

Shared Decision Making
Teresa Miceli, RN, BSN, OCN
International Myeloma Foundation InfoLine Advisor & Nurse Leadership Board; Mayo Clinic-Rochester
Shared Decision Making: Be An Active
Member
Of Your Health Care Team
Teresa Miceli, RN BSN OCN
International Myeloma Foundation - InfoLine Advisor, NLB Member, Support Group Leader (MMSS, Smolder Bolder)
Mayo Clinic – Myeloma Nurse Navigator
National Cancer Institute - Myeloma Patient Advocate


Goals
• Review Share Decision Making (SDM) Concepts
• Identify Influencing Factors To Treatment Decision Making
• Discuss Strategies To Enhance Patient Empowerment & Promote Shared Decision Making

Individual Beliefs & Preferences
Transplant
Eligible Patients
Individual Care Partner
Family
Initial Therapy
A Person With `

Treating Myeloma
Transplant (ASCT) Maintenance
Transplant
Ineligible Patients
Everyone
Social Network & Obligations
Treatment of Relapsed disease
Consolidation / Maintenance Continued therapy
Myeloma Symptoms & Treatment
Options
Supportive Care
Employme nt & Finances
the clinical-trial setting: understanding the balance between efficacy, safety and tolerability, and quality

Terpos E, Mikhael J, Hajek R, Chari A, Zweegman S, Lee HC, Mateos MV, Larocca A, Ramasamy K, Kaiser M, Cook G, Weisel KC, Costello CL, Elliott J, Palumbo A, Usmani SZ. Management of patients with multiple myeloma beyond
SDM: Patient-Centered Care
“The aim of shared decisionmaking is to ensure that:
- Patients understand their options and the pros and cons of those options.
- Patient's goals and treatment preferences are used to guide decisions.”

https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/c ommunication/strategy6i-shared-decisionmaking.html#6i1

Steps in Shared Decision-Making


Identify that a decision is needed: The HCP informs the patient that a decision is to be made and that the patient's opinion is important (Choice talk).
Understand the options:
The HCP explains the evidence-based options and their pros and cons. The patient expresses their preferences, and the HCP supports the patient in decision-making (Option talk). Come to a decision:
The HCP and patient discuss the patient's wish to take part in the decision making and incorporate the patient's values and preferences into the decision (Decision talk
Follow-up: Review and evaluate the decision, adjust as needed

Advantages to Partaking in SDM

Patients, regardless of age, want to be a part of treatment decision-making
Requires staying informed
Reduces uncertainty and alleviates concerns
Decisions reflect personal and family values
Promotes patient and care partner engagement and sense of empowerment
Positive impact on QOL and continuation on therapy

“The 'efficacy' of treatment means different things to different patients, and treatment decision-making in the context of personalized medicine must be guided by an individual's composite definition of what constitutes the best treatment choice.” Terpos, et al. Terpos, et al. 2021
https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/ 6-strategies-for-improving/communication/strategy6i-shared-decision making.html#6i1


Influencing Factors to Treatment DecisionMaking
• Disease-derived
• Time: Stage, risk stratification, Urgent intervention needed vs time to consider options
• Treatment: Availability/access, effectiveness, toxicity, current research
Choon-Quinones, Mimi, Hose D, Kaló Z, Zelei T, Harousseau JL, Durie B, Keown P, Barnett M, Jakab I. Patient and Caregiver Experience Decision Factors in Treatment Decision Making: Results of a Systematic Literature Review of Multiple Myeloma Decision Aids. Value Health. 2023 Jan;26(1):39-49. doi: 10.1016/j.jval.2022.04.003. Epub 2022 May 22. PMID: 35613958.
Patient-derived
Provider-derived
Time limitations
Support for patient involvement
Provider bias and preference
Understanding complex treatment options
Physical and emotional wellness
Comfort in speaking up “Doctor knows best”
Financial, Cultural and Religious factors
Care partner & social network, transportation
https://www.valueinhealthjournal.com/action/showFullTableHTML?isHtml=true&tableId=tbl4&pii=S1098-3015 %2822%2900198-X
https://www.ahrq.gov/sites/def ault/files/wysiwyg/cahps/qualit y-improvement/improvement-g uide/6-strategies-for-improving /communication/cahps-strateg y-section-6-i.pdf


















Strategies for Patient Empowerment

Consider your priorities
Consider your goals/values/preferences
Include your care partner/network in the discussion
Be a part of the conversation, create a dialog
Ask questions & Express your goals/values/preferences
Ask for time to consider options, if needed
Arrive at a treatment decision together
Arrange follow up to review and adjust the plan, if needed




Strategies for Patient Empowerment

Know the members of your care teamUnderstand their different roles
Myeloma specialist and General Heme/Onc
Primary care: for health screening, general check ups, vaccinations
Sub-specialists: specialty needs
Keep a contact list of your providers

Care Provider (PCP)


Subspecialists



Health Staff


Allied
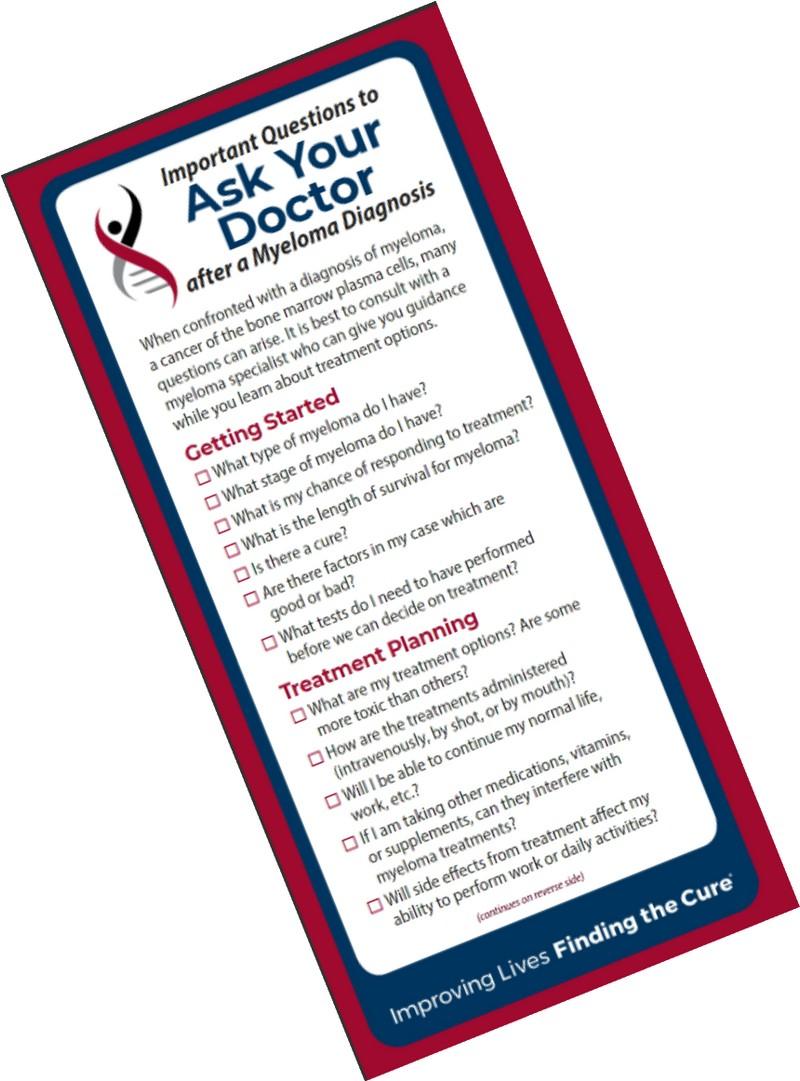
Strategies: Prepare For Medical Visits
Prepare
Medications: Bring a current list of prescribed and over-thecounter
Questions: Prioritize questions & concerns including financial issues
Paperwork needing medical signature (ex FMLA, prior authorizations)
Inform
Updates: Medical or life changes since your last visit
Symptoms: How have they changed (improved, worsened, stable)? Keep a symptom diary. Bring it along
Communicate effectively so your health care team can help
Follow Up
“Next Steps”: Future appointments, medication changes, plan of care. Ask for the information in writing or on your patient portal
Include a care partner, especially for pivotal appointments

Consider Telemedicine
Strategies: Prepare For Tele-Med Visits
Check with your healthcare team –
Is telemedicine an option?
What is the process and what technology is needed?
Are labs needed in advance? Do you need an order?
Preparation is similar for “in-person” appointment PLUS:
Location: quiet, well-lit location with strong Wi-Fi is best
Yourself: Do you need to show a body part - wear accessible clothing
Vital signs (blood pressure, temp, heart rate, weight) selfserve blood pressure cuff is available at many pharmacies and for purchase
Include a care partner, especially for pivotal appointments

Create a Care Network
Myeloma causes the highest burden of symptoms, most commonly effecting people of older age with other medical issues. Care partner support is valuable in SDM
Care partners assist in many ways
Attending medical appointments, being present to learn and discuss possible treatment options and alert the medical team of side effects to treatment
Some treatment options available only if care partner support exists
Care partners can be one person or a rotation of many people
Building a partnership is based in good communication
Finding the balance:

- helping the patient with needed activities while maintaining a sense of independence
- allowing the care partner to have time for good self-care
Care Partner Tip Card https://www.myeloma.org/resource-library/tip-cardcare-partners
Terpos, et al. 2021; Soong, et al., 2023
Credit: https://www.mmtoldtrue.com/community/care-partner-corner




Key
Take-Aways - Think About It ….
Over the next two days:
Evaluate where you are at in the process (What decisions need to be made?)
Absorb the information being presented (What are the options?)
Consider how the information impacts you and your family (What are your preferences?)
Create questions that will lead to better understanding (What more do I need to know before making a decision?)
Become an active member of your health care team
Share Decision Making

Resource List
Bylund CL, Eggly S, LeBlanc TW, Kurtin S, Gandee M, Medhekar R, Fu A, Khurana M, Delaney K, Divita A, McNamara M, Baile WF. Survey of patients and physicians on shared decision-making in treatment selection in relapsed/refractory multiple myeloma. Transl Behav Med. 2023 Apr 15;13(4):255-267. doi: 10.1093/tbm/ibac099. PMID: 36688466.
Chari A, Romanus D, DasMahapatra P, Hoole M, Lowe M, Curran C, Campbell S, Bell JA. Patient-Reported Factors in Treatment Satisfaction in Patients with Relapsed/Refractory Multiple Myeloma (RRMM). Oncologist. 2019 Nov;24(11):1479-1487. doi: 10.1634/theoncologist.2018-0724. Epub 2019 Aug 1. PMID: 31371520; PMCID: PMC6853123.
Choon-Quinones, Mimi, Hose D, Kaló Z, Zelei T, Harousseau JL, Durie B, Keown P, Barnett M, Jakab I. Patient and Caregiver Experience Decision Factors in Treatment Decision Making: Results of a Systematic Literature Review of Multiple Myeloma Decision Aids. Value Health. 2023 Jan;26(1):39-49. doi: 10.1016/j.jval.2022.04.003. Epub 2022 May 22. PMID: 35613958.
Rifkin RM, Bell JA, DasMahapatra P, Hoole M, Lowe M, Curran C, Campbell S, Hou P, Romanus D. Treatment Satisfaction and Burden of Illness in Patients with Newly Diagnosed Multiple Myeloma. Pharmacoecon Open. 2020 Sep;4(3):473-483. doi: 10.1007/s41669-019-00184-9. PMID: 31605300; PMCID: PMC7426337.
3718 Cytokine Release Syndrome: The Patient, Caregiver and Healthcare Professional Experience. Janelle Soong, Giuseppe De Carlo, Naziah Lasi-Tejani, Sumanjit K. Sethi, Natacha Bolaños, Martine Elias, Yelak Biru, Solène Clavreul, G. Scott Chandler, Klaus Finzler, Yann Nouet, Antonio Giuseppe Del Santo. Blood (2023) 142 (Supplement 1): 3718
Terpos E, Mikhael J, Hajek R, Chari A, Zweegman S, Lee HC, Mateos MV, Larocca A, Ramasamy K, Kaiser M, Cook G, Weisel KC, Costello CL, Elliott J, Palumbo A, Usmani SZ. Management of patients with multiple myeloma beyond the clinical-trial setting: understanding the balance between efficacy, safety and tolerability, and quality of life. Blood Cancer J. 2021 Feb 18;11(2):40. doi: 10.1038/s41408-021-00432-4. PMID: 33602913; PMCID: PMC7891472.
https://www.ahrq.gov/health-literacy/professional-training/shared-decision/index.html
https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/communication/strategy6i-shared-decisionmaking.html #6i1

