and the Developing Brain

EMERGING IDEAS IN BRAIN SCIENCE • SPRING 2022
FEATURES
12 Poverty and the Developing Brain
From a team that studies this issue at Washington University School of Medicine, our authors explain the challenges and necessary steps to build a healthier, more productive society.
By Joan L. Luby, M.D., Deanna M. Barch, Ph.D., and John N. Constantino, M.D.
18 Managing Pain: Ancient Ideas and New Frontiers
A cognitive psychologist and head of Dartmouth College’s Cognitive and Affective Neuroscience Lab, our author examines what pain looks like in the brain, and how new research findings are leading to new treatments for pain.
By Tor Wager, Ph.D.
26 The Miracle of Light
A Q&A with Karl Deisseroth, a winner of the 2021 Lasker Prize in Basic Medical Research for his pivotal work in optogenetics and author of the widely praised book, Projections: A Story of Human Emotions.
By Carl Sherman
32 Sleep’s Dark and Silent Gate
Neuroscientists across the globe have new tools to study the integral role that sleeps plays in memory. But they agree that there are still many questions to be answered.
By Kayt Sukel
38 Poetry of the Brain
This year’s winning entries on the 20th anniversary of the annual Neuroscience for Kids Poetry Contest, which is designed to educate kids about the brain through creative writing.
By Bill Glovin
SECTIONS
6 Advances • Notable brain science findings
7 Briefly Noted • By the Numbers, Brain in the News
8 Clinical Corner • Mental Health for Refugees, By Anne Glowinski, M.D., M.P.E. 10 Neuroethics • The Debate Over Safe Injection Sites, By Philip M. Boffey
4 From the Editor | 5 Contributors | 40 Advisory Board | 42 Cerebrum Staff
COVER ILLUSTRATION: LUISA JUNG
SPRING 2022 | VOLUME 3, ISSUE 2
2 DANA FOUNDATION CEREBRUM | Spring 2022
Dana.org 3 ILLUSTRATION: SHUTTERSTOCK
A Final Good-Bye
BY BILL GLOVIN Editor-in-Chief

To our many faithful subscribers and other readers who have been with us since the early 1990s—through many iterations and, for the past three years, as an expanded e-magazine and regular podcast—I’m sorry to report that Cerebrum is ending after this last issue. The Dana Foundation is shifting its focus away from publications to increased grant-giving on how brain science impacts society. These future grants will aim to strengthen neuroscience’s positive role in the world through interdisciplinary programs and public engagement.
Putting the magazine together has been a true team effort. First and foremost, I’d like to give an enormous shoutout to Bruce Hanson, our freelance art director who helped bring the text to life and worked closely with the many talented illustrators whose work has graced our pages. If you have enjoyed our presentation, I have Bruce mainly to thank.
Associate Editor Seimi Rurup was always instrumental in suggesting visual concepts and contributing to our editorial content. Our Copy Editor, Carl Sherman, also authored features and worked tirelessly behind the scenes to make sure that our science was delivered clearly. Nicky Penttila and Brandon Barrera always did great work on our Advances and Books columns, respectively, and our regular contributors Kayt Sukel and Brenda Patoine wrote extraordinary long-form journalism from the beginning.
Finally, a huge note of thanks to my scientific advisory board, who suggested topics and authors, vetted articles, and brought their wisdom and experience in neuroscience to the table. I’ll surely miss our Zoom calls. Our recently retired in-house scientific adviser/ advisory board member Carolyn Asbury was a major sounding board through thick and thin, and recently retired Executive Vice President Barbara Gill, former Acting President Burt Mirsky, and the Dana Board helped me realize my vision and allowed for the expansion to a quarterly magazine. I’m eternally grateful to them.
Corny as it may sound, editing Cerebrum has been an awesome learning experience—and even fun sometimes. To get to work with all these gifted individuals and all our neuroscientist authors has truly been an absolute privilege. Best of luck to new President Caroline Montojo and all my other wonderful colleagues at Dana as they transition to their new and important direction.
Enjoy this final effort, and thanks for your time and attention. l
Bill Glovin Editor-in-Chief
Bruce Hanson
Art Director
Seimi Rurup Associate
Editor
Brandon Barrera Staff Writer
Carl Sherman Copy Editor
Khara M. Ramos, Ph.D. Scientific Consultant
Cerebrum is published by the Charles A. Dana Foundation, Incorporated. DANA is a federally registered trademark owned by the Foundation.
© 2022 by The Charles A. Dana Foundation, Incorporated. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the publisher, except in the case of brief quotations embodied in articles.
Letters to the Editor
Cerebrum Magazine
10 Rockefeller Plaza, 16 Floor New York, NY 10020 or cerebrum@dana.org
Letters may be edited for length and clarity. We regret that we cannot answer each one.
4 DANA FOUNDATION CEREBRUM | Spring 2022 FROM THE EDITOR
EMERGING IDEAS IN BRAIN SCIENCE
Poverty
> Page 14
JOAN L. LUBY, M.D., is the Samuel and Mae S. Ludwig Professor of Psychiatry (Child) at the Washington University School of Medicine, where she had founded and leads the Early Emotional Development Program. Luby specializes in infant/ preschool psychiatry and her clinical and research program has focused on early childhood psychopathology and emotional development, specifically in application to the risk trajectory for early onset depressive disorders. Her clinical expertise is on early childhood psychopathology in the mood and affective domain and how this relates to alterations in emotion development.

DEANNA M. BARCH, Ph.D., is Couch Professor of Psychiatry and a professor of radiology and chair of the Department of Psychological & Brain Sciences at Washington University School of Medicine. Her research focuses on understanding the mechanisms that give rise to the challenges in behavior and cognition found in illnesses such as schizophrenia and depression, and utilizing psychological, neuroimaging and computational approaches. She is deputy editor at Biological Psychiatry, editor-in-chief of Biological Psychiatry: Global Open Science, and president of the Psychology Section of the American Association for the Advancement of Science.

JOHN N. CONSTANTINO, M.D., is the Blanche F. Ittleson Professor of Psychiatry and Pediatrics and Director of the Division of Child and Adolescent Psychiatry at the Washington University School of Medicine in St. Louis. He previously served as chair of the Mental Health Commission of the State of Missouri and is currently psychiatrist-In-chief of St. Louis Children’s Hospital. Constantino’s work focuses on understanding genetic and environmental influences on disorders of social development in childhood, for the purpose of reducing risk for lifelong impairment. He and his team have worked to understand and offset the influence of early adverse environmental experience on social development in children, particularly in relation to the prevention of child maltreatment.
> Page 18
TOR WAGER, Ph.D., is the Diana L. Taylor Distinguished Professor in Neuroscience at Dartmouth College and the director of Dartmouth’s Cognitive and Affective Neuroscience laboratory, the Dartmouth Brain Imaging Center, and the Dartmouth Center for Cognitive Neuroscience. He received his Ph.D. from the University of Michigan in cognitive psychology and served as an assistant and associate professor at Columbia University, and as associate and full professor at the University of Colorado, Boulder. Since 2004, he has directed the Dartmouth lab devoted to research on the neurophysiology of affective processes—pain, emotion, stress, and empathy—and how they are shaped by cognitive and social influences. Wager also teaches courses and workshops on fMRI analysis and has co-authored Principles of fMRI



> Page 26
CARL SHERMAN has written about neuroscience for the Dana Foundation for ten years. His articles on science, medicine, health, and mental health have appeared in national magazines including Psychology Today, Self, Playboy, and Us. He has been a columnist for GQ and Clinical Psychiatry News, and is the author of four books. He holds a doctorate in English literature and has taught at various universities. When not writing about the mind, the brain, and the interesting things people do with them, he enjoys travel, listening to music, looking at art, and copyediting. He lives and works in New York City.
Sleep's Dark and Silent Gate
> Page 32
KAYT SUKEL‘s work has appeared in the Atlantic Monthly, the New Scientist, USA Today, the Washington Post, Parenting, National Geographic Traveler, and the AARP Bulletin. She is a partner at the award-winning family travel website Travel Savvy Mom, and is also a frequent contributor to the Dana Foundation’s science publications. She has written about out-of-body experiences, fMRI orgasms, computer models of schizophrenia, the stigma of single motherhood, and why one should travel to exotic lands with young children. She is the author of Dirty Minds: How Our Brains Influence Love, Sex and Relationships and The Art of Risk: The New Science of Courage, Caution & Chance

Dana.org 5
CONTRIBUTORS
and
the Developing Brain
Managing Pain: Ancient Ideas and New Frontiers
The Miracle of Light
ADVANCES
Notable brain-science findings
EVERY YEAR IN THE US, about 100,000 young people will experience a first episode of PSYCHOSIS, which can include hallucinations, paranoia, delusions, disordered speech and behavior, and significant impairment at home and school. In a study and clinical trial led by Kelly Allott from the University of Melbourne, the youth who got placebos and those who got antipsychotics had similar levels of improvement in their social and occupational functioning. The findings support the need for careful consideration of the risks and benefits of various antipsychotics and the importance of accounting for their cognitive effects in longitudinal research. l
FOLLOWING A CORONAVIRUS INFECTION, even mild cases of Covid-19 are associated with subtle tissue damage and accelerated losses in brain regions tied to sense of smell, as well as a small loss in the brain’s overall volume, a new British study finds. The paper, published in Nature and led by University of Oxford investigators, is the first study of the disease’s potential impact on the brain that is based on brain scans taken both before and after participants contracted the coronavirus. l
BY EMPLOYING ARTIFICIAL INTELLIGENCE (AI) and robotics to formulate therapeutic proteins, a team led by Rutgers researchers has successfully stabilized an enzyme able to degrade scar tissue resulting from spinal cord injuries and promote tissue regeneration. The study, recently published in Advanced Healthcare Materials, details the team’s groundbreaking stabilization of the enzyme Chondroitinase ABC (ChABC), offering new hope for patients coping with spinal cord injuries. l

In a study led by Cedars-Sinai Medical Center and part of a multi-institutional BRAIN Initiative consortium funded by the National Institutes of Health, researchers discovered two types of BRAIN CELLS that play a key role in dividing continuous human experience into distinct segments that can be recalled later. The discovery—published in the peer-reviewed journal Nature Neuroscience—provides new promise as a path toward developing novel treatments for memory disorders such as dementia and Alzheimer’s disease. l
California Governor Gavin Newsom has proposed to address the overlapping MENTAL HEALTH AND HOMELESSNESS

CRISIS facing Los Angeles and other cities. The proposal, which would need approval by the Legislature—is called Community Assistance Recovery and Empowerment, or “CARE Court.” It would enable people with severe untreated mental illness or substance use disorders to be placed under court-ordered psychiatric care at the request of family members, clinicians, and others who work closely with them. l
NOSTALGIA decreases activity in pain-related brain areas and decreases subjective ratings of thermal pain, according to research recently published in Journal of Neuroscience. Researchers from the Chinese Academy of Sciences measured the brain activity of adults with fMRI while the participants rated the nostalgia levels of images and rated the pain of thermal stimuli. Viewing nostalgic images reduced pain ratings compared to viewing control images, with the strongest effect on low-intensity pain. It also reduced activity in the left lingual gyrus and parahippocampal gyrus, two brain regions implicated in pain perception. l
6 DANA FOUNDATION CEREBRUM | Spring 2022
ILLUSTRATIONS: SHUTTERSTOCK
BRAIN IN THE NEWS
Links to brain-related articles we recommend


> The Economist: Video game makers must address worries about addictiveness



> New York Times: How Exercise May Tame Our Anxiety
> CNN Health News: Dogs can recognize different languages and nonsense words, study says
> NBC News: Even mild Covid is linked to brain damage, brain scans show
> New York Times: Wildlife Personalities Play a Role in Nature
> Brain + Life: Smart Ways to Make Playing Video Games Healthier
> New York Times: We Will Forget Much of the Pandemic. That’s a Good Thing
> Washington Post: This is why it’s hard to find mental health counseling right now
> Star-Ledger: ‘We must act’ on kids’ mental health crisis, experts say

> American Scholar: Footage from a war and the effects on your brain

> New York Times: Is Geometry a Language Only Humans Know?



> Psyche: Bias in mental health diagnosis gets in the way of treatment
The strategy the White House has laid out in its fact sheet is a necessary beginning—and it will save lives. Their approach will meet people where they are and will reduce disparities and promote equity across the mental health landscape.”
BY THE N UMBERS
1% percent of people in indigenous groups in the Bolivian Amazon suffer from dementia, in contrast to 11 percent of people over 65 in the US.

FIVE neuromyths, including the “silent cortex” theory that a person uses only 10 percent of his or her brain, have been debunked by researchers.
140 MILLION people around the world now play Minecraft, a video game that a neuroscientist in Scotland uses to explain neuroscience and biological principles.

10



of these natural have been shown to combat anxiety and depression.

credits are the maximum number (down from 23) engineering majors can now take each semester at Cornell University. The new threshold is an to improve student mental health.
$700,000,000






is the investment President Biden has proposed for programs that provide clinicians with the tools to treat mental health and substance use treatment in rural and underserved communities.

Dana.org 7
“ BRIEFLY NOTED
— Schroeder Stribling, president and CEO of Mental Health America
TWENTY
Mental Health for Refugees
BY ANNE GLOWINSKI, M.D., M.P.E.

LAST MONTH, AGAINST THE backdrop of tens of thousands of refugees fleeing Ukraine, the US formally accused Myanmar of committing genocide against its minority Rohingya population. This genocide was evident during two trips I and younger colleagues made in 2018 to Bangladesh to provide mental health training and support to relief workers on the frontlines of the refugee camps. Depression, anxiety, distrust, post-traumatic stress disorder, and substance abuse were among the problems.
Invited by a Non-Governmental Organization (NGO), our first visit took place about a few months after hundreds of thousands of Rohingya refugees—many of them children—had perilously crossed the Myanmar border into south-eastern Bangladesh. In my role as a professor of child and adolescent psychiatry, I engaged in myriad activities, which included visiting NGO headquarters and refugee camps. We observed living conditions, spoke to Rohingya people of all ages, and listened to the stories of villagers—several of which had been at the epicenter of massacres by Myanmar’s military-led government. One particularly vivid memory is having long conversations with three wonderful brothers ages 8, 14, and 21, who were the sole survivors among a sibship that included initially 15 brothers.
I kept a journal throughout the visit, and here is some of what I wrote to
express what my experience was like on my very first day in Bangladesh:
After two days and three flights through Dubai and Dhaka, Dr. Ali Anwar (one of my chief child and adolescent psychiatry fellows at Washington University) and I arrive at the Friends in Village Development Bangladesh (FIVDB) headquarters in Sylhet, a northeastern Bangladesh city. We started our 1 to 5 p.m. workshop almost an hour late. We were jetlagged and nervous but exhilarated.
the leaders and main coordinators from FIVDB—that the NGO’s vision is “A vibrant society based on justice, equity, democracy, and environmentally sound principles.”
Like almost everywhere around the world, education does not necessarily translate to mental health literacy. That is why we have been invited.: Mental health problems are plaguing the refugees. So, Ali and I start, daunted and yet reassured by the outstanding reputation of FIVDB. They understand adult learning; it is not just about content. It is about inspiring by tapping into pre-existing relevance for the adults, who, unlike children, do not always integrate novelty with abundant enthusiasm.
Our presentation stresses concepts such as depression or the impact of trauma on the mind and body, and we find it especially impactful to have the audience participate and role play. We quickly attain a high level of trust, candor, and (according to participants’ feedback) a true consolidation or awakening that mental health, an area of taboo in Bangladesh and many other parts of the world, must be heeded and integrated into healthcare.
Tomorrow, we will conduct a more intimate in-training session for their refugee camps’ staff in Cox’s Bazaar, where we will be heading later today. The rest of our time we will visit remote Rohingya refugee camps near the Myanmar border. FIVDB has helped to organize help for many refugees through the educational programs that they are famous for, such as community theater (e.g., to inform the Rohingya about the risks of child marriage).
At yesterday’s workshop, during obligatory computer issues, Ali and I learn from our audience—mainly
Ali and I cannot offer many specialized resources, so we demonstrate basic skills, especially those recommended by the World Health Organization and others for psychological first aid by lay people. We focus particularly on active listening, a skill that can also facilitate self-care and community support for a work force at enormous risk for burnout.
This is especially true for the refugee camp workers we will meet tomorrow. We are also listening actively and learn that access to remote camps built on slopes requires daily back and forth walking for several kilometers in heat and humidity. Also, the monsoon
8 DANA FOUNDATION CEREBRUM | Spring 2022 CLINICAL CORNER
“It is clear that all refugees fleeing armed conflict and danger share the same almost unbearable human anguish, thirst for justice, and for the fraternity of others more fortunate.”
season is near, with its flooding and cyclones; half of the refugees, or almost 400,000 people, will need to be relocated. However, no firm plans have been proposed yet, creating a toxic level of anxiety among the relief workers.
We hear about the challenges of working with refugees who have partially unfamiliar customs in this new country and have been acutely traumatized recently, but also chronically for decades before that. We hear about leadership challenges and that the refugee crisis is leading to an unprecedented level of scrutiny by NGOs from all over the world. So, FIVDB is getting a lot of well-meaning expert advice—some contradictory.
Afterwards, we are exhausted yet rich with new connections and grateful for what our learners have taught us, too. We fall asleep underestimating mosquitoes and a few other things that we will encounter in the week ahead.
Traveling forward to 2022, present day: Despite heroic efforts by NGOs and their workers and their many innovative programs, the situation in Rohingya refugee camps continues to be harrowing. This is not a complete surprise: Refugees are the fastest growing population in the world, and the average time spent in a camp by a refugee is 10 to 20 years. Justice, even symbolical, is slow: evidence is the five years it has taken for the US to recognize the Rohingya as victims of genocide.
Much is being said about the sentimental discrepancy between our average emotional reactions to the plight of Ukrainians (many now refugees), and our less intense average reactions to the plight of other refugees, such as the Rohingya and many others. It is clear that all refugees fleeing armed conflict and danger share the same, almost unbearable human anguish, thirst
for justice, and for the fraternity of others more fortunate.
In a conversation I had with Rohingya elders in 2018 when we gathered to discuss their cultural identity before making any substantial mental health recommendations, one of the men told me: “If you have a cow that is brown, you call it brown cow. If you have one with spots, you call it a spotted cow. We are like a cow without a name. To the world we don’t have a name.” l

Dana.org 9 PHOTO COURTESY OF
ANNE GLOWINSKI, M.D., M.P.E., is the Robert Porter Professor of Child and Adolescent Psychiatry and Division Director for Child and Adolescent Psychiatry at the UCSF Child, Teen, and Family Center in San Francisco. Glowinski previously worked as Professor and Associate Chief of Child and Adolescent Psychiatry at Washington University in St. Louis.
ANNE GLOWINSKI
Anne Glowinski observes a group of kids at a child safe place within a refugee camp as they learn rudimentary new Bangla vocabulary through song.
The Debate Over Safe Injection Sites
BY PHILIP M. BOFFEY

IN THE FINAL WEEKS OF HIS administration, Bill de Blasio, then mayor of New York, opened the nation’s first two overdose prevention centers to save the lives of people with substance use disorders who inject dangerous narcotics. Such sites are almost certainly illegal under an outdated federal law designed to close places where drug use is prevalent. But is it also unethical or immoral to operate the new sites? Or would it be even more unethical to close them down and leave people struggling with addiction to the mercy of the streets?
The section of federal law that seemingly prohibits such sites makes it a felony to own, rent, or operate a location for the purpose of facilitating illegal drug use. Violators can be punished by up to 20 years in prison and served hefty fines. Simply raising that threat was enough to deter Philadelphia from opening a planned site.
There were more than 95,000 drug overdose deaths in the year ending in February 2021, an all-time record, according to the Centers for Disease Control and Prevention. The chief culprits were opioids, including fentanyl, heroin, and prescription opioids, among others.
The federal statute—dating back to the Anti-Drug Abuse Act of 1986— was designed to close buildings where people would shoot up and often die in shadowy corners in scenes worthy of a Dickens novel.
But the clean, modern facilities that federal authorities are targeting seem a much better option. The new facilities are sometimes called “safe injection sites” or “overdose prevention sites’” to underscore their important public health mission.
Shortly after New York City’s first two sites opened in November 2021, reporters for the New York Times described the scene inside. People brought their own drugs to the sites, were provided with clean needles to use, and if they overdosed, were quickly given naloxone to reverse the overdose and save their lives. They were also told about options to receive treatment for their addiction, often crucial information for people struggling with substance use disorders. The sites have been supported by four of the city’s five district attorneys and by Eric Adams, the new mayor, who has a strong police background. The local law enforcement authorities can draw on their experience to understand what cities desperately need to combat rising addiction rates.
The arguments against such sites were laid out by Rod Rosenstein, then deputy attorney general for the Trump administration, in an
opinion piece in the New York Times on August 27, 2018. He called the sites “very dangerous” and said they “would only make the opioid crisis worse.” He claimed drug dealers would flock to the area, destroying the surrounding community. People “do not need a tax-payer sponsored haven to shoot up,” he said. “Injection sites normalize drug use and facilitate drug addiction by sending a powerful message to teenagers that the government thinks illegal drugs can be used safely.”
Some opponents of injection sites also raise moral arguments—saying that injection drug use is

NEUROETHICS 10 DANA FOUNDATION CEREBRUM
intrinsically evil because it is nontherapeutic and causes serious harm to the user. They believe injection sites entice some users to continue by providing them a site to shoot up. Interestingly, Rod Rosenstein did not make a moral or ethical argument but rather predicted dire consequences if sites are opened.
Regardless, observers on both sides of the discussion need to choose appropriate language to reduce stigma and avoid undermining the likelihood that people will seek help. A paper published in Neuropsychopharmacology
indicates that “stigma—negative attitudes toward people based on distinguishing characteristics— contributes in multiple ways to poorer health outcomes; consequently, it has been identified as a critical focus for research and interventions.”
On the opposite side of this debate, William F. Haning III, a physician in Hawaii, made a strong case for supporting injection sites in a September 29, 2021, opinion piece
the spread of blood-borne infectious diseases.
The trend nationwide is running toward greater use of injection sites. Rhode Island last year became the first state to enact a law to open sites with local approval under a
for STAT news. Writing as president of the American Society of Addiction Medicine, he cited great value in opening sites where people can consume previously obtained drugs in a hygienic monitored environment without fear of arrest. The American Medical Association has also endorsed such sites.
Haning cited research in other nations which showed that injection sites did not increase drug use, trafficking, or crime. Instead of destroying the surrounding community, the sites reduced the volume of public injecting as well as the number of syringes discarded on streets and sidewalks. On the plus side, the sites achieved important health goals by reducing harm among drug users and connecting some to health and social services. The sites are no panacea, of course, and can’t solve all the societal factors that contribute to drug use. But they can at least reduce deaths and provide clean needles to prevent
two-year pilot program. San Francisco is poised to open a site later this year, and other cities are expected to join the parade. The Boston Globe editorial board called for their own mayor to follow quickly on the heels of New York.
Whether the Biden administration will be more receptive than the Trump administration to safe injection sites and other harm reduction approaches is not yet clear. The president may be too preoccupied with a host of domestic and foreign crises and political battles to pay much attention to this issue. His staff and cabinet appointees would be wise to recognize that the most ethical course of action would be to open more of these sites and pledge not to arrest their staff or clientele working to combat addiction and save lives. l
PHIL BOFFEY is former deputy editor of the New York Times Editorial Board and editorial page writer, primarily focusing on the impacts of science and health on society. He was also editor of Science Times and a member of two teams that won Pulitzer Prizes
The views and opinions expressed are those of the author and do not imply endorsement by the Dana Foundation.
in poverty show tangible alterations. Our authors, all part of needed to build a healthier and more productive society.
By Joan L. Luby, M.D., John N. Constantino, M.D., & Deanna M. Barch, Ph.D.
Numerous studies of children in the US across decades have shown striking correlations between poverty and less-thanoptimal physical and mental health and developmental outcomes. Trauma, poor health care, inadequate nutrition, and increased exposures to psychosocial stress and environmental toxins—all of which have significant negative developmental impact—are likely to be involved.
 Illustration by Luisa Jung
Illustration by Luisa Jung

Dana.org 13 of
The effects of elevated stress on child-caregiver relationships appear to be particularly detrimental, unsurprising in that nurturing and supportive caregiver relationships are foundational for healthy development in early childhood. For adults whose job options are unconducive to their role as parents (such as working multiple jobs or night shift hours), or for whom family support is unavailable, or for those do not have the material resources they need, the resulting stress may result in sleep disruption, depression, and anxiety—all of which translate to poor developmental trajectories for their children.
Other health and developmental risks often associated with poverty include lead and other pollutants in air and water, poor nutrition (often related to living in “food desert” areas where healthy foods such as fresh fruits and vegetables are scarce), neighborhood violence, and trauma. “Toxic stress” that exceeds a child’s ability

to adapt can occur when the burden of stressful life experience overwhelms the brain’s regulatory capacity, or when the compensatory abilities of brain and body are compromised. A lack of cognitive stimulation (due to such factors as the absence of books and educational materials in the home, poor immersion in language, and a lack of after school or other enrichment activities) or disruption of sleep and circadian rhythms (by neighborhood noise or parents’ irregular work schedules) is likely to impact brain development and emotional and behavioral regulation when these systems are rapidly developing.
How the Environment Shapes the Developing Brain
Building on a robust body of literature in the behavioral sciences, developmental neuroscientists have begun to investigate whether tangible effects of poverty and adversity can be detected in the structure and function of the developing brain. A growing body of evidence demonstrates quantifiable relationships between adverse environmental exposures and alterations in neurodevelopment visible in brain scans.
Work in animal models has shown that environmental exposures influence the sculpting of neural circuits, particularly during early developmental “sensitive” periods when the brain is uniquely malleable. This sculpting occurs through processes such as neurogenesis (the sprouting of new brain cells), synaptogenesis (the growing of new connections between brain cells), and synaptic pruning (the elimination of less-used connections between brain cells to enhance efficiency of communication among neurons and in brain circuits). The environmental influence
14 DANA FOUNDATION CEREBRUM | Spring 2022
A growing body of evidence demonstrates quantifiable relationships
on this shaping process is thought to prepare the organism for adaptation to experiences and challenges it is likely to encounter in the future.
In human studies during childhood, developmental neuroscientists have used tools such as electroencephalography (EEG) and both structural and functional magnetic resonance neuroimaging (sMRI/fMRI) to show an association between early exposure to poverty and changes in brain structures critical for emotion regulation and cognitive function. For example, research has linked early poverty to a reduction in the size of the hippocampus, a brain region critical for healthy stress response and memory function. Further, studies using both EEG and fMRI have shown different patterns of brain activation in response to stimuli that evoke emotion or the need for emotional regulation.
Children growing up in poverty showed greater amygdala
activity in response to threatening stimuli. Researchers have also found an association between early poverty and alterations in brain circuits that are important for experiencing emotions, generating adaptive behavior patterns, and learning. These changes include reduction in the connections between the hippocampus and other brain regions, such as the prefrontal cortex and the anterior cingulate, that support cognition.
As environmental shaping helps prepare an organism for its expected future, such stress-related differences in brain structure and function might be adopted to help a child manage uncertainty or respond to difficult circumstances later on. Over time or in response to chronic exposure to stress, however, adversity may also contribute to enduring disruptions in physical and mental health or in cognitive and emotional function.
There is evidence suggesting that the link between early poverty and later psychopathology is mediated through some of the alterations in brain structure and function described above. Findings of this nature have re-ignited public health attention to the problem of child poverty; their insights into the mechanistic pathways of poverty’s deleterious effects on the brain pave the way to more directed targets for prevention and early intervention.
Studies of Mechanisms
As with brain development, while the association between exposure to poverty and negative developmental child outcomes have been apparent for many decades, the underlying cellular-level and psychosocial processes are more elusive. Numerous mechanisms appear to
be involved. For example, work in both humans and animals has shown that early exposure to enriched versus depleted environments, as well as variations in maternal care, can change the expression of key genes (i.e., turning on and off the production of proteins encoded by each gene) that are involved in brain development and function.
Such epigenetic mechanisms represent an interface at which nature and nurture interact. For example: A healthy response to stress requires activation of a brain system called the hypothalamic pituitary adrenal axis (HPA axis); it regulates the release of the brain hormone cortisol, which helps prepare the body for adaptive coping. Excessive or prolonged HPA activation (such as the chronic stress that commonly accompanies poverty), generates too much cortisol, and can change gene expression in a way that causes lasting disruptions in hippocampal structure and function.
A similar process has been described in immune system reactivity, where chronic exposure to poverty and related stresses results in a “pro-inflammatory” state where the immune system remains activated, even without microbial threats. This chronic low level of elevated inflammation poses long-term health risks.
In addition, living in poverty is associated with disruptions in the sleep-wake cycle; noise and light and patterns of household function that accompany challenging work hours (e.g., late shift work) can reduce the amount of sleep for children as well as adults. These disruptions have their own impact on brain circuits, interfering with neural restorative processes that accompany regular sleep and are critical for learning and emotion.
As noted above, poverty is frequently associated with exposure to environmental toxins known to harm brain development, such as lead, polycyclic aromatic hydrocarbons (produced when oil, gas, and tobacco are burned), and nitrogen dioxide (present in air pollution). All too frequently, poverty also means reduced access to adequate nutrition, green space, and health care, all of which can directly and indirectly impact brain and overall development.
Understanding the mechanisms of risk is complicated by the fact that poverty typically brings many risks at once, making it difficult to determine which risk factor drives which specific negative outcome (e.g., emotion dysregulation, failure to achieve potential), or whether multiple exposures have synergistic effects. And while causality may be suggested by association, it can be
Dana.org 15
relationships between adverse environmental exposures and alterations in neurodevelopment visible in brain scans.
clearly established only with experimental designs that measure key outcomes before and after exposure to risk factors. Such studies are very rare but have been possible in the face of an environmental change (e.g., income increases brought out by an economic boon to a community, a pandemic, or policy change, or natural or man-made disasters that bring about social adversity in a previously well-resourced community).
Knowledge gaps notwithstanding, the robust evidence for a connection between poverty and poor physical and developmental outcomes, and the high proportion of US children born into poverty, argue an ethical imperative to determine whether ensuring economic equity would bring benefits comparable to avoidance of toxic exposures and iron deficiency, which is now the standard of care and practice. Further enhancing income may also be a first step towards ameliorating other negative social forces
and psychosocial support of parents during their children’s first years of life (Early Head Start and Healthy Families America); and educational support of preschoolers (Head Start). Each program has overwhelmingly demonstrated incremental improvements in the average outcomes of the children such as overall achievement and lower rates of psychopathology. But they have not been nearly enough to close the developmental and mental health gap between children who grow up in underprivileged environments and those who do not.
Interventions designed to enhance the parent-child relationship and reduce the likelihood of severe adverse experiences, such as child abuse and neglect, have proven a feasible and effective next-line-of-defense in the roster of federal programs for children in poverty. Ranging from home-visiting programs to live coaching during parent-child interactions, they aim to enhance emotional
such as environmental and racial injustices associated with low SES. Studies that provide income transfers to young families living in poverty have provided some promising initial results, but most have not followed children long enough to show the enduring neural and mental health benefits.
Understanding the pathways and mechanisms of poverty’s negative effects on the developing child is essential if we are to understand the importance of alleviation of risks associated with poverty and develop more cost-effective and targeted preventions and early interventions. That the direct consequences of economic insufficiency on brain development are entirely avoidable in the US, given its wealth as a nation, underscores the importance of these scientific endeavors.
Interventions to Protect Developing Children
Despite the growing knowledge base, there has been surprisingly little sustained public interest or investment in supporting robust programs to interrupt poverty’s deleterious impact on children. A notable exception is the “War on Poverty” with its federal programs for children living below the poverty line, initiated by President Lyndon Johnson in 1964 and still operational in all 50 states.
Temporary Assistance for Needy Families (TANF) and the annual Child Tax Credit, contemporary mechanisms for direct cash transfers to impoverished families, evolved from the War on Poverty. Other federal programs have focused on consequences of poverty that damage the development of children, including nutritional support (the Women, Infants, and Children program WIC); educational
connection and warmth between parent and child and teach caregivers how to set nurturing but firm limits. These strategies have shown strong efficacy in buffering the negative emotional impact of poverty.
Such interventions may be delivered in clinical settings or in the home or, more recently, by video conferencing. Extending them through community settings such as school or primary care sites will facilitate access to high-risk populations. There are now a number of empirically tested (and proven effective) models of this type of preventive intervention whose low cost makes them feasible for broad delivery with minimal social investment (through taxpayer dollars into social programs) and a high return on that investment. The question becomes: How to emphasize the importance of these interventions and their effectiveness to administrators responsible for child health and well-being?
Science Policy Gap
In regard to the above question, the gap between scientific advances and changes in social policy and healthcare practices is well-known. The field of implementation science was developed to address it by identifying barriers to the uptake of advances in medicine, social science, and psychology by practitioners and healthcare systems. This gap can be even more daunting in the area of public policy, where political perspectives and agendas can obstruct the integration of scientific findings.
In the area of poverty and child development, the science-policy gap is strongly influenced by political philosophies and belief systems about the merits and liabilities of social safety nets. Even tangible economic
16 DANA FOUNDATION CEREBRUM | Spring 2022
Despite the growing knowledge base, there has been surprisingly little sustained public interest or investment in supporting
benefits—compelling data that early interventions for children living in poverty result in a high return on investment and significant savings in tax-payer dollars over the long-term when they are used to fund these social programs—often fail to influence policy in a logical manner.
Changing Social Attitudes
More generally, stereotypes about poverty continue to thwart progress in this area. The idea that people live in poverty because they are unmotivated to work, or fail to take responsibility for themselves, or are genetically destined to fail, often drives social investment or lack thereof, even when it affects the well-being of young children. The commonly held misconception that people living in poverty are predominantly racial/ethnic minorities in cities may fuel beliefs based on implicit or explicit bias. In fact, the majority of people in poverty in the
supporting robust programs to interrupt poverty’s impact on children.

US are white and live in rural areas. This is because even though the percentage of racial and ethnic minorities living in poverty is higher than the percentage of white individuals, there are a larger number of white individuals in the US. For example, in 2020, 15.6 percent of white non-Hispanic households were living on $24,999 or less a year, with 29.7 percent of household identifying as black were living at or below the same income levels. However, in terms of numbers of households, this reflects 13.3 million households identifying as white non-Hispanic and 5.2 million households identifying as Black. This is not to suggest that we should only care about poverty if it happens to majority culture individuals, but simply to point out that poverty affects people of all racial and ethnic identities in our society.
We need to develop interventions that support people facing poverty across all racial, ethnic, geographic, and other identity lines. Greater attention to the forces that drive individuals into poverty, such as a lack of intergenerational transmission of wealth, systemic racism and discrimination, social rejection, drug and alcohol abuse, and limitations in opportunity, is of paramount importance when addressing this problem on a larger scale.
Otherwise, the unacceptably high proportion of young children—the next generation of adults— growing up in poverty represents our future. An understanding of how powerfully early life experiences shape the development of their minds and brains provides compelling evidence of what can and needs to be protected, and points to a great opportunity for building a healthier and more productive society. The public needs to know. l
Dana.org 17
More than suffer from pain. Our psychologist College’s Cognitive Neuroscience relationship feelings, and the actual what pain and how new leading to
PAIN IS AN INCONVENIENT REALITY. It is the most common reason people seek medical attention, affecting more people than diabetes, heart disease, and cancer combined. It exacts enormous costs in quality of life, not just for the pain sufferer, but for their families, caregivers, and communities. It is a symptom in hundreds of disorders, cutting across virtually every specialty in medicine. It is also intimately related to the ongoing opioid epidemic in America and beyond.
18 DANA FOUNDATION CEREBRUM | Spring 2022
Managing
than 20 percent of US adults from some form of chronic author, a cognitive psychologist and head of Dartmouth Cognitive and Affective Neuroscience Lab, examines the relationship among our thoughts, and beliefs about pain and actual physical pain that we feel, pain looks like in the brain, new research findings are to effective new treatments.
By Tor D. Wager, Ph.D.
Dana.org 19
ng
Patients are routinely prescribed opioids for acute pain after injury or surgery, and a substantial fraction of them will go on to become chronic opioid users. For some of these, the effects are devastating: In 2021, America saw over 100,000 drug overdose-related deaths, 75 percent of them caused by opioids, and the numbers have been climbing each year. For those who survive, opioid use takes a toll as well, causing changes in the brain that make it more difficult to work and to find enjoyment in daily life. Pain and pleasure are two fundamental forces that motivate us. Our history with pain goes back to our most ancient ancestors: Protozoa, sponges, insects, crustaceans, and more possess the same families of ion channels that enable pain in humans. These channels sense harmrelated signals in the environment, like noxious chemicals, and turn them into electrical signals in the nervous system, providing the basis for escape, avoidance, and learning. The dual teachers of pain and reward are at the core of our brain’s ability to rewire itself to avoid threats and pursue opportunities in changing environments.
Pain Falls Between the Cracks
In spite of its fundamental importance, pain has fallen between the cracks in our scientific disciplines and healthcare systems. Most medical schools provide only a handful of hours of pain education, distributed across four years. If a peripheral cause cannot be determined and eliminated, chronic pain patients are shuttled across departments, their pain “managed” but with little hope for a cure. They are often referred to psychiatrists, but few psychiatrists are equipped
to deal with chronic pain. Pain barely appears in the Diagnostic and Statistical Manual of Mental Disorders and is absent from the Research Domain Criterion framework, although in real life it co-occurs substantially with depression and anxiety. In fact, there is evidence that links between pain and mental illness are causal and bidirectional Psychology also has a blind spot when it comes to pain. Pain researchers are uncommon in academic psychology departments and neuroscience programs. And though many forms of chronic pain are treatable with behavioral methods, clinical training programs equip newly minted psychologists to treat anxiety, depression, obsessivecompulsive disorder, panic disorder, personality disorders and more— but not pain. There is no National Institute of Pain.
Pain is a central part of being human: Many of our oldest philosophical and spiritual traditions address ways to manage, avoid, and sometimes accept it. The Bhagavad Gita, for instance, instructs us to be at peace “in cold and heat, in pleasure and pain, in honor and dishonor.” The Roman stoic Marcus Aurelius wrote in the book Meditations, “Pain is neither intolerable nor everlasting, if thou bearest in mind that it has its limits, and if thou addest nothing to it in imagination…” These traditions teach us how to think about suffering and how to tap into our brains’ innate capacity to self-regulate. Although our ancestors knew nothing of the brain pathways that create pain, the central principles they taught and lived by have been rediscovered and adapted by modern approaches to pain treatment.
The Oldest Cure in the Book
Morphine–derived from the opium poppy–is the oldest drug in modern medicine’s pharmacopeia. Its medicinal use dates to ancient Egypt. It also has long been known that morphine and other opioids are addictive. One of the earliest synthetic drug formulations— developed by Bayer in the 1890s— was designed to make morphine less addictive and marketed as a “soothing syrup” to help children sleep. That drug is heroin, which is illegal in the US because of its high risk for abuse.
The evidence from randomized clinical trials of opioid treatment shows that its benefits are surprisingly modest. In the most recent meta-analysis, pain control was less than one point on a ten-point scale, and its efficacy declined with prolonged treatment. Meanwhile, basic research indicates that opioids can sensitize nociceptive neurons in the spinal cord, increase neuroinflammation, and increase pain in the long-term. The dose required to maintain the same degree of pain
20 DANA FOUNDATION CEREBRUM | Spring 2022
ILLUSTRATIONS: BRUCE HANSON AND SHUTTERSTOCK
control rises dramatically (there is a 40-fold difference between the lowest and highest doses offered by some manufacturers), because the nervous system desensitizes to opioids when they are used continuously.
Desensitization to opioids is a powerful example of an opponent process, in which short-term effects (pain relief and possibly a “high”) are counteracted by long-term adaptations (desensitization). The net result with opioids is short-term pain relief but long-term anhedonia— reduced joy and motivation, also called hyperkatifeia—along with uncontrolled pain. The longer one takes the drug, the lower the benefits and greater the costs. After taking opioids even for a short period of time in some studies, individuals experience increases in both pain sensitivity and negative emotion unless the drugs are actively “on board.”
Other popular “painkillers” don’t work as well as it might seem, either. How about an ibuprofen or acetaminophen for low back pain? Their effects are barely better than taking a placebo pill. With regard to neuropathic pain, which is caused by a lesion or disease in the central nervous system (e.g., diabetes, stroke, or nerve injury), antidepressants, gabapentinoids, and even opioids are prescribed. But whichever drug is used, the effects are modest on average. How about cannabinoids? It’s taken as established truth that they are good for pain. But in a recent meta-analysis, they provided only a three-to-four percent improvement over placebo.
The pharmaceutical industry has spent billions of dollars developing pain treatments, with (at least so far) unimpressive results. Every drug has side
effects; many are ineffective. Many drug companies have simply stopped trying to advance new therapeutics for managing pain. Clinical trials are expensive, so most pain treatments will never be vetted as extensively as drugs or reported in major medical journals, particularly if the treatments are principles and practices that are freely available. All this work has given us some good ideas about what doesn’t work very well.
Clues from the Brain
Research across sensory modalities has found that our perceptions are constructions: The brain interprets sensory input through a lens of memory, logic, and emotion. Our perception is not a veridical reflection of the world, but rather a guess, an inference, about what is really there based on multiple context clues. That’s why we see faces, effortlessly and automatically, in particular configurations of clouds. And it is why people with some pain conditions feel pain when they look at emotionally distressing pictures These “biases” help us act not just on what is immediately presented to our senses, but what is likely to be there, and they help us predict and respond to situational demands in advance: They alter our pain sensitivity to prepare for action in a dangerous situation.
Because pain is a construction based only partly on input from the body, the brain has the capacity to alter pain and the feelings and motivations surrounding it in multiple ways. Descending modulatory systems can enhance or inhibit pain-related signals in the spinal cord before they even reach the brain. The brain maintains a balance between promoting and inhibiting pain, and nerve injuries can shift the balance towards a pain facilitation state
Dana.org 21
Essentially, the brain has “decided” that when an injury is perceived, it should feel pain, which can promote recovery. Pain also drives decisionmaking at several levels: what we escape now, what we avoid in the future, for which threats we should be vigilant, and what cues signal danger. Pain is the experience that drives fear-conditioning and other
forms of threat-learning. The activity in these systems is also subject to construction, as the brain “decides” which sensations are truly threats to the body and what defensive adaptations are necessary to prevent future harm.
These principles suggest why pain-related brain activity is sensitive to context, past experiences,
and suggestion. Giving a placebo treatment—e.g., a sugar pill or inert ointment—can reduce activity in brain areas involved in constructing the pain experience and induce the release of endogenous opioids and dopamine. In some studies, placebo treatments coupled with suggestions about increases and decreases in pain can affect pain-related activity in the human spinal cord. These neurobiological effects play out in real life: Clinically, placebo treatments can reduce pain related to migraines and other headaches, osteoarthritis, gastrointestinal pain, and more.
Placebo treatments and interventions based on manipulation of the social and environmental context don’t all affect pain by the same neurological pathways. For example, suggestions about social context (how other people perceive pain) and classical conditioning can both exert substantial effects on the experience of pain and even autonomic responses to painful events. But their effects on pain are mediated by different brain systems; prefrontal cortical systems are involved in social cognition, and hindbrain systems in associative learning. There appears to be no “final common pathway.” But behind all these interventions is the brain’s mental model of the painful event and whether it is conceived of as damaging or dangerous, now or in the future.
Emerging research on underlying brain systems supports the idea that chronic pain, even more strongly than pain evoked acutely by somatic stimuli, is an integrative construction that extends beyond the detection of painful stimuli. Neuroimaging of pain sensations in hypersensitive patients has found enhanced activity in brain regions that also encode pain in healthy people. Moreover, new
22 DANA FOUNDATION CEREBRUM | Spring 2022
studies have found that chronic pain induces changes in affective and motivational circuits that don’t respond to noxious input—that is, their activity doesn’t increase as one turns up the level of painful heat or pressure applied to the body. These circuits include the ventromedial prefrontal cortex (vmPFC), posterior cingulate, nucleus accumbens, and hippocampus.
Whether back pain progresses from acute to chronic, for example, appears to be related to the strength of functional connectivity between the vmPFC and the nucleus accumbens, as measured with
fMRI. Stronger correlations between activity in the vmPFC and pain encoding regions have been found in chronic back pain, fibromyalgia, failed back surgery, and more. Other studies suggest that pain is not localized to any one brain network but is instead an altered global brain state that is defined by a pattern of interconnections across many regions spanning the brain.
Some of the key brain areas for chronic pain intersect with what has come to be known as the “default mode network” (DMN), so named because it is primarily active when a person is simply resting without any external stimulation (i.e., daydreaming, mind-wandering, etc.). This network seems to encode, in various ways, our conception of situations—mental conceptions of the environment and our capacity to act in it—particularly as they relate to the self and future well-being. The vmPFC is a key “node” in the DMN. Patterns of activity in the vmPFC encode our personal memories, the value we place on rewards, imagined futures, the hidden causes to which we attribute rewarding or punishing outcomes, and the meaning we ascribe to events. But the vmPFC is also a primary driver of autonomic activity and hormone release; its response during stress determines heart rate increases and the brainstem activity that controls autonomic output. It is also among the brain areas most strongly associated with immune responses My colleagues and I have proposed that the DMN plays a central role in constructing situational meaning, linking conceptual thought with the mobilization of physiological resources to meet the demands that bear on one’s personal well-being. This hypothesis gives vmPFC and the DMN a critical role in avoidance
learning, linking actions and other cues (sensations, places) to danger, and guiding actions to avoid threats. This inherently requires inference or guesswork because no two situations are the same. If you injure your back alpine skiing, should you be afraid of skiing again?
More broadly, the vmPFC helps determine how we generalize our experiences, which, in turn, depends on what we think was the underlying cause and whether it will recur in new scenarios. For example, in the case of back surgery for chronic pain, our brain contains a mental model of this situation—local injury and inflammation, with the expectation that the pain will last for a few months and decrease gradually as the injury heals. When you feel local back pain, you are not surprised because you attribute it to the model. You take a walk and feel some pain, but this is normal—it fits within the model. But what happens if the pain starts to get worse again or spreads to other parts of the body? This might prompt a more sinister interpretation: that the body is and will remain dysregulated in ways unexplainable by medicine.
This view might be reinforced by physicians who are unable to identify a physiological cause for the pain. As one patient described it, “I’ve always been told that I’m broken.”
Once pain has persisted for a long time, clinicians might say that until a cause is found, the patient will always be in pain. Others might say that pain is a sign of bodily injury, so he or she should avoid doing something if it hurts. While these statements may be reasonable guesses, they have powerful nocebo (the opposite of placebo) effects: The suggestion of ongoing harm can enhance threat signaling in brain and body. More perniciously, they
Dana.org 23
reinforce maladaptive beliefs about the meaning of pain, as a sign of bodily harm or dysfunction and an indicator of future dysfunction. My colleagues and I think that such mental constructs are maintained in the DMN, forging the link between this system and chronic pain.
What Works
A family friend recently wrote me about her experience with Complex Regional Pain Syndrome, a form of neuropathic pain that she developed after a cycling accident. She tried over 20 unsuccessful treatments, including three stellate ganglion blocks, 200 hours of physical therapy, yoga, direct current microstimulation, and pulsed electromagnetic field therapy. At the end of this odyssey, she has been able to substantially reduce her pain, return to work, and eliminate all of the invasive interventions. What worked? It’s not clear that any single treatment was a magic bullet. In this journey, she established a “new brainbased belief system,” thinking of her pain and its peripheral signs— including inflammation and other visible signs—as the result of an unconscious threat response in her brain. She framed recovery as an “argument with the body,” an attempt to convince her brain that the injury is healed and there is no longer a need to mount a threat response. And “when the argument was won, acceptance. Relief.”
What works may be different for each individual, but a common principle may be changing those systems in the brain that maintain the belief that the body is under threat. But what is convincing to one person (or one person’s unconscious brain) may not be to another. I’ve heard many stories of people who have been in chronic pain for years,
finding substantial relief in a single session of therapy, or after reading a book whose ideas resonate. Others need more support and personalized guidance.
My laboratory has recently completed a study of a treatment called Pain Reprocessing Therapy (PRT), a combined psychological and behavioral treatment that is designed to do two things. The first step is to help patients realize that pain does not reflect tissue damage or harm. It is a “false alarm” created by the brain, unpleasant but not dangerous. The second step is to put that realization into practice by performing the movements and exposing oneself to the situations that created pain and fear in the past. In a randomized clinical trial, patients who received PRT achieved remarkable reductions in pain. Though the participants had been in pain for ten years on average, two thirds were pain-free or nearly so after four weeks of treatment (eight sessions). Patients randomized to placebo or usual care showed much more modest gains.
Like other psychological treatments, PRT gives people principles to practice in their daily lives, so benefits didn’t end after the eight sessions were finished. They were nearly as large a year later. Using fMRI after treatment, we found reductions in pain-encoding parts of the anterior insula and anterior cingulate, the two areas most strongly associated with sensing pain and regulation of the autonomic nervous system. And while there were many auxiliary benefits (improved mood, sleep, and function), the strongest predictor of pain reduction was change in beliefs about the causes and meaning of pain.
Recent studies have also found substantial improvements with
other psychological and behavioral treatments. Some methods, such as Emotional Awareness and Expression Therapy, focus on associations between emotional trauma and pain. Others, like Mindfulness-Oriented Recovery Enhancement (MORE), aim to change the meaning of pain and stressors. In one recent study, MORE substantially reduced both pain and opioid use. The effects were larger the longer the follow-
24 DANA FOUNDATION CEREBRUM | Spring 2022
up; at nine months, MORE cut opioid use in half.
These approaches, which combine methods used in cognitive behavioral therapy (CBT) in a novel way, are not yet standard practice in the psychological treatment of pain. But they appear to work substantially better: While standard psychological modalities yield only modest effects (comparable to or weaker than the drug effects mentioned above), these new treatments have shown substantial and durable benefits, at least in initial studies. Many questions remain about the types of chronic pain for which each of the new treatments is helpful, who will benefit most, how extensive the treatment must be, and how easily people can be trained to deliver it.
As for CBT and other standard psychological approaches to pain, the lack of compelling data does not mean they cannot be important treatment avenues for many people. Such treatments
are not standardized the way that drug treatment is: They are tailored to the individual patient, and many individual practitioners have converged on principles similar to those in PRT or MORE. This suggests that the optimal ingredients of CBT for pain remain to be discovered.
Several principles underlying psychological treatments like PRT depart from standard pain psychology. First, they provide an explanation for chronic pain that acknowledges its reality while affirming that it is not a sign of damage to the body but the result of sensitization in neural circuits, drawing on findings in neuroscience. The belief that “pain does not equal damage” helps patients see that pain, while unpleasant, can be safe. Second, it encourages them to turn their attention back to the body by practicing mindful attention to the physical sensations of emotion and of pain, and even engage in painful movements deliberately.
These clinical effects dovetail with findings from my laboratory that focusing on the non-affective aspects of pain (i.e., treating it as an “interesting sensory experience”) can produce more pain relief than turning attention away from the body (e.g., distraction). By the same token, we’ve found that mindful acceptance of pain is one of the most potent interventions for reducing painrelated brain activity. If pain is viewed as fundamentally safe, it’s okay to perform painful movements; this pain exposure may be a key to re-training the brain towards a less sensitive state.
Exposure has two other advantages: Putting nascent beliefs into practice, it amplifies commitment to the idea that pain is safe. And it provides somatosensory input to help the brain recognize
pain signals as part of the normal sensory landscape. Beyond overcoming negative beliefs, some emerging treatments focus on reengaging positive experiences—like the practice of “savoring” positive experiences (cultivating enjoyment) in MOST or exploring pain sensations with a curious or even playful attitude in PRT (“wow, look at my brain tricking me!”)— ideas antithetical to regarding pain as a threat.
We have a long way to go in understanding how to help those who suffer from chronic pain find their individual paths to recovery. But advances in that direction have been significant, demonstrating that such pain is real but that its root causes are in the brain rather than in local tissue—i.e., “where it hurts.” Innovations in pain psychology have shown that even with acute paininducing pathology after an injury, cognitive approaches can re-shape neural circuits to minimize suffering and promote recovery.
At the same time, researchers into the biology of chronic pain are developing biomarkers to sharpen diagnosis and prognosis, and track treatment response on a larger scale than ever before. Toward that end, the UK Biobank has gathered genetic, clinical, neuroimaging, and other measures on approximately 500,000 individuals, including those with dozens of pain disorders. The Acute to Chronic Pain Signatures program is taking a comprehensive approach to understanding vulnerability to post-surgical chronic pain, using neuroimaging, metabolomics, transcriptomics, lipidomics, and systemic inflammation data in more than 2,000 patients followed over time. All in all, the future of pain treatment is looking brighter than it ever has—and there is not a moment to lose in moving forward. l
Dana.org 25
The
26 DANA FOUNDATION CEREBRUM | Spring 2022
The Miracle of Lıght
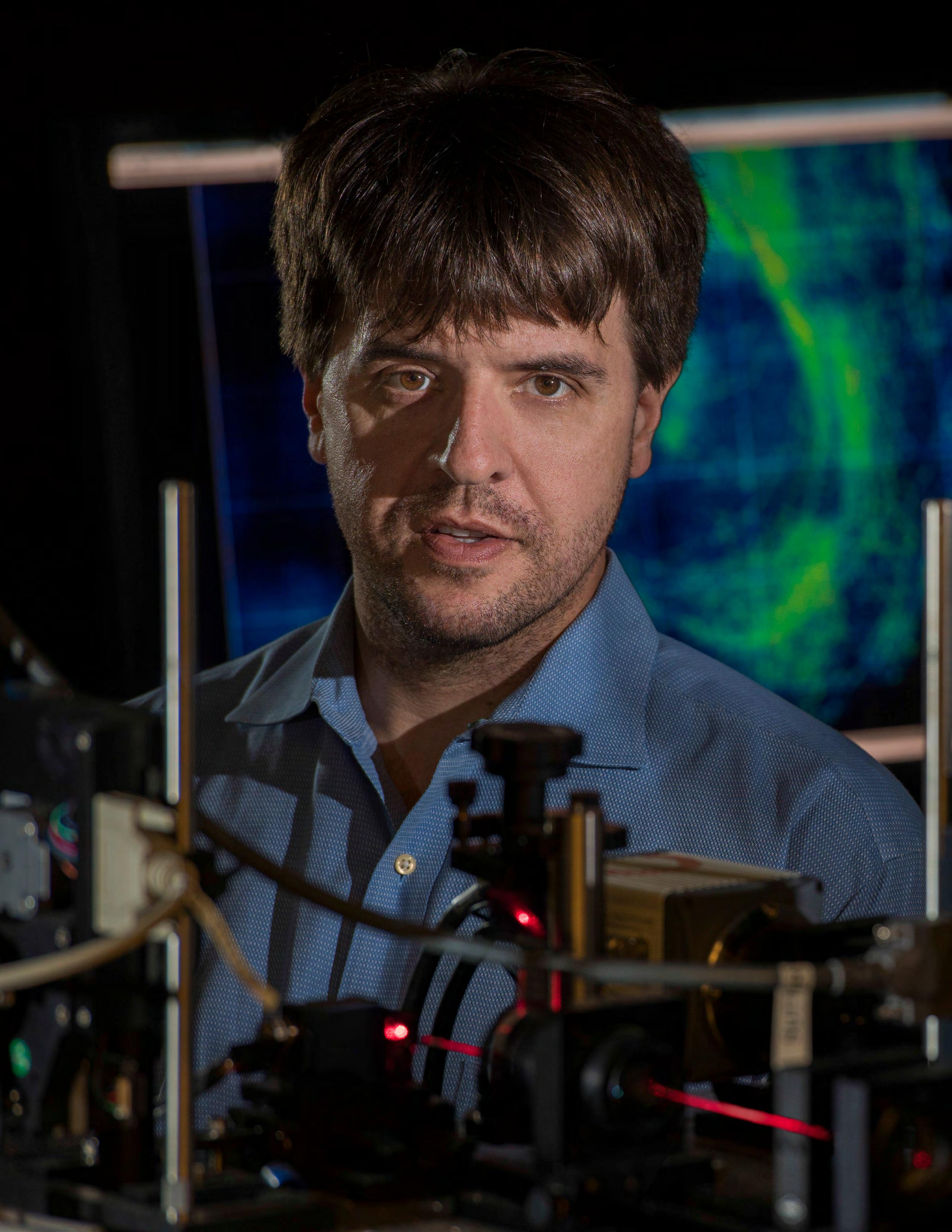
Karl Deisseroth, a winner of the 2021 Lasker Prize in Basic Medical Research for his pivotal work in optogenetics and author of the widely praised book, Projections: A Story of Human Emotions, explains this new instrument in a neuroscientist’s toolkit, its potential to help people, and what he’s learned as a practicing psychiatrist.
 By Carl Sherman
By Carl Sherman
Dana.org 27
Photograph by Steve Fisch
OW IS THE BRAIN PUT TOGETHER?
HOW DOES IT WORK—WHAT HAPPENS WHEN WE THINK, FEEL, ACT?
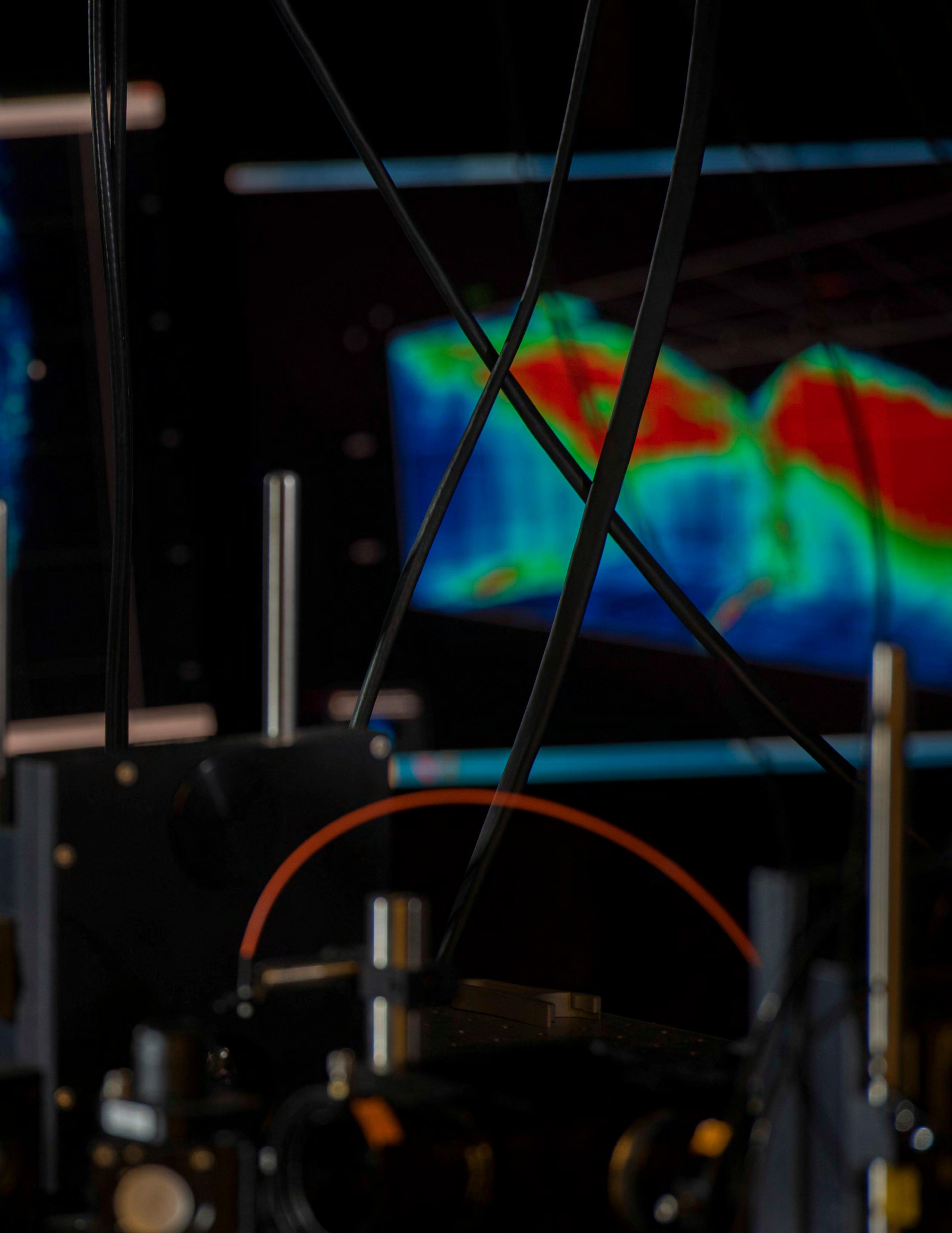
What goes wrong in psychiatric and neurological illness? A giant step toward answering these central questions of neurobiology emerged over the last 15 years with the development of optogenetics. This now-essential instrument in the neuroscientist’s toolkit represents a convergence of botany, microbiology, proteomics, genomics, and optics, and an accordingly wide array of contributions by an impressive cast of researchers.
A leader of the pack is unarguably Karl Deisseroth, M.D., Ph.D., professor of bioengineering and of psychiatry and behavioral sciences at Stanford University, one of three scientists awarded the 2021 Lasker Prize in Basic Medical Research for his pivotal work. Deisseroth, a practicing psychiatrist as well as a researcher, hit another milestone last year with the publication by Random House of Projections: A Story of Human Emotions, his widely-praised book that brings bench and bedside together with a detailed, empathic account of his work with patients, in the context of the brain dynamics underlying their difficulties—according to optogenetics.
CARL SHERMAN: Let’s talk about optogenetics. Can you give me a capsule version of just what it is?
KARL DEISSEROTH: Optogenetics is a way of using light to study how a biological system works. But it’s the opposite of how we normally use light, which is to collect information, to look at something and see what happens. Instead, optogenetics uses light to control what happens.
The way we do this is make some cells responsive to light, so we can turn them on or off with it. Then we can see what kinds of activity, what kinds of cells, and what connections between cells actually matter for the mysterious and wonderful things that the brain accomplishes; for sensation, cognition, action.
More specifically, how do you transform these cells?
DEISSEROTH: We use genes from microbes, single-celled organisms, that for their own reasons have evolved to make light-activated ion channels, little molecules that sit in the cell membrane and move ions—charged particles— across it. They create a current in response to light.
In evolving these beautiful, light-sensitive proteins, these microorganisms have done an important job for us, because we can use genetic tricks with viruses to put their genes into neurons, and neurons use electricity to turn themselves on and off. Then we can guide light into the brain, and only the cells that have this gene will be turned on or off by it, depending on which microbial gene we put in.
It can get very fancy. We can use holographic techniques to guide dozens or hundreds of spots of light to individual cells and control them.
I understand that discoveries by a number of scientists went into the development of this technique, starting with
the identification of these light-sensitive proteins 150 years ago. What was your lab’s contribution?
DEISSEROTH: I’m a neuroscientist, but I’m also a biochemist by training. All through my career I’ve taken a molecular approach to systems-level questions. What my lab did was figure out how these molecules work, bridging all the way to their implementation in neuroscience. A lot of real basic science that enabled the applications came later.
First, we discovered the structures of channelrhodopsins, these light-activated proteins, which allowed us to see how they work, and exactly which atoms and which movements are important. That let us redesign them, to change the colors of light that they respond to, and the kind of ions that they let through. Along the way we discovered major new types of channelrhodopsins.
And we built the tools to make optogenetics work—the viral vectors to put these genes into neurons in the brains of mammals, and the fiberoptic methods to guide light and target cells and connections in different parts of the brain.
Just how do you target and activate specific neurons? You’re introducing the viral vector into an area of the brain, yet it only affects certain cells in that area. How do you make this happen?
DEISSEROTH: The virus gets the gene into all the nearby cells, but the genes are not turned into functional protein (channelrhodopsins) in all of them. That step is achieved with bits of DNA called promoters and enhancers, which regulate gene function, and we design the virus so that the protein is only made by the specific, targeted type of cell. We achieve additional specificity by guiding light spots
28 DANA FOUNDATION CEREBRUM | Spring 2022
to a subset of the cells in which the protein is made. And then finally, we developed projection targeting, where you deliver the opsin—the light-sensitive protein—to one part of the brain and deliver the light to another.
The reason this works is that the opsin protein fills the whole neuron; it gets trafficked out into the long axons that extend from one part of the brain to another. If you put your fiber optic in that other brain region, the only thing that’s sensitive to light will be the axons that started from where you injected your virus. So you get specificity by connection type.

So you can use optogenetics to discover neural connections that hadn’t been mapped before and delineate them with more precision?

DEISSEROTH: Exactly. You could demonstrate functional connectivity very efficiently, and on different scales. On a local circuit scale, you can zip your light around to all the cells individually or in combination, while listening to or recording activity. You can see which of the cells you stimulate, which types of cells, which locations, which combinations give rise to the activity of interest.
On the other hand, if you test all the cells and combinations of cells with the broad, high-content recording technologies we’ve developed, you can be quite global and unbiased about the kind of information you collect.
Also, there have long been ways to slowly ramp up or ramp down the activity of individual neurons—chemical methods, for example. But with those methods you don’t
have naturalistic timing information, which turns out to be critical. With optogenetics you can be very, very rapid and swift.
Why is timing so important?
DEISSEROTH: The brain is designed to work on millisecond time scales. The speed, the brevity of action potential transmission, is important for survival. We see this all over neuroscience. If you give a stimulus the frequency of 10 Hertz, you’ll get a totally different result than if you stimulate at 80 or 100 Hertz.
Could you give me examples how optogenetics has been applied in neuroscience? Some discoveries it’s facilitated, processes it’s clarified, etc.
DEISSEROTH: One thing is anxiety. We all know anxiety; we know it’s got these different parts to it. We know it feels bad. We know it affects our body: It makes us breathe more quickly and our heart beat faster. And we know it affects our choices: When we’re anxious, we don’t do the risky things that might otherwise happen. All these features, that are so different, come on together and go away together. So somehow our brain has built a way to create this state, to make it coherent and unitary, to have anxiety happen and then go away.
Dana.org 29
PHOTO: JIM GENSHEIMER
matters in the brain—which cells, which activity, and which connections are
We used optogenetics in my lab to sort out how this happens, how the different features are obtained and wrapped up together. This was done using projection targeting. You can show that there’s a part of the extended amygdala called the bed nucleus of the stria terminalis (BNST) and that different projections coming out from the BNST, going to different parts of the brain, access these different features. There’s a projection that goes to the parabrachial nucleus, part of the brainstem that controls respiratory rate, the breathing changes associated with anxiety. But it doesn’t affect the behavioral decisions, or the positive or negative feeling-state, at all.
There’s another projection that goes from the BNST to the lateral hypothalamus, and that controls the behavioral decisions but doesn’t affect the breathing rate at all, or the subjective valence, the feeling-state.
And there’s a third that goes to the ventral tegmental area. This is the part of the brain where dopamine neurons live, that seems to set the negativity of anxiety and the positivity that comes from the release of anxiety. But it doesn’t affect respiratory rate or behavioral decisions. So, these different features can be cleanly broken apart, and they’re assembled by these projections.
Just how did you parse the anxiety response—how did you show projections from the BNST to different brain regions to be responsible for distinct facets of anxiety?
DEISSEROTH: We did this in mice, which have many of the same structures that we have and exhibit robust anxiety responses, using the projection targeting method that I described. We delivered excitatory or inhibitory channelrhodopsins to the BNST, and then we delivered fiberoptics to different downstream regions that we knew were connected to it but didn’t know how. And we explored what the causal impact was on which parts, which behaviors were elicited. We observed this clean deconstruction of the different features of anxiety, as a result of controlling these different projections from the anxiety control region of the BNST.

To take another example, Catherine Dulac at Harvard did the same kind of thing five years later for parenting. This is quintessential: There’s not much that’s more important to a mammal than parenting, right? As it turns out, as complex a state as it is, aspects of parenting can be broken down into component parts that map onto physical structures in the brain. What Catherine Dulac showed, using optogenetic projection targeting, was that there’s a connection that starts from one part of the brain and goes to another, that mediates the grooming of the young, the physical care that all mammals do. But it
doesn’t affect the motivation to go out and retrieve the young that had strayed from the nest. That was controlled by a different connection, a different projection, which didn’t affect grooming at all. And there are many such examples.
You’re also a practicing psychiatrist. What kind of work do you do?
DEISSEROTH: Well, I really do three kinds of work. There are the extremely acute cases that come to the emergency room. They’ve been brought in by police, or by family, or they bring themselves in because they know they’re in danger. I’m the attending physician, and I work with the emergency room doctors and others, to sort out the right care.
I also run an outpatient clinic. I see those patients once a month, or some, if they’re quite ill, more often, even every week. I focus on very severe cases, hard-totreat illnesses, particularly two things: treatment-resistant depression and autism.
And finally—and this is more recent—we’re doing clinical trials, trying to understand the internal brain processes, the dynamics that underlie complex altered brain states like dissociation, which is a very important and mysterious brain state that shows up all across psychiatry.
How does your clinical work relate to your research? In your book, you suggest a kind of synergy between them.
DEISSEROTH: It’s so important to be able to go to my trainees in the lab, my students and postdoctoral fellows, and to tell them, “Look, this is what anxiety is really like. This is what depression is really like. This is what matters to someone with autism. It isn’t just one symptom from a list; it really disrupts their life, and this is how they feel about it.” That is so helpful to guide the research in the lab.
It works the other way, too. In the lab, we found this very interesting altered brain state that was associated with dissociation, and we were able to go and find that
30 DANA FOUNDATION CEREBRUM | Spring 2022
Optogenetics, first and foremost is a discovery tool. It lets us understand what actually and action, whether healthy and adaptive, or maladaptive. This is so powerful because once you understand at that level, then any kind of treatment becomes much more grounded.
important for sensation, cognition,
same exact state happening in a human being. That’s now guiding our ongoing clinical work, including the clinical trial that I mentioned. So it really works both ways. The science enhances the patient work. The patient work enhances the science. I wouldn’t do it any other way now.
Speaking of the connection between clinical work and science, have there been any clinically relevant applications of optogenetics?
DEISSEROTH: Optogenetics, first and foremost is a discovery tool. It lets us understand what actually matters in the brain—which cells, which activity, and which connections are important for sensation, cognition, and action, whether healthy and adaptive, or maladaptive. This is so powerful because once you understand at that level, then any kind of treatment becomes much more grounded. It could be a pill. It could be a brain stimulation treatment: Now you can target specific? components. That would be the broadest and biggest impact, you could call it indirect application, guiding treatment. But my colleague and friend, Botond Roska in Switzerland, just published the first direct application of optogenetics in the human central nervous system this past year, in Nature Medicine. It was used to treat someone who was blind, and he was able to confer new light sensitivity onto the retina of this person with optogenetics. It’s pretty amazing. You can see videos of this on the journal site: A person sitting at a table who had been unable to see objects was now able to reach for them in a directed way.
Are there any clinical trials under way?
DEISSEROTH: There are a bunch involving the retina. There’s some work percolating, exploring pain treatment. And then there are a lot of optogenetics-guided clinical trials—where people have discovered something using optogenetics and are using that to design brainstimulation therapies, medication therapies, and so on.
What are your thoughts about the immediate or intermediate-term future of optogenetics?
DEISSEROTH: Thousands of discoveries have been made with optogenetics, all over the world. It’s been applied in essentially every experimental animal system, to many different kinds of cells and questions. And just in the past couple of years it’s made this leap from the level of cell types to the level of single cells. That’s very exciting— mammalian behavior controllable at the single-cell level. And so the future will be understanding how many cells are needed for a sensation, or a cognition, or an action.
Which cells, and which regions, work together? What’s essential, what’s not at the single cell level?
The other development is all the way at the other end of the scale—at the whole, intact-brain level. Getting to all the cells. We can now do this in the zebra fish, which is a small, transparent vertebrate. It’s small enough and transparent enough that we can see all the way through it, see all the cells during behavior, and during optogenetic control.
Of course, there’s a huge amount of data. Basically, the people in the lab have to become near-professional data scientists. But it’s got the appeal of not missing anything. We can take global, unbiased perspectives, which we definitely need in neuroscience because there are so many unknowns. In many cases, we can’t even frame hypotheses well. We want to take the big picture. We want to play the role of an astronomer centuries ago who built a new telescope and was pointing it at part of the sky to see what could be seen.
And this is already bearing fruit, this approach. The dissociation question I mentioned earlier: nobody really knew—we certainly didn’t—how dissociation might be implemented in the brain. What it actually is, physically, materially. And by taking that very broad, unbiased approach, we were able to see a signal that nobody anticipated. It popped out at us and turned out to be really important, both in mouse and in human for dissociation.
How did you do this?
DEISSEROTH: We used what we call wide-field imaging, where you can see almost across the entire brain. We gave a range of different strong, psychoactive drugs, including dissociative agents. We saw an amazing pattern that we hadn’t predicted: a rhythm in one part of the brain that all the dissociative drugs elicited, but none of the non-dissociative drugs. And then optogenetics came in, because then we could say “does it matter?” We provided that rhythm to those cells, and we saw if it caused the dissociative behavior. And it did. Then we were able to go and look for the same rhythm in human beings who were dissociating, and we found it.
Final thoughts about optogenetics?
After a study abroad experience, Perry switched her focus from neuroscience to microbiology.
DEISSEROTH: It highlights how important basic, curiositydriven research is. The deepest roots of optogenetics are in botany, 150 years ago. If people weren’t poking around with weird microorganisms a century or more ago, we wouldn’t be where we are today. l
are
Dana.org 31
PHOTO: COURTESY OF STANFORD UNIVERSITY
Dark Silent Gate Sleeps and
Neuroscientists across the globe have new tools to help them study the integral role that sleeps plays in memory. But they agree that there are still many questions to be answered.

’

32 DANA FOUNDATION CEREBRUM | Spring 2022
By Kayt Sukel


Dana.org 33
Illustration by Amy Lauren
EACH NIGHT,
AS YOU
TRANSITION
INTO DEEP SLEEP FROM WAKEFULNESS,
your body undergoes a remarkable transformation. Your muscles relax. Your breathing slows. Your temperature and blood pressure drop. Even your brain activity changes, decelerating into slow, coordinated waves. Despite these remarkable physiological changes, scientists are now learning that the brain is far from idle during sleep. Rather, it remains hard at work, facilitating memory and learning while uncoupled from the external world.
“For a long time, we believed that being awake all day depleted you and that sleep was what was required to restore and reinvigorate the whole body, including the brain,” says Robert Stickgold, a pioneering sleep researcher at Harvard Medical School. “It turns out that rest has very little to do with the function of sleep—rather, our brain is sorting and consolidating the information we learned during the day so we can better access it when it’s needed.”
Anyone who has ever pulled an all-nighter knows the effect that sleep deprivation can have on cognitive function, including one’s ability to learn and retain new information. Yet, over the last few decades, neuroscientists across the globe have learned that sleep plays an integral role in memory—and it is a role that is highly conserved across the animal kingdom. To better understand how sleep helps us remember, these researchers have been working to characterize not only the physiological changes observed during sleep, but also the neural mechanisms underlying them.
Sleep Stages and Memory Consolidation
Nearly every animal on earth, from fruit flies to nonhuman primates, experiences some form of sleep, a naturally recurring state of altered consciousness and inhibited sensory activity. And while the exact amount of time spent in slumber, and the patterns of neural activity, differ from animal to animal, humans are no different. We need sleep to thrive.

While it is too easy to associate sleep with some sort of biological “off button,” it is actually a dynamic process that, in human beings, repeatedly cycles through four distinct stages. You have likely heard of the two main types of sleep: rapid eye movement (REM) sleep, characterized by quick back-and-forth eye movements; and non-rapid eye movement (NREM) sleep, a deeper
stage of sleep which contains three unique stages, each with its own pattern of brain activity. Neuroscientists are particularly interested in one of those NREM stages, deep or slow-wave sleep (SWS), where the neurons fire in a slow, high-amplitude wave of activity called a delta wave.
Jan Born, a sleep researcher at Germany’s University of Tübingen, was one of the first scientists to show that the spatio-temporal pattern of neural firing seen in SWS is critical to consolidating memories for long-term storage. The specific pattern of activity is a crucial aspect of helping us to remember.
“During NREM sleep, the brain reactivates and reorganizes memories that were encoded when you were awake. And in many cases—not all—when you test recall, it is better after sleep than if you test after wakefulness,” he explains. “My theory is that, during wakefulness, you experience an event in a context. [After sleeping], you have a more generalized, episodic representation of that event. We hypothesize the brain abstracts certain aspects of that memory and puts it into the long-term store. These changes in neural activity help with that.”
Dozens of studies have now demonstrated that most animal species show better recall on a variety of memory tasks after sleep. In humans, this is the case whether it’s a task involving learning nonsense syllables (numerous letter combinations without meaning, used in learning experiments) or a new motor skill. And researchers in different labs are tirelessly working to better understand what neural processes in sleep facilitate this kind of learning.
34 DANA FOUNDATION CEREBRUM | Spring 2022
Research decades has memory are influenced system’s ability it encountered waking hours.
Finding Balance
Of course, our brains are not primed to consolidate and store everything we have learned or experienced during waking hours. The energetic cost of doing so would likely be too much to bear. To help explain how the brain can find this crucial energy balance, where the brain is not always in a state of learning overdrive, Giulio Tononi and Chiara Cirelli, researchers at the University of WisconsinMadison’s Center for Sleep and Consciousness, proposed the synaptic homeostasis hypothesis of sleep nearly 20 years ago.
“The brain mainly learns from strengthening of synapses,” said Cirelli. “That means there’s a need for synaptic re-normalization because you can’t just keep strengthening more and more synapses. Synaptic activity is just too expensive in terms of the brain’s energy budget. So, to keep things in check, the brain weakens some of those connections when we sleep. We couldn’t learn and remember things if it didn’t.”
She and Tononi have shown, using a variety of different molecular and genetic approaches, that synaptic strength, on the whole, is depressed during sleep. This synaptic depression helps to remove unnecessary information— remove the noise, so to speak—as well as prepare the brain for learning the next day. Yet, their work has shown some synapses appear to be protected from this weakening process. Were those preserved synapses strengthened by sleep as part of the consolidation process? In a recent Nature Communications paper, the researchers used two-photon imaging to track synapses in the mouse cortex in sleep after a motor learning task to find out.
“We found that sleep doesn’t provide any special treatment to the synapses involved with the learned information. They stay at the same level of strength,” she says. “But it does bring down the strength of all the other synapses around them. And we see this balancing of synaptic strength is directly correlated with how well animals performed on the later memory task.”
Sleep Facilitates Many Types of Memory
Many of the earliest studies of sleep-dependent memory have focused on motor learning. But research over the past two decades has shown that all manners of memory are influenced by sleep—even the immune system’s ability to recognize a pathogen it encountered during waking hours. But beyond helping to consolidate and store the gist or essence of an event, sleep is instru-


Dana.org 35
Research over the past two shown that all manners of influenced by sleep—even the immune to recognize a pathogen encountered during hours.
mental in encoding emotions associated with it.
A recent study by Sara Aton and colleagues at the University of Michigan, published in Nature Communications, showed that sleep is vital to encode fear connected to a visual stimulus in a mouse model. The researchers paired a visual image with a mild foot shock to help the animals learn fear of the stimulus. After learning, the researchers observed, neurons in visual cortex associated with the event were more active during sleep, helping the animals retain the association between the stimulus and emotion. But when the team disassociated the sensory stimulus from the emotion, by selectively activating the neurons in visual cortex without showing the animals the image, they found those animals that slept still held on to their fear.
“What was amazing to me was that when we disrupted the visual cortex so the animal could no longer discriminate between the different stimuli, if the animals are sleeping, they retain that fear. They remembered that they should be afraid, but instead of it being attached to a specific stimulus, it’s just this generalized fear,” Aton says. “But if you do the same thing and sleep-deprive the animals, they don’t have any fear at all.”
These results, Aton maintains, demonstrate that sleep is also vital to remembering the emotional aspects of an experience. The hippocampus must coordinate with both the neocortex and the limbic system to consolidate memories into long-term storage. This more expansive coordination, she says, makes a lot of sense.
“We need both the memory and the emotions, good or bad, to function properly. [Consolidating both the emotional and sensory aspects of an experience] gives us a much fuller context of what we’ve learned—whether it’s a person or place or some other thing—and why it should matter to us so we know how to deal with it when we encounter it again.”
Moving Forward
While researchers have made great strides in understanding sleep’s role in memory consolidation, they largely agree that many questions still need to be answered.
“What does good sleep really mean? And if we figure that out and can learn how to improve sleep, can we improve memory? We know that poor sleep is associated with a lot of psychological and psychiatric problems—could we find a way to go in there and change what kind of memories people are reactivating and consolidating to help with those conditions?” asks Ken Paller, a sleep researcher at Northwestern University. “There are a lot of potential applications if we can figure this stuff out.”
But while the idea of such applications is appealing, Stickgold says scientists are still tirelessly working on more basic mechanistic questions about the relationship between sleep and memory.
“One of the biggest problems with understanding what sleep does for memory is that we don’t really know what a memory looks like. We don’t know how a memory gets encoded. We certainly don’t know how a memory gets found,” he says. “We can talk about the hippocampus and synapses and cell activity all day but if you ask me, ‘Bob, what’s your mother’s name?’ I still can’t tell you exactly what my brain is doing to get you the answer.”
But Stickgold is optimistic that neuroscientists will get there—eventually. Aton concurs.
“We’re getting new tools all the time where we can start looking at different questions, whether it’s looking at how these different stages of sleep are involved with memory consolidation, to understanding what might be happening when we dream and whether that’s involved with memory, too,” she says. “As we get these tools, put together the findings that are out there, and start to test new ideas, I think the coming decades will have quite an impact on our understanding of sleep and why it’s so important to memory as well as to our survival.” l

36 DANA FOUNDATION CEREBRUM | Spring 2022 ILLUSTRATION: SHUTTERSTOCK
" We can talk about the hippocampus and synapses and cell activity all day but if you ask me, ‘Bob, what’s your mother’s name?’ I still can’t tell you exactly what my brain is doing to get you the answer.”
Sigmund Freud, the 19th century Austrian neurologist who fathered the field of psychoanalysis, once said that the ability to interpret dreams is “the royal road to a knowledge of the unconscious activities of the mind.” Anyone who has read his seminal book The Interpretation of Dreams knows that Freud believed dreams essentially manifested repressed or unconscious desires. Thinking has changed in the century since Freud’s classic, however, and today, research connecting sleep with memory has inspired new theories regarding the function of dreams.
To wit, Robert Stickgold of Harvard University, and Antonio Zadra, of the Center for Advanced Research in Sleep Medicine at the University of Montreal, proposed in their book, When Brains Dream: Understanding the Science and Mystery of Our Dreaming Minds, that dreams play a critical role in memory consolidation. Their theory, Network Exploration to Understand Possibilities (NEXTUP), suggests that when we dream, our brains are looking to find connections between what we learned during the day and what is already present in our stored memory.

“We’ve known for a long time that if you wake someone from REM sleep after a learning task, they are much faster at identifying links between weakly-associated word pairs,” Stickgold says. “So, if you presented ‘wrong and right’ and ‘wrong and thief,’ they will be better at remembering ‘wrong and thief.’ We believe, based on the studies, that when you are in REM sleep, you are actually in a hyperassociative state where the brain is taking these looser associations, building them into a narrative structure of some sort, and letting those narratives play out to see if you have any emotional response to them. If you do have an emotional response, then the brain knows that association is potentially valuable.”

And what about that time just before you fall asleep, when your brain conjures up that item on your to-do list that must get done the next day—or, the perfect comeback to a comment made by your archnemesis earlier in the day? Stickgold contends that such activity during the period between consciousness and sleep is the brain sorting through the day’s learning to identify important items for consolidation.
“These aren’t dreams—they really are just thoughts and snapshots,” he says. “We believe what’s happening is that these thoughts are being tagged with some sort of label so, once you are in deeper sleep, the brain can ensure that important information is put into memory.”
The Dream Factor
Stickgold concedes that it has been hard to find the tools to test the NEXTUP theory at the molecular or cellular level. Yet, Aton says that while the model is theoretical, current research looking at sleep and memory consolidation supports these ideas.
“We still need to do a lot of digging to say, yes, this is what sleep looks like and how it’s different from wakefulness,” she says. “We also still need to do quite a bit of work to see how non-REM sleep is different from REM sleep and what the two offer to our overall cognition. But it is entirely possible that REM sleep is there to prepare your brain for consolidation. Maybe dreaming is a way for us to adapt, to come up with new answers to problems, and to sort things out in a way that just isn’t possible when you are awake. It’s going to be exciting to do the experimental work to test these new ideas in the future.” l
Dana.org 37
Poetry Braın of the E
ducating kids about the brain through creative writing has been the goal of the annual Neuroscience for Kids Poetry Contest for 20 years. Sponsored by the Center for Neurotechnology at the University of Washington, some teachers throughout the world use the contest as a classroom exercise. For the 2022 contest, 232 entries were received from 20 different states in the US and five countries—and are divided into five groups by grade level.
“The contest provides people with the opportunity to express their thoughts and knowledge about neuroscience in a creative form,” says neuroscientist Eric Chudler, executive director/education director of the center, a research associate professor in the Department of Bioengineering, and founder of the contest. “Writers must choose their words carefully, so their ideas are conveyed in an imaginative and scientifically accurate way.”
Winners are awarded a certificate and a book about neuroscience. More details of the contest and an entry form are available on Neuroscience for Kids, a site overseen by Chudler. Also, an announcement of the contest is sent out to subscribers of the monthly Neuroscience for Kids Newsletter. Have a look at this year’s winning entries.
—Bill Glovin

38 DANA FOUNDATION CEREBRUM | Spring 2022
ILLUSTRATION: MILLIE BAKER
Kindergarten to Grade 2
Requirements: Poem can be in any style
Winner: Cullen S.
Inverness, IL (Grade 2)
My smart brain
Thinks fast like a train. The wheels on the train go fast. When I use my brain, I have a blast. My brain is good at math, like a train is good on a path.
Grade 6 to Grade 8
Requirements: Poem must be in the form of a haiku.
Winner: ShreyaR. Kowloon, Hong Kong (Grade 8) Synapses shooting, Neurons buzzing here and there, Thoughts bloom in mybrain.
Grade 9 to Grade 12
Requirements: Poem must be in the form of a limerick.
Winner: Maya M. Silver Spring, MD (Grade 4) All aboard the Impulse Train! We start our journey at a station in the brain, then zoom expeditiously from nerve cell to cell, transmitting the brain’s many messages to tell the human body what to move, say, or do. From axons to dendrites, we nimbly make our way So,through! the next time you hear, taste, touch, smell, or see, know that our electrical signals are moving rapidly. Our train hurtles forward, and we will not derail, as we leap over synapses to deliver your impulse mail.
Grade 3 to Grade 5
Requirements: Poem must rhyme.
Winner: Jaiden M. LagunaHills, CA(Grade 10)
Billions of neurons, countless connections
Sending out signals, in alldirections
Rapid impulses conduct Neurochemicals instruct Responsible forourthoughts and actions.
Adults
Requirements: Poem must rhyme and explain why it is important to learn about the brain.
Winner: Janna H. Bellevue, WA
To comprehend our stellar planet and civilizations, Understand our brain’s molecular sonnet and mutations
Bridging the neurosciences and the humanities
Reshapes the vanities to myriad capacities
What is means to be human, What constitutes a good life, These are the life-long questions that serve you in pursuit of a life.
Dana.org 39
ADVISORY BOARD
JOSEPH T. COYLE, M.D.
Joseph T. Coyle is the Eben S. Draper Chair of Psychiatry and Neuroscience at Harvard Medical School. A graduate of the Johns Hopkins School of Medicine in 1969, he was a research fellow at the National Institute of Mental Health with Nobel Laureate, Julius Axelrod. After psychiatric residency at Hopkins, he joined the faculty in 1975. In 1982, he became the director of the Division of Child and Adolescent Psychiatry. From 1991 to 2001, he was chairman of the Department of Psychiatry at Harvard Medical School. His research interests concern the causes of neuropsychiatric disorders. He is the past-president of the Society for Neuroscience (1991), a member of the National Academy of Medicine (1990), a fellow of the American Academy of Arts and Sciences (1993), a fellow of the American Association for the Advancement of Science (2005), and the former editor of JAMA Psychiatry
MARTHA J. FARAH, Ph.D.

Martha J. Farah is the Walter H. Annenberg Professor of Natural Sciences at the Center for Neuroscience & Society, University of Pennsylvania. She is a cognitive neuroscientist who works on problems at the interface of neuroscience and society. Her recent research has focused on socioeconomic status and brain development. Farah grew up in New York City, was educated at MIT and Harvard, and taught at Carnegie-Mellon University before joining the University of Pennsylvania. She is a fellow of the American Academy of Arts and Sciences, a former Guggenheim Fellow and recipient of honors including the National Academy of Science’s Troland Research Award and the Association for Psychological Science’s lifetime achievement award. She is a founding and current board member of the International Society for Neuroethics.
PIERRE MAGISTRETTI, M.D., Ph.D.

Pierre Magistretti is the dean of the Division of Biological and Environmental Science and Engineering at King Abdullah University of Science and Technology and professor emeritus in the Brain Mind Institute, EPFL and Center for Psychiatric Neuroscience, Department of Psychiatry–CHUV/UNIL, Switzerland. Magistretti received his M.D. from the University of Geneva and his Ph.D. from the University of California at San Diego. Magistretti’s research team has made significant contributions in the field of brain energy metabolism. His group has discovered some of the cellular and molecular mechanisms that underlie the coupling between neuronal activity and energy consumption by the brain. This work has considerable ramifications for the understanding of the origin of the signals detected with the current functional brain imaging techniques used in neurologic and psychiatric research.
HELEN S. MAYBERG, M.D.
Helen S. Mayberg is a neurologist renowned for her study of brain circuits in depression and for her pioneering deep brain stimulation research, which has been heralded as one of the first hypothesis-driven treatment strategies for a major mental illness. She is the founding director of Mount Sinai Health System’s The Nash Family Center for Advanced Circuit Therapeutics. Mayberg received an M.D. from the University of Southern California, trained at the Neurological Institute of New York at Columbia University, and was a post-doctoral fellow in nuclear medicine at Johns Hopkins Medicine. Immediately prior to joining Mount Sinai, Mayberg was Professor of Psychiatry, Neurology, and Radiology and held the inaugural Dorothy C. Fuqua Chair in Psychiatric Neuroimaging and Therapeutics at Emory University School of Medicine. She is a member of the National Academy of Medicine, The American Academy of Arts and Sciences, and the National Academy of Inventors. She is on the board of the International Society for Neuroethics and won the society’s Steven E. Hyman for Distinguished Service to Neuroethics (2018).

40 DANA FOUNDATION CEREBRUM | Spring 2022
ADVISORY BOARD
RICHARD M. RESTAK, M.D.


Richard Restak is clinical professor of neurology at George Washington Hospital University School of Medicine and Health Sciences, a member of the clinical faculty at St. Elizabeth’s Hospital in Washington, DC, and also maintains a private practice in neurology and neuropsychiatry. A graduate of Georgetown University School of Medicine, Restak has written over 24 books on the human brain and has penned articles for the Washington Post, The New York Times, the Los Angeles Times, and USA Today; and presented commentaries for both Morning Edition and All Things Considered on National Public Radio. He is a past recipient of the Claude Bernard Science Journalism Award, given by the National Society for Medical Research.
HARALD SONTHEIMER, Ph.D.
Harald Sontheimer is I. D. Wilson Chair and professor and founder and executive director of the Virginia Tech School of Neuroscience. He is also Commonwealth Eminent Scholar in cancer research and director of the Center for Glial Biology in Health, Disease & Cancer and the Fralin Biomedical Research Institute. A native of Germany, Sontheimer obtained a master’s degree in evolutionary comparative neuroscience, where he worked on the development of occulomotor reflexes. In 1989, he obtained a doctorate in Biophysics and Cellular & Molecular Neuroscience form the University of Heidelberg. He moved to Yale University for post-doctoral studies and later founded Transmolecular Inc., which was acquired by Morphotec Pharmaceuticals. He is the author of Diseases of the Nervous System (Elsevier, 2015).
STEPHEN WAXMAN, M.D., Ph.D.


Stephen Waxman is the Bridget Flaherty Professor of Neurology, Neurobiology, and Pharmacology at Yale University, and served as chairman of neurology at Yale from 1986 until 2009. His research uses tools from the “molecular revolution” to find new therapies that will promote recovery of function after injury to the brain, spinal cord, and peripheral nerves. A member of the National Academy of Medicine, Waxman has been honored in Great Britain with the Physiological Society’s annual prize, an accolade that he shares with Nobel Prize laureates Andrew Huxley, John Eccles, and Alan Hodgkin. In 2018, Waxman received the Julius Axelrod Prize from the Society for Neuroscience.
CHARLES F. ZORUMSKI, M.D.
Charles Zorumski is the Samuel B. Guze Professor and head of the Department of Psychiatry and Professor of Neuroscience at Washington University School of Medicine in St. Louis. Zorumski is also Psychiatrist-in-Chief at Barnes-Jewish Hospital and founding director of the Taylor Family Institute for Innovative Psychiatric Research. Zorumski’s laboratory studies synaptic transmission in the hippocampus. Since 1997, he has served on the steering committees of the McDonnell Center for Cellular and Molecular Neurobiology and the McDonnell Center for Systems Neuroscience and was director of the Center for Cellular and Molecular Neurobiology from 2002 to 2013. Zorumski has also served on the editorial boards of JAMA Psychiatry, Neurobiology of Disease, and served on the board of Scientific Counselors for the NIMH Intramural Research Program from 2009 to 2013. Since 2011, he has also served on the scientific advisory board of Sage Therapeutics, a publicly-traded company developing neurosteroids and oxysterols as treatments for neuropsychiatric illnesses.
Dana.org 41
Bill Glovin Editor-in-Chief


Glovin has been a working journalist for more than 30 years. He is executive editor at the Dana Foundation and hosts the Cerebrum Podcast. He has served as editor of Cerebrum since 2012. Previously, he was senior editor at Rutgers Magazine, managing editor of New Jersey Success, editor for New Jersey Business and a staff writer for The Bergen Record. Glovin graduated from George Washington University with a degree in journalism. He sometimes escapes from in front of the monitor to enjoy basketball, biking, and guitar.
Bruce Hanson Art Director

Hanson is responsible for the design and production of Cerebrum. A graduate of Rutgers University’s journalism program, he has worked in a variety of capacities in publishing and media for more than 30 years. In 1991, he founded EGADS, a studio which specializes in graphic design for education, arts and culture, publishing, and technology. When away from his desk, he'll most likely be playing guitar in a live music venue or plotting with his wife about how to book cheap flights to distant destinations.
 Seimi Rurup Associate Editor
Seimi Rurup Associate Editor

Rurup oversees the production of all digital and print content at the Dana Foundation. She previously served as editor of Brain in the News, which was the Foundation’s longest running print publication, and utilizes her background in fine arts to contribute to current publications and social media. She also contributes to the Foundation’s Neuro News section. Rurup graduated from Sarah Lawrence College with a degree in writing. When she is not in the office, she can be found in one of NYC’s many museums, Brooklyn cafés, or at home cooking with friends.
Brandon Barrera Staff Writer
Barrera is a New York City journalist, born and raised in Queens and living in Manhattan. A public affairs assistant at the Dana Foundation, he is the host of the Dana Foundation’s Communicating Brain Science podcast and writes about books for the magazine. Before coming to Dana, he helped produce content for Bronx Net, a public access television channel. When not enthralled by all things sci-fi, Barrera is fond of cycling, film, and arguing the finer points of tabletop gaming.

CEREBRUM STAFF
42 DANA FOUNDATION CEREBRUM | Spring 2022 Subscribe to our newsletter: Dana.org/subscribe THANK YOU FOR READING! FALL 2020 EMERGING IDEAS IN BRAIN SCIENCE Neuroscience Expansion Putting treatment and technology into place across the globe using cultural and ethical guidelines EMERGING IDEAS IN BRAIN SCIENCE FALL 2021 THE PRESSURE TO PERFORM SPRING 2020 The Mind of a EMERGING IDEAS IN BRAIN SCIENCE A Renaissance in Canine Cognitive Science Sheds Light on How They See the World and Bond with Humans DOG EMERGING IDEAS IN BRAIN SCIENCE SUMMER 2021 AGEISM THE BRAIN STRIKES BACK AGAINST WISDOM EXPERIENCE PLASTICITY EMPATHY Podcast WINTER 2020 How the Brain CREATES EMERGING IDEAS IN BRAIN SCIENCE Brain imaging and behavioral experiments can now examine how creative thinking works in different contexts and domains.






































 Illustration by Luisa Jung
Illustration by Luisa Jung



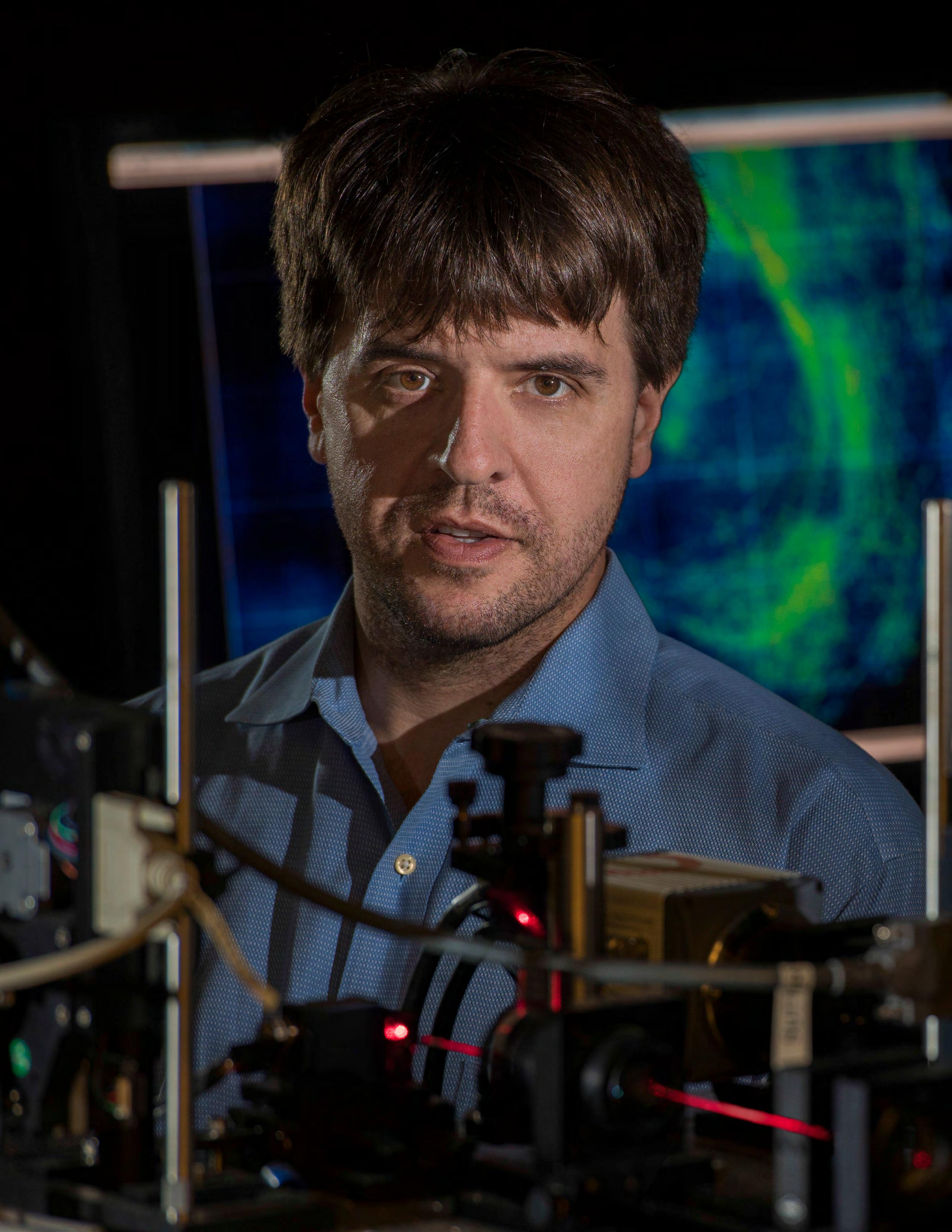
 By Carl Sherman
By Carl Sherman




















 Seimi Rurup Associate Editor
Seimi Rurup Associate Editor


