EDITORS-IN-CHIEF:
Kristen Ashworth
Iciar Iturmendi Sabater
Suraiya Mangra

By Yu-Wen Jan, MScBMC Candidate (2T5)
Kyla Trkulja
EXECUTIVE DIRECTORS:
Niki Akbarian
Kevan Clifford
Mahbod Ebrahimi
Kiko Huang
Alyona Ivanova
Elizabeth Karvasarski
Nayaab Punjani
Lizabeth Teshler
SOCIAL MEDIA TEAM:
Elizabeth Karvasarski (Outgoing Director)
Lizabeth Teshler (Incoming Director)
JOURNALISTS & EDITORS:
Beatrice Acheson
Ilakkiah Chandran
Anthaea-Grace Patricia
Dennis
Sipan Haikazian
Karan Patel
Hania Siddiqui
Kowsar Teymouri
Beatrix Wang
DESIGN EDITORS:
Stefanie Jinyin Wang (Co-Director)
Nichole Zhou (Co-Director)
Emily Huang
Yu-Wen Jan
Lauren Jones
Jeah Kim
Anaiah Reyes


Just as the vibrant foliage signals a season of change, the IMS Magazine is also embracing new beginnings as we welcome new members of our 2024-25 leadership team. We are thrilled to announce the addition of our two incoming Editors-in-Chief, Kristen Ashworth and Suraiya Mangra, who will be joining the role with Kyla Trkulja (returning Co-Editor-in-Chief). We bid a fond farewell to our outgoing Co-Editor-in-Chief, Iciar Iturmendi-Sabater, as we turn the page to this new chapter. Iciar has been a member of the IMS Magazine since Fall 2021, and served as a Co-Editor-in-Chief this past 2023-24 school year. Iciar had some farewell words to share:
“Co-directing the IMS Magazine has given me a unique opportunity to gain a broad perspective on the innovative research and ideas emerging from our inspiring IMS community. It has helped me recognize that all research exists within a social context, where scientists thrive when they feel connected to their communities. Working with Kyla and leading a talented team of writers, editors, and designers has strengthened my belief that collaboration in interdisciplinary research improves science. Lastly, I am deeply grateful for the trust Dr. Mingyao Liu and the IMS team have placed in their students to spearhead innovative projects like the IMS Magazine. Serving as a Co-Editor-in-Chief has made me a more well-rounded scientist and I am proud to have contributed to the IMS community in this role.” - Iciar Iturmendi-Sabater
Kristen Ashworth and Suraiya Mangra, also wanted to share a few words of welcome:
“For the past two years, I have had the pleasure of working with the IMS Magazine team, first as a journalist and then as an Executive Editor. One of the most meaningful aspects of being part of this team has been knowing the impact we have on the Institute of Medical Science (IMS) community. Through the stories we tell, I feel fortunate to have come to know IMS–and the faculty and students who make it such a special institute–in a profound way. I am thrilled to extend my leadership this year as Co-Editor-in-Chief to continue fostering this impact and elevate the magazine’s role in our community. Here’s to a fantastic year ahead!” - Kristen Ashworth
“My motivation for joining IMS Magazine in 2023 was to explore new and interesting topics in medical science that were outside the scope of my thesis. In the past year, our magazine’s viewpoint articles have allowed me to dive into fascinating research that I would have otherwise never learned about. I have had the privilege of collaborating with a dedicated team of writers, photographers,

Kyla Trkulja
Kyla is a PhD student studying the mechanism of action of novel therapies for lymphoma under the supervision of Dr. Armand Keating, Dr. John Kuruvilla, and Dr. Rob Laister.
@kylatrkulja
Iciar Iturmendi-Sabater
Iciar is a PhD student investigating how to promote adaptive social behaviors in youth with neurodevelopmental conditions such as autism and attention-deficit/hyperactivity disorder under the supervision of Dr. Meng-Chuan Lai and Dr. Hsiang-Yuan Lin.
@iciar_itur


designers, and fellow editors that all share an inspiring passion for bringing science to a wider audience. As one of the three Editors-inChief for this year, I am thrilled to be continuing with the magazine in a more substantial role.” - Suraiya Mangra
Our Fall 2024 issue is all about cardiovascular health. From a young age, we learn that our heart is the drumbeat of our bodies: the vital organ that keeps us alive. With that considered, do we truly take care of our hearts the way that we should?
As the weather turns colder and the bustle of the school year picks up, it can be easy to fall into habits that compromise our heart health. Our Viewpoint articles touch upon the detrimental impacts of sedentary behaviour, excessive screen time, and vaping–common habits associated with colder weather and increased stress and workload–on our cardiovascular systems. We also explore a positive counterpoint to these habits: exercise and endurance training. Our Faculty Feature articles highlight some of the foremost cardiovascular research taking place within the IMS right now, from the labs of Dr. Paaladinesh Thavendiranathan, Dr. Keyvan Karkouti, and Dr. Osami Honjo. Our spotlighted IMS members for this issue include Dr. Tony George, Dr. Aadil Ali, and Alex Boshart–each of whom have touched the lives of others through leadership, innovation, and mentorship. Their stories remind us of the non-physical part of the heart: the part we use to care for others.
Whether you are pipetting all day at the lab bench, analyzing patient data, or finishing your next grant application at the office, remember to take care of your heart this school year, in every sense. We hope these articles provide valuable and inspiring insights on how to do just that. On behalf of both the outgoing and incoming Editors-in-Chief, we would like to extend our thanks to all the journalists, editors, and designers who have made this issue’s production possible.

Kristen Ashworth
Kristen is a PhD student studying the use of a human-based retinal organoid model to investigate cell therapies for genetic eye disease under the supervision of Dr. Brian Ballios at the Krembil Research Institute.
@K_Ashworth01

Suraiya Mangra
Suraiya is a 2nd year MSc student investigating the effects of neuromodulation interventions on brain morphology in patients with neurodegenerative disorders at the Krembil Research Institute under the supervision of Dr. Andres Lozano.

Director, Institute of Medical Science
Professor, Department of Surgery Senior Scientist, Toronto General Hospital Research Institute, University Health Network
With the new academic year upon us, I would like to give a warm welcome to all new IMS students and faculty–and for returning members of our community, welcome back. The fall semester is a meaningful time for new beginnings, as well as learning, growing, and reflecting on the progress we have made over the years and preparing for where we want the future to take us. This sentiment is in line with the Fall 2024 issue of the IMS Magazine, which focuses on cardiovascular health–a topic originally covered over 10 years ago in the Winter 2014 issue of the magazine. It is a privilege to witness how far our research has come since then, and it brings me great excitement to think of where the field will progress over the next 10 years.
This issue features individuals that have conducted innovative research in the field of cardiovascular health and disease. Dr. Paaladinesh Thavendiranathan is developing new models to predict and diagnose cardiovascular toxicity in patients undergoing cancer treatments. Dr. Keyvan Karkouti is investigating strategic ways to minimize blood loss in perioperative bleeding to improve the recovery of patients undergoing surgery. Lastly, Dr. Osami Honjo is researching how to improve the quality of damaged donor hearts so they can be effectively used in transplants. These impressive researchers are improving both the quality and duration of life in those with various cardiovascular conditions around the world, and it is wonderful to see them featured in this issue of the magazine.
The Fall 2024 issue of the IMS Magazine also shares the personal journeys of several influential members of the IMS community. Alex Boshart shares how his experiences navigating his PhD have turned him into the impactful student leader he is today. Dr. Aadil Ali, a 2021 IMS alum, highlights how he was able to turn his PhD research into an organ preservation device that has changed the standard of care for transplants around the world. Finally, Dr. Tony George describes how he took the leap from a small town in Nova Scotia to becoming an influential psychiatrist, scientist, and award-winning professor here at the IMS.
With the new academic year, there are also new leaders for the IMS Magazine. I would like to extend a sincere thank you to Iciar Iturmendi Sabater for her dedication to the magazine over the last several years and wish her the best of luck as in the new learning and leadership opportunities that await her. I would also like to welcome two new Co-Editors in Chief, Kristen Ashworth and Suraiya Mangra, who will be working with current Co-Editor in Chief Kyla Trkulja to tirelessly move the magazine forward. As always, I would also like to thank the journalists, editors, and design team for their contributions that allow us to showcase our community’s accomplishments in this issue. I hope you enjoy reading about how we have advanced cardiovascular research over the last 10 years.
Sincerely,
Dr. Mingyao Liu
Director, Institute of Medical Science

Beatrice Acheson is a first-year MSc student working under the supervision of Dr. Peter St George Hyslop at the Tanz Centre for Research in Neurodegenerative Disease (CRND), where she investigates the genetic and molecular mechanisms underlying microglial dysfunction in Alzheimer’s Disease. When she is not in the lab, Beatrice is likely reading a book, attending a yoga class, or playing beach volleyball.
bea.acheson

Niki Akbarian is a second-year MSc student under the supervision of Dr. James Kennedy. Her research focuses on the genomic analyses of the relationship between neuroticism and Alzheimer’s Disease. Outside of academia, Niki enjoys photography, playing the piano, and watching sitcoms.

Ilakkiah Chandran is a PhD student at IMS supervised by Dr. Danielle Andrade at the Krembil Brain Institute. Her thesis aims to understand the phenotypic and genotypic presentation of infantileonset developmental and epileptic encephalopathies in adults. In her free time, she enjoys reading, going on impromptu adventures and tuning into some true-crime!

Kevan Clifford is a PhD candidate in the IMS program, with a crossappointment at the Centre for Addiction and Mental Health. Working under the supervision of Dr. Yuliya Nikolova, his research combines bioinformatics and neuroimaging to characterize mechanisms of brain aging at the genetic level, and outcomes on brain structure and function. Outside of the lab, Kevan enjoys trail running, photography, and a good book.

Mahbod Ebrahimi is a second-year MSc student investigating the association between immune gene expression and schizophrenia subphenotypes under the supervison of Dr. James Kennedy. Outside of research, Mahbod enjoys a good book, playing chess, and listening to Jazz music. Mahbod is also a member of our social media team.
mahbooli99

Sipan Haikazian is a second-year MSc student researching the efficacy and safety of maintenance ketamine infusions for relapse prevention in patients with treatment-resistant bipolar depression, under the supervision of Dr. Joshua Rosenblat. Outside of research, Sipan enjoys playing the piano, exercising, and being around good company.
sipan_haikazian

Kiko Huang is a second-year MSc student studying glaucoma epidemiology and public health under the supervision of Dr. Yaping Jin. Her work aims to investigate various trends in ophthalmology and vision care to gain a better understanding of the health landscape and guide health policy. During her free time, she’s likely out exploring all the food that the city has to offer!
k.huangs

Alyona Ivanova is a first-year PhD student investigating the molecular signature of glioblastoma at the Hospital for Sick Children under the supervision of Dr. Sunit Das. Alyona is a figure skater, equestrian rider and a model. She enjoys traveling, cooking and reading.
_alyonaivanova_

Samuel Lasinski is a second-year MASc student supervised by Professor Axel Guenther in the Institute of Biomedical Engineering at the University of Toronto. His research focuses on the scalable formation of ultra-thin aligned collagen sheets for tissue engineering applications. Outside of the lab, he enjoys dancing tango, cooking, and swimming.

Karan Patel is a second-year MSc student under the supervision of Dr. Michael Fehlings at the Krembil Research Institute. He is investigating the synaptic integration of neural progenitor cells into the lesioned corticospinal tract to restore forelimb function following cervical spinal cord injury. Outside of research, he enjoys playing basketball, traveling to new countries, and spending time with family and friends.
karan_patel01

Nayaab Punjani is a fifth-year PhD student at the Krembil Research Institute in Dr. Michael Fehlings’ Lab. She is studying a neuroprotective peptide drug therapy to treat cervical traumatic spinal cord injury. In her free time she enjoys digital art and nature photography, as well as watching mystery, action, and sci-fi TV shows and movies.
nayaab_punjani

Hania Siddiqui is a second-year MSc student working under the supervision of Dr. Steve Lin and Dr. Rohit Mohindra at St. Michael’s Hospital. Her thesis work focuses on the identification of opioid-induced cardiac arrest. Outside of her research, Hania enjoys running, discovering new cafes, and spending time with family and friends.

Kowsar Teymouri is a third-year PhD student working under the supervision of Dr. James Kennedy at the Centre for Addiction and Mental Health (CAMH). Kowsar is investigating the role of the immune system genes in schizophrenia and how they are associated with different subgroups of schizophrenia. If not at CAMH, you can find Kowsar running along the lakeshore, creating content for her travel blog, hiking in new trails or painting.
kowsar_teymouri

Elizabeth Karvasarski (Outgoing Lead) is a PhD candidate at the Mount Sinai Catheterization Laboratory under the supervision of Dr. Susanna Mak. Her research involves investigating right ventricular and pulmonary arterial interactions in patients with pulmonary hypertension and heart failure. Outside of research, Elizabeth practices martial arts and is a 4th degree black belt.
ekarvasarski

Lizabeth Teshler (Incoming Lead) is a PhD student supervised by Dr. Brian Feldman at The Hospital for Sick Children. Her research investigates how to improve the clinical examination of musculoskeletal health for people with Hemophilia. Outside of research, Lizabeth loves biking, spending time outdoors and exploring new cities.
Anthaea-Grace Patricia Dennis Beatrix Wang
The IMS Design Team is a group of second year MSc students in the Biomedical Communications (BMC) program. Turning scientific research into compelling and effective visualisations is their shared passion, and they are thrilled to contribute to the IMS Magazine.

Stefanie Wang (Co-director) stefaniejyw

emilyhuangart
emilyhuang.ca


Zhou (Co-director) niczhouart

dinosaur.visuals
lauren.sciart yuwenjan.myportfolio.com

fabulaurora
fabulaurora. myportfolio.com

areyes_visuals
References







By Karan Patel
Cancer patients treated with chemotherapies are at an elevated risk of developing cancer therapy-related cardiovascular toxicity (CTR-CVT) and long-term cardiovascular disease.1 The imminent need to treat the cancer often takes priority over the risk of developing cardiovascular-related side effects. The predisposing factors involved in developing cardiac complications are poorly understood and the ability to identify which patients are at risk has been challenging. The current approach has been to treat the cardiovascular disease with established cardiac medications as symptoms arise; however, this approach fails to proactively mitigate risk.
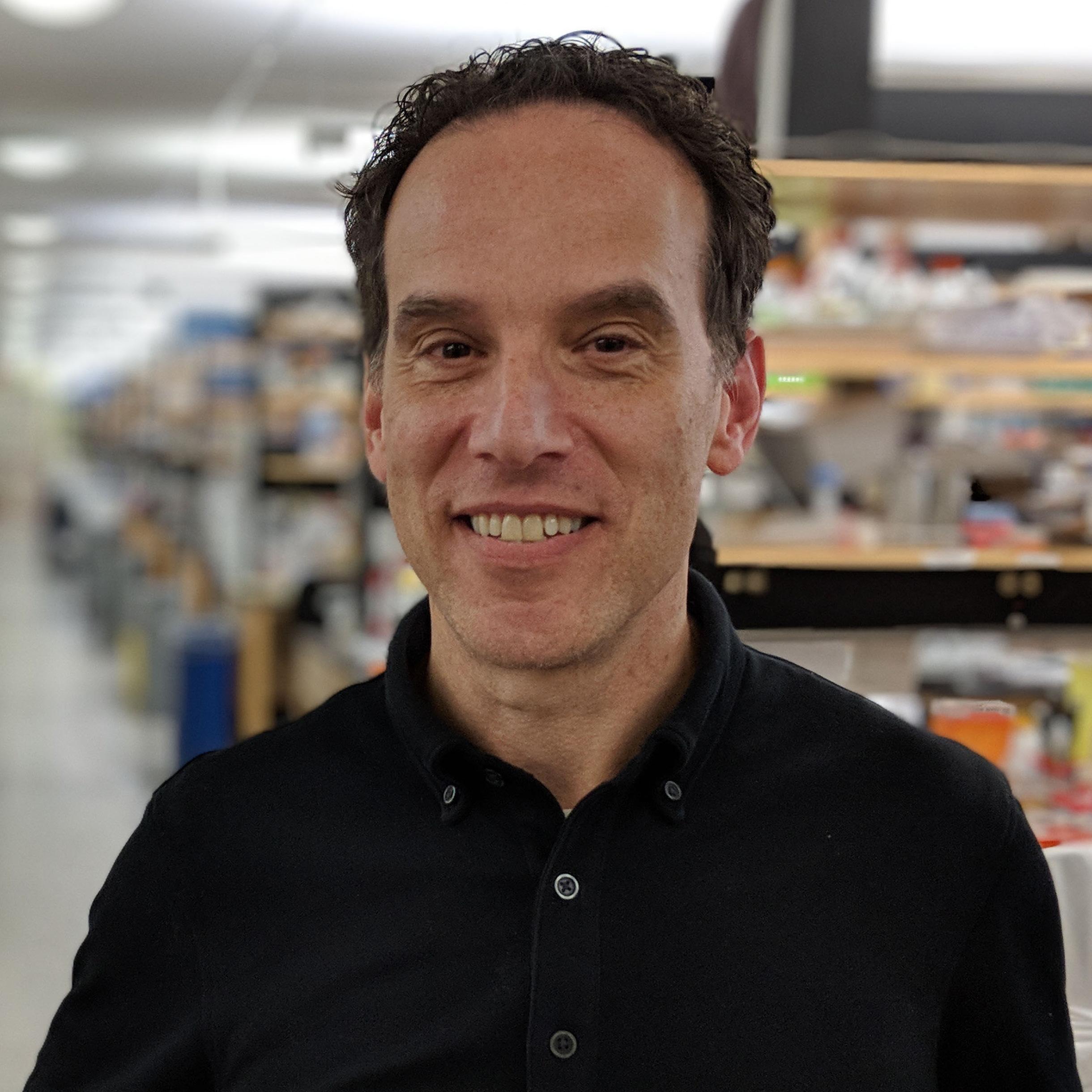
Dr. Paaladinesh Thavendiranathan is a cardiologist and senior scientist at the Toronto General Hospital (TGH), a professor of medicine at the Institute of Medical Science (IMS), the Director of the Ted Rogers Program in Cardiotoxicity Prevention, and the Canada Research Chair in Cardio-Oncology. His laboratory group investigates the use of cardiac imaging and biomarkers circulating in the blood for the detection of cardiac toxicity. The team creates risk prediction models to determine the likelihood of a cancer patient developing cardiac complications in the future.
Dr. Thavendiranathan completed his medical school education and cardiology residency at the University of
Toronto, followed by fellowships at the Ohio State University Medical Center (Columbus, Ohio) and the Cleveland Clinic (Cleveland, Ohio). During his fellowship, he learned about the field of cardio-oncology. At that time, as Dr. Thavendiranathan explains, the field was interested in “early markers of heart injury and imaging markers [to] identify patients at risk of heart failure.” Given his prior training in advanced cardiac imaging methods, “it was a perfect fit” for Dr. Thavendiranathan to pursue this niche area of medicine. Thereafter, he returned to the University Health Network (UHN) in Toronto for an attending position at a time when “nobody was actively practicing full time in [cardio-oncology].” He was intrigued by the opportunity to lead the UHN’s cardio-oncology program, which serves patients from the largest cancer centres in the nation, for both adults (Princess Margaret Cancer Centre (PMCC)) and children (the Hospital for Sick Children (SickKids)).
Today, Dr. Thavendiranathan leads a large research team including other physicians, clinical fellows, research coordinators, sonographers, and kinesiologists. Together, their goal is to “reduce the burden of cardiovascular disease in cancer survivors.” Over the years, his laboratory group has widely focused on epidemiology, retrospective and perspective trials, randomized control trials, and collaborations with other labs for basic science investigations.
Notably, their group has investigated the long-term incidence of cardiac failure in women treated for breast cancer, and the use of cardiac MRI-mediated tissue characterization for detection of early cardiac injury. Moreover, his team is working on artificial intelligencebased risk prediction algorithm that will incorporate cardiac imaging data, circulating biomarkers, and other relevant metrics to predict future risk of heart failure. Dr. Thavendiranathan expects a global footprint for this algorithm; however, he is aware that the comprehensive input parameters may not be accessible for all hospital systems, elaborating that they plan to “create a parsimonious model that can be more universally usable around the world” in developing nations.
Further to their clinical research investigations, Dr. Thavendiranathan has established collaborations with several basic science laboratories at the University of Toronto, including that of Dr. Jason Fish, Dr. Phyllis Billia, and Dr. Slava Epelman. His group understands the need for collaboration to accelerate their research interests. Their recent collaboration with Dr. Fish’s lab led to the identification of six novel biomarkers of future cardiac failure in cancer patients as they undergo therapy. The patents for this work are pending as they prepare to translate the findings to clinical use. Dr. Thavendiranathan believes that this is just the beginning of the discovery phase, noting that they have “banked [patient]


Dr. Paaladinesh Thavendiranathan
MD
Cardiologist, Toronto General Hospital
Senior Scientist, Toronto General Hospital Research Institute (TGHRI) Professor at the University of Toronto
blood in the PMCC biobank” over the “past eight to nine years.” They anticipate that there will be distinct biomarkers of heart failure for different cancers, emphasizing the need for continued investigatory research. Moreover, they anticipate these insights to drive future therapeutic development for cardio-protection.
Cancer therapies are moving towards targeted delivery methods including chimeric antigen receptor (CAR) T-cells and lipid nanoparticle delivery systems. Despite the dream of targeted therapies
that minimize cardiovascular toxicity, Dr. Thavendiranathan feels that “we are still far away.” Furthermore, in cases of some malignancies and particular primary cancers including melanoma, targeted delivery is not always possible. Therefore, there will be an ongoing need for cardiovascular risk assessment and cardiac surveillance in patients with cancers being treated systemically with certain potentially cardiotoxic therapies.
Patients being treated for cancer should be “active,” “aware,” and “[motivated],” says Dr. Thavendiranathan, adding that patients often get demotivated throughout their cancer journey, are not engaged in physical activity resulting in a tendency to lose muscle mass—a long term risk factor for cardiovascular disease. He advises patients to engage in exercise, maintain a healthy diet, engage in “whatever helps [their] mind relax”, including yoga, and to read and participate in cancer learning sessions. He emphasizes the need for patients to be aware of the risk for future cardiac events; however, he cautions that patients should focus foremost on dealing with the current problem—the cancer— before worrying about the future risk for cardiac events.
Dr. Thavendiranathan encourages students interested in the field of cardiooncology to “think where you can succeed” when entering a new field, and to find the right mentors. He feels that the field of “cardiology naturally leads itself to research,” and that “those who push
the field forward are researchers.” He enjoys splitting his roles as a clinician and scientist and cherishes his interactions with patients, many of whom have agreed to blood draws which have been banked for potential future research—an ideal opportunity for bedside-to-bench discovery.
The field of cardio-oncology is nascent and relatively unexplored. Dr. Thavendiranathan is optimistic for a future where cardiac complications in cancer survivors can be accurately predicted and minimized proactively. Despite the primary focus for cancer patients being the cancer treatment, he advises patients to understand the risk of long-term cardiac complications and engage in lifestyle decisions that can minimize their risks. In the meantime, his team continues to work relentlessly to investigate protocols to not only minimize future risk, but to prevent CTRCVT altogether.
...those who push the field forward are researchers. “ “
References

By Kowsar Teymouri
Perioperative bleeding can occur before, during, or after surgery, and depending on severity, can lead to the need for blood transfusions and increased rates of morbidity and mortality.1 Cardiac surgery, in particular, is a major consumer of blood products due to the extent of surgical trauma and influence of the cardiopulmonary bypass system on the coagulation system. Post-operative management of bleeding in cardiac surgery often involves transfusions of allogeneic blood products (blood obtained from a compatible donor), such as frozen plasma (FP), platelet concentrates, or red blood cells. Despite improvements in transfusion medicine, blood transfusions are still associated with adverse outcomes, such as mortality.2 Thus, there is a need to further mitigate postoperative bleeding in patients undergoing cardiac and other types of high-blood-loss surgeries.
Dr. Keyvan Karkouti is a professor of anesthesiology and pain medicine at the University of Toronto and the head of the Department of Anesthesia and Pain Management at University Health Network (UHN), Sinai Health, and Women’s College Hospital. He is a globally-recognized clinician-scientist in his field. Dr. Karkouti completed his medical training and anesthesia residency at the University of Toronto, followed by a fellowship in anesthesia at St. Michael’s Hospital under the supervision of Dr. Keith Rose. He later obtained a master’s degree in Clinical Epidemiology, Health Care Research, and Health Administration at the University of
Toronto. Working alongside his team–Dr. Jeannie Callum, Dr. Stuart McCluskey, and Dr. Justyna Bartoszko–his research focus has been on advancing the perioperative management of bleeding in cardiac surgery, focusing on minimizing blood loss and enhancing patient outcomes.
Dr. Karkouti’s motivation to focus his research on perioperative bleeding management stems from his understanding that bleeding carries a heavy burden of illness for surgical patients. Cardiac surgery offers a unique opportunity to study this problem because it provides for a relatively homogeneous, high-risk setting, which allows for easier identification of the effectiveness of interventions in clinical trials (as opposed to other settings such as trauma, where the causes of bleeding and patient population are very heterogeneous). Moreover, he underscores his passion in this field of research for the ability to collaborate with a robust network of hospitals and multidisciplinary teams across Canada, enhancing the quality and impact of the research conducted.
Dr. Karkouti reflected on his clinical experience from his time in the CVICU (Cardiovascular ICU), over 20 years ago, which further shaped his research focus. Despite their best efforts to address bleeding using the standard diagnostic assays and interventions available at the time, patients frequently had to return to surgery to control postoperative bleeding. In some cases, even returning to surgery did not address the problem, leaving the
patients with refractory bleeding that would invariably lead to very poor outcomes, including major organ failure and death.
Today, we have access to far more effective therapies for managing refractory bleeding and diagnosing coagulation abnormalities, reflecting significant progress in this field. Traditional lab assays such as complete blood count (CBC), partial thromboplastin time (PTT), and international normalized ratio (INR) have been superseded by advanced point-of-care (POC) assays. These modern tools enhance our ability to better identify the cause of bleeding, predict its occurrence, and tailor targeted therapies for patients. This progress has also provided numerous research opportunities to explore the roles of clotting factor concentrates. Dr. Karkouti and his team have spearheaded several studies aimed at eliminating the need for allogeneic blood product transfusions, leading to substantial changes in clinical practice.
As noted earlier, coagulopathic bleeding is a frequent complication of cardiac surgeries that consumes a large proportion of our blood supply. Moreover, it is directly linked with increased morbidity and mortality rates.3 POC hemostatic assays, with their faster turnaround times and superior ability to identify the causes of coagulopathy compared to standard tests, are particularly useful in the dynamic environment of surgery. To investigate the efficiency of the POC assays, Dr. Karkouti led a multicentre study across 12 hospitals, recruiting almost 8,000


Professor of Anesthesiology and Pain Medicine at the University of Toronto and Chief of the Department of Anesthesia and Pain Management at University Health Network (UHN), Sinai Health, and Women’s College Hospital
patients. This research demonstrated that the implementation of POC hemostatic assays significantly reduced major bleeding and the need for blood product transfusions after cardiac surgery, resulting in a substantial change in clinical practice across Canada.
Providing evidence for the adaptation of POC assays as a means of diagnosing coagulation abnormalities set the stage for Dr. Karkouti’s team to next investigate novel interventions in treating these conditions. In one major study, they compared the safety and effectiveness of
an older blood product – cryoprecipitate – with a newer, purified product –fibrinogen concentrate. Cryoprecipitate is derived from FP and has long been used to treat fibrinogen deficiency, which is a crucial coagulation factor, in bleeding patients. However, cryoprecipitate is not a purified product and contains additional factors, some of which may increase the risk of complications. Following Dr. Karkouti’s study demonstrating that fibrinogen concentrate is as effective as cryoprecipitate, use of fibrinogen concentrates has largely replaced cryoprecipitate across Canada.4 Dr. Karkouti is now leading another study with the aim of reducing the reliance on frozen plasma, another allogeneic blood product that carries significant risks to some patients, by assessing the relative safety and effectiveness of another purified product, prothrombin complex concentrate (PCC), which contains significantly higher concentrations of clotting factors compared to FP. If this study demonstrates that PCC is superior to FP, it will have a tremendous impact on the practice as it may largely phase out the use of FP for management of coagulopathic bleeding in surgery and possibly other settings. He hopes to conclude the study by November and publish it by next year.
Lastly, Dr. Karkouti highlights the high prevalence of anemia among cardiac surgery patients, noting, “about 30% of patients present with anemia at the time of surgery.” He emphasizes that lower hemoglobin levels are associated
with poorer postoperative outcomes and an increased likelihood of needing transfusions. To address this, hospitals across Ontario have implemented programs to diagnose anemia before surgery and intervene by increasing hemoglobin levels through intravenous iron or erythropoietin treatments prior to the procedure.
As advice to future clinician-scientists, Dr. Karkouti underscores the importance of teamwork and collaboration, stating, “all ships rise with a rising tide.” He also highlights the need for adaptability in research in response to emerging opportunities and challenges. Embracing these principles, Dr. Karkouti, who has become a trailblazer in bleeding management research, exemplifies how success in science depends not just on individual effort, but also on the collective strength and adaptability of the team. As for ongoing research on bleeding, he believes that research is advancing well and is confident that exceptional researchers across Canada will continue to drive progress in this field.
References
1. Ghadimi K, Levy JH, Welsby IJ. Perioperative management of the bleeding patient. Vol. 117, British Journal of Anaesthesia. 2016.
2. Dyke C, Aronson S, Dietrich W, et al. Universal definition of perioperative bleeding in adult cardiac surgery. Vol. 147, Journal of Thoracic and Cardiovascular Surgery. 2014.
3. Karkouti K, Callum J, Wijeysundera DN, et al. Point-of-Care Hemostatic Testing in Cardiac Surgery: A Stepped-Wedge Clustered Randomized Controlled Trial. Circulation. 2016;134(16).
4. Callum J, Farkouh ME, Scales DC, et al. Effect of Fibrinogen Concentrate vs Cryoprecipitate on Blood Component Transfusion after Cardiac Surgery: The FIBRES Randomized Clinical Trial. JAMAJournal of the American Medical Association. 2019;322(20).

By Niki Akbarian
Congenital Heart Disease (CHD) encompasses a wide variety of abnormalities in the structure of the heart that occur before birth in the fetus while it is developing during pregnancy.1 CHD is the most common birth defect, with an annual prevalence of 12.3 per 1,000 births in Canada.2 Some CHDs, such as atrial septal defect or ventricular septal defect, may have minimal impact on heart function and can sometimes resolve on their own without requiring treatment. On the other hand, other forms of CHDs, such as single ventricle defects or hypoplastic left heart syndrome, are severe diseases that significantly impair the structure and function of the heart, necessitating urgent medical care and intervention to ensure the survival of affected newborns.
Professor Osami Honjo, a cardiovascular surgeon at The Hospital for Sick Children (SickKids) and a Senior Associate Scientist in the Translational Medicine program at the SickKids Research Institute, aims to optimize heart transplantation and mechanical circulatory support for neonates and infants with severe, life-threatening CHDs. Dr. Honjo completed his medical education at the Shimane Medical University and completed cardiovascular surgery residency and a PhD in Cardiovascular Physiology at the Okayama University in Japan. In 2004, he joined the University of Toronto as a Congenital Heart Surgery Research Fellow, where he has since led
groundbreaking research at both the University of Toronto and the SickKids Research Institute.
With extensive experience in treating various forms of CHD, Dr. Honjo notes that single ventricle physiology presents the most severe outcomes, often resulting in irreparable heart damage and end-stage heart failure. “Patients with single ventricle physiology require three operations to sustain long-term heart function,” Dr. Honjo explains. “Despite these interventions, they may still experience circulatory failure, and the only options for ensuring their survival are mechanical circulatory support or heart transplantation.” Yet, these life-saving measures are confronted with several challenges, including a shortage of heart donors, post-transplant rejection, and the lack of feasible mechanical circulatory support devices for the neonatal and infant populations. Hence, Dr. Honjo’s research is dedicated to overcoming these limitations, aiming to optimize heart transplantation and mechanical circulatory devices for pediatrics with single ventricle physiology.
Over the past five years, Dr. Honjo and his team have concentrated on advancing ex-vivo heart perfusion for pediatric patients—a technique designed to resuscitate and rehabilitate donor hearts for transplantation. Donor hearts can be obtained through two primary methods: donation after brain death (DBD), which is more commonly used in clinical settings; or donation after circulatory death
(DCD), where the heart must be arrested before retrieval. Hearts retrieved through DCD are often more damaged due to prolonged ischemia (lack of blood supply), making rehabilitation essential before transplantation. This is where ex-vivo heart perfusion plays a critical role in providing mechanical support to reanimate the heart in a controlled environment using a small circulatory device, thus protecting the heart by minimizing ischemic time.
Given the smaller size of infant hearts, ex-vivo perfusion of DCD hearts presents unique challenges in pediatric care, particularly in determining the optimal perfusion rate—the amount of blood that needs to be circulated to the heart for effective rehabilitation. Dr. Honjo and his team have explored these challenges using large animal models, including piglets, to identify the best methods for setting the perfusion rate. Specifically, the rate can be adjusted by either controlling the flow or the pressure of blood circulation to the heart. In their studies, Dr. Honjo and his team observed that a flow-targeted perfusion rate leads to less swelling and edema of the heart muscle, which, in turn, preserves the heart’s function and enhances both systolic and diastolic ventricular performance.4




Dr. Osami Honjo
Surgical Director, Heart Transplantation and Mechanical Circulatory Support, Senior Associate Scientist, SickKids / Professor of Surgery, University of Toronto, Full Member at Institute of Medical Science
Photo Credit: Dr. Honjo
The working theory behind this observation is that, when a donor’s heart is retrieved through DCD, it suffers from ischemic injury. Once connected to the ex-vivo perfusion device, the heart experiences a secondary injury known as ischemia-reperfusion injury, which occurs when blood flow is restored to previously ischemic tissues, leading to further cellular dysfunction and death. During this reperfusion phase, the micro-vessels in the heart exhibit unpredictable constrictions and relaxations, causing fluctuations in
coronary vascular resistance. If the ex-vivo perfusion is solely based on maintaining a specific coronary artery pressure, these fluctuations can result in the heart muscle receiving too much or too little blood flow. However, flow-targeted perfusion ensures consistent coronary blood flow regardless of changes in coronary vascular resistance. Indeed, Dr. Honjo and his team were pioneers in highlighting the advantages of flow-targeted over pressure-targeted perfusion rates for the pediatric population.
Another key area of research in Dr. Honjo’s lab, in collaboration with Dr. Mansoor Husain’s lab at Toronto General Hospital, focuses on identifying pharmacological therapies that aid in the recovery of DCD hearts. In their recent publication, the team highlighted the protective effects of Exenatide, a glucagon-like peptide-1 receptor agonist, for enhancing cardiac function and reducing reperfusion injury in DCD hearts.5
Despite significant advancements, Dr. Honjo emphasizes that future studies must address certain limitations that challenge the clinical applicability of their findings. Firstly, important structural and anatomical differences remain that limit the direct translation of results from piglet models to human patients. Additionally, due to the substantial time and resources required for in-vivo transplantation after ex-vivo perfusion, most animal studies in the field of ex-vivo heart perfusion assess heart function using an ex-vivo
device rather than by transplanting the heart back into the animal, challenging the clinical relevance of the findings. Addressing these limitations could lead to a more effective evaluation of strategies and therapeutic agents aimed at minimizing reperfusion injury during the ex-vivo phase, ultimately improving outcomes for pediatric patients following the transplantation of DCD hearts.
Indeed, DCD hearts have revolutionized adult cardiac care by expanding the pool of heart donors, including those from greater distances and with borderline cardiac function, thereby reducing the high waiting list mortality among adults with heart disease. Dr. Honjo hopes that their research will bring about a similar transformation in pediatric heart transplantation. “We are hoping that our work will make some difference in the pediatric heart transplantation world,” Dr. Honjo says.
References
1. Sun R, Liu M, Lu L, et al. Congenital heart disease: Causes, diagnosis, symptoms, and treatments. Cell Biochemistry and Biophysics. 2015 Feb 1;72(3):857–60. doi:10.1007/s12013-015-0551-6
2. Miao Q, Dunn S, Wen SW, et al. Association between maternal marginalization and infants born with congenital heart disease in Ontario Canada. BMC Public Health. 2023 Apr 28;23(1). doi:10.1186/s12889-023-15660-5
3. Congenital heart defects in children [Internet]. Mayo Foundation for Medical Education and Research; 2024 [cited 2024 Aug 19]. Available from: https://www.mayoclinic.org/diseases-conditions/ congenital-heart-defects-children/symptoms-causes/syc-20350074
4. Kobayashi J, Luo S, Akazawa Y, et al. Flow-targeted pediatric ex vivo heart perfusion in donation after circulatory death: A porcine model. The Journal of Heart and Lung Transplantation. 2020 Mar;39(3):267–77. doi:10.1016/j.healun.2019.11.023
5. Kadowaki S, Siraj MA, Chen W, et al. Cardioprotective actions of a glucagon‐like peptide‐1 receptor agonist on Hearts donated after circulatory death. Journal of the American Heart Association. 2023 Feb 7;12(3). doi:10.1161/jaha.122.027163

Geneviève Groulx
Geneviève is a medical and scientific illustrator from Ottawa, ON. She specializes in creating accessible educational materials for patients and healthcare professionals, and in designing visuals for researchers in the fields of science, medicine, history, and art.






In response to the growing need for comprehensive and accessible sexual health education materials for individuals with Intellectual and Developmental Disabilities (IDDs), the website Growing UP: Understanding Puberty was created. This digital puberty education resource was primarily designed for preteens and teens and can be accessed on tablet and desktop applications. By following SIECCAN’s and the Government of Ontario’s guidelines on sexual health education for youth, accessible graphic design guidelines, web accessibility guidelines, as well as Plain Language and Easy Read principles, this resource provides its targeted users with comprehensive and concise overviews on the topics of puberty and sexual health. Growing UP: Understanding Puberty is meant to empower its target audience with accessible health knowledge as they physically and emotionally transition to adulthood.

Nicole Arizala is a Medical Illustrator dedicated to creating beautiful, educational, and accurate medical and scientific illustrations. With a background in fine arts, Kinesiology, Fitness and Health Promotion, and now in Biomedical Communications, she strives to create educational materials for patients, students, and clinicians alike - helping bridge gaps in knowledge transfer and facilitating learning.


Throughout my life, I have found a connection between my interest in the sciences and my passion for visual arts. Through the MScBMC program, my goal is to improve my skills to help bridge the gap between the scientific community and the public in a way that is inclusive and accessible. Outside of work and school, I love reading with hot chocolate and a blanket, petting allergy-prone cats and dogs, and hiking west coast mountains if it’s not too cold out.



By Ilakkiah Chandran, PhD Candidate, Institute of Medical Science, Toronto Western Hospital
oday, we are fortunate to benefit from technology that enhances the efficiency of our daily lives and improves our overall quality of life. We depend on innovative devices to better our lives, from using Netflix to skip television advertisements to using smartwatches to track our activity patterns.
In 2007, vaping using electronic cigarettes (e-cigarettes) was introduced in North America. Marketed as a safer alternative to smoking cigarettes, vaping soon became a popular substance.1 In comparison to traditional cigarettes that are known to cause multiple chronic and acute health complications, e-cigarettes were perceived to be effective in curbing the desire to smoke a cigarette while allowing consumers to experience a similar sensation. Soon after their introduction, the uptake of e-cigarettes increased and the use of traditional cigarettes decreased.1 However, with time, a growing body of research has associated e-cigarettes with harmful effects at both the systemic and cellular levels.2 The concern about e-cigarette use continues to grow, along with their popularity-especially among youth, with e-cigarette use increasing by almost 14 times between 2011 and 2018 among that demographic due to their user-friendly functionality, design, unique flavours, and ability to be used discretely.3

So, what exactly does this uptake of vaping among youth mean? “ “
Vapes are largely unregulated and are often purchasable via the internet, making them easily accessible. Recent research reveals that the toxic components often found in vapes include formaldehydewhich is associated with some cancers-, as well as acetaldehyde and acrolein-which are associated with reduced respiration and irritation to the lungs at greater concentrations.4 Similarly, other studies have suggested that acute lung injuries and ocular health deficits are often seen among those who vape.5,6 The use of vapes also makes youth more susceptible to nicotine addiction, as early exposure to nicotine can make it difficult to tolerate and cease the use of nicotine. Nicotine addiction can then serve as a gateway to using other substances, including traditional cigarettes.
Despite the preliminary research on the health effects of vaping, the long-term impacts are difficult to know given that this is a fairly new substance with variable technology associated. This uncertainty is particularly concerning regarding young people at critical development stages.
Aside from the direct health consequences of vaping on youth, it also poses challenges in the public health domain. Firstly, the increase in health consequences increases the public health burden by increasing expenditure both at the patient and systematic levels. It also creates the need for social structures to adapt to this usage. Another challenge concerns how the public health system will direct the messaging around vaping to ensure that the public is adequately educated on the topic, given the limited understanding on this substance.
Moreover, when considering this growing challenge from a health equity perspective, it is likely that, like other substances, individuals of lower socioeconomic status and those with a poor relationship with social determinants of health are more likely to be impacted by the risks of vaping-thus contributing to a rise in health disparities.




“ “
...a growing body of research has associated e-cigarettes with harmful effects at both the systemic and cellular levels
The ease of purchasing e-cigarettes through online and in-person vendors makes it difficult to curb the increasing incidence of vaping among youth. The various types of vaping products available online are often difficult to regulate, making the concentrations of ingredients unclear. Additionally, vaping products are often marketed as being available in flavours that resemble candy, with distinct colouring that makes them desirable for youth. In 2021, the Canadian government introduced a proposal to ban these ‘desirable’ flavours, instead limiting vape flavours to mint or tobacco.7 However, this proposal has yet to be approved.
It remains a challenge to enforce vaping policies and regulations, especially when features such as USB charging, sleek designs, and inconspicuous smells make it challenging to impose vaping restrictions in spaces with existing policies.
Vaping currently poses many risks and challenges to youth, including the possibility of reversing the progress made to cease the smoking of traditional cigarettes, thereby creating more serious long-term consequences. There is therefore a need to protect youth from the harms of e-cigarettes to ensure the well-being of future generations.
At a policy level, this includes enforcing more strict age restrictions and limiting marketing strategies that target youth. From a public health perspective, this can include building modules on the harms of vaping into school curriculums, while also creating broader campaigns to handle the information that is spread on vaping. Finally, by increasing health surveillance and research on vaping, we as a society can be better informed of the harms of vaping and prepared to handle the risks associated with this new, mysterious substance.
1. Lichtenberg, K. E-Cigarettes: Current Evidence and Policy. Mo Med 114, 335–338 (2017).
2. Münzel, T., Daiber, A. & Hahad, O. Are e-cigarettes dangerous or do they boost our health: no END(S) of the discussion in sight. Eur J Prev Cardiol 30, 422–424 (2023).
3. Fadus, M. C., Smith, T. T. & Squeglia, L. M. The rise of e-cigarettes, pod mod devices, and JUUL among youth: Factors influencing use, health implications, and downstream effects. Drug Alcohol Depend 201, 85–93 (2019).
4. Kaisar, M. A., Prasad, S., Liles, T. & Cucullo, L. A decade of e-cigarettes: Limited research & unresolved safety concerns. Toxicology 365, 67–75 (2016).
5. Martheswaran, T., Shmunes, M. H., Ronquillo, Y. C. & Moshirfar, M. The impact of vaping on ocular health: a literature review. Int Ophthalmol 41, 2925–2932 (2021).
6. Traboulsi, H. et al. Inhalation Toxicology of Vaping Products and Implications for Pulmonary Health. Int J Mol Sci 21, 3495 (2020).
7. Health Canada. Health Canada announces new restrictions to prevent youth vaping . Government of Canada (2021).

By Hania Siddiqui
We live in a digital age where nearly everyone has access to electronic devices, and this exposure begins at increasingly younger ages. A Canadian study found that almost all children in Canada are exposed to screens by the age of two, and only 15% of children aged three to four meet the recommended screen time guidelines of less than one hour per day.1
It’s no surprise that electronics consume much of our daily lives, impacting both children and adults. However, excessive electronic use comes with significant risks. One major concern is that increased screen time displaces physical activity, leading to more sedentary behaviour. Sedentary behaviour is defined as any activity involving ≤1.5 metabolic equivalents of task (METs) of energy expenditure while in a seated, reclined, or lying posture.2 It’s important to distinguish sedentary behaviour from physical inactivity. A person can still be considered active by meeting the recommended 150 to 300 minutes of moderate-intensity physical activity per week, as outlined by the World Health Organization (WHO), yet still engage in sedentary behaviour due to work or leisure activities that involve prolonged sitting. 3
A recent study published in The Lancet examined physical activity reports from adults across 163 countries and found that nearly one-third (31%) of the world’s
“ “
...onethird (31%) of the world’s population does not engage in sufficient physical activity.4
population does not engage in sufficient physical activity.4
Advanced technology has undoubtedly made daily tasks more convenient, with apps and online services for nearly everything. However, the increased reliance on motorized transport and screen time for both recreational, education, and work purposes has contributed to more sedentary lifestyles.3 The COVID-19 pandemic
exacerbated this issue and was associated with greater physical inactivity.5,6 Confinement to the indoors and feeling unsafe outdoors potentially served as a barrier for many people to get active during the pandemic.
The dangers of prolonged screen time and sedentary behaviours are numerous. Excessive screen time is well-known to contribute to mental health issues such as anxiety and stress, as well as physical health problems like obesity, type 2 diabetes, and even cancer.7,8 But did you know that sedentary behaviours, such as scrolling through your phone or sitting in front of a laptop for hours, can also negatively impact your heart health? In fact, the negative effects of inactivity on cardiovascular function can manifest within a short period, with studies showing that 3-6 hours of uninterrupted sitting can cause deterioration in vascular function. 9
Common cardiovascular diseases, including coronary artery disease, heart failure, and ischemic heart disease, are closely linked to metabolic activity.10 A study using Mendelian randomization—a technique that uses genetic variants to establish causal relationships between exposure factors and outcomes—found a significant causal association between screen time (specifically mobile phone and TV use) and cardiovascular diseases.10 Interestingly, computer use

References was not significantly associated with cardiovascular disease.
A survey of 2,000 remote and hybrid workers in the United States conducted by the Upright Pose team revealed some alarming findings.11 Fifty-four percent of these workers estimated that they had reduced their mobility during work hours by 50% or more in the past year, with 63% reporting that they only walked to the bathroom or kitchen during a typical remote workday. While the flexibility of working from home is convenient and life-changing for many, prolonged inactivity can be problematic if one does not make an effort to exercise. Sitting for long periods, as
many remote workers do, can increase the risk of developing blood clots, which can travel through the veins, block blood flow to the heart, and potentially cause a heart attack. 12
Fortunately, physical inactivity and sedentary behaviour are modifiable risk factors, meaning that measures can be taken to reduce the chances of developing cardiovascular disease and other conditions.13 Taking proactive steps to ensure adequate daily physical activity can make a significant difference in your overall health and well-being. Your heart will thank you for it!
physical inactivity and sedentary behaviour are modifiable risk factors, meaning that measures can be taken to reduce the chances of developing cardiovascular disease and other conditions.13 “ “
1. Ponti, M. Screen Time and preschool children: Promoting health and development in a Digital World. Paediatrics & Child Health. 2023; 28(3):–192. https://doi.org/10.1093/pch/pxac125
2. What is sedentary behaviour?. The Sedentary Behaviour Research Network (SBRN) [Internet]. 2017 June https://www.sedentarybehaviour.org/what-is-sedentary-behaviour/#:~:text=Sedentary%20 behavior%20is%20any%20waking,are%20engaging%20in%20 sedentary%20behaviour
3. World Health Organization. Physical activity. World Health Organization [Internet]. https://www.who.int/news-room/fact-sheets/ detail/physical-activity
4. Strain, T., Flaxman, S., Guthold, R., et al. National, regional, and global trends in insufficient physical activity among adults from 2000 to 2022: A pooled analysis of 507 population-based surveys with 5·7 million participants. The Lancet Global Health. 2024 Aug; 12(8): e1232-e1243. https://doi.org/10.1016/s2214-109x(24)00150-5
5. Peçanha T, Goessler K. F, Roschel, H, et al. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. American Journal of Physiology-Heart and Circulatory Physiology. 2020; 318(6); . https://doi. org/10.1152/ajpheart.00268.2020
6. Kinoshita, K., Ozato, N., Yamaguchi, T. et al. Association of the COVID-19 pandemic with changes in objectively measured sedentary behaviour and adiposity. International Journal of Obesity. 2023 Feb 16; 47, 375–381.. https://doi.org/10.1038/s41366-023-01274-9
7. Nakshine VS, Thute P, Khatib MN, et al. Increased Screen Time as a Cause of Declining Physical, Psychological Health, and Sleep Patterns: A Literary Review. Cureus. 2022 Oct 8;14(10):e30051. doi: 10.7759/cureus.30051.
8. Hunter RF, Murray JM, Coleman HG. The association between recreational screen time and cancer risk: findings from the UK Biobank, a large prospective cohort study. Int J Behav Nutr Phys Act. 2020 Aug 03;17(1):97. doi: 10.1186/s12966-020-00997-6.
9. Thosar SS, Bielko SL, Mather KJ, et al. Effect of prolonged sitting and breaks in sitting time on endothelial function. Med Sci Sports Exerc 47: 843–849, 2015. doi: 10.1249/MSS.0000000000000479.Qiu, Z., Jia, X., Fu, Y., et al. Screen Time in the development of cardiovascular diseases: A two-sample mendelian randomization study. Nutrition, Metabolism and Cardiovascular Diseases, 2024 Oct 03; 34(3), 706–717. https://doi.org/10.1016/j.numecd.2023.09.029
10. Qiu, Z., Jia, X., Fu, Y. Screen Time in the development of cardiovascular diseases: A two-sample mendelian randomization study. Nutrition, Metabolism and Cardiovascular Diseases, 2024 Oct 03; 34(3), 706–717. https://doi.org/10.1016/j.numecd.2023.09.029
11. The health dilemma of the work from Home Era. UPRIGHT Posture Training Device [Internet]. (2021, May 28). https://www. uprightpose.com/the-health-dilemma-of-the-work-from-home-era/ 12. O’Connell-Domenech, A. Remote work poses risks to physical health. The Hill [Internet]. (2023a, July 4). https://thehill.com/ changing-america/well-being/4076569-remote-work-poses-risksto-physical-health/
13. Lavie, C. J., Ozemek, C., Carbone, et al. Sedentary behavior, exercise, and Cardiovascular Health. Circulation Research, 2019; 124(5), 799–815. https://doi.org/10.1161/circresaha.118.312669

By Kyla Trkulja
We have all heard of developing a workout “routine”, but contrary to what many believe, this goes far beyond picking your favourite form of physical activity and deciding when you’ll slot it into your busy schedule. Exercise can be broken down into four main types–strength, balance, flexibility, and endurance training–and not all are created equal.1 For example, strength training involves building up muscle throughout the body, whereas flexibility training combines stretches with deep breathing to increase oxygen flow and elasticity in the muscles. As a result, a healthy workout routine ideally includes all four types of exercise.1
Out of all exercise types, endurance training captures the attention of many. This form of workout, also known as aerobic exercise or “cardio” training, involves activities that increase breathing and heart rate.1 A wide variety of exercises can be captured under this umbrella, including running, biking, jumping rope, and the newly popular “High Intensity Interval Training” (HIIT) workouts being offered at specialized fitness centres. Personally, HIIT workouts are what have made me passionate about endurance training, as different exercises can be incorporated into each session, making no two sessions identical and allowing me to overcome my selfperceived boredom of running.
It’s no secret that regular endurance training is good for the body’s
cardiovascular system. We’ve all probably heard at some point that this type of exercise reduces blood pressure and cholesterol, lowering the risk of heart disease, heart attacks, and other cardiovascular conditions.2 Other benefits include a minimised risk of type 2 diabetes and metabolic syndrome, as well as reduced inflammation and stress hormones.2,3 These benefits are made possible by changes that happen within the heart, blood vessels, and other cells in the body when engaging in regular aerobic activity. Let’s explore these changes a little bit further:
How Does Regular Endurance Training Lower Risk of Type 2 Diabetes (T2D)?
T2D is a form of diabetes that develops in adulthood due to insulin resistance. This is due, in part, to poor eating habits resulting in chronic insulin signalling that the body eventually learns to ignore.4 Regular endurance training, however, helps those with T2D manage their blood sugar and also lowers the risk of developing the disease in the first place. This is due to the effects of frequent muscle contractions during exercise, which requires a substantial amount of energy; as a result, muscle cells will increase the expression of surface proteins that take up sugar from the blood, such as GLUT4 transporters, to increase their energy supply.5 As a result, blood
sugar is lowered, and cells become more responsive to insulin due to the increased expression of these surface proteins, which helps maintain healthy blood sugar levels even after exercise is complete.
How Does Regular Endurance Training Lower Blood Pressure?
There is no singular way regular aerobic activity reduces blood pressure, but one of the most well-understood mechanisms involves the release of a compound called nitric oxide (NO).6 NO acts as a vasodilator, meaning that it causes blood vessels to widen. Wider blood vessels allow the blood to become less dense, reducing the pressure put on the vessel walls, ultimately decreasing blood pressure. While NO is released during endurance exercise in response to signals released from the muscles requiring increased blood flow, long-term exercise training can actually increase NO release even while the body is resting, leading to an overall reduction in blood pressure.




Heart attack, heart disease, heart failure, and arrhythmia risk are all lowered by regular endurance training. Increased NO release that lowers blood pressure results in reduced clumping of blood cells throughout the vessels, lowering the risk of blood clots and heart attacks.3 Levels of triglycerides, a type of fat that very easily stacks on top of blood vessels and increases the risk of blood clots, are also decreased.3 Regular aerobic exercise also increases the amount of “good” cholesterol in the body, known as High-Density Lipoprotein (HDL), while decreasing the amount of “bad” cholesterol, Low-Density Lipoprotein (LDL), which lowers the risk of heart disease.6 Whereas LDL builds up in the blood vessels, HDL removes LDL, improving cardiovascular health and reducing the risk of cardiovascular disease.

Physical changes also occur in the heart as a consequence of regular endurance training. During intense exercise, increased blood flow is required to meet the energetic demands of cells throughout the body, such as muscle cells. To meet these demands and minimize stress on the body, the heart will structurally adapt to make it more efficient at pumping blood throughout the body.6 Cardiac myocytes, the muscle cells in
the heart, will increase in size, leading to an increase in the overall mass of the heart–especially in the heart’s pumping chambers known as the ventricles.6 This makes the heart contract in a more powerful and effective way, preventing conditions such as heart failure and arrhythmia. The impacts of these effects on cardiovascular health are quite evident, as regular endurance exercise has been found to reduce cardiovascularrelated deaths by up to 40%.3
Surprisingly, there is no true consensus on how much exercise is needed to achieve these health benefits. The World Health Organization (WHO) recommends a minimum of 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity physical activity each week,7 but some studies have suggested 3-5 times this amount.8 There is also some evidence that too much exercise, 15-20 times higher than the amount recommended by the WHO, can actually be detrimental to cardiovascular health due to chronic stress on the body, exaggerated blood pressure rises, and inflammatory processes that occur during exercise.3 As a result, there is no “magic number”, but the most common guidelines suggest 30 minutes of physical activity each day, five days each week.1 That being said, any amount of physical
activity is better than nothing, so even if this target isn’t possible to reach, you can still experience the benefits of regular exercise with shorter workouts–listen to your body, and create a routine that works for you.

1. American Heart Association. Endurance exercise (aerobic) [Internet]. 2024. Available from: https://www.heart.org/en/healthy-living/ fitness/fitness-basics/endurance-exercise-aerobic
2. Johns Hopkins Medicine. Exercise and the heart [Internet]. 2023. Available from: https://www.hopkinsmedicine.org/health/wellness-and-prevention/exercise-and-the-heart
3. Parry-Williams G, Sharma S. The effects of endurance exercise on the heart: Panacea or Poison? Nature Reviews Cardiology. 2020 Mar 9;17(7):402–12. doi:10.1038/s41569-020-0354-3
4. Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, Uribe KB, et al. Pathophysiology of type 2 diabetes mellitus. International Journal of Molecular Sciences. 2020 Aug 30;21(17):6275. doi:10.3390/ijms21176275
5. Nystoriak MA, Bhatnagar A. Cardiovascular effects and benefits of exercise. Frontiers in Cardiovascular Medicine. 2018 Sept 28;5. doi:10.3389/fcvm.2018.00135
6. Kuru O, Şentürk ÜK, Koçer G, Özdem S, Başkurt OK, Çetin A, et al. Effect of exercise training on resistance arteries in rats with chronic nos inhibition. Journal of Applied Physiology. 2009 Sept;107(3):896–902. doi:10.1152/japplphysiol.91180.2008
7. World Health Organization. Global recommendations on physical activity for health [Internet]. 2010. Available from: https://www. who.int/dietphysicalactivity/factsheet_recommendations/en/
8. Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: Systematic review and dose-response meta-analysis for the global burden of disease study 2013. BMJ. 2016 Aug 9;i3857. doi:10.1136/bmj.i3857
By Iciar Iturmendi-Sabater
It is often said that getting a PhD is like running a marathon. As someone who tends to take things literally, I’ve embraced this metaphor wholeheartedly. Now, as I enter the third year of my PhD, I am also training for my first marathon.
Completing a marathon, a gruelling 42.195 km, is an achievement that parallels earning a PhD in terms of exclusivity: about 1% of Canada’s population have a PhD,1 while less than 1% globally have finished a marathon.2 I suspect that the percentage of marathon finishers amongst PhD holders is higher than in the general population. Here’s my reasoning: being able-bodied, having the time management skills to accommodate four to five runs a week, work on multiple research projects, and being long termoriented are just some of the factors that facilitate success in both marathon running and PhD completion. Of course, these are my own untested hypotheses—hence the lack of citations, which I’ve grown so accustomed to providing as my academic career progresses.
Running has precisely taught me to balance reason and intuition: to listen to my body, harness its power, and follow my instinct. Following this principle, I would also argue that while the predispositions presented earlier are facilitating factors, they are not sufficient to train for a marathon, nor to defend a PhD. Again, based on my own subjective experience, a strong sense of commitment and responsibility, perhaps even stubbornness, are also indispensable to long distance running and completing

a PhD. These traits are often fuelled by a competitive drive—primarily with oneself. The runner is excited by increasing their mileage and improving their strength. For PhD candidates, the thrill comes from running further experiments or testing their findings through alternative analysis pipelines.
More attributes are shared between these journeys, with organization and planning being crucial to both pursuits. A PhD student must learn to structure experiments and plan years in advance to produce a thesis. Similarly, a runner needs to plan their training, balancing both strength exercises with diverse types of running workouts, to avoid injuries and fit them into their daily schedule. For example, I am currently following a specific 14-week marathon plan, but I am not starting from scratch. In fact, I have been consistently running an average of 25 km weekly for one year and have completed three halfmarathons in the past three months, increasing my mileage in the lead-up to each race. My marathon plan is structured such that in the first four weeks, I focus on building strength through anaerobic exercise, which does not require oxygen to power muscle contractions. Strength training prepares me to increase my running mileage progressively, averaging 35 to 40 km per week during this period.
Much like how pacing oneself through the persistent but gradually increasing demands of a PhD leads to success, the key to training for a marathon is mostly running slowly
during training. Running slowly primarily engages the aerobic system teaching your body to efficiently use oxygen. Training at 60-70% of maximum heart rate like this is referred to as ‘heart rate zone 2 cardio’, which helps us build our base of endurance necessary to complete a marathon. When running slowly, your body relies more on fat as a fuel source instead of carbohydrates, increasing the ability to burn fat for energy preserves of glycogen stores for the later stages of the marathon when you need them most.3 Similar to marathon training, building new academic experiences and skills at a sustainable pace is necessary for a large portion of the journey.
On weeks four to twelve, my mileage keeps progressively increasing up to 60-65km a week. I mostly run slow but also introduce interval training and ‘fartlek’ sessions. Fartlek, meaning ‘speed play’ in Swedish, involves alternating speeds during a running session, such as changing my pace every minute during a one-hour run. Similarly, interval training involves running faster in short bursts, like doing ten series of 800 meters, each faster than the last. This reminds me of how a PhD student’s workload fluctuates throughout the year. How is it possible that, in the same week, I have a funding application deadline, a Program Advisory Committee meeting, a request to peer-review for a journal, and an invitation to revise and resubmit a manuscript that’s been dormant for months? These weeks certainly feel like an interval training session. Similar to how these busy periods of work as a

student likely increase my stress tolerance and efficiency as an academic, fartlek and interval training improve one’s lactate threshold—the point at which lactic acid starts accumulating in the muscles, causing fatigue. A higher lactate threshold allows you to maintain a faster pace during the marathon without getting tired as quickly. Overall, these types of training enhance both running speed and form, harnessing aerobic and anaerobic energy.3
Every week there is a long-distance run at a pace that feels comfortable. The longest distance I plan on running is 32km, about three weeks before the marathon. Lastly, the final three to four weeks before the race are for ‘tapering’, when one reduces the volume and intensity of training to recover from fatigue and be in perfect shape leading up to the race.4 I am afraid that my academic tapering time will mostly come once I defend my thesis, although travelling to international conferences has definitely provided me with energy and motivation along the way. I would argue it is equally important for students and academics to find small bits of ‘taper’ time throughout our busy schedules to prevent us from burning out.
Overall, running requires such a similar skill set as pursuing a PhD that I sometimes find myself using one as an excuse to procrastinate on the other. I would delay writing a manuscript to go for a run or consider skipping a training session to read a newly published article in my field. Since both require a nearly
equivalent effort, it feels as if substituting one activity with the other won’t make me feel unproductive or lazy. Ridiculous, I know. But why else would anyone want to train for a marathon while pursuing a PhD (other than to justify one’s procrastination drive)?
Running helps you learn better and faster. When I travel to a new place, I go on a run. I run through the streets or paths that I would otherwise cover in a car or on the subway, which blind you from the everyday, ‘not-so-touristy’ details of the place. This helps my orientation and makes me comfortable in the unknown. I enjoy passing as a local. While running, I learn to listen to my body and appreciate what I am physically capable of doing. I connect better with my thoughts and understand my mood, which is usually lifted after I run—thank you, endorphins. Through running I have met new friends of different ages and backgrounds who encourage me to be my best, and to whom
I can complain to when I am feeling lazy or exhausted. Running empowers me.
In the midst of paper rejections, null findings, failed funding applications, frustrating code debugging sessions, and endless corrections to address after my supervisor reviews my writing, which make up the not so well recognised reality of a PhD student’s daily life, running has, most of all, helped me remain confident when I would have otherwise doubted myself.
References
1. Government of Canada. Occupational profile and work tasks of Canadian PhDs: Gender and field of study differences [Internet]. 2022 [cited 2024 Aug 20]. Available from: https://www150.statcan. gc.ca/n1/pub/36-28-0001/2022012/article/00002-eng.htm
2. RunRepeat - Athletic shoe reviews [Internet]. [cited 2024 Aug 20]. The State of Running 2019. Available from: https://runrepeat.com/ state-of-running
3. Seiler S, Tønnessen E. Intervals, Thresholds, and Long Slow Distance: the Role of Intensity and Duration in Endurance Training. | Sportscience | EBSCOhost [Internet]. Vol. 13. 2009.
4. Smyth B, Lawlor A. Longer Disciplined Tapers Improve Marathon Performance for Recreational Runners. Front Sports Act Living. 2021 Sep 28 [cited 2024 Aug 20];3.



Dr. April Khademi is Canada Research Chair in Artificial Intelligence (AI) for Medical Imaging, associate professor of Biomedical Engineering at Toronto Metropolitan University, and principal investigator of the Image Analysis in Medicine Lab (IAMLAB). Her research focuses on the design, development, and deployment of AI algorithms for medical imaging.
Dr. Ian M. Rogers is a professor at the University of Toronto and scientist at the LunenfeldTanenbaum Research Institute. His lab is focused on developing ex vivo organ perfusion bioreactors, stem cell differentiation systems and engineered organ scaffolds to study disease, repair and regeneration.

Dr. Lorenzo Del Sorbo is an Intensive Care attending physician at Toronto General Hospital and associate professor at the University of Toronto. His main academic interests focus on the application of innovative strategies to prevent the injury induced by invasive mechanical ventilation.

Dr. Rohit Mohindra’s research team is interested in improving care for refugee patients, providing equitable care to cardiac arrest patients, and using artificial intelligence (AI) to make the Emergency Department experience a little more human for patients.

Dr. Errol Colak is an associate professor in the Department of Medical Imaging and is an abdominal radiologist at St. Michael’s Hospital. His research focuses on machine learning applications in medical imaging.

Dr. Linda Hiraki is a rheumatology physician and scientist in Genetics & Genome Biology at SickKids Hospital. She is coordinating a large, international cohort of lupus patients followed over years to understand the genetics of lupus, its manifestations, disease course, and outcomes. Dr. Hiraki holds a Canada Research Chair in Genetics of Rare Systemic Inflammatory Diseases.

Dr. Linda Mah is a clinician-scientist at the Rotman Research Institute and a geriatric neuropsychiatrist at Baycrest. Her research focuses on early detection and prevention of Alzheimer’s disease (AD) through development of clinical markers of AD risk and evaluation of neuromodulation therapies for older adults at risk for AD.



Dr. Joshua Rosenblat is a psychiatristresearcher conducting clinical trials evaluating novel interventions for mood disorders. He is now conducting federally funded clinical trials evaluating ketamine and psilocybinassisted psychotherapy for unipolar and bipolar depression.

Dr. Jennifer Crosbie is a senior associate scientist in the Neuroscience and Mental Health Program at SickKids and associate professor in the Department of Psychiatry at the University of Toronto. Her research investigates the etiology of childhood mental health

Dr. Alexandre Boutet attended medical school at McGill University and developed his passion for neuroscience at the Montreal Neurological Institute. He now works as a neuroradiologist at the University Health Network in Toronto. His main interest is to use neuroimaging to improve patient care. Outside of work, he enjoys travelling and social gatherings with friends.

Dr. Robert Vanner is a medical oncologist at the Princess Margaret Cancer Centre with the Gastrointestinal and Clonal Hematopoiesis programs. His team uses genomics, cellular and animal models to define how clonal

Dr. Ewan Goligher is an associate professor of Medicine and Physiology at the University of Toronto. His research program focuses on characterizing the mechanisms and impact of injury to the lung and diaphragm during mechanical ventilation and on the use of innovative clinical trial designs to test lung and diaphragmprotective ventilation strategies.

Dr. Sanjeev Kumar is a geriatric psychiatrist. His research focuses on developing novel biomarkers and treatment interventions for patients with Alzheimer’s disease (AD) using brain stimulation,

By Beatrice Acheson
I would work in the lab for free. It’s that love for it that keeps me going. Sometimes [when experiments don’t work] I think ‘well that sucked,’ but I know I’ll be back tomorrow.
These words capture the dedication of Alex Boshart, a fifth-year PhD candidate at the Institute of Medical Science (IMS) investigating the role of antibody-mediated rejection (ABMR) in kidney transplant failure. Under the supervision of Dr. Ana Konvalinka at Toronto General Hospital, Alex conducts research aimed at improving outcomes for kidney transplant patients. His impact is not confined to the lab, Alex takes on many roles in the IMS precinct. As the Senior Advisor for the IMS Student Association (IMSSA) and Prospective Student Ambassador for IMS, he dedicates his time to helping new students and enhancing their academic experience.
When we sat down for coffee in the sleek lobby of the MaRS Centre, I asked him to tell me a bit about what he does. Before I knew it, he was describing the intricacies of ABMR, the leading cause of allograft failure five years after transplant and emphasizing the dire need for new therapies to improve patient outcomes following kidney transplants. His passion for all facets of his research, from the underlying science to its clinical applications, was immediately apparent.
told her] that I am a quick learner. I am interested and I am willing.” Alex suggests to new and current IMS students that this mentality is “all you need because you are here to learn anyways.”
“
But Alex was not always so certain of his path. After completing his undergraduate degree in Health Sciences at Wilfrid Laurier University in 2019, he had to delay his IMS start date from September 2019 to January 2020.
“[After graduating university] I didn’t get into medical school. I was like, ‘Okay, what’s next?’ I took the summer to figure that out, which is why I started in January. I couldn’t collect everything in time for September,” Alex said.
The process was daunting and intimidating, and Alex recalled the questions that plagued him: “What happens if I don’t find [a supervisor]? Can I still come [in January]? How does this work?”
After a few anxious calls to the IMS admissions office, Alex connected with Dr. Konvalinka, who invited him to complete a placement in her laboratory that fall, allowing both parties to decide if it was the right fit. “I was lucky that I found Dr. Konvalinka, and that she was willing to take a chance on a kid that had never done cell work,” Alex said, attributing his success in securing the role to his keen attitude and commitment to learning. “[I
Despite finding his footing in the Konvalinka lab, Alex stressed that obstacles continued to arise in his PhD, and they still sometimes do. He learned adaptability and resilience early on in his graduate career. In 2020, during his first Program Advisory Committee (PAC) meeting, Alex received a dreaded question: “‘What if [your experiments] don’t work? How will you pivot?’” Alex was initially caught off guard, stating, “I wanted to cry. I didn’t know what I would do if it didn’t work.”
However, Alex bounced back quickly, gaining confidence in his identity as a researcher after returning to the lab in person following the COVID-19 pandemic. “Only after the first year, once I got back to the lab after COVID-19, did I hit my stride. I told myself, ‘I’m doing science. I am a scientist,’” Alex said.
In taking his research by storm, Alex obtained vast and diverse technical skills, but he stresses that, most importantly, he has learned the importance of resolve, determination, and curiosity to succeed in graduate studies. “I like to say that the P in PhD stands for problem-solving,” he noted. “You aren’t just learning how to learn, but also how to roll with the punches. If one door doesn’t work, how do you open the window? How do you pick the lock?”



“We answer questions. But the questions are never tough ones, they’re more like, ‘Am I going to be okay?’ and ‘I’m really worried about this,’” Alex explained. He hopes to provide incoming students with answers to the questions that he himself had nearly five years ago.
significant contributions to the academic experience of other graduate students.
Alex suggests that creative problemsolving is key to success in graduate studies, and he wasn’t kidding when he said to “roll with the punches.” In his free time, he enjoys watching mixed martial arts (MMA) with his friends. He added that his time watching the sport has taught him valuable lessons and drew a parallel to the inevitable setbacks of research: “You get hit, but you keep moving because this is our sport, and this is what we like to do.”
Alex’s academic journey is a testament to perseverance and has inspired him to assist other new IMS students in their journey to graduate school. As the Prospective Student Ambassador for IMS, Alex is responsible for calming the inevitable nerves of incoming IMS students.
Alex stresses that his work would not be possible without support, emphasizing the importance of his friendship and collaboration with Co-Prospective Student Ambassador Sajeevan Sujanthan, a fourthyear PhD candidate at IMS. “He and I fill each other’s niches because I work in a wet lab, and he works in a dry lab. When we have [new students] come in, they can get both perspectives. We can delegate based on our areas of expertise,” Alex said. “We are really close. There’s no one else I’d want to work in this position with. We work very well together.”
Alex maintains this collaborative attitude in the lab as well, crediting much of his success as a researcher to the teamwork in the Konvalinka Lab. “We’re a very collaborative lab. We all do everything for each other. The synergy is amazing. We all discuss results because maybe in your thought process, you’re missing something that someone else will see. It adds another layer,” he highlighted.
Alex’s holistic commitment to IMS through research, advocacy, and leadership, has not gone unrecognized. In 2024, Alex was awarded the Roncari Prize, which acknowledges IMS students who have made
Throughout our conversation, Alex’s message remained strong: be fearless, take advantage of what is in front of you, and have fun while you do it. As an incoming student myself, I left the interview inspired and motivated to begin my graduate journey in IMS, but I was struck mostly by Alex’s commitment to humility in his work despite his significant accomplishments.
“When you’re green, you grow and when you’re ripe, you rot,” Alex mentioned. “Everyone wants to be at the peak, but if you stay green, then there is always space to grow.”
As Alex continues his journey in IMS, his story serves as a powerful reminder of the importance of resilience, collaboration, and community. Much like in the MMA fights he enjoys watching, Alex’s approach to his research is about rolling with the punches, adapting to challenges, and staying in the fight no matter what. With unyielding curiosity and humility, Alex is not only advancing the field of kidney transplant research but also inspiring the next generation of scientists to approach their work with passion, perseverance, and the readiness to keep moving forward.

By Kyla Trkulja
Graduates from IMS take on diverse career paths, with no two trajectories being identical. In these roles, alums make an impact on the communities around them in their unique ways. Recently, I had the privilege to meet with 2021 alumnus Dr. Aadil Ali, where we sat down in the MaRS Discovery District and discussed his experiences over coffee. Dr. Ali’s journey is a testament to the power of collaboration and innovation. His contributions to science have earned him several academic awards, including the IMS Emerging Leader Award at this year’s Scientific Day, and international recognition on the Forbes 30 Under 30 list.
Dr. Ali completed his PhD at IMS under the supervision of Dr. Marcelo Cypel at Toronto General Hospital (TGH). With an area of focus in lung transplantation, Ali benefited greatly from the expertise and guidance of his mentors at a worldrenowned center for transplantation medicine, where TGH had performed the world’s first successful lung transplant in 1983. “There’s so much history, so many exciting things that come from the team here,” Dr. Ali highlighted. “The team at the Toronto Lung Transplant program really understands the urgency and importance of going bench-to-bedside for the benefit of patients. Good things happen when you are a part of such an amazing team.”
Dr. Ali still had the chaotic research journey that most PhD students embark on, regardless of their research site and supervisor, where “you start with one thing
and then end up gearing off into a different pathway.” He initially started his research with the intent of focusing on gene therapies for organs before transplantation, but after some time, he began looking at strategies to improve the way donor lungs were preserved outside of the body.
One of the team’s key discoveries challenged the conventional wisdom that colder is always better for preservation. Many of us are used to thinking that if you want to preserve something longer, you should put it in the fridge or freezer–and for years, this rationale was used to preserve organs outside of the body before transplant, as they were kept on ice. However, the team of researchers learned that keeping organs on ice leads to accumulated damage from ice injuries, ultimately causing cell death within the organ. As a result, organs such as the lungs could only be preserved for a maximum of six to eight hours outside of the body. Building off this, they later found that preserving the organ at a slightly warmer temperature of ten degrees Celsius prevents this damage, allowing it to be stored outside of the body for longer.
After completing his PhD, Dr. Ali worked closely with commercial partners to help transform this discovery into a practical innovation that could revolutionize transplant care worldwide. Collaborating with Traferox Technologies, a Canadian biomedical device company, Dr. Ali played a pivotal role in the development of a preservation device that keeps the organs

at a ten-degree Celsius temperature. Dr. Ali credits the entire team at Traferox Technologies for recognizing this critical clinical need and for their dedication in driving the development of this innovative technology forward. This small change in storage conditions has had remarkable effects, as lungs are now able to be stored for as long as 24 hours outside of the body–four times longer than they were able to be stored on ice. This device is now used routinely as a method for preserving organs prior to transplant not just in Canada, but also in medical centres in the United States, Europe, Australia, India

and Israel, and the technology is also being expanded so it can store other organs such as the heart, liver, kidney, and pancreas. Not only does this have a direct impact on patients, but transplant surgeons have benefitted as well, as the increased window of time the organs can survive outside of the body has improved their workflow: “A lot of residents and fellows don’t want to go into transplant because of the intensive work schedule and how complicated it is,” Dr. Ali explained. “If you get a call that you have a donor lung, you have to pick up the call at 9 pm and you do the transplant at 2 am, stay up the whole night, and then do your elective surgeries the next morning … Now, you have 24 hours to make your schedule more flexible.” As a result of this, overnight transplants are no longer done in Toronto and many parts of the world, easing some of the intensive scheduling on physicians. Hopefully, as transplant scheduling becomes less vigorous, residents and fellows will become more inclined to choose this specialty for their career path.
Currently, Dr. Ali is the Director of Clinical Development at Traferox, where he
continues to contribute towards innovative work on organ preservation. He has played a crucial role in the collaborative effort of expanding these preservation devices to other organs and spreading this technology to other countries, allowing patients and medical professionals all around the world to be impacted by the benefits of these extended times where the organs remain viable. “When I did my research, even after publishing it, it felt very confined within the walls of the institution and the facility,” Dr. Ali says. “But now … my favourite part is just being able to spread all this technology, spread all work that I’ve done, and have people use it to benefit patients around the world.”
When reflecting on his journey throughout his PhD, Dr. Ali credits IMS with providing him with the skills and resources he needed to take part in something so original. “Being in a cutting-edge environment, that definitely was one of the huge things that IMS offered me on top of the other things, such as time management skills, being able to have relations with people, and critical thinking,” he explained.
“ “ You have to go through the exercise of trying, failing, and problem solving. I think that’s where the real value of doing a PhD comes from.
He learned the value of collaboration and forming meaningful relationships with those around him, and, just as important to the success of his device, how to work with industry partners to commercialize an innovative idea. “I think that as things progress, there definitely has to be more conversations that will facilitate those healthy relationships between research and industry because it is the new way that things are going and to move things forward,” Dr. Ali mentioned, expressing the importance of industry support in getting the appropriate regulatory approvals so that this scientific concept could be made into a viable device that would impact the world around him.
In addition to learning how to conduct research and make discoveries as meaningful as possible, Dr. Ali also shared that learning to overcome failures was a crucial skill he developed during his PhD. “It’s more about the process [of research], and people don’t realize that,” he explained. “You have to go through the exercise of trying, failing, and problem solving. I think that’s where the real value of doing a PhD comes from.” By combining research skills with resilience and relationships, one can work towards success in whichever career path they choose and use their strengths to touch the lives of those around them. In the case of Dr. Ali, he did exactly that, and the results of his efforts are a direct representation of UofT’s goals for their impacts: to be boundless.

By Kristen Ashworth
“Don’t forget where you came from, and pay it forward.” This guiding principle has helped to shape Dr. Tony George’s career, from his roots in small-town Nova Scotia, to his current position as a leading scientist in psychiatric research at The Centre for Addiction and Mental Health (CAMH). He attributes the meaningful connections he has built throughout his life in paving his professional (and personal) success, and now places a strong emphasis on mentoring the next generation of scientists.
Dr. George is a psychiatrist and senior scientist at CAMH, and professor at the Department of Psychiatry at the University of Toronto. He completed his medical training at Dalhousie University, followed by a psychiatry residency and fellowship in Translational Neuroscience at Yale School of Medicine. After pursuing a near-decade-long position as a physician-scientist at Yale where he established his first laboratory, Dr. George came back to Canada, joining the University of Toronto as a faculty member in 2007. His lab at CAMH, called BACDRL–the Biobehavioural Addictions & Concurrent Disorders Research Laboratory–is focused on investigating the mechanistic relationships between drugs of abuse, such as nicotine and cannabis, and the psychiatric disorders with which they are associated, such as schizophrenia and depression.
Dr. George is now a leading psychiatrist and scientist in the field of behavioural addiction research, but his path into psychiatry was not a linear one. He grew up in Kentville, Nova Scotia–a town with a population of less than 6000. His parents, who had immigrated to Canada from India, supported and encouraged him to aim high academically. His father, a psychiatrist himself, helped to provide Dr. George with an understanding of the field of medicine from a young age. After high school, Dr. George moved to Halifax to attend Dalhousie University, first to complete his Bachelor of Science, and then, his medical training.
Upon entering medical school, he was still unsure of the field of medicine about which he was most passionate. At the time, he was working in a laboratory studying the metabolic organization of lipid pathways–a field outside the realm of psychiatry. But, it was through the experience at this lab that his passion for scientific research was first sparked. By the end of his medical school education, Dr. George had become deeply interested in the workings of the brain, and decided psychiatry would be the right path for him. To combine both passions–scientific research, honed from his lab experience, and psychiatry–he chose Yale to complete his clinical residency and fellowship in Translational Neuroscience. There, he was mentored by Dr. Robert Roth and conducted research on the effects of drugs, like nicotine, on the brain dopamine function in rats.
He reflects on his time with Dr. Roth as a pivotal experience in his research career, because it launched him into a whole new network of scientists that enabled his growth at Yale and further, to this day. In a full-circle moment, he reflects on the serendipity of one of his first publications from Dr. Roth’s lab: a paper published in Neuropsychopharmacology, the very journal where he now serves as co-principal editor.
Dr. George explained how he transitioned from rat research with Dr. Roth, to clinical research at Yale, first by developing a rat model that could be translated to humans to study the effects of nicotine on working memory. As a psychiatrist, he found that working with a human-translational model resonated deeply, bringing his work closer to the clinic. He was able to garner significant funding for this research, and was able to carve his own path in an increasingly competitive field at the time. “It was called the decade of the brain,” Dr. George explains, recalling the 1990s, when neuroscience and psychiatry were at the forefront of scientific advancement.
In conjunction with this research while a faculty member at Yale, Dr. George established a translational research program called the Program for Research in Smokers with Mental Illness (PRISM).
Dr. George explains how PRISM helped segue his research at his current lab, BACDRL, when he moved back to Canada and started his position at the University


of the Institute of Medical Science (IMS). The graduate-level IMS course that he has developed, called The Biopsychosocial Basis of Mental Health and Addictive Disorders (MSC1089), covers the complex intersections of behavior, addiction, and mental illness. Throughout the course, Dr. George brings in a diverse group of colleagues and guest speakers who offer perspectives on several topics of behaviour and addiction–including aspects of genetics, pathophysiology, clinical phenomenology and diagnostics, and treatment. In 2021, he was awarded an IMS Course Director Award in recognition of his excellence in teaching, and the impact MSC1089 has made in the IMS course portfolio, with its highly relevant and engaging content on mental health and addiction.
having a mentor that cares about your success is critical... “ “
of Toronto and CAMH in 2007: “[PRISM was] my first attempt to study addictions in people with serious mental illness, and focused on tobacco. It morphed into the BACDRL program at CAMH when I came to Toronto, which now studies a broader range of addictions (cannabis, nicotine, alcohol) and co-occurring mental illness (schizophrenia, mood and anxiety disorders).”
Outside of the BACDRL lab, Dr. George has made a significant impact as a member
Reflecting on what he enjoys most about being a part of UofT and IMS, Dr. George says, “UofT and IMS offer a diverse and dynamic research environment, and access to a large number of excellent graduate students which is unmatched at other centers, including at Yale. It is a collegial and collaborative place, whether mentoring my own grad students or teaching my course in IMS.”
As a trailblazer in the field, Dr. George credits his parents, his wife, and his daughter, as key sources of inspiration and support in helping him reach where he is today. In addition, he emphasizes the role
his mentors have played along the way throughout medical school, residency, and fellowship as he sought to establish himself as a physician-scientist. Now, he explains, he is committed to “paying it forward” by sustaining a meaningful, mentoring presence for his own students–whether they are graduate students in his lab, medical students and residents shadowing him through rotations at CAMH, or his course students who take a vested interest in the material. He believes that having a mentor that cares deeply about your success is critical, and advises IMS students to seek out mentors who can propel them to new and exciting opportunities in academia and beyond.
Dr. George’s journey illustrates that true success–whether in science, medicine, or any other aspect of life– is achieved not only through hard work and determination, but also by the people in your life that support you in getting there. And, by coming together to nurture the next generation of scientists, he is confident that the future of addiction research will be left in capable hands.

By Samuel Lasinski
When most people think of tissue engineering, they envision the creation of solid organs; sci-fi scenes of ethereal lungs languidly pulsating in neon suspension readily spring to mind. While engineered solid organs remain a distant goal, a more immediate target is of critical clinical and scientific relevance: small diameter vascular grafts. Although these apparently simple structures may not capture the imagination like more complex tissues, they could drastically improve the care of thousands and represent a crucial stepping stone towards engineered solid organs.
Blood vessels are classified as a type of connective tissue that, along with the heart, make up the structural components of the circulatory system. Small arteries— those with outer diameter between one and six millimeters—play a critical role in this system. Their primary function is to transport blood from the large arteries to smaller arterioles and capillaries, ensuring sufficient perfusion of vital organs and peripheral tissues. They also help regulate blood pressure by adjusting their diameter through processes known as vasodilation (widening) and vasoconstriction (narrowing).
Given their role as conduits, it should come as no surprise that the most critical diseases affecting small arteries impede blood flow. Chief among these flow-limiting conditions are coronary artery disease, peripheral artery disease, and cerebrovascular disease.1 All are characterized by a progressive narrowing of vessels by deposited plaques, risking oxygen deprivation and death of downstream tissues. In the case of coronary artery disease, this results in a myocardial infarction or heart attack.1
When pharmacological treatment is insufficient to address these conditions, alternative interventional methods are required. One such example is the use of a vascular graft to bypass the occluded region and restore blood flow to the tissues.
Autologous grafts are the current standard of care for bypassing diseased small arteries.2, 3 These grafts are harvested from elsewhere on the patient’s body depending on the treatment site. For example, vessels for coronary artery bypass grafting (CABG) may be harvested from the internal thoracic artery in the chest, radial artery in the arm, or the saphenous vein in the leg.1 These grafts can be effective multiple years post-implantation, helping to alleviate symptoms of vessel occlusion and offering significant improvements to patients’ quality of life.4
However, the use of autologous grafts is not without its drawbacks. The secondary procedure to harvest the graft introduces risks of scarring, infection, nerve damage, and reduced blood flow which can result in permanent damage to the donor region. In rare cases, these complications may necessitate the amputation of the limb altogether.5 The act of harvesting itself may compromise the graft resulting in later occlusion and failure.6 Moreover, prior harvesting or widespread damage to the cardiovascular system due to systemic disease can render potential donor sites unviable and limit the amount of material available for harvest; this is especially true in severe cases requiring multiple bypasses where greater amounts of vascular material are necessary. In contrast to the repair and replacement of large arteries, no alternative grafts—synthetic or otherwise—have
been found to be clinically viable for small vessel applications.3 It is here that the promise of tissue engineered vascular grafts comes into play.
Tissue-engineered vascular grafts (TEVGs) are biological constructs intended for the repair or replacement of damaged vascular tissue. They are typically composed of endothelial, smooth muscle, and fibroblast cells seeded within synthetic or biological scaffolds which provide structural organization, mechanical strength, and sites for cell adhesion. These living and non-living components are carefully selected and assembled to replicate the properties of native tissues, aiming to integrate seamlessly into the cardiovascular system. By mimicking natural vascular structures, TEVGs seek to promote tissue regeneration and improve upon existing synthetic grafts.
An understanding of the mechanical and biological characteristics of small diameter grafts best highlights the unique suitability of tissue-engineered constructs for this application. Grafts must have sufficient burst pressure, elasticity, and resilience to withstand the cyclical pressurization of the cardiovascular system driven by the heart’s pulse.3 They must also possess sufficient strength to hold a suture and ensure proper implantation.3 To further complicate matters, properties exceeding those of the native vessels are not suitable as the mismatch of mechanical properties has been found to contribute to disturbed blood flow at the site of anastomosis (vessel joining). This causes excess growth of endothelial cells lining the vessels (intimal hyperplasia) and eventual graft failure.7 Simply implanting an exceedingly

strong tube is not a viable approach. Graft materials must also be chosen to minimize the risk of immune rejection; biological building blocks like collagen are preferable to synthetic polymeric materials which have been shown to provoke an elevated immune response, and biological materials of human origin are preferred to those of another species.3 Moreover, the graft’s materials should allow for progressive invasion of cells from native tissues and remodeling of the structure to facilitate complete integration into the native architecture.3 Evidently, any cells included within the graft should be of human origin as well.3 Finally, properties of the inner surface of the graft should be carefully selected to minimize the risk of blood-interactions resulting in thrombosis (blood clots).3
Taken together, these design considerations help reveal why previous attempts at synthetic small diameter grafts have largely failed and how tissue engineered grafts are uniquely suited to fill the gap. Where synthetic materials provoke immune response and rejection, a biologically engineered graft may facilitate complete integration. Where differences in mechanical properties induce pathological cell growth and vessel occlusion, a construct made from native materials allows remodeling and even growth. Most insightfully, an overview of these criteria highlights the absolute necessity of an interdisciplinary, collaborative approach between the engineering, health, and biological sciences to the successful generation of such a graft.
Such tissue-engineered grafts may be closer to clinical use than ever before. Humacyte, a biotech company out of Dr.
Laura Niklason’s lab at Yale University, recently announced positive phase 2/3 clinical results for its “Human Acellular Vessel (HAV)” for the treatment of vascular trauma and arteriovenous access for hemodialysis.8,9 In the trauma repair trial, HAV treatment resulted in a patency rate of 90.2% and an amputation rate of only 9.8% 30 days after treatment, compared to 81.1% and 20.6% for existing synthetic alternatives.8 Meanwhile, the arteriovenous access trial showed an HAV 12-month patency rate of 68.3%, slightly higher than the 62.2% seen for standard arteriovenous fistula treatment, although the HAV treatment group did experience a higher incidence of adverse events.9 Following the promising vascular trauma data, the US FDA accepted Humacyte’s Biologics License Application for review in February 2024.10 In August 2024, Humacyte revealed that the FDA required additional time to review its application; as of this publication, the FDA’s decision remains under review.11
Even as implantable tissue-engineered vascular grafts remain just out of reach, research in this area is highly significant for the broader field of tissue engineering. Insights gained from developing vascular grafts will directly inform the creation of other tubular structures, such as bile ducts, segments of the gastrointestinal tract, branches of the airway, and components of the urinary and reproductive systems. Additionally, advances in bioreactor design and perfusion techniques derived from vascular graft research will be crucial for developing perfusion systems for engineered solid organs. More broadly, work in vascular engineering will enhance the understanding of all
soft load-bearing tissues as well as the interaction of biological and mechanical aspects in engineered constructs. Thus, the impact of tissue-engineered grafts extends beyond their direct clinical benefits to the development of the field as a whole.
The development of small diameter vascular grafts represents a critical area of research in tissue engineering. With implications far beyond the field of cardiovascular health and disease, the complex, even contradictory challenges posed by the project highlight the strength and requirement of interdisciplinary collaboration in biomedical research. While perhaps not as glamorous as ideas of 3D printed kidneys or xenograft hearts, the deceptively simple vascular graft represents both a stepping stone towards complex tissues and a potentially life-saving intervention. For thousands of patients worldwide, their arrival is eagerly awaited.
1. Hernandez-Sanchez D, Comtois-Bona M, Muñoz M, et al. Manufacturing and validation of small-diameter vascular grafts: A mini review. iScience. 2024;27(6):109845.
2. Naegeli KM, Kural MH, Li Y, et al. Bioengineering Human Tissues and the Future of Vascular Replacement. Circulation Research. 2022;131(1):109-26.
3. Niklason LE, Lawson JH. Bioengineered human blood vessels. Science. 2020;370(6513):eaaw8682.
4. Abdallah MS, Wang K, Magnuson EA, et al. Quality of Life After PCI vs CABG Among Patients With Diabetes and Multivessel Coronary Artery Disease: A Randomized Clinical Trial. JAMA. 2013;310(15):1581-90.
5. Paletta CE, Huang DB, Fiore AC, et al. Major leg wound complications after saphenous vein harvest for coronary revascularization. Ann Thorac Surg. 2000;70(2):492-7.
6. Schanzer A, Hevelone N, Owens CD, et al. Technical factors affecting autogenous vein graft failure: Observations from a large multicenter trial. Journal of Vascular Surgery. 2007;46(6):1180-90.
7. Post A, Diaz-Rodriguez P, Balouch B, et al. Elucidating the role of graft compliance mismatch on intimal hyperplasia using an ex vivo organ culture model. Acta Biomater. 2019;89:84-94.
8. Humacyte Global, Inc [Internet]. Durham: Globe Newswire; 2023 Sept 12. Humacyte Announces Positive Top Line Results from Phase 2/3 Trial of Human Acellular Vessel™ (HAV™) in Treatment of Patients with Vascular Trauma [cited 2024 Aug 26]. Available from: https:// investors.humacyte.com/news-releases/news-release-details/humacyte-announces-positive-top-line-results-phase-23-trial-0
9. Humacyte Global, Inc [Internet]. Durham: Globe Newswire; 2024 July 31. Humacyte Acellular Tissue Engineered Vessel (ATEV™) Meets Primary Endpoints in V007 Phase 3 Clinical Trial in Arteriovenous Access for Hemodialysis [cited 2024 Aug 26]. Available from: https://investors. humacyte.com/news-releases/news-release-details/humacyte-acellular-tissue-engineered-vessel-atevtm-meets-primary

By Sipan Haikazian
Cardiovascular disease (CVD) refers to a group of diseases of the heart and blood vessels, including angina, myocardial infarctions (heart attacks), strokes, heart failures, and arrhythmias.1 CVDs continue to be a leading cause of morbidity and mortality in Canada, with approximately one in 12 Canadians over the age of 20 living with one or more CVDs. As with many other medical conditions, there are significant disparities in outcomes, which are particularly influenced by numerous racial and socioeconomic factors. This article will bring attention to the factors responsible for some of the most significant disparities in CVD across Canada, discuss some driving factors of these disparities, and finally, offer a look into what is being done to address these differences.
In Canada, incidences and prevalences of CVD vary greatly across ethnic groups. In one study of over 350,000 Canadians, hypertension, which is a risk factor for numerous CVDs, was found to be significantly greater in Filipino, South Asian, and Afro-Caribbean communities, as compared to the greater white population.2 The prevalence of CVDs was higher among South Asian-born immigrant communities as compared with Native-Born Canadians.3 Additionally, the Cardiovascular Health in Ambulatory Care Research Team (CANHEART) Immigrant Study investigated incidence rates of cardiovascular symptoms and events over ten years, including a population of just under 825,000 immigrants in Canada.4
They found that immigrants of Black and Southeast Asian heritage had some of the highest rates of diabetes in the population. Rates of hypertension were also greatest in these communities. Both diabetes and hypertension are significant risk factors for CVDs. From this research, the increased risk seen in these communities is due in part to higher rates of diabetes and hypertension.
Studies of these discrepancies have outlined a few key risk factors that may be unique to ethnic groups. For example, low fluency in English may present barriers to reporting cardiovascular symptoms and seeking help from the healthcare system. The lack of formal education around these topics may also play a role. Furthermore, the overlap between the challenges above and the possibility that members of these communities may begin their lives in Canada at a relatively lower socioeconomic status are also important considerations.
Indigenous peoples also face a higher burden of cardiovascular disease as compared with non-Indigenous peoples. According to a 2001 analysis published in the Lancet, Indigenous Peoples who identify as First Nations had a 250% increase in the prevalence of CVDs, as compared with non-First Nations individuals.5 Risk factors and prodromes are more prevalent in these populations than non-Indigenous peoples. Rates of congestive heart failure, hypertension, and stroke were found to be significantly higher in a sample of Métis Indigenous
peoples as compared with a nonIndigenous sample.6
Multiple contributing factors have been explored. Looking from a historical lens, the impact of colonization, widespread oppression, and healthcare biases that continue to persist to this day all play essential roles. For a large part of Canada’s history, Indigenous peoples received subpar care as compared with their non-Indigenous counterparts. While much legislation has been passed to provide greater care to these communities, challenges remain. The geographical isolation of many of these communities, lack of adequate resources and infrastructure, and preponderance of Western-style medicine continue to play a role in exacerbating medical disparities for many individuals. As a simple example, healthcare in rural and remote areas, largely composed of Indigenous communities, are typically very sparsely staffed. Many of these hospitals and health centers are lucky to get 24/7 coverage from a family physician, so it is unlikely that they would receive a cardiologist with extensive training and expertise in treating CVDs.

Despite Canada’s universal healthcare system, disparities still exist. “ “
Socioeconomic status is also a key determinant of cardiovascular health outcomes in Canada. Individuals with lower socioeconomic status often face higher risks of hypertension, coronary artery disease, and other cardiovascular conditions. A systematic review and meta-analysis of 31 studies conducted in the Journal of Public Health found that socioeconomic inequalities contribute significantly to differences in cardiovascular health.7 The results showed that the lower a person’s socioeconomic status, the more likely they are to present cardiovascular risk factors and associated CVD outcomes. Lower-income individuals experienced higher rates of risk factors such as smoking, obesity, and physical inactivity.7
Furthermore, access to healthcare is a critical factor that may influence cardiovascular health outcomes more globally. Despite Canada’s universal healthcare system, disparities still exist.
For instance, a lack of affordable transportation may reduce access to care for many, especially if there is no robust public transit infrastructure. While general medical care may be covered by provincial healthcare plans, other services such as prescription coverage, eye care, and dental treatment are typically covered by private insurance plans. The lack of prescription coverage is particularly damning for those with CVD, as rates of medication usage are high for those with these diseases. These barriers can lead to delays in diagnosis and treatment, exacerbating cardiovascular health disparities.
In terms of interventional strategies, several are being implemented to improve cardiovascular-related outcomes for affected populations. As with other areas of medicine and healthcare, there is currently a shift towards culturally sensitive care and accessibility. Improving literacy has been a central focal point for intervention. For example, one interventional trial attempted to incorporate Indigenous traditions and culturally sensitive material for Indigenous patients presenting with CVDs and found that rates of medication and treatment understanding had significantly improved compared with before the intervention.8 Combining such strategies with broader policy changes and systemic improvements can result in not only a bridging of a gap in disparities in CVD outcomes but also a reduction in such outcomes.
1. Olvera Lopez E, Ballard BD, Jan A. Cardiovascular Disease. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 [cited 2024 Aug 22]. Available from: http://www.ncbi.nlm.nih.gov/ books/NBK535419/
2. Liu R, So L, Mohan S, Khan N, King K, Quan H. Cardiovascular risk factors in ethnic populations within Canada: results from national cross-sectional surveys. Open Med. 2010;4(3):e143-153.
3. Sebastian SA, Sethi Y, Padda I, Johal G. Ethnic Disparities in the Burden of Cardiovascular Disease Among Immigrants in Canada. Current Problems in Cardiology. 2024 Jan;49(1):102059.
4. Tu JV, Chu A, Rezai MR, Guo H, Maclagan LC, Austin PC, et al. The Incidence of Major Cardiovascular Events in Immigrants to Ontario, Canada: The CANHEART Immigrant Study. Circulation. 2015 Oct 20;132(16):1549–59.
5. Anand SS, Yusuf S, Jacobs R, Davis AD, Yi Q, Gerstein H, et al. Risk factors, atherosclerosis, and cardiovascular disease among Aboriginal people in Canada: the Study of Health Assessment and Risk Evaluation in Aboriginal Peoples (SHARE-AP). The Lancet. 2001 Oct;358(9288):1147–53.
6. Atzema CL, Khan S, Lu H, Allard YE, Russell SJ, Gravelle MR, et al. Cardiovascular Disease Rates, Outcomes, and Quality of Care in Ontario Métis: A Population-Based Cohort Study. Zhang W, editor. PLoS ONE. 2015 Mar 20;10(3):e0121779.
7. Wang T, Li Y, Zheng X. Association of socioeconomic status with cardiovascular disease and cardiovascular risk factors: a systematic review and meta-analysis. J Public Health (Berl) [Internet]. 2023 Jan 21 [cited 2024 Aug 22]; Available from: https://link.springer.com/10.1007/s10389-02301825-4
8. Crengle S, Luke JN, Lambert M, Smylie JK, Reid S, Harré-Hindmarsh J, et al. Effect of a health literacy intervention trial on knowledge about cardiovascular disease medications among Indigenous peoples in Australia, Canada and New Zealand. BMJ Open. 2018 Jan;8(1):e018569.

By Kiko Zi Yi Huang
Earlier this year, I had the privilege of attending The Association for Research in Vision and Ophthalmology’s (ARVO) 2024 Annual Meeting in Seattle, Washington, with my supervisor, Dr. Ya-ping Jin. This was particularly special for me, as it marked both my first international conference and my first time travelling to Seattle.
The highlight of my trip was undoubtedly the conference itself. ARVO 2024 took place at the expansive Seattle Convention Center, which is composed of two grand, multi-story buildings. The venue was brimming with people and buzzing with activity, proudly hosting a diverse mix of physicians, researchers, students, and other field professionals. There was never a dull moment during this conference, with a variety of activities available, ranging from attending insightful lectures, exploring the exhibition hall, to participating in the lighthearted ARVO scavenger hunt sidequest.

Outside the main building, Arch, of the Seattle Convention Center. This picture does not do the scale of the building justice, but it was truly massive!

The weather in Seattle was perfect during my four-day visit in May, with clear skies throughout. This photo captures a view from Pike Place Market, featuring the iconic Ferris wheel.
Perhaps my favourite part of the conference was the poster hall. Having my research on display gave me a unique opportunity to connect with a wide range of individuals from a range of different backgrounds and universities. I was extremely nervous, but this quickly eased as I realised that everyone was incredibly friendly! Engaging in conversations about their experiences and sharing my own research was deeply rewarding and fun. Meeting people from all around the world and learning about the diverse range of research being conducted was truly eye-opening (pun intended)!
Beyond the conference, I spent my time wandering around the city with no set destination in mind. The famous Pike Place Market, conveniently located just a 15-minute walk from the convention centre, quickly became one of my favourite spots. Whether I was grabbing a quick coffee, enjoying a bite
to eat, or picking up souvenirs for friends, the market’s bright atmosphere was a delightful pit-stop, no matter the time of day. Its carefree vibe offered a perfect counterbalance to the intensity of the conference, providing moments to recharge and savour the city’s charm.
I also have to give a special mention to the absolutely delightful Din Tai Fung restaurant, which we sadly don’t have in Toronto. This restaurant serves the most incredible steamed soup dumplings, and I’d return to Seattle solely for the chance to indulge in a hundred more of these little bites of heaven.
I’m eager to see where future ARVO meetings will lead me next, but for now, I’m just incredibly grateful to have had this opportunity. I would highly recommend anyone who hasn’t yet visited Seattle to do so—it’s a vibrant city teeming with countless experiences and delicious eats that deserves to be explored!