Property marketplace...



Innovation...
Expert analysis...
March 2023





Property marketplace...



Innovation...
Expert analysis...
March 2023




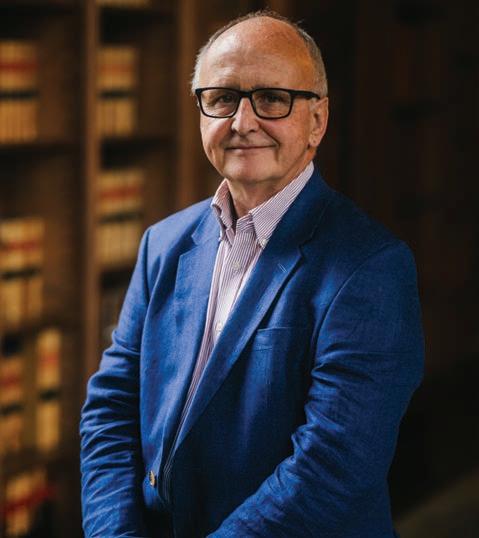
Professor Vic Rayner OBE, chief executive of the National Care Forum, argues it’s time to look beyond our borders.
ALSO IN THIS ISSUE
Leader’s spotlight
Berkley Care Group chief executive Andrew Winstanley

CT on the road
Memory care the Montessori way
Legal & regulatory
To refer or not to refer?
30 June – 01 July 2023




NEC Birmingham
Free CPD
Free tickets
See page 24
Hosted by Davina McCall




Chief executive Andrew Winstanley explains what makes Berkley Care Group stand out from the pack in the crowded luxury care home market

23 LEGAL & REGULATORY
Launching a new monthly column analysing the hot legal and regulatory topics in social care, Ridouts examines when to make a misconduct referral to the Nursing and Midwifery Council

8 COVER STORY
Professor Vic Rayner, chief executive of the National Care Forum, argues it’s time for a long hard look at care delivery through a global lens, to help address the challenges we face in the UK

Robert Kilgour, founder and executive chairman of Renaissance Care, looks at Scottish proposals for a National Care Service

Chief executive officer
Alex Dampier
Chief operating officer
Sarah Hyman
Editor-in-chief
Lee Peart
Features editor
Charlotte Goddard
Subeditor
Charles Wheeldon
Advertising & event sales director
Caroline Bowern 0797 4643292 caroline.bowern@nexusgroup.co.uk
Exhibition sales manager
Nijeesh Hareendranath nijeesh.h@nexusgroup.co.uk
Event operations manager
Carly McGowan
Operations executive
Sophia Chimonas
Senior conference producer
Teresa Zargouni
Head of digital content
Alice Jones
Marketing design manager
Craig Williams
Marketing campaign manager
Sean Sutton Lead developer Jason Hobbs Web developer
It’s the time of year to celebrate the amazingly talented people who make up the care home workforce.
Submissions for this year’s Care Sector’s Got Talent show are due this month. Organised by Championing Social Care, the flagship event is the perfect opportunity to showcase your singing, dancing, comedy, magic and musical talents.
Last year’s hugely successful finals event was watched live online by more than 400 people with 1,175 people watching on YouTube.
The event was won by Bollywood sensation, Sarabdeep Singh, of Hallmark Care Homes.
After triumphing, Sarabdeep was awarded a £500 LoveToShop voucher and performed at a prestigious awards event and The Care Show.
If you have a special talent you would
like to share this year, the deadline for submissions is 19 March.
The event is a great way to have fun and spread some joy in these tough times.
The final extravaganza, which is expected to be even bigger and better than last year, will take place on 20 April at the Derby Arena.
Care Sector’s Got Talent is one of a string of celebratory, marquee events run by Championing Social Care this year.
Other key dates for your diary include Care Home Open Week (26 June - 2 July), #SparkleforSocialCare (July) and the Care Sector Ball (30 September).
You can find out more about how to get involved and celebrate our sector at: championingsocialcare.org.uk/
Lee Peart Editor-in-chief Caring TimesRobert



The Liberal Democrats called for a Carers’ Minimum Wage set at £2 above the National Minimum Wage. The move would mean carers earning a minimum of £12.42 an hour from this April.

MPs backed a bill that would guarantee minimum service levels during strike action. The bill, which was approved by MPs by 315 votes to 246, would mean some workers would be required to work during industrial action and would face the sack if they did not comply.

A coalition of more than 50 organisations called on the government to protect the legal right of people in vulnerable situations to be supported by their carers, friends and families. The new right would give anyone who needs care access to a care supporter – a relative or friend who can help them wherever they need it, such as in hospitals, care homes or GP surgeries.
National learning disabilities care provider, Hft, will launch its annual Sector Pulse Check report at this year’s Care England Conference. Since 2016, Hft’s Sector Pulse Check report has provided an annual snapshot of the
financial health of the learning disability sector, as well as exploring other relevant issues and challenges.
Norfolk County Council approved a £30 million rise in care fees. The 9% increase, which comes into effect in April, is the council’s highest ever annual increase in fees.
This year’s £60 billion local government finance settlement for local services included access to a £2 billion social care grant. The settlement for the 2023/24 financial year represented a £5.1 billion (9.4%) increase on last year.
The Local Government and Social Care Ombudsman issued a guide to help care providers on good record-keeping. The new guide focuses on a number of case studies highlighting the common issues
the Ombudsman sees, and also includes good practice tips to help providers avoid the problems from occurring in their own settings.
Five people suspected of recruiting and exploiting Indian students working in care homes in North Wales were handed Slavery and Trafficking Risk Orders. The defendants were originally from the state of Kerala in India and have links to care homes in Abergele, Pwllheli, Llandudno and Colwyn Bay, either by working there themselves or having a direct family link to someone who works in them.
Council leaders urged the government to engage fully with local government and its partners on its £200 million hospital discharge programme. In a letter to secretary of state for health and social care, Steve Barclay, the leaders of Association of Directors of Adult Social Services, the Local Government Association and Solace laid out conditions for making the discharge of hospital patients to care homes a success.
Nadra Ahmed, executive chairman of National Care Association and chairman of The Care Provider Alliance called on care homes to “hold firm” against pressures to take Covid-positive hospital discharges.
Ahmed told Caring Times it was “deeply disturbing” that lessons from the pandemic had not been learnt and that NHS colleagues were putting providers under pressure to take unsafe discharges.

Just over half of 300 interim care home beds funded by the Scottish government to ease hospital pressures have been taken up by health boards, it was revealed. The Scottish government said 162 people had so far entered the interim care facilities it recently funded.
A health board in South Wales launched an investigation into allegations that safeguarding procedures were bypassed when discharging two patients to a local care home. The Aneurin Bevan University Health Board, which runs Royal Gwent Hospital in Newport, launched the probe following complaints from Aria care home which is run by Arcadia Care Homes.
Four staff members were arrested following an incident at a Dorset care home. The incident took place at Signature House in Dorchester, which is operated by Amica Care Trust, on 8 January.
Team members from Oakland Care’s eight care homes have joined a range of volunteer tree planting events in Essex. Oakland Care has committed to planting 1,000 trees a year as part of its commitment to sustainability and combating climate change.

Orchard Care Homes, a care provider across the north of England, launched a new initiative which aims to shift attitudes towards dementia care across the UK. The ‘Dementia Promise’ is part of Orchard Care Homes’ commitment to challenge the negativity and inequalities
often experienced by people living with dementia in care homes.
HC-One enhanced its dementia strategy to meet the rising demand for care. The strategy has been developed by HC-One’s specialist dementia care team led by director of dementia Professor Graham Stokes, a leading thinker and academic authority in dementia care in the UK.

platform providing a range of services from clinical best practice to activitybased programmes. The organisation plans to roll the system across other care sectors internationally.
The government launched a competition for businesses to bid for a share of £1 million to stimulate innovation in occupational health. Small and medium enterprises are being invited to bid for up to £100,000 to back their projects from 19 May.

Bupa Care Homes was fined £400,000 after an eight-year-old girl suffered major injuries from a falling tree. The care home provider pleaded guilty at West Hampshire Magistrates Court to failing to provide a system to manage trees at Oak Lodge Care Home in Bitterne, Southampton following the incident on 8 July 2021.
Person Centred Software, provider of a digital care planning system, acquired Oomph Wellness, a wellbeing business for older adults. Following the acquisition, more than 5,000 care homes will have access to a multi-functional digital

Entries opened for Championing Social Care’s Care Sector’s Got Talent 2023 show. All talented people, whether in the field of singing, dancing, comedy, magic or music, are urged to apply for this year’s show to share their talents with everyone by visiting the Championing Social Care website.

In 2019, there were 703 million people aged 65 and over in the world. That number is predicted to double to 1.5 billion in 2050, with one in six people in the world aged 65 or older..
While we should of course celebrate the increase in longevity that we will hopefully all enjoy, it also is not a population shift that can be managed without significant changes to the way in which we all live. Climate goals are firmly embedded in our psyche, but the call for a transformation in approaches to ageing does not get anywhere near the same profile, yet the impact on communities, people, economies and rights all require our attention. ‘Zero ageism’ should be our 2050 slogan, as a focus on the rights of older people will lead to a care system fit for the future.
However, much like the climate challenge, despite the irrefutable demographic data, the time frame for change far outstrips any incumbent political party's ambitions for tenure in office. Governments know that complex and far-sighted attempts to address societal agendas are often trumped by the electorate’s drive for actions that impact on the here and now. This must change.
That is why I am very pleased to be part of the Global Ageing Network which has published a ‘call to governments’ across the world to think about how long-term care needs to transform in order to ensure that
those ageing have not only the care they need, but also receive it in a way that embodies the rights and dignity to live a full and positive life.
Organisations representing care providers and the voices of people receiving care and support have come together under the Global Ageing Network banner to call on governments to take action now, and have highlighted key areas which each and every government needs to have in mind.

The focus on the UK workforce is unrelenting. The pay, terms and conditions of the workforce are the subject of endless reports and short-term approaches to address the ever-increasing levels of vacancies. However, if we only see this as a UK-wide issue, we are missing the bigger picture. In recent months the government has turned its attention to the opportunities that international recruitment brings, with new funding to increase the ability of care and health providers to recruit from overseas following the inclusion of both senior and front line care workers on the Shortage Occupation List. However, it is clear that not only will the UK need to be able to compete with multiple other countries seeking a care workforce to support their ageing population, but increasingly we will be competing with other countries such as Australia and Canada which have both indicated their desire to bring in a migrant workforce from the UK, alongside other countries, in order to address their shortfall in care staff. Migration of the care workforce is a reality, and looking for ways which recognise the portability of skills, expertise and workers’ rights need to be seen as international priorities. Solutions to labour shortages must be both ethical and underpinned by a constant drive to increase quality.
Economies across the world need to be identifying new ways to support the ageing population. The growing number of older people means there will be fewer working age people to contribute to the economy, and therefore a reduction in the ability of countries to rely on taxation or other sources of public funding to deliver long-term care. If this leads to increased reliance on unpaid carers, then there’s a well-documented correlation between increases in unpaid carer commitment leading to a reduction in their ability to engage in paid employment. In addition, the shrinking ratio between working age adults and older people will mean those available to provide unpaid care, even if that was their wish, will be reducing year-on-year. Models of care delivery across the globe are moving towards home-based approaches, with a strong focus on the potential for technology to meet needs. There is much to learn from each other, and we need the same ambition around global approaches to innovations in health, science and technology to tackle the future of care delivery.
While there have been many medical and societal advances that enable a longer and healthier life, it’s still the likelihood that at least half of the growing population of older adults will need some long-term care services for a period of time in their lives. Working together as a global group, it’s clear to see that the experience of the UK is replicated across the world, with similar unsatisfactory outcomes. Care coordination everywhere is hampered by a fragmented patchwork of funding
“Migration of the care workforce is a reality, and looking for ways which recognise the portability of skills, expertise and workers’ rights need to be seen as international priorities.”
sources, budgets protected within silos, and all contribute to insufficient and inefficient care coordination. Integration of care is thwarted by the differential values, culture and
training of health professionals and care professionals, leading to a lack of familiarity or understanding about what each other does. Too often, across the world, there’s a failure to understand the complexity of the delivery of care for older adults, leaving it outside the academic curriculum, and meaning that society rarely appreciates or acknowledges much-needed professional expertise and knowledge as core to the role of long-term care.

We need a new vision for the future, and that should encompass our desire for all to be able not just to live longer, but to live high-quality lives with
dignity, respect, self-determination and independence. The Global Ageing Network is committed to challenging governments to help shape this vision and will be working with NCF and Scottish Care at the Global Ageing Conference in Glasgow on 7-8 September to this end. We are at a crossroads. As the ageing population grows, more of the same is not an option. It’s vital that governments across the globe take note and work together to ensure a sustainable future for long-term care. The electorate must make it clear that while individual governments come and go, the decisions they make in relation to ageing and care matter to us all.
“Care coordination everywhere is hampered by a fragmented patchwork of funding sources, budgets protected within silos, and all contribute to insufficient and inefficient care coordination.”
Chief executive Andrew Winstanley explains to Caring Times what makes Berkley Care Group stand out from the pack in the crowded luxury care home market.

Tell us about your background and how you joined Berkley.
Upon graduating from university, I established and developed a successful sports training business, which I grew and subsequently sold. I then moved into the hospitality industry, and specifically, high-end luxury hotels.
After four years at Ralph Trustees, the largest family-owned, privately run hotel group in the UK, I moved into the adult social care sector taking up the role of regional business manager at Caring Homes Group. I brought to the role a clear commercial mindset through the application of the knowledge and understanding I had secured from my time in the luxury hotel industry as well as the theoretical and practical business understanding I gained from my MBA.
I was initially responsible for 10 homes in the London and Southeast region with overall responsibility for the care, clinical, operational, property and financial performance of the homes. A particular focus of the role was increasing home managers’ awareness of business performance and implementing key performance indicators around this. In 2011, my remit was increased to 16 homes and as of 2012 my role changed to encompass financial, business and sales responsibility for all 32 homes across the South division.
In 2013 I moved to Sovereign Care as group operations director where I took direct responsibility for the operational and business performance of the group’s homes and care villages.
In February 2015 I was appointed managing director of Baycroft Care Homes where I reported to the executive board with a remit to meet One Housing's corporate plan targets through the delivery of 10 aspirational consumer-led care homes to the private market by 2019. I also established the operating brand Baycroft with direct responsibility for all stages of commissioning new care homes, including site finding and acquisition,
design and development, through to reaching operational maturity, achieving occupancy targets and EBITDARM performance.
Finally, in February 2020 I was recruited to my current role as chief executive of Berkley Care Group.
How many care homes do you have and what services do you provide?
We have 11 homes in our portfolio with our 12th due to open in Leamington Spa in April. Those currently in operation (or due to open imminently) are shown below.
nursing, dementia Outstanding
Grange Bromsgrove, Residential, dementia, respite Outstanding Worcestershire
Burcot Lodge Bromsgrove, Residential, dementia, respite Good Worcestershire
Cumnor Hill House Oxford
Residential, nursing, dementia Requires improvement
Jubilee House Leamington Spa, Residential, dementia n/a (scheduled to Warwickshire open in April)
Portobello Place Chesham, Residential, dementia n/a Buckinghamshire
Shinfield View Reading, Berkshire
Residential, dementia, Outstanding respite, day care
Blenheim House Melksham, Wiltshire Residential, nursing, dementia Good Cedar Mews Leicester Residential, dementia, day care Good
Fernhill House Worcester Residential, nursing, dementia Good Leycester House Warwick
dementia Good
nursing, dementia Good Ryefield Court
Tell us about the geographical footprint of your homes and how this has evolved.
Our homes are located across the Midlands area and the South and Southwest of England. Five are located in the West Midlands (including Jubilee House), two are based in the Southwest, and five are based in the South of England.
Berkley Care Group was first setup in May 2010 by Seamus Halton who quickly established a portfolio of six luxury homes designed specifically for the self-pay market. The portfolio was acquired by Korian Group in March 2021.

How do you differentiate yourselves from other luxury providers?
All our homes offer outstanding care and state-of-the-art facilities, but what really distinguishes our provision from that of our competitors is our simple,
transparent, all-inclusive pricing model and our truly bespoke and tailored approach to the customer journey.
In terms of pricing, we understand the worries that residents and families face when it comes to care fees. Their anxiety is only compounded if they’re uncertain how much they will pay from one month to the next. So, instead, our all-inclusive model gives residents and their families the knowledge that everything is included in just one fee.
This includes person-centred activities as well as regular trips out or a weekly visit to the in-house hairdresser and barber for a cut or blow dry, relaxing treatments in our hair beauty salons, private dining with family or friends, or being chaperoned to appointments or even a visit to a friend in our chauffeured car. These services are offered at no extra charge.
We also pride ourselves on our commitment to customer care. We
“We also pride ourselves on our commitment to customer care. We guide residents and their families throughout their journey right from the moment they step through the door.”
guide residents and their families throughout their journey right from the moment they step through the door. We understand that choosing and moving into a care home can be a daunting process, so we hold their hand throughout. Our staff are personal and caring in their interactions with our residents and their families. Care is bespoke and tailored to the needs and experiences of each resident. We also work hard to ensure that our homes are alive and vibrant with activity rather >
than being subdued and isolated from the wider community in which they’re located.
What is your average weekly fee?
Our average weekly fee across all 11 homes is just over £1,500. The fees range widely with a mix of fairly independent residents with low need who see their stay in our homes as a lifestyle choice, to those with much higher physical or cognitive need that require round-theclock support and care.
What is your current profit margin as measured by EBITDAR and how has this changed over the last year?
EBITDAR is obviously impacted depending on the service being offered and the required staffing levels and skill sets, as well as the maturity level of the homes. We had two homes in commissioning stage last year which will affect the overall EBITDAR as occupancy ramps up, but as a group we achieved an EBITDAR of 26% which is in line with our budget and expectations for the year
What is your current level of occupancy?
Across our mature homes we are running at 91%, with our two new homes in ramp up running at 70%. Overall occupancy rate is 88%.

How challenging is the current recruitment climate?
The ongoing sector-wide recruitment challenge is undoubtedly a struggle, but fortunately our above industry-average rates of pay, matched with our generous employee benefits package, has meant our rate of staff retention is high
and we are seeing strong numbers of applications for each role we advertise.
Agency staffing has been required, but this has been kept to a minimum thanks to our innovative embrace of technology to, for example, encourage existing staff to refer friends and family to apply for advertised roles.
Furthermore, we’ve been pioneers in the application of improvements in the understanding of neurodiversity to encourage those who might not otherwise apply for positions in the adult social care sector based on their misperceived unsuitability for roles.
How do you seek to recruit and retain staff?
As well as traditional recruitment strategies, we’re also passionate believers in the application of technology to solve some of the challenges facing the sector.
We’ve enthusiastically rolled out the use of the Care Friends app among our staff. The app works by incentivising a care provider’s existing staff to share job vacancies listed on the app, which works
like a job board. In return for sharing the vacancies within their personal network, staff receive points which can then be exchanged for money. The rate of exchange is determined by the provider. At Berkley one point is equal to £1. As well as earning a point for each job advert they share across their social media network, any expressions of interest resulting from their shares of the advert earn them two points. Candidates’ progression through the various stages of the recruitment process earns staff further points. Staff have the potential to earn up to £365 if their referral results in a successful appointment. Due to the importance of attracting talent from outside the industry, an additional 50 bonus points is awarded if the individual is new to the care sector.
We believe that referrals by our staff are often a more effective way to attract high-quality candidates. Evidence suggests that personal referrals not only deliver higher-quality applicants, but that those recruited also stay for longer. The system was initially implemented in two of our care homes: Blenheim House in Wiltshire and Fernhill House in Worcester. We have gradually rolled out the app across our 950 employees since May 2022. We passed the 250 sign-ups mark at the end of August 2022.

So far, the system has resulted in over 100 applications to roles across Berkley Care Group. 22 new staff have joined because of the app, with more than 28 interviews currently pending and five more successful applicants waiting to start work with the group.
We are also passionate believers in staff wellbeing and satisfaction. In
accordance with Maslow’s hierarchy of needs, we understand that employee satisfaction isn’t simply derived from levels of pay. Instead, we work hard to engage with our employees, and create a listening and feedback culture to drive engagement and wellbeing. Technological innovation supports us with this too.
Last year we began using employee engagement platform Winningtemp. The app-based platform enables us to quickly capture employee feedback through weekly ‘pulse surveys’ that typically take a matter of seconds to complete. These empower our employees to provide valuable ideas and suggestions that we can in turn use to better understand their needs and take actions to drive positive engagement and wellbeing. The technology also encourages peer-to-peer praise and recognition through the platform, helping us to develop a culture of recognition at all levels. Winningtemp automatically analyses the results in real time, translating them into actionable insights meaning we can be proactive, rather than reactive.
There are two key advantages to the software: first, it allows us to gain feedback from our employees in real time, rather than having to wait for an annual review. This means we can act on this feedback much more quickly. Second, it enables us to identify –using the software’s visual ‘heat maps’ technology – key trends more easily across the employee experience in key categories such as job satisfaction, autonomy and personal development and break this down by teams.
The insights we’re gaining from the technology are helping to inform our decision-making on a regular basis. For example, through the feedback we gained, we learned that our employees wanted more formal recognition for some of their work and achievements. This led to us staging Berkley Care Group’s very first employee awards reception, called ‘B:Celebrated’ on 24 February. Held at an exclusive hotel, the event showcased the excellent work our team members perform day in and day out.
It is obviously role-dependant, but we guarantee to be paying comfortably
above the National Minimum Wage and also benchmarking regularly to ensure we are not only competitive with other social care providers in the locality of our homes, but also with out of sector benchmarking with restaurants, supermarkets, high street retail, etc.
Tell us about your acquisition by Korian and what benefits this has brought the business?

Berkley Care Group was acquired by Korian in 2021. The working relationship has been fantastic. Korian has provided the resources to enable Berkley to grow while also affording us the autonomy to take the nuanced decision-making that rests on our understanding of the domestic UK market. Korian acquired Berkley in the knowledge that the company is founded upon a successful business model, for example, our inclusive pricing structure. There has been no attempt to dilute this and bring it in line with its operating model across Europe. Instead, Korian has sought to complement our existing operations through the provision of additional resources and financial investment, while also providing counsel and advice on business strategy and development. We also have the huge benefit of exposure to the operating practices of the largest care provider in Europe, so we have a significant amount of trading data and best practice from across France, Germany, the Netherlands, Italy and Spain.
What digital technology do you use?
In addition to Care Friends and Winningtemp, many of our homes
operate state-of-the-art technologies to support residents and the care team to make our residents even safer. Acoustic monitoring and non-intrusive, secure live feed camera technology, for example, are deployed to offer residents and their loved ones additional peace of mind every day.
All our staff rostering and payroll – time and attendance – is digital, as well as our care planning and clinical compliance software so that all auditing can be achieved at any point in time from any location.
We use Found through Lottie for our CRM software, so that all enquiry management is captured and that allimportant customer journey is logged from the very first interaction we have.
How has your business grown over the past year and what are your ambitions going forward?
In January and April 2022 we acquired Blenheim House and Fernhill House from Majesticare, and in August 2022 we completed our acquisition of Burcot Grange, Burcot Lodge and Cedar Mews care homes from Cinnamon Care Collection.
On 1 April we are opening Jubilee House in Leamington Spa, our latest purpose-built home that at full capacity will provide 78 rooms and create 150 jobs in the local area. We are continuing to work closely with Korian’s M&A team to identify further acquisition opportunities across the UK over the next 24 months in order to grow Berkley’s presence further and cement its standing as one of the leading providers of luxury care in the country.
A new report has called for a social care wage floor set at £2 above the minimum wage.
The proposal comes in the Resolution Foundation’s ‘Who cares?’ report which says care workers are paying for their dedication with unsafe working conditions and unlawful minimum wage underpayment.
FIGURE 3: Care workers express similar levels of job satisfaction to the average worker, and higher satisfaction levels than other low-paid workers
FIGURE 3: Care workers express similar levels of job satisfaction to the average worker, and higher satisfaction levels than other low-paid workers
Proportion of workers who say they are satisfied (‘completely’, ‘very’ or ‘fairly’) with their job, by occupation: UK
Proportion of workers who say they are satisfied (‘completely’, ‘very’ or ‘fairly’) with their job, by occupation: UK
The report finds typical hourly pay for front line care workers was £10.90 as of April 2022, below the economy-wide average of £14.47 and less than some low-paid jobs, including transport and call centres, as well as average pay for public sector nursing assistants (£11.14).
Additionally, it says the ‘pay premium’ social care workers receive relative to other low-paid jobs for additional skills and challenges shrank from 5% in 2011 to 1% in 2021.
Who cares? | The experience of social care workers, and the enforcement of employment rights in the sector workers). This data is set out in Figure 10. As we will discuss in depth later, however, it’s important to note that these measures of pay don’t account for domiciliary workers’ travel time and so will over-estimate workers’ true pay. Unfortunately this is a common problem across pay datasets, and so these estimates are the best we can offer.
rights
The research also says a domiciliary care worker earning £11.07 an hour is typically being paid an effective hourly rate of £9.20, 30p below the minimum wage, because they are rarely paid for their travel time between homes.
workers). This data is set out in Figure 10. As we will discuss in depth later, however, it’s important to note that these measures of pay don’t account for domiciliary workers’ travel time and so will over-estimate workers’ true pay. Unfortunately this is a common problem across pay datasets, and so these estimates are the best we can offer.
NOTES: Jobs are defined according to SOC 2000 classification. ‘Social care’ is SOC code 611. ‘Other low-paid jobs’ include the following SOC codes: 543, 612, 622, 623, 629, 711, 712, 721, 811, 812, 813, 814, 821, 822, 911, 912, 913, 914, 921, 922, 923, 924, 925. These include jobs such as cleaning, childcare, hairdressing, housekeeping, retail assistants, process jobs in factories, transport drivers, and jobs with lower skill requirements in agriculture, construction, storage, administration, and security.
NOTES: Jobs are defined according to SOC 2000 classification. ‘Social care’ is SOC code 611. ‘Other low-paid jobs’ include the following SOC codes: 543, 612, 622, 623, 629, 711, 712, 721, 811, 812, 813, 814, 821, 822, 911, 912, 913, 914, 921, 922, 923, 924, 925. These include jobs such as cleaning, childcare, hairdressing, housekeeping, retail assistants, process jobs in factories, transport drivers, and jobs with lower skill requirements in agriculture, construction, storage, administration, and security.
SOURCE: RF analysis of ONS, Skills and Employment Survey.
Less than half (47%) of job moves by front line care workers were out of the sector, compared with two-thirds for storage, leisure, call centre and cleaning workers.
SOURCE: RF analysis of ONS, Skills and Employment Survey.
Median hourly pay among frontline care workers is well below the economy-wide level (£14.47), and also lower than in some other low-paid job categories, including low-paid work in offices and call centres, in transport, and perhaps more relevantly, among nursing assistants in the public sector (£11.14). But high rates of part-time work in the sector (38 per cent, versus 25 per cent economy-wide11) means that social care workers are closer the bottom of a pay ranking if we instead measure weekly pay. Median gross weekly pay in April 2022 was £374 among frontline social care workers (slightly higher among residential workers - £383, compared to £350 among domiciliary workers). This compares £415 among nursing assistants in the public sector, and £567 across the economy as whole. As discussed earlier, the care workers we spoke to mostly felt that there was demand for them to work more hours, suggesting that to a significant extent the highrate of part-time work among care workers reflects workers’ preferences.
For care workers in residential homes, the report highlights issues around understaffing and resultant safety breaches, with tasks requiring at least two people often being carried out by one worker.
Median hourly pay among frontline care workers is well below the economy-wide level (£14.47), and also lower than in some other low-paid job categories, including low-paid work in offices and call centres, in transport, and perhaps more relevantly, among nursing assistants in the public sector (£11.14). But high rates of part-time work in the sector (38 per cent, versus 25 per cent economy-wide11) means that social care workers are closer to the bottom of a pay ranking if we instead measure weekly pay. Median gross weekly pay in April 2022 was £374 among frontline social care workers (slightly higher among residential workers - £383, compared to £350 among domiciliary workers). This compares to £415 among nursing assistants in the public sector, and £567 across the economy as a whole. As discussed earlier, the care workers we spoke to mostly felt that there was demand for them to work more hours, suggesting that to a significant extent the highrate of part-time work among care workers reflects workers’ preferences.
An additional important positive aspect of caring that was highlighted was the job security. Care workers recognise that they are in demand, and many pointed out that it is a sector where work would always be readily available if they needed it. This was summed up in the comment from one focus group participant that ‘there’s always a job for you in care’.
Despite these challenges, the report highlights that in the most recent study in 2017, 88% of social care workers said they were satisfied with their job, compared to 83% in other low-paid roles.
FIGURE
An additional important positive aspect of caring that was highlighted was the job security. Care workers recognise that they are in demand, and many pointed out that it is a sector where work would always be readily available if they needed it. This was summed up in the comment from one focus group participant that ‘there’s always a job for you in care’.
There are that many jobs out there … the care homes are so desperate. The good jobs are out there, it is just a case of finding them.
Front line care workers are more likely than workers in the wider economy to move jobs in a given quarter. From 2011 to 2020, 3.3% of front line care workers moved jobs per quarter, versus 2.3% across the economy as a whole. Among the low-paid job categories shown, only low-paid workers in leisure (4.3% per quarter), call centres (4.8% per quarter), and hospitality (6% per quarter) make job moves at a higher rate.
There are that many jobs out there … the care homes are so desperate. The good jobs are out there, it is just a case of finding them.
But an important difference between front line care workers and other low-paid workers (and workers in the wider economy) is that care workers’ job moves are more likely to be within their job category rather than to a job in a different sector or occupation. From 2011 to 2020, 1.5% of front line social care workers made a job move away from front line care work, lower than the (at least) 3% of workers in low-paid hospitality, leisure and call centre jobs who made job moves away from those categories per quarter.
They need me more than I need them.
They need me more than I need them.
FIGURE 10: Frontline social care jobs are low-paid, though typically slightly above the minimum wage
Median hourly and weekly pay by low-paid job categories: GB, April 2022
Median hourly and weekly pay by low-paid job categories: GB, April 2022
Personal assistant.
Personal assistant.
Domiciliary care worker.
Domiciliary care worker.
High levels of job security in care work are borne out in the data. Care workers are less likely to face redundancy or dismissal than across the economy as a whole, and
High levels of job security in care work are borne out in the data. Care workers are less likely to face redundancy or dismissal than across the economy as a whole, and
Data from the Skills and Employment Survey shows front line social care workers have in the last two waves been more likely than other workers (including other low-paid workers, but especially workers in the wider economy) to agree that they have ‘very little’ loyalty to their employer. Interestingly this employer-level disloyalty among the social care workforce has been rising – from 13% in 1992 to 31% in 2012 and 31% again in 2017. Employer disloyalty has also risen among workers in other low-paid job categories, but not as significantly; it has also risen among the wider workforce, but only slightly.
Social care workers are more likely than workers in the wider economy, and even more so than workers in other low-
NOTES: Job categories are all low-paid jobs (apart from the ‘all’ and ‘other’ categories) and are based on the Low Pay Commission’s categorisation of low-paid jobs, and frontline care is defined based on Migration Advisory Committee approach; see Annex for details. Hourly pay measure is derived from weekly pay (excluding overtime and shift premiums) divided by basic weekly paid hours. Weekly pay measure is gross weekly pay, including overtime and incentive payments as well as any shift premiums.
NOTES: Job categories are all low-paid jobs (apart from the ‘all’ and ‘other’ categories) and are based on the Low Pay Commission’s categorisation of low-paid jobs, and frontline care is defined based on Migration Advisory Committee approach; see Annex for details. Hourly pay measure is derived from weekly pay
divided by basic weekly paid hours. Weekly pay measure is gross
to a different sector. This is set out in Figure 6, which shows the proportion of workers who between 2011 and 2020 made a job move in the last quarter, broken down by those who made a job move within their job category (shown in bars to the left of the vertical axis) and those who a job move to a different job category (shown in bars to the right of the vertical axis). The total size of the bars represents the proportion of workers who made any job move in the past quarter.
to a different sector. This is set out in Figure 6, which shows the proportion of workers who between 2011 and 2020 made a job move in the last quarter, broken down by those who made a job move within their job category (shown in bars to the left of the vertical axis) and those who made a job move to a different job category (shown in bars to the right of the vertical axis). The total size of the bars represents the proportion of workers who made any job move in the past quarter.
FIGURE 6: Social care workers make large numbers of within-sector job moves, but are relatively unlikely to move to a job outside the sector
FIGURE 6: Social care workers make large numbers of within-sector job moves, but are relatively unlikely to move to a job outside the sector
Proportion of workers who moved jobs in the past quarter, either within their job category, or to a different job category, by job category in the previous quarter: UK, 20112020
Proportion of workers who moved jobs in the past quarter, either within their job category, or to a different job category, by job category in the previous quarter: UK, 20112020
a real difference to people’s lives. That’s why they love their jobs more than other low-paid workers do.
“But the danger is this sense of vocation and commitment comes with a high price, including unlawful underpayment of the minimum wage and unsafe working conditions for some.
Total bar size = proportion of workers making any job move
NOTES: For frontline social care, moving to a different job category is defined as leaving frontline social care (i.e. moving from residential to domiciliary care is coded as a ‘within’ job category move). Job categories are all low-paid jobs and are based on the Low Pay Commission’s categorisation of low-paid jobs. Frontline care is defined based on Migration Advisory Committee approach; see Annex for details.
NOTES: For frontline social care, moving to a different job category is defined as leaving frontline social care (i.e. moving from residential to domiciliary care is coded as a ‘within’ job category move). Job categories are all low-paid jobs and are based on the Low Pay Commission’s categorisation of low-paid jobs. Frontline care is defined based on Migration Advisory Committee approach; see Annex for details.
“Addressing these problems isn’t costfree but it is urgent given the chronic shortage of care workers. Improving working conditions in the care sector is the only route to making it more attractive for new recruits and giving our ageing society the level of care it deserves.”
SOURCE: RF analysis of ONS, Two-Quarter Longitudinal Labour Force Survey.
paid roles, to say that they put in more effort than their job requires. In 2017, for example, more than three-in-four (76%) social care workers said they went above and beyond at work, compared to 65% of all workers, and 58% of workers in other low-paid roles.
SOURCE: RF analysis of ONS, Two-Quarter Longitudinal Labour Force Survey.
FIGURE 7: Despite being relatively attached to their sector, care workers do not tend to feel loyalty towards their employer
FIGURE 7: Despite being relatively attached to their sector, care workers do not tend to feel loyalty towards their employer
Proportion of workers who say they feel ‘very little’ loyalty to their organisation: UK
Proportion of workers who say they feel ‘very little’ loyalty to their organisation: UK
To address the care sector’s recruitment challenges the reports calls for:
• A higher, sector-specific wage floor for care work, with minimum pay set at £2 above the adult minimum wage. This would be £12.42 an hour from April this year (when the minimum wage will increase to £10.42). This would improve the pay of over half the existing number of front line care workers, and provide a sufficient buffer to reduce the risk of minimum wage underpayment. This social care wage floor will require higher spending and taxation in the public sector, and higher prices in the private sector, which the Foundation says are costs worth paying.
Who cares? | The experience of social care workers, and the enforcement of employment rights in the sector
Who cares? | The experience of social care workers, and the enforcement of employment rights in the sector
18
FIGURE 8: Care workers are more likely than other workers to put in extra effort at work
NOTES: Jobs are defined according to SOC 2000 classification. ‘Social care’ is SOC code 611. ‘Other low-paid jobs’ include the following SOC codes: 543, 612, 622, 623, 629, 711, 712, 721, 811, 812, 813, 814, 821, 822, 911, 912, 913, 914, 921, 922, 923, 924, 925. These include jobs such as cleaning, childcare, hairdressing, housekeeping, retail assistants, process jobs in factories, transport drivers, and jobs with lower skill requirements in agriculture, construction, storage, administration, and security.
NOTES: Jobs are defined according to SOC 2000 classification. ‘Social care’ is SOC code 611. ‘Other low-paid jobs’ include the following SOC codes: 543, 612, 622, 623, 629, 711, 712, 721, 811, 812, 813, 814, 821, 822, 911, 912, 913, 914, 921, 922, 923, 924, 925. These include jobs such as cleaning, childcare, hairdressing, housekeeping, retail assistants, process jobs in factories, transport drivers, and jobs with lower skill requirements in agriculture, construction, storage, administration, and security.
FIGURE 8: Care workers are more likely than other workers to put in extra effort at work
SOURCE: RF analysis of ONS, Skills and Employment Survey.
SOURCE: RF analysis of ONS, Skills and Employment Survey.
Proportion of workers who say that they put ‘a lot’ more effort into their job than what is required, by selected occupation: UK
Proportion of workers who say that they put ‘a lot’ more effort into their job than what is required, by selected occupation: UK
Having set out some of the positive experiences of working as a carer, we now move onto some of the ‘bad’ aspects – including low pay and high workloads.
• Introducing measures to ensure domiciliary care workers are paid for their travel time, instead of just receiving a mileage reimbursement. One solution would be to calculate travel time on the basis of the distance between jobs, with an appropriate formula based on typical travel speeds in the area and the time of day.
Having set out some of the positive experiences of working as a carer, we now move onto some of the ‘bad’ aspects – including low pay and high workloads.
The high level of attachment that many social care workers show to their jobs is illustrated once again in Figure 8, which shows that social care workers are more likely than workers in the wider economy, and even more so than workers in other low-paid roles, to say that they put in more effort than their job requires. In 2017, for example, more than three-in-four (76 per cent) social care workers said they went above and beyond at work, compared to 65 per cent of all workers, and 58 per cent of workers in other low-paid roles.
Nye Cominetti, senior economist at the Resolution Foundation, said: “Social care workers fulfil a skilled and hugely necessary role in our society and make
The high level of attachment that many social care workers show to their jobs is illustrated once again in Figure 8, which shows that social care workers are more likely than workers in the wider economy, and even more so than workers in other low-paid roles, to say that they put in more effort than their job requires. In 2017, for example, more than three-in-four (76 per cent) social care workers said they went above and beyond at work, compared to 65 per cent of all workers, and 58 per cent of workers in other low-paid roles.
jobs
NOTES: Jobs are defined according to SOC 2000 classification. ‘Social care’ is SOC code 611. ‘Other low-paid jobs’ include the following SOC codes: 543, 612, 622, 623, 629, 711, 712, 721, 811, 812, 813, 814, 821, 822, 911, 912, 913, 914, 921, 922, 923, 924, 925. These include jobs such as cleaning, childcare, hairdressing, housekeeping, retail assistants, process jobs in factories, transport drivers, and jobs with lower skill requirements in agriculture, construction, storage, administration, and security.
NOTES: Jobs are defined according to SOC 2000 classification. ‘Social care’ is SOC code 611. ‘Other low-paid jobs’ include the following SOC codes: 543, 612, 622, 623, 629, 711, 712, 721, 811, 812, 813, 814, 821, 822, 911, 912, 913, 914, 921, 922, 923, 924, 925. These include jobs such as cleaning, childcare, hairdressing, housekeeping, retail assistants, process jobs in factories, transport drivers, and jobs with lower skill requirements in agriculture, construction, storage, administration, and security.
SOURCE: RF analysis of ONS, Skills and Employment Survey.
SOURCE: RF analysis of ONS, Skills and Employment Survey.
Richard Humphries, senior adviser to The Health Foundation sets out his thoughts to William Walter, managing director of social care PR consultancy, Townsend Communications, regarding the government’s hospital discharge programme and his analysis of longer-term plans to keep people out of hospital through care in the community.
News headlines have been dominated by stories of besieged acute hospitals, whose front doors are bursting with very poorly people queuing to get in, some waiting in ambulances outside, while many of the patients inside cannot get out because of delays to their discharge. Away from the media glare, there’s an equally serious but far less visible crisis involving many thousands of people waiting for social care in their own homes. When hospitals are full, the community is usually ‘full’ too. The human consequences of our failing health and care system are immense.
It is to the government’s credit that in five months it has found £750 million to tackle the problem of delayed discharges. But it has been tardy in getting the money out to systems, the funding route has been fragmented between councils and the NHS, and the short-term approach – the latest tranche of money has to be spent within weeks – has stifled progress. Far more could have been achieved if providers and commissioners had been brought together a year or more ago to plan what could be done with such a substantial sum of public money. There would have been no shortage of practical ideas and solutions.
Amid an almost desperate drive to relieve the pressures on hospitals, it is worth remembering that delayed discharges are but one symptom of the failure of the NHS and social care system to offer people the right care, in the right place, at the right time. Attributing the problem to social care alone overlooks the fact many delays are due to internal hold-ups within hospitals such as waiting for prescriptions, transport, referral letters and decision-making ward rounds. The Department of Health and Social Care’s own guidance estimates that at least half of people leaving hospital are ‘simple’ discharges not dependent on further
care or support. Less than 5% will need residential care. There are some awkward questions about why some hospitals still struggle with these basic operational issues 20 years after good practice guidance on hospital discharge (which I helped to write). And why the NHS has consistently underinvested in basic community services, intermediate care and rehabilitation that achieve better outcomes for people and reduce the need for acute and long-term care.
It is encouraging that some of these issues are acknowledged in the NHS’s new plan for recovering urgent and emergency care that sets out over the
next two years to increase capacity, deliver more out-of-hospital care such as the virtual ward initiative and improving discharge through more step-up and step-down care. All laudable aims, but whether they go far enough in tackling the deeper and long-standing problems afflicting health and social care is questionable. A record number of 165,000 vacancies in social care alongside critical shortages in general practice and district nursing begs the question of where staff will come from. Quick fixes are no substitute for a good long-term plan, including the longpromised reform of social care.
How effective has the hospital discharge programme been at improving capacity in the social care sector and increasing the hospital discharge rate?
The extra investment was undoubtedly needed, but the money hasn’t been as effective as the government would have hoped for. That’s why additional funding has subsequently been required. But it’s naïve to believe short-term injections of funding alone are the solution to the problem. Instead, much more needs to be done to achieve parity of esteem, opportunity, and pay between a career in the social care sector and that of the NHS.

Also, integrated care pathways aren’t as developed as they should be. There needs to be more streamlining both in
terms of funding, but also the discharge process. The communication and assessment between health and social care is still too disjointed.
Do you believe slow hospital discharge rates are primarily because of shortcomings in the social care or secondary care sector?
Forty per cent of hospital discharges are delayed awaiting a social care package, the remainder are down to other factors. We need to get a better handle on what drives these ‘other’ factors.
But, and in terms of those waiting to access social care, I know from my work in Parliament and in my constituency that these problems aren’t unique to NHS England.
Access to social care in rural areas is a particular challenge and is often a symptom of the chronic workforce crisis facing the sector. Care providers, including those in my constituency, often tell me how they invest significant resources recruiting, training and trying to retain carers only to find that they leave the sector in favour of other higher-paid jobs. Tackling the social care recruitment crisis is a key issue.
Will improved intermediate care, such as community health services, and increased ‘virtual ward’ capacity free up hospital capacity?
Community health services have an important role to play. But they present another workforce issue. Is the manpower required to provide these services going to drain staff away from areas such as primary care, social care and the NHS? How will training be delivered? Effective long-term workforce planning is required.
But we also need to address barriers preventing people from accessing primary care services. Improved access to primary and community care will improve early intervention and alleviate demand for secondary care.
Diagnostic centres and mental health hubs based in the community could play a valuable role in alleviating pressure on hospitals and mental health services, but, again, it’s about having appropriately trained staff to service them.
Technology is another important part of the jigsaw. Robotics, patient screening, virtual wards etc. Technology can carry some of the load. The complete digital integration of community health must be a priority.
Bureaucracy in the NHS has often stifled innovation. Covid demonstrated that by cutting out this red tape the results can be transformative. We must nurture digital innovation in the health service, but doctors and nurses and other experts need to be involved in the development process.
Parklands, which acquired the home six months ago, said it had been faced with a “wave of rising costs” which meant the expense of operating and upgrading the service to the required quality was “simply not sustainable over the long term”.
Ron Taylor, managing director of Parklands Care Homes, said: “We regret that Mo Dhachaidh care home in Ullapool will close in April, despite our best efforts to ensure its long-term future.
“We will work closely with residents, families and NHS Highland to secure alternative care provision for all residents. Where there is capacity, Mo Dhachaidh residents will be given priority access to our other care homes. Existing employees will be offered career opportunities elsewhere in the Parklands group. Eligible employees who choose not to accept another role will be offered a redundancy package.
“This is not a decision we have taken lightly; in 30 years as a care provider, it is the most difficult decision we have ever had to take. However, working with the NHS, we are determined to secure the best possible outcome for our residents and employees.”
Mo Dhachaidh has capacity for 19 residents but is currently home to 14 residents. The home has 18 members of staff.
Parklands has nine other homes in Tain, Muir of Ord, Fortrose, Grantown on Spey, Aberlour, Keith and Buckie.
Kate Earnshaw, NHS Highland’s district manager for Skye, Lochalsh and South West Ross, said: “This is a sad time for residents, families and staff at Mo Dhachaidh. The home has provided excellent care to the local community for many years.
“We will remain in close contact with residents and their relatives, as well as staff working in the home, to ensure they are kept up to date with developments.”
Louise Bussell, chief officer at NHS Highland, said: “I am saddened by this news but understand the challenges that
have been experienced by Parklands after they took over the running of the care home last year.
“NHS Highland is working closely with The Highland Council within the partnership arrangements in the development of our strategic plan with a focus on ensuring we have the right balance of services across Highland and will continue to work with all of the independent care providers as we plan for future service provision.”
Aplomb Care has purchased Aldersmead Care Home in Bognor Regis, West Sussex, a Good-rated home which provides nursing, residential and dementia care for 38 residents occupying en suite bedrooms.

The vendor is Casco Finance, which trades as Balcombe Care Homes. Business property advisor Christie & Co facilitated the sale. Charles Phillips, director, healthcare at
Christie & Co, said: “The sale of this home demonstrates the strong level of activity within the care market in this region.”
Aldersmead Care Home was sold for an undisclosed price.

Barchester Healthcare has opened its latest luxury care home in Purley, South London.

The grand opening of Chestnut Gardens was performed by the executive mayor of Croydon, Jason Perry, in front of invited guests from the local community.

Perry said: “It is very good to see Barchester investing with such confidence in the future of care in the county – that investment will ensure not only topquality facilities and world-class care, but also jobs, training and a boost to the local economy.
“It is clear from everyone I have met today how dedicated the Barchester teams are to the people that they care for, and it’s reassuring to know that the people of Purley and beyond will receive a warm welcome at Chestnut Gardens, and that their needs will be met with respect and dignity.”
Barchester’s chief executive Dr Pete Calveley and general manager Krystyna Bosko hosted the event and invited guests
to view the care home which is now open and welcoming its first residents.
Dr Calveley said: “Chestnut Gardens is going to be a wonderful home. Krystyna and her team here will offer personalised care for the people of Purley in this lovely setting. We’re thrilled to add Chestnut Gardens to our Barchester family of quality care homes and hospitals.”
Bosko commented: “We are delighted our home is now open. Our residents are at the heart of everything we do at Chestnut Gardens, and we look forward to welcoming them and their families, becoming an intrinsic part of the local community and delivering seamless personalised care in partnership with other local organisations.
“We take pride in really getting to know each of our residents to provide tailored care and support, ensuring dignity and choice in every aspect of daily life.”
Barchester Healthcare has opened its Shawford Springs luxury care home in Otterbourne to visitors.
The home, which will welcome its first residents in early spring, will offer residential, dementia and respite care.
General manager Julie House said: “We are thrilled our stunning new home is ready to welcome visitors. It’s a wonderful way for people to come and find out about the exceptional care we provide and meet the friendly team who will be looking after our residents.
“Personalised care really is at the heart of everything we do and we are looking forward to meeting new friends from within the local community and to
welcoming our new residents and their loved ones.”
Facilities at the home will include a café to socialise and enjoy freshly baked treats, spa bathrooms, en-suite bedrooms with smart TVs, a choice of comfortable lounges and an in-house hair salon.
The Barchester home will provide a dedicated life enrichment programme which includes a choice of daily activities for residents and the home’s chefs will prepare nutritious home-cooked meals from seasonal menus, catered towards individual preferences.


First residents, Colin and Joyce Smith, marked the occasion by cutting a ribbon on their arrival at the home.
Home manager of Chartwell House, Diane Collins, said: “Welcoming Colin and Joyce to their new home is an immensely proud moment for all of us here at Chartwell House. It has been an incredible journey working with the team to get the home to this moment, but this is just the start. We’re ever so excited to welcome further residents to Chartwell House and create a truly special community.”
Admissions manager Jude Coveney added: “It has been an honour to support Joyce and Colin on their journey to find Chartwell House and it was a pleasure and a very emotional moment to welcome them today. I am very proud to be able
to guide and help people to find the very best care home for their loved ones.”
Chartwell House offers facilities including a bistro café, a family celebrations room and landscaped gardens. Future residents will enjoy spacious accommodation of 20 square metre bedrooms which all come with additional space of private en suite rooms.
Ameet Kotecha, managing director and head of Boutique Care Homes, said: “Today is a big moment for all of us here at Boutique Care Homes. Chartwell House is the third home in our family and I am incredibly proud of all of the team
involved in getting us to this moment. Chartwell House completely embodies our values and is at the forefront of innovation in care. I am excited to see this home develop and supporting the whole team and residents on their journey.”
Specialist care provider Exemplar Health Care is recruiting for more than 100 positions at its newest Liverpool-based specialist care home.
Roseside in Belle Vale is a 32-bed, four-unit specialist care home supporting those living with complex needs.
Exemplar Health Care is recruiting for roles including health care assistants, registered nurses and unit managers.
Charlotte Lloyd, director of commissioning, said: “We are delighted to be opening our fourth home in Merseyside, bringing over 100 jobs to the local area. Our aim at Roseside is to help our residents with everyday living skills and empower them to live as fulfilled and independent lives as possible.
“Our high staffing levels enable us to work at people’s own pace and build
trust, which leads to improved personcentred and longer-term outcomes. There are plenty of opportunities for progression in the company and we offer a range of rewards and benefits including exclusive retail and lifestyle discounts, an employee assistance programme, car salary sacrifice scheme for registered nurses, and access to wages before payday through fastPAYE.”
Exemplar Health Care’s most recent
refurbishment in the Northeast, Tyne Grange, achieved an Outstanding rating from the Care Quality Commission just 18 months after opening.
A newly established care group, Nisi Dominus Frustra, has purchased St Cecilia care home in Poole, Dorset, a Good-rated care home registered for 15 service users in the category of old age, dementia and mental health.
The business occupies a two-storey detached Edwardian former family home. Since 1988, the home has been owned and operated by Robert and Ruth Eshelby, who are selling in order to retire from the sector.

Business property advisor Christie & Co facilitated the sale.
Charles Phillips, director, healthcare at Christie & Co, said: “With the seller living in France, the buyer living in Hong Kong, and the care home and agent in England, this was, at times, a challenging process. The sale of St Cecilia shows that there is demand for UK care homes from buyers all around the world.”
St Cecilia was sold for an undisclosed price.
Nisi Dominus Frustra translates as ‘Without God, [it is] in vain’.
Elevation Development Partners, a real estate fund advised by Elevation, in partnership with PGIM Real Estate and elderly care operator Care Concern Group (CCG), has completed the development and sale of a new-build luxury care home in Didcot, Oxfordshire, to a European asset manager.
Valerian Court Care Home comprises 70 en-suite wetroom bedrooms and offers 24-hour comprehensive care with facilities including a cinema, hairdressers and rooftop garden. It also has electric vehicle charging points and cycle storage.

PGIM Real Estate partnered with Elevation to source and structure investments with developer-operators, and to provide ongoing asset and development management services.
Elevation and PGIM Real Estate have so far committed to six new purpose-built care homes, in partnership with CCG.
Charles Crowe, head of UK transactions at PGIM Real Estate, said: “During this challenging time, the importance of highquality senior housing has never been more apparent. Long-term demographic trends in the UK are strongly favourable,
with increasing demand from a rapidly ageing population.”
Andrea Auteri, managing partner at Elevation commented: “We are thrilled to see the realisation of our first project in our investment joint venture with PGIM Real Estate and CCG, which is providing modern, high-quality care environments to an undersupplied market. This innovative investment partnering product allows operators to incubate freehold developments on their balance sheet to retain development upside while reducing their equity requirements, enabling efficient scaling of multiple
developments at once. The sale of this first care home is a vote of confidence in the UK healthcare real estate market and shows the value in quality accommodation for investors, as well as residents, staff and the local community.”
Amrit Dhaliwal, chief executive of homecare provider Walfinch, looks at why care operators need to build sustainable, ethical businesses which make a profit in order to pay carers fairly and provide quality care.

Profit. There, I’ve said it. For too many businesses in the homecare sector, profit has been something of a dirty word.
Everyone in the care sector talks about the importance of high-quality care –and they are right – but we should not be ashamed to talk about money too. Because without making a profit we can’t deliver quality care – in fact we may not be able to deliver care at all.
We are not in the care sector for the money, but money is the lifeblood of any industry, and the care industry is no different. It enables care providers to hire qualified staff and pay them properly, purchase necessary equipment and supplies, and keep facilities running smoothly.
It’s our responsibility, too I’m not just talking about funding from local authorities and the NHS, though it is not enough, partly because the money they receive from the government falls short of what’s needed.
I’m talking about how care sector businesses approach the issue of money themselves.
Some homecare businesses focus too little on money. It’s bad business practice,
but worse, it can endanger their services to clients. The overall average rate offered by local authorities and the NHS is £18.57 an hour, but we have heard of some offering only £13 an hour. This is not enough to pay carers a decent wage and run a sustainable business that makes even a modest profit.
The importance of saying “No” Faced with unsustainable rates, providers must not be afraid to say “No”. Yes, it sounds callous, and we all hate doing it, but realistically, if we don’t make a decent income, we risk restricting the quality and growth of our services. With more than 500,000 people awaiting social care, restricted growth is bad news for them and our businesses. We need to ensure that we have enough income to run a business capable of delivering a high standard of care. We can’t do that on ridiculously low margins.
The key to taking the guilt out of saying no is knowing the minimum revenue our individual business requires to operate a sustainable service. Any rate below that level is unacceptable.
At Walfinch, our franchisees typically
“Profit. There, I’ve said it. For too many businesses in the homecare sector, profit has been something of a dirty word.”
serve a mixture of local authority, NHS and private clients.
Some of them are using one client group to effectively cross-subsidise another. The Homecare Association currently estimates the minimum cost of providing care is £23.22 an hour, so if, for instance, we charge private clients £30 an hour, then we are making enough profit –without being extortionate – to enable us to absorb or discount fees for those most in need. This goes some way towards ensuring that people need not go without the care they need.
There are no easy answers but without new ideas in the industry, quality of care will suffer. For the sake of our services, our carers and not least our clients, we must not be ashamed to talk about money.
Launching a new monthly column analysing the hot legal and regulatory topics in social care, Nicola Wheater, a solicitor at Ridouts, examines when to make a misconduct referral to the Nursing and Midwifery Council (NMC).

Having reviewed some of the most recent NMC fitness to practise decisions, it appears care home providers continue to make referrals to the NMC. While some misconduct exhibited by nurses or nursing associates is relatively clear cut, some conduct or competency concerns fall below the threshold for referral and lead providers to question whether they should make a referral or not.
In accordance with its website, the NMC states that a provider should make a referral if there are:
1) Concerns that pose a serious risk to service users and would be difficult for the provider to put right - examples of this could include:
• Verbally, physically, or sexually abusing service users
• Stealing money from service users and/or taking advantage of them
• Deliberately falsifying service user records
• Causing avoidable clinical harm to service users
• Falsifying their nursing qualifications and incorrectly stating they are NMC registered.
2) Concerns where localised action is unable to manage effectively ongoing risks to service users - this largely applies to competency concerns where localised action taken by the provider has not worked or the nurse has suddenly left its employment. Practical examples of this could include:
• A nurse managing a health condition with the knowledge and support of the provider but thereafter fails to engage/ take medication impacting the safety of service users
• A nurse required to undergo further training and supervision to remediate clinical concerns but suddenly quits without notice. In doing so, and without restriction of practice, the nurse poses a
risk of harm to future service users when starting new employment.
3) Concerns requiring the NMC to take action to protect public confidence in the profession and to uphold standards - examples could include:
• Stealing from the care home
• Obtaining a criminal conviction and intentionally failing to notify the provider or the NMC
• Posting homophobic, sexist or racist content online or exhibiting such behaviour towards colleagues in the care home.
In most cases, it is likely the provider (in the employer/employee context) would have commenced and completed its own internal disciplinary or conduct and capability proceedings prior to referring the concern to the NMC. However, and where the conduct or competency concerns raised are serious, a referral should be made straight away. Any conduct or competency concerns
which do not meet the threshold for a referral, and are therefore considered low level, should be dealt with using the provider’s own internal disciplinary, conduct and capability processes, or through further training and supervision.
Referral to the NMC may also coincide with notification to the CQC under Regulation 18 of the CQC (Registration) Regulations 2009 (Notification of other incidents) and failure to do so can result in prosecution. A safeguarding investigation may also arise out of the same set of factual particulars and any notifiable safety incidents will need to be disclosed to the service user and/or their family in accordance with Regulation 20 of the of the Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 (Duty of Candour).
While deciding whether to make a referral to the NMC can be a daunting decision, the NMC has provided detailed guidance on its website to assist providers. The NMC has also established an Employer Link Service which enables employers to speak with the service where they remain uncertain whether to make a referral or not. Providers can also seek independent legal advice.
"Where the conduct or competency concerns raised are serious, a referral should be made straight away."
30 JUNE – 01 JULY 2023 NEC BIRMINGHAM
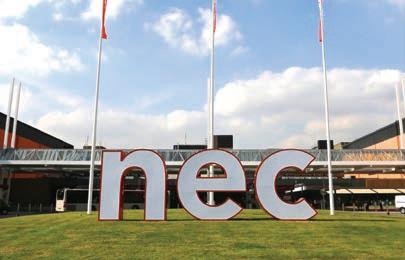
HOSTED BY DAVINA M c CALL

Join Caring Times for the largest show in the UK dedicated to care managers.
Over 4,000 managers, employers and sector specialists attending.

• Care managers
• Assistant care managers
• Care group executives and owners
• Care suppliers
• Representatives of industry bodies and associations
Our host Davina McCall will celebrate key figures in the industry and interview guests with first-hand experience of care.
Prioritise your health with interactive relaxation workshops and panel discussions.


Benefit from a best-in-class programme of free CPD. Access information on career progression and funded apprenticeships.
Learn about the latest technology and how it could impact the way managers and teams operate.


Ensure best practice. Workshops and panels on HR, recruitment, staff morale and managing risk.
GET YOUR FREE TICKETS TODAY

Athena Care Homes appointed Richard Shaw as project manager to lead the estates team, overseeing the larger refurbishment projects, assisting with service contracts, tenders and capital expenditure projects, as well as future expansion developments for the business. Shaw qualified as a building surveyor 25 years ago and has experience working for both care providers and construction companies. He has more than 20 years’ experience in the healthcare sector, working as property and estates manager.
activity programme for residents at Wilmslow Manor, including one-toone and group sessions. She will also work to integrate the care home into the community and organise enjoyable events with family participation.
Senior Lifestyle appointed Michelle Gray as general manager of Signature at Reigate Grange, which supports up to 95 residents. Gray has more than 30 years’ experience in social care and nursing, having worked in the private sector and the NHS in clinical and management roles. She previously worked for Queen Elizabeth’s Foundation for Disabled People, Kingston Hospital, and Basildon and Thurrock University Hospitals.
Scottish care provider Meallmore appointed William Narvaez as the new care home manager of Grove Care Home in Kemmay. Narvaez started his career at Meallmore four years ago and returns after a two-year hiatus. He first joined the care home company as charge nurse at Kynnaird House Care Home in Fraserburgh, and then worked as deputy manager at Bayview Care Home in Cruden Bay.

Luxury care provider Boutique Care Homes has appointed David Lobb as land director to support its continued growth. Lobb joined the Boutique Care Homes team with more than 30 years’ experience in land and property and of purchasing new sites for the development of care homes and retirement schemes.

Parklands Care Home in Alloa, part of the Meallmore group, appointed Shelley Watters as its care home manager. Watters has almost 20 years of experience in the care sector, starting her career as a care assistant. Since then, she has become well established in the industry, with a total of seven years care home management experience.
New Care appointed Helen Hartley to manage its Bramhall Manor Care Centre in Stockport, Greater Manchester. Hartley will manage a team of 80 nurses and care professionals. She has a first class honours degree in adult nursing and has worked in healthcare since 2010, first as a care support worker for Salford Royal Evening District Nurses and then as a community nurse within the urgent response team progressing to Band 6 level.
New Care appointed a wellbeing coordinator at its Wilmslow Manor Care Centre to develop community links and create a varied and fulfilling activity programme. Sarah Wild’s role will include the creation of a weekly person-centred




Orchard Care Homes, which provides care homes in the North of England and the Midlands, appointed Richard Wormwell as head of recruitment to lead the company’s talent and acquisition programme across its 23 homes, based at Orchard’s headquarters in Harrogate. Wormwell has experience of the talent and acquisition arena across the healthcare sector, heading recruitment divisions within specialist eating disorder services, mental health and acute NHS providers.


Proposals for a National Care Service in Scotland are the “nanny state on steroids,” says Renaissance Care founder Robert Kilgour.
The government has described the plans, which are scheduled to be introduced by the end of the current Parliament, as one of the most ambitious reforms of public services since the creation of the National Health Service.
The plans, which are designed to deliver consistency and quality of care and support nationally and to make the Scottish government directly accountable for services, are estimated to cost £1.25 billion and include a pledge to increase adult social care funding by at least 25%, or £840 million.
Robert Kilgour, founder and executive chairman of Renaissance Care, told Caring Times: “I am in favour of it if it means more funds for social care and if it means an improved service at the front line. I have yet to be convinced on either.”

Kilgour described the proposals, which include visiting rights for residents, as “woolly”, and “a blatant power grab by the Scottish government from local authorities”.
“Local authorities in Scotland work very well with the independent sector on delivering 85% of care home beds at the front line,” Kilgour said. “They are just desperately short of funding. This is not the time for the biggest reorganisation in 70 years.”
The care leader said that the £1.25 billion estimate for the reforms was “way out” citing analysis by the national auditor.
Kilgour added: “I am hopeful and optimistic that they will engage more
with stakeholders on this because it’s common sense. It’s not going to be a success if they just impose it and more central control because the people who are going to be responsible for making it a success are going to feel ignored and not included.”
The Scottish government’s minister for social care Kevin Stewart said: “We are committed to establishing the National Care Service by the end of the current Parliament and ending the postcode

“I am hopeful and optimistic that they will engage more with stakeholders on this because it’s common sense.”
lottery in care provision.
“This is the biggest public service reform since the introduction of the NHS 75 year ago. Given the scale of this undertaking we will, as would be expected, take the time necessary to make sure we get it right.
“The voices of people who are service users are key in these changes, and as we have been clear from the outset, we will be working closely with them as the plans develop.
“But we are also working to deliver improvements here and now so that social care continues to service and support the people of Scotland long into the future.”
In December last year, a third of all new cars sold in the UK were electric vehicles (EVs) – a staggering increase from just three years earlier when the equivalent figure was less than 2%. The unprecedented fuel price increases triggered by the Ukraine conflict have tipped the cost-benefit analysis decisively in favour of low-carbon vehicles.
Globally, transport accounts for around 25% of carbon emissions and road vehicles account for almost three-quarters of this total. In the UK and US, the transport sector is now responsible for emitting more greenhouse gases than any other sector, with the average petrol car in the UK producing 180g of carbon every kilometre. And let’s also not forget the serious impact of combustion engine vehicles on air quality.
Figures on vehicle numbers and mileage across the social care sector are hard to come by. The majority of services will have at least one vehicle for transporting those in their care to appointments, visits etc. So that’s probably something like 20,000 vehicles. With an average UK annual car distance of 7,400 miles, that’s approximately 43,000 metric tonnes of carbon emitted each year.

But that’s just from vehicles for residential homes. The Homecare Association recently suggested that UK homecare workers travel more than four million miles a day; that equates to a further 423,000 metric tonnes of carbon emitted each year.
You’d have to plant almost 2.8 million trees every year to offset the impact on the environment of car miles in social care. And we haven’t even yet looked at the impact of the hundreds of thousands of care professionals commuting to work every day by car.
The case for change is overwhelming. So, what’s holding us back?
The first issue is, inevitably, cost. The up-front costs of EVs are still significantly higher than combustion engine equivalents. The average pre-tax price of a medium-sized electric car was £29,000 in 2022, compared with £16,500 for a

petrol car. Given the financial challenges of the social care sector, who can argue with those figures? Well, I can. When you look at the wholelife costs, the latest research shows that EVs are now slightly cheaper to run than their petrol equivalents. That is certainly what we found at CareTech; when we factored in lower maintenance, fuel, road tax, congestion charges etc, we found that transitioning our fleet to EVs will save us money over a pretty short timeframe.
Secondly, many people still suffer from ‘EV range anxiety’. I was told recently that EVs were fine if you only want to do up to 80 miles a day. But nearly 99% of all driven journeys are under 100 miles and every EV on the market is capable of handling this distance on a limited charge. Today’s EVs have an average battery range of 257 miles compared with 74 miles in 2011, with predictions that 400 miles will soon be the norm. While there is undoubtedly investment required in the public charging infrastructure, the number of charging stations is increasing exponentially – and the time taken to charge is reducing too, thanks to new technology. For all but a tiny minority, range anxiety is simply unjustified. It wouldn’t be a social care article unless we mentioned recruitment and retention. Taking advantage of new EV salary sacrifice schemes can play a really useful part of your benefits package. At no cost
to the organisation – indeed, most will actually save money – providers can offer their staff access to EV leased cars that, thanks to their tax efficiency, can instantly make EV ownership a reality for many staff. Most of us lease our cars these days, so why not provide your staff with this option to get an EV car, reducing their fuel bills significantly as well as their carbon impact?
There are some great examples of social care providers already seizing the initiative, such as Northern Ireland’s domiciliary care provider Connected Health which has introduced a fleet of electric cars and electric bicycles as part of its carbon neutral care initiative.
Transition to EV cars is critical to becoming net zero and the government will ban the sale of new petrol and diesel vehicles by 2030. But why wait? Surely, it’s time to join the EV party.
Athena Care Homes shares how Flavia Hansell progressed through the company to manage her own residential community

Stow Healthcare shares its pioneering Montessori memory care model
Dr Shelley James explains how lighting can improve wellbeing for care home residents


Sleep therapist Dr Kat Lederle explains how sleep deprivation affects care workers and what can be done to help
 31 CPD
CARE FOR TOMORROW
46 WELLBEING
31 CPD
CARE FOR TOMORROW
46 WELLBEING
31 CPD IN FOCUS
Athena Care Homes shares how Flavia Hansell progressed through the company to manage her own residential community

32 C T ON THE ROAD
Stow Healthcare shares its pioneering Montessori memory care model

36 CHEF OF THE MONTH


National Care Award winner Lorna Parsons of Colten Care’s Bourne View in Poole
37 FOOD AND NUTRITION
Chris Burdett, Signature Senior Lifestyle’s head of food and beverage, on veganism in care homes

40 NORRMS’ BLOG
Dementia columnist Norrms McNamara looks at the year ahead

41 CREATIVE CARING
The latest fun and innovative activities taking place in care homes

43 CARE FOR TOMORROW
Dr Shelley James explains how lighting can improve wellbeing for care home residents and Digitalising Social Care at NHS England offers advice on where to start when going digital
45 10 QUESTIONS WITH Victoria Read, general manager of Signature at Barnet

46 WELLBEING
How sleep deprivation affects care workers and what can be done to help
47 END OF LIFE CARE
Orchard Care Homes on the importance of discussing end of life care at a critical time in a person’s life
Athena Care Homes shares how Flavia Hansell progressed through the company to manage her own residential community.
It was the hours that first attracted Flavia Hansell to the job of housekeeper at Amberley Hall Care Home back in 2010.
"I was a single mum so the hours were ideal," explains Flavia, who joined in May 2010 as a housekeeper before Athena Care Homes took over the site.
She would work from 8am to midday weekdays, sometimes taking on longer shifts at weekends when she had childcare covered.
Since then she has progressed through the company and now runs the residential community at the Kings Lynn home.
“It was brought to my manager’s attention that I really enjoyed talking to the residents when I was cleaning in the rooms, and I really did,” Flavia says. “I said I wanted to do more so I was encouraged to apply to become a carer, something I never would have thought of previously.”
Flavia was given induction training and later studied for her NVQ Level 2 in adult health and social care while working with Athena. She has also completed leadership courses, end-of-life training and the CHAPS scheme.

With the support of her colleagues and managers at Athena, Flavia has in more recent years passed her NVQ Levels 3 and 5.
During this time she became team leader then community lead before going on to work as a regional trainer for Athena, travelling across East Anglia to work with staff at all five of its
residential and nursing homes. When the pandemic hit, travel was restricted and she returned to base at Amberley Hall, where there was a vacancy for a residential care manager. The mum-of-two feels privileged to have been given these opportunities and
“To have been approached by different managers and encouraged to take the next step has always felt so rewarding, it shows the management recognise the work we do. ”
to have been able to continue her career with Athena.
She says: “To have been approached by different managers and encouraged to take the next step has always felt so rewarding, it shows the management recognise the work we do. I am happy here, it feels like a family. The company has really invested in me and my development throughout my career in care.”
Group operations director Katherine Foley says: “We are proud to be able to support our colleagues as they progress in their careers and offer ongoing training and support to enable them to do this. At Athena our moto is ‘Our family caring for yours’ and while that applies to each and every one of our residents, it also applies to our team members.”
“It was brought to my manager’s attention that I really enjoyed talking to the residents when I was cleaning in the rooms, and I really did”
For Stow Healthcare director Ruth French Montessori proved the perfect fit when looking to develop a new care ethos for its Maple Memory Centre at Brandon Park Nursing Home in Suffolk.
Nursing homes are not the first thing to spring to mind when thinking about Montessori education. The teaching model focused on hands-on learning and developing real-world skills is usually linked with educating children.
“We wanted to have a specialist centre for people living with memory issues,” French told Caring Times. “We didn’t want it to be a standard dementia unit because you can find that pretty much anywhere. We felt there was a real opportunity here to create a different type of memory care provision.
“We feel there’s such a stigma in this country around the word ‘dementia’. I don’t want to put my loved one in a ‘dementia unit’. It feels like we are labelling and really treating people as though they have nothing more to give and don’t have a value or purpose. We wanted to create a centre that supported people with memory issues and didn’t
write them off.”
Having spent a lot of time researching different models of memory care, French and fellow director Roger Catchpole chose the Montessori method.
“While Montessori is associated with the early developmental stage of life the principles are the same for the other end of life,” French noted. "It’s about putting useful objects into someone’s hands and for that to add value and purpose and redevelop and relearn skills or learn some skills for the first time.
“We are not very good at letting people take risks in dementia care in the UK. People move into a care home and suddenly we are doing everything for them and we are taking away every possible risk. When we do that, we are actually taking away people’s sense of their own personal worth and sense of purpose.
“When people move into a care home they are having their tea made for

them, we are buttering their toast when previously they did that for themselves –they are being unintentionally deskilled.”
When setting up the memory centre, French and her team deliberately made sure there was a usable kitchen so that people could prepare their own meals, wash up and feel normal.
Stow Healthcare uses a different terminology for its memory care centre to reflect its non-hierarchical nature.
“We don’t have residents, we have ‘family members’ and we don’t have carers we have ‘home makers’,” French explained. It’s not about having a carer, a kitchen assistant and a cleaner with everyone coming in and having a different uniform.
“None of the staff wear a uniform and all family members and home makers wear a name badge so that everyone can remember each other’s names.”
Home makers are carers, cleaners, kitchen assistants and activities co-
“When people move into a care home they are having their tea made for them, we are buttering their toast when previously they did that for themselves – they are being unintentionally deskilled.”

ordinators all rolled into one.
“They live the full course of the day with the family members,” French explained. “They go in in the morning and support them in whatever way they need to get up and encourage them to make their bed and do light cleaning in their rooms and to come and live as a family community together.”
Family members are encouraged to choose their breakfasts from the selection of available options and do their own washing up.
“One family member has made it her job to do the washing at the end of the day,” French said. “Another lady who has memory impairment because of a stroke has been supported to make her own cup of tea. Sometimes she puts in apple juice instead of milk but she can make a cup of tea now.”
Another special family member, Pat,
who chose to come to the centre after visiting with her daughter has relearnt to iron and sew and has the certificates on her wall to prove it.
Pat told Caring Times that relearning ironing had given her her confidence back.
“I achieved something and that was good for me,” Pat said. “I am person who likes to be independent.”
In another example of how the team has empowered family members to regain their independence, a gentleman who was particularly proud of his appearance was taught to shave again by using a potato and a vegetable peeler. “It’s about supporting those fine motor skills,” French noted.
Care support levels are high with the 13 family members treated as though they are high-dependency residents with five-and-a-half to six hours of dedicated one-to-one care each day.
As French notes quality memory care doesn’t come cheap with average weekly fees of around £1,500 a week, £200 to £300 above typical residential care fees.
The results of such high levels of care have been startling, with falls and antipsychotic medicine use dramatically down, and family members allowed to live more independently for longer.
Since the introduction of the centre, Brandon Park has gone from two to three Outstanding CQC key lines of enquiry ratings, adding Caring to
Responsive and Well-led.
One relative told inspectors: "My (person’s relative) has Alzheimer's and is now living in the Maple Memory Centre. It is wonderful, they have got their freedom back. They are encouraged to be independent, can now make a drink when they want to, get up when they choose to. How they live their daily life is their choice, and their independence is encouraged in a safe, well-staffed environment."
Having seen the success of Maple, Stow Healthcare will be creating a similar memory centre at its newly acquired home in Colchester, as well as rolling out its care practices at its other residential and dementia homes.
“We have started to look at lessons we can learn from the memory centre that can be applied to any of our homes,” French told us. “We are looking at setting up kitchenette spaces in dining rooms across our homes where we have space to do that so that people can help themselves.
“Some of this stuff is so easy to do and I think in general in social care we need to be looking at what’s working with this kind of approach because we all need a reason to get out of bed each day.”
Led by French, Stow Healthcare looks set to continue to be a pioneer in developing a more effective model of memory care for years to come.
Ontex has teamed up with Caring Times once again to reward those working in care homes who are always ready to go that extra mile.
There are thousands of people working in UK care homes that make a real difference, whether it’s behind the scenes in the laundry room, preparing meals in the kitchen, or direct personal care of the residents. We’re looking for those that go beyond the job description. For example, it could the gardener who brings a resident their favourite cookies, or a housekeeper who helps a resident to rediscover their hobbies – we’re searching for those who bring a little bit of extra joy into the care world. Your unsung hero may be a colleague or someone else you know, and now is the time to reward those individuals that have made a genuine impact on their particular place of work!
If you know of anyone that fits the bill, entries can be made online at: caring-times.co.uk/care-home-heroes
So go to this link and tell us, in 400 words or less, why you think your nominated person deserves to win. Make sure to include an example of when they have gone the extra distance to make a difference.
All winners will be announced in June and will be presented with their certificate and Love2Shop vouchers or similar gift card on Friday 30 June at the Care
Managers Show at the NEC.
Three runner-up winners will each receive £250 Love2Shop vouchers or similar gift card, and the Overall Winner will receive a £500 Love2Shop voucher or similar gift card.
The three runner-up winners will feature in the September, October and November issues of Caring Times magazine, and the Overall Winner will feature in a special feature in the December issue of Caring Times
This prize draw is organised by Ontex, Weldon House, CorbyGate Business Park, Priors Haw Road, Corby, NN17 5JG. It is governed by the laws of England and Wales and it is subject to the following conditions:
• The prize draw is not open to employees or contractors of Ontex or any person directly or indirectly involved in the organisation and running of the competition or their direct family members.
• No purchase is necessary to take part in the prize draw.
• The prize draw is open to UK residents only who are aged 18 or over.
• Closing date for entry is Friday 19th May . Winners will be notified by 1st June 2023
• All winners will be presented with their Award at the Care Managers Show if they are able to attend on Friday 30th June .- otherwise they will be sent a certificate
• Permission will be required for Ontex to contact the winners and visit them to hand deliver the prizes when possible.
• If the winners do not confirm acceptance of his/her prize within 7 days he/she will automatically forfeit the rights to claim for the prize. In the event of the prize not being claimed, Ontex reserves the right to select an alternative winner via any means that Ontex feel appropriate.
• By participating in the prize draw, you declare that you accept these terms and conditions unconditionally. There is no cash alternative.
Care Homes Heroes 2023 offers a unique chance to celebrate the dedication of all those who go above and beyond to keep care homes running. It’s a brilliant way to shine the spotlight on people who get on with their jobs unseen and unheard, but make a real difference.
“This is the fifth year we’ve worked with Caring Times for the Care Home Heroes and we absolutely love it because it’s important to shine a light on those who go above and beyond for their residents,” commented Angela Gillespie, distributor channel manager at Ontex. “And it doesn’t have to be a grand gesture - it’s the little, consistent things that really have an impact on someone’s life.”


Last year, we received over 350 entries and it took a panel of five to decide the finalists. Gillespie continued: “It’s a difficult competition to judge because each person is so deserving. My top tip when nominating somebody is to use a particular example with lots of detail for how they have made a difference and how this impacted others – good luck to all nominees!”
Overall Winner 2022: Nicola Mould, home manager, Orchard Mews, HC-One Care Home Heroes 2022 Overall Winner was Nicola Mould. Nicola was nominated by community nurse, Jennifer Dodds, whose mum was a resident at Orchard Mews. “My Mum suffered from Alzheimer’s and was discharged from hospital post-Covid with deteriorated condition for palliative care,” says Jennifer. “Nicola made every effort to support my Mam, myself and my siblings during such a traumatic and sad time. She went above and beyond her role to support and help us all, often staying at work hours past her shift ending when mum deteriorated to wait for the GP to review and implement a plan and ensure Mam was comfortable and pain free.”
“The Care Home Heroes competition is a great opportunity for us to recognise and reward those working in our care homes who are always ready to go that extra mile and have made a real impact to the lives of residents,” says James Tugendhat,
chief executive at HC-One. “We are always on the lookout for opportunities to celebrate our colleagues’ achievements. We were delighted that Nikki Mould, home manager at HCOne’s Orchard Mews Care Home, was selected as the overall winner of the Care Home Heroes competition in 2022,” he continues. “Nikki was nominated for being professional, empathetic and knowledgeable, and in recognition of how she delivers high quality nursing care and excels in the management of her amazing care team whose care philosophy is completely person-centred.”
Runner-up 2022: Karen Jones, domestic, Park House Care Home, Eastgate Care Karen Jones has been with Park House Care Home for just under 10 years, and her standards have never slipped. “Nothing is too much trouble for this lady who always clocks up to 50 hours a week making sure our home is extremely clean,” says Park House. “No speck of dirt escapes her.” During the pandemic Karen was fastidious in ensuring all recommended measures were put in place and the home received a glowing CQC Infection Prevention and Control report. Karen spends her spare time with the people who live at Park House, singing, playing board games and chatting.

Runner-up 2022: Paul Bond, housekeeper, Fremantle Trust
As housekeeper, Paul gets involved with most of the residents. After noticing a fishing magazine in the room of one resident, “RS”, Paul decided to make his wish to go fishing again come true. Along with RS’ daughter Tracey, he arranged everything from obtaining a fishing licence, sorting out a suitable venue, carrying out a risk assessment and organising a carer to accompany the two of them. Paul ensured that RS had an amazing day out, and took a photograph of the fish he caught and landed. “We were so pleased that we could fulfil RS’ dream,” says Fremantle Trust. “He has been to fish three times now and further plans have been made.”

“I treat all my residents as individuals with different tastes and dietary needs and also know exactly what foods they have a passion or particular fondness for.”
within the company and by meeting with the clinical lead on a monthly basis regarding the residents’ nutritional health status.
How do you cater for residents with dementia?
We speak with our residents’ relatives upon arrival to discuss dishes they enjoy. We also offer visual choices on brightly coloured crockery and ensure the food is vibrant in appearance.
What’s your most popular dish?
Tell us about your background and how you joined Colten Care
My journey started with Colten Care in 1998 when I was 14 years old. I was employed to wash up and gained experience by making sandwiches and supporting the chef. This helped to inspire my passion for food and I was offered the opportunity to enrol in the local catering college. Here I gained my NVQ level 2/3 in professional cookery. I am always eager to learn more, so I enhanced my skills and experience by attending cake decorating courses and also by undertaking a patisserie and confectionery course at Brockenhurst College. This has helped me to create delicious treats for the residents in our café.

What is special about working at Colten Care?
The most special part of my job is being able to make a difference to the residents’ lives by using my food to keep
them healthy and happy. I treat all my residents as individuals with different tastes and dietary needs and also know exactly what foods they have a passion or particular fondness for.
How do you vary your menu to provide choice for residents?
I enjoy being able to interact with the residents on a daily basis to find out more about their meal preferences and to gain feedback from them, which helps shape future menus.
What does your typical weekly menu look like?
Our menus are well balanced and full of nutritional choices. We also cater for vegetarian options and other religious diets, and allergen-specific diets.
How do you meet residents’ nutritional and health needs?
I ensure this is achieved by keeping up to date with my nutritional training
Our residents are very traditional in the choices that they make, with fish and chips and roast dinners big favourites.
What’s your own favourite dish?
My own personal favourite dish would have to be sushi and sashimi. Whenever this is on a menu while I am out, it’s always a go to.
How do you make the dining experience special for residents and their families?
I take time to introduce myself to each new resident and their relatives when they first arrive at Bourne View. We greet residents and their families with a warm welcome when entering the dining room. Greeting residents on a first name basis and getting to know them helps me to understand their individual needs and give them the best quality dining experience. They also receive first-class service from our front of house team and a delightful general ambience in our beautiful dining room.
With the rising popularity of veganism over the past decade Chris Burdett, Signature Senior Lifestyle’s head of food and beverage, says this global shift is here to stay
What was once seen as a fad, adopting a plant-based diet is now a prevalent lifestyle choice. This can be reflected by the number of vegan options available in supermarkets and restaurants, the growth of scientific research into meat and dairy alternatives, or trends such as Veganuary – a 31-day challenge which sees hundreds of thousands of people adopt a plant-based diet throughout January.
While 18 to 24-year-olds are frequently seen to be the most likely to adopt a vegan or vegetarian diet, it is in fact the older generation who are more willing to take a plant-based approach to the contents of their plates, as research by Green Chef, a meal box company suggests. It revealed a fifth of British adults aged 55-plus follow a vegan or vegetarian diet, whereas only one-in-25 (4%) of millennials revealed they eat a strictly vegan diet.
These outcomes are an important catalyst behind Signature Senior Lifestyle’s dining and nutrition strategy supporting more than 2,000 residents. The sector needs to be acutely aware of how to support reduced meat and meatfree residents with nutritious, tasty and ultimately exciting meals.
The next steps
Offering choice and variety is fundamental to ensuring residents fully enjoy their dining experience. It’s essential that food is prepared using high-quality ingredients for a wellbalanced and nutritious diet for all. Doing so requires an acute awareness of up-to-date lifestyle choices, dietary requirements and the food industry more broadly – plus a collective emphasis on not only taking the minimum steps to align with these changes, but going above and beyond to remain at the cutting edge.

Our own research has identified 3% to 5% of our residents are vegetarian, while 10% will actively choose a vegetarian or vegan option. Whether a menu is in a restaurant, a hospital or a care home, 30% of it should be vegetarian as a minimum. Doing so requires ambition and creativity.
Doing so need not be as burdensome as one might assume, the solutions can even stare right at us. Take the old idea
“There are many considerations when developing vegetarian and vegan options. One of the most fundamental is meeting vital protein requirements and other key nutritional needs.”
of sponge and custard – in theory, a simple dish that is adaptable to both vegetarian and vegan diets. Yet, for many elderly people who adopt this lifestyle choice, and others looking to do so, this is not an exciting, nor appealing option.
Instead, we encourage our chefs to think differently and bring fresh ideas to the table that hit all three of our targets, not only in terms of nutrition, but taste and quality for our residents.
Naturally, this is not always a guaranteed success, and requires trial and error. Last year we tested the use of a range of meat replacement products. While some were less appealing, for the most part the others enabled us to develop delicious dishes that were thoroughly enjoyed by residents and have shaped many of our menu options since.
Our commitment to champion vegetarianism comes as Signature Senior Lifestyle partners with Vegetarian for Life. As our partnership progresses, Vegetarian for Life will review our menu plans and help support us through its rating scheme and provide suggestions to bolster our offering further.
There are many considerations when developing vegetarian and vegan options. One of the most fundamental is meeting vital protein requirements and
other key nutritional needs.
The care sector being cognisant that this is very much the topic of the day, rather than of tomorrow, will certainly make a big difference moving forward.
For many chefs the progression towards veganism and plant-based diets presents a new and sometimes daunting transition in their profession. Yet, to achieve success and remain future-proofed for the journey ahead, it’s important to upskill chefs by encouraging them to embrace the challenge, rather than shy away.
At Signature we place a strong emphasis on the provision of training and development opportunities, and each year we look to deliver dedicated days towards honing these skills and their understanding of dietary needs.
Just last year, we led a pasta-making
programme in which our 18 chefs were able to learn different techniques, including how they can substitute ingredients for vegan or vegetarian alternatives within their pasta and pie recipes.

Adapting to and utilising a resident’s own background with food is a key factor in meeting their care needs. To illustrate this, we even had a resident at our care home, Signature at Wandsworth Common, who taught our chefs how to cook traditional Balinese food, which was predominately vegetarian and vegan and added another string to their culinary bows.
This is ultimately the binding factor behind any success in this space. To remain at the cutting edge when it comes to supporting resident’s lifestyle choices and diet it needs the right people, with the right skillset, to make it happen.
Achieving clean, infection-free laundry involves more than just high-performance machines. It also requires efficient design and processes as well as regular staff training.
For some inspiration on what can be achieved, WASHCO, the commercial laundry specialist, catches up with the joint winner of its Love Laundry Hero Award, Sarah Williamson, laundry manager from Canwick House Care Home in Lincoln, whose changes have improved infection control and staff engagement.
What changes have you made to Canwick House’s laundry facility since joining the home?
Since becoming part of the team, I’ve introduced many small improvements to the laundry. In particular, I enjoy assisting staff to maintain a new culture and understanding of the importance of infection control within the laundry room environment.
But the biggest change has been to the layout of the laundry room. The home is located in a beautiful listed building and the laundry room is in a small space. Changing the design and layout of the room has meant a more user-friendly experience as well as total IPC (infection prevention and control) compliance. We’ve removed old pipe work and a butler sink, as well as introduced splash back tiles, new colour coordinated systems and regular staff training around laundry management.
You mentioned you enjoy helping the team; what training has been put in place?
After completing a ‘Train the Trainer’ course which management suggested, I now undertake regular training for all staff. This means we can go through relatable in-house experiences and discuss challenges laundry staff may be facing. I am on hand daily to support staff and give that motivation and encouragement.
How have your changes positively impacted the team and your laundry results?
All members of staff have shown a greater confidence around laundry
management. Where previously, the wrong washes were used – often a ‘hot wash’, we now have a better understanding of the programmes available and how our machines operate, so we can use them to the most efficient and correct procedure.
Staff feedback that they feel confident when entering the laundry room and are able to solve any issues, whereas before they would have needed to call on others for help.
Looking to achieve the same in your care home? WASHCO can help!
WASHCO’s aim is to work with your care home to find the right cost-effective laundry solution that meets your needs.


From conducting site surveys to helping establish the optimum working environment to installing energyefficient laundry equipment and delivering staff training, WASHCO has helped care homes across the UK transform both their laundry facilities and their processes.
To help keep laundry simple, WASHCO has introduced a comprehensive rental package. With no upfront cost, predictable monthly
payments and servicing and maintenance included as standard, it’s a great alternative for care homes that may not have the capital to purchase machines outright.
There are many things to consider when running a care home laundry, so WASHCO has compiled a library of handy resources to give you a helping hand. These include a laundry capacity calculator, equipment buyer’s guide, laundry room poster and much more. Scan the QR code to access WASHCO’s care resources.

Alternatively, visit washco.co.uk/freecare-home-resources
To start transforming your laundry, call WASHCO’s expert team on 08000 546 546 or email: info@washco.co.uk
Well, we are now well and truly into 2023 and the year ahead is stretching out in front of us, so what of the year to come?
It’s going to be a tough one for all I think, that, as they say, is a ‘given’, so this year I’m going to explain all I know and all I have learned for making the lives of those with dementia and their families just that little bit better and try to improve the wellbeing of all those affected by this awful disease as well as explain what it’s like to live with dementia and also provides updates from the Purple Angel Dementia Campaign and all it’s up to. I will also chat about nutrition and hydration, as well as things going on for carers around Torbay to help them get some much-needed ‘me time’.
After the euphoria (or not) of Christmas and New Year we sometimes come down to earth with a bump. I know I do, as Christmas festivities are a huge thing in our house and, dementia or not, we try and make the best of it.
But there’s always that little empty feeling at the beginning of January with the dread of the coming months and facing another year of not knowing where to go or what to do when dementia touches your lives, especially for the first time, so we will start at the very beginning as Julie Andrews once sang.
I am so often asked how come I have managed to live so long with this disease and yet others sadly pass away after only a few years and my answer is always the same. At the very first sign of forgetfulness becoming a problem please seek a diagnosis. Go straight to your doctor with your concerns and ask

for an appointment to see someone in the memory clinic or the equivalent in your part of the world.
You see we all have forgetfulness, even kids forget things, but when it comes to forgetting how to get dressed, where you live, being lost when out or how to use a knife and fork, then you must please act quickly. I had a very early diagnosis along with a scan of my brain and even though it took a while to get the medication right, though not a cure, it certainly helped me, but a very early diagnosis is such a must. When all’s said and done, if your results come back as
clear, just think of the relief you will feel; if not, I promise you, once you have got your head around it, a feeling of relief also ensues as at least you know what’s going on and you’re not just becoming more forgetful as they say.
It’s the not knowing that can hurt the most, the confusion, the ‘fog’ as they call it in front of your eyes and the frustration when everybody keeps telling you, you are getting things wrong, trust me, even for someone as placid as myself it used to drive me up the wall. I was convinced the whole world was wrong and I was right, when it turned out it was the other way around, but once you know, you can start to understand it, even if only a little, it does help.
Living with dementia for both the diagnosed and families is without doubt a very grey area and a quagmire of emotions and frustrations, but hopefully, month by month I will try to make it a little easier for you as clear and simply as I can, but please remember “if you are unsure about your memory in any way? Seek a diagnosis please!”
Till next time...
As always, carers have been demonstrating their creativity through fun and innovative events for their residents…

Leicester were all a flutter when some friendly feathered visitors came to visit. Elvis, a Eurasion eagle owl and Fletcher, a tawny owl, were brought to the RMBI home by local organisation Bird on the Hand. Home activities coordinator, Fiona Collins, said: “It was a fantastic way of bringing nature and the outdoors into the home on a cold winter’s day.”

When resident Nalini Bhagwat asked staff at Colten Care’s St Catherine’s View dementia care home if she could revisit some Bollywood dance moves, companionship team leader Laura Sheldrake reached out on social media. Dance teacher Vaishnavi Singh responded and danced with Nalini for nearly an hour. Nalini learned classical Indian dancing as a child.

Residents and staff at Liverpool’s Oak Springs Care Home, part of Sandstone Care Group, teamed up with members of the community to knit the city’s longest scarf. The 104-metre woolly creation, as long as ten double-decker buses, was knitted to celebrate Dignity Action Day, an annual opportunity to uphold people’s rights to dignity.

Residents at the Royal Alfred Seafarers’ Society’s specialist maritime care home welcomed a group of sea cadets to share stories and learn about how life at sea has changed over the years. During the visit, the first in an ongoing partnership, many of the residents wore their uniforms and medals and shared stories about each award.

The Year of the Rabbit kicked off with a celebration at Sandstone Care Group’s St Helens Hall Care Home. Activity coordinator Jackie Smith and her team worked with residents to create colourful Chinese lantern decorations, and the home’s chef prepared a Chinese banquet with everything from prawn toast to a selection of curries and noodle dishes.
Residents at Devonshire Court in
Priesty Fields Care Home in Cheshire
has launched a nutritional scheme based on popular TV show Come Dine with Me. Residents rate their dishes with scorecards, giving chef Barry Moorcroft a better understanding of likes and dislikes. The ‘Care Dine with Me’ scheme aims to promote independence and a sense of control among residents.

Knutsford-based care home MHA The Willows took residents to China from their armchairs as part of its Chinese New Year celebrations. Residents’ names were printed in Chinese and put on the walls along with decorations prepared during the craft club. The day included traditional Chinese food, activities and a ‘tour of China’ with videos of famous landmarks.

Residents at Barchester Healthcare’s Meadowbeck Care Home celebrated International Flower Day with activities


including flower arranging and a quiz. Annaliza Kemp, general manager, said: “Our garden is a much loved space. We don’t have many flowers at the moment so our residents very much enjoying the escapism of virtually visiting some of the most famous gardens in the world.”
Cinnamon Luxury Care is rolling out drum fit classes across all of its homes, after successful sessions in four settings. Fully trained and qualified drum base exercise leaders support residents through seated, drum-based exercises – a great way to get less active people moving. Geoff Pride, activities support consultant, said: “This workout class encourages participants to release the popstar within!”

MHA Oak Manor has created a ‘remembrance fence’ where residents and members of the community can remember their loved ones by placing a padlock. Home manager Fay Gooch was inspired by the lovelocks on the Great Wall of China. “Because of where the fence is, it’s something that will catch the eye of people when they go past,” she said.

Aberdeen care home residents celebrated Burns Night with the help of local pipers and school children. Renaissance Care’s Cowdray Club, Jesmond and Persley Castle Care Homes all hosted traditional Burns suppers of haggis, neeps and tatties, followed by a dram of whisky for those who fancied it and recitations of some of Burns’ most iconic works.
with the residents. After a creative afternoon at the home, Super Freak, also known as Dan Whitehouse, auctioned the artwork via Instagram, raising £1,000.
Wokingham-based Prince Philip Duke of Edinburgh Court has joined the Unit Award Scheme, allowing residents to engage with learning and have their achievements formally recognised. Irene Muggeridge, aged 104, took up arts and crafts lessons to create her own woollen pom-pom, an accomplishment that came with an official certificate.



Staff at Plymouth’s Butterfly Lodge escorted residents living with dementia to see the Eden Project’s immersive winter music and light experience. Sarah McCaffrey, deputy manager at the Camelot Care home, said: “A sensory experience like this offers an immediate reward to people living with dementia and can also remind them of happy times in their past.”

Freak out
Birmingham-based artist Super Freak, who has more than a million followers on Instagram, visited Field House Care Home in Stourbridge to create artwork
Therapy guinea pig Poppy visited Thetford’s Buckingham Lodge Care Home with other pigs from Cuddly Cavies. The furry friends enable the use of fine motor skills, prompt memories, encourage vocalisation and provide a fun sensory experience. Diana Taylor, owner of Cuddly Cavies, said: “One gentleman doesn't speak much, but he absolutely lights up when we bring a guinea pig in and will happily sit with her for the whole hour.”

Lowestoft care home The Dell has transformed a day care centre, empty since the pandemic, into an activity centre. The Wellbeing Care home created a space for residents and assisted living tenants to enjoy activities such as a breakfast club, providing an opportunity to socialise and enjoy food outside the typical care setting.
The lighting industry has coined the term ‘human-centred lighting’ to describe lighting systems that reflect the day-night cycle: bright ‘cool’ days, ‘campfire glow’ evenings and dark, peaceful nights. This logical approach builds on NASA’s billion-dollar investment in lighting systems to help astronauts on the space station get a good night’s sleep.
There is exciting evidence that this principle can effectively transform the quality of sleep for older adults in longterm residential care too. Studies from around the world consistently show a significant reduction in falls due to night-time wandering and reduced ‘sundowning’ agitation. Evidence also points to reduced medication and night-time staffing levels, improved working conditions and a more relaxed environment for loved ones to visit.
A growing number of care homes are adopting this approach and seeing the benefits. In the UK, Ed Russell, chief executive of WCS Care in Warwickshire, noted significant improvement in
mood, almost complete elimination of sundowning and increased resilience during the Covid-19 pandemic. Kim Crowe, chief executive of the Parkhaven Trust in Liverpool, was able to focus care teams on daytime activities. Michelle Borreson, administrator at the Tweeten Care Centre in Minnesota in the US tracked a 62% reduction in energy use and a significant cut in maintenance costs. She was delighted to see a 30% reduction in falls and a 10% cut in antianxiety and anti-psychotic medication too. Borreson estimates a return-oninvestment within six-and-a-half years from energy savings alone. All these care providers say their facilities enjoy significantly higher occupancy rates than the average in their local area, with the potential to charge a premium for their facilities thanks to the improved environment of care they provide.
This brings us to the critical question – does it cost more? These lighting solutions do cost more upfront than basic products, partly because they are designed to change brightness and

colour from bright ‘cool’ to soft warm from daytime to evening. These systems also demand more sophisticated controls than ‘on-off' and motion sensors that may be in place today. However, systems can be designed to retrofit with phases in implemention to minimise disruption. Many run on an open ‘bluetooth mesh’ so that there’s no need to rewire, or sign up for a proprietary system or an ongoing maintenance contract which can be more expensive over time. But the additional costs can be offset in two ways. First, the energy costs. LEDs are more efficient than fluorescent lights, so they use less energy when they're on. This approach also means that they are dimmed or switched off entirely for a significant part of the day, representing additional savings. The second is a reduction in operational costs: medication, staff absence and turnover can all make a significant difference to the bottom line.
Human-centred lighting is not rocket science. These down-to-earth solutions have the power to create a brighter future for us all.
Digitalising Social Care at NHS England offers advice on where to start when going digital.
Moving from paper-based systems to digital systems can be daunting. With so much information out there it’s hard to know where to start and, if you describe yourself as a technophobe, it might all feel pretty overwhelming.

Breaking it down into manageable stages is definitely the best approach; it’s a marathon, not a sprint after all.
When considering new technology for your service it’s best to ask yourself some fundamental questions: are our current systems fit for purpose, both now and looking to the future? What positive changes can technology help us achieve? How will we know that it’s been successful?
For many care providers the first step to digital transformation is the move from paper-based care planning to using digital care records.
But there are some other elements to consider before getting to that point. How good is your Wi-Fi? Have you thought about data security and cyber protection? Is everyone on your team on board with the proposed change?
Decent internet connectivity is essential for any business these days and that applies to care businesses too. There’s guidance to help you get set up and the good news is things like digital care record systems can still work well even if you don’t have superfast internet connectivity.
Making sure you’re managing confidential information properly is important for any business. The Better Security, Better Care programme is there to help care providers store and share information safely and this applies to both paper and digital records. Completing the Data Security and Protection Toolkit will help you to evaluate and improve your data and cybersecurity and ensure you have met the standards needed to handle data safely and transition from paper to digital.
And last, but definitely not least, digital transformation needs to start from the ground up. It’s vital that
“For many care providers the first step to digital transformation is the move from paper-based care planning to using digital care records.”
everyone in your team is onboard with the change. Do they understand the benefits of digital working and the role they play in making it happen? Most importantly, everyone needs the skills and confidence to use the technology effectively. The good news is there’s lots of free training to support you and your team in gaining and developing those digital skills.
Once you’ve got these fundamentals in place then it’s time to think about moving away from paper to digital care planning.
We can help you with all of this. We manage a list of companies that have passed our rigorous assurance processes for provision of digital care plan solutions. There’s even an online tool to help you select the right system for your needs.
When it comes to paying for it all it’s important that you set your budget and understand both the upfront and ongoing costs, including aspects such as the time it will take to transfer care information over. There’s matched funding available to help you get up and running with going digital and make that initial investment.
What if you’ve already got a digital care plan in place? Now you’ve made that leap there’s lots of other ways you can continue to digitalise. We can help with funding to support you to make further investments in technologies that improve the quality, safety and personalisation of care, such as sensors to ensure staff are alerted if someone falls.
There’s lots of help and support, wherever you are on your digital journey. With funding support, help to develop your team’s digital skills and resources and opportunities to learn from other providers there’s never been a better time to take that first step into digital care.
For more info, contact us at: england.adultsocialcare.nhs.net
You’ll also find lots of information about funding, training as well as useful resources including our list of assured suppliers by visiting digitalsocialcare.co.uk
In our monthly feature showcasing our amazing care home managers we talk to Victoria Read, general manager of Signature at Barnet

Why did you join the social care sector?
I worked in the leisure, health and fitness industry for more than 25 years, but made the decision to take a completely different direction in career and join the care sector after my experience caring for my mum before she sadly passed away. I was inspired by this part of my life and wanted to continue making a difference in the lives of others. This was one of the best decisions I have ever made. While it was not easy to begin with, and for the first two to three years an immense learning curve, I knew as soon as I walked into my first care home as the manager, I was at home and where I was supposed to be.
What do you enjoy most about your job?
I love being part of a team and organisation that truly believes in providing the best care. It is a real privilege to help our residents be who they are, enjoying life, being happy, making friendships, and remaining independent and active. My job is never boring, and no day is ever the same, which allows me to keep learning and striving to be the best I can be.
Who is your social care hero and why?
I don’t have one person. I am in awe of anyone that specialises in end-of-life care. Their empathy, patience and ability to go above and beyond to deliver care with dignity right to the very end is admirable and takes a very special person to be able to do it.
What is the one thing you would change about social care?
I think there should be greater funding to support residents to go to the care homes of their choice, whatever their circumstances.
What, in your opinion, makes a great care worker?
I believe to be a great care worker you need to be able to communicate effectively, have clear goals and targets,
be motivational and inspiring to those around you, and always make time for your residents, relatives and their families. To achieve all of this you ultimately need to love what you do.
What do you do when life all gets a bit too much?
I absolutely love my Peloton bike and can often be found taking a virtual spin class, even at 4am when they are being broadcast live from New York. I also love taking my dog Barney on long walks, which gives me time away to relax, think and reset.
What advice would you give your younger self?
Life is going to throw some real curve balls at you, so believe in yourself –you’ve got this!
Which three famous people would you have to dinner and why?
I absolutely love a dinner party, so three is certainly a struggle. Pink – she is amazing. She holds strong opinions and beliefs which I would want to find out more about, and she can also
“I think there should be greater funding to support residents to go to the care homes of their choice, whatever their circumstances.”
really sing so would provide some great entertainment.
Barack Obama, he has lived an incredible life. I would have so many questions to ask and I am sure he has some fascinating stories to tell.
And Dame Judi Dench, she’s an amazing actress, and one that has had a remarkable career which would be great to hear more about.
What three items would you bring with you on a desert island?
A portable solar panel charger with cables, a mobile phone and a big knife.
What is your secret talent?
I can tell a good joke!
More than a third of the population aren’t sleeping enough. Charlotte Goddard finds out how sleep deprivation affects care workers and what can be done to help
Only 37% of people in the UK get enough sleep, according to Nuffield Health’s Healthier Nation index. Care workers can be particularly vulnerable, according to Karolina Gerlich, chief executive at the Care Workers Charity. “Some issues are related to work patterns, which might include waking or sleep-in shifts,” she says. Care workers are often woken more than they should be during so-called ‘sleep-in’ shifts, she explains, leading to disturbed sleep. “There are also liferelated issues that can impact on care workers’ sleep, such as anxiety,” she says.
Difficulties with sleep is a particular issue for people with stressful jobs, combined with a demanding home life. “When there is no place to process anxieties during the day, that processing may take place at night,” says sleep therapist Dr Kat Lederle. “You are either unable to get to sleep or wake up worrying at 3am.”

“If you have just one bad night's sleep, you're four times more likely to catch a cold the next day.”

Shorter sleep times have been linked to a wide range of health issues, including heart disease and diabetes. “During sleep, we optimise our immune system,” says Dr Neil Stanley, independent sleep expert. “If you have just one bad night's sleep, you're four times more likely to catch a cold the next day.”
There are links between sleep deficiency and depression, anxiety, social isolation and poor emotional wellbeing. Lack of sleep can affect cognitive skills such as planning, problem solving, concentration and memory. “Your ability to do your job lessens, your judgement is affected and your reaction time is slower,” says Stanley. “You will feel less empathy and become less able to interpret body language and tone of voice.”
Given that a lack of sleep has such a devastating impact, what can be done to help? General tips for getting a good night’s sleep include ensuring your bedroom is calm and dark, avoiding caffeine, alcohol and electronic devices before bedtime, and establishing a relaxing wind-down routine. However, what happens during the waking day, including in the workplace, is just as important as what happens at night, says Lederle. “We can't just work on the hour before you go to bed.”
Advice for creating a sleep-friendly workplace includes encouraging staff to set up a blue filter on mobile devices, since the light they emit can disrupt the sleep-wake rhythm. Non-caffeinated drinks and healthy food options should be readily available, including during night shifts.
Managers who act as ‘sleep leaders’, promoting and modelling the importance of sleep, can play a vital role, says Lederle. “The supervisor needs to be checking in with the team about sleep,” she explains. “They also need to send a strong message that it is OK to prioritise your sleep.”
Mindfulness techniques and meditation can help with stress and anxiety at bedtime. Therapeutic techniques can also help – cognitive
behavioural therapy has been shown to be as effective as sleeping tablets and to last longer, Stanley says.
“It’s important to make the link between poor sleep and poor outcomes. Remember that good sleep is one of the best things you can do for yourself.”
In a society that doesn’t necessarily value sleep, it’s essential for employers and managers to show that they do. “We live in a society that doesn’t see sleep as important,” concludes Stanley. “It’s important to make the link between poor sleep and poor outcomes. Remember that good sleep is one of the best things you can do for yourself.”
Find out how to maximise your sleep from Dr Neil Stanley at the Care Managers Show at NEC Birmingham, 30 June – 1 July.

Jamie Ashton, Orchard Care Home’s clinical lead at its Three Bridges home in Warrington, talks to Caring Times about the importance of families discussing end of life care at a critical time in a person’s life.

By specialising in end of life care, Ashton chose what could be considered quite an unusual career path for someone starting out in nursing. After qualifying as a nurse at Chester University and undertaking a post in intensive care for two years, he realised that his passion lay in caring for the elderly and sought to develop end of life care practices within Orchard.

Having grown up around care, often visiting his grandmother in a care home in Workington, Ashton knew that often the difference to a positive end of life experience, where everyone feels informed and able to contribute their needs, can bring so much comfort to the person and their families.
“Often talking about death is a bit taboo,” Ashton says. “Many people feel uncomfortable either talking about their own end of life wishes or feel anxious bringing the subject up."
“Often talking about death is a bit taboo,” Ashton says. “Many people feel uncomfortable either talking about their own end of life wishes or feel anxious bringing the subject up.
“At Orchard Care Homes, we believe that everyone should have a voice when it comes to their end of life care plans,” he continues. “It’s important to decide who the person wants by their side in the final hours and what symptom management they prefer. Some of the people we have helped have requested more contemporary methods of relaxation such as aromatherapy, which can help to ease the anxiety around such a difficult event.”
The Covid pandemic was a bit of a turning point for Ashton and his team as social distancing restrictions meant that often he had to become the conduit for the sick person and their family, so he sought to bring everyone together through a bespoke questionnaire.
“This approach was a bit of a game changer for us,” comments Ashton. “It really helped to address the visitation issues at the time and it prompted questions between the family which they may not have thought about or were too worried to ask.”
While a difficult role emotionally, end of life care is something that Ashton and his team continue to adapt and develop as they learn more about what each individual needs. Quality of care and best practice is at the forefront of Orchard Care Homes’ strategy and end of life care is no exception, with the team often going the extra mile to gain a positive result for the families.
“I’m always thinking how I can do more to help to make such a difficult event more comfortable for everyone."
“I’m always thinking how I can do more to help to make such a difficult event more comfortable for everyone. Some days it’s really hard, and I go home taking the job away with me, thinking what else can be done to make a family’s experience as positive as possible.
“It can be a difficult, emotional job,” he adds. “But I wouldn’t change it for the world. I’m really proud of our achievements and the caring, respectful work we do for our people at a time when they need a lot of reassurance and hand holding.”
Hillcrest
Redruth
Closed care home
Kerensa Care and Support
Achieve Together
£295,000
Christie & Co
Simon Harvey – 07764 241310
The Old Vicarage


Otterton, near Budleigh Salterton
26, Residential
Transfer of Shares in Glebefield Care

£2.65 million
Christie & Co
Simon Harvey – 07764 241310
Dorset
Transfer of shares in Bymead House

3.25 million
Christie & Co
Hertfordshire
Nursing Home
IF YOU’RE THINKING OF SELLING YOUR CARE BUSINESS, SPEAK TO THE EXPERTS: Contact our award-winning team on: 0207 448 8826 | care@christie.com
Name of property sold:
Treetops Residential Home Margate 24, Residential Undisclosed


Undisclosed
Undisclosed
Christie & Co
John Harrison – 07764241296
Learning Disability
Undisclosed
Undisclosed
Undisclosed
Christie & Co
John Harrison – 07764 241296
Name of property sold:
Duckyls Farm Centre West Hoathly

10, Learning Disability
Undisclosed
Undisclosed
Undisclosed
agent: Contact person:
Christie & Co
John Harrison – 07764 241296


Malvern House Nursing Home, Saltash

Freehold, £1,350,000
Registered for 22
Detached and extended home
3270341
T: 07764 241310
Care Home, Devon
Freehold, £1,450,000

LOOKING TO SELL? TALK TO THE EXPERTS. We have a large pool of buyers ready to invest in the UK social care sector.




Drayton House, Bridport, Dorset
Freehold, £699,000
• Former care home premises
• Previously registered for 19 3270341
T: 07764 241310
• Grade II listed care home


• Registered for 24
3270262
T: 07764 241310
Care Home, Cornwall
Freehold £1,150,000
• Run by registered manager
• Registered for 19
3270366
T: 07764 241310
Confidential Property
Care Home, Bridgend
Freehold £1,100,000
• Registered for 31
• Long established home run under management
3470707
T: 07702 809198
Care Home, Glamorgan
Freehold, £650,000
• Registered for 27
• Excellent reputation
4770015
Manor House, Cornwall
Freehold, £995,000
• Registered for 16
• Adjacent detached two bedroom cottage
3270297
T: 07764 241310
T: 07702 809198
Confidential Property
Former Llanyravon Court Nursing Home, Gwent
Freehold, £1,250,000
• Purpose built care home

• Previously registered for 53 3470704
T: 07702 809198
24 November 2023 | Platinum Suite, London
The National Care Awards returns in 2023 for its 25th year. We can’t wait to celebrate our silver anniversary event with all the gold star employees in the social care sector.

Whether you’re new to the industry or have joined us before, get ready to submit your entry when we open submissions, then secure your place at the prestigious and fun-filled National Care Awards.
Shop