It’s given me the chance to see my boy grow up.





The most effective method of cancer treatment is preventive. Comprehensive Cancer Centers’ goal is to help patients detect cancer before it strikes, or while it is still early enough to deploy the most successful treatments. Comprehensive is increasing the quality of life for our patients and their families, and most importantly giving them the opportunity to live their lives to the fullest. Screening and early detection save lives. Ask your doctor today to learn more.



































































Our philosophy is centered around personalized care that addresses the unique needs of each patient.

osteopathicmedical@embarqmail.com
5410 West Sahara Avenue,Las Vegas, NV 89146

SERVICES INCLUDE:
On-site lab, X-Ray, ultrasound, dietitian, hearing tests, minor surgeries, skin services, CDL and immigration physicals
MOST MAJOR INSURANCE PLANS ACCEPTED.
Including: Aetna Medicare, Aetna HMO, Aetna Choice Plus, Aetna PPO, Champva/Champus, Cigna, First Health, Humana Gold Plus, GEHA, SCAN Medicare Advantage, Humana PPO, Medicare/Railroad Medicare, Tricare, United Healthcare PPO, United Healthcare POS, United AARP Medicare Advantage, Universal Health Network, Wellportal, Select Health, Prominence, MGM PPO
MEDICAL STAFF
Peter J. Licata, D.O.
George Gabriel Toldness, APRN-C
Charmaine Coronado, APRN-C
Donna Gould, M.S., R.D., L.D.
Special Publications Editor SIERRA SMART
Managing Editor/News DAVE MONDT
Staff Writers KYLE CHOUINARD
GRACE DA ROCHA, HILLARY DAVIS, HAAJRAH GILANI, KATIE ANN MCCARVER, ILANA WILLIAMS
Copy Editor ABRAHAM KOBYLANSKI
Photo Coordinator BRIAN RAMOS
Staff Photographers CHRISTOPHER DEVARGAS, STEVE MARCUS, WADE VANDERVORT
Publisher of Digital Media KATIE HORTON
Senior Advertising Manager MIKE MALL, ADAIR MILNE, SUE SRAN
Account Executives CRISTAL BLAKEMAN, LAUREN JOHNSON, GIANNA PUCCI
Web Content Specialist CLAYT KEEFER
Vice President of Manufacturing MARIA BLONDEAUX
Production Director PAUL HUNTSBERRY
Production Manager BLUE UYEDA
Associate Marketing Art Director BROOKE EVERSON
Marketing Graphic Designer CARYL LOU PAAYAS
Senior Traffic Coordinator DENISE ARANCIBIA
Traffic Coordinator KIMBERLY CHANG
Production Artist MARISSA MAHERAS
Route Administrator KATHY STRELAU
Fulfillment Operations Coordinator CASANDRA PIERCE
Distribution Relations Liaison JIDAN SHADOWEN
Events Director SAMANTHA PETSCH
Events Manager HANNAH ANTER
Events Coordinator APRIL MARTINEZ
Event Sales Coordinator MELINA TAYLOR




















CEO , Publisher & Editor BRIAN GREENSPUN
Chief Operating Officer ROBERT CAUTHORN
Managing Editor RAY BREWER







Associate Publisher ALEX HAASE
VEGAS INC





2275 CORPORATE CIRCLE, SUITE 300 HENDERSON, NEVADA 89074 | 702.990.2550





Sometimes reality hits me like a ton of bricks and I have a renewed realization that I have a lot to learn. It’s humbling. I feel it often working on this publication. As contradictory as it may seem, I do not have any formal health care training. However, I am passionate about many health care issues. Especially the ones that affect our community.
As the health care landscape and our community rapidly evolve, we must evolve to facilitate that growth. This issue is full of exciting growth. The Notes section highlights new hires, practices and graduates. And, on the heels of Intermountain Health’s announcement of its upcoming children’s hospital, we have an article about what a children’s hospital is and exactly what community needs it aims to meet here in Southern Nevada.
In the cover story, you can learn all about goal-setting and the science behind it. Included are several goal-setting methods that you can test for yourself to help you achieve success.
treat all her patients and their concerns equally, hold her peers accountable and advocate for women to fight for and find the care they need.
If you’ve ever been curious about vitamin D, you can read about how our bodies synthesize this vitamin from the sun and the important role of this nutrient.
You will also find articles on exciting applications of technology, specifically wearable devices like smartwatches and virtual reality, for more effective injury prevention and health treatment.

A valuable commodity to established and burgeoning communities is perspective. At VEGAS INC we value diverse voices, the unique illumination they provide for key issues and the solutions they supply.
For example, a young man moved to Nevada several years ago only to discover that there was no school specifically for blind and visually impaired children. Fortunately, this young man found the resources available through the Nevada Blind Children’s Foundation. His experiences helped guide him to give back and advocate for greater resource availability for a still-widely underserved community.
A local doctor found new purpose in her work when she had a health incident of her own that opened her eyes to gender disparity in health care. Her experience instilled in her a renewed drive to
Health care thrives on collaboration, and Health Care Quarterly aims to be a platform for ongoing dialogue, helping to foster the exchange of knowledge and ideas that lead to better outcomes for all. I hope you will value curiosity and new perspectives as your personal and professional circles of influence grow and as you participate in and learn about our local health care industry.
I am so grateful for all that I have learned from the generous and knowledgeable health care professionals who write for Health Care Quarterly. I encourage anyone with health care expertise to write in and share your insights.
I hope you find this issue informative and inspiring. The future of health care is full of promise, and we’re proud to be part of your journey as we all work toward a healthier tomorrow.
Wishing you health and happiness,
Sierra Smart Special Publications Editor sierra.smart@gmgvegas.com
National Cancer Institute-designated cancer centers, including Dana-Farber Cancer Institute, Fred Hutch Cancer Center, Memorial Sloan Kettering Cancer Center, and The Sidney Kimmel Comprehensive Cancer Center and Whiting School of Engineering at Johns Hopkins, joined forces and secured funding from AI technology leaders AWS, Deloitte, Microsoft and NVIDIA, to create the Cancer AI Alliance in fall 2024. The alliance will apply responsible AI to the collective power of the participating cancer centers’ data to unlock insights while protecting data security, all to identify more ways to transform cancer research and care.

Cosmetic and reconstructive dentist Dr. Joe Willardsen died Jan. 26 at 53 years old. Willardsen founded True Dentistry in Las Vegas, Nevada. As an innovator, Willardsen developed new educational systems to teach and train other dentists around the world in the latest techniques in cosmetics, occlusion and biomimetic dentistry. Willardsen was often sought after by professionals in the modeling and entertainment industries for his advanced techniques and proven record of successful cosmetic dental rejuvenation.

Sunrise Hospital & Medical Center announced the opening of ER at Boulder’s Edge, a freestanding emergency room servicing Henderson and southeast Las Vegas. Valley Health Systems announced the ER at South Summerlin, an extension of Summerlin Hospital. These freestanding ERs will provide the community with more choices and shorter wait times in case of emergencies. Both facilities, and several others already established throughout the valley, will have testing capabilities including on-site laboratories, CT scanner and imaging equipment, along with multiple treatment rooms and exam rooms. These 24/7 facilities are staffed with emergency trained personnel and can easily transfer patients who need further care to affiliated hospitals.
16
Exploring the crucial role that vitamin D plays in the human body
20
Unlocking your inner success: The science behind goal setting
28 Gender disparities create huge health care risks
44
News and updates from the Las Vegas medical community
The cardiac experts at Dignity Health want your heart to keep beating strong for your loved ones. When it comes to cardiovascular disease, people often don’t know their personal risk. Early detection of heart problems means treatment can start earlier, so you’ll live healthier longer. A renowned and trusted team of cardiovascular physicians offers leading-edge cardiovascular care, state-of-the-art technology, and breakthrough clinical research—close to where you live and work.
Learn more and find a cardiologist near you at DignityHealth.org/NVHeart to learn more.






BY LAURINE TIBALDI, MD
Pregnancy and childbirth are often celebrated as incredible events in a woman’s life; yet, for some, it can be anything but joyful. Pregnancy-related mental health conditions affect 1 in 5 women. Of those, 20% will face suicidal thoughts or attempt to harm themselves. Maternal mental health challenges are the number one cause of maternal mortality, primarily due to suicide.
Most women experience “baby blues” to varying degrees but some are more likely to experience severe mental health issues. Women with a history of anxiety or mood disorders, or those with a family history of postpartum depression, have a higher risk. Women from under-resourced communities, those with little to no social support, and those who use substances like drugs or alcohol also face higher risks, as do women who have experienced fertility challenges, an unwanted pregnancy or a difficult birth.
Further, within communities of color, stigma and judgment often prevent women from seeking mental health treatment.
The time has come to recognize that pregnancy-related mental health conditions are not only prevalent but largely preventable. Here are a few tips to help combat maternal mental health challenges: Inform yourself. Take some time to familiarize yourself with emotional changes that can come with pregnancy and the postpartum period. This knowledge not only helps in setting your own expectations but also empowers you to communicate effectively with health care providers.
Talk to your doctor about treatment options. When exploring medication options for treating postpartum depression, it’s important to understand the benefits and potential side effects. Be sure to speak with your health care provider to understand the best option for you and check
with your health coverage plan to make sure the medication is covered.
Destigmatize mental health. It’s okay to talk about how you’re really feeling. Whether you’re pregnant, a new parent, a supportive partner or friend, speaking up about mental health challenges should be as normal as talking about a backache. Opening up makes it easier for everyone to seek the help they might need.
Monitor your well-being. Changes in mood, energy levels or thoughts can be subtle clues that you need some extra care.
Call your health plan provider: Your health insurer can also help you access care. Some insurers like UnitedHealthcare have specially trained advocates to support members who might be struggling, help members understand their benefits and guide them to timely care.
Take advantage of your Employee Assistance Program. These programs typically offer services of which few employees take advantage. Depending on your situation, you may not need to seek additional behavioral health support with a care provider if your EAP offers personalized guidance.
Seek support. A trusted health care provider can guide you to the right level of support, such as talking to an expert in-person or virtually, or joining a network or discussion group about this issue. Your family and friends can be there for you in many ways, including by listening, offering personal experiences or even helping with household chores to allow you time to rest. Remember that acting early is a proactive step toward maintaining your mental health.
Together, we can break the silence, prioritize maternal mental health and ensure that no mother faces this challenge alone. It is time to unite, embrace compassion and empower all women to embark on their motherhood journey with strength and resilience.
BY RACHEL BOWERS, PA-C
Bioidentical hormone replacement therapy uses fabricated hormones identical to the ones found in someone’s body to adjust hormone levels in individuals who experience changing, low or unbalanced hormones—often common for women going through perimenopause and menopause. Bioidentical hormone replacement therapy is more than just a fix for weight gain, hair loss and hot flashes—it can improve quality of life and extend longevity. Despite its benefits, misconceptions rooted in flawed research have discouraged its use for decades.
It’s important for women to recognize that many symptoms they experience during perimenopause and menopause—such as fatigue, mood swings and loss of libido—are valid medical concerns. However, many providers, including gynecologists and endocrinologists, lack the specialized education needed to address hormone-related concerns women face.
Although hormonal changes are gradual, the symptoms often feel as if they happened overnight. Three of the most common symptoms patients notice as their hormone levels decline are poor sleep, increased anxiety/moodiness, and a lack of sex drive. But mostly, patients describe that they simply don’t feel like themselves.
Testosterone is just as important for women as it is for men. Sadly, women face barriers to the treatment of low testosterone due to a lack of
FDA approval. There are currently no FDA-approved testosterone medications for women, so if women want treatment, they must use compounded forms or microdose commercially available testosterone for men.
As women age, the appearance of the skin on their faces changes. Laxity sets in and wrinkles develop, which causes some women to seek expensive treatments to reverse the signs of aging. Skin integrity is largely estrogen-dependent, so if you see changes on your face, you likely have changes to the vulvovaginal area’s skin. Topical estradiol can rejuvenate this tissue, improving sexual health and preventing urinary tract infections and incontinence.
Declining estrogen levels contribute to systemic inflammation, often leading to joint pain and conditions like frozen shoulders in postmenopausal women. Early intervention with bioidentical hormone replacement therapy can mitigate these symptoms and preserve musculoskeletal health.
Menopause is a universal experience, but its symptoms should not be accepted as inevitable. Many women suffer in silence, assuming these issues are normal because they’re common, but there are solutions and preventive measures and you do not have to settle.
That’s why Halcyon Health was started: to help women find better answers to their health questions.
For more information, visit halcyonoptimized.com.

Rachel Bowers , PA-C, is a provider at Halcyon Health with expertise in Bioidentical Hormone Replacement Therapy

Saad Jahangir , MD, is director of research and clinical trials—Nevada at Optum Cancer Care
BY K. SAAD JAHANGIR, MD
Significant advances are being made to ensure quality health care is being delivered in Southern Nevada, and Optum Cancer Care’s clinical research team is at the forefront of this movement.
Clinical trials are research studies performed on patients, with the goal of evaluating a new medical treatment (e.g., a new drug, medical device or other proposed treatment), and determining if it is safe and effective. Further, researchers want to learn if such treatments are more effective or have fewer side effects than standard treatments.
For example, a recent study on the treatment of Stage 4 bladder cancer explored the combination of immunotherapy with antibody-drug conjugates, which bind to specific proteins or receptors found on certain types of cells, including cancer cells. This allows the linked drug to enter cancer cells and kill them without harming other cells.
Patients of the study reported preserved or improved quality of life, and following the research, this study—which was a multinational trial within the Optum Cancer Care precision medicine program—received FDA approval and updated medical practice guidelines as the first-line treatment for certain Stage 4 bladder cancer patients.
In our precision medicine program, our mantra is “the right treatment for the right patient at the right time.” Currently, it takes us two to three weeks to open a clinical trial, which is significantly faster than the three- to six-month industry average. We are involved in more than 50 clinical trials, and we recently launched three trials in 16, 18 and 21 days, respectively.
Among our cutting-edge, technology-based treatments, we use immunotherapy, targeted
therapy and antibody-drug conjugates to treat various forms of cancer. We can also genetically sequence each patient’s tumor types and create custom-made treatments that yield better clinical outcomes with reduced toxicity. Additionally, in our various clinical trials, we are searching for circulating tumor DNA in the blood, a biomarker which can help us detect cancer early and allow us to diminish the duration of cancer treatments. This technology is at the forefront of current clinical research in oncology.
One of the greatest advantages of participating in a clinical trial is that it often covers most of the treatment and treatment-related expenses, therefore reducing financial barriers to accessing high-quality health care services. As a result, we’ve been able to provide meaningful treatment options for our patients in the Las Vegas area.
Having already attracted patients from prestigious providers such as MD Anderson Cancer Center, Mayo Clinic and Cleveland Clinic to participate in clinical trials, Optum Cancer Care’s precision medicine program is reversing the trend of Nevadans traveling to other states for a higher level of medical care.
While significant advances continue, we’re still in the developing stages of our clinical trials program. As we move forward, we want our patients and the community to become part of this journey with us. Our philosophy is a holistic approach where mind, body and soul must be in synergy to get the best therapeutic outcomes.
For information, please visit optum-cancer.com/clinical-trials
BY KATHERINE SPECHT, DO
Imoved to Las Vegas in 2017 after matching into the general surgery program at the Sunrise Health Medical Education Consortium, based out of MountainView Hospital. At the time, the general surgery program was relatively new, and I had the unique opportunity to grow alongside it as the program developed.
On my first night of trauma call at Sunrise Hospital, I was tasked with triaging trauma patients and mobilizing care alongside my attending and fellow residents. That night left an indelible mark on me. Over the following weeks and months, I witnessed how the entire community came together on a moment’s notice—not only to provide care for critically injured patients but also to support the caregivers at the hospital.
During my residency, I discovered a passion for colorectal surgery—a field that perfectly combines technical expertise, patient-centered care and impactful outcomes. They say you find your people, and I truly did. I was drawn to the supportive, collaborative nature of colorectal surgeons and the opportunity to make a profound difference in patients’ lives. After completing residency, I pursued advanced surgical training at AdventHealth in Orlando, Florida, where I specialized in colorectal surgery. This further honed my skills in treating both benign and malignant conditions affecting the colon, rectum and anus.
Colorectal cancer remains a significant health concern, with incidence rates alarmingly on the rise among younger populations. This trend underscores the urgent need for increased awareness and timely screening. Colonoscopy is a life-saving tool in this fight, as it allows for early detection and removal of precancerous polyps, preventing progression to cancer. When caught early, colorectal cancer is not only treatable but
often curable, offering patients a much better prognosis.
With Las Vegas’s rapid population growth in recent years comes an increasing demand for skilled health care providers to meet the diverse and evolving needs of the community. The strain on health care systems, particularly in specialties like surgery, underscores the importance of cultivating local talent and retaining skilled physicians in the region.
One of the primary goals of the Graduate Medical Education program is to address this need by training the next generation of physicians who will not only deliver excellent care but also contribute to the long-term health of the community. GME programs are vital in fostering a pipeline of dedicated, well-trained health care providers who understand the unique challenges and needs of the populations they serve.
I am excited to bring my expertise in colorectal care to the community. My practice incorporates advanced, minimally invasive techniques, including robotic-assisted surgeries, which provide greater precision, quicker recovery times and better patient outcomes. I am also passionate about raising awareness of the importance of colon cancer screening and offering compassionate, high-quality care tailored to each patient’s unique needs.
Joining the exceptional team at Las Vegas Complex Surgical Specialists, we are dedicated to providing comprehensive, patient-centered care while mentoring and guiding the next generation of surgical residents. Teaching and training residents is a responsibility I take to heart because it ensures the continued growth of skilled surgeons who will go on to make a lasting impact. It is incredibly fulfilling to contribute to the development of future physicians while simultaneously improving the overall health and well-being of this vibrant and rapidly expanding community.

For parents and caregivers, there are few things worse than a sick kid. Even a simple flu can bear unique challenges for children, let alone the devastating effects of acute and chronic pediatric diseases that require ongoing care. Children’s hospitals are vitally important to any community because they are optimized to treat the physiological and emotional needs of children in a developmentally appropriate setting. The treatment teams available at children’s facilities ensure the very best care for the child and their family, and often contribute to improved health outcomes.
Pediatric care is complex work. Infants and children have rapidly changing bodies, varying developmental stages and unique physical and emotional considerations. Children’s organ function, metabolism and immune system are vastly different than that of an adult, and they face different health challenges including different types of cancer, genetic disorders and infections. Pediatric facilities require specialized tools that are suitable for children’s anatomy and often a broader swath of professionals in the care team, including pediatricians, pediatric specialists, child psychologists and therapists, social workers, nutritionists and child life specialists.
Children’s hospitals provide a holistic, thoughtfully tailored approach that is essential when treating such a vulnerable population. Here are some of the qualities that make children’s hospitals unique.
Specialized, comprehensive care: Pediatric
patients are cared for with a comprehensive, multidisciplinary approach, ensuring that every aspect of the child’s health is addressed, especially for long-term chronic conditions.
A focus on pediatric diseases: Children tend to face different diseases and health challenges than adults do. Children’s hospitals focus on conditions that are more prevalent in childhood, and often use cutting-edge research and treatments that are not available in general hospitals.
Developmentally appropriate environment: Children’s hospitals offer a child-friendly environment that includes comforting spaces, child-sized equipment, toys and activities that are designed to help put children at ease and make the hospital experience less scary.
Family-centered care: Children’s hospitals often prioritize family involvement in the patient care process. Family-centered care supports parents and caregivers, offers education and resources to the family, and provides emotional support. Further, because children are not always able to communicate their needs or understand their treatment, the family is considered a partner in care.
Emotional support: Emotional support is a necessary component in maintaining a child’s mental health and well-being and fostering resilience during hospital stays. For this reason, many children’s hospitals offer emotional and psychological support, including child life specialists to help children understand and cope with their circumstance using age-appropriate methods like play and art therapy.
Continued on page 14
The future site of Intermountain Health’s standalone children’s hospital at UNLV’s Harry Reid Research and Technology Park (Courtesy)


Mitch
Cloward is president of Intermountain Health’s Desert Region, including Southern Nevada and Southwest Utah.
Intermountain Health is building Nevada’s first standalone children’s hospital. Recently, dignitaries and community members gathered at the future building site as Governor Joe Lombardo unveiled the sign alongside the Hernandez family.
The Hernandezes are one of many families who have had to travel out of state for advanced pediatric care. When their son was diagnosed with pediatric cancer that required immediate treatment, including a bone marrow transplant, the Hernandez family was faced with the difficult decision to leave Nevada for care. Because Las Vegas does
not currently offer a comprehensive, stand-alone care facility geared to children’s health, the Hernandez family moved to California for their son’s treatment. Today, he is cancer-free after finding a bone marrow match with his brother, and they were able to move back to Southern Nevada.
This is a story too many families relate to, but soon Nevadans will be able to receive advanced care by specialists in our own community. The comprehensive, subspecialty care in our backyard will greatly reduce strain on families already burdened by emotionally and physically
challenging health conditions.
The forthcoming children’s hospital is the result of 40 years of hard work by many in the Las Vegas community, long before Intermountain Health began caring for patients in Southern Nevada.
Pediatricians, caregivers, hospitals and other organizations have dedicated themselves to caring for children and contributed to this milestone. Over the next few years, the children’s hospital will begin to take shape. Currently, the design phase is in progress and the groundbreaking is expected in late 2025.
— Mitch Cloward
Continued from page 12
Advocacy and research: Pediatric medical research can be challenging for several reasons, including ethical considerations in treating children. Many children’s hospitals are at the forefront of research, offering new treatments, medications and interventions designed specifically for children. This work improves outcomes for patients and children around the world.
Pediatric patients may present complex medical conditions, challenges in diagnostics and treatment, the need for increased psychological and emotional support and more.
Anatomical and physiological differences: There are many differences in a child’s anatomy that may present obstacles in diagnosis and care.
Smaller airways and lungs: Children, especially infants, have smaller airways that can make respiratory issues more critical and difficult to manage. Conditions like asthma or respiratory infections can progress quickly.
Higher metabolic rate: Children have faster metabolisms, which affects how they absorb, process and eliminate medications.
Immature immune systems: A child’s immune system is still developing, which makes them more vulnerable to infections and illnesses, and they may respond differently to infections compared with adults.
Rapid growth and development: Children’s bodies are constantly growing and developing. Medications or treatments that work well in adults may not be safe or effective in children, and dosages often need adjustment based on the child’s age, weight and growth stage.
Diagnostic challenges: Many diseases present differently in children than they do in adults, and children are often unable to express what they are feeling, making it harder to assess their symptoms. Further, many pediatric diseases share symptoms such as fever, irritability and vomiting, which can make for a longer diagnostic process.
Medication management: Because children process medicine differently than adults, there are limited drug options and precise dosage calculations required to avoid under- or over-dosing. Especially for young children and infants, the consequences of incorrect dosing can lead to serious complications. Children may also experience side effects of medication differently, and the long-
term impacts of medication on a child’s development may not be fully understood.
Psychological and emotional effects: Hospitals can be frightening places for all of us, but they can be especially upsetting for children. Fear and separation anxiety can lead to distress and can cause a range of behavioral issues. Tending to the child’s psychological needs is integral to their treatment plan.
Chronic and complex conditions: Many child patients are faced with lifelong or complex medical issues such as congenital heart defects, cystic fibrosis or childhood cancers. Conditions like these may require extra support.
Long-term treatment plans: Children with chronic conditions may require ongoing treatment that may affect their normal development or schooling. In addition to medical and psychological care, these patients often need educational and social support as well.
Transition to adulthood: As children with chronic conditions reach adulthood, transitioning from pediatric to adult health care can present challenges. It requires planning and continuity of care to ensure that adolescents continue to receive appropriate treatment as their needs change.
Vulnerability to infections: Children are more susceptible to infections, partly because their immune systems are still developing. Infections can also spread quickly in pediatric populations, especially in hospital settings. This leaves them at a higher risk for complications.
Social and developmental factors: Treating children requires attention to their social and developmental context, as medical treatment can affect their growth, education and overall development.
Impact on schooling and development:
Prolonged illness or hospitalization can interfere with a child’s education and development. Specialized educational support and therapies are often required to address developmental delays caused by illness or treatment.
Social isolation: Hospitalized children may feel isolated from their peers, affecting their mental and emotional health. Keeping a child socially engaged during treatment is important but often difficult.
Ethical considerations: Pediatric care often involves complex ethical issues.
Parental consent vs. child’s autonomy: The need to balance parental authority with a child’s emerging ability to make decisions can create eth -

ical dilemmas. For instance, older children may have opinions on their treatment, but they may not be legally able to make medical decisions.
When children are faced with terminal illnesses, making decisions about treatment options and end-of-life care can be emotionally and ethically challenging for both health care providers and families.
According to the Agency for Healthcare Research and Quality, there were 5.2 million pediatric hospitalizations in 2019, and 76.7% of them were newborns and infants under 1 year old. Respiratory conditions were common reasons for hospitalizations among younger children, with acute bronchitis being the most common principal diagnosis for children under 5 years old. Mental disorders were the most common reasons among older children, with depressive disorders being the most common principal diagnosis among children 10 years old and older.
Sources: Children’s Hospital Association, American Academy of Pediatrics, Agency for Healthcare Research and Quality
Vitamin D is vitally important for our bodies to function. According to the Mayo Clinic, vitamin D has antiinflammatory, antioxidant and neuroprotective properties that support bone health, muscle function, brain cell activity, immune health and more. We get it from sunshine, diet and supplementation, and yet the Cleveland Clinic reports that at least 35% of adults in the United States are vitamin D deficient. Here is everything you need to know about this complex nutrient.
Vitamin D is fat soluble vitamin that is sometimes referred to as a hormone because it regulates biological processes in the body. Calcitriol, the active form of vitamin D, travels through the bloodstream and targets different organs to help different physiological processes including calcium absorption in the intestines, bone mineralization, kidney function and immune function. It also plays a role in regulating cell growth and repair.
The skin contains a compound called 7-dehydrocholesterol that UVB radiation from the sun interacts with and causes to convert into previtamin D3.

Previtamin D3 is then converted to vitamin D3 and enters the bloodstream where it is carried to the liver.
For many people, the primary source of vitamin D comes from sunlight. It is the only vitamin that the body can synthesize on its own from sunlight, whereas most other vitamins only come from food sources.
The liver converts it into 25-hydroxyvitamin D (calcidiol), which is the primary circulating form of vitamin D in the body. It then travels to the kidneys.
In the kidneys, 25-hydroxyvitamin D is converted to 1,25-dihydroxyvitamin D (calcitriol), the active form of vitamin D. This is the one that has physiological effects on various organs and biological systems.
With shorter days and less sunlight, people may be more prone to vitamin D deficiency during the winter. According to the National Institutes of Health, low levels of vitamin D are often found in people with seasonal affective disorder but more research is necessary to conclude whether vitamin D supplementation can help relieve SAD symptoms.

Unlike most vitamins, vitamin D is fat-soluble, which means your body can store it in your fat cells for later use. If you get more than you need during summer months, your body can hold on to it for use during winter when sunlight is less abundant. This is also why you can get nauseous taking vitamin D on an empty stomach— your body needs fat to absorb it.
Several factors affect vitamin D synthesis in the skin, including:
n Geographic location: People living closer to the equator, where sunlight is more direct year-round, can produce more vitamin D compared to people living in areas with less sunlight, especially in the winter.
n Skin type: People with darker skin have more melanin, which can reduce the skin’s ability to produce vitamin D. Melanin absorbs UVB radiation and reduces its effectiveness in vitamin D synthesis.
n Time of day: UVB rays are strongest between 10 a.m. and 4 p.m., so exposure during these hours is more effective for vitamin D production.
n Duration of exposure: The amount of time spent in the sun affects how much vitamin D is synthesized. 10–30 minutes of sun exposure a few times a week is sufficient for many people, but this varies depending on skin type and environmental conditions.
Most animals can’t make vitamin D from sunlight
Unlike humans, most pets, including dogs and cats, cannot synthesize vitamin D from sunlight, so they need it in their diet. Pet foods are often fortified with vitamin D for this reason.
n Age: Older adults may have less efficient skin synthesis of vitamin D.
n Sunscreen: Sunscreens with high SPF block UVB rays and can reduce vitamin D production. Limited sun exposure without sunscreen is often recommended for producing adequate vitamin D while still protecting skin from damage.
Beyond sunlight, food and supplements also offer vitamin D. Some foods naturally contain vitamin D, including fatty fish like salmon and sardines, beef liver, egg yolks and mushrooms, while some foods are fortified with it, including dairy. Vitamin D supplements are commonly used to correct deficiencies, especially for those who have limited sun exposure or dietary intake.
Vitamin D2
This form is typically found in plantbased sources, such as mushrooms exposed to sunlight.
Vitamin D3
This form is found in animal-based sources, like fatty fish, egg yolks, and liver, and is also produced by the skin when exposed to sunlight.
When choosing a vitamin D supplement, its generally recommended to get a vitamin D3 supplement because it is considered more potent.
The Mayo Clinic generally recommends:
n 400 IU/day for children up to 12 months
n 600 IU/day for people ages 1-70
n 800 IU/day for people over 70 years old
However, people who are deficient or at risk of deficiency should consider taking more at their doctors’ recommendation. Regular monitoring of vitamin D levels through blood tests can help ensure an appropriate dose.

Can you take too much?
Yes, excessive supplementation can lead to toxicity that can result in high calcium levels. This can cause nausea, vomiting, weakness, kidney stones, and calcification of soft tissues.
While most people can get enough vitamin D through a combination of sunlight and diet, people who are at a higher risk of deficiency may benefit from vitamin D supplementation.
n People with limited sunlight exposure: This includes people who live in areas with long winters, people who spend most of their time indoors and nightshift workers.
n Older adults: As people age, their ability to produce vitamin D in the skin decreases and older adults may have reduced dietary intake of vitamin D.
n People with dark skin: People with darker skin produce less vitamin D when exposed to sunlight because melanin absorbs UVB radiation. Individuals with dark skin, especially those living in regions with limited sunlight, may need to take supplements to ensure adequate vitamin D levels
n People with some medical conditions: Certain medical conditions can impair the body’s ability to produce or absorb vitamin D, including osteoporosis, malabsorption disorders, kidney disease, liver disease and obesity.
n Pregnant and breastfeeding women: Pregnant and breastfeeding women are at an increased risk of vitamin D deficiency, which can affect both her health and the health of her baby. The American College of Obstetricians and Gynecologists recommends that pregnant women take vitamin D supplements to ensure they meet their needs.
n Infants: Breastfed infants may need vitamin D supplements because breast milk is generally low in vitamin D. The American Academy of Pediatrics recommends that breastfed infants receive 400 IU of vitamin D per day starting soon after birth. Formula fed infants who drink less than 32 ounces of formula should also supplement.
n People who follow certain diets: Vegans and vegetarians may be a higher risk of deficiency since natural sources of vitamin D are primarily animal-based.

Symptoms of vitamin D deficiency include bone pain, muscle weakness, fatigue and an increased risk of fractures. In severe cases, it can lead to conditions like rickets (in children) or osteomalacia (in adults), where bones become soft and weak.
Sources: Harvard School of Public Health, Columbia University, Oregon State University, Johns Hopkins University

PREFRONTAL CORTEX
Goal setting occurs in many forms. It’s embedded in our daily tasks—I will fold the laundry; I will not hit snooze. It’s part of our long-term planning— I will get a promotion by the end of the year; I will work out four times a week. It’s also part of our lifetime benchmarks—I will retire comfortably; I will travel the world.
Setting goals, big or small, is what drives us forward and allows us to become the people we want to be. An entire field of study is dedicated to goal setting. Psychologists, neuroscientists, behaviorists and more work to identify the most effective methods to achieving and maintaining goals. With more resources than ever, finding success may simply be about finding the right technique for you.
Goal setting is a process that activates areas of the brain that manage motivation, reward and decision making. One key area involved in this process is the prefrontal cortex, which is responsible for higher cognitive functions such as planning, problem-solving and self-control, according to a 2001 article in the Annual Review of Neuroscience. When setting goals, the prefrontal cortex helps us develop strategies, anticipate outcomes and make choices that align with our objectives. The dopaminergic system also plays a critical role in the motivation and reward processing involved in goal pursuit. According to a 1998 article in Journal of Neurophysiology, dopamine, a neurotransmitter associated with pleasure and motivation, is released when we achieve milestones or make progress toward a goal. This
release of dopamine reinforces behavior, making it more likely that we will continue working toward our goals. Further, Edwin Locke and Gary Latham, pioneers in goal setting research, claim that breaking larger goals into smaller, more achievable steps can prevent overwhelm and maintain motivation because it provides frequent rewards that activate dopamine release. This feedback loop sustains focus and drives continued effort.
A 2004 article published in Nature Reviews Neuroscience reports that the striatum, a region in the brain involved in habit formation and reward, is also activated during goal-directed activities. When goals are perceived as rewarding or intrinsically motivating, the brain strengthens neural pathways that support continued goal-directed behavior.

Where neuroscience studies the brain and its functions in the body, psychology studies the mind and how thoughts affect behaviors. The psychology of goal setting is well-researched, and it delves into how individuals set, pursue and achieve goals. Several psychological theories provide insight into this process and offer practical applications for improving goal achievement. One of the most influential psychological theories is Locke and Latham’s Goal Setting Theory, which asserts that clear, specific and challenging goals lead to higher achievement. They found that the act of setting specific goals rather than vague, general intentions provides direction and focus, which increases effort and persistence. Challenging goals, ones that are considered within reach but require effort, tend to boost performance. Locke and Latham’s five principles that maximize success in accomplishing goals:
1 CLARITY
Successful goals are specific.
2 CHALLENGE
The degree of difficulty for a goal, goals require growth and stretching.
3 COMMITMENT
Dedication to a goal and what benefit it will have to a person.
4 FEEDBACK
Accountability and recognition from a trusted loved one or peer.
5 COMPLEXITY
The difficulty and execution of plans and tasks that a person must accomplish to reach the goal.
There are other important psychological concepts in goal setting, including Edward Deci’s self-determination theory, which emphasizes the importance of intrinsic and extrinsic motivation in goal setting. Deci theorized that goals which align with personal interests and values (intrinsic motivation) are more likely to encourage sustained effort than goals driven solely by external rewards (extrinsic motivation). Goals often reflect our values, and those that do are more likely to succeed.
Narrowing in on motivation in goal setting is crucial to success. There are many possible motivating factors, including:
Clarity and direction: Setting goals gives us a path and a sense of direction. It helps focus our energy and resources on something meaningful and gives us something to aim for.
Sense of accomplishment: Achieving a goal may create a feeling of accomplishment and satisfaction, which could fuel more goal setting. This creates a cycle of motivation where each success builds momentum for future achievements.
Avoiding regret: People may set goals to avoid regret later in life. The fear of looking back and wishing we had done more motivates some to start setting and working toward goals.
Personal values: Some goals are driven by deeper core values, like the desire to help others, make a difference or live a life that aligns with personal beliefs.
These goals can be especially motivating because they provide meaning beyond just the goal itself—they’re rooted in something larger than accomplishment.
Some people may know exactly what drives them and have a clear vision of what they would like their lives to look like. Others may struggle to set meaningful goals because they are still learning what motivates them and still considering who they want to be. When setting goals, you might consider the following questions to help determine your core values:
What accomplishments have you felt the greatest pride in? What made that accomplishment meaningful? Why do you think that is?
What situations make you feel frustrated, angry or defeated? How do you react in these situations? Why do you respond the way you do?
When you make a difficult decision, what factors guide you?
The answers to these questions may help guide both your long-term and short-term goals.
Businessman George T. Doran coined the term SMART goals in 1981. Placing goals into a framework like this helps create a plan for execution and evaluation, and allows people to track their progress. Industry professionals later expanded on SMART goals to include evaluation and revision. The acronym stands for goals that are:
SCENARIO
Sarah wants to be healthier by exercising consistently.
Sarah sets a goal to go to the gym twice a week with a set workout plan.
She uses a calendar to chart the days she attends each week.
Sarah makes sure this goal is manageable with her work schedule and social commitments.
Developed by Mark Murphy in 2009, HARD goals are geared toward corporate environments and are designed to be challenging. The core belief of this goal structure is that to accomplish great things, you have to grow outside of your comfort zone. HARD stands for heartfelt, animated, required and difficult—each category has a corresponding question. Here is an example of how the HARD goals method could play out:
SCENARIO
Sarah is a marketing professional, and she wants to double her number of clients from 2024 to 2025.
What are three reasons you want this goal?
Sarah loves her job and wants to increase her capabilities, she wants to grow financially, and she believes she can help more people reach their goals.
Where do you want your career to be?
She wants to double her number of clients this year. This will set her business up for success over the next three years and allow her business to grow.
There are many methods for goal achievement. Some traditional methods were developed from Locke and Latham’s five principles, whereas others look at habit-based goal setting. Some may encourage visualization, some may focus on prioritization, and some may use a combination of different methods. They all aim to implement meaningful infrastructure around goal setting to maximize success.
This goal pushes Sarah to work harder but isn’t such a drastic change that she will become easily disheartened.
Sarah commits to this plan for 3 months.
Sarah completes her goals and evaluates their effectiveness. She asks herself how well she is executing her plan and considers its sustainability.
Based on her evaluation, Sarah revises her goals. She can determine to set a more challenging goal or to continue her newly created habit.
What milestones do you need to keep on track to achieve this goal?
She needs to reach out to a target number of new contacts every month and fulfill a quota of contracts each quarter to keep her on track for her yearly goal.
What are the three to five most important skills you’ll need to develop to achieve this goal and how will you do that?
Sarah will need to improve her networking skills. She can buy a book on client acquisition and retention, and attend conferences where she can meet people and expand her knowledge.
This is one example of an ambitious goal that would be well adapted within the HARD goal framework. Sarah’s vision is backed by concrete plans and an awareness of her shortcomings in order to address them.
A good option for visual learners, the goal pyramid method breaks down large goals into distinct levels and manageable tasks. By establishing a hierarchy, this method can also give people a sense of accomplishment as they “climb” towards their goals.
Example: Sarah wants to go back to school for a master’s degree. Her goal pyramid might look like this:

TOP TIER GRADUATING WITH HONORS!
SECOND TIER MASTER’S THESIS
THIRD TIER TAKING CLASSES
FOURTH TIER STUDYING FOR INDIVIDUAL EXAMS AND PROJECTS
FIFTH TIER TAKING ENTRY EXAMS AND FILLING OUT APPLICATIONS
When goals are broken down into smaller, more manageable tasks, it may help prevent overwhelm and burnout. This method allows people to develop the baseline foundation of the goal and then explore higher tiers as their goal-based skills grow.
Visualization is a popular tool in goal setting because it may help prepare the mind for success and strengthen the connection between the goal and the reward. It can also help build confidence and reinvigorate the motivation for setting the goal to begin with.

Developed by psychologist Gabriele Oettingen, the WOOP acronym stands for wish, outcome, obstacles and plan. Oettingen’s research found that this method leads to more successful goal attainment because it blends positive visualization with a realistic assessment of potential barriers.
Wish: Clearly define what you want to achieve Outcome: Visualize the best possible outcome of achieving that goal.
Obstacles: Identify internal obstacles that might prevent success.
Plan: Create a concrete plan to overcome those obstacles.
EXAMPLE
Wish: Sarah wants to be taken more seriously at work.
Outcome: Sarah visualizes helping her colleagues, gaining the respect of her peers and earning a promotion.
Obstacles: Sarah does not speak up in meetings.
Plan: Sarah decides to contribute three ideas in each meeting, and she plans her talking points in advance. She is prepared with notes and does not hesitate to share her thoughts.
James Clear, author of Atomic Habits, encourages people to implement identity-based habits as a way of changing behavior and achieving goals. Instead of focusing on an outcome-based goal (i.e., I want to lose weight), Clear suggests reframing it as an identity shift (i.e., I will be the type of person who moves every day). From there, focus on small wins toward the goal, such as taking the stairs and increasing your step count.

Nathalie Majorek, MD , is an internal medicine physician at CarePartnersMD with more than 25 years of experience. For more information about Majorek and her practice, visit CarePartnersMD.com.
BY NATHALIE MAJOREK, MD
The 2022 KFF Women’s Health Survey found that 29% of women ages 18-64 reported that their health concerns were dismissed by a doctor and 15% felt their doctor did not believe them. These statistics showcase a broader issue that negatively affects women everywhere, including myself.
In my 30s, I experienced severe pelvic pain. A colleague suggested I see a gynecologist at another hospital, as I preferred not to be evaluated by someone I work with. Just like every other woman, I went into the exam room and introduced myself. Unlike others, I did so as a physician expecting professional discussion about my condition. The response I was met with was a wakeup call about how women are treated in health care.
Despite explaining my ongoing and intense pain, the doctor insisted that fibroids were unlikely to cause such discomfort and suggested I only return if my symptoms worsened. I was speechless and baffled that I was made to feel as though I was exaggerating or fabricating my pain. I consulted another gynecologist who performed surgery, finding that the fibroids were so large and invasive that several physicians were shocked I had endured the pain for so long. Finally, I felt validated. But I asked myself: How many women never receive that confirmation?
Scientific and medical advancements are evident, yet women continue to be disproportionately affected by many diseases and conditions. Women’s health care concerns are often dismissed, and female-specific conditions remain under-researched. In 2020, McKinsey Global Health Institute found that only 1% of health care research and innovation was invested in female-specific conditions beyond oncology.
Less research and less understanding prioritize male perspectives. This leads to women encountering missed diagnoses, less effective treatment and more side effects with treatments. For example, heart attacks in women often present with atypical symptoms such as nausea, fatigue or abdominal pain, whereas men typically experience more accepted symptoms such as chest and left arm pain. As a result, women under 55 are 50% more likely than
men to be initially misdiagnosed for a heart attack, and any delay in treatment increases the risk of serious consequences, including death.
Women’s pain is also more likely to be minimized. A 2001 study in The New England Journal of Medicine found that women are less likely to receive adequate pain management compared with men. Furthermore, women are more frequently prescribed psychiatric medication, and their physical symptoms are more likely to be blamed on psychological causes leading to further misdiagnosis, repeated doctor visits and delayed diagnosis.
Beyond medical bias, women face financial barriers to health care access. The 2017 Kaiser Women’s Health Survey found, “roughly 1 in 4 (26%) women and 1 in 5 (19%) men have had to delay or forego care in the past year due to cost. Because of costs, approximately 1 in 5 women postponed preventive care (19%), skipped a recommended test or treatment (20%) or made medication tradeoffs such as not filling a prescription or cutting dosages (17%).”
Women of color and LGBTQ+ women face even greater disparities in care, often receiving less adequate treatment due to stigma and discrimination. For example, “Overview of maternal mortality in the United States,” an article published in Seminars in Perinatology, found that Black women are three to four times more likely than white women to die from childbirth-related complications, regardless of their income or education level.
To address these disparities, major changes are necessary, including policy reforms, improving medical education, promoting sex-specific research and raising awareness of cultural competency and implicit bias among health care providers. The health care system needs an overhaul, including how physicians are educated and trained as well as how research is conducted.
In the meantime, the key is that all patients, regardless of gender, feel heard and respected by their physician. If that’s not the case, patients have the right to seek another provider. To women everywhere: advocate for yourself and, if possible, bring a trusted friend or family member to appointments who can also advocate on your behalf.

BY VANDHANA WADHWA, MD

Wadhwa, MD , is the West regional chief medical officer at Carelon Health
More than half a billion people worldwide live with diabetes. That’s 1 in 10 adults, making it one of the leading causes of death and disability. Nearly 1 in 2 adults with diabetes go undiagnosed.
In the United States, 29 million people have diabetes and nearly 98 million have prediabetes—almost 38% of the population. Globally, the disease is growing. According to the World Health Organization:
n Individuals living with diabetes increased from 200 million in 1990 to 830 million in 2022.
n It’s increasing more rapidly in low- and middle-income countries than in high-income countries.
n Diabetes can cause serious damage to the body, especially to the nerves and blood vessels. A wide range of other health concerns, such as blindness, kidney failure, heart attacks, stroke and lower limb amputation are possible if left untreated.
Diabetes can be caused by the dual influence of genetics and lifestyle:
Type 1 diabetes is an autoimmune disease where the body’s immune system attacks and destroys the cells in the pancreas that produce insulin, resulting in the body not being able to make its own insulin.
Type 2 diabetes occurs when the body either doesn’t produce enough insulin or the cells become resistant to the insulin it does produce, meaning the body can’t use insulin effectively.
Type 1 diabetes typically requires daily insulin injections while Type 2 diabetes can often be managed with lifestyle changes and oral medications. Type 2 diabetes prevention is crucial because 90-95% of all diabetes diagnoses are for Type 2 diabetes.
While Type 1 diabetes is more of an autoimmune problem, Type 2 diabetes is caused by insulin resistance that’s affected by diet and lifestyle. If you’re obese, sedentary or eat mostly processed foods, it leads you to a predisposition to developing diabetes.
Technology can eventually help navigate the dif-
ficulties of treating diabetes. There is definitely the cost factor and the adherence to treatment. It can range from not being able to afford the medication to not wanting to give themselves the injection. We have advances in technology like glucose monitors that are making it easier to manage and get in control of your condition.
Some of the ways to keep diabetes in check are through practical strategies that focus on lifestyle changes like weight loss, exercise, diet, stress management and smoking cessation. Through Carelon Health, patients can take part in our Nifty after Fifty by Encore Wellness program. Located in our Nevada care centers, this program includes fitness evaluations, screenings and physical activities, which can all play an important role in diabetes prevention and overall health management.
n Check your blood sugar often and take your prescribed medication. Knowing your blood sugar numbers can help you make better food choices and adhering to medication can help you manage your blood sugar and prevent complications.
n See your doctor regularly. Talk to your care team often. They can help you track your health and change treatments if needed.
n Be mindful of your carb intake. Too many carbs can make your blood sugar go up quickly. Instead, eat more whole grains, fruits and vegetables.
n Stay active. Even light exercise can help keep your blood sugar stable. It can also promote weight loss, give you more energy and reduce stress.
n Keep stress at bay. Stress can affect your blood sugar. Things like yoga, meditation or mindfulness can help you stay calm and keep your diabetes under control.
n Keep moving and drink water. Exercise and drinking lots of water can help keep your blood sugar at a healthy level.
Early intervention, lifestyle changes, and medical and social support systems are important components to successfully manage the disease.
Sources: Harvard University, Centers for Disease Control and Prevention, World Health Organization


Hamilton, MEd , is an early childhood outreach educator at The Las Vegas-Clark County Library District
BY ANGELA HAMILTON, ME d
According to the Center on the Developing Child at Harvard University, critical brain development is supported by nurturing interactions with caregivers starting at birth. At the Las Vegas-Clark County Library District, we are taking steps to support and encourage nurturing experiences using books aimed at ages birth through 5. The Library District, besides offering books and story times for our little ones, has also created the My First Library and 1,000 Books Before Kindergarten initiatives to support the youngest community members
Chatting with your baby as you go about your daily routine may seem like a one-sided conversation but it is critical to building life-long language skills. During years 1-5 in a baby’s life, the brain is building important connections needed to develop language-processing skills. Language is one of our most necessary learned skills, and reading and understanding the spoken and written word opens the doorway to learning throughout your child’s life. Time spent reading a book, or just identifying and describing its pictures, is the first step toward your child’s ability to communicate.
Early learning development was the inspiration behind the Library District’s My First Library box, which is given to new parents/ caregivers at the Sunrise Children’s Hospital. The box includes soft-sided books, a guide to early reading to encourage families to read together starting at birth and more.
Reading to your baby is not about the amount of time you spend. It’s about establishing a special time for the joy of discovery that is found in reading and making it a habit that they look forward to each day.
Presenting books as a fun activity that is associated with play and bonding time with a beloved caregiver makes positive memories that last a lifetime. Reading will then become a source of knowledge and solace as they grow.
The Library District offers another engaging program for little ones called 1,000 Books Before Kindergarten. It allows families to record their time together reading books and earn exciting prizes along the way. It might seem like reading 1,000 books with your child before they start kindergarten is a big ask but think about it this way: If you start reading to your baby as soon as they enter the world, you will have 1,825 days of reading before your child turns five and starts kindergarten. This is plenty of time to complete 1,000 books—duplicate reads count—and build a little reader for life.
The Library District website includes community resources, reading support, links to story time events, home learning and more at thelibrarydistrict.org/baby-and-me. You will also find a link to the 1,000 Books Before Kindergarten program on the Let’s Read Together page.
The Library District offers two other annual programs to help reach the 1,000-books goal: n Summer Challenge (which includes reading and activities from May 15-July 31) n Winter Reading Challenge (which runs from January 2-31)
Both programs give participants the opportunity to earn prizes for babies, elementary-age children, teens and adults. During our story times at the library, we encourage each child to engage in their own way as we read. We talk together, sing songs, get up and dance, play with puppets and do other fun activities. Caregivers can do these same activities during at-home story times.

The early years of reading are not about following a book from beginning to end. Just enjoy the interactive experience, have fun and be responsive to your child’s interest in a picture or a character or the sound that an animal in the story might make. Let them hold the book and manage the pages to find out what is fun for them. If your infant or child touches something in the book, identify it, describe it and tell them what you know about it. You are building their understanding of the world when you do this.
If they are active, choose a book that has movements. If they are learning to speak, choose a book that has repetitive language so they can read with you by repeating the words.
You can go to the library and let them explore our board book collection for something that catches their eye. It may be that your child likes informational books more than they like storybooks. You can make up your own story together using something from an image in whatever book they have chosen. If traditional books don’t engage them at first, ask a librarian for pop-up, lift-the-flap or other interactive books. A librarian can also help you find books that explore specific topics of interest.
There are no fees for damaged board books at the Library District. The value of a book is in its use, and we expect little ones to use books in a more physical way. If your little one tears a page

or a cover, just return the book to your library, as you normally would, so that we can record it and replace the titles that seem to be the tastiest to our little ones. Then feel free to pick out some new books for them to devour.
Did you know that using multiple languages with your child supports retention of more brain connections as they get older? The Library District has books in many languages. If you need help, ask your librarian.
There is so much to discover at your local library for every member of the family. STEAM learning, college test prep, and spooky fun TeenTober are some of the offerings for teens. For adults, there are options for earning a diploma, learning a language, changing careers, engaging with new technologies and more.
Find out what our libraries offer at thelibrarydistrict.org and visit the library today.

Shannon Martin , OTR/L, OTD, BCG, is professor and program director at the School of Occupational Therapy at Touro University Nevada
BY SHANNON MARTIN, OTR/L, OTD, BCG
Falls are often a major concern for aging people and can have potentially catastrophic consequences. According to the Centers for Disease Control and Prevention, more than 14 million adults aged 65 and older in the United States report falling each year, which is about 1 in 4 older adults.
Approximately 37% of those suffered injuries that required medical treatment or restricted their activity for at least one day. However, falls are preventable and many risk factors can be modified. One innovative approach to fall prevention is wearable technology. Utilizing common and often relatively inexpensive devices, such as smartwatches and fitness trackers, has the potential to support older adults aging independently in their homes and prevent falls.
Approaches to fall prevention often include exercises directed at improving muscle strength and balance, being evaluated for appropriate durable medical equipment as needed, and reducing clutter and hazards within the home. There are several evidence-based fall-prevention programs backed by the CDC that are widely available in many communities and address many of the most common risks associated with falls. While these efforts can be effective in increasing awareness of fall risk and improving strength and balance, wearable technology can provide additional insight and support into fall prevention.
Wearable technology describes electronic devices, designed to be worn on the body as an accessory, that are equipped with sensors to collect, analyze and transmit data, often in real-time. This data can be shared with health care providers. Because the use of wearable technology is common across generations, these devices are not typically associated with stigma around aging and are widely accepted by older adults. Key features
like step tracking and exercise duration in these devices are particularly beneficial for older adults as they provide insights into their daily physical activity levels and overall health. This can be beneficial in noticing trends as one ages or sustains an injury, and provides important insight to health care providers regarding one’s risk factors associated with falling.
Particularly useful features of these devices are the ability to detect falls using accelerometers and alert caregivers or emergency services if the individual wearing the device needs help.
One of the most serious consequences of a fall for an older adult is being unable to get up from the ground for a significant period following the incident, increasing the potential for injury and complications. Even if the device is not set to automatically call emergency services in the event of a fall, the wearer may be able to use the device to make a phone call or send a text message to alert someone of their situation if needed.
Additional features related to mobility that many users are not familiar with include the device’s ability to track walking speed, walking step length and walking asymmetry. This information gives an estimate of stability while walking which is an indication of how likely you are to fall at any given moment. Tracking this information over long periods is one of the most powerful tools to track fall risk as one ages. Devices can additionally be set so that the wearer can receive notifications to alert them of elevated fall risk. Further, many wearable technologies worn at night can monitor sleep patterns and sleep quality. Poor sleep and frequent night arousal are associated with increased falls.
Beyond fall prevention, these devices can also track important health information that can be indicative of potential health concerns. This includes heart rate monitoring which can help detect irregularities and potentially prevent

cardiac events, and temperature monitoring which can help identify early detection of infection or other health issues. Some wearable devices are able to measure blood oxygen levels which can indicate potential respiratory conditions as well.
Data collected by wearable technology, in addition to other personal information, can support health care providers’ understanding of the individual’s current health status and physical fitness. Occupational therapists and other health care professionals have the potential to integrate these devices into their practices to enhance client outcomes and promote quality of life. Occupational therapists play a vital role in enhancing the health and well-being
of older adults by providing individualized client-centered recommendations for preventing falls and ensuring home safety.
Wearable technologies are a common, cost-effective approach to collecting and understanding a wealth of health-related information. Trends in this information can show changes in overall health and potential concerns, particularly as we age. Currently, wearable technology is a powerful tool in preventing falls and the potentially life-altering consequences of a fall. Wearable technology provides untapped potential in the future of health care and aging, and should be considered for a better understanding of your health and wellness.
BEYOND FALL PREVENTION, THESE DEVICES CAN ALSO TRACK IMPORTANT HEALTH INFORMATION. ... THIS INCLUDES HEART RATE MONITORING, WHICH CAN HELP DETECT IRREGULARITIES AND POTENTIALLY PREVENT CARDIAC EVENTS AND TEMPERATURE MONITORING, WHICH CAN HELP IDENTIFY EARLY DETECTION OF INFECTION OR OTHER HEALTH ISSUES. SOME WEARABLE DEVICES ARE ABLE TO MEASURE BLOOD OXYGEN LEVELS WHICH CAN INDICATE POTENTIAL RESPIRATORY CONDITIONS AS WELL.

BY AARMONI RAFTERY
In a state where support for visually impaired children is scarce, finding your way can feel impossible. I discovered this firsthand in 2018 when, at 12 years old, my family moved to Southern Nevada. Born with retinopathy of prematurity and no peripheral vision, I was used to navigating challenges. Too often, my community needs to fight to be noticed. But nothing prepared me for moving to one of only seven states without a school for the blind.
Services are sparse and often challenging to access. Things changed for my family when we found Nevada Blind Children’s Foundation, as it did for so many of my peers and their families that shared similar experiences.
Like most communities, the visual impairment community represents a diverse spectrum of experiences and needs. At NBCF, each student’s journey is unique—from those with low vision to those who are completely blind, and everything in between. Understanding this diversity is crucial, as each child’s experience with vision loss is distinctly personal and often complex.
Kevin Spilsbury founded NBCF in 2006 with the sole goal of empowering students ages 2 to 22 with the skills they need to gain employment and graduate from high school and college. In the beginning, the foundation was little more than a support group based in Kevin’s home for parents to discuss common issues. Today, it serves 25% of the population of children who are blind or visually impaired in Clark County. All of the programs are focused on the goal of empowering students to reach their full potential, providing them with the tools they need to succeed. They provide programs like early childhood intervention,
life skills and adaptive annual experiences like summer and spring break camps. All are designed to build a community and support system around students with visual impairments to succeed in education, employment and life.
The foundation’s holistic approach focuses on practical, everyday independence. Students learn to confidently manage their personal finances, develop crucial organizational skills and learn basic hygiene upkeep. Through carefully structured activities, from the early childhood program through early adult years, students build the fundamental abilities needed for future employment and higher education. Perhaps most importantly, NBCF creates an environment where students can freely express their needs and challenges, fostering self-advocacy skills that are essential for lifelong success.
My story with NBCF began with its summer camp in 2018. I was blown away by the support and community provided to the students by the staff. There are still staff members at NBCF today from when I was a student in 2018 and 2019. After summer camp in 2018, I joined NBCF’s teen robotics program, one of its innovative after-school activities that showed me how STEAM could be accessible for students with visual impairments.
This program is designed to demonstrate that science and technology are accessible to everyone. Additionally, adaptive recreation programs build physical confidence and spatial awareness. These programs interweave fun with learning, which was an important part of my NBCF experience. While I briefly stepped away in mid-2019, I found myself drawn back to NBCF to volunteer, eager to give back to my community and help students with similar experiences to mine.
In October 2023, I started a program called


EMPOWER, with the help of Megan, the Family Advocate and in-house social worker; Ashley, the Digital Media Coordinator; and Rena, a paraprofessional with her own personal experiences within the visually impaired community. The program is about guiding current students with vision impairments to advocate for their wants and needs. This provides them with an extra safe space where they could speak freely about their experiences, building confidence and learning how to identify and navigate unique challenges with the help of their peers.
I enjoyed every moment I spent at NBCF as a student and volunteer. Because of itsfantastic support, I am now attending UNLV as a business major.
The value of NBCF’s services is immeasurable. The foundation doesn’t just provide programming; it builds a community where every child with a visual impairment is able to reach their full potential. From those early meetings in Kevin Spilsbury’s garage to today’s comprehensive programs, NBCF continues to prove that with the right support, there are no limits to what we can achieve. As I prepare for my next chapter at UNLV, I know that somewhere in Southern Nevada, another 12-year-old is finding their way through NBCF’s doors, about to discover just how bright their future can be.

Virtual reality may be a future treatment option for individuals suffering from trauma, depression, anxiety, sleep disorders, pain and more
BY SHAN PADDA
ccording to market intelligence group
Open Minds, the United States spent approximately $329 billion on behavioral health in 2022, with Nevada’s per-citizen spending up 47% since 2015. The State of Mental Health in America Report, published by Mental Health America, ranked Nevada No. 51 in the country for mental health. This challenging landscape is compounded by the fact that nearly 88% of the state’s population lives in federally designated mental health provider shortage areas, according to the Nevada Health Workforce Research Center. Such conditions underscore the need for innovative solutions in trauma and behavioral health care.
One solution gaining momentum is the integration of virtual reality therapy with cognitive behavioral techniques, a novel approach that has shown promise in addressing the mental and physical aspects of trauma, particularly in patients suffering from chronic pain, anxiety, depression, sleep and PTSD-related symptoms. At the forefront of this innovation is Harvard MedTech, a Las Vegas-based health care technology company that is harnessing VR to create a remote, effective therapy model known as Vx Therapy.
Vx Therapy is a multifaceted program that combines VR technology with behavioral health coaching to manage both physical injury and psychological distress, including those caused by accidents, work-related injuries and combat exposure. The program, which has already served more than 4,500 patients, offers an immersive, at-home therapy experience designed to address the intersecting nature of mental health, chronic pain and PTSD-related symptoms. Unlike traditional treatments, Vx Therapy allows patients to experience calming, nature-based VR environments and guided cognitive behavioral therapy sessions from the comfort of their homes.

The program is structured to offer weekly support from behavioral health professionals who guide patients through VR-based interventions. These immersive experiences aim to calm the nervous system, promote sleep, reduce anxiety and improve mood regulation.
Additionally, they work to reframe patients’ perceptions of pain, helping them become more resilient to their injuries and trauma.
Continued on page 40

One of the most significant advantages of Vx Therapy is its ability to improve access to care. By offering a home-based solution, Vx Therapy reduces barriers such as stigma, travel difficulties and the need for in-person visits. This is particularly important for veterans, many of whom live in remote locations, which makes regular visits to health care facilities a major logistical challenge. In fact, the program has been integrated into veterans’ treatment plans at both local and national VA centers, providing an accessible and complementary solution for the VA providers to use by itself or in combination with traditional therapy.
Beyond veterans, Vx Therapy has been utilized in workers’ compensation and rural health markets. The program’s ability to provide targeted support for individuals experiencing both physical and psychological trauma has made it a valuable tool for helping people recover from their injuries, pain and often undiagnosed trauma-related symptoms such as anxiety, depression and sleep disorders. For injured workers and employers, this leads to a better overall experience by helping avoid contentious or legal interactions, ultimately improving return-to-work goals for the employee and employer. Vx Therapy helps employers save time and money managing a claim while enhancing engagement and retention of their employee.
The effectiveness of Vx Therapy in improving these outcomes has been substantiated by multiple studies. Research published in Pain News Network and the North American Spine Society Journal has demonstrated how Vx Therapy is improving patients’ pain levels, anxiety and depression. A study of 145 patients with chronic spondylitic pain found that after 14 weeks of treatment, participants experienced significant reductions in pain, anxiety and depression. Specifically, pain intensity was reduced by 33%, and anxiety scores dropped by nearly 46%. These findings underscore the potential of VR therapy as a non-pharmacological solution to pain management, particularly in the post-opioid epidemic era.
The power of VR in pain management lies in its ability to provide immersive distraction. VR-based interventions can significantly reduce the perception of pain by engaging patients in immersive, calming environments. This distraction technique is akin to mindfulness and meditation, but with the added benefit of deeper engagement through sensory immersion.
For patients with psychological trauma or PTSD-related symptoms, VR therapy offers a safe space to confront their
triggers in a controlled manner, reducing the emotional and psychological intensity often associated with exposure therapies. By helping patients recalibrate their stress response, VR therapy fosters greater emotional resilience and better coping strategies.
Additionally, VR has been shown to improve sleep quality, a critical area of concern for many individuals suffering from trauma and PTSD. A 2021 study published in the Sleep journal demonstrated the importance of improving sleep to mitigate PTSD symptoms. By creating a calming and immersive bedtime routine, VR helps patients reduce anxiety before sleep, promoting better sleep quality and continuity.
The clinical studies highlight the effectiveness of VR therapy in managing both pain and trauma-related symptoms. These therapeutic benefits are not only reflected in statistical data but also in the personal experiences of patients, who consistently report improvements in their emotional and physical well-being.
Patients who have participated in Vx Therapy have shared testimonials about their experiences. For example, a firefighter and veteran described how the program allowed him to manage pain and anxiety better, offering a sense of control over his recovery. One patient noted that VR experiences were so immersive that they were able to forget about their pain, making the process of managing anxiety and depression feel more proactive.
Success stories highlight the effectiveness of Vx Therapy in not only treating pain but also improving the quality of life for patients dealing with mental health challenges. Patients consistently report a reduction in pain and anxiety, increased sleep quality and a renewed sense of agency over their health.
As VR technology becomes more accessible and the health care landscape continues to evolve, digital tools like Vx Therapy are poised to play a central role in mental health care. With ongoing research and refinement, VR simulations can be tailored to meet the unique needs of patients suffering from specific traumas, phobias or chronic pain conditions. This evolution will further enhance the precision and effectiveness of digital therapeutics in managing mental health.
As more health care institutions, insurers and advocacy organizations partner with technology developers, therapies like Vx Therapy will become even more accessible. Harvard MedTech is helping shape a future where trauma recovery is more effective and accessible than ever before by using the combined power of VR technology and behavioral health support.




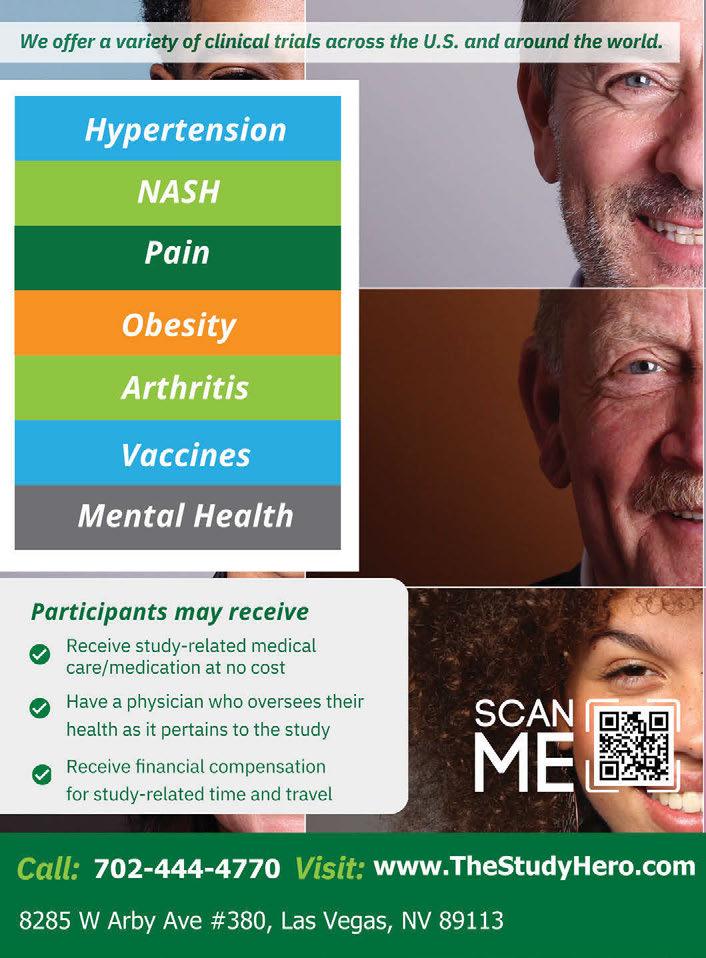

Karen Rubel is president and CEO of Nathan Adelson Hospice
BY KAREN RUBEL
The landscape for hospice care across the United States has grown increasingly competitive in recent years. Regulatory and compliance requirements are also increasing, and our organization is seeing patients present more complex needs. On the heels of a 45-year anniversary of providing care to the Southern Nevada community, we must consider what the next 45 years as a legacy organization looks like.
What is Nathan Adelson Hospice and what services or programs do you offer Nevadans?
Nathan Adelson Hospice is the largest and longest-established hospice in Southern Nevada. We were founded in 1978, following the death of Mr. Nathan Adelson, a beloved hospital administrator at Sunrise Hospital who cared deeply for his patients and employees. During his long, painful battle with cancer, family and friends close to him realized the need for specific health care to pain management, and responded to that need. Now, more than 45 years later, we provide comprehensive end-oflife care to more than 400 patients and families every day across Southern Nevada including Las Vegas, Henderson, Pahrump and Amargosa Valley communities. Our vision is that no one should end the journey of life alone, afraid or in pain, regardless of their ability to pay.
With our two inpatient facilities, we offer homecare services, where we see and care for most of our patients. The choice of where to spend one’s final days is so important, and we’re proud to offer compassionate bedside care no matter the location. In addition to excellent hospice and palliative care, through our foundation we provide bereavement and spiritual care services, compli-
mentary therapies including pet therapy, aroma therapy, art therapy, reflexology and more.
What does an affiliation mean and who else has joined in this new partnership?
An affiliation is very different from an acquisition or merger. Unlike an acquisition or a merger, an affiliation refers to a looser partnership between organizations where no ownership is transferred. Instead, organizations collaborate and align to achieve shared goals while maintaining separate identities. In partnership with Hospice East Bay (Pleasant Hill, California), Hospice of Santa Cruz County (Santa Cruz, California) and Willamette Vital Health (Salem, Oregon), we announced a groundbreaking affiliation agreement to join Chapters Health West, a newly launched division of Chapters Health System; it’s the largest not-for-profit chronic illness management and hospice organization in the country. This landmark partnership ushers in a new era within nonprofit hospice care across the Western United States, blending innovation with a commitment to compassionate, community-based care.
Why is now a critical time for this affiliation agreement?
Now more than ever, we’re seeing the hospice industry face challenges, including fraudulent hospice operators, increased regulatory scrutiny, increased costs and lower reimbursement. Hospices all over the country are exploring opportunities to address growing competition, workforce challenges and the need to stay relevant within their communities. As we also anticipate unprecedented growth in the Medicare population, we want to be ready to meet the needs of the community, integrating hospice care with palliative care and expanding to provide more home-based services

now and in the future.
With enhanced regulatory burdens, increasing competition in our market and the rising costs of delivering care, this affiliation allows us to gain efficiencies in all areas of operations. In essence, allowing us to create savings, increase opportunities for growth and have the scale needed to reduce costs.
What is the significance of this partnership in the eyes of the patients and families you serve in Southern Nevada?
While this affiliation opens new opportunities for innovation and sustainability, our commitment to the community remains the same.
Nathan Adelson Hospice will not see a change in its ability to provide quality end-of-life care to those in our community. We will continue to create best practices for hospice and
palliative care, as well as growth in payor contracts, operating efficiency and innovative and collaborative programs and services.
The affiliation of Chapters Health West will strengthen our organization by enhancing our ability to compete in an increasingly challenging marketplace. Through sharing best practices, joint contracting and other cost-sharing benefits, the affiliation will help ensure our organization’s long-term success.
Through this affiliation we are still a 501(c)(3) nonprofit, our Medicare number doesn’t change, our business model doesn’t change, and o ur board of trustees stays in place. Also, all philanthropy to the hospice stays local. We are part of a larger structure, but we keep our independence, identity and connection to our community.
In what ways should affiliations be a consideration for other nonprofit health care organizations?
Affiliations are an important consideration for nonprofit health care organizations, because they influence a range of operational, financial and strategic factors. They open access to resources which, in turn, can increase efficiencies, stabilize financial hardships, provide guidance within regulatory environments and even help navigate rising costs and workforce challenges since the fall out of COVID. While affiliations are very common in the for-profit world, nonprofits don’t often consider this option. This partnership allows us to think of our future and growth—all of which is better together.
In your opinion, will this partnership expand or elevate care in the Valley?
Through our affiliation and formation of Chapters Health West, the standard of care we provide at the bedside will not change. We will remain a hospice of choice, employer of preference, training center of excellence and the community’s trusted partner for comprehensive end-oflife care. However, by becoming part of a larger organization, we have the ability to create more efficiencies and share best practices, all of which benefit our patients and their families.
We’re not just coming together for today—we’re building a future where we can do more, expand innovation, and grow our market. By preserving the best parts of our independent paths and aligning them, each organization within Chapters Health West will create a future that honors our past while taking bold steps forward. Nathan Adelson Hospice will continue to build on the legacy of Irwin and Susie Molasky and prominent members of our community who founded our hospice so “no one ends the journey of life alone, afraid or in pain.”
Southern Hills Hospital and Medical Center completed the renovation and expansion of its operating room space. The $37 million project broke ground in May 2023, added 16,905 square feet of new operating space and imaging devices, and renovated 10,535 square feet of existing space. The improvements will accommodate more surgeries, reduce wait times and provide patients and sta with a more comfortable and e cient environment.
Molina Healthcare of Nevada, in collaboration with the MolinaCares Accord, announced a $350,000 grant to UNLV Health, expanding access to care at UNLV Health’s ear, nose and throat clinic in Las Vegas. UNLV Health will service more ENT patients with 15 fully equipped and operational clinic procedure rooms. The grant also supports the purchase of cutting-edge equipment needed for patient procedures requiring specialized care, including ear microscopes and laryngoscopies to examine patients’ voice boxes.
CarePartnersMD, led by internal medicine physician Nathalie Majorek, MD, opened its practice near Summerlin. Majorek and the CarePartnersMD wellness team o er prioritized primary care medicine, tailored wellness plans, advanced health screenings, medical assessments, diagnostic tests to enhance early issue detection and additional measures outside the scope of a traditional primary care visit.
Comprehensive Cancer Centers nurses Kelly Trigueros, Havana Lopez, Carla Juarez and Amber Bustamante passed the oncology nursing examination. Nurse practitioner Jewel Torres completed the advanced oncology nursing certification examination.
Molina Healthcare of Nevada partnered with Women’s Health Associates of Southern Nevada to provide a $250,000 grant to expand access to obstetrics and gynecology services. The partnership supports the recruitment of new physicians and advanced practice providers that will enhance access to high-quality OB/GYN care and improve outcomes for fetal and maternal health amid a severe shortage of specialty care statewide. Four physicians and two advanced practice providers committed to join the practice in the second quarter of this year. Two are former UNLV School of Medicine residents.
Cure 4 The Kids Foundation welcomed

Dristhi Ragoonanan, MD. As a board-certified pediatric hematology-oncology physician, Dr. Ragoonanan joined 18 other providers at the clinic, treating children and young adults a ected by pediatric cancer, blood and bleeding disorders, and rare diseases.
Comprehensive Cancer Centers hired oncologist, Janson Trieu, MD, and advanced nurse practitioners Ti any F. Show, Jan Kathleen Stanek and Damaris Kiptoo. Trieu is a medical oncologist and hematologist at Comprehensive’s Central Valley–Twain treatment center, located at 3730 S. Eastern Ave. Show, MSN, APRN, FNP-BC, sees patients at Comprehensive’s Horizon Ridge–Henderson treatment center, located at 2460 W. Horizon Ridge Parkway, where she provides oncology care and follow-up care to patients. Stanek, MSN, APRN, FNP-C, FNP-BC, CMSRN, works out of Comprehensive’s Henderson–Siena treatment center, located at 10001 S. Eastern Ave., where she helps manage the care and treatment plans for patients with cancer and blood disorders. Kiptoo, MSN, APRN, FNP-C, provides patient care at Comprehensive’s Northwest treatment center, located at 7445 Peak Drive.
Blessing Enudu, MD joined Southwest Medical’s Tenaya Health Care Center at 2704 N. Tenaya Way, specializing in adult medicine.
Nicole Wessendorf was appointed as director of communications and public relations at Touro University Nevada College of Osteopathic Medicine and Health and Human Services. In this role, Wessendorf oversees all aspects
Continued on page 46




Ensuringeverystudentwithavisual impairmentreachestheirfullpotential. Educate.Employ.Empower.
NBCFoffersafter-schoolprogramsforblind andvisuallyimpaired students, promotingindependencethroughrecreationand essential skills.
NBCFofferstop-tierearlyinterventionprograms, ensuringreadiness for visuallyimpairedstudentsandpeerswithexcellence.
NBCFpartnerswithfamiliesandcommunities to support students, fostering success andinclusivitytogether.





info@nvblindchildren.org www.nvblindchildren.org 702-735-6223
























If stress, anxiety, and overwhelm are running your life, it’s not your fault—you just need better tools.
Elite athletes, CEOs, and top professionals don’t just “manage” stress—they master their mindset. Now, you can too with Mental Wellness Unlocked Masterclasses
Science-backed techniques to control stress & anxiety
Rewire your thinking for emotional resilience
No fluff—just proven tools from Dr. Tiffany M. Smith, DNP


Stop guessing. Start thriving. Scan the QR code now—spots are filling fast! 702.907.7924 | www.Wellness.Vegas

of the communications strategy, including media relations, corporate messaging, crisis communication and public outreach.
West Henderson Hospital opened in December. Located at 1155 Raiders Way, the 150-bed hospital is equipped to care for patients with a variety of medical needs. Services include emergency care, cardiac care, neurology care, surgery, gastroenterology and inpatient care.
The Centers for Disease Control and Prevention designated Intermountain Health in Nevada as a 2024 Million Hearts Hypertension Control Champion for the health system’s e orts to enhance the health of patients by reducing blood pressure in patients with hypertension. This is the first time any health system has earned this distinction in Nevada.
MountainView Hospital welcomed Nelly P. Chow, DO, a highly trained cardiothoracic surgeon to MountainView Hospital and its patient clinic, Cardiovascular & Thoracic Surgery Associates. Chow is recognized for her expertise in minimally invasive thoracic surgery, including robotic procedures for lung cancer resection and mediasti-

nal mass removal, and for her work in hyperhidrosis management.
MDMeals, a Las Vegas-based online delivery service o ering dietitian-approved meals specifically curated for chronic health conditions, launched and is serving select states across the Western U.S. Founded by doctors with firsthand experience in how proper nutrition plays a critical role in treating illnesses, the company is setting a new standard with a health care-first approach to the meal delivery service industry.
Continued on page 48
NUTRITION EDUCATION






HOLIDAY HELPINGS



In-class healthy eating instruction at Title I elementary schools


Groceries, nutrition, and fitness guidance for families during school breaks


COOKIN’ UP BREAKFAST




Free breakfast for CCSD Title I Schools
MICHAEL TY CULINARY AWARD




Scholarships for culinary students






































Sunrise Health System’s four Nevada hospitals— MountainView Hospital, Southern Hills Hospital & Medical Center, Sunrise Hospital and Sunrise Children’s Hospital achieved accolades for clinical excellence from Healthgrades, including four excellence awards. The hospitals are among the nation’s top 10% across an expansive list of specialties, including stroke care, pulmonary care, neurosciences and outpatient prostate care. The four hospitals were also ranked among the top 100 hospitals in America for cardiac care, critical care, gastrointestinal care, gastrointestinal surgery, prostate surgery, pulmonary care, surgical excellence, orthopedic surgery, spine surgery and stroke care.

MountainView Hospital and Southern Hills Hospital integrated the latest surgical system into their operations. The newest robotic surgery system will support a wide range of procedures, enhance workflows, and provide precision and e ciency for patients and medical teams. The system is equipped with:
■ Revolutionary force-sensing technology: Surgeons can sense push and pull forces at the instrument tip, minimizing tissue damage and improving surgical precision.
■ Enhanced 3D vision system: This system delivers a realistic view, enabling surgeons to perform procedures with heightened accuracy.
■ Streamlined e ciency: More than 150 design innovations were incorporated for faster procedures and greater autonomy for surgical teams.
■ Advanced AI integration: This system evolves through AI, providing insights and continuously improving outcomes as it learns and adapts.
Touro University Nevada’s Michael Tang Regional Center for Clinical Simulation was granted full accreditation by the Society for Simulation in Healthcare’s Board of Review, making it the first simulation center in Nevada to receive this distinction. Touro Nevada’s simulation center is a comprehensive learning environment that supports the College of Osteopathic Medicine and the College of Health and Human Services, providing students across health care programs with hands-on experience, the opportunity to practice teamwork and the chance to encounter various stages of medical procedures or situations.
Molina Healthcare of Nevada and Birth Collaborative LV were selected to participate in the Institute for Medicaid Innovation’s National Doula Learning and Action Collaborative, a new multi state, three-year initiative to increase access to community-based doula
services for families of color who have Medicaid health coverage.
Nevada Donor Network and the Nevada Department of Education collaborated to launch the first statewide curriculum for teachers and students to raise awareness about organ, eye and tissue donation. The curriculum was developed in response to a requirement adopted in 2017 under Nevada Revised Statutes 389.021, requiring that organ, eye and tissue donation be taught in middle- and high school health education classes. The material discusses statistics, in-depth information about the donation process and local donor and recipient stories to share in their classrooms. The curriculum is designed to help students make an informed decision as they prepare to visit the Department of Motor Vehicles and consider registering as organ, eye and tissue donors. All of Nevada’s more than 260 middle and high schools will have access to the materials.




































































Whether you need specialized care for hereditary heart disease, or you’re experiencing chest pains, UMC is here to provide the complete cardiovascular care you deserve. Our world-class teams bring the power of the latest clinical breakthroughs and advanced technology to you. From innovative minimally invasive procedures to the most complex surgeries, when you choose UMC, rest assured your heart is in the right place.

Interventional Cardiology • Open Heart Surgery Program • Cardiac Rehabilitation Heart Failure Clinic • Nevada’s Only Cardiology Fellowship Program • Serving Nevada Since 1931




Roseman University is training the next generation of compassionate and highly competent healthcare providers in pharmacy, nursing, dental medicine and graduate studies to thrive in the ever-changing world of healthcare.







Developed Roseman Dental Clinics, offering reduced-cost, high-quality Dental and Orthodontic care to adults and children and specialized care for children with cancer and other systemic diseases and those with cleft lip and palate deformities

With more than two decades of building from a firm foundation to a broad universe of healthcare education, Roseman continues to develop innovative programs that train a diverse student body to be exceptional leaders in their chosen fields. We look ahead to the limitless promise of the future, in providing our communities unparalleled patient care, scientific discovery, and commitment to improving healthcare outcomes in our region and beyond.

Via Roseman Medical Group, offering high-value evidence-based family medicine to adults as well as GENESIS, offering household-centered care, and EMPOWERED, supporting pregnant and post-partum mothers with substance abuse disorders


Through thousands of dollars annually of donated care to underserved populations in Nevada and Utah

Learn more at roseman.edu
Transforming Education. Reimagining Healthcare. Embracing Discovery. Committed to Community.

roseman.edu | @rosemanuhs