






Seamless Operation Patient Friendly User Friendly Affordable EC90 VOL.15 NO 11 PAGES 44 DECEMBER2022,`50 PUBLIC HEALTH Can India afford Universal Health Coverage (UHC)? MEDTECH Make in India making India a global medtech hub
TransasiaHouse,8ChandivaliStudioRoad,Andheri(E),Mumbai-400072. T:(022)40309000,Fax:(022)28573030www.erbamannheim.com responses@transasia.co.in StayConnected: 7304448818





















VOL.15 NO 11 PAGES 44
















Chairman of the Board
ViveckGoenka


Sr.Vice President-BPD Neil Viegas
Asst.Vice President-BPD Harit Mohanty


Editor
Viveka Roychowdhury*
BUREAUS Mumbai Lakshmipriya Nair,Kalyani Sharma Delhi Akanki Sharma
DESIGN Art Director Pravin Temble Senior Designer Rekha Bisht Senior Artist Rakesh Sharma Digital Team Viraj Mehta (Head of Internet) Marketing Team
Rajesh Bhatkal Ambuj Kumar Ashish Rampure
Debnarayan Dutta Production Co-ordinator DhananjayNidre Scheduling & Coordination Pushkar Waralikar
Mohan Varadkar

Healthcare® Regd.With RNI No.MAHENG/2007/22045.Postal Regd.No.MCS/162/2022 - 24.Printed and Published byVaidehi Thakar on behalf of The Indian Express (P) Limited and Printed at The Indian Express Press,Plot No.EL-208,TTC Industrial Area,Mahape,Navi Mumbai-400710 and Published at Mafatlal Centre,7th floor,Ramnath Goenka Marg,Nariman Point,Mumbai 400021.
Viveka Roychowdhury.* (Editorial & Administrative Offices: Mafatlal Centre,7th floor,Ramnath Goenka Marg,Nariman Point,Mumbai 400021)

CONTENTS December 2022 EXPRESS HEALTHCARE 7
* Responsible for selection of news under the PRB Act.Copyright © 2017.The Indian Express (P) Ltd.All rights reserved throughout the world. Reproduction in anymanner,electronic or otherwise,in whole or in part,without prior written permission is prohibited. 27 5G ROLLOUTIN INDIAAND OPPORTUNITYFOR TELEMEDICINE 28 CYBER SECURITY CHALLENGES IN THE HEALTHCARE INDUSTRY 12 MAKE IN INDIA MAKING INDIAA GLOBALMEDTECH HUB DBS therapyfor movement disorders has gained acceptance and widespread clinical use in recent years P10: INTERVIEW MADAN KRISHNAN VP& MD,Medtronic India HEALTHCARE IT 24 CAN INDIA AFFORD UNIVERSAL HEALTH COVERAGE (UHC)? PUBLIC HEALTH MEDTECH P22: INTERVIEW PRABAKAR SUKUMARAN Regional Director-West, GE Healthcare COVER STORY
CIRCULATION
Express
Editor:
Learnings from the IHH-Fortis saga
The competition for a slice of India's healthcare pie continues with a fierce bidding war for Kolkata-based AMRI Hospitals. The latest buzz is that Max Health has added Rs 900 crore to Manipal Health Enterprises’ (MHE) bid, making it a total bid of Rs 2700 crore.
This counteroffer has reportedly forced MHE to take legal action, moving the Delhi High Court on November 29, to block AMRI’s promoters, the Emami Group, from backing out of the purchase agreement signed between MHE and Emami way back in June this year.
Will this become another prolonged legal tangle, like the IHH Healthcare-Fortis saga? In November 2018, Malaysia’s IHH Healthcare purchased a 31.17 per cent stake in Fortis Healthcare from the original promoters Malvinder Singh and Shivinder Singh. The Malaysian group invested about Rs 4,000 crores of fresh capital to grow its presence in India through the Fortis network.
However, IHH Healthcare’s mandatory open offer (MTO) of December 2018, to acquire an additional 26.1 per cent stake in Fortis, is in limbo since the past four years. A Supreme Court order took cognisance of Japanese pharma company Daichii Sankyo’s allegation that the IHH Healthcare-Fortis deal violates the former promoters’ undertaking that they would not sell shares in any of their companies. The SC order relates to the pending settlement of a Rs 3,500-crore arbitration award to the Japanese company, alleging the Singh brothers withheld crucial information when they sold Ranbaxy Laboratories to Daichii Sankyo in 2008.
The current management of Fortis and IHH Healthcare has always tried to ring fence themselves from the actions of the former promoters and management. When asked on a concall on November 9, what would it take for IHH Healthcare to walk away from Fortis, (the way Daichii Sankyo cut its loses when it sold Ranbaxy to Sun Pharma in 2015), Dr Kelvin Loh, MD and CEO, IHH Healthcare reiterated that “Fortis is IHH’s main platform in India.” He also indicated that plans to re-brand Fortis to the Parkway brand would also happen in due course of time.
In a press statement that followed on November 11, Dr Loh addressed investor sentiment saying, “We certainly understand the frustration Fortis investors have felt over the past four years around the uncertainty of the IHH open offer.” He ended his statement, “…hopeful for a positive outcome so that we can explore more avenues to work with Fortis to accelerate its growth plans,…”
Whether IHH Healthcare is an ‘innocent bystander’ suffering ‘collateral damage’ due to the alleged misdeeds of the past promoters/management, the fact remains that it stands to gain immensely by sticking to its guns and waiting till the courts give the green signal for the MTO. As per the terms of the MTO framed in 2018, IHH Healthcare would pay Rs 170 per share, which is substantially lower than the current share price of Fortis
Healthcare. (Rs 288.55 on December 2, 2022). On the November 9 concall, Dr Loh indicated that there was no requirement to change this offer price.
The rise in the Fortis stock price reflects the steady improvement in its operating margins over the past four years, thanks to the fresh capital from IHH Healthcare and guided by the current management. Fortis’ contribution to IHH Healthcare’s revenues is also on the rise. While the Q32022 results of IHH Healthcare Berhad, posted on November 30, showed a disappointing over 50 per cent drop in net income, in part due to a high base in Q32021 and forex losses, the numbers from India were encouraging. In terms of revenue and EBITDA at the IHH Healthcare Group level, India operations contributed 22 per cent and 18 per cent respectively. India operations clocked a 6 per cent revenue growth and one per cent de-growth in EBITDA compared to other markets.
Fortis is thus once again an attractive takeover target. Rumours that other hospital groups and strategic investors have tried to muscle in have also done the rounds from time to time.
The interest is a reflection of the opportunities in India's healthcare sector, seen as a recession proof sector. Patients and their caregivers may postpone but cannot totally avoid hospital stay, especially if they are part of India's growing demographic prone to lifestyle conditions, which need prolonged and repeated care.
So how will history view the IHH-Fortis saga? One learning is the need to improve corporate governance standards of India’s largely promoter-driven hospitals sector. There is also the need to improve ease of doing business and speed up the legal process to give more confidence to overseas investors. While investors vie for a slice of India's hospital pie, which is only set to increase with an ageing demographic, well on the way to becoming the diabetes/NCD capital of the world, how can policy makers balance patient needs with corporate interests?
Meanwhile on the public health front, pockets of India are seeing outbreaks of measles among children who missed their vaccinations during the COVID pandemic. Hopefully, these outbreaks will result in more budgetary allocation to immunisation in the upcoming budget. Healthcare experts are in fact pushing for increased allocation for adult vaccinations as well. The recent cyber attack at AIIMS Delhi is the latest warning that there are many weak links in our public health infrastructure, which can be easily exploited.
As we near the end of 2022 and plan for 2023, we hope some of these learnings convert into action in the year ahead.
VIVEKA ROYCHOWDHURY Editor viveka.r@expressindia.com viveka.roy3@gmail.com

EDITOR’S NOTE EXPRESS HEALTHCARE December 2022 8
One learning is the need to improve corporate governance standards of India’s largely promoter-driven hospitals sector

MEDTECH
DBS therapyfor movement disorders has gained acceptance and widespread
clinical use in recent years
,VP& MD,Medtronic

Tell us about your company's recent collaboration with Aster Medcity? What is the objective behind this partnership?
The aim of the partnership with Aster Medcity is to take Parkinson’s management to the next level by empowering surgeons to make faster and more accurate treatment decisions using Deep Brain Stimulation (DBS) therapy. Clinicians can deliver truly data-driven, personalised therapy that fits the needs of Parkinson’s and movement disorder patients who need the treatment, especially to those with relatively early onset (under 45 years) or youngonset of Parkinson’s disease so that they get back their mobility and functional capacity in the most productive years of their lives.
The partnership supports the Aster Centre for Parkinson’s and Movement Disorder by bringing together Aster's teams with their medical and surgical expertise in DBS therapy and Medtronic’s complete suite of DBS technologies along with technical expertise and support. DBS uses a small pacemaker-like device, placed under the skin of the chest, to send electrical signals through extensions and very thin wires (leads) to an area in the brain that controls movement. These signals block some of the brain messages that cause the movement symptoms of Parkinson’s.
Can you throw some light on the current prevalence of Parkinson's disease in India?
Parkinson's is a progressive disease, which means that symptoms get worse over time. In the more advanced stages, it causes severe disability due to the increasing severity of
movement-related problems, and balance and cognitive functions symptoms. Overall, movement disorders constitute 3-8 per cent of neurological disorders in India with a crude prevalence rate (CPR) varying from 31 to 45/100,000 above 60 years of age.1 In 2016, it was estimated that 6.1 million people worldwide had Parkinson’s disease. The prevalence in India was estimated to be 10% of the global burden, that is, 5.8 lakhs.2
How effective is DBS therapy in treating Parkinson's disease? What is the need of the hour for its further strengthening?
Parkinson’s disease may have a significant impact on a patient’s quality of life. DBS is a well-established, safe and effective therapy for the treatment of motor symptoms in Parkinson’s disease, including tremor (shaking); slowed movement (bradykinesia); and stiffness (rigidity) when medications aren't as effective as they used
to be. For over 30 years, Medtronic’s Deep Brain Stimulation (DBS) technology has been helping Parkinson’s patients around the world. It is backed by our decades of research, innovation, and experience. We’d recently launched the latest and advanced DBS system in India where in the technology is designed to capture brain signals while simultaneously delivering therapeutic stimulation, inside and outside the clinic.
DBS therapy for movement disorders has gained acceptance and widespread clinical use in recent years. However, there is a need to raise adequate awareness about the disease and the therapy so that more patients can benefit from it in India. We understand that no one entity can address the challenges of healthcare alone, hence we forge partnerships that can help advance access to quality care for more people across India.
As part of our partnership with Aster Medcity, we
introduced the latest version of Microelectrode recording system for DBS surgeries –NeuroNav MER system at Aster Medcity Kochi, making it the first centre in South Asia to bring in this technology. Microelectrode recording (MER) has been considered the gold standard in ensuring accuracy for the deep brain stimulation procedure. The NeuroNav MER system has been developed by an Israelbased Medtech company, Alpha Omega Engineering. *
It is a compact, field-proven MER system, used clinically in the localisation of surgical targets for the implantation of DBS electrodes for the treatment of neurological and psychiatric diseases.
What is the current scalability and acceptance of this therapy in India?
First case of DBS in India happened more than 20 years back (1999). Today, there are many centers across the country that are equipped to perform DBS procedures. In 2019, IRDAI included advanced treatment for Parkinson’s into the approved treatment protocols. This has given a good boost to the acceptance of DBS therapy in India. However overall awareness is still a barrier.
Are there any challenges at the training level that you feel need to be addressed and how?
The importance of continuous training and education is critical in the field of healthcare technology. While providing new tools and technologies for surgeons is important to improve access to quality care, it is also imperative to stay abreast with the latest techniques to perform safer, faster, and less
invasive surgeries that improve clinical outcomes. Skill gap is a major barrier for the broader adoption of DBS therapy among Neurologists and Neurosurgeons. Very few teaching institutions perform DBS surgeries and there are also very limited fellowship opportunities available in India.
DBS procedure requires high level of skill and training to perform the procedure with precision.
Healthcare technologies are rapidly changing and being a physician requires focus and adaptability as therapies and procedures evolve. At Medtronic, we know the world’s greatest tool is only as effective as the skilled clinicians who use it. That’s why we’re committed to empowering surgeons and healthcare professionals through high-quality clinical education and immersive programs with our technologies.
Reference
1- Das SK, Ghosh B, Das G, Biswas A, Ray J. Movement disorders: Indian scenario: A clinico-genetic review. Neurol India 2013;61:457-66
2- Dorsey ER, Elbaz A, Nichols E, Abd-Allah F, Abdelalim A, Adsuar JC, et al. Global, regional, and national burden of Parkinson's disease, 1990–2016: A systematic analysis for the global burden of disease study 2016.
*Alpha Omega NeuroNav System is intended to be used in assisting neurosurgeons in the operating room during functional neurosurgery and to record from and stimulate brain motor and sensory neurons to aid in the placement of depth electrode.
Kalyani.sharma@expressindia.com journokalyani@gmail.com
EXPRESS HEALTHCARE December 2022 10
INTERVIEW
Madan Krishnan
India in an interaction with Kalyani Sharma talks about his company’s recent collaboration with Aster Medcity and highlights the objective behind it

























































































Make in India making India a global medtech hub
The global medical devices industry was valued at USD 455.3 billion in 2021. Medical devices market in India stood at USD 12 billion in 2020 and is expected to grow at a CAGR of 15 per cent. It is among the top 20 medical device markets and is the fourth largest medical device market in Asia.
Recently, the Indian medical devices sector’s contribution has become even more prominent as India supported the global battle against COVID-19 pandemic through the production of medical devices & diagnostic kits, e.g., ventilators, RT-PCR kits, IR Thermometers, PPE Kits & N95 masks.
Over the years, Indian Government has undertaken structural and sustained reforms to strengthen the healthcare sector and has also announced conducive policies for encouraging FDI.
The medical devices sector was recognised as a focus sector by the Government of India as part of Make in India campaign in 2014. Since then, the industry has evolved in terms of deepening its ability in the value chain across device-segments ranging from low-tech segment to highend equipment. Government relied on the domestic manufacturers to meet the rising demand of essential healthcare equipments & devices, encouraging the Indian medical devices sector to become more self-reliant. PreCOVID there were approximately 1000 domestic medical devices manufacturers in India, these doubled to over 2000.
The Atmanirbhar Bharat program driving the self- sufficiency campaign of the government holds immense opportunities for foreign investors. From ever- increasing investment in medical device parks and clustering projects vide the medical devices park scheme with the view to develop world-class infrastructure and testing facilities,
to the Production Linked Incentive (PLI) scheme allowing incentives for the manufacturers on incremental sales. Medical Devices
Parks will play the catalytic role to extend an integrated medical device manufacturing ecosystem set up. The PLI scheme has been notified to boost domestic manufacturing and attract large investments in the industry. The

scheme has a total outlay of about Rs 3,420 Cr whereas The Scheme for Promotion of Medical Device Parks has been notified to develop common infrastructure facilities (CIF) which in turn will reduce production cost of medical devices manufactured in the country.
India has become a leading destination for high-end diagnos-
tic services and is a growing market for diagnostic kits, reagents, hand-held equipment, and stimulation for operation rooms. The demand for the medical devices industry has mainly been met through multinationals and home-raised players. The latter have made enormous contributions topromote manufacturing as part of government’s vision of
Make in India for the world.
The Indian medical devices sector presents an unparalleled growth opportunity backed by inherent growing demand arising from increasing healthcare needs along with government’s commitment towards providing an enabling policy-environment for domestic manufacturing.
The proposed National Medical Device Policy by the government aims to accelerate an orderly growth of the medical device sector to meet the primary objectives of accessibility, affordability, safety, and quality, while ensuring focus on self-sustainability and innovation. Through this policy, they are determined to help the sector realise its full potential by creating a robust regulatory framework with feedback mechanisms, building an enabling ecosystem for medical device manufacturing within the country, focusing on innovation for high end technology, extending support in training and capacity building programs and promoting higher education to foster fresh talent and skilled resources in line with the industry requirements. Encouraging domestic production of medical devices is in conformity with the government’s ‘Atmanirbhar Bharat Abhiyan’ and ‘Make in India’ campaign.
The medical devices sector will be placed on an accelerated growth path to increase access and affordability of products & services of excellent quality to meet the evolving health care needs of patients, by building a globally competitive industry in India, supported by best of class infrastructure, quality manpower, enabling ecosystem and streamlined regulatory framework. This would enable India to emerge as the leader in the manufacturing of medical device products, The pharmacy of the world can also become the global hub of medical device and equipment.
EXPRESS HEALTHCARE December 2022 12 MEDTECH
Himanshu Baid,Managing Director,Poly Medicure emphasises that the Indian medical devices sector presents an unparalleled growth opportunity backed by inherent growing demand arising from increasing healthcare needs along with government’s commitment towards providing an enabling policy-environment for domestic manufacturing
Over the years,Indian Government has undertaken structural and sustained reforms to strengthen the healthcare sector and has also announced conducive policies for encouraging FDI
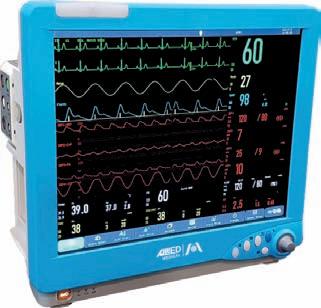
AMLaims to revolutionise criticare
When it comes to a vision for the future of healthcare organisations, and government, both are recognising the need for many changes in the way we care for patients. The critical care setting is a high-tension environment with a large number of users interacting with an even larger number of devices. The use of devices in medical care was introduced for many reasons, the primary ones being related to patient monitoring and automation of procedures in order to save time and increase accuracy. The devices were not intended to replace human caregivers but to supplement their tasks. The effectiveness of these devices relied largely on how well the user operated them. The concept of including patient safety measures in medical devices slowly evolved as the impact of errors due to the improper design, mplementation, and use, of medical devices, started being recognised.
From a general standpoint, when a new device is invented, the primary concern at the time is to achieve the desired functionality. With constant use, shortcomings or possible improvements for the device become evident; with modifications, subsequent generations of the device evolve into much better contraptions. Similarly, medical devices and instruments have evolved in functionality by incorporating more and more features and automaticity. With the development of more programmable and independently operating devices, it became imperative that they not compromise patient safety in any way.
Considering the fact that medical devices do not work in isolation but interact with various other entities and personnel working in the same
setting, the next evolutionary stage in terms of patient safety measures should account for these factors as well. From the time a clinician decides on a plan of action to the actual exe-
cution of this plan, several cognitive processes and sequential events occur. The communication cascade triggered by this situation is mostly concentrated around nurses and
physicians. Performing a cognitive task analysis of real clinical settings and understanding the peculiarities of the health care system can provide cues for new design principles in device development.
At Allied Medical Limited (AML), we have realised that technology adoption in the field of health care has accelerated at a very faster rate. Companies that provide new innovative medical solutions to hospitals and physicians which can help them to embrace this new paradigm will emerge much stronger. As a result of that, we have come up with

India’s largest critical manufacturing plant which is operational in full swing. The new facility is five times bigger than the current factory and has a dedicated R&D department consisting of more than thirty engineers who are constantly working on the existing product development and many new ventures that will make it easier for the medical fraternity to have a more ingenious approach for treating the patients. For incessant and effective delivery of prolific diagnostic and treatment solutions for the healthcare providers the government, the medical device industry and other stakeholders like educational institutions, research facilities, and funding agencies must all work in tandem with one another to encourage local manufacturing.
The Indian government is a key contributor in creating favourable policy and regulatory requirements, as well as putting up a framework for the development of indigenous medical device production. As a reciprocal, the medical industry must coordinate with the government to encourage the generation of novel ideas and localisation among its member, consequently, facilitating access to cost-effective and superior healthcare services. AML is consistently working on critical care devices like ventilators, infusion pumps, and patient monitors having an intuitive and simple user interface with quick operational readiness and automatic device check that give confidence to the user and reduces training time. Simple user interface and effortless operation make AML devices to be innate and require a minimum amount of training for the medical and nursing staff thus reducing the errors related to devices or users in the healthcare setup.
December 2022 EXPRESS HEALTHCARE 13 MEDTECH
Aditya Kohli,CFO & Director-Sales,Allied Medical Limited (AML) emphasises that AMLis consistently working on critical care devices having an intuitive and simple user interface with quick operational readiness and automatic device check that give confidence to the user and reduces training time
Companies that provide new innovative medical solutions to hospitals and physicians which can help them to embrace this new paradigm will emerge much stronger



EXPRESS HEALTHCARE December 2022 14 cover )
Renewed focus to prevent,detect,control and treat NCDs is the need of the hour

 ByKalyani Sharma
ByKalyani Sharma
December 2022 EXPRESS HEALTHCARE 15
NCDs are the leading cause of death and disability around the world. The United Nations’ Sustainable Development Goal 3.4 focuses on reducing mortality from NCDs by a third by 2030. The pandemic slowed down the process of achieving this goal. Considering the scale and speed at which they are rising, it’s time to re-consider some of the interventions that are important to prevent them.
Non-Communicable Diseases (NCDs) threaten progress towards the 2030 Agenda for Sustainable Development, which includes a target of reducing the probability of death from any of the four main NCDs between ages 30 and 70 years by one-third by 2030.
Dr Gautam Wankhede, Director-Medical Affairs, Mylab Discovery Solutions emphasises thatthe burden of NCDs exceeds the burden of communicable diseases. He said, “NCDs are the leading cause of morbidity and premature mortality around the world, which were primarily due to cardiovascular diseases, diabetes, cancers and chronic respiratory diseases. India is in the midst of an epidemiological transition as the burden of NCDs exceeds the burden of communicable diseases. The pandemic has significantly worsened outcomes for many NCDs.”
Current status: Where do we stand?
As per WHO recent data, “NCDs kill 41 million people each year, equivalent to 74 per cent of all deaths globally. Also, cardiovascular diseases account for most NCD deaths, or 17.9 million people annually, followed by cancers (9.3 million), chronic respiratory diseases (4.1 million), and diabetes (2.0 million including kidney disease deaths caused by diabetes).”
Dr Grace E. Terrell, Chief Product Officer, IKS Health said, “The pandemic unleashed many unanticipated tragedies
India is in the midst of an epidemiological transition as the burden of NCDs exceeds the burden of communicable diseases
Dr Gautam Wankhede Director-Medical Affairs, Mylab Discovery Solutions


The pandemic unleashed many unanticipated tragedies with magnitudes of unprecedented scale and impact.While the world gradually comes out of the pandemic phase,the last couple of years or so have led to dilution and diversion of attention required towards reducing NCDs which continue to plague society at large with an immensity of higher proportion compared to the pandemic
Dr Grace E.Terrell Chief Product Officer, IKS Health

We have seen in the recent COVID-19 pandemic that people with co-morbidities had higher mortality compared to those who did not.This makes prevention and control of NCDs all the more important
Dr Preeti Kabra Chief of Lab, Neuberg Diagnostics

The development of diagnostic tools allows for the rapid detection of NCDs biomarkers with high sensitivity to help detect diseases at their early stages,which subsequently contributes to the easier treatment and fast cures
Vikram Thaploo CEO, Apollo Telehealth
EXPRESS HEALTHCARE December 2022 16 cover )
with magnitudes of unprecedented scale and impact. While the world gradually comes out of the pandemic phase, the last couple of years or so have led to dilution and diversion of attention required towards reducing NCDs which continue to plague society at large with an immensity of higher proportion compared to the pandemic.”
“About a hundred years ago the most common causes of death were communicable diseases and our health care systems worldwide were designed and developed to treat these acute diseases. With the advent of antibiotics and vaccines, lifespans have increased and chronic diseases have become an increasingly significant proportion of the disease burden. Currently, 73 per cent of global deaths are the result of chronic diseases and 60 per cent of the global disease burden. Prior to the pandemic, cardiovascular diseases, cancer, diabetes and chronic respiratory diseases made up most of the causes of premature death worldwide. With the impact of the pandemic subsiding, it is time to refocus our efforts on these non-communicable diseases. The prepandemic data from 2019 shows that the top three countries' total incidence of diabetes (China, India, US) is 224.4 million but without any intervention, it will be 318.2 million people by 2045. Additionally, worldwide noncommunicable diseases collectively will cost $47 trillion by 2030. The United Nations’ goal of reducing premature mortality from non-communicable diseases by one-third by 2030 is now running behind due to the pandemic. It is essential to apply focused efforts on the main causes (poor diet, inadequate physical exercise, tobacco use and excessive alcohol use) through designing models of care that are person-centered and preventative, with early diagnostics and cost-effective, accessible therapies”, she added.
Access to high-quality diagnostics to manage the burden of NCDs
Unlike communicable diseases where diagnostic tools have played an important role in




addressing the disease, the diagnostic landscape of NCDs still needs more attention. The diagnosis of NCDs at an early stage can help avert a potential fatality.
Dr Preeti Kabra, Chief of Lab, Neuberg Diagnostics shares some numbers. She said, “In the survey conducted by ASSOCHAM titled “NonCommunicable Diseases in
India” more than 40 per cent of the respondents suffering from CVD and hypertension accepted that they were not aware of having their respective diseases for more than
PORTABLE CT Bringing the Power of Imaging to Your Patient 8-slicePortable Head&NeckCTScanner CereTomElite 32-SlicePortable WholeBodyCTScanner BodyTomElite 16-SlicePortable CTScanner OmniTomElite December 2022 EXPRESS HEALTHCARE 17
3 years. The report highlighted that for the heart ailment over 70 per cent of respondents stated that they were diagnosed after 1 year of suffering. The survey further showed that over 52 per cent of CVD/heart disease patients seek medical advice only in the case of an emergency.”
Although, there are substantial advances in the diagnostics ecosystem of the NCDs, innovating on the ways that can make early diagnosis more possible still needs attention.
Vikram Thaploo, CEO, Apollo Telehealth also believes, “The development of diagnostic tools allows for the rapid detection of NCDs biomarkers with high sensitivity to help detect diseases at their early stages, which subsequently contributes to the easier treatment and fast cures.”
While innovating new diagnostic solutions is an important factor, accessibility and availability of these solutions is also crucial.
Stressing on the same, Dr Yogesh Gupta, MD Medicine, Consultant Physician & Geriatrician, Sterling Hospitals stresses, “Despite substantial advances, it is still not possible to prevent or completely cure NCDs. For years, people with diabetes may go undiagnosed, and with the current state of cancer diagnostics, patients may not find out they have the disease until it is in its latter stages. We need to have highquality, integrated, and peoplecentered primary health services for all and an appropriate well-trained, equipped health workforce which will be beneficial to increase access to early and advanced diagnostics. It has been discovered that NCD diagnostic and monitoring technologies are either not available inside health systems or are too expensive for individuals to obtain for self-monitoring.”

Dr Vikram, MS-General Surgery, Aarvy Healthcare Super speciality hospital said, “It is often too late when these diseases are diagnosed by the
Despite substantial advances,it is still not possible to prevent or completely cure NCDs.For years,people with diabetes may go undiagnosed,and with the current state of cancer diagnostics,patients may not find out they have the disease until it is in its latter stages
Dr Yogesh Gupta


MD Medicine, Consultant Physician & Geriatrician, Sterling Hospitals
It is often too late when these diseases are diagnosed by the physician,during which they set in often leading to devastating consequences for the patients.It would not be an exaggeration to state that if COVID is termed as a pandemic,NCDs in patients running parallelly with COVID caused a syndemic
Dr Vikram
MS-General Surgery, Aarvy Healthcare Super speciality hospital
As health is a state concern in India,a joint strategy between the state and central government is necessary to boost cervical cancer screening penetration
Venkatraman V Commercial Director, Hologic South Asia
There is a dire need to improve surveillance,monitoring and reporting tools and methodologies.Disease-specific surveillance and monitoring tools would have to be employed. Given the innate role of baseline data,mobile phones and internet technologies can be used for data collection
Dr Nitendra Sesodia Senior Director-Medical Communications & Corporate Sales, Thieme Group

EXPRESS HEALTHCARE December 2022 18 cover
)
physician, during which they set in often leading to devastating consequences for the patients. It would not be an exaggeration to state that if COVID is termed as a pandemic, NCDs in patients running parallelly with COVID caused a syndemic. The loss of immunity due to COVID in relatively healthy individuals made them vulnerable to a plethora of dormant diseases. COVID not only lowered immunity but also aggravated the severity of NCDs. Therefore, it is pivotal that the diagnosis of NCDs is done at an early stage, to ensure holistic treatment and avoidance of chronic recurrence. The clinical handling of NCDs requires a 360-degree approach in terms of their diagnostics.”
“From the perspective of healthcare providers, it should be their endeavor to tap into logistics and modern-day technology enabling support for ease of specimen collection, real-time connectivity to provide required test data to clinicians and users and provision of sensitive and specific diagnostic technology to avoid false positive and negative results”, he added.
Venkatraman V, Commercial Director, Hologic South Asia throws light on cervical cancer surveillance and currently available technologies. He said, “It is important to ward off the disease through regular screening along with the HPV vaccination (most cervical cancer is caused by HPV). Awareness and prevention are the two most effective weapons against this disease. As health is a state concern in India, a joint strategy between the state and central government is necessary to boost cervical cancer screening penetration. Today, there are various non-invasive and convenient screening tests available in the market like Visual Inspection with Acetic Acid (VIA), Pap smear, Liquid-based cytology (LBC), HPV testing, etc., each has benefits and limitations. The VIA has a lot of false positives, the Pap test misses many cases. Globally,
Liquid-based cytology (LBC)-an improved liquid-based collection method was created, which increases the chance of detection. The Liquid-based cytology (LBC) test consists of rapid
fixation, an exact monolayer depiction of the complete material, and diminished obscuring components. This test has enhanced the detection of aberrant cervical cells since its
implementation. Liquid-based cytology (LBC) solution is the most widely used test globally, as it has the advantage of allowing a single specimen to be used for HPV testing, sexually trans-
mitted disease screening, and cytology. This alternative not only allows providers to reduce manpower and supply costs but can also reduce the frequency of repeat appointments for add-on

December 2022 EXPRESS HEALTHCARE 19
testing and thus, making it more convenient for both patients and doctors. LBC filtration technology has shown enhanced identification of adenocarcinomas, as well as the capacity to undertake out-ofvial testing, such as co-testing for HPV or sexually transmitted infections, without the need for an additional specimen.”
Disease surveillance and technology
Tracking the disease trends and systematically evaluating the interventions are some of the necessary factors for effective NCD surveillance.
Dr Kabre explains that we have seen in the recent COVID-19 pandemic that people with co-morbidities had higher mortality compared to those who did not. This makes prevention and control of NCDs all the more important.
She added, “India has a National Program for Control of Cancer, Diabetes, Cardiovascular diseases and Stroke (NPCDCS). MPW (Multi Purpose Workers) play a major role in population screening, identification of cases for referral, Follow-ups and treatments, recognition of complications and prevention and health promotion. ANM/MPW need to closely work with ASHA in their areas and this can really make a difference in managing these NCDs at the grassroot level. Proper awareness, training and guidance to these people can help India combat NCDs at a larger level. Proper monitoring, evaluation and surveillance of this program as well as proper analysis of data at all levels is the need of the hour. Just like we had a national level data collection during COVID, we need to have such use of digitisation at all levels for managing national level programs.”
Dr Wankhede opines, “Monitoring of epidemiological trends for modifiable risk factors including tobacco use, harmful alcohol use, physical inactivity and eating unhealthy diets is crucial to accurately
estimate disease burden, and also for policy/program implementation and evaluation. it will also provide a huge boost to the economic development of the country. Big data and data analytics, other cuttingedge technologies could be used to collect NCD surveillance data. Including behavioral, environmental and community data into the surveillance of NCDs could lead to opportunities for interventions
Multiple factors have impacted the risks and outcomes of non-communicable diseases,and there is an imperative need for an integrated approach from all associated players to tackle the severity of the ailments overshadowed during the pandemic
Dr Sushrut Pownikar

Head-Quality Assurance Department & Deputy Director, Oncquest Laboratories
Strengthening of cancer registries and improvement of linkages between different healthcare levels with the incorporation of task-shifting,adding digital technology and supporting programs that promote women’s welfare and health will also provide synergy to cancer control programs
Sumit Bagaria
Managing Director and CEO, Hemogenomics
To prevent and control NCDs,NPCDCS (National Programme for Prevention and Control of Cancer,Diabetes, Cardiovascular Diseases,and Stroke) was launched in 2010 with the sole vision of focusing on strengthening the existing infrastructure
Srinivasa Vivek Co-Founder, Resolute

aimed at improving population health.”
Due to the complex nature of NCDs, having a multiple surveillance approach in place is also required.
Vikas Gupta, Co-Founder and Chief Product Officer, MyDiagnostics stresses that the advancements in technology have enabled researchers to investigate the root cause of these diseases, rather than just focusing on treating them.

He said, “In the past, doctors and scientists have been able to identify diseases by studying the signs and symptoms of a patient. However, the advancements in technology have enabled researchers to investigate the root cause of these diseases, rather than just focusing on treating them. This has led to a new era of diagnosis where doctors can pinpoint what is causing health issues by analysing
data from various sources such as blood samples and stool samples etc.”
Highlightening the importance of disease surveillance and technology, Dr Nitendra Sesodia, Senior DirectorMedical Communications & Corporate Sales, Thieme Group said, “There is a dire need to improve surveillance, monitoring and reporting tools and methodologies. Disease-specific surveillance
EXPRESS HEALTHCARE December 2022 20 cover
)
and monitoring tools would have to be employed. Given the innate role of baseline data, mobile phones and internet technologies can be used for data collection.”
Infrastructure to deal with NCDs
The pandemic has highlighted the gaps in India's healthcare system that needs to be filled and has prompted calls for reform. The same reforms and learnings can also be used in enhancing the current healthcare infrastructure for NCDs.
Dr Wankhede says, “Both private and public primary care facilities and public secondary facilities are currently not adequately prepared to comprehensively address the burden of NCDs in India. The need of the hour is to develop strong healthcare systems. Primary care is the best avenue for delivering NCD care in the most comprehensive way. Public health facilities should be strengthened for providing services of screening.”
Dr Yogesh also says, “The healthcare system has improved dramatically, thus facilities must be sanitary, safe, and cost-effective. Improvements have been made to the infrastructure, but more can be done. There are now a greater number of hospitals with specialisation in services and technology that allow hospitals to treat noncommunicable conditions like cancer. The pandemic has highlighted the many ways in which India's healthcare system falls short and has prompted calls for reform.”
Policyinterventions
At the policy level, strategies and programs to combat NCDs are already in place.
Dr Sushrut Pownikar, HeadQuality Assurance Department & Deputy Director, Oncquest Laboratories said, “During the pandemic, India witnessed severe morbidity and high mortality associated with the prior affliction of the NCDs, making it a public health emergency.
According to experts, there is an immediate need for a concerted global effort with policy instruments to promote health, detect and control risk factors early and effectively treat diseases in a cost-effective manner to significantly prevent untimely deaths. With increased financial allocations and initiatives to strengthen the health system, the government should make addressing the NCDs a priority, with an enhanced focus on primary healthcare.”
Dr Pownikar also shares, “The unprecedented pandemic has created havoc across the globe for over two years, with thousands of people getting infected by the novel virus and many having lost their lives. Governments and the healthcare system in almost all countries aggressively focused on combating the pandemic and
Though the focus still remains on recovering from the pandemic, the government and healthcare system should also find ways to curb the impact of the NCDs during this period. Multiple factors have impacted the risks and outcomes of non-communicable diseases, and there is an imperative need for an integrated approach from all associated players to tackle the severity of the ailments overshadowed during the pandemic”, he added.
Srinivasa Vivek, CoFounder, Resolute throws light on theinitiatives by the government to control NCDs.He said, “To prevent and control NCDs, NPCDCS (National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases, and Stroke) was
accessibility and availability of policies at the public level, Dr Yogesh said, “Many strategies have been developed to improve the treatment of noncommunicable illnesses since everyone should have equal access to excellent health; any disparity should not be accepted. To promote pharmaceutical accessibility, affordability, and acceptance for those in need, policies should bridge the gap between resources and influence. Policies should be inclusive of everyone and accessible to everyone. More resources should be directed into the health sector in general, and chronic diseases in particular, by the federal and state governments.”
Emphasising on the policies and need of the hour specifically for cervical cancer in India, Sumit Bagaria,
the socio-economic burden owing to the treatment of cervical cancer at a late stage. In the current pandemic era, HPVassisted self-sampling can be an ideal method for screening, and if co-testing is combined with liquid-based cytology, it can provide the highest sensitivity and increase the chances of detection.
Professional organizations like FOGSI, Asia-Oceania Research Organization in Genital Infection and Neoplasia (AOGIN-India), Indian Society of Colposcopy and Cervical Pathology (ISCCP) and Association of Gynaecologic Oncologists of India (AGOI) have contributed to cervical cancer prevention strategies by developing screening guidelines, conducting screening outreach camps and conducting awareness talks across the country, using innovative strategies like the Lifeline Express to reach remote areas and collaborating with corporate and paramedical organisations.”
normalizing the healthcare crisis. In this disturbing scenario, it should be remembered that the concurrent threat of people being vulnerable to noncommunicable diseases still exists and complicates and already troublesome situation. During the pandemic, while the world witnessed millions of people getting affected by COVID-19, a communicable disease, the vulnerability of people to non-communicable diseases (NCDs) also escalated parallelly. The pandemic has also managed to significantly disrupt NCD services, the impact of which has been severe for people already living with that disease.”
“Now, as the turmoil caused by the pandemic has significantly normalised, a renewed focus on prioritising non-communicable diseases and their solutions has become the need of the hour.
launched in 2010 with the sole vision of focusing on strengthening the existing infrastructure. NPCDCS looks over human resource development, health promotion, early diagnosis, management, and referral to an appropriate level of the healthcare facility for the treatment of non-communicable diseases. Under this initiative, NCD cells are being established at the district, state, and national levels for program management and to provide facilities for early diagnosis, treatment, and follow-up for common NCDs. There is additionally a provision to provide free diagnostic facilities and drugs for patients attending such clinics. Also, Cardiac Care Units (CCUs) are being established for providing emergency care along with daycare centers for cancer care.”
Sharing his views on the
Managing Director and CEO, Hemogenomics said, “The approach of organising outreach clinics and camps was followed over decades where women voluntarily approach the camp for screening when provided with awareness regarding cervical cancer. It was useful for women who actively participated in the screening programs. It did not, however, translate into active community participation. The apprehension to undergo travel and internal examination during testing led to poor acceptance and participation. The initial screening approach, using VIA and sometimes the Pap test, also led to multiple dropouts at various steps. There is a need to advocate policy support for early screening and its impact. It is imperative to ensure a higher number of women are screened, which will result in the overall reduction of
“In 2020, all member states endorsed the global strategy towards the Elimination of Cervical Cancer at the World Health Assembly - the first elimination strategy for cancer in WHO’s history. India, a signatory, has to have a national program while active participation of the states should be incentivised.
Strengthening of cancer registries and improvement of linkages between different healthcare levels with the incorporation of task-shifting, adding digital technology and supporting programs that promote women’s welfare and health will also provide synergy to cancer control programs”, he added.
Wayforward
In the aftermath of the pandemic, renewed focus to prevent, detect, control and treat NCDs is the need of the hour. We don’t want another pandemic!
Kalyani.sharma@expressindia.com journokalyani@gmail.com
December 2022 EXPRESS HEALTHCARE 21
Tracking the disease trends and systematically evaluating the interventions are some of the necessary factors for effective NCD surveillance
Collaborations are pivotal to scale healthcare across India

Prabakar Sukumaran,Regional Director-West,GE Healthcare in an interaction with Express Healthcare highlights the importance of early diagnosis of Non-Communicable Diseases (NCDs).He also emphasises that Public-Private Partnerships (PPPs) are an important solution to reach larger communities in India,especially to grow rural accessibility and exposure to medical technologies
Across the NonCommunicable Diseases (NCDs) affecting India, we know that early detection and diagnosis are crucial. How do you think diseases can be diagnosed earlier and better?
According to United Nations Institute for Training and Research, roughly 6 million people die from NCDs like diabetes, cancer, cardiovascular diseases, and chronic respiratory diseases, every year in India. These are on the rise across the globe as well, with roughly 41 million deaths attributed to NCDs annually.
It is clear that early detection and diagnosis is crucial, which can help patients get access to the treatment they may require sooner. For more diseases to be diagnosed earlier and better, a few key gaps must be overcome. These include low awareness about the disease and lifestyle issues that exacerbate it. Late diagnosis can result in the disease advancing, which can be the case with cancer, for example. Many also neglect their health, or continue to adopt unhealthy lifestyle habits, including excessive alcohol intake, smoking, and more, which can especially create problems with cardiovascular diseases. Raising awareness on the problems that
unhealthy lifestyle patterns perpetuate is also important, so people stop overlooking health and wellness. Further, to support early disease detection, screening programs are important. For instance, if an individual goes to a healthcare practitioner with symptoms like fatigue, recurrent pain, new black spots appearing and other signs, they may be referred to get a PET Scan. This can rule out or indicate cancer and give you a clear picture of where the cancer is localized.
Early detection is also vital for cardiovascular diseases. To spearhead this, cardiac angiography CT scans, for instance, are one key measure that should be increasingly adopted. These offer a non-invasive approach to comprehensive cardiovascular disease screening. Scaling adoption of this nationwide is vital. At GE Healthcare, we are also providing the Made-in-India ‘Revolution™ Maxima,’ which is a powerful, highperforming, and reliable CT with a 128-slice scanner, which can be used as a screening tool for cardiac angiographies.
One area where we can address this, for example, is tackling the challenge of people suddenly collapsing during marathons. This can be due to several reasons,
including a sudden pressure on the heart, making it pump more oxygen, which results in collapsing. To address this, we welcome the plans that if the government can establish a new rule, stating that anyone who is going to run a marathon, or any longdistance physical competition will first need a cardiac CT scan done and must produce the certificate to qualify.
What key measures can the healthcare industry take to broaden the scope of accessible and quality care delivery, particularly to reach rural and remote areas of the country?
As we look at how we can move forward in healthcare in India, our emphasis remains on ensuring affordability, availability, and accessibility of key healthcare solutions and services. To reach larger communities in India, PublicPrivate Partnerships (PPPs) are an important solution, especially to grow rural accessibility and exposure to medical technologies. Skilling efforts are also crucial alongside this. For instance, we can advance quality care nationwide by installing medical devices, such as CT scanners, PET Scans, Cath Labs and MRIs, across Indian medical colleges through PPPs. This can be done where
EXPRESS HEALTHCARE December 2022 22 cover )
INTERVIEW
Collaborations are pivotal to scale healthcare across India, and these have been instrumental to GE Healthcare’s efforts to advance accessibility to medical devices nationwide
students and doctors have not previously had access to high-end medical devices and technologies. Such installation efforts must also be paired with skilling initiatives to teach them how to use these devices to address various complex cases and non-communicable diseases.
Such initiatives are a great step forward – for instance, 20 to 25 years ago, medical colleges only had ultrasound and X-Ray in radiology departments. However, the National Medical Council has since made it compulsory for medical colleges to have MRIs, CT scans, Cath Labs, high-end X-rays and more. PPPs have helped make this possible, ensuring more people are trained to operate medical devices effectively. Such partnerships also ensure these initiatives are sustained and run in the longterm.
To broaden access to care, Wipro GE Healthcare also launched a mission to accelerate ‘Yogya Bharat’ or ‘Skilled India,’ in partnership with healthcare and education experts.
Could you discuss what steps GE Healthcare has taken to expand access to the latest healthcare solutions and technologies,
including what kind of collaborations it has explored?
Collaborations are pivotal to scale healthcare across India, and these have been instrumental to GE Healthcare’s efforts to advance accessibility to medical devices nationwide. For instance, by collaborating with key partners, we have installed several medical imaging devices nationwide in medical colleges, which offer great value to diagnose diseases effectively. We have successfully led initiatives to do this with our valued PPP players across India. Wipro GE Healthcare has been strengthening Indian healthcare infrastructure with PPP projects for a long time. One of our first PPP initiatives was at Netaji Subash Chandra Bose College in Jabalpur in 2006, driven by one of our national PPP partners. This involved a radiology set-up in a government medical college, and our device was one of the
first 1.5 T high end MRIs that was introduced to the town. Now, Jabalpur has many 1.5 TESLA machines running.
We find the shift from a focus only on radiology to specific imaging for oncology and cardiovascular diseases particularly promising, such as with Cath Labs being installed nationwide. PPPs are vital to introduce quality equipment like MRIs, CT and PET-CT Scanners, Cath Labs and more for rural areas and smaller villages.
Industry collaborations also scale access to care and training. Earlier this year, we also collaborated with global medical device manufacturer Boston Scientific to provide end-to-end innovative interventional cardiac care solutions in India. This involved combining our strong interventional cardiology portfolios.
Looking ahead from a longterm perspective, what measures do you foresee could have a significant
impact on the health of the nation? What more can be done to support customers and patients across India? In the long term, the future of health will be driven by a number of key trends across the healthcare ecosystem. This includes industry-wide collaborations, such as with PPPs, and the need to sustain a conducive policy ecosystem that enables access to care for all. PPPs play an important role in medical education, skilling, and support investments in healthcare infrastructure and manpower. These can also ensure care advancements and newer technologies and tools are installed and adopted across the wider population. Another supporting measure with a great impact on healthcare is digitalization – especially with digital data transfers becoming more common. For instance, key machines are installed in a central hub, and imaging data is often analysed and sent from there to local practitioners and physicians
who can guide the patient along their treatment pathway.
Other important measures with long-term impact are policies like Ayushman Bharat and the Pradhan Mantri Jan Arogya Yojana, which are extremely promising. We must urge more hospitals, including a larger set of private hospitals, to embrace and adopt such schemes, as it can ensure affordable healthcare for more patients. This can have important implications across therapy areas, such as oncology, for which the cost of treatment is especially burdensome for patients. More measures must also be introduced across the continuum of care to streamline and fasten processes, like introducing eapprovals for equipment installation. This can address traditional pain points with medical device installation and help reduce delays, so the needed facilities can be quickly adopted across regions, including rural and remote areas.
We aim to continue working towards advancing healthcare for all, to support more customers, patients, and practitioners across the nation and strengthen the country’s healthcare ecosystem.
December 2022 EXPRESS HEALTHCARE 23
As we look at how we can move forward in healthcare in India,our emphasis remains on ensuring affordability,availability,and accessibility of key healthcare solutions and services
Can India afford Universal Health Coverage (UHC)?
On 10 October 2019, the UN General Assembly adopted a resolution committing member nations to achieving Universal health Coverage (UHC) by 20301. The Indian Government has signalled its intent to implement Universal Healthcare in India over the next decade. India’s National Health Policy (NHP 2017)2 includes this goal “...the attainment of the highest possible level of health and wellbeing for all at all ages, through a preventive and promotive health care orientation in all developmental policies, and universal access to good quality health care services without anyone having to face financial hardship as a consequence. ”. The roadmap towards achieving this goal is work in progress. One of the concerns is that Universal Healthcare is not affordable for Low and Middle Income Countries like India. In our research, we have triangulated evidence from multiple sources to build a cost estimate for UHC. Based on this estimate, we conclude that UHC is an achievable objective for India, although it may require deep structural changes in the extant healthcare ecosystem. In this article, we discuss these issues.
Beyond the moral, ethical and constitutional imperatives that drive the state to care for its citizens, there are also practical considerations: in the absence of UHC, families get pushed into poverty and become a greater burden on the state. Furthermore, productivity is impaired, denting GDP growth. India is among the countries with high Out-of-Pocket Expenditures (OOPE; percentage of national health expenditure that is spent by individuals and families from their own resources) on healthcare, as seen in Table 1.
In this table, select countries have been ranked by UHC serv-
ice coverage index (UHC-SCI), a composite score obtained as the geometric mean of 14 tracer indicators of health service coverage3. Broadly, for the countries in Table 1 there is an inverse rela-
tionship between UHC service coverage index and OOPE on healthcare. India with a UHCSCI of 61 and OOPE per cent of 63 per cent is at the bottom, just above Bangladesh.
Apart from economic costs, what difference does UHC make to health outcomes? Table 2 shows UHC-SCI against life expectancy at birth.
Again, there is a clear trend for countries with high UHCSCI to also have better life expectancy. In general, countries with high UHC-SCI also have high per capita healthcare ex-
UHC-SCI, broken down into its components, shows that over the years India has dramatically improved in the areas of infectious disease and reproductive health, but not so much in the areas of NCDs and Service Access (Table 3).
struggles to bring NCDs under control (US DALYs are comparable to India because of the huge burden of NCDs), then unless India takes drastic measures, the future can be catastrophic.
penditures, as might be expected. The outlier is the US, which has a significantly higher per capita healthcare spend compared to Canada and the UK and yet performs worse on
Through focused mission oriented programs, India has drastically brought down DALYs due to perinatal disease, but the trend of growing DALYs due to non-communicable diseases (NCDs) which are much more complex and expensive to manage portends a grim future. If a wealthy country like the US
In the journey towards UHC, the government has initiated measures that include schemes like Ayushman Bharat, alongside state specific schemes. These schemes attempt to universalise healthcare coverage by covering fixed treatment costs at empanelled hospitals, including private hospitals, for certain procedures. For treatments not eligible under these schemes, patients who cannot afford private care have to rely solely on hospitals run by the government. The capacity of government run hospitals falls far short of the load of patients they are burdened with. Furthermore, even in Ayushman Bharat the expenses covered by the scheme are the barest minimum acceptable to private delivery institutions and does not compensate the patient for lost wages, travel to the hospital, accommodation for an accompanying attendant etc. These are significant barriers to accessing care for someone below the poverty line. This partially explains the low uptake of such schemes. Offering a bouquet of incoherent schemes with plenty of gaps is not the solution or a desirable path towards UHC.
The extant model of healthcare, which is dominated by private fee for service players, is poorly suited to cost-effectively provide UHC. If there is one lesson to be learnt from the experience of other nations implementing UHC, it is to strengthen government operated or managed primary healthcare and make it available as close to citizens as possible. Primary health-


EXPRESS HEALTHCARE December 2022 24
PUBLIC HEALTH
UHC-SCI and life expectancy. Clearly, the method of implementation of UHC impacts the efficiency of healthcare delivery and resultant clinical outcomes.
gatekeeper
care should serve a
Aparajithan Srivathsan,CEO,Intent Health Technologies and Swami Subramaniam,CEO, Ignite Life Science Foundation in their research triangulated evidence from multiple sources to build a cost estimate for UHC.Based on this estimate,they concluded that UHC is an achievable objective for India,although it may require deep structural changes in the extant healthcare ecosystem.In this article,they discuss these issues AparajithanSrivathsanSwamiSubramaniam Table 2: UHC SCI and Life Expectancyat Birth (All data for 2019) S.No Country UHC Service Coverage Index Life Expectancyat Birth (Years) DALYs/1000 (Years) Health Expenditure per Capita ($PPP) As %age of GDP 1 Canada 89 81.8 273.4 5476 10.8% 2 UK 88 80.9 293.2 4765 10.2% 3 USA 83 77.3 338.7 11027 16.8% 4 China 82 77.1 268.7 815 5.4% 5 Mexico 74 75.1 272.0 1058 5.4% 6 India 61 69.9 336.4 242 3.0% 7 Bangladesh 51 72.9 270.8 130 2.5% Table 1: UHC SCI and OOPE Country UHC Service Coverage Index % OOPE share of national healthcare expenditure Households with OOPE >10% of annual income 1 Canada 89 14.8% 3.8% 2 UK 88 16.5% 2.2% 3 USA 83 10.9% 4.5% 4 China 82 35.5% 24.0% 5 Mexico 74 41.6% 1.6% 6 India 61 63.0% 17.3% 7 Bangladesh 51 78.5% 24.4%
function that ensures that patients are referred only when appropriate for specialist, secondary, or tertiary care. While all villages in India may not be close enough to a suitably equipped Primary Health Centre (PHC), care at the door step should be possible through a
health worker tethered to the nearest PHC using the tools of telemedicine. Emergency care may also need to be redesigned to be as accessible as possible in the remotest regions of the country. Building such a comprehensive network will require significant upfront investments,
as well as systems and procedures to integrate existing private players.
In order to estimate the cost of providing UHC for the Indian population, we need estimates of consumption and costs per unit of consumption. The National Sample Survey Organization (NSSO) data5 provides estimates of both. But both being retrospective data based on a pre-UHC situation can only be taken as baselines and not as targets to meet. To estimate consumption, we can look at consumption data for a country like Canada which has one of the more successful models of UHC. But this data on consumption has to be adjusted for differences with respect to India in terms of demographics and DALYs. Canada has an older demographic. But India has a higher DALY number, suggesting that despite a younger population, Indians in general have higher levels of morbidity. The only way to address these countervailing consumption drivers is to look at consumption data in a situation in India that may be closest to what UHC in practice may look like. The Indian Railways with its 1.3 million employees spread across the country, with access to healthcare close to their homes through a net-
work of railway hospitals and clinics, comes close to being ideal in terms of healthcare provision in India6. If we look at healthcare consumption among railway employees and their families, we can see that it is close to the current consumption rates in Canada for hospitalisation, but still only 50 per cent of Canadian consumption in terms of OPD visits.
Using information from these sources, we have estimated consumption under UHC in India (Table 4).
We have increased the target OPD visits to 4 per year (from 1.9 in the general population and 3 among Railway employees and families). This is to account for an increase in consumption (as seen in Canada for OPD visits) as part of a preventive approach to health under UHC. We have bumped up consumption of hospitalisation only marginally, since we have assumed that hospitalisation among railway employees/families is at near ideal levels (a patient sick enough to be hospitalised is unlikely to defer or delay treatment when the employer is paying for care). Thus, the figure of 8 hospitalisations per 100 per year is slightly higher than rates currently prevalent in the railway employee population and slightly
lower than what is seen in Canada.
Once we have triangulated estimates of consumption (Table 4), we need to look at costs per unit consumed for both OPD visits and hospitalisations. Here the Railways' data again has a normative value. We have estimated OPD costs of Rs 1000 per visit and hospitalisation cost of Rs 50000 per admission. Based on annual consumption rates, the total annual cost of healthcare per Indian works out to Rs 6600 (at 2018-2020 prices). At current population and GDP levels this works out to an aggregate amount of Rs 900000 crores or 5.2 per cent of GDP, which is 80 per cent higher than current spending levels, or 3 per cent of GDP. Targeting such costs may be unrealistic today. However, if we were to project a comprehensive UHC system to be implemented by 2035, the same level of spending would account for 23 per cent of projected GDP (at 2018-2020 prices) and by 2050 only around 1 per cent of GDP. While this estimate is only a rough approximation, even a doubling may not be a significant burden on costs. If consumption stays where we project it to be, UHC would be a highly affordable public good.
One item not accounted for in
December 2022 EXPRESS HEALTHCARE 25
Table 4: Estimating consumption,unit costs and total per capita costs of UHC (based on data for 2017-18) CONSUMPTION COST/UNITCONSUMED (INR) COST/PER PERSON/PER YEAR (INR) OPD visits per person per year Hospitalisations per 100 persons per year OPD Visit Hospitalisation OPD Visits Hospitalisation Total Healthcare consumption India In Govt facilities 0.57 2.36 918 27353 523 646 1169 In Private Facilities 1.33 2.44 888 51130 1181 1248 2429 TOTAL 1.9 4.8 1704 1893 3597 Healthcare consumption in Indian Rlys In own facilities 3 5.9 918 27353 2754 1614 4368 In other hospitals 1.9 51130 0 971 971 TOTAL 3 7.8 2754 2585 5339 Healthcare consumption in Canada 6.7 8.3 Assuming consumption for India is as in Canada 6.7 8.3 18 27353 6151 2270 8421 Estimating comsumption based on DALYdata and actual consumption in RailwayHospitals In government facilities 3 7.2 1000 30000 3000 2160 In private facilities 1 0.9 1000 50000 1000 450 TOTAL 4 8 4000 2610 6600 Table 3: UHC SCI trend for India 2000-2019 2000 2010 2019 UHC SCI Overall 31 48 61 Infectious Diseases 8 30 71 Reproductive Health 56 73 72 NCD 46 57 63 Service Access 44 41 44 Global Rankon UHC SCI 143 135 121 India (DALYs/1000) Overall 501.7 399.9 336.4 Infectious Diseases 169.8 103.4 58.1 Reproductive Health 74.5 52.5 33.1 NCD 183.4 184.3 194.9 Healthcare Expenditure Per Capita (INR) 986 2464 3708 % of GDP 4.7% 4.1% 3.0% Govt Share as % of GDP 0.9% 1.2% 1.0%
PUBLIC HEALTH
this estimate is the likelihood that the establishment of new methods of operation required for UHC can create significant front loaded capital expenditures. Another is the concurrent spend on social determinants of health, such as public health and civic infrastructure, which could provide a multiplier effect to the direct spending on health. On the other hand, we have also not specifically accounted for savings that will result from avoiding wasteful expenditures (through a gatekeeper mechanism rendered through primary and community care clinics, and near-universal substitution of generics in the place of branded products).
The analysis presented here is a beginning. Given that UHC should be a compulsory public good, we have attempted to
show that it is also an affordable public good. While our estimates may lack the precision that can only be arrived at by conducting a large-scale bottom up exercise, it holds out hope that UHC is feasible, and therefore it should provide the needed impetus to taking definitive actions to making UHC a reality. The most difficult structural element to execute will be the establishment of a comprehensive network of primary/community health centres whose staff are charged with being the first point of call for patients for their healthcare needs. The second structural change will be the necessity in any UHC system to build a strong backbone of government led delivery mechanisms (the gatekeeper mechanism and emergency care being core to this element) that can work with and get the best
out of private players.
For a large country like India with wide income inequalities, UHC is an imperative and not a choice. By adopting new structures and institutions, the cost of UHC should be well within the means of the Indian economy. The gains in productivity resulting from a population that is healthy can outweigh the cost of implementing UHC (we estimate the cost of lost productivity at Rs 765000 crores in the year 2050 (at 2018-20 prices) based on a reduction of DALYs by 30 under a UHC regime. This figure would represent almost 1 per cent of GDP.
The necessity for deep structural changes in how healthcare is operated is unavoidable. It is a bullet the government must bite, if UHC in any form is to be realised. We have not in this piece
covered initiatives in the area of public health that can contribute to significant improvements in the health of the population, e.g. control of air pollution or the plentiful availability of recreation areas for exercise. Any move towards UHC must take a comprehensively inclusive view of health.
In summary, UHC is a necessary public good that is affordable for a resurgent India with an expanding GDP. The rightful question to ask is - “can India’s aspiration to become a developed country on the back of a productive labour force afford NOT to have UHC?”
References
1. Political Declaration of the High-Level Plenary Meeting on Universal Health Coverage (2019), UN General Assembly
2. National Health Policy 2017, published by the Ministry of Health and Family Welfare
3. WHO - Global Health Observatory
4. National Health Accounts Estimates for India 2017-18, published in 2021 by the Ministry of Health and Family Welfare
5. NSS 75th Round 2017-18, Key Indicators of Social consumption in India-Health, published by the Ministry of Statistics and Program
Implementation
6. Feroz Ikbal, Rudrani Ghosh and Praveen Bhide; Indian Railway Health Service: A model for Universal Health Coverage, Economic and Political Weekly, Vol. 57, Issue No. 34, 20 Aug, 2022
7. Institute for Health Metrics and Evaluation | (healthdata.org)

EXPRESS HEALTHCARE December 2022 26
E m a i l : r a j e s h b h a j n i k @ e x p r e s s i n d i a c o m ■ C o n t a c t N o 9 8 6 7 1 4 5 0 2 8 C o m p a n y N a m e T h e I n d i a n E x p r e s s ( P ) L t d , C o m p a n y A d d r e s s M a f a t l a l C e n t r e , 7 t h F l o o r , R a m n a t h G o e n k a M a r g , N a r i m a n P o i n t t , M u m b a i 4 0 0 0 2 1 B a n k N a m e H D F C B a n k L t d ● B a n k A d d r e s s C 5 / 3 2 , S a f d a r j u n g D e v e l o p m e n t A r e a ( S D A ) , N e w D e l h i 1 1 0 0 1 6 ● A c c o u n t 0 0 3 2 8 6 3 0 0 0 0 0 7 5 ● S w i f t C o d e H D F C I N B B ● I F S C H D F C 0 0 0 0 0 3 2 A c c o u n t T y p e C u r r e n t
HEALTHCARE IT
5G rollout in India and opportunityfor telemedicine
India faces several challenges in providing quality healthcare in the coming decades with the second highest population in the world, increasing life expectancy and uneven geographical distribution of medical resources across urban and rural areas. Telemedicine is all about delivering healthcare services by medical professionals leveraging digital technology for the exchange of relevant information for diagnosis, treatment and prev ention of diseases and injuries all across the world. Rollout of telemedicine can be crucial in providing quality healthcare services at reasonable rates and to overcome the challenges limited medical resources and infrastructure. Through telemedicine and 5G enabled mobile medical units, primary healthcare services and specialist advice can be effectively brought to the doorsteps of people in the remote locations of the country.
The network support for telemedicine must be robust to effectively support near real-time data and high-quality images and video. The important characteristics of 5G which are of most value to healthcare include high speed data transfer rate, low latency, high reliability and high device connection density which are significantly higher than 4G. 5G will drive near real-time, high-quality video required for remote medical consultations. The high speed will offer faster diagnostics while the low latency will offer quick transfers of images and files thus enhancing remote monitoring of patients and improving the efficiency of the administrative processes. With extending health care providers’ reach with the help of 5G beyond
hospitals, telemedicine will improve access to quality care, helping patients access specialists who are otherwise not available in a shorter time span.
The need for a real-time
network with higher bandwidth and high-speed internet access has been also driven by the development of data hungry artificial intelligence healthcare applications. This involves for exam-
ple using machine learning algorithms to analyse large amounts of medical data to identify patterns and trends that can be used to provide the appropriate treatment and improve patient care online. Wearable medical devices using 5G enables instantaneous patient monitoring across the globe. The incorporation of 5G with these devices can further open up new opportunities to provide personalised and holistic patient care. Telemedicine is constantly evolving and has come a long way in terms of both service delivery and infrastructure as it incorporates new advancements in technology and adapts to the changing health requirements and contexts of societies. Research studies have supported telemedicine services as a promising solution to improve several chronic medical conditions such as diabetes, obesity, hypertension, depression, and cancer. It can help healthcare professionals bring a proactive approach toward healthcare, thus minimising the chances of a health issue occurring.
Telemedicine in India has huge potential to grow from its nascent stages. The market size for telemedicine in India is expected to grow at a compound annual growth rate of 31 percent from 2020 to 2025. To reap the maximum benefits from 5G, telemedicine needs to be integrated as a key component of healthcare delivery in India with well-defined telemedicine model covering diagnostics, prescriptions, and care delivery supported by a partner ecosystem. This requires close collaboration between government agencies, hospitals, technology infrastructure partners and telemedicine service providers

including startups. Such collaboration can bring down the cost of upgrading legacy hospital systems and the cost of connected medical devices and services.
There are of course several challenges that need to be addressed starting with reengineering of clinical process flows. The frontend and backend processes for patient connection, diagnosis, treatment and follow ups need to be relooked and made telemedicine centric as possible. Healthcare agencies and hospitals need to accelerate collaboration with industry partners to develop 5G enabled telemedicine applications aligned to these new clinical processes and leveraging shared data across various platforms including mobile phones and wearables. Possessing adequate digital literacy skills is critical for medical practitioners moving forward.
There is already effort put in this regard during the COVID-19 pandemic as various organisations and medical professionals came together to successfully collaborate to monitor infection rates and do contact tracing through shared data obtained via mobile phone applications.
Telemedicine application designers and developers need to ensure that such applications are user friendly and accessible through multiple platforms ensuring data privacy and security and with clear payment models for reimbursement of cost incurred.
Telemedicine services with 5G connectivity, has the power to elevate healthcare to the next level with personalised services across the country thus relieving the severe resource restraints faced by India and saving precious lives.
December 2022 EXPRESS HEALTHCARE 27
Dr Karippur Nanda Kumar,Professor-IT,SPJain School of Global Management explains that through telemedicine and 5G enabled mobile medical units,primary healthcare services and specialist advice can be effectively brought to the doorsteps of people in the remote locations of the country
5G will drive near real-time,highquality video required for remote medical consultations.The high speed will offer faster diagnostics while the low latency will offer quick transfers of images and files thus enhancing remote monitoring of patients and improving the efficiency of the administrative processes
Cyber securitychallenges in the healthcare industry
&
As cybercriminals continue to become more sophisticated by the day, the number of breaches across industries is climbing. In the healthcare space, however, a cybersecurity lapse can be life-threatening. Stolen or modified patient information, misdiagnosis, delay in treatment, or diverting ambulances can all jeopardise human life.
Unfortunately, by the end of 2020, the breaches amounted to $6 trillion, which cost the industry $10 million per breach. While healthcare players must prioritise cybersecurity, it is also particularly tough for this sector.
Here is a list of the top ten cybersecurity challenges in the healthcare industry:
Data breaches: As mentioned before, the average and aggregate cost of data breaches is enormous and can prolong the entire treatment process. Healthcare organisations must follow the highest standards for security information related to the patients by investing in device management and monitoring and encryption of sensitive data.
Ransomware and malware:
Ransomware attacks are one of the most common ways of data theft. Secured systems are attacked with this malware in which attackers take the data on a victim's computer through encryption and demand payment for decryption and access return. Training hospital employees about the seriousness of such threats is critical to secure information and avoid mishaps.
Vulnerability of legacy systems: The legacy or traditional systems running on old codes and operating systems are prone to cyberattacks as they have negligible layers of security compared with the current systems. While there are cutting-edge medical facilities that run on the latest standards, many others use software and security systems that are dated. Hence, upgrading systems should be an integral part of the cybersecurity process.
Insecure medical devices and equipment: In modern times, many devices and equipment run through IoT or IoMT, meaning that providing secure access to such devices is critical. However, decision-makers can easily miss this point, leav-
ing the entire organisation vulnerable to attacks.
Insider threats: There can be circumstances of distressed or unhappy employees leaking out sensitive information to the attackers on purpose. Hence, insider threats must be addressed with the utmost care, as employees have massive amounts of data available to them.
Distributed Denial of Service (DDoS) attack: It is a common technique used by attackers wherein many requests are forwarded to the server to bring it down. Healthcare services can-
not remain down for long, and such attacks can cause massive panic among the stakeholders.
Lack of documented cybersecurity and governance policies: There is a severe lack of documentation, codification, and record management, as far as cybersecurity and governance policies of healthcare organisations are concerned.
Since healthcare organisations might not have the expertise needed for such compliances, it is recommended to hire thirdparty experts for the job.

Cloud-based threats: With the emergence of the cloud as the most preferred platform by healthcare organisations, there is a significant risk as the volume of data and number of users interacting on the cloud are enormous. With an increased number of stakeholders on the cloud, the chances of attacks also increase.
Phishing attack: These attacks induce users to provide their passwords and other personal information to the attackers who pose as a legit website or information source. This is quite a common way of attacking users, and one of the ways to control these attacks is by
constant vigilance.
Lack of cyber awareness: Besides the business-related updates, a healthcare organisation should create an environment that educates the employees about the threats and ways attackers generally attempt to enter a secured system. A comprehensive training module should be designed based on which do's, and don'ts are crafted.

Summing up
With the increase in digital processes and asset usage, the overall risk of cyberattacks on healthcare systems has increased. Hospitals are prone to lose sensitive information about treatment and patient history, which could be catastrophic for the entire critical care process. Despite improved cybersecurity measures, the number of attacks on healthcare organisations continues to rise yearly. From the perspective of a healthcare organisation, besides awareness, alertness, preparedness, and quick response, codification and documentation of cybersecurity best practices could be the way to counter these challenges.
EXPRESS HEALTHCARE December 2022 28 HEALTHCARE IT
Shashidhar Rachuri,Director-Innovation
Growth,Noventiq India emphasises that with the emergence of the cloud as the most preferred platform by healthcare organisations,there is a significant risk as the volume of data and number of users interacting on the cloud are enormous. With an increased number of stakeholders on the cloud,the chances of attacks also increase
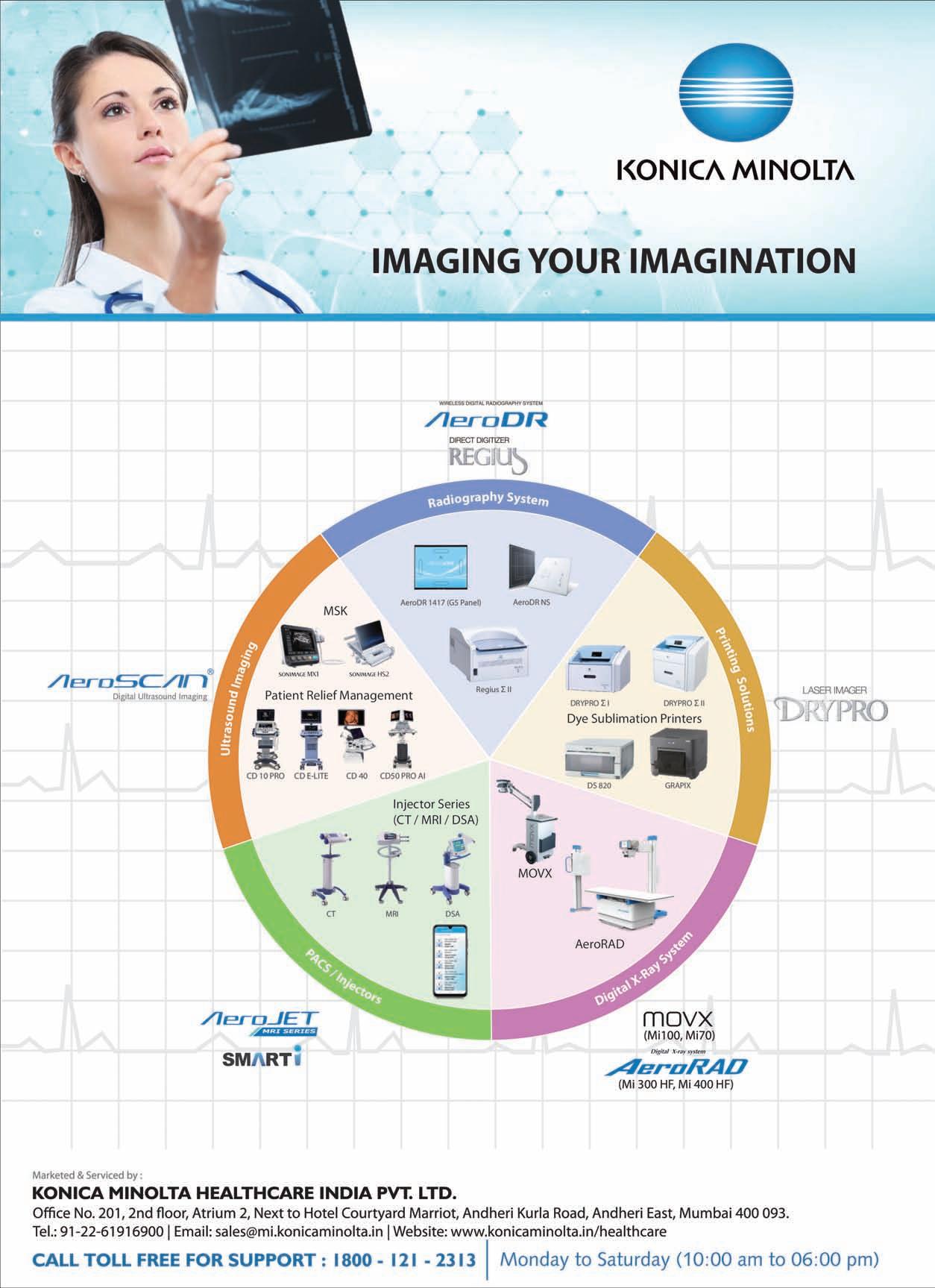
BUSINESS AVENUES EXPRESS HEALTHCARE EXPRESS HEALTHCARE December 2022 29

BUSINESS AVENUES EXPRESS HEALTHCARE December 2022 EXPRESS HEALTHCARE 30
BUSINESS AVENUES EXPRESS HEALTHCARE EXPRESS HEALTHCARE December 2022 31


BUSINESS AVENUES EXPRESS HEALTHCARE December 2022 EXPRESS HEALTHCARE 32









BUSINESS AVENUES EXPRESS HEALTHCARE EXPRESS HEALTHCARE December 2022 33 BlueHeaven SILICONETRANSPARENTTUBING M.K.SiliconeProductsPvt.Ltd. E-mail:sales@mksilicone.com 205&206HillViewIndustrialPremises,AmrutNagar, Ghatkopar(W),Mumbai-400086,India.Tel.:022-25004576 fortheQualityConscious…. INDIA QM002 AnISO9001-2015COMPANY Quality Products Since 1997 CERTIFIED CLEA N ROOM IS08 To Advertise in Business Avenues Email: rajesh.bhatkal@expressindia.com rbhatkal@gmail.com





















BUSINESS AVENUES EXPRESS HEALTHCARE December 2022 EXPRESS HEALTHCARE 34
HEALTHCARE TRACKER
MISPAi3 –The third generation patented specific protein analyser from Agappe
Thomas John,MD,Agappe highlights that when Agappe introduced the Mispa I series in 2011,it could completely improvise on the traditional latex method for protein measurement by integrating nephelometry and immunoturbidimetry technologies.This unique technology offers a wide range of results with excellent sensitivity,and higher linearity at a reasonable price
In its 27 years of service to the IVD segment of medical devices, Agappe has consistently maintained on the cutting edge of technology throughput its journey to handhold its customers and offer patients a faster, reasonably priced, and precise diagnostics of highest quality standards.
It’s a moment of great pride and privilege for Agappe to receive the award of technology patent in respect of Mispa i3New Technology as Patent No: 409768 from Indian Patent Office on October 25 2022. The title of patent is “APPARATUS AND METHOD TO MEASURE CONCENTRATION OF PARTICULATES IN SOLUTION”. Mispa i3 had received three other design registrations during 2016 itself.
Nearly 35 per cent of estimates for individual proteins were made using the latex approach 10 years before. The latex methods have their own restrictions and a more time-consuming results generation process. Due to these latex testing limitations, results were not certain, particularly in the borderline ranges.
When Agappe introduced the Mispa I series in 2011, it could completely improvise on the traditional latex method for protein measurement by integrating nephelometry and immunoturbidimetry technologies. This unique technology offers a wide range of results with excellent sensitivity, and higher linearity at a reasonable price.

Later on, another semiautomatic protein analyzer called Mispa-i2 was introduced with the proprietary "UCS" technology, for which patent was awarded in 2018 as Patent No: 303381.
The third-generation equipment of the family of Mispa I series, the Mispa-i3, is an automated cartridge based specific protein analyzer that provides higher precision and quick turnaround results for all pro-
tein assays in blood. It covers a broader assay panel of 23 parameters and supports greatly in clinical management of a number of disorders. It is a wholly indigenously manufactured nephelometry equipment
which assists in quantitatively estimating individual proteins utilising a combination of nephelometry and turbidimetry techniques, which are recognised to be the gold standard. Besides, Mispa i3 uses unique technology to offer the highest linearity and best sensitivity, employing channel shift in order to produce high-quality results.
Higher sensitivity and linearity in the results allow Mispa i3 equipment for an easy and one step laboratory testing at a low cost. The assay panel includes a cardiovascular risk profile, allergy profile, COVID profile, diabetes profile, rheumatology profile, osteoporosis screen profile, etc. Doctors can easily identify disorders and monitor patients' progress thanks to numerous and broad test panels available with the machine. Cystatin C is a more accurate predictor of early renal failure than enzymatic creatinine. The cardiovascular risk profile includes the indicators hs-CRP, Lp(a), D Dimer, Apo A1, and Apo B. The diabetes profile includes the HbA1c and Microalbumin tests. Instances of infections or inflammation brought on by viral or bacterial responses can be precisely estimated through biomarkers like CRP, RF, ASO, Ferritin, PCT, C3, or C4 using the powerful UCS Technology of Mispa i3. Mispa i3 can accurately estimate elevated levels of IgG, IGA, IgE, and IgM due to immune responses, with zero reagent waste and the quickest reporting time. This new type of instrument, with pre-calibrated reagent pack and extensive automation, make the usage so simple to any unskilled technicians with minimum training. Mispa i3 stands out
from other instruments due to its lower pack sizes for all special parameters and inexpensive equipment cost.
Within a short period of five years, Mispa i3 became the game-changer in specialised protein testing due to the rising trend of automation and the avoidance of manual errors on a global scale. Customers in more than 75 countries now choose it as their first choice for protein estimation.
10 per cent of the total work force in Agappe works for R&D section at Agappe, which comprises of multiple PhDs and master’s degree holders. They play the pivotal role in developing innovative technologies in Agappe, spend around 6 per cent of its total revenue for research, while average Indian figure is below 1 per cent.

Patents have a strong positive effect on society as well as science as they promote innovation. The afore-mentioned new technology patent proves that Mispa i3 is a revolutionary product.
Agappe was honoured with the prestigious award from the former President of India, Ram Nath Kovind as the winner of National Awards 2018 for the “Indigenous Development of Technology and Commercialization” of Mispa-i3, the Automated Cartridge Based Specific Protein Analyzer, in the presence of Dr Harsh Vardhan, former Union Minister for S&T and ES.
Customers today are better informed. Both patients and doctors expect quick, precise, economical, and simple technology for their diagnostic tools. Agappe is always committed in offering such cutting-edge technologies, in pursuit of better patient care and wellness.
December 2022 EXPRESS HEALTHCARE 35
Mindraylaunches BC-700 series: Compact,integrated CBC & ESR hematologyanalyzer for small-to-mid sized labs
Mindray a global leading medical solution provider, has launched the newBC-700 Series in India, a revolutionary hematology analyzer series that incorporates both Complete Blood Count (CBC) and Erythrocyte Sedimentation Rate (ESR) tests. This series, including two open vial models BC-700/BC-720 and two autoloader models BC760/BC-780, is designed to empower medium-volume laboratories with advanced diagnostics technologies that are applied in the premium products.


SFCube 3D analysis technology
Striving to benefit more laboratories worldwide, the BC-700 series adopts Mindray’s core hematology technology of SF Cube 3D analysis and is built from the same platform as its high-end BC-6000 Series, but in a smaller footprint. In SF Cube technology, target cells are subject to a 3D analysis using bi-angular laser scatter signals and fluorescence. The 3D scattergrams generated with the cellular information can help clinical experts to identify and differentiate cell populations, in particular abnormal clusters, providing a morereliable result to the doctor.
Integrated CBC + ESR solution
The erythrocyte sedimentation rate, also known as ESR, is a blood test that measures how quickly red blood cells (RBCs) settle in diluted plasma over a specified period of time. Although ESR is a nonspecific test, it can effectively reveal inflammatory activities in the body. ESR test results alongside other clinical information can help doctors to diagnose and monitor the progress of an inflammatory disease.
Traditionally, ESR tests are performed on an independent analyzer, and can take up to 60 minutes to get the results. A
thorough survey conducted by Mindray in more than 30 countries and regions reveals a demand for integrated testing for CBC and ESR. Now, the BC-700 Series is engineered to meet that demand, being the first all-inone hematology solution that combines 5-part differential with ESR analysis. With just one test, it yields both CBC and ESR results in mere1.5 minutes, significantly improving workflow and
testing efficiency while benefiting patients with quicker blood test reports.
Optical PLTin everyCBC & DIFFtest
Powered by the SF Cube analysis technology, Mindray has developed many useful hematology parameters. With the new parameter, PLT-H, the BC-700 Series can more easily address the challenges that were previously
inadequately met by conventional hematology analyzers, providing an accurateoptical platelet count result in every CBC and DIFF test. By using patented reagents with cuttingedge technology, the BC-700 Series also allows the platelet clumps to be de-aggregated, offering laboratories a complete solution for reliable platelet analysis.

"We designed and built this
analyzer series, because Mindray believes all labs matter. Every laboratory needs solutions that empower trust and accurate results, and this is what drives us to develop technologies and innovations that go above and beyond your requirements."
Mindray is committed to providing high quality, reliable IVD solutions to empower trust, delivering accurate results while meeting laboratories’ demands on efficiency worldwide. With our continuous investment in R&D, we will keep advancing healthcare technologies to meet the evolving needs of our customers.
EXPRESS HEALTHCARE December 2022 36 HEALTHCARE TRACKER
Kshama Nandode,Marketing Manager-IVD,Mindray India gives an overview of Mindray’s newly launched CBC & ESR hematology analyzer
The winged BCS and ease of blood collection
Among the many pieces of equipment that medical professionals use, the winged blood collection Set (BCS) stand out. Also known as butterfly set, they are used to draw blood or deliver intravenous therapy through veins.
The components of a winged BCS are a slim needle, two flexible and colored wings, transparent tubing, and a connector. There can also be a plastic covering on the needle to prevent needlestick injuries. While drawing blood, a tube can be attached to the connector and blood samples can be collected with ease.
Blood collection is an irreplaceable method to diagnose as well as monitor health issues. Other means can be highly invasive and painful for the patient. But collecting blood has its own set of challenges as well. At least it did before Hindustan Syringes & Medical Devices Ltd (HMD) introduced the Vaku 8-winged blood collection set.
HMD’s Vaku 8-winged blood collection set is designed for safe,fast, easy& efficient blood sampling

Offered by one of India’s most promising medical devices manufacturers, Vaku 8 is a closed system that facilitates the safe collection of specimens with minimum pain. The set also contains disposable tubes and needles. This reduces the possibility of blood exposure and cross-contamination. Let us look at the features and benefits of winged BCS in detail.
The winged BCS Vaku 8 solves problems faced by healthcare workers
Healthcare workers have a heavy schedule and often need to stay on their toes throughout their day. And with blood samples required frequently, inefficient blood collection can cause unnecessary delays, stress or even a misdiagnosis.
Healthcare workers must al-
ways keep patient health and safety as a top priority. Patients with low blood pressure might suffer adversely during blood collection.
But not with the Vaku 8. Its winged set is a closed system that obtains blood through a complete vacuum draw. This way, it maintains the sample's integrity and prevents air from filling during blood collection.
The trauma that patients have to endure due to subpar medical equipment is also a consideration. The possibility of issues like cross penetration and incorrect angle of the nee-
dle is also eliminated with the use of the Vaku 8 blood collection set.
While collecting blood, healthcare workers might need to make multiple attempts for correct venipuncture, which results in the loss of vacuum in the tube and the underfilling of specimens.
But the Vaku 8 eliminates this possibility with its evacuated tube system.
Safe and easycollection of blood with
Vaku 8 HMD puts safety first. Vaku 8’s flashback visualisation ensures
accurate needle insertion, and its superior hypodermic needle allows for a safe shallow angle insertion. With its ease of cannulation, chances of cross-vein perforation are significantly reduced as well.
Lastly, Vaku 8 makes blood collection truly easy by allowing multiple tubes with a single insertion. Its flexible tubing tolerates more patient movement. So, whether the patient is an adult or a child, Vaku 8 will enable efficient drawing of blood.
The takeaway
The winged BCS makes
blood collection safe, fast, easy & efficient.
HMD provides winged blood collection sets under its proprietary brand Vaku-8. They come with high-quality plastic wings and are safety-engineered for secure blood drawing processes. They are also available in various sizes for different treatment purposes.
So, stock your medical institutions with winged blood collection set for routine blood collection and provide quality treatment to patients.
Make sure you ask for Vaku-8 when getting a blood test done.
December 2022 EXPRESS HEALTHCARE 37 HEALTHCARE TRACKER
Hindustan Syringes & Medical Devices,HMD’s Vaku 8-winged blood collection set is designed for safe,fast,easy & efficient blood sampling
Medikabazaar launches corporate vaccination drive to beat absenteeism & improve productivity
Winter is coming and it marks the start of influenza or flu. The pandemic has taught us that prevention is always better than cure. CDC & WHO recommends flu vaccination for all eligible persons, including pregnant and lactating individual.
Gauzing the trends worldwide, Medikabazaar has taken up the initiative to contain the spread of influenza and stop it from becoming a menace. With influenza vaccine readily available, it is possible to limit the spread of virus and minimise the spread of infections at workplace and to infants and elderly who could be possible carriers. The safest, economic and readily available solution is the influenza vaccine.
Medikabazaar
Increasing number of corporates have realised this and are going for corporate vaccination camps. All one needs is a commitment to contribute to employee welfare and the rest you can leave it on Medikabazaar.
Medikabazaar is committed to bring healthcare to all. They are the largest and the fastest growing online platform work-
ing in the B2B space and have the experience and the expertise to manage corporate vaccination end to end.
Medikabazaar is making influenza vaccination administering for employees and their dependents easy, safe and convenient.
Medikabazaar’s achievements include successfully
driving COVID-19 vaccination drives in the corporates for their employee and loved ones. The costs for such drives are the cost of the vaccine plus a service charge for administering it. Also keep the following in mind ◆ H1N1, MERS, SAARS are influenza variants 80 per cent of infected employees continue to come to the office
◆ Vaccination is a small cost as compared to the hospitalisation expenses.
Other important vaccinations which we recommend and are in scope of our proposition for adults at workplace are
◆ Pneumococcal (>50 years)
◆ HPV-Human Papillomavirus (Girl & Women 18-45 Years)
◆ Td- Tetanus Diphtheria (19 years onwards)
◆ MMR- Measles Mumps Diphtheria (19-60 years)
◆ Meningococcal vaccine for frequent travelers to abroad
The flu is costing corporates MILLIONS in lost productivity and Medikabazaar has taken the responsibility to address this issue and reduce illness in the corporate world.
● Express Healthcare accepts editorial material for the regular columns and from pre-approved contributors/columnists.
● Express Healthcare has a strict non-tolerance policy towards plagiarism and will blacklist all authors found to have used/referred to previously published material in any form,without giving due credit in the industryaccepted format.
● As per our organisation’s guidelines,we need to keep on record a signed and dated declaration from the author that the article is authored by him/her/them, that it is his/her/their original work,and that all references have been quoted in full where necessary or due acknowledgement has been given.The declaration also needs to state that the article has not been published before and there exist no impediment to our publication.Without this declaration we cannot proceed.
● If the article/column is not an original piece of work, the author/s will bear the onus of taking permission for re-publishing in Express Healthcare.The final decision to carry such republished articles rests with the Editor.
● Express Healthcare’s prime audience is senior management and professionals in the hospital industry.
Editorial material addressing this audience would be given preference.
● The articles should cover technology and policy trends and business related discussions.
● Articles by columnists should talk about concepts or trends without being too company or product specific.
● Article length for regular columns: Between 1300 - 1500 words.These should be accompanied by diagrams,illustrations,tables and photographs, wherever relevant.
● We welcome information on new products and services introduced by your organisation for our Products sections.Related photographs and brochures must accompany the information.
● Besides the regular columns,each issue will have a special focus on a specific topic of relevance to the Indian market.You may write to the Editor for more details of the schedule.
● In e-mail communications,avoid large document attachments (above 1MB) as far as possible.
● Articles may be edited for brevity,style, relevance.
● Do specify name,designation,company name, department and e-mail address for feedback, in the article.

● We encourage authors to send a short profile of
professional achievements and a recent photograph, preferably in colour,high resolution with a good contrast.
Email your contribution to: viveka.r@expressindia.com viveka.roy3@gmail.com
Editor, Express Healthcare
EXPRESS HEALTHCARE December 2022 38 HEALTHCARE TRACKER
Gauzing the trends worldwide,Medikabazaar has taken up the initiative to contain the spread of influenza and stop it from becoming a menace
is committed to bring healthcare to all.They are the largest and the fastest growing online platform working in the B2B space and have the experience and the expertise to manage corporate vaccination end to end
CONTRIBUTOR’S CHECKLIST
w w w.mindray.com/in info.in@mindray.com






















































































OnemoreMilestoneofAgappeR&D, Mispai3 isPatented(409768)byits UniqueTechnology. CartridgeBasedSpecificProteinAnalyser Quality isnotanact, it’sahabit... BarcodedReagentsCartridge AutoSaveCalibration NGSPCertifiedHbA1cReagents UCSTechnology CARDIACINFECTIOUSALLERGYAUTOIMMUNE DIABETIC BONEMETABOLISMANEMIA SEPSIS COVIDPROGNOSIS AVAILABLEPROFILES 18004257151/18008917251/18002707151 Toll Free ScanHere formoreinfo AWARDED WITHMULTIPLE TECHNOLOGY PATENTS&DESIGN REGISTRATIONS “AgappeHills”,Pattimattom(PO),Dist.Ernakulam,Kerala-683562,India. TEL:+914842867000|productcorp@agappe.in|www.agappe.com REGD.WITH RNI NO.MAHENG/2007/22045,POSTAL REGD.NO.MCS/162/2022 – 24,PUBLISHED ON 8TH EVERY MONTH, POSTED ON 14TH,15TH,16TH EVERY MONTH,POSTED AT MUMBAI PATRIKA CHANNEL SORTING OFFICE,MUMBAI – 400001
















































































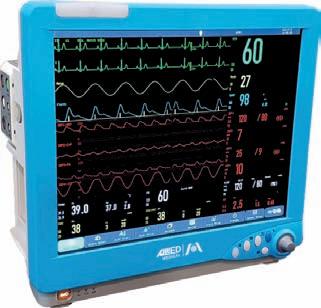

























 ByKalyani Sharma
ByKalyani Sharma