




EDITORS-IN-CHIEF:
Kyla
Iciar
EXECUTIVE DIRECTORS:
Janet Li
Kristen Ashworth
Elizabeth Karvasarski
Niki Akbarian
Mahbod Ebrahimi
PHOTOGRAPHERS:
Niki Akbarian (Director)
DESIGN EDITORS:
Jayne Leggatt (Director)
Josephine Choi
Genevieve Groulx
Brendan Lazar
Andrew Janeczek
Anne McGrath
SOCIAL MEDIA TEAM:
Elizabeth Karvasarski (Director)
Lizabeth Teshler
Mahbod Ebrahimi
JOURNALISTS & EDITORS:
Ilakkiah Chandran
Kevan Clifford
Anthaea-Grace Patricia Dennis
Bahar Golbon
Sipan Haikazian
Kiko Huang
Vanessa Ip
Alyona Ivanova
Nikou Kelardashti
Lauren Levy
Eileen (Xiao Yu) Liu
Jennifer Ma
Suraiya Mangra
Karan Patel
Samantha Ricardo
Denise Sabac
Sara Shariati
Beatrix Wang
Rachel Yang



This Spring 2024 issue of the IMS Magazine is a celebration of how advances in surgery are flourishing at the IMS.
We shine a spotlight on the creative and innovative spirit of IMS faculty whose perseverent efforts are advancing surgical interventions, despite their invasiveness, high risk, and potential complications. An example of this determination is Dr. Victor Pereira’s work, dedicated to the development of cutting-edge robotic technologies to aid the surgical treatment of neurovascular conditions. We further discuss the history and implications of robotic surgeries as well as human enhancement in two different viewpoints.
We also showcase Dr. David Gomez’s work, motivated by his realization that barriers to surgical care were not only an issue in his native Colombia, but also in high income countries like Canada. His research is now devoted to examining who was most affected by the millions of procedures that were halted during the COVID-19 pandemic in Ontario, which is relevant to guide future action-plans. In two other viewpoint articles, our writers originally illustrate the barriers to surgical access through a case series, and consider the economic factors driving medical tourism, and its subsequent ethical consequences. In a continued examination of the existing barriers to access health services, the Diversity in Science piece discusses 2SLGBTQ+ Communities’ difficulties to obtain mental health care.
Advances in surgery also involve the development of new diagnostic tools to avoid invasive surgical interventions in favor of less harming procedures. We feature Dr. Gelareh Zadeh, first female chair of neurosurgery at the University of Toronto, whose team has found that blood and immune samples can be used to discriminate between intracranial tumors and glioblastomas, respectively, leading to the development of new and more effective brain tumor classification systems. The use of artificial intelligence and neural networks to classify tumors is also commented on in the viewpoints section.
The Spotlight on Dr. Pascal Tyrrel serves to emphasize that both academia and industry share equally important roles in promoting the innovative spirit that feeds surgical advances. He embodies this idea by leading the Health Care Innovation Challenge at the IMS. In fact, our graduate research does not happen in the void, but within the thriving IMS and broader UofT communities. The Spotlights on IMS students Ergi Duli and Carly Davenport also exemplify how students can get involved by leading IMS Scientific Day, becoming a mentor for new students, or carrying out meaningful environmental action. We are glad to include again in this issue a piece by the spoken voice of the IMS, RawTalk Podcast. Last but not least, a student shares her academic experience beyond the streets of Toronto attending the American Society of Nephrology’s Kidney Week in Philadelphia.

We thank all writers, copy-editors, and designers involved in the production of this issue, which we hope can water our readers’ innovative minds!
Kyla TrkuljaKyla is a PhD student studying the mechanism of action of novel therapies for lymphoma under the supervision of Dr. Armand Keating, Dr. John Kuruvilla, and Dr. Rob Laister.
@kylatrkulja
Iciar Iturmendi SabaterIciar is a PhD student under the supervision of Dr. Meng-Chuan Lai and Dr.Hsiang-Yuan Lin. She investigates social adaptive behaviors in children and adolescents with neurodevelopmental conditions such as autism, attention-deficit hyperactivity disorder, and obsessive-compulsive disorder.
@iciar_itur

Director, Institute of Medical Science
Professor, Department of Surgery Senior Scientist, Toronto General Hospital Research Institute, University Health Network
After a long and grey winter, I’m sure we are all warmly welcoming the Spring season, which represents a fresh start for many. The Spring 2024 issue of the IMS Magazine coincides nicely with this theme – this issue highlights advances in surgery, which allows many individuals to have a new beginning with their health.
This issue features IMS faculty that are working to improve the landscape of surgeries across Canada. Dr. Kazuhiro Yasufuku and Dr. Gelareh Zadeh are making great strides towards the development of non-invasive techniques for diagnosing and treating lung and brain cancers, respectively. Dr. Vitor Pereira shares how his team has pioneered the use of robotic-assisted surgery for neurovascular conditions such as stroke and aneurysms. Lastly, Dr. David Gomez is ensuring equitable access to healthcare among Canadians by working to address the surgical backlog across the country and investigating how to best improve wait times.
We also put the spotlight on 3 individuals within the IMS community that have made wonderful contributions to the natural, academic, and professional environments here at the University. Carly Davenport, a student at IMS, shares her motivations behind creating Birdsafe UofT, an initiative that aims to protect other life forms that share the campus with us. Ergi Duli discusses his involvement with IMS throughout his graduate studies and what shaped him to becoming the student leader he is today. Dr. Pascal Tyrrell shares his journey about his career path that led him through both academic and industry jobs, providing reassurance to students that a career is not always linear. Lastly, this issue shares highlights from the 13th Annual Ori Rotstein Lecture in Translational Research.
On behalf of the IMS community, I extend my heartfelt congratulations to the new faculty joining IMS and members that have been promoted this year. I would also like to thank the Editors-in-Chief Kyla and Iciar, as well as the journalists, editors, photographers, and design team for putting together another exciting issue of the IMS Magazine. I hope you enjoy reading about the incredible accomplishments our community has made!
Dr. Mingyao Liu Director, Institute of Medical Science DR. MINGYAO LIU




Niki Akbarian is a second-year MSc student under the supervision of Dr. James Kennedy. Her research focuses on the genomic analyses of the relationship between neuroticism and Alzheimer’s Disease. Outside of academia, Niki enjoys photography, playing the piano, and watching sitcoms.

Ilakkiah Chandran is a second-year MSc student at IMS supervised by Dr. Danielle Andrade at the Krembil Brain Institute. Her thesis aims to understand the phenotypic and genotypic presentation of pediatric-onset developmental and epileptic encephalopathies in adults. In her free time, she enjoys reading, going on impromptu adventures and tuning into some true-crime!

Kiko Huang is a first-year MSc student studying glaucoma epidemiology and public health under the supervision of Dr. Yaping Jin. Her work aims to investigate various trends in ophthalmology and vision care to gain a better understanding of the health landscape and guide health policy. During her free time, she’s likely out exploring the city and trying new restaurants!

Alyona Ivanova is a first-year PhD student investigating the molecular signature of glioblastoma at the Hospital for Sick Children under supervision of Dr. Sunit Das. Alyona is a figure skater, equestrian rider and a model. She enjoys traveling, cooking and reading.

Janet Z. Li is a second-year MSc student studying the brain-behavior relationships between conditioned pain modulation capability and functional connectivity of key pathways within the dynamic pain connectome, namely the descending antinociceptive pathway. She is supervised by Dr. Karen Davis at the Krembil Brain Institute in Toronto Western Hospital. Outside of research, she can be found practicing piano, figure skating, creating fashion content, and café hopping.
Kristen Ashworth is an MSc student working under the supervision of Dr. Brian Ballios at the Donald K. Johnson Eye Institute and Krembil Research Institute. Her thesis work is focused on developing a retinal organoid model in which to evaluate stem cell therapies for USH2A- and CRB1-related inherited retinal diseases. Kristen loves cross country running, reading a good book, going to Marshalls, and most importantly, doting on her two adorable golden retrievers.
Bahar Golbon is a third-year MSc student investigating the surgical outcomes of primary hyperparathyroid patients in Ontario under the supervision of Dr. Jesse Pasternak. In her free time, you can find Bahar completing a puzzle and drinking a cup of coffee!

Vanessa Ip is a first-year MSc student working with Dr. Vicky Stergiopulos in General Psychiatry and Health Systems Division at CAMH. She is investigating the characteristics of forensic patients designated ALC in the last 5 years, the housing needs and preferences of this population, and their challenges and barriers to accessing housing. Aside from research, Vanessa has a passion for dogs, photography, and espresso.
Nikou Kelardashti is a second-year MSc student under the supervision of Dr. Karen Davis. Her research focuses on the relationship between neural oscillations and pain-attention interaction. Outside of academia, Nikou enjoys reading poetry and classic literature, watching old movies, and going for long walks.

Eileen (Xiao Yu) Liu is currently supervised by Dr. Sunit Das and Dr. Vitor Pereira at St. Michael’s Hospital. Her research project focuses on the use of endovascular radiosurgery as a way to treat brain tumors. Outside of academia, Eileen enjoys running, bouldering, playing badminton, exploring new activities and trying new food.
_jenniferma_



Jennifer Ma is a second-year MSc student investigating the functional neural networks involved in suicide, and their relation to pain perception as a potential biomarker of suicide risk. She is under the supervision of Dr. Sakina Rizvi at the Arthur Sommer Rotenberg Suicide and Depression Studies Program at St. Michael’s Hospital. Outside of the lab, she enjoys crochet, painting and acting in local theatrical productions.
Denise Sabac is a second-year MSc student working with Dr. Felsky in the Krembil Centre for Neuroinformatics at CAMH. Her work aims to subtype mental illnesses in treatment-seeking youth using Similarity Network Fusion analysis of the Toronto Adolescent & Youth CAMH Cohort Study data. Aside from research, Denise enjoys playing sports, walking along sandy beaches, and drinking lots of coffee.
Soha Usmani is a second-year MSc student researching the ability of mitochondrial genomes to act as DNA barcodes for cryptic and understudied malaria vector species, under the supervision of Dr. Doug Norris at the Bloomberg School of Public Health. Outside labwork, she enjoys science and history podcasts, going through her “ToWatch” list of movies, and museums.
The IMS Design Team is a group of second year MSc students in the Biomedical Communications (BMC) program. Turning scientific research into compelling and effective visualisations is their shared passion, and they are thrilled to contribute to the IMS Magazine.



Genevieve Groulx






Samantha Ricardo is a first-year MSc student studying mechanisms of Alport Syndrome under the supervision of Dr. Moumita Barua at PMCRT. Outside of the lab, you can catch her biking around the city, trying new cuisines, or attempting to play chess.
Sara Shariati is a second-year MSc student, investigating gene expression changes in mesothelioma patients post-radiotherapy under the supervision of Dr. Marc de Perrot at Toronto General Hospital. Outside of research, she enjoys swimming, cafe hopping, writing, and reading about sociology.
Rachel Yang is a first-year MSc student studying the capability of a nanoparticle for precise tumor magnetic resonance imaging and its potential to reduce hypoxia to complement radiotherapy. She is conducting her research under the supervision of Dr. Michael Milosevic at the Princess Margaret Cancer Research Tower. In her spare time, she takes pleasure in taking walks, running outdoors, playing songs on the piano, and trying out new restaurants.


Elizabeth Karvasarki (Lead) is a PhD IMS at Mount Sinai Catheterization Laboratory under the supervision of Dr. Susanna Mak. Her research involves investigating right ventricular and pulmonary arterial interactions in patients with pulmonary hypertension and heart failure. Outside of research, Elizabeth practices martial arts and is a 4th degree black belt.
Mahbod Ebrahimi is a second-year MSc student investigating the association between immune gene expression and schizophrenia subphenotypes under the supervison of Dr. James Kennedy. Outside of research, Mahbod enjoys a good book, playing chess, and listening to Jazz music. Mahbod is also a member of our social media team.
Kevan Clifford Anthaea-Grace Patricia Dennis Sipan Haikazian
Lauren Levy Suraiya Mangra Karan Patel Beatrix Wang
1 Minimally Invasive Surgery (MIS)1
What is it?
What is it?
What are the advantages?
What are the advantages?
What surgeries is MIS used for?
What surgeries is MIS used for?
Example of MIS:
Example of MIS:
Making small incisions with specialized instruments to minimize tissue damage
Making small incisions with specialized instruments to minimize tissue damage.
Less risk and pain, quicker recovery time, reduced scarring.
Less risk and pain, quicker recovery time, reduced scarring.
Brain, heart, colon, kidney, and orthopedic surgery, amongst others.
Brain, heart, colon, kidney, and orthopedic surgery, amongst others.
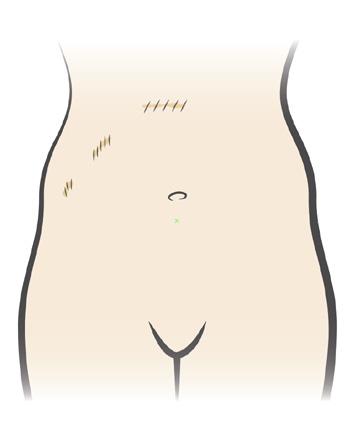
Laparoscopic cholecystectomy: Removing the gallbladder by making key-hole incisions via a laparoscope.
Laparoscopic cholecystectomy: Removing the gallbladder by making key-hole incisions via a laparoscope.
What is it?
What is it?
What are the advantages?
What are the advantages?
What surgeries is RAS used for?
What surgeries is RAS used for?
Example of RAS:
Example of RAS:
What is it?
What is it?
What are the advantages?
What are the advantages?
What surgeries is 3D printing used for?
What surgeries is 3D printing used for?
Example of 3D printing in surgery:
Example of 3D printing in surgery:
Creates patient-specific models, implants, prosthetics and surgical guides using 3D printing technology
Creates patient-specific models, implants, prosthetics and surgical guides using 3D printing technology
Can enable more personalized treatment and improved surgical accuracy and long-term outcomes.
Can enable more personalized treatment and improved surgical accuracy and long-term outcomes.
Craniofacial, oromaxillofacial, cardiothoracic and orthopedic surgeries, amongst others.
Craniofacial, oromaxillofacial, cardiothoracic and orthopedic surgeries, amongst others.
Patient-specific knee replacement: The prosthetic joint used for knee replacement is custom-designed and 3D-printed to precisely fit the patient’s knee
Patient-specific knee replacement: The prosthetic joint used for knee replacement is custom-designed and 3D-printed to precisely fit the patient’s knee
A type of MIS using advanced robotic systems (controlled by surgeons) to direct the execution of precise surgical maneuvers.
A type of MIS using advanced robotic systems (controlled by surgeons) to direct the execution of precise surgical maneuvers.
Allows for greater range of motion and dexterity, therefore improved surgical outcomes.
Allows for greater range of motion and dexterity, therefore improved surgical outcomes.
Colorectal, heart, head and neck, urologic and thoracic surgery, amongst others.
Colorectal, heart, head and neck, urologic and thoracic surgery, amongst others.
da Vinci Surgical System: Provides a surgeon-guided system console with robotic hands (with a built-in tremor-filtration) that hold the instruments; and a 3D high-definition camera view of the surgical area.
da Vinci Surgical System: Provides a surgeon-guided system console with robotic hands (with a built-in tremor-filtration) that hold the instruments; and a 3D high-definition camera view of the surgical area.

org/tests-procedures/minimally-invasive-surgery/about/pac-20384771
2. What is robotic surgery? [Internet]. [cited 2024 Feb 9]. Available from: https://www uclahealth.org/medical-services/robotic-surgery/what-robotic-surgery#:~:text=During%20a%20robotic%2Dassisted%20procedure,surgeon%20moves%2C%20inside%20your%20body
2. What is robotic surgery? [Internet]. [cited 2024 Feb 9]. Available from: https://www uclahealth.org/medical-services/robotic-surgery/what-robotic-surgery#:~:text=During%20a%20robotic%2Dassisted%20procedure,surgeon%20moves%2C%20inside%20your%20body
3. What is da Vinci Robotic Surgery? A Complete Overview [Internet]. [cited 2024 Feb 9]. Available from: https://www.intuitive.com/en-us/patients/da-vinci-robotic-surgery
3. What is da Vinci Robotic Surgery? A Complete Overview [Internet]. [cited 2024 Feb 9]. Available from: https://www.intuitive.com/en-us/patients/da-vinci-robotic-surgery
4. Hoang, D., Perrault, D., Stevanovic, M., & Ghiassi, A. (2016). Surgical applications of three-dimensional printing: a review of the current literature & how to get started Annals Of Translational Medicine, 4(23), 456. doi:10.21037/atm.2016.12.18
4. Hoang, D., Perrault, D., Stevanovic M., & Ghiassi, A. (2016). Surgical applications of three-dimensional printing: a review of the current literature & how to get started Annals Of Translational Medicine, 4(23), 456. doi:10.21037/atm.2016.12.18
5. Image guided surgery [Internet]. 2021 [cited 2024 Feb 9]. Available from: https://www.neurosurgery.columbia.edu/patient-care/treatments/image-guided-surgery#:~:text=Image%20guided%20surgery%20is%20any,was%20a%20technique%20called%20fluoroscopy
5. Image guided surgery [Internet]. 2021 [cited 2024 Feb 9]. Available from: https://www.neurosurgery.columbia.edu/patient-care/treatments/image-guided-surgery#:~:text=Image%20guided%20surgery%20is%20any,was%20a%20technique%20called%20fluoroscopy
6. What is image-guided therapy? [Internet]. [cited 2024 Feb 9]. Available from: https://www brighamandwomens.org/research/amigo/image-guided-therapy-at-bwh
6. What is image-guided therapy? [Internet]. [cited 2024 Feb 9]. Available from: https://www brighamandwomens.org/research/amigo/image-guided-therapy-at-bwh
7. Asiri, A., AlBishi, S., AlMadani, W., ElMetwally A., & Househ, M. (2018). TheUse of Telemedicine in Surgical Care: a Systematic Review Acta
7. Asiri, A., AlBishi, S., AlMadani, W., ElMetwally, A., & Househ, M. (2018). TheUse of Telemedicine in Surgical Care: a Systematic Review Acta informatica medica : AIM journal of the Society for Medical Informatics of Bosnia & Herzegovina : casopis Drustva za medicinsku informatiku BiH, 26(3), 201–206. https://doi org/10.5455/aim.2018.26.201-206
medicinsku informatiku BiH, 26(3), 201–206. https://doi org/10.5455/aim.2018.26.201-206
Image-Guided Surgery5,6
What is it?
What is it?
What are the advantages?
What are the advantages?
What surgeries is image-guided surgery used for?
What surgeries is image-guided surger y used for?
Example of image-guided surgery:
Example of image-guided surger y:
Smart surgical lights
Smart surgical lights
Adaptive lamps that adjust the colour temperature and intensity in the surgical room to eliminate shadows, optimize visibility, and reduce eye strain for the surgical team9.
Adaptive lamps that adjust the colour temperature and intensity in the surgical room to eliminate shadows, optimize visibility, and reduce eye strain for the surgical team9
Using real-time images of the inside of the body (produced by a combination of X-rays, CT scans, computers and other technology) to help visually inform the surgeon and guide the surgical procedure as it is being carried out
Using real-time images of the inside of the body (produced by a combination of X-rays, CT scans, computers and other technology) to help visually inform the surgeon and guide the surgical procedure as it is being carried out.
Enhances precision, accuracy and safety of the surgery.
Enhances precision, accuracy and safety of the surgery.
Most commonly for brain surgery, but can be applied to others too
Most commonly for brain surgery, but can be applied to others too
Brain tumor removal: Uses live-imaging MRI to identify and target the area of the brain that requires tumor removal, without disrupting other critical structures.
Brain tumor removal: Uses live-imaging MRI to identify and target the area of the brain that requires tumor removal, without disrupting other critical structures.
What is it?
What is it?
What are the advantages?
What are the advantages?
What surgeries is telemedicine used for?
What surgeries is telemedicine used for?
Example of telemedicine:
Example of telemedicine:
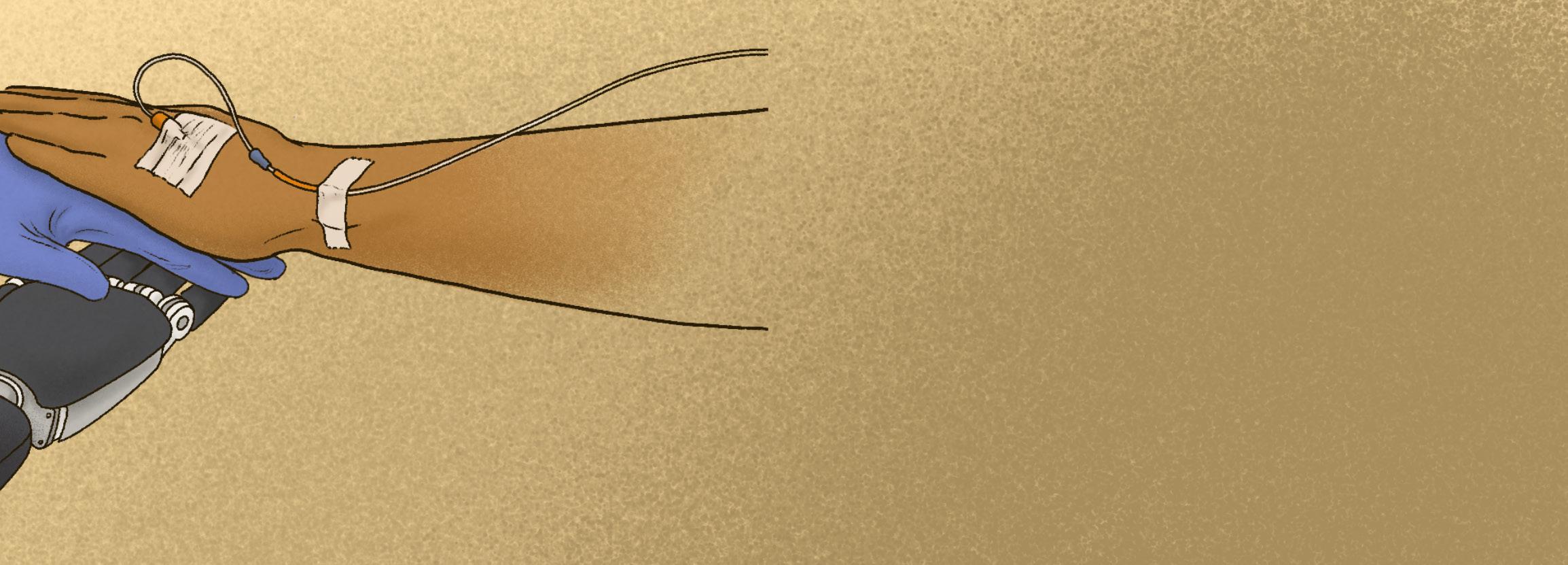
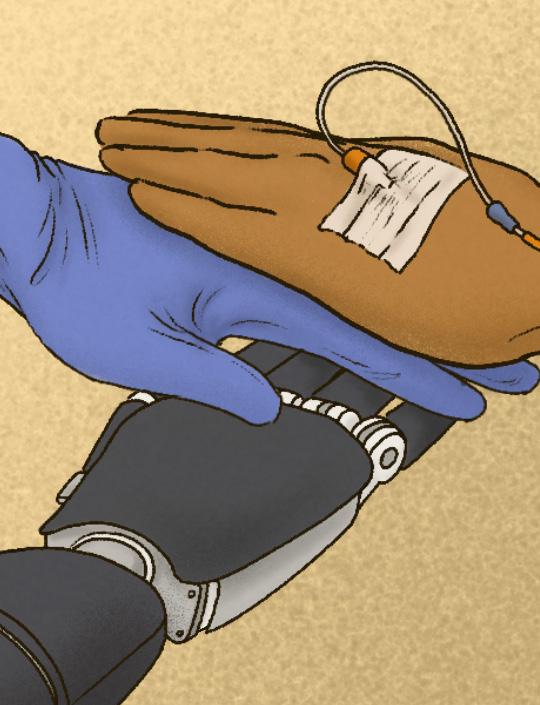
Remote physician-patient communication via telecommunication technologies; used in pre- and post-operative surgical consultation, monitoring, and even some types of surgical procedures (telesurgery).
Remote physician-patient communication via telecommunication technologies; used in pre- and post-operative surgical consultation, monitoring, and even some types of surgical procedures.
Expands the access to specialized care and expertise, particularly in underserved areas, while minimizing travel requirements.
Expands the access to specialized care and expertise, particularly in underserved areas, while minimizing travel requirements.
Most types (general surgery, bariatric surgery, appendectomy, etc.).
Most types (general surgery, bariatric surgery, appendectomy, etc.).
Telesurgery: Doctor uses a wireless network and robotic technology to perform surgery on a patient that is in a physically different location.
Telesurgery: Doctor uses a wireless network and robotic technology to perform surgery on a patient that is in a physically different location.
3D surgical camera
3D surgical camera
Live capturing of the surgical area to provide depth perception and enhance visualization for the surgeon, commonly used in minimally invasive procedures13
Live capturing of the surgical area to provide depth perception and enhance visualization for the surgeon, commonly used in minimally invasive procedures13
Laser scalpel
Laser scalpel
built with hollow core optic fibre technology that deliver laser pulses to carry out ultraprecise cutting and cauterization of tissue10.
built with hollow core optic fibre technology that deliver laser pulses to carry out ultraprecise cutting and cauterization of tissue10.
8. Choi P J Oskouian, R J., & Tubbs, R. S. (2018). Telesurgery: Past Present and Future Cureus, 10(5), e2716. https://doi org/10.7759/cureus.2716
9. Iled 7 surgical light [Internet]. [cited 2024 Feb 9]. Available from: http://www.hillrom.ca/en/products/iled-7-surgical-light/ 10. Precision Laser scalpel [Internet]. Heriot-Watt University; 2021 [cited 2024 Feb 9]. Available from: http://www hw.ac uk/uk/research/global/medical-technology/precision-laser-scalpel htm
11. Gani, A., Pickering, O., Ellis, C., Sabri, O., & Pucher, P. (2022). Impact of haptic feedback on surgical training outcomes: A Randomised Controlled Trial of haptic versus non-haptic immersive virtual reality training. Annals of medicine and surgery (2012), 83, 104734. https://doi org/10.1016/j amsu.2022.104734
Iled 7 surgical light [Internet]. [cited 2024 Feb 9]. Available from: http://www.hillrom.ca/en/products/iled-7-surgical-light/ 10. Precision Laser scalpel [Internet]. Heriot-Watt University 2021 [cited 2024 Feb 9]. Available from: http://www hw.ac uk/uk/research/global/medical-technology/precision-laser-scalpel htm 11. Gani, A., Pickering, O., Ellis, C., Sabri, O., & Pucher, P. (2022). Impact of haptic feedback on surgical training outcomes: A Randomised Controlled Trial of haptic versus non-haptic immersive virtual reality training. Annals of medicine and surgery (2012), 83, 104734. https://doi org/10.1016/j amsu.2022.104734
12. Ntakakis, G., Plomariti, C., Frantzidis, C., Antoniou P. E., Bamidis, P D., & Tsoulfas, G. (2023). Exploring the use of virtual reality in surgical education. World journal of transplantation, 13(2), 36–43. https://doi org/10.5500/wjt.v13.i2.36
13. Baum, S., Sillem, M., Ney J T Baum, A., Friedrich, M., Radosa, J Kramer K. M., Gronwald B Gottschling, S., Solomayer, E. F Rody A., & Joukhadar R. (2017). What Are the Advantages of 3D Cameras in Gynaecological Laparoscopy?. Geburtshilfe und Frauenheilkunde 77(1), 45–51. https://doi org/10.1055/s-0042-120845
12. Ntakakis, G., Plomariti, C., Frantzidis, C., Antoniou P. E., Bamidis, P D., & Tsoulfas, G. (2023). Exploring the use of virtual reality in surgical education. World journal of transplantation, 13(2), 36–43. https://doi org/10.5500/wjt.v13.i2.36 13. Baum, S., Sillem, M., Ney, J T., Baum, A., Friedrich, M., Radosa, J., Kramer, K. M., Gronwald, B., Gottschling, S., Solomayer, E. F., Rody, A., & Joukhadar R. (2017). What Are the Advantages of 3D Cameras in Gynaecological Laparoscopy?. Geburtshilfe und Frauenheilkunde, 77(1), 45–51. https://doi org/10.1055/s-0042-120845

Lung cancer continues to be the leading cause of cancer-related deaths in Canada.1 Despite this, health professionals, including physicians and surgeons must adhere to established standards of care even if there are instances where current technology or techniques fall short in delivering the optimal care and outcomes for patients. This underscores the need for continuous efforts aimed at researching and establishing new standards, to ensure an ongoing progression in improving care for patients affected by this prevalent and challenging disease.
Dr. Kazuhiro Yasufuku, the Head of Thoracic Surgery at Toronto General Hospital (TGH), goes beyond the confines of direct patient care. Engaged in both clinical practice and research, he seeks to extend his impact outside of the operating room. Driven by a commitment to make a broad impact, he aims to “make a difference for many more patients than what [he] can actually do as only a surgeon.” Dr. Yasufuku is also a senior scientist at the Latner Thoracic Surgery Research Laboratory, Professor of Surgery at the University of Toronto, Director of Endoscopy and Director of the Interventional Thoracic Surgery Program at the University Health Network (UHN). After completing his medical education at Japan’s Chiba University School of Medicine in 1992, he continued practicing medicine and conducting research at TGH and has become a pioneer and leader in the field of minimally invasive diagnostics and therapeutics for thoracic malignancy.
One key focus of Dr. Yasufuku’s research involves advancing image-guided diagnosis and surgical approaches for lung cancer patients. When he initially began practicing medicine, “minimally invasive thoracic surgery was still in its infancy; we weren’t using thoracoscopes, we weren’t using minimally invasive approaches,” Dr. Yasufuku recalls. Traditionally, clinicians used a thin, flexible tube, called a bronchoscope, inserted through the nose or mouth and down the throat, to visualize the airways in the lungs. However, these bronchoscopes only allowed visualization of what was directly in the airway, and sometimes the airways themselves were normal; as a result of these limitations, it was reported that only 29% of carcinoma in situ and 69% of microinvasive tumors were detectable using these white light bronchoscopes.2 A tremendous advancement in the field of lung cancer diagnosis and staging came with the introduction of the Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration (EBUS-TBNA), co-developed by Dr. Yasufuku and the biotechnology company Olympus in 2002.3 Explaining how EBUS-TBNA came to be, Dr. Yasufuku says that he drew from personal experience: “as a surgeon, you’re seeing patients, and you understand what the issues are and what current technology does not provide.” It encouraged him to design a tool that could serve as an effective diagnosing instrument that had yet to be discovered. EBUS-TBNA involves a very small ultrasound probe tethered at the end of a bronchoscope; it enters the
airway in a minimally invasive fashion, and instead of only seeing the airways, it enables the visualization of important structures under the airways, including potentially abnormal lymph nodes and large vessels.3 Once lymph nodes are identified, a needle can be inserted into the bronchoscope, piercing through the airway and directly into the lymph node to collect a sample. This sample is then examined by a pathologist to determine whether the lymph node is involved in cancer – critical to the decisions that will be made in creating treatment plans for patients.
One of Dr. Yasufuku’s ongoing projects includes utilizing micro-samples collected from EBUS-TBNA for diagnosis and staging, as well as genetic profiling to assess if patients are suitable for specific molecular-targeted agents in the treatment of lung cancer. For instance, EBUS-TBNA samples can be used to assess for genetic variants such as in the epidermal growth factor receptor to create personalized chemotherapy treatment for patients.4 Furthermore, there are also emerging
biomarkers for predictive or diagnostic purposes, such as using the concentration of cytokeratin-19 mRNA in lymph nodes as a marker for metastasis.4 With its ability to collect high-quality biopsy samples in a minimally invasive manner for histopathological and molecular analyses, EBUS-TNBA has become the standard of care for minimally invasive modality in sampling mediastinal lymph nodes and lung cancer staging.5


Head, Division of Thoracic Surgery, Toronto General Hospital, University Health Network (UHN), Director of Endoscopy, UHN, Director, Interventional Thoracic Surgery Program, UHN
with Techna and OK Fiber Technology, the Yasufuku lab has developed a remarkably small fiberscope capable of fluorescing tumor nodules and simultaneously performing photothermal therapy.6 This fiberscope (less than a millimeter in size) can reach much deeper in the lung compared to earlier, less flexible fiberscopes. Dr. Yasufuku is continually evaluating the use of the fiberscope in conjunction with the porphysome nanoparticle, aiming to concurrently visualize and treat lung tumors that are not discernible macroscopically. “The ultimate goal is to treat lung cancer nodules without making an incision,” says Dr. Yasufuku.
References
1. Public Health Agency of Canada. Government of Canada [Internet]. / Gouvernement du Canada; 2023 [cited 2024 Feb 13]. Available from: https://www.canada.ca/en/public-health/services/chronic-diseases/cancer/lung-cancer.html
2. Andolfi M, Potenza R, Capozzi R, et al. The role of bronchoscopy in the diagnosis of early lung cancer: A Review. J Thorac Dis. 2016 Nov [cited 2024 Feb 13];8(11):3329–37. Available from: https:// www.ncbi.nlm.nih.gov/pmc/articles/PMC5179455/ doi:10.21037/ jtd.2016.11.81
3. Yasufuku K, Chiyo M, Sekine Y, et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest [Internet]. 2004 Jul [cited 2024 Feb 19];126(1):122–8. Available from: https://www.sciencedirect.com/ science/article/pii/S0012369215329044?via%3Dihub doi:10.1378/ chest.126.1.122
4. Oezkan F, Khan AM, Zarogoulidis P, et al. Efficient utilization of EBUS-TBNA samples for both diagnosis and molecular analyses. OncoTargets and Therapy [Internet]. 2014 Nov [cited 2024 Feb 19];2061. Available from: https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC4234164/#:~:text=Dividing%20EBUS%2DTBNA%20 samples%20for,needle%20passes%20for%20molecular%20analyses. doi:10.2147/ott.s72974
Dr. Yasufuku is committed to exploring the potential of employing this minimally invasive approach in lung cancer treatment. He states, “My ultimate goal for lung cancer treatment is to use a very small bronchoscope to approach nodules for a diagnosis, and subsequently, employing different energy modalities to treat and cure the cancer.” Pursuing this objective, one of his ongoing projects, in collaboration with Dr. Gang Zheng, focuses on using porphysomes, nanoparticles that preferentially accumulate and fluoresce in tumors, to guide surgeons to precise locations of tumor nodules.6 Collaborating
Dr. Yasufuku emphasizes, “At the end of the day, it’s all about identifying what we lack in medicine and doing our best to address these challenges.” He remains dedicated to scrutinizing current standards of care through a patient-centric lens, focusing on research that makes positive and direct impacts on patients. Through his groundbreaking work on the EBUS-TBNA, he has revolutionized the lives of lung cancer patients globally, providing an alternative to invasive surgeries. Dr. Yasufuku’s ongoing research of using micro-samples for personalized patient treatments and incorporating porphysome nanoparticles with photothermal therapy strives to offer minimally invasive treatment alternatives for lung cancer patients. He envisions a future for the field of thoracic surgery where the diagnosis and treatment of lung cancer patients can be achieved entirely in a minimally invasive manner.
5. Torre M, Reda M, Musso V, et al. Diagnostic accuracy of endobronchial ultrasound-transbronchial needle aspiration (EBUS-TBNA) for mediastinal lymph node staging of lung cancer. Mediastinum. 2021 Jun 25 [cited 2024 Feb 13];5(15). Available from: https:// www.ncbi.nlm.nih.gov/pmc/articles/PMC8794299/ doi:10.21037/ med-21-2
6. Kinoshita T, Effat A, Gregor A, et al. A novel laser fiberscope for simultaneous imaging and phototherapy of Peripheral Lung Cancer. Chest. 2019 Sept [cited 2024 Feb 13];156(3):571–8. Available from: https://pubmed.ncbi.nlm.nih.gov/31034817/ doi:10.1016/j. chest.2019.04.010

 By Nikou Kelardashti
By Nikou Kelardashti
In the intricate world of neurosurgery, Dr. Gelareh Zadeh stands as a beacon of innovation, reshaping patient care and pushing the boundaries of scientific inquiry. As a Professor at the Department of Surgery at University of Toronto, Head of Neurosurgery at Toronto Western Hospital, and Senior Scientist at Princess Margaret Cancer Research Institute, Dr. Zadeh’s impact in the field of neurosurgery and neuro-oncology is vast and transformative.
The desire to have a direct, tangible impact in the world emerged as the primary motivation guiding Dr. Zadeh toward a career in medicine. However, her interest and motivation to pursue research deepened as she started to pursue the field of neurosurgery. Dr. Zadeh explains “the field has a lot of potential. It is in its infancy and has room to grow in how we treat patients, advances that will directly impact patients and change how we practice.” Driven by these insights, she embarked on a journey that led to her pursuit of a PhD at University of Toronto, where she actively engaged in “learning the new language of research.”
During her PhD, Dr. Zadeh focused on tumour angiogenesis, a process characterized by the growth of new blood vessels within a tumour. These blood vessels play a crucial role in growth and progression of cancerous tumours. Dr. Zadeh’s focus was to investigate the factors influencing this blood vessel development and understand its implications for
diseases, vascular malformations, and other complications. During her PhD work, Dr. Zadeh maintained a broad approach, remaining open to different subspecialties within the field of neurosurgery.
When Dr. Zadeh established her own laboratory, molecular genomics and epigenomic profiling had gained significant popularity. Reflecting on this era, Dr. Zadeh draws a parallel to current times, stating, “I think what molecular biology was then is what AI [artificial intelligence] is now”. Consequently, her lab focused on establishing markers of brain tumours. It was then that she focused on researching tumours which were relevant to her clinical practice, including meningioma, schwannoma, and glioma. These tumours differ in the types of cells from which they originate. Meningiomas originate from the meninges, which are the tissue layers that cover the brain. Schwannomas originate from Schwann cells, which produce myelin (the protective covering around peripheral nerves). Lastly, gliomas originate from the glial cells, which are the supportive cells of the central nervous system.1 For tumour research associated with these three cell types, Dr. Zadeh and her lab focused on establishing multiplatform understanding of tumour biology. This approach facilitated improvements in diagnosis, development of predictors for treatment response, and overall advancements in understanding and managing these tumour conditions.
Meningiomas are one of the most prevalent types of brain tumours.2 Traditionally, the classification of the specific subtypes of these tumours relied on histopathology according to the World Health Organization. However, this classification has proven inadequate in accurately representing the clinical behavior of all meningiomas.2 Dr. Zadeh and her team have combined various molecular genomic techniques and pioneered a new classification system, which demonstrates a more reliable prediction of tumour behavior and recurrence compared to histopathology-based classification. The implementation of this innovative approach holds the potential to enhance therapeutic decision-making significantly.
Despite being a prevalent type of brain tumour, meningiomas have unfortunately received insufficient attention due to a lack of awareness and advocacy for further research. To address this gap, in 2016, Dr. Zadeh co-founded and currently leads the International Consortium on Meningiomas (ICOM). ICOM is a multidisciplinary and multi-institutional collaborative group with the aim of increasing awareness of meningiomas. ICOM brings international institutions together to optimize research by pooling data, samples, and patient information. Dr. Zadeh reflects on the success of the consortium, stating it “allowed us to build that momentum to the point that when we introduced it in 2016 to now it has become the mainstay of the scientific meeting that happens every year at society of neuro-oncology. More than


Professor at the Department of Surgery at University of Toronto, Head of Neurosurgery at Toronto Western Hospital, and Senior Scientist at Princess Margaret Cancer Research Institute
Photo Credit: Dr. Zadeh
120 members work together, collaborate, and produce publications.”
Dr. Zadeh and her team have also made significant strides in the development of non-invasive diagnostic tools. Traditionally, accurate diagnosis of intracranial tumours required invasive surgery to obtain tissue samples. However, Dr. Zadeh’s groundbreaking research has demonstrated that plasma obtained from a blood sample contains DNA-methylation profiles that can enable the discrimination of common intracranial tumours.3 This non-invasive approach mitigates the risks associated
with invasive surgery for tissue sampling. Consequently, this innovative method, through a simple blood test, facilitates risk assessment for tumour development, enables early detection, and, by classifying the tumour, empowers clinicians to choose the most effective treatment approach.
All these research projects are meticulously designed to efficiently address the needs of both patients and clinicians, ensuring that the findings seamlessly translate into clinical practice. The success of this integration is attributed to Dr. Zadeh’s dual role, actively engaged in both clinical and research fields. As a clinician-scientist, Dr. Zadeh holds a unique position, shaping her research questions based on invaluable insights gained from daily experiences in clinical settings and operating rooms. Dr. Zadeh emphasizes, “it is that day-to-day in clinical and operating room that I see these questions that are presented to us and how do we do better because there are gaps and limitations in what we can do. So having that perspective of a clinician is very helpful.”
Additionally, Dr. Zadeh and her team are at the forefront of innovative clinical trials aimed at enhancing treatment for glioblastoma, an exceptionally malignant form of glioma with a challenging prognosis.4 Notably, Dr Zadeh’s team has successfully classified different types of glioblastomas based on their immune microenvironment. Within this classification, a subset of glioblastomas exhibit an immunosuppressive
microenvironment, which makes them resistant to traditional immunotherapy. Dr. Zadeh explains, “the emerging technology is for us to change the method by which we have been trying to make advances and that is to change the mechanism by which we deliver treatment into the tumour.” In response, to tackle this subtype of glioblastoma tumours, they inject the tumour with oncolytic viruses to infect cancer cells and stimulate an immune response.4 This strategic shift to a more immunogenic microenvironment enhances the effectiveness of immunotherapy.
In conclusion, Dr. Zadeh’s profound contributions to the field of neurosurgery underscore her unwavering commitment to advancement. As the first female chair of neurosurgery at the University of Toronto, she breaks barriers leaving a significant mark on the scientific and medical landscape. Dr. Zadeh’s legacy extends beyond her ground-breaking research, resonating in the inspiration and guidance she provides to the next generation of medical professionals, setting a powerful example for inclusivity and excellence in the ever-evolving field of neurosurgery.
References
1. Mayo Clinic. “Brain Tumor - Symptoms and Causes.” Mayo Clinic, 21 Apr. 2023, www.mayoclinic.org/diseases-conditions/brain-tumor/symptoms-causes/syc-20350084.
2. Nassiri F, Liu J, Patil V, et al. A clinically applicable integrative molecular classification of meningiomas. Nature. 2021 Sep 2;597(7874):119-25.
3. Nassiri F, Chakravarthy A, Feng S, et al. Detection and discrimination of intracranial tumors using plasma cell-free DNA methylomes. Nature medicine. 2020 Jul;26(7):1044-7.
4. Nassiri F, Patil V, Yefet LS, et al. Oncolytic DNX-2401 virotherapy plus pembrolizumab in recurrent glioblastoma: a phase 1/2 trial. Nature Medicine. 2023 May 15:1-9.
 By Eileen (Xiao Yu) Liu
By Eileen (Xiao Yu) Liu
Recently, I interviewed Dr. Vitor Pereira, a renowned neurointerventionist currently working at St. Michael’s Hospital. Our conversation revealed the transformative journey that led him to the field of medicine. Growing up in an island in northeastern Brazil and studying computating science, Dr. Pereira shifted towards a career towards medicine as a result of his father’s illness.
As a medical student, Dr. Pereira became captivated by the neuro field and neurosurgery. He acknowledged the significant role played by Professor Pierre Lasjaunias, who emphasized the importance of neuroangiographic anatomy, embryology, disease pathomechanisms, and genetics. Professor Lasjaunias recommended a continuation of Dr. Pereira's training under the guidance of Jacques Moret, a renowned neurointerventionist. This opportunity allowed Dr. Pereira to gain profound knowledge on the anatomy and technical skills to navigate each procedure with care and precision. To this day, he is greatful for the transformative influence that Professor Lasjaunias and Professor Moret have had on shaping not only his practice, but also the broader field of neurointervention.
In the beginning of his career, the impact of stroke lingered in his mind as there was a lack of effective treatments available for these patients. “The fact that we couldn’t do anything for our patients stroked me,” Dr. Pereira explained. “I always carried that in the back of my mind thinking that if we are
developing minimally invasive treatments for brain aneurysms, we should be able to do something similar for stroke as well.”
Few years later in 2009, after his fellowship where he saw the infancy of endovascular stroke, he works in a pioneer project together with few centers in Europe to develop a transformative technology to remove clot from bain vessels, devices called stent retrievers. He also led first prospective trials as well as randomized controlled trials that, in 2015, made endovascular stroke treatment standard of care. During our discussion, Dr. Pereira brought up some of the challenges that occurred in the early phases of introducing innovative techniques, particularly in stroke treatment: “In society, not only medicine, innovation and novelty drives fear. There was quite a lot of resistance from a conservative group of academics but this was all overcome after the randomized controlled trials.
Since he started his practice in Canada 10 years ago, one of Dr. Pereira’s proudest achievements is the RADIS Lab, which was co-founded by him self and Ms. Nicole Cancelliere. It is dedicated to translating pioneering research and the application of cutting-edge technologies in treating neurovascular diseases. RADIS is an acronym that highlights the technologies used to tacle the clinical challenges he and his team face in the neurovascular clinic at St Michaels Hospital. It stands for Robotics, Artificial intelligence, Dynamic flow, Imaging and Simulation. as it fosters collaboration between clinicians
and scientists, driving innovations in robotics, artificial intelligence, procedure simulation, and new imaging technologies. Dr. Pereira highlighted groundbreaking projects, including the world's first robotic aneurysm treatment and contributions to the development of novel devices like the Surpass EVOLVE flow diverter and the BossStent venous stenosis treatment device. The Surpass EVOLVE flow diverter is used to treat brain aneurysms, while the BossStent is a stent being used to treat symptomatic cerebral venous diseases, including venous stenosis. Also, the RADIS lab was a pioneer in the use of OCT (optical coherence tomography) to diagnosis neurovascular diseases and to assist interventional neuroradiology procedures.
"Improve accessibility and expertise in patient care"
A major area of focus for Dr. Pereira and his lab is the development of remote robotics. Surgical robots are already known to enhance precision in neurointervention. In neurointervention, the use of robots to manipulate the different devices emerged over the last decade driven by goals of radiation protection and precise manipulation of the neurointerventional devices. In 2019, Dr. Pereira and his team performed the world's first cases of brain aneurysms treatment using robotic assistance, which marked a significant milestone in the field of neurointervention. “Even with this first generation of robotic,

Director of Endovascular Research and Innovation, St. Michael’s Hospital, Lead Scientist, Li Ka Shing Knowledge Institute, Professor of Surgery and Medical Imaging, University of Toronto
we already saw that we can be more precise placing coils and stents for brain aneurysm treatment,” Dr. Pereira explained. Results from additional studies demonstrated the robot’s enhanced technical skills, which potentially could be a great tool for the less-experienced neurointerventionalists. Dr. Pereira foresees the integration of artificial intelligence (AI) and automation in the next generation of robotic neurointervention, further refining capabilities.
A significant benefit of remote robotics is to expand access to care to patients with acute conditions, such as stroke that require urgent care in remote locations. In vast geographical regions like Canada, the United States, China, and Russia, where access to neurointerventional expertise is limited, remote robotics may offer a solution by reducing the transfer time for patients in need of immediate treatment. Dr. Pereira believes that the use of remote robotics will have more societal impact in areas where there is a lack of material resources and human support available and accessible to patients. While the current affordability of devices remains a challenge, the ongoing development of these devices will allow them to become a more cost-effective solution. Dr. Pereira emphasizes that while robots will never replace human expertise, their cost-effectiveness and potential to function with low maintenance make them a pragmatic and impactful addition to neurointerventional practices. He hopes that this addition will help to improve accessibility and expertise in patient care.
Looking ahead to the next five to ten years, Dr. Pereira shared insights into emerging technologies within the field of neurointervention. In stroke treatment, he emphasized the potential of remote robotics as a way to improve access to care. For brain aneurysms, Dr. Pereira envisions leveraging coated devices to further reduce complication rates. Exploring new frontiers, he emphasized the use of dedicated devices for conditions like venous stenosis and idiopathic intracranial
hypertension, as well as the intravascular delivery of chemothereapy or radiation for brain tumors. On the technological front, Dr. Pereira sees a growing role for MRI in interventions, with ongoing studies and device developments that will allow us to shift from using traditional angiography with X-ray to perform interventions, to instead us MRI machines. Overall, Dr. Pereira see a future where the “trend is to use more technology to better triage and help patients to make treatment decisions.” He strongly believes understanding more about the disease and ensuring the safety and reliability of treatment is crucial for improving patient outcomes and advancing medical sciences.

Growing up during a period of tension between the Betancur and Barco administrations, guerilla insurgents, and rising Colombian drug cartels, Dr. David Gomez bore witness to high levels of violence and civil conflict throughout his home country, provoking his interest in trauma surgery.
At that time, Colombia’s healthcare system had three sectors: public, social insurance, and private insurance. Pre-existing socioeconomic inequalities intersected with the mix of public and private care to create barriers in access, leaving about 15% of the population with no access to acceptable healthcare services at all.1 The subsequent gradient in access to timely and quality surgery became evident to Dr. Gomez, a medical student at the time, who was driven to examine broad aspects of surgical access in his research career. While completing his medical and research training in Sydney, Australia and Toronto, Canada respectively, he noticed the patterns he identified in Colombia were not unique.
“Even in a high-income, well-funded public healthcare system, there were still high inequalities in access,” he noted. “If you’re able to identify interventions [to the way we provide care at a systems level], you are going to have very profound impacts on large aspects of the population – for generations sometimes.”
Today, Dr. Gomez devotes approximately 65% of his time to research as an Assistant Professor in the University of Toronto Department of Surgery and Scientist at the Li Ka Shing Knowledge Institute. In his research, he is dedicated to understanding the factors that drive access from a patient perspective, striving to design systems that provide better and more equitable care. His remaining time is spent in his clinical practice, as an acute care and trauma surgeon at St. Michael’s Hospital.
As a Level I trauma centre in downtown Toronto, St. Michael’s Hospital is in the heart of need in the city. In his day-today as a clinician, Dr. Gomez sees many barriers in healthcare access, such as inability to pay or interpret language. However, he recognizes the limitations of his individual experiences. His collaborators help to fill in some of those gaps, coming from a range of backgrounds, such as obstetrics and gynaecology, ophthalmology, and neurology.
“Be bold, be broad,” is his advice to trainees. “Being uncomfortable, reaching across the aisle to other fields is a way to be much more impactful…and you will bear the fruit of that, because you will be a more resilient scientist, able to pivot and collaborate across fields.”
His current research examines the surgical backlog: approximately one million procedures across Canada that would have been completed if not for the COVID-19 pandemic.2 The pandemic necessitated
large public health interventions, where “for the first time ever, governments told all hospitals they had to halt nonessential surgical care” – three separate times. This further weakened an already-strained system. For example, only 50% of knee replacement and 57% of hip replacement patients received surgery within the recommended time frame in 2022. This was a dramatic decrease in timely care from pre-pandemic levels, where about 70% of knee replacements and 75% of hip replacements were completed within the recommended period.2 As patients are left waiting, many will be continuously impacted by symptoms like loss of mobility or chronic pain, and some will become ineligible for surgery altogether, leading to worsened outcomes.
“We have barely been able to recover to numbers [of surgical cases] we were doing before the pandemic, but have never been able to over-perform in any significant way […] so we have never been able to catch up,” explains Dr. Gomez.
Furthermore, the pandemic’s impact was not the same throughout time and space. For example, Northern Ontario experienced lower rates of COVID19 at the beginning, allowing surgical capacity to remain relatively resilient. However, surges from high caseloads later in the pandemic eliminated this benefit. Dr. Gomez is therefore mapping out these regional variations, to examine if “areas less impacted by COVID-19 were more resilient and [better able to]

Acute Care and Trauma Surgeon, St. Michael’s Hospital, Unity Health Toronto
Assistant Professor, Department of Surgery, University of Toronto
Adjunct Scientist, Institute for Clinical Evaluative Sciences
Scientist, Li Ka Shing Knowledge Institute, Unity Health Toronto
catch up on surgical care.” Indeed, urban neighbourhoods with high immigrant populations and low socioeconomic statuses experienced higher rates of COVID-19 and lower rates of vaccination. In these areas, not only is the backlog of cases larger, but the capacity to recover is smaller. The most complex cases were transported from suburban and rural regions to urban centres, further straining their hospitals, which are now operating with less staff who are less experienced.
The pandemic unearthed and worsened these pre-existing inequities, and has indicated that those who will face the greatest health burden are likely also those in the greatest need.
Dr. Gomez believes that fluid and topdown public health responses will be necessary in future pandemic response, allowing “geographical areas with no impact [to continue] to provide routine care in a safe way”, and adjusting. Otherwise, the system may find itself back where it is now: with one million surgical cases left unaddressed.
“We are at a tipping point right now, particularly in Ontario, because the provincial government is proposing to open a large number of for-profit surgical centres,” he cautioned. “When driving surgical recovery will be about recouping profits, the things that will be impacted [are] quality and equity. For-profit centres will choose healthy, young patients that they can treat quickly, and complex care will be off-loaded to an alreadyunderfunded public healthcare system; that will lead to further inequalities.”
Adamantly opposed to the expansion of for-profit clinics as a strategy to cope with the surgical backlog, he points to the evidence, emphasizing his own background working within the Colombian, Australian, and Canadian health systems. Privatized healthcare has not only been associated with lower equity, accessibility, and quality of care, but
also does not improve health outcomes.3 As such, Dr. Gomez is also modelling gradients in access to private cataract centres with healthcare engineers at the University of Toronto. Together, they are taking a holistic view of recovery times by various increments of increased surgical capacity, as well as potential inequalities, with the goal of building an evidence base to further strengthen the public healthcare system and examine equitable alternatives, such as not-for-profit surgical centres.
“Part of the foundation of Canada is you should be able to access the same care as everyone else because you live, work, or study here,” he said. “The way we are heading right now [is] eliminating what we have built over decades, but there is still time.”
As Canadians re-evaluate the core values of the public healthcare system, Dr. David Gomez is identifying the gaps at a broad scale, in hopes that systemic policy changes can help patch them to improve equitable access for all – no matter who, no matter where.
References
1. Esteves RJ. The quest for equity in Latin America: a comparative analysis of the health care reforms in Brazil and Colombia. International Journal for Equity in Health. 2012 Feb 2;11(1):6.
2. Canadian Institute for Health Information. Canadian Institute for Health Information. 2023 [cited 2024 Feb 9]. Surgeries impacted by COVID-19: An update on volumes and wait times.
3. Lee SK, Rowe BH, Mahl SK. Increased Private Healthcare for Canada: Is That the Right Solution? Healthc Policy. 2021 Feb;16(3):30–42.


Jeah Kim
Cellular Aging in a Morphological Aspect
I’ve always loved simplifying complex concepts and combining unrelated ideas. This 3D illustration was also created to enhance the visual interest and clarity of how we can notice the biological time of the cell by incorporating the concept of gravitational time dilation. My goal is to create visually digestible and impactful illustrations that can boost the meaning of research and inspire others. Join me on this exciting journey as I endeavor to bridge the realms of art and science! (Instagram:@fabulaurora)


Yu-Wen Jan
More than a drug: Cannabis
Hi, I’m Yu-Wen Jan. I’ve spent several years as a bench researcher at the Institute of Plant and Microbial Biology in Taiwan. Recently, I embarked on a new journey by enrolling in the MScBMC program to pursue my passion for scientific visualization. Combining my scientific background with a deepseated love for design and fine art, I specialize in creating precise and practical scientific visualizations and illustrations. My focus primarily lies in vector illustrations and graphic designs, aiming to deliver concise and informative pieces that effectively communicate complex scientific concepts.


Emily Huang

As the scientific world grows and evolves so must the avenues in which we express and teach the knowledge uncovered. I and my many talented peers are honing the skills to create and share new and innovative ways to communicate science. It is with great pride that I have the privilege to expand my capabilities in the Biomedical Communications program at the University of Toronto. I am excited to continue to create approachable and informed visual aids to accompany scientific information and discovery!
Show me the unseeable: Right Kidney
While completing my HBSc in Biomedical Science at the University of Ottawa, I had the opportunity to work alongside healthcare researchers to design logos and illustrations. Coupled with taking a few English electives, I was sure that science communication was a path I needed to follow. Now at BMC, I’m excited to develop my skills in graphic medicine, and 2D illustration and animation to create visuals that have the ability to inform and educate audiences.



The Unseeable: The Liver
As a student in the Biomedical Communications program, it has been incredible to be able to see the science in our world through a different lens. I’m so grateful to be in a field that constantly challenges me to problem solve creatively, while also applying the knowledge that I’ve gained through my experiences in clinical lab settings and university. I hope to one day realize a goal of enhancing patient education through meaningful contributions to the field of medical visualization!
 By Ilakkiah Chandran
By Ilakkiah Chandran
The 2023 Fraser Institute report revealed that wait times from general practitioner referral to receipt of treatment has increased by 198% between 1993 and 2023.1 Aside from the general increase in wait times across the country, this report also identified that the province of care and specialty are factors for wait times and, inadvertently, negatively impacting the care and patient’s quality of life. Wait times were significantly high for surgery across all specialties, with patients waiting an average of 10 months for neurosurgery since receiving a referral from their general practitioner.1 Notably, patients in New Brunswick waited 46 times longer than those in Quebec for neurosurgery.1 This report raises an interesting question regarding additional factors that impact one’s care and treatment in Canada. If a patient’s geographic location can affect their care, how do social determinants of health (SDOH) such as one’s socioeconomic status, gender, or race factor into patient wait times and overall care?
SDOH has been studied in the past, including understanding how education impacts health promotion, the racial disparities in health access and the role of housing on healthcare access. There’s an overwhelming amount of research that explores how SDOH impacts people’s healthcare
and surgical experiences. This viewpoint shows how two fictional characters, Alisha and Aiden, may navigate their surgical experience from diagnosis to recovery.
Alisha is a 45-year-old African Canadian woman. She is a single mother with 2 young boys, and also of low-income status. She lives with her older sister in an apartment building in Scarborough and works at a local grocery store. After a workplace injury, Alisha requires knee surgery.
Aiden is a 23-year-old White man. He is a single man who recently moved from British Columbia after completing his undergraduate degree and lives alone in downtown Toronto. He works a 9-5 PM job at a well-established marketing firm and is of middle-high income. Due to tears in Anterior Cruciate Ligament (ACL), Aiden is also looking to get knee surgery.
As the Fraser Institute report reveals, having access to timely surgery remains a challenge for all. However, there is a notable challenge in accessing healthcare among individuals of different SDOH statuses. A recent study conducted in 2020 revealed that despite the accessibility of hospitals in major metropolitan cities across
Canada, the suburbs around these cities experienced the lowest accessibility.2 Similarly, financial challenges such as the inability to take time off from work, the lack of paid time off, and temporary employment make it challenging for individuals to prioritize their health and wellbeing.3 Aside from these factors, it’s also important to consider the roles individuals play in others’ lives. Caregivers are more likely to prioritize the person they are caring for over their own health.4 Given these two factors, Alisha was more likely to experience challenges getting to her appointments, given the challenges with accessibility and the lack of flexibility in her job and her responsibilities as a caregiver. Now even after finally making it to their general practitioner, the nature of both their procedures would’ve required them to wait 24-29 weeks to receive treatment.1
Now, after finally being scheduled for surgery, there are additional barriers one may experience while undergoing the procedure. Experiences of racism and sexism have been described as impacting the quality of life and the health outcomes experienced. Research in obstetrics reveals that black women have experienced manifestations of racism, including instances of discrimination, loss of

agency, being objectified and being mistreated in Canada.5 Similarly, a recent study identified that surgeons were reimbursed at significantly lower rates in 8 Canadian provinces when performing surgeries on female patients.6 This may impact their willingness to take on female patients and inadvertently impact the care female patients receive. These factors impact the care Alisha will receive during her surgery compared to what Aiden may experience.
Patients are often discharged from the hospital after being monitored for a few days to weeks.7 Previous research identifies that having social support plays a significant role in the postoperative recovery of patients who have undergone surgery and can significantly impact their mental and functional health outcomes.8,9 Between Alisha and Aiden, although being single may impact their recovery and health outcomes, Alisha’s access to her sister may warrant greater social support. However, Aiden may be able to hire in-home support if necessary. In contrast, Alisha’s sister may have to work to support their day-to-day expenses. Another key factor that impacts surgical recovery is an individual’s socioeconomic status, which includes access to time off work and prioritized health. For example, previous research identifies
that absences after surgery are often associated with lower household income.10 Another study recognizes that the lack of financial resources and lower social connectivity can reduce successful surgeries and influence readmission in some surgeries.11 In this case, we can anticipate that Alisha may have more difficulty staying on course with her recovery, given her job and her lower income status. Similarly, it’s less likely that Alisha is part of a union at her job, and being in a more precarious role may require her to be ready to work earlier than she is healed.
The various factors point to Alisha facing additional barriers and challenges when navigating her surgery experience. But what does this mean? Despite wait times being a challenge experienced by the two of them, SDOH have a significant role on the overall health status of patients and their recovery. This reveals the dire need to ensure systems are equipped with adequate tools to improve accessibility, care and health outcomes as part of the interest in improving wait times is necessary.
1. Moir, M., Barua, B. & Wannamaker, H. Waiting your Turn 2023: Wait Times for Health Care in Canada, 2023 Report. (2023).
2. Boisjoly, G. et al. Measuring accessibility to hospitals by public transport: An assessment of eight Canadian metropolitan regions. J Transp Health 18, 100916 (2020).
3. DeRigne, L., Stoddard-Dare, P. & Quinn, L. Workers Without Paid Sick Leave Less Likely To Take Time Off For Illness Or Injury Compared To Those With Paid Sick Leave. Health Aff 35, 520–527 (2016).
4. Acton, G. J. Health-Promoting Self-Care in Family Caregivers. West J Nurs Res 24, 73–86 (2002).
5. Boakye, P. N. et al. Obstetric racism and perceived quality of maternity care in Canada: Voices of Black women. Women’s Health 19, (2023).
6. Chaikof, M. et al. Surgical sexism in Canada: structural bias in reimbursement of surgical care for women. Canadian Journal of Surgery 66, E341–E347 (2023).
7. Canadian Association of General Surgeons. After your Surgery. (2023).
8. Orlas, C. P. et al. Perceived social support is strongly associated with recovery after injury. Journal of Trauma and Acute Care Surgery 91, 552–558 (2021).
9. Kulik, J. A. & Mahler, H. I. Social support and recovery from surgery. Health Psychol 8, 221–38 (1989).
10. Gbolahan, O. O., Fasola, A. O., Ayantunde, A. A. & Olaopa, O. I. Evaluation of causes and predictors of non-attendance at review appointments following treatment of Maxillofacial injuries. Niger Dent J 23, 181–189 (2020).
11. Holbert, S. E. et al. Social Determinants of Health Influence Early Outcomes Following Lumbar Spine Surgery. Ochsner Journal 22, 299–306 (2022).
 By Nikou Kelardashti
By Nikou Kelardashti
From the first crude attempts at surgery to the precision of today’s robotic arms, the evolution of surgical technology reflects an unwavering pursuit of perfection in the operating room.
Historically, open surgery with large incisions was the predominant surgical method. This method allowed the surgeons to directly visualize the surgical site and made the problem more tangible. However, this invasive approach comes with drawbacks such as increased risk of infection, post-surgical pain, increased blood loss, and prolonged recovery time.1 The invention of video laparoscope in the 1980s marked a pivotal shift towards minimally invasive surgery.1 Laparoscope, a tube equipped with a camera and a light source, is inserted through a small incision into the abdominal or pelvic cavity. This enables the surgeon to visualize and examine the affected area. Consequently, laparoscopic surgery has gained popularity as a form of minimally invasive surgery.
Despite overcoming some of the disadvantages associated with open surgery, laparoscopic surgery introduced some of its own challenges. Notably, these include extended procedure times and the necessity for general anesthesia as opposed to local. In addition, a significant drawback of traditional laparoscopic surgery was the counterintuitive movement of surgical instruments, where hand movements were in the opposite direction of instruments’ motion.1 Moreover, the two-dimensional nature of its video display hindered depth perception. All these
factors rendered traditional laparoscopy challenging for inexperienced surgeons. Recognizing these limitations, robotic surgery or robot-assisted surgery has emerged as a novel minimally invasive surgery method aimed at overcoming the setbacks of the previous surgical methods.
Applications of robotic surgery span a wide range of medical specialties. In cardiac procedures like coronary artery bypass surgery and mitral valve replacement, robotic surgery has become a viable option eradicating the need for extensive incisions and ribcage openings. Within the realm of urology, many surgeries including those for prostate, kidney, and bladder can be performed robotically. Similarly, in gynecology, hysterectomy or removal of uterus is among the procedures benefiting from robotic surgery. Beyond these domains, robotic surgery is used in colorectal, general, and thoracic surgeries. The adaptability of robotic systems to various anatomical structures and surgical challenges underscores their potential to redefine the standards of care across a broad spectrum of medical interventions, marking a paradigm shift in the way surgeons approach and execute intricate procedures.
The inception of robotic surgery finds its roots in the military domain. This was prompted by challenges faced in military combat zones where access to healthcare assistance is often limited.2 Consequently, the concept of teleoperation
emerged as a solution. This would have allowed the surgeons to operate a surgical robot from a distance thereby enhancing surgical capabilities in the battlefield. Another catalyst for teleoperation came from the extended stays of astronauts in spaceships, highlighting the anticipated need for surgical expertise in space.2 All these underscored the significance of telepresence as a driving force for improving laparoscopic surgeries.
Later on, the concepts developed for military teleoperation found commercial applications making pivotal movement in the evolution of robotic surgery. The first application of a robot in surgery occurred in 1988 when Dr. Kwoh and his team at California’s Memorial Medical Center performed a neurosurgical biopsy using PUMA 560, the first flexible robotic arm.3 This innovation aimed to increase precision and guidance during procedures surpassing the capabilities of the surgeon’s hand. Afterwards, for an extended period of time, the da Vinci system, a robotic-assisted set by Intuitive Surgical (Sunnyvale, CA) dominated the field of robotic-assisted surgery. However, in recent years, other companies have tried to challenge da Vinci’s dominance, introducing an element of competition and choice to the realm of robotic surgery.
Unveiling Robotic Surgery
Robotic surgical systems are categorized into three primary types: active, semiactive, and master-slave systems.⁴ Active
systems are preprogrammed and function autonomously under the supervision of a surgeon. Semi-active systems perform pre-programmed tasks and incorporate a surgeon-driven element. The most prevalent are the master-slave systems which lack any pre-programmed tasks and depend entirely on the surgeon’s control. These systems are composed of three components. The tower (slave) is equipped with multiple arms featuring instruments such as hooks, forceps, and needle-drivers with an additional arm housing a high-resolution camera. The console (master), where the surgeon sits, is placed in the same surgical room. It gives the surgeon the ability to remotely control the tiny laparoscopic surgical instruments with a wide range of motion. The system translates the surgeon’s hand movements at the console in real time offering a 3D highdefinition view of surgical site.
In addition to mitigating the disadvantages associated with open surgery, robotic surgery has many advantages over laparoscopic surgery. These include tremor fixation, a ten-fold magnification capability, stereoscopic vision, heightened precision, and motion scaling.⁴ In addition, robotic surgery puts less physical strain on the surgeon in comparison to the alternative surgical methods.⁴
While robotic surgery offers many advantages, its utilization comes with certain drawbacks that warrant consideration. Primarily, the initial cost of purchasing and implementing the robotic
systems can be substantial.⁵ The necessity for recurrent maintenance and specialized training of surgeons further amplifies the costs associated with this type of surgery. For example, the da Vinci robot costs US$2 million, rendering it financially inaccessible for many institutions.⁵ Beyond the financial considerations, the large and obstructive nature of robotic arms present practical challenges.3 This complicates surgical procedures even in standard-sized operating rooms, frequently leading to collisions. Additionally, certain procedures require undocking and redocking of robotic arms during surgery, resulting in increased time of surgery and increased anesthesia time.3 Another drawback is the lack of tactile feedback for the surgeon and an inability to regulate the applied force effectively. Moreover, the long-term outcomes of robot-assisted surgeries remain inadequately documented. While preliminary research indicates superior short-term results in cancer operations, such as reduced blood loss and enhanced recovery times, the equivalency of longterm outcomes remains a subject of ongoing investigation.⁵ This highlights the importance of comprehensive research on long-term benefits of robot-assisted surgery.
In summary, the evolving trends in robotic surgery indicate a relentless pursuit of innovation in surgical systems. The next generation of robotic platforms is expected to achieve several key objectives including the reduction of instrument and robotic
arm sizes, the facilitation of automatic instrument exchange, the integration of tissue feedback technology, and the incorporation of artificial intelligence and machine learning. The integration of artificial intelligence stands to offer various advantages such as providing intraoperative guidance based on real-time surgical data and automating repetitive tasks, enhancing the overall efficiency of surgeons. This convergence of cutting-edge technologies signifies a paradigm shift towards precision and personalized patient care, ushering in a new era in the field of surgery.

References
1. 1. Gharagozloo F, Najam F. Robotic Surgery. New York, NY: McGraw-Hill Medical; 2008.
2. 2. Morrell ALG, Morrell-Junior AC, Morrell AG, et al. The history of robotic surgery and its evolution: when illusion becomes reality. Rev Col Bras Cir. 2021;48:e20202798.
3. 3. Kalan S, Chauhan S, Coelho RF, Orvieto MA, Camacho IR, Palmer KJ, et al. History of robotic surgery. J Robot Surg. 2010;4(3):141–7
4. 4. Bramhe S, Pathak SS. Robotic surgery: A narrative review. Cureus. 2022 Sept 15;14(9).
5. 5. Crew B. Worth the cost? A closer look at the da Vinci robot’s impact on prostate cancer surgery. Nature. 2020;580(7804):S5–7.
 By Alyona Ivanova
By Alyona Ivanova
Central nervous system (CNS) tumors, especially in children, are considered highly lethal cancers.1 The primary approach to treatment involves surgically removing the tumor; a procedure that necessitates a delicate balance between maximizing resection extent and minimizing the risk of neurological damage and associated complications.2 Unfortunately, surgeons often lack precise information about the tumor type before surgery. The current standard practice relies on preoperative imaging and intraoperative histological analysis, but their conclusiveness is not guaranteed and can sometimes be inaccurate.3
In response to this diagnostic uncertainty, there is a growing exploration of innovative technologies to augment surgical decision-making processes. Notably, the integration of neural network (NN) technologies for tumor classification during surgery emerges as a promising avenue. These advanced computational models have the potential to revolutionize the field by providing real-time insights into the molecular characteristics of tumors. By leveraging rapid sequencing for real-time analysis of genomic DNA and employing sophisticated NNs there is an opportunity to enhance the accuracy and efficiency of tumor classification, facilitating more informed and precise surgical interventions.5-7 For instance, the developed Sturgeon model is a patient-agnostic transfer-learned
neural network that enables molecular subclassification of CNS malignancies based on sparsity profiles.4 This introduction sets the stage for an exploration into the benefits and challenges associated with utilizing NN in the intricate landscape of CNS tumor surgery.
The use of NNs is just one application of artificial intelligence (AI) technologies in the operating room (OR). AI use during surgery for tumor classification offers several potential benefits, with the greatest being real-time diagnosis. AI algorithms can rapidly analyze data, providing real-time classification of tumors. This enables surgeons to make informed decisions on the spot, potentially improving the efficiency of the procedure.3 Furthermore, machine learning models can analyze complex datasets, including genomic and molecular information, with a high degree of accuracy. This can lead to more precise tumor classification compared to traditional methods, reduce the likelihood of misdiagnosis, and improve treatment planning.4 AI algorithms can also learn from a large volume of data, continually improving their accuracy and performance over time. This adaptive nature can contribute to ongoing advancements in tumor classification and surgical decision-making.4
Precision medicine, also known as personalized medicine, involves
tailoring medical treatment and interventions to the individual characteristics of each patient.9 In the case of tumor classification, precision medicine aims to customize treatment plans based on the unique molecular and genetic profile of the tumor. This personalized approach may enhance the effectiveness of therapies. Moreover, accurate intraoperative tumor classification can help surgeons achieve optimal resection during the initial surgery, potentially reducing the need for additional surgeries. This can lead to quicker recovery times and improved patient outcomes.4 Finally, by providing timely and accurate information about the tumor type, AI can assist surgeons in striking a balance between maximizing the extent of resection and minimizing the risk of neurological damage.4 This is particularly crucial in CNS surgeries.
While these benefits are promising, it’s important to note that the integration of AI technologies into surgical workflows requires careful validation, ethical considerations, and collaboration between medical professionals and AI experts to ensure patient safety and the effectiveness of these technologies in clinical settings.10 AI models heavily rely on the quality and representativeness of the training data. If the training data is biased or lacks diversity, the AI algorithm may produce biased results or struggle to generalize to diverse patient populations. While an AI model may perform well on a specific dataset, its performance on new,
unseen data is crucial.10 Establishing the reliability of these models across diverse patient populations and clinical settings requires rigorous validation. Additionally, many AI models, especially complex deep learning models, are often considered “black boxes”11 because their decision-making processes are not easily interpretable. This lack of transparency can be a concern for medical professionals seeking to understand and trust the AI-generated recommendations. However, striking the right balance between the expertise of healthcare professionals and the capabilities of AI systems is crucial. Over-reliance on AI or the neglect of clinician expertise can lead to suboptimal patient care.
The use of AI in healthcare also raises ethical issues related to patient privacy, consent, and the responsible use of sensitive medical data.12 Legal frameworks and guidelines must be in place to address these concerns and protect patient rights. Regulatory frameworks for the approval and deployment of AI technologies in healthcare are still evolving.12 Navigating regulatory hurdles and ensuring compliance with standards and guidelines can be a complex process.
Finally, incorporating AI technologies into existing surgical workflows may pose challenges. Surgeons and healthcare professionals need to adapt to these new tools seamlessly, and integration
must not disrupt the efficiency and effectiveness of clinical practices.10 Furthermore, implementing AI technologies in healthcare settings may require significant financial investments in infrastructure, training, and maintenance.10 This could be a barrier for some healthcare institutions, particularly those with limited resources.
In conclusion, the integration of AI, particularly NN technologies, in the realm of CNS tumor surgery holds immense promise for revolutionizing diagnostic precision and treatment personalization. The challenges and benefits associated with employing AI in this critical medical domain underscore the transformative potential of technology in enhancing patient outcomes. In essence, the journey toward incorporating AI technologies into CNS tumor surgery represents a dynamic intersection of innovation, medical expertise, and ethical responsibility. Ongoing research, collaborative efforts, and the establishment of robust frameworks will be instrumental in navigating the complexities, fostering trust, and ultimately realizing the transformative potential of AI in improving patient care and outcomes in the challenging landscape of neurosurgical interventions.
1. Cohen AR. Brain tumors in children. N. Engl. J. Med. 2022;386(20):1922-1931.
2. Yong RL, Lonser RR. Surgery for glioblastoma multiforme: striking a balance. World Neurosurg. 2011;76(5):528-530.
3. Djirackor L, Halldorsson S, Niehusmann P, et al. Intraoperative DNA methylation classification of brain tumors impacts neurosurgical strategy. Neurooncol Adv. 2021;3:vdab149.
4. Vermeulen C, Pagès-Gallego M, Kester L, et al. Ultra-fast deep-learned CNS tumour classification during surgery. Nature. 2023;622:842-849. https://doi.org/10.1038/s41586-023-06615-2
5. Gorzynski JE, Goenka SD, Shafin K, et al. Ultrarapid nanopore genome sequencing in a critical care setting. N Engl J Med. 2022;386:700-702.
6. Sagniez M, Simpson SM, Caron M, et al. Real-time molecular classification of leukemias. Preprint at medRxiv. 2022 https://doi.org /10.1101/2022.06.22.22276550
7. Guo C, Pleiss G, Sun Y, et al. On calibration of modern neural networks. In Proc. 34th International Conference on Machine Learning, Vol. 70 (eds Precup D, Teh YW). Proceedings of Machine Learning Research. 2017;1321-1330.
8. Kuschel LP, Hench J, Frank S, et al. Robust methylation-based classification of brain tumors using nanopore sequencing. Preprint at bioRxiv. 2021 https://doi.org/10.1101/2021.03.06.21252627
9. Naithani N, Sinha S, Misra P, et al. Precision medicine: Concept and tools. Med J Armed Forces India. 2021;77(3):249-257. https://doi. org/10.1016/j.mjafi.2021.06.021
10. Kelly CJ, Karthikesalingam A, Suleyman M, et al. Key challenges for delivering clinical impact with artificial intelligence. BMC Med. 2019;17(1):195. Published 2019 Oct 29. https://doi.org/10.1186/ s12916-019-1426-2
11. Rudin C, Radin J. Why Are We Using Black Box Models in AI When We Don’t Need To? A Lesson From an Explainable AI Competition. Harvard Data Science Review. 2019;1(2). https://doi. org/10.1162/99608f92.5a8a3a3d.
12. Jobin A, Ienca M, Vayena E. The global landscape of AI ethics guidelines. Nat Mach Intell. 2019;1:389-399. https://doi. org/10.1038/s42256-019-0088-2.
 By Janet Z. Li
By Janet Z. Li
Surgical and restorative technologies, such as organ transplantation and graft procedures, have increased immensely in frequency over the last few decades. In 2020, there were an estimated 1.4 million cases of restorative intervention in the US, representing a 19% increase compared to 2019.1,2 In the past, the vast majority of physical or surgical restorations have occurred out of necessity, such as in cases of injury, illness, or handicap at birth.3 However, there is increasing demand for aesthetic or abilityenhancing medical applications. Put simply, the process of human enhancement is evolving towards the goal of bypassing natural human limitations instead of creating equity.⁴
This trend comes with notable benefits but equally as many concerns. People like the idea of boosting human productivity by creating efficient workspaces, better work-life balance, and improving overall quality of life satisfaction.3,⁴ However, human enhancement also comes with many potential ethical issues, including the endangerment of individual autonomy in the face of surgical improvement. Parents may opt to make their children “better than well” in a number of ways, ranging from biochemistry of height to aesthetics of eye color.⁴ Unjustified and irreversible changes could be forced upon individuals while others may experience the exact opposite, living in the unhappiness of unaltered normality. Yet, beyond ethics and social repercussions, there is an equally if not more significant concern in
the psychological component of human enhancement that is less addressed.
The rules of nature are ever evolving, changing, and adapting. We exist, as human beings, within the context of an environment that is in constant motion. And yet, humans tend to relentlessly strive for perfection. This idea in itself is an oxymoron, since the attainment of a “perfect” form would require us to live in static and highly controlled environment, which we know cannot succeed or sustain for long on a larger scale.⁵ Therefore, by holding tightly to the ideals of perfection, we are setting ourselves up to experience the frustration, self-judgement, and exhaustion of unattainable, unrealistic goals.
More critically, we can consider the lens of negative perfectionism. As we know, a perfectionist mindset itself can be highly beneficial when applied appropriately and in moderation. However, unrestricted human enhancement may be dangerous in the face of such perfectionist tendencies, leading one down a path that follows destructive patterns of failure, selfcriticism, and emotional (and even physical) pain.⁶ Some psychologists refer to this phenomenon as an addiction, appropriately so given that they share many neurological and physiological traits in common.⁶ Of course, considering behavior as an illness is an extreme. As such, the majority of cases are more likely to fall into a milder category and can be address via a mindset shift.
The Precautionary Principle is a commonly used guide for assessing projects that pose strong environmental risks.⁷ While it has been re-written and devised in different ways, the iteration most often associated with the idea of human enhancement is as follows: when a project or policy is associated with a serious risk, it should not be pursued, regardless of its expected benefits.⁷ In other words, a “better safe than sorry” approach may be the most rational approach to this problematic question. The negative effects of self-oriented perfectionism are dangerous and may feed addictive behavior tendencies even in less radical situations. Research shows that more than 60% of patients undergoing minimally invasive cosmetic procedures are repeat patients.⁸ Coupled with statistics showing that over 15% of patients presenting for aesthetic treatments meet diagnostic criteria for body dysmorphic disorder,⁸ there is increasing reason to be

References hesitant about the normalization of surgical human enhancement.
With the existing amount of legal and well-viewed modifications, we are already seeing a tendency for humans to stray farther and farther from satisfaction with their appearances.⁹ One driving force is the field of cosmetic surgery, one that is growing at exponential rates and, as of 2020, was valued at nearly 17 billion dollars in the US alone.1⁰ A 2012 study by Frederick et al. showed that up to 40% of women and 30% of men are dissatisfied with their body appearance,1⁰ a number that has only since increased rapidly;
certain recent studies have shown body image dissatisfaction to be as high as 79% in 2023.11 Non-surgical measures such as medication for weight-loss are already prominent within the general population. Studies have shown that adults who use anabolic steroids for body image purposes are 3-4 times more likely to experience clinical depression and anxiety when compared to those who don’t.12 Furthermore, social media and movies have a prolific influence on young people’s concept of body image. Studies have shown that as little as 30 minutes of daily social media use can negatively impact young women’s views on their own bodies,12 and that girls who read beauty magazines can be 6 times more likely to engage in extreme and dangerous weight control behaviors such as taking diet pills and force vomiting.12 There is also no shortage of celebrities who have spoken out about their cosmetic regrets. A popular
case is Khloe Kardashian regretting her face fillers, saying that even after having them dissolved she felt like she looked crazy and that the “effects were still in there.”13,1⁴ From my personal experience, I’ve even heard stories about people who have gotten small-scale cosmetic surgeries such as blepharoplasty, better known as double eyelid surgery, and been so unhappy after multiple attempts to reach their ‘ideal’ look that suicide ensued.
So yes, while surgical human enhancements have the allure of promised beauty and perfection, it’s important to remember that perfection is a man-made idea. Because the concept only exists in our minds, it cannot simply be actualized in real life. We are constrained by reality, and therefore, perfection is impossible to achieve fully. As such, as we strive to become better and better, we may ultimately end up burning ourselves out in the process. In the end, we have to consider if what we want is worth losing what we have, because sometimes it really is better to be safe than sorry.
1. Wilson, J. (n.d.). Cosmetic Surgery Is On The Rise With Technology And Hollywood Is At The Center Of It. Forbes. Retrieved January 10, 2024, from https://www.forbes.com/sites/joshwilson/2023/01/18/cosmetic-surgery-is-on-the-rise-with-technologyand-hollywood-is-at-the-centre-of-it/?sh=4f2e65b01d91
2. The American Society of Plastic Surgeons ® Procedural Statistics Data Insights Partners: 2022 ASPS Procedural Statistics Release. https://www.plasticsurgery.org/documents/News/Statistics/2022/ plastic-surgery-statistics-report-2022.pdf
3. Human enhancement: Is it good for society? (2019). ScienceDaily. https://www.sciencedaily.com/releases/2019/02/190211114300.htm
4. Almeida, M., & Diogo, R. (2019). Human enhancement: Genetic engineering and evolution. Evolution, medicine, and public health, 2019(1), 183–189. https://doi.org/10.1093/emph/eoz026
5. Pascal, S. (2019, March 31). Why Perfectionism Isn’t Nature’s Way. Maria Shriver. https://mariashriver.com/perfectionism-natures-way/ 6. Krull, E. (2021, July 21). What’s the Relationship Between Perfectionism and Addiction? GoodRx; GoodRx. https://www.goodrx. com/conditions/substance-use-disorder/perfectionism-and-addiction
7. Douglas T. (2015). The harms of enhancement and the conclusive reasons view. Cambridge quarterly of healthcare ethics : CQ : the international journal of healthcare ethics committees, 24(1), 23–36. https://doi.org/10.1017/S0963180114000218
8. Sarwer, D. B. (2021). Returning for Aesthetic Procedures: Compliance or Compulsion? Aesthetic Surgery Journal, 41(6), 744–745. https://doi.org/10.1093/asj/sjab157
9. Grossman, S. (2021, March 24). Nature and Perfectionism. Medium. https://medium.com/@stevegrossman821/nature-and-perfectionism-f56d5d2979d4
10. Frederick, D. A., Jafary, A. M., Gruys, K., Daniels, E. A. Surveys and the epidemiology of body image dissatisfaction. In: Encyclopedia of body image and human appearance. Amsterdam: Academic Press; (2012). p. 766–74.
11. American Society of Plastic Surgeons. (2020). PLASTIC SURGERY STATISTICS REPORT 2020. https://www.plasticsurgery.org/ documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf
12. Gestsdottir, S., Kristjansdottir, H., Sigurdsson, H., & Sigfusdottir, I. D. (2021). Prevalence, mental health and substance use of anabolic steroid users: a population-based study on young individuals. Scandinavian journal of public health, 49(5), 555-562
13. Chandler, K. (2023, June 22). Women and Body Image StatisticsNew 2023 Data. Healthcare Data Management Software & Services | Harmony Healthcare IT. https://www.harmonyhit.com/womenand-body-image-statistics-new-2023-data/#:~:text=Body%20 Image%20Issues%20in%202023&text=Overall%2C%2079%25%20 have%20dealt%20with
14. Plastic Surgery Gone Wrong: Celebs Who Regret Going Under the Knife and Other Cosmetic Procedures. (2023, November 28). Yahoo Entertainment. https://www.yahoo.com/entertainment/plastic-surgery-gone-wrong-celebs-195707948.html

Medical tourism, which refers to individuals traveling abroad to seek healthcare, is a booming industry with a global market worth billions of dollars.1 While the concept of traveling for medical treatment has existed since the 20th century–primarily involving individuals from less affluent countries seeking advanced care and technology in more developed nations–a new trend has lately emerged.2 In recent years, there has been a significant increase in individuals from developed countries traveling to developing nations for medical purposes, giving rise to a form of “reverse globalization” where markets from developing nations expand autonomously and become increasingly popular.1
One of the challenges in comprehending the scale of medical tourism lies in the difficulty of accurately quantifying the number of medical tourists. Many individuals do not explicitly state that healthcare is their primary reason for travel on official forms. Some immigrants and dual citizens, for instance, undergo elective or cosmetic surgeries when visiting their home countries, but this may not be documented as the primary purpose of their trip. Similarly, tourists often combine vacation with minor medical procedures, such as dental care, which might not be reported. Consequently, the reported figures likely underestimate the true extent of medical tourism. Despite these challenges in acquiring accurate statistics, the available data shows that the market for
medical tourism grew from less than ten billion dollars in 2000 to over 100 billion dollars in 2012.1
Although precise statistics are elusive, certain destinations have emerged as wellknown hubs for medical tourism, with countries in Asia and Latin America–such as India, Thailand, Turkey, Singapore, Malaysia, the Philippines, Cuba, Mexico, Argentina, and Brazil–being the preferred choices for many medical tourists.3 These countries have become popular hubs for medical tourists by offering a wide variety of medical, surgical, and dental services in modern, well-equipped facilities and affordable accommodations.3
The motivations behind medical tourism are diverse, but two major factors stand out: reduced wait times and cost-effective treatments. Patients often choose to travel abroad to bypass lengthy waiting lists in their home countries. Additionally, elective and cosmetic procedures are typically more affordable in destination countries. For instance, the cost of medical services in India could be as low as 10% of prices in the United States.3 Given that cosmetic and elective treatments are often not covered by public healthcare or private insurance plans, cost is a significant consideration for many patients. Furthermore, specific medical procedures, such as certain fertility treatments, may not be accessible to patients in their home countries.
Numerous medical tourism packages are now available, providing all-inclusive options for patients seeking treatment abroad. For example, breast implant or liposuction packages in Thailand on the website placidway.com start from a few thousand dollars.4
Medical tourism serves as a vital economic stimulant for destination countries, creating a ripple effect that benefits various sectors. Beyond job creation and revenue generation, it promotes investments in healthcare infrastructure, thereby raising the overall standard of medical care in these nations.
Destination countries recognize the potential of medical tourism in bolstering their healthcare systems. They often allocate resources to improve medical facilities, adopt advanced technologies, and provide specialized training for healthcare professionals.5 Some governments have
also utilized medical tourism to bring back healthcare workers who had previously emigrated, thereby reversing the brain drain from their countries.5
Moreover, medical tourism encourages investments in the hospitality industry, leading to the construction of hotels, resorts, and other accommodations. These developments create employment opportunities, stimulate local economies, and contribute to the growth of the tourism
sector. The synergistic relationship between healthcare and tourism bolsters the nation’s economic stability, reducing its dependence on traditional industries.
It is important to note that the length of stay for medical tourists varies depending on the complexity of their procedures. While simpler treatments, like dental care, may require only a few days of stay, more complex surgeries could necessitate several weeks or even months of residence in the destination country, thereby bringing in more funds for these nations.
As the medical tourism industry flourishes, it becomes imperative to address the ethical dilemmas associated with it comprehensively. One of the primary concerns revolves around access inequality. The majority of medical tourists belong to the middle class, which means that the lower-income population may be unable to afford such travel, exacerbating access inequality issues in the home countries of medical tourists.3
Additionally, the outsourcing of patients to other countries can lead to complacency within the healthcare systems of the home countries of medical tourists. Instead of addressing systemic issues, such as prolonged wait times or limited access to specialized treatments, governments may become less motivated to enact reforms when they perceive a temporary relief in demand.
Within destination countries, the preferential treatment of medical tourists can result in unequal access to healthcare services for the local population. Immediate attention and resources may be directed towards tourists, pushing local patients onto waitlists, creating disparities, and engendering frustration among residents.5 Furthermore, experienced and highly trained physicians in destination countries may be drawn to work in hospitals and medical facilities catering to tourists, due to competitive salaries and more advanced equipment; this would further reduce the quality of public healthcare for the local residents of destination countries.5
Quality of care is another ethical concern. The standards and regulations governing medical practice can vary widely between countries. Thus, patients may not have the same level of legal protection or recourse in the event of malpractice in destination countries as they do in their home countries. Given the transient nature of medical tourists’ stays, complications arising from procedures may also be challenging to address, potentially putting patients’ health at risk.3
Furthermore, cultural and ethical differences can affect the overall patient experience in medical tourism destinations, impacting patient-provider communication and informed consent processes. Ensuring that patients are adequately informed and prepared for such cultural and ethical variations is crucial to maintaining ethical standards in healthcare delivery.
In conclusion, medical tourism is a multifaceted phenomenon with far-reaching economic and ethical implications. While it offers advantages, such as opportunities for economic growth in developing countries, increased investments in healthcare infrastructure, and higher affordability of treatment, it also raises ethical concerns related to access inequality, complacency in home countries, health disparities within destination countries, and quality of care. Navigating these challenges requires stringent regulation, ethical awareness, and a commitment to upholding patient rights and well-being. In an interconnected world, addressing the ethical dimensions of medical tourism is essential to ensure that healthcare remains accessible, affordable, and of high quality for all, transcending geographical boundaries. Addressing these ethical issues requires dialogue, discussion, and cooperation between healthcare professionals and medical experts in home and destination countries.
1. Sun X. Research on the Model of Cross-Border Medical Tourism Decision-Making under the Background of Globalization. Open J. Soc. Sci. 2018;6:230-246. doi: 10.4236/jss.2018.69016.
2. Meng CK, Piaralal SK, Islam MA et al. International medical tourists’ expectations and behavioral intention towards health resorts in Malaysia. Heliyon. 2023;9:e19721. doi: 10.1016/j.heliyon.2023. e19721.
3. Horowitz MD, Rosensweig JA, Jones CA. Medical Tourism: Globalization of the Healthcare Marketplace. MedGenMed. 2007;9:33.
4. All-Inclusive Medical Treatments Packages in Thailand. PlacidWay. [https://www.placidway.com/search-medical-packages/All/Thailand/1.]
5. Smith R, Martínez Álvarez M, Chanda R. Medical tourism: A review of the literature and analysis of a role for bi-lateral trade. Health Policy. 2011;103:276-282. doi: 10.1016/j.healthpol.2011.06.009.

Promoted to Full Member

Dr. Moraes is Division Head of Respiratory Medicine and a senior scientist at SickKids. He has a broad interest in pediatric lung disease. He is the Toronto site PI for CHILD, a National Birth Cohort and has expertise in airway epithelial cell biology with research focused on cystic fibrosis, asthma, vaping and respiratory viral infections.

Dr. Saharan is an assistant professor of Biomedical Communications. His research focuses on understanding the complex interplay and mutual influences of design strategy, visual treatment, scientific accuracy and pedagogical goals, particularly in the context of engineering education.

Dr. Vogel’s scientific focus is on translational and clinical research in the field of gastrointestinal cancers. Since 2004, he has headed a translational research group focusing on the pathogenesis of hepatobiliary carcinomas and precision medicine. Dr. Vogel has been working as a clinical investigator in oncology since 2006 and has been involved in numerous clinical trials as Principal Investigator.

Dr. Nikolova is a scientist in the Neurobiology of Depression & Aging Program at CAMH. Her work combines translational neuroimaging and genetics to study mechanisms of risk for mental illness across the lifespan.

The Zheng research group focuses on the development and application of innovative radiopharmaceuticals for the diagnosis and assessment of treatment in neuropsychiatric and neurodegenerative disorders. Dr. Zheng’s research program involves integrating disciplines such as medicinal chemistry, radiochemistry, quantitative PET imaging from in vitro and preclinical in vivo studies, and pharmacology.

Dr. Dickie’s research program that bridges the newest advances in human brain mapping with psychiatry research. She builds novel software tools to advance the way that researchers store and analyze neuroimaging data. She applies these novel techniques to the study of complex brain disorders (such as Autism and Schizophrenia Spectrum Disorders) and youth mental health.

Dr. Tyrrell is a data scientist—a combination of research methodologist, computer/database solutions architect and innovator. His research aims to introduce statistically sound and innovative artifical intelligence and machine learning approaches to the study of medical images in healthcare.

Dr. Diaconescu leads the Cognitive Network Modeling team at CAMH, advancing computational psychiatry. As an assistant professor at the University of Toronto, Dr. Diaconescu’s research is centered on the clinical validation of computational models for predicting psychosis risk.

Dr. Kloiber is a clinicianscientist and psychiatrist at CAMH working on understanding neurobiological mechanisms and novel treatments in mood and anxiety disorders through clinical trials, PET imaging and biomarker studies with specific interests in endocannabinoid system and effects of cannabinoids.

Alfonso Fasano
Dr. Fasano holds the Chair in Neuromodulation at the University of Toronto and University Health Network. His main areas of interest are the treatment of movement disorders with advanced technology (infusion pumps and neuromodulation), pathophysiology, and treatment of tremor and gait disorders.

Dr. Courtney’s research focus is on the treatment of adolescent depression through the use of a collaboratively developed treatment pathway based on high-quality clinical practice guidelines. He also has an interest in the management of concurrent disorders, where young people are affected by both primary psychiatric disorders and substance use disorders.

As the Neuropsychology lead in the Harquail Centre for Neuromodulation, Dr. Rabin’s research characterizes cognitive, behavioural, and psychosocial changes associated with novel neuromodulation strategies. Dr. Rabin also combines multimodal neuroimaging with sensitive cognitive measures to better understand risk factors for Alzheimer’s disease.

Dr. Anirban Das is a paediatric neuro-oncologist and cancer geneticist working as a staff physician at SickKids and an assistant professor at the University of Toronto. His research focus is to unearth the germline underpinnings of deadly brain tumors in children and young adults and translate these discoveries to improve diagnostics and clinical care for these young patients globally.

Dr. Lee is a clinician-scientist at the Inflammatory Bowel Disease Centre at Mount Sinai Hospital. His research focues in using novel omics to better understand the host microbe, metabolomic, and immune interaction that contribute to the pathogenesis of IBD.

Dr. Taylor’s research is focused on developing mathematical models that predict tumour response to radiotherapy in order to give the right dose to the right patient at the right time (ie. personalised cancer medicine). To do this, he applies simple models of tumour microenviromental factors to images (MR, CT, and PET) acquired of patients during radiotherapy.

Dr. Charlotte Anderson is a registered physiotherapist and researcher focusing on clinical management and treatment for patients with concussion injuries.

If you are a graduate student at the Institute of Medical Science (IMS), you must have heard of Ergi Duli , a senior Ph.D. candidate. His research focuses on understanding the cellular pathways and anatomical structures involved in atypical hemolytic uremic syndrome (aHUS), a rare genetic clotting disorder that affects the kidneys. As his clinical collaborators begin promising plasma infusions in patients, Ergi’s work highlights the fascinating translation from basic science lab work to patient care. Yet, it is his passion outside the lab that has made him a pillar in the IMS community.
Like many other graduate students, Ergi’s story is far from linear. He began his post-secondary studies in the Medical Sciences program at Western University. After graduating, he worked as a summer research student at the Peter Gilgan Centre for Research and Learning at the Hospital for Sick Children under Dr. Mathieu Lemaire, a pediatric nephrologist. Once he discovered his interest in research, Ergi entered the IMS to complete a master’s degree with Dr. Lemaire. Considering the many graduate departments at the University of Toronto, Ergi explains his decision to pick the IMS, “I find that the larger your institution, the more opportunities you have. For example, the IMS exceeds what other graduate departments offer for extracurriculars and opportunities to start your own initiatives.” However,
as a new graduate student, Ergi’s mindset differed from what it is today. At the time, he believed that more hours spent in the lab equated to better and faster results. After spending nearly 12 hours a day in the lab, Ergi recalls, “I learned how slow wet lab research moves. It’s easy to get frustrated and lose sight of having some balance.” When the pandemic struck, and he encountered a roadblock in pursuing medicine, Ergi took advantage of the unique circumstances and transferred to a Ph.D. But this time around, he had a more sustainable plan in mind.
Ergi’s experience as an immigrant inspired his extracurricular involvement as he understood the difficulty in securing mentors within one’s community. “You face many problems with finding people who can help you figure out what you need to do to reach whatever goal you’ve set for yourself. I think that’s very characteristic of not just my story but many other students at IMS.” This experience encouraged Ergi to engage in various groups within the department to improve the student experience by facilitating new connections and opportunities.
Over the past two years, Ergi has been the student lead responsible for arranging the IMS event of the year, the Scientific Day. Despite limited experience in event organization,
he excelled by acquiring practical experience and now urges students to venture beyond their comfort zone. “I think the more you take on and challenge yourself, the more you’ll realize how capable you are not just of what you can do now but what you can learn to do.” Ergi also acts as a mentor for new IMS students through the Peer-to-Peer (P2P) Mentorship program. The program pairs incoming students with senior IMS students to ease the transition into graduate studies and foster a sense of community. Furthermore, as the IMS Alumni Engagement Coordinator, he was recently involved with the launch of the Career Mentorship Program (CMP). While the P2P mentorship program focuses on matching new graduate students, the CMP seeks to establish connections between upper-year students and IMS alums. As graduate work comes to an end, there can be a daunting uncertainty about what to pursue next. The CMP aims to offer students the opportunity
to explore their career of interest and receive individualized guidance. Ergi highlights, “There’s a lot of great options, but you’re burdened by choice.” Currently comprising of 100 mentors from academia and industry, the CMP team is actively working to enhance the diversity and representation of career options. Through all these positions, Ergi has played an integral role in assisting IMS students at various


stages of their graduate careers. His significant contributions to the academic experience of graduate students have been rewarded with the 2023 Roncari Prize and the 2023 Student Contribution to Graduate Education Award. The Roncari Prize was established in 1995 after Dr. Daniel Roncari, a historical Director of the IMS, and the recipient is nominated by the leaders of the Student, Staff, Alumni and Faculty Engagement (SAFE) committee based on their notable contributions to the experience of graduate students. 1
By pursuing a Ph.D., Ergi bought himself some time for introspection. He discovered that medicine is still the career that he would like to pursue despite its arduous nature. Ergi notes, “I enjoy the feedback of medicine, where you are seeing patients, coming up with a treatment plan, and you can see the effects of those treatments within a few weeks, if not the same treatment session. I think that’s very emotionally rewarding.” Although science can be intellectually fulfilling, individuals often experience extremely delayed gratification, and one’s impact may be difficult to measure. “Medicine still offers something unique compared to a pure science career. That’s why I’m not going to give up on it.” Ergi’s determined mindset is inspirational, considering the challenges of medical training and the passion required to succeed in the long-term. “A Ph.D. was more like an interesting detour than something I had set my sights on since childhood. It gave me time to work on my application and learn more about my career path. I will find creative ways to use it as I move through my future.”
Ergi, who will graduate with his doctoral degree shortly, shared some valuable insights for current and prospective IMS students. “You really want to start early, build connections, and understand the day-to-day life in a certain field. That will alleviate a lot of stress from your shoulders.
Understand that everything comes at its own pace, take it step by step, have a clear idea of your goals, and avoid thinking 30 steps ahead.” He continues to encourage students to attend diverse career events to explore and broaden their networking circles. Though securing a Ph.D. was not initially in Ergi’s plan, his legacy and contribution will continue to positively impact the IMS community. Your IMS family wishes you the best of luck in your medical aspirations!

 By Iciar Iturmendi-Sabater
By Iciar Iturmendi-Sabater
I believe research does not take place in a vacuum; I can’t ignore the climate and biodiversity crisis unfolding around me “ “
Shares Carly Davenport, a master’s student at the Institute of Medical Science (IMS) and the co-founder of BirdsafeUofT. She researches the restingstate functional connectivity in people with neurodegenerative syndromes under the supervision of Prof. Carmela Tartaglia in the Tanz Centre for Research on Neurodegenerative Disease. We meet over Zoom and in less than five minutes she creates a safe environment where tips on how to learn functional neuroimaging from scratch are shared and the salience network is discussed, an intrinsically connected network of cortical and subcortical brain structures. “Reduced functional connectivity in this network is associated with clinical symptoms of neurodegenerative syndromes, like loss of empathy or reduced socioemotional sensitivity”, Carly explains. Her research is meaningful to both patients and caregivers, since symptoms of impaired social cognition in patients with dementia frequently relate to burden and depression amongst caregivers as well.
Just as passionately as Carly talks about her master’s research, she strongly advocates

for preventing bird-window collisions at the University of Toronto (UofT)’s St. George campus. One wonders if Carly’s artistic side had anything to do with designing the illustrations seen in some of UofT’s windows aimed at preventing these collisions. She studied drawing and painting at OCAD and worked as an Assistant Art Director in the film and television industry for over a decade before embarking on a second career in science and starting her postgraduate studies at the IMS. Humbly, Carly answers she wishes she had the time and ability
to design these illustrations herself. Her friend, artist and BirdsafeUofT co-founder Laurna Germscheid deserves all the credit, while Carly contributes from an art direction angle. In the Fall of 2023 only, they completed window retrofits at Victoria University, New College, and the Ramsay Wright building. This work is just the cherry topping of the efforts they make to ensure UofT is a bird-safe campus. As it turns out, Carly has indeed found the time to complement her postgraduate research with meaningful environmental action.

an“Because of the green spaces on campus, there’s a lot of birds that trickle up from the waterfront, forage, and spend some time on campus before moving on with their migration”. Combined with the unsustainable architecture on campus, this leads to a lot of fatal collisions happening here. After taking a 4-year ornithology course during her undergraduate degree, Carly joined Canada’s Fatal Light Awareness Program (FLAP, flap.org), the principal charity in Canada with the goal of preventing the over 25 million bird-building collisions that happen every year in our country. FLAP has a bird-safe campus programme which Carly has brought to UofT. They collect data for the Global Bird Collision Mapper (birdmapper.org), where over 90,000 collisions have been reported so far. They also rescue and rehabilitate birds injured in window collisions, advocate for improved policy and guidelines, and organize education and outreach events.
Right now, a lot of buildings on campus have a mirrored quality to the glass. “They’re treated on the inside, which is an obstacle that I keep running up against over and over. You must disrupt the outside, the first surface, if you want to disrupt the reflection”. Unfortunately, there is no legislation in Toronto, Ontario, or Canada to mandate treating windows with bird-deterrent markings yet. Although Carly explains that “FLAP is advocating for the adoption of the CSA A460:19 bird safety guidelines into the Ontario Building code, so perhaps
soon”. New York, for instance, does have it. What we have in Toronto is the green standard. However, since it has gone through a number of different iterations and considering how early site plan applications are submitted before construction starts, architects often comply with outdated versions. “This is very frustrating for me. I see UofT spend thousands of dollars on glass that is treated on the interior, like for example Robarts Common by Diamond and Schmitt Architects. The bird-deterrent pattern needs to be the exterior surface to break up the reflective property of glass. It also needs to be 2” x 2” spacing, Robarts is 4” x 4”—this does nothing for hummingbirds that collide or some of the smaller warblers”, says Carly. She explains that BirdsafeUofT is “working with UofT’s Sustainability Office to hopefully adopt the Canadian standard for bird friendly windows into the university’s design standards, which are currently being revised”.
If you see a dead or injured bird at the base of a building on campus, you can email birdsafeuoft@gmail.com or DM @ birdsafeuoft on Instagram with a photo and some information about the bird and collision. Anyone can also log in to the Global Collision Mapper and map their own observations. Carly reminds us that “it is illegal to harass, possess or transport a migratory bird in North America without a permit”. You need to be a FLAP volunteer to be covered by their scientific permit.
“I’m a FLAP volunteer. My friend, Laurna, the talented artist, she’s a FLAP volunteer. We both are on campus here and there. So we thought, there’s no one actively patrolling campus right now. There are a lot of glass buildings. Let’s patrol it and see what we find.” In this way, Carly transformed her daily walks to campus into patrolling outings. She and Laurna then thought: “Here’s a university that has a School of the Environment. They have a big Ecology and Evolutionary Biology program. They have an Architectural Studies program. This will be a slam dunk, we’ll get the campus treated”. Although change is achieved slowly, Carly is already setting an example of collaboration across different schools at UofT. She shows resilience in her belief that the social and environmental context where our research takes place matters, and we have the responsibility to take action.

 By Denise Sabac
By Denise Sabac
Dr. Pascal Tyrrell is an Associate Professor and Director of Data Science in the Department of Medical Imaging with appointments with the Department of Statistical Sciences and the IMS at the University of Toronto. He is also a generous, curious, and passionate individual whose academic and personal journey sheds light on how to navigate the abundance of postgraduate opportunities.
When I asked Dr. Tyrrell about his career path, he answered that it is “very long and convoluted”. He continued by stating that his academic journey started with roughly 18 years of university studies. Dr. Tyrrell’s relationship with academia began at Concordia University, where he completed his undergraduate studies in cellular and molecular biology. During this time, he met his eventual graduate research supervisor, who he followed to UofT to complete his master’s studies on cyanobacterial physiology. However, this initial interest was short-lived. Despite almost completing a PhD at the same lab, he described feeling that he “was not in the right place.” He did not see a career for himself in academia, and subsequently chose to enter the corporate world. Excited by the demand for computer programmers in the new age of Y2K, Dr. Tyrrell chose to become one himself. Shortly afterwards, he pivoted into a new job as an IT recruiter. Despite the excitement of industry, Dr. Tyrrell now found himself back in academia as a Data Manager at SickKids in the Division of Rheumatology. As you can imagine, the story does not end there.
In fact, after his department underwent budget cuts that terminated his position, he chose to commence another PhD in clinical epidemiology and biostatistics in the IMS. After successfully acquiring his PhD, he hoped this time to stay in academia, but this proved to be a difficult task. Dr. Tyrrell shares that “getting a job as a professor was too hard, and still is.” Instead, he became a financial advisor at Edward Jones Investments, but this was only temporary. The rapid emergence of data science and Dr. Tyrrell’s passion for academics prompted his return to UofT as an associate professor in the Department of Medical Imaging, where he conducts pioneering research on the use of AI and data science in healthcare.
After reflecting on his experiences, Dr. Tyrrell expressed that the interesting part about his journey is that he “did none of this intentionally.” Rather, it is possible to follow what you enjoy and have things work out without the need for a rigid plan. Despite his overall success, Dr. Tyrrell conveys that the greatest challenge for him was finding “a job that fit him right, a job to grow in and be successful at”. For him, this job was data science.
As a motivated data scientist, Dr. Tyrrell describes his role as “studying different ways to leverage the information contained in data in order to help improve patient outcomes.” He also shows great appreciation for the breadth of data science, which he believes made this field a good fit for him. Dr. Tyrrell explains
that while he is not formally trained in computer science, statistics, or medicine, he gained the ability to conduct medical research as a data scientist. He learned computer science through programming involved with data analysis, gained a foundation in medicine through medical research, and learned statistics as a PhD student. He further shared that this type of informal training is common in data science because you never know the content that it will be applied to. Dr. Tyrrell explained that data science is made of three pillars: math/statistics, computer science, and content. He describes content as “understanding the data, understanding what the data is for, and understanding how you are leveraging the information that's contained in the data in order to better something.” As such, he encourages students to consider what type of content they find intriguing and ensure that they
get a good mix of all three pillars if they want to pursue a career in data science. Overall, Dr. Tyrrell is grateful for the emergence of his current field, but also explains that he “worked hard to be in a position to be lucky.”
Furthermore, Dr Tyrrell’s hard work has led him through both academic and industry positions; thus, I asked if he was willing to elaborate on the differences between the two. Dr. Tyrrell eagerly started explaining that we should do both and that they are not completely separate. In academia, the research “provides theories to things that can be applied.” He also explained that there


necessarily a “bad” thing. He explained that while many graduate students enjoy and excel in academia, they should be prepared for the differing values and work structure at for-profit organizations. Overall, Dr. Tyrrell stressed that the main difference between for-profit (industry) and academic institutions are their missions. Academia predominantly applies theoretical research in the pursuit of uncovering ‘ultimate truths,’ whereas industry often relies on applied research driven by profit. Lastly, he shared that the biggest misconception is that theoretical research is the most important component to innovation. Rather, he believes that both industry and academia are fundamental to this goal.
available in this work, he encourages graduate students to participate in this line of work. He does so by leading the Healthcare Innovation Challenge at IMS, and teaching the new Startups in Medical Sciences course, which was offered for the first time in Winter 2024.
is more flexibility while working in academia—you are responsible for how and when your work gets done. On the other hand, he describes industry as relying more on applied research, and that “it aims to take an idea and turn it into a commercializable product, which is extremely difficult.” Additionally, in terms of the work structure, he mentions that there is a lot less independence. Staff are often assigned work that aims to benefit the company at large, and do not have a say in what project they work on. Dr. Tyrrell emphasized that this is not
In addition to academic and industrybased research, Dr. Tyrrell is very passionate about startups. He describes these organizations as “the middle ground between research and large corporations,” and that they represent a large percentage of business in Canada. Despite being largely involved in many startups over the years, today he is primarily involved with the software startup company SofTx Innovations Inc. as the CEO and co-founder. He describes this work as a type of hobby for him that he can do in addition to his responsibilities as a professor. In fact, being at the intersection between academia and industry also provides him with opportunities to translate his research into real-world applications. Given his strong interest in startups, and the learning opportunities
Given his abundance of experiences, I wondered what advice Dr. Tyrrell would share with current graduate students. His response to this inquiry emphasized the importance and beauty of always learning. He encourages students to be engaged and to never stop learning. With science and technology changing so rapidly, he advised that “it's inconceivable to think that you're not going to continue to learn.” Lastly, he concluded by reflecting that learning is a journey that should be enjoyed without placing too much emphasis on the destination.
 By Kiko Zi Yi Huang
By Kiko Zi Yi Huang
On November 15, 2023, the Li Ka Shing Auditorium at St. Michael’s Hospital was filled with field experts, academics, and graduate students for the 13th Annual Ori Rotstein Lecture in Translational Research. Hosted by the Institute of Medical Science, the event offered a captivating exploration into the world of medical innovation and serendipitous breakthroughs, with the keynote speaker, Dr. Robert Montgomery, providing a narrative that transcended the technicalities of his achievements.
Dr. Montgomery, Professor and Chair of the Department of Surgery and Director of the NYU Langone Transplant Institute, brought a unique perspective to the lecture. While his achievements in the field of kidney transplantation are widely celebrated, it was his encounters with countless life-or-death situations that set him apart. Dr. Montgomery’s journey unfolded as a testament to the resilience and determination required in medical research. The lecture shed light on Dr. Montgomery’s pivotal role in developing the laparoscopic procedure for live kidney donation, which has become the global standard. It was truly amazing to learn about advancements in the field of transplantation surgeries and the future of transplantation! The lecture was quite interesting, sparking numerous questions for Dr. Montgomery during the engaging Q&A session that followed.
The open panel discussion that followed Dr. Montgomery’s presentation featured prominent figures in medical research, including Drs. Shaf Keshavjee, Ana Konvalinka, Mamatha Bhat, and Olivia Hough. Dr. Ori Rotstein initiated the discussion with questions for the panelists, followed by an opportunity for all audience members to engage. The panelists shared profound insights into the unpredictable nature of scientific discovery. Dr. Montgomery, recounting moments in his career when chance played a decisive role, emphasized the importance of embracing unexpected turns in the pursuit of knowledge.
The remaining panelists echoed this sentiment, each weaving their tales of discovery influenced by unplanned events. The panel discussion became a platform for emphasizing the value of curiosity, resilience, and openness to unexpected opportunities in the research journey. As a member of the audience, it was truly inspiring to hear the way that the panelists painted science as an ever-evolving, dynamic field where unpredictability is not a hindrance, but rather, a catalyst for innovation.
In conclusion, the 13th Annual Ori Rotstein Lecture in Translational Research was more than a recounting of achievements; it was an exploration of the human spirit in the face of challenges. Dr. Montgomery’s anecdotes of resilience and the panelists’ reflections
on the unpredictability of research left an indelible mark, inspiring students to embark on their scientific journeys with an open mind and a readiness to embrace the unexpected. The stories shared underscored the importance of embracing the unknown, and questioning what one is told—although we may not necessarily recommend walking out of the hospital immediately after being advised to rest!
As we reflect on this enriching event, we extend our heartfelt gratitude to Dr. Ori Rotstein for his visionary leadership and commitment to advancing translational research. Our appreciation extends to the esteemed panelists for sharing their wisdom and experiences, which enriched the discourse with valuable insights. A sincere thank you also goes to the planning committee members whose dedication and meticulous efforts ensured the success of the lecture. Lastly, a warm thank you to everyone who attended the lecture— your presence contributed to the vibrant exchange of ideas. We hope to see you all again at the next Ori Rotstein lecture!

This past November, I had the pleasure of attending my first nephrology conference as a graduate student. I visited Philadelphia for the American Society of Nephrology’s (ASN) 2023 Kidney Week. From November 2nd to 5th, scientists, clinicians, and trainees researching kidney disease gathered to discuss the latest findings in nephrology, from kidney transplantation to rare genetic diseases, and diabetes.
Despite a somewhat rocky start – I had the unfortunate experience of losing my luggage in the airport – the conference was an incredible opportunity to be immersed in kidney research from across the world.
Each day started with a plenary session, featuring addresses by the ASN President and guest speakers. Notably, Dr. Ardem Patapoutian, a Nobel laureate known for his groundbreaking work on receptors related to temperature and touch, gave one of the addresses. These plenary sessions were followed by poster presentations. Given the focus of my lab’s research is Alport Syndrome, a very specific and rare genetic kidney disorder, it can be challenging to find other researchers whose work closely relates to my own. However, at the ASN Kidney Week 2023 poster session, there was entire section dedicated to the study of Alport Syndrome, connecting me to a much larger network of both established and early-career researchers within the field.

The rest of the day included sessions on specific topics including collagen IV variants and their relation to kidney disorders, the correlation of data science and nephrology, and the exploration of genetic therapies for kidney disease. Particularly interesting was the discussion on the use of specific oligonucleotide inhibitors as a genetic treatment for autosomal dominant polycystic kidney disease – a rather novel approach considering the limited specificity of targeted genetic therapies for kidney diseases.
One of the most touching aspects of this conference was the interference between clinical and basic science. As someone who spends most of her days in the lab or working with rodents, this conference was an extremely important reminder that all the work we do as scientists is ultimately aimed at improving the quality of life and wellbeing of patients. This theme tied together the connection between basic research, clinical trials, and future commercial therapies.
One of my biggest take-aways from this conference is the importance of collaboration within research. Perhaps no one at your institute studies your research topic, however, it is likely that someone, somewhere does. To this end, it is incredibly important to keep updated in your research field. Another important take-away from this conference is the connection that exists between disparate scientific fields. This message was brought into focus by Dr. Patapoutian, whose research on touch receptors, while initially focused on the brain, likely extends beyond neuroscience,
and may impact other organs including the kidneys. This serves as an important reminder to never underestimate the potential relevance of research unrelated to your field of study, and to keep an open mind to learning from peers, including peers within the Institute of Medical Science. I am excited to continue learning from others through conferences and programs which connects students including IMS Scientific Day!
Although our schedule was incredibly busy, my lab mates and I did get the opportunity to explore parts of Philadelphia, particularly the food scene! The loss of my luggage also granted me the ability to walk through downtown Philadelphia and appreciate the city’s charm.
I am incredibly grateful for the opportunity to have attended this conference and am looking forward to applying all the knowledge learned to future kidney disease research!

 By Vanessa Ip
By Vanessa Ip
Two-spirit, lesbian, gay, bisexual, trans, and queer (2SLGBTQ+) individuals experience greater risk of mental health challenges compared to their heterosexual and cisgender counterparts.1 This includes increased general anxiety, depressive symptoms, substance misuse and suicide risk, compared to the national average.2 Research suggests that these effects have been worsened amidst the COVID-19 pandemic.2,3 Prior to the pandemic, the Canadian Mental Health Association (CMHA) disclosed that one-third of 2SLGBT+ Canadians experience poor mental health.3 This ratio increased drastically over the pandemic, with over three-fourths of 2SLGBTQ+ respondents reporting poor mental health.
This marginalized community continues to face barriers while accessing appropriate healthcare including service delivery gaps, access to resources, and knowledgeable providers.3 2SLGBTQ+ individuals struggle to find gender affirming care and healthcare providers often lack the training to treat this diverse and intersectional group.2,3 Notably, 2SLGBTQ+ individuals who face such barriers varied significantly in socioeconomic brackets, including income and education level.2 The top barriers faced are finances and not knowing where to get help.4 In fact, many prefer to manage their substance use themselves simply because it is more convenient than going through the healthcare system. 2SLGBTQ+ youth who also identify with other marginalized
groups (i.e. lower socio-economic status, homelessness) are further disadvantaged from accessing telehealth services due to lack of a reliable and private internet connection.2 These results are in line with previous findings that low socioeconomics status, regardless of their identity, is associated with decreased mental health services access.2 A greater percentage of 2LSBGTQ+ respondents accessed virtual mental health services during the pandemic, while only 7% accessing both virtual and in-person substance-use services.4 This lack of use is thought to be caused by stigma, living in unsupportive home environments, and nature of care through virtual platforms (e.g., gender affirming care).2,3
“ “
Perhaps a “whole person” concept of care would help create a holistic point of view.
For those experiencing difficulty in attaining housing, 2SLGBTQ+ adults experience discrimination from landlords, lack of safety, and lack of awareness of services.5 2SLGBTQ+ couples reported being targeted by landlords, as they may
unconsciously choose a heteronormative couple. Some may feel a need to hide their identity to increase their chance of attaining housing. This ties into interpersonal challenges with accepting one’s identity. A “one-size-fits-all” model would not be helpful in these cases and for 2SLGBTQ+ adults experiencing homelessness, it is important to develop housing models and services that attend to their needs. 5 Perhaps a “whole person” concept of care would help create a holistic point of view. 1,5
Aside from sociodemographic variables, differences in gender identity, sexual orientation, and education significantly impacted whether individuals expressed a need for care or not. 2 Those who identify as gender non-binary, gender non-conforming/Two-Spirit and women are more likely to express a need for
care. This is because those who identify as men may be pressured to conform to gender norms traditionally associated with masculinity. For instance, expressing a need for mental health care or expressing feelings would go against these norms. Due to heteronormative counterparts not experiencing the same barriers, they do not have as high a need of care. In addition, individuals who identified with non-monosexual labels (i.e. bisexual or pansexual) are more likely to express a need for care. This may lead to isolation and difficulty assimilating with a group. 2 This further emphasizes the separation and comfort level between patients and physicians.

The complications of these barriers to mental health care further stresses the need for proper training of health professionals and providers with lived experience. Pasanan6 emphasizes on the need to create an inclusive and safe environment for learning about LGBT issues. Policies should be put in place for healthcare providers to be informed about how to best serve the community and combat heteronormative, heterosexist, and homophobic thinking.1,6
Heterosexist, cis-normative, transnegative and homonegative attitudes in formal and informal practice are barriers to promoting healthy 2SLGBTQ+ communities. 6 These barriers are deeply rooted in health policy history, discrimination, and stigmatization. 7 Progress has been made, as shown by the Canadian Human Rights Act in 1966 that included sexual orientation as one of the prohibited grounds of discrimination. 8 However, there continues to be stigma attached to queer identities and prejudice against 2SLGBTQ+ groups, as they experience twice as much public violence and harassment as heterosexual Canadians. 4 A 2019 forum identified emerging themes and future action items.1 Creating safe spaces for 2SLGBTQ+ in healthcare should aim to be traumainformed, use a harm-reduction lens, provide anti-racist and anti-oppressive frameworks, and assure respect for confidentiality and informed consent. 1,6 A patient’s previous experience with
providers may have been negative and it is important to work towards building trust and rapport through acknowledging these barriers. 2 Building cultural competency and genderaffirming care 7 is urgently required for providers, so “we can let the client be the client”. 3 Current examples of care that implement these recommendations include LGBTQ cultural competency training, 7 family intervention approach, trans lived experience programs, and sexual-health-focused programs. 9
Long-term action items include raising awareness of the important of safe spaces for 2SLGBTQ+ persons, prioritizing intersectionality, and spreading change through policy makers, service providers, and other decision makers. 1,6 Notably, it is important to educate and connect with allies in healthcare, so that they can adequately listen to and support the voices of the 2SLGBTQ+ community.1 A community approach would help reduce social isolation and exclusion for queer people and help create a voice for them. 6 This includes hiring providers with lived experience and incorporating person-centred care. 3,5 Educating mental healthcare providers about the struggles of this marginalized population and taking this into consideration when tailoring treatment interventions, are the first steps towards improving accessibility to mental health care for 2SLGBTQ+ individuals. Specific interventions for 2SLGBTQ+ individuals have been proposed for not only
promoting mental health care, but also self-affirmation practices. 9 Future mental health care for 2SLGBTQ+ persons include creating a safe space, offering resources, and trauma- and culturalinformed treatment and interventions.
1. Mental Health Commission of Canada, Wisdom2Action. Creating Safer Spaces for 2SLGTBQ+ Emerging Adults in Health-care (Forum Report) [Internet]. 2019 Jul 11 [cited 2023 Dec 30]. Available from https://mentalhealthcommission.ca/ resource/mhcc-w2a-rainbow-youth-health-forum-report/
2. Chaito M, Musani I, Pullman M, et al. Access to Mental Health and Substance Use Resources for 2SLGBTQ+ Youth during the COVID-19 Pandemic. Int J Environ Res Public Health. 2021 Oct 28; 18(21):11315. Available from: https://doi.org/10.3390/ ijerph182111315
3. Canadian Mental Health Association, Sherbourne Health. 2SLGBTQ+ mental health and wellness [Internet]. Available from: https://ontario.cmha.ca/wp-content/uploads/2023/06/ Amplifying-Voices-Recommendations-for-MH-Organizations. pdf
4. Leger, Canadian Centre on Substance Use and Addiction, Mental Health Commission of Canada. Mental Health and Substance Use During COVID-19 - Summary Report 6: Spotlight On 2SLGBTQ+ Communities in Canada [Internet]. 2022 Aug 2 [cited 2023 Dec 30]. Available from: https:// mentalhealthcommission.ca/resource/mental-health-and-substance-use-during-covid-19-spotlight-on-2slgbtq-communities-in-canada/
5. Ecker J. Facilitators and barriers to attaining housing among 2SLGBTQ+ adults with experiences of homelessness. J Gay Lesbian Soc Serv. 2023 Aug 28. Available from: https://doi.org/ 10.1080/10538720.2023.2251132
6. Pasanen PR. 2SLGBTQ+ Community Health Needs: An Advanced Practicum Report. [Internet]. 2022 [cited 2023 Dec 30]. Available from: https://zone.biblio.laurentian.ca/ handle/10219/4008
7. Organek AJ, Weisdorf T. Supporting 2SLGBTQ+ patients in your practice. Can Fam Physician. 2023 June; 69(6):377. Available from: https://doi.org/10.46747/cfp.6906377
8. Canadian Human Rights Commission. Human Rights Milestones [Internet]. [cited 2023 Dec 30]. Available from: https:// www.chrc-ccdp.gc.ca/en/about-human-rights/milestones
9. Higgins R, Hansen B, Jackson BE, et al. At-a-glance – Programs and interventions promoting health equity in LGBTQ2+ populations in Canada through action on social determinants of health. Health Promot Chronic Dis Prev Can. 2021 Dec; 41(12):431-5. Available from: https://doi.org/10.24095/hpcdp.41.12.04
 Primary Author: Soha Usmani
Primary Author: Soha Usmani
Contributors:
WSonika Kumari, Hannah Shuster-Hymanhen one hears or talks about weight loss, the most common associations tend to be for aesthetic or health purposes—and with good reason. Health professionals commonly prescribe weight loss as a treatment measure for numerous medical conditions, including obesity, type II diabetes, hypertension, and cardiovascular disease. However, what’s considered a healthy weight and the best way to achieve that weight loss varies depending on who you ask. “We prescribe weight loss to people to support so many conditions and illnesses,” registered dietician Ali Eberhardt states, “yet we do not have one sustainable way to have people achieve that.” Unlike other noncommunicable diseases, many view larger bodies and fatness as a result of moral failure and poor life choices, leading to bad health. However, Dr. Catherine Sabiston from the UofT Department of Kinesiology clarifies that the actual body of research shows that a heavier body isn’t inherently unhealthy nor linked to worse health outcomes. “The link between weight and health has been long-standing,” noted Dr. Sabiston. “It’s tied to this idea that if you are in a larger body, there have to be some health consequences. Yet [...] we don’t find the effects that these perceptions are based on,” she said.
This belief of heavier bodies being inherently unhealthy ties back to the persistent weight stigma and bias in healthcare and society as a whole,
alongside widespread misinformation. Within healthcare, a major driver of this misconception is the continued reliance on the body mass index (BMI) scale, an unreliable health indicator and diagnostic measure. 1 BMI calculations do not inform on the location of fat within the body, nor do they incorporate differences in age groups, race/ethnicity, or biological sex. 1 This has important health implications as fat in the waist and surrounding organs is more associated with health conditions such as insulin resistance and cardiovascular disease than fat under the skin. 1 It also doesn’t differentiate muscle mass or consider body composition, as muscular individuals can have the same BMI as obese individuals, and those who appear thin can still have excess visceral fat. 1
Beyond the healthcare setting, modern diet culture and the diet industry perpetuate misconceptions about weight and health, specifically, the promotion of fad diets such as the Atkins regimen, fruitarian lifestyles, and juice cleanses. With a net worth of around USD 72.6 billion, the diet industry is unavoidable in today’s social climate due to its marketing incorporated into celebrity endorsements, media outlets, and influencers.2 The packaging of these diets or cleanses as quick and easy fixes for weight loss helps promote that fatness can be dealt with by individual choice and willpower alone. The solutions offered are often not based on accurate scientific information and promote extreme systems of consumption (or lack
thereof) that may be harmful.2,3 These diets promote inaccurate information that may make sense intuitively but have the opposite effect.3 Examples include decreasing calorie intake leading to cravings for higher-calorie foods, and demonizing entire food groups such as carbohydrates and fats. Alongside fad diets, pharmaceuticals have become a noteworthy ‘magic bullet’ weight loss strategy recently.
Societal perceptions around weight and health are only further complicated by the increasing popularity of weight loss drugs. With a current market size of over USD 2 billion expected to grow to $77100 billion by 2030, it’s clear that weight loss drugs are, and will continue to be, major players in the pharmaceutical industry.4,5 Recent popular classes of weight loss pharmaceuticals have arisen from antidiabetic drugs designed to mimic metabolic hormones such as glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP).6,7 Their similar molecular structures allow the drug to bind and activate receptors that stimulate and elevate insulin production, which decreases blood sugar levels and appetite.7 One of the most notable drugs is semaglutide, also known as Novo Nodirsk’s Ozempic, a GLP-1 analog approved by the FDA in 2017 for type II diabetes.6 In 2021, the FDA approved a higher-dose version of Ozempic specialized for obesity and weight-related conditions known as Wegovy. In 2022-23, Eli Lilly launched Tirzepatide, the first to target GLP-1 and
GIP, in two versions with different dosages: Zepbound for weight loss and Mounjaro for diabetes.7 Both pharmaceutical companies are forecasted to control 80% of the obesity drug market by 2030.4 While Ozempic was only tested and approved for type II diabetes, there has been an increasing rise in its off-label use as a drug for weight loss.
A significant appeal of weight loss drugs is the view that they provide a faster, more straightforward pathway to weight loss compared to dieting and exercise strategies that also run a higher risk of failing. The growing popularity is primarily driven by effective marketing tactics, including television and online advertising and endorsements from influencers and celebrities. The semantics and language in lay media are also noteworthy, as the term ‘weight loss drugs’ may be attractive to many people aiming to lose weight, rather than the more specific ‘antiobesity or antidiabetic drugs.’ The rapid rise in popularity of using Ozempic for weight loss has created numerous challenges regarding drug availability and manufacturing. There have been ongoing semaglutide shortages in Canada and the U.S., which are significantly impacting diabetic patients alongside reports of unlicensed manufacturing and distribution.6 In 2023, the New York Times reported seizures of counterfeit Ozempic injectors and unapproved but cheaper semaglutide ‘generics’ and falsely labelling brand medications.6
The perception of these drugs as instant panaceas and the rampant anti-fat bias present in our culture often lead individuals to underestimate or undervalue the adverse effects associated with weight loss drugs. The general side effects of weight loss drugs include gastrointestinal issues and the increased risk of kidney failure, pancreatitis, and medullary thyroid carcinoma.7 Endorsements also don’t clarify that clinical trials have only been conducted on patients diagnosed with obesity and diabetes, so the impact on individuals without these conditions is still unknown.6 While no drug is devoid of side effects, off-label and unprescribed users tempted by a quick fix or under pressure to conform to a specific body type are at serious risk. The ever-increasing use of weight loss drugs will have enduring consequences on perceptions of weight, fatness, and weight loss in both healthcare settings and general society.
Weight loss pharmaceuticals are an ongoing point of discussion in healthcare and public health discourse. How these drugs will play into the future of care for obesity and type II diabetes, as well as more general conversations about the intersection of weight and health, remain to be seen. The long-term effects, the health consequences of unlicensed usage, and the development of novel pharmaceuticals will also be hot topics for current and prospective practitioners and researchers. Readers interested in learning
more about the societal implications of weight loss drugs can listen to Raw Talk episode #120: The Era of Ozempic: AntiFat Bias and Body Image, where the team talks further with Ali Eberhardt and Dr. Catherine Sabiston!
A big thank you to the episode team for their help and support
1. 1. Prillaman M. Why BMI is flawed — and how to redefine obesity. Nature. 2023 Oct 11;622(7982):232–3.
2. 2. St KRNC 151 WL, Collins S 1400 8022 CDF. Kendall Reagan Nutrition Center. [cited 2024 Jan 17]. I spy a fad diet! Your guide to critically evaluating diet and wellness trends. Available from: https:// www.chhs.colostate.edu/krnc/monthly-blog/i-spy-a-fad-diet-yourguide-to-critically-evaluating-diet-and-wellness-trends/
3. 3. www.heart.org [Internet]. [cited 2024 Jan 17]. Research says fad diets don’t work. So why are they so popular? Available from: https://www.heart.org/en/news/2022/02/18/research-says-fad-dietsdont-work-so-why-are-they-so-popular
4. 4. Why the anti-obesity drug market could grow to $100 billion by 2030 [Internet]. [cited 2024 Jan 17]. Available from: https://www. goldmansachs.com/intelligence/pages/anti-obesity-drug-market. html
5. 5. Morgan Stanley [Internet]. [cited 2024 Jan 17]. Obesity Drugs’ Accelerating Growth. Available from: https://www.morganstanley. com/ideas/obesity-drugs-investment-opportunity
6. 6. Blum D. What Is Ozempic and Why Is It Getting So Much Attention? The New York Times [Internet]. 2022 Nov 22 [cited 2024 Jan 17]; Available from: https://www.nytimes.com/2022/11/22/well/ ozempic-diabetes-weight-loss.html
7. 7. Suran M. As Ozempic’s Popularity Soars, Here’s What to Know About Semaglutide and Weight Loss. JAMA. 2023 May 16;329(19):1627–9.

