Election time

Dan Hayes, chief executive of Order of St John’s Care Trust, the UK’s most historic care provider, details his ‘asks’ from the next government as polling day looms Opinion: Nadra Ahmed gives her take on the upcoming General Election
Politics & policy: CQC’s Ian Trenholm breaks down the Single Assessment Framework so far Care Managers Show: Everything you need to know about the show’s return to Birmingham this June
06/2024 June Edition caring-times.co.uk








Outstanding stain removal and cleaning on the toughest professional stains
Contains specific whiteness technologies which keeps your whites, white for longer
Great cleaning results even without pre-washing or pre-soaking to help you save water and energy
Gentle to sensitive skin, hypoallergenic and dermatologically tested
Contains specific softness technologies that protect the fibers from damage to help extend linen life Makes linen easier to iron

*85% of the ingredients contributing to Lenor’s softness are plant-based. **Stain removal tested among professional detergents. Safe, simple,
key
an exceptional clean
Visit our P&G Professional website to discover more. Lenor
Enhancer Senstitive 3.8L Ariel
Regular 4.05L
effective professional cleaning solutions to meet your
business needs and help deliver
for your customers.
Professional Fabric
Professional Liquid Detergent
Designed
extra softness to
laundry No.1 for professional cleaning even at 30°C** ODY BLE TES TED D E RMATO L OGICA L L Y ODY BLE
to bring
your


10 LEADER'S SPOTLIGHT
In the hotseat this month is Dan Hayes, chief executive of Order of St John’s Care Trust

14 POLITICS & POLICY
The Single Assessment Framework so far, with Ian Trenholm (CQC) and Nikki Walker (QCS)
8 OPINION
Nadra Ahmed gives the National Care Association’s take on the upcoming General Election

16 SURVEYS & DATA
The UK has seen a 76% decline in visa applications from health and care workers
business
Chief executive officer
Alex Dampier
Chief operating officer
Sarah Hyman
Chief marketing officer
Julia Payne
Editor-in-chief
Sam Lewis
Features editor Charlotte Goddard
Subeditor Charles Wheeldon
Advertising & event sales director
Caroline Bowern
0797 4643292
caroline.bowern@nexusgroup.co.uk
Business development director
Mike Griffin
Business development executive
Kirsty Parks
Event manager
Conor Diggin
Marketing content manager
Sophie Davies
Publisher Harry Hyman
Investor Publishing Ltd, 3rd Floor, 10 Rose and Crown Yard, King Street, London, SW1Y 6RE
Tel: 020 7104 2000
Website: caring-times.co.uk
Caring Times is published 10 times a year by Investor Publishing Ltd. ISSN 0953-4873
© Investor Publishing Limited 2023
The views expressed in Caring Times are not necessarily those of the editor or publishers.
Caring Times™ and the CT® logo are registered trademarks of Nexus Media Group
@Caring_Times

Hit the ground running
Hello! If you hadn’t already noticed, I’m not Lee Peart!
Yes, this marks my first issue as editor of Caring Times, and it’s an honour to have been entrusted with such an esteemed and long-running title, and a pleasure to be able to continue my work with you, the good people of social care.
But there’s no time for sentimentality, because no sooner did I join than Rishi Sunak made the announcement that the UK General Election would be taking place on 4 July. (It never rains but it pours, right?)
Nevertheless, after months of speculation, I couldn’t be happier to finally have an election date on the horizon. The outcome might feel like a formality, but that doesn’t mean any of us knows what the post-election landscape is going to look like, especially for care. My gut feeling is that Labour knows it’s a hot-button topic, and with the Lib Dems and Greens making it a pivotal part of their campaigns, Labour will be under pressure to deliver. However, we’ve been here before: Boris Johnson famously promised to “fix” social care, and on his departure from Downing Street claimed to have succeeded, much to the outrage of most. So, how do we know Labour won’t pull a similar stunt?
Well, we don’t. That’s the scary part. But that doesn’t mean it’s out of our
Our round-up of last month’s big stories 8
Nadra Ahmed is in the hotseat in this month’s opinion pages 10 LEADER'S
SPOTLIGHT
Charlotte Goddard sits down with OSJCT’s Dan Hayes 14
Ian Trenholm and Nikki Walker review the Single Assessment Framework
Health and Care Worker visa applications
plummeting
control. The sector has been shouting about the need for reform and more funding for years, and – with an election incoming and the parties no doubt working on their manifestos as I write –now is the time to redouble our efforts and shout louder than ever. We know that the quality of life of our most vulnerable individuals relies on the victorious party taking the social care crisis seriously; now it’s time to make sure they understand that too.
I can’t predict what will happen, but I do feel like it’s going to be a rocky ride, so strap in and get ready. I look forward to bringing you all the biggest news, interviews and more over the coming months and years, and continuing my work with friends old and new in the care sector.
(To get in touch with news, pitches, queries or just to say hello, email me at sam.lewis@nexusgroup.co.uk.)
Sam Lewis, Editor-in-chief Caring Times

With CareTech and Hartford Care
We round up last month’s big deals
The major people moves from the last month
&
With Mills & Reeve
business | welcome 4 | JUNE 2024 CARING-TIMES.CO.UK
linkedin.com/company/caring-times business contents 6 NEWS IN BRIEF
OPINION
POLITICS & POLICY
SURVEYS & DATA
16
18 SUSTAINABILITY MATTERS
20 PROPERTY
& DEVELOPMENT
24 PEOPLE MOVES
LEGAL
REGULATORY
26

News in brief
POLICY & POLITICS
More than £9.2 million is being given to third-sector organisations in Scotland over the next three years to provide independent support, information, advice and advocacy to people using social care and their carers. The Support in the Right Direction fund (2024-27) is managed by Inspiring Scotland and will support the delivery of the Scottish government’s Self-Directed Support Improvement Plan 2023-27 by empowering people to have choice and control over their social care support. A call for evidence has been launched by the government to capture and consider views about how the duty of candour system is honoured, monitored and enforced in health and social care settings. The review was launched amid concerns there is some inconsistency in how the system is being applied with it having been in place for a decade. Minister for mental health and women’s health strategy, Maria Caulfield, said: “I spent 20 years working as a nurse in the NHS, and I know how important it is that health and care providers are open with patients and their loved ones –especially if something has gone wrong. I want to ensure that our system of duty of candour is kept up to date, so I urge anyone with views or experience to respond to the call for evidence to help inform our review, which will ensure that honesty and integrity remain at the heart of our health and social care services.”


LEGAL & REGULATORY
An Ombudsman investigation has found evidence a company failed to provide adequately trained live-in carers. Promedica24 was asked to pay £550 and ensure its carers met the needs of service users following a complaint about its live-in care in Lancashire between April and November 2022. The Ombudsman said Promedica24 had acknowledged some of its care was below an acceptable standard and appeared to accept some workers didn’t have sufficient training or experience to meet service users’ needs, including their dietary requirements. The complainant terminated his contract on the ground of unsatisfactory service and has refused to pay a termination fee of almost £4,000.
New guidance has been published by the Information Commissioner’s Officer to improve health and social care transparency. The guidance by the UK data protection regulator is designed to help organisations understand the definition of, and assess appropriate levels of, transparency. It also provides practical steps to developing effective transparency information.
An Aberdeen care worker was given a six months’ suspension order for poking a resident on the shoulder and twisting their finger. A Scottish Social Services Council issued the sanction to Gabriel David who was as care assistant at Caring Homes when the incident took place in June last year. A care home resident told the panel that David had poked them on the shoulder
three or four times after they had made a joke about him not responding when they asked for assistance. The resident said David then pointed a finger in their face. He then grabbed the resident’s finger and twisted it.
PROVIDER NEWS
Thousands of care services are expected to open their doors for this year’s Care Home Open Week, taking place from 24 to 30 June. A launch event in London will include a visit from social care minister Helen Whately. Events will take place across the country during the week with Friday 28 June branded MP Engagement Day. Last year’s Care Home Open Week saw around a third of care homes register to take part, with more than 150 MPs visiting a home. Event organiser Championing Social Care anticipates another successful campaign of public engagement.
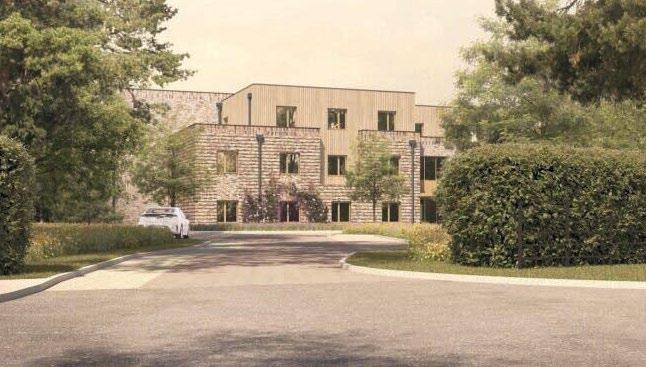
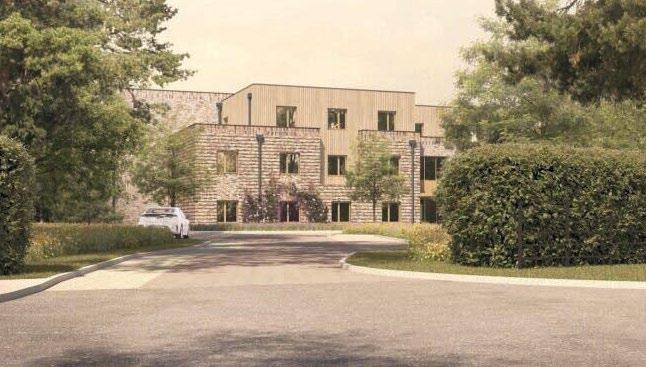
Oyster Care Homes hosted a topping out ceremony for Somer Valley House in Midsomer Norton, Somerset, a 66-bed care home scheduled to open in October. Somer Valley House is equipped with solar panels, a battery store capable of holding two days’ energy, and ground-source heating. The topping out ceremony marked the completion of the roofing stage, paving the way for the next phases of construction. It was attended by Dan Norris, mayor of the West of England. Ideal Carehomes has topped out its newest eco-friendly care home in Cheltenham as the building prepares to open in September in what will be the provider’s 37th home. A solar
business | news 6 | JUNE 2024 CARING-TIMES.CO.UK
Maria Caulfield
Preparing for Care Home Open Week

panel was added to the home’s roof in a ceremonial topping out to mark the next stage of construction. The Energy Performance Certificate A-rated care
home has been built to be energy efficient and environmentally friendly. Ground source heat pump technology allows the home to operate as a carbonfree green home running without the use of gas.
FUNDRAISING
Avnish Goyal, chair of Hallmark Luxury Care Homes, abseiled down the Empire State Building as part of a fundraising event in early May. Goyal, who also founded charities the Hallmark Foundation and the Goyal Foundation, was one of 20 fundraisers to take part in the Big Rappel event which is raising funds for education and charitable network Outward Bound. The group, which included actor and musician Jared Leto, abseiled nearly 900 feet from the building’s iconic spire down to the 30th floor.
Supporting care home operators in the UK
• Dedicated healthcare specialist relationship manager to provide tailored expertise
• Commercial mortgages for first-time buyers up to £5 million, and experienced elderly care/
learning disability care home operators up to £10 million
The event was supported by Outward Bound trustee Princess Beatrice, and donations so far exceed £2.4 million.









news | business CARING-TIMES.CO.UK JUNE 2024 | 7
Speak with our dedicated healthcare specialist: hello@allica.bank allica.bank/info/find-your-relationship-manager Allica Bank Limited is authorised by the Prudential Regulation Authority and regulated by the Financial Conduct Authority and the Prudential Regulation Authority (FRN: 821851). Registered office at 4th Floor, 164 Bishopsgate, London EC2M 4LX. Incorporated under the laws of England and Wales with company number 7706156. Copyright © Allica Bank Limited. All rights reserved. 0330 094 3333 Allica Bank Limited is authorised by the Prudential Regulation Authority and regulated by the Financial Conduct Authority and the Prudential Regulation Authority (FRN: 821851). Registered office: 4th Floor, 164 Bishopsgate, London EC2M 4LX. Registered in England and Wales with company number 07706156. © 2024 Allica Bank Limited. All rights reserved.
specialist
Topping out at Somer Valley House
Avnish Goyal at the top of the Empire State Building
Under pressure
Nadra Ahmed, executive co-chairman of the National Care Association (NCA), paints a picture of a sector that has grown used to being under immense pressure, a sector that needs actions, not words, from the next government
Having worked in the world of social care for over four decades I have been on the receiving end of the pressures of being a provider, which far outweigh the role of a sector representative. At no time during this period have a I felt completely comfortable in the knowledge that social care is valued for the enormous contribution that it makes in the lives of those who need it.
The importance of social care for those who use it continues to grow, while in the political area, where decisions need to be made, it remains firmly in the toodifficult-to-solve pile. Despite promises from every prime minister since Tony Blair, standing on the steps of Downing Street telling the country that they have the solution for social care, they have all left office without making any sustainable difference.
We seldom hear about the contribution social care makes to the wellbeing of people when they face unexpected or critical challenges, or the support it gives to families and friends at times of despair. Sadly, these things are not often highlighted because a
“Despite promises from every prime minister since Tony Blair, standing on the steps of Downing Street telling the country that they have the solution for social care, they have all left office without making any sustainable difference.”
poor portrayal of care is what interests journalists and sells papers. We know there are sympathetic politicians and journalists, but the impact they can make is often negligible. No one person stands out in my mind who has consistently championed the role of social care while in office: notably, when they are in a position to do something tangible, amnesia sets in.
It is always frustrating, for those working in social care, to be constantly portrayed as unscrupulous employers ‘deliberately’ paying poorly to ensure huge profits. The reality is that over 82% of providers are classed as small and medium-sized enterprises (SME) and will be working in their business in some capacity. SMEs are often familyrun services with substantial borrowings, which means that they will be affected by every rise in interest rates, utility bills or cost of living. A substantial number of these services will have local authority contracts which means that they are systematically underfunded and so subsidising the state. Their business models will be complex, and any resilience will be tested in the current climate.
We must never forget that the role of social care is an ever-evolving one and has historic roots. Definitions have changed in modern days, but the ethos of the service remains, which is to support those who need it. Control of the services and the funding of them has always remained a substantial issue since I have been in working in social care, and the distribution of funds gives commissioners a dominant position which plays out differently across the country. This means that there isn’t a nationally acceptable level of fee for individuals in their own homes or in a care setting. Fees are set by the local authority and providers are increasingly moving towards privately-funded placements to ensure business viability: inadvertently, we have allowed a two-tier
“In the 1980s people used to walk into our services; today they often arrive in an ambulance and come with complex health care needs.”
system to emerge – a postcode lottery. There is no doubt that social care delivers so much more than the tin says. According to the term ‘social care’ we are deemed to be supporting people with social needs to counter social isolation and age-related ailments which make living alone in your own home undesirable or risky. The reality today is that we are caring for people who, less than two decades ago, were supported by the NHS in long-term wards or specialist hospitals. I recall doing work experience in the early 1980s in an establishment where people with disabilities were housed. When that service was closed a decade later many of the residents were dispersed to private settings.
In the 1980s people used to walk into our services; today they often arrive in an ambulance and come with complex health care needs.
The delivery model is such that we are caring for people with increasingly complex care needs. As a sector we are creating services which will enable people to live in homely environments despite some very challenging conditions. To do this, we need a confident and competent workforce which means we are upskilling them to levels akin to health care assistants in hospitals, but sadly we cannot match the pay thresholds they deserve. The irony is that we do this at a cost well below the true cost of care: all we need to look at
8 | JUNE 2024 CARING-TIMES.CO.UK business | opinion

“Our reliance on foreign nationals in social care and health is purely because we do not have a domestic workforce in sufficient numbers to meet the growing need.”
is the comparison of keeping someone in hospital at the cost of over £2300 per week, as opposed to a week in a social care setting of £700-900.
As we all acknowledge, the sector would be nowhere without our amazing workforce. They are seldom valued or acknowledged publicly for the work they do, but regularly criticised. The image of our sector is tarnished by stories of poor
care, even when the issues were raised in an NHS setting like Winterbourne View; press referred to it as social care setting and that it was how the optics stayed. We have a regulator who appears to be ever less capable of proactive support hiding behind desktop analysis.
There is a critical shortage of staff, well debated across many forums. The reality is that social care is a highly skilled role which is not valued or rewarded appropriately. How do we square the circle of insufficient funding for the delivery of care and valuing our workforce through pay and conditions which recognise their skills, training and commitment to the role.
Our reliance on foreign nationals in social care and health is purely because we do not have a domestic workforce in sufficient numbers to meet the growing need. Despite warnings, decision-makers have consistently chosen to neglect the impact of workforce shortages on care delivery. Commitments given are short-lived, and any recruitment
support from overseas is overshadowed by the discussions framed by the wider immigration debate, not in the interest of those we care for.
The solution lies in nurturing and developing a domestic workforce. The reality is, until and unless we improve the status of the role and create professionally recognised pathways, we will continue to struggle; the workforce is needed today, not in five years’ time, and it has to be people who cherish the role, not ones who are forced into it. We are looking after people, not widgets. Compassion and care should be paramount for everyone who choses to work in our sector.
Going forward, we have to ensure that we value the role of social care and recognise it as a key partner in the solution of the challenges faced by the NHS. Decisions made must not be on how social care can help the NHS targets, but about how social care can grow and support people, so they don’t have to turn to the NHS.
CARING-TIMES.CO.UK JUNE 2024 | 9
‘Asks’ from a new government
Charlotte Goddard talks to The Orders of St John Care Trust’s chief executive Dan Hayes about his top requests from a new government
There are not many care providers that can lay claim to a history of care stretching back almost 1,000 years, but not-for-profit organisation The Orders of St John Care Trust (OSJCT) does just that. One of its sponsoring organisations, the Order of Malta, started out by providing a hospice for sick pilgrims in 1099. The other, the Venerable Order of St John, is the organisation behind St John’s Ambulance.
While the charity is rooted in history, chief executive Dan Hayes is in the mood to look forwards, not backwards. On the morning we meet, Labour leader Sir Keir Starmer has just revealed the six actions his party would prioritise if it wins the general election, with social care conspicuous by its absence.
“It isn’t a manifesto, but it is clearly the things they see as their most important messages, and the fact that social care is missing sends a message to everybody about the importance they attach to it,” says Hayes.
Hayes has been part of OSJCT for more than 20 years, joining in 2003 in a human resources role after spending some time working for the NHS. “I joined having only ever stepped inside one care home in my life, which bizarrely enough happened to be an OSJCT care
“It isn’t a manifesto, but it is clearly the things they see as their most important messages, and the fact that social care is missing sends a message to everybody about the importance they attach to it.”
home which my great aunt was living in,” he says. “I've been at the trust ever since. Wherever you are in the trust, whether you are a leader, or work in invoice processing or health and safety, you are so close to the delivery of the main service that you can see the impact you have.”
As well as being chief executive of OSJCT, Hayes is a board member of the National Care Forum (NCF), which last year announced its “social care musthaves” for the next government. These five proposed reforms are:
• Think social care first – Ensure that people care about social care like they do the NHS and understand its central role in joined up health and care.
• Improve the pay, terms and conditions of the workforce.
• Invest in people, not profit.
• Create an economic growth strategy for adult social care.
• Enshrine rights, fairness and choice for people in a National Care Covenant. Hayes says that his own “social care asks” are broadly aligned with the membership body, which he sees as playing a vital role in the sector. The first 100 days is a key time for any incoming government, and while he admits his expectations are low, he would like to see an immediate commitment to social care.

“Make a commitment to return to the reform agenda, with a principle of a fairer, better-funded system,” he says. “The one thing that will make the NHS work a lot better, even better than pouring a load of money into it, would be to get social care working properly and fairly – the NHS would be strengthened as a result of that.”
Whichever party is governing after the next election, it needs to take a cross-party approach to social care, Hayes believes. “It's a major fix that is required and that is only really going to be achieved by some sort of cross-party

business | leader’s spotlight 10 | JUNE 2024 CARING-TIMES.CO.UK
Dan Hayes
OSJCT Edwardstow Court in Stow on the Wold

“Make a commitment to return to the reform agenda, with a principle of a fairer, better-funded system,”
solution,” he says. “As a priority, any incoming government should say ‘let’s start to work together straightaway on a solution’, right at the beginning of the new government. Any fix is clearly going to spread over more than one electoral cycle, and other parties need to commit to not changing the foundations drastically.”
A new government can take some confidence in the public reaction to the temporary increase in the National Insurance Levy, which was raised by 1.25 percentage points in April 2022 to fund health and social care – even though this was then reversed in November 2022. “The first thing is to take some confidence from what's happened in recent years,” he says. “In the last two years, the National Insurance Levy was raised to fund social care in the future and there were no riots on the streets. The only public pushback I saw was the fact that people didn't trust it was going to be spent where the government said it was going to be spent. I hope that an incoming government sees that as a massive confidence boost that people will pay for a fairer system.”
However, since the publication of the adult social care reform White Paper ‘People at the Heart of Care’ in 2021, little has changed. “We were within touching distance of some moves that would have fundamentally improved social care but, three years later, it has just been forgotten,” he says. “I think we've got a good minister in Helen Whately, who is somebody that I think is committed to the sector, and there have been some


CARING-TIMES.CO.UK JUNE 2024 | 11 >
OSJCT is committed to providing a nurturing environment where residents and colleagues thrive
Birmingham, Northampton & Market Harborough Email us at charlotte.macfarlane@catolex.law to arrange your initial telephone consultation 0121 387 4410 catolex.law Reliable, clear advice on what to do and why Specialist in the Care Sector 38 years of experience in Conflict Resolution Owner of a care company with 90+ employees John Cato Solicitor-Advocate Reshaping The Business Of Law

good attempts at reform, but we end the term further behind than when we started it.”
Hayes is calling for a move away from “short-termism” in social care planning, with decisions based entirely on finances. “What we're seeing as a provider are things like short stay rehabilitative beds being pulled by the integrated care boards, not because it is the least used service – in fact it is probably the most beneficial service – but because it's the easiest thing to pull,” he says.
While he believes well-delivered home care can be the best option for many people, he is cynical about a move away from rehabilitative beds in care homes and towards care in the home, believing it is motivated by finances rather than care quality. “If what's happening is a genuine growth in high-quality care packages delivered at home, I think that's fantastic,” he says. “But I think we'd all be cynical about a service that goes from being pretty substantial to almost nothing overnight. Have we really created a system that is providing loving, rehabilitative care for all those people who were with us yesterday? Are they all receiving that care in their own homes today to the same standards? It makes me slightly concerned about what might be going on behind the front doors of a percentage of those people.”
The NCF’s social care ‘asks’ include “improve the pay, terms and conditions of the workforce”. As an employer committed to paying the Real Living Wage, this is something that Hayes is very much behind. “Labour has been
talking about a new deal for workers, with an initial focus on social care,” he says. Labour has said it will establish a Fair Pay Agreement in adult social care to improve terms and conditions across the sector.
“In my humble opinion nobody is more deserving of a better deal than social care workers,” says Hayes. “I think the majority of employers want to give that better deal and are only held back by the current funding model. We pay above the Real Living Wage, we give great sickness benefits and pensions, and this all comes at the cost of a sustainable surplus each year.”
With many care workers held back by lack of qualifications, Hayes would like to see a new emphasis on the value of experience within the sector, enabling practitioners to progress into roles in nursing and social work. “Often the barrier is the GCSEs and A-levels required,” he says. “It is important to recognise that lots of people in social care haven’t had a great academic experience,
but the experience they have gained while working in social care is invaluable. Let’s continue to work to recognise that as a route into these other professions. You can say social care is then losing people to other professions, but actually you are creating a career pathway in the sector –and the people who then occupy those professions will have a wholly different regard for social care, as it is where they came from. That will change the status of the sector over time.”
Under Hayes’ leadership the OSJCT has gone from strength to strength. In February the organisation merged with charity The Fremantle Trust, gaining facilities including 11 care homes for older people and residential and supported living services for people with learning disabilities. In March it acquired private provider Elmfield Care which offers residential, dementia and respite care for around 200 residents across three purpose-built luxury care homes in Wiltshire and Gloucestershire.

12 | JUNE 2024 CARING-TIMES.CO.UK >
OSJCT Grace Care Centre in Thornbury
While some not-for-profit providers, such as Anchor, have acquired private companies, this is the first such move for the OSJCT. The acquisition will support the charity’s sustainability, as well as providing a source of best practice that can be rolled out across OSJCT’s homes, says Hayes.
“Charities and not-for-profit organisations rely very much on people that pay for their own care to be sustainable – none of us would be here without cross-subsidy,” says Hayes. “As a group we have had a strategy for a long time to increase the number of people who fund their own care within the trust. More recently we have developed self-funded services with a higher degree of discretionary choice within them.”
Elmfield’s value base is a good fit with OSJCT, says Hayes. “The acquisition does strengthen our financial performance, which is better for everybody, but more than that that, we've bought into practices that we can apply across the rest of the organisation
OSJCT at a glance
• The Orders of St John Care Trust (OSJCT) is a not-for-profit charity providing care across 62 care homes and eight extra care housing schemes for older people.
• OSJCT offers dementia care supported by specialist Admiral nurses, residential, nursing, intermediate, respite, day and extra care.
• OSJT caters to nearly 3,000 older people, employs just over 4,400 staff and manages more than 500 volunteers.
• OSJCT is part of The Orders of St John Care Trust Group, which includes The Fremantle Trust and Elmfield Care. The group caters to nearly 6,000 people and employs more than 5,700 staff in 75 care homes, eight extra care housing schemes, and residential and supported living services for people with learning disabilities across Buckinghamshire, Gloucestershire, Lincolnshire, Oxfordshire, Suffolk, West Sussex and Wiltshire.
that make us better,” he states. “For example, the way they use their digital platforms, and the integration of their enquiry management services.”
While the OSJCT’s two sponsoring orders have a Christian background, the organisation is entirely secular on a day-to-day basis. However, there is an emphasis on transparency, and
on the provision of loving care. “I genuinely consider myself as one of the most fortunate chief executives out there, because the only thing that the sponsoring orders challenge me and my colleagues to deliver is loving care to anybody that needs it, that comes across our threshold,” says Hayes. “And that's what we endeavour to do.”
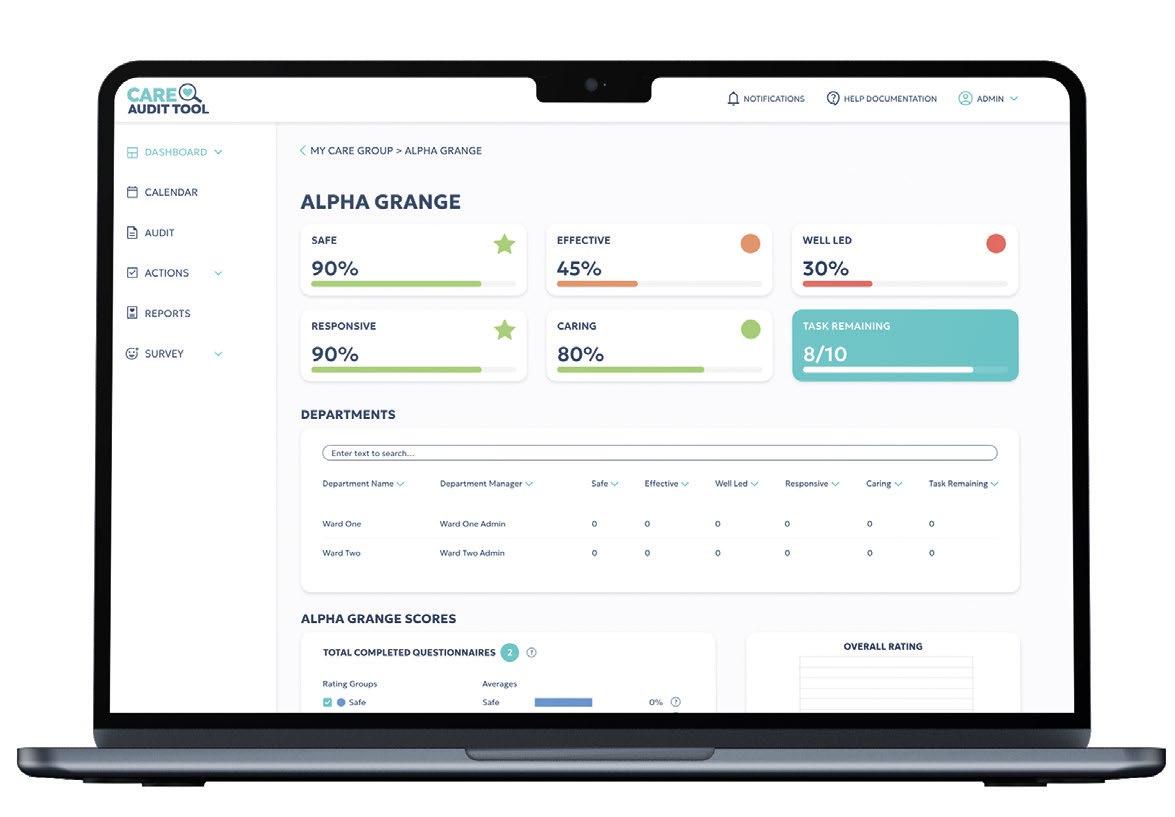
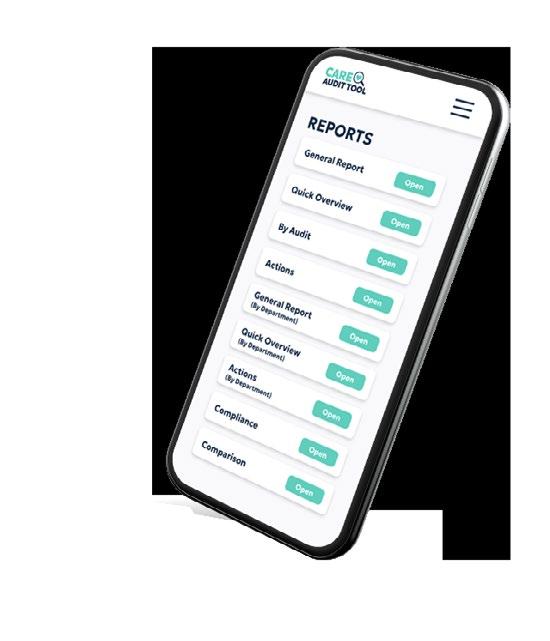
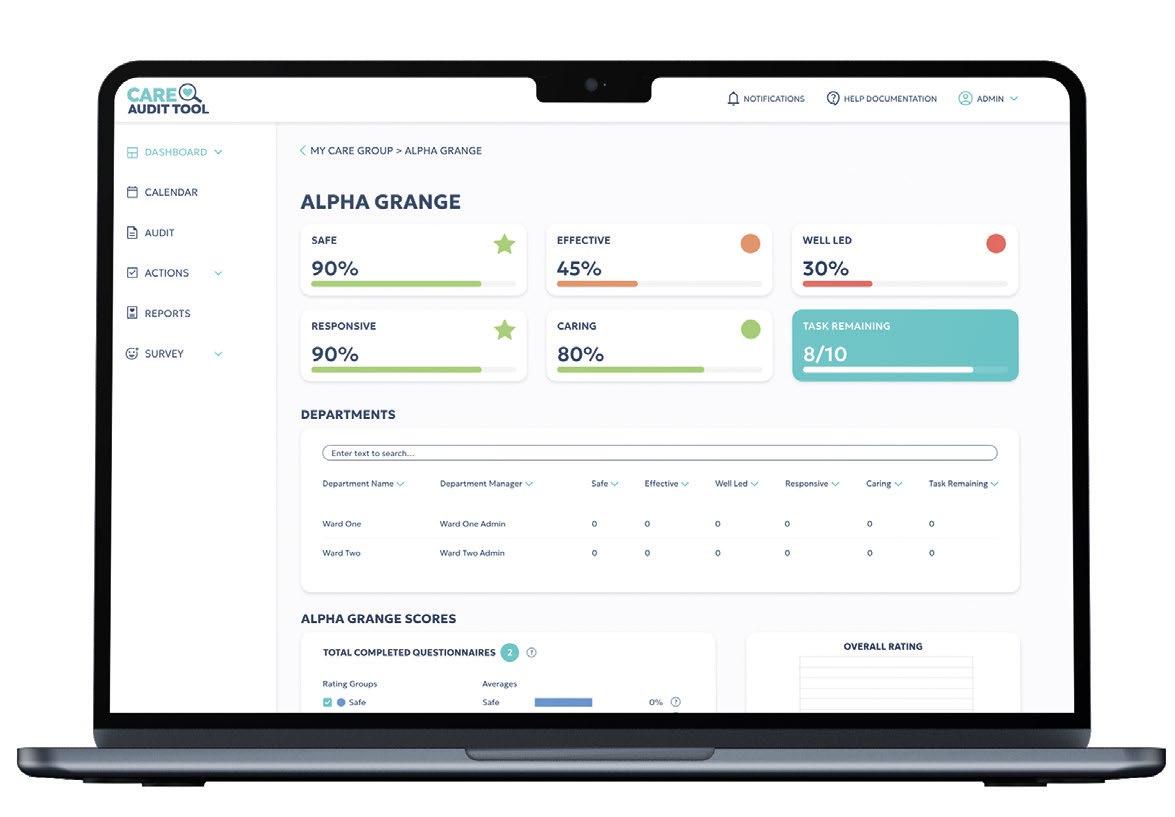
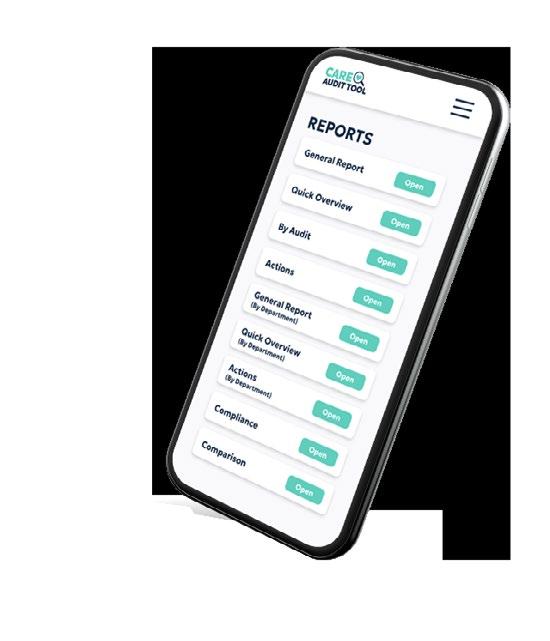
Avoid “inadequate” or “requires improvement” ratings!
Fundamentally changing the way, you manage your quality and governance processes, we make sure you get compliant and remain compliant.
A new and better system built by healthcare professionals for healthcare professionals.
We fully understand the pressures associated with CQC inspections and the ratings system. Based on decades of knowledge and expertise, our audits ask the right questions in every aspect of your activities and provides solutions and actions to create lasting impact and positive change.
No more CQC headaches and stresses.
Come and see us at the show next month, have a demo, pick our brains, and see the amazing benefits for yourself.
CARING-TIMES.CO.UK JUNE 2024 | 13 leader’s spotlight | business
Find out more at careaudittool.co.uk
Single Assessment Framework – is it working?
This month, William Walter, managing director of Bridgehead Communications, sits down with Nikki Walker, chief executive of Quality Compliance Systems (QCS), to discuss the ongoing implementation of the CQC’s Single Assessment Framework.
We begin by discussing the feedback QCS received from its customers regarding the new Single Assessment Framework. Walker explains that it’s been a mixed bag: “The theory of it was received positively, and providers are pleased that [the guidance and framework] are being simplified.”
But the change has brought challenges. She explains: “We have had a lot of feedback from customers who were frustrated with the lack of information and resources available at the beginning, which was difficult for providers.”
Overall, though, Walker hopes that the problems in adapting to the CQC’s new framework are short-term and “teething problems from having to go through the steps of implementation and getting [the new framework] to come alive”. There are, however, clear frustrations particularly with access to the new portal and inconsistency in inspections. These need to be resolved for providers to see the benefits of the new framework.
However, while simplicity has been
“There are, however, clear frustrations particularly with access to the new portal and inconsistency in inspections. These need to be resolved for providers to see the benefits of the new framework.”
helpful, some parts of social care remain shrouded in regulatory blind spots, she explains. “I think there are other spaces which aren’t regulated sufficiently, particularly dementia,” Walker says. She adds: “There is an opportunity for further thinking about what regulation is needed to ensure that those living with dementia consistently receive the right care and how we enable people to stay living at home longer.”
This need for continued serious conversations between regulators, policymakers and care providers is compelling for Walker, who believes only through addressing this can dementia care be “delivered really well and done safely”.
Digitally driven
What is clear is that an essential feature of the new framework has been a prioritisation of digitally driven continuous assessment. When pressing Walker specifically on whether this reliance on digital data is harmful for social care, where the human element is so important, she believes it does not have to be.
She says: “If it’s done well, no ... it is possible for providers to make everything digital. [The pandemic] helped create an impetus to become more digital, and we see almost completely digital providers. Obviously, care is all about the human element, so this is not about being robotic … it’s about using technology to support service users to give the best care most efficiently.”
The future of care regulation
As we near the end of our discussion, we look forward to the future of regulation in the sector. Given the UK’s ageing population and rising demand for adult social care, Walker believes this

“I think part of this has been recognising that the really detailed framework we had wasn’t going to be workable as we go forward.”
may have influenced the changes in the framework. She comments: “I think part of this has been recognising that the really detailed framework we had wasn’t going to be workable as we go forward.”
The overriding message from our discussion is that while the new Single Assessment Framework has faced problems, simplification is good news for providers. As we wrap up, Walker highlights the exciting changes in the sector and draws attention to the “vision-led businesses” operating within it who are determined to innovatesomething that QCS, at the forefront of technology in the care sector, is spearheading.
business | politics & policy 14 | JUNE 2024 CARING-TIMES.CO.UK
Nikki Walker
How can it be better?
Ian Trenholm, chief executive of the Care Quality Commission (CQC), explains the implementation of the new Single Assessment Framework so far, and what improvements can be made. (Interview conducted by Bridgehead Communications’ William Walter. The following is based on a blog post published at the end of March, available on Medium.)
The CQC is changing. We've developed and introduced a new assessment framework that provides a single vision of quality for the whole health and care system. This framework draws heavily on our experience of regulation over the last decade, including lessons learned during the pandemic and our Key Lines of Enquiry.
Our ambition for the new assessment approach is to use the data we collect more effectively, enabling us to more frequently update our view of quality across services and systems. This will give people who receive care and providers a clear view of the quality of care and areas for improvement.
Transformation of this scale has required extensive planning and development. Over the last three years, we've worked with people who use services and the people who care for them to ensure that the new framework represents and supports individuals and their needs.
At the same time, transformation of this scale is, of course, neither linear nor simple. We've taken a staged approach, and we're learning and refining through
“We've taken a staged approach, and we're learning and refining through the feedback we receive from colleagues across health and social care.”
the feedback we receive from colleagues across health and social care.
Quality statements
We know how important it is for the public, providers and stakeholders to share an up-to-date view of quality. Our new approach allows us to work in smaller packages over shorter time frames, working on and off-site, which providers will find less disruptive.
Frequency of assessments
We also know that providers are keen to understand the planned frequency of assessments. We're building that information using the feedback and data we gather during this transition period. We aim to publish timelines in the summer.
Relationships with providers
Another concern we're hearing from providers is that they will no longer have a dedicated relationship holder. Our new assessment team structure means there will always be someone you can contact and speak to with knowledge about your service. We are reviewing how this assessment team structure works in practice and will keep providers updated on any changes from this work.
Clarity of guidance
We heard that the website's guidance section needed to be more straightforward. We've created a new "guidance and regulation" landing page and an index page for assessment, setting out a clear running order and allowing providers to download all our assessment content from a single page.
Provider portal
Our new provider portal is now available. We're continuing to work towards further improvements, such as developing how providers upload and

“I'm confident that as we continue to assess services against the new framework and as our technology changes mature and become embedded, the strategic aims behind our transformation will be realised.”
share information with us, for a better experience.
I'm confident that as we continue to assess services against the new framework and as our technology changes mature and become embedded, the strategic aims behind our transformation will be realised. These aims — regulation driven by people's needs and experiences, smarter regulation, safety through learning, and accelerated improvement – underpin everything we're collectively working for.
politics & policy | business CARING-TIMES.CO.UK JUNE 2024 | 15
Ian Trenholm
Visa rule changes hit sector hard
The UK has seen a 76% decline in overseas visa applications from overseas health and care workers since the announcement of new rules denying migrants the right to bring dependants with them to the country.
Government data shows that, from January to April of this year, there were around 12,400 applications for the Health and Care Worker visa.
This represents a 76% drop from the 50,900 who applied during the same period last year.
With the changes coming into effect in March, data from April (the first full month of data) shows a 58% drop in applications from health and care dependants.
Meanwhile, the study visa also saw a similar drop in applicants, however the skilled worker visa has rocketed in popularity.
James Cleverly, Home Secretary, said the restrictions on visa applicants were "working" to reduce immigration to the UK, adding: "The British people deserve an immigration system that puts their interests first.
"Our approach is about control and fairness - to the highly skilled coming here who deserve a decent wage, to taxpayers who shouldn't be relied on to support them, and to British workers who shouldn't be undercut.
"We will continue to keep these measures under close review and if
"Our approach is about control and fairness - to the highly skilled coming here who deserve a decent wage, to taxpayers who shouldn't be relied on to support them, and to British workers who shouldn't be undercut.”
January to April of this year, there were around
12,400
applications for the Health and Care Worker visa
50,900 applied during the same period last year
58% drop in applications from health and care dependants.
over 150,000
unfilled roles in our social care sector
76% fall
in the number of visa applications from overseas health and care workers between January and April 2024 compared with the same period in 2023
needed, we will not hesitate to go further."
Responding to a 76% fall in the number of visa applications from overseas health and care workers between January and April 2024 compared with the same period in 2023, Pat Cullen, RCN general secretary and chief executive, said: “Blocking care workers and their families from coming to the UK is detrimental to the care of those in need and cruel to the people
who can provide it.
“There are over 150,000 unfilled roles in our social care sector and it is illogical for ministers to celebrate making this situation worse. An overburdened NHS will continue to pay the price for a failing care sector. Many of the patients lining corridors in hospitals should be supported properly at home instead.
“A safely staffed social care sector requires rule changes, clear investment and improving pay and conditions.”
16 | JUNE 2024 CARING-TIMES.CO.UK business | surveys & data

Commitment to staff
Quality director Nicky Barnes explains how Hartford Care’s focus on employee wellbeing and career development led to a substantial reduction in agency use
It’s no secret that recruitment is one of the biggest challenges facing the care sector, and yet carers do one of the most important jobs there is. While it sounds like a cliché, our people are truly the heart of Hartford Care; investing in their career development and wellbeing is one of our fundamental commitments as a business. Our continued focus on improving recruitment and retention has meant that we have decreased the use of agency staff by 140% in the past 12 months alone.
Our philosophy is one of a ‘home from home’, and our residents feel as if the team supporting them are
“The team also has access to a free counsellor-led helpline, and we’ve set up a crisis fund which provides interest-free loans to staff in case of an emergency..”
members of their own family. With more than 850 staff, we are proud to be an accredited Living Wage Employer, and all employees have access to an app which has tools to help improve financial health where needed, including having the opportunity to speak with expert financial coaches.
We are dedicated to setting the best example in the care sector and our pioneering initiatives include being the first operator to introduce a winter fuel contribution of up to £600 for all staff when the energy crisis hit. This initiative cost the business £400,000, but the benefits of protecting the mental health and wellbeing of our team so they could continue to provide the high quality of service to our residents, far outweighs the cost to the company.
The team also has access to a free counsellor-led helpline, and we’ve set up a crisis fund which provides interest-free loans to staff in case of an emergency.
To celebrate our much-valued employees, we also host an annual awards ceremony, with categories ranging from ‘Carer of the year’ to ‘Team of the year’, with residents, family members, visitors and team members voting for their winners.


At Hartford Care, we champion career progression, whether that’s through ‘learning on the job’ and gaining promotions, or partnerships such as with the University of Winchester on an apprentice nursing associate course. This enables staff to study for a fully funded foundation degree and upon completion they can then take on a nursing associate role, or continue with their studies and convert the qualification into a full nursing degree. This additional 18-month course is also fully funded and following successful completion, they can take on the role of registered general nurse within one of our homes.
Importantly, we are also a resettlement partner with Communities for Ukraine and through this, we’ve already helped several families flee the war in Ukraine. On the programme, all new team members and their families are given free accommodation, including utility costs for six months, in our staff accommodation. Those who have joined us so far, have taken up roles from care assistants to general assistants, and we look forward to welcoming more new team members under the initiative.
business | sustainability matters 18 | JUNE 2024 CARING-TIMES.CO.UK
Nicky Barnes
Collaboration is key
Jonathan Freeman, group sustainability director at CareTech Group, provides his monthly take on how social care is adopting a green agenda, asking how a competitive care sector can work together to tackle sustainability challenges
Let’s be honest, until relatively recently the social care sector could not describe itself as being at the cutting edge of technological innovation – paper-based care records, for example, were the norm for most providers – and still are for many. Deployment of (and funding for) technological assistive devices is growing but is still relatively rare. And, when the Covid pandemic struck, the lack of infrastructure to enable digital connectivity for those in care with their loved ones and with external agencies became painfully obvious.
TRightly or wrongly, the social care sector is a complex patchwork of provision from local authority-run, to charity operators, to private provision. That was the political decision taken by successive governments and it’s unlikely this mixed economy will change soon, but it does pose some serious questions as to how best to tackle sustainability challenges.
With commissioners driving everharder funding decisions, all of us in social care tend to default to competition. How can we deliver more than our competitors? How can we deliver at a lower cost? How can we get people to work for us, not our competitors?
Where does sustainably fit into that mix? In particular, how can we square the baked-in competitive nature of the sector with environmental sustainability, when tackling the climate crisis effectively requires collaborative effort of the like not seen before?
First, we need to work with commissioners – particularly those in local authorities – on our sustainability efforts. Local authorities are increasingly seeking to drive pressure on their providers to achieve their own sustainability targets. And the government is under pressure to support local authorities to up their game. For social care providers with NHS contracts, the sustainability requirements are increasingly stringent with all contracts for £5 million requiring the operator to set out a public
carbon reduction plan. A collaborative approach between the sector to drive collective change is essential.
Each commissioner appears to have its own approach and its own asks of providers, creating unnecessarily complicated and wasteful work. We need to work together, agree our shared priorities, streamline and make consistent the asks of commissioners on providers. We need to work together with the Local Government Association and the Association of Directors of Adult Social Services to agree on expectations on sustainability that will support the ambitions of local authorities and the social care sector alike.
Second, we need to collaborate with our suppliers, all of whom are, of course, on their own sustainability journey. To address our indirect emissions, known as Scope 3, we have to work with all of our suppliers to drive down our carbon emissions. These emissions include, for example, all of the products that operators buy, use and dispose of from suppliers. As those operators looking at their indirect emissions are discovering, the majority (typically, around 70% but often as high as 85% to 95% of an organisation’s indirect carbon emissions are driven by these Scope 3 emissions.
It is inevitable that suppliers to the sector will want to address their own carbon emissions as regulators, national and international, up the ante on these issues. Consumer demand, however, is likely to drive the pace more quickly. At CareTech, we have found just asking a simple set of questions of our suppliers about their approach has unlocked some mutually beneficial opportunities. Our stationary providers, for example, have swapped in a new range of recycled and more environmentally-sensitive products at no extra cost. Our cleaning products supplier is piloting a range of new products that promise to reduce plastic waste dramatically – again, at no extra cost. And this is just from opening up the conversation with our suppliers.

Third, we need to start working together more as operators. That’s why a group of us came together to establish the Social Care Sustainability Alliance. The Alliance brings together senior leaders in providers across the social care sector to pool their thinking on sustainability, to work together on the tricky issues with which we are all grappling, and to support more providers to start or accelerate their sustainability journeys. The Alliance has already published a comprehensive ‘Business case for sustainability in social care’. Other papers on the way include those on retrofitting for older properties, the expectations of investors, a guide to statutory and voluntary requirements on sustainability, and best practice on measuring and reporting on carbon emissions. By working together in this way, we will all make faster progress on key issues and we will all benefit as a result. All too often, social care providers look to succeed by competing with other providers. That approach will simply not work when it comes to sustainability. Sustainability gives us a very real and pressing opportunity for the sector to come together behind a shared objective to make a deep and lasting change for the better – together. Perhaps, this might even be a lesson that we could apply more generally to tackling the challenges facing the social care sector.
CARING-TIMES.CO.UK JUNE 2024 | 19 sustainability matters | business
Jonathan Freeman
Property news

Boutique care home group Welford Healthcare has purchased Ivybank House Care Home in Bath, Somerset, which provides residential, respite and day care for up to 45 residents. The vendor is care home operator brighterkind.

We Care Group has acquired long-term leases on three homes in Bradford from Impact Healthcare REIT. The homes have been operated by Melrose Holdings following their transfer from the Silverline Group as part of a recovery plan announced by Impact Healthcare last June. Impact has granted a rent-free period to We Care and lease incentives of £1.46 million of which £0.25 million is additional cash for direct investment in the homes.

Danforth Care has opened Harbour Manor, a purpose-built 66-bed care home in Felixstowe, Suffolk, with rooms available for one inclusive fee. The home, built by LNT Developments, provides 24-hour residential and dementia care, personalised activity programmes, restaurant-quality food, a cinema, salon, café and library. Each private room has an en suite wetroom, a flat screen TV, a mini fridge and underfloor heating.

Care home owners Sally and David Price have purchased the freehold of White Rock Nursing Home in Barton-on-Sea, Hampshire, a 30-registered care home with 24 bedrooms which specialises in dementia care. The Prices own another care home in Hampshire, as well as a domiciliary care agency. The sale was facilitated by business property advisor Christie and Co, with funding sourced through Christie Finance.

HC-One’s £12 million Bluebell View Care Home has opened its doors in Oswestry, Shropshire. The purpose-built threestorey home features residents’ lounges, tranquil reading rooms and a comfortable reception and bar area, along with private gardens with courtyards. Bluebell View has been developed in conjunction with contractor Greenchurch Developments.

Agincare has confirmed it has exchanged contracts to acquire two Somerset Care homes previously threatened with closure. The two providers began talks in March after Somerset Care had
20 | JUNE 2024 CARING-TIMES.CO.UK business | real estate & development
real estate & development | business
begun a consultation on closure citing “financial challenges”. An Agincare spokesperson said: “Agincare can confirm that we have exchanged contracts with Somerset Care regarding Critchill Court in Frome and Sunnymeade in Chard.”
Foundation Partners Asset Management and Deer Capital have acquired Hartford Care for more than £100 million. Hartford Care provides residential, dementia and nursing care and operates 20 care homes in the South of England delivering services to more than 1,000 people. Real estate company Knight Frank advised Hartford Care on the transaction.

McCarthy Stone, a developer and manager of retirement communities, has launched a retirement village in Wimborne, Dorset, comprising 100 new specialist retirement properties. The new community, with a total gross development value of £45 million, features 68 apartments, 22 bungalows and 10 chalets, designed for the over-65s. The properties are being offered for outright sale and shared ownership. First occupations will be in the autumn.

Care home developer Morrison Community Care Group has acquired a development site for an 81-bedroom care home in Ewell, Surrey. Planning consent was achieved in February and
the development will provide accommodation for local elderly people. It will feature wetrooms, balconies, a cinema, champagne bar, spa, bistro, private dining room and landscaped gardens. Construction is scheduled to complete in 2026. Business property advisor Christie & Co facilitated the sale.

Real estate fund Elevation Healthcare Properties has acquired Abbey Wood Lodge, a 60-bed, purpose-built care home in Ormskirk, Lancashire, which will now be operated by Torwood on a long-term lease with RPI-linked escalator with cap and collar. Abbey Wood Lodge offers full en suite wetrooms.

Care provider Anavo Group has acquired five Scottish care homes which it has managed since 2021 following their entering administration. The homes are: Burnside in Laurencekirk, Cochrane in Johnstone, Newark in Port Glasgow, Ranfurly in Johnstone, and Spiers in Beith.

Hallmark Luxury Care Homes has celebrated the opening of the £22 million Hallmark Willingdon Park Manor in Eastbourne which features a cinema, café, hair salon, cocktail bar and ninesuite retirement living offering called The Residences.
CARING-TIMES.CO.UK JUNE 2024 | 21


IMPACT FUTURES

Hey! We need an advert for CT Magazine that showcases the new Level 2 Adult Social Care Certificate. Could you work your magic?


Of course, could you let me know a bit more about it, and the benefits for employers?
So, the Department for Health & Social Care will be providing up to £53.91m of funding to support 37,000 individuals in direct adult social care roles, and we will be one of the first to bring it to market!
It will replace the current care certificate, and employers can get on the workforce development register and then claim back up to £1,500 per person
Essentially, it’s going to pave a way for care providers to upskill existing staff, including overseas care workers, for FREE*!
To be fair, that’s actually unbelieveable.

Could you let me know where to signpost employers?
They can get in touch via email on info@impactfutures.co.uk, give us a call on 01753 596 004, or they can scan the QR code!
(Oh yeah, we need a QR code please.)
All sorted.
impactfutures.co.uk SCAN HERE *Terms and conditions apply, please see website
People moves
Achieve together, a provider of specialist support in adult social care, has appointed Zak Houlahan as chief executive. Houlahan has 20 years’ senior management experience, most recently as acting chair and chief executive at Enerveo Group, the former multidisciplinary contracting business of European energy utility SSE. Before that, he led business units at Amey local government, TCR Group and several environmental businesses.

Langford Park Care Home, outside Exeter in Devon, has appointed Ed Courtney as home manager, responsible for 50 staff at the 35-bed home. Courtney’s first care job at 16 was as an activities co-ordinator in a care home. He later worked for a care consultancy, visiting hundreds of homes across the country advising managers about staffing, introducing new systems, and developing a positive working culture. More recently Courtney has been a change manager, supporting struggling homes.

Sandstone Care Group has appointed Rachelle White to the new role of regional head of catering and hospitality. White joined Sandstone in 2017 as chef at Oak Springs Care Home in Liverpool. She will oversee catering at Sandstone’s nine care homes, ensuring menus are varied and suitable for all diets, and will look at ways to improve the dining experience.
Residential and domiciliary care services provider Healthcare Homes has appointed Martin Hill as operations director of its Manorcourt Homecare and Live-in care services. Hill has more
in association with



than two decades experience of the care industry, beginning in 2003 with Craegmoor and later working at Summercare, Affinity Trust and Sussex Healthcare in turnaround, development and leadership roles.
Aria Care Group has appointed Paul Wright as its group hospitality manager, focusing on laundry and housekeeping. Aria Care operates 50 homes located in England, Scotland and Jersey. Wright has had a long career in the hospitality and care industries. Having previously worked in hotels and restaurants, he spent a

business | personnel 24 | JUNE 2024 CARING-TIMES.CO.UK
Achieve together - Zak Houlahan
Langford Park - Ed Courtney
Healthcare Homes - Martin Hill
Aria Care Group - Paul Wright
Sandstone Care Group - Rachelle White
large part of his career at Unilever as a senior development chef, latterly looking after the elderly care sector, designing food for people living with dementia, as well as designing courses for care groups. Most recently, he was regional hospitality manager at Sanctuary Group.

Social care company HICA Group has appointed Ed Robinson as manager at Prospect House in Goole in the East Riding of Yorkshire. Prospect House cares for adults with learning disabilities and specialises in supporting those with complex needs. Robinson has extensive experience of social care and previously worked at Moorview Care in Hull. He has qualifications in social care and positive behaviour support.

Aurem Care, a care provider for older people, has appointed Daryl Martin as regional director for the North to oversee five homes. Martin has 21 years’ specialised healthcare experience with a focus on the care of older people He is a registered general nurse and has worked in the NHS and for various private sector companies, including one of the largest care providers in the UK. His qualifications include a Level 6 organisational leadership course and a Level 6 care of the elderly course. He has also completed a degree module in elderly care.

Aurem Care also appointed Richard Lawson as regional director for the South to oversee seven care homes. Lawson previously worked as a home manager after working in the hospitality and entertainment industry, including roles with P&O Cruises, Greene King, and Haven Holidays.

Michaela O’Brien and Octavia Ndlovu have been appointed as home manager and deputy home manager at New Care’s Ashlands Manor in Sale, Greater Manchester, a 57-bed care facility offering residential, dementia and 24-hour nursing care services. O’Brien has a diploma in health and social care and has worked in the health sector for more than 25 years. Ndlovu has worked in healthcare for 23 years in a variety of roles and has a diploma in general nursing and a postgraduate diploma in general management.

personnel | business CARING-TIMES.CO.UK JUNE 2024 | 25
HICA Group - Ed Robinson
Aurem Care - Daryl Martin
Aurem Care - Richard Lawson
New Care - Michaela O'Brien (left) & Octavia Ndlovu
Inspection review
Amanda Narkiewicz, regulatory partner at Mills & Reeve, provides an update on the government’s planned review of the Care Quality Commission’s new inspection methodology.
The government has launched a review of the Care Quality Commission, and has appointed North West London Integrated Care Board chair Penny Dash to lead it, according to a Health Service Journal article which first reported the story.
The full terms of reference for the review are not yet available although the Health Service Journal report says the review will examine how well the regulator’s new Single Assessment Framework is working as well as:
• Whether the CQC's ratings are properly rewarding and incentivising the improvement of care.
• Whether it is properly taking into account patient voices.
• Whether the CQC has the leadership and staffing it needs to review local authority adult social care functions.
Purpose and scope of the review
The terms of the full scale review has been launched under the Cabinet Office Public Bodies Review Programme with the findings of the review expected before autumn. The review forms part of the Cabinet Office’s review programme launched in April 2022, which aims to review periodically the governance, accountability, efficacy and efficiency
"Reviews are intended to be “constructive and challenging”, identifying areas in need of improvement and providing tangible recommendations for addressing them."
of existing arm’s length bodies (ALBs), including in response to significant changes in approach. Reviews are intended to be “constructive and challenging”, identifying areas in need of improvement and providing tangible recommendations for addressing them. For the first time, review teams are required to examine the wider “delivery system” within which ALBs operate, not just the body in isolation.
It is unclear what has triggered the review as the regulator was not included in the list of bodies scheduled for review in 2024/25.
The CQC was established in April 2009 under the Health and Social Care Act 2008. Since its inception it has operated as the sole regulator of health and adult social care in England and Wales. While the CQC as regulator has endured, the regime under which it regulates services has evolved over time and in 2021 it launched its new regulatory approach as part of its new strategy to rely less on set-piece inspections and instead becoming more risk-based and data driven.

Concerns about CQC registration delays and assessments
We expect this review will be welcomed by providers across the health and social care sector who have expressed concerns about several issues, including technical issues with accessing the provider portal, delays in registration

26 | JUNE 2024 CARING-TIMES.CO.UK business | legal and regulatory
Amanda Narkiewicz

and inspection, issues with the way that the CQC is conducting and reporting on inspections, and loss of dedicated relationship managers. We are also aware that providers are not receiving auto responses upon submitting notifications.
Evidence-gathering and stakeholder engagement
According to Cabinet Office guidance, reviews of public bodies usually involve a combination of both internal selfassessment and external research, as well as inspections and interviews with the leadership and staff of the body, and with key stakeholders, including the public where appropriate. The guidance further explains that “key stakeholders should have the opportunity to provide input into the review. Departments and lead reviewers are strongly encouraged to consider whether users or customers are considered in this. Review teams may consider approaching key stakeholders directly. This should be noted in the terms of reference and can
also be reflected in the review report and recommendations.” In this context, we hope the review team will engage and call for evidence from provider representatives.
Commenting on the announcement, Professor Martin Green, chief executive of Care England said: “It is vital that the review spans all the sectors regulated by the CQC, including not just healthcare, but social care too. The NHS is already treated differently by the regulator, so it is imperative this disparity does not extend to the review conducted by government.
“We have heard concerns from providers about a number of issues, including the CQC’s overreliance on outdated data, the lack of transparency in their regulatory approach, and vast inconsistencies between assessments. It would be remiss of the review not to examine these issues carefully.
The announcement of the ministerial review is the first step towards progress, but for it to be deemed a success, we need action.”
“It is vital that the review spans all the sectors regulated by the CQC, including not just healthcare, but social care too.
The NHS is already treated differently by the regulator, so it is imperative this disparity does not extend to the review conducted by government."
If you’d like to discuss any of the issues raised in this article or require CQC support, please get in touch with Amanda Narkiewicz.
CARING-TIMES.CO.UK JUNE 2024 | 27

















































because...
your pandemic story, to help us learn lessons for the future. Search:
Share
Every Story Matters
my story
Charmaine, Care worker








care
32 10 QUESTIONS WITH… …
34
30
MANAGERS’
GUIDE TO… …
music! Colten Care’s Fiona Pritchard explains how music can be healing for those with dementia
Jan Daly, registered manager at Friends of the Elderly’s Redcot Residential Care Home
ON THE ROAD Charlotte Goddard visits CHD Living’s
Kings
Lodge Care Centre 40 CARE MANAGERS SHOW We preview everyone’s favourite care sector trade show
Managers, guide to… music and dementia
For people with dementia, music can be a powerful way to activate and promote positive feelings and connection with others. Fiona Pritchard, music and arts partner at Colten Care, offers advice on how to incorporate music into your care home
Music has an important role to play in our lives from the very beginning to the very end and musical memories that are deep and long-lasting can greatly benefit people with dementia.
Music can help people with dementia because it encourages a complex skill involving the engagement of multiple brain mechanisms to recognise and distinguish pitch and rhythm, activating focused and undivided attention.
1. People don’t have to take part to benefit from music. There may be some people who don’t want to sing, or use an instrument, but like to feel included. They can share in the music just by being there. Music is accessible because it is non-verbal and the experience can be appreciated and shared passively as well as in an interactive participatory way.
2. Singing can encourage speech. Music is stored in our semantic memory, like riding a bike or knowing the alphabet – things you can do that you don’t have to think about very much. If you ask people with dementia if they would like a cup of tea they may not reply, but if you sing it to them, they may respond. After a singing session, people might be able to say more than before as their mind has been activated.
3. Musical preferences are retained in people with dementia, so make sure you have life story documents that include favourite songs or tracks.
4. You don’t have to be a musician to introduce music into your care home. Just listen to music on the radio or smart speaker and sing along. You don’t have to be the world’s best singer, but singing together can make people feel part of a community. I have started to say “if you can’t remember the word, singing ‘la la la’is welcome”, so people are reminded
they can do that – including staff. Think of how music is used in the military, or at football matches, when people want to feel unified. Residents are often pleased when other staff members, not just the activity team, join in with music activities –including the manager.
5. Lots of homes have smart speakers like Alexa, which are game-changing, as opposed to searching for CDs. It is so easy to say “shall we have some music? Gentle or jolly?” Have residents request songs and present the activity as a chart countdown: “at number 10, Gladys chose Pretty Woman”. Or you can put song names in a hat and get residents to choose like a raffle.
6. Musical bingo can be a great activity to introduce, where you cross off a square when a particular song plays. You could make your own 50s or 60s version. ‘Name that tune’ also goes down well. Or hold a themed music day: “today we are going to visit the 1950s”.
7. Introduce props like pom poms, scarves and ribbons, which make people feel more playful. You can join scarves in a circle, wave them up and down – it is a way of connecting. Think about introducing unusual instruments like singing bowls or tongue drums, which make lovely shimmering sounds.
8. You can clap to anything, or use a shaker or a tambourine, or jingle bells at Christmas, or drums. It might be simply that the characteristic of music stimulates an instinctive or spontaneous subconscious physical response such as tapping. Make sure instruments are not too childish – I have seen other groups where activity leaders have velcroed handbells onto people’s hands – residents have to have the opportunity of letting go

and stop playing if they want to. Try tapping or shaking to the rhythm of different words like the names of things such as ‘ginger biscuits’ or ‘choco-late bour-bons’ or ‘hob-nobs’, or drinks – ‘gin-and-ton-ic’, ‘red-wine’.
9. Music is not for everyone. Having said all this, there may be residents who cry “turn that racket off” and their wishes should also be respected.
10. Music has a role to play in end of life care, helping to regulate mood, reassure and comfort. Familiar music creates a secure or familiar environment. Personal preferences may further enhance this experience, increasing this reassurance as the positive emotions associated with the music are released. The opportunity for live music, song, the sound of a voice and the touch of a hand, or sitting with someone offers additional comfort, as the presence of another person can be identified by breathing and warmth close by.
30 | JUNE 2024 CARING-TIMES.CO.UK care | registered managers
Chef of the month
Dylan Jay, second chef at Care UK’s Bourley Grange care home in Fleet, Hampshire, shares his experience of providing a great dining experience for residents
Tell us about your background in care I started my career working in a pub as a kitchen porter alongside being in college, and then went on to try something different working at a garden centre for a while before realising that I missed being in a kitchen environment. I wasn’t sure what to expect working in a care home’s kitchen, but once I had my interview with one of the chefs at Bourley Grange, I could see how passionate he was and that passion becomes contagious.
What’s special about working at Bourley Grange?
I had never worked under such incredible management before joining Bourley Grange. I think how my colleagues and I are cared for – even outside of fulfilling our job roles is extremely special. I also get to provide residents with great food. I have the privilege of interacting with them on a daily basis and building bonds with them – you don’t get that in any other kitchen environment. It means you feel so much more involved in making a difference to their lives in the home.
How do you vary your menu to provide choice for residents?
We hold weekly residents’ meetings where they can bring up anything they would like us to make for them. Often it will be something they ate in their younger years, like in Care UK’s recent ‘Recipes to remember’ campaign where we discovered that 65% of the nation no longer cook recipes that the older generation would have eaten, and to help save these recipes we asked residents to help put together a cookbook full of their favourites.
How do you meet residents’ nutritional and health needs?
We keep their diet as varied as possible throughout the week, strictly following our care plans to ensure that any individual nutritional needs are met. We specialise in following IDDSI

guidelines, making many meals for residents at a level 5 and level 4 which is minced and moist foods, and pureed foods.
How do you care for residents with dementia?
I personally pipe the pureed foods fresh, so I get to deliver these meals to the dining rooms and to our residents living with dementia. I also take our trolleys full of fresh fruits, and other snacks to the dementia suite daily, which I really enjoy as I get to see and speak to the same residents. I have been holding ‘Cooking with Dylan’ classes every two weeks, where residents enjoy learning about the dishes we make, and the passion that goes into them. It’s something that residents, especially those living with dementia, seem to really look forward to.
What’s your most popular dish?
Bourley Grange residents recently really enjoyed a bacon and onion suet pudding I made. We’ve had a lot of requests to make that again already, so I’m sure that’s going to be one of their firm favourites.
What’s your favourite dish?
I really like making sweet and sour chicken – residents have great reactions to it every time.
How do you make the dining experience special for residents and their families? Relatives are often invited to dine with their loved ones, especially to celebrate occasions such as birthdays and other milestones. We will ask them beforehand what they would like to eat together, and then we’ll set up a dining area for them exclusively.
CARING-TIMES.CO.UK JUNE 2024 | 31 catering | care
Dylan Jay
10 questions with…
We speak to Jan Daly, registered manager at Friends of the Elderly’s Redcot Residential Care Home in Haslemere, Surrey

Why did you join the social care sector?
From a very young age, I knew I wanted to work in the care sector, either as a nurse, midwife or carer. I just felt this deep need to help people. I grew up in a nursing environment, as my mum was a nurse at St Thomas’ Hospital in London. At the age of five I had my own nurse’s uniform and doctor’s bag and I used to love listening to mum’s stories about what she’d been doing at the hospital each day. After leaving school I went to Guildford College to begin my nursing journey. I then decided to specialise in midwifery and worked hard to become a registered midwife. After qualifying, I worked at the Royal Surrey County Hospital, delivering many beautiful, bouncing babies. After having my own family, I returned to work in care and nearly five years ago, I joined Friends of the Elderly as the registered care home manager at Redcot.
What do you enjoy most about your job? I have an amazing and caring team who are devoted to our residents, making sure that they are happy, safe, engaged and motivated every day. Our residents are wonderful and I thoroughly enjoy spending time with them, whether we are taking part in one of our many wide and
varied activities or simply sitting down with a cup of tea and having a chat. Their life stories are fascinating and some of the tales they tell me are absolutely hilarious.
Who is your social care hero and why?
Florence Nightingale – the Lady with the Lamp. She was a pioneer of her time and the founder of modern nursing. Her quote “The very first requirement in a hospital is that it should do the sick no harm” is so true, and still stands true today. She did so much for so many – I admire her drive and dedication.
What is the one thing you would change about social care?
I would like to see a nationwide high standard of care for older people living with dementia. At Friends of the Elderly, we have 66 dementia champions – of which I am one. They focus on encouraging independence, giving reassurance, supporting and helping, inspiring communication, creativity and interactions, and providing highquality care with dignity that meets each individual’s needs. They spend time with every resident or day care client supporting, caring for, and getting to really know them, finding out about their
backgrounds, likes, dislikes, interests and hobbies, building trust and friendship. Each dementia champion is continually learning and developing thanks to our dementia training programme. It would be wonderful to see our high standards of caring for those living with dementia implemented throughout the country.
What in your opinion makes a great care worker?
Kindness, empathy and dedication.
What do you do when life all gets a bit too much?
I go on holiday as I can totally relax and recharge. I also spend as much time as possible with my family and I do enjoy a good book. I’m a bit of a bookworm.
What advice would you give your younger self?
Travel more and see the world. I only really started travelling as I got older. Perhaps if I’d travelled in my younger years, I would still have had a career in the care sector, supporting and caring for people, but maybe as an Army medic.
Which three famous people would you have to dinner and why?
Nobel Prize winner, Marie Curie – what a fascinating and amazing woman. She not only discovered radium and polonium and contributed so much towards treatments for cancer, but back in 1914, during World War I, she created Little Curies, mobile X-Ray units which enabled doctors to see any broken bones or bullets in wounded soldiers. Dolly Parton, as I think she’d be hilarious and have everyone in hysterics –and Elvis, for the entertainment.
What three items would you bring with you on a desert island?
My radio, books (so I guess that’s more than three) and my tweezers.
What is your secret talent?
I am fantastic at lip syncing to all Tina Turner’s songs. I do quite a good impression, even if I do say so myself.
32 | JUNE 2024 CARING-TIMES.CO.UK care | manager in focus
Jan Daly
Take care with inductions
Jon Kerr, head of workforce capacity at Skills for Care, says organisations should be clear about the learning and development opportunities they offer new employees.
There’s a clear link between the training and development opportunities you offer your staff and how likely they are to remain with you in the long term.
In adult social care, we know that qualified staff have an average turnover rate of 26.5%, whereas staff with no qualifications have a turnover rate of 37% – developing your staff makes them more likely to remain in post.
Similarly, we also know that the quality of your induction process is another relevant factor when it comes to retention. Organisations with more rigorous inductions that make people feel confident and effective in their roles from day one tend to retain staff at a higher rate.
So, where do these two factors intersect? That answer is in how organisations induct their staff and how they communicate development opportunities and expectations with new staff.
A learning and development plan is a crucial part of any effective induction. This plan lays out the expectations that organisations have of their new employees, such as the completion of mandatory training, but it also gives them insight into the development milestones they may reach and how they can continue to develop their career.
The goal in this respect is to take your new starter through a planned
"The goal in this respect is to take your new starter through a planned learning and development session while ensuring not to overload them with new information."
learning and development session while ensuring not to overload them with new information.
Being clear on the mandatory elements and deadlines for any training, while also allowing time for the participant to query any issues, will ensure they are able to achieve their learning and development objectives on time and minimise any unnecessary pressure or stress.
Additional development opportunities make staff feel like their employer is invested in their career and knowledge. Outlining any learning and development that your staff can complete, and how this can potentially benefit them, is another important factor to consider during induction.
This could include topics such as how to access funding that is used to pay for industry qualifications, or where they can access online materials to support further learning.
Regardless of what your new staff member’s learning and development plan looks like, it’s important to communicate the details clearly during this initial phase, while ensuring they are not overwhelmed.

To assist adult social care providers in delivering the most effective induction possible, including what to consider when you’re planning your new staff’s learning and development road map, we’ve created an induction toolkit to help managers plan and deliver a highquality induction that fully supports new starters to quickly settle into their roles.
You can find out more about these new resources at: skillsforcare.org.uk/ induction.

cpd | care
CARING-TIMES.CO.UK JUNE 2024 | 33
Jon Kerr
King of care homes
Charlotte Goddard visits CHD Living’s Kings Lodge Care Centre in West Byfleet, Surrey, and finds out about the home’s role in supporting local hospitals to free up beds
It is the anniversary of VE Day, and residents at CHD Living’s Kings Lodge Care Centre in West Byfleet gather in the lounge to watch costumed performers singing period songs. The residents have created some fantastic decorations, including cut-out Spitfires and bunting, and are discussing rationing.
The home supports a number of people with high levels of complex needs from multiple sclerosis to Parkinson’s to advanced dementia. Posters, photographs and displays on the walls of the corridors recall past activities and promote future events, with residents’ preferences kept front and centre. “The residents wanted a pantomime dame in, so we got a dame and they performed for us,” recalls manager Josh Barlow, indicating pictures of the event. “Our receptionist holds a book club twice a week, they have read some Charles Dickens and now they have gone on to a more modern one.” Events yet to come include a magician and a holiday campstyle music show.
Barlow has been manager of 43-bedroom Kings Lodge for the past two years, having joined CHD Living in 2019 as a team leader. “I have always tried to soak up all the knowledge I can within the service, and made it known I had a desire to progress in the industry,” he says. He quickly moved to the role of deputy manager at another Surrey CHD
“We
support people out of hospital who have been deemed medically fit for discharge, but where it is uncertain as to what the next best step might be,”

home, The Summers in West Molesey, and during the pandemic became manager at St Catherine’s in Guildford, taking it from Requires Improvement to Good. Shortly after becoming manager at Kings Lodge, the CQC paid a visit and again Barlow was able to secure an overall rating of Good.
He's not resting on his laurels though, and is full of plans to improve the home, from extending the lounge area to improve engagement, to partnering with local colleges that run agricultural courses to enhance the outdoor environment. About to compete his Level 5 diploma in leadership and management for adult care, Barlow also oversees CHD Living’s work with the Surrey Heartlands Health and Care Partnership which aims to free up beds in hospitals. For the past three years the partnership has funded 60 beds across three CHD Living Homes, including Kings Lodge.
“We support people out of hospital who have been deemed medically fit for discharge, but where it is uncertain as to what the next best step might be,” says Barlow. Individuals will move from hospital and spend up to four weeks in a CHD Living home while they are assessed and supported to their next step. CSH Surrey, which delivers services on behalf of the NHS, works with CHD Living, local authorities
and residents’ families to decide on that next step, which may be returning home with a care package, live-in carers, or a residential or nursing placement. As well as freeing up beds, the scheme also prevents hospital readmission, by ensuring people do not return to an unsafe environment.
The Kings Lodge team has had to get used to a new way of working, with a rapid turnaround of residents in the block beds. “Sometimes it takes longer than four weeks due to different complications, sometimes it can be as quick as within a week,” says Barlow. “A resident can leave like they did yesterday, and then we have a new admission coming in today.”
On occasion an individual who has arrived to take up one of the block beds ends up staying at the home. Others come back to visit or to take part in events.
“We have had one or two relatives who really enjoyed their loved one’s stay in our environment, who have come back in and spoken to residents they had developed a relationship with,” says Barlow. “It doesn’t always end with discharge.”
Although residents in the block beds are only there for a short period of time, it’s important not to differentiate them from permanent residents when it comes to care, says Barlow. The team will try to get as much information as they can
care | ct on the road 34 | JUNE 2024 CARING-TIMES.CO.UK


about needs and preferences. “We look at the same information for a short-term care plan that we would look at from a permanent perspective, there is no difference in terms of the content,” he explains.
The initiative is currently being redeveloped to bring in CHD Living’s home care expertise, with a view to supporting more hospital leavers at home. Not one to miss an opportunity, Barlow is taking advantage of the reduced number of block beds to refurbish the rooms, ready for more permanent residents.
Barlow is clearly a hands-on manager and is enthusiastic when talking about the improvements he has made and plans to make in the future. A library has been transformed into a sensory
room for residents living with a more advanced level of dementia. “They may not be able to take part in the activities our wellbeing co-ordinator has on offer, but here is a space for them and their loved ones where they can be stimulated by sound, touch, and so on,” says Barlow. The room includes a well-stocked fish tank, musical instruments and toggle blankets to fiddle with.
Also on the ground floor is Kings Lodge’s own pub, complete with bar, sofas, and doors leading out onto a large grassy space. Usually open to residents, the pub is currently full of staff undergoing moving and handling training.
Training and development plays an important role in building a successful team, says Barlow. “Giving the staff opportunities and support to develop themselves means I have a team that are able to manage situations – whoever is on duty, whatever the scenario, there is a team there that can manage that.”
Some team members don’t want to progress, in which case Barlow finds training to help them upskill within their existing role, perhaps improving their knowledge of dementia care for example. “Others who identify they want to progress into another role, it is about giving them the chance to experience what that would look like,
so maybe working alongside some of the team leaders or the nurses, and giving them some responsibility so if they decide they want to progress into that role, they already have an understanding,” says Barlow
One example of supporting staff to progress is newly appointed wellbeing coordinator Christine. “She was already working in the service as a laundry assistant, but was identified as someone we felt would be great in the wellbeing role, so we posed the idea to her,” says Barlow. “She was a little bit dubious at first, but she has done amazing work, has really enjoyed the job, and the residents are responding well to her.” So well that Christine was voted the home’s first employee of the month, as part of a scheme she helped to set up.
Navigating through the ground floor of Kings Lodge takes you on a journey around the home and returns you back where you started. “We recently had the local authority come out to review the home, because it had been identified as a good layout, and a standard for potential new builds,” says Barlow. “It is essentially a rectangle, but it doesn’t feel like that when you walk round it. It means people who like to walk with purpose, who may get confused from time to time, are essentially going to come back around to where they started.”
CARING-TIMES.CO.UK JUNE 2024 | 35
On hand to hold your hand
Writing on behalf of NHS England’s Digitising Social Care programme, Gina Trimble, provider relationship manager at Suffolk and North East Sussex Integrated Care System (ICS) says she loves helping adult social care providers go digital
First, I start by asking how, and when, people prefer to be contacted. In my experience registered managers in adult social care are flat out, all the time, usually pulled in several directions all at once. I always ask if now is a good time to talk. What’s most important to me is ensuring I support adult social care providers with everything they need to make the switch to digital social care records as smooth and painless as possible. So whether it’s help to apply for funding (and as DiSC’s current campaign highlights, ‘the clock is ticking’ before the application window closes), to choose the right supplier, or to reassure a dedicated team of carers that it will all be worth it – I’m only too happy to help.
At last count, I was supporting 225 adult social care providers in Suffolk and North East Essex. I tell them about what funding is available and help them through the process. It’s actually very straightforward but if they have any hiccups, for example with filling out online forms or answering particular questions, they know they can give me a call. I understand that provider staff work exceptionally long and variable hours, I therefore adopt a flexible approach for them to contact me when they might get that rare moment of calm. That applies to help with getting started once they have their funding and are getting set up too, or with any
“I’ve met most of the suppliers too, so if care providers are having teething problems I can often point them in the right direction.”
admin or governance issues like getting the Data Security and Protection Toolkit (DSPT) over the line.
I’ve met most of the suppliers too, so if care providers are having teething problems I can often point them in the right direction. There are currently 26 assured solutions for social care records (managed by the Digitising Social Care programme and available on its website) – 20 of which I have regular contact with. Admittedly I’ve got a bit of catching up to do to meet the six new ones! I often say to care providers – I’m your middle person. If you can’t reach the supplier I will help.
But I’m not just waiting for the phone to ring. I have a full list of adult social care providers in this area and contact them for regular check-ins and to discuss their plans to go digital, or see how they are progressing.
What I love most is getting out there into care settings and understanding first-hand what they are looking for and how they are getting on. As I travel around, I can share that learning with others who might have similar aims or challenges – and am able to

share that experience, which much as they’d love to support their fellow care organisations, they simply don’t have time for. And after all, they are only going to do this once, but they can tap into the knowledge I’ve built up from working with others.
Last week, one of our smaller care providers called me to ask about their new digital social care record app. We tried a Teams call, but she was still struggling so I said I’m down your way

36 | JUNE 2024 CARING-TIMES.CO.UK care | care for tomorrow
Gina Trimble

“I get so much valuable feedback to pass on to others, and I think they feel valued and appreciate that their experience can be shared.”
on Monday, I’ll pop in. We got it sorted over a cuppa. I try to be there to hold their hand and to address their fears. I can even help set up or attend their demos with digital suppliers. I always remain impartial, because ultimately it has to be the care provider and their team’s decision – but I know my way around lots of the solutions these days so can often make comparisons or suggestions.
We also make sure we’re in touch once they are up and running with a benefits survey six months after implementation. I get so much valuable feedback to pass on to others, and I think they feel valued and appreciate that their experience can be shared. They almost always have great advice for other care providers considering or planning the switch to digital.
I just love working with people, getting things done and giving them an opportunity to grow. And I try to be the first to congratulate managers and teams when they secure funding or select their supplier – they are stepping into their digital future.
To find out more search NHS digitising social care









CARING-TIMES.CO.UK JUNE 2024 | 37
AM , Partners that Care “We have just renewed again. Such an easy system to use for managers and care staff” caretutor.org Over 75 interactive video-based courses Endorsed by Skills for Care, CPD accredited Best in eLearning for Care Home and Home Care staff eLearning that offers Solutions Visit us at STAND H32 27 - 28 June 020 3129 5667 Annual subscription, pay-asyou-go or license for own LMS
Creative Caring
As always, carers have been demonstrating their creativity through fun and innovative events for their residents

And they’re off!
Residents at Oak Springs Care Home in Liverpool got into the spirit of the Grand National. Rescue pony Merlin paid a visit from Woodlands Animal Sanctuary, and everyone had a chance to place their bets and cheer on their horses. Earlier in the week, residents of the Sandstone Care Group home created homemade hats and fascinators, with prizes for the ‘best dressed’.

Flying visit
Birds of prey including kestrels, owls and falcons thrilled residents at Colten Care’s Avon Reach home in Mudeford, Dorset, when they visited with experienced handler Colin Sutherland. The visit was a wish come true for resident Elizabeth Longley who had told carers how much she would like to see such birds close up.

home in Doncaster hosted ‘Fashion through the years’, taking attendees on a journey through iconic styles and moments from the 1940s to the 1990s.
Resident Joyce’s dream of experiencing a fashion show was realised as she graced the red carpet in a stunning dress.

Well well
In Worcestershire, Friends of the Elderly’s Malvern’s three residential, nursing and dementia homes decorated the historic well located in their grounds as part of the Malvern Waters and Well Dressing Festival. Pupils from a local school coloured leaves to make bunting, while residents judged the best colouring and presented prizes.

Veteran honoured
In Newmarket, Suffolk, Brampton Manor resident Peter Powney-Jones was presented with the Nuclear Test Medal, a symbol of gratitude and recognition for his invaluable service, during a ceremony at the care home. The medal honours the contributions of veterans and civilians who participated in the British nuclear testing programme between 1952 and 1967. Mr Powney-Jones’s family joined in celebrating this momentous occasion with afternoon tea.
Generations together HC-One’s Abermill Care Home in

Abertridwr, Caerphilly, welcomed children from Nant Y Parc Primary School as it celebrated Global Intergenerational Week. Children enjoyed a movement to music session hosted by the home’s wellbeing coordinators and a teacher. Resident Jane Lewis said: “I really enjoyed interacting with the children, including speaking to them about the history of the village.”

Tea break
Centrum Care Group’s Beacon House Care Home in Dartmouth, Devon, raised £1,278 for Dementia UK with its annual ‘Time for a cuppa’ event. The day included fun activities, a bake sale and a raffle, creating a memorable event for residents, their families and local supporters.

In Woodham Ferrers, Essex, staff members at Eastham care home shared
38 | JUNE 2024 CARING-TIMES.CO.UK care | activities news
Ageless style Runwood Homes’ Liberty House care
Diverse dress
their Indian heritage with residents during an event aimed at fostering a deeper sense of community and understanding. The cultural showcase included a display of traditional Indian attire worn by staff members.

Friday walkabout
Goodwins Hall Care Home in Kings Lynn, Norfolk, has introduced weekly Friday wellness walks. Every team member, from managers to kitchen staff, are asked to take 15 minutes or more to take a resident outside for a walk. Home manager Flavia Hansell said: “We have wonderful gardens at Goodwins Hall which everyone likes to get out into and enjoy.”

Football fun
David Fuller and Joe Swindon, residents at Orchard Care Homes’ Green Lodge Care Home in Stockton-on-Tees, County Durham, were treated to a visit to Middlesbrough Football Club, their favourite team, for a VIP tour. The visit was made possible by the MFC Foundation, which offers anyone living with dementia special assistance to enjoy visiting the stadium while feeling safe and comfortable.

Puppy partnership
Gibson, a five-month-old German Shepherd-Golden Retriever cross, has been visiting residents at Abbeyfield Winnersh in Berkshire every other week, thanks to a partnership with the Guide Dogs charity. The visits are part of Gibson’s training to become a fulltime guide dog. Gibson is accompanied by puppy development supervisor and current owner Rakesh, who has the pup for just over a year before he moves on to more training.

Blackburn Buccaneer
Gordon Walsh, a 98-year-old veteran and aircraft construction worker from Ebor Court Care Home in Nether Poppleton, York, was invited to the Yorkshire Air Museum to commemorate the anniversary of the Blackburn Buccaneer’s withdrawal from service. Gordon, who began working on the Blackburn Buccaneer Royal Navy Aircraft in 1953, took part in a special evening dinner at the museum, which houses three surviving Buccaneer planes.

The cup that cheers
Residents from Oakland Care’s 10 care homes have been celebrating National Tea Day with a unique series of tea events in partnership with Twinings. After hearing about the fascinating history of the company, residents were given the opportunity to taste and rate a range of blends. Residents were also given the opportunity to get stuck into some baking, with a specially prepared Earl Great Tea bread recipe provided by Oakland Care’s executive chef.

Spiritual support
Stafford Hall care home in South Benfleet, Essex, helped resident Anne after she told the home’s wellbeing lead she would like to be baptised. Father Ben from St Mary the Virgin Church visited the care home to officiate the baptism. “The staff really made it special for me,” said Anne.

Award winner
In Kidderminster, Worcestershire, Foley Grange Care Home resident, John Clarke, has been recognised by the Ideal Care Awards in the ‘Outstanding resident contribution’ category. The awards recognise Ideal Carehomes’ staff and residents across its 36 care homes. John’s win was announced at a glitzy ceremony hosted by Eastenders actor Shaun Williamson.

Furry friends
MHA Priceholme in Scarborough, North Yorkshire, had some furry visitors as members of the Butterwick Alpaca Retreat came to the home. Alpacas Sunny and Sandstorm, rabbits Pickles and Pom Pom and guinea pigs Peanut and Grillo visited the home, along with their owners, Anna and Chris Ramsey. “Some of our residents would have been animal owners themselves so for them it's a reconnection with their past,” said administration manager Pippa Lees.
CARING-TIMES.CO.UK JUNE 2024 | 39 activities news | care
Care Managers Show
The first Care Managers Show of 2024 once again looks set to be the pinnacle of the events calendar when it comes to care sector trade shows, thanks to another outstanding lineup at Birmingham’s NEC this 27 and 28 June.
Yes, every care manager’s favourite trade show is back bigger and better than ever before, kicking off on Thursday, 27 June. Spanning two full days, the show will see the cream of the crop in care converge on Birmingham’s National Exhibition Centre (NEC). There, visitors will find an all-star agenda of guest speakers and panel sessions, as well as a jawdropping exhibitor list, showing off all the best products and services for care businesses in 2024.
Exhibitors
The aim with putting together the Care Managers Show is to bring as much value to attendees as possible. On the speakers and panels side, visitors can find engaging, informative sessions full of useful tips and tricks for care companies. When it comes to exhibitors, just as with the speakers, expect quality and quantity. Find the full list of exhibitors and their stand numbers below:
Blue Sky Social Care Card, Stand: G23
Care Audit Tool, Stand: G12
Care Home Life, Stand: A12
Care Quality Commission (CQC), Stand: E21
Care Tutor, Stand: H32
Carebeans, Stand: D11
Charles Bloe Training, Stand: B20
Connect2Care, Stand: A30
CoolCare, Stand: A10
Croner-I, Stand: A33, A31
Croslyn Healthcare, Stand: G13
Fallsaver/ComServe, Stand: B23
Get Borderless, Stand: D10
Hamptons, Stand: D21
Impact Futures/
The Childcare Company, Stand: E30, E32
Insignia Global, Stand: E20
Leicestershire Training Team, Stand: TBD
Lifetime Training, Stand: E44
Lifeways Group, Stand: B11
Newcross Healthcare, Stand: D22
Paragon Skills, Stand: B30
Rotacloud, Stand: C13
Staffscanner, Stand: A20
T150 Energy, Stand: B12
UK Fire Group, Stand: C11
Workforce, Stand: C12

care | care managers show 40 | JUNE 2024 CARING-TIMES.CO.UK

What’s on
Day one will begin with a talk titled ‘Hear from CQC: Understanding the single assessment framework’, as senior specialist for adult social care, Julia Spencer Ellis, takes to the stage to continue the regulator’s recent spate of appearances at sector events.
Visiting Angels founder and CEO Dan Archer will explain ‘Why recruitment and retention needs to start with a carer-first culture’ in his session.
Also taking to the stage will be Skills for Care CEO Oonagh Smyth, who tackles the weighty issue of staffing in her talk, ‘Developing a workforce strategy for adult social care – and what it means for managers’, before Ebury Court Care Home’s Beverley Manzar is invited to the stage for ‘Delivering outstanding care from a care home manager’.
The rest of the show will promises to provide invaluable information on a wide range of topics – the likes of falls management, complaints, marketing, training, rostering, diversity and the intriguingly titled panel ‘Managing and supporting the safety of lone workers’ – all discussed by the biggest names in the sector, including Amrit Dhaliwal

(CEO, Walfinch), Liz Blacklock, (CEO, National Association of Care and Support Workers), Charlie Jones (COO, BKR Care Consultancy) and Samantha Crawley, (CEO, Bracebridge Care Group and director, The Outstanding Society).
And as though all that weren’t enough, visitors to the Care Managers Show 2024 will also be treated to: a performance from iconic boy band Five; a free lunchtime cooking demonstration from a certain celebrity chef; two free holiday giveaways and much, much more.
We can’t wait to see you there.


Contact
If you haven’t already, get your free ticket at caremanagersshow.co.uk. For commercial opportunities such as sponsoring a speaker slot or booking a stand at the show, please head to the website or contact new editor Sam Lewis at sam.lewis@nexusgroup.co.uk >
CARING-TIMES.CO.UK JUNE 2024 | 41
Dan Archer
Liz Blacklock
Amrit Dhaliwal








42 | JUNE 2024 CARING-TIMES.CO.UK care | care managers show






CARING-TIMES.CO.UK JUNE 2024 | 43 care managers show | care
Enjoy a life less retiring at Riverstone

Riverstone redefines later livingwith its thriving communities in the capital exclusivelyfor people over65. With two prime residences, both offering 1, 2 and 3-bedroom apartments for sale, take yourpick between elegant, cultural Kensington orthe riverside charm of Fulham —with more locations coming soon.
New residents automatically join our exclusive members’ community, The Riverstone Club, and regularly invite friends and family to enjoy our extensive suite of amenities on o er. Whether that’s relaxing in the Pool, watching a lm in the Private Cinema or enjoying classic brasserie dishes at Maria G’s, our neighbourhood Restaurant and Bar.
The Riverstone Club curates a lively calendar of informal gatherings, special guest speakers and exclusive events thanks to our partnerships with the Royal Albert Hall, Royal Philharmonic Orchestra, English National Opera, Glyndebourne Opera Festival and many more.
Our dedicated team works with every resident to help them achieve their wellbeing goals. From exercise classes and bespoke workouts through to our unique Health Concierge Service, we create tailored wellbeing programmes for every individual. Riverstone also offers wider health support and care through selected expert partners, should you need it.

Whether you want to stay living in the same area that has so much to o er but are keen to ‘right size’, wish to move closer to family, or simply seek a place where you can lock up and leave, safe in the knowledge that someone is looking after your home, we have all your needs covered.


Bookyour viewingtoday. Explore ourstunning show apartmentsandamenities, and meet theteam.
Call 020 3839 8543; or visit riverstoneliving.com




Alternatively, scan the QR code using your smartphone camera or QR reader to visit the website.
Prices start from £810,000*. Ts & Cs apply/ *Otherfees apply. Prices correct at timeof publication.
44 | JUNE 2024 CARING-TIMES.CO.UK
Dementia with Lewy bodies
Regular columnist Norrms’ McNamara reflects on what it’s like to live with dementia
During the night last night, I sat up in my bed, I looked down and saw my wife who was sleeping peacefully besides me, apparently unaware that the computer screen was flashing on and off. I sat upright in bed and rubbed my eyes as it flashed and flashed, sometimes quickly, sometimes slowly, then the screen came on a brilliant white.
After a few seconds, I was just about to get up to see what was going on when all sorts of jumbled up letters began appearing across the screen, jetting backward and forwards, not making any sense, not making any words, just random letters zig-zagging up and down. Then the zig-zagging stopped and a sentence appeared. I strained my eyes to see what it said and the sentence just grew bigger and bigger. Then it started to roll down like an old-fashioned music box on top of an old piano that used to play music by itself. I couldn't believe my wife hadn't even moved as she is such a light sleeper.
Then, just as I made a move to get out of bed, I felt it. It was only light at first, but then felt like something was grabbing me. It felt so small, almost like a baby's hands, then another, then another, until all I could feel were tiny hands clawing at the small of my back

and sides, nipping me, scratching me, and even more terrifying trying to pull me into the mattress below.
My own hands went around the back of me as I tried to swat the hands away. I looked at the computer screen, which was going crazy now, and all sorts of

noises were coming from it. I screamed, and screamed again, and then – as quickly as it had happened, it stopped, and Elaine was by my side holding me, reassuring me and telling me it was all a hallucination. I could do nothing but shake and weep for the next 10 minutes saying over and over again: "Nobody knows, nobody knows…” while Elaine held me.
I have been through this so many times of late, once even in the afternoon a couple of weeks ago while out and about and it never gets any easier. Some I remember. Some I don't. This one has stayed with me all day and even as I type I can almost feel the hands around my waist and it makes me shudder. Till next time…
CARING-TIMES.CO.UK JUNE 2024 | 45 norrms’ blog | care
Norrms McNamara
Housekeeper of the month
Louise Alexander, head housekeeper
at Porthaven’s Thirlestaine Park Care Home in Cheltenham, Gloucestershire, tells us how she goes the extra mile
How did you get into care housekeeping?
I have worked in care for more than 25 years in different roles, including senior care assistant, activities, hospitality/ housekeeping and home administration. I realised that although I loved other roles, I had a real passion for housekeeping and love making sure the environment is the best it can be. The experience I gained in other roles helps me as head housekeeper – I have great organisational skills, high standards and an eye for detail, which has led me to help out in other Porthaven homes within the company’s housekeeping departments. One home had a change of staff, for example, so asked me to go and assist.
How do you go about meeting residents’ needs?
I always make sure our role is personcentred. I try to speak to our residents daily, as a team I always encourage my staff to get to know the residents as this makes a huge difference to them. With a consistent housekeeping team the residents become familiar with the staff members and can build a good rapport.
What’s a typical day like?
I allocate my team members daily tasks. I check which areas need deep cleaning – we prioritise our ‘residents of the day’. We have a mixture of residents including people living with dementia and those with nursing needs, so this can be interesting especially when a resident with dementia wants to help.
"With a consistent housekeeping team the residents become familiar with the staff members and can build a good rapport."

We have a couple of ladies who like to clean, and I am more than happy to give them a cloth and to chat to them as we go around. One of them can set up a table better than I can, she folds the napkins.
What is the most challenging part of your job?
It can be challenging to fit everything into one day sometimes. I am responsible for ensuring we have all the supplies we need for our daily tasks and that they are ordered in time.
Is there anything that would surprise people about your job?
I think people would be surprised at how essential being a housekeeper is, from the first impressions people get when they come into the home, to ensuring the smooth running of the home with continued high standards.
Has anything changed since you started your role?
In the last 25 years the standards of care
have become higher and very personcentred. This is really noticeable.
What’s special about the care home you work for?
They really recognise staff when they have done a good job. I myself was nominated for care housekeeper of the year in the National Care Awards, in which I was a finalist in 2023. Management support is always excellent, the home manager is always approachable and takes the time to speak to staff and residents.
What skills and talents do you need to be a great housekeeper?
I have a very strong team in our housekeeping department who are longstanding members and when I asked them this question, they said I had the following attributes: “highly organised, approachable, understanding, a team player, fair, flexible and empathetic”. Kevin Peck, the home manager, agreed and is looking at ways for me to develop further in my role.
care | support staff 46 | JUNE 2024 CARING-TIMES.CO.UK
Louise Alexander


Oliver McGowan Mandatory Training for Care Providers
Autism Community Network CIC, trading as Autism Somerset, and our sister company Award Training, are approved providers of both the Part 2, Tier 1 and Tier 2 Oliver McGowan training on learning disabilities and autism. We are also Tier 2 Train the Trainers offering the ability to train Tier 2 facilitators and experts with lived experience, allowing organisations to create their own trios to deliver.

All health and social care staff must receive this training to be CQC compliant.
Conversations changing culture
Since July 2023 our passionate team of experts with lived experience have trained over 2500 staff across the country.
The training is quality assured, fully interactive, and embeds our 15 years experience working in the field with the standardised training content.


https://www.autismsomerset.org/ https://www.award.training/

For more information contact: Jai Ward contact@award.training 07507 861388

Registered Company Numbers: Autism Community Network 7894336 / Award Training 15480139