



Our Contributors





















Our aim is clear - to provide you, our audience with indepth insights into these critical facets of the health tech landscape.
Dear Readers and Health Tech Enthusiasts, Happy 63rd Independence Day to fellow Nigerians, and welcome to the promising month of October! As we celebrate the strides of our nation, I am delighted to introduce the 6th Edition of Health Tech Insider, marking a significant step forward in our journey to explore the cutting edge of health technology.



This edition is a testament to our commitment to exploring the forefront of health technology. We’ve refined our focus to bring you 5 distinct segments: Digital Health Transformation, Emerging Technologies, Data Analytics and Insights, Regulatory and Ethics, and Industry Perspective and Case studies.
In this edition, you can expect thought-provoking articles, expert interviews, and case studies that delve into the heart of digital health, exploring the innovations that are shaping the future of healthcare. We'll be unravelling the potential of emerging technologies, examining the power of data analytics to drive informed decisions, providing keen insights and case studies across the industry and navigating the complex web of regulatory and ethical considerations in our field.
Beyond the pages, Health Tech Insider is more than a publication it's a thriving community. With over 2K engaged readers spanning Asia, Europe, North America, South America and Africa, we are gradually becoming a trusted source of information for healthcare professionals, thought leaders, innovators, and decision-makers in the health and tech sphere.
Now, we invite you to be a part of our journey. If you have groundbreaking health tech solutions that deserve the spotlight, consider showcasing your products and services in Health Tech Insider. Join us in reaching a highly engaged audience eager to embrace the future of healthcare.
Thank you for being a part of our community and for your unwavering support. Together, let's shape the future of health tech and pave the way for a healthier tomorrow.
Happy reading, and here's to a future where technology and healthcare seamlessly intertwine for the betterment of all.
Wishing you a month filled with groundbreaking discoveries and inspiration!
Warm regards,
Ayo-Olagunju Munachimso Editor-in-Chief


In recent years, the healthcare industry has undergone a digital transformation, with technological advancements reshaping the way medical services are delivered. One such innovation that has gained significant attention is the chatbot symptom checker a tool designed to assist individuals in evaluating their health concerns and determining the appropriate course of action. This article delves into the evolution, benefits, challenges, and ethical considerations surrounding chatbot symptom checkers in healthcare.

The concept of utilizing technology to assess health symptoms dates back to the early days of the Internet when rudimentary websites offered basic symptom checklists However, the emergence of artificial intelligence (AI) and natural language processing (NLP) has propelled this idea to new heights. Modern chatbot symptom checkers leverage advanced algorithms to engage in dynamic conversations with users, asking targeted questions to gather relevant information about their symptoms.
Accessibility and Convenience: One of the primary advantages of chatbot symptom checkers is their availability 24/7 Users can access these tools from the comfort of their homes, eliminating the need for immediate in-person medical attention for minor concerns.
Healthcare Triage: Chatbots play a crucial role in healthcare triage, assisting users in determining the urgency of their symptoms. They guide individuals towards seeking prompt medical attention if their symptoms warrant it, thus potentially reducing unnecessary visits to emergency rooms
Medical Information: Chatbot symptom checkers provide users with valuable information about the potential causes of their symptoms. This empowers individuals to engage in informed discussions with healthcare professionals, promoting a more productive doctor-patient relationship
Public Health Monitoring: Aggregate data from chatbot interactions can offer insights into emerging health trends and potential outbreaks. This data can aid health authorities in early detection and response.
Accuracy and Reliability: While chatbots have come a long way in understanding natural language, they can still struggle with accurately interpreting complex or ambiguous descriptions of symptoms Ensuring a high level of accuracy is crucial to prevent misdiagnoses and unnecessary anxiety.
Liability and Legal Issues: If a chatbot provides incorrect advice that leads to harm, questions of liability and legal responsibility arise. Establishing clear terms of use and disclaimers is vital to mitigate these concerns.

Data Privacy and Security: Chatbots collect sensitive health information, making data privacy and security paramount Healthcare providers must adhere to strict regulations, such as HIPAA, to protect user data.

Overreliance and Underutilization:
Users might over-rely on chatbot advice, dismissing the need for professional medical evaluation when necessary. Conversely, some individuals might underutilize these tools, potentially ignoring symptoms that require attention
Informed Consent: Users must be informed about the limitations of chatbot symptom checkers and be aware that these tools do not replace professional medical advice
Transparency: Developers need to be transparent about how chatbots arrive at their recommendations Users should know if the advice is based on AI algorithms, expert guidelines, or a combination of both
Equity and Accessibility: Developers should ensure that chatbot symptom checkers are accessible to diverse populations, including those with disabilities or limited access to technology

As AI and NLP technologies continue to advance, the capabilities of chatbot symptom checkers are likely to improve. Integrations with electronic health records, wearable devices, and telehealth platforms could enhance their accuracy and relevance However, striking the right balance between AI assistance and human medical expertise will remain a critical challenge.
In conclusion, chatbot symptom checkers represent a transformative development in healthcare, offering accessible and convenient tools for individuals to evaluate their health concerns. While they bring several benefits, ensuring accuracy, addressing legal concerns, and upholding ethical standards are vital to their successful integration into the healthcare landscape As these tools evolve, they have the potential to play a significant role in shaping the future of medical diagnosis and patient care.


In recent years, there has been a transformational change in the healthcare industry toward more patient-centric treatment, and one key breakthrough in this direction is Remote Patient Monitoring (RPM). RPM is a healthcare approach that leverages technology to monitor patients' health conditions remotely, allowing for proactive and personalized care. While, Remote Patient Monitoring holds enormous promise for improving patient outcomes and lowering healthcare costs, but there are complicated regulatory issues that must be addressed. Remote Patient Monitoring (RPM) is a healthcare practice that allows healthcare providers to remotely monitor patients' vital signs, symptoms, and other health data This is typically achieved through the use of wearable devices, mobile apps, and other digital tools that collect and transmit patient data to healthcare professionals.
RPM has gained popularity due to its potential to improve patient outcomes, enhance the quality of care, and reduce hospital admissions. RPM offers numerous advantages. Early detection of health conditions proper care of chronic illnesses, and increased adherence to drugs
provided by health providers Furthermore, RPM enables patients with mobility difficulties or living in remote places to receive timely medical assistance by allowing patients and healthcare professionals to communicate in real-time.
As with any innovative healthcare practice, RPM is subject to a complex regulatory landscape. The regulatory framework includes rules and regulations aimed at assuring patient safety, data security, and the quality of care supplied via remote monitoring, albeit these may differ from nation to country Compliance with regulations in RPM is essential, as non-compliance has serious consequences, including legal penalties, adverse publicity, and

most importantly, risks to patient safety. Healthcare organizations, technology developers, and other stakeholders must understand and strive toward effective regulatory solutions. The regulatory challenges in RPM are multifaceted. They encompass issues related to data privacy, security, interoperability, reimbursement policies, and adherence to local healthcare regulations. Ensuring that remote monitoring technologies comply with these regulations is a significant challenge for healthcare providers and technology developers alike One of the key complexities in compliance with RPM regulations is the evolving nature of technology. As there continues to be technological advancement with devices and software solutions, regulators often struggle to keep pace with these innovations.
Non-compliance with RPM regulations can have severe repercussions. Legal consequences, such as fines and sanctions, can be crippling for healthcare organizations.
Therefore, healthcare organizations must invest time and resources in staying up-to-date with the latest regulations and adapting their practices accordingly. Moreover, RPM data contains sensitive patient information, raising concerns about data security and privacy Healthcare providers must implement robust cybersecurity measures to safeguard patient data, adding another layer of complexity to compliance. Non-compliance with RPM regulations can have severe repercussions. Legal consequences, such as fines and sanctions, can be crippling for healthcare organizations. Additionally, patient trust can be eroded if data breaches or privacy violations occur, potentially leading to a loss of patients and a damaged reputation.
Beyond regulatory challenges, RPM also raises ethical questions. The collection and use of patient data in remote monitoring may involve ethical dilemmas related to patient autonomy, consent, and the responsible use of information. Healthcare providers must strike a balance between monitoring patient health for their benefit and respecting their privacy and autonomy.

Patients often find themselves in a vulnerable position when it comes to remote monitoring. The continuous collection of health data may raise concerns about the invasion of privacy and the potential for surveillance. Balancing the benefits of RPM with the protection of patient autonomy requires careful consideration and ethical decisionmaking.

While RPM comes with ethical challenges, it also offers numerous benefits, including improved healthcare access, better disease management, and enhanced patient engagement. Weighing these benefits against the potential risks is a crucial ethical undertaking for healthcare providers and policymakers. Addressing the regulatory complexities in RPM requires a multifaceted approach. Healthcare organizations should establish clear policies and procedures that align with regulatory requirements and ensure ongoing compliance. This includes regular training for staff and technology users to maintain awareness of the evolving regulatory landscape.
Technology itself can play a significant role in facilitating compliance with RPM regulations. Developers of remote monitoring solutions should prioritize data security, encryption, and user authentication features to protect patient information. Additionally, the use of standardized data formats and interoperable systems can help ensure that RPM devices and applications can seamlessly integrate with existing healthcare infrastructure. Collaboration among healthcare providers, technology developers, regulators, and patient advocacy groups is essential for navigating the regulatory challenges in RPM. Regular communication and cooperation can help shape regulations that strike the right balance between innovation and patient protection. Engaging with patients and obtaining their input on remote monitoring practices can also lead to more ethically sound and patient-centred solutions
In conclusion, Remote Patient Monitoring holds tremendous potential to revolutionize healthcare by providing more personalized and proactive patient care. However, the regulatory challenges in RPM cannot be underestimated. Compliance with regulations is not only a legal requirement but also a moral obligation to protect patient privacy, autonomy, and safety. As RPM continues to evolve and gain prominence in healthcare, regulatory considerations will remain a dynamic and evolving field. In view of these obstacles, healthcare institutions, technology developers, regulators, and patients should collaborate to create a future where Remote Patient Monitoring is not only technologically advanced but also ethically and legally sound. Increased awareness, education, and commitment to compliance with regulations are the keys to unlocking the full potential of RPM while safeguarding patient interests. By addressing regulatory complexities and ethical concerns, we can ensure that RPM truly delivers on its promise of improving healthcare outcomes and enhancing the quality of life for patients worldwide.

 by Uchechi Amilo
by Uchechi Amilo
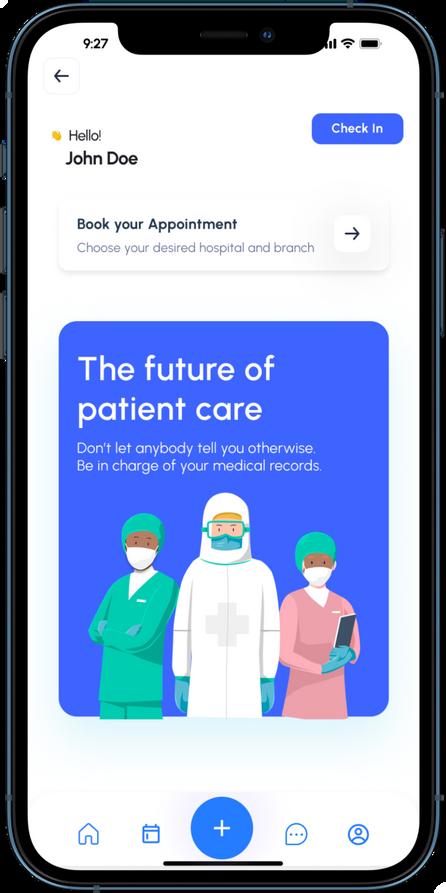
Healthcare is a significant aspect of our society and human life. Quality health care cannot be complete when patients are not involved in their care. As healthcare providers, it is paramount that both the patient and their caregiver are comprehensively informed about all aspects of their care. One of the fundamental rights of the patient in healthcare is autonomy. Patient autonomy is the right of competent adults to make informed decisions about their medical care, informed decision-making suggests information is made available and patients are active stakeholders in their health, this can be made possible ONLY when they have unfettered access to their health records.
Patient access refers to the ability of individuals to obtain and use healthcare services, information, and resources.
It is a crucial aspect of the healthcare system, as it affects the quality and availability of care for patients. Improving patient access is a critical goal of the healthcare system, as it can lead to better health outcomes and improved quality of life for patients.
Democratising access to patient health records aims at making health records accessible and inclusive to patients. This means ensuring that individuals have the right to access and manage their health information, empowering them to make informed decisions about their care. It also involves implementing secure and user-friendly systems that enable patients to easily access and share their health records with healthcare providers. This approach promotes patient autonomy, transparency, and collaboration in healthcare.
These three terms are important in the delivery of quality care. Since healthcare takes an interdisciplinary approach that involves nurses, doctors, and medical laboratory scientists among other healthcare professionals it is expected that these professionals have access to the necessary health records of patients in other to understand patients' conditions and facilitate quality patient care.
With the increase in the number of people leaving the country, there is a need for patients to have access to their health records, so they can be empowered and enlightened about matters pertaining to their health even when they start their healthcare journey anew with a different healthcare provider. It is amazing to know that with the advent of electronic health records, patient health records can now be stored in a
well-organized manner and retrieved without any stress, they can also be transferred or shared with ease this has made access to patient health records seamless both for patients and healthcare professionals.
Nonetheless, with the wonderful role technology has to play in democratizing access to patient health records, we cannot neglect the fact that confidentiality is an integral part of healthcare, so patients' health records should still be kept private regardless to prevent issues of litigation or information falling into the wrong hands. Furthermore, the fact that patients have access to health records might not necessarily mean they understand, the healthcare provider can do a good job of explaining and guiding them about what their health records entail so they can make informed decisions as regards their care.

In summary, democratising access to patient health records would do a lot of good for both the patients and the health care professionals but it is important to know that sometimes access can be abused so measures should be put in place to ensure that despite the accessibility and inclusivity of patient to their health records there is also heightened confidentiality to prevent harm.


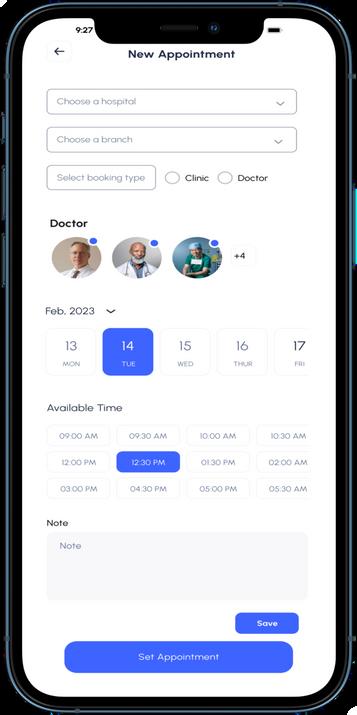
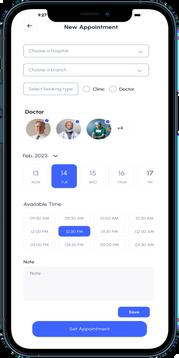
We live in an era dominated by technological breakthroughs, HealthTech is transforming the healthcare scene, bringing forth technologies that make receiving medical services and maintaining our well-being more convenient than ever before. From the Genesys patient app, with its teleconsultation offering, which allows patients to connect with healthcare professionals from the comfort of their homes to wearable devices that monitor vital signs like heart rate and blood pressure, these technologies have the potential to improve our overall health and well-being.
However, amid the promise of HealthTech, new challenges are lurking that demand our attention and careful consideration. One of these pressing issues pertains to the handling of our health data a topic of paramount importance in the digital age.
Health data ownership is a concept that bestows individuals with the power to control their health information. It not only grants the right to dictate who can access, use, and benefit from one's health data but also enables the correction, deletion, or transfer of this data as desired. The significance of this concept reverberates through several crucial aspects of our lives: privacy, autonomy, and trust in others. Privacy acts as the shield that guards our personal information against prying eyes, autonomy empowers us to make independent decisions regarding our well-being, and trust forms the bedrock of our interpersonal relationships.
However, the intricacies of health data ownership become more delicate as we engage with health-related software applications. A variety of parties, including healthcare providers, technology companies, researchers, and insurers, are involved in the collection, storage, and dissemination of human health data. Each participant brings their own motivations and goals to the table, creating ethical concerns regarding consent, transparency, and the benefits of sharing health data.
Some HealthTech companies have already taken steps to address these concerns and implement controls to protect patients' information. These efforts align with regulations like the Nigerian Data Protection Regulation (NDPR) of 2019 under Section 4.1, which discusses the concept of "Further Processing."


This section stipulates that when a Data Controller intends to use Personal Data for a purpose other than its initial collection, they must inform the Data Subject about this new purpose and provide relevant additional information.
To ascertain whether further processing is appropriate, the Data Controller must consider various factors, such as the connection between the original purpose and the proposed one, the context in which data was initially collected, the nature of the Personal Data, the potential impact on the Data Subject, and the presence of safeguards for the data. Crucially, this information must be communicated to the Data Subject before any further processing takes place. Further processing may proceed if the Data Subject consents based on the new information if it serves scientific, historical, or statistical purposes in the public interest, or if it is required to comply with a legal obligation. (NITDA, 2021)
One remarkable example of this implementation in action is the "Patient Record Release" feature introduced by Genesys Health Management Systems. This innovative feature empowers patients by giving them full autonomy over their health data. Patients can request the transfer of their records from Health Provider A to Health Provider B within the Partner network of Genesys Health System and even to Health Providers outside the Genesys Health Systems network.
The data is securely released to various destinations in an encrypted manner, following a series of approvals. This feature epitomizes the power of individuals to influence the fate of their health data, allowing them to determine what information is shared and how it is collected, stored, and utilized.
Nevertheless, balancing individual rights and societal interests remains a central challenge. While it is essential we advocate patient data autonomy, we also believe that sharing health data can have significant benefits, such as advancing medical research, enhancing public health, and lowering healthcare costs. Striking this balance necessitates constant ethical debate, raising key questions about how much control individuals should have over their health data and how much power they are willing to give up for the greater good.
As HealthTech continues to transform the healthcare environment, stakeholders such as regulators, healthcare providers, and patients must work together to set ethical principles and practices. These guidelines should prioritize data protection, consent, transparency, and the responsible use of health data, ensuring that the potential of HealthTech is harnessed while preserving individual rights and societal well-being. In this journey, the ethical compass guiding us through the HealthTech era is fundamental to building a healthier and more connected world. This ensures that patient data remains securely guarded, deeply confidential, and firmly in the hands of its rightful owners, in my opinion: the patients themselves.
One remarkable example of this implementation in action is the "Patient Record Release" feature introduced by Genesys Health Management Systems This innovative feature empowers patients by giving them full autonomy over their health data.




I N D U S T R Y P E R S P E C T I V E & C A S E S T U D I E S
 By Adeyinka Adenikinju
By Adeyinka Adenikinju
In recent years, the healthcare landscape in Nigeria, a country with a population of more than 213 million people with a good percentage of them living in rural areas, has witnessed a transformational shift towards digitalization, while urban areas have been quick to embrace these technologies, rural healthcare is also making strides in improving access to healthcare services. The adoption of econsultation and patient self-service portals has played a pivotal role in bridging the healthcare gap in remote regions of the country. Here we explore industry insights and present case studies highlighting the positive impact of these technologies in rural healthcare settings.

Nigeria, a country known for its diverse culture and vast geography, faces significant challenges in providing accessible healthcare services to its rural populations. However, advancements in telemedicine and healthcare technology have begun to change this narrative.
E-consultation platforms and patient self-service portals are empowering rural healthcare facilities by enabling virtual consultations, remote monitoring, and streamlined administrative processes. These digital tools are designed to enhance the overall healthcare experience, ensuring that patients receive timely and quality care regardless of their geographical location.
1. Increased Access to Healthcare
E-consultation platforms have extended the reach of healthcare services to remote areas. Patients no longer need to travel long distances to consult with specialists or access essential healthcare information. This increased accessibility has significantly reduced the burden on rural healthcare facilities and improved overall patient outcomes.
Patient self-service portals have streamlined administrative tasks such as appointment scheduling, billing, and medical record management. This efficiency allows healthcare providers to focus more on patient care, reducing the time spent on paperwork and administrative hassles.
Digital health technologies provide much data for population health management and targeted interventions. This data-driven approach enables healthcare providers to identify trends, monitor disease outbreaks, and allocate resources more effectively, improving healthcare outcomes.

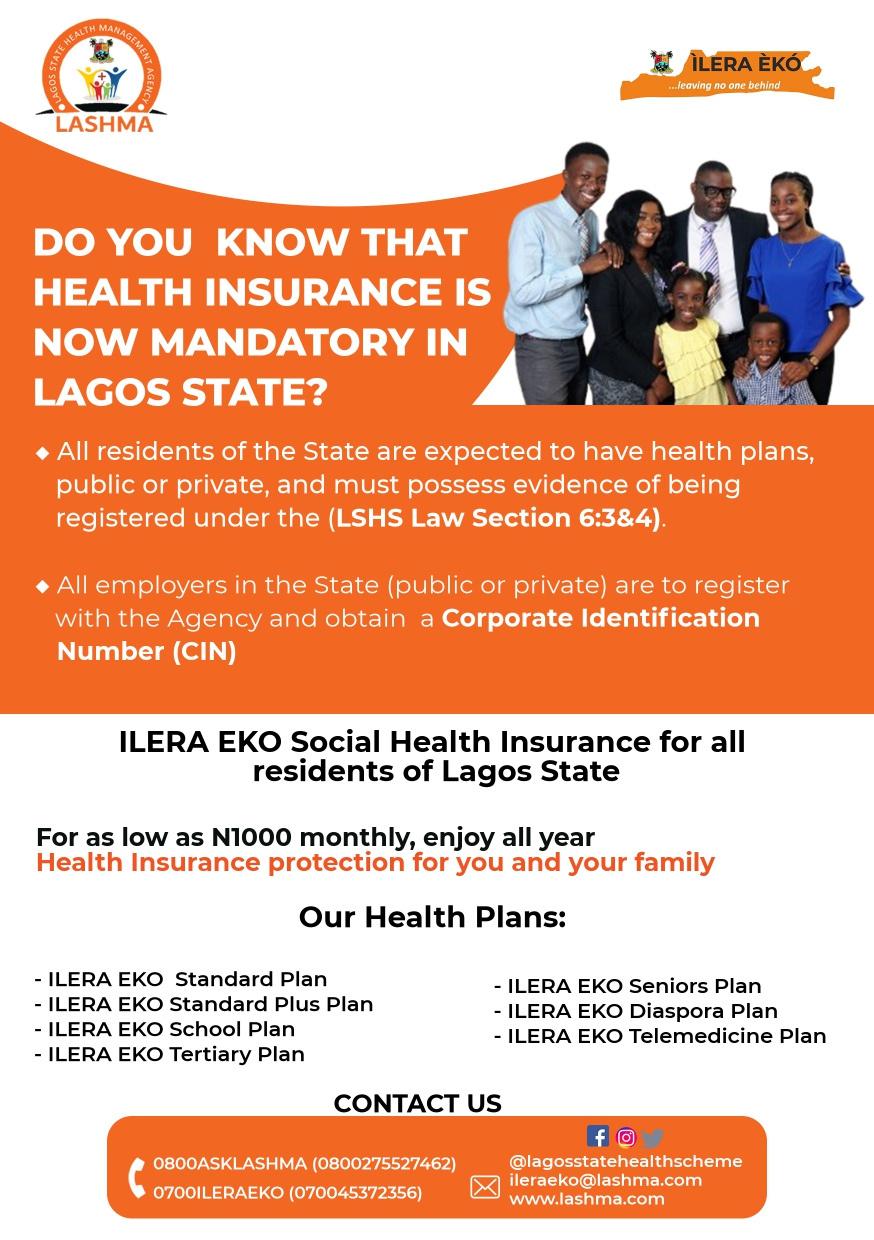
4. Government Initiatives: The Nigerian government has recognized the potential of digital healthcare solutions in improving healthcare access. Initiatives such as the National Health Insurance Scheme (NHIS) and the National Primary Health Care Development Agency (NPHCDA) are promoting the integration of technology in rural healthcare.
5. Collaboration with Telemedicine Providers: Many rural healthcare facilities are partnering with telemedicine providers to offer Econsultation services. This collaboration extends the reach of specialized healthcare services to remote areas.
6. Covid 19 as a catalyst: The onset of the COVID-19 pandemic prompted a rapid shift in how healthcare services were delivered. Social distancing measures and lockdowns made traditional in-person doctor visits challenging. In response to these limitations, the adoption of econsultation and patient self-service portals gained momentum. These platforms allow patients to connect with healthcare providers remotely, enabling access to medical advice and consultations from the safety of their homes.

Northern Nigeria is known for its picturesque landscapes and rich cultural heritage. However, when it comes to healthcare access, the region has faced significant challenges. Sparse population densities, limited healthcare infrastructure, and a shortage of skilled medical professionals have historically resulted in poor healthcare outcomes. Rural residents often had to travel long distances to reach a healthcare facility, leading to delayed treatment, exacerbated health conditions, and increased healthcare costs. Insecurity and attacks on medical facilities including pharmacy outlets have contributed to the continuous shortage of access to healthcare in the region. The need for a more accessible and cost-effective healthcare model became evident.
In Gombe State, a “GoHealth mobile App” initiative was launched to connect rural patients with specialists in urban areas. The state used the mobile application to encourage Universal Health Coverage across all strata. This enabled patients with medical conditions enroll into the health scheme, book appointments with their care providers, make enquiries, receive expert advice, treatment plans as well as provide feedback to enable the government to take necessary measures to improve the quality of service.” This initiative has not only improved health outcomes but also reduced the need for costly and timeconsuming travel. The initiative saw more than 25,000 poor and vulnerable access healthcare service in the state.


Abia, another Nigerian state, implemented a patient self-service portal to digitize its healthcare administration. Patients can now schedule appointments, access their medical records, and receive billing information through a secure online platform. The Tele-health initiative is Abia state’s own contribution to progressing the Universal Health Coverage mandate of the Federal Government of Nigeria, based on the e-Health policy of Nigeria as it is foundation, after its adoption at the 58th NCH in Sokoto in 2016, the state became the pioneer state for the Project. Abia state’s largest telecommunication network provider Glo, which played in a market that caters to almost 3.5 million active subscribers, was partnered with, thus making it the single largest provider of services in the state. The telecommunication call center through the local healthcare workers serves as an avenue to render prompt consultations, health information and education to people in the comfort, convenience, and confidentiality of their own spaces, homes, offices, and shops. This has reduced wait times and improved the overall patient experience while increasing the accuracy of medical records.


eHealth Africa, a nonprofit organization, implemented a telemedicine program in several rural areas of Nigeria. Through mobile clinics equipped with telehealth technology, they provided virtual consultations and educational resources to remote communities. Their strength in good coverage of the regions where they are presence has helped in ensuring that Kaduna state Bureau of statistics have up-todate data to take pre-informed decisions through their support in the development of GRID3 project.
It should be stated that the project's overarching objective is to ensure that the people of Nigeria, particularly those who are economically disadvantaged, can benefit from improved resource allocation based on evidence and data-driven policy decisions made by policymakers. This will be achieved through three primary objectives:
Enhancing the quality of public primary healthcare facilities to meet national and international standards for maternal and child health.
Strengthening the supply chain for essential health commodities. Enhancing eHA's ability to promptly respond to public health emergencies.
The adoption of e-consultation and patient self-service portals in rural Northern Nigeria is undoubtedly a step in the right direction. However, several challenges remain to be addressed:

Infrastructure: Ensuring reliable internet connectivity and access to digital devices is crucial for the success of these initiatives.

Healthcare Literacy: Efforts must be made to educate the rural population about the benefits and usage of these digital healthcare tools.

Protecting patients' sensitive health data is paramount, and robust cybersecurity measures must be in place.
The adoption of e-consultation and patient self-service portals in rural Northern Nigeria is undoubtedly a step in the right direction. However, several challenges remain to be addressed:
The adoption of e-consultation and patient self-service portals in rural healthcare settings in Nigeria has ushered in a new era of healthcare accessibility and efficiency. These technologies are instrumental in improving patient outcomes, streamlining administrative processes, and enabling data-driven healthcare decisions.
As Nigeria continues to embrace digital health solutions, the industry will undoubtedly witness even more innovative approaches to address the unique challenges faced by rural healthcare facilities. With increased collaboration between the public and private sectors, it is expected that healthcare in rural Nigeria will continue to improve, setting an inspiring example for other countries facing similar challenges.

Ensuring that digital healthcare services are accessible and affordable for all, regardless of socio-economic status, is a continuous challenge.

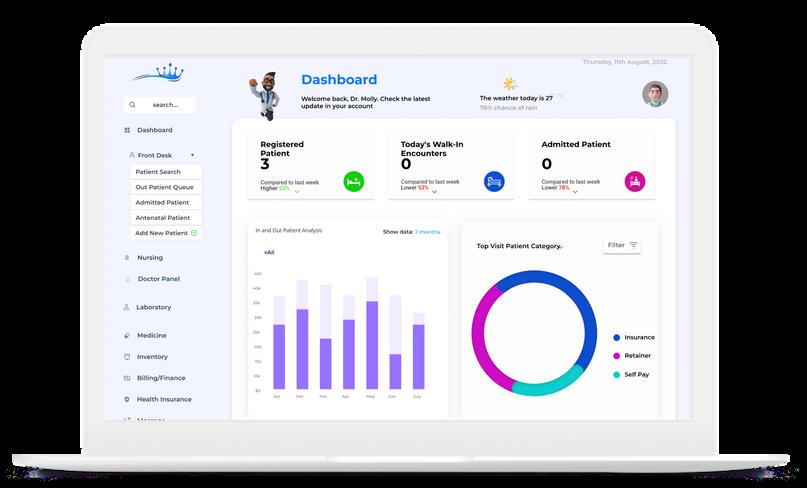
In recent times, Nigerian healthcare has seen a remarkable transformation with the introduction of Electronic Medical Records (EMRs) or Electronic Health Records (EHRs) in leading hospitals. This exciting shift is driven by a commitment to enhance healthcare services, improve patient care, streamline administrative processes, safeguard sensitive medical data, and address evolving ethical and legal considerations. One definition of an Electronic Medical Records (EMRs) or Electronic Health Records (EHRs) is that it is the application of health information technology (HIT), encompassing patient health data, clinical decision support, results management, central data storage, and order entry technologies like computerized physician order entry (CPOE). It can also be simply defined as a digital version of the traditional paper-based medical record for an individual. This aids in organizing and providing healthcare services, allowing for the ongoing collection of electronic health information for individual patients and populations (Gabriel Alobo et al., 2020). In this edition, we delve into the adoption of EMRs in Nigeria's leading healthcare institutions and the multifaceted impact it brings. The rapid trend of adoption of EMRs may suggest that some hospitals just want to imitate the echelons in the health sector by adopting EMRs so as not to be seen as being left behind. This trend, however, is a positive as against the backdrop of poor health information system singled out as a key challenge in developing countries healthcare system, which includes Nigeria (Sani et al., 2017).
The real time use of systems to automate record taking and aid decision support in Nigerian hospitals used to largely be a hit and miss and lead to a failed implementation because of several obstacles;
Infrastructure and Connectivity: Insufficient IT (Information Technology) infrastructure and connectivity issues which present hurdles to seamless EMR (Electronic Medical Record) adoption. The cost of getting and supporting these infrastructures is the major obstacle; most leading hospitals can afford to invest in such assets.
Resistance to Change: Staff resistance to modern technology which usually requires comprehensive training and educational programs to ease the transition and most importantly handholding of users until familiarization.
It would be good to say how the myth that computers are coming to take their jobs plays a role in staff resistance, though not the only reason, one that the management must take good consideration of. Other reasons include fear of being exposed if they have been partaking in nefarious acts like theft in the facility especially those in “juicy offices” like the storeroom, pharmacy and finance/billing unit.
Implementation Costs: Initial costs can be significant, potentially limiting adoption, particularly in smaller healthcare facilities. Hospital management must think of the cost of on-premises servers, internet and intranet cabling and connectivity concerns. The advent of cloud servers was also helpful, especially for hospitals with a network of branches initially, but with the ever-widening gap in the foreign exchange rates, it is now becoming a recurrent cost that is using up financial resources.
Data Migration: The migration from paper-based records to electronic format can be time-consuming and resource-intensive.
Interoperability: Ensuring EMR systems work seamlessly with other healthcare systems and devices is a complex but necessary challenge. If hospitals had their preferences, they would look to dominate their services, prompting the need for in-depth examination. They would aim to take part in various medical specialties and would generally refer patients to other healthcare facilities only when they are unable to supply the necessary care themselves.
Adaptability: Continued failure in the implementation of Electronic Medical Records (EMRs) in Nigerian hospitals will persist unless there is a concerted effort to customize and adapt the fragmented foreign EMR components to local needs and requirements. One of such ways most of the big hospitals have solved this is having to go with an indigenous health tech company to develop the EMR that suits their processes.

Enhanced Patient Care: Reddington Hospital Ikeja in Lagos, a pioneer in EMR adoption, reported significant improvements in patient care. EMRs allow their healthcare providers

preventive care reminders have empowered healthcare professionals to make informed choices, improving patient safety.
Decision Support: KAAF MLMC in Lagos, a leading Mother and child hospital, has utilized EMRs' decision support tools effectively. Appointment and medication expiry dates alerts and to access comprehensive patient information promptly, leading to precise diagnoses and enhanced treatment outcomes.
Data Security: At Subol hospitals ltd in Lagos, robust EMR security measures have been instrumental in safeguarding patient data. These features protect against unauthorized access, ensuring the utmost confidentiality.
Efficient Record
Keeping: RNZ

Occupational Hospital in Port Harcourt has experienced a


significant reduction in paperwork since adopting EMRs. This shift has simplified data retrieval, reduced the risk of misplacement, and saved valuable time and resources.
Streamlined
Administration: Molly hospital in Ibadan has seamlessly integrated EMRs with its financial systems. This integration has led to streamlined billing processes, reducing administrative costs and enhancing revenue management

Enables Quality Practice & Collaborative Care: Lagoon hospital, one
of the early adoptersof EMR in Lagos, were able to see significant decreased medical errors, adverse drug events, prescription errors and improved prescribing practice. This has upheld the safety, effectiveness and appropriateness pillars for quality healthcare in their facility (Ojo, 2013).

THE USE OF EMRS BY HOSPITALS HAVE YIELDED A LOT OF BENEFITS, FOR A FEW BELOW ARE SOME TESTAMENTS OF EMR ADOPTION:
We must also reflect the Impact of EMRs on Healthcare Delivery in Nigeria:
Improved Quality: EMRs empower healthcare providers to make informed decisions, ultimately enhancing patient care and outcomes.
Error Reduction: Life Support Eye Clinic, Lagos saw that for a period of study of EMR use in 11 years, the system minimized record and medication errors, promoting patient safety Ogundipe (2011)
Cost Savings: Over time most of the major hospitals adopted EMR implementation, so it led to large savings by reducing paperwork and administrative burdens.
Patient Engagement: Patients can access their records, fostering greater engagement in their healthcare decisions.
Research and Public Health: EMRs provide valuable data for research and public health initiatives, enabling better healthcare planning.
EMRs have also brought about significant changes in medical litigations and raised ethical concerns:
Legal Documentation: EMRs provide a detailed, time-stamped record of patient interactions, which can be pivotal in medical malpractice lawsuits. Proper documentation is essential to protect both patients and healthcare providers
Privacy and Consent: Ethical concerns revolve around patient consent for sharing their electronic medical data. Healthcare institutions must establish clear policies to keep patient trust and data security.
Data Accuracy: Ensuring the accuracy of data input is crucial, as inaccuracies can lead to incorrect diagnoses or treatments. Ethical responsibility lies in keeping the integrity of patient records.
In conclusion, the adoption of electronic medical records in Nigeria's leading hospitals represents a significant leap forward in healthcare delivery. However, alongside enjoying the advantages of EMRs, healthcare institutions must also manage the intricate realm of legal and ethical concerns. To achieve a more efficient, patient-centered, and legally compliant future, this requires ongoing investments in technology infrastructure, staff training, and the use of indigenous health tech companies with over a decade of expertise in crafting tailored EMRs.
Although there are other areas we could delve into, we'll keep this brief to serve its intended purpose. Please remain connected for further updates on healthcare innovations in our upcoming newsletters.


 BY AYO-OLAGUNJU MUNA
BY AYO-OLAGUNJU MUNA

In today's data-driven world, predictive analytics has emerged as a powerful tool with the potential to transform various industries, including healthcare. Its promises are enticing and the possibilities alluring, but to fully understand its implications in healthcare, we must first embark on a journey to demystify what predictive analytics is and isn’t
Predictive analytics is a subset of a larger branch of data analytics – which is the practice of Examining data to answer questions, identify trends and extract insights to provide necessary information for informed business decision-making. There are four types of data analytics; Descriptive analytics, which answers the question, “What happened?” Diagnostic, which answers the question, “Why did this happen?” Prescriptive analytics, which answers the question, “What next?” and lastly, our subject of interest, Predictive analytics
Predictive analytics is a branch of data analytics that makes predictions on future outcomes using historical data combined with statistical modelling, data mining techniques, artificial intelligence and machine learning (IBM, 2023). It attempts to answer the question, “What happens next?” Organizations can use historical and current data to forecast trends and behaviours second, days, or years into the future, with a great deal of precision. It leverages a variety of techniques, to sift through vast amounts of data and identify patterns that may not be immediately apparent to human analysts.
Predictive analytics in healthcare is not fortune-telling! It doesn't provide crystal-clear prophecies of what will happen but rather offers probabilities based on historical data and current trends.

It's akin to weather forecasting, where meteorologists use data to predict the likelihood of rain, but they can't guarantee with 100% certainty that it will rain. The bane of Netflix’s “Because You Watched…” list is equally hinged on this, Netflix collects various users’ past viewing history and behaviour data to determine suitable content suggestions. Within the healthcare domain, predictive analytics takes on a profound role. Imagine a scenario where healthcare providers can anticipate disease outbreaks, allocate resources efficiently, and even predict patient health deterioration before it occurs.
According to IBM (2023), Geisinger Health used predictive analytics to mine health records to learn more about how sepsis is diagnosed and treated. They created a predictive model based on the health records of more than 10,000 patients who had been diagnosed with sepsis in the past. The model yielded impressive results, correctly predicting patients with a high rate of survival. This is the promise that predictive analytics holds.
It is NOT an alternative or replacement for Healthcare Professionals: This happens to be one of the most widely believed myths, and one can easily see where the source of concern stems from. Unfortunately, this is far from the truth, as we’ve seen with the inclusion of robotics and automation in other industries. Predictive analytics is a complementary tool that merely assists healthcare professionals in decision-making. It enhances their ability to make informed choices by providing valuable insights from data. While predictive analytics has made significant strides and advancements, it cannot replace the comprehensive roles of physicians, as they bring the vital ‘human element’ to healthcare. They not only consider clinical data but incorporate a patient’s mental state, cultural factors and beliefs in decision-making, which is valued by patients and crucial during sensitive times.
 We will now proceed to dispel some common myths surrounding predictive analytics in healthcare
We will now proceed to dispel some common myths surrounding predictive analytics in healthcare
2. Analytics is NOT only for executives and management: While it's true that business intelligence and analytics initially served the needs of corporate leaders, healthcare is experiencing a transformation. In today's healthcare landscape, analytics is no longer confined to the boardroom. Recent advancements in clinical information systems have brought analytics to the front lines of healthcare. Clinical staff now interact with electronic patient records and diagnostic systems daily, generating a wealth of valuable data. This data is not just for executives but serves as a powerful resource for healthcare transformation. Effective communication is paramount to quality improvement initiatives. Analytics tools can play a vital role in engaging front-line staff. Instead of burying insights in complex reports, organizations are adopting userfriendly visualizations and "quality boards" that display key performance indicators. These accessible tools empower staff to monitor progress, understand performance targets, and actively participate in improvement initiatives.
3. The combination of big data and brilliant data scientists DOES NOT always equal success: While domain experts and big data are invaluable and essential, that alone cannot guarantee success or accuracy.
The quality of the data, coupled with a deep understanding of it is what is most crucial to the success of any predictive analytics endeavour in healthcare. In determining the quality of the data, it is vital to answer the question of how the data was gathered. For instance, the adoption of electronic health records (EHRs) can lead to more comprehensive data, but without acknowledging this change, one might draw incorrect conclusions about patient health. It is important to put context around the purpose for which the data was collected. For instance, data collected for specific purposes, such as lab data in a hospital, may not represent the broader population accurately. It's biased toward sick individuals seeking health care. Another important consideration is the limitations of the data since variations would typically occur when dealing with data from multiple organizations, despite using similar systems. Of course, data’s meaning can evolve with time, a practical example would be the representation of gender. Staying current with evolving concepts is crucial. True success necessitates a holistic understanding of data, domain expertise, and the recognition that a combination of ML and human expertise often produces the best results in healthcare predictive analytics.
Having dispelled the myths, let's shift our focus to some real-world applications of predictive analytics in healthcare:
Disease Outbreak Prediction: Predictive analytics can help in disease surveillance by analyzing factors such as; population density, travel patterns, and disease transmission rates to predict, prepare and possibly avert a pandemiclevel disease outbreak.



Readmission Risk Prediction: Healthcare providers can use predictive models to identify patients at a higher risk of hospital readmission, allowing for proactive interventions and improved patient outcomes. According to research (Kennedy, 2023) Corwell Health, through a recent initiative that uses predictive analytics to forecast risks and reduce readmissions, has kept 200 patients from being re-admitted, saving over $5 Million in the process, since January 2021.
Resource Allocation: Hospitals can optimize resource allocation by predicting patient admissions, enabling them to better allocate staff, beds, and supplies more effectively. Beth Israel Deaconess Medical Centre (BIDMC) in Boston leveraged predictive analytics to create an application that predicts the discharge date, with a high degree of accuracy (Haas et al., 2019).
Predictive analytics in healthcare isn't without its challenges. Data privacy and security concerns are paramount, and the potential for bias in algorithms must be addressed. Moreover, the interpretation of predictive results requires a deep understanding of both data and medical context.
Privacy Concerns: One of the significant concerns in predictive analytics in healthcare is the privacy of patient data. To make accurate predictions, algorithms need access to vast amounts of patient information, which raises pertinent questions about how this data is collected, stored, and used. Patients must trust that their personally identifiable sensitive information is handled with the utmost care.
Bias and Fairness: Algorithms used in predictive analytics can inherit biases present in historical data. For example, if a healthcare system historically provided unequal care to different demographic groups, predictive models trained on that data may perpetuate these inequalities. Addressing bias and ensuring fairness in predictive analytics is a critical ethical consideration.
Interpretability: Predictive models, especially complex ones like deep learning neural networks, can be difficult to interpret. This lack of interpretability raises questions about how decisions are made and whether healthcare professionals can trust these models when making critical decisions.
Predictive analytics holds immense promise in revolutionizing healthcare. It empowers healthcare professionals with valuable insights, enhances patient care, and optimizes resource allocation. However, it is crucial to approach it with a realistic understanding of its capabilities and limitations.

As we move forward in the age of data, healthcare providers and researchers must embrace predictive analytics responsibly, harnessing its potential while safeguarding patient privacy and ensuring equitable access to its benefits. In doing so, we can navigate the path from myth to reality, where predictive analytics becomes an indispensable tool in the pursuit of healthier communities and better patient outcomes.
In summary, predictive analytics in healthcare is not a crystal ball, but a powerful ally in the hands of healthcare professionals. Its ability to analyze data, identify trends, and make predictions has the potential to transform healthcare delivery. However, we must remain vigilant in addressing privacy, bias, and interpretability concerns to fully unlock its benefits. In the end, the true power of predictive analytics lies in its responsible and ethical use to improve the health and well-
 BY AYO-OLAGUNJU MUNA
BY AYO-OLAGUNJU MUNA
In the rapidly evolving realm of healthcare, a profound shift is underway one driven by the convergence of data and technology. Hospital operations, once guided by intuition and experience, are now being revolutionized by datadriven decision-making. This article delves into the dynamic synergy between data insights and hospital operations, exploring how this collaboration is reshaping the healthcare landscape.
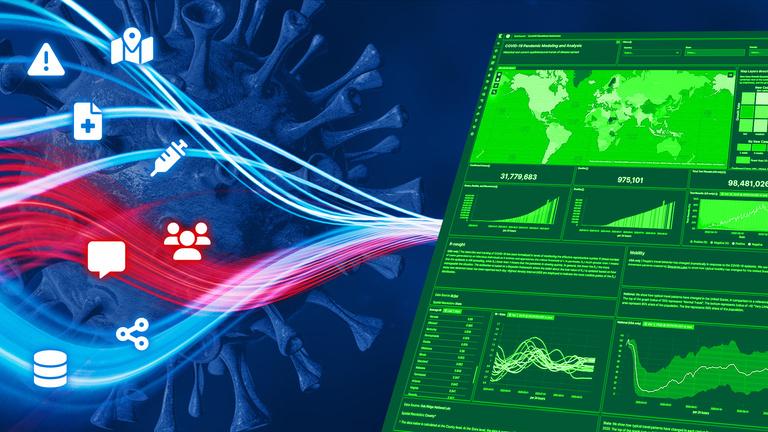
The COVID-19 pandemic exposed the vulnerabilities in the health sector the world over, as its impacts weighed heavy on even the perceived robust health systems. Suffice it to say, that no amount of resources can wholly tackle a fullblown pandemic outbreak. Healthcare leaders recognized the significance of promptly gathering and comprehending data to guide their responses and adaptations. Hospitals and health systems effectively utilized data and analytics solutions to gain insights into the transmission of COVID-19 within their communities and anticipate the influx of COVID-19 patients in their emergency wards. The present healthcare landscape has equally been marred by labour shortages – especially in developing, under-developed, and Lowand-middle-income countries, rapidly shifting care trends, and professional burnout. To fully optimize their operations, researchers and healthcare professionals must broaden their horizons beyond time-consuming and costly randomized controlled trials and explore the ever-evolving realm of real-world data and operational excellence.
The era of manual processes and fragmented information in hospital operations is gradually fading into the background. The emergence of datadriven decision-making enables healthcare institutions to leverage the wealth of data generated daily to enhance their operations. An example of this trend is the integration of advanced Electronic Medical Record (EMR) systems that streamline patient data, treatment strategies, and administrative workflows. Providers gain valuable insights from patient data analysis, enabling the identification of patterns, trends, and risk factors. By identifying bottlenecks, streamlining workflows, and reducing costs, healthcare organizations can enhance their efficiency. Additionally, data analytics supports inventory management, resource allocation, and staff scheduling. Detecting patterns indicative of fraudulent or abusive practices becomes possible through the analysis of healthcare claims data, which helps prevent financial losses and safeguards patients. Moreover, healthcare data analytics facilitates medical research by providing valuable insights into disease patterns, treatment effectiveness, and the development of new drugs. Through the application of data analytics, healthcare organizations can achieve deliverables that would otherwise require extensive manpower and process transformations.
We would highlight four key areas where hospitals can leverage data insights in optimizing their operations to achieve operational excellence:
providers continually strive to provide the right care for their ique patient needs, they are constantly shuffling between aluating patients’ needs accurately while managing hospital sources effectively. While providers are often equipped and ained for the former, they are usually found wanting in the latter, which is a challenging task — especially given the pressure on the health system that’s even more pronounced with the rising brain drain.
At the provider level, data-driven operational decision-support systems can provide valuable insights to aid in making these triage, admission, and discharge decisions. For example, when a patient arrives and a provider is unsure whether the patient should be sent to the ICU or a general ward, a decision-support algorithm can provide recommendations based on the predicted benefit of ICU admission for that particular patient. According to (Kim & Song, 2022), research using patient-level operational data from more than 190,000 hospitalizations across 15 U.S. hospitals shows that when patients who had a clinical need for admission to the ICU are instead admitted to another unit of the hospital (e.g., a general ward), it often results in longer hospital stays and higher readmission rates.

When the capacity of the desired ICU is constrained, the provider may consider different options such as; placing the patient in another unit (e.g., a surgical ICU as against ICU) or discharging patients who are currently in the ICU to make room for new ones. According to (Song et al., 2020), the same research using hospital operational data reveals both strategies have critical tradeoffs and unintended consequences that need to be accounted for. Decision-support algorithms can be designed to incorporate these tradeoffs, weigh the costs and benefits of the different choices, and provide appropriate recommendations.
At the ward level, machine learning and decision-support algorithms can equally be used to predict the expected number of admissions, discharges, and transfers to and from the ward, which in turn can inform subsequent actions based on these predictions. This can facilitate the bed turnover process, leading to improved patient flow and reduced length of stay. The predictions for individual wards can serve as inputs to a hospital-wide bed management dashboard, which can be used not only to display the current status of each ward but also to provide predictions for the expected future status throughout the hospital. According to (Bertsimas et al., 2021) similar systems are already in play at Beth Israel Deaconess Medical Centre in Boston and Boston’s Children's Hospital (Siwicki, 2018).
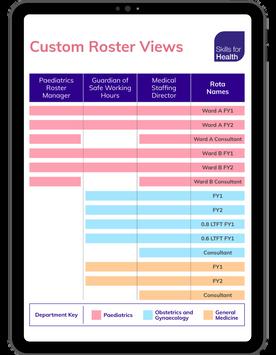
Data insights from operations can equally help with the supply side, in better managing clinical roaster and staff needs, especially with the shortage of healthcare workers. Personnel costs account for a significant portion of hospitals’ costs. Instead of relying on phone calls, text messages, and other manual means, to make ad-hoc staffing decisions that often change at the very last minute, hospital administrators can utilize analytics to improve this process.
Algorithms can predict staff absenteeism and attrition rates and the need for surge staffing to preemptively determine the right number of locum staff to bridge the gap. According to research (Green et al., 2013) in emergency department operations, both can be modelled, even in environments where demand is highly uncertain. A key advantage is the ability of these systems to preempt and respond more quickly, which can in turn improve the consistency and predictability of the clinical work schedule. This aspect is highly important as hospitals and other healthcare providers work on reducing notoriously high clinical turnover rates. Research examining nursing turnover in one of the largest home health agencies in the United States shows that employer-driven inconsistency in workers’ schedules increases workers’ likelihood of quitting (Bergman et al., 2021).
While the adoption of digital capturing and storing of patient records is on the increase, the scheduling of various other resources such as; theatre and surgical scheduling, and scans in radiology suites, to mention a few are still largely manually driven. This is another area where technology flourishes and can bring substantial improvements not only by better predicting resource needs and effortlessly incorporating last-minute alterations and cancellations, but also by optimizing schedules based on data insights
For illustration purposes, predictive and machine-learning algorithms can be used to better predict the duration of procedures such as the length of a surgery or an MRI, by so doing, optimally manage resource allocation. The projected duration of a procedure is a function of the patient's characteristics, their unique clinical needs, and other variable operational factors. For instance, the length of a surgical procedure tends to increase as a function of larger team sizes, higher workloads, and the sequence of the operation in the operating room. Algorithms are better equipped than humans to account for the effects of such operational factors in making predictions. According to Tozzi (2019), at the Beth Israel Deaconess Medical Center, tools developed by Amazon are being used to book operating room times more precisely.
Insights drawn from data, coupled with machine learning can also be used to predict the time required for each patient to spend in the post-anesthesia care unit (PACU) following a surgery. Since PACU congestion often leads to delays in the operating theatres, this is another area where data insights can be useful.
In the United States, hospitals spent an average of $11.9 million each on medical and surgical supplies in 2018, accounting for up to a third of the total operating expenses in some of these facilities (Kim & Song, 2022). Despite this, enhancing supply chain and inventory management is not often on their priority list, as they tend to focus more on the processes surrounding direct patient care. Yet, having these supplies is necessary for delivering high-
quality care. Pooling and coordinating supplies across different units and departments within a hospital can significantly reduce the amount of inventory required to meet a given service level. While physical centralization is one way to achieve this, information centralization, which can be easily achieved with a digitized supply-chain-management system, may be sufficient to reap the same benefits.

According to Digital Supply Chain Transformation (2022), digitally transforming the supply chain across many industries has been shown to reduce process costs by 50% and increase revenue by 20% and hospitals are no exception! EMR insights on hospital consumption patterns and utilization can feed into an automated procurement process of medical, surgical, and pharmaceutical supplies, hospitals can significantly reduce supply chain and inventory management-related costs. Improving agility and resilience to demand and supply-side shocks has become even more critical, and hospital managers are increasingly looking for ways to leverage data and technology to gain insight into inventory, pricing, lead times, and demand trends.
Radio-frequency identification (RFID) technologies and internet-connected trackers can be used to better track and locate supplies in real time. For example, Mayo Clinic’s Saint Marys Hospital rolled out an RFID system for their emergency room operations in 2015, which led to improved care and patient experience as well as lower costs (Kim & Hummy, 2015).
The intersection of data insights and hospital operations is only beginning to reveal its potential. As technology continues to evolve, hospitals can anticipate even deeper integration, predictive capabilities, and AI-driven insights. The journey toward optimized operations is ongoing and will be steered by pioneers who recognize the transformative power of data in reshaping the healthcare landscape.
In conclusion, the fusion of data insights and hospital operations marks a turning point in healthcare. By harnessing the potential of data, hospitals can streamline operations, elevate patient care, and embark on a path toward operational excellence and patient-centricity.





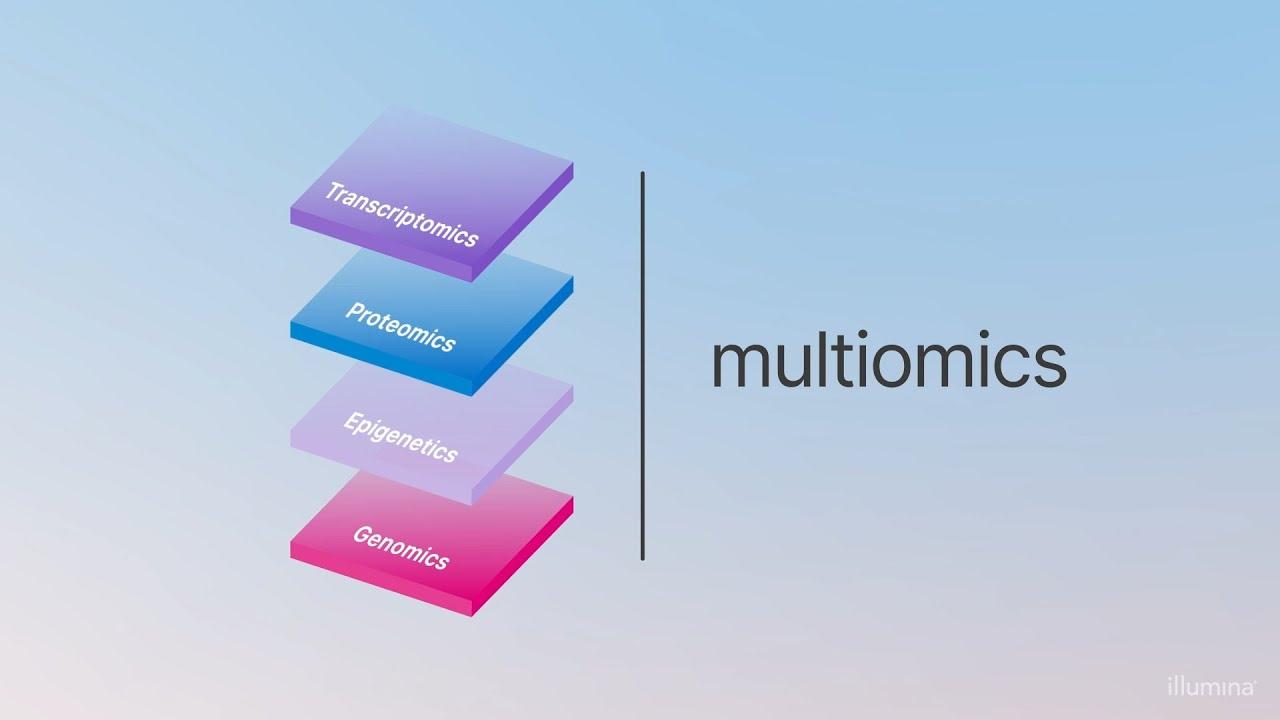
Multi-omic technologies refer to the comprehensive analysis of multiple biological data types, often on a genome-wide scale, to gain insights into the intricate workings of an organism.
Peter OwolabiIn recent years, the field of healthcare has witnessed remarkable advancements, and one of the key driving forces behind this progress is the integration of multi-omic technologies. These cutting-edge approaches have revolutionized our understanding of diseases, personalized medicine, and treatment strategies. This discussion delves into the significance of multi-omic technologies, their current applications, and the promising breakthroughs they hold for the future of healthcare.
Multi-omic technologies refer to the comprehensive analysis of multiple biological data types, often on a genome-wide scale, to gain insights into the intricate workings of an organism. These data types can include genomics (study of genes and their variations), transcriptomics (study of gene expression), proteomics (study of proteins), metabolomics (study of small molecules involved in metabolism), and epigenomics (study of chemical modifications to DNA that regulate gene activity). Integrating these various omics layers allows researchers and clinicians to obtain a holistic view of an individual's health and disease state.
Currently, one of the most promine applications of multi-omic technologi is in the realm of precision medicin This approach tailors medic treatments to the unique gene makeup and molecular characterist of each patient. By analyzing individual's genome, transcriptome, an proteome, clinicians can ident specific genetic mutations, ge expression patterns, and protein profil that may contribute to disea susceptibility and progression. Arm with this information, they can devel personalized treatment strategies th are more effective and have fewer si effects.
Furthermore, multi-omic technologi have been instrumental in unravelli the underlying mechanisms of complex diseases. For example, cancer, once thought of as a single disease, is now recognized as a diverse group of diseases with distinct molecular profiles. Multi-omic analyses have revealed the genetic mutations, altered gene expression, and aberrant protein signalling pathways that drive different types of cancer. This knowledge has led to the development of targeted therapies that specifically target the molecular vulnerabilities of cancer cells, improving patient outcomes.
In addition to diagnosis and treatment, multi-omic technologies have shown promise in disease prevention and early detection. By monitoring an individual's omics data over time, healthcare providers can identify subtle changes that may indicate the onset of disease even before clinical symptoms appear.

This proactive approach allows for early interventions and better disease management, ultimately leading to improved patient outcomes and reduced healthcare costs.
Looking ahead, the future of healthcare is brimming with exciting possibilities for multi-omic technologies. One of the most anticipated breakthroughs is the integration of artificial intelligence (AI) and machine learning into omics data analysis. These advanced algorithms can sift through vast datasets to identify complex patterns and correlations that may not be apparent to human researchers. AI-driven omics analyses have the potential to accelerate drug discovery, identify novel therapeutic targets, and predict patient responses to treatment with unprecedented accuracy.
Furthermore, the advent of single-cell omics technologies is poised to revolutionize our understanding of cellular heterogeneity and disease progression. Traditional omics analyses often rely on bulk tissue samples, which can mask the distinct characteristics of individual cells. Single-cell omics, on the other hand, allow researchers to study the genetic, transcriptomic, and proteomic profiles of individual cells, providing insights into cell-to-cell variation within tissues and organs. This level of granularity is invaluable in fields such as immunology, where understanding the diversity of immune cell populations is critical for developing targeted immunotherapies.
Another promising avenue for multiomic technologies is the study of the microbiome, which consists of trillions of microorganisms residing in and on the human body. Multi-omic approaches can decipher the complex interactions between the host genome, microbiome, and environmental factors, shedding light on how the microbiome influences health and disease. This knowledge may lead to innovative treatments that modulate the microbiome to prevent or treat a wide range of conditions, from gastrointestinal disorders to autoimmune diseases.
In conclusion, multi-omic technologies have already made significant contributions to the field of healthcare by enabling precision medicine, uncovering disease mechanisms, and advancing disease prevention and early detection. As we look to the future, the integration of AI, single-cell omics, and microbiome research holds tremendous promise for even greater breakthroughs.
With these evolving technologies, healthcare is on the cusp of a transformative era where treatments are increasingly personalized, diseases are better understood, and innovative interventions become a reality. As we continue to adapt and harness the power of multi-omic technologies, the prospects for improving human health and well-being are brighter than ever before.

 By Ngozi Nweke
By Ngozi Nweke
According to the International Association for the Study of Pain (2011), “Pain is defined as an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”. This definition emphasizes the subjective and multidimensional nature of pain, incorporating both the sensory and emotional components of the experience. Pain motivates organisms to withdraw from damaging situations, to protect a damaged body part while it heals and to avoid similar experiences in the future. In simple terms, Pain is a distressing feeling
often caused by intense or damaging stimuli.
Pain management and treatment are hot topics in the healthcare industry. With medication being the most effective approach to alleviating pain, traditional pain relievers like opioids have been widely used. However, the negative consequences and tolerance that may result from their use have made it imperative to find alternative ways to ease pain. It is essential to understand that pain is a personal experience influenced by various nonphysical factors, such as social and cultural influences, gender, and
individual characteristics (Michaelides & Zis, 2019).
Non-pharmacologic techniques like hypnosis, cognitive behavioural therapy, and music can complement drug treatment for procedural pain. However, mainstream science has only partially recognised their benefits. Doctors are exploring alternative and unconventional methods to alleviate pain, including virtual reality (VR). VR is a technology that stimulates multiple senses and has been used in medical situations for over two decades (Satava, 1993; Rothbaum et al., 1999 & Weiss et al., 2006). It is known for its non-drug-based approaches that can help manage pain through distraction or VR analgesia. Additionally, it can promote emotional processing and reduce the reluctance towards treatment.
Virtual Reality (VR) is an advanced technology that creates a fully immersive experience, transporting users to another world. To experience it, all one needs to do is put on a VR headset, which allows the view of a 360° virtual environment. One can move his or her head in any direction, and the view will change accordingly Additionally, one can hear sounds from the headset's built-in speakers or headphones, making the experience even more realistic. Within the context of pain management, several strategies can be employed when using virtual reality (VR), such as mindfulness (focusing on the present moment), meditation, guided imagery, and cognitive behavioural therapy (redirecting negative thoughts to positive ones). These approaches aim at managing stress and moods, as stress, anxiety, depression, and fear are all factors that contribute to pain The experience of pain is a complex and ever-changing phenomenon.
According to Melzack's Neuromatrix Theory, factors such as cognition, sensation, and emotions can affect how pain is perceived. Unlike many painkillers that disrupt the transmission of signals to the brain, this theory suggests that distraction can also effectively reduce pain. Pain is a crucial protective mechanism, but when a significant distraction occurs, it can reduce the attention given to the pain to the point of being ignored. Virtual reality is an effective distraction for patients experiencing pain. By dividing their attention, patients cannot process the pain signals, resulting in less focus on the pain and a subsequent reduction in the pain experience. Virtual reality enhances immersion and distraction by appealing to multiple senses and capturing the patient's attention.

Virtual environments employ headtracking systems, tactile feedback, and highly stimulating visual and auditory sensations, allowing the individual to be fully engrossed in a virtual world, thereby reducing pain perception.
Hunter Hoffman and David Patterson, pain specialists and virtual reality (VR) pioneers, have been conducting research at the University of Washington for over 20 years to prove VR's unique ability to alleviate acute pain. Their seminal work was performed with burn patients, and they developed a virtual reality (VR) game called SnowWorld. Patients use wide-view goggles, audio headphones, and a simple hand controller to interact with snowmen, igloos, penguins, woolly mammoths, and flying fish by throwing snowballs (Kenny, 2018). By immersing themselves in SnowWorld and focusing on the game during treatments, burn patients reported 35-50% reductions in procedural pain. Brain scans using fMRI also showed associated reductions in pain-related brain activity during the virtual reality (VR) game, this shows the ability of virtual reality (VR) to alter the perception of pain by diverting the attention of the patients from the physical pain and placing focus on the game.
In a study conducted by Hoffman et al. on healthy individuals, exposure to thermal stimulation revealed that virtual reality significantly reduced pain. The researchers identified five brain regions of interest: the anterior cingulate cortex, primary and secondary somatosensory cortex, insula, and thalamus. They also conducted a randomized control study (RCS) that supports the observational case studies. The randomized control study (RCS) involved investigating pain intensity in
burn patients undergoing a range of motion physical therapy. The study results showed a significantly lower pain rating in the analgesia-plus-VR group compared to the analgesia-only group, with the former group also showing a more excellent range of motion. Additionally, fMRI scans revealed that the pain reduction experienced using VR was like the analgesic effect of a moderate hydromorphone pain medication (Sharar et al., 2007).
Early studies on virtual reality (VR) and pain targeted burn patients as participants due to the high pain, discomfort, and anxiety they experienced. These studies focused mainly on the physical sensation and reporting of pain, while some also explored the emotional states associated with pain. Later studies have shown positive results in reducing pain in various settings, including pain from chemotherapy port access, lumbar punctures, gastrointestinal endoscopy, and rehabilitation of upper limbs of patients with Duchenne muscular dystrophy, headaches, and fibromyalgia. These later studies have also broadened their focus to include emotional states such as anxiety, fatigue, and depression. Virtual Reality (VR) application extends beyond pain management into the realm of rehabilitation, particularly in physical and neurological recovery. Patients often struggle with adhering to rehabilitation regimes due to monotony and lack of motivation Virtual reality (VR) addresses this challenge by introducing interactive exercises and simulations that transform rehabilitation into an engaging and enjoyable activity. Through these interactive experiences, patients are encouraged to actively take part in their recovery process, leading to improved
compliance and better outcomes (Laver et al., 2015).
Furthermore, Virtual Reality (VR) holds great promise in neurological rehabilitation. Stroke survivors and individuals with traumatic brain injuries face intricate challenges in restoring cognitive and motor functions. Virtual Reality (VR) supplies a unique platform to recreate real-life scenarios in a controlled environment, offering patients the opportunity to practice essential skills while receiving help from immediate feedback. Research proves that VR-based interventions can significantly improve motor skills and cognitive functions, contributing to enhanced quality of life for patients (Laver et al., 2015).
VR has been proven helpful in conjunction with other pain management methods. The notable discoveries discussed in this article highlight how VR can treat pain. VR is recommended for use in severe medical and less severe cases if the advantages outweigh the costs. By reducing the need for medication and potentially replacing or reducing the use of opioids, VR can offer significant benefits to doctors and patients. Although many studies have yielded positive results, it is essential to note that many have small sample sizes and are case studies. Additionally, these studies often do not control extraneous variables like the relationship between pain and anxiety and the type and dosage of VR technology. Mixed results have also been seen for using VR in treating chronic and acute and chronic pain in pediatric populations. Larger randomized controlled trials are necessary to better understand the most effective use cases for VR.
Future studies should evaluate the proper dosage of VR exposure compared to other pain analgesia therapies (such as pain medications, visual illusions, mirror box therapy, etc.) for both short and long-term outcomes.
Due to its high cost, VR studies are primarily done in clinical environments. However, as VR becomes more affordable and widespread, it is worth exploring the possibility of incorporating it into homebased care. For VR to be a helpful complementary intervention, it needs to be accessible outside of clinical settings and applicable to the real world. Therefore, it is crucial to ensure its generalizability and relevance. A significant amount of research has been conducted on the use of virtual reality (VR) in pain management and treatment. This shows significant interest in this development area and its potential effectiveness. As technology advances and the quality of VR experiences improve, its efficacy will likely increase further. Additionally, VR paired with other technology-based Interventions such as AI, biofeedback, or hypnosis to decide if a compounding positive effect could have long-lasting benefits. With the expanding knowledge of VR as a complementary pain management tool, the use of VR is expected to rise as virtual reality (VR) empowers patients and healthcare professionals alike to collaborate in achieving holistic pain relief and comprehensive rehabilitation.


Our just concluded webinar saw you delve into the potential of mobile health apps in enhancing patient experience. The webinar was graced by various multidisciplinary healthcare stakeholders, health tech enthusiasts, techies and of course patients. Our external panellists were occupied by the very dynamic and seasoned duo of Dr. Wale Adeosun (MD), a medical doctor with years of experience developing and implementing digital health solutions and Dr. Ololade Diya, a highly respected medical professional with a passion for excellence in the healthcare sector in Nigeria, Africa and beyond.


Dr. Adeosun opened with a take on the challenges preventing patients' consistent use of mobile health apps. Putting this into the African and Nigerian context, he opined that the reality is patients are not keen on embracing digital health solutions, due to low digital literacy levels and from his experience, a pragmatic way to galvanize this is by showing them the inherent benefits within. From a patient perspective, he stressed that patients are always looking for ways to improve their experience as hospital visits are often associated with unpleasant experiences. So, once they . associate these mobile health apps with something of value, it would help in driving adoption and consistent use. He further went on to highlight some of the technological limitations that might hinder adoption, which include poor user experience, unfriendly user interface, privacy and/or security concerns and infrastructure challenges, to mention a fewHe further touched on some of the regulatory and ethical considerations that need to be put in place in building mobile health apps, which include things like; data privacy, informed consent, and accessibility, which is getting more coverage in recent times. You want to ensure equity is being put into consideration on your platform and you are not actively trying to marginalize a certain demographic or cohort. Additionally, you want to make sure that you conform to local regulations. If you operate within Europe, that would be the GDRP. If within America, HIPAA (Health Insurance Portability and Accountability) and within Nigeria, NDPR (Nigeria Data Protection Regulation). It is vital to ensure that your solution is accessible to all users and most importantly, that your users are fully aware and fully informed, having sought informed consent as to how their data will be used.
In terms of cultural, religious, and demographic considerations, Dr. Adeosun shared experiences from a practical perspective, from one of his digital health implementations, stating that the earliest consideration should be given to localizing the solution, such that it supports as many languages as your target market. He further stated that some other appropriate considerations need to be put in place that align with the societal and religious beliefs of your intended demography.


Regarding how effective collaboration can be fostered between the tech providers and critical healthcare stakeholders, towards ensuring the incorporation of mobile health apps into the care continuum. Sharing his wealth of personal experience, he expressed that it boils down to the issue of trust. He feels that the typical Nigerian doctor, even in the elite niche, feels technology might make an already laborious process cumbersome. But stressed that transparency, clearly defined objectives and deliverables, would help in managing expectations and overcoming


the trust factor. Prioritizing the patient is also one of the ways both parties can ensure these, since the patient is centred around why they exist and lastly, providing adequate support all goes a long way in fostering effective collaboration.
The COO (Chief Operating Officer) of Genesys Health brought his perspective on the integrated approach of making not only the patient front and centre in terms of design considerations, but every focal system actor. He stressed the need for userfriendly and intuitive designs and incorporating features that appeal to the key stakeholders. This further buttressed Dr. Adeosun's point on the role of patient feedback in mobile health app development, towards meeting their evolving needs.
The webinar wrapped up with a response by Dr. Wale to the question of What level of due diligence is given to onboarding doctors on telemedicine platforms, given there are doctors who are willing to offer their services at ridiculously cheap rates. He acknowledged that the scenario is unique to a platform and is heavily dependent on the checks the vendors have put in place to guarantee the authenticity of a registered physician, some common examples cited were; manual or automated credential verification, professional screenings and sometimes a combination of all. He wrapped up by saying pricing alone cannot be the ultimate litmus test to guarantee the genuineness and efficacy of a doctor, as doctors can offer their services pro bono for altruistic reasons.
If you enjoyed this highlight and are looking forward to our next edition, use these links, to keep up to date with us;
https://facebook.com/genesyshmis
https://instagram.com/genesyshmis

https://twitter.com/genesyshmisng
https://linkedin.com/company/genesys-health-information-systems-ltd

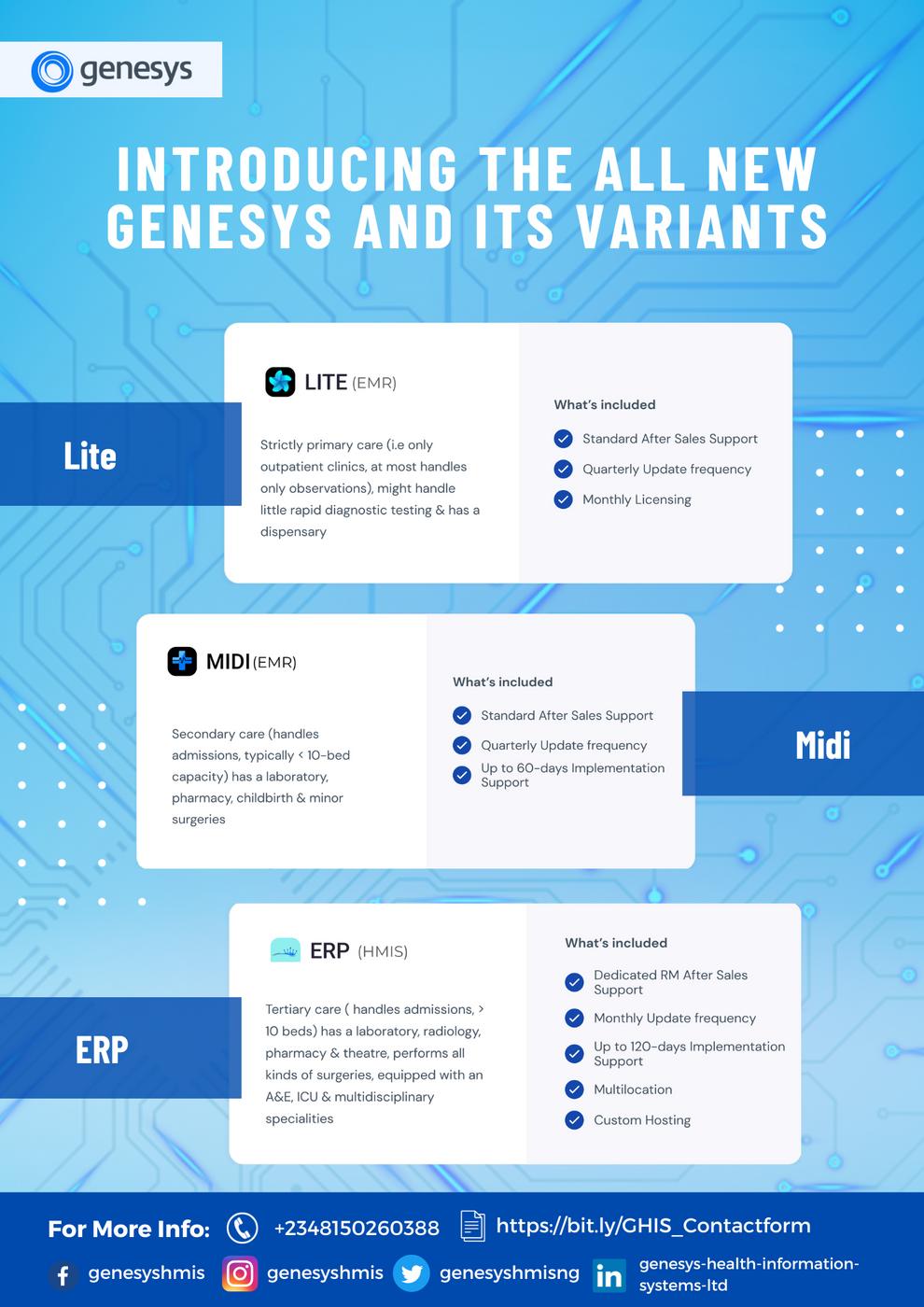

 BY PETER OWOLABI
BY PETER OWOLABI
Coconut is often referred to as the "tree of life". A versatile and incredible fruit that has been cherished for centuries across various cultures. This tropical gem offers an array of benefits, ranging from its delicious taste to its numerous health and beauty advantages. This article reveals the awesome benefits of coconut and why you should consider incorporating it into your daily life.

Coconut is a rich source of essential nutrients. It contains vitamins such as vitamin C, B vitamins (B1, B2, B3, B5, B6), and minerals like potassium, magnesium, and iron. These nutrients are vital for maintaining overall health, supporting immune function, and promoting strong bones and teeth.

Despite its high saturated fat content, coconut has been shown to have potential benefits for heart health. The type of saturated fats found in coconut, known as medium-chain triglycerides (MCTs), may actually raise HDL (good) cholesterol levels and improve the overall lipid profile, reducing the risk of heart disease.

MCTs in coconut have gained attention for their ability to boost metabolism and promote weight loss. They provide a quick source of energy and can help control appetite, making you feel fuller for longer.

Coconut oil is renowned for its exceptional moisturizing properties. It's a natural, chemical-free alternative to many skincare products. When applied topically, it can help hydrate the skin, treat dryness, and even soothe skin conditions like eczema and psoriasis. Additionally, coconut oil can work wonders for your hair, making it shinier, smoother, and more manageable.

Coconuts are packed with antioxidants, which can help strengthen your immune system by neutralizing harmful free radicals. Lauric acid, found in coconut oil, also has antibacterial, antiviral, and antifungal properties, further contributing to immune support.

The fibre content in coconut supports digestive health by promoting regular bowel movements and preventing constipation. It also contains compounds that can help soothe the digestive tract and reduce inflammation.

The fibre content in coconut supports digestive health by promoting regular bowel movements and preventing constipation. It also contains compounds that can help soothe the digestive tract and reduce inflammation.

Oil pulling, a practice where you swish coconut oil in your mouth, has gained popularity for its potential benefits in oral hygiene. It may help reduce harmful bacteria, improve gum health, and freshen your breath.

Coconut adds a unique and delicious flavour to a wide range of dishes, from curries and desserts to beverages like coconut water and coconut milk. It's a staple ingredient in many Southeast Asian and tropical cuisines, adding depth and richness to the flavour profile.

Coconut trees are highly sustainable and eco-friendly. They require minimal water and pesticide use, making them an environmentally responsible choice.

The coconut is truly a remarkable gift from nature. Its incredible versatility, coupled with a myriad of health and beauty benefits, makes it a valuable addition to your daily life. Whether you enjoy it in your cooking, or for its numerous other applications, the coconut is a true symbol of both nourishment and wellbeing. So, go ahead and embrace the awesomeness of coconut in all its forms!






APROKO DOCTOR (Egemba Chinonso Fidelis) an alum of Nnamdi Azikiwe University is a Nigerian boardcertified medical doctor, an awardwinning content creator, a public speaker and chief editor of aprokodoctor.com and thehealthythreads.com.
Aproko Doctor uses storytelling via social media to combat health misinformation and influence healthy lifestyle practices in Africa evident in his OKIRIKIRI series, TIME OUT series etc.

Chinonso is passionate about health information dissemination in Africa and wants to make positive contributions towards improving health care delivery and health ignorance by leveraging on health education.

s
rds in recognition of blic health education
ers Award 2021
a Award for Health
Award for Health
tion 2021
u se a ard for Health
Influencing 2021
Nominee, The Future Africa

Award for health 2021
Nominee: Rising star. Africa Healthcare summit awards

Laughter is Medicine: Laughing is not only fun but also has health benefits. It can boost your mood, reduce stress, and even improve your immune system.
Brain Power: The human brain generates about 20 watts of electrical power when awake, enough to power a dim light bulb
Fingerprints: No two people have the exact same fingerprints. Even identical twins have different fingerprint patterns
Heartbeats: Your heart beats around 100,000 times a day, pumping blood through your body's 60,000 miles of blood vessels
Blinking: On average, a person blinks about 15-20 times per minute. That's over 1,000 blinks per hour!
Blood Cells: Your body produces millions of new red blood cells every second. That's around 2 5 million every second.
Healthy Eating: The human body is made up of around 7,000,000,000,000,000,0 00,000,000,000 atoms. Eating a variety of foods helps provide the raw materials for these atoms.
Healthy Fats: Not all fats are bad Omega-3 fatty acids, found in fish like salmon and walnuts, are essential for brain health and reducing inflammation
Muscle Power: The human body has over 600 muscles Smiling uses 17 muscles, while frowning uses 43
Bone Strength: Pound for pound, human bone is stronger than steel. A cubic inch of bone can bear a load of 19,000 pounds.
What is the current edition of this publication?
A) 4th Edition B) 6th Edition
C) 3rd Edition D) 1st Edition
Who’s the founder of Genesys Health?
A) Charles Onu B) Vivian Nwakah
C) Ayo - Olagunju Munachimso
D) Adereti Francis

What was the feature article of the maiden edition of Health Tech Insider?
A) Genesys Electronic Medical Records
B) physical File C) Clinical Specialized Packages D) Stand-alone Packages
What is the medical term for high blood pressure?
A) Hypertension B) Hypotension
C) Hyperglycemia D) Hyperactivity
When was Genesys Health Information Systems Limited founded?
A) 2010 B) 2018
C) 2020 D) 2017
In which city is Genesys Health Information Systems Limited headquartered?
A) Lagos, Nigeria B) Nairobi, Kenya
C) Accra, Ghana D) Johannesburg, South Africa
Our Values at Genesys Health Information Systems Limited are?
A) Integrity B) Diligence
C) Empathy D) All of the above
What is the recommended daily water intake for an average adult?
A) 1 litre B) 4 liters
C) 8 glasses (approximately 2 litres) D) 10 liters
What is the primary function of red blood cells?
A) Fighting infections B) Transporting oxygen
C) Storing nutrients
D) Producing hormones
Which of the following is a major source of vitamin C?

A) Spinach B) Orange
C) Eggs D) Chicken
You, Yue, and Xinning Gui. “Self-Diagnosis through AI-Enabled Chatbot-Based Symptom Checkers: User Experiences and Design Considerations.” AMIA Annual Symposium Proceedings, vol. 2020, 25 Jan. 2021, pp. 1354–1363, www.ncbi.nlm.nih.gov/pmc/articles/PMC8075525/.
Adewale, O. S. (2004). An internet-based telemedicine system in Nigeria. International Journal of Information Management, 24(3), 221–234. https://doi.org/10.1016/j.ijinfomgt.2003.12.014
Adewara, F. (2023, August 22). Telehealth start-up bridges healthcare gap in Nigeria. Africa Renewal. https://www.un.org/africarenewal/magazine/august2023/telehealth-start-bridges-healthcare-gap-nigeria
Azubuike, C. (2022, April 1). Gombe launches an app to aid universal health coverage. Punch Newspapers. https://punchng.com/gombe-launches-app-toaid-universal-health-coverage/ eHealth Africa. (2019, April 8). GRID 3. EHealth Africa - Building Stronger Health Systems in Africa. https://www.ehealthafrica.org/grid-3
Okezie, V. I., Ahukannah, G. J., Onuka, O., Omas, S. U., Kanu, C., Tega, A., Macaulay, A., & Folu, A. (2021). Abia State Telehealth Initiative: A Novel Ingenuity. E-Health Telecommunication Systems and Networks, 10(03), 75–82.
https://doi.org/10.4236/etsn.2021.103004
Gabriel Alobo, I., Soyannwo, T., Ukponwan, G., Akogu, S., Matthew Akpa, A., & Ayankola, K. (2020). Implementing electronic health system in Nigeria: perspective assessment in a specialist hospital. African Health Sciences, 20(2), 948–954. https://doi.org/10.4314/ahs.v20i2.50
Ogundipe, O. (2011). Electronic Medical Record Keeping: Eleven Years
Experience at Life Support Eye Clinic, Lagos, Nigeria. Nigerian Journal of Ophthalmology, 19(1). https://doi.org/10.4314/njo.v19i1.70771
Ojo, Dr. O. (2013). SUSTAINING QUALITY HEALTHCARE IN A PAPERLESS ENVIRONMENT -EMR AT LAGOON HOSPITALS. http://sqhn.org/wpcontent/uploads/2013/04/007-EMR-Lagoon.pdf
Sani, N., Manohar, DR. R. K., & Alkali, M. .A. (2017). FACTORS HINDERING THE ADOPTION OF DIGITAL RECORD IN NIGERIA; A SYSTEMATIC REVIEW OF SOME LITERATURE. International Research Journal of Management Science & Technology, 8(10). https://www.academia.edu/36225015/FACTORS HINDERING THE ADOPTION OF DIGITAL RECORD IN NIGERIA A SYSTEMATIC REVIEW OF SOME LITER ATURE
Bergman, A., David, G., & Song, H. (2021). “I Quit”: The Role of Schedule Volatility in Employee Turnover. SSRN Electronic Journal. https://doi.org/10.2139/ssrn.3910077
Bertsimas, D., Pauphilet, J., Stevens, J., & Tandon, M. (2021). Predicting Inpatient Flow at a Major Hospital Using Interpretable Analytics. Manufacturing & Service Operations Management. https://doi.org/10.1287/msom.2021.0971
Digital Supply Chain Transformation. (2022, June 25). Home. MIT Digital Supply Chain Transformation. https://digitalsc.mit.edu/
Green, L. V., Savin, S., & Savva, N. (2013). “Nursevendor Problem”: Personnel Staffing in the Presence of Endogenous Absenteeism. Management Science, 59(10), 2237–2256. https://doi.org/10.1287/mnsc.2013.1713
Kim, S.-H., & Hummy, S. (2015, December 31). How RFID Technology Improves Hospital Care. Harvard Business Review. https://hbr.org/2015/12/how-rfidtechnology-improves-hospital-care
Kim, S.-H., & Song, H. (2022, January 18). How Digital Transformation Can Improve Hospitals’ Operational Decisions. Harvard Business Review.
https://hbr.org/2022/01/how-digital-transformation-can-improve-hospitalsoperational-decisions
Siwicki, B. (2018, February 16). Boston Children’s builds dashboard to better manage patient capacity and beds. Healthcare IT News. https://www.healthcareitnews.com/news/boston-childrens-builds-dashboardbetter-manage-patient-capacity-and-beds
Song, H., Tucker, A. L., Graue, R., Moravick, S., & Yang, J. J. (2020). Capacity Pooling in Hospitals: The Hidden Consequences of Off-Service Placement. Management Science, 66(9), 3825–3842. https://doi.org/10.1287/mnsc.2019.3395
Tozzi, J. (2019, March 4). Amazon Gives AI to Harvard Hospital in Tech’s Latest Health Push. BQ Prime. https://www.bqprime.com/onweb/amazon-gives-ai-toharvard-hospital-in-tech-s-latest-health-push
NITDA. (2021). NDPR-Implementation-Framework. In NITDA.
https://nitda.gov.ng/wp-content/uploads/2021/01/NDPR-ImplementationFramework.pdf
Piasecki, J., & Cheah, P. Y. (2022). Ownership of individual-level health data, data sharing, and data governance. BMC Medical Ethics, 23(1). https://doi.org/10.1186/s12910-022-00848-y
Cote, C. (2021, October 26). What is predictive analytics? 5 examples | HBS online. Business Insights - Blog. https://online.hbs.edu/blog/post/predictiveanalytics
Google Cloud. (2023). What is predictive analytics and how does it work? Google Cloud. https://cloud.google.com/learn/what-is-predictiveanalytics#:~:text=started%20for%20free-
Haas, D. A., Makhni, E. C., Schwab, J. H., & Halamka, J. D. (2019, November 13). 3 myths about machine learning in health care. Harvard Business Review. https://hbr.org/2019/11/3-myths-about-machine-learning-in-health-care IBM. (2023). What is predictive analytics? | IBM. Www.ibm.com.
https://www.ibm.com/topics/predictive-analytics
Kennedy, S. (2023, February 3). Predictive Analytics Tool Identifies Readmission Risk, Reduces Costs. Health IT Analytics; HealthITAnalytics. https://healthitanalytics.com/news/predictive-analytics-tool-identifiesreadmission-risk-reduces-costs
Stromme, T. (2014). Top five healthcare analytics myths that prevent effective adoption and reduce return on data. In HealthcareAnalytics.info. http://healthcareanalytics.info/downloads/special reports/SR Healthcare Imp rovement _Analytics_Myths.pdf
Prasad, A. (2022). What is Remote Patient Monitoring (RPM)? - Devices & Solutions. Www.revenuexl.com. https://www.revenuexl.com/resources/whatis-remote-patient-monitoring-benefits-solutions
Vegesna, A., Tran, M., Angelaccio, M., & Arcona, S. (2017). Remote Patient Monitoring via Non-Invasive Digital Technologies: A Systematic Review. Telemedicine and E-Health, 23(1), 3–17. https://doi.org/10.1089/tmj.2016.0051
Hadjiat, Y., & Marchand, S. (2022). Virtual Reality and the Mediation of Acute and Chronic Pain in Adult and Pediatric Populations: Research Developments.
Frontiers in Pain Research, 3. https://doi.org/10.3389/fpain.2022.840921
International Association for the Study of Pain. (2011). Terminology | International Association for the Study of Pain. International Association for the Study of Pain (IASP). https://www.iasp-pain.org/resources/terminology/ Kenny, T. (2018, February 24). SnowWorld melts away pain for burn patients, using virtual reality snowballs. GeekWire. https://www.geekwire.com/2018/snowworld-melts-away-pain-burn-patientsusing-virtual-reality-snowballs/
Laver, K. E., George, S., Thomas, S., Deutsch, J. E., & Crotty, M. (2015). Virtual reality for stroke rehabilitation. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.cd008349.pub3
Michaelides, A., & Zis, P. (2019). Depression, anxiety and acute pain: links and management challenges. Postgraduate Medicine, 131(7), 438–444. https://doi.org/10.1080/00325481.2019.1663705
Satava, R. M. (1993). Virtual reality surgical simulator. Surgical Endoscopy, 7(3), 203–205. https://doi.org/10.1007/bf00594110
Sharar, S. R., Carrougher, G. J., Nakamura, D., Hoffman, H. G., Blough, D. K., & Patterson, D. R. (2007). Factors Influencing the Efficacy of Virtual Reality Distraction Analgesia During Postburn Physical Therapy: Preliminary Results from 3 Ongoing Studies. Archives of Physical Medicine and Rehabilitation, 88(12), S43–S49. https://doi.org/10.1016/j.apmr.2007.09.004
Weiss, P. L., Kizony, R., Feintuch, U., & Katz, N. (2006). Virtual reality in neurorehabilitation (F. Gage, L. Cohen, M. Selzer, P. Duncan, & S. Clarke, Eds.). Cambridge University Press; Cambridge University Press. https://www.cambridge.org/core/books/abs/textbook-of-neural-repair-andrehabilitation/virtual-reality-inneurorehabilitation/9458A95AA6B9988A1691F0EC61AF5A1E
https://eastafricamonitor.com/
https://e4sv.org/can-telemedicine-revolutionise-rural-healthcareafrica/?doing wp cron=1695487485.7197680473327636718750
https://www.telecomreviewafrica.com/
https://edition.cnn.com/2020/04/10/africa/african-leaders-healthcarecoronavirus-intl/index.html
https://www.mytechmag.com/how-data-analytics-is-empowering-thehealthcare-sector/
https://www.bcbs.com/the-health-of-america/articles/4-ways-we-aredemocratizing-health-data
https://cms.officeally.com/blog/electronic-medical-records-patientcare
https://heliumhealth.com/what-are-the-pros-and-cons-of-electronicmedical-records/
https://images.app.goo.gl/HQgSuJoKa8PBjTbi8
https://images.app.goo.gl/TuZf8tfabA1tyazM6
https://images.app.goo.gl/HHN8ZAraMTCPxiaj7
https://www.vccircle.com/will-the-covid-19-crisis-infuse-a-fresh-leaseof-life-into-health-tech-startups
https://www.businesscompilerng.com/2022/05/big-data-analytics-inhealthcare.html
https://pngtree.com




