Uropatholog y
FRCPATH COURSE PART1 – JANUARY 2025


FRCPATH COURSE PART1 – JANUARY 2025

RCC – staging, grading
Familial RCC syndromes
Malakoplakia
Prostate carcinoma – staging and Gleason grading
Testicular tumours – classification of germ cell tumours, staging
Bladder cancer - staging
Penile tumours

Rules for classification with the procedures for assessing T, N and M categories; additional methods may be used when they enhance the accuracy of appraisal before treatment
Anatomical sites and subsites where appropriate
Definition of the regional lymph nodes
Distant metastasis
TNM Clinical classification
pTNM Pathological classification
G Histopathological grading where applicable
Stage grouping
Summary

Tx – Primary tumour cannot be assessed
T0 – No evidence of primary tumour
T1 – Tumour 7.0 cm or less, limited to kidney
T1a: Tumour 4cm or less
T1b: Tumour 4-7cm
T2 – Tumour more than 7.0 cm, limited to kidney
T2a – Tumour more than 7cm but not more than 10cm
T2b – Tumour more than 10cm limited to the kidney
T3 – Tumour directly invades into perinephric tissues (not beyond Gerota’s fascia) or extends into major veins
T3a: Tumour directly invades perinephric tissues (perirenal fat, renal sinus fat)
T3b: Tumour grossly extends into vena cava below diaphragm
T3c: Tumour infiltrates vena cava above diaphragm
T4 – Tumour directly invades beyond Gerota’s fascia or into ipsilateral adrenal gland

Nx – Regional lymph nodes cannot be assessed
N0 – No regional lymph node metastasis
N1 – Metastasis in regional lymph node(s)
Regional lymph node groups – Hilar, abdominal para-aortic, pre-aortic, precaval, retro-caval and retro-aortic nodes.

Select the appropriate pathological tumour stage from the options for each of the renal tumours described. Each option may be used once, more than once or not at all.
A. pT0
B. pT1a
C. pT1b
D. pT2a
E. pT2b
F. pT3a
G. pT3b
H. pT3c
I. pTx
J. pT4
1. Tumour 3 cm confined to the kidney.
2. Tumour 5cm, invasion into perinephric fat.
3. Tumour 4 cm with direct extension into the renal sinus fat. The major tributaries of the renal vein show macroscopic tumour invasion.
4. Tumour 7cm with invasion of the adrenal gland.
5. Tumour 6 cm with invasion beyond Gerota’s fascia.

Tumour 3 cm confined to the kidney – pT1a
Tumour 5cm, invasion into perinephric fat – pT3a
Tumour 4 cm with direct extension into the renal sinus
fat. The major tributaries of the renal vein show
macroscopic tumour invasion – pT3a
Tumour 7cm with invasion of the adrenal gland – pT4
Tumour 6 cm with invasion beyond Gerota’s fascia – pT4
Stage I: T1 N0 M0
Stage II: T2 N0 M0
Stage III
◦ T3 N0 M0
◦ T1, T2, T3 N1 M0
Stage IV
◦ T4 N0, N1 M0
◦ Any T N2 M0
◦ Any T Any N M1
Stage I – 60% to 80%
Stage II – 40% to 70%
Stage III – 10% to 40%
Stage IV - < 5%


Prognostic difference between T1 and T2 tumours?
Tumour size matters only if size less than 4 cm or more than 10 cm.
Recurrence and survival for T1N0M0 and T3aN0M0 tumours are equivalent.
Grade 1 Round, Uniform None
Grade 2 Slightly irregular Visible at x400 magnification
Grade 3 Very irregular outlines Visible at x100 magnification
Grade 4 Bizarre, multilobed or spindle Prominent
(Based on highest grade that occupies a high power field.
Validated in clear cell and papillary RCC only)
G1 - Nucleoli absent or inconspicuous and basophilic at x400 magnification
G2 - Nucleoli conspicuous and eosinophilic at x400 magnification but inconspicuous at x100 magnification
G3 - Nucleoli conspicuous and eosinophilic at x100 magnification
G4 - Marked nuclear pleomorphism and/or multinucleate giant cells and/or rhabdoid and/or sarcomatoid differentiation

A renal tumour on histology shows solid sheets of clear cells with a prominent vascular network. The majority of the tumour cells have slightly irregular nuclei with nucleoli visible at X400 magnification. A focal area with spindled, highly pleomorphic cells is also noted. What is the ISUP grade of the tumour?
A. Grade 1
B. Grade 2
C. Grade 3
D. Grade 4
E. Grade 2 and Grade 3

A renal tumour on histology shows solid sheets of clear cells with a prominent vascular network. Most of the tumour cells have slightly irregular nuclei with nucleoli visible at X400 magnification. A focal area with spindled, highly pleomorphic cells is also noted. What is the ISUP grade of the tumour?
A. Grade 1
B. Grade 2
C. Grade 3
D. Grade 4
E. Grade2 and Grade 3

Most (>95%) renal tumour sporadic, but…
Von Hippel–Lindau disease
Hereditary leiomyomatosis and renal cell carcinoma
Hereditary papillary renal cell carcinoma
Birt-Hogg Dube’ syndrome
Tuberous sclerosis
Multiple tumours, FH, young pts


Type of renal carcinoma distinct in each inherited syndrome
Regular screening of carriers mandatory
Germline mutations of VHL tumour suppressor gene (3p25-26)
VHL protein associated with cell cycle regulation and angiogenesis
Renal manifestations – Clear cell renal carcinomas, renal cysts
Extra-renal manifestations – Retinal and CNS haemangioblastomas, phaeochromocytomas, pancreatic cysts, neuroendocrine tumours
Type I – With phaeochromocytoma
Type II – Without phaeochromocytoma
IIa: Renal cell carcinoma present
IIb: No renal cell carcinoma


Mutations of the met oncogene (7q31)
Multiple type I papillary renal carcinomas
Usually before 55 years of age
No known extra-renal manifestations.
Mutations in the FH (fumarate hydratase) gene (1q42-43)
Renal manifestations – Type II papillary renal cell carcinomas
Extra–renal manifestations –Cutaneous leiomyomas, uterine leiomyomas and leiomyosarcomas.

BHD gene (17p11.2), folliculin
Renal manifestations – Chromophobe carcinomas, clear cell carcinomas, oncocytoma
Extra-renal manifestations – Benign skin lesions including fibrofolliculomas, trichodiscomas and acrochordons.
TSC1 (9q34) and TSC2 (16p13) genes
Renal – angiomyolipomas, lymphangioleiomyomatosis
Extra-renal: Subungual fibromas, cutaneous angiofibromas, cardiac rhabdomyomas, SEGA (subependymal giant cell astrocytoma), adenomatous polyps
A 30 year old male presents with bilateral renal clear cell carcinoma. Investigations also reveal a posterior fossa CNS tumour with histological appearances of a haemangioblastoma.
Abnormalities of which of the following chromosomes leads to this condition? A. 7q31 B. 3p25 C. 17p11.2
9q34
1q42

A 30 year old male presents with bilateral renal clear cell carcinoma. Investigations also reveal a posterior fossa CNS tumour with histological appearances of a haemangioblastoma. Abnormalities of which of the following chromosomes leads to this condition?



A 56-year-old female undergoes cystoscopy for investigation of haematuria. Multiple nodular thickenings of the mucosa are seen near the trigone, which are biopsied. Histology reveals sheets of CD68+ cells with intracytoplasmic concentrically layered inclusions. Which of the following histochemical stains demonstrates these inclusions?
A. Alcian blue
B. Rubeanic acid
C. Orcein
D. Von Kossa
E. PTAH




A 56-year-old female undergoes cystoscopy for investigation of haematuria. Multiple nodular thickenings of the mucosa are seen near the trigone, which are biopsied. Histology reveals sheets of CD68+ cells with intracytoplasmic concentrically layered inclusions. Which of the following histochemical stains demonstrates these inclusions?



Inflammatory condition
Unknown aetiology
Infections? Gram negative coliform bacilli
Causes defective function of histiocytes; chronic inflammatory state; fibrosis and scarring
Intracellular deposition of iron and calcium –Michaelis-Guttman bodies
TX – Primary tumour cannot be assessed
T0 – No evidence of primary tumour
Ta – Non-invasive papillary carcinoma
Tis – Carcinoma in situ: ‘flat tumour’
T1 – Tumour invades subepithelial connective tissue
T2 – Tumour invades muscle
T2a – Tumour invades superficial muscle (inner half)
T2b – Tumour invades deep muscle (outer half)

T3 – Tumour invades perivesical tissue:
T3a – microscopically
T3b – macroscopically (extravesical mass)
T4 – Tumour invades any of the following: prostate stroma, seminal vesicles, uterus, vagina, pelvic wall, abdominal wall
T4a – Tumour invades prostate stroma, seminal vesicles, uterus or vagina
T4b – Tumour invades pelvic wall or abdominal wall

You can put a comment regarding
category but not pT

E. pT2b F. pT2C G. pT3a H. pT3b
I. pT4 J. pT2
1. A 73 year old male with PSA levels of 8.4. Histology shows adenocarcinoma invading into the right seminal vesicle.

2. A 62 year old male undergoes radical prostatectomy for cancer. On histology, the carcinoma extends beyond the prostate into the periprostatic fat.
3. A 68 year old male with elevated PSA levels has a normal prostate on clinical and radiological examination. Needle core biopsies from both lobes however, reveal an adenocarcinoma.
4. A 52 year old male with obstructive symptoms undergoes radical prostatectomy. On histology, an adenocarcinoma involving both lobes, but confined to the prostate is seen.
5. A 58 year old male with obstructive symptoms and a PSA of 38, undergoes a CT scan of the pelvis, which reveals a prostatic tumour extending into the levator muscles.
The classification applies only to adenocarcinomas.
Transitional cell carcinoma of the prostate is classified as a urethral tumour. There should be histological confirmation of the disease.

Tx – Primary tumour cannot be assessed
T0 - No evidence of primary tumour
T1 – Clinically inapparent tumour
T1a: Incidental tumour <5% of total tissue
T1b: Incidental tumour >5% of total tissue
T1c: Tumour identified by needle biopsy
T2 – Tumour confined to the prostate
T2a: Tumour involving not more than one half of one lobe
T2b: Tumour involving more than one half of one lobe
T2c: Tumour involving both lobes
T3 – Tumour with extra-prostatic extension
T3a: Extracapsular extension (including bladder neck)
T3b: Tumour invades seminal vesicle(s)
T4 – Tumour invades adjacent structures other than seminal vesicles (ie. external sphincter, rectum, levator muscles and/or pelvic wall)


N – Regional Lymph Nodes
NX – No regional lymph node metastasis
N0 – No regional lymph node metastasis
N1 – Regional lymph node metastasis
M – No distant metastasis*
M1 – Distant metastasis
M1a – Non-regional lymph node(s)
M1b – Bone(s)
M1c – Other site(s)
Note: *When more than one site of metastasis is present, the most advanced category is used. pM1c is the most advanced category.

A 73 year old male with PSA levels of 8.4. Histology shows adenocarcinoma invading into the right seminal vesicle
A 62 year old male undergoes radical prostatectomy for cancer. On histology, the carcinoma extends beyond the prostate into the peri-prostatic fat
A 68 year old male with elevated PSA levels has a normal prostate on clinical and radiological examination. Needle core biopsies from both lobes however, reveal an adenocarcinoma
A 52 year old male with obstructive symptoms undergoes radical prostatectomy. On histology, an adenocarcinoma involving both lobes, but confined to the prostate is seen
A 58 year old male with obstructive symptoms and a PSA of 38, undergoes a CT scan of the pelvis, which reveals a prostatic tumour extending into the levator muscles

A 73-year-old male with PSA levels of 8.4. Histology shows adenocarcinoma invading into the right seminal vesicle – pT3b
A 62-year-old male undergoes radical prostatectomy for cancer. On histology, the carcinoma extends beyond the prostate into the peri-prostatic fat – pT3a
A 68-year-old male with elevated PSA levels has a normal prostate on clinical and radiological examination. Needle core biopsies from both 52-58-year-old however, reveal an adenocarcinoma - pT1c
A 52-year-old male with obstructive symptoms undergoes radical prostatectomy. On histology, an adenocarcinoma involving both lobes, but confined to the prostate is seen – pT2
A 58-year-old male with obstructive symptoms and a PSA of 38, undergoes a CT scan of the pelvis, which reveals a prostatic tumour extending into the levator muscles – pT4


A 66-year-old man undergoes radical prostatectomy for a needle core detected adenocarcinoma. The tumour predominantly shows raggedly infiltrating single and separate glands of varying sizes. Approximately 5% of the carcinoma also shows rounded tumour masses with central necrosis. Which of the following best represents the grade of the tumour?
A. Gleason’s 3 + 3 = 6
B. Gleason’s 3 + 4 = 7
C. Gleason’s 4 + 3 = 7
D. Gleason’s 3 + 5 = 8
E. Gleason’s 4 + 5 = 9

In the 1960’s and 1970’s, Donald F Gleason and collaborators characterized various architectural patterns of prostatic cancer and grouped them into 5 grades or patterns, thus establishing the Gleason grading system
More than 4 decades since its introduction, the Gleason system remains the key prognostic factor in patients with prostatic cancer
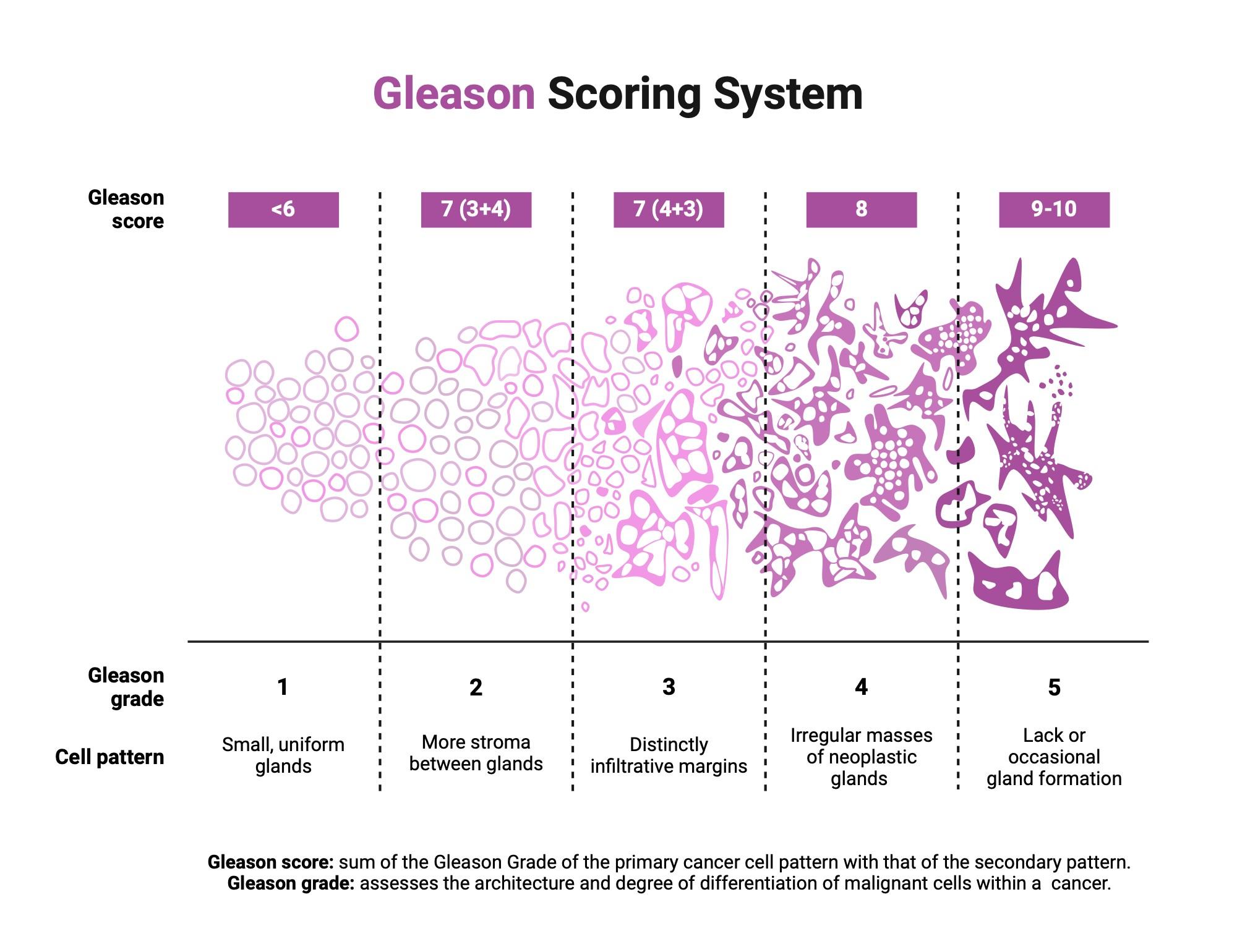
Thus, a 2005 ISUP modified Gleason system was proposed, outlining the morphological patterns 1-5, which were accompanied by a modified diagram, similar to the original Gleason system
It was reiterated that GP1 and GP2 are quite rare on biopsy and prostatectomy. The most significant modifications pertained to patterns 3 and 4
GP3 was restricted to discrete glandular units and to smoothly circumscribed but only small cribriform tumour nodules
Pattern 4 included fused glands and large cribriform glands or cribriform glands with border irregularities, as well as hypernephromatoid glands
Additionally, a category of ill-defined glands or glands containing poorly formed glandular lumina was introduced under GP4
GP5 was reserved for cancers containing essentially no glandular differentiation, composed of solid sheets, cords, and single cells. Comedocarcinoma with central necrosis was also retained in pattern 5

Pattern 3:
Discrete glandular units
Infiltrates in and amongst nonneoplastic prostate acini
Marked variation in size and shape
Pattern 4:
Fused microacinar glands
Ill-defined glands with poorly formed glandular lumina
Cribriform glands
Glomeruloid
Pattern 5:
Essentially no glandular differentiation, composed of solid sheets, cords, or single cells
Comedocarcinoma with central necrosis
surrounded by papillary, cribriform, or solid masses

Cribriform prostate cancer with perineural invasion.
Cribriform glands with round border (arrow)
Cribriform glands with irregular border (arrowhead) – both now Gleason 4











Grade obtained by adding the most prevalent (primary) and the second most prevalent (secondary) pattern +/- any tertiary pattern (if 4 or 5)*
Needle biopsy:
Grade obtained by adding the most prevalent (primary) and the highest Gleason’s grading tutorial – pathology.jhu.edu/prostate
*A pattern is secondary if it accounts for at least 5% of the tumour, and tertiary if it is < 5% of the tumour

A 66 year old man undergoes radical prostatectomy for a needle core detected adenocarcinoma. The tumour predominantly shows raggedly infiltrating single and separate glands of varying sizes. Approximately 5% of the carcinoma also shows rounded tumour masses with central necrosis. Which of the following best represents the grade of the tumour?
A. Gleason’s 3 + 3 = 6
B. Gleason’s 3 + 4 = 7
C. Gleason’s 4 + 3 = 7
D. Gleason’s 3 + 5 = 8
E. Gleason’s 4 + 5 = 9


The classification applies to germ cell tumours of the testis. There should be histological confirmation of the disease and division of cases by histological type. Histopathological grading is not applicable.
The presence of elevated serum tumour markers, including alphafetoprotein (AFP), hCG and LDH, is frequent in this disease. Staging is based on the determination of the anatomic extent of disease and assessment of serum tumour markers.
Serum tumour markers are obtained immediately after orchidectomy and if elevated, should be performed serially after orchidectomy according to the normal decay for AFP (half-life 7 days) and HCG (half-life 3 days).
The serum level of LDH (but not its half-life levels) has prognostic value in patients with metastatic disease and is included for staging.
Choose the WHO classification category from the options for each of the testicular tumours described below. Each option may be used once, more than once or not at all.
A. Embryonal carcinoma
B. Seminoma
1. Nests of tumour cells separated by fibrous septae, infiltrated by lymphocytes. A few syncytiotrophoblast like cells are seen.
C. Teratoma with somatic transformation
2. Diffuse sheets of anaplastic cells, positive for CD30
D. Spermatocytic tumour
E. Mixed germ cell tumour
F. Dermoid cyst
G. Mature teratoma
3. A child with a cystic lesion containing keratin and lined by squamous epithelium. The wall contains cutaneous adnexal structures.
4. Haemorrhagic tumour showing admixture of atypical syncitio and cytotrophoblastic cells.
H. Yolk sac tumour
I. Choriocarcinoma
5. Diffuse sheets of CD30 + anaplastic cells admixed with areas showing well differentiated glandular structures and islands of mature cartilage

WHO system based on identification of different germ cell components
The BTTP category should no more be used
All teratomas in adults are potentially malignant with the exception of dermoid cyst.
(J Clin Pathol 2008;61:20-24)

Choose the WHO classification category from the options for each of the testicular tumours described below. Each option may be used once, more than once or not at all.
A. Embryonal carcinoma
B. Seminoma
C. Teratoma with somatic transformation
D. Spermatocytic tumour E. Mixed germ cell tumour
Dermoid cyst G. Mature teratoma H. Yolk sac tumour
I. Choriocarcinoma
1. Nests of tumour cells separated by fibrous septae, infiltrated by lymphocytes. A few syncytiotrophoblast like cells are seen. B
2. Diffuse sheets of anaplastic cells, positive for CD30. A
3. A child with a cystic lesion containing keratin and lined by squamous epithelium. The wall contains cutaneous adnexal structures. No GCNIS present F
4. Haemorrhagic tumour showing admixture of atypical syncytio and cytotrophoblastic cells. I
5. Diffuse sheets of CD30 + anaplastic cells admixed with areas showing well differentiated glandular structures and islands of mature cartilage E
pTx Primary tumour cannot be assessed
pT0 No evidence of primary tumour (e.g. histological scar in testis)
pTis Germ cell neoplasia in-situ (carcinoma in-situ)
pT1 Tumour limited to testis and epididymis without vascular/lymphatic invasion; tumour may invade tunica albuginea but not tunica vaginalis
pT2 Tumour limited to testis and epididymis with vascular/lymphatic invasion, or tumour extending through tunica albuginea with involvement of tunica vaginalis
pT3 Tumour invades spermatic cord with or without vascular/lymphatic invasion

pT4 Tumour invades scrotum with or without vascular/lymphatic invasion

pNx – Regional lymph nodes cannot be assessed
pN0 – No regional lymph node metastasis
pN1 – Metastasis with a lymph node mass 2cm or less in greatest dimension and 5 or fewer positive nodes, none more than 2cm in greatest dimension
pN2 – Metastasis with a lymph node mass more than 2cm but not more than 5cm in greatest dimension; or more than 5 nodes positive, none more than 5cm; or evidence of extranodal extension of tumour
pN3 – Metastasis with a lymph node mass more than 5cm in greatest dimension
pM
pM1 – Distant metastasis microscopically confirmed
Note: *pM0 and pMX are not valid categories
SX – Serum marker studies not available
S0 – Serum marker study levels within normal limits
LDH HCG (Miu/ML) AFP (ng/ml)
S1 - <1.5xN and <5000 and <1000
S2 - 1.5-10xN or 5000-50000 or 100010000
S3 - >10xN or >50000 or >10000
Note: N indicates the upper limit of normal for the LDH assay


A biopsy of a cryptorchid testis shows atrophy with a few seminiferous tubules containing atypical germ cells with clear cytoplasm. These cells are positive for PLAP.
Which other immunostain is routinely used to confirm the diagnosis?
A biopsy of a cryptorchid testis shows atrophy with a few seminiferous tubules containing atypical germ cells with clear cytoplasm. These cells are positive for PLAP.
Which other immunostain is routinely used to confirm the diagnosis?

Can be seen in
Residual testis harbouring germ cell tumour
Contralateral testis
Undescended testis
Specific types:
Intratubular seminoma
Intratubular embryonal carcinoma


Germ cell neoplasia insitu (GCNIS)


Prepuce
Glans penis
Body of penis
The regional lymph nodes are the superficial and deep inguinal and the pelvic nodes




