






Complications are related to surgical procedures, followed by adverse drug events, infections and hospital-related problems like falls or pressure ulcers
More than a third of surgical patients develop complications as a result of their procedure, a new study shows.
About 38% of adult patients suffer an adverse event during or following their surgery, researchers reported Nov. 13 in the BMJ.
Nearly half of these complications result in serious, life-threatening or fatal harm, results showed.
What’s more, about 60% of the complications were potentially preventable and 21% were definitely or probably preventable, researchers report.
“Adverse events remain widespread in contemporary healthcare, causing substantial and preventable patient harm during hospital admission,” concluded the research team led by physician Andre Duclos, a professor of public health with the University Claude Bernard Lyon in France.
However, surgeons aren’t the only reason why these complications occurred, the researchers found.
“These incidents were not solely a concern for surgeons in operating rooms, but involved healthcare
professions throughout the hospital,” their report noted.
For the study, researchers analyzed more than 1,000 admissions for surgery at 11 Massachusetts hospitals that took place in 2018.
Complications developed in 383 (38%) of surgeries, with major adverse events occurring in 160 (16%), results show.
About half (49%) of the complications were related to surgical procedures, followed by adverse drug events (27%), healthcare-associated infections (12%) and hospital-related problems like falls or pressure ulcers (11%).
Half of the complications cropped up in general care units, compared with 26% in operating rooms and 13% in intensive care units.
Worse, many of these complications could have been avoided, researchers said.
“About one-fourth of all patients experienced potentially preventable adverse events, with one in 10 concerning events that were probably or definitely preventable,” the researchers concluded in a journal

About 38% of adult patients suffer an adverse event during or following their surgery, researchers reported Nov. 13 in the BMJ.
news release.
Possible reasons for these complications could involve doctor burnout, inadequate nurse staffing and failure to utilize technology that could detect and prevent the health problems, according to an accompanying editorial written by Helen Haskell, president of Mothers Against Medical Error.
But these events also keep oc-
curring because little progress has been made in recruiting patients and families to help unravel the causes of complications, Haskell added.
“If we are truly interested in advancing patient safety, patients and families need to be empowered to weigh in on the accuracy of the accounts of their own care and participate in finding solutions,” Haskell concluded.


One day of the week has highest suicide risk
A“case of the Mondays” is more perilous than just the returnto-work blues, a new study warns.
Suicide risk is highest on Monday in the United States and around the world, an international team of researchers has discovered.
“Mondays and New Year's Day were both associated with increased suicide risk in most countries,” concluded the team led by Yoonhee Kim, an associate professor with the University of Tokyo's Department of Global Environmental Health.
Mondays constitute 15% to 18% of total suicides, compared with other days, researchers found.
Results also show that weekend suicide risk varies greatly between countries.
Suicide risk is lowest on Saturdays or Sundays in many countries across North America, Asia and Europe. However, suicide risk increases during the weekend in South and Central American Countries, Finland and South Africa.
For the study, researchers analyzed suicide data for 740 locations in 26 countries and territories from 1971 to 2019, including more than 1.7 million suicides.
Previous studies have shown that suicide risk differs by day of the week, but results have been inconsistent, researchers said in background
notes.
Suicide risk increased on New Year's Day in all countries, especially in men, the results showed.
The researchers said there are several potential explanations for the increased suicide risk on Mondays and New Year's Day.
One is the “broken-promise effect theory,” which holds that people experience a negative mood when things don't go as planned. In essence, a bad weekend or a trying year causes an intense feeling of depression or despair that increases suicide risk.
The beginning of the week might also increase work pressure and stress, a phenomenon called “Blue Monday,” researchers said.
It also could be that people drink more on the weekends and on New Year's Day, which is considered a major risk factor for suicide, researchers added.
“Notably, our study showed that men who died by suicide were more affected by the day of the week and New Year's Day compared with women,” the researchers wrote.
The new study was published Oct. 23 in the BMJ.
Men are more susceptible to isolation and stress, while women typically have a bigger and more diverse social support system, researchers said.
A monthly newspaper published by Local News, Inc. 20,000 copies distributed. To request home delivery ($21 per year), call 315-749-7070.
In Good Health is published 12 times a year by Local News, Inc. © 2024 by Local News, Inc. All rights reserved. 4 Riverside Drive, # 251, Utica, NY 13502 Phone: 315-749-7070 • Email: IGHmohawkvalley@gmail.com
Editor & Publisher: Wagner Dotto • Associate Editor: Stefan Yablonski
Contributing Writers: Barbara Pierce, Deb Dittner, Gwenn Voelckers, David Podos, Deborah Jeanne Sergeant, Anne Palumbo, Jolene Cleaver
Advertising: Amy Gagliano: 315-402-3370 • Email: amyIGHmv@gmail.com
Layout & Design: Angel Campos-Toro • Office Manager: Allison Lockwood
No material may be reproduced in whole or in part from this publication without the express written permission of the publisher. The information in this publication is intended to complement — not to take the place of — the recommendations of your healthcare provider.

Immediate openings for:
• LICENSED PRACTICAL NURSES
• CERTIFIED NURSING ASSISTANTS at Valley Health Services and Valley Residential Services in Herkimer, NY.
Work on a team that is:
• Focused on high-quality care and resident safety
• Patient-focused and dedicated to making a difference
• Inspiring and innovative
• Committed to continual improvement
Plus:
• Comprehensive health benefits
• Retirement benefits
• Generous paid time off
• and more!

APPLY NOW Bassett.org/Careers


By George W. Chapman

House Speaker Mike Johnson has more than once threatened to repeal the Affordable Care Act. President-elect Trump baselessly calls it "lousy healthcare," which must make our hard working physicians, nurses and ancillary professionals feel really appreciated. After 10 years, 45 million people are covered by the ACA, giving them access to the same hospitals and providers as the rest of us. By significantly reducing (almost eliminating) the uninsured, it has provided sorely needed revenue to hospitals and physicians virtually saving providers
CMS (Medicare) has proposed to cut, yes cut, physician reimbursement by 2.5% next year, despite its own medical economic index showing 3.5% inflation. The cut is tantamount to an in flation-adjusted 6.3% reduction in reimburse ment. Recognizing this absurdity, a bipartisan committee has hurriedly proposed a bill eliminating the possible cut and proffering a 4.7% update to the physician reimbursement schedule. The committee wants to push the bill before Congress goes on recess. The ridiculous and untenable cut would be further compounded and exacerbated by copy cat cuts from commercial insurers. The pandemic has created incomparable increases in staff and supply costs for physician practices.
serving inner cities and remote rural areas from closing. It is by no means "lousy healthcare." The ACA was carefully crafted by the AHA, the AMA, commercial insurance carriers, CMS and various industry experts. It was bipartisan and non-political. It works effectively in both red and blue states alike. Congress has enough things to fix, including inflation, immigration, public safety, women's reproductive rights and infrastructure. Like everything else, the ACA could be tweaked. But in no way is it "lousy healthcare" screaming for repeal.

No, not as in Halloween. It refers to provider directories that list non-participating or even non existent providers. Individual consumers and businesses typically base their purchasing decision primarily on premiums, benefits and the plan's provider network. An inflated
directory of providers has created legal problems for NYS plan Anthem BCBS. The case is centered around "ghost" mental health providers listed in the iAnthem directory. With increasing mental health problems, especially among younger adults, provider participation can be paramount to plan selection. Attorneys for the plaintiffs called the first 100 mental health providers listed in the Anthem directory. Only seven providers out of the 100 were actual participants. The other 93 providers did not accept Anthem insurance, were retired or never existed. Plaintiffs argue that this deception caused them undue anguish and financial hardship by having to seek out and use more expensive out -of-network care. (The Anthem directory lists a total of 4,300 providers.) The Departments of Labor and Health have promulgated rules to protect and expand equitable access to mental health services. Provider directories are updated annually as older physicians retire, newer physicians join the plan, office affiliations or addresses change, the provider is not accepting new patients or the provider has opted out altogether. Normally, this activity would account for maybe 5% of the listings from year to year. It becomes a ghost or false network when 93% of providers don't participate or even exist. When changing plans,
experience, reduce costs and improve quality. (Not exactly an innovative concept.) By directing members to "high-quality" providers (Just how is that determined? I am skeptical. Are high-quality providers the ones that will accept a lower fee from Aetna in exchange for higher volume and year end profit sharing? Just saying.) Aetna claims it will save the client money. So far, they claim a 60% increase in the use of high-quality providers saves the self-insured plan about 12%. Members can search for the high-quality providers via an app. Aetna-CVS seems to be a victim of over-diversification having to divest or shrink certain lines of business that are not profitable. Aetna might want to stick with selling insurance and CVS with selling drugs.
The ACA impacts all of us. It ended pre-existing conditions. It capped commercial insurer profits at 15%. If a carrier spends less than 85% of premiums on claims, it must rebate the difference to members. It eliminated the confusion in comparing plans by establishing minimum benefits for three levels of coverage: bronze, silver and platinum. The ACA was not an issue in the election this year because it works. Trump inexplicitly attempted to repeal the ACA more than 60 times. He failed every time. I'm concerned he still doesn't get the message.
especially for mental health, it is recommended you call the particular provider office you are considering and verify they are accepting new patients AND accept the insurance.

There is no doubt in the technical pow er of artificial intel ligence in medicine. Billions of dollars are being invested in AI development. (Even the ubiquitous Elon Musk is get ting involved.) AI innovations have improved care and future AI applications are endless. However, while the technical aspects of AI are a given, AI must also engender patient trust, be transparent, offer choices and protect privacy and autonomy. Otherwise, success will be compromised. For example, patients want to know when they are talking to either a real human being or a chatbot. We don't want to be "catfished." Providers need to keep the patient's experience personal, not cookie cutter, especially in times of crisis.
Aetna-CVS is offering self-insured businesses and organizations a product that will simplify the patient
Dating back to the end of the Civil War, Black Americans have lagged far behind whites when it comes to overall health and life expectancy. Study after study has concluded there has been little to no progress even in the last two decades. Lingering racism in government, intentional or not, bears a lot of the blame. South Carolina's notorious "corridor of shame," 17 predominately Black poverty-stricken rural counties along interstate 95, has some of the nation’s worse outcomes. According to the few providers serving the area, most of the residents cannot afford care, so they don’t seek care. South Carolina is one of the few states to refuse Medicaid expansion which would have given the residents at least some insurance. The Black residents living in the corridor suffer much higher rates of high blood pressure, diabetes and heart disease than whites. The National Academies of Sciences, Engineering and Medicine concluded our fragmented and uneven system of healthcare results in millions of preventable deaths and the loss of billions in economic benefit. Many states, Louisiana for example, allow residents to carry concealed and unregistered guns. Gun violence is the No. 1 killer of kids and young adults. Blacks are 18 times more likely to die by gun than whites. Adding to the disparity, 80% of all solid waste incinerators are located in low income communities. An AMA study in 2023 calculated that in the last 20 years there have been 1.63 million excess deaths among Blacks versus Whites, resulting in 80 million years of lives lost. America is still caught up, consciously or not, in our deep seeded racial history and government decisions regarding gun control, expanded medical insurance or even incinerators contribute to the continuing disparity in health among Blacks.

George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse.
Middle-aged folks facing a colon cancer screening now have a blood test they can choose over a standard colonoscopy.
However, the blood test isn't as effective as colonoscopy at detecting and preventing colon cancer, a new review finds.
About two and a half times more colon cancer deaths can be expected to occur in people taking the blood test every three years as recommended, compared to those who undergo colonoscopy once a decade.
Colon cancer death rates will increase if too many people choose the blood test over either colonoscopy or stool-based tests, researchers predicted.
“The first generation of blood tests are a really exciting development in the colorectal cancer screening paradigm,” said lead researcher, physician Uri Ladabaum, a professor of gastroenterology with Stanford Medicine. “But for now, if you're willing and able to do a colonoscopy or stool-based test, don't switch to a blood test.”
The U.S. Food and Drug Administration in July approved the first blood test for screening colon cancer in people at average risk of
the disease.
The FDA based its approval on a clinical trial involving nearly 8,000 people, which found that the test detected colon cancer in more than 83% of people with a colorectal tumor.
However, the test only was able to detect precancerous colon polyps in about 13% of people.
Colonoscopy is not an easy procedure. People must take powerful laxatives ahead of time to completely empty their bowels and are put under sedation while doctors use a thin tube to examine the inside of the entire colon.
However, colonoscopy makes colon cancer one of the only fully preventable cancers, because doctors can remove any precancerous polyps they come across during the examination.
“This makes colonoscopy a unique cancer screening method because you also have the possibility of cancer prevention,” Ladabaum said. “Despite that, there are many people who are not getting screened at all, or who are not getting screened as often as they should.”
Patients who get a positive result from a fecal or blood test are urged to undergo colonoscopy, to dou-






ble-check whether they have either cancer or polyps.
For the study, researchers pooled together data on six commercially available or in-development bloodand stool-based screening tests, as well as on gold-standard colonoscopy.
Using this data, they estimated the relative rate of colon cancer cases and deaths among people who used each screening approach.
The estimated case and death rate for every 100,000 people who choose:
• Colonoscopy: 1,543 cases and 672 deaths
• Stool tests: about 2,200 to 2,500 cases and 904 to 1,025 deaths
• Blood tests: about 4,300 cases and 1,600 deaths
• No screening: 7,500 cases and 3,600 deaths
Researchers also found that colonoscopies and stool tests are more cost-effective than blood tests.
The study was published Oct. 28 in the Annals of Internal Medicine.
“The blood tests are certainly much better than nothing, but you'll worsen the population outcomes
and raise health care costs if you see people switching from colonoscopies to first-generation blood tests,” Ladabaum said in a Stanford Medicine news release.
The best-case scenario will be if most people continue to use colonoscopy or fecal tests, and resort to a blood test only if they find those two options so repellant they would otherwise not be screened, researchers said.
“Ideally, we want as many people as possible to get screened for colorectal cancer, and that's likely going to mean a combination of different tests being used across the population,” Ladabaum said.
However, the blood test is still so new that it isn't covered by existing colon cancer screening guidelines, and it's not clear how many people will choose it, researchers noted.
“It remains to be seen who will really use the blood tests,” Ladabaum said. “Will it be people who have never been screened using any other method? And will they be willing to get a follow-up colonoscopy if indicated?”


By Barbara Pierce
Twenty-seven-year-old Samuel Rivers of New York Mills is a radiation therapist for Mohawk Valley Health System. He is employed by the MVHS Cancer Center at the outpatient Faxton Campus in Utica.
The MVHS Cancer Center offers care and treatment for patients who have been diagnosed with a variety of cancers. Their personalized approach to care is based on the belief that every patient and their needs are unique. From treatment options to symptom management, the care that is provided is individually tailored to each patient.
Treatment of cancer may involve many different types of treatments, such as surgery, chemotherapy, radiation therapy or hormone therapy. The type of treatment recommended depends on the type and stage of the cancer, the overall health of the patient and their personal preferences. Patients may receive a combination of treatments or may only need one.
Hearing a diagnosis of cancer can be overwhelming. And the treatment can be a very difficult time to go through. Every member of the cancer care team must be sensitive to what patients are dealing with.
I spoke with Samuel Rivers about his decision to pursue this specialty.
Q: How did you become interested in a career as a radiation therapist?
A: I was in and out of the hospital as a child. This gave me the experience of what health care is really like. I wanted to give back to the community that cared for me. Also, in 2016, a close friend died of can-
cer and that sparked my interest in cancer. I began as a volunteer for an ambulance company, then I worked at a dialysis clinic as a patient technician. At that job, I stumbled into X-ray, found that it appealed to me and went to school to get a degree in radiology. I settled into radiation therapy because I wanted to see patients, to be involved with people. I’ve been employed at the outpatient Faxton campus for the past two and a half years. This is my first job in radiation therapy.
Q: What training did it take for you to begin work as a radiation therapist?
A: I received a bachelor’s degree in professional studies at SUNY Upstate Medical University, with a focus on radiation therapy. Also, I have an AA degree as a radiation technician from Mohawk Valley Community College.
Q: What is your job like on a dayto-day basis? Can you describe the technical side of radiation therapy? We understand it’s one of the most common treatments for cancer, using special equipment to aim high doses of radiation at cancer cells that damages the cancer cells and causes them to die. Radiation therapy may be used alone, or in combination with other treatments such as surgery or chemotherapy.
A: On the technical side, the treatment depends on the type of cancer. Radiation therapy uses high-energy radiation to shrink tumors by killing the cancer cells. I get people lined up, set them up for their treatment from the machines. The

treatments last from 15 to 20 minutes. Patients come in once a day. Some come in just one time; some come for up to 30 days. I work with the doctors and a great team of people.
Q: How effective is radiation therapy in killing cancer cells?
A: How many people survive cancer depends on where the tumor is and how much it’s progressed. Everybody is different. I don’t see a lot of people coming back for more radiation treatments and that’s a good sign that the treatment has worked.
Q: Isn’t it difficult to help people through this terrible time in their life?
A: I find it very rewarding. I get to help people in their time of need, I provide comfort. People are going through the most difficult time in their life. And it’s very rewarding to
help them through this time in their life.
Q: How do you do this? How to you deal with people whose world has been turned upside down in every way?
A: I always try to come to them with a smile; I leave my personal problems as the door so I can be there for the patient.
Yes, it’s challenging. It does take an emotional toll on you when you’re dealing with patients at the worst time of their life. I often have serious conversations with them about what they’re going through. And these conversations are emotionally stressful. But I’m glad I can be there for people and do this.
It’s certainly not a job for everybody. But if you really want to make a difference, you can.











By Barbara Pierce
“Maybe we should see someone,” suggested Donald, the man I live with. “A therapist? I’m not happy with the way my life is going. I just watch TV all day; you’re never here.”
I was stunned. I’m a retired therapist. How could he be suggesting we see a therapist? I should be keeping us both happy.
I thought about it. And came to the conclusion: “He’s right. How could he be happy with such a limited life? I’m not really happy either, if I’m honest with myself.”
We’d been living together for close to a year. Living in a new area, neither of us knew anyone when we moved in. I began doing activities to get to know other people. Donald chose not to come with me.
As he’s in the early stages of dementia, he avoids things that he finds too complex. He sits home and watches tennis on TV while I run around in my search to find a community of people. I had to admit that I wasn’t finding that and I really wasn’t happy either. I wasn’t depressed, but I wasn’t thriving. This isn’t the life I want, I admitted.
I decided couples counseling wasn’t the solution. Our relationship was working. We coped reasonably well with each other’s weirdnesses. It was just that neither of us were happy with our lives.
If you’re thinking about sharing your issues with someone, it’s most important to find the right therapist for you. Here’s how I looked: I researched online. As I had been a licensed clinical social worker, I felt someone with this training and
expertise would be best for me.
There are several categories of psychotherapists: LCSWs, licensed marriage and family counselors, psychologists. Anyone would have been OK, really. It’s more a matter of fitting with the individual doing the therapy. (Psychiatrists prescribe medication; they usually don’t do therapy. Life coaches don’t do therapy.)
Credentials are important. A credible mental health professional will be transparent about their training, licensure and areas of expertise.
Credentials and licensing were what I looked for, first of all. Next, I needed someone who took my insurance. As I have Medicare, they usually said this on their website. In the past, I had other insurance. I started with my insurance plan. Asked them who was on their list. And it’s important to know how much they’ll pay. Some plans cover a limited number of sessions.
I looked at how each therapist described their areas of expertise — how they worded what they offer. I avoided those with jargon-heavy language, like “inner-child work,” boundaries, unresolved trauma, etc. I wanted a person who could speak ordinary everyday language. Their photo was important also. I trusted my gut to see if I would feel comfortable sharing with this person. Did they look open and accepting or judgmental and critical? Would I click with this person?
I read the reviews with much skepticism, of course.

I selected one who appeared to be what I was looking for. No, it isn’t a quick process, but it’s necessary. And it’s necessary to trust your gut instinct. When we need help getting through a tough time, more and more of us are finding a therapist on social media. Social media platforms are filled with experts, offering their advice and attracting millions of people.
If you’re not seeing much information, search the person online. If they’re legitimate, they’ll come up on Psychology Today, LinkedIn or their own private practice website. If they’re trying to sell you something, like online courses or books they’ve written, that may be a red flag. If their content keeps leading you back to what they’re selling, this means they’re more concerned about making you a customer than helping you get through a tough time in your life.
Getting back to my search, I clicked on “Schedule an appointment,” was asked to briefly describe my goals, what I was seeking from therapy. I had to think about that. And it was good for me to think it through. I decided on “I haven’t got the life I want to have.
And my partner is unhappy with me” or something basic like that.
I meet with the therapist I chose a few times. He helped me identify the four or five problems I was juggling. I set goals for each area and made several changes in my life. Life is better for both Donald and I.
That therapist turned to be great for me. But if you find the person you first choose isn’t working for you, you don’t click with them, try another.
Larger companies have an employee assistance program, free short-term counseling with a licensed therapist. It’s confidential; your employer won’t know you used the program.
In addition to what I mentioned above, proceed with caution if you choose a ‘therapist’ you find on social media, say many experts. It can be difficult to know who is credible and whether their information is trustworthy.
Check their biographies. That’s where they specify whether they have credentials.

Barbara Pierce is a retired licensed clinical social worker with many years of experience helping people. If you would like to purchase a copy of her book, “When You Come to the Edge: Aging” or if you have questions for her, contact her at barbarapierce06@yahoo.com.


◘ Conducting
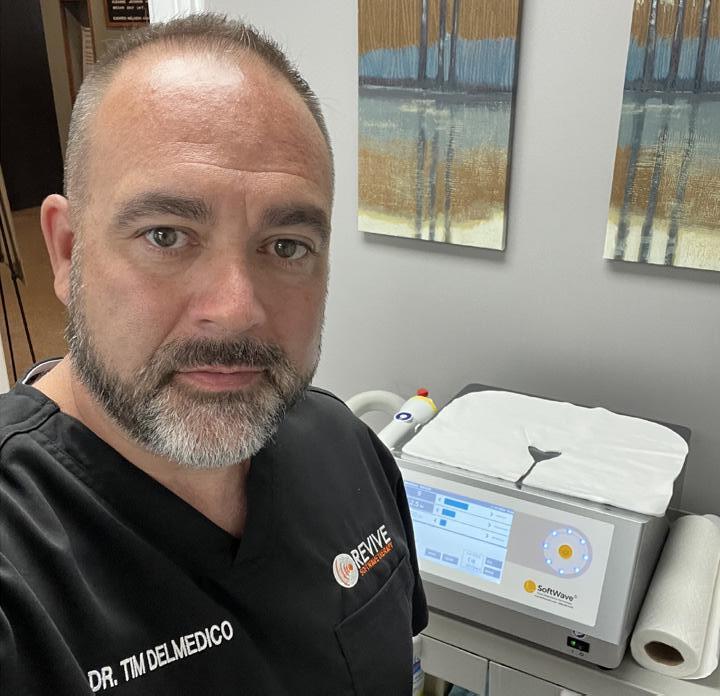
LMain focus of local surgeon is to offer minimally evasive treatments for the spine, nerves
By David L. Podos
iving with chronic pain can be debilitating. In a 2021 research study, the CDC estimated that close to 21% of United States adults (more than 51 million people), experienced chronic pain. Almost 7% or 17.1 million experienced high-impact chronic pain — pain that was so severe that it restricted most daily activities.
Additionally, the economic impact from people dealing with chronic pain is significant, An estimate is that, due to reduced productivity and the associated health care costs, it costs the country between $560 billion and $635 billion annually.
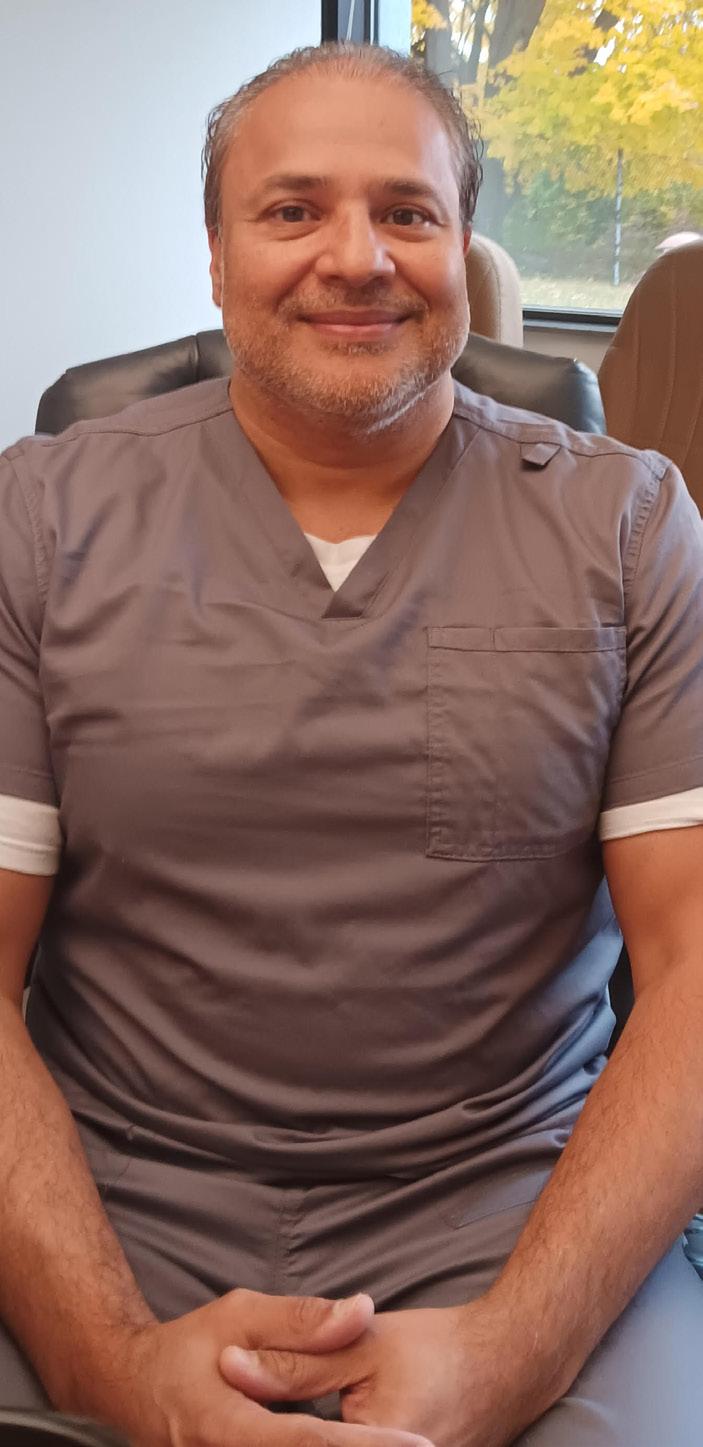
New and promising innovations in the treatment of pain are giving hope to many who suffer day in and day out, giving them their lives back. Here in the Utica area patients have the opportunity to be treated by a renowned surgeon — physician Nameer R. Haider.
Haider is a graduate of King Ed-
ward Medical University, completed his surgical internship at East Carolina University School of Medicine. His residency was at Northshore University – Long Island Jewish Medical Center in New York—where he was chief resident. He completed his fellowship training in interventional pain management at the Spinal and Skeletal Pain Institute in New York. He is triple board certified in physical medicine and rehabilitation, pain medicine and interventional pain management.
Haider is the principal at Omni Pain and Precision Medicine in Utica.
“My main focus of practice is in minimally evasive surgical treatments specifically for the spine. However, we also offer orthopedic treatments and nerve treatments for various nerve and orthopedic conditions,” he said.
He also utilizes a number of innovative modalities to treat a host of medical conditions from depression,
too nerve pain, such as transcranial magnetic stimulation, radio frequency and spinal cord stimulators to name just a few.
While that may sound like something out of a science fiction magazine, that is far from the truth.
“In medical practice doctors often use medications for the treatment of mental health issues. Oftentimes they work. However, they do have side effects and sometimes the medication doesn’t work. So, for example, I was looking for something that would help people with mental health problems,” he said. “Transcranial magnetic stimulation is a treatment that is non evasive, not painful, where we actually use magnetic waves to target a specific part of the brain that is sensitive to the transmission of those signals (abnormal signals when someone is depressed) or someone who has PTSD or an obsessive-compulsive disorder. We have a very high efficacy rate in our treatments with patients, and it is FDA approved.”
Medicine is evolving rapidly and alongside this evolution is the use of medical implants. Haider invented and was the first in the world to utilize the HALO procedure using surgically implanted peripheral cranial nerve stimulation for the treatment of chronic headache (killmigriane.com) and the Bio Disc procedure for the treatment of spinal disc disease.
Additionally, off-label use of medicines and or procedures for “other” conditions is becoming more common. An article from the Mayo Clinic and authored by endocrinologist Sumit Bhagra, mentions that there are risks and benefits of off-label use. However, the popularity is growing.
“There are examples of widely practiced off-label medications in every specialty of medicine and, in some cases, these have become predominate treatments for specific health conditions,” Haider said. “An example of this is aspirin. It has FDA approval for pain, fever, rheumatic diseases, heart disease and other conditions. Yet, aspirin was never studied in people with both diabetes and heart disease. Therefore, a low-dose aspirin regime for someone with Type 2 diabetes is considered a mainstream, yet off -label recommendation.”
Haider also incorporates off-label use as well.
“We have to look at what is

FDA-approved. So, right now the FDA has approved the use of transcranial magnetic stimulation for depression, obsessive compulsive disorder and for smoking cessation. However, off-label use it has been studied and proven that it is effective for chronic pain and even for post COVID conditions.”
Medical devices that are implanted just under the skin have also seen an increase in the use of managing pain.
“For example, there is a new procedure called Sprint PNS (peripheral nerve stimulation), it works to treat pain coming form a specific area. So, say that you have shoulder pain or hip pain; on an out-patient basis we put a very thin wire under the skin. What happens is, that wire has micro electrodes on it made of platinum and iridium. They send an electric signal, sort of the way that a pacemaker works to control the heart, this works to control pain wherever that might be, like your shoulder or your hip,” Haider explained.











By Barbara Pierce Pain
“I woke up each day in pain,” said 74-year-old Donald Kozlowski of Bradenton, Florida. “Pain in my back and neck. Some days it was worse than others. When it was bad, I just sat in my recliner with an ice pack and watched tennis matches on TV all day. It wasn’t a good life.
“I tried everything. I was in the ER for my pain a few times, but all it got me was a referral to a pain specialist and a huge bill to my insurance. The pain specialist prescribed medication. My primary physician said not to take it because it could affect my brain in ways I wouldn’t want. Acupuncture helped some, but it was only a temporary fix and expensive, so I stopped.
“Then a friend suggested physical therapy had helped her chronic back pain. After my first session, I felt much better. I’ve been going once or
twice a week for about four months. I’ve got my life back. My pain is a horrible thing of the past!”
Pain does seem to be part of aging. Some studies show that up to 85% of adults older than 60 experience regular pain that disrupts their daily lives, according to the Cleveland Clinic.
And, yes, in my opinion physical therapy is the best way to stop certain types of pain. A much better alternative than medication or surgery, for certain cases.
The beauty of physical therapy lies in the fact that it’s non invasive, affordable and simple when compared to more invasive solutions like surgeries.
Physical therapy is a combination of hands-on techniques (a therapist moving part of your body) and exercises or movements that you perform
under the direction of the physical therapist. It can include stretching, massage, heat or cold therapy or the use of a TENS unit (transcutaneous electrical nerve stimulation unit; a small, battery-powered device that uses electrical currents to relieve pain).
The therapist will probably want you to come two or three times week for six weeks or so and will suggest exercises you can do at home to optimize your recovery.
Physical therapists are highly trained in assessing a patient’s pain and looking for its cause.
They are experts in functional movement and have a range of noninvasive treatment options. It is rooted in scientific principles and evidence-based practice.
The goal of physical therapy is for you to be able to get on with your life. The functioning that you’ve lost because of your pain can be fixed so your life can go on as before.
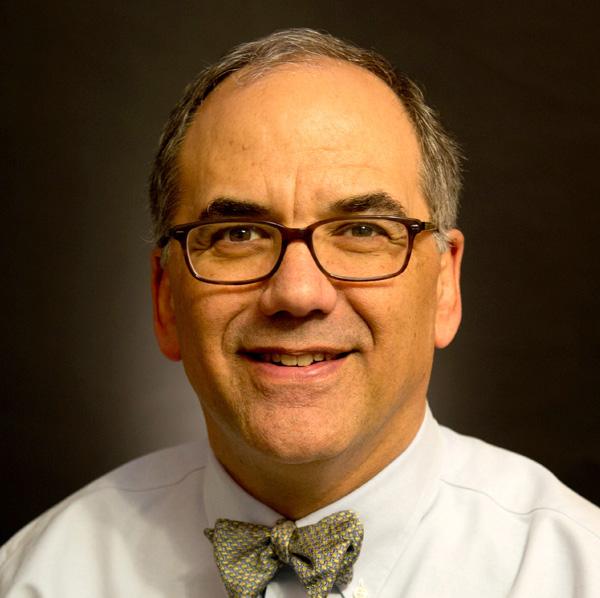
I asked board-certified family physician Benjamin Friedell, chief of primary care at Bassett Healthcare
ENetwork in Oneonta about the best ways to prevent and relieve pain.
Movement can decrease your pain and stiffness, improve your range of motion, strengthen your muscles and increase your endurance, he said.
Regular physical activity is the most potent and least invasive pain reliever available.
“It’s important to stay active!” he said. “Stay active with things that won’t cause you pain. For example, if your hip is affected, walk as much as you can. If you can’t walk because it’s too painful, ride a bike or use a stationary bike.”
“Keep active, find an activity you like and keep doing it,” he continued. “Swimming is great. Even walking in the pool, as the buoyancy of the water supports you, that can be most helpful.”
Do daily, gentle stretches that move your joints through their full range of motion. A physical or occupational therapist can help you develop an exercise program that’s right for you.
Avoid activities that involve high impact or repetitive motion, like running, high-impact aerobics, tennis.
“It’s important to keep your range of motion,” Friedell said. “For example, your shoulder hurts so you don’t lift it up for several days. Then you go to lift it up and it’s gotten frozen because you didn’t move it. It’s difficult to get your range of motion back. Stay active. Avoid freezing your joints.”
How long you’ll need physical therapy depends on which injuries or health conditions you have and which area of your body needs help moving better. Some people only need a few weeks of physical therapy to help with a short-term issue. Others need it for months or years to manage symptoms of a chronic (long-term) condition.
xcellus BlueCross BlueShield honored Bassett Healthcare Network’s New York Center for Agricultural Medicine and Health (NYCAMH) with a Circle of Excellence Award for its high-quality and innovative health care delivery and patient care.
NYCAMH received the health plan’s 2024 Circle of Excellence Innovation Award, recognizing the health care organization for its meaningful impact in the quality of patients’ lives through clinical leadership and vision to promote continuous improvement in the health care system. Led by clinical case worker Heather Chauncey, the NYCAMH Farm Partners Program (FPP) provides free and confidential case management and therapeutic counseling to the farming community and individuals with occupational health issues.
In addition to connecting members of the farming community with a wide array of resources and assists in filing and applying for needed services, FPP provides funding and resources to assist with living ex-

From left: Erika Scott, deputy director, NYCAMH; Sue Ackerman, center manager, NYCAMH; Shannon Campbell, value-based payment clinical consultant, Excellus BCBS; Jennifer Barretta, value-based payment account manager, Excellus BCBS; Heather Chauncey, clinical case worker, NYCAMH; Mary Stubley, director of value based payment account management and payments, Excellus BCBS; and Julie Sorenson, director, NYCAMH.
penses, shelter, medical expenses and emergencies for farm families. Chauncey has also advocated for the agricultural community with the NewYork legislature and state organizations as well as the NYS Education Department to obtain the first farm vehicle modification for a disabled farmer in 20 years.
“NYCAMH’s programs strive to improve the lives, health, safety and well-being of New York’s farmers, their families, and their employees,” says Chauncey. “Farmers work hard for long hours, so we meet them where they are—on their land and by conducting trainings and support groups in their milking parlors and
barns. It’s a model that reminds me of the old-fashioned house calls.
“Getting to know farmers, farm families and farm workers, I see how grateful they are for the help my coworkers and I provide them. I also see the challenges they face. They motivate me to work harder and go above and beyond to help.”
Internal Medicine Associates of Auburn are also recipients of a Circle of Excellence Innovation Award for it Innovation and cxcellence program which features a determined and systematic approach toward managing our patient population with an “all in” team commitment at the practice level, as well as thoughtful collaboration with patients.
“We developed the Circle of Excellence awards to recognize those who work in partnership with us to look at different ways to deliver high-quality care, and we’re very happy to recognize Bassett Healthcare and NYCAMH for their innovative work and community impact,” says Tony Vitagliano, senior vice president provider network and Utica regional president, Excellus BCBS.
By Anne Palumbo

Raise your hand if you only eat oats for breakfast. Now, raise your other hand if you were raised on single-serving packets of instant oatmeal.
Both hands up? Mine, too.
Just thinking about the maple and brown sugar flavor fills me with dreamy nostalgia.
But that was then.
These days, I go for healthier versions of oats, including savory dishes.
Yes, savory! What’s more, I consume this superfood daily.
Like many Americans, I suffer from high LDL cholesterol, the bad kind that clogs the arteries that feed the heart and brain. This stealthy buildup, as many studies have shown, can lead to heart attack, stroke and other health problems. While my level isn’t high enough for cholesterol-lowering medication, it is high enough for lifestyle changes.
According to Harvard Health, adding foods that lower artery-clogging LDL cholesterol is the best way to achieve a low-cholesterol diet.
And the food at the top of many lists? Oats!
Loaded with whole-grain goodness, oats stand out for their soluble fiber, the coveted fiber that binds cholesterol in the digestive system and drags it out of the body before it gets into circulation. This type of fiber also keeps you feeling full for hours, which can help with weight control. Carrying extra weight raises your chances of having too much bad cholesterol in your blood, with every 10 extra pounds producing as much as 10 milligrams of extra cholesterol daily.
Multiple studies suggest that those who have or are concerned with Type 2 diabetes could benefit from a daily dose of oats. Why oats over other whole grains, like whole wheat or brown rice? Oats (and barley) are the only whole grains
that carry a distinctive kind of soluble fiber — beta-glucan — which forms a thick gel that delays the emptying of the stomach and absorption of glucose into the blood.
Nutrient-dense oats boast a unique combination of vitamins, minerals, and antioxidants. A few superstars include manganese, which improves brain function, lowers inflammation, and is vital to bones; and vitamin B1 (thiamine), which helps turn food into energy, boost memory, and fight depression. One cup of cooked oats has 150 calories, 6 grams of protein, 4 grams of fiber, 28 grams of carbs, and scant sugar.

Since the nutrition profiles are quite similar for the three main types of oats — steel-cut, rolled, and quick — choose the oatmeal whose texture and method of preparation suit you. Steel-cut, the least processed, have a firmer bite while rolled and quick have a smoother, creamier texture. All forms now come in instant versions. Do check the nutrition facts of your preferred oats, especially flavored instant oatmeal. Remember that maple and brown sugar flavored instant oatmeal I adored?
A measly ½ cup has 12 grams of added sugars!

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
Ingredients
2 hard-boiled eggs
1 avocado, sliced lemon juice
3 teaspoons olive oil, divided
3 cups spinach or other greens
¼ cup finely chopped onion or shallot
1 garlic clove, minced
Instructions
1. Peel and slice hard-boiled eggs; set aside. If making fried, fry up right before serving. Slice avocado, drizzle with lemon juice, and set aside.
2. Heat 1 teaspoon olive oil in small saucepan over medium-low heat. Add the greens, lightly sauté until wilted (about 1 minute), remove, and set aside. In same pan, heat remaining oil over medium heat; add shallot or onion and cook until softened, about 2 minutes.
¾ cup instant rolled oats (or preferred oats)
1¼ cups water
Salt and coarse black pepper
½ cup black beans cherry tomatoes, sliced ¼ cup cheese of choice
Hot sauce or pesto
Add-ons: toasted nuts or seeds, fresh herbs
3. Add the oats and garlic and stir to coat in oil; then add the water and bring to a boil. Reduce the heat and simmer, stirring occasionally until the oats are thick and creamy, about 5 minutes. Season to taste with salt and pepper.
4. Remove from the heat and portion into bowls. Top with the sautéed greens, egg, avocado slices, beans, cherry tomatoes, and sprinkle of cheese. Serve with drizzles of hot sauce, a squeeze of lemon juice, and other add-ons.










By Deborah Dittner

Where does the time go? It seems like only yesterday I was planning for the holidays … last year. But here we are. Another year … another season of holiday gift giving, parties, planning and more.
Most importantly, you must first take care of yourself.
Self-care by being conscious of what you are eating (whole nutrient dense foods), restorative sleep (between seven to nine hours nightly), physical movement (a minimum of 30 minutes most days of the week) and the everyday routines that keep you healthy the rest of the year. By taking care of YOU first, you will be able to provide for family and friends with more comfort and ease. Set the intention.
With the rising costs of food, clothing and other everyday necessities, finances are a concern especially for those on a strict or limited budget. Making a list and checking it twice (where have I heard that phrase before?) will provide you with insight as to who you may be gift giving followed by suggestions as to what that person on your list may truly need. Be realistic when it comes to “needs” and “wants.” You may “want” a new outfit for family gatherings or parties or “want” a new car or “want” to give expensive or many gifts to a loved one. However, reality may not allow for such extravagances. Consider adding accessories to an outfit previously worn or leasing a car or asking your loved one what they may actually “need.”
Families may need a variety of items that would be helpful and necessary for their family life.
Remember to be conscious of your financial concerns and setting limitations when gifting as there is no need to overdo.
It’s the thought that counts.

• Gift cards from food stores that are frequented.
• A subscription to a meal company providing prepared meals on a weekly basis for one person to a family. This not only will provide nutrition but also creates family time in preparation.
• A homemade meal for someone who has been ill or has had surgery.
• A CSA membership.
• Basket for cooks (recipe book, tools needed, ingredients for a specific recipe), for tea or coffee lovers, chocolate lovers.
• A subscription for a child as a budding sous chef. A child in the kitchen from an early age prepares them for years of cooking and experimenting in the kitchen.
• A bread basket (a loaf or two of special breads, jams or jellies, a towel to wrap the bread when warm).
• Babysit the children so Mom and Dad can have a date night and possibly add movie tickets or dinner.
• House clean for a friend or relative who has been ill or had surgery. If this becomes an extended amount of time, consider going in with another friend or two to acquire a cleaning service.
• Walk the dog.
• Offer to pick up groceries at the store.
• Everyone needs self-care. However not everyone will spend this on themselves.
• Basket for sleep (Epsom salt and lavender essential oil for a soothing bath, bath mitt or loofah, calming tea with a special tea cup, a journal
for gratitude writing at the end of the day).
• Basket for the athlete (a gym membership, handheld weights, yoga mat and blocks).
• Basket for the reader (the next read in a series that is loved, special bookmark, night reading light).
• Never too early to start planning for the garden come spring.
• Gardening journal.
• Gardening books on different ways to maximize your yield of veggies.
• Basket with garden tools (gloves, trowel, clippers, seed markers, weeder).
• Garden magazine subscription.
• Seed sorter or saver.
Finding the right gift for those on your list can be a challenge, so it is very important to listen when in conversation. You may be told exactly what that person or family may need or some special little thing that they may want. Making mental notes from conversations when with family or friends that you plan to gift can often provide you with the inspiration needed for the perfect gift.
Wishing you all a happy and healthy holiday season!

Deborah Dittner is a family nurse practitioner and health consultant. Her mission is to transform as many individuals as possible through nutrition and lifestyle changes. www. debdittner.com




By Barbara Pierce
The holidays are supposed to be a time of joy, of celebrating, cheerfully getting together with family and friends.
Generally, we’re supposed to feel happy.
Some years, that’s not easy for many of us. The holidays bring a lot more stress when we’re already on overload. Sometimes they bring sadness, memories of those we have lost. Or they might heighten our feelings of loneliness. Loved ones pass away, people get sick, money is tight, friends move away. It can be especially hard to feel joy this time of year.
If the holidays are feeling tough for you this year, Jim Davis, executive director of Samaritan Counseling Center of the Mohawk Valley, offers ways to help lessen the stress and pain of the holidays:
Make plans: “With all of the holiday activities and events going on, I suggest planning,” said Davis. “Make a to-do list and prioritize the tasks on it. Break what needs to be
done into chunks to avoid feeling overwhelmed.”
Pace yourself.
It’s okay to say no: “Be selective about the activities you’re invited to. Limit your commitments,” he advised.
There are only so many activities you can go to; trying to do them all will become overwhelming. Prioritize the most important activities or schedule get-togethers for after the holidays. Learn to say no when you need to.
Set realistic expectations: “Remember it’s OK if things don’t go exactly as planned. Don’t aim for perfection,” he added and be OK with that.
Use a budget for gifts, food and activities to avoid financial stress,” he added.
If finances are a problem for you, turn down gift exchanges in favor of low-cost activities.
Giving to others is not about spending money. Offer to have someone over for a home-cooked meal or

plan a coffee date. It’s not unreasonable to set spending limits or make homemade gifts if you can’t avoid a gift exchange. Sometimes personal gifts — like a poem, framed photo, homemade cookies — are the best ones.
Consider how much money you can comfortably spend and stick to the amount. If purchasing gifts for everyone is difficult, consider having a Secret Santa or White Elephant exchange to reduce the number of items everyone needs to buy. You can also simply let people know you are unable to give gifts this year.
Take time for yourself. “Exercise, read or simply take a moment to breathe. Do activities that are relaxing. Don’t forget hobbies,” Davis suggested.
Practice self-care. Schedule time for activities that recharge you, like reading, working out or spending time in nature. You can also try stress management techniques like meditation or deep breathing.
Get outside. Fresh air and sunlight can help you relax and improve your mood.
Avoid numbing yourself with alcohol or other drugs. They will impact your mood and will make the stress feel worse when the alcohol wears off.
Keep your perspective, Davis suggested. Remember the holidays are not about things; focus on connections instead of material things. Connect with loved ones.
Keeping your perspective during the holidays means staying focused on the true meaning and importance of the holiday season, avoiding getting caught up in the stress, materialism and pressures that can accompany it. Instead prioritize the positive aspects like spending time with loved ones and appreciating the moment.
Dealing with grief and loss: “Acknowledge your feelings,” he said. “It’s OK to feel sadness and or grief. It’s OK to have mixed emotions.”
Honor the memory of the person you’ve lost: Create new traditions. “Start a new tradition that honors your loved ones. A new tradition could be lighting a candle and sharing stories about a loved one,” he added.
There’s no way to replace the presence of a loved one who has passed away. But one way of coping is to honor their memory rather than mourn their absence. Find meaningful ways to remember your loved one, like creating a scrapbook or making a donation in their name or carrying on a tradition that the departed used.
If holiday celebrations don’t seem right for you at this time, you don’t need to force yourself to attend. Instead, connect with a support group, a therapist, a faith community or friends who understand. Sharing your emotions and feelings can help.
“The Good News Center in Utica offers a grief group run by volunteers,” said Davis. “Seek professional help if your grief becomes overwhelming.
“Remember the holidays may not feel the same and that it is OK to adjust your expectations. Focus on the moment. Focus on activities that bring you joy and help you stay grounded in the moment. It could be a walk in nature, reading a favorite book, watching a favorite movie or going for a car ride.”


By Kimberly Blaker
Are you tired of spending hours, days, or weeks scouring the planet for just the right gift? Only to find yourself giving the usual standby, such as a sweater or bottle of cologne? After a while, doling out the same boring gift feels like giving a worn-out consolation prize.
This year, try one of these gift ideas that'll elicit surprise and enthusiasm for your thoughtfulness.
• Concert tickets. Whether the person on your list is a rock-n-roller or symphony fan, a pair of concert tickets will be a sure pleaser, especially if you can swing the best seats.
• Dinner at a posh restaurant. The old adage goes, the way to a man's heart is through his stomach. Women enjoy gourmet dinners just as much. So give a gift certificate to a top-notch restaurant that your recipient's reluctant to splurge on. It's the perfect way for the person on your list to enjoy a gourmet meal without guilt.
• Golf package. Give a round of golf at an elite course or a weekend
en only? Men who enjoy playing chef will appreciate the tools to create their gourmet dishes. Consider a top-quality butcher block knife set, rotisserie, food processor, blender, or crockpot.
• Sporting event tickets. Whatever your gift recipient's favorite sport, a pair of tickets, particularly to a top rival game, is sure to be a hit.
• Remote car starter. This is an excellent gift for both hot and cold climates. With a remote starter, your recipient can heat or cool their car before stepping out into uncomfortable temperatures.
• Magazine subscription. Whether the person on your list is a sports fan, outdoors person, world traveler, hobbyist, professional, or business owner, there's a magazine out there for every niche.
• Gadgets. A person can never have too many of these. How about a Bluetooth speaker or headphones, multi-device charging valet, night vision binoculars, heated ice scraper,

vintage record stores, antique malls, or online.
• Audiobook subscription. If the person on your list loves to read but just doesn't have time for it, an audio subscription may be the perfect alternative. Your recipient can download books to his or her smartphone or iPod. Then they can listen while working out or on the drive to work.
• Music download subscription. One can never have too much music. Find subscriptions for music downloads at Amazon, Napster, iTunes, eMusic, and Spotify, to name a few.




American Humane Society, or another organization that fits their interest. Most organization memberships include periodicals, among many other benefits.
• A trip or weekend away. This gift could be as simple as a nearby weekend away for rest and relaxation or a week-long adventure to a favorite destination. Watch for travel deals at Travelzoo, Travelocity, Google Flights, Airfairwatchdog, and Kayak.

• Annual nonprofit membership. Make the person on your list a card-carrying member of the National Audubon Society, Earth Policy Institute, Republican National Committee, Democratic National Committee, National Coalition for the Homeless,
• Museum membership. Is the person on your list an art enthusiast or history buff? If so, look for museum memberships in your recipient's nearby metropolitan area. In addition to free entrance, museum memberships typically include extra perks such as entry into special exhibitions, discounts on special events, and periodic newsletters.




By Jolene Cleaver
Is there a nursing and physician shortage across Central New York and the Mohawk Valley?
Hospital system leaders in the region say, “yes.”
But the reasons why are complicated.
According to data by the Health Resources and Services Administration, an agency of the U.S. Department of Health and Human Services, as of Sept. 27, in select Central New York counties based on local populations, Herkimer County needs 4.83 full time primary care workers; Madison County needs 4.82; Oneida County needs 18.58; Oswego County needs 7.35 and Onondaga County needs 17.95.
These data points represent the number of full-time equivalent practitioners needed in the health professional shortage area so that it will achieve the population to practitioner target ratio.
When it comes to medical care shortages, patients are sounding off and some have found their own solutions.
“Finding a good doctor in itself is a huge hurdle and then you find one and don’t like them but you just deal because who wants to go through that process again? … I would say start with your insurance, but even their resource lists aren’t updated,” said one Mohawk Valley woman in a social media post.
However, while data can point to immediate needs, healthcare officials say finding a long-term solution requires more analysis.
“Anecdotally we have heard that the staffing shortages are being felt across the state, but are certainly more significant in some areas [more of the rural areas] than others. Factors that are impacting staffing numbers include the aging and retirement of the nursing workforce,
In an effort to fight shortage of health professionals, hospitals offer sign-on bonus, flexible schedules, onsite training, tuition reimbursement … and more
limited capacities in nursing education pipeline due to lack of clinical placement sites and lack of nursing faculty, the stress on the nursing workforce post COVID causing nurses to leave the profession,” said Jeanine Santelli, executive director of American Nurses Association, New York, in a statement.
The nursing shortage issue is not new.
A December 2023 release by the NYS Nurses Association notes:
“Decades of underfunding and staffing shortages across New York have plunged the state’s healthcare workforce into crisis, requiring healthcare workers to push themselves past the point of exhaustion, working mandatory overtime with skeleton crews. Meanwhile, hospitals throughout the state are having to work with negative or unsustainable operating budgets, incentivizing the further reduction of healthcare workers, exacerbating short staffing, worsening quality of care and further destabilizing the workforce. In New York state, only 53% of actively licensed nurses are actively working as nurses, demonstrating that the state is facing more of a shortage of good healthcare jobs than healthcare workers themselves.”
In recent interviews, hospital leaders spoke to staffing challenges for both the nursing and primary care physicians in their systems.
Charleen Ryan, interim chief nursing officer at the Syracuse-seated St. Joseph’s Health system said in a statement:
“...We are lucky to have St. Joseph’s College of Nursing because it acts as a pipeline for those looking to pursue a degree in nursing. It offers traditional and non traditional programs, tuition assistance, and flexible schedules. Students undergo on-site training and preparation so once they complete their schooling they can immediately join the St. Joseph’s Health team.
“Our talent acquisition team works hard to find creative ways to reach nursing candidates. There are sign-on bonuses and other incentives; team members regularly visit local colleges that graduate nurses; we attend in-person and virtual job fairs and think outside the box as much as possible to reach nursing candidates. We have added to our talent acquisition team and started our own travel nursing program.”
Physician Michael Trevisani, interim chief medical officer, St. Joseph’s Health Hospital, added:
“St. Joseph’s has been committed to providing training for family medicine residents in Central New York for nearly 60 years. We are home to one of the original six family medicine residencies nationally and have a strong retention rate of our graduates to St. Joseph’s and the CNY region. St. Joseph’s also hosts a transitional year residency [for doctors pursuing training in fields such as radiology, dermatology, radiation oncology, etc.], a family medicine-surgical OB fellowship, as well
as a general practice dental residency.
“St. Joseph’s is a clinical training site for dozens of graduate medical education programs across New York state (and beyond) for nurse practitioners, physician assistants, medical students, perfusionists, registered nurse anesthetists, midwives, marriage and family therapists, etc.
“In addition, we engage physician recruitment firms to get the message out and screen for possible applicants. Our outreach program includes advertising in specialty medical journals about the practice opportunities offered at St. Joseph’s Health. At times we also engage staffing firms to contract with physicians for shorter periods of time in particular physician-need areas. Telehealth is also utilized to tap into the expertise of physicians who do not live in our area but are licensed by New York state.”
In the Cooperstown-based Bassett Healthcare Network, there is a nursing and doctor shortage, officials there said.
In a recent interview, Bassett officials talked regional perspective, noting that the reality of medical staff shortages — such as nursing — are often not always what people think.
There, shortages mostly translate to in-patient care nurses.
Compounding the issue is that there are simply not enough nurses, and many seeking an education for nursing are on a waitlist because there are not enough instructors for nursing educational programs.
To the crew at Bassett, getting a nursing degree can open the door for numerous possibilities.
Once someone graduates a nursing program, “Some are going right on to further education or seeking a specialty,” said Melanie Craig, director of nursing at Bassett.
There’s also a split in this issue across the state in how urban nurses and rural nurses are working. Nurses can hop from hospital to hospital in an urban setting. However, in rural communities, they are looking at advancement opportunities, Craig said.
In an example of creating a longterm supply and fostering a growth strategy in local healthcare professionals, work at Bassett Healthcare includes teaming with high schools and foundations to find students who are interested in medicine and foster their path to a career in medicine.
Bassett engages in a practice transition accreditation program (PTAP), which is a yearlong nursing residency program; a pipeline of sorts.
Right now, there are 40-50 graduates of the program every year, which constitutes a drop in enrollment numbers in the wake still rippling from COVID-19. At one time, there would have been double the number of students in any given year.
“Without educators, nursing programs are really paralyzed,” Craig said, pointing out issues that Bassett officials also said include teaching being cost-prohibitive for many instructors.
Also after the pandemic, some questioned whether they wanted to
Continued the next page
remain in the field after apparent burnouts. So, some left and then there were diminishing class sizes. And now, many nurses are seeking spots in the critical care, ICU and dialysis specialties.
In the Bassett network, despite the nursing shortages, the picture is not all gloom and doom and shouldn’t be cause for alarm if there is ever a large-scale health event. Bassett officials point to events such as COVID-19 as proof that when there is a catastrophe, the nursing community steps up.
At the Mohawk Valley Health System in Utica, the picture is very similar. As people live longer, there is an increasing demand for healthcare leading to a “very acute issue in central New York with an aging population and a lack of nursing and doctors,” said Darlene Stromstad, MVHS president.
The picture at Rome Health is similar, and so when it comes to the recruitment and retention of nurses. Rome Health has implemented strategies to prepare and support new nurses as they transition from the classroom to the bedside, according to the hospital.
“At Rome Health, we created the nurse extern program for senior student nurses to foster resiliency and clinical excellence,” said Chief Nursing Officer-VP Clinical Services Ashley Edwards, MSN, RN, NE-BC. “Physical and emotional burnout are lead contributors to newly licensed nurse turnover. Job stress, lack of support, inadequate training, worklife balance and low job satisfaction all contribute to burnout.”
“Retention rates double for new nurses that participate in the extern program,” Edwards said, citing retention rates of 80 to 100 percent since 2021 for externs. “At Rome Health, we are committed to setting people up for success and fostering ongoing professional development throughout their career.”


At Rome Health, student nurses are hired to work as patient care technicians throughout the health care organization and there are tuition reimbursement opportunities for those meeting certain criteria.
“When the student nurse externs begin their senior year of nursing school, they receive an increase in pay and participate in monthly education sessions with the transitions to practice director. This includes communication, delegation and resiliency skills, didactic training and individualized support,” notes a statement.
When it comes to attracting nurses and physicians to the region,

hospital systems are finding themselves doing a bit of promotion of the area above and beyond the job.
Hospital officials say there’s sometimes more to recruitment than educational offerings.
“This part of New York is very beautiful,” MVHS’s Stromstad said. “When you recruit, you spend a lot of time trying to recruit people to the area.”
The recruitment challenge can also be impacted by generational differences.
Stromstad said that younger generations are more open to being fluid and traveling. Nurses from older generations were more prone to stay in a position for decades.
Looking even more broadly, while rural medical physicians are hard to get, Stromstad said, there are medical residencies, but specialties like OB-GYN are hard to recruit doctors for.
In a solution, MVHS began its physician residency program in 1975 and that program continues to grow today. Also helping to create a pipeline of providers is the hospital system’s St. Elizabeth’s College of Nursing. If they stay for three years after graduation, their tuition gets waived.
“We have a lot of travel nurses coming in,” Stromstad said. “We have a stronger staff, but now we are more reliant on travel nurses, which at any point in time, can be about 20% of the nursing staff at the hospital.”
Travel nursing has also become even more commonplace in the years since COVID-19.
The benefit of travel nursing is it is an opportunity to have a broader experience by working in different communities with different needs, as well as elevated pay. Travel nurses typically stay in a location from 13 weeks to a year.
Still, despite the staffing challenges, the hospital systems all reported they are making progress and achieving upward growth for their communities.
New York state healthcare shortage solutions
In addition to hospital systems positioning themselves to grow the next generation of healthcare professionals, the state is also stepping in.
In recent months, New York Gov. Kathy Hochul announced select workforce investment organizations would receive awards totaling up to $646 million over the next three years to implement the career pathways training program, to recruit and train thousands of new health, mental health and social care workers across New York.







Screening for cancer saves lives, but a new report shows it comes with a hefty price tag: The United States spends at least $43 billion annually on tests that check for five major cancers.
Published in August in the Annals of Internal Medicine, the new analysis focused on screenings for breast, cervical, colon, lung and prostate cancers.
Study lead author Michael Halpern, a medical officer in the National Cancer Institute's health care delivery research program, told the New York Times that his team was surprised by the high cost.
And some critics of the country's current amount of screening questioned whether the price tag was justified.
“What are we actually getting of value for that amount of money?” Adewole Adamson, a dermatology researcher at the University of Texas at Austin who studies screening, asked the Times.
“If it was actually doing something I could say, 'Yes, it is justified,'” he said. However, studies have repeatedly failed to show that people live longer if they are screened, he said, and some cancers are just deadly from the start.
“People have an outsized idea of what the benefits are,” Adamson said.
But Karen Knudsen, chief executive of the American Cancer Society, stressed the value of cancer screening is clear.
“We are talking about people's lives,” she said. “Early detection allows a better chance of survival. Full stop. It's the right thing to do for individuals.”
“We screen for cancer because it works,” Knudsen added. “The cost is small compared to the cost of being diagnosed with late-stage disease.”
Still, other experts say the finding, which was based on 2021 data, supports their contentions that screening is overused.
Colonoscopies were a big source of screening costs, accounting for 55 percent of the total.
Physician David Lieberman, a specialist in colon cancer screening from Oregon Health & Science University, told the Times that while the cost of colonoscopies are high, the test can prevent cancer as well as detect it because doctors can slice out growths on the colon wall that can turn into cancers.
While preventive testing against cancer could be carried out more efficiently, advocates for screening maintain it still saves lives.
“Too many people undergo screening who are unlikely to benefit, but many more who could benefit have never been screened or are not screened regularly,” Knudsen said.
She added that “the value of screening is settled science.”
But Gilbert Welch, a senior researcher in the Center for Surgery and Public Health at Brigham and Women's Hospital who wrote an editorial that accompanied the new study, said falling cancer rates can't be chalked up solely to cancer screening.
For example, earlier research from Welch showed the death rate for colon cancer has declined for 40 years, falling by nearly 50 percent from the 1980s — when few were screened — to today, when about 50 percent of eligible adults are screened.
“I'm not saying there is no effect from screening, but it is so small that something else is going on,” Welch told the Times. Instead, better colon cancer treatments and healthier diets among Americans might be fueling the drop, he noted.
We’ve listened to your feedback concerning your preference to do business with us online. You want the option to submit forms, evidence and other information electronically. You also want to sign documents electronically before submitting them.
This year we released eSignature/Upload Documents as an option to submit documents. This new online service option allows our employees to electronically request, and our customers to electronically submit, 50 forms and nearly 80 types of evidence. This option eliminates the need to mail, fax or deliver information to a local Social Security office. By streamlining our document submission process and reducing mail, we are improving the way you do business with us.
How Does it Work?
1. Our employee sends the customer a link with the request for the forms and evidence we need to process their application.
2. The customer authenticates by signing in to, or creating, their personal My Social Security account at www.ssa.gov/myaccount. The customer then reviews the request, completes the form, electronically signs (when signatures are required) and uploads the completed forms and any supporting evidence to our portal.
Customers have 30 days to electronically submit requested information and may receive an email reminder. If the electronic request expires, they can contact our office to ask for a new request or submit the forms and information by mail, fax, or by visiting an office.
To learn more about Upload Documents, visit our FAQ webpage at faq.ssa.gov/en-US/Topic/?id=-
Q.: I worked for the last 10 years, and I now have my 40 credits. Does this mean that I can get the maximum Social Security retirement benefit?
A.: The 40 credits are the minimum number you need to be eligible for retirement benefits. However, we do not base your benefit amount on those credits, but on your earnings over a lifetime of work. To learn more about how you earn Social Security credits and how they work, read, or listen to our publication How You Earn Credits, available at www.ssa. gov/pubs/EN-05-10072.pdf.
In addition to the eSignature/ Upload Documents option, we are converting many of our frequently used forms to more convenient online versions. Customers will have the option to complete a user-friendly, fillable online form, then electronically sign and submit it.
Some of our frequently used forms now available to sign and submit electronically include:
• SSA-827, Authorization to Disclose Information to Social Security Administration.
• SSA-820/821, Work Activity Reports.
• SSA-632, Request for a Waiver of Overpayment Recovery.
• SSA-634, Request for Change in Overpayment Recovery Rate.
We have removed the signature requirement for 12 of our most used forms. These forms include:
• SSA-L4201, Employer Requesting Wage Information.
• SSA-789, Request for Reconsideration/Disability Cessation Right to Appear.
• SSA-787, Statement of Patient’s Capability to Manage Benefits.
To learn more about the removal of signature requirements from certain Social Security forms, check out our YouTube video Signature Removal from SSA Forms at www.youtube. com/watch?v=vmben-skPo4&t=2s.
Whether you do business with us online, by phone, or in person, we’re committed to making it easier for you. We continue to explore more opportunities to make doing business with us easier. Please share this information with others.
Q.: Will my Social Security disability benefit increase if my condition gets worse or I develop additional health problems?
A.: No. We do not base your Social Security benefit amount on the severity of your disability. The amount you are paid is based on your average lifetime earnings before your disability began. If you go back to work after getting disability benefits, you may be able to get a higher benefit based on those earnings. In addition, we have incentives that allow you to work temporarily without losing your disability benefits. For more information about disability benefits, read our publications “Disability Benefits and Working While Disabled — How We Can Help.” Both are available online at www.ssa. gov/pubs.
By Jim Miller
Dear Savvy Senior,
Can a person in their early fifties have osteoporosis? When I fell and broke my wrist last winter the doctor that treated me told me I might have osteoporosis.
Surprised Susan
Dear Susan,
While osteoporosis is much more common in adults over age 60, it can strike younger people too. In fact, according to the Bone Health & Osteoporosis Foundation, half of women and up to 25 percent of men in the U.S. over age 50 will break a bone due to osteoporosis.
According to the Bone Health & Osteoporosis Foundation, all women over 65 and men over 70 should have a baseline dual energy X-ray absorptiometry (DXA) scan, which is a painless measurement of the calcium in your bones. But those at high risk should start around age 50. Factors that make a good case for early screening include having a family history of osteoporosis, a broken bone after age 50, vitamin D deficiency, a smoking habit, medical conditions such as diabetes or rheumatoid arthritis or previous or current use of medications that can weaken bones, like steroid prednisone and certain antidepressants.
checked to see if you need a supplement.
• Exercise: Low impact weight-bearing exercises like walking, and strength training with light weights or resistant bands several times a week can actually help build bone strength, as well as improve balance and muscle strength.
• Don’t smoke: Women who smoke a pack of cigarettes per day as adults have less dense bones at menopause.


osteopenia (lower than normal bone density) — 80 percent of whom are women.
Most bone density tests are covered by health insurance companies including Medicare, and are done in hospital radiology departments, private radiology practices and standalone clinics.
If, however, your bone density test finds that you have osteoporosis your doctor will probably recommend medications. The first line of treatment is usually bisphosphonates such as alendronate (Binosto and Fosamax), risedronate (Actonel and Atelvia), and ibandronate (Boniva). These oral or injectable drugs slow the breakdown of bone but won’t build it back.
Here’s what you should know.
Most people, by the time they reach their late 30’s, gradually start losing some of their bone mass, but for women, the biggest decline happens in the five to seven years following menopause, when levels of estrogen, which helps to keep bone strong, plummets. Bone loss for men occurs much more gradually. How-
If your bone scan finds that you have osteopenia but have a low to moderate 10-year fracture risk, lifestyle measures are usually the best course of action. Three important things you can do to boost your bone health include:
• Get enough calcium and vitamin D: Calcium helps keep bones strong, and vitamin D helps us absorb calcium. Women older than 50 and men over 70 need at least 1,200 mg of calcium per day ideally from foods like dairy, canned sardines, kale and fortified orange juice. Adults over 50 need 870 to 1,000 IU of vitamin D each day, but that’s hard to get from food. Have your levels
For severe osteoporosis your doctor may instead prescribe an anabolic: teriparatide (Forteo), abaloparatide (Tymlos), or romosozumab (Evenity). These are typically given as daily or monthly injections and they increase the amount and strength of bones.



A new 21,000 square foot Cancer Center and Community Wellness Center is now open in Camillus at 5490 Cobbler Way! This modern, spacious new office replaces our Onondaga Hill location and Camillus Community Wellness Center – and offers a comprehensive range of services under one roof, with plenty of free parking. Use the QR code to learn more and see the services at our new Camillus location!


By Barbara Pierce
Tis the season to get sick. Colds, flu and respiratory illnesses will be at their peak this winter. We’re traveling more, spending more time with others, inside more. All these mean viruses pass more easily from one person to another. Babies, older folks and those with compromised immune systems are especially susceptible.
William McCue, regional chief of primary care, Bassett Healthcare Network, suggests tips to prevent some of the most common illnesses common during the holiday season. Outsmart germs with these simple strategies:

1. Wash your hands frequently: “The simplest of things are the most effective,” said McCue. “That’s the case with all these illnesses. The simplest thing to do is hand-washing.”
Colds are typically infections of the nose and throat, caused by more than 200 different respiratory viruses. Colds are highly contagious.
Hand-washing is the easiest way to prevent the spread of cold germs. If soap and water aren’t available, use an alcohol-based hand sanitizer. Avoid touching commonly touched surfaces, including pens, pencils, public doorknobs and light switches, grocery carts, etc. unless necessary. If others use your work station, wipe down your keyboard, phone and mouse after them. Germs can be transmitted by spray from coughs and sneezes.
Avoid touching your eyes, nose and mouth with unwashed hands. Viruses live on your hands and easily enter your body this way.
Though there’s no cure for a cold, rest and keeping hydrated will help you feel better. Most colds reach the peak of their severity between three to five days. Over-the-counter
medicines can ease your symptoms. Always ask your doctor or pharmacist before starting a new medication, including OTC medications. Not all medications are safe to take. Always read the label and use medications only as directed. Antibiotics are not useful to treat a cold.
2. Get a flu shot: “A flu shot is the most important thing I do for the people I treat,” said McCue.
It works by caus ing the body to develop antibodies that provide protection against the flu.
as your immune system is more sluggish,” said McCue. “If you’re over 50 and have a risk factor like diabetes, COPD, congestive heart failure, get vaccinated.”
“Treatment for COVID works extremely well,” he added. “Start treatment within the first five days to reduce illness. Most pneumonia are bacterial. Therefore, getting vaccinated is important.”

CDC recommends that everyone six months and older get a flu vaccine every year to reduce the risk of getting the flu and its complications. As well as reducing the risk that you’ll get the flu, the shot decreases the risk of serious illness, hospitalization and death from the flu.
The flu is a viral infection of the nose, throat and lungs. Often mistaken for a cold, flu tends to present quickly and severely. Coughing, sore throat, headaches, body aches and high fever are common flu symptoms. OTC fever reducing medication helps.
“Tamiflu helps to reduce the length and severity of the flu,” added McCue.
Tamiflu is a prescription medication.
3. Get vaccinated: “Get vaccinated for COVID and pneumonia if needed,” advised McCue.

The pandemic may be over, but we’ve still got COVID worry about. New variants of the disease continue to pop up.
“If you’re over 70, It’s highly recommended that you get vaccinated
RSV (respiratory syncytial virus) is a risk for older adults and infants younger than 12 months. RSV is a common virus that usually causes mild, cold-like symptoms, including nasal congestion, cough, fever, wheezing and dehydration. It can last one to two weeks and has the potential to become serious.
“Pregnant women should get vaccinated for RSV at 36 weeks to protect the infant,” advised McCue.
Norovirus, also known as stomach flu, is extremely contagious and rages during the winter, leading to severe vomiting and diarrhea.
“There’s no vaccine or treatment,” said McCue. “Push fluids with electrolytes and eat a bland diet.”
(Fluids with electrolytes: Gatorade, Pedialyte, etc.; bland foods include foods that are easy to digest — eggs, broth, pudding, cream of wheat, tofu, lean meat.)
Symptoms tend to last only one to three days. If anyone in your family has this bug, avoid contact as much as possible and wash your hands frequently.
4. Other preventive actions: “Get adequate sleep, eat healthy and stay active,” suggested McCue. “Cardio activities help boost our immune system.”
Tired, run-down people are more susceptible germs. Drink

plenty of fluids.
5. When to see your health care professional: While most of these illnesses will run their course without intervention, see a professional if your symptoms worsen. Monitor your temperature if you’re getting sick. For adults, a high fever is one that is above 100.5 degrees. “See your health care professional if you have fever for a week,” suggested McCue. Contact your health care professional if you have difficulty breathing; a cough that gets worse while other cold symptoms improve; or flare-up of any chronic lung condi-


If your child is younger than 3 months old and has a fever of 100.4 °F or higher, call your health care professional right away.
We’re in your corner in the fight against breast cancer.
“Being able to take away a breast cancer patient’s financial stress is huge.”
As someone who deals directly with breast cancer patients – and as a cancer survivor herself – AnnMarie Gianno, from CancerConnects, has seen first-hand the positive impact Saint Agatha Foundation’s support has on CNY breast cancer patients. By helping with unmet financial needs – like transportation costs, co-pays, specialized garments, and much more – the CancerConnects/ Saint Agatha Foundation partnership helps alleviate financial strains for those already fighting a breast cancer diagnosis. If your medical or non-medical organization would like to provide financial support to CNY breast cancer patients, too – visit s saintagathafoundation org/ for-providers to learn more and watch an interview with AnnMarie. New provider partners are always welcome!
saintagathafoundation.org

AnnMarie Gianno Patient Program Coordinator, CancerConnects




Excellus BlueCross to improving maternal health outcomes. Through investments in local nonprofits and creating our Bright Beginnings program, we’re supporting expecting parents in our communities. reduce racial disparities in maternal health visit ExcellusBCBS.com