Introduction
This Emergency Preparedness Procedures manual is designed to guide you during emergencies such as fires, disasters, bomb threats or medical emergencies. Keep this manual in a visible location so that it is readily accessible when needed. This manual can also be used to answer questions of inspectors and surveyors during accreditation surveys.
Anyone wishing for more information regarding emergency procedures should contact the Environmental Safety & Emergency Management Dept. during normal working hours at (602) 528-1207. Become familiar with the information contained in this manual.
Card 1 Front Introduction
FACILITY ALERT: Earthquake
FACILITY ALERT: Earthquake
If a Tremor Strikes When You Are Inside:
• Stay inside. Watch out for falling debris. Stay away from windows and mirrors.
• Either crawl under a table or desk, sit or stand against an inside wall away from windows, or stand inside a strong doorway.
After the Tremor Is Over:
• Check for injured people. Do not move seriously injured people unless they are in immediate danger.
• If you think the building has been damaged, evacuate. After-shocks can level severely damaged buildings.
• Do not use the telephone except to report an emergency. If a call is necessary, dial the emergency number x5999 to report the emergency. Be sure to give your name, location and telephone extension.
• Do not use plumbing or anything electrical until after the utility and electrical lines have been checked.
• Open doors carefully, watching for objects that may fall.
• Do not use matches or lighters. Watch for fires that may have started.
• Be prepared for additional after-shocks.
• Facilities Management will inspect all damage from the earthquake and determine priority of repair work needed.
• The Emergency Operations Plan will be activated, if necessary. The Operator will announce, “Facility Alert + Activation of Emergency Operations Plan + Event.”
FACILITY ALERT: Earthquake
Card 1 Rear
FACILITY ALERT: Fire Alarm/Fire Drill
Smoke or Fire Sighted:
R A C E:
R Remove anyone in immediate danger.
A Alarm:
• Pull nearest pull station.
• Call x5999. Operator will announce “Facility Alert + Fire Alarm/Drill + Location.”

C Close any open doors and windows.
• Do not turn off oxygen, unless told to by the Charge Nurse in conjunction with Facilities Management, The Safety Officer and the Fire Department and ONLY after all oxygen dependent patients are provided with portable oxygen or moved to areas where they can be served.
E
Extinguish the fire, if safe to do so, and evacuate the building.
• Know where your department’s nearest extinguishers are.
• Evacuate the building to your designated area.
• Report any damaged or malfunctioning safety equipment.
Complete an Occurrence Report before the end of the shift.
Card 2 Front FACILITY ALERT: Fire Alarm/Fire Drill
FACILITY ALERT: EOP (Disaster Plan)
FACILITY ALERT: Activation of the Emergency Operations Plan (Disaster Plan)
Definition:
Any emergency situation in which the Clinic expects to receive more patients that they can accommodate at once with the regular number of staff from an external event or to minimize and accommodate casualties resulting from internal events, such as fires, hostage situations, explosions, bomb threats, vital utility system failures, natural disasters or hazardous waste incidents.
Staff Response:
• Upon activation of the Emergency Operations Plan, the Operator will announce, “Facility Alert + Activation of Emergency Operations Plan + Event”, all staff on duty will report to their departments and stand by (i.e., being ready, willing and able to perform assigned duties) for further instruction.
• Staff away from their department or duty station, who cannot report physically to the department, will communicate with the department and identify their current location and status of activity.
• Patient care activities will continue until a point of completion is reached.
• Staff will notify their Department Heads of the location of their patients and Staff members.
• Department Heads will report to the Command Center to receive a briefing.
• Each Department Head, or designee, will identify available resources, such as beds, personnel, and equipment, which could be allocated to the emergency response.
• The Department Head will provide information to the Command Center staff when requested.
• When deemed appropriate, the Incident Commander will initiate the recovery phase and call for an “ All Clear.”
Evacuation:
For specific procedures, see: Policy ER.440.11 Emergency Operations Plan Activation.
Note: Specific instructions are listed under each specific policy available on the Intranet or in the Emergency Operations Plan. FACILITY ALERT: EOP (Disaster Plan)
Card 2 Rear
FACILITY ALERT: Hazardous Material Spill
Chemical Spill: Incident: Small Spills
Spill does not pose a threat to human health and the environment and can be mitigated at the time of release by employees in the immediate release area. A small spill can be cleaned up by the person discovering it without any special equipment beyond what they normally use. These spills should be cleaned up promptly; and no further action is needed. Example: A few drops of blood, or a few drops of a normally used chemical.
Actions:
1. Personal Protection: The personal protection indicated is that normally used for handling of these materials or wastes (e.g., gloves, apron, eye protection, etc.). The personal protective equipment used is that normally available for general use in that area of the facility, or used normally by that person.
2. Spill Kits: Where spill kits are available, and staff is trained to use them, the kit may be used.
3. An Occurrence Report will be completed before the end of the shift.
Incident: Large Spills
A major spill is a significant spill that is greater in quantity or risk than the staff has been trained to contain and clean up; or a spill that exceeds the limits of the personal protection available and for which staff is trained. Example(s): A gallon of Xylene; a 5 pint jug of Formalin.
Actions:
1. Immediately evacuate the area, and close all of the doors as you go. This will help contain the vapors and odor.
2. Call the emergency phone number x5999 report a major spill. The Operator will announce, “Facility Alert + Spill Team + Location.”
3. Contact Facilities Management to shut off recirculating ventilation in the affected area.
4. Contact Security to assist in securing the area.
5. During normal business hours, contact the Safety Officer and the Director of Facilities Management who will evaluate the situation. Their backup is Security.
Spill
Card 3 Front
FACILITY ALERT: Hazardous Material
6. An Occurrence Report will be completed before the end of the shift.
7. Continue to secure the area, and assure (to the extent practical without personal protection) that all people are out of the area; all staff, visitors, and patients are accounted for and that all entrances have someone to keep people out. If noxious smells extend out of the area, secure a larger area. If necessary, use the GRHC Evacuation Plan to move patients and staff to alternate sites.
8. When the designated environmental contractor arrives, provide them with full cooperation. If possible, have a Safety Data Sheet for the chemical spilled available for their use. Attempt to have floor plans of the area available to let them see the areas involved, and the access points.
9. If practical, have the person that discovered the spill available to explain the situation to the environmental contractor.
10. Staff must NOT try to clean up spills for which they have not been trained, or are not equipped. EVS and Facilities Management staff members are not trained to control or clean up major spills.
11. The area should not be reoccupied for normal use until the Safety Officer, Director
of Facilities Management or Administrator on Call determines that there are no remaining hazards from the cleanup process.
12. All significant chemical incidents should be documented by a narrative discussion of what is known to have happened; and by employee injury and/or Occurrence Report forms. All significant chemical spill incidents will be reported to the Safety/EOC Committee, and evaluated for the potential for improving the process.
Mercury Spill:
Actions:
1. Minor spills (less than 500 grams) of liquid (Metallic) mercury can be cleaned up by EVS staff who have been trained and equipped to handle such spills. They should be notified immediately, and the mercury spill contained under water or under wet towels until they arrive and begin cleanup. NOTE: If the spill occurs on a carpet, it may be necessary to extract the carpet, or remove sections of carpet to remove the hazard. This is beyond a normal spill and may require outside assistance, in which case it becomes a Major Spill.
2. An Occurrence Report will be completed before the end of the shift.
Card 3 Rear
FACILITY ALERT: Utilities Systems Failure
Failure of: What to Expect: Who to Contact: Initial Response: Secondary Response: Computer Systems System down. IT: x4357 Proceed with Departmental System Downtime Procedures. Contact the Administrator on Call (AOC).
If outage is expected to last longer than 3 hours, contact the Administrator-On-Call (AOC) to activate the Emergency Operations Plan.
Electrical Power –Emergency Generators Work
Electrical Power – Total Failure
Most lights out. RED outlets work.
Facilities Management: x1221
Ensure that life-support systems on Emergency Power (RED outlets). Use flashlights. Complete all procedures ASAP. Contact the Administrator on Call (AOC).
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
Failure of all Electrical Systems, including Chiller Plant for cool air.
Facilities Management: x1221
Use flashlights and battery lanterns; manually regulate IVs; supply patients with fans and extra fluids; monitor for heat exposure. Contact the Administrator on Call (AOC).
Fire Alarm System No fire alarms or sprinklers. Facilities Management: x1221
Medical Gases Gas alarms; no Oxygen (O2), medical air or Nitrous Oxide (NO2).
Medical Vacuum No vacuum; system failure and alarm.
Facilities Management: x1221
Overhead announcement; use runners or telephones to report fires. Contact the Administrator on Call (AOC).
Use portable gases; transfer patients, if necessary; order extra portable gas tanks. Contact the Administrator on Call (AOC).
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
If outage is expected to last longer than 4 hours, implement Interim Life Safety Measures.
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
Facilities Management: x1221
Nurse Call System No patient contact. Facilities Management: x1221
Use portable vacuum; finish cases in progress; don’t start new cases. Contact the Administrator on Call (AOC).
Use bedside telephone; move patients; obtain and use hand bells, cell phones, and two-way radios. Contact the Administrator on Call (AOC).
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
Utilities Systems Failure
Card 4 Front
FACILITY ALERT:
Failure of: What to Expect: Who to Contact: Initial Response: Secondary Response:
Natural Gas Failure or Leak Odor, no flames on Burners, etc.
Patient Care Equipment/ System
Equipment does not function properly.
Facilities Management: x1221
Facilities Management: x1221
Sewer –Stoppage Drains backing up. Facilities Management: x1221
Steam No building heat, hot water, sterilizers.
Facilities Management: x1221
Open windows to ventilate, turn off gas equipment; don’t use spark-producing equipment.
Remove from service and tag defective equipment. Obtain alternate unit or initiate alternate care process. Complete Work Order. Complete incident report.
Do not flush toilets; Do not use water. Use Red Bags in toilets.
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
Follow up on work orders/recall alerts.
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
Conserve sterile materials and all linens, provide extra blankets, prepare cold meals.
Telephones No phone service. IT: x4357 Use overhead paging, pagers, cellular phones, 2-way radios or email.
Ventilation/ HVAC No ventilation; no heating or cooling.
Water Sinks & toilets don’t work. Chillers will not supply cool air. Tap water unsafe to drink. RO system not functioning.
Facilities Management: x1221
Open windows or obtain blankets if needed; restrict use of odorous/hazardous materials.
Facilities Management: x1221
Conserve water, turn off water in sinks, and use Red Bags in toilets. Supply patients with fans and extra fluids, monitor for heat exposure. Place “Non-Potable Water. Do Not Drink” signs at all drinking fountains and wash basins. Obtain additional water supply. Follow RO Water emergency procedures.
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
If outage is expected to last longer than 3 hours, contact the AOC to activate the Emergency Operations Plan.
Card 4 Rear
SECURITY ALERT: Bomb Threat/Suspicious Package
If You Receive a Telephone Bomb Threat:
1. Do not hang up.
2. Remain calm.
3. Try to prolong the conversation and get as much information as possible.
4. Questions to ask (remain calm and talk distinctly): Use the “Bomb Threat Checklist” found in this Guide.
a. When is the bomb going to explode?
b. Where is the bomb right now?
c. What kind of bomb is it?
d. What does it look like?
e. Where are you calling from?
f. Why did you place the bomb?
g. Who is calling?
5. Description of caller’s voice:
a. Male/Female
b. Young/Middle Age/Older
c. Accent
d. Tone of voice
e. Background noise
f. Is voice familiar?
g. If so, who does it sound like?
h. Other voice characteristics
i. Time caller hung up
j. Remarks
6. Immediately notify the Operator by dialing x5999 and relay all of the information you were able to obtain. The Operator will announce, “Security Alert+ Suspicious Package + Instructions”.
7. Evacuate the area while keeping observant for anything that may be suspicious or out of place that could be helpful to the Police Dept.
8. Evacuate to your department’s designated meeting area.
If You Discover a Bomb or a Suspicious Item:
1. Leave it untouched and secure area until police arrive.
2. Dial x5999 to report a suspicious item. The Operator will announce, “Security Alert+ Suspicious Package + Instructions”.
3. Evacuate the area while keeping observant for anything that may be suspicious or out of place that could be helpful to the Police Dept.
4. Evacuate to your designated area
Complete an Occurrence Report before the end of the shift.
Card 5 Front
SECURITY ALERT: Bomb Threat/Suspicious Package SECURITY ALERT: Missing Person
SECURITY ALERT: Missing Person
During regular business hours, as soon as it becomes known that there is a missing Person, dial the emergency number x5999 and give the operator a description of the missing person.
The Operator will announce, “Security Alert + Missing Person + Description of Missing Person.”
a. Monitor assigned exits to assure that persons leaving the facility are not carrying or concealing an infant within a package, bag, coat or other container if the missing person is a child.
b. Ask the person to open any package, bag, coat or other container for your inspection.
c. Ask anyone leaving the facility to stop until the All Clear is announced. Do not attempt to restrain anyone. If they refuse to stop, dial the emergency number x5999 immediately with a description and other identifying information.
d. Inform patients that they may leave the facility once the department has been cleared.
e. Resume patient care as soon as possible once the department has been cleared.
f. Continue to man and monitor assigned exits until the All Clear is announced.
Complete an Occurrence Report before the end of the shift.
Card 5 Rear
SECURITY ALERT: Missing Person
SECURITY ALERT: Emergency Assistance From Security
Any staff member may implement the Emergency Assistance From Security procedure when concerned about their own safety and the safety of others due to abusive or assaultive behavior.

1. Dial the emergency number (x5999) to ask for Emergency Assistance from Security.
2. The Operator will announce, “Security Alert + Security Assistance Requested + Location.”
3. The Emergency Response Team as well as any available staff who are in the area that have had de-escalation training will respond to the area of the emergency and assist staff in managing and/or de-escalating the situation.
4. If the incident is criminal in nature, Security staff will take control and release all other staff. If the incident involves a patient, available clinical staff will stay on scene to assist and other staff may be released.
Complete an Occurrence Report before the end of the shift.
Card 6 Front
SECURITY ALERT: Security Assistance SECURITY ALERT: Active Assailant
SECURITY ALERT: Active Assailant
Any staff member may implement the Active Assailant procedure in the event of a real or perceived threat made with a weapon.
1. Should an individual be detected displaying a weapon in a hostile manner, employees will immediately move away from the individual and call the emergency number (x5999) and give the Operator as much information as safely possible (location, description, etc.). The Operator will announce, “Security Alert + Active Assailant + Location.”
2. Call 911 to report the incident to the appropriate authorities. Do not assume that someone else has reported the incident. Be persistent; phones may be jammed.
3. Calmly identify yourself and your exact location. Remain calm and answer the dispatcher’s questions. The dispatcher is trained to obtain the necessary and required information for an appropriate emergency response.
4. If safe to do so, stop and take time to get a good description of the individual. Note the person’s height, weight, sex, race, approximate age, clothing, method and direction of travel, and his/ her name, if known.
5. If the suspect is entering a vehicle, note the license plate number, make and model, color, and outstanding characteristics. All of this takes only a few seconds and is of the utmost help to the responding officers.
• AVOID
Pay attention to your surroundings.
Have an exit plan. Move away from the source of the threat as quickly as possible; the more distance between you and the threat, the better.
Leave belongings behind but take your cell phone if it is handy.
• DENY the assailant’s access by Finding a hidden location.
– Find protection behind furniture if possible.
– Find a room that locks if you can.
– If possible, close and lock the outside door to the room. Blockade the door.
Keep distance between you and the source. Do not peek out to see what may be happening.
Turn the lights off. Remain out of sight and quiet by hiding behind large objects. Silence your phone. Make a plan with others in the room about what you will do if the shooter enters. If possible and safe to do so, report the location of the individual.
• DEFEND because you have the right to protect yourself.
If you cannot Avoid or Deny; be prepared to defend yourself. Be aggressive and committed to your actions. Do not fight fairly. THIS IS ABOUT SURVIVAL.
Card 6 Rear
SECURITY ALERT: Missing Person
MEDICAL ALERT: Cardiac Arrest – Code Blue & Rapid Response
A. Cardiac Arrest – Code Blue – Situation that requires initiation of cardiopulmonary resuscitation due to cardiac and/or respiratory arrest.
EXCEPTION: instances with individuals who have, at hand, documented physician orders withholding resuscitation.
1. Code Blue events shall not be managed in the Clinic. Call 911.
B. Rapid Response – Unexpected Changes in Condition that may require Rapid Response, include (but are not limited to):
1. Loss of consciousness/fainting without loss of pulse or breathing.
2. Sudden complaint of severe, debilitating pain.
3. Sudden onset of significant shortness of breath or difficulty breathing. 4. Fall outside of clinical setting (such as waiting room or bathroom). 5. Seizure-like activity.
Dial x5999 and request “Rapid Response” to the location. Dial 911 as well. (NOTE: E. Dialysis, VLJ Admin, New Beginnings, RTC, Ak-Chin Clinic, Shegoi, and W. Dialysis will only dial 911.)
Staff will not utilize the option of making the announcement themselves, since this will render the Operator incapable of using the paging function.
Personnel assigned to the Rapid Response Team shall respond to the call.
Primary Care shall be in charge of the event.
Complete an Occurrence Report before the end of the shifts.
Card 7 Front
TEAM COMPOSITION
Rapid Response Team • 1 PCD Physician • 1 PCD Nurse • 1 Security Officers • 1 PCD MA • Clinicians are BLS certified •
Bag • Ambu Bag • Oxygen Tank • Automatic External
(AED) •
MEDICAL ALERT: Cardiac Arrest – Code Blue & Rapid Response
ASSIGNMENT EQUIPMENT
RRT
Defibrillator
Glucometer
Card 7 Rear
WEATHER ALERT: Severe Weather

Definitions:
A. Severe Weather Watch
Issued by the National Weather Service when conditions are right for severe thunderstorms. Be alert for changing conditions.
B. Severe Weather Warning
Issued by the National Weather Service when storms with strong winds, rain, and hail are expected in the area. A severe thunderstorm warning may last for up to one hour.
General Procedures:
A. Dial the emergency number (x5999) and give the Operator information about the incoming severe weather. The Operator will announce, “Weather Alert + Type of Weather + Instructions.”
B. Employees must be prepared to move all individuals to a safe area per the departmental plan and move unsecured equipment and hazardous chemicals to a safe area (if time allows).
C. A damage assessment team will be formed by Facilities Management to assess damage and determine priority of repair work needed.
D. Report structure damage (area involved, type, and extent of damage) to Facilities Management via phone, if possible. If phone service is interrupted, a verbal message is taken to the Command Center.
E. Depending upon the extent of damage and number of injuries, it may be necessary to implement the Emergency Operations Plan.
Card 8 Front
WEATHER ALERT: Severe Weather
Card 8 Rear
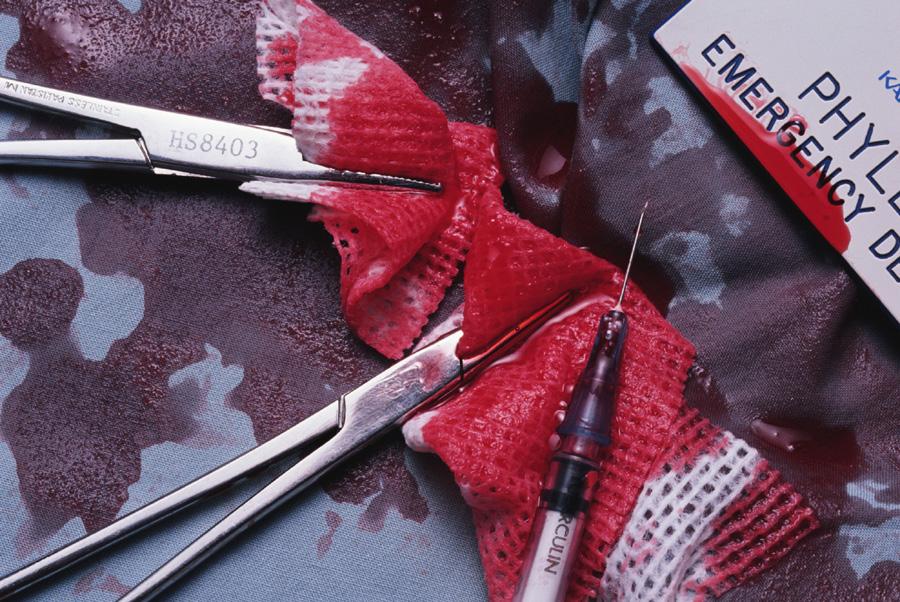
Body Fluid Exposure
In the event an employee has an exposure to body fluid, either through the skin (for example, a needle stick) or onto a mucous membrane (e.g., eyes, nose, mouth):
1. Provide immediate first aid:
• For a splash into eyes, flush eyes with lots of water.
• For a needlestick, cut, wound, or splash onto the body or mucous membrane other than the eyes, wash the exposed body part with lots of soap and water.
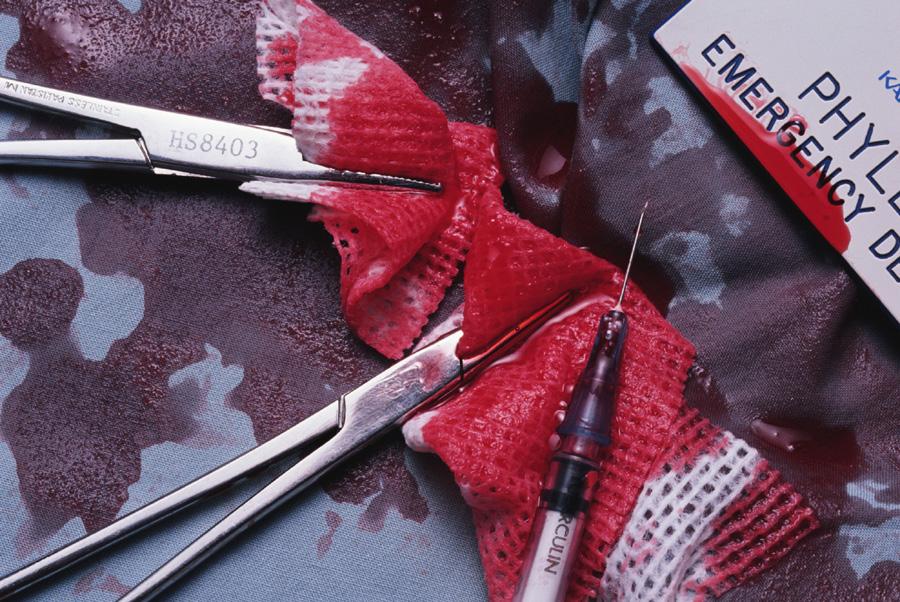
• Remove soiled clothing, wash skin, and change to clean clothing.
2. Inform supervisor.
3. Report as soon as possible (preferably within 1-2 hours) to the Employee Health Department during regular business hours. After hours, report to the Emergency Department and fill out the appropriate forms.
• Bloodborne Exposure Hotline: x1254. Are you an employee who’s had a needlestick or has blood come in contact with your mucous membranes (e.g., eyes, nose, mouth), or an open cut, scratch, wound? Health Care Practitioners caring for exposed staff or patients can also get treatment guidelines and information by selecting option 1.
4. Follow up with any recommended treatment and/or evaluation.
Card 9 Front Body Fluid
Exposure
Card 9 Rear
Bioterrorism Quick Reference Guide
Introduction:
Bioterrorism is defined by the Center for Disease Control (CDC) as “The intentional or threatened use of viruses, bacteria, fungi, and toxins from living organisms, or other chemicals, to produce death or disease in humans, animals or plants.” This guide will provide a brief summary of clinically relevant information dealing with the recognition, reporting, treatment and infection control/public health implications of several of the potential biological, chemical or radiological agents that could be utilized.
Clinical Recognition and Management of Suspected Events:
Healthcare providers should be alert to illness patterns and diagnostic clues that might signal an unusual infectious disease outbreak due to the intentional release of a biological agent and should report these concerns immediately to the County Department of Public Health.
Unlike a chemical or nuclear release, the covert release of a biological agent will not have an immediate impact because of the delay between exposure and illness onset. Consequently, the first indication of a biological attack may only be identified when ill patients present to physicians or other healthcare providers for clinical care.
Look for the following clinical and epidemiological clues that may be suggestive of a possible bioterrorist event:
1. Any unusual increase or clustering in patients present with clinical symptoms that suggest an infectious disease outbreak (e.g., greater than two patients presenting with an unexplained febrile illness associated with sepsis, pneumonia, adult respiratory distress, mediastinitis, rash, or a botulism-like syndrome with flaccid muscle paralysis, especially if occurring in otherwise healthy individuals).
2. Any case of a suspected or confirmed communicable disease due to a Category A bioterrorism agent (e.g., anthrax, plague, tularemia, smallpox or viral hemorrhagic fever).
3. Any unusual age distributions for common disease (e.g., severe chickenpox-like illness among adult patients).
4. Any unusual temporal and/or geographical clustering or illness (e.g., persons who attended the same public event or religious gathering).
5. Any sudden increase in the following non-specific syndromes, especially if illness is occurring in previously healthy individuals and if there is an obvious common site of exposure:
• Respiratory illness with fever
• Gastrointestinal illness
• Encephalitis or meningitis
• Neuromuscular illness (e.g., botulism)
• Fever with rash
• Bleeding disorders
6. Simultaneous disease outbreaks in human and animal populations.
Some infections caused by potential bioterrorist agents present with distinctive signs that can provide valuable diagnostic clues. In previously healthy persons presenting with a febrile illness, the following signs and symptoms are highly suggestive of infection with certain biological agents:
Diagnostic Sign: Disease:
Widened mediastinum with fever and sepsis
Inhalation anthrax Pneumonia with hemoptysis Pneumonic plague
Vesicular/pustular rash starting on face and hands, with all lesions at the same stage of development
Smallpox
Card 10 Front Bioterrorism Quick Reference Guide Lockdown Procedure: Bioterrorism Event
Lockdown Procedure During Bioterrorism Event
The Administrator On Call (AOC) must approve a lockdown of the Clinic if there is evidence of possible harm to staff or patients.
The procedure for the lockdown is as follows:
1. Security and members of Facilities Management will secure all doors leading into the Clinic by placing one person at each entrance.
2. All persons wishing to enter the Clinic will be questioned as to the purpose of their visit. Anyone who states that they have been exposed to a harmful agent or have a possible harmful agent in their possession will be directed to the decontamination area outside of the North exit near the secured parking area.
3. People/staff wishing to leave the facility may do so.
4. If contamination occurs in the Clinic, lockdown will be initiated so as to allow no one in or out until released by the Decontamination Team or the GRIC FD HazMat Team
Card 10 Rear
Lockdown Procedure: Bioterrorism Event
General Information on Bioterrorism
Most Likely Agents:
• Anthrax
• Plague
• Tularemia • Smallpox
• Botulism • Viral hemorrhagic fevers
• Nerve Agents • Radiological
Most Common Symptoms:
• Acute respiratory distress with fever
• Influenza-like illness
• Gastrointestinal illness
• Skin lesions
• Acute onset neuromuscular symptoms/signs
Bio-agent Infection Control Measures:
Standard Precautions:
Standard Precautions are employed in the care of ALL patients, under ALL circumstances:
• Wash hands after each patient contact.
• Wear gloves when touching blood, body fluids, secretions, excretions and contaminated items.
• Wear a mask and eye protection, or a face shield, during procedures likely to generate splashes or sprays of blood, body fluids, secretions or excretions.
• Handle used patient-care equipment and linens in a manner that prevents the transfer of microorganisms to people or equipment.
• Use care when handling sharps and use oneway valve airway device when performing rescue breathing.
Airborne Precautions: Use Standard Precautions plus:
• Place the patient in a private room that has monitored negative pressure, a minimum of six air changes/hour, and appropriate filtration of air before it is discharged from the room.
• Wear respiratory protection when entering the room.
• Limit movement and transport of the patient. Place a surgical mask on patient if he/she needs to be moved.
Conventional Diseases Requiring Airborne Precautions:
• Measles
• Varicella
• Pulmonary tuberculosis
Bio-threat Diseases Requiring Airborne Precautions:
• Smallpox
• Viral hemorrhagic fevers
Droplet Precautions: Use Standard Precautions plus:
• Place the patient in a private room or cohort them with someone with the same infection. If not feasible, maintain at least three feet between patients.
• Wear a mask when working within three feet of the patient.
• Limit movement and transport of the patient. Place a mask on the patient if he/she needs to be moved.
General Information on Bioterrorism
Card 11 Front
Conventional Diseases Requiring Droplet
Precautions:
• Invasive haemophilus influenza and meningococcal disease.
• Drug-resistant pneumococcal disease. • Diphtheria • Pertussis • Mycoplasma
Contact Precautions: Use Standard Precautions plus:

• Place the patient in a private room or cohort them with someone with the same infection if possible.
• Wear gloves when entering the room. Change gloves after contact with infective material.
• Wear a gown when entering the room if contact with patient is anticipated or if the patient has diarrhea, a colostomy or wound drainage not covered by a dressing.
• Limit the movement or transport of the patient from the room.
Biothreat Diseases Requiring Droplet
Precautions: • Pneumonic plague • Viral hemorrhagic fevers
• Ensure that patient-care items, bedside equipment, and frequently touched surfaces receive daily cleaning.
• Dedicate use of non-critical patient-care equipment (such as stethoscopes) to a single patient, or cohort of patients with the same pathogen. If not feasible, adequate disinfection between patients is necessary.
Conventional Diseases Requiring Contact
difficile
RSV
Para influenza
Enteroviruses
Enteric infections in the incontinent host
Skin infections (SSSS, HSV, impetigo, lice, scabies) • Hemorrhagic conjunctivitis
Bio-threat Diseases Requiring Contact Precautions: • Viral hemorrhagic fevers
Card 11 Rear
• GABHS • Influenza • Mumps • Rubella • Parvovirus
•
•
Precautions: • MRSA • VRE • Clostridium
•
•
•
Ten Critical Steps for Handling Possible Bioterrorist Events
1. Maintain an index of suspicion.
In an otherwise healthy population, some associations are very suggestive, especially when seen in clusters, high numbers, or unusual presentations.
Clustered Symptoms Potential Bioagent
Hemoptysis
Plague
Flaccid Paralysis Botulism
Centripetal Rash Smallpox
Wide mediastinum Anthrax
Purpura Viral Hemorrhagic Fevers (VHF)
2. Protect yourself and your patients.
Use appropriate personal protection equipment (PPE). Prophylaxis: vaccines, if available; or antibiotics, if risks are known.
3. Adequately assess the patient.
Review and assess the patient’s history. Also ask:
• Are others ill?
• Were there any unusual events?
• Was there an uncontrolled food source or other environmental factor?
• Has the patient been traveling?
• What is the patient’s immunization record?
Perform a physical examination with special attention to the respiratory system, nervous system, skin condition, and hematologic and vascular status.
4. Decontaminate as appropriate.
Do not use bleach on exposed people. A 1:10 dilution of bleach may be used on hard surfaces. Soap, water and shampoo are perfectly adequate for all biological and most chemical agents. Chemically contaminated clothes should be removed and discarded safely.
Biologically contaminated clothes can be laundered with soap, water and perhaps bleach.
5. Establish a diagnosis.
Think clinically and epidemiologically; always send specimens for culture.
Symptom (Individuals) Possible Diagnosis
Pulmonary Tularemia, plague, staph enterotoxin B (SEB)
Neuromuscular Botulism, Venezuelan equine encephalitis (VEE)
Bleeding/purpura VHF, ricin, plague (late) Rash (various) VHF, T2 mycotoxin, smallpox, plague
Flu-like symptoms Varies
Immediate Symptoms (Large Numbers) Possible Diagnosis
Pulmonary SEB, mustard, Lewisite, phosgene, cyanide
Neurological Nerve gases, cyanide
Delayed Symptoms
(Large Numbers)
Possible Diagnosis
Pulmonary Biological agents, mustard, phosgene
Neurological Botulism, VEE, other encephalitis
Card 12 Front
Ten Critical Steps for Handling Possible Bioterrorist Events
6. Render prompt treatment.
Airway, Breathing, Circulation.
7. Provide good infection control.
• Gown, gloves, mask and hand washing, and eyewear if necessary, are sufficient.
• Recommend isolation precautions for biological agents include:
Standard Precautions – For all individuals/ patients.
Contact Precautions – Viral Hemorrhagic Fevers.
Droplet Precautions – Pneumonic plague and Tularemia.
Airborne Precautions – Smallpox.
8. Alert the proper authorities.
GRIC Office of Emergency Management (OEM) (520) 610-8120
GRIC Tribal Health Department (520) 652-5100
GRIC Fire Department 911
GRIC Police Department 911 GRIC EMS 911
Pinal County Sheriff’s Department (800) 420-8689
Pinal County Office of Emergency Management (520) 866-6095
Pinal County Public Health Services District (520) 866-6239
Maricopa County Health Department (602) 372-2651
Arizona Department of Health Services (602) 542-1023
ADHS On-Call Epidemiologist (602) 839-5040
FBI Field Office – Phoenix (602) 279-5511
Bioterrorism Emergency Number – CDC Emergency Response Office
9. Assist in the epidemiological investigations. Steps in an epidemiological investigation so as to determine who may be at risk.
• Count cases
• Relate to the at-risk population
• Make comparisons
• Develop hypotheses
• Test hypotheses
• Make interfaces
• Conduct studies
• Interpret and evaluate
10. Know and spread this information.
(770) 488-7100
CDC Hospital Infections Program (404) 639-6413
Card 12 Rear
How to Handle Anthrax and Other Biological Agent Threats
Do Not Panic:
Anthrax organisms can cause infection in the skin, gastrointestinal system, or the lungs. To do so, the organism must be rubbed into abraded skin, swallowed, or inhaled as a fine, aerosolized mist. Disease can be prevented after exposure to the anthrax spores by early treatment with the appropriate antibiotics. Anthrax is not spread from one person to another person.
For anthrax to be effective as a covert agent, it must be aerosolized into very small particles. This is difficult to do, and requires a great deal of technical skill and special equipment. If these small particles are inhaled, life-threatening lung infection can occur, but prompt recognition and treatment are effective.
Follow These Procedures if You Receive a Suspicious Unopened Letter or Package Marked with a Threatening Message Such as “Anthrax”:
1. Do not shake or empty the contents of any suspicious envelope or package.
2. Place the envelope or package in a plastic bag or some other type of container to prevent leakage of contents.
3. If you do not have a container, then cover the envelope or package with anything (e.g., clothing, paper, trash can, etc.) and do not remove this cover.
4. Leave the room and close the door, or section off the area to prevent others from entering (i.e., keep others away).
5. Wash your hands with soap and water to prevent spreading any powder to your face.
6. What to do next:
• If you are at home, report the incident to the local police—dial “911.”
• If you are at work, notify your supervisor immediately.
7. List all people who were in the room or area when this suspicious letter or package was recognized. Give this list to both the local public health authorities and law enforcement officials for follow-up investigations and advice.
If Envelope with Powder Spills Out Onto Surface:
1. Do not try to clean up the powder. Cover the spilled contents immediately with anything (e.g., clothing, paper, trash can, etc.) and do not remove this cover!
2. Leave the room and close the door, or section off the area to prevent others from entering (i.e., keep others away).
3. Wash your hands with soap and water to prevent spreading any powder to your face.
4. What to do next:
• If you are at home, report the incident to the local police—dial “911.”
• If you are at work, notify your supervisor immediately.
5. Remove heavily contaminated clothing as soon as possible and place in a plastic bag, or some other container that can be sealed. This clothing bag should be given to the emergency responders for proper handling.
6. Shower with soap and water as soon as possible. Do not use bleach or other disinfectant on your skin.
7. If possible, list all people who were in the room or area, especially those who had actual contact with the powder. Give this list to both the local public health authorities so that proper instructions can be given for medical follow-up, and to law enforcement officials for further investigation.
How to Handle Anthrax and Other Biological Agent Threats
Card 13 Front
Question of Room Contamination by Aerosolization:
For example: small device triggered, warning that air-handling system is contaminated, or warning that biological agent was released in a public space.
1. Turn off local fans or ventilation units in the area.
2. Leave the area immediately.
3. Close the door, or section off the area to prevent others from entering (i.e., keep others away).
4. What to do next:
• If you are at home, dial 911 to report the incident to local police and the local FBI field office.
• If you are at work, dial 911 to report the incident to local police and the local FBI field office, and notify your supervisor immediately.
5. Shut down air handling system in the building, if possible.
6. If possible, list all people who were in the room or area. Give this list to both the local public health authorities so that proper instructions can be given for medical follow-up, and to law enforcement officials for further investigation.
How to Identify Suspicious Packages and Letters:
Some characteristics of suspicious packages and letters include the following:
• Excessive postage
• Handwritten or poorly typed addresses
• Incorrect titles
• Title, but no name
• Misspellings of common words
• Oily stains, discolorations or odor
• No return address
• Excessive weight
• Lopsided or uneven envelope
• Protruding wires or aluminum foil
• Excessive security material such as masking tape, string, etc.
• Visual distractions
• Ticking sound
• Marked with restrictive endorsements, such as “Personal” or “Confidential”
• Shows a city or state in the postmark that does not match the return address
Card 13 Rear
Acute Radiation Syndrome
Acute Radiation Syndrome (ARS) (sometimes known as radiation toxicity or radiation sickness) is an acute illness caused by irradiation of the entire body (or most of the body) by a high dose of penetrating radiation in a very short period of time (usually a matter of minutes). The major cause of this syndrome is depletion of immature parenchymal stem cells in specific tissues.
The Required Conditions for Acute Radiation Syndrome (ARS) Are:
• The radiation dose must be large: greater than 0.7 Gray (Gy) or 70 rads. (Mild symptoms may be observed as low as 0.3 Gy or 30 rads.)
• The dose usually must be external (i.e., the source of radiation was outside of the patient’s body).
Radiation materials deposited inside the body have produced some ARS effects only in extremely rare cases.
• The radiation must be penetrating (i.e., able to reach the internal organs).
High energy X-rays, gamma rays and neutrons are penetrating radiations.
• The entire body (or a significant portion of it) must have received the dose.
Most radiation injuries are local, frequently involving the hands, and these local injuries seldom cause classical signs of ARS.
• The dose must have been delivered in a short time (usually a matter of minutes).
Fractionated doses are often used in radiation therapy. These are large total doses delivered in small daily amounts over a period of time.
Fractionated doses are less effective at inducing ARS than a single dose of the same magnitude.
The Three Classic ARS Syndromes Are:
Bone Marrow Syndrome: the full syndrome will usually occur with a dose between 0.7 and 10 Gy (70–1000 rads) though mild symptoms may occur as low as 0.3 Gy or 30 rads.
• The survival rate of patients with this syndrome decreases with increasing doses. The primary cause of death is the destruction of the bone marrow, resulting in infection and hemorrhage.
Gastrointestinal (GI) Syndrome: the full syndrome will usually occur with a dose between 10 and 100 Gy (1000–10,000 rads) though some symptoms may occur as low as 6 Gy or 600 rads.
• Survival is extremely unlikely with this syndrome. Destructive and irreparable changes in the GI tract and bone marrow usually cause infection, dehydration and electrolyte imbalance. Death usually occurs within two weeks.
Cardiovascular (CV)/Central Nervous System (CNS) Syndrome: the full syndrome will usually occur with a dose greater than 50 Gy (5000 rads) though some symptoms may occur as low as 20 Gy or 2000 rads.
• Death occurs within three days. Death is likely due to collapse of the circulatory system as well as increased pressure in the confirming cranial vault as the result of increased fluid contact caused by edema, vasculitis and meningitis.
Special Considerations for Radioactive Agent Decontamination:
1. If the possible threat involves Radioactive material or radiation exposures, the Radiation Safety Officer (RSO) and Employee Health will be contacted immediately, to assist in determining the type of radiation, extent of dose and framing out our best, safest course of action and contingencies.
2. The RSO will determine the type and extent of injury/exposure (i.e., external irradiation, absorption through the skin, inhaled, introduced through wounds, etc.).
3. Conventional exposure prevention methods to protect staff and physicians.
• Time – Assessment, decontamination, treatment, etc., must be performed quickly and efficiently. The shorter the time in a radiation field, the less the radiation exposure.
• Distance – The farther from the source of radiation the lower the dose. Establish “hot” and “cold” zones to allow for the clear discernment of the hazardous area, and promote strict isolation precautions and safe distances. Use brooms and implements with long handles to move contaminated materials to avoid physical contact.
• Shielding – Although not always practical in an emergency, barriers can reduce radiation exposure.
Acute Radiation Syndrome
Card 14 Front
Patients known or suspected of being contaminated should be decontaminated with soap and water without delay. Open wounds should be irrigated first and covered with sterile dressing. Following decontamination, patients should be reevaluated and, if negative, admitted to the hospital for assessment and treatment. Evidence of continued contamination will require additional washing.
Syndrome Dose Prodromal Stage Latent Stage Manifest Illness Stage Recovery
Bone Marrow
• 0.7 – 10 Gy (70 – 1000 rads).
• Mild symptoms may occur as low as 0.3 Gy or 30 rads.
• Anorexia, nausea and vomiting.
• Occurs one hour to two days after exposure.
• Lasts for minutes to days.
• Stem cells in bone marrow are dying, though patient may appear and feel well.
• Lasts one to six weeks.
• Drop in all blood cell counts for several weeks.
• Anorexia, fever, and malaise.
• Primary cause of death is infection and hemorrhage.
• Survival decreases with increasing dose.
• Most death occur within a few months after exposure.
• In most cases, bone marrow cells will begin to repopulate the marrow.
• There should be full recovery for a large percentage of individuals from a few weeks up to two years after exposure.
• Death may occur in some individuals at 1.2 Gy (120 rads).
• The LD 50/60 is about 2.5 to 5 Gy (250 to 500 rads).
Gastrointestinal (GI)
• 10 – 100 Gy (1000 – 10,000 rads).
• Some symptoms may occur as low as 6 Gy or 600 rads.
• Anorexia, severe nausea, vomiting, cramps and diarrhea.
• Occurs within a few hours after exposure.
• Lasts about two days.
• Stem cells in bone marrow and cells lining the GI tract are dying, though patient may appear and feel well.
• Lasts less than one week.
• Malaise, anorexia, sever diarrhea, fever, dehydration, electrolyte imbalance.
• Death is due to infection.
• The LD 100 is about 10 Gy (1000 rads).
Cardiovascular (CV)
Central Nervous System (CNS)
• Greater than 50 Gy (5000 rads).
• Some symptoms may occur as low as 20 Gy or 2000 rads.
• Extreme nervousness; confusion; severe nausea, vomiting, and watery diarrhea; loss of consciousness; burning sensations of the skin.
• Occurs within minutes of exposure.
• Lasts for minutes to hours.
• Patient may return to partial functionality.
• May last for hours, but often is less.
• Return of watery diarrhea, convulsions, coma.
• Begins five to six hours after exposure.
• Death within three days of exposure.
• No recovery.
Card 14 Rear
Chemical Agents Reference Chart
Chemical Symptoms Treatment
Nerve Agents
• Tabun
• Sarin
• Soman
• VX (V Agents)
• Salivation (spit)
• Lacrimation (tears)
• Urination
• Defecation
• Gastric-
• Emptying (vomiting)
• Pinpoint pupils (everything looks dark)
• Seizures
Cyanides
• Hydrogen Cyanide
• Cyanogen Chloride
Vesicants
• Mustard
• Lewisite
• Non-specific: anxiety, hyperventilation, respiratory distress.
• Cherry-red skin, though classic, is seldom seen.
• Lactic acidosis and increased concentration of venous oxygen.
• Redness and blisters.
• Inhalation injury may result in respiratory distress.
• Leukopenia to pancytopenia.
Pulmonary Intoxicants
• Chlorine
• Phosgene
• Delayed onset of non-cardiogenic pulmonary edema.
• Atropine – Initial dose 2 mg. Additional doses until symptoms resolved (will not reverse miosis).
• Pralidoxime chloride – 1 gram IV over 20-30 minutes.
• Benzodiazepines – for seizure control or to prevent seizures in severely intoxicated patients.
Riot Control Agents
• Pepper Spray
• Mace
• Tear Gas
• Ear, nose, mouth and eye irritation.
• Cyanide Antidote Kit.
• Amyl nitrite ampul first aid until IV established. Crush and place inside mask of Bag-Valve-Mask (BVM); 15 seconds of inhalation, then 15 second break; repeat until IV established.
• Sodium nitrite – 300 mg over 2-4 minutes.
• Sodium thiosulfate – 12.5 g over 5 minutes.
• Decon within 2 minutes exposure ideal.
• Topical antibiotics.
• Systemic analgesics.
• Fluid balance (do not overhydrate; not a thermal burn).
• Bronchodilators and steroids for pulmonary symptoms, only if Lewisite is the poison, then BAL is the antidote.
• Treat hypertension with fluid; no diuretics.
• Ventilate with positive end expiratory pressure (PEEP).
• Bronchodilators.
• Patient exposed to liquid phosgene can gas-off and contaminate others.
• Patient exposed to phosgene or chlorine gas do NOT pose a risk of secondary contamination.
• No specific antidote for phosgene or chlorine.
• Irrigate.
• Treat bronchospasm with bronchodilators and steroids, as needed.
Card 15 Front Biological Agents Chart
Chemical Agents Chart
Biological Agents Detection and Treatment Chart
Agent Detection Treatment
Anthrax
I: 1-6 days of flu-like symptoms. Possible widened mediastinum. Gram stain (grampositive rod) of blood and blood culture (late).
• TBI: treatment may be delayed 24 hours until cultures from incident site available.
• Post-exposure prophylaxis (only if instructed by government officials): ciprofloxacin or doxycycline by mouth x eight weeks.
• Severe cases: ciprofloxacin, doxycycline or penicillin IV.
Cholera
I: 4 hours – 5 days. Severe gastrointestinal with “rice water” diarrhea.
• Oral rehydration with WHO solution or IV hydration.
• Tetracycline, docycycline (dosage as below or 300 mg one time) by mouth for three days. Ciprofloxacin or norfloxacin by mouth for 3 days if resistant strains.
Plague
I: 2-3 days of flu-like symptoms. Chest X-ray: patchy infiltrates or consolidation. Gram strain of lymph node aspirate, sputum, or cerebrospinal fluid (gram negative, non-spore forming rods).
Tularemia
Q Fever
Smallpox
Viral Encephalitides
Viral Hemorrhagic Fevers
I: 2-10 days of flu-like symptoms.
I: 10-14 days of flu-like symptoms.
7-17 (avg. 12) days. Later erythematous rash that progresses to pustular vesicles. Electron or light microscopy of pustular scrapings. PCR.
1-6 days flu-like symptoms. Immunoassay.
4-21 days flu-like symptoms. Easy bleeding and petechiae. Enzyme immunoassay.
Botulism
Staphylococcus
Enterotoxin B
Ricin
T-2 Mycotoxins
1-5 days. Descending bulbar, muscular and respiratory weakness.
3-12 hours flu-like symptoms.
18-24 hours flu-like symptoms, pulmonary edema, and severe respiratory distress.
2-4 hours. Sink, respiratory and GI symptoms.
• Isolation.
• Post-exposure prophylaxis: doxycycline or ciprofloxacin for seven days.
• Symptomatic: gentamicin or doxycycline IV for 10-14 days.
• Meningitis: chloramphenicol.
• Gentamicin for 10-14 days.
• Most cases self-limited.
• Tetracycline or doxycycline by mouth for 5-7 days.
• Isolation.
• Post-exposure prophylaxis: vaccinia vaccine scarification and vaccinia immune globulin IM.
• Supportive.
• Isolation.
• Supportive care.
• Some respond to ribavirin.
• Supportive.
• Post-exposure prophylaxis: toxoid.
• Symptomatic: anti-toxin.
• Supportive.
• Supportive.
• Supportive.
Card 15 Rear
Biological Agents Chart
Biological Agents Reference Chart
Description Clinical Features Transmission Modes
Anthrax
• An acute infectious disease caused by Bacillus anthracis
• Disease occurs most frequently in sheep, goats and cattle by eating contaminated soil.
Can occur in three forms:
Pulmonary – Nonspecific flu-like symptoms followed by a brief period of improvement then an abrupt onset of respiratory failure after two to four days.
Cutaneous – Local skin involvement fol lowing direct contact with spores (lesions commonly seen on head, forearms and hands).
Gastrointestinal –Abdominal pain, nausea, vomiting, bloody stool; typically following the ingestion of contaminated food.
• Skin contact, inhalation of spores (e.g., from contaminated animals – “wool sorter’s disease”).
• Ingestion of contaminated food. Transmission of Anthrax from person to person is unlikely.
• Airborne transmission does not occur, but transmission could occur through direct contact with skin lesions.
Decontamination IC – Isolation
• The risk of reaerosolizing Bacillus anthracis is extremely low.
• In situations where risk of gross exposure to actual spores exists, consider cleaning skin with soap and water to reduce risk of cutaneous transmission.
• Instruct patients to remove clothing and handle with minimal agitation.
• Decontaminate surfaces using approved disinfectant.
• Standard/Universal Precautions should be applied for care of patients, transport and management of equipment.
Private room placement is NOT necessary.
Botulism
• Clostridium botulinum, an anaerobic gram positive bacillus, produces a potent neurotoxin (botulinum toxin).
• Food-borne botulism is characterized by gastrointestinal symptoms.
• Inhalational and food-borne botulism share the following symptoms:
a. Blurred vision.
b. Symmetric descending weakness and paralysis.
c. Drooping eyelids, difficulty swallowing or speaking, weakened jaw clench, etc.
• Respiratory dysfunction.
• Usually transmitted by ingestion.
• Aerosolization of botulism may be a mechanism for bioterrorism.
Botulism is NOT transmitted from person to person.
• There is no risk of dermal exposure or reaerosolization.
Decontamination is NOT required.
• Standard/Universal Precautions should be applied for care of patients exposed to botulism and for the cleaning and disinfection of surfaces and equipment.
Patient-to-patient transmission does NOT occur.
Card 16 Front
Biological Agents Reference Chart
Description Clinical Features Transmission Modes
Plague
• An acute infectious bacterial disease caused by the gram negative bacillus Yersinia pestis
• Bioterrorism outbreak may be airborne causing pneumonic plague.
• Fever, cough and chest pain.
• Muco-purulent or watery sputum.
• Evidence of bronchopneumonia in X-ray.
• Typically transmitted to humans by an infected flea from an infected rodent.
• Bioterrorism related outbreaks could be caused by dispersion of an aerosol.
• Person-to-person transmission possible through large aerosol droplets.
Decontamination IC – Isolation
• The risk of reaerosolization of the bacteria is low.
• Removal of clothing and decontamination with soap and water may be considered in situations of gross exposure.
• Aerosolized droplet precautions (such as TB measures) should be employed in addition to Universal Precautions.
• Infected patients should be placed in designated rooms with atmospheric isolation.
Smallpox
Possible viral biological exposure.
• The Variola virus causes both major and minor forms of the disease.
• The virus could be relatively simple to disseminate as a biological agent.
• While smallpox was declared eradicated in 1980s, concerns remain over possible stockpiling.
Tularemia
• The bacteria Fracisella tularensis typically causes disease in animals. Humans may be infected by handling fluids from diseased animals or through the bite of infected deer flies or ticks.
• Latent onset of flulike symptoms.
• Initial macules progress to pustular vesicles that scab over within 10 days.
• The disease is highly contagious (contact with vesicles and fluid). Affected patients are communicable until scabs are healed over.
• Removal of clothing and self-decontamination with water may be considered in situations of gross exposures.
• Patients must be quarantined and kept in isolation.
• The disease is characterized by inflammation and necrosis in the lungs, throat, eyes and skin (progressing seven to fourteen days).
• While initial diagnosis is generally difficult to confirm, patients may present with fever, chills, headache, nonproductive cough, muscle pain and pneumonia. Cutaneous ulcers can eventually progress to secondary pleuro-pulmonary infections.
Inhalation of tularemia is the most deadly route of exposure.
Person-to-person transmission does not occur.
• The risk of reaerosolization of the bacteria is low.
• Removal of clothing and decontamination with soap and water may be considered in situations of gross exposures.
• Routine universal precautions should be followed.
Card 16 Rear
LEFT SIDE PANEL Bomb Threat Checklist The following is a checklist to be utilized by a person receiving a Bomb Threat. Checklist: (Complete all possible items immediately following the call.) 1. Caller’s Name and Address (if known): 2. Sex: Male Female 3. Age: Adult Child 4. Bomb Facts: a. When will it go off? b. In what building is it placed? c. Exact location? 5. Call Was: Local Long-Distance Unknown 6. Voice Characteristics: Tone Speech Language Loud Fast Excellent Soft Slow Good High Pitch Distorted Fair Low Pitch Cursing Poor Stutter Slurred Raspy Lisp Nasal Disguised Pleasant Accent Manner Local Poor Grammar Emotional Not Local Well-Spoken Laughing Foreign Taped Irrational Ethnicity: Message Read Deliberate 7. Background Noise: Office Machines Voices Quiet Factory Machines Music Party Cellular Phone Animals Static PA System Radios Bedlam Street Traffic Airplanes Trains
Emergency Information
REPORT AN EMERGENCY ........................ x5999
Biomedical Engineering (480) 216-2598 Dietary x1213 Emergency Department x1215 Facilities Management x1221/(480) 216-2598 (480) 216-2319
IT.......... x4357/(602) 528-4357 Security .HHK: x1189 ................................. KHC: x6510/(602) 568-9758 RTTHHC: x2700/(520) 610-0618 TCH: (602) 904-3258
HHK Hospital Command Center (VLJ Conference Room A&B)
Incident Commander .........................(602) 528-7200 Operations (602) 528-7201 Planning (602) 528-7202 Logistics (602) 528-7203 Finance (602) 528-7204
KHC Command Center
Administration Conference Room
RTHHC Command Center Administration Conference Room
Other Important Phone Numbers
Arizona Department of Health Services (602) 542-1023 ADHS On-Call Epidemiologist (602) 839-5040
CDC Emergency Response Office Bio-terrorism Emergency Number (770) 488-7100
CDC Hospital Infections Program (404) 639-6413
FBI Field Office – Phoenix (602) 279-5511
GRIC EMS ............................................................ 911
GRIC Fire Department 911
GRIC Tribal Health Department. (520) 652-5100
GRIC Office of Emergency Management (OEM) (520) 610-8120
GRIC Police Dept. 911
Maricopa County Health Department (602) 372-2651
Pinal County Office of Emergency Management (520) 866-6095
Pinal County Public Health Services District (520) 866-6239
Pinal County Sheriff’s Department (800) 420-8689
RIGHT SIDE PANEL