ORIGINAL PAPERS
1 Luciano Giuliani (1928-1994): Great master and founding father of moder n Italian Urolog y Mariano Martini, Giuseppe Martorana
7 New concept in urologic surger y: The total extended genital sparing radical cystectomy in women
Antonio Cisternino, Lorenzo Capone, Antonio Rosati, Costanzo Latiano, Nicola Sebastio, Antonio Colella, Giuseppe Cretì
14 Effectiveness and safety of spinal anesthesia in patients undergoing open radical retropubic prostatectomy
Salvatore Blanco, Angelica Grasso, Endrit Sulmina, Marco Grasso
18 The use of renal biopsy in the kidney tumor management: A retrospective analysis of consecutive cases in a refer ral center
Andrea Benedetto Galosi, Marco Macchini, Roberto Candelari, Virgilio De Stefano, Silvia Stramucci, Vanessa Cammarata, Omar Al Ayoubi, Andrea Cicconofri, Carlo Giulioni
23 HER2/neu expression status of post BCG recur rent non-muscle-invasive bladder urothelial carcinomas in relation to their primar y ones
Mohamed Yousef Ali, Ahmed Yousef Aboelsaad, Ahmed M Abdel Gawad, Tamer A Abouelgreed, Ahmed A El Gammal, Osama M Ghoneimy, Eman M El-Dydamony, Ahmed A Alrefaey, Eslam Mohamed, Sherif Azzam, Ayman Abdelmohaymen, Yasien Mohammed, Mohammed S Abdelwahed, Ahmed Fawzi A Elsayed, Basem A Fathi, Nosaiba M Abd Alrahim, Abeer S Farag, Alaa R Mahmoud, Hasan Ismail Mohamed, Seth Horsu, Abdulkarim Hasan
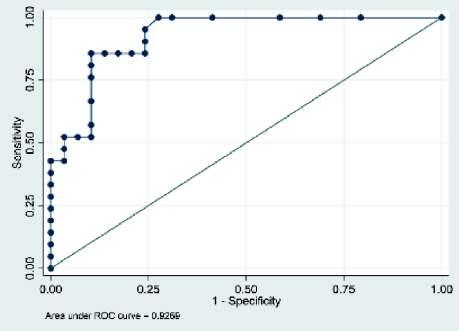
28 The association between ser um hypoxia inducible factor-1α level and urothelial bladder cancer : A preliminar y study
Ginanda Putra Siregar, Ida Parwati, Bambang Sasongko Noegroho, Ferry Safridai, Gerhard Reinaldi Situmorang, Raden Yohana, Astrid Feinisa Khairani
31 68Ga-PSMA PET/CT evaluation in men enrolled in prostate cancer Active Sur veillance
Pietro Pepe, Ludovica Pepe, Marinella Tamburo, Giulia Marletta, Francesco Savoca, Michele Pennisi, Filippo Fraggetta
35 Safety and tolerability of biodegradable balloon spacers in patients undergoing radiotherapy for organ-confined prostate cancer
Luca Topazio, Federico Narcisi, Fabio Tana, Cosimo Ciotta, Iossa Vincenzo, Pasquale Perna, Francesco Chiaramonti, Federico Romantini
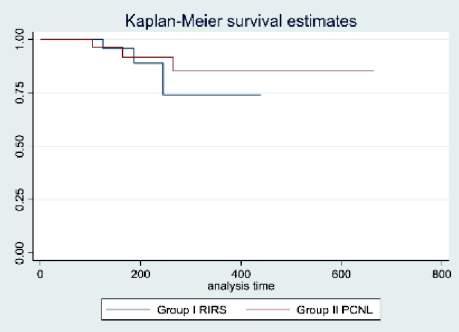
39 Enhanced recover y after retrograde intra-renal surger y (RIRS) in comparison with mini-percutaneous nephrolithotomy (Mini-PCNL) for renal stone treatment
Vladimir Vorobev, Vladimir Beloborodov, Temirlan Hovalyg, Igor Seminskiy, Andrey Sherbatykh, Igor Shaderkin, Mikhail Firsov
47 Comparison of commonly utilized ureteral access sheaths: A prospective randomized trial
Mohamed Elsaqa, Zain Hyder, Kim Thai, Katherine Dowd, Amr El Mekresh, Kristofer Wagner, Belur Patel, Patrick Lowry, Marawan M El Tayeb
51 Variation of inflammator y indexes in patients with chronic abacterial prostatitis treated with an herbal compound/extract

Luca Cindolo, Andrea Fabiani, Daniele Vitelli, Filippo Cianci, Lorenzo Gatti, Nicola Ghidini, Nikolas Niek Ntep, Rosario Calarco Piazza, Alessandra Filosa, Giovanni Ferrari
57 Oncological outcomes of papillar y versus clear cell renal cell carcinoma in pT1 and pT2 stage: Results from a contemporar y Turkish patient cohor t
Taha Cetin, Serdar Celik, Sinan Sozen, Bulent Akdogan, Volkan Izol, Guven Aslan, Evren Suer, Yildirim Bayazit, Nihat Karakoyunlu, Haluk Ozen, Sumer Baltaci, Fatih Gokalp, Ilker Tinay, Members of Turkish Urooncology Association
61 Chronic prostatitis as possible risk factor for Peyronie's disease: Psychological, sexual and prostatitis-like symptoms in patients with PD
Gianni Paulis, Andrea Paulis
69 Treatment outcome of Four nier's gangrene and its associated factors: A retrospective study
Khaled Al-Kohlany, Khaled Baker, Faisal Ahmed, Murtadha Mohamed, Majdi Alshami, Mohamed Badheeb
74 Sexual dysfunctions of rheumatological patients are a neglected issue: Results from a national sur vey of Italian Society of Rheumatolog y Luigi Napolitano, Ilenia Pantano, Lorenzo Romano, Luigi Cirillo, Celeste Manfredi, Francesco Mastrangelo, Giovanni Maria Fusco, Daniele Mauro, Lorenzo Spirito, Roberto La Rocca, Davide Arcaniolo, Corrado Aniello Franzese, Carmine Sciorio, Marco Romano, Marco De Sio, Vincenzo Mirone, Francesco Ciccia
continued on page III
Vol. 95; n. 2, June 2023
ISSN 1124-3562








PRESENTANO Costo di copertina € 180,00 Sconto del 50% Indicando il Codice: AIUA2023 Prezzo finale: € 90,00* L’opera è acquisabile inviando un’e-mail a: atlantediecografia@gmail.com * IVA e Spese di spedizione comprese 124 autori 592 pagine + di 1500 immagini ecografiche 61 video Hardcover Cofanetto ATLANTE di ECOGRAFIA UROLOGICA, ANDROLOGICA e NEFROLOGICA PASQUALE MARTINO
EDITORIAL BOARD
ASSOCIATE EDITORS
EDITOR IN CHIEF
Alberto Trinchieri (Milan, Italy)
Emanuele Montanari, Department of Urology, IRCCS Foundation Ca’ Granda Ospedale Maggiore Policlinico, University of Milan, Italy – Gianpaolo Perletti, Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy; Department of Human Structure and Repair, Ghent University, Ghent, Belgium - Angelo Porreca, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy
EXECUTIVE EDITORIAL BOARD
Alessandro Antonelli, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Antonio Celia, Department of Urology, San Bassiano Hospital, Bassano del Grappa, Italy - Luca Cindolo, Department of Urology, Villa Stuart Hospital, Rome, Italy - Andrea Minervini, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Bernardo Rocco, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Riccardo Schiavina, Department of Urology, University of Bologna, Bologna, Italy
ADVISORY EDITORIAL BOARD
vasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy - Fabrizio Di Maida, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Antonio Galfano, Urology Unit, Niguarda Hospital, Milan, Italy - Michele Marchioni, Department of Medical, Oral and Biotechnological Sciences, "G. d'Annunzio" University of Chieti, Laboratory of Biostatistics, Chieti, Italy - Andrea Mari, Department of Urology, University of Florence, Unit of Oncologic Minimally-Invasive Urology and Andrology, Careggi Hospital, Florence, Italy - Luigi Napolitano, Unit of Urology, Department of Neurosciences, Reproductive Sciences, and Odontostomatology University of Naples “Federico II”, Naples, Italy - Antonio Porcaro, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Stefano Puliatti, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Daniele Romagnoli, Robotic Urology and Mini Invasive Urologic Surgery Unit, Abano Terme Hospital, Abano Terme, Italy - Chiara Sighinolf, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy - Tommaso Silvestri, Urology Clinic, Department of Medical, Surgical and Health Science, University of Trieste, Trieste, Italy - Petros Sountoulides, Aristotle University of Thessaloniki, Department of Urology, Thessaloniki, Greece - Alessandro Tafuri, Department of Urology, Vito Fazzi Hospital, Lecce, Italy
SIEUN EDITOR
Pasquale Martino, Department of Emergency and Organ Transplantation-Urology I, University Aldo Moro, Bari, Italy
SIEUN EDITORIAL BOARD
Giovanni Colpi, Retired Andrologist, Milan, Italy
Pier Francesco Bassi, Urology Unit, A Gemelli Hospital, Catholic University of Rome, Italy – Francesca Boccafoschi, Health Sciences Department, University of Piemonte Orientale in Novara, Italy – Alberto Bossi, Department of Radiotherapy, Gustave Roussy Institute, Villejuif, France –Tommaso Cai, S Chiara Hospital, Trento, Italy –Paolo Caione, Department of Nephrology-Urology, Bambino Gesù Pediatric Hospital, Rome, Italy – Luca Carmignani, Urology Unit, San Donato Hospital, Milan, Italy –Liang Cheng, Department of Urology, Indiana University School of Medicine, Indianapolis, IN; Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, Indianapolis, IN
– Giovanni Corona, Department of Urology, University of Florence, Careggi Hospital, Florence, Italy – Antonella Giannantoni, Department of Surgical and Biomedical Sciences, University of Perugia, Italy – Paolo Gontero, Department of Surgical Sciences, Molinette Hospital, Turin, Italy – Steven Joniau, Organ Systems, Department of Development and Regeneration, KU Leuven, Belgium – Frank Keeley, Bristol Urological Institute, Southmead Hospital, Bristol UK – Laurence Klotz, Division of Urology, Department of Surgery, Sunnybrook Health Sciences Centre, University of Toronto, Toronto, Ontario, Canada – Börje Ljungberg, Urology and Andrology Unit, Department of Surgical and Perioperative Sciences, Umeå University, Umeå, Sweden –Nicola Mondaini, Uro-Andrology Unit, Santa Maria Annunziata Hospital, Florence, Italy – Gordon Muir, Department of Urology, King's College Hospital, London, UK –Giovanni Muto, Urology Unit, Bio-Medical Campus University, Turin, Italy – Anup Patel, Department of Urology, St Mary's Hospital, Imperial Healthcare NHS Trust, London, UK – Glenn Preminger, Division of Urologic Surgery, Duke University Medical Center, Durham, NC, USA – David Ralph, St. Peter's Andrology Centre and Institute of Urology, London, UK – Allen Rodgers, Department of Chemistry, University of Cape Town, Cape Town, South Africa – Francisco Sampaio, Urogenital Research Unit, State University of Rio de Janeiro, Rio de Janeiro, RJ, Brazil – Kemal Sarica, Department of Urology, Kafkas University Medical School, Kars, Turkey – Luigi Schips, Department of Urology, San Pio da Pietrelcina Hospital, Vasto, Italy – Hartwig Schwaibold, Bristol Urological Institute, Southmead Hospital, Bristol, UK – Alchiede Simonato, Department of Urology, University of Verona, Azienda Ospedaliera Universitaria Integrata, Verona, Italy – Carlo Terrone, Department of Urology, IRCCS S Martino University Hospital, Genova, Italy – Anthony Timoney, Bristol Urological Institute, Southmead Hospital, Bristol, UK – Andrea Tubaro, Urology Unit, Sant’Andrea Hospital, “La Sapienza” University, Rome, Italy – Richard Zigeuner, Department of Urology, Medical University of Graz, Graz, Austria
BOARD OF REVIEWERS
Maida Bada, Department of Urology, S Pio da Pietrelcina Hospital, ASL 2 Abruzzo, Vasto, Italy - Lorenzo Bianchi, Department of Urology, University of Bologna, Bologna, Italy - Mariangela Cerruto, Department of Urology, Azienda Ospedaliera Universitaria Integrata (A O U I ), Verona, Italy - Francesco Chessa, Department of Urology, University of Bologna, Bologna, Italy - Daniele D’Agostino, Robotic Urology and Mini In-
Emanuele Belgrano, Department of Urology, Trieste University Hospital, Trieste, ItalyFrancesco Micali, Department of Urology, Tor Vergata University Hospital, Rome, ItalyMassimo Porena, Urology Unit, Perugia Hospital, Perugia, Italy – Francesco Paolo Selvaggi, Department of Urology, University of Bari, Italy – Carlo Trombetta, Urology Clinic, Cattinara Hospital, Trieste, Italy – Giuseppe Vespasiani, Department of Urology, Tor Vergata University Hospital, Rome, Italy – Guido Virgili, Department of Urology, Tor Vergata University Hospital, Rome, Italy
UrOP EDITOR
Carmelo Boccafoschi, Department of Urology, Città di Alessandria Clinic, Alessandria, Italy
UrOP EDITORIAL BOARD
Renzo Colombo, Department of Urology, San Raffaele Hospital, Milan, Italy – Roberto Giulianelli, Department of Urology, New Villa Claudia, Rome, Italy – Massimo Lazzeri, Department of Urology, Humanitas Research Hospital, Rozzano (Milano), Italy – Angelo Porreca, Department of Urology, Polyclinic Abano Terme, Abano Terme (Padova), Italy –Marcello Scarcia, Department of Urology, "Francesco Miulli" Regional General Hospital, Acquaviva delle Fonti (Bari), Italy – Nazareno Suardi, Department of Urology, San Raffaele Turro, Milano, Italy
GUN EDITOR
Arrigo Francesco Giuseppe Cicero, Medical and Surgical Sciences Department, Sant’Orsola-Malpighi University Hospital, Bologna, Italy
GUN EDITORIAL BOARD
Gianmaria Busetto, Department of Urology, Sapienza University of Rome, Italy –Tommaso Cai, Department of Urology, Santa Chiara Regional Hospital, Trento, Italy –Elisabetta Costantini, Andrology and Urogynecological Clinic, Santa Maria Hospital of Terni, University of Perugia, Terni, Italy – Angelo Antonio Izzo, Department of Pharmacy, University of Naples, Italy – Vittorio Magri, ASST Nord Milano, Milano, Italy – Salvatore
Micali, Department of Urology, University of Modena and Reggio Emilia, Modena, Italy –



Gianni Paulis, Andrology Center, Villa Benedetta Clinic, Rome, Italy – Francesco Saverio Robustelli della Cuna, University of Pavia, Italy – Giorgio Ivan Russo, Urology
Department, University of Catania, Italy – Konstantinos
Stamatiou, Urology Department, Tzaneio Hospital, Piraeus, Greece – Annabella Vitalone, Department of Physiology and Pharmacology, Sapienza University of Rome, Rome, Italy
O f f i c i a l J o u r n a l o f S I E U N , U r O P , S S C U a n d G U N
–
NOVITÀ
Un’opera nuova e completa sul microbiota, il complesso consorzio di o malattia. Centinaia di illustrazioni a colori, contenuti multimediali, aggiornati in progress continuo ed accessibili mediante QR code. Un Trattato imprescindibile per chi si occupa di salute interpretando i referti sul microbiota.
Costo di copertina €120,00, IVA e spese di spedizione incluse. Per informazioni ed eventuali ordini, scrivere a: info@edizioniscriptamanent.eu

ORIGINAL PAPERS
78 Single-incision needleless mini-sling technique for female stress urinar y incontinence: A comparative study with standard transobturator inside-out technique
Eman Ali, Salah E Shebl, Sayeda Ibrahim
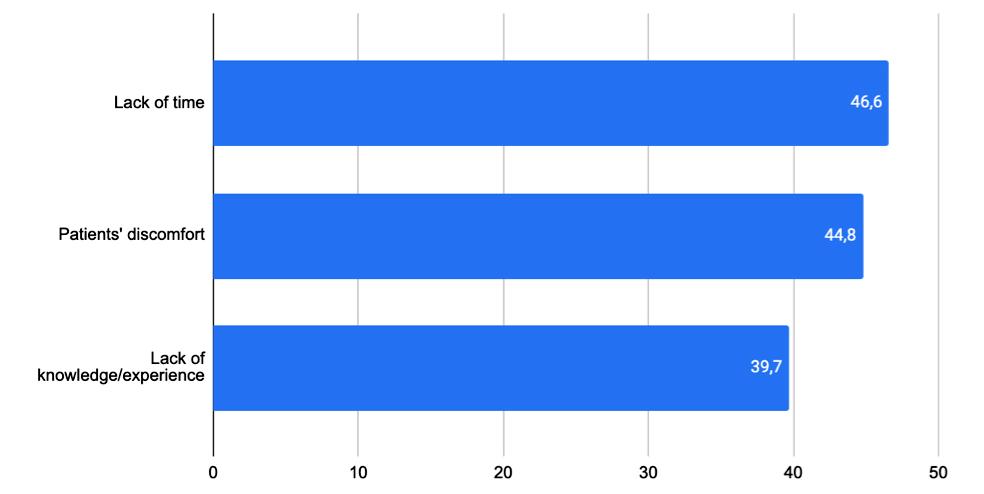
85 Telemedicine and YouTube™: V ideo quality analysis before and after COVID-19 pandemic
Vincenzo Mirone, Marco Abate, Giovanni M Fusco, Luigi Cirillo, Luigi Napolitano, Simone Morra, Francesco Di Bello, Gianluigi Califano, Claudia Mirone, Roberto La Rocca, Massimiliano Creta, Giuseppe Celentano, Marco Capece, Francesco Mangiapia, Nicola Longo, Claudia Collà Ruvolo
91 Analysis of transurethral resection of prostate videos on YouTube™: Educational quality assessment
Yavuz Karaca, Emre Burak Sahinler, Didar Ilke Karaca, Orhun Sinanoglu
95 Histor y of infantile BCG immunization did not predict lamina propria invasion and/or high-grade in patients with non-muscle invasive bladder cancer
Anastasia MacDonald, Vahid Mehrnoush, Asmaa Ismail, Livio Di Matteo, Ahmed Zakaria, Waleed Shabana, Ashraf Shaban, Mohammed Bassuony, Hazem Elmansy, Walid Shahrour, Owen Prowse, Ahmed Kotb
98 Psychological and sexual problems of cancer sur vivors
Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti, Rudi Rudi, Riri Maria
108 Knowledge, attitude and practice towards pelvic floor muscle training among childbearing women
Nur Fairuz Mohd Fauzey, Siti Mariam Muda, Haliza Hasan, Zalina Nusee, Muzaitul Akma Mustapa Kamal Basha
REVIEWS
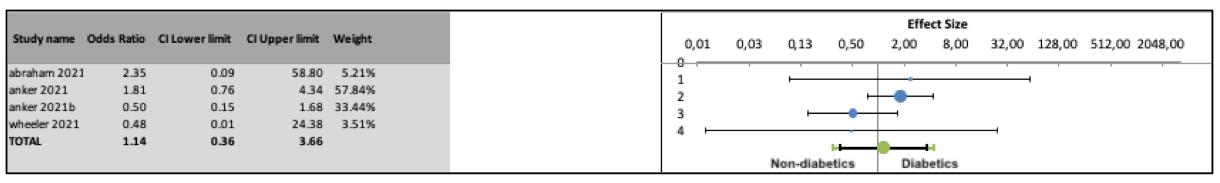
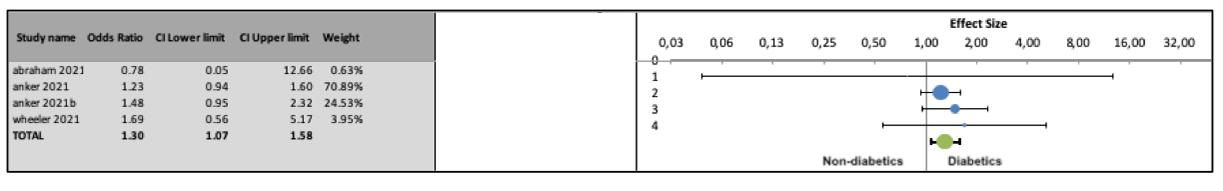
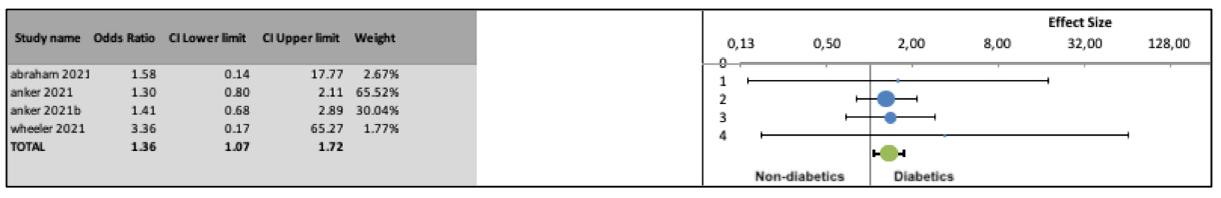
112 Risk of urogenital infections in non-diabetic patients treated with sodium glucose transpor ter 2 (SGLT2) inhibitors. Systematic review and meta-analysis
Rawa Bapir, Kamran Hassan Bhatti, Ahmed Eliwa, Herney Andrés García-Perdomo, Nazim Gherabi, Derek Hennessey, Vittorio Magri, Panagiotis Mourmouris, Adama Ouattara, Gianpaolo Perletti, Joseph Philipraj, Konstantinos Stamatiou, Musliu Adetola Tolani, Lazaros Tzelves, Stefan D Anker, Alberto Trinchieri, Noor Buchholz
120 The presentation and outcomes of penile fracture with associated urethral injur y: A systematic literature review
Salah
E Shebl
LETTERS TO EDITOR
126 Role of spinal anesthesia in robot-assisted radical prostatectomy: Gamble or oppor tunity?
Lorenzo Spirito, Annachiara Marra, Vincenzo Mirone, Celeste Manfredi, Ferdinando Fusco, Luigi Napolitano, Giuseppe Servillo, Nicola Logrieco, Pasquale Buonanno
129 Recreation use of phosphodiesterase type 5 inhibitors, the other side of erectile dysfunction
Giovanni Maria Fusco, Luigi Cirillo, Francesco Mastrangelo, Francesco Romano, Ernesto di Mauro, Gianluigi Cacace, Gianluca Spena, Annamaria Iannicelli, Corrado Aniello Franzese, Vincenzo Mirone, Roberto La Rocca, Luigi Napolitano
Edizioni Scripta Manent s.n.c.
Via Melchiorre Gioia 41/A - 20124 Milano, Italy
Tel +39 0270608060
e-mail: scriman@tin.it
web: www edizioniscriptamanent eu
Registrazione: Tribunale di Milano n 289 del 21/05/2001
Direttore Responsabile: Pietro Cazzola
Direzione Marketing e PR: Donatella Tedeschi
Comunicazione e Media: Ruben Cazzola
Grafica e Impaginazione: Stefania Cacciaglia
Affari Legali: Avv Loredana Talia (MI)
Ai sensi della legge 675/96 è possibile in qualsiasi momento opporsi all’invio della rivista comunicando per iscritto la propria decisione a: Edizioni Scripta Manent s n c - Via Melchiorre Gioia, 41/A - 20124 Milano
The Publisher is not liable for the opinion expressed by the Authors of the articles and for images used by them
GENERAL INFORMATION
AIMS AND SCOPE
“Archivio Italiano di Urologia e Andrologia” publishes papers dealing with the urological, nephrological and andrological sciences
Original articles on both clinical and research fields, reviews, editorials, case reports, abstracts from papers published elsewhere, book rewiews, congress proceedings can be published

III Archivio Italiano di Urologia e Andrologia 2023, 95, 2
Questo Trattato nasce dall’esigenza di offrire evidenze scientifiche della letteratura in diversi àmbiti clinici, riguardo alla Nutraceutica in Pediatria, in un contesto attuale dove è molto forte da parte della società la propensione a ricorrere a “prodotti naturali”.

I temi trattati sono a sostegno di scelte mirate da parte del Pediatra, che possono essere di supporto dal punto di vista preventivo e terapeutico, per la salute di bambini e adolescenti.
25 Capitoli
64 Autori
480 Pagine a cura di Gianvincenzo Zuccotti
Enza D’Auria
Elvira Verduci
Prezzo di copertina € 100,00
Per l’acquisto inviare una e-mail a: info@edizioniscriptamanent.eu
ORIGINAL PAPER
Luciano Giuliani (1928-1994): Great master and founding father of modern Italian Urology
 Mariano Martini 1, 2 , Giuseppe Martorana 3
Mariano Martini 1, 2 , Giuseppe Martorana 3
1 Department of Health Sciences, University of Genoa, Genoa, Italy;
2 UNESCO Chair Anthropology of Health Biosphere and Healing System, University of Genoa, Genoa, Italy;
3 University of Bologna, Bologna, Italy
Summary
Luciano Giuliani was born near Arezzo, in Tuscany (Italy) in 1928 After taking his Degree cum Laude in Medicine and Surgery at the University of Florence in 1951, he became a voluntary assistant at the Institute of General Clinical Surgery and Surgical Therapy. He then took a diploma in Urology and General Surgery, having demonstrated his great technical and surgical ability, and was subsequently appointed assistant in charge and then extraordinary assistant. Endowed with uncommon surgical skills and a forceful personality, Giuliani tirelessly carried out his clinical and surgical activity, covering several roles and rapidly earning profound esteem and recognition in the field of urology As a pupil of the great luminary of Italian surgery, Ulrico Bracci, Dr Giuliani keenly followed his master, embracing his teachings and surgical techniques, until 1969, when he was appointed to run the 2nd Urology Division at San Martino Hospital in Genoa He subsequently took up the chair of Urology at the University of Genoa and became Director of the Specialty School in Urology Within a few years, he earned a solid reputation both nationally and internationally through his innovative surgical techniques He also gave considerable impetus to the Genoese School of Urology, reaching the highest echelons of the Italian and European Societies of Urology At the beginning of the 1990s, he designed and founded a new urology clinic in Genoa; this imposing, avant-garde building was subdivided into four floors and equipped with 80 beds. In July 1994, he won the prestigious “Willy Grégoir Medal”, an accolade awarded to eminent personalities in European urology. In August of the same year, he died in the Institute that he himself had created at San Martino Hospital in Genoa.
KEY WORDS: Luciano Giuliani; History of Medicine; History of Urology; Italian Urology; Genoese Urology School
Submitted 22 March 2023; Accepted 23 March 2023
LUCIANO GIULIANI: THE FIRST STEPS
Dr Luciano Giuliani was bor n in Paindiscò (Arezzo) on 3 July 1928 (Figure 1)
Having matriculated at the Faculty of Medicine of the University of Florence in the academic year 1945-46, he enthusiastically and assiduously devoted himself to his studies In the years 1949-50 and 1950-51, he regularly frequented the departments and the laboratories of the Surgical Clinic as a student inter n
On 25 July 1951, at the University of Florence, he took his
Degree in Medicine and Surgery, having discussed an experimental thesis entitled “Intracardiac pressure variations after interruption of the inferior caval circulation” and ear ning top marks: 110/110 with distinction (1)
- Endowed with great talent, Giuliani was appointed voluntary Assistant at the Institute of General Clinical Surgery and Surgical Therapy of the University of Florence a few months later, on 1 November 1951 He immediately became known for his ability and diligence in carrying out his activities and for his outstanding skills, and his position was confirmed until 1954 In the period between 15 January 1952 and 31 May 1953, he carried out his obligatory military service; having achieved first place in his course (out of 302 candidates) (2) in the final examinations of the 10th Course for Additional Trainee Medical Officers, he was appointed Medical Officer with the rank of Second Lieutenant (3)
Subsequently, Giuliani first served as an Assistant at the Institute of War Traumatology and Surgery of the School of Military Health in Florence from 15 June 1952 to 15 June 1953 One of the first publications of his long career was “L’ibernazione” (“Hibernation”), which was published in the Gior nale di Medicina Militare (Jour nal of Military Medicine) in 1953 (4) In it, he outlined the biological, physiological and clinical bases of the practice of hibernation and offered some considerations regarding the purposes, indications and limitations of its application, particularly in the field of surgery (Figure 2) On 1 November 1954, Giuliani continued his career at the Surgical Clinic of the University of Florence, where he
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 1
DOI: 10 4081/aiua 2023 11329
Figure 1. Prof Luciano Giuliani (1928-1994)
Figure 2
S Ten Med Dott
L. Giuliani. L’ibernazione Extract of Giornale di Medicina Militare (Journal of Military Medicine).

remarkable tenacity and determination, were evident right from the first years of his training Indeed, during his military service, he dealt with military traumatology and surgery from both a theoretical and practical standpoint, without ever interrupting his university activities Moreover, for several years, and consistently until 1956, he served as an assistant surgeon at the Ospedale Civile di Empoli during the summer closure of the University clinics, which enabled him to “stay on form” and to hone his surgical skills even during the summer period!
In the early period of his career, Giuliani actively devoted himself to the various branches of surgery, acquiring extensive knowledge of thoracic, urological, orthopaedic, gynaecological and obstetric surgery, in addition to general surgery Moreover, in 1956, when still academically very young (28 years old), he was given responsibility for the practical training in Clinical Urology of sixth-year students at the University of Florence, where he subsequently taught the following subjects at the Specialty School in Urology:
- functional diagnostics in urology (1st year);
- functional pathology of the excretory pathway
was appointed “Extraordinary Assistant” , a position that he held until 1 November 1956, when he moved to the newly-founded Urology Clinic
During this period, Giuliani also took a Specialty Diploma in Urology at the University of Pisa (18 July 1955), achieving a mark of 70/70 (5)
Following the establishment of the new Urology Clinic of the University of Florence in 1956, Giuliani was immediately appointed Extraordinary Assistant The following year (1957), he further consolidated his training by taking a Specialty Diploma in General Surgery, achieving the top mark of 70 with distinction
The year 1957 was a particularly important one for Dr Giuliani; in addition to ear ning the above-mentioned Specialty Diploma in General Surgery (29 July) with distinction, he was appointed for the academic year 1957/58 as Designated Assistant to the Chair of the Urology Clinic (6), a position that was confirmed for the years 1958/59, 1959/60 and 1960/61
These were fundamental years and constituted the foundations on which he would later build his long and fruitful academic pathway in the field of urology
LUCIANO GIULIANI: A VERSATILE SURGEON AND A YOUNG ACADEMIC
On 18 April 1958, following a public competition, Giuliani qualified for the position of Ordinary Assistant to the Chair of Urology of the University of Florence The following month, however, he interrupted this tenure in order to be reconfirmed Extraordinary Assistant His title of Extraordinary Assistant was also confirmed for the academic year 1958-59
Dr Giuliani carried out his clinical and surgical activities in a continuous manner: first during his service at the Surgical Clinic in Florence as an assistant in the various departments of general and thoracic surgery and then in the urology department Subsequently, he held the position of Head of Department with the function of “Vicechief” at the Urology Clinic Giuliani's temperament and versatility, coupled with his
During those years, Giuliani wrote several scientific articles Notable for its originality, methodological rigour and scientific impact, was “On the extra-hepatic biliary pathways” , published in 1954 in the jour nal “La Chirurgia Generale” (7) (Figure 3)
Figure 3. “On the extrahepatic biliary pathways” (1954)“La Chirurgia Generale” (General Surgery) in Rivista di Biologia
In it, the young author made innovative anatomical, physiological and pathophysiological observations (8) However, the young Giuliani was still fascinated by the urological activity carried out in the dedicated department and coordinated by Prof Bracci, Prof Fedeli's assistant; he therefore began to participate more closely in this work
For his part, Prof Bracci, with the encouragement and approval of his mentor Prof Fedeli, had long been oriented towards the entire field of urology, working first in the surgical clinic in Perugia and then, after 1947, in Florence
Indeed, after first qualifying to teach Surgical Pathology and Surgical Anatomy, he became a freelance teacher of Urology in 1942 Moreover, while still a young assistant, and a few years after following Prof Fedeli to Florence, he wrote a book

Archivio Italiano di Urologia e Andrologia 2023; 95, 2 M Martini, G Martorana 2
on urological semiotics (1950) and introduced an innovative method regarding “access pathways in the surgery of the urinary apparatus” (which would be published in 1956)
In 1955 (the year in which Giuliani took his specialty diploma in Urology), Prof Bracci was chosen as one of the three winners (together with Prof Pavone in Palermo, and Prof Pisani in Milan) of the first national competitive examination for the post of Ordinary Prof of Urology
The following year, he was appointed Director of the Institute of Clinical Urology of the University of Florence, the first university chair of urology in Italy, and in 1957 the specialty school in Urology was instituted Thus began a new era for Florentine urology in particular, and also for Italian urology in general
Bracci brought to urology all his knowledge of general surgery, developing themes which

albeit previously described and implemented
had, for various reasons, never been widely adopted, e g the use of the intestine in urology Hitherto, the standard procedure had been ureterosigmoidostomy (USS); urinary infection was the most frequent cause of severe complications sometimes more “malignant” than neoplastic disease progression
This aspect soon became the principal theme to investigate (as is well described in Bracci's report, published in 1959 in Chirurgia Urologica) (Figure 4)
teachings of their mentor In those years, the Urology Clinic of the University of Florence was made up of:
– ordinar y assistants with "vice-chief" responsibilities: Alfiero Costantini, Luciano Giuliani, Mario Polito, Mario Tacciuoli;
– o rd i n a r y a s s i s t a n t s a n d v o l u n t e e r s : Tu l l i o L o t t i , Francesco Micali, Nicola Cer ulli, Michelangelo Rizzo, Alessandro Basso, et al ;
physicians from different specialties who collaborated with the Chair of Urology: Elia Vernaglione, Anna Martini (anaesthetists) Gianfranco Bruscagli (cardiologist) Bruno Fedi (pathologist) Imola Rossi (chemist) Giancarlo Masini (radiologist)
Among these, was Luciano Giuliani, who (as we have already mentioned above) became “extraordinary university assistant” at the newly founded Urology Clinic on 1st November 1957 (9)
Giuliani soon became one of Bracci's closest collaborators:
– from the surgical point of view: he was one of Bracci's favourite assistants in the operating theatre;
– from the teaching point of view: he was entrusted with the practical training in Clinical Urology of sixth year students at the University of Florence;
from the scientific point of view: he immediately manifested his propensity for research; specifically, he supported his mentor and conducted important studies in experimental surgery and urodynamics of the urinary derivations (10, 11)
As the author of numerous publications of a clinical, radiological, pathological, surgical and experimental nature, generally in the field of urology, Dr Giuliani was awarded the prestigious “prize for scientific diligence” for the academic years 1956/57 and 1958/59 at the University of Florence Moreover, at the 32nd Congress of the Italian Society of Urology in September 1959, he received the “Premio Itala IV°” for the best urology publication of the year for his paper entitled: “Gastrocystoplasty: from the experimental idea to some practical considerations concerning plastic and replacement surgery of the bladder” (10)
From 1959 onwards, Dr Giuliani also worked systematically in the departments of general and thoracic surgery directed by his mentor Ulrico Bracci at the Sanatorium of the Anti-tuberculosis Consortium in Florence, were he was able to increase his surgical skills and his clinical experience (12)
T h e m a i n o b j e c t i v e w a s t o a b a n d o n t h e p re v i o u s approach, which involved the mixing of faeces and urine, and to create a reservoir that displayed the following characteristics:
sufficient capacity to allow almost normal frequency of urination;
– in the filling phase, the patient could feel the stimulus and would be prompted to urinate;
– complete emptying and explorability;
– no negative impact on the upper urinary apparatus
As the rectal neo-bladder met these requirements, it was adopted, in its variants, for years
Bracci proved to be a great innovator and succeeded in promoting his discipline, bringing together a group of young physicians, who enthusiastically embraced the
Prof Ulrico Bracci was one of the great luminaries of 20th century Italian surgery and the founder of the first true Italian school of urology at the end of the 1950s in Florence and subsequently in Rome Prof Bracci played a fundamental role as an innovator and promoter of specialisation in urology, becoming a dominus and a point of reference for Italian urologists for over 30 years
After again winning the “prize for scientific diligence” (1959/60), in 1960 Giuliani deservedly obtained his qualification as untenured lecturer in Urology (Special Surgical Pathology and Clinical Propedeutics), achieving first place among the candidates
In the same year, he actively collaborated in the Italian Society of Urology's official report (Brescia-Bergamo) on “Surgery for renal hypertension” (Figure 5)
A year later, 1961, he took part in the report of the annual Congress on the “Surgical treatment of prostate cancer”
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 3
Luciano Giuliani (1928-1994), pioneer of history of Urology
–
–
–
–
–
Figure 4. Bracci U Chirurgia Urologica (Urologic Surgery), 1959
Figure 5.
Atti della Società italiana di UrologiaUrology's official report (Oberholtzer A, a cura di), XXXIII Congresso, Bergamo-Brescia, 13-16 Ottobre, 1960


the intestine in urology (13); – radical prostatectomy (14);
– pathways of access in the surgery of the urinary apparatus
All this involved demanding and innovative research work, all of which was designed and implemented during this fruitful Florentine period Subsequently, it was developed during Giuliani's Roman period Indeed, in 1963, Prof Bracci was called to Rome to take up the first official chair of urology in the history of the capital
This marked the beginning of the so-called “Roman School of Urology” , a development that had considerable impact on the history of Italian urology
The Urology Clinic in Florence was left under the direction of Alfiero Costantini, while Bracci was followed by his pupils Giuliani and Tacciuoli, who supported their master in his teaching Subsequently, Lotti, Micali and Polito also moved to Rome, followed later by Cerulli and Calderini
and just the surgery of prostate cancer is another example of Prof Bracci's boost to “ more complex” urological surgery
This had previously been rarely undertaken, as the subtle course of the disease meant that the tumour was almost always discovered when it was no longer operable This was the first time in Italy that the issue of radical prostatectomy had been presented in such an organic, complete and didactic manner Thus, its anatomo-surgical foundations were laid (Figure 6)
Bracci U, Giuliani L, Costantini A, Tacciuoli M. The Surgical Treatment of Prostate Cancer 1961 Vallecchi ed Officine Grafiche. Firenze
The years spent in Rome enabled the young Giuliani to grow and to acquire vast experience in the various areas of urology
Of the several scientific works produced during that fecund Roman period, we may cite the important contribution entitled “The functional recovery of excluded kidneys” (Figure 7) presented at the 40th Congress of the Italian Society of Urologia held in Bologna in October 1967 (15)
Bracci U, Giuliani L, Polito M La ripresa funzionale dei reni esclusi (The functional recovery of excluded kidneys) (1967) Ente Fiuggi, Cappelli Editore, Bologna.

Giuliani, together with his mentor, played a central role in both the anatomo-surgical study and the writing of the text, with the collaboration of Prof Costantini and Prof Tacciuoli
These were fundamental years for Giuliani and constituted the foundations on which he would later build his long and fruitful academic pathway in the field of urology
These were precisely crucial years for Giuliani, as is demonstrated by his “prizes for scientific diligence” They were also very productive years for Prof Bracci's whole team, of which Giuliani was a member, both from the clinical and scientific standpoints and from that of the promotion of the discipline of urology Indeed, it was in those years that Italian urology laid down the foundations for the use of:
THE GREAT LEAP FORWARD: GIULIANI IN GENOA
The experience gained by Giuliani during the fruitful years in which he worked alongside his mentor Prof Bracci in Rome, summed to his tireless activity during the previous Florentine period, enabled him to reach such a level of maturity as to warrant his autonomous direction of a clinic The opportunity soon materialised – at one of Europe's largest hospitals of the day: San Martino Hospital in Genoa
Indeed, in 1969, the Department of Urology of San Martino Hospital was divided into two large branches:
- 1st Urology Division, headed by Prof Germinale, already tenured at San Martino Hospital;
- 2nd Urology Division, directed by Prof Giuliani
This was Giuliani's first fully autonomous position in
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 M Martini, G Martorana 4
–
Figure 6.
Figure 7.
which he had sole responsibility for direction At that time, he was working at the Urology Clinic in Rome as “University Vice-chief” to Prof Ulrico Bracci, and had already emerged as a “ternate winner” in a competition for professors
- A couple of years after being given responsibility for the Urology Division at San Martino, in March 1971, Giuliani was unanimously declared Extraordinary Professor of Urology at the Faculty of Medicine and Surgery of the University of Genoa; thus, he became the first tenured professor of the Chair of Urology in Genoa and in Liguria
The 2nd Urology Division was thus renamed “Urology Clinic” and, over the years, Genoa became the capital of Italian urology

A short time later, in 1972, the Specialty School in Urology was also instituted at the University of Genoa, and was immediately entrusted to the direction of Prof Giuliani
Prof Giuliani was endowed with great intelligence and competence and possessed extraordinary surgical skills that enabled him to develop innovative, ground-breaking techniques Naturally enough, he rapidly emerged on the national and inter national scientific scene, distinguishing himself through his forceful personality and great authoritativeness Thus, he imparted an enormous thrust to the Genoese urology school, which soon became a point of reference for the scientific sector nationwide
In 1973, Giuliani was appointed President of the 46th National Congress of the Italian Society of Urology, which was held in Genoa A few years later (1978) he was elected President of the Italian Society of Urology (SIU), a post he held until 1982, when he was elected to the Executive Committee of the European Society of Urology (ESU)
The year 1986 was an important one not only for the Genoese School of Urology, the city of Genoa and the Liguria region, but also for the whole of Italian urology Indeed, it was in that year that Giuliani succeeded in founding and inaugurating the Centre for Calculosis of the Genoese Urology Clinic He equipped this facility with an extracorporeal lithotriptor (a very moder n apparatus that shattered calculi by means of an extracorporeal approach); a truly extraordinary event, since this was the first public facility in Italy to be so equipped!
Moreover, the “Genoese school” , directed by Prof Giuliani and featuring a team made up of Belgrano, Carmignani, Giberti, Martorana, Puppo et al , also distinguished itself through the production of a sort of “graphic-editorial exercise” in urological surger y, which was designed to aid and improve teaching activities
Indeed, 1986 saw the publication of a complete “Atlas of surgery of kidney cancer ” , probably the first such atlas in the history of Italian publishing; it was subsequently translated into English and distributed inter nationally

The Atlas provided an analytical and highly detailed presentation – in a rational, schematic and realistic form (as far as this was possible in an atlas of surgical techniques) – of the times and sequences most characteristic of the principal operations involved in the surgical treatment of kidney cancer (Figure 8)
And a couple of years earlier, on the occasion of the National Congress of Urology, held in Bari in 1984, a scientific text was published for the Proceedings of the Italian Society of Urology (SIU) under the title: “Pathways of access in urology” , a volume featuring ample drawings (16-19)
In 1988, with the retirement of Prof Germinale, and after a brief interim period of direction by another Ligurian colleague, the Urology Division was merged with the Urology Clinic and Giuliani became responsible for the single facility, which was very extensive and equipped with numerous beds (20)
This newly instituted single facility was a truly evocative retur n to the past, in that it brought urology back to the original structure directed by the great master Giorgio Nicolich Jr, which extended for almost 30 years, from 1938 to 1966 (21)
In April 1992, Giuliani succeeded in an enterprise that was, at that time, truly extraordinary and titanic: the inauguration of the new Genoese Urology Clinic (Figure 9)!
The entire operation was personally drawn up and directly supervised by Giuliani himself, with considerable financial support from the Genoese banking institution Ca Ri Ge Thus, Prof Giuliani achieved his objective of constructing an imposing, modern, complete facility consisting of: - a 4-storey building equipped with 80 beds;
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 5
Luciano Giuliani (1928-1994), pioneer of history of Urology
Figure 8 Giuliani L La Chirurgia del Carcinoma Renale (The surgery of kidney cancer) Atlas Urology Clinic of the University of Genoa (1990), Mazzucchelli ed
Figure 9.
The new Genoese Urology Clinic, inaugurated in 1992.
- a semi-intensive post-operative therapy department;
- a surgical block devoted exclusively to urology;
- a centre for calculosis;
- a centre for urodynamics;
- an outpatient clinic;
- a teaching centre
CONCLUSIONS
During the Congress of the European Society of Urology in Berlin in July 1994, Prof Giuliani was awarded the highly prestigious Willy Grégoir Medal, an accolade conferred upon eminent personalities in European urology
A month later, on 18 August 1994, following a brief illness, Giuliani died in the very Institute that he himself had created in Genoa; he was 66 years old
In December of the same year, the Institute was named in his honour, thus becoming the “Luciano Giuliani Institute of Clinical Urology”
Luciano Giuliani was a distinguished scientist and one of the most renowned scholars of urology in the inter national scientific firmament Nicknamed “Grand Master” , Giuliani struck very deep roots and ploughed a furrow that ran uninterruptedly through the generations of his pupils, who were truly numerous and of high quality When faced with a clinical problem, every urologist should remember that things are what they are today because in the past there have been people like the Maestro Giuliani and clinical experiences that have, thanks also to advances in technology, pharmacology and biomaterials, allowed constant evolution, thereby enabling us to achieve ever-better results (da prefazione di Marco Carini) (13)
ACKNOWLEDGEMENTS
- Thanks to Prof Carlo Terrone (University of Genoa) for the photo number 9 and for reading the text
- Thanks to Gianmaria Martini (independent scholar) for the help in bibliographic data
REFERENCES
1 Private Archive “Luciano Giuliani”
2 Circular N° 360 of G M 1951 Military School of Health, Florence
3 Military School of Health, Florence D M N° 2598/C of prot Doc of 13 October 1953, Prof Col G Piazza (Giuliani Private Archive)
4 Giuliani L L’ ibernazione G Med Milit 1953; 103:335-344
5 University of Pisa Certificate N° 3211, Matriculation N° 7/259
6 Rector's Decree N° 2544 of 18 November, 1957 (Official Bulletin of the Ministry of Education, Part II, N° 36 of 4 September, 1958, p 5048
7 Giuliani L Sulle vie biliari extraepatiche (nota anatomica) La Chirurgia Generale 1954; 3:189-207
8 Fedeli F University of Florence Institute of General Clinical Surgery and Surgical Therapy Florence, 6 June 1959
9 Rector's Decree N° 2544 of 18 November, 1957 (Official Bulletin of the Ministry of Education, Part II, N° 36 of 4 September, 1958, p 5048
10 Giuliani L La gastrocistoplastica: dall'idea sperimentale ad alcune considerazioni pratiche in tema di chirurgia plastica e sostitutiva della vescica Urologia 1958; 25 (suppl 7)
11 Giuliani L, Pisani E L'intestino nella chirurgia plastica e sostitutiva della vescica: valutazione cistografica e cistomanometrica dei risultati Arch It Urol 1959; 32:164
12 Luciano Giuliani Private Archive
13 Martorana G L’uso dell’intestino in urologia (The use of the intestine in urology) Bononia University Press Bologna, 2021
14 Bracci U, Giuliani L, Costantini A, Tacciuoli M The Surgical Treatment of Prostate Cancer Vallecchi ed Officine Grafiche Firenze, 1961
15 Bracci U, Giuliani L, Polito M La ripresa funzionale dei reni esclusi (The functional recovery of excluded kidneys) Relazione ufficiale al congresso della Società Italiana di Urologia, Capelli ed Bologna, 1967
16 Bracci U Le vie d’accesso nella chirurgia dell’apparato urinario Le vie d’accesso al rene Macrì, Firenze, 1956
17 Giuliani L, Carmignani G, Belgrano E, Martorana G Le vie d’accesso in chirurgia urologica Relazione ufficiale LVI Congresso, SILI, Bari, 3-6 ottobre 1984
18 Giuliani L, Giberti C, Martorana G Atlas of surgery for renal cancer 2nd ed Zambeletti S p A , Milano, 1989
19 Giuliani L, Giberti C, Martorana G, Rovida S Radical extensive surgery for renal cell carcinoma: long-term results and prognostic factors J Urol 1990; 143:468 5
20 Malinaric R, Mantica G, Martini M, et al The Lifetime History of the First Italian Public Extra-Corporeal Shock Wave Lithotripsy (ESWL) Lithotripter as a Mirror of the Evolution of Endourology over the Last Decade Int J Environ Res Public Health 2023; 20:4127
21 Carmignani G, Traverso P (Durand F) Brief history of Ligurian urology Tipografia Araldica Genova, 1997
Correspondence
Mariano Martini, MD, PhD (Corresponding Author)
mariano martini@unige it
mariano yy@gmail
Department of Health Sciences, University of Genoa
Largo R Benzi 10, 16132 Genoa, Italy
Giuseppe Martorana, MD
University of Bologna, Bologna, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 M Martini, G Martorana 6
New concept in urologic surgery: The total extended genital sparing radical cystectomy in women
Department of Urology, Fondazione IRCCS Casa Sollievo della Sofferenza, San Giovanni Rotondo, Italy
Summary
Introduction and objectives: The aim of the study was to evaluate genital sparing radical cystectomy surgery in female patients from the point of view of both oncologic and functional outcomes (with emphasis on urinary and sexual outcomes) in a single high-volume center for the treatment of muscular invasive bladder cancer
Materials and methods: Between January 2014 and January 2018, 14 female patients underwent radical cystectomy with preservation of genital organs (the entire vagina, uterus, fallopian tubes, ovaries) and orthotopic urinary neobladder (Padua neobladder) Inclusion criteria were recurrent T1G3 tumors; refractory tumors after BCG therapy without associated carcinoma in situ (CIS); T2 or T3a tumors entirely resected at endoscopic transurethral resection of the bladder and not involving urethra/bladder trigone Exclusion criteria were: T3b or higher bladder cancer, associated CIS and involvement of urethra or bladder trigone Oncological and histopathological outcomes
(Overall Survival - OS, Recurrence Free Survival - RFS), urinary outcomes (day and night incontinence, intermittent catheterization use, Sandvik Score) and sexual outcomes (Female Sexual Function Index 19 FSFI-19) were considered
The average follow-up time was 56 months.
Results: Considering oncological outcomes, histologic examination reported urothelial carcinoma in 13/14 patients; 8/13 patients (61 5%) had high grade T1 stage, 3/13 patients (23%) had high grade T2 stage and finally 2/13 patients (15.5%) had high-grade T3 stage One patient presented with embryonal rhabdomyosarcoma completely excised after surgery (PT2aN0M0) No patient developed local or metastatic recurrence (RFS 100%); OS was 100%. Considering urinary continence outcomes, 12/14 patients retained daytime and nighttime continence (85.5%); 2/14 (14.5%) complained of low stress urinary incontinence daily and nighttime urinary leakage
The Sandvik Score showed complete continence in 7/14 patients (50%); mild degree incontinence in 6/14 patients without use of incontinence devices (43%); moderate degree of incontinence in one patient (7%) The FSFI administered at 1 year from the surgery showed sexual desire in all patients (100%); subjective arousal, achievement of orgasm and sexual satisfaction in 12/14 patients (85 5%); sufficient lubrication in 11/14 patients (78 5%) Only one patient (7%) complained about dyspareunia during sexual intercourse
Conclusions: Our study aims to demonstrate that genital-sparing radical cystectomy is a safe surgery in terms of oncologic outcomes and, most importantly, that it is beneficial in terms of urinary and sexual function Indeed, patients’ quality of life together with their psychological and emotional health should be put on the same level as oncological safety However, it is a
treatment reserved for selected patients who are strongly motivated to preserve fertility and sexual function and thoroughly informed about the benefits and complications of such a procedure
KEY WORDS: Muscle-invasive bladder cancer; High risk non-muscle invasive bladder cancer; Total extended genital sparing; Oncologic outcomes; Sexual life; Post-operative continence; Quality of life
Submitted 4 December 2022; Accepted 20 December 2022
INTRODUCTION
Bladder cancer is the 13th most common cancer worldwide when both sexes are considered If only the male population is taken into account, the incidence rises to sixth place with a mortality rate of 3 3 per 100 000 population (1) However, cancer incidence is about four times lower in women than in men (2) Nevertheless, female gender is an independent risk factor for the disease, which is associated with a higher stage at diagnosis (3) Radical cystectomy with urinary diversion and possibly neoadjuvant chemotherapy is the treatment of choice for patients with muscle-invasive bladder cancer or high-risk non-muscleinvasive bladder cancer In men, this involves removal of the bladder, prostate, seminal vesicles and loco-regional lymph nodes In women, it is a true anterior pelvic exenteration with removal of the bladder, urethra, uterus, ovaries, adnexa, anterior wall of the vagina and locoregional lymph nodes (4) This surgery has a detrimental effect on both the quality of life and the psychology of the patient, and many high-volume centers have considered it being less disruptive for female patients, especially in the pre-menopausal phase (5) Initially, cystectomy with urethral sparing and urinary diversion was performed, but nowadays selected patients undergo cystectomy with genital sparing, which can preserve fertility and a sexually active life (6) In this article we describe our genital organ preservation technique and examine the oncological and functional results at 56 months of follow-up
MATERIALS AND METHODS
Between January 2014 and January 2018, 14 female patients were admitted to the Urology Department of the IRCCS Casa Sollievo della Sofferenza Foundation in San Giovanni Rotondo All patients underwent radical cystecto-
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 7
ORIGINAL PAPER
Antonio Cisternino, Lorenzo Capone, Antonio Rosati, Costanzo Latiano, Nicola Sebastio, Antonio Colella, Giuseppe Cretì
DOI: 10 4081/aiua 2023 11058
my and bilateral pelvic lymphadenectomy with preservation of genitalia (vagina, uterus, fallopian tubes and ovaries) and orthotopic urinary diversion Prior to surgery, they were carefully counseled about the procedure, possible long-term and short-term complications, and finally signed an informed consent

In accordance with the most recent guidelines, we placed as inclusion criteria for surgery: recurrent high-grade T1 tumors, tumors relapsed after BCG therapy without the presence of concomitant Carcinoma in situ (CIS), T2 and T3a tumors completely excised at endoscopic transurethral resection of the bladder (TURB) and not involving the urethra or bladder trigone All patients were sexually active and were younger than 65 years of age Before surgery, each patient was evaluated by accurate clinical history (with special attention to urinary and sexual function), physical examination, complete abdominal ultrasound, cystoscopy, and bladder biopsy in order to exclude CIS or concomitant dysplasia; they also had gynecological examination to exclude tumors or papilloma of the cervix, uterus, or ovaries Finally, all patients were staged by abdominal and pelvic CT with contrast and sequential bone scintigraphy to exclude extension to the peri-vesical fat (T3b), lymph nodes, and/or adjacent organs (T4) Exclusion criteria were bladder cancer T3b or higher, concomitant CIS, and urethral and/or trigone involvement All patients had bowel preparation and antibiotic prophylaxis the day before surgery
Surgical open technique
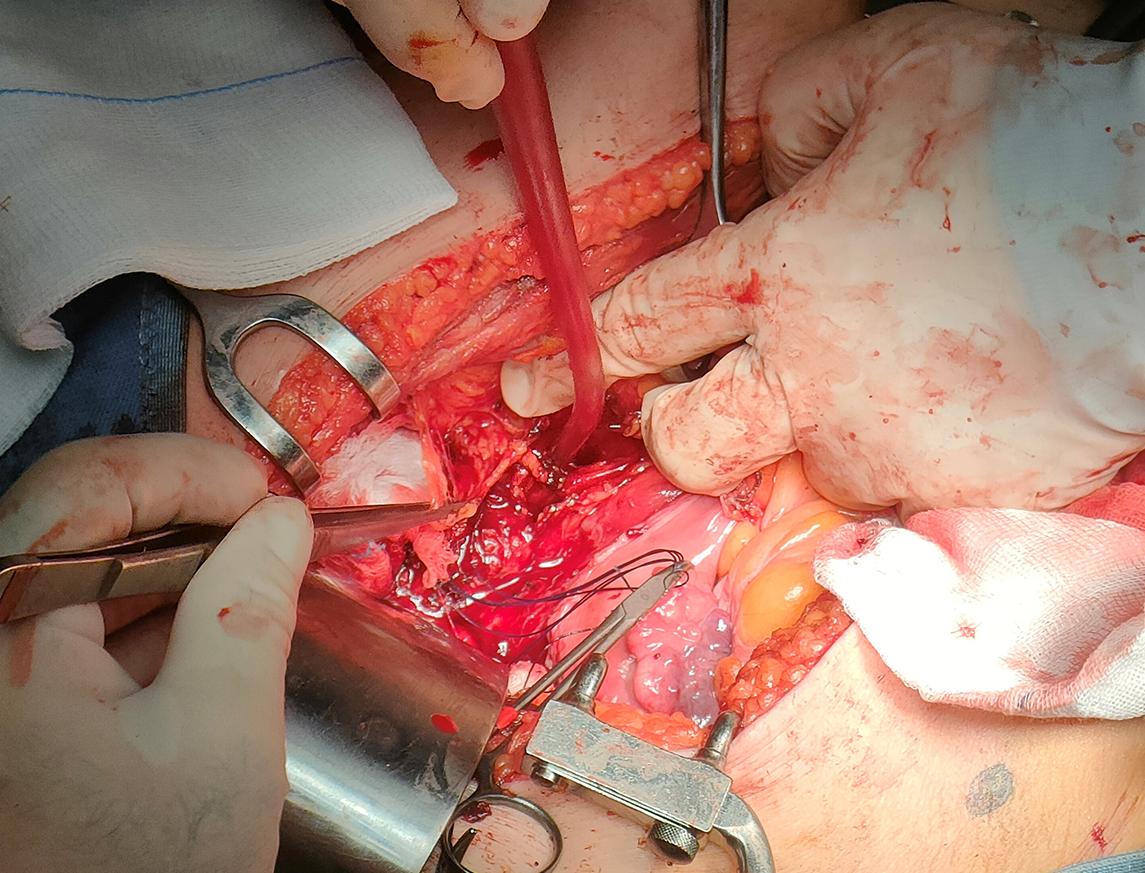
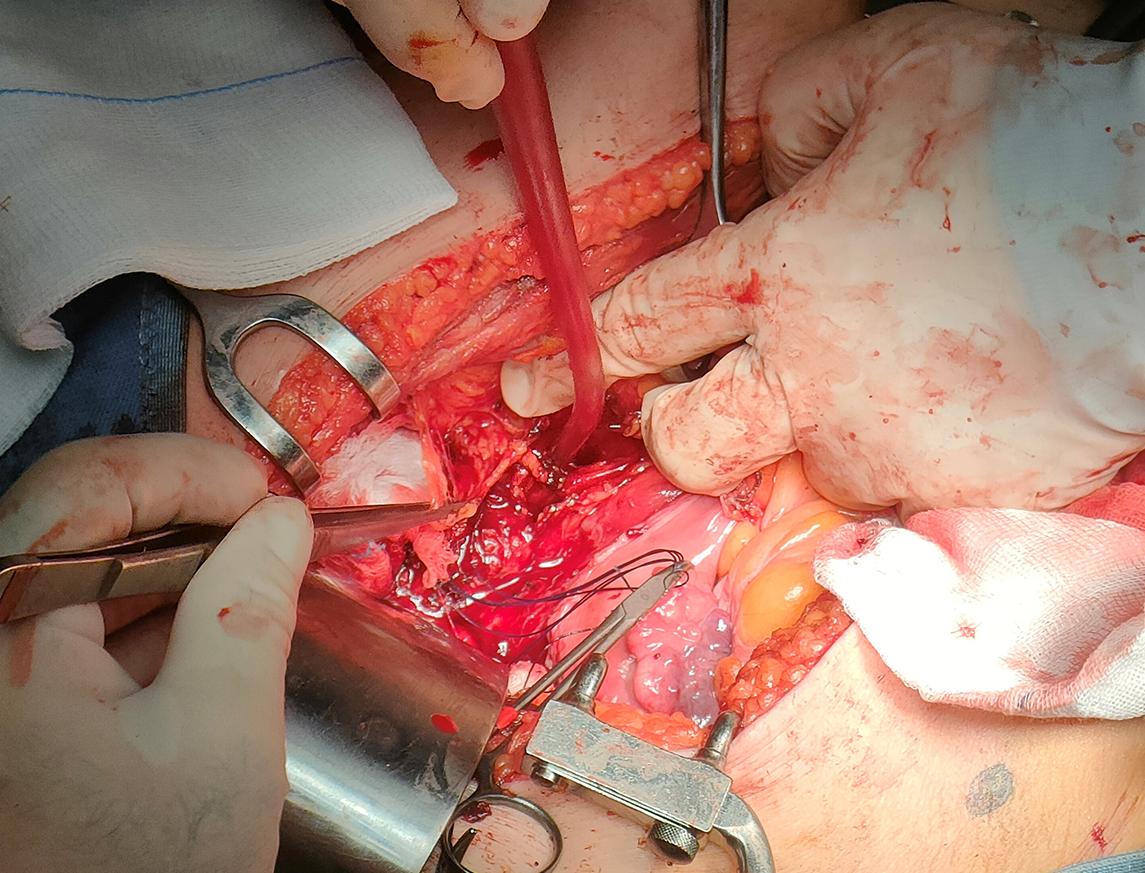
Patients were placed in the Trendelenburg supine position with pelvic hyperextension An incision was made on the midline from the pubis to the umbilicus, after dividing the muscular-aponeurotic planes, the peritoneal sac was opened Lysis of any bowel-omental adhesions was performed, and the bowel was cranially dislocated to expose the pelvis The bladder was then mobilized to the lateral walls of the pelvis The residual urachus was circumscribed – paying attention not to injure the lower epigastric vessels –, to be removed with the entire bladder A careful and systematic examination was carried out to determine the extent of the disease and the possible presence of metastases or massive retroperitoneal lymphadenopathy At this point the bowel was mobilized from the ascending colon, which was moved medially to gain access to the right ureter The mesentery was reversed until the retroperitoneal part of the duodenum was exposed The left colon and sigmoid were then mobilized to the inferior pole of the left kidney to give access to the left ureter The ureters were then isolated at their entrance to the bladder, were they were ligated and dissected To exclude neoplastic involvement, the distal margin was sent for extemporaneous histopathology The umbilical, uterine, superior, and inferior bladder arteries were carefully dissected bilaterally The bladder was mobilized and the junction between the cervix and the anterior wall of the vagina was identified along the anterior wall of the uterus The vaginal wall was then dissected at the level of the anteroventral plane of the vagina, at 2 o'clock and 10 o'clock, as close as possible to the bladder wall, in order to preserve the paravaginal tissues con-
taining the autonomic nerves that reach the proximal sphincter The superior and inferior bladder arteries were dissected at their origin, at the level of the hypogastric arteries, while the uterine arteries and vaginal branches to the paravaginal tissues were spared Once the retropubic space was created and opened, the endopelvic fascia was incised very close to the bladder neck to reduce the risk of inadvertent injury to the paraurethral neurovascular structures, which are crucial for sexual function and continence (Figures 1, 2) The urethra was carefully prepared, exposed and divided, and a specimen was sent for extemporaneous histopathological examination (Figure 3) At this time, careful dissection of the retroperitoneal lymph nodes was performed The margins of the resection were cranially defined by the common iliac artery,
Archivio Italiano di Urologia e
2
8
Andrologia 2023; 95,
A
Cisternino, L Capone, A Rosati, C Latiano, N Sebastio, A Colella, G Cretì
Figure 1.
Development of the plane between uterus and bladder
Figure 2.
Genital sparing cystectomy with sparing of the uterus, ovaries, tubes and vagina
laterally by the genito-femoral nerves, inferiorly by the Cooper's ligament, caudally by the obturator canal, medially and laterally by the hypogastric vessels
Mini-invasive technique
Out of the 14 patients who underwent radical cystectomy with genital sparing, 3 underwent removal of the bladder using the robot-assisted laparoscopic technique with the Da Vinci robot (Ab Medica) During the procedure, patients were placed in the supine position with abducted lower limbs A catheter was placed This was followed by a supraumbilical skin incision to access to the abdomen using the Hasson open technique, opening of the peritoneum under direct vision, positioning of the first optical trocar and induction of pneumoperitoneum at 12 mmHg Patients were placed in Trendelenburg position (> 25°), and the peritoneal cavity and viscera were inspected to exclude adhesions or metastatic pathology
Two additional 8 mm robotic surgical ports were placed approximately 8 cm from the optical trocar, 2 cm lateral to the rectus abdominis muscle, at the level of the inferior border of the umbilicus Two further laparoscopic ports were introduced, one 12 mm, 5 cm above the anterior superior iliac spine, on the right mid-axillary line for the surgical tractions; another 5 mm, approximately 2 5 cm above the right robotic ports for the surgical aspirator Finally, the robot was docked with monopolar curved scissors on the right and bipolar ProGrasp forceps on the left The steps for radical cystectomy were the same as for open surgery At the end of the robotic procedure, a suprapubic Pfannenstiel incision was made, the surgical
piece previously placed in the endobag was removed and finally the orthotopic urinary diversion was packed

Orthotopic neobladder
At a distance of 15-20 cm from the ileocecal valve, a 40 cm ileal segment is isolated Intestinal continuity is restored with a latero-lateral anastomosis Mechanical sutures are used The distal loop (approximately 20 cm in length) is lowered to form a 'U' to reach the membranous urethra
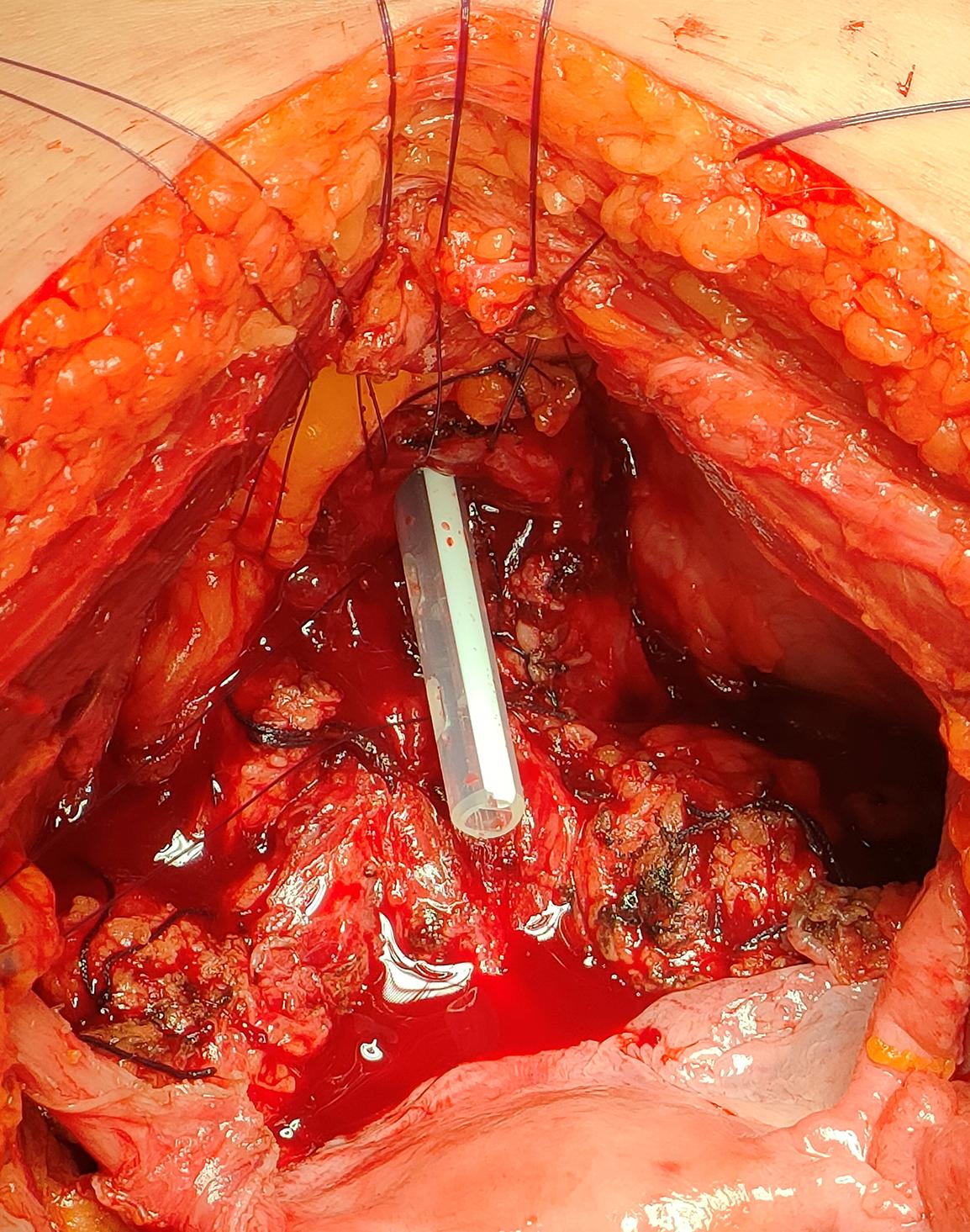
The ileal segment is then opened along the antimesenteric border A 3/0 V-Loc suture is used to tunnel the lower part of the ileal loop posteriorly and anteriorly The proximal loop is folded medially into an inverted U-shape and the opposite inner edges are then sutured from side to side to form an upper ileal cup This is then inverted at the edges of the lower ileal pouch to create an oval reservoir The urethro-intestinal anastomosis is packed with 6 detached stitches of resorbable 3/0 glyconate monofilament suture on a 20-ch 3-way neobladder catheter The uretero-neovesical anastomosis is then exteriorized at the level of the left iliac fossa using Bracci ureteral catheters as a guide A hydraulic leak test of the neobladder is performed and a 24 c tube drain is placed in the Retzius excavation at the level of the right iliac fossa
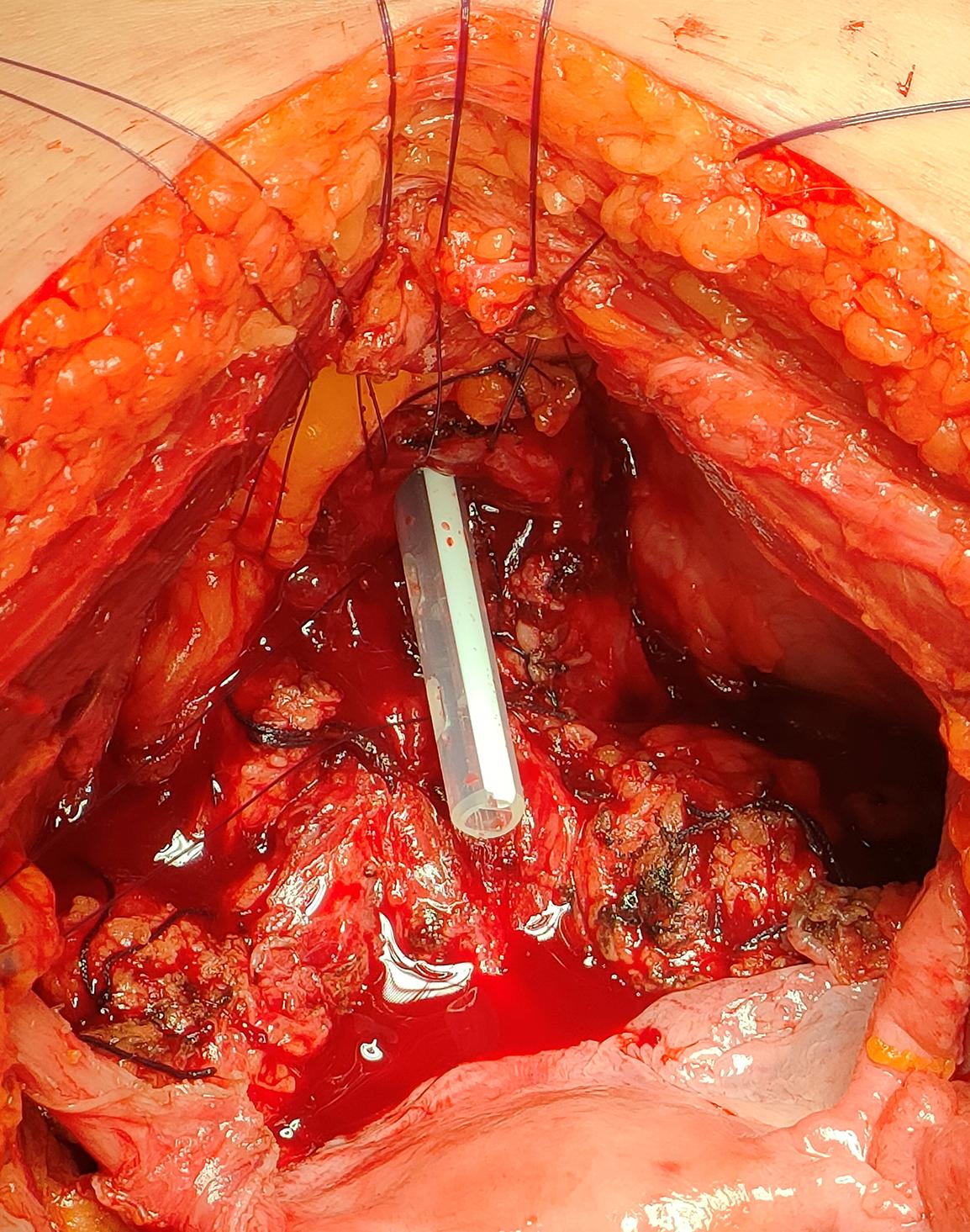
Finally, the abdominal wall is closed in layers (Figure 4)
Post-operative assessment
Patients were evaluated according to age, Body Mass Index (BMI), American Society of Anesthesiology (ASA) score, preoperatively measured hemoglobin and creatinine
Surgical outcomes were operative time, discharge hemoglobin and creatinine, days in hospital and perioperative complications in accordance with the Clavien-Dindo classification system (7) Patients were functionally and oncologically followed by outpatient visits quarterly in the first year and biannually thereafter with a program including b
,
i n e c y t o l o g y , abdominal and pelvic CT, urethrocystoscopy and chest X-ray The study evaluated the following oncological outcomes: Recurrence Free Survival (RFS local or metastatic)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 9 Total extended
genital sparing radical cystectomy in female patients
l o o d t e s t s , a b d o m i n a l u l t r a s o u n d
u
r
Figure 3
Preparation of the urethra
Figure 4. Final configuration of the neobladder
and Overall Survival (OS) both measured at more than 56 months of follow-up and finally anatomopathological outcomes In terms of functional outcomes, sexual function was measured using a standardized questionnaire: The Female Sexual Function Index (FSFI-19) (8) This is a quick and effective questionnaire that structures female sexual function into 6 different aspects: desire, subjective arousal, lubrication, orgasm, satisfaction, and pain, with a score ranging from a minimum of 2 to a maximum of 36 We administered it both 3 and 12 months after surgery Urinary function was evaluated by the patient's level of continence (day and night) and the use of urinary incontinence devices; the severity of urinary leakage was calculated using the Sandvik score (9) Finally, urinary retention requiring intermittent urethral catheterization was assessed
RESULTS
The mean age of the 14 patients who underwent genital sparing radical cystectomy was 57 6 years (range 30-65)
The preoperative clinicopathological characteristics of the patients are shown in Table 1 Regarding surgical outcomes (Table 2), the mean operative time for the entire procedure, including cystectomy, bilateral pelvic lymphadenectomy and neobladder reconstruction, was 260 minutes (range 220-396 minutes) for the open procedure
Table 1.
characteristics.
and 318 minutes (range 258-432 minutes) for the robotic one The mean blood loss during surgery was 400 ml (230-710 ml) Patients' mean hospital stay was 18 days (15-24 days), and discharge hemoglobin and serum creatinine were 9 3 g/dL (8 9-14 8 g/dL) and 1 2 mg/dL (0 8-1 6 mg/dL), respectively Perioperative complications such as loss of ileo-ileal anastomotic seal, bleeding, or loss of neobladder seal were not observed in any of the patients
None of the patients had complications requiring surgery (grade ≥ 3 according to the Clavien-Dindo classification of postoperative complications); only one patient had postoperative acute pancreatitis, which was successfully treated with medical therapy
Final histopathological examination revealed urothelial carcinoma in 13 patients, of which 8/13 (61 5%) had low grade T1 stage, 3/13 (23%) had high grade T2 stage and, finally, 2 (15 5%) had high grade T3 stage Botryoid variant embryonal rhabdomyosarcoma localized to the bladder and completely excised after surgery (PT2aN0M0) was found in one patient at final histopathological exam-
Table 2
Surgical and oncologic outcomes
Archivio Italiano di Urologia e Andrologia 2023; 95, 2
10
A Cisternino, L Capone, A Rosati, C Latiano, N Sebastio, A Colella, G Cretì
Patient
Patient characteristics Mean (range) Age (years) 57 6 (30-65) Body Mass Index 26 1 (20-30 5) Preoperative Creatinine (mg/dL) 0 86 (0 72-1 1) Preoperative Hemoglobine (g/dL) 12 7 (11 2-14 3) No. of patients (%) Status Married 13 (93) Unmarried 1 (7) Menopause Premenopausal 6 (43) Postmenopausal 8 (57) ASA Score I 8 (57) II 6 (43) Previous abdominal surgery Cesarean section 1 (7) Appendicectomy open 1 (7) Location of the tumor Posterior wall 6 (43) Anterior wall 1 (7) Lateral wall 6 (43) Dome of the bladder 1 (7) Pathological type Urothelial carcinoma 13 (93) Other (Embryonal rhabdomyosarcoma) 1 (7) Grading of the tumor Low grade 0 (0) High grade 14 (100) Staging TNM T1 N0 M0 8 (57) T2 N0 M0 4 (29) T3 N0 M0 2 (14)
Surgical and oncologic outcomes Mean (range) Operative time (min) Open 260 (220-396) Robot-assisted 318 (258-432) Mean Blood Loss (ml) 400 (230-710) Hospital stay (days) 18 (15-24) Postoperative creatinine (mg/dL) 1 2 (0 8-1 6) Postoperative hemoglobine (gr/dL) 9 3 (8 9-14 8) No of patients (%) Complications Clavien low grade (0-2) 14 (100) Clavien high grade (3-5) 0 (0) Cystectomy Robotic-assisted cistectomy 3 (21) Open cystectomy 11 (79) Postoperative pathologic stage Ta, Tis, T1 8 (57 5) T2aN0M0 1 (7) T2bN0M0 3 (21 5) T3aN0M0 1 (7) T3bN0M0 1 (7) T4 0 (0) Pathologic nodal stage N0 14 (100) N+ 0 (0) Tumor grading Low grade 0 (0) High grade 14 (100) Positive surgical margins 0 (0) Follow-up 12 months Recurrence-free survival 14 (100) Overall survival 14 (100) Follow-up 24 months Recurrence-free survival 14 (100) Overall survival 14 (100) Follow-up 36 months Recurrence-free survival 14 (100) Overall survival 14 (100)
Table 3 Functional outcomes
DISCUSSION
ination Resection margins were free of neoplastic pathology in all patients, and all resected lymph nodes were free of tumor pathology All patients were followed for at least 56 months During this period, no patient developed local recurrence (urethral and/or neovesical) or metastatic recurrence (RFS 100%) with a 100 % OS The oncological findings are presented in Table 2 Out of the 14 patients, 12 (85 5%) maintained complete continence both during the day and at night, 2 (15 5%) complained about urine leakage at night, and only 1 required the use of 1-2 pads The Sandvik Score showed a state of complete continence in 7 patients (50%), mild incontinence in 6 patients (43%) without the use of urinary incontinence devices, moderate incontinence in 1 patient (7%) with the use of 1-2 pads during the night Only one patient developed urethral-neovesical stenosis after 6 months, which was treated by endoscopic surgery During the follow-up period, no patient developed hydronephrosis, urethro-neovesical reflux or deterioration of renal function Of the 14 patients who underwent surgery, 13 (93%) were married, 1 was single (7%) but had a stable partner; 6 women (43%) were fertile at the time of surgery, while the other 8 (57%) were already menopausal; all patients were sexually active As mentioned above, sexual function was assessed using the FSFI-19 This was administered 3 months and 1 year after surgery One year postoperatively, FSFI showed sexual desire in all patients (100%); subjective arousal, orgasmic attainment and sexual satisfaction in 12/14 patients (85 5%); sufficient lubrication in 11/14 patients (78 5%) Dyspareunia during intercourse was reported by only one patient (7%) One year after surgery, all patients were sexually active Finally, when we compared patients' test scores at 3 months and 12 months postoperatively, we found that all patients had higher final test scores after one year, due to improved sexual comfort These data were also in line with the findings of the outpatient survey (total FSFI 3 months 18 3, range 15-21; total FSFI 12 months: 29 1, range 25-33) Functional outcomes are shown in Table 3
For more than half a century, radical cystectomy has globally been the procedure of choice for all male and female patients with muscle-invasive bladder cancer or high-risk non-invasive bladder cancer However, it is an invasive procedure whose main target was, and still is, oncological radicality, aimed to improve the prognosis of patients, which is already poor (5-year survival rate of 63% in stage II patients and 48% in stage III patients) (10) At the same time, an attempt was made to mitigate the clinical and psychological consequences to which a patient undergoing radical cystectomy was subjected by reconstructing the lower urinary tract and in particular by orthotopic urinary diversions Nowadays, there is also an increasing focus on the patient's quality of life, and minimally invasive surgical techniques or the search for organ-sparing techniques are a direct consequence of this (11, 12) Female gender is considered a protective factor in the epidemiology of many oncological diseases, but this is not the case for bladder cancer where being female means not only having a higher risk of cancer-specific mortality than men, but it is also considered an independent risk factor for bladder cancer-specific death (13, 14) The causes of this universally accepted statistic have been investigated in the underestimation of hematuria due to a false diagnosis of cystitis rather than bladder cancer, resulting in the absence of more accurate examinations (15) Another cause is to be identified in anatomy: in women there is no natural anatomical barrier between the bladder and the uterus capable of preventing extraorgan invasion of the bladder tumor, thus leading to a higher rate of diagnosis of advanced-stage tumors (16) For these reasons, radical cystectomy in women with orthotopic urinary diversion developed later than in men (it was only in the early 2000s that the genital organ-sparing cystectomies were performed in women) Numerous studies have been conducted to assess the oncological feasibility of sparing first the urethra, then the vagina and finally the genital organs in toto Ali-El-Dein et al. in a 1999 study were among the first to show that sparing the urethra and making a neobladder was oncologically safe (17) He again reviewed 609 cystectomy patients for bladder cancer in 2004 and reported a 2 6% incidence of secondary genital co-invasion and a 0% incidence of primary genital cancer (18) Groutz et al in a 1999 study performed 37 radical cystectomies and found genital organ involvement in only one patient (19) In a more recent study in 2019 Huang and colleagues showed out of 112 radical cystectomies the presence of uterine invasion in only 5 patients (4 5%) (20)
In our institution, we developed a technique with the aim of respecting oncological radicality and totally sparing the genital organs The diversion used was the Padua neobladder because of its favorable urodynamic characteristics (adequate compliance and low pressures) and the use of a relatively short ileum segment During genital organ sparing, we took special attention to sparing the neurovascular bundles along the lateral wall of the vagina with the aim of preserving not only the patients' fertility but also their sexual function On the oncological side, none of our patients had genital organ recurrence or lymph node and/or extra lymph node metastases In
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 11 Total extended genital sparing radical cystectomy in female patients
Functional outcomes No of Patients (%) Continence Day-time 14 (100) Night-time 12 (85.5) Sandvik score 0 (continent) 7 (50) 1-2 (mild incontinence) 6 (43) 3-6 (moderate incontinence) 1 (7) 8-9 (severe incontinence) 0 (0) 12 (very severe incontinence) 0 (0) Neobladder complications Uretral stricture 1 (7) Female Sexual Function Index (FSFI) at 12 months Sexual desire 14 (100) Sexual arousal 12 (85 5) Lubrication 11 (78 5) Orgasm 12 (85 5) Satisfaction 12 (85 5) Pain 1 (7)
terms of continence and sexuality, we have had satisfactory results about daytime and nocturnal continence as well as the fertility and sexuality of the patients As far as complications, except for a single episode of urethral stenosis resolved by surgery, no patient developed prolapse, fistulas between the neobladder and vagina, or alteration of the upper urinary tract The results of our study, in line with the literature, show that a total extended genital sparing radical cystectomy with sparing of the neurovascular bundle and the pubo-urethral ligaments strongly reduces the risk of vaginal fistulas, pelvic prolapse, neobladder prolapse secondary to an angulation of the uretero-intestinal anastomosis through the anterior wall of the vagina, and chronic urinary retention (21-23) Above all, it allows maintenance of good continence, satisfactory sexual function and not least the maintenance of fertility In fact, in their papers, both Ali-El-Dein et al. and Niver et al described a patient who became pregnant after the surgery, one of whom was also able to have a child (24, 25)
Finally, an interesting 2005 case report by Puppo et al presented a patient with cystocele and stress incontinence secondary to subtotal hysterectomy The patient underwent radical cystectomy with ileal reservoir followed by reconstruction of pelvic floor integrity by colposacropxy using mesh The hysterectomy with vaginal sparing and fixation of vaginal wall to adjacent structures or sacropexy may be a valid solution both oncologically and functionally
Nevertheless, from our point of view, anatomical support to the neobladder secondary to genital sparing, preservation of the neurovascular bundle, and maintenance of fertility are to be pursued in highly motivated and selected patients (26)
CONCLUSIONS
Total extended genital sparing cystectomy appears to be a safe treatment for high-risk non-muscle invasive or muscle invasive bladder cancer in terms of oncological radicality and it is also beneficial in terms of urinary continence, fertility and sexual function, quality of life and psychological and emotional health However, it is a treatment that should be reserved for carefully selected patients who are highly motivated by the preservation of fertility and sexual function and who are fully informed about the advantages and disadvantages of this procedure
REFERENCES
1 Sung H, Ferlay J, Siegel RL, et al Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries CA Cancer J Clin 2021; 71:209-249
2 Ferlay J, Colombet M, Soerjomataram I, et al Cancer statistics for the year 2020: An overview Int J Cancer 2021
3 Scosyrev E, Noyes K, Feng C, Messing E Sex and racial differences in bladder cancer presentation and mortality in the US Cancer 2009; 115:68-74
4 Babjuk M, Burger M, Compérat E, et al Guidelines on Non-muscle-invasive Bladder Cancer (Ta, T1 and CIS) EAU Guidelines Office, 2022 European Association of Urology Guidelines Office Arnhem, The Netherlands
5 Varkarakis IM, Pinggera G, Antoniou N, et al Pathological review of internal genitalia after anterior exenteration for bladder cancer in women Evaluating risk factors for female organ involvement Int Urol Nephrol 2007; 39:1015-1021
6 Kulkarni JN, Rizvi SJ, Acharya UP, et al Gynecologic-tract sparing extra peritoneal retrograde radical cystectomy with neobladder Int Braz J Uro 2008; 34:180-7
7 Dindo D, Demartines N, Clavien PA Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey Ann Surg 2004; 240:205-213
8 Rosen R, Brown C, Heiman J, et al The Female Sexual Function Index (FSFI): A multidimensional self-report instrument for the assessment of female sexual function J Sex Marital Ther 2000; 26:191-208
9 Sandvik H, Seim A, Vanvik A, Hunskaar S A severity index for epidemiological surveys of female urinary incontinence: comparison with 48-hour pad-weighing tests Neurourol Urodyn 2000; 19:137-45
10 Witjes JA, Bruins HM, Carrión A, et al EAU Guidelines on Muscle-invasive and Metastatic Bladder Cancer 2022 Edn presented at the 37th EAU Annual Congress Amsterdam European Association of Urology Guidelines Office Arnhem, The Netherlands
11, Tang K, Li H, Xia D, et al Laparoscopic versus open radical cystectomy in bladder cancer: a systematic review and meta-analysis of comparative studies PLoS One 2014; 9:e95667
l Cystectomy in Female Patients - Improving Outcomes Curr Urol Rep 2019; 20:83
13 Kluth LA, Rieken M, Xylinas E, et al Gender-specific differences in clinicopathologic outcomes following radical cystectomy: an international multi-institutional study of more than 8000 patients Eur Urol 2014; 66:913-9
14 Messer JC, Shariat SF, Dinney CP, et al Female gender is associated with a worse survival after radical cystectomy for urothelial carcinoma of the bladder: a competing risk analysis Urology 2014; 83:863-7
15 Cohn JA, Vekhter B, Lyttle C, et al Sex disparities in diagnosis of bladder cancer after initial presentation with hematuria: a nationwide claims-based investigation Cancer 2014; 120:555-61
16 Weissbart SJ, Smith AL Hysterectomy in the Urologist's Practice Curr Urol Rep 2017; 18:4
17 Ali-el-Dein B, el-Sobky E, Hohenfellner M, Ghoneim MA Orthotopic bladder substitution in women: functional evaluation J Urol 1999; 161:1875-80
18 Ali-El-Dein B, Abdel-Latif M, Mosbah A, et al Secondary malignant involvement of gynecological organs at radical cystectomy specimens in women: is it mandatory to remove these organs routinely? J Urol 2004; 172:885-7
19 Groutz A, Gillon G, Konichezky M, et al Involvement of internal genitalia in female patients undergoing radical cystectomy for bladder cancer: a clinicopathologic study of 37 cases Int J Gynecol Cancer 1999; 9:302-306
20 Huang H, Yan B, Shang M, et al Is hysterectomy beneficial in radical cystectomy for female patient with urothelial carcinoma of bladder? A retrospective analysis of consecutive 112 cases from a single institution BMC Urol 2019; 19:28
21 Moursy EE, Eldahshoursy MZ, Gamal WM, Badawy AA Orthotopic genital sparing radical cystectomy in pre-menopausal women with muscle-invasive bladder carcinoma: A prospective study Indian J Urol 2016; 32:65-70
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 A
12
Cisternino, L Capone, A Rosati, C Latiano, N Sebastio, A Colella, G Cretì
1 2 K a l a m p o k i s N , G r i v a s N , Ö l s c h l ä g e r M , e t a l R a d i c a
22 Roshdy S, Senbel A, Khater A, et al Genital Sparing Cystectomy for Female Bladder Cancer and its Functional Outcome; a Seven Years' Experience with 24 Cases Indian J Surg Oncol 2016; 7:307-11
23 Borghi C, Manservigi M, Milandri ES, et al The impact of orthotopic reconstruction on female sexuality and quality of life after radical cystectomy for non-malignant bladder conditions Arch Ital Urol Androl 2021; 93:255-261
24 Ali-El-Dein B, Mosbah A, Osman Y, et al Preservation of the internal genital organs during radical cystectomy in selected women
with bladder cancer: a report on 15 cases with long term follow-up Eur J Surg Oncol 2013; 39:358-64
25 Niver BE, Daneshmand S, Satkunasivam R Female reproductive organ-sparing radical cystectomy: contemporary indications, techniques and outcomes Curr Opin Urol 2015; 25:105-10
26 Puppo P, Introini C, Calvi P, Naselli A Pelvic floor reconstruction before orthotopic bladder replacement after radical cystectomy for bladder cancer Urology 2005; 65:174
Correspondence
Antonio Cisternino, MD (Corresponding Author) antonio cisternino@libero it
Lorenzo Capone, MD (Corresponding Author) lorenzocapone@msn com
Antonio Rosati, MD
Costanzo Latiano, MD
Nicola Sebastio, MD
Antonio Colella, MD
Giuseppe Cretì, MD
Department of Urology, Fondazione IRCCS Casa Sollievo della Sofferenza, via dei Cappuccini, 71013, San Giovanni Rotondo (Italy)
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 13 Total
genital sparing radical cystectomy in female patients
extended
ORIGINAL PAPER
Effectiveness and safety of spinal anesthesia in patients undergoing open radical retropubic prostatectomy
Summary
Objective: Prostate cancer is one of the most widespread neoplasms affecting the male gender. The most commonly used procedures in various urological centers are laparoscopic and robotic surgery because they are considered minimally invasive techniques. We present our experience in traditional open radical prostatectomy performed under spinal anesthesia.
Materials and methods: We reviewed the clinical courses of 88 consecutive patients who underwent open radical prostatectomy performed under spinal anesthesia at our Institution
Results: Median age: 67.7 years. Median follow up duration: 48 months Median pre-operative PSA: 15,9 ng/ml, median Prostate weight: 44.5 gr, median surgical time: 96.5 minutes (range 55138) Perioperative complications were recorded The most frequent complication was anemia, 9 cases need blood transfusion after surgery Complications directly related to spinal anesthesia were not observed Most patients were discharged within 5 days from the procedure After two weeks we observed a quick recovery of total continence in 90% of patients After 6 months all patients were perfectly continent Erectile dysfunction after 6 months was reported by 48 patients
Conclusions: The reasons why the gold standard of radical prostatectomy surgery has been considered general anesthesia are essentially two: the long duration of the surgical procedure and the associated significant blood loss Multiple evidences show that radical retropubic prostatectomy can be safely performed under spinal anaesthesia with various advantages It is therefore no longer justified to consider general anesthesia as the gold standard for radical prostatectomy with an open technique.
KEY WORDS: Prostate cancer; Radical prostatectomy; Spinal anesthesia
Submitted 28 February 2023; Accepted 20 March 2023
INTRODUCTION
Prostate cancer is one of the most widespread neoplasms affecting the male gender all over the world with variable incidence in relation to the geographical area considered The gold standard remains in most cases the radical surgical removal of the prostate and district lymph nodes The anatomical characteristics of the surgical field have made radical prostatectomy the most performed surgical procedure in the world with robotic-assisted laparoscopic technique; this is due to the search for less invasiveness and
better surgical accuracy The lack of comparative studies between the different surgical approaches has not allowed for many years to establish which of open, laparoscopic or robotic surgery guarantees better oncological and functional long-term results Today, the most commonly used procedures in various urological centers are laparoscopic and robotic surgery because they are considered minimally invasive techniques but open radical prostatectomy (ORP) remains well established and commonly performed in many parts of the world (1) Recently Alexander Haese et al in a comparative study of robot-assisted and open radical prostatectomy in 10 790 men conclude that: “Both surgical approaches, performed in a high volume centre by the same surgeons, achieve excellent, comparable oncological and functional outcomes” (2) We present in this study our experience in traditional open radical prostatectomy surgery performed under spinal anesthesia
MATERIALS AND METHODS
For analysis in this study, we reviewed the clinical courses of 88 consecutive patients who underwent ORP between 05/2016 and 06/2021 at our Institution
Preoperatively, after diagnostic assessment of prostate cancer with transrectal eco-guided biopsy, an abdominal computerized tomography and bone scintigraphy were performed for staging the disease Pathology results in all patients confirmed adenocarcinoma of the prostate gland However, some patients with prostate cancer diagnosed elsewhere were also referred to our hospital for further definite treatment Preoperative investigations included a complete blood count, serum coagulation, electrolytes, creatinine, electrocardiogram, and chest x-ray We have placed the indications for the surgical treatment following the European Guidelines 2020, edition 2021 Morbidity influenced the choice of the anesthetic regimen Patients with a history of myocardial infarction, previous cerebrovascular accident, transient ischemic attack from the study within a year preoperatively and extensive spinal surgery were considered cases of contraindication for regional anesthesia and the patients were excluded from the study Instead, we considered eligible for the study patients with previous prostate surgery or endoscopic prostate procedures subjected to subsequent open radical prostatectomy Each patient was informed in detail about
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 14
Salvatore Blanco 1 , Angelica Grasso 2 , Endrit Sulmina 3 , Marco Grasso 1
1 Department of Urology, Fondazione IRCCS San Gerardo dei Tintori, Monza, Italy;
2 Department of Urology, ASST Santi Paolo e Carlo, University of Milan, Milan, Italy;
DOI: 10 4081/aiua 2023 11281
3 Department of Anesthesia and Intensive Care Medicine, Fondazione IRCCS San Gerardo dei Tintori, Monza, Italy
the advantages and disadvantages of spinal anesthesia and the accompanying risk factors
We have not considered patients’ BMI, although adiposity could influence the outcomes of prostatectomy We might evaluate this topic in a different work
Spinal anesthesia method
Subarachnoid or spinal anesthesia is a central locoregional anesthesia technique in which the anesthetic, whether or not combined with opiates or alpha agonists, is injected into the subarachnoid space, into the cephalorachid fluid surrounding the spinal cord, reversibly inhibiting sensory and motor nerve conduction
To perform the spinal anesthesia, the patient is positioned seated with knees flexed to 90° and relaxed shoulders, chin touching the chest, trying to bend the lumbar vertebrae outwards, causing the intervertebral space to open allowing the needle to pass through Careful disinfection of the skin with alcoholic solution or iodopovidone is performed
A sterile drape with a central slit is placed and the intervertebral space is searched by palpating the spinous processes of the lumbar vertebrae, then local anesthesia of the skin and the inter spinous and yellow ligaments is applied For radical prostatectomy the space usually chosen is L2-L3 where hyperbaric Bupivacaine is injected at a dosage of 0 12-0 15 mg/kg for a total of 12-14 mg with the addition of an opiate, Disufen 2-4 mcgr or Morphine 100200 mcg, which prolongs both the duration of anesthesia and postoperative pain control The drug is injected in a cephalic direction to achieve a level of anesthesia of at least T9-T10, sufficient to cover the skin metameres at the surgical incision site, sub umbilical-pubic Mild or deep sedation is combined for the duration of the operation with benzodiazepines or hypnotics while maintaining spontaneous breathing The duration of spinal anesthesia is approximately 2-3 hours after which the motor and sensory blockade is slowly resumed, which is prolonged up to 4 hours with the addition of opioids Intraoperative monitoring is done with a 5-lead ECG, with non invasive blood pressure monitoring every 5' and measurement of peripheral saturation It is useful to place 2 venous accesses of at least 18 G, to perform loading with 500-1000 ml crystalloid and to have blood available as it is an operation with important fluid shift The side effects of this anesthesia are usually hypotension and bradycardia, easily reversible
Time in surgery
We defined time of surgery as the period between start of cut on the suprapubic skin and the end of agraffes skin affixing To reduce variations in surgical skill and experience of the surgeon, all patients in this series of open radical prostatectomies with spinal anesthesia were operated by two surgeons
Surgical procedure
We describe the technique of open radical prostatectomy developed on the basis of a personal series of more than 1500 procedures We perform a conventional median surgical incision starting under umbilicus with pelvic space exposure We performed a bilateral pelvic lymphadenectomy in all patients independently of value Gleason grade biopsies or prostate specific antigen (PSA) level The opera-
tion was carried out using some variants with respect to the original technique described by Walsh (3) Our approach results from surgical experience observations collected since 1995 with patients subjected to radical prostatectomy with bladder neck preservation (4) and also using our particular experience in radio guided radical prostatectomy with sentinel lymph node dissection (5) During detachment of the prostate from the bladder, an electro incision was made in the demarcation point between the bladder and the gland, which was highlighted by palpating the balloon of a Foley catheter inflated to 10 cc and tautened Following an electro incision extended by about 270° (i e from one lateral peduncle to the other in order to spare the ventral area), detachment of the prostatic gland on an anatomic plane was carried out manually by the surgeon At the end of this operation, urethral and periurethral muscle fibers sectioning were performed by means of scissors During this stage, particular attention should be paid to the prevention of lesions of the prostatic capsule, or lacerations in the bladder wall, especially in the ventral area Having removed the prostate-vesicular block, bladder neck biopsies were carried out in all quadrants; the urethrovesical anastomosis was performed with the aid of a urethral protractor (6) with 6 single 3/0 monocryl suture The catheter was removed on the 11th day without the need of any radiological check Patients were discharged usually in the fourth day after surgery In this study, we focused on findings useful to evaluate if spinal anesthesia could be an efficient and suitable technique for this procedure Particularly we evaluated the abdominal and pelvic muscle relaxation throughout the procedure on a scale of 1 to 4, with 1 indicating poor muscle relaxation and 4 excellent muscle relaxation as already indicated in other experiences of the efficacy of spinal anesthesia on muscle relaxation throughout the operative period (7) We also want to underline the good control of pain in the first postoperative hours which allowed to avoid or reduce the use of opiate drugs
Postoperative period
Postoperatively all patients were monitored in the post anesthesia care unit (PACU) Post anesthetic management of the patient included periodic assessment and monitoring of function of the lower urinary tract (urine output, drainage and bleeding), of respiratory function, cardiovascular function, neuromuscular function, temperature, pain (especially the ability of the patient to communicate breakthrough pain or if the feelings of tension is present in the abdominal- pubic area), mental status, nausea and vomiting, fluid assessment Postoperative pain management was easily controlled with oral analgesics (FANS) since spinal anesthesia demonstrated excellent pain control for at least four to five hours after surgery Therefore, an early mobilization was still guaranteed
Hospital stay
In order to compare time of hospital stay, minimum and maximum values and median values were calculated
Low-weight heparin was administered in the post-operative period (at the end of the hemorrhagic risk) every day of hospitalization, at midnight, and then at home for at least fifteen days
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 S
15
Blanco, A Grasso, E Sulmina, M Grasso
Overall functional follow up
The follow-up of the patients monitored the degree of urinary continence achieved during the immediate postoperative period (two weeks after the operation), then at three months, six months and one year after the operation The degree of continence was assessed during the immediate post-operative period by compilation of a previously validated questionnaire (7), in which patients were invited to annotate actual urine leaks, as well as the need for protective pads In this study, we defined “dry or continent” patients who did not use pads or just used a safety pad in a day because many patients used a pad as a precautionary measure, despite their sufficient continence Those patients who were completely dry or only subject to a sporadic leakage of drops of urine due to micturition urgency, or on straining or coughing, were defined as continent Finally, we evaluated intraoperative and postoperatively early and late complications of open radical prostatectomy and spinal anesthesia Early complications were defined as those that developed within one month postoperatively, and late ones those observed at least 1 month after operation
RESULTS
We retrospectively screened 88 patients undergoing open radical prostatectomy for clinically localized prostate cancer (pCa) Median age was 67 7 years (range from 46 to 81 years) and median follow up duration was 48 months (6 to 54 months) Median pre-operative PSA was 15 9 ng/ml (range 2 1-80), median prostate weight (as reported by pathologist) was 44 58 g (range 12-86) Median preoperative Hb was 14 3 mg/dl, at hospital discharge Hb was 10 3 mg/dl, and 9 patients have been transfused Median surgical time (calculated by surgical incision until closure of the skin) was 96 5 minutes (range 55-138) Clinical-pathological stage were recorded in Table 1 The
throughout the operative period has been always judged adequate by the surgeon In all cases the surgery lasted less than two hours and the use of spinal anesthesia was more than sufficient Perioperative complications (intrapostoperatively) were recorded The most frequent complication was post-operative anemia which was observed in 9 cases out of 88 requiring blood transfusion during stay in hospital and always after surgery Other early comp
patients that required prolonged drainage for more than 2 w
Surgical site infection was observed in 3 patients, in all cases the infections were superficial and did not need specific treatment, surgical drainage being not required in any case Early complications directly related to spinal anesthesia were never observed Late complications were only related to surgical procedure: anastomotic stricture with poor urinary stream (< 10 ml/sec in Qmax by uroflowmetry) was observed in 5 patients, requiring an endoscopic incision; more than half of them occurred within 6 months after operation No case of lymphocele that required specific therapy Anterior urethral stricture was observed in 2 patients Most patients were discharged within 5 days from the procedure (range 3-17) Following an anamnestic assessment conducted two weeks after the operation, we observed a quick recovery of total continence in 90% of patients At six months visit all patients were perfectly continent Erectile dysfunction after 6 months was reported by 48 patients (not considering in this work the pre-operative status, the comorbidities and the correct intake of post-operative PDE5 inhibitors) Patients’ satisfaction was high; most of them confirmed that they were very happy with this anesthesia
DISCUSSION
Open radical retropubic prostatectomy is an effective treatment for localized prostate cancer but adequate anesthesiologic management is mandatory Spinal anesthesia is a form of regional anesthesia, which indications include lower abdominal and perineal surgery as are many genitourinary surgeries The use of spinal anesthesia during radical prostatectomy is not usually considered as it is judged not suitable for long-term surgery with significant blood loss (8) In fact, it is generally considered not advisable to employ spinal anesthesia for surgeries lasting for more than 2 hours On the other hand, time required for the performance of the open radical prostatectomy procedure varies depending on surgeon skill and competence
The advantages of this anesthesia technique for this type of operation are: patient comfort/satisfaction, less sedation score, faster postoperative recovery flatus passing, and mobilization/ambulation and pain control in the first hours postoperatively (8)
Other advantages are less effective surgical time, less use of amines and fluids, shorter post-anesthesia care unit stay as well as less hospital stay (9) and good muscle relaxation comparable to general anesthesia (10) Studies demonstrated that in spinal anesthesia blood loss is less than with general anesthesia (12) although others do not sustain this finding (11) Patients with locoregional anesthesia had significantly decreased risk of cardiac arrhythmia, deep vein thrombosis, respiratory depression, intubation risk, atelectasis, pneumonia, ileus, and postoperative nausea and vomiting (4), may have reduced risk of delirium in elderly ages (14) and had better overall survival after radical prostatectomy (14) The disadvantages are the limited duration of anesthesia in case of prolonged interventions, difficulties in the management of hemodynamics in case of significant blood loss as well as the need of conversion to general anesthesia in urgent care with an awake patient
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 16 Spinal
anesthesia for open radical retropubic prostatectomy
f fi c a c y o f s p i n a l a n e s t h e s i a o n m u s c l e r e l a x a t i o n
l i c a t i o n s o b s e r v e d w e r e a n a s t o m o t i c l e a k a g e i n 2
e
e e k s w i t h c o n s e q u e n t e x t e n s i o n o f h o s p i t a l s t a y
Table 1. pT2: 42pts pT3: 46pts N1: 8pts R+: 51pts T2a:5pts, T2b:2pts, T2c:35pts T3a:33pts, T3b:11pts T2aN0R0:4pts T3aN0R0:9pts T2aN0R1:1pt T3aN0R1:19pts T2bN0R0:1pt T3aN0R2:3pts T2bN0R1:1pt T3aN1R1:3pts T2cN0R0:18pts T3bN0R0:3pts T2cN0R1:17pts T3bN0R1:4pts T3bN1R0:1pt T3bN1R1:4pts
Spinal anesthesia is not always successful for long surgical procedures and is often associated with undesirable complications (15, 16) In our study the surgery procedure time was brief (median time 95 minutes) Advantages of spinal anesthesia were also confirmed in our experience: reduced risk of respiratory complications and quick restoration of bowel function The combination of the surgeon's experience (17, 18) able to perform the procedures with very limited laparotomies, and the known advantages of spinal anesthesia in terms of better control of postoperative pain, longer control of detrusor contractility, and no impact on the mental state of the patient in addition to the reduction of blood loss and the incidence of thromboembolic events (4), allows, in our opinion, to consider this surgical procedure as a minimally invasive procedure In fact, these patients, as for other minimally invasive techniques, are characterized by a smooth postoperative time and early discharge, within 4 to 5 days
Finally, we consider this procedure to be further advantageous not only in terms of costs for the national health service, but above all in terms of reducing the risk of postoperative delirium and cognitive impairment, given the large number of patients, including elderly ones, who are operated on today In our opinion, we are recently creating a confused concept of invasiveness that cannot be measured with the length of a cut but with other parameters such as duration of surgery, blood loss, postoperative pain, absence of cognitive disorders, etc
CONCLUSIONS
We want to strongly emphasize that in choosing the type of anesthesia to use, the comparison with the prostatic adenomectomy surgery is crucial In fact, all over the world and after many evaluations published and validated about 40 years ago, if there are no specific contraindications, prostatic adenomectomy is performed under spinal anesthesia
The reasons why the gold standard of radical prostatectomy surgery has been considered general anesthesia are essentially two: the long duration of the surgical procedure and the associated significant blood loss It is known that, with the standardization of the surgical technique in highvolume surgical centers like our, the two types of surgery can be equated for bleeding risk and duration
Multiple evidences show that radical retropubic prostatectomy can be safely performed under spinal anesthesia with various advantages (19), therefore it is no longer justified to consider general anesthesia as the only gold standard for radical prostatectomy with an open technique Our experience with spinal surgery could, of course, not be transferred to laparoscopic or robotic-assisted surgery where general anesthesia is currently mandatory due to patient’s positioning
REFERENCES
1 Pereira R, Joshi A, Roberts M, et al Open retropubic radical prostatectomy Transl Androl Urol 2020; 9:3025-3035
2 Haese A, Knipper S, Isbarn H, et al A comparative study of robotassisted and open radical prostatectomy in 10 790 men treated by highly trained surgeons for both procedures M BJU Int 2019; 123:1031-1040
3 Walsh PC, Retik AB, Vaughan ED Anatomic radical retropubic prostatectomy In: Campbell’s Urology, 7th ed , Philadelphia: W B Saunders, Co , 1998; vol 3, chapt 86, pp 2565-2588
4 Grasso M, Torelli F, Lania C, Blanco S The role of bladder neck preservation during radical prostatectomy: clinical and urodynamic study Arch Ital Urol Androl 2012; 84:1-6
5 Grasso M, Blanco S, Grasso AAC, et al Radio guided radical prostatectomy: evaluation of feasibility, safety and clinical outcomes Minerva Urol Nefrol 2016; 68:3-8
6 Fröhlich G, Wördehoff A The urethral protractor A new instrument for facilitating the anastomosis between urethra and bladder in radical prostatectomy and urethro-intestinal anastomoses following cystectomy Urologe A 1990; 29:155-7
7 Donovan JL, Abrams P, Peterset TJ The ICS-‘BPH’ Study: The psychometric validity and reliability of the ICS male questionnaire Br J Urol 1996; 77: 554-563
8 Salonia A, Crescenti A, Suardi N General versus spinal anesthesia in patients undergoing radical retropubic prostatectomy: results of a prospective, randomized study Urology 2004; 64:95-100
9 Kofler O, Prueckner S, Weninger E Anesthesia for Open Radical Retropubic Prostatectomy: A Comparison between Combined Spinal Epidural Anesthesia and Combined General Epidural Anesthesia Prostate Cancer 2019; 2019:4921620
10 Bajwa SJ, Kulshrestha A Anaesthesia for laparoscopic surgery: General vs regional anaesthesia J Minim Access Surg 2016; 12:4-9
11 Wong RP, Carter HB, Wolfsonet A, et al Use of spinal anesthesia does not reduce intraoperative blood loss Urology 2007; 70:523-6
12 Pöpping DM, Elia N, Van Aken HK et al Impact of epidural analgesia on mortality and morbidity after surgery: systematic review and meta-analysis of randomized controlled trials Ann Surg 2014; 259:1056-67
13 European Geriatric Medicine, 2013; vol 4, pp S17-S18
14 Lee BM, Ghotra VS, Karam JA, et al Regional anesthesia/analgesia and the risk of cancer recurrence and mortality after prostatectomy: a meta-analysis Pain Manag 2015; 5:387-395
15 Hartmann B, Junger A, Klasen J, et al The incidence and risk factors for hypotension after spinal anesthesia induction: an analysis with automated data collection Anesth Analg 2002; 94:1521-9
16 Bromage PR Neurological complications of subarachnoid and epidural anaesthesia Acta Anaesthesiol Scand 1997; 41:439-44
17 Begg CB, Riedel ER, Bachet PB Et al Variations in morbidity after radical prostatectomy N Engl J Med 2002; 346:1138-44
18 Gershman B, Meier SK, Jeffery MM, et al Redefining and Contextualizing the Hospital Volume-Outcome Relationship for RobotAssisted Radical Prostatectomy: Implications for Centralization of Care J Urol 2017; 198:92-99
19 Pikramenos K, Zachou M, Apostolatou E, et al The effects of method of anaesthesia on the safety and effectiveness of Radical Retropubic Prostatectomy Arch Ital Urol Androl 2022; 94:396-400
Correspondence
Salvatore Blanco, MD - sblanco 74@yahoo it
Marco Grasso, MD - grasso m@virgilio it
Department of Urology, Fondazione IRCCS San Gerardo dei Tintori, Monza, Italy
Angelica Grasso, MD - angelicagrasso84@gmail com
Department of Urology, ASST Santi Paolo e Carlo, University of Milan, Italy
Endrit Sulmina, MD - e sulmina@asst-monza it
Department of Anesthesia and Intensive Care Medicine, Fondazione IRCCS San Gerardo dei Tintori, Monza, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 S
17
Blanco, A Grasso, E Sulmina, M Grasso
The use of renal biopsy in the kidney tumor management: A retrospective analysis
of consecutive cases in a referral center
Summary
Introduction: Ultrasound-guided renal masses biopsy (RMB) is a useful and underestimated tool to evaluate suspected renal tumors This study aimed to assess the safety and feasibility of this technique
Materials and Methods: Data of 80 patients with suspected primary or secondary kidney tumors who underwent RMB between January 2012 and December 2020 were included in this retrospective study. Twelve patients were excluded due to incomplete data Biopsy outcomes were collected through our electronic medical records system and then compared with definitive pathology
Results: RMB was performed in 68 cases. Pathological examination reported 43 (63%) malignant cases, while RMB was negative in 15 (22%) samples. On the other hand, a benign lesion was present in 8 (12%) cases, and 2 (3%) biopsies were non diagnostic. One major and one minor post-procedure complication were reported among the patients A total of 31 patients underwent renal surgery including 19 partial and 12 radical nephrectomies Out of them, 4 patients had a negative biopsy, but radiological imaging strongly suggested malignancy. The concordance between biopsy and definitive pathology occurred in 22 out of 31 (71%) cases, with a higher rate among the masses greater than 4 cm, 9/11 (82%) compared to smaller ones 13/20 (65%) Pathologic examination of the 4 cases with negative biopsy showed 3 renal cell and a translocation renal cell carcinoma
Conclusions: Ultrasound-guided biopsy for renal masses is a safe and effective procedure Its ability to identify malignancy is evident, especially for primary renal tumors However, low concordance between biopsy and definitive pathology in cases with negative biopsies, especially for tumors < 4 cm, does not reliably guarantee the absence of tumor and, therefore, strict follow-up or repeat biopsy may be indicated.
KEY WORDS: Kidney tumors; Renal masses biopsy; Ultrasound; Small renal mass; Nephron-sparing surgery; Active surveillance
Submitted 26 December 2022; Accepted 20 March 2023
INTRODUCTION
Since the past few decades, the incidence of clear cell renal cell carcinoma has dramatically increased, and currently counts approximately 431 000 new cases per year worldwide (1) Furthermore, it is the cause of death of over
179 000 people annually (1) This phenomenon reflects the development of advanced diagnostic imaging, which determines a greater detection rate In a retrospective study involving 3001 consecutively registered asymptomatic adults, a renal mass of at least 1 cm occurred in nearly 15% of examinations (2)
Currently, there is an increased number of diagnoses of small renal masses (SRM), which consists of cystic or solid lesion measuring < 4 cm on cross-sectional imaging and with features suspicious of a cT1a RCC (3) Nowadays, several therapeutic options may be offered, in particular nephron-sparing surgery (NSS) is preferable to radical nephrectomy for tumors up to cT1b stage due to the preservation of renal function (4, 5) Furthermore, partial nephrectomy is associated with a decrease in cardiovascular events and overall mortality (6) Cryoablation is a valid option in patients with several comorbidities and low life expectancy, due to minimum effect on renal function and low post-procedure complication rate, despite the high treatment failure rates (7) Alternatively, active surveillance has demonstrated cancer-specific survival similar to primary intervention for patients with SRM (8) The most appropriate treatment decision for the patient is based first on the patient's general condition (including comorbidities, renal function, and life expectancy) and the nature of the renal tumor However, traditional diagnostic imaging provides data on mass characteristics, but it cannot determine whether the lesion is benign or malignant yet There is evidence that dynamic magnetic resonance imaging may differentiate tumor subtypes (9), but tumor aggressiveness cannot be defined For the latter, the details from ultrasound-guided renal mass biopsy (RMB) are crucial This procedure plays a key role in approximately 60% of patients (10), guiding them toward the most appropriate therapy, whether medical or surgical
This study aimed to describe our experience with RMB, evaluating its safety and feasibility
MATERIALS AND METHODS
An institutional retrospective review was conducted with data analysis of 80 patients with suspected primary or secondary kidney tumors who underwent RMB between January 2012 and December 2020 Twelve cases were
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 18
ORIGINAL PAPER
Andrea Benedetto Galosi 1 , Marco Macchini 2 , Roberto Candelari 2 , Virgilio De Stefano 1 , Silvia Stramucci 1 , Vanessa Cammarata 1 , Omar Al Ayoubi 1 , Andrea Cicconofri 1 , Carlo Giulioni 1
1 Department of Urology, Polytechnic University of Marche, Azienda Ospedaliera Universitaria della Marche, Ancona, Italy;
DOI: 10 4081/aiua 2023 11115
2 Interventional Radiology, Department of Radiology, Azienda Ospedaliera Universitaria della Marche, Ancona, Italy
(A) An axial CT image of a left superior mesopolar renal mass

(B) An ultrasound image of the renal mass biopsy with the needle guide
described using the median and interquartile ranges IBM SPSS (V26) was used as statistical software
RESULTS
The median age of the patients was 71 years (36-85), and the median BMI was 27 5, as shown in Table 1 Median core needle samples per biopsy were 2 Tumor characteristics were reported in Table 2 Forty-four cases had an SRM (< 4 cm), and 24 had masses ≥ 4 cm RMB in our series was performed in 68 cases The histological outcomes of all the biopsies are listed in Table 3 The biopsy outcome was malignancy in 43 (63%) cases, and the renal cell carcinoma (RCC) was the most frequent tumor; 15 biopsies were negative, a benign lesion was present in 8 (12%) cases, and 2 (3%) biopsies were non diagnostic Two patients experienced complications after the biopsy procedure: 1 case of a subcapsular renal haematoma that
Patients and samples characteristics
excluded due to the lack of complete data in the database
A l l p a t i e n t s h a d p re v i o u s l y p e r f o r m e d a c o n t r a s te n h a n c e d c o m p u t e d t o m o g r a p h y ( C T ) s c a n o f t h e abdomen, which allowed for tumor characteristics evaluation (Figure 1A) Renal biopsy was indicated in the following cases: patients with various comorbidities in whom surgery is planned, patients with imaging findings suggestive of unresectable renal cancer, suspected metastasis in the kidney, and indeterminate cystic renal mass
Two experienced radiologists performed all the RMB guided by ultrasound machine LOGIQ S8 XDclear (GE Healthcare®, Chalfont St Giles, UK) after the analysis of contrast-enhanced CT imaging Specimens were obtained through an automated biopsy gun with an 18-Gauge needle (Figure 1B) One to four cores were collected per biopsy, giving an average of two Patients’ characteristics, including age, gender, body mass index (BMI), skin-to tumor distance and thickness of subcutaneous fat, were calculated through the radiology Moreover, several radiological tumor characteristics were evaluated, such as size, location, endophyticity, cortical location and cystic component
All data regarding post-procedure complications following primary intervention were reported and ranked according to Clavien-Dindo (CD) Classification (11) as collected through our electronic medical records system
Qualitative variables were described using absolute frequencies and percentages
Quantitative variables were
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 A B Galosi, M Macchini, R Candelari, et al 19
Table 1.
No (%) Median (range) Age, years 71 (36-85) Gender Male 49 (72%) Female 19 (28%) Patient BMI 27 5 (18 6-44 2) < 30 46 (68%) ≥ 30 22 (32%) Core needle samples, n 2 (1-4) Skin-to-tumor distance, cm 5 8 (15-120) < 7 cm 43 (63%) ≥ 7 cm 25 (37%) Thickness of subcutaneous fat, cm 1 9 (2 -54) < 3 cm 50 (74%) ≥ 3 cm 18 (26%)
Figure 1.
Table
Tumor characteristics No (%) Side Left 25 (37) Right 43 (63) Tumor size < 4 cm 44 (65) ≥ 4 cm 24 (35) Mass location Mesorenal 22 (32) Upper pole 26 (38) Lower pole 18 (27) Renal pedicle 2 (3) Cortical location Anterior cortex 18 (27) Posterior cortex 32 (47) Neither 18 (27) Endophytic vs exophytic Completely endophytic 10 (15) < 50% exophytic 29 (43) ≥ 50% exophytic 29 (43) Cystic vs solid Cystic component ≥ 50% 5 (7) Cystic component < 50% 10 (15) No cystic component 53 (78)
2.
3
Histological outcomes of diagnostic biopsies
Chemo- or immunotherapy was proposed to the seven patients with locally advanced disease or primary tumor in another location Active surveillance was offered to the 8 cases of oncocytoma, while 3 cases of watchful waiting occurred
As shown in Table 5, the overall concordance between RMB and definitive pathology was 22/31, with a higher rate for masses greater than 4 cm Ultrasound-guided biopsy demonstrated its reliability in diagnosing RCC, both for small and large masses Tumor subtype was confirmed by definitive pathology in 82% of cases (22/27) However, in two cases of unspecified carcinoma, after excision, one had a histological outcome of skeletal muscle metastases and the other urothelial cell carcinoma
Four patients with negative biopsies underwent surgery because of highly suspicious lesions for tumor on radiological imaging Biopsies reported only necrosis in two of them and solid component of a cystic lesion in the other two The final diagnosis was RCC in three patients and translocation renal cell carcinoma in one
not required treatment (CD 1), and 1 case of renal bleeding, who required Super-Selective Embolization (CD 3), occurred
Table 4 reported the treatment offered to the patients
In summary, the overall sensibility was 71%, with a higher value for masses greater than 4 cm than the smaller ones (82% vs 65%, respectively) Furthermore, the positive predictive value was 96%
DISCUSSION
According to EAU guidelines, surgery is the first-line choice therapy for patients with a localized renal mass, preferring, whenever feasible, the NSS to radical nephrectomy (12)
Nowadays, there is a trend toward a conservative approach for renal surgery also for increasingly challenging cases In a multicenter study involving 410 patients with high complexity masses, partial nephrectomy showed satisfactory long-term oncological and functional outcomes despite an acceptable rate of perioperative complications (13, 14) However, 20-50% of the definitive pathologies of this surgery find benign tumors, which might be managed by active surveillance (15) On the other hand, a multidisciplinary strategy is necessary for metastatic diseases or locally advanced renal cancer, which provides a palliative cytoreductive nephrectomy and systemic treatments (12) Moreover, microRNAs were proposed as a non-invasive biomarker for various roles in RCC management, although no definitive conclusions emerged from the literature (16) Therefore, a histological diagnosis is essential to guide the best therapeutic management
Although ultrasound-guided biopsy may have other hints, as in glomerulonephritis, its more frequent use is in the field of oncology RMB indication occurs in several cases, such as the diagnosis of tumor metastasis, unresectable renal cancer, indeterminate cystic or multiple renal mass, and in patients not fit for surgery (17)
The biopsy was proposed for SRM, although an i n v e r s e re l a t i o n s h i p w a s re p o r t e d b e t w e e n tumor size and its risk of malignancy (18)
Ultrasound-guided biopsy showed good accuracy in defining the nature of the renal tumor In our series, a concordance of tumor malignancy between biopsy and definitive pathology always
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 20 Safety and feasibility of US guided renal
biopsy
mass
Table
Therapeutic management No (%) < 4 cm ≥ 4 cm Nephron sparing surgery (NSS) RCC 9 (13) 81 Others 10 (15) 73 Radical Nephrectomy RCC 8 (12) 26 Others 4 (6) 31 Active Surveillance RCC 1 (1) 10 Oncocytoma 8 (12) 62 Others 2 (3) 2 0 Oncologic treatment (chemo or immunoterapy) RCC 2 (3) 02 Others 5 (7) 23 Watchful waiting RCC 1 (1) 01 Others 2 (3) 11 Patients lost during follow-up 16 (24) 12 4 RCC 2 (3) 11 Others 14 (21) 11 3 RCC: renal ce l carcinoma
4.
Table 5.
Concordance with Concordance with Concordance with definitive patholog y definitive patholog y definitive patholog y in all masses in masses < 4 cm in masses ≥ 4 cm Overall, n (%) 22/31 (71) 13/20 (65) 9/11 (82) RCC, n (%) 22/23 (96) 13/14 (93) 9/9 (100) Unspecified carcinoma, n (%) 0/3 (0) 0/2 (0) 0/1 (0) Others, n (%) 0/1 (0) 0/1 (0) 0/0 (0) Negative, n (%) 0/4 (0) 0/3 (0) 0/1 (0) RCC: renal ce l carcinoma
Concordance between biopsy and definitive pathology.
Table
Histological subtype at RMB No. (%) Clear cell RCC 21 (29) Papillary RCC 9 (13) Oncocytoma 8 (12) Unspecified carcinoma 3 (4) Oncocytic RCC 2 (3) Lymphoma 3 (4) Urothelial carcinoma 1 (1) Skeletal muscle cancer (metastasis) 1 (1) Collecting (Bellini) duct carcinoma 1 (1) Translocation Renal Cell Carcinoma 1 (1) Lung cancer (metastasis) 1 (1) Non diagnostic 2 (3) Negative 15 (22) RMB: rena mass biopsy; RCC: renal cel carcinoma
occurred Moreover, the concordance of RCC between RMB and definitive pathology was 96% In a large metaanalysis involving 5228 patients, its sensitivity and specificity were 99 1% and 99 7%, respectively (19)
Furthermore, the authors showed a concordance rate between tumor histotype on biopsy and surgical specimen of 90 3%, while concordance rates of tumor grade ranged from 43% to 93% The last data raises several doubts about biopsies, especially for SMR Similarly, Pierorazio et al reported high percentages in terms of sensitivity and specificity, while the negative predictive value was 68 5% and non-diagnostic rates ranged from 0% to 22 6% for masses less than 4 cm (20) In the same way, in the present study, the concordance rate between biopsy and definitive pathology of all SRM dropped up to 65%
The most critical aspect that emerged from our analysis is the specificity of RMB Indeed, there was low concordance between biopsy and definitive pathology for negative or unspecified carcinoma diagnoses in our results
Abel et al reported that when carrying out a biopsy of a metastatic lesion or primar y tumor, as opposed to nephrectomy specimen examination, it is likely that only one subpopulation of cells is sampled, and prognostic information is based on only one subpopulation of cells (21) Therefore, high false-negative rates raise concerns about the reliability of the procedure However, RMB may be repeated on all patients with unspecified masses or non-diagnostic cases to increase the diagnostic rate (22) Furthermore, renal biopsy is not without complications, due to the procedure invasiveness, especially bleeding, although they are considered rare events According to Lane et al., minor and major complications after RMB are, respectively, less than 5% and 1% (23) Of these, the most common is undoubtedly bleeding, which often tends to present subclinically and requires transfusion in about 1 5% of cases (24) Indeed, both post-procedure complications were related to haemorrhage in the present study
Another frequent complication is the intrarenal arteriovenous fistulae occurred According to Rollino et al., the development of this clinical condition has an incidence of up to 5% when colour-coded Doppler sonography is used (25) However, no case was reported in our analysis
The limitations of the present study are evident First, it is a retrospective study and biases linked to its nature are predictable Second, the pathological specimens were not reviewed independently for the current study Moreover, a considerable number of subjects dropped out from our analysis: in fact our radiology department also accepts patients referred from other hospitals and, therefore, a loss of some of them in the follow-up is inevitable At last, a relatively small sample size is involved in this analysis, not allowing to obtain definitive data
CONCLUSIONS
Ultrasound-guided biopsy for renal masses demonstrated satisfactory ability to distinguish benign and malignant tumors Concordance between biopsy and definitive pathology was high for RCC, particularly for masses greater than 4 cm However, the low concordance in the negative biopsies, especially for tumors < 4 cm, may require a second biopsy In any case, the procedure
proved to be safe and effective in referring patients to the most appropriate therapeutic management Considering the low prevalence of this procedure in routine clinical practice, its use is recommended whenever an indication occurs
REFERENCES
1 Global Cancer Observatory International Agency for Research on Cancer World Health Organization
2 O'Connor SD, Pickhardt PJ, Kim DH, et al Incidental finding of renal masses at unenhanced CT: prevalence and analysis of features for guiding management AJR Am J Roentgenol 2011; 197:139-45
3 Finelli A, Ismaila N, Bro B, et al Management of Small Renal Masses: American Society of Clinical Oncology Clinical Practice Guideline J Clin Oncol 2017; 35:668-680
4 Dell'Atti L, Scarcella S, Manno S, et al Approach for Renal Tumors With Low Nephrometry Score Through Unclamped Sutureless Laparoscopic Enucleation Technique: Functional and Oncologic Outcomes Clin Genitourin Cancer 2018; 16:e1251-e1256
5 Giulioni C, Di Biase M, Marconi A, et al Clampless Laparoscopic Tumor Enucleation for Exophytic Masses Greater Than 4 cm: Is Renorrhaphy Necessary? J Laparoendosc Adv Surg Tech A 2022; 32:931-937
6 Huang WC, Elkin EB, Levey AS, et al Partial nephrectomy versus radical nephrectomy in patients with small renal tumors--is there a difference in mortality and cardiovascular outcomes? J Urol 2009; 181:55-61
7 Zargar H, Atwell TD, Cadeddu JA, et al Cryoablation for Small Renal Masses: Selection Criteria, Complications, and Functional and Oncologic Results Eur Urol 2016; 69:116-28
8 Pierorazio PM, Johnson MH, Ball MW, et al Five-year analysis of a multi-institutional prospective clinical trial of delayed intervention and surveillance for small renal masses: the DISSRM registry Eur Urol 2015; 68:408-15
9 Sun MR, Ngo L, Genega EM, et al Renal cell carcinoma: dynamic contrast-enhanced MR imaging for differentiation of tumor subt y p e s - - c o rre l a t i o n w i t h p a t h o l o g i c f i n d i n g s R a d i o l o g y 2 0 0 9 ; 250:793-802
10 Maturen KE, Nghiem HV, Caoili EM, et al Renal mass core biopsy: accuracy and impact on clinical management AJR Am J Roentgenol 2007; 188:563-70
11 Clavien PA, Barkun J, de Oliveira ML, et al The Clavien-Dindo classification of surgical complications: five-year experience Ann Surg 2009; 250:187-196
12 B Ljungberg (Chair), L Albiges, J Bedke, et al Volpe Guidelines on Prostate Cancer Edn presented at the EAU Annual Congress Milan 2021 978-94-92671-13-4 EAU Guidelines Office, Arnhem, Netherlands
13 Sciorio C, Prontera PP, Scuzzarella S, et al Predictors of surgical outcomes of retroperitoneal laparoscopic partial nephrectomy Arch Ital Urol Androl 2020; 92:165
14 Mari A, Tellini R, Porpiglia F, et al Perioperative and Mid-term Oncological and Functional Outcomes After Partial Nephrectomy for C o m p l e x ( PA D U A S c
: A
e
t i v e Multicenter Observational Study (the RECORD2 Project) Eur Urol Focus 2021; 7:1371-1379
15 Russo P, Uzzo RG, Lowrance WT, et al Incidence of benign versus malignant renal tumors in selected studies J Clin Oncol 2012; 30, 92
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 A B
al 21
Galosi, M Macchini, R Candelari, et
a l Tu
o re ≥ 1 0 ) R e n
m o r s
P ro s p
c
16 Napolitano L, Orecchia L, Giulioni C, et al The Role of miRNA in the Management of Localized and Advanced Renal Masses, a Narrative Review of the Literature Applied Sciences 2023; 13:275
17 Sahni VA, Silverman SG Biopsy of renal masses: when and why Cancer Imaging 2009; 6; 9:44-55
18 Frank I, Blute ML, Cheville JC, et al Solid renal tumors: an analysis of pathological features related to tumor size J Urol 2003; 170:2217-20
19 Marconi L, Dabestani S, Lam TB, et al Systematic Review and Meta-analysis of Diagnostic Accuracy of Percutaneous Renal Tumour Biopsy Eur Urol 2016; 69:660-673
20 Pierorazio PM, Johnson MH, Patel HD, et al Management of Renal Masses and Localized Renal Cancer: Systematic Review and Meta-Analysis J Urol 2016; 196:989-99
21 Abel EJ, Carrasco A, Culp SH, et al Limitations of preoperative biopsy in patients with metastatic renal cell carcinoma: comparison to surgical pathology in 405 cases BJU Int 2012; 110:1742-6
22 Lim A, O'Neil B, Heilbrun ME, et al The contemporary role of renal mass biopsy in the management of small renal tumors Front Oncol 2012; 2:106
23 Lane BR, Samplaski MK, Herts BR, et al Renal mass biopsy--a renaissance? J Urol 2008; 179:20-7
24 Tang S, Li JH, Lui SL, et al Free-hand, ultrasound-guided percutaneous renal biopsy: experience from a single operator Eur J Radiol 2002; 41:65-9
25 Rollino C, Garofalo G, Roccatello D, et al Colour-coded Doppler sonography in monitoring native kidney biopsies Nephrol Dial Transplant 1994; 9:1260-3
Correspondence
Andrea Bendetto Galosi, MD andreabenedettogalosi@ospedaliriuniti marche it
Virgilio De Stefano, MD
virgilio destefano@gmail com
Silvia Stramucci, MD
silvia stramucci@gmail com
Vanessa Cammarata vanessa cammarata@gmail com
Omar Al Ayoubi, MD
omar alayoubi@gmail com
Andrea Cicconofri, MD andrea cicconofri@gmail com
Carlo Giulioni, MD (Corresponding Author) carlo giulioni9@gmail com
Department of Urology, Polytechnic University of Marche
Azienda Ospedaliero Universitaria delle Marche
71 Conca Street, 60126 - Ancona (Italy)
Marco Macchini, MD
marco macchini@ospedaliriuniti marche it
Roberto Candelari, MD
roberto candelari@ospedaliriuniti marche it
Interventional Radiology, Department of Radiology, Azienda Ospedaliera Universitaria della Marche, Ancona (Italy)
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 22 Safety
and feasibility of US guided renal mass biopsy
HER2/neu
expression status
of post BCG recurrent non-muscle-invasive bladder urothelial carcinomas in relation to their primary ones
Mohamed Yousef Ali 1 , Ahmed Yousef Aboelsaad 2 , Ahmed M Abdel Gawad 2 , Tamer A Abouelgreed 3 , Ahmed A. El Gammal 3 , Osama M. Ghoneimy 3 , Eman M. El-Dydamony 3 , Ahmed A. Alrefaey 4 , Eslam Mohamed 5 , Sherif Azzam 5 , Ayman Abdelmohaymen 6 , Yasien Mohammed 1 , Mohammed S. Abdelwahed 1, 7 , Ahmed Fawzi A. Elsayed 2 , Basem A. Fathi 3 , Nosaiba M. Abd Alrahim 8 , Abeer S. Farag 9 , Alaa R. Mahmoud 10 , Hasan Ismail Mohamed 4 , Seth Horsu 11 , Abdulkarim Hasan 1
1 Pathology Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
2 Urology Department, Damietta Faculty of Medicine, Al-Azhar University, Damietta, Egypt;
3 Urology Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt;
4 Urology Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
5 Clinical Oncology Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
6 Surgical Oncology Department, Faculty of Medicine, Al-Azhar University, Cairo, Egypt;
7 Pathology Department, Faculty of Medicine, University of Jeddah, Jeddah, Saudi Arabia;
8 Clinical pathology Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt;
9 Pathology Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt;
10 Urology Department, Faculty of Medicine, Al-Azhar University, Assiut, Egypt;
11 Histopathology Department, St Vincent’s University Hospital, Dublin, Ireland
Summary
Background: Transurethral resection (TUR) followed by adjuvant therapy is still the treatment of choice of Non-Muscle-Invasive Bladder Urothelial Carcinoma (NMIBUC) However, recurrence is one of the most troublesome features of these lesions. Early second resection and adjuvant BCG therapy has been shown to improve the outcome
Objective: To evaluate the prognostic value of C-erbB-2 (HER2/neu) expression status in Non-Muscle-Invasive Bladder Urothelial Carcinoma cases, before and after intravesical Bacillus Calmette Guerin (BCG immunotherapy)
Materials and methods: HER2/neu expression was studied in 120 (Ta-T1) Non-Muscle-Invasive Urothelial Carcinoma cases
The expression was evaluated and compared to the expression after Bacillus Calmette Guerin (BCG) immunotherapy
Results: HER2/neu expression in low and high grade of the NonMuscle-Invasive Urothelial Carcinoma was (38%) and (83%) respectively. The difference of the expression rates by tumor grade was statistically significant In recurring lesions post BCG therapy, C-erbB-2 expression was markedly decreased (31 6%) when compared to its expression before therapy (65%)
Conclusions: The HER2/neu expression increased as the tumor grade rose The reduction in expression following BCG treatment in Non-Invasive transitional cell carcinoma cases could reflect a reduction of the potential malignancy of the tumor
KEY WORDS: Transurethral resection; Non-Muscle-Invasive Urothelial Carcinoma; C-erbB-2; Bacillus Calmette Guerin; Immunohistochemistry
Submitted 14 March 2023; Accepted 1 April 2023
INTRODUCTION
Non-Muscle-Invasive Bladder Urothelial Carcinoma (NMIBUC) is the most common type of urinary bladder carcinoma It
accounts for approximately 75% of all BC lesions at initial presentation; this percentage is even greater in younger patients (< 40) The high prevalence of NMIBUC can be attributed to its long-term survival and reduced risk of cancer-specific mortality compared to muscle-invasive (T2-4 stages) tumors (1) These tumors are restricted to the mucosa (Ta, CIS) or submucosa (T1), and are treated by trans-urethral resection Although trans-urethral resection of bladder tumors (TURBT) by itself can totally remove Ta/T1 lesions, they frequently recur and can progress to MIBC The recurrence rate of such tumors is 50 to 70% As a result, all patients should be considered for adjuvant intravesical instillation (IVI) therapy and surveillance, based on their risk stratification (2) The most important step in the management of NMIBUC is the transurethral resection procedure This procedure is crucial for the complete removal of all visible/suspicious lesions and for proper grading and staging by sampling of detrusor muscle; thus, determining the next appropriate treatment (2) Because of the high risk of recurrence and progression following primary resection, adjuvant therapy and long-term surveillance should be considered in all patients (3) There is evidence that treatment with Bacillus Calmette-Guérin immunotherapy following primary resection can lower cancer recurrence rates and progression to more advanced stages (4)
C-erbB-2 is a tyrosine kinase transmembrane protein that is related to epidermal growth factor receptor (EGFR) family and it is known as HER2/neu (human epidermal growth factor receptor-2) Its expression in urinary bladder transitional cell carcinoma has been described, and it has been proposed that its expression increases with tumor grade and recurrence of urothelial cancer Bladder urothelial carcinomas with C-erbB-2 expression have poor prognosis, hence
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 23
ORIGINAL PAPER
DOI: 10 4081/aiua 2023 11313
it can be used as a prognostic clinical biomarker (5) The goal of this study is to evaluate the C-erbB-2 (HER2/neu) immunostaining status in Non-Muscle-Invasive Bladder Urothelial Carcinoma cases, before and after intravesical Bacillus Calmette Guerin (BCG) immunotherapy
PATIENTS AND METHODS
This work was conducted at our institution over the period between March 2016 to February 2020 It included 120 cases (86 men and 34 women; mean age 52 3 ± 11 4, range 41-70 years) with recurrent urothelial tumors confined to the bladder All patients had a history of transurethral resection of bladder tumor (TURBT) and full dose BCG therapy for primary NMIBUC lesions Before removal of the tumor, each patient had a history taken, physical examination, urinalysis, an ultrasound scan (USS), and CT scan TURBT was performed under classical white light using the 26-Fr continuous-flow Karl Storz resectoscope with distilled water for irrigation The aim of resection was complete removal of all visible/suspicious lesions and their underlying muscularis propria The tumor and its related underlying muscle were sent separately labelled for histopathologic assessment Tumors were staged and graded according to the WHO/ISUP classification 2016 with external consultation when indicated We selected patients who had NMIBUC (Ta-T1) without carcinoma in situ (Cis) after pathological examination A second look cystoscopy was then performed after 2 weeks of the initial resection to ensure no residual lesion Patients were then followed up for intravesical instillation (IVI) of BCG BCG was instilled for six consecutive weeks, as an induction dose, starting 15-21 days after TURBT to enable surface urothelium to recover (6) Two weeks after the last instillation, surveillance cystoscopy was carried out, with random cold-cup biopsies taken from the ex-tumor site and its vicinity, as well as from other regions of the bladder, to detect recurrence The emergence of histopathologically confirmed urothelial tumor in the bladder, regardless of stage, was characterized as recurrence Since the biopsies were negative, our patients received a maintenance dose of BCG (3-weekly instillations, given at 3, 6, 12, 18, 24, 30 and 36 months)
Histopathology
Prepared H&E slides were analyzed and examined microscopically by the histopathologists to confirm the diagnosis according to the diagnostic criteria defined by the latest WHO/ISUP classification 2016
Immunohistochemistry
HER2/neu Immunostaining
An automatic immunohistochemical staining device (Benchmark XT; Ventana Medical System, Tucson, Arizona, USA) was used to stain formalinfixed paraffin-embedded tissue sections, according to the manufacturer's instructions
Briefly, 5-mm-thick sections were cut on Poly-Llysine-coated adhesive slides and dried for 30 minutes at 62°C After epitope retrieval by standard heat treatment for 30 minutes in ethylene diamine tetra acetic acid (pH 8 0) in an autostain-
er, the samples were incubated with mouse polyclonal antibodies to C-erbB-2 (dilution1: 500, cloneA0485; Labvision/Neomarker, Fremont, California, USA) The slices were then counterstained with Harris hematoxylin after being treated with biotinylated anti mouse immunoglobulins, peroxidase-labeled streptavidin (LSAB Kit; Labvision), and 3 30-diaminobenzidine Breast cancer slices fixed in paraffin were used as positive controls Membrane staining was assessed This step was evaluated independently and jointly by the histopathologists
HER2/neu expression
The percentage of stained cells and intensity of staining were ranged from 0 to 3+, as follows: no staining (0), low intensity and incomplete membrane staining in less than 10% of cells (1+), low intensity and full membrane staining in more than 10% of cells (2+), and high intensity and total membrane staining in more than 10% of cells (3+) Tumors with scores 0 and 1+ were considered to be negative, while those with scores 2+ and 3+ were considered positive (7)
Statistical analysis
The collected data were arranged, tabulated, and statistically analyzed using SPSS software statistical computer package version 16 (SPSS Inc , Chicago, Illinois, USA) Student's t-test was used to evaluate the difference between two means The Mann-Whiney test was used to compare two different groups, while the Wilcoxon signed rank test was used to compare two related groups The threshold for significance was set at less than 0 05
RESULTS
The 120 included patients had NMIBUC lesions, with a tumor size of 8-20 mm The lesions were detected by USS in 58 patients and by CT in the remaining 62 patients
Immunohistochemical findings
C-erbB-2 expression was found in 77 of 120 primary NMIBUC cases (64 16%) (Table 1) with expression ranging from weak (score 2 +) in 29 cases to strong (score 3 +) in 48 cases (Figures 1 and 2) When the score and tumor grade were compared, it was observed that C-erbB-2 was expressed in 19 out of 50 in low-grade cases (38%) In high grade cases, C-erbB-2 was expressed in 58 out of 70 instances (83%), with expression ranging from weak (score 2 +) in 19 cases to strong expression (score 3 +) in 39 cases C-erbB-2 expression in high grade urothelial
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 M
A
24
Yousef Ali,
Yousef Aboelsaad, A M Abdel Gawad, et al
Table 1
Groups No C-erbB-2 expression -VE +VE NO (%) Total/NO (%) 0 +1 +2 +3 Non-invasive urothelial carcinoma Low grade 50 21 10 10 9 19/50 (38%) 77/120 (64 2%) High grade 70 12 0 19 39 58/70 (83%) P value < 0 05 Mann-Whitney
C-erbB-2 expression in of the primary NMIBC lesions
test used BCG, Bac l us Ca mette Guer n
Non-Muscle-Invasive Bladder Urothelial Carcinoma (NMIBUC) limited to lamina propria - (Low grade T1)

(a) H&E X200, (b) Positive (score +2) for C-erbB-2 (membranous) - 200, (c) The same cases after B C G therapy negative for C-erbB-2 (score zero) x 200
Non-Muscle-Invasive Bladder Urothelial Carcinoma (NMIBUC) limited to lamina propria - (High grade T1)
(a) H&E X200, (b) Strong positive (score + 3) for C-erbB-2 (membranous) - x 100, (c) The same cases after B C G therapy negative for C-erbB-2 (score 1) x 100
carcinoma was significantly higher when compared to low grade one (p < 0 05) Hence, with increasing tumor grade, there was a statistically significant rise in C-erbB-2 expression
C-erbB-2 was found in 38 out of 120 cases (31 6%) of recurring lesions post BCG therapy with expression ranging from weak (score 2 +) in 28 cases to strong (score 3 +) in 10 cases Interestingly, its expression was found only in 8 only out of 50 low grade (16%), and in 30 out of 70 high grade (42 9%) recurring lesions This drop in C-erbB-2 expression in recurring cases after BCG therapy was statistically significant (p < 0 005) when compared to its expression in the same group before therapy
DISCUSSION
Histologically, 90% of bladder cancer lesions are of urothelial origin At the time of diagnosis, 20-25% of these lesions are Muscle-Invasive (stageT2 or higher); the rest are NonMuscle-Invasive, previously called superficial bladder cancer Only (8-12%) of all NMIBC tumors may progress to Muscle-Invasive Bladder Urothelial Carcinoma (MIBUC) (8)
The commonly employed scoring systems for initial risk stratification of NMIBUC lesions and for prediction of their risk of recurrence and progression after IVI of BCG, are based on clinicopathologic factors: age, gender, tumor
(number, diameter, grade, and staging), prior recurrence status, and concurrent CIS (9) Aside from these clinicpathologic criteria, it would be advantageous if biological markers could contribute in the risk categorization of NMIBUC lesions and in predicting their risk of recurrence and progression after IVI therapy Molecular biomarkers such as FGFR3, p53, p63 and Epidermal Growth Factors, and their prognostic role have been investigated in many studies (10, 11, 12) According to the latest EAU guidelines, the role of these biomarkers in the current era of personalized cancer management is promising, especially in the patients' categorization based on molecular classification (2) Regrettably, existing evidence is still inconclusive, and these biomarkers are not yet ready for routine use in clinical practice (13) C-erbB-2 is a tyrosine kinase receptor that belongs to the epidermal growth factor receptor family It regulates the cell cycle and promotes cell growth C-erbB-2-positivity rates have been found to vary between populations in studies The majority of C-erbB-2 expression investigations in bladder cancer have been conducted on MIBC, with expression ranging from 9% to 81% (14)
Another tyrosine kinase dysregulation of Axl receptor and its ligand growth arrest specific gene was also studied in urinary bladder carcinoma and showed a close relation to tumor stage and tumor grade, but still further

Archivio Italiano di Urologia e Andrologia 2023; 95, 2 25 HER2/neu expression after BCG for bladder carcinomas
Figure 1
Figure 2.
A B C A B C
studies are recommended to assess its role in tumor prognosis (15, 16)
However, there are few reports of C-erbB-2 status in NMIBUC C-erbB-2 protein overexpression has been found in 4-13% of NMIBUCs in a few studies (12, 17) In the current study, we investigated the immunohistochemistry expression of C-erbB-2 in 120 patients with recurrent NMIBUC, comparing it with the expression of their primary lesions We found that C-erbB-2 expression was seen in 64 16% (77 cases) of the primary tumors and there was a significant relationship between C-erbB-2 expression, in both recurrent and initial lesions, with tumor grade There is a statistically significant increase in C-erbB-2 expression as tumor grade rises These results were in line with those of Hegazy et al in 2015 and Agrawal et al in 2020 (10, 12), who found a relation between greater tumor grade and increased C-erbB-2 expression BCG immunotherapy post TURBT remains the most effective treatment for reducing the risk of NMIBUC recurrence and progression Patients with recurrent NMIBUC (with or without Cis) are frequently administered adjuvant intravesical BCG (18) According to Hegazya et al and Morgan et al (10, 19), BCG adjuvant therapy for NMIBUC lowered the incidence of C-erbB-2 expression with favorable outcomes In our research, we observed a significant drop in C-erbB-2 expression in recurrent lesions (38/120) when compared to their primary ones (77/120) (p < 0 05) Overall, an accurate a s s e s s m e n t o f C - e r b B - 2 s t a t u s i s r e c o m m e n d e d i n NMIBUC lesions for proper patient selection to BCG therapy In primary lesions, the C-erbB-2 immunoreactivity should be assessed before initiation of BCG immunotherapy If there is recurrence, the C-erbB-2 expression of the recurring lesion should be performed and compared with the primary one In case of down expression, one can consider adjuvant BCG therapy
Future studies, particularly ongoing C-erbB-2 targeted therapy trials, will undoubtedly shed further light on the significance of C-erbB-2 in bladder cancer management and treatment However, BCG production has shown its limits, with recent worldwide BCG shortage (20)
CONCLUSIONS
This study contributes to our understanding of C-erbB-2 expression in urothelial carcinoma It supports the role of C-erbB-2 immunostaining in NMIBUC lesions since the expression increased with increase tumor grade Our findings also suggest the importance of BCG therapy in the treatment of these cases although further studies on the role of this marker in recurrent lesions are highly recommended
Ethical Approval: Provided from Damietta Faculty of Medicine Under Id number: DFM-IRB-00012367 - 23-03003
REFERENCES
1 Compérat E, Larré S, Roupret M, et al Clinicopathological characteristics of urothelial bladder cancer in patients less than 40 years old Virchows Arch 2015; 466:589
2 Babjuk M, Burger M, Compérat EM, et al European Association of Urology guidelines on non-muscle-invasive urothelial carcinoma of the bladder (TaT1 and carcinoma in situ) - 2019 update Eur Urol 2019; 76:639-657
3 de Goeij L, Westhoff E, Witjes JA, et al The UroLife study: protocol for a Dutch prospective cohort on lifestyle habits in relation to non-muscle-invasive bladder cancer prognosis and health-related quality of life
BMJ Open 2019; 9:e030396
4 Malmström PU, Sylvester RJ, Crawford DE, et al An individual patient data meta-analysis of the long-term outcome of randomised s t u d i e s c o m p
Calmette-Guérin for non-muscle-invasive bladder cancer Eur Urol 2009; 56:247-256
5 Zhao J, Xu W, Zhang Z, et al Prognostic role of HER2 expression in bladder cancer: a systematic review and meta-analysis Int Urol Nephrol 2015; 47:87-94
6 Babjuk M, Burger M, Compérat E EAU guidelines on non-muscle-invasive bladder cancer Arnhem, The Netherlands: European Association of Urology; 2022 https://uroweb org/guideline/non-muscle-invasive-bladder-cancer/
7 Ramezani M, Siami, S, Rezaei M, et al Immunohistochemical Study of c-erbB2/HER2 Tumor Marker in Primary Malignant Brain Tumors Preprints org 2018, 2018120017 https://doi org/10 20944/ preprints 201812 0017 v1
8 Ali MY, El-Esawy BH Her2/neu expression in urothelial dysplasia, carcinoma in situ, and superficial urothelial carcinoma and its value in assessing the response to BCG therapy Egyptian Journal of Pathology 2014; 34:25-31
9 Remy E, Rebouissou S, Chaouiya C, et al A Modeling Approach to Explain Mutually Exclusive and Co-Occurring Genetic Alterations in Bladder Tumorigenesis Mathematical Model of Bladder Tumorigenesis Cancer Res 2015; 75:4042-4052
10 Hegazy R, Kamel M, Salem EA, et al The prognostic significance of p53, p63 and Her2 expression in nonmuscle- invasive bladder cancer in relation to treatment with bacille Calmette-Guerin Arab J Urol 2015; 13:225-230
11 Kumar S, Prajapati O, Vaiphei K, et al Human epidermal growth factor receptor 2/neu overexpression in urothelial carcinoma of the bladder and its prognostic significance: is it worth hype? South Asian J Cancer 2015; 4:115-117
12 Agrawal V, Bharti N, Pandey R Human epidermal growth factor receptor 2 (HER2) gene amplification in non-muscle invasive urothelial bladder cancers: Identification of patients for targeted therapy Arab Journal of Urology 2020; 18:267-72
13 Eriksson P, Rovira C, Liedberg F, et al A validation and extended description of the Lund taxonomy for urothelial carcinoma using the TCGA cohort Sci Rep 2018; 8:1-2
14 Bellmunt J, Werner L, Bamias A, et al HER2 as a target in invasive urothelial carcinoma Cancer Med 2015; 4:844-852
15 Akgül M, Baykan Ö, Çagman Z, et al Gas6 expression and Tyrosine kinase Axl Sky receptors: Their relation with tumor stage and grade in patients with bladder cancer Arch Ital Urol Androl 2021; 93:148-152
16 Mitrakas L, Gravas S, Karasavvidou F, et al Endothelin-1 indicates unfavorable prognosis in primary high-grade non-muscle-invasive urothelial bladder cancer Arch Ital Urol Androl 2021; 93:143-147
17 Lim SD, Cho YM, Choi GS, et al Clinical significance of substaging and HER2 expression in papillary non-muscle invasive urothelial cancers of the urinary bladder J Korean Med Sci 2015; 30:1068-1077
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 M
A
26
Yousef Ali,
Yousef Aboelsaad, A M Abdel Gawad, et al
n g i n t r a v e s i c a l m i t o m y c i n C v e r s u s b a c i l l u s
a r i
18 Sylvester RJ, Brausi MA, Kirkels WJ, et al Long-term efficacy results of EORTC genito-urinary group randomized phase 3 study 30911 comparing intravesical instillations of epirubicin, bacillus Calmette-Guerin, and bacillus Calmette-Guerin plus isoniazid in patients with intermediate-and high-risk stage Ta T1 urothelial carcinoma of the bladder Eur Urol 2010; 57:766-773
19 Morgan BE, Salup R, Morgan MB Differential C-erbB-2 and VEGF expression following BCG immunotherapy in superficial papillary transitional cell carcinoma of the bladder Urol Oncol 2002; 7:67-72
20 Trigo S, Gonzalez K, Di Matteo L, et al Bacillus Calmette-Guerin vaccine and bladder cancer incidence: Scoping literature review and preliminary analysis Arch Ital Urol Androl 2021; 93:1-8
Correspondence
Mohamed Yousef Ali, MD
mohamedyousef79@gmail com
Abdulkarim Hasan, MD (Corresponding Author)
abdulkarim hasan@azhar edu eg
Pathology Department, Faculty of Medicine, Al-Azhar University, 11884 Cairo, Egypt
Telephone & fax: 0020224012932
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 27 HER2/neu
expression after BCG for bladder carcinomas
The association between serum hypoxia inducible
factor-1α level and urothelial bladder cancer: A preliminary study
Ginanda Putra Siregar 1, 2 * , Ida Parwati 3 * , Bambang Sasongko Noegroho 4 * , Ferry Safridai 4 * , Gerhard Reinaldi Situmorang 5 , Raden Yohana 6 , Astrid Feinisa Khairani 7
1 Doctoral Study Program, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia;
2 Division of Urology, Department of Surgery, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia;
3 Department of Clinical Pathology, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia;
4 Department of Urology, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia;
5 Department of Urology, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia;
6 Division of Oncology, Department of Surgery, Faculty of Medicine, Padjadjaran University, Bandung, Indonesia;
7 Department of Biomedical Sciences, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
* These authors contributed equally to this paper
Summary
Introduction: We aim to evaluate the association between serum hypoxia inducible factor (HIF)-1α level and stage and grade of urothelial bladder cancer (UBC)
Methods: A case-control study was conducted at Haji Adam Malik Hospital Medan, Indonesia Inclusion criteria for case group was subject aged 18 years or older and diagnosed with UBC based on histopathological examination Control group consisted of gender and age matched healthy subjects. Serum HIF-1α level was determined using ELISA method Data was analyzed with chi square, Mann Whitney, and independent T tests
Results: A total of 80 subjects were enrolled and divided into case and control groups equally Most subjects were males with mean age of 69 65 years for case group and 68 25 years for control group Most subjects had advanced primary tumor and lymph node stages Only 30% subjects had metastasized UBC Higher serum HIF-1α level was observed in case group (p < 0 001) Serum HIF-1α level was strongly associated with metastasis stage (p < 0.001), followed by lymph node (p = 0.005) and primary tumor (p = 0 013) stages Serum HIF-1α level was not associated with grading (p = 0.134).
Conclusions: Serum HIF-1α level is associated with staging but not grading of UBC.
KEY WORDS: HIF-1α; Grade; Stage; Urothelial bladder cancer
Submitted 5 March 2023; Accepted 2 April 2023
INTRODUCTION
Urothelial bladder cancer (UBC) is the 7th and the 17th most common cancer globally in men and women, respectively (1) This subtype is responsible for more than 90% bladder cancer cases (2, 3) Annually, there are 110 500 men and 70 000 women diagnosed with new UBC cases worldwide The disease is more frequent in developed countries (1) Every year, 38 200 cases were diagnosed in European Union and 17 000 subjects died due to UBC (1, 2) Smoking is the most important risk
factor for UBC Exposure to chemical compounds, particularly aromatic amines and polycyclic aromatic hydrocarbons, parasitic infection, along with genetic predisposition are also considerable risk factors (1, 4)
Approximately 25% of newly diagnosed UBC are invasive, requiring radical surgery or radiotherapy (1, 2, 5) Unfortunately, the disease outcome is still poor despite systemic therapy (1) Five-year overall survival (OS) and disease-specific survival (DSS) rates for UBC are 57 2% and 77 3%, respectively (2) Early detection of UBC is important to improve patient’s outcome, since the treatment can be delivered aggresively Hypoxia inducible factor (HIF)-1α is a regulatory protein produced in hypoxic microenvironment that consists of two subunits Its expression is found in several solid tumors including UBC, lung, breast, ovary, prostate, and kidney cancers The binding of HIF-1α with its receptor initiates cell proliferation, migration, and invasion in UBC (3, 6, 7) Additionally, HIF-1α is also closely related to angiogenesis (3, 7-9) In this study, we aimed to evaluate the association between HIF-1α and stage and grade of UBC Our findings may provide insight regarding earlier diagnosis, prompt management, improved outcome, and possible therapeutic method for UBC
METHODS
This was a case-control study conducted in JanuaryDecember 2022 at Haji Adam Malik Hospital Medan, Indonesia The inclusion criteria for case group was subject aged 18 years or older and diagnosed with UBC based on histopathological examination Beside diagnosing UBC, biopsy specimen from case group underwent hematoxylin and eosin staining to determine stage and grade of disease All histopathological examinations were conducted at Department of Pathology of Universitas Sumatera Utara Control group included healthy subjects who came to the hospital for general check-up or healthy hospital employers Exclusion criteria was previous history of
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 28
PAPER
ORIGINAL
DOI: 10 4081/aiua 2023 11292
malignancy, bladder lesion due to methastasis from distant primary cancers, patients receiving systemic therapy for badder cancer, patients with diabetes mellitus, chronic kidney disease, and cerebrovascular disease We did gender and age mathcing between the two groups All subjects received explanation regarding this study and were asked to sign informed consent Subjects unwilling to participate in this study were excluded
Serum sample was obtained from each subject in case group Evaluation of serum HIF-1α level was conducted at Research and Esoteric Laboratory Jakarta, Indonesia
We used HIF-1α Human ELISA kit (Ther mo Fisher Scientific Inc , Waltham, USA) to determine serum HIF-1α level in this study Data was analyzed using Statistical Package for Social Science (SPSS) software Categorical data was presented in frequency and percentage while numerical data was presented in median and range if it was not normally distributed Otherwise, it was presented in mean and standard deviation Chi square test was utilized to determine relationship between categorical variables while Mann Whitney and independent T tests were used to determine the relationship between categorical and numerical data All statistical analyses were conducted at confidence interval of 95% A p value of < 0 05 was considered significant
RESULTS
A total of 80 subjects were enrolled in this study All subjects were divided into the two groups equally In case group mean age of subjects was 69 65 years and males subjects were prevalent Most subjects had advanced primary tumor and lymph node involvement Only 30% s u b j e c t s i n t h e c a s e g ro u p h a d m e t a s t a s i z e d U B C Significantly higher serum HIF-1α level was observed in case group compared to control group (Table 1) From statistical analysis, we found that serum HIF-1α l e v e l w a s s t ro n g l y a s s o c i a t e d w i t h m e t a s t a t i c U B C (p < 0 001), followed by UBC with lymph node involvement (p = 0 005) and primary tumor (p = 0 013) stage
Table
Baseline characteristics of subjects
Table 2. Association between serum HIF-1α level and staging and grading of UBC
Overall, serum HIF-1α level was associated with UBC staging (p = 0 008) but not grading (p = 0 134) (Table 2)
DISCUSSION
As most solid tumors grow, the need of oxygen for their metabolism is increased This situation creates hypoxic condition (6, 10) Hypoxic condition upregulates several proteins including HIF-1α that it is important for adaptation of tumor, including UBC, in hypoxic condition Angiogenesis or neovascularization is the end point of this adaptation (3, 4, 6), Hypoxia is also the culprit of treatment resistance in many cancers (8, 10) and HIF-1α is one of the underlying etiologies (11-13) Binding of HIF-1α with its receptor in the nucleus promotes cell proliferation, migration, and invasion Overexpression of HIF-1α is associated with progression and recurrence of UBC (4, 6) The expression of HIF-1α in bladder cancer cells is also influenced by several other factors, such as elevated serum copper level and decreased serum zinc level (4)
In UBC, HIF-1α expression was higher compared to normal tissue (4, 8) The expression of HIF-1α in patients with bladder cancer was in line with the expression of vascular endothelial growth factor (VEGF) (r = 0 606) We know that VEGF is important in neovascularization and growth of malignant tissue (4) This finding was confirmed by Theodoropoulos et al who found in their study that HIF-1α was positively associated with histological grade of UBC This association was mediated by VEGF expression and microvessel density (MVD) Patients with high HIF-1α expression tended to have advanced disease and unfavorable outcome (8) Badr et al also reported similar findings showing that HIF-1α expression is significantly higher in patients with bladder cancer despite its etiology The level of urinary HIF-1α was also able to discriminate between malignant and non-malignant tumor with sensitivity and specificity of 82 1% and 63 3%, respectively In contrast with our results, this study failed to demonstrate significant relationship between HIF-1α and UBC stage and grade (9)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 G
29
Putra Siregar, Ida Parwati, B Sasongko Noegroho, et al
1
Characteristics Case Control P (n = 40) (n = 40) Mean age, years ± SD 69.65 ± 7.01 68.25 ± 7.74 0.400 a Gender, n (%) Male 30 (75%) 32 (80) 0 592 a Female 10 (25%) 8 (20%) Primary tumor stage (T), n (%) NA NA T1+T2 10 (25%) T3+T4 30 (75%) Lymph node stage (N), n (%) NA NA N0 18 (45%) N1 22 (55%) Metastasis stage (M), n (%) NA NA M0 28 (70%) M1 12 (30%) Median HIF-1α level, pg/mL (range) 345 (142-587) 123 (94-234) < 0 001 * b SD: standard deviat on; a chi square test; b Mann Wh tney test; * p < 0 05
Variables Mean HIF-1 α levels, pg/mL ± SD P Primary tumor stage (T) T3+T4 389 ± 126 66 0 013 * T1+T2 273 4 ± 103 89 Lymph node stage (N) N1 410 45 ± 115 4 0 005 * N0 298 56 ± 123 42 Metastasis stage (M) M1 477 ± 95 16 < 0 001 * M0 310 ± 110.34 Staging 3+4 395 67 ± 124 11 0 008 * 1+2 273 4 ± 103 89 Grading High grade 378 ± 131.42 0.134 Low grade 306 4 ± 117 04 SD: standard deviat on; * p < 0 05
Most patients with UBC expressed high HIF-1α Tumor size, histological grade, tumor invasion, and recurrence of UBC were also associated with high HIF-1α expression In line with previous study, this effect was linked to VEGF and MVD Disease free survival (DFS) of UBC was independently influenced by HIF-1α (p = 0 011) (7) Deniz, et al supported these findings with their study Immunoreactivity of HIF-1α was in concordance with stage and histologic grade of UBC Immunoreactivity of HIF-1α was also related to VEGF (p < 0 001) and MVD (p = 0 002) (14) Another study by Theodoropoulos, et al in 2005 reported that HIF1α expression is more common in high grade UBC It was also positively correlated with increased proliferative activity, apoptotic rate, and MVD However, they found no association between HIF-1α alone and prognosis of UBC The prognosis of UBC was associated with both HIF-1α and mutation in p53 nuclear protein (5) A study conducted by Fus, et al reported a contradictive result They found that the expression of HIF-1α is significantly lower in high grade UBC Negative correlation was also reported between the expression of HIF-1α and MVD (3)
We found that serum level of HIF-1α in case group is significantly higher compared to control group (p < 0 001) Serum HIF-1α was also higher in advanced UBC stage, including primary tumor, lymph node, and metastasis stage Higher serum HIF-1α was also observed in advanced UBC grade but the difference was not statistically significant There were several limitations in our study We did not analyze risk factors for UBC other than gender and age We also did not analyze variables that influence the level of serum HIF-1α The kit we used to determine serum HIF1α level was also different which may have given different result Additional study, preferably a meta-analysis, is requested to determine the association between serum HIF-1α level and progression of UBC
CONCLUSIONS
There was a significant association between serum HIF1α level and staging of UBC Serum HIF-1α level may aid in early diagnosis, prompt management, and improved outcome of patients with UBC
REFERENCES
1 Burger M, Catto JWF, Dalbagni G, et al Epidemiology and risk factors of urothelial bladder cancer Eur Urol 2013; 63:234-41
2 Martin JW, Jefferson FA, Huang M, et al A California cancer registry analysis of urothelial and non-urothelial bladder cancer subtypes: epidemiology, treatment, and survival Clin Genitourin Cancer 2020; 18:e330-6
3 Fus LP, Pihowicz P, Koperski L, et al HIF-1α expression is inversely associated with tumor stage, grade and microvessel density in urothelial bladder carcinoma Pol J Pathol 2018; 69:395-404
4 Mortada WI, Awadalla A, Khater S, et al Copper and zinc levels in plasma and cancerous tissues and their relation with expression of VEGF and HIF-1 in the pathogenesis of muscle invasive urothelial bladder cancer: a case-controlled clinical study Environ Sci Pollut Res Int 2020; 27:15835-41
5 Theodoropoulos VE, Lazaris AC, Kastriotis I, et al Evaluation of hypoxia-inducible factor 1 alpha overexpression as a predictor of
tumour recurrence and progression in superficial urothelial bladder carcinoma BJU Int 2005; 95:425-31
6 Xue M, Li X, Li Z, Chen W Urothelial carcinoma associated 1 is a hypoxia-inducible factor-1α-targeted long noncoding RNA that enhances hypoxic bladder cancer cell proliferation, migration, and invasion Tumour Biol 2014; 35:6901-12
7 Chai C, Chen W, Hung W, et al Hypoxia-inducible factor-1alpha expression correlates with focal macrophage infiltration, angiogenesis and unfavourable prognosis in urothelial carcinoma J Clin Pathol 2008; 61:658-64
8 Theodoropoulos VE, Lazaris AC, Sofras F, et al Hypoxia-inducible factor 1 alpha expression correlates with angiogenesis and unfavorable prognosis in bladder cancer Eur Urol 2004; 46:200-8
9 Badr S, Salem A, Yuosif AH, et al Hypoxia inducible factor-1alpha and microvessel density as angiogenic factors in bilharzial and nonbirharzial bladder cancer Clin Lab 2013; 59:805-12
10 Darmadi D, Ruslie RH Association between Prothrombin Induced by Vitamin K Absence-II (PIVKA-II) and Barcelona Clinic Liver Cancer (BCLC) Stage, Tumor Size, Portal Venous Thrombosis in Hepatocellular Carcinoma Patients Sains Malays 2021; 50:475-80
11 Shigeta K, Hasegawa M, Hishiki T, et al IDH2 stabilizes HIF1α-induced metabolic reprogramming and promotes chemoresistance in urothelial cancer EMBO J 2023; 42:e110620
12 Darmadi D, Ruslie RH, Pakpahan C Vascular endothelial growth factor levels difference among hepatocellular cancer patients based on Barcelona clinic liver cancer staging Open Access Maced J Med Sci 2021; 9:797-800
13 Ruslie RH, Darmadi D, Siregar GA Vascular endothelial growth factor (vegf) and neopterin levels in children with steroid sensitive and steroid-resistant nephrotic syndrome Med Arch 2021; 75:133-7
14 Deniz H, Karakok M, Yagci F, Guldur ME Evaluation of relationship between HIF-1α immunoreactivity and stage, grade, angiogenic profile and proliferative index in bladder urothelial carcinomas Int Urol Nephrol 2010; 42:103-7
Correspondence
Ginanda Putra Siregar, MD (Corresponding Author) ginandasir@gmail com
Doctoral Study Program, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia and Division of Urology, Department of Surgery, Faculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia
Ida Parwati, MD
Department of Clinical Pathology, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
Bambang Sasongko Noegroho, MD
Ferry Safridai, MD
Department of Urology, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
Gerhard Reinaldi Situmorang, MD
Department of Urology, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia
Raden Yohana, MD
Division of Oncology, Department of Surgery, Faculty of Medicine, Padjadjaran University, Bandung, Indonesia
Astrid Feinisa Khairani, MD
Department of Biomedical Sciences, Faculty of Medicine, Universitas Padjadjaran, Bandung, Indonesia
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 30 Serum
and
bladder
hypoxia inducible factor-1α level
urothelial
68Ga-PSMA PET/CT evaluation in men enrolled in prostate cancer Active Surveillance
Summary
Introduction: To evaluate the accuracy of 68Ga-prostate specific membrane antigen (PSMA) positron emission tomography/computed tomography (PET/CT) in the diagnosis of clinically significant prostate cancer (csPCa: Grade Group ≥ 2) in men enrolled in Active Surveillance (AS) protocol.
Materials and methods: From May 2013 to December 2021 200 men aged between 52 and 74 years (median age 63) with very low risk PCa were enrolled in an AS protocol study During the follow up 48/200 (24%) men were upgraded and 10/200 (5%) decided to leave the AS protocol After five years from confirmatory biopsy (range: 48-60 months) 40/142 (28.2%) consecutive patients were submitted to mpMRI and 68Ga-PSMA PET/CT imaging examinations before scheduled repeated biopsy. All the mpMRI (PI-RADS ≥ 3) and 68Ga-PET/TC standardized uptake value (SUVmax) ≥ 5 index lesions underwent targeted cores (mpMRI-TPBx and PSMA-TPBx) combined with transperineal saturation prostate biopsy (SPBx: median 20 cores).
Results: Multiparametric MRI and 68Ga-PSMA PET/CT showed 18/40 (45%) and 9/40 (22.5%) lesions suspicious for PCa. In 3/40 (7 5%) men a csPCa (GG2) was found; 68Ga-PSMA-TPBx vs mpMRI-TPBx vs SPBx diagnosed 2/3 (66 6%) vs 2/3 (66 6%) vs 3/3 (100%) csPCa, respectively In detail, mpMRI and 68Ga-PSMA PET/TC demonstrated 16/40 (40%) vs 7/40 (17 5%) false positive and 1 (33 3%) vs 1 (33 3%) false negative results
Conclusion: Although 68PSMA PET/CT did not improve the detection for csPCa of SPBx (1 false negative result equal to 33 3% of the cases), at the same time, would have spared 31/40 (77 5%) scheduled biopsies showing a better diagnostic accuracy in comparison with mpMRI (83.3% vs. 70.2%).
KEY WORDS: Prostate cancer; 68Ga-PSMA PET/CT; Active Surveillance; PCa
Submitted 18 March 2023; Accepted 28 March 2023
INTRODUCTION
Active surveillance (AS) has become an alter native to radical treatment of low/very low risk prostate cancer (PCa), reducing the risk of overtreatment and improving quality of life of the patients (1-3) However, the time of confirmatory biopsy has been established within one year from initial diagnosis (4) there are no data regarding the num-
ber of systematic needle cores and the best imaging procedure to use for omitting or postponing scheduled re p e a t e d b i o p s i e s ; i n t h i s re s p e c t , M u l t i p a r a m e t r i c Magnetic Resonance Imaging (mpMRI) is strongly recommended in AS follow up (4, 5)
R e c e n t l y, P ro s t a t e - s p e c i f i c m e m b r a n e a n t i g e n ( P S M A ) inhibitors conjugated with the radionuclides 68Gallium (68Ga) and 18fluoride (18F) have been well-explored and successfully translated for the clinical diagnosis of PCa (6, 7) Moreover, tumour uptake, which represents PSMA expression (standardised uptake value “SUVmax), resulted highly correlated with the Gleason score of the primary prostatic tumour (9) However, a limited number of studies have focused on the primary prostatic lesion (8, 9) 68Ga-PSMA positron emission tomography/computed tomography (PET/CT) has shown to be sensitive for the detection of primar y prostatic lesions and regional lymphadenopathy (10, 11) Recently, the use of 68Ga-PSMA PET/CT combined with mpMRI has been suggested to improve the accuracy to identify men suitable for active surveillance (12)
The aim of this study is to prospectively evaluate the diagnostic accuracy of 68Ga-PSMA PET/CT in the diagnosis of csPCa (Grade Group ≥ 2) (13) in men enrolled in AS protocol
MATERIALS AND METHODS
From May 2013 to December 2021 200 men aged between 52 and 74 (median age 63) with very low risk PCa were enrolled in an AS protocol study After institutional review board and ethical committee approval were granted, informed consents were obtained from all participants included in the study Presence of the following criteria defined eligibility: life expectancy greater than 10 years, clinical stage T1c, PSA below 10 ng/ml, PSA density (PSA-D) < 0 20, ≤ 2 unilateral positive biopsy cores, Gleason score 6/International Society of Urologic Pathology (ISUP) Grade Groups (GG) 1, maximum core percentage of cancer (GPC) ≤ 50% (3) All the patients underwent confirmatory biopsy 6-12 months later the PCa diagnosis previous mpMRI evaluation During the follow up 48/200 (24%) men were upgraded and 10/200 (5%) men autonomously decided to leave the AS protocol After five
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 31
ORIGINAL PAPER
Pietro Pepe 1 , Ludovica Pepe 1 , Marinella Tamburo 2 , Giulia Marletta 2 , Francesco Savoca 1 , Michele Pennisi 1 , Filippo Fraggetta 3
DOI: 10 4081/aiua 2023 11322
1 Urology Unit, Cannizzaro Hospital, Catania, Italy; 2 Radiotherapy Unit, Cannizzaro Hospital, Catania, Italy; 3 Pathology Unit, Cannizzaro Hospital, Catania, Italy
Figure 1.
68Ga-prostate-specific membrane antigen (PSMA) PET/CT: presence of high vs low suspicious area of clinically significant prostate cancer in the right (A) vs. left lobe (B) of prostate gland (axial valuation) with a standardized uptake value (SUVmax) equal to 88 8 vs 6 5, respectively
A. B.
ed to the clinical data The location of focal uptake on 68Ga-PSMA PET/TC (Figure 1), three-dimensional size, and SUVmax values were reported on a per-lesion basis with a sextant scheme (apex, midgland, and base, each split into left and right) (4)
All the mpMRI (PI-RADS score ≥ 3) and 68GaPET/TC index lesions (SUVmax ≥ 5) (14) underwent cognitive targeted cores (mpMRITPBx and PSMA-TPBx: four cores) combined with saturation prostate biopsy (SPBx: median 20 cores; range 18-22) The procedure was performed transperineally using a tru-cut 18 g a u g e n e e d l e ( B a rd ; C o v i n g t o n , G A , U S A ) under sedation and antibiotic prophylaxis (15) The prostate targeted cores were done using an Hitachi 70 Arietta ecograph, Chiba, Japan) supplied by a bi-planar trans-rectal probe (16) performing a free-hand cognitive approach

years from confirmatory biopsy (range: 48-60 months), also in the presence of stable clinical parameters, the last 40/142 (28 2%) consecutive patients were submitted to mpMRI and 68Ga-PET/CT imaging examinations before scheduled repeated biopsy
All mpMRI examinations were performed using a 1 5 or 3 0 Tesla scanner, equipped with surface 16 channels phased-array coil placed around the pelvic area with the patient in the supine position; multi-planar turbo spinecho T2-weighted (T2W), axial diffusion weighted imaging (DWI) and axial dynamic contrast enhanced (DCE) were performed for each patient The mpMRI lesions characterized by Prostate Imaging Reporting and Data System (PIRADS) version 2 (4) scores ≥ 3 were considered suspicious for cancer; two radiologists blinded to pre-imaging clinical parameters evaluated the mpMRI data separately and independently; moreover, one urologist with more than 25 years of experience performed the biopsy procedure (4)
PET/CT imaging was performed using a CT-integrated PET scanner (Biograph 6; Siemens, Knoxville, TN, USA) 68GaPSMA was prepared with a fully automated radiopharmaceutical synthesis device based on a modular concept (Eckert & Ziegler Eurotope, Berlin, Germany) 68Ga-PSMA-11 was given to patients via an intravenous bolus (mean, 144 ± 12 MBq; range, 122-188 MBq), and the PET acquisition was started at a mean of 58 ± 12 min (range, 50-81 min) afterward Scans were acquired in 3-dimensional mode with an acquisition time of 3 min per bed position Emission data were corrected for randoms, dead time, scatter, and attenuation and were reconstructed iteratively using ordered-subsets expectation maximization (4 iterations, 8 subsets) followed by a postreconstruction smoothing gaussian filter (5 mm in full width at half maximum) For attenuation correction, a low dose unenhanced CT scan was performed from the skull base to the middle of the thigh Images were processed to obtain PET, CT, and PET-CT fusion sections in the axial, coronal, and sagittal planes with a thickness of approximately 0 5 cm by two experienced nuclear medicine specialists, who were blind-
RESULTS
The clinical parameters of the 40 men enrolled in Active Surveillance protocol are listed in Table 1
Multiparametric MRI and 68Ga-PSMA showed 18/40 (45%) and 9/40 (22 5%) lesions suspicious for PCa those were submitted to targeted cores combined with SPBx In detail, mpMRI PI-RADS score resulted ≤ 2 vs 3 vs 4 in 22 (55%) vs 15 (37 5%) vs 3 (7 5%) men The average intraprostatic SUVmax and tumor dimension was 4 6 g/mL (range: 3 2-19 8) and 7 0 mm (range 4-12 mm), respectively; only 9/40 (22 5%) men had a SUVmax ≥ 5 (range: 5 1-19 8), moreover, 68Ga-PSMA PET/TC showed two suspicious areas in correspondence of iliac ala and spinal cord those resulted negative for metastases at targeted MRI for bone evaluation In 3/40 (7 5%) men a csPCa (GG2) was found: both patients had a GPC equal to 20% with a number of positive cores equal to 3 and 4, respectively, moreover PSA density was 0 15, 0 16 and 0 18, respectively 68Ga-PSMA-TPBx vs mpMRI-TPBx vs SPBx diagnosed 2/3 (66 6%) vs 2/3 (66 6%) vs 3/3 (100%) csPCa, respectively In detail, mpMRI and 68Ga-PSMA PET/TC
Table 1.
Clinical parameters of 40 men enrolled in Active Surveillance protocol submitted to scheduled biopsy
Clinical and biopsy findings GG1 40 patients
GG: Internat onal Society of Urolog ca Patho ogy Grade Group; mpMRI: mu t parametr c magnet c resonance imag ng; PSA: prostate spec fic ant gen; GPC: greatest percentage of cancer; PSMA: Prostate specific membrane antigen; PI-RADS: Prostate imag ng report ng and data system; PET/TC: positron emission tomography/computed tomography
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 P
32
Pepe, L Pepe, M Tamburo, G Marletta, F Savoca, M Pennisi, F Fraggetta
Median PSA (range: 4 5-12 5 ng/ml) 4 8 Median PSA density (range: 0 10-0 20) 0 15 Median GPC (range: 10-50%) 40% Median number of positive cores 2 Percentage of positive cores 98% mpMRI 18 PI-RADS score ≥ 3 (45%) 68Ga-PSMA PET/CT 9 suspicious for PCa (22 5%)
demonstrated 16/40 (40%) vs 7/40 (17 5%) false positive and 1 (33 3%) vs 1 (33 3%) false negative results; in detail, one patient had PI-RADS score 2 and SUVmax of 6 8 and the second patient had PI-RADS score 3 and SUVmax equal to 4 5 g/mL In addition, mpMRI and 68Ga-PSMA PET/TC showed a diagnostic accuracy in the diagnosis of csPCa equal to 70 2 and 83 3%, respectively
DISCUSSION
The estimated risk-free treatment at 15 years in men enrolled in AS with GG1 PCa is equal to 58% (1) Although mpMRI is strongly recommended in the revaluation of men in AS (2, 5, 6), still today, scheduled systematic repeated prostate biopsies are recommended to reduce the false negative rate for csPCa of mpMRI equal to 15-20% of the cases (16); At the same time, the number of cores performed at initial and repeat evaluation is directly correlated with a lower risk of reclassification (6) during the follow up allowing to postpone scheduled repeated prostate biopsy in favour of clinical findings (i e , PSA density, risk calculator) (17-19) and imaging revaluation (mpMRI) (5, 6)
In the last years, 68Ga-PSMA-PET/CT has been suggested to improve the clinical staging of high-risk PCa and disease recurrence (20, 21); at the same PSMA PET/CT has been proposed for the diagnosis of primary intraprostatic cancer (22, 23) The presence of focal uptake on PSMAPET/CT (SUVmax) and the maximal dimensions of PETavid lesions have been correlated with the presence of csPCa (24, 25) There is a range of proposed cut-offs to detect csPCa from SUVmax 3 15 to up SUVmax 9 1 (26, 2 7 ) ; t h e c o n c o rd a n c e b e t w e e n p re o p e r a t i v e P S M A PET/TC evaluation (SUVmax, dimension of the lesion) and definitive prostate specimen ranges from 81 2% (28) to 96% (29); moreover, PSMA PET/MRI seems reduce false positive rate of PET/CT (about 8% of cases) (30)
In our series, 68Ga-PSMA-TPBx vs mpMRI-TPBx vs SPBx diagnosed 2/3 (66 6%) vs. 2/3 (66 6%) vs. 3/3 (100%) csPCa, respectively In detail, mpMRI and 68Ga-PSMA PET/TC demonstrated 16/40 (40%) vs 7/40 (17 5%) false positive and 1 (33 3%) vs 1 (33 3%) false negative results In addition, mpMRI and 68Ga-PSMA PET/TC showed a diagnostic accuracy in in the diagnosis of csPCa equal to 70 2 and 83 3%, respectively In definitive, still today, diagnostic imaging should not replace scheduled prostate biopsy but is mandatory to detect targeted lesions suspicious for csPCa; in addion, several biochemical parameters, such as germline evaluation or PHI (prostate health index), could be helpful in decrease the ratio of scheduled biopsy
Among our results some considerations should be made
First, the number of patients evaluated was low Secondly, the results should be evaluated in the entire prostate specimen and not in biopsy histology; a more detailed histological evaluation of patients who underwent biopsy upstaging would be of interest, for example by adding supplementary staining for PSMA on the biopsy samples
Third, the low rate of reclassification (7 5% of the cases) could be explained because the patients previously underwent SPBx plus mpMRI evaluation before confirmatory biopsy Four, 68Ga-PSMA PET/TC evaluation could be pro-
posed in men with negative mpMRI or in the presence of claustrophobia, severe obesity or cardiac pacemaker (13); moreover, a 68Ga-PSMA PET/TC fusion platform would have increased the accuracy of targeted prostate biopsy In conclusion, although 68PSMA PET/CT did not improve the detection for csPCa of SPBx (1 false negative result equal to 33 3% of the cases), at the same time, would have spared 31/40 (77 5%) scheduled biopsies showing a better diagnostic accuracy in comparison with mpMRI (70 2% vs 83 3%)
REFERENCES
1 Carlsson S, Benfante N, Alvim R, et al Long-Term Outcomes of Active Surveillance for Prostate Cancer: The Memorial Sloan Kettering Cancer Center Experience J Urol 2020; 203:1122-1127
2 Briganti A, Fossati N, Catto JWF, et al Active Surveillance for Low-risk Prostate Cancer: The European Association of Urology Position in 2018 Eur Urol 2018; 74:357-368
3 Pepe P, Cimino S, Garufi A, et al Confirmatory biopsy of men under active surveillance: extended versus saturation versus multiparametri c mag n e ti c reson an ce i mag i n g /tran srectal u l trasou n d fusion prostate biopsy Scand J Urol 2017; 51:260-263
4 Pepe P, Pepe L, Pennisi M, Fraggetta F Which Prostate Biopsy in Men Enrolled in Active Surveillance? Experience in 110 Men Submitted to Scheduled Three-Years Transperineal Saturation Biopsy Combined With Fusion Targeted Cores Clin Genitourin Cancer 2021; 19:305-308
5 Pepe P, Garufi A, Priolo GD, et al Is it time to perform only MRI targeted biopsy? Our experience in 1032 men submitted to prostate biopsy J Urol 2018; 200:774-778
6 Caglic I, Sushentsev N, Gnanapragasam VJ, et al MRI-derived PRECISE scores for predicting pathologically-confirmed radiological progression in prostate cancer patients on active surveillance Eur Radiol 2021; 31:2696-2705
7 Perera M, Papa N, Roberts M, et al Gallium-68 prostate-specific membrane antigen positron emission tomography in advanced prostate cancer-updated diagnostic utility, sensitivity, specificity, and distribution of prostate-specific membrane antigen-avid lesions: A systematic review and meta-analysis Eur Urol 2020; 77:403-417
8 Privé BM, Israël B, Schilham MGM, et al Evaluating F-18PSMA-1007-PET in primary prostate cancer and comparing it to multi-parametric MRI and histopathology Prostate Cancer Prostatic Dis 2021; 24:423-430
9 Uprimny C, Kroiss AS, Decristoforo C, et al 68Ga-PSMA-11 PET/ CT in primary staging of prostate cancer: PSA and Gleason score predict the intensity of tracer accumulation in the primary tumour Eur J Nucl Mol Imaging 2017; 44:941-949
10 Zhang Q, Zang SM, Zhang CE, et al Comparison of 68GaPSMA11 PET-CT with mpMRI for preoperative lymph node staging in patients with intermediate to high-risk prostate cancer J Transl Med 2017; 15:230-38
11 Pepe P, Pepe L, Cosentino S, et al Detection Rate of 68Ga-PSMA PET/CT vs mpMRI Targeted Biopsy for Clinically Significant Prostate Cancer Anticancer Research 2022; 42:3011-3015
12 Raveenthiran S, Yaxley WJ, Franklin T, et al Findings in 1,123 Men with Preoperative 68Ga-Prostate-Specific Membrane Antigen Positron Emission Tomography/Computerized Tomography and Multiparametric Magnetic Resonance Imaging Compared to Totally Embedded Radical Prostatectomy Histopathology: Implications for
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 33 68Ga-PSMA PET/CT and Active Surveillance
the Diagnosis and Management of Prostate Cancer J Urol 2022; 207:573-580
13 Pepe P, Pepe L, Tamburo M, et al Targeted prostate biopsy: 68GaPSMA PET/CT vs mpMRI in the diagnosis of prostate cancer Arch Ital Urol Androl 2022; 94:274-277
14 Pepe P, Roscigno M, Pepe L, et al Could 68Ga-PSMA PET/CT evaluation reduce the number of scheduled prostate biopsy in men enrolled in active surveillance protocols? J Clin Med 2022; 16:3473
15 Pepe P, Pennisi M, Fraggetta F How many cores should be obtained during saturation biopsy in the ra of multiparametric magnetic resonance? Experience in 875 patients submitted to repeat prostate biopsy Urology 2020; 137:133-37
16 Pepe P, Garufi A, Priolo G, Pennisi M Can MRI/TRUS fusion targeted biopsy replace saturation prostate biopsy in the re-evaluation of men in active surveillance? World J Urol 2016; 34:1249-53
17 Roscigno M, Stabile A, Lughezzani G, et al The Use of Multiparametric Magnetic Resonance Imaging for Follow-up of Patients Included in Active Surveillance Protocol Can PSA Density Discriminate Patients at Different Risk of Reclassification? Clin Genitourin Cancer 2020; 18:e698-e704
18 Roscigno M, Stabile A, Lughezzani G, et al Multiparametric magnetic resonance imaging and clinical variables: Which is the best combination to predict reclassification in active surveillance patients? Prostate Int 2020; 8:167-172
19 Pepe P, Dibenedetto G, Pepe L, Pennisi M Multiparametric MRI Versus SelectMDx Accuracy in the Diagnosis of Clinically Significant PCa in Men Enrolled in Active Surveillance In Vivo 2020; 34:393396
20 Pepe P, Pennisi M Should 68Ga-PSMA PET/CT Replace CT and Bone Scan in Clinical Staging of High-risk Prostate Cancer? Anticancer Res 2022; 42:1495-1498
21 Kwan TN, Spremo S, Teh AYM, et al Performance of Ga-68 PSMA PET/CT for diagnosis and grading of local prostate cancer Prostate International 2021; 9:107-112
22 Ma L, Zhang WC, Ya-Xin Hao YX, Hao YX Current state of prostate-specific membrane antigen PET/CT imaging-targeted biop-
sy techniques for detection of clinically significant prostate cancer J Med Imaging Radiat Oncol 2022; 66:776-780
23 Perera M, Papa N, Roberts M, et al Gallium-68 Prostate-specific Membrane Antigen Positron Emission Tomography in Advanced Prostate Cancer-Updated Diagnostic Utility, Sensitivity, Specificity,
Lesions: A Systematic Review and Meta-analysis Eur Urol 2020; 77:403-417
24 Demirci E, Kabasakal L, Sahin OE, et al Can SUVmax values of Ga-68-PSMA PET/CT scan predict the clinically significant prostate cancer? Nucl Med Commun 2019; 40:86-91
25 Rüschoff JH, Ferraro DA, Muehlematter UJ, et al What's behind 68Ga-PSMA-11 uptake in primary prostate cancer PET? Investigation of histopathological parameters and immunohistochemical PSMA expression patterns Eur J Nucl Med Mol Imaging 2021; 48:4042-4053
26 Franklin A, Yaxley WJ, Raveenthiran S, et al Histological comparison between predictive value of preoperative 3-T multiparametric MRI and 68Ga-PSMA PET/CT scan for pathological outcomes at radical prostatectomy and pelvic lymph node dissection for prostate cancer BJU Int 2021; 127:71-79
27 Liu Y, Yu H, Liu J, et al A Pilot Study of 18 F-DCFPyL PET/CT or PET/MRI and Ultrasound Fusion Targeted Prostate Biopsy for Intra-Prostatic PET-Positive Lesions Front Oncol 2021; 11:612157
28 Kalapara AA, Nzenza T, Pan HYC, et al Detection and localisation of primary prostate cancer using 68 gallium prostate-specific membrane antigen positron emission tomography/computed tomography compared with multiparametric magnetic resonance imaging and radical prostatectomy specimen pathology BJU Int 2020; 126:83-90
29 Xue AL, Kalapara AA, Ballok ZE, et al 68Ga-Prostate-Specific M
Standardized Uptake Value as a Predictor of Gleason Pattern 4 and Pathological Upgrading in Intermediate-Risk Prostate Cancer J Urol 2022: 207:341-349
30 Bhanji Y, Rowe SP, Pavlovich CP New imaging modalities to consider for men with prostate cancer on active surveillance World J Urol World J Urol 2022; 40:51-59
Correspondence
Pietro Pepe, MD (Corresponding Author) piepepe@hotmail com
Ludovica Pepe, MD ludopepe97@gmail com
Francesco Savoca, MD
Michele Pennisi, MD
michepennisi2@virgilio it
Urology Unit, Cannizzaro Hospital
Via Messina 829, Catania, Italy
Marinella Tamburo, MD
marinellatamburo@virgilio it
Giulia Marletta, MD
marlettagiulia1@gmail com
Radiotherapy Unit, Cannizzaro Hospital, Catania, Italy
Filippo Fraggetta, MD
filippofra@hotmail com
Pathology Unit, Cannizzaro Hospital, Catania, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 P
L
M
34
Pepe,
Pepe,
Tamburo, G Marletta, F Savoca, M Pennisi, F Fraggetta
a n d D i s t r i b u t i o n o f P ro s t a t e - s p e c i f i c M e m b r a n e A n t i g e n - a v i d
e m b r a n e A n t i g e n P o s i t ro n E m i s s i o n To m o g r a p h y M a x i m u m
ORIGINAL PAPER
Safety and tolerability of biodegradable balloon spacers in patients undergoing radiotherapy for organ-confined prostate cancer
Summary
Introduction: Radiotherapy is a common treatment for prostate cancer, and can be administered in various ways, including 3D conformal radiotherapy (3DCRT), intensity-modulated radiotherapy (IMRT) and hypo-fractionated radiation therapy. During treatment the gastrointestinal tract may be exposed to radiation and the rectal wall may be exposed to high doses of ionizing radiation, which can lead to rectal bleeding, ulcers or fistulas, and an increased risk of rectum cancer Various strategies to minimize these complications have been developed in the last decade; one of the most promising is to use a rectal balloon to fixate the prostate gland during treatment or to inject biodegradable spacers between the prostate and rectum to reduce the rectal dose of radiation Aim of our paper is to evaluate the safety and tolerability of spacers implantation
Materials and methods: From January 2021 to June 2022 all patients with a diagnosis of prostate cancer with unfavorable/intermediate risk - poor prognosis and programmed hypofractionated radiation therapy were enrolled.
In all patients biodegradable balloons spacers were placed posteriorly to the prostate to increase the separation between prostate and rectum The duration of the procedure, observation time, the appearance of early and late complications and their severity (according to Charlson comorbidity index) and tolerability of the device were recorded at the time of positioning and after 10 days.
Results: 25 patients were enrolled in our study. Two patients (8%) underwent acute urine retention resolved with catheterization and one patient (4%) developed a mild perineal hematoma that did not require any treatment As regards late complications 1 patient (4%) developed hyperpyrexia (> 38°C) the day after the procedure requiring continuation of antibiotic regimen. At T1 visit we recorded no medium-high grade complications. As for the tolerability of the device, it was optimal with no perineal discomfort or alterations of bowel function
Conclusions: Biodegradable balloon spacers appears to be safe and well tolerated and its positioning does not present any technical difficulties or risks of major complications
KEY WORDS: Prostate cancer; Spacer; Radiotherapy; Hypo-fractionated radiotherapy
Submitted 14 January 2023; Accepted 22 April 2023
INTRODUCTION
Prostate cancer (PCa) is the second most commonly diagnosed cancer in men, with approximately 1 1 million diagnoses worldwide each year, accounting for 15% of all cancers diagnosed (1) The incidence of PCa increases with age, with over 25% of men over the age of 75 years being affected (1) Low-risk PCa (PSA < 10 ng/ml, ISUP 1, T2a) can be managed through several different modalities, including the non-operative approach of “active surveillance” , which involves laboratory and clinical monitoring of tumor progression and active treatment if necessary (2) Other active treatments, such as radiotherapy or surgery, are also options Intermediate/high-risk organconfined prostate cancers require active treatment, which may include surgery and/or radiotherapy (exter nal beam or brachytherapy) Approximately 40% of people with prostate cancer undergo radiotherapy as part of their treatment, which can serve various purposes such as curative intent, post-operative adjuvant, post-operative rescue intent, or palliative intent (3) Conventional radiotherapy is delivered as external beam radiotherapy (EBRT), and conformal radiotherapy, including 3D confor mal radiotherapy (3DCRT) and intensity-modulated radiotherapy (IMRT), is commonly used in high-income countries During treatment, despite recent advances in techniques and technologies that allow precise delivery of radiation on the focus organ, pelvic radiotherapy inevitably exposes the surrounding normal gastrointestinal tract to some degree of radiation, potentially causing rectal bleeding, ulcers or fistulas and increasing the risk of rectal cancer by 105% over the following decade (4)
Different strategies have been recently adopted and implemented to minimize these complications; one technique aims to fixate the prostate gland during radiation treatment via a rectal balloon to reduce the prostate motion and to make sure the dose delivered to the target volume is efficient , allowing a safer and smaller planning target volume margin as stated elsewhere (5, 6) By using a rectal balloon, the dose exposure to the posterior rectal wall is decreased as opposed to an increased dose to the anterior rectal wall
Biodegradable balloon spacers are three-dimensional scaffolds that can be implanted between the prostate gland
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 35
Luca Topazio 1 , Federico Narcisi 1 , Fabio Tana 2 , Cosimo Ciotta 2 , Iossa Vincenzo 2 , Pasquale Perna 2 , Francesco Chiaramonti 2 , Federico Romantini 1
1 ASL Teramo, U O C di Urologia, Teramo, Italy;
DOI: 10 4081/aiua 2023 11156
2 University of L'Aquila, Department of Life, Health and Environmental Sciences, L'Aquila; U O C di Urologia, P O Mazzini, Teramo, Italy
and rectum to protect the rectum from radiation during radiotherapy They are commercially available in Europe
A further clinically available technique reduces the rectal dose of radiations using the injection of materials such as hydrogel, hyaluronic acid gels, and collagen between the prostate and rectum, remarkably lessening late-rectum toxicity Spacers implantation is indeed a minimally invasive surgical procedure guided by transrectal ultra-sound that permit the positioning of biodegradable balloons that can be placed posteriorly to the prostate to increase the separation between prostate and rectum thus protecting the latter from radiations during RT sessions It demands attendance of a trained physician, qualified to perform this kind of surgery The procedure takes from 10 to 30 min and can be carried out under local or general anesthesia
As reported in the EAU 2022 guidelines, “ a meta-analysis including one RCT and six cohort studies using the hydrogel spacer demonstrated a 5-8% reduction in the rectal volume receiving high-dose radiation ” (7) Spacers can be implanted in outpatient setting, using local, epidural, or general anesthesia

A recent study, evaluated the correlation between the use of prostate spacers and the incidence of erectile dysfunction in men with organ-confined prostate cance submitted to hypofractionated radiotherapy (8) The use of spacers allowed to keep pretreatment sexual potency in 62 5% of the cases (8)

A biodegradable balloon spacer is a three-dimensional scaffold made of biocompatible material that is designed to be implanted between the prostate gland and the rectum, prior to the beginning of a radiotherapy program It is biodegradable and it is actually commercialized in Europe (Figure 1) With the patient in the lithotomy position, and under transrectal ultrasonography (TRUS) guidance, an 18-gauge needle is inserted between Denonvilliers’ fascia and the anterior rectal wall (Figure 2) Once the needle is in the correct position, saline water is injected to carry out hydro-dissection and to create a potential space between the prostate and rectum Implantation time is relatively short, with a mean overall procedure time of 16 minutes (7 8 min) from time of TRUS insertion to TRUS removal; moreover, the biodegradable
gel takes an average of 6 to 12 months to absorb once injected in the patients’ regions of interest Reported complications of spacers positioning, although rare, are prostatic abscess, fistulae and sepsis The aim of this study is to evaluate the safety and efficacy of biodegradable balloon spacer placement in prostate cancer patients who are candidates for radiation treatment
MATERIALS AND METHODS
This is a prospective observational study that enrolled patients with a diagnosis of prostate cancer (PCa) who had unfavorable/intermediate risk (poor prognosis) and were receiving hypofractionated radiation therapy between January 2021 and June 2022 Patients who had previously received pelvic irradiation for rectum morbidities were also included in the study, and no exclusion criteria were used in the patient selection phase The timing of the procedure, related complications, and the tolerability of the device were evaluated at two time points: T0 (the day of spacer placement) and T1 (an ambulatory control visit at 10 days) The spacer (BIOPROTECT® biodegradable spacer) was placed in an outpatient setting with the patient in a lithotomic position Cefazoline 1 gram was administered intravenously and local anesthesia was given to the perineal area and levator ani muscles with 2% mepivacaine The procedure was performed using transrectal ultrasound with a biplanar probe A cutaneous incision was made at the perineal level, 1 cm above the anus, and the dilator was inserted behind the prostate at the level of the Denonvilliers’ fascia Hydrodissection was performed to create a well-defined plane from the prostate apex to the seminal vesicles The device containing the balloon was then inserted and advanced to the level of the seminal vesicles, inflated with physiological solution (16-23 ml), and released The correct positioning of the device was confirmed using transrectal ultrasound (TRUS) The patient was observed for any early complications during the post-procedural observation period before being dismissed Late complications and the tolerability of the device were evaluated at T1 The duration of the procedure (in minutes), observation time (in minutes), and the appearance and severity (according to the Charlson comorbidity index) of early and late complications were
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 L Topazio, F Narcisi, F Tana, et al 36
Figure 1.
Illustration of a biodegradable balloon spacer positioning
Figure 2
Illustration of the 18-gauge needle needed for the implantation of the spacer.
recorded The tolerability of the device was evaluated using a scale from 0 to 10 for discomfort (0 = no discomfort, 10 = severe discomfort) and by assessing pelvic-perineal encumbrance and changes in bowel function After the T1 visit, the patient was sent for radiotherapy
RESULTS
From January 2021 to June 2022, 25 patients were enrolled Their baseline epidemiological data are shown in Table 1 The procedure was performed in an outpatient setting following the protocol described in the previous section The average time of the procedure was 18 minutes [10-25 min] All patients were then discharged within two hours of the procedure (average post-op observation time: 90 minutes [45-110 min]), after the resumption of spontaneous micturition and the absence of early complications Two patients (8%) experienced acute urine retention that was resolved with catheterization, a n d o n e p a t i e n t ( 4 % ) d e v e l o p e d a m i l d p e r i n e a l hematoma that did not require treatment As for late complications, one patient (4%) developed fever (> 38°C) the day after the procedure, requiring continuation of the antibiotic regimen At the T1 visit, no medium-high grade complication was recorded The tolerability of the device was optimal, with an average score of 2 and a range of 04 on the previously described discomfort scale
No patients reported disturbances in defecation, changes in intestinal transit, or a sense of encumbrance in the pelvic-perineal area Results are listed in Table 2
DISCUSSION
Prostate cancer (PCa) is the second most common cancer among men worldwide, ranking first in developed countries According to the World Research Fund International, there were over 1 4 million new diagnoses of PCa in 2020 worldwide The incidence and mortality of PCa are correlated with age, with the average age of diagnosis being 66 years There is a higher incidence of PCa in AfricanAmerican men compared to white men, with 158 3 new cases diagnosed per 100 000 men and double the mortality While the lethality of PCa is not as severe as other types of cancer, the number of yearly deaths due to PCa is high due to its high incidence
PCa diagnosis is based on standardized protocols that involve prostate specific antigen (PSA) testing, digital rectal examination (DRE), and the newly implemented multiparametric magnetic reonance imaging (mpMRI) as an additional diagnostic tool before biopsy, allowing for the specific targeting of possible malignant lesions
There are various treatment options for organ-confined PCa, ranging from active surveillance to active treatment with surgery or radiotherapy Radiotherapy (RT) can be performed in various settings, such as external beam RT (EBRT) and intensity-modulated RT (IMRT) IMRT delivers a precise beam of modulated intensity that delivers radiation with higher selectivity to prostatic tissue, minimizing exposure to proximal organs
An hypofractionated RT protocol uses a higher dose of radiation per session, reducing the number of necessary sessions The major drawback of RT is the incidental irradiation of proximal anatomical areas, such as the rectum, which is mostly inevitable due to the anatomical relationship between the rectum and prostate Spacers provide a solution to this problem by inserting a device between the prostate and rectum, separating the target of the radiation beam from a contiguous organ In addition, the procedure can be performed in an outpatient setting via a dayhospital regimen, resulting in reduced costs and minimal operative time (9)
Overall, the implantation of spacers has been shown to be safe and fast, with optimal tolerability of the device (10, 11) No severe complications were observed in the postprocedural time (T0), allowing the procedure to be performed in an outpatient setting and at T1 follow-up outpatient visit Mild complications related to the implantation procedure have been documented, but they are relatively uncommon We recorded one episode of acute urinary retention (AUR) in a patient with a voluminous enlarged prostate, a risk factor commonly associated with prostate biopsies
The incidence of urinary tract infections (UTIs) is comparable to that of transperineal prostate biopsies, so adherence to the most recent guidelines is recommended (12) Even among the most unfavorable cases (patients who have already undergone radiation treatment and need another cycle of IMRT), no complications ranging from mild to severe were reported, in contrast to what is suggested in the EAU guidelines about this topic (fistulas, abscesses, sepsis)
Our overall experience is in line with the European consensus, as we did not encounter acute or delayed intermediate-severe complications, despite having modest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 37
Tolerability of biodegradable balloon spacers
Table
Baseline
Patients’ characteristics Number of patients 25 pts Age 68 yo (range 59-77) Tumor stage cT1c: 10 pts cT2a: 8 pts cT2b: 7 pts cT2c: o pts (0%) PSA level 14 ng/ml (8-27 ng/ml) ISUPP ISUPP 1: 4 pts ISUPP 2: 6 pts ISUPP 3: 15 (%) pts ISUPP 4: 0 (0%) pts ISUPP 5: 0 (0%) pts
1.
epidemiologic data
Table 2
Average duration of the procedure 18 minutes (10-25 minutes) Average duration of observation 90 minutes (45-110 minutes) Early complications Acute urinary retention 2 pz (10%) Hematoma 1 pz (5%) Late complications Fever 1 pz (5%) Spacer tolerability score 2 (0-4) Reported bowel symptoms 0 pz Perineal bulk sensation 0 pz
Data obtained after the spacer placement
previous experience with these types of devices and transperineal procedures This highlights the low lear ning curve for this procedure
CONCLUSIONS
Biodegradable balloon spacers appear to be safe and well tolerated and their positioning does not present any technical difficulties or risks of major complications Its usage can and must be discussed when dealing with patients diagnosed with prostate cancer and scheduled to undergo radiation therapy in order to increase the selectivity of such treatment by protecting the rectum via mechanical separation from the prostate The device is designed to be left in place as it is biodegradable and does not require any additional maintenance or monitoring
There are several potential benefits to using a biodegradable balloon spacer in the treatment of prostate cancer In addition to potentially improving the effectiveness of radiation therapy, it may also reduce the risk of side effects such as rectal bleeding and discomfort It may also help to reduce the risk of long-term complications such as bowel and urinary incontinence
Overall, the biodegradable balloon spacers are promising tools in the treatment of prostate cancer, offering the potential for improved outcomes and fewer side effects for patients It is an important advancement in the field of cancer treatment and continues to be studied and refined in order to optimize its effectiveness and safety
Nonetheless, further data must be gathered as more of these devices are effectively used in everyday clinical practice to improve our understanding of its efficacy in protecting the rectum from radiation beams and their effects on the quality of life of patients, thus requiring a longer follow-up
REFERENCES
1 Wang L, Lu B, He M, et al Prostate Cancer Incidence and Mortality: Global Status and Temporal Trends in 89 Countries From 2000 to 2019 Front Public Health 2022; 10:811044
2 EAU Guidelines Edn presented at the EAU Annual Congress Amsterdam 2022 ISBN 978-94-92671-16-5
3 Hummel S, Simpson EL, Hemingway P, et al Intensity-modulated radiotherapy for the treatment of prostate cancer: a systematic review and economic evaluation Health Technol Assess 2010; 14:1108, iii-iv
4 Nilsson S, Norlén BJ, Widmark A A systematic overview of radiation therapy effects in prostate cancer Acta Oncol 2004; 43:316-81
5 Navaratnam A, Cumsky J, Abdul-Muhsin H, et al Assessment of Polyethylene Glycol Hydrogel Spacer and Its Effect on Rectal Radiation Dose in Prostate Cancer Patients Receiving Proton Beam Radiation Therapy Adv Radiat Oncol 2019; 5:92-100
6 Mok G, Benz E, Vallee JP, et al Optimization of radiation therapy techniques for prostate cancer with prostate-rectum spacers: a systematic review Int J Radiat Oncol Biol Phys 2014; 90:278-88
7 Miller LE, Efstathiou JA, Bhattacharyya SK, et al Association of the Placement of a Perirectal Hydrogel Spacer With the Clinical Outcomes of Men Receiving Radiotherapy for Prostate Cancer: A Systematic Review and Meta-analysis JAMA Netw Open 2020; 3:e208221
8 Pepe P, Tamburo M, Panella P, et al Erectile dysfunction following hydrogel injection and hypofractionated radiotherapy for prostate cancer: Our experience in 56 cases Arch Ital Urol Androl 2022; 94:166-168
9 Fathy MM, Hassan BZ, El-Gebaly RH, Mokhtar MH Dosimetric evaluation study of IMRT and VMAT techniques for prostate cancer based on different multileaf collimator designs Radiat Environ Biophys 2023; 62:97-106
10 Thompson AB, Hamstra DA Rectal Spacer Usage with Proton Radiation Therapy for Prostate Cancer Int J Radiat Oncol Biol Phys 2020; 108:644-648
11 Sanei M, Ghaffari H, Ardekani MA, et al Effectiveness of rectal displacement devices during prostate external-beam radiation therapy: A review J Cancer Res Ther 2021; 17:303-310
Complications following Prostate Biopsy: A Systematic Review and Meta-Analysis J Urol 2021; 205:653-663
Correspondence
Luca Topazio, MD (Corresponding Author) luca topazio@aslteramo it
Federico Narcisi, MD federico narcisi@aslteramo it
Federico Romantini, MD federico romantini@aslteramo it
ASL Teramo, U O C di Urologia (Teramo), Italy
Fabio Tana, MD fabiotana21@gmail com
Cosimo Ciotta, MD ciottacosimo@live it
Vincenzo Iossa, MD vincenzoiossa@msn com
Pasquale Perna, MD pasquper@gmail com
Francesco Chiaramonti, MD
francesco tr92@virgilio it
University of L'Aquila (L'Aquila), Department of Life, Health and Environmental Sciences; U O C di Urologia, P O Mazzini, (Teramo), Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 L Topazio, F Narcisi, F Tana, et al 38
1 2 P r a d e re B , Ve e r a t t e r a p i l l a y R , D i m i t ro p o u l o s K , e t a l N o n a n t i b i o t i c S t r a t e g i e s f o r t h e P re v e n t i o n o f I n f e c t i o u s
Enhanced recovery after retrograde intra-renal surgery (RIRS) in comparison with mini-percutaneous nephrolithotomy (Mini-PCNL) for renal stone treatment
Vladimir Vorobev 1 , Vladimir Beloborodov 1 , Temirlan Hovalyg 1 , Igor Seminskiy 2 , Andrey Sherbatykh 3 , Igor Shaderkin 4 , Mikhail Firsov 5
1 Department of General Surgery, Irkutsk State Medical University, Krasnogo Vosstaniya str , 1, Irkutsk, 664003, Russian Federation;
2 Department of Pathology, Irkutsk State Medical University, Krasnogo Vosstaniya str , 1, Irkutsk, 664003, Russian Federation;
3 Department of Faculty Surgery, Irkutsk State Medical University, Krasnogo Vosstaniya str , 1, Irkutsk, 664003, Russian Federation;
4 E-Health Laboratory, I M Sechenov First Moscow State Medical University, Pirogovskaya str , 2, Moscow, 119296, Russian; Federation;
5 Department of Urology, Andrology and Sexology, Krasnoyarsk State Medical University named after Professor V F Voino-Yasenetsky, Partizan Zheleznyaka str , 1, Krasnoyarsk, 660022, Russian Federation
Summary
Objectives. The study presents a comparative analysis of the mini-percutaneous nephrolithotripsy (mini-PCNL) and retrograde nephrolithotripsy (RIRS) with a logistic analysis of outcomes and complications
Material and methods. The prospective study included 50 patients diagnosed with urolithiasis from 2018 to 2021 in the urological hospitals in Irkutsk. Patients were divided into two groups: RIRS (group I, n = 23) and Mini-PCNL (group II, n= 27). The comparison groups are statistically homogeneous. Results Both procedures equally lead to high stone free rates (SFR > 1 mm, 91.3% vs 85.1%; p = 0.867; SFR > 2 mm, 95.6% vs 92 5%; p = 0 936) The intergroup analysis of the total operation time (and lithotripsy) demonstrated similar times (p > 0 05) Postoperative complications of classes II-III (Clavien-Dindo) in the early and late postoperative period developed rarely and were comparable (p > 0 05) Class I complications were predominant in the PCNL group (p = 0.007). Some parameters demonstrated the superiority of RIRS over PCNL: less pronounced pain syndrome (p = 0 002), less drainage time (p < 0 001), no postoperative hematuria (p = 0 002), shorter hospitalization and total treatment period (p < 0 001)
Conclusions The study highlighted the positive effect of the oneday surgery principle on the risk of developing postoperative hematuria, urinary infection, or severe postoperative pain RIRS and mini-PCNL have similar effectiveness, but RIRS meets the criteria of the enhanced recovery program more than PCNL
KEY WORDS: Fast track surgery; RIRS; PCNL; mini-PCNL; Enhanced recovery
Submitted 4 November 2022; Accepted 17 February 2023
INTRODUCTION
Enhanced recovery is the conventional name of various protocols or programs for optimizing the perioperative period (for example, fast track surgery, Enhanced Recovery
After Surgery or ERAS) aimed at restoring health, working capacity, and improving the quality of treatment
Urolithiasis is a widespread disease affecting up to 12% of the human population, with pronounced social and eco-
nomic significance The social aspect is related to the long duration of the illness, the high recurrence rate (up to 50%), and its frequent urgent presentation, leading to sudden disability (1) The economic aspect is related to high personal and government costs for treatment, and loss of working activity Mortality from urolithiasis has recently increased (2, 3)
The multifactorial process of stone formation leads to a wide variety of clinical presentations One of the most common forms of urolithiasis is the formation of calcium oxalate stones (4) The increased concentration of salts in the urine, inflammation, the presence of papillary plaques and plugs in the collecting system of the kidney, and other factors contribute to the development of the disease (5) A complex of metaphylactic measures, such as lifestyle changes, hyperhydration, dietary modifications, correction of concomitant diseases and hormonal disorders, is considered extremely important to prevent relapses after surgical treatment In addition, the prevention of postoperative recurrence depends on minimizing intraoperative trauma, reducing the risk of infectious complications, and avoiding residual fragments that can act as initial nucleus of stone formation (6)
It is important to note that the recommendations for stone treatment have been changed in the context of the pandemic The International Endourological Society has reached a consensus on several recommendations for urolithiasis treatment Thus, it was recommended to conduct remote counseling, avoid intubation methods of anesthesia, reduce indications for surgical treatment of asymptomatic concretions, etc (7)
Currently, there are two most effective alternative methods for minimally invasive removal of kidney stones with a high level of stone-free rate (SFR) that are the retrograde nephrolithotripsy or retrograde intra-renal surgery (RIRS) and the percutaneous nephrolithotomy (PCNL) using flexible optics (8, 9) These methods are superior to the alternative method, shock-wave lithotripsy, in terms of SFR and complications (10, 11) An effective combination of both methods is possible in complex cases (12, 13) Both
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 39 ORIGINAL PAPER
DOI: 10 4081/aiua 2023 10991
methods lead to several postoperative complications, such as hematuria, fever, extravasation, pain However, complications after RIRS are less pronounced and less likely to require surgical treatment (14, 15) Nevertheless, reducing the diameter of the working tool can reduce the severity of complications after PCNL and even surpass RIRS (10)
There is a small number of publications devoted to RIRS (according to PubMed, 601 works on 02 02 2022 from 1988 to 2022), and only 48 comparative studies of RIRS and PCNL (according to PubMed, 48 works on 02 02 2022 from 2008 to 2022) Moreover, there are practically no comparative studies on optimization of the perioperative period to improve the treatment effectiveness and enhance recovery
The study presents a comparative analysis of the use of mini-percutaneous nephrolithotripsy (mini-PCNL) and retrograde nephrolithotripsy (RIRS) with a logistic analysis of outcomes and complications
METHODS Research design
The local ethics committee of the Irkutsk State Medical University (ISMU) of the Ministry of Health of the Russian Federation approved the clinical trial It was a prospective, blind, randomized study in Irkutsk urological hospitals
The study included an analysis of perioperative data and treatment outcomes in patients with urolithiasis who underwent one of the surgical methods established by the protocol from January 2018 to October 2021
Surgical operations were performed using one of two endourological methods:
mini-PCNL or RIRS
All the features of the planned treatment methods were explained to the patient
Inclusion criteria:
– planned surgery for kidney stones;
– indications for the operation meeting the criteria of the approved protocol;
– operation was planned to use one of the methods approved in the study;
age over 18 years;
patient signed a voluntary informed consent to participate in the study
Non-inclusion criteria:
– no indication to treatment;
– presence of concomitant diseases that significantly affect the general conditions of the patient (decompensated diabetes mellitus, heart failure, gross neurological deficits, etc );
– inability to comply with the protocol of the study
Exclusion criteria:
– deviation from the study protocol;
– deviation from the criteria of the group
The inclusion of patients in the study was carried out prospectively and continuously, until reaching the minimum sample size (20 patients in each group) and then within the planned timeframe of the study Finally, there were 77 patients recruited to participate in
the study, out of them 50 patients completed the study
All the included patients were randomized into two groups based on the approved study protocol The groups were not artificially aligned The first group was treated with RIRS, the second group with mini-PCNL
Deviations from the protocol
Of the 77 patients included in both groups in the study, 27 were excluded (17 - due to deviation from the protocol, and 10 - for personal reasons) The evaluation of the results (per-protocol) included 50 patients who meet all the criteria of the study RIRS group included 23 patients (group I) and mini-PCNL group included 27 patients (group II)
Outcomes
Primary outcomes of the study were: absence of residual fragments in the postoperative period, not earlier than a month later; need for re-operation, migration of the stone into the ureter during surgery Secondary outcomes: p o s t o p e r a t i v e e x a m i n a t i o n d a t a ; r e n a l c o l i c ; u r ohematomas; urine leakage; recurrence of stone formation
Comparison of study groups
Table 1 presents the preoperative parameters of patients
The statistical analysis established the homogeneity of the two groups (p > 0 05) according to the initial status
Diagnostic methods
Evaluation included clinical history (history of stone disease, concomitant diseases, etc ), physical examination,
Table 1
Preoperative status
Parameter Group I Group II P (n = 23) (n = 27)
Age, years
Weight, kg
Height, cm
BMI, units
Female, n (%)
Disease duration, days
Emergency intervention, n (%)
Re-stenting, n (%)
Leukocytosis, n (%)
Anemia, n (%)
Ischemic heart disease, n (%)
Hypertension, n (%)
Diabetes mellitus, n (%)
Prostate hyperplasia, n (%)
Urinary tract cancer, n (%)
Kidney cysts, n (%)
Chronic urinary infection, n (%)
Area of the largest concretion, mm2
HU density, units
Concretion > 20 mm, n (%)
More than one concretion, n (%)
Calcium oxalates, n (%)
60 (51; 63)
88 2 ± 20 8
1 66 ± 0 1
31 (27; 37)
16 (69.5%)
15 (4; 36)
2 (8 6%)
0 (0%)
3 (13 0%)
1 (4 3%)
10 (43 4%)
14 (60 8%)
3 (13.0%)
6 (26 0%)
1 (4 3%)
4 (17 3%)
8 (34 7%)
135 (117;195)
948 (± 298)
5 (21 7%)
8 (34 7%)
15 (65.2%)
12 (44 4%)
13 (5; 26)
5 (18 5%)
2 (7 4%)
4 (14 8%)
2 (7 4%)
11 (40 7%)
11 (40 7%)
3 (11 1%)
1 (3 7%) 0 (0%)
1 (3 7%)
15 (55.5%)
120 (90;228)
909 (± 394)
8 (29 6%)
11 (40 7%)
19 (70 3%)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 V
40
Vorobev, V Beloborodov, T Hovalyg, I Seminskiy, A Sherbatykh, I Shaderkin, M Firsov
–
–
15 7
70 ± 0 08
51 (39; 55) 81 1 ±
1
28 (25; 30)
0 413 0 173 0 147 0 052 0 345 0 847 0.384 0 199 0 875 0 668 0 900 0 414 0 852 0 049 0 284 0 147 0 367 0 602 0 697 0 626 0 771 0 864
biochemistry, imaging (ultrasound, tomography, X-ray) and endoscopy
The analysis of the composition of the calculi was performed by spectroscopy in a specialized laboratory after surgery
Multi-slice computer tomography (MSCT) examination helped to assess the urinary system status, including the density and size of concretions
The severity of postoperative pain syndrome was assessed according to the Visual Analog Scale (VAS) of pain
Before removal of the urethral catheter, nephrostomy, and stent an ultrasound examination was performed to rule out possible uro-hematomas No earlier than one month after the operation and no later than two months, there was the first control by MSCT to assess SFR After the first follow up visit after surgery, patients regularly (once every six months) underwent the examinations established by the protocol of the study: consulta-
Table 2.
tion of the operating doctor, blood and urine tests, ultrasound MSCT
There were several criteria for evaluation of treatment effectiveness: SFR, no re-operation, no complications > Class II according to Clavian-Dindo SFR was evaluated according to two criteria: fragments > 1 mm and fragments > 2 mm
The perioperative period was evaluated separately by assessing the length of hospital stay, the total period of disability, the functional status in the postoperative period (pain, temperature, etc )
The cost-effectiveness of treatment was not evaluated
Surgical treatment
During the study, a common protocol of enhanced recovery for patients with planned endourological intervention foe renal stones was followed in both groups
Table 2 presents the protocol scheme
The enhanced recovery protocol for endourological surgery for kidney stones
PREOPERATIVE
– Informing the patient about the disease, treatment options, and possible outcomes, indicating the average effectiveness, risks of complications, typical postoperative condition, timing of catheterization, hospitalization, possible methods of pre-rehabilitation, and further rehabilitation methods
– One-day concept: the patient undergoes most of the preoperative examinations in one day, without the need for multiple re-preparation; the order of examinations and tests is optimized and sorted to achieve the desired outcome
– Rigorous evaluation of indications for surgical treatment: symptomatic concretions; chronic urinary infection; concretions > 15 mm; progressive size growth; obstructive disorders; recurrent course
– Assessment of the possibility of patient compliance with the protocol and its feasibility in the medical institution
– Preventive administration of antihistamines and antacids drugs
– Avoiding of preoperative sedation
– Pre-rehabilitation based on indications: age group; obesity; exhaustion; sarcopenia; impaired carbohydrate tolerance or diabetes mellitus
– Preoperative antibiotic therapy according to the indications: latent or obvious infection of the genitourinary system (according to the results of bacteriological research)
– Multidisciplinary examination of patients: Urologist; Anesthetist; General Practitioner/Cardiologist; Radiologist; And other specialists as needed
– CT/MRI of the urinary system, with 3D modeling and contrast, including angiography
A rich carbohydrate and protein meal (if there are no contraindications) and 200 ml of liquid 2.5 hours before surgery
– The last meal (if the operation is in the morning) at 10 P.M. the day before, if in the afternoon no later than 6 hours before the operation
– Antibiotic prophylaxis 60 minutes before surgery with 3rd generation cephalosporins with a negative result of a urine culture examination
– No shaving of the surgical area
– Preparation of the intestine with laxatives or single micro-clysm
– Prevention of thromboembolic complications by compression of the lower extremities and administration of low-molecular-weight heparins
– No cleansing enemas
– Avoiding of pre-stenting/pre-catheterization
INTRAOPERATIVE
– Preferred method of anesthesia: regional anesthesia/multimodal anesthesia
– Heating of the patient during the operation with the control of normothermia
– Heating of infusion solutions and inhalation gases
– RIRS or mini-(micro)-PCNL using flexible endoscopes
– Using a small diameter access sheath (up to 12-14Fr with RIRS; up to 14Fr with PCNL)
– Laser application in low power mode (up to 10W)
– Avoiding of popcorning Spraying of fragments > 1 mm with difficult extraction
– Avoiding of the ureteral access sheath for single concretions < 10 mm with RIRS
– Avoiding of multi-access with PCNL
– Administration of tranexamic acid before puncturing during PCNL
– Avoiding of nephrostomy/stenting if possible
– Reduced fluid pressure in the kidney
– Adhesive bandage on the skin
– Intraoperative euvolemia
– Urethral catheters 12-14Ch
– Sealed cosmetic skin suture without loose ends and knots on the skin, adhesive bandages with PCNL
POSTOPERATIVE
– Early fluids intake (2–3 hours after surgery) and food (6 hours after surgery)
– Early activation (2–4 hours after surgery, after evaluation by an anesthesiologist and urologist)
– Physical therapy (breathing exercises, walking, and other exercises)
– Multimodal prevention of nausea and vomiting (Metoclopramide+Ondansetron)
– Early ultrasound control to exclude hematomas and urinomas in the first 3-6 hours after surgery
– Removal of the urethral catheter, nephrostomy, stent after ultrasound control no later than 3 (for PCNL) and 1 (after RIRS) day after surgery, followed by re-evaluation
– Hemostatic drugs (tranexamic acid) in intraoperative or detected postoperative bleeding
– Continuation of prevention of thromboembolic complications by compression of the lower extremities and the use of low-molecular-weight heparins
– Multimodal analgesia for pain control (dexketoprofen + paracetomol)
– Use of alpha blockers
– Chewing gum on the first and second day after surgery
– Monitoring of blood and urine parameters on the first day after surgery
–
Strict glycemic control in case of impaired carbohydrate tolerance and diabetes mellitus
– A detailed discussion of the behavior of the patient and the rehabilitation plan before the discharge
– Detailed written instructions in the discharge documents
– Strict plan of control examinations in the postoperative period
– Strict postoperative hygiene of the genitals and postoperative wounds (with an adhesive bandage, the patient is recommended to take a hygienic shower daily from the first day without additional processing)
– Discharge from the hospital within 1-3 days after the operation with the outpatient observation or the recovery
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 41 The
retrograde intra-renal surgery
–
The final surgical treatment method was chosen before the operation by randomization
The operating time was estimated from the beginning (including patient positioning) to the complete end of all the actions of the surgical team
A thulium laser with a power mode up to 10W was used for lithotripsy
After both procedures, pyeloureterography was done at the end of the operation to assess the need for kidney stenting/nephrostomy
The main types of operations were mini-perc PCNL with access sheath up to 14 Fr (for multiple and large concretions) and use of flexible optics (to avoid multi-access and to search for possible residual fragments) Puncture of renal cavities was done under Emergency Operations Center (EOC) and ultrasound control, after preliminary route planning based on the MSCT angiography results
The patient could be in any position at the discretion of the surgeon, avoiding prone position Nephrostomy was maintained in most cases for a period of 1 to 3 days
Tubeless procedure was preferred for single, uninfected stones, without ongoing hematuria
RIRS was performed under EOC control; when ureteral access sheath was not placed, the surgeon inserted the endoscope into the ureter up to the kidney with a guidewire In absence of signs of perforation or fragments migration, a ureteral catheter was maintained for up to 12 hours from the end of surgery whereas in other situations, a ureteral stent was placed
After the operation, all patients stayed in the intensive care unit for 2-3 hours
All patients received multimodal analgesia, prevention of thromboembolic complications (low molecular weight heparin), and protection from stress ulcers (proton pump blockers) On the first day after surgical treatment patients were assessed the pain level
Statistical analysis
The pre-operative data and the results of surgical treatment were analyzed using STATISTICA software for Windows version 10 0 (Statsoft, Inc, USA), SPSS Statistics version 23 0 (IBM, USA), and Stata version 16 0 (StataCorp, USA)
The significance level for all the methods was set at p ≤ 0 05 (except multiple logistic regression)
Data of the two groups (RIRS vs mini-PCNL) were compared
RESULTS
Peri-and postoperative results
In the peri-and postoperative periods, there were no cases of lethality, anesthesiologic complications or critical deterioration of the state of health due to concomitant diseases in both groups
All registered complications corresponded to classes I-IIIb Clavien-Dindo following the recommendations of the European Association of Urology (16, 17) There was one IIIb complication in the PCNL group associated with an increasing paranephric hematoma
The average surgery duration in groups I and II were 67 ± 34 and 75 ± 21 minutes, respectively (p = 0 350) The
time of direct lithotripsy and evacuation of fragments for I and II was 41 ± 31 and 49 ± 20 minutes, respectively (p = 0 276)
Table 3 shows the postoperative status of patients
Table 3. Postoperative status of patients
Parameter Group I Group II P (n = 23) (n = 27)
Clavien-Dindo complications, n (%):
I class
II class
IIIa class
IIIb class
Migration of concretions fragments, n (%)
Paranephral hematoma > 100 ml, n (%)
Blood transfusion, n (%)
Postoperative hematuria up to 1 day, n (%)
Subfebrility 1s day after surgery, n (%)
Febrility 1st day after surgery, n (%)
Pyelonephritis after surgery, n (%)
Stenting (I)\nephrostomy (II), n (%)
Timing of kidney catheterization\nephrostomy, days
Perforation, n (%)
Re-operation, n (%)
VAS more than 5 points on the first day after surgery, n (%)
Postoperative pain, points
Average duration of hospitalization, bed-day
1-day stay, n (%)
Total treatment period, days
SFR > 1 mm, n (%)
SFR > 2 mm, n (%)
VAS: visua analog scale; SFR: stone-free rate
Significant postoperative complications (Clavien-Dindo ≥ 3) rarely developed in both groups There is a significant statistical difference in the level of mild and minor complications: in group II, class I complications occurred with a higher frequency (p = 0 007) Migration of concretions fragments was more frequent in group II (p = 0 009), which was probably due to worse visualization caused by the development of intraoperative hematuria In general, hemorrhagic complications in group II are significantly more common
An objective examination in the late postoperative period established the groups' comparability (p > 0 05) and a significant difference in the risks of complications, postoperative status, and duration of treatment (p < 0 05)
It should be noted that the development of complications of classes IIIa-b was isolated
Univariate logistic regression analysis of these complications revealed no relationship with perioperative parameters (p > 0 05)
Table 4 partially presents the data of the performed regression analysis
of predictors of postoperative complications
A significant predictor of residual concretions was the duration of lithotripsy for more than one hour (HR 2 40; 95% CI -0 21; 5 02; p = 0 072) The remaining factors were not significant (p > 0 1)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 V
42
Vorobev, V Beloborodov, T Hovalyg, I Seminskiy, A Sherbatykh, I Shaderkin, M Firsov
1 (4 3%) 1 (4 3%) 1 (4 3%) 0 0 0 0 0 0 0 0 10 (43 4) 1 (1; 1) 1 (4 3%) 0 0 4 (4; 4) 1 (1; 1) 13 (56 5%) 1 (1; 2) 21 (91 3%) 22 (95 6%) 13 (48 1%) 6 (22 2%) 1 (3 7%) 1 (3 7%) 9 (33 3%) 1 (3.7%) 2 (7 4%) 13 (48 1%) 4 (14 8%) 3 (11 1%) 1 (3 7%) 17 (62 9) 2(2; 4) 1 (3.7%) 2 (7 4%) 21 (77 7%) 6 (6; 7) 3 (2; 4) 0 10 (3; 14) 23 (85 1%) 25 (92 5%) 0 007 0 115 0 911 0 360 0 009 0 360 0.199 0 002 0 073 0 118 0 360 0 448 < 0 001 0 911 0 199 0 002 < 0 001 < 0 001 0 005 < 0 001 0 867 0 936
Table 4.
Analysis of predictors of complications in the early and late postoperative period.
Figure 1 shows a model with a very good predict i v e v a l u e ( a r e a u n d e r curve, AUC = 0 88) presented as a ROC curve
C o n s e q u e n t l y , t h e l o n g duration of the operation (lithotripsy) increases the p r o b a b i l i t y o f r e s i d u a l fragments by 2 4 times
Baseline anemia (HR 3 13; 95% CI 0 02; 6 24; p = 0 048; AUC = 0 72) and urinary tract perforation (HR 3 85; 95% CI 0 44; 7 25; p = 0 027; AUC = 0 73) were reliable predictors of the need for reoperation with one-factor regression
I t w a s n o t p o s s i b l e t o build a reliable multivariate regression model
Significant predictors of postoperative hematuria were male gender (HR 2 14; 95% CI -0 27; 4 56; p = 0 082), duration of lithotripsy more than an hour (HR 3 53; 95% CI -0 31; 7 38; p = 0 072), chronic pyelonephritis (HR 3 09; 95% CI -0 48; 6 67; p = 0 090) and severe postoperative pain VAS > 5 points (HR 3 35; 95% CI 0 34; 6 35; p = 0 029)
Figure 2 shows a model with excellent predictive value (area under curve, AUC = 0 93) presented as a ROC curve
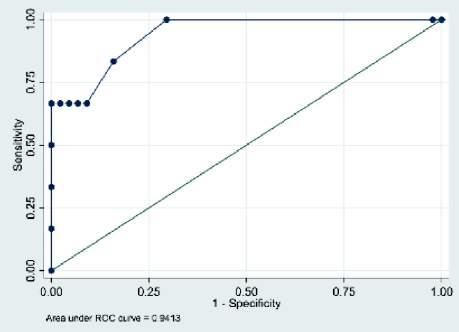

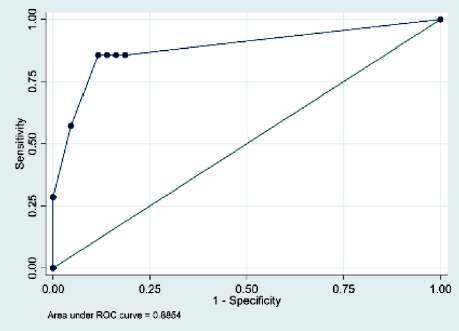
The remaining factors were not significant (p > 0 1)
Significant predictors of postoperative exacerbation of urinary infection were chronic hepatitis (HR 3 93; 95% CI 0 15; 7 72; p = 0 041), baseline bacteriuria (HR 2 64; 95% CI -0 40; 5 69; p = 0 089) and any migration of concretion intraoperatively (HR 2 86; 95% CI -0 48; 6 22; p = 0 094) Figure 3 shows a model with excellent predictive value (area under curve, AUC = 0 94) presented as a ROC curve
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 43 The retrograde intra-renal surgery
Figure 1. ROC curve for multivariate logit regression of predictors of postoperative residual concretions
Figure 2. ROC curve for multivariate logit regression of postoperative hematuria predictors
Figure 3 ROC curve for multivariate logit regression of predictors of exacerbation of urinary infection
Complication Predictor Univariate analysis Multivariate analysis χ2 OR (95% CI) P OR (95% CI) P Residual concretion Lithotripsy time > 60 minutes 14 61 3 61 (1 32; 5 89) 0 002 2 40 (–0 21; 5 02) 0 072 Multivariate Logit Regression: Intraoperative hematuria 3 62 1 61 (–0 05; 3 28) 0 057 χ2 = 16.89; p = 0.0007 Any concrement migration 6.67 2.31 (0.55; 4.07) 0.010 1.21 (–1.07; 3.50) 0.299 Area > 500 m2 9 17 2 8 (0 97; 4 77) 0 003 1 69 (–0 61; 4 00) 0 150 Reoperation Multivariate Initial anemia 3 30 3 13 (0 02; 6 24) 0 048 Logit Regression: χ2 –; p – Perforation 4 30 3 85 (0 44; 7 25) 0 027 Coagulopathy 2 20 2 39 (– 055; 5 35) 0 112 Postoperative pain syndrome, Increasing experience of the surgeon 9 59 –0 72 (–1 21; –0 23) 0 004 –0 51 (–1 7; 0 69) > 5 points on the VAS scale Lithotripsy time is more than 30 minutes 8 24 1 79 (0 47; 3 11) 0 008 2 28 (0 26; 4 31) Prescription of acute illness, day 9 44 0 68 (0 20; 1 16) 0 005 0 03 (–0 07; 0 15) Multivariate Logit Regression: 1-day surgery 6 96 –1 66 (–2 95; –0 37) 0 011 3 51 (–1 27; 8 31) χ2 = 34 38; p < 0 0001 Preoperative waiting > 3 days 7 14 1 87 (0 39; 3 34) 0 013 1 73 (–1 74; 5 21) Intraoperative hematuria 13 69 2 69 (1 02; 4 37) 0 002 1 78 (–0 88; 4 45) Stenting 15 60 –2 74 (–4 38; –1 10) 0 001 –3 4 (–5 93; 0 87) Any concrement migration 5 85 1 90 (0 21; 3 60) 0 028 1 48 (–1 71; 4 68) VAS: V sual ana og scale
Significant predictors of postoperative pain syndrome were lithotripsy time of more than half an hour (HR 2 28; 95% CI 0 26; 4 41; p = 0 027) Postoperative kidney stenting was a protective factor (HR -3 4; 95% CI -5 93; -0 87; p = 0 008) Figure 4 shows a model with excellent predictive value (area under curve, AUC = 0 92) presented as a ROC curve
Long-term results
General results were reported according to the last observation
True relapse was considered only when newly identified concretions were observed in patients who were previously considered stone free with a 1 mm cut off (SFR > 1 mm)
Successful primary SFR > 1 mm was observed in 21 (91 3%) vs 23 (85 1%) (p = 0 867); false relapse in 2 (8 6%) vs 4 (14 8%) (p = 0 555); and true relapse in 2 (9 5%) vs 3 (13 0%) (p = 0 742) in group I and II, respectively
The average clinical observation period was 251 days (95% CI 98-146 days) and maximum duration of follow up was 664 days For group I, the average follow-up period was 218 days (95% CI 61-112 days) and maximum period of follow up was 440 days For group II, the average follow-up period was 279 days (95% CI of 108-189 days) and maximum period of follow up was 664 days
Due to the absence of cases of lethality, survival analysis was not performed, the survival rate for both groups being 100% There were no significant complications in the long-term postoperative period
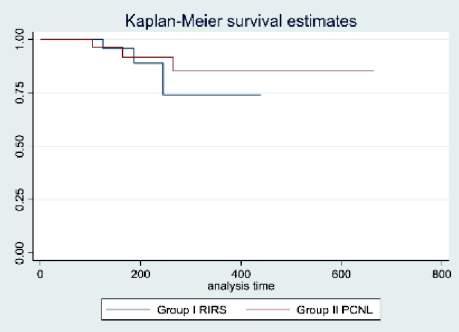
In group I, Kaplan-Meyer's estimate of freedom from true stone recurrence was 95 6 ± 4 25% after the first six months (95% CI 72 9; 99 3%), 88 8 ± 7 6% (95% CI 60 9; 92 2%) after 9 months and 74 0 ± 14 9% (95% CI 32 5; 92 2%) after a year and a half
In group II, freedom from true stone recurrence was 96 3 ± 3 6% (95% CI 76 4; 99 4%) after the first six months, 91 7 ± 5 6% (95% CI 70 4; 97 8%) after 9 months, and 84 9 ± 8 3% (95% CI 58 6; 95 1%) after a year and a half The sta-
Freedom from a true relapse of stone formation according to the Kaplan-Meyer method
tistical uniformity of the likelihood ratio (Likelihood-ratio test statistical of homogeneity) is comparable (p = 0 620; χ2 = 0 24)
The log-rank criterion did not reveal statistical differences (p = 0 582; χ2 = 0 30) in the frequency of relapse over the entire follow-up period, which is graphically expressed by the Kaplan-Meyer method in Figure 5
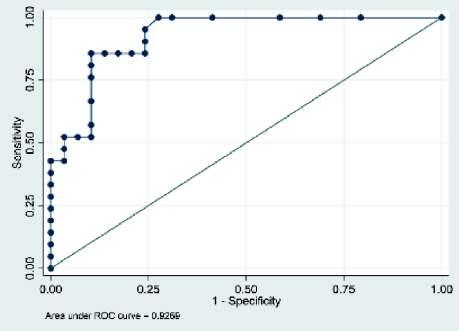
Table 5 presents the regression model of proportional Cox risks describing the influence of various factors on the development of relapse
Multivariate regression analysis of proportional Cox risk (sample from p < 0 05) demonstrated the significance of postoperative fever (HR 23 45; 95% CI 2 14; 256 5; p = 0 010) and initial stone density > 600 HU (HR 0 04; 95% CI 0 004; 0 49; p = 0 010) in predicting possible recurrence of urolithiasis
The treatment results showed statistical equality for stone free rate (SFR), freedom from stone recurrence during the entire follow-up period, and rate of complications of classes II-III Clavien-Dindo (p > 0 05)
Meanwhile, a significant superiority of group I (RIRS) was demonstrated for shorter duration of hospitalization and overall disability, and better objective condition in the early postoperative period
Economic efficiency was not evaluated
Consequently, RIRS meets the criteria of the enhanced recovery program more than PCNL with a similar perioperative protocol
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 V Vorobev, V
T
I
A
I
M
44
Beloborodov,
Hovalyg,
Seminskiy,
Sherbatykh,
Shaderkin,
Firsov
Figure 4
ROC curve for multivariate logit regression of predictors of moderate postoperative pain
Figure 5
Table 5.
Variable Univariate Cox analysis Multivariate Cox analysis, χ2 = 12 66; p = 0 0018 Valda χ2 HR (95% CI) P HR (95% CI) P Febrility after surgery 3 59 6 77 (1 21; 37 9) 0 029 23 45 (2 14; 256 5) 0 010 Concretion density > 600, HU 6 12 0 12 (0 022; 0 683) 0 016 0 04 (0 004; 0 49) 0 010 Body Mass Index > 25 7.19 2.24 (0.88; 5.70) 0.090 Duration of postoperative follow-up 4 99 0 88(0 785; 1 00) 0 056
Regression model of urolithiasis recurrence
Limitations
Limitations of the study were the relatively small sample size, the average postoperative follow-up period less than two years, mixing of various surgical techniques within the framework of the protocol (PCNL, RIRS)
DISCUSSION
In the presented study, the outcomes for SFR, I-III class c o m p l i c a t i o n s d e v e l o p m e n t , a n d s u r g e r y d u r a t i o n (lithotripsy) were similar to the data of other authors and meta-analyses of these data
The problem of a longer hospitalization and general treatment period and a more pronounced pain syndrome also corresponds to what reported in previous papers (18-21) A possible solution to align the results of the two procedures and improve compliance with the enhanced recovery program is the transition from mini-PCNL to micro-PCNL (22, 23)
In general, analyzing the results of PCNL and RIRS comparison presented by different authors, attention is drawn to the pronounced spread of SFR indicators, the lack of a clear definition of SFR by the size of the fragments, the lack of a clear definition of the operation duration and its pronounced spread Probably, such differences are due to different technical conditions, the experience of the surgical team, and other similar reasons In general, our own experience demonstrates greater ease of implementation and convenience for RIRS patients in comparison with mini-PNCL
Both treatment protocols are safe, effective, and accompanied by minimal risks of complications They equally lead to high stone free rates (SFR > 1 mm, 91 3% vs 85 1%; p = 0 867; SFR > 2 mm, 95 6% vs 92 5%; p = 0 936)
Intergroup analysis of the total operation duration (and lithotripsy) demonstrated a similar duration in the two group (p > 0 05) Postoperative complications (ClavienDindo) in the early and late periods developed rarely and were comparable (p > 0 05) although class I complications were predominant in the PCNL group (p = 0 007) Some parameters demonstrated the superiority of RIRS over PCNL: less pronounced pain syndrome (p = 0 002), less drainage time (p < 0 001), no postoperative hematuria (p = 0 002), lower average duration of hospitalization, and total time spent on treatment (p < 0 001)
The analysis of predictors of the complication development based on the results of multivariate analysis showed that exceeding the lithotripsy time by more than one hour increases by 2 4 times (HR 2 40; 95% CI -0 21;5 02; p = 0 072) the risk of presence of residual fragments (SFR > 1 mm) This indicates the expedience of discussing a possible second stage of treatment in certain groups of patients Postoperative hematuria can be triggered by the following factors: male gender (HR 2 14; 95% CI -0 27; 4 56; p = 0 082), duration of lithotripsy more than an hour (HR 3 53; 95% CI -0 31; 7 38; p = 0 072), chronic pyelonephritis (HR 3 09; 95% CI -0 48; 6 67; p = 0 090) and severe postoperative pain (VAS > 5 points) (HR 3 35; 95% CI 0 34; 6 35; p = 0 029) Significant predictors of postoperative exacerbation of urinary infection are chronic hepatitis (HR 3 93; 95% CI 0 15; 7 72; p = 0 041), baseline bacteriuria (HR 2 64; 95% CI -0 40; 5 69; p = 0 089) and migration of concretions intraoperatively (HR
2 86; 95% CI -0 48; 6 22; p = 0 094) Lithotripsy time of more than half an hour is a significant predictor of severe postoperative pain syndrome (HR 2 28; 95% CI 0 26; 4 41; p = 0 027) whereas a protective factor is postoperative kidney stenting (HR -3 4; 95% CI -5 93; -0 87; p = 0 008)
Special attention should be paid to the prognostic protective effect of the one-day surgery principle and the effect of improvement of the operating surgeon skills on the risk of complications such as postoperative hematuria, exacerbation of chronic urinary infection, severe postoperative pain syndrome (p < 0 05)
Both treatment protocols have a high safety profile without the risk of mortality or relapse The log-rank criterion did not reveal statistically significant differences in the frequency of survival (p = 1), or relapse (p = 0 582)
The advantages of the performed study are its prospective design, randomization, homogeneity of groups, mandatory strict protocol of the study, in-depth statistical analysis of outcomes, description of the algorithm of patient management with a detailed presentation of the materials and results of the study
CONCLUSIONS
The results of the study have high practical and scientific significance The design of the study according to a strict protocol, compliance with the good clinical practice (GCP) criteria, a clear presentation of diagnostic, surgical, and statistical techniques, specific and objective parameters allowed us to obtain reliable results
The results led to important conclusions for the selection of treatments RIRS and mini-PCNL have similar effectiveness, but the path to recovery using retrograde surgery is somewhat simpler and shorter RIRS meets the criteria of the enhanced recovery program more than PCNL with a similar perioperative protocol
REFERENCES
1 Zeng J, Wang S, Zhong L, et al A retrospective study of kidney stone recurrence in adults J Clin Med Res 2019; 11:208-212
2 Lang J, Narendrula A, El-Zawahry A, et al Global trends in incidence and burden of urolithiasis from 1990 to 2019: an analysis of global burden of disease study data Eur Urol Open Sci 2022; 35:37-46
3 Hill AJ, Basourakos SP, Lewicki P, et al Incidence of kidney stones in the United States: The Continuous National Health and Nutrition Examination Survey J Urol 2022; 207:851-856
4 Skolarikos A, Straub M, Knoll T, et al Metabolic evaluation and recurrence prevention for urinary stone patients: EAU guidelines Eur Urology 2015; 67:750-763
5 Alhasan KA, Shalaby MA, Albanna AS, et al Comparison of renal stones and nephrocalcinosis in children: findings from two tertiary centers in Saudi Arabia Front Pediatr 2021; 9:736308
6 Streltsova OS, Vlasov VV, Grebenkin EV, et al Controlled fragmentation of urinary stones as a method of preventing inflammatory infections in the treatment of urolithiasis (experience in successful clinical use) Sovrem Tekhnologii Med 2021; 13:55-61
7 Scotland K, Tailly T, Chew BH, et al Consensus statement on uri-
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 45 The retrograde intra-renal surgery
nary stone treatment during a pandemic: a delphi process from the endourological society TOWER Research Initiative J Endourol 2022; 36:335-344
8 Buyko EE, Ivanov VV, Kaidash OA, et al Hypolipidemic activity of the polysaccharide L-rhamnopyranosyl-6-O-methyl-galacturonan in combined administration with HMG-CoA reductase and cholesterol absorption inhibitors Drug Dev Registr 2022; 11:57-63
9 Zolotov SA, Demina NB, Ponomarev ES, et al Study of the technological methods effect on dissolution of the X-ray amorphous Efavirenz-mesoporous carrier system Drug Dev Registr 2022; 11:84-89
10 Datta SN, Chalokia RS, Wing KW, et al Ultramini-percutaneous nephrolithotomy versus retrograde intrarenal surgery in the treatment of 10-30 mm calculi: a randomized controlled trial Urolithiasis 2022; 50:361-367
11 Fayad MK, Fahmy O, Abulazayem KM, Salama NM Retrograde intrarenal surgery versus percutaneous nephrolithotomy for treatment of renal pelvic stone more than 2 centimeters: a prospective randomized controlled trial Urolithiasis 2022; 50:113-117
12 Su B, Hu W, Xiao B, et al Needle-perc-assisted endoscopic surgery for patients with complex renal stones: technique and outcomes Urolithiasis 2022; 50:349
13 Dossanov B, Trofimchuk V, Lozovoy V, et al Evaluating the results of long tubular bone distraction with an advanced rod monolateral external fixator for achondroplasia Sci Rep 2021; 11:14727
14 Shrestha A, Gharti BB, Adhikari B Perirenal extravasation after retrograde intrarenal surgery for renal stones: a prospective study Cureus 2022; 14:e21283
15 Senel S, Ozden C, Aslan Y, et al Can the stone scoring systems
be used to predict infective complications after retrograde intrarenal surgery? Med Princ Pract 2022; 31:231-237
16 Mitropoulos D, Artibani W, Biyani CS, et al Validation of the clavien-dindo grading system in urology by the European Association of urology guidelines ad hoc panel Eur Urol Focus 2018; 4:608-613
17 Mitropoulos D, Artibani W, Graefen M, et al Reporting and grading of complications after urologic surgical procedures: an ad hoc EAU guidelines panel assessment and recommendations Eur Urol 2012; 61:341-349
18 Dossanova A, Lozovoy V, Wood D, et al Reducing the risk of postoperative genital complications in male adolescents Int J Environ Sci Educ 2016; 11:5797-5807
19 Ghazala SG, Saeed Ahmed SM, Mohammed AA Can mini PCNL achieve the same results as RIRS? The initial single center experience Ann Med Surg (Lond) 2021; 68:102632
20 Erkoc M, Bozkurt M, Danis E, Can O Comparison of miniPCNL and retrograde intrarenal surgery in the treatment of kidney stone over 50 years old patients Urologia 2022; 89:575-579
21 Nogaeva UV, Naumova AA, Novinkov AG, et al Comparative study of rheological properties of gels and creams on different carrier bases Drug Dev Registr 2022; 11:121-129
22 Jain M, Manohar CS, Nagabhushan M, Keshavamurthy R A comparative study of minimally invasive percutaneous nephrolithotomy and retrograde intrarenal surgery for solitary renal stone of 12 cm Urol Ann 2021; 13:226-231
23 Pillai SB, Chawla A, de la Rosette J, et al Super-mini percutaneous nephrolithotomy (SMP) vs retrograde intrarenal surgery (RIRS) in the management of renal calculi ≤ 2 cm: a propensity matched study World J Urol 2021; 40:553-562
Correspondence
Vladimir Vorobev, MD (Corresponding Author) vorobevr782192@rambler ru
Vladimir Beloborodov, MD vbeloborodov391@rambler ru
Temirlan Hovalyg, MD temirlan hovalyg@rambler ru
Department of General Surgery, Irkutsk State Medical University, Krasnogo Vosstaniya str , 1, Irkutsk, 664003, Russian Federation
Igor Seminskiy, MD
Department of Pathology, Irkutsk State Medical University, Krasnogo Vosstaniya str , 1, Irkutsk, 664003, Russian Federation seminskiy igor@rambler ru
Andrey Sherbatykh, MD andsherbatykh3@rambler ru
Department of Faculty Surgery, Irkutsk State Medical University, Krasnogo Vosstaniya str , 1, Irkutsk, 664003, Russian Federation
Igor Shaderkin, MD igshaderkin@rambler ru E-Health Laboratory, I M Sechenov First Moscow State Medical University, Pirogovskaya str , 2, Moscow, 119296, Russian Federation
Mikhail Firsov, MD m firsov31@rambler ru
Department of Urology, Andrology and Sexology, Krasnoyarsk State Medical University named after Professor V F Voino-Yasenetsky, Partizan Zheleznyaka str , 1, Krasnoyarsk, 660022, Russian Federation
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 V
46
Vorobev, V Beloborodov, T Hovalyg, I Seminskiy, A Sherbatykh, I Shaderkin, M Firsov
Comparison of commonly utilized ureteral access sheaths: A prospective randomized trial
Summary
Objective: We aimed to evaluate and compare the functional characteristics, safety profile and effectiveness of two commonly used ureteral access sheaths (UAS) during flexible ureteroscopy
Methods: After institutional review board approval, patients with proximal ureteral or kidney stones requiring flexible ureteroscopy and UAS were prospectively randomized to group I or group II according to the type of access sheath used Primary outcome was incidence of intraoperative complications. Results: Eighty-eight patients were enrolled in the study, 44 patients in each group. Sheath size 12/14 FR was used in both cohorts Median (IQR) stone size was 10 mm (7-13 5) and 10 5 mm (7.37-14) in group I and II respectively (p = 0.915). Nineteen and twenty patients, in group I and II respectively, were pre-stented. Subjective resistance with insertion of the UAS was observed in 9 and 11 patients in group I and II respectively (p = 0.61) while failed insertion was encountered in one patient in group I Traxer grade 1 ureteral injury was noted in 5 and 6 patients in group I and II respectively while grade 3 injury was seen in 1 patient for both cohorts (p = 0 338) There was less resistance for UAS placement in pre-stented patients (p = 0 0202) but without significant difference in ureteric injury incidence (p = 0.175). Emergency department visits were encountered in 7 (group I) and 5 patients (group II) (p = 0 534) Conclusions: The studied UASs were comparable regarding safety and efficacy in the current study Pre-stented and dilated ureters had less resistance to insertion although this was not reflected on incidence of ureteric injury
KEY WORDS: Ureteroscopy; Urolithiasis; Ureteral Access sheath; Ureteral trauma
Submitted 11 January 2023; Accepted 22 January 2023
BACKGROUND
Ureterorenoscopy continues to be one of the most common procedures performed in urology practice, being a minimally invasive option for treatment of nephrolithiasis and ureterolithiasis Technological advances in both the size and flexibility of ureteroscopes have been integral to removing larger stones with a higher stone free rate The continued advancement of the technology surrounding Holmium: YAG lasers, graspers, and baskets have continued to widen the application of ureteroscopy (1, 2) There are multiple instruments available on the market to aid in the performance of ureteroscopy (3) One tool in the
urologist armamentarium is the ureteral access sheath (UAS), to access the proximal collecting system The use of UAS has the proposed advantages of lowering the intrarenal pressure that probably decreases the complications related to infection, increasing irrigation flow and facilitating multiple reinsertions and withdrawals of the ureteroscope during surgery (4, 5) However, these benefits are associated with the cost of increased insertion forces and greater risk for ureteral wall injury, and possible failed insertion Proposed higher stone free rates with UAS use and cost-effectiveness are too much debated (6-8)
Although safety has been demonstrated, there have been few studies comparing designs of different companies in the hands of practicing urologists in vivo We aimed to compare two commonly used UASs regarding functional characteristics, safety profile and effectiveness of each This information will help guide urologists in product selection when performing ureteroscopy
METHODS
After institutional review board (IRB) and ethical committee approval, patients with proximal ureteral or kidney stones requiring flexible ureterorenoscopy and UAS placement in our tertiary center were enrolled in the prospective clinical trial after signing the informed consent Patients less than 18 years old or patients with ureteric stricture were excluded Patients were randomized to the use of Boston Scientific Navigator HDTM (NHD) (Group I) or of Cook FlexorTM (CF) (group II) UAS Randomization was performed by investigator using closed envelope technique
The data of both cohorts were prospectively obtained and analyzed Traxer grading system for UAS-related injuries was used for classification and comparison of intraoperative ureteric injuries (8) Primary outcome was incidence of sheath related intraoperative complications while the difficulty of UAS placement, length of procedure (LOP), p
plaints/phone calls/Emergency Department (ED) visits, postoperative hydronephrosis were Secondary outcomes
The two UAS brands have a design of outer hydrophilic sheath and smooth-tapered inner coaxial dilator The CF outer sheath is specialized with coil construction core The inner dilator of NHD has a stiff body and a more flex-
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 47 ORIGINAL PAPER
U A S h a s m u l t i p l e d e s i g n s a c r o s s m u l t i p l e b r a n d s
o s t - o p e r a t i v e c o m p l i c a t i o n s , p a t i e n t - r e p o r t e d c o m
Mohamed Elsaqa 1,2 , Zain Hyder 1 , Kim Thai 1 , Katherine Dowd 1 , Amr El Mekresh 1 , Kristofer Wagner 1 , Belur Patel 1 , Patrick Lowry 1 , Marawan M. El Tayeb 1
DOI: 10 4081/aiua 2023 11149
1 Baylor Scott & White Medical Center, Temple, TX USA; 2 Alexandria University Faculty of Medicine, Alexandria, Egypt
ible tip while CF inner dilator has a stiff tip tapered to 6 Fr diameter The NHD is available in 3 sizes of 11/13 Fr, 12/14 Fr, and 13/15 Fr whereas CF is available in 12/14 and 14/16 in addition to smaller diameters of 9 5/11 5 and 10 7/12 5 Fr
Statistical analysis
All statistical analysis was performed using the commercially available SAS Version 9 4 ( Statistical Analysis Software) (SAS Institute Inc , Cary, NC, USA) Frequencies and percentages were used to describe categorical variables while medians and interquartile ranges (or means and standard deviations where appropriate) were used to describe continuous variables A chi-square test or Fisher’s exact test were used to test for comparison of categorical variables according to the expected cell counts while two-sample t-test (or Wilcoxon rank-sum test when appropriate) was used for comparison of quantitative variables The significance level was set at a p-value < 0 05
RESULTS
Between February 2017 and February 2020, 88 patients were prospectively enrolled in the study Forty-four patients were included in each group Sheath of 12/14 French was used in both cohorts Patients' demographics were comparable with no statistical significance between both cohorts except for higher rate of preoperative alpha blocker use in group II Median (IQR) stone size was 10 (7-13 5) mm and 10 5 (7 37-14) in group I and II respectively (p = 0 915) Thirty-nine patients had ureteric stents previously inserted (pre-stented) at the time of flexible ureteroscopy, nineteen and twenty patients, in group I and II respectively (Table 1)
Median (IQR) operative time was 54 (41-78) and 51 (3672) minutes in group I and II respectively (p = 0 302)
Subjective resistance with insertion of the UAS was observed in 9 patients in Group I vs 11 patients in group II (p = 0 61) There was one failure of insertion of the UAS in group I There was a statistically less resistance for placement of the UAS noted in pre-stented patients’ cohort (p = 0 0202) It was also noted that patients with preoperative
Table 2.
Perioperative outcome data
hydronephrosis had significantly less resistance to UAS placement (p = 0 0493) There was no significant difference in resistance to insertion between patients who had preoperative alpha blocker use or not (p = 0 34)
Regarding sheath-related ureteric trauma, a total of 13 (16%) injuries were observed; 7 and 6 injuries in group I and II respectively Out of 13 patients with ureteric injury, 8 patients were not previously stented (p = 0 175)
Taxer grade 1 ureteral injury was noted in 6 patients in the group I vs 5 patients in Group II Taxer Grade 3 injury was seen in 1 patient for both cohorts (p = 0 338) (Table 2)
Need for opioid analgesia and patients’ phone calls were comparable between both groups (p = 0 247, 0 669 respectively) Return to the ED was encountered in 7 and 5 patients from group I and II respectively (p = 0 534) The complains were mainly related to pain and hematuria There was no association with sheath complication and return to ED Within follow up of 3 months, one p a t i e n t i n g r o u p 2 h a d p e r s i s t e n t h y d r o n e p h r o s i s although imaging has excluded occurrence of ureteric stricture
DISCUSSION
The benefits of the UAS in ureteroscopy and retrograde intrarenal surgery (RIRS) are still controversial De Coninck et al , in their systemic review, showed that UAS helps increasing flow of irrigation and decreasing intrarenal pressure but the impact of UASs on stone-free rates, ureteroscope protection or damage, postoperative pain, risk of ureteral strictures, and cost-effectiveness are still controversial (4)
In another recent review article, Wong et al have concluded that no evidence exists for higher stone free rate with the use of UAS but facilitates multiple and rapid pass a g e s o f t h e u r e t e r o s c o p e d u r i n g t h e p r o c e d u r e According to Wong et al, larger UAS diameters > 12/14 Fr were associated with lower intrarenal pressure and greater efficacy at the cost of increased forces during insertion, greater risk for ureteral wall injury, and lower insertion success rates (6)
Regarding the UAS size choice, Yoshida et al have evaluat-
Archivio Italiano di Urologia e Andrologia 2023; 95, 2
48
Mohamed Elsaqa, Zain Hyder, Kim Thai, et al
Table 1.
Group I (n = 44) Group II (n = 44) P value Age, years, mean (SD) 59 1 (2 3) 53 9 (2 5) 0 13 Sex, n (%) Male 21 (48%) 25 (57%) 0 393 Female 23(52%) 19(43%) Stone size, mm, median (IQR) 10 (7-13 5) 10 5 (7 37-14) 0 915 Stone side, n (%) Right 18 (40%) 14 (32%) 0 414 Left 24 (54 5%) 27 (61 3%) Bilateral 2 (4 5%) 3 (6 8%) Alpha blocker use, n (%) 15 (34%) 28 (63%) 0.005 Stone location, n (%) Renal 41 45 0 305 Upper ureter 7 13 Mid ureter 01 Lower ureter 23 Hydronephrosis, n (%) 23 (52%) 30 (68%) 0 127 Preop UTI, n (%) 6 (13 6%) 12 (27 2%) 0 112 Pre-stenting, n (%) 19 (43 1%) 20 (45 4%) 0 83
Preoperative patient criteria in both groups
Group I (n = 44) Group II (n = 44) P value Operative time, min, median (IQR) 54 (41-78) 51 (36 5-72 25) 0 302 Anesthesia time, min, median (IQR) 100 (74 5-121 5) 104 (76 5-118 5) 0 779 Resistance to introduction, n (%) 9 (20 4%) 11 (25%) 0 61 Failed insertion, n (%) 1 (2 27%) 0 0 314 String on stent 23 (52%) 25 (56 8%) 0 66 Op sheath complication, n (%) 7 (15 9%) 6 (13 6%) 0 763 Ureteral injury grade, n (%) Garde 1 6 (13 6%) 5 (11 3%) 0 338 Grade 2 00 Grade 3 1 (2.27%) 1 (2.27%) Need for Opioid analgesia, n (%) 16 (36 3%) 11 (25%) 0 247 Phone calls, n (%) 22 (50%) 20 (45 4%) 0 669 ED-return, n (%) 7 (15 9%) 5 (11 36%) 0 5344 PO Hydronephrosis, n (%) 0 1 (2 27%) 0 314
ed different UAS ≤ 10/12 F regarding the intrapelvic pressure in an ex-vivo porcine kidneys They showed that 9 5/11 5 F UAS were associated with excessive intrapelvic pressure (10) Sener et al have recommended sheath size 10/12 F as the first choice during flexible ureterorenoscopy for good irrigation and lower rate of ureter injury than 12/14 F UAS (11)
De et al compared the physical characteristics of NHD, CF and other two new single-wire system UASs in ex-vivo study They reported that NHD is more slippery and more rigid with larger outer diameter while CF had shorter and stiffer tip and appeared less traumatic (more force was required for tip perforation) (12) In a similar ex-vivo study, Patel et al also compared the physical and mechanical characteristics of NHD UAS versus GlidewayTM and PathwayTM UASs supplied by Terumo They reported superiority for NHD regarding safety and ease of use (13) Loftus et al have compared the same two investigated UAS brands in a randomized clinical trial In contrary of our study, all the patients included in their study were not pre-stented Loftus et al used different UAS sizes and they crossed over patients who fail insertion of one UAS type to the other They reported overall sheath placement success rate of 87 8% with no difference between both types although NHD was subjectively easier to insert and was successful in 3 out of 7 (43%) patients who failed insertion of CF They have reported some factors associated with high-grade (grade 2 or 3) ureteral injury as male gender, difficult subjective insertion, longer time of sheath insertion and high stone burden (14)
In the current study, the insertion success rate was 98 8% with no significant difference between both groups The two UASs appeared comparable on many fronts, including ease of placement, ureteral injury rates, operative times, and return to ED rates Of note, our results showed less resistance to insertion was seen with preoperative hydronephrosis and ureteric stenting although no difference regarding ureteric injury Similarly, Yuk et al have reported that pre-stenting was associated with higher UAS placement success although had no effect on overall operative outcomes (15)
Other studies have investigated the use of alpha blockers on UAS force of placement Koo et al have reported that preoperative use of alpha blockers was associated with lower UAS insertion force (16) However, contradictory results were reported by Erturhan et al in another study (17) In our cohort, the preoperative usage of alpha blockers prior to UAS placement was not associated with an easier subjective UAS clinical placement
Study by Stern et al demonstrated that high-grade injury due to UAS placement has around a 1 8% stricture rate and this rate was similar to that reported without use of UAS (8) Aykant et al , in a prospective randomized study, have recently reported the rates of low-grade ureteral injury rate of 23 1% while high-grade injury rate was 8 9% After 1-year, the ureteral stricture was 1 6% They reported that use of 12/14 F UAS was associated with higher risk of high-grade injuries although there was no difference in ureteral stricture formation compared to use of 9 5F/11 5 F sheath (18)
There were only two high grade ureteral injuries noted in the current study All ureteral injuries were treated with
stent placement for 2-4 weeks On follow up, only 1 patient had persistent hydronephrosis and no patients were noted to have ureteral stricture at follow up of 3 months Our study adds to growing literature that the NHD and CF have similar safety profiles and have a broad range of clinical application
Limitations of the study include small study group and lack of stone-free rate assessment Further studies could be used to target stone size and determine the effect of sheath usage on stone clearance rates
CONCLUSIONS
The two commonly utilized ureteral access sheath brands are equally safe and effective for utilization during flexible ureteroscopy and retrograde intrarenal surgery Prestented and dilated ureters show less resistance to insertion although this was not associated with lower incidence of associated ureteric injury
Informed consent: The study and informed consent were approved by Baylor Scott & White Institutional review board (IRB No: 18-4720) All patients have signed an informed consent prior to participation to the study
REFERENCES
1 Doizi S, Traxer O Flexible ureteroscopy: technique, tips and tricks Urolithiasis 2018; 46:47-58
2 Rodríguez-Monsalve Herrero M, Doizi S, Keller EX, et al Retrograde intrarenal surgery: An expanding role in treatment of urolithiasis Asian J Urol 2018; 5:264-273
3 Inoue T, Okada S, Hamamoto S, Fujisawa M Retrograde intrarenal surgery: Past, present, and future Investig Clin Urol 2021; 62:121-135
4 De Coninck V, Keller EX, Rodríguez-Monsalve M, et al Systematic review of ureteral access sheaths: facts and myths BJU Int 2018; 122:959-969
5 Auge BK, Pietrow PK, Lallas CD, et al Ureteral access sheath provides protection against elevated renal pressures during routine flexible ureteroscopic stone manipulation J Endourol 2004; 18:33-6
6 Wong VK, Aminoltejari K, Almutairi K, et al Controversies associated with ureteral access sheath placement during ureteroscopy Investig Clin Urol 2020; 61:455-463
7 Meier K, Hiller S, Dauw C, et al Understanding Ureteral Access Sheath Use Within a Statewide Collaborative and Its Effect on Surgical and Clinical Outcomes J Endourol 2021; 35:1340-1347
8 Stern JM, Yiee J, Park S Safety and efficacy of ureteral access sheaths J Endourol 2007; 21:119-23
9 Traxer O, Thomas A Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery J Urol 2013; 189:580-4
10 Yoshida T, Inoue T, Abe T, Matsuda T Evaluation of Intrapelvic Pressure When Using Small-Sized Ureteral Access Sheaths of ≤ 10/12F in an Ex Vivo Porcine Kidney Model J Endourol 2018; 32:1142-1147
11 Sener TE, Cloutier J, Villa L, et al Can We Provide Low Intrarenal Pressures with Good Irrigation Flow by Decreasing the Size of Ureteral Access Sheaths? J Endourol 2016; 30:49-55
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 49 Ureteral access sheaths
12 De S, Sarkissian C, Torricelli FC, et al New ureteral access sheaths: a double standard Urology 2015; 85:757-63
13 Patel N, Monga M Ureteral access sheaths: a comprehensive comparison of physical and mechanical properties Int Braz J Urol 2018; 44:524-535
14 Loftus CJ, Ganesan V, Traxer O, et al Ureteral Wall Injury with U r e t e r a l A c c e s s S h e a t h s : A R a n d o m i z e d P r o s p e c t i v e T r i a l J Endourol 2020; 34:932-936
15 Yuk HD, Park J, Cho SY, et al The effect of preoperative ureteral stenting in retrograde Intrarenal surgery: a multicenter, propensity score-matched study BMC Urol 2020; 20:147
16 Koo KC, Yoon JH, Park NC, et al The impact of preoperative αadrenergic antagonists on ureteral access sheath insertion force and the upper limit of force required to avoid ureteral mucosal injury: a randomized controlled study J Urol 2018; 199:1622-30
17 Erturhan S, Bayrak Ö, Sen H, et al Can alpha blockers facilitate the placement of ureteral access sheaths in retrograde intrarenal surgery? Turk J Urol 2019; 45:108-112
18 Aykanat C, Balci M, Senel C, et al The Impact of Ureteral Access Sheath Size on Perioperative Parameters and Postoperative Ureteral Stricture in Retrograde Intrarenal Surgery J Endourol 2022; 36:1013-1017
Correspondence
Mohamed Elsaqa, MD (Corresponding Author) mohamed elsaqa@alexmed edu eg
Division of Urology, Department of Surgery, Baylor Scott & White Health, 2401 S 31st Street, Temple, TX 76508
Zain Hyder, MD zain hyder@bswhealth org
Kim Thai, MD kthai88@gmail com
Katherine Dowd, MD katiedowd12@gmail com
Amr El Mekresh, MD elsaqa2020@yahoo com
Kristofer Wagner, MD
kristofer wagner@bswhealth org
Belur Patel, MD
belur patel@bswhealth org
Patrick Lowry, MD patrick lowry@bswhealth org
Marawan M El Tayeb, MD
marawan eltayeb@bswhealth org
Baylor Scott & White Medical Center, Temple, TX, USA
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e
95, 2
Andrologia 2023;
50
Mohamed Elsaqa, Zain Hyder, Kim Thai, et al
Variation of inflammatory indexes in patients with chronic abacterial prostatitis treated with an herbal compound/extract
Summary
Introduction: Inflammation is a highly prevalent finding in the prostate Men with inflammation have higher IPSS score and increased prostate size For men with prostatic inflammation, there is a significantly increased risk of developing acute urinary retention and the need of a surgical approach to the disease Some laboratory tests (i e fibrinogen, C-reactive protein), can play a role in identifying patients at greatest risk of complications and adverse outcomes after surgery There have been several experiences exploring the role of nutraceutical approach to the prostate inflammation Aim of our study were to describe the variation in symptoms and inflammatory indexes in men affected by chronic abacterial prostatitis, treated with an herbal extract containing Curcuma Longa 500 mg, Boswellia 300 mg, Urtica dioica 240 mg, Pinus pinaster 200 mg and glycine max 70 mg
Materials and methods: A prospective multicenter study was conducted from February 2021 and March 2022 One hundred patients, with a diagnosis of Chronic Prostatitis were enrolled in a multicentric phase III observational study They were treated with the herbal extract, one capsule per day, for 60 days. No placebo arm was included In each patient, inflammatory indexes, PSA, prostate volume, IIEF-5, PUF, uroflowmetry (Qmax), IPSS-QoL, NIH-CPPS were registered and statistically compared at baseline and at the follow up visit.
Results: The variation obtained on the inflammation indexes showed a global improvement after treatment, including the PSA reduction We also recorded a significant improvement on IPSS-QoL, NIH-CPPS, PUF and Qmax scores
Conclusions: The herbal extract considered in our study may represent a promising and safe therapeutic agent leading to a reduction of inflammation markers, and could be used in the treatment of prostatitis and benign prostatic hyperplasia
KEY WORDS: Nutraceuticals; Inflammation; Inflammatory indexes; PSA
Submitted 1 May 2023; Accepted 11 May 2023
INTRODUCTION
In recent years many authors highlighted the central role of inflammation in the pathogenesis of urological diseases In particular, in patients with some neoplastic diseases, it has been shown that the presence of locoregional chronic
inflammation is involved in carcinogenesis (1, 2) In the field of prostate diseases, recent studies have shown that patients with chronic inflammation of the prostate are at greater risk of more severe voiding symptoms, acute urinary retention and prostate surgery (3, 4) The gold standard for the diagnosis of tissue inflammation is represented by histological examination of tissue specimen A biopsy cannot always be performed for both ethical and procedural issues (5) For this reason, in recent years, several studies attempted to identify a serological marker of inflammation for the various neoplastic and benign urological pathologies (6) However, most of the markers used at preclinical and in vitro levels have poor diagnostic specificity, significant variability over time or high costs
In recent years, several authors have shown how some laboratory tests (Complete Blood Count/CBC, albumin, fibrinogen, C-protein reactive/PCR and procalcitonin/PCT), that are routinely performed in preparation for various urological surgeries, can play a role in identifying patients at greatest risk of complications and adverse outcomes after surgery (7) In particular, these markers can be considered as proxies of inflammation of the organism and are related to an increased risk of mortality in numerous diseases
The role of these inflammation markers in urology is still unclear today and the scientific evidence comes mainly from retrospective studies (8) There is currently no consensus on the pharmacological management of inflammatory prostatic diseases in a unique way
Nonsteroidal anti-inflammatory drugs (NSAIDs) are typically prescribed together with antibiotics without clear evidence The use of herbal remedies is very common, but the clinical evidence remains scarce (9) Above all, it remains unclear whether the use of such preparations can affect the reduction of the inflammatory state inferred on blood chemistry tests The primary purpose of this multicenter study is to describe the variation in subjective, objective and biochemical inflammatory indexes in men affected by chronic abacterial prostatitis, treated with herbal extracts, containing Curcuma Longa 500 mg, Boswellia 300 mg, Urtica dioica 240 mg, Pinus pinaster 200 mg and glycine max 70 mg, for each administration, as described in the manufacturer’s instructions (Naturneed, Macerata, Italy)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 51
ORIGINAL PAPER
Luca Cindolo 1 , Andrea Fabiani 2 , Daniele Vitelli 1 , Filippo Cianci 1 , Lorenzo Gatti 1 , Nicola Ghidini 1 , Nikolas Niek Ntep 1 , Rosario Calarco Piazza 1 , Alessandra Filosa 3 , Giovanni Ferrari 1
1 Cure Group, Hesperia Hospital, Modena, Italy;
2 Urology Unit, Surgical Dpt, AST Macerata, Macerata Hospital, Macerata, Italy;
DOI: 10 4081/aiua 2023 11441
3 Pathological Anatomy, Politechnic University of Marche Region, Ancona, Italy
MATERIALS AND METHODS
From February 2021 and March 2022, all 100 consecutive patients, with prostatitis-like symptoms (10) attending each one of participating urologic centers, were enrolled in a multicentric phase III observational study The patients were treated with an herbal extract, containing Curcuma Longa 500 mg, Boswellia 300 mg, Urtica dioica 240 mg, Pinus pinaster 200 mg and glycine max 70 mg (PROSTAFLOG®), taking one capsule at bedtime every 24h for 60 days No placebo arm was included The demographic characteristics were studied using descriptive analysis tables and the calculation on the sample size has not been determined because the sample will be a "convenience sample" Inclusion criteria were: age more than 18 years, diagnosis of diagnosis of chronic abacterial prostatitis, any prostatic volume, Qmax between 11 and 25, post voiding volume < 50 ml Exclusion criteria were patient under 18 years old, history of neurological or psychiatric disorders which may impair evaluation of urinary symptoms, patients with urethral stricture or history of bladder or prostatic cancer or concomitant bladder stones, previous pelvic radiation therapy, inability to assess urinary symptoms, chronic opioid or opioid derivatives (for any reason) or cortisone therapy, alpha blockers or 5-alpha-reductase therapies, phosphodiesterase-5 inhibitors (PDE5i) or NSAIDs assumption during the study period, intolerance/allergies to the ingredients of the herbal extracts After the diagnosis of chronic prostatitis, all patients who met the inclusion criteria signed a written informed consent and underwent baseline questionnaires: Inter national Prostatic Symptoms Score-Quality of Life (IPSS-QoL), National Institutes of Health
Chronic Prostatitis Symptom Index (NIH-CPSI), P e l v i c P a i n a n d U rg e n c y / F re q u e n c y ( P U F )
Patient Symptom Scale, International Index of Erectile Function-5 (IIEF-5) (11, 14) A urological examination using the expressed prostatic secrete (EPS) culture or seminal fluid culture and a prostatic transrectal ultrasound (TRUS) were performed Uroflowmetry, CBC, inflamm a t i o n i n d i c e s ( e r y t h ro c y t e s e d i m e n t a t i o n rate/ESR; PCR; prothrombin time/PT; partial thromboplastin time/PTT; fibrinogen; PSA) were tested The first follow-up visit was scheduled at 2 months from starting therapy, with a urol o g i c a l a n d m i c ro b i o l o g i c a l e x a m i n a t i o n , questionnaire collection, transrectal ultrasound (TRUS), Treatment Benefit Scale (TBS) questionnaire compilation (15)
The softwares used for statistical analyses were Excel 2019, StatPlus Pro 7 6 5 (Med Calc to confirm) Mean, standard deviation, median, differences were calculated for the quantitative variables interquartile
The scores obtained in the responses to the IPSS, NIH CPSI, PUF and IIEF 5 questionnaires were assimilated to variables quantitative, but IPSS and IIEF 5 were also evaluated b a s e d o n t h e f re q u e n c y d i s t r i b u t i o n f o r expected score ranges, which is perhaps a more correct way of considering them, since there is a division into interpretation classes
For the QOL questionnaire, the frequency distributions recorded in the baseline versus follow up visit were evaluated, for the 5 scheduled answers For TBS, the distribution of frequencies recorded in each of the 4 responses was equally evaluated as provided in the questionnaire For each quantitative variable examined, the normality of the distribution of data was preliminarily evaluated, using Shapiro Wilk's test In case of confirmed H0 and of normal distribution, parametric tests were used in the evaluation of the statistical significance of the differences between the different variables at baseline and after follow up (ANOVA within subjects) In case of data non-normally distributed, the evaluation of the differences between the variables (baseline vs follow-up) was performed using nonparametric tests (Wilcoxon Signed Rank Test) The differences between the frequency distributions were evaluated by Pearson's Chi-square test
RESULTS
One hundred patients were included in the study The main characteristics were: mean age 52 1 ± 12 0 yeras, mean Body Mass Index 25 5 ± 2 8 Essential systemic arterial hypertension, dyslipidemia and diabetes mellitus occurred in 37%, 37% and 13%, respectively
The changes in baseline vs follow up clinical and biochemical variables were reported in Table 1 and 2 These changes between visit 1 and visit 2 were significant for prostate volume, Qmax and for all the questionnaires but the IIEF score variation which showed was not significant (Table 1) The TBS score revealed an interesting improve-
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 L
et
52
Cindolo, A Fabiani, D Vitelli,
al
Table 1.
Baseline Follow-up Variable Mean ± SD Median Mean ± SD Median Baseline vs follow-up (p) Prostate Volume (ml) 35 58 ± 15 98 33 50 33 82 ± 15 64 30 00 < 0 001 Uroflowmetry Qmax (ml/s) 17 74 ± 5 40 17 00 19 00 ± 5 41 18 00 < 0 001 IPSS 15.94 ± 5.01 17.5 13.78 ± 4.89 14.00 < 0.001 QOL 2 60 ± 0 89 3 00 2 16 ± 0 94 2 00 0 003 NIH CPSI 17 34 ± 5 43 18 00 14 56 ± 5 83 14 00 < 0 001 PUF 12 77 ± 4 36 15 00 10 74 ± 4 8 10 00 < 0 001 IIEF 5 18 ± 4 19 18 ± 4 19 0 909
The clinical variables at baseline visit and follow-up
Table 2
Baseline Follow-up Variable Mean ± SD Median Mean ± SD Median Baseline vs follow-up (p) WBC (10^3/mL) 6 36 ± 1 76 6 17 6 02 ± 1 30 5 80 0 0039 Lymphocyte count (10^3/mL) 2 08 ± 0 55 2 05 1 96 ± 0 53 1 95 < 0 001 Neutrophil count (10^3/mL) 3 97 ± 1 25 3 86 3 64 ± 0 90 3 60 < 0 001 ESR (mm/h) 7 76 ± 7 99 6 00 5 98 ± 5 40 5 00 < 0 001 CRP 2 40 ± 2 92 0 80 2 22 ± 2 90 0 50 < 0 001 Fibrinogen (mg/dL) 261 33 ± 57 28 246 00 250 56 ± 57 27 230 00 < 0 001 Total serum PSA (ng/ml) 3 57 ± 3 70 2 80 2 37 ± 1 73 2 20 < 0 001
Variation of inflammation indices
ment of perceived clinical status At follow up visit, the patients declared an improvement (great also) in 76% of cases No changes were declared in 22% and a worsened situation only in 2% (Figure 1) For the IIEF-5 questionnaire the differences are not significant both if we evaluate the scores or if we consider it a quantitative variable dividing the patients into categories based on the score intervals (Figure 2a, b) The variation obtained on the biochemical inflammation indexes was reported in Table 2, showing a global improvement of all parameters at follow-up visit, including a significant reduction in PSA as proxy of inflammatory status



DISCUSSION
Inflammation is a highly prevalent finding in the prostate, both at histological and biochemical level Men with inflammation have higher IPSS scores and increased prostate size, even if these differences appear to be imperceptibly small For men with prostatic inflammation, there is a significantly increased risk of developing acute urinary retention and the need of a surgical approach to
the disease (4) In recent years, several authors have shown how some laboratory tests (CBC, albumin, ESR, fibrinogen, PCR) that are routinely performed in preparation for various urological surgeries can play a role in identifying patients at greatest risk of complications and adverse outcomes after surgery (6) The effects of systemic inflammatory conditions, most notably metabolic syndrome, and their role in lower urinary tract symptoms (LUTS) have also been examined When the data are examined at a clinically relevant level, we must take into high consideration that inflammation is a common process in the prostate and that the clinically significant impact of ingland inflammation is variable and difficult to define For a long time, we know that the location of inflammation is important and that there are subsets of inflammation that are more frequently associated with the development of urinary symptoms or the prostate growth (16) In recent years, there was several experiences exploring the role of nutraceutical approach to the prostate inflammation In particular, Cai and co-workers (17) evaluated the efficacy of a combination of soyabean extracts associated with Curcuma Longa, Boswellia, Pinus pinaster and Urtica dioica ( P R O S TA F L O G ® ) i n p a t i e n t s a ff e c t e d b y C P / C P P S , through the evaluation of interleukin-8 (IL-8) plasma seminal levels All patients diagnosed with CP/CPPS, attending the same urologic center, were enrolled in this randomized, controlled phase III study Participants were randomized to receive oral capsules of PROSTAFLOG® (two capsules at bedtime every 24 h) or Ibuprofen 600 mg (1 tablet daily), lasting for a period of four weeks NIHCPSI and SF-36 questionnaires in association with urological evaluations with TRUS, Meares-Stamey test, and IL-8 dosage in seminal plasma were performed at baseline and at 3 months follow-up A total of 77 patients were enrolled [PROSTAFLOG® (n = 39); ibuprofen (n = 38)] in t h e s t u d y a n d f o l l o w e d f o r 3 m o n t h s I n t h e PROSTAFLOG® series, 69 2% of patients showed a significant reduction in the NIH-CPSI score, compared with 34 2% in the ibuprofen group (p < 0 0001) The mean IL8 levels were significantly lower in the PROSTAFLOG®
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 53 Herbal compound/extract in chronic abacterial prostatitis
Figure 1. Treatment benefit scale (TBS) after therapy
Figure 2a, b. No improvement of IIEF score after therapy. a. b.
cohort compared with the ibuprofen series (p < 0 0001), while a significant reduction in the IL-8 level between the e n ro l l m e n t a n d l a s t f o l l o w - u p e v a l u a t i o n w a s a l s o
observed in this group (p < 0 0001) Additionally, a significant reduction in the volume of the seminal vesicles assessed by TRUS was also found in the PROSTAFLOG® series during the observational timeframe The Authors concluded that PROSTAFLOG® significantly improves the QoL in patients affected by CP/CPPS and provides a significant reduction in IL-8 seminal levels as the overall seminal vesicles volume In our present study, the same observation in terms of QoL improvement was made (Figure 3) Especially in case of moderate QoL alteration, patients declared a positive impact from therapy on symptoms These data are confirmed at the follow up evaluation with TBS questionnaire The 20% of population studied reported a great improvement after treatment The rate moves to 76%
considering improvement to any extent
The statistically significant amelioration recorded at the follow-up visit after two months of therapy in IPSS, NIH CPPS and PUF scores (Figures 4a-b, 5, 6) confirms how the control of prostatic inflammation is correlated closely with a better perception of urinary symptoms characteristic of chronic prostatitis The IIEF-5 scores registered before treatment did not improve This finding could be related to the markedly multifactorial nature of the etiology of erectile dysfunction (ED) Given the age of the patients




Archivio Italiano di Urologia e Andrologia 2023; 95, 2 L Cindolo, A Fabiani, D Vitelli, et al 54
Figure 3. QoL improvement after therapy
Figure 4a, b
IPSS global score improvement at follow up visit, but not in cases with severe basal symptoms
Figure 5
NIH-CPSI score improvement at follow up visit
a. b.
enrolled and the presence of known risk factors for ED, such as systemic hypertension and diabetes mellitus, the lack of improvement after treatment is not surprising as the therapy is aimed at the management of the prostatic inflammatory process which is only one of the possible causative factors of ED Considering inflammation indicators, we preferred to investigate laboratory tests more accessible in daily clinical practice than seminal IL-8 levels The routinely determined markers of inflammation showed a statistically significative improvement between the first visit and the visit performed at the follow-up This clearly depends on prostatic inflammation etiology and confirm the anti-inflammatory role of the nutraceutical product The first experience with PROSTAFLOG® was by Fabiani et al. (18) They described their real-life experience with this anti-inflammatory mixture on PSA levels and, in a prospective mono-institutional study of 50 patients, admitted for a first PSA raising, reported a lowered PSA value in 80% of cases, with a mean of reduction of 2 94 ng/ml (0 26-16 2 ng/ml) in one month therapy (two pill per day) No differences were reported in term of prostate volume variation They concluded that PROSTAFLOG® use was able to lower the value of PSA, inviting to evaluate in appropriate studies the nutraceuticals products use in the treatment of prostatic pathology In our present experience, we can confirm the lowering effect on PSA value by the PROSTAFLOG® administration After 60 days of treatment, with one pill per day, we observed, at followup visit, a mean PSA levels of 2 74 ng/ml, starting from a 4 63 ng/ml mean value (Figure 7) Moreover, in our results, we reported a statistically significant reduction on prostate volume (38 01 ml vs 35 86 ml), presumably linked to the anti-inflammatory effect of prolonged administration (Figure 8) From a functional point of view, we found a significant improvement on flow parameters (Figure 9) The Qmax registered at the enrollment visit was significantly increased after PROSTAFLOG® treatment This is evidently the effect induced by the reduction of the static and dynamic factors which underlie the typical symptoms of BPH (9)
CONCLUSIONS
PROSTAFLOG® treatment employed in case of chronic prostatitis may significantly increase QoL, providing a sig-

nificant improvement of symptomatic scores A critical reduction in PSA level may be eventually take into account in clinical decision making PROSTAFLOG® may represent a promising and safe therapeutic agent leading to a reduction of inflammation markers, able to interrupt the pathophysiological mechanism of benign prostatic hyperplasia


REFERENCES
1 Lloyd GL, Marks JM, Ricke WA Benign Prostatic Hyperplasia and Lower Urinary Tract Symptoms: What Is the Role and Significance of Inflammation? Curr Urol Rep 2019; 20:54
2 Vasavada SR, Dobbs RW, Kajdacsy-Balla AA, et al Inflammation on Prostate Needle Biopsy is Associated with Lower Prostate Cancer Risk: A Meta-Analysis J Urol 2018; 199:1174-1181

Archivio Italiano di Urologia e Andrologia 2023; 95, 2 55 Herbal compound/extract in chronic abacterial prostatitis
Figure 7. Decreased PSA level from baseline after 2 months of treatment
Figure 8
Prostate volume decrease after therapy
Figure 9. Qmax improvement at follow up visit.
Figure 6. PUF score improvement after therapy
3 De Nunzio C, Voglino O, Cicione A, et al Ultrasound prostate parameters as predictors of successful trial without catheter after acute urinary retention in patients ongoing medical treatment for b e n i g n p ro s t a t i c h y p e r p l a s i a : a p ro s p e c t i v e m u l t i c e n t e r s t u d y Minerva Urol Nephrol 2021; 73:625-630
4 Gandaglia G, Briganti A, Gontero P, et al The role of chronic prostatic inflammation in the pathogenesis and progression of benign prostatic hyperplasia (BPH) BJU Int 2013; 112:432-41
5 Vela-Navarrete R, Alcaraz A, Rodríguez-Antolín A, et al Efficacy and safety of a hexanic extract of Serenoa repens (Permixon®) for the treatment of lower urinary tract symptoms associated with benign prostatic hyperplasia (LUTS/BPH): systematic review and metaanalysis of randomised controlled trials and observational studies BJU Int 2018; 122:1049-1065
6 Wang Q, Zhu SR, Huang XP, et al Prognostic value of systemic immune-inflammation index in patients with urinary system cancers: a meta-analysis Eur Rev Med Pharmacol Sci 2021; 25:1302-1310
7 Alazawi W, Pirmadjid N, Lahiri R, Bhattacharya S Inflammatory and Immune Responses to Surgery and Their Clinical Impact Ann Surg 2016; 264:73-80
8 Paulis G Inflammatory mechanisms and oxidative stress in prostatitis: the possible role of antioxidant therapy Res Rep Urol 2018; 10:75-87
9 Cicero AFG, Allkanjari O, Busetto GM, et al Nutraceutical treatment and prevention of benign prostatic hyperplasia and prostate cancer Arch Ital Urol Androl 2019; 91
10 Krieger JN, Nyberg L Jr, Nickel JC NIH consensus definition and classification of prostatitis JAMA 1999 Jul; 282:236-7
11 Hopland-Nechita FV, Andersen JR, Beisland C IPSS "bother
Correspondence
Luca Cindolo, MD, PhD lucacindolo@virgilio it
Daniele Vitelli, MD doc vitelli@gmail com
Filippo Cianci, MD filippocianci3p@hotmail com
Lorenzo Gatti, MD dottor102@gmail com
Nicola Ghidini, MD info@nicolaghidini it
Nikolas Niek Ntep, MD nicolas22it@yahoo fr
Rosario Calarco Piazza, MD iaiiopiazza@gmail com
Giovanni Ferrari, MD giogioferrari@yahoo it
Cure Group, Hesperia Hospital, Modena, Italy
Andrea Fabiani, MD (Corresponding Author) andreadoc1@libero it
Surgery Dpt, Section of Urology ASUR Marche Area Vasta 3, Macerata Hospital, Italy Via Santa Lucia, 2; 62100 Macerata (Italy)
Alessandra Filosa, MD PhD alessandrafilosa@yahoo it
Pathology Unit, ASUR MARCHE Area Vasta 5, Ascoli Piceno (Italy)
question" score predicts health-related quality of life better than total IPSS score World J Urol 2022; 40:765-772
12 Giubilei G, Mondaini N, Crisci A, et al The Italian version of the National Institutes of Health Chronic Prostatitis Symptom Index Eur Urol 2005; 47:805-11
13 Brewer ME, White WM, Klein FA, et al Validity of Pelvic Pain, Urgency, and Frequency questionnaire in patients with interstitial cystitis/painful bladder syndrome Urology 2007; 70:646-9
14 Rosen RC, Cappelleri JC, Smith MD, et al Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction Int J Impot Res 199; 11:319-26
15 Viktrup L, Hayes RP, Wang P, Shen W Construct validation of patient global impression of severity (PGI-S) and improvement (PGII) questionnaires in the treatment of men with lower urinary tract symptoms secondary to benign prostatic hyperplasia BMC Urol 2012; 12:30
16 Kohnen PW, Drach GW Patterns of inflammation in prostatic hyperplasia: a histologic and bacteriologic study J Urol 1979; 121:755-60
17 Cai T, Anceschi U, Tamanini I, et al Soybean Extracts (Glycine Max) with Curcuma, Boswellia, Pinus and Urtica Are Able to Improve Quality of Life in Patients Affected by CP/CPPS: Is the ProInflammatory Cytokine IL-8 Level Decreasing the Physiopathological Link? Uro 2022; 2:40-48 https://doi org/10 3390/ uro2010006
18 Fabiani A, Morosetti C, Filosa A, et al Effect on prostatic specific antigen by a short time treatment with a Curcuma extract: A real life experience and implications for prostate biopsy Arch Ital Urol Androl 2018; 90:107-111
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 L Cindolo, A Fabiani, D Vitelli, et al 56
Oncological outcomes of papillary versus clear cell renal cell carcinoma in pT1 and pT2 stage: Results from a contemporary Turkish patient cohort
Taha Cetin 1 , Serdar Celik 1 , Sinan Sozen 2 , Bulent Akdogan 3 , Volkan Izol 4 , Guven Aslan 5 , Evren Suer 6 , Yildirim Bayazit 4 , Nihat Karakoyunlu 7 , Haluk Ozen 3 , Sumer Baltaci 6 , Fatih Gokalp 8 , Ilker Tinay 9 ,
Members of Turkish Urooncology Association
1 Izmir Bozyaka Research and Training Hospital Urology Department, Izmir, Türkiye;
2 Gazi University Faculty of Medicine Urology Department, Ankara, Türkiye;
3 Hacettepe University Faculty of Medicine Urology Department, Ankara, Türkiye;
4 Cukurova University Faculty of Medicine Urology Department, Adana, Türkiye;
5 Dokuz Eylul University Faculty of Medicine Urology Department, Izmir, Türkiye;
6 Ankara University Faculty of Medicine Urology Department, Ankara, Türkiye;
7 University of Health Sciences Dıskapi Yildirim Beyazit Research and Training Hospital Urology Department, Ankara, Türkiye;
8 Mustafa Kemal University Tayfur Ata Sokmen Medicine Faculty Urology Department, Hatay, Türkiye;
9 Marmara University Faculty of Medicine Urology Department, Istanbul, Türkiye
Summary
Objectives: To compare overall survival (OS), recurrence free survival (RFS), and cancer-specific survival (CSS) in the long-term follow-up of T1 and T2 clear-cell-Renal Cell Carcinoma (ccRCC) and papillary Renal Cell Carcinoma (pRCC) patients, as well as to determine the risk factors for recurrence and overall mortality.
Material and method: Data of patients with kidney tumors obtained from the Urologic Cancer Database - Kidney (UroCaD-K) of Turkish Urooncology Association (TUOA) were evaluated retrospectively. Out of them, patients who had pathological T1-T2 ccRCC and pRCC were included in the study
According to the two histological subtype, recurrence and mortality status, RFS, OS and CSS data were analyzed
Results: RFS, OS and CSS of pRCC and ccRCC were found to be similar Radiological local invasion was shown to be a risk factor for recurrence in pRCC, and age was the only independent factor affecting overall mortality
Conclusions: There were no differences in survivals (RFS, OS and CSS) of patients with localized papillary and clear cell RCC. While age was the only factor affecting overall mortality, radiological local invasion was a risk factor for recurrence in papillary RCC.
KEY WORDS: Kidney cancer; Renal cell carcinoma; Clear cell RCC; Papillary type RCC; Recurrence, Survival
Submitted 26 January 2023; Accepted 17 February 2023
INTRODUCTION
Almost twenty years ago the Heidelberg classification system recognized the histological subtypes of Renal Cell Carcinoma (RCC) as clear cell (cc)-RCC, with a frequency of 70-88% in most series, papillary (p)-RCC accounting for 10-15% and other RCC accounting for less than 10% (1, 2) Several studies have uniformly reported that a pRCC histology is associated with a favorable prognosis compared with clear cell RCC (ccRCC) (3-6) In other studies, pRCC
was a significant risk factor (7, 8) However, the results of multivariable analyses assessing the prognostic significance of type2 pRCC histological subtype are incoherent (9, 10) In this context, outcomes may vary depending on the pRCC type and tumor stage
The aim of this study was to compare OS, CSS and RFS of patients diagnosed with pRCC and ccRCC and define the factors affecting survival in the patient population with localized disease
MATERIALS AND METHODS
Patients with renal cell carcinoma (RCC), who underwent radical or partial nephrectomy due to renal tumors, whose data were obtained from a series of 5300 patients with kidney tumors included in the Urologic Cancer DatabaseKidney (UroCaD-K) of Turkish Urooncology Association (TUOA) were evaluated retrospectively Pathological stage and grade were determined according to the 2002 Union Internationale Contre le Cancer TNM Classification, and Fuhrman classification (G1-G4), respectively Tumor size was measured using the computed tomography (CT) and taking the largest diameter
Histological subtypes were classified according to the Heidelberg classification (1): ccRCC, pRCC, chromophobe, Bellini duct, and unclassified RCC Patients from UroCaD-K database, who had pathological T1-T2 ccRCC and pRCC were evaluated in the study According to the two histological subtype, recurrence and mortality status, recurrence free survival (RFS), overall survival (OS) and cancer-specific survival (CSS) data were analyzed The follow-up protocol of the patients was arranged according to the EAU-RCC guideline
Statistical analysis
Analyses were performed by the using of Statistical Package for the Social Sciences (SPSS) version 22 0 Chi-
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 57
ORIGINAL PAPER
DOI: 10 4081/aiua 2023 11218
square and Student t-tests were used to compare categorical and continuous data, respectively The relationship between tumor size and histological subtype was analyzed with logistic regression models The Kaplan-Meier method was used to estimate tumor specific survival, and c o m p a r i s o n w a s p e r f o r m e d b y t h e l o g - r a n k t e s t
Multivariate Cox proportional hazard models were used to detect independent variables with a p < 0 05 considered to indicate statistical significance
1
RESULTS
The clinical, pathological and oncological data of the patients are shown in Table 1 Among 5300 patients, 2129 patients who had pathological T1-T2 ccRCC and pRCC were included in the study The mean age was 57 7 ± 11 8 years and two-thirds of the patients were male There were 1700 patients with ccRCC, while the pRCC was observed in 429 patients
Patients in the ccRCC group were younger and had a higher BMI (p values were < 0 001 and 0 004, respectively)
Radiological tumor size was statistically found to be smaller in pRCC than ccRCC group (mean size were 4 7 cm vs 5cm, p = 0 001)
We detected that radiologically < 4 cm tumors were more frequent in the pRCC group that ccRCC (p = 0 034) The finding of radiological local invasion was also more common in ccRCC, but there was no statistically difference (5 4% vs 3 5%) There was no statistically difference between the groups when we evaluated them in terms of pathological tumor size and Fuhrman grade Considering the postoperative follow-up periods, the mean follow-up time for ccRCC and pRCC were 25 2 months and 26 1 months, respectively (p = 0 613)
Pathological T stage and radiological local invasion were found to be risk factors for recurrence in ccRCC Age, radiological local invasion and Fuhrman grade 3-4 were found to be independent risk factors affecting overall mortality in patients with ccRCC In pRCC patients, radiological local invasion was found to be an independent risk factor for recurrence and age was a risk factor for overall mortality (Table 2)
In addition, RFS, OS and CSS were not statistically different between the groups (Figure 1)
DISCUSSION
Factors affecting recurrence and overall mortality in ccRCC and pRCC groups
We aimed to discuss OS, CSS and RFS of patients diagnosed with pRCC and ccRCC and define the factors affecting survival in patient population with pT1 and pT2 disease It was observed that ccRCC was seen in younger patients and in patients with higher BMI, and that pRCC was more common in males
P a p i l l a r y t y p e p a t h o l o g y w a s r a d i o l o g i c a l l y smaller and was more frequently evaluated as pT1a than clear cell type Radiological local invasion and age were found to be independent risk factors for recurrence and overall mortality, respectively for both groups Pathological stage was also a risk factor for recurrence in ccRCC
In addition, during the follow-up, OS, CSS and RFS were not statistically different for both groups in pT1 and pT2 disease
The two most important factors determining the outcome of RCC are nuclear grade and tumor stage (11) According to some authors, apart from these two factors, histological subtype was also an independent prognostic factor (12)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 T Cetin, S Celik, S Sozen, et al 58
Table
data of the patients ccRCC (n = 1700) pRCC (n = 429) P Age (year) 56 7 ± 12 59 6 ± 11 8 < 0.001 Sex, n (%) Female 641 (37 9) 72 (16 8) < 0 001 Male 1048 (62 1) 356 (83.2) BMI (kg/m2) 28.3 ± 5 27 ± 4 0.004 Radiological tumor size (cm) 5 ± 3 4 7 ± 3 0 001 Tumor diameter, n (%) < 4 cm 787 (46 4) 226 (52 6) 0.034 4-7 cm 626 (36 8) 126 (29 4) 7-10 cm 209 (12 3) 55 (12 8) > 10 cm 77 (4 5) 22 (5 2) Radiological Organ confined, n (%) Localized 1609 (94 6) 414 (96 5) 0 114 Locally invasive 91 (5 4) 15 (3 5) Pathological tumor size (cm) 5±2 8 5 2±3 2 0 155 Pathological T stage, n (%) T1a 806 (37 1) 216 (43 4) 0 05 T1b 606 (28 4) 129 (25 7) T2a 214 (10 9) 55 (11 6) T2b 74 (4 1) 29 (6 3) Fuhrman Grade, n (%) 1-2 986 (70 4) 177 (67 8) 0 385 3-4 413 (29.6) 70 (32.2) Relapse, n (%) 33 (1 94) 10 (2 33) 0 608 Overall mortality, n (%) 37 (2 17) 11 (2 6) 0 629 Cancer specific mortality, n (%) 10 (0 6) 2 (0 5) 0 556 Mean follow-up time (months) 25 2 ± 30 3 26 1 ± 30 7 0 613
Clinical, pathological and oncological
Table 2.
Histologic subtype Recur rence Overall mor tality Univariate Multivariate Univariate Multivariate P value OR (CI) P value OR (CI) ccRCC Age 0 958 - 0 002 1 056 (1 023-1 090) Sex 0 370 - 0 084BMI 0 279 - 0 471Pathological tumor size 0 071 - 0 105Pathological stage 0 044 1 447 (1 006-2 081) 0 091Radiological local inv 0 007 4 136 (1 663-10 287) 0 044Fuhrman 3-4 0 952 - 0.033pRCC Age 0 444 - 0 026 1 066 (1 009-1 127) Sex 0 069 - 0 128BMI 0 270 - 0 131Pathological tumor size 0 776 - 0 275Pathological stage 0.423 - 0.474Radiological local inv 0 044 7 808(1 507-40 450) 0 673Fuhrman 3-4 0 406 - 0 681 -
Type 1 pRCC is associated with MET alteration or trisomy of chromosome 7 where the MET gene is located, while Type2 pRCC shows allelic imbalance on chromosomes 1p, 3p, 5, 6, 8, 9p, 10, 11, 15, 18 and 22 (13, 14)
According to the study shared by Waldert et al 5-year CSS was 94% in type 1 pRCC and 74% in type 2 pRCC (p = 0 027) During the follow-up, the overall CSS for M0 patients with pRCC and ccRCC (90% vs 84% respectively) was not significantly different) Steffens et al evaluated long-term survival of pRCC versus ccRCC In this series, patients with pRCC had significantly higher 5-yr CSS rate (85 1% vs 76 3%; p = 0 001) Notably, at multivariable analysis, the papillary subtype was significantly associated with favorable oncologic outcome in localized RCC but was an independent negative prognostic factor in metastatic patients
These results could be evaluated separately for papillary type 1 and type 2, but this was not evaluated in the study (14)
In addition, authors have shown that type 1 and type 2 RCC have similar clinical and histopathological features, but lymphovascular invasion (LVI) in type 2 pRCC worsened CSS rate, compared to type1 pRCC (5)
In a multicenter study involving more than four thousand patients from eight international centers, patients with pRCC had better 5-year CSS than patients with ccRCC in univariate analysis (73% versus 79% respectively) In multivariate analysis, the histological subtype was not an independent prognostic factor (15)

Five studies with 32 158 patients indicated that pRCC had a better prognosis than ccRCC (3, 6, 16-18), while other 5 studies including 3674 patients showed that pRCC was an independent predictor of poor outcomes (4, 7, 8, 19, 20) According to the results of the metaanalysis including these studies, pRCC was associated with better outcomes than ccRCC in patients with nonmetastatic disease, but not in patients with metastatic disease Type 2 pRCC had worse prognosis than ccRCC, but no significant difference was found with type 1 pRCC
In this study, it was observed that the tumor size was smaller in pRCC In the study of Waldert et al tumor size was also smaller in pRCC (mean 4 5 cm) compared to ccRCC (mean 5 5 cm) (p = 0 013) (14)
Traditionally, p-RCC is divided into 2 types: type 1 is characterized by a basophilic cytoplasm and is classified as a low-grade tumor, while type 2 displays a bulky eosinophilic cytoplasm and pseudostratified tumor cell nuclei and is considered a high-grade tumor (3)
Compared to type 1 p-RCC, type 2 p-RCC presents more frequently as a locally advanced disease and is associated with more aggressive clinicopathologic features and significantly worse outcome (9, 10, 14, 21)
Our study had some limitations Most important limitations are the retrospective analysis and the multi-centered design with pathological evaluation not performed in a single centre Evaluation of the patients by experts in urooncology may reduce the disadvantage of multi-center data analysis In addition, not taking into the account the pRCC subtypes can be considered among the limitations of the study
CONCLUSIONS
In conclusion, RFS, OS and CSS were similar between p R C C a n d c c R C C p a t i e n t s w i t h l o c a l i z e d d i s e a s e Although it was not statistically significant, it is obvious that the histopathological and therefore cancer biology of the most common RCC subtypes are different The management of patients should be planned according to the stage and subtype of the disease
REFERENCES
1 Kovacs G, Akhtar M, Beckwith BJ, et al The Heidelberg classification of renal cell tumours J Pathol 1997; 183:131-3
2 Pantuck AJ, Zisman A, Belldegrun AS The changing natural history of renal cell carcinoma J Urol 2001; 166:1611-1623
3 Wagener N, Edelmann D, Benner A, et al European Association of Urology (EAU) Young Academic Urologists (YAU) Kidney Cancer Group Outcome of papillary versus clear cell renal cell carcinoma varies significantly in non-metastatic disease PLoS One 2017; 12:e0184173
4 Nguyen DP, Vertosick EA, Corradi RB, et al Histological subtype of renal cell carcinoma significantly affects survival in the era of partial nephrectomy Urol Oncol 2016; 34:259 e1-8
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 59 Papillary clear cell carcinoma outcomes
Figure 1. Kaplan-Meier Survival analysis of recurrence-free survival (RFS), Overall survival (OS), cancer specific survival (CSS) between pathological T1-T2 ccRCC and pRCC
5 Steffens S, Janssen M, Roos FC, et al Incidence and long-term prognosis of papillary compared to clear cell renal cell carcinoma--a multicentre study Eur J Cancer 2012; 48:2347-52
6 Teloken PE, Thompson RH, Tickoo SK, et al Prognostic impact of histological subtype on surgically treated localized renal cell carcinoma J Urol 2009; 182:2132-6
7 Yoo S, You D, Jeong IG, et al Histologic subtype needs to be considered after partial nephrectomy in patients with pathologic T1a renal cell carcinoma: papillary vs clear cell renal cell carcinoma J Cancer Res Clin Oncol 2017; 143:1845-1851
8 Kondo T, Ikezawa E, Takagi T, et al Negative impact of papillary histological subtype in patients with renal cell carcinoma extending into the inferior vena cava: single-center experience Int J Urol 2013; 20:1072-7
9 Delahunt B, Eble JN, McCredie MR, et al Morphologic typing of papillary renal cell carcinoma: comparison of growth kinetics and patient survival in 66 cases Hum Pathol 2001; 32:590-5
10 Pignot G, Elie C, Conquy S, et al Survival analysis of 130 patients with papillary renal cell carcinoma: prognostic utility of type 1 and type 2 subclassification Urology 2007; 69:230-5
11 Gudbjartsson T, Hardarson S, Petursdottir V, et al Histological subtyping and nuclear grading of renal cell carcinoma and their implications for survival: a retrospective nation-wide study of 629 patients Eur Urol 2005; 48:593-600
12 Cheville JC, Lohse CM, Zincke H, et al Comparisons of outcome and prognostic features among histologic subtypes of renal cell carcinoma Am J Surg Pathol 2003; 27:612-24
13 Jiang F, Richter J, Schraml P, et al Chromosomal imbalances in papillary renal cell carcinoma: genetic differences between histological subtypes Am J Pathol 1998; 153:1467-73
14 Antonelli A, Tardanico R, Balzarini P, et al Cytogenetic features, clinical significance and prognostic impact of type 1 and type 2 papillary renal cell carcinoma Cancer Genet Cytogenet 2010; 199:128-33
15 Waldert M, Haitel A, Marberger M, et al Comparison of type I and II papillary renal cell carcinoma (RCC) and clear cell RCC BJU Int 2008;102:1381-4
16 Patard JJ, Leray E, Rioux-Leclercq N, et al Prognostic value of histologic subtypes in renal cell carcinoma: a multicenter experience J Clin Oncol 2005; 23:2763-71
17 Lee WK, Lee SE, Hong SK, et al Characteristics and prognostic value of papillary histologic subtype in nonmetastatic renal cell carcinoma in Korea: a multicenter study Urol J 2014; 11:1884-90
18 Keegan KA, Schupp CW, Chamie K, et al Histopathology of surgically treated renal cell carcinoma: survival differences by subtype and stage J Urol 2012; 188:391-7
19 Beck SD, Patel MI, Snyder ME, et al Effect of papillary and chromophobe cell type on disease-free survival after nephrectomy for renal cell carcinoma Ann Surg Oncol 2004; 11:71-7
20 Simone G, Tuderti G, Ferriero M, et al Papillary type 2 versus clear cell renal cell carcinoma: Survival outcomes Eur J Surg Oncol 2016; 42:1744-1750
21 Kim KH, You D, Jeong IG, et al Type II papillary histology predicts poor outcome in patients with renal cell carcinoma and vena cava thrombus BJU Int 2012; 11:E673-8
Correspondence
Taha Cetin, MD, FEBU (Corresponding Author) tahacetin88@gmail com
Serdar Celik, MD serdarcelik84@hotmail com
Izmir Bozyaka Research and Training Hospital Urology Department, Izmir, Türkiye
Sinan Sozen, MD sinansozen@usa net
Gazi University Faculty of Medicine Urology Department, Ankara, Türkiye
Bulent Akdogan, MD blntakdogan@yahoo com
Haluk Ozen, MD drhalukozen@gmail com
Hacettepe University Faculty of Medicine Urology Department, Ankara, Türkiye
Volkan Izol, MD volkanizol@yahoo com
Yildirim Bayazit, MD ybayazit@yahoo com
Cukurova University Faculty of Medicine Urology Department, Adana, Türkiye
Conflict of interest: The authors declare no potential conflict of interest
Guven Aslan, MD drguvenaslan@gmail com
Dokuz Eylul University Faculty of Medicine Urology Department, Izmir, Türkiye
Evren Suer, MD drevrensuer@gmail com
Sumer Baltaci, MD baltacisumer@gmail com
Ankara University Faculty of Medicine Urology Department, Ankara, Türkiye
Nihat Karakoyunlu, MD nkarakoyunlu@gmail com
University of Health Sciences Dıskapi Yildirim Beyazit Research and Training Hospital Urology Department, Ankara, Türkiye
Fatih Gokalp, MD fatihgokalp85@gmail com
Mustafa Kemal University Tayfur Ata Sokmen Medicine Faculty Urology Department, Hatay, Türkiye
Ilker Tinay, MD ilker tinay@yahoo com
Marmara University Faculty of Medicine Urology Department, Istanbul, Türkiye
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 T Cetin, S Celik, S Sozen, et al 60
Chronic prostatitis as possible risk factor for Peyronie's disease:
Psychological, sexual and prostatitis-like symptoms in patients with PD
Gianni Paulis 1 , Andrea Paulis 2
1 Peyronie’s Care Center, Department of Uro-Andrology, Castelfidardo Clinical Analysis Center, Rome, Italy;
2 Neurosystem Center for applied Psychology and Neuroscience, Janet Clinical Centre, Rome, Italy
Summary
Objective: This study aims to investigate a possible relationship between chronic prostatitis (CP) and Peyronie's disease (PD) and to characterize the psychological profile of patients suffering from PD, with or without concomitant CP.
Methods: We included 539 patients with PD, of which 200 were found to have underlying CP. As a comparator population, we selected 2201 patients without PD, referring to our tertiary care clinic. In this population, we detected 384 subjects with CP. All 539 PD patients underwent photographic documentation of the penile deformation, and dynamic penile eco-color Doppler with plaque and volume measurements and answered the following questionnaires: the Generalized Anxiety Disorder-7, the Patient Health Questionnaire-9, the Visual Analog Scale for penile pain measurements, the International Index of Erectile Function (IIEF), and the NIH-Chronic Prostatitis Symptom Index
Results: The overall prevalence of chronic prostatitis in PD patients was 37 1% compared to a prevalence of 17 4% in the non-PD control population (OR = 2 79 and p < 0 0001) The severity of CP symptom total scores (NIH-CPSI) correlated significantly with the severity of erectile dysfunction (p < 0 0001)
Significant anxiety was present in 89 2% of PD patients and it is more prevalent in PD patients with CP than in PD patients without CP (93 0% vs 87 0%, respectively; p = 0 0434)
Significant depression was detected in 57 1% of PD patients and it is more prevalent in PD patients with CP than in PD patients without CP (64 0% vs 53 09%, respectively; p = 0 0173)
Conclusion: Chronic prostatitis (CP) and Peyronie's disease (PD) are frequently associated Our results demonstrate the strong impact of chronic prostatitis on the mental status of PD patients Anxiety and depression were significantly more pronounced in PD patients with CP than in PD patients without CP.
KEY WORDS: Chronic prostatitis; Peyronie’s disease; Risk factors
Submitted 12 April 2023; Accepted 11 May 2023
INTRODUCTION
Prostatitis is a pathological condition that is often observed in patients with Peyronie's disease (PD)
This clinical association is often present in specialist outpatient practice and is also described in the literature (15) With this study, we set out to ascertain whether there are common factors between the two pathologies that could justify this relationship
Inflammatory features common to two pathologies: PD and CP
In both diseases, there is a chronic inflammatory process in which pro-inflammatory cytokines and oxygen and nitrogen reactive species (ROS/RNS) play an important role (6-10) Furthermore, there are studies in the literature that have confirmed the therapeutic efficacy of the use of antioxidant substances in both diseases (10-15) We also know that pro-inflammatory cytokines, Tumor Necrosis Factor (TNF), and interleukin 1 and 6 (IL-1 and IL-6) are present at high levels in the inflammatory process of PD and chronic prostatitis (CP) (6, 7)
In both diseases, as well as in other chronic inflammator y
increased; therefore, these can act systemically in other organs, including the nervous system (16-19) It has been ascertained that pro-inflammatory cytokines can determine various effects at this level and particularly by reducing serotonin levels This mechanism, as is known, is also strongly involved in the development of depression Pro-inflammatory cytokines are also capable of causing an additional pro-depression effect as they cause changes in glucocorticoid function via the hypothalamicpituitary-adrenal axis (20) Cytokines are also capable of having effects on the amygdala and hippocampus, which are areas widely involved in stress and anxiety (21, 22)
Thanks to this knowledge from the literature, we can better understand the causes of anxious-depressive symptoms in patients with PD and CP
Pro-inflammatory cytokines are also involved in neurogenic inflammation causing pelvic pain in patients with prostatitis/chronic pelvic pain syndrome (CPPS) (22) Pelvic pain in CP is therefore the consequence of neurogenic inflammation in the nervous system (central and peripheral)
An important signaling molecule implicated in neurogenic inflammation is Nerve Growth Factor neurotrophin (NGF) Neurotrophins are proteins that determine the survival, development, and function of neurons NGF is a signaling molecule that is produced in the case of neuronal suffering, which in our case is caused by inflammation NGF appears to be induced by IL-10, a cytokine that possesses anti-inflammatory activity by inhibiting the synthesis of pro-inflammatory cytokines (23-25)
Several studies have demonstrated that NGF together with some cytokines (IL-6 and IL-10) that regulate inflamma-
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 61
ORIGINAL PAPER
d i s e a s e s , t h e c i r c u l a t i n g l e v e l s o f c y t o k i n e s a r e
DOI: 10 4081/aiua 2023 11406
tion can play a role in the pain of patients with CPPS; furthermore, NGF directly correlates with pain severity (2325) We also know that IL-10 is a known inducer of NGF and a suppressor of IL-6 and IL-8 expression (23, 25) The association of increased levels of NGF in other inflammatory states (inflammatory bowel disease and arthritis) has also been demonstrated (25)
Although no studies exist in the literature, it is likely that NGF also plays a role in PD and associated erectile dysfunction, since some studies demonstrate a protective role of this neurotrophin on erectile function (26-28) Kalisch et al , in one of their studies, demonstrated that the NGF neurotrophin increases NOS activity expression (in all three of its isoforms: nNOS, eNOS, and iNOS) and nitric oxide (NO) production, the principal mediator of penile erection (29)
In an experimental study on diabetic rats, the induction of IgC (anti-NGF) was detected with related erectile dysfunction caused by a decrease in the tissue level of NGF (neutralizing effect of anti-NGF) (26) It is in fact known that in patients with diabetes mellitus, the incidence of erectile dysfunction is significantly higher than in the general male population In another experimental study on diabetic rats with erectile dysfunction, the presence of high concentrations of NGF was found in the penis, and the authors hypothesized that the significant presence of NGF, in the presence of erectile nerves that are severely damaged by diabetes, would not be sufficient to compensate for the reproductive needs of nerve fibers (27) Another study found elevated concentrations of NGF in urine in patients with type 2 diabetes mellitus and associated erectile dysfunction (28)
Considering that several pro-inflammatory biological factors and other signaling molecules are present in CP, it may be hypothesized that CP could represent a risk factor for PD
The present study aimed at studying the relationship between a history of CP and PD The psychological impact of PD, in the presence or absence of concomitant CP, was also investigated in depth
Psychological consequences of PD and CP
The penile deformation present in patients with PD inevitably determines a significant impact on the psychic sphere of these patients, their quality of life (QoL), and their psycho-social relationships In fact, these patients show depressive symptoms in about 48% of cases (30) In these patients, bowing can frequently lead to a loss of personal body image, lower self-esteem, and a lower ability to achieve satisfactory sexual intercourse; furthermore, sexual performance anxiety with secondary psychogenic erectile dysfunction is often present (31) Other possible consequences are as follows: the tendency to lose confidence in their sexual abilities; decreased sex drive or even sexual aversion; concern about further sexual trauma; and curtailing or canceling appointments with prospective sexual partners (32-34) Although there is no specific incidence of anxiety symptoms in PD in the literature, some studies report the presence of "emotional difficulties" and "distress" in about 80-81% of cases (34, 35) In our recent study, we found that moderate-to-severe anxiety was present in 89 4% of PD patients (36)
Chronic prostatitis such as PD is characterized by a strong component of frustration with related anxious-depressive symptoms (21) Depression and catastrophizing about pain are often present; in this regard, some authors believe that depression and catastrophism represent a strong factor in the development, prolongation, and perpetuation of prostatic symptoms and, particularly, chronic pelvic pain (37, 38) Patients who have more pain tend to amplify it and have more catastrophic thoughts, resulting in a poorer physical QoL and a tendency towards depression (39) In their recent study, Bai et al found a higher incidence of depression, anxiety, somatization disorder, and obsessive-compulsive behavior in patients with ED associated with CP/CPPS (40)
The literature is quite scarce regarding the incidence of anxiety and depression in patients with CP/CPSS; however, in the few studies analyzed, the incidence of anxiety symptoms in patients with CP/CPPS was found in about 60-90% of cases (41, 42), while with respect to the incidence of depressive symptoms, these were found to be present in approximately 27-90% of cases in patients with CP/CPPS (42-44)
This study aims to investigate a possible relationship between CP and PD and to characterize the psychological profile of patients suffering from PD, with or without concomitant CP
PATIENTS AND METHODS
Study design
We performed a retrospective analysis of the clinical database of a single andrology clinic From the database, we considered two separate cohorts of patients observed between January 2013 and January 2023 In this study, one cohort included 539 patients diagnosed with PD As a comparator population, we considered a cohort of 2201 urological patients referred to our clinic for any disease but not PD Among our cohorts of patients, we identified patients with a diagnosis of long-standing CP (CP, Category II chronic bacterial prostatitis or Category III chronic prostatitis/chronic pelvic pain syndrome, NIH criteria)
All data were obtained from patient records This retrospective observational study was conducted in compliance with the principles contained in the Declaration of Helsinki ; all study subjects were contacted and provided informed consent for the study Sensitive data were anonymized to warrant patients’ privacy according to Legislative Decree 10 August 2018, n 101, published in the Official Gazette of the Italian Republic, General Series, issue 205, 09/04/2018
Inclusion criteria
The inclusion criteria for both groups were as follows: age between 18 and 75 years and availability of data that report the results of thorough clinical history examination (comprising all diseases, including prostatitis)
The diagnosis of PD was made as follows: performing penile palpation for all PD patients and by a (i) photo-
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 G Paulis, A Paulis 62
I n t h e S u p p l e m e n t a r y M a t e r i a l s w e p u b l i s h e d a n "Addendum"" as a deeper insight into the two diseases CP and PD
(according to Kelâmi) with a goniometric measurement of the angulation and evaluation with respect to the possible presence of the multiplanarity of the curvature (29) and a (ii) dynamic penile eco-color Doppler ultrasound with plaque measurements and volume calculation (in the three dimensions) using an ellipsoid formula (volume = 0 524 x width x length x thickness) (45, 46)
Exclusion criteria
The exclusion criteria were as follows: – for both groups, PD patients and non-PD patients an age under 18 years and over 75 years; – for the comparison control cohort (2201 non-PD patients) a diagnosis of PD, without excluding all other associated diseases including a possible erectile dysfunction
Clinical data
Patients with PD were asked to complete of the following questionnaires: (i) the Visual Analog Scale (VAS) for penile pain measurement, (ii) the International Index of Erectile Function (IIEF), (iii) the NIH-Chronic Prostatitis Symptom Index (NIH-CPSI), (iv) the Generalized Anxiety Disorder-7 (GAD-7, focusing on anxiety), and (v) the Patient Health Questionnaire-9 (PHQ-9, focusing on depression) (4751)
The VAS score range varies from 0 (no pain) to 10 (most intolerable pain) (48)
The IIEF score interpretation is as follows: severe ED = from 0 to 10; moderate ED = from 11 to 16; mild-tomoderate ED = from 17 to 21; mild ED = from 22 to 25; no ED, from 26 to 30 (49)
The GAD-7 score interpretation is as follows: minimal anxiety = 0-4; mild anxiety = 5-9; moderate anxiety = 1014; and severe anxiety = 15-21 (50) We considered the presence of significant anxiety when GAD-7 score > 9
The PHQ-9 score interpretation is as follows: minimal depression = 0-4; mild depression = 5-9; moderate depression = 10-14; moderately severe depression = 1519; and severe depression = 20-27 (51) We considered significant depression when PHQ-9 score > 9
NIH-CPSI is assessed in 3 domains with the following severity levels: pain (from 0 to 21), urinary symptoms (from 0 to 10), and impact on QoL (from 0 to 12) (47)
Chronic prostatitis was diagnosed in patients with prostatitis-like symptoms according to the following examinations: clinical history, thorough physical examination, including the digital rectal exam, prostate ultrasound, and microbiological assessment (pre- and post-massage urine and sperm cultures)
Study endpoints
The primary endpoint of the study was the association between a diagnosis of CP and the occurrence of PD in a patient population referring to a single tertiary care andrology center
The secondary endpoints are as follows:
The impact of prostatitis on the psychological status of patients and, particularly, on anxiety, which was assessed with the GAD-7 test, and depression which was assessed with the PHQ-9 test;
The impact of prostatitis on the presence and severity of erectile dysfunction;
– The impact of prostatitis on the presence and severity of penile pain;
– The impact of prostatitis on the severity of penile curvature;
– The impact of prostatitis on the PD plaque volume; – The impact of prostatitis on the multiplanarity of penile curvature;
– The impact of prostatitis on plaque multifocality;
– The impact of prostatitis on plaque calcification
Statistical analysis
The central tendency and dispersion data for continuous or interval variables were expressed as means and standard deviations (SDs) or medians and interquartile ranges (IQRs), respectively
Intergroup unpaired comparisons for continuous or interval variables were performed using a 2-tailed t-test (heteroscedastic) or a 2-tailed Mann–Whitney–Wilcoxon (rank-sum) test, respectively
Differences between proportions in unpaired groups were analyzed by both a Z-test and Pearson’s chi-square test Correlations between questionnaire scores were analyzed by non-parametric tests (Spearman’s rho and Kendall’s tau) Analyses were performed in the “R” environment for statistical computing
We planned a post hoc analysis of the statistical power achieved for the crude odds ratio calculation using the G*Power 3 1 software (52)
A 5% threshold for the alpha error was used to define statistical significance (significant p-value < 0 05)
RESULTS
A Table (Supplementary Materials) summarizes the clinical characteristics of the two groups (PD patients and non-PD control population) and the relative statistical study Cases and controls did not differ in age, and most associated pathologies However, for some associated diseases such as diabetes mellitus, erectile dysfunction, hypertension, benign prostatic hyperplasia (BPH), and CP, there was a statistically significant difference between the two groups
Prevalence of CP in PD patients
From our general patient database, we extracted a cohort of 539 PD patients, with a mean age of 49 68 years (± 12 16 SD), that met our inclusion criteria Within this cohort, 200 patients (37 1%) were diagnosed with CP
The median total score of the NIH-CPSI test in this cohort was 9 (IQR = 10) The cohort of urological patients without PD meeting our inclusion criteria consisted of 2201 subjects, with a mean age of 50 53 years (± 12 04 SD), of which 384 (17 4%) were diagnosed with CP The statistical comparison between the mean age of the two patient cohorts (unpaired t test) was not significant (p value = 0 1088)
The difference between the proportions of CP patients in the two cohorts is statistically significant (p < 0 0002, two-tailed Z-test: p < 0 0001 and two-tailed chi-square test; chi-square = 98 6) We generated a contingency
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 63 Chronic prostatitis as possible risk factor for Peyronie's disease g r a p h i c d o c u m e n t a t i o n o f t h e p e n i l e d e f o r m a t i o n
–
–
table comparing the presence/absence of a history of prostatitis in patients diagnosed or not with PD
The resulting significant crude odds ratio (OR) for prostatitis was 2 79 (95% CI, 2 27 to 3 43, p < 0 0001) (see Table 1) The post hoc analysis showed an achieved power equal to 0 99 for the magnitude of effect (odds ratio) and 95% CI
Assessment of prostatitis symptoms (NIH-CPSI test) in PD patients with or without PC
Median NIH-CPSI scores were significantly higher in PD patients with CP (n = 200) (median NIH-CPSI = 9, IQR = 10) compared to PD patients without CP (n = 339) (median NIH-CPSI = 2, IQR=2; P = < 0 0001, two-tailed Mann-Whitney-Wilcoxon test)
Psychological profiling of PD patients with or without CP
All included PD patients completed the Generalized Anxiety Disorder-7 questionnaire Median anxiety scores of GAD-7 in patients with or without CP were identical and not significantly different at the statistical level (CP = 14, IQR = 7; no-CP = 14, IQR = 7, p = 0 21, two-tailed Mann-Whitney-Wilcoxon test)
However, the severity of total CP symptom scores assessed with the NIH-CPSI test correlated positively and significantly with GAD-7 anxiety scores (Spearman’s rho, 0 21, p = 0 0031; Kendall’s tau, 0 163, p = 0 018) PHQ-9 depression scores were significantly higher in CP
Table
patients (median = 14; IQR = 4) compared to patients without CP (median = 12 5; IQR = 4, p = 0 0017, twotailed Mann-Whitney-Wilcoxon test)
However, the severity of total CP symptom scores assessed with the NIH-CPSI test did not significantly correlate with PHQ-9 depression scores (Spearman’s rho, 0 072, p = 0 309; Kendall’s tau, 0 054, p = 0 28)
Table 2 summarizes data of GAD-7, PHQ-9, NIH-CPSI, and IIEF in PD patients with and without prostatitis
Erectile dysfunction in PD patients with or without CP
We evaluated the median scores of the IIEF test in PD patients with erectile dysfunction with or without prostatitis In these patients, erectile dysfunction developed concomitantly with PD
Median IIEF scores were not significantly different in PD patients with (median IIEF = 23, IQR = 4 5) or without CP (median IIEF = 23, IQR = 5; P = 0 98, two-tailed MannWhitney-Wilcoxon test) However, the severity of total CP symptom scores assessed with the NIH-CPSI test correlated significantly and inversely with IIEF scores (Spearman’s rho, -0 9, p < 0 0001; Kendall’s tau, -0 77, p < 0 0001)
Penile pain assessments in PD patients with or without CP
We evaluated the median VAS scores in PD patients with penile pain with or without prostatitis
Prevalence of CP in PD patients compared to the non-PD control population.
Median VAS scores were not significantly different in patients with (median VAS = 2, IQR = 5) or without CP (median VAS = 1, IQR = 4; p = 0 784, two-tailed MannWhitney-Wilcoxon test) (see Table 2)
Severity of the penile curve and fibrotic plaque in PD patients with or without CP
Patients with prostatitis showed a less pronounced penile curve (29 ± 34 degrees) compared with patients without CP (34 ± 21 degrees, p = 0 0066, two-tailed t-test)
Table 2.
Summary of data of GAD-7, PHQ-9, NIH-CPSI, IIEF and VAS in PD patients with and without chronic prostatitis
Questionnaire score PD patients with prostatitis (CP) PD patients without prostatitis (CP) Mann-Whitney test (n cases = 200) (n cases = 339)
No significant differences were found between the mean volumes of fibrotic plaques in PD patients with (809 6 ± 563 9 mm^3) or without CP (mean = 908 4 ± 618 6 mm^3; p = 0 063, twotailed t-test)
Characteristics of PD in patients with or without CP
NIH-CPSI Nat onal Institutes of Hea th Chronic Prostat t s Symptom Index is assessed n 3 domains w th the fol owing severity levels: pain (from 0 to 21), urinary symptoms (from 0 to 10), and impact on qua ity of l fe (QoL) (from 0 to 12) (47)
IIEF = Internationa Index of Erecti e Function (IIEF) questionna re, score range = 0-30 Interpretation: severe erecti e dyisfunct on (ED) = from 0 to 10; moderate ED = from 11 to 16; mild-to-moderate ED = from 17 to 21; mi d ED = from 22 to 25; no ED, from 26 to 30 (49)
GAD-7 = Generalized Anx ety D sorder-7 questionna re, score range = 0-21 Interpretation: 0-4, minima anxiety; 5-9, mild anxiety; 10-14, moderate anxiety; 15-21, severe anxiety “S gn ficant anxiety” (moderate-to-severe anxiety) when GAD-7 score > 9 (50)
PHQ-9 = Patient Hea th Quest onnaire-9, score range = 0-27
Interpretat on: 1-4, min ma depress on; 5-9, m ld depression; 10-14, moderate depress on; 15-19, moderately severe depression; 20-27, severe depression “signif cant depression” (moderate to severe depression) when PHQ-9 score > 9 (51)
VAS Visua Ana og Scale quest onnaire for pa n measurement Score range 0-10 Interpretation: 1-5, mi d–moderate pa n; 6-7, severe pain; 8-10, very severe pain (48)
Table 3 summarizes the findings relative to plaque calcification and plurifocal lesions and relative to curve complexity (multiplanar curve deformity)
No significant differences were found i n a n y o f t h e c o n s i d e r e d fi n d i n g s between patients with or without CP
Psychological profile (anxiety and depression) of PD patients
The results showing the psychological profile (anxiety and depression) of PD
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 G
A
64
Paulis,
Paulis
1.
Cohor t of patients with Non-PD control Statistical analysis Peyronie's disease (PD) population odds ratio (OR) - P value Chronic prostatitis (CP) 200 384No chronic prostatitis (CP) 339 1817TOTAL 539 2201Prevalence of CP (%) 37 1 17 4 OR = 2 79 - P < 0 0001
Median score Median score P value NIH-CPSI 92 < 0 0001 IIEF 23 23 0 98 GAD-7 14 14 0 21 PHQ-9 14 12
0 0017 VAS
0 784
5
21
Table 3.
Summary of findings related to plaque calcification and multifocal lesions and curve complexity (multiplanar curve deformity)
Table 4
Psychological profile of 539 patients with Peyronie’s disease
presence of CP compared to patients with PD alone (6 5% vs 4 6%, respectively) (see Table 5)
DISCUSSION
The scientific literature is rich in studies that have demonstrated the presence of numerous risk factors able to favor the onset of PD These studies include the following risk factors: penile trauma, erectile dysfunction, congenital penile curvature, Dupuytren's disease, diabetes mellitus, dyslipidemia, obesity, hypertension, smoking, alcohol consumption, rheumatoid arthritis, psoriasis, and psoriatic arthritis (36, 53-58)
= Generalized Anx ety D sorder-7 questionna re, score range = 0-21 Interpretat on: 0-4, m n ma anxiety; 5-9, m ld anxiety; 10-14, moderate anx ety; 15-21, severe anxiety
“Sign f cant anxiety” (moderate-to-severe anxiety) when GAD-7 score > 9 (50)
PHQ-9 Patient Hea th Quest onnaire-9, score range 0-27
Interpretat on: 1-4, m n ma depression; 5-9, m ld depression; 10-14, moderate depress on; 15-19, moderately severe depression; 20-27, severe depress on
Sign f cant depress on” (moderate to severe depression) when PHQ-9 score > 9 (51)
Table 5. Psychological profile of PD patients with or without chronic prostatitis (PC)
This is the first study that specifically investigates the association between PD and CP
Our results show that the overall prevalence of CP in patients with PD was significantly higher (37 1%) compared to the prevalence in a non-PD control population (17 4%) Our data suggest that CP and PD are frequently associated Another study on this topic identified PD as a risk factor for prostatitis (3)
CP = Chron c prostatit s
GAD-7 = Genera ized Anx ety Disorder-7 questionna re, score range = 0-21
Interpretation: 0-4, m nimal anx ety; 5-9, mild anx ety; 10-14, moderate anxiety; 15-21, severe anxiety
“Signif cant anxiety” (moderate-to-severe anxiety) when GAD-7 score > 9 (50)
PHQ-9 Pat ent Hea th Questionnaire-9, score range 0-27
Interpretation: 1-4, m nimal depression; 5-9, mi d depression; 10-14, moderate depress on; 15-19, moderate y severe depression; 20-27, severe depress on
Signif cant depression” (moderate to severe depression) when PHQ-9 score > 9 (51)
patients are illustrated in Table 4 Notably, “significant anxiety” is more prevalent in PD patients showing the concomitant presence of CP compared to patients with PD alone (93 0% vs 89 2%, respectively) We also found that severe anxiety is more prevalent in PD patients showing the concomitant presence of CP compared to patients with PD alone (43 5% vs 39 3%, respectively) (see Table 5) It should be also noted that “significant depression” is more prevalent in PD patients showing the concomitant presence of CP compared to patients with PD alone (64 0% vs 57 1%, respectively) We also found that severe depression is more prevalent in PD patients showing the concomitant
In our study, median IIEF scores were n o t s i g n i fi c a n t l y d i f f e r e n t i n P D patients with or without CP although the severity of CP symptom total scores ( N I H - C P S I ) c o r r e l a t e d s i g n i fi c a n t l y with the severity of erectile dysfunction (p < 0 0001)
Some studies published in the literature have already argued or demonstrated the correlation between prostatic symptoms and erectile dysfunction (59-65)
In our study, median VAS scores were not significantly different in PD patients with or without CP
Furthermore, the presence of CP in patients with PD does not affect the following: severity of penile curvature, complexity of penile curvature (multiplanarity), penile plaque volume, plaque plurifocality, and plaque calcification presence
In their study, Smith and colleagues reported that 81% of PD patients suffered from "emotional difficulties" (35) Our results revealed that “significant anxiety” was present in 89 2% of PD patients
Furthermore, our study found that “significant anxiety” is more prevalent in PD patients showing the concomitant
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 65 Chronic prostatitis as possible risk factor for Peyronie's disease
Prostatitis (n = 200) No Prostatitis (n = 339) P, F isher’s exact test P, Pearson’s chi-square No of patients with a complex (multiplanar) curve 62 (31%) 105 (31%) 0 99 0 99 Number of patients with multifocal plaque 46 (23%) 58 (17%) 0 11 0 094 Number of patients with calcifications 61 (30 5%) 81 (24%) 0 105 0 092
Psychological questionnaire Mental state N cases Prevalence (%) Mean test score GAD-7 Minimal anxiety 6 1 1 2 5 Mild anxiety 52 9 6 6 7 Moderate anxiety 269 49 9 13 06 Severe anxiety 212 39 3 19 7 “Significant anxiety” 481 89 2 15 9 TOTAL 539 - 14 9 PHQ-9 Minimal depression 62 11 5 3 3 Mild depression 169 31 3 7 08 Moderate depression 194 35.9 12.1 Moderately severe depression 89 16 5 16 6 Severe depression 25 4 6 21 64 “Significant depression” 308 57 1 14 19 TOTAL 539 - 10 7
GAD-7
Psychological Mental state PD patients with CP PD patients without CP Statistical analysis questionnaire N cases out 200 cases N cases out 339 cases P-value (χ2 test ) Prevalence (%) Prevalence (%) GAD-7 “Significant anxiety” 186 (93 0) 295 (87 0) 0 0434 Severe anxiety 87 (43 5) 125 (36 8) 0 1526 PHQ-9 “Significant depression” 128 (64 0) 180 (53 09) 0 0173 Severe depression 13 (6 5) 25 (7 3) 0 8344
presence of CP compared to PD alone (93% vs 89 2%, respectively) We also found that severe anxiety is more prevalent in PD patients showing the concomitant presence of CP compared to PD alone (43 5% vs 39 3%, respectively) Our findings show that prostatitis symptomatology affects PD patients' anxiety status; in fact, the severity of total CP symptom scores, assessed with the NIH-CPSI test, correlates positively and significantly with GAD-7 anxiety scores (p < 0 05) These results demonstrate the strong impact of CP on the anxiety state of PD patients
Nelson and coworkers, in their study about depression in men with PD, demonstrated that 48% of patients show clinically meaningful depression (30) In our study “significant depression” was reported in a higher fraction of patients (57 1%) Furthermore, our study found that “significant depression” is more prevalent in PD patients showing the concomitant presence of CP compared to PD alone (64 0% vs 57 1%, respectively) We also found that severe depression is more prevalent in PD patients showing the concomitant presence of CP compared to PD alone (6 5% vs 4 6%, respectively)
Overall, our results demonstrate the strong impact of PD and CP on the mental status of patients
CONCLUSIONS
Chronic prostatitis (CP) and PD are frequently associated
Although the present study has the limitations of a retrospective analysis performed on a patient database, the size of the odds ratio (= 2 79), and its statistical significance (p < 0 0001) support the relative certitude of our results
Patients with PD and CP showed a significantly higher prevalence of more severe depression and anxiety
In urological and andrological clinical practice, the involvement of psychologists is desirable in order to provide the patient with psychological support treatment and to mitigate the psychological impact of these two physically and psychologically devastating diseases (PD and CP) Our study suggests that patients with PD and/or CP should always be studied by administering specific psychological questionnaires because depressive and anxious symptoms may be unknown or at least underestimated in terms of severity and prevalence Further studies are needed not only to confirm CP as a risk factor for PD but also to further investigate the psychological effects of CP and PD
ACKNOWLEDGEMENTS
We thank Prof Gianpaolo Perletti (Insubria University, Varese, Italy) for advice and assistance in statistical analysis
REFERENCES
1 Billig R, Baker R, Immergut M, et al Peyronie's disease Urology 1975; 6:409-418
2 Solakhan M, Kısacık B Is Peyronie's an IgG4-related disease? Eur J Rheumatol 2021; 8:27-30
3 Pastuszak AW, Rodriguez KM, Solomon ZJ, et al Increased Risk of Incident Disease in Men with Peyronie's Disease: Analysis of U S Claims Data J Sex Med 2018; 15:894-901
4 Paulis G, Romano G, Paulis A Prevalence, psychological impact, and risk factors of erectile dysfunction in patients with Peyronie's disease: a retrospective analysis of 309 cases Res Rep Urol 2016; 8:95103
5 Casabé A, Bechara A, Cheliz G, et al Risk factors of Peyronie's disease What does our clinical experience show? J Sex Med 2011; 8:518-523
6 Paulis G, Conti E, Voliani S, et al Evaluation of the cytokines in genital secretions of patients with chronic prostatitis Arch Ital Urol Androl 2003; 75:179-186
7 Liang W, Wu Z, Zhang G, et al A urine-based biomarker for chronic prostatitis/chronic pelvic pain syndrome: a retrospective multi-center study Transl Androl Urol 2020; 9:2218-2226
8 Paulis G Inflammatory mechanisms and oxidative stress in prostatitis: the possible role of antioxidant therapy Res Rep Urol 2018; 10:75-87
9 Sikka SC, Hellstrom WJ Role of oxidative stress and antioxidants in Peyronie's disease Int J Impot Res 2002; 14:353-360
10 Paulis G, De Giorgio G, Paulis L Role of Oxidative Stress in P e y r o n i e ' s D i s e a s e : B i o c h e m i c a l E v i d e n c e a n d E x p e r i e n c e s o f Treatment with Antioxidants Int J Mol Sci 2022; 15; 23:15969
11 Paulis G, Barletta D, Turchi P, et al Efficacy and safety evaluation of pentoxifylline associated with other antioxidants in medical treatment of Peyronie's disease: a case-control study Res Rep Urol 2015; 8:1-10
12 Franco JV, Turk T, Jung JH, et al Pharmacological interventions f o r t r e a t i n g c h r o n i c p r o s t a t i t i s / c h r o n i c p e l v i c p a i n s y n d r o m e Cochrane Database Syst Rev 2019; 10:CD012552
13 Yaryari AM, Mousavibahar SH, Amirhassani S, et al Men suffering from category III chronic prostatitis may benefit from Nacetylcysteine as an adjunct to alpha-blockers Low Urin Tract Symptoms 2022; 14:199-207
14 Wagenlehner FM, Schneider H, Ludwig M, et al A pollen extract (Cernilton) in patients with inflammatory chronic prostatitis-chronic pelvic pain syndrome: a multicentre, randomised, prospective, double-blind, placebo-controlled phase 3 study Eur Urol 2009; 56:544551
15 Vicari E, Arancio A, Catania VE, et al Resveratrol reduces i n
17:1864-1870
16 Zimmermann RP, Feil G, Bock C, et al Significant alterations of serum cytokine levels in patients with Peyronie's disease Int Braz J Urol 2008; 34:457-466
17 Drachenberg DE, Elgamal AA, Rowbotham R, et al Circulating levels of interleukin-6 in patients with hormone refractory prostate cancer Prostate 1999; 41:127-133
18 John H, Barghorn A, Funke G, Sulser T, et al Noninflammatory chronic pelvic pain syndrome: immunological study in blood, ejaculate and prostate tissue Eur Urol 2001; 39:72-8
19 Bai J, Wang S, Liu J, et al Characterization of circulating CD4+CD25high regulatory T cells in men with chronic prostatitis/ chronic pelvic pain syndrome Urology 2010; 75:938-942
20 Jeon SW, Kim YK The role of neuroinflammation and neurovascular dysfunction in major depressive disorder J Inflamm Res 2018; 11:179-192
21 Kwon JK, Chang IH Pain, catastrophizing, and depression in chronic prostatitis/chronic pelvic pain syndrome Int Neurourol J 2013; 17:48-58
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 G Paulis, A Paulis 66
m m a t i o n - r e l a t e d P r o s t a t e F i b r o s i s I n t J M e d S c i 2 0 2 0 ;
fl a
22 Revest JM, Dupret D, Koehl M, et al Adult hippocampal neurogenesis is involved in anxiety-related behaviors Mol Psychiatry 2009; 14:959–967
23 Pontari MA, Ruggieri MR Mechanisms in prostatitis/chronic pelvic pain syndrome J Urol 2004; 172:839-845
24 Watanabe T, Inoue M, Sasaki K, et al Nerve growth factor level in the prostatic fluid of patients with chronic prostatitis/chronic pelvic pain syndrome is correlated with symptom severity and response to treatment BJU Int 2011; 108:248-251
25 Miller LJ, Fischer KA, Goralnick SJ, et al Nerve growth factor and chronic prostatitis/chronic pelvic pain syndrome Urology 2002; 59:603-608
26 Yohannes E, Chang J, Tar MT, et al Molecular targets for diabetes mellitus-associated erectile dysfunction Mol Cell Proteomics 2010; 9:565-578
27 Dai YT, Chen Y, Yao LS, et al Expression of nerve growth factor in cavernous tissue and its effects on the treatment of rats with diabetic erectile dysfunction Zhonghua Nan Ke Xue 2005; 11:748-751
28 Wang CC, Liao CH, Liu HT, et al Association of urinary nerve growth factor levels with erectile function in young men with type 2 diabetes mellitus Int J Impot Res 2017; 29:101-104
29 Kalisch BE, Bock NA, Davis WL, Rylett RJ Inhibitors of nitric oxide synthase attenuate nerve growth factor-mediated increases in choline acetyltransferase expression in PC12 cells J Neurochem 2002; 81:624-635
30 Nelson CJ, Diblasio C, Kendirci M, et al The chronology of depression and distress in men with Peyronie's disease J Sex Med 2008; 5:1985-1990
31 Rosen R, Catania J, Lue T, et al Impact of Peyronie's disease on sexual and psychosocial functioning: qualitative findings in patients and controls J Sex Med 2008; 5:1977-1984
32 Hartzell R Psychosexual Symptoms and Treatment of Peyronie's Disease Within a Collaborative Care Model Sex Med 2014; 2:168177
33 Nelson CJ, Mulhall JP Psychological impact of Peyronie's disease: a review J Sex Med 2013; 10:653-660
34 Terrier JE, Nelson CJ Psychological aspects of Peyronie's disease Transl Androl Urol 2016; 5:290-295
35 Smith JF, Walsh TJ, Conti SL, et al Risk factors for emotional and relationship problems in Peyronie’s disease J Sex Med 2008; 5:2179-2184
36 Paulis G, Paulis A, Perletti G Congenital penile curvature as a possible risk factor for the onset of Peyronie's disease, and psychological consequences of penile curvature Arch Ital Urol Androl 2023; 95:11328
37 Ahn SG, Kim SH, Chung KI, et al Depression, anxiety, stress perception, and coping strategies in korean military patients with chronic prostatitis/chronic pelvic pain syn- drome Korean J Urol 2012; 53:643-648
38 Miller HC Stress prostatitis Urology 1988; 32:507-510
39 Krsmanovic A, Tripp DA, Nickel JC, et al Psychosocial mechanisms of the pain and quality of life relationship for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) Can Urol Assoc J 2014; 8:403-408
40 Bai J, Gu L, Chen Y, et al Evaluation of psychological stress, cortisol awakening response, and heart rate variability in patients with chronic prostatitis/chronic pelvic pain syndrome complicated by
lower urinary tract symptoms and erectile dysfunction Front Psychol 2022; 13:903250
41 Zhang GX, Bai WJ, Xu T, et al A preliminary evaluation of the psychometric profiles in Chinese men with chronic prostatitis/chronic pelvic pain syndrome Chin Med J (Engl) 2011; 124:514-518
42 Anderson RU, Orenberg EK, Chan CA, et al Psychometric profiles and hypothalamic-pituitary-adrenal axis function in men with chronic prostatitis/chronic pelvic pain syndrome J Urol 2008; 179:956-960
43 Egan KJ, Krieger JN Psychological problems in chronic prostatitis patients with pain Clin J Pain 1994; 10(3):218-226 Katz J, Melzack R Measurement of pain Surg Clin North Am 1999; 79:231-252
44 Sugimoto M, Hijikata Y, Tohi Y, et al Low quality of life in men with chronic prostatitis-like symptoms Prostate Cancer Prostatic Dis 2022; 25:785-790
45 Eri LM, Thomassen H, Brennhovd B, Håheim LL Accuracy and repeatability of prostate volume measurements by transrectal ultrasound Prostate Cancer Prostatic Dis 2002; 5:273-278
46 Lee JS, Chung BH Transrectal ultrasound versus magnetic resonance imaging in the estimation of prostate volume as compared with radical prostatectomy specimens Urol Int 2007; 78:323-327
47 Litwin MS, McNaughton-Collins M, Fowler FJ Jr, et al The National Institutes of Health chronic prostatitis symptom index: development and validation of a new outcome measure Chronic Prostatitis Collaborative Research Network J Urol 1999; 162:369375
48 Kahl C, Cleland JA Visual analogue scale, numeric pain rating scale and the McGill pain Questionnaire: an overview of psychometric properties Phys Ther Rev 2005; 10:123-128
49 Rosen RC, Riley A, Wagner G, et al The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction Urology 1997; 49:822-830
50 Spitzer RL, Kroenke K, Williams JB, Löwe B A brief measure for assessing generalized anxiety disorder: the GAD-7 Arch Intern Med 2006; 166:1092-1097
51 Kroenke K, Spitzer RL, Williams JB The PHQ-9: validity of a brief depression severity measure J Gen Intern Med 2001; 16:606613
52 Faul F, Erdfelder E, Lang AG, Buchner A G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences Behav Res Methods 2007; 39:175-91
53 Bjekic MD, Vlajinac HD, Sipetic SB, et al Risk factors for Peyronie's disease: a case-control study BJU Int 2006; 97:570-574
54 Carrieri MP, Serraino D, Palmiotto F, et al A case-control study on risk factors for Peyronie's disease J Clin Epidemiol 1998; 51:511-515
55 La Pera G, Pescatori ES, Calabrese M, et al SIMONA Study Group Peyronie's disease: prevalence and association with cigarette smoking A multicenter population-based study in men aged 50-69 years Eur Urol 2001; 40:525-530
56 Tal R, Heck M, Teloken P, et al Peyronie's disease following radical prostatectomy: incidence and predictors J Sex Med 2010; 7:1254-1261
57 El-Sakka AI Prevalence of Peyronie's disease among patients with erectile dysfunction Eur Urol 2006; 49:564-569
58 Ventimiglia E, Capogrosso P, Colicchia M, et al Peyronie's dis-
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 67 Chronic prostatitis as possible risk factor for Peyronie's disease
ease and autoimmunity a real-life clinical study and comprehensive review J Sex Med 2015; 12:1062-1069
59 Brookes ST, Link CL, Donovan JL, McKinlay JB Relationship between lower urinary tract symptoms and erectile dysfunction: results from the Boston Area Community Health Survey J Urol 2008; 179:250-255
60 Magri V, Perletti G, Montanari E, et al Chronic prostatitis and erectile dysfunction: results from a cross-sectional study Arch Ital Urol Androl 2008; 80:172-1755
61 Hao ZY, Li HJ, Wang ZP, et al The prevalence of erectile dysfunction and its relation to chronic prostatitis in Chinese men J Androl 2011; 32:496-501
62 Shoskes DA The challenge of erectile dysfunction in the man with chronic prostatitis/chronic pelvic pain syndrome Curr Urol Rep 2012; 13:263-267
63 Zhang Z, Li Z, Yu Q, et al The prevalence of and risk factors for prostatitis-like symptoms and its relation to erectile dysfunction in Chinese men Andrology 2015; 3:1119-1124
64 Zhang Y, Zheng T, Tu X, et al Erectile Dysfunction in Chronic Prostatitis/Chronic Pelvic Pain Syndrome: Outcomes from a MultiCenter Study and Risk Factor Analysis in a Single Center PLoS One 2016; 11:e0153054
65 Magri V, Boltri M, Cai T, et al Multidisciplinary approach to prostatitis Arch Ital Urol Androl 2019; 90:227-248
Correspondence
Gianni Paulis, MD (Corresponding Author)
paulisg@libero it
Peyronie’s Care Center, Department of Uro-Andrology, Castelfidardo Clinical Analysis Center, Rome, Italy
Andrea Paulis, MD
andrea fx 94@gmail com
Neurosystem Center for applied Psychology and Neuroscience, Janet Clinical Centre, Rome, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 G Paulis, A Paulis 68
ORIGINAL PAPER
Treatment outcome of Fournier's gangrene and its associated factors: A retrospective study
Khaled Al-Kohlany 1 , Khaled Baker 2
Faisal Ahmed 3 , Murtadha Mohamed 4 , Majdi Alshami 4 , Mohamed Badheeb 5
1 Department of Urology, College of Medicine, Sana'a University, Sana'a, Yemen;
2 Department of Urology, Sanus Hospital, Hradec Kralove, Czech Republic;
3 Department of Urology, College of Medicine, Ibb University, Ibb, Yemen;
4 Department of Urology, General Military Hospital, Sana'a, Yemen;
5 Department of Internal Medicine, College of Medicine, Hadhramaut University, Mukalla, Yemen
Summary
Introduction: Fournier's gangrene (FG) is a rapidly progressive necrotizing infection that affects the perineal and abdominal regions and is known for its high mortality rate. This study aims to present the practical experience of managing FG patients and identify factors that may affect their clinical outcomes.
Materials and methods: A retrospective study was conducted from April 2009 to December 2020 at General Military Hospital in Sana'a, Yemen including 26 patients who were diagnosed with FG and treated on. Data on demographic characteristics, time to admission, surgical intervention, and treatment outcomes were collected. Univariate analysis was performed to determine factors that affect patient outcomes
Result: The mean age of the patients was 65.77 ± 5.04 years, and 65 4% of them were over the age of 65 Most patients (57 7%) presented after five days of experiencing symptoms, and 65 4% were in septic conditions Of the patients, 17 (65 4%) survived, and the total mortality rate was 34 6% Univariate analysis showed that delayed presentation (p = 0 001), a history of diabetes mellitus (p < 0 001), end-stage renal disease (p < 0 001), heart failure (p < 0 001), cerebrovascular accident (p = 0 032), liver cirrhosis (p < 001), presence of multiple comorbidities (p < 001), involvement of lager area (p < 001), septic conditions (p = 0 009), advanced age (p = 0 018), and intensive care unit admission (p = 0.002) were found to be risk factors for mortality in patients with FG
Conclusions: FG is a potentially life-threatening medical condition, even with aggressive and specialized treatment Our study revealed a mortality rate of 34.6%. Factors such as older age, the presence of multiple comorbidities, septic conditions, the abdominal spread of the disease, intensive care unit admission, and delayed presentation contribute to higher mortality rates
KEY WORDS: Fournier's gangrene; Necrotizing fasciitis; Risk factor; Mortality; Outcome
Submitted 15 March 2023; Accepted 25 March 2023
INTRODUCTION
Fournier's gangrene (FG) is a devastating, progressive, and polymicrobial inflammation of the external genitalia and perineum (1) Also known as necrotizing fasciitis of the genitalia (NFG), it is a life-threatening urologic emergency that requires urgent admission and surgical intervention (1)
Typically, FG is characterized by severe necrosis of the soft tissues of the genitalia and perineum However, it can extend to the lower abdomen, flank, and even the axilla, cervical region, and upper limbs (2) Although the necrosis usually remains limited to the fascial layers of the pelvis, perineum, thighs, and tunica albuginea of the penis and testes, it can sometimes spread beyond these barriers to involve deeper structures such as the anal sphincter, rectum, thighs, penis, and testicles, necessitating more aggressive procedures such as fecal diversion, orchiectomy, and even limb amputation (2)
While FG is typically diagnosed easily by clinical examination without additional laboratory or radiological investigations, the treatment course represents a significant challenge (3) This is especially true in developing countries, where healthcare systems are under-resourced and less organized Typically, these patients are elderly and immune-compromised, with associated comorbidities, and require admission to intensive care units (ICU) or isolation in separate rooms (4) It is common in such communities for hospitals to reject FG patients due to a shortage of beds and facilities or a lack of staff expertise in dealing with such patients (5) Several comorbidity indexes, such as the Charlson Comorbidity Index and Fournier's Gangrene Severity Index, have been utilized to predict the prognosis and mortality in FG (6, 7) However, the mortality rate remains high, and their reliabilities are not yet clear This report aims to share the experience of handling FG patients admitted to our hospital and identify the factors that affect the outcome of these patients
MATERIAL AND METHODS Study design and setting
This retrospective study included 26 patients diagnosed with Fournier's gangrene at General Military Hospital, between April 2009 and December 2020 The Ethics Research Committees of General Military Hospital, Sana'a, Yemen provided their approval for the study (ID: 23-008, on 1,3,2023), which adhered to the ethical principles outlined in the Declaration of Helsinki
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 69
,
DOI: 10 4081/aiua 2023 11318
Inclusion criteria
Patients diagnosed with FG and treated at General Military Hospital were included in the study The diagnosis of FG was based on clinical criteria, including the presence of fever (> 38°C), erythema and swelling in the perianal or scrotal region, purulent-malodorous discharge, and the detection of fluctuation or crepitation at the wound site Prior to inclusion, all patients were assessed to confirm their eligibility for the study (1)
Exclusion criteria
Patients treated at other hospitals and those with abscesses confined to the scrotal, periurethral, and perianal regions with no fascial or soft tissue extension were excluded
Surgical procedure and postoperative care
All participants in the study received immediate aggressive debridement under general or spinal anesthesia to remove necrotic tissue until healthy tissue was observed In addition, cystostomy catheters were placed, limiting the contact of the urethra with urine Empiric intravenous antibiotic therapy, including Ceftriaxone (1 g every 12 hours) and metronidazole (500 mg every 12 hours), was a d m i n i s
u r e r e s u l t s w e r e o b t a i n e d Dressings were changed three times daily with sterile gauze soaked in a solution of povidone-iodine, 0 2% nitrofurazone ointment, and 250 mg rifampicin ampoule
A colostomy was performed in cases where the perirectal and anal regions were affected, while an orchiectomy was performed in testicular involvement cases Patients were transferred to the Plastic and Reconstructive Surgery Clinic once their general health status and wound cleanliness had improved
Data collection and study outcome
Patient demographic characteristics, including age, time to admission, location of the initial lesion, the extent of the disease, comorbidities, number of surgical debridements, intensive care unit (ICU) admission, colostomy diversion, length of hospital stay, and mortality rate, were extracted from patient's medical records for analysis
Patients were stratified into two groups based on their survival status: survivors and non-survivors Mortality refers to all-cause mortality and any cause of FG-related death during the initial admission (1) To assess the extension of FG, we used a modified body surface area nomogram commonly used for estimating the extension of burn injuries (7) This involved assigning a value of 1% for penile, scrotal, and perineal involvement, and 2 5% for ischiorectal fossa involvement
Statistical analysis
The study utilized descriptive statistics to present quantitative variables in terms of means and standard deviations, while qualitative variables were presented as frequencies and percentages The normality of the data was assessed using the Kolmogorov-Smirnov test To compare patients in the survivor and non-survivor groups, univariate analysis was performed using either independent samples T-Test or Mann-Whitney test to compare means for quantitative variables and Chi-square or Fisher's exact test for qualitative variables Statistical significance was set at p < 0 05 The statistical analysis was carried out using IBM SPSS version 18 software (IBM Corp , Armonk, New York)
Table 1.
Demographic characteristics of patients
Showing A: Fournier’s gangrene involving the scrotum;
B: Fournier’s gangrene involving both the penis and scrotum;
C: Fournier’s gangrene involving the penis, scrotum, and ischiorectal fossa;
D: Partially debrided Fournier’s gangrene

Archivio Italiano
95, 2
70
di Urologia e Andrologia 2023;
K
Al-Kohlany, K Baker, F Ahmed, M Mohamed, M Alshami, M Badheeb
t e r e d u n t i l c u l t
Variable N (%) Age (year), mean ± SD 65 77 ± 5 04 Age groups < 65 years 9 (34 6) ≥ 65 years 17 (65 4) Time to admission (days), mean ± SD 6 15 ± 2 71 Time to admission ≤ 5 days 11 (42.3) > 5 days 15 (57 7) Source of infection Urinary tract infection 12 (46 2) Perianal or perirectal infection 4 (15 4) Unknown 10 (38 5) Septic condition 17 (65 4) History of Diabetes mellitus 13 (50) History of heart failure 6 (23 1) History of ESRD 6 (23 1) History of CVA 3 (11 5) History of anorectal surgery 3 (11 5) History of liver cirrhosis 6 (23 1) Total affected body surface area ≤ 3% 18 (69 2) > 3% 8 (30 8) Number of debridements One time 11 (42 3) 2 times or more 15 (57 7) Needs ICU admission 8 (30 8) Hospital stays (day), mean ± SD 5 42 ± 1 88 Needs for colostomy 3 (11 5) Needs for orchiectomy 2 (7 7) Outcome Survivors 17 (65 4) Non-survivors 9 (34 6) ICU: ntens ve care unit; CVA: cerebrovascular acc dent; ESRD: End-Stage Rena Disease
Figure 1.
RESULT
Baseline clinical characteristics
The mean age of patients was 65 77 ± 5 04 years, and most (65 4%) were over 65 years The mean time to hospital admission was 6 15 ± 2 71 days, and the majority (57 7%) presented after five days of symptom onset 65 4% of patients were in septic conditions A history of diabetes mellitus, heart failure, renal failure with hemodialysis, cerebrovascular accident (CVA), anorectal surgery, and liver cirrhosis was present in 13 (50%), 6 (23 1%), 6 (23 1%), 3 (11 5%), 3 (11 5%), and 6 (23 1%) patients, respectively The mean total affected body surface area was 3 02 ± 1 41%, and in 18 (69 2%) patients, the total affected area was 3% or less The infection involved only the scrotum in 6 (23 1%) patients (Figure 1A), while penile, scrotal, and perineal involvement was seen in 11 (42 3%) patients (Figures 1B and 1C) Most patients (57 7%) required more than one surgical debridement (Figure 1D)
Table 2.
Comparison between survivors and non-survivors for quantitative variables
Orchiectomy and colostomy proc e d u r e s w e r e p e r f o r m e d i n 3 (11 5%) and 2 (7 7%) patients, respectively The mean hospital stay was 5 42 ± 1 88 days and 8 ( 3 0 8 % ) p a t i e n t s r e q u i r e d I C U a d m i s s i o n O f t h e p a t i e n t s , 1 7 (65 4%) survived and the total m o r t a l i t y r a t e w a s 3 4 6 % T h e baseline clinical characteristics of the study population are summarized in Table 1
F a c t o r s a s s o c i a t e d w i t h m o r t a l i t y i n p a t i e n t s w i t h
Fournier’s gangrene:
Univariate analysis showed that a long time to hospital admission (p < 0 001), history of diabetes mellitus (p < 0 001), history of end-stage renal disease (ESRD) (p < 0 001), history of heart failure (p < 0 001), history of CVA (p = 0 032), history of liver cirrhosis (p < 0 001), presence of multiple comorbidities (p < 0 001), involvement of larger area (p < 0 001), presentation in septic conditions (p = 0 009), advanced age (p = 0 018), and need for ICU admission (p = 0 002) were found to be risk factors for mortality in patients with FG (Table 2 and 3)
DISCUSSION
FG is a life-threatening condition that involves necrotizing fasciitis in
Table 3.
the genitourinary areas and the perineum It is typically a polymicrobial infection caused by anaerobic and facultative aerobic bacteria (8) The rapid progression of FG is linked to impaired cellular immunity, which permits suppurative bacterial infection, and the synergetic polymicrobial nature, which causes a substantial release of bacterial toxins Eventually, small subcutaneous vessels experience obliterative thrombosis, resulting in gangrene of the involved
Comparison between survivors and survivors for quantitative variables
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 71 Fournier's gangrene outcomes
struc-
Variable Sub variable Total (n = 26) Outcome Univariate analysis N (%) Sur vivor N (%) Died N (%) OR (95 % CI) P-value* 17 (65 4) 9 (34 6) Age (year) < 65 9 (34 6) 7 (77 8) 2 (22 2) 0 40 (0 06-2 58) 0 341 ≥ 65 17 (65.4) 10 (58.8) 7 (41.2) Reference group History of Diabetes mellitus Yes 13 (50) 4 (30 8) 9 (69 2) - 0 000 No 13 (50) 13 (100) 0 (0 0) Reference group Number of debridements ≤ 1 11 (42 3) 6 (54 5) 5 (45 5) 2 29 (0 44-11 91) 0 324 > 2 15 (57 7) 11 (73 3) 4 (26 7) Reference group Time to presentation (day) ≤ 5 11 (42 3) 11 (100) 0 (0 0) - 0 002 > 5 15 (57 7) 6 (40 0) 9 (60 0) Reference group Total affected BSA (%) ≤ 3 18 (69 2) 17 (94 4) 1 (5 6) - 0 000 > 3 8 (30 8) 0 (0 0) 8 (100) Reference group Comorbidity number ≤ 1 19 (73 1) 17 (89 5) 2 (10 5) - 0 000 > 1 7 (26 9) 0 (0 0) 7 (100) Reference group Need colostomy Yes 3 (11 5) 2 (66 7) 1 (33 3) 0 93 (0 07-11 99) 0 960 No 23 (88 5) 15 (65 2) 8 (34 8) Reference group Need orchiectomy Yes 2 (7 7) 1 (50 0) 1 (50 0) 2 00 (0 11-36 30) 0 639 No 24 (92 3) 16 (66 7) 8 (33 3) Reference group Septic condition Yes 17 (65 4) 8 (47 1) 9 (52 9) - 0 009 No 9 (34 6) 9 (100) 0 (0 0) Reference group History of heart failure Yes 6 (23 1) 0 (0 0) 6 (100) - 0 000 No 20 (76 9) 17 (85 0) 3 (15 0) Reference group History of ESRD Yes 6 (23.1) 0 (0.0) 6 (100) - 0.000 No 20 (76 9) 17 (85 0) 3 (15 0) Reference group History of CVA Yes 3 (11 5) 0 (0 0) 3 (100) - 0 032 No 23 (88 5) 17 (73 9) 6 (26 1) Reference group History of anal surgery Yes 3 (11 5) 2 (66 7) 1 (33 3) 0 93 (0 07-11 99) 0 960 No 23 (88 5) 15 (65 2) 8 (34 8) Reference group History of liver cirrhosis Yes 6 (23 1) 0 (0 0) 6 (100) - 0 000 No 20 (76.9) 17 (85.0) 3 (15.0) Reference group Need ICU admission Yes 8 (30 8) 1 (12 5) 7 (87 5) 56 00 (4 33-724) 0 002 No 18 (69 2) 16 (88 9) 2 (11 1) Reference group
ESRD: End-Stage Rena Disease
BSA: body surface area; CI: confidence interval; ICU: intensive care un t; OR: odds rat o; CVA: cerebrovascular accident;
*P-values of < 0 05 were considered sign f cant
Variable Outcome Mean Difference t & z P-value* Sur vivors Died (95 % CI) Mean (SD) Mean (SD) Age (year) 64 11 (3 98) 68 88 (5 55) -4 77 (-8 65 to -0 88) -2 53 0 018 Number of debridements 1 76 (0 66) 1 77 (1 56) -0 01 (-0 90 to 0 88) -0 39 0 711 Time to hospital presentation (days) 4 94 (2 13) 8 44(2 18) -3 50 (-5 33 to -1 67) -3 94 0 001 Total BSA (%) 2 29 (0 98) 4 16(1 39) -1 87 (-2 83 to -0 90) -3 99 0 001 Hospital stays (days) 5 82 (1 81) 4 66 (1 87) 1 15 (-0 40 to 2 71) 1 53 0 138 BSA: body surface area; CI: confidence nterval; ICU: intensive care unit; OR: odds rat o; CVA: cerebrovascular acc dent; ESRD: End-Stage Rena D sease
of < 0 05 were cons dered s gn ficant
*P-values
tures (1, 9) The bacterial access usually results from a cutaneous breakdown (e g , local trauma) or the spread of urinary or perineal infections In our study, urinary tract infection was the most common cause of FG (46 2%) Our result was similar to Tahmaz et al 's study, which reported that 33% of FG cases were due to urinary tract infections (10) Nevertheless, no identifiable cause was observed in onequarter of the patients in El-Qushayri et al study (11) There is a discrepancy in the literature regarding several independent prognostic factors in patients with FG For example, some studies have shown that younger age is associated with improved survival (1, 12, 13), while other studies have not found a significant difference in disease onset between various age groups (5, 14) In our study group, advanced age was noticed among non-survival and was found to be a risk factor for mortality This suggests that the average age of those affected by Fournier's gangrene is rising as reported by Hong et al (15) Similarly, there are inconsistent findings regarding the duration between the onset of FG symptoms and hospitalization, ranging from 1 to 30 days (15) Our study showed a statistically significant difference between survivors and non-survivors in the time it took to seek medical care, with survivors presenting earlier (4 94 ± 2 13 days) compared to non-survivors (8 44 ± 2 18 days) (p = 0 001) These findings are consistent with the results of other studies, such as those conducted by Doluog lu et al and Yeniyol et al (1, 14), and are further supported by a systematic review that identified a positive correlation between time to treatment and patient survival (16) However, some studies have reported no significant difference in time to admission between survivors and nonsurvivors (15, 17) These inconsistencies may be attributed to variations in study settings, patient demographics, hospital accessibility, income, and educational levels FG is a multifactorial disease with a mortality rate ranging from 3% to 67% (15) The variable outcomes of the disease suggest the involvement of various underlying conditions that can contribute to the FG occurrence, aggravation, and mortality rate Certain conditions such as DM, alcohol consumption, immunocompromised status, malignancy, heart failure, hepatic disease, and renal insufficiency are reported to be positively associated with FG mortality (1, 10, 15, 16, 18) In this study, despite meticulous and specialized management and selective antibiotic therapy, the mortality rate was 34 6%, and patients with a history of DM, ESRD, heart failure, cerebrovascular accident, and liver cirrhosis were found to suffer poorer outcomes with a higher mortality rate DM was the most common comorbidity, affecting 50% of patients, and was significantly associated with a higher mortality rate in our cohort However, the relationship between DM and mortality remains controversial, as some studies have reported an association with both incidence and mortality (18, 19), while others have shown an association with incidence but not with FG mortality (1, 15, 20) The increased incidence and higher mortality rate of FG in diabetics may be attributed to the small-vessel diseaseinduced propensity to tissue ischemia and the decreased phagocytic and intracellular bactericidal activity and neutrophil dysfunction that attenuate bacterial microbes’ clearance (18) Similarly, immunocompromised patients (e g , HIV) and patients on immunosuppressive medications are
at higher risk (16) Doluog˘lu et al reported that severe sepsis and multiple organ failure, chronic renal failure, and pulmonary embolism were the major mortality-associated etiologies in FG patients, with a reported mortality of 20 5% (1) We found that septic conditions and having multiple comorbidities at the time of admission were significant predicting factors for mortality and outcome, which goes in trend with prior reports (13, 21)
This study found a significant difference in the average extent of body surface area affected by necrotizing tissue between patients who survived and those who did not (2 29 ± 0 98 versus 4 16 ± 1 39, respectively) (p = 0 001) The number of surgical debridements, on the other hand, did not have a significant impact on patient outcomes (p = 0 711), which is in line with the findings of Yeniyol et al (14) However, the results reported by Spirnak et al differ from these findings, as they showed a higher mortality rate among patients who underwent more frequent operations due to more extensive disease (22) Generally, prompt surgical intervention (aggressive and often repeat debridement), broad-spectrum antibiotics, and appropriate resuscitation are crucial in these patients (23) As expected, patients with large involved body surface areas usually died during the hospital course, and the chance of undergoing multiple debridements subsequently decreased in this group
In our study, the need for ICU admission was associated with non-survival, and our result was similar to a study by Azmi et al (8) In contrast, in the study by Yilmazlar et al , survivors stayed in the hospital significantly longer than non-survivors (24) We explain that high-risk patients with multiple underlying diseases had a low probability of survival and died within a few days of ICU admission
This study has several limitations Firstly, the retrospective design and the small sample size are potential sources of bias that might limit the generalizability of our findings Secondly, due to the nature of the study, some relevant factors, such as laboratory data, Charlson Comorbidity Index, and Fournier's Gangrene Severity Index, were not included in our analysis Future studies with larger sample sizes and prospective multicenter designs are recommended to strengthen the validity and generalizability of our findings
CONCLUSIONS
Fournier's gangrene represents a critical medical condition with notable morbidity and mortality rates Our investigation unveiled a mortality rate of 34 6%, despite the implementation of maximum multidisciplinary therapy in a specialized center Notably, increased mortality rates were associated with advanced age, underlying diseases, delayed hospital presentation, the presence of multiple comorbidities, septic conditions, the abdominal spread of the disease, and intensive care unit admission
REFERENCES
1 Doluoglu Ö G, Karagöz MA, Kılınç MF, et al Overview of different scoring systems in Fournier's Gangrene and assessment of prognostic factors Turk J Urol 2016; 42:190-6
Archivio Italiano di Urologia e
2023; 95, 2
72
Andrologia
K Al-Kohlany, K Baker, F Ahmed, M Mohamed, M Alshami, M Badheeb
2 Misiakos EP, Bagias G, Papadopoulos I, et al Early Diagnosis and Surgical Treatment for Necrotizing Fasciitis: A Multicenter Study Front Surg 2017; 4:5
3 Milanese G, Quaresima L, Dellabella M, et al A conservative approach to perineal Fournier's gangrene Arch Ital Urol Androl 2015; 87:28-32
4 Benjelloun el B, Souiki T, Yakla N, et al Fournier's gangrene: our experience with 50 patients and analysis of factors affecting mortality World J Emerg Surg 2013; 8:13
5 Wetterauer C, Ebbing J, Halla A, et al A contemporary case series of Fournier's gangrene at a Swiss tertiary care center-can scoring systems accurately predict mortality and morbidity? World J Emerg Surg 2018; 13:25
6 Charlson ME, Pompei P, Ales KL, MacKenzie CR A new method of classifying prognostic comorbidity in longitudinal studies: development and validation J Chronic Dis 1987; 40:373-83
7 Laor E, Palmer LS, Tolia BM, et al Outcome prediction in patients with Fournier's gangrene J Urol 1995; 154:89-92
8 Azmi YA, Alkaff FF, Purba AKR, et al Factors for In-Hospital Mortality in 145 Male Patients with Fournier's Gangrene: A 10-Year Observational Study from a Single Tertiary Referral Center in Indonesia Med Sci Monit 2022; 28:e938578
9 Olivieri V, Ruggiero G, Abate D, et al Fatal infections in andrology Atypical clinical presentation of a Fournier's disease Arch Ital Urol Androl 2020; 92:213
10 Tahmaz L, Erdemir F, Kibar Y, et al Fournier's gangrene: report of thirty-three cases and a review of the literature Int J Urol 2006; 13:960-7
11 El-Qushayri AE, Khalaf KM, et al Fournier's gangrene mortality: A 17-year systematic review and meta-analysis Int J Infect Dis 2020; 92:218-25
12 Tuncel A, Keten T, Aslan Y, et al Comparison of different scoring systems for outcome prediction in patients with Fournier's gangrene: experience with 50 patients Scand J Urol 2014; 48:393-9
13 Martinschek A, Evers B, Lampl L, et al Prognostic aspects, survival rate, and predisposing risk factors in patients with Fournier's gangrene and necrotizing soft tissue infections: evaluation of clinical outcome of 55 patients Urol Int 2012; 89:173-9
14 Yeniyol CO, Suelozgen T, Arslan M, Ayder AR Fournier's gangrene: experience with 25 patients and use of Fournier's gangrene severity index score Urology 2004; 64:218-22
15 Hong KS, Yi HJ, Lee RA, et al Prognostic factors and treatment outcomes for patients with Fournier's gangrene: a retrospective study Int Wound J 2017; 14:1352-8
16 Lewis GD, Majeed M, Olang CA, et al Fournier's Gangrene Diagnosis and Treatment: A Systematic Review Cureus 2021; 13:e18948
17 McCormack M, Valiquette AS, Ismail S Fournier's gangrene: A retrospective analysis of 26 cases in a Canadian hospital and literature review Can Urol Assoc J 2015; 9:E407-10
18 Korkut M, Içöz G, Dayangaç M, et al Outcome analysis in patients with Fournier's gangrene: report of 45 cases Dis Colon Rectum 2003; 46:649-52
19 Cakmak A, Genç V, Akyol C, et al Fournier's gangrene: is it scrotal gangrene? Adv Ther 2008; 25:1065-74
20 Meki CS, Mangwiro TI, Lazarus J Fournier's gangrene: outcome analysis and prognostic factors S Afr J Surg 2018; 56:43-6
21 Mulla ZD, Gibbs SG, Aronoff DM Correlates of length of stay, cost of care, and mortality among patients hospitalized for necrotizing fasciitis Epidemiol Infect 2007; 135:868-76
22 Spirnak JP, Resnick MI, Hampel N, Persky L Fournier's gangrene: report of 20 patients J Urol 1984; 131:289-91
23 Auerbach J, Bornstein K, Ramzy M, et al Fournier Gangrene in the Emergency Department: Diagnostic Dilemmas, Treatments and Current Perspectives Open Access Emerg Med 2020; 12:353-64
24 Yilmazlar T, Ozturk E, Ozguc H, et al Fournier's gangrene: an analysis of 80 patients and a novel scoring system Tech Coloproctol 2010; 14:217-23
Correspondence
Khaled Al-Kohlany, MD kalkohlani@gmail com
Murtadha Mohamed, MD ahmedmurtadha386@gmail com
Majdi Alshami, MD dr majdialshami@yahoo com
Urology Office, General Military Hospital, Sana'a, Yemen
Khaled Baker, MD bakerkhaled9@gmail com
Urology Office, Sanus Hospital, Hradec Kralove, Czech Republic
Faisal Ahmed, MD (Corresponding Author) fmaaa2006@yahoo com
Urology Office, Al-Thora General Hospital, Alodine street, Ibb, Yemen, Mohamed Badheeb, MD badheeb2009@gmail com
Internal Medicine Office, Hadhramaut University, Mukalla, Yemen
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 73 Fournier's gangrene outcomes
patients are a neglected issue: Results from a national survey of Italian Society of Rheumatology
Luigi Napolitano 1 , Ilenia Pantano 2 , Lorenzo Romano 1 , Luigi Cirillo 1 , Celeste Manfredi 3 , Francesco Mastrangelo 1 , Giovanni Maria Fusco 1 , Daniele Mauro 2 , Lorenzo Spirito 3 , Roberto La Rocca 1 , Davide Arcaniolo 3 , Corrado Aniello Franzese 4 , Carmine Sciorio 5 , Marco Romano 6 , Marco De Sio 3 , Vincenzo Mirone 1 , Francesco Ciccia 2
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples "Federico II", Naples, Italy;
2 Department of Precision Medicine, University of Campania "Luigi Vanvitelli", Naples, Italy;
3 Unit of Urology, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli", Naples, Italy;
4 ASL Napoli 3 Sud, Naples, Italy;
5 Urology Unit, Ospedale Alessandro Manzoni, Lecco, Italy;
6 Department of Precision Medicine and Hepatogastroenterology Unit, AOU University Luigi Vanvitelli, Naples, Italy
Summary
Introduction: Sexual dysfunctions (SD) are frequently encountered in patients with rheumatologic diseases In this scenario, a multidisciplinary approach to rheumatologic diseases is often mandatory
The aim of this survey was to assess whether Italian rheumatologists routinely explore sexual health of their patients, their knowledge on the topic, and the barriers to discussing SD in clinical practice.
Methods: A 32-items anonymous questionnaire was mailed to members of the Italian Society of Rheumatology (rheumatologists and residents in rheumatology training) in February 2023 The questionnaire aimed to determine attitudes, knowledge, and practice patterns regarding the discussion of SD with rheumatologic patients. A descriptive analysis of responses was performed.
Results: A total of 162 responses were received Overall, 50 0% of respondents occasionally asked patients about SD related to their rheumatologic pathologies, while 37 1% never did so Respondents declared that patients occasionally (82 3%) or never (16 1%) reported SD related to rheumatologic diseases
The main barriers to discussing sexual health were lack of time during medical examination (46.6%), patients’ discomfort (44 8%), and lack of knowledge/experience (39 7%) Overall, 41 9% and 33 9% of respondents respectively totally and partially agreed that rheumatologists should routinely investigate patients' sexual health Most of the respondents (79 0%) thought that discussing sexual health problems could help patients cope with their rheumatologic diseases. Of all respondents, 74.2% felt the need to broaden their personal knowledge about SD. Finally, 45 9% and 34 4% of respondents respectively partially and totally agreed that training courses for rheumatologists could be helpful in the management of sexual health in rheumatological patients
Conclusions: SD was not routinely discussed in rheumatology practice, still remaining a neglected issue. The most frequent explanations for the lack of attention toward SD were lack of time, patients’ discomfort, and lack of knowledge/experience
Most of the respondents expressed the possible usefulness of attending SD courses to improve knowledge about these conditions
KEY WORDS: Sexual dysfunction; Rheumatology; Barrier; Rheumatological disorders
Submitted 26 March 2023; Accepted 30 March 2023
INTRODUCTION
Sexual dysfunctions (SD) are a broad spectrum of conditions such as decreased sexual desire, ejaculatory disorders, erectile dysfunction, orgasmic changes, painful intercourse, and insufficient vaginal lubrication (1-3) They are very common worldwide and have a negative impact on male and female quality of life (QoL) (4) The etiopathogenesis of SD is multifactorial and it can be related to age, comorbidities, psychological or emotional state, hormonal imbalance, couple difficulties, and medical therapies (5)
Several studies reported the frequent association between SD and rheumatic diseases (RD) (6, 7) Although many hypotheses have been proposed to explain this association, the exact mechanism is not identified yet In patients with rheumatoid arthritis (RA), SD ranged from 31% to 76% of all cases (8) Pain and depression seem to be the principal factors involved in SD in rheumatoid arthritis (9) Vaginal discomfort or pain during intercourse occur in women affected by Sjogren syndrome, systemic lupus erythematosus, and systemic sclerosis (10, 11)
Depression, pain, and fatigue can affect the sexual function of patients with fibromyalgia (12), premature ejaculation, erectile dysfunction and global sexual dysfunction i n p a t i e n t s w i t h R A ( 1 3 , 1 4 ) A m u l t i d i s c i p l i n a r y approach to rheumatic diseases is therefore often mandatory Consequently, rheumatologists should know and
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 74
ORIGINAL PAPER
Sexual dysfunctions of rheumatological
DOI: 10 4081/aiua 2023 11337
explore the sexuality of their patients for proper management, including referral to the appropriate health professionals (15) Despite this, sexual counseling in patients with RD is a neglected issue nowadays Most of the evidence shows that it is also a neglected problem in other specialist fields such as cardiology, neurology and gastroenterology Several reasons such as lack of knowledge/training, lack of time during visits, and embarrassment have been reported (16-20)
To the best of our knowledge, there are no study evaluating how the rheumatologists discuss and manage their patients' sexual problems The aim of this survey was to assess whether Italian rheumatologists routinely explore sexual health of their patients, their knowledge on the topic, and the barriers to discussing SD in clinical practice
MATERIALS AND METHODS
The questionnaire
A national cross-sectional anonymous online questionnaire was sent to all members (specialists and residents) of Italian Society of Rheumatology (SIR) in February 2023
The questionnaire was designed by two authors (I P and L R ) and structured according with questionnaires used in other studies after a literature review (11,15) A full professor of rheumatology (F C ) was interviewed to analyze the survey, which was adjusted according to his feedback and comments The questionnaire was designed using Google Forms (Google LLC, Mountain View, CA, USA) A brief letter explaining the objectives of the study was sent with the questionnaire All respondents had to fully complete the questionnaire before submission, since all questions were flagged as mandatory After submission, users could not review neither amend their answers Reminder e-mails were sent to non-responders 1 and 2 months after the initial mailing No incentives were offered for participation in the survey
The questionnaire comprised 30 questions focusing on: demographic data of respondents; frequency of discussing sexual health with patients during visit; rheumatologist’s level of knowledge on sexual dysfunction; rheumatologist’s level of knowledge on phosphodiesterase type 5 inhibitors (PDE5Is); perceived barriers to address sexual issues; knowledge about referring patients with SD Some questions had only one possible answer, others gave the possibility of multiple answers A part of questions had multiple selectable options, others had an open answer The questionnaire was detailed in Supplementary Table 1 Given the nature of the study, it was not necessary to obtain Ethics Committee approval All respondents consented to the publication of the collected data A descriptive analysis of the results of survey was performed Categorical variables were presented as frequencies and percentages, continuous variables were reported as means and ranges No normality test or power analysis was performed
RESULTS
Demographic data of respondents
A total of 162 responses were received Overall, 50 0% of respondents were female, 48 4% male, and 1 subject did
not declare gender (1 6%) Age was mainly between 30 and 40 years old (56 4%) Most of the respondents were rheumatologists (77 4%), while a minority consisted of rheumatology residents (22 6%) Regarding the workp
Hospitals, 17 2% in non-University Hospitals, and 12 9% were self-employed Work experience was reported > 10 years by 51 6% of respondents
Frequency of discussing sexual health with patients during visit
Overall, 50 0% of respondents occasionally asked patients about SD related to their rheumatologic pathologies, while 37 1% never did so On the other hand, respondents declared that patients occasionally (82 3%) or never (16 1%) reported SD related to rheumatologic diseases Subjects reporting SD were mainly men < 50 years old (40 3%), men < 40 years old (35 5%), men whose age was between 40-50 years old (30 6%), and women < 40 years old (30 6%) Men mainly complained about erectile dysfunction (57 4%) and loss of libido (27 9%) Women mainly complained about sexual pain (including dyspareunia, vaginismus, and noncoital pain disorder) Fibromyalgia was the rheumatologic disease most associated with SD (58 3%), followed by systemic sclerosis and dermatomyositis (21 7%) and Sjogren syndrome (11 7%)
Management of SD and Perceived barriers to discussing sexual health
Overall, 41 9% and 33 9% of respondents respectively totally and partially agreed that rheumatologists should routinely investigate patients' sexual health Most of the respondents (79 0%) thought that discussing sexual health problems could help patients cope with their rheumatologic diseases Related to this, 37 1% and 22 6% of respondents respectively totally and partially disagreed that discussing sexual health was only the responsibility of andrologists and gynecologists Besides, 37 7% and 29 9% of respondents respectively occasionally and often suggested patients to undergo an andrological/gynecological evaluation for sexual health problems The main barriers to discussing sexual health were lack of time during medical examination (46 6%), patients’ discomfort (44 8%), and lack of knowledge/experience (39 7%) (Figure 1)
Rheumatologist knowledge about SD and sexually impacting drugs
Of all respondents, 74 2% felt the need to broaden their personal knowledge about SD Besides, 43 5% believed that medicine courses lack sufficient knowledge about sexual health Finally, 45 9% and 34 4% of respondents respectively partially and totally agreed that training courses for rheumatologists could be helpful in the management of sexual health in rheumatological patients
Overall, 71 0% of respondents said they were aware that some rheumatologic drugs have the potential to cause SD The drugs most associated with SD were antidepressants (82 8%) and immunosuppressors (24 1%) Moreover, 61 3% of respondents reported that patients occasionally relate SD to rheumatologic therapy, but 71 0% of physicians did not change therapy when SD were reported Of all respondents, 78 7% always referred to specialists in
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 L
75
Napolitano, I Pantano, L Romano, et al
l a c e , 6 2 9 % o f r e s p o n d e n t s w o r k e d i n U n i v e r s i t y
case of patients who need pharmacological treatment for SD Besides, 41 9% and 33 9% respectively reported that patients never or rarely used PDE5Is autonomously Finally, 88 5% of respondents were aware of PDE5Is inhibitors side effects that most of them (75 4%) identified only with flushing and headache
DISCUSSION
SD have been reported to be common in rheumatologic patients and several risk factors as well as pain, fatigue, stiffness, disability, psychological state, hormonal imbalance, or side effects of medications can contribute to these conditions There is no doubt that sexuality impacts on the QoL, and represents a fundamental part of medical history, with a great significance in the lives of patients with RD The reasons for SD are multifactorial and comprise diseaserelated factors, physiological factors, and therapy Despite this, SD in rheumatologic settings remains a neglected issue This study represents the first Italian nationwide survey to investigate the attitude, knowledge, practice, and barriers among rheumatologists in discussing SD in patients with rheumatologic disorders We reported a gap between rheumatologists' attitudes and their daily practices regarding SD Indeed, although rheumatologists agreed with the importance of discussing sexual issues with their patients, they did not address it in their clinical practice These data corroborated findings of previous published studies: 87 1% of rheumatologists addressed SD in their patients and 16 1% of patients did not refer to SD In our recent publication about SD and gastroenterological disease, we reported that 71% of gastroenterologists never or infrequently addressed SD in patients with gastrointestinal disorders, and only 4% of patients refer their SD to their own gastroenterologist (20) Similar results were reported by Nicolai et al and Van Ek et al in cardiology and nephrology practice respectively (16, 21), while Sobecki et al , reported that 63% of obstetrician and gynecologists routinely assess patients’ sexual activities but only 40% investigate their SD (22) Insufficient time during visits (46 6%), followed by patients’ embarrassment (44 8%), and lack of training, are the most important reasons that contributed to not assess SD in the daily practice On the contrary other healthcare professionals as well as gastroenterologists, car-
diologists, nephrologists, neurologists, and neurosurgeons reported that the most important reasons are lack of knowledge and training, insufficient time during the visits and embarrassment (19) Despite these, 34 4% of rheumatologists are conscious that a specific training in sexual medicine could be useful in SD treatments These findings confirmed the data reported by Romano et al among gastroenterologists Adequate and standardized training should be mandatory to help healthcare in management of SD, in fact nowadays the lack of education represents a widespread problem for several healthcare Fibromyalgia represents the most frequent rheumatologic disorder (58 3%) related to SD (20) Collado-Mateo at al reported a prevalence of 76% of sexual problems among women with fibromyalgia compared to 15% in healthy controls, in particular among those aged 50 or over (23) It is associated with menopause, psychiatric comorbidities, and high degree of musculoskeletal pain (24)
One of the most important therapies in RD consist of antidepressants, that are notoriously related to SD (2526) Our responders reported that antidepressants represent the most common drugs related to SD (82 8%), followed by immunosuppressive medication (24 1%) Due to this, sometimes a multidisciplinary approach in SD is necessary (26-29)
To the best of our knowledge, this is the first study focused on the behavior and knowledge of rheumatologists regarding the SD of their patients However, our results should be read and interpretated according to several limitations, mainly including the small sample size, the use of a non-validated questionnaire, and the inclusion of a limited sample of respondents by country and age Future research is therefore needed to confirm and further our findings on the topic
In conclusion, SD is not routinely discussed in rheumatology practice, still remaining a neglected issue The most frequent explanations are lack of time, patients’ discomfort, and lack of knowledge/experience However, sexual health remains an essential issue in the lives of patients with RD, which should always be addressed by rheumatologists in order to start a correct counseling and an adequate multidisciplinary management Specific training on SD could be one of the most important steps to improve the practice of rheumatologists in this regard
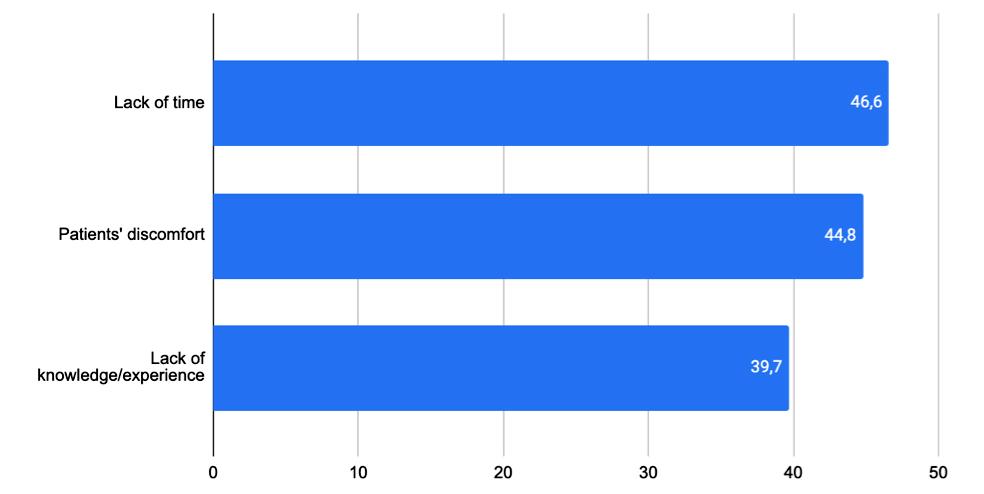
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 76 Rheumatologists and sexual dysfunction
Figure 1. Perceived barriers to discussing sexual health by rheumatologists.
REFERENCES
1 Manfredi C, Fortier É, Faix A, Martínez-Salamanca JI Penile Implant Surgery Satisfaction Assessment J Sex Med 2021; 18:868-874
2 Garrido-Abad P, Senra-Bravo I, Manfredi C, et al Combination therapy with topical alprostadil and phosphodiesterase-5 inhibitors after failure of oral therapy in patients with erectile dysfunction: a prospective, two-arm, open-label, non-randomized study Int J Impot Res 2022; 34:164-171
3 Mirone V, Napolitano L, D'Emmanuele di Villa Bianca R, et al A new original nutraceutical formulation ameliorates the effect of Tadalafil on clinical score and cGMP accumulation Arch Ital Urol Androl 2021; 93:221-226
4 Meyer M, Brunner P, Geissmann L, et al Sexual Dysfunctions in Patients Receiving Opioid Agonist Treatment and Heroin-Assisted Treatment Compared to Patients in Private Practice-Identifying Group Differences and Predictors Front Psychiatry 2022; 13:846834
5 Bay LT, Graugaard C, Nielsen DS, et al Sexual Health and Dysfunction in Patients With Rheumatoid Arthritis: A Cross-sectional Single-Center Study Sex Med 2020; 8:615-630
6 Anyfanti P, Pyrpasopoulou A, Triantafyllou A, et al Association between mental health disorders and sexual dysfunction in patients suffering from rheumatic diseases J Sex Med 2014; 11:2653-60
7 Tristano AG The impact of rheumatic diseases on sexual function Rheumatol Int 2009; 29:853-60
8 Tristano AG Impact of rheumatoid arthritis on sexual function World J Orthop 2014; 5:107-11
9 Yılmaz V, Umay E, Gündogdu I, et al Rheumatoid Arthritis: Are psychological factors effective in disease flare? Eur J Rheumatol 2017; 4:127-132
10 van Nimwegen JF, Arends S, van Zuiden GS, et al The impact of primary Sjögren's syndrome on female sexual function Rheumatology (Oxford) 2015; 54:1286-93
11 Moghadam ZB, Rezaei E, Faezi ST, et al Prevalence of sexual dysfunction in women with systemic lupus erythematosus and its related factors Reumatologia 2019; 57:19-26
12 Toussaint LL, Vincent A, McAllister SJ, et al A Comparison of Fibromyalgia Symptoms in Patients with Healthy versus Depressive, Low and Reactive Affect Balance Styles Scand J Pain 2014; 5:161-166
13 Tanski W, Dudek K, Tomasiewicz A, et al Sexual Dysfunction and Quality of Life in Patients with Rheumatoid Arthritis Int J Environ Res Public Health 2022; 19:3088
14 Azab M, Abdellatif MA, Abdelnaby MM Evaluation of sexual dysfunction and its predictive factors in female and male patients with rheumatoid arthritis Egypt Rheumatol Rehabil 2021; 48:38
15 Tsimtsiou Z, Hatzimouratidis K, Nakopoulou E, et al Predictors of physicians' involvement in addressing sexual health issues J Sex Med 2006; 3:583-588
16 Nicolai MP, Both S, Liem SS, et al Discussing sexual function in the cardiology practice Clin Res Cardiol 2013; 102:329-36
17 Sobecki JN, Curlin FA, Rasinski KA, Lindau ST What we don't talk about when we don't talk about sex: results of a national survey of U S obstetrician/gynecologists J Sex Med 2012; 9:1285-94
18 Korse NS, Nicolai MP, Both S, et al Discussing sexual health in spinal care Eur Spine J 2016; 25:766-73
19 Laldjising E, Sekercan A, Gadjradj PS Neurosurgeons' opinions on discussing sexual health among brain tumor patients: Room for improvement? J Clin Neurosci 2021; 94:292-297
20 Romano L, Zagari RM, Arcaniolo D, et al Sexual dysfunction in gastroenterological patients: Do gastroenterologists care enough? A
nationwide survey from the Italian Society of Gastroenterology (SIGE) Dig Liver Dis 2022; 54:1494-1501
21 van Ek GF, Krouwel EM, Nicolai MP, et al Discussing Sexual Dysfunction with Chronic Kidney Disease Patients: Practice Patterns in the Office of the Nephrologist J Sex Med 2015; 12:2350-63
22 Sobecki JN, Curlin FA, Rasinski KA, Lindau ST What we don't talk about when we don't talk about sex: results of a national survey of U S obstetrician/gynecologists J Sex Med 2012; 9:1285-94
23 Collado-Mateo D, Olivares PR, Adsuar JC, Gusi N Impact of fibromyalgia on sexual function in women J Back Musculoskelet Rehabil 2020; 33:355-361
24 Mutti GW, de Quadros M, Cremonez LP, et al Fibromyalgia and sexual performance: a cross-sectional study in 726 Brazilian patients Rheumatol Int 2021; 41:1471-1477
25 DeRubeis RJ, Hollon SD, Amsterdam JD, et al Cognitive therapy vs medications in the treatment of moderate to severe depression Arch Gen Psychiatry 2005; 62:409-16
26 Higgins A, Nash M, Lynch AM Antidepressant-associated sexual dysfunction: impact, effects, and treatment Drug Healthc Patient Saf 2010; 2:141-50
27 Cirillo L, Fusco GM, Di Bello F, et al Sexual dysfunction: Time for a multidisciplinary approach? Arch Ital Urol Androl 2023; 95:11236
28 Napolitano L, Fusco GM, Cirillo L, et al Erectile dysfunction and mobile phone applications: Quality, content and adherence to European Association guidelines on male sexual dysfunction Arch Ital Urol Androl 2022; 94:211-216
29 Romano L, Granata L, Fusco F, et al Sexual Dysfunction in Patients With Chronic Gastrointestinal and Liver Diseases: A neglected Issue Sex Med Rev 2022; 10:620-631
Correspondence
Luigi Napolitano, MD - dr luiginapolitano@gmail com
Lorenzo Romano, MD (Corresponding Author) - loryromano@hotmail it
Luigi Cirillo, MD - cirilloluigi22@gmail com
Francesco Matrangelo, MD - f mastrangelo91@gmail com
Giovanni Maria Fusco, MD - giom fusco@gmail com
Roberto La Rocca, MD - robertolarocca87@gmail com
Vincenzo Mirone, MD - mirone@unina it
Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples "Federico II", Naples, Italy
Ilenia Pantano, MD - ileniapantano@gmail com
Daniele Mauro, MC - dranielmar@gmail com
Francesco Ciccia, MD - francesco ciccia@unicampanaia it
Department of Precision Medicine, University of Campania "Luigi Vanvitelli", Naples, Italy
Celeste Manfredi, MD - manfredi celeste@gmail com
Lorenzo Spirito, MD - lorenzospirito@msn com
Davide Arcaniolo, MD - davide arcaniolo@gmail com
Marco De Sio, MD - marco desio@unicampania it
Unit of Urology, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli", Naples
Corrado Aniello Franzese, MD - corradofranzese@libero it
ASL Napoli 3 Sud, Naples, Italy
Carmine Sciorio, MD - carmine sciorio@gmail com
Urology Unit, Ospedale Alessandro Manzoni, Lecco, Italy
Marco Romano, MD - marco romano@unicampania it
Department of Precision Medicine and Hepatogastroenterology Unit, AOU University Luigi Vanvitelli, Naples, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 L
77
Napolitano, I Pantano, L Romano, et al
Single-incision needleless mini-sling technique for female stress urinary incontinence: A comparative study with standard transobturator inside-out technique
Eman Ali, Salah E Shebl, Sayeda Ibrahim Urology Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
Summary
To evaluate the safety and efficacy of surgeon-tailored polypropylene mesh (STM) through a needle-less single incision mini-slings (SIMS) vs standard trans-obturator tape (TOT) in the treatment of female stress urinary incontinence (SUI)
Methods: We conducted an open-label randomized controlled trial that included women with SUI. Eligible women were randomized in a 1:1 ratio to receive either standard TOT or SIMS techniques. All procedures were performed using a surgeon-tailored polypropylene mesh and monofilament tape
Results: A total of 60 women were included. The mean operative time was significantly longer in the standard TOT group The mean bleeding rate was significantly higher in the standard TOT group (87 6 ± 10 6 cc) compared to the SIMS group (60.0 ± 8.1 cc). There was no urethral injury in both groups. Transient thigh pain occurs in 12 cases (40 %) of the standard TOT and no cases in the SIMS group (p < 0.001). After three months, there was no significant statistical difference between the result of the two groups as regard to cure or improvement rate No failed cases were reported in both groups (p = 0 64) Likewise, there was no significant difference between the two groups regarding patients' satisfaction rate
Conclusions: SIMS was not inferior to standard TOT. STM SIMS is a mini-invasive, relatively safe, reproducible, easy to perform in a short time, with excellent patient tolerability and minimal pain, allowing early return to work and economically effective surgical procedure for the treatment of female stress urinary incontinence
KEY WORDS: Contasure-needleless; Single-incision needleless minisling; Stress urinary incontinence; Transobturator inside-out
Submitted 28 March 2023; Accepted 30 April 2023
INTRODUCTION
Stress urinary incontinence (SUI) is a complaint of involuntary urine leakage triggered by coughing, sneezing, exertion, or effort According to age, geographic location, and race, SUI prevalence varies from 5 to 61%, with yearly incidence rates of 4-11% and remission rates of only 4-5% (13) Particularly in developing countries, SUI continues to be a substantial health burden (3) There have been several surgical methods developed throughout time to treat female SUI, including tension-free vaginal tape (TVT) and trans-obturator tape (TOT) (4, 7) Both of these surgical approaches are widely accepted for the treatment of SUI However, TOT became more popular owing to its same
cure rate and lower incidence of complications, such as urinary tract infections, pelvic hematoma, and bladder/vaginal perforation (8, 9) The TOT sling method is regarded as the gold standard in the treatment of female SUI (10) Retropubic polypropylene mesh supports the urethra without tension, which was originally used in the initial approach, has now been modified to provide the same therapeutic benefits with fewer complications (11, 12) By avoiding the retropubic area, the TOT helps prevent hematoma and bladder perforation development in this area (13) These mid-urethral slings (MUS) procedures, however, also have complications owing to the blind transit of the introducer needles via obturator foramen Although groin pain has been reported to occur at a rate of 2-7 5% in certain studies, more significant complications such as vascular injury may also occur (11) A novel minimally invasive technique for treating SUI, known as single incision minislings (SIMS), was proposed as a way to reduce postoperative pain and eliminate blind passing trocars via the Retzius space and obturator canal with less mesh (14, 15) In this study, we aimed to evaluate the safety and efficacy of surgeon-tailored polypropylene mesh (STM) through a needleless SIMS vs standard TOT in the treatment of female SUI
METHODS
The local ethics committee approved the protocol of the current trial of Faculty of Medicine for girls, Al-Azhar University (FMG-IRB) met at Faculty of Medicine for Girls, Nasr City, Cairo, Egypt (Registration Number: 29042019) Only women who were able to read and sign the informed consent were included All procedures run in compliance with the standards of the Declaration of Helsinki (16) The reporting of the present manuscript followed the CONSORT statement (17)
Study design and patients
We conducted an open-label randomised controlled trial that included women with SUI, who were scheduled to undergo surgical management at Al Zahraa University Hospital in Cairo, Egypt, from February 2019 to June 2022 Adult women with a confirmed diagnosis of SUI through a positive stress test were included if they exhibited no response to pelvic floor exercise There were no restrictions regarding the severity of SUI or the presence of cystocele We excluded women with tumours of the
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 78
ORIGINAL PAPER
DOI: 10 4081/aiua 2023 11342
genitourinary organs, infection, neurogenic bladder, and pregnant women Eligible women were randomised in a 1:1 ratio to receive either standard TOT or SIMS techniques All procedures were performed using a surgeontailored polypropylene mesh and monofilament tape

Preoperative assessment
Preoperatively, all women were assessed for the presentation, duration, and severity of SUI through the questionnaire described by Sand et al (18) Besides, patients were evaluated for associated genitourinary or neurological conditions and bowel habits General medical, obstetric, and gynaecological histories were evaluated as well All women underwent routine physical examination and preoperative laboratory assessment, including complete blood count (CBC), liver and renal functions, bleeding profile, and urine culture Abdominopelvic ultrasonography was performed for all women to assess post-void residual urine All patients underwent cytometry preoperatively via Andromeda Urodynamic apparatus
Surgical procedures
In both groups:
– patients received prophylactic antibiotics one hour before the procedure (1gm 3rd generation cephalosporin intravenously);
– procedures were performed under spinal anesthesia and in lithotomy position, with a 16 F bladder catheter insertion;
– labia were retraced using a 3 0 silk stay suture;

– a vaginal incision was done;
– Allis clamps were applied at each side of the midline to suspend the anterior vaginal wall;
hydrodissection of the vaginal mucosa was performed;

– vaginal wall was incised 1 cm on the sagittal line starting 1 cm below the urethral meatus
In the standard TOT group:
– the mesh was prepared using a 30 x 30cm monofilament mesh;
– periurethral fascia was dissected laterally using Metzenbaum scissors toward the inferior pubic ramus at each side;
– a skin incision was made at the adductor longus tendon base parallel to the clitoris;
– a needle was passed from this incision to the vaginal incision;





– surgeon-tailored mesh was fixed to the needle and guided throughout the thigh;
to obtain a tension-free procedure a non-toothed forceps was placed between the sling and the urethra to avoid twisting of the tape;
A Paraurethral space was bluntly dissected (at 2 o’clock position) until the descending ischiopubic ramus was reached
B Tape applicator (needle) passing through tract created using out-in technique by supination movement
E Receiving the needle on index finger through tract
Suburethral straightening of the tape by using the back of
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Eman Ali, Salah E Shebl, Sayeda Ibrahim 79
Figure 1 (A-H). Standard transobturator tape (TOT) procedure
C Needle through tract with its tip out of vaginal incision
G Removal of excess tape outside the skin and closure of incision by vicryl 3/0.
H Closure of vaginal incision by vicryl 3/0 in interrupted manner.
D Mesh was fixed to the needle and drawn out through the thigh by pronation movement
F.
a toothed forceps that was placed between the tape and the urethra
–
–
Single-incision needleless mini-sling technique for female stress urinary incontinence
the patient was asked to cough to assess the correction of stress incontinence;
a 3-0 vicryl suture was used to close the skin and vaginal incisions in sub-cuticular and interrupted fashions, respectively;
– the vagina was packed with a povidone-iodine-soaked pack, and the urethral catheter was connected to closed-bag drainage (Figure 1)
In the SIMS:
– the mesh was prepared using 15 x 15 cm monofilament mesh (polypropylene mesh; Prolene, Ethicon Ltd , UK) to prepare T-pocket shaped strips of a total length of 12 5 cm;

Needle-less single incision mini-sling (SIMS)
dissection was made bilaterally to reach the ischiopubic ramus;
– the T-pocket shaped mesh was then folded into surgical forceps, which were introduced at 45 degrees to the dissected paraurethral space until the internal obturator fascia was penetrated;

– the surgeon opened the forceps to extend the T-pocket shaped mesh and removed the pulling sutures after full positioning;
– a 3-0 vicryl suture was used to close the vaginal incisions in an interrupted fashion The vagina was packed with a povidone-iodine-soaked pack, and the urethral catheter was connected to closed-bag drainage (Figure 2)
B Polypropylene strips or tapes (surgical tailored mesh) each one 1 cm x 30 cm prepared for package and sterilization by plasma machine

D Paraurethral space blunt dissection at 2 o’clock position until the descending ischiopubic ramus was reached
H By hyperextension and closure of the forceps the STM was folded into surgical forceps by placing the forceps inside the T- Pocket followed by opening and closing the forceps
I Forceps with the folded mesh was introduced by a controlled push at 45° from the horizontal plane in the previous dissected paraurethral space until a “crack” was felt that signified the penetration of the internal obturator fascia
J The T-pocket was then extended inside the internal obturator muscles by opening the forceps The forceps were then closed and pulled off the vagina.
L Closure of vaginal incision by vicryl 3/0 interrupted suture







F

Archivio Italiano di Urologia e Andrologia 2023; 95, 2 80
–
–
Figure 2 (A-L)
C. Suburethral longitudinal midline incision of anterior vaginal wall in presence of urethral catheter
E. Paraurethral spaces blunt dissection (at 10 o’clock position) until the descending ischiopubic ramus was reached.
Hyperextention of the STM T pocket by the forceps
G. Hyperextention of the T pocket of STM by the forceps at other end of the STM tape.
K. Visualization of suburethral tape untwisted before closure of the wound.
A. Polypropylene mesh 30 x 30 cm that will be tailored as tapes.
–
Women in both groups received routine postoperative care, and the vaginal pack and catheter were removed 12 hours after the operation in uneventful cases
Follow-up and study's outcomes
All women were followed biweekly in the first postoperative month, then every month for three months The follow-up visits consist of subjective assessment of SUI symptoms through the SUI questionnaire and urodynamic studies The surgical outcome was categorized according to the questionnaire and abdominal leak point pressures (ALLP) into: success, in which there is no urinary leakage with stress and patient's satisfaction; improve; in which there was leakage with severe exertion only; and failed, in which there is a persistent leakage and patient's dissatisfaction
Statistical analysis
Retrieved data were summarized and processed with IBM SPSS statistical software (version 25) Descriptive statistics were used to describe continuous and categorical data, respectively The hypothesis of significant difference between the techniques regarding postoperative outcomes and complications was tested using the Chi-square test, with Fisher exact whenever needed The association between technique and continuous data was tested using the Mann-Whitney test P-value < 0 05 was regarded as statistically significant
RESULTS
A total of 60 women were included in the present study
The mean age of the standard and SIMS groups was 45 6 ± 7 9 and 42 3 ± 6 6 years old, respectively None of the patients was nulliparous The mean number of deliveries in the standard group was 3 6±1 7, compared to 3 9 ± 1 1 deliveries in the SIMS group Two patients had cesarean section (CS) in addition to their vaginal deliveries Seven cases had associated preoperat i v e u r i n a r y t r a c t i n f e c t i o n
Almost 90% of the patients had n o p r e v i o u s s u r g e r y , t h r e e p a t i e n t s ( 5 % ) u n d e r w e n t a n a b d o m i n a l h y s t e r e c t o m y , a n d three patients (5%) underwent previous vaginal prolapse repair surgery Nine (30%) patients had grade I cystocele in the standard group, and six (20%) patients h a d g r a d e I I c y s t o c e l e F i v e (16 6%) patients had grade I cystocele on examination in the SIMS group The mean duration of symptoms was 2 73 ± 1 36 years (range 1-5 years) Four c a s e s o n l y ( 6 6 7 % ) i n b o t h groups had an ALPP less than 50 m l , w h i c h i n d i c a t e i n t r i n s i c sphincteric deficiency The preo p e r a t i v e u r o d y n a m i c s t u d i e s showed a mean bladder capacity of 382 76 ± 34 26 ml No patient
had detrusor overactivity or significant residual urine preoperatively (Table 1)
The mean operative time was significantly longer in the standard TOT group (17 0 ± 2 9 min) compared to the SIMS group (10 7 ± 1 8 min) The mean bleeding rate was significantly higher in the standard TOT group (87 6 ± 10 6 cc) compared to the SIMS group (60 0 ± 8 1 cc)
One case (3 33%) had bladder injury in the SIMS group, which needed cystoscopy revealing a small bladder injury that was repaired immediately by vicryl 4/0 in two layers There was no urethral injury in both groups None of the studied patients developed intraoperative vaginal wall laceration (Table 2)
Concerning early complications, re-catheterisation was not needed in any patient as there was no retention of urine or significant residual urine postoperatively The incidence of postoperative urinary tract infection (UTI) was 10% and was treated medically according to culture and sensitivity Three patients (two in the standard TOT and one in the SIMS group) developed a vaginal discharge Postoperative wound infection was not found in any cases None of the studied patients developed urine retention In terms of late complications, transient thigh pain occurs in 12 cases (40%) of the standard TOT and no cases in the SIMS group (p < 0 001) After three months from operation, vaginal discharge was reported in two cases (6 7%) treated with the appropriate antibiotics, antifungals, and frequent vaginal douches Five cases (20%) had urinary tract infection which was treated medically according to culture and sensitivity Dyspareunia, vaginal erosions and de novo urgency were not reported during postoperative follow up (Table 2)
After three months, there was no significant statistical difference between the result of the two groups as regard to cure or improvement rate, wherein the standard TOT group, 27 cases (90%) and three cases (10%) were succeeded and improved, respectively, compared to 28 cases (93 33%) and two cases (6 66%) in the SIMS group No
Table 1. Preoperative data of both groups
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Eman Ali, Salah E Shebl, Sayeda Ibrahim 81
Variables STM standard TOT STM SIMS P-value N = 30 % N = 30 % Age (years) Mean ± SD 45 6 ± 7 9 42 3 ± 6 6 P 0 086 Delivery Normal vaginal delivery 3 6 ± 1 7 3 9 ± 1 1 P 0 561 Cesarean section 0 07 ± 0 25 0 03 ± 0 18 Menopausal status Pre menopause 20 (66 7%) 24 (80%) P = 0 243 Post menopause 10 (33 3%) 6 (20%) Surgical history Patients with no previous surgery 25 (83 3%) 29 (96 7%) P = 0 163 Previous vaginal prolapse repair surgery 3 (10%) 0 (0%) Previous abdominal hysterectomy 2 (6 7%) 1 (3 3%) Per vaginal examination Normal 15 (50%) 25 (83 3%) P = 0 008* Mild cystocele 9 (30%) 5 (16 7%) Moderate cystocele 6 (20%) 0 (0%) Severity of preoperative incontinence rate Mild (0-1 pad/day) 2 (6 7%) 3 (10%) P 0 707 Moderate (2-3 pad/day) 14 (46 7%) 16 (53 3%) Severe (4-5 or more pad/day) 14 (46 7%) 11 (36 7%) ALLP < 50 ml 2 (6 66%) 2 (6 66%) 51-100 ml 12 (40%) 16 (53 33%) 101-150 ml 14 (46 66%) 12 (40%) 151-200 ml 2 (6 66%) 0 (0%)
Table 2
Operative
and complication of both groups
In our study, the early postoperative complications were more common in the standard TOT, including groin pain, UTI, and vaginal infection However, intraoperative complications and late postoperative complications were similar in both groups Likewise, in the Hasan et al trial, there was no significant difference in iatrogenic organ injury and postoperative complications between the two groups (5) When Amati et al completed their investigation, they found that just one patient in each group had a bladder injury that could be attributed to the simultaneous surgery In the group of standard TOT, there was one case (3 3%) catheterized for two weeks due to intraoperative bladder injury (24) Navazo et al reported a mean catheterization time of 2 02 days (20) Cabrera et al mentioned that after the standard TOT, the mean catheterization time was 1 52 days in 5 patients with acute retention (19) Retention that needed catheterization for more than 24 hours following routine TOT resolved spontaneously in less than two days in one case described by Magon and Chopra (21) It has been found that the prevalence of dyspareunia after SIMS ranges from 3 to 8% (Richter et al ) (25) In our study, it was observed that neither group suffered from urge incontinence, voiding difficulties, urine retention, urethral or bladder erosions, or dyspareunia
failed cases were reported in both groups (p = 0 64) (Figure 3) Likewise, there was no significant difference between the two groups regarding patients' satisfaction rate In the standard TOT group, 23 cases (76 7%) were very satisfied, compared to 22 cases (73 3%) in the SIMS group (p = 1 00)
DISCUSSION
In this study, we included two comparable groups of women with no significant differences in terms of age, BMI, parity, or menopausal status In addition, there were no significant differences in results of pelvic examination or cough stress test between women of both groups before surgery However, in terms of operative time, STM SIMS needed a mean operative time of 10 7 minutes, which was significantly less than the mean operative time (17 minutes) needed by the STM standard TOT procedure Similarly, Hasan et al , demonstrated that the mean operative time of the mini-sling procedure was 8 3 minutes compared to 16 5 minutes in the standard TOT procedure (5) The mean operative time of the single incision TOT procedure was nine minutes and seven minutes in the studies conducted by Cabrera et al (19) and Navazo et al (20), respectively
Regarding intraoperative blood loss, our findings showed that the standard TOT was associated with significantly higher procedure-related blood loss compared to STM SIMS In the Hasan et al study, single incision TOT patients had a lower average than regular TOT patients (51 5 vs 123 1 ml), respectively (5) According to a study done by Magon and Chopra on 51 individuals, the average volume of blood loss in the conventional TOT was 78 76 ml (21) Dobson et al showed that the blood loss was more than 100 ml in 71% of cases (22) Moore et al reported an average intraoperative blood loss of 57 ± 22 ml in the standard TOT and 36 ml in the single incision TOT (23)
According to Karakeçi et al , postoperative dyspareunia occurred in 21% of patients in the midurethral sling (MUS) group and 20% of patients in the SIMS group (26)
According to several clinical trials, the percentage of voiding problems after SIMS ranged from zero to eight percent (27, 29) The proportion of patients experiencing pain after the procedure was reported to reach up to 15 5% (25) Although the groin and leg pain spontaneously resolved within a few weeks in many cases, it may be prolonged in some patients During the short mid-term follow-up, Karakeçi et al preferred the SIMS technique since it caused less groin pain (26) Also, SIMS was preferred a n d r e c o m m e n d e d b y m o r e i n c o n t i n e n c e - s u f f e r i n g women (30, 31) SIMS has reduced complication rates due to little retropubic dissection and the absence of blind needle and mesh path in the groin region (26)
Patients were released from the hospital within 24 hours following surgery in our study with no significant differences in postoperative hospital stays between the two techniques In the study of Magon and Chopra, the average hospitalization time was 1 6 days; 45 8% of patients were released within 24 hours after surgery, 50 88% were discharged between 24 and 72 hours after surgery, and only 3 4% of patients had to remain in the hospital for more than three days because of intraoperative complications (21) Postoperative hospital stay was not significantly different between the two procedure (standard TOT: 2 95 days and single-incision TOT: 2 65 days), with a mean of 1 04 days including both procedures when there were no concomitant operations and of 2 65 days when there were concomitant operations (24)
STM standard TOT patients had an objective cure rate of 90% after three months, with a 10% improvement and no failed cases reported, while STM SIMS patients had an objective cure rate of 93 33% after three months, with a 6 6 6 %
undergone single incision TOT and found that 86% of them were
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 82 Single-incision needleless mini-sling technique for female stress urinary incontinence
i m p r o v e m e n t a n d n o f a i l e d c a s e s r e p o r t e d Cabrera et al studied 230 women who had
time
Variables STM standard TOT STM SIMS P-value N = 30 % N = 30 % Operative time (minutes) P = 0 000* 8-11 0 0 0 20 66 7 12-18 22 73 3 10 33 3 19-25 8 26 7 0 0 0 Operative time (minutes), Mean ± Sd 17.0 ± 2.9 10.7 ± 1.8 P = 0.000* Intra-operative complications P = 0 313 Bladder injury 1 (3 3%) 0 Bleeding rate (CC), Mean ± SD 87 6 ± 10 6 60 0 ± 8 1 P = 0 000* Vaginal wall laceration 00 Early postoperative complications P = 0.000* Groin pain 12 (40%) 0 (0%) Urinary tract infection 2 (6 7%) 1 (3 3%) Vaginal infection 2 (6 7%) 1 (3 3%) Urine retention 0 (0%) 0 (0%) Late postoperative complications P = 0.554 Mesh erosions 00 De novo urgency 00 Dyspareunia 00 Vaginal discharge 1 (3 34%) 1 (3 34%) Urinary tract infection 3 (10%) 2 (6.7%)
objectively cured after a year, with 6% showing improvement and 8% being classified as failures (19), while Navazo et al studied 120 women who had undergone single incision TOT and found that 84% were objectively cured after a year, with 8% showing improvement (20) There were no failed cases in the initial case series performed by Delorme et al on 32 women who had undergone the conventional TOT and had a cure rate of 90 6% at one year (32) At one year following the standard TOT operation, the objective cure rate was 88-92% and the subjective cure rate was 68-90%, according to published studies (33)
In conclusion, our study showed that SIMS was not inferior to standard TOT STM SIMS is a mini-invasive, relatively safe, reproducible, and economically effective surgical procedure for the treatment of female stress urinary incontinence The STM for SIMS was easy to insert in a short time operation It demonstrated excellent patient tolerability with minimal pain, early return to work and normal activity, and low morbidity when compared to STM standard TOT STM SIMS should be considered as a low-cost alternative to the available commercial kits in the treatment of female SUI, mainly for public health systems with few financial resources Randomized controlled studies with a longer duration of follow-up are needed to confirm our results
REFERENCES
1 Luber KM The definition, prevalence, and risk factors for stress urinary incontinence Rev Urol 2004; 6(Suppl 3):S3-S9
2 Aoki Y, Brown HW, Brubaker L, et al Urinary incontinence in women Nat Rev Dis Prim 2017; 3:17042
3 Reynolds W, Dmochowski R, Penson D Epidemiology of Stress Urinary Incontinence in Women Curr Urol Rep 2011; 12:370-376
4 Shirvan MK, Rahimi HR, Darabi Mahboub MR, Sheikhi Z Tension-free vaginal tape versus transobturator tape for treatment of stress urinary incontinence: A comparative randomized clinical trial study Urol Sci 2014; 25:54-57
5 Hasan MRA, AbdelMagid ME, Tagreda IA Sub-urethral Mini Sling versus Transobturator Vaginal Tape for Treatment of Female Stress Urinary Incontinence, One Year Follow-up Egypt J Hosp Med 2019; 76:3176-3183
6 Nerli RB, Kumar AG, Koura A, et al Transobturator vaginal tape in comparison to tension-free vaginal tape: A prospective trial with a minimum 12 months follow-up Indian J Urol 2009; 25:321-325
7 Zyczkowski M, Nowakowski K, Kuczmik W, et al Tension-free vaginal tape, transobturator tape, and own modification of transobturator tape in the treatment of female stress urinary incontinence: comparative analysis Biomed Res Int 2014; 347856
8 Rajamaheshwari N, Varghese L Transobturator tapes are preferable over transvaginal tapes for the management of female stress urinary incontinence: For Indian J Urol 2009; 25:550-553
9 Gomes CM, Carvalho FL, Bellucci CHS, et al Update on complications of synthetic suburethral slings Int Braz J Urol 2017; 43:822-834
10 Khan FN, Hamid A, Wazir BS, et al An Evaluation of Use of Trans-Obturator Tape (TOT) Sling Procedure in the Current
Surgical Management of Female Stress Urinary Incontinence Int J Health Sci (Qassim) 2008; 2:118-125
11 Ford AA, Rogerson L, Cody JD, et al Mid-urethral sling operations for stress urinary incontinence in women Cochrane database Syst Rev 2017; 7:CD006375-CD006375
12 Sergouniotis F, Jarlshammar B, Larsson P-G Urethral complications after tension-free vaginal tape procedures: A surgical management case series World J Nephrol 2015; 4:396-405
13 Wu E, High R, Lewis C, et al Retropubic mid-urethral slings and de novo urinary urgency and frequency: The role of retropubic hematomas Neurourol Urodyn 2021; 40:1686-1694
14 Leanza V, Intagliata E, Leanza A, et al Comparison between three mini-sling surgical procedures and the traditional transobturator vaginal tape technique for female stress urinary incontinence G Chir 2014; 35:80-84
15 Abdel-Fattah M, MacLennan G, Kilonzo M, et al The SIMS trial: adjustable anchored single-incision mini-slings versus standard tension-free midurethral slings in the surgical management of female stress urinary incontinence A study protocol for a
7:e015111-e015111
multi-
16 JAVA Declaration of Helsinki World Medical Association
Declaration of Helsinki Bull world Heal Organ 2013; 79:373-374
17 Schulz KF, Altman DG, Moher D, et al CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials (Chinese version) J Chinese Integr Med 2010; 8:604-612
18 Sand PK, Winkler H, Blackhurst DW, Culligan PJ A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling for treatment of genuine stress incontinence with low-pressure urethra Am J Obstet Gynecol 2000; 182:30-34
19 Cabrera J, Puyol M, Sousa A, et al Minimal invasive surgical technique without Needles (Contasure Needleless) for the surgical treatment of stress urinary incontinence: a multicentric trial Eur Urol Suppl - Eur Urol Suppl 2008; 7:147
20 Navazo R, Sierra J, Hidalgo C, et al Contasure needleless: A single incision TOT for the surgical treatment of stress urinary incontinence Arch Esp Urol 2009; 62:719-723
21 Magon N, Chopra S Transobturator Tape in Treatment of Stress
Urinary Incontinence: It is Time for a New Gold Standard N Am J Med Sci 2012; 4:226-230
22 Dobson A, Robert M, Swaby C, et al Trans-obturator surgery for stress urinary incontinence: 1-year follow-up of a cohort of 52 women Int Urogynecol J Pelvic Floor Dysfunct 2007; 18:27-32
23 Moore RD, JR M, M C Monarc Transtobturator sling: Combined analysis of one-year followup in nine countries with 266 patients Int Urogynecol J Pelvic Floor Dysfunct 2006; 17:203-207
24 Amati LT ME and LJ Contasure-Needleless® compared with transobturator-TVT® for the treatment of stress urinary incontinence Int Urogynecol J 2001; 22:827-33
25 Richter HE, Albo ME, Zyczynski HM, et al Retropubic versus transobturator midurethral slings for stress incontinence N Engl J Med 2010; 362:2066-2076
26 Karakeçi A, Eftal TC, Keles ¸ A, et al Single-incision midurethral sling shows less pain and similar success rate in a short-term followup compared to the transobturator tape method in the treatment of stress urinary incontinence Turkish J Urol 2020; 46:63-68
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Eman Ali, Salah E Shebl, Sayeda Ibrahim 83
c e n t r e , n o n - i n f e r i o r i t y r a n d o m i s e d c o n B M J O p e n 2 0 1 7 ;
pragmatic,
Single-incision needleless mini-sling technique for female stress urinary incontinence
27 Maturana AP, Palos CC, Ghersel FR, et al Randomized controlled trial comparing mini-sling with transobturator sling for the treatment of stress urinary incontinence Int Urogynecol J 2020; 31:1925-1931
28 Djehdian LM, Araujo MP, Takano CC, et al Transobturator sling compared with single-incision mini-sling for the treatment of stress urinary incontinence: a randomized controlled trial Obstet Gynecol 2014; 123:553-561
29 Pascom ALG, Djehdian LM, Bortolini MAT, et al Randomized controlled trial comparing single-incision mini-sling and transobturator midurethral sling for the treatment of stress urinary incontinence: 3-year follow-up results Neurourol Urodyn 2018; 37:2184-2190
30 Sangsawang B, Sangsawang N Stress urinary incontinence in pregnant women: a review of prevalence, pathophysiology, and treatment Int Urogynecol J 2013; 24:901-912
31 de Vries AM, Heesakkers JPFA Contemporary diagnostics and treatment options for female stress urinary incontinence Asian J Urol 2018; 5:141-148
32 Delorme E, Droupy S, de Tayrac R, Delmas V Transobturator tape (Uratape) A new minimally invasive method in the treatment of urinary incontinence in women Progr Urol 2003; 13:656-659
33 Deval B, Ferchaux J, Berry R, et al Objective and subjective cure rates after trans-obturator tape (OBTAPE) treatment of female urinary incontinence Eur Urol 2006 49:373-377
Correspondence
Salah E Shebl, MD (Corresponding Author)
salahshebl@yahoo com
salahshebl@azhar edu eg
Urology Department, Faculty of Medicine for Girls Al-Azhar University, Al Zahraa University Hospital, Al-Azhar University, Abbasia, Cairo, Egypt
Sayeda Ibrahim, MD
Soso uro@yahoo com
Eman Aly, MD
dr emanaly200@gmil com
Urology Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 84
Telemedicine and YouTube™: Video quality analysis before and after COVID-19 pandemic
Vincenzo Mirone 1 , Marco Abate 1 , Giovanni M Fusco 1 , Luigi Cirillo 1 , Luigi Napolitano 1 , Simone Morra 1 , Francesco Di Bello 1 , Gianluigi Califano 1 , Claudia Mirone 2 , Roberto La Rocca 1 , Massimiliano Creta 1 , Giuseppe Celentano 1 , Marco Capece 1 , Francesco Mangiapia 1 , Nicola Longo 1 , Claudia Collà Ruvolo 1
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples “Federico II”, Naples, Italy;
2 Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania "Luigi Vanvitelli", Naples, Italy
Summary
Objective: To assess the quality content of YouTubeTM videos on telemedicine during COVID-19 pandemic
Materials and methods: First, the frequency of worldwide YouTube™ and Google™ searches for telemedicine was analyzed. Second, we queried YouTube™ with telemedicine-related terms Third, the Patient Education Materials Assessment Tool for Audiovisual Materials (PEMAT A/V), the Global Quality Score (GQS), and the Misinformation tool were used for the quality assessment.
Results: According to selection criteria, 129 videos were collected for the analysis. From January 2018 to January 2022, the peak relative interest on YouTube™ and Google™ occurred in March 2020. Of all, 27.1 and 72.9% were uploaded before (Jan 2018-Feb 2020) and after (Mar 2020-Mar 2022) the COVID-19 outbreak, respectively. According to the PEMAT A/V, the overall median understandability and actionability was 50 0% (33 3 [IQR 0-66.7] vs 50.0 [27.1-75], p = 0.2) and 66.7% (63.6 [IQR 50 0-75 7] vs 67 9 [50 0-79 2],p = 0 6), respectively According to GQS, 3.9%, 17.8%, 24.0%, 26.4% and 27.9% were classified as excellent, good, medium, generally poor, and poor-quality videos, respectively The highest rate of poor-quality videos was recorded in videos uploaded before COVID-19 pandemic (37 1 vs 24 5%) According to overall misinformation score, a higher score was recorded for the videos uploaded after COVID-19 pandemic (1 8 [IQR 1 4-2 3] vs 2 2 [1 8-2 8], p = 0 01)
Conclusions: The interest in telemedicine showed a significant peak when the COVID-19 pandemic was declared However, the contents provided on YouTubeTM were not informative enough In the future, official medical institutions should standardize telemedicine regulation and online content to reduce the widespread of misleading information
KEY WORDS: Telehealth; Virtual healthcare; Healthcare technology; COVID-19; Social media
Submitted 24 January 2023; Accepted 17 February 2023
INTRODUCTION
The terms telehealth and telemedicine are often used interchangeably Telehealth is the provision of health care remotely by means of a variety of telecommunication tools, such as smartphones, and mobile wireless devices,
with or without a video connection (1, 2) Telemedicine has been defined as the communication of medical information among users through electronic devices, referring to specific clinical services (2-4)
D u r i n g t h e C O V I D - 1 9 p a n d e m i c , t h e r e q u e s t f o r telemedicine activities increased exponentially (4-7) Indeed, the World Health Organization and the Centers for Disease Control and Prevention (USA) encouraged the use of telemedicine with the aim of limiting people’s mobility and reducing the chance of infection, without compromising patients’ care (8-10)
Nowadays, the Internet is deeply used for professional networking, medical education, research recruitment, and patient information (11-13) Among Internet sources, YouTube™ is the second most used website and over 2 6 billion people worldwide use it at least once a month (14) The open-access material on this platform, which is not peer-reviewed as scientific materials published on PubMed, might spread misleading information Consequently, a quality information analysis must be required
The aim of the current study was to evaluate the overall quality of YouTube™ telemedicine-related videos and how it changed before and after COVID-19 pandemic
MATERIALS AND METHODS
Web interest assessment
We evaluated the interest of the worldwide web users in telemedicine We queried Google™ Trends (15) with the terms “Telemedicine” and “Telehealth” , using the following search settings: “worldwide” , “period from 01/01/2018 to 01/01/2022” , a n d “ all the categories” T h e t r e n d s o f Google™ and YouTube™ search were independently recorded: the data was depicted as a 0 to 100 scale The value 100 indicates the highest search frequency of the term, and 50 indicates half of the searches A score of 0, on the other hand, indicates that not enough data was found for the term
Search strategy, selection criteria, and videographic characteristics
We queried YouTube™ with 19 keyword combinations (Supplementary Table 1) The search was performed in
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 85 ORIGINAL PAPER
DOI: 10 4081/aiua 2023 11341
incognito status to minimize the search history and the geographically related biases
The first 30 videos were examined for each of the 19 keyword combinations A total of 570 videos was achieved The following exclusion criteria were applied: duplicates, non-English language, off topic, video length > 30 minutes, and video with marketing purpose
The videos published after the 1st of January 2018 were included A total of 129 videos were eligible for the analyses (Figure 1)
For each of the 129 videos included, the following variables were collected on the 25th of March 2022: length (minutes), views, persistence time on YouTube™ (days), view ratio (defined as the ratio between the number of views and the persistence time on YouTube™), likes, subscribers, number of videos with or without disabled comments, authoring entity (private users, medical doctor, hospitals [such as academic hospitals and academic institutions, or non-academic hospitals and institutions, health-care centers, private practice hospitals], and others [such as news channels, general communication channel, talks]) and target audience (healthcare workers, patients and other [such as general public])
According to the recent YouTube™ rules, dislikes are not visible anymore for general Internet users
The YouTube™ videos were further stratified according to the date of the upload before and after the COVID-19 outbreak (March 2020) (16, 17)
Strategies and instruments for the assessment of videos content
Video contents were assessed independently by two medical doctors [L C and G M F ]
A third investigator, a senior urology resident [C C R ], adjudicated any differences, and the consensus was achieved among all reviewers
The reviewers were blinded to each other’s evaluations
The Patient Education Materials Assessment Tool for Audiovisual Materials (PEMAT A/V), the Global Quality Score (GQS), and the Misinformation tool were used for the video quality assessment

First, the PEMAT A/V is a systematic tool designed to be completed by professionals, including healthcare providers, health librarians, and others, who provide high-quality materials to patients or consumers It consists of 17 items developed to evaluate and compare the Understandability (questions 1-13) and Actionability (questions 14-17) of patient education materials Three answers were permitted (agree = 1, disagree = 0, not available = NA) The total score was presented as a percentage obtained by the sum of all points, divided by the number of the items judged as agree or disagree Higher scores detect more understandable and actionable content (12, 18, 19)
Second, The GQS is a validated tool assessing the quality, feasibility, and clinical utility of each video Five possible scores from 1 (poor quality, poor flow, most of the information missing, not at all useful) to 5 (excellent quality, excellent flow, completely accurate information, very useful) were assigned (20)
Third, the Misinformation tool consists of 5 questions appositely created for the porpoise of the study, as previously done (21-24) The aim of this tool is to examine relevant aspects not investigated with the other validated tools The questions are as follows: 1 Is the telemedicine definition correctly provided? 2 Is the telemedicine aim correctly described? 3 Are the instruments used for telemedicine correctly described? 4 The patients’ consent regulation in telemedicine is correctly described? 5 Are the limits of telemedicine well explained? The possible scores range from 1 (extreme misinformation) to 5 (no misinformation)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 V Mirone, M Abate, G M Fusco, L Cirillo, et al 86
Figure 1. PRISMA diagram depicting inclusion and exclusion criteria of YouTube™ video search.
Statistical analysis
Descriptive statistics were presented as medians and interquartile ranges (IQR) for continuously coded variables or counts and percentages for categorically coded variables
Kruskal-Wallis test, Chi-square test, and proportion test examined the statistical significance in medians and proportions differences In all statistical analyses, the R software (www rproject org) environment for statistical computing and graphics (R version 4 0 0) was used All tests were two-sided with a level of significance set at p < 0 05
RESULTS
Worldwide Web interest
From January 2018 to January 2022, the relative interest on YouTube™ ranged from 5 to 19 and from 13 to 20, using respectively the “Telehealth” and “Telemedicine” keywords (Figure 2) For both keywords, the peak occurred in March 2020 (100 and 63, respectively) From January 2018 to January 2022, the relative interest on GoogleTM ranged from 6 to 22 and from 5 to 9, using respectively the “Telehealth” and “Telemedicine” keyword For both keywords, the peak occurred in March 2020 (100 and 47 respectively)
Videographic characteristics
Of 129 videos (Table 1), 35 (27 1%) a n d 9 4 ( 7 2 9 % ) w e r e u p l o a d e d before (Jan 2018-Feb 2020) and
Figure 2
Chart-line plot depicting relative frequency of worldwide search for “Telehealth” (red) and “Telemedicine” (blue) on both YouTube™ and Google™ searches, observed between the January 1, 2018 and the January 31, 2022

after (Mar 2020-Mar 2022) the COVID-19 outbreak, respectively The overall median length was 4 5 minutes (Jan 2018-Feb 2020: 3 [IQR 1 5-4 5] vs Mar 2020-Mar 2022: 5 5 [2 4-10 9], p < 0 001), the overall median number of views was 2428 (Jan 2018-Feb 2020: 7783
pandemic declaration date (the 9th of March 2020).
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 87 Telemedicine and YouTube™
Table 1.
Overall Jan 2018-Feb 2020 Mar 2020-Mar 2022 p-value n = 129 n = 35 (27.1) n = 94 (72.9) Length, min < 0 001 Median 4 5 3 5 5 IQR 2 2-10 0 1 5-4 5 2 4-10 9 Views, n 0 02 Median 2428 7783 1576 IQR 375-10022 897 5-21220 5 328 5-6526 2 Persistence time on YouTube™ < 0 001 Median 663 1264 600 IQR 400-853 1055 5-1369 5 321 8-676 5 View ratio 0 7 Median 3 5 5 3 IQR 0-12 0-8.5 0-12.5 Likes, n 0 7 Median 16 19 5 15 5 IQR 3-62 5 1-136 3-48 2 Comments, n 0 8 Median 000 IQR 0-4 0-5 5 0-4 Subscribers, n 0 2 Median 3250 2425 4460 IQR 380 5-29600 107 8-26125 524-30900 Disabled comments, n (%) No 110 (85 3) 25 (71 4) 85 (90 4) 0 01 Yes 19 (14.7) 10 (28.6) 9 (9.6) 0.01 Authoring entity, n (%) Private user 31 (24 0) 7 (20 0) 24 (25 5) 0 7 Medical doctor 14 (10 9) 5 (14 3) 9 (9 6) 0 6 Hospital 4 (3 1) 2 (5 7) 2 (2 1) 0 6 Other 80 (62 0) 21 (60 0) 59 (62 8) 0 9 Target audience, n (%) Healthcare workers 45 (34 9) 13 (37 1) 32 (34 0) 0 9 Patients 36 (27 9) 12 (34 3) 24 (25 5) 0 4 Other 48 (37 2) 10 (28 6) 38 (40 4) 0 3
Videographic characteristics of 129 YouTube™ telemedicine-related videos, recorded on the 25th of March 2022, stratified according to the COVID-19
Table 2. Quality assessment with The Patient Education Materials Assessment Tool for Audiovisual Materials (PEMAT A/V) and Global Quality Score (GQS) in overall videos (n = 129) and stratifying according to the COVID-19 pandemic declaration date (the 9th March 2020)
was 66 7% (Jan 2018-Feb 2020: 63 6 [IQR 50 0-75 7] vs Mar 2020-Mar 2022: 67 9 [50 0-79 2], p = 0 6)
According to GQS (Table 2B), of all 3 9% (n=5), 17 8% (n=23), 24 0% (n=31), 26 4% (n=34) and 27 9% (n=36) were classified as excellent, good, medium, generally poor, and poor-quality videos, respectively
According to the uploaded date (Jan 2018-Feb 2020 vs Mar 2020-Mar 2022), the highest rate of excellent quality videos was recorded in videos uploaded after COVID-19 outbreak (0 0 vs 5 3%, p = 0 4) The highest rate of poor-quality videos was recorded in videos uploaded before COVID-19 pandemic (37 1 vs 24 5%, p = 0 2)
Table 3.
Quality assessment with the Misinformation tool in overall videos (n = 129) and stratifying according to the COVID-19 pandemic declaration date (the 9th March 2020).
According to the Misinformation tool (Table 3), the lowest median score w a s r e c o r d e d f o r t h e q u e s t i o n 1 (defined as “Is the Telemedicine definition correctly provide?”), question 4 (defined as “The patients’ consent regul a t i o n i s c o r r e c t l y d e s c r i b e d ? ” ) a n d question 5 (defined as “Are the limits of Telemedicine well explained?”) The highest median score was recorded for questions 2 (defined as “Is the telemedicine aim correctly described?”) and 3 (defined as “Are the instruments u s e d f o r T e l e m e d i c i n e c o r r e c t l y described?”) According to the mean misinformation score, a statistically significant difference was recorded for question 2 (median: 2 [IQR: 1-30] vs 3 [IQR: 2-4], p = 0 01)
[IQR 897 5-21220 5] vs Mar 2020-Mar 2022: 1576 [328 5-6526 2], p = 0 02), the overall median view ratio was 2 (Jan 2018-Feb 2020: 5 5 [IQR 0-8 5] vs Mar 2020Mar 2022: 3 [0-12 2], p = 0 7) and the median number of likes was 16 (Jan 2018-Feb 2020: 19 5 [IQR 1-136] vs Mar 2020-Mar 2022: 15 5 [3-48 2], p = 0 7) Moreover, the median number of comments and subscribers was 0 (Jan 2018-Feb 2020: 0 [IQR 0-5 5] vs Mar 2020-Mar 2022: 0 [0-4 4], p = 0 8), and 3250 (Jan 2018-Feb 2020: 2425 [IQR 107 8-26125] vs Mar 2020-Mar 2022: 4460 [524-30900], p = 0 2), respectively Of all videos, 24 0% (20 0 vs 25 5%), 10 9% (14 3 vs 9 6%), 3 1% (5 7 vs 2 1%), and 62 0% (60 0 vs 62 8%) were produced by private users, medical doctor, hospitals or other, respectively Additionally, 34 9% (37 1 vs 34 0%), 27 9% (34 3 vs 25 5%) and 37 2% (28 6 vs 40 4%) were targeted to healthcare workers, patients and other, respectively (all p > 0 05)
Videos content results
According to the PEMAT A/V (Table 2A), the overall median Understandability was 50 0% (Jan 2018-Feb 2020: 33 3 [IQR 0-66 7] vs Mar 2020-Mar 2022: 50 0 [27 1-75], p = 0 2) and the overall median Actionability
According to the overall misinformation score, a higher score was recorded for YouTube videos uploaded after the COVID-19 pandemic (median 1 8 [IQR 1 4-2 3] vs 2 2 [1 8-2 8], p = 0 01)
DISCUSSION
The current study aimed to evaluate the overall quality of Y o u T u b e ™ t e l e m e d i c i n e - r e l a t e d v i d e o s a n d h o w i t changed before and after COVID-19 outbreak To the best of our knowledge, no previous investigators examined this topic We addressed this void and identified several noteworthy observations
First, as clearly shown by the trend analysis, the web interest in telemedicine impressively increased when the COVID-19 pandemic was declared (16, 17)
Furthermore, the interest is keeping high from the outbreak to date, compared to the past Additionally, we revealed a higher interest on the YouTube™ , relative to the Google™ website In consequence, most of the users interested in the topic obtained information from videos uploaded on the web This observation further corroborates the intent of the current study, which consisted of examining the quality content on YouTube™ videos in
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 V Mirone, M Abate, G M Fusco, L Cirillo, et al 88
Overall Jan 2018-Feb 2020 Mar 2020-Mar 2022 p-value n = 129 n = 35 (27.1) n = 94 (72.9) A) PEMAT A/V, % Actionability 0 02 Median 50 33 3 50 IQR 0-75 0-66 7 27 1-75 Understandability 0 06 Median 66 7 63 6 67 9 IQR 50-77 6 50 0-75 7 50 0-79 2 B) GQS, n (%) Excellent 5 (3 9) 0 (0 0) 5 (5 3) 0 4 Good 23 (17 8) 7 (20 0) 16 (17 0) 0 9 Medium 31 (24.0) 7 (20.0) 24 (25.5) 0.7 Generally poor 34 (26 4) 8 (22 9) 26 (27 7) 0 7 Poor 36 (27 9) 13 (37 1) 23 (24 5) 0 2 IQR: Interquarti e range
Overall Jan 2018-Feb 2020 Mar 2020-Mar 2022 p-value n = 129 n = 35 (27 1) n = 94 (72 9) 1 Is the telemed cine def n tion Median 112 0 1 correctly defined? IQR 1-3 1-2 1-3 2 Is the telemed cine aim Median 323 0 01 correctly described? IQR 2-4 1-3 2-4 3. Are the instruments used for Median 323 0.1 telemedicine correct y described? IQR 2-4 1-3 5 2-3 8 4 The patients’ consent regulat on Median 111 0 6 in te emedicine is correctly described? IQR 1-2 1-2 1-2 5 Are the l mits of telemedicine Median 111 < 0 01 wel explained? IQR 1-2 1-1 1-2 8 Misinformation score Median 2 2 1 8 2 2 0 01 IQR: Interquarti e range
order to make aware Internet users on the dangerous possibility of acquiring misleading information
Second, we recorded a higher number of videos uploaded after the COVID-19 outbreak (35 vs 94) This data may indicate that the general community is becoming more aware regarding the importance of using the Internet, and specifically YouTube™ , as an instrument for getting and spreading information However, we did not observe differences in terms of authoring entity or target between videos uploaded before and after the COVID-19 outbreak This observation is against our expectations
Indeed, we expected that more videos would be produced by healthcare providers and official entities in order to guarantee good quality information to general community For example, among the medical fields, neurophysiologists intensively used telemedicine to ensure for neurological disorders care during the pandemic
Indeed, Stipa et al published a study in the 2020 providing recommendations for guidelines development in this field (9) This study should represent an example for the other specialties to encourage the development of specific guidelines
Third, according to the quality assessment tools used in the current study, poor-quality video content was recorded Specifically, according to the PEMAT A/V tools, both A c t i o n a b i l i t y ( 5 0 % ) a n d U n d e r s t a n d a b i l i t y ( 6 6 7 % ) scores were low, regardless the year of upload
The Understandability reflects how viewers could process the information displayed in the videos, while the A c t i o n a b i l i t y r e fl e c t s h o w v i e w e r s c o u l d u s e t h e m
According to Shoemaker et al , a PEMAT A/V score < 70% is considered poorly understandable or poorly actionable (25) In consequence, based on our results, we recorded poor quality content Furthermore, according to the GQS tool, more than half of the videos were classified as generally poor or poor quality The same observation was noticed in the videos uploaded before or after the COVID-19 pandemic In consequence, despite a higher number of videos uploaded after the pandemic outbreak, low-quality content was uploaded Unfortunately, we were the first to examine YouTube™ video content related to telemedicine and no comparisons was possible Fourth, interesting results emerged from the Misinformation tool, which allowed us to investigate other aspects, not well examined by the other validated quality assessment tools used Thanks to that, we discovered that relevant telemedicine aspects were underestimated during the YouTube™ video making For example, we did not record any video explaining the differences between telecollaboration, tele-treatment, tele-monitoring, or tele-support (26) Additionally, scant information was provided on the informed consent that should be obtained by healthcare providers (27) Last, but not least, the physicians’ roles and responsibilities were rarely provided (28) However, we recorded an improvement of the Misinformation tool items score in the videos uploaded after the pandemic declaration, compared to the ones recorded before These observations may proof that the community is increasingly using the Internet as a spreading information instrument on telemedicine, due to the higher requests and unexperienced needs caused by the pandemic However, with this tool, we also highlighted that all the
possible risks behind the telemedicine use were dangerously hidden
Taken together, we observed that the telemedicine interest peak occurred in March 2020 on both Google™ and YouTube™ websites, concordantly with the first pandemic wave It confirms how YouTube™ was highly used to promptly acquire information on telemedicine
Moreover, overall reliability and quality of YouTube™ videos on this topic were inadequate, as evidenced by a low PEMAT A/V score and a high number of poor and generally poor quality videos Additionally, important aspects, such as the limited and fragmented insurance coverage of telemedicine, the lower quality of patientphysician relationships, the legal issues, and the differential access to telecommunication technologies based on social and geographic factors, were underestimated In the future, considering the essential importance of telemedicine in the modern era, it will be mandatory for the official entity to develop proper guidelines to provide the best information to Internet users
The current study is not devoid of limitations
First, some reliable or non-reliable videos might be missed, due to our search terms However, we used 19 keyword combin
d , o n l y English-language videos were included in the final sample Other language videos could provide different information Third, quality assessment videos were subjectively evaluated However, three investigators were independently involved to analyse video contents and were
, YouTube™ is a constantly expanding multimedia platform and the contents may rapidly change significantly with new updates over time
CONCLUSIONS
The interest in telemedicine showed a significant peak when the COVID-19 pandemic was declared Despite the importance of telemedicine in the modern era, the contents provided were not informative enough and not verified by an official entity In the future, official medical institutions should standardize telemedicine regulation and online contents to reduce the widespread of misleading information
REFERENCES
1 Dorsey ER, Topol EJ State of Telehealth Campion EW, editor N Engl J Med 2016; 375:154-61
2 Gajarawala SN, Pelkowski JN Telehealth Benefits and Barriers J Nurse Pract 2021; 17:218-21
3 Kichloo A, Albosta M, Dettloff K, et al Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA Fam Med Community Health 2020; 8:e000530
4 Mirone V, Creta M, Capece M, et al Telementoring for communication between residents and faculty physicians: Results from a survey on attitudes and perceptions in an Academic Tertiary Urology Referral Department in Italy Arch Ital Urol Androl 2021; 93:450-4
5 Hollander JE, Carr BG Virtually Perfect? Telemedicine for Covid19 N Engl J Med 2020; 382:1679-81
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 89 Telemedicine and YouTube™
a t i o n s t o m i n i m i z e s e l e c t i o n e r r o r s S e c
e a c h o t h e r b l i n d e d d u r i n g t h e e v a l u a t i o n F o u r t h
o n
6 Novara G, Checcucci E, Crestani A, et al Telehealth in Urology: A Systematic Review of the Literature How Much Can Telemedicine Be Useful During and After the COVID-19 Pandemic? Eur Urol 2020; 78:786-811
7 Mirone V, Celentano G, Collà Ruvolo C, et al Perceptions and attitudes toward the use of telemedicine for the postoperative outpatient urological care during the COVID-19 pandemic in an Academic Hospital in Southern Italy Arch Ital Urol Androl 2022; 94:375-9
8 Monaghesh E, Hajizadeh A The role of telehealth during COVID19 outbreak: a systematic review based on current evidence BMC Public Health 2020; 20:1193
9 Stipa G, Gabbrielli F, Rabbito C, et al The Italian technical/ administrative recommendations for telemedicine in clinical neurophysiology Neurol Sci 2021; 42:1923-31
10 Creta M, Sagnelli C, Celentano G, et al SARS-CoV-2 infection affects the lower urinary tract and male genital system: A systematic review J Med Virol 2021; 93:3133-42
11 Turco C, Collà Ruvolo C, Cilio S, et al Looking for cystoscopy on YouTube: Are videos a reliable information tool for internet users? Arch Ital Urol Androl 2022; 94:57-61
12 Collà Ruvolo C, Califano G, Tuccillo A, et al “YouTube™ as a source of information on placenta accreta: A quality analysis” Eur J Obstet Gynecol Reprod Biol 2022; 272:82-7
13 Loeb S, Reines K, Abu-Salha Y, French W, et al Quality of Bladder Cancer Information on YouTube Eur Urol 2021; 79:56-9
14 Alexa - Top sites [Internet] [cited 2022 Apr 18] Available from: https://www alexa com/topsites
15 Google Trends [Internet] Google Trends [cited 2021 Dec 30] Available from: https://trends google it/trends/?geo=IT
16 Cucinotta D, Vanelli M WHO Declares COVID-19 a Pandemic Acta Bio Medica Atenei Parm 2020; 91:157-60
17 Coronavirus Disease (COVID-19) Situation Reports [Internet] [cited 2022 Jun 7] Available from: https://www who int/emergencies/diseases/novel-coronavirus-2019/situation-reports
1 8 S j S P a t i e n t E d u c a t i o n M a t e r i a l s A s s e s s m e n t T o o l f o r Audiovisual Materials (PEMAT-A/V) :4
19 Di Bello F, Collà Ruvolo C, Cilio S, La Rocca R, et al Testicular cancer and YouTube: What do you expect from a social media platform? Int J Urol 2022; 29:685-691
20 Gerundo G, Collà Ruvolo C, Puzone B, et al Personal protective equipment in Covid-19: Evidence-based quality and analysis of YouTube videos after one year of pandemic Am J Infect Control 2021 Nov; S0196655321007586
21 Morra S, Collà Ruvolo C, Napolitano L, et al YouTube™ as a source of information on bladder pain syndrome: A contemporary analysis Neurourol Urodyn 2022; 41:237-245
22 Melchionna A, Collà Ruvolo C, Capece M, et al Testicular pain and youtube™: are uploaded videos a reliable source to get information? Int J Impot Res 2023; 35:140-146
23 Capece M, Di Giovanni A, Cirigliano L, et al YouTube as a source of information on penile prosthesis Andrologia 2022; 54:e14246
24 Cilio S, Collà Ruvolo C, Turco C, et al Analysis of quality information provided by ‘Dr YouTube™’ on Phimosis Int J Impot Res 2022; 24:1-6
25 Shoemaker SJ, Wolf MS, Brach C Development of the Patient Education Materials Assessment Tool (PEMAT): A new measure of
understandability and actionability for print and audiovisual patient information Patient Educ Couns 2014; 96:395-403
26 National Telemedicine Guidelines [Internet] 2015 Available from: https://www moh gov sg/docs/librariesprovider5/resources-stat
lines-rev pdf
27 Becker CD, Dandy K, Gaujean M, et al Legal Perspectives on Telemedicine Part 1: Legal and Regulatory Issues Perm J 2019; 23:18-293
28 National Telemedicine Guidelines [Internet] 2020 Available from: https://www mohfw gov in/pdf/Telemedicine pdf
Correspondence
Vincenzo Mirone, MD mirone@unina it Marco Abate, MD marcoabate5@gmail com
Giovanni Maria Fusco, MD giom fusco@gmail com
Luigi Cirillo, MD cirilloluigi22@gmail com
Luigi Napolitano, MD (Corresponding Author) dr luiginapolitano@gmail com
Simone Morra, MD simonemorra93@gmail com
Francesco Di Bello, MD fran dibello12@gmail com
Gianluigi Califano, MD gianl califano2@gmail com
Roberto La Rocca, MD robertolarocca87@gmail com
Massimiliano Creta, MD max creta@gmail com
Giuseppe Celentano, MD dr giuseppecelentano@gmail com
Marco Capece, MD drmarcocapece@gmail com
Francesco Mangiapia, MD mangiapiaf@gmail com
Nicola Longo, MD nicolalongo20@yahoo it
Claudia Collà Ruvolo, MD c collaruvolo@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples Federico II, Via Sergio Pansini n°5, 80138 Naples
Claudia Mirone, MD claudiamirone@outlook it
Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania "Luigi Vanvitelli", Naples
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 V Mirone, M Abate, G M Fusco, L Cirillo, et al 90
i s t i c s / g u i d e l i n e s / m o h - c i r - 0 6 2 0 1 5 3 0 j a n 1 5 t e l e m e d i c i n e - g u i d e -
Analysis of transurethral resection of prostate videos on YouTube™: Educational quality assessment
Summary
Background: Our aim was to evaluate the educational value of transurethral resection of prostate (TURP) videos on YouTube.
Methods: A comprehensive search was conducted for TURP videos on YouTube. Based on the Laparoscopic Surgery Video Educational Guidelines we created a checklist which includes 20 items for evaluation of the videos. IBM SPSS statistics was used for analysis
Results: A total of 104 surgical videos were assessed. The mean view count was 15647 3 (21-324 522, SD 47556 4) Video image quality found as low for 57 7% of videos Both staff (76%) and resident (75%) rated most of the videos low educational quality No statistically significant difference was found between staff’s total points (mean 4 35 ± SD 2 9) and resident’s total points (mean 4 63 ± SD 3 3) (p: 0 761) Positive correlation was found between view count and staff’s total points (r: 0 242 p < 0 05), resident’s total points (r: 0 340 p < 0 01) There was also positive correlation between number of likes and staff’s total points (r: 0 375 p < 0 01) and resident’s total points (r: 0.466 p < 0.01).
Conclusions: Most TURP surgical videos on YouTube are low quality. Higher educational quality videos with detailed explanation of the procedure are needed on this subject We believe this study could be a guide for future high quality TURP videos.
KEY WORDS: Transurethral resection of prostate; Benign prostatic hyperplasia; Social media; Video recording; Data quality
Submitted 11 April 2023; Accepted 27 April 2023
INTRODUCTION
Benign prostatic hyperplasia (BPH) is a histologic diagnosis which is characterized by proliferation of smooth muscle and epithelial cells of the periurethral prostatic tissue Its prevalance increases with age reaching 90% by the ninth decade of life at autopsy studies (1) BPH is the leading cause of male lower urinary tract symptoms (LUTS) (2) Most men after 45 suffer at least one component of LUTS and symptoms are mostly mild (3) With aging global population and high prevelance of LUTS especially in elderly men, treatment of male LUTS will become even more important in the future
Treatment options for BPH related male LUTS are cons e r v a t i v e t r e a t m e n t , p h a r m a c o t h e r a p y a n d s u r g e r y
Surgical management of BPH can basically divided into three main groups; open prostatectomy, minimally inva-
sive techniques (laparoscopic, robotic prostatectomy) and endoscopic interventions First resectoscope and the first transurethral resection of prostate (TURP) procedure was introduced by Maximilian Stern in 1926 (4) With technological advances, TURP became more and more popular and has been considered the reference technique for the surgical management of BPH Despite the decline in the rate of TURP for BPH surgery due to development of various alternative techniques such as Holmium laser enucleation of prostate (HoLEP), TURP is still the most frequently taught and performed surgical technique for BPH (5)
The internet's baby steps began to be taken in the 1960’s and accelerated in the 80’s (6) Nowadays, 60% of the world’s population has access to internet (7) With portable electronic devices online resources have become an important part of education in general Videos are easily accessible, allow creating personal time and space for learning By watching videos online, one can learn different techniques from various surgeons, interact with colleagues around the world, exchange ideas and improve skills With fewer opportunities being found lately by trainees in the operating rooms due to work hour restrictions, high costs, patient safety measures (8), videos became a crucial learning method in surgical training Many surgical videos are avaliable online and advantages of these videos in surgical education have been shown in various studies (9, 10)
YouTube™ (Google, LLC) which was founded on 2005, is the second most popular website in the world with over 33 billion total visits in June 2022 (11) and the biggest source of videos on the internet Studies showed that YouTube™ is the most widely used platform by both residents and surgeons for surgical education (12, 13) There is a great opportunity to learn about surgical techniques and improving skills with watching videos on YouTube™ However, since there is lack of professional p e e r r e v i e w a n d q u a l i t y c h e c k o f t h e v i d e o s o n YouTube™ , surgical videos may be untrustworthy In this study we aimed to evaluate the educational quality of TURP videos on YouTube™
MATERIALS AND METHODS
In this study we evaluated TURP surgery videos which are avaliable for the public Therefore, no ethical approval is
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 91
ORIGINAL PAPER
Yavuz Karaca 1 , Emre Burak Sahinler 1 , Didar Ilke Karaca 2 , Orhun Sinanoglu 1
DOI: 10 4081/aiua 2023 11404
1 Department of Urology, Sancaktepe Sehit Prof Dr Ilhan Varank Research and Training Hospital, Istanbul, Turkey; 2 Department of Public Health, Marmara University School of Medicine, Istanbul, Turkey
required A comprehensive search was performed in October 31, 2022 on YouTube™(https://www.youtube.com) using the search terms “tur prostate” , “tur prostatectomy” , “tur p ” , “monopolar tur p ” , “bipolar tur p ” seperately The videos were selected by the first author based on following criterias: traditional resection of the prostate must be performed either with monopolar or bipolar systems, live surgery recorded by endoscopic camera systems, videos made by professionals and videos in English language Videos including multiple surgeries, externally recorded videos, commercial videos, slide based presentation videos and animation videos and non- English videos were excluded from the study 104 videos met these criterias and were included the study (Figure 1) Characteristics of the videos were view count, number of likes, days online, video length, region, video image quality (480p resolution: low, 720p resolution: medium, 1080p resolution: high)
There are several reports assessing YouTube™ videos from patient’s perspective, rating their understandibility and patient educational value (14, 15) In this report, we tried to evaluate TURP videos on YouTube™ as tools for surgical education No guideline for assessing the educational value of TURP videos were present First author which is a junior staff urologist and the third author which is a senior staff urologist created a video quality checklist based on the checklist that was developed for the evaluation of laparoscopic surgery videos (16) The checklist included five major categories which were author’s information, case presentation, critical steps of the procedure, outcomes of the procedure, supplementary contents with a total of 20 items Each item represented one point (Table 1) First author and second author which was a junior res-

The checklist for the evaluation of TURP surgical videos' educational quality
Items of checklist
Author’s Information
1 Author’s information
2 Title of the video including the procedure
3 Conflict of interest disclosure
Case Presentation
4 Patient privacy protection
5 Patient characteristics
6 Preoperative work-up
7 Prostate volume
Critical steps of the procedure
8 Introduction of the equipments
9 Setting of cut and coagulation
10 Anatomic demonstration
11 Step by step explanation
12. Explanation of the critical steps
Outcomes of the procedure
13 Operating time
14 Volume of resected specimen
15. Length of hospitalization
16 Intraoperative and postoperative complications
17 Functional outcomes
Supplementary contents
18 Educational tables and photos
19 Audio commentary
20 Video commentary
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Y Karaca, E Burak Sahinler, D Ilke Karaca, O Sinanoglu 92
Table 1
Figure 1. PRISMA diagram showing the selection of the videos
ident evaluated the videos and scored each video from 1 to 20 Videos were divided into 4 educational quality groups according to their total score; low quality (0-5 points), medium quality (6-10 points), high quality (1116 points) and very high quality (16-20 points) With scoring videos separately by a staff surgeon and a resident we aimed to not only evaluate the educational quality of the videos but to determine if there is a difference between a resident’s and a surgeon ’ s evaluation
Statistical analysis
Statistical analysis was performed with IBM SPSS software (version 26 for MacOS, IBM Corporation, NY, USA) The characteristics of the videos were presented as mean, median, ranges, standard deviation (SD) The distribution of the variables was measured by Kolmogorov- Smirnov test Mann Whitney U test was used for the comparison of two reviewers mean points Pearson’s correlation coefficient was used to evaluate the correlations between variables P < 0 05 was considered statistically significant
RESULTS
Total of 104 videos were evaluated The mean view count was 15647 3 (range 21-324 522, SD 47556 4) Mean like count was 30 8 (range 0-285, SD 54 7) The median days avaliable online was 1856 5 (137-5943) (Table 2) Videos w e r e s o u r c e d f r o m A s i a ( 6 5 3 % ) , E u r o p e ( 1 5 3 % ) , Unknown region (14 4%), USA (2 8%) and Australia (1 9%) 73 (70 1%) videos were uploaded by private users, 15 (14 4%) videos by medical organizations and 16 (15 3%) videos by unknown users Video image quality was found as low for 60 (57 7%), medium for 25 (24%) and high for 19 (18 3%) videos No statistically significant difference was found between staff’s total points (mean 4 35 ± SD 2 9) and resident’s total points (mean 4 63 ± SD 3 3) for the evaluation of the videos (p: 0,761) (Table 3) No video received full points from the checklist Both staff urologist (79/104, 76%) and resident (78/104, 75%) rated most of the videos low educational quality Resident rated 8 (7 7%) videos high quality while staff urologist rated 5 (4 8%) Only one video rated very high quality and it was by the staff urologist
The correlation test showed positive correlation between view count and number of likes (r: 0 787 p < 0 01), staff’s total points (r: 0 242 p < 0 05), resident’s total points (r:0 340 p < 0 01) and days online (r: 0 477 p < 0 01) There was also positive correlation between number of likes and staff’s total points (r: 0 375 p < 0 01) and resident’s total points (r: 0 466 p < 0 01)
There was a positive correlation between staff’s total points and resident’s total points (r: 0 887 p < 0 01) Negative correalation was found between days online and video lenght (r: 0 207 p < 0 05) and staff’ total points (r: 0 195 p < 0 05) (Table 4)
DISCUSSION
In this study our purpose was to evaluate TURP videos on YouTube™ to estimate their educational value, define the pros and cons of the videos and try to set a standard for future high quality videos To our knowledge, this is the first report to review the quality of TURP videos on YouTube™
In this report we demostrated that most of the TURP videos on YouTube™ have low educational quality In the majority of videos; there was limited information regarding patient’s data Most videos consisted of edited or unedited footage of the surgery and did not include any explanation of the critical steps regarding the procedure Very few of the videos have mentioned outcomes of the procedure Additionally image quality were low in most videos These major defects resulted in videos that were not suitable for educational purpose
There are several studies in the literature assessing surgery videos on YouTube™ A study on videos about surgical treatment of LUTS/BPH indicated low quality content in the vast majority of the videos (17) Yang et al evaluated 70 ThuLEP videos on YouTube™ and concluded that there is lack of high educational valued videos on this topic (18) A review of 32 mid urethral sling videos on YouTube™ showed that none of the videos demonstrated the complete list of critical steps of the procedure (19) Loeb et al reported that overall information quality was moderate to poor in 67% of 150 bladder cancer videos on YouTube™ and moderate to high misinformation was present in 21% of the videos (20) Haslam et al assessed 23 robotic pyeloplasty videos on YouTube™ and found out that only 6 videos included all critical steps of the procedure (21) These studies along with our ’ s outlined that, although
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 93 Quality evaluation of TURP videos on YouTube™
Table 3 Comparison of staff’s and residents' mean points Staff Urologist’s points Resident’s points P-value Mean ± SD 4 35 ± 2 9 4 63 ± 3 3 0 761 Median (min-max) 3 (2-16) 3 (2-15)
Characteristics
videos Mean ± SD Median (min-max) View count (n) 15647 3 ± 47556 4 894 (21-324522) Video length (m) 864 ± 988 6 528 (77-6236) Like (n) 30 8 ± 54 7 7 (0-285) Days online (d) 1961.1 ± 1297.4 1856.5 (137-5943) Number (n); Minute (m); Days (d)
4
Table 2.
of the
Table
123456 1 View count 1 2 Video lenght 0 150 1 3 Like 0 787** 0 190 1 4 Point 1 0 242* -0 072 0 375** 1 5 Point 2 0 340** 0 004 0 466** 0 887** 1 6 Days online 0 477** -0 207* 0 086 -0 195* -0 134 1 * Correlation is s gnificant at the 0 05 leve (2-ta led) ** Correlation is significant at the 0 01 leve (2- tai ed)
Correlation analysis of between video features and scores
YouTube™ has a wide variety of medical videos, there are great heterogeneity in their quality Great care must be taken when using YouTube™ videos as a source of information, because most of the videos contain inaccurate and incomplete information about the procedures, which may prove to be harmful than educational, especially for inexperienced learners Videos from academic institutions tend to be more high quality than videos from single users (22) Sources with rigorous review processes like official websites of urological associations (i e American Urological Association, European Association of Urology) or video sections of certain urology journals may be used for more credible information
Our study has limitations Firstly, we evaluated videos on YouTube™ solely hence more websites should be included for more comprehensive view of the quality of TURP videos But since YouTube™ is the most popular source for surgical videos we believe these results have great value Secondly, the fact that one of the reviewer was a junior resident with little experience on TURP could have introduced bias into the study However no statistically significant difference was found between two reviewers evaluations thus this suggests that his inexperience did not have any effects on our findings and our findings are reliable Lastly we were obligated to create a checklist for evaluation of TURP videos because no other study has addressed this subject before More studies are needed to develop a standardizied and validated checklist
CONCLUSIONS
YouTube™ lacks high educational quality videos of transurethral resection of the prostate It is important to detect high quality videos and verify the information with multiple sources We believe that this study can guide future high educational quality videos
REFERENCES
1 Berry SJ, Coffey DS, Walsh PC, Ewing LL The development of human benign prostatic hyperplasia with age J Urol 1984; 132:474-9
2 Parsons JK Benign Prostatic Hyperplasia and Male Lower Urinary Tract Symptoms: Epidemiology and Risk Factors Curr Bladder Dysfunct Rep 2010; 5:212-218
3 McVary KT BPH: epidemiology and comorbidities Am J Manag Care 2006; 12(5 Suppl):S122-8
4 https://www baus org uk/ user files/pages/files/Museum/20%20%20TURP pdf
5 Malaeb BS, Yu X, McBean AM, Elliott SP National trends in surgical therapy for benign prostatic hyperplasia in the United States (2000-2008) Urology 2012; 79:1111-6
6 https://www britannica com/story/who-invented-the-internet
7 https://data worldbank org
8 Pugh CM, Watson A, Bell RH Jr, et al Surgical education in the internet era J Surg Res 2009; 156:177-82
9 Friedl R, Höppler H, Ecard K, et al Development and prospective evaluation of a multimedia teaching course on aortic valve replacement Thorac Cardiovasc Surg 2006; 54:1-9
10 Pape-Koehler C, Immenroth M, Sauerland S, et al Multimedia-
based training on Internet platforms improves surgical performance: a randomized controlled trial Surg Endosc 2013; 27:1737-47
11 https://www similarweb com/top-websites/
12 Rapp AK, Healy MG, Charlton ME, et al YouTube is the Most Frequently Used Educational Video Source for Surgical Preparation J Surg Educ 2016; 73:1072-1076
13 Mota P, Carvalho N, Carvalho-Dias E, et al Video-Based Surgical Learning: Improving Trainee Education and Preparation for Surgery J Surg Educ 2018; 75:828-835
14 Shoemaker SJ, Wolf MS, Brach C Development of the Patient Education Materials Assessment Tool (PEMAT): a new measure of understandability and actionability for print and audiovisual patient information Patient Educ Couns 2014; 96:395-403
15 Morra S, Napolitano L, Collà Ruvolo C, et al Could YouTube™ encourage men on prostate checks? A contemporary analysis Arch Ital Urol Androl 2022; 94:285-290
16 Celentano V, Smart N, McGrath J, et al LAP-VEGaS Practice Guidelines for Reporting of Educational Videos in Laparoscopic Surgery: A Joint Trainers and Trainees Consensus Statement Ann Surg 2018; 268:920-926
17 Betschart P, Pratsinis M, Müllhaupt G, et al Information on surgical treatment of benign prostatic hyperplasia on YouTube is highly biased and misleading BJU Int 2020; 125:595-601
18 Yang K, Meng Y, Zhang K Educational value of YouTube Surgical Videos of Thulium Laser Enucleation of The Prostate (ThuLEP): the quality assessment Transl Androl Urol 2021; 10:2848-2856
19 Larouche M, Geoffrion R, Lazare D, et al Mid-urethral slings on YouTube: quality information on the internet? Int Urogynecol J 2016; 27:903-8
20 Loeb S, Reines K, Abu-Salha Y, et al Quality of Bladder Cancer Information on YouTube Eur Urol 2021; 79:56-59
21 Haslam RE, Seideman CA Educational Value of YouTube Surgical Videos of Pediatric Robot-Assisted Laparoscopic Pyeloplasty: A Qualitative Assessment J Endourol 2020; 34:1129-1133
22 Sahin Y, Paslanmaz F, Ulus I, et al Quality and content analysis
o f f e m a l e u re t h ro p l a s t y v i d e o s o n Yo u Tu b e L o w U r i n Tr a c t Symptoms 2023; 15:24-30
Correspondence
Yavuz Karaca, MD mdyavuzkaraca@gmail com
Emre Burak Sahinler, MD emre sahinler@yahoo com
Orhun Sinanoglu, MD orhundr@hotmail com
Department of Urology, Sancaktepe Sehit Prof Dr Ilhan Varank Research and Training Hospital, Istanbul, Turkey
Didar Ilke Karaca, MD karacailke@yahoo com
Department of Public Health, Marmara University School of Medicine, Istanbul, Turkey
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Y
E
94
Karaca,
Burak Sahinler, D Ilke Karaca, O Sinanoglu
with non-muscle invasive bladder cancer
Summary
Objective: To evaluate the utility of infantile BCG vaccination history in predicting stage and grade of tumours in non-muscle invasive bladder cancer (NMIBC)
Materials and methods: We retrospectively analyzed data from patients from a single center who were diagnosed with new NMIBC and underwent transurethral resection of bladder tumour (TURBT) between 2017 and 2022 We assessed BCG immunization status with various demographics and comorbidities, as well as tumour recurrence, progression, stage, and grade
Results: A total of 188 patients met the inclusion criteria for our study The mean age of patients at the time of diagnosis was significantly lower in those that had been immunized with BCG (71 ± 9) than those who had not (77 ± 10) (p < 0 0001) History of BCG immunization did not correlate with sex, history of diabetes mellitus (DM), prior history of intravesical BCG treatment, and tumour recurrence, progression, stage, and grade.
Conclusions: History of infantile BCG vaccination did not correlate with the depth of invasion and/or the grade in patients with non-muscle invasive bladder cancer Patients that received infantile BCG vaccination were significantly younger at the time of diagnosis of NMIBC
KEY WORDS: BCG; Non-muscle invasive bladder cancer (NMIBT); Bladder cancer
Submitted 11 April 2023; Accepted 26 May 2023
INTRODUCTION
Bladder cancer is the tenth most common malignancy worldwide, with increasing incidence, particularly in developed nations (1) Approximately 80% of bladder cancers arise in individuals aged 65 or older with the mean age being 73 years old (2, 3) This is thought to reflect a disease process requiring many decades of development following exposure to risk factors, such as tobacco (2) Urothelial carcinoma (UC) accounts for 90% of bladder cancers (4) At the time of presentation, approximately 70% of UC cases are non-muscle invasive (NMIBC), while 30% are muscle invasive (MIBC) (4) Initial management of NMIBC is transurethral resection of bladder tumor (TURBT) (4) For those with NMIBC who are deemed to be at high risk for
progression, intravesical Bacillus Calmette-Guérin (BCG) is the gold standard adjuvant therapy (4)
The use of intravesical instillation of BCG for high risk NMIBC demonstrates a role for immunotherapy in UC BCG, originally used as a vaccine against tuberculosis (TB), contains live-attenuated Mycobacterium bovis (4)
The specific mechanism of BCG in NMIBC treatment continues to be studied, however, its role is attributed to both local immunological efforts and systemic immune responses (5) Some work has suggested that BCG vaccination may be associated with a lower rate of bladder cancer incidence (6) Despite this relationship, research on BCG immunization as a possible predictive factor in NMIBC has been limited In the present study, we evaluated the relationship between history of infantile BCG vaccination with the depth of invasion and the grade in patients with NMIBC
METHODS
Data were retrospectively collected between 2017 and 2022 Inclusion criteria included all patients with a new diagnosis of NMIBC at the Thunder Bay Regional Health Sciences Centre (TBRHSC), for whom complete clinical, lab, and pathological data could be retrieved Data collected included the history of infantile BCG as well as the patients’ age, sex, comorbid status, CBC, vaccination, history of intravesical BCG instillation, pathological data, recurrence, and progression Vaccination status was correlated with these variables Institutional ethical approval was obtained from the TBRHSC research ethics board (RP741) Correlations between continuous variables were done using Student’s t-test Categorical variables were compared using Fisher Exact test A p-value of < 0 05 was used to define significance
RESULTS
A total of 188 patients met the inclusion criteria for our study No patients were lost to follow up The mean follow-up time was 26 ± 7 months Of the 188 individuals meeting the eligibility criteria, 113 individuals had received the infantile BCG immunization and 75 did not
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 95
ORIGINAL PAPER
History of infantile BCG immunization did not predict lamina propria invasion and/or high-grade in patients
Anastasia MacDonald 1 , Vahid Mehrnoush 1 , Asmaa Ismail 1 , Livio Di Matteo 2 , Ahmed Zakaria 1 , Waleed Shabana 1 , Ashraf Shaban 1 , Mohammed Bassuony 1 , Hazem Elmansy 1 , Walid Shahrour 1 , Owen Prowse 1 , Ahmed Kotb 1
DOI: 10 4081/aiua 2023 11380
1 Northern Ontario School of Medicine, Thunder Bay, ON, Canada; 2 Department of Economics, Lakehead University, Thunder Bay, ON, Canada
A s t a t i s t i c a l l y s i g n i f i c a n t d i ff e re n c e w a s i d e n t i f i e d between the age of individuals who had received the immunization and those who did not (p < 0 0001) The mean age at the time of diagnosis for those immunized was 71 ± 9 years, and 77 ± 10 in the non-immunized group There was no statistically significant difference found between immunization status and other patient characteristics including sex, history of diabetes mellitus (DM), or history of intravesical BCG treatment History of immunization did not correspond with tumour recurrence, progression, stage, or grade in this population
The results are summarized in Table 1
strated that BCG immunotherapy in NMIBC patients induced TI and provided protection against respiratory infections (9) This suggests that intravesical BCG therapy can produce similar systemic immune responses as the BCG vaccination Given that our data demonstrated that immunization status did not impact the tumour progression characteristics and risk stratification, this may suggest increased importance in the role of the local immune response in intravesical BCG in preventing the progression of NMIBC
Our findings may also be explained by the waning protection from immunization over time While bladder cancer incidence increases in the elderly (10), individuals immunized with BCG are typically immunized as infants It has been well documented that protection from this immunization against TB infections wanes over time (7) Studies have identified that a positive purified protein derivative (PPD) skin test, an indication of BCG immunity, was associated with a better response to intravesical BCG therapy than those with a negative reaction (11, 12) Niwa et al (2017) demonstrated that the recurrence-free survival (RFS) in patients with a slightly positive or negative PPD skin test reaction was significantly diminished compared to the RFS in those with a strongly positive response This may suggest that a reduced immune response from BCG immunization does not generate the same benefit in BCG treatment Given that the mean age of those vaccinated with BCG in our study was 71 years, and our study specifically looked at infantile BCG immunization, this may also explain why individuals with waning immunity from remote immunization did not influence tumour characteristics or risk stratification in patients with NMIBC
DISCUSSION
Studies assessing the relationship between NMIBC and BCG immunization have been limited One scoping literature review identified a 35-37% lower age-standardized rate of bladder cancer incidence in individuals with BCG immunizations, suggesting an association between the two (6)
We demonstrated that BCG immunization did not correlate with tumour characteristics in NMIBC, including stage, grade, and risk stratification This may be explained by the routes of administration and subsequent immune responses elicited The anti-tumour activity of intravesical BCG therapy is attributed to non-specific immune mechanisms related to the direct interaction with urothelial cells, as well as a contribution of systemic immune response, though specific mechanisms have yet to be fully elucidated (7) BCG immunization is also associated with non-specific immune mechanisms that provide protection against tuberculosis, however, given the nature of vaccinations, this response is exclusively systemic (8) Interestingly, this generalized immune response from immunization has been shown to confer protection against other respiratory infections through a mechanism referred to as trained immunity (TI) (8, 9) It was demon-
In our study, the mean age of patients diagnosed with new N M I B C w a s s i g n i f i c a n t l y l o w e r i n i n d i v i d u a l s w h o received the infantile BCG vaccination (71 ± 9) compared to those who did not (77 ± 10) (p < 0 0001) Increased age is a risk factor for developing UC, largely attributed to a disease course that develops decades after exposure to risk factors (2) Countries with the lowest incidence of bladder cancer are typically those found to be below average on the human development index (HDI), which may be attributable to less industrial chemical exposure and access to tobacco, major risk factors for UC (1)
Interestingly, such countries tend to have a higher incidence of tuberculosis and subsequently higher rates of infantile BCG immunization (13) This may imply that non-immunized individuals were likely raised in countries with low TB incidence, yet above-average HDI Such individuals would likely have had a higher risk of exposure to industrial chemicals and tobacco, leading to the slow development of bladder cancer and presentation at a later age Those immunized and likely raised in countries with less exposure to common risk factors may have developed UC earlier on due to other reasons, such as genetics, diets, or other lifestyle factors
Older age at presentation has been shown to be a poor prognostic factor in NMIBC (4) Consequently, the older age of presentation with NMIBC in non-immunized individuals poses a significant healthcare concer n The incidence of bladder cancer has been steadily increasing, particularly in developed countries (1) Such countries do not tend to implement routine immunization against TB
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 A MacDonald, V Mehrnoush, A Ismail, et al 96
Table 1
No infantile BCG Infantile BCG P value Age (mean + SD) 77 + 10 71 + 9 0 0001 Sex Males 60 77 0 09 Females 15 36 Recurrence No 34 57 0 5 Yes 41 56 Progression No 72 108 1 Yes 35 Intravesical BCG No 44 68 0 9 Yes 31 45 DM No 61 86 0 5 Yes 14 27 Stage Ta 58 86 1 T1 17 27 Grade Low 54 81 1 High 21 32 SD: standard deviation BCG: Baci lus Calmette–Guér n DM: Diabetes Mell tus
Correlation of clinical and tumour data with history of infantile BCG immunization.
given the low incidence Consequently, there is a growing population of non-immunized individuals presenting with NMIBC and potentially at older ages This may result in overall more complicated patients with poorer prognostics Further research in this area would be of utility given the growing aging population and potentially increased demands on healthcare systems
There are several limitations to our study First, it is a retrospective study completed at a single center Therefore, selection bias was inevitable, and our study represents a relatively small sample size of patients This study also limited by the relatively short follow up period (26 + 7 months) for assessing recurrence and progression Additionally, we did not account for the various demographic factors that may influence the risk factors for developing NMIBC
CONCLUSIONS
Infantile BCG immunization was not associated with higher risk stratification in patients with NMIBT The mean age of patients diagnosed with NMIBC was significantly lower in patients who received the infantile BCG vaccination
REFERENCES
1 Bray F, Ferlay J, Soerjomataram I, et al Global cancer statistics 2018: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries CA Cancer J Clin 2018; 68:394
2 Mushtaq J, Thurairaja R, Nair, R Bladder cancer Surgery (Oxf) 2019; 37:529
3 Siegel RL, Miller KD, Jemal A Cancer statistics, 2019 CA Cancer J Clin 2019; 69:7
4 Saginala K, Barsouk A, Aluru JS, et al Epidemiology of Bladder Cancer Med Sci 2020; 8:15
5 Taniguchi K, Koga S, Nishikido M, et al Systemic immune response after intravesical instillation of Bacille Calmette-Guérin (BCG) for superficial bladder cancer Clin Exp Immunol 1999; 115:131
6 Trigo S, Gonzalez K, Di Matteo L, et al Bacillus Calmette-Guerin vaccine and bladder cancer incidence: Scoping literature review and preliminary analysis Arch Ital Urol 2021; 93:1
7 Mukherjee N, Julián E, Torrelles JB, Svatek RS Effects of Mycobacterium bovis Calmette et Guérin (BCG) in oncotherapy: Bladder cancer and beyond Vaccine 2021; 39:7332
8 Covián C, Fernández-Fierro A, Retamal-Díaz A, et al BCGInduced Cross-Protection and Development of Trained Immunity: Implication for Vaccine Design Front Immunol 2019; 10:2806
9 van Puffelen J H, Novakovic B, van Emst L, et al Intravesical BCG in patients with non-muscle invasive bladder cancer induces trained immunity and decreases respiratory infections J Immunother Cancer 2023; 11:e005518
10 Martinez L, Cords O, Liu Q, et al Infant BCG vaccination and risk of pulmonary and extrapulmonary tuberculosis throughout the life course: a systematic review and individual participant data metaanalysis Lancet Glob Health 2022: 10:e1307
11 Niwa N, Kikuchi E, Matsumoto K, et al Purified protein derivative skin test reactions are associated with clinical outcomes of
patients with nonmuscle invasive bladder cancer treated with induction bacillus Calmette-Guérin therapy Urol Oncol 2018; 36e15
12 Biot C, Rentsch CA, Gsponer JR, et al Preexisting BCG-specific T cells improve intravesical immunotherapy for bladder cancer Sci Transl Med 2012; 4:72
13 Centers for Disease Control and Prevention BCG Vaccine Fact Sheet 2016 Retrieved from https://www cdc gov/tb/publications/ factsheets/prevention/bcg htm
Correspondence
Anastasia MacDonald, MD anamacdonald@nosm ca
Vahid Mehrnoush, MD vahidmehrnoush7@gmail com
Asmaa Ismail, MD asmaaismail0782@gmail com
Ahmed Zakaria, MD aszakaria81@yahoo com
Waleed Shabana, MD waleed shabana@gmail com
Ashraf Shaban, MD ashraf shaban@tbh net
Mohammed Bassuony, MD mohammed bassuony@tbh net
Hazem Elmansy, MD hazem elmansy@tbh net
Walid Shahrour, MD walid shahrour@tbh net
Owen Prowse, MD owen prowse@tbh net
Ahmed Kotb, MD, PhD, FRCSC, FRCS Urol, FEBU (Corresponding Author)
Associate Professor drahmedfali@gmail com
Northern Ontario School of Medicine (NOSM) and Thunder Bay Regional Health Research Institute (TBRHRI)
Thunder Bay, ON, Canada
Livio Di Matteo, MD ldimatte@lakeheadu ca
Department of Economics, Lakehead University, Thunder Bay, ON
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 97
Infantile BCG vaccination in patients with NMIBC
Psychological and sexual problems of cancer survivors
Ida Ayu Made Ari Santi Tisnasari 1 , Tuti Nuraini 2 , Yati Afiyanti 3 , Rudi Rudi 4 , Riri Maria 5
1 Faculty of Nursing, Universitas Indonesia, Depok, Indonesia;
2 Department of Basic Science and Fundamental Nursing, Faculty of Nursing Universitas Indonesia, Depok, Indonesia;
3 Department of Maternity Nursing, Faculty of Nursing Universitas Indonesia, Depok, Indonesia
4 Master of Nursing Program, Faculty of Nursing Universitas Indonesia, Depok, Indonesia;
5 Department of Medical Surgical Nursing, Faculty of Nursing Universitas Indonesia, Depok, Indonesia
Presented as conference papers at the 8th V-BINC at FON Universitas Indonesia
Summary
Objective: To explore: 1) the unmet needs of breast cancer patients; 2) the sexual needs experienced by breast cancer survivors; 3) the experiences of cancer patients at the time of relapse, including the biopsychosocial-spiritual aspects of their experiences
Materials and Methods: Interpretative phenomenological qualitative research by conducting direct in-depth interviews with participants who met the inclusion criteria.
Sample analyzed were breast cancer survivors who had experiences related to unmet needs (14 participants) or sexual problems (12 participants); adult cancer patients who experienced recurrences (10 participants).
Results: Themes identified for breast cancer patients with unmet needs were i) overcoming health problems in breast cancer survivors; ii) need to access the best health services; iii) women’s unmet information needs concerning cancer treatment. For breast cancer survivors: i) information is needed to overcome sexual problems, ii) family support is needed to get sexual information, and iii) health care facilities need to provide sexual information. For patients experiencing recurrences: i) the reaction that occurs when receiving bad news; ii) efforts made during a relapse, iii) self-concept during a relapse
Conclusions: Health-related problems of breast cancer survivors, such as fatigue and fear of cancer recurrence, can lead them to have trouble with social relationships, question their spirituality, and struggle with sex and sexuality Oncology nurses and other professionals need to be aware of the unmet needs of breast cancer survivors, especially in relation to resolving the sexuality issues of cancer survivors Understanding of the experiences of patients with relapse of different types of cancer should be improved.
KEY WORDS: Cancer patients; Cancer recurrence; Cancer therapy; Relapse; Resilience; Breast cancer; Unmet needs; Sexuality; Survivors
Submitted 10 March 2023; Accepted 18 March 2023
BREAST CANCER SURVIVORS' UNMET NEEDS FOLLOWING CHEMOTHERAPY *
(Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti)
Introduction
Breast cancer is the most common malignancy in women worldwide, accounting for almost one in four cancer
cases The number of breast cancer sufferers increases annually (1), and there were an estimated 2 261 419 new cases worldwide in 2020 (2) In Indonesia, there is a high incidence of breast cancer in Bali Province Based on data reported by Hospital in Denpasar about patient visits for breast cancer ts from August to November 2020, out of a total of 1380 patient visits, 285 were cancer patients Breast cancer greatly affects a woman's life, and a recent study noted the importance of carrying out follow-up health checks, addressing post-treatment concerns, and improving the wellbeing and quality of life of cancer survivors (3) A high level of unmet needs in cancer survivors is associated with a poor quality of life This condition can be attributed to the low attendance to care, which is rarely accepted by cancer survivors in Indonesia To remedy the situation, healthcare professionals, especially nurses, should be trained to identify various problems and unmet needs experienced by breast cancer survivors so they can provide holistic nursing care (medical, psychological, social, spiritual, and cultural) for cancer survivors (4) Another study suggested that of all cancer care today, breast cancer patients represent the largest patient group with high supportive care needs (5) Accordingly, it is important to strive to better understanding breast cancer survivors’ unmet needs, which should be explored in-depth To do so, we must explore the experiences of breast cancer survivors, especially the Balinese breast cancer survivors
Materials and methods
The research design used in this study was an interpretative phenomenological qualitative research design to examine the unmet needs of breast cancer survivors following cancer therapy Participants in this study were selected using a purposive sampling method The sample in this study were breast cancer survivors who had experiences related to unmet needs according to inclusion criteria set by the researcher The inclusion criteria in this study were: i) female breast cancer survivors from various age groups, both young adults and elderly adults; ii) breast cancer survivors who wish to discuss unmet needs The number of subjects included in this qualitative descriptive study was of 14 participants Data was collected through in-depth interviews with all participants
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 98 ORIGINAL PAPER
DOI: 10 4081/aiua 2023 11473
This research was conducted in March-June 2022 The study was conducted at the Hospital in Bali Province, Indonesia This study used the researcher himself as the research instrument The researcher collected the data by himself without a research assistant or co-researcher The data analysis process in this study was carried out based o n t h e r e s e a r c h p r o t o c o l , r e g a r d i n g t h e t h e m a t i c approach to analysis, namely identifying, analyzing, and reporting patterns (themes) of the data (6)
Results
Theme 1: overcoming health problems in breast cancer survivors
Theme 2: need to access the best health services
Theme 3: unmet information needs about cancer treatment (Details are available in Supplementary Materials)
Discussion
Several themes were obtained from the data analysis The three main themes were: i) overcoming health problems in breast cancer survivors; ii) need to access the best health services; iii) unmet information needs about cancer treatment
Each of those themes were below discussed in more detail in comparison of the existing literature
Overcoming health problems in breast cancer survivors
The first theme that emerged through this work was the challenge that women must face as a result of the health problems they experience as breast cancer survivors Such challenges can be physical, psychological, social, spiritual, and sexual
Physical problems reported included memory loss and stiff joints, although the most common physical problem reported by participants was fatigue Breast cancer survivors reported a lower quality of life than other women even years after completing their treatment due to experiencing disturbing and long-lasting side effects, including cancer-related fatigue, which can affect breast cancer survivors for many years after their treatment is completed (5) Another physical challenge experienced by the participants was memory loss There are various research results on how memory decline or cognitive impairment can occur in breast cancer survivors A study reported that memory loss in breast cancer survivors can be more severe in patients undergoing chemotherapy as a side effect of treatment (6) Another study similarly concluded that memory decline in breast cancer survivors could occur for years with significantly impact on the quality of life (7) Memory loss due to side effects of cancer treatment is known generally as “chemo fog” or “chemo brain” or in medical terms as cancer-related cognitive impairment It can be exacerbated by hormonal treatment, commonly taken after breast cancer therapy (8) It is recommended that nurses are trained to provide interventions to overcome memory loss problems, such as teaching mindfulness-based stress-reduction exercises (9) A further physical challenge experienced by participants was stiffness in their hands According to research among breast cancer survivors in Africa, stiffness in the hands is widely experienced, along with pain (10) Another study described side effects caused by cancer treatment includ-
ing problems in the hands and shoulders and muscle strength in breast cancer survivors (11) These effects can reduce the quality of life of survivors by creating barriers to carrying out daily activities, such as dressing, combing their hair, working, shopping, exercising, etc
Accordingly, nurses should provide interventions to help women reduce the stiffness in their hands, such as by teaching them arm and shoulder muscle exercises (12)
A further physical health-related challenge breast cancer survivors often face is changes in their appearance, such as weight loss According to research, cancer therapy causes weight fluctuations, as well as changes in skin and nail color (13) Breast cancer survivors often feel embarrassed, lose their confidence, and have body image problems due to their changed appearance To provide support, various nursing interventions may be directed toward increasing the confidence of women with breast cancer and survivors to breast cancer, such as running beauty care activities, holding discussions with cancer survivors, or offering cognitive behavioral therapy to women with body image problems (12)
Another challenge experienced by breast cancer survivors after chemotherapy was psychological, largely constituted by fear of recurrence The fear was greatest when the participants felt unwell, when going to the hospital for restaging, or when they heard of others with a diagnosis or metastasis (14) They explained that after receiving cancer treatment, the transition to the life of a breast cancer survivor brings a series of challenges, the most important being the worry that remission will not last and they will one day need to resume treatment This worry causes w o m e n
Commonly, after chemotherapy, breast cancer survivors also experience social challenges due to their increased sensitivity, which prompts them to limit how much they socialize The participants in this study stated that they assumed other people did not fully understand the situation they were facing, which implies that they were now quickly irritated and easily angered because of the chemotherapeutic drugs they had taken This, of course, affected the participants’ relationships with the people around them They notably socialize less than they had in the past and had feelings of being unproductive Such an outcome is in accordance with the results of other research that showed that the treatment of subjects with cancer also impacts on the people closest to them (14) All participants in this study also faced spiritual challenges, such as questioning their faith or wanting to end their life because they felt alone, despairing, like they had failed to achieve their life goals, or overcome family problems Other participants stated they were disappointed with the hand they had been dealt or felt as if all they ever got out of life were problems This was different from the research finding who suggested that individuals tend to turn to spirituality to overcome cancer (15) Greater overall spirituality was associated with fewer depressive symptoms and a better quality of life in individuals living with cancer or other illnesses The researchers noted that for Latinx breast cancer survivors, in particular, religion and spirituality are essential for overcoming cancer Although a cancer diagnosis increases feelings of vulnerability in Latinx breast cancer survivors, the cancer event strengthens their spirituality
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti, Rudi Rudi, Riri Maria 99
e s s a n d a f f e c t s t h e i r q u a l i t y o f l i f e
t o s t r
Spirituality is a helpful source of coping for Latinx cancer patients during both the treatment phase and the ensuing long-term survivor phase
The benefits of spirituality include a feeling of satisfaction, a sense of peace or harmony with life, and the comfort of feeling accompanied by a spiritual presence The different findings in this study may have resulted due to factors that affected the participants’ spirituality, for instance, economic factors or life events that caused the participants to fall into despair and feel disappointed with this turn in their lives To prevent that from happening, nurses should lead spiritual-based interventions such as preparing a spiritual care program that is tailored to a patient’s beliefs, supporting their spiritual well-being both as a patient and later as a breast cancer survivor (16)
Some of the participants in this study also faced challenges around sex and their sexuality, namely relationship problems with their husbands in married breast cancer survivors, or self-acceptance problems with potential sexual partners for unmarried breast cancer survivors (17) Cancer treatment can cause reduced vaginal lubrication, impaired sexual desire and arousal, pain during sexual activity, and the stigmatization of a woman as "cancer contagious" Such effects are hugely significant and detrimental to a women ’ s sense of fulfillment since sex and sexuality are basic elements of human life, regardless of whether or not someone has a long-term sexual partner
The need to access the best health services
The second key theme that emerged from this research was a need to access the best health services, with accu-
Participants explained the importance of having a PET scanner and bone-scanning equipment available at the nearest hospital so that cancer survivors who wish to use these facilities do not need to travel outside the area to obtain accurate staging results Such tools are valuable for preventing errors when detecting cancer metastases in breast cancer survivors according to research showing that bone-scanning tools are very useful for detecting the incidence of bone metastases at an early stage (18) An article previously highlighted the importance of the introduction of accurate cancer-detection tools in regional hospitals so that survivors do not have to travel far for examinations, especially those concerning the incidence of metastases, and we support that request (19) In addition, we must note the importance of nurses adopting a caring attitude for patients and cancer survivors Care for each survivor must be specific, based on their history of treatment Survivorship services are usually offered in Indonesia to every patient who completes cancer treatment seeing as each therapy has short- and long-term impacts that affect the quality of life of cancer survivors (20) To improve the current offering, nurses must be trained to help cancer survivors overcome health-related challenges such as fatigue, cognitive disorders, depression, and issues around sex Oncology nurses should understand the stages of breast cancer care so they can better understand survivors and adopt a caring attitude to meet the needs of breast cancer survivors
Unmet information needs about cancer treatment
A final theme identified in this study was the participants’
unmet needs regarding cancer care information, such as information on the treatment stages, how to cope with the side effects of the therapy, the latest treatment information, and signposting to information technology resources to accompany their cancer care In the research conducted among breast cancer survivors in South Korea, their greatest unmet need was in the domain of information, comprising a need for information about examinations and treatment, symptoms that need to be referred to the hospital, and how to see a doctor quickly and easily when needed (21) Paired with the results of this study, these findings should provide valuable resources for those developing new interventions in the nursing field It is vital that health information technology is made soon applied to make it easier for breast cancer survivors to obtain the information they need regarding their cancer care
Conclusions
The research results from this qualitative study exploring health problems and unmet needs in breast cancer survivors after chemotherapy lead us to highlight three key takeaways: i) breast cancer survivors must overcome various challenges associated with health problems; ii) they are highly motivated to access the best health services; iii) these survivors have unmet information needs about cancer treatment A key consideration is how survivors’ health-related challenges, such as fatigue, fear of cancer recurrence, issues with social and romantic relationships, and spiritual distress, can create barriers to these women attending appointments for restaging To increase their life expectancy and the survival rate after cancer treatment in Indonesia, oncology nurses and other healthcare professionals must strive to understand better the challenges breath cancer survivors face, and accordingly, adapt their nursing practice to meet survivors’ needs better
SPECIAL INFORMATION TO DISCUSS SEXUALITY
PROBLEMS: A BALINESE BREAST CANCER SURVIVOR'S UNMET NEED **
(Ida Ayu Made Ari Santi, Yati Afiyanti, Tuti Nuraini)
Introduction
Breast cancer is the most common malignancy in women worldwide, accounting for almost one in four cases of cancer The number of breast cancer sufferers is increasing every year (1) It was estimated that in 2020, there were
2 261 419 new cases of breast cancer worldwide (22)
In Indonesia, Bali is one of the provinces with the highest incidence of breast cancer Based on data from Sanglah Hospital Denpasar, of a total of 1 380 patient visits to Sanglah Hospital between August and November 2020, 285 visits were made by cancer patients
The experience of breast cancer greatly affects a woman's life Recent studies confirm the importance of carrying out regular health checks, addressing post-treatment concerns, and improving the well-being and quality of life (QoL) of cancer survivors (3)
The development of technology and public awareness of the importance of early detection of breast cancer has led to an increase in the survival rate of breast cancer patients (23) An increased survival rate should be accompanied by
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 100 Problems of cancer survivors
r a t e c a n c e r - d e t e c t i o n t o o l s a n d f r i e n d l y n u r s e s
an increased QoL However, in many breast cancer survivors, sexual problems affect their QoL Sexual health concerns have been reported in 50% of cancer survivors, and the situation, if not addressed, is likely to worsen (24) Sexual issues can be complex Problems that are often reported include pain during intercourse, difficulty achieving orgasm, and psychological struggles, such as impaired body image, accompanied by reduced feelings of femininity and sexual attractiveness, which cause the partner to be less interested Feelings of femininity and attractiveness generally improved only after 10 months to three years after surgery Sexual attractiveness and feeling comfortable during sexual intimacy are major problems in the first one to two years after breast surgery (23) In Indonesian society, which includes that of Bali, a woman ’ s sexuality is not considered a basic need when she is first diagnosed with breast cancer The situation can cause her husband (or life partner) to look for other ways to fulfill his sexual needs This can lead to complex problems if not resolved, and a better solution needs to be discussed from the beginning Balinese women want to display perfect breasts as they symbolize their beauty and sexual attractiveness When they develop breast cancer, many problems follow, especially for their spouses Balinese women are required to perform many tasks, including satisfying their spouses sexually However, there are many things a woman cannot do when she has had breast cancer Information about sexual needs is still a taboo topic, even though these needs are very present to Balinese women In this study, the problem of sexual needs is explored, especially the information needed by cancer survivors to enable them to overcome their sexual issues
Materials and methods
Research design
The design used in this study was interpretative phenomenological qualitative research, designed to explore the sexual needs of breast cancer survivors following their cancer therapy
Sample and sampling
The participants in this study were selected using the purposive sampling method The sample was composed by breast cancer survivors who had experienced sexual needs The inclusion criteria were: i) female breast cancer survivors of various ages; ii) breast cancer survivors who finished their primary treatment The sample for this qualitative descriptive study comprised 12 participants
Data collection
Data were collected through in-depth interviews This research was conducted between March and August 2022 The study was conducted at the oncology polyclinic of Sanglah Hospital Denpasar The researcher collected the data by interviewing all the participants without any research assistant, so that, in this study, the researcher was the research instrument
Data analysis
The data analysis process in this study was based on Braun and Clarke’s (2006) description of the thematic analysis
approach, which involves identifying, analyzing, and reporting patterns (themes) of the data In the first phase the researcher begins to record or transcribe data in written form Then, the researcher read the results of the transcript repeatedly to find out and record emerging ideas for the next coding process The second phase is to generate the initial coding The third phase is developing a theme: in this phase, all the collected and coded research data are analyzed into a larger theme The fourth phase is reviewing the requested theme: in this phase, several themes can be grouped together if they are too different The fifth phase is defining and naming the theme: here, the researcher determines the essence of each generated theme and then refines the resulting theme for analysis
The sixth phase is reporting: this phase begins when the researcher has fully defined and analyzed a theme and writes a report on the research results obtained (6)
Rigor
The validity of the data in this study included the aspects of credibility, transferability, and confirmability The researcher confirmed and clarified various items that have been expressed by participants The researcher also observed participants during the interview process The researcher confirmed data by reflecting on research results in comparison with related papers, consulting expert researchers, and confirming information with participants The researcher also presented the results of the verbatim transcript in the research report so that the reader could assess the accuracy of the way the researcher transferred the research results to the readers and other researchers
Ethical principles
This study had the potential to cause psychological disc o m f o r t o r p s y c h o l o g i c a l f a t i g u e i n p a r t i c i p a n t s Therefore, the researcher applied the principles of beneficence, respect for human dignity, and confidentiality
This meant that the identity of the participants was not included, or only the initial code on the informed consent form was included This research design was approved by the ethics committee of Sanglah Hospital Denpasar
Results
1 Information is needed to overcome sexual problems
2 Family support is needed to get information on sexuality
3 Healthcare facilities need to provide sexual information (Details are available in Supplementary Materials)
Discussion
Sexuality is a normal part of life Therefore, as there has been a substantial increase in the number of breast cancer survivors, it is critical to address their QoL after treatment (23) The survival rate for women with breast cancer is increasing Treatment regimens are accompanied by a range of physical, psychological, existential, and social concerns (23) Balinese breast cancer survivors have different issues from others in relation to meeting sexual needs since they have a distinctive culture Nevertheless, the fulfillment of their sexual needs remains an important part of their lives
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti, Rudi Rudi, Riri Maria 101
Based on the results of the data analysis, three main themes emerged: i) the need for information to overcome sexual problems and meet the partner’s sexual needs; ii) the need for support from the extended family to meet the need for information about sexuality; iii) the need for health care practitioners to provide information on sexuality
Information needed to overcome sexual problems
Informant 1 explained her need for information on sexuality The informants discussed the problems experienced in fulfilling their own and their husband’s sexual needs, such as pain during intercourse The informants were told that there is a gel that can help reduce pain during intercourse Interventions using technology to increase relational intimacy and a sexual enhancement intervention for couples experiencing sexual difficulties following breast cancer have been shown to be acceptable, with a high level of satisfaction (25)
Informant 2 explained that she didn't care that her husband was cheating on her because she was more focused on her own health treatment However, she was still annoyed with her husband and demanded him to end the affair and stay away from her She was successful in her demands because her caste level in Bali was higher than her husband's Informant 2 felt that her partner was no longer interested in her She no longer wanted to serve her partner This would have a complex impact on the integrity of the family This couple needed counseling and information about their sexuality so that their QoL problems would not become even more complex The husbands of women with breast cancer need support to improve their sexual and marital relationships Education and counseling about sexual activity during treatment for breast cancer should be incorporated into healthcare programs (26)
Family support is needed to get information on sexuality
Balinese women lack support and advice from their families in relation to their sexual needs Therefore, healthcare providers play an essential role These women do not have the support they need They believe that sexuality is a shameful issue, and they are reluctant to ask questions about it Healthcare professionals need to talk about the possibility of sexual problems arising due to the changes in women ’ s bodies caused by cancer and its treatments These women need to be encouraged to talk about these problems, with due consideration for their religious and cultural positions (27)
Healthcare facilities need to provide sexual information
Informants 3 and 11 stated that they were ashamed to discuss their sexual needs Indonesian society considers it taboo to discuss sexuality, even though it is a normal basic need that must be met The attitudes of healthcare providers and survivors concerning what constitutes helpful and unhelpful communication behaviors when discussing sexual health concerns were misaligned in nuanced and significant ways (24) Providers should make an effort to find ways to communicate effectively with survivors Informant 4 felt that the nurses and healthcare workers did not care about whether the sexual needs of survivors were met Therefore, health workers
need sufficient information to help survivors Zhang et al explained that there is a significant gap between the providers’ perceptions and the patients’ needs regarding discussions on sexual health More effort should be made to promote the communication needed regarding sexual health (28) A study showed that there is a need for healthcare providers to discuss sexual health after breast cancer with all their patients, as it is a concern that both single and partnered breast cancer survivors have to face after treatment (29)
Research implications and limitations
Breast cancer survivors have unmet needs for information, including information about their sexual needs Cancer nursing services should be equipped to provide this information The results of this study can provide an overview for nurses and other healthcare workers regarding the unmet needs of breast cancer survivors, especially the information needed about sexuality This would enable nurses and other healthcare professionals to improve the quality of the healthcare services they provide by offering supportive care services that are in alignment with the needs of breast cancer survivors, thereby achieving a more holistic quality of service In addition, the findings of this study raise the hope that there will be consultation on the problems experienced by cancer patients and survivors, which will trigger awareness of the importance of specialist oncology nurses being present in cancer care structures Furthermore, it is recommended that more comprehensive nursing care should be provided by healthcare providers to assist cancer survivors in meeting their needs This would result in an increased life expectancy or survival rate for cancer surv i v o r s i n I n d o n e s i a R e c o m m e n d a t i o n s f o r f u r t h e r research are that the unmet needs of cancer survivor couples be investigated so that new concepts relating to supportive care can emerge
The researcher realized that there were limitations and shortcomings in this study, namely that the participants felt embarrassed to express complaints relating to the services they received at the hospital
Conclusions
Sexuality is still a basic need of breast cancer survivors Inaccurate information or poor communication can affect the fulfillment of survivors’ sexual needs, which will have a negative impact on their QoL Therefore, oncology nurses and other professionals need to understand the problems of breast cancer survivors, especially those in Bali, so that they can enable them to fulfill their sexual needs
LIFE EXPERIENCES OF INDONESIAN CANCER PATIENTS WITH CANCER RECURRENCES: INTERPRETATIVE PHENOMENOLOGY ***
(Rudi Rudi, Yati Afiyanti, Riri Maria)
Introduction
A patient is considered to have had a cancer recurrence when the same type of cancer cells as when first diagnosed are found either in the same or a different place
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 102 Problems of cancer survivors
after at least 1 year from receiving primary treatment (30) There is no time limit for determining whether the cancer is recurrent or developing, but most clinicians consider it as a recurrence if it reappears after one year of no signs or symptoms (30)
Each type of cancer has a recurrence rate that varies according to the stage, histology, genetic factors, patientrelated factors, and treatment It is believed that many recurrence rates do not take into account the latest cancer treatment options, especially when new cancer therapies are being used for certain types of cancer Therefore, recurrence rate estimates can vary between individuals and include both high and low recurrence rates
Some cancers have low recurrence rates if treatment occurs at an early stage For example, patients with breast cancer who receive an initial treatment with receptor therapy followed by maintenance therapy have a recurrence rate of 5% to 9% (31)
For cancer patients, the World Health Organization has created evaluation criteria for classifying clinical recurrence and remission in solid tumors called the Response Evaluation Criteria in Solid Tumors, which consists of several definitions including complete response, partial remission, progressive disease, and stable disease (32)
The definitions are used to assess the extent of the response obtained by cancer patients who have received different modalities of treatment such as chemotherapy, radiation, and surgery
When a patient has a cancer recurrence, several problems can arise For example, in a phenomenological study conducted by Finlayson et al , on ovarian cancer patients who consider recurrence as a chronic disease, the patients were unable to make treatment decisions and had longlasting emotional distress (33) According to Shao et al , other issues, such as a poor financial situation, can make an impact on the quality of life (QoL) of patients with cancer recurrence (34) Good coping strategies are needed to overcome the problems arising after that a patient is informed to have had a cancer recurrence In ovarian cancer recurrence, the coping strategies used have been based more on emotions and personal beliefs (35) There are no definitive data on cancer recurrence in Indonesia regarding new cases and cancer deaths However, cancer recurrence is a significant health issue for cancer patients who experienced this problem after treatment In addition, data regarding the varied experiences of cancer survivors in Indonesia who have had recurrences are also scarce Therefore, data regarding the experiences of cancer patients who experience recurrences should be the subject of in-depth study in order to make able oncology nurses and other health care professionals to understand the problems and needs of these patients and to develop interventions to solve them
Materials and methods
Participants
A total of 13 patients treated and followed at Dharmais Cancer Hospital who had experienced a recurrence were recruited and included according to the following inclusion criteria: i) male or female adult cancer patient who had experienced a recurrence after at least 2 months from
the declared relapse; ii) could communicate well
Three patients were not interviewed for the following reasons: one patient was afraid of trauma when talking about the recurrence, one patient had a worsening condition and had to be admitted to the emergency room, and one patient could not be contacted again after being confirmed In total only 10 patients participated in the study
Data collection
RD (first author) conducted data collection from March 2022 to May 2022 Data were collected via in-depth direct interviews with seven patients (one patient was recruited at the Dharmais Hospital as an outpatient, two patients were recruited through home visits, and the rest were inpatients), and three patients were interviewed by telephone The researcher and each patient agreed on location and methods of interview With the consent of the participants, interviews were recorded for 60 to 75 minutes Interview guidelines are shown in Table 1
Table 1.
Interview guidelines
No Question
1 What did you experience when you had a recurrence?
2 What efforts have you made to overcome the recurrence of cancer?
3 What are the things that affect your resilience when experiencing a recurrence?
Thematic analysis
The data analysis process was performed according to six steps (6) RD and YA did the data transcription separately Then, after obtaining the transcript, they read it repeatedly and recorded or marked keywords for the coding process
The researchers used the NVivo 12 application with serial number NVP12-LU001-ED03O-25004-LOBI This application was used to perform the initial coding of each interview transcript The initial coding activity was carried out by RD with YA The two authors then compiled the themes; namely, all the research data that had been coded and collected was analyzed to determine larger themes The next stage was to review the generated themes and group them into sub-themes This process was carried out by peer debriefing
In the fifth stage, the themes were defined and named to determine the essence of each generated theme, and then these themes were refined The final stage determined the final themes of the results of this study
Results
Theme 1: the reaction when information about recurrence or when bad news were received
Theme 2: the efforts made during a recurrence
Theme 3: the patient’s self-concept during a recurrence (Details are available in Supplementary Materials)
Discussion
Reaction when information of recurrence was received or when bad news was received
A recurrence can be detected by the onset of symptoms like those of early cancer These symptoms reappear at
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti, Rudi Rudi, Riri Maria 103
least one year after an initial diagnosis of cancer (36)
Some participants in this study expressed psychological reactions when experiencing a recurrence, such as shock, sadness, disappointment, and shame The participants who expressed disappointment felt that they had taken care of themselves as best as they could, so why did other people who did not take such good care of themselves not experience a recurrence? Those participants felt that God was mistreating them These experiences of the participants are similar to those conveyed in the research conducted by Thornton et al , who mentioned that one of the themes found in their research was an emotion with a sub-theme of anger caused by feelings of envy because the patients felt that they had done everything correctly according to the doctors’ instructions (37) This is also as stated by Economou et al , who indicated that patients who received bad news felt anger and sadness early during a recurrence (38) Psychological responses to bad news can affect the QoL of patients For example, the results of the research by Kugimoto et al , showed that psychological responses to stress that can affect QoL occur in cancer patients from news about terminal conditions, disease names, and recurrences (39) Bad news must be delivered by professional health personnel, such as nurses, who must pay attention to the room's condition, time, and atmosphere so that the patient does not become emotionally stressed (40)
The efforts made during a recurrence
Some participants chose alternative treatments such as cupping or hypnotherapy before taking conventional medical treatments when they were declared to be recurrent Some of them had used herbal treatment before the recurrence, such as drinking soursop leaves, which are believed to cure cancer When interviewed, participants said they received information on the benefits of herbal medicines from the internet The recurrences experienced by the participants made them stop taking soursop leaf herbal medicine as they then considered it useless The impressions regarding treatments and herbal medicines that participants conveyed were in line with the results of a previous study that found that an average of 51% of cancer patients used alternative and complementary therapies to improve their health and treat the complications from cancer or treatments (41) A qualitative study conducted by Abu Sharour, on patients with colorectal cancer in Jordan found that participants sought complementary treatments when experiencing a recurrence (42)
It takes the participation of health workers, especially nurses, to convey that there are alternative and complementary therapies that are safe and recommended for patients with cancer One of the participants in this study had difficulty urinating and drank a decoction of kumis kucing leaves as suggested by a friend After drinking the decoction of kumis kucing leaves, the participant could urinate but continued to go to the hospital because the participant considered the kumis kucing treatment only temporary Research by Madyastuti et al stated that the kumis kucing plant (Orthosiphon aristatus Blume) that is easily found in Indonesia has flavonoid ingredients with diuretic activity (43)
The conventional medical therapies received by the 10
participants consisted of surgery, chemotherapy, and radiation, with no other therapies besides these were found Previous studies have suggested that the available cancer treatments apart from surgery, chemotherapy, and radiation also include immunotherapy, hormone therapy, bone marrow transplantation, and targeted drug therapy that are conventionally administered metastatic breast cancer treatment (44)
As stated by Birmingham Children’s Hospital, patients need to be prepared physically and mentally for chemotherapy, surgery, and radiation treatments (45) Chemotherapy is a serious medical procedure, and it must be ensured that the patient is otherwise in good health Mental preparation creating self-efficacy has been shown to reduce emotional stress, such as in patients who are about to undergo surg e r y ( 4 6 ) P a r t i c i p a n t s w h o r e c e i v e d g e n e r a l o r a l chemotherapy experienced a weight loss because of the effects of chemotherapy can cause nausea, vomiting, and diarrhea After chemotherapy, the participants experienced difficulties eating and persistent diarrhea until they were given drugs to stop the diarrhea (47) After mastectomy patients are at risk for lymphedema, which is soft tissue swelling due to the accumulation of protein-rich fluid in the extracellular space, with swelling usually in the arm or hand on the side of the body that was operated on (48) Swelling in the hands after surgery was also experienced by one of the participants, who received an explanation from a medical rehabilitation doctor that this condition can occur as a side effect
Some participants maintained the recommended diet by consuming foods that contain protein, such as fish, meat, tofu, and tempeh, and not eating satay In another study, it was stated that one of the causes of the occurrence and recurrence of cancer is foods that contain carcinogens, such as salted fish (30)
In addition to maintaining the diet, the participants also revealed the efforts they made in maintaining a healthy lifestyle, such as exercise, routine checks, self-checking their breasts, and not smoking Cancer patients are recommended to continue physical activity because routine physical activity can prevent cancer recurrence (30) This opinion is in accordance with research conducted by Rock et al , which recommended that to prevent cancer, adults should perform a physical activity of a moderate-to-heavy intensity, depending on physical condition Not smoking is also part of maintaining a healthy lifestyle because cigarettes have tobacco as primary ingredient that is an agent that causes cancer
Getting closer to God when suffering from illness is another part of the efforts made for healing by asking for His help In this study, the participants revealed the efforts that they made to get closer to God through better prayer and worship For someone who has been able to maintain their life despite experiencing a cancer recurrence, the next stage is then personal growth At the individual post-traumatic growth stage, the result is an increase in spiritual well-being
Self-concept during a recurrence
This study explored various factors that can affect survival at the time of a recurrence In this study, it was found that some participants expressed the reasons that they believed could enable them to survive their recurrences Namely
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 104 Problems of cancer survivors
they believed that they could recover, by having a strong motivation to recover and enthusiasm for undergoing treatment, obtaining support when undergoing treatment, and eating food appropriate for treating a recurrence The participants who said that they believed that they were sure to recover demonstrated their optimism, while those participants who said they had the motivation to recover demonstrated their hope The support for undergoing treatments can come from family or from sources other than family; in this study, it came from husbands, wives, children, parents, and neighbors Patients who experience a relapse need to be given support and hope from everyone, especially their closest family members who act as caregivers while the patients are undergoing treatment Thus, support from families (parents or children) is very important for cancer patients and those who experience a recurrence For example, if the cancer patient is a father, they especially need support from their children
Optimism, hope, and support are part of the direct path to fostering the survival of someone who has just undergone a stressful event, such as receiving news of a cancer recurrence, while how one interprets a recurrence can be an indirect pathway to building resilience If the meaning is positive, then survival can be achieved, but if the meaning is negative, it will be a warning that makes the patient uncomfortable Achieving resilience requires evaluation
If the evaluation results are positive, they will produce optimism, hope, and will ultimately have survival
The results found in this study can be used as a basic data source for education, nurses, and hospitals to provide nursing care to cancer patients who experience recurrence Hospitals need to prepare a special room for patients who will be given bad information such as news of recurrence so that patients can convey all their feelings after hearing this information From this research data, oncology nursing specialists can also provide information about fact-based complementary therapies so that they can be used by patients who experience relapse Cancer patients need to involve the palliative team from the start so that when cancer patients experience a relapse, their self-concept and quality of life are good For future researchers, the results of this study can provide the latest information about cancer recurrence, so that it becomes data to quantitatively measure the problems and needs of cancer patients when they experience a recurrence
The researcher realizes that there are limitations and deficiencies in this study, namely the setting of the place used when collecting data in the hospital, that was not s dedicated room because of limited space
Conclusions
When patients receive information that they are experiencing a recurrence, psychological reactions, such as shock, sadness, and disappointment, occur Many efforts have been made by patients to cope with recurrences, namely through non-medical activities, medical activities, lifestyle changes, and getting closer to God This study also found a variety of factors that can influence patients when experiencing a recurrence, such as having the confidence to recover, strong motivation to recover, enthusiasm for undergoing treatment, support in undergoing treatment, and understanding of relapse This study can help increase
our understanding of the experiences of patients with different types of cancer during a recurrence phase
Acknowledgments: We are grateful to Universitas Indonesia for supporting our research
Acknowledgement of financial support:
* The study “Breast cancer survivors' unmet needs following chemotherapy” was supported by the Universitas Indonesia under Grant PUTI 2022 (Publication International Indexed 2022) No: NKB-99/UN2 RST/HKP 05 00/2022
** The study “Special information to discuss sexuality problems: a Balinese breast cancer survivor's unmet need” was supported by Tesis Magister Grant from The Minister of National Research and Technology, Culture, and Education, Republic of Indonesia No NKB-903/UN2 RST/HKP 05 00/2022
*** The study “Life experiences of Indonesian cancer patients with cancer recurrences: interpretative phenomenology” was supported by the Universitas Indonesia under Grant PUTI 2022 (Publication International Indexed 2022) No: NKB101/UN2 RST/HKP 05 00/2022
References
1 Lee JW, Lee J, Lee MH, et al Unmet needs and quality of life of caregivers of Korean breast cancer survivors: A cross-sectional study Ann Surg Treat Res 2021; 101:69-78
2 International Agency for Research on Cancer WHO Glob Cancer Observatory 2020 Available from: https://gco iarc fr/today/data/ factsheets/populations/900-world-fact-sheets pdf
3 Runowicz CD, Leach CR, Henry NL, et al American cancer society/American society of clinical oncology breast cancer survivorship care guideline CA Cancer J Clin 2016; 66:43-73
4 Afiyanti Y, Besral, Haryani The quality of life of Indonesian women with gynecological cancer Enferm Clin 2020; 30:65-9
5 Amane HY, Tessema AM, Seid KA, et al Factors associated with unmet supportive care needs of oncology patients at Dessie Referral Hospital, 2020 Ecancermedicalscience 2021; 15:1300
6 Braun V, Clarke V Qualitative Research in Psychology Using thematic analysis in psychology Using thematic analysis in psychology Qual Res Psychol 2006; 3:77-101
7 Maurer T, Jaskulski S, Behrens S, et al Tired of feeling tired – The role of circulating inflammatory biomarkers and long-term cancer related fatigue in breast cancer survivors Breast 2021; 56:103-9
8 Ng T, Dorajoo SR, Cheung YT, et al Distinct and heterogeneous trajectories of self-perceived cognitive impairment among Asian breast cancer survivors Psychooncology 2018; 27:1185-92
9 Bellens A, Roelant E, Sabbe B, et al A video-game based cognitive training for breast cancer survivors with cognitive impairment: A prospective randomized pilot trial Breast 2020; 53:23-32
10 Lambert M, Ouimet LA, Wan C, et al Cancer-related cognitive impairment in breast cancer survivors: An examination of conceptual and statistical cognitive domains using principal component analysis Oncol Rev 2018; 12:90-7
11 Boucheron P, Anele A, Zietsman A, et al Self-reported arm and shoulder problems in breast cancer survivors in Sub-Saharan Africa: the African Breast Cancer-Disparities in Outcomes cohort study Breast Cancer Res 2021; 23:109
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti, Rudi Rudi, Riri Maria 105
12 Bruce J, Williamson E, Lait C, et al Randomised controlled trial of exercise to prevent shoulder problems in women undergoing breast cancer treatment: Study protocol for the prevention of shoulder problems trial (UK PROSPER) BMJ Open 2018; 8 e019078
13 Esteban-Simón A, Díez-Fernández DM, Artés-Rodríguez E, et al Absolute and relative handgrip strength as indicators of self-reported physical function and quality of life in breast cancer survivors: The efican study Cancers (Basel) 2021; 13:5292
14 Kang D, Choi EK, Kim IR, et al Distress and body image due to altered appearance in posttreatment and active treatment of breast cancer patients and in general population controls Palliat Support Care 2018; 16:137-45
15 Morales-Sánchez L, Luque-Ribelles V, Gil-Olarte P, et al Enhancing self-esteem and body image of breast cancer women through interventions: A systematic review Int J Environ Res Public Health 2021; 18:1-20
16 Soriano EC, Perndorfer C, Otto AK, et al Does sharing good news buffer fear of bad news? A daily diary study of fear of cancer recurrence in couples approaching the first mammogram post-diagnosis Psychooncology 2021; 18:1640
17 Garduño-Ortega O, Morales-Cruz J, Hunter-Hernández M, et al Spiritual Well-Being, Depression, and Quality of Life Among Latina Breast Cancer Survivors J Relig Health 2021; 60:1895-907
18 Khezri E, Bagheri-Saveh MI, Kalhor MM, et al Nursing care based on the Support-Based Spiritual Care Model increases hope among women with breast cancer in Iran Support Care Cancer 2022; 30:423-9
19 Kowalczyk R, Nowosielski K, Cedrych I, et al Factors Affecting Sexual Function and Body Image of Early-Stage Breast Cancer Survivors in Poland: A Short-Term Observation Clin Breast Cancer 2019; 19:e30-9
20 James J, Teo M, Ramachandran V, et al Looking for metastasis in early breast cancer: does bone scan help? A retrospective review Clin Breast Cancer 2021; 21:e18-21
21 High B, Bohnenkamp S, Mulligan S What you need to know about caring for breast cancer survivors Medsurg Nurs 2019; 28:189-93
22 Ferlay J, Ervik M, Lam F, et al International agency for research on cancer 2020 Glob Cancer Obs Cancer Today 2020; 419:1-2
23 Almeida NG De, Knobf TM, Oliveira MR De, et al A pilot intervention study to improve sexuality outcomes in breast cancer survivors Asia Pac J Oncol Nurs 2020; 7:161-6
24 Rose M, Garcia D, Fisher CL, et al Communication about sexual health with breast cancer survivors : Variation among patient and provider perspectives Patient Educ Couns 2016; 99:1814-20
25 Cullen K, Fergus K Acceptability of an online relational intimacy and sexual enhancement (iRISE) intervention after breast cancer J Marital Fam Ther 2021; 47:515-32
26 Maleki M, Mardani A, Ghafourifard M, Vaismoradi M Changes and challenges in sexual life experienced by the husbands of women with breast cancer: a qualitative study BMC Womens Health 2022; 22:1-12
27 Mofrad SA, Nasiri A, Rad GHM, Shandiz FH Spousal sexual life issues after gynecological cancer: a qualitative study Support Care Cancer 2021; 29:3857-64
28 Zhang X, Sherman L, Foster M Patients’ and providers’ perspectives on sexual health discussion in the United States: A scoping review Patient Educ Couns 2020; 103:2205-13
29 Tat S, Doan T, Yoo GJ, Levine EG Qualitative exploration of sexual health among diverse breast cancer survivors J Cancer Educ 2018; 33:477-84
30 American Cancer Society Can I Do Anything to Prevent Cancer Recurrence? Available from: https://www cancer org/content/dam/ CRC/PDF/Public/8423 00 pdf 2016; 1-5
31 Colleoni M, Sun Z, Price KN, et al Annual hazard rates of recurrence for breast cancer during 24 years of follow-up: Results from the international breast cancer study group trials I to V J Clin Oncol 2016; 34:927-35
32 Widhiarta PR, Mahendra INB, Dwi Aryana, MB, Megaputra IG Faktor-faktor klinikopatologi kekambuhan kanker serviks stadium IIIA2 pasca histerektomi radikal di RSUP Sanglah periode 20192020 Intisari Sains Medis 2021; 12:196-200
33 Finlayson CS, Fu MR, Squires A, et al The Experience of Being Aware of Disease Status in Women with Recurrent Ovarian Cancer: A Phenomenological Study J Palliat Med 2019; 22:377-84
34 Shao Z, Zhu T, Zhang P, et al Association of financial status and the quality of life in Chinese women with recurrent ovarian cancer Health Qual Life Outcomes 2017; 15:1-8
35 Lee Y, Praveena K, Woo Y, Ng C Coping Strategies among Malaysian Women with Recurrent Ovarian Cancer: A Qualitative Study Asia-Pacific J Oncol Nurs 2021; 8:40-5
36 Society AC What is cancer recurrence? Am Cancer Soc [Internet] Available from: https://www cancer org/treatment/sur-
recurrence/what-is-cancer-recurrence html 2016; 1-4
37 Thornton LM, Levin AO, Dorfman CS, et al Emotions and social relationships for breast and gynecologic patients: A qualitative study of coping with recurrence Psychooncology 2014; 23:382-9
38 Economou D, Walshe C, Brearley SG Exploring the experience of recurrence with advanced cancer for people who perceived themselves to be cancer free: a grounded theory study Support Care Cancer 2021; 29:3885-94
39 Kugimoto T, Katsuki R, Kosugi T, et al Significance of psychological stress response and health-related quality of life in spouses of cancer patients when given bad news Asia-Pacific J Oncol Nurs 2017; 4:147-54
40 Matthews T, Baken D, Ross K, et al The experiences of patients and their family members when receiving bad news about cancer: A qualitative meta-synthesis Psychooncology 2019; 28:2286-94
41 Keene MR, Heslop IM, Sabesan SS, Glass BD Complementary and alternative medicine use in cancer: A systematic review Complement Ther Clin Pract [Internet] 2019; 35:33-47
42 Abu Sharour L Lived experience of Jordanian colorectal cancer patients with recurrence: an interpretative phenomenological analysis Psychol Heal Med [Internet] 2019; 00:1-9
43 Madyastuti R, Ietje wientarsih, Setyo Widodo, Erni H Purwaningsih, Eva Harlina Aktivitas Diuretik dan Analisa Mineral Urin Perlakuan Ekstrak Tanaman Kumis Kucing (Orthosiphon Stamineus Benth) pada Tikus Jantan Acta Vet Indones 2020; 8:16-23
44 Al-Mahmood S, Sapiezynski J, Garbuzenko OB, Minko T Metastatic and triple-negative breast cancer: challenges and treatment options Drug Deliv Transl Res 2018; 8:1483-507
45 Birmingham Children’s Hospital Guidelines for the administration of chemotherapy for malignant disease NHS Found Trust [
h s u k / m i d seast/wp-content/uploads/sites/7/2018/04/guidelines-administrationchemotherapy-for-malignant-disease-v2-1-0 pdf 2015; 1–17
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 106 Problems of cancer survivors
v i v o r s h i p - d u r i n g - a n d - a f t e r - t r e a t m e n t / u n d e r s t a n d i n g -
e t ] A v a i l a b l e f r o m : h t t p s : / / w w w e n g l a n d n
I n t e r n
46 Marinelli V, Danzi OP, Mazzi MA, et al PREPARE: PreoPerative Anxiety REduction One-Year Feasibility RCT on a Brief Psychological Intervention for Pancreatic Cancer Patients Prior to Major Surgery Front Psychol 2020; 11:1-14
47 Amjad MT, Chidharla A, Kasi A Cancer Chemotherapy In Treasure Island (FL) 2022
48 Wanchai A, Armer JM, Stewart BR, Lasinski BB Breast cancerrelated lymphedema: A literature review for clinical practice Int J Nurs Sci [Internet] 2016; 3:202-7
49 Rock CL, Thomson CA, Sullivan KR, et al American Cancer Society nutrition and physical activity guideline for cancer survivors CA Cancer J Clin 2022; 72:230-262
Correspondence
Ida Ayu Made Ari Santi Tisnasari
Faculty of Nursing, Universitas Indonesia, Depok, Indonesia
Tuti Nuraini (Corresponding Author) tutinfik@ui ac id
Department of Basic Science and Fundamental Nursing, Faculty of Nursing, Universitas Indonesia, Depok, 16424, West Java, Indonesia
Yati Afiyanti (Corresponding Author) yatikris@ui ac id
Department of Maternity Nursing, Faculty of Nursing, Universitas Indonesia, Depok, 16424, West Java, Indonesia
Rudi Rudi
Master of Nursing Program, Faculty of Nursing Universitas Indonesia, Depok, Indonesia
Riri Maria
Department of Medical Surgical Nursing, Faculty of Nursing Universitas Indonesia, Depok, Indonesia
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti, Rudi Rudi, Riri Maria 107
Knowledge, attitude and practice towards pelvic floor muscle training among childbearing women
1 Kulliyyah of Nursing, International Islamic University Malaysia, Kuantan, Malaysia;
2 Department of Special Care Nursing, Kulliyyah of Nursing, International Islamic University Malaysia, Kuantan, Malaysia;
3 Department of Obstetrics & Gynecology, Kulliyah of Medicine, International Islamic University Malaysia, Kuantan, Malaysia
Presented as conference papers at the 8th V-BINC at FON Universitas Indonesia
Summary
Objectives: This study aims to identify knowledge, attitude, and practice of pelvic floor muscle training (PFMT) and to identify the prevalence of urinary incontinence
Materials and methods: The method used was a cross-sectional study Self-administered knowledge, attitude, and practice questionnaires were distributed among childbearing women attending Maternal & Child Health Clinics in the East Coast region of Malaysia
Results: The findings revealed that most respondents (N = 896) had good or moderate knowledge (80 1%) and attitudes (77 3%) regarding PFMT but most of them (87.2%) still lacked practice. However, there was no association between urinary incontinence and PFMT practice. On the contrary, married women showed a higher risk of urinary incontinence
Conclusions: The practice of pelvic floor muscle training should be recommended and emphasized to childbearing women by healthcare professionals.
KEY WORDS: Attitude; Knowledge; Pelvic floor muscle training; Practice; Urinary incontinence; M-ISI
Submitted 10 March 2023; Accepted 18 March 2023
INTRODUCTION
Urinary incontinence (UI) is one of the worldwide health problems but is not considered life-threatening (1) Most of the victims did not share their problems and kept silent until they were interviewed by healthcare professionals A study identified factors that affect help-seeking behavior: not accepting incontinence as a disease, shame, non-optimal health care system, negative support of essential others and reduced quality of life (2) The risk factors for UI include menopause, increased body mass index, straining hard during defecation, coffee consumption and depression (3)
The management of UI was divided into two, which are conservative and non-conservative treatment The nonconservative treatment is the medical or surgical treatment, whereas the conservative treatment is non-costly One of the conservative treatments is, pelvic floor muscle training, or known as Kegel’s exercise In 1948, Dr Kegel, who invented the Kegel exercise, stated that the cure rate after training pelvic floor muscles for women with different types of incontinence was 84% Besides, pelvic floor
muscle training is the most recommended treatment method, especially for stage 1 stress urinary incontinence (4) Thus, pelvic floor muscle training (PFMT) has been recognized as the first-line therapy for urinary incontinence (5) Women with the symptom of stress and mixed urinary incontinence who had the treatment of PFMT showed improvement in their symptoms of UI (4) The rationale for doing PFMT is to maximize the urethral pressure and improve the voluntary contraction of the muscle by improving pelvic floor muscle strength (6)
In Malaysia, the prevalence of UI among women was 17 3% while for antenatal cases it was 34 3% during their third trimester (3) However, compared with Turkey, the prevalence of UI among pregnant women was high, with almost 80% with stress urinary incontinence (7) A study among antenatal women in Kelantan showed women had a low level of knowledge regarding PFMT with only 5 8% doing PFMT (8)
The result showed that the women knew the information regarding PFMT (9) Whereas another finding in Selangor stated that 46 6% of pregnant women had a good attitude towards PFMT (10)
There is no standardized measurement tool that can be used to discern the type, severity, or bother attributed to UI at one time In government hospitals and clinics throughout Malaysia, a variety of forms of UI screening were identified Presently, to identify all the symptoms, women had to complete multiple questionnaires in one setting, and the healthcare professionals then had to determine how to interpret and assimilate the results of these different measures One of the instruments with high accuracy levels to discern the types of urinary incontinence is Michigan Incontinence Symptom Index (M-ISI) (11) Unlike other UI questionnaires, the M-ISI covers different aspects of UI that were essential for women's care and research It also has been proved that the threshold scores for the M-ISI could be used to screen for clinically relevant urinary incontinence (11)
This study provided a simple and comprehensive instrument to measure types, severity, and bother related to UI among childbearing women The aims were to identify the knowledge, attitude, and practice towards pelvic floor muscle training, to measure the UI using a validated MISI questionnaire, and to identify the association between the UI and PFMT among childbearing women
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 108
PAPER
ORIGINAL
Nur Fairuz Mohd Fauzey 1 , Siti Mariam Muda 2 , Haliza Hasan 2 , Zalina Nusee 3 , Muzaitul Akma Mustapa Kamal Basha 2
DOI: 10 4081/aiua 2023 11298
MATERIALS AND METHODS
The study used a quantitative research method with crosssectional design It was conducted at five government Maternal & Child Health Clinics in the East Coast Region in Malaysia (Kelantan, Terengganu, Pahang) The populations were childbearing women who attended the Maternal and Child Health Clinic The inclusion criteria were Malaysian women, aged 18 to 45 years old, and able to read in M a l a y T h e e x c l u s i o n c r i t e r i a i n c l u d e d m e n o p a u s a l women, a history of mental health problems, and diagnosed chronic illness The study included 2 parts: the first part was the recruitment process, and the second was the administration of two sets of questionnaires, M-ISI screening test and a survey on knowledge, attitude, and practice of pelvic floor muscle training Figure 1 shows the process of recruitment of participants in this study
Table 1. Socio-demographic characteristics
The sample size was calculated using the open-source calculation OpenEpi Version 3 using the Odds Ratio (OR) from a previous study (10) Using a 20% non-response factor, it was decided to have a total of 1219 childbearing women involved in the study
All the data obtained from the study were recorded and statistically analysed using Statistical Package for Social Science Software, version 26 0 Basic details of the participants and urinary incontinence were analysed using descriptive statistics, including mean and standard deviation or median with interquartile range for non-normally distributed data A Chi-square test was used to identify the association between urinary incontinence and pelvic floor muscle training and logistic regression was done to identify the predictors of urinary incontinence among childbearing women

This study obtained approval from the Research Committee at International Islamic University Malaysia (IIUM) (IREC 2021-008) and National Medical Research Register (NMRR) (NMRR-19-4172-51098) All participants consented and were involved in this study on a voluntary basis
RESULTS
A total of 896 participants answered all questions yielding a 74% completion rate, with the power of the study being 100% Age distribution is shown in Table 1 There were 506 participants (58 0%) who were multigravida (usually 3-5 pregnancies), while 30% were primigravida
who had first-time experience in pregnancy The majority of the participant were Malay (99 5%), and the highest educational level was diploma/degree holder (48 8%)
More than half of the participants (52 6%) were housewives, and in terms of monthly income, the majority of the participants (78 2%) were categorized in the lower h
RM4,850 per month
The number of women with UI using the M-ISI questionnaire was 173, with an estimated prevalence of 19 3% (Table 2) As reported in table 3, 43 0% of the respondents had good knowledge of PFMT Most of the childbearing women had a moderate attitude toward PFMT (55 9%) and poor practice toward PFMT (87 2%)
As reported in Table 3, 43 0% of the respondents had good knowledge of PFMT Most of the childbearing women had
Archivio Italiano di Urologia e Andrologia 2023; 95, 2
109
Nur Fairuz Mohd Fauzey, Siti Mariam Muda, Haliza Hasan, Zalina Nusee, Muzaitul Akma Mustapa Kamal Basha
o u s e h o l d i n c o m e g r o u p ( B 4 0 ) , e a r n i n g l e s s t h a n
Characteristics Frequency Percentage (%) Age (years) (n = 887) < 20 28 3 2 21-30 432 48 7* 31-40 361 40 7 > 41 66 7 4 Marital status (n 883) Single 23 2 6 Married 850 96 3* Widow 10 1.1 Gravida (n = 873) Nulligravida 14 1 6 Primigravida 262 30 0 Multigravida 506 58 0* Grand multigravida 91 10 4 Ethnicity (n = 885) Malay 881 99 5* Chinese 2 0 2 India 2 0 2 Educational level (n = 864) Primary school 17 2 0 Secondary school 401 46 4 Diploma/Degree 422 48 8* Master/PhD 24 2.8 Occupation (n = 854) Housewife 449 52 6* Self-employed 92 10 8 Government sector 175 20 5 Private sector 135 15 8 Student 3 0 4 Monthly income** (n 832) B40 (bottom 40%) 651 78 2* M40 (middle 40%) 168 20 2 T20 (top 20%) 13 1.6 *The highest score n each item; **Malays an household ncome c assification
Urinar y incontinence Frequency Percentage (%) Yes 173 19 3 No 723 80.7
Table 2. The prevalence of urinary incontinence
Figure 1
The process of recruitment of participants
a moderate attitude toward PFMT (55 9%) and the majority reported a poor practice of PFMT (87 2%)
Table 4 depicted that there was a significant association between the level of knowledge of PFMT and UI (p = 0 001); it also showed a significant association between the level of attitude toward PFMT and UI (p = 0 009) but no significant association between level of practice of PFMT and UI (p > 0 05)
Good knowledge of PFMT (adjusted OR = 0 69; 95% CI 0 41-1 19) and moderate knowledge of PFMT (adjusted OR = 0 70, 95% CI 0 43-1 14) were negative predictors of UI, meaning that women with good/moderate knowledge are less likely prone to UI compared to those with poor knowledge However, other socio-demographic factors, such as being married women, showed to be statistically significant towards the risk to be UI (p = 0 040)
place, population, and questionnaire that have been used
The various definitions of incontinence, the use of different questionnaires, settings, procedures, and the validity of self-report data all contributed to the variation in epidemiological data about the prevalence rate of UI (5) This study found that most of the childbearing women had a good knowledge of PFMT, similar to the previous study conducted at one of the teaching hospitals in Malaysia (13) However, the respondents demonstrated a moderate attitude towards PFMT, contrary to the findings previously observed among antenatal women in Kelantan (14) The pregnant women felt that PFMT had positive effects on their health, such as improved incontinence, pelvic organ prolapse, quality of life and increased sexual satisfaction (15) There was a positive change in attitude score after attending antenatal class (16), and as a result, education was a critical factor in improving women ’ s attitudes and motivation towards PFMT
The finding from this study showed that married women had a significant association with UI Married women were more likely to have UI than single women because they tend to have an older age, which becomes a risk factor for UI (17) Being married women, earlier age at marriage, high parity, and old age were associated with the increase in UI among women in Lahore (18) Women do not practice PFMT, possibly due to a lack of information or awareness about doing this exercise during antenatal or postnatal periods This can be seen in another study in which 44% of them reported lack of knowledge about the exercise and 96% stated that there was no guidance from healthcare professionals during the postpartum period in promoting PFMT (19)
CONCLUSIONS
This study revealed that, although overall knowledge and attitude towards PFMT were good, women did not practice the exercise regularly Thus, it is recommended to healthcare professionals to play an essential role by providing more information as well as raising awareness about PFMT The best method to give the information effectively is during consultation sessions and the antenatal class
Acknowledgments: We would like to thank all participants involved in this study for their help and support
Funding: This study was supported by the Fundamental Research Grant Scheme for Research Acculturation of Early Career Researchers (RACER) under Ministry of Higher Education Malaysia
Acknowledgement of financial support: This work was supported by Fundamental Research Grant Scheme for Research Acculturation of Early Career Researchers (RACER) under Ministry of Higher Education Malaysia
DISCUSSION
The prevalence of UI among childbearing women in this study, which included the East Coast region of Malaysia, was lower than the one reported in a previous study, which evaluated the rate of UI among women aged > 18 years (12) However, the prevalence may vary with the
REFERENCES
1 Mohd Yusoff D, Awang S, Kueh YC Urinary incontinence among pregnant women attending an antenatal clinic at a tertiary teaching hospital in North-East Malaysia J Taibah Univ Med Sci 2019; 14:39
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 110 Pelvic floor muscle training among childbearing women
Level Frequency Percentage (%) Knowledge towards pelvic floor muscle training Good 385 43 0 Moderate 332 37 1 Poor 179 20 0 Attitude towards pelvic floor muscle training Good 192 21 4 Moderate 501 55 9 Poor 203 22 7 Practice towards pelvic floor muscle training Good 32 3 6 Moderate 81 9 2 Poor 772 87 2
Table 3. The level of knowledge, attitude and practice towards pelvic floor muscle training.
floor
incontinence. Variable Urinar y incontinence χ2 P-value Yes (n = 173) n (%) No (n = 723) n (%) Knowledge Good 61 (35 3) 324 (44 8) 14 195 0 001 Moderate 60 (34 7) 272 (37 6) Poor 52 (30 1) 127 (17 6) Attitude Good 30 (17 3) 162 (22 4) 9 368 0 009 Moderate 89 (51 4) 412 (57 0) Poor 54 (31 2) 149 (20 6) Yes (n = 169) n (%) No (n = 716) n (%) Practice Good 1 (0 6) 31 (4 3) 5 851 0 054 Moderate 18 (10 7) 63 (8 8) Poor 150 (88 8) 622 (86 9) S gnificant value, P-value < 0 05
Table 4. Association between level of knowledge, attitude, and practice towards
pelvic
muscle training with urinary
2 Fakari FR, Hajian S, Darvish S, Alavi Majd H Explaining factors affecting help-seeking behaviors in women with urinary incontinence: a qualitative study BMC Health Serv Res 2021; 21:1-10
3 Kaur Dhillon H Urinary incontinence amongst Malaysian women in Selangor: prevalence, types and risk factors World J Public Health 2019; 4:10
4 Ptak M, Cie´cwiez S, Brodowska A, et al The Effect of Pelvic Floor Muscles Exercise on Quality of Life in Women with Stress Urinary I n c o n t i n e n c e a n d I t s R e l a t i o n s h i p w i t h V a g i n a l D e l i v e r i e s : A Randomized Trial Biomed Res Int 2019; 2019:5321864
5 Abrams P, Smith AP, Cotterill N The impact of urinary incontinence on health-related quality of life (HRQoL) in a real-world population of women aged 45-60 years: results from a survey in France, Germany, the UK and the USA BJU Int 2015; 115:143
6 Malhotra N, Chahal A The effectiveness of pelvic floor exercises on symptoms in females with stress urinary incontinence Biosci Biotechnol Res Commun 2018; 11:681
7 Özdemir K, S¸ahin S, Özerdog ˘ an N, Ünsal A Evaluation of urinary incontinence and quality of life in married women aged between 20 and 49 years (Sakarya, Turkey) Turk J Med Sci 2018; 48:100-9
8 Ahmed Ibrahim W Assess levels of knowledge, attitude and practice of the married women about pelvic floor muscles exercise Int J Sci Res 2015; 6:2319
9 Rosediani M, Nik Rosmawati NH, Juliawati M, Norwati D Knowledge, attitude and parctice towards pelvic floor muscle exercise among pregnant women attending antenatal clinic in Universiti Sains Malaysia Hospital, Malaysia Int Med J 2012; 19:37
10 Jaffar A, Mohd-Sidik S, Nien FC, et al Urinary incontinence and its association with pelvic floor muscle exercise among pregnant women attending a primary care clinic in Selangor, Malaysia PLoS One 2020; 15:e0236140
11 Suskind AM, Dunn RL, Morgan DM, et al A screening tool for clinically relevant urinary incontinence Neurourol Urodyn 2015; 34:332-5
12 Baykus¸ N, Yenal K Prevalence of urinary incontinence in women aged 18 and over and affecting factors J Women Aging 2020; 32:578-90
13 Jarni MF, Mohamad MY, Kamarudzaman N Knowledge, attitude, and practice (KAP) towards pelvic floor muscle exercise among the female population attending the Obstetrics and Gynaecology Clinic at Sultan Ahmad Shah Medical Centre (SASMEC@IIUM) International Journal of Allied Health Sciences 2021; 5:2521-2529
14 Muhammad J, Muhamad R, Husain NRN, Daud N Pelvic floor muscle exercise education and factors associated with implementation among antenatal women in Hospital Universiti Sains Malaysia Korean J Fam Med 2019; 40:45 1 5 T
Chongsomchai C Knowledge, attitude, and practices (KAP) survey towards pelvic floor muscle training (PFMT) among pregnant women Int J Womens Health 2020; 12:295-9
16 Habib M, Sohail I, Nasir M, Nasir F Awareness, knowledge and practices of pakistani women towards pelvic floor muscle exercises (PFMES) during pregnancy J Soc Obstet Gynaecol Pak 2020; 10:121
17 Al Kiyumi MH, al Belushi ZI, Jaju S, al Mahrezi AM Urinary incontinence among omani women prevalence, risk factors and impact on quality of life Sultan Qaboos Univ Med J 2020; 20:45
18 Jawad Z, Malik A, Khan S Prevalence of Urinary Incontinence in Women in Lahore: severity, associated factors and impact on daily life Age 2021; 15:5
19 Alharqi HM, Albattawi JA Assessment of Knowledge and Attitude of Women Towards Postpartum Exercise J Nurs Health Sci 2018; 7:16
Correspondence
Nur Fairuz Mohd Fauzey
Kulliyyah of Nursing, International Islamic University Malaysia, Kuantan, Malaysia
Siti Mariam Muda (Corresponding Author)
sitimariam@iium edu my
Haliza Hasan
Muzaitul Akma Mustapa Kamal Basha
Department of Special Care Nursing, Kulliyyah of Nursing, International Islamic University Malaysia, Kuantan, 25200, Malaysia
Zalina Nusee
Department of Obstetrics & Gynecology, Kulliyah of Medicine, International Islamic University Malaysia, Kuantan, Malaysia
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2
111
Nur Fairuz Mohd Fauzey, Siti Mariam Muda, Haliza Hasan, Zalina Nusee, Muzaitul Akma Mustapa Kamal Basha
m t a n a k i t p a i s a
T
B
n y a v e j c h e v i n S , B u p p a s i r i P ,
e
n
,
u
Risk of urogenital infections in non-diabetic patients treated with sodium glucose
transporter 2 (SGLT2) inhibitors. Systematic review and meta-analysis
Rawa Bapir 1, 16 , Kamran Hassan Bhatti 2, 16 , Ahmed Eliwa 3, 16 , Herney Andrés García-Perdomo 4, 16 , Nazim Gherabi 5, 16 , Derek Hennessey 6, 16 , Vittorio Magri 7, 16 , Panagiotis Mourmouris 8, 16 , Adama Ouattara 9, 16 , Gianpaolo Perletti 10, 16 , Joseph Philipraj 11, 16 , Konstantinos Stamatiou 12, 16 , Musliu Adetola Tolani 13, 16 , Lazaros Tzelves 8, 16 , Stefan D. Anker 14 , Alberto Trinchieri 15, 16 , Noor Buchholz 16
1 Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq;
2 Urology Department, HMC, Hamad Medical Corporation, Qatar;
3 Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt;
4 Universidad del Valle, Cali, Colombia;
5 Faculty of Medicine Algiers 1, Algiers, Algeria;
6 Department of Urology, Mercy University Hospital, Cork, Ireland;
7 Urology Unit, ASST Fatebenefratelli Sacco, Milan, Italy;
8 2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece;
9 Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso;
10 Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy;
11 Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India;
12 Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece;
13 Division of Urology, Department of Surgery, Ahmadu Bello University/Ahmadu Bello University Teaching Hospital, Zaria, Kaduna State, Nigeria;
14 Department of Cardiology and BCRT (Campus CVK), Charité Universitätsmedizin Berlin, Germany;
15 Urology School, University of Milan, Milan, Italy;
16 U-merge Ltd (Urology for emerging countries), London-Athens-Dubai *
Authors 1-16 have equally contributed to the paper and share first authorship
* U-merge Ltd (Urology for Emerging Countries) is an academic urological platform dedicated to facilitate knowledge transfer in urology on all levels from developed to emerging countries U-merge Ltd is registered with the Companies House in London/ UK www U-merge com
Summary
Although SGLT2 inhibitors have been initially employed in the treatment of type 2 diabetes, their clinical use was later extended to the treatment of other conditions such as heart failure, chronic kidney disease and obesity In patients with type 2 diabetes, the administration of SGLT2 inhibitors has been associated with an increased incidence of urogenital infections, which may be linked to high glucose levels in the urine The rate of urogenital side effects may be different in non-diabetic patients. The aim of this study was to review the risk of urogenital infections in non-diabetic patients taking SGLT2 inhibitors.
Materials and methods: We conducted a systematic review and meta-analysis by searching PubMed and EMBASE for randomized controlled trials (RCTs) reporting urogenital adverse effects in non-diabetic patients treated with SGLT2 inhibitors. Odds ratios for urogenital infections were calculated using random effect Mantel-Haenszel statistics.
Results: Out of 387 citations retrieved, 12 eligible RCTs were assessed for risk of bias and included in the meta-analysis.
Compared to placebo, SGLT2 inhibitors were associated with increased odds of genital infections (OR 3.01, 95% CI: 1.934 68, 9 series, 7326 participants, Z = 5 74, p < 0 0001, I 2 = 0%) as well as urinary tract infections (OR 1.33, 95% CI: 1.13-1.57,
9 series, 7326 participants, Z = 4 05, p < 0 0001, I2 = 0%)
When four trials investigating the effects of SGLT2 inhibitors in populations including both diabetic and non-diabetic patients were considered, administration of SGLT2 inhibitors in diabetic patients was associated with significantly higher odds of genital infections but not urinary tract infections compared to patients without type 2 diabetes In patients taking placebo, the odds for urinary tract infections were significantly increased in diabetic patients compared to non-diabetic patients.
Conclusions: The risk of genital infections is increased also in non-diabetic patients taking SGLT2 inhibitors although at a lesser extent that in diabetics A careful assessment of the local anatomical conditions and of the history of previous urogenital infections is desirable to select those patients who need more intense follow-up, possibly combined with prophylactic measures of infections during treatment with SGLT2 inhibitors.
KEY WORDS: Sodium glucose transporter 2 (SGLT2) inhibitors; Urinary tract infections; Genital infections; Candidiasis; Heart failure; Chronic kidney disease; Obesity
Submitted 4 June 2023; Accepted 5 June 2023
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 112 REVIEW
DOI: 10 4081/aiua 2023 11509
INTRODUCTION
Sodium glucose transporter 2 (SGLT2) inhibitors have been recently introduced in the treatment of type 2 diabetes (T2DM)
The most frequently administered SGLT2 inhibitors are canagliflozin, dapagliflozin, and empagliflozin The SGLT2 transporter is responsible for reabsorption of more than 90% of renal glucose from the urine filtered by renal glomeruli In diabetic patients, administration of a SGLT2 inhibitor reduces the renal glucose threshold, resulting in glycosuria and in the lowering of plasma glucose levels In patients with T2DM, administration of SGLT2 inhibitors as monotherapy or in combination with other antidiabetic agents was shown to lower HbA1C, to induce weight loss and to decrease blood pressure (1)
Somehow unexpectedly, SGLT2 inhibitors were found to be potentially useful in the management of heart failure (2) In addition, studies in patients with chronic kidney disease, showed that SGLT2 inhibitors reduced the risk of a decline of renal function or end-stage kidney disease regardless of the presence or diabetes (3, 4) Due to these favorable characteristics, SGLT 2 inhibitors are increasingly prescribed not only in patients with type 2 diabetes mellitus, but also in patients with cardiovascular and renal diseases Interestingly, SGLT2 inhibitors have also proven to be effective in lowering body weight in obese patients without type 2 diabetes (5)
Although SGLT2 inhibitors are generally well tolerated, increased rates of genital and urinary tract infections have been reported (6, 7) The increased frequency of genital infections in diabetic patients treated with SGLT-2 inhibitors may be explained by high urinary glucose concentrations that can promote the growth of fungi on the surface of the genital mucous membranes
However, the concentration of glucose in the urine of diabetic patients taking SGLT-2 inhibitors may be lower compared to the one measured in non-diabetic patients who are receiving SGLT-2 inhibitors for other conditions For this reason, the risk of genital infections in patients taking SGLT-2 inhibitors for conditions other than type 2 diabetes may be different compared to patients with type 2 diabetes
The aim of this systematic review and metanalysis was to evaluate the evidence describing the prevalence of genitourinary infections in non-diabetic patients receiving SGLT2 inhibitors for different conditions
MATERIALS AND METHODS
Protocol and registration
The review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and MetaAnalyses (PRISMA) guidelines (8) The protocol for this review was registered on the PROSPERO platform (registration number: CRD42022375951)
Types of studies
We considered articles written in English, reporting randomized controlled trials (RCTs) evaluating the side effects of SGLT2 inhibitors, administered to diabetic or non-diabetic patients (i) for prevention of heart failure, (ii) for
preserving renal function in end-stage kidney disease or (iii) for weight loss
Types of patients
Participants of both sexes were involved irrespective of their age or ethnicity
Types of interventions administered to patients
Patients on treatment with SGLT2 inhibitors or placebo were included in the present review
Outcomes
The outcome considered for this review was the assessment of the prevalence of genital or urinary infections in subjects taking SGLT2 inhibitors compared to those not taking this treatment
Search strategy
Two electronic databases (PubMed and EMBASE) were searched for records published up to January 31st, 2023 Broad search strings, based on MeSH terms, were used (e g , [sodium glucose co-transporter-2 OR canagliflozin OR dapagliflozin OR empagliflozin) AND (urinary tract infections OR genital infections OR balanitis OR vulvov
Relevant data were also hand-searched by browsing reference lists of reviews and trial reports, or other sources Duplicate references were excluded
Data collection and analysis - selection of studies and data extraction
Title and abstract screening to exclude documents that did not meet the inclusion criteria was performed independently by four authors (two for each database) Selected titles were downloaded for full-text reading, for final inclusion and for extraction of relevant information Controversies were resolved by one independent researcher A PRISMA flow diagram was drawn to summarize the process of study selection Data extraction was performed by four authors using a standardized form The following data were extracted from each study report: author(s), publication year, study design, population, intervention, prevalence of genital and urinary infections In case of missing or insufficient information, we considered the impact of missing data on the meta-analysis results
Quality evaluation on methodology
Three authors independently performed the quality assessment by identifying potential biases using the Cochrane risk of bias tool (9) The following potential sources of bias were considered: randomization process (D1), deviations from the intended interventions (D2), missing outcome data (D3), measurement of the outcome (D4) and selection of the reported result (D5)
Disagreements were resolved by discussion Risk of bias was not used to exclude studies
Statistical analysis
Statistical analysis was performed using the MetaEssentials-1 software (Rotterdam School of Management, Erasmus University, The Netherlands) Dichotomous data (presence/absence of urinary or genital stone disease) and number of subjects
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 R Bapir, K
A Eliwa, et al 113
Hassan Bhatti,
a g i n i t i s O R c a n d i d i a s i s O R F o u r n i e r g a n g r e n e ] )
Urogenital infection and SGLT2 inhibitors
were extracted to calculate odds ratios (OR), confidence intervals (CI) to odds-ratios, and Z statistics (Random-effects model, Mantel-Haenszel method)
Assessment of heterogeneity
Study heterogeneity was assessed by the I2 statistic, reported with 95% CIs, and interpreted as of lesser importance (I2 ≤ 40%), moderate (I2 = 30%-60%), substantial (I2 = 50%-90%) or considerable (I2 ≥ 75%), according to Cochrane criteria Sensitivity analysis was planned if considerable heterogeneity of pooled analyses including at least 4 studies was detected
Assessment of reporting bias
Publication bias was assessed by funnel plot in the presence of at least 4 trials in each meta-analysis If a potential bias was suspected by visual inspection of the plots, the Begg’s and Egger’s tests were used to test funnel plots symmetry and to confirm or exclude the presence of publication bias The ‘trim and fill’ missing study imputation approach was applied to funnel plots; if missing studies were imputed by this procedure, adjusted overall effect sizes (odds ratios) were calculated and presented in the
plots Publication bias analysis was performed using the MetaEssentials-1 software (Rotterdam School of Management, Erasmus University, The Netherlands)
RESULTS
(Medline = 104, EMBASE = 283) Subsequent screening of title and abstract restricted the number of records to 42 Four additional studies were retrieved by handsearching the references of selected studies After removal of 5 duplicates, we considered 41 articles for full-text evaluation Full-text evaluation resulted in the exclusion of 29 articles for the following reasons: one review article, 15 reports dealing only with type-2 diabetes patients, 2 articles reporting a comparison of SGLT2 inhibitors with other drugs, one letter to the Editor, 5 papers reporting the results presented in other included studies, 2 studies reporting short-term administration of SGLT2 inhibitors, one article dealing with cost-benefit of SGLT2 inhibitors treatment, 3 reports non presenting safety data
The remaining 12 articles were included in the qualitative systematic review Out of them, nine were included in the meta-analysis
Included studies
Three studies included overweight or obese patients without DM type 2 receiving (i) canagliflozin or (ii) canagliflozin plus phentermine or (iii) dapagliflozin plus exenatide (10-12) In the DIAMOND trial, dapagliflozin w a s a d m i n i s t e r e d t o n o n - d i a b e t i c patients with chronic kidney disease and proteinuria (13)

I n a n o t h e r s t u d y , t h e e f f e c t o f dapagliflozin was evaluated in nondiabetic patients with heart failure and reduced ejection fraction (14) In the remaining 7 studies, SGLT2 inhibitors were administered in populations that included both patients with type 2 diabetes and non-diabetic patients with heart failure (EMPERORPreserved, EMPEROR-Reduced, EMPERIAL, DAPA-HF, DELIVER) or chronic kidney disease (DAPA-CKD, EMPA-Kidney) (15-21)
Data divided by diabetic status were available in two studies in the primary publication (16, 21) In two other studies we obtained from the Authors data presented according to diabetes status (22, 23)
Data extracted by the studies are presented in Supplementary Table 1
Quality assessment and risk of bias analysis
Of the 12 included studies, only one was classified as high risk (14), two studies were classified as having some
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 114
D a t a b a s e s e a r c h r e s u l t e d i n 3 8 7 r e t r i e v e d r e c o r d s
Figure 1. PRISMA flow diagram of the record retrieval and selection process
Odds for urinary tract infections in non-diabetic patients taking SGLT2 inhibitors Odds ratios of single studies and of the pooled analysis are presented The values at the right of the no-effect bar show higher odds of infection in patients treated with SGLT2 inhibitors
concerns (11, 16), and nine studies (10, 12, 13, 15, 17-21) were assessed as low risk of bias (Supplementary Figure 1)
The study classified as high risk was assessed as having high risk of bias for the randomization process and presented some concerns with regard to deviations from intended intervention The other two studies presented some concerns about randomization
Meta-analysis
Meta-analysis was performed on 9 trials in which data were presented separately according to diabetes status
Non-diabetic patients - Urinary tract infectionsSGLT2 inhibitors vs placebo (9 studies)
There was a statistically significant difference in the odds of urinary tract infections in patients treated with SGLT2 inhibitors compared to placebo (OR 1 33, 95% CI: 1 131 57, 9 series,7326 participants, Z = 4 05, p < 0 0001, I2 = 0%) (Figure 2) Although publication bias analysis did not detect a significant asymmetry of the funnel plot (p = 0 31, Egger’s test; p = 0 14, Begg’s test ), the “trim and fill” strate-
gy imputed three missing studies on the left side of the funnel plot (shown in the Supplementary Figure 2); the resulting adjusted odds ratio was 1 30 (95%CI, 1 1-1 55)


Genital infections - SGLT2 inhibitors vs placebo
Similarly, a statistically significant difference in the odds of genital infections was observed when SGLT2 inhibitors were compared to placebo (OR 3 01, 95% CI: 1 93-4 68, 9 series, 7326 participants, Z = 5 74, p < 0 0001, I2 = 0%) (Figure 3) Publication bias analysis did not detect a significant asymmetry of the funnel plot (p = 0 95, Egger’s test; p = 0 29, Begg’s test )

Non-diabetic vs diabetic patients - Urinary tract and genital infections - Treatment with SGLT2 inhibitors (4 studies)
In four studies comparing diabetic vs non-diabetic patients taking SGLT2 inhibitors for heart failure or chronic kidney disease, we did not find a statistically significant difference of the odds for urinary tract infection (OR 1 34, 95% CI: 0 83-1 59, 4 series, 7317 participants, Z = 1 34,
Odds for genital infections in non-diabetic patients taking SGLT2 inhibitors Odds ratios of single studies and of the pooled analysis are presented The values at the right of the no-effect bar show higher odds of infection in patients treated with SGLT2 inhibitors
Odds for urinary tract infection in diabetics vs non-diabetics taking SGLT2 inhibitors Odds ratios of single studies and of the pooled analysis are presented The values at the right of the no-effect bar show higher odds of infection in diabetic patients
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 R Bapir, K Hassan Bhatti, A Eliwa, et al 115
Figure 2.
Figure 3.
Figure 4.
Figure 5.
Odds for genital infection in non-diabetics vs diabetics taking SGLT2 inhibitors Odds ratios of single studies and of the pooled analysis are presented The values at the right of the no-effect bar show higher odds of infection in diabetic patients
Figure 6.
Odds for urinary tract infection in non-diabetics vs diabetics on placebo. Odds ratios of single studies and of the pooled analysis are presented The values at the right of the no-effect bar show higher odds of infection in diabetic patients
Figure 7.
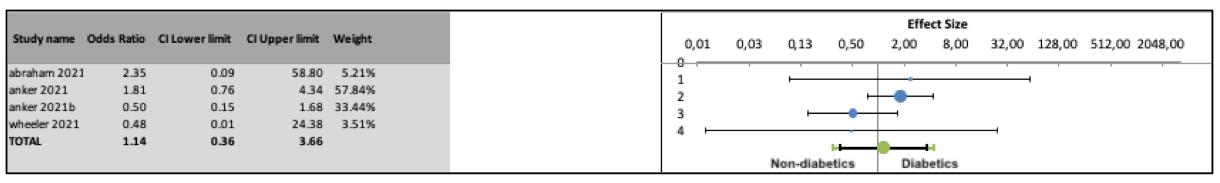
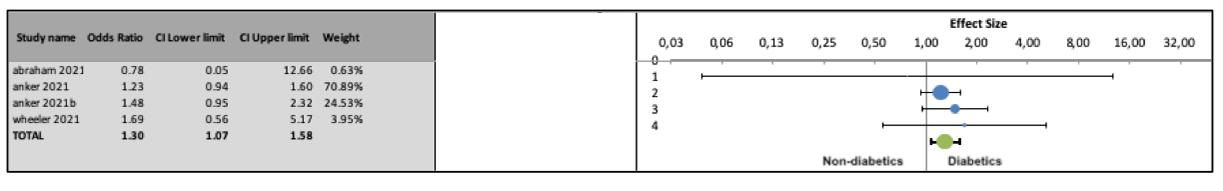
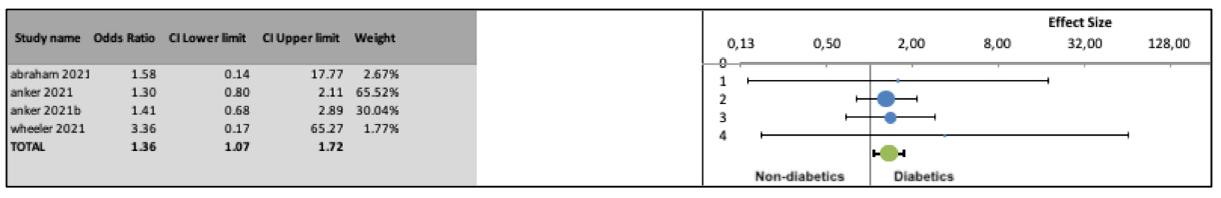
Odds for genital infection in non-diabetics vs diabetics on placebo. Odds ratios of single studies and of the pooled analysis are presented The values at the right of the no-effect bar show higher odds of infection in diabetic patients
p = 0 091, I2 = 0%) (Figure 4) However, significantly higher odds were found in diabetic patients for genital infections (OR 1 36, 95% CI: 1 07-1 72, 4 series, 7317 participants, Z = 4 08, p < 0 0001, I2 = 0% (Figure 5) Although publication bias analysis of the odds for urinary tract infections did not detect a significant asymmetry of the funnel plot (p = 0 09, Egger’s test; p = 0 49, Begg’s test), the “trim and fill” strategy imputed two missing studies on the left side of the funnel plot (shown Supplementary Figure 2); the resulting adjusted odds ratio was 1 11 (95%CI, 0 861 43) Funnel plots of the odds for genital infections showed asymmetry (p = 0 13, Egger’s test; p = 0 042, Begg’s test); two missing studies on the left side of the funnel plot were imputed by “trim and fill” (shown in the Supplementary material); the resulting adjusted odds ratio is significant (1 33; 95%CI, 1 08-1 63)
Urinary tract and genital infections - Placebo (4 studies)
In the same four studies including diabetic vs non-diabetic patients with heart failure or chronic kidney disease taking placebo, we found a statistically significant odds ratio for urinary tract infections (OR 1 30, 95% CI: 1 071 58, 4 series,7312 participants, Z = 4 29, p < 0 0001, I2 = 0%) (Figure 6) Publication bias analysis did not detect a significant asymmetry of the funnel plot (p = 0 75, Egger’s test; p = 0 99, Begg’s test )
The odds for genital infection were not significantly higher in diabetic versus non-diabetic patients taking placebo
(OR 1 14, 95% CI: 0 36-3 66, 4 series,7312 participants, Z = 0 37, p = 0 35, I2 = 7 15%) (Figure 7)
DISCUSSION
The effect of high urinary levels of glucose on the risk of urinary tract and genital infections is not fully investigated Although it is well known that diabetes is an important risk factor for urinary tract infections (24), the possible role of high urine glucose concentrations in the pathogenesis of urinary tract infections has not been confirmed The causes of the increased risk of urinary tract infections in diabetic patients has been attributed to multiple factors including alterations in the immune response, metabolic abnormalities and neurological and nephrological complications (25) In an in-vitro study, addition of glucose (up to a concentration of 1000 mg/dl) to urine enhanced the growth rate of pathogenic urinary isolates (26) In a clinical study higher levels of glucosuria were associated with higher rate of asymptomatic bacteriuria (27), although this finding was not confirmed by other Authors (28) and in a large series of women with either type 1 or type 2 diabetes, glucosuria was not associated with the development of symptomatic urinary tract infections (29)
Treatment with SGLT2 inhibitors of patients with type 2 diabetes was associated with a small increase in incidence of urinary tract infections, with no increase in serious or upper urinary tract infections (30)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 116 Urogenital infection and SGLT2 inhibitors
The role of high urine glucose levels in the pathogenesis of genital mycotic infections in men and women is based on more robust considerations
Candida species are polymorphic fungi that may colonize s
pathogens (31, 32) The first phase of infection is adhesion of yeast forms to receptors on epithelial cells, which is mediated by adhesins and invasins (33) Subsequently, the filamentous hyphae are responsible for the formation of a biofilm on the superficial mucosa of the host (34)
Colonization is favored by a carbohydrate-rich environment, which is a source of energy for producing biofilms that protect fungal cells from external agents (35-37)
The high incidence of genital infections in patients with uncontrolled glycemia can be attributed to different pathophysiological mechanisms (38) Infection can be favored by glucose, a viable nutrient for the growth of the fungi in the urine and in the secretions Furthermore, in vitro studies have shown that high glucose levels facilitate the adhesion of Candida to cells through intercellular adhesion molecule 1 expression (39)
In addition, infections are more frequent in diabetic patients also due to compromised cellular immunity and to functional changes in polymorphonuclear cells, monocytes, and lymphocytes (40)
Meta-analyses including large populations of patients with type 2 diabetes treated with SGLT2 inhibitors demonstrated an up-to-four times increased risk of genital yeast infections for both genders in comparisons with placebo or other anti-hyperglycemic medications (41) According to some authors, the risk of Candida colonization and infection after SGLT2 inhibitors is even higher in real world practice (42)
Yokoyama et al (42) found that among the patients who were initially negative for Candida, 37% converted to a positive culture after treatment with SGLT2 inhibitors and 16% developed symptomatic vulvovaginitis This finding can be explained by urinary glucose excretion and the subsequent deposition of urine with high glucose content on the genital mucosa On the other hand, the magnitude of the glucosuric effect of SGLT2 inhibitors in non-diabetic patients may be less pronounced than the one observed in diabetic patients In a phase 1 study in healthy men, canagliflozin (i) decreased in a dosedependent fashion the renal threshold for glucose, with maximal reduction to approximately 60 mg/dl, (ii) increased mean 24-h urinary glucose excretion and (iii) reduced postprandial plasma glucose (43) In another phase 1 study, canagliflozin significantly increased 24-h urinary glucose excretion in obese patients, but there were no significant changes in fasting plasma glucose and mean 24-h plasma glucose (44) In a phase 2b study in overweight and obese subjects without type 2 diabetes, mean 24-h urinary glucose excretion of 45-60 g was observed after canagliflozin administration (10) The effect of SGLT2 inhibitors on glucose excretion may be different in euglycemic subjects compared to diabetic patients because of SGLT1 activity SGLT1 is a low-capacity, high-affinity transporter that mediates approximately 5% of glucose reabsorption in the S3 (distal) segment of the proximal tubule whereas SGLT2 is a high-capacity, low-affinity glucose transporter which is responsible for
the reabsorption of approximately 90-95% of glucose in the S1 and S2 segments of the proximal tubule (45)
Conversely, when SGLT2 is inhibited, a larger rate of glucose is reabsorbed by SGLT1, resulting in excretion of only 50-60% of filtered glucose (46) In fact, animal studies confirmed that the contribution of SGLT1 to renal glucose reabsorption is greater under lower glycemic conditions than under hyperglycemic conditions (47)
In our meta-analysis, the risk of genital infections and, to a lesser extent, of urinary tract infections was increased also in non-diabetic patients taking SGLT2 inhibitors Similarly, a previous meta-analysis showed no statistically significant different rates of genital and urinary tract infections in large series of patients taking SGLT2 inhibitors for treating type 2 diabetes or heart failure or chronic renal disease (48)
Our meta-analysis also demonstrated that odds of genital infection after taking SGLT2 inhibitors are higher in diabetic patients than in non-diabetics
Diabetic status is therefore a risk factor for genital infections in patients taking SGLT2 inhibitors, although a primary care database study did not find an increased risk of infection in patients with higher HbA1c levels (49) However, even non-diabetic patients treated with SGLT2 inhibitors must be carefully monitored for the onset of genital infections, especially in the presence of risk factors such as female gender, higher BMI and history of previous genital infection that are independently associated with risk for genital infection in patients treated with SGLT2 inhibitors (49) Similarly, male patients with foreskin phimosis may be at increased risk of developing a fungal infection because the moist, warm space underneath the foreskin promotes yeast growth, especially when hygiene is poor
CONCLUSIONS
Genital infections in patients taking SGLT2 inhibitors are usually easily treated with appropriate antimycotic treatment However, SGLT2 inhibitors may significantly increase the risk of serious infections For this reason, it is advisable to adequately inform patients, who must be aware of the possible risks of genital infection Increased hygiene measures should be recommended (e g , frequent washing of the genital area, if possible after each urinat i o n ) S u b g r o u p s o f p a t i e n t s s h o w i n g a m a r k e d l y increased risk of genital infections when treated with SGLT2 inhibitors should be identified for closer follow up; prophylactic administration of antimycotic drugs to prevent candidiasis should be considered (50) Circumcision surgery may be suggested in selected cases
REFERENCES
1 Monami M, Nardini C, Mannucci E Efficacy and safety of sodium glucose co-transport-2 inhibitors in type 2 diabetes: a meta-analysis of randomized clinical trials Diabetes Obes Metab 2014; 16:457-66
2 Butler J, Usman MS, Khan MS, et al Efficacy and safety of SGLT2 inhibitors in heart failure: systematic review and meta-analysis ESC Heart Fail 2020; 7:3298-3309
3 Hallow KM, Helmlinger G, Greasley PJ, et al Why do SGLT2
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 R
K
A Eliwa, et al 117
Bapir,
Hassan Bhatti,
i
a n d m u c o s a l s u r f a c e s a c t i n g a s o p p o r t u n i s t i c
k
n
Urogenital infection and SGLT2 inhibitors
inhibitors reduce heart failure hospitalization? A differential volume regulation hypothesis Diabetes Obes Metab 2018; 20:479-487
4 Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al DAPACKD Trial Committees and Investigators Dapagliflozin in Patients with Chronic Kidney Disease N Engl J Med 2020; 383:1436-1446
5 Zheng H, Liu M, Li S, et al Sodium-Glucose Co-Transporter-2 Inhibitors in Non-Diabetic Adults With Overweight or Obesity: A Systematic Review and Meta-Analysis Front Endocrinol (Lausanne) 2021; 12:706914
6 Puckrin R, Saltiel MP, Reynier P, et al SGLT-2 inhibitors and the risk of infections: a systematic review and meta-analysis of randomized controlled trials Acta Diabetol 2018; 55:503-514
7 Li D, Wang T, Shen S, et al Urinary tract and genital infections in patients with type 2 diabetes treated with sodium-glucose co-transporter 2 inhibitors: A meta-analysis of randomized controlled trials Diabetes Obes Metab 2017; 19:348-355
8 Moher D, Liberati A, Tetzlaff J, et al Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement PLoS Med 2009; 6:e1000097
9 Sterne JAC, Savovic J, Page MJ, et al RoB 2: a revised tool for assessing risk of bias in randomised trials BMJ 2019; 366:l4898
10 Bays HE, Weinstein R, Law G, Canovatchel W Canagliflozin: effects in overweight and obese subjects without diabetes mellitus Obesity (Silver Spring) 2014; 22:1042-9
11 Hollander P, Bays HE, Rosenstock J, et al Coadministration of C a n a g l i fl o z i n a n d P h e n t e r m i n e f o r W e i g h t M a n a g e m e n t i n
Overweight and Obese Individuals Without Diabetes: A Randomized Clinical Trial Diabetes Care 2017; 40:632-639
12 Lundkvist P, Pereira MJ, Katsogiannos , et al Dapagliflozin once daily plus exenatide once weekly in obese adults without diabetes: Sustained reductions in body weight, glycaemia and blood pressure over 1 year Diabetes Obes Metab 2017; 19:1276-1288
13 Cherney DZI, Dekkers CCJ, Barbour SJ, et al DIAMOND investigators Effects of the SGLT2 inhibitor dapagliflozin on proteinuria in non-diabetic patients with chronic kidney disease (DIAMOND): a r a n d o m i s e d , d o u b l e - b l i n d , c r o s s o v e r t r i a l L a n c e t D i a b e t e s Endocrinol 2020; 8:582-593
14 Reis J, Teixeira AR, Gonçalves AV, et al Dapagliflozin Impact on the Exercise Capacity of Non-Diabetic Heart Failure with Reduced Ejection Fraction Patients J Clin Med 2022; 11:2935
15 Anker SD, Butler J, Filippatos G, et al EMPEROR-Preserved Trial Investigators Empagliflozin in Heart Failure with a Preserved Ejection Fraction N Engl J Med 2021; 385:1451-1461
16 Abraham WT, Lindenfeld J, Ponikowski P, et al Effect of empagliflozin on exercise ability and symptoms in heart failure patients with reduced and preserved ejection fraction, with and without type 2 diabetes Eur Heart J 2021; 42:700-710
17 The EMPA-KIDNEY Collaborative Group; Herrington WG, Staplin N, Wanner C, et al Empagliflozin in Patients with Chronic Kidney Disease N Engl J Med 2023; 388:117-127
18 McMurray JJV, Solomon SD, Inzucchi SE, et al DAPA-HF Trial Committees and Investigators Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction N Engl J Med 2019; 381:1995-2008
19 Packer M, Anker SD, Butler J, et al EMPEROR-Reduced Trial Investigators Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure N Engl J Med 2020; 383:1413-1424
20 Solomon SD, McMurray JJV, Claggett B, et al DELIVER Trial
Committees and Investigators Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction N Engl J Med 2022; 387:1089-1098
21 Wheeler DC, Stefánsson BV, Jongs N, et al DAPA-CKD Trial Committees and Investigators Effects of dapagliflozin on major adverse kidney and cardiovascular events in patients with diabetic and non-diabetic chronic kidney disease: a prespecified analysis from the DAPA-CKD trial Lancet Diabetes Endocrinol 2021; 9:22-31
22 Anker SD, Butler J, Filippatos G, et al Effect of Empagliflozin on Cardiovascular and Renal Outcomes in Patients With Heart Failure by Baseline Diabetes Status: Results From the EMPEROR-Reduced Trial Circulation 2021; 143:337-349
23 https://www g-ba de/bewertungsverfahren/nutzenbewertung/810/ Nutzenbewertungsverfahren zum Wirkstoff Empagliflozin (Neues Anwendungsgebiet: chronische Herzinsuffizienz mit linksventrikulärer Ejektionsfraktion LVEF > 40 %) - Gemeinsamer Bundesausschuss (g-ba de)
24 Fünfstück R, Nicolle LE, Hanefeld M, Naber KG Urinary tract infection in patients with diabetes mellitus Clin Nephrol 2012; 77:40-8
25 Nicolle LE, Capuano G, Fung A, Usiskin K Urinary tract infection in randomized phase III studies of canagliflozin, a sodium glucose co-transporter 2 inhibitor Postgrad Med 2014; 126:7-17
26 Geerlings SE, Brouwer EC, Gaastra W, et al Effect of glucose and pH on uropathogenic and non-uropathogenic Escherichia coli: studies with urine from diabetic and non-diabetic individuals J Med Microbiol 1999; 48:535-539
27 Turan H, Serefhanoglu K, Torun AN, et al Frequency, risk factors, and responsible pathogenic microorganisms of asymptomatic bacteriuria in patients with type 2 diabetes mellitus Jpn J Infect Dis 2008; 61:236-8
28 Geerlings SE, Stolk RP, Camps MJ, et al Asymptomatic bacteriuria may be considered a complication in women with diabetes Diabetes Mellitus Women Asymptomatic Bacteriuria Utrecht Study Group Diabetes Care 2000; 23:744-9
29 Geerlings SE, Stolk RP, Camps MJ, et al Diabetes Women Asymptomatic Bacteriuria Utrecht Study Group Risk factors for symptomatic urinary tract infection in women with diabetes Diabetes Care 2000; 23:1737-41
30 Nicolle LE, Capuano G, Fung A, Usiskin K Urinary tract infection in randomized phase III studies of canagliflozin, a sodium glucose co-transporter 2 inhibitor Postgrad Med 2014; 126:7-17
31 Gunther LS, Martins HP, Gimenes F, et al Prevalence of Candida albicans and non-albicans isolates from vaginal secretions: comparative evaluation of colonization, vaginal candidiasis and recurrent vaginal candidiasis in diabetic and non-diabetic women Sao Paulo Med J 2014; 132:116-20
32 Ciurea CN, Kosovski IB, Mare AD, et al Candida and Candidiasis-Opportunism Versus Pathogenicity: A Review of the Virulence Traits Microorganisms 2020; 8:857
33 Mukaremera L, Lee KK, Mora-Montes HM, Gow NAR Candida albicans Yeast, Pseudohyphal, and Hyphal Morphogenesis Differentially Affects Immune Recognition Front Immunol 2017; 8:629
34 Nikou SA, Kichik N, Brown R, et al Candida albicans Interactions with Mucosal Surfaces during Health and Disease Pathogens 2019; 8:53
35 Rodrigues CF, Rodrigues ME, Henriques M Candida sp Infections in Patients with Diabetes Mellitus J Clin Med 2019; 8:76
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 118
36 Van Ende M, Wijnants S, Van Dijck P Sugar Sensing and Signaling in Candida albicans and Candida glabrata Front Microbiol 2019; 10:99
37 Chandra J, Kuhn D, Mukherjee P, et al Biofilm formation by the fungal pathogen Candida albicans: Development, architecture, and drug resistance J Bacteriol 2001; 183:5385-5394
38 Talapko J, Meštrovic T, Škrlec I Growing importance of urogenital candidiasis in individuals with diabetes: A narrative review World J Diabetes 2022; 13:809-821
39 Mikamo H, Yamagishi Y, Sugiyama H, et al High glucose-mediated overexpression of ICAM-1 in human vaginal epithelial cells increases adhesion of Candida albicans J Obstet Gynaecol 2018; 38:226-230
40 Calvet HM, Yoshikawa TT Infections in diabetes Infect Dis Clin N Am 2001; 15:407-421
41 Alexander JT, Staab EM, Wan W, et al Longer-term Benefits and Risks of Sodium-Glucose Cotransporter-2 Inhibitors in Type 2 Diabetes: a Systematic Review and Meta-analysis J Gen Intern Med 2022; 37:439-448
42 Yokoyama H, Nagao A, Watanabe S, Honjo J Incidence and risk of vaginal candidiasis associated with sodium-glucose cotransporter 2 inhibitors in real-world practice for women with type 2 diabetes J Diabetes Investig 2019; 10:439-445
43 Sha S, Devineni D, Ghosh A, et al Canagliflozin, a novel inhibitor of sodium glucose co-transporter 2, dose dependently reduces calculated renal threshold for glucose excretion and increas-
Correspondence
Rawa Bapir, MD Dr rawa@yahoo com
Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq
Kamran Hassan Bhatti, MD kamibhatti92@gmail com Urology Department, HMC, Hamad Medical Corporation, Qatar
Ahmed Eliwa, MD ahmedeliwafarag@gmail com
Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt
Herney Andrés García-Perdomo, MD herney garcia@correounivalle edu co Universidad del Valle, Cali, Colombia
Nazim Gherabi, MD ngherabi@gmail com
Faculty of Medicine Algiers 1, Algiers, Algeria
Derek Hennessey, MD derek hennessey@gmail com
Department of Urology, Mercy University Hospital, Cork, Ireland
Vittorio Magri, MD vittorio magri@asst-fbf-sacco it Urology Unit, ASST Fatebenefratelli Sacco, Milan, Italy
Panagiotis Mourmouris, MD thodoros13@yahoo com
Lazaros Tzelves, MD lazarostzelves@gmail com
2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece
Conflict of interest: The authors declare no potential conflict of interest
es urinary glucose excretion in healthy subjects Diabetes Obes Metab 2011; 13:669-672
44 Sarich T, Devineni D, Ghosh A, et al Canagliflozin, a novel inhibitor of sodium glucose co-transporter 2, increases 24-hour urinary glucose excretion and reduces body weight in obese subjects over 2 weeks of treatment Diabetologia 2010; 53(Suppl 1):S349-S350
45 Novak LM, Kruger DF Bolstering your armamentarium with SGLT2 inhibitors Nurse Pract 2017; 42:28-34
46 Rieg T, Masuda T, Gerasimova M, et al Increase in SGLT1mediated transport explains renal glucose reabsorption during genetic and pharmacological SGLT2 inhibition in euglycemia Am J Physiol Renal Physiol 2014; 306:F188-93
47 Nagata T, Fukazawa M, Honda K, et al Selective SGLT2 inhibition by tofogliflozin reduces renal glucose reabsorption under hyperglycemic but not under hypo- or euglycemic conditions in rats Am J Physiol Endocrinol Metab 2013; 304:E414-23
48 Staplin N, Roddick AJ, Emberson J, et al Net effects of sodiumglucose co-transporter-2 inhibition in different patient groups: a m e t a - a n a l y s i s o f l a r g e p l a c e b o - c o n t r o l l e d r a n d o m i z e d t r i a l s EClinicalMedicine 2021; 41:101163
49 McGovern AP, Hogg M, Shields BM, et al MASTERMIND consortium Risk factors for genital infections in people initiating SGLT2 inhibitors and their impact on discontinuation BMJ Open Diabetes Res Care 2020; 8:e001238
50 Cooke G, Watson C, Deckx L, et al Treatment for recurrent vulvovaginal candidiasis (thrush) Cochrane Database Syst Rev 2022; 1:CD009151
Adama Ouattara, MD adamsouat1@hotmail com
Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso
Gianpaolo Perletti, Dr Biol Sci M Clin Pharmacol Gianpaolo Perletti@uninsubria it
Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy
Joseph Philipraj, MD josephphilipraj@gmail com
Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India
Konstantinos Stamatiou, MD stamatiouk@gmail com
Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece
Musliu Adetola Tolani, MD adetolatolani@yahoo com
Division of Urology, Department of Surgery, Ahmadu Bello University/ Ahmadu Bello University Teaching Hospital, Zaria, Kaduna State, Nigeria
Stefan D Anker, MD s anker@cachexia de
Department of Cardiology and BCRT (Campus CVK), Charité Universitätsmedizin Berlin, 13353 Berlin, Germany
Alberto Trinchieri, MD (Corresponding Author) alberto trinchieri@gmail com
Urology School, University of Milan, Milan (Italy) ORCID 0000-0002-9394-8292
Noor Buchholz, MD noor buchholz@gmail com
Sobeh's Vascular and Medical Center, Dubai Health Care City, Dubai, United Arab Emirates
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 R
119
Bapir, K Hassan Bhatti, A Eliwa, et al
The presentation and outcomes of penile fracture with associated urethral injury: A systematic literature review
Salah E Shebl
Urology Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
Summary
Purposes: Penile fracture (PF) with associated urethral injury has been described as a rare condition yet a serious urological emergency. We conducted this systematic review to address the current literature concerning the etiology, presentations, intra-operative findings, site of injury, and complications of PF with associated urethral injury, Materials and Methods: The present systematic review was limited to human-based studies published in English language, and reporting clinical data on PF cases with associated urethral injuries A comprehensive search of the literature was conducted on five electronic databases from their inception to May 2022: Medline via PubMed, Web of Science, Google Scholar, Scopus, and EBSCO host.
Results: A total of 15 studies were included encompassing 1671 patients with PF. Out of 1665 patients with PF retrieved from the case series studies, 65 patients had associated urethral injuries giving a point prevalence of 3.9%. The vast majority of the patients had blood on the meatus and hematuria suggestive of urethral injury (57/59; 96 6%) Forty patients had partial urethral disruption and the rest of the patients had a complete rupture All patients received primary urethroplasty as the main modality of treatment The median hospital stay was two days and the median duration of transurethral catheterization was 21 days Five patients (8 5%) developed urethral stricture; other complications included penile curvature (6 7%), palpable fibrosis (6 7%), and erectile dysfunction (3 4%)
Conclusions: Urethral injuries are uncommon, but serious findings, in patients with PF. Primary urethroplasty appears to achieve satisfactory outcomes with a low incidence of short and long-term complications.
KEY WORDS: Penile fracture; Urethra; Urethral injury; Systematic review
Submitted 12 December 2022; Accepted 7 April 2023
INTRODUCTION
Penile fracture (PF) with associated urethral injury has been described as a rare condition yet a serious urological emergency (1) PF is characterized by signification injury of corpus cavernosum anatomy due to profound trauma or manipulation of an erect penis; while traumas to the flaccid penis or the suspensor ligament are not usually considered as PF (2, 3) Commonly, PF is caused by severe bending of the erect penis during sexual intercourse, masturbation, rolling over during sleep, and powerful methods of sexual arousal To a lesser extent, PF can result from direct trauma or fall onto the erect penis The basal and
midshaft penis are the most commonly affected sites by PF (1, 4) Clinically, the onset of PF is usually accompanied by a loud cracking sound, followed by penile localized swelling, bruises, pain, and immediate detumescence Many reviews report that the diagnosis of penis fractures can depend exclusively on clinical findings, based on patient history and physical examination (2, 5)
Multiple studies have reported that a wide diversity of investigations are useful in the diagnosis of PF as X-ray imaging, Doppler ultrasound, retrograde urethrocystography (RGU), flexible cystoscopy, and magnetic resonance imaging (MRI) (6-8) However, it is unnecessary to use radiological investigations in most cases where the history and the clinical examination are sufficient to confirm the diagnosis The X-ray imaging may still be required in some cases, especially in patients with atypical clinical presentation (9) Some authors consider the Doppler ultrasound as the preferred radiological tool for investigating penile trauma cases given that it is a non-invasive and inexpensive procedure On the other hand, MRI is the most accurate test in diagnosing the PF as it shows high contrast resolution between tissues and identifies the pathological processes of soft tissues Studies also reported that it can be used in the evaluation of the urethral injury, although it is not commonly used because of its low cost-effectiveness and long execution time (10, 11) RUG is the gold standard for urethra evaluation The RUG is easy to perform on trauma patients at the bedside: 20 to 30 mL of diluted watersoluble contrast is injected into the urethral meatus, before x-raying A positive RUG will show contrast outside the urethral serpentine cylinder Retrograde urethrograms are sensitive in detecting urethral injuries but can't pinpoint their location and are operator-dependent (12)
Previous reports demonstrated that urethral injuries are present in 1-38% of the PF cases Patients with an associated urethral injury can present with blood at the meatus, leading to hematuria and urinary retention (5, 13, 14) However, these findings are not specific as previous case reports indicated that some PF cases with associated urethral injuries had no suspected symptoms Thus, investigations, particularly urine analysis and retrograde urethrogram (RGU), are of paramount importance for identifications of associated urethral injuries (15) Accurate identification of urethral injuries is critical before PF repair to avoid the risk of postoperative complications, including urethral stricture and urethrocutaneous fistula (16) However, due to the rarity of the disease, little literature has been published so
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 120
REVIEW
DOI: 10 4081/aiua 2023 11082
far concerning the presentation and outcomes of PF with associated PF Therefore, we conducted this systematic review to address the current literature concerning the etiology, presentations, intra-operative findings, site of injury, and complications of PF with associated urethral injury
MATERIALS AND METHODS
The present systematic review receives PROSPERO ID 342298 and adhered to the recommendations of the recent version of the Cochrane Collaboration Handbook and the MOOSE statement (17, 18)
Eligibility criteria and literature search
The present systematic review was limited to human-based studies, published in the English language, and reporting clinical data on PF cases with associated urethral injuries There were no limitations regarding the date of publication or study design Studies were excluded if they were review articles, duplicate datasets, or they had no separate data on patients with associated urethral injuries Besides, we excluded conference abstracts with no available full texts

A comprehensive literature search was conducted on five electronic databases from their inception to May 2022
These bibliographic databases were: Medline via PubMed, Web of Science, Google Scholar, Scopus, and EBSCO host Various combinations of the following queries were utilized: penile, penis, fracture, injury, urethra Following the literature search, retrieved citations were imported to EndNote X7 for duplicates removal Unique records were then screened through two stages: the first stage was a screening by titles and abstracts, while the second stage was an full-text evaluation of potentially eligible abstracts for final inclusion in the present systematic review
Quality assessment
The quality assessment of the included case reports and case series was conducted using Murad's tool (19), which is specifically designed to evaluate the methodological quality of case reports and case series
This tool consists of eight criteria that cover four primary domains: selection, ascertainment, causality, and reporting
Two independent reviewers conducted the quality assessment of the included studies, in case of any discrepancies
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 S E Shebl 121
Figure 1 PRISMA flow diagram.
The presentation and outcomes of penile fracture with associated urethral injury
between the reviewers, a consensus was reached through discussion or, if necessary, by involving a third reviewer
Data extraction
Standardized data extraction was done using Excel software for data retrieval and processing The following data were extracted from each eligible study: year of publication, country, study design, number of patients with PF, number of cases with confirmed urethral injuries, cause of PF, presentation of urethral injury, location of the injury, intraoperative findings, need for supra-pubic cystostomy tube, treatment, complications, hospital stay, and duration of follow-up
RESULTS
A total of 7242 records were retrieved from online search and 12 records were identified by manual searching Of them, 4201 records were screened after duplicates removal After the initial screening, 55 full texts were retained for a full evaluation Out of them, 40 studies were excluded as they were narrative or systematic review (n = 8), animal models (n = 3), irrelevant (n = 16), simulation-based studies (n = 6), or they had no data on urethral injuries (n = 7) Finally, 15 studies were included in the present systematic review (See PRISMA flow diagram; Figure 1)
General characteristics of the included studies and prevalence of urethral injuries
Six retrospective studies (20-25), two prospective study (26, 27), and seven case reports were included in the present systematic review (21, 28-34) Two from India, two from Egypt, two from the United States, and one from Serbia, Italy, Slovenia, Canada, China, Peru, Tunisia, Brazil and UK each The median time from injury to presentation was six hours (range 1-48 5 hours) and the median time of follow-up was 21 months (1-107 months) A total of 1671 patients with PF were retrieved from the included studies Out of them, 65 patients had associated urethral injuries giving a point prevalence of 3 9% (Table 1)
Quality assessment of included studies
The quality assessment of the included studies was conducted using Murad's tool In terms of selection, eight studies did not report that this was their whole experience on penile fracture or provide a clear selection process Regarding ascertainment, the majority of the studies (14 out of 15) adequately ascertained exposure and outcomes, while one study failed to do so Alternative causes that could explain the observation were clearly ruled out in 12 of the included studies Most studies (10 out of 15) adequately followed their patients, while five studies lacked sufficient follow-up period
Reporting: The majority of the studies (11 out of 15) provided sufficient details to allow other investigators to replicate the research or practitioners to make inferences related to their own practice However, four studies did not provide enough details in their reports Overall, the quality assessment revealed that most studies had adequately ascertained exposure and outcome, and provided sufficient reporting details However, some studies did not meet all the causality criteria (Supplementary Table 1)
Presentation of the included cases
Among the 65 patients with associated urethral injuries, the most common cause of fracture was sexual intercourse (41/65; 69%), followed by masturbation (8/65; 13 5%) and rolling over (6/65; 10 1%) With regard to the classic presentation of PF, the most common presentations were hematoma (34/65; 57%) and penile swelling (33/65; 55 9%), followed by Aubergine sign/egg-plant deformity (30/65; 50 8%) and crackling sound (29/65; 49 1%) The vast majority of the patients had blood on the meatus and hematuria suggestive of urethral injury (57/65; 87 6%) The most commonly affected location of the included patients was proximal shaft (21/65; 35 5%) followed by midshaft (19/65; 32 2%) The vast majority of the patients had unilateral corporal involvement (54 2%), mainly on the right side (30 5%) Forty patients had partial urethral disruption and the rest of the patients
Table 1.
General characteristics of the included studies
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 122
Authors, Year Countr y Study design Median time from the time Mean Hospital Total cases Confir med of injur y to the time of follow-up stay of penile urethral presentation to the Hospital (months) (days) fracture injur y Am t et al, 2013 (20) India Retrospective case series NA 34 3 2 34 8 Kasaraneni et al, 2019 (27) India Prospective observational 6 24 2 75 12 Derouiche et al, 2007 (22) Tunisia Retrospective case series 10 18 14 312 10 Raheem et al, 2014 (6) Egypt Retrospective case series 5 5 72 6 2 1 246 12 Ibrah em et al, 2010 (23) Egypt Retrospective case series 48 5 107 2 3 155 14 Barros et a , 2018 (26) Brazil Prospective observational NA NA NA 175 27 Mercado-Olivares et a , 2018 (34) Peru Case Report 19 NA NA 281 1 Ouanes et al, 2021 (24) Tunisia Retrospective case series 1 to 5 12 NA 138 15 Hughes et al, 2021 (33) UK Case Report NA NA NA 11 Boncher et al, 2010 (39) USA Case Report 8 48 NA 11 Tang et a , 2018 (25) USA Retrospective case series 1 2 ± 1 03 21 (1-73) NA 62 13 Ge et al, 2021 (31) China Case Report NA 12 NA 11 Garofalo et al, 2015 (30) Italy Case Report 1 12 211 Jagod c et al, 2007 (29) Slovenia Case Report 6 12 13 11 Hoag et al, 2011 (28) Canada Case Report 11211
Table 2.
The distribution of causes and presentations among the included patients.
had a complete rupture Two studies reported the utilization of RGU for the evaluation of PF and associated urethral injuries (Tables 2 and 3)
Treatment and outcomes of the included cases
All patients received primary urethroplasty as the main modality of treatment
Besides, 15 patients needed a supra-pubic cystostomy tube Fifty-one patients received medications to prevent erection in the form of estradiol, diazepam, sildenafil, and amyl nitrite The median hospital stay was two days and the median duration of transurethral catheterization was 21 days Five patients (8 5%) developed urethral stricture; other complications included penile curvature (6 7%),
palpable fibrosis (6 7%), and erectile dysfunction (3 4%) (Table 4)
DISCUSSION
Urethral injuries can concurrently occur in patients with PF and a considerable proportion of these injuries are missed at initial diagnosis, despite being widely considered as a serious complication If not discovered and managed early, associated urethral injuries can dramatically lead to short and long-term complications in patients with PF (2) However, due to the rarity of the disease, little literature has been published so far concerning the presentation and outcomes of PF with associated urethral injury
Table 3
The distribution of intraoperative findings and location of injury among the included patients
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 S E Shebl 123
Authors, year Intra operative findings Location of injur y Par tial Complete Proximal Midshaft Distal Bilateral Unilateral Right Left urethral urethral shaft shaft corporal corporal corporal corporal disr uption disr uption of penis of penis involvement involvement involvement involvement Am t et al, 2013 (20) 716 NA NA 1752 Kasaraneni et al, 2019 (27) 11 16241 11 46 Derouiche et al, 2007 (22) 10 05410 10 64 Raheem et al, 2014 (6) 1 11 0 12 0 12 000 Ibrah em et al, 2010 (23) 11 3 NA NA NA NA NA NA NA Barros et a , 2018 (26) NA NA NA NA NA NA NA NA NA Mercado-Olivares et a , 2018 (34) NA NA 0010110 Ouanes et al, 2021 (24) NA NA 118 0 20 0 138 NA NA Hughes et al, 2021 (33) NA NA 0010101 Boncher et al, 2010 (39) NA NA 0010110 Tang et a , 2018 (25) NA NA 23 18 21 NA NA NA NA Ge et al, 2021 (31) 01100 NA NA NA NA Garofalo et al, 2015 (30) 011000110 Jagod c et al, 2007 (29) 01100 NA NA NA NA Hoag et al, 2011 (28) 011001000
Authors, year Causes of penile fractures Presentation of penile fracture Sexual Rolling Blunt Forced Masturbation Urethral Hematoma Crackling Penile Bladder Aubergine Retention intercourse over injur y penile bleed or sound swelling palpable sign/egg-plant of urine pending eccymosis defor mity Amit et al, 2013 (20) 600026060 NA 6 NA Kasaraneni et al, 2019 (27) 92100 11 0703 12 3 Derouiche et al, 2007 (22) 04006 10 0 10 02 10 2 Raheem et al, 2014 (6) 11 0010 12 12 0 12 003 Ibrahiem et al, 2010 (23) 7 NA NA 0 NA 13 14 NA 14 00 NA Barros et al, 2018 (26) 69 005 16 NA NA NA NA NA NA NA Mercado-Ol vares et al, 2018 (34) 100000100000 Ouanes et al, 2021 (24) 47 NA NA 62 NA NA NA NA NA NA NA NA Hughes et al, 2021 (33) 100001110000 Boncher et al, 2010 (39) 100000111010 Tang et al, 2018 (25) 41 00 19 2 12 44 34 62 000 Ge et al, 2021 (31) 100001111000 Garofalo et al, 2015 (30) 101001111000 Jagodic˘et al, 2007 (29) 100001111101 Hoag et a , 2011 (28) 101001101000
Table 4.
The treatment and outcomes of injury among the included patients.
Therefore, we conducted this systematic review to address the current literature concerning the PF with associated urethral injury Our results highlighted that there are currently 65 published cases of PF with associated urethral injuries giving a point prevalence of 3 9% Such findings are in line with a large case-series of 312 PF cases from the Middle East, in which ten cases had associated urethral injuries (22) Other reports from the Middle East reported similar findings (35) On the contrary, reports from Europe and the United States demonstrated a much higher prevalence of associated urethral injuries, affecting up to onethird of PF cases (36-38) It is not clear why patients from the Middle East had a lower prevalence of associated urethral injuries; however, it was reported that a large number of PF in the Middle East is attributed to the widespread practice of “taghaandan” , which is a low-energy trauma with a low possibility of urethral injuries (35, 32) We also postulated that the low prevalence of associated urethral injuries can be attributed to a large number of pooled cases with PF from the Middle East and the dependence on clinical examination, without further investigations, which might have led to under-detection of associated urethral injuries
As previously mentioned, the proximal and midshaft penis are the most commonly affected sites by PF; while sexual intercourse and masturbation account for the vast majority of PF (1, 4) These findings appear to apply also to patients with associated urethral injuries; in this review, we found that the most common cause of fracture was sexual intercourse, followed by masturbation and rolling over; while the majority of the cases had proximal and midshaft fractures Clinically, the presence of urethral injuries is suspected when there is blood at the meatus, with or without hematuria, on examination; besides, urine analysis and RGU can be useful for identifications of associated urethral injuries (15) However, as demonstrated by this systematic review, some PF cases may not exhibit specific symptoms for urethral injuries (see Table 3) Besides,
urine analysis and RGU exhibited false-negative results in some case-series (15, 39) Thus, a careful intraoperative inspection of the urethra is recommended in all cases with PF to avoid missed injuries
To our knowledge, there is no published systematic review that has attempted to explore the presentation and outcomes of PF cases with associated urethral injuries; nonetheless, we acknowledge the existence of several limitations in our review All included studies suffered from substantial methodological flaws that can affect the quality and generalizability of our findings The outcome measurements are subjective and postoperative erectile and voiding functions have not been assessed using validated tools In conclusion, urethral injuries are uncommon, but serious findings, in patients with PF The clinical presentation of patients with urethral injuries usually involves urethral bleeding and hematuria The diagnosis of associated urethral injuries can be established by clinical examination with the limited role of imaging studies Thus, a careful intraoperative inspection of the urethra is recommended in all cases with PF in order to avoid missed injuries Primary urethroplasty appears to achieve satisfactory outcomes with a low incidence of short and longterm complications Nonetheless, the current published literature is still limited by the low number of published cases and low quality of published reports; thus, further studies are needed to characterize the presentation and outcomes of PF with association urethral injuries
ACKNOWLEDGMENT
The authors thank the study participants, trial staff, and investigators for their participation
REFERENCES
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 124 The presentation and outcomes of penile fracture with associated urethral injury
1 Mahapatra RS, Kundu AK, Pal DK Penile Fracture: Our Experience in a Tertiary Care Hospital World J Mens Health 2015; 33:95
Authors, year Treatment Supra-pubic Medication Median duration Hospital Complications cystostomy to prevent of transurethral stay Penile Palpable Erectile Stricture UTI tube erection catheterization (days) (days) cur vature fibrosis dysfunction urethra Amit et al, 2013 (20) Primary urethroplasty Not used Estradiol 21 200100 Kasaraneni et al, 2019 (27) Primary urethroplasty Not used Estradiol 21 210012 Derouiche et al, 2007 (22) Primary urethroplasty Used Diazepam 13 14 00000 Raheem et al, 2014 (6) Primary urethroplasty Used in 5 patients Sildenafil® 22 5 2 1 23110 Ibrahiem et al, 2010 (23) Primary urethroplasty Not used PGE1 NA 2 3 NA 1 NA 10 Barros et al, 2018 (26) NA NA NA NA NA NA NA NA NA NA Mercado-Olivares et al, 2018 (34) Primary urethroplasty NA NA NA NA 00000 Ouanes et al, 2021 (24) Primary urethroplasty NA NA NA NA NA NA NA NA NA Hughes et al, 2021 (33) Primary urethroplasty NA NA NA NA NA NA NA NA NA Boncher et al, 2010 (39) Primary urethroplasty NA Diazepam 28 NA 00000 Tang et al, 2018 (25) Primary urethroplasty Used amyl nitate NA NA 00000 Ge et al, 2021 (31) Primary urethroplasty NA NA 12 NA NA NA NA NA NA Garofalo et al, 2015 (30) Primary urethroplasty Used NA NA 210010 Jagodic et al, 2007 (29) Primary urethroplasty Used Diazepam 12 13 00010 Hoag et a , 2011 (28) Primary urethroplasty Used NA 28 2 NA NA NA NA NA
2 Eke N Fracture of the penis Br J Surg 2002; 89:555-65
3 El-Sherif AE, Dauleh M, Allowneh N, Vijayan P Management of Fracture of the Penis in Qatar Br J Urol 1991; 68:622-5
4 Ateyah A, Mostafa T, Nasser TA, et al Penile fracture: Surgical repair and late effects on erectile function J Sex Med 2008; 5:1496502
5 Zargooshi J Sexual function and tunica albuginea wound healing following penile fracture: An 18-year follow-up study of 352 patients from Kermanshah, Iran J Sex Med 2009; 6:1141-50
6 Raheem AA, El-Tatawy H, Eissa A, et al Urinary and sexual functions after surgical treatment of penile fracture concomitant with complete urethral disruption Arch Ital Urol Androl 2014; 86:15-9
7 Kamdar C, Mooppan UMM, Kim H, Gulmi FA Penile fracture: Preoperative evaluation and surgical technique for optimal patient outcome BJU Int 2008; 102:1640-4
8 Saglam E, Tarhan F, Hamarat MB, et al Efficacy of magnetic resonance imaging for diagnosis of penile fracture: A controlled study Investig Clin Urol 2017; 58:255-60
9 Pavan N, Tezzot G, Liguori G, et al Penile fracture: retrospective analysis of our case history with long-term assessment of the erectile and sexological outcome Arch Ital Urol Androl 2014; 86:359-70
10 Choi MH, Kim B, Ryu JA, et al MR imaging of acute penile fracture Radiographics 2000; 20:1397-405
11 Murray KS, Gilbert M, Ricci LR, et al Penile fracture and magnetic resonance imaging Int Braz J Urol 2012; 38:287-8
12 Rosenstein DI, Alsikafi NF Diagnosis and Classification of Urethral Injuries Urol Clin North Am 2006; 33:73-85
13 Koifman L, Cavalcanti AG, Manes CH, et al Penile fractureExperience in 56 cases Int Braz J Urol 2003; 29:35-9
14 Mydlo JH Surgeon experience with penile fracture J Urol 2001; 166:526-9
15 Gedik A, Kayan D, Yamis S, et al The diagnosis and treatment of penile fracture: our 19-year experience Ulus Travma Acil Cerrahi Derg 2011; 17:57-60
16 Shaeer O Methylene blue-guided repair of fractured penis J Sex Med 2006; 3:349-54
17 Higgins JPT, Thomas J, Chandler J, et al Cochrane handbook for s y s t e m a t i c r e v i e w s o f i n t e r v e n t i o n s C o c h r a n e H a n d b o o k f o r Systematic Reviews of Interventions 2019, pp 1-694
18 Stroup DF, Berlin JA, Morton SC, et al Meta-analysis of Observational Studies in EpidemiologyA Proposal for Reporting JAMA 2000; 283:2008-12
19 Murad MH, Sultan S, Haffar S, Bazerbachi F Methodological quality and synthesis of case series and case reports BMJ Evid Bas Med 2018; 23:60-3
20 Amit A, Arun K, Bharat B, et al Penile fracture and associated urethral injury: Experience at a tertiary care hospital J Can Urol Assoc 2013; 7:E168-70
21 Raheem AA, El-Tatawy H, Eissa A, et al Urinary and sexual functions after surgical treatment of penile fracture concomitant with complete urethral disruption Arch Ital Urol Androl 2014; 86:15-9
22 Derouiche A, Belhaj K, Hentati H, et al Management of penile fractures complicated by urethral rupture Int J Impot Res 2008; 20:111-4
23 Ibrahiem EHI, El-Tholoth HS, Mohsen T, et al Penile fracture: long-term outcome of immediate surgical intervention Urology 2010; 75:108-11
24 Ouanes Y, Saadi MH, Haj Alouene H, et al Sexual Function
Outcomes After Surgical Treatment of Penile Fracture Sex Med 2021; 9:100353
25 Tang Z, Yang L, Wei Q, et al Management and outcomes of penile fracture: a retrospective analysis of 62 cases with long-term assessment Asian J Androl 2018; 20:412
26 Barros R, Silva MIS, Antonucci V, et al Primary urethral reconstruction results in penile fracture Ann R Coll Surg Engl 2018; 100:21-5
27 Kasaraneni P, Mylarappa P, Gowda RD, et al Penile fracture with urethral injury: Our experience in a tertiary care hospital Arch Ital Urol Androl 2019; 90:283-7
28 Hoag NA, Hennesse K, So A Penile fracture with bilateral corporeal rupture and complete urethral disruption: case report and literature review Can Urol Assoc J 2011; 5:E23
29 Jagodic K, Erklavec M, Bizjak I, et al A case of penile fracture with complete urethral disruption during sexual intercourse: a case report J Med Case Rep 2007; 1:14
30 Garofalo M, Bianchi L, Gentile G, et al Sex-related penile fracture with complete urethral rupture: A case report and review of the literature Arch Ital Urol Androl 2015; 87:260-1
31 Ge G, Wang H, Chen Y, et al Complete urethral injury in the penile fracture: a case report and literature review Transl Androl Urol 2021; 10:969
32 Boncher NA, Vricella GJ, Jankowski JT, et al Penile Fracture w
2010:791948
33 Hughes S, Elbaroni W, O’donoghue J, Williams M Atypical presentation of a vertical penile fracture BMJ Case Reports CP 2021; 14:e243353
34 Mercado-Olivares F, Antonio Grandez-Urbina J, Farfan-Daza G, et al Case Report: Double penile fracture F1000Research 2018; 7 F1000Res 2018; 7:1828
35 Zargooshi J Penile fracture in Kermanshah, Iran: report of 172 cases J Urol 2000; 164:364-6
36 Fergany AF, Angermeier KW, Montague DK Review of Cleveland Clinic experience with penile fracture Urology 1999; 54:352-5
37 Bitker MO, Belin J, Jardin A, Chatelain C “Faux pas du coit” with associated rupture of corpora cavernosa and urethra Urology 1988; 32:447-8
38 Agarwal MM, Singh SK, Sharma DK, et al Fracture of the penis: a radiological or clinical diagnosis? A case series and literature review Can J Urol 2009; 16:4568-75
39 Mydlo JH, Hayyeri M, Macchia RJ Urethrography and cavernosography imaging in a small series of penile fractures: A comparison with surgical findings Urology 1998; 51:616-9
Correspondence
Salah E Shebl, MD (Corresponding Author) salahshebl@yahoo com salahshebl@azhar edu eg Urology Department, Faculty of medicine for girls Al-Azhar University Urology Department, Alzahraa University Hospital, Cairo, Egypt
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 S E Shebl 125
i t h A s s o c i a t e d U r e t h r a l R u p t u r e C a s e R e p M e d 2 0 1 0 ;
Role of spinal anesthesia in robot-assisted radical prostatectomy: Gamble or opportunity?
1 Urology Unit, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli", Naples, Italy;
2 Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples “Federico II”, Naples, Italy;
3 Urology Unit, Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples
II", Naples
Submitted 14 March 2023; Accepted 23 March 2023
To the Editor,
Although postoperative pain associated with robot-assisted radical prostatectomy (RARP) is less than pain following the open technique, it remains a fundamental issue as it can be a significant source of discomfort for the patient and lengthen recovery times after surgery The optimal management of pain after RARP is far from being fully elucidated and many factors have to be evaluated to choose the best analgesic approach (1) Pain management in the postoperative period is classically achieved through the administration of intermittent or continuous intravenous drugs; opioids and non-steroidal anti-inflammatory drugs (NSAIDs) represent the cor nerstones of this approach These drugs have many potential adverse effects (AEs) NSAIDs can affect renal and platelet function leading to kidney injury and significant bleeding, while opioids can be associated with delayed recovery of gut motility, urinary retention, dizziness, nausea, vomiting, and immunosuppression (2) Spinal anesthesia is emerging as an alter native technique to control the postoperative pain or even to avoid general anesthesia not only in urological but also in cardiac, gynecological, and spine laparoscopic and robotic surgery (Table 1) (3-6) It allows to reduce the drugs dosage and, consequently, their AEs However, several additional advantages can be identified Spinal anesthesia is performed before the induction of general anesthesia and its analgesic effect covers also the intraoperative period, so lower dosage of intraoperative opioids can be used along with lower minimum alveolar concentration of inhalational anesthetics, thus leading to an important reduction of postoperative nausea and vomiting along with a faster recovery of consciousness after general anesthesia; furthermore, the reduction of analgesic drugs during anesthesia can contribute to the hemodynamic stability Recently, some concer ns have been raised about the immunosuppressive effect of opioids and, consequently, the potential risk of promoting metastatic spread of cancer cells; therefore, reducing opioid administration in the perioperative period is even more important (7) Pikramenos et al reported their experience in 60 men, underwent combined spinal/epidural anaesthesia during radical retropubic prostatectomy: They showed that combined spinal/epidural anaesthesia is a safe procedure to perform and is associated with less intraoperative blood loss and potentially reduced risks of postoperative complications (8)
The role of spinal anesthesia should also be considered in the management of the bladder spasm and the discomfort due to urethral catheter which can impact on the patient satisfaction and on the ability to early recover autonomous walking, with possible dramatic consequences on the risk of thromboembolism and on the length of hospital stay (9) Interestingly, several adjuvants can be added to the solution injected in the subarachnoid space thus increasing the ability to achieve the desired effects with very small amounts of drugs Ketamine, dexmedetomidine, midazolam, and clonidine are some examples of drugs which are commonly used with or without opioids to prolong and/or potentiate the effect of the local anesthetic Many combinations of these drugs for spinal anesthesia have so far been reported in literature and appropriate use of their different pharmacological properties can be employed to manage not only postoperative pain but also intraoperative analgesia, allowing RARP to be performed only with spinal anesthesia and light sedation No study is currently available on the topic, however, as part of a clinical trial, we have begun performing the first cases of RARP under spinal anesthesia in our center, with encouraging preliminary results demonstrating the feasibility and potential of this novel technique
Some authors have expressed concerns regarding the risk-benefit ratio of spinal anesthesia, as this technique can cause severe AEs An accidental puncture of an epidural blood or a spinal nerve can lead to permanent injuries such as motor and sensory loss of the lower limbs, loss of sphincters continence, and typical neuropathic symptoms These complications are actually very rare; for example, the reported incidence of spinal hematoma is about 1:220,000 cases and a careful medical history along with appropriate management of anti-platelet and anticoagulant drugs can significantly reduce the risk (10)
Absolute contraindications to spinal anesthesia are patient refusal, injection site infection, increased intracranial pressure (except for pseudotumor cerebri), allergy to the drugs to be injected, and uncorrected hypovolemia (as spinal anesthesia
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 126 LETTER TO EDITOR
Lorenzo Spirito 1 , Annachiara Marra 2 , Vincenzo Mirone 3 , Celeste Manfredi 1 , Ferdinando Fusco 1 , Luigi Napolitano 3 , Giuseppe Servillo 2 , Nicola Logrieco 2 , Pasquale Buonanno 2
DOI: 10 4081/aiua 2023 11311
"Federico
Table 1.
Use of spinal anesthesia and analgesia in robotic and laparoscopic surgery (see Supplementary material for references)
Ar ticle Study design Surger y Groups
Duration of inter vention Outcomes
Beilstein CM et al, 2022 RCT Urological/RARP or open General anesthesia associated with: Group SSS: 282 min [240; 322] No differences in QoR; radical prostatectomy Subarachnoid analgesia (SSS) Group TAS: 270 min [240; 300] no differences in postoperative pain Transversus abdomnis plane block (TAP) Group SA: 274 min [240; 312]
Gontero P et al, 2022 Case report
Systemic lidocaine (SA)
Urologicalc/robotic partial Continuous subarachnoid anesthesia 2h 45 min
Patient hemodinamically stable; nephrectomy no intraoperative desaturation; optimal postoperative analgesia
Dhawan R et a , 2021 RCT Cardiac/robotic totally endoscopic General anesthesia without (groups GA) Group GA: 290 (238–346) min Group SA showed less postoperative pain, coronary artery bypassor with subarachnoid analgesia (group SA) Group SA: 315 (235–366) min less need for postoperative morphine, and less cough
Shim JW et al, 2021 RCT
Urological/RARP General anesthesia with (group non-ITMB) group non-ITMB: 120 (108-143)) min
Group ITMB less postoperative pain or without (group ITMB) intrathecal group ITMB: 120 (115-130 min and opioids consumption morphine and bupivacaine
Shim JW et al, 2020 Prospective Urological /RALP General anesthesia with: Group IV-PCA: 123 (109-145) min
Group ITMB required less intraoperative observational Group IV-PCA: intravenous Group RSB: 123 (100-141) min opioids and showed less postoperative patient-controlled analgesia Group ITMB: 123 (114-138) min pain with a lower postoperative Group RSB: rectus sheath bupivacaine block consumption of opioids, better QoR Group ITMB: intrathecal morphine and bupivacaine
Bae J et al, 2017 RCT
Urological/RALP
General anesthesia with Group ITM: Group ITM: 171 ± 42 min Group ITM showed less postoperative pain intrathecal morphine+ intravenous Group IV-PCA: 164 ± 41 min and morphine consumption atient-controlled analgesia Group IV-PCA: only intravenous patient-controlled analgesia
Segal D et al, 2014 RCT
Urogynecological/robotic
Ross SB et al, 2013 RCT
General anesthesia without (group GA)
Group SA showed less postoperative pain, sacrocervicopexy or with subarachnoid anesthesia (SA) lower postoperative consumption of opioids, and a higher satisfaction of patients and nurses
General surgery/Laparo-endoscopic
QoR: quality of recovery; RALP: robot-assisted laparoscopic prostatectomy; RCT: randomized control tr al
General anesthesia (group GA) Group GA: 65 2 ± 25 1 min
Group EA showed less postoperative pain single-site (LESS) cholecystectomy vs Epidural anesthesia (group EA) Group EA: 64 5 ± 21 5 min
causes vasodilation due to sympathetic block) Relative contraindications are sepsis, coagulopathy, fixed cardiac output states, aortic stenosis (previously considered an absolute contraindication), indeterminate neurological disease, multiple sclerosis and other demyelinating diseases (as demyelinated nerves seem more susceptible to local anesthetic toxicity (11) In conclusion spinal anesthesia to perform RARP can be a gamble or an opportunity depending on the players who take part to the match: the appropriate assessment and selection of the patient, the correct management of the drugs affecting coagulation and platelet function, and the proper use of adjuvants in the solution to be injected are essential for a successful and safe spinal anesthesia However, the role of spinal anesthesia in the context of RARP needs to be evaluated in randomized controlled trials with adequate sample size and follow-up Not only the impact on the postoperative pain but also on other sources of possible discomfort for the patient should be investigated The feasibility and relative advantages and disadvantages of spinal anesthesia when used as a replacement for general anesthesia should be clarified with adequate comparative studies Moreover, future studies should compare the spinal anesthesia with novel techniques of regional analgesia such as erector spinae plane and transversus abdominis plane blocks, which are less invasive and consequently safer than the intrathecal administration of drugs
REFERENCES
1 Joshi GP, Jaschinski T, Bonnet F, Kehlet H PROSPECT collaboration Optimal pain management for radical prostatectomy surgery: what is the evidence? BMC Anesthesiol 2015; 15:159
2 Koh JC, Lee J, Kim SY, et al Postoperative Pain and Intravenous Patient-Controlled Analgesia-Related Adverse Effects in Young and Elderly Patients: A Retrospective Analysis of 10,575 Patients Medicine (Baltimore) 2015; 94:e2008
3 Gontero P, Oderda M, Calleris G, et al Awake Da Vinci robotic partial nephrectomy: First case report ever in a situation of need Urol Case Rep 2022; 42:102008
4 Giampaolino P, Della Corte L, Mercorio A, et al Laparoscopic gynecological surgery under minimally invasive anesthesia: a prospective cohort study Updates Surg 2022; 74:1755-1762
5 Dhawan R, Daubenspeck D, Wroblewski KE, et al Intrathecal Morphine for Analgesia in Minimally Invasive Cardiac Surgery: A Randomized, Placebo-controlled, Double-blinded Clinical Trial Anesthesiology 2021; 135:864-876
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 L Spirito, A Marra, V
C
F
L
G
N
P
127
Mirone,
Manfredi,
Fusco,
Napolitano,
Servillo,
Logrieco,
Buonanno
Spinal anesthesia and robot-assisted radical prostatectomy
6 Gao S, Wei J, Li W, et al Accuracy of Robot-Assisted Percutaneous Pedicle Screw Placement under Regional Anesthesia: A Retrospective Cohort Study Pain Res Manag 2021; 2021:6894001
7 Lee BM, Singh Ghotra V, Karam JA, et al Regional anesthesia/analgesia and the risk of cancer recurrence and mortality after prostatectomy: a meta-analysis Pain Manag 2015; 5:387-95
8 Pikramenos K, Zachou M, Apostolatou E, et al The effects of method of anaesthesia on the safety and effectiveness of Radical Retropubic Prostatectomy Arch Ital Urol Androl 2022; 94:396-400
9 Morgan MS, Ozayar A, Friedlander JI, et al An Assessment of Patient Comfort and Morbidity After Robot-Assisted Radical Prostatectomy with Suprapubic Tube Versus Urethral Catheter Drainage J Endourol 2016; 30:300-5
10 Moen V, Dahlgren N, Irestedt L Severe neurological complications after central neuraxial blockades in Sweden 1990-1999 Anesthesiology 2004; 101:950-9
11 Carpenter RL, Caplan RA, Brown DL, et al Incidence and risk factors for side effects of spinal anesthesia Anesthesiology 1992; 76:906-16
Correspondence
Lorenzo Spirito, MD lorenzospirito@msn com
Celeste Manfredi, MD manfredi celeste@gmail com
Ferdinando Fusco, MD ferdinando-fusco@libero it
Urology Unit, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli", Naples
Annachiara Marra, MD dottmarraannachiara@gmail com
Giuseppe Servillo, MD
giuseppe servillo@unina it
Nicola Logrieco, MD nicola logrieco@unina it
Pasquale Buonanno, MD pasquale buonanno@unina it
Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples “Federico II”, Naples, Italy
Vincenzo Mirone, MD mirone@unina it
Luigi Napolitano, MD (Corresponding Author) dr luiginapolitano@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology
University of Naples “Federico II”
Via Pansini 5, 80131 Naples, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 128
Recreation use of phosphodiesterase type 5 inhibitors, the other side of erectile dysfunction
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples "Federico II", Naples, Italy;
2 Department of Translational Medical Sciences, University of Naples "Federico II", Naples, Italy;
3 ASL Napoli 3 Sud, Naples, Italy
KEY WORDS: Erectile dysfunction; PDE5i; Recreational drug.
Submitted 2 April 2023; Accepted 6 April 2023
To the Editor,
In 1998 Sildenafil was approved by the Food and Drug Administration as first line therapy for erectile dysfunction Since then, phosphodiesterase type 5 inhibitors (PDE5i) represent the first-line treatment of erectile dysfunction (ED), improving physiological erectile function, sexual orgasmic function, psychological self-esteem, couples’ relationship, and quality of life (1) Sildenafil represents the most used recreational drugs (2, 3) This could be due to its popularity/familiarity, the presence of more than 30 generic sildenafil and to the significantly lower costs compared to other PDE5i as well as tadalafil (2) The population of PDE5i users is different in terms of demographics, sexual behaviors, attitudes in general/sexual health, and demands for ED treatments (4) Nowadays PDE5i are very popular drugs and one of the most important problems is their recreational use (5) Mostly young men bypassed health care prescriptions (HCP) and obtained these drugs through uncontrolled sources, on the inter net market (6, 7) There are several risks related to recreational use of PDE5i: a certain portion of drugs available on the inter net are contaminated by counterfeits and unapproved generics (1, 8) Alshahrani et al reported that in Saudi Arabia population, the most important reason in using PDE5i for recreational use is curiosity (38 5%) followed by enhancing self-confidence (25 6%), increasing erection duration (10 3%) and improving ejaculation problems (5 1%) All these people bought the PDE5i from drug stores (73 9%), without a medical prescription (9) Similar data were reported by Attia et al. in Egyptian males: in 58 35% of cases PDE5i were used for pleasure, followed by increasing intercourse duration/frequency (15 6%) In 62% of cases Egyptian males obtained them from friends, relatives, and colleagues (62%) or by themselves (25%) or from pharmacists (6 7%), and only 5 4% after medical consultation (1, 10) Bechara et al reported that 21 5% of healthy men between 18 and 30 years old used PDE5i as a recreational drug, mostly associated with alcohol or other drugs as well as illicit drugs, and psychotropic medications This could explain the high incidence of adverse events, mainly related to vasodilator effects (6, 11) with the use of the cannabis, an inhibitor of the cytochrome P450 3A4 hepatic microsomal isoenzyme that is involved into PDE5i metabolism (12, 13) Kimura et al. reported that 45 4% of Japanese men bypassed HCP interaction to obtain PDE5i, 23 4% of men obtained it from friends and 22 0% obtained it via the Inter net (8) Korkes et al reported a recreational use in 9% of young men, although they considered themselves with perfect erectile function Of these, 46 7% had used PDE5i more than three times, and 71 4% had mixed them with alcohol (7) Harte et al reported the same effect in users and nonusers, with a lower erectile confidence and overall satisfaction in the first group (14) In this scenario it should be necessary to provide more education with the aim to decrease the number of PDE5i users without prior HCP consultation (7, 15) Further work on the risk or potential health problems in such conditions is encouraged to improving the information in the general population, creating a collaborative effort between pharmacists, health professionals, and policy makers is necessary to avoid selling medication without a medical prescription and to give adequate and scientific information regarding PDE5i use and misuse
REFERENCES
1 Attia AA, Abdel-Hameed AKS, Amer MAEM, et al Study of the prevalence and patterns of phosphodiesterase type 5 inhibitor use among sexually active Egyptian males: A National Cross-sectional Survey Andrologia 2019; 51:e13364
2 Huang SA, Lie JD Phosphodiesterase-5 (PDE5) Inhibitors In the Management of Erectile Dysfunction P T 2013; 38:407-19
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 129 LETTER TO EDITOR
Giovanni Maria Fusco 1 , Luigi Cirillo 1 , Francesco Mastrangelo 1 , Francesco Romano 1 , Ernesto di Mauro 1 , Gianluigi Cacace 1 , Gianluca Spena 1 , Annamaria Iannicelli 2 , Corrado Aniello Franzese 3 , Vincenzo Mirone 1 , Roberto La Rocca 1 , Luigi Napolitano 1
DOI: 10 4081/aiua 2023 11350
3 Atsbeha BW, Kebede BT, Birhanu BS, et al The Weekend Drug; Recreational Use of Sildenafil Citrate and Concomitant Factors: A CrossSectional Study Front Med (Lausanne) 2021; 8:665247
4 Mulhall JP, Hassan TA, Rienow J Sexual habits of men with ED who take phosphodiesterase 5 inhibitors: a survey conducted in 7 countries Int J Clin Pract 2018; 72:e13074
5 Cirillo L, Fusco GM, Di Bello F, et al Sexual dysfunction: Time for a multidisciplinary approach? Arch Ital Urol Androl 2023; 95:11236
6 Bechara A, Casabé A, De Bonis W, et al Recreational Use of Phosphodiesterase Type 5 Inhibitors by Healthy Young Men J Sex Med 2010; 7:3736-42
7 Korkes F, Costa-Matos A, Gasperini R, et al Recreational Use of PDE5 Inhibitors by Young Healthy Men: Recognizing This Issue Among Medical Students J Sex Med 2008; 5:2414-2418
8 Kimura M, Shimura S, Kobayashi H, et al Profiling Characteristics of Men Who Use Phosphodiesterase Type 5 Inhibitors Based on Obtaining Patterns: Data from the Nationwide Japanese Population J Sex Med 2012; 9:1649-1658
9 Alshahrani S, Ahmed AF, Gabr AH, Al Ansari A, El-feky M, Elbadry MS Phosphodiesterase type 5 inhibitors: Irrational use in Saudi Arabia Arab Journal of Urology 2016; 14:94-100
10 Mirone V, Napolitano L, D’Emmanuele di Villa Bianca R, et al A new original nutraceutical formulation ameliorates the effect of Tadalafil on clinical score and cGMP accumulation Arch Ital Urol Androl 2021; 93:221-226
11 Ahmed AF, Alshahrani S, Morgan A, et al Demographics and sexual characteristics of sex-enhancing medication users: Study of a web-based cross-sectional sample of sexually active men Arab Journal of Urology 2017; 15:366-371
12 Napolitano L, Fusco GM, Cirillo L, et al Erectile dysfunction and mobile phone applications: Quality, content and adherence to European Association guidelines on male sexual dysfunction Arch Ital Urol Androl 2022; 94:211-216
13 Schnetzler G, Banks I, Kirby M, et al Original Research ED Pharmacotherapy: Characteristics, Behaviors, and Attitudes of Men Bypassing the Healthcare System When Obtaining Phosphodiesterase Type 5 Inhibitors J Sex Med 2010; 7:1237-1246
14 Harte CB, Meston CM Recreational Use of Erectile Dysfunction Medications and Its Adverse Effects on Erectile Function in Young Healthy Men: The Mediating Role of Confidence in Erectile Ability J Sex Med 2012; 9:1852-1859
15 Napolitano L, Cirillo L, Fusco GM, et al Natural treatments for erectile dysfunction: A focus on mobile health applications Arch Ital Urol Androl 2022; 94:373-374
Correspondence
Giovanni Maria Fusco, MD giom fusco@gmail com
Luigi Cirillo, MD cirilloluigi22@gmail com
Francesco Mastrangelo, MD f mastrangelo91@gmail com
Francesco Romano, MD romanofrancesco92@libero it
Gianluca Spena, MD spena dr@gmail com
Ernesto Di Mauro, MD ernesto dimauro@unina it
Gianluigi Cacace, MD Naples cacace gianlu@gmail com
Vincenzo Mirone, MD mirone@unina it
Roberto La Rocca, MD robertolarocca87@gmail com
Luigi Napolitano, MD dr luiginapolitano@gmail com
Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples "Federico II", Naples, Italy
Annamaria Iannicelli, MD
annamaria iannicelli@unina it
Department of Translational Medical Sciences, University of Naples "Federico II", Via Pansini 5, 80131, Naples, Italy
Corrado Aniello Franzese, MD corradofranzese@libero it
ASL Napoli 3 Sud, Naples, Italy
Conflict of interest: The authors declare no potential conflict of interest
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 G M Fusco, L Cirillo, F Mastrangelo, F
et al 130
Romano,
Chronic prostatitis as possible risk factor for Peyronie's disease: Psychological, sexual and prostatitis-like symptoms in patients with PD
Gianni Paulis 1 , Andrea Paulis 2
1 Peyronie’s Care Center, Department of Uro-Andrology, Castelfidardo Clinical Analysis Center, Rome, Italy;
2 Neurosystem Center for applied Psychology and Neuroscience, Janet Clinical Centre, Rome, Italy
Supplementary Table 1.
Clinical characteristics and basic demographics of patients in the two groups (PD patients and non-PD patients)
APPENDIX (TO THE INTRODUCTION SECTION)
Chronic prostatitis
This article refers to chronic prostatitis (CP) and not to its acute form Symptoms of prostatic inflammation are very frequent in young adult males; however, they often also affect males over 50 years of age The prevalence of prostatic symptoms varies between 8 0 and 14 2% with respect to the adult male population (1, 2) Chronic prostatitis refers to a series of heterogeneous clinical states where the presence of inflammation has often not been ascertained due to inadequate diagnostics and the absence of recognized standardized therapy The symptoms that refer to this condition are very heterogeneous, and often, only some of these are present: dysuria, micturition burning, increased micturition frequency, nocturia, micturition urgency, difficulty emptying the bladder, post-micturition dripping, hematospermia When pain is present, it can be isolated or is present in multiple locations (testes, hypogastric, inguinal, perineal, perianal, penile, and sacral regions) Other possible symptoms are premature ejaculation and scrotal and/or penile post-orgasmic pain and erectile dysfunction Anxiety and depression are often present and greatly affect the quality of life (QoL) of these patients (3-5)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 61 A ORIGINAL
- SUPPLEMENTARY
PAPER
MATERIAL
Variable PD patients Non-PD control population Statistical analysis (539 cases) (2201 cases) P-value (t-test) Mean age 49 6 (± 12 16 SD) 50 5 (± 12 04 SD) 0 108 Variable PD patients Non-PD control population Statistical analysis n cases (%) n cases (%) P-value (χ2 test ) Varicocele 13 (2 4) 62 (2 8) 0 711 Hydrocele 6 (1 1) 23 (1 04) 0 889 Hypercholesterolemia 48 (8 9) 151 (6 8) 0 121 Thyroid disease 27 (5 00) 111 (5 04) 0 974 History of myocardial infarction 13 (2 4) 50 (2 2) 0 972 History of malignant urological neoplasm 43 (7 97) 176 (7 99) 0 988 History of non-urological malignancy 11 (2 04) 48 (2 18) 0 971 History of urinary stones 52 (9 6) 207 (9 4) 0 927 Urogenital infections 19 (3 5) 120 (5 4) 0 085 Diabetes mellitus 32 (5 9) 77 (3 49) 0 0134 Hypertension 101 (18.7) 299 (13.5) 0.0030 Erectile dysfunction (ED) 216 (40 07) 529 (24 03) < 0 0001 Benign prostatic hyperplasia (BPH) 119 (22 07) 298 (13 5) < 0 0001 Cronich prostatitis (CP) 200 (37 1) 384 (17 4) < 0 0001
In case of the exacerbation of prostatitis, fever, arthralgia, and myalgia may be present
In 1999, the National Institute of Health (NIH) proposed a classification of prostatitis into four categories, which is still accepted and shared (6): Category I, acute bacterial prostatitis (current bacterial infection); Category II, chronic bacterial prostatitis (recurring bacterial infections); Category III, chronic non-bacterial prostatitis/chronic pelvic pain syndrome (CPPS) (absence of infection), which is then divided into two sub-categories: III A inflammatory (with clear laboratory signs referable to inflammation = presence of leukocytes (WBC) in semen or expressed prostatic secretion (EPS) or postprostatic massage urine) and III B, non-inflammatory (with the absence of leukocytes in semen or expressed prostatic secretion (EPS) or post-prostatic massage urine); Category IV, asymptomatic inflammatory prostatitis
This classification has proved to be very useful because a laboratory diagnostic study (Meares-Stamey test) is essential to find the type of category to which the observed patient belongs (7) Excluding category IV, our opinion on this classification is that it does not represent a list of different pathological conditions; we think that categories I, II, and III A and III B represent nothing more than four different types of the "clinical state" of the patient observed at that given moment
In practice, every patient with chronic prostatitis in their clinical life almost always finds themselves in each of the different I, II, and III categories of the NIH classification
It is certainly an excellent classification in which different states of "clinical presentation" of the same disease are listed
In fact, it is known that about 5% of patients with acute prostatitis (Cat I) evolve towards chronic prostatitis, which can sometimes flare up due to a bacterial infection (Cat II) or become evident and correspond clinically to Cat IIIA or IIIB
The Meares-Stamey test still maintains its important diagnostic effectiveness, and it is very useful compared to the other method available, which uses the dosage of IL-6 and IL-8 (in semen or expressed prostatic secretion (EPS) or post-prostatic massage urine) in order to be able to differentiate clinical situation III A from situation III B (8, 9) The compilation of the NIH-CPSI (Chronic Prostatitis Symptom Index) questionnaire is very useful in the classification of the patient and in the evaluation of the symptoms after treatment (10)
Peyronie's disease
PD is a fibrogenic inflammatory disease that involves the tunica albuginea of the corpora cavernosa for determining the deformation of the penis (bending, shortening, hollowing, torsion, hourglass, etc ) Its genetic component with autosomal dominant transmissions seems established, and it is also known with respect to its analogy with Dupuytren's disease and Ledderhose disease (11,12) The prevalence of PD varies from 0 6% to 13% in relation to the geographical area, although PD prevalence seems higher in the Western world and lower in Asian countries (13-18) Even if its etiopathogenesis is still much debated, an almost unanimous consensus prevails in the literature on the traumatic origin of the disease (19, 20) The clinical presentation of PD includes the following: penile deformation, penile pain, erectile dysfunction (in about 1/3 of cases), and anxious-depressive symptoms (21, 22) The diagnosis includes penile palpation and diagnostic investigation with dynamic penile color Doppler and photographic documentation of the deformation (according to Kelâmi) (23-25) The conservative medical treatment of PD is indicated in the active phase of the disease and includes the following: vitamin E and other antioxidants; tamoxifen; potaba; non-steroidal anti-inflammatory drugs (NSAIDs); penile injections with verapamil, pentoxifylline, interferon-α2b, cortisone substances, collagenase, hyaluronic acid, etc ; and physical therapies (iontophoresis, shockwave therapy, and vacuum penile and traction devices) (2529) Surgical therapy is reserved for cases of disease stabilization or when erectile dysfunction and/or severe curvature do not allow for complete sexual intercourse (28-30)
REFERENCES
1 Krieger JN, Lee SW, Jeon J, et al Epidemiology of prostatitis Int J Antimicrob Agents 2008; 31(Suppl 1): S85-S90
2 Mehik A, Hellström P, Lukkarinen O, et al Epidemiology of prostatitis in Finnish men: a population-based cross-sectional study BJU Int 2000; 86:443-448
3 Kwon JK, Chang IH Pain, catastrophizing, and depression in chronic prostatitis/chronic pelvic pain syndrome Int Neurourol J 2013; 17:48-58
4 Krsmanovic A, Tripp DA, Nickel JC, et al Psychosocial mechanisms of the pain and quality of life relationship for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) Can Urol Assoc J 2014; 8:403-408
5 Bai J, Gu L, Chen Y, et al Evaluation of psychological stress, cortisol awakening response, and heart rate variability in patients with chronic prostatitis/chronic pelvic pain syndrome complicated by lower urinary tract symptoms and erectile dysfunction Front Psychol 2022; 13:903250
6 Nickel JC, Nyberg LM, Hennenfent M Research guidelines for chronic prostatitis: consensus report from the first National Institutes of Health International Prostatitis Collaborative Network Urology 1999; 54:229-233
7 Stamey TA Prostatitis J Royal Soc Med 1981; 74:22-40
8 Paulis G, Conti E, Voliani S, et al Evaluation of the cytokines in genital secretions of patients with chronic prostatitis Arch Ital Urol Androl 2003; 75:179-186
9 Liang W, Wu Z, Zhang G, et al A urine-based biomarker for chronic prostatitis/chronic pelvic pain syndrome: a retrospective multi-center study Transl Androl Urol 2020; 9:2218-2226
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 G Paulis, A Paulis 61 B
10 Eri LM, Thomassen H, Brennhovd B, Håheim LL Accuracy and repeatability of prostate volume measurements by transrectal ultrasound Prostate Cancer Prostatic Dis 2002; 5:273-278
11 Bias WB, Nyberg Jr LM, Hochberg MC, et al Peyronie's disease: a newly recognized autosomal-dominant trait Am J Med Genet 1982; 12:227-235
12 Dolmans GH, Werker PM, de Jong IJ, et al WNT2 Locus Is Involved in Genetic Susceptibility of Peyronie’s Disease J Sex Med 2012; 9:1430-1434
13 Dibenedetti DB, Nguyen D, Zografos L, et al A Population-Based Study of Peyronie's Disease: Prevalence and Treatment Patterns in the United States Adv Urol 2011; 2011:282503
14 Stuntz M, Perlaky A, des Vignes F, et al The Prevalence of Peyronie's Disease in the United States: A Population-Based Study PLoS One 2016; 11:e0150157
15 La Pera G, Pescatori ES, Calabrese M, et al SIMONA Study Group Peyronie's disease: prevalence and association with cigarette smoking A multicenter population-based study in men aged 50-69 years Eur Urol 2001; 40:525-530
16 Schwarzer U, Sommer F, Klotz T, et al The prevalence of Peyronie's disease: results of a large survey BJU Int 2001; 88:727-730
17 Shiraishi K, Shimabukuro T, Matsuyama H The prevalence of Peyronie's disease in Japan: a study in men undergoing maintenance hemodialysis and routine health checks J Sex Med 2012; 9:2716-2723
18 Wong A, Tsang SS, O RY, et al Prevalence of Peyronie’s disease and its psychosexual impact in the chinese population: A large cohort population-based cross-sectional study J Urol 2020; 203(Suppl 4):e499, Mp33-12
19 Devine CJJ, Somers KD, Jordan GH, et al Proposal: trauma as the cause of the Peyronie's lesion J Urol 1997; 157(1):285-290
20 Jarow JP, Lowe FC Penile trauma: an etiologic factor in Peyronie's disease and erectile dysfunction J Urol 1997; 158:1388-1390
21 Nelson CJ, Diblasio C, Kendirci M, et al The chronology of depression and distress in men with Peyronie's disease J Sex Med 2008; 5:19851990
22 Pryor JP, Ralph DJ Clinical presentations of Peyronie's disease Int J Impot Res 2002; 14:414-417
23 Kadioglu A, Tefekli A, Erol H, et al Color Doppler ultrasound assessment of penile vascular system in men with Peyronie’s disease Int J Impot Res 2000; 12:263-267
24 Kelâmi A Autophotography in evaluation of functional penile disorders Urology 1983; 21:628-629
25 Levine LA, Larsen S Diagnosis and management of Peyronie disease In: Wein AJ, Kavoussi LR, Partin AW, Peters CA, editors CampbellWalsh Urology, 11th ed Philadelphia: Elsevier Saunders, 2015; 722-748
26 Yousif A, Natale C, Hellstrom WJ Conservative Therapy for Peyronie’s Disease: a Contemporary Review of the Literature Curr Urol Rep 2021; 22:1-12
27 Natale C, McLellan DM, Yousif A et al Review of intralesional collagenase clostridium histolyticum injection therapy and related combination therapies in the treatment of Peyronie's disease (an update) Sex Med Rev 2021; 9:340-349
28 Chung E, Ralph D, Kagioglu A, et al Evidence-based management guidelines on Peyronie's disease J Sex Med 2016; 13:905-923
29 Nehra A, Alterowitz R, Culkin DJ, et al Peyronie’s disease: AUA guideline J Urol 2015; 194:745-753
30 Osmonov D, Ragheb A, Ward S, et al ESSM Position Statement on Surgical Treatment of Peyronie's Disease Sex Med 2022; 10:100459
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 61 C
Chronic prostatitis as possible risk factor for Peyronie's disease
Sexual dysfunctions of rheumatological patients are a neglected issue: Results from a national survey of Italian Society of Rheumatology
Luigi Napolitano 1 , Ilenia Pantano 2 , Lorenzo Romano 1 , Luigi Cirillo 1 , Celeste Manfredi 3 , Francesco Mastrangelo 1 , Giovanni Maria Fusco 1 , Daniele Mauro 2 , Lorenzo Spirito 3 , Roberto La Rocca 1 , Davide Arcaniolo 3 , Corrado Aniello Franzese 4 , Carmine Sciorio 5 , Marco Romano 6 , Marco De Sio 3 , Vincenzo Mirone 1 , Francesco Ciccia 2
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples "Federico II", Naples, Italy;
2 Department of Precision Medicine, University of Campania "Luigi Vanvitelli", Naples, Italy;
3 Unit of Urology, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli", Naples, Italy;
4 ASL Napoli 3 Sud, Naples, Italy;
5 Urology Unit, Ospedale Alessandro Manzoni, Lecco, Italy;
6 Department of Precision Medicine and Hepatogastroenterology Unit, AOU University Luigi Vanvitelli, Naples, Italy
Supplementary
Tables 1. Questionnaire
1 Age, years
2 Gender
a. Male
b Femal
3 Are you Resident or Rheumatologist?
4 Practice setting
a Community Hospital
b Academic Hospital
c Private Hospital
5 In which region do you practice your work?
6 Practice duration (years)
7 How often do you discuss SD with your patients?
a Never
b Infrequently
c Sometimes
d Frequently
e Always
8 Why do not you investigate SD in patients during visit?
a I do not have enough knowledge or experience
b There are dedicated specialists
c Patient will ask the specialist on his/her own
d Sexual function is private matter
e I do not have enough time
f The patient may feel embarrassed
g The partner of the patient may feel embarrassed
9 How often do patients refer SD related to their rheumatological disorders?
a Never
b Infrequently
c Sometimes
d Frequently
e Always
10 Which kind of patients tell you about his/her SD:
a Women < 40 years old
b Women 40–50 years old
c Women ≥ 50 years old
d. Men < 40 years old
e Men 40–50 years old
f Men ≥ 50 years old
11 What is the most reported SD by male patients?
a Low libido
b Erectile dysfunction
c Premature ejaculation
d Late ejaculation
e None of them
12 What is the most reported SD by female patients?
a Sexual arousal disorder
b Orgasmic disorder
c Dyspareunia
d Low sex drive
e None of them
13 What is in your experience the rheumatological disorder most frequently associated with SD?
a Rheumatoid arthritis
b Spondyloarthritis
c Systemic lupus erythematosus
d Systemic sclerosis and dermatomyositis
e Sjogren's syndrome
f Fibromyalgia
g Vasculitis
14 How often does the female partner of your patient report SD due to GI disease?
a Never
b Infrequently
c Sometimes
d Frequently
e Always
15 How often does the male partner of your patient report SD due to GI disease?
a Never
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 74 A ORIGINAL PAPER - SUPPLEMENTARY MATERIAL
b Infrequently
c Sometimes
d Frequently
e Always
16 Do you know, which kind of rheumatological drugs are related to SD?
a Yes
b No
17 What are the drugs that generally, in your experience, are the most common cause of SD?
a Immunosuppressant
b Antidepressant
c Biological drugs
d Corticosteroids
18 How often do patients refer that their SD is apparently related to the therapy you have prescribed?
a Never
b Infrequently
c Sometimes
d Frequently
e Always
19 Have you ever changed your therapy after referred SD?
a No
b Yes
20 If the answer is Yes to question 19, indicate the therapy you suspended due to iatrogenic SD
21 Do rheumatologists have the responsibility to discuss SD with their patients? I do not know
a Totally agree
b Partially agree
c I do not know
d. Partially disagree
e Totally disagree
22 Do you think that assessing SD in clinical practice can help patients?
a No, it would have no impact on therapeutic diagnostic process
b Yes, it would improve the diagnostic and/or therapeutic pathway
c Yes, it would improve the relationship with patients
23 Discussing SD pertains only to andrologist or gynecologist, sexologist, or endocrinologist
a. Totally agree
b Partially agree
c I do not know
d Partially disagree
e Totally disagree
24 How often do you refer your male patients to andrologist for their sexual problems?
a Never
b. Infrequently
c Sometimes
d Frequently
e Always
25 Which specialists should treat SD?
a Urologist/andrologist for men
b Gynecologist for women
c Sexologist
d Endocrinologist
26 Do you know PDE5i side effect?
a Yes
b No
27 Which is a side effect of PDE5i?
a Dyspeptic symptoms
b Flushing and headache
c Lumbar pain
d None of the previous
e All of the previous
28 Have you ever prescribed PDE5i or other treatments to your patients?
a No, I refer patients to the andrologist
b Yes, I have prescribed supplements
c Yes, I have prescribed 5-PDEi
d Yes, I have prescribed both
29 How often do your patients refer using PDE5i independently?
a Never
b Infrequently
c Sometimes
d Frequently
e. Always
30 Do you feel the need to broaden your knowledge about sexual disorders?
a Yes
b No
31 Do you feel that your education has given you enough knowledge to discuss sexual problems with your patients:
a No knowledge
b. Enough knowledge
c Little knowledge
d More Knowledge
32 It would be useful for gastroenterologists to attend courses on SD:
a Totally agree
b Partially agree
c I do not know
d. Partially disagree
e Totally disagree
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 L Napolitano, I Pantano, L Romano, et al 74 B
Telemedicine and YouTube™: Video quality analysis before and after COVID-19 pandemic
Vincenzo Mirone 1 , Marco Abate 1 , Giovanni M Fusco 1 , Luigi Cirillo 1 , Luigi Napolitano 1 , Simone Morra 1 , Francesco Di Bello 1 , Gianluigi Califano 1 , Claudia Mirone 2 , Roberto La Rocca 1 , Massimiliano Creta 1 , Giuseppe Celentano 1 , Marco Capece 1 , Francesco Mangiapia 1 , Nicola Longo 1 , Claudia Collà Ruvolo 1
1 Department of Neurosciences, Reproductive Sciences and Odontostomatology, University of Naples “Federico II”, Naples, Italy;
2 Multidisciplinary Department of Medical, Surgical and Dental Sciences, University of Campania "Luigi Vanvitelli", Naples, Italy
Supplementary Table 1 Search keyword combinations used on YouTube™ on the 25th of March, 2022
Search keyword combinations
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 85 A ORIGINAL PAPER - SUPPLEMENTARY MATERIAL
1 Telemedicine 2 Telehealth 3 Teleconsultation 4 Televisit 5 Telemonitoring 6 Telesupport 7 Telemedicine and COVID 8 Telemedicine and Coronavirus 9 Global Health Telemedicine 10 Telemedicine and Technology 11 Telemedicine and Healthcare 12 Telemedicine and Physicians 13 Telemedicine and Doctor 14 Telemedicine and Patients 15 Telemedicine and Monitoring Service 16 Telemedicine and Medical Devices 17 Healthcare on demand 19 Video consultation
Psychological and sexual problems of cancer survivors
Ida Ayu Made Ari Santi Tisnasari 1 , Tuti Nuraini 2 , Yati Afiyanti 3 , Rudi Rudi 4 , Riri Maria 5
1 Faculty of Nursing, Universitas Indonesia, Depok, Indonesia;
2 Department of Basic Science and Fundamental Nursing, Faculty of Nursing Universitas Indonesia, Depok, Indonesia;
3 Department of Maternity Nursing, Faculty of Nursing Universitas Indonesia, Depok, Indonesia
4 Master of Nursing Program, Faculty of Nursing Universitas Indonesia, Depok, Indonesia;
5 Department of Medical Surgical Nursing, Faculty of Nursing Universitas Indonesia, Depok, Indonesia
Presented as conference papers at the 8th V-BINC at FON Universitas Indonesia
BREAST CANCER SURVIVORS' UNMET NEEDS FOLLOWING CHEMOTHERAPY *
(Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti)
Results
Theme 1: overcoming health problems in breast cancer survivors
The first theme that emerged was a need for breast cancer survivors to overcome health problems they were experiencing, along with physical, psychological, social, spiritual, and sexual challenges that resulted All participants experienced health problems that left them physically challenged, such as experiencing fatigue, memory loss, joint stiffness, and changes in physical appearance
“I get tired quickly, you know, easily getting tired It's easy to get tired when you carry it around I'm still actively working I've been brought to work for one hour and two hours I'm already tired I'm so tired ” (P5)
“Yes, sometimes what you want to say is forgotten. For example, when you want to say something like this, it comes out differently Forget about it for a moment Sometimes I ask my father why he keeps forgetting, and friends say maybe it's because of the chemo factor ” (P7)
“In 2019, I had stiffness in my right hand that I felt was going to be almost 5 years after chemotherapy ” (P5)
“After chemo, I lost weight. Because we don't know yet, we think about eating "oh this one can't be; that's also not allowed" It's like stress from eating ” (P4)
Particularly after chemotherapy, breast cancer survivors have often experienced psychological challenges, chiefly fear of recurrence
“There is a sense of worry every time I go for restaging Every time I go for restaging, I get nervous A week before restaging, my husband didn't like to eat, and he was restless at bedtime That happened because we overthink about the bad results; we are afraid that cancer will come back again ” (P3)
“Right now, I'm still worried Moreover, when friends have a recurrence, it's very influential Listening to him metastasize, it feels like our bodies are sick Start by reflecting on yourself ” (P5)
“Worried about the cancer cells coming back or recurrence
I think the survivors must be worried about that too I think so I hope not I really hope it doesn't ” (P11)
Breast cancer survivors, especially after chemotherapy, also reported challenges associated with socializing They felt sensitive, which led them to reduce their social activities
“Yes, due to chemo, sometimes our minds are more sensitive, easily angered, and easily offended I've never been like that before, but I’ve changed a lot since the chemo If someone says something bad, I get offended ” (P14)
“Sometimes I often feel sensitive when the chemo is finished Then if there is a problem, what should be said first to the husband?” (P4)
“After chemo until now, the activity has decreased Now that I have reduced my activities, I feel that I am not as productive as I used to be In terms of social relations, I reduce socialization activities more I don't participate in social activities very often, right?” (P1)
“From a social perspective, if you don't feel confident, you go out to meet friends, reduce your activities with friends outside. So I prefer to stay at home if there are no important activities, maybe go out just for family events or deliver food orders After that, I usually rest at home ” (P3)
All participants in this study faced spiritual challenges, such as questioning their faith or wanting to end their life because they felt alone, despairing, like they had failed to achieve their life goals, or overcome family problems Other participants stated they were disappointed with the hand they had been dealt or felt as if all they ever got out of life were problems
One participant, a 54-year-old woman who was unmarried and childless, stated that she had considered ending her life because she felt alone
“Cancer causes death, it's true I think about death I'm alone: I don't have children, and I don't have a husband So, if no one in this world wished for my existence, it seems better just to die ” (P1)
Another participant, a woman who is 48 years old, has 2 children and is currently experiencing metastases, stated that she had problems with her partner, who is currently having another woman Here's the expression:
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 98 A
PAPER - SUPPLEMENTARY MATERIAL
ORIGINAL
“Oops, I'm too lazy to get the treatment It's a thought to die I cried all the times when I found out my husband was cheating on me I feel like dying, especially when I remember my husband and family, who didn't support me My husband's family supported my husband with another woman even though I was undergoing cancer therapy at the time My heart was broken at that time I just wanted to die ” (P8)
The next participant, a 34-year-old young woman who works as a notary, stated that she felt hopeless because of the pain she was experiencing and felt better returning to the creator along with her statement I felt like I was desperate because of this pain I had a feeling that I wanted to just die like that I think it would be better if I were taken like that That's how I felt The important thing is that I've tried If, for example, it's time, I'll leave it to God I always think that way (P11)
Another participant, a 42-year-old woman, a housewife, expressed her disappointment with the fate that is currently happening to her This participant shared that she often helps her friends and prays for charity; however, she still experiences a bad fate in her life, as follows: Yes, I used to want to die, but I also thought that the children were still young and my husband was too In fact, I was desperate to kill myself (P14)
A 49-year-old female participant, who works as a housewife, expressed disappointment when she experienced cancer because the participants felt they had tried to maintain their health but turned out to have cancer Participants feel unfairly towards other people who do not take care of their health but do not have cancer
Following her expressions:
“Disappointed maybe I was shocked and disappointed when I found out that I had cancer because I am one of those people who maintain a regular diet while my younger siblings eat carelessly How come they don't get cancer?” (P8)
The female participant, aged 43 years, working as a housewife, felt disappointed because of the problems that came repeatedly, many of which added to the pain experienced, so that the situation felt even worse Here's the story:
“There's a feeling of disappointment How come we live like this? There is a problem of persistent pain that doesn't go away. She thought, "Why did God give me this ordeal?" There have been many problems, plus pain too But I try to live it all sincerely even though it's hard ” (P12)
All participants in this study had experienced challenges among sex and their sexuality, largely materializing as relationship problems with their partner or a lack of selfacceptance, which prevented them from bearing their bodies to others
One participant, a 48-year-old woman who was married and had two children, explained that she experienced physical changes resulting from cancer and its treatment, which made it difficult for her to find sex with her husband pleasurable anymore She described how they found themselves in a desperate situation:
“Initially, after chemotherapy, the relationship between husband and wife was very difficult, until finally we searched for
additional information via Google so that it could be resolved I also had time to ask the doctor, but they only explained things briefly and concisely “You can search on Google and find the answer, ” he said ” (P3)
Participant 4, a 44-year-old woman who is married and does not have children, explained that there was an impact on her relationship with her husband, namely a reduction in the attractiveness of having sex The following are participant statements:
“There is an impact on intimate relationships with husbands, so it's not like normal people He's a little less passionate than before The feeling of interest is reduced, which is usually the same as often asking if one wants But since the chemotherapy, sometimes I don't want to have sex with my husband In the past, I used to ask first, but now it's not like that ” (P4)
Participant 8, a 49-year-old woman who is married and has two children, revealed that she had problems with her husband because he had turned to another woman The participant stated that her husband wanted to remarry since he was sick The following are statements from the participant:
“When it comes to my relationship with my husband, personally, I have had ups and downs as well When I was sick, my husband had an affair with another woman So, I had to go to the ER myself Well, one day, I was caught last year, in August So I was sick, and my husband wanted to remarry ” (P8)
Participant 9, a 33-year-old woman who works as a notary public, revealed that since she had cancer, she could not cover up her inner defects, so she hoped that her current partner would accept her condition as it is The following are the expressions given by participant about her sexual problems:
“I told you, I don't want to cover up my hidden flaws in my partner I have to be sporty When I start a relationship, I don't want to start with doubts that hiding my identity and past is really bad, really bad perception. So when my partner wanted to be serious, I immediately sat at the table saying I was sick, accept me or not If he doesn't accept my condition, we go back If he accepts my situation, we go forward I said so ” (P9)
Another participant, a 34-year-old woman, reported that she feared a lack of acceptance from the man She felt insecure about her imperfections after undergoing cancer treatment The following of her statement:
“So, I feel like I'm being shunned When I'm sick, I feel like I'm being shunned or left out I feel more like that than normal, and it affects my confidence anyway Today, I'm still learning to cope I am aware that the opposite sex, men, want the perfect partner, right? So, if I am self-assured and bare myself to the opposite sex, I always wonder whether or not he will accept my condition as it is now, not to mention my status as a survivor ” (P11)
Theme 2: the need to access the best health services
A second theme that appeared in this investigation was the need to access the best health services, which women considered to involve accurate cancer-detection tools and friendly nurses
Several participants expressed their desire to access
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti, Rudi Rudi, Riri Maria 98 B
health services with more accurate cancer-detection tools than those currently at their disposal
One participant, a 48-year-old woman, explained the importance of introducing PET scanning equipment at the nearest hospital so that cancer survivors who wish to use this facility do not need to travel far for an examination The participant expressed herself as follows:
“I just want a PET scan You can't use Indonesian Government Health Insurance, and the scanner's not here; it's only in Jakarta So, why is a PET scan important? Because we, as survivors, need to know where else this cancer cell is hiding Well, it can only be known through a PET scan We can't get one here; we have to go to Jakarta and it is costly ” (P3)
Participant 6, a 55-year-old woman who works as a housewife, explained the need for a nearby bone scan because the results are more accurate than using only X-rays for accurate staging results This tool is expected to exist to prevent errors in detecting cancer metastases in breast cancer survivors
“The only thing that needs to be fixed is the Oncology Polyclinic, actually If there is a bone scan tool in Local Hospital, that would be amazing Because at that time, in the results of the bone survey, there was an incident that I was thought to have had metastases to the brain at that time I'm paranoid When the results are in, I go straight to Jakarta for a bone scan Bone scan accuracy is higher than x-rays At least it's a relief if you have a result like that, right? So that's why we need a second opinion with such a sophisticated tool ” (P6)
Meanwhile, participant 12, a 43-year-old woman who works as a housewife, explained the need for a bone scan or pet scan so that the results of the examination are not erroneous as in previous experiences
“From the beginning, I didn't know what the examination was going to be like At first, when I was caught sick, I was told to check the FNAB from a regional hospital, where it was said that I had a malignant tumor. Then I was referred to Hospital and X-rayed The results were good Then he asked to do a biopsy After the biopsy, he said no disease was found That's how it was again re-checked at the biopsy Suddenly, at the operation, he said there was a malignant tumor, and her breast was immediately removed So, I want there to be a bone scan or a pet scan here so that the results of the examination are not as wrong as before. I used to also have to go to Jakarta to check by bone scan ” (P12)
Several participants expressed the hope that any future treatment of theirs would be provided by nurses who were friendly to patients and cancer survivors
One participant, a 54-year-old woman, commented that she had been treated unkindly by the existing nurses: “In the oncology polyclinic, there are some nurses who are not friendly So, the nurses ’ words are often firm, but sometimes, I mean the nurse is really mean ” (P1)
Another participant, a 48-year-old woman, described older nurses as feistier than those who were younger “If the nurse is from the old school, they will be lazier and more aggressive They tend to not like seeing patients spoiled
If you are in the oncology polyclinic, do not be surprised if there are nurses who are very fierce But maybe they are fierce because of the pressure they face due to the very large number of patients, right?” (P3)
Participant 7, a 50-year-old woman who works as a housewife, explained that there are nurses who are emotional
“Indeed, my friends say that there are nurses, especially those who are on duty at the oncology polyclinic, so fierce that they have shouted at the control person at the oncology polyclinic ” (P7)
Participant 8, a 48-year-old woman who works as a housewife, stated that she wanted the unfriendly nurse service she had experienced to be changed to a morefriendly service because, according to the participant, the attention of a patient was not only physical but also a patient's comfort
“In the inpatient room, a nurse came in, the nurse grumbled, saying she didn't like messy rooms Why is the nurse being so bitchy? Such services must be changed The nursing profession should pay attention not only to the physical condition of the patient but also to their comfort ” (P8)
Theme 3: unmet information needs about cancer treatment
Several cancer survivors expressed that they wanted more information, including about the stages of treatment, how to overcome the side effects of cancer therapy, and information technology resources to accompany their cancer treatment One participant, a woman aged 48 years, remarked that healthcare workers do not explain the stages of treatment unless they are asked This leaves some, especially women from remote areas, confused about or unaware of the treatment stages they will undergo The following is a related excerpt:
“So, if we don't ask, the staff don't talk and don't tell us about t h e s t a g e s o f t r e a t m e n t P e o p l e f r o m v i l l a g e s s u c h a s Karangasem and Tabanan don't understand what they are going to do after this. They don't know because not every patient is accompanied Not every patient understands what is being explained ” (P3)
Participant 10, a 37-year-old woman who works as a private employee, explained that patients must ask first or find out on their own to get the necessary information Some participants even said they had to eavesdrop on other patients' conversations to get useful information to overcome the side effects of the therapy they felt
“
So far, this is my experience We have to ask first, especially if you are dealing with the side effects of chemo So that's my trick I heard from friends there too From the results of my eavesdropping with those friends, I finished chemo looking for the food I wanted first For maybe a few days, I will not be able to eat That's very helpful You can eat a little bit of it ” (P10)
Several participants expressed the need for detailed health information Participant 5, a 47-year-old woman who works as an entrepreneur, explained that the health information provided to patients must be detailed Participants felt that it was necessary to explain the latest treatment information The following are participant statements:
“If we don't ask, the officers only follow the medical history
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 98 C Problems of cancer survivors
according to the medical record If I asked for additional treatment, the staff would not be there There are additional checks that sometimes we are not informed about, even though they are covered by government health insurance ” (P5)
Participant 9, a 33-year-old woman who works as a notary public, explained that it is necessary to provide information technology for cancer treatment This is considered important by participants to speed up the examination process so that participants are expected not to feel tired with the existing queues The following are statements from participants:
“It is enough with technology such as mobile applications; the examination files should be ongoing If I wait at the hospital, first I'm tired, and second, I'm full That was before COVID19 That's incredible exhaustion Imagine at the time of COVID-19 what the treatment would be I think the world of health must learn to use technology as a means of efficiency in carrying out health actions ” (P9)
SPECIAL INFORMATION TO DISCUSS SEXUALITY
PROBLEMS: A BALINESE BREAST CANCER SURVIVOR'S UNMET NEED
(Ida Ayu Made Ari Santi, Yati Afiyanti, Tuti Nuraini)
Results
Information needed to overcome sexual problems
Informant 1 was a 45-year-old woman who worked as a housewife and owned a salon, was married and had two children She stated that in the first year of treatment, she did not want to engage in sexual activity because her vagina felt dry
“I need information about how to solve my sexual problem It's dry It's like a razor blade, ma'am, during intercourse It feels very dry Yes, as a wife, yes he also understands Sometimes, I feel sorry for that Sometimes, I don't feel forced I'm also a woman as well... but sometimes, ma'am, after chemo, sometimes we want to do that I do not understand Even though it's dry, the vagina is really dry, but I want us to have sex I don't know, or maybe this is what medicine I want hahaha ”
(Informant 1)
Informant 10 told the researcher that since her illness, her h u s b a n d h a d b e c o m e c l o s e r a n d m o r e c o n c e r n e d However, as a cancer survivor, she was unable to serve her husband sexually although she still wanted to; the pain was severe
Informants 1 and 10 both stated that they had pain during intercourse but still felt obliged to provide sexual services to their husbands Therefore, information on how to meet their sexual needs were urgently needed to solve their sexual problems
According to these informants' experiences, the first year of treatment was very heavy going, and they had no desire for sexual activity, possibly due to the chemo treatment However, after a year of treatment, their desire for sexual activity returned
Informant 2 was 48 years old, had two children, and currently had metastases She stated that she was having problems with her husband, who currently had another woman
“About sexual things? No, it's just them sometimes Maybe it's because they're already sick so don't worry about that anymore, ma'am Let's focus on our health Sometimes, it's okay if he wants to look outside; what's more important, the important thing is that I'm healthy, sometimes my friends especially those who are still on drug therapy, like that Have you thought about that again?” (Informant 2)
Informant 2 focused more on her own treatment and said she didn't care about her husband's sexual needs In fact, she added that she had found her husband with another woman in his room
“But sex with a physical problem due to chemotherapy side effects was extremely upsetting to me The husband acted not that interested in sexual activities, hahaha It looks like I'm the only one who wants to do it that's why I'm sharing about cancer don't feel hopeless ” (Informant 2)
Informant 2 stated that her husband was no longer interested in her; in fact, she had to sleep on the sofa so she could sleep separately from her husband As a result, she experienced lower back pain because she didn't sleep in bed
Informant 5 stated that she did not want to display her body parts when in intimate contact with her husband She could not display her breasts to her spouse when engaging in sexual activities
“I could not engage in normal sexual activity with my husband I had to cover my breast area with a shirt because I was embarrassed to show it to my husband I feel like an imperfect wife to my husband ” (Informant 5)
Family support is needed to get information on sexuality Participants explained that family support greatly influenced the good relationship between participants and their partners Information about sexuality issues provided by the family is very meaningful for building good relationships with partners
“If you marry into a different clan, there is a problem: you cannot return to your family because you are not considered as their family member again ” (Informant 6)
“Family harmony has changed since my illness ” (Informant 7)
“In the family, it is really taboo to discuss sexual needs If there is a problem, it must not be told because it is a matter of shame ” (Informant 8)
“The problem must just be self-contained. That's better.” (Informant 9)
Informants 6, 7, 8, and 9 all stated that they needed support from their families The cancer survivors did not feel any bond with their partner’s family
Healthcare facilities need to provide sexual information
“Well then, there are many ways we can connect To begin with, it seems that many are shy to talk about sex I need more opportunities to discuss my sexual problems with people who are more experts in dealing with sexual problems after cancer therapy ” (Informant 3)
“If you want a discussion about sexual needs, you must ask in a kidding way ” (Informant 11)
Informants 3 and 11 stated that they felt ashamed to discuss their sexual needs Survivors feared discussing their
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Ida
Riri
98 D
Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti, Rudi Rudi,
Maria
sexual problems due to the taboo around this information
“Yes at least in the community, there is one nurse who is very close to us She was stationed in Sarjiwani She is such a good nurse; she continues to support us, but it seems that for something like that, about sex, she never did ” (Informant 4)
“We need a means for supporting our sexuality needs, a consultant ” (Informant 12)
Informants 4 and 12 stated that there had never been a nurse with whom they could discuss sexuality, and they needed someone with whom they could consult The informants were confused about the information they had received from the general environment relating to sexual problems The cancer survivors needed a discussion about sexual problems, which should be conducted with both the patients and their partners
LIFE EXPERIENCES OF INDONESIAN CANCER PATIENTS WITH CANCER RECURRENCES: INTERPRETATIVE PHENOMENOLOGY
(Rudi Rudi, Yati Afiyanti, Riri Maria)
Results
Theme 1: the reaction when information about recurrence was received or when bad news were received
Reaction of some participants to bad news included the surprise that their cancer had recurred For example, participant 4, who was 36 years old and had nasopharyngeal cancer, experienced a recurrence in August 2021 and said: “I was also surprised At first, Dr H stated that I had completely recovered, but I was suddenly surprised when the CT s c a n r e s u l t s s h o w e d a n o t h e r r a d i a t i n g t o t h e l i v e r ”
(Participant 4)
Participant 3, a woman 58 years old with breast cancer, experienced a recurrence in June 2020 When she received the bad news, she felt sad because her breast cancer had recurred and spread to her lungs and brain, stating: “Sad for sure, yes, yes, that's the most (crying) just giving up, other than trying to find a way, I just follow it, that's all ”
(Participant 3)
Participant 7, a man 43 years old with breast cancer, was disappointed after receiving information that his disease had recurred because of all the time he had put in trying to maintain his health through a healthy diet and regular exercise, but cancer kept coming back The participant said:
“Yes, I think I'm disappointed as long as it's been taken care of as much as possible, but why did I get cancer? Why did the others with random eating patterns, just healthy, just like that, when I thought like that, I protested; it's like it's not fair ”
(Participant 7)
Theme 2: the efforts made during a recurrence
All participants made efforts to overcome their recurrences
For example, participant 7, who was 43 years old when he was informed to have had a recurrence, tried having alternative treatments, namely cupping, hypnotherapy, and drinking herbs, stating:
“ I tried an alternative way The alternative was cupping and
hypnotherapy At that time, I had a fever, so I was taken to the therapy place there ” (Participant 7)
“At least, I prefer herbs I drink turmeric, ginger If I don't feel well, I drink ginger If that's the case, it's better just to make it myself and brew it myself ” (Participant 7)
Participant 9, a woman 58 years old with nasopharyngeal cancer, regularly consumed soursop leaves to treat her cancer The information about traditional medicine was obtained from browsing on the internet Participant 9 said:
“I used to browse on the internet that a traditional medicine to cure cancer is soursop leaves, so I regularly consume nine soursop leaves The containers range from a big bowl to a 3cup jar, and then one glass is the final There is no other medicine, there is no such thing as herbal medicine It's just that, just drink the leaves In the village, sir, there are many soursop leaves, only maumah ” (Participant 9)
Participant 6, a man 65 years old with bladder cancer that had recurred, when he had difficulty urinating drank boiled orthosiphon aristatus leaves based on a friend's suggestion After trying it, he could immediately urinate, stating:
“ my friend has bought it for me Once, I remembered boiled kumis kucing leaves When you drink it, it really comes out Wuuh, beeeerr ” (Participant 6)
The conventional medical treatments that the participants received were performed by healthcare workers in accordance with cancer treatment programs These treatments i
i o n Participant 7, after trying the next alternative, received conventional medical treatment as chemotherapy eight times after surgery and said:
“I got chemo after being in Dharmais from the surgeon who ordered chemo After that, eight rounds of chemo, followed by surgery ” (Participant 7)
After experiencing a recurrence, participant 8, 65 years old with back lippy sarcoma cancer, went back to the doctor and underwent surgery again, stating:
“Yes, eeh, the first time I said three surgeries, but suddenly the doctor was great, the mother was great, the mother was strong, and so we took everything Thank God, in 3 days, we went home straight away Thank God, we didn't feel anything ” (Participant 8)
Participant 3 was found to have had a recurrence in June 2020, and then in July 2020, the doctor gave instructions for a ray Here is his statement:
“ The main thing was that I was exposed to the light around the end of July, which means I found out it was around June if I'm not mistaken ” (Participant 3)
Lifestyle changes were also part of the participants' efforts to overcome their recurrences through having a healthier lifestyle, such as maintaining a healthy diet and cooking at home This was expressed by participant 1 when stating:
“If we cook our own food, we know we can't eat this, we can't wash it, we have to clean it, we have to eat vegetables too When we eat, we just cook; that's for ourselves, so the problem is I never buy food At least I buy fruit too; I haven't peeled it yet ” (Participant 1)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 98 E Problems of cancer survivors
n c l u d e d c h e m o t h e r a p y , s u r g e r y , a n d r a d i a t
Through the maintenance of a healthy lifestyle, an effort was made by the participants to overcome recurrence by controlling their routine based on the advice of medical personnel For example, the following was as stated by participant 9:
“ So, every December, the report card ends up being a check-up holiday after the class increase, and it's a check-up holiday, so we take the check-up from December to January and December to June school holidays every half year ”
(Participant 9)
After it was determined that participant 1 had a recurrence, her husband and children refrained from smoking in order to help her avoid another recurrence, stating:
“No, the husband doesn't smoke, and the children don't smoke If there's a friend playing, a friend of the father or a friend of the child, I'll go straight up ” (Participant 1) Getting closer to God was also part of the participants' efforts to regain health by praying to make their treatments easier, which was expressed by participant 2 when stating:
“Then what is more certain is that you pray more to God, so to ask for an easier treatment so that you can prolong your life so you can worship more ” (Participant 2)
Theme 3: the patient’s self-concept during a recurrence
Participant 1, a woman 49 years old with leukemia, hoped that after chemotherapy, she would not experience a recurrence, saying:
“Yes, if it's okay now, I'll just follow it, hopefully after the chemo Hopefully, it won't come back Maybe this chemo hasn't happened yet, bro. Can you do it one more time or two more times?” (Participant 1)
One indicator of the strong motivation of the participants to survive was seen in their continuation of cancer treatments that have side effects One important reason for this strong motivation for continuing to undergo treatments was found in their desire to live with their children until they grow up and get married or to see their grandchildren grow up This was expressed by both participant 2 and participant 1 as follows:
“Well, I don't know what for sure Maybe it's family, maybe
it's family I also want to be like my parents, so I can play with their grandchildren, hahaha ” (Participant 2)
“Yes, bro, I want to see my children, see my grandson grow up (while crying), and that's just how it is Look at my family I have to be strong and have to be excited to see my grandchildren just like that (crying while taking a deep breath) ”
(Participant 1)
The spirit of undergoing treatment was in the desire of each participant to immediately get help to become healthy and recover soon For example, participant 1 and participant 10 each stated:
“ I want to rush to chemo at home, so I said, yes, I want to rush to chemo so that I can treat my illness ” (Participant 1)
“Yes, the pain is not playing, so I just want to have another surgery If you don't remove it, it will interfere with eating It's really annoying ” (Participant 10)
Both moral and material support for patients undergoing treatment was obtained from family members This was as expressed by participant 8 when saying:
“Yes, the support is to be given back and forth from Jakarta You have to pay for it, and you have to give encouragement so that the mother gets better So, leaving for Jakarta, the motivation comes from their children Yes, there is encouragement from their children, brothers, and sisters There are also
(Participant 8)
Support from people outside the family, such as friends, neighbors, and neighborhood administrators, was also important as participant 2 and participant 8 both said:
“ and also with friends like that, friends who are close to you or for example, I also rarely say hello, but because we have, for example, what are we like, like the WA group for example, we need a donor It comes like that It means that God's help is also like that, right?” (Participant 2)
“Yes, there was also moral material that was donated yesterday. People received donations from something, such as a foundation, and then to the RW from the RT, who gave the expenses for the expenses there The community supports it from the outside; there is a lot of support; it encourages a speedy recovery ” (Participant 8)
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 Ida Ayu Made Ari Santi Tisnasari, Tuti Nuraini, Yati Afiyanti, Rudi Rudi, Riri Maria 98 F
e i g h b o r s w h o w a n t t o s e e k m y r e c o v e r y i n J a k a r t a ”
n
Risk of urogenital infections in non-diabetic patients treated with sodium glucose transporter 2 (SGLT2) inhibitors. Systematic review and meta-analysis

Rawa Bapir 1, 16 , Kamran Hassan Bhatti 2, 16 , Ahmed Eliwa 3, 16 , Herney Andrés García-Perdomo 4, 16 , Nazim Gherabi 5, 16 , Derek Hennessey 6, 16 , Vittorio Magri 7, 16 , Panagiotis Mourmouris 8, 16 , Adama Ouattara 9, 16 , Gianpaolo Perletti 10, 16 , Joseph Philipraj 11, 16 , Konstantinos Stamatiou 12, 16 , Musliu Adetola Tolani 13, 16 , Lazaros Tzelves 8, 16 , Stefan D. Anker 14 , Alberto Trinchieri 15, 16 , Noor Buchholz 16
1 Smart Health Tower, Sulaymaniyah, Kurdistan region, Iraq;
2 Urology Department, HMC, Hamad Medical Corporation, Qatar;
3 Department of Urology, Zagazig University, Zagazig, Sharkia, Egypt;
4 Universidad del Valle, Cali, Colombia;
5 Faculty of Medicine Algiers 1, Algiers, Algeria;
6 Department of Urology, Mercy University Hospital, Cork, Ireland;
7 Urology Unit, ASST Fatebenefratelli Sacco, Milan, Italy;
8 2nd Department of Urology, National and Kapodistrian University of Athens, Sismanoglio Hospital, Athens, Greece;
9 Division of Urology, Souro Sanou University Teaching Hospital, Bobo-Dioulasso, Burkina Faso;
10 Department of Biotechnology and Life Sciences, Section of Medical and Surgical Sciences, University of Insubria, Varese, Italy;
11 Department of Urology, Mahatma Gandhi Medical College and Research Institute, Sri Balaji Vidyapeeth, Puducherry, India;
12 Department of Urology, Tzaneio General Hospital, 18536 Piraeus, Greece;
13 Division of Urology, Department of Surgery, Ahmadu Bello University/Ahmadu Bello University Teaching Hospital, Zaria, Kaduna State, Nigeria;
14 Department of Cardiology and BCRT (Campus CVK), Charité Universitätsmedizin Berlin, Germany;
15 Urology School, University of Milan, Milan, Italy;
16 U-merge Ltd (Urology for emerging countries), London-Athens-Dubai *
Authors 1-16 have equally contributed to the paper and share first authorship
* U-merge Ltd (Urology for Emerging Countries) is an academic urological platform dedicated to facilitate knowledge transfer in urology on all levels from developed to emerging countries U-merge Ltd is registered with the Companies House in London/ UK www U-merge com
Supplementary Table 1.
Data extracted from the included studies (PICO Tables).
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 112 A REVIEW - SUPPLEMENTARY
MATERIAL

Archivio Italiano di Urologia e Andrologia 2023; 95, 2 R Bapir, K
Bhatti, A Eliwa, et al 112 B
Hassan

Archivio Italiano di Urologia e Andrologia 2023; 95, 2 112 C Urogenital infection and SGLT2 inhibitors

Archivio Italiano di Urologia e Andrologia 2023; 95, 2 R Bapir, K
A Eliwa, et al 112 D
Hassan Bhatti,
REFERENCES
1 Anker SD, Butler J, Filippatos G, et al EMPEROR-Preserved Trial Investigators Empagliflozin in Heart Failure with a Preserved Ejection Fraction N Engl J Med 2021; 385:1451-1461
2 Abraham WT, Lindenfeld J, Ponikowski P, et al Effect of empagliflozin on exercise ability and symptoms in heart failure patients with reduced and preserved ejection fraction, with and without type 2 diabetes Eur Heart J 2021; 42:700-710
3 Bays HE, Weinstein R, Law G, Canovatchel W Canagliflozin: effects in overweight and obese subjects without diabetes mellitus Obesity (Silver Spring) 2014; 22:1042-9
4 Cherney DZI, Dekkers CCJ, Barbour SJ, et al DIAMOND investigators Effects of the SGLT2 inhibitor dapagliflozin on proteinuria in nondiabetic patients with chronic kidney disease (DIAMOND): a randomised, double-blind, crossover trial Lancet Diabetes Endocrinol 2020; 8:582-593
5 The EMPA-KIDNEY Collaborative Group; Herrington WG, Staplin N, Wanner C, et al Empagliflozin in Patients with Chronic Kidney Disease N Engl J Med 2023; 388:117-127
6 Hollander P, Bays HE, Rosenstock J, et al Coadministration of Canagliflozin and Phentermine for Weight Management in Overweight and Obese Individuals Without Diabetes: A Randomized Clinical Trial Diabetes Care 2017; 40:632-639
7 Lundkvist P, Pereira MJ, Katsogiannos P, et al Dapagliflozin once daily plus exenatide once weekly in obese adults without diabetes: Sustained reductions in body weight, glycaemia and blood pressure over 1 year Diabetes Obes Metab 2017;19:1276-1288

Archivio Italiano di Urologia e Andrologia 2023; 95, 2 112 E Urogenital infection and SGLT2 inhibitors
8 McMurray JJV, Solomon SD, Inzucchi SE, et al DAPA-HF Trial Committees and Investigators Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction N Engl J Med 2019; 381:1995-2008
9 Packer M, Anker SD, Butler J, et al EMPEROR-Reduced Trial Investigators Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure N Engl J Med 2020; 383:1413-1424
10 Reis J, Teixeira AR, Gonçalves AV, et al Dapagliflozin Impact on the Exercise Capacity of Non-Diabetic Heart Failure with Reduced Ejection Fraction Patients J Clin Med 2022;11:2935
11 Solomon SD, McMurray JJV, Claggett B, et al DELIVER Trial Committees and Investigators Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction N Engl J Med 2022; 387:1089-1098
12 Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al DAPA-CKD Trial Committees and Investigators Effects of dapagliflozin on major adverse kidney and cardiovascular events in patients with diabetic and non-diabetic chronic kidney disease: a prespecified analysis from the DAPA-CKD trial Lancet Diabetes Endocrinol 2021; 9:22-31
13 Nutzenbewertungsverfahren zum Wirkstoff Empagliflozin (Neues Anwendungsgebiet: chronische Herzinsuffizienz mit linksventrikulärer Ejektionsfraktion LVEF > 40%) https//www g-ba de /bewertungsverfahren/nutzenbewertung/810/
14 Anker SD, Butler J, Filippatos G, et al Effect of Empagliflozin on Cardiovascular and Renal Outcomes in Patients With Heart Failure by Baseline Diabetes Status: Results From the EMPEROR-Reduced Trial Circulation 2021; 143:337-349
Archivio Italiano di Urologia e Andrologia 2023; 95, 2
112 F
R Bapir, K Hassan Bhatti, A Eliwa, et al
Supplementary Figure 1
RISK OF BIAS
Risk of Bias (RoB) 2 assessment of risk of bias in randomised control trialspresented The values at the right of the no-effect bar show higher odds of infection in diabetic patients
REFERENCES
1 Sterne JAC, Savovic J, Page MJ, et al RoB 2: a revised tool for assessing risk of bias in randomised trials BMJ 2019;366:l4898
2 Lundh A, Gotzsche PC Recommendations by Cochrane Review Groups for assessment of the risk of bias in studies BMC Med Res Methodol 2008;8:22

Archivio Italiano di Urologia e Andrologia 2023; 95, 2 112 G Urogenital infection and SGLT2 inhibitors
R Bapir, K Hassan Bhatti, A Eliwa, et al
Tools to assess study quality were tailored to study design The risk of bias in randomised control trials was assessed using the Risk of Bias (RoB) 2 assessment tool as prescribed by the Cochrane Methods 1,2 Data is shown in table S2 (Supplementary Table 2) Study quality was independently assessed by two reviewers (DH and HP) against pre-defined criteria Disagreements were resolved by discussion Risk of bias was not used to exclude studies We anticipated identifying too few studies to assess publication bias
COMMENTS
Abraham - Slight differences between the two groups Domain 1 slight concer ns
Anker - No concer ns
Bays - No concer ns
Cherney - No concer ns
Herrington - No concer ns
Hollander - Single blinded study Domain 1 slight concer ns Small sample sizes
Lundquist - No concer ns
McMurray - No concer ns
Packer - No concer ns
Reis - Not blinded I am not sure the allocation sequence concealed until participants were enrolled and assigned to interventions also carers and people delivering the interventions were aware of participants' assigned intervention during the trial
Salomon - No concer ns
Wheeler - No concer ns
Archivio Italiano di Urologia e Andrologia 2023; 95, 2
112 H
Urogenital infection and SGLT2 inhibitors
FUNNEL PLOTS
Supplementary Figure 2
Publication bias assessment in pooled analyses including at least 4 trials The effect size is presented as the logarithm of the odds ratios If missing studies (open orange circles) are imputed by the “trim-and-fill” analysis, adjusted odds ratios (red dots) and 95% confidence intervals are presented in the plots



UTI in non-diabetics; SGLTi vs Placebo Genital infections in non-diabetics; SGLTi vs Placebo
UTI – Diabetics vs Non Diabetics; patients on SGLTi
Genital infections – Diabetics vs Non Diabetics; patients on SGLTi
UTI – Diabetics vs Non Diabetics; patients on Placebo
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 112 I
SUMMARY OF FINDINGS
Supplementary Table 2
Effect of SGLT2 inhibitors or placebo on urogenital infections
Patient or population: male or female patients with or without diabetes
Settings: outpatient
Comparison: placebo Outcome:
The corresponding intervention risk (and ts 95% conf dence interva ) s based on the assumed control r sk n the compar son group and the relative effect of the intervent on (and its 95% CI)
It is calcu ated from the odds ratio us ng the formu a: OR x ACR/[1-ACR + (OR x ACR)]
CI: Conf dence Interval; OR: Odds Ratio; ACR: Assumed Control Risk
GRADE Work ng Group grades of ev dence
High qua ity: Further research is very unl ke y to change our conf dence in the estimate of effect
Moderate qual ty: Further research is l ke y to have an mportant impact on our confidence in the estimate of effect and may change the estimate
Low qual ty: Further research is very likely to have an important impact on our confidence in the estimate of effect and s likely to change the estimate
Very low quality: We are very uncertain about the estimate
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 R
112 L
Bapir, K Hassan Bhatti, A Eliwa, et al
Intervention: SGLT2 inhibitors (SGLT2i)
onset of urinary tract infections (UTI) or genital infections (GI) Endpoint, Comparison, Condition Illustrative comparative risks (95% CI) Relative effect No of Par ticipants Quality of the e vidence Comments (95% CI) (studies or comparisons) (GRADE) Assumed control risk Corresponding intervention risk Comparison Intervention Urinary tract infections, SGLT2i 44 41 per 1000 58 21 per 1000 OR 1 33 7326 ⊕⊝⊝⊝ Reasons for downgrad ng: vs. placebo, non-diabetic subjects (47.78 to71.21) (1.08 to 1.65) (9) Very low - risk of bias
probable publication bias
Indirectness of evidence (Surrogate endpoint) Genital infections, SGLT2i 5 34 per 1000 16 42 per 1000 OR 3 11 7326 ⊕⊕⊕⊝ Reasons for upgrading: vs placebo, non-diabetic subjects (10 04 to 26 80) (1 89 to 5 13) (9) Moderate - large magnitude of effect Reasons for downgrad ng: - risk of bias - Indirectness of evidence (Surrogate endpoint) Urinary tract infections, diabetic 58 81 per 1000 67 03 per 1000 OR 1 15 7317 ⊕⊕⊝⊝ Reasons for downgrad ng: vs non-diabetic subjects treated (55 47 to 80 96) (0 94 to 1 41) (4) Low - probable publication bias with SGLT2i - Indirectness of evidence (Surrogate endpoint) Genital infections, diabetic 13.33 per 1000 18.05 per 1000 OR 1.36 7317 ⊕⊕⊝⊝ Reasons for downgrad ng: vs non-diabetic subjects treated (14 26 to 22 72) (1 07 to 1 72) (4) Low - probable publication bias with SGLT2i - Indirectness of evidence (Surrogate endpoint) Urinary tract infections, diabetic 45 89 per 1000 58 85 per 1000 OR 1 30 7312 ⊕⊕⊕⊝ Reasons for downgrad ng: vs non-diabetic subjects taking placebo (477 64 to 72
Moderate - Indirectness of evidence (Surrogate endpoint)
infections,
4 86
1000 5 49 per 1000 OR 1 13 7312 ⊕⊕⊕⊝ Reasons for downgrad ng: vs non-diabetic
placebo (2 09 to 14 35) (0 43 to 2 98) (4) Moderate - Indirectness of evidence (Surrogate
-
-
29) (1 04 to 1 62) (4)
Genital
diabetic
per
subjects taking
endpoint)
The presentation and outcomes of penile fracture with associated urethral injury: A systematic literature review
Salah E. Shebl Urology Department, Faculty of Medicine for Girls, Al-Azhar University, Cairo, Egypt
1 Does the patient(s) represent(s) the whole experience of the investigator (centre) or is the selection method unclear to the extent that other patients with similar presentation may not have been reported?
2 Was the exposure adequately ascertained?
3 Was the outcome adequately ascertained?
4 Were other alternative causes that may explain the observation ruled out?
5 Was there a challenge/ rechallenge phenomenon?
6 Was there a dose–response effect?
7 Was follow-up long enough for outcomes to occur?
8 Is the case(s) described with sufficient details to allow other investigators to replicate the research or to allow practitioners make inferences related to their own practice?
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 120 A REVIEW - SUPPLEMENTARY MATERIAL
Supplementary Table 1 Quality assessment of included studies Study ID Selection Ascer tainment Causality Repor ting Amit et al, 2013 (20) Yes Yes Yes Yes N/A N/A Yes Yes Kasaraneni et al, 2019 (27) Yes Yes Yes Yes N/A N/A Yes Yes Derouiche et al, 2007 (22) No No No Yes N/A N/A Yes No Raheem et al, 2014 (6) Yes Yes Yes Yes N/A N/A Yes Yes Ibrahiem et al, 2010 (23) Yes Yes Yes Yes N/A N/A Yes Yes Barros et al, 2018 (26) Yes Yes Yes Yes N/A N/A Yes Yes Mercado-Olivares et al, 2018 (34) No Yes Yes No N/A N/A No Yes Ouanes et al, 2021 (24) Yes Yes Yes Yes N/A N/A No No Hughes et al, 2021 (33) No Yes Yes No N/A N/A No No Boncher et al, 2010 (39) No Yes Yes No N/A N/A Yes No Tang et al, 2018 (25) Yes Yes Yes Yes N/A N/A Yes Yes Ge et al, 2021 (31) No Yes Yes Yes N/A N/A No Yes Garofalo et al, 2015 (30) No Yes Yes Yes N/A N/A Yes Yes Jagodic et al, 2007 (29) No Yes Yes Yes N/A N/A Yes Yes Hoag et a , 2011 (28) No Yes Yes Yes N/A N/A No Yes N/A: Not applicable
LETTER TO EDITOR - SUPPLEMENTARY MATERIAL
Role of spinal anesthesia in robot-assisted radical prostatectomy: Gamble or opportunity?
Lorenzo Spirito 1 , Annachiara Marra 2 , Vincenzo Mirone 3 , Celeste Manfredi 1 , Ferdinando Fusco 1 , Luigi Napolitano 3 , Giuseppe Servillo 2 , Nicola Logrieco 2 , Pasquale Buonanno 2
1 Urology Unit, Department of Woman, Child and General and Specialized Surgery, University of Campania "Luigi Vanvitelli", Naples, Italy;
2 Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples “Federico II”, Naples, Italy;
3 Urology Unit, Department of Neurosciences, Reproductive Sciences and Odontostomatology, Urology Unit, University of Naples "Federico II", Naples
Submitted 14 March 2023; Accepted 23 March 2023
REFERENCES
Bae J, Kim HC, Hong DM Intrathecal morphine for postoperative pain control following robot-assisted prostatectomy: a prospective randomized trial J Anesth 2017; 31:565-571
Beilstein CM, Huber M, Furrer MA, et al Impact of analgesic techniques on early quality of recovery after prostatectomy: A 3-arm, randomized trial Eur J Pain 2022; 26:1990-2002
Dhawan R, Daubenspeck D, Wroblewski KE, et al Intrathecal Morphine for Analgesia in Minimally Invasive Cardiac Surgery: A Randomized, Placebo-controlled, Double-blinded Clinical Trial Anesthesiology 2021;135:864-876
Gontero P, Oderda M, Calleris G, et al Awake Da Vinci robotic partial nephrectomy: First case report ever in a situation of need Urol Case Rep 2022; 42:102008
Ross SB, Mangar D, Karlnoski R, et al Laparo-endoscopic single-site (LESS) cholecystectomy with epidural vs general anesthesia Surg Endosc 2013; 27:1810-9
Segal D, Awad N, Nasir H, et al Combined spinal and general anesthesia vs general anesthesia for robotic sacrocervicopexy: a randomized controlled trial Int Urogynecol J 2014; 25:369-74
Shim JW, Cho YJ, Kim M, et al Comparison of analgesic efficacy between rectus sheath blockade, intrathecal morphine with bupivacaine, and intravenous patient-controlled analgesia in patients undergoing robot-assisted laparoscopic prostatectomy: a prospective, observational clinical study BMC Anesthesiol 2020; 20:291
Shim JW, Cho YJ, Moon HW, et al Analgesic efficacy of intrathecal morphine and bupivacaine during the early postoperative period in patients who underwent robotic-assisted laparoscopic prostatectomy: a prospective randomized controlled study BMC Urol 2021; 21:30
Archivio Italiano di Urologia e Andrologia 2023; 95, 2 126 A
INSTRUCTIONS TO AUTHORS – ARCHIVIO ITALIANO DI UROLOGIA E ANDROLOGIA
OPEN ACCESS
Open access publishing does have its costs. Information regarding authors’ payment are not made available to editors and reviewers ensuring that they cannot be influenced in their selection of papers for publication by payment conditions or limitations.
The Article Processing Charge for publication in this journal is EUR 300,00 (plus VAT, if applicable).
Our fees cover the costs of peer review, copyediting, publication, different format of publication (HTML, PDF), inclusion in many Open Access databases.
All bank charges shall be borne by the payer.
Please note that our fees do not include taxes (VAT):
- Private or public ITALIAN customers (individuals, universities, hospitals, other organizations) must ALWAYS add VAT (IVA) at standard rate (4%);
- European Union PRIVATE customers must add the standard rate of their own country VAT tax;
- European Union private/public ORGANIZATIONS (universities, hospitals, others with regular VAT number) should not add any taxes at standard rate, provided that they indicate their VAT number;
- Outside the European Union, individuals and organizations should not add any taxes at standard rate.
Important: Authors are NOT required to pay at the moment of submission. If the paper is accepted, the Managing Editor of Open Access Edition will guide the Authors through the payment procedure. No article will be published before waiver or payment.
According to the United Nations list of Least Developed Countries (LCDs) available from: http://www.un.org/en/development/desa/policy/cdp/ldc2/ldc_countries.shtml
Authors coming from those countries are entitled to ask for a discount.
A “Formal Request for discount” has to be forwarded to the Managing Editor of Open Access Edition, after receiving the acceptance letter. The Editorial Committee will then evaluate the merits of each individual case. Any other informal request (such as comments at the moment of submission, or made in the covering letter of the revised version) will not be taken into consideration.
FAST-TRACK
PEER REVIEW
All papers published in Archivio Italiano di Urologia e Andrologia (AIUA) are peer reviewed. Fast-track peer review (4 weeks) can be obtained by supplementary fee of € 488 (VAT included).
in Italian language can be published after translation (expenses will be charged to the Authors). Manuscripts should be typed double spaced with wide margins. They must be subdivided into the following sections:
TITLE PAGE
It must contain: a) title; b) a short (no more than 40 characters) running head title; c) first, middle and last name of each Author without abbreviations; d) University or Hospital, and Department of each Author; e) last name, address and e-mail of all the Authors; f) corresponding Author; g) acknowledgement of conflict of interest and financial support.
SUMMARY
Authors must submit a summary (300 words, 2000 characters) divided by subheadings as follows: Objective(s), Material and method(s), Result(s), Conclusion(s). After the summary, three to ten key words must appear, taken from the standard Index Medicus terminology.
TEXT
For original articles concerning experimental or clinical studies, the following standard scheme must be followed: Summary - Key Words - Introduction - Material and Methods - Results - Discussion - Conclusions - References - Tables - Legends - Figures.
Case Report should be divided into: Summary - Introduction (optional) - Case report(s) - Conclusions - References
Supplementary Materials can be added for online publication.
SIZE OF MANUSCRIPTS
Literature reviews, Editorials and Original articles should not exceed 3500 words with 3-5 figures or tables, and no more than 30 references.
Case reports, Notes on surgical technique, and Letters to the editors should not exceed 1000 words (summary included) with only one table or figure, and no more than three references. No more than five authors are permitted.
REFERENCES
Authors can pay their fees by: PayPal is the most recommended and secure payment system. It enables you to pay getting your payment receipt immediately and without sharing your financial information. Other methods of payment are:
METHODS OF PAYMENT
Bank transfer
BANK NAME: Banca Popolare di Sondrio, Branch #1, Strada Nuova 75, I-27100 Pavia, Italy
ACCOUNT HOLDER: PAGEPress Srl
BIC/SWIFT: POSOIT22
IBAN: IT85Y0569611301000005086X83
Credit Card The credit card form to be filled and returned either via e-mail or via fax is available for download here. http://www.pagepress.org/journals/public/credit_card.pdf
Check sent by surface mail Checks must be made payable to PAGEPress Srl and must be sent to our full postal address: PAGEPress Publications, via A. Cavagna Sangiuliani 5, 27100 Pavia, Italy.
Note: In any method of payment you choose, kindly specify: 1. journal name; 2. paper ID number; 3. first author.
IMPORTANT TO KNOW
REGISTERED DRUGS, DIET SUPPLEMENTS, NUTRACEUTICALS, MEDICAL DEVICES
Authors of papers that contain references to registered drugs, diet supplements, nutraceuticals and medical devices are requested to buy a minimum amount of 100 reprints at a cost of € 1.500 (1 to 4 pages) or € 2.000 (5 to 8 pages). Prices for the purchase of number of reprints greater than 100 can be negotiated with Edizioni Scripta Manent At present, Edizioni Scripta Manent let everyone to read, print and download papers from website, but retains copyright for republishing and distribution rights for commercial purpose.
TRANSLATION
Translation of manuscripts in Italian language is offered on payment.
Translation and reprints can be requested to Edizioni Scripta Manent by e-mail to info@edizioniscriptamanent.eu
AUTHORS’ RESPONSIBILITIES
Manuscripts are accepted with the understanding that they have not been published or submitted for publication in any other journal.
Authors must submit the results of clinical and experimental studies conducted according to the Helsinki Declaration on clinical research and to the Ethical Code on animal research set forth by WHO (WHO Chronicle 1985; 39:51).
The Authors must obtain permission to reproduce figures, tables and text from previously published material. Written permission must be obtained from the original copyright holder (generally the Publisher).
MANUSCRIPT PRESENTATION
Authors must submit their manuscripts (MAC and WINDOWS Microsoft Word are accepted) after registration and login to the link: http://www.aiua.it. Surface or e-mail submission are not accepted.
Manuscripts must be written in English language in accordance with the “Uniform Requirements for Manuscripts submitted to biomedical journals” defined by The International Committee of Medical Journal Editors (http://www.ICMJE.org). Manuscripts
References must be sorted in order of quotation and numbered with arabic digits between parentheses. Only the references quoted in the text can be listed. Unpublished studies cannot be quoted, however articles “in press” can be listed with the proper indication of the journal title, year and possibly volume. References must be listed as follows.
JOURNAL ARTICLES
All Authors if there are six or fewer, otherwise the first three, followed by “et al.”. Complete names for Work Groups or Committees. Complete title in the original language. Title of the journal following Index Medicus rules. Year of publication; Volume number: First page. Example: Starzl T, Iwatsuki S, Shaw BW, et al. Left hepatic trisegmentectomy Surg Gynecol Obstet. 1982; 155:21.
BOOKS
Authors - Complete title in the original language. Edition number (if later than the first). City of publication: Publisher, Year of publication. Example: Bergel DIA. Cardiovascular dynamics. 2nd ed. London: Aca de mic Press Inc., 1974.
BOOK CHAPTERS
Authors of the chapters - Complete chapter title. In: Book Editor, complete Book Title, Edition number. City of publication: Publisher, Publication year: first page of chapter in the book. Example: Sagawa K. The use of central theory and system analysis. In: Bergel DH (Ed), Cardiovascular dynamics. 2nd ed. London: Aca demic Press Inc., 1964; 115.
TABLES
Tables must be numbered in Arabic digits and referred to in the text by progressive numbers. Every table must be accompanied by a brief title. The meaning of any abbreviations must be explained at the bottom of the table itself.
FIGURES
(Graphics, algorithms, photographs, drawings). Figures must be numbered and quoted in the text by number. The meaning of symbols or abbreviations must be indicated. Histology photograph legends must include the enlargement ratio and the staining method. Legends must be collected in one or more separate pages.
• Do not include any illustrations as part of your text file. • Do not prepare any figures in Word as they are not workable. • Line illustrations must be submitted at 600 DPI. • Halftones and color photos should be submitted at a minimum of 300 DPI. • Power Point files cannot be uploaded. • If possible please avoid transmitting electronic files in JPEG format or save the JPEG at the highest quality available • PDF files may be uploaded.
MANUSCRIPT REVIEW
Manuscripts are evaluated by the Editorial Board and/or by two referees designated by the Editors. The Authors are informed in a time as short as possible on whether the paper has been accepted, rejected or if a revision is deemed necessary. The Editors reserve the right to make editorial and literary corrections with the goal of making the article clearer or more concise, without altering its contents. Submission of a manuscript implies acceptation of all above rules.
PROOFS
Authors are responsible for ensuring that all manuscripts are accurately typed before final submission. Galley proofs will be sent to the first Author. Proofs should be returned within seven days from receipt.
que è u n st’aque tt p n u ti per i p bbona proge lut a no e o in tiien az p ti.it it t tutti.i te.en per tua la el sa /a p ’aspet pe la i s va fo er in

da quest’anno salutepertutti.it è un progetto ind ipendente. abbonati per i pazienti della tua sala d’aspetto.



10,00€/anno per 3 numeri per info vai su www.salutepertutti.it






Una raccolta di foto e curiosità, sul mondo della Salute e dello stare bene.
ti.i

tto. tt no per 3 nu n w.s w w u i s eri m tuluteper a t ti i it t tutti.i






www.salutepertutti.it
www.salutepertutti.it

I l podcast d ella rIvIsta












Salutepertutti.it non è più solo la rivista della sala d’aspetto.




In questo podcast parliamo sì di salute, ma lo facciamo legandola
ta anche alla cultura pop, al cinema, ai social e all'attualità.

Le voci di Salutepertutti.it sono
Ruben Cazzola e Alessia Bisini.
















 Mariano Martini 1, 2 , Giuseppe Martorana 3
Mariano Martini 1, 2 , Giuseppe Martorana 3