9 minute read
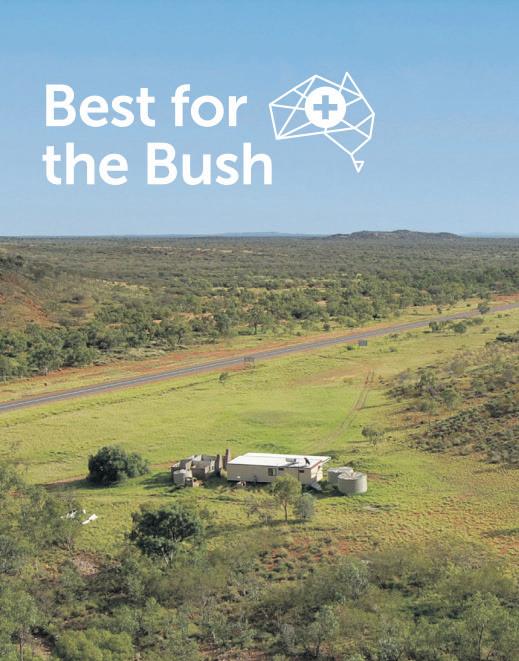
Primary care access vital for better health outcomes in remote Australia
The second annual Royal Flying Doctor Service ‘Best for the Bush, Rural and remote Health Base Line’ report was released today.
Presenting the latest data on the health of rural and remote Australians and evidence on service gaps, the report identifes the issues that most urgently need attention from service providers, funders, partners and policy makers.
Poorer health outcomes
This report again demonstrates signifcantly poorer health outcomes and more limited access to primary health services in rural and remote Australia. This results in people from these areas getting sicker and requiring more urgent attention.
As compared with those in major cities, the report details that rural and remote residents are;
• 2.9x more likely to be hospitalized
• 2.8x more likely to be hospitalized for reasons that are potentially preventable
• 2.7x more likely to die from potentially avoidable causes
High post-COVID demands
An analysis of RFDS emergency aeromedical retrievals shows a 9% increase in the last (fnancial) year, transporting people from rural and remote areas to larger, metropolitan centres for urgent hospital care. The most common reason for retrievals remains heart, stroke and vascular disease.
Leading causes of death and illness are preventable
The leading causes for death in Australia, by remoteness are heart disease (1.9x higher than in major cities), and Diabetes (2nd leading cause of death in remote areas, while only seventh in major cities). People living in remote areas are 1.4X more likely to die from lung cancer and in very remote areas, 1.6X more likely.
Heart disease and diabetes can be prevented through effective primary healthcare. Lung cancer and other cancers can be detected (and then treated) through screening services. Unless more comprehensive primary healthcare services are expanded into rural and remote areas, people in these communities will continue to experience higher levels of illness, avoidable hospitalisation, and earlier death.
Compared to those in major cities
• Females in very remote areas are likely to die 16 years earlier;
• Males in very remote areas are likely to die 13 years earlier; and
• Males and females have a mortality rate 1.6 times as high;
Indigenous health
Almost 60% of Aboriginal and Torres Strait Islander Australians live in rural or remote Areas of Australia and there is not only a gap in life expectancy between Indigenous Australians and non-Indigenous Australians of up to 12.5 years that increases with increasing remoteness, but there is a further gap amongst Indigenous people depending on where they live:
• Life expectancy for Indigenous males living in remote and very remote areas was 5.2 years lower than that of Indigenous males living in major cities (67.3 years compared with 72.5 years).
• The equivalent comparison for Indigenous females was 4.2 years lower (71.3 years compared with 76.5 years).
• 26.9% of retrieval patients were Indigenous, refecting the high proportion of Indigenous Australians living in rural and remote areas.
The Royal Flying Doctor Service
In 2022-23, the Royal Flying Doctor Service conducted 36,937 aeromedical retrievals, equivalent to 101 aeromedical retrievals per day, or four per hour. There were 137,995 RFDS face-to-face primary health consultations conducted, 28,889 primary health clinics held, 19,946 mental health consultations and 10,881 dental health consultations conducted.
“Our postcode should not be what determines access to health services”, says Frank Quinlan, Federation Executive Director of the Royal Flying Doctor Service. “All Australians should expect reasonable access to primary healthcare services no matter where they live.
For Australians living in rural, remote and regional Australia, access simple services such as a nurse-led clinic, a GP, a dentist or a specialist is so much harder.”
The National Rural Health Alliance recently released a report detailing the comparative Government health spend between major city residents and rural and remote Australia. This shows a gap of $6.55 billion, which is a health spend shortfall of $848 per person in rural and remote Australia. Given the challenges, those that live in rural and remote Australia should be seeing a greater investment in health service expenditure and not struggling to have a parity with those in our major cities.
“As we look to reform Medicare across the country, we need help people living outside the reach of mainstream services, who rely on services outside the Medicare system.
“This report recognises “rural and remote communities need rural and remote solutions” that are designed with local communities to respond to need.
“The RFDS Best for the Bush report can bring government, service partners and communities together to solve these problems and ensure better health outcomes for our rural and remote communities.”
“Working alongside government, service partners and communities, this Best for the Bush report is continuation of the RFDS’ 100year commitment to delivering evidencebased healthcare in regional, rural and remote Australia”, said RFDS Federation Executive Director Frank Quinlan. “This will only be achieved through accessible primary healthcare”.





By Helen Trustum

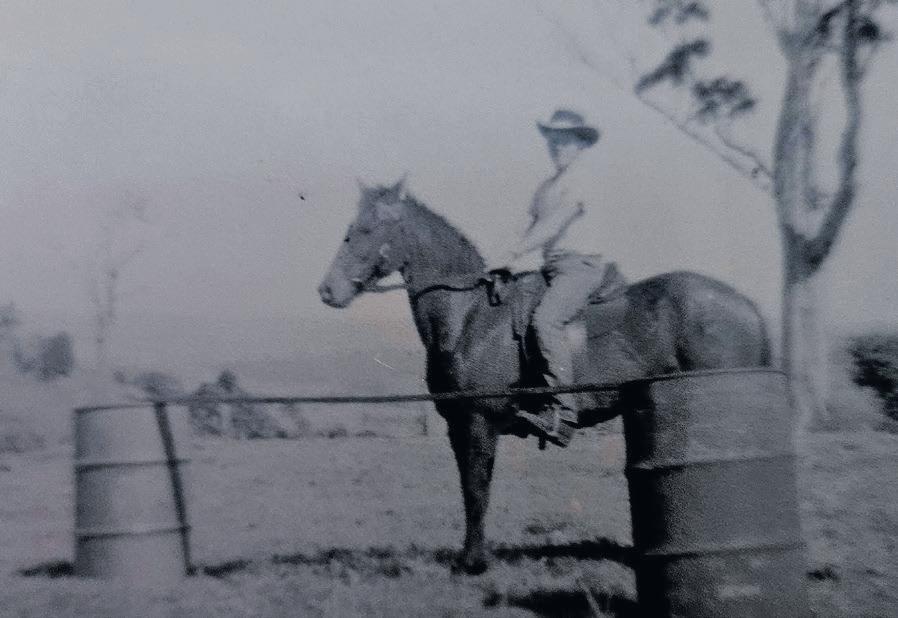
Spencer Maxwell Maher, known as Max, was born 18th January 1943, to parents Spencer known as “Penny” and Enid Maher of Goolmangar. Their family – Valerie, Nola, Max, Glen and Darryl. As Max was the eldest boy, he was given the Spencer name just like his father and Grandfather, Spencer Wesley Maher. A family trait that is handed down over the years and still carried on. Each boy in the Maher Family Tree that is born frst carries the “Spencer” name. Max grew up on the family farms at Koonorigan and Goolmangar. He always had a love for horses where he rode to school at Coffee Camp then later competing at Country Shows. Max remembers the February 1954 cyclone when raging waters from the River tore the Coffee Camp School and the local Community Hall at Coffee Camp from their stumps then fowed down the river out of site. Mr Lake, teacher in charge at Coffee Camp School and his wife Mrs Lake recalled the day when they were watching from the schoolhouse and saw it all unfold before their eyes. A document written by Mrs Lake stated: “The school went frst tipping over in the water then hitting a tree and breaking up. The hall was shuddering and groaning, it did not want to go. Suddenly the walls opened up and out came the stools and wooden tables. Cups and plates bobbed up and down in the water and then the piano came out”. School lessons were held on the side verandah of the schoolhouse, the teachers dwelling. The piano was found, it was high up a tree further down the river on Reg Parmenter’s farm. The Honour Roll from the hall along with the Union Jack were rescued. A new hall and school were built.

Max remembers one day after school when he and Nola were saddling up their horses to ride home and Nola threw the saddle on where the stirrup hit their teacher

Mr Blake on the head. He certainly had a bad knock. The schoolhouse was next door to Max’s Grandparents Percy and Casandra Swift. Shows were a feature of the Maher home, where it was not long before Max and Valerie were competing at the Nimbin Show. They would share the pony “Wally” between them. Their father would take them to the show in his 1948 Single Wheel Bedford. The vehicle was green with black mud guards purchased from W Robinson and Son in Lismore. Max and Valerie would compete for School Boy and School Girl of the Show. Many ribbons were won. Later Max’s father purchased a hunting mare for Max. Her name was “Silka”. Max was 12 years of age at the time. Jumps were set up on the farm where Max would practice. The pair competed at many shows around the district.
Eventually this horse was sold to Earl Creighton for his son Guy to ride. Guy was 10 years of age at the time. They competed at Pony Club events and shows. Guy went on to be Australia’s Champion competing at Commonwealth Games. Penny, Max’s father, was no stranger to the showground as he raced trotters for years. A few of the men that Max can remember are Charlie Langley, Barry King, Ned Coleman, Ray
Essery Snr., Barry Troy, Cec Knight and Butcher Dunn. These men would always meet at Dave Wotherspoons Saddlery in North Lismore (near the Winsome Hotel) during the 1950’s. The family loved attending functions in the Goolmangar Hall. Fancy dress or Christmas Tree concerts were always held.
Max always loved country music and from an early age he would be glued to the radio every Saturday morning at 10am listening to Radio Ranch on 2LM Lismore.
Kevin Knapp was the announcer on Radio Ranch. Kevin went on to Tamworth where he started the Tamworth Country Music Festival.

His cousin and good friend Ken Parmenter at that stage purchased a guitar, so Max was always up at the Parmenters farm learning to play the guitar. He would ride his push bike up to Kens and stay overnight. One particular weekend, Ken’s mother, Phyllis, who was Max’s Aunty, beckoned Max to have a look on his bed. There was a guitar waiting for him. What a

By Helen Trustum
great thrill. He was eight years old at the time. In later years his mother and father purchased him a guitar and one he still has (see photo). There was no stopping him now going from hall to hall singing and playing. Max would also sing and play at the concerts at Brunswick Heads, Ballina and Evans Head each Christmas. These concerts would raise money for the Life Saving Clubs in the district.
always held to this day. Ray went on to be one of the best known and loved poets in Australia. His humour and history of the area is second to none.
Max only attended one year at High School then
At frst a horse drawn plough was used on the farm then later a tractor was purchased to plough the paddocks for a paddock of corn. Max was so small on the tractor his head was hard to see above the

When it came time for High School in 1956 Max attended Lismore High along with good friend Ray Essery who lived at Booerie Creek. A friendship he has returned to the family farm. The 125 Jersey cows were milked and the cream was picked up and taken to Norco in Lismore, by cream carrier Dick Hayes. mudguard on the back of the tractor.

In 1960 Max decided to give the farming life away and began working at Smith Ingots buying scrap metal. The frm gave Max a new Bedford as the job took him as far as Rockhampton in the north to Coffs Harbour in the south. After two years employment at Smiths Ingots, he began working at Bytheway’s BMC dealers in Lismore, selling cars.
Continued next issue.

National Rural Health Alliance
The Best for the Bush: Rural and Remote Health Baseline 2023 released by the Royal Flying Doctor Service (RFDS) today, shows the alarming health disparities between the 30 per cent of the Australian population living in rural, regional and remote areas and those living in cities, which aligns with the National Rural Health Alliance’s (the Alliance) call for geographic health equity.
“The Best for the Bush report demonstrates the massive health underspend in rural areas that contributes to a heavy burden of disease and shorter life expectancy. Most of these diseases are preventable with better access to primary health care,” said the Alliance Chief Executive Susi Tegen.
The report refers to the Alliance’s Evidence base for additional investment in rural health in Australia (Nous report) which shows that rural Australians are missing out on $6.55 billion ($850 per person) each year in health care.
“The government needs to step up in its funding for rural health in a sustainable and fexible manner, without having ad hoc projects on the ground that only become band-aids.
“We stand with the RFDS in its recommendations for expanded health funding that would help remove barriers to healthcare access. It’s important to agree on a defnition for ‘reasonable access’ to health care. The Alliance and others are working to develop minimum standards for healthcare access and we’re keen on taking this project forward with the government.
“We propose the Primary care Rural Integrated Multidisciplinary Health Services (PRIM-HS) model, which addresses the complexities in rural and remote community health service delivery, as each rural community has different health needs. The PRIM-HS model should be one of the targeted plans for rural and remote healthcare, as the Best for the Bush report recommends, ensuring local planning and leadership in healthcare delivery.”
The Alliance also calls for a National Rural Health Strategy that aligns with the RFDS recommendation for a National Compact on Rural and Remote Health. This would be a transparent agreement to bring rural healthcare delivery under one umbrella and oversee the implementation and funding of a sustainable plan to improve health outcomes for rural, regional and remote Australia. We see great beneft in the Australian and state/ territory governments being collaborative and equitable in how they are investing in rural and remote health.
“The Best for the Bush report is evidence that we need to set benchmarks and measure these annually so that we are accountable to rural communities for funding and to ensure that our policymakers are reminded of the dire state rural communities are in concerning healthcare accessibility. We are yet to see rural Australians enjoying the same health benefts as their city counterparts. The Best for the Bush report provides further evidence for the government to implement, not only the recommendations of the RFDS but also the many recommendations made through their own reform and reviews of the healthcare workforce, health access and fexible funding for rural and remote communities,” Ms Tegen concluded.







The National Rural Health Alliance (the Alliance) comprises 51 national organisations committed to improving the health and wellbeing of the 7 million people in rural and remote Australia. Our diverse membership includes representation from the Aboriginal and Torres Strait Islander health sector, health professional organisations, health service providers, health educators and students.















