

Advanced Care Planning
Wendy Thomas, RN, MSN, CHPN
Palliative Care Nurse Specialist, Kansas University Medical Center
KC Area Support Group Leader
Advance Care Planning

Wendy Thomas, RN, MSN, CHPN

Wendy Thomas, RN MSN CHPN
• Outpatient Palliative Care
Nurse Navigator
• Kansas City Area Myeloma
Support Group Leader
About me:
• Nurse 27 years
• 14 years in blood and marrow transplant
• 8 years in palliative care
• 10 years as a myeloma support group leader
• Worked for the University of Kansas Health System for 17 years
• Based at the Bloch Cancer Care Pavilion, Westwood Kansas
Advance Care Planning
What is Advance Care Planning?
• Discussing and preparing for future medical care decisions
• Important at any stage of life
• Crucial for anyone with a serious illness
• Goes into effect ONLY when you are unable to speak for yourself

Do you have an Advance Directive?

• Who would you want to speak for you if you were unable to speak for yourself?
• Do your family/loved ones know what your wishes would be in a healthcare emergency?
• Do you know what your wishes would be?
• Are you confident they could carry out your wishes?
Advance Care Planning
DPOA & Healthcare Directive
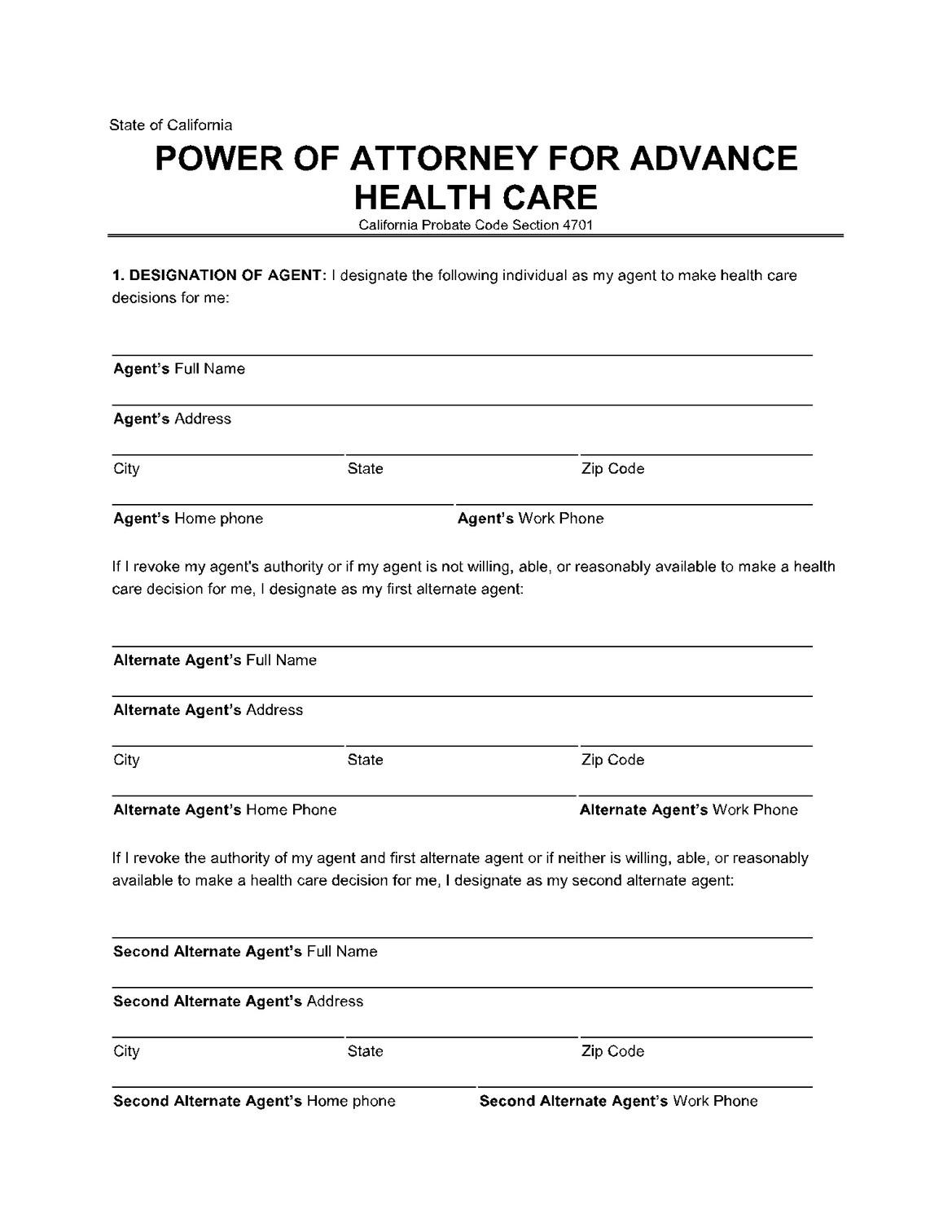

CA requires notary or two adult witnesses to signature
What are your wishes?

Code Status
• What is a Code Status?
• Cardiopulmonary Resuscitation or CPR
• Why do they keep asking?
• Code status expires at discharge
• Out of hospital DNR
• Living will
• How aggressive do you want care to be?
• ICU
• Mechanical Ventilation
• Medically administered nutrition
Deciding about CPR
CPR
• No pulse, not breathing
• One of the few treatments that patients must choose to NOT have performed
• A physician order is REQUIRED to NOT perform CPR
• Older people and people with cancer may have survival & quality of life after CPR
• You can CHOOSE to allow a NATURAL death if you prefer

Level of Medical Interventions?

Pulse present &/or still breathing
• Full treatment – most aggressive ICU and intubation with mechanical ventilation
• Midlevel treatment – less aggressive Antibiotics, fluids, medication to support blood pressure, transfusions
• Best supportive care – least aggressive Treat with dignity and respect, comfortfocused medical treatment
• DNR doesn’t equal non-aggressive care
Out of hospital DNR
• Patients should complete with your healthcare provider
• Requires healthcare provider signature
• Original form stays with patient
• Copy should be provided to all of your healthcare providers/health systems
• Some states have transportable DNR laws

POLST

• Physician Orders for Life-Sustaining Treatment
• Provides more control over endof-life care to seriously-ill patients
What to do with Forms & Documents?

• Make certain your family/loved ones know the location
• Give a copy to your healthcare providers/health systems
• Easy to find in case of emergency
• These documents DO NOT belong in your safe deposit box
• Fridge and beside table good locaitons
Other Practical issues
Planning ahead
• Eases the burden for family/loved ones
• Protects your assets
• Allows you to manage your personal effects

Finances
• Bank Accounts
• Bill Pay

• Property Cell Phone
• Access
• Contacts
New Complications
• The electronic era brings new challenges
• Cellphones, computers, online accounts, social media and photos

• Photos Passwords
• Account Log-in
• Social Media
• EVERYTHING!

The Most Important Part

Talking with your loved ones about your healthcare wishes brings comfort
prepareforyourcare.org

National Healthcare Decision Day: April 16th

• Go Wish Cards
• ACP Bubble Map
• Coalition for Compassionate Care of CA
• Social Worker
