EMERGING IDEAS IN BRAIN SCIENCE



Putting treatment and technology into place across the globe using cultural and ethical guidelines

Ilina Singh, Ph.D.
Neuroscience for Global Mental Health
Page 12

Frank R. Lin, M.D., Ph.D.
Hear and Now
Page 20

Kayt Sukel
Adapting to the (Not So) New Age of Computer Learning
Page 26

Brenda Patoine
Pandemic Brain: Parsing the Mental Health Toll:
Page 32
Ilina Singh, Ph.D., is Professor of Neuroscience & Society at the University of Oxford and co-director of the Welcome Trust Center for Ethics and Humanities. Her core research examines the psychosocial and ethical implications of advances in biomedicine and neuroscience for young people and families. She received a Wellcome Trust Senior Investigator Award in 2015 on the ethics of early intervention in child psychiatry. Since 2016, Singh has led a global collaborative project on the science and ethics of psychiatric genomics in Africa. She is the academic lead for Patient and Public Involvement and Engagement in the Oxford Health Biomedical Research Center and sits on the UK Research and Innovation Covid-19 Rapid Response Taskforce. Singh is also treasurer of the International Neuroethics Society. She received her doctorate in human development and psychology from Harvard University.
Frank R. Lin, M.D., Ph.D., is professor and director of the Cochlear Center for Hearing and Public Health at Johns Hopkins University. As an otologic surgeon and epidemiologist, he has translated his experiences caring for older adults with hearing loss into foundational public health research and federal policy. His research established the association of hearing loss with cognitive decline and dementia, and he now leads two ongoing, National Institutes of Health-funded randomized trials that are evaluating the efficacy of hearing interventions. In parallel, Lin has collaborated with the National Academies, the White House, and Congress to develop policies to ensure hearing loss can be effectively and sustainably addressed in society.
Kayt Sukel‘s work has appeared in the Atlantic Monthly, the New Scientist, USA Today, the Washington Post, Parenting, National Geographic Traveler, and the AARP Bulletin. She is a partner at the award-winning family travel website Travel Savvy Mom, and is also a frequent contributor to the Dana Foundation’s science publications. She has written about out-of-body experiences, fMRI orgasms, computer models of schizophrenia, the stigma of single motherhood, and why one should travel to exotic lands with young children. She is the author of Dirty Minds: How Our Brains Influence Love, Sex and Relationships and The Art of Risk: The New Science of Courage, Caution & Chance
Brenda Patoine is a freelance science writer, reporter, and blogger who has been covering neuroscience research for more than 30 years. Her specialty is translating complex scientific findings into writings for the general public that address the question of “what does this mean to me?” She has interviewed hundreds of leading neuroscientists over three decades, including six Nobel Laureates. She founded ScienceWRITE Medical Communications in 1989 and holds a degree in journalism from St. Michael’s College. Other areas of interest are holistic wellness, science and spirituality, and bhakti yoga. Brenda lives in Burlington, V.T., with her cat Shakti.
Our author—Professor of Neuroscience & Society at the University of Oxford and codirector of the Wellcome Trust Center for Ethics and Humanities—reflects on efforts to grow recognition of neuroscience in low- and middle-income countries.
By Ilina Singh, Ph.D.As a practicing otologic surgeon with a Ph.D. in epidemiology, our author tells us what we’ve learned and what we still need to know about the relationship between hearing loss and cognitive decline in older adults.on education and personal development.
By Frank R. Lin, M.D., Ph.D.Schools have had no choice but to embrace virtual learning. But the question remains: How does it work when compared to traditional, face-to-face instruction?
By Kayt SukelMany experts have sounded the alarm for an approaching tsunami of psychological maladies that could sink an already overburdened mental healthcare system.
By Brenda PatoineShowcasing the works and stories of talented, under-the-radar artists with developmental disabilities.
By Seimi Rurup5 Briefly Noted • By the Numbers, Brain on the Web, Reading Is Fundamental
6 Advances • Notable brain science findings
7 Bookshelf • A few brain science books that have recently caught our eye
8 Neuroethics: Neuroscience Confronts Racism • By Philip M. Boffey
9 In Memoriam • Leslie Iversen, Masakazu Konishi, Frederick Goodwin, Stephen Lieber
10 Clinical Corner: The Normally Abnormal • By Michael P.H. Stanley, M.D.
11 Talking Neuroscience • A Sampler of Cerebrum Podcast Episodes

NOTABLE FACTS IN THIS ISSUE
4 The overwhelming majority of what we know about the human brain is derived from research on people of Anglo-European descent living in Western countries.
Neuroscience for Global Mental Health, Page 12
4 For those who obtained effective treatment for their hearing loss with hearing aids or a cochlear implant, the effects were often equally dramatic.
Hear and Now, Page 20
4 “We’ve learned the average attention span of a high schooler lasts for about a six-minute video. You get even less time for the little ones. So, you need to create the kind of structure and routine for kids so they can stay engaged and motivated.”
Adapting to the (Not So) New Age of Computer Learning, Page 26
4 While the Covid-19 pandemic rages on worldwide, the immediate mental health impact of this collective trauma is coming into focus even as the outlook for long-term psychological effects remains considerably fuzzier.
Pandemic Brain: Parsing the Mental Health Toll, Page 32
4 The Arc Westchester provides support for more than 2,000 individuals with intellectual and developmental disabilities, and its gallery provides opportunities for artists to develop their talents alongside a community where artistic expression is cultivated and supported.
Art on the Spectrum, Page 38
2 Contributors | 4 From the Editor | 42 Advisory Board | 44 Editorial Staff
 BY BILL GLOVIN Executive Editor, Dana Foundation
BY BILL GLOVIN Executive Editor, Dana Foundation
While Cerebrum has published individual articles and book reviews since 1998, this issue signifies our first year of publishing Cerebrum as a magazine. We’ve enjoyed bringing it to you and hope you’ve found it useful. The objective is to provide a visually appealing mix: first and foremost, articles by neuroscientists who tell us why their area of research has the potential to help people, as well as the topic’s funding and publicpolicy implications.
We also offer articles by science journalists on subjects we think are of interest. Since reliable information on Covid-19’s relationship to the brain and mental health continues to slowly unravel, we examine two related topics in this issue: live instruction versus computer learning and collective trauma’s impact on mental health.
Front and center in recent months has also been the Black Lives Matter movement, and inclusion and diversity in the neuroscience field are the focus of both our cover story and neuroethics column. We’ve asked Ilina Singh, Ph.D., Professor of Neuroscience & Society and co-director of the Wellcome Centre for Ethics and Humanities at the University of Oxford, to tell us why neuroscience is mostly invisible in some parts of the world and the strategies by leadership to expand outreach. Our neuroethics columnist, Phil Boffey, confronts diversity with his column titled, “Neuroscience Confronts Racism.”
We are also offering a feature on a topic that has been under the radar for far too long: hearing loss and its link to dementia and cognitive function. Frank Lin, M.D., Ph.D., professor and director of the Cochlear Center for Hearing Loss and Public Health at Johns Hopkins University, tells us what we’ve learned and what we still need to know about an issue that effects millions of people and their families. Additionally, assistant editor Seimi Rurup helps us showcase the art of talented, under-the-radar artists with developmental disabilities.
With this issue, we also introduce a new regular column, “Clinical Corner,” a first-person account from someone on the frontlines of neurodegenerative or mental health treatment. The idea is to help humanize some of the complex research that is often at the heart of some of our stories. In this first column, “The Normally Abnormal,” neurologist Michael P.H. Stanley, M.D., addresses the challenges of treating a patient with multiple neuropsychiatric symptoms. We hope you find this new column informative.
Meanwhile, our new Cerebrum magazine welcomes your feedback; whether it be on our content, what we should consider covering, or how you feel about anything at all. l
Bill Glovin Executive Editor
Seimi Rurup Assitant Editor
Podcast
Brandon Barrera Editorial Assistant
Carl Sherman Copy Editor
Carolyn Asbury, Ph.D. Scientific Consultant
Bruce Hanson Art Director
Cerebrum is published by the Charles A. Dana Foundation, Incorporated. DANA is a federally registered trademark owned by the Foundation.
© 2020 by The Charles A. Dana Foundation, Incorporated. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the publisher, except in the case of brief quotations embodied in articles.
Letters to the Editor
Cerebrum Magazine
505 Fifth Avenue, 6th Floor New York, NY 10017 or cerebrum@dana.org
Letters may be edited for length and clarity. We regret that we cannot answer each one.
ILLUSTRATION:
A few brain-related articles we recommend:
> CNN Health: Americans over 30 have been drinking more during the coronavirus pandemic, research shows

> Washington Post: Creators call digital game prescription for ADHD the future of medicine. Critics call it a marketing ploy.
> CNN: Scientists find intact brain cells in skull of man killed in Vesuvius eruption nearly 2,000 years ago
> New Scientist: Cyborg grasshoppers have been engineered to sniff out explosives
> The Guardian: Researchers find a western-style diet can impair brain function
> Brain Facts/SfN: How Microdosing Psychedelic Drugs Affects Mental Health
> New York Times: The Brain Implants That Could Change Humanity
> Smithsonian Magazine: What Neuroscientists Are Discovering About Stuttering
> New York Times: How the Coronavirus Attacks the Brain
> AARP’s The Daily: 3 Reasons the Pandemic Is Ruining Your Sleep—And What to Do About It

$3 million was awarded by the Breakthrough Prize Foundation earlier this year to Virginia M.Y. Lee, Ph.D., at Pennsylvania State University, for discovering protein aggregates in frontotemporal dementia and amyotrophic lateral sclerosis.
02.20.2020 was the date for the first shipping of Buzz, a wearable wristband that allows people to sense sound through their skin. The technology was conceived in neuroscientist David Eagleman’s lab at Stanford University and is sold through his company, Neosensory.
23% of preschool children ages two to five with family dogs were less likely to have social interaction problems than children whose households do not have a dog. The “mere presence of a family dog was associated with many positive behaviors and emotions,” said one of the researchers.
25 of October 2020 is the deadline for submissions to an annual visual storyteller photography competition that documents Alzheimer’s disease and dementia. Sponsored by the Bob and Diane Fund, the competition awards a $5,000 grant in mid-November during National Caregivers Month.
55% of coronavirus patients still have neurological problems three months later, according to a study published in Lancet
Reading is fundamental
“[Print reading] is kind of like meditation—focusing our attention on something still. And it’s a whole different kind of immersion than responding to [digital] stimuli. I think it’s healthy for us as human beings to sit down with something that doesn’t move, ping, or call on our attention.”

— Anne Mangen, a literacy professor at the University of Stavanger in Norway
80% of kids who stutter grow up to have normal speech patterns, while the other 20 percent continue to stutter into adulthood.
1,000 is the number of older adults in their 70s and 80s recruited for the Aging and Cognitive Health Evaluation in Elders (ACHIEVE) trial.
8,557 is the number of subscribers to the Neuroscience for Kids newsletter, which has been published by neuroscientist Eric Chudler, Ph.D. and colleagues at the University of Washington since 1997.
 BY NICKY PENTTILA
BY NICKY PENTTILA
The effects of high blood pressure and diabetes can already be seen among middle-aged people, who appear otherwise healthy, as reduced scores on tests of COGNITIVE FUNCTION and in altered brain structure, according to a review of health data from 22,000 people in the UK Biobank project. Researchers found the effect was strongest in people ages 44-69 and increased in proportion to how far above 140mm a person’s systolic blood pressure (BP) was. Earlier studies have shown that midlife troubles with blood pressure and diabetes increase the risk of dementia in older age; this study suggests that people with “mildly” high BP try to keep their number below 140. l
PARKINSON’S DISEASE (PD) may originate in two separate ways: A “brain-first” (top-down) type that starts in the brain and spreads into motor and other systems, or a “body-first” (bottom-up) type that starts in the autonomic nervous system in the gut and spreads to the brain. Using PET brain imaging and CT colon imaging from 37 volunteer patients with Parkinson’s and 22 volunteers who had one symptom (Isolated REM sleep behavior disorder) but not PD, the researchers could trace the two pathways. The sleep symptom is an early signal for the body-first subtype, they reported in the journal Brain l
Studying living brains is tough: They are dense and well-protected by skull and other materials. To investigate at the molecular level, magnetic resonance imaging (MRI) uses contrast agents, which often contain metals that are foreign to the body. Now, researchers have described a method that uses something already in our bodies: AIR. Our cells contain gas vesicles, tiny genetically encodable protein structures filled with air, which read on scans differently than water and can be tracked as they move through the brain. Best of all, turning them from “on” to “off” can be safely done via ultrasound; a calibrated soundwave will burst the vesicle, and the air drains out, changing the image and showing that the effect a researcher is studying is real, not just a mistake in the scan. l
Psychosocial interventions—especially COGNITIVE BEHAVIORAL THERAPY (CBT)—may also result in improvements in how the human immune system works. A meta-analysis of 56 randomized controlled studies found that after people underwent one of eight interventions, including psychotherapy, psychoeducation,

Research supported in part by donations from the Ice Bucket Challenge, the social media sensation that raised more than $200 million worldwide, has led to an experimental medication that may slow the progression of amyotrophic lateral sclerosis, or ALS, according to a study at Massachusetts General Hospital’s Sean M. Healey & AMG Center for ALS. The drug is not a cure, but it may help slow the inexorable disability caused by ALS, which rapidly destroys the nerve cells that control the muscles that allow us to move, speak, eat, and even breathe. l
bereavement therapy, CBT, and others, they showed significant improvement in measures of immune system function. Beneficial immune system functions showed an increase for at least six months after the intervention, while harmful immune system functions showed a decrease. l
The Food and Drug Administration (FDA) has approved another use of the anesthetic and party drug KETAMINE: as a nasal spray for suicidal patients with major depression. The drug, Spravato, which contains esketamine, a chemical cousin of ketamine, was approved last year for people with major depression who had not responded to other treatments. Now, the FDA has extended its approved use to people who are having suicidal thoughts or have recently attempted self-harm. The drug’s advantage over other depression treatments is its speed: People report relief from some symptoms within 24 hours, compared with weeks for other drugs. l
Another reminder for researchers to take care to describe their analysis: REPRODUCIBILITY. A study led by researcher Russel Poldrack asked 70 teams of scientists to analyze the same set of fMRI data. Using different software, steps, and setting different thresholds for results, the groups came to different conclusions more than half the time. “There was something about going from the intermediate steps of analysis workflow, to determining the right threshold, to denoting a final yes/no answer that changed things,” Poldrack told a reporter. “It was really striking.” He suggests researchers describe their methods precisely and consider running multiple analyses before they submit results for publication. l
A few brain science books that have recently caught our eye
 BY BRANDON BARRERA
BY BRANDON BARRERA

Discovering and implementing strategies to cultivate your personal and professional well-being is invaluable, especially during tumultuous times. This latest volume in the Norton Series on Interpersonal Neurobiology invites readers to join scientists, clinicians, and mindfulness instructors in conversation—the transcribed format of the book is meant to preserve the flow of engagement, exercises, and human moments found in the live sessions. Across 15 presentations, experts with backgrounds in psychology, neuroscience, neurobiology, law, and physics share their perspectives on the science of self-compassion; the value of positive emotions and social connections in nurturing a naturally antidepressant brain; social justice and interconnectedness; bridging science and spirituality with physics and yoga; what Alzheimer’s can teach us about the mind and who we are; and many other thought-provoking reflections. Anyone interested in wellness, mental training, and consciousness will find this compilation to be a valuable resource.

fMRI by Peter A. Bandettini (MIT Press)
With close to three decades of fMRI (functional magnetic resonance imaging) research shaping his perspective, Peter A. Bandettini, Ph.D., leans on his experience to discuss the history and fundamental concepts of fMRI—the non-invasive and high-sensitivity technique for measuring brain activity that has helped reshape brain science over the last two decades. Bandettini, chief of the section on functional imaging and director of the Functional MRI Facility at the National Institute of Mental Health, infuses fMRI with insights that are unique to pioneers of the field like himself. The book includes a brief primer of the brain imaging landscape and mostly concerns itself with fMRI methods: hardware and acquisition, brain activation experiments, and the crucial processing of data. One chapter is dedicated to fMRI controversies and challenges, chronologically cataloging more than 20 scientific debates that consider the various views and issues which inevitably surface. fMRI is a worthy companion for, as Bandettini puts it, the “curious layperson” and the “sophisticated developer and user.”

Livewired: The Inside Story of the EverChanging Brain by David Eagleman (Penguin Random House)
The brain is a dynamic structure, changing in response to both internal and external factors. Neuroscience refers to this as neuroplasticity—in essence, experience sculpts our “plastic” neural landscape, and our brains retain these changes in a continuous process with no end. It is because of this ever-present flux that David Eagleman, Ph.D., professor of neuroscience at Stanford University and host of the acclaimed television series The Brain, shies away from relying on the term "plastic" and its association with a final, landfill-bound end product. Instead, Eagleman introduces a new concept: livewired. This framework, Eagleman writes, recognizes the brain as the extraordinary self-configuring organ it is. Remove a limb and the corresponding cortical region in the brain will cede ground to its neighbors, essentially reorganizing the brain map to reflect the new, current form of the body. Introduce a new data stream, one captured and converted into electrical signals by novel sensors, and the brain will figure out how to use the data. Eagleman’s book lays out these livewiring principles, illustrating why he considers the concept to be “quite possibly the most gorgeous phenomenon in biology.”

Mind to Matter: The Astonishing Science of How Your Brain Creates Material Reality by Dawson Church (Hay House)
When scientific principles brush against the metaphysical, it is possible to become disoriented—where once you stood on solid ground, you may find yourself wading out into the ethereal. It is this space, where science probes the limits of knowledge, at times blurring into the fantastical, that author Dawson Church, Ph.D., chooses to explore. A self-described mystic and scientific researcher, Church’s interests lie in the power of thought and discovering the limits of “intention.” Church’s book addresses the research into the mind’s influences on the objective, external world. Neuroplasticity, emotional regulation, and what is known about the different frequencies of brainwaves are presented in ways that empower readers to benefit from potential health and therapeutic qualities associated with each. To be sure, the book concerns itself with much of the metaphysical and spiritual realms as well. While all are presented with references, many claims merit further investigation, such as the ability to alter a radioactive substance’s rate of decay through intent alone. Nevertheless, the curious will find much to consider and may find a new appreciation of the power of their mind. l
 BY PHILIP M. BOFFEY
BY PHILIP M. BOFFEY
The Black Lives Matter protests have triggered an intense bout of soul-searching and frantic efforts to erase all vestiges of racism from institutions around the nation. With all this ferment, it is not surprising that the tides of re-evaluation have lapped into the field of neuroscience. Webinars sponsored by the Society for Neuroscience (SfN) in July and September laid bare the appalling lack of diversity in neuroscience and called for reforms to do something about it.
Just as there was a moral obligation to end slavery in the 19th century and there is a moral obligation today to end police brutality against Black people, so too is there a moral and ethical obligation to increase the representation of minorities in neuroscience as part of a national effort to rectify the injustices still permeating many aspects of American life. There would even be a scientific advantage to doing so. But there is clearly a long way to go.
Joanne Berger-Sweeney, Ph.D., the president of Trinity College, who moderated the SfN webinar, cited a startling and depressing statistic. She said that over the past 60 years, the percentage of Black, tenured professors in all fields (not just in neuroscience or other technical fields) increased by only two percent, suggesting that there is “clearly a problem in the system.”
The percentage for neuroscience was almost certainly even worse than the two percent overall average, which would have been buoyed by faculty hired to teach social science and political science courses focused on race-related issues.
A commentary in the July 23 issue of the journal Cell by an African American neuroscientist at Duke University asserted that “Even now, only one to two percent of scientists awarded major grants by the National Institutes of Health are Black.” He complained that the review systems used to select winners of these grants are biased against Black people.
The National Science Foundation published the number of neuroscience degrees awarded to various racial minorities and white people each year from 2008 through 2018. At all levels, Black students showed minimal gains over that recent decade. Meanwhile, a report from the Association of American Medical Colleges on “Diversity in Medicine” said that in 2018, only 3.6 percent of the full-time faculty positions in medical schools were held by Black people, who comprised 14.7 percent of the population in 2019. The Black share was well below the 63.9 percent held by white faculty and the 19.2 percent held by Asian faculty, the two largest contingents.
Bachelor's degrees
Total: 6,191

Advanced degrees
Total: 865

The most distressing findings were analyses showing that years-long efforts to promote greater diversity by recruiting more "minority" applicants and using “holistic” measures, not just test scores, to evaluate them had made only a marginal difference in advancing diversity in medical education, with the number of Black faculty members noticeably lagging.
Once on the job, practicing physicians from non-white backgrounds often confront racism and bias not only from peers and superiors but also from patients. Such implicit and explicit bias can only be countered by an all-out effort to develop an inclusive, equity-minded environment.
A timely place to start would be to include many more Black subjects and physicians in the ongoing clinical trails for a vaccine to combat Covid-19. Four Black medical leaders have persuasively argued that participation by the groups most severely infected by the pandemic could build trust in the results and detect side effects not seen in white participants.
The editors of Cell pledged to do their part to highlight Black authors and perspectives in an editorial entitled, “Science Has a Racism Problem.” They acknowledged that Black scientists were underrepresented among their authors, reviewers, and on the advisory board, and they pointed to the “extreme disparity” in the genetic and clinical databases that scientists have built. The overwhelming majority of data comes from white Americans of European descent, resulting in a dearth of understanding of health and disease in Black individuals.
Meanwhile, the editor-in-chief of the Journal of the American Heart Association retracted a viewpoint article that had argued against affirmative action on the grounds that Black and Latino trainees in medicine were supposedly inferior to white and Asian trainees. He said that he and the
association “condemn discrimination and racism in all forms” and that much more needs to be done to increase diversity in medicine and cardiology, including the publication of viewpoints recommending alternate approaches.
An apology for even more appalling past racism has been issued by the American Academy of Pediatrics, which repeatedly rejected Black physicians applying for membership starting in 1939 because, a member of the all-white executive board explained, “if they became members they would want to come eat with you at the table. You cannot hold them down.” To atone for past sins, the Academy’s board published a resolution apologizing for contributing to the racism that Black pediatricians had endured and stressed that Academy membership does not discriminate on the basis of race or multiple other categories.
A key federal agency published its strategies for enhancing the diversity of neuroscience researchers. The agency will search for talent at every level, from high school on up, and will provide resources and guidance to help them succeed until they reach faculty positions. One key element is meaningful mentorship all along the way.
A collateral benefit is that diversity would help scientists solve many of the tough questions within neuroscience, the article said. It pointed to research showing that teams from diverse backgrounds outperform homogeneous teams in addressing complex scientific problems because they bring different perspectives and more innovative ideas to bear on the problem.
A positive development is that many universities and health care systems are launching efforts to diversify, including a particularly ambitious program established at Trinity College by Berger-Sweeney. Among multiple “action steps,” Trinity will (1) require all campus members and trustees to complete anti-racist and unconscious bias educational training this fall and (2) create six “special opportunity hires” (preferably at senior tenured positions) each year for the next three years to increase faculty diversity.
The college also established a task force that will provide “key metrics” to monitor its progress toward its goals. That could show whether a vigorous campus-wide effort to eradicate racism and promote diversity can succeed when so many previous efforts have fallen short. Other institutions need to follow Trinity’s example. l
Phil Boffey is former deputy editor of the New York Times Editorial Board and editorial page writer, primarily focusing on the impacts of science and health on society. He was also editor of Science Times and a member of two teams that won Pulitzer Prizes.
The views and opinions expressed are those of the author and do not imply endorsement by the Dana Foundation.

Leslie Iversen, Ph.D., a neuropharmacologist at the University of Oxford and a member of the Dana Alliance for Brain Initiatives (DABI) — Iversen, along with DABI members Ed Kravitz and Zach Hall, were the first to demonstrate that GABA was released from inhibitory nerve terminals. During his career, he headed the United Kingdom drug discovery unit for Merck and was a member of UK’s Advisory Council on the Misuse of Drugs Committee. He was awarded the Lifetime Achievement Award of the British Association for Psychopharmacology in 2005.

Masakazu Konishi, Ph.D., a neuroethologist at Caltech and member of DABI, was a leader in the field of avian neuroethology— the neurobiological study of natural behavior — Konishi became the Bing Professor of Behavioral Biology in 1980. Konishi’s autobiography, written for the Society for Neuroscience’s The History of Neuroscience, Volume 6, can be found here

Frederick Goodwin, M.D., worldrenowned psychiatrist, former director of the National Institutes of Mental Health, and a founding member of DABI — The second edition of his 1990 seminal text, Manic Depressive Illness, was awarded the 2008 Best Medical Book Award from the American Medical Writers Association. He also headed the Alcohol Drug Abuse & Mental Health Administration and hosted the popular Infinite Mind weekly radio show on National Public Radio.

Stephen Lieber, chairman of the Brain and Behavior Research Foundation (BBRF) and an advocate for mental health research — Lieber helped grow a modest philanthropic group known as the National Alliance for Research on Schizophrenia & Depression (NARSAD) into today’s BBRF—the largest private supporter of psychiatric research grants in the country. His philanthropy helped create the Lieber Recovery and Rehabilitation Clinic for Psychotic Disorders and the Lieber Schizophrenia Clinic at Columbia University, as well as the Lieber Institute for Brain Development (affiliated with Johns Hopkins University) in Baltimore.
 BY MICHAEL P.H. STANLEY, M.D.
BY MICHAEL P.H. STANLEY, M.D.
Ifeel old,” said Jane. “I see the pillbox every morning and think it’s my parents’ pillbox, not mine!” To her students, she still looks like the same warm, engaged young teacher, but in between the jokes she cracks and the details of her upcoming lessons, there is still a catch in her voice. Jane is recovering from an unnamed inflammation of the brain. Peculiar symptoms of falling out of bed and mistaking names progressed into odd trembling at the whiteboard and clumsiness in sports, before finally culminating into such profound incoordination and incoherence that, by the third or fourth emergency room visit, physicians could no longer attribute it to a woman with an “extensive psych history.”
As Jane kept reaching out for care, her ER visits provided further fodder to reluctant doctors to anchor upon an expedient psychiatric excuse. But to Jane, these symptoms could not be explained by her personal experience with anxiety or obsessive-compulsive disorder (OCD). “I know what my normally abnormal feels like, but the way I was feeling was abnormally abnormal for me.” It was not until subtle, objective signs coalesced around these enigmatic, traditionally “psychogenic” phenomena of inconsistent tremor and distractible weakness that a neurologist suspected her problem wasn’t “just in her head,” but precisely in her head. Jane's presentation suggested an encephalitis. The shift from a complaint of the mind to a condition of the brain illustrates that the provinces of psychiatry and
Every day, hospitalized patients ask when they can go home, and Jane was no different. Inherent in home is the past life before illness and back to the familiar.
neurology are more porous than our system is prepared to address.
She started on prednisone, a steroid to quell the inflammation, and as the confusion abated, Jane couldn’t tell if hours or months had gone missing. She kept reintroducing herself to doctors who had seen her daily for two weeks. Once she rallied to pun off one of the doctor’s dry statements, an attempt to show herself and her doctors that— despite the hospital gown—she still retained a sense of humor. When no one laughed, self-doubt crept back in. “Am I sicker than they thought?” she wondered.
She was making progress against the inflammation, but when the brain
and address all three if we are aiming for wellness.
Every day, hospitalized patients ask when they can go home, and Jane was no different. Inherent in home is the past life before illness and back to the familiar. Jane explained that after the near constant reevaluation of attentive physicians and nurses abruptly stopped, “I’m home. I go to work. I’m suddenly supposed to feel well. My friends have stopped calling because I look like myself, but I’m not quite myself. I don’t want to be a burden, to admit that I could still use that support. I don’t know what to expect because no one knows what to expect with what I’ve got, and I don’t want to bother my doctors over what might be nothing.”
is inflamed, the intact networks are like frustrated hostages witnessing the networks still perturbed. And when that observation is focused through a lifelong lens of anxiety and compulsion, doctors need to reframe what (and whom) they’re caring for. Jane’s case illustrates the wisdom of that Hippocratic axiom, “cure sometimes, treat often, comfort always.” Drugs like prednisone affect the course of diseases, but healing is an ongoing negotiation between a patient and their body, with doctors as guides. Patients suffer and recover from the experience of illness—a complex feature of identity formulated in equal parts biology, psychology, and culture—and physicians must remember to assess
For those with concomitant psychiatric illness, such as OCD, it is doubly difficult—at first for the initial diagnosis, but now in preventing relapse. OCD can reinforce the anxieties surrounding the neuropsychiatric manifestations of an encephalitis like Jane’s, leaving doctor and patient bewildered as to which disease is flaring up. For many with dual diagnoses, the possibility of being considered a “problematic patient” to a doctor is paralyzing. No one wants to be dreaded, and patients with psychiatric disease are all too familiar with the dread of being dreaded.
Hearts beat. Lungs breathe. Brains who and what and why. When people like Jane suffer brain injuries, their sense of Self can change. Some of that is an organ’s defect, but the rest is our response to it—that “our” exists where the brain meets the mind and especially where psychiatric illness is concerned, organic or otherwise. Recovery is not just repairing the cerebrum but renovating someone’s sense of self as we make our way towards a new “normally abnormal.” l
Michael P.H. Stanley, M.D., is a neurology resident of the Massachusetts General Hospital and the Brigham & Women’s Hospital.
Aselection of some of Bill Glovin’s engaging and memorable interviews with top neuroscientists who discuss their Cerebrum articles, their personal stories, and how their work has the potential to make a difference in people’s lives. Subscribe to Cerebrum here or on your favorite platform.






Ilina Singh, Ph.D., Professor of Neuroscience & Society and co-director of the Wellcome Center for Ethics and Humanities at the University of Oxford, and author of this issue’s cover story on global neuroscience expansion.





PREVIOUS EPISODES
Gregory Bern, M.D., Ph.D., director of the Center for Neuropolicy and Facility for Education & Research in Neuroscience at Emory University, on his Spring 2020 cover story, “Decoding the Canine Mind.”
Jerold Chun, M.D., Ph.D., senior VP of Neuroscience Drug Discovery at Sanford Burnham Prebys, on his January 2019 article, “The Gene Conundrum in Alzheimer’s Disease.”
Thomas R. Insel, M.D., former director of NIMH and co-founder and president of Mindstrong Health, on his November 2018 article, “Building the Thermometer for Mental Health.”
Howard Hurtig, M.D., co-founder of the Parkinson's Disease and Movement Disorders Center at the University of Pennsylvania, on his August 2019 article, “The Many Faces of Parkinson’s Disease.”




Frank R. Lin, M.D., Ph.D., director of the Cochlear Center for Hearing and Public Health at Johns Hopkins University and author of this issue’s feature on the link between hearing loss and dementia.
Lee Alan Dugatkin, Ph.D., a biologist at the University of Louisville and coauthor of How to Tame a Fox (and Build a Dog), on his Spring 2020 article, “Jump-Starting Evolution.”
Maheen Mausoof Adamson, Ph.D., senior scientific research director for Defense and Veterans Brain Injury Center in Palo Alto, CA, on her November 2019 article, “Rewiring the Brain: Zapping with Precision.”
Michael L. Lipton, M.D., Ph.D., associate director of the Gruss Magnetic Resonance Research Center at Einstein College of Medicine, on his September 2019 article, “Rethinking Youth Sports.”
Karen Moxon, Ph.D., director of the Neurorobotics Laboratory at UC-Davis, on her June 2019 article, “Mind Over Matter: Cognitive Engineering.”

author—Professor of Neuroscience & Society at the University of Oxford and co-director of the Wellcome Trust Center for and Humanities—reflects on efforts to grow recognition of neuroscience in low- and middle-income countries.

ARLY IN 2016, I WAS INVITED TO JOIN THE LANCET COMMISSION on Global Mental Health and Sustainable Development to work on a report that followed up the seminal 2007 series of articles in the journal Lancet that launched the field of global mental health. I was excited and honored. The Lancet reports are multi-authored and rigorously evidencebased; they also frequently contribute to shaping global health policy. At last, I thought, my discipline, neuroethics, would contribute analysis of substantive ethical challenges that arise when addressing mental health needs in a global context, such as the dignity and care of persons with mental and neurological disorders; equitable access to treatments; and the problem of stigma.
As it turned out, while the Commission wanted to address and tackle these concerns, my role would not just be to contribute ethical thinking. Rather, I was to represent the potential for neuroscience, and, more broadly, biological psychiatry, to help position mental health as a development priority in efforts to reduce the global burden of disease. The World Health Organization (WHO) had explicitly acknowledged mental health as a global development issue in a summit hosted jointly with the World Bank in 2016; in the WHO Comprehensive Mental Health Action Plan; and in the inclusion of mental health in the WHO High Level Commission on Non-Communicable Diseases.
The desire to integrate biological approaches to mental health and illness in the Commission represented an important progression from the original 2007 Lancet series. In working with Commission colleagues, I began to understand that a core challenge that lay before us could be construed as ethical: to confront the contention that
a biomedical model of mental disorder is reductive and essentialist, and potentially harmful to interests of dignity and justice. I have argued for many years that such a hard-line critique of “the biomedical model” is not a useful or necessarily accurate account of scientific thinking. However, suspicions about biological approaches linger, particularly in the form of concerns about “medicalization” of mental health and overuse of biological treatments. Such concerns are especially resonant in low- and middle- income country (LMIC) contexts, where medicalization of mental health has been associated with studied indifference to culture and context. Promotion of dehumanizing, essentialist ideas about non-Western brains and minds and persons is part of a painful history of colonialism and oppression. So if the discoveries of biological psychiatry were to inform the Commission’s report, it would be important and right to acknowledge these critiques, while also evidencing the value of biological approaches to the high-level aims of the report: improving mental health at the population level and reducing the contribution of mental illness to the global burden of disease.
My working group included some of the world’s leading biological psychiatrists and neuroscientists, and we ultimately convinced fellow commission members to give biological dimensions of mental health more airtime in the final report. The value of biological research was clearest when we could demonstrate identifying targets for effective interventions. Digital mental health, for example, is often positioned as a technology that could revolutionize global mental health— there are currently about 10,000 mental health “wellness” apps available for a broad range of conditions. But most of these apps do not leverage mechanistic understanding of underlying behaviors and cognitions, as, for example, reward
processing deficits in schizophrenia; or regulation of affective and cognitive pathways in depression
One thing that we did was to fundamentally change the trajectory of the Commission: we drew on emerging evidence from neuroscience and genomics to describe brain development as a function of convergent, multi-level factors: environmental, psychosocial, and biological. We relied heavily on research on the correlations between socioeconomic status and its associated variables (such as malnutrition, lack of stimulation, and chronic stress), and early brain development. We also drew on brain plasticity research that depicted current knowledge about sensitive periods during childhood and adolescence. We wanted to stimulate further research in this area and help support arguments to health policymakers to develop early intervention and prevention strategies.
One overall message was, instead of supporting categorical claims about ultimate causes of mental disorder, or about the presence or absence of mental illness, genomic neuroscience research could be used to help illuminate the highly complex and dynamic pathways to mental health and in illness across the life course. Another important point was to emphasize some of the similarities between “Global
n working with that a core challenge to confront essentialist, justice in global
with Commission colleagues, I began to understand challenge that lay before us could be construed as ethical: the contention that biological psychiatry is reductive, essentialist, and potentially harmful to the interests of dignity and global mental health.

North” and the “Global South” in relation to the political economy of mental health. These descriptive terms are used by the United Nations and World Bank to point to political and economic differences in LMIC countries (Global South) as compared to other countries (Global North). However, all countries are vulnerable, to some extent, to economic, political, and environmental conditions that contribute to health inequalities, such as conflict and displacement, urbanization, income inequalities, and climate change. Better understanding of the contributions of these “social determinants” in the pathophysiology of mental illness, and proportionate action to improve health inequalities, is therefore crucial to progress in all countries.
As part of the Lancet Commission, we explored the question: Should neuroscience find its way into LMIC settings, in the context of global mental health? Our conclusion was “yes”; but in order to meet the ethical challenges of relevance and utility, neuroscience research needed to more clearly speak to challenges arising in LMIC contexts. I hope that in the future we will do better at demonstrating that relevance and utility.
Since the Commission, my own work with LMIC partners has expanded considerably, which has convinced me of the need to keep asking that should question to illuminate ethical concerns and ensure benefits. Increasingly we have also focused on a secondary question: If biological research is to inform our understanding of human brain development and functioning in LMIC contexts, how should this happen?
The overwhelming majority of what we know about the human brain is derived from research on people of Anglo-European descent living in Western countries. If we agree that
My working group included some of the world’s leading biological psychiatrists and neuroscientists, and we ultimately convinced fellow commission members to give biological dimensions of mental health more airtime in the final report.
human brain development is a dynamic “eco-bio-developmental” process, as a highly cited recent model suggests, then this limited evidence base means that we likely have limited epidemiological understanding of patterns of risk and resilience in brain development.
Moreover, most of the brain research that has been done in LMICs was conducted by Western researchers. This reality raises a range of ethical considerations, including the relevance and accessibility of neuroscience knowledge and interventions in LMICs, and the need to build capacity among local researchers to participate in and to lead LMIC-based research projects.
Compounding these challenges is the fact that human biological research by Western researchers in LMICs has a long history of unethical behavior. For example, biological materials, such as saliva, blood, and tissue, derived from research on the African continent, have for centuries been transported to the West. Despite the transformations in Western research ethics following the 1979 UK Belmont Report, the flow of such research materials still involves significant risk of ethical violations, such as lack of valid consent, biological material transfer agreements, and benefit sharing. As recently as last year, the UK Wellcome Sanger Center was accused of “bio-piracy” for allegedly planning to commercialize a gene chip
that used DNA from indigenous African tribes. Groups like H3Africa (Human Heredity and Health in Africa) are a robust response to historic injustices, focused on African leadership and facilitation of sustainable research infrastructure and ethical guidelines.
This history and such LMIC responses as H3Africa have guided us in developing NeuroGenE, a global initiative in psychiatric ethics. The endeavor grew out of a partnership with the Stanley Center at the Broad Institute of Harvard University and MIT in a project called “Neuropsychiatric Genetics in African Populations” (NeuroGAP). Although all human beings are genetically very similar, African populations have the greatest genetic diversity in the world but are, for historical, practical, and cultural reasons, severely underrepresented in genetic studies. The genetic architecture of psychiatric illnesses is highly complex and still not well understood; large-scale collections from African and other underrepresented populations in genetic studies of neuropsychiatric disorders may accelerate genetic discovery and drive development of targeted therapeutics

Led by principal investigator Karestan Koenen and a team of African co-researchers, NeuroGAP encompasses scientific
research, local capacity building and training, and ethics. Each arm of the project works collaboratively to facilitate responsible, relevant, and meaningful outcomes. At the core of the project sits the Africa Ethics Working Group, made up of bioethicists and social scientists across the African sites in which NeuroGAP operates: South Africa, Kenya, Uganda, Ethiopia. As NeuroGenE has grown, we have been joined by researchers from Zimbabwe and Ghana.

With these colleagues, we are addressing challenges and opportunities for development of responsible and relevant neuropsychiatric and genetic research in LMIC contexts. Along with innumerable lessons learned thus far, Caesar Atuire, a philosopher at the University of Ghana, has inspired us to consider a metaphysical challenge to take African cosmology seriously. Consider these (fictional) scenarios:
A woman who donated saliva, after consenting according to protocol, returns after a few days in some distress. She has consulted family and elders and realizes that part of her spirit resides in the saliva. She asks if she can have her saliva back. Even if researchers were to agree to the request, the sample has already been anonymised.
During the consenting process, a man asks to take the consent forms home, in order to consult his ancestors about his participation in research that requires donation of a biological sample. The research ethics protocol requires participants to give their consent on location.
If one accepts that what Atuire calls local “cosmological visions” are worthy not just of respect, but of equal explanatory status, then research ethics protocols need to consider these perspectives in anticipating the potential
harms of research. This is a provocative proposal even for local committees in LMICs, since much of the practical ethics applied by those committees is based on Western philosophy. However, there is currently active discussion and debate about the development of an "African bioethics" that draws upon traditional philosophical frameworks. In my view, this debate should rightly and deeply scrutinize both the generalizability of our Western bioethical concepts, and the practices we researchers have constructed, albeit with good intentions, that impose Western interpretations of these concepts in LMIC research settings.
If that all seems to impossibly complicate how neuroscience and broader biological brain research is to be done in LMICs, let me offer another discovery from ongoing work: Local beliefs in these settings can and do co-exist with an acceptance of the biological underpinnings of mental health and illness. As scholars of cultural psychiatry have illustrated, people around the world access health systems in more or less traditional ways: There is a range rather than a dichotomy. Many of us live in global societies in which we reconcile contrasting belief systems; for example, by simultaneously pursuing Western and non-Western approaches to health, by visiting a Western medical clinic, an acupuncturist, and a meditation teacher for a chronic illness.

Recent research led by Atuire and public health researcher
Violet Naanyu in Kenya aims to better understand help-seeking preferences for a set of cognitions and behaviors that, from a Western perspective, would be labelled “schizophrenia.” Preliminary analyses suggest that people would prefer to consult both a local healer or spiritual practitioner, and a doctor trained in biological psychiatry. Such research
also helps to reveal the complexities of stigma associated with mental disorder and neurodevelopmental conditions.
Across Western and non-Western settings, a narrative of biological blame for such conditions can both reinforce stigma, particularly familial stigma; or reduce it, particularly self-stigma. Whether the impact is positive or negative often depends on context, such that a person can have different stigma experiences in the course of their day. Consequently, one cannot assume the value of a biological account in efforts to defeat stigma; rather, one needs to work to understand stigma locally and enable appropriate mental health literacy.
A broader issue concerns community engagement and involvement in research on the human brain in LMICs. Researchers agree that community engagement is important for its practical benefits, such as better recruitment, more compliance with protocols, and lower dropout rates. But there are additional important human rights benefits. These derive from the long and troubled history, both in the Global North and Global South, of viewing people with mental illness, neurodevelopmental conditions, and neurological conditions as unworthy of rights, respect, and dignity normally accorded to human beings.
In recognition of this history, influential funders have called for “experts by experience” to be included in global research into human brain development and function. Ironically, about a decade ago, I struggled to get funding for a project on the experiences of moral agency and personal authenticity among young people taking stimulant medication for ADHD. That study, ultimately funded by the Wellcome Trust, was rejected multiple times due largely to concerns that these "experts by experience" were unreliable sources who were unable to form independent
Our approach has been to build capacity in young people to participate meaningfully in research and get involved in research and health policy decision-making.
views. Subjective experience, particularly that of children, was deemed largely irrelevant to the progress of scientific understanding.
It is a good thing, then, that experts by experience are now in vogue. Still, the work of integrating this “expertise” into the scientific enterprise is difficult and needs to respond to significant objections, even if this critique is now more muted. An effective response requires theoretical rigor: One must be able to say convincingly why this kind of expertise matters. It also demands methodological innovation and moral seriousness: the involvement of experts by experience and their communities cannot be simply a well-intentioned exercise in “vox pop” or an assertion of public preferences. Mere “voices” are too easily ignored or, worse, appropriated to promote particular research or health policy agendas.
Working with colleagues at University of Oxford and enlisting groups of young people as advisors and coresearchers, our approach has been to build capacity in young people to participate meaningfully in research and to get involved in research and health policy decision-making. To meet the requirements of methodological rigour, we draw on techniques for balanced arguments, perspective taking, deliberation, and decision-making. The advocacy work of young people in LMICs can have significant impacts on mental health literacy and stigma in their communities and in the world, and we want to empower them to become such advocates. We hope it will help move more national resources into positive
mental health policies.
A wonderful example of the power of young people is the Lancet Young Leaders for Global Mental Health, who created an award-winning social media campaign, #mymindourhumanity, to help disseminate the findings of the Lancet Commission Report on Global Mental Health. Since 2018, we have worked with and learned from these young leaders as they engage in dialogues about mental health experiences in their communities, foster research, and advocate for policy change on international stages with the leaders of the WHO, UNICEF, the World Bank, and other globally influential institutions.
It is worth noting that neuroscience has a significant international presence through global brain projects in the European Union, the U.S., China, Japan, Korea, Australia, and Canada. Because I focused here on biological approaches in LMICs, I omitted any mention of these enormous international investments. One might argue that these investments are hardly relevant in LMIC contexts, given that their scale exceeds the gross domestic product of many such countries. But should a technologydriven neuroscience agenda be more engaged in LMICs? Should there be LMIC leadership of a global brain project?
The scale of investments in these projects highlights economic disparities in global brain research, and risks leaving LMIC scientists behind through gaps in knowledge, capacity, and technology. Even as global mental health grapples with legacy of the biological model,
global human brain projects risk going down the same road. Richer countries might build human and technological infrastructure and pursue research goals that have relevance to and potential benefits for those countries, but fail to address the basic, sizable neurological and mental health problems that arise as a consequence of the social determinants of health.
Recently, global uprisings around diversity and in inequality have shown us that a lack of diverse representation of human actors, interests, and experiences can result in blind spots. As noted by the National Institute of Neurological Disorders and Stroke and other institutions, in science such blind spots impact our evidence and hamper our ability to turn knowledge into meaningful interventions for a significant subset of the global population. Thanks to leadership by Karen Rommelfanger (director of Emory University’s neuroethics program), working with a group of international colleagues, global human brain projects have embraced ethics as a core dimension of their work. This development, alongside active work to support neuroscience in the Global South by prominent organizations such as the International Brain Research Organization, presents a promising platform for LMIC interests to be included and heard.
In short, to answer the question of how biological research on human brain development and function should venture forth in LMICs: through intentional partnerships; with humility, abundant care, and respect for persons, history, and ethics; and with curiosity and an open mind. l
The Lancet Commission on Global Mental Health report was completed after three years by a group of 28 commissioners from across the globe to guide action in reducing the global burden of mental health problems.
Vikram Patel, Ph.D., the Pershing Square Professor of Global Health, Harvard Medical School
Shekhar Saxema, M.D., visiting professor at Harvard T H Chan School of Public Health and former director of the Department of Mental Health and Substance Abuse, WHO
Crick Lund, Ph.D., professor of Global Mental Health and Development, Kings College, London
Sir Graham Thornicroft, Ph.D., professor of Community Psychiatry, Kings College, London
Florence Baingana, M.Sc., psychiatrist, public health specialist, and former mental health advocate for WHO in Nigeria, Sierra Leone, and Liberia
Paul Bolton, M.B.B.S., senior scientist in the Center for Humanitarian Health, Johns Hopkins University Bloomberg School of Public Health
Dan Chisholm, Ph.D., Program Manager for Mental Health, WHO Regional Office for Europe
Pamela Y. Collins, M.D., director of Global Mental Health, University of Washington
Janice L. Cooper, Ph.D., senior project advisor on Global Mental Health, Emory University
Julian Eaton, MRCPsych, Global Mental Health advisor for CBM International and co-director of the Center for Global Mental Health, London School of Hygiene and Tropical Medicine
Helen Herrman, M.D., president of the World Psychiatric Association and director of the WHO Collaborating Center for Mental Health, Melbourne
Mohammad M. Herzallah, Ph.D., founder and director of the Palestinian Neuroscience Initiative, Al-Quds University
Yueqin Huang, Ph.D., director of the Division of Social Psychiatry and Behavioral Medicine, Peking Institute
Mark Jordans, Ph.D., professor in Child and Adolescent Global Mental Health, University of Amsterdam
Arthur Kleinman, M.D., professor of medical anthropology, Harvard Medical School
Maria Elena Medina-Mora, Ph.D., director-general of the National Institute on Psychiatry (Mexico) a WHO Collaboration Center
Ellen Morgan, M.Phil., Program Officer with Templeton World Charity Foundation

advisory board, The Lancet Psychiatry International and adjunct professor, Dow University of Health Sciences, Karachi
Olayinka Omigbodun, FMCPsych, professor and head of psychiatry at the College of Medicine, University of Ibadan and University College Hospital, Ibadan, Nigeria
Martin Prince, M.D., Professor of Epidemiological Psychiatry and co-Director of the Centre for Global Mental Health at King’s College London
Atif Rahman, Ph.D., professor of child psychiatry at the University of Liverpool and chairs the Academic child mental health unit at Alder Hey Children’s Hospital, Liverpool
Benedetto Saraceno, M.D., Secretary General of the Lisbon Institute for Global Mental Health
Bidyut K. Sarkar, Ph.D., project director of PRIDE Project, (a collaboration between Sangath, India; and the Public Health Foundation of India)
Mary De Silva, Ph.D., head of Population Health at The Wellcome Trust
Ilina Singh, Ph.D., Professor of Neuroscience & Society and co-director of the Wellcome Centre for Ethics and Humanities, University of Oxford
Dan J. Stein, FRCPC, professor and chair of the psychiatry and mental health, University of Cape Town
Charlene Sunkel, a leading South African voice for the rights of people with mental health problems
JÜrgen UnÜtzer, M.D., professor and chair of psychiatry and behavioral sciences at the University of Washington
 By Frank R. Lin, M.D., Ph.D.
By Frank R. Lin, M.D., Ph.D.
As a practicing otologic surgeon with a Ph.D. in epidemiology and a leader in research that examines hearing loss as a potent risk factor for dementia, our author tells us what we’ve learned and what we still need to know about the relationship between hearing loss and cognitive decline in older adults.
WHEN I WAS GOING THROUGH
my otolaryngology residency at Johns Hopkins in the early 2000s, I was struck by the disparity between how hearing loss was managed in children and in older adults. In the case of the child, it was a medical priority to ensure access to a hearing aid so he or she could communicate optimally at home and in school, and such devices were covered by insurance. This approach was justified based on extensive research demonstrating that hearing loss could have a substantial impact on a child’s cognitive and brain development, with lifetime consequences for educational and vocational achievement.
For the older adult, the approach was radically different, even if the degree of hearing impairment was the same as in the child. The adult would be reassured that the deficit was to be expected, based on his or her age, and told that a hearing aid, if desired, would represent an out-of-pocket expense averaging about $4,000. Medicare provided no coverage for hearing aids. There was no robust research demonstrating meaningful consequences of hearing loss for older adults, as there was for children, and the clinical approach was typically guided by the notion that it was a very common, and hence inconsequential, aspect of aging.
But this approach didn’t make sense, given what I had observed clinically. Older adults with hearing loss recounted to me their sense of isolation and loneliness, and the mental fatigue of constantly concentrating in trying to follow conversations. Family members would often describe a decline in patients’ general well-being and mental acuity as they struggled to hear. For those who obtained effective treatment for their hearing loss with hearing aids or a cochlear implant, the effects were often equally dramatic. Patients spoke of reengaging with family, no longer
Every young academic clinician is looking for was excited to have hit upon
getting fatigued from straining to listen, and becoming their “old selves” again. If hearing was fundamentally important for children and represented a critical sensory input that could affect brain function, wouldn’t loss of hearing have corresponding implications for the aging brain and its function?
Around this time, I happened across a small study, published in 1989, in the Journal of the American Medical Association (JAMA), that suggested a link between hearing loss and the risk of dementia. The relationship intuitively made sense to me, but the study was relatively limited in size and riddled with potential holes. For example, did older adults with hearing loss do more poorly on cognitive tests because they simply misheard what the examiner said? Or perhaps, could the co-occurrence of hearing loss and dementia be explained by a common pathologic cause? Finally, maybe hearing loss didn’t contribute to dementia risk at all, but dementia led to problems with hearing (the old chickenand-egg conundrum).
Most surprising was that in the two

decades since the article was published, there hadn’t been a substantive attempt to replicate these findings in a larger study that might address the limitations of the original one. Every young academic clinician is looking for a niche in which to make an impact, and I was excited to have hit upon one that could be of real importance, based on my clinical experiences.
Hunches that come from caring for patients are helpful, but scientific theories supported by evidence are a lot better. Over the past decade, my research has focused on understanding how hearing loss in older adults might contribute to cognitive decline and dementia, drawing on research done over the past half-century by giants in the disparate fields of cognitive psychology, auditory science, and other disciplines.
To elucidate the link between hearing loss and cognitive impairment, one has
Older adults with hearing loss recounted to me their sense of isolation and loneliness, and the mental fatigue of constantly concentrating in trying to follow conversations.
for a niche in which to make an impact, and I upon one that could be of real importance,
to start by understanding the realities of hearing and hearing loss. At the most fundamental level, our ability to hear depends on two steps—peripheral encoding of sound into a neural signal by the cochlea in the inner ear, and central decoding of the signal into meaning by the brain. The hearing loss commonly associated with aging results from accumulated damage to the cochlea that adversely affects the encoding end of the process. Because many of the cells in the inner ear that enable the cochlea to encode sounds can’t regenerate, damage done by such factors as noise exposure and oxidative stress can’t be undone.
With this in mind, one of the first hypothesized mechanisms linking hearing loss with impaired cognition is that hearing loss poses an additional cognitive load on the brain. We all experience that it’s often harder to do two things at once—commonly called “multitasking.” (Try doing a difficult mental math problem when walking quickly.) It’s not your imagination. Nearly 50 years ago, Daniel Kahneman, a psychologist and behavioral economist, who would later go on to win the Nobel Prize, postulated the idea of cognitive resource capacity—that for any individual, there’s a finite pool of cognitive resources available for thinking, memory, coordinating body movements, and so on. In the years since, the implications of multitasking on cognitive performance has been well established across multiple studies.
This concept of cognitive resource capacity applies to hearing as well. When hearing is normal, sounds are encoded with high fidelity, and the resulting neural signal can be effortlessly decoded by the brain. But with hearing loss, the signal produced by the cochlea is distorted, and the decoding process requires greater cognitive effort. Research over the past several decades confirms what
based on my clinical experiences.
theory suggests: that the predicted reallocation of cognitive resources to aid in decoding sound actually occurs and comes at the expense of other cognitive abilities. Functional imaging studies on individuals with hearing loss have demonstrated that brain areas critical for higher order planning and cognitive tasks but not ordinarily used for auditory processing are being activated with auditory stimuli.
Likewise, psychological studies conducted in the 1960s and replicated numerous times since have demonstrated the impact of impoverished and garbled auditory signals on cognitive performance. Importantly, the cognitive load hypothesis suggests that hearing loss doesn’t cause any actual brain pathology that leads to dementia but impacts brain function in a way that may contribute to earlier unmasking of dementia symptoms. Scientists have long known that there is not a precise one-to-one correlation between brain pathology and dementia and that various factors may buffer against brain pathology manifesting clinically. Hearing loss may be one of the factors that erodes this buffer.
But this does not exclude the possibility that hearing loss leads to pathological brain changes associated with cognitive impairment and dementia through another mechanism: auditory deprivation. Support for this hypothesis comes from experiments showing that if an animal is partially deafened, functional reorganization of the brain occurs, along with atrophy in areas that process sound. Epidemiological studies that followed older adults in the community with sequential brain scans for many years demonstrated similar findings: rates of atrophy over portions of the temporal
 Frank R. Lin
Frank R. Lin
lobe important for sound processing were accelerated in those with hearing loss. Importantly, these brain regions are also critical for other aspects of cognitive function such as semantic memory. These findings lead to the hypothesis that hearing loss may act as an additional trigger (along with common causes of dementia such as Alzheimer’s and microvascular disease) for brain atrophy and other pathological changes that could directly contribute to the risk of dementia in older adults.
But hearing loss is more than a matter of possible effects on neural mechanism—it has a social dimension as well. A final mechanism hypothesized to explain how auditory deficits contribute to dementia relates to the social isolation and loneliness experienced by many individuals with hearing loss. While the exact mechanism through which loneliness may increase dementia risk is not yet known, there are plenty of clues, and multiple factors may be involved. Individuals who are isolated tend to be less active, more often depressed, and less likely to adhere to medical treatments—all of which could potentiate the risk of dementia over time. Most intriguingly, research over the past decade has suggested loneliness may lead to greater inflammation in the body, which would physiologically explain many of the adverse health events that have been linked with it, including heart attacks and increased mortality as well as dementia.
These mechanistic theories linking hearing loss to dementia are plausible, consistent with clinical observations, and supported by half a century of research across all fields. But even if ongoing findings continue to bear them out, does it really matter? Do these mechanisms exert a meaningful enough impact on the risk of cognitive decline and dementia over time that hearing loss is something to worry about?
To answer this question, we must draw on large epidemiological studies that follow older adults living in the community for many years. Such studies allow us to account for factors that might explain in simple terms the correlation between hearing and dementia. For example, they may be linked by advanced age, which is strongly associated with both. Likewise, cardiovascular risk factors such as hypertension and diabetes, or general predictors of health, such as low levels of education, could potentially have negative consequences for both hearing and the brain. In a large epidemiological study consisting of hundreds to thousands of participants, we can

In 2017, the federal Over-the-Counter the hearing aid market
statistically control these variables to assess whether hearing loss is an independent risk factor for dementia.
A large epidemiological study also allows us to overcome other limitations of earlier studies. By following participants over a period of many years rather than just at one point in time, we can observe if the hearing loss preceded cognitive changes (and hence may have contributed to it) rather than following after cognitive impairment. A carefully designed epidemiological study of older adults can also benefit from precise measures of hearing and cognitive function. Such studies often incorporate calibrated tests of the peripheral auditory system rather than relying solely on participants’ subjective ratings of their hearing, which may be highly variable depending on personality, lifestyle, and other factors.
Rigorous protocols for the assessment of cognitive function and dementia also guard against cognitive results being biased by hearing loss. Testers are specifically trained to communicate in ways that ensure the participant’s ability to hear and understand them, and testing batteries incorporate a wide range of tests (both auditory and non-auditory) to precisely assess different aspects of cognitive function such as memory, processing speed, and language abilities.
In collaboration with researchers at the National Institute on Aging, we carried out such an epidemiological study in 2010 to see if we could replicate the intriguing results of the 1989 JAMA study. Using data from the Baltimore Longitudinal Study of Aging, the longest ongoing study of older adults in the U.S., we investigated whether hearing levels in a sample of adults measured in the early 1990s were associated with the risk of being diagnosed with dementia over the subsequent 15 years.
In the study, we found that individuals with mild, moderate, and severe hearing loss, respectively, had a two-fold, threefold, and five-fold increased risk of dementia, compared to those with normal hearing. These results were surprising to us in the magnitude of the associations—we weren’t seeing a modest 5-10 percent increase in dementia risk but an astronomical 100, 200 and 400 percent increase. Such an effect for a single risk factor was extremely large, and we didn’t quite believe our findings (and neither did others) when the study was published in 2011.
Since then, the wheels of science have continued to turn, and other investigators who have conducted similar studies using large epidemiological datasets and precise measures of hearing and cognitive function have found comparable results. This research is perhaps best summarized in a report published in 2017 by a commission on dementia convened by the journal Lancet to review the literature on major, potentially treatable risk factors for dementia. In this review, which was updated in 2020, the authors concluded that age-related hearing loss may account for nine percent of all cases of dementia, making it the single largest, potentially modifiable risk factor for the condition, far outstripping the contribution of
Over-the-Counter
Hearing Aid Act was passed, which, by 2021, will open up market
to the
such well-recognized risk factors as smoking (five percent) and hypertension (two percent).
This conclusion, while striking, comes with a substantial caveat—potentially modifiable. Although hearing loss tops the Lancet list of risk factors, how much it matters depends on whether treating hearing loss makes an actual difference. In early studies investigating hearing-aid use in older adults, some investigators have shown a reduced risk of dementia, but these findings must be interpreted with caution: individuals who choose to use hearing aids (and more importantly, have the financial means and are sufficiently health conscious to do so) are different from those who don’t use them.
consumer technology industry, incentivizing companies like Bose and Apple to innovate and sell hearing aids and related technologies directly to consumers.
older adults with hearing loss?
Whether it’s the use of hearing aids, or the factors underlying their use, that drives the association with better outcomes cannot be fully disentangled even with the most sophisticated epidemiological models. To isolate the specific effect of hearing loss treatment on cognition would require a clinical trial in which a large group of older adults are randomly assigned to hearing intervention or a control condition.
I’m involved in such a trial, which is now in progress and led by the Johns Hopkins Bloomberg School of Public Health in collaboration with six other universities and supported by the National Institute on Aging. For this trial (the Aging and Cognitive Health Evaluation in Elders (ACHIEVE), we recruited nearly 1,000 older adults in their 70s and early 80s with mild-to-moderate hearing loss (approximately half of all older adults in this age range have such deficits) and randomly assigned them to receive hearing intervention or a healthy aging education control intervention. When this study is completed in 2023, after all participants have been followed for three years, we’ll have a clearer sense of whether treating hearing loss can actually reduce cognitive decline and dementia risk.
As a practicing otologic surgeon, I see patients weekly who are concerned about their hearing and seeking advice and solutions. One question often stated bluntly is, “Doc, are you telling me that I’m going to develop dementia?” The answer, of course, is no—epidemiological studies provide insights about average effects across populations, but individual prediction is impossible. What often follows is, “Doc, will hearing aids reduce my risk of dementia, and if so, how am I going to afford them?” The answers to these questions are unsatisfying for all concerned: “We don’t know yet. And I’m sorry that the costs of hearing aids are so high.”
My best efforts to relieve their concerns are of little help to patients who are struggling to hear, isolated from family. As a surgeon used to making clinical decisions from a risk-benefit perspective, I also find it frustrating: Hearing aids for older adults may well carry benefits for cognitive health and appear to pose zero medical risk. Wouldn’t that argue for treating all
The problem is that while hearing aids carry no medical risk, the barriers to care are substantial. They are rarely covered by insurance, and with the average cost in the U.S. of at least $4,000, they represent for many people the third largest material purchase in life after a house and a car. This cost is coupled with the time needed to make multiple visits to a hearing-care provider to get tested and fitted. And all this for a condition that is prevalent in nearly two-thirds of older adults over 70.
With this in mind, over the past five years, through collaborations with the National Academy of Medicine and the White House (ending in 2017), and using epidemiological data to demonstrate the potential effect of hearing loss on cognitive health in older adults, my collaborators and I have begun to have an impact on systemic policy barriers, which may ultimately reduce the personal and societal costs of treating hearing loss. Presently, only licensed healthcare professionals are allowed to sell hearing aids, according to federal regulations, and the entire worldwide hearing aid marketplace is dominated by just six companies, keeping costs high.
In 2017, the federal Over-the-Counter Hearing Aid Act was passed, which beginning in 2021 will open up the hearing aid market to the consumer technology industry, incentivizing companies like Bose and Apple to innovate and sell hearing aids and related technologies directly to consumers. In parallel, we’ve begun to advance federal legislation through the House of Representatives to require Medicare to cover hearing-related services.
As a clinician, I can’t reduce the medical risk of hearing aids beyond zero, but our research is spurring changes to federal policies that will reduce their personal and societal costs. Between this progress and the results from the ACHIEVE trial coming in 2023, I’m hopeful that the gaping disparity between the management of pediatric and adult hearing loss that I first noted over ten years ago may start to narrow. More importantly, I’m hugely relieved that rather than providing my patients with a diagnosis that only leads to further health and financial concerns, I’ll soon be able to provide them with evidence-based answers to questions they’ve been asking me for years and steer them toward accessible solutions. l
The pandemic has forced educators to embrace virtual learning,
 By Kayt Sukel
By Kayt Sukel
learning, but can it measure up to in-class instruction?

EEVEN AS COVID-19 INFECTIONS CONTINUE TO slow in the New Jersey area where she lives and works, Rebecca DeSimone, a 9th grade Spanish teacher, will start all of her classes online this fall. As a 22-year public school educator—who has already used technology regularly in her in-person classes—she now finds herself struggling, unsure how to structure her courses so they will facilitate learning. Precious little of her professional development, to date, has looked at how kids learn best when being taught remotely.
“I would love a list of ideas that will really engage the kids while they are home—something that people already know works and will help the kids pay attention and actually learn what they need to learn,” she says. “But I feel like we are the blind leading the blind here. I’m not sure how to make my classes work online. I’m not even sure what my expectations for my students should be.”
DeSimone is not alone in that sentiment. Both teachers and parents across the country are wondering just how effective online instruction will be this school year. Barbara Means, Ph.D., executive director at Digital Promise, a nonprofit organization created by Congress to accelerate innovation in education, has spent her career studying how digital technologies can enhance traditional learning. She says it’s

Like classroom instruction, not all and the heterogeneity software used (as well as how
 Barbara Means / Digital Promise
Barbara Means / Digital Promise
important not to equate the “remote emergency instruction” that took place last spring with “intentional” online courses created using key principles of instructional design.
“There are many reasons—and vulnerabilities—that may lead to a student doing more poorly in an online class than in a traditional, face-to-face environment,” she says. “But learning is learning. And when instructors can design courses that help support students as they learn, online instruction can be quite effective.”
According to National Center for Education Statistics, nearly 7 million students were enrolled in online courses at postsecondary institutions in 2018. Colleges, however, were not the only ones to offer students the opportunity to log-on to learn. Twenty-one percent of primary and secondary public schools also offered certain classes online. Most public schools across the country rely on other forms of technology, including the use of personal smart phones or library computer stations, to supplement traditional classroom instruction, too.
For many years, educators hoped that advances in technology would help bridge disparities in educational outcomes—connecting students of all backgrounds and in all locations with the best teachers in the world. Yet while they do provide increased access, it’s unclear whether online courses are as effective as in-person learning. Some studies link online education with poorer outcomes in both engagement and achievement. Others find the opposite. But such studies are often quite narrowly designed, looking at very specific tasks or groups of children. It’s hard to know when and where their results can and should be applied to online instruction as a whole.
For example, there are numerous studies from the 1990s that suggest people are able to more easily attend to—and thus retain information from—paper books versus e-readers or computer screens. Many of those studies suggest those differences are due to the lack of additional tactile input to the brain as you turn papers and navigate the text. Yet, as anyone who has ever tried to solely rely on a textbook to cram for an exam after skipping too many classes knows, education is much more than simply comprehending texts. Today’s online learning platforms employ a variety of different activities, ranging from streaming video lectures to interactive games, to help students better consume new material.
all virtual learning is created equalheterogeneity in both the hardware and how "learning" is measured) makes it hard to directly compare on-premise to remote instruction.
Like classroom instruction, not all virtual learning is created equal—and the heterogeneity in both the hardware and software used (as well as how “learning” is measured) makes it hard to directly compare on-premise to remote instruction. And since most research has been done on older students—generally high school and college students—it is also difficult to translate online strengths and shortcomings to school-age children. What works for 10th graders may not for kindergarteners. This is definitely a situation where one size will not fit all—and it makes it very challenging to compare online instruction to classroom learning in an “apples to apples” way.
 June Ahn / University of California, Irvine
June Ahn / University of California, Irvine
“Unfortunately, online instruction isn’t as simple as throwing a textbook online—and, in my opinion, online education platforms have focused too much on just putting content up online,” says June Ahn, Ph.D., a member of the Connected Learning Lab at the University of California, Irvine. “We have decades of education research that shows us that content is not the sole factor for promoting learning. That’s why we just don’t hand kids textbooks and leave it at that. We need to find ways to help students engage, inquire, and connect to new information.”
Most educational technology experts agree that the same principles of effective instruction apply whether you are learning in-person or remotely—learning, after all, is a process that can occur in a wide variety of different circumstances. For example, as noted in a recent Journal of Neuroscience study, listening to narrative stories activates the same emotional and language areas in the brain as consuming them on paper. As scientists delve into the nitty gritty of learning, it appears there are many ways that students can effectively engage with content. Yet, researchers are discovering, there are features of an in-person environment that naturally support engagement, inquiry, and connection—and they are also understanding, more and more, that such elements can be challenging to recreate in a virtual setting.
“A lot of what teachers do each day involves classroom management,” says Betsy DiSalvo, director of the Culture and


Technology Lab at the Georgia Institute of Technology. “They are experts in managing a group of children and keeping them on task, especially when you are talking about younger students who don’t have the self-regulation needed to do it on their own. It’s hard to do that kind of management remotely. And, unfortunately, being able to do so has significant impact on getting students to follow along long enough to understand new concepts.”
John Danner, a former middle school teacher who now is the managing partner of Dunce Capital, a venture capital firm that specializes in educational technology start-ups, points out that computer scientists have been designing massive open online courses for decades. But he refers to them as “version 1.0” of online learning efforts.

“Options like Khan Academy and Coursera are great resources, but they don’t really map to anything I saw in the classroom with regards to how kids actually learn, especially when they are used by themselves,” he says. “We know

"Unfortunately, we see quite a bit of evidence resources we see online, particularly
“You need to find ways to chunk lessons into smaller sections,” she says. “We’ve learned the average attention span of a high schooler lasts for about a six-minute video. You get even less time for the little ones. So, you need to create the kind of structure and routine for kids so they can stay engaged and motivated. That starts with breaking up lessons into shorter, digestible sections.”
To foster engagement, she adds, it is also important for educators to think long and hard about how to create a sense of community and provide opportunities for socialization between students. For example, a teacher could record a short lesson via video and then meet with kids later using video conference tools to engage in “inquiry, problem-solving, or instructions for a hands-on activity” to be completed after they’ve watched it. The students could then break up into groups to continue discussion or work on a project together, with the teacher periodically checking in with each group to answer specific questions.
that kids learn in many different ways. And we also know that they are very familiar with technology and social media. So, the question now becomes, ‘Can you create an online learning environment better than YouTube?’ I think we can—but there aren’t hard and fast rules on what that should look like.”
Ahn says to create such an environment, teachers must follow the same general principles they know to support learning in the classroom.
“We already have a lot of information on what makes for a good learning experience,” he continues. “You need to find ways to make the content interesting and relevant. You need interaction. You need kids to do some work on their own— but not all of it on their own. Students need to be able to ask questions. So it’s important to find ways to support these principles in online environments, too.”
 Kerry Rice / Boise State University
Kerry Rice / Boise State University
Kerry Rice, Ph.D., a professor in educational technology at Boise State University and author of Making the Move to K-12 Online Teaching::Research-Based Strategies and Practices, argues that teachers can’t just expect to record a lesson, post it online, and call it a day—especially when they are working with younger students. And, too often, that’s what online courses try to do.
“You want to make the face-to-face time you have with kids, even when it’s happening over Zoom, really count,” she says. “Save that time for active learning [defined as learning where students are experientially involved in the learning process]. That face-to-face time is where you can make connections with kids, see how they’re thinking and feeling, and have those important discussions that are at the heart of learning something new and then applying what you’ve learned.”
DiSalvo adds that teachers shouldn’t try to reinvent the wheel. There are many resources online that can be enlisted— think Khan Academy, as well as other educational games and websites—to augment a lesson.
“The exciting thing about online learning is that it offers an opportunity to provide multimodal learning,” she says. “Some students are visual learners. Some need to do an art project or other hands-on activity to understand the lesson. Teachers can pull together multiple resources that teach the same concept in different ways—so if one option doesn’t work for a particular student, they can go to others, perhaps even created by other teachers, to help. There is a lot of room for creativity here.”
As for classroom management, Ahn suggests that much of that duty will fall on families, especially parents or the older siblings of younger students. Teachers should be able to control the audio and video content of online learning platforms from afar—but they can’t make kids stay in their seats. And, Ahn adds, while parents shouldn’t be expected to “teach” per se, helping students stay on task during class and talking to them later about what they’ve learned will be important in helping them retain information.
“Groundbreaking studies looking at how kids learn from Sesame Street, a television show, demonstrated that learning was most effective when children and parents were watching
together or children and parents took time to talk about the program after the kids watched it,” he says. “It was those everyday conversations that helped make the content stick. That principle applies in online environments, too. Good content is the first step. But the next step involves those conversations and interactions you have with others to illuminate the content and help you remember it.”
Much of the research looking at online instruction has been done in resource-rich environments that can offer the latest hardware, reliable connectivity, and even technical support. DiSalvo reports that not even her graduate students always have all those luxuries when working from home, so it’s unlikely every American student will. Many families have several children who need to share a single device for online school, limiting how much time each can spend on their schoolwork. Some students will only have a smart phone, making it difficult to see and hear the content presented on a smaller screen—or to maintain focus if the phone is always pinging with alerts from other apps. Others may have to go to the library or even to their local McDonald’s for a reliable broadband signal to even access that content in the first place. Such inequities need to be addressed for success. If they aren’t, it becomes even harder for teachers to engage all their students—and to assess their progress as they learn.
“Unfortunately, we see quite a bit of evidence that the resources we see online, particularly for informal learning, has widened the gap between educational outcomes for the wealthy and the poor,” says DiSalvo. “It’s not just a matter of technical access, though that remains a problem in many cases. It’s also understanding, as a parent or teacher, what assets are out there and how they can be used to help students learn more effectively. Many people just don’t know what kind of key words or search terms will bring up resources to help with math or other types of classes. And not knowing can leave them behind.”

There is still much to learn about effective online instruction, says Michelle Miller, Ph.D., a professor of psychological sciences at Northern Arizona University, and author of Minds Online: Teaching Effectively with Technology; she hopes that this fall will offer new insights that can be used to promote effective course design in the future and believes that
for the wealthy and the poor."
teachers who go into virtual instruction with open minds will find success.
“There isn’t one template that will work for every teacher or every class,” she believes. “But teachers already know that they can’t teach the same way to every class anyway. So much depends on the content, the kids, and the resources you have available. But this fall will offer teachers a unique opportunity to explore new techniques and teaching resources that can benefit students—things they might not have tried if they were still teaching in a traditional classroom.”
Overall, while educators and parents may worry about potential learning loss for children who only have online instruction available to them, Ahn is more circumspect.
“It’s important to remember that children are learning all the time outside the classroom—it just happens to be information that we don’t traditionally test them on,” he says. “They are going to continue to learn this fall, too. It may look different— or happen a little less efficiently. But they are going to learn.” l



N RECORD NUMBERS, AMERICANS ARE anxious, worried, sleep-deprived, distracted, and depressed. The Covid-19 pandemic’s triple whammy of an invisible and omnipresent threat (coronavirus infection), profound disruptions in daily life, and uncertainty for the future has thrust many people into a chronic, high-stress state that is, let’s just say, less than optimal for rational thinking or any other sort of higher-order cognitive functioning.
While the Covid-19 pandemic rages on worldwide, the immediate mental health impact of this collective trauma is coming into focus even as the outlook for long-term psychological effects remains considerably fuzzier.
Are we experiencing a pandemic of mental illness? Much has been reported about the ill-termed “mental health pandemic” that seems to be surging through the U.S. and other countries in lockstep with lockdowns and the death, societal disruption, and economic devastation of the viral pandemic. Many experts have sounded the alarm for an approaching tsunami of psychological maladies that could sink an already overburdened mental healthcare system.
A growing cache of data seems to bear out those fears. One of the most recent, a population survey conducted in April and May, found a three-fold increase in depression since the pandemic began. The researchers examined mental health problems relative to 13 pandemic-specific stressors, including loss of a job, death of someone close to you due to Covid-19, and financial problems (see box for full list). The more stressors people reported, the more likely they were to also report symptoms of anxiety and depression.
Other studies show similar rises. From April to June, the
In one study of the Boston Marathon who watched the most had the highest stress levels, who directly experienced
Census Bureau tracked anxiety and depression symptoms among Americans in weekly emergency surveys, finding a sharp rise in both. In a Kaiser Family Foundation Health Tracking Survey conducted in July, more than half of U.S. adults (53 percent) said worry and stress related to coronavirus has had a negative impact on their mental health, up from 39 percent in May.
A key question is whether, and to what degree, pandemicrelated symptoms of anxiety and depression will progress into serious mental illness and increased rates of suicide and addiction, or if all this angst and gloom is more accurately seen as a normal adaptive response to the amped-up stress that many people are experiencing during Covid.
The evolving field of disaster mental health requires that practitioners (clinicians and indigenous helpers) work with individuals and whole communities in the field rather than in an office. Among the lessons it has taught us is that largescale traumatic events such as 9/11 or Hurricane Katrina trigger
people experienced the traumatic event.
immediate and persistent psychological symptoms in large swaths of the affected population. It tells us that stressors generally have a cumulative effect both during and after disasters: the more life stressors people experience, the more likely they are to have persistent symptoms of depression and anxiety, and/or suffer consequences years later in the form of cardiovascular problems or other stress-related diseases. And it tells us that not everyone reacts the same to the same event, and that many factors—environmental, social, cultural, as well as an individual’s personality traits—interact to determine how each person responds.
Media exposure seems to play a critical role, with greater exposure to coverage of a disaster consistently linked to higher stress levels. In one study of the Boston Marathon bombing, people who watched the most news about the event also had the highest stress levels, higher even than people who directly experienced the traumatic event. This can create a “self-perpetuating cycle of distress,” the authors noted, with people seeking out more news as their anxiety increases.
Data from a population survey by Sondro Galea of Boston University and colleagues suggests that the impact of the Covid-19 pandemic on Americans may be substantially larger than that of previous large-scale events—a reflection, the authors speculated, of its ubiquity. “The reason is probably that this is not one event,” Catherine Ettman, the paper’s lead author, wrote in an email. “This is both Covid, and the fear and anxiety around Covid, as well as the dramatic economic consequences. Evidence for that comes, in particular, from the disproportionate burden of depression on people with fewer resources.”
A greater burden of deleterious effects is consistently seen in predictably vulnerable populations, such as those who have directly suffered financial loss, are at direct risk of harm, or have lost a loved one. Women, minorities, the elderly, and the poor have historically been hit the hardest by large-scale collective traumas. The Covid data so far echo and amplify these trends,


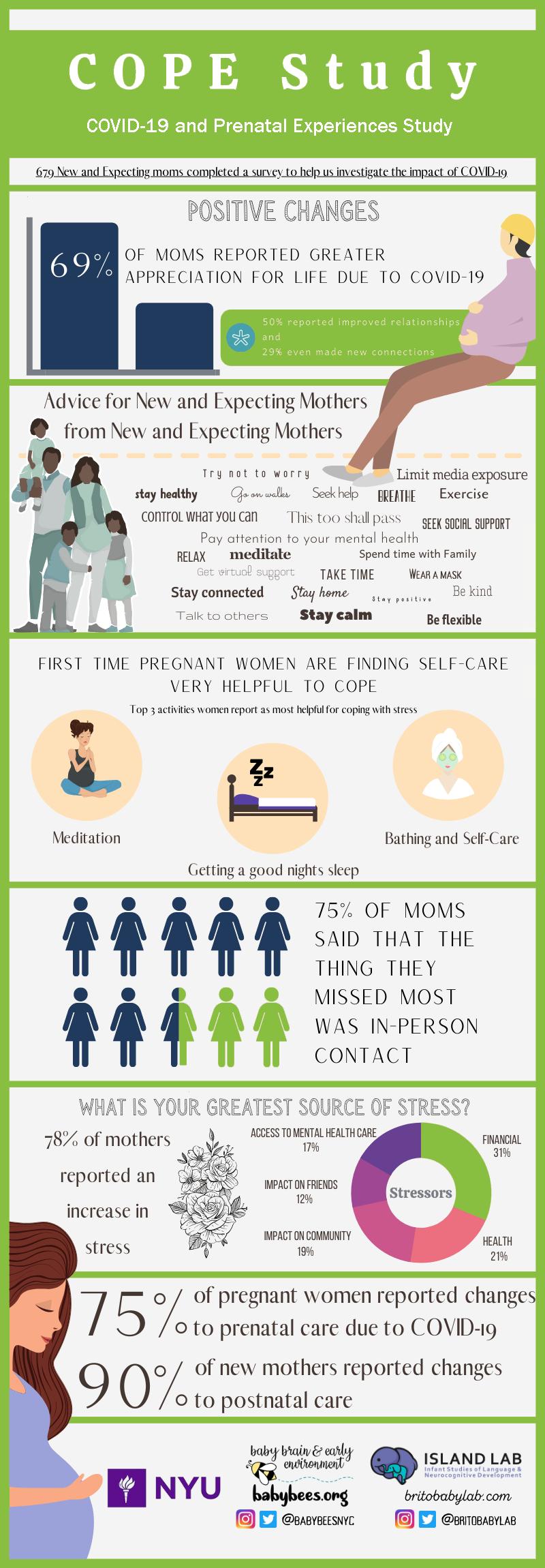
with one interesting exception: younger adults are reporting more stress than older adults in the current crisis.
Clearly, the mere presence of stress-related psychological symptoms does not by itself signal mental illness. In its guidebook, Protecting Mental Health During Epidemics, the Pan American Health Organization (PAHO) notes that the majority of psychological and social problems that occur during an epidemic are “normal reactions to an abnormal situation” rather than diseases. Signs that differentiate a “normal” reaction from a potentially pathological one, PAHO says, are prolonged or intense suffering, the presence of associated complications such as suicidal behavior, and problems that significantly impact an individual’s routine and social functioning.
Only time—and research—will tell where the lines are drawn between “normal” and “pathological” mental health responses to a global pandemic. In September, six months into lockdown in the U.S., the National Institute of Mental Health started enrolling volunteers in a large-scale clinical trial to assess mental health outcomes over time, and to identify risk and resilience factors. Ten thousand participants, including healthy volunteers and people with a history of mood or anxiety disorders, will self-track their psychological symptoms online every two weeks for six months. The study will examine how Covid stressors relate to mental health symptoms and distress, and how pre-existing mental health concerns affect this relationship.
Moriah Thomason, Ph.D., a developmental neuroscientist at NYU Langone, is extending this inquiry into the next generation, asking what effect today’s stress will have on babies born in the midst of the pandemic. Her team has recruited 1,000 women in New York City to be part of a longitudinal study, the so-called Coronavirus Outbreak Psychological Outcomes study, examining the relationship between a mother’s Covidrelated stress during pregnancy and the neurodevelopmental health of her children. Initial unpublished data from 679 new and expecting mothers finds that the vast majority—78 percent—reported an increase in stress during Covid; financial woes, personal health, and the impact of Covid-19 on their communities were the top three sources (see "COPE Study", at left).
The study’s first babies were born in late summer, and Thomason hopes to begin doing magnetic resonance imaging scans of the infants’ brains by the end of the year—pandemic permitting. Researchers will track brain development in the babies and how that relates to the mother’s stress levels and resilience-oriented behaviors during pregnancy. One of the things she is particularly interested in is the toll of stress related to the uncertainty surrounding Covid.
The late Bruce McEwen of Rockefeller University, an expert on the physiological consequences of stress, argued that what we call “stress” is really the brain’s effort to resolve uncertainty. The brain operates by making predictions about the world based on what it can ascertain through the senses. When it can’t resolve the uncertainty, it has to work harder to find a resolution. This makes uncertainty stress “bioenergetically expensive,” says Thomason. The brain is a greedy organ—it gobbles up 20 percent of the body’s overall metabolic energy and prioritizes its own needs at the expense of other organ systems. If the brain is “always on” to figure out an uncertainty, it is constantly pulling energetic resources from the body. Physically, this can result in fatigue, sleep disruptions, fluctuations in overall energy levels—the kinds of things that are hallmarks of chronic stress.
The brain is well equipped to deal with acute stress, having evolved to flee the tiger or fight the foe in order to survive. Under threat, the amygdala kicks off a well-characterized stress response, releasing cortisol and other powerful hormones that activate the autonomic nervous system.
Heart rate speeds up, breathing quickens, and blood flows to muscles and limbs. Organs unneeded for the immediate
In September, six months into lockdown in the U.S., the National Institute of Mental Health started enrolling volunteers in a largescale clinical trial to assess mental health outcomes over time, and to identify risk and resilience factors.
For more findings about effects of the COVID-19 pandemic on mental health, visit the KFF website.
response, like the gastrointestinal tract, are put on hold. When the stressor has passed, the whole system relaxes, returning to its balanced baseline performance.
It’s when the stressor doesn’t pass that things can get ugly. Or when it keeps rearing its head, or is compounded by other stressors. Then the system can’t return to baseline. Stress hormones keep pouring out. The brain stays in a hypervigilant, energy-hogging, toxin-producing state.
That’s because repeated exposure to cortisol, the stress hormone, can be toxic to nerve cells. One of its effects is to cause changes in ion channels that regulate neuronal firing in the prefrontal cortex, the thinking part of the brain. The prefrontal cortex exerts inhibitory control over more evolutionarily primitive circuits like the amygdala and basal ganglia, which govern instincts, habits, and emotions. Animal research in Amy Arnsten’s laboratory at Yale has shown how synaptic connections in the prefrontal cortex first weaken and eventually wither away under conditions of chronic stress, unleashing the primitive, instinctual brain from its executive overseer.
“Without this top-down regulation by the prefrontal cortex, the amygdala and basal ganglia are free to act in these more primitive ways, so you become more irritable or impulsive, acting in a habitual rather than a thoughtful way,” she says. Arnsten recently released a YouTube video that describes this biological effect, with the hope of helping people understand the neural events behind their behaviors. Says Arnsten, “When you understand the neurobiology, it helps you be compassionate with yourself, instead of getting into a vicious cycle where you blame yourself for your cognitive and emotional errors.” l
TO THE INDIVIDUAL, ART IS AN ENDEAVOR OF SKILL AND imagination, but in its broader sense, it is a form of communication. The works on these pages were made by artists who practice art not only as a creative outlet or pastime, but as a mode of self-expression when verbal communication is limited. Featured in various New York exhibitions, these artworks are part of the permanent collection of gallery265 , a space founded by The Arc Westchester to offer a unique perspective into the personalities of artists with developmental disabilities. Since opening in 2009, gallery265 has had 24 rotations and a permanent collection composed of 87 pieces by 25 artists.
The Arc Westchester is a nonprofit organization that provides support for more than 2,000 individuals with intellectual and developmental disabilities, and its gallery provides opportunities for artists to develop their talents alongside a community where artistic expression is cultivated and supported.
By Seimi Rurup

Alex Masket’s artistic abilities became clear early on, at age two. Alex, 33, has severe autism and is unable to communicate verbally with others. Alex uses art to express himself through the use of bold colors, typography, shape, and form. At first glance, his mixed media collages may seem random or disordered, an aesthetic akin to action painting (a style made popular in the 1950s that defined artists such as Jackson Pollock and Franz Kline). But if you take a closer look, it becomes clear that his work is made with great intent and precision. His artwork has been displayed in galleries and sold commercially over the years, and was the focus of an award-winning, short documentary by Dennis Connors called “Breaking Boundaries: the Art of Alex Masket,” which can be found on sproutflix.org




Antoine Hawkins is 30 years old and living with autism. When he was a toddler, he discovered a love for drawing and has continued to make artwork since.
Over the years, Antoine has collected hundreds of images clipped from newspapers, magazines, or sourced from the internet. He draws inspiration from these images and recreates them incorporating his own artistic style. According to his family, Antoine is happiest when sharing his artwork with family and friends. His work has been displayed in local art exhibitions, and he loves seeing other people smile when they look at his drawings. Through the support of The Arc Westchester, Antoine also received job skill training and is currently employed at a local electronic fabrication business.
“Lady Gaga”
Art pencil and chalk



John Israel is 66 years old and living with developmental disabilities that inhibit his ability to communicate verbally. Despite this, the pride he takes in his work is evident when sharing with his community. John, whose particular focus is on watercolors and acrylics, has created over 100 paintings, many of which appeared in local exhibitions. Common themes in his paintings are fish and water. John’s mother was a recognized artist, and it is clear that he has inherited her talent and fondness for certain color schemes and styles.
“Rainbow Fish” (22” x 14”)
Acrylic on art paper


Susan Green began her formal studies as an artist in 2006, demonstrating a keen interest in painting from the start. Now, at 59, she has had her artworks featured in multiple exhibitions over the past few years. Susan is an artist with developmental disabilities, and her interest in painting arose from a desire for creative self-expression through the use of shapes, forms, bright colors, and faces. She often expresses her shapes in a series of circles that dance across the canvas.
Untitled (22” x 14”)




Rafael Reis is a 22-year-old artist who is on the autism spectrum and was able to explore his love for art through a day program at The Arc Westchester after graduating from high school. He attended weekly art classes where he was able to use different mediums and work alongside fellow artists to create detailed, colorful works. He also volunteered at a local senior center where he worked with residents on a variety of art projects for the local community.
Untitled (22” x 14”)

Joseph T. Coyle is the Eben S. Draper Chair of Psychiatry and Neuroscience at Harvard Medical School. A graduate of the Johns Hopkins School of Medicine in 1969, he was a research fellow at the National Institute of Mental Health with Nobel Laureate, Julius Axelrod. After psychiatric residency at Hopkins, he joined the faculty in 1975. In 1982, he became the director of the Division of Child and Adolescent Psychiatry. From 1991 to 2001, he was chairman of the Department of Psychiatry at Harvard Medical School. His research interests concern the causes of neuropsychiatric disorders. He is the past-president of the Society for Neuroscience (1991), a member of the National Academy of Medicine (1990), a fellow of the American Academy of Arts and Sciences (1993), a fellow of the American Association for the Advancement of Science (2005), and the former editor of JAMA Psychiatry


Martha J. Farah is the Walter H. Annenberg Professor of Natural Sciences at the Center for Neuroscience & Society, University of Pennsylvania. She is a cognitive neuroscientist who works on problems at the interface of neuroscience and society. Her recent research has focused on socioeconomic status and brain development. Farah grew up in New York City, was educated at MIT and Harvard, and taught at Carnegie-Mellon University before joining the University of Pennsylvania. She is a fellow of the American Academy of Arts and Sciences, a former Guggenheim Fellow and recipient of honors including the National Academy of Science’s Troland Research Award and the Association for Psychological Science’s lifetime achievement award. She is a founding and current board member of the International Society for Neuroethics.
PIERRE MAGISTRETTI, M.D., Ph.D.
Pierre Magistretti is the dean of the Division of Biological and Environmental Science and Engineering at King Abdullah University of Science and Technology and professor emeritus in the Brain Mind Institute, EPFL and Center for Psychiatric Neuroscience, Department of Psychiatry–CHUV/UNIL, Switzerland. Magistretti received his M.D. from the University of Geneva and his Ph.D. from the University of California at San Diego. Magistretti’s research team has made significant contributions in the field of brain energy metabolism. His group has discovered some of the cellular and molecular mechanisms that underlie the coupling between neuronal activity and energy consumption by the brain. This work has considerable ramifications for the understanding of the origin of the signals detected with the current functional brain imaging techniques used in neurologic and psychiatric research.

HELEN S. MAYBERG, M.D.
Helen S. Mayberg is a neurologist renowned for her study of brain circuits in depression and for her pioneering deep brain stimulation research, which has been heralded as one of the first hypothesis-driven treatment strategies for a major mental illness. She is the founding director of Mount Sinai Health System’s The Nash Family Center for Advanced Circuit Therapeutics Mayberg received an M.D. from the University of Southern California, trained at the Neurological Institute of New York at Columbia University, and was a post-doctoral fellow in nuclear medicine at Johns Hopkins Medicine. Immediately prior to joining Mount Sinai, Mayberg was Professor of Psychiatry, Neurology, and Radiology and held the inaugural Dorothy C. Fuqua Chair in Psychiatric Neuroimaging and Therapeutics at Emory University School of Medicine. She is a member of the National Academy of Medicine, The American Academy of Arts and Sciences, and the National Academy of Inventors. She is on the board of the International Society for Neuroethics and won the society’s Steven E. Hyman for Distinguished Service to Neuroethics (2018).

JOHN H. MORRISON, Ph.D.
John H. Morrison is UC Davis Distinguished Professor, director of the California National Primate Research Center (CNPRC), Professor of Neurology in the School of Medicine, and professor in the Center for Neuroscience at UC Davis. Morrison earned his bachelor’s degree and Ph.D. from Johns Hopkins University and completed postdoctoral studies in the laboratory of Dr. Floyd E. Bloom at the Salk Institute for Biological Studies. Morrison’s research program focuses primarily on the neurobiology of aging and neurodegenerative disorders. His laboratory is particularly interested in age-related synaptic alterations that compromise synaptic health, lead to cognitive decline, and potentially leave the brain vulnerable to Alzheimer’s Disease. Morrison is a member of the National Academy of Medicine.




RICHARD M. RESTAK, M.D.
Richard Restak is clinical professor of neurology at George Washington Hospital University School of Medicine and Health Sciences, a member of the clinical faculty at St. Elizabeth’s Hospital in Washington, DC, and also maintains a private practice in neurology and neuropsychiatry. A graduate of Georgetown University School of Medicine, Restak has written over 24 books on the human brain and has penned articles for the Washington Post, The New York Times, the Los Angeles Times, and USA Today; and presented commentaries for both Morning Edition and All Things Considered on National Public Radio. He is a past recipient of the Claude Bernard Science Journalism Award, given by the National Society for Medical Research.
HARALD SONTHEIMER, Ph.D.
Harald Sontheimer is I. D. Wilson Chair and professor and founder and executive director of the Virginia Tech School of Neuroscience. He is also Commonwealth Eminent Scholar in cancer research and director of the Center for Glial Biology in Health, Disease & Cancer and the Fralin Biomedical Research Institute. A native of Germany, Sontheimer obtained a master’s degree in evolutionary comparative neuroscience, where he worked on the development of occulomotor reflexes. In 1989, he obtained a doctorate in Biophysics and Cellular & Molecular Neuroscience form the University of Heidelberg. He moved to Yale University for post-doctoral studies and later founded Transmolecular Inc., which was acquired by Morphotec Pharmaceuticals. He is the author of Diseases of the Nervous System (Elsevier, 2015).
Stephen Waxman is the Bridget Flaherty Professor of Neurology, Neurobiology, and Pharmacology at Yale University, and served as chairman of neurology at Yale from 1986 until 2009. His research uses tools from the “molecular revolution” to find new therapies that will promote recovery of function after injury to the brain, spinal cord, and peripheral nerves. A member of the National Academy of Medicine, Waxman has been honored in Great Britain with the Physiological Society’s annual prize, an accolade that he shares with Nobel Prize laureates Andrew Huxley, John Eccles, and Alan Hodgkin. In 2018, Waxman received the Julius Axelrod Prize from the Society for Neuroscience.
CHARLES
Charles Zorumski is the Samuel B. Guze Professor and head of the Department of Psychiatry and Professor of Neuroscience at Washington University School of Medicine in St. Louis. Zorumski is also Psychiatrist-in-Chief at Barnes-Jewish Hospital and founding director of the Taylor Family Institute for Innovative Psychiatric Research. Zorumski’s laboratory studies synaptic transmission in the hippocampus. Since 1997, he has served on the steering committees of the McDonnell Center for Cellular and Molecular Neurobiology and the McDonnell Center for Systems Neuroscience and was director of the Center for Cellular and Molecular Neurobiology from 2002 to 2013. Zorumski has also served on the editorial boards of JAMA Psychiatry, Neurobiology of Disease, and served on the board of Scientific Counselors for the NIMH Intramural Research Program from 2009 to 2013. Since 2011, he has also served on the scientific advisory board of Sage Therapeutics, a publicly-traded company developing neurosteroids and oxysterols as treatments for neuropsychiatric illnesses.

Carolyn Asbury has worked in health philanthropy for more than two decades, directing neuroscience-related health programs at the Robert Wood Johnson Foundation and directing the Pew Charitable Trusts’ Health and Human Services Program prior to consulting with the Dana Foundation. Her own research, through the University of Pennsylvania’s Leonard Davis Institute, concerns policies to facilitate development and market availability of drugs and biologics for “orphan” (rare) diseases. She undertook pro bono research and helped to design the Orphan Drug Act; authored “Orphan Drugs: Medical vs Market Value,” and has authored several journal articles and book chapters on these topics. She has served on the boards of several nonprofit health-related organizations, including the National Organization for Rare Disorders, U.S. Pharmacopeia, College of Physicians of Philadelphia, and Treatment Research Institute.
 Bill Glovin Executive Editor
Bill Glovin Executive Editor
Glovin has been a working journalist for more than 30 years. He is executive editor at the Dana Foundation and hosts the Cerebrum Podcast. He has served as editor of Cerebrum since 2012. Previously, he was senior editor at Rutgers Magazine, managing editor of New Jersey Success, editor for New Jersey Business and a staff writer for The Bergen Record. Glovin graduated from George Washington University with a degree in journalism. He sometimes escapes from in front of the monitor to enjoy basketball, biking, and guitar.
 Seimi Rurup Assistant Editor
Seimi Rurup Assistant Editor
Rurup oversees the production of all digital and print content at the Dana Foundation. She previously served as editor of Brain in the News, which was the Foundation’s longest running print publication, and utilizes her background in fine arts to contribute to current publications and social media. She also contributes to the Foundation’s Neuro News section. Rurup graduated from Sarah Lawrence College with a degree in writing. When she is not in the office, she can be found in one of NYC’s many museums, Brooklyn cafés, or at home cooking with friends.

Brandon Barrera Editorial Assistant
Barrera is a New York City journalist, born and raised in Queens and living in Manhattan. A public affairs assistant at the Dana Foundation, he is the host of the Dana Foundation’s Communicating Brain Science podcast and writes about books for the magazine. Before coming to Dana, he helped produce content for Bronx Net, a public access television channel. When not enthralled by all things sci-fi, Barrera is fond of cycling, film, and arguing the finer points of tabletop gaming.