SURVIVING BREAST CANCER
Rate of cancer in NYS is higher than the national average. It Upstate, the situation is even worse. Find out why



Wednesday,
•
• Light
• To






Rate of cancer in NYS is higher than the national average. It Upstate, the situation is even worse. Find out why



Wednesday,
•
• Light
• To





Afew cups of coffee each morning can help protect a person against heart disease, stroke and Type 2 diabetes, a new study says.
Drinking three cups of coffee a day — or about 200 to 300 milligrams of caffeine — lowered the risk of health problems linked to the heart or metabolism, researchers found.
“The findings highlight that promoting moderate amounts of coffee or caffeine intake as a dietary habit to healthy people might have far-reaching benefits,” said lead researcher physician Chaofu Ke, a medical statistician with Suzhou Medical College of Soochow University in China.
For the study, researchers analyzed data on more than 500,000 people aged 37 to 73 participating in the long-term U.K. Biobank research project.
Out of that group, they identified more than 172,000 people who’d reported their caffeine intake, and another 188,000 who’d reported their coffee or tea consumption.
The researchers compared people’s caffeine intake to whether they had developed two or more signs of cardiometabolic disease. That term
relates to risk factors that can harm heart health, such as diabetes, high cholesterol, high blood pressure and excess body weight.
Results showed that any level of coffee or caffeine intake lowered a person’s risk of suffering multiple health problems related to heart or metabolism.
But the best results came with moderate intake of coffee or caffeine, they found.
People who drank three cups of coffee a day had a 48% lower risk of heart or metabolic disease, compared to those who drank no coffee.
And those who got 200 to 300 milligrams of caffeine daily had a 41% reduced risk compared to those who consumed none or less than 100 milligrams, researchers found.
The new study was published Sept. 17 in the Journal of Clinical Endocrinology & Metabolism.
Any lower risk would help protect a person’s health, as people with heart or metabolic diseases are four to seven times more likely to die from any cause, researchers said in a journal news release. They also have higher risk of disability and mental stress.
A monthly newspaper published by Local News, Inc. 20,000 copies distributed. To request home delivery ($21 per year), call 315-749-7070.
In Good Health is published 12 times a year by Local News, Inc. © 2024 by Local News, Inc. All rights reserved. 4 Riverside Drive, Suite 251, Utica, NY 13502 Phone: 315-749-7070 • Email: IGHmohawkvalley@gmail.com
Editor & Publisher: Wagner Dotto • Associate Editor: Stefan Yablonski
Contributing Writers: Barbara Pierce, Deb Dittner, Gwenn Voelckers, David Podos, Deborah Jeanne Sergeant, Anne Palumbo, Jolene Cleaver
Advertising: Amy Gagliano: 315-402-3370 • Email: amyIGHmv@gmail.com
Layout & Design: Angel Campos-Toro • Office Manager: Allison Lockwood


When it comes to breast cancer, monthly self-exams and regular mammograms can save your life.
Time for your next mammogram? Don’t wait! Contact your healthcare practitioner for a referral or call (607) 547-3600 to schedule an appointment.

Excellus BlueCross BlueShield is accepting applications for its 2024 Health Equity Innovation Awards, which provide funding to community-based organizations to support health and wellness programs that address racial and ethnic health disparities in Upstate New York.
The online application portal will close at 11:59 p.m. on Friday, Oct. 4,
“The Health Equity Innovation Award funding is designed to support initiatives that confront the fundamental causes of health disparities, particularly those linked to structural racism. By providing funding for projects that tackle social, economic, and systemic issues, we aim to create a healthcare system that is fair and equitable for everyone,” said Simone E. Edwards, vice president of health equity and community investments at Excellus BCBS.
Nonprofit 501(c)(3) organizations in the Excellus BCBS’ service area can apply for funding of up to $30,000.
Applications should propose innovative projects with measurable outcomes, expansion potential and clearly outlined goals to reduce health disparities and address social disadvantages. Funding is dependent upon a project’s ability to demonstrate tangible improvement in racial and ethnic health equity.
Priority categories for the Health Equity Innovation Awards include:
• Improved maternal health outcomes
• Behavioral health or mental health conditions
• Acute and chronic disease management
• Social determinants of health such as economic stability; education access, and quality; health care access and quality; neighborhood and built environment; and social and community context
For more information and to apply, go to www.excellusbcbs.com and type “community-investments-partnerships” in the search menu.

By Barbara Pierce
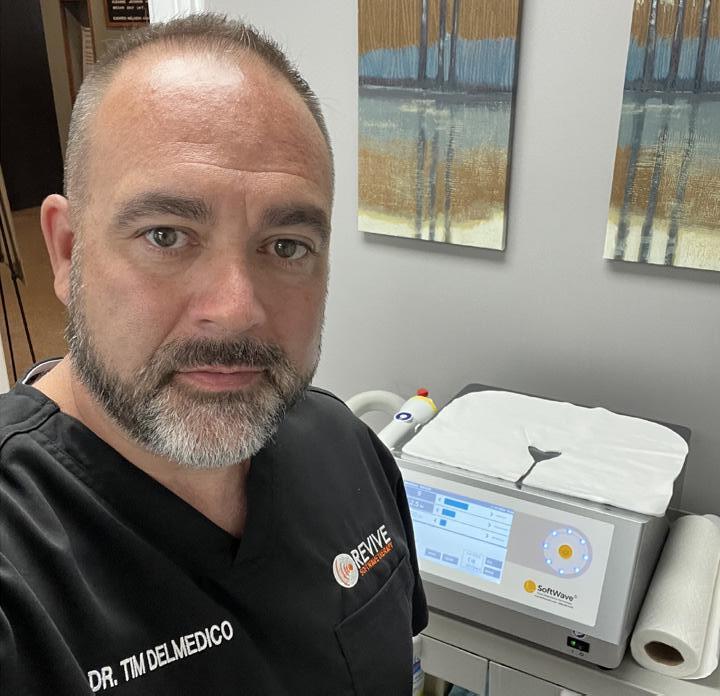
DelMedico, Doctor of Chiropractic
Owner and operator of Revive SoftWave Therapy in Utica discusses how he uses FDA-approved softwave therapy, a noninvasive, drug-free treatment for chronic pain, inflammation and joint issues
Q: A non-invasive treatment for chronic pain sounds like a great development! Tell us more about it.
A: The machine delivers sound waves — high energy sound waves at 3,000 miles per hour — to the area of the pain. This promotes the body to make stem cells that go to the area of the pain to reduce it. Softwave therapy also decreases inflammation, often a cause of pain. Stem cells are cells with the potential to develop into many different types of cells in the body. They serve as a repair system for the body. They are the body’s natural way of healing by repairing the underlying problem for long-term results. The big advantage is that it’s non-invasive; it doesn’t require surgery or a pill. It uses the body’s natural resources to
heal the pain.
Q: Just how does it work?
A: Gel is applied to the treatment area and the machine releases harmless sound waves over the treatment area. The over 3,000 mile per hour sound waves cause the body to make stem cells that go to the area to heal your issue. It turns on the body’s natural healing process. The treatment takes 10 minutes; there’s no down time; you can go back to work right afterwards. There’s no taking pills. It’s completely safe.
Q: How about results?

Q: Can anyone use the therapy?
A.: This technology can’t be used for people with pacemakers, pregnancy, cancerous tumors or infections.
Q: How did you learn about this?
A: Sound wave therapy has been used in Europe for 20 years; here in the U.S. for only a few years. I first saw it on social media. I went to the website to do research and also researched what the FDA said. I was so impressed with it, I sold my chiropractic business [Realm Chiropractic] and started Revive SoftWave Technology as a separate business here in Utica.
Q: You have a doctor of chiropractic degree. How did you become interested in this field?
A: I was treated by a chiropractor at a young age for an injury and that influenced my decision to pursue this career. After I got my doctorate degree, I started my own practice, Realm Chiropractic, where I practiced for 23 years. I sold it so I can focus on this new business that I started a couple years ago.
Q: What else would you like us to know about softwave therapy?
A: Most people see results in one or two treatments. Typically, people have six to eight visits. Most elect to come back every month or so. The number of treatments needed depends on the condition that is being treated. A big advantage is that it has no side effects. You can go back to work right afterwards.
Q: What conditions can be treated with softwave therapy?
A.: I mostly use the machine on joint issues, like a torn rotator cup, hip pain, knee pain, plantar fasciitis, arthritis, fibromyalgia, any many more. See our website www.revivesoftwave.com for details. It’s helpful for conditions, like neuropathy, that there has not been any treatment for before this.
We have an 80% success rate overall. For knees, the success rate is over 90%.
Applying high-energy sound waves to injured, degenerated or painful areas of the body is very effective in reducing pain and increasing mobility and function. It fast-tracks the healing process in the body. The big advantage is that this treatment is safe; it doesn’t require surgery, drugs, or needles and helps reduce pain, speed up recovery and regenerate tissue. It’s definitely impressive!
A: I was trained by the company, trained so that I can now sell the machine and train others to use it. I believe in it so much that I’ve begun distributing it throughout the U.S. Any health care provider can get it. I’ve opened four offices to do the treatment; Utica is the flagship. We also have offices in Albany, Saratoga and Syracuse. Other doctors are in charge in those offices; I’ve trained them and I oversee these offices.
Q: What has been the response of the community response to this new technology?
A: Word is getting out there. We’ve quadrupled our business since we opened. At this time, insurance doesn’t cover this treatment, not yet anyway.
Q: Summing up:
A: The big buzz is that softwave therapy makes a massive amount of stem cells, the body’s natural way of healing as the cells internally migrate to the area that needs healing. You can get relief from pain without pills or surgery. This is a game changer! It’s so valuable they use it in open heart surgery to increase blood flow to the heart. And for Alzheimer’s, they send shock waves through the skull to the brain to improve the functioning of the brain.
Name: Tim DelMedico, D.C
Position: Owner and operator of Revive SoftWave Therapy, 2709 Genesee St., Utica
Hometown: New Hartford
Education: Doctorate from Northeast College of Health Sciences (formally New York Chiropractic College) in Seneca Falls
Family: Wife (Lori); three children
Hobbies: Enjoys the outdoors, the Adirondacks, real estate investing, reading, baseball and spending time with family.
For more information, visit website www.revivesoftwave.com or call 315725-8427.
By Barbara Pierce
“Nobody told me how incredibly painful it would be. The commercials where the parents dance around and turn their kids’ rooms into something else was the complete opposite for me. I found myself practically in a fetal position for days,” said one woman on the internet.
Said another: “I always thought I’d be aggrieved when the kids inevitably moved away and into adult life. So, I was rather surprised when all I felt was a sense of relief, like I had been given a little bit less to worry over.”
An a third: “I missed them when they went off to college. But at the same time I liked the peace and quiet. Also, they weren’t really ‘gone’, they came home on breaks and that was a lot of fun.”
If you’re a parent, you may face this situation sooner or later.
Whether they’ve gone off to college, they’re traveling the world or they’ve joined the military or started a new job, the result is the same for you: an empty nest.
It doesn’t matter if you had one child or several: the house definitely feels quieter.
After years of raising a family and perhaps putting your marriage on the back burner while you tended to your kids, you and your spouse might feel strange in a suddenly quiet house. Some couples find it exhilarating to be just the two of them again, while others are overcome with a feeling of loss. It’s common to have both feelings, as well as everything in between.
Reactions to the time when your kids move on can have a wide range of feelings — from elation to depression and a mix of both ends of the spectrum.
While everyone reacts differently to coping with an empty nest, it’s important to recognize those feelings of loss and take steps to cope. The parenting road you’ve traveled for 18 years is turning a corner, headed for a bridge. What’s on the other side of the bridge? How can you get through this time of transition?
We asked author, speaker and mentor Jenny Garufi of Oneonta for her suggestions.
Q: Is dealing with an empty nest a common problem for women?
A: I’ve seen this as an issue with about half the women I work with when their kids leave home. They feel an emptiness and aren’t sure what to do without that role of “mom” being an everyday job.
Q: How do you help them get through this difficult transition?
A: I help them by having them remember they are soooo much more than mom. It’s important to remember who they are and who they were before and who they want to be right now. I get them back in touch with hobbies they loved and things they might have always wanted to try but never had the time.

Q: What can a woman do to ease her way through this transition?
A: Connect with yourself to find what brings you joy other than your kids. Nature? Music? Dance? Other hobbies?
Now is definitely the time to finally write the book you have been talking about for years, start the business, study a new language, painting or pottery, learn to sew, take a garden design course or fulfill another long held dream.
Or join gym, redecorate, adopt a pet. Try volunteering, plan a vacation. Try to revive romance in your life.
This isn’t the end of your life. This is a new beginning for your life to open up.
Connect with other women or at least one other, advised Garufi. Maybe women who are also empty nesters. Or other people with similar interests to yours. Meetup.com is always an awesome place to find people in your area interested in the same things you are. If not, try online communities.
Being an empty nester means you have more ownership of your life. That can be both exciting and frightening. Taking care of the kids is no longer your primary responsibility. They’re no longer a reason or a convenient excuse. Now you have the time to do the things you’ve been putting off, maybe you’ve put them off for years and even forgotten about them. It’s time to pull them from out of the back of your mind and start putting them into action.
Q: Have you gone through this yourself?
A: I had my sad moments when my kids left. But I mostly felt joy. Joy for them and their next steps and for me for my freedom of time. As long as your kids know you are still there for them and you’re in touch with yourself, this can be a very beautiful time — the next stage in life.





By George W. Chapman

The CDC still recommends we get the updated vaccine, but advises us to not jump the gun and wait until later fall.
The protection afforded by the vaccine wanes after a few months so you don’t want this to hap-

The vote in the Senate to pass the Inflation Reduction Act, which authorized Medicare to finally negotiate drug prices on behalf of its 40 million mem- bers, passed by just one vote. Not one Republican voted to pass the IRA. Not one. Vice president Harris had to cast the deciding vote. However, the “good” news is that both presidential candidates are in favor of controlling drug prices. Consequently, drug manufacturers have hedged their bets. Historically, prior to the IRA, the drug lobby has fended off all attempts by Medicare to negotiate prices. While most of our elected representatives on both sides of the aisle accepted money from drug lobbyists, three to four times more money went to Republican reps than Democratic reps. This year, however, total contributions to members of the two parties are just about even.
Over the past several decades, drug costs have increased from 3% of the total cost of care to almost 10% of the total cost of care. The trend can be attributed to our increasing dependence on drugs (most per capita in the world) and to unregulated
pen during winter months when COVID-19 tends to peak. Thankfully, as more of us are immunized, deaths and hospitalizations are rarer. There were about 2,000 COVID-related deaths this past July compared to 26,000 deaths in July 2020. Virol-
costs versus physician and hospital costs which are set. GLP-1 drugs used to treat diabetes and weight like Ozempic, Jardiance and Wegovy are having a significant impact on our premiums and copays be they Medicare, commercial or private or on the government exchange. Any of these drugs could be on Medicare’s “hit list” for 2026 but will remain uncontrolled for private insurers. 57 million people or 40% of those covered by their employer could potentially be eligible for GLP-1 drugs. The eventual economic impact on premiums and copays for employees will ultimately be determined by the plan your employer selects and by arbitrary coverage limitations. Initially developed to treat diabetes, only 5% of GLP-1 drugs are prescribed to treat just diabetes. Forty-two percent of these drugs are prescribed to treat obesity. The balance of prescriptions are for other conditions. Medicare spent $57 million on GLP-1 drugs in 2018. Spending jumped to a staggering $5.7 BILLION in 2022, due to a combination of price gouging and treatment of obesity. Employees, unfortunately, are virtually locked into the plan their employer selects and are subject to whatever drug coverage attached to that plan. On the other hand, Medicare beneficiaries and those on the government exchange can use navigators to help them find a plan with the best
ahead of the game but lifted a ban in 2015. As with regulating drug costs, fortunately, both political parties are in sync when it comes to the negative impact of smartphones on student mental health and that something has to be done. Overlooked if not lost in the discussion surrounding the impact of smartphones on students is the impact on teacher morale and retention especially in districts serving predominantly underprivileged students.

ogists suggest the current variant may be less virulent this year, but still recommend getting vaccinated. Waste water analysis shows that, currently, COVID is worse in western and southern states. The CDC recommends annual updated shots because of the ever-evolving variants.
coverage of a particular drug they are on. CMS has granted $100 million to navigators who can assist seniors select an advantage plan or individuals not covered at work select a plan on the exchange.

There is little disagreement among parents, teachers and legislators that smartphones have negatively impacted student learning, student mental health and even teacher retention. Student cyber bullying, loneliness, anxiety, depression, body dissatisfaction, eating disorders have approached epidemic proportions. Numerous studies found 50% of all students spend more than four hours a day on their phone. It’s basically an addiction and rehab will not be easy. 90% of schools report cyberbullying and 40% report the negative impact on learning when smartphones are unchecked. Seven states have banned smartphone use in schools with some exceptions for emergencies. They are Florida, Indiana, Louisiana, Minnesota, Ohio, South Carolina and Virginia. It is too soon to draw conclusions, but it is still worth gath ering evidence. Once results are in, implementing any kind of restriction or total ban will be difficult. Teachers now have to worry about guns and cell phones. New York state was way
By 2030, just six years from now, 42 of our 50 states will face a severe nursing shortage. Interestingly, of the eight states that expect to be alright, six are in the northeast: Vermont, Rhode Island, Maine, Pennsylvania, Connecticut and New Hampshire. Rural hospitals are most vulnerable to a shortage of nurses which can be a major factor leading to an outright closure. About 300 rural hospitals are on the brink. 10% are in Texas and Kansas, both states with large rural populations. The closure of a rural hospital, many hundreds from the nearest hospital, impacts far more than access to acute care. More than likely, unless affiliated with or supported by another healthcare system, physicians, pharmacists and other health professionals may abandon the community as well. The lack of a local hospital will also impact schools and local businesses. The local chamber of commerce will have a difficult time attracting new businesses. Half of nurses leave their job within two years as compared to four years for all industries. A study of 50,000 nurses found that on any given day, more than half of all nurses feel a sense of depletion, emotional exhaustion or fatigue. The double whammy of the pandemic and our aging population has exacerbated the shortage. Thousands of applicants to nursing schools have to be rejected every year because there are not enough professors in the schools to teach. Since the pandemic, most health care providers (well, the smart ones anyway) are much more attuned to their cultures, working environment and stresses facing their staff. Hopefully resulting in far less turnover and dissatisfaction. Nurse salaries have increased considerably since the pandemic. Nursing schools are receiving subsidies helping them attract and retain professors. Finally, 18% of healthcare workers are immigrants. Legal immigrants. That’s almost one in five employees. So, as in many other industries, staff shortages would be FAR worse without the steady flow of immigrants.

George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.

End-of-life doula services is one of the services Madison County Rural Health Council Inc. provides in Mohawk Valley, explains agency’s deputy director
By David Podos
Q: Your agency is located in Madison County, however, the services you offer go beyond this county. What other counties do you serve and what are the core programs you offer?
A: Well, we offer different services to different counties. We have some programs that are specific only to Madison County. For example, we have a transportation program that offers services to Madison County residents that are 60-plus. This service provides transportation to medical appointments as well as other necessary quality of life appointments. We have other programs like our mental health first aid program. Trainings for the mental health first aid program while generally held in person here in Madison County, through interactive technology, virtually anyone can attend. This also is the same for our diabetes prevention program.
Q: Let’s talk a bit about what services you provide for Oneida County, what would they be?
A: So, we serve Oneida County with our for birth Doula program and our end-of-life Doula program. The funding we receive for those services are earmarked for both Madison and Oneida county. For our end-of-life doula program we provide companionship, comfort and guidance to a dying person, their loved ones and family.
Q: Does this take place in the person’s home or other facilities?
A: The doula can meet in their
Q: Let’s switch to the opposite spectrum. Talk about your for-birth doula program, what services do you provide?
A: The doula for birth is a partnership program with three other organizations. Herkimer County Public Health, Seven Valleys Health Coalition, Cayuga Community Health Network. We started our birth doula program two and half years ago. We initially offered this service to just Madison County residents, then we saw the need for Oneida County. So our agency sought out additional funding to bring the service there. We provide emotional and physical support to women who are pregnant. Our trained professionals actually will meet with the client and provide three prenatal visits. They will talk about their birth plan, for example, they will ask if you want an epidermal, who are you going to have in the room with you once you give birth, what positions you want to be in, etc.
Q: Will the doula actually be with the woman as she is giving birth?
A: Absolutely. Whether it is a home birth and or a hospital birth, they will be there providing any assistance that is needed.
Q: Are there any fees associated with these doula services.
A: No. Both the end-of-life and doula for birth services are completely free of charge.
Q: If these services were not available, what do you think would happen?
home or if they are in a facility we can go to that facility.
Q: So, doula is an interesting word, I have to say, I never heard of it before, is it an acronym?
A: No, it is not an acronym. These are trained non medical professionals that provide educational, informational, physical and emotional support to a person with a terminal diagnosis. These services are an addition to whatever hospice might be providing for that person. We are not a substitute for what hospice does; rather, our services are an added complement to what hospice is already providing. In regards to the name, it derives from the Greek word doule, which translates to a female helper or maid servant. However, today those services have expanded as well as having both male and female trained doulas.
Q: What other services does the end-of-life doula provide?
A: We have conversations asking the client what do they want their end of days to be like. Do they want lots of family members and friends visiting them, perhaps they want only a select few. We do our best to help them get their affairs in order, for example, any paperwork they need to finalize, we even ask them if there is any special music they would like played. Everything we do points how we can assure they will pass in dignity.
A: Without the doula the birth process could be more difficult. There certainly are benefits to people who receive these services. For instance, a birth doula can help to shorten the duration of labor, they can help decrease the risk of a caesarean birth, decrease the use of pain medications and it provides an overall positive experience. For the end-of-life doula program those services provide much needed communication between the dying person and their family and most importantly to help the family understand the stages of a dying person. It also gives the family members a respite for them to do some personal errands while they know their loved one is being comforted. Without these supports the death could be much harder on everyone.
Q: How long have you been the deputy director?
A: I have been the deputy director for the past two and half years, but with the agency for five years, starting off as a program assistant, then to program coordinator and eventually my current position as deputy director.
Q: What is your educational background?
A: I have a bachelor’s degree in sociology and my employment background before coming here has always been in the human services social services arena, working in the nonprofit sector for the past 20 years.
Q: What number can someone call if they are interested in your services and do you have a website?
A: Our number is 315-815-4141. www.mcrualhealthcouncil.org





















By Barbara Pierce
Over the past decade there has been a huge increase in the number of children diagnosed with special needs, according to data from the CDC. There is an alarming rise in the number of children who are given a mental health diagnosis.
In New York state, 20.5% of our children are in special ed — the highest percentage in the nation. One out of every five! Experts suggest that emerging evidence implies that perhaps children are being over-diagnosed.
This stunning information can be found in an article in the August issue of In Good Health.
As parents, we should all be concerned about this. Very concerned!
In another article earlier this year, I learned that a 2022 survey of our children, aged 13-18, found that about 77% of them in Herkimer and Oneida counties had sad, empty, angry or anxious feelings; 86% had
investigative journalist says: “When asked, our kids said they were miserable. Our kids didn’t want to leave their rooms. Our kids didn’t date. Our kids moved home and stayed. They didn’t want to get married or have kids. Our kids were on five or six different psychotropic drugs. None of it seemed to make them feel better. None of it seemed to make them feel anything at all.”
As a licensed therapist, I’m not the intended audience for this book. It’s written for those skeptical of mental health care and mental health terminology directed at kids. But I found myself agreeing more than I expected to.
And those numbers? The overwhelmingly high percentage of kids reporting they have sad, empty, angry or anxious feelings? Shrier blames the surveys themselves as responsible for the inordinately large numbers of children reporting they have mental health problems.
The questions seem to presume levels of distress and depression that ought to be relatively rare in middle school. ’Do you ever feel sad or hopeless? Do you ever feel angry or anxious?’ the surveys ask.
Though there is no proof that asking kids repeatedly about selfharm will encourage them to attempt it, it does imply that it is normal to have suicidal thoughts or thoughts of cutting. Because suicide and cutting are so contagious among teens, adults must be extremely careful not to ask kids leading questions. But when you ask ‘When was the last time you thought about cutting yourself?’ the implications are that people do this. You could be doing this.
“It’s almost as if school survey authors decided to deliberately to include suicidal thoughts and cutting behaviors as something adolescents often do as a means of coping with personal problems. The surveys are jam-packed with details of how one might do this.” Shrier said.
Let me be clear on one thing: It’s important to let you know that I haven’t been able to determine just what questions they asked our kids. I don’t know if our kids are being asked if they have thoughts of suicide or cutting. I haven’t been able to find out information about the surveys that
challenges into a cause for concern. The purpose of childhood is to allow kids to take risks — things that involve getting all kinds of hurt — and to practice skills they will need as adults while they are still safely under their parents’ roof. Childhood exists to allow kids to hazard an unpredictable friend. To lose a ball game, stand up to a bully, pick themselves up, offer another kid a hand. We want them to venture out and get their hearts broken, try and fail and at last succeed —all while we’re still in the next bedroom, Shrier said. Childhood is experiencing all of the pains of adulthood in smaller doses, so that they build up immunity to the poison of heartache and loss. And when they stumble, they need to see in our eyes, not worry, but faith they they’re going to be just fine. We want all this to happen when they’re young. If they find themselves facing disappointment or rejection for the first time as adults, something has gone terribly wrong.


The U.S. Preventive Services
Task Force this year lowered the age recommendation for when individuals should begin getting screened for breast cancer.
The task force now advises eligible individuals who are not at high risk and who don’t have a family history of breast cancer to get screened every other year starting at age 40, which is 10 years earlier than its previous recommendation. Regular screenings are recommended to continue through age 74.
Breast cancer is the second most common cancer among women, accounting for about 30% of all new cancers diagnosed, according to the American Cancer Society. It is the second leading cause of cancer death in women, behind lung cancer. Early detection is key, and a mammogram can detect a tumor up to two years before it can be felt by the patient or a health care provider.
“Screening for breast cancer saves lives, so it is important for everyone who is eligible to be screened to follow these new recommendations,” says physician Nicholas Massa, vice president of medical affairs at Excellus BlueCross BlueShield. “Unfortunately, not everyone who is eligible is getting a mammogram.”
About 20% of individuals in New York state who are eligible for breast cancer screening are not getting screened, according to an Excellus BCBS review of the most recent data from the National Cancer Institute. Among eligible individuals between the ages of 50 and 74, 81.4% had a mammogram in 2022.
Obstacles that may prevent someone from having routine breast cancer screening can include lack of transportation, inconvenient screening facility hours, and/or patient apprehension about screening discomfort and safety.
To combat the transportation barrier, some hospitals and medical practices bring a mobile mammography van out into the community. Many hospitals and clinics also offer extended hours for on-site mammography screenings, so appointments can fit most schedules.
“Screening for breast cancer can be uncomfortable, but the test only takes a few minutes,” says Massa. “The potential benefits of early cancer detection outweigh any discomfort or concerns.”
Routine breast cancer screening is a preventive service that is among the essential benefits included in all Marketplace health plans and many other plans, at no cost to the patient, even if a yearly deductible has not yet been met. Note: These services are free to the patient only when delivered by a doctor or other provider in your health plan’s network.
An individual’s risk factors determine when they should begin getting screened for breast cancer.
Learn more about breast cancer and screening by visiting the U.S. Preventive Services Taskforce website at https://uspreventiveservicestaskforce.org and typing “Breast Cancer Screening” in the search box.
Submitted by Excellus BlueCross BlueShield.
Final government data finds the number of U.S. births falling by 2% last year compared to 2022, continuing a decades-long decline.
Overall, annual U.S. birth numbers have fallen by 17% since peaking in 2007, according to the new report from the U.S. Centers for Disease Control and Prevention. The general fertility rate (births per 1,000 women) has also tumbled by 21% over that time period, the report found.

Births to females in their teen years (ages 15 to 19) are part of this trend, declining by 4% from 2022 to 2023, say a team led by Joyce Martin, of the CDC’s National Center for Health Statistics (NCHS).
In total, there were 3,596,017 births recorded in the United States last year, compared to 3,667,758 the year previously.
In other CDC birth data, fewer pregnant women received adequate care in 2023 compared to 2022.
The number of women who
received prenatal care during their first trimester fell by 1%, and the percentage who got no prenatal care at all rose by 5%, continuing a trend noted in 2021 to 2022.
“Late and no-care levels have risen steadily since 2016,” Martin’s team noted in the report.
About 10.4% of births were premature in 2023; about the same as 2022. Early-term births (during the 37th and 38th week of pregnancy) rose by 2%.
“Since the most recent low in 2014, preterm birth rates have risen 9% and early-term births by 21%, while full-term and late- and post-term births have declined,” the NCHS team wrote.
The new findings were published Aug. 20 as an NCHS Data Brief.
Analysis of millions of births shows one-third of birth complications occur during the six weeks following discharge and disproportionately affect
New data shows that dangerous, unexpected birth complications often emerge weeks after the patient and baby have left the hospital, with Black patients experiencing these events at a rate 87% higher than white patients. Moreover, New York state has the highest number of these events in the nation, according to a new Blue Cross Blue Shield (BCBS) analysis.

The analysis of these birth complications, known as severe maternal morbidity (SMM), draws on nationwide data from more than 700,000 BCBS commercially insured births and data from the Centers for Medicare & Medicaid Services on more than 1.5 million Medicaid births.
Across New York state, the data revealed the rates of SMM events are higher than the national average, both overall, and for each ethnic group (Black, Hispanic, white), particularly for Medicaid members. The data also confirms racial and ethnic disparities in SMM events in New York state.
“The statistics are alarming, but they’ve also presented an opportunity and a responsibility to confront this national crisis,” says Excellus BlueCross BlueShield’s physician Simone Edwards, vice president, health equity and community investments. “Excellus BCBS is committed to collaborating with local commu-
nity organizations to support safe pregnancies and childbirth, eliminate pregnancy-related health disparities, and improve health outcomes for new mothers and babies.”
Excellus BCBS’s Bright Beginnings program is stepping in to fill necessary gaps in care like transportation, resources, and provider referrals to help new parents effectively care for themselves and their mental health.
The program, led by Kara Traverse, manager, maternity care management, includes a team of licensed social workers and registered nurses who meet with members referred by area doctors and hospitals, family, and even members themselves.
“They contact the member, listen to their concerns and screen for depression and anxiety. From there, the case manager assesses and makes
appropriate recommendations, providing resources for transportation, education, mental health support and more,” Traverse explains.
The Bright Beginnings team also collaborates with community-based partners committed to increasing maternal health care awareness and availability. From breast pump and pregnancy education to mental health screenings and arranging hospital and pediatrician visits, the Bright Beginnings program aims to help parents stay on track caring for themselves and their children.
Excellus BCBS also supports programs for maternal mental health run by community-based organizations across its operating area. Some of these efforts include Cortland-based Seven Valleys Health Coalition’s Post Partum Doula Support and Doula Partnership, Syracuse-based Contact Community Services’ Maternal Mental Health Follow Up Support, and Utica-based Integrated Community Alternatives Network’s (ICAN) Maternal Health Equity for Pregnant Homeless Teens.
Read the full report, “Improving Postpartum Maternal Health Outcomes,” part of the BCBS Health of America Report series, here: http:// bcbsa.co/6046YtIzI.
Submitted by Excellus BlueCross BlueShield.
By Deborah Dittner

As we age, many will read about the need to increase protein in your diet.
Protein helps in building and maintaining muscle which many tend to lose with the aging process especially if you become less active. If you have incorporated a healthy nutritional intake of animal and plant-based foods, you should be able to achieve your daily protein goals.
Then there are those of you who do not partake in animal sources of
protein and need to be more aware of protein from other sources.
Do note though that there are many professional athletes who are vegan or vegetarian, and able to achieve the necessary protein requirements. Also, healthy animal proteins may be out of your food budget range as these have skyrocketed in price.
Let’s look at healthy, plant-based foods to incorporate into your daily nutritional needs that are high in protein:


1. Lentils — my favorite. Not only are lentils rich in protein but also vitamins and minerals such as potassium, magnesium, folate and iron. One cup of lentils provides 17.9 grams of protein and can be added to soups and salads. One of my favorite meals is a recipe from Kris Carr’s book Crazy Sexy Kitchen. On page 183, you’ll find Lentil and Chard Ragout which is also gluten-free. It’s so good, I could eat the entire pot which is supposed to serve 4-6. Fortunately, I do leave some for leftovers. Lentil burgers (from my book “Body Balance Empowering Performance “on page 119) is another yummy addition of protein.
2. Asparagus — my second favorite. One cup of cooked asparagus provides 4.32 grams of protein and can be added to soups, salads, pasta dishes, and egg dishes such as a frittata. This non starchy vegetable is also rich in vitamins A, C, K, and folate. An easy favorite on the grill as well.
3. Green peas — Rich in protein at 8.58 grams per 1 cup cooked and vitamins A, C, K and B’s. Incorporated into rice and pasta dishes and on its own, peas will add color, abundant flavor and fiber. Peas are reasonably priced when purchased frozen.
4. Black beans —Per 1 cup cooked, you will receive 15.2 grams protein and also rich in magnesium which aids in sleep and stress reduction. High in fiber, black beans are very versatile in making soups, toppings or stuffing for sweet potatoes (also high in protein - see below), chili (also made with kidney beans high in protein - see below), and veggie burgers
5. Kidney beans — Did I happen to mention chili? One cup of cooked kidney beans provides 15.3 grams of protein and is a wonderful source of folate and high in fiber. With fall weather, chili can become a favorite meal to warm you both inside and out.
6. Sweet potatoes — A root veg-
etable, also high in fiber, provides 4.02 grams protein per 1 cup mashed. Sweet potato burgers (recipe also in my book on page 120) is another favorite meal. Toppings for baked sweet potatoes can include black beans (see above) and spinach (see below) for additional protein.
7. Spinach — A one cup cooked non-starchy vegetable provides 5.35 grams of protein and is an excellent source of vitamins and minerals, including vitamins A, C, K, calcium, iron and magnesium. When combined with black beans on top of a sweet potato – Yum! If you make smoothies, add a couple handfuls of spinach. You can also add spinach to salads, sauteed with onions and garlic for a side dish, soups, and frittatas.
8. Peanuts — Thought of as a nut, the peanut is actually a legume. One ounce provides 7.43 grams of protein and is a good source of vitamin E, magnesium and folate. Peanuts can be added to soups, salads, trail mix and Asian dishes.
Other high protein vegetables include:
• Artichoke hearts
• Edamame
• Navy beans
• Brussel sprouts
• Broccoli
• Russet potatoes
• Red potatoes
• Beets
• Rutabaga
As you can see, there are many plant-based protein options to choose from: legumes, non starchy vegetables, and root vegetables. With so many possibilities, you will be able to meet the protein requirements your body needs.
MP Order Proposal#

Deborah Dittner is a family nurse practitioner and health consultant. Her mission is to transform as many individuals as possible through nutrition and lifestyle changes. www. debdittner.com






By Anne Palumbo
Ever since I discovered that kefir

— a fermented milk product with more probiotics than yogurt — could benefit my achy gut, I jumped on it.
From the health benefits to the tangy taste to the ease of consumption, it checks all the boxes.
Plus, I’m tired of skipping activities because of my finicky gut, and, so far, kefir is doing the trick.
Fermented foods — like kefir, yogurt, sauerkraut, kimchi and kombucha — teem with probiotics, the “good” bacteria that can help restore the natural balance of bacteria in your gut and decrease signs of gut inflammation. Reducing inflammation is important, especially since longterm gut inflammation can increase the risk of chronic diseases over time.
What’s more, a healthy gut can boost the immune system, help keep blood glucose levels stable, and may even influence moods and mental health, according to the Mayo Clinic.
I’m also hooked on kefir because it’s a rich source of calcium, protein and B vitamins.
Forever seeking ways to strengthen my bones and prevent loss, I look forward each day to the 300-400 mg of calcium per cup that kefir provides. Same goes for the impressive dose of protein that kefir delivers per cup: 9 grams. Protein is a building block for muscles, cartilage, skin, and — yes! — bones.
Kefir is rich in energy-boosting
vitamins, most notably vitamins B2 (riboflavin) and B12. This powerhouse combo helps turn food into fuel, build red blood cells and minimize the risk of birth defects. Also, both vitamins can help slow cognitive decline as well as nuke toxic free radicals, whose buildup in our bodies can cause chronic disease and premature aging. Especially good news for those seeking stronger bones: Both vitamins may support bone health and prevent osteoporosis.
Not a big fan of bananas, the go-to food for potassium? Reach for kefir, whose potassium levels rival a banana’s. An essential mineral for all body functions, potassium is your heart’s best friend: it keeps the beat regular, reduces the effect of sodium (present in table salt) on blood pressure and lowers your risk of cardiovascular disease.

Anne Palumbo lifestyle columnist, food guru, and sea soned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
Read nutrient labels carefully (some flavors have more sugar than others). Pair kefir with foods high in “prebiotics” — such as bananas, apples, and berries — for a synergistic combo that optimizes gut health function. Some kefir brands (like Lifeway low-fat kefir) are up to 99% lactose-free, which may make them tolerable for those with mild lactose intolerance.

1 cup kefir of choice (I used Lifeway low-fat vanilla)
½ cup blueberries
½ cup sliced strawberries
½ cup sliced peaches
Folks dieting to drop pounds should consider eating a fistful of nuts here and there, a new review suggests.
People who ate 1.5 to 3 ounces of almonds, peanuts, pistachios or walnuts daily as part of a calorie-cutting diet wound up losing more weight than those on the same diet without nuts, researchers said.
In fact, people on “nut-enriched” diets lost an extra 3 to 16 pounds compared to folks on nut-free diets, results show.
“People often avoid nuts when trying to lose weight because they think that the energy and fat con-
tent in nuts can contribute to weight gain,” said senior researcher Alison Coates, dean of research in allied health and human performance with the University of South Australia. Instead, it looks like nuts might help curb hunger more effectively.
“Nuts are rich in healthy unsaturated fats, plant protein and dietary fiber, all of which play a role in promoting satiety and reducing excess calorie consumption,” Coates said in a university news release. “Nuts are associated with improved cardiovascular and metabolic health, better gut health and enhanced cognitive performance.”
For the review, researchers analyzed the findings of seven randomized controlled trials involving diets that cut food intake between 240 and 1,000 calories a day. The studies lasted from a month to a year, and involved 676 people who were overweight or obese.
None of the studies showed that nuts hampered weight loss, researchers found, and four of the studies found that nuts actually caused folks to drop even more weight.
The review, which was not funded by the nut industry, was published recently in the journal Nutrition Research Reviews.
sprinkling of favorite toasted nuts or granola
Place everything in a bowl and enjoy! Or make a smoothie with kefir and your favorite fruits.
“Nuts are an important part of many people’s diets because they provide a taste and texture you can’t find in other food groups, while also being a healthy, on-the-go snack,” said study co-author Sharaya Carter, an adjunct research fellow with the University of South Australia.
“For people who enjoy eating nuts, knowing that they can help meet weight-loss goals while also improving your overall health is a huge plus,” Carter said. “It’s also great for health professionals who can be confident in recommending nuts, in the context of a healthy diet, without concerns of an adverse effect on weight.”
By Deborah Jeanne Sergeant
Arecent study by an organization affiliated with Columbia University indicates that compared with the rest of the nation, New York showed higher incidence rates for prevalent cancers, especially among those aged 25 to 49 for several cancers, including breast, colorectal, thyroid, kidney, renal pelvis and leukemia.
A few answers as to why were offered by Christopher P. Morley, Ph.D., chairman of the department of public health and preventive medicine and professor at Upstate Medical University.
“This is a complicated question because the broad mapping data combine all cancer types,” said Morley, who also serves as editor-in-chief of peer-reviewed Reports in Medical Education Research (PRiMER). “However, we know that disparities, in cancer incidence and in outcomes, exist between rural and urban populations. One issue is that we often see markers of health behavior that increase risk for cancer as higher in rural populations. In New York state, for example, you can simply visually compare the maps of where smoking rates are higher with the cancer incidence maps and you can visually discern the connection.”
Tobacco use has been implicated
as a factor in causing numerous types of cancer. Morley added that areas where more people consume higher levels of red meat, fried foods and alcohol tend to have poorer health, as do those who have fewer food choices.
“Many health behaviors follow an educational and socio-economic gradient, with those who are less well-off having higher rates of tobacco and alcohol use and obesity,” Morley said.
It’s not that any one particular factor makes all the difference. It’s the stressors added up that can tip a person from reasonably good health into illness.
to face higher levels of what some social scientists call ‘allostatic load’ or the overall levels of stress that impact health outcomes.”
Morley also blamed the poor access to preventive services in rural areas. Typically, cancer that is caught and treated later is more likely to become fatal.
In addition to avoiding tobacco, reducing consumption of alcohol, red meat and processed and sugary foods, Morley encourages people to maintain a healthy weight.
“That can mean engaging in intentional exercise, but people don’t need gym memberships,” he said. “You can increase physical activity, even if it means going for a walk, taking the stairs instead of an elevator or making other small choices throughout the day that improve your physical stamina.”

Morley explained that “people in lower socio-economic strata also tend
As a new federal regulation that requires mammography centers to tell their patients how dense their breasts are takes effect, experts explain what breast density is and why it is important.
The American College of Surgeons’ National Accreditation Program for Breast Centers (NAPBC) standards, revised last year to focus on personalized care, also require mammography centers to educate patients on breast density. Here, radiologists on the NAPBC board offer insight into what women should know about breast density, and why it matters.
• Breast density is the ratio of fatty and fibrous tissue in the breast. Breast density, which is unique to each woman, is important for several reasons. First, having dense breast tissue may mask small masses on a mammogram. Fatty tissue tends to appear as dark areas, while dense breast tissue and cancerous changes often show up as white areas, making it harder for radiologists to distinguish between suspicious lesions
or benign changes.
“Another way to think about breast density on a mammogram is like looking at a cloudy sky and trying to differentiate things that are coming through in the sky. You’re not going to see things as well when the sky is cloudy versus when it’s clear,” explained Dr. Georgia Spear, division chief of breast imaging at Endeavor Health/NorthShore University HealthSystem and an NAPBC board member representing the American College of Radiology Imaging Network.
In addition to making it hard to detect cancerous changes during mammograms, breast density raises a woman’s risk of developing breast cancer by four to six-fold. Spear noted breast cancer tends to develop in fibrous and glandular tissue, which is more abundant in women with dense breasts.
• Only imaging can measure breast density. According to the National Cancer Institute (NCI), four categories of breast density may be noted on a woman’s imaging report:
He added that it’s easier to make lasting change through small, achievable steps rather than trying to make sweeping changes in lifestyle habits that can affect health.
Physician Haider Khadim, an oncologist with St. Joseph’s Health, explains to his patients that there are some nonmodifiable risks such as age and genetics and some that are modifiable, such as lifestyle factors and preventive health measures for some types of cancer, such as screenings and tests.
“There are a few cancers we can screen for like prostate cancer and
(1) entirely fatty breast tissue, (2) scattered fibroglandular breast tissue, (3) heterogeneously dense breast tissue, and (4) extremely dense breast tissue.
• Women with dense breasts may benefit from additional screening. Women with increased breast density may receive supplemental screening with ultrasound or breast MRI. These screening techniques can help radiologists spot cancerous changes that may be masked by dense breast tissue.
“Density is just one factor that we look at when we decide what’s the best way to screen a patient,” said physician Lora Barke, chief of breast imaging at Invision Sally Jobe in Denver and an NAPBC board member representing the American College of Radiology on Breast Imaging Commission. “When we look at density, it helps us decide on some other tools that would be beneficial for that patient along with mammography. Knowing breast density provides patients with a bigger picture to make more informed decisions.”
While mammograms remain the gold standard of breast cancer screening, Barke noted that MRI and/or ultrasound may be superior in detecting small masses or other subtle changes that may be more
breast cancer,” Khadim said. “For prostate cancer, have a blood test after 50. There’s colonoscopy for colorectal cancer. It’s appearing more in younger people so we lowered the age to start screening at 45, not 50. Women should also get mammograms done at age 40 and sooner if a close family relative who had breast cancer. Young men should get screened if their mothers had cancer younger. There’s a perception that BRCA mutation perception that only women can get breast cancer, but men can get it as well. Families with BRCA positivity are prone to prostate cancer and pancreatic cancer. A family should consult with a geneticist.”
Physician Tarek Sousou, a medical oncologist and hematologist who is the board president of Hematology-Oncology Associates of CNY, said that genetic risk from hereditary mutations causes up to 10% of cancers.
“Through screening tests, these patients can undergo enhanced screening and other risk reductive strategies to avoid developing cancer or diagnose it at earlier stages when it can be more readily cured,” Sousou said. “Adjustment of controllable risk factors such as avoidance of tobacco, enhanced cancer screening and maintaining a healthy lifestyle and weight can help reduce genetic and age-related risk for cancer.”
Maintaining a healthy weight can be challenging in New York. In a CDC study from 2017 to 2020, New York ranked among states with a self-reported sedentary rate of 25% to 29%. A handful of Southern states ranked worse. However, New York ranked worst in the Northeast.
Long, cold winters may help explain the low rates of physical activity in the area. However, sedentary lifestyle should be avoided for many reasons, including the fact that it contributes to higher rates of obesity. Obesity is a risk factor for many diseases and illnesses, including cancer.
Choosing an activity that is enjoyable and also meets health goals can help people stick with it.
difficult to see on a mammogram, especially in women with dense breast tissue.
Unfortunately, insurance coverage for supplemental screening varies widely, so breast MRIs and ultrasound may not be fully covered for some women.
• A woman’s breast density level may change over time.
Women should not panic if they are told they have dense breasts, as it is extremely common. Nearly half of women over the age of 40 have dense breast tissue, according to the NCI. While breast density can remain constant, the tissue can also become less dense after childbirth and as women age.
“We record the category of breast density every single time a patient visits us, so it’s something that we monitor from year to year on a mammogram,” said physician Jocelyn Rapelyea, associate director of breast imaging at GW Medical Faculty Associates in Washington, D.C. “If you are informed that you have dense breast tissue on your mammogram report, my advice is to discuss that finding with the radiologist as to what it means for you and what additional screening may be right for you.”

When Lynne Browne of Rome was diagnosed with stage 2 breast cancer at 43 after a routine mammogram in February 2006, she had no symptoms. There was no sickness. No soreness. Nothing.
“That is why mammograms are so important,” she said in September, adding that education, treatments, advancements in medicine and community togetherness are constantly being cultivated.
With October being Breast Cancer Awareness Month, residents across the Mohawk Valley step up to support their loved ones and raise money through community events that boosts medical research and provides resources for those in treatment and recovery.
In measuring statistics, according to information from the Susan G. Komen Foundation there will be an estimated 310,720 new cases (not recurrences) of invasive breast cancer among American women by the end of 2024 and 42,250 breast cancer deaths. Among men in the United States there is expected to be 2,790 new cases (not counting recurrences) of invasive breast cancer and 530 breast cancer deaths by the end of 2024.
This is Lynne Browne’s fight
Browne recalls her personal call to action after additional post-imaging testing revealed she was positive for the HER2 gene.
HER2, or human epidermal growth factor receptor 2, is a protein that helps control cell growth in normal cells. However, some types of cancer cells produce too much HER2, which can cause them to grow and spread more quickly.
To fight her occurrence, Browne opted for a lumpectomy that was

By Jolene Cleaver
followed by chemotherapy, radiation and other treatments that included taking courses of Herceptin, which works by binding to HER2 receptors on the surface of cancer cells and prevents them from receiving growth signals which allows the body’s immune system to destroy them.
She shaved her head in March of that year after hair loss began to become apparent.
But by the end of the year — and multiple tests — she was in the clear and began healing. Her hair grew
minutes here and there,” she said, emphasizing that some people may opt for stepping away from their job while getting treated. “It’s all about how the individual feels physically and mentally. … How their body responds to treatment.”
But having a goal got her through. That and humor. Being able to share a joke and have a good laugh with her husband, Michael Browne, helped immensely.
“I don’t have children, but my husband was fantastic,” she said,
There will be an estimated 310,720 new cases of invasive breast cancer among American women by the end of 2024 and 42,250 breast cancer deaths, according to Susan G. Komen Foundation.
back within a year.
To this day, she hasn’t had a recurrence, she said.
Browne’s thoughts on life during treatment
She worked partial weeks while getting chemotherapy. The same with radiation.
“Everybody is different. I think I needed work to have something to focus on while I went through treatment. Of course I cried for 10
adding that allowing friends and family to help care for you and being open with your symptoms can make the process more hopeful.
Leaning on her community while she was sick is what leads her to continue giving back today. Browne mans tables at events in the area for the American Cancer Society. Over the years, she has come to know others in the area who have had diagnoses, which in turn creates a support system for others.
Lynne and her husband are now retired and enjoying their life. As she observes her current day to day, she thinks about how her diagnosis reshaped her.
“I felt — they always talk about the journey — but when you’re done, the sky is a little bit bluer,” she said. “I try to say ‘yes’ to things that I would have passed on before my illness. One of the big things I said yes to was taking photos of some of our refugee friends at events in Utica. These photos led to an exhibit in Munson [in Utica] during an exhibit. It was an opportunity of a lifetime and if I said no I never would have gotten that chance.”
If she gives any advice to young women, it would be to stress the importance of mammograms. She said to not be afraid of the procedure or of the discomfort it might cause.
The brief discomfort goes away, she said.
“And get your bloodwork done on a regular basis,” she added.
Over the years, she has come to know others in the area who have had diagnoses and has had a few revelations about how families can come together and contribute to prevention and health maintenance.
“Families should talk more openly about their health history. … Share information about common illnesses in a group document,” she said.
Pointing to her own situation, she said the reason she had been getting a mammogram in her early 40s was because she knew that her grandmother and an aunt also had breast cancer diagnoses.
For those just learning they are diagnosed, Browne again emphasized to reach out for support and not go through care and treatment alone.
“I would not wish this on my enemy,” she said.

Hematology-Oncology Associates of CNY (HOA) presents an educational forum on prostate cancer care from 6-7 p.m., Oct. 9 at HOA’s East Syracuse location, 5008 Brittonfield Parkway.
It is free and open to the public, and a light dinner will be served. Reservations are requested at rsvp@hoacny.com or 315-472-7504, extension 1303.
HOA’s experts in treating prostate cancer will lead the forum. They are medical oncologists, Steven Duff and Ajeet Gajra, and radiation oncologist, Shing Chin. Attendees will have the opportunity to ask questions and engage in a discussion with the presenters.
“We are excited to offer this educational opportunity to our community,” said CEO Maryann Roefaro, HOA CEO. “It is important for prostate cancer patients and their loved ones to learn about all of their treatment options directly from a medical oncologist who can manage all of their cancer care.”
HOA is a private community cancer center established in 1982 with a mission provide the highest level of quality care in a healing environment for the mind, body and spirit of patients dealing with cancer and blood disorders. A member of the Community Oncology Alliance, HOA has offices in Auburn, East Syracuse and Camillus.

By David L. Podos
Nancy Cunningham grew up in Arkport, a small rural village in Steuben County with a rich agricultural history and a notable farming community. It is located in the town of Hornellsville, north of the city of Hornell.
Eventually Cunningham moved to Utica and lived here from 1989 to 1991. She is a licensed cosmetologist and worked for a number of prominent hair salons in Utica and in New Hartford. In 2015, she moved to Florida where she continues to live to this day.
Her life changed abruptly when she found out she had cancer.
“I was diagnosed with breast cancer in 2004 and had to have a right-side mastectomy. When I was on the operating table the doctors took four nodes from me and tested them,” she said. “Everything seemed good. So, the medical staff went back to my mom and said, ‘your daughters’ nodes are clear.’ But a few days later I received a call that after pathology it was discovered there were microscopic amounts of cancer cells in one node. The medical staff want-
treatments I had surgery,” she said. “I was cancer free once again, but sadly it returned just four months later.”
Once again, she made the decision to return to an alternative and natural protocol in an attempt to treat her returning cancer. But she was never able to become cancer-free again. At that time her alternative doctor said things weren’t working. Cunningham returned to chemotherapy.
“[I] think the main thing for me is my faith. I feel I am guided and protected; I really just believe that here I am after all of what I have been through; yet, I am still alive and no one knows the exact time when they will pass from this life,” she said. “I heard a great joke the other day from the famous actor and comedian Woody Allen. He said, ‘none of us knows when we are going to die, I just don’t want to be there when it happens.’”
She continues to receive treatment for her ovarian cancer as she journeys forward.
“I just don’t feel like it’s my time to go. Yet, there is a part of me that says, ‘alright, if I have to go then it is OK.’ With all that I have been through and what I am still going through, I have a beautiful life,” she said. “I don’t know how or why I got these cancers, who knows for sure? Back in my small town where I grew up in I remember playing outside as a young girl and this yellow crop duster plane would fly over spraying the entire area. Did that have anything to do what happened to me? Maybe, but it might have been something else entirely.”
ed me to do chemo and radiation and I opted not to do that. I wanted to go the natural route.”
As she puts it, she “discovered” a more natural life style in 2000. In a health food store that she visited one day when shopping, she spotted a pamphlet on a display table; on the front it said, “If you want overall health and wellness call this number.” She called and the person she spoke to was an herbalist. That was her first introduction into alternative healing. Slowly, but inevitably, from that point forward, through the years, she became more involved in natural healing. She started to do more of her own research into a holistic lifestyle, eventually incorporating things like massage, acupuncture, yoga, vitamins and herbs to maintain health.
For nearly 20 years Cunningham was cancer free and she attributes this to her lifestyle change — [but] then she received some troubling news.
“I was diagnosed with ovarian cancer in November of 2021. I decided to do chemo and after my chemo
Her advice to anyone who may be going through something similar is this. “I would say to them, we are all miracles and we all have the ability to heal in whatever way that healing comes to us. That is how we were created. Listen to your body and the inner wisdom that comes to you. Stay as positive as possible. It is one day at a time. Recently I said to my Mom, ‘mom, today is a good day, I am here, when it starts to not get so good, then we can worry.’ Do the best you can each day and stay in the moment. There is much to be grateful for,” she said.
In 2024, an estimated 2,001,140 new cases of cancer will be diagnosed in the United States and 611,720 people will die from the disease. The most common cancers (listed in descending order according to estimated new cases in 2024) are breast cancer, prostate cancer, lung and bronchus cancer, colon and rectum cancer, melanoma of the skin, bladder cancer, kidney and renal pelvis cancer, non-Hodgkin lymphoma, endometrial cancer, pancreatic cancer, leukemia, thyroid cancer, and liver cancer. These statistics come from the National Cancer Institute.
The foundation gives away thousands of dollars to support breast cancer patients — but some still don’t know about it, the chairwoman says
By Stefan Yablonski
The Saint Agatha Foundation is a nonprofit that provides financial support to qualified breast cancer patients across seven CNY and Mohawk Valley counties. It means it gives free money to some cancer patients.
But, according to its chairwoman, many women are unaware of it.
Born in Manlius on June 10, 1968, Laurie Mezzalingua was the third of six children. She graduated from Manlius Pebble Hill in 1986 and Boston University in 1990.
In 1997, Laurie was diagnosed with breast cancer at 29. As she battled the disease, she became a passionate and vocal advocate for patient support.
A breast cancer patient for 12 years, she established the Saint Agatha Foundation in 2004.
She died on July 4, 2009.
But her spirit lives on.
The foundation partners with local hospitals and agencies to support patients in Onondaga, Cortland, Cayuga, Madison, Oneida, Oswego and Jefferson counties.
“We are trying to raise more awareness — because we are still finding out that many women aren’t aware of our foundation that is helping them with their breast cancer bills,” said Kathy Mezzalingua, chairwoman of the foundation and Laurie’s mother. “It’s hard to believe that after all these years, but it is true. Somehow we fall through the cracks when we can help so many women; we have money to give them.”
The foundation is dedicated to providing “support, comfort and care to breast cancer patients through financial assistance programs — allowing patients to focus on their treatment, not their bills,” she explained.
Funds are distributed to patients via both medical and non medical
Saint Agatha Foundation has provided $17.5 million in financial support to more than 10,000 breast cancer patients in Central New York
service providers who apply on behalf of their patients or clientele.
Bills the foundation can assist with, once insurance has done its part, can include everything from clinical items like lab tests, infusion, radiation therapy, doctor’s appointments to non medical items like child care, transportation, household and legal expenses, she added.
“We originally had a base amount that was generated by my daughter before she died. She had some money and we have fundraised. We have been able to increase the fund as well as give the money away. So we have done pretty well,” Kathy said. “We have a place on our website (www.saintagathafoundation.org) where people can go to make donations. We’ve grown to the point where we can give away about a quarter of a million dollars a year.”
Over the last decade, the foundation has provided financial assistance to more than 7,035 breast cancer patients by providing grants in excess of $13.5 million to local hospitals and partner organizations.
Overall, it has provided $17.5 million in financial support to more than 10,000 breast cancer patients in Central New York, she added.
“We are in seven counties —
When cancer strikes, you could easily go into debt, even with health insurance in place, according to a new survey from the American Cancer Society.
The survey, based on responses from nearly 1,300 cancer patients and survivors from March 18 through April 14, found that 47% had medical debt. Half of those respondents said that debt exceeded $5,000.
Two-thirds had struggled with debt for more than a year and a third had dealt with it for more than three years.
Almost all — 98% — said they had health insurance when their debts began mounting.
“While people are insured, sometimes they don’t have very good insurance,” Arthur Caplan, head of the division of medical ethics at NYU Langone Medical Center in New York City, told NBC News.
He said many cancer patients with medical debt have high-deductible insurance plans in which a lot of expenses need to be paid out-ofpocket before coverage kicks in.
But cancer care can stretch even

Kathy Mezzalingua, Saint Agatha Foundation chairwoman: “We are trying to raise more awareness — because we are still finding out that many women aren’t aware of our foundation that is helping them with their breast cancer bills.”
Oswego being one of our excellent partners and Onondaga County of course. We are extending north, south, east, west. We don’t want to go as far as the major cities like Rochester or Buffalo or Albany,” she said. “We want to stay within Central New York because there is so much need there. That’s our focus; that’s our goal; to help these women, help them, as my daughter said to concentrate on their healing and not their bills.”
As she battled the disease, Laurie became a passionate and vocal advocate for patient support, according to her mother.
“A breast cancer diagnosis is a
tough one. The first thing you think of is what about my job, my family, how am I going to afford all these expenses? So we take care of that so they can just heal, get better and move on,” Kathy said. “Laurie just felt so badly; she said, ‘we have got to help these people so they have the same opportunities that I do.’”
Saint Agatha Foundation joins many other institutions in Central New York in recognizing National Breast Cancer Awareness Month as a way to draw attention to the continuing and critical fight against breast cancer,
“We take this opportunity to spotlight our unique mission of providing financial support to breast cancer patients in our community, to help patients focus on overcoming their diagnosis instead of worrying about unmet financial stress they may be facing,” she said.
“We don’t actually do things on our own a lot. The only thing we really do on our own is the gala,” she said. “Some of the individual regions will have their own individual fundraisers. This gala is our major fundraiser, but we are hoping to do more for more visibility in the future.”
This year’s gala is set for Oct. 24 at the Syracuse OnCenter. For more information, visit their website.
“We have our administrative office in Pennsylvania — that is our national headquarters.
I’m still the president. I oversee the board. We meet three times a year; vote on all the decisions, all the grants,” she said. “I work on things weekly with my administrator. We have a woman in Syracuse through CancerConnects who helps with all the local things. With the regional, we leave it up to your organizers. We also give to places like the Y, support groups and we give to legal aid ... we have a wide range of services.”
CancerConnects, Inc., is a nonprofit 501(c)(3) organization incorporated in New York in 2006, under the guidance and support of physicians, staff and cancer survivors patients of Hematology-Oncology Associates of Central New York, P.C.
Saint Agatha tags on with other events to help raise awareness, she explained.
“I’m going to keep doing this for as long as I can, absolutely! And then one of my children is going to take over,” she said. “It’s a healthy, very healthy endowment that we want to continue in perpetuity.”
gold-plated insurance plans, Caplan added.
“These cancer treatments can go on and on,” he said. “They can also cost a lot of money for diagnostic testing, genetic testing, and pretty soon you say, ‘Well, I have a policy of a million dollars and it’s gone.’ “
Karen Knudsen is CEO of the American Cancer Society. Speaking with NBC News, she noted that the new survey uncovered significant disparities, with Black and Hispanic patients more likely to fall into medical debt than whites.
Medical debt also hits the young particularly hard: Nearly three-quarters of patients aged 35 to 44 were behind on health care bills, the survey
found.
“We were really dismayed to see that,” Knudsen said. “That strain has been shown to be durable in their lifetime, impacting their choices, their ability to take jobs and of their choice to have a life that they would like.”
Besides the financial and emotional strain that debt incurs, health care can also suffer, she said. Many patients end up skipping cancer screenings or medications due to cost, Knudsen explained.
The bottom line, she said, is that even with insurance, “cancer care is really devastating to people’s financial position.”
Breast care physician at Rome Health discusses how technology and screenings have helped treat breast cancer.
Breast cancer is the most commonly diagnosed cancer among U.S. women after skin cancers, according to www.breastcancer.org.
Each year, about 30% of all newly diagnosed cancers in women are breast cancer. In 2024, approximately 311,000 women and 2,800 men will be diagnosed with invasive breast cancer.
James Cesare is a board-certified surgeon, receiving his certification from the American Board of Surgery. A breast care specialist, Cesare is the director of the Breast Care Center at Rome Health. Cesare has been practicing medicine post-residency for 32 and for the last 19 years has specialized in breast care. Cesare practiced breast care at Slocum Dickson Medical Group for many years; this will be his first year bringing his medical expertise in breast care to Rome Health.
“When I left Slocum Dickson, I wanted to look for a place that was patient-friendly and that could accommodate a breast care center. So, when I came here to visit, and met the CEO and the people who work here, I was really overwhelmed how — and it may sound a little cliched’ — how nice people were, how caring they were about patient care. When you have that type of mentality and that type of culture, which starts from the top down, that is the kind of place I wanted to be at,” he said.
When asked if that type of environment helps him as a physician to utilize his skills in the most efficient and effective way for patient care, Cesare eagerly agrees.
“Of course. But not only that, you want an environment that you believe in, that you want to be part of and certainly that is the same type of attitude and presentation that I want my office to show to patients to make them comfortable and let them know that we respect and care about
them,” he said.
From physicianspractice.com, physician Peminda K. Cabandugama said: “Patient-positive healthcare environments might not get as much airtime as treatment approaches and emerging research, but they can be just as vital for improving patient health. When patients feel comfortable, engaged and respected, they are better equipped to achieve their long-term health objectives.”
Oftentimes and with most people, when mentioning breast cancer, they immediately think of a woman, not realizing that men can and do get breast cancer.
Cesare said, “Here at our breast care center, we take care of both benign and malignant disease. We see men, woman and even young children. Anyone with a breast issue we see and men have breasts. Presently I am seeing seven male breast cancer patients. It is, however, much rarer for a man to get breast cancer than a woman. But they do in fact get it.”
With advancements in diagnostic technologies, cancers of the breast can be detected early and appropriate treatments provided. Cesare said that at one time and not that long ago, a diagnosis of breast cancer often meant a death sentence.
“Not a death sentence anymore. What we have done in regards to breast cancer, which is different than any other cancer that people get, such as colon, melanoma and lung cancer, for example, it is the only cancer where the death rate has drastically gone down,” he said. “There are two main reasons why the death rates have fallen off. First is early detection through technology, such as mammograms and ultrasound. Secondly, with all the money that is put into cancer research, we have better medicines for treating cancer, so, we are not only able to detect and find cancers early, but we are able to treat

the disease state more effectively.”
Cesare utilizes a team approach when treating his patients. For example, he will perform the surgical biopsies, as well as the ultrasound guided biopsies. When needed, he has a radiologist on staff to further assist. In regards to removing a lump in the breast if detected and warranted to remove, in the past Cesare would perform all the surgeries, but now takes a multi-disciplinary approach using local surgeons and local oncologists as well.
“Breast cancer is easier to treat today than years ago. We have technology that shows us that we look at the pathology and now we can look at certain markers of cancers
With November as Lung Cancer Awareness Month, Hematology/ Oncology Associates of CNY (HOA) and CRA Medical Imaging (CRA) are offering free lung cancer screenings 8 a.m. to 2 p.m., on Saturday, Nov. 2, in three locations:
• HOA, 5008 Brittonfield Parkway, East Syracuse, NY 13057
• HOA, 5490 Cobbler Way, Camillus, NY 13031
• Diagnostic Imaging Center, 37 West Garden Street, Auburn, NY 13021
Appointments are required by calling 315-472-7504, extension 1301. Walk-ins are not allowed.
Who qualifies for a free screening?
This free lung cancer screening is available for people at high risk for lung cancer, meaning they must meet all the following criteria:
• Are 50 to 80 years old
• Are currently a heavy smoker or one who has quit within the last 15 years. Heavy smoking is defined as: one pack of cigarettes per day for 20 years; two packs of cigarettes per day for 10 years
• Have not previously received
a free lung cancer screening through this program Anyone unsure if they meet the guidelines can take asimple quiz at hoacny.com/lungscreening.
Is it really free?
This annual clinic is absolutely free as a community service from HOA and CRA. However, anyone who meets the above criteria can contact HOA or CRA at any time to arrange a lung cancer screening at a time convenient for them. In most cases
and certain biological markers on the tumors and that enables us to target treatments much, much better,” he explained.
When posed with the question how A.I. (artificial intelligence) might be used in the diagnosis of breast cancer, Cesare feels strongly that with A.I. it will allow medical professionals to see even better-quality imaging.
“Maybe even new types of imaging will be available perhaps even on the molecular level, so we can see a molecular change in the breast and that type of scan could replace everything else,” he said. “It truly is an exciting time in science and medicine.”
insurance will pay for the procedure. The procedure also can be paid outof-pocket for approximately $250.
What does it involve?
The only recommended screening test for lung cancer is low-dose computed tomography (also called a low-dose CT scan, or LDCT). During an LDCT scan, the patient lies on a table fully clothed and the CT scanner uses a small amount of radiation to make detailed 3D images of their lungs. The scan takes less than five minutes and is not painful. While this scan will expose you to a low-dose of radiation, LDCT uses 75% less radiation than a traditional CT scan and shows more detail than a standard chest X-ray.
ELEMENTAL MANAGEMENT GROUP
Hybrid Nurse Aide Training Program
Hybrid Nurse Aide Training Program
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMEN UP





Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP















OUP
MANAGEMENT GROUP

Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
CONTACT:

Peg Reith BSN, RN
CONTACT:
Peg Reith BSN, RN
CONTACT:
Phone: 315-529-3267
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
CONTACT:
Peg Reith BSN, RN
Email: CNA_Training@elementalmgt.com
Peg Reith BSN, RN
Phone: 315-529-3267
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com
Email: CNA_Training@elementalmgt.com






















Alive and kicking: Seventyseven year-old Clifford Crandall Jr. is the grandmaster at his New Hartford martial arts studio, the American Martial Arts Institute in New Hartford. He now produces his own video series and columns dubbed “Still Alive and Kicking.”
In 1998, Clifford Crandall Jr. became an entry in the Guinness Book of World Records with a skydive of 11,000 feet in the skies above Schenectady.
During the dive, he successfully split a wooden board by hand that was being held by another diver.
He had a goal that day.
“I was jumping to promote child safety,” he said.
His overall statement being that he would be able to safely jump 11,000 feet, cloud to ground, while throwing a stunt in the middle; and would “be safer than many children walking along a neighborhood street on their way to school.”
At the time of the jump, Crandall had already long been training and teaching martial arts and finding creative ways to inspire people of all ages to make and maintain healthy living life goals.
For Crandall, that page in his life story of planning and achieving goals was equally as important as the page that came before it and the page to come after.
As life throws you obstacles, how do you stay motivated to stay active and continue to set healthy living goals?
The answer centers on assessing obstacles and setting life goals, Crandall said.
In a 2020 study by the United

By Jolene Cleaver
States Center for Disease Control, “...24.2% of adults aged 18 and over met the 2018 Physical Activity Guidelines for Americans for both aerobic and muscle-strengthening activities.
…”
With statistics like that in mind, “health is just so important,” said the 77-year-old Crandall, who is the grandmaster at his New Hartford martial arts studio, the American Martial Arts Institute, located at 8382 Seneca Turnpike in New Hartford.
Clifford Crandall’s goal work
Fifty-seven years ago, Crandall committed to his goal of healthy living.
He started training in martial arts and later began teaching and growing the healthy living spirit in the community with not just fitness classes and training, but competition, written columns, videos that has grown to include all wellness activities: golf, scuba, skydiving … anything to stay active.
As a teacher, Crandall said the most common struggle people have is finding the one activity people can focus on and achieve success.
“If you just do some activity but you have none you are passionate
about it won’t take,” he said, “You don’t have to be good at it. … This is new. This is going to be a challenge. Everything has a learning curve.”
To get started, Crandall advises you have a serious conversation with yourself.
What’s the ultimate motivation? What are the goals?
“What’s a goal? It’s a deadline. Put a date on things to make it a goal,” said Crandall. “Everything is a dream until you put a deadline on it.”
Then, when you have settled all of that, tell someone else your goals. That adds an extra layer of determination.
“We have excuses. One million excuses. The promise you make to yourself is one you shouldn’t break,” Crandall said.
When starting a new activity, don’t be discouraged by phrases like “easy” or “simple.” Give yourself time to adapt to the activity. “Give yourself time to break down the movements, otherwise you’re going to look like a newborn giraffe,” he said.
Work on your form. Research and teach the brain. Learn. Focus.
Oftentimes, when young people attend martial arts classes, they have underdeveloped goals. Typically among any martial arts classes, there is an 80% drop out rate within the first two years, but the ones who make it past two years begin a transformation.
“It’s about the journey,” he said.
Still alive and kicking
About three years ago, Crandall started producing his own video series and columns dubbed “Still Alive and Kicking,” which goes into depth about wellness and staying active. Check him out here: https:// stillaliveandkicking.org.
Like many other things, he said he planned it out and decided on his message.
“It wasn’t a flash in the pan,” he said.
“We’ve all got things that are going to be obstacles … our mind is sharp enough, our body can be taught to compensate. … Good health is about what you can do with the parts that still work. … You are the center of your universe. We revolve around each other. We can’t take care of the universe unless you take care of yourself.”
As a service to our community, Hematology-Oncology Associates of CNY and CRA Medical Imaging are offering a free lung cancer screening to qualified participants.
Saturday, November 2, 8:00 a.m. to 2:00 p.m.
HOA’s East Syracuse, Auburn and Camillus locations
Free screenings are available to individuals 50-80 who:
- are heavy smokers (e.g. 1 pack a day for 20 years or 2 packs a day for 10 years)
- OR are former heavy smokers who quit in the last 15 years
- AND have not previously received a free lung cancer screening from us.
To make an appointment, call 315-472-7504, extension 1301.
This free screening event is co-sponsored by:


Excellus BlueCross® BlueShield® is working to make quality care more accessible. With low or no cost plans and programs that support families, we are focused on improving access in your community.
To find coverage that’s right for your family, visit ExcellusBCBS.com


