
28 minute read
Survivor Stories
By Jerry Grillo
n Photos by Jack Kearse
Black communities have been hit hard by COVID-19. Here, four families share their experience with the novel coronavirus and what it’s like to come out on the other side, alive and grateful.

CLAUDETTE HIMES HAD JUST SPENT 12 AND A HALF DAYS IN AN ISOLATED HOSPITAL BED AS A VENTILATOR PUSHED AIR IN AND OUT OF HER LUNGS WHILE HER HUSBAND, LEONARD, WAITED ANXIOUSLY FROM A SAFE DISTANCE, WONDER-
ING IF SHE WOULD LIVE OR DIE. Though Claudette’s body had been slipping toward the latter, she rallied suddenly on the 13th day, emerging from an induced coma with tears on her face and a prayer on her lips.
“It was Psalm 91. When I woke up, I was saying that prayer,” recalls Claudette, a 63-year-old accountant who spent several weeks in Emory Saint Joseph’s Hospital battling COVID-19. It was a prayer she and Leonard, associate pastor at Beulah Baptist in Decatur, said together every morning before they went to work and every night before they went to sleep.
“The prayer of protection. It was part of our life,” Claudette says. It was a prayer the couple had been saying together for months, long before an unexplained high fever and breathing trouble sent her to the hospital on March 16.
She doesn’t remember many of the days that followed. “The next thing I know, my eyes are open and a lady is telling me, ‘Ms. Himes, don’t cry. We thought we’d lost you.’ She also said, ‘You are our miracle.’ ”
Lost her? Miracle? Claudette had no idea what her nurse meant; at the time she didn’t even know what it was that had tried to kill her. These were the early days of the global pandemic, and she was an unfortunate pioneer. Health care providers and patients alike were grappling with a massive medical mystery.
Several Atlanta-area families who have been acutely affected by COVID-19 agreed to speak with us about their experiences. The patients are a diverse group: a PhD psychotherapist infected while working on the frontline of the pandemic; a kidney transplant recipient who fought the virus in the hospital while his wife recovered at home; the beloved grandmother of a close-knit family; and the Himeses.
The families share a few common threads: their illness was severe enough to require hospitalization at one of Emory’s facilities in metro Atlanta; the patients all are African Americans, which places them in a high-risk group during the pandemic; and they credit their deep faith with pulling them through. {
Claudette Himes (above, with husband Leonard Himes) credits her care team, her deep faith, and Leonard’s help and support for her recovery from COVID-19.
Black Americans are more likely to be infected by COVID-19 and, once infected, are more likely to die. In fact, they have been dying at about 2.4 times the rate of white Americans. As emerging data continues to show that African Americans are disproportionately harmed by the pandemic, it reflects an entrenched reality of health and health care disparity.
“Social determinants of health that are deeply rooted in structural racism have created a lot of gaps,” Tracey Henry, assistant professor of medicine at Emory, told a virtual audience during a webinar in June hosted by Emory School of Medicine about the impact of COVID-19 in communities of color.
“Specifically, I’m talking about the poverty gap—in the US, race and ethnicity is very much tied to poverty,” said Henry, a physician at Grady Memorial Hospital in Atlanta and a health policy expert. “People of color are much more likely to have less access to basic resources for health and wellness. So Black people were generally starting at a disadvantage at the onset of this pandemic, in terms of getting the care they need and being able to successfully overcome the virus.”
Henry and other panelists shared information, statistics, and anecdotes that told the grim story of health and health care inequity in Georgia and the US, illustrating the challenges that a global pandemic has brought.
Panelist Janice Newsome, director of Interventional Radiology and Image Guided Medicine at Emory Hospital Midtown, said the pandemic has uncovered, “a lot of small cracks that turned out to be gaping holes. This disease has humbled us quite a bit.”
That was Friday. She was isolated in a hospital room before her virus was confirmed. On Sunday she was discharged and told to quarantine at home. On one hand, she was relieved to be well enough to go home. On the other, there was the matter of Chico, her beloved shih tzu— what would happen if she exposed him to the virus? “My doctor wasn’t sure of how COVID-19 would affect animals, and I really love my animal. But I had to send him away for a few weeks,” she says. “That was hard on both Chico and me.”
When she got home, Andrea put herself on a regimen of, “hot tea, all day and night. I’m convinced I would not be here without it. All kinds of tea. And the only medicine I took was Tylenol and blood thinner.” Her get-well program also included liquid B-12 and zinc supplements every day, “the natural approach,” she says.
As her appetite returned (“That was the worst symptom,” Andrea says), she got back into exercising. Being active made a difference for her, she says, along with her deep faith. “I’m a very spiritual woman,” she says. “I take no credit for my healing. I prayed for that to happen.”

A persistent fever and breathing problems sent psychotherapist Andrea Young (above) to the hospital, where COVID-19 was confirmed.
HERE BECAUSE OF LOVE Psychotherapist Andrea Young was working “THE DISPARTIES WE’RE SEEING IN THIS in the emergency room with a mental health patient who was in isolation for COVID-19. PANDEMIC ARE NOT NEW. WE’VE HAD
Within two to three weeks, she started feeling ENORMOUS HEALTH CARE DISPARITIES IN symptoms, which she figured was an allergic reaction to March’s high pollen count. But a THIS COUNTRY WE HAVE NOT ADDRESSED. persistent fever and breathing trouble sent her to Emory Decatur Hospital. MY HOPE IS THAT, AS A RESULT OF THE Andrea drove herself. “It was an excellent set-up, I was impressed,” she says. “They had PANDEMIC, WE’RE GOING TO IMPROVE something like a MASH unit outside the ER—it THE RACIAL AND ETHNIC DISPARITIES THAT took me back to my military days. I remember thinking, ‘Somebody here really knows what HAVE BEEN SO UNACCEPTABLE.” they’re doing.’ It was all very orderly.” —Carlos del Rio, NPR Health, Sept. 13, 2020
PHOTO COURTESY OF ANDREA YOUNG
When she retested as negative, Andrea was able to get a long-awaited hug from her son, Julian, and cried in his arms. Chico came home and Andrea insists she feels better now than before she got sick.
She returned to work the first of June and is adamant about the importance of wearing proper Personal Protective Equipment (PPE). “If you love your community, you’ll wear a mask,” she says.
“I’m here because of love and compassion,” she says. “The love and compassion given to me by other human beings, and also God’s love. I am alive because of love.”
A LONELY DISEASE
You don’t have to be an expert in risk management, like Walter Gilstrap, to realize that he was the classic high-risk patient to develop COVID-19.
At 65, he’d had a kidney transplant in 2007 as a result of polycystic kidney disease, and he has a heart murmur. And thanks to his suppressed immune system, he battled a case of pneumocystis pneumonia (PCP) so severe in 2010 that he spent a month in the hospital.
At one point during that stay, the hospital chaplain called for Walter’s wife, Theresa. “He told her she’d better get to the hospital fast,” Walter says. “Of course, I pulled through.”
Walter spent almost another month in the hospital during his COVID-19 ordeal, which began in late February. He had symptoms of a urinary tract infection, and took antibiotics and kept tabs on the fever, which would never quite leave. By the weekend of March 13, when it was obvious that he wasn’t getting better—now he was experiencing low energy and diarrhea, too—he went to the emergency room at Emory University Hospital, where he spent the night.
His son, Justin, stayed with Walter through the weekend. On Monday, Walter was diagnosed with COVID-19—and a urinary tract infection. “And from there, it was like a long roller coaster ride,” Walter says. “I wasn’t having any noticeable respiratory symptoms of COVID-19 or anything to suggest my lungs were impaired. But my oxidation numbers were very low.”
Several days later he was placed on a ventilator. That lasted for two days. But his breathing was still troublesome, and he was placed on the ventilator again for several days. It looked bad. “My numbers were not good,” he says. “Then literally overnight, my oxygen levels went from precarious to 100 percent. I started feeling better.”
For Walter Gilstrap (below, far right, with his family) recovery from COVID-19 was “like a long roller coaster ride.” His wife, Theresa (in pink), had a milder case.

than whites.
In fact, Blacks have
been dying at about 2.4 times the rate
of whites during the pandemic.
Other communities of color, including Latino
and Native American populations, have also been hard hit by the virus.
The CDC attributes this difference to health in-
equities, such as poverty and health care access, discrimination, more crowded housing, and more underlying health conditions, such as high blood pressure and diabetes.
Also, ethnic and racial minority groups are
disproportionately represented in essential work settings such as health care, farms, factories, grocery stores, and
public transport, and thus at higher risk of getting the virus.
He was taken off the ventilator; the virus was diminishing, but he had dangerously high levels of a protein called creatine kinase (CK), which happens in about 14 percent of COVID-19 patients. To avoid going on dialysis he was put on an IV therapeutic cocktail that eventually brought his CK levels down from the danger zone (high CK levels can lead to renal failure). “I was finally able to go home after 27 days in the hospital, 17 of those in the ICU,” he says.
Meanwhile, Theresa had also tested positive for COVID-19. She was able to isolate at home, in her own bed. Their children, wearing PPE, became caregivers. Justin lives just minutes away and their daughter, Janna, flew home from New York and spent several months in her parents’ Decatur home, helping to care for Theresa. Theresa and Walter communicated, when they were able, via Facetime. By the time Walter went home on April 10, Theresa had recovered.
But after so many days in a bed, the muscles in Walter’s legs had atrophied, and he couldn’t walk. “I went from a wheelchair to a walker, then completed six weeks’ worth of physical therapy in three weeks. I had some catching up to do,” says Walter, who retired several years ago after 40 years in risk management with a Fortune 50 client list that included Coca-Cola and UPS, among others.
The Gilstraps believe they were infected while visiting Walter’s younger sister in the hospital (for a non-COVID issue) in early February. Walter seldom leaves home now and, when he does, he wears a mask.
He thinks back on his four weeks in the hospital: “What a lot of people miss is, this is a very lonely disease, which makes it mentally challenging, in addition to the physical and emotional toll. Not being able to see your loved ones makes it even more difficult than it would be otherwise.”
PRAYER FOR PROTECTION
The trouble started on Friday the 13th. Claudette Himes felt like she had the flu, but her fever wouldn’t go down and her primary care physician sent her to the emergency room at Emory Saint Joseph’s, where she was tested for COVID-19. They should have the results in a few days, the Himeses were told. Go home and rest.
Leonard Himes, who has been married to Claudette for eight years, picks up the story: “Her symptoms only got worse, and then late that Sunday night, she had trouble breathing. She was confused. I found out later that confusion is part of the COVID course of events for some people.”
On Monday he brought his very sick wife back to the hospital. With low blood-oxygen saturation and failing lung capacity, Claudette was placed on a ventilator. Leonard was sent home alone but spoke with her physician every day, and called the ICU nurse regularly, for almost two weeks. Her test had come back positive for COVID-19. “That was the toughest part, not being there with her,” he says. “She seemed to be getting steadily worse. For every step forward, two steps back. She was having kidney issues, and her lungs were full of pneumonia. Her physician said we needed to discuss palliative care.”
On Friday, March 27, through a baby monitor placed in Claudette’s room by the hospital chaplain, Leonard spoke with his wife for what he believed could be the last time. He hoped that Claudette could hear him saying, “I love you.”
Saturday morning, Leonard met virtually with Claudette’s attending physician, as well as the chaplain, an epidemiologist, a pulmonologist, and several others, including his niece, who works in infectious diseases. They were going to discuss his wife’s end-of-life plan.
That’s when Leonard’s phone started ringing. The nurse was calling. Claudette was sitting up in bed. Several days later, on April 2, she celebrated her birthday in a different hospital room, surrounded by joyful hospital staff. The next day, still testing positive for the virus, she went home. Leonard wouldn’t consider a rehab facility. He was going to care for her. Having been a firefighter and paramedic, he felt well suited to the difficult task. “I had some great nurses in the hospital, but my husband was the best nurse I had,” Claudette says. “The Bible talks about no greater love than a man who will lay down his life for a friend. I am so thankful and grateful to have a husband who loves me so much he would put his own life in jeopardy to care for me.”
As she started feeling better, the Himeses were able to celebrate their wedding anniversary with a quiet dinner at home.
“Don’t take your health for granted, please, I implore you,” Claudette says. “Wear your mask, social-distance. I am just so glad that I can see my husband, I can sit at the table and eat dinner with him, we can pray, we can sit on the back porch and enjoy looking out at the birds and just being together.” n
Three generations—(l to r) Barbara Johnson, Elizabeth Matthews, and Mikisha Johnson—supported each other during 83-year-old Elizabeth’s recovery from COVID. “I thank the Lord I made it through,” she says.
MIKISHA JOHNSON HAD JUST HUNG UP THE PHONE. On the call, her 83-yearTHREE GENERATIONS OF Today, more than 300 studies from around the world have looked at links old grandmother, Elizabeth Matthews, had struggled to string words together CARING between neurological problems and COVID-19. More are under way. and sounded disoriented. “Grandmama doesn’t sound right,” Mikisha told her By Shannon McCaffrey “We are now recognizing COVID-19 disease actually has a significant mother, Barbara. neurological implication or neuro-
When Barbara Johnson arrived logic effect,” says Byron Milton III, a the following morning at her parents’ physiatrist in physical medicine and home in the southwest Atlanta neighborhood of Collier rehabilitation at Emory University Hospital who has helped Heights, her mother didn’t look right either. Barbara COVID patients cope with dementia-like symptoms and told her, “Mama, you’re slurring your words, your mouth other neurological problems. is twisted, and your hand is trembling. You are going to Even as they care for patients, researchers and health the hospital.” care providers at the Emory Brain Health Center are among
Elizabeth already had a pretty good idea what was those leading the way toward understanding the short- and wrong, but she didn’t want to worry her daughter. “I said to long-term neurological implications of the pandemic on my husband, ‘I believe I had a stroke,’ ” she recalled. the brain and the mind.
She was right. But that wasn’t all. At that visit in early Those efforts are featured in Season 2 of the “Your FanAugust, doctors at Emory Saint Joseph’s Hospital told tastic Mind” television series from Georgia Public BroadElizabeth she’d also tested positive for COVID-19. “I got real casting and Emory, at pbs.org/show/your-fantastic-mind/. emotional when they told me that,” she says. “I was think- Elizabeth spent six days at Emory Saint Joseph’s Hospiing, ‘Am I going to die?’ ” tal battling COVID-19 and recovering from a stroke. Once
Since the COVID-19 outbreak began late last year, it has back home, she was told to quarantine for 14 days, although largely been understood as an assault on the respiratory she did 17 days for good measure. She doesn’t know whether system. Telltale symptoms are often a fever, hacking cough, COVID-19 contributed to her stroke. Retired as a factory and difficulty breathing; patients in the worst shape end worker at the now defunct General Motors plant in Doraup on respirators. What is still less understood but just as ville, she’s taking it easy these days. Her breathing can still alarming is the damage the virus may be doing to the brain, be labored; she gets winded easily. The trio miss their T.J. from strokes to reports of headaches, seizures, and confu- Maxx shopping trips together. But they’re also grateful that sion. And that doesn’t take into account the staggering toll Elizabeth will be around when her granddaughter has of the pandemic on our mental health. her first baby. n


09:24:20 | A COVID-19 FIRESIDE CHAT WITH DR. ANTHONY FAUCI

CUTTING THROUGH THE CHAOS
DURING THE PANDEMIC, SCHOOL OF MEDICINE FACULTY HAVE BEEN CALLED ON TO WRITE OP-EDS, APPEAR ON LIVE NEWS BROADCASTS, AND SERVE AS EXPERT ADVISERS. THEY’VE TURNED HOME OFFICES INTO TEMPORARY STUDIOS AND USED SOCIAL MEDIA TO GET HEALTH FACTS OUT. HERE ARE JUST A FEW OF OUR PUBLIC SCHOLARS:

| CARLOS DEL RIO
Executive Associate Dean for Emory at Grady Memorial Hospital, Carlos del Rio, Distinguished Professor of Medicine in the Division of Infectious Diseases and professor of global health and epidemiology in Rollins School of Public Health, is a sought-after expert on COVID-19.
And he doesn’t pull any punches on what he sees as the mishandling of the pandemic in this country. “While this is heartbreaking, what has to be said over and over is that this did not need to happen,” he says. “What drops my stomach through the floor is the irresponsible political leadership during this pandemic that has us in a crisis.”
From appearing live on CNN and MSNBC’s “The Rachel Maddow Show,” to coauthoring several viewpoint articles on the novel coronavirus in the Journal of the American Medical Association, to serving on the National Collegiate Athletic Association’s (NCAA) COVID-19 advisory panel, to his more than 33,000 followers on Twitter, del Rio doesn’t back away from challenging misinformation and calling out poor decisions. This is not the first pandemic del Rio has battled publicly and clinically. Since his days as a physician in training, del Rio has worked to reduce the spread of HIV on multiple fronts, directing the NIH-sponsored HIV Prevention Trials Network at Emory and codirecting the Emory Center for AIDS
Research. He also serves as Foreign Secretary of the National Academy of Medicine.
Del Rio has turned his office into a broadcast studio of sorts, with improved lighting and an abstract painting of lungs on the wall behind him, painted by his daughter. “She did a series some years ago on the organs—the lungs, the heart, and the brain—which I loved. Now it turns out they are the three organs most impacted long term by COVID-19.”
He understands the power of social media to reach people directly. Del Rio has done several Facebook live webinars and tweets nearly every day. Del Rio’s tweets sometimes highlight an upcoming media engagement: “Will be joining @ JohnKingCNN in @CNNPolitics tomorrow to talk about how quickly a vaccine can be approved, public trust about safety and questions of political pressure on @US_FDA to fast track a #SARSCoV2 vaccine before the election.”
Or he may simply remind people of basic protective measures: “As health care workers, we are tired, we are frustrated, and we are mad. If March–April was a wave this is a tsunami and could have been prevented. Please everyone #WearAMask #WatchYourDistance & #WashYourHands.”—Mary Loftus
| SANJAY GUPTA
Perhaps the Emory physician with the most airtime during the pandemic is Associate Professor of Neurosurgery Sanjay Gupta, CNN’s chief medical correspondent and host of “Sanjay Gupta MD,” for which he has won multiple Emmy awards. Gupta continues to see patients as a general neurosurgeon at Grady Memorial in Atlanta.
He is a frequent contributor to numerous CNN shows covering the crisis, and hosts a weekly town hall with CNN anchor Anderson Cooper.
Each week, on CNN Health, the father of three answers kids’ questions about COVID-19, such as “Why do some people get the coronavirus but don’t feel sick?” and “When can I hang out with Grandma and Grandpa again and not have to worry about giving them coronavirus?”
Gupta also hosts a “Coronavirus: Fact or Fiction” podcast, (cnn.com/audio/ podcasts/corona-virus) where he covers such topics as frontline workers at the breaking point, Doctors without Borders helping American nursing homes, and how this pandemic compares with the 1918 influenza pandemic.
As a trusted medical journalist, viewers look to Gupta for understandable medical explanations and implications of the ever-evolving discoveries about COVID-19, such as the recent finding that up to 35 percent of Big Ten athletes who had the virus now show signs of heart inflammation. “This is pretty frightening,” he says, before describing the fact in more detail.
Gupta (@drsanjaygupta on Twitter) sees his role as “setting the record straight” on inaccurate information that is circulated, much of the time on social media.
“Since I started reporting on the coronavirus, I’ve heard a lot of myths and theories about it,” Gupta says. “The
outbreak has unleashed so much information, the World Health Organization has called it an infodemic. And there’s so much misinformation that goes along with it.”
One specific appearance by Gupta on the big screen has gone viral—when he portrayed himself in the 2011 movie Contagion. “In one scene, Dr. Sanjay Gupta is featured on a TV news program discussing preventive measures [against a fast-spreading, lethal virus]. Now, nine years later, he’s doing it for real on CNN,” says an article in Variety.— Mary Loftus
| DAVID HOLLAND
Associate Professor of Infectious Diseases David Holland spent years working on HIV, tuberculosis, sexually transmitted infections, and viral hepatitis with the Fulton County Board of Health. “The strongest public health agencies in the US maintain strong connections with academia, and I am very grateful to be in this position,” he says.
But when the novel coronavirus pandemic came to the US, Holland’s role as chief of Medical and Preventive Services for Fulton County pivoted to focus on COVID19—a disease that would need to be managed through testing and contact tracing, with no vaccine available. “In a lot of ways this was not a pandemic that we planned for,” says Holland, who oversees the board’s COVID-19 testing activities. But they adapted. Holland said that by July, the Board of Health and its partners were testing up to 25,000 people per week at fixed and mobile sites within the county. “We’re hoping sometime in the not-toodistant future, we’ll be able
to convert testing to vaccine administration,” Holland says. Holland’s work during
the HIV crisis taught him a crucial lesson: The most effective testing strategy is to engage the community
from the start. “For any sort of intervention to work,” he says, “it has to be something that is meaningful to the people.”
Working closely with minority communities that experience disproportionate impact from disease, Holland says, is a responsibility to which public health agencies have recommitted during this time of national awareness of systemic racism.
“I’m proud to work for two organizations—Fulton
and Emory—that are engaged in definitive anti-racist activities, particularly around health care,” he says. “We can never achieve any of our goals in public health until we assure health equity for everyone.”—Emily Weyrauch
| NADINE KASLOW
Professor of Psychiatry and Behavioral Sciences Nadine Kaslow is often called on by the media to comment on effective coping strategies during times of crisis. So, understandably, she has been called on frequently during the pandemic, by everyone from CNN to Georgia Public Broadcasting. She has written op-eds for CNN.com, done Q&As on social media on the topic of mental health and COVID-19, and speaks about how children are being impacted by COVID-19. “It’s
really, really hard on kids. And they don’t developmentally have the same coping strategies as adults do. There’s no way they can.”
Kaslow suggests families have at least one meal together a day and “try to build in pleasurable activities. I do think our kids are picking up on our anxieties, so we need to be mindful of that. . . . Now is the time to say, ‘I’ll bet this must be hard for you, not getting to see your friends.’ Be patient and tolerant, and remember what our kids need most from us right now is our love.”
Kaslow is often called on to help health care providers who are stressed or experiencing PTSD. At Emory she launched a series of support groups—Caring Communities for COVID Caregivers—held in ICUs and hospital units treating COVID-19 patients. The groups use a peer- support framework to help medical workers share coping strategies.
Kaslow and her colleagues also run support groups for medical workers who have tested positive for COVID-19 and for those who are grieving. In addition, she has partnered with the World Health Organization–Africa and the US Department of State to offer education, guidance, and support to frontline medical providers in Africa and other regions with a shortage of mental health care providers.
She encourages everyone to embrace compassion. “All of us having to change our normal routines is extremely stressful, and we’re all scared of getting sick and dying or losing people we care about,” Kaslow says. “I think escapism is absolutely fine, even if it involves Netflix and snacks. Be easy on yourself as well as those around you.”—Mary Loftus
| COLLEEN KRAFT
Associate Professor of Infectious Diseases and Pathology Colleen Kraft is no stranger to pandemics. Five years ago, she played a lead role in treating Ebola patients who came to Emory during the 2014–16 outbreak. Now she’s helping to coordinate her hospital’s response to COVID-19 as an associate chief medical officer at Emory University Hospital.
Kraft is helping to shape the national conversation—


04:09:20 | LIFE WITH COVID-19 CALMING THE MIND

09:01:20 | CNN NEWSROOM

09:14:20 | CNN NEWSROOM

and public health policies— on the coronavirus pandemic. She’s made appearances on CNN, NBC, and NPR programs; written op-ed pieces; and was profiled in the Los Angeles Times and the AJC. Kraft also was named to the NCAA COVID-19 advisory panel, and serves on Georgia Governor Brian Kemp’s coronavirus task force. “I’ve learned to enjoy this public-facing aspect of the job,” she says. “I look at
these opportunities as a way to get the truth about COVID-19 out there to as many people
as possible. I work hard to try and make challenging topics understandable and
accessible, yet I’m not afraid to challenge the audience with a little bit more complexity than most people usually see on social media and the news. It’s a different form of teaching for me, on a larger scale.”
When stress is running high, she does what many of us do: “I read novels. I try to get some exercise or a walk in every day. And I love spending time with my kids. We’ve been watching Disney’s The Mandalorian. It’s a fun, grounding ritual, because everything else is so upside down right now. Most important, when we’re together, we try not to talk about the coronavirus.” —Kelley Freund and Roger Slavens
| KIMBERLY MANNING
Professor of Medicine Kimberly Manning decided for her birthday this year, she wanted one thing: to raise money for Grady Memorial Hospital in downtown Atlanta. So she posted on social media: “2020 has been a year that many of us would soon prefer to forget. Along with all the tragedy, I am reminded that this year also includes two major milestones in my life: the start of my 20th year as a Grady doctor, and my 50th year. Here is my
birthday dream: To raise $50,000 for the Grady Health Foundation, specifically targeting our Grady COVID-19 Response Fund.
Given the disproportionate impact that COVID-19 has had on the Black community, this is personal to me. I hope you’ll let it be personal to you, too.”
Manning’s Twitter handle is @gradydoctor, and for the past 11 years, she’s been writing the blog “Reflections of a Grady Doctor,” in which she tells about her experiences as a physician and clinical educator with honesty, poignancy, and humor. It was named a top medical blog by O, the Oprah Magazine. She has more than 50,000 followers on Twitter. “I impulsively decided to start a blog,” says Manning, who joined Emory’s faculty in 2001 after training at Case Western Reserve’s MetroHealth Medical Center in internal medicine and pediatrics. “In my time at Grady, I’ve realized just how much magic is happening there and how much
humanity is inside. But that isn’t what people see when they turn on the news. I tell stories that show the positive and beautiful aspects of a safety-net hospital.”
If Manning experiences something that impacts her, “particularly if the person is underrepresented in medicine, I’m going to use my position to get that voice out. I care about diversity, equity, inclusion, and humanizing patients who are underserved. I care about kindness. If that’s something that makes someone an influencer, I think we can all be influencers.” —Camile Matthews
| INGRID PINZON
Assistant Professor of Hospital Medicine Ingrid Pinzon, a physician at Emory Saint Joseph’s Hospital, became concerned when she saw a jump in younger Hispanic patients coming into the hospital with COVID-19. Many had no underlying health conditions but “because they came in sicker, they developed more complications,” she says.
Indeed, like other people of color, Latinos and Hispanics are more likely to contract COVID-19. While making up 19% of the US population, they make up nearly 31% of all US COVID-19 cases.
Because language can be a barrier for teaching Spanish-speaking residents how to protect themselves from the virus, Pinzon and other bilingual Emory Healthcare physicians are working to reach Atlanta’s Latinx community, reaching out to them in areas where they live, work, shop, and socialize, and making signs with prevention tips in Spanish. “This population needs specific guidelines in Spanish, I think that’s the key,” Pinzon told Fox5 Atlanta.—Mary Loftus
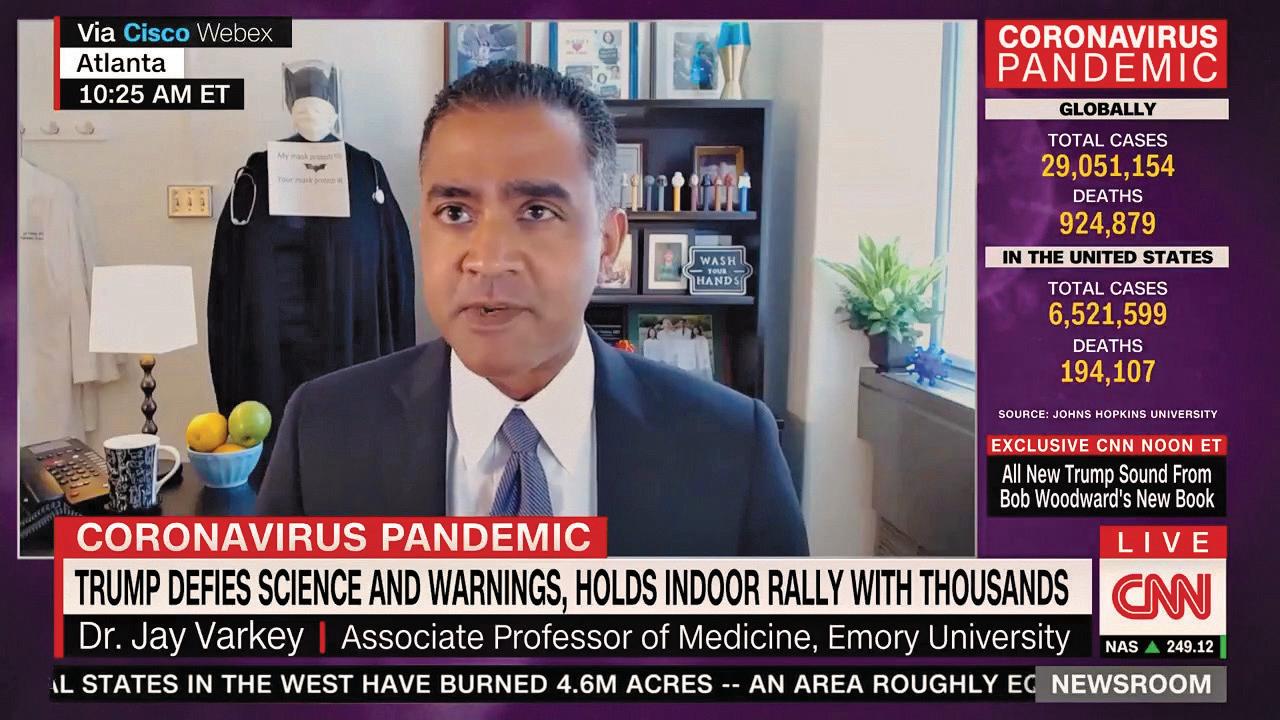
| JAY VARKEY
Associate Professor of Infectious Diseases Jay Varkey was also on Team Ebola, helping to care for the first Ebola patients on US soil in 2014, in the serious communicable diseases unit at Emory University Hospital. Varkey, a hospital epidemiologist, addressed how lessons from Ebola can help fight COVID-19 in US News & World Report: “The first is that caring for a patient with COVID-19 is clearly a team sport.
“Certainly, there’s been a lot of focus on frontline health care workers within the hospital itself, but given how prevalent this infection is, it’s really impacted everyone, including those who keep our hospital environments safe by cleaning up every day in areas where there is environmental contamination, where they are putting themselves at risk.
“The last piece where there’s a really important parallel with Ebola is that the key to preventing COVID-19 is strict adherence to basic infection prevention principles. Personal protective equipment, or PPE (such as masks, gloves, gowns), works. It’s strict attention to the basics that keeps us safe.”
Varkey has done a series of Q&As on social media called “COVID-19: What You Need to Know,” with his ever-present Batman costume draped with a stethoscope in the background. He’s answered questions on vaccine, therapies, and school openings on SiriusXM with Olivier Knox. He’s active on Twitter (@jaybvarkey), mixing in a good dose of humor with COVID science and medical information.
And he has appeared on CNN Newsroom, where he said on February 27, near the beginning of the pandemic: “This notion of community spread is not a reason to panic, it’s a reason to prepare.”—Mary Loftus








