11/2024
NOVEMBER-DECEMBER

Why we need to rethink our approach to healthcare design and delivery
How private capital can bring longterm solutions for the health estate
RAAC hospitals to be rebuilt despite Labour's spending review






NOVEMBER-DECEMBER

Why we need to rethink our approach to healthcare design and delivery
How private capital can bring longterm solutions for the health estate
RAAC hospitals to be rebuilt despite Labour's spending review





This edition of Healthcare Property was completed just days before the annual government Spending Review.
Each year the much-anticipated policy statement sets out public spending plans for government departments, including the Department of Health and Social Care (DHSC).
And this year, in particular, the sector is waiting to see whether the new government will put its money where its mouth is in terms of properly funding both the health and social care systems in order to reduce waiting lists and deliver widespread operational and service improvements.

While Wes Streeting’s promised shift from a reactional to a preventative service — with primary care improvements at its heart — is widely welcomed, there is arguably a need to overhaul every area of both health and social care to properly achieve reform.
And this includes the estate, which we know is suffering from a plethora of issues, most notably ongoing safety concerns over RAAC; huge backlog maintenance problems; and the need to think differently about the environments from which we deliver health and care services due to the increasing innovation in technology.
Siva Anandaciva, interim co-director of policy, events, and partnerships at health think tank, The Kings Fund, wrote just last week that ‘capital investment in buildings and equipment — often maintained in real terms at best — is often earmarked for specific national priorities like the New Hospital Programme’.
And he added: “The Autumn Budget may only be the prelude to the wider Comprehensive Spending Review next year, which will set longer-term budgets for this parliament. But it is still an opportunity to send
About Jo: Jo is the editor of Healthcare Property, having joined Nexus Media in November.
She has been specialising in design and construction best practice within the health and care sector for the past 15 years, working on the Building Better Healthcare
an early signal that this government is approaching things differently.
“An early indication that the public health grant could increase in real terms, allocating more capital investment outside of hospital, giving local systems more freedom over how capital spending is prioritised, greater use of central grants rather than local taxes to support social care… any of these actions would represent a turning of the page and a real demonstration of the Government’s commitment to its stated reforms.”
You can read about some of the challenges health and social care operators are currently facing in this edition, including news that issues with the estate are contributing to ‘widespread failings’ in maternity services; and a report by Prime Plc which highlights the cost of inaction on NHS and GP buildings (News, P6).
Elsewhere, in our Design and Build section (p28) we look at why people with dementia need to be more involved in the design process; how designing health services with more focus on integrated community facilities offers a more-holistic, preventative view of health and wellbeing; and we explore why a rethink is needed in our approach to the delivery of hospital schemes.
And Property and Finance features (p18) include calls for a review of the current NHS funding system so private capital can be used to address the many problems facing the estate.
If you have any news or would like to comment on key issues facing the healthcare property sector, please contact joanne.makosinski@nexusgroup.co.uk
Jo Makosinski Editor, Healthcare Property
Awards and editing both Building Better Healthcare and Healthcare Design & Management magazines. She has a special interest in the design of mental health and dementia care settings and in modern methods of construction and energy efficiency.


Chief executive officer
Alex Dampier
Chief operating officer
Sarah Hyman
Chief marketing officer
Julia Payne
Editor
Joanne Makosinski
joanne.makosinski@nexusgroup.co.uk
Reporter and subeditor
Charles Wheeldon
Advertising & event sales director
Caroline Bowern
Business development executive
Kirsty Parks
Publisher Harry Hyman

We round up the latest big stories, including a new King’s Fund report which highlights the role of the estate in NHS staff recruitment; how failing estates are contributing to flaws in maternity services; and the Government’s commitment to ridding the NHS of RAAC

A cross-party commission unveils bold plans for 21st-century health services; industry leaders welcome delays to the publication of the Procurement Act 2023; and the Government pledges to strengthen patient safety

Exploring the idea of designing healthcare facilities with less reliance on acute hospitals; why people living with dementia should be involved in building design; and how the revamp of Hythe and Dibden War Memorial Hospital has impacted the staff and patient experience

38-40
Estates takeover at Cumbria trust; FM firm wins Scottish hospital contract; and how security experts are helping to protect
Investor Publishing Ltd, 3rd Floor, 10 Rose & Crown Yard, King Street, London, SW1Y 6RE
Tel: 020 7104 2000
Website: www.healthcare-property.com
Healthcare Property is published six times a year by Investor Publishing Ltd.
ISSN 3029-0627
© Investor Publishing Limited 2024
The views expressed in Healthcare Property are not necessarily those of the editor or publishers.
@HCprop

linkedin.com/company/healthcare-property/
A new Christie & Co report shows an uptick in the care home property market; and there are calls for private capital to be used to address NHS estate issues


42-48
Government unveils new NHS waste roadmap; hospitals win heat network funding; and we look at why sustainability is critical for the social care sector
49-50
The latest company recruitment news from across the sector
The Government has been warned it will need to increase NHS capital spending after ‘unsuitable estates’ were ruled to be contributing to ‘widespread’ failings in maternity services.
A major review by the Care Quality Commission (CQC) revealed that failings in NHS maternity services are so ‘widespread’ they risk becoming ‘normalised’.
It found that dire care is ‘not isolated’ to high-profile scandals like East Kent and Shrewsbury and Telford, where hundreds of babies and mothers died or suffered preventable harm.
And it stressed that many trusts are not learning from mistakes, instead choosing to treat incidents as ‘inevitable’ rather than accepting accountability.
The CQC said two thirds of services either ‘require improvement’ or are ‘inadequate’ for the safety of mothers and their babies.
In an unprecedented move, the regulator called for ‘increased

national action’ and ring-fenced investment to tackle the shortfalls.
One area of concern in the report was around estates and the environment.
It states: “Unsuitable maternity estates emerged as another key barrier to high-quality care.
“We found some maternity units were not fit for purpose, as they lacked space and facilities and, in a small number of cases, appropriate levels of potentially life-saving equipment.
“Additional capital investment is
needed to ensure women receive safe, timely care in an environment that meets their needs.”
Health Secretary, Wes Streeting, described the situation as a ‘national shame’ and vowed to fix services, insisting that the current state of affairs keeps him ‘awake at night worrying’.
He added: “These findings are cause for national shame.
“Women deserve better — childbirth should not be something they fear or look back on with trauma.
A hard-hitting new report has highlighted the important role of the estate in helping to address the ongoing workforce shortage across the health service.
Mandated minimum standards for healthcare facilities as part of improving working conditions for staff is one of the recommendations made by the King’s Fund’s policy adviser, Jessica Holden, in a new briefing to address NHS workforce challenges.
The paper calls for the provision of adequate space and time for all staff to take breaks, rest, and, where necessary, sleep.
It further calls for guaranteed access to functioning lockers, bathroom facilities, and nourishing food and drink in appropriate settings, and says that employers should receive funding to meet the mandated standard.

working risks long-term NHS vacancies becoming a permanent fixture, as the number of UK workers expecting flexible working options continues to rise,” the briefing warns.
As of May 2024, there were more than 100,000 vacancies across the NHS
“It is simply unacceptable that nearly half of maternity units the CQC reviewed are delivering substandard care.”
NHS maternity care has been under increased scrutiny following several high-profile inquiries, including more than 200 baby deaths at the Shrewsbury and Telford Hospital NHS Trust, and the investigation into maternity services in East Kent.
Inspectors visited 131 units between August 2022 and December 2023 as part of a national programme to reverse the trend.
The report also blamed poor management with limited learning when things go wrong, failure to ensure safe and timely assessment at triage, a lack of oversight from trust boards, and significant challenges in recruiting and retaining staff.
It concludes: “Without action, the danger is that poor care and preventable harm will become normalised.
“We cannot, and must not, let that happen.”
workforce in England, excluding primary care vacancies such as GPs.
Holden said: “Improving staff working conditions will take time and effort across the health and care system and at all levels.
“This briefing focuses on immediate actions that can be taken by one group, the new government, to start bringing muchneeded improvements.
“While this is not a comprehensive list of actions, the recommendations are early measures new ministers can take to improve working conditions and lay the foundations for more comprehensively addressing chronic staff shortages and increasing retention.
“The ultimate goal is to improve staff wellbeing and productivity, and therefore improve patients’ access to high-quality, safe, effective care.”
A new report has shed light on the growing financial and operational crisis facing NHS estates, with data revealing that delaying vital healthcare infrastructure projects can increase costs by over 140% in a decade.
The report by Prime, entitled Deliver or Delay? The Escalating Cost of Inaction on NHS trusts and GP estates, reinforces the urgent need for decisive action.
Five years ago, it was noted that a three-year delay in NHS estates projects could spike costs by more than 40%.
However, recent challenges — including a global pandemic, economic turmoil, and geopolitical tensions — have exacerbated these risks.
The maintenance backlog for NHS facilities has doubled in the past decade, with high-risk backlog items skyrocketing by 500%.
According to an indepth study by the Institute for Fiscal Studies, the required investment to eliminate the NHS England maintenance backlog has soared from £5.5bn in 2013-14 to a staggering £12.5bn in 2022-23.
This underscores the immense financial burden that delays impose on the healthcare system.

The period from March 2020 to March 2024 saw dramatic increases in building material costs, with pre-cast concrete up by 85%, insulating materials up by 58%, and metal doors and windows up by 53%.
These rising costs further stress the importance of timely investments.
Healthcare leaders are navigating complex funding rules, which hampers their ability to maintain equipment and buildings.
And this inaction leads to severe operational

…transformational change is achievable if leaders focus on solutions within their control
challenges, affecting patient safety and staff satisfaction.
Deteriorating infrastructure — evident in broken lifts, leaking roofs, and structural risks from materials like reinforced autoclaved aerated concrete (RAAC) — poses significant threats to both patients and staff.
Poor working conditions and inadequate staff facilities are also exacerbating the NHS’s recruitment and retention issues.
Navigating the labyrinth of funding streams, approvals, and competing priorities can make building new NHS infrastructure feel like an overwhelming task
Post-pandemic, healthcare professionals are leaving the field for better working conditions and pay, with the NHS currently facing a staggering shortage of 121,000 fulltime-equivalent staff, with only 25% of the workforce believing there are enough staff at their organisation.
The reliance on agency staff to cover shortages diverts critical funds from infrastructure projects, creating a vicious cycle.
And, although the NHS Long Term Workforce Plan aims to bolster workforce numbers over the next six years, the necessary infrastructure to support new staff remains insufficient.
The newly-released report delves into the current challenges and proposes solutions to break free from the cycle of short-term fixes.
It also highlights successful projects across the country that demonstrate transformative change is possible.
With bold leadership and a revised approach, the report argues, the NHS can achieve significant progress.

Upgrades to hospital estates affected by reinforced autoclaved aerated concrete (RAAC) will ‘proceed at pace’ despite the Labour government’s ongoing spending review.
The new administration announced in July it would review the Conservative's flagship New Hospital Programme (NHP), which pledged to build or expand 40 hospitals by 2030.
This prompted concerns that redevelopment work and the removal of RAAC would be stalled.
But Health Secretary, Wes Streeting, has told MPs that the seven hospitals in the programme which were constructed largely of RAAC, will not be considered under the scope of the review and redevelopment work will go ahead.
The hospitals are:
• Queen Elizabeth Hospital, King’s Lynn
• Leighton Hospital, Crewe
• James Paget Hospital, Great Yarmouth
• Frimley Park Hospital, Camberley
• Hinchingbrooke Hospital, Huntingdon
• Airedale Hospital, Keighley
• West Suffolk Hospital
A spokesman for Frimley Health NHS Foundation Trust, which runs Frimley Park Hospital, said of the announcement: “We are delighted that the Government has
confirmed that all RAAC schemes are exempt from its review of the national New Hospital Programme.
“This means the new Frimley Park Hospital has been formally confirmed as sitting outside of the broader review and given the green light to continue to move forward as planned.
“We are being actively supported by the national NHP to maintain progress to ensure the new hospital will be open as soon as possible.
“While we were always confident that our new hospital would remain a priority, we know the announcement of the review into the national NHP raised questions and uncertainty in our community, and so we welcome this additional clarity and renewed commitment.
“This is an exciting once-in-a-generation opportunity for us to transform the future of healthcare for our staff, patients, and local communities.”
Hannah Coffey, chief executive of North West Anglia NHS Foundation Trust, which runs Hinchingbrooke Hospital in Huntingdon, added: “This is excellent news for our patients and staff as it enables us to eradicate RAAC from our hospital site for good.
“We are incredibly fortunate to be able to
While we were always confident that our new hospital would remain a priority, we know the announcement of the review into the national NHP raised questions and uncertainty in our community, and so we welcome this additional clarity and renewed commitment
We are incredibly fortunate to be able to forge ahead with our build programme and are excited to be able to provide a hospital that will meet the needs of our future patients for many decades to come

forge ahead with our build programme and are excited to be able to provide a hospital that will meet the needs of our future patients for many decades to come.”
On 20 September, The Department of Health and Social Care (DHSC) published the terms of reference for the NHP review.
And it stated that the probe will assess ‘the appropriate schedule for delivery of schemes in the context of overall constraints to hospital building and wider health infrastructure priorities, while also looking at where improvements can be made’.
Out of scope will be schemes that have approved full business cases, and any associated phases that have specific commitments.
The review assumes these will continue to their current delivery timelines.
Also out of scope will be the critical seven hospitals with RAAC, which will ‘proceed at pace due to the substantive safety risks associated with these’.
Instead the review will consider all remaining hospitals in the programme without full business case approvals for their main build phase.
The review will present a full range of options to be taken forward for the overall size and ambition of the programme to provide a clear approach for the programme going forward.
The review will also feed into the spending review process, where decisions on the outcome will be taken in the round and the Government will confirm the outcome of the

The review was requested by Streeting and the Chancellor of the Exchequer and will be jointly led and resourced across the DHSC, NHS England, and HM Treasury (HMT).
It will be led by the director for delivery, performance, and assurance in the DHSC’s New Hospital Programme sponsor team, along with senior colleagues from the NHS England delivery team and HMT.
A steering group, including representation from HMT, the Cabinet Office, and the Infrastructure and Projects Authority (IPA), will be convened to oversee the review, directed by the senior responsible owner for the NHP, the chief financial officer at NHS England, the director general for finance at the DHSC, and senior officials in HMT, reporting to the Permanent Secretary of the DHSC.
It will conclude ‘as soon as possible’ and will be submitted to Streeting and the Treasury
Under the review, key data will be collated for each of the hospitals, including criteria around clinical outcomes, deliverability, cost, and estate condition.
Data will be drawn from existing sources where possible. Where the information is not held, or not up to date, further data may be requested from NHS trusts or regional teams.
The hospitals in scope will be prioritised according to the criteria.
The review will look at the possible timelines for delivery for each scheme, along with clinical considerations, risk, and cost profiles and present a range of options to be taken forward. Options and recommendations for phasing of the programme will then be established for ministers to consider.
The recommended options for scope, size, and phasing will be supported by confirmation of the optimum approach for delivery, underpinning clinical assumptions and the associated commercial strategy.

West Cumberland Hospital in Whitehaven, part of North Cumbria Integrated Care NHS Foundation Trust (NCIC), has opened its doors following a £40m redevelopment.
The milestone marks the completion of a new 55,860sq ft, two-storey extension delivered by GRAHAM through the ProCure22 framework.
Designed by Gilling Dod Architects, the state-of-the-art facility incorporates up to 70% modern methods of construction (MMC), demonstrating a successful integration of innovative building techniques into healthcare infrastructure.
It includes specialised wards and units that cater to a diverse range of healthcare needs, including:
• Specialist palliative care unit and stepdown community ward (Loweswater Suite and Copeland Unit): Located on the ground floor, this unit offers private
rooms and access to a tranquil courtyard, providing a calming environment for patients and their families
• Children and young people’s wards: wards feature upgraded rooms with en-suite facilities, creating a welcoming and safe environment for children and young people

• Care of the elderly ward: Designed with dementia-friendly features, this ward includes six four-bedded bays, eight ensuite side rooms, and communal spaces to promote social interaction
• Stroke rehabilitation unit: Situated on the ground floor, this unit provides an outdoor rehabilitation area, private family room, and a mix of single rooms and bays to accommodate varying patient needs The building integrates advanced medical facilities with patient-centric design to enhance both the quality of care and the overall patient experience, with private
this project to life over the last four years, none more so than our own staff who have been integral in getting the right design approved and over the line for their patients.
“This will make a huge difference to our patient experience and we hope our patients and visitors and the rest of the team will agree it has been a great project and certainly worth all the hard work.”
Peter Reavey, regional director at GRAHAM, added: “The new facilities at West Cumberland Hospital will greatly improve the provision of healthcare services locally.
“Using modern methods of construction, we’ve delivered a building that not only meets, but exceeds, current healthcare standards.”
The paediatric radiology department at Queen’s Medical Centre in Nottingham has re-opened after an upgrade to improve facilities and increase capacity.
Nottingham University Hospitals NHS Trust invested £3m into the improvement works, which have created 50% more space, with a new waiting area and two larger X-ray rooms.
The increased size of rooms also allows for easier hoisting of patients and access for beds and wheelchairs.
And the department is equipped with new state-of-the-art Fuji X-ray equipment, including a long imaging detector which uses a low radiation dose, an important factor when imaging children, and allows the whole spine and lower body to be captured in one image. The technology is one of only four across the country.
The walls of the new rooms have been painted with themed murals to help provide a calm and stimulating environment for patients, their families, and staff.
Commenting on the improvements, Sumit Jagani, head of radiology services, said: “It is fantastic to see the new department reopen.
“The larger footprint and X-ray rooms allows us to perform over 16,000 examinations a year.
“We also now have a dedicated quiet room to support difficult conversations with our patients and carers and the new waiting area can accommodate beds, hoists, and supportive medical equipment, which allows us to be inclusive in the care we deliver.
“Having the equipment, environment, and space complements the skill and enthusiasm of our team and creates the excellent patient experience we strive for.”

supporters, we’ve been able to fund special additions for the new paediatric radiology department, such as colourful wall art and privacy screens, to help make appointments less daunting for young patients.
“We hope the jungle and space-themed wall art will provide a welcome distraction for children undergoing X-rays and scans, helping to reduce their anxiety and speed up appointments.”
The first first phase of restoration works at the historic Grade I-listed Finsbury Health Centre in Clerkenwell have been completed.
The building, designed by Berthold Lubetkin in 1935, opened to patients in 1938. It received partial restoration works in the 1990s, but required further repair due to water damage.
Building owner, NHS Property Services (NHSPS), commissioned Avanti Architects and worked alongside NHS colleagues at North Central London Integrated Care System (ICS) to initiate remedial works on the centre, with the first phase of works completed in May this year.
A total investment of £1.5m will be injected into the restoration scheme, including £1.4m from NHSPS and £100,000 of Community Infrastructure Levy (CIL) funds from Islington Council.
Following full heritage assessments, the first phase has now been completed, undertaken sympathetically to respect the building’s unique significance while keeping disruption to services and patient access to a minimum. Works on the roof were carried out in 2021, during which a waterproof membrane was applied.
The recently-completed works include repairs to the façades, replacement windows, curtain walling, and tiling to the clinical wings, replacement of heavily-damaged glass blockwork screens, and render and concrete repairs at the rear.
Belinda Cameron, senior capital manager

for London at NHSPS, said: “Following on from the roof works in 2021, the initial phase of facade replacement at Finsbury Health Centre is now complete.
“This marks a key milestone in the restoration of the health centre and will ensure that this seminal building is preserved for future generations.”
Avanti Architects carefully sourced materials to replicate the building’s aesthetic, preserving the historic look and feel.
Previous restorations in 1990 were led by architect, John Allan, an authority on the building and friend of original architect, Berthold Lubetkin.
Maintaining these ties, works have been
led by Avanti Architects’ director and project leader, Fiona Lamb, with consultancy input from Allan.
The building currently features on the Historic England Heritage ‘At Risk’ register. However, following the delivery of the first two phases of works, NHSPS is liaising with Historic England regarding the downgrading of the risk rating of the building, with the aim to remove it from the At Risk register entirely in the longer term.
Lamb said: “The work undertaken to date has involved every type of repair and upgrade required at the centre and we look forward to overseeing the further phases needed to achieve the complete restoration of this internationally-renowned building.”
Work has started on the construction of a new £11m health centre on the outskirts of Norwich.
NHS Property Services (NHSPS); NHS Norfolk & Waveney; and developer, Darwin Group, have begun groundworks at the site of the new Rackheath Health Hub, which is due to open next year.
The hub will house primary care and community services and will be delivered through offsite construction methods.
The building will be made up of 45 modules making up around 16,000sq ft of internal floor space.
The scheme will provide essential new infrastructure to the local area, where it is also expected that additional housing will be delivered over the coming months and years.
Barry Clark, capital manager for national major projects at NHSPS, said:
“The new centre will offer both existing and future residents in Rackheath a state-of-the-art facility that, to its core, is sustainable and modern.
“Through our partnership we will be able to help health professionals deliver the care that patients deserve in space that is welcoming, sustainable, and fit for purpose.”
The new facility will include modernised consultation and examination rooms, community areas, and district nurse facilities, as well as back-office and shared space.
Paul Higham, associate director of estates at NHS Norfolk and Waveney, said “We are pleased to be working together with local partners to continue to progress the planned development for a new healthcare facility in the Rackheath area that will further improve residents’ access to health and care services now, and for the future.
“The planned Hub at Rackheath will help to transform how health and care services are delivered, bringing services closer to where people live, enabling more-joined-up care, and supporting residents to access information and wider services that will help them to live healthy and well.”
Darwin Group was appointed by NHSPS and NHS Norfolk & Waveney to deliver the build.
The company’s deputy chief executive, Jim Pierce, said: “This has been in the planning for some time now and, when open, it will offer patients a state-of-the-art medical facility with excellent working conditions for all staff.
“We also understand how important this medical facility will be for the growing population of Rackheath and the wider community as it will help with future demand and medical care in the area for many years to come.”
NHS Property Services (NHSPS) has partnered with MSI Reproductive Choices to repurpose Woodfarm Health Centre and Chess Medical Centre in Oxford to deliver state-of-the-art reproductive services.
The previously-vacant sites, retained by NHS Buckinghamshire, Oxfordshire, and Berkshire West Integrated Care Board (ICB), have been leased for 10 years following a competitive bidding process and MSI Reproductive Choices has been commissioned by the ICB to deliver essential reproductive services to Oxfordshire.
The organisation opened its first clinic in central London in 1976 and has grown into one of the world’s-largest providers of contraception and safe abortion services.
MSI Reproductive Choices is investing £500,000 to refurbish Woodfarm Health
Centre – which has been vacant for over a decade, with NHSPS also involved in delivering some of the improvements.
These include implementing net carbon zero sustainability measures by installing new roofmounted solar panels.
The solar PV system is designed to optimise the building’s estimated energy consumption, with estimated yearly savings of 6,160kWph — equivalent to charging a smartphone once a day 3,366 times, or the same impact as planting 55 trees a year.
Given MSI's wider requirements in the region, the organisation has also agreed to acquire space at the previously-vacant first floor of Chess Medical Centre.
MSI will be running a service from three clinical rooms alongside reactivating a reception area and waiting room.

Kirsty Goddard, head of operations at MSI Reproductive Choices UK, said: “These sites have enabled us to expand access to abortion and contraception services in the area — ensuring people can make an informed choice about their body and future.”
David Lloyd, senior estates manager at NHSPS, added: “We’re truly proud to announce this partnership. It not only optimises the use of available spaces in the facilities, but also aligns with our commitment to deliver excellent patient care.
“By securing these leases, we’re supporting MSI’s valuable work while ensuring that our sites are utilised to their fullest potential.”
Work on new staff accommodation at the emergency department at Stepping Hill Hospital in Stockport has been completed.
Tilbury Douglas has handed over the newly-completed development to Stockport NHS Trust.
The modern accommodation includes offices, meeting rooms, and welfare facilities, designed to enhance team collaboration, professional development, and overall staff wellbeing.
This improved environment is expected to boost staff satisfaction and retention, ultimately supporting the trust in delivering high-quality patient care.

The scheme is part of a larger project that includes extensive remodelling of the emergency department, with 2,600sq m of refurbished space and 1,300sq m
department, mental health services, and same-day emergency care.
Additionally, the ambulance drop-off area has been redesigned for better accessibility and efficiency.
Martin Horne, regional director for the
A £2.6m minor operations suite has opened at Spire Claremont Hospital, delivering shorter waiting times and a wider range of treatments to NHS and private patients across Sheffield and the surrounding areas.
The suite mainly accommodates minor operations that do not require a general anaesthetic and is expected to facilitate over 5,000 procedures a year.
The space freed up by the move will
North West at Tilbury Douglas, said: “We are incredibly proud to have reached this important milestone at Stepping Hill Hospital.
“The new staff accommodation is about more than just modern facilities; it’s about enhancing the wellbeing and efficiency of the emergency department team, enabling them to deliver even better care to patients during critical moments.”
Jackie McShane, executive director of operations for Stockport NHS Foundation Trust, added: “It was fantastic to both see and celebrate these new facilities.
“They are already providing a greatlyimproved environment from which our emergency and urgent care colleagues can provide care for our patients.”
enable the hospital to perform almost 800 more-complex procedures every year in its existing theatres.
And the eight recovery bays in the new minor treatment suite will help to release more space on the ward for patients requiring longer stays.
Tim Smith, hospital director, said: “By increasing our capacity to deliver more minor and complex procedures, we will be reducing waiting times and improving the overall local healthcare services.”

A six-bed discharge lounge and five-bed palliative care ward have been created in a newly-constructed facility at the Queen Elizabeth Hospital (QEH) in King’s Lynn by MTX Contracts using modern methods of construction (MMC).
The two-storey facility is a stand-alone building which has been designed to be reused when the planned new hospital is built, with bespoke ground-floor and first-floor corridors linking back to the main building and hospital ‘street’.
The discharge lounge was commissioned to support the ongoing reinforced autoclaved aerated concrete (RAAC) failsafe programme of works within the QEH site.
It provides care for patients who are ready to leave hospital as they wait to go home or receive further care in the community.
The existing discharge lounge will be demolished as part of the RAAC eradication works.
The five-bed palliative care unit on the first floor of the new building provides patients with a dignified and comfortable place to receive end-of-life care.
And it has been specially designed to provide a calming and peaceful space away from busy hospital wards.
Each of the rooms is ensuite and sympathetically equipped so family members can be comfortable as they spend precious time with their loved ones.
The two-storey building is located in a courtyard at the rear of the hospital site, which allows easier access for patients and staff and will take high volumes of site traffic away from the busy hospital ‘front door’ and emergency department areas of the site.
It will also enhance privacy for patients being discharged.
The design includes a new bedlift for

discharge area.
Internal fitout of the new building included HTM-compliant air handling systems along with power, medical gases, and other bedside services.
The contract was awarded by the Queen Elizabeth Hospital King's Lynn NHS Foundation Trust and MTX worked closely with the trust’s multi-disciplinary design and construction consultancy partner, exi, which is managing the RAAC failsafe programme.
MTX and its MMC methodology was chosen following the company’s successful delivery of the new endoscopy building on the QEH site in 2023.
MTX managing director, David Hartley, explained: “The new building was fabricated offsite while complex enabling works and site preparation was undertaken prior to the factory-manufactured structural units arriving on site.

services and building within the constraints of a tight courtyard site surrounded by live hospital wards and the Macmillan Centre.
“This meant craning in modules was the best solution because it reduced overall site/ construction time and fit within the tight RAAC programme, while minimising disruption to the existing site operation and services.
“Using MMC principles enables us to maximise offsite manufacturing opportunities and the use of precisely-engineered structural modules to build faster, safer, greener, and more cost effectively.”
Simon Illingworth, the trust’s chief operating officer, added: “The discharge lounge will have a positive impact on flow through our hospital.
“Every patient who is ready to be discharged that we can get home or into community has a positive impact on other patients waiting for treatment and frees up beds on our wards for people who need acute medical care.”


Leading figures from health, politics, and wider society propose most-ambitious blueprint for the nation’s health since the Beveridge Report
Acomprehensive plan for a modern 21st-century health creation system has been unveiled in a major report aimed at kickstarting a once-in-a-generation rethink of national health policy to revitalise wellbeing and the UK economy.
The Institute for Public Policy Research’s (IPPR) cross-party Commission on Health and Prosperity — chaired by top surgeon, Lord Ara Darzi, and Professor Dame Sally
Davies, former chief medical officer for England, has concluded its almost-threeyear enquiry into the interaction between health and the economy.
The commissioners — who include Andy Burnham, Manchester mayor and a former health secretary; and Lord James Bethell, a former Conservative health minister, find that the UK’s worsening public health crisis is linked to the country’s faltering
There is a limit to which pushing the NHS’s workforce, equipment, and estate to its limit — ‘running it hot’ — works before productivity falls off a cliff
economic performance.
And they say that better health is the most-important medicine the economy needs for the faster growth that the new government has identified as one of its five key missions.
The final report — which comes shortly after Lord Ara Darzi’s review into the state of the NHS — conducted new analysis which shows health could solve many of Britain’s most-pressing economic challenges, including low growth and productivity.
The findings include:
• If trends continue, economic inactivity due to sickness could hit 4.3 million by the end of this parliament, up from 2.8 million today. As of the end of 2023, an estimated 900,000 extra workers are missing from work
• These 900,000 missing workers could mean an estimated £5bn in lost tax receipts
in 2024, while better population health could save the NHS £18bn per year by the mid-2030s
• Some occupations — including caring roles — have seen particularly-high rates of workers becoming inactive due to sickness. The rate of inactivity due to sickness is highest among the workingage populations of Northern Ireland, the North East, and Wales
The commission, which began working in early 2022 and was first to identify economic inactivity due to sickness as a major postpandemic challenge, has concluded that better health is Britain’s greatest untapped path to prosperity.
At the core of its recommendations is to move from a reactive, sickness-orientated 20th-century healthcare system into a pro-active 21st-century health creation system, working in parallel to the NHS’s ‘sickness service’.
The overarching goal for the health creation system would be to add 10 years to healthy life expectancy by 2055 and to halve regional health inequalities.
To do that, the commission sets out an ‘ovenready’ first parliament policy programme for the new government’s health mission — covering a bold new childhood health programme, a comprehensive health industrial strategy to penalise polluters and support innovators, nationwide restoration of critical community infrastructure, higher standards for health at work, and more-integrated health and employment support services.
And proposed measures will also include developing a new ‘neighbourhood health centre’ in every part of the country: a onestop shop for diagnostics, primary care, mental health, and public health with a focus on prevention.
This will mean a need for increased capital investment in the estate.
The report says: “There is a limit to which pushing the NHS’s workforce, equipment, and estate to its limit — ‘running it hot’ — works before productivity falls off a cliff.
“It is this that explains why more money and more staff in recent years have delivered very little extra activity.
“To ensure the NHS works for public health and public finances — that is, to ensure it is both a high-quality and sustainable sickness service — demands a new approach to productivity.
“We propose a strategy of ensuring the foundations of more and better outputs are in place, as opposed to simply constraining

If we do not get prevention and productivity right, and if we do not achieve on the other health creation shifts proposed by this report, the future of the NHS looks very uncertain
resource. This would mean investing in the workforce to reboot staff motivation after the pandemic; boosting NHS investment in capital and the estate; and ensuring better use of digital, technology, and innovation.
“If we do not get prevention and productivity right, and if we do not achieve on the other health creation shifts proposed by this report, the future of the NHS looks very uncertain.”
Lord Darzi added: “Our commission was among the first to identify the rising sickness as a major and immediate postpandemic fiscal challenge.
“Now, as the Government sets up its health mission, our final report provides a ready-made policy vision for a new approach to public health.”
And Lord Bethell said: “For too long, the default political answer to this country’s health crisis has been more of the same: more doctors, more hospitals, rinse and repeat.
“This commission now proves that disease and bankruptcy beckon if we unthinkingly continue with this ineffective approach.
"It’s time to think differently. There is no more exciting vision for the future of Britain than in the reform agenda put forward by this report.
“It’s time for a new health policy where we all play our par — businesses, employers, investors, individuals, communities, and families alike.” n
For too long, the default political answer to this country’s health crisis has been more of the same: more doctors, more hospitals, rinse and repeat

Industry leaders have welcomed the Cabinet Office’s decision to delay implementation of the Procurement Act 2023 to enable a policy statement to be produced.
The Act, which received royal assent on 26 October 2023, will be delayed from 28 October 2024 to 24 February 2025 to allow the Government to provide a new National Procurement Policy Statement.
Announcing the decision, Georgina Gould, Parliamentary Secretary for the Cabinet Office, said: “Under the Act, the previous administration published a National Procurement Policy Statement to which contracting authorities will have to have regard.
“But this statement does not meet the challenge of applying the full potential of public procurement to deliver value for money, economic growth, and social value.
“I have therefore taken the decision to begin the vital work of producing a new National Procurement Policy Statement that clearly sets out this Government’s priorities for public
procurement in support of our missions.
“It is crucial that the new regime in the Act goes live with a bold and ambitious statement that drives delivery of the Government’s missions and, therefore, I am proposing a short delay to the commencement of the Act to February 2025 so this work can be completed.
“I am confident that the extra time to prepare will allow for a more-seamless transition, ensuring a smoother and more-effective implementation process for both contracting authorities and suppliers.”
The Procurement Act 2023 aims to create a simpler and more-transparent regime for public sector procurement that will deliver better value for money and reduce costs for business and the public sector.
It will also act as a framework to drive economic growth and open up public procurement to new entrants such as small businesses and social enterprises.
Welcoming the delay, Louise Bennett, senior associate specialising in public procurement at UK and Ireland law firm, Browne Jacobson, told Healthcare Property: “A four-month delay to the implementation of the Act gives much-needed
breathing space to public authorities, a large number of which understandably weren’t ready for the significant changes it brings due to the late arrival of statutory guidance.
“This legislation will fundamentally transform how the public sector purchases goods and services, with an overarching principle of ensuring it delivers value for money, maximises public benefit, and acts with integrity throughout a procurement exercise that should also continue to focus on equal treatment to bidders.
“It places a greater emphasis on transparency, supplier performance, and non-financial criteria such as quality, local job creation, and environmental impact.
“This requires public authorities to review procedures and skillsets within their organisation before the Act comes into force, while contract management should be top of the ongoing strategic considerations in order to run smooth procurement exercises.
“They would be wise to use the extra time afforded by the Government to ensure they are up to speed on the new regulations and have everything in place so they are now ready from 24 February next year.”
Patient safety across health and social care is set to be bolstered as the Government takes action to improve the effectiveness and efficiency of key organisations.
The move, aimed at ensuring the country has the best system in place to keep patients safe, comes as a major review of the Care Quality Commission’s (CQC’s) operational effectiveness is published in full.
The report, led by Dr Penny Dash, chair of the North West London Integrated Care Board, identifies significant internal failings at the regulator which are hampering its ability to identify poor performance at hospitals, care homes, and GP practices.
Its interim conclusions, published in July, prompted the Health and Social Care Secretary to order immediate action to restore public confidence in the effectiveness of health and social care regulation.
The full report confirms significant failings at the CQC in regard to its operational effectiveness, including poor performance in relation to inspections and a lack of capacity and capability to deliver improvements. And it provides seven specific
recommendations for improvement, which the new Secretary of State for Health and Social Care, Wes Streeting, fully supports.
This includes recommending that the CQC formally pauses the implementation of its assessments of integrated care systems as it works to restore public confidence in health and care regulation.
This will allow the CQC to focus on getting the basics right when assessing the organisations it regulates.
The Health and Social Care Secretary has now asked Dr Dash to conduct two further reviews moving her focus from operational effectiveness to patient safety and quality.
The first review will examine the roles and remits of six key organisations and make recommendations on whether patient safety could be bolstered through a different approach.
These are:
• CQC, including the Maternity and Newborn Safety Investigations programme (MNSI)
• National Guardian’s Office (NGO)
• Healthwatch England (HWE) and the Local Healthwatch (LHW) network
• Health Services Safety Investigations Body (HSSIB)
• Patient Safety Commissioner (PSC)
• NHS Resolution (quality and safety functions only)
A further review will focus on quality and its governance. This will guide the Government’s next steps as it continues its drive for positive cultural change across health and social care.
All findings will also inform the Government’s 10-year Health Plan to transform the NHS and social care services and make them fit for the future.
Streeting said: “Patient safety is the bedrock of a healthy NHS and social care system. That’s why we are taking steps to reform the CQC, to root out poor performance, and ensure patients can have confidence in its ratings once again.
“This government will never turn a blind eye to failure. An overly-complex system of healthcare regulation and oversight is no good for patients or providers.
“We will overhaul the system to make it effective and efficient, to protect patient safety.”

We look at the take-home points from Christie & Co’s annual Care Home Market Review 2024
Operators and investors in the care home sector are reporting a rise in confidence in the property market, according to a new report from specialist business property adviser, Christie & Co.
The Care Market Review 2024 report analyses a range of topics relating to the UK healthcare business market, including capital markets, land, and development; the transactional market; shifts in local authority fee rates; operator sentiment; the finance landscape; and includes a Q&A with Matt Lowe, chief executive of LNT Care Developments.
Here, we look at the main findings from this paper.
Due to the strong needs-driven underpin and defensive characteristics of the sector, healthcare remains a highly-attractive asset class to investors.
However, the higher cost of capital has been a key issue for investors.
This is illustrated at a macro level by the increase in the Bank of England base rate from 3.5% at the start of 2023 to 5.25% at the end of the year.
This increase was driven by wider inflationary pressures, with other important metrics like 10-year UK Government gilt yields increasing to a high of 4.6% in August 2023.
As we move further into the second half of 2024, there are clear signs that yields have stabilised with market activity picking up — with a steady increase in the volume of investment activity, a number of major processes being launched, and more funds looking to actively participate as buyers.
This reflects a combination of new capital entering the market and existing funds becoming more acquisitive.
And it is illustrated well by both real estate investment activity and wider corporate/private equity transactions.
The UK planning system continues to be unpredictable and protracted, with refusals occurring at a local level often for political reasons or simply-poor processing

of applications due to under-resourced planning departments.
Market participants are also now having to navigate recent planning policies such as Biodiversity Net Gain (BNG) and Nitrate Neutrality, which can be both challenging and costly to adhere to.
In addition, a recent update to Part L Building Regulations is placing moreonerous standards relating to the energy performance of new buildings, which has also increased construction costs.
However, the Christie & Co report notes a general stabilisation of construction costs following a period of significant inflation, and recent tender pricing has pointed to a settling down of this key component, which is allowing confidence to return.
Despite a correction in land values across many property sectors, land values for care home development sites are faring better, with operators increasingly recognising the value in the certainty that consented sites provide, and the supply continues to be constrained by the planning system.
Additional value creation continues to take place in the UK by way of Opco multiples being achieved by high-quality leasehold platforms, and Christie & Co anticipates seeing more evidence of transactions to support this over the next 12 months.
The supply of purpose-built senior housing is significantly behind that of other developed countries, but delivery volumes and planning activity are now steadily increasing in the UK.
Recent schemes in the UK have generally catered for either the luxury or affordable ends of the market, but newer entrants are
targeting the mid market, where there is the attraction of mass demand.
Established retirement living providers have continued to bring forward schemes of 50-80 units in urban areas close to high street amenities.
However, Christie & Co is increasingly seeing successful applications for larger Integrated Retirement Communities (IRC) products.
An analysis of Christie & Co’s transactional data revealed an increase in the proportion of larger care home sales in the first half of 2024, with the sale of assets over 40 beds comprising 58% of its total volume, compared with 52% in 2023.
Meanwhile, the percentage of sales of homes with under 20 beds dropped to 11% of its volume, broadly similar to 2022 figures.
And the proportion of transactions concluded to new entrants in the first half of 2024 was over double that of 2023, at 9%.
However, the number of first-time buyers was at an all-time low in 2023, reflecting a tough lending environment in 2022 together with a sector that was still recovering from the pandemic.
Small and medium groups were the most-active buyer group in the first half of 2024, representing 33% of Christie & Co’s completions.
However, the number of deals concluded to larger groups declined, shifting from 36% in 2023 to 29% in the first half of 2024. This is likely to be due to the softening of yields in 2023, reducing activity in the saleand-leaseback market.
An analysis of the vacant possession deals transacted in 2023 shows that 58% were sold to care-related buyers.
Twenty four per cent of the transactions were to buyers seeking to convert the property to a specialist care facility, and 20% of buyers sought to reconfigure the property and re-open as an elderly care facility. And 27 per cent of closed care homes sold through the broker went to residential developers.
Christie & Co analysed a Freedom of Information Act survey, covering all 174 local authorities across England, Wales, and Scotland. It found an average residential fee increase in England of 9% compared with 9.5% in 2023/24.
Fee rate levels remain a challenge in some areas, with the increases being insufficient to offset inflationary cost pressures, and Christie & Co expects that the burden on the self-funded client base is likely to rise, with the majority of providers achieving private fee increases of between 5%-10% or more.
Christie & Co interviewed a cross-section of local and regional care providers throughout the UK to gather their sentiments on the sector. The survey revealed:
• 60% of operators in the UK have a reduction in agency usage over the last 12 months, whereas only 13% stated agency usage had increased. 75% of providers in Wales reported a reduction in agency usage with only 50% of Scottish providers reporting a decline
• 59% of operators reported an increase in local authority fee rates
• In Wales, 88% of providers reported local authority fee increases of between 5%-10%. As in England there is a huge disparity in baseline local authority fees, with a 29% difference between the highest-paying authority in Wales to the lowest
• Private fee rates increased across all country regions, with 63% of operators reporting a 5%-10% increase. 18% of respondents reported increases of over 10%, compared with 36% with local authority fees, suggesting there has been some improvement on the LA side to align fees
• 62% of surveyed operators from England reported a 5%-10% increase in private fee rates, and 27% of Welsh-based providers surveyed increased their private fee rates by over 10%
• In England and Scotland, over 40% of respondents are looking to expand their portfolios, while sentiment is stronger in Wales where 67% of respondents are looking to acquire in the next 12 months
• Given the uncertainty around interest rates, there remained some degree of caution from operators, with a quarter still unsure over their appetite going forward
In a section on the finance landscape, Christie Finance notes a positive sentiment from funders lending into the sector and an increase in demand for finance, with the broker having completed 23% more transactions in the


offers of finance.
There has also been an increase in operators seeking unsecured business loans and asset finance to support refurbishment, upgrade and improvement projects which, in some cases, have been put off due to external pressures and a perceived lack of access to finance of this nature.
These types of projects made up 40% of lending within the sector in H1 2024.
Additionally, in a survey of lenders, when asked about the key challenges they face when underwriting a transaction, 18% said regulation and 22% said client income/turnover.
When asked about their bank’s opinion of the UK economy over the next 12 months, 65% of lenders said they expect to see growth.

Richard Lunn, managing director for care at Christie & Co, said of the report: “We’re seeing a renewed appetite from both buyers and investors in the market, which has resulted in a strong level of transactional activity across the whole of our team, with a big emphasis on trying to conclude deals ahead of the Budget in late October.
Our average deal time from acceptance
of an offer to completion of the transaction has materially increased from five and a half months to nearly eight months; the reasons for this are numerous, including greater diligence, insurance cover challenges, and regulatory registration implications.
“Clearly, changes in the Budget, such as important tax regimes including IHT and CGT, could materially impact both deal times and the seller’s desire to transact.”
The British Property Federation calls on the Government to work with the real estate industry to investigate avenues for private capital to deliver long-term solutions for the health estate

The British Property Federation (BPF) is calling on the Government to review the current NHS funding system so private capital can be used to address maintenance backlog, upgrade existing estates, and invest in new buildings.
According to the BPF report, Building Healthy Futures: Strengthening our Healthcare Estates, the private sector has readily-available resource and expertise to improve the NHS estate, helping the Government deliver on its growth ambitions, while simultaneously addressing funding challenges.
BPF chief executive, Melanie Leech, said: “NHS estates are a critical part of ensuring Britain has an efficient and effective healthcare system.
“By delivering much-needed new facilities, upgrading existing buildings, and tackling maintenance issues, communities can receive better and more-accessible care, ultimately improving health outcomes.
“The private sector has the resources and capacity to be rapidly deployed in
the construction and maintenance of NHS buildings, but the current system isn’t enabling this investment to be fully realised and, without it, NHS services will continue to suffer.
“Reforming existing barriers to inward investment would enable constrained public finances to be spent elsewhere in the NHS, including on staff and equipment, while also helping the NHS reach its sustainability targets.”
A lack of investment in NHS buildings means that 21% of primary care premises are described as not fit for purpose by GPs, while secondary care facilities have an £11.6bn maintenance backlog.
At the same time, delivery of the New Hospitals Programme (NHP) has been delayed amid questions over funding.
Leech said: “NHS buildings, from local GP surgeries to hospitals and specialist and acute care facilities, are critical to the health and wellbeing of communities.
“Effective primary care can reduce pressure and the cost of secondary and acute care by aiding illness prevention and alleviating waiting lists.
“Private capital will reduce the burden on public funding, allowing it to be used elsewhere within the NHS; will ensure properties are well maintained and occupiable; and enable investment in the decarbonisation of buildings.
“The Government urgently needs to work
Private capital will reduce the burden on public funding, allowing it to be used elsewhere within the NHS; will ensure properties are well maintained and occupiable; and enable investment in the decarbonisation of buildings

with the real estate industry to investigate innovative approaches to funding to enable private investment to upgrade NHS buildings, improve care outcomes, and help with staff retention.”
To unlock this private capital the BPF recommends the Government works with them to explore:
• Enabling NHS organisations to effectively utilise their budgets and private capital funding by reviewing spending limits and capital allocations
• Reviewing the primary care valuations process to ensure viable rents that deliver an appropriate return for investors and value for money for the NHS
• Facilitating third party partnership between the NHS and the private sector for the construction and modernisation of both primary and secondary care estates
• Decentralising estate planning to enable local decision-making, guided by clear national objectives and frameworks that can better respond to local community need
Leech said: “Despite record levels of public investment, the gap between capital need and capital investment continues to widen.
“This has very-real effects on NHS capacity and the ability for healthcare professionals to deliver preventative care.”
Elevation Advisors LLP has announced that its real estate fund, Elevation Healthcare Properties, has completed the acquisition of land and agreed forward funding to support the development of two care homes in Gravesend and Pagham, with Simply Care as developer and Simply Develop as the builder.
Once completed, the homes will be let on a long-term lease with RPI-linked escalator with cap and collar to Simply’s Morar Living brand, a new operator relationship for EHP.
The first development is a 75-bed care home in Gravesend, Kent, a large commuter town with strong transport links into London.
The second is in Pagham, West Sussex, a highly-sought-after coastal location.
Both homes have been designed to a high specification to enhance the wellbeing of residents, relatives, and staff, and will have wetroom en-suites throughout and amenities including a cinema, bistro, and family room.

Simply is a care home contractor, developer, and operator, with 14 operating care homes and a further seven developments under construction.
Construction on both new homes has begun and they are set to open in late 2025, with an emphasis placed on environmental performance in their design.
The developments will achieve an EPC ‘A’ rating, focusing on the eradication of fossil fuels to deliver carbon reductions, with an all-electric power supply comprising air source heat pumps and the inclusion of PV.
It is anticipated that the homes will achieve a BREEAM In-Use rating of ‘Excellent’ on completion.
Furthermore, the homes will each create 6080 jobs for the local communities.
Thomas Meany, investment manager at Simply, said: “We are delighted to start our relationship with Elevation and excited about further ventures with them in the future.

great additions to the group and are being constructed to our typical high-quality standard which, along with the great calibre of facilities each home provides, helps us achieve 90%plus occupancy across the group in a short space of time.”
James Giles, investment director at Elevation, added: “We are thrilled to begin our partnership with Simply by adding two homes
Sullivan Street Partners, a UK-based midmarket buy-out specialist, has announced the acquisition of UKAT, the UK’s leading residential addiction treatment group.
UKAT operates more than 200 beds across eight residential facilities in the UK, all of which will now transfer to Sullivan Street Partners.
Daniel Gerrard, chief executive and founder of UKAT, said: “We’re thrilled to welcome new ownership under Sullivan Street Partners.
“We have a positive history with the team
and they know the industry, our business, and, most importantly, our desire and drive to help as many people suffering with addiction as possible, and they’ll undoubtedly be able to help us achieve our mission.”
Layton Tamberlin, managing partner at Sullivan Street, added: “We are pleased to have completed this acquisition.
“Over the course of our involvement, we developed a comprehensive understanding of the business, its aims, and have built a strong relationship with the
“The homes will be built to exceed the latest environmental standards and serve the needs of the local area, then will be operated by a team committed to high-quality care and engagement with their community.
“We are excited to support Simply and fulfil the market need for care homes which are built for longevity and make a positive impact on their wider communities.”
management team.
“We have deep respect for Daniel and his drive to provide the best-possible outcomes for UKAT’s patients and stakeholders, and persevering through challenging periods of fraught ownership.
“We are confident in UKAT’s resilience and growth prospects and we look forward to bringing out the company’s full potential over the years to come.”
Connell Consulting produced vendor commercial due diligence to support the sale.
A High Court ruling into the unwinding of a care home group which was funded through a collective investment scheme could see investors recovering some of their money.
The High Court ruled that the former investors into St Mary’s Nursing Home in Moston, Manchester, a Qualia Care home with 77 residents and 85 members of staff, could surrender their leases which were purchased under ‘fractional ownership’ in order for the property to be sold — and enabling care for elderly and vulnerable residents to continue.

Stephen Hunt of Griffins, the appointed administrator of the Qualia Group, and solicitors, Gateley Legal, made an application to the High Court under the Financial Services and Markets Act 2000 (FSMA) in relation to the home, which is being marketed by Colliers’ healthcare team.
Qualia Care Properties Ltd and Qualia Care Developments Ltd were funded by a Ponzi scheme which took £57m from individual investors between February 2016 and September 2020.
Individuals invested between £50-70,000 on purchasing a longterm lease on a room in a care home and sub-let the room back to the other Qualia companies. In a previous case bought by the
Financial Conduct Authority last year, the High Court ruled that the former director of the company Robin Forster had made false and misleading statements, promising investors returns of between 8-10% of the purchase price, which were never likely to be achievable.
Qualia Care Properties Ltd and Qualia Care Developments Ltd were both liquidated in the summer of 2022, while Qualia Care Ltd went into administration in October of that year.
Some of the group’s 14 care homes have since closed. However, nine are still in operation providing approximately 476 care home places.
The portfolio is estimated to have a value in excess of £20m and could achieve greater uplift following asset management.
This latest High Court ruling unlocks the way for the Qualia
Care assets to be sold to new owners and operators and could see former investors receive around a third of their investment recovered through the sales process.
Hunt said: “It is rare for an insolvency practitioner to obtain a happy outcome for all concerned.
“This case marks the culmination of two years of hard work by a number of professionals and stakeholders to obtain a remarkable outcome for investors, staff, and vulnerable residents.
“I was appointed to a lossmaking care home group formed by a Ponzi scheme soon after the end of COVID and during the energy crisis caused by the Ukraine war.
“Qualia had no access to funding as it had no free assets to borrow against.
“From this unpromising start we
have turned round the business and implemented a novel legal solution to unlock returns to investors and creditors of up to £20m. Everyone involved should be very proud of that.”
Nick Hammond, head of Colliers’ advisory and restructuring team, added: “There are so many vulnerable parties who have been caught up in this whole scheme, from the investors, to the residents and the staff at these care homes.
“This court ruling unlocks the opportunity to safeguard the operational homes by allowing them to be marketed to a new owner and operator.”
And Ali Willoughby from Colliers’ healthcare team said: “We received lots of interest in St Mary’s and following the due legal process will be able to complete its sale next month.
“We anticipate continued interest in the majority of the remaining Qualia Care assets, which will provide certainty to both the staff and residents, as well as the potential to recover some of the funds for the individual investors, many of whom ploughed their life savings into this scheme.”
The court hearing was led by barristers Eleanor Temple KC (Kings Chambers) and FSMA specialist Ruth Bala (4 Pump Court).
A vacant dental practice in Frimley Road in Camberley, Surrey, is set to reopen following the sale of the building. Formerly under corporate ownership, this two-surgery practice ceased trading several years ago.
The building occupies a prominent roadside position in the Surrey town of Camberley and, following a confidential sales process with Tony Walker at Christie & Co, the practice has been sold to husband-and-wife first-time buyers, Sreecharan Poosala and Dr Aishwarya Gadde, who plan to refurbish the property and to purchase this property and beyond

thrilled to bring a new dental practice to the community, providing a welcoming environment where patients of all ages can feel comfortable, informed, and confident to seek dental care, which will open its doors to all patients in 2025.”
Walker added: “We’re delighted to have completed the sale of the practice.
“This is a wonderful opportunity for the new owners to create a great practice and I have no doubt they will make a great success of it.”
The practice was sold for an undisclosed price.

Christie & Co has announced the sale of a development site in Nettleham, Lincolnshire, which benefits from planning permission for a 65-bedroom care home.
Leading care home developer, Frontier Estates, has secured the planning consent for a specialist 65-bedroom dementia care home development scheme (Use Class C2) inclusive of 100% en-suite bathrooms and accommodated over 2.5 storeys.
The site sits on a circa 1.4-acre plot in the Lincolnshire village of Nettleham.
Following a sales process with Jordan Rundle and Sara Hartill at Christie & Co, it has been purchased by award-winning care provider, Country Court, which plans to complete construction in 2026.
Matt Croger, land director at Frontier Estates, said: “Nettleham is an attractive village with good transport links to Lincoln that doesn't
currently have any care facilities.
“Through the planning process, and with the positive feedback from local residents and businesses, Frontier and the council both recognised this would be a great scheme appreciated by the community.
“Country Court is an excellent operator with an exciting development pipeline which we look forward to working closely with.
“Frontier is very pleased to have passed the scheme in Nettleham onto them and looks forward to it being a hub of the community once built.”
Al-Karim Kachra, co chief executive at Country Court Care, adds: “We’re pleased to secure an excellent site and expand our presence in Lincoln and surrounding areas and we hope to be onsite by the end of Q1 2025, with a view to opening in late 2026.”
And Rundle, director of healthcare
investment and development at Christie & Co, said: “Nettleham presents a superb opportunity for a new-build care home, underpinned by strong affluence indicators for the area.
“The site itself benefits from a highlyprominent roadside location and will provide the local community with a state-of-theart care facility.
“Following several other planning approvals this year, Frontier Estates has secured another excellent consent in what continues to be a challenging planning environment.
“With a significant presence in the region already, Country Court Care will be exceptionally placed to deliver outstanding care for the growing need of Lincolnshire’s elderly demographic.”
The development site was sold for an undisclosed price.
Digital bank, OakNorth, has provided a £2.25m loan to a new joint venture between Kyte Property and Grosvenor Hill to fund a new supported living development in Bedfordshire.
Kyte Property is a London-based property development company specialising in creating unique boutique living spaces across the South East of England.
Headquartered in Finchley, north London, the firm’s current and previous projects include the conversion and extension of an old warehouse to 23 apartments and 3,000 ft of commercial space in Queen’s Park, and a major residential scheme in Acton Park.
Formed in 2022, Grosvenor Hill is a real
estate investment and development group specialising in social housing and facilities.
The firm is managed by Abel Leaman and Dion Michael, who have a track record and experience within the real estate, investment banking, and social housing sectors.
The £2.25m loan from OakNorth will be used to acquire a former NHS health centre in Bedfordshire and convert it into a new supported living scheme, consisting of 18 onebedroomed flats.
The site is located a short walk from the high street and will offer residents large indoor and outdoor communal areas.
Max Kyte, chairman of Kyte Property, said: “Following our launch 15 years ago, we’ve
been devoted to our simple mission – to build homes that resonate with the dreams of our clients, and craft environments where memories can flourish.
“Our latest supported living scheme in Dunstable is the perfect example of this and we look forward to continuing our partnership with Grosvenor Hill moving forward.”
Michael, director of Grosvenor Hill, added: “We believe that everyone should have equal access to safe, affordable, and comfortable housing and our new partnership with Kyte Property means we’re set to deliver a greater number of truly-transformative solutions to tackle the social housing and care crisis.”

The finalists of the 2024 National Care Awards have been announced.
Now in its 26th year, the annual competition is organised by Healthcare Property publisher, Nexus Media Group.
And this year there are 26 trophies up for grabs, with the winners due to be announced at a ceremony in London on 29 November.
The finalists are:
BUSINESS INITIATIVE OF THE YEAR
SPONSORED BY SANCTUARY CARE
• Brandon Park and Horkesley Manor Memory Centres, Stow Healthcare Group
• Community Integrated Care & Okta
• Maplewood Court, Oakland Care
• Nexus Events, Nexus Care Services
• OSCE Nurses Initiative/Overseas recruitment, Nellsar
• Our Approach to Dementia Care, Four Seasons Healthcare Group
CARE HOME OF THE YEAR
SPONSORED BY ONTEX
• Charrington Manor, Hamberley Care Homes
• Danecroft Residential Home, St Andrews Care Homes
• Fitzwilliam House, Excelcare Holdings
• Hill Brow Residential Home
• Holmwood Care
• Sandown Park, Healthcare Homes
• Tudor Bank Nursing Home, We Care Group
• Wiltshire Heights Care Home, Porthaven Care Homes
CARE HOME GROUP (SMALL)
• Boutique Care Homes
• Danforth Care Homes
• Hengoed Care
• KRG Healthcare
• Majesticare
• Olea Care
To book your place at the awards,


CARE HOME GROUP (MEDIUM)
• Black Swan Care Group
• Hallmark Care Homes
• Hamberley Care Homes
• Hartford Care Group
• Oakland Care
• Stow Healthcare Group
CARE HOME GROUP (LARGE) SPONSORED BY STAFFSCANNER
• Aria Care
• Care UK
• Healthcare Homes
• Minster Care Group
• Sanctuary Care
CARE PERSONALITY OF THE YEAR
SPONSORED BY CARE SHOP
To be announced on the night

CARE ACTIVITIES
CO-ORDINATOR/ FACILITATOR OF THE YEAR
SPONSORED BY TLC CARE
• Julia Constandache, Fordmill Nursing Home, Barchester Health Care
• Ben Line, St Johns Court, Amica Care Trust
• Herve Boscher, Maplewood Court, Oakland Care
• Kate Lockwood, Westmead Residential Care Home, Sanctuary Care
• Raquel Rena Aristizabal, Home of Compassion, Aria Care
• Robert Speker, Sydmar Lodge
• Sarah Savidge, Admiral Court Care Home, Hallmark Care Homes
• Shobha Lakshminarayan, Southborough Nursing Home, The Future Care Group
CARE HOME MANAGER OF THE YEAR
SPONSORED BY WE CARE GROUP
• Anca Markley, Hunters Down Care Home — Excelcare Holdings Ltd
• Beverley Manzar, Ebury Court Care Home — Ebury Court Residential Home Limited
• Gigi Jacob, Highclere Care Home, HC-One
• Jagpal Singh, Liberham Lodge — Care UK
• Jeanette Fairclough, Jasmine Court — Amicura
• Josi George, Mundy House, Larchwood Care
• Louise Blezzard, Loveday Kensington — Loveday
• Sandra O’Grady, Holmwood Residential Home — Holmwood Care Limited

CARE OPERATIONS/AREA MANAGER OF THE YEAR
SPONSORED BY COMPASS ASSOCIATES
• Michelle Bolton, CareTech
• Diane Smith, Eleanor Nursing & Social Care
• Sarah Parkins, By Your Side Home Care
• Lukasz T.-Bustos, Sanctuary Care
• Lynne John, Hengoed Care
• Sue Astill, Porthaven Care Homes
THE SARA BERRIO CARE CHAMPION AWARD
SPONSORED BY BLUELEAF
• Amanda Keeler, Walfinch
• Amy Croker, Seymour Court Nursing Home
• John Lil, County Care
• Mark Panto, Nightingale Hammerson
• Rita Schofield, Sanctuary Care
• Sarah Jeneson, Hampshire County Council
• Tim Williams, Hengoed Care
• Yasmin Bloor, Platinum Healthcare
CARE CHEF OF THE YEAR
• Aneil Manmohan, Nesbit House, Hamberley Care Homes
• Cosmin Cristea, Nellsar Princess Christian Care Centre, Nellsar Ltd
• Daniel Street, Hartismere Place, Care UK
• Emilio Pascucci, Astbury Manor Care Home, Avery Healthcare
• Majinda Ndoj, Cooperscroft Care Home, TLC Care
• Sam Armstrong, Heffle Court, Aria Care
• Samantha Heal, Falkland Grange Care Home, Porthaven Care Homes

CARE HOME
DESIGN OF THE YEAR
SPONSORED BY VIRGIN MONEY
• Abbots Wood Manor, Hamberley Care Homes
• Angmering Grange Care Home, Hallmark Care Homes
• Ashton Manor, Evermore Care
• Brook House, Aria Care
• Brownscombe Care Res, CHD Living
• Chartwell House, Boutique Care Homes
• Hengoed Park, Hengoed Care
• Loveday Abbey Road, Loveday
TECH INNOVATION OF THE YEAR
• CareTech Services by CareTech
• Cavendish Park by Majesticare
• Claire Fances Fuller, Cera Care App
• Cleva Card by Cleva
• Elsyng House, Oakland Care
• PredicAire by PredicAire
CARE LEADERSHIP OF THE YEAR
SPONSORED BY DOMUS RECRUITMENT
• Ann Ayris, Ebury Court Care Home
• Donald Morris, Canford Healthcare
• Louise Damms, Cheviot Court, Care UK
• Marie-Claire Foale, Seymour Court Nursing Home
• Nancy Walters, Mumbys Live in Care
• Nuno Santos Lopes, Nightingale HammersonRuth French, Stow Healthcare Group
• Sarah Larden, Home Instead Bromley, Chislehurst & Orpington


CARE REGISTERED NURSE OF THE YEAR SPONSORED BY CARE UK
Charlotte Cole, We Care Group
Chris Winkley, Briardene, Barchester Healthcare
Daisy Delgado, Halden Heights Care Community, Eleanor Nursing & Social Care
Kyleigh Hardy, Maplewood
Molcy Mathew, Ty Enfys Care Home, Hallmark Care Homes
Sheeba Lalson, Wisteria Lodge, Waterlooville, Wisteria Lodge Ltd
Silpa Paul, Cooperscroft Care Home, TLC Care
LIFETIME ACHIEVEMENT
Alison Lee, Woodlands & Hill Brow Bashir Jamal, Oakland Care
Emma Hodges, Avante Care & Support
Helena Shelton, County Care Group
Julie Rayner, Hallmark Care Homes
Kathleen Norris, Wisteria
Patricia Roche, Borough Care
Wendy Lane, Doddington Lodge


Senior Lifestyle
• Wiltshire Heights Care Home, Porthaven Care Homes


TRAINING & DEVELOPMENT OF THE YEAR
SPONSORED BY PORTHAVEN
Ebury Court Care Home
Healthcare Homes Academy, Healthcare Homes
Infection Prevention & Control Team, Birmingham Community Healthcare NHS Trust
Landermeads
Sanctuary Care
Stow Healthcare Group
Tricuro
Walfinch Halesowen and Redditch, Spice of Life (South West Midlands)
CARE HOUSEKEEPER OF THE YEAR
SPONSORED BY P&G PROFESSIONAL
Derek Tilley, Ashridge Court Care Centre, Canford Healthcare
Jodi Holland, Arlington Manor Care Home, Hallmark Care Homes
Louise Alexander, Thirlestaine Park, Porthaven Care Homes
Marina Holder, Stowlangtoft Hall
Nursing Home, Stow Healthcare Group
• Cera Care
• Fulcrum Care
• Ontex
• PLMR Group
• Quality Compliance Systems
Marzena Chmielewska, Mill House, Aria Care
• Melissa Harvey Pemberton, Highmarket House, Care UK
• Shaun May, Cambridge Manor Care Home, TLC Care

Michael Woodford, director of White Arkitekter, speaks to Jo Makosinski about why good hospital design is fundamental to the recovery and long-term success of our NHS estates
The recent collapse of ISG is devastating for the staff who worked there; and serves as a wake-up call for the construction industry and the public sector which relies on it to deliver vital infrastructure.
In January 2018, Carillion suffered a similar fate, leading to the loss of over 3,000 jobs and causing a major crisis across public sector projects that included hospitals, schools, and prisons.
The ripple effect from the failure of these construction giants exposes the industry’s dependence on large firms and highlights the vulnerability of the extensive network of subcontractors and consultancies.
Against this backdrop, the new Labour government is currently undertaking a ‘terms of reference’ review of the ambitious £20bn New Hospital Programme (NHP),

the NHS estate.
The review aims to put the programme on a ‘deliverable footing’.
At the same time, the Darzi Report has laid bare the challenges faced by the NHS, including a staggering £11.6bn in backlog maintenance and a pressing need to decarbonise healthcare estates.
Industry is reacting to Hospital 2.0, a template hospital system, which aims to standardise hospital design with repeatable rooms and a focus on dFMA, MMC, and offsite fabrication to increase speed and reduce cost.
The question is: does the UK have the capacity to overcome these monumental challenges? Or should we look at alternative models to ensure these critical infrastructures are delivered and built to last?
The ISG collapse underscores the potential over reliance on key players who, when they fall, take entire networks down with them.
This raises concerns about whether the construction industry has the capacity to deliver the NHP as currently envisioned.
While there are firms who might be willing to step in should businesses fail, a shift toward smaller, more-diversified project delivery could mitigate risks and prevent repeating past mistakes.
One solution is to rethink the scale of some healthcare projects, with the NHP shifting towards smaller, community-based health hubs located in our struggling high streets.
These facilities could bring healthcare closer to people’s homes, reducing the strain on large hospitals and offering earlier interventions in a community setting.
Health hubs could also play a crucial role in revitalising underused urban spaces, breathing life into failing high streets while delivering essential care.
As the Darzi Report states: “Performance standards are focused on hospitals, not on primary care, community services, or mental health.
However, while smaller health hubs may provide a solution for routine care and preventative services, they cannot entirely replace the need for large hospital facilities.
The increasing complexity of healthcare, particularly in areas such as cancer care and paediatrics, necessitates specialised facilities that smaller hubs simply cannot provide. Such is the case for Cambridge Children’s Hospital and Moorfields Eye Hospital, two large hospitals dedicated to specialised care for entire regions.
At White Arkitekter we are fortunate to be involved in recent healthcare projects that are pushing boundaries and innovation, with the aim of seeking new solutions to provide the UK with public health infrastructure that lasts.
Cambridge Children’s Hospital offers a glimpse into the future of integrated healthcare.



Bringing together two NHS trusts — Cambridge University Hospitals NHS Foundation Trust and Cambridgeshire and Peterborough NHS Foundation Trust — and the University of Cambridge, this project combines physical and mental health under one roof, alongside University of Cambridge research to treat the whole child.
The emphasis on both types of care, combined with state-of-the-art research, offers a new level of innovation as well as showcasing the benefits of collaboration across sectors to provide healthcare that is fit for the future.
Another approach to delivery is looking at alternative financing models.
Given the mixed legacy of PFI, there is understandable scepticism about returning to public-private financing models. Nevertheless, public-private partnerships can play a valuable role in delivering

healthcare infrastructure.
The Velindre Cancer Centre in Cardiff provides an example of how this can be employed.
In this case, the Welsh Government adopted the Mutual Investment Model, a public-private partnership (PPP), allowing the project to be jointly financed.
PFI may have left many NHS trusts burdened with debt and facilities difficult to maintain, yet, as the Velindre Cancer Centre shows, when structured properly, and with careful management, PPPs can still provide viable financing solutions.
The key is in ensuring that these projects are designed with sustainability, flexibility, and long-term resilience in mind.
The NHS has made significant progress in addressing sustainability, particularly through its net-zero standard, but decarbonising the estate remains a monumental task.
With £11.6bn in backlog maintenance, retrofitting existing hospitals will play a
critical role in meeting these targets.
And transformation of existing building stock has to be carefully considered.
Successful projects, such as the Bromma Hospital in Stockholm, demonstrate how the transformation of existing buildings can deliver high-quality healthcare environments, sustainable design, and stimulate the circular economy.
The integration of low-carbon and lowenergy design strategies, from the earliest stages of design, combined with the use of technology to track energy performance, will be essential to decarbonising the NHS estate.
As the UK embarks on the next stage of the £20bn New Hospital Programme, the evidence is clear: the healthcare system needs to be decentralised. It must adopt a more-flexible, diversified approach to project delivery that embraces collaboration, creativity, and innovation, and not rely on the monopolisation of large construction firms to deliver vital public infrastructure. n

Heriot-Watt University research calls for greater involvement of people living with dementia in building design
People living with dementia should have more power and creative freedom in collaborative design projects, new research from Heriot-Watt University suggests.
This includes using their own ideas and actions to shape, lead, and deliver projects, rather than always having projects given to them.
Dr Euan Winton, a design expert at the University’s School of Textiles and Design in Galashiels in the Scottish Borders, has proposed a new framework that outlines this way of working.
It follows six years of working with members of an Alzheimer Scotland Dementia Resource Centre who designed projects and services including printed textiles, ceramics, tabletop gardens, lighting, travel postcards, sculptural signage for a community allotment, and a photo scanning service.
Collaborative design — shortened to co-design — helps communities and groups contribute to design projects with guidance from professional designers.
And it is a growing field in settings
including health, community development, innovation, public sector, and charities.
But there are huge variations in the extent to which participants are involved in these projects, Dr Winton argues.
His research paper, The co-design participatory power pyramid, formally defines these different levels of involvement and illustrates them as a pyramid with four layers — ‘to’, ‘for’, ‘with’, and ‘by’, with ‘to’ at the base of the pyramid and ‘by’ at the top.
“Good collaborative design is about helping people play a significant role in rethinking things that inform or shape their lives,” he said.
“And really that should mean you’ve collaborated on more than 50% of the project.
“Your thoughts, your actions, your ideas, and the content you generate is important and you should have quite a bit of agency in making changes.
“We see a lot of co-design projects being done to, for, or with participants. But the most-empowering model is co-design ‘by’
— when designs for products or services are generated entirely by people living with dementia.
“It’s about reinforcing the idea that people need to be recognised for what they can do, recognised for having rights, and that they should be listened to.”
Dr Winton’s maternal and paternal grandmothers both had dementia.
Co-author, Paul Rodgers, Professor of Design, Manufacturing and Engineering Management at the University of Strathclyde, also had dementia.
Dr Winton started his research as part of a PhD focused on design for dementia and over six years has worked on collaborative design projects with around 20 members of the Glasgow Dementia Resource Centre, which supports people with dementia and is run by Alzheimer Scotland, Scotland’s national dementia charity.
The participants were aged between 40-70 and diagnosed with early-onset dementia, when symptoms develop before the age of 65.
The research included walking tours and visits to museums and art galleries with people living with dementia to get ideas for designs.

We see a lot of co-design projects being done to, for, or with participants. But the most-empowering model is co-design ‘by’ — when designs for products or services are generated entirely by people living with dementia
“One of the very first conversations I had was with a man who said he used to quite like photography, but no one would give him a camera these days,” Dr Winton said.
“I replied — that’s the first thing I’m going to do when we go out walking. You’re all going to have cameras — and will be collecting the images and things that inspire you.”
The inclusive approach, which also involved working with a dementia group in Edinburgh, generated 15 design projects which are outlined in the research paper.
And some of the products created were sold in a pop-up shop in Glasgow and the projects overall promoted ‘self-belief’, ‘free thinking’, and a ‘stronger sense of capability, belonging, and independence’.
The products and services that were co-designed by people living with dementia include:
• Printed textiles inspired by murals in Glasgow of comedian Billy Connolly. These were turned into products including cushions, bags, and lampshades
• Ceramic plates with face designs inspired by a ‘floating head’ exhibit at the Kelvingrove Art Gallery and Museum in Glasgow
• Tabletop gardens inspired by outdoor walks that the participants designed and created themselves
• A decorative light inspired by Charles Rennie Mackintosh, made with coloured lighting gels
• A concrete sign for Bellahouston Park Allotments in Glasgow that was designed
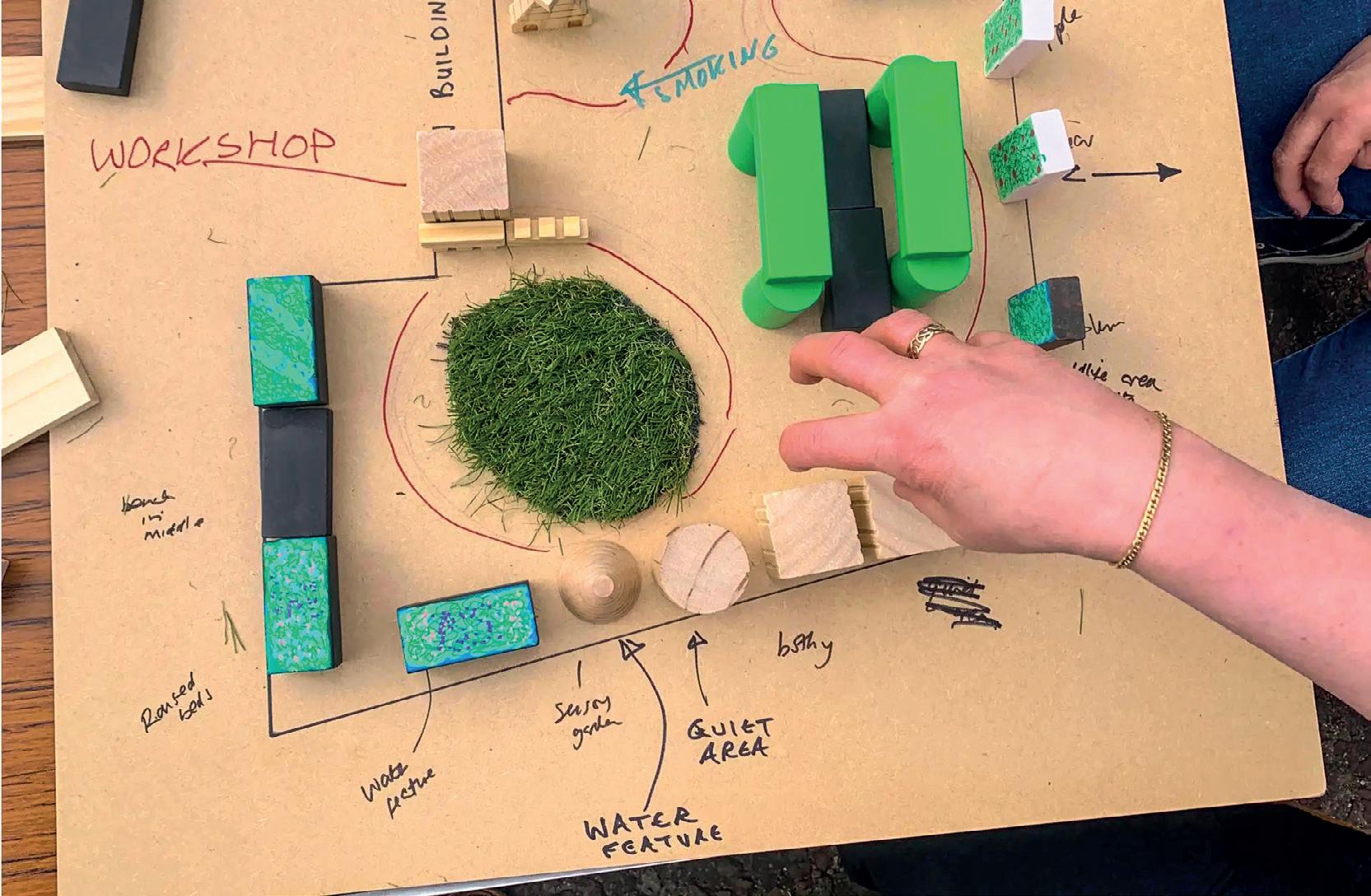
by the participants and then crafted by a stone specialist
• A photo scanning service to help other people living with dementia revive memories from old photographs
Dr Winton said the participants all took enthusiastic ownership of their projects and ‘regularly expressed elation’ with their abilities and a ‘sense of disbelief’ at what they had achieved. They also learned about design practices and took projects in their own direction.
The research paper concludes that people living with dementia should be involved as much as possible in as many stages of the design process as possible.
These stages include background research; developing the product design brief based on customer needs; generating ideas and concepts; developing technical drawings and prototypes and then detailed design, incorporating exploration of

materials and manufacturing techniques.
Dr Winton said the co-design participatory power pyramid could be applied to collaborative design projects in any sector.
And he is bidding for funding to further develop his research and presented his paper in June in Boston in the US to the Design Research Society, a learned society committed to promoting and developing design research. n

As Hythe and Dibden War Memorial Hospital celebrates its first anniversary, we look back at how the building has revolutionised the delivery of health and wellbeing services
Hythe and Dibden War Memorial Hospital has marked its first anniversary, having reopened to patients last year following a £10m rebuild. Bringing together previously-dispersed services including specialist dentistry, X-ray, physiotherapy, audiology, MSK, community maternity, and GP services; the building has enabled more than 52,000 appointments since its completion.
And at a recent ceremony patients and NHS staff spoke about the impact the new facility has had on care delivery.
Dr Nicky Sheppard, who works at the centre, said: “It has revolutionised my working day.
“I was able to visit two palliative patients in one afternoon and spend time with them
and their families, explaining what happens now and offering them support.
“I can’t remember the last time I had the time available to do that in the manner I can now.”
A patient at the centre added: “I was dealt with by a very friendly and efficient receptionist who gave me an appointment at Hythe Hospital.
“A practitioner saw me before my appointment and I picked up a prescription from the pharmacy. What an excellent service.”
The redevelopment was designed to provide the local community with a place that provides efficient, flexible, modern accommodation which houses existing services, as well as opening up new

opportunities, increasing integration and co-ordination of care, and reducing pressure on nearby hospitals, both now and in the years to come.
The project involved collaboration across a number of organisations, including NHS Property Services (NHSPS), Hampshire and Isle of Wight Integrated Care Board, Kier, GBP consultants, and the NHS providers who use the building, including the local Primary Care Network, Southern Health NHS Foundation Trust, and University Hospitals Southampton NHS Foundation Trust.
Various local commissioning and estate strategies highlighted the need to redevelop Hythe and Dibden War Memorial Hospital, finding:
• The site needed major repairs and upgrades to continue offering quality patient care, particularly since the inpatient beds closure in April 2010
• The outpatient facility was not suitable to deliver modern standards of care
• Void space was costing the CCG £186,000 per year and there was no demand for this space
• Lack of strategic oversight and service integration was not meeting the needs of the local population
The project was identified as a priority due to the escalating healthcare needs of the 80,000-plus population within the Totton and Waterside area, coupled with the outdated and non-compliant state of the existing facilities.
As well as improving site quality, there was also a significant opportunity for streamlining operations and achieving cost efficiencies.
Sustainability was a key decisionmaking factor throughout the design and construction phase, aligning with the NHS goal of achieving net zero carbon by 2040. As such, the project received a BREEAM ‘Excellent’ rating.
NHSPS and West Hampshire Clinical Commissioning Group (WHCCG) pro-actively looked for a solution, intensifying efforts to deliver a modern, fit-for-purpose, health and wellbeing centre for the community.
NHSPS’s portfolio optimisation team developed and assessed a range of options for the project, scoping out requirements and supporting the then Clinical Commissioning Group (CCG) through public consultation.
The decision was then taken to pursue a new-build option, rather than consolidating services into either of the existing buildings.
In the interim, the old hospital building was decommissioned, with all services run through the medical centre.
NHSPS’s town planning team supported the application, with planning consent granted in 2018. It then helped the CCG further develop its Outline Business Case to secure the funding, which was approved by NHS England in 2019.
Delays to project development and approvals caused construction costs to increase — for example, the impact of Brexit on the availability of materials and then the COVID-19 pandemic changing how contractors worked on site.
The £1m shortfall was bridged by NHSPS’s capital recycling scheme, with funds generated from the sale of surplus land onsite reinvested in the project.
NHSPS also worked with the CCG to secure additional Estates, Technology and Transformation funding (ETTF) to support the primary care expanded offering at the new hospital, which added an additional capital injection into the project.
NHSPS and WHCCG secured Full Business Case approval in June 2020.
The project progressed in two phases:
1. Pre-construction: Including site setup, ground surveys, the demolition of the old building and site preparation took around six months
2. Construction: The new build took around 19 months, slightly longer than planned due mainly to the COVID-19 pandemic NHSPS used the Southern Construction Framework (SCF) to ensure a local Tier 1


contractor undertook the works.
Ensuring each contactor possesses a regional office within Hampshire was a strategic decision by NHSPS to guarantee the chosen provider had a vested interest and commitment to the success of the project. A series of panel interviews were then held to assess the contractors’ proposals and capabilities, with Kier Construction selected to carry out the works.
The NHSPS construction lead held regular monthly meetings with the CCG and customer representatives to keep them up to date on activities, with key decisions undertaken via the steering board. Additionally, site visits were arranged for the CCG and end users to observe progress.
Particular challenges with the build included a significant slope and a well that both needed to be filled; the discovery of unknown services that needed to be moved, including underground electrical and gas supplies; and consultants and sub contractors which went into administration.
The COVID-19 pandemic also posed a significant challenge for the project due to restrictions on how many sub contractors could work on site at any one time, as well as adjustments to working practices to comply with Government regulations.
This included expanding the size of site offices and welfare facilities — incurring an additional cost to the budget of approximately £200,000.
In the first month of opening the hospital had 7,500 on-the-day appointments booked.
And the new hospital provides patients with direct access to more services, closer to home.
Additionally, provisions were made for mobile diagnostic services on the site, such as breast screening and MRI.
Designed to be inviting, inclusive, and built to the highest quality, the building creates a positive, welcoming experience for patients, visitors, and staff.
The hospital operates on a significantlyreduced footprint, making it more efficient.
And this enabled the release of surplus land for responsible disposal, which was sold to New Forest District Council for housing, and the proceeds were reinvested into the new build.
Through optimising space and employing flexible room booking and a seven-day schedule, the new facility can accommodate existing services while creating room for an expanded range of health and wellbeing services. n

Bob Wills, director of Medical Architecture, explores the idea of designing health services with less reliance on acute hospitals and more focus on integrated community facilities offering a more-holistic, preventative view of health and wellbeing
Published earlier in the year, a report by The King’s Fund offers a fresh perspective on a challenge that the national health service has faced for many years.
Titled Making care closer to home a reality, the report states that: “Since at least 1974, and arguably earlier, successive governments have aimed to make the health and care system less hospital focused and more focused on primary and community care.”
It cites the World Health Organization (WHO) in its view that this approach is the most-inclusive, effective, and efficient way to enhance people’s physical and mental health and wellbeing.
This is about ‘improving both the experience and the quality of care that people receive, while boosting prevention or, at the very least, reducing the speed of onset of disease. It is also about meeting people’s needs and making sure each part of the health and care system is freed up to
In terms of our approach to healthcare facility design, this is an important shift in thinking, and one that we have seen embraced in pioneering community health schemes in recent years
provide the care it is best placed to offer’.
Many of us will recognise this as a proactive, preventative approach to health, as opposed to a reactive, treatment-based approach, with care delivered closer to people’s homes.
Despite this long-held ambition, the report highlights a mismatch in action, with the proportion of Department of Health and Social Care spending on primary care falling in recent years from 8.9% in 2015-16 to 8.1% in 2021-22.
Similarly, while the NHS has received additional funding in recent years, acute hospital trusts have seen 27% funding growth since 2016-17, compared to community trusts, which have experienced just half that level of growth, at 14%.
The King’s Fund report goes on to suggest reasons for the lack of change, before setting out a solution for refocusing of the health and care system, which is detailed and far reaching, covering policy, leadership, funding, and workforce.
A critical element to this is cultural change: “The increasing complexity of people’s health and care needs requires an integrated, holistic response, rather than a ‘body part’ or single condition response.

“There needs to be more of a focus on people and outcomes, rather than processes and outputs”.
In terms of our approach to healthcare facility design, this is an important shift in thinking, and one that we have seen embraced in pioneering community health schemes in recent years.
One example where this approach has proven to be successful is The Jean Bishop Integrated Care Centre (JBICC) in Hull.
Prior to the project commencing, Hull and North Yorkshire ICB faced numerous challenges.
Hull had around 25,000 residents living with frailty, and 3,200 with severe frailty.
As a result, the health system was overwhelmed with non-elective hospital admissions, struggling to find beds for elderly patients amid peak admissions and growing demands from the aging population.
A 2012 study found that a third of older patients admitted to hospital in an emergency had no clinical need to be in a hospital bed, and that admission quickly reduced the ability for vital rehabilitation and reablement.
In response, and informed by engagement with residents, Humber and North Yorkshire ICS developed an anticipatory care model that completely redesigned the approach to create an out-of-hospital service to help people to stay at home and out of hospital.
We were commissioned to work with the stakeholders to develop the first facility which could deliver the care model effectively.
Adopting an entirely-new way of delivering health services, the centre brings together a range of specialist services to provide a more-holistic approach to health, care, and social support.
Unlike regular community health facilities, where patients receive assessment and treatment for a single health complaint or condition, at the JBICC patients receive a full physical and mental health check, as well as help with other social challenges. They may spend an entire day there, but they leave treated and with a care plan.
The type of facilities offered reflect this extended visit and include a café run by Inspire Hull, a charity which aims to improve physical and mental wellbeing through the development of friendships and feelings of purpose. Activities are curated which bring people together to tackle feelings of social isolation.
The therapeutic and non-institutional character of the design, with views to

gardens and landscape from many areas of the building, create a comfortable environment to support patients during these extended visits.
A recent study, led by researchers from the Wolfson Palliative Care Research Centre at the University of Hull, assessed the wellbeing of patients who received this more-holistic, person-focused assessment at the centre compared to those who did not.
It showed, for those living in their own home, a 15-20% reduction in emergency department (ED) attendances and a 1025% reduction in emergency admissions for the 12 months after their assessment compared to the 12 months prior.

their assessment, there is consistently over-50% reduction in ED attends and admissions in the following 12 months.
Also, for residents in care homes, there has been a 20-25% reduction in ED attends, and for the frail cohort who had more than five ED attends in the 12 months preceding
Clearly then, long-term investment in the right kind of community-focused facilities can reduce demand for acute services and bring about savings to the wider healthcare system, as well as improving the wellbeing of individuals.


The King’s Fund points to a need to invest in primary and community healthcare estates to promote joined-up, integrated working locally between public partners across health, social care, and community services.
However, despite a number of recent initiatives to bring forward innovation in the delivery of community health, investment remains weighted towards capital investment in acute services, with the New Hospital Programme a prominent example.
The Cavell Centre programme, named after Edith Cavell, a British nurse during World War I, is one such initiative that looks to the future.
The programme began after Medical Architecture, with John Cooper Architects, proposed the development of a blueprint for the transformation of primary and community care facilities in England.
Developed with NHS England and NHS Improvement (NHSE/I), the aim was
to optimise and standardise the briefing, planning, and design process to allow the business case process to be streamlined, increasing quality and reducing design costs at each project stage.
The proposed ‘Cavell Centres’ that emerged pioneered an approach to standardised-yet-adaptable planning, with a specific approach to MMC, net-zero carbon design, and high-quality patient environments for health and wellbeing.
Following on from this work, we were commissioned alongside Passivhaus design specialist, Architype, to co-design one of six pilot schemes for the programme, and the only one to be designed to Passivhaus standards.
Like The Jean Bishop Integrated Care Centre, the strategic vision for the Cavell Centres recognises that social factors in health are as significant as clinical factors, and therefore
We are hopeful that initiatives such as the Cavell Centre programme will be able to demonstrate the benefit of a long-term investment in a preventative approach to healthcare in relieving pressure on an already-overstretched system
combines both models to pro-actively address the barriers to improved community health and wellbeing.
This formed a central feature of the pilot scheme design.
Setting a new standard for community health facilities, the building hosts a varied health and wellbeing offering, including multiple GP practices, community diagnostics, therapy services, outpatient services, third-sector social prescribing organisations, and a health-centred commercial offer.
The building is designed to be highly flexible to allow this mix of services and tenants to adapt over time.
Strong internal connections to quality external landscaping with lawns, planting, and water features; and inviting, noninstitutional internal spaces; enable a variety of wellbeing activities. This, combined with access to local authority support, links patients with opportunities for social prescribing, integrating health and wellness into the community.
Currently, NHSE has paused the development of the project business cases to focus on developing the programme business case ahead of a bid for capital funding for the programme at upcoming spending reviews.
We are hopeful that initiatives such as the Cavell Centre programme will be able to demonstrate the benefit of a long-term investment in a preventative approach to healthcare in relieving pressure on an already-overstretched system.
In its report, The King’s Fund describes ‘hierarchies of care’ — urgent problems taking priority over longer-term issues — as a reason for underinvestment in community healthcare. For example, treatments for urgent medical problems taking priority over services that prevent the development of problems.
It recommends that leaders need to be clear about why a change in focus is needed ‘which is to deliver improved care and improved outcomes, and to ensure the health and care system is sustainable for the future, rather than to deliver cost savings in the short term’.
Clearly, the challenges the health service faces are complex and multifaceted, and no quick solution exists. However, successful pioneering projects like The Jean Bishop Integrated Care Centre demonstrate the value of a person-focused, preventative approach, which the Cavell Centre programme is well placed to continue, if funded as a priority. n
• This article was first published in Architect’s Datafile magazine in May 2024.


Serco has retained its contract to provide soft facility management (FM) services that support the delivery of care for patients at Forth Valley Royal Hospital for the next seven years.
The contract follows a comprehensive market test exercise conducted in partnership with Forth Health and NHS Forth Valley.
Serco has been responsible for providing both soft and hard FM services at Forth Valley Royal Hospital since 2010.
The latest award will see the company continue to provide soft FM services, including cleaning, catering, and portering services at the hospital for a further seven years, while the provision of hard services, including building maintenance, will continue through to 2042.
Petra Moss, managing director of Serco’s health business, said: “We are delighted to have been given the opportunity to continue to support patient care with the provision of soft services at Forth Valley Royal Hospital.
“We have provided these services, along with hard services, since 2010 and are extremely proud of our team which performs a challenging and difficult role with great professionalism.
“We believe that our approach and values

make a real impact and bring about positive change for patients, supporting their recovery when they need it the most.”
Forth Valley Royal Hospital is the only acute hospital facility serving the local community across Forth Valley.
And Serco’s primary purpose is to provide a
NTW Solutions has taken over the operation of estates services across Cumbria from Cumbria, Northumberland, Tyne and Wear NHS Foundation Trust (CNTW).
While the estates team has been part of CNTW for some time, this latest move will further enhance the management and maintenance of key healthcare facilities such as the Carleton Clinic near Carlisle.
Improvements include the introduction of an online proactive and reactive maintenance system.
An NTW Solutions spokesman said: “The response from clinical teams has been fantastic and they have already seen an improvement in the condition of the site.
“One unexpected consequence has been that more maintenance requests were coming in as staff see an improvement in the responsiveness.
clean, safe, and well-maintained environment for patients, visitors, and staff.
The company has a team of 750 people who deliver a 24/7 service, 365 days a year.
In addition the team also provides full patient catering to NHS Forth Valley’s four community hospitals.

“It is a positive step forward and hopefully the start of a virtuous cycle of improvement of the estate.”
includes maintaining hospital buildings, ensuring compliance with safety standards, and creating a better environment for both patients and staff.
“The transition will bring about more-
NTW Solutions is a subsidiary of CNTW and was established in 2017. It now provides a wide range of support services, including estates management to partners in the NHS and beyond.




In response to the increased demand for oxygen supplies following the 2020 COVID-19 pandemic and the subsequent rise in respiratory-related conditions, Jacksons Fencing recently completed a key project to safeguard vital oxygen storage facilities at a leading UK hospital.
The COVID-19 pandemic highlighted the critical role of oxygen in treating patients, leading to a surge in its use across hospitals.
Some facilities even declared major incidents due to oxygen shortages, prompting a significant government investment of over £15m to upgrade oxygen supplies and prevent future disruption.
As part of these improvements, many larger hospitals now feature onsite liquid oxygen storage facilities, where vast industrial tankers convert liquid oxygen to gas as needed.
But, given the stringent safety requirements associated with liquid oxygen – due to its extremely-low temperatures, precise pressure needs, and related fire and explosion risks – securing and managing these supplies is paramount.
To address these needs, Jacksons Fencing provided and installed a comprehensive security solution for a new oxygen storage compound.
The installation includes 38m of Securi-Mesh fencing, standing at a height of 2.4m.
This is mounted on concrete hardstanding and is complemented by two cantilever sliding gates and a single-leaf pedestrian gate with a pushpad exit and key entry.
Securi-Mesh fencing features a tightlywoven mesh pattern designed to deter climbing attempts, and its small apertures significantly improve resistance to cutting.
Additionally, the mesh provides an ‘invisible screen’ effect that allows for effective

The cantilever sliding gates installed are particularly well suited for the restricted space in front of the facility.
Unlike traditional swing gates, these slide parallel to the fenceline, requiring minimal space both in front of, and behind, the fence.

This design not only maximises space efficiency, but also enhances security, with quick operational cycles, allowing for faster vehicle and goods transit, reducing the time the gates remain open and minimising security risks.
Furthermore, the absence of ground tracks for the cantilever gates reduces maintenance needs by preventing issues related to debris or track damage, leading to fewer repairs and reduced downtime.
In addition to these features, the fencing and gates are backed by a 25-year guarantee, ensuring long-term durability and minimal maintenance.
And the green polyester powder coating provides extra corrosion resistance and contributes to lower long-term costs for the hospital.
Sections of the fencing, installed at varying heights, are further secured with a Barbican vertical bar fan panel, which offers both a physical barrier to intrusion and a visual deterrent.
Peter Jackson, managing director of Jacksons Fencing, said: “The pandemic highlighted the crucial role of oxygen and we must safeguard these resources effectively.
“The integration of our Securi-Mesh fencing and cantilever sliding gates reflects our commitment to providing both superior protection and operational efficiency.
“By addressing the specific security needs of these vital resources, we help ensure that hospitals can focus on delivering high-quality patient care without disruption.”
The World Health Organization (WHO) has published a new operational guide for managing infectious diarrhoea in healthcare settings.
The guide is intended for hospital administrators, water sanitation and hygiene specialists, food safety and nutrition service managers, infection prevention and control professionals, occupational health managers, and health and care workers.
It is structured into three parts: water, sanitisation and hygiene (WASH) and waste management; food safety management; and infection prevention and control.
Detailed procedures are set out as each of these areas requires dedicated planning, staffing, training, and resources to mitigate the entry points, transmission risks, and reservoirs of infection that can cause infectious
diarrhoea in healthcare settings. The key messages of the guidance are to:
• Evaluate and improve water, sanitation and hygiene (WASH) infrastructure and waste management systems
• Implement food safety management measures for safe handling, preparation, and serving of food
• Screen all patients — inpatient and outpatient — for diarrhoea
symptoms upon initial contact in any healthcare setting and use contact precautions when infectious diarrhoea is suspected
In addition to the detailed sections on these key messages, the operational guide also has sections on health and care training — monitoring and exposure management, and healthcare-associated infection (HCAI) surveillance.

Inside issue 03, May-June 2024
• Milestone for £85m maternity hospital development in Belfast
• Spotlight on best practice for dementiainclusive design
• Framework agreements provide support for next-generation healthcare buildings
• Designing mental health facilities closer to home Scan to read now

Inside issue 04, July-August 2024
• Advocating a simpler approach to the healthcare planning process
• The implications of a new accountancy treatment on NHS leases
Inside issue 05, September-October 2024
• Contractor appointed to build £15m community health centre
• Keyworker housing model supports recruitment and retention of staff
• Investors and property developers remain interested in health and care sector

Helping care companies with the growing need to be sustainable by improving efficiency in the supply chain has been a mission for Kerry Southern-Reason, chief executive of the Care Home Interiors Group. Here, she speaks about how her latest company, Care Home Rental Furniture, is doing just that
Waste is a huge problem; we only have to turn the news on to see the devasting sights of waves of plastic washing up on beaches right around the world.
However, closer to home, our obsession with the throw-away culture is contributing to tonnes and tonnes of unnecessary waste entering landfill. From waste food, packaging, clothing — you name it.
Shocking statistics reveal that an average of 22 million pieces of furniture are discarded per year in the UK, much of which goes straight to landfill.
And annual statistics produced by the Wood Recyclers’ Association show that the amount of waste wood processed in the UK rose from 4.17 million tonnes in 2021 to 4.31 million tonnes in 2022.
In the care home sector, we have to try and do our bit and adopt more-sustainable and environmentally-friendly supply chain practices to stop this.
Care homes face a pressing need to offer their services in top-notch facilities.
But worn-out fabrics, chipped and scratched furniture, and overall dated interiors will not cut it in this increasinglycompetitive market.
Even worse, once a care home has got to this dishevelled level, a dip in occupancy tends to follow, and once that happens it
becomes very hard to secure the necessary funding to invest in its refurbishment.
In fact, many care providers are discovering that funders require moresustainable fit-out strategies for a chance of securing funding. Between a rock and hard place sustainable practices become a pipe dream for most as they balance limited resources with offering the best service in the conditions they have.
…once a care home has got to this dishevelled level, a dip in occupancy tends to follow, and once that happens it becomes very hard to secure the necessary funding to invest in its refurbishment
Between a rock and hard place sustainable practices become a pipe dream for most as they balance limited resources with offering the best service in the conditions they have

New care home constructions have the luxury of prioritising eco-friendly designs and materials.
Incorporating efficient floorplans, optimising insulation, and sustainable energy features such as solar panels and motion sensor LED lighting, can lower energy consumption and costs.
Additionally, sustainable building practices can enhance the overall wellbeing of residents by creating healthier living environments with improved air quality and natural light.
Whether starting from a blank canvas or retrofitting, we have focused on being more supportive of sustainability goals.
Mindful of the cost pressures operators face, we have developed a service that can reduce direct costs while enabling greater efficiency of resources via a renting model.
Our rental system from Care Home Rental Furniture not only allows care homes to upgrade without the high costs associated with refurbishment, but also helps reduce their environmental footprint.
With this model, care homes benefit from timeless designs that never date, and our furniture is manufactured in the UK and FSC certified, so also benefits from a waste-avoidance approach through our ‘repair and reuse’ approach.
With its 30-year lifecycle, the furniture is tough and robust, more so than general domestic furniture, and is offered with a five-year refurbishment service where a technician will remove and repair scratches, chips, dints, and any other defects.
The additional bonus of leasing is it doesn’t affect EBITDAR (earnings before interest, taxes, depreciation, amortisation, and restructuring or rent costs) due to new accounting reporting of leases.
The furniture is refurbished in our UK solar-powered workrooms, stripped back to its bare bones, resprayed, and offered back into the market for use.
This approach not only provides modern and fit-for-purpose furniture, but also embodies the very essence of re-using and recycling.
And it dismisses the concept of singleuse furniture and represents good value for money above anything else.
Environmentally-friendly supply chain management can be achieved in many ways. But this method ensures products are sourced from suppliers that meet a strict eco criteria, reducing energy use and minimising waste.
By embracing these practices, care homes can make significant steps in reducing their environmental impact while improving the quality of the environment they provide care in.
Implementing a greener purchasing strategy, optimising supply chains, and adopting a holistic approach to caring for the environment are essential steps toward a more-financially-sustainable future for the care sector.


Mindful of the cost pressures operators face, we have developed a service that can reduce direct costs while enabling greater efficiency of resources via a renting model
For those who live in care homes, don’t they deserve to live in a home that’s well furnished?
This model ensures a comfortable space that is consistently updated to meet modern standards, contributing to a better quality of life. n




University Hospital of Hartlepool will harvest energy from the ground and sun to power the site
Ahospital in Teesside will become one of the first in the country to use greenfriendly technology to heat the site.
The University Hospital of Hartlepool will use a combination of renewable energy from the ground and from the sun to provide heating and electricity.
Work has begun to drill deep boreholes into the ground for a new ground-source heat pump system, which collects energy from water stored in an aquifer.
And solar panels will also be installed on the building’s roof and to the back of the site to provide electricity for large periods of the year.
When the works are completed by contractor, Veolia, over the next year, the hospital is anticipated to meet its NHS 80% carbon reduction target ahead of schedule.
North Tees and Hartlepool NHS Foundation Trust has been granted more than £13m funding to help carry out the improvements.
Steve Taylor, group director of estates for the trust, said: “These works will make the University Hospital of Hartlepool one of the first in the country to use an aquifer-based ground-source heat pump system.
“This involves a mix of the latest renewable technology and local geology to help heat the building for many months of the year.
“Solar panels are also going to be included to give green electricity to the building and reduce the need to import electricity from the Grid.
“These improvements will mean we are making huge reductions to our carbon footprint, while providing the best care for our patients and protecting our environment for our local community.”
The new scheme will combine a 1,400kW ground-source heat pump system, with a 70,000l thermal store.
The works will also include upgrading the hospital’s air handling units and installing new LED lighting.

To make a real difference and limit the damaging effects of climate change needs innovation, and this latest hospital upgrade shows what we can do for the vital healthcare sector …
John Abraham, chief operating officer for industrial, water, and energy at Veolia, said: “We have been delivering energy management to University Hospital of Hartlepool for over 20 years, and this new project will further extend efficiency and the carbon savings.
“To make a real difference and limit the damaging effects of climate change needs innovation, and this latest hospital upgrade shows what we can do for the vital
healthcare sector as part of our Green Up strategic programme.
“This will help the NHS meet the net zero target and we look forward to working in partnership with the teams at Hartlepool and achieving their environmental goals.”
The funding was approved last year by Salix, an organisation which administers funds on behalf of the Department for Energy Security and Net Zero. n

Relocation and replacement of cooling infrastructure on mission-critical live data centre at the Royal Free Hospital
Secure I.T. Environments Ltd (SITE) has completed an air conditioning upgrade project on the main mission-critical data centre at the Royal Free Hospital, part of the Royal Free London NHS Foundation Trust.
The project, which was completed in nine weeks, was commissioned to replace endof-life cooling infrastructure and improve the energy efficiency of the data centre.
Originally built in 2010 by Secure I.T. Environments, the data centre serves the Royal Free Hospital’s patients receiving acute and specialist services, including hundreds of transplant patients.
As part of the project the existing cooling infrastructure was removed and replaced with four GEA 18D Multi-DENCO down flow close control direct expansion air handling systems and four DENCO ambient aircooled condensers.
The new installation now achieves PUE values of 1.15 or less.
This solution also achieves a sensible heat ratio (SHR) of 1.0, meaning that air is cooled
without dehumidifying it.
This combined optimised use of the inverter compressor, electronic expansion valve (EEV), and fans as part of the climate control system, reduces energy costs, improves energy efficiency, and extends the life of the humidifier cylinder.
The changing cooling requirements of the data centre meant the relocation of the external condensing units needed to be housed in a completelydifferent location. This required considerable effort to ensure compliance with building and planning regulations, including acoustic surveys and aesthetic considerations.
The condensers are now located outside on a balcony away from existing services, requiring the installation and weatherproofing of new pipework and ensuring it would be accessible and safe for ongoing maintenance.
Commenting on the project, Chris Wellfair, projects director at Secure I.T. Environments, said: “At all times we had to

consider that this was a fullyoperational hospital, with a tight project window.
“We installed temporary cooling to ensure concurrent maintainability of existing services at all times, as well as carefully managing all logistics through multi-departmental planning at the trust across
SITE will now embark on a project to implement cold aisle containment in the same data centre and provide UPS and AC upgrades at another.
Secure I.T. Environments also provides ongoing maintenance support for five rooms at the trust. n
Two health trusts are among 33 schemes to benefit from a £2.7m moneypot aimed at optimising heat networks across England and Wales.
Croydon Health Services NHS Trust and Hywel Dda University Health Board in Wales will share in the cash, awarded to heat networks in the sixth round of funding allocated under the Government’s Heat Network Efficiency Scheme (HNES).
The revenue funding will support studies to identify issues with efficiency levels at Croydon University Hospital and Bronglais Hospital respectively.
Minister for Energy Consumers, Miatta Fahnbulleh MP, said: “Heat
network customers should be able to expect a good-quality service — delivering regular, reliable heating and hot water.
“Today’s £2.7m funding boost will transform 33 old and inefficient heat networks across the country.
“This is part of our wider efforts through the Heat Network Efficiency Scheme — with more projects set to benefit in the near future.”
Louise Singleton, principal consultant at Gemserv, added: “It is great to see HNES continuing to provide vital funding to old, inefficient heat networks across England and Wales.
“It is particularly encouraging to see applicants being proactive once receiving the output of their HNES-funded optimisation studies.”

New strategy will radically cut the number of single-use medical devices in the health service
The Government is launching a major crackdown on waste in the NHS to save millions of pounds a year, helping to divert more resources to frontline care.
The Design for Life roadmap is being published to radically cut the number of single-use medical devices in the health service and reduce the reliance on foreign imports.
Disposable medical devices substantially contribute to the 156,000 tonnes of clinical waste that the NHS produces every year in England alone.
And the roadmap paves the way to slashing this waste and maximising reuse, remanufacture, and recycling in the NHS.

jobs and help transform the country into a life sciences superpower.
As it stands, millions of devices, such as walking aids and surgical instruments, are thrown away after just one use.
Harmonic shears — surgical devices which seal patients’ wounds using ultrasound waves — each cost more than £500 and around 90% of them are binned after a single use.
But innovative companies are already purchasing these used devices and safely remanufacturing them at a lower price.
The Government will now encourage more of this kind of innovation to safely remanufacture a wider range of products and drive costs down, including by changing procurement rules to incentivise reusable products and rolling out examples where hospitals are already leading the way on cutting wasteful spending and practices.
Approximately £10bn a year is spent on medical technology like this in the NHS, but too much of it is imported via vulnerable
routes that risk disrupting patient care.
A Circular Economy Taskforce has already been created to foster more highly-skilled green jobs and smarter use of our resources.
An economy-wide shift to a circular economy could add £75bn to the economy and create 500,000 jobs by 2030.
Health and Social Care Secretary, Wes Streeting, said: “The NHS is broken. It is the mission of this government to get it back on its feet, and we can’t afford a single penny going to waste.
“Because the NHS deals in the billions, too often it doesn’t think about the millions. That has to change.
“This government inherited a £22bn black hole in the public finances, so we will have a laser-like focus on getting better value for taxpayers’ money.
“Every year, millions of expensive medical devices are chucked in the bin after being used just once. We are going to work closely with our medical technology industry to eliminate waste and support homegrown MedTech and equipment.”
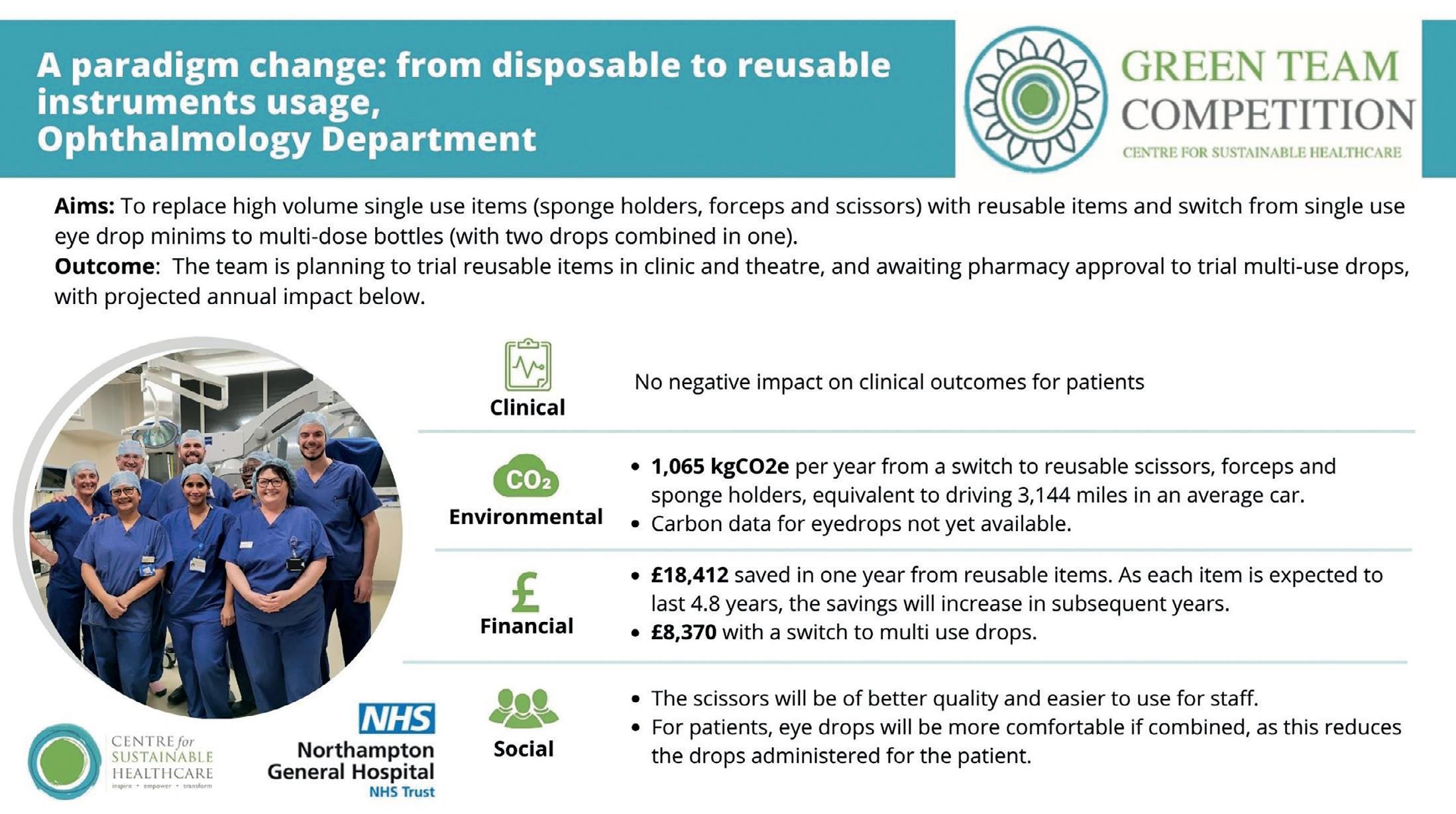

The below case studies illustrate the potential savings:
• Mid Yorkshire Teaching NHS Trust uses 330,000 single-use tourniquets in a year, but a single reusable tourniquet can be used 10,000 times. In a one-year trial, reusable alternatives saved £20,000 in procurement costs and 0.75 metric tonnes of plastic waste
• At Northampton General Hospital NHS Trust, a single ophthalmology department saved 1,000 pairs of disposable scissors and £12,000 in a year by switching to reusable pairs. Single-use scissors are often used in surgical settings and NHS procurement data shows that several million pairs of single-use scissors were purchased by the NHS in a single year (2022 to 2023). That is the equivalent of hundreds of pairs of scissors thrown away every hour
• The Leeds Teaching Hospitals NHS Trust saved £76,610 in costs purchasing 604 remanufactured electrophysiology (EP) catheters, and generated a further £22,923 for selling used devices for collection. If the same approach were to be scaled up across the UK, the NHS could save millions of pounds per year on EP catheters alone, just a few product lines among hundreds of thousands
• Harmonic shears are complex devices for performing surgical procedures and cost more than £500 each, yet around 90% are binned after a single use. The
Leeds Teaching Hospitals NHS Trust has demonstrated that companies can safely remanufacture them, giving up to 50% cost savings
The Design for Life programme will reduce this kind of waste and achieve an NHS-wide move to sustainable alternatives — also supporting the Government’s net zero goals.
The new roadmap sets out 30 actions to achieve this shift, including how the Government will work with companies to encourage the production of more-sustainable products, along with training for NHS staff on how to use them.
Taking this approach will mean more money can be spent in the UK, driving growth and creating more engineering, life sciences, and research jobs, all while securing savings for the NHS budget.
Many of these products include precious metals such as platinum and titanium, which are in high demand but go to landfill when they could be recovered and sold.
A reduction in the amount of disposed single-use devices will also reduce the country’s carbon footprint and plastic pollution.
The Government will encourage industry figures to innovate by making sure benefits of reusable MedTech are part of how the NHS chooses the products it buys.
Health Minister, Baroness Gillian Merron, recently visited University
College London Hospital, a member of the Circular Economy Healthcare Alliance, which advocates for sustainable practices within the NHS.
She said: “Design for Life doesn’t just deliver on the Health Mission, to build an NHS fit for the future, it also delivers on our Growth Mission to make the UK a life science superpower and our commitment to get the NHS to net zero by 2045.”
During her visit she toured a mock operating theatre and was shown various sustainable products its NHS staff use — from simple products like gowns and scissors to sophisticated, expensive products like harmonic shears.
Professor Sir Stephen Powis, national medical director of NHS England, said: “While the NHS is treating record numbers of patients, we know there is much more to do to ensure taxpayers get value for money.

worth of efficiency savings last year and is targeting a further £9bn of savings for 2024/2025. But we are rightly still looking for ways to get our money’s worth for every penny we spend.”
The Design for Life programme was
from the UK MedTech industry, the health and care system, and research organisations. It forms part of the Government’s ambition to transform the UK into a life sciences superpower and ensure sustainability. n
Soft plastics donated by Tesco have been recycled into decking and accessible picnic tables for the grounds of John Scott Health Centre in north London.
Tesco, Veolia, Groundwork, and NHS Property Services (NHSPS) have joined forces to recycle soft plastics into outdoor furniture for upcoming social prescribing green spaces.
Since 2019, NHSPS has delivered 100 hubs and gardens across the country with the aim of promoting community wellbeing and connectivity through naturecentric environments.
And over six tonnes of soft plastics – or 155,500 individual items – were donated by Tesco and transformed into a sustainable 100%-recycled plastic lumber, known as Smartawood.
This lumber was accredited by BBA with a life expectancy of 120 years, requires little maintenance, and is designed not to rot or rust.
Overall, this process resulted in approximately 15.5kg of CO2 savings.
John Scott Health Centre was the first purpose-built medical centre in Britain and was once home to an active gardening group which lost its space to a pop-up vaccination centre during the COVID-19 pandemic.
Now NHSPS has reinstated the garden area, making it a welcoming and usable area with decking and accessible picnic tables.
Further projects are planned at Maghull

something new that will benefit communities and help give young people a stronger start in life.
Dr Min Rodriguez, head of social impact at NHSPS, said: “This collaboration highlights the potential of innovative partnerships to not only create vibrant spaces for public benefit, but also to drive positive change in healthcare and environmental sustainability. And it’s particularly special that we are repurposing soft plastics instead of increasing waste.”
Tony McElroy, Tesco head of campaigns, added: “It’s fantastic to see the soft plastic that our customers are returning being turned into
“It’s still our absolute priority to remove and reduce as much plastic as possible and make sure everything we use is recycled and kept out of the environment.”
And Adam Wylie, managing director of commercial at Veolia, said: “Utilising recycled materials in green spaces and collaborating across private and public bodies to deliver these social prescribing gardens is a testament to how we can, and must, all work together to deliver ecological transformation.”

Specialist healthcare property investor and developer, Assura, has appointed Steven Noble to the newlycreated role of chief investment officer (CIO) to support the business’ short and long-term growth strategy.
Noble joins the business immediately and will be responsible for implementing Assura’s investment strategy across all healthcare markets, including delivery of capital recycling initiatives.
He was most recently chief investment officer at Atrato Group, the investment adviser to Atrato Onsite Energy (ROOF) and
Supermarket Income REIT (SUPR), where he negotiated and executed over £2bn of property transactions and played an important role in taking SUPR from IPO to the FTSE250.
Prior roles include nine years at Lloyds in origination and risk management with a focus on commercial real estate, and KPMG where he qualified as a chartered accountant.
Jonathan Murphy, Assura chief executive, said: “Steven’s appointment is an important strategic step for Assura to support our ambitious growth plans.
“The UK healthcare crisis continues to worsen, with an immense need for improved access to healthcare services across the country.
“These factors are driving demand for infrastructure across an increasingly-diverse range of healthcare markets, to which Assura is best placed to respond owning to

Aura Care Living has appointed two new senior figures to its award-winning group.

The care and retirement specialist, which has sites in Cirencester, Gloucestershire, and Camberley in Surrey, has brought in Richard Scarth as its new chief operations officer, and Colleen Joubert as the care home general manager.
They will both operate from Cirencester’s Stratton Court Retirement Village and Care Home.
Scarth has over 20 years experience within the health and social care sector and previously held senior positions with Sunrise Senior Living, Barchester
Healthcare, and Care UK.
Between 2015-2022 he broadened his experience by working in the NHS at director and chief executive level, during which time he was instrumental in developing schemes to support the patient journey from acute care into residential and nursing care.
Most recently, he left the NHS for an operational role within a fire and rescue service and currently splits his time between life on shift and time spent driving the provision of the highest-possible standard of care at Stratton Court.
He said of his new position: “My greatest passion is making a difference to people living with, and families affected by, memory loss and dementia.”
Joubert qualified as a nurse 28 years ago before going on to become a community nurse, midwife, and psychiatric nurse.
She said: “My passion is palliative care; I truly believe that everyone deserves a dignified death.
“I’ve been a turnaround home manager for 17 years, assisting providers to receive good and outstanding outcomes for their homes.
“I enjoy the challenges of finding solutions for problems and ensuring all staff are empowered to deliver the highest quality of care.”
our market position, sector expertise and capabilities, and our strong corporate culture.
“Steven’s skills and expertise will complement those already within the executive committee to deliver against this demand and our long-term growth strategy."
Noble adds: “I am delighted to be joining Assura at such an exciting time, with the business strategically positioned to capture the significant growth opportunities across broader healthcare markets.
“The business’ recent acquisition of 14 private hospitals and its JV with USS are a clear indication of the group’s ambition and I am incredibly excited to be part of Assura's next stage of growth.
“I look forward to working as part of an exceptionally-skilled and experienced team at the UK’s leading listed healthcare property investor.”

The Welsh Government has seen its third cabinet reshuffle this year, including a new Cabinet Secretary for Health and Social Care.
Mark Drakeford, former First Minister, has now left his role as interim health secretary, with Jeremy Miles being instated as health minister.
Miles, a Labour Co-op politician, moves from the role of Cabinet Secretary for Economy, Energy and
He also ran in the Welsh Labour Leadership election at the end of last year, but was ultimately defeated by short-lived First Minister, Vaughan Gething.
Now Vaughan’s successor as First Minister, Eluned Morgan, has appointed Miles to the health secretary job.
Drakeford, meanwhile, becomes finance minister — a role he held before becoming First Minister in 2018.
Commenting on his new role, Miles said via X (formerly Twitter): “I am delighted to take up the health and social care portfolio working… as part of Eluned’s team.”
On her Cabinet reshuffle, Morgan adds: “The changes I am announcing today offer stability, draw on experience, and bring our collective talents together.
“The new portfolios reflect modern Wales and are designed to address the key challenges that face us all.”
Knight Frank’s healthcare team has recruited four new members.
William Freston, Sara Lightfoot, Ella Davenport, and Elisa Linu have all recently joined the 23-strong specialist team.
Freston and Davenport will focus on corporate healthcare and fund valuations, Lightfoot on commercial healthcare and bank lending valuations, and Linu joins the development consultancy team to specialise in care home development.


Medical Premises Consultants (MPC) has announced the appointment of Georgina Silk as director of lease consultancy.
A highly-skilled and qualified surveyor, Silk brings extensive experience in the healthcare real estate industry, further strengthening MPC’s commitment to delivering expert property consultancy services to the primary care sector.

With over six years of experience at Aitchison Raffety, she has developed a strong reputation for working effectively with both landlords and GPs, particularly in the areas of lease consultancy and valuation.
And her expertise aligns seamlessly with MPC’s mission to provide innovative, sustainable solutions for healthcare premises while supporting the ongoing evolution of the UK healthcare landscape.
Rob Hearle, managing director at MPC, said: “Georgina’s proven track record and deep understanding of the healthcare property sector make her an invaluable addition to our team.
“As MPC continues to grow, her expertise will play a crucial role in expanding our lease consultancy services and supporting our clients’ needs.”
Silk’s appointment comes at a time of strategic growth for MPC as the firm continues to expand its national reach and strengthen its multi-disciplinary approach to healthcare property consultancy.
“I am excited to join MPC at such a pivotal time in the company’s growth,” said Silk.
“I look forward to contributing to the continued success of MPC and working closely with our clients to deliver tailored, innovative solutions that meet the evolving demands of the healthcare sector.”

Specialist healthcare property adviser, Christie & Co, has appointed Kevin Strain as a senior business agent in its dental team in Scotland.
Strain is a qualified member of the Royal Institution of Chartered Surveyors (RICS), with extensive knowledge of the Scottish commercial property market and over four years experience in real estate agency working for a large corporate consultancy.
His new role as a senior business agent at Christie & Co will see him handle key dental sales across the length and breadth of Scotland alongside the company’s head of dental, Joel Mannix.
He joins at what is a busy time for the dental market, with significant activity across the region, particularly from the independent market.
Mannix said: “Kevin’s extensive expertise will be crucial as we continue to provide an unparalleled service to our clients and his appointment reinforces our growing business in Scotland’s dental sector.”
Browne Jacobson is now providing HR services to health and social care clients after making a key hire.
Laura Chinyere-Ezeh has joined the UK and Ireland law firm as HR consultant in health and social care to lead the new offering for residential care homes, nursing homes, domiciliary care providers, and hospices.
With more than a decade of experience as an HR generalist, Chinyere-Ezeh brings expertise in CQCregulated environments.
Prior to joining Browne Jacobson, she was an HR business partner at Ramsay Healthcare and was part of senior leadership teams for three neurological rehabilitation centres’ clinical support functions for acute care and central corporate teams.
She has also held several HR management positions, including with a domiciliary care provider for local authorities.
Based at the firm’s Birmingham office, she works with clients nationally.

She said: “It is a brilliant time to be joining Browne Jacobson as the firm continues to grow its clients, teams, and services, proving that the expertise in law firms goes far beyond legal advice into various other practical and strategic matters.
“The health and social care sector is experiencing a lot of change right now, with retention and recruitment among its greatest challenges.
“By thinking outside the box, employers can showcase the rewarding nature of working in this sector and ensure they have a sustainable supply of talent to meet future demands.”
Working closely with the firm’s employment law specialists, Chinyere-Ezeh’s team will provide advice on matters such as workforce planning, dealing with complex grievances and disciplinaries, managing allegations against staff, team restructures, organisational development, TUPE transfers and indemnities on outsourcing, and exit agreements. It will also support clients with HR audits to ensure compliance with the Care Quality Commission (CQC), bespoke and off-the shelf-training for all levels of staff, and developing HR policies.







