 24), while “VaricoHealth” produced by “Varicocele Healing Ltd” , received the lowest mean score of 2 46 (0 68)
Subjective quality
The subjective quality section consisted of 4 items The score was 2 18 (0 54) The “YO Sperm Test Wi-Fi” app produced by “Medical Electronic System, LLC” received the highest score of Subjective quality section of 3 5
EAU adherence checklist
EAU guidelines adherence was evaluated and the EAU adherence scores were reported in Table 3 The mean Definition score was 0 6 (0 84), with 60% (n = 6) apps reporting a score of zero; the mean Physiopathology score was 0 7 (1 05) with 60% (n = 6) apps reporting a score of zero; the mean risk factors’ scores was 1 4 (1 17) with 30% (n = 3) apps reporting a score of zero; the mean diagnosis score was 1 2 (1 03) with 30% (n = 3) apps reporting a score of zero; the mean treatment score was 1 1 (0 87) with 30% (n = 3) apps reporting a score of zero The highest score was reported by “Infertilità” produced by “Nature Healthy Care” with an overall EAU Adherence score of 12 points The lowest score was reported by “Fertility Diet Guide” , produced by “Prestige Worldwide Apps, Inc” with an overall EAU Adherence score of zero points
Variable correlations
A Pearson correlation coefficient was computed to assess the linear relationship between variables and number of
downloads The only statistically significant correlation was found between the number of download and the section on “risk factors” of the adherence to the EAU guidelines scoring system, with r = -0 928, p = 0,001
DISCUSSION
The aim of the present study was to give an overview of MHAs for MI, currently available on the market in order to assess their quality and adherence to EAU guidelines To the best of our knowledge, no previous studies examined this topic, so we addressed this void and identified several noteworthy observations
First, of all 10 apps on MI eligible for the analyses, the majority were present on Google Play Store and 80% reported general information on MI However, only half of the apps reported information on diagnosis and treatment options Therefore, the developer of apps should improve the quality of the content present in the apps in order to allow a greater understanding of the phenomenon of MI
Second, according to MARS score criteria, the lowest mean score was reported for the “Engagement” section, while the highest mean score was reported for the “Functionality” section These findings are in agreement with O’Connor et al (28) and indicate that the apps were generally better designed in terms of their usability but may have lacked behavioral and design features associated with sustained usage
Third, according to EAU Guidelines Adherence scoring system, the lowest mean score was reported in the “Definition” section, while the highest score was reported in the “Risk Factors” section The overall scores of this tool are very low These results are corroborated by other published studies highlighting a dramatically low adherence to guidelines This is due to lack of involvement of healthcare MHAs development, representing a great limit, that should be addressed in their future development On the other side collaboration with healthcare does not meaning high quality In fact, as reported by Dantas et al in MHAs for rheumatic disease, not developed for commercial purposes, but created with a partnership between industry/developers and academic institutions, the quality was still low (29)
Fourth, according to MARS, the best MHA currently present on the market is represented by “YO Sperm Test WiFi” developed by “Medical Electronic System, LLC” This app reported the highest score in every single section of this quality tool It’s noteworthy that this app reported the highest score in the “Engagement” section (4 2), followed by Information (4 17), and Functionality (4) To the best of our knowledge no previous studies reported this finding in Engagement, which generally is the lowest reported score, because MHAs are better designed for their usability (efficient and easy to use) and lacked behavioral and design features This is corroborated by the Functionality score which is the highest reported score
YO Sperm Test Wi-Fi can make patients feel that they are participating in the management of their disease The
473 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Male infertility and mobile health applications
Name Definition Physiopatholog y Risk factors Diagnosis Treatment YO Sperm Test Wi-Fi 11232 VaricoHealth 01100 Infertility solutions 20212 Fertility treatment 10012 Sperm count advice 00001 Infertility and its management 02321 Fertility diet guide 00000 Infertility 23322 How to get pregnant fast 00121 How to get pregnant fast 00210 Mean (SD) 0 6 (0 84) 0 7 (1 05) 1 4 (1 17) 1 2 (1 03) 1 1 (0 87) SD = standard dev ation
most reported findings suggest developing MHAs with these characteristics
Taken together, MHAs have a great potential to control the spread of misinformation, raise awareness, helping and informing patients (9) Given the rising role of new technologies in the various health-care services, a formal standardization of contents addressed to nonmedical users would be desirable The majority MHAs currently present in the market are not good enough to be used as reliable source of information on MI However, Kruglova et al developed a MHA, Infotility XY, to promote men ’ s reproductive health (31) Their study showed evidence of the feasibility of MHAs to improve men ’ s knowledge about fertility, about risks factor In fact, men involved in the study, identified more risk factors after using the app (M = 17 14, SD = 4 32) compared to before (M = 11 12, SD = 4 53) Despite this, nowadays there were a multitude of MHAs lacking in quality and correct information This study has several strengths: this is the first study evaluating the content, the quality, and the adherence to EAU guidelines about MI; we performed a rigorous search, screening, and analysis on iTunes and Google Play Store; reviewer had experience in MARS using Our research is not avoided by some limitation: reproducibility of the research turns out to be complex due to the working method of the App Store and Google Play Store (the visibility of apps depends on the device and on the country where the search is performed); the exclusion criteria, which led to the exclusion of paid apps; the guidelines developed for healthcare and not for patients and the constant production of new MHAs
CONCLUSIONS
Nowadays, MHAs present in the market are not a reliable source of information on MI An improvement by the app developers would be welcome, in order to make the apps good both in terms of content and in terms of compliance with the guidelines Therefore, an ideal MHAs should be based on scientific evidence, user friendly, respecting privacy and security laws, making patients feel capable and confident to change personal behavior or attitudes
Interesting, it could be the involvement of patients in the development, design, and validation of MHAs
REFERENCES
1 Mirone V, Creta M, Capece M, et al Telementoring for communication between residents and faculty physicians: Results from a survey on attitudes and perceptions in an Academic Tertiary Urology Referral Department in Italy Arch Ital Urol Androl 2021; 93:450-4
2 Vaggers S, Puri P, Wagenlehner F, Somani BK A Content analysis of mobile phone applications for the diagnosis, treatment, and prevention of urinary tract infections, and their compliance with European Association of Urology guidelines on urological infections Eur Urol Focus 2021; 7:198-204
3 Morra S, Collà Ruvolo C, Napolitano L, et al YouTubeTM as a source of information on bladder pain syndrome: A contemporary analysis Neurourol Urodyn 2022; 41:237-45
4 Capece M, Di Giovanni A, Cirigliano L, et al YouTube as a source of information on penile prosthesis Andrologia 2022; 54:e14246
5 Creta M, Sagnelli C, Celentano G, et al SARS-CoV-2 infection affects the lower urinary tract and male genital system: A systematic review J Med Virol 2021; 93:3133-42
6 Turco C, Collà Ruvolo C, Cilio S, et al Looking for cystoscopy on YouTube: Are videos a reliable information tool for internet users? Arch Ital Urol Androl 2022; 94:57-61
7 Melchionna A, Collà Ruvolo C, Capece M, et al Testicular pain and youtubeTM: are uploaded videos a reliable source to get information? Int J Impot Res 2022 Feb 8 doi: 10 1038/s41443-02200536-w Epub ahead of print
8 mHealth: new horizons for health through mobile technologies: second global survey on eHealth [Internet] [cited 5 September 2022] Available at https://apps who int/iris/handle/10665/44607
9 Davalbhakta S, Advani S, Kumar S, et al A systematic review of Smartphone applications available for Corona virus disease 2019 (COVID19) and the assessment of their quality using the mobile application rating scale (MARS) J Med Syst 2020; 44:164
10 Napolitano L, Fusco GM, Cirillo L, et al Erectile dysfunction and mobile phone applications: Quality, content and adherence to European Association guidelines on male sexual dysfunction Arch Ital Urol Androl 2022;94:211-6
11 Hull MG, Glazener CM, Kelly NJ, Conway DI, Foster PA, Hinton RA, et al Population study of causes, treatment, and outcome of infertility Br Med J Clin Res Ed 1985; 291:1693-7
12 Salonia A, Bettocchi C, Boeri L, et al European Association of Urology guidelines on sexual and reproductive health-2021 update: Male Sexual Dysfunction Eur Urol 2021; 80:333-57
13 GBD 2017 Population and Fertility Collaborators Population and fertility by age and sex for 195 countries and territories, 19502017: a systematic analysis for the Global Burden of Disease Study 2017 Lancet 2018; 392:1995-2051
14 Di Bello F, Creta M, Napolitano L, et al Male sexual dysfunction and Infertility in spinal cord injury patients: state-of-the-art and future perspectives J Pers Med 2022; 12:873
15 The influence of varicocele on parameters of fertility in a large g r o u p o f m e n p r e s e n t i n g t o i n f e r t i l i t y c l i n i c s W o r l d H e a l t h Organization Fertil Steril 1992; 57:1289-93
16 Napolitano L, Barone B, Morra S, et al Hypogonadism in patients with Prader Willi Syndrome: a narrative review Int J Mol Sci 2021; 22:1993
17 Foresta C, Garolla A, Bartoloni L, et al Genetic abnormalities among severely oligospermic men who are candidates for intracytoplasmic sperm injection J Clin Endocrinol Metab 2005; 90:152-6
18 Rastrelli G, Lotti F, Reisman Y, et al Metabolically healthy and unhealthy obesity in erectile dysfunction and male infertility Expert Rev Endocrinol Metab 2019; 14:321-34
19 Creta M, Arcaniolo D, Celentano G, et al Toxicity of antioxidant supplements in patients with male factor infertility: a systematic review and meta-analysis of randomized controlled yrials Antioxid 2021; 11:89
20 Bisht S, Faiq M, Tolahunase M, Dada R Oxidative stress and male infertility Nat Rev Urol 2017; 14:470-85
21 Reifsnyder JE, Ramasamy R, Husseini J, Schlegel PN Role of optimizing testosterone before microdissection testicular sperm extraction in men with nonobstructive azoospermia J Urol 2012; 188:532-6
22 Fusco F, Verze P, Capece M, Napolitano L Suppression of spermatogenesis by exogenous testosterone Curr Pharm Des 2021; 27:2750-3
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 G M Fusco, L
M
et al 474
Cirillo,
Abate,
23 Practice Committee of the American Society for Reproductive Medicine in collaboration with the Society for Male Reproduction and Urology Electronic address: asrm@asrm org The management of obstructive azoospermia: a committee opinion Fertil Steril 2019; 111:873-80
24 Amor-García MÁ, Collado-Borrell R, Escudero-Vilaplana V, et al Assessing apps for patients with genitourinary tumors using the Mobile Application Rating Scale (MARS): systematic search in app stores and content analysis JMIR MHealth UHealth 2020; 8:e17609
25 Stec MA, Arbour MW, Hines HF Client-centered mobile health c a r e a p p l i c a t i o n s : u s i n g t h e M o b i l e A p p l i c a t i o n R a t i n g S c a l e Instrument for evidence-based evaluation J Midwifery Womens Health 2019; 64:324-9
26 Stoyanov SR, Hides L, Kavanagh DJ, et al Mobile app rating scale: a new tool for assessing the quality of health mobile apps JMIR MHealth UHealth 2015; 3:e27
27 Trecca EMC, Lonigro A, Gelardi M, et al Mobile applications in
Otolaryngology: a systematic review of the literature, Apple App Store and the Google Play Store Ann Otol Rhinol Laryngol 2021; 130:78-91
28 O’Connor SR, Kee F, Thompson DR, et al A review of the quality and content of mobile apps to support lifestyle modifications following a transient ischaemic attack or «minor» stroke Digit Health 2021; 7:20552076211065270
29 Dantas LO, Carvalho C, Santos BL de J, et al Mobile health technologies for the management of urinary incontinence: A systematic review of online stores in Brazil Braz J Phys Ther 2021; 25:387-95
30 Vega M, Mckay ER, Halani PK Evaluation of mobile applications for patients with fecal incontinence using a modified APPLICATIONS scoring system Int Urogynecology J 2021; 32:2529-36
31 Kruglova K, Gelgoot EN, Chan P, et al Risky Business: increasing fertility knowledge of men in the general public using the mobile h
l t h a p p l i c a t i o n i n f o t i l i t y X Y A m J M e n s H e a l t h 2 0 2 1 ; 15:15579883211049028
Correspondence
Giovanni Maria Fusco, MD giom fusco@gmail com
Luigi Cirillo, MD cirilloluigi22@gmail com
Marco Abate, MD marcoabate5@gmail com
Simone Morra, MD (Corresponding Author) simonemorra93@gmail com
Vincenzo Morgera, MD vincemorgera87@gmail com
Biagio Barone, MD biagio barone@unina it
Felice Crocetto, MD felice crocetto@unina it
Gianluigi Cacace, MD cacace gianlu@gmail com
Francesco Di Bello, MD fran dibello12@gmail com
Alessandro Palmieri, MD info@alessandropalmieri it
Vincenzo Mirone, MD mirone@unina it
Ciro Imbimbo, MD
ciro imbimbo@unina it
Luigi Napolitano, MD luiginap89@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples "Federico II", Naples, Italy
Via Sergio Pansini n 5, Naples (NA), Campania (Italy)
Lorenzo Spirito, MD lorenzospirito@msn com
Celeste Manfredi, MD
manfredi celeste@gmail com
Davide Arcaniolo, MD
davide arcaniolo@unicampania it
Urology Unit, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli", Naples, Italy
475 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Male infertility and mobile health applications
a
e
Department of Urology, Athens, Greece
Summary
Objective: To assess the role of Cytoreductive Nephrectomy for synchronous metastatic Renal Cell Carcinoma patients in the Systemic Therapy era and beyond regarding the Overall Survival, the optimal sequence between Systemic Therapy and Cytoreductive Nephrectomy and prognostic factors
Methods: The systematic review was conducted in accordance with the PRISMA guidelines Bibliographic search was performed in Medline (PubMed), ClinicalTrials.gov, and Cochrane Library-Cochrane Central Register of Controlled Trials (CENTRAL) Studies included were those indexed from 2005 in an attempt to limit those conducted in the cytokine era Risk of bias assessment was performed by two authors (K S and T L) using the Cochrane Collaborative Risk of Bias tool for randomized trials, the Cochrane Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) tool for nonrandomized studies
Results: Cytoreductive nephrectomy was associated with improved overall survival in all but one of the observational studies While in all of these studies the unvariable analysis showed improved overall survival in favor of the cytoreductive nephrectomy group in some studies the subgroup analysis showed no benefit. Regarding the optimal sequence, deferred cytoreductive nephrectomy demonstrated better results in more studies than upfront cytoreductive nephrectomy but a advantage was not clearly certain In the analysis of possible prognostic factors for overall survival with cytoreductive nephrectomy, most common prognostic factors found were age (in 8 studies), tumor histology (in 7 studies), number of metastasis (in 6 studies), and T stage
Conclusions: Cytoreductive nephrectomy can still play an important role in wisely selected patients, although the role of cytoreductive nephrectomy in the new immunotherapy era needs to be defined
KEY WORDS: Cytoreductive nephrectomy; Metastatic renal cell carcinoma; Systemic therapy; Immune check point inhibitors
Submitted 4 September 2022; Accepted 2 October 2022
INTRODUCTION
During the last two decades, the role of cytoreductive nephrectomy (CN) in the treatment of synchronous metastatic renal cell carcinoma (mRCC) has been reevaluated many times according to the newly discovered different oncological therapies In the cytokine era, due to lack of significant effectiveness of medical therapies, CN
was considered the standard of treatment justified by two randomized phase 3 trials (SWOG 8949, EORTC30947) (1, 2) Both trials showed an overall survival (OS) benefit of CN followed by interferon-alpha (IFN-a) 2b versus interferon alone (1-3) Since 2005, systemic therapies (ST), s u c h a s v a s c u l a r e n d o t h e l i a l g r o w t h f a c t o r r e c e p t o r s (VEGFR)-tyrosine kinase inhibitors (TKI) and mammalian target of rapamycin (mTOR) inhibitors, replaced cytokines as they have been proven superior to cytokines (4, 5) CN was evaluated, regarding possible advantages on OS in mRCC patients treated with ST, through multiple retrospective studies The CARMENA trial (6) and the SURTIME trial (7), are the only randomized controlled trials (RCT) investigating the role of CN in the ST era These two studies reduced the enthusiasm on upfront CN and opened a discussion about which patients treated with ST could benefit more by CN Furthermore, new therapeutic agents such as immune check point inhibitors (ICI), presented as superior to TKI in recent studies (8-10) These controversial observations prompted us to conduct a systematic review in order to examine the role of CN for synchronous mRCC patients in the ST era and beyond regarding the overall survival (OS), the optimal sequence between ST and CN and prognostic factors
METHODS
The systematic review was conducted in accordance with the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) (11)
Bibliographic search was performed in Medline (PubMed), ClinicalTrials gov, and Cochrane Library-Cochrane Central Register of Controlled Trials (CENTRAL) Studies included were those indexed from 2005 in an attempt to limit those conducted in the cytokine era The last search date was March 14, 2022
The following medical subject heading terms were used in combination with Boolean operators (AND, OR, NOT): (“cytoreductive nephrectomy”) AND ("targeted therapy" OR "
Two independent reviewers (K S, T L) screened all articles retrieved by the initial search All disagreements were
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 476 REVIEW No conflict of interest
declared
s y s t e m i c t h e r a p y " O R “ i m m u n e o n c o l o g y [ I O ] ” O R immunotherapy OR "immune checkpoint inhibitor*" OR “ i m m u n o o n c o l o g y ” ) N O T ( R e v i e w [ P u b l i c a t i o n T y p e ] ) NOT (Meta-analysis[Publication Type]) NOT (Systematic review[Publication Type])
Cytoreductive nephrectomy for synchronous metastatic renal cell carcinoma. Is there enough evidence?
Stamatios Katsimperis, Lazaros Tzelves, Themistoklis Bellos, Konstantinos Pikramenos, Ioannis Manolitsis, Ioannis Tsikopoulos, Iraklis Mitsogiannis
DOI: 10 4081/aiua 2022 4 476
Figure 1. PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only
resolved with discussion, and final decision was reached by consensus with a third reviewer (M I ) Reference lists were systematically searched for relevant articles in a snowball procedure
An ethical approval is not required because this study is a review of the existing international literature
Study criteria
Clinical trials, cohort studies, and case-control studies were considered for inclusion (Figure 1)
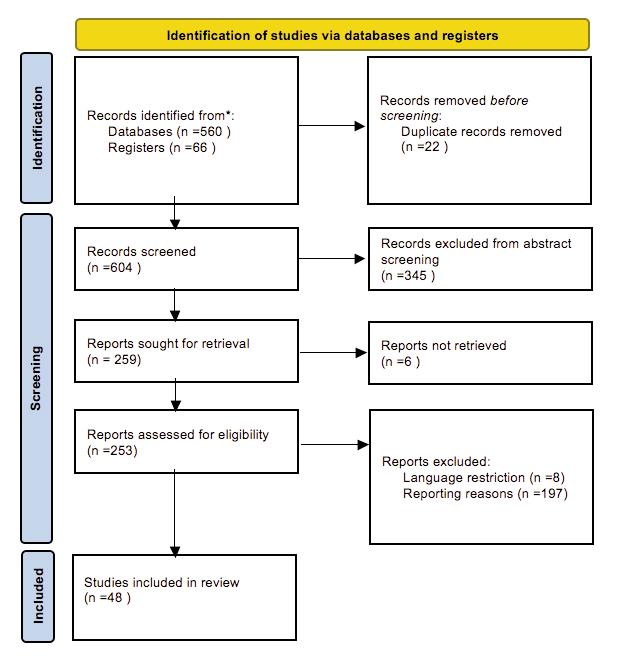
Excluded studies met ≥ 1 of the following criteria: (1) irrelevant to the subject studies, (2) studies published in a nonEnglish language, (3) case reports, case series including less than 10 patients, systematic reviews and meta-analyses, and (4) editorials, perspectives, and letters to the editors, (5) studies including only drugs from cytokine era (studies excluded are summarized in Supplementary Table 1)
Types of participants and exposure
Patients diagnosed with synchronous mRCC, who underwent CN Studies with patients undergoing partial nephrectomy, ablative procedures or nephrectomy for palliative reasons were not included Primary research question was the effect of CN in the OS Secondary ques-
tions were the optimal sequence between systemic therapies and CN, and possible prognostic factors
Risk of bias assessment
Risk of bias assessment was performed by two authors (K S and T L) using the Cochrane Collaborative Risk of Bias tool for randomized trials (12), the Cochrane Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool for nonrandomized studies (13) (Table 1) Most common reasons for the studies evaluating the relationship between CN and OS to be classified as having moderate or serious risk of bias were the unmeasured differences between CN and control groups and the inadequate adjustment for confounding factors The inability to adjust for differences between groups was also found in the studies assessing the prognostic factors and the role of sequence between ST and CN Moreover, the studies assessing the sequence between ST and CN also demonstrated selection bias
RESULTS
Cytoreductive nephrectomy and overall survivor
Thirty studies were included in the analysis of the rela-
477 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Nephrectomy for metastatic renal cell carcinoma
Table 1
Risk of bias assessment for non-randomized studies
tionship between CN and OS (14-42, 65) (Table 2) All of the studies except for one (41), which was a prospective randomized trial, were retrospective cohort studies
Ten of them were from the Surveillance, Epidemiology, and E n d R e s u l t s ( S E E R ) d a t a b a s e , 4 f r o m I n t e r n a t i o n a l Metastatic RCC Database Consortium (IMDC), two from National Cancer Database (NCDB) and the rest were sin-
gle or multi-center studies Most common systemic agent used was sunitinib (Table 1), while there were three studies (2, 40, 42) comparing CN with the use of ICIs These studies are of great importance, as they are the first retrospective studies on the role of CN in the immunotherapy era and demonstrated an OS benefit in patients treated with ICI plus CN compared to ICI alone (HR 0 23-0 39,
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
478
S Katsimperis, L Tzelves, T Bellos, K Pikramenos, I Manolitsis, I Tsikopoulos, I Mitsogiannis
F irst author Confounding Par ticipant Inter vention Deviation from Missing Outcome Selected Overall (year) selection classification inteended treatment data measurement repor r ting bias Day (2016) Moderate Moderate Low Low Moderate Low Low Moderate de Groot (2016) Moderate Serious Low Low Moderate Low Low Serious Hanna (2016) Moderate Serious Low Low Moderate Low Low Serious Heng (2014) Moderate Serious Low Low Low Low Low Serious Klatte (2018) Moderate Serious Low Low Low Low Low Serious Patel (2017) Serious Moderate Low Low Moderate Moderate Low Serious Tatsugami (2015) Moderate Moderate Low Low Moderate Low Low Moderate You (2011) Moderate Moderate Low Low Low Low Low Moderate Abern (2014) Serious Moderate Low Low Low Low Low Serious Conti (2014) Serious Moderate Low Low Low Low Low Serious Marchioni (2019) Serious Moderate Low Low Low Low Low Serious Patel (2017) Serious Moderate Low Low Moderate Moderate Low Serious Aizer (2014) Serious Moderate Low Low Low Moderate Low Serious Song (2016) Serious Serious Low Low Low Low Low Serious Abel (2017) Moderate Moderate Low Low Moderate Low Low Moderate Corcoran (2014) Moderate Moderate Low Low Low Low Low Moderate Culp (2010) Moderate Moderate Low Low Low Low Low Moderate Culp (2014) Moderate Moderate Low Low Low Low Low Moderate Kalogirou (2017) Serious Moderate Low Low Low Low Low Serious Sakai (2014) Moderate Moderate Low Low Low Low Low Moderate Sharma (2015) Moderate Moderate Low Low Moderate Low Low Moderate You (2015) Serious Moderate Low Low Low Low Low Serious MacLeod (2017) Moderate Moderate Low Low Moderate Low Low Moderate Stroup (2013) Serious Moderate Low Low Low Low Low Serious Wood (2009) Serious Moderate Low Low Low Low Low Serious Luzaggo (2021) Moderate Moderate Low Low Low Low Low Moderate Singla (2020) Moderate Moderate Low Low Low Low Low Moderate Palumbo (2020) Moderate Moderate Low Low Low Low Low Moderate Choi (2018) Moderate Serious Low Low Low Low Low Serious Janish (2020) Moderate Serious Low Low Moderate Low Moderate Serious Alnimer (2021) Moderate Moderate Low Low Low Low Low Moderate Vaishampayan (2019) Serious Moderate Low Low Low Low Low Serious Graham (2019) Moderate Serious Low Low Low Moderate Low Serious You (2014) Moderate Moderate Low Low Low Low Low Moderate Zhao (2019) Serious Moderate Low Low Low Low Low Serious Poprach (2020) Moderate Moderate Low Low Low Low Low Moderate Bakouny (2020) Serious Moderate Low Low Low Low Low Serious Dragomir (2021) Serious Moderate Low Low Low Moderate Low Serious Ljungberg (2020) Serious Serious Low Low Low Low Low Serious Mcintosh (2020) Moderate Moderate Low Low Low Low Low Moderate Rosiel o (2019) Serious Serious Low Low Low Low Low Serious Teishima (2018) Serious Moderate Low Low Low Low Low Serious Adashek (2021) Moderate Moderate Low Low Low Low Low Moderate Bh ndi (2020) Moderate Moderate Low Low Low Low Low Moderate De Bruijn (2020) Serious Serious Low Low Low Low Low Serious Uprety (2018) Moderate Moderate Low Low Low Low Low Moderate Study Random Allocation Blinding of par ticipants Blinded outcome Incomplete Selective Other Overall sequence generation concealment and personnel assessment outcome data repor ting bias risk of bias Bex (2017) Low Low Low Low Low Low Moderate Moderate Mejean (2018) Low Low Low Low Low Low Moderate Moderate Risk of bias assessment for randomized studies.
Nephrectomy for metastatic renal cell carcinoma
Table 2.
Studies evaluating the association between CN and OS
N (total) = 15390 NR CN before or after ST 17 1 vs 7 7, HR 0 49USA (NCDB) 2006-2013
(CN) 5374 (95% CI 0 46–0 52) N (no CN) = 10016
Singla (2020) (24), Retrospective cohort,
(total) = 391 Upfront CN = 197, No CN = 11 6
Median OS was not reached in the CN group USA (NCDB) 2015-2016
(CN) = 221 ST before CN = 24 HR 0 23 (95% CI 0 15–0 37)
0 24–1 15)
N (no CN) = 33
Graham (2019) (28), Retrospective cohort, N (total) 353 Sunitinib (54%) CN before ST 16 3 vs 8 6, HR 0 62 Metastatic Papillary Renal Cell international (IMDC) 2005-2017 N (CN) = 244 Temsirolimus (23%) (95% CI 0.45–0.85) Carcinoma studied
N (no CN) = 109 Pazopanib (11%)
Sorafenib (2 8%)
Klatte (2017) (29), Retrospective cohort, N (total) = 261 Sunitinib (60 5%) CN before ST Unadjusted:UK (Single center), 2006-2017 N (CN) 97 Pazopanib (28 4%) 25 6 vs 12 4, HR 0 46
N (no CN) = 164 cabozantinib or (95% CI 0.34–0.62)
Nivolumab (8 4%)
IPTW-adjusted: 20 9 vs 12 6, other (34 5%) HR 0 63 (95% CI 0 46–0 84)
You (2014) (30), Retrospective cohort, N (total) = 171 Sunitinib (70%), CN before ST 19 9 vs 11 7Korea (Single center) 2006-2012 N (CN) 96
Sorafenib(19%), HR: NR
N (no CN) = 75 Pazopanib (4%), Temsirolimus (7%)
Tatsugami (2015) (31), Retrospective cohort, N (total) = 330 NR NR
N (no CN) 76
27 4 vs 10 3, HR 0 40
Mixed population of approximately half Japan (multicenter) 2001-2015 N (CN) = 254 (95% CI 0 29–0 57) patients receiving Cytokines and half
Subgroup analysis for patients receiving Systemic Therapy receiving only ST: 30.9 vs 15.5, HR 0 48 (95% CI 0 28–0 90)
479 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Study Number Systemic agents CN-systemic therapy Median OS (CN vs no CN) Supplementary info of patients used sequence OS HR (95% CI) for the study Conti (2014) (14), Retrospective cohort, N (total) 20104 NR NR 15 vs 4, HR 0 41 Non–clear cell renal cell carcinoma studied USA (SEER) 1993-2010 N (CN) = 6915 (95% CI 0.37–0.55) N (no CN) = 13819 Aizer (2014) (15), Retrospective cohort, N (total) = 591 NR NR 14 vs 6, HR 0 45 Cytokines + ST USA (SEER) 2000-2009 N (CN) = 384 (95% CI 0 39–0 43) N (no CN) 207 Abern (2014) (16), Retrospective cohort, N (total) = 7143 NR NR HR 0.33 Median OS in months: NR USA (SEER) 2005-2009 N (CN) = 2629 (95% CI 0 31–0 36) N (no CN) = 4514 Vaishampayan (2019) (17), Retrospective cohort, N (total) = 18422 NR NR 18 vs 3, HR 0 39USA (SEER) 2010-2016 N (CN) 7660 (95% CI 0 30–0 33) N (no CN) =10762 Zhao (2019) (18), Retrospective cohort, N (total) = 1113 NR NR 26 vs 9, HR 0 40USA (SEER) 2010-2014 N (CN) = 618 (95% CI 0 35–0 47) N (no CN) = 415 Marchioni (2019) (19), Retrospective cohort, N (total) 851 NR NR HR 0 38 Median OS in months: NR USA (SEER) 2001-2014 N (CN) = 575 (95% CI 0.30–0.47) Non-clear Cell Renal Cell Carcinoma studied N (no CN) = 276 Palumbo (2020) (20), Retrospective cohort, N (total) = 2241 NR NR 28 vs 12, HR 0 49USA (SEER) 2010-2015 N (CN) = 1168 (95% CI 0 41–0 58) N (no CN) 1073 Luzzago (2021) (21), Retrospective cohort, N (total) = 1573 NR CN before ST No treatment = 3 USA (SEER) 2006-2015 N (no-treatment) = 350 ST alone = 7 N (ST alone) = 387 CN = 9 N (CN) = 396 CN+ST = 13 N (CN+ST) 440 HR NR Non–clear cell renal cell carcinoma studied Alnimer (2021) (22), Retrospective cohort, N (total) = 5483 NR NR 24 vs 6, HR 0.33USA (SEER) 2010-2016 N (CN) = 2991 (95% CI 0 28–0 40) N (no CN) = 2483 Hanna (2016) (23), Retrospective cohort,
N
N
N
Patients were treated with immune N (no CN) = 170 checkpoint inhibitors Choi (2018) (25), Retrospective cohort, N (total) 294 Sunitinib (52 4%) ST before CN 29 vs 11, HR 0 40Korea (Single center) 2005-2015 N (CN) = 109 Pazopanib (26.2%) (95% CI 0.28–0.58) N (no CN) = 105 Sorafenib (10 9%) Temsirolimus (4 4%) Janish (2020) (26), Retrospective cohort, N (total) = 262 Sunitinib (66%) CN before ST 27 months for the CN group No difference in OS between the two groups Germany (Single center) 2000-2016 N (CN) 104 Sorafenib (20%) P > 0 05 N (no CN) = 158 Pazopanib (10%) You (2011) (27), Retrospective cohort, N (total) = 78 Sunitinib (81%) CN before ST 21 6 vs 13 9, HR 0 53Korea (Single center) 2006-2009 N (CN) = 45 Sorafenib (19%) (95% CI
Day (2016) (32), Retrospective cohort, N (total) 91 Sunitinib (74%) CN before ST 23 vs 10 9, HR 0 33Australia (multicenter) 2006-2012 N (CN) = 46 Pazopanib (4%) (95% CI 0 20–0 55)
N (no CN) = 45 Everolimus (4%)
Bevacizumab (2%)
Interferon (2%)
Temsirolimus (1%)
Choueiri (2011) (33), Retrospective cohort, N (total) = 314 Sunitinib (63%) CN before ST 19 8 vs 9 4, HR 0 68Canada and USA (multicenter) 2004-2008 N (CN) = 201 Sorafenib (30%) (95% CI 0 46–0 99) N (no CN) = 113 Bevacizumab (7%)
Heng (2014) (34), Retrospective cohort, N (total) = 1658 CN; no CN NR 20 6 vs 9 6, HR 0 60international (IMDC), years not specified N (CN) 982 Sunitinib (67%; 79%) (95% CI 0 52–0 69)
N (no CN) = 676
Sorafenib (20%; 8 6%)
Axitinib (0 4%; 0 4%)
Bevacizumab (4%; 1 5%)
Temsirolimus (3 6%; 6 4%)
Pazopanib (2 8%; 2 8%)
Everolimus (1%; 1%)
Other (0 7%; 0 3%)
De Groot (2016) (35), Retrospective population N (total) = 146 Sunitinib CN before ST 17 9 vs 8 8, HR 0 61based matched cohort, The Netherlands 2008-2010 N (CN) = 73 (95% CI 0 41–0 92)
N (no CN) 73
Poprach (2020) (36), Retrospective cohort, N (total) = 730 Sunitinib (78 8%) CN before ST 27 2 vs 14 2, HR 0 55Czech Republic (National registry) 2007-2018 N (CN) = 458 Pazopanib (21 2%) (95% CI 0 45–0 68)
N (no CN) = 272
Song (2016) (37), Retrospective cohort, N (total) = 74 Sunitinib (44 6%) CN before ST 32 2 vs 23 -
China (single center) 2006-2014 N (CN) 51 Sorafenib (29 7%) HR: NR
N (no CN) = 23 Famitinib (18 9%)
Pazopanib (6 7%)
Bhindi (2020) (38), Retrospective cohort, N (total) = 1541 Sunitinib CN before or after ST CN+sunitinib vs sunitinib Comparative analyses of upfront CN+ sunitinib
IMDC 2006-2018 N (CN+Sunitinib) = 805 vs sunitinib+dCN 19 vs 10 vs 46 vs sunitinib+ dCN vs sunitinib
N (no CN) 651
N (Sunitinib+dCN) = 85
Upfront CN+sunitinib vs sunitinib
HR 0 89 (95% CI 0 71–1 1)
Sunitinib+dCN vs sunitinib
HR 0 89 (95% CI 0 71–1 1)
Sunitinib+dCN vs Upfront CN +sunitinib
HR 0 52 (95% CI 0 39–0 70)
Patel (2017) (39), Retrospective cohort, N (total) = 1062 NR NR HR 1 90 (95% CI 1 61–2 25) OS in months NR Australia 2001-2009 N (CN) = 289 Includes cytokine era
N (no CN) = 773
Dragomir (2021) (40), Retrospective cohort, N (total) = 788 Sunitinib (51 1%) CN before CN+ST vs ST 36 vs 18, HR 0 65 One of few studies including patients treated Canada (multicenter) 2011-2020 N (CN) 80 Pazopanib (16 8%) or after ST (95% CI 0 52–0 82) with ICI
N (CN+ST) = 383 Ipilimumab/ ST+CN vs ST 48 vs 18, HR 0 41
N (ST+CN) = 73 Nivolumab (13 8%) (95% CI 0 28–0 60)
N (ST only) = 282 other (18 9%) CN (only) vs ST (only) 24 vs 18, HR 0 75 (95% CI 0 48–1 17)
CN+ST vs ST+CN 36 vs 48, HR 0 66 (95% CI 0 42–1 04)
Mejean (2018) (41), Prospective Randomized trial, N (total) = 450 Sunitinib CN before or after ST 13 9 vs 18 4, HR 0 89 17% of patients in the sunitinib-only France, Norway, England, Scotland, N (CN) = 226 (95% CI 0 71–1 1) arm received subsequent CN
Sweden 2009-2017
N (no CN) 224
Bakouny (2020) (42) Retrospective cohort, N (total) = 4054 NR CN before or after ST CN+ ICI vs ICI
One of few studies including patients treated international (IMDC) 2009-2019
N (TT only) = 1386 53 6 vs 21 4, HR = 0 44 with ICI
N (CN+TT) = 2470 (95% CI 0 30-0 64)
N (CN+ICI) = 143
CN+ TT vs TT 26 5 vs 10 3, HR = 0 48
N (ICI only) 282 (95% CI 0 45-0 52)
Uprety (2018) (65), Retrospective cohort, N (total) = 3376 NR NR 18 vs 4
USA (SEER) 2006-2012
N (CN) = 1110
N (no CN) = 2266
CN Cytoreduct ve nephrectomy; dCN Deferred CN; OS Overa l surv val; HR hazard rat o; ST Systemic therapy; NR Not reported; CI Conf dence interva ; SEER Surve llance, Ep demiology, and End Resu ts; NCDB Nationa Cancer Database; IMDC Internat onal Metastatic Rena Cel Carc noma Database Consort um
with 95% CI 0 15-0 37 and 0 19-0 83) Regarding the sequence of CN and ST, CN was administered before ST in 12 studies (21, 26-30, 32, 33, 35-37), before or after in 5 (23, 38, 40-42), after in one study (25) while sequence was not specified in the rest
CN was associated with improved OS in all but one of the observational studies (26), with HRs ranging from 0 23 to 1 90 (Table 1) In all of these studies (14-25, 27-42) the univariable analysis showed improved OS in favor of the CN group although in some studies subgroup analysis
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
480
S Katsimperis, L Tzelves, T Bellos, K Pikramenos, I Manolitsis, I Tsikopoulos, I Mitsogiannis
showed no benefit (33, 34) Choueiri et al (33) stratified patients according to the IMDC prognostic factors and demonstrated that poor-risk patients had no significant benefit in OS (HR 0 67 95% CI 0 44-1 01, p = 0 06) Also, Heng et al (34), in a similar subgroup analysis showed absence of OS benefit for poor risk patients (OS 6 vs 5 4 months, p > 0 1)
The CARMENA trial (41), the only prospective trial in this review, compared sunitinib plus CN versus sunitinib alone in mRCC patients and showed for the first time the non-inferiority of systemic therapy compared to upfront CN plus sunitinib, with OS 18 4 months vs 13 9 months (HR 0 89 95% CI 0 71-1 1) Results were similar in the intermediate risk (HR 0 92 95% CI 0 68-1 24) and poor-
Table 3.
Studies evaluating the sequencing of CN and ST.
risk (HR 0 86 95% CI 0 62-1 17) patients However, the study has some serious limitations In the sunitinib alone arm, 17% of the patients underwent subsequent CN and 7% of patients in the CN plus sunitinib arm did not receive surgery The study also included only poor-risk Memorial Sloan Kettering Cancer Center (MSKCC) and intermediate-risk MSKCC patients that have been shown before not to benefit from CN (33, 34)
Sequencing of cytoreductive nephrectomy and systemic therapies
Ten studies were included in the analysis of the sequencing of CN and ST (Table 3) Nine studies were retrospective cohorts (23, 38, 40, 43-48), and one was a prospec-
Study Number of patients Comparison F indings
Wood (2009) (43), Retrospective cohort, N (total) = 102 CN followed by TT versus TT followed by CN
Unadjusted KM analysis revealed similar median CSS USA (single center) 2005-2007 N (CN+TT) = 58 31 vs 27 7 mo, p = 0 697
N (TT+CN) = 44
Stroup (2013) (44), Retrospective cohort, N (total) 35 CN followed by Sunitinib versus Sunitinib followed by CN
Unadjusted KM analysis revealed no difference in OS
USA (multi center) 2005-2009 N (CN+Sunitinib) = 17 p = 0 579
N (Sunitinib+ CN) = 18
Hanna (2016) (23), Retrospective cohort, N (total) = 4223 CN followed by TT versus TT followed by CN
Unadjusted KM analysis revealed, 1-, 2-, and 3-year OS rates were: 61 2%, USA (NCDB) 2006-2013 N (CN+TT) = 3733 37 8%, 26 6% for CN+TT patients versus 73 3%, 48 1%, 35 3%
N (TT+CN) 490 for TT+CN patients log-rank p < 0 001
Macleod (2017) (45), Retrospective cohort, N (total) = 537 CN followed by TT versus TT followed by CN
Median OS of CN+TT vs TT+CN: 17 4 vs 9 2 months
USA (SEER) 2006-2011 N (CN+TT) = 190 HR 0 50 (95% CI 0 38-0 65) In propensity score matching: 5 8 N (TT+CN) = 347 months advantage for immediate CN
Bex (2018) (7), Prospective RCT, N (total) = 99 CN followed by Sunitinib versus Sunitinib followed by CN In the ITT population, no difference in PFR at 28 weeks
The Netherlands, Canada, UK, Belgium 2010-2016 N (CN+Sunitinib) 50 (CN+Sunit 42% vs Sunit +CN 43% p 0 61)
N (Sunitinib+ CN) = 49
Median OS of CN+Sunit vs Sunit +CN: 15 vs 32 4 months
HR 0 57 (95% CI 0 34-0 95) p = 0 032
In the PPP the OS was greater in deferred CN but not statistically significant p = 0 23
Bhindi (2018) (46), Retrospective cohort, N (total) 15068 CN followed by TT versus TT followed by CN In IPTW analysis, median OS of CN+TT vs TT+CN: 16 5 vs 9 2 months USA (NCDB) 2006-2013
N (CN+TT) = 6731 HR 0 61 (95% CI 0 59-0 64) p < 0 001
N (TT+CN) = 8337
Bhindi (2020) (38), Retrospective cohort, N (total) = 1541 CN followed by Sunitinib versus Sunitinib followed by CN Median OS of CN+Sunitinib vs Sunitinib+deferred CN: 19 vs 46 months USA (IMDC) 2006-2018
N (CN+Sunitinib) = 805
N (no CN) 651
N (Sunitinib+dCN) = 85
HR 0 52 (95% CI 0 39–0 70) p < 0 001
Median OS of CN+TT vs TT+CN: 30 7 vs 36 9 months Canada (single center) 2009-2016
Kapoor (2019) (47), Retrospective cohort, N (total) = 54 CN followed by TT versus TT followed by CN
N (CN+TT) = 32
N (TT+CN) = 22
De Bruijn (2020) (48), Retrospective analysis, N (total) 338
Pooled data from prospective trials 2006-2016
N (CN+TT) = 149
N (TT+CN) = 189
CN followed by TT versus TT followed by CN
When stratified by number of metastatic sites (< 3 vs ≥ 3 sites)
median OS was significantly longer in the upfront TT group with ≥ 3 metastasis sites: 33 vs 12 1 months
HR 4 65 (95% CI 1 18–18 39) p = 0 03
In intermediate-risk patients, upfront TT group had longer OS: 70 5 vs 30 7 months
HR 3 25 (95% CI 1 16–9 08) p = 0 03
In unselected for risk group
Median OS of CN+TT vs TT+CN: 18 4 vs 24 3 months
HR 0 78 (95% CI 0 59–1 04) p = 0 09
In intermediate-risk group
Median OS of CN+TT vs TT+CN: 22 8 vs 33 months
HR 0 72 (95% CI 0 52–0 99) p 0 047
Dragomir (2021) (40), Retrospective cohort, N (total) = 788
CN followed by ST versus ST followed by CN
Median OS of CN+ST vs ST+CN: 36 vs 48 months Canada (multicenter) 2011-2020
N (CN) = 80 ST includes TT or immune check point inhibitors HR 0 66 (95% CI 0 42–1 04)
N (CN+ST) = 383
N (ST+CN) = 73
N (ST only) 282
CN Cytoreductive nephrectomy; OS Overal surv val; CSS Cancer specific surv val,; HR Hazard rat o; ST System c therapy; TT Ttargeted therapy; CI Confidence interval; KM Kap an Meier; ITT Intention to treat; PPP Per protocol popu ation; SEER Surve l ance, Ep demiology, and End Resu ts; NCDB Nationa Cancer Database; IMDC International Metastat c Renal Ce l Carcinoma Database Consortium
481 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
metastatic renal
carcinoma
Nephrectomy for
cell
Figure 2
Prognostic factors
tive randomized controlled trial (RCT) (7) Out of retrospective studies, two were population based (45, 38), three studies used a national hospital-based database (46, 23, 40), two were from a single institution (43, 47), one study was multicenter (44) and one study pooled data from 4 prospective trials (48)
In two studies (45, 46), CN prior to ST found to have an advantage in OS Macleod et al (45) showed that median OS of immediate CN was 17 4 months vs 9 2 in the deferred CN group, with HR 0 50 (95% CI 0 38-0 65) An advantage of 5 8 months for the immediate CN group was also found in propensity score matching There was no survival benefit regarding the sequencing of CN and ST in three studies (40, 43, 44) Unadjusted Kaplan Meier (KM) analyses from both Wood et al and Stroup et al did not reveal a benefit in survival in neither the upfront nor the differed CN group (p = 0 697 and p = 0 579 respectively)
In the only prospective RCT from Bex et al (7) median OS in the deferred CN group was greater than in the immediate one in the intention to treat population (32 4 vs 15 months, HR 0 57; 95% CI 0 34-0 95, p = 0 032) but not in the per protocol population (HR 0 71; 95% CI 0 401 24, p = 0 23) Similar results with advantage of deferred CN were reported in four more studies (23, 38, 47, 48)
Interestingly, Bhindi et al (38, 46), in two studies reported contradictory results for the role of deferred CN
When initial treatment with CN, with or without subsequent targeted therapy (TT) was compared to initial treatment with TT, with or without subsequent CN in a sample population pooled from National Cancer Data Base (NCDB) (46), Authors found an OS benefit for the first group (HR 0 61; 95% CI 0 59-0 64, p < 0 001) However, in a more recent study (38), a retrospective cohort with d a t a f r o m I n t e r n a t i o n a l m R C C D a t a b a s e C o n s o r t i u m (IMDC), comparison of CN followed by Sunitinib versus
Sunitinib followed by CN, favored the latter (HR 0 52; 95% CI 0 39-0 70, p < 0 001) Another study of notable mention comes from Dragomir et al (40), as it is the only one that included in the ST arm patients who were also treated with ICI This study also favors deferred than initial CN (HR 0 66; 95% CI 0 42-1 04)
Prognostic factors for OS with CN
Twenty-four studies were included in the analysis of possible prognostic factors for OS with CN In Figure 2 independent prognostic factors are demonstrated with green color, those found not to be independent prognostic factors are demonstrated with red, while those not assessed are the ones in the white cells Most common prognostic factors found in the analysis were age (in 8 studies) (15, 18, 23, 27, 30, 39, 52, 53, 57), tumor histology (in 7 studies) (15, 18, 26, 27, 32, 51-53), number of metastasis (in 6 studies) (18, 30, 45, 51, 55, 60), and T stage (in 6 studies) (18, 31, 51-53, 57, 58) Other factors were, sarcomatoid histology, IMDC or M S K C C c l a s s i fi c a t i o n , s y s t e m i c s y m p t o m s , l y mphadenopathy, hemoglobin and albumin level, levels of serum calcium or creatinine or platelets, C-reactive protein (CRP) level, absolute neutrophil count and neutrophillymphocyte ratio, bone metastasis, lymph node metastasis, visceral metastasis or liver metastasis, tumor grade, sex, body mass index (BMI), marital status, race, level of thrombus, if existing, and other comorbidities From the factors mentioned above, those associated with poor overall survival after CN are high T stage and number of m e t a s t a s

h i s t o l o g y , b o n e m e t a s t a s i s , lymph node metastasis, visceral metastasis or liver metastasis, thrombus level above the diaphragm, existing comorbidities, presence of systemic symptoms, poor IMDC or MSKCC classification, unmarried status, poor

Archivio Italiano di Urologia e Andrologia 2022; 94, 4
482
S Katsimperis, L Tzelves, T Bellos, K Pikramenos, I Manolitsis, I Tsikopoulos, I Mitsogiannis
c o
i s , s a r
m a t o i d
performance status, hemoglobin level less than the lower limit of normal, LDH level above the upper limit of normal and a neutrophile/lymphocyte ratio ≥ 4 Female gender, thrombocytosis, CRP level ≥ 1 ng/ml, good performance status, and good/intermediate IMDC or MSKCC classification were considered having an OS benefit
DISCUSSION
T r e a t m e n t o f s y n c h r o n o u s m R C C h a s f a c e d m a n y changes in recent years, due to the ongoing development of new drugs, making the therapeutic choice a complex task The two well-known RCTs that were published regarding the role of CN in mRCC patients, CARMENA and SURTIME, changed what we thought to be the standard of care The role of CN was deeply questioned, and systemic therapies were found to be more effective Results from SURTIME and CARMENA (6, 7) demonstrated an absence of benefit in immediate CN, while deferred CN showed an OS benefit in intermediate risk patients However, their results should be interpreted with caution as both CARMENA and SURTIME, are found to have certain pitfalls For instance, in CARMENA there was a significant crossover with 17% of patients in the sunitinib alone arm undergoing subsequent CN, and 7% of patients in the CN plus sunitinib arm not receiving surgery SURTIME on the other hand, suffered from poor accrual, changing the primary endpoint from progression free survival (PFS) to progression free rate (PFR) A discordance was also found, between the intention to treat and per protocol population, OS outcome For that reason, the selection of patients who might benefit from CN is of great importance In our review, most of the studies evaluating the effect of CN in OS showed a benefit of CN (1425, 27-42) Although most of these studies are retrospective and observational, their results cannot be overlooked In three studies that used ICIs (2, 40, 42), CN demonstrated an OS benefit Given the absence of prospective studies with patients treated with ICIs, these results underline the importance of CN in the mRCC treatment
Prognostic factors have been described, with age, tumor histology, number of metastasis and T stage being the most common There are also two prognostic models allowing patient risk stratification: MSKCC and IMDC risk scores (34, 63) These models stratify patients in favor, intermediate and poor risk categories, using performance status (PS), time from diagnosis to treatment, hemoglobin concentration, calcium level and lactate dehydrogenase level as criteria According to current evidence, poor MSKCC/IMDC risk patients do not seem to benefit from upfront CN (33, 34) while other patients such as those with good risk prognosis and good PS seem to benefit the most from CN It should be noted however, that MSKCC/IMDC prognostic scores were originally designed to predict OS in patients with mRCC, and not the OS benefit associated with CN (65) That shows the need for new validated prognostic models Among patients that were found to benefit from CN, the optimal sequence between CN and TT is not yet well established, as was also documented in our review
Deferred CN demonstrated better results, in more studies
than upfront CN (7, 23, 38, 47, 48) but a certain advantage was not clear
Despite the new insights into the treatment of mRCC patients that CARMENA and SURTIME provided, TKIs are not anymore considered the standard of care as ICIs have been established as first-line therapy in mRCC patients Three randomized trials: The CheckMate-214 (nivolumab plus ipilimumab vs sunitinib), KEYNOTE426 (pembrolizumab plus axitinib vs sunitinib), and JAVELIN Renal 101 (avelumab plus axitinib vs sunitinib) demonstrated the superiority of ICIs in the treatment of m R C C w h e r e a s s u n i t i n i b a n d o t h e r V E G F R - T K I monotherapies are reserved for those who cannot tolerate ICI combination or have no access to these drugs(9-11)
What we already know from CARMENA and SURTIME has to be re-evaluated Singla et al (24) in the first retrospective analysis of the role of CN in the immunotherapy era, demonstrated an OS benefit for those patients treated with ICI plus CN compared to ICI alone (HR 0 23; 95% CI 0 15-0 37) In this regard, further data from high level of evidence studies are required in order to define the role of CN in the modern immune oncology (IO) era Currently there are two RCTs underway, to guide us to that The PROBE trial (NCT04510597) will evaluate the combination of CN followed by IO or TKI+ IO compared to no CN The NORDIC-SUN trial (NCT03977571) will evaluate the role of deferred CN in patients receiving combination IO
We acknowledge that the present study had several limitations The major limitations were the retrospective nature of the studies included and the small number of studies having ICIs as the main agent used The retrospective nature could have resulted in selection bias in performance of CN Moreover, many studies come from an era when systemic therapies were not well established
CONCLUSIONS
The role of CN on mRCC treatment remains a controversial issue Data from most recent studies have questioned the benefit from CN, shifting the first line treatment from surgical to medical CN can still play an important role in wisely selected patients, although the role of CN in the new immunotherapy era still needs to be defined
REFERENCES
1 Flanigan RC, Salmon SE, Blumenstein BA, et al Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer N Engl J Med 2001; 345:1655-9
2 Mickisch GH, Garin A, van Poppel H, et al Radical nephrectomy plus interferon-alfa-based immunotherapy compared with interferon alfa alone in metastatic renal-cell carcinoma: a randomised trial Lancet 2001; 358:966-70
3 Flanigan RC, Mickisch G, Sylvester R, et al Cytoreductive nephrectomy in patients with metastatic renal cancer: a combined analysis J Urol 2004; 171:1071-6
4 Motzer RJ, Hutson TE, Tomczak P, et al Sunitinib versus interferon alfa in metastatic renal-cell carcinoma N Engl J Med 2007; 356:115-24
5 Coppin C, Le L, Porzsolt F, Wilt T Targeted therapy for
483 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Nephrectomy for metastatic renal cell carcinoma
S Katsimperis, L Tzelves, T Bellos, K Pikramenos, I Manolitsis, I Tsikopoulos, I Mitsogiannis
advanced renal cell carcinoma Cochrane Database Syst Rev 2008:CD006017
6 Méjean A, Ravaud A, Thezenas S, et al Sunitinib alone or after nephrectomy in metastatic renal-cell carcinoma N Engl J Med 2018; 379:417-427
7 Bex A, Mulders P, Jewett M, et al Comparison of immediate vs deferred cytoreductive nephrectomy in patients with synchronous metastatic renal cell carcinoma receiving sunitinib The SURTIME Randomized Clinical Trial JAMA Oncol 2019; 5:164-170
8 Motzer RJ, Tannir NM, McDermott DF, et al Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma N Engl J Med 2018; 378:1277-1290
9 Rini BI, Plimack ER, Stus V, et al Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma N Engl J Med 2019; 380:1116-1127
10 Motzer RJ, Penkov K, Haanen J, et al Avelumab plus axitinib versus sunitinib for advanced renal-cell carcinoma N Engl J Med 2019; 380:1103-1115
11 Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement J Clin Epidemiol 2009; 62:1006-1012
12 Higgins JP, Altman DG, Gotzsche PC, et al The Cochrane Collaboration's tool for assessing risk of bias in randomised trials BMJ 2011; 343:d5928
13 Sterne JA, Hernan MA, Reeves BC, et al ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions BMJ 2016; 355:i4919
14 Conti SL, Thomas IC, Hagedorn JC, et al Utilization of cytoreductive nephrectomy and patient survival in the targeted therapy era Int J Cancer 2014; 134:2245-52
15 Aizer AA, Urun Y, McKay RR, et al Cytoreductive nephrectomy in patients with metastatic non-clear-cell renal cell carcinoma (RCC) BJU Int 2014; 113:E67-74
16 Abern MR, Scosyrev E, Tsivian M, et al Survival of patients undergoing cytoreductive surgery for metastatic renal cell carcinoma in the targeted-therapy era Anticancer Res 2014; 34:2405-11
17 Vaishampayan U, George J, Vigneau F Predictors of Cytoreductive Nephrectomy for Metastatic Kidney Cancer in SEER and Metropolitan Detroit Databases J Kidney Cancer VHL 2019; 6:13-25
18 Zhao Z, Wu W, Duan X, et al The value of cytoreductive nephrectomy on the survival of metastatic renal carcinoma patients based on the number of site-specific metastases PLoS One 2019; 14:e0215861
19 Marchioni M, Bandini M, Preisser F, et al Survival after Cytoreductive Nephrectomy in Metastatic Non-clear Cell Renal Cell Carcinoma Patients: A Population-based Study Eur Urol Focus 2019; 5:488-496
20 Palumbo C, Mistretta FA, Knipper S, et al Contemporary Cytoreductive Nephrectomy Provides Survival Benefit in Clear-cell Metastatic Renal Cell Carcinoma Clin Genitourin Cancer 2020; 18:e730-e738
21 Luzzago S, Palumbo C, Rosiello G, et al Association Between Systemic Therapy and/or Cytoreductive Nephrectomy and Survival in Contemporary Metastatic Non-clear Cell Renal Cell Carcinoma Patients Eur Urol Focus 2021; 7:598-607
22 Alnimer Y, Qasrawi A, Yan D, Wang P Prognostic Impact of Cytoreductive Nephrectomy in Patients with Metastatic Renal Cell Carcinoma: Data from a Large Population-Based Database Urol J 2021; 19:111-119
23 Hanna N, Sun M, Meyer CP, et al Survival Analyses of Patients With Metastatic Renal Cancer Treated With Targeted Therapy With or Without Cytoreductive Nephrectomy: A National Cancer Data Base Study J Clin Oncol 2016; 34:3267-75
24 Singla N, Hutchinson RC, Ghandour RA, et al Improved survival after cytoreductive nephrectomy for metastatic renal cell carcinoma in the contemporary immunotherapy era: An analysis of the National Cancer Database Urol Oncol 2020; 38:604 e9-604 e17 25
26 Janisch F, Hillemacher T, Fuehner C, et al The impact of cytoreductive nephrectomy on survival outcomes in patients treated with tyrosine kinase inhibitors for metastatic renal cell carcinoma in a real-world cohort Urol Oncol 2020; 38:739 e9-739 e15
27 You D, Jeong IG, Ahn JH, et al The value of cytoreductive nephrectomy for metastatic renal cell carcinoma in the era of targeted therapy J Urol 2011; 185:54-9
2 8 G r a h a m J , W e l l s J C , D o n s k o v F , e t a l C y t o r e d u c t i v e Nephrectomy in Metastatic Papillary Renal Cell Carcinoma: Results from the International Metastatic Renal Cell Carcinoma Database Consortium Eur Urol Oncol 2019; 2:643-648
29 Klatte T, Fife K, Welsh SJ, et al Prognostic effect of cytoreductive nephrectomy in synchronous metastatic renal cell carcinoma: a comparative study using inverse probability of treatment weighting World J Urol 2018; 36:417-425
30 You D, Jeong IG, Song C, et al Analysis of pre-operative variables for identifying patients who might benefit from upfront cytoreductive nephrectomy for metastatic renal cell carcinoma in the targeted therapy era Jpn J Clin Oncol 2015; 45:96-102
31 Tatsugami K, Shinohara N, Kondo T, et al Role of cytoreductive nephrectomy for Japanese patients with primary renal cell carcinoma in the cytokine and targeted therapy era Int J Urol 2015; 22:736-40
32 Day D, Kanjanapan Y, Kwan E, et al Benefit from cytoreductive nephrectomy and the prognostic role of neutrophil-to-lymphocyte ratio in patients with metastatic renal cell carcinoma Intern Med J 2016; 46:1291-1297
33 Choueiri TK, Xie W, Kollmannsberger C, et al The impact of cytoreductive nephrectomy on survival of patients with metastatic renal cell carcinoma receiving vascular endothelial growth factor targeted therapy J Urol 2011; 185:60-6
34 Heng DY, Wells JC, Rini BI, et al Cytoreductive nephrectomy in patients with synchronous metastases from renal cell carcinoma: results from the International Metastatic Renal Cell Carcinoma Database Consortium Eur Urol 2014; 66:704-10
35 de Groot S, Redekop WK, Sleijfer S, et al Survival in Patients With Primary Metastatic Renal Cell Carcinoma Treated With Sunitinib With or Without Previous Cytoreductive Nephrectomy: Results From a Population-based Registry Urology 2016; 95:121-7
36 Poprach A, Holanek M, Chloupkova R, et al Cytoreductive Nephrectomy and Overall Survival of Patients with Metastatic Renal Cell Carcinoma Treated with Targeted Therapy-Data from the National Renis Registry Cancers (Basel) 2020; 12:2911
37 Song Y, Du CX, Zhang W, et al Impact of Cytoreductive Nephrectomy on Survival in Patients with Metastatic Renal Cell Carcinoma Treated by Targeted Therapy Chin Med J (Engl) 2016; 129:530-5
38 Bhindi B, Graham J, Wells JC, et al Deferred Cytoreductive Nephrectomy in Patients with Newly Diagnosed Metastatic Renal Cell Carcinoma Eur Urol 2020; 78:615-623
39 Patel MI, Beattie K, Bang A, et al Cytoreductive nephrectomy for metastatic renal cell carcinoma: inequities in access exist despite improved survival Cancer Med 2017; 6:2188-2193
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
484
Cytoreductive Nephrectomy for Patients with Metastatic Renal Cell Carcinoma: Real World Data from Canadian Centers Eur Urol Focus 2021:S2405-4569(21)00276-5
41 Méjean A, Ravaud A, Thezenas S, et al Sunitinib Alone or after Nephrectomy in Metastatic Renal-Cell Carcinoma N Engl J Med 2018; 379:417-427
42 Bakouny Z, Xie W, Dudani S, et al Cytoreductive nephrectomy (CN) for metastatic renal cell carcinoma (MRCC) treated with immune checkpoint inhibitors (ICI) or targeted therapy (TT): A propensity score-based analysis Journal of Clinical Oncology 2020; 38(6 suppl): 608-608
43 Wood CG, Margulis V Neoadjuvant (presurgical) therapy for renal cell carcinoma: a new treatment paradigm for locally advanced and metastatic disease Cancer 2009; 115(10 Suppl):2355-60
44 Stroup SP, Raheem OA, Palazzi KL, et al Does timing of cytoreductive nephrectomy impact patient survival with metastatic renal cell carcinoma in the tyrosine kinase inhibitor era? A multi-institutional study Urology 2013; 81:805-11
45 Macleod LC, Odisho AY, Tykodi SS, et al Comparative Effectiveness of Initial Surgery vs Initial Systemic Therapy for Metastatic Kidney Cancer in the Targeted Therapy Era: Analysis of a Population-based Cohort Urology 2018; 113:146-152
46 Bhindi B, Habermann EB, Mason RJ, et al Comparative Survival following Initial Cytoreductive Nephrectomy versus Initial Targeted Therapy for Metastatic Renal Cell Carcinoma J Urol 2018; 200:528-534
47 Kapoor A, Wong ECL, Fang W, Wong NC Upfront cytoreductive nephrectomy vs upfront systemic therapy in metastatic kidney cancer Can Urol Assoc J 2019; 13:E377-E381
48 de Bruijn R, Wimalasingham A, Szabados B, et al Deferred Cytoreductive Nephrectomy Following Presurgical Vascular Endothelial Growth Factor Receptor-targeted Therapy in Patients with Primary Metastatic Clear Cell Renal Cell Carcinoma: A Pooled Analysis of Prospective Trial Data Eur Urol Oncol 2020; 3:168-173
49 Abel EJ, Spiess PE, Margulis V, et al Cytoreductive Nephrectomy for Renal Cell Carcinoma with Venous Tumor Thrombus J Urol 2017; 198:281-288
50 dashek JJ, Zhang Y, Skelton WP 4th, et al Dissecting Outcomes: Should Cytoreductive Nephrectomy Be Performed for Patients With Metastatic Renal Cell Carcinoma With Sarcomatoid Dedifferentiation? Front Oncol 2021; 10:627025
5 1 C o r c o r a n A T , K a f f e n b e r g e r S D , C l a r k P E , e t a l Hypoalbuminaemia is associated with mortality in patients undergoing cytoreductive nephrectomy BJU Int 2015; 116:351-7
52 Culp SH, Tannir NM, Abel EJ, et al Can we better select patients with metastatic renal cell carcinoma for cytoreductive nephrectomy? Cancer 2010; 116:3378-88
53 Culp SH, Karam JA, Wood CG Population-based analysis of factors associated with survival in patients undergoing cytoreductive nephrectomy in the targeted therapy era Urol Oncol 2014; 32:561-8
54 Kalogirou C, Mulfinger P, Sokolakis I, et al Preoperative CReactive Protein Values as a Potential Component in Outcome Prediction Models of Metastasized Renal Cell Carcinoma Patients Receiving Cytoreductive Nephrectomy Urol Int 2017; 99:297-307
55 Kapoor A, Wong ECL, Fang W, Wong NC Upfront cytoreductive nephrectomy vs upfront systemic therapy in metastatic kidney cancer Can Urol Assoc J 2019; 13:E377-E381
56 Klatte T, Fife K, Welsh SJ, et al Prognostic effect of cytoreduc-
tive nephrectomy in synchronous metastatic renal cell carcinoma: a comparative study using inverse probability of treatment weighting World J Urol 2018; 36:417-425
57 Ljungberg B, Sundqvist P, Lindblad P, et al Survival advantage of upfront cytoreductive nephrectomy in patients with primary metastatic renal cell carcinoma compared with systemic and palliative treatments in a real-world setting Scand J Urol 2020; 54:487-492
58 McIntosh AG, Umbreit EC, Holland LC, et al Optimizing patient selection for cytoreductive nephrectomy based on outcomes in the contemporary era of systemic therapy Cancer 2020; 126:39503960
59 Rosiello G, Knipper S, Palumbo C, et al Unmarried status is a barrier for access to treatment in patients with metastatic renal cell carcinoma Int Urol Nephrol 2019; 51:2181-2188
60 Sharma P, Zargar-Shoshtari K, Caracciolo JT, et al Sarcopenia as a predictor of overall survival after cytoreductive nephrectomy for metastatic renal cell carcinoma Urol Oncol 2015; 33:339 e17-23
61 Sakai I, Miyake H, Hinata N, Fujisawa M Improved survival in patients with metastatic renal cell carcinoma undergoing cytoreductive nephrectomy in the era of targeted therapy Int J Clin Oncol 2014; 19:674-8
62 Teishima J, Ohara S, Shinmei S, et al Normalization of C-reactive protein levels following cytoreductive nephrectomy in patients with metastatic renal cell carcinoma treated with tyrosine kinase inhibitors is associated with improved overall survival Urol Oncol 2018; 36:339 e9-339 e15
63 Motzer RJ, Bacik J, Schwartz LH, et al Prognostic factors for survival in previously treated patients with metastatic renal cell carcinoma J Clin Oncol 2004; 22:454-63
64 Westerman ME, Shapiro DD, Tannir NM, et al Survival following cytoreductive nephrectomy: a comparison of existing prognostic models BJU Int 2020; 126:745-753
65 Uprety D, Bista A, Smith AL, et al Cytoreductive Nephrectomy in Elderly Patients with Metastatic Renal Cell Carcinoma in the Targeted Therapy Era Anticancer Res 2018; 38:3013-3018
Correspondence
Stamatios Katsimperis, MD stamk1992@gmail com
Lazaros Tzelves, MD lazarostzelves@gmail com
Themistoklis Bellos, MD bellos themistoklis@yahoo com
Konstantinos Pikramenos, MD k pikramenos@gmail com
Ioannis Manolitsis, MD giannismanolit@gmail com
Ioannis Tsikopoulos, MD Ioannistsikopoulos@yahoo com
Iraklis Mitsogiannis, MD imitsog@med uoa gr
Department of Urology, Athens, Greece
485 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Nephrectomy for metastatic renal cell carcinoma 4 0 D r a g o m i r A , N a z h a S , T a n g u a y S , e t a l O u t c o m e s o f
Diagnosis and management of intradiverticular bladder tumours: A pooled analysis of 498 cases
Stamatios Katsimperis, Lazaros Tzelves, Themistoklis Bellos, Panagiotis Angelopoulos, Ioannis Tsikopoulos, Iraklis Mitsogiannis, Athanasios Papatsoris
Summary
Objective: Intradiverticular bladder tumors (IDBT) are uncommon clinical entities We reviewed the literature for clinical presentation, diagnosis and therapeutic options to establish recommendations for diagnostic and therapeutic management.
Methods: Bibliographic research was performed using PubMed from database inception until October 15, 2022. A pooled analysis was performed of 498 patients with IDBT presented in the literature. The evaluation included patient sex, age, diagnostic methods, symptoms, localization of the tumor, tumor staging, tumor histopathology, treatment, and the presence of recurrence To express results, descriptive statistics were used appropriately
Results: The mean age at diagnosis was 64 81 years (range 49 days to 84 years) The ratio between men and women was ≈ 24:1, suggesting a male predominance (85% male, 3 6% female) The most common presenting symptom was gross hematuria (60 88%) Most of the patients had cystoscopy (56 85%) and intravenous or computed tomography urography (52 01%) Regarding tumor staging, most of the patients were diagnosed with pT1 tumors For the histopathology of IDBT, 87 95% of the specimens were transitional cell carcinomas and in 10.84% there were concomitant CIS Regarding the treatment, radical cystectomy was chosen in 34.34%, partial cystectomy in 26.66%, diverticulectomy in 15 95% and transurethral resection of bladder tumour (TURBT) in 16.36% of the patients.
Conclusions: Most common diagnostic tool for IDBT seems to be cystoscopy followed by computerized tomography urogram. Due to the absence of muscle layer in the diverticulum and the highgrade histology of most of them at diagnosis, cystectomy is the first therapeutic choice However, for patients that are not considered appropriate candidates or for those presenting with lowgrade and low volume tumors, TURBT is a good option
KEY WORDS: Intradiverticular bladder tumors; Bladder diverticular carcinoma; Urothelial carcinoma; Bladder diverticulum
Submitted 15 November 2022; Accepted 7 December 2022
INTRODUCTION
Bladder diverticula are outpouchings of the bladder wall devoid of a functional muscularis propria lining (1) The lack of a muscle layer results in a loss of contractility, which in turn results in urine stasis in the diverticulum This chronic irritation can lead to chronic inflammation and an increased risk of neoplasms, owing to a prolonged
exposure to carcinogens such as aromatic amines from cigarette smoke (1) Intradiverticular bladder tumours (IDBT) account for approximately 1% of all urinary bladder tumors (2) Therefore, they pose a unique diagnostic and therapeutic challenge Considering the scarceness of intradiverticular bladder tumours it is not surprising that there are no standard guidelines for the diagnosis and management We performed a pooled analysis of 498 cases of intradiverticular bladder tumours collected from the international literature, in order to completely characterize the entity in relation to epidemiological, medical and surgical aspects
METHODS
This review was conducted in accordance with the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) (3) Bibliographic research was performed using PubMed from database inception until October 15, 2022 The following medical subject heading terms were used in combination with Boolean operators (AND, OR, NOT): bladder diverticulum, bladder diverticula, intradiverticular, bladder tumor, bladder cancer, carcinoma Two independent reviewers (K S, T L) screened all the articles retrieved by the initial search All disagreements were resolved with discussion, and final decision was reached by consensus with a third reviewer (P A ) Reference lists were systematically searched for potentially eligible, missed studies Fifty-nine articles were found in total Among these, we spotted 498 welldocumented cases of intradiverticular bladder tumors (Figure1) (1, 4-61) Retrieved articles were carefully studied and a database with the patients’ characteristics was made (see Supplementary Materials) The database included sex, age, diagnostic methods, symptoms, localization of the tumor, tumor staging, tumor histopathology, treatment and recurrence The cases that fulfilled most of these criteria have been included in the statistical analysis Excluded studies met ≥ 1 of the following criteria: (a) irrelevant to the subject studies, (b) studies published in a non-English language, (c) reviews and metaanalyses, and (d) editorials, perspectives, and letters to the editors An ethical approval is not required because this study is a review of the existing international literature To express results, descriptive statistics were used appropriately
declared
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 486 REVIEW No conflict of interest
DOI: 10 4081/aiua 2022 4 486
Second Department of Urology, National and Kapodistrian University of Athens, Sismanogleio General Hospital, Athens, GRC
RESULTS
Characteristics of IDBT were determined concerning sex, age diagnostic methods, symptoms, localization of the tumor, tumor staging, tumor histopathology, treatment and recurrence
Gender
Concerning gender, 85% of the patients were male (431 patients), while 3 6% were female (18 patients) There were no data regarding gender for 49 patients The ratio between men and women was ≈ 24:1, suggesting a male predominance in the reported IDBT population
Age
Mean age of the population was 64 81 years, ranging from 49 to 84 years It is concluded that IDBT most frequently appeared in age range from 60 to 70 years
Diagnostic methods
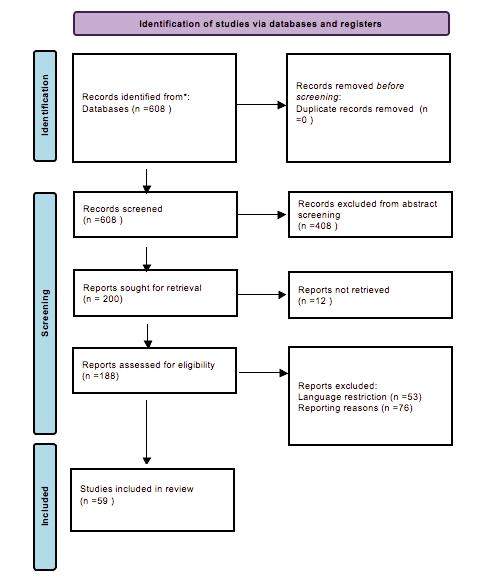
The most useful tool was cystoscopy (141/248 patients, 56 85%), followed by intravenous/computed tomography
urography (IVU/CTU) (129/248 patients, 52 01%) as shown in Figure 2 Other imaging techniques used were c o m p u t e d t o m o g r a p h y ( C T ) s c a n ( 4 6 / 2 4 8 p a t i e n t s ,
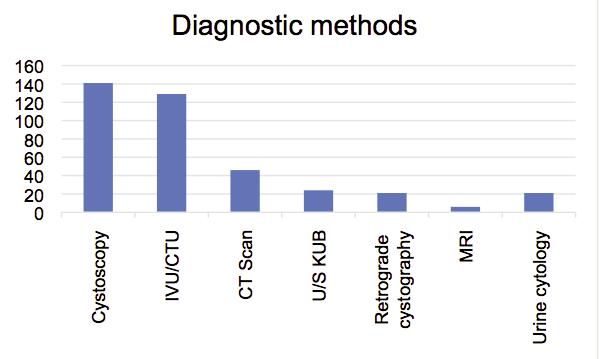
487 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Intradiverticular bladder tumours
Figure 1. Flow chart of papers selection
Figure 2.
Diagnostic methods
S Katsimperis, L Tzelves, T Bellos, P Angelopoulos, I Tsikopoulos, I Mitsogiannis, A Papatsoris
18 54%) and ultrasound (U/S) of Kidneys, Ureters, and Bladder (KUB) (24/248 patients, 9 67%); retrograde cystography (21/248 patients, 8 46%) is still of great importance for the diagnosis of IDBT Last but not least, magnetic resonance imaging (MRI) can be a helpful tool for the differential diagnosis of IDBT In the laboratory tests, 21 of 248 patients (8 46%), underwnt a urine cytology test for the detection of IDBT
Presenting symptoms
IDBT can present with a wide variety of symptoms, ranging from gross hematuria to symptoms of urinary tract infections (UTI) Our statistical analysis has shown that the most frequent symptom is gross hematuria (151/248 patients 60 88%) Eight patients presented with microhematuria (3 22%), 8 patients had frequency (3 22%) and 11 had dysuria (4 43%) Lower urinary tract symptoms ( L U T S ) , o b s t r u c t i v e s y m p t o m s , u r i n a r y r e t e n t i o n , hydronephrosis, pain, loss of weight and UTI were found in 23 (9 27%), 15 (6 04%), 2 (0 8%), 7 (1 4%), 6 (2 82%), 2 (0 8%) and 14 (5 64%) patients respectively
Tumor localization
Pooled analysis included limited data concerning tumor localization that was mentioned in only 66 patients Most common site was right lateral wall (19/66 patients, 28 78%), while left lateral wall was the second one (16/66 patients, 24 24%) IDBT appeared above right and left orifice in 9 and 8 patients respectively (13 63% and 12 12%) Nine patients (13 63%) had an IDBT in the posterior wall The base of the bladder (2/66 patients, 3 03%), dome (1/66 patients, 1 51%), anterior wall (1/66 patients, 1 51%) and trigone (1/66 patients, 1 51%) represent rarer locations of IDBT
Tumor staging
Regarding tumor staging, most of the patients were diagnosed as pT1 tumors (117 patients), followed by those diagnosed with pT2 tumors (33 patients) Patients with pTa, pT3 and pT4 tumors were 2, 19 and 1 respectively Pooled analysis of tumor grade using low grade (LG)/high grade (HG) and G1/G2/G3 classification resulted in 28 patients with LG tumors, 128 patients with HG tumors, 15 patients with G1 tumors, 24 patients with G2 tumors and 31 patients with G3 tumors
Tumor histopathology
In relation to histopathology of IDBT, most of them presented as transitional cell carcinomas (TCC) (438 patients, 87 95%) Squamous cell carcinomas come followed with 26 patients (5 22%) Small cell carcinomas, adenocarcinomas and sarcomatoid carcinomas were 8, 6 and 8 cases respectively Worth of mention is the presence of concomitant carcinoma in situ (CIS) in 54 patients (10 84%)
Treatment
Regarding the treatment applied, radical cystectomy has been chosen in 170 of 495 patients (34 34%), whereas partial cystectomy in 132 patients (26 66%) Seventynine (79) patients underwent diverticulectomy (15 95%) Transurethral resection of bladder tumor (TURBT) was performed in 81 patients (16 36%) and out of them 14
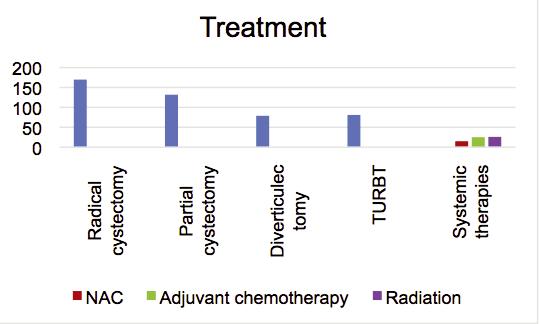
(2 82%) had also intravesical therapy as part of their t r e a t m e n t S y s t e m i c t h e r a p i e s s u c h a s n e o a d j u v a n t chemotherapy, adjuvant chemotherapy and radiation were applied in 15 (3 03%), 25 (5 05%) and 26 (5 25%) patients respectively Figure 3 summarizes all the above treatments
Recurrence
Pooled analysis resulted in a recurrence rate of 19 07% (95 patients)
DISCUSSION
Intradiverticular bladder tumors are uncommon clinical entities, with only few studies reported in the literature Their rarity make diagnosis and management a unique challenge They were first described by Targett in 1896 (62) and account for approximately 1% of bladder tumors IDBT seem to have a male predilection (male: female ratio, 24:1) and they more frequently appear in the sixth decade
The diagnosis of IDBT is usually like that used for other tumors of the bladder, based on the cystoscopy and imaging findings In some patients the anatomy of the bladder diverticulum may not help to perform a cystoscopy (narrow neck of the diverticulum) However, in most cases cystoscopy is the main diagnostic test used and cannot be excluded from the diagnostic procedure A variety of imaging techniques can be used to evaluate IDBT Ultrasonographically, IDBT present as a mostly echo-free outpouching that protrudes outside the urinary bladder outlines with an echogenic soft-tissue lesion projecting inside it It has been found that ultrasonography is useful for diagnosing larger tumors but its sensitivity is poor if the IDBT is < 1 cm in diameter (63) In our review ultrasonography was reported as a useful tool for the first assessment of hematuria related with IDBT but further imaging techniques were usually needed such as CT scan and CT urography CT gives further details regarding extravesical extension and tumor stage Among laboratory tests, urine cytology, due to its low sensitivity for lowgrade tumors, has not been used very often (8 46%)
IDBT display a great variety of symptoms
The majority of cases present with gross hematuria Hydronephrosis and pain can also appear due to obstruction ofe ureteric orifices LUTS and symptoms of urinary tract infections are
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
488
Figure 3
Treatment
common mostly because of the presence of the diverticulum rather than the tumor itself Our study supported the assumption that the most common clinical manifestation of IDBT is gross hematuria, while LUTS are the second most frequent clinical presentation
Regarding location of IDBT, it extends from lateral wall to the dome The majority arise from right and left lateral wall followed by those above the ureteric orifices Most of the tumors reported in our study were TCC high grade and more specifically pT1 ones Although squamous cell carcinomas were not even close in numbers to the TCC they cannot be overlooked, as they represent a not so rare manifestation (5 22%)
Regarding treatment all scientists agree that IDBT should be excised when diagnosed The main surgical approach was radical cystectomy (34 34%) followed by partial cystectomy (26 66%) The predominance of high-grade, that was mentioned before and the recurrence rate of 18 67% which many times resulted in an upstaging of the tumor were the main reason for that choice Interestingly, Voskuilen et al (11), in their retrospective study, presenting the largest series of IDBT published so far, showed that although upstaging was frequent in the patients that underwent partial rather than radical cystectomy, there was no difference in overall survival In another study from Kong et al (12) including 36 patients, 28 of them had partial cystectomy or diverticulectomy as primary treatment without compromising cancer related survival Similar results are presented in two more studies (13, 16) Golijanin et al (16), supported that patients with low or high grade Ta tumors may be treated conservatively (either by complete TUR or partial cystectomy) providing a close surveillance after treatment In a more recent study Bourgi et al (13), concluded that conservative management is feasible even in high grade tumors or in patients presenting with CIS In view of these facts, a fair n u m b e r o f p a t i e n t s w e r e t r e a t e d w i t h l e s s r a d i c a l approaches such as diverticulectomy (15 95%) or TURBT (16 36%) They usually presented with low-grade and low volume tumors
In our review, most of the studies included were case reports or small case series with insufficient case number and short follow-up time Multiple case reports indicated that poor outcome was the result of difficult and delayed diagnosis, leading to early invasion and advanced disease at presentation That was the reason for the predominance of radical cystectomy as therapeutic approach There was also a correlation of the year of published studies and the treatment applied In the past it was widely accepted that IDBT had an ominous prognosis so the management was more radical Data from most recent studies have questioned the benefit of radical approach for IDBT, shifting the primary treatment to less invasive techniques
We acknowledge that the present study had several limitations The major limitations were the retrospective nature of the studies included, the large numbers of case reports and the lack of long follow-up time in most of them However, to the best of our knowledge this is the first attempt to present a thorough review of a clinical entity that was much overlooked in the published literature
CONCLUSIONS
Most common diagnostic tool for IDBT seems to be cystoscopy followed by CTU The relative rarity of IDBT makes their management challenging because as there is no clear consensus about it Although cystectomy seems a much more morbid procedure compared to less invasive techniques such as TURBT, the absence of muscle layer in the diverticulum and the high-grade histology of most of them, makes it the most likely therapeutic choice However, it has been proved that less invasive techniques such as partial cystectomy, diverticulectomy or TUBT can be applied in wisely selected patients with similar clinical outcomes
REFERENCES
1 Kelalis PP, McLean P The treatment of diverticulum of the bladder J Urol 1967; 98:349-52
2 Walker NF, Gan C, Olsburgh J, Khan MS Diagnosis and management of intradiverticular bladder tumours Nat Rev Urol 2014; 11:383-90
3 Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement J Clin Epidemiol 2009; 62:1006-12
4 Knappenberger ST, Uson AC, Melicow MM Primary neoplasms occurring in vesical diverticula: a report of 18 cases J Urol 1960; 83:153-9
5 Baniel J, Vishna T Primary transitional cell carcinoma in vesical diverticula Urology 1997; 50:697-9
6 Garzotto MG, Tewari A, Wajsman Z Multimodal therapy for neoplasms arising from a vesical diverticulum J Surg Oncol 1996; 62:46-8
7 Montague DK, Boltuch RL Primary neoplasms in vesical diverticula: report of 10 cases J Urol 1976; 116:41-2
8 Redman JF, McGinnis TB, Bissada NK Management of neoplasms in vesical diverticula Urology 1976; 7:492-4
9 Raheem OA, Besharatian B, Hickey DP Surgical management of bladder transitional cell carcinoma in a vesicular diverticulum: case report Can Urol Assoc J 2011; 5:E60-4
10 Faysal MH, Freiha FS Primary neoplasm in vesical diverticula A report of 12 cases Br J Urol 1981; 53:141-3
11 Voskuilen CS, Seiler R, Rink M, et al ; Young Academic Urologists’ Working Group on Urothelial Carcinoma of the European A s s o c i a t i o n o f U r o l o g y U r o t h e l i a l C a r c i n o m a i n B l a d d e r Diverticula: A Multicenter Analysis of Characteristics and Clinical Outcomes Eur Urol Focus 2020 Nov 15; 6:1226-1232
12 Kong MX, Zhao X, Kheterpal E, et al Histopathologic and clinical features of vesical diverticula Urology 2013; 82:142-7
1 3 B o u r g i A , A y o u b E , M e r h e j S D i v e r t i c u l e c t o m y i n t h e Management of Intradiverticular Bladder Tumors: A Twelve-Year Experience at a Single Institution Adv Urol 2016; 2016:2345306
14 Melekos MD, Asbach HW, Barbalias GA Vesical diverticula: etiology, diagnosis, tumorigenesis, and treatment Analysis of 74 cases Urology 1987; 30:453-7
15 Di Paolo PL, Vargas HA, Karlo CA, et al Intradiverticular bladder cancer: CT imaging features and their association with clinical outcomes Clin Imaging 2015; 39:94-8
16 Golijanin D, Yossepowitch O, Beck SD, et al Carcinoma in a
489 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Intradiverticular bladder tumours
S Katsimperis, L Tzelves, T Bellos, P Angelopoulos, I Tsikopoulos, I Mitsogiannis, A Papatsoris
bladder diverticulum: presentation and treatment outcome J Urol 2003; 170:1761-4
17 Zhong H, George S, Kauffman E, et al Clinicopathologic characterization of intradiverticular carcinoma of urinary bladder - a study of 22 cases from a single cancer center Diagn Pathol 2014; 9:222
18 Hu B, Satkunasivam R, Schuckman A, et al Urothelial carcinoma in bladder diverticula: outcomes after radical cystectomy World J Urol 2015; 33:1397-402
19 Yu CC, Huang JK, Lee YH, et al Intradiverticular tumors of the bladder: surgical implications--an eleven-year review Eur Urol 1993; 24:190-6
20 Md Noh MS, Abdul Aziz AF, Mohd Ghani KA, et al Giant Intradiverticular Bladder Tumor Am J Case Rep 2017; 18:212-216
21 Sah AK, Maharjan B, Adhikari MB, et al Radical Cystectomy for Intradiverticular Bladder Carcinoma: A Case Report JNMA J Nepal Med Assoc 2021; 59:1069-1071
22 Al-Hajjaj M High-grade intradiverticulum bladder tumor: A case report Int J Surg Case Rep 2021; 83:106057
23 Dong WX, Ping YX, Liang WC, et al Small cell carcinoma of the urinary bladder diverticulum: a case report and review of the literature J Cancer Res Ther 2013 Jan-Mar; 9:151-3
24 Grubišic I, Lenicek T, Tomas D, et al Primary osteosarcoma of bladder diverticulum mimicking intradiverticular calculus: a case report Diagn Pathol 2011; 6:37 doi: 10 1186/1746-1596-6-37
25 Thwaini A, McLeod A, Nambirajan T Laparoscopic bladder diverticulectomy J Laparoendosc Adv Surg Tech A 2008; 18:849-51
2 6 A b d u l r a h m a n S A , M u h a m m a d I , A b d u l r a h m a n A , e t al Urothelial carcinoma arising within a congenital bladder diverticulum in an adult male: A rare case report and literature review Ann Med Surg (Lond) 2022; 77:103666
27 Sousa Escandón A, Garcia R, Argüelles M, et al Carcinosarcoma in a bladder diverticulum A case report and literature review Urol Int 2000; 65:169-72
28 Rabin JM, Hirschfield L, Badlani GH Type IX Ehlers-Danlos syndrome: bladder diverticula with transitional cell carcinoma Urology 1991; 38:563-6
29 Shah B, Rodriguez R, Krasnokutsky S, et al Tumour in a giant bladder diverticulum: a case report and review of literature Int Urol Nephrol 1997; 29:173-9
30 Moussa M, Abou Chakra M Urothelial carcinoma arising from a bladder diverticulum containing multiple stones: A case report Urol Case Rep 2018; 20:80-82
31 Tonzi M, Watson MJ, Singh A Bladder diverticulectomy using a pre-peritoneal, trans-vesicle approach with the SP platform: A novel approach Urol Case Rep 2021; 39:101753
32 Tsuboi I, Maruyama Y, Sadahira T, et al Inflammatory myofibroblastic bladder tumor with divergent behavior in a patient with spinal cord injury IJU Case Rep 2019; 2:212-214
33 Elands S, Vasdev N, Tay A, Adshead JM Robot-Assisted L a p a r o s c o p i c B l a d d e r D i v e r t i c u l e c t o m y a n d U r e t e r a l R eI m p l a n t a t i o n f o r a D i v e r t i c u l u m C o n t a i n i n g H i g h G r a d e Transitional Cell Carcinoma Curr Urol 2015; 8:104-8
34 Haecker A, Riedasch G, Langbein S, et al Diverticular carcinoma of the urinary bladder: diagnosis and treatment problems A case report Med Princ Pract 2005; 14:121-4
35 El Abiad Y, Bakloul F Squamous cell carcinoma in a giant bladder diverticulum Pan Afr Med J 2015; 20:378
36 Omeroglu A, Paner GP, Wojcik EM, Siziopikou K A carcinosarcoma/sarcomatoid carcinoma arising in a urinary bladder diverticulum Arch Pathol Lab Med 2002; 126:853-5
37 Durfee SM, Schwartz LH, Panicek DM, Russo P MR imaging of carcinoma within urinary bladder diverticulum Clin Imaging 1997; 21:290-2
38 Matta EJ, Kenney AJ, Barré GM, Vanlangendonck RM Jr Best c a s e s f r o m t h e A F I P : i n t r a d i v e r t i c u l a r b l a d d e r c a r c i n o m a Radiographics 2005; 25:1397-403
39 Madison BB Papillary carcinoma of a bladder diverticulum treated by transurethral resection J Urol 1948; 59:42
40 García Figueiras R, Sousa Escandón A, García Figueiras A, et al Unusual retrovesical masses in men Eur Radiol 2000; 10:1639-43 4 1 L e m b o F , S u b b a E , L a g a n à A S , e t a l I n t r a d i v e r t i c u l a r Sarcomatoid Carcinoma of The Bladder: An Overview Starting From A Peculiar Case Urol J 2016; 13:2800-2
42 Dragsted J, Nilsson T Urothelial carcinoma in a bladder diverticulum evaluated by transurethral ultrasonography Scand J Urol Nephrol 1985; 19:153-4
43 Knezevic M, Grubisic I, Soipi S, et al C202: A rare case of squamous cell carcinoma in urinary bladder diverticulum successfully treated by bladder - sparing surgery European Urology Supplements 2014; 13:1371
44 Fu LY, Adeniran AJ Adenocarcinoma Arising from a Bladder Diverticulum J Urol 2015; 194:527-8
45 Labanaris AP, Zugor V, Smiszek R, et al Small cell carcinoma encountered in a urinary bladder diverticulum Urol J 2009; 6:546
46 Ozguven S, Maleki R, Ones T, et al Invasive urothelial carcinoma detected in bladder diverticulum with FDG PET/CT: a rare case with negative cystoscopy Rev Esp Med Nucl Imagen Mol 2014; 33:399-400
47 Nanbu A, Tsukamoto T, Kumamoto Y, et al Squamous cell carcinoma of bladder diverticulum with initial symptoms produced by metastasis to maxillary sinus Eur Urol 1988; 15:285-6
48 Siegel WH Neoplasms in bladder diverticula Urology 1974; 4:411-3
49 Muellner SR Cancer in diverticulum of the bladder; a pitfall to the resectionist J Urol 1946; 56:427
50 Wang CK, Chueh SC Laparoscopic partial cystectomy with endo-GIA stapling device in bladder diverticular carcinoma J Endourol 2007; 21:772-5
51 Holck S, Jørgensen L Verrucous carcinoma of urinary bladder Urology 1983; 22:435-7
52 Tudor J, Cantley RL, Jain S Primary small cell carcinoma arising from a bladder diverticulum J Urol 2014; 192:236-7
53 Evans AJ, Al-Maghrabi J, Tsihlias J, et al Primary large cell neuroendocrine carcinoma of the urinary bladder Arch Pathol Lab Med 2002; 126:1229-1232
54 Moinzadeh A, Latini J, Hamawy KJ Clear cell adenocarcinoma of the urinary bladder within a diverticulum Urology 2003; 62:145
55 Cramer SF, Aikawa M, Cebelin M Neurosecretory granules in small cell invasive carcinoma of the urinary bladder Cancer 1981; 47:724-30
56 Pearlman CK, Bobbitt RM Carcinoma within a diverticulum of the bladder J Urol 1948; 59:1127-9
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
490
57 Bjerklund Johansen TE Primary neoplasms in vesical diverticula Reports of two cases Scand J Urol Nephrol 1988; 22:347-8
58 Mayer RF, Moore TD Carcinoma complicating vesical diverticulum J Urol 1954; 71:307-15
59 Shigehara K, Taya T, Hisazumi H Primary adenocarcinoma in the bladder diverticulum Scand J Urol Nephrol 2008; 42:481-3
60 Agarwal M, Azzopardi A, Mufti GR Pyrexia of unknown origin in association with bladder diverticulum tumour Postgrad Med J 1993; 69:403-5
Sarcomatoid Carcinoma with Osseous Metaplasia from Urinary Bladder Diverticulum Indian J Surg Oncol 2017; 8:436-439
62 Targett JH Diverticula of the bladder associated with vesical growths Trans Path Soc Lond 1896; 47:155, 1896
63 Neuzillet Y, Comperat E, Rouprêt M, et al ; Membres du Comité de cancérologie de l’Association française d’urologie Tumeurs de vessie intradiverticulaires: revue du Comité de cancérologie de l'Association française d'urologie Prog Urol 2012; 22:495-502
Correspondence
Stamatios Katsimperis, MD (Corresponding Author) stamk1992@gmail com
Lazaros Tzelves, MD lazarostzelves@gmail com
Themistoklis Bellos, MD bellos themistoklis@yahoo com
Panagiotis Angelopoulos, MD angelopoulospanag@gmail com
Ioannis Tsikopoulos, MD ioannistsikopoulos@yahoo com
Iraklis Mitsogiannis, MD imitsog@med uoa gr
Athanasios Papatsoris, MD agpapatsoris@yahoo gr
Second Department of Urology, National and Kapodistrian University of Athens, Sismanogleio General Hospital, Athens, GRC
491 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Intradiverticular bladder tumours
6 1 M i t t a l V , R u p a l a K K , Y a d a v R , S u r y a v a n s h i M G i a n t
Efficacy of overactive neurogenic bladder treatment: A systematic review of randomized controlled trials
Rawa Bapir 1, 14 , Kamran Hassan Bhatti 2, 14 , Ahmed Eliwa 3, 14 , Herney Andrés García-Perdomo 4, 14 , Nazim Gherabi 5, 14 , Derek Hennessey 6, 14 , Vittorio Magri 7, 14 , Panagiotis Mourmouris 8, 14 , Adama Ouattara 9, 14 , Gianpaolo Perletti 10, 14 , Joseph Philipraj 11, 14 , Konstantinos Stamatiou 12, 14 , Alberto Trinchieri 13, 14 , Noor Buchholz 14
1 Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq;
2 Urology Department, HMC, Hamad Medical Corporation, Qatar;
3 Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt;
4 Universidad del Valle, Cali, Colombia;
5 Faculty of Medicine Algiers 1, Algiers, Algeria;
6 Department of Urology, Mercy University Hospital, Cork, Ireland;
7 ASST Nord Milano, Milan, Italy;
8 2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece;
9 Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso;
10 Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy;
11 Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India;
12 Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece;
13 Urology School, University of Milan, Milan, Italy;
14 U-merge Ltd (Urology for emerging countries), London-Athens-Dubai *
Authors 1-14 have equally contributed to the paper and share first authorship
* U-merge Ltd (Urology for Emerging Countries) is an academic urological platform dedicated to facilitate knowledge transfer in urology on all levels from developed to emerging countries U-merge Ltd is registered with the Companies House in London/ UK www U-merge com
Summary
Background: Overactive bladder (OAB) symptoms of frequency, urgency and urge incontinence are frequently associated with known neurological diseases like multiple sclerosis (MS), spinal cord injury (SCI), Parkinson’s disease (PD), stroke
Objective: The aim of our study was to review the efficacy of pharmacological and non-pharmacological treatments for neurogenic overactive bladder
Materials and methods: We searched two electronic databases (PubMed and EMBASE) for randomized controlled trials focusing on pharmacological and non-pharmacological medical treatments for overactive bladder symptoms associated with neurological diseases published up to 30 April 2022
Results: A total of 157 articles were retrieved; 94 were selected by title and abstract screening; after removal of 17 duplicates, 77 records were evaluated by full-text examination. Sixty-two studies were finally selected The articles selected for review focused on the following interventions: anticholinergics (n = 9), mirabegron (n = 5), comparison of different drugs (n = 3), cannabinoids (n = 2), intravesical instillations (n = 3), botulinum toxin (n = 16), transcutaneous tibial nerve stimulation (TTNS) (n = 6), acupuncture (n = 2), transcutaneous electrical nerve stimulation TENS (n = 4), pelvic floor muscle training (PFMT) (n = 10), others (n = 2).
Anticholinergics were more effective than placebo in decreasing the number of daily voids in patients with PD (mean difference
[MD]- 1 16, 95 % CI - 1 80 to - 0 52, 2 trials, 86 patients, p< 0 004), but no significant difference from baseline was found for incontinence episodes and nocturia Mirabegron was more
effective than placebo in increasing the cystometric capacity in patients with MS (mean difference [MD] 89 89 mL, 95 % CI 29.76 to 150.01, 2 trials, 98 patients, p < 0.003) but no significant difference was observed for symptom scores and bladder diary parameters. TTNS was more effective than its sham-control in decreasing the number of nocturia episodes (MD -1 40, 95 % CI -2.39 to -0.42, 2 trials, 53 patients, p < 0.005) but no significant changes of OAB symptom scores were reported PFMT was more effective than conservative advice in decreasing the ICIQ symptom score (MD, -1 12, 95 % CI -2 13 to -0 11, 2 trials, 91 patients, p = 0 03), although the number of incontinence episodes was not significantly different between groups Conclusions: The results of the meta-analysis demonstrate a moderate efficacy of all considered treatments without proving the superiority of one therapy over the others Combination treatment using different pharmacological and non-pharmacological therapies could achieve the best clinical efficacy due to the favorable combination of the different mechanisms of action This could be associated with fewer side effects due to drug dosage reduction These data are only provisional and should be considered with caution, due to the few studies included in metaanalysis and to the small number of patients.
KEY WORDS: Overactive bladder; Urinary incontinence, Urge; Multiple sclerosis; Ischemic stroke; Parkinson disease; Anticholinergics; Mirabegron; Cannabinoids; Transcutaneous tibial nerve stimulation (TTNS); Pelvic floor muscle training (PFMT)
Submitted 5 November 2022; Accepted 15 November 2022
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 492 REVIEW No conflict of interest declared
DOI: 10 4081/aiua 2022 4 492
INTRODUCTION
Voiding dysfunction often develops in patients with underlying neurological diseases Patients may present with overactive bladder (OAB) symptoms of frequency, urgency and urge incontinence OAB in patients with known neurological diseases (neurogenic overactive bladder) is related to disturbances of the neurological control of micturition
OAB symptoms are highly prevalent among patients with multiple sclerosis (MS), spinal cord injury (SCI), Parkinson’s disease (PD), various neurological diseases, and stroke This was shown by a recent study demonstrating OAB symptoms in over 50% of these patients (1) Symptoms vary from mild lower urinary tract symptoms (LUTS), that are often poorly recognized or misdiagnosed in men as prostatic disease, to severe clinical conditions like those observed after spinal cord injury (SCI) The severity of symptoms depends on the type and degree of damage to the nervous system As the neurological condition progresses, the bladder function progressively deteriorates, and becomes more difficult to treat Incontinence frequently develops as a consequence of disease progression
Conservative management includes pharmacological treatment to reduce the contractility of the detrusor muscle, behavioral therapy and biofeedback, electrical stimulation, or chemical denervation procedures (instillation of capsaicin and resiniferatoxin or intradetrusorial injection of Botulinum toxin) No single treatment exists for neurogenic OAB due to the complexity and individual variability of the underlying neurological diseases Treatment should be tailored to the individual patient, also considering that conventional treatment programs for non-neurogenic OAB could lack clinical efficacy in neurogenic patients
Several systematic reviews have been published in the last 15 years to evaluate the evidence concerning the different treatments for neurogenic OAB (2-13)
In 2012, Madhuvrata and coworkers (2) published a systematic review and meta-analysis on anticholinergic treatment of adult neurogenic OAB, which updated and completed a previous systematic review assessing the efficacy and tolerability of anticholinergic agents in patients with OAB associated to multiple sclerosis (3) A more recent systematic review evaluated the effectiveness and safety of intravesical oxybutynin therapy for patients with neurogenic OAB (4) Two recent systematic reviews addressed the results of pelvic floor muscle training (PFMT) for bladder dysfunction in patients with multiple sclerosis (5, 6) One of these systematic reviews extended its analysis to the results of peripheral tibial nerve stimulation (PTNS) (6)
A systematic review addressed the outcomes of PTNS in the treatment of lower urinary tract dysfunction including neurogenic bladder PTNS was found to be effective in up to 100% of patients with neurological pathologies, although this review was based on non-randomized studies (7)
A meta-analysis evaluated the results of studies focusing on sacral neuromodulation (SNM) in patients with neurogenic lower urinary tract dysfunction (8)
Finally, several systematic reviews with metanalysis evaluated the treatment of overactive bladder syndrome with Botulinum toxin injection (9-15)
Although a relevant bulk of information from previous systematic reviews is available, certain specific aspects, such as
efficacy mirabegron and new anticholinergic agents in neurogenic bladder have not yet been addressed Other issues, such as efficacy of PTNS in neurogenic bladder, need to be corroborated by randomizes studies
The aim of our study was to review the efficacy of treatments for neurogenic OAB focusing on recent clinical evidence, including studies focusing on mirabegron and on new anticholinergic agents
MATERIALS AND METHODS
The review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (16) It has been registered o n t h e P R O S P E R O p l a t f o r m ( r e g i s t r a t i o n n u m b e r : CRD42022347165)
Types of studies, inclusion criteria
We considered randomized controlled trials (RCTs), with single/double blinded design without time constraints
We included studies involving adult patients of both sexes subjected to pharmacological and non-pharmacological medical treatment for overactive bladder symptoms associated with neurological diseases including post-ischemic stroke, Parkinson’s disease and multiple sclerosis
Outcomes
The following outcomes were considered: number of daytime voids and night-time voids (nocturia); number of incontinence and urgency episodes; modification of scores measuring urinary symptoms and quality of life; change of urodynamic measurements (cystometric capacity, peak pressure, volume at 1st contraction)
The Overactive Bladder Symptom Score (OAB-SS) is a diagnostic tool divided in four domains, administered to patients for self-evaluation of voiding symptoms The score ranges between 0 and 15 (15 = most severe symptoms)
The International Consultation on Incontinence Questionnaire Overactive Bladder (ICIQ) is a questionnaire for evaluating overactive bladder and related impact on quality of life (QoL) and outcome of treatment in men and women in research and clinical practice across the world It is based on a 0-16 overall score with greater values indicating increased symptom severity
Search strategy
Two electronic databases (PubMed and EMBASE) were searched for articles in English, published up to 30 April 2022 Record search and retrieval was performed using strings based on the combination of various MeSH terms: (Urinary Bladder, Overactive; Urinary Incontinence, Urge; Multiple Sclerosis; Ischemic Stroke; Parkinson Disease): (treatment) AND (urge urinary incontinence OR overactive urinary bladder OR detrusor overactivity) AND (multiple sclerosis OR Parkinson disease OR ischemic stroke)
Relevant data were also hand searched by browsing various sources (e g , reference lists from reviews and study reports, congress abstracts, clinical trial registers such as www clinicaltrials gov, www clinicaltrialsregister eu, etc )
Selection of studies
Retrieved papers were independently screened by two
493 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
authors by title and abstract to exclude documents that did not meet the inclusion criteria Duplicate references were deleted Full texts of selected papers were downloaded to confirm/reject inclusion and to extract relevant information
Controversies were resolved by a third researcher A PRISMA flow diagram summarizes the study selection process (Figure 1)
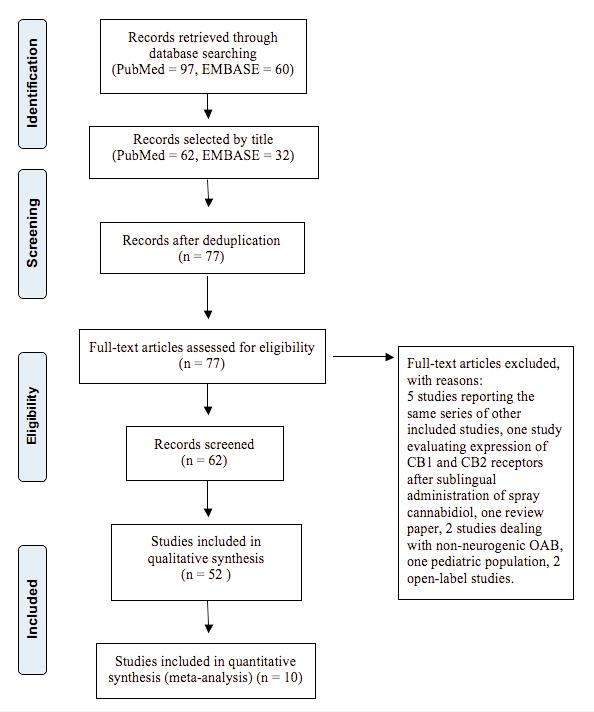
Data extraction (Supplementary Materials PICO tables)
Data extraction was performed by four authors using a standardized form The following information was obtained from each study: author(s), publication year, study design, population, interventions, comparisons, outcomes/endpoints In case of missing or insufficient information, we analyzed the reason for incompleteness and considered the impact of missing data on the meta-analysis results
Quality evaluation
(Supplementary Materials RoB evaluation)
Two authors independently performed the quality assessment by identifying potential biases using the 2019 Cochrane risk of bias tool (RoB) 2 (17) Study quality was assessed against pre-defined criteria in relation to randomization process (D1), deviations from the intended interventions (D2), missing outcome data (D3), measurement of the outcome (D4) and selection of the reported result (D5)
Disagreements were resolved by discussion
The presence of high risk of bias was not used as a criterion to exclude studies from analysis
Publication bias was planned to be assessed by funnel plot in the presence of at least 5 trials in each metaanalysis If a potential reporting bias was found by visual inspection of the plots, the Berg and Egger tests were used to test funnel plots symmetry and to confirm the presence/absence publication bias
A summary of findings table was generated, and the quality of the evidence emerging from meta-analyses including at least 3 studies was rated according to GRADE criteria
Statistical analysis
Statistical analysis was performed using the RevMan5 software
Mean differences, 95% confidence intervals (CI) and Z statistics were calculated (Random-effects model, inverse variance method)
Study heterogeneity was assessed by calculating the I^2 (and 95% CI), which was interpreted as of lesser importance (I^2 ≤ 40%), moderate (I^2 = 30%-60%), substantial (I^2 =
50%-90%) or considerable (I^2 ≥ 75%), according to Cochrane criteria Sensitivity analysis was planned in case substantial or considerable heterogeneity of pooled analyses including at least 5 studies
RESULTS
In total, 157 records (97 from Medline, 60 from EMBASE) were retrieved by database searching; 94 papers were included after title and abstract screening (62 from Medline, 32 from EMBASE)
After removal of 17 duplicates, we evaluated 77 papers by full-text reading Twelve studies were excluded: five studies reported data contained in other included studies, a study evaluated the expression of CB1 and CB2 receptors after sublingual administration of spray cannabidiol, an article contained a review of the literature, two studies focused on non-neurogenic OAB, one study addressed a pediatric population, two studies were open-label
Sixty-two studies were finally selected (Figure 1)
Table 1 lists the 62 studies included in this review, according to underlying disease and type of treatment
Quantitative analysis was limited to the comparisons of mirabegron vs placebo, anticholinergics vs placebo, TTNS
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
494
Figure 1. Flow diagram
Table 1. Studies retrieved divided by treatment
vs sham intervention, and PFMT vs controls Other outcomes were not analyzed quantitatively because several extensive meta-analyses were previously published
Anticholinergics
We found 9 papers evaluating the effects of anticholinergics (18-26)
Three papers compared anticholinergic agents with placebo for treatment of overactive bladder in patients with Parkinson disease (n = 2), multiple sclerosis or spinal cord injury (n = 1) (18-20)
Quantitative analysis of two studies (18, 19) in patients with Parkinson disease demonstrated that anticholinergics were more effective than placebo in decreasing the number of day voids (mean difference [MD], -1 16, 95% CI - 1 80 to - 0 52, 2 trials, 86 patients, Z = 3 56, p < 0 004) Changes from baseline number of incontinence and nocturia episodes were not significantly different between anticholinergics and placebo (MD, -0 44, 95% CI -1 23 to 0 35, 2 trials, 86 patients, Z = 1 08, P = 0 28, and MD, -0 36, 95% CI -1 17 to 0 45, 2 trials, 86 patients, Z = 0 87, p = 0 39, respectively) (Figure 2)
Adverse events associated with anticholinergics as dry mouth, constipation, and blurred vision are well known and may lead to therapy discontinuation
In a study comparing solifenacin or oxybutynin with placebo the most common treatment emergent side effects were dry mouth and urinary tract infections although most events were considered mild in severity (20) Dry mouth was observed more frequently in patients taking oxybutyinin (17%) then in those receiving solifenacin (4 2-7 8%) or placebo (2 3%) Changes from
baseline in VAS dry mouth score were significantly higher in the oxybutynin group than in placebo whereas there was no difference of VAS dry mouth score between solifenacin group and placebo In another study, solifenacin was well tolerated but a case of urinary retention was observed in the treatment group (11%) Xerostomia and constipation were also observed (18)
During the treatment with fesoterodine 4 mg there was no serious adverse event and no urinary retention episode in both fesoterodine and placebo groups Xerostomia (3%) and constipation (3%) were observed in the treatment group (19)
One study demonstrated that short-term treatment using oral extended-release oxybutynin 5 mg once daily was safe and well tolerated compared to placebo (with no onset of delirium) in older female nursing home participants with mild to severe dementia (21)
Four studies compared the outcome of the treatment with anticholinergic agents administered at different dose, or as different formulations, or via different routes (22-25)
Oral trospium chloride at standard dosage was compared with oral trospium chloride administered at adjustable doses A therapeutic response was achieved in 58% of patients in the adjustable dose group and in 72% of those in the standard dose group (p = 0 23) Rates of side effects were similar between groups (35% vs 37%) (22)
Oral treatment with oxybutynin immediate release was compared to intravesical oxybutynin or atropine
The increase in maximum bladder capacity was higher with intravesical application, also causing less frequent and less severe side effects (23, 24)
Propiverine extended-release
495 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
(ER) was
compared with
Treatment Design N° of studies Disease Mirabegron Compared to placebo 5 PD (3), MS or SCI (2) Anticholinergics Compared to placebo 3 PD (2), MS or SCI (1) Compared to placebo to evaluate the cognitive effects of oxybutynin 1 Old people with cognitive impairment Oral trospium, standard vs adjustable dose 1 Neurogenic detrusor overactivity Oral oxybutynin IR vs intravesical oxybutynin or atropin 2 Neurogenic detrusor overactivity Propiverine IR vs ER 1 Neurogenic detrusor overactivity Propiverine vs Oxybutynin 1 Neurogenic detrusor overactivity Comparison of drugs Mirabegron vs darifenacin 1 Poststroke Oxybutyinin+trospium vs oxybutynin+solifenacin 1 Neurogenic detrusor overactivity Milnacipran vs paroxetine 1 Neurogenic detrusor overactivity Cannabinoids Compared to placebo 2 MS Intravesical instillations Capsaicin compared to saline 2 Spinal cord lesions Neurogenic detrusor overactivity Nociceptin/orphanin FQ 1 Neurogenic detrusor overactivity Botulinum toxin Compared to placebo 13 Neurogenic detrusor overactivity Trigone excluding vs trigone including 2 Comparison of different doses 1 Transcutaneous tibial nerve stimulation (TTNS) Compared to sham 3 Compared to pelvic floor muscle training 1 Compared to oxybutynin 2 Acupuncture 2 PD, poststroke Transcutaneous electrical nerve stimulation (TENS) Compared to sham 3 Poststroke (3) Compared to oxybutynin 1 Pelvic floor muscle training (PFMT) Compared to controls 6 PD (2), MS (2), poststroke (2) PFMT+electrostimulation vs PFMT 3 MS (3) Compared to intravaginal neuromuscular electrical stimulation or to TTNS 1 Others Deep brain stimulation/ Intradetrusor adipose stem cells (ADSC) injections 2 PD
Figure 2
A, changes from baseline number of incontinence in patients with Parkinson disease treated with anticholinergics vs placebo;
B, changes from baseline number of night voids in patients with Parkinson disease treated with anticholinergics vs. placebo;
C, changes from baseline number of day voids in patients with Parkinson disease treated with anticholinergics vs placebo
Diamonds on the left side of the no-effect line indicate decreased numbers of episodes in patients treated with active drugs (anticholinergics) compared to placebo
Mean differences with 95% confidence intervals and heterogeneity statistics (I^2) are shown
propiverine immediate-release (IR) The latter showed slightly better tolerability compared to propiverine ER (25) The effects of propiverine and oxybutynin were compared in a study by Stöhrer et al Both treatments increased maximum cystometric capacity and lowered maximum detrusor pressure during the filling phase with no significant differences between treatment groups Adverse events were reported less frequently in the propiverine arm compared to the oxybutynin group (63 0% versus 77 8%) (26)
Mirabegron
We retrieved five RCTs comparing mirabegron vs placebo in patients with OAB and Parkinson disease (n = 3) (27-29) or spinal cord injury/multiple sclerosis (n = 2) (30, 31)
Three studies evaluated the clinical results of mirabegron treatment in patients with Parkinson disease Changes from baseline values of the OAB-SS score, day void rates or of incontinence and urgency episodes were not significantly different between mirabegron and placebo (MD, -2 01, 95% CI -4 24 to 0 21, 2 trials, 212 patients, Z = 1 78, p = 0 08; MD, -0 80, 95% CI, -3 04 to 1 43,2 trials, 227 patients, Z = 0 71, p = 0 48; MD, -0 11, 95% CI -3 12 to 2 91, 2 trials,195 patients, Z = 0 07, p = 0 94; MD, -0 56, 95 % CI -1 88 to 0 75, 3 trials, 227 patients, Z = 0 84, p = 0 40; respectively) (Figure 3, panels A, B, C and D)
Two studies evaluated changes of urodynamic values in patients with spinal cord injury/multiple sclerosis treated with mirabegron Mirabegron was more effective than placebo in increasing cystometric capacity (MD, 89 89 mL, 95% CI 29 76 to 150 01, 2 trials, 98 patients, Z = 2 93, p < 0 003) Changes from baseline values of peak pressure and volume at first contraction were not significantly different between mirabegron and placebo (MD,13 34 cm2, 95% CI -55 70 to 29 01, 2 trials, 97 patients, Z = 0 62, P = 0 54 and MD, 22 92 mL, 95 % CI - 20 78 to 66 63,2 trials, 98 patients, Z = 1 03, p = 0 30, respectively) (Figure 4 A, B and C)
In general, the rate of treatment emergent adverse events was similar in the mirabegron and placebo groups and the degree of adverse events was mild or moderate in most cases
A major safety concern with mirabegron is cardiovascular safety because of beta-adrenergic stimulation In three studies changes in cardiovascular parameters were actively assessed demonstrating no significant changes of mean systolic and diastolic blood pressure, pulse rate, and QTc interval during mirabegron treatment (28, 30, 31)
The risk of urinary retention is another concern associated to mirabegron treatment Data from two studies (27, 31) showed no significant change of mean post-voiding residual volume or proportion with PVR > 100 ml,

Archivio Italiano di Urologia e Andrologia 2022; 94, 4 R Bapir, K
Bhatti,
Eliwa, et al 496
Hassan
Ahmed
A. Day voids
B. Incontinence
C. Nocturia
Figure 3.
A, changes from baseline values of OAB-SS scores after mirabegron vs placebo in patients with Parkinson disease;
B, changes from baseline number of day voids after mirabegron vs placebo in patients with Parkinson disease;
C, changes from baseline number of urgency episodes after mirabegron vs placebo in patients with Parkinson disease;
D, changes from baseline number of incontinence episodes after mirabegron vs placebo in patients with Parkinson disease
Diamonds on the left side of the no-effect line indicate decreased numbers of episodes or symptom scores in patients treated with mirabegron compared to placebo Mean differences with 95% confidence intervals and heterogeneity statistics (I^2) are shown
whereas in a study a case with PVR > 100 was described in mirabegron group but not in placebo (28)
Comparison between various drugs
Three studies compared the efficacy and safety of different drugs used for treatment of neurogenic OAB
In patients who had ischemic stroke, mirabegron and darifenacin showed similar improvement of bladder diary parameter without deterioration of cognitive function (32)
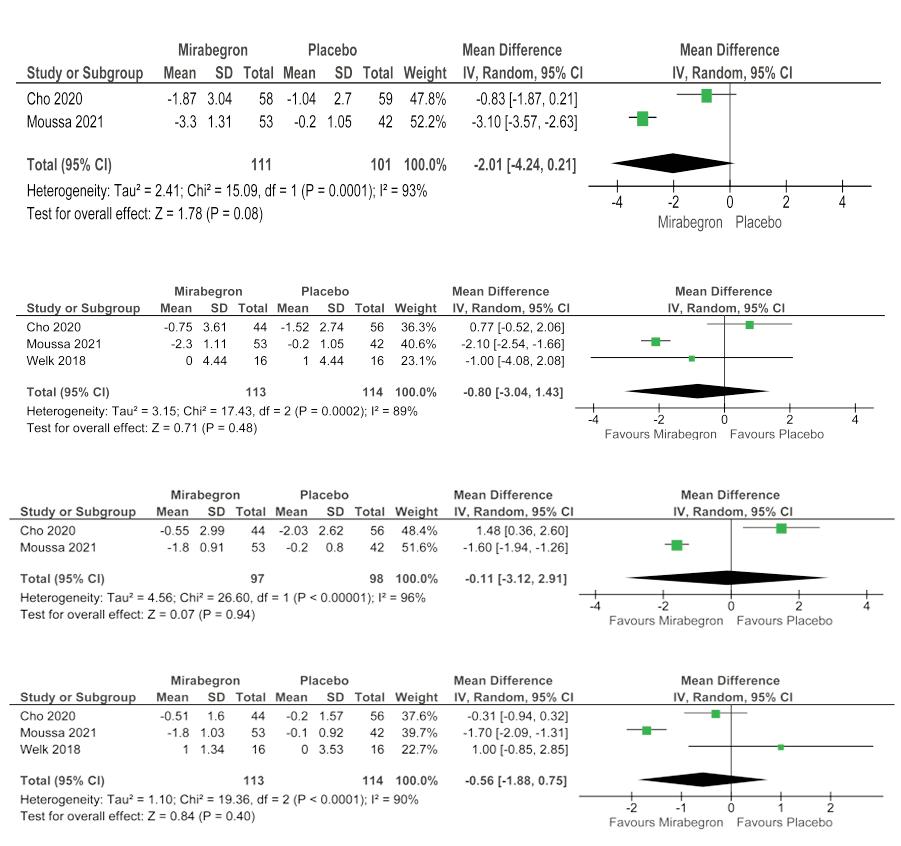
Both combination of trospium chloride with oxybutynin, and solifenacin with oxybutynin improved subjective
and urodynamic urinary parameters, though side effects were higher in patients taking oxybutyinin plus solifenacin (33)
A study proposed the use of serotonin and noradrenaline reuptake inhibitors (SNRIs) as an alternative to anticholinergic treatment in order to minimize antimuscarinic or cardio-suppressive effects SNRIs are currently used for treatment of depression, though the SNRI duloxetine has been used to treat stress urinary incontinence thanks to its activity on the urinary sphincter, presumably via serotoninergic and adrenergic receptors of the sacral Onuf’s nucleus SNRIs lack anticholinergic properties, unlike conventional
497 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
C. Urgency
B. Day voids
A. OAB-SS
D. Incontinence
Figure 4
A, changes of cystometric capacity values in patients with spinal cord injury/multiple sclerosis treated with mirabegron vs placebo;
B, changes of peak pressure values in patients with spinal cord injury/multiple sclerosis treated with mirabegron vs. placebo;
C, changes of volume at 1st contraction values in patients with spinal cord injury/multiple sclerosis treated with mirabegron vs placebo Diamonds on the right side of the no-effect line indicate increased cystometric capacity (A) and volume at first contraction (C) in patients treated with mirabegron compared to placebo Diamonds on the right side of the no-effect line indicate decreased peak pressure in patients treated with mirabegron compared with placebo Mean differences with 95% confidence intervals and heterogeneity statistics (I^2) are shown.
antidepressants, and stimulation of serotoninergic receptors seems to suppress bladder contractility For this reason, SNRIs could have a role in the treatment of neurogenic OAB A study compared the effect of the SNRI milnacipran on OAB symptoms compared to paroxetine, a selective serotonin reuptake inhibitor (SSRI) lacking adrenergic effect Milnacipran, but not paroxetine, improved the quality of life of patients by reducing daytime urinary frequency and by increasing the bladder capacity (34)
Cannabinoids
Two studies reported the effect of cannabis-containing medicines in patients with overactive bladder and multiple sclerosis (35, 36)
Cannabinoids (cannabis extract, Δ9-tetrahydrocannabinol or THC, nabiximols or Sativex) were used to treat OAB in patients with MS Cannabis extract and THC reduced incontinence episode rates by 38% and 33%, respectively Sativex, an endocannabinoid system modulator, significantly reduced nocturia episodes and daytime voids Dizziness (16%), disorientation (6%) and dissociation (6%) were observed during treatment
Intravesical instillations
In two studies, a single intravesical instillation of capsaicin significantly decreased voiding frequency and incontinence episodes, increased the maximum cystometric capacity and decreased the maximum detrusor pressure (37, 38) Capsaicin diluted in ethanol solvent caused significant side effects in 70% of cases, whereas side effects were limited using a glucidic solvent
The therapeutic effect of capsaicin is time-limited with no significant efficacy observed after three months
Intravesical instillations of nociceptin/orphanin FQ also decreased urine leakages and increased the voiding bladder capacity without significant side effects (39)
Botulinum toxin
Thirteen studies evaluated the effect of Botulinum toxin intra-detrusor injection compared to saline injection in patients with neurogenic detrusor overactivity associated with spinal injury or multiple sclerosis (40-52) Intravesical Botulinum toxin treatment proved to be effective and safe for the treatment of neurogenic detrusor overactivity Transient adverse events were urinary retention,
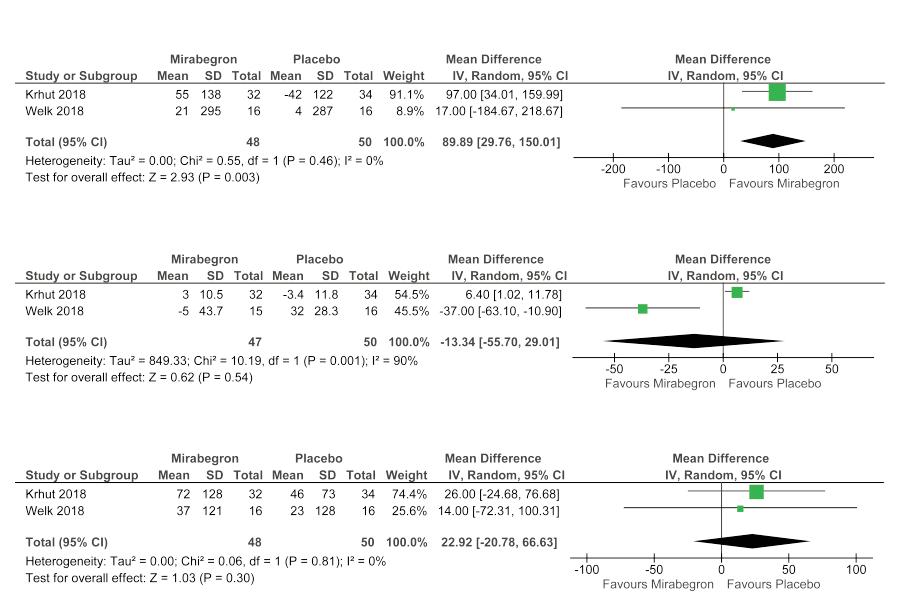
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al 498
Cystometric capacity Peak pressure Volume at first contraction
hematuria, muscle weakness, and urinary tract infection
Two studies compared the effect of injections in the detrusor excluding the trigone with injections including the trigone (53, 54)
A study compared the effect of the administration of two different doses of Botulinum toxin type A (55)
Most of these studies were included in recently published meta-analyses
Our search added to published systematic reviews three studies which were published after 2017 Kennelly et al reported pooled data from two phase 3 studies assessing the safety and efficacy of abobotulinumtoxinA (aboBoNTA) in patients with neurogenic detrusor overactivity who were routinely performing clean intermittent catheterization Treatment with aboBoNT-A significantly reduced incontinence episodes per week in comparison to placebo (p < 0 001) and significantly increased the volume per v o i d D e n y s e t a l c o m p a r e d t h e a d m i n i s t r a t i o n o f abobotulinumtoxinA by 15 intra-detrusor injections in comparison to 30 injections (43)
Both 15 and 30 injections administration modes decreased the daily number of incontinence episodes and improved urodynamic parameters in patients with NDO
Honda et al described the results of the administration of onabotulinumtoxinA in Japanese patients with neurogenic detrusor overactivity, demonstrating reduction of urinary incontinence episodes and improvement of urodynamic parameters (47)
Transcutaneous tibial nerve stimulation (TTNS)
Six studies reported the results of TTNS in neurogenic OAB Three studies compared active treatment with sham treatment (56-58) and 3 compared TTNS with other treatments such as pelvic floor muscle training (59) or oral anticholinergics (n = 2) (60, 61)
TTNS reduced urinary frequency, urgency, and incontinence episodes in comparison to placebo
Quantitative analysis of two studies comparing TTNS with sham treatment in patients with Parkinson disease shows that TTNS was more effective than sham in decreasing the number of nocturia episodes (MD, -1 40, 95% CI -2 39 to -0 42, 2 trials, 53 patients, Z = 2 79, p < 0 005) Changes from baseline of OAB scores were not significantly different between TTNS and sham (MD2 87, 95% CI -17 25 to 11 51, 2 trials, 53 patients, Z = 0 39, p = 0 70) (Figure 5A, B)
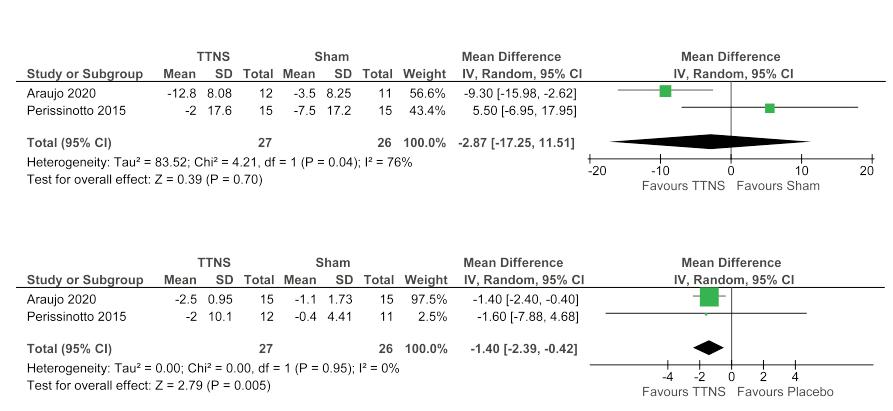
In a study including patients with multiple sclerosis, quality of life scores (SF-Qualiveen), overactive bladder symptom scores (USP) and rates of urgency episodes were improved after both PFMT and TTNS but no differences between the two groups were observed (59) TTNS was compared to oxybutynin (5 mg BID) in patients with OAB and multiple sclerosis TTNS showed a less significant reduction of OAB-S (overactive bladder symptoms) and OAB-Q (overactive bladder quality of life) scores in comparison to oxybutynin, though the latter was associated with a higher rate of side effects (35%) (60)
In another study including women with neurogenic bladder, the association of TTNS with tolterodine 4 mg improved urgency symptoms (61)
Acupuncture
The effect of acupuncture and electroacupuncture was reported in 2 studies in patients with Parkinson’s disease and post-stroke OAB In PD patients, acupuncture associated with a low dose of tolterodine (1 mg BID) improved daily rates of frequency and incontinence as well as mean urine volumes more than full-dose tolterodine (2 mg BID) (62) In post-stroke patients, electroacupuncture treatment improved the perceived severity of OAB symptoms in com-
A, changes from baseline of OAB scores in patients with Parkinson disease treated with TTNS vs sham treatment;
B, changes from baseline of the number of night voids in patients with Parkinson disease treated with TTNS vs sham treatment
Diamonds on the left side of the no-effect line indicate decreased numbers of episodes or symptom scores in patients treated with TTNS compared to sham treatment Mean differences with 95% confidence intervals and heterogeneity statistics (I^2) are shown
499 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
Figure 5.
A. OAB-SS
B. Nocturia
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
parison with standard care, though no significant differences were observed in bladder diary parameters and quality of life scores (SSQoL) Both acupuncture and electroacupuncture were well tolerated (63)
Transcutaneous electrical nerve stimulation (TENS)
Transcutaneous electrical nerve stimulation has been used to treat post-stroke neurogenic overactive bladder
Positive pads were usually placed in the region of the second sacral level of the vertebral column and negative pads were placed at the level of the middle and lower third of the junction between the posterior superior iliac spine and the ischial node Treatments were administered 30 minutes once a day for 60-90 days, in the form of unidirectional square waves with different combinations of pulse duration and frequency
In three studies, TENS was compared to sham treatment for treatment of post-ischemic stroke urinary incontinence, whereas one study compared TENS to anticholinergic drugs (64-67)
TENS improved symptom scores, voiding diary parameters (daily micturition, nocturia, urgent urination, and urge UI), and urodynamic findings (maximum cystometry volume, flow rate, pressure of detrusor in the end of the filling phase)
In the study comparing TENS with anticholinergics, the former was superior than the latter
Pelvic floor muscle training
Six studies evaluated the outcome of behavioral therapy, including pelvic floor muscle training (PFMT) in comparison with controls (2 in Parkinson disease, 2 in incontinence post-stroke, 2 in multiple sclerosis) (68-73)
The quantitative analysis of the results of two studies in patients with Parkinson disease comparing pelvic floor muscle training with conservative advice, demonstrated that PFMT was more effective than the latter in decreasing the values of the ICIQ score (MD -1 12, 95% CI -2 13 to -0 11, 2 trials, 91 patients, Z = 2 17, p = 0 03) The number of incontinence episodes from baseline was not significantly different between PFMT and controls (MD,0 41, 95% CI -2 84 to 2 03, 2 trials, 91 patients, Z = 0 33, p = 0 74) (Figure 6) Other studies compared PFMT plus vaginal electrostimulation to home PFMT in patients with multiple sclerosis (74-77)
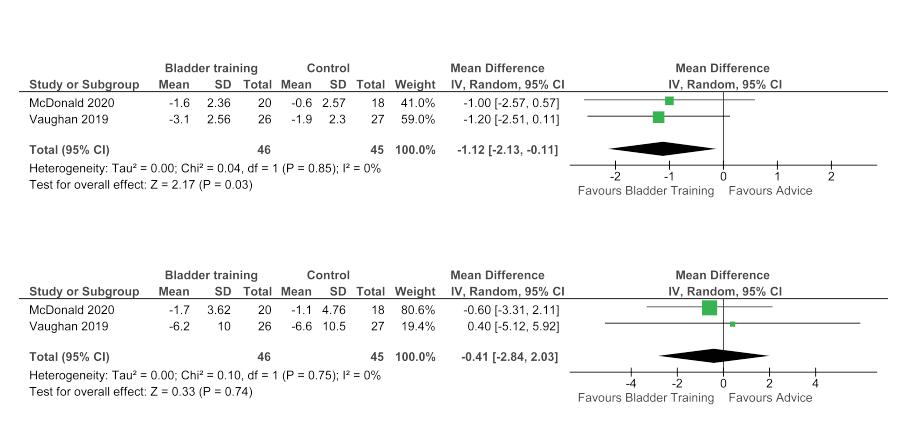
In patients with multiple sclerosis and LUTS, the association of PFMT (with EMG feedback) and intravaginal NMES significantly improved pelvic floor muscle assessment findings and OAB-V8 scores more than PFMT alone and the association of PFMT with TTNS
Three studies from the same group compared outcomes of PFMT alone with PFMT with vaginal electrostimulation in women with LUTS in multiple sclerosis OAB-V8 scores, quality of life and perineal musculature contraction were improved after both treatments, although a greater increase was obtained with the addition of electrostimulation
Other studies
Deep brain stimulation (DBS), a surgical treatment for motor symptoms in advanced PD, showed improvement of LUTS in PD patients (78)
Intra-detrusor injections of adipose stem cells (ADSC) were also used to treat PD-related OAB symptoms A single ADSC injection significantly improved symptom scores and voiding diary parameters (79)
A, changes from baseline of ICIQ-OAB scores in patients with Parkinson disease treated with pelvic floor muscle training vs conservative advice;
B, changes from baseline of the incontinence episodes in patients with Parkinson disease subjected to the same treatments Diamonds on the left side of the no-effect line indicate decreased numbers of episodes or symptom scores in patients treated with PFMT compared to advice. Mean differences with 95% confidence intervals and heterogeneity statistics (I^2) are shown.
B. Incontinence
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
500
Figure 6.
A. ICIQ score
DISCUSSION
Anticholinergics
Anticholinergics are the first-line choice for the pharmacologic treatment of OAB They are used to stabilize the d e t r u s o r m u s c l e a n d i m p r o v e b l a d d e r c o m p l i a n c e because detrusor smooth contraction is initiated via release of acetylcholine The major disadvantage of oral anticholinergics are the side effects that result in treatment discontinuation in up to 70% of patients, depending on the duration of treatment Furthermore, a potential risk of cognitive decline and worsening of gait in patients with PD has been recently suggested
In 2009, a Cochrane systematic review assessed the efficacy and tolerability of anticholinergic agents in patients with overactive bladder associated to multiple sclerosis (MS) (3) Only three RCTs were considered suitable for analysis An older randomized cross-over study compared methantheline bromide, flavoxate chloride and meladrazine tartrate (Hebjorn 1977) (81) A more recent study found reduced symptoms after oxybutynin compared to propantheline (Gajewski 1986) (82) Finally, a study found no significant difference in term of efficacy b e t w e e n o r a l o x y b u t y n i n a n d i n t r a v e s i c a l a t r o p i n e , although side effects and quality of life were in favor of the latter (Fader 2007) (83) The Authors concluded that evidence was insufficient to demonstrate any benefit from the administration of anticholinergics for urinary symptoms in multiple sclerosis In addition, high rates of adverse effects were reported, with 20% of patients who had to withdraw from oral treatment
In a systematic review by Madhuvrata et al. (2), eight RCTs comparing anticholinergic drugs with placebo in adult neurogenic OAB were included The metanalysis of three studies showed higher maximum cystometric capacity, higher volume at first contraction, and lower maximum detrusor pressure after anticholinergics compared to placebo On the contrary, no significant changes in frequency of micturition or incontinence episodes per 24 hours were observed
The present review included three RCTs (18-20) comparing anticholinergics with placebo, which were published after the review of Madhuvrata et al In patients with Parkinson disease, anticholinergics were more effective than placebo in decreasing the number of day voids, though the number of incontinence episodes and nocturia were not significantly decreased
The most frequent side effect was dry mouth which was observed in 17% of the patients taking oxybutynin Similarly, the meta-analysis of Madhuvrata et al (2) showed statistically significantly higher dry mouth with anticholinergic drugs compared with placebo (32 vs 7%), but did not report any statistically significant difference in any other adverse event, nor in withdrawal rates due to adverse events (8 vs 2%) There were no statistically significant differences in any of the outcomes between oxybutynin and other anticholinergics nor among different doses and preparations of anticholinergic drugs
A meta-analysis of RCTs on the efficacy and safety of anticholinergic drugs for non-neurogenic overactive bladder ( 8 3 ) c o n c l u d e d t h a t e x t e n d e d - r e l e a s e f o r m u l a t i o n s showed some advantages when compared to immediate
release ones, both in terms of efficacy and safety No significant advantage was observed after transdermal delivery compared to oral intake
In general, dose escalation obtained some improvements in term of efficacy, although it was associated with a significant increase in the rate of adverse events Tolterodine IR was associated with less adverse events than oxybutynin IR
In our review, we included three studies comparing the effect of the treatment with anticholinergic agents administered at different doses or with different formulation
O r a l t r o s p i u m c h l o r i d e a t s t a n d a r d d o s e s a n d a t adjustable doses showed similar therapeutic responses and similar rates of side effects (22) Similarly, when compared to propiverine IR, propiverine ER showed a slightly better tolerability (25)
A comparison of propiverine vs oxybutynin showed no significant differences in the increase of maximum cystometric capacity and decrease of maximum detrusor pressure during the filling phase Adverse events were reported less frequently in the propiverine arm compared to the oxybutynin group (63 0% versus 77 8%) (26)
Shen et al (4) recently reviewed randomized and non-randomized studies evaluating effectiveness and safety of intravesical oxybutynin therapy for patients with neurogenic detrusor overactivity compared to oral oxybutynin In studies in adults, maximum bladder capacity increased and detrusor pressure at maximum bladder decreased more after intravesical oxybutynin than after oral treatment After treatment, 76 9% of adult patients were considered “dry or improved” Side effects were reported in 13 5% of cases and 6 6% of patients withdraw for side effects
Our review did not add any new study on intravesical anticholinergic administration to Shen’ s meta-analysis
Combined administration of two different anticholinergic drugs instead of standard of care (a single antimuscarinic drug administered at maximum of recommended dosage) was proposed to improve efficacy without affecting tolerability Combined administration of trospium chloride with oxybutynin and solifenacin with oxybutynin (33) improved subjective and urodynamic urinary parameters, although side effects were higher in patients taking oxybutyinin plus solifenacin
Mirabegron
Mirabegron is a beta-3 adrenoceptor agonist that mediates bladder relaxation and facilitates the filling phase by stimulating beta-3 adrenoceptors Mirabegron is commonly used for idiopathic OAB treatment because of its efficacy, comparable to that of anticholinergic drugs, but with a better tolerability profile (84, 85) However, mirabegron may affect the cardiovascular system causing hypertension, increased heart rate, arrhythmias, and headache (86) Patients with neurogenic OAB could be more exposed to such side effects because of potential disturbances of the vegetative nervous system In particular, this could be the case in patients with SCI above the T6 level that is above the outflow of splanchnic sympathetic fibres Our meta-analysis partially supported the efficacy of mirabegron in patients with neurogenic overactive bladd e r T h e c y s t o m e t
501 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
a p a c i t y w a s i n c r e a s e d a f t e r
r i c c
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
mirabegron in patients with MS, although peak pressures and volume at 1st contraction were not significantly increased Symptom scores and bladder diary parameters were not significantly changed in patients with PD Cardiovascular parameters were not significantly affected by mirabegron treatment although patients at risk for cardiovascular disease were excluded from most trials Mirabegron was compared to darifenacin in the treatment of OAB in patients with a history of cerebrovascular accident (32) No differences in bladder diary parameters were observed between groups No patients developed intolerable severe adverse effects and no deterioration in the cognitive function assessed using MoCA-B scores was observed in either arm
Cannabis-containing medicines
Cannabis-containing medicines were used in the treatment of OAB in patients with multiple sclerosis The potential mechanism of action of those medicines is not fully elucidated, although it could be mediated by CB1 receptors or by transient receptor potential vanilloid 1 (TRPV1) receptor in the bladder In our review, two RCTs were included, showing that treatment with THC or cannabidiol (CBD) reduced episodes of incontinence, daytime voids and nocturia
Other oral treatments
A possible alternative to anticholinergics is milnacipran, a serotonin and noradrenaline reuptake inhibitor (SNRI) which can suppress bladder contractility by stimulating serotoninergic receptors In a single study, this drug was able to reduce daytime urinary frequency and to increase bladder capacity (34)
Intravesical instillations
Prevention of micturition reflex to trigger bladder overactivity represents a possible alternative to drugs blocking smooth muscle contraction like anticholinergics Drugs like capsaicin, RTX, and nociception/orphanin FQ have an effect on the unmyelinated C-fiber afferent limb of the micturition reflex
Instillations of both capsaicin and nociceptin/orphanin FQ were able to decrease incontinence rates and to improve urodynamic parameters in patients with neurogenic OBA (37-39)
Botolinum toxin injections
Botulinum toxin has been used for many years in the treatment of severe neurogenic overactive bladder refractory to standard treatment In 2007, Duthie et al published a systematic review on the treatment of overactive bladder syndrome with botulinum toxin injections The review, which was updated in 2011 (9), included patients affected by either neurogenic OAB or idiopathic OAB
Botulinum toxin injection was superior to placebo in all studies included in the analysis, with an effect lasting for several months depending on the dose and the type of toxin used Other systematic reviews with meta-analysis were subsequently published to confirm the efficacy and safety of this treatment
Zhang et al (10) retrieved eight RCTs focusing on efficacy and safety of onabotulinumtoxinA in patients with
neurogenic detrusor overactivity (NDO), published up to September 2012 Infiltrations with onabotulinumtoxinA improved maximum cystometric capacity and decreased maximum detrusor pressure compared to placebo The treatment was more frequently associated with UTIs than placebo No dose-related differences of efficacy and side effects were observed when regimens based on 300 U or 200 U doses were compared
Similarly, Zhou et al (11) searched databases (up to November 2013) to identify RCTs focusing on the effect of onabotulinumtoxinA for treatment of NDO
The authors included four studies in their analysis, which confirmed a dose-independent reduction of the number of urinary incontinence episodes per week, the increase of maximum cystometric capacity, and the reduction of m a x i m u m
o
l a c e b o OnabotulinumtoxinA was more often associated with the onset of UTIs, hematuria and urinary retention
Mehta et al (12) retrieved 14 studies from 1980 to June 2012, demonstrating improvements of postvoid residual urine volume, reflex detrusor volume, bladder capacity, bladder compliance, and catheterization frequency (p < 0 01) after administration of botulinum toxin type A (BTX-A)
Wu et al (13) searched the literature up to May 2017 and included five RCTs in their analysis BTX-A intra-detrusorial infiltrations reduced the number of urinary incontinence episodes per day and per week compared to placebo and increased maximum cystometric capacity and decreased maximum detrusor pressure at week 6 BTX-A administration was more frequently associated with urinary tract infections
Ni et al (14) searched the literature up to June 2016 for papers reporting the outcomes of studies focusing on repeated BTX-A injections in adult patients with NDO They included 18 retrospective or prospective cohort studies, but no RCT The meta-analysis demonstrated t h a t r e p e a t e d B T X - A i n j e c t i o n s a l l o w e d s u s t a i n e d improvements in patients with NDO, with a stable and low rate of adverse events Jo et al (15) searched for RCTs assessing the efficacy and safety of onabotulinumtoxinA, administered in different injection sites, for treatment of OAB The authors included studies performed in adults treated for both neurogenic detrusor overactive bladder a n d i d i o p a t h i c O A B T r i g o n e - i n c l u d i n g i n j e c t i o n s demonstrated more significant improvement in symptom score, higher complete dryness rates, and lower rates of incontinence episodes compared to trigone-sparing injections Moreover, lower detrusor pressure and higher volume at first desire to void were observed with trigoneincluding injection
We added three recently published studies assessing the effect of abobotulinumtoxinA in patients with NDO on clean intermittent catheterization (49), comparing the performance of abobotulinumtoxinA by 15 intra-detrusor injections with a 30-injection regimen (43), and describing the results of the administration of onabotulinumtoxinA in Japanese patients (47) AbobotulinumtoxinA showed its efficacy in treating patients with NDO compared to placebo even when the number of injections was reduced and the efficacy of onabotulinumtoxinA was confirmed in an Asian population
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
502
p r e s s u
e c
m
d e t r u s o r
r
o
p a r e d t
p
Pelvic floor muscle training (PFMT) and non-invasive electrical stimulation
A recent metanalysis addressed studies that evaluated PFMT in multiple sclerosis patients with LUTS in the period between 1990 and 2019 Kajbafvala et al (5) found that PFMT significantly reduced urinary incontinence episodes and neurogenic bladder symptoms measured according to OAB-VS scores According to the PERFECT scheme for assessment of pelvic floor muscle function, PFMT increased the overall endurance and power of the pelvic floor musculature
One metanalysis by Vecchio and coworkers evaluated the effectiveness of peripheral tibial nerve stimulation (PTNS) and pelvic floor muscle training (PFMT) for bladder dysfunction in MS, on the basis of data retrieved up to October 2021 (6) The authors found no significant differences in voided volume after PFMT However, according to the PERFECT scheme assessed at 3 months, endurance and fast contraction of pelvic floor muscles were significantly improved (p = 0 002)
Papers on PFMT (without or with electrostimulation) in patients with MS which were retrieved in our review were also previously included in these reviews
We retrieved four additional studies reporting about PFMT in patients with PD (n = 2) or with post-stroke OAB (n = 2) Meta-analysis of two studies in patients with PD, showed that PFMT could improve OAB symptoms in PD, though the number of episodes of incontinence was not significantly decreased In men and women with post-stroke OAB symptom scores, bladder diary parameters and pelvic floor function and strength were improved
Gaziev et al (7) reviewed the efficacy of TTNS in the treatment of lower urinary tract dysfunction, including overactive bladder The authors found that TTNS was effective in 37-100% of patients with OAB Four RCTs were retrieved; importantly, these studies did not distinguish between neurogenic and idiopathic OAB The above cited metanalysis by Vecchio et al. (6) showed significant improvements of daytime frequency, nocturia, urgency incontinence and voided volume after three months of PTNS (p < 0 001) in patients with MS A significant improvement in maximum cystometric capacity was also observed Our review added three studies evaluating the effect of PTNS in patients with PD or post-stroke OAB Quantitative analysis of two studies comparing TTNS with sham treatment in patients with PD tentatively indicates that TTNS is more effective than sham in decreasing the number of nocturia episodes TENS improved urinary symptoms also in patients with post-ischemic stroke by reducing urinary urgency and frequency
Acupuncture and electroacupuncture also proved to be effective in patients with PD and in post-stroke patients Finally, transcutaneous electrical nerve stimulation (TENS) was successfully used to treat post-stroke neurogenic OAB Treatment improved voiding diary parameters and urodynamic findings and showed to be superior to anticholinergics
Sacral neuromodulation
A systematic review evaluated the results of studies on sacral neuromodulation (SNM) in patients with neurogenic
lower urinary tract dysfunction Data published between 1998 to March 2020 were retrieved The review included retrospective or prospective clinical studies, cohort studies, and case reports A meta-analysis of 21 studies demonstrated a 66 2% success rate of SNM test stimulation; another meta-analysis of 24 studies reported a 84 2% success rate of permanent SMN Loss of effectiveness, infection, pain at implant site, and lead migration were observed in 4 7%, 3 6%, 3 2%, and 3 2% of cases, respectively The clinical effect of SMN for neurogenic lower urinary tract dysfunction was comparable to the outcomes obtained in idiopathic populations
CONCLUSIONS
Although all treatments have proven efficacy, there is no therapy that can be considered clearly superior to the others In fact, the treatment of neurological bladder must be tailored to the individual patient, and often requires the combination of different forms of complementary treatment Combination of different pharmacological treatments, or associating pharmacological treatments and non-pharmacological treatments, can allow reduction of the dosage of drugs, thus minimizing the side effects which represent a limitation of their usage in therapy
A caveat: evidence from our quantitative analysis is fragmentary and does not allow to draw robust conclusions Our data are only provisional and should be considered with caution, due to the few studies included in metaanalysis and to the small number of patients included in each study
REFERENCES
1 Przydacz M, Chlosta M, Golabek T, Chlosta P Population-based study of prevalence, bother and behavior related to treatment for lower urinary tract symptoms and overactive bladder among polish neurogenic patients Brain Sci 2021; 11:712
2 Madhuvrata P, Singh M, Hasafa Z, Abdel-Fattah M Anticholinergic drugs for adult neurogenic detrusor overactivity: a systematic Review and Meta-analysis Eur Urol 2012; 62:816-830
3 Nicholas RS, Friede T, Hollis S, Young CA Anticholinergics for urinary symptoms in multiple sclerosis Cochrane Database of Systematic Reviews 2009, Issue 1 Art No : CD004193
4 Shen S-H, Jia X, Peng L, et al Intravesical oxybutynin therapy for patients with neurogenic detrusor overactivity: a systematic review and meta analysis
5 Kajbafvala M, Ashnagar Z, Lucio A, et al Pelvic floor muscle training in multiple sclerosis patients with lower urinary tract dysfunction: A systematic review and meta-analysis Mult Scler Relat Disord 2022; 59:103559
6 Vecchio M, Chiaramonte R, Di Benedetto P Management of bladder dysfunction in multiple sclerosis: a systematic review and meta-analysis of studies regarding bladder rehabilitation European Journal of Physical and Rehabilitation Medicine 2022; 58:387-96
7 Gaziev G, Topazio L, Iacovelli V, et al Percutaneous Tibial Nerve Stimulation (PTNS) efficacy in the treatment of lower urinary tract dysfunctions: a systematic review BMC Urol 2013; 13:61
8 van Ophoven A, Engelberg S, Lilley H, Sievert KD Systematic Literature Review and Meta-Analysis of Sacral Neuromodulation (SNM) in Patients with Neurogenic Lower Urinary Tract Dysfunction
503 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
(nLUTD): Over 20 Years' Experience and Future Directions Adv Ther 2021; 38:1987-2006
9 Duthie JB, Vincent M, Herbison GP, et al Botulinum toxin injections for adults with overactive bladder syndrome Cochrane Database of Systematic Reviews 2011, Issue 12 Art No : CD005493
10 Zhang R, Xu Y, Yang S, et al OnabotulinumtoxinA for neurogenic detrusor overactivity and dose differences: a systematic review Int Braz J Urol 2015; 41:207-19
11 Zhou X, Yan HL, Cui YS, et al Efficacy and safety of onabotulinumtoxinA in treating neurogenic detrusor overactivity: a systematic review and meta-analysis Chin Med J (Engl) 2015; 128:963-
12 Mehta S, Hill D, McIntyre A, et al Meta-analysis of botulinum toxin A detrusor injections in the treatment of neurogenic detrusor overactivity after spinal cord injury Arch Phys Med Rehabil 2013; 94:1473-81
13 Wu SJ, Xu YQ, Gao ZY, et al Clinical outcomes of botulinum toxin A management for neurogenic detrusor overactivity: meta-analysis Ren Fail 2019; 41:937-945
14 Ni J, Wang X, Cao N, et al Is repeat Botulinum Toxin A injection valuable for neurogenic detrusor overactivity-A systematic review and meta-analysis Neurourol Urodyn 2018; 37:542-553
15 Jo JK, Kim KN, Kim DW, et al The effect of onabotulinumtoxinA according to site of injection in patients with overactive bladder: a systematic review and meta-analysis World J Urol 2018; 36:305-317
16 Moher D, Liberati A, Tetzlaff J, et al Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement PLoS Med 2009; 6:e1000097
17 Sterne JAC, Savovic J, Page MJ, et al RoB 2: a revised tool for assessing risk of bias in randomised trials BMJ 2019; 366:l4898
18 Zesiewicz TA, Evatt M, Vaughan C, et al Randomized, controlled pilot trial of solifenacin succinate for overactive bladder in Parkinson's disease Parkinsonism Relat Disord 2015; 21:514-20
19 Yonguc T, Sefik E, Inci I, et al Randomized, controlled trial of fesoterodine fumarate for overactive bladder in Parkinson's disease World J Urol 2020; 38:2013-2019
20 Amarenco G, Sutory M, Zachoval R, et al Solifenacin is effective and well tolerated in patients with neurogenic detrusor overactivity: Results from the double-blind, randomized, active- and placebo-controlled SONIC urodynamic study Neurourol Urodyn 2017; 36:414-421
21 Lackner TE, Wyman JF, McCarthy TC, et al Randomized, placebo-controlled trial of the cognitive effect, safety, and tolerability of oral extended-release oxybutynin in cognitively impaired nursing home residents with urge urinary incontinence J Am Geriatr Soc 2008; 56:862-70
22 Menarini M, Del Popolo G, Di Benedetto P, et al Trospium chloride in patients with neurogenic detrusor overactivity: is dose titration of benefit to the patients? Int J Clin Pharmacol Ther 2006; 44:623-32
23 Fader M, Glickman S, Haggar V, et al Intravesical atropine compared to oral oxybutynin for neurogenic detrusor overactivity: a doubleblind, randomized crossover trial J Urol 2007; 177:208-13
24 Schröder A, Albrecht U, Schnitker J, et al Efficacy, safety, and tolerability of intravesically administered 0 1% oxybutynin hydrochloride solution in adult patients with neurogenic bladder: A randomized, prospective, controlled multi-center trial Neurourol Urodyn 2016; 35:582-8
25 Stöhrer M, Mürtz G, Kramer G, et al Efficacy and tolerability of propiverine hydrochloride extended-release compared with immediaterelease in patients with neurogenic detrusor overactivity Spinal Cord 2013; 51:419-23
26 Stöhrer M, Mürtz G, Kramer G, et al Propiverine compared to oxybutynin in neurogenic detrusor overactivity--results of a randomized, double-blind, multicenter clinical study Eur Urol 2007; 51:23542
27 Cho SY, Jeong SJ, Lee S, et al Mirabegron for treatment of overactive bladder symptoms in patients with Parkinson's disease: A doubleblind, randomized placebo-controlled trial (Parkinson's Disease
Overactive bladder Mirabegron, PaDoMi Study) Neurourol Urodyn 2021; 40:286-294
28 Moussa M, Chakra MA, Dabboucy B, et al The safety and effectiveness of mirabegron in Parkinson's disease patients with overactive bladder: a randomized controlled trial Scand J Urol 2022; 56:66-72
29 Ray S, Burdick D, Griffith A, Agarwal P Preliminary report on the MAESTRO study: A pilot study of mirabegron and behavioral modification including pelvic floor exercise for overactive bladder in Parkinson's disease Movement Disorders 2017; 32(Suppl 2):945-946
30 Krhut J, Borovicka V, Bilkova K, et al Mirabegron in the treatment of neurogenic detrusor overactivity due to spinal cord injury and multiple sclerosis International Journal of Urology 2017; 24(Suppl 1):18-19
31 Welk B, Hickling D, McKibbon M, et al A pilot randomized-controlled trial of the urodynamic efficacy of mirabegron for patients with neurogenic lower urinary tract dysfunction Neurourol Urodyn 2018; 37:2810-2817
32 Vasudeva P, Kumar A, Yadav S, et al Neurological safety and efficacy of darifenacin and mirabegron for the treatment of overactive bladder in patients with history of cerebrovascular accident: A prospective study Neurourol Urodyn 2021; 40:2041-2047
33 Nardulli R, Losavio E, Ranieri M, et al Combined antimuscarinics for treatment of neurogenic overactive bladder Int J Immunopathol Pharmacol 2012; 25(1 Suppl):35S-41S
34 Sakakibara R, Ito T, Uchiyama T, et al Effects of milnacipran and paroxetine on overactive bladder due to neurologic diseases: a urodynamic assessment Urol Int 2008; 81:335-9
35 Freeman RM, Adekanmi O, Waterfield MR, et al The effect of cannabis on urge incontinence in patients with multiple sclerosis: a multicentre, randomised placebo-controlled trial (CAMS-LUTS) Int Urogynecol J Pelvic Floor Dysfunct 2006; 17:636-41
36 Kavia RB, De Ridder D, Constantinescu CS, et al Randomized controlled trial of Sativex to treat detrusor overactivity in multiple sclerosis Mult Scler 2010; 16:1349-59
37 De Sèze M, Wiart L, Joseph P-A, et al Capsaicin and neurogenic detrusor hyperreflexia: A double-blind placebo- controlled study in 20 patients with spinal cord lesions Neurourology and Urodynamics 1998; 17:5 (513-523) Cited by: 97
38 de Sèze M, Gallien P, Denys P, et al Intravesical glucidic capsaicin versus glucidic solvent in neurogenic detrusor overactivity: a double blind controlled randomized study Neurourol Urodyn 2006; 25:752-7
39 Lazzeri M, Calò G, Spinelli M, et al Daily intravesical instillation of 1 mg nociceptin/orphanin FQ for the control of neurogenic detrusor overactivity: a multicenter, placebo controlled, randomized exploratory study J Urol 2006; 176:2098-102
40 Del Popolo G, Denys P, Keppenne V, et al Efficacy and safety of onabotulinumtoxina 100u for treatment of urinary incontinence due to neurogenic detrusor overactivity in non-catheterising multiple sclerosis patients Neurourology and Urodynamics 2016; 35(Suppl 3):S53-S54
41 Chancellor MB, Patel V, Leng WW, et al OnabotulinumtoxinA improves quality of life in patients with neurogenic detrusor overactivity Neurology 2013; 81:841-8
42 Cruz F, Herschorn S, Aliotta P, et al Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neu-
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
504
8
rogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial Eur Urol 2011; 60:742-50
43 Denys P, Del Popolo G, Amarenco G, et al Efficacy and safety of two administration modes of an intra-detrusor injection of 750 units dysport® (abobotulinumtoxinA) in patients suffering from refractory neurogenic detrusor overactivity (NDO): A randomised placebo-controlled phase IIa study Neurourol Urodyn 2017; 36:457-462
44 Ehren I, Volz D, Farrelly E, et al Efficacy and impact of botulinum toxin A on quality of life in patients with neurogenic detrusor overactivity: a randomised, placebo-controlled, double-blind study Scand J Urol Nephrol 2007; 41:335-40
45 Ginsberg D, Gousse A, Keppenne V, et al Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity J Urol 2012; 187:2131-9
46 Herschorn S, Gajewski J, Ethans K, et al Efficacy of botulinum toxin A injection for neurogenic detrusor overactivity and urinary incontinence: a randomized, double-blind trial J Urol 2011; 185:2229-35
47 Honda M, Yokoyama O, Takahashi R, et al Botulinum toxin injections for Japanese patients with urinary incontinence caused by neurogenic detrusor overactivity: Clinical evaluation of onabotulinumtoxinA in a randomized, placebo-controlled, double-blind trial with an openlabel extension Int J Urol 2021; 28: 906-912
48 Sussman D, Patel V, Del Popolo G, et al Treatment satisfaction and improvement in health-related quality of life with onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity Neurourol Urodyn 2013; 32:242-9
49 Kennelly M, Cruz F, Herschorn S, et al Efficacy and Safety of AbobotulinumtoxinA in Patients with Neurogenic Detrusor Overactivity Incontinence Performing Regular Clean Intermittent Catheterization: Pooled Results from Two Phase 3 Randomized Studies (CONTENT1 and CONTENT2) European Urology 2022
50 Grise P, Ruffion A, Denys P, et al Efficacy and tolerability of botulinum toxin type a in patients with neurogenic detrusor overactivity and without concomitant anticholinergic therapy: Comparison of two doses Eur Urol 2010; 58:759-766
51 Schurch B, De Sèze M, Denys P, et al Botulinum toxin type A is a safe and effective treatment for neurogenic urinary incontinence: Results of a single treatment, randomized, placebo controlled 6-month study J Urol 2005; 174:196-200
52 Schurch B, Denys P, Kozma CM, et al Botulinum toxin A improves the quality of life of patients with neurogenic urinary incontinence Eur Urol 2007; 52:850-8
53 Abdel-Meguid TA Botulinum toxin-A injections into neurogenic overactive bladder--to include or exclude the trigone? A prospective, randomized, controlled trial J Urol 2010; 184:2423-8
54 Hui C, Keji X, Chonghe J, et al Combined detrusor-trigone BTX-A injections for urinary incontinence secondary to neurogenic detrusor overactivity Spinal Cord 2016; 54:46-50
55 Grise P, Ruffion A, Denys P, et al Efficacy and tolerability of botulinum toxin type a in patients with neurogenic detrusor overactivity and without concomitant anticholinergic therapy: Comparison of two doses Eur Urol 2010; 58:759-766
56 Araujo TG, Schmidt AP, Sanches PRS, et al Transcutaneous tibial nerve home stimulation for overactive bladder in women with Parkinson's disease: A randomized clinical trial Neurourol Urodyn 2021; 40:538-548
57 Perissinotto MC, D’Ancona CA, Lucio A, et al Transcutaneous tibial nerve stimulation in the treatment of lower urinary tract symptoms and its impact on health-related quality of life in patients with
Parkinson disease: a randomized controlled trial J Wound Ostomy Continence Nurs 2015; 42:94-9
58 Monteiro ÉS, de Carvalho LB, Fukujima MM, et al Electrical stimulation of the posterior tibialis nerve improves symptoms of poststroke neurogenic overactive bladder in men: a randomized controlled trial Urology 2014; 84:509-14
59 Gaspard L, Tombal B, Opsomer RJ, et al Kinésithérapie et symptômes du bas appareil urinaire chez des patients atteints de la sclérose en plaques : étude contrôlée randomisée [Physiotherapy and neurogenic lower urinary tract dysfunction in multiple sclerosis patients: a randomized controlled trial] Prog Urol 2014; 24:697-707
60 Zonic-Imamovic M, Imamovic S, Cickušic A, et al Effects of Treating an Overactive Urinary Bladder in Patients with Multiple Sclerosis Acta Med Acad 2019; 48:271-277
61 Eftekhar T, Teimoory N, Miri E, et al Posterior tibial nerve stimulation for treating neurologic bladder in women: a randomized clinical trial Acta Med Iran 2014; 52:816-21
62 Chen YL, Feng WJ, Zhang XL Parkinson's disease combined with overactive bladder syndrome treated with acupuncture and medication Zhongguo Zhen Jiu 2012; 32:215-8
63 Chen H, Wang C, Zhou M, et al Electroacupuncture for post-stroke overactive bladder: a multi-centre pilot randomized controlled trial Acupunct Med 2021; 39:175-183
64 Guo ZF, Liu Y, Hu GH, et al Transcutaneous electrical nerve stimulation in the treatment of patients with poststroke urinary incontinence Clin Interv Aging 2014; 9:851-6
65 Guo GY, Kang YG Effectiveness of neuromuscular electrical stimulation therapy in patients with urinary incontinence after stroke: A randomized sham controlled trial Medicine (Baltimore) 2018; 97:e13702
66 Liu Y, Xu G, Luo M, Teng HF Effects of Transcutaneous Electrical Nerve Stimulation at Two Frequencies on Urinary Incontinence in Poststroke Patients: A Randomized Controlled Trial Am J Phys Med Rehabil 2016; 95:183-93
67 Liu Y, Xu G, Geng J Efficacy of Transcutaneous Electrical Nerve Stimulation in the Management of Neurogenic Overactive Bladder: A Randomized Controlled Trial Am J Phys Med Rehabil 2022; 101:2-10
68 McDonald C, Rees J, Winge K, et al Bladder training for urinary tract symptoms in Parkinson disease: A randomized controlled trial Neurology 2020; 94:e1427-e1433
69 Vaughan CP, Burgio KL, Goode PS, et al Behavioral therapy for urinary symptoms in Parkinson's disease: A randomized clinical trial Neurourol Urodyn 2019; 38:1737-1744
70 Tibaek S, Gard G, Jensen R Pelvic floor muscle training is effective in women with urinary incontinence after stroke: a randomised, controlled and blinded study Neurourol Urodyn 2005; 24:348-57
71 Tibaek S, Gard G, Dehlendorff C, et al Is Pelvic Floor Muscle Training Effective for Men With Poststroke Lower Urinary Tract Symptoms? A Single-Blinded Randomized, Controlled Trial Am J Mens Health 2017; 11:1460-1471
72 Khan F, Pallant JF, Pallant JI, et al A randomised controlled trial: Outcomes of bladder rehabilitation in persons with multiple sclerosis Journal of Neurology, Neurosurgery and Psychiatry 2010; 81:9 (10331038)
73 Lúcio AC, Perissinoto MC, Natalin RA, et al A comparative study of pelvic floor muscle training in women with multiple sclerosis: its impact on lower urinary tract symptoms and quality of life Clinics (Sao Paulo) 2011; 66:1563-8
74 Botini D, Lucio A, Domingos J, et al Pelvic floor muscle training in the treatment of lower urinary tract symptoms in women with multiple
505 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
sclerosis and myelopathy associated with HTLV-I (HAM/TSP): A randomized controlled trial Neurourology and Urodynamics 2019; 38 (Suppl 3):S455-
75 Ferreira AP, Pegorare AB, Salgado PR, et al Impact of a Pelvic Floor Training Program Among Women with Multiple Sclerosis: A Controlled Clinical Trial Am J Phys Med Rehabil 2016; 95:1-8
76 Silva Ferreira AP, de Souza Pegorare ABG, Miotto Junior A, et al A Controlled Clinical Trial on the Effects of Exercise on Lower Urinary Tract Symptoms in Women With Multiple Sclerosis Am J Phys Med Rehabil 2019; 98:777-782
77 Lúcio A, D’ancona CA, Perissinotto MC, et al Pelvic Floor Muscle Training With and Without Electrical Stimulation in the Treatment of Lower Urinary Tract Symptoms in Women With Multiple Sclerosis J Wound Ostomy Continence Nurs 2016; 43:414-9
78 Witte LP, Odekerken VJJ, Boel JA, et al Does deep brain stimulation improve lower urinary tract symptoms in Parkinson's disease? Neurourol Urodyn 2018; 37:354-359
79 Moussa M, Abou Chakra M, Dabboucy B, et al Single intradetrusor injection of autologous adipose-derived stem cells in Parkinson's disease patients with overactive bladder: A pilot study Neurourology and Urodynamics 2021; 40(Suppl 2):S93-S95
80 Hebjorn S Treatment of detrusor hyperreflexia in multiple sclerosis: a double-blind, crossover clinical trial comparing methantheline
Correspondence
Rawa Bapir - Dr rawa@yahoo com
Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq
Kamran Hassan Bhatti - kamibhatti92@gmail com
Urology Department, HMC, Hamad Medical Corporation, Qatar
Ahmed Eliwa - ahmedeliwafarag@gmail com
Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt
Herney Andrés García-Perdomo - herney garcia@correounivalle edu co
Universidad del Valle, Cali, Colombia
Nazim Gherabi, MD - ngherabi@gmail com
Faculty of Medicine Algiers 1, Algiers, Algeria
Derek Hennessey, MD - derek hennessey@gmail com
Department of Urology, Mercy University Hospital, Cork, Ireland
Vittorio Magri, MD - vittorio magri@virgilio it
ASST Nord Milano, Milan, Italy
Panagiotis Mourmouris, MD - thodoros13@yahoo com
2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece
Adama Ouattara, MD - adamsouat1@hotmail com
Division of Urology, Souro Sanou University Teaching Hospital, BoboDioulasso, Burkina Faso
Gianpaolo Perletti, Dr Biol Sci M Clin Pharmacol
Gianpaolo Perletti@uninsubria it
Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy
Joseph Philipraj, MD - josephphilipraj@gmail com
Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India
Konstantinos Stamatiou, MD - stamatiouk@gmail com
Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece
Alberto Trinchieri, MD - alberto trinchieri@gmail com
Urology School, University of Milan, Milan (Italy)
Noor Buchholz, MD - noor buchholz@gmail com
Sobeh's Vascular and Medical Center, Dubai Health Care City, Dubai, United Arab Emirates
bromide (Banthine), flavoxate chloride (Urispas) and meladrazine tartrate (Lisidonil) Urol Int 1977; 32:209-17
81 Gajewski JB, Awad SA Oxybutynin versus propantheline in patients with multiple sclerosis and detrusor hyperreflexia J Urol 1986; 135:966-68
82 Fader M, Glickman S, Haggar V, et al Intravesical Atropine
Overactivity: A Double-Blind, Randomized Crossover Trial J Urol 2007; 177:208-13
83 Novara G, Galfano A, Secco S, et al A systematic review and metaanalysis of randomized controlled trials with antimuscarinic drugs for overactive bladder Eur Urol 2008; 54:740-63
84 Rossanese M, Novara G, Challacombe B, et al Critical analysis of phase II and III randomised control trials (RCTs) evaluating efficacy and tolerability of a β3-adrenoceptor agonist (Mirabegron) for overactive bladder (OAB) BJU Int 2015; 115:32-40
85 Chapple CR, Kaplan SA, Mitcheson D, et al Mirabegron 50 mg once-daily for the treatment of symptoms of overactive bladder: an overview of efficacy and tolerability over 12 weeks and 1 year Int J Urol 2014; 21:960-967
86 Rosa GM, Ferrero S, Nitti VW, et al Cardiovascular safety of β3adrenoceptor agonists for the treatment of patients with overactive bladder syndrome Eur Urol 2016; 69:311-323
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
506
R
C o m p a r e d t o O r a l O x y b u t y n i n f o r N e u r o g e n i c D e t r u s o r
Risk of urinary stone formation associated to proton pump inhibitors: A systematic review and metanalysis
Rawa Bapir 1, 15 , Kamran Hassan Bhatti 2, 15 , Ahmed Eliwa 3, 15 , Herney Andrés García-Perdomo 4, 15 , Nazim Gherabi 5, 15 , Derek Hennessey 6, 15 , Vittorio Magri 7, 15 , Panagiotis Mourmouris 8, 15 , Adama Ouattara 9, 15 , Gianpaolo Perletti 10, 15 , Joseph Philipraj 11, 15 , Konstantinos Stamatiou 12, 15 , Musliu Adetola Tolani 13, 15 , Lazaros Tzelves 8, 15 , Alberto Trinchieri 14, 15 , Noor Buchholz 15
1 Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq;
2 Urology Department, HMC, Hamad Medical Corporation, Qatar;
3 Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt;
4 Universidad del Valle, Cali, Colombia;
5 Faculty of Medicine Algiers 1, Algiers, Algeria;
6 Department of Urology, Mercy University Hospital, Cork, Ireland;
7 ASST Nord Milano, Milan, Italy;
8 2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece;
9 Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso;
10 Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy;
11 Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India;
12 Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece,
13 Division of Urology, Department of Surgery, Ahmadu Bello University / Ahmadu Bello University Teaching Hospital, Zaria, Kaduna State, Nigeria;
14 Urology School, University of Milan, Milan, Italy;
15 U-merge Ltd (Urology for emerging countries), London-Athens-Dubai*
Authors 1-14 have equally contributed to the paper and share first authorship
* U-merge Ltd (Urology for Emerging Countries) is an academic urological platform dedicated to facilitate knowledge transfer in urology on all levels from developed to emerging countries U-merge Ltd is registered with the Companies House in London/ UK www U-merge com
Summary
Objective: Proton pump inhibitors are widely used as treatment of acid-related disorders. They are considered safe although their long-term use has been associated with some adverse effects including an increased propensity for urinary calculi formation The aim of this study was to systematically review available data from studies evaluating the association of PPIs and nephrolithiasis
Materials and methods: We searched two electronic databases (PubMed and EMBASE) for cohort studies or case-control studies evaluating the relationship between treatment with proton pump inhibitors and the risk of stone formation published up to 31 October 2022 The overall association of PPIs and urinary calculi was analyzed using a random effects model (RevMan5) The quality of the included studies was assessed using the Newcastle-Ottawa Quality Assessment Scale.
Results: A total of 550 studies were retrieved; 7 were selected by title and abstract screening; after removal of duplicates, 4 records were evaluated by full-text examination An additional study was retrieved by handsearching the references included in screened studies In the unadjusted analysis, the odds of urinary calculi were greater in subjects taking PPIs compared to controls (unadjusted OR = 2.10, 95% CI 1.74-2.52, p < 0.00001). The pooled odds ratio of two case-control studies confirmed that use of PPIs increased the odds of urinary calculi compared with non-use (OR 2 44, 95% CI 2 29 to 2 61) Pooled analysis of three cohort studies evaluating incident nephrolithiasis showed
an overall hazard ratio estimate of 1.34 (95% CI = 1.28-1.40). One study found lower urinary citrate and urinary magnesium levels in subjects exposed to PPIs The Newcastle-Ottawa Quality Assessment Scale scores ranged between 6 and 8 Conclusions: PPIs showed an association with urinary calculi in patients included in the studies included in this review If these data will be confirmed in adequately powered randomized trials, clinicians may consider limiting the long-term use of PPIs, to avoid unnecessary prolongation of treatment Urinary magnesium and citrate should be evaluated in renal stone forming patients taking PPIs to supplement their intake when requested
KEY WORDS: Proton pump inhibitors; Urinary calculi; H2-receptor blockers; Magnesium; Citrate
Submitted 1 December 2022; Accepted 15 December 2022
INTRODUCTION
Proton pump inhibitors (PPIs) reduce the gastric acid production by irreversibly blocking the H+/K+ ATPase, also known as the proton pump, located in the parietal cells of the gastric wall PPIs are widely used for the treatment of gastroesophageal reflux disease (GERD), Zollinger-Ellison syndrome, erosive esophagitis, duodenal or gastric ulcers
507 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 REVIEW
of
No conflict
interest declared
DOI: 10 4081/aiua 2022 4 507
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
including those caused by non-steroidal anti-inflammatory drugs (NSAIDs), and for the eradication of Helicobacter pylori in combination with antibiotics
They have emerged as first-line treatment of acid-related disorders, traditionally treated with histamine type 2 receptor antagonists/blockers (H2RAs), that inhibit gastric acid secretion by blocking the histamine stimulation of gastric parietal cells (1)
PPIs are considered safe, though their long-term use has been associated with some serious adverse effects including community acquired pneumonia (2), risk for osteoporosisrelated fractures (3, 4), enteric infection (5), Clostridium difficile-associated diarrhea (6, 7), myocardial infarction (8), chronic kidney disease (9), Alzheimer’s dementia (10), and hypomagnesemia (4)
In 2019, the analysis of post-marketing safety data from FDA Adverse Event Reporting System (FAERS) suggested an increased propensity for nephrolithiasis in subjects taking proton-pump inhibitors (11) Two studies, presented as congress communications but never published as full-text reports, demonstrated that the use of PPIs and H2 blockers was associated with an increased risk of kidney stones (12, 13) More recently, three articles were published, evaluating in three different large population from the United States (N = 2) and Korea (N = 1) the risk of stone formation in patients taking PPIs (14-16) The aim of this study was to systematically review the data from studies evaluating the association of PPIs and nephrolithiasis and, where possible, to perform a pooled analysis of the prevalence of urinary stone disease in patients taking PPIs Particular attention was devoted to the assessment of the risk of bias in the studies included in the analysis
MATERIALS AND METHODS
Protocol and registration
The review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (17) It was registered on the PROSPERO platform as CRD42022375951
Types of studies
We considered articles written in English, reporting cohort studies, case-control studies and randomized controlled trials evaluating the relationship between the treatment with PPIs or H2RAs and the risk of kidney stone formation, without time constraints
Types of patients
Adult participants (> 18 years) of both sexes were involved irrespective of their age or ethnicity
Types of interventions
Proton pump inhibitors (PPIs) and histamine-2 receptor antagonists (H2RAs)
Outcomes
The main outcome considered for this review was the assessment of the prevalence rate of urinary stones in subjects taking PPIs compared to those not taking this treatment A secondary outcome was the comparison of renal
stone prevalence between subjects taking compared to those non-taking H2Ras
Search strategy
Two electronic databases (PubMed and EMBASE) were searched for articles published up to 31 October 2022 Search was performed using the following string based on MeSH terms: (proton pump inhibitors OR histamine H2 antagonists OR omeprazole OR esomeprazole OR lansop
rabeprazole) AND urinary calculi Relevant data were also hand searched by browsing various sources (e g , reference lists from reviews and study reports, congress abstracts, clinical trial registers such as www clinicaltrials gov, www clinicaltrialsregister eu, etc )
Data collection and analysis
Selection of studies
Title and abstract screening to exclude documents that did not meet the inclusion criteria was performed independently by two authors Duplicate references were deleted Full texts were downloaded for full-text screening and to extract relevant information Controversies were resolved by a third researcher
A PRISMA flow diagram was drawn to illustrate the results of study selection process (Figure 1)
Data extraction
Data extraction was conducted by four authors using a s t a n d a r d i z e d f o r m T h e f o l l o w i n g i n f o r m a t i o n w a s obtained from each study: author(s), publication year, study design, population, intervention, prevalence of stone disease In case of missing or insufficient information, we considered the impact of missing data on the meta-analysis results
Risk of bias analysis
Two authors independently performed the assessment of quality of the included studies using the NewcastleOttawa Scale (NOS), a risk of bias assessment tool for o b s e r v a t i o n a l s t u d i e s t h a t i s r e c o m m e n d e d b y t h e Cochrane Collaboration (18) The NOS evaluates three quality parameters (selection, comparability, and outcome) divided across eight specific items It can be scored a maximum of one ‘star’ for each item within the ‘Selection’ and ‘Exposure/Outcome’ categories and a maximum of two ‘stars’ for ‘Comparability’ The maximum NOS score is 9 A study with score ranging between 7 and 9 is rated as being high quality, between 4 and 6 as medium quality, and between 0 and 3 as low quality The overall evaluation of the quality of pooled evidence was performed according to GRADE criteria
Publication bias assessment by Funnel plot analysis was performed in the presence of at least 4 studies If a potential reporting bias was suspected, the Begg/Mazumdar and Egger’s regression tests were used to assess the significance of funnel plot asymmetry and potential publication bias
Statistical analysis
Statistical analysis was performed using the RevMan5
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
508
r a z o l e O R d e x l a n s o p r a z o l e O R p a n t o p r a z o l e O R
software Dichotomous data (presence/absence of stone disease) and number of subjects were extracted to calculate odds ratios (OR), hazard ratios (HR), confidence intervals (CI), and Z statistics Pooled analyses were performed using the generic inverse-variance random-effects model Random effect model was used due to high heterogeneity of included studies
Assessment of heterogeneity
Heterogeneity was assessed by I^2 statistics, reported with 95% CIs, and interpreted as of lesser importance (≤ 40%), moderate (30%-60%), substantial (50%-90%) or considerable (≥ 75%), according to Cochrane criteria
RESULTS
We retrieved 550 records, 539 from EMBASE and 11 from Medline
After title and abstract screening of retrieved records and deduplication, we selected 7 articles After full text reading, we considered 4 articles for meta-analysis An additional study was retrieved by handsearching the references included in screened studies
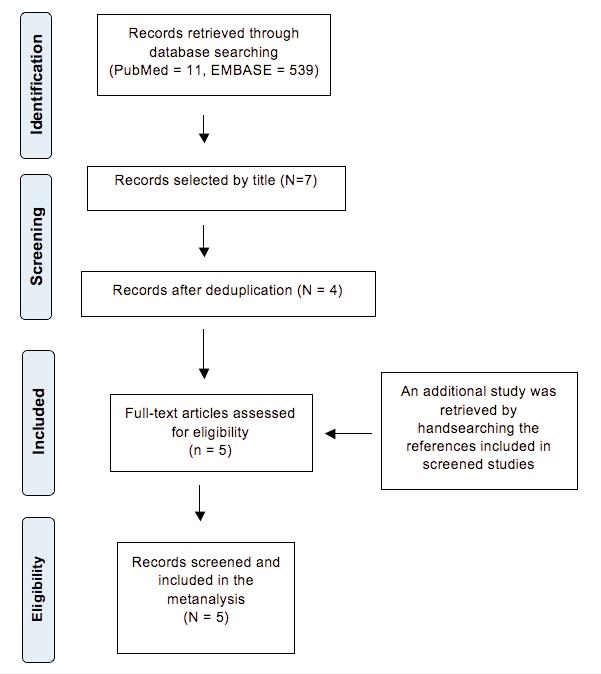
Description of studies
A description of the selected studies, including retrieved data, is shown in the Supplementary Materials
Ferraro et al (12) evaluated cohorts of health professionals participating to the H e a l t h P r o f e s s i o n a l s F o l l o w - u p S t u d y (HPFS), and Nurses’ Health Study (NHS)
I and II (n = 187 330) Incident stone episodes were prospectively evaluated during a follow up > 10 years Urinary excretion risk factors for stone formation was evaluated in a subgroup of 6 520 participants
Kwak et al (13) evaluated a cross-sectional sample of the US population in the c o n t e x t o f t h e N a t i o n a l H e a l t h a n d Nutrition Examination Survey (NHANES), providing a variety of health and nutrition measurements in men and nonpregnant women age > 20 (n = 13836)
Kim et al (14) conducted a nested casecontrol study using the National Health Insurance Service-National Health Screening Cohort in Korea, that included unselected men and women from the general population, older than 40 years Renal stone formers and controls were randomly matched for age, sex, income, and region of residence A total of 28 962 urolithiasis participants and 115 848 control participants were enrolled
Simonov et al (15) retrospectively evaluated incident stones in participants to the Women Veterans Cohort Study (WVCS), i n c l u d i n g m e n a n d w o m e n v e t e r a n s who were discharged from military service as of October 2001 and who elected to utilize the Veteran Administration medical care (n = 465 891) Subjects with diagnosis of nephrolithiasis or a history of PPI usage prior pre-observation were excluded from the study A subset of subjects taking PPIs or not (86 264 in each group) were considered for a propensity-matched model The median observation time was 4 years A limitation of this study was the younger age of the population, which limited the generalizability of the study findings to other populations
Sur et al (16) evaluated the records of the database of clinical data Vanderbilt Research and Synthetic Derivative Medical center electronic health records from 1993 to 2020 were obtained for over three million patients
The researchers identified a cohort of 55 765 adults with GERD, who were PPI naïve and had no history of nephrolithiasis Incident nephrolithiasis was retrospectively evaluated using the first PPI use as the date of first GERD diagnosis The median follow up was 3 years Urinary 24-hour risk factors for stone formation were evaluated in a subset of 593 patients with GERD
Quantitative analysis
Unadjusted data from four studies showed that PPIs use was significantly associated with urinary calculi (OR = 2 10, 95% CI 1 74-2 52, p < 0 00001) (Figure 2A) The study of Ferrero and coworkers was excluded from this analysis because it was presented as an abstract lacking crude data to be used for quantitative analysis No addi-
509 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Proton pump inhibitors and urinary calculi
Figure 1. Flow diagram
A – Rates of urinary calculi in patients taking PPIs and controls (unadjusted data); B – pooled odds ratios of case-control studies investigating urinary calculi in patients taking PPIs compared to controls; C – pooled hazard ratios of incident nephrolithiasis in patients on PPIs treatment compared to controls Data are adjusted for comorbidities and concurrent medications
Diamonds on the right side of the no-effect line indicate greater odds and hazard ratios in patients treated with PPIs compared to controls placebo Odds ratio and hazard ratio with 95% confidence intervals and heterogeneity statistics (I^2) are shown
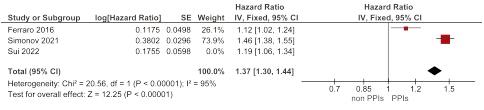
tional information was obtained from the Authors When pooled analyses were performed using data adjusted for comorbidities and concurrent medications, the association between PPIs and urinary calculi remained significant The pooled odds ratio of two case-control studies confirmed that the use of PPIs increased the odds of urinary calculi compared with non-use (OR 2 44, 95% CI 2 29 to 2 61) (Figure 2B) The pooled hazard ratios of three studies evaluating incident nephrolithiasis showed an overall pooled HR estimate of 1 34 (95% CI = 1 281 40) (Figure 2C) Considerable heterogeneity was found in all analyses (I2 = 96%, 92%, and 88% respectively)
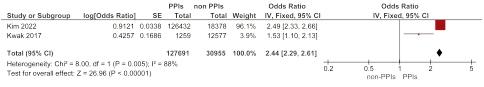
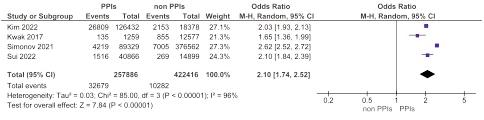
Length and dose of treatment
Results concerning the effect of the duration of PPI treatment on the risk of stone formation are controversial Kim et al (14) found higher odds for urolithiasis when treatment with PPI was extended to 365 days or longer (OR 2 32) compared to shorter periods (30-364 days: OR 1 97, 1-19 days: OR 1 65) This confirms the finding of Kwak et al (13) who reported higher rates of urinary calculi in subjects taking PPIs for more than 5 years Conversely, Ferraro et al (12) observed that HRs were
independent of duration of use Simonov et al (15) observed that higher doses of PPIs were associated with an increased risk of kidney stones formation
H2 blockers
Ferraro et al (12) found that the use of H2 blockers is also associated to higher risks of renal stone formation (HR 1 13, 95% CI 1 02, 1 24, p-value = 0 02) Simonov et al (15) confirmed an increased risk for renal stone upon treatment with H2 blockers (adjusted HR, 1 47; CI 1 311 64) Pooled hazard ratios of the two studies evaluating incident nephrolithiasis showed an overall pooled HR estimate of 1 27 (95% CI = 1 18-1 37) (Figure 3) Heterogeneity was 91% Kwak et al (13) reported greater odds for combined PPI/antacid use (OR: 2 03, 95% CI: 1 28-3 23, p = 0 049) and combined PPI/H2 blocker use (OR: 3 18, 95% CI: 1 12-9 07, p = 0 031)
Urinary risk factors
Sur et al (16) observed significantly lower mean levels of urinary citrate and urinary magnesium in the PPI-exposed group compared to non-exposed subjects Ferraro et al (12) found lower urinary excretion of calcium in PPI users
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al 510
Figure 2
A.
B.
C.
Pooled hazard ratios of incident nephrolithiasis in patients on treatment with H2-blockers compared to controls Diamonds on the right side of the no-effect line indicate greater hazard ratios in patients treated with H2-blockers compared to controls placebo Hazard ratio with 95% confidence intervals and heterogeneity statistics (I^2) are shown.

Risk of Bias, quality of the evidence
According to the quality assessment of NOS, all the studies were characterized by high quality, with scores ranging between 6 and 8 (Supplementary Materials)
According to GRADE criteria, the quality of the evidence is low Downgrading criteria are the observational design of the studies, the presence of moderate risk of bias and the inconsistency due to heterogeneity The large magnitude of effect (Odds ratio > 2) was considered as criterion for upgrading
Publication bias assessment by Funnel plot analysis resulted in no statistically significant asymmetry (P = 0 190, Egger’s test; P = 0 497, Begg’s test) The funnel plot is shown in the Supplementary Materials section The “trim-and-fill” strategy imputed zero missing studies
DISCUSSION
Urinary stone disease has a complex pathogenesis involving different aspects of the metabolism and depending on the chemical composition of the stones A non-negligible fraction of cases is caused by the intake of different kinds of drugs that can lead to the formation of stones containing amounts of the same drugs Other drugs cause alterations of different metabolic steps, resulting in the modification of the urinary excretion of risk factors for stone formation (19)
The potential risk of kidney stone formation in subjects treated with PPIs is still debated, and the factors causing an increased risk have not been fully elucidated In general, PPI-related increases of gastric pH may lead to deficiencies of minerals (iron, calcium and magnesium) and vitamins (B12 and C) which need a low gastric pH for their absorption and bioavailability (20) However, a specific effect of long-term PPI treatment on mineral metabolism is the reduction of serum magnesium levels resulting from its reduced intestinal absorption Intestinal absorption of magnesium depends on both active transcellular transporters and passive paracellular absorption mediated by claudins Active transportation of magnesium through enterocyte cell membranes is mainly mediated by transient receptor potential melastatin 6 and 7 (TRPM6 and TRPM7), whose activity is regulated by intracellular magnesium and pH levels whereby a more acidic milieu increases TRPM6 activity (21) PPIs may alter transporter transcription or channel function by increasing the luminal pH, thus affecting hydrogen pro-
ton secretion The decrease of TRPM6 and TRPM7 activity results in decreased magnesium absorption (22) In vitro studies suggested the concomitant inhibition of passive magnesium absorption by PPIs (23) The extent of the decrease of intestinal magnesium absorption during PPI treatment seems to be minor, but it may cause longterm cumulative deficiency The effect of PPIs on magnesium metabolism is also enhanced by other medications acting on magnesium metabolism, such as loop diuretics (24) Severe hypomagnesaemia can manifest with musculoskeletal, neurological, or cardiac arrhythmic symptoms, b
d e r f o r m s m a y r e m a i n u n d e t e c t e d ( 2 5 ) Hypomagnesemia induced by PPIs is often associated w i t h m u l t i p l e e l e c t r o l y t e d i s t u r b a n c e s , i n c l u d i n g hypocalcemia, hypophosphatasemia, and hypokalemia
Low serum magnesium levels interfere with calciumsensing receptors suppressing parathyroid hormone (PTH) secretion and increasing organ resistance to PTH by inhibiting receptor binding and intracellular signaling (26) Hypoparathyroidism results in turn in low serum and urinary calcium levels Hypomagnesemia also causes hypokalemia by inducing kaliuresis (27) Reduced intestinal absorption of magnesium is balanced by changes in renal reabsorption of magnesium resulting in a reduction of urinary magnesium The reduction of urinary excretion of both calcium and magnesium during PPI treatment may have conflicting effects on the overall risk of kidney stone formation, because the reduced urinary calcium excretion decreases urinary saturation with respect to calcium oxalate and calcium phosphate, but the reduced magnesium excretion increases the risk of stone formation due to the decrease of urinary inhibitory activity of crystallization Studies focused on the effect of PPIs on the urinary excretion of citrates, which are potent crystallization inhibitors, whose decline in the urine can increase the risk of kidney stone formation (28-30) The urinary levels of citrate are reduced in conditions of acidosis, which induces an increase in the metabolism of citrate in the renal proximal tubule cells with a consequent decreased excretion of citrate in the urine (31) An initial study performed on a small sample of subjects treated for a short time with omeprazole did not demonstrate changes in the daily urinary electrolyte output and urine pH in response to ammonium chloride load (32) However, a case report described metabolic acidosis associated with hypomagnesaemia in a patient receiving omeprazole (33) A recent study in a larger population of
511 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Proton pump inhibitors and urinary calculi
u t m i l
Figure 3.
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
renal stone patients receiving PPIs showed that patients tended to show decreased citrate levels (28) This finding was explained by the net gastric acid loss due to reduced gastric acid production by proton pump inhibition, r e s u l t i n g i n r e d u c e d b i c a r b o n a t e g e n e r a t i o n a n d decreased renal excretion of citrate In this study, the decrease of urinary citrate was not associated to a decrease of urinary magnesium in stone patients taking PPIs On the contrary, William et al demonstrated reduced urinary magnesium in renal stone patients taking PPIs but a non-statistically significant trend of reduction of urinary citrate (29, 30) Penniston et al also showed lower urinary magnesium in renal stone formers taking omeprazole, but they were not able to show any other change in urinary risk factors (34) Finally, in a large series of patients with GERD, Sui et al demonstrated that patients taking PPIs had significantly lower mean urinary levels of both citrate and magnesium (16) In conclusion, the decrease of inhibitors of urinary crystallization in subjects taking PPIs represents a potential risk for renal stone formation
Limitations
A major limitation of the studies that were considered in this meta-analysis is represented by the selection of subjects to be assigned to the PPI-exposed group and to the PPI-non exposed group Exposure to PPIs depends on the presence of acid-related diseases that in themselves may be risk factors for renal stone formation The indications for treatment with PPIs approved by the FDA are healing and maintenance of healing of erosive esophagitis (EE), H pylori eradication to reduce the risk of recurrence of duodenal ulcer (DU), symptomatic gastroesophageal reflux disease (GERD), risk reduction of nonsteroidal anti-inflammatory drug (NSAID)-associate gastric ulcer (GU) and pathological hypersecretory conditions These acid-related diseases have not been directly associated with kidney stone formation, though the stomach plays an important role in the metabolism of calcium and oxalate (20, 35) On the other hand, acid-related diseases are not associated with other enteric diseases that can promote renal stone formation A study by Sonnenberg et al (36) demonstrated that gastro-esophageal reflux disease (GERD) is inversely associated with all forms of inflammatory bowel diseases that are associated with an increased risk of stone formation due to increased urinary oxalate caused by fat mala b s o r p t i o n O n t h e c o n t r a r y , s u b j e c t s w i t h g a s t r oesophageal reflux-type symptoms showed an higher risk of irritable bowel syndrome that has not been associated with renal stone disease (37) However, acid-related diseases and renal stone diseases share several risk factors
Obesity has been associated with both the presence of symptoms of gastroesophageal reflux disease (38, 39) and the formation of kidney stones (40)
Similarly, a diet rich in proteins and animal fats and low in vegetables and fruit can predispose to both gastroesophageal reflux (41) and kidney stones (42)
Furthermore, concomitant use of antacids may increase the risk of stone formation Antacids are still used for the treatment of acid-related disorders because they are easily available over the counter and may also be more affordable than prescription medications These preparations
contain magnesium trisilicate, that may cause the formation of silicate calculi, and calcium carbonate that -when administered outside meals- may cause peaks of serum and urinary calcium with an increased risk of calcium crystallization in the urine Finally, reflux patients tend to avoid citrus fruits that can trigger reflux but are a source of citrates that act as crystallization inhibitors
In our review, four studies evaluated populations including subjects on treatment with PPIs or not To rule out an assignment bias, most authors compared patients taking or non-taking PPIs for the presence of comorbidities and dietary patterns and adjusted their analyses for potential confounders Ferraro et al (12) used Cox proportional hazards regression models adjusted for age, race, body mass index (BMI), physical activity, smoking status, comorbidities, use of medications and intake of nutrients, whereas Kwak et al (13) found no difference in dietary or supplemental calcium, vitamin D, liquid, protein, sodium, and potassium intake in subjects taking PPIs or not The latter adjusted their multivariate analysis for male gender, middle to old age, white ethnicity, obesity, diabetes, and elevated creatinine levels Similarly, Kim et al (14) adjusted their multivariable logistic regression analysis for age, sex, income, region of residence, total cholesterol, SBP, DBP, fasting blood glucose, CCI score, prescription dates within 1 year of each H2 blocker and NSAID, and number of GERD treatments, and performed subgroup analyses according to age, sex, income, region of residence, obesity, smoking, alcohol consumption, total cholesterol, systolic blood pressure, and fasting blood glucose Simonov et al (15) used a time-varying Cox proportional hazards model adjusted for baseline covariates including sex, race/ethnicity, age, creatinine, medications (H2RAs, thiazide diuretics, loop diuretics, gout medications), medical history (gastroesophageal reflux disease, peptic ulcer disease, Barrett’s disease, gastrointestinal bleed, gastritis, functional dyspepsia, gastrointestinal surgical history, diabetes, gout) and total number of inpatient/outpatient encounters in the previous year Finally, Sur et al. used multivariable Cox models with time-varying covariates after adjusting for age, BMI, gender, history of hypertension, coronary artery disease, hyperlipidemia and type 2 diabetes (16)
Only the study by Sui et al (16) restricted its investigation to subjects with GERD, thus reducing the selection bias of assignment to treatment Selection bias is known to affect the quality of studies performed on large general populations However, even in this study a bias related to assignment to treatment with PPIs is still present, because subjects who did not take PPIs may have had a less severe disease than those who were on PPIs
In general, observational studies are thought to tend to overestimate intervention effects and to have a lower grade of evidence in the hierarchy of research design compared to randomized controlled trials (RCTs) In an editorial, the results of observational studies showing an increased risk of renal stones and other diseases in subjects taking PPIs were critically commented (43) It was highlighted that randomized studies are “the most powerful design to determine whether PPIs may cause long-term harm” In fact, the results of a study of over 17 500 aspirin and/or apixaban users randomized to treatment with pantoprazole did not support the results of observational data suggesting that
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
512
small increases of risk for some diseases in subjects taking PPIs could be due to confounding factors or biases (44) This randomized controlled study was not included in our analysis because kidney stone formation was not included among the safety outcomes of the trial Furthermore, the population studied was not representative of the subjects most frequently affected by calcium renal stones, which occur more frequently between the ages of 30 and 50, whereas the study inclusion criteria were stable coronary and arterial disease in patients older than 65 years or arterial disease involving 2 cardiovascular beds and/or had 2 additional risk factors in younger subjects
A randomized study to evaluate the risk of stone formation in subjects taking PPis should require the evaluation of a population of subjects aged between 20 and 60 who can be randomized to treatment with PPIs over a period of several years Ethical issues and financial considerations make such a study unlikely to be accomplished On the other hand, previous comparisons of randomized controlled studies with cohort or case-control studies assessing a specific intervention demonstrated that welldesigned observational studies do not overestimate the effects of the intervention as compared to randomized controlled studies (45)
CONCLUSIONS
Our meta-analysis identified a potentially increased risk of kidney stone formation in patients taking PPIs However, the observational design of included studies points to a strong risk of assignment bias Consequently, these results must be considered with great caution and do not justify a restriction of the use of PPIs when they are administered in accordance with guidelines recommendations, avoiding unjustified long-term prolongation of the therapy In fact, PPIs are frequently purchased over the counter, are often used without correct indications, are rarely deprescribed, thus being often used for longer periods than necessary Administration of magnesium and citrate supplements and/or periodical evaluation of serum and urinary magnesium and urinary citrate levels should be considered for patients on long-term PPI treatment, and especially in stone forming patients on treatment with these drugs
REFERENCES
1 Zamburak RD, Schubert ML Control of gastric acid secretion
Histamine H2-receptor antagonists and H+K(+)-ATPase inhibitors
Gastroenterol Clin North Am 1992; 21:527-50
2 Laheij RJ, Sturkenboom MC, Hassing RJ, et al Risk of community-acquired pneumonia and use of gastric acid suppressive drugs
JAMA 2004; 292:1955-1960
3 Yang YX, Lewis JD, Epstein S, et al Long-term proton pump inhibitor therapy and risk of hip fracture JAMA 2006; 296:2947-2953
4 Ito T, Jensen RT Association of long-term proton pump inhibitor therapy with bone fractures and effects on absorption of calcium, vitamin B12, iron, and magnesium Curr Gastroenterol Rep 2010; 12:448-57
5 Leonard J, Marshall JK, Moayyedi P Systematic review of the risk of enteric infection in patients taking acid suppression Am J Gastroenterol 2007; 102:2047-2056
6 Dial S, Delaney JAC, Barkun AN, et al Use of gastric acid-suppressive agents and the risk of community-acquired Clostridium difficile-associated disease JAMA 2005; 294:2989-2995
7 Trifan A, Stanciu C, Girleanu I, et al Proton pump inhibitors therapy and risk of Clostridium difficile infection: Systematic review and meta-analysis World J Gastroenterol 2017; 23:6500-15
8 Charlot M, Grove EL, Hansen PR, et al Proton pump inhibitor use and risk of adverse cardiovascular events in aspirin treated patient with first time myocardial infarction: a nationwide propensity score matched analysis BMJ 2011; 342:d2690
9 Lazarus B, Chen Y, Wilson FP, et al Proton pump inhibitor use and risk of chronic kidney disease JAMA Intern Med 2016; 176:238-246
10 Gomm W, von Holt K, Thome F, et al Association of proton pump inhibitors with risk of dementia: a pharmacoepidemiological claims data analysis JAMA Neurol 2016; 73:410-416
11 Makunts T, Cohen IV, Awdishu L, Abagyan R Analysis of postmarketing safety data for proton-pump inhibitors reveals increased p r o
Sci Rep 2019; 9:2282
12 Ferraro PCG, Gambaro G, Taylor E Proton Pump Inhibitors, Histamine Receptor-2 Blockers and the Risk of Incident Kidney Stones American Society of Nephrology Kidney Week; Chicago, IL 2016; p 467A
13 Kwak YE, Buller G, Masoud A Increased risk of nephrolithiasis in patients using chronic proton pump inhibitor and antacid agents Gastroenterology 2017; 152:5(Suppl 1)(S273-)
14 Kim SY, Yoo DM, Bang WJ, Choi HG Association between Urolithiasis and History Proton Pump Inhibitor Medication: A Nested Case-Control Study J Clin Med 2022; 11:5693
15 Simonov M, Abel EA, Skanderson M, et al Use of Proton Pump I n h i b i t o r s I n c r e a s e s R i s k o f I n c i d e n t K i d n e y S t o n e s C l i n Gastroenterol Hepatol 2021; 19:72-79 e21
16 Sui W, Miller NL, Gould ER, et al Proton pump inhibitors use and risk of incident nephrolithiasis Urolithiasis 2022; 50:401-409
17 Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and MetaAnalyses: The PRISMA Statement PLoS Med 2009; 6:e1000097
18 Wells G, Shea B, O’Connell D, et al The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses; 2013 https://www ohri ca/programs/clinical epidemiology/oxford asp
19 Daudon M, Frochot V, Bazin D, Jungers P Drug-Induced Kidney Stones and Crystalline Nephropathy: Pathophysiology, Prevention and Treatment Drugs 2018; 78:163-201
20 Shkembi B, Huppertz T Calcium Absorption from Food Products: Food Matrix Effects Nutrients 2021; 14:180
21 Voets T, Nilius B, Hoefs S, et al TRPM6 forms the Mg2+ influx channel involved in intestinal and renal Mg2+ absorption J Biol Chem 2004; 279:19-25
22 Li M, Du J, Jiang J, Ratzan W, et al Molecular determinants of Mg2+ and Ca2+ permeability and pH sensitivity in TRPM6 and TRPM7 J Biol Chem 2007; 282:25817-25830
23 Thongon N, Krishnamra N Apical acidity decreases inhibitory effect of omeprazole on Magnesium(2+) absorption and claudin-7 and -12 expression in Caco-2 monolayers Exp Mol Med 2012; 44:684-93
513 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Proton
and urinary
pump inhibitors
calculi
p e n s i t y f o r r e n a l i n j u r y , e l e c t r o l y t e a b n o r m a l i t i e s , a n d nephrolithiasis
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
24 Kieboom BC, Kiefte-de Jong JC, Eijgelsheim M, et al Proton pump inhibitors and hypomagnesemia in the general population: a population-based cohort study Am J Kidney Dis 2015; 66:775-82
25 Atkinson NS, Reynolds DJ, Travis SP 'Lemonade Legs': Why do Some Patients Get Profound Hypomagnesaemia on Proton-Pump Inhibitors? Intest Res 2015; 13:227-32
26 Fatuzzo P, Portale G, Scollo V, et al Proton pump inhibitors and s y m p t o m a t i c h y p o m a g n e s e m i c h y p o p a r a t h y r o i d i s m J N e p h r o l 2017; 30:297-301
27 Negri AL, Valle EE Hypomagnesaemia/hypokalemia associated with the use of esomeprazole Curr Drug Saf 2011; 6:204-6
28 Patel PM, Kandabarow AM, Aiwerioghene E, et al Proton-pump inhibitors associated with decreased urinary citrate excretion Int Urol Nephrol 2021; 53:679-683
29 William JH, Nelson R, Hayman N, et al Proton-pump inhibitor u s e i s a s s o c i a t e d w i t h l o w e r u r i n a r y m a g n e s i u m e x c r e t i o n Nephrology 2014; 19:798-801
30 William JH, Danziger J Proton-Pump inhibitor-induced hypomagnesemia: current research and proposed mechanisms World J Nephrol 2016; 5:152
31 Simpson DP Citrate excretion: a window on renal metabolism Am J Physiol 1983; 244:F223-34
32 Howden CW, Reid JL Omeprazole, a gastric 'proton pump inhibitor': lack of effect on renal handling of electrolytes and urinary acidification Eur J Clin Pharmacol 1984; 26:639-40
33 Isse N, Hashimoto M Omeprazole-induced hypomagnesaemia, causing renal tubular acidosis with hypokalaemia, hypocalcaemia, hyperlactacidaemia and hyperammonaemia BMJ Case Rep 2020; 13:e235385
34 Penniston KL, Li S, Nakada SY, Jhagroo RA Omeprazole lowers 24-hour urinary magnesium excretion in patients with a history of urolithiasis: Single center experience J Urol 2021; 206(Suppl 3): e143
35 Hautmann RE The stomach: a new and powerful oxalate absorption site in man J Urol 1993; 149:1401-4
36 Sonnenberg A, Turner KO, Genta RM Decreased risk for microscopic colitis and inflammatory bowel disease among patients with reflux disease Colorectal Dis 2018; 20:813-820
37 Lovell RM, Ford AC Prevalence of gastro-esophageal reflux-type symptoms in individuals with irritable bowel syndrome in the community: a meta-analysis Am J Gastroenterol 2012; 107:1793-801
38 Jacobson BC, Somers SC, Fuchs CS, et al Body-mass index and symptoms of gastroesophageal reflux in women N Engl J Med 2006; 354:2340-8
39 Locke GR 3rd, Talley NJ, Fett SL, et al Risk factors associated with symptoms of gastroesophageal reflux Am J Med 1999; 106:642-9
40 Aune D, Mahamat-Saleh Y, Norat T, Riboli E Body fatness, diabetes, physical activity and risk of kidney stones: a systematic review and meta-analysis of cohort studies Eur J Epidemiol 2018; 33:10331047
41 Zhang M, Hou ZK, Huang ZB, et al Dietary and Lifestyle Factors Related to Gastroesophageal Reflux Disease: A Systematic Review Ther Clin Risk Manag 2021; 17:305-323
42 Taylor EN, Fung TT, Curhan GC DASH-style diet associates with reduced risk for kidney stones J Am Soc Nephrol 2009; 20:2253-9
43 Moayyedi P Leaving No Stone Unturned in the Search for
Adverse Events Associated With Use of Proton Pump Inhibitors Clin Gastroenterol Hepatol 2021; 19:41-42
44 Moayyedi P, Eikelboom JW, Bosch J, et al ; COMPASS
Investigators Safety of Proton Pump Inhibitors Based on a Large, Multi-Year, Randomized Trial of Patients Receiving Rivaroxaban or Aspirin Gastroenterology 2019; 157:682-691 e2
45 Concato J, Shah N, Horwitz RI Randomized, controlled trials, observational studies, and the hierarchy of research designs N Engl J Med 2000; 342:1887-92
Correspondence
Rawa Bapir - Dr rawa@yahoo com
Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq
Kamran Hassan Bhatti - kamibhatti92@gmail com
Urology Department, HMC, Hamad Medical Corporation, Qatar
Ahmed Eliwa - ahmedeliwafarag@gmail com
Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt
Herney Andrés García-Perdomo - herney garcia@correounivalle edu co
Universidad del Valle, Cali, Colombia
Nazim Gherabi, MD - ngherabi@gmail com
Faculty of Medicine Algiers 1, Algiers, Algeria
Derek Hennessey, MD - derek hennessey@gmail com
Department of Urology, Mercy University Hospital, Cork, Ireland
Vittorio Magri, MD - vittorio magri@virgilio it
ASST Nord Milano, Milan, Italy
Panagiotis Mourmouris, MD - thodoros13@yahoo com
2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece
Adama Ouattara, MD - adamsouat1@hotmail com
Division of Urology, Souro Sanou University Teaching Hospital, BoboDioulasso, Burkina Faso
Gianpaolo Perletti, Dr Biol Sci M Clin Pharmacol
Gianpaolo Perletti@uninsubria it
Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy
Joseph Philipraj, MD - josephphilipraj@gmail com
Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India
Konstantinos Stamatiou, MD - stamatiouk@gmail com
Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece
Musliu Adetola Tolani, MD - adetolatolani@yahoo com
Division of Urology, Department of Surgery, Ahmadu Bello University/Ahmadu Bello University Teaching Hospital, Zaria, Kaduna State, Nigeria
Lazaros Tzelves, MD - lazarostzelves@gmail com
2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece
Alberto Trinchieri, MD - alberto trinchieri@gmail com
Urology School, University of Milan, Milan (Italy)
Noor Buchholz, MD - noor buchholz@gmail com
Sobeh's Vascular and Medical Center, Dubai Health Care City, Dubai, United Arab Emirates
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
514
The Discipline of Pediatric Urology: Prerogatives and Necessities
“Position Paper” written by the Italian Society Urology (Società Italiana Urologia, SIU) and the Italian Society Pediatric Urology (Società Italiana Urologia Pediatrica, SIUP)
Walter Artibani 1 , Luca Carmignani 2 , Giuseppe Carrieri 3 , Marco Castagnetti 4 , Giuseppe Cretì 5 , Mario De Gennaro 6 , Gianantonio Manzoni 7 , Lorenzo Masieri 8 , Francesco Porpiglia 9 , Roberto M. Scarpa 10
1 Segretario Generale SIU 2018-2021;
2 Comitato Esecutivo SIU 2018-2021, Responsabile Ufficio Ricerca;
3 Comitato Esecutivo SIU 2018-2021, Responsabile Ufficio Educazionale;
4 GdL SIU Urologia Pediatrica 2018-2021 e Consiglio Direttivo SIUP 2020-21;
5 Consiglio Direttivo SIUP, Presidente Eletto 2022-23;
6 Coordinatore GdL SIU Urologia Pediatrica 2018-2021;
7 Presidente SIUP 2020-21;
8 GdL SIU Urologia Pediatrica 2018-2021 e Consiglio Direttivo SIUP 2020-21;
9 Comitato Esecutivo SIU 2018-2021, Responsabile Ufficio Scientifico;
10 Presidente SIU 2021
KEY WORDS: Pediatric urology; Urology; Children; Italy; Position paper
Submitted 4 April 2022; Accepted 6 April 2022
To the Editor,
The aim of this “position paper” is to describe the discipline of Pediatric Urology with its clinical and cultural competencies, represent the reasons for legitimizing its existence, and reinforce its importance in the “scenario” of the National Italian Healthcare System The requisites and the educational requirements were defined by both the Italian Ministry of Health with the State-Regions Conference, and the European Union
Definition and requirements
Pediatric Urology (Discipline code 48 - Ministerial Decree 05 December 2006) deals with the congenital and acquired diseases and disorders of the urinary and genital systems, at every pediatric age, from the fetal and neonatal age as far as the adolescence In collaboration and synergy with adult specialties, pediatric urology continues to deal with the assistance of the patients “becoming adults” , in their process of “transitional care” and thereafter long-life (1)
The national needs for Pediatric Urology services in Italy have been defined in the Ministerial Decree of 02 April 2015 (Italian Official Gazette n. 70 of 04 June 2015) (2): it was recognized as “medium” level of healthcare regarding the allocation of human resources (doctors, nurses), similarly to others surgical specialties It was also calculated a population basin of 4-6 millions of inhabitants for each pediatric urology unit, therefore a total of 10-15 units nationwide, a parameter that substantially matches the current existing situation (16 units) The same 2015 ministerial document indicates the need for pediatric surgery units, which are currently twice as many as expected
A further consideration comes from the international definitions of the pediatric Networks, and of the pathways to treat uro-genital malformations by reconstructive/substitution surgery There is a tendency to refer the complex and “rare” conditions to a few “hub” Centers, which are able to provide the needed specialized services and reference sub-disciplines This trend has been acknowledged by the Italian State-Regions Conference (Agreement of December 21, 2017Guidelines to promote and ameliorate the quality, security, and appropriateness of treatment interventions in the pediatric-adolescent area)
PEDIATRIC UROLOGY AS A SUB-SPECIALTY
The origin of Pediatric Urology is traced back to Great Britain during the 1960s, while a more structured development occurred also in North America and northern Europe during the seventies (3) At that time, the necessities were mainly dictated by the young age of the patients (children and newborns), requiring expertise in working with fragile structures,
515 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 LETTER TO EDITOR No conflict of interest declared
DOI: 10 4081/aiua 2022 4 515
W Artibani, L Carmignani, G Carrieri, M Castagnetti, G Cretì, M De Gennaro, G Manzoni, L Masieri, F Porpiglia, R M Scarpa
in “small” surgical fields, using “small” instruments; while another limitation was the high risk for general anesthesia
Furthermore, the principle to be followed was the correction of any congenital malformations, at any age, thus falling under the competence of General Pediatric Surgeons They were the experts of embryology (the fetus), of neonatal and pediatric development, of changes at adolescence Moreover, Pediatric Surgeons had also greater support from advanced neonatal/pediatric anesthesia and specialized radiology, and availability of miniaturized instruments But, newborns and children’s survival was, at that time, the only (or main) objective when correcting congenital anomalies: little consideration was given to the dysfunction of a malformed organ and system, which on the contrary could result in clinical complications, impairments (even fatal in the long-term) and disabilities leading to poor quality of life
More recently, gradually the various pediatric surgical specialists were able to benefit from more specific training, coupled with the advent of advanced technologies within their “parent” specialties (i e Cardiac Surgery, Neurosurgery, Orthopedics, Plastic Surgery, Urology, etc ) Regarding Urology, in parallel, some medical pediatric specialties related to Urology (i e Nephrology, Endocrinology) grew up, and supported pediatric urology itself by their specific competencies, as for renal transplant and the disorders of gender differentiation Thus, in the end, pediatric urology separated from pediatric surgery, to become a subspecialty in its own right, similarly to the previous development of Urology as a specialty distinct from General Surgery (4)
By this way, most Pediatric Urologists could fully work with pediatric patients, paying attention to the emerging necessities of the affected children and adolescents, who legitimately were looking for a reasonable quality of life In general, patients with congenital anomalies aspire to achieve a “normal” life, playing sports, having fun with friends and getting a fulfilling job Conversely those with genito-urinary malformations disabilities, also, wish a reasonable urinary (and fecal) continence, a regular sexual activity, sufficient fertility, and adequate maternity and paternity For the above reasons, nowadays, the surgical correction of malformations of the genital and urinary systems has to firmly take into account the preservation of affected organs and functions The initial purpose of saving life has changed into the perspective of the adulthood, in view of lifelong maintenance of the primary functions and continuous management of the condition itself Clinical pathways and regular follow-up toward adulthood are of paramount importance and should be shared among the different pediatric and adult specialists This process of moving from pediatric to adult healthcare, known as “transition of care ” , is even more compelling, as is the training of general urologists in the reconstructive and corrective surgery of malformations in functional terms (5, 6)
Related disciplines
The principal relationship of Pediatric Urology is with Urology, due to technological innovations and for the competence in adults looking at the transitional care; while the collaboration with Pediatric Surgery relates to the association between genito-urinary and other apparatus malformations, such as anorectal anomalies
Furthermore, clinical relationships with the following medical sub-specialties are required, to obtain a complete and firstclass assistance:
– Pediatric Nephrology, for renal function aspects and kidney replacement therapy (transplant)
Neonatology, for specific neonatal assistance of patients with complex anomalies
Fetal Medicine, for antenatal diagnosis/counselling and selective fetal interventions
Pediatric Endocrinology, for genital diseases in general, and especially for differences of sex development (DSD)
The advanced center of Pediatric Urology should also offer availability for some specialized activities and procedures which are very common for adults but rarely used for children: they should have easy and structured access to endourology (stone centers), neuro-urology (spinal units, incontinence referral centers), robotic surgery, interventional radiology
Uro-genital diseases and malformations
The urinary and genital malformations are the most frequent (3 1 0/00 live births), following cardiac (6 5 0/00) and limbs (3 8 0/00) defects [data from the Eurocat 2010 study, conducted on 1 5 million of births in 22 European countries] They may affect continence and fertility The most complex anomalies are exstrophy-epispadias, posterior urethral valves, neurogenic bladder, ano-rectal malformations, all affecting continence; while the most frequent are hypospadias and cryptorchidism, potentially affecting fertility Surgical correction should save functions of the patient becoming adult, who has the hope to enjoy his/her own social, sportive, working, procreative and emotional life
Other fields of interest are the not-malformative urinary and genital diseases: neuropathic bladder and neurogenic dysfunction, urinary calculi, tumors of urogenital tracts, vesicoureteral reflux, vesical and perineal dysfunctions, urinary incontinence, nocturnal enuresis
Guidelines for principal and more frequent diseases pertinent to pediatric urology are jointly elaborated by the European Association of Urology (EAU) and the European Society for Pediatric Urology (ESPU), and are published on the website of both SIU e SIUP
PEDIATRIC UROLOGY IN ITALY
In Italy, the development of pediatric urology began in the 1980s within the fields of general urology (i e Padua, Florence, Varese) and pediatric surgery (i e Vicenza, Bologna, Rome), and this led to the subsequent establishment of the first autonomous pediatric urology departments in Children's Hospitals, and also in general and teaching Hospitals
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
516
–
–
–
Table 1.
Formalized Units of Pediatric Urology in Italy - January 2022
Firenze
Roma-Palidoro
Napoli
Hospital
Vicenza “San Bortolo” Hospital
UOSD Maternal Pediatric Dep Pediatric Urology Gen Drsa L Reali
UOS Pediatric Surgery Div Pediatric mini-invasive Urology Gen Dr F Chiarenza (int)
Alessandria “Arrigo” Pediatric Hospital UOS Pediatric Surgery Div Pediatric Urology Ped Dr L. Sangiorgio
Milano “Buzzi” Pediatric Hospital UOS Pediatric Surgery Div Pediatric Urology Ped Dr G Selvaggio
Milano “San Raffaele” Hospital UOS Urology Division Pediatric Urology Gen Drsa A Lesma
S Giovanni Rotondo (FG) “Casa Sollievo Sofferenza” Hospital
UOSD Dep Surgery Pediatric Urology Gen Dr G Cretì
UOC = Comp ex Operative Un t; UOS = S mp e Operat ve Unit; UOSD = Simple Departmental Un t; Dep = Department; D v = D vision; Hosp = Hosp tal; Gen = General Hospita ; Ped = Pediatric hosp tal; ( nt) = ad interim
* Neonatology, Pediatric nephrology and renal transplant ava lable at the Institut on
RESULTS OF THE SIU/SIUP CENSUS (2021)
The Italian Society of Urology, in collaboration with the Italian Society of Pediatric Urology in 2020 and 2021 conducted a census of the pediatric urology units in the nation, taking into consideration their assignment to general urology and/or pediatric surgery divisions, or if they were independent and affiliated to general departments, as surgery or pediatrics
The results showed a sufficient yet in-homogeneous distribution across Italy Of the 16 formal departments, 10 are located in the North of the country, while 11 Regions are totally devoid of a service The majority of the pediatric Hospitals have a department of pediatric urology, specifically eight out of the eleven ones nationwide (Turin, Milan, Alessandria, Trieste, Florence, Rome, Naples, Bari), with the exclusion of Genoa, one of the largest pediatric Institutions Of the aforementioned 16 pediatric urology departments, 11 are autonomous and 5 are divisions of pediatric surgery (3) or general urology (2) departments There are only 4 units (Milan, Padua, Turin, Rome) offering renal transplantation within a context of tertiary care (Table 1)
Organization and education in Italy and European Union Organization
Since 2013, with the objective of reducing healthcare inequalities for everyone with rare and complex diseases, the European Reference Networks of Centers of Expertise (ERN) has been identifying Centers of excellence (HCP), primarily those with larger case-loads including the more complex cases The ERN on uro-recto-genital diseases and conditions, eUROGEN, comprises three workstreams with their own disease areas (malformative, reconstructive/functional, oncological) and provides pathways of clinical care from birth to adulthood; Workstream 1 focuses on rare congenital urogenital anomalies
These Centers of excellence have been recognized due to their experience, expertise, and volume of activity within the urological area, and area quite distinct from pediatric surgery
Education
The European Union of Medical Specialists (UEMS), jointly with urologists and pediatric surgeons, has established a qualification in pediatric urology, which involves a biennial period of training in European Board Pediatric Urology (EBPU) Accredited Training Centers, and Fellowships in European Pediatric Urology Academy (FEAPU)
In Italy, we have 2 of the above accredited Centres: the Bambino Gesù Children Hospital in Rome and the Foundation IRCCS Cà Granda Policlinico Maggiore Hospital in Milan In addition, several academic Schools of Urology provide brief educational programs in pediatric urology inside the entire general urology program, involving periods of active training in pediatric urology departments And the Universities of Milan and Florence provided a professional Master’s course in pediatric nephron-urology It would be desirable that the Urological Society contributes to the development of the international fellowship EBPU and FEAPU programs The desire is to reinforce the educational academic offer in general, in order to ensure that in Italy, as in other European countries, will be possible to obtain a more structured educational program in the field of pediatric urology and transitional urological care
517 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 The Discipline of Pediatric Urology: Prerogatives and Necessities
City Institution Unit Depar tment/Division Name of the Unit Hosp Head Padova University Hospital * UOC Dep Surgery Pediatric Urology Gen Prof F Del Moro (int)
“Regina Margherita” Hospital * UOC Dep Pediatrics Pediatric Urology Ped Drsa S Gerocarni Nappo Milano Foundation “Cà Granda Maggiore” Hospital * UOC Maternal Pediatric Dep Pediatric Urology Gen Dr G A Manzoni
Torino
“Meyer” Pediatric Hospital UOC Multidisciplinary Dep Pediatric Urology Ped Prof L Masieri
”Bambino Gesù” Children Hospital * UOC Dep Surgery Pediatric Urology Ped Prof M Castagnetti
Roma
”Bambino Gesù” Children Hospital * UOC Dep Surgery Continence Surgery and Neurourology Ped Dr G Mosiello
“Santobono” Hospital UOC Dep Surgery Pediatric Urology Ped Dr G Di Iorio Bari “Papa Giovanni XXIII” Pediatric Hospital UOC Pediatric Surgical Sciences Dep Pediatric Surgery Urological Ped Dr N Laricchiuta Trieste “Burlo Garofalo” Pediatric Hospital UOSD Maternal Pediatric Dep Pediatric Surgery and Urology Ped Dr J Schleef (int) Bolzano “Centrale” Hospital UOS Urology Division Pediatric Urology Gen Drsa E Comploj Varese “Del Ponte”
W
Artibani, L Carmignani, G Carrieri, M Castagnetti, G Cretì, M De Gennaro, G Manzoni, L Masieri, F Porpiglia, R M Scarpa
CONCLUSIONS
This document was designed looking at the following objectives:
– maintain and sustain the Italian pediatric urology credit, on a national and international level
– clarify the affinity of the sub-specialty Pediatric Urology with the discipline general urology and also its proximity to the pediatric surgery discipline, even emphasizing its own autonomy
– defend the existence and operativity of the already formalized Pediatric Urology Units, its diffusion nationwide, and natural placement in Children’s Hospitals; and promote the institution of other units where required, on a regional and national basis
implement the educational offer, according to European standards, and encourage and help international attendance at accredited training centers in Italy
– promote a culture of the "referral center” for rare pathologies (e g bladder exstrophy) and for advanced technologies (robotic surgery, neuromodulations)
– contribute to the identification of "hubs" to refer for more complex pathologies (e g North, Centre, South), with their requirements
REFERENCES
1 Lambert SM Transitional care in pediatric urology Seminars in Pediatric Surgery 2015; 24:73-78 doi:10 1053/j sempedsurg 2015 01 004
2 D M 70/02 04 2015: Regolamento recante definizione degli standard qualitativi, strutturali, tecnologici e quantitativi relativi all’assistenza ospedaliera venerdì 5 giugno 2015
3 Innes Williams D The history of paediatric urology: personal recollections 1948-1978 BJU Int 2003; 92(Suppl 1):1-3 doi:10 1046/j 1464410x 92 s1 7 x
4 Lebowitz RL Paediatric urology and uroradiology: changes in the last 25 years: PAEDIATRIC UROLOGY and URORADIOLOGY BJU International 2003; 92:7-9 doi:10 1046/j 1464-410X 92 s1 3 x
5 Ritchey ML Pediatric Urology: A “Grown-Up” Subspecialty Journal of Urology 2012; 187:7-8 doi:10 1016/j juro 2011 10 050
6 Van Batavia JP, Shukla AR, Joshi RS, Reddy PP Pediatric Urology and Global Health Urologic Clinics of North America 2018; 45:623-631 doi:10 1016/j ucl 2018 06 009
Correspondence
Walter Artibani, MD prof artibani@gmail com
Luca Carmignani, MD luca carmignani@unimi it
Giuseppe Carrieri, MD
giuseppe carrieri@unifg it
Francesco Porpiglia, MD
francesco porpiglia@unito it
Roberto Mario Scarpa, MD r scarpa@unicampus it
Società Italiana di Urologia, Via Giovanni Amendola 46, 00185 Roma
Giuseppe Cretì, MD urologia@operapadrepio it
Gianantonio Manzoni, MD
gianantonio manzoni@policlinico mi it
Lorenzo Masieri, MD
lorenzo masieri@meyer it
Marco Castagnetti, MD
marco castagnetti@unipd it
Mario De Gennaro, MD (Corresponding Author) dott mariodegennaro@gmail com
Società Italiana Urologia Pediatrica
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
518
–
Increased exfoliation of immature germ cells detected in semen analysis routine and its clinical significance
Fernando Tadeu Andrade-Rocha 1 , Walter D Cardona Maya 2
1 Lisa Andrology Lab, Petrópolis, RJ, Brazil;
2 Reproduction Group, Department of Microbiology and Parasitology, Faculty of Medicine, Universidad de Antioquia UdeA, Medellín, Colombia
Submitted 18 July 2022; Accepted 24 July 2022
To the Editor,
Currently, semen analysis is the unique test to evaluate men ’ s fertility potential Semen analysis provides valuable information on sperm production and quality In addition to the conventional assessment of the sperm characteristics in a basic semen analysis routine, performing a differential diagnosis of leukocytes and sperm precursors immature germ cells (IGC) is also pivotal (1-3), due to adding valuable and clinically suitable information to the semen report While increased leukocyte count may indicate infections (4), increased exfoliation of IGC from seminiferous tubules suggests abnormal spermatogenesis (5, 6) Even the inflammation could induce exfoliation of IGC from seminiferous tubules (7) In semen analysis, a global and differential count of all seminal round cells can improve the diagnosis (8) and treatment options to achieve a successful pregnancy (9) A high count of IGC in semen would represent different seminal and reproductive alterations and would be an essential indicator for detecting testicular alterations (6) Therefore, an index could be developed comparing IGC count/mL vs sperm count/mL In some instances, this index would be paramount for estimating, for example, the negative impact of varicocele on the germinal epithelium in increased exfoliation of IGC in semen The normal is to find one IGC for every 40 spermatozoa, values between 20/1 and 40/1 are indeterminate, and values lower than 20/1 indicate increased exfoliation of IGC, which suggests a loss of integrity of the germinal epithelium Occasionally, ratios greater than 1/1000 are also found, mainly in ejaculate with high sperm count (Andrade-Rocha FT, Unpublished data) The lower this index, the worse is the integrity of the germinal epithelium The cells are sloughed off before completing the spermatogenesis process and spermatozoa production For example, the conventional semen parameters routinely evaluated in a 32 years old man in Lisa Andrology Lab (Petrópolis, RJ, Brazil) for investigating male infertility showed the ratio was six IGC for each sperm; it was even worse, showing an inversion in the index (Table 1 and Figure 1) show a representative aggregate of IGC in the semen specimen
Table
Figure 1.
Unequal aggregation of immature germ cells regarding to sperm
The semen smear used for the microphotograph shown in this editorial was made with concentration to show the proportionality between IGC and sperm in the analyzed semen specimen
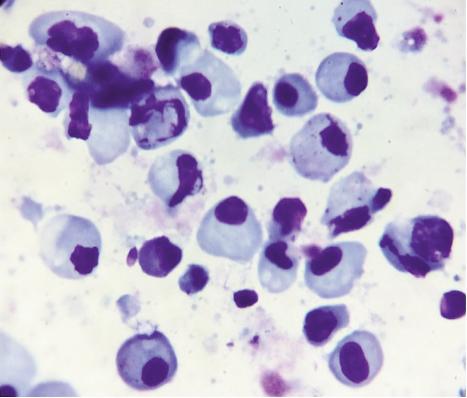
519 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
EDITOR No conflict of interest declared
LETTER TO
DOI: 10 4081/aiua 2022 4 519
1.
semen characteristics and lower reference limit Parameter Outcomes Lower reference limit –percentile 5th (11) Semen volume 6.1 mL 1.4 mL Sperm count/mL 317 000 16 x 106/mL Total sperm count 1 931 710 39 x 106 per ejaculate Vitality 20% 54% Total motility 10% 42% Progressive motility (a) 0 30% Slow/irregular motility (b) 9%Non-progressive motility (c) 1% 1% Immotile (d) 90% 20% Normal morphology 0 53 4% Amorphous sperm 11%Tapered sperm 7%Sperm immature germ cells vs sperm 1/6 1/40 Hypo-osmotic swelling 18% 58% pH 8.2 > 7.2
Patient
This assessment measures the intensity of the famous seminal stress pattern that John MacLeod proposed in the 1960s (10) According to MacLeod, the stress pattern is characterized by an increase of amorphous and tapered and exfoliated IGC in semen and is usually diagnosed in some varicocele men Unlike previous observations by MacLeod (10), it has been observed that varicocele men can cause structural changes in sperm, like amorphous and tapered sperms, increased exfoliation of sperm precursors and both Therefore, further studies are needed to expand knowledge on this issue, which is practically unexplored in clinical and laboratory practice
REFERENCES
1 Jassim A, Festenstein H Immunological and morphological characterisation of nucleated cells other than sperm in semen of oligospermic donors J Reprod Immunol 1987; 11:77-89
2 Tomlinson MJ, Robert Barratt CL, Bolton AE, et al Round cells and sperm fertilizing capacity: the presence of immature germ cells but not seminal leukocytes are associated with reduced success of in vitro fertilization Fertil Steril 1992; 58:1257-9
3 Fedder J, Askjaer SA, Hjort T Nonspermatozoal cells in semen: relationship to other semen parameters and fertility status of the couple Arch Androl 1993; 31:95-103
4 Sharma R, Gupta S, Agarwal A, et al Relevance of leukocytospermia and semen culture and its true place in diagnosing and treating male infertility World J Mens Health 2022; 40:191-207
5 Andrade-Rocha FT Semen analysis in laboratory practice: an overview of routine tests J Clin Lab Anal 2003; 17:247-58
6 Palermo GD, Neri QV, Cozzubbo T, et al Shedding light on the nature of seminal round cells PLoS One 2016; 11:e0151640
7 Gandini L, Lenzi A, Lombardo F, et al Immature germ cell separation using a modified discontinuous Percoll gradient technique in human semen Hum Reprod 1999; 14:1022-7
8 Patil PS, Humbarwadi RS, Patil AD, Gune AR Immature germ cells in semen - correlation with total sperm count and sperm motility J Cytol 2013; 30:185-9
9 Ariagno J, Curi S, Mendeluk G, et al Shedding of immature germ cells Arch Androl 2002; 48:127-31
10 MacLeod J Seminal cytology in the presence of varicocele Fertil Steril 1965; 16:735-57
11 World Health Organization WHO Laboratory Manual for the Examination and Processing of Human Semen 6th ed WHO Press; Geneva, Switzerland 2021 (accessed on 15 July 2022)
Correspondence
Fernando Tadeu Andrade-Rocha, BS (Corresponding Author) lisalabrescenter@gmail com
Lisa Andrology Lab, Petrópolis, RJ (Brazil)
Walter Darío Cardona Maya, PhD wdario cardona@udea edu co
Grupo Reproducción, Facultad de Medicina, Universidad de Antioquia, Medellin (Colombia)
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 F T Andrade-Rocha, W D Cardona Maya 520
Outcomes of dutasteride discontinuation in patients with benign prostatic hypertrophy
Hiroshi Masuda,
Department of Urology, Teikyo University Chiba Medical Center, 3426-3 Anesaki, Ichihara, Chiba 299-0111, Japan
KEY WORDS: Benign prostatic hypertrophy; Nocturia; Discontinuation; 5-alpha reductase inhibitor; Polypharmacy
Submitted 30 October 2022; Accepted 19 November 2022
To the Editor,
Benign prostatic hyperplasia (BPH) is a common cause of lower urinary tract symptoms (LUTS) in elderly males The current guidelines recommend the use of a 5-alpha reductase inhibitor (5ARI) to treat males with moderate-to-severe LUTS and an enlarged prostate (1) Combination therapy with an alpha blocker and a 5ARI has proven effective at ameliorating LUTS and reducing the total prostate volume (TPV) and the risk of the disease progression (2-5)
With the aging of the Japanese population, it is expected that the frequencies of various chronic diseases will increase, and as a result, it is assumed that the number of oral medications being taken by older people will rise It has been reported that the incidence of adverse drug events is higher among the elderly than among younger patients, and adverse drug event rates of 15-20% per year have been reported in nursing homes in the United States (6) The higher adverse drug event rates seen in elderly patients are caused by greater drug sensitivity due to age-related changes in pharmacokinetics and the higher number of drugs being taken by each patient
As mentioned above, elderly people are prone to polypharmacy, as they have many comorbidities In a multicenter study, it was reported that the elderly subjects were taking an average of 4 5 different medications (7) Polypharmacy is associated with increases in drug costs and drug interactions In addition, it has been reported that the risk of adverse drug events was increased in patients taking ≥ 6 drugs (8), and furthermore, that the incidence of falls was high among patients taking ≥ 5 drugs (9) Therefore, among elderly people, even if only one type of medication is discontinued, the risk of adverse drug events can be expected to decrease, which may help to reduce healthcare costs in the long term
It has been reported that when an alpha-1 blocker is combined with dutasteride, symptom relief can be maintained with dutasteride alone after the discontinuation of the alpha-1 blocker (10) However, it has also been reported that 60% of patients who stop taking dutasteride resume taking it within 1 year (11) Recently, it was suggested that 5ARI may induce suicidal behavior and depression and that the discontinuation of 5ARI should be considered (12) However, there are no studies involving a follow-up period of 2 years after discontinuation of dutasteride
The purpose of this study was to investigate the predictors of restarting dutasteride in a real-world setting in the era of polypharmacy At the beginning of 2016 a shortage of the drug forced us to stop dutasteride treatment in a group of patients The drug returned to be available after four months Nevertheless, some patients did not restart dutasteride but remained on treatment with alpha-blockers alone We aimed to evaluate reasons for restarting or not dutasteride after a period of discontinuation
MATERIAL AND METHODS
Study subjects
We retrospectively reviewed the medical records of patients with LUTS secondary to BPH who were treated with an alpha-1 blocker and dutasteride (0 5 mg/d) from September 2010 to December 2015 From January 2016, dutasteride was discontinued, and the patients were only prescribed an alpha-1 blocker A total of 39 patients were included in this study
The patients were divided into two groups: patients who restarted dutasteride (DR) and patients who remained on discontinuation of dutasteride (DD) group In both groups, age, body mass index (BMI), International Prostate Symptom Score (IPSS), quality-of-life (QoL) score, Overactive Bladder Symptom Score (OABSS), duration of dutasteride treatment before
521 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
TO EDITOR No conflict of interest declared
LETTER
Kosuke Mikami, Kotaro Otsuka, Kyokusin Hou, Takahito Suyama, Kazuhiro Araki, Satoko Kojima, Yukio Naya
DOI: 10 4081/aiua 2022 4 521
H Masuda, K Mikami, K Otsuka, K Hou, T Suyama, K Araki, S Kojima, Y Naya
discontinuation, number of different types of medications being taken by the patients, prostate volume, rate of reduction in prostate volume, post-void residual volume (PVR), and presence or absence of comorbidities were evaluated
Prostate volume and the PVR were evaluated by using transabdominal ultrasound All data were collected prior to the discontinuation of dutasteride
The follow up period after the discontinuation of dutasteride lasted 24 months Alpha-1 blocker monotherapy was continued during this period
IPSS, OABSS, prostate volume (PV), and PVR were evaluated at 1, 3, 6, 12, 18, and 24 months after the discontinuation of dutasteride
Patients were allowed to restart dutasteride during the follow-up period according to their desires and the judgement of the attending physician
Statistical analysis
Statistical analyses were carried out to identify clinical parameters that differed significantly between the DR and DD groups The results are shown as the mean ± standard error (SE) The Mann-Whitney U test and Chi-squared test were used for the statistical analyses The Cox proportional hazards model was used to estimate the relative risk of dutasteride being restarted associated with each parameter Rate estimates were calculated using the Kaplan-Meier method The logrank test was used to evaluate differences in rates between the groups All analyses were performed with JMP version 10 (SAS Institute Inc , Cary, NC, USA) Probability values of < 0 05 were considered statistically significant
Ethical approval
The institutional review board of Teikyo University approved this study (TUIC-COI 21-179)
RESULTS
Out of 39 eligible patients, 36 were analyzed at 24 months, and 13 patients (13/36, 36%) restarted dutasteride
The remaining 23 patients (64%) discontinued dutasteride within 24 months as shown by the Kaplan-Meier curve in Figure 1
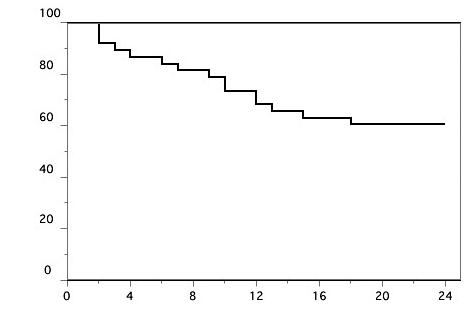
Neither the type nor dose of alpha-1 blocker was changed during the follow-up period in any patient
The mean number of different types of medications being taken by the patients in the DR and DD groups was 6 5 and 5 7, respectively The mean number of nocturia events experienced per day before the discontinuation of dutasteride was significantly higher in the DR group than in the DD group (2 8 vs 1 8, respectively; p = 0 005) The mean duration of dutasteride treatment prior to discontinuation was significantly longer in the DR group (37 months) than in the DD group (25 months) (p = 0 0261) (Table 1)
Dutasteride discontinuation rate during the 2-year follow-up period as determined using a Kaplan-Meier curve The discontinuation rates at 6, 12, 18, and 24 months were 87%, 74%, 64%, and 64%, respectively
Table 1
Patient characteristics
The PVR before the discontinuation of dutasteride was not significantly different in the DR group (59 ml) compared to the DD group (35 ml) (p = 0 0868) Total IPSS and total OABSS were also not significantly higher in the DR group than in the DD group
Multivariate analysis showed statistically significant differences in the duration of dutasteride treatment before discontinuation and the frequency of nocturia between the groups
In DD group, the change from baseline of mean IPSS values (Δ-IPSS) at 1, 3, 6, 12, 18, and 24 months were ±0, +0 6, +0 3, +0 6, +0 9, and +0 6, respectively (p = 0 9985), the Δ-OABSS values at 1, 3, 6, 12,18, and 24
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
522
Variables DR group DD group P-value (n=13) (n=23) Age (mean ± SE), years 79 ± 2 2 76 ± 1 3 0 2283 BMI (mean ± SE), kg/m2 23 3 ± 0 9 23 3 ± 0 6 0 6523 Prostate volume (mean ± SE), ml 46 3 ± 7 3 45 ± 3 6 0 781 Hypertension, n (%) 9 (75%) 12 (52%) 0 1907 Diabetes mellitus, n (%) 2 (17%) 2 (9%) 0 4817 Dyslipidemia, n (%) 0 (0%) 6 (26%) 0 0519 No of types of medications being taken (mean ± SE) 6 5 ± 2 2 5 7 ± 2 2 0 3334 Duration of dutasteride treatment (mean ± SE), months 37 ± 4 6 24 ± 3 5 0 0261 No of nocturia events per night (mean ± SE) 2 8 ± 0 3 1 7 ± 0 2 0 0050 Total IPSS (mean ± SE) 14 3 ± 1 7 11 7 ± 1 3 0 1294 Urinary symptom score (mean ± SE) 6 0 ± 1 0 5 5 ± 0 7 0 7005 Irritative symptom score (mean ± SE) 5 5 ± 1 2 4 4 ± 0 6 0 31 QOL score (mean ± SE) 2 8 ± 0 6 3 2 ± 0 3 0 6329 Total OABSS (mean ± SE) 5 3 ± 1 5 4 2 ± 0 6 0 7391 PVR (mean ± SE), ml 59 ± 16 35 ± 7 3 0 0868 Reduction rate (mean ± SE), % 12 4 ± 4 3 14 4 ± 4 1 0 8894 Overactive Bladder Symptom Score; PVR: Post-vo d res dual vo ume; SE: Standard error
Figure 1.
P r o b a b i l i t y o f d i s c o n t i n u a t o n ( % ) Time since discontinuation (months)
months were +0 1, +0 5, +0 4, +0 1, ±0, and +0 6, respectively (p = 0 9927), and the mean Δ-PVR values at 1, 3, 6, 12,18, and 24 months were -6 4, -3 0, -6 3, -1 4, +0 3, and -3 3, respectively (p = 0 9920) In DD group, the mean ΔPV values at 1, 3, 6, 12, 18, and 24 months were +4 1, +2 7, +5 7, +9 2, +11 7, and +8 9 respectively (p = 0 3945)
The reasons why dutasteride was restarted were as follows: choice of the patient in 4 cases, macrohematuria in 2 cases, nocturia in 1 case, symptom exacerbation in 4 cases, and the judgment of the physician in 2 cases
DISCUSSION
In the present study, it was suggested that nocturia and a long period of dutasteride treatment prior to the discontinuation of dutasteride are predictors of restarting dutasteride in the real-world setting Consequently, in patients that do not exhibit nocturia before the discontinuation of dutasteride, the withdrawal of dutasteride should be considered feasible
Discontinuation of drugs for BPH treatment
There have been a few prospective studies on the discontinuation of dutasteride Shindo et al evaluated the possibility of discontinuing dutasteride after it was used in combination with an alpha-1 blocker for BPH (11) After 6 months of combination therapy, 60% of the patients in whom dutasteride was discontinued restarted taking dutasteride within 12 months The degree of prostatic enlargement seen after the discontinuation of dutasteride differed among patients
According to this study, rapid regrowth of the prostate leads to the deterioration of storage symptoms and a tendency to restart dutasteride and the baseline intraprostatic architecture may be a predictor of whether a patient is a good candidate for dutasteride discontinuation
Victor et al investigated the outcomes of discontinuing one medication after 2 years of combined alpha-blocker and 5ARI therapy for BPH/LUTS in a randomized multicenter study (13) They concluded that the discontinuation of either drug caused the progression of BPH However, they suggested that the risk of resuming medication or undergoing transurethral resection of the prostate was greater in patients who discontinued 5ARI
Jeong et al reported that the discontinuation of 5ARIs during combination therapy induced prostate regrowth and symptom aggravation in males with BPH (14) Therefore, they suggested that the life-long use of 5ARIs should be considered to prevent BPH progression
In the current study it was demonstrated that the temporary discontinuation of dutasteride was feasible, and in selected cases it was possible to discontinue dutasteride for 2 years
Polypharmacy
Regarding polypharmacy in the elderly, it was suggested that the temporary discontinuation of medications could be a good option, and it is expected that reducing the number of medications being taken could potentially reduce healthcare costs In the present study, the number of different types of oral medications being taken by the patients was higher in the DR group Basically, it is assumed that patients want to reduce the number of different types of oral medications they are taking, and hence, to maintain discontinuation However, when the number of different types of oral medications being taken exceeds a certain level, one less medication does not really change the patient’s condition In fact, the restarting of oral medications may be related to the types of oral medications being taken, rather than the number of medications being taken by itself
Length of previous treatment
This study suggested that a longer period of dutasteride treatment before discontinuation was associated with a greater likelihood of restarting dutasteride, whereas previous administration of dutasteride for a shorter period (approximately 2 years) was associated with persistent discontinuation of dutasteride A longer dutasteride treatment before discontinuation could be associated with a greater effect of prostate shrinkage that could be maintained for a longer period after dutasteride discontinuation so delaying restarting of dutasteride treatment, on the contrary we observed the opposite in this study It has been reported that the main reason for restarting dutasteride is the regrowth of the prostate due to the discontinuation of the drug (11) although in this study dutasteride was mainly restarted because of hematuria or the choice of the patient
Nocturia
Nocturia before the discontinuation of dutasteride was identified as another predictor of restarting dutasteride treatment
In a recent study involving a follow-up period up to 21 years, it was reported that males with BPH have a persistently higher risk of Alzheimer’s disease and all-cause dementia compared with males in the general population (15) The study identified BPH (and associated sleep disturbances) as a common, potentially curable, disorder associated with dementia risk Therefore, it seems that controlling nocturia is an important issue for urologists
Risk of depression
Moreover, it is important to prescribe appropriate medication Associations between 5ARIs and suicidality and depression have been reported In a large cohort of males aged ≥ 66 years, it was found that the risk of self-harm and depression were higher than in males that were treated with 5ARIs Therefore, it was suggested that the discontinuation of 5ARIs in these circumstances may be appropriate (12)
523 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Dutasteride discontinuation in BPH
Limitations
We would like to emphasize several limitations of our study Firstly, it was a retrospective cohort study, which involved the extraction of electronically stored clinical data, and it had a small sample size Secondly, we could not assess the effects of the discontinuation of dutasteride on QoL Thirdly, we examined the types of other medications (in general) the patients were taking, but we should also have examined the actual daily amounts of other medications that they were taking It was suggested that if the daily amounts of other medications being taken by a patient is high, the patient may not restart taking discontinued medications because they may want to reduce the daily amounts of other medication that they are taking
CONCLUSIONS
The present study suggested that the temporary discontinuation of dutasteride can be considered in cases who present a low frequency of nocturia and a relatively short period of dutasteride treatment before discontinuation In addition, temporary discontinuation of dutasteride may be useful for dealing with polypharmacy in the elderly
REFERENCES
1 Gratzke C, Bachmann A, Descazeaud A, et al EAU Guidelines on the Assessment of Non-neurogenic Male Lower Urinary Tract Symptoms including Benign Prostatic Obstruction Eur Urol 2015; 67:1099-1109
2 McConnell JD, Roehrborn CG, Bautista OM, et al Medical Therapy of Prostatic Symptoms (MTOPS) Research Group: The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia N Eng J Med 2003; 349:2387-2398
3 Roehrborn CG, Siami P, Barkin J, et al CombAT Study Group: The effects of dutasteride, tamsulosin and combination therapy on lower urinary tract symptoms in men with benign prostatic hyperplasia and prostatic enlargement: 2-year results from the CombAT study J Urol 2008; 179:616-621
4 Roehrborn CG, Siami P, Barkin J, et al CombAT Study Group: The influence of baseline parameters on changes in international prostate symptom score with dutasteride, tamsulosin, and combination therapy among men with symptomatic benign prostatic hyperplasia and an enlarged prostate: 2-year data from the CombAT study Eur Urol 2009; 55:461-471
5 Roehrborn CG, Siami P, Barkin J, et al CombAT Study Group: The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study Eur Urol 2010; 57:123-131
6 Rothschild JM, Bastes DW, Leape LL Preventable medical injuries in older patient Arch Intern Med 2000; 160:2717-2728
7 Suzuki Y, Akishita M, Arai H, et al Multiple consultations and polypharmacy of patients attending geriatric outpatient units of university hospitals Geriatr Gerontol Int 2006; 6:244-247
8 Kojima T, Akishita M, Kameyama Y, et al High risk of adverse drug reactions in elderly patients taking six or more drugs: analysis of inpatient database Geriatr Gerontol Int 2012; 12:761-762
9 Kojima T, Akishita M, Nakamura T, et al Polypharmacy as a risk for fall occurrence Geriatr Gerontol Int 2012; 12:425-430
10 Barkin J, Guimaraces M, Jacobi G, et al Alpha-blocker therapy can be withdrawn in the majority of men following initial combination therapy with the dual 5alpha-reductase inhibitor dutasteride Eur Urol 2003; 44:461-466
11 Shindo T, Hashimoto K, Shimizu T, et al Significance of intraprostatic architecture and regrowth velocity for considering discontinuation of dutasteride after combination therapy with an alpha blocker: a prospective, pilot study KJU 2015; 56:305-309
12 Welk B, McArthur E, Ordon M, et al, Association of Suicidality and Depression With 5alpha-Reductase Inhibitors JAMA Intern Med 2017; 177:683-691
13 Lin VC, Liao CH, Kuo HC Progression of lower urinary tract symptoms after discontinuation of 1 medication from 2-year combined alphablocker and 5-alpha-reductase inhibitor therapy for benign prostatic hyperplasia in men--a randomized multicenter study Urology 2014; 83:416-421
14 Jeong YB, Kwon KS, Kim SD, Kim HJ Effect of discontinuation of 5alpha-reductase inhibitors on prostate volume and symptoms in men with BPH: a prospective study Urology 2009; 73:802-806
15 Nørgaard M, Horváth-Puhó E, Corraini P, et al Sleep disruption and Alzheimer's disease risk: Inferences from men with benign prostatic hyperplasia EClinical Medicine 2021; 32:100740
Correspondence
Hiroshi Masuda, MD, PhD (Corresponding Author) hrsmasuda@yahoo co jp
Kosuke Mikami, MD
Kotaro Otsuka, MD
Kyokusin Hou, MD
Takahito Suyama, MD
Kazuhiro Araki, MD
Satoko Kojima, MD
Yukio Naya, MD
Department of Urology, Teikyo University Chiba Medical Center - 3426-3 Anesaki, Ichihara, Chiba, 299-0111 (Japan)
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
524
H Masuda, K Mikami, K Otsuka, K Hou, T Suyama, K Araki, S Kojima, Y Naya
AB0 blood groups and oncological and functional outcomes in bladder cancer patients treated with radical cystectomy
Alessandro Tafuri 1, 2* , Andrea Panunzio 1,3* , Antonio Soldano 1* , Giovanni Mazzucato 1 , Paola Irene Ornaghi 1 , Giacomo Di Filippo 4 , Alessandra Gozzo 1 , Nicola De Maria 1 , Francesco Cianflone 1 , Aliasger Shakir 5 , Zhe Tian 3 , Matteo Brunelli 6 , Antonio Benito Porcaro 1 , Vincenzo Pagliarulo 2 , Walter Artibani 1 , Pierre I Karakiewicz 3 , Alessandro Antonelli 1 , Maria Angela Cerruto 1
1 Department of Urology, University of Verona, Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Italy;
2 Department of Urology, “Vito Fazzi” Hospital, Lecce, Italy;
3 Cancer and Prognostics Health Outcomes Unit, Division of Urology, University of Montreal Health Center, Montreal, Quebec, Canada;
4 Department of General and Hepatobiliary Surgery, University of Verona, Azienda Ospedaliera Universitaria Integrata Verona, Verona, Italy;
5 USC Institute of Urology, Catherine and Joseph Aresty Department of Urology, Keck School of Medicine, University of Southern California (USC), Los Angeles, CA;
6 Department of Pathology, University of Verona, Azienda Ospedaliera Universitaria Integrata di Verona, Verona, Italy
* These Authors contributed equally to the manuscript
Supplementary Figure 1.
Line plot illustrating median eGFR trend over time (pre-operative vs post-operative day [POD] 1 vs discharge vs. 6-months follow up) according to AB0-blood groups system.

428-1 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 ORIGINAL PAPER - SUPPLEMENTARY MATERIAL No conflict of interest declared
Supplementary Table 1
Univariable and multivariable logistic regression models addressing renal function decline (eGFR < 60 mL/min) at post operative day 1, at discharge and at 6-months follow up, according to AB0-blood groups system
UNIVARIABLE
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 A Tafuri, A Panunzio, A Soldano, et al 428-2
MULTIVARIABLE
day 1 eGFR < 60 mL/min OR (95% CI) 1 p-value OR (95% CI) 1 p-value A vs 0 0 79 (0 48, 1 29) 0 3 0 59 (0 31, 1 12) 0 1 B vs 0 0 46 (0 19, 1 07) 0 08 0 44 (0 14, 1 32) 0 2 AB vs 0 2 71 (0 97, 8 80) 0 07 2 89 (0 80, 11 64) 0 1 Discharge eGFR < 60 mL/min OR (95% CI) 1 p-value OR (95% CI) 1 p-value A vs 0 1 30 (0 75, 2 27) 0 4 1 26 (0 60, 2 70) 0 5 B vs. 0 0.63 (0.20, 1.69) 0.4 0.70 (0.16, 2.69) 0.6 AB vs 0 3 27 (1 16, 9 42) 0 025 4 28 (1 04, 18 65) 0 047 6 months eGFR < 60 mL/min OR (95% CI) 1 p-value OR (95% CI) 1 p-value A vs 0 1 02 (0 48, 2 13) 0 9 0 86 (0 28, 2 54) 0 8 B vs 0 0 50 (0 13, 1 63) 0 3 0 71 (0 12, 3 68) 0 7 AB vs 0 2 25 (0 58, 9 61) 0 2 1 69 (0 28, 11 56) 0 6 1 OR Odds Ratio; CI Confidence Interva
comp ications
* Post-operative
* Models adjusted for age, Charlson Comorbid ty Index, pre-operative eGFR, ur nary derivat on type, post-operative
Stamatios Katsimperis, Lazaros Tzelves, Themistoklis Bellos, Konstantinos Pikramenos, Ioannis Manolitsis, Ioannis Tsikopoulos, Iraklis Mitsogiannis
Department of Urology, Athens, Greece
476-1 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 REVIEW - SUPPLEMENTARY MATERIAL No conflict of interest declared
Cytoreductive nephrectomy for synchronous metastatic renal cell carcinoma. Is there enough evidence?
F irst author Year Reason Bensalah 2018 Article in French Nayak 2021 Case series with < 10 patients Pilie 2017 Review Finelli 2020 Guidelines Verzoni 2018 Ongoing clinical trial Gilbert 2017 Article in German Capitanio 2019 Editorial Tabakin 2020 Review Balssa 2018 Article in French Dursun 2021 Not relevant Tenold 2020 Review Shao 2021 Not relevant Esdaille 2021 Editorial Guo 2020 No outcome of interest Shuch 2008 Data before TT ST era Dalloglio 2011 Case series with < 10 patients Russo 2007 before TT era Ho 2016 No outcome of interest Khochikar 2017 Review Belmunt 2014 Guidelines Laru 2021 No outcome of interest Park 2013 Cytokine therapy Bosse 2019 No CN data Shaw 2012 No overallsurvival data Blick 2010 Not matching criteria Smalodone 2014 No outcome of interest Zhang 2021 No outcome of interest Culp 2014 Editorial Stewart 2017 Editorial Wald 2014 No outcome of interest Shuch 2009 No outcome of interest Dizaman 2017 No outcome of interest Birkhauser 2013 Interleukin therapy Reimers 2020 Case report Albiges 2022 No outcome of interest Mir 2021 Case report
Table 1. Excluded studies
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
476-2 Camai 2021 No outcome of interest Singh 2017 No outcome of interest Bhat 2010 Review Richey 2011 No cytoreductive nephrectomy Miyake 2018 Interferon used Patel 2016 No outcome of interest Nishimura 2017 Case report Bex 2008 Cytokines Courcier 2021 No CN data Claeys 2017 Did not report effect estimate of interest Laukhtina 2020 No outcome of interest Psutka 2015 No outcome of interest Nizam 2020 Review Kikuchi 2022 No outcome of interest Watanabe 2019 Case report Koga 2019 Editorial Lyon 2018 No outcome of interest Zhou 2021 Case report Cost 2011 No outcome of interest Tornberg 2018 No outcome of interest Schulman 2017 Case report Margulis 2008 Editorial Gershman 2016 No outcome of interest Marconi 2018 No outcome of interest Graafland 2021 No outcome of interest Meerveld-eggink 2022 No outcome of interest Abel 2011 No outcome of interest Dason 2013 Review Albiges 2020 No outcome of interest Battaglia 2015 Editorial Kubler 2015 Editorial Kinsey 2020 Review Gu 2016 No outcome of interest Thomson 2020 No outcome of interest Urasaki 2021 No outcome of interest Brecheteau 2017 No outcome of interest Matin 2006 Cytokine era Chapin 2011 No outcome of interest Furubayashi 2022 Case report Harshmann 2013 No outcome of interest Tsao 2012 No outcome of interest Papavassilis 2014 Article in german Yoon 2013 No outcome of interest Mejean 2017 Article in french Massari 2019 Comment to article Ganeshappa 2010 No outcome of interest Griffioen 2012 No outcome of interest Laguna 2020 No outcome of interest Maestroni 2021 Case report Agarwal 2016 Editorial Eisenberg 2006 No outcome of interest Amin 2008 Small number of patients Bigot 2015 Editorial comment Bex 2018 Guidelines Lee 2016 No CN Algarra 2020 Case report
S Katsimperis, L Tzelves, T Bellos, K Pikramenos, I Manolitsis, I Tsikopoulos, I Mitsogiannis
476-3 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Chertin 2009 No outcome of interest Shinohara 2012 No CN +Interferon Kim 2019 No outcome of interest Fuchizawa 2021 Case report Zarrabi 2019 Case report Okazaki 2020 Case report Benamran 2022 Review Billon 2019 Case report Jonasch 2010 Review Bex 2016 Guidelines Biswas 2017 Comment to article Tam 2020 Case report Safriadi 2020 Case report Bex 2011 Editorial Vento 2019 Case report Nelson 2013 No outcome of interest Castillo 2008 Article in spanish+ case report Procopio 2015 Metachronous mRCC Sazuka 2021 Case report Otsuka 2022 Case report D'aniello 2014 Case report Peters 2012 Case report Marzouk 2014 Case report Shah 2015 Case report Lebret 2010 Article in french Ikehata 2013 Case report in japanish Nosov 2015 Article in russian Velasco 2020 Case report Hayata 2018 Case report Zubairi 2016 Case report Bhat 2019 Case report Giannarini 2016 Case report Li 2012 Case report Ficarra 2016 Case report Ueda 2011 Case report McKiernan 2013 Review Locatelli 2010 Case report Moslemi 2010 Case report Pan 2006 Case report Larcher 2020 No outcome of interest Roussel 2020 No outcome of interest Vaishampayan 2019 Duplication of study cohort Cao 2022 Not clear differentiation between synchronous and metachronous mRCC groups Kim 2017 No outcome of interest Liu 2020 Overall survival outcome not reached in CN group Manley 2017 Did not report effect estimate of interest Tsao 2012 No outcome of interest Mutlu 2014 Did not report effect estimate of interest Janisch 2021 No outcome of interest Xiao 2015 No overall survival rates Kassouf 2007 Did not report effect estimate of interest Rosiello 2021 Did not report effect estimate of interest Macleod 2015 Review Berg 2018 Did not report effect estimate of interest Westesson 2014 No outcome of interest
Nephrectomy for metastatic renal cell carcinoma
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
476-4 Qi 2017 No outcome of interest Zhao 2020 No outcome of interest Minervini 2019 Editorial Commentary Fristrup 2019 Upcoming trial Southwest Oncology Group 2020 Upcoming trial Zequi 2020 Editorial Comment Psutka 2019 Review Pantuck 2017 Review Carver 2009 Article comment Graham 2019 Review Grassi 2017 Terminated trial Neill 2008 Review Ontario Clinical Oncology Group - No outcome of interest Westerman 2020 No outcome of interest Massari 2019 Comment to article De Velasco 2018 No outcome of interest Kokorovic 2019 Review Arora 2019 No outcome of interest Jonasch 2009 No outcome of interest Gao 2019 No outcome of interest Patel 2016 No outcome of interest Jamshidi 2016 No outcome of interest Powles 2011 No outcome of interest Albiges 2019 No outcome of interest Woldu 2018 No outcome of interest Gao 2017 No outcome of interest Runcie 2021 Trial under enrollmnet Jäger 2010 No outcome of interest Capitanio 2016 Review Landman 2017 Trial closed due to extremely low accrual Bayer Study Director 2018 No outcome of interest Jonasch 2022 No results posted Kapoor 2018 No results posted Finelli 2015 No results posted Venturini 2013 No results posted Sharma 2020 No results posted Flaherty 2014 No results posted Amiel 2016 Only 9 participants Oh 2022 No results posted Ishihara 2021 No CN performed Kato 2022 The non-upfront CN group included also patients who did not receive CN Woldu 2018 No outcome of interest De Bruijn 2017 No outcome of interest De Bruijn 2019 No outcome of interest Jiang 2021 No outcome of interest Kim 2019 No outcome of interest Kim 2020 No outcome of interest Kutikov 2009 No outcome of interest Noe 2016 No outcome of interest O’Malley 2011 No outcome of interest Pal 2013 No outcome of interest Powles 2016 No outcome of interest Roussel 2020 No outcome of interest Stellato 2021 No outcome of interest
S Katsimperis, L Tzelves, T Bellos, K Pikramenos, I Manolitsis, I Tsikopoulos, I Mitsogiannis
Diagnosis and management of intradiverticular bladder tumours: A pooled analysis of 498 cases

Stamatios Katsimperis, Lazaros Tzelves, Themistoklis Bellos, Panagiotis Angelopoulos, Ioannis Tsikopoulos, Iraklis Mitsogiannis, Athanasios Papatsoris
Second Department of Urology, National and Kapodistrian University of Athens, Sismanogleio General Hospital, Athens, GRC
DATA BASE EXTRACTED BY STUDIES INCLUDED IN THE SYSTEMATIC REVIEW
486-1 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
- SUPPLEMENTARY
No conflict of interest declared
REVIEW
MATERIAL
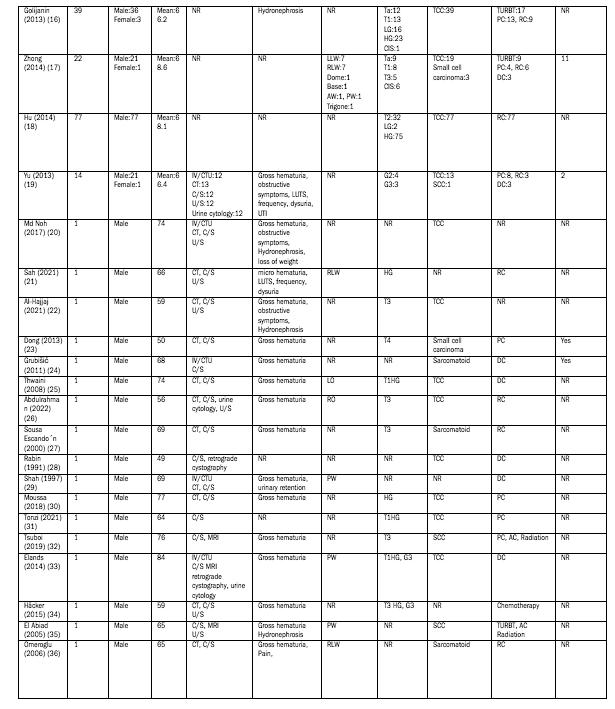
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
486-2
S Katsimperis, L Tzelves, T Bellos, K Pikramenos, I Manolitsis, I Tsikopoulos, I Mitsogiannis
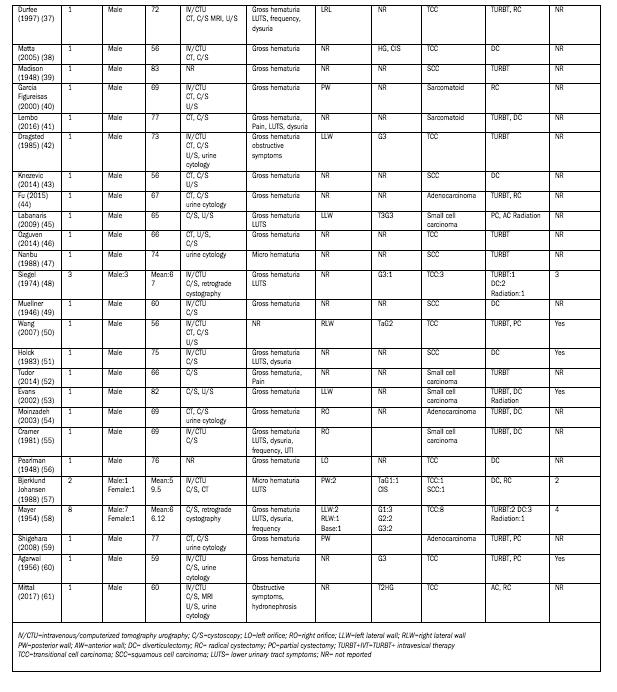
486-3 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Nephrectomy for metastatic renal cell carcinoma
Efficacy of overactive neurogenic bladder treatment: A systematic review of randomized controlled trials
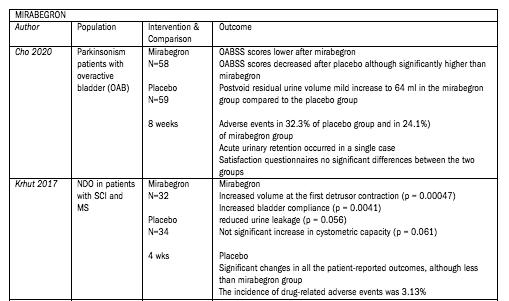
Rawa Bapir 1, 14 , Kamran Hassan Bhatti 2, 14 , Ahmed Eliwa 3, 14 , Herney Andrés García-Perdomo 4, 14 , Nazim Gherabi 5, 14 , Derek Hennessey 6, 14 , Vittorio Magri 7, 14 , Panagiotis Mourmouris 8, 14 , Adama Ouattara 9, 14 , Gianpaolo Perletti 10, 14 , Joseph Philipraj 11, 14 , Konstantinos Stamatiou 12, 14 , Alberto Trinchieri 13, 14 , Noor Buchholz 14
1 Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq;
2 Urology Department, HMC, Hamad Medical Corporation, Qatar;
3 Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt;
4 Universidad del Valle, Cali, Colombia;
5 Faculty of Medicine Algiers 1, Algiers, Algeria;
6 Department of Urology, Mercy University Hospital, Cork, Ireland;
7 ASST Nord Milano, Milan, Italy;
8 2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece;
9 Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso;
10 Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy;
11 Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India;
12 Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece;
13 Urology School, University of Milan, Milan, Italy;
14 U-merge Ltd (Urology for emerging countries), London-Athens-Dubai *
Authors 1-14 have equally contributed to the paper and share first authorship
* U-merge Ltd (Urology for Emerging Countries) is an academic urological platform dedicated to facilitate knowledge transfer in urology on all levels from developed to emerging countries U-merge Ltd is registered with the Companies House in London/ UK www U-merge com
PICO TABLES
492-1 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 REVIEW - SUPPLEMENTARY MATERIAL No conflict of interest declared
Cho SY, Jeong SJ, Lee S, et al Mirabegron for treatment of overactive bladder symptoms in patients with Parkinson's disease: A double-blind, randomized placebo-controlled trial (Parkinson's Disease Overactive bladder Mirabegron, PaDoMi Study) Neurourol Urodyn 2021; 40:286294

Krhut J, Borovicka V, Bilkova K, et al Mirabegron in the treatment of neurogenic detrusor overactivity due to spinal cord injury and multiple sclerosis International Journal of Urology 2017; 24(Suppl 1):18-19
Moussa M, Chakra MA, Dabboucy B, et al The safety and effectiveness of mirabegron in Parkinson's disease patients with overactive bladder: a randomized controlled trial Scand J Urol 2022; 56:66-72
Ray S, Burdick D, Griffith A, Agarwal P Preliminary report on the MAESTRO study: A pilot study of mirabegron and behavioral modification including pelvic floor exercise for overactive bladder in Parkinson's disease Movement Disorders 2017; 32:(Suppl 2):945-946
Welk B, Hickling D, McKibbon M, et al A pilot randomized-controlled trial of the urodynamic efficacy of mirabegron for patients with neurogenic lower urinary tract dysfunction Neurourol Urodyn 2018; 37:2810-2817
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
492-2
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
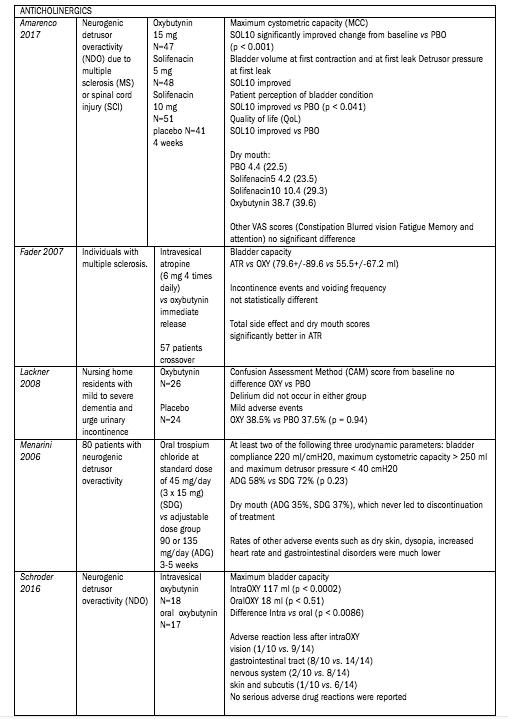
492-3 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
Amarenco G, Sutory M, Zachoval R, et al Solifenacin is effective and well tolerated in patients with neurogenic detrusor overactivity: Results from the double-blind, randomized, active- and placebo-controlled SONIC urodynamic study Neurourol Urodyn 2017; 36:414-421
Fader M, Glickman S, Haggar V, et al Intravesical atropine compared to oral oxybutynin for neurogenic detrusor overactivity: a double-blind, randomized crossover trial J Urol 2007; 177:208-13
Lackner TE, Wyman JF, McCarthy TC, et al Randomized, placebo-controlled trial of the cognitive effect, safety, and tolerability of oral extended-release oxybutynin in cognitively impaired nursing home residents with urge urinary incontinence J Am Geriatr Soc 2008; 56:862-70
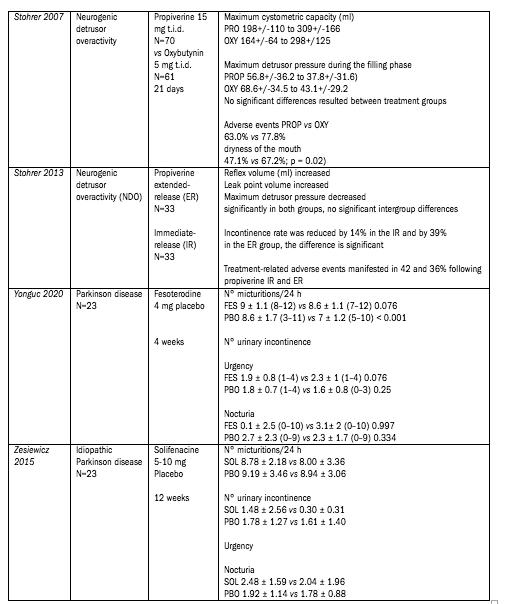
Archivio Italiano di Urologia e Andrologia 2022; 94, 4 R
492-4
Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
Menarini M, Del Popolo G, Di Benedetto P, et al Trospium chloride in patients with neurogenic detrusor overactivity: is dose titration of benefit to the patients? Int J Clin Pharmacol Ther 2006; 44:623-32
Schröder A, Albrecht U, Schnitker J, et al Efficacy, safety, and tolerability of intravesically administered 0 1% oxybutynin hydrochloride solution in adult patients with neurogenic bladder: A randomized, prospective, controlled multi-center trial Neurourol Urodyn 2016; 35:582-8
Stöhrer M, Mürtz G, Kramer G, et al Propiverine compared to oxybutynin in neurogenic detrusor overactivity--results of a randomized, double-blind, multicenter clinical study Eur Urol 2007; 51:235-42
Stöhrer M, Mürtz G, Kramer G, et al Efficacy and tolerability of propiverine hydrochloride extended-release compared with immediate-release in patients with neurogenic detrusor overactivity Spinal Cord 2013; 51:419-23
Yonguc T, Sefik E, Inci I, et al Randomized, controlled trial of fesoterodine fumarate for overactive bladder in Parkinson's disease World J Urol 2020; 38:2013-2019
Zesiewicz TA, Evatt M, Vaughan CP, et al Randomized, controlled pilot trial of solifenacin succinate for overactive bladder in Parkinson's disease Parkinsonism Relat Disord 2015; 21:514-20
Nardulli R, Losavio E, Ranieri M, et al Combined antimuscarinics for treatment of neurogenic overactive bladder Int J Immunopathol Pharmacol 2012; 25(1 Suppl):35S-41S
Sakakibara R, Ito T, Uchiyama T, et al Effects of milnacipran and paroxetine on overactive bladder due to neurologic diseases: a urodynamic assessment Urol Int 2008; 81:335-9
Vasudeva P, Kumar A, Yadav S, et al Neurological safety and efficacy of darifenacin and mirabegron for the treatment of overactive bladder in patients with history of cerebrovascular accident: A prospective study Neurourol Urodyn 2021; 40:2041-2047
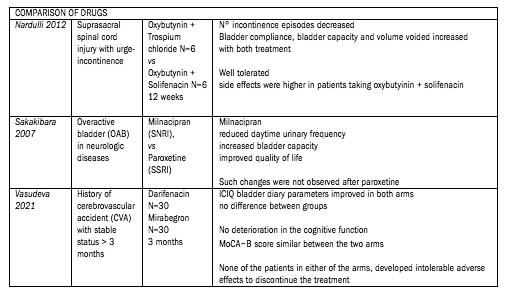
492-5 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
Freeman RM, Adekanmi O, Waterfield MR, et al The effect of cannabis on urge incontinence in patients with multiple sclerosis: a multicentre, randomised placebo-controlled trial (CAMS-LUTS) Int Urogynecol J Pelvic Floor Dysfunct 2006; 17:636-41
Kavia RB, De Ridder D, Constantinescu CS, et al Randomized controlled trial of Sativex to treat detrusor overactivity in multiple sclerosis Mult Scler 2010; 16:1349-59

Archivio Italiano di Urologia e Andrologia 2022; 94, 4
492-6
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
De Sèze M, Wiart L, Joseph P-A, et al Capsaicin and neurogenic detrusor hyperreflexia: A double-blind placebo- controlled study in 20 patients with spinal cord lesions Neurourology and Urodynamics 1998; 17:5(513-523) Cited by: 97
de Sèze M, Gallien P, Denys P, et al Intravesical glucidic capsaicin versus glucidic solvent in neurogenic detrusor overactivity: a double blind controlled randomized study Neurourol Urodyn 2006; 25:752-7
Lazzeri M, Calò G, Spinelli M, et al Daily intravesical instillation of 1 mg nociceptin/orphanin FQ for the control of neurogenic detrusor overactivity: a multicenter, placebo controlled, randomized exploratory study J Urol 2006; 176:2098-102

492-7 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
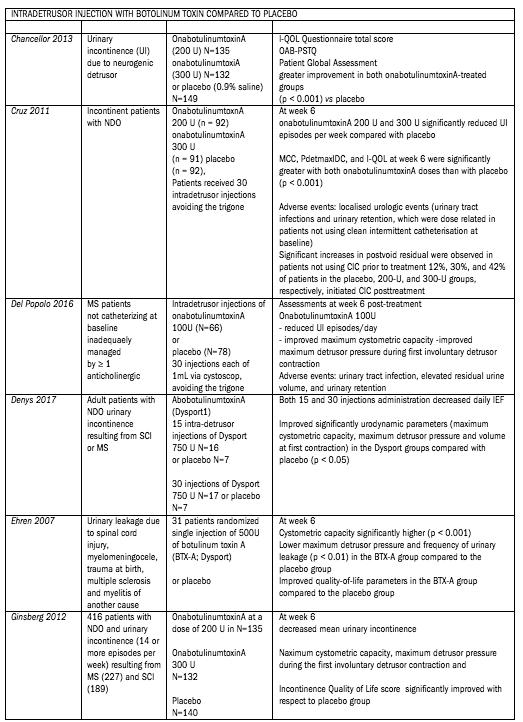
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
492-8
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
Del Popolo G, Denys P, Keppenne V, et al Efficacy and safety of onabotulinumtoxina 100u for treatment of urinary incontinence due to neurogenic detrusor overactivity in non-catheterising multiple sclerosis patients Neurourology and Urodynamics 2016; 35(Suppl 3):S53-S54
Chancellor MB, Patel V, Leng WW, et al OnabotulinumtoxinA improves quality of life in patients with neurogenic detrusor overactivity Neurology 2013; 81:841-8
Cruz F, Herschorn S, Aliotta P, et al Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial Eur Urol 2011; 60:742-50

492-9 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
Denys P, Del Popolo G, Amarenco G, et al Efficacy and safety of two administration modes of an intra-detrusor injection of 750 units dysport® (abobotulinumtoxinA) in patients suffering from refractory neurogenic detrusor overactivity (NDO): A randomised placebo-controlled phase IIa study Neurourol Urodyn 2017; 36:457-462
Ehren I, Volz D, Farrelly E, et al Efficacy and impact of botulinum toxin A on quality of life in patients with neurogenic detrusor overactivity: a randomised, placebo-controlled, double-blind study Scand J Urol Nephrol 2007; 41:335-40
Ginsberg D, Gousse A, Keppenne V, et al Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity J Urol 2012; 187:2131-9
Herschorn S, Gajewski J, Ethans K, et al Efficacy of botulinum toxin A injection for neurogenic detrusor overactivity and urinary incontinence: a randomized, double-blind trial J Urol 2011; 185:2229-35
Honda M, Yokoyama O, Takahashi R, et al Botulinum toxin injections for Japanese patients with urinary incontinence caused by neurogenic detrusor overactivity: Clinical evaluation of onabotulinumtoxinA in a randomized, placebo-controlled, double-blind trial with an open-label extension Int J Urol 2021; 28:906-912
Kennelly M, Cruz F, Herschorn S, et al Efficacy and Safety of AbobotulinumtoxinA in Patients with Neurogenic Detrusor Overactivity Incontinence Performing Regular Clean Intermittent Catheterization: Pooled Results from Two Phase 3 Randomized Studies (CONTENT1 and CONTENT2) European Urology 2022
Schurch B, De Sèze M, Denys P, et al Botulinum toxin type A is a safe and effective treatment for neurogenic urinary incontinence: Results of a single treatment, randomized, placebo controlled 6-month study J Urol 2005; 174:196-200
Schurch 2007
Evaluation of QoL in the same series of Schurch 2005
Sussman D, Patel V, Del Popolo G, et al Treatment satisfaction and improvement in health-related quality of life with onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity Neurourol Urodyn 2013; 32:242-9
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
492-10
Abdel-Meguid TA Botulinum toxin-A injections into neurogenic overactive bladder--to include or exclude the trigone? A prospective, randomized, controlled trial J Urol 2010; 184:2423-8
Hui C, Keji X, Chonghe J, et al Combined detrusor-trigone BTX-A injections for urinary incontinence secondary to neurogenic detrusor overactivity Spinal Cord 2016; 54:46-50
Grise P, Ruffion A, Denys P, et al Efficacy and tolerability of botulinum toxin type a in patients with neurogenic detrusor overactivity and without concomitant anticholinergic therapy: Comparison of two doses Eur Urol 2010; 58:759-766
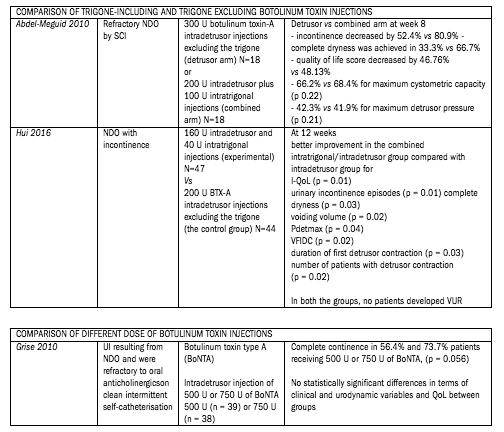
492-11 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
Araujo TG, Schmidt AP, Sanches PRS, et al Transcutaneous tibial nerve home stimulation for overactive bladder in women with Parkinson's disease: A randomized clinical trial Neurourol Urodyn 2021; 40:538-548
Monteiro ÉS, de Carvalho LB, Fukujima MM, et al Electrical stimulation of the posterior tibialis nerve improves symptoms of poststroke neurogenic overactive bladder in men: a randomized controlled trial Urology 2014; 84:509-14

Archivio Italiano di Urologia e Andrologia 2022; 94, 4
492-12
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
Perissinotto MC, D’Ancona CA, Lucio A, et al Transcutaneous tibial nerve stimulation in the treatment of lower urinary tract symptoms and its impact on health-related quality of life in patients with Parkinson disease: a randomized controlled trial J Wound Ostomy Continence Nurs 2015; 42:94-9
Gaspard L, Tombal B, Opsomer RJ, et al Kinésithérapie et symptômes du bas appareil urinaire chez des patients atteints de la sclérose en plaques: étude contrôlée randomisée [Physiotherapy and neurogenic lower urinary tract dysfunction in multiple sclerosis patients: a randomized controlled trial] Prog Urol 2014; 24:697-707
Eftekhar T, Teimoory N, Miri E, et al Posterior tibial nerve stimulation for treating neurologic bladder in women: a randomized clinical trial Acta Med Iran 2014; 52:816-21
Zonic-Imamovic M, Imamovic S, Cickušic A, et al Effects of Treating an Overactive Urinary Bladder in Patients with Multiple Sclerosis Acta Med Acad 2019; 48:271-277
Chen YL, Feng WJ, Zhang XL Parkinson's disease combined with overactive bladder syndrome treated with acupuncture and medication Zhongguo Zhen Jiu 2012; 32:215-8
Chen H, Wang C, Zhou M, et al Electroacupuncture for post-stroke overactive bladder: a multi-centre pilot randomized controlled trial Acupunct Med 2021; 39:175-183

492-13 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
of overactive neurogenic bladder
Treatment
Guo ZF, Liu Y, Hu GH, et al Transcutaneous electrical nerve stimulation in the treatment of patients with poststroke urinary incontinence Clin Interv Aging 2014; 9:851-6
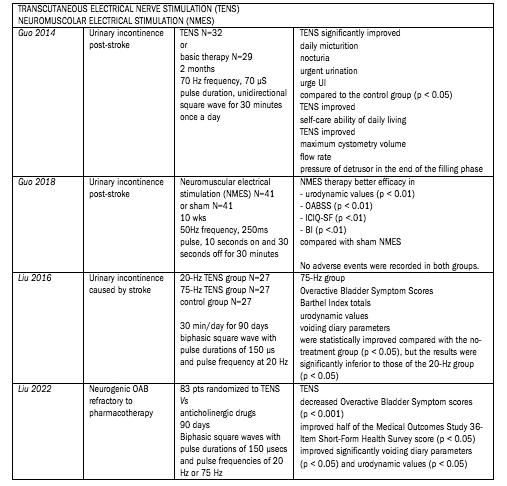
Guo GY, Kang YG Effectiveness of neuromuscular electrical stimulation therapy in patients with urinary incontinence after stroke: A randomized sham controlled trial Medicine (Baltimore) 2018; 97:e13702
Liu Y, Xu G, Luo M, Teng HF Effects of Transcutaneous Electrical Nerve Stimulation at Two Frequencies on Urinary Incontinence in Poststroke
Patients: A Randomized Controlled Trial Am J Phys Med Rehabil 2016; 95:183-93
Liu Y, Xu G, Geng J Efficacy of Transcutaneous Electrical Nerve Stimulation in the Management of Neurogenic Overactive Bladder: A Randomized Controlled Trial Am J Phys Med Rehabil 2022; 101:2-10
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
et
492-14
R Bapir, K Hassan Bhatti, Ahmed Eliwa,
al
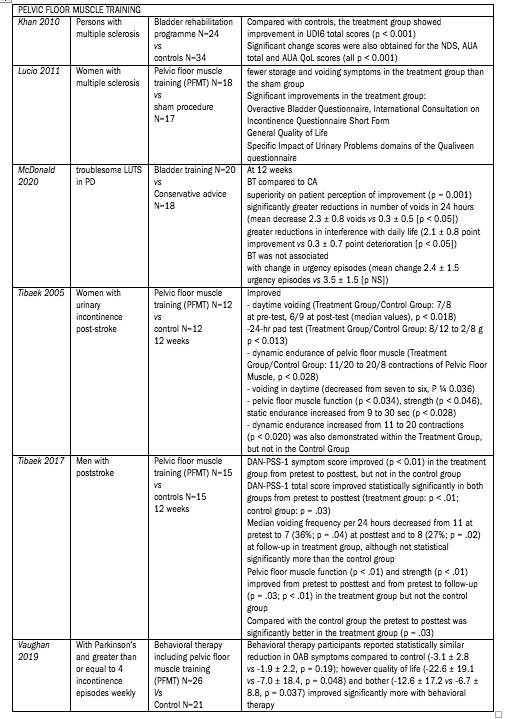
492-15 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
Khan F, Pallant JF, Pallant JI, et al A randomised controlled trial: Outcomes of bladder rehabilitation in persons with multiple sclerosis Journal of Neurology, Neurosurgery and Psychiatry 2010; 81:9 (1033-1038)

Lúcio AC, Perissinoto MC, Natalin RA, et al A comparative study of pelvic floor muscle training in women with multiple sclerosis: its impact on lower urinary tract symptoms and quality of life Clinics (Sao Paulo) 2011; 66:1563-8
McDonald C, Rees J, Winge K, et al Bladder training for urinary tract symptoms in Parkinson disease: A randomized controlled trial Neurology 2020; 94:e1427-e1433
Tibaek S, Gard G, Jensen R Pelvic floor muscle training is effective in women with urinary incontinence after stroke: a randomised, controlled and blinded study Neurourol Urodyn 2005; 24:348-57
Tibaek S, Gard G, Dehlendorff C, et al Is Pelvic Floor Muscle Training Effective for Men With Poststroke Lower Urinary Tract Symptoms? A Single-Blinded Randomized, Controlled Trial Am J Mens Health 2017; 11:1460-1471
Vaughan CP, Burgio KL, Goode PS, et al Behavioral therapy for urinary symptoms in Parkinson's disease: A randomized clinical trial Neurourol Urodyn 2019; 38:1737-1744
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
492-16
Botini D, Lucio A, Domingos J, et al Pelvic floor muscle training in the treatment of lower urinary tract symptoms in women with multiple sclerosis and myelopathy associated with HTLV-I (HAM/TSP): A randomized controlled trial Neurourology and Urodynamics 2019; 38(Suppl 3): S455-
Ferreira AP, Pegorare AB, Salgado PR, et al Impact of a Pelvic Floor Training Program Among Women with Multiple Sclerosis: A Controlled Clinical Trial Am J Phys Med Rehabil 2016; 95:1-8
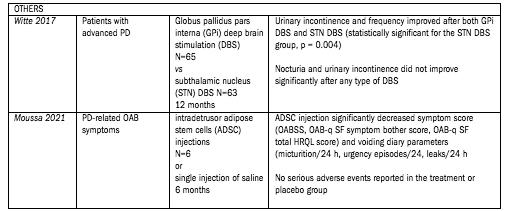
Silva Ferreira AP, de Souza Pegorare ABG, Miotto Junior A, et al A Controlled Clinical Trial on the Effects of Exercise on Lower Urinary Tract Symptoms in Women With Multiple Sclerosis Am J Phys Med Rehabil 2019; 98:777-782
Lúcio A, D’Ancona CA, Perissinotto MC, et al Pelvic Floor Muscle Training With and Without Electrical Stimulation in the Treatment of Lower Urinary Tract Symptoms in Women With Multiple Sclerosis J Wound Ostomy Continence Nurs 2016; 43:414-9
Witte LP, Odekerken VJJ, Boel JA, et al NSTAPS study group Does deep brain stimulation improve lower urinary tract symptoms in Parkinson's disease? Neurourol Urodyn 2018; 37:354-359
Moussa M, Abou Chakra M, Dabboucy B, et al Single intradetrusor injection of autologous adipose-derived stem cells in Parkinson's disease patients with overactive bladder: A pilot study Neurourology and Urodynamics 2021; 40(Suppl 2):S93-S95
492-17 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Treatment of overactive neurogenic bladder
RISK OF BIAS
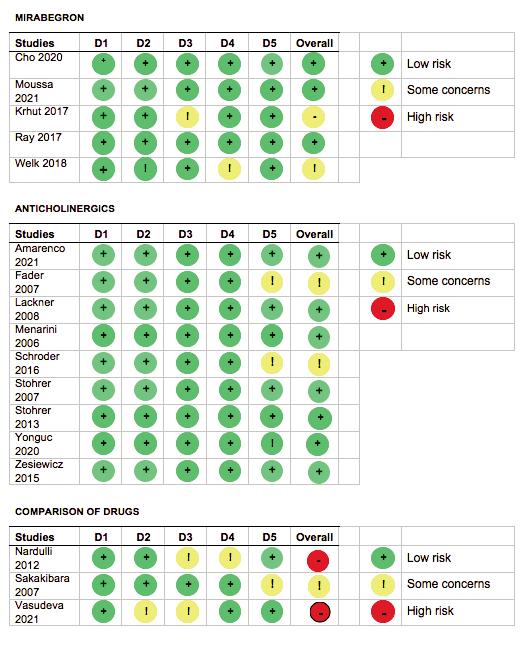
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
492-18
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
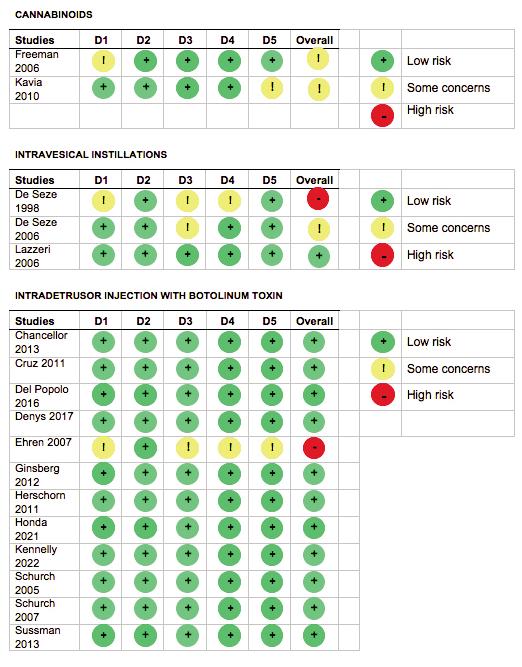
492-19 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
Treatment of overactive neurogenic bladder
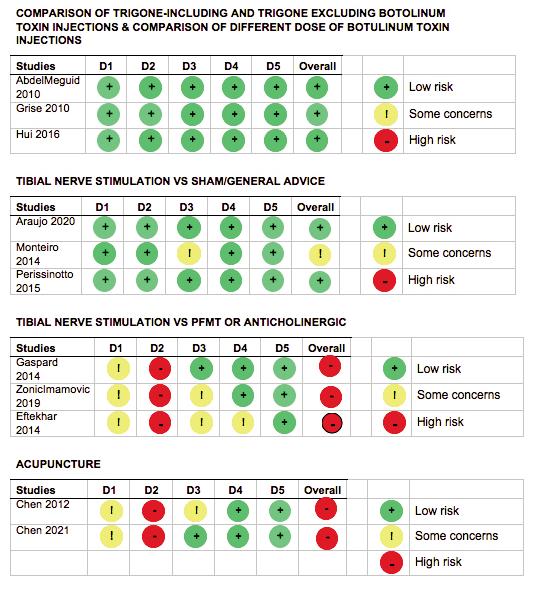
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
492-20
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
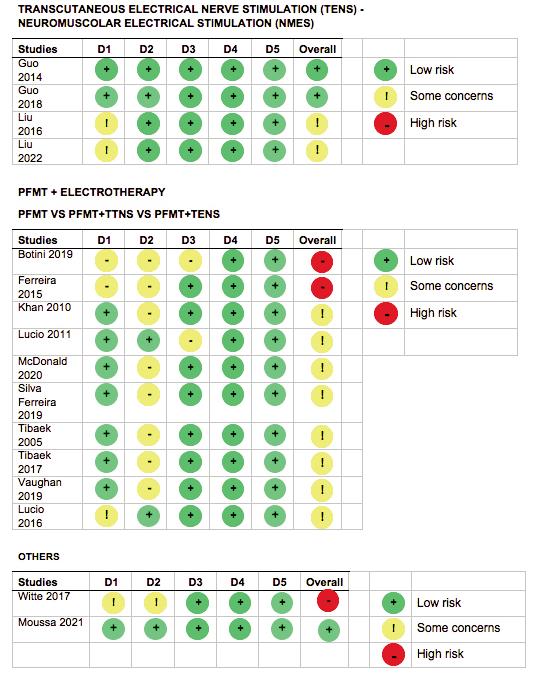
492-21 Archivio Italiano di Urologia e Andrologia 2022; 94, 4
of overactive neurogenic bladder
Treatment
SUMMARY OF FINDINGS
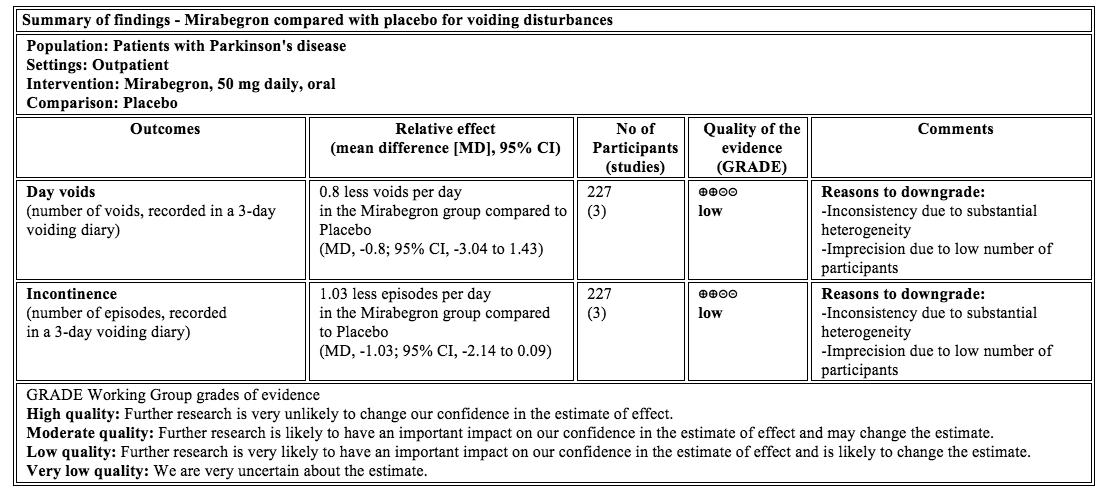
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
492-22
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
Risk of urinary stone formation associated to proton pump inhibitors: A systematic review and metanalysis of observational studies
Rawa Bapir 1, 15 , Kamran Hassan Bhatti 2, 15 , Ahmed Eliwa 3, 15 , Herney Andrés García-Perdomo 4, 15 , Nazim Gherabi 5, 15 , Derek Hennessey 6, 15 , Vittorio Magri 7, 15 , Panagiotis Mourmouris 8, 15 , Adama Ouattara 9, 15 , Gianpaolo Perletti 10, 15 , Joseph Philipraj 11, 15 , Konstantinos Stamatiou 12, 15 , Musliu Adetola Tolani 13, 15 , Lazaros Tzelves 8, 15 , Alberto Trinchieri 14, 15 , Noor Buchholz 15
1 Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq;
2 Urology Department, HMC, Hamad Medical Corporation, Qatar;
3 Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt;
4 Universidad del Valle, Cali, Colombia;
5 Faculty of Medicine Algiers 1, Algiers, Algeria;
6 Department of Urology, Mercy University Hospital, Cork, Ireland;
7 ASST Nord Milano, Milan, Italy;
8 2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece;
9 Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso;
10 Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy;
11 Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India;
12 Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece,
13 Division of Urology, Department of Surgery, Ahmadu Bello University / Ahmadu Bello University Teaching Hospital, Zaria, Kaduna State, Nigeria;
14 Urology School, University of Milan, Milan, Italy;
15 U-merge Ltd (Urology for emerging countries), London-Athens-Dubai*
Authors 1-14 have equally contributed to the paper and share first authorship
* U-merge Ltd (Urology for Emerging Countries) is an academic urological platform dedicated to facilitate knowledge transfer in urology on all levels from developed to emerging countries U-merge Ltd is registered with the Companies House in London/ UK www U-merge com
INCLUDED STUDIES
Ferraro PCG, Gambaro G, Taylor E Proton Pump Inhibitors, Histamine Receptor-2 Blockers and the Risk of Incident Kidney Stones American Society of Nephrology Kidney Week; Chicago, IL 2016, p 467A
Kwak YE, Buller G, Masoud A Increased risk of nephrolithiasis in patients using chronic proton pump inhibitor and antacid agents Gastroenterology 2017; 152:(5 Supp 1)(S273-)
Kim SY, Yoo DM, Bang WJ, Choi HG Association between Urolithiasis and History Proton Pump Inhibitor Medication: A Nested Case-Control Study J Clin Med 2022; 11:5693
Simonov M, Abel EA, Skanderson M, et al Use of Proton Pump Inhibitors Increases Risk of Incident Kidney Stones Clin Gastroenterol Hepatol 2021; 19:72-79 e21
Sui W, Miller NL, Gould ER, et al Proton pump inhibitors use and risk of incident nephrolithiasis Urolithiasis 2022; 50:401-409
507-1 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 REVIEW - SUPPLEMENTARY MATERIAL No conflict of interest declared
PICO TABLES

Archivio Italiano di Urologia e Andrologia 2022; 94, 4
507-2
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al

507-3 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Proton pump inhibitors and urinary calculi
RISK OF BIAS
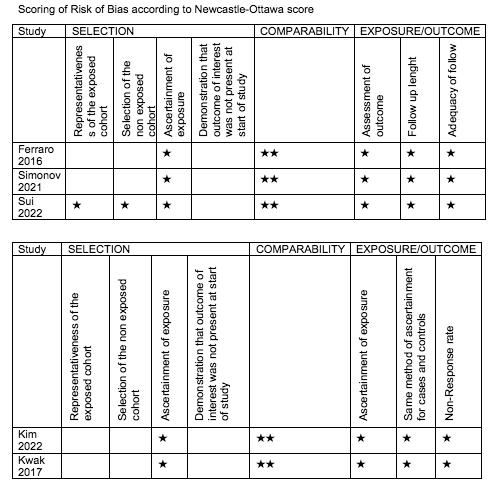
Archivio Italiano di Urologia e Andrologia 2022; 94, 4
507-4
R Bapir, K Hassan Bhatti, Ahmed Eliwa, et al
“TRIM-AND-FILL” STRATEGY
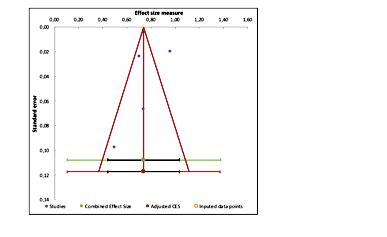
507-5 Archivio Italiano di Urologia e Andrologia 2022; 94, 4 Proton pump inhibitors and urinary calculi
INSTRUCTIONS TO AUTHORS – ARCHIVIO ITALIANO DI UROLOGIA E ANDROLOGIA
OPEN ACCESS
Open access publishing does have its costs. Information regarding authors’ payment are not made available to editors and reviewers ensuring that they cannot be influenced in their selection of papers for publication by payment conditions or limitations.
The Article Processing Charge for publication in this journal is EUR 300,00 (plus VAT, if applicable).
Our fees cover the costs of peer review, copyediting, publication, different format of publication (HTML, PDF), inclusion in many Open Access databases.
All bank charges shall be borne by the payer.
Please note that our fees do not include taxes (VAT):
- Private or public ITALIAN customers (individuals, universities, hospitals, other organizations) must ALWAYS add VAT (IVA) at standard rate (4%);
- European Union PRIVATE customers must add the standard rate of their own country VAT tax;
- European Union private/public ORGANIZATIONS (universities, hospitals, others with regular VAT number) should not add any taxes at standard rate, provided that they indicate their VAT number;
- Outside the European Union, individuals and organizations should not add any taxes at standard rate.
Important: Authors are NOT required to pay at the moment of submission. If the paper is accepted, the Managing Editor of Open Access Edition will guide the Authors through the payment procedure. No article will be published before waiver or payment.
According to the United Nations list of Least Developed Countries (LCDs) available from: http://www.un.org/en/development/desa/policy/cdp/ldc2/ldc_countries.shtml
Authors coming from those countries are entitled to ask for a discount.
A “Formal Request for discount” has to be forwarded to the Managing Editor of Open Access Edition, after receiving the acceptance letter. The Editorial Committee will then evaluate the merits of each individual case. Any other informal request (such as comments at the moment of submission, or made in the covering letter of the revised version) will not be taken into consideration.
FAST-TRACK
PEER REVIEW
All papers published in Archivio Italiano di Urologia e Andrologia (AIUA) are peer reviewed. Fast-track peer review (4 weeks) can be obtained by supplementary fee of € 488 (VAT included).
in Italian language can be published after translation (expenses will be charged to the Authors). Manuscripts should be typed double spaced with wide margins. They must be subdivided into the following sections:
TITLE PAGE
It must contain: a) title; b) a short (no more than 40 characters) running head title; c) first, middle and last name of each Author without abbreviations; d) University or Hospital, and Department of each Author; e) last name, address and e-mail of all the Authors; f) corresponding Author; g) acknowledgement of conflict of interest and financial support.
SUMMARY
Authors must submit a summary (300 words, 2000 characters) divided by subheadings as follows: Objective(s), Material and method(s), Result(s), Conclusion(s). After the summary, three to ten key words must appear, taken from the standard Index Medicus terminology.
TEXT
For original articles concerning experimental or clinical studies, the following standard scheme must be followed: Summary - Key Words - Introduction - Material and Methods - Results - Discussion - Conclusions - References - Tables - Legends - Figures.
Case Report should be divided into: Summary - Introduction (optional) - Case report(s) - Conclusions - References
Supplementary Materials can be added for online publication.
SIZE OF MANUSCRIPTS
Literature reviews, Editorials and Original articles should not exceed 3500 words with 3-5 figures or tables, and no more than 30 references.
Case reports, Notes on surgical technique, and Letters to the editors should not exceed 1000 words (summary included) with only one table or figure, and no more than three references. No more than five authors are permitted.
REFERENCES
METHODS OF PAYMENT
Authors can pay their fees by: PayPal is the most recommended and secure payment system. It enables you to pay getting your payment receipt immediately and without sharing your financial information. Other methods of payment are:
Bank transfer
BANK NAME: Banca Popolare di Sondrio, Branch #1, Strada Nuova 75, I-27100 Pavia, Italy
ACCOUNT HOLDER: PAGEPress Srl
BIC/SWIFT: POSOIT22
IBAN: IT85Y0569611301000005086X83
Credit Card The credit card form to be filled and returned either via e-mail or via fax is available for download here. http://www.pagepress.org/journals/public/credit_card.pdf
Check sent by surface mail Checks must be made payable to PAGEPress Srl and must be sent to our full postal address: PAGEPress Publications, via A. Cavagna Sangiuliani 5, 27100 Pavia, Italy.
Note: In any method of payment you choose, kindly specify: 1. journal name; 2. paper ID number; 3. first author.
IMPORTANT TO KNOW
REGISTERED DRUGS, DIET SUPPLEMENTS, NUTRACEUTICALS, MEDICAL DEVICES
Authors of papers that contain references to registered drugs, diet supplements, nutraceuticals and medical devices are requested to buy a minimum amount of 100 reprints at a cost of € 1.500 (1 to 4 pages) or € 2.000 (5 to 8 pages). Prices for the purchase of number of reprints greater than 100 can be negotiated with Edizioni Scripta Manent At present, Edizioni Scripta Manent let everyone to read, print and download papers from website, but retains copyright for republishing and distribution rights for commercial purpose.
TRANSLATION
Translation of manuscripts in Italian language is offered on payment.
Translation and reprints can be requested to Edizioni Scripta Manent by e-mail to info@edizioniscriptamanent.eu
AUTHORS’ RESPONSIBILITIES
Manuscripts are accepted with the understanding that they have not been published or submitted for publication in any other journal.
Authors must submit the results of clinical and experimental studies conducted according to the Helsinki Declaration on clinical research and to the Ethical Code on animal research set forth by WHO (WHO Chronicle 1985; 39:51).
The Authors must obtain permission to reproduce figures, tables and text from previously published material. Written permission must be obtained from the original copyright holder (generally the Publisher).
MANUSCRIPT PRESENTATION
Authors must submit their manuscripts (MAC and WINDOWS Microsoft Word are accepted) after registration and login to the link: http://www.aiua.it. Surface or e-mail submission are not accepted.
Manuscripts must be written in English language in accordance with the “Uniform Requirements for Manuscripts submitted to biomedical journals” defined by The International Committee of Medical Journal Editors (http://www.ICMJE.org). Manuscripts
References must be sorted in order of quotation and numbered with arabic digits between parentheses. Only the references quoted in the text can be listed. Unpublished studies cannot be quoted, however articles “in press” can be listed with the proper indication of the journal title, year and possibly volume. References must be listed as follows.
JOURNAL ARTICLES
All Authors if there are six or fewer, otherwise the first three, followed by “et al.”. Complete names for Work Groups or Committees. Complete title in the original language. Title of the journal following Index Medicus rules. Year of publication; Volume number: First page. Example: Starzl T, Iwatsuki S, Shaw BW, et al. Left hepatic trisegmentectomy Surg Gynecol Obstet. 1982; 155:21.
BOOKS
Authors - Complete title in the original language. Edition number (if later than the first). City of publication: Publisher, Year of publication. Example: Bergel DIA. Cardiovascular dynamics. 2nd ed. London: Aca de mic Press Inc., 1974.
BOOK CHAPTERS
Authors of the chapters - Complete chapter title. In: Book Editor, complete Book Title, Edition number. City of publication: Publisher, Publication year: first page of chapter in the book. Example: Sagawa K. The use of central theory and system analysis. In: Bergel DH (Ed), Cardiovascular dynamics. 2nd ed. London: Aca demic Press Inc., 1964; 115.
TABLES
Tables must be numbered in Arabic digits and referred to in the text by progressive numbers. Every table must be accompanied by a brief title. The meaning of any abbreviations must be explained at the bottom of the table itself.
FIGURES
(Graphics, algorithms, photographs, drawings). Figures must be numbered and quoted in the text by number. The meaning of symbols or abbreviations must be indicated. Histology photograph legends must include the enlargement ratio and the staining method. Legends must be collected in one or more separate pages.
• Do not include any illustrations as part of your text file. • Do not prepare any figures in Word as they are not workable. • Line illustrations must be submitted at 600 DPI. • Halftones and color photos should be submitted at a minimum of 300 DPI. • Power Point files cannot be uploaded. • If possible please avoid transmitting electronic files in JPEG format or save the JPEG at the highest quality available • PDF files may be uploaded.
MANUSCRIPT REVIEW
Manuscripts are evaluated by the Editorial Board and/or by two referees designated by the Editors. The Authors are informed in a time as short as possible on whether the paper has been accepted, rejected or if a revision is deemed necessary. The Editors reserve the right to make editorial and literary corrections with the goal of making the article clearer or more concise, without altering its contents. Submission of a manuscript implies acceptation of all above rules.
PROOFS
Authors are responsible for ensuring that all manuscripts are accurately typed before final submission. Galley proofs will be sent to the first Author. Proofs should be returned within seven days from receipt.









































www.salutepertutti.it ancheseguiciqui!! Il podcast d ella rIvIsta ici segu a hg nche q i!! qu www l I t di benesser cezione non è solo assenza di malattia, ma anche per salute La d pod o bene più pr nostr menti quotidiani per mantener ovar su come tr Ogni settimana parliamo di salute, e, sentirsi bene ed occuparsi di cose benesser ezioso. o e il -gi e piccoli accorLe voci di Salutepertutti.it sono utili e belle. Alessia Bisini e Ruben Cazzola.