






Higginbotham Public Sector (800) 583-6908 www.mybenefitshub.com/snyderisd
The Standard Group #160-763263 (800) 877-7195 www.standard.com
The Hartford (800) 523-2233 www.TheHartford.com
Higginbotham (866) 419-3519 https://flexservices.higginbotham.net
CHUBB
Group #100000226 (888) 499-0425 www.chubb.com/
Experian (855) 797-0052 www.experian.com
Important
BCBSTX (866) 355-5999 www.bcbstx.com/trsactivecare
CHUBB
Group #100000226 (888) 499-0425 www.chubb.com/
CHUBB
Group #100000226 (888) 499-0425 www.chubb.com/
CHUBB (888) 499-0425 www.chubb.com
CHUBB
Group #100000226 (888) 499-0425 www.chubb.com/
Group #FBS (888) 365-1663 www.consultmdlive.com
Lincoln Financial Group Group #snyderisd (800) 423-2765 www.lfg.com
The Hartford Group #VAC-888367 (800) 523-2233 www.TheHartford.com
EECU (817) 882-0800 www.eecu.org/
5Star Group #2596 (866) 863-9753 www.5starlifeinsurance.com/
MASA
Group #MKSNYISD (800) 423-3226 www.masamts.com/
Clever RX (800) 873-1195 www.cleverrx.com
Enrollment assistance is available by calling Higginbotham Public Sector at (866) 914-5202 to speak to a representative. Spanish speaking representatives are also available. Hours are Monday—Friday 8:00 AM - 6:00 PM.
Annual Open Enrollment Benefit elections will become effective 9/1/2024 (elections requiring evidence of insurability, such as life Insurance, may have a later effective date, if approved). After annual enrollment closes, benefit changes can only be made if you experience a qualifying event (and changes must be made within 31 days of event).


1 www.mybenefitshub.com/snyderisd
2
CLICK LOGIN
3 Enter your Information
• Last Name
• Date of Birth
• Last Four (4) of Social Security Number
NOTE: THEbenefitsHUB uses this information to check behind the scenes to confirm your employment status.
4
5
Once confirmed, the Additional Security Verification page will list the contact options from your profile. Select either Text, Email, Call, or Ask Admin options to receive a code to complete the final verification step.
Enter the code that you receive and click Verify. You can now complete your benefits enrollment!
During your annual enrollment period, you have the opportunity to review, change or continue benefit elections each year. Changes are not permitted during the plan year (outside of annual enrollment) unless a Section 125 qualifying event occurs.
• Changes, additions or drops may be made only during the annual enrollment period without a qualifying event.
• Employees must review their personal information and verify that dependents they wish to provide coverage for are included in the dependent profile. Additionally, you must notify your employer of any discrepancy in personal and/or benefit information.
• Employees must confirm on each benefit screen (medical, dental, vision, etc.) that each dependent to be covered is selected in order to be included in the coverage for that particular benefit.
All new hire enrollment elections must be completed in the online enrollment system within the first 30 days of benefit eligible employment. Failure to complete elections during this timeframe will result in the forfeiture of coverage.
For supplemental benefit questions, you can contact your Benefit Office or you can call Higginbotham Public Sector at (866) 914-5202 for assistance.
For benefit summaries and claim forms, go to your benefit website: www.mybenefitshub.com/snyderisd Click the benefit plan you need information on (i.e., Dental) and you can find the forms you need under the Benefits and Forms section.
For benefit summaries and claim forms, go to the Snyder ISD benefit website: www.mybenefitshub.com/snyderisd. Click on the benefit plan you need information on (i.e., Dental) and you can find provider search links under the Quick Links section.
If the insurance carrier provides ID cards, you can expect to receive those 3-4 weeks after your effective date. For most dental and vision plans, you can log in to the carrier website and print a temporary ID card or simply give your provider the insurance company’s phone number, and they can call and verify your coverage if you do not have an ID card at that time. If you do not receive your ID card, you can call the carrier’s customer service number to request another card.
If the insurance carrier provides ID cards, but there are no changes to the plan, you typically will not receive a new ID card each year.
A Cafeteria plan enables you to save money by using pre-tax dollars to pay for eligible group insurance premiums sponsored and offered by your employer. Enrollment is automatic unless you decline this benefit. Elections made during annual enrollment will become effective on the plan effective date and will remain in effect during the entire plan year.
Marital Status
Change in Number of Tax Dependents
Change in Status of Employment Affecting Coverage Eligibility
Gain/Loss of Dependents’ Eligibility Status
Judgment/ Decree/Order
Eligibility for Government Programs
Changes in benefit elections can occur only if you experience a qualifying event. You must present proof of a qualifying event to your Benefit Office within 30 days of your qualifying event and meet with your Benefit Office to complete and sign the necessary paperwork in order to make a benefit election change. Benefit changes must be consistent with the qualifying event.
A change in marital status includes marriage, death of a spouse, divorce or annulment (legal separation is not recognized in all states).
A change in number of dependents includes the following: birth, adoption and placement for adoption. You can add existing dependents not previously enrolled whenever a dependent gains eligibility as a result of a valid change in status event.
Change in employment status of the employee, or a spouse or dependent of the employee, that affects the individual’s eligibility under an employer’s plan includes commencement or termination of employment.
An event that causes an employee’s dependent to satisfy or cease to satisfy coverage requirements under an employer’s plan may include change in age, student, marital, employment or tax dependent status.
If a judgment, decree, or order from a divorce, annulment or change in legal custody requires that you provide accident or health coverage for your dependent child (including a foster child who is your dependent), you may change your election to provide coverage for the dependent child. If the order requires that another individual (including your spouse and former spouse) covers the dependent child and provides coverage under that individual’s plan, you may change your election to revoke coverage only for that dependent child and only if the other individual actually provides the coverage.
Gain or loss of Medicare/Medicaid coverage may trigger a permitted election change.
Supplemental Benefits: Eligible employees must work 20 or more regularly scheduled hours each work week.
Eligible employees must be actively at work on the plan effective date for new benefits to be effective, meaning you are physically capable of performing the functions of your job on the first day of work concurrent with the plan effective date. For example, if your 2024 benefits become effective on September 1, 2024, you must be actively-at-work on September 1, 2024 to be eligible for your new benefits.
Dependent Eligibility: You can cover eligible dependent children under a benefit that offers dependent coverage, provided you participate in the same benefit, through the maximum age listed below. Dependents cannot be double covered by married spouses within the district as both employees and dependents.
Please note, limits and exclusions may apply when obtaining coverage as a married couple or when obtaining coverage for dependents.
Potential Spouse Coverage Limitations: When enrolling in coverage, please keep in mind that some benefits may not allow you to cover your spouse as a dependent if your spouse is enrolled for coverage as an employee under the same employer. Review the applicable plan documents, contact Higginbotham Public Sector, or contact the insurance carrier for additional information on spouse eligibility.
FSA/HSA Limitations: Please note, in general, per IRS regulations, married couples may not enroll in both a Flexible Spending Account (FSA) and a Health Savings Account (HSA). If your spouse is covered under an FSA that reimburses for medical expenses then you and your spouse are not HSA eligible, even if you would not use your spouse’s FSA to reimburse your expenses. However, there are some exceptions to the general limitation regarding specific types of FSAs. To obtain more information on whether you can enroll in a specific type of FSA or HSA as a married couple, please reach out to the FSA and/or HSA provider prior to enrolling or reach out to your tax advisor for further guidance.
Potential Dependent Coverage Limitations: When enrolling for dependent coverage, please keep in mind that some benefits may not allow you to cover your eligible dependents if they are enrolled for coverage as an employee under the same employer. Review the applicable plan documents, contact Higginbotham Public Sector, or contact the insurance carrier for additional information on dependent eligibility.
Disclaimer: You acknowledge that you have read the limitations and exclusions that may apply to obtaining spouse and dependent coverage, including limitations and exclusions that may apply to enrollment in Flexible Spending Accounts and Health Savings Accounts as a married couple. You, the enrollee, shall hold harmless, defend, and indemnify Higginbotham Public Sector from any and all claims, actions, suits, charges, and judgments whatsoever that arise out of the enrollee’s enrollment in spouse and/or dependent coverage, including enrollment in Flexible Spending Accounts and Health Savings Accounts.
If your dependent is disabled, coverage may be able to continue past the maximum age under certain plans. If you have a disabled dependent who is reaching an ineligible age, you must provide a physician’s statement confirming your dependent’s disability. Contact your Benefit Office to request a continuation of coverage.
Description
(IRC Sec. 223)
Approved by Congress in 2003, HSAs are actual bank accounts in employees' names that allow employees to save and pay for unreimbursed qualified medical expenses tax-free.
Employer Eligibility A qualified high deductible health plan
Contribution Source Employee and/or employer
Account Owner Individual
Underlying Insurance
Requirement
Minimum Deductible
Maximum Contribution
High deductible health plan
$1,600 single (2024)
$3,200 family (2024)
$4,150 single (2024)
$8,300 family (2024) 55+ catch up +$1,000
Permissible Use Of Funds
Cash-Outs of Unused Amounts (if no medical expenses)
Year-to-year rollover of account balance?
Does the account earn interest?
Portable?
Employees may use funds any way they wish. If used for non-qualified medical expenses, subject to current tax rate plus 20% penalty.
Flexible
(IRC Sec. 125)
Allows employees to pay out-of-pocket expenses for copays, deductibles and certain services not covered by medical plan, taxfree. This also allows employees to pay for qualifying dependent care tax-free.
All employers
Employee and/or employer
Employer
None
N/A
$3,200 (2024)
Reimbursement for qualified medical expenses (as defined in Sec. 213(d) of IRC).
Permitted, but subject to current tax rate plus 20% penalty (penalty waived after age 65). Not permitted
Yes, will roll over to use for subsequent year’s health coverage.
Yes
Yes, portable year-to-year and between jobs.
No. Access to some funds may be extended if your employer’s plan contains a 2 1/2-month grace period or $500 rollover provision.
No
No
Major medical insurance is a type of health care coverage that provides benefits for a broad range of medical expenses that may be incurred either on an inpatient or outpatient basis.
For full plan details, please visit your benefit website: www.mybenefitshub.com/snyderisd



Learn the Terms.
• Premium: The monthly amount you pay for health care coverage.
• Deductible: The annual amount for medical expenses you’re responsible to pay before your plan begins to pay.
• Copay: The set amount you pay for a covered service at the time you receive it. The amount can vary based on the service.
• Coinsurance: The portion you’re required to pay for services after you meet your deductible. It’s often a specified percentage of the costs; e.g., you pay 20% while the health care plan pays 80%.
• Out-of-Pocket Maximum: The maximum amount you pay each year for medical costs. After reaching the out-of-pocket maximum, the plan pays 100% of allowable charges for covered services.
TRS contracts with HMOs in certain regions to bring participants in those areas additional options. HMOs set their own rates and premiums. They’re fully insured products who pay their own claims.
Blue Essentials - South Texas HMOSM Brought to you by TRS-ActiveCare
You can choose this plan if you live in one of these counties: Cameron, Hildalgo, Starr, Willacy
Blue Essentials - West Texas HMOSM Brought to you by TRS-ActiveCare
You can choose this plan if you live in one of these counties: Andrews, Armstrong, Bailey, Borden, Brewster, Briscoe, Callahan, Carson, Castro, Childress, Cochran, Coke, Coleman, Collingsworth, Comanche, Concho, Cottle, Crane, Crockett, Crosby, Dallam, Dawson, Deaf Smith, Dickens, Donley, Eastland, Ector, Fisher, Floyd, Gaines, Garza, Glasscock, Gray, Hale, Hall, Hansford, Hartley, Haskell, Hemphill, Hockley, Howard, Hutchinson, Irion, Jones, Kent, Kimble, King, Knox, Lamb, Lipscomb, Llano, Loving, Lubbock, Lynn, Martin, Mason, McCulloch, Menard, Midland, Mitchell, Moore, Motley, Nolan, Ochiltree, Oldham, Parmer, Pecos, Potter, Randall, Reagan, Reeves, Roberts, Runnels, San Saba, Schleicher, Scurry, Shackelford, Sherman, Stephens, Sterling, Stonewall, Sutton, Swisher, Taylor, Terry, Throckmorton, Tom Green, Upton, Ward, Wheeler, Winkler, Yoakum
Dental insurance is a coverage that helps defray the costs of dental care. It insures against the expense of routine care, dental treatment and disease.
For full plan details, please visit your benefit website: www.mybenefitshub.com/snyderisd
Employer Paid Benefit for Employee Only
Benefits At-A-Glance
With the Lincoln Dental Mobile App
• Find a network dentist near you in minutes
• Have an ID card on your phone
• Customize the app to get details of your plan
• Find out how much your plan covers for checkups and other services
• Keep track of your claims
Calendar (Annual) Deductible
The Lincoln DentalConnect® PPO Plan:
• Covers many preventive, basic, and major dental care services
• Also covers orthodontic treatment for children
• Features group coverage for Snyder Independent School District employees
• Allows you to choose any dentist you wish, though you can lower your out-of-pocket costs by selecting a contracting dentist
• Does not make you and your loved ones wait six months between routine cleanings
Individual: $50 Family: $150 Waived for: Preventive
Individual: $50 Family: $150 Waived for: Preventive
Deductibles are combined for basic and major Contracting Dentists’ services. Deductibles are combined for basic and major Non-Contracting Dentists’ services. Annual Maximum
MaxRewards® lets you and your covered family members roll a portion of unused dental benefits from one year into the next. So you have extra benefit dollars available when you need them most.
• Eligible Range (claim threshold): $500
• Rollover Amount: $250 per calendar year
• Rollover Amount with Preferred Provider: $350 per calendar year
• Maximum Rollover Account Balance: $1,000
Lifetime Orthodontic Max
Orthodontic Coverage is available for dependent children.
Waiting Period
• 0 months for basic services
• 0 months for major services
• 0 months for orthodontic services
If you had dental coverage through Snyder Independent School District’s previous group plan for 12 months or more and enroll in this plan when it is first offered, your benefit waiting period for this plan will be reduced accordingly. This plan includes a waiting period if you do not enroll when it is first offered to you.
• 0 months for basic services
• 12 months for major services
• 12 months for orthodontic services
• Routine oral exams
• Bitewing X-rays
• Full-mouth or panoramic X-rays
• Other dental X-rays (including periapical films)
• Routine cleanings
• Fluoride treatments
• Space maintainers for children
• Sealants
• Problem focused exams
• Consultations
• Palliative treatment (including emergency relief of dental pain)
• Injections of antibiotics and other therapeutic medications
• Fillings
• Prefabricated stainless steel and resin crowns
• Simple extractions
• Biopsy and examination of oral tissue (including brush biopsy)
• Surgical extractions
• Oral surgery
• General anesthesia and I.V. sedation
• Prosthetic repair and recementation services
• Endodontics (including root canal treatment)
• Periodontal maintenance procedures
• Non-surgical periodontal therapy
• Periodontal surgery
• Bridges
• Full and partial dentures
• Denture reline and rebase services
• Crowns, inlays, onlays and related services
• Build-ups/post & core
• Implants
• Implant related services
• Implants & implant related service
• Orthodontic exams • X-rays • Extractions • Study models
Appliances
To find a contracting dentist near you, visit
This plan lets you choose any dentist you wish. However, your out-of-pocket costs are likely to be lower when you choose a contracting dentist. For example, if you need a crown…
…you pay a deductible (if applicable), then 50% of the remaining discounted fee for PPO members. This is known as a PPO contracted fee.
… you pay a deductible (if applicable), then 50% of the usual and customary fee, which is the maximum expense covered by the plan. You are responsible for the difference between the usual and customary fee and the dentist’s billed charge.
Help protect your eye health with coverage for exams, glasses and contacts.

This summary of benefits and coverage shows how you and The Standard would share the cost for covered vision care services.
NOTE: This is only a summary; for detailed information on coverage, please consult your certificate of coverage.
Plan 1: Balanced Care Vision I Plan Summary
Deductibles
$10 Exam
Effective Date: 9/1/2024
$10 Exam
$25 Eye Glass Lenses or Frames* $25 Eye Glass Lenses or Frames
Annual Eye Exam Covered in full
Lenses (per pair)
Single Vision Covered in full
Bifocal Covered in full
Trifocal Covered in full
Lenticular Covered in full
Progressive See lens options NA
Contacts
Fit & Follow Up Exams
to $45
to $30
to $50
to $65
to $100
Participant cost up to $60 Not covered
Elective Up to $150
Medically Necessary Covered in full
Frame Allowance $150**
Frequencies (months)
Exam/Lens/Frame
Based on date of service
*Deductible applies to a complete pair of glasses or to frames, whichever is selected.
**The Costco and Walmart allowance will be the wholesale equivalent.
Lens Options (participant cost)*
Progressive Lenses
to $105
Based on date of service
VSP Choice Network + Affiliates Out of
(Other than Costco)
Up to provider’s contracted fee for Lined Bifocal Lenses. The patient is responsible for the difference between the base lens and the Progressive Lens charge. Up to Lined Bifocal allowance.
Std. Polycarbonate Covered in full for dependent children
$33 adults Not covered
Solid Plastic Dye $15 (except Pink I & II)
Plastic Gradient Dye
Photochromatic Lenses
(Glass & Plastic)
Scratch Resistant Coating
Anti-Reflective Coating
Ultraviolet Coating
$31-$82
$17-$33
$43-$85
*Lens Option participant costs vary by prescription, option chosen and retail locations.
Rates
Additional Balanced Care Vision I Choice Network Features
Contact Lenses Elective
Additional Glasses
Frame Discount
Laser VisionCare
Low Vision

Allowance can be applied to disposables, but the dollar amount must be used all at once (provider will order 3 or 6 month supply). Applies when contacts are chosen in lieu of glasses. For plans without a separate contact fitting & evaluation (which includes follow up contact lens exams), the cost of the fitting and evaluation is deducted from the allowance.
20% off additional complete pairs of prescription glasses and/or prescription sunglasses.*
VSP offers 20% off any amount above the retail allowance.*
VSP offers an average discount of 15% off or 5% off a promotional offer for LASIK Custom LASIK and PRK. The maximum out-of-pocket per eye for participants is $1,800 for LASIK and $2,300 for custom LASIK using Wavefront technology, and $1,500 for PRK. In order to receive the benefit, a VSP provider must coordinate the procedure.
With prior authorization, 75% of approved amount (up to $1,000 is covered every two years).
Based on applicable laws, reduced costs may vary by doctor location.
Balanced Care Vision I from The Standard features the money -saving eye care network of VSP. Customer service is available to plan participants through VSP's well -trained and helpful service representatives. Call or go online to locate the nearest VSP network provider, view plan benefit information and more.
VSP Call Center: 800.877.7195
⚫ Service representative hours: 5 a.m. to 7 p.m. Pacific Monday through Friday, 6 a.m. to 2:30 p.m. Pacific Saturday
⚫ Interactive Voice Response available 24/7
Locate a VSP provider at: www.standard.com/services
For more than 100 years, we have been dedicated to our core purpose: to help people achieve financial well -being and peace of mind. Headquartered in Portland, Oregon, The Standard is a nationally recognized provider of group employee benefits. To learn more about products from The Standard, visit us at www.standard.com
The Standard is a marketing name for StanCorp Financial Group, Inc. and subsidiaries. Insurance products are offered by Standard Insurance Company of Portland, Oregon, in all states except New York. Product features and availability vary by state and are solely the responsibility of Standard Insurance Company.
This form is a benefit highlight, not a certificate of insurance. This policy has exclusions, limitations, reductions of bene fits, and terms under which the policy may be continued in force or terminated. Please contact The Standard or your employer for additional information, including costs and complete details of coverage.
Cancer insurance offers you and your family supplemental insurance protection in the event you or a covered family member is diagnosed with cancer. It pays a benefit directly to you to help with expenses associated with cancer treatment.
For full plan details, please visit your benefit website: www.mybenefitshub.com/snyderisd

A cancer diagnosis and treatment can be an emotionally and physically difficult time. Chubb is there to help support you by providing cash benefits paid directly to you. Benefits are paid if you are diagnosed with cancer, but also help cover many other cancer-related services such as doctor’s visits, treatments, specialty care, and recovery. However, there are no restrictions on how to use these cash benefits—so you can use them as you see fit.
Choose the right level of coverage during the enrollment period to better protect your family.
Diagnosis of cancer
Hospital confinement
Hospital confinement ICU
Alternative care
Medical imaging
Skin cancer initial diagnosis
$5,000 employee or spouse
$7,500 child(ren)
Waiting period: 0 days
Benefit reduction: none
$200 per day – days 1 through 30
Additional days: $400
Maximum days per confinement: 31
$600 per day – days 1 through 30
Additional days: $600
Maximum days per confinement: 31
$75 per visit
Maximum visits per calendar year: 4
$500 per imaging study
Maximum studies per calendar year: 2
$100 per diagnosis
Lifetime maximum: 1
$10,000 employee or spouse
$15,000 child(ren)
Waiting period: 0 days
Benefit reduction: none
$300 per day – days 1 through 30
Additional days: $600
Maximum days per confinement: 31
$600 per day – days 1 through 30
Additional days: $600
Maximum days per confinement: 31
$75 per visit
Maximum visits per calendar year: 4
$500 per imaging study
Maximum studies per calendar year: 2
$100 per diagnosis
Lifetime maximum: 1
First bone marrow transplant: $6,000
Additional transplant: 50%
Lifetime maximum transplant(s): 2
Bone marrow or stem cell transplant
First stem cell transplant: $600
Additional transplant: 50%
Lifetime maximum transplant(s): 2
$50 per treatment
Hormonal therapy
National Cancer Institute designated comprehensive cancer treatment center evaluation/consultation
First bone marrow transplant: $9,000
Additional transplant: 50%
Lifetime maximum transplant(s): 2
First stem cell transplant: $900
Additional transplant: 50%
Lifetime maximum transplant(s): 2
Maximum treatments per calendar year: 12 $50 per treatment Maximum treatments per calendar year: 12
maximum consultations: 1
Maximum visits per calendar year: 6
$150
2
maximum number of devices: 1
maximum consultations: 1
per visit Maximum visits per calendar year: 6
2
maximum number of devices: 1 Recovery at home
Therapy
Transportation and lodging
Genetic tumor testing
$150 per day not to exceed the number of days confined
Maximum days per calendar year: 15
$25 per day of therapy
$150 per day not to exceed the number of days confined
Maximum days per calendar year: 15
Maximum days per calendar year: 40 $25 per day of therapy
Transportation: $100 per trip
Maximum trips per calendar year: 12
Lodging: $100 per day
Maximum days per calendar year: 100
Maximum days of service, per covered person per calendar year: 1 day(s)
Follow-up test benefit amount: $100
Waiting period: 0 days
$50 per test
Maximum tests per calendar year: 2
Maximum days per calendar year: 40
Transportation: $100 per trip
Maximum trips per calendar year: 12
Lodging: $100 per day
Maximum days per calendar year: 100
Maximum days of service, per covered person per calendar year: 1 day(s)
Follow-up test benefit amount: $100
Waiting period: 0 days
$50 per test
Maximum tests per calendar year: 2
Do you have kids playing sports, are you a weekend warrior, or maybe accident-prone? Accident plans are designed to help pay for medical costs associated with accidents and benefits, are paid directly to you. For full plan details, please visit your benefit website: www.mybenefitshub.com/snyderisd

SPECIFIED INJURY & SURGERY
ASKED & ANSWERED
You are eligible for this insurance if you are an active full-time employee who works at least 20 hours per week on a regularly scheduled basis, and are less than age 80.
Your spouse and child(ren) are also eligible for coverage. Any child(ren) must be under age 26 (or under age 26 if a full-time student).
This insurance will end when you or your dependents no longer satisfy the applicable eligibility conditions, or when you reach the age of 80, premium is unpaid, you are no longer actively working, you leave your employer, or the coverage is no longer offered.
CAN I KEEP THIS INSURANCE IF I LEAVE MY EMPLOYER OR AM NO LONGER A MEMBER OF THIS GROUP?
Yes, you can take this coverage with you. Coverage may be continued for you and your dependent(s) under a group portability policy. Your spouse may also continue insurance in certain circumstances. The specific terms and qualifying events for portability are described in the certificate.
This insurance coverage includes certain limitations and exclusions. The certificate details all provisions, limitations, and exclusions for this insurance coverage. A copy of the certificate can be obtained from the benefits portal www.mybenefitshub.com/snyderisd
Disability insurance protects one of your most valuable assets, your paycheck. This insurance will replace a portion of your income in the event that you become physically unable to work due to sickness or injury for an extended period of time.
For full plan details, please visit your benefit website: www.mybenefitshub.com/snyderisd

What is Educator Disability Income Insurance?
Educator Disability insurance combines the features of a short-term and long-term disability plan into one policy. The coverage pays you a portion of your earnings if you cannot work because of a disabling illness or injury. The plan gives you the flexibility to choose a level of coverage to suit your need.
You can purchase Disability Insurance through your employer. This highlight sheet is an overview of your Disability Insurance. Once a group policy is issued to your employer, a certificate of insurance will be available to explain your coverage in detail on your employers benefits website.
Why do I need Disability Insurance? Coverage?
More than half of all personal bankruptcies and mortgage foreclosures are a consequence of disability1
1 Facts from LIMRA, 2016 Disability Insurance Awareness Month
The average worker faces a 1 in 3 chance of suffering a job loss lasting 90 days or more due to a disability2
2Facts from LIMRA, 2016 Disability Insurance Awareness Month
Only 50% of American adults indicate they have enough savings to cover three months of living expenses in the event they’re not earning any income3
3Federal Reserve, Report on the Economic Well-Being of U.S. Households in 2018
Eligibility
Enrollment
Effective Date
You are eligible if you are an active employee who works at least 20 hours per week on a regularly scheduled basis.
You can enroll in coverage within 31 days of your date of hire or during your annual enrollment period.
Coverage goes into effect subject to the terms and conditions of the policy. You must satisfy the definition of Actively at Work with your employer on the day your coverage takes effect.
Actively at Work You must be at work with your Employer on your regularly scheduled workday. On that day, you must be performing for wage or profit all your regular duties in the usual way and for your usual number of hours. If school is not in session due to normal vacation or school break(s), Actively at Work shall mean you are able to report for work with your Employer, performing all the regular duties of Your Occupation in the usual way for your usual number of hours as if school was in session.
Benefit Amount
Elimination Period
You may purchase coverage that will pay you a monthly benefit of 45%, 55%, 65% of your monthly income, to a maximum of $8,000. Earnings are defined in The Hartford’s contract with your employer.
You must be disabled for at least the number of days indicated by the elimination period that you select before you can receive a disability benefit payment. The elimination period that you select consists of two numbers. The first number shows the number of days you must be disabled by an accident before your benefits can begin. The second number indicates the number of days you must be disabled by a sickness before your benefits can begin.
For those employees electing an elimination period of 30 days or less, if you are confined to a hospital for 24 hours or more due to a disability, the elimination period will be waived, and benefits will be payable from the first day of hospitalization.
Maximum Benefit Duration Benefit Duration is the maximum time for which we pay benefits for disability resulting from sickness or injury. Depending on the age at which disability occurs, the maximum duration may vary. Please see the applicable schedules below based on the Premium benefit option.
Premium Option: Table below shows Max Benefit resulting from sickness or injury
Age Disabled Maximum Benefit Duration
Prior to 63
Age 63
To Normal Retirement Age or 48 months if greater
To Normal Retirement Age or 42 months if greater
Age 64 36 months
Age 65
months
Age 66 27 months
Age 67 24 months
Age 68 21 months
Age 69 and older 18 months
Mental Illness, Alcoholism and Substance Abuse, Self-Reported or Subjective Illness
You can receive benefit payments for Long-Term Disabilities resulting from mental illness, alcoholism, and substance abuse for a total of 24 months for all disability periods during your lifetime.
Any period of time that you are confined in a hospital or other facility licensed to provide medical care for mental illness, alcoholism and substance abuse does not count toward the 24-month lifetime limit.
Partial Disability Partial Disability is covered provided you have at least a 20% loss of earnings and duties.
Other Important Benefits Survivor Benefit - If you die while receiving disability benefits, a benefit will be paid to your spouse or child under age 26, equal to three times your last monthly gross benefit.
The Hartford's Ability Assist service is included as a part of your group Long Term Disability (LTD) insurance program. You have access to Ability Assist services both prior to a disability and after you’ve been approved for an LTD claim and are receiving LTD benefits. Once you are covered you are eligible for services to provide assistance with child/elder care, substance abuse, family relationships and more. In addition, LTD claimants and their immediate family members receive confidential services to assist them with the unique emotional, financial, and legal issues that may result from a disability. Ability Assist services are provided through ComPsych®, a leading provider of employee assistance and work/ life services.
Travel Assistance Program – Available 24/7, this program helps employees and their dependents who travel 100 miles from their home for 90 days or less. Services include pre-trip information, emergency medical assistance and emergency personal services.
Identity Theft Protection – An array of identity fraud support services to help victims restore their identity. Benefits include 24/7 access to an 800 number; direct contact with a certified caseworker who follows the case until it’s resolved, and a personalized fraud resolution kit with instructions and resources for ID theft victims.
Workplace Modification provides for reasonable modifications made to a workplace to accommodate your disability and allow you to return to active full-time employment.
Definition of Disability Disability is defined as The Hartford’s contract with your employer. Typically, disability means that you cannot perform one or more of the essential duties of your occupation due to injury, sickness, pregnancy, or other medical conditions covered by the insurance, and as a result, your current monthly earnings are 80% or less of your pre-disability earnings.
One you have been disabled for 24 months, you must be prevented from performing one or more essential duties of any occupation, and as a result, your monthly earnings are 65% or less of your predisability earnings.
Pre-Existing Condition Limitation
Your policy limits the benefits you can receive for a disability caused by a pre-existing condition. In general, if you were diagnosed or received care for a disabling condition within the 3 consecutive months just prior to the effective date of this policy, your benefit payment will be limited, unless: you have been insured under this policy for 12 months before your disability begins.
If your disability is a result of a pre-existing condition, we will pay benefits for a maximum of 6 weeks.
Continuity of Coverage
If you were insured under your district’s prior plan and not receiving benefits the day before this policy is effective, there will not be a loss in coverage, and you will get credit for your prior carrier’s coverage.
Recurrent Disability What happens if I Recover but become Disabled again?
Periods of Recovery during the Elimination Period will not interrupt the Elimination Period, if the number of days You return to work as an Active Employee are less than one-half (1/2) the number of days of Your Elimination Period. Any day within such period of Recovery, will not count toward the Elimination Period.
Benefit Integration
For the first 12 months your benefit may be reduced by other income you receive or are eligible to receive due to your disability, such as Workers' Compensation Law, the Jones Act, occupational disease law, similar law or substitutes or exchanges for such benefits.
After 12 months, your benefit may be reduced by other income you receive or are eligible to receive due to your disability, such as:
• Social Security Disability Insurance
• State Teacher Retirement Disability Plans
• Workers’ Compensation
• Other employer-based disability insurance coverage you may have:
• Unemployment benefits
• Retirement benefits that your employer fully or partially pays for (such as a pension plan)
Your plan includes a minimum benefit the greater of 10% of elected benefit or $100.
General Exclusions You cannot receive Disability benefit payments for disabilities that are caused or contributed to by:
• War or act of war (declared or not)
• Military service for any country engaged in war or other armed conflict.
• The commission of or attempt to commit a felony.
• An intentionally self-inflicted injury
• Any case where Your being engaged in an illegal occupation was a contributing cause to your disability.
• You must be under the regular care of a physician to receive benefits.
Life insurance is an important part of your employee benefits package. Chubb Term Life and Accidental Death and Dismemberment (AD&D) insurance provides the protection your family needs if something were to happen to you. Your family can receive cash benefits paid directly to them that they can use to help cover expenses like mortgage payments, credit card debt, childcare, college tuition, and other household expenses.
Voluntary Term Life and AD&D Insurance is made available for purchase by you and your family. Employees must be actively at work for at least 20 hours per week.
Life Insurance/AD&D
Life and AD&D: $10,000 increments up to a maximum of $500,000
For Your Spouse
Life: $5,000 increments up to a maximum of $500,000, not to exceed 100% of employee amount
AD&D: 50% of employee amount up to maximum of $250,000
For Your Dependent Children
Life: Live birth to 6 months, $1,000; 6 months to age 26: $10,000
AD&D: 10% of employee amount to a maximum of $10,000
Reduction Schedule
50% at age 70
Accelerated Death Benefit for Long Term Care
Accelerated Death Benefit for Terminal Illness
Guaranteed Issue
Employee: $300,000 Spouse: $50,000 Child: $10,000
Newly eligible employees and dependents: You and your eligible dependents may elect coverage up to the guaranteed issue amounts without answering health questions. Elections over the guaranteed issue amounts will require medical underwriting.
Current employees: At subsequent annual enrollments if you or your eligible dependents are currently enrolled in the plan, you may increase your coverage up to the guaranteed issue amounts without answering health questions. All amounts over the guaranteed issue will require medical underwriting.
*Please note that if you or your dependents did not elect coverage when first eligible, then you are considered a late entrant. Late entrants will be medically underwritten and will have to answer health questions for any amount of coverage elected.
4% of Death Benefit per month up to 75% of Death Benefit, not to exceed $200,000
75% of Death Benefit, not to exceed $500,000
Employee Assistance Program 6 face-to-face visits
Travel Assistance Included
AD&D Covered Losses and Benefits
The AD&D plan provides additional protection for you and your dependents in the event of an accidental bodily injury resulting in death or dismemberment. In addition to standard dismemberment coverage, the following benefit provisions are included:
• Air Bag Benefit – The lesser of 5% of AD&D benefit or $5,000
• Child Care Expense Benefit – 5% of employee’s AD&D benefit up to $12,000 per year for 4 years
• Child Education Expense Benefit – 6% of employee’s AD&D benefit up to $6,000 for 6 years; maximum benefit of $24,000
• Common Carrier Benefit – Included
• Elder Care Expense Benefit – The lesser of 1% of AD&D benefit or $500
• Exposure and Disappearance Benefit– Included
• Repatriation Expense Benefit – The lesser of $1,000 or the actual expense incurred
• Seatbelt Benefit – The lesser of 10% of AD&D benefit or $25,000
• Spouse Education Benefit – The lesser of 1% of AD&D benefit, $1,000, or the actual tuition expenses incurred
• Workplace Felonious Assault Benefit – 5% of AD&D benefit up to $10,000
A Health Savings Account (HSA) is a personal savings account where the money can only be used for eligible medical expenses. Unlike a flexible spending account (FSA), the money rolls over year to year however only those funds that have been deposited in your account can be used. Contributions to a Health Savings Account can only be used if you are also enrolled in a High Deductible Health Care Plan (HDHP).
www.mybenefitshub.com/snyderisd
For full plan details, please visit your benefit website: www.mybeneitshub.com/sampleisd
A Health Savings Account (HSA) is more than a way to help you and your family cover health care costs – it is also a tax-exempt tool to supplement your retirement savings and cover health expenses during retirement. An HSA can provide the funds to help pay current health care expenses as well as future health care costs.
A type of personal savings account, an HSA is always yours even if you change health plans or jobs. The money in your HSA (including interest and investment earnings) grows tax-free and spends tax-free if used to pay for qualified medical expenses. There is no “use it or lose it” rule — you do not lose your money if you do not spend it in the calendar year — and there are no vesting requirements or forfeiture provisions. The account automatically rolls over year after year.
You are eligible to open and contribute to an HSA if you are:
• Enrolled in an HSA-eligible HDHP (High Deductible Health Plan) Not covered by another plan that is not a qualified HDHP, such as your spouse’s health plan
• Not enrolled in a Health Care Flexible Spending Account, nor should your spouse be contributing towards a Health Care Flexible Spending Account
• Not eligible to be claimed as a dependent on someone else’s tax return
• Not enrolled in Medicare or TRICARE
• Not receiving Veterans Administration benefits
You can use the money in your HSA to pay for qualified medical expenses now or in the future. You can also use HSA funds to pay health care expenses for your dependents, even if they are not covered under your HDHP.
Your HSA contributions may not exceed the annual maximum amount established by the Internal Revenue Service. The annual contribution maximum for 2024 is based on the coverage option you elect:
• Individual – $4,150
• Family (filing jointly) – $8,300

You decide whether to use the money in your account to pay for qualified expenses or let it grow for future use. If you are 55 or older, you may make a yearly catch-up contribution of up to $1,000 to your HSA. If you turn 55 at any time during the plan year, you are eligible to make the catch-up contribution for the entire plan year.
If you meet the eligibility requirements, you may open an HSA administered by EECU. You will receive a debit card to manage your HSA account reimbursements. Keep in mind, available funds are limited to the balance in your HSA.
• Always ask your health care provider to file claims with your medical provider so network discounts can be applied. You can pay the provider with your HSA debit card based on the balance due after discount.
• You, not your employer, are responsible for maintaining ALL records and receipts for HSA reimbursements in the event of an IRS audit.
• You may open an HSA at the financial institution of your choice, but only accounts opened through EECU are eligible for automatic payroll deduction and company contributions.
• Online/Mobile: Sign-in for 24/7 account access to check your balance, pay bills and more.
• Call/Text: (817) 882-0800 EECU’s dedicated member service representatives are available to assist you with any questions. Their hours of operation are Monday through Friday from 8:00 a.m. to 7:00 p.m. CT, Saturday 9:00 a.m. to 1:00 p.m. CT and closed on Sunday.
• Lost/Stolen Debit Card: Call the 24/7 debit card hotline at (800)333-9934.
• Stop by a local EECU financial center: www.eecu.org/ locations.
A Flexible Spending Account allows you to pay for eligible healthcare expenses with a pre-loaded debit card. You choose the amount to set aside from your paycheck every plan year, based on your employer’s annual plan limit. This money is use it or lose it within the plan year.
For full plan details, please visit your benefit website: www.mybenefitshub.com/andrewsisd
www.mybenefitshub.com/snyderisd

The Health Care FSA covers qualified medical, dental and vision expenses for you or your eligible dependents. You may contribute up to $3,200 annually to a Health Care FSA and you are entitled to the full election from day one of your plan year. Eligible expenses include:
• Dental and vision expenses
• Medical deductibles and coinsurance
• Prescription copays
• Hearing aids and batteries
You may not contribute to a Health Care FSA if you contribute to a Health Savings Account (HSA)
The Higginbotham Benefits Debit Card gives you immediate access to funds in your Health Care FSA when you make a purchase without needing to file a claim for reimbursement. If you use the debit card to pay anything other than a copay amount, you will need to submit an itemized receipt or an Explanation of Benefits (EOB).
The Dependent Care FSA helps pay for expenses associated with caring for elder or child dependents so you or your spouse can work or attend school full time. You can use the account to pay for day care or baby sitter expenses for your children under age 13 and qualifying older dependents, such as dependent parents. Reimbursement from your Depend ent Care FSA is limited to the total amount deposited in your account at that time. To be eligible, you must be a single parent or you and your spouse must be employed outside the home, disabled or a full-time student.
• Overnight camps are not eligible for reimbursement (only day camps can be considered).
• If your child turns 13 midyear, you may only request reimbursement for the part of the year when the child is under age 13.
• You may request reimbursement for care of a spouse or dependent of any age who spends at least eight hours a day in your home and is mentally or physically incapable of self-care.
• The dependent care provider cannot be your child under age 19 or anyone claimed as a dependent on your income taxes.
• The maximum per plan year you can contribute to a Health Care FSA is $3,200. The maximum per plan year you can contribute to a Dependent Care FSA is $5,000 when filing jointly or head of household and $2,500 when married filing separately.
• You cannot change your election during the year unless you experience a Qualifying Life Event.
• In most cases, you can continue to file claims incurred during the plan year for another 90 days after the plan year ends.
• Your Health Care FSA debit card can be used for health care expenses only. It cannot be used to pay for dependent care expenses.
• Review your employer's Summary Plan Document for full details. FSA rules vary by employer.
Health care reform legislation requires that certain over-the-counter (OTC) items require a prescription to qualify as an eligible Health Care FSA expense. You will only need to obtain a one-time prescription for the current plan year. You can continue to purchase your regular prescription medications with your FSA debit card. However, the FSA debit card may not be used as payment for an OTC item, even when accompanied by a prescription.
Higginbotham Portal
The Higginbotham Portal provides information and resources to help you manage your FSAs.
• Access plan documents, letters and notices, forms, account balances, contributions and other plan information
• Update your personal information
• Utilize Section 125 tax calculators
• Look up qualified expenses
• Submit claims
• Request a new or replacement Benefits Debit Card
Register on the Higginbotham Portal
Visit https://flexservices.higginbotham.net and click Register. Follow the instructions and scroll down to enter your information.
• Enter your Employee ID, which is your Social Security number with no dashes or spaces.
• Follow the prompts to navigate the site.
• If you have any questions or concerns, contact Higginbotham:
∗ Phone – 866-419-3519
∗ Questions – flexsupport@higginbotham.net
∗ Fax – 866-419-3516
∗ Claims- flexclaims@higginbotham.net
Life insurance is an important part of your employee benefits package. Chubb Term Life and Accidental Death and Dismemberment (AD&D) insurance provides the protection your family needs if something were to happen to you. Your family can receive cash benefits paid directly to them that they can use to help cover expenses like mortgage payments, credit card debt, childcare, college tuition, and other household expenses.

Employer Term Life and AD&D Insurance is provided by your employer. Employees must be actively at work for at least 20 hours per week. There is no premium paid by you for this life insurance.
Life Insurance/AD&D
For You
$50,000
Guaranteed Issue All coverage amounts
Accelerated Death Benefit for Terminal Illness
AD&D Covered Losses and Benefits
Reduction Schedule 50% at age 70
75% of Death Benefit, not to exceed $500,000
The AD&D plan provides additional protection for you and your dependents in the event of an accidental bodily injury resulting in death or dismemberment. In addition to standard dismemberment coverage, the following benefit provisions are included:
• Air Bag Benefit – The lesser of 5% of AD&D benefit or $5,000
• Child Care Expense Benefit – 5% of employee’s AD&D benefit up to $12,000 per year for 4 years
• Child Education Expense Benefit – 6% of employee’s AD&D benefit up to $6,000 for 6 years; maximum benefit of $24,000
• Common Carrier Benefit – Included
• Elder Care Expense Benefit – The lesser of 1% of AD&D benefit or $500
• Exposure and Disappearance Benefit – Included
• Repatriation Expense Benefit – The lesser of $1,000 or the actual expense incurred
• Seatbelt Benefit – The lesser of 10% of AD&D benefit or $25,000
• Spouse Education Benefit – The lesser of 1% of AD&D benefit, $1,000, or the actual tuition expenses incurred
• Workplace Felonious Assault Benefit –5% of AD&D benefit up to $10,000
Group Term Life Insurance to age 121 with Quality of Life

Make a smart choice to help protect your loved ones and your future.
Help protect your family with the Family Protection Plan Group Level Term Life Insurance to age 121. You can get coverage for your spouse even if you don’t elect coverage on yourself. And you can cover your financially dependent children and grandchildren (14 days to 26 years old). The coverage lasts until age 121 for all insured,* so no matter what the future brings, your family is protected.
Buying life insurance when you’re younger allows you to take advantage of lower premium rates while you’re generally healthy, which allows you to purchase more insurance coverage for the future. This is especially important if you have dependents who rely on your income, or you have debt that would need to be paid off.
Portable
Coverage continues with no loss of benefits or increase in cost if you terminate employment after the first premium is paid. We simply bill you directly.
Life moves fast so having a portable life insurance allows you to keep your coverage if you leave your school district. Keeping the coverage helps you ensure your family is protected even into your retirement years.
44% of American households would encounter significant financial difficulties within six months if they lost the primary family wage earner. 28% would reach this point in one month or less.

Group Term
illness acceleration of benefits
Coverage pays 30% (25% in CT and MI) of the coverage amount in a lump sum upon the occurrence of a terminal condition that will result in a limited life span of less than 12 months (24 months in IL).
Protection you can count on
Within one business day of notification, payment of 50% of coverage or $10,000 whichever is less is mailed to the beneficiary, unless the death is within the two-year contestability period and/or under investigation. This coverage has no war or terrorism exclusions.
Convenient
Easy payment through payroll deduction.
Quality of Life benefit
Optional benefit that accelerates a portion of the death benefit on a monthly basis, up to 75% of your benefit, and is payable directly to you on a tax favored basis* for the following:
•Permanent inability to perform at least two of the six Activities of Daily Living (ADLs) without substantial assistance; or
•Permanent severe cognitive impairment, such as dementia, Alzheimer’s disease and other forms of senility, requiring substantial supervision.
Many individuals who can’t take care of themselves require special accommodations to perform ADLs and would need to make modifications to continue to live at home with physical limitation. The proceeds from the Quality of Life benefit can be used for any purpose, including costs for infacility care, home healthcare professionals, home modifications, and more.
2024 Enrollment Plan Year
Guaranteed Issue is offered to all eligible applicants regardless of health status. No Doctor exams or physicals.
Employee: $100,000 | Spouse: $30,000 | Child: $10,000
Enroll to provide peace of mind for your family
To do an initial enrollment or if you have questions please call our customer service at 866-914-5202. Monday - Friday | 8:00 am-6:00 pm CST

The Family Protection Plan offers a lump-sum cash benefit if you die before age 121. The initial death benefit is guaranteed to be level for at least the first ten policy years. Afterward, the company intends to provide a nonguaranteed death benefit enhancement which will maintain the initial death benefit level until age 121. The company has the right to discontinue this enhancement. The death benefit enhancement cannot be discontinued on a particular insured due to a change in age, health, or employment status.
It’s not easy to pay hospital bills, especially if you have a high-deductible medical plan. Chubb Hospital Cash pays money directly to you if you are hospitalized so you can focus on your recovery. And since the cash goes directly to you, there are no restrictions on how you use your money. average three-day hospitalization cost.¹ average hospital stay.²
5.4 days $30,000 ¹

First Hospitalization Benefit
This benefit is payable for the first covered hospital confinement per certificate.
Hospital Admission Benefit
This benefit is for admission to a hospital or hospital sub-acute intensive care unit.
Hospital Admission ICU Benefit
This benefit is for admission to a hospital intensive care unit.
Hospital Confinement Benefit
This benefit is for confinement in hospital or hospital sub-acute intensive care unit.
Hospital Confinement ICU Benefit
This benefit is for confinement in a hospital intensive care unit.
Newborn Nursery Benefit
This benefit is payable for an insured newborn baby receiving newborn nursery care and who is not confined for treatment of a physical illness, infirmity, disease, or injury.
Observation Unit Benefit
This benefit is for treatment in a hospital observation unit for a period of less than 20 hours.
Rehabilitation Unit Admission Benefit
This benefit is for admission to a rehabilitation unit as an inpatient.
• $500
• Maximum benefit per certificate: 1
• $1,500
• Maximum benefit per calendar year: 5
• $3,000
• Maximum benefit per calendar year: 2
• $100 per day
• Maximum days per calendar year: 30
• $200 per day
• Maximum days per calendar year: 30
• $500 per day
• Maximum days per confinementnormal delivery: 2
• Maximum days per confinementcaesarean section: 2
• $500
• Maximum benefit per calendar year: 2
• $500
• Maximum benefit per calendar year: 3
• $500
• Maximum benefit per certificate: 1
• $3,000
• Maximum benefit per calendar year: 5
• $6,000
• Maximum benefit per calendar year: 2
• $200 per day
• Maximum days per calendar year: 30
• $400 per day
• Maximum days per calendar year: 30
• $500 per day
• Maximum days per confinementnormal delivery: 2
• Maximum days per confinementcaesarean section: 2
• $500
• Maximum benefit per calendar year: 2
• $500
• Maximum benefit per calendar year: 5
Waiver of Premium for Hospital Confinement
This benefit waives premium when the employee or spouse is confined for more than 30 continuous days.
Included
We will not pay for any Covered Accident or Covered Sickness that is caused by, or occurs as a result of 1) committing or attempting to commit suicide or intentionally injuring oneself; 2) war or serving in any of the armed forces or units auxiliary; 3) participating in an illegal occupation or attempting to commit or actually committing a felony; 4) sky diving, hang gliding, parachuting, bungee jumping, parasailing, or scuba diving; 5) being intoxicated or being under the influence or any narcotic or other prescription drug unless taken in accordance with Physician’s instructions 6) alcoholism; 7) cosmetic surgery, except for reconstructive surgery needed as the result of an Injury or Sickness or is related to or results from a congenital disease or anomaly of a covered Dependent Child; 8) services related to sterilization, reversal of a vasectomy or tubal ligation, in vitro fertilization, and diagnostic treatment of infertility or other related problems.
A Physician cannot be You or a member of Your Immediate Family, Your business or professional partner, or any person who has a financial affiliation or business interest with You.

Contact the FBS Benefits CareLine via the QR code or (833) 453-1680.
*Please refer to your Certificate of Insurance at https://www.mybenefitshub.com/snyderisd for a complete listing of available benefits, limitations and exclusions. Underwritten by ACE Property & Casualty Company, a Chubb company. This information is a brief description of the important benefits and features of the insurance plan. It is not an insurance contract. This is a supplement to health insurance and is not a substitute for Major Medical or other minimal essential coverage. Hospital indemnity coverage provides a benefit for covered loss; neither the product name nor benefits payable are intended to provide reimbursement for medical expenses incurred by a covered person or to result in any payment in excess of loss.
Critical illness insurance can be used towards medical or other expenses. It provides a lump sum benefit payable directly to the insured upon diagnosis of a covered condition or event, like a heart attack or stroke. The money can also be used for non-medical costs related to the illness, including transportation, child care, etc.
For full plan details, please visit your benefit website: www.mybenefitshub.com/snyderisd

Heart attacks and strokes happen every day and often unexpectedly. They don’t give you time to prepare and can take a serious toll on both your physical and financial well- being. Chubb Critical Illness pays cash benefits directly to you that you can use to help with your bills, your mortgage, your rent, your childcare—you name it—so you can focus on recovery.
Employee
Spouse
$10,000, $20,000, $30,000 or $40,000 face amounts
$10,000, $20,000, $30,000 or $40,000 face amounts
Child coverage Included in the employee rate
No benefits will be paid for a date of diagnosis that occurs prior to the coverage effective date. There is no pre-existing conditions limitation. All amounts are Guaranteed Issue — no medical questions are required for coverage to be issued.
Occupational Package
Pays 100% of the face amount; Benefits payable for HIV or Hepatitis B, C, or D, MRSA, Rabies, Tetanus, or Tuberculosis contracted on the job.
Childhood Conditions
Pays 100% of the dependent child face amount.
Provides benefits for childhood conditions (Autism Spectrum Disorder; Cerebral Palsy; Congenital Birth Defects; Heart, Lung, Cleft Lip, Palate, etc.; Cystic Fibrosis; Down Syndrome. Gaucher Disease; Muscular Dystrophy; and Type 1 Diabetes).
Recurrence Benefit
Benefits are payable for a subsequent diagnosis of Aneurysm –Cerebral or Aortic, Benign Brain Tumor, Coma, Coronary Artery
Obstruction, Heart Attack, Major Organ Failure, Severe Burns, Stroke, or Sudden Cardiac Arrest.
Advocacy Package
Best Doctors Physician Referrals
• Ask the Expert Hotline provides 24-hour advice from experts about a particular medical condition.
• In-Depth Medical Review offers a full review of diagnosis and treatment plan.
Diabetes Benefit
Diabetes Diagnosis Benefit
• Pays a benefit once for Covered Person’s Diabetes diagnosis.
Additional Benefits
Miscellaneous Diseases Rider + COVID-19
The Miscellaneous Disease Rider is payable once per covered condition.
Covered conditions include: Addison’s disease; cerebrospinal meningitis; COVID-19, diphtheria; Huntington’s chorea; Legionnaire’s disease; malaria; myasthenia gravis; meningitis; necrotizing fasciitis; osteomyelitis; polio; rabies; scleroderma; systematic lupus; tetanus; tuberculosis.
COVID-19 means a disease resulting in a positive COVID-19 diagnostic screening and 5 consecutive days of hospital confinement.
Waiver of premium
Waives premium while the insured is totally disabled.
Wellness benefit – payable once per insured per year. $50
Comprehensive coverage and care for emergency transport.
Our Emergent Plus membership plan includes:
Emergency Ground Ambulance Coverage1
Your out-of-pocket expenses for your emergency ground transportation to a medical facility are covered with MASA.
Your out-of-pocket expenses for your emergency air transportation to a medical facility are covered with MASA.
When specialized care is required but not available at the initial emergency facility, your out-of-pocket expenses for the ground or air ambulance transfer to the nearest appropriate medical facility are covered with MASA.
Should you need continued care and your care provider has approved moving you to a hospital nearer to your home, MASA coordinates and covers the expense for ambulance transportation to the approved medical facility.

Did you know?
51.3 million emergency responses occur each year
MASA protects families against uncovered costs for emergency transportation and provides connections with care services.
Source: NEMSIS, National EMS Data Report, 2023
MASA is coverage and care you can count on to protect you from the unexpected. With us, there is no “out-of-network” ambulance. Just send us the bill when it arrives and we’ll work to ensure charges are covered. Plus, we’ll be there for you beyond your initial ride, with expert coordination services on call to manage complex transport needs during or after your emergency — such as transferring you and your loved ones home safely.
Protect yourself, your family, and your family’s financial future with MASA.

protects families against out-of-pocket costs for emergency transportation and provides connections with care. Gain peace of mind and shield your finances knowing there’s a MASA plan best suited for your needs.
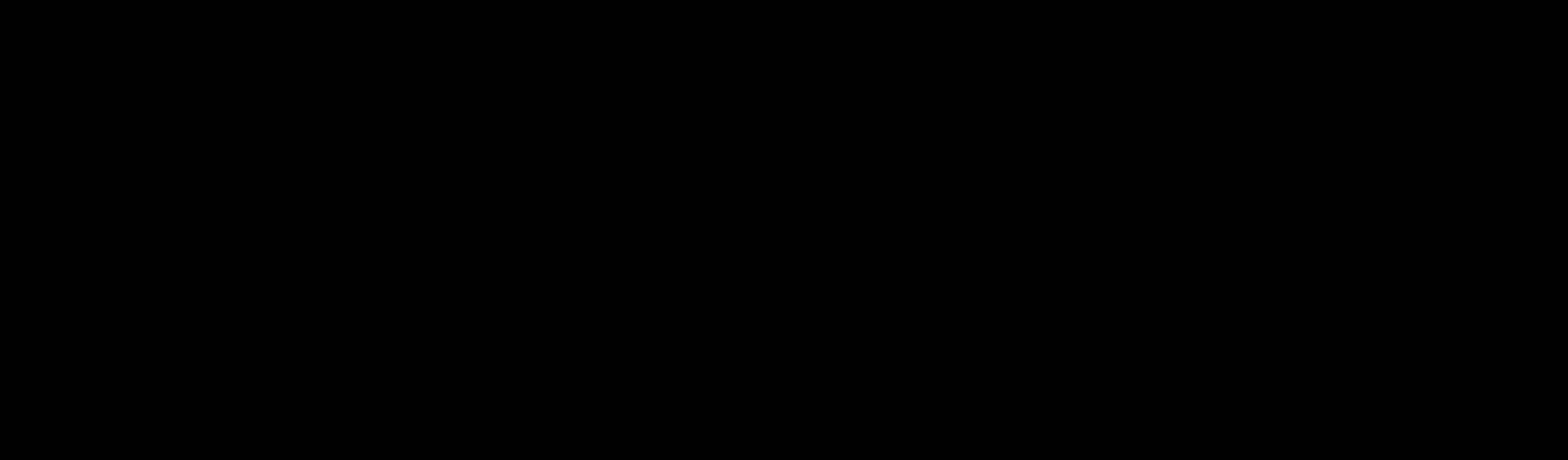
As identity theft and fraud continue to increase, an evolving suite of products helps you monitor any potential threats to your identity and alerts you if there are any areas of concern. You will also have access to a full financial wellness platform and proactive digital privacy tools that can help you keep passwords and other personal information private and secure while surfing the web.

For full plan details, please visit your benefit website: www.mybenefitshub.com/snyderisd




part of your health plan.
Getting sick is always a hassle. When you need care fast, talk to a board-certified MDLIVE doctor in minutes. Get reliable care from the comfort of home instead of an urgent care clinic or crowded ER. MDLIVE is open nights, weekends, and holidays. No surprise costs.
Convenient and reliable care.
MDLIVE doctors have an average of 15 years of experience and can be reached 24/7 by phone or video.
Affordable alternative to urgent care clinics and the ER. MDLIVE treats 80+ common conditions like flu, sinus infections, pink eye, ear pain, and UTIs (Females, 18+). By talking to a doctor at home, you can avoid long waits and exposure to other sick people. Prescriptions.
Your MDLIVE doctor can order prescriptions1 to the pharmacy of your choice. MDLIVE can also share notes with your local doctor upon request.

MDLIVE cares for more than 80 common, non-emergency conditions, including:

• Pink Eye
• Sinus Problems
• Cough
• Ear Pain
• Headache
• Prescriptions
• Sore Throat
• UTI (Females, 18+)
• Yeast Infections
• And more





1Prescriptions are available at the physician’s discretion when medically necessary. A renewal of an existing prescription can also be provided when your regular physician is unavailable, depending on the type of medication.
Download your Clever RX card or Clever RX App to unlock exclusive savings.
Present your Clever RX App or Clever RX card to your pharmacist.
ST EP 1:
Download the FREE Clever RX App. From your App Store search for "Clever RX" and hit download. Make sure you enter in Group ID and in Member ID during the on-boarding process. This will unlock exclusive savings for you and your family!
ST EP 2 :
Find where you can save on your medication. Using your zip code, when you search for your medication Clever RX checks which pharmacies near you offer the lowest price. Savings can be up to 80% compared to what you're currently paying.
FREE to use. Save up to 80% off prescription drugs and beat copay prices.
Accepted at most pharmacies nationwide ST AR T SA VI NG TOD AY W
100% FREE to use
Unlock discounts on thousands of medications
Save up to 80% off prescription drugs – often beats the average copay
Over 7 0% of peopl e c an benefi t fro m a pre sc rip ti on sav ing s c ard due t o high dedu ct ible heal t h plan s, high c opa ys , and being unde r in s ured or u ni ns ur ed
ST EP 3 :
Click the voucher with the lowest price, closest location, and/or at your preferred pharmacy. Click "share" to text yourself the voucher for easy access when you are ready to use it. Show the voucher on your screen to the pharmacist when you pick up your medication.
ST EP 4:
Share the Clever RX App. Click "Share" on the bottom of the Clever RX App to send your friends, family, and anyone else you want to help receive instant discounts on their prescription medication. Over 70% of people can benefit from a prescription savings card.
TH A T IS N O T ONLY CL EVER, I T IS CL EVE R RX .
DID Y OU KNOW?
Ov er 3 0 % of
Enrollment Guide General Disclaimer: This summary of benefits for employees is meant only as a brief description of some of the programs for which employees may be eligible. This summary does not include specific plan details. You must refer to the specific plan documentation for specific plan details such as coverage expenses, limitations, exclusions, and other plan terms, which can be found at the Snyder ISD Benefits Website. This summary does not replace or amend the underlying plan documentation. In the event of a discrepancy between this summary and the plan documentation the plan documentation governs. All plans and benefits described in this summary may be discontinued, increased, decreased, or altered at any time with or without notice.
Rate Sheet General Disclaimer: The rate information provided in this guide is subject to change at any time by your employer and/or the plan provider. The rate information included herein, does not guarantee coverage or change or otherwise interpret the terms of the specific plan documentation, available at the Snyder ISD Benefits Website, which may include additional exclusions and limitations and may require an application for coverage to determine eligibility for the health benefit plan. To the extent the information provided in this summary is inconsistent with the specific plan documentation, the provisions of the specific plan documentation will govern in all cases.