






Higginbotham Public Sector (800) 583-6908 www.mybenefitshub.com/ lifeschoolofdallas
Mayda Falcon Central Office (469) 850-5433 benefits@lifeschools.net
EECU (817) 882-0800 www.eecu.org
Cigna Group #HC110473 (800) 754-3207 www.mycigna.com
Superior Vision Group #037494 (800) 507-3800 Superior National Network www.superiorvision.com
Lincoln Financial Group (800) 423-2765 www.lfg.com
MASA
Group # MKLIFE (800) 423-3226 www.masamts.com
(800) 858-6843
STD Group #419941 LTD Group #419942 www.unum.com
OneAmerica Financial Partners, Inc.
Group #00617146 (800) 537-6442 www.oneamerica.com
Experian (855) 797-0052
www.experian.com
Blue Cross Blue Shield (800) 521-2227
BCBS HSA: 360498_0001
BCBS Base HMO: 360757_0002
BCBS Enhanced HMO: 360757_0003 www.bcbstx.com
Lincoln Financial Group (800) 423-2765
Dental Low Plan: 0001D040928
Dental High Plan: 0001D040929
Dental HMO: 0001D040930 www.lfg.com
Lincoln Financial Group (800) 423-2765 www.lfg.com
5 Star Life Insurance Company (866) 863-9753 www.5starlifeinsurance.com
National Benefit Services (855) 399-3035 www.nbsbenefits.com EMPLOYEE ASSISTANCE
ComPsych Guidance Resources Program
Group #ONEAMERICA3 (855) 387-9727
https://www.guidanceresources.com/
NBS Retirement Service Center (800) 274-0503 ext 2,5
https://nbsbenefits.com/non-erisa403b-forms/


1
2
www.mybenefitshub.com/lifeschoolofdallas
3
4
Enter your Information
• Last Name
• Date of Birth
• Last Four (4) of Social Security Number
NOTE: THEbenefitsHUB uses this information to check behind the scenes to confirm your employment status. CLICK LOGIN
Once confirmed, the Additional Security Verification page will list the contact options from your profile. Select either Text, Email, Call, or Ask Admin options to receive a code to complete the final verification step.
5
Enter the code that you receive and click Verify. You can now complete your benefits enrollment!
During your annual enrollment period, you have the opportunity to review, change or continue benefit elections each year. Changes are not permitted during the plan year (outside of annual enrollment) unless a Section 125 qualifying event occurs.
• Changes, additions or drops may be made only during the annual enrollment period without a qualifying event.
• Employees must review their personal information and verify that dependents they wish to provide coverage for are included in the dependent profile. Additionally, you must notify your employer of any discrepancy in personal and/or benefit information.
• Employees must confirm on each benefit screen (medical, dental, vision, etc.) that each dependent to be covered is selected in order to be included in the coverage for that particular benefit.
All new hire enrollment elections must be completed in the online enrollment system within the first 30 days of benefit eligibility employment. Failure to complete elections during this timeframe will result in the forfeiture of coverage.
For supplemental benefit questions, you can contact your Benefit Office or you can call Higginbotham Public Sector at (866) 914-5202 for assistance. Where can I find forms?
For benefit summaries and claim forms, go to your benefit website: www.mybenefitshub.com/ lifeschoolofdallas. Click the benefit plan you need
information on (i.e., Dental) and you can find the forms you need under the Benefits and Forms section.
For benefit summaries and claim forms, go to the Life School of Dallas benefit website: www.mybenefitshub. com/lifeschoolofdallas. Click on the benefit plan you need information on (i.e., Dental) and you can find provider search links under the Quick Links section.
If the insurance carrier provides ID cards, you can expect to receive those 3-4 weeks after your effective date. For most dental and vision plans, you can log in to the carrier website and print a temporary ID card or simply give your provider the insurance company’s phone number, and they can call and verify your coverage if you do not have an ID card at that time. If you do not receive your ID card, you can call the carrier’s customer service number to request another card.
If the insurance carrier provides ID cards, but there are no changes to the plan, you typically will not receive a new ID card each year.
The amount of coverage you can elect without answering any medical questions or taking a health exam. Guaranteed coverage is only available during initial eligibility period. Actively-at-work and/or preexisting condition exclusion provisions do apply, as applicable by carrier.
Applies to any illness, injury or condition for which the participant has been under the care of a health care provider, taken prescription drugs or is under a health care provider’s orders to take drugs, or received medical care or services (including diagnostic and/or consultation services).
A Cafeteria plan enables you to save money by using pre-tax dollars to pay for eligible group insurance premiums sponsored and offered by your employer. Enrollment is automatic unless you decline this benefit. Elections made during annual enrollment will become effective on the plan effective date and will remain in effect during the entire plan year.
Marital Status
Change in Number of Tax Dependents
Change in Status of Employment Affecting Coverage Eligibility
Gain/Loss of Dependents’ Eligibility Status
Judgment/ Decree/Order
Eligibility for Government Programs
Changes in benefit elections can occur only if you experience a qualifying event. You must present proof of a qualifying event to your Benefit Office within 30 days of your qualifying event and meet with your Benefit Office to complete and sign the necessary paperwork in order to make a benefit election change. Benefit changes must be consistent with the qualifying event.
A change in marital status includes marriage, death of a spouse, divorce or annulment (legal separation is not recognized in all states).
A change in number of dependents includes the following: birth, adoption and placement for adoption. You can add existing dependents not previously enrolled whenever a dependent gains eligibility as a result of a valid change in status event.
Change in employment status of the employee, or a spouse or dependent of the employee, that affects the individual’s eligibility under an employer’s plan includes commencement or termination of employment.
An event that causes an employee’s dependent to satisfy or cease to satisfy coverage requirements under an employer’s plan may include change in age, student, marital, employment or tax dependent status.
If a judgment, decree, or order from a divorce, annulment or change in legal custody requires that you provide accident or health coverage for your dependent child (including a foster child who is your dependent), you may change your election to provide coverage for the dependent child. If the order requires that another individual (including your spouse and former spouse) covers the dependent child and provides coverage under that individual’s plan, you may change your election to revoke coverage only for that dependent child and only if the other individual actually provides the coverage.
Gain or loss of Medicare/Medicaid coverage may trigger a permitted election change.
Supplemental Benefits: Eligible employees must work 32 or more regularly scheduled hours each work week.
Eligible employees must be actively at work on the plan effective date for new benefits to be effective, meaning you are physically capable of performing the functions of your job on the first day of work concurrent with the plan effective date. For example, if your 2024 benefits become effective on September 1, 2024, you must be actively-at-work on September 1, 2024 to be eligible for your new benefits.
Dependent Eligibility: You can cover eligible dependent children under a benefit that offers dependent coverage, provided you participate in the same benefit, through the maximum age listed below. Dependents cannot be double covered by married spouses within the district as both employees and dependents.
Please note, limits and exclusions may
when obtaining coverage as a married couple or when
Potential Spouse Coverage Limitations: When enrolling in coverage, please keep in mind that some benefits may not allow you to cover your spouse as a dependent if your spouse is enrolled for coverage as an employee under the same employer. Review the applicable plan documents, contact Higginbotham Public Sector, or contact the insurance carrier for additional information on spouse eligibility.
FSA/HSA Limitations: Please note, in general, per IRS regulations, married couples may not enroll in both a Flexible Spending Account (FSA) and a Health Savings Account (HSA). If your spouse is covered under an FSA that reimburses for medical expenses then you and your spouse are not HSA eligible, even if you would not use your spouse’s FSA to reimburse your expenses. However, there are some exceptions to the general limitation regarding specific types of FSAs. To obtain more information on whether you can enroll in a specific type of FSA or HSA as a married couple, please reach out to the FSA and/or HSA provider prior to enrolling or reach out to your tax advisor for further guidance.
Potential Dependent Coverage Limitations: When enrolling for dependent coverage, please keep in mind that some benefits may not allow you to cover your eligible dependents if they are enrolled for coverage as an employee under the same employer. Review the applicable plan documents, contact Higginbotham Public Sector, or contact the insurance carrier for additional information on dependent eligibility.
Disclaimer: You acknowledge that you have read the limitations and exclusions that may apply to obtaining spouse and dependent coverage, including limitations and exclusions that may apply to enrollment in Flexible Spending Accounts and Health Savings Accounts as a married couple. You, the enrollee, shall hold harmless, defend, and indemnify Higginbotham Public Sector from any and all claims, actions, suits, charges, and judgments whatsoever that arise out of the enrollee’s enrollment in spouse and/or dependent coverage, including enrollment in Flexible Spending Accounts and Health Savings Accounts.
If your dependent is disabled, coverage may be able to continue past the maximum age under certain plans. If you have a disabled dependent who is reaching an ineligible age, you must provide a physician’s statement confirming your dependent’s disability. Contact your Benefit Office to request a continuation of coverage.
Description
Health
(IRC Sec. 223)
Approved by Congress in 2003, HSAs are actual bank accounts in employee’s names that allow employees to save and pay for unreimbursed qualified medical expenses tax-free.
(IRC Sec. 125)
Allows employees to pay out-of-pocket expenses for copays, deductibles and certain services not covered by medical plan, taxfree. This also allows employees to pay for qualifying dependent care tax-free.
Employer Eligibility A qualified high deductible health plan All employers
Contribution Source Employee and/or employer Employee and/or employer
Account Owner Individual
Underlying Insurance Requirement High deductible health plan None
Minimum Deductible
Maximum Contribution
Permissible Use Of Funds
Cash-Outs of Unused Amounts (if no medical expenses)
$1,600 single (2024)
$3,200 family (2024) N/A
$4,150 single (2024)
$8,300 family (2024)
Employees may use funds any way they wish. If used for non-qualified medical expenses, subject to current tax rate plus 20% penalty.
$3,200 (2024)
Reimbursement for qualified medical expenses (as defined in Sec. 213(d) of IRC).
Permitted, but subject to current tax rate plus 20% penalty (penalty waived after age 65). Not permitted
Year-to-year rollover of account balance? Yes, will roll over to use for subsequent year’s health coverage.
Does the account earn interest?
Portable?
Yes
Yes, portable year-to-year and between jobs.
No. Access to some funds may be extended if your employer’s plan contains a 2 1/2 –month grace period or $500 rollover provision.
No
No
A Health Savings Account (HSA) is a personal savings account where the money can only be used for eligible medical expenses. Unlike a flexible spending account (FSA), the money rolls over year to year however only those funds that have been deposited in your account can be used. Contributions to a Health Savings Account can only be used if you are also enrolled in a High Deductible Health Care Plan (HDHP). For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas
A Health Savings Account (HSA) is more than a way to help you and your family cover health care costs – it is also a tax-exempt tool to supplement your retirement savings and cover health expenses during retirement. An HSA can provide the funds to help pay current health care expenses as well as future health care costs.
A type of personal savings account, an HSA is always yours even if you change health plans or jobs. The money in your HSA (including interest and investment earnings) grows tax-free and spends tax-free if used to pay for qualified medical expenses. There is no “use it or lose it” rule — you do not lose your money if you do not spend it in the calendar year — and there are no vesting requirements or forfeiture provisions. The account automatically rolls over year after year.
You are eligible to open and contribute to an HSA if you are:
• Enrolled in an HSA-eligible HDHP (High Deductible Health Plan) Not covered by another plan that is not a qualified HDHP, such as your spouse’s health plan
• Not enrolled in a Health Care Flexible Spending Account, nor should your spouse be contributing towards a Health Care Flexible Spending Account
• Not eligible to be claimed as a dependent on someone else’s tax return
• Not enrolled in Medicare or TRICARE
• Not receiving Veterans Administration benefits
You can use the money in your HSA to pay for qualified medical expenses now or in the future. You can also use HSA funds to pay health care expenses for your dependents, even if they are not covered under your HDHP.
Your HSA contributions may not exceed the annual maximum amount established by the Internal Revenue Service. The annual contribution maximum for 2024 is based on the coverage option you elect:
• Individual – $4,150
• Family (filing jointly) – $8,300

You decide whether to use the money in your account to pay for qualified expenses or let it grow for future use. If you are 55 or older, you may make a yearly catch-up contribution of up to $1,000 to your HSA. If you turn 55 at any time during the plan year, you are eligible to make the catch-up contribution for the entire plan year.
If you meet the eligibility requirements, you may open an HSA administered by EECU. You will receive a debit card to manage your HSA account reimbursements. Keep in mind, available funds are limited to the balance in your HSA.
• Always ask your health care provider to file claims with your medical provider so network discounts can be applied. You can pay the provider with your HSA debit card based on the balance due after discount.
• You, not your employer, are responsible for maintaining ALL records and receipts for HSA reimbursements in the event of an IRS audit.
• You may open an HSA at the financial institution of your choice, but only accounts opened through EECU are eligible for automatic payroll deduction and company contributions.
• Online/Mobile: Sign-in for 24/7 account access to check your balance, pay bills and more.
• Call/Text: (817) 882-0800 EECU’s dedicated member service representatives are available to assist you with any questions. Their hours of operation are Monday through Friday from 8:00 a.m. to 7:00 p.m. CT, Saturday 9:00 a.m. to 1:00 p.m. CT and closed on Sunday.
• Lost/Stolen Debit Card: Call the 24/7 debit card hotline at (800)333-9934.
• Stop by a local EECU financial center: www.eecu.org/ locations.
HSA

https://policy-srv.box.com/s/iabvrkcmqvrrzptpbf7lo97g63cs4ph1.

T he Summary of Benefits and Coverage (SBC) document will help you choose a health plan . The SBC shows you how you and the plan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium ) will be provided separately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, call 18005212227 or at For general definitions of common terms, such as allowed amount, balance billing , coinsurance , copayment , deductible , provider , or other underlined terms, see the Glossary. You can view the Glossary at www.healthcare.gov/sbcglossary/ or call 18557564448 to request a copy. Important Questions Answers Why
Generally, you must pay all of the costs from providers up to the deductible amount before this plan begins to pay. If you have other family members on the pla n , each family member must meet their own individual deductible until the total amount of deductible expenses paid by all family members meets the overall family deductible . Are there services covered before you meet your deductible ?
You don’t have to meet deductibles for specific services.
Yes. Certain preventive care is covered before you meet your deductible .
What is the overall deductible ?
This plan covers some items and services even if you haven’t yet met the deductible amount. But a copayment or coinsurance may apply. For example, this plan covers certain preventive services without cost sharing and before you meet your deductible . See a list of c overed preventive services at www.healthcare.gov/coverage/preventivecarebenefits/ . Are there other deductibles for specific services?
No.
The outofpocket limit is the most you could pay in a year for covered services. If you have other family members in this plan , they have to meet their own outofpocket limits until the overall family outofpocket limit has been met.
What is the outofpocket limit for this plan ? InNetwork : $5,000 Individual / $15,000 Family OutofNetwork : $18,000 Individual / $54,000 Family
This plan uses a provider network . You will pay less if you use a provider in the plan ’s network . You will pay the most if you use an outofnetwork provider , and y ou might receive a bill from a provider for the difference between the provider ’s charge and what your plan pays ( balance billing ).
Be aware, your network provider might use an outofnetwork provider for some services (such as lab work). Check with your p rovider before you get services.
Even though you pay these expenses, they don’t count toward the outofpocket limit . Will you pay less if you use a network provider ? Yes. See www.bcbstx.com or call 18008102583 for a list of network providers .
You can see the specialist you choose without a referral .
What is not included in the outofpocket limit ? Premiums , balancebilling charges, and health care this plan doesn’t cover.
Do you need a referral to see a specialist ? No.
please refer to your
for more details.
copayment and coinsurance costs shown in this chart are after your deductible has been met, if a deductible applies.

You may have to pay for services that aren’t
the
what your
more information about limitations and exceptions, see the plan or policy document at
You Will Pay
OutofNetwork Provider (You will pay the most)
InNetwork Provider (You will pay the least)
You May Need
Retail covers a 30day supply. With appropriate prescription, up to a 90day supply is available. Mail order covers a 90day supply. OutofNetwork mail order is not covered. Payment of the difference between the cost of a brand name drug and a generic may be required if a generic drug is available. For OutofNetwork pharmacy, member must file claim . Certa in drugs require approval before they will be covered. The costsharing for insulin included in the drug list will not exceed $25 per prescription for a 30day supply, regardless of the amount or type of insulin needed to fill the prescription.
For InNetwork benefit, specialty drugs must be obtained from InNetwork specialty pharmacy provider . Specialty drugs are limited to a 30day supply except for certain FDAdesignated dosing regimens . Mail order is not covered.
Ground and air transportation covered.
You may have to pay for services that are not covered by the visit fee. For an example, see “If you have a test” on page 2.
more information about limitations and exceptions, see the plan or policy document at
Certain services must be preauthorized; refer to your benefit booklet* for details. Virtual visits are available, please refer to your plan policy for more details.
Cost sharing does not apply for preventive services . Depending on the type of services, a coinsurance or deductible may apply. Maternity care may include tests and service described elsewhere in the SBC (i.e. ultrasound).
Limited to 60 visits per calendar year. Preauthorization is required.
Limited to 90 visits combined for all therapies per calendar year . Includes, but is not limited to, occupational, physical, and manipulative therapy.
Limited to 60 visits per benefit period.
more information about limitations and exceptions, see the plan or policy document
Generally Does NOT Cover (Check your policy or plan document for more information and a list of any other
Services Your
• Acupuncture • Bariatric surgery • Cosmetic surgery • Dental care (Adult)
• Infertility t reatment • Longterm care • Nonemergency care when traveling outside the U.S. • Privateduty nursing • Routine foot care • Weight loss programs Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.)
• Hearing aids ( 1 per ear p er 36month period)
• Chiropractic care
• Routine eye care (Adult) https://policy-srv.box.com/s/iabvrkcmqvrrzptpbf7lo97g63cs4ph1.
*For more information about limitations and exceptions, see the plan or policy document
Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: For group health coverage contact the plan , Blue Cross and Blue Shield of Texas at 18005212227 or visit www.bcbstx.com . For group health coverage subject to ERISA, contact the U.S. Department of Labor’s Employee Benefits Security Administration at 1866444EBSA (3272) or www.dol.gov/ebs a/healthreform . For nonfederal governmental group health plans , contact Department of Health and Human Services, Center for Consumer Information and Insurance Oversight, at 18772672323 x61565 or www.cciio.cms.gov . Church plans are not covered by the Federal COBRA continuation coverage rules. If the coverage is insured, individuals should contact their State insurance regulator regarding their pos sible rights to continuation coverage under State law. Other coverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace . For more information about the Marketplace , visit www.HealthCare.gov or call 18003182596 . Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim . This complaint is called a grievance or appeal . For more information about your rights, look at the explanation of benefits you will receive for that medica l claim . Your plan documents also provide complete information to submit a claim , appeal , or a grievance for any reason to your plan . For more information about your rights, this notice, or assistance, contact: For group health coverage subject to ERISA: B lue Cross and Blue Shield of Texas at 18005212227 or visit www.bcbstx.com , the U.S. Department of Labor's Employee Benefits Security Administration at 1866444EBSA (3272) or www.dol.gov/ebsa/healthreform , and the Texas Department of Insurance, Consumer Protection at 18002523439 or www.tdi.texas.gov . For nonfederal governmental group health plans and church plans that are group h ealth plans , Blue Cross and Blue Shield of Texas at 18005212227 or www.bcbstx.com or contact the Texas Department of Insurance, Consumer Protection at 18002523439 or www.tdi.texas.gov . Additionally, a consumer assistance program can help you file your appeal . Contact the Texas Department of Insurance’s Consumer Health Assistance Program at 18002523439 o r visit www.cms.gov/CCIIO/Resources/ConsumerAssistanceGrants/tx.html .
Does this plan provide Minimum Essential Coverage ? Yes . Minimum Essential Coverage generally includes plans , health insurance available through the Marketplace or other individual market pol icies, Medicare, Medicaid, CHIP, TRICARE, and certain other coverage. If you are eligible for certain types of Minimum Essential Coverage , you may not be eligible for the premium tax credit .
Does this plan meet the Minimum Value Standards ? Yes . If your pl an doesn’t meet the Minimum Value Standards , you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace .
Langua ge Access Services: Spanish (Español): Para obtener asistencia en Español, llame al 18005212227. Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 18005212227.
Chinese ( 中文 ): 如果需要中文的帮助, 请拨打这个号码 18005212227.
Navajo (Dine): Dine k'ehgo shika at'ohwol ninisingo, kwiijigo holne' 18005212227.
To see examples of how this plan might cover costs for a sample medical situation, see the next section.
About these Coverage Examples: This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the costsharing amounts ( deducti bles , copayments and coinsurance ) and excluded services under the plan . Use this information to compare the portion of costs you might pay under different health plans . Please note these coverage examples are based on selfonly coverage.

covered services.
The plan would be responsible for the other costs of these

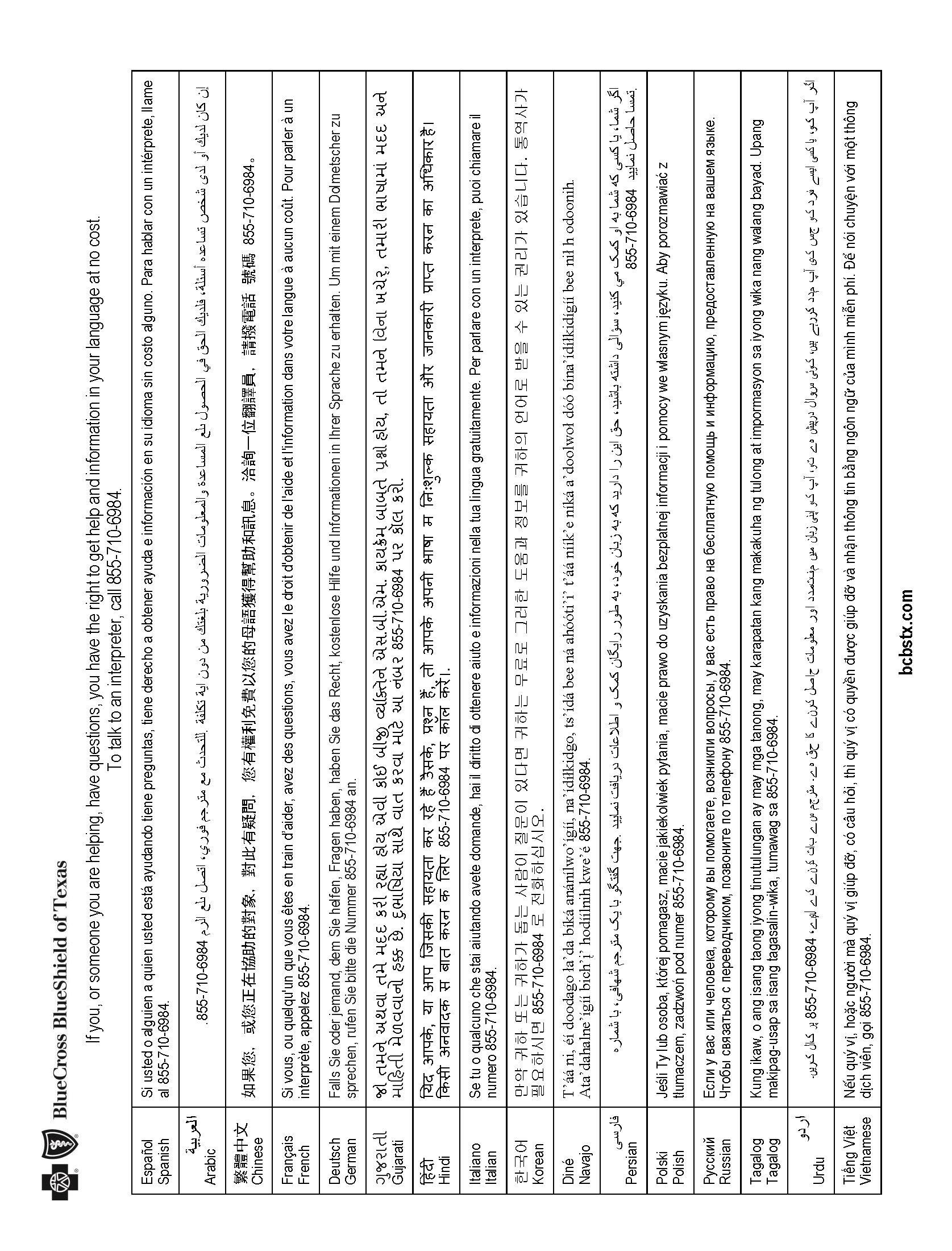
Health care coverage is important for everyone. We provide free communication aids and services for anyone with a disability or who needs language assistance. We do not discriminate on the basis of race, color, national origin, sex, gender identity, age, sexual orientation, health st atus or disability.
To receive language or communication assistance free of charge, please call us at 8557106984.
If you believe we have failed to provide a service, or think we have discriminated in another way, contact us to file a grievance .
Phone: 8556647270 (voicemail)
Office of Civil Rights Coordinator
300 E. Randolph St.
Fax: 8556616960
TTY/TDD: 8556616965 35th Floor
Chicago, Illinois 60601
You may file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights, at:
Phone: 8003681019
TTY/TDD: 8005377697
U.S. Dept. of Health & Human Services
200 Independence Avenue SW
Room 50 9F, HHH Building 1019
Complaint Forms: http://www.hhs.gov/ocr/office/file/index.html
Complaint Portal: https://ocrportal.hhs.gov/ocr/portal/lobby.jsf Washington, DC 20201
bcbstx.com

https://policy-srv.box.com/s/0wasy3ktn8r0knttb0ulevzvutx0bw2b.

T he Summary of Benefits and Coverage (SBC) document will help you choose a health plan . The SBC shows you how you and the plan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium ) will be provided separately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, call 18772992377 or at For general definitions of common terms, such as allowed amount, balance billing , coinsurance , copayment , deductible , provider , or other underlined terms, see the Glossary. You can view the Glossary at www.healthcare.gov/sbcglossary/ or call 18557564448 to request a copy. Important Questions Answers Why
Generally, you must pay all of the costs from providers up to the deductible amount before this plan begins to pay. If you have other family members on the plan , each family member must meet their own individual deductible until the total amount of deductible expenses paid by all family members meets the overall family deductible .
$3,500 Individual / $10,500 Family
Yes. Services that charge a copayment , prescription drugs , and preventive care are covered before you meet your deductible .
You must pay all of the costs for these services up to the specific deductible amount before this plan begins to pay for these services.
What is the overall deductible ?
This plan covers some items and services even if you haven’t yet met the deductible amount. But a copayment or coinsurance may apply. For example, this plan covers certain preventive services without cost shari ng and before you meet your deductible . See a list of covered preventive services at www.healthcare.gov/coverage/preventivecarebenefits/ . Are there other deductibles for specific services?
Are there services covered before you meet your deductible ?
The outofpocket limit is the most you could pay in a year for covered services. If you have other family members in this plan , they have to meet their own outofpocket limits until the overall family outofpocket limit has been met.
Yes. $500 Individual / $1500 Family prescription drug deductible for brand name drugs . There are no other specific deductibles .
$7,500 Individual / $18,200 Family
What is the outofpocket limit for this plan ?
Even though you pay these expenses, they don’t count toward the outofpocket limit .
What is not included in the outofpocket limit ? Premiums , balancebilling charges, and health care this plan doesn’t cover.
This plan uses a provider network . You will pay less if you use a provider in the plan ’s network . You will pay the most if you use an outofnetwork provider , and you might receive a bill from a provider for the difference between the provider ’s charge and what your plan pays ( balance bil ling ).
Be aware, your network provider might use an outofnetwork provider for some services (such as lab work). Check with your provider before you get services.
Will you pay less if you use a network provider ? Yes. See www.bcbstx.com or call 18008102583 for a list of network providers .
Do you need a referral to see a specialist ? Yes. This plan will pay some or all of the costs to see a specialist for covered services but only if you have a referral before you see the specialist .
costs shown in this chart are after your deductible has been met, if a deductible applies.
please refer to your

Virtual visits are
for more details.
You may have to pay for services that aren’t preventive . Ask your provider if the services needed are preventive . Then check what your plan will pay for.
Individual $1500 Family Retail covers a 30day supply. With appropriate prescription, up to a 90day supply is available. Mail order covers a 90day supply. Payment of the difference between the cost of a brand name drug and a generic may be required if a generic drug is available. Certain drugs require approval before they will be covered. The costsharing for insulin included in the drug list will not exceed $25 per prescription for a 30day supply, regardless of the amount or type of insulin needed to fi ll the prescription.
after
$130 retail/ $300 mail order/prescription after deductible Not Covered
Specialty drugs must be obtained from InNetwork specialty pharmacy provider . Specialty drugs are limited to a 30day supply except for certain FDAdesignated dosing regimens . Mail order is not covered. If you have
$500 /prescription after deductible
more information about limitations and exceptions, see the plan or policy document at
You may have to pay for services that are not covered by the visit fee. For an example, see “If you have a test” on page 2.
Certain services must be preauthorized; refer to your benefit booklet* for details. Virtual visits are available, please refer to your plan policy for more details.
Copay ment applies to first prenatal visit (per pregnancy). Cost sharing does not apply for preventive services . Depending on the type of services, a copayment , coinsurance , or deductible may apply. Maternity care may include tests and service described elsewhere in the SBC (i.e. ultrasound).
(Check your policy or plan document for more information and a list of any other excluded services
• Routine foot care • Weight loss programs Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.)
• Infertility t reatment ( diagnosis of infertility covered; invitro not covered.)
• Routine eye care (Adult)
• Dental care (Adult, limited coverage) • Hearing aids ( 1 per ear p er 36month period)
• Chiropractic care • Cosmetic surgery (limited coverage)
more information about limitations and exceptions, see the plan or policy document at
Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: For group health coverage contact the plan , Blue Cross and Blue Shield of Texas at 18772992377 or visit www.bcbstx.com . For group health coverage subject to ERISA, contact the U.S. Department of Labor’s Employee Benefits Security Administration at 1866444EBSA (3272) or www.dol.gov/ebs a/healthreform For nonfederal governmental group health plans , contact Department of Health and Human Services, Center for Consumer Information and Insurance Oversight, at 18772672323 x61565 or www.cciio.cms.gov . Church plans are not covered by the Federal COBRA continuation coverage rules. If the coverage is insured, individuals should contact their State insurance regulator regarding their pos sible rights to continuation coverage under State law. Other coverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace . For more information about the Marketplace , visit www.HealthCare.gov or call 18003182596 . Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim . This complaint is called a grievance or appeal . For more information about your rights, look at the explanation of benefits you will receive for that medica l claim . Your plan documents also provide complete information to submit a claim , appeal , or a grievance for any reason to your plan . For more information about your rights, this notice, or assistance, contact: For group health coverage subject to ERISA: B lue Cross and Blue Shield of Texas at 18772992377 or visit www.bcbstx.com , the U.S. Department of Labor's Employee Benefits Security Administration at 1866444EBSA (3272) or www.dol.gov/ebsa/healthreform , and the Texas Department of Insurance, Consumer Protection at 18002523439 or www.tdi.texas.gov . For nonfederal governmental group health plans and church plans that are group h ealth plans , Blue Cross and Blue Shield of Texas at 18772992377 or www.bcbstx.com or contact the Texas Department of Insurance, Consumer Protection at 18002523439 or www.tdi.texas.gov . Additionally, a consumer assistance program can help you file your appeal . Contact the Texas Department of Insurance’s Consumer Health Assistance Program at 18002523439 o r visit www.cms.gov/CCIIO/Resources/ConsumerAssistanceGrants/tx.html .
Does this plan provide Minimum Essential Coverage ? Yes . Minimum Essential Coverage generally includes plans , health insurance available through the Marketplace or other individual market pol icies, Medicare, Medicaid, CHIP, TRICARE, and certain other coverage. If you are eligible for certain types of Minimum Essential Coverage , you may not be eligible for the premium tax credit .
Does this plan meet the Minimum Value Standards ? Yes . If your pl an doesn’t meet the Minimum Value Standards , you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace .
Langua ge Access Services: Spanish (Español): Para obtener asistencia en Español, llame al 18772992377. Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 18772992377.
Chinese ( 中文 ): 如果需要中文的帮助, 请拨打这个号码 18772992377.
Navajo (Dine): Dine k'ehgo shika at'ohwol ninisingo, kwiijigo holne' 18772992377.
To see examples of how this plan might cover costs for a sample medical situation, see the next section.
About these Coverage Examples: This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the costsharing amounts ( deducti bles , copayments and coinsurance ) and excluded services under the plan . Use this information to compare the portion of costs you might pay under different health plans . Please note these coverage examples are based on selfonly coverage.
Simple Fracture

covered services.
The plan would be responsible for the other costs of these

Health care coverage is important for everyone. We provide free communication aids and services for anyone with a disability or who needs language assistance. We do not discriminate on the basis of race, color, national origin, sex, gender identity, age, sexual orientation, health st atus or disability.
To receive language or communication assistance free of charge, please call us at 8557106984.
If you believe we have failed to provide a service, or think we have discriminated in another way, contact us to file a grievance .
Phone: 8556647270 (voicemail)
Office of Civil Rights Coordinator
300 E. Randolph St.
Fax: 8556616960
TTY/TDD: 8556616965 35th Floor
Chicago, Illinois 60601
You may file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights, at:
Phone: 8003681019
TTY/TDD: 8005377697
U.S. Dept. of Health & Human Services
200 Independence Avenue SW
Room 50 9F, HHH Building 1019
Complaint Forms: http://www.hhs.gov/ocr/office/file/index.html
Complaint Portal: https://ocrportal.hhs.gov/ocr/portal/lobby.jsf Washington, DC 20201
bcbstx.com

https://policy-srv.box.com/s/x5aq54czhv0qvss2djtz8crz2slqsxs4.

T he Summary of Benefits and Coverage (SBC) document will help you choose a health plan . The SBC shows you how you and the plan would share the cost for covered health care services. NOTE: Information about the cost of this plan (called the premium ) will be provided separately. This is only a summary. For more information about your coverage, or to get a copy of the complete terms of coverage, call 18772992377 or at For general definitions of common terms, such as allowed amount, balance billing , coinsurance , copayment , deductible , provider , or other underlined terms, see the Glossary. You can view the Glossary at www.healthcare.gov/sbcglossary/ or call 18557564448 to request a copy. Important Questions Answers Why
Generally, you must pay all of the costs from providers up to the deductible amount before this plan begins to pay. If you have other family members on the plan , each family member must meet their own individual deductible until the total amount of deductible expenses paid by all family members meets the overall family deductible .
$1,250 Individual / $3,750 Family
Yes. Services that charge a copayment , prescription drugs , and preventive care are covered before you meet your deductible .
You must pay all of the costs for these services up to the specific deductible amount before this plan begins to pay for these services.
What is the overall deductible ?
The outofpocket limit is the most you could pay in a year for covered services. If you have other family members in this plan , they have to meet their own outofpocket limits until the overall family outofpocket limit has been met.
Even though you pay these expenses, they don’t count toward the outofpocket limit .
This plan uses a provider network . You will pay less if you use a provider in the plan ’s network . You will pay the most if you use an outofnetwork provider , and you might receive a bill from a provider for the difference between the provider ’s charge and what your plan pays ( balance bil ling ).
Be aware, your network provider might use an outofnetwork provider for some services (such as lab work). Check with your provider before you get services.
Yes. $250 Individual / Family
This plan covers some items and services even if you haven’t yet met the deductible amount. But a copayment or coinsurance may apply. For example, this plan covers certain preventive services without cost shari ng and before you meet your deductible . See a list of covered preventive services at www.healthcare.gov/coverage/preventivecarebenefits/ . Are there other deductibles for specific services?
Are there services covered before you meet your deductible ?
$750 prescription drug deductible for brand name drugs . There are no other specific deductibles .
$5,000 Individual / $15,000 Family
What is the outofpocket limit for this plan ?
What is not included in the outofpocket limit ? Premiums , balancebilling charges, and health care this plan doesn’t cover.
Will you pay less if you use a network provider ? Yes. See www.bcbstx.com or call 18008102583 for a list of network providers .
Do you need a referral to see a specialist ? Yes. This plan will pay some or all of the costs to see a specialist for covered services but only if you have a referral before you see the specialist .
costs shown in this chart are after your deductible has been met, if a deductible applies.
Virtual visits are available, please refer to your
for more details.
You may have to pay for services that aren’t preventive . Ask your provider if the services needed are preventive . Then check what your plan will pay for.

$750 Retail covers a 30day supply. With appropriate prescription, up to a 90day supply is available. Mail order covers a 90day supply. Payment of the difference between the cost of a brand name drug and a generic may be required if a g eneric drug is available. Certain drugs require approval before they will be covered. The costsharing for insulin included in the drug list will not exceed $25 per prescription for a 30day supply, regardless of the amount or type of insulin needed to fil l the prescription.
after
$80 retail/ $200 mail order/prescription after deductible Not Covered
Specialty drugs must be obtained from InNetwork specialty pharmacy provider . Specialty drugs are limited to a 30day supply except for certain FDAdesignated dosing regimens . Mail order is not covered. If you have
$500 /prescription after deductible
more information about limitations and exceptions, see the plan or policy document at
You may have to pay for services that are not covered by the visit fee. For an example, see “If you have a test” on page 2.
Certain services must be preauthorized; refer to your benefit booklet* for details. Virtual visits are available, please refer to your plan policy for more details.
Copay ment applies to first prenatal visit (per pregnancy). Cost sharing does not apply for preventive services . Depending on the type of services, a copayment , coinsurance , or deductible may apply. Maternity care may include tests and service described elsewhere in the SBC (i.e. ultrasound).
(Check your policy or plan document for more information and a list of any other excluded services
• Routine foot care • Weight loss programs Other Covered Services (Limitations may apply to these services. This isn’t a complete list. Please see your plan document.)
• Infertility t reatment ( diagnosis of infertility covered; invitro not covered.)
• Routine eye care (Adult)
• Dental care (Adult, limited coverage) • Hearing aids ( 1 per ear p er 36month period)
• Chiropractic care • Cosmetic surgery (limited coverage)
more information about limitations and exceptions, see the plan or policy document at
Your Rights to Continue Coverage: There are agencies that can help if you want to continue your coverage after it ends. The contact information for those agencies is: For group health coverage contact the plan , Blue Cross and Blue Shield of Texas at 18772992377 or visit www.bcbstx.com . For group health coverage subject to ERISA, contact the U.S. Department of Labor’s Employee Benefits Security Administration at 1866444EBSA (3272) or www.dol.gov/ebsa/healthreform For nonfederal governmental group health plans , contact Department of Health and Human Services, Center for Consumer Information and Insurance Oversight, at 18772672323 x61565 or www.cciio.cms.gov . Church plans are not covered by the Federal COBRA continuation coverage rules. If the coverage is insured, individuals should contact their State insurance regulator regarding their possible rights to continuation coverag e under State law. Other coverage options may be available to you too, including buying individual insurance coverage through the Health Insurance Marketplace . For more information about the Marketplace , visit www.He althCare.gov or call 18003182596 . Your Grievance and Appeals Rights: There are agencies that can help if you have a complaint against your plan for a denial of a claim . This complaint is called a grievance or appeal . For more information about your rights, look at the explanation of benefits you will receive for that medical claim . Your plan documents also provide complete information to submit a claim , appeal , or a gri evance for any reason to your plan . For more information about your rights, this notice, or assistance, contact: For group health coverage subject to ERISA: Blue Cross and Blue Shield of Texas at 18772992377 or visit www.bcbstx.com , the U.S. Department of Labor's Employee Benefits Security Administration at 1866444EBSA (3272) or www.dol.gov/ebsa/healthreform , and the Texas Department of Insurance, Consumer Protection at 18002523439 or www.tdi.texas.gov . For nonfederal governmental group health plans and church plans that are group health plans , Blue Cross and Blue Shield of Texas at 18772992377 or www.bcbstx.com or contact the Texas Department of Insurance, Consumer Protection at 18002523439 or www.tdi.texas.gov . Additionally, a consumer assistance program can help yo u file your appeal . Contact the Texas Department of Insurance’s Consumer Health Assistance Program at 18002523439 or visit www.cms.gov/CCIIO/Resources/ConsumerAssistanc eGrants/tx.html .
Does this plan provide Minimum Essential Coverage ? Yes . Minimum Essential Coverage generally includes plans , health insurance available through the Marketplace or other individual market policies, Medicare, Medicaid, C HIP, TRICARE, and certain other coverage. If you are eligible for certain types of Minimum Essential Coverage , you may not be eligible for the premium tax credit .
Does this plan meet the Minimum Value Standards ? Yes . If your plan doesn’t meet the Minimum Value Standards , you may be eligible for a premium tax credit to help you pay for a plan through the Marketplace .
Langua ge Access Services: Spanish (Español): Para obtener asistencia en Español, llame al 18772992377. Tagalog (Tagalog): Kung kailangan ninyo ang tulong sa Tagalog tumawag sa 18772992377.
Chinese ( 中文 ): 如果需要中文的帮助, 请拨打这个号码 18772992377.
Navajo (Dine): Dine k'ehgo shika at'ohwol ninisingo, kwiijigo holne' 18772992377.
To see examples of how this plan might cover costs for a sample medical situation, see the next section.
About these Coverage Examples: This is not a cost estimator. Treatments shown are just examples of how this plan might cover medical care. Your actual costs will be different depending on the actual care you receive, the prices your providers charge, and many other factors. Focus on the costsharing amounts ( deducti bles , copayments and coinsurance ) and excluded services under the plan . Use this information to compare the portion of costs you might pay under different health plans . Please note these coverage examples are based on selfonly coverage.
Simple Fracture

covered services.
The plan would be responsible for the other costs of these

Health care coverage is important for everyone. We provide free communication aids and services for anyone with a disability or who needs language assistance. We do not discriminate on the basis of race, color, national origin, sex, gender identity, age, sexual orientation, health st atus or disability.
To receive language or communication assistance free of charge, please call us at 8557106984.
If you believe we have failed to provide a service, or think we have discriminated in another way, contact us to file a grievance .
Phone: 8556647270 (voicemail)
Office of Civil Rights Coordinator
300 E. Randolph St.
Fax: 8556616960
TTY/TDD: 8556616965 35th Floor
Chicago, Illinois 60601
You may file a civil rights complaint with the U.S. Department of Health and Human Services, Office for Civil Rights, at:
Phone: 8003681019
TTY/TDD: 8005377697
U.S. Dept. of Health & Human Services
200 Independence Avenue SW
Room 50 9F, HHH Building 1019
Complaint Forms: http://www.hhs.gov/ocr/office/file/index.html
Complaint Portal: https://ocrportal.hhs.gov/ocr/portal/lobby.jsf Washington, DC 20201
bcbstx.com
This is an affordable supplemental plan that pays you should you be inpatient hospital confined. This plan complements your health insurance by helping you pay for costs left unpaid by your health insurance.
For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas
Rates are subject to change when enrolled in Medical.

Available Coverage: The benefit amounts shown in this summary will be paid regardless of the actual expenses incurred and are paid on a per day basis unless otherwise specified. Benefits are only payable when all policy terms and conditions are met. Please read all the information in this summary to understand the terms, conditions, state variations, exclusions, and limitations applicable to these benefits. See your Certificate of Insurance for more information.
Benefit Waiting Period:* None, unless otherwise stated. No benefits will be paid for a loss which occurs during the Benefit Waiting Period.
Newborn Nursery Care Admission
Limited to 1 day, 1 benefit per newborn child. This benefit is payable to the employee even if child coverage is not elected.
Newborn Nursery Care Stay*
Limited to 30 days, 1 benefit per newborn child. This benefit is payable to the employee even if child coverage is not elected.
How do I submit a claim?
Complete the claim form with the link provided below: https://www.cigna.com/static/www-cigna-com/docs/individuals-families/member-resources/hospital-care-claim-form.pdf
Options for filing the Claim Form:
• Call (800) 754-3207 to speak with one of our dedicated customer service representatives.
• Email your scanned documents to: SuppHealthClaims@Cigna.com
Benefit Amounts Payable: Benefits for all Covered Persons are payable at 100% of the Benefit Amounts shown, unless otherwise stated. Late applicants, if allowed under this plan, may be required to provide medical evidence of insurability.
NOTE: The following are some of the important policy provisions, terms and conditions that apply to benefits described in the policy. This is not a complete list. See your Certificate of Insurance for more information.
Benefit-Specific Conditions, Exclusions & Limitations (Hospital Care):
Hospital Admission: Must be admitted as an Inpatient due to a Covered Injury or Covered Illness. Excludes: treatment in an emergency room, provided on an outpatient basis, or for re-admission for the same Covered Injury or Covered Illness (including chronic conditions)
Hospital Chronic Condition Admission: Must be admitted as an Inpatient due to a covered chronic condition and treatment for a covered chronic condition must be provided by a specialist in that field of medicine. Excludes: treatment in an emergency room, provided on an outpatient basis, or for re-admission for the same Covered Injury or Covered Illness (including chronic conditions).
Hospital Stay: Must be admitted as an Inpatient and confined to the Hospital, due to a Covered Injury or Covered Illness, at the direction and under the care of a physician. If also eligible for the ICU Stay Benefit, only 1 benefit will be paid for the same Covered Injury or Covered Illness, whichever is greater. Hospital stays within 90 days for the same or a related Covered Injury or Covered Illness is considered one Hospital Stay.
Intensive Care Unit (ICU) Stay: Must be admitted as an Inpatient and confined in an ICU of a Hospital, due to a Covered Injury or Covered Illness, at the direction and under the care of a physician. If also eligible for the Hospital Stay Benefit, only 1 benefit will be paid for the same Covered Injury or Covered Illness, whichever is greater. ICU stays within 90 days for the same or a related Covered Injury or Covered Illness is considered one ICU stay
Hospital Observation Stay: Must be receiving treatment for a Covered Injury or Covered Illness in a Hospital, including an observation room, or ambulatory surgical center, for more than 24 hours on a non-inpatient basis and a charge must be incurred. This benefit is not payable if a benefit is payable under the Hospital Stay Benefit or Hospital Intensive Care Unit Stay Benefit
Newborn Nursery Care Admission and Newborn Nursery Care Stay: Must be admitted as an Inpatient and confined in a hospital immediately following birth at the direction and under the care of a physician.
Dental insurance is a coverage that helps defray the costs of dental care. It insures against the expense of routine care, dental treatment and disease.
For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas
Rates shown include the Disrict Contribution
Lincoln DentalConnect® Plan
Benefits At-A-Glance - Group# 0001D040929
• Plan cover many preventive, basic, and major dental care services. (See Below)
• Both plans allow you to choose any dentist you wish, though you can lower your out-of-pocket costs by selecting a contracting dentist.
• Does not make you and your dependents wait six months between routine cleanings.
Dentists
Individual: $50 Family: $150
Plan Year Deductible
Waived for: Preventive
Dentists
Individual: $50 Family: $150
Waived for: Preventive
Deductibles are combined for basic and major Contracting Dentists’ services.
Deductibles are combined for basic and major Non-Contracting Dentists’ services.
Plan Year Maximum
$2,000
$2,000
Plan Year Maximums are combined for preventive, basic, and major services.
Waiting Period There are no benefit waiting periods for any service types
Lifetime Orthodontic Max
Basic Services
$1,000
$1,000 Orthodontic Coverage is available for dependent children. Age 19
• Palliative treatment (including emergency relief of dental pain) Injections of antibiotics and other therapeutic medications Fillings
• Simple extractions Surgical extractions Oral surgery
• Biopsy and examination of oral tissue (including brush biopsy) General anesthesia and I.V. sedation
• Prosthetic repair and recementation services Endodontics (including root canal treatment) Periodontal maintenance procedures
• Non-surgical periodontal therapy Periodontal surgery
• Denture reline and rebase services
• Occlusal guard
Lincoln DentalConnect® Plan
Benefits At-A-Glance - Group# 0001D040928
You can request your dental ID card by contacting Lincoln Financial Dental directly at (800) 423-2765 and mention Group ID: LIFESCHDAL
Plan Year Deductible
Deductibles are combined for basic and major Contracting Dentists’ services.
Deductibles are combined for basic and major Non-Contracting Dentists’ services. Plan Year Maximum
Plan Year Maximums are combined for preventive, basic, and major services.
Waiting Period There are no benefit waiting periods for any service types Basic Services
• Palliative treatment (including emergency relief of dental pain) Injections of antibiotics and other therapeutic medications Fillings
• Biopsy and examination of oral tissue (including brush biopsy) Prosthetic repair and recementation services
• Denture reline and rebase services
You can also go to www.lfg.com and register/login to access your account and Downloand the Lincoln Dental Mobile App.
• Find a network dentist near you in minutes
• Have an ID card on your phone
• Customize the app to get details of your plan
DHMO Plan
Lincoln DentalConnect® Plan
Benefits At-A-Glance - Group #0001D040930
• Find out how much your plan covers for checkups and other services
• Keep track of your claims
Trips to the dentist are a little less scary when you know how much you’ll pay ahead of time. And easier, too, with no claim forms or deductibles.
Here’s how this important coverage works.
• You choose your primary-care dentist when you enroll. To find a participating dentist, visit http://ldc.lfg.com and select Find a Dentist. (You can also print your dental ID card from this site once your coverage begins.)
• This dental plan offers a detailed list of covered procedures, each with a dollar copayment (see the Summary of Benefits for details). You pay for services provided during your visit.
• Emergency care away from home is covered up to a set dollar limit.
• You can change your primary-care dentist at any time by calling the customer service number listed on your dental ID card.
Vision insurance provides coverage for routine eye examinations and can help with covering some of the costs for eyeglass frames, lenses or contact lenses.
For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas

You can request your vision id card by contacting Superior Vision directly at (800) 507-3800. You can also go to www.superiorvision.com and register/login to access your account by clicking on “Members” at the top of the page. You can also download the Superior Vision mobile app on your smart phone.
Look for providers in the provider directory who accept discounts, as some do not; please verify their services and discounts (range from 10%-30%) prior to service as they vary.
Discounts on covered materials
Frames: 20% off amount over allowance
Lens options: 20% off retail
Progressives: 20% off amount over retail lined trifocal lens, including lens options
Speciality contact lens fit: 10% off retail, then apply allowance
Discounts on non-covered exam, services and materials
Exams, frames, and prescription lenses: 30% off retail
Lens options, contacts, miscellaneous options: 20% off retail
Disposable contact lenses: 10% off retail
Retinal imaging: $39 maximum out-of-pocket
The following options have out-of-pocket maximums5 on standard (not premium, brand, or progressive) lenses.
5. Discounts and maximums may vary by lens type. Please check with your provider.
Superior Vision has a nationwide network of independent refractive surgeons and partnerships with leading LASIK networks who offer members a discount. These discounts range from 10%-50%, and are the best possible discounts available to Superior Vision.
Disability insurance protects one of your most valuable assets, your paycheck. This insurance will replace a portion of your income in the event that you become physically unable to work due to sickness or injury for an extended period of time.
For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas
Who is eligible?
You are eligible for Long Term Disability (LTD) coverage if you are an active employee in the United States working a minimum of 32 hours per week. This benefit is employer paid.
What is my monthly benefit amount?
Your employer is providing a benefit of 60% of your monthly earnings to a maximum of $9,500.
How long do I have to wait to receive benefits?
The elimination period is the length of time you must be continuously disabled before you can receive benefits.
You could begin receiving LTD benefits if, after 90 days of disability, you are still disabled (as described in the definition of disability).
If you return to work while satisfying the elimination period and are no longer disabled, you may satisfy the elimination period within the accumulation period – you don’t have to be continuously disabled through the elimination period, if you are satisfying the elimination period under this provision. If you don’t satisfy the elimination period within the accumulation period, a new period of disability will begin.
Accumulation Period is the period of time from the date the disability begins during which you must satisfy the elimination period. The accumulation period is two times your elimination period.
During your elimination period, you will be considered disabled if you are limited from performing the material and substantial duties of your regular occupation due to your sickness or injury, and you are under the regular care of a physician. You are not required to have a 20% or

more earnings loss to be considered disabled during the elimination period due to the same sickness or injury.
The duration of your benefit payments is based on your age when your disability occurs. Your LTD benefits are payable for the period during which you continue to meet the definition of disability. If your disability occurs before age 62, benefits could be payable up to the Social Security Normal Retirement Age. If your disability occurs at or after age 62, your benefits would be paid according to the benefit duration schedule.
What is my maximum monthly benefit amount?
Your total monthly benefit (including all benefits provided under this plan) will not exceed 100% of your monthly earnings, unless the excess amount is payable as a Cost of Living Adjustment.
Can my benefit be reduced?
Your disability benefit may be reduced by deductible sources of income and any earnings you have while disabled. Deductible sources of income may include such items as disability income or other amounts you receive or are entitled to receive under: workers’ compensation or similar occupational benefit laws; state compulsory benefit laws; automobile liability and no fault insurance; legal judgments and settlements; certain retirement plans; other group or association disability programs or insurance; and amounts you or your family receive or are entitled to receive from Social Security or similar governmental programs.
When would I be considered disabled?
During the first 24 months, you are disabled when Unum determines that:
• You are unable to perform the material and substantial duties of your regular occupation* due to sickness or injury and are not working; or
• You have a 20% or more loss of indexed monthly earnings while working.
• After 24 months of payments, you are disabled when Unum determines that due to the same sickness or injury:
• You are unable to perform the duties of any gainful occupation for which you are reasonably fitted by education, training or experience.
Can I receive rehabilitation and return-to-work services?
If you are deemed eligible and are participating in the program, Unum will pay an additional benefit of 10% of your gross disability payment to a maximum of $1,000 per month.
What other services are available?
If you are disabled, participating in the rehabilitation and return-to-work assistance program, and have dependent care expenses, you may also receive the dependent care expense benefit — $350 per dependent per month, to a monthly maximum of $1,000 for all eligible dependents combined.
Disability insurance protects one of your most valuable assets, your paycheck. This insurance will replace a portion of your income in the event that you become physically unable to work due to sickness or injury for an extended period of time.
For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas
Rates shown are calculated by using your annual salary. Please refer to the plan summary for a more detailed explanation.
Who is eligible?
You are eligible for Short Term Disability coverage if you are an active employee in the United States working a minimum of 32 hours per week.
What is my weekly benefit amount?
You can elect to purchase a benefit of 60% of your weekly earnings to a maximum of $500 per week.
How long do I have to wait to receive benefits?
The elimination period is the length of time you must be continuously disabled before you can receive benefits. If your disability is the result of a covered injury or sickness, you could begin receiving benefits after 7 days.
When would I be considered disabled?
• You are disabled when Unum determines that, due to sickness or injury:
• You are limited from performing the material and substantial duties of your regular occupation
• You have a 20% or more loss in weekly earnings due to the same sickness or injury.
• You must be under the regular care of a physician to be considered disabled.
*Unless the policy specifies otherwise, as part of the disability claims evaluation process, Unum will evaluate your occupation based on how it is normally performed in the national economy, not how work is performed for a specific employer, at a specific location, or in a specific region.

How long will my benefits last?
If you continue to meet the definition of disability, you may receive benefits for 12 weeks.
Do you have kids playing sports, are you a weekend warrior, or maybe you’re accident-prone? Accident plans are designed to help pay for medical costs associated with accidents and benefits are paid directly to you.
full plan details, please visit your benefit website: www.mybenefitshub.com/

Based upon the need for and length of sutures
follow-up visits (up to six visits)
Alternative care/rehabilitative confinement
Epidural/cortisone pain management (up to one injection)
Wheelchair (expected use one year or more)
driver injury/death: Motor vehicle helmet
Safe rider: Other helmet (bicycle, scooter, skateboard, etc.)
*Fracture benefits listed are nonsurgical. Treatment for the fracture must occur within 90 days of the accident. The combined maximum of all fractures is two times the highest fracture payable.
**Dislocation benefits listed are nonsurgical. Treatment for the dislocation must occur within 90 days of the accident. The combined maximum of all dislocations is two times the highest dislocation payable.
***Benefits will be paid up to two times the highest surgical benefit payable for all surgeries.
Critical illness insurance can be used towards medical or other expenses. It provides a lump sum benefit payable directly to the insured upon diagnosis of a covered condition or event, like a heart attack or stroke. The money can also be used for non-medical costs related to the illness, including transportation, child care, etc.
For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas

Employee Guaranteed coverage amounts
Spouse Guaranteed coverage amount
Children Guaranteed coverage amount
$10,000, $20,000 or $30,000
$10,000, $20,000 or $30,000 (up to 100% of the employee coverage amount)
$5,000, $10,000 or $15,000 (up to 100% of the employee coverage amount)
cancer (in situ)
Skin Cancer (other than melanoma) $500 per lifetime
ALS/Lou Gehrig’s disease
Benign brain tumor
Loss of sight, hearing and/or speech
Severe burns, permanent paralysis or traumatic brain injuries (includes coma)
Group term life is the most inexpensive way to purchase life insurance. You have the freedom to select an amount of life insurance coverage you need to help protect the well-being of your family.
Accidental Death & Dismemberment is life insurance coverage that pays a death benefit to the beneficiary, should death occur due to a covered accident. Dismemberment benefits are paid to you, according to the benefit level you select, if accidentally dismembered.
For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas
What you need to know about your Basic Life and AD&D Benefits
Guaranteed Issue: Employee: $20,000
Accidental Death and Dismemberment (AD&D): Additional life insurance benefits may be payable in the event of an accident which results in death or dismemberment as defined in the contract. Additional AD&D benefits include seat belt, air bag, repatriation, child higher education, child care, paralysis/loss of use, severe burns, disappearance, and exposure.
Accelerated Life Benefit: If diagnosed with a terminal illness and have less than 12 months to live, you may apply to receive 25%, 50% or 75% of your life insurance benefit to use for whatever you choose.
Reductions: Upon reaching certain ages, your original benefit amount will reduce to the percentage shown in the following schedule.
Basic Employee Life and AD&D Coverage
Your Life and AD&D insurance coverage amount is $20,000. This is an employer paid benefit to full time employees. Coverage is provided at no cost to you.
What you need to know about your Voluntary Term Life Benefits and AD&D Benefits
Flexible Options:
Employee: $10,000 to $500,000, in $10,000 increments.
Spouse: $10,000 to $500,000, in $5,000 increments, not to exceed 100% of the employee’s amount.
Guaranteed Issue:
Employee: $200,000
Spouse: $50,000
Child: $10,000

Dependent Life Coverage: Optional dependent life coverage is available to eligible employees. You must select employee coverage in order to cover your spouse and/or child(ren).
Accelerated Life Benefit: If diagnosed with a terminal illness and have less than 12 months to live, you may apply to receive 25%, 50% or 75% of your life insurance benefit to use for whatever you choose.
Guaranteed Increase In Benefit: You may be eligible to increase your coverage annually until you reach your maximum amount without providing evidence of insurability.
Accidental Death and Dismemberment (AD&D): You must select Life coverage in order to select any AD&D coverage. Additional life insurance benefits may be payable in the event of an accident which results in death or dismemberment as defined in the contract.
Group Term Life Insurance to age 121 with Quality of Life

Make a smart choice to help protect your loved ones and your future.
Help protect your family with the Family Protection Plan Group Level Term Life Insurance to age 121. You can get coverage for your spouse even if you don’t elect coverage on yourself. And you can cover your financially dependent children and grandchildren (14 days to 26 years old). The coverage lasts until age 121 for all insured,* so no matter what the future brings, your family is protected.
Buying life insurance when you’re younger allows you to take advantage of lower premium rates while you’re generally healthy, which allows you to purchase more insurance coverage for the future. This is especially important if you have dependents who rely on your income, or you have debt that would need to be paid off.
Portable
Coverage continues with no loss of benefits or increase in cost if you terminate employment after the first premium is paid. We simply bill you directly.
Life moves fast so having a portable life insurance allows you to keep your coverage if you leave your school district. Keeping the coverage helps you ensure your family is protected even into your retirement years.
44% of American households would encounter significant financial difficulties within six months if they lost the primary family wage earner. 28% would reach this point in one month or less.

Group Term
Terminal illness acceleration of benefits
Coverage pays 30% (25% in CT and MI) of the coverage amount in a lump sum upon the occurrence of a terminal condition that will result in a limited life span of less than 12 months (24 months in IL).
Protection you can count on
Within one business day of notification, payment of 50% of coverage or $10,000 whichever is less is mailed to the beneficiary, unless the death is within the two-year contestability period and/or under investigation. This coverage has no war or terrorism exclusions.
Convenient
Easy payment through payroll deduction.
Quality of Life benefit
Optional benefit that accelerates a portion of the death benefit on a monthly basis, up to 75% of your benefit, and is payable directly to you on a tax favored basis* for the following:
•Permanent inability to perform at least two of the six Activities of Daily Living (ADLs) without substantial assistance; or
•Permanent severe cognitive impairment, such as dementia, Alzheimer’s disease and other forms of senility, requiring substantial supervision.
Many individuals who can’t take care of themselves require special accommodations to perform ADLs and would need to make modifications to continue to live at home with physical limitation. The proceeds from the Quality of Life benefit can be used for any purpose, including costs for infacility care, home healthcare professionals, home modifications, and more.
2024 Enrollment Plan Year
Guaranteed Issue is offered to all eligible applicants regardless of health status. No Doctor exams or physicals.
Employee: $100,000 | Spouse: $30,000 | Child: $10,000
Enroll to provide peace of mind for your family
To do an initial enrollment or if you have questions please call our customer service at 866-914-5202. Monday - Friday | 8:00 am-6:00 pm CST

The Family Protection Plan offers a lump-sum cash benefit if you die before age 121. The initial death benefit is guaranteed to be level for at least the first ten policy years. Afterward, the company intends to provide a nonguaranteed death benefit enhancement which will maintain the initial death benefit level until age 121. The company has the right to discontinue this enhancement. The death benefit enhancement cannot be discontinued on a particular insured due to a change in age, health, or employment status.
Medical Transport covers emergency transportation to and from appropriate medical facilities by covering the out-of-pocket costs that are not covered by insurance. It can include emergency transportation via ground ambulance, air ambulance and helicopter, depending on the plan.
For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas

A MASA MTS Membership provides the ultimate peace of mind at an affordable rate for emergency ground and air transportation service within the United States and Canada, regardless of whether the provider is in or out of a given group healthcare benefits network. If a member has a high deductible health plan that is compatible with a health savings account, benefits will become available under the MASA membership for expenses incurred for medical care (as defined under Internal Revenue Code (“IRC”) section 213 (d)) once a member satisfies the applicable statutory minimum deductible under IRC section 223(c) for high-deductible health plan coverage that is compatible with a health savings account.
Emergent Air Transportation In the event of a serious medical emergency, Members have access to emergency air transportation into a medical facility or between medical facilities.
Emergent Ground Transportation In the event of a serious medical emergency, Members have access to emergency ground transportation into a medical facility or between medical facilities.
Non-Emergency Inter-Facility Transportation In the event that a member is in stable condition in a medical facility but requires a heightened level of care that is not available at their current medical facility, Members have access to nonemergency air or ground transportation between medical facilities.
Repatriation/Recuperation Suppose you or a family member is hospitalized more than 100-miles from your home. In that case, you have benefit coverage for air or ground medical transportation into a medical facility closer to your home for recuperation.
Should you need assistance with a claim contact MASA at (800) 643-9023. You can find full benefit details www.mybenefitshub.com/lifeschoolofdallas
Only $14.00 per month to cover you and your family!


As identity theft and fraud continue to increase, an evolving suite of products helps you monitor any potential threats to your identity and alerts you if there are any areas of concern. You will also have access to proactive digital privacy tools that can help you keep passwords and other personal information private and secure while surfing the web.
Identity Theft insurance1
Get help when things go bad. Generous insurance is there to cover up to $1M of fraud recovery expenses.

Identity Restoration
Get back on track with help from a trained agent that can walk you through the process of reclaiming what’s yours.
Digital Identity Manager™
Reclaim exposed info from people finder sites to help reduce your risk of ID theft and potential fraud.
Experian® CreditLock
Block fraudsters from getting new credit with your info to help prevent ID theft. Unlock when applying for credit.
Secure VPN
Helps to prevent people and companies from collecting your personal information and data.

Password Manager
Safely store and protect your logins and payment info in one place with airtight security features.

Dark Web Monitoring
We’ll alert you if we detect any threats on the millions of data points we scan, so you can protect your information.
Safe Browser
Get alerted when you visit unsafe websites, block ads and help prevent tracking of your personal data.

1 The Identity Theft Insurance is underwritten and administered by American Bankers Insurance Company of Florida, an Assurant company under group or blanket policy(ies). The description herein is a summary and intended for informational purposes only and does not include all terms, conditions and exclusions of the policies described. Please refer to the actual policies for terms, conditions, and exclusions of coverage. Coverage may not be available in all jurisdictions.



Take control and improve how lenders see you with a credit education experience from Experian®. Innovative features provide you direct access to the reports and scores lenders use to make credit approval decisions.
Unlimited Account Link (Checking, Credit, 401k etc.)
Automated Budgets powered by Artificial Intelligence
Digital Wallet (Venmo®, Apple Pay®, PayPal®, etc.)
Transaction & Spending Categorization
Spending Summaries & Payment Reminders
Debt & Cashflow Management
Financial Goal Planning & Tracking
Net Worth & Investment Tracking
Financial Health Analysis & Score
Account Activity & Transaction Alerts
Credit & Financial Improvement Insights
50+ unique recommendations to help achieve financial goals sooner including activity, spending, budgeting, and VantageScore®* improvements.
Innovative Money Management Features
Link all your accounts to stay on top of your daily spending with recommended budgets powered by AI and machine learning of past transactional behavior.



Automated Budgeting Transaction Monitoring Cashflow Analysis

1 Calculated on the VantageScore 3.0 model. Your VantageScore 3.0 from Experian® indicates your credit risk level and is not used by all lenders, so don’t be surprised if your lender uses a score that’s different from your VantageScore 3.0. Click here to learn more
2 Child credit freeze assistance via call center by legal parent or guardian.



returns); (b) your taxable compensation; (c) your spouse’s actual or deemed earned income.
“Register” in the top right corner, and follow the




An Employee Assistance Program (EAP) is a program that assists you in resolving problems such as finding child or elder care, relationship challenges, financial or legal problems, etc. This program is provided by your employer at no cost to you.
For full plan details, please visit your benefit website: www.mybenefitshub.com/lifeschoolofdallas
Personal issues, planning for life events or simply managing daily life can affect your work, health, and family. Your Guidance Resources program provides support, resources, and information for personal and work-life issues. The program is companysponsored, confidential, and provided at no charge to you and your dependents. This explains how Guidance Resources can help you and your family deal with everyday challenges.
Counseling
3 Session Plan
This no-cost counseling service helps you address stress, relationship and other personal issues you and your family may face. It is staffed by GuidanceConsultantsSM—highly trained master’s and doctoral level clinicians who will listen to your concerns and quickly refer you to in-person counseling (up to 3 sessions per year) and other resources for:
› Stress, anxiety and depression
› Relationship/marital conflicts
› Problems with children
› Job pressures
› Grief and loss
› Substance abuse
Financial Information and Resources
Discover your best options.
Speak by phone with our Certified Public Accountants and Certified Financial Planners on a wide range of financial issues including:
› Getting out of debt
› Credit card or loan problems
› Tax questions
Legal Support and Resources
Expert info when you need it.
› Retirement planning
› Estate planning
› Saving for college
Talk to our attorneys by phone. If you require representation, we’ll refer you to a qualified attorney in your area for a free 30-minute consultation with a 25% reduction in customary legal fees thereafter. Call about:
› Divorce and family law transactions
› Debt and bankruptcy
› Real estate
› Civil and criminal actions
› Contracts

Delegate your “to-do” list.
Our Work-Life specialists will do the research for you, providing qualified referrals and customized resources for:
› Child and elder care
› Moving and relocation
› Making major purchases
GuidanceResources® Online
Knowledge at your fingertips.
› College planning
› Pet care
› Home repair
GuidanceResources Online is your one stop for expert information on the issues that matter most to you… relationships, work, school, children, wellness, legal, financial, free time and more.
› Timely articles, HelpSheetsSM, tutorials, streaming videos and self-assessments
› “Ask the Expert” personal responses to your questions
› Child care, elder care, attorney and financial planner searches
Online Will Preparation
Get peace of mind.
EstateGuidance® lets you quickly and easily write a will on your computer. Just go to www.guidanceresources.com and click on the EstateGuidance link. Follow the prompts to create and download your will at no cost. Online support and instructions for executing and filing your will are included. You can:
› Name an executor to manage your estate
› Choose a guardian for your children
› Specify your wishes for your property
› Provide funeral and burial instructions
Call Your ComPsych Guidance Resources program anytime for confidential assistance.
Call: (855) 387-9727 TDD: (800) 697-0353
Go online: guidanceresources.com
Your company Web ID: ONEAMERICA3
Enrollment Guide General Disclaimer: This summary of benefits for employees is meant only as a brief description of some of the programs for which employees may be eligible. This summary does not include specific plan details. You must refer to the specific plan documentation for specific plan details such as coverage expenses, limitations, exclusions, and other plan terms, which can be found at the Life School of Dallas Benefits Website. This summary does not replace or amend the underlying plan documentation. In the event of a discrepancy between this summary and the plan documentation the plan documentation governs. All plans and benefits described in this summary may be discontinued, increased, decreased, or altered at any time with or without notice.
Rate Sheet General Disclaimer: The rate information provided in this guide is subject to change at any time by your employer and/or the plan provider. The rate information included herein, does not guarantee coverage or change or otherwise interpret the terms of the specific plan documentation, available at the Life School of Dallas Benefits Website, which may include additional exclusions and limitations and may require an application for coverage to determine eligibility for the health benefit plan. To the extent the information provided in this summary is inconsistent with the specific plan documentation, the provisions of the specific plan documentation will govern in all cases.