Hartford Care invests in sustainability
Mike Padgham urges the main political parties to seize the moment for social care reform

How CQC inspections will change
Daisy Cooper shares the Lib Dems' vision for social careChief executive officer
Alex Dampier
Chief operating officer
Sarah Hyman
Chief marketing officer
Julia Payne
Editor-in-chief
Lee Peart
Features editor
Charlotte Goddard
Subeditor
Charles Wheeldon
Advertising & event sales director
Caroline Bowern 0797 4643292 caroline.bowern@nexusgroup.co.uk
Business development director
Mike Griffin
Sales manager
Luke Crist
Business development executive
Kirsty Parks
Business development researcher
Robert Drummond
Delegate relationship manager
Sharifa Marshall
Event manager
Conor Diggin
Marketing content manager
Sophie Davies
Marketing campaign manager
Sean Sutton
Publisher
Harry Hyman
Investor Publishing Ltd, 3rd Floor, 10 Rose and Crown Yard, King Street, London, SW1Y 6RE
Tel: 020 7104 2000
Website: caring-times.co.uk
A major new report on the NHS and social care last month provided a timely reminder to politicians ahead of the general election on the urgent need for reform.
The Times Health Commission, which is made up of experts, including clinicians, business leaders and academics, aims to help inform policy on how the NHS and social care are run.
In a 10-point plan for health and social care the commission backed the creation of a National Care System (NCS), which similarly to Labour’s tentative proposals for a National Care Service, would be administered locally and delivered by a mixture of the public and private sectors.
As well as providing a much-needed single brand, similar to the NHS, which would help improve recognition and pride in the sector, the NCS would set national guidelines to establish baseline standards for care quality and workforce terms and conditions.
As social care has persistently called for, care staff would be better recognised and suitably remunerated by integrating their pay scales with equivalent NHS bands.
In terms of service user reforms, the commission recommends the immediate adoption of the delayed £86,000 lifetime cap on care costs.
The experts also recommend raising the current £23,500 level on which people no
longer qualify for state support for social care.
So how this will all be paid for?
The commission suggests around half the money required for reform could be raised from older rather than working age people. Proposed measures to achieve this include shifting from the pension triple lock to a simple earnings uprating which would raise £14 billion a year and means testing the winter fuel payment.
In addition, the commission suggests making all employees and employers pay national insurance , or as in Japan, having people pay a higher tax rate when they reach 40 to reflect the rising costs of social care.
With Labour already rowing back on its commitments to social care in advance of the general election, the commission’s report provides a timely reminder that the next government cannot shirk the need for urgent, long-term social care reform.

6
We round-up last month's big stories
8
10
Daisy

12
Christie
14
Hartford Care invests in green environments and Jonathan Freeman calls for sharing of best
16
Last month's big deals
18
Last month's personnel moves
20
Mills & Reeve flags up changes to CQC inspections

Join our mission to bring people together and end loneliness.
Support a socially driven, charitable organisation committed to reducing feelings of loneliness and isolation, by encouraging intergerational bonding through the pairing of volunteers with the older persons' community.
How can you help?
Download our app Sign up as a volunteer today!

Register your care home!
Our initiative is endorsed by CQC and we would love to have more care homes and older people to pair with our volunteers!

Become a Sponsor!


Help us to grow our charity - find out more on our website!
With thanks to our sponsors and partners:




hello@adoptagrandparent.org.uk

“Speaking to Ruby has become the highlight of my week; I always look forward to receiving her calls ” Iris, ‘Grandparent’




www.adoptagrandparent.org.uk
A £600 million support package, including £500 million for social care, was announced by the government. The £500 million, which comes in addition to the £64 billion provisional Local Government Finance Settlement for 2024-25, will be added to the Social Care Grant to bolster social care budgets.
The government announced that overseas care workers will no longer be able to bring dependants to the UK as of 11 March. The news came as the government rolled-out the timeline for measures designed to reduce net migration announced by home secretary James Cleverley in December.

The Home Office ruled out raising English language care worker requirements despite the tragic death of a care home resident after foreign staff failed to explain the seriousness of her condition to emergency services. Coroner Samantha Marsh wrote to the Home Office calling for action after the death of Barbara Rymmell at Ashley House in Somerset on 8 August 2022.
A commission set up to address the most urgent challenges facing health and social care called for the formation of a National Care System. In a 10-point plan following a year-long investigation, the commission called for a National Care System that was “equal but different from the NHS”, that would be administered locally and delivered by a mixture of the public and private sectors.
Social care providers gave a guarded

welcome to the Labour Party’s reported priorities for the sector in the coming general election. The comments followed a report in The Observer which said Labour would delay National Care Service legislation if elected but prioritise securing a fair pay deal for care workers.
Care charities The Orders of St John Care Trust and The Fremantle Trust, announced a merger. In a joint statement, the charities said the move would help achieve greater benefits for residents through shared size, pooling of resources and economies of scale.
Residents and families expressed relief after two councils abandoned plans to close three care homes. Private buyers are being sought by Kirklees Council in West Yorkshire for Claremont House in Heckmondwike and Castle Grange in Huddersfield, and by West Berkshire Council for
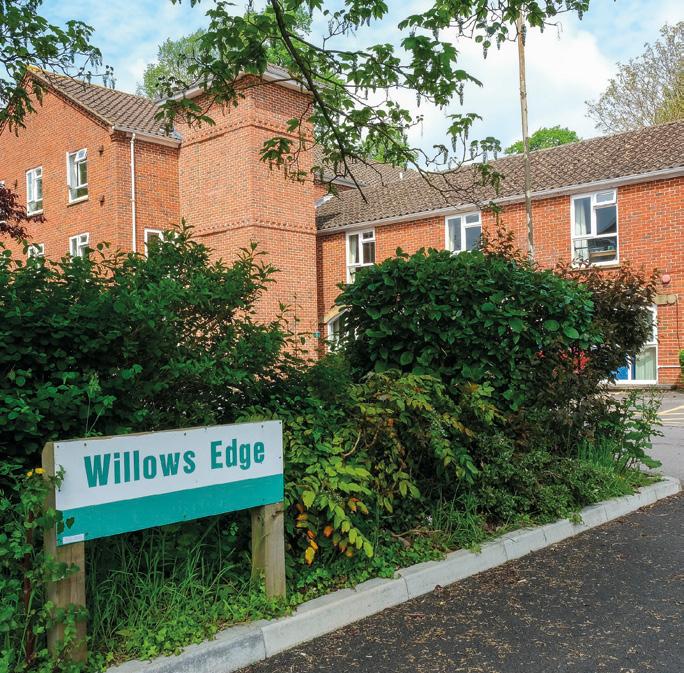
Willows Edge in Newbury, following public consultations.
A luxury home care service focused on integrating with clients’ lifestyles was launched in London by founder and chief executive Louise Blezzard, who was previously group director of wellbeing and membership at Loveday. Vivant incorporates a concierge service, tailored care support and companionship.

Research revealed a more than sixfold rise in the number of international students coming into the care sector. A report published by The Migration Observatory at the University of Oxford showed there were more than 26,000 international students recruited into the care sector in the year ending June 2023, compared with around 3,900 in the year-earlier period.
Signature Senior Lifestyle celebrated record-breaking colleague retention of 96%. The milestone came 12 months after the luxury residential and specialist care group launched its Regional Carers flexible workforce programme.
Lovett Care said it will continue to pay all staff a minimum of the Real Living Wage of £12 an hour, regardless of age or role. The commitment followed the government’s announcement that the Real Living Wage will increase by 10.1% in 2024 and that the National Minimum Wage will rise by 9.8%.
Championing
Social Care’s Christmas Lunch in December raised more than £20,000 for Adopt a Grandparent.
The annual flagship event, which had Virgin Money as its headline partner, was also supported by carehome. co.uk, Dormy Care Communities, Catalyst Interiors and Caring Times.


Target Healthcare, a real estate investment trust which invests in modern, purpose‐built care homes, reported rental growth supported by tenant profitability in the final quarter of 2023. Contractual rental income increased by 1.3% over the quarter, comprising a 1.1% like-for-like increase from 25 inflation-linked upwards-only rent reviews, with an average uplift of 4%.
Lovett Care unveiled a new robotic team member at its Fairfax Manor flagship care home in Harrogate. Alfred, a Servi+ foodservice solution developed by Bear Robotics, can be seen weaving his way through the home’s orangery and dining areas. The state-of-the-art system can perform a number of tasks, including collecting and returning cups and plates, or delivering a cup of tea to a resident’s bedroom.



The Independent Care Group’s chair Mike Padgham urges the main political parties to priortise care as the general election looms
Never has there been a greater opportunity to make now-ornever changes to social care and to the happiness and welfare of many hundreds of thousands of older and vulnerable people.
The sector is currently on its knees but this year, and the general election we will have, offers a once-in-ageneration opportunity to change things and we mustn’t throw it away.
William Shakespeare wrote in Julius Caesar: “There is a tide in the affairs of men which, taken at the flood, leads on to fortune.” His meaning was “seize the day” and that is what we, as a country, must do in 2024. Social care’s time has come.
The election looks like being later this year unless things improve so dramatically that the prime minister is persuaded towards a May dash to the polls.
As an apolitical organisation, the Independent Care Group doesn’t endorse any political party. When you look at the past 30 years there have been endless promises from all the parties on social care and none has yet delivered.
We need change. To begin with, we must ensure social care reform is in the main political parties’ manifestos with some concrete proposals and an end to the sticking plaster politics – a few
"The election looks like being later this year unless things improve so dramatically that the prime minister is persuaded towards a May dash to the polls."
million here, a few million there – that has made zero difference to the sector.
Take the £500 million for social care announced to much cheering by the government just a few weeks ago, for example. Welcome money I am sure, but it has had no impact on the front line.
Going forward, we deserve better. We need the election to bring root and branch reform, a National Care Service and a minimum of £7 billion a year extra into social care to make meaningful change to social care delivery and to the pay and conditions of those we employ.
We deserve to know what’s in the politicians’ thinking before we go to the polls and this time there must be a legally binding way to hold them to account if they fail to deliver. Should there be, I wonder, some social care candidates with that single issue on their nomination papers to stand and make that point?
In more than 30 years, the climate in social care is the worst I have known it. Providers are struggling, handing back contracts, closing services and closing down. We are losing capacity in the sector.
A lack of social care hurts our hospitals, and some 14,000 people can’t be discharged even though they are well enough. Our own hospital here in Scarborough is at breaking point partly because some 20-25% of beds are occupied by people who could be discharged. Much of this is down to a lack of available care.
For example, the number of home care packages is falling, with the Homecare Association reporting that the number handed back in 202223 was an average of 81 per council or HSC trust. And many home care providers are reporting a reduction of 25 to 35% in hours available to them – putting their viability at risk. This is a damaging decline in a government flagship policy, the desire to have people cared for in their own home.
The Care Quality Commission reported that at the end of 2023 there were 518 fewer care homes in England than at the same time the previous year – a closure of 14,169 beds. Care England and Hft similarly reported that some 43% of providers had been forced to close in part or hand back contracts and 18% of care providers offered care to fewer people than the previous year.
This much we know. What we don’t know is what our politicians are going to do about it if they become the next government?
Will they seize the day or kick the can down the road again? Because we should remember that the Shakespeare quote continues: “Omitted, all the voyage of their life is bound in shallows and in miseries.” In other words, if we don’t take this opportunity the chance will be lost. Without action we will sleepwalk into creating social care deserts.
As I write this, the Conservatives are saying very little on social care, while Labour is said to be looking at better pay for the social care workforce but delaying plans for a National Care Service. The Liberal Democrats promise free personal care for some, a Carer’s Minimum Wage and greater support for unpaid carers.
Overall though, I fear the main political parties fail to see social care
" Overall though, I fear the main political parties fail to see social care as a genuine priority or even as an opportunity."
as a genuine priority or even as an opportunity.
They worry about how previous promises of social care reform backfired during the run-up to elections. Or they wrongly believe that there are no votes in it, gambling that people only take an interest in care when they or a family member needs it. That is wrong. More and more people do recognise how important social care is to the efficient running of the NHS and to the overall wellbeing of the country. Let’s start by renaming it the Department of Social Care and Health, run by a secretary of state for social care and health, to give the sector the better billing it deserves.
Reforming it offers a great opportunity, a chance to be the political party that finally grasped the nettle of social care and created something special. Something that, on a social level, meets the needs of the 1.6 million who currently can’t get care
and the hundreds of thousands more who will need it in the coming years and something that eases the intense pressure on the NHS. Something that properly rewards care staff, on a par with their colleagues in the NHS and local authorities. And on a financial level, something that adds to the £55.7 billion the sector contributes to the England economy each year.
And it needn’t cost the earth. The Health Foundation has reported that introducing an £86,000 cap on care costs would only cost the government some £4.25 per household per week. It argued that social care reform was therefore both affordable and urgently needed. Money invested in social care saves money for the NHS in the long run through preventative intervention which hopefully keeps people out of hospital for longer or even altogether. So, the extra investment needed doesn’t all have to be new money, but could be redirected from the NHS.
I accept that politicians can’t do it all. As a sector we must speak louder, with a unified voice and set aside our differences – like the current profit versus not-for-profit debate, for example, for the greater good of social care. Care providers have a role in raising awareness of social care and the vital role it plays in the care of the nation. The government should also call upon the expertise and experience in the sector to contribute to the solution.
We can work with them and with care commissioners to streamline the system and reduce bureaucracy, red tape and delays in the system that prevent care getting to where it is needed quickly enough. We should begin by having social care providers’ voices heard much louder on the integrated care boards.
Local authorities must make care a priority for their citizens and invest in it, rather than driving down fee levels, as they have done for the past two decades, squeezing the life out of care providers in the process.
We need a more understanding and supportive regulator. The Care Quality Commission can learn much from the lessons learned by Ofsted and reduce the pressures over inspection, for example.
We have to take a stand. I have heard people speak about social care strikes and I have heard talk of providers withholding their registration fees. I’m not sure we are there yet, but we can’t be far off. We need decision-makers to sit up and listen.
Above all, we must persuade our politicians that creating a wonderful National Care Service, with a thriving, fit for purpose and sustainable social care element within it, would be something to be proud of, something that would set them apart from their predecessors who have fudged and failed these past 30 years. Now that would be something worth voting for.
Townsend Communications managing director, William Walter, interviews Daisy Cooper, Liberal Democrat spokesperson for health and social care, to hear her party’s “ambitious but credible” plans for the future of adult social care
Often interviews with politicians can prove to be a dry formulaic one-way flow of information. Cooper is not like that. She conveys sincerity and a genuine passion for her brief.
We kick off by discussing her thoughts on the shortcomings of the current government’s approach to social care. “Simply put, it’s just not a priority for them,” she asserts. “What we’ve seen time and time again is that the government seems to wait until there’s a crisis in the NHS” before throwing “large sums of money at the problem, hoping to solve it. There’s never a longterm plan to look at the issue”.
As to how the Liberal Democrats would approach these issues, the St Albans MP is equally clear: “We want to put social care at the absolute heart of our manifesto and the general election campaign.” Her party would be “open and honest about the scale of our ambitions in this area, along with the associated costs”.
Proposals vary across the board. First, one of the Liberal Democrats’ priorities is to introduce free personal care for both over 65s and working age adults, which encompasses support with nursing care, personal hygiene, mobility problems and the taking of medication. The party has estimated that introducing free personal care would cost the Treasury £5 billion, but savings to the NHS as a result would mean the net cost
"We
want
this plan to be seen as both ambitious and credible, based on numbers that have been crunched by the experts."
of the proposal would be just £3 billion.
Cooper is keen to point out these numbers are based on independent analysis: “We’ve used a lot of different authoritative sources on this – the IPPR [Institute for Public Policy Research] has calculated that [the £2 billion in savings figure] is the net saving that can be made across the NHS,” she says. This figure does not factor in other potential savings that could be made elsewhere as a result of fewer people requiring hospital treatment – having been looked after in their own homes under the scheme. “We want this plan to be seen as both ambitious and credible, based on numbers that have been crunched by the experts,” she says.
Among other proposals is a higher minimum wage for care workers across the country, a part of a larger plan to “make sure that care workers themselves are really valued”. Particularly during Covid, care workers “made enormous sacrifices, and there hasn’t been a proper reward or recognition of the enormous contribution they have made”, Cooper argues. She suggests that the current failure to appreciate properly the skilled nature of care work, and support employees with sufficient renumeration, was partly responsible for the “mass exodus” of care workers to other sectors, including the NHS, hospitality and retail roles.
A key aspect of the Liberal Democrats’ plan for social care is the introduction of a Royal College of Care Workers. Noting the success of Royal Colleges in the health sector in promoting the interests of their members so effectively, Cooper argues that the introduction of a similar body for care workers would provide “the status, the voice, the pay and the career progression that many carers really want to see”. As the care sector changes, as the needs of care users change, and as the care workforce itself changes, she hopes that the Royal College would ensure care workers “always have a voice at the table”.

“A lot more support for the millions and millions of unpaid carers” across the country is also an important pillar of the Liberal Democrats’ plan for adult social care. Cooper’s parliamentary colleagues have made recent progress in legislating for further support, not least Wendy Chamberlain MP, whose Carers Leave Act is scheduled to come into force in April this year. Under the provisions of the Act, employees who balance work with caring responsibilities will be entitled to at least one week of unpaid leave annually. Cooper explains that the Liberal Democrats would commit to making this leave paid, rather than unpaid, if elected.
Also proposed is an increase to the carers allowance provision of around £1,000 a year, and the Liberal Democrats plan to increase the weekly income threshold at which people become ineligible for Carer’s Allowance.
Asked about how the Liberal Democrats plan would provide support for care home providers, Cooper argues that “stability and long-term security” are key, where providers know that the government has got a longer-term plan. The Liberal Democrats would, she states, not only introduce a social care workforce plan “to provide some certainty to the sector that actually we

"At its heart and root, social care should
there
be
to enable people to live their lives as they choose – happy, long lives, living in dignity, with as much independence as possible. I feel incredibly passionate about that.”
are serious about recruiting the staff we need across the sector”, but would also propose a long-term funding settlement.
Cooper is clear that the money for
these proposals would not come from taxes on struggling families; it would come from “big companies who have done really well over the last few years who can afford to pay to support our public services”.
Cooper is also optimistic about the potential for technology in the care sector, though she is keen to point out that many care users prefer to discuss the topic on the premise of “living tech-enabled lives”, rather than simply discussing “tech-enabled care”.
She offers several examples of where technological innovation could, and does, play a significant role in supporting the social care sector. Sometimes, she argues, “it’s as simple as having an electronic tablet box that reminds you when to take tablets. That can be lifechanging”. Cooper discusses The Tribe Project, a technology-based organisation
that aims to increase social action in the care sector through the use of applied technology, reducing pressure on public services across the UK. She nonetheless suggests that a lack of synchronisation between integrated care boards across the country is making the wider expansion of technological innovation in the sector “really hard”. “If we could try to harmonise that,” she continues, “we have a much better chance of rolling out tech innovations that would lead people to have tech-enabled lives”.
Concluding the conversation, Cooper stresses the overarching importance of prioritising social care. “At its heart and root, social care should be there to enable people to live their lives as they choose – happy, long lives, living in dignity, with as much independence as possible. I feel incredibly passionate about that.”
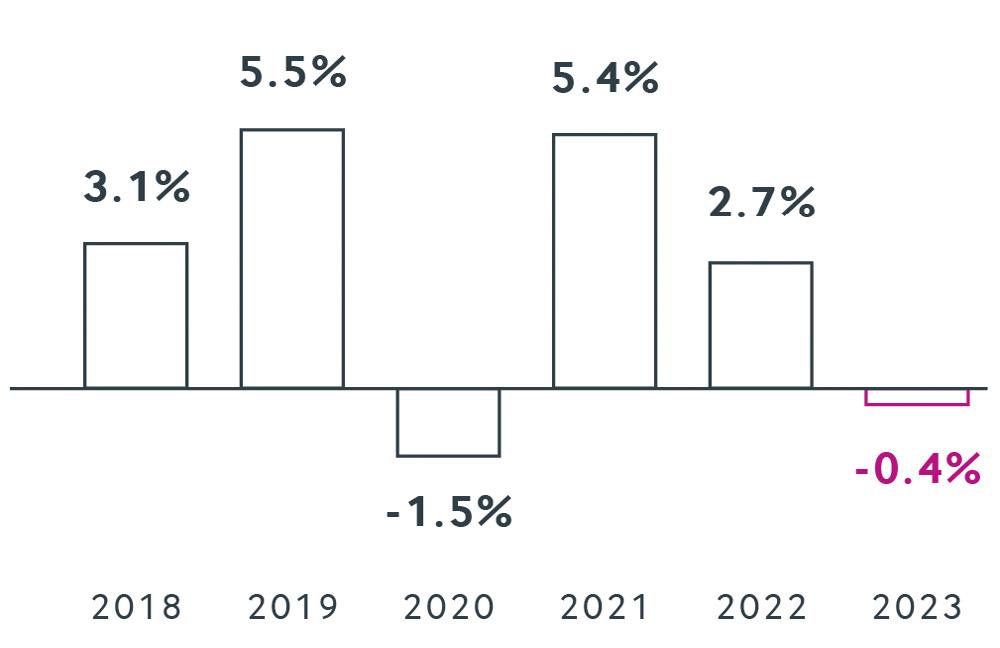
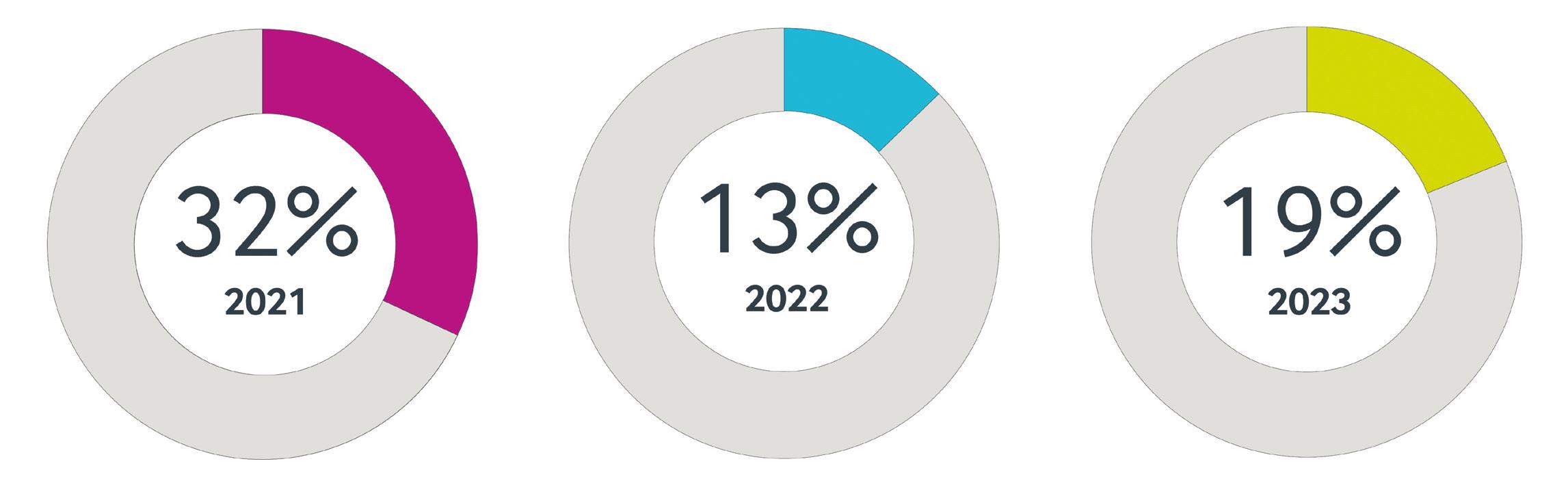
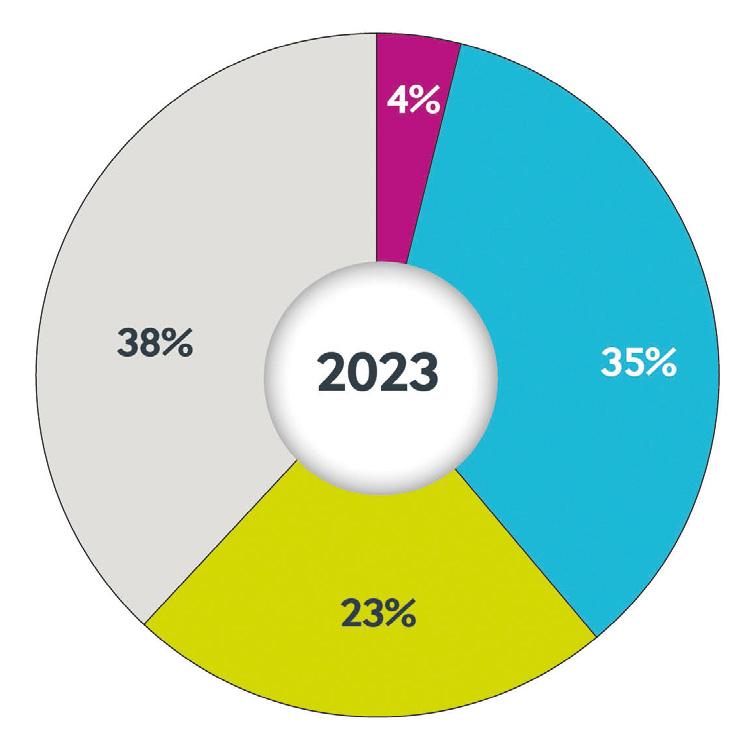
Christie & Co has reported “robust” deal volumes along with a rise in care homes closures in 2023.
In its ‘Business Outlook 2024’ report, the business property advisor reported a 14% rise in completions last year.
Wider cost pressures had a significant impact on providers of smaller, converted care homes which lack economies of scale and are less energyefficient, the report said. This increased the rates of care home closures at a time when demand for bed spaces should be increasing. The proportion of closed care homes sold rose to 19% of deal volumes in 2023, compared with 13% in 2022. Christie & Co said new-builds were not keeping pace with closures with its number of distressed sales rising by 7%.
More positively, the company didn’t see a material deterioration in asset values for going-concern deals – noting a 0.4% decrease in its annual price index – and the performance of the sector fared well compared with other asset classes.
The development market faced stronger headwinds due to construction cost inflation and the availability of debt , Christie & Co said. However, the need for future-proof care beds remained undiminished and the underlying ESG credentials, together with future bed demand needs, remained compelling for investors. Christie & Co saw a greater number of developments in the regions last year
and expects this to continue this year.
Christie & Co also identified other economic pressures, operational challenges, sector funding and sustainability as key themes influencing the sector.
The care sector continued to be well supported by both traditional and alternative funders; with the level of finance Christie Finance generated for its clients having increased by 28% between 2022 and 2023. Income potential and cash flows were seen as particularly reliable due to the sector's needs-driven nature, however there are now more intense audits, assessments, and monitoring from lenders around how operators will manage the effects of the rising cost of living and increase in debt costs on their business.
This year, Christie Finance is hoping for a more stable economic environment which, when combined with currently reducing inflation and the increased cost of living mostly now absorbed by operators, should lead to a more fluid finance market.
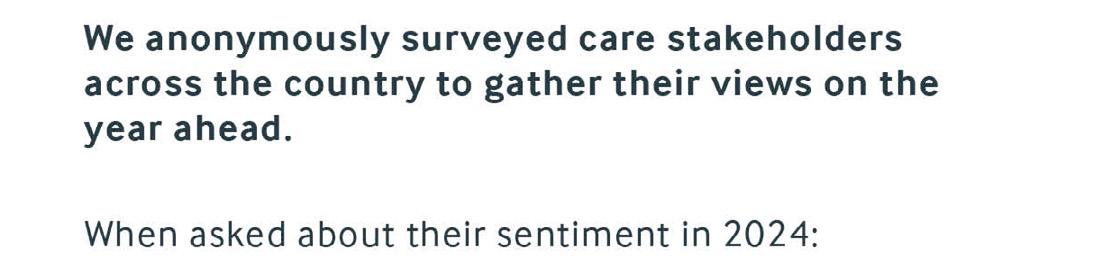
In its survey of healthcare professionals, 48% felt positive about the year ahead – a 14% rise on the previous year – while 9% felt negative. When asked about their sale and acquisition plans in 2024, 77% said they were planning to buy and/or sell.
The company made the following predictions for 2024:
• Capital values will remain stable with strong occupancy levels and investor demand offsetting higher debt costs.
• Capital markets activity will increase
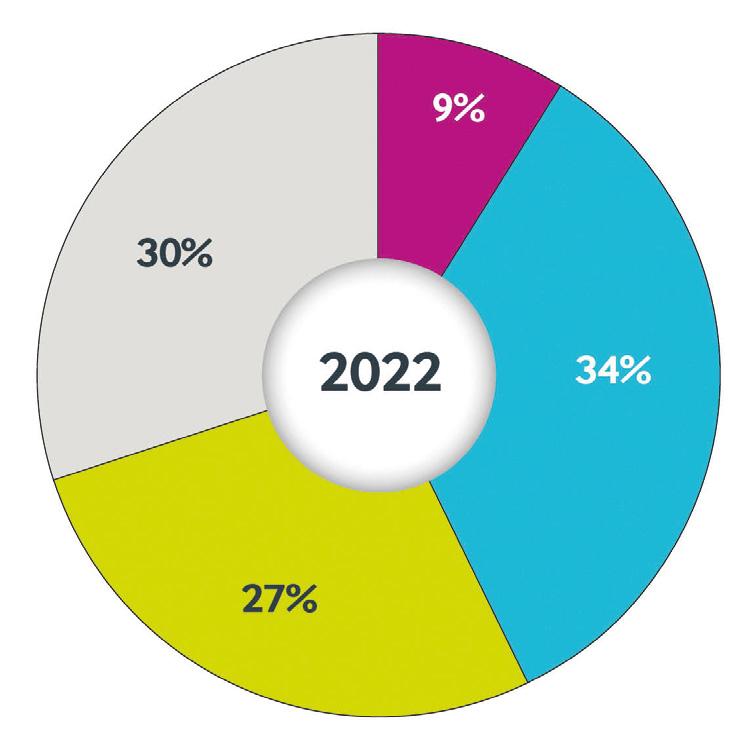
l NEW MARKET ENTRANTS
l INDEPENDENTS
l REGIONAL MULTIPLES
l NATIONAL PROVIDERS/FUNDS
with a more stable interest rate environment.
• There will be an increased number of OpCo transactions as operators seek to expand their portfolios without tying up capital in real estate.
• Growing distress for smaller assets with rising staffing and capital costs, largely driven by the increasing minimum wage.
• New-build development activity will increase across broader geographical regions as operators seek less competitive operating markets.
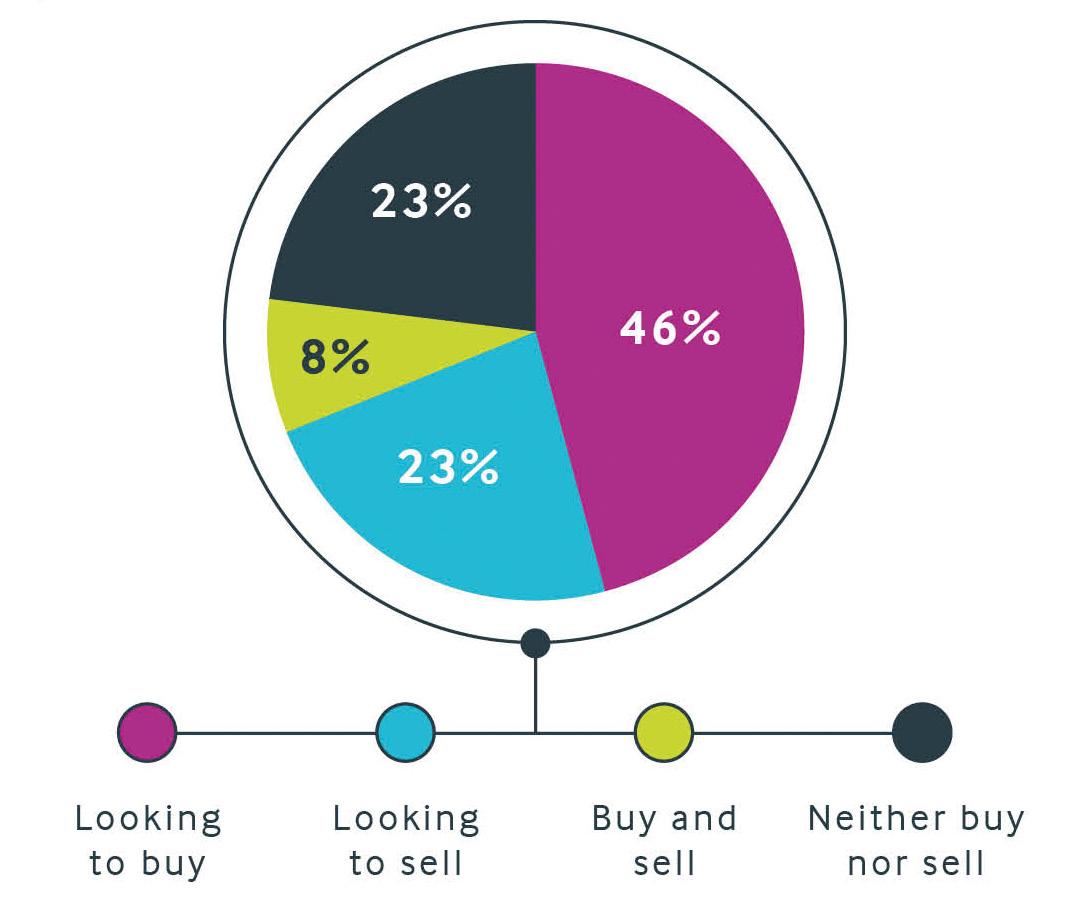
• Ongoing rationalisation from larger providers and third sector providers.
• Continued protractions and uncertainty in the planning system will constrain the supply of consented care home development sites.
Richard Lunn, managing director,
care at Christie & Co, said: “Despite the undoubted economic headwinds, the care sector remained resilient through 2023. Good levels of demand and a limited availability of stock enabled pricing to hold up well. Moving into 2024, we are positive about the prospects for the year ahead.”
Quality director Nicky Barnes explains how Hartford Care is investing in
Committed to building a sustainable future, we are continually investing in our homes and improving our green credentials. With sustainability key to our growth strategy, we have already invested more than £8 million in reducing our carbon footprint and futureproofing our homes.
So far, £2 million has been spent on the installation of solar panels at 11 of our homes, with a further five due to be completed this year. On average, where already installed, around 30% of each homes’ energy is now being produced from the solar panels.
In addition, we are undertaking refurbishment projects across our homes, including installing loft and cavity wall insulation, and changing all lighting to low-energy LEDs. All new home extensions are being built using energy efficient structural insulated panels (SIPs), a technology used in passive house design, which requires less time and fewer tradespeople onsite, resulting in less travel and wastage during the build process.
We educate our staff and residents about sustainability. This grassroots effort, where everyone comes together in every care home, collectively makes small, everyday wins, in-turn supporting our larger goal.
Each home takes part in an energy consumption league table, to encourage healthy competition. In the lead so far, Springfield Nursing Home on the Isle
“So far, £2 million has been spent on the installation of solar panels at 11 of our homes, with a further five due to be completed this year.”
of Wight has achieved 55% less energy use in December 2023 than they did in December 2022, which is a great feat given it’s one of our older buildings.
Further sustainable initiatives have been put in place, including electric vehicle charging points being installed on all newly built care homes and extensions, a car sharing scheme for staff, new recycling facilities and a rewilding biodiversity programme. Our central support team has also recently been issued a survey on commuting methods to encourage proactive thinking to reduce carbon.
Certain aspects of sustainability, which may be taken for granted elsewhere, can be very difficult in a care home environment, such as recycling. Each home has a lot of medication –and packaging from this – and this waste needs to be disposed of safely and within regulations.
Going forward, most new homes will be newly built, which helps hugely as sustainability is part of the process from the outset. The acquisition of older homes still proves challenging, but sustainability is part and parcel of any new deal, with investigations taking place into how the buildings efficiency can be improved.
We are constantly exploring new ideas in energy saving technology and we’re currently investigating the benefits of smart thermostats and voltage optimisation. The latter would mean that as electricity is drawn from the grid, anything that isn’t used –rather than going to waste – is stored and then sold back to the grid, saving both cost and waste.
While more and more care home brands are prioritising sustainability, Hartford Care was one of the first to take action, bringing on board a sustainability consultant and with the arrival of our chief executive, Kevin Shaw in 2022, our approach was ‘less talking, more doing’ and we hit the ground running implementing new initiatives.

“We are constantly exploring new ideas in energy saving technology and we’re currently investigating the benefits of smart thermostats and voltage optimisation.”
Sustainability is increasingly at the forefront of people’s minds, and many families and potential recruits are showing an interest and prioritising it. Investing now helps us to continue to attract the best talent and create homes which meet the expectations of residents and families.
Over the long term, the investment Hartford Care is making into sustainability may see a cost saving, however we are investing heavily now to ensure we’re playing our part to create the best future for everyone.
CareTech group sustainability director Jonathan Freeman calls on care providers to share their experience of promoting green policies and practices so the whole sector can improve
Management gurus regularly trot out the line that “what gets measured gets managed”, attributing this aphorism to the legendary management theorist Peter Drucker. Unfortunately, as my research for this article taught me, Drucker didn’t say this at all. And, in any event, it’s not really true anyway. There are loads of things that are important to business that are really tricky to measure (or, at least, to measure well).
When it comes to promoting sustainability within our organisations, while there is an ever-growing army of ESG and sustainability consultants ready to advise, the truth is that we are all trying to find our way. Okay, there’s a lot we have learned on how to measure, for example, our carbon emissions. And there is increasing evidence of the steps that can be taken to reduce our environmental impact. But much of this field is in its infancy and we have so much to learn.
Given the fragmented and competitive nature of the social care provider infrastructure, our default approach tends to be one of secrecy and insularity. Why share the recipe for your special sauce with your competitor, after all? But that approach doesn’t really work for sustainability.
Let’s remind ourselves of the bigger picture. Addressing sustainability is a global challenge and only collective efforts will address the issues involved.
"Given the fragmented and competitive nature of the social care provider infrastructure, our default approach tends to be one of secrecy and insularity."
In the long-term, this is not a zerosum game of winners and losers – only concerted effort by all stakeholders will avoid all of us, eventually, being losers in the catastrophic climate emergency.
While it is undoubtedly the case that those moving more quickly on addressing sustainability challenges will get first mover advantage, this is unlikely to result in longer-term benefit. And, even it did, is this the sort of game that you would want to win?
So, for me (and – shameless plug – the other growing number of members of the Social Care Sustainability Alliance that I chair), the only rational and moral choice is for us to share our experience, both successes and failures, with our colleagues across the sector so that we can all make quicker and better progress.
It is for this reason that we at CareTech have published our annual ‘Purpose report’ for the past three years. To support our headline commitments for each aspect of our CARE4 Sustainability Strategy, we have identified a set of ambitious supporting targets to galvanise our efforts.
While the ‘management by measurement’ approach is in many ways flawed, the galvanising effect on individuals and organisations of public targets shouldn’t be underestimated.
As Dan Ariely in the Harvard Business Review states: “Human beings adjust behaviour based on the metrics they’re held against. Anything you measure will impel a person to optimize his score on that metric. What you measure is what you’ll get. Period.”
If we simply measure business success by short-term profitability, then that will be what business leaders will fixate on. As Ariely argues: “If we want to change what they care about, we should change what we measure.” Which is why establishing sustainability targets and reporting on progress is so important.
For us at CareTech, our sustainability journey is a long-term one and we recognise we will not meet each target

"For us, the direction of travel, and building momentum to become a truly sustainable business, is what matters most."
on that journey. For us, the direction of travel, and building momentum to become a truly sustainable business, is what matters most. Our ‘Purpose report’, therefore, tries to provide an honest account of the progress we’re making and, really importantly, how we are doing it.
Our ‘Purpose report’ reminds us and our stakeholders of the journey we are on and just how far we’ve travelled on that journey. The report shares a variety of case studies to acknowledge and celebrate some fantastic achievements across the organisation.
Hopefully, this ‘show and tell’ exercise enthuses our people to recommit themselves to this agenda and offers some ideas for other organisations to help them on their own sustainability journeys. If others can benefit from our efforts, then we are more than happy that they ‘borrow with pride’ from our experience. In that way, we will all benefit.

Aurem Care is investing £1 million in Beech House, part of its Hailsham House care home in East Sussex. The refurbishment will include 32 en suite rooms, each equipped with a full wetroom, a full kitchen refurbishment and digital care planning.

HC-One opened a marketing suite at its £12 million Bluebell View Care Home in Oswestry, Shropshire. Bluebell View, which is scheduled to open in the coming months, is the latest home to be built in HC-One’s new-build programme, which saw three homes open in 2021: in York, Bingham and Telford.

Handsale announced the closure of Bierley Court care home in Bradford due to the difficult economic climate. The care home operator told the BBC that “exorbitant energy prices and high interest rates” led to the decision to close the service.
Lidder Care secured planning permission for the extension and improvement of Newgate Lodge Care Home in Mansfield. The works will see the facility grow from 60 to 84 beds to meet growing demand for dementia care. PKL Investments, the construction arm of Lidder Care, will take the helm as main contractor for the project with work expected to get under way in the spring.

Wallacea Living marked a significant milestone in the construction of its first integrated retirement community. Representatives from Wallacea Living and developer Berkeley were joined by key stakeholders from the local community, as well as members of the project team for the ‘topping out’ ceremony in London at Wallacea Living Marylebone within Berkeley’s West End Gate development.


BN Care Holdings purchased Court House care home in Cullompton, Devon, which caters to up to 33 elderly residents. The vendors were Marcus Lyward and Lorna Turner who purchased the home in 2014 and added more bedrooms. They sold in order to retire from the sector. BN Care Holdings operates five care homes providing 171 beds across Exeter, East Devon, and West Dorset.

Lovett Care is developing a purpose-built care home in Northern Moor, Manchester, offering nursing and dementia care, and treatments for other mental health conditions. The home will comprise 59 en suite rooms, lounge and dining facilities, a hair and beauty salon, a café and activity room. OakNorth Bank provided a loan for the development.
RMBI Care Co is investing £16 million in a new-build care home on the site of its existing Outstanding-rated Cornwallis Court in Bury St Edmunds, Suffolk. The phased new-build, which has received planning approval, will commence in April with targeted completion by 2027.

Care home entrant Afir Homes purchased The Willows Care Centre in Margate, a mental health and dementia care home registered for 40 service users, which occupies five three-storey Victorian houses which have been converted, interconnected and extended. The vendor was Premiere Care Homes which purchased the business in 2012.

Angela Boxall replaced Avnish Goyal as the chair of Care England. New trustees of the association include: Joanne Balmer, chief executive of Oakland Care; Aneurin Brown, managing director of Hallmark Care Homes; Russell Brown, chief executive of Shaw healthcare (group); Simon McCall, commercial director at Barchester Healthcare and Jake Rollin, director of commissioned care and commercial support for HC-One. They join existing board trustees James Allen, chief executive of National Care Group and Vishal Shah, founder and managing director of Banyan Care Group.

Sarah Beshir became the franchisee and managing director of Right at Home’s office in Westminster, central London, having recently received her Care Quality Commission registration. Beshir started her career as a biomedical scientist at the NHS blood transfusion department in 2005, before becoming a registered nurse and working for various hospitals across London. When the Covid-19 pandemic hit, Beshir was placed in charge of infection prevention and control at St John and St Elizabeth Hospital in London.


Craigielea Care Home in Gateshead promoted two staff members to leadership positions. Sarah Johnson, a member of the Craigielea team since 2019, was appointed care home manager and Sarah Hoey, who began working at Craigielea in 2003 as a care assistant, was appointed deputy manager.

Law firm RWK Goodman appointed Anna Fee to its health and social care team to focus on regulation and contentious matters based in the firm’s London office. Fee is a regulatory solicitor with experience supporting health and social care providers in challenging Care Quality Commission and Ofsted inspection reports and other enforcement action including warning notices, notices of proposal and notices of decision to impose conditions or cancel providers’ registrations. Fee will also advise providers about local authority contract matters, safeguarding investigations, and inquests. She joined RWK Goodman from Ridouts.



Dan Scott-Elder joined family-owned care group Westgate Healthcare as operations director. With more than 20 years’ experience in social care, Scott-Elder previously worked with Runwood Homes where he was promoted from senior home manager to regional operations director in June 2022.

Cornerstone Healthcare Group, a provider of specialist and complex care in the UK, announced the appointment of Paul Hayes as the company's new chief executive, after Johann van Zyl stepped down in January.

Voyage Care appointed Mike McKessar as chief executive. McKessar will take up his role in early summer. Jayne Davey, chief operating officer, will become interim chief executive when Andrew Cannon leaves this month.


Katherine Wackett, senior associate from Mills & Reeve, explains the expected effect of the Care Quality Commission’s new single assessment framework on in-person inspections
As healthcare providers will be aware, the Care Quality Commission is introducing its new ‘single assessment framework’ in April. The practical detail of how this will work is not entirely clear and no doubt the CQC will need to refine the process once it begins rolling it out.
However, what’s clear is there is a shift away from in-person inspections and a move towards evidence collection and reliance on third-party intelligence. The CQC is changing its process from ‘inspection’ to ‘assessment’ and away from its ‘boots on the ground’ approach.
The CQC is replacing its current ‘Key Lines of Enquiry’ with 34 ‘Quality Statements’ or QS. These QS relate to areas across the five key questions of: safe, effective, responsive, caring and well-led.
In order to assess services against these QS, the CQC has set out six categories of evidence that it will assess, and each evidence category will be scored from 1 to 4.
The six evidence categories are:
1. People’s experiences of health and care services.
2. Feedback from staff and leaders.
3. Feedback from partners.
4. Observation.
5. Processes.
6. Outcomes.
"As healthcare providers will be aware, the Care Quality Commission is introducing its new ‘single assessment framework’ in April."
Observation is the fourth evidence category in the CQC’s new inspection regime and includes both off-site and on-site observations.
It’s clear from these evidence categories that the CQC is moving away from its traditional approach based on inspection of services on site, with only one category out of six being directly based on what CQC inspectors observe at a service. The evidence category of ‘Observation’ will, however, include off-site observations gathered from local Healthwatch and other partners and via the Experts by Experience programme. Where evidence from these other bodies is about the care environment, this will be included in Observation rather than the Feedback categories.
The other five evidence categories all rely on non-observational evidence.
As a result, we expect physical inspections of services to take place only where there are concerns or where evidence gathering can only be done on site.
This new approach means care homes need to be more proactive in their approach to CQC regulation. Rather than responding to a CQC inspection that may take place once every two or three years, providers will need to provide evidence proactively to the CQC on an ongoing basis. The idea behind this is to allow the CQC to provide a dynamic up-to-date

assessment of risk and enable it to reassess service providers much more frequently than it does under the current inspection framework.
The CQC’s provider portal is likely to play a pivotal role in this new framework and is, according to the CQC, going to allow the easy exchange of information.
As each of the 34 QS are going to be scored, it would be prudent for care providers to map what evidence can be used to demonstrate that each of these QS are met and ensure that such evidence is readily available to provide to the CQC.
To ensure care homes are ready for this change, systems may need to be updated to ensure this information can be exchanged with the CQC on an ongoing basis.

The direction of personalised home care is ever-evolving, offering new ways to provide a bespoke approach that goes beyond the conventional norms of traditional caregiving. As the founder and chief executive of Vivant, a luxury home care provider, I have witnessed first-hand the recent transformation in caregiving practices, which is shifting the way we perceive and experience home care.
The integration of cutting-edge technology is reshaping luxury care, allowing caregivers to utilise intelligent home care systems and leverage artificial intelligence and other devices to monitor health indicators, ensure medication adherence and uphold client safety. These recent advancements in technology not only provide caregivers with real-time insights, but also empower individuals to engage actively in their own care, developing a sense of autonomy and control.
Care service technology has also evolved, with virtual consultations, remote health monitoring and interactive therapy sessions now widely available to home care recipients. This both heightens accessibility and ensures individuals receive prompt and effective care without the necessity of physical presence.
" Care service technology has also evolved, with virtual consultations, remote health monitoring and interactive therapy sessions now widely available to home care recipients."
In addition, the commitment to continuous learning technology reflects a dedication to providing care recipients with the highest standards of care in an ever-changing healthcare landscape. Looking ahead, new technology offering even more capabilities will become a hallmark of the home care industry.
This year, the paradigm of luxury home care extends beyond the boundaries of medical assistance, embracing a holistic perspective that caters to emotional, social and lifestyle needs. From thoughtful wellness programmes and bespoke nutrition plans to specialised fitness regimes, our services go far beyond the conventional scope of caregiving, contributing to a comprehensive sense of wellbeing.
A notable shift lies in the recognition of the importance of mental health. Our caregivers are not merely versed in medical procedures, they are attuned to the emotional wellbeing of our clients. Moving forward, there will be a pronounced emphasis on mental health support, companionship and activities geared towards instilling joy and fulfilment, constituting an intrinsic part of the personalised care experience.
The future of personalised care revolves around the concept of curated experiences. Each home care recipient is distinct and services should be meticulously designed to mirror and honour that distinctiveness. From personalised care plans that adapt with evolving needs, to a concierge-style approach that anticipates and fulfils every requirement, our commitment is to deliver an experience that is as unique as the individual themselves.
Personalisation also extends to cultural nuances, preferences and lifestyle choices. Whether it involves creating an environment that resonates with a person’s cultural heritage or

"
Whether it involves creating
an environment that resonates with a person’s cultural heritage or curating activities aligned with their interests, care should integrate into the fabric of every individual’s life."
curating activities aligned with their interests, care should integrate into the fabric of every individual’s life.
Ultimately, the future of home care brings together the threads of technology, holistic wellbeing and individualised experiences. As the owner of Vivant, I am excited by the transformative journey that awaits us in 2024 and beyond, celebrating the uniqueness of each individual.



 36 CARE SECTOR'S GOT TALENT
Care Sector's Got Talent winners Charlene Reeves and Michael Gallagher look back on an unforgettable year
38 CT ON THE ROAD
Charlotte Goddard visits The Royal Naval Benevolent Trust
46 CARE HEROES 2024
Nominations open for your Care Heroes 2024
25 LEADER'S SPOTLIGHT Bracebridge chief executive Samantha Crawley on heart-centred care
36 CARE SECTOR'S GOT TALENT
Care Sector's Got Talent winners Charlene Reeves and Michael Gallagher look back on an unforgettable year
38 CT ON THE ROAD
Charlotte Goddard visits The Royal Naval Benevolent Trust
46 CARE HEROES 2024
Nominations open for your Care Heroes 2024
25 LEADER'S SPOTLIGHT Bracebridge chief executive Samantha Crawley on heart-centred care
Apprenticeships help attract, develop and retain a skilled workforce, says Susan Beasley, apprenticeship and qualifications manager at HC-One and Allison Gill, home manager at Priory Gardens
Apprenticeships help individuals develop the skills and knowledge to access rewarding careers, which in turn helps organisations to develop, build and retain a talented workforce equipped with the right skills to meet current and future demand. Apprenticeships are designed to deliver the skills and behaviours employers need and are continually reviewed. They are quality assured and delivered through providers that are Ofsted inspected. HC-One has been named as one of the Department for Education’s Top 100 Apprenticeship Employers for the past two years, offering apprenticeship opportunities to newly recruited and existing colleagues.
1. Apprenticeships have a role to play in retention, they are not just about attracting new workers. Giving people career opportunities at every level encourages them to remain in the sector and helps develop a pipeline of professionals. HC-One currently offers apprenticeships from Level 2 to Level 7, and the number of different levels available means the training can act as stepping stones to reaching career goals.
2. Apprenticeships are not just aimed at care staff. HC-One recently launched apprenticeships for registered nursing associates and registered nurses. Our apprenticeships cover a plethora of roles including hospitality, administration, procurement, IT and leadership. One of our youngest apprentices, Bradley Taylor, is now a chef at Priory Gardens. He completed his production chef Level 2 apprenticeship and is looking to progress to Level 3 senior production chef.
3. Encouraging employees to complete an apprenticeship grows their confidence as well as their
skills. A lot of people don’t believe in themselves, but if you support and encourage them, they see what they are capable of.
4. There is no age restriction on apprenticeships and apprentices can be paid above the Apprenticeship Minimum Wage. Our apprentices range from 19 to over 60. We pay according to the role. If you start an apprenticeship with HC-One your salary and terms and conditions do not change.
5. Apprenticeships are not only for people who work 37 hours a week or more. This is a common misconception; models of delivery can be adapted for part-time workers, which is important in our sector.

6. Apprenticeships allow people to earn and learn at the same time, without incurring extra debts, which is a good retention tool when the cost of going to university is so high.
7. Be mindful that ‘off the job learning’ is an essential part of the apprenticeship journey. Apprentices need to spend a percentage of the time ‘off the job’ during paid working time. ‘Off the job’ doesn’t mean away from the care home – it can include work shadowing, having a professional discussion with a colleague, learning about a new piece of equipment, or undertaking an inhouse training programmes relevant to the apprenticeship..
8. Communication is key. An apprenticeship is a threeway partnership between the employer, training provider and apprentice. Maintaining effective communication between everyone
supports your apprentice to have the best experience and helps to identify any barriers that may be stopping apprentices reaching their goals early so you can support them – for example do they need transport because they can’t drive or help to access the online platform they use for studying?
9. Identify potential mentors among your team. Apprentices are assigned workplace mentors, but this doesn’t have to be the manager’s role. Find people who are good at listening, building rapport, and sharing their experiences, and see if they can take on this role. It’s a good way to develop team members and keeps their skills up to date.
10. Check in on apprentices’ wellbeing. Apprenticeships are flexible, and there is an option for individuals to take a break in learning and return at a later date, for example in cases of maternity leave or long-term sickness.

Tell us about your background in care I started my career in Kenya at a culinary school. At this point in my life I had not yet considered working in care. I worked in different kitchens including a five-star hotel, the African Nazarene University, where we catered for both students and the missionaries. When I moved to the UK in 2007, I worked for a holiday resort in North Wales.
I moved to Harrogate in 2012, working at several different hotels in the region until I joined a catering agency and worked in hotels across the UK. I moved back to Harrogate in 2018 and joined Vida Healthcare. What was supposed to be a three-week cover placement working in the kitchen has become a three-year career journey. I am now head chef at Vida’s newest care home, Vida Court –it’s a place I absolutely love and I feel very lucky to have a career that I’m passionate about too.
What’s special about working in care?
It is honestly a privilege to cater for individuals who are going through a different and more difficult phase of their lives. Having previously worked in hotels where profit was often the focus, I feel I can now give back to
the community and provide residents with the best-quality meals that meet their nutritional needs.
How do you vary your menu to provide choice for residents?
At Vida our menus vary depending on the season and what produce will be at its best at the time. We always keep our menus diverse and visually appealing, with the inclusion of traditional and nostalgic meals, as this is beneficial for our residents.
In the summer we usually cook lighter dishes with a variety of fresh fruits, whereas in winter our menus may include more hearty hot meals like stews. We always ensure all our meals are both nourishing and delicious.
What does your typical menu look like?
There isn’t a typical menu at Vida; we have meals we may cook more regularly, but we ensure that everything is centred around the residents and their needs. You have to consider what they like, their texture preferences and the different colours within meals.
How do you meet the nutritional and health needs of your residents?
Vida Healthcare is committed to providing the most nutritious meals to its residents, which is why the Vida team works in conjunction with Harrogate District Hospital to deliver regular courses via its in-house training academy, Vida Academy. These courses focus on nutrition specifically, to ensure that Vida’s residents are offered the healthiest and most nutritious meals.
No two residents are the same, so we also work closely with team leaders and
care staff to tailor our menus to each of our residents’ individual needs. Some may need to be eating more healthily, some residents need to be eating a high-calorie diet, and others, further along in their dementia journeys, may have pureed diets. We must consider all of these and provide all residents with balanced meals.
How do you cater to residents living with dementia?
When catering for residents living with dementia you have to make decisions in their best interest. It’s important to make meals as easy to consume as possible; meat should be cooked for longer so it's softer and easier to chew and vegetables should be cut up into smaller pieces.
Presentation is also important; the meals must be presented beautifully and there shouldn't be too much food on a plate as residents may feel overwhelmed.
What is your most popular dish?
I recently wanted to make something different for the residents and followed a new recipe for a fish curry with coconut rice which was a winner. Mushroom and red pepper stroganoff is always a favourite too.
What’s your favourite dish?
I love baking, especially making birthday cakes for all the residents. It feels more personal and it is an opportunity to make their day special.
How do you make the dining experience special for residents and their families?
I want to make food that everyone genuinely likes and I know everyone on my team feels the same. Our meals have got to be perfect for all residents. After mealtimes I visit the houses at Vida Court to speak to carers and enable residents to see how each meal has been received. Communication is key, menus and recipes change with time and I want my cooking to be interesting and enjoyed.
Samantha Crawley joined new startup care company Bracebridge in 2022 when she was approached by the company’s founders.
“They had already started building three care homes and were looking for somebody who understood care,” says Samantha.
When asked what her vision for Bracebridge was, Crawley says: “My vision came from years of making mistakes. Every mistake I have made I have tried to create a vision to enable us not to make those same mistakes again, maybe make different ones, but not those same ones.
“We wanted to make a space where people with really complex needs can live which feels like home and not like hospital, with an engaged team who are really heart-centred.
“I know everyone talks about personcentred care, but the original philosophy was never about the person getting the care, it was about the person who is giving the care. It was meant to come from the centre of the carer.”
With more than 20 years’ experience in care homes and being a director of The Outstanding Society, few people could have been better qualified for starting a
“We wanted to make a space where people with really complex needs can live which feels like home and not like hospital, with an engaged team who are really heartcentred.
new care business than Crawley who was then Excelcare’s director of care quality and transformation.
With the build of the company’s three care homes, The Maples in Telford, The Oaks in Bromsgrove and The Rowans in Wigan, well under way, Crawley immediately went about helping to make their design feel more homely.
“We had the opportunity to redesign them and make them feel more like home and much less clinical than the original design – really thinking about how people use space, especially people living with dementia,” Crawley says.
“The business as it is today wasn’t set up at all. We had to build a business, a brand, a website and everything. There was a lot of work to do in a short amount of time.”
Crawley gives her designers a typically idiosyncratic and unorthodox brief that is succinct and to the point.
“There needs to be sofas,” Crawley laughs. “In your living room you have sofas, you don’t have a load of chairs. They need to be somewhere where somebody can put their feet up, the dog can come and jump on them and the grandkids can play around and it feels like home.
“The designers kind of look at me like ‘are you insane or what?’ but that’s how we live isn’t it? We don’t live in hotel style places with lots of chairs around.
“If you treat somebody like an animal and cage them, they will act like one. If we treat somebody with kindness and give them a home they have more chance of feeling human and being human. You need to keep the stuff of life around people and not take it away. If you live with dementia you need stuff to pick up and engage you. If that’s not there, then there will be issues as people will be bored and unfulfilled.”
Crawley says plans are in the pipeline for each care home to have its own dog to further supplement their homely environment. Bracebridge also makes every effort to accommodate people’s pets to help them feel at home.

People are also given full licence to personalise their bedrooms as well as their communal spaces.
“We need to make the living spaces be places where people can have their own things,” Crawley sayd. “Traditionally in care homes we have restricted people to just their bedroom space.”
At Bracebridge, people are encouraged to decorate their living rooms with their family pictures.
“If they want pictures of their grandkids by the fireplace because that’s where they always were, then let’s do that,” Crawley says.
Led by Crawley, Bracebridge takes an innovative and creative approach to keeping people engaged. Visitors to their homes may be surprised to find props such as wedding dresses hanging in hallways.
“We use tools and props to help divert different situations,” Crawley explains. “When people get angry because there’s something going on with their dementia, a team member slipping on a wedding dress can de-escalate that really quickly by making it a very different situation because they will then be thinking ‘why is there a girl in a wedding dress?’ and the team member will be saying ‘I am going to be late for my wedding, how can I get there?’ All of a sudden that human who has been arguing now

“If they want pictures of their grandkids by the fireplace because that’s where they always were, then let’s do that,” Crawley says.
wants to help that person get married.”
Care through role play was something Crawley learned through her work with professor of emotional intelligence at York University, Dr David Sheard. “I remember seeing David on TV and thinking ‘this is exactly what I thought care should be like’,” Crawley laughs. “David schooled me in how really to approach team members and then people living with dementia and more
complex care needs. He taught me that the team members are everything. If we focus on the team being well and happy in their roles and equipped to manage something, then the people who live there will definitely be okay. If we focus on that, the people who live with us will feel that too. It’s essentially all about who we are and how we show up to the person in our care.”
Innovative recruitment
Crawley takes an innovative approach to recruitment in order to find the right people with the right values. In the first step of the process, people applying on Bracebridge’s website are confronted with unorthodox questions devised by Crawley such as: “Would you dance with a stranger in the rain?” and “Would you talk to a stranger at a bus stop?” Depending on their answer, they may then be invited to take part in an informal assessment session where they are able to get to know the Bracebridge team.
The assessment has a focus on fun and allowing people to be themselves. Candidates are asked to bring along something that is really important to them that they can talk about.
“We are looking for people who will listen to other people, people who will see a shy person and pull them into the group and also for potential leaders,” Crawley explains. “It’s not always the mouthy people like me but people who can influence the group without being overbearing that we are looking for. It might be someone who has come in for a kitchen assistant role. but who you can see has a real ability to influence people and you can see they have a career trajectory to offer.”
During the assessment session, members of the interview team will test candidate’s responses to care situations. For example, a team member may pretend to trip and fall.
“We see people who giggle, people who respond, and people who check in
“Our care teams don’t wear uniforms to prevent any ‘them and us’ feelings. “There’s people who live in our care homes and people who work in our care homes and they’re all just people. We don’t use the word staff at all.”
with that person an hour or so later to see how they are,” Crawley explains.
The assessment team also leave rubbish
around the bin to test the responses of candidates. Those who pass the initial assessment then go on to be interviewed.
When asked to name the qualities she looks for in team members, Crawley put “integrity” first and foremost. “Integrity is everything because it’s about what you do when no one is looking,” she notes. “In care there are a lot of things done when no one is looking.”
Secondly, Crawley highlights someone who’s willing to share who they are and not be scared about it, who is willing to have conversations with residents and families that might be uncomfortable and who would not pass by when someone is in need.
“I also ask people to tell me who they are,” Crawley says. “They say
‘personally or professionally?’ and I always say ‘there’s no difference, you are you’. I think we have stop telling people ‘you have got to be professional’ when actually we need people to turn up as they are so that they can build relationships.
“Our care teams don’t wear uniforms to prevent any ‘them and us’ feelings. There’s people who live in our care homes and people who work in our care homes and they’re all just people. We don’t use the word staff at all.”
Crawley says all her homes took a certain amount of people who had never worked in care.
“They are the best candidates because we can mould them into the way we care,” she laughs.
People have joined the business from all sorts of backgrounds, including >


Amazon, Morrisons, Tesco and even engineering. When asked what brought these people into care, Crawley says: “A lot of the people who are right for us are completely unfulfilled in what they do. They go to work and it doesn’t really count. You get an ‘extra pay check’ in care from really enhancing somebody’s life.”
Crawley also takes a risk positive approach to working with challenging people while maintaining a strong safety culture.
“We will take a chance and work with people,” she says. “We know things will occasionally go wrong and there will be incidents that happen, but if we can learn from them, then we can all go forward and learn in the future. Our ultimate vision is to have a place that someone can call home and understand that regardless of what their dementia will make them do it will still be their home. That’s a tough ask but it’s what we want.”
Crawley has taken a hands-on approach by leading training for her teams and bringing in a training company to help embed her innovative approach to care.
“I want to give our people as many tools as I can depending on what the situation is,” she says.
The new approach begins with the
language used by her teams, Crawley explains. “We have a dictionary that says this is the language you may have used before and this the language we use,” she highlights. Words such as ‘challenging behaviour’ are taboo.
The chief executive says honesty and transparency is fundamentally important in creating a healthy working culture for her teams. “They will tell us what’s working and what’s not working, which is perfect,” she says. “I would never pretend that we are perfect and we have it all sorted.”
Learning from mistakes is a key component of Bracebridge’s culture. Crawley runs a ‘lessons learned’ lab every month with an invite to everyone in the company.
“We talk about safeguardings that have been raised and talk openly about them,” Crawley says.
The reports are shared openly with the Care Quality Commission. “I think they appreciate we are giving them as much information as we have,” Crawley says.
Complaints are also covered in the meetings as well as examples of outstanding care, and team members create case studies each month of outstanding outcomes for people.
"Our ultimate vision is to have a place that someone can call home and understand that regardless of what their dementia will make them do it will still be their home."
Crawley says it’s the people on the front line who really matter in care. “Some of us leaders might get caught up with how important we are, but to the person in room 90, it’s the carer that matters,” she concludes. “Keeping people happy is much more important than any pay rate. As a leader, that’s about being willing to ask the question, often when you don’t have the time, and being really willing to listen to the answer especially if it’s something we could have done better. That means you have an engaged workforce who then feel listened to and valued and who feel happy and who will go into room 90 feeling that way. It’s a chain reaction.”
Wise words Samantha. Wise words.


Charlotte Goddard talks to Blue Sky Social Care Card founder Raj Johal about the benefits the service offers to care workers
When care workers feel undervalued, both in terms of financial reward and the value placed on their role by society, the sector struggles to recruit and retain staff. Carers often feel they lack the recognition given to staff in the health sector, for example. When retailers and other organisations offer discounts to ‘forces and front line workers’, care workers may struggle to offer identification to prove they qualify.
That’s why Raj Johal, executive director at Blue Sky Brokers, decided to launch the Blue Sky Social Care Card, which acts as both an employee ID card and a passport to discounts and offers aimed at front line workers. Care workers undergo a robust vetting process to ensure they are eligible before being issued the card, which is open to everyone providing care, including personal assistants, unpaid carers and all those working in care homes and home care companies.
“We have checks in place to ensure carers are verified and vetted, and we find the card is accepted and recognised by retailers because of that,” says Johal. “It has been a good way for unpaid carers to be recognised as official carers.”
For many carers, just being recognised for what they do can give a
“We have checks in place to ensure carers are verified and vetted, and we find the card is accepted and recognised by retailers because of that.”
real emotional boost, even without the discounts and offers they can access. Last year Blue Sky created a card for TV presenter Kate Garraway, as she was caring for her husband Derek Draper who sadly died earlier this year after a battle with Long Covid. “Her reaction proved how important recognition really is,” says Johal. “She was so happy and felt appreciated, and to see that was lovely, because she deserved it. That is what we feel about all the unpaid carers.”
“Self-employed carers are often overlooked when it comes to being recognised in social care,” says Maria Tomlinson, founder of the Professional Carers Network. “For example, the Blue Light discount scheme allows carers to join, but not self-employed carers, so it was great to find a company that values self-employed carers and offers them the chance to get discounts too.”
Care home and home care workers can also purchase the card, which costs £5 a year, on an individual basis. Alternatively, employers can provide it to staff as an incentive and form of identification, adding their own logo and taking it back when employees leave the company. “The Blue Sky Card has truly been indispensable for our staff, serving not only as a dependable form of identification but also providing substantial discounts,” says Vanessa Morales, care co-ordinator at Nationwide Care Services, which provides home care and supported living facilities.
Blue Sky Card holders are able to access an app with offers and discounts from retailers such as The Body Shop, Parkdean Resorts and JD Sports. The card is usually accepted by high street retailers and other services which offer ‘forces and front line’ discounts, says Johal. Users have been flagging up successful uses of the card across the UK in specific locations on an interactive map, which currently shows more than 200 individual outlets where

the card has been accepted, including branches of Starbucks, River Island, Nando’s, New Look and The Perfume Shop.
Blue Sky Card, which is recognised by Skills for Care and the Local Government Association, has signed up a number of partners. “When we partner with an organisation, we can issue cards to members once we verified their membership, because they have already been vetted by the partner organisation,” explains Johal. Partners include the National Association of Care and Support Workers and ILF Scotland, which provides funding for disabled people in Scotland and Northern Ireland to help them lead a more independent life. ILF Scotland has signed up to reimburse its funding recipients who buy the card as a perk for their personal assistants.
However, Johal is keen to get the bigger care home providers signed up to the scheme. “We are waiting for the bigger fish to come forward,” she says. “It is a tax-deductible cost, because this is seen as a work ID card, so it is a work expense. Care managers have told me they give their team vouchers for Christmas – but with the card you can give £5 and it goes a lot further in terms of savings.”
Eduardo Buglosa Jr, home manager at New Care’s Guiseley Manor Care Centre in Leeds, tells us what he loves about care
Why did you join the social care sector?
My previous experience prior to coming to the UK was hospitalbased. I wanted a change so opted for social care in 2016, working in a care home setting. I really enjoyed the experience.
What do you enjoy most about your job?
I get to practise my leadership, clinical, communication and caring skills. But what I enjoy most about my job is seeing our residents looked after with the highest standard of care and enjoying their day-to-day lives as much as they can. I also like to see the people that I have worked with, coached and mentored progress in their career.
Who is your social care hero and why?
I guess everyone working in the social care sector are heroes. We all try and work hard every day to make positive changes as well as enhance the lives of our residents as best we can.
What is the one thing you would change about social care?
Better funding perhaps and greater access to care provisions.
What, in your opinion, makes a great care worker?
Patience and being a good listener is important. Being passionate in caring for others is essential, and I would also say being able to look into the situation from a resident’s perspective.
What do you do when life all gets a bit too much?
Take some time off to recharge. I know it’s easier said than done to not think about work as much as we can. Also, although there is still a lot that I can do and learn, I need to remind myself of the things that I have achieved so far, and use them as inspiration to keep going, and improve my performance even further to make a greater impact on our residents' lives.
What advice would you give your younger self?
Do what scares you. Never be afraid to learn new things and you are only one decision away to a completely different life. Better to try and learn, than not to try at all.
Which three famous people would you have to dinner and why?
Simon Sinek, Mark Cuban and Carlo Ancelotti. All great leaders, businessmen and speakers. I would like to learn more about leadership, business, people management and life in general from them.
What three items would you bring with you on a desert island? Bowie/hunting knife, lighter and waterproof jacket.
What is your secret talent?
Turning concerns into compliments.
Our columnist Norrms McNamara reflects on what it’s like to live with dementia
Goodness me, that’s a question that perplexes us all when it comes to dementia. It’s a bit like at the age-old chicken and the egg question, but it’s one that’s discussed and debated over so many times.
Well, here’s my take/view on it – and before I explain myself I’d just like to state that I am, in no way, an expert on medical matters. Some say because we live with dementia we are ‘experts by experience’, but again in my very humble opinion I think that’s stretching it a bit, but here goes anyway.
As for a cure, I think they are looking in the wrong place. I know, this may shock some, but I really do and here’s why. When researching dementia the emphasis is always on the Alzheimer’s type, and rightly so as it’s the most prevalent and makes good old-fashioned common sense (remember that), but my question is: What type of Alzheimer’s are they looking for? “What?” you say, “is there more than one type of Alzheimer’s?” In my humble opinion yes there is and when I say “what type?”, I mean what strain of Alzheimer’s is it? and the reason for thinking there are many different types of it is because if we look at the common cold, and research how many strains there are, why cannot the same apply to Alzheimer’s?
I really believe the evidence is right in front of our noses because those who

have Alzheimer’s never have the exact same symptoms. They don’t act the same or do the same things. Their lifespans are totally different. Even though it’s an incurable disease, some live only for a few years after diagnosis, whereas others live for more than 25 years. And this is well documented all over the world, so if anybody thinks that a diagnosis means the end, it doesn’t.
The best explanation I’ve ever heard is the saying: “When you’ve met one person with dementia, you have met one person with dementia”, and never a truer word was spoken. The same applies to
all different types of dementia in general as far as I’m concerned. I really do think there are so many differing types of strains when it comes to dementia and therein lies the problem as to why a cure hasn’t been found yet. Radical? Some will think so, but I truly believe if more research was done on this and one prevalent type of strain was concentrated on, instead of a named type, we might just get there.
I myself was diagnosed with Alzheimer’s before I met a consultant who had joined the practice who had researched Lewy bodies dementia in Newcastle and who said very quickly “This gentleman does not have Alzheimer’s, but Lewy bodies dementia” and from that day on I have to say I have met so many people who have told me they have similar symptoms to me but have also been diagnosed with Alzheimer’s dementia when all the signs point to Lewy bodies. Hopefully we have progressed away from: “Oh well, you’re 85, it’s your age, what do you expect.” But have we progressed from doctors saying it’s Alzheimer’s because it’s easier? Or are those with dementia still being put into boxes and packed away for ease? Makes you think, doesn’t it?
Till next time…
Journalist Philip Fairclough shares how staff at a rehabilitation home helped him walk again and reintegrate back into society after he suffered brain damage from a work-related accident
Brain damage! Perhaps no two words are more likely to instil fear. Why? Because they are perceived to represent a living death for the victim. Is that true?
On 4 November 1994 I suffered brain damage as a result of a workrelated accident. ‘Dying’ twice in the air ambulance and, once in the hospital, being given 24 hours to breathe unaided , I have since written a book about my life, Living with Brain Injury, and written numerous articles for health-related journals among others and given talks to healthcare professionals, medical staff, litigators, victims of brain injury and their families and carers. Am I superhuman, a rare case? By no means. Along with others I had an amazing surgical team, a loving and supportive family and a great rehab team at the Rosehill Rehabilitation Centre in Torquay (now Priory’s Notts Hill House) who helped me get my life back.
Has it been easy? By no means. At first being paralysed down one side, suffering loss of hearing in one ear with subsequent balance difficulties, vision problems in one eye, incontinence and
"You may not know where we are, and we may not know your whereabouts, but we and our families remember your tireless efforts on our part and know that for many, it’s not just a job.

epilepsy, it has taken determination, being unwilling to take things lying down, motivation, a willingness to learn and relearn things once taken for granted. It has also required patience, acceptance, time and a strong faith, a belief that I survived for a reason and that every day is a bonus not to be squandered and much more to be desired than the alternative.
As a healthcare professional, you may feel somewhat helpless, that you can do little for people like me but make our days as pleasant as possible, offering platitudes to us and our families and that once we pass from your care we will forget you. Rest assured, nothing could be further from the truth. I dedicated my book to the team at Rosehill who spent 18 months teaching me to walk again, reintegrate with society, manage my fatigue, relearn skills I thought I’d lost and by means of six-monthly reviews helped me set goals which, once achieved were not simply
dismissed but reassessed to see what further improvement could be made and then new targets set.
At no time did I sense frustration from them or an impatience from my slowness to grasp or apply their suggestions. And there was no ‘onesize-fits-all’; each client was treated as an individual with personal needs and problems. The OTs became like a second family, they told me and my family to call if we needed help, invited me back to give talks to the staff, fellow sufferers and their families, and encouraged me to write the first book of its kind in the UK.
So are you forgotten? No way. You may not know where we are, and we may not know your whereabouts, but we and our families remember your tireless efforts on our part and know that for many, it’s not just a job. You really are carers because you care. From all those with brain injury especially, a big thank you.
As always, carers have been demonstrating their creativity through fun and innovative events for their residents

It’s a sign
Healthcare Homes Group’s Bedhampton Court in Havant, Hampshire, has introduced a British Sign Language course. Activities coordinator Wendy Bennett is behind the weekly sessions which have fostered a sense of community and stimulated learning among residents. “It’s wonderful to see how much our residents are enjoying the course, and even more special to have family members joining in," said Bennett.

Residents at Bracebridge Court, Runwood Homes Senior Living’s care home in Atherstone, Warwickshire, spent the day at the Royal Air Force Museum. They were able to explore the history of aviation and take a close-up look at aircraft, rounding off the day with a winter picnic in the museum grounds.

Down under
Residents from Care South’s Wickmeads care home in Bournemouth
celebrated National Australia Day with a week of activities. The celebration kicked off with an exploration of Aboriginal language, history and culture, and included art sessions, a quiz and an armchair travel adventure. Residents enjoyed an array of tucker, including an Aussie meat pie.

Residents of Simonsfield Care Home in Anfield celebrated the Chinese New Year, which heralded the Year of the Dragon, symbolising strength, good luck and prosperity. They crafted decorations, including traditional lanterns and paper dragons, to adorn their communal spaces. Manager Karen Evans said: "It's heartwarming to see our residents so engaged.”

Residents at 21 Colten Care homes across the South celebrated Burns Night with poetry recitals, songs, games, whisky tasting and dancing, along with haggis, neeps and tatties. The haggis was piped into Braemar Lodge in Salisbury by pipe sergeant Keith Turner of the Wiltshire Caledonian Pipes & Drums, and the ceremonial address to the haggis was performed by companionship team leader Graham Ballard.

Ideal Carehomes’ Cadley Hill View in Swadlincote, Derbyshire banished the winter blues by transforming its vintage tea room into a seaside haven, complete with beach umbrellas and a seascape backdrop. Staff members sported oldfashioned long swimwear and residents were served fish and chips, cockles, crab sticks and ice cream.

Residents at Camelot House and Lodge in Somerset enjoyed the great outdoors despite the cold weather by watching birds through the windows and taking part in bird-related activities. Manager Zillah Oakes said: “Many of our residents regularly enjoy the Great Garden Birdwatch on TV, but it’s a big ask for them to keep reliable notes on what they see, so we came up with a bundle of more easily achievable birdthemed activities.”

Barchester Healthcare’s Meadowbeck care home in York was transformed into Graceland to mark what would have been Elvis Presley’s 89th birthday earlier this year. Residents were treated to live entertainment from Glen Booth as Elvis. General manager Annaliza
Kemp said: “We’ve had a fantastic day listening to all his hits, finding out about his early life and what influenced him and watching old Elvis movies.”

Staff at Excelcare’s Windmill Care Lodge in South London have learned circus skills as part of a five-week training course with contemporary circus company Upswing. During the introductory session, the team learned the basics of juggling, using scarves instead of balls at first to improve their coordination skills. They will use their newfound skills to perform at the home as well as passing them on to residents.

Pat Shepherd, 77, a resident at Hallmark’s Admiral Court in Leighon-Sea, Essex, has been an amateur singer ever since she joined the school choir at primary school. The Hallmark team helped Pat to spend the morning singing with ‘Dolly Parton’ – or someone very like her. Pat said: “I know many of her songs but ‘Coat of Many Colors’ will always be very special to me and so to have her perform it here is a memory I will treasure for a long time.”

encouraging residents to plant and grow their own fruit, vegetables and herbs. It is one of 10 MHA homes taking part in a project with Pot Gang, which provides seeds, pots, compost and guidance to grow seasonal fruit, vegetables and herbs. Stephen Hill, home manager said: “In our first delivery we received seeds for pepper, aubergines and parsley and they have gone down really well.”

Ashwood care home in Ware, Hertfordshire hosted a silent disco to celebrate the birthday of Monica, a resident at the home. Monica’s daughter donated the setup, transforming the lounge into a dance floor decorated with glow sticks and an array of party food while residents boogied to music they listened to through headphones. Hanna Anderson, home manager, said: “The silent disco was a big hit, and we’re planning to organise more events like this in the future.”

Residents at Stow Healthcare’s Mansion House care home in Bury St Edmonds, Suffolk became cover stars, inspired by actress Miriam Margolyes who appeared on the front cover of Vogue magazine aged 82 years. The ‘Stowgue’ (a pun on Vogue) photo shoot aimed to celebrate and value residents and challenge preconceived notions about life in a care home.
Residents at Renaissance Care Group homes have put out a call for pen pals

in care homes overseas, after taking part in language lessons with Glasgow-based charity Lingo Flamingo. The project aims to promote language learning and build meaningful friendships among seniors in both communities. Charles Menzies, 86, said: “I look forward to our weekly lessons. They get your brain engaged and challenge you to think outside the box.”

Daisy the miniature Shetland pony paid a visit to Larchwood Care’s Diamond House in Downham Market in Norfolk. Daisy, accompanied by handlers from Miniature Dreams, was able to visit less mobile residents upstairs as well as trotting through communal areas. While the home has welcomed everything from creepy crawlies to lizards and rabbits, Daisy is the first-ever pony visitor.

Wellbeing Care’s The Dell in Lowestoft, Suffolk invited the local community to take advantage of residents’ experience in the world of love by submitting relationship dilemmas and questions. Residents were filmed answering the questions, with videos appearing on the organisation’s social media channels in the run-up to Valentine’s Day.
Being crowned winner of Care Sector's Got Talent was just the beginning of an amazing year for Glasgow’s Hill View Care Home’s Charlene Reeves and Michael Gallagher. Caring Times caught up with the singing duo to discover what they’ve been up to
Care Sector's Got Talent is a showcase of diverse talent from across the care sector. Run by Championing Social Care, it’s a chance for care staff, or those who receive care, to showcase their talent and a way of celebrating and supporting the sector. Finalists get the opportunity to perform in front of a live audience at a glamorous professional event, that’s also live streamed to care homes across the UK.
Last year Glasgow’s Hill View Care Home’s Charlene Reeves and Michael Gallagher were voted winners of Care Sectors Got Talent by the panel of judges – but that was just the beginning of a year-long journey.
April
Care Sectors Got Talent final –and beyond
Michael and Charlene both work at Hill View Care Home, where Charlene is wellbeing co-ordinator and Michael is a senior care assistant. Before entering the competition they had never sung together, and Charlene had never sung in public, but the pair blew the judges away with their rendition of Bradley Cooper and Lady Gaga’s ‘Shallow’. “It was completely out of my comfort zone, but it was amazing,” says Charlene. “The organisers make you feel so special.”
When the pair arrived back at Hill View, they realised they had become local celebrities. “Our care home is made up of five separate units, and they all had a finals party, and watched the final online,” says Charlene. “It was nice to bring the whole home together for the day. Even residents we don’t work with knew who we were – family members were coming up and congratulating us, and saying how proud they were of us; we did feel like a wee bit of a celebrity.”
The duo were interviewed for a piece in Caring Times, but there was also local media interest in their story. “The local newspaper, the Clydebank Post,

did an interview with us and took some photos,” says Michael.
At the end of June, Charlene and Michael travelled to London to perform at Priscilla Wakefield House at the launch of Care Home Open Week, which sees care homes throw open their doors to the local community for special events. “That was really good,” remembers Michael.
The duo performed an emotional duet, then travelled back up to Glasgow to entertain guests at their own Open Week event, themed around the Mad Hatters’ Tea Party. They were reunited with fellow finalist Craig Smith from Newcarron Care Home in Falkirk who reprised his performance as Elvis.
Care Sector Fundraising Ball
September saw Michael and Charlene perform for more than 600 people at the glamorous Care Sector Fundraising Ball at the Grosvenor House Hotel on London’s Park Lane. They were joined by other finalists from the show including pianist Robert Speker and singer Kayleigh Morgan.
“The Fundraising Ball was something else,” says Michael. “It was beautiful. The standing ovation we got blew my mind.”
“A whole different world,” agrees Charlene. “We watched the venue transform as we rehearsed into a glittering ballroom with beautiful food and drink. It was brilliant to be invited as a guest, but to be part of it all and perform for everyone was amazing. The event was raising money for two

charities so it was great to be part of that. It was spinetingling.”
In October it was off to Birmingham NEC to perform at the Leaders in Care Awards and the Care Show.
November
The National Care Awards
Unfortunately Charlene came down with Covid towards the end of last year, but Michael stepped up to the plate, travelling to London again to perform at the National Care Awards at London Excel alongside other finalists. The event was hosted by TV presenter Kate Garraway.
“It’s been living the life,” says Michael. “There has been something every month, it has been fantastic, they treat you so well.”
December
Care Sector Christmas Lunch
To round off the year, Charlene and Michael performed a medley of Christmas songs at the Care Sector Christmas Lunch, which took place at the glamorous Royal Automobile
Club in London’s Pall Mall. “It was very fancy,” says Michael. “We were asked to sing in-between courses and do some Christmas songs, then we kept being asked if we could sing some more so we just pulled whatever we could out of the hat. It was a good laugh,” says Charlene.
During the year Michael and Charlene managed to fit in practice between the demands of their day job. “We would steal half an hour’s rehearsal time while we were working,” says Charlene. “We
got good at practising individually and sending voice notes to each other. We have got used to each other’s voices; we have become the best of friends so we know what to harmonise before we have even started practising.”
April 2024
Rounding off a year like no other, Michael and Charlene will be performing at the final of this year’s Care Sector’s Got Talent at Coventry Building Society Arena on April 16.
Even if you didn’t enter this year, you could still be part of this celebration of the sector by lending your support at the grand final. Care Sector's Got Talent serves as a unique platform for individuals within the care sector to display their diverse talents, whether through singing, dancing, comedy, musical performances or unconventional acts. The event also aims to support the mental health of those in the care sector, providing a memorable and positive experience.
The event takes place on 16 April at the Coventry Building Society Arena and will be presented by chair of Care England and chief executive of Majesticare Angela Boxall. Last year's event featured eight spectacular finalists, and the live stream was watched by 1,780 people.
Tickets are free and available through Eventbrite. Car parking is available at the arena and can be pre-booked.
For details visit: championingsocialcare.org.uk/care-sectors-got-talent
The Royal Naval Benevolent Trust’s Admiral Jellicoe House cares for veterans of the Royal Navy and their dependents. Charlotte Goddard visited the Portsmouth home to find out how its team builds on a shared culture to support residents’ wellbeing
Residents of Admiral Jellicoe House (AJH) in Portsmouth can go to sea without leaving the grounds. A wooden boat, fitted with instruments and a virtual screen, allows them to steer their ship through storms and sunny weather. This ‘dementia boat’, inspired by a similar simulator in a care home in Europe, is the only one of its kind in the UK.
The dementia boat is particularly important to the residents of AJH because they share a naval background. Run by charity The Royal Naval Benevolent Trust (RNBT), AJH is a purpose-built care home which opened in June 2022, offering residential, nursing and dementia care to veterans of the Royal Navy and the Royal Marines and their dependants. It is open to those of warrant officer rank and below, as commissioned officers have their own charitable organisations.
The home is full of nods to the shared history and culture of residents, from collages of naval photographs from different eras to the ships’ crests that adorn the walls of the bar. A flagpole flies the White Ensign, usually only flown by commissioned ships and naval establishments.
Many of the home’s team are veterans, including Corinne Day, RNBT events and publicity officer, and home manager Jade Delaney, who was a naval medic. This allows them to build strong relationships
“It is not essential to have that background in order to work here, but veterans have a very special relationship with other veterans,”

with residents and their families.
“It is not essential to have that background in order to work here, but veterans have a very special relationship with other veterans,” says Delaney. “You can have that banter with the residents, and know what sort of things they might have done in the Navy. For example, we used to play a game called uckers, which is very much like ludo, so we have an uckers club.”
AJH’s wellbeing team embraces traditional naval celebrations such as Pickle Night, which involves beer, rum and sea shanties. “HMS Pickle was the ship that came back from the Battle of Trafalgar to tell the country that we had won,” explains Day.
AJH is run as a business, with fees varying depending on the level of care needed. However, the RNBT can provide financial assistance with care home topup fees as part of its general remit. Typical fees for residential care start from £1,250 a week for new residents.
AJH came into existence when the RNBT decided to mark its centenary by building a care home that could deliver dementia care as well as the residential and nursing care offered by its existing home, Pembroke House. Pembroke House was converted from an orphanage in 1952 but AJH was purpose-built by LNT Care Developments. “It was a turnkey home, so it was built with all the furniture and decorating done,” says Delaney.

On the ground floor a reception area leads to a spacious, light-filled loungediner, where residents eat, take part in activities and watch TV, and a relaxing garden room.
“Each floor has its own lounge-diner and residents can come and go as they please,” says Delaney. “We have got six married couples who live here, and five of them live on separate floors to each other – mostly because they have different needs, although in one case they just don’t want to be on the same floor.”
Named by residents, the Atlantic community is on the ground floor, the Jutland community on the top floor, and the middle floor is the Ganges community, a reference to HMS Ganges where many residents trained as young men.
The Ganges floor houses the home’s dementia community, and includes a ‘quiet lounge’ with nostalgic items such as an old phone. Staff are encouraged to support residents to maintain independence, rather than stepping in to do everything for them. One resident, for example, likes to be busy and have jobs to do, so the cleaners have got him his own trolley so he can accompany them on their rounds.
In the Navy, the shops run on ships and shore bases are known as the NAAFI (Navy, Army, and Air Force Institutes). AJH has created its own NAAFI, where residents and staff can


buy small items like shampoo and sweets. Further along the corridor, a pretty tea room contains an interactive table which can be used to play games, and a piano donated by one of the residents. “Music is very beneficial to those living with dementia, and can stir up memories or feelings,” explains Delaney. “They might not remember who or where they are, but they can remember exactly how to play the piano.” The wellbeing team runs activities in the tea room including cookie and chocolate making, arts and crafts and table-top games.
Murals along the corridors aim to give visual stimulation. “We asked residents if they would prefer a beach or dockyard scene and they chose the beach – they said they had spent long enough in the dockyard, they didn’t want to see it anymore!” remembers Delaney. A sound machine usually plays soothing
sea sounds, but it’s so popular it has gone missing today – probably a resident has taken it to their room.
The top floor is a mix of nursing and residential care. A library gives a good view of the neighbouring cricket pitch, and the diner is occupied by a small group sitting at a table and having an in-depth chat. “On this floor they really love a glass of wine with their lunch, and they will sit and chat for hours and put the world to rights,” says Delaney.
In the cinema room, residents have just watched the film ‘Dunkirk’, and a member of staff is ‘selling tickets’ for this afternoon’s music show. Further along the corridor is the bar. “People come here whenever they like, the bar is stocked and it is all-included in their fees,” says Delaney. “On Thursday afternoon the wellbeing team will be there to serve drinks. The men have beer and sausage sessions in here, the ladies have afternoon tea – although both sessions are open to both men and women, we are inclusive.”
Most of residents are from Portsmouth, but the home attracts people from a wider area, drawn by the camaraderie. “They have come away from their usual support networks because they want to be around people who have been through the same sort of things they have – we have got a few Falkland War veterans, for example,” says Delaney. Naval spouses also tend to form

a close bond with each other.
There are strong links with the local community. A group of local schoolchildren file into reception, on their way to read to residents, followed by a man carrying colourful hoops who has arrived to lead a music and movement session. Veterans and serving personnel are keen to offer support, visiting and volunteering. Students at training establishment HMS Collingwood often come to lend a hand, and the Royal Marines Drums Corp recently played for a resident who turned 100.
Recruitment is not an issue for AJH, which employs 106 staff. “Our salaries are good, and we won’t take just anyone who applies; we probably employ one out of every eight people we interview,” says Delaney. “They have to display the RNBT values of courage, community, clarity and commitment, and show care and compassion on a level that isn’t just for everybody.”
Future plans for the home include the creation of a day centre for people living with dementia, located in the grounds. “There are a lot of veterans outreach programmes, and they could host those at the day centre,” says Delaney. “That is my vision.”
Geraint Thomas, founder of tech consultancy Guided Innovation, explores the benefits of sensor assistive technology
In the ever-evolving landscape of social care, technological plays an increasingly growing role in revolutionising the way care is delivered. One topic often spoken about is the promise assistive technology holds. These sophisticated solutions are reshaping the social care sector by enhancing safety, promoting independence and improving the overall quality of life for individuals receiving care.
Assistive technology encompasses a wide range of solutions tailored to meet the diverse needs of individuals across various care settings. I am going to hone in on just two, although perhaps three if you merge these technologies together. Why? Because I am commonly asked
“Assistive technology encompasses a wide range of solutions tailored to meet the diverse needs of individuals across various care settings."
what assistive tech care organisations should invest in, and I jump to those that not only provide risk reduction, and quality increases, but may offer the elusive ‘return on investment’.
There are two or three areas of tech that hold great benefits for social care.
Sensors
Sensors, often referred to as the eyes and ears of modern technology, play a pivotal role in capturing real-world data and transforming it into actionable insights. These ingenious devices come in a myriad of forms, each tailored to serve a specific purpose and function. From temperature sensors monitoring environmental conditions, to motion detectors detecting movement within a space, the applications of sensors are vast and diverse.
What sets modern sensors apart is their ability to leverage advanced technologies such as the Internet of Things (IoT) and artificial intelligence to enhance their capabilities. IoT sensors, for instance, are interconnected devices that can communicate with each other and transmit data over a network, enabling seamless integration and interoperability. Similarly, AIpowered sensors possess the ability to analyse complex data patterns and make predictive insights.
Sensors can be used in the following ways:
- At night in residents’ rooms to alert if they get up, are restless or may have fallen.
- In domiciliary client’s homes for staff to see when they are waking and when is best to visit.
- In any environment to show family how their loved one is getting on.
- In reablement services you can track activity and activities of daily living. Example solutions include AVERio
Remote communication tools
Remote communication tools form the backbone of modern connectivity, enabling seamless interaction and collaboration across geographical boundaries. From videoconferencing platforms to instant messaging applications, these tools facilitate realtime communication and information exchange among individuals and organisations.
In the healthcare sector, remote communication tools have become indispensable for telemedicine consultations, enabling healthcare providers to deliver care remotely and reach patients in underserved areas. In social care there was a burst of this technology during the recent pandemic to reach people in rural areas and for
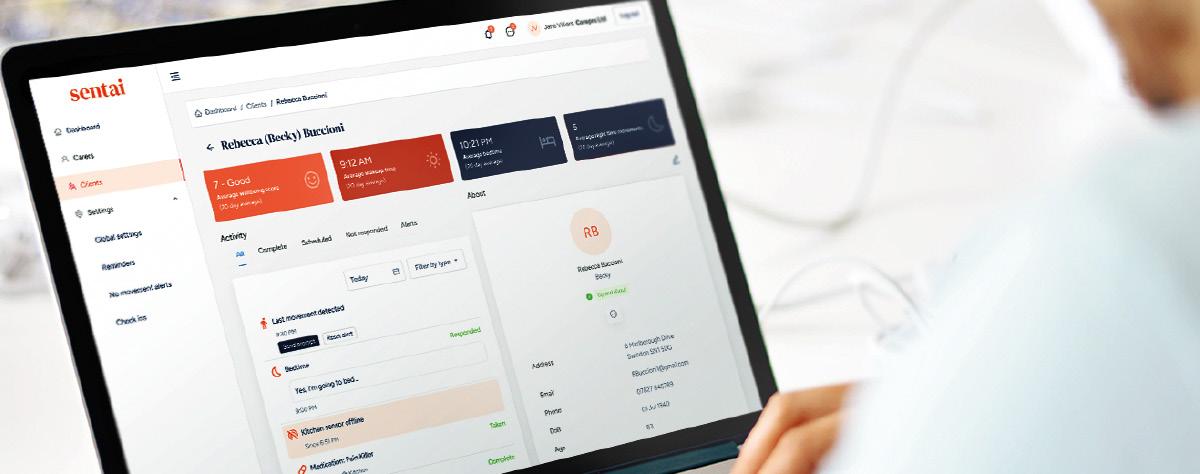
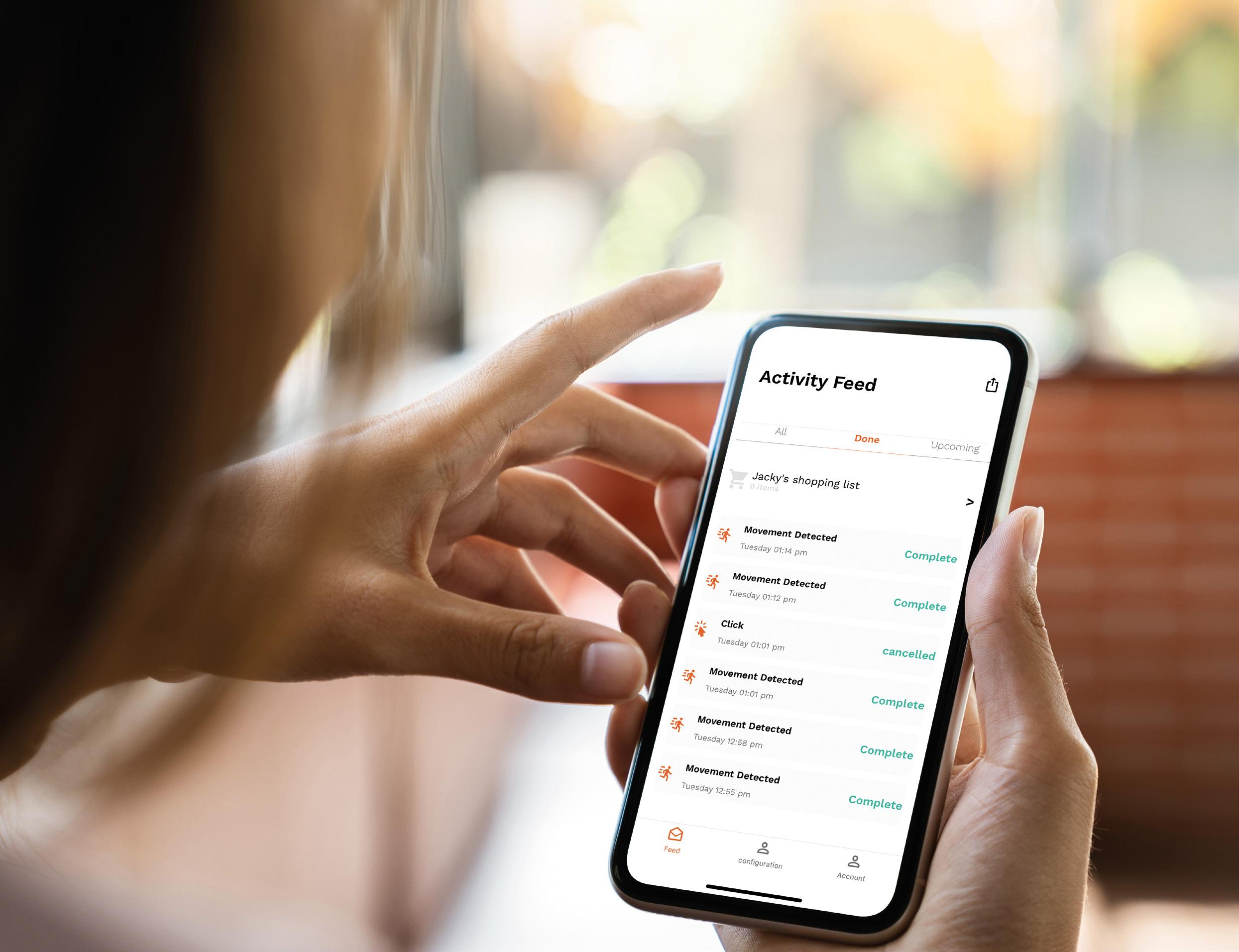
"For social care, the integration of sensor technology and communication tools holds immense promise in revolutionising the way care is delivered and experienced."
families to come face to face with their loved ones in a home.
Remote communication tools can be used in the following ways:
- An Alexa show in someone’s room for them to communicate with staff without pulling the nurse call pendant.
- Families being able to ‘call’ into their loved one’s rooms without them having to find and answer a phone.
- Staff can contact domiciliary clients without having to drive there.
Example solutions include DiscVision and Genie Connect
Solutions that do both The convergence of sensor technology and communication solutions has given rise to a new breed of intelligent systems that not only collect data but also facilitate real-time communication and decision-making. These integrated solutions leverage sensors to gather valuable insights from the physical world and use communication tools to relay information to stakeholders in real-time.
The true power for me comes when you adopt both sensors and remote communication tools. Sensors alerting and gathering data and then play those alerts and insights back though communication tools to the care staff, those they support, and families. You can procure each solution and use them in tandem. Or look for integrated
solutions.
Solutions that do both can be used in the following ways:
- A sensor picks up that someone has got out of bed; an Alexa prompts them to take their time before standing up.
- Bathroom sensors detect someone has been in there far longer than normal and alerts staff to check on them.
- Physios can consult someone via a video call and then use sensors to see if they are doing their exercises.
Example solutions include Sentai
For social care, the integration of sensor technology and communication tools holds immense promise in revolutionising the way care is delivered and experienced. By harnessing the power of sensors to monitor individual wellbeing and utilising communication tools to facilitate timely interventions and remote support, staff can enhance safety, promote independence and improve the overall quality of life for those under their care.
Dr Gill Horne outlines the difference the Topol Digital Fellowship is making to her hospice team and the people cared for and their families
As a registered nurse and programme director of care services at Rowcroft Hospice in Devon, I was one of the first adult social care leaders to take part in the Topol Digital Fellowship – a programme designed to equip and inspire professionals in the NHS and social care to lead person-centred, digital transformation projects and services.
Whether you’re an early adopter or a slightly nervous new arrival, there’s no denying that digital is the future when it comes to providing safer, more effective and more personalised care.
In all honesty, I was pretty new to digital. That’s why I was thrilled to be accepted onto the Topol Digital Fellowship run by the NHS Digital Academy to support health and social care leaders to design and deliver digital projects and initiatives to improve care. I may be a couple of months away from completing the course, but I’ve already put the learning into practice in my role as programme director at the hospice.
I am one of four fellows focusing specifically on social care solutions. As a result of learning and discussions on the programme, I have been working with people who have experience of dementia and motor neurone disease to co-design a new, decision-
"Whether you’re an early adopter or a slightly nervous new arrival, there’s no denying that digital is the future when it comes to providing safer, more effective and more personalised care."
making tool for choosing the right digital and artificial intelligence in care home settings. This tool, still in testing, guides care home managers, staff, residents and other stakeholders by asking questions that help them consider the potential impact on people (residents and staff), operations and governance. The journey we have taken together has been so rewarding and has led me to apply for and secure funding for two other digital projects.
One of these is enabling our hospice community team to design a new app for use at home to explore and meet the needs and challenges of people at the end of their life, with input from their families, carers and hospice staff. Funded by The Health Foundation's ‘Tech for Better Care Programme’, and using human-centred design principles, this is already shaping up to potentially make a real difference for planning and delivering care specifically tailored to individuals and their families. This proactive approach simply won’t be possible without the interactive technology and the ability to collate and synthesise the various perspectives, be they from patients, carers or professionals.
The other piece of work involves developing two new AI concepts, one of which will use AI-enabled doors in our future care home to create a more open environment and avoid a sense of confinement. The other will use AI technology to monitor and prevent dehydration, a common concern in elderly people that’s hard to spot at an early stage, and linked to infection and other health challenges. This work has been funded by a Amazon Web Services Imagine Grant which launched for the first time in the UK last year.
These grants, discovered through my Topol Digital Fellowship, are enabling us to deliver truly transformational work. The programme has helped me understand technical language, set up and run digital projects, and importantly develop ideas and discuss

"The journey we have taken together has been so rewarding and has led me to apply for and secure funding for two other digital projects."
plans with other fellows in both clinical and non-clinical roles. I have learned about everything from machine learning to human-centred design.
It has allowed me to make connections with new digital networks and organisations, including the South West CNIO digital nursing network, AI developers and digital companies.
Some of my colleagues here at Rowcroft Hospice have suggested I am now a ‘digital guru!’ Very clearly, I’m not, but being a Topol fellow has truly opened my eyes to the endless possibilities of digital technology and programmes to improve health and social care services. I am so thankful for this amazing opportunity.




Blue Light Card is offering those working in the social care sector the opportunity to take advantage of thousands of exclusive deals, discounts and savings from big name brands as part of its exclusive membership.
More than just a discount provider; Blue Light Card is a testament to your commitment to supporting staff wellbeing both inside and outside of working hours, by offering staff a vast array of benefits and perks. Offering a portfolio of over 13,000 partner retailers - including big name brands such as Jet2Holidays, Nike, Apple, Schuh and Hotels.com, Blue Light Card membership presents a surefire way of enhancing your employee benefits program and standing out as an employer of choice.
Encouraging a healthy and sustainable work-life balance, Blue Light Card also grants members access to the hottest tickets in town. Blue Light Tickets hosts members only ballots, as well as firstcome-first-served ticket launches to events up and down the country - offering your staff a chance to get free access to attractions, gigs, music venues, sporting events, festivals and more.
As the UK’s number one discount service for emergency services, NHS, armed forces and social care workers, Blue Light Card allows over three million members across the country to take full advantage of savings, discounts and benefits that are often unavailable to the general public. In 2023, Blue Light Card saved its members a huge total of over £330 million across retail, travel, entertainment, and more.
With more than 850,000 Blue Light Card members already registered as working in the social care sector, don’t miss out on your chance to partner with the country’s leading specialist discount provider, aligning your organisation with a brand that resonates with the values of care, appreciation and recognition.
Registering for Blue Light Card membership as part of your employee benefit scheme is quick and easy. A card costs £4.99 and includes access to the Blue Light card app where members can easily find information about all live offers. Membership is valid for two years, giving members access to exclusive offers and discounts on shopping, tech, meals out and more, all year round.
If you’re working within social care for a company that appears on one of the below registers, you’re eligible for a Blue Light Card:



Ontex has teamed up with Caring Times once again to reward those working in care who are always ready to go that extra mile
There are thousands of people working in UK care homes who make a real difference, whether it’s behind the scenes in the laundry room, preparing meals in the kitchen, or providing direct personal care for the residents. We’re looking for those who go beyond the job description. Whether it’s the gardener who brings residents their favourite cookies, or a housekeeper who helps residents to rediscover their hobbies – we’re searching for those who bring a little bit of extra joy into the care world.
Your unsung hero may be a colleague or someone else you know, and now is the time to reward those individuals who have made a genuine impact on their particular place of work.
If you know of anyone that fits the bill, entries can be made online at: caring-times.co.uk/care-home-heroes
So go to this link and tell us, in 400 words or less, why you think your nominated person deserves to win.
Terms and conditions

Make sure to include an example of when they have gone the extra distance to make a difference.
All winners will be announced in June and will be presented with their certificate and Love2Shop vouchers on Friday 28 June at the Care Managers Show at the NEC Birmingham. Three runner-up winners will each
This prize draw is organised by Ontex, Weldon House, CorbyGate Business Park, Priors Haw Road, Corby, NN17 5JG. It is governed by the laws of England and Wales and it is subject to the following conditions:
• The prize draw is not open to employees or contractors of Ontex or any person directly or indirectly involved in the organisation and running of the competition or their direct family members.
• The prizes are up to the value of £250 of Love2Shop Vouchers for the three runner-up winners and £500 Love2Shop voucher for the one overall winner. The Love2Shop vouchers may be substituted to an alternative gift card chosen by Ontex to the same value if required. There is no cash alternative. The vouchers will be presented to the winners on stage at the Care Managers Show at the NEC on Friday 27 June.
• The three runner-up winners will be included in the Caring Times publication during the September 2024, October 2024 and November 2024 issues. The overall winner will be included in the Caring Times publication during the December 2024 issue.
• No purchase is necessary to take part in the prize draw.
• The prize draw is open to UK residents only who are aged 18 or over.
• Closing date for entry is Friday 19 May. Winners will be notified by 1 June.
• The overall winner will receive two tickets to the National Care Awards on Friday 29 November in London.
• All winners will be presented with their award at the Care Managers Show and must be available to attend the Show on Friday 27 June.
• If the winners do not confirm acceptance of his/her prize within seven days he/she will automatically forfeit the rights to claim for the prize. In the event of the prize not being claimed, Ontex reserves the right to select an alternative winner via any means that Ontex feel appropriate.
By participating in the prize draw, you declare that you accept these terms and conditions unconditionally.
receive £250 Love2Shop vouchers, and the Overall Winner will receive a £500 Love2Shop voucher. The three runner-up winners will feature in the September, October and November issues of Caring Times magazine, and the overall winner will feature in a special feature in the December issue of Caring Times.

Care Homes Heroes 2024 offers a unique chance to celebrate the dedication of all those who go above and beyond to keep care homes running. It’s a brilliant way to shine the spotlight on people who get on with their jobs unseen and unheard, but make a real difference.
“This is the sixth year we’ve worked with Caring Times for the Care Home
Overall Winner 2023:
Heroes and we absolutely love it because it’s important to shine a light on those who go above and beyond for their residents,” comments Angela Gillespie, distributor channel manager at Ontex. “And it doesn’t have to be a grand gesture – it’s the little, consistent things that really have an impact on someone’s life.”
Last year, we received over 350 entries
David Fielding, handyman, Forest Care, Cedar Lodge Care Home
David’s love for his residents and his commitment to Cedar Lodge’s values drives him to perform brilliantly in his role as handyman, always exceeding his remit. He drives residents to hospital appointments, collects prescriptions from pharmacies and delivers blood samples to medical practices. He supports and contributes to the wellbeing of residents, shopping for personal items on their behalf, taking them out for shopping trips and willingly involving himself in activities on themed days.
David carries out all health and safety, induction and fire training for staff on an ongoing basis. He literally goes the extra mile to collect colleagues from home to ensure they can attend training if they do not have access to transport.
and it took a panel of five to decide the finalists. Gillespie continued: “It’s a difficult competition to judge because each person is so deserving. My top tip when nominating somebody is to use a particular example with lots of detail for how they have made a difference and how this impacted others – good luck to all nominees.”

“David is a good listener and takes the time to stop and chat with residents and colleagues,” says Nenita Jopson, care home manager. “If you need something doing, he replies enthusiastically straight away ‘yes, I can do that.’ David is our unsung hero.”

Runner-up 2023:
Runner-up 2023:
Vincent Doherty, facilities manager, The White House Nursing Home
Vincent has been The White House’s facilities manager for more than 30 years. Although he has been diagnosed with cancer and undergone treatment in recent years, Vincent has still shown up to work between treatments ready to support the home and his colleagues. He regularly escorts the activities team on trips so he can help residents on and off the home’s van. Vincent is much-loved by everyone at the home and makes time to talk to residents and their families ensuring they are happy with the facilities provided for their residents. He is an extremely talented carpenter, creating a dedicated visiting pod during Covid to keep residents and families safe, and even making a bar for the residents’ lounge.
Joy Clark, receptionist, The Burlington Care Home, Boutique Care Homes
As a receptionist, Joy’s role goes beyond greeting visitors and answering phone calls. She takes the time to get to know each resident, their interests and their preferences. Joy goes above and beyond to make the residents’ day-to-day experiences more enjoyable. She hosts them in the café for coffee and cake, taking the time to chat and listen to their stories. She has also set up a music club for the residents in the bistro, bringing in her own soundbar and putting together a playlist of old songs. This has been a huge hit.

Runner-up 2023:

Marcia Hughes, activities co-ordinator, Thorp House Nursing Home, Kingsley Healthcare
Marcia’s drive and enthusiasm is infectious. She uses Facebook and local community pages to showcase the home, with posts shared by local dignitaries such as the mayor, councillors and the local MP. She forges strong relationships to involve the home in the community, and thanks to her there are regular mentions in the local paper. Marcia works hard to ensure no resident feels isolated, and breaks activities down so that everyone can take part even if they can’t leave their room. Through a Wishing Tree she has encouraged residents to find new zest for life. Marcia sends monthly newsletters and activities planners to all the families ensuring they know what’s going on, and to see if they wish to attend anything.
Marzena Chmielewska-Akinola, head housekeeper at Aria Care’s Mill House Nursing Home in Gloucestershire, shares how she goes the extra mile
Tell us a bit about your background –how did you get into care housekeeping? I started my journey in the care sector in 2010 when I first came to UK and started working as a healthcare assistant at Mill House. I was a care assistant for about five years. When I lost my grandma in Poland, I was angry with myself that I hadn’t been with her as much as I wanted. Instead of caring for my grandma, I had been caring for everybody else, and I was no longer happy as a care worker. I stayed with Mill House but moved to housekeeping, as I didn't want to leave this place, and I was happy again. It was a different job, but I could still be close to our residents. I was a domestic assistant for another six years, working mostly in my favourite role, laundry, and eventually became head housekeeper.
How do you go about meeting the needs of residents?
I always ask our residents how they would like things to be done. For example, if they tell me that they like their room to be done in the morning while they are out for breakfast, I will do that for them. If they would like an extra pillow for a good night’s sleep, I will make sure they have it. If a resident is unable to tell me about their needs, I speak to their family and friends, and our carers and nurses are also good source of information.
What’s a typical day like?
Every day is different, with new challenges and different tasks. We try to
"People are usually surprised with how magically and quickly we can make a room look good and clean again."

keep things running smoothly by having one housekeeping assistant on each floor and one in the laundry. I provide extra help on both floors and in the laundry. I make sure that we have enough products in stock, and that carers and nurses have their wipes, gloves and red bags and yellow bags in place for different kinds of waste. I check and answer emails, prepare show rooms or prepare rooms for new arrivals. We also help to prepare tables in dining rooms after lunch and occasionally help with activities.
What is the most challenging part of your job?
When a resident is not happy with us. Sometimes this is through no fault of our own, someone is just in a mood and we have to accept it. We don't always have to clean a room straight away, we can wait for a better moment, but sometimes it is a must and we have to come in and clean even if the resident is not happy about it. However, we make sure to respect them and have a chat with them while we work.
Is there anything that would surprise people about your job?
People are usually surprised with how
magically and quickly we can make a room look good and clean again. They are also surprised by how much laundry we do in a day.
Has anything changed since you started your role?
We do more e-learning now, which has enabled me to learn new skills and expand my knowledge across various subjects.
What is special about the care home you work for?
Mill House is like my second home. It is not just a place of work, it’s a place where I spend so much time with people I like to work with and with residents who are like my own grandparents.
What skills and talents do you need to be a great head housekeeper?
You need to be fit to be a good head housekeeper, as it’s not a job where you sit much at a desk. You need to be happy in your job, because our job is also giving a smile to our residents. You need to have a good eye for detail and be quick. You also need to be a good leader, as you are in charge of a small group of people.
In the quest for achieving clean and infection-free laundry in care homes, the focus naturally turns to having the right washing machines and dryers in place to do the job. However, success doesn't solely depend on the machines but also on the people involved
Amanda Symmons, care expert at WASHCO, provides practical steps to help your team optimise laundry processes for the best results.
Separating laundry in the residents’ rooms, ready for washing, is key to protecting staff and making processes more efficient.
Investing in a trolley with 4 containers makes it easy to separate sheets, towels, personal items and red bags. Laundry can then be placed straight from the container into the washing machine, making it easier to select the appropriate programmes.
We recognise that in a busy laundry environment, the priority is to keep pace with the continuous piles of washing, but it’s important not to overfill or underfill your machines.
Overfilling prevents the laundry from being agitated sufficiently to effectively remove dirt and stains, often meaning that items need rewashing. On the other hand, underfilled machines take more time to process the laundry (vs a full load).
Some machines have technology which can be a real benefit in this area. For example, WASHCONNECT machines feature a dynamic weighing system which adjusts the cycles, energy and detergent used based on the amount of laundry loaded. It’s easy to see if machines are constantly under or overfilled, highlighting potential training needs.
Not all laundry requires thermal disinfection, including personal non-soiled clothing. Instead, staff should be trained in selecting the appropriate cycles and pairing these with the correct chemicals in order to help avoid damage to clothes, reduce wash times and save energy.

To help improve efficiency in your laundry, you could also consider introducing auto-dosing, which will automatically select the detergent needed and ensure the right amount is dispensed.
Once your laundry has been washed, ideally staff should touch the laundry as little as possible, aiming for no more than four times.
• Touch 1: Transferring laundry from the washing machine to the dryer.
• Touch 2: Folding laundry. To minimise the risk of contamination, no laundry should be stored in the laundry room.
• Touch 3: Storing laundry. This is another area where training staff can make a difference. Avoid the temptation to put freshly laundered linen on top of other linens, clean items should go to the bottom to ensure regular rotation.
• Touch 4: Returning laundry to the residents straight away, minimising unnecessary handling. With the right training, tools and existing teamwork, making minor
changes to your laundry operations will empower your team to provide an even better service for your residents.
WASHCO have a library of handy resources to give you a helping hand with managing your care home’s laundry. Scan the QR code to check it out.
Alternatively, visit washco.co.uk/ free-care-home-resources
For support improving your care home’s laundry service, contact WASHCO’s highly qualified team on 08000 546 546 or info@washco.co.uk
Launching her new column, Riverstone’s wellbeing director Dr Zoe Wyrko, an expert on living and ageing well, offers a fresh take on later-living
Riverstone is revolutionising retirement for people over 65, so that they continue to enjoy interesting and active lives right in the heart of London.
When I’m asked about the main difference between my former life as a physician in the NHS, and my current job as wellbeing director for Riverstone, my answer often surprises people. It’s not about the beautiful surroundings or being respected by my employers, but rather that I now have the opportunity to help older people to stay well instead of just picking up the pieces once things have gone wrong.
Working as part of a frailty-focused multidisciplinary team in a busy inner-city A&E department meant my colleagues and I could often see the tipping point in a person’s life approaching, but were completely powerless to stop it, knowing that we would shortly be dealing with a full-blown crisis for that individual and their loved ones. We could often identify where a timely care, support or health intervention would have made all the difference, were it able to be accessed.
Protecting our own health, preventing illness where possible, and being fit to face what comes at us as we get older is a step that everyone should be able to take – and for those of us working in the care sector, it’s something that we should be
supporting our clients with.
It’s a way to be able to maintain a degree of power over what life throws at us, and a sense of control is important for both physical and mental health.
Scientific research has shown that genetics account for about 25% of how we age, which means that we are able to exert an influence on the rest. Some aspects will still be out of our control, for example, our childhoods, personal circumstances and employment (the social determinants of health that cause inequalities) but there is still scope for change, and it’s never too late in life to start.
Public health campaigns mean we know not to smoke, not to drink too much alcohol, to eat a healthy balanced diet, and to do 150 minutes of moderate exercise (including two sessions of 30-minute strength training) each week. However, ‘knowing’ is different to ‘doing,’ and unfortunately exercise and a good diet are not within the reach of many in 21st century Britain.
There are then vital aspects of prevention which require interaction with a health professional, such as getting blood pressure checked and treated, receiving scheduled vaccinations, seeing a dentist, getting eyes and ears tested (correcting sensory impairments has been proved to reduce loneliness, isolation and subsequent depression and cognitive impairment).


Dr Zoe Wyrko
"Scientific research has shown that genetics account for about 25% of how we age, which means that we are able to exert an influence on the rest. "
These basic interventions are becoming harder to access for many people due to availability, or cost, or simply the ability physically to get to the services.
And finally, it’s much harder to measure things that don’t happen, compared to things that do. We know that a timely support package, with long enough care calls, can prevent the decline that leads to falls, fractures and ultimately much higher costs and a poor quality of life. But all that will be seen on the balance sheet is the cost of that care for a person not in desperate need, with none of the benefits that occur as a result of it.
For more information on Riverstone and its revolutionary ‘Wellbeing Journey’, visit riverstoneliving.com
Are you a registered manager of an adult social care service? Come join us to be part of a membership community that helps increase the professional recognition of registered managers and champions the values for delivering compassionate, person-centred care.
Skills for Care is the membership organisation for registered managers in England. As a member, you will keep up-to-date with sector developments and access benefits that enhance your learning, development and wellbeing.
Membership benefits include:
■ a printed copy of our Social care manager’s handbook, an essential resource for registered managers
■ a dedicated monthly newsletter full of practical information and guidance
■ access to the Good and outstanding care guide (Single Assessment Framework version) including 34 Quality Statement Recommendation checklists
■ an exclusive resource when you renew your annual membership
■ the chance to train to become a mentor or receive mentoring
Is your organisation looking to invest in your registered managers?
Membership adds value and demonstrates a commitment to investing in your managers. Buy 10 or more memberships and receive a 10% discount.