Property marketplace... Innovation... Expert analysis...

September 2023


Property marketplace... Innovation... Expert analysis...

September 2023

Ron Taylor, managing director of Parklands Care Homes, warns Scotland’s care home sector is leaning into a precipice
ALSO IN THIS ISSUE
Care Managers Show
We look back on this summer’s smash hit event
Opinion
Integrated Care Systems could be a game changer
CT's Top Five Picks
Our top five food service providers revealed


Skills for Care’s annual report highlights the key role of migrant workers in filling the social care workforce shortfall




Chief executive officer
Alex Dampier
Chief operating officer
Sarah Hyman
Executive assistant
Kirsty Parks
Editor-in-chief
Lee Peart
Features editor
Charlotte Goddard
Subeditor
Charles Wheeldon
Advertising & event sales director
Caroline Bowern 0797 4643292 caroline.bowern@nexusgroup.co.uk
Business development manager
Steven Godleman steven.godleman@nexusgroup.co.uk
Business development researcher
Robert Drummond
Operations executive
Sophia Chimonas
Senior conference producer
Teresa Zargouni
Head of digital content
Alice Jones
Marketing design manager
Craig Williams
Marketing campaign manager
Sean Sutton
CRM database manager
Annalisa La Manna
Lead developer
Jason Hobbs
Publisher Harry Hyman Investor
In our lead story this month, Ron Taylor, chief executive of Parklands Care Homes, graphically illustrates the huge challenges facing Scottish care home providers in terms of inadequate funding, recruitment shortages and soaring costs.
One care home closes every week in Scotland, according to Scottish Care, a clearly unsustainable situation.
Care home operators in England, Wales and Northern Ireland face the same perfect storm. Skills for Care estimates there are around 152,000 care vacancies in England alone.
Faced with this critical situation, urgent action from government is clearly required in order to prevent the whole social care system collapsing with disastrous consequences for the NHS.
Instead of government action on relieving recruitment pressures on providers, however, we were treated this summer to the insane demand from the New Conservatives splinter group for an end to social care migrant visas in order to help put a brake on soaring migration.
Skills for Care’s latest workforce report (also in this issue) graphically illustrates how the migrant workforce has kept the social care sector afloat with around 70,000 people recruited from abroad last year.
While no one is advocating that heavy reliance on overseas recruitment is a longterm solution, it’s clear there’s a desperate need for migrant workers currently, particularly in rural parts of the country where there are simply not enough local care workers.
Until we see a significant rise in care worker salaries and a long-term workforce plan designed to make care a career of choice for far more people, access to overseas workers will remain crucial to the sector.
Instead of stopping overseas workers as advocated by the loony right, the government needs to provide easy access to migrants, including our much neglected friends in Europe.
Lee Peart Editor-in-chief Caring Times
The government unveiled a £600 million package to help with recruitment and retention in social care. The fund will support the social care workforce and boost capacity in social care, supporting the NHS ahead of winter and through into next year.

moved to alternative accommodation after an inspection found serious fire safety risks. The evacuation was carried out following an inspection of Springfield Cottage Care Home by the Care |Quality Commission and Lancashire Fire and Rescue Service.

The NHS announced a number of measures to prepare for winter, including rolling out care ‘traffic control’ centres to speed up discharge. The measures, which were set out at an NHS England board meeting in Birmingham, aim to boost capacity and resilience across the NHS.

Residents at a Blackburn care home were

HC-One was named among the top 100 apprenticeship employers for the second consecutive year, in recognition of its commitment to the career boosting opportunities provided by apprenticeships over the past 12 months. The care home operator joined major household names in the top 100 of the independently assessed rankings, which are developed by the Department for Education in conjunction with High Fliers Research.
North West Leicestershire District Council rejected Exemplar Health Care’s plans for a 36-bed care home in Coalville. The planning application submitted in April was for a home for those with neuro-disabilities, brain injuries and dementia which was to be located opposite the listed Snibston Colliery. A council report said: “The public benefits overall are not considered to outweigh the significant but less than substantial harm to heritage assets. The scale, layout and appearance of the proposed development would erode the setting which contributes positively to the significance of the scheduled ancient monuments that form part of Snibston Colliery.”
NHS and Care Volunteer Responders is now open to all adult social care providers in eligible residential and domiciliary settings across England. This expansion grants easier access and simplifies the process for care providers to request helpful volunteer support.
NHS and Care Volunteer Responders is a flexible volunteering programme. Built on a digital platform the ‘GoodSAM’ app, this programme links an available pool of volunteers to local live tasks. Volunteers are readily available to offer a range of services:
Check In and Chat volunteers provide telephone support to people who need a chat and some encouragement to improve their mental health and wellbeing.
Check In and Chat Plus volunteers provide regular telephone calls for more vulnerable people - 3 calls a week over a 6-week period from the same volunteer.
Pick-Up and Deliver volunteers transport medication or small items of medical equipment to people’s homes from NHS sites and equipment between sites.
Community Response volunteers are available to collect and deliver essential shopping and prescriptions to people in receipt of care support.
Volunteer Responders do not undertake staff duties but instead complement the existing workforce. This allows care staff to focus on providing quality care to those who need it most.
Volunteer Responders have had the appropriate checks and receive the required guidance and support for these activities. They are co-ordinated centrally and deployed locally. Their expenses are paid by the programme.
With volunteering available seven days a week, there is comprehensive wrap-around support and assurance. Safeguarding and problem-solving teams, and a helpline are available every day from 8 am to 8 pm.
The programme offers numerous benefits to individuals and the sector as a whole:
Benefits to the people being supported
Adding value to their care experience
Reducing isolation and loneliness and improving wellbeing and sense of connection.
Enhancing quality of life.
Supporting the ASC workforce
Quick access to a free pool of available volunteers.
Volunteers free up staff to support individuals with more complex needs to live independently.
Research shows that care staff, supported by volunteers, report greater job satisfaction and reduced stress levels.*
Enhancing sector provision
Providing short-term support for up to six weeks. After which, people can be re-referred.
Complementing existing volunteering programmes and increasing overall capacity.
Facilitating ASC staff and volunteer recruitment
Volunteer Responders attracts newcomers into volunteering due to its flexibility, acting as a stepping stone to ongoing volunteering participation.
The programme creates a helpful pool of individuals with care experience, supporting recruitment into social care.
* www.royalvoluntaryservice.org.uk/about-us/our-impact/our-research-policy-work/ reimagining-social-care/
To make a referral, visit our website at nhscarevolunteerresponders.org, call 0808 196 3646 (Between 8am and 8pm, 7 days a week) or scan the QR code for more information.
Service provided by:
“It’s immensely helpful to be able to offer people emotional wellbeing support and the opportunity to have a friendly phone call as part of their care package... I would recommend the programme to other social care providers, it’s quick and easy to use.”
Samantha Aylott, Specialist Advisor for Adult Social Care at Essex County Council

Avery Healthcare Group acquired 29 care homes from Signature Senior Lifestyle increasing its portfolio to 99. The homes will become part of the company’s new luxury brand, Avery Collection.

Exemplar Health Care has marked the official opening its £5 million Roseside care home in Liverpool. Local comedian and actress Pauline Daniels and former Lord Mayor of Liverpool, Frank Prendergast cut the ribbon to launch the home officially.

Grade II listed Birchley Hall Care Home in Billinge, Merseyside is to close after being placed into administration last year after operating for 50 years. After the administration, the home was managed by Healthcare Management Solutions (HMS), one of 10 care homes managed by the company since Qualia Care went into administration last October.
Deputy lieutenant of Sevenoaks
Nicholas Hely-Hutchinson cut the ribbon to open Oakland Care’s ninth care home in Hildenborough, Kent. Caring Times joined residents, staff and children from local Stocks Green School for a day of celebration to mark the day’s opening.

Care Concern acquired two care homes in Cannock, Staffordshire: Barton House and Needwood House, which cater for a total of 48 service users requiring mental health support. The business has been owned and operated by John and Ann Mansell since 1995 who recently decided to sell as part of their retirement plans. The two homes were sold for an undisclosed price. Business property advisor Christie & Co facilitated the sale.
Care home owners Sunjay Rai and Ash Sharma purchased Sunnyhill Residential Care Home in Eastbourne, East Sussex. The vendor was Raj Madlani of Amba Care Homes Group. Sunnyhill is a threestorey, 20-bedroom dementia care home with a Good Care Quality Commission rating.


Specialist provider Eden Futures has opened a supported living service for adults with learning disabilities, mental ill-health or autism in Stoke-on-Trent. The facility has been developed in partnership with Stoke City Council, Staffordshire County Council, North Staffordshire Combined NHS Trust, a specialist supported housing developer, and housing provider Blue Square.
Resicare Alliance, a provider of specialist children’s residential services and family assessment centres, has acquired three children’s homes in Birmingham, previously trading as part of Aston Children’s Care Holdings.


Czajka Care Group began work to extend Currergate Nursing Home in Steeton, West Yorkshire after planning approval was granted for the first phase of development. Currergate currently has 34 fully occupied rooms, and will now invest £1.5 million in the development and refurbishment.
Boutique Care Homes has purchased a care home development site in Maidenhead, Berkshire. The company is applying for planning permission for a luxury care home featuring spacious bedrooms with en suite wet rooms, a bistro, beauty salon, cinema lounge, hobby craft room, and tree-lined gardens. The care home will also create more than 70 jobs.

Care England’s chief executive Professor Martin Green says it’s time to shift the dial in the conversation about what true health and social care integration means


We have been talking about the benefits of health and social care integration for a long time, and it is important to remember there have been many attempts to deliver this, all of which have failed to a greater or lesser extent. I can remember when we had joint appointments between health and social care; we also had co-location where health and social care staff were working out of the same office. After this came a range of structural changes. We have had health and wellbeing boards, primary care trusts, and clinical commissioning groups, and now we are in an era of integrated care systems. What’s clear from this history is that people don’t
“We have had health and wellbeing boards, primary care trusts, and clinical commissioning groups, and now we are in an era of integrated care systems. ”
learn from it, and every time the system goes into a spasm of reorganisation, there’s so much hope for a change in how services are delivered. Yet, much of this hope is dashed by the reality of what happens on the ground.
One of our biggest challenges is that nobody understands what integration means. There is so much talk about organisations, systems and processes, yet integration should be about people and outcomes. We need to shift the dial from talking about the NHS, local authorities or care providers and focus on the experience of people using the service. There also needs to be more acknowledgement about integrating systems with vastly different resource bases and public perceptions. The NHS swallows up vast amounts of taxpayers’ money and there’s little left for social care. Another challenge is that the different bits of the system have widely different statuses and knowledge among the public. For 70 years, the public has been fed a diet of how wonderful the NHS is, which is in marked contrast to the little public recognition of social care.
It’s also impossible to integrate systems with significantly different success measures. If we are going to have truly integrated health and social care services, we need to be clear that everyone has to be measured in the same way. The current system requires an integrated approach to measurement. In some cases, the measures of success in different parts of the system are incompatible and in conflict with



one another. If you take the example of measures of success in the NHS, these are often tied to activity when they should be about prevention and enabling people to live well. This is brought into stark contrast where the measure of failure for a local authority adult services director may be the admission to the hospital of a citizen, yet this is a measure of success in the NHS, where measurement systems tend to work on activity rather than outcome.
I think we should work on three very high-level sets of measures. First, we should measure the person experience; we need to know how the person experiences the service and be clear that it delivers what they need and want from the intervention. Second, we must measure the outcomes of an intervention. Every single intervention, whether it’s health or social care, should have a clearly defined and measurable outcome, and any intervention should leave people with a better outcome than would have been delivered had they not been in contact with health and social care. These measures can be very broad and include medical treatments, improved wellbeing, or better capacity to manage their lives and long-term health conditions. The third measure is about the effective and efficient use of human and financial resources. If we were to recalibrate services on the basis of the most effective use of resources, there would likely be a significant transfer of money from health into social care and into prevention. It is sad that in all the attempts to deliver an
integrated system, we see little attention given to the measures of success across that system.
It is also essential to think about how people live their lives, and we often have conversations about integrated systems which begin and end with health and social care. While these are very important aspects of an integrated approach, people live their lives within communities. So real integration would go far beyond health and social care and would think about housing, transport, community services and connectivity with community family and friends. All these elements lead to a healthy and happy life for the citizen, and in many ways to address only two of them, and forget the other aspects of people’s lives, is to miss the point of an integrated approach.
Despite my fairly healthy cynicism about previous reorganisations, the move towards integrated care systems could be a game changer, but it has to be accompanied by a significant amount of culture change within the current system. If history has taught us anything, it’s that just by changing structure, you don’t necessarily change the outcomes or transform the system. It’s often said that culture eats structure for breakfast, and we see this so graphically illustrated in health and social care reorganisations. We often see structures, names and organisations changing, but we find huge numbers of the same people just shunted into different jobs with little or no focus on how they are going to deliver something differently and how they are going to change their approach to be fit for purpose in the 21st century, or indeed, how they will be measured in terms of their success.
I distinctly remember meeting senior leaders in South London’s health and social care sectors many years ago. I was in a room with 30 people and I asked them to introduce themselves and tell me about their job and immediate previous roles. What was so evident was that every single one of those people had
had senior positions in the last structure and had just been moved sideways into a new structure. I then asked the question, how were they going to deliver on this objective of integrated care? I got lots of wonderful fluffy rhetoric, but they could have gone into detail about how the money would flow, how efficiency would be measured, or how people would move seamlessly across the system to ensure their needs were met effectively. There also needed to be a conversation about the huge differential in remuneration, training and status between the staff in one part of the system and the other. I also witnessed some interesting power dynamics where NHS staff saw themselves as being the lead in everything related to this new system and social care staff were relegated to second place. There is a desperate need to have an integrated system, but I’m concerned that we’re not learning from previous experience, and I don’t see the culture change that needs to happen to deliver a different system fit for purpose in the 21st century. I am still waiting for an ICS with a clear grasp of integrated success measures and integrated approaches to value and outcomes for citizens. When I see that, I will believe that we might get to where we need to be. As demographic change starts to happen and there are more pressures on our system, we cannot afford to fail, and we cannot afford to do what we have always done because we will not have the financial or human resources available for business as usual. This is our moment for a paradigm shift; I only hope some are brave enough to take it.
“It’s also impossible to integrate systems with significantly different success measures. If we are going to have truly integrated health and social care services, we need to be clear that everyone has to be measured in the same way."
“As demographic change starts to happen and there are more pressures on our system, we cannot afford to fail, and we cannot afford to do what we have always done because we will not have the financial or human resources available for business as usual. "
Is your care home being held back by endless piles of laundry and struggling with outdated processes? It may be time to embrace a fresh approach to laundry management.
WASHCO's care expert, Amanda Symmons, is here to guide you through a Laundry Health Check that will help to identify areas where you can enhance efficiency and boost productivity.
Evaluate your capacity
The capacity of your laundry machines directly impacts how much laundry your home can handle.

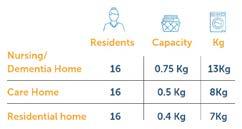
The general rule is that a care home will need 0.5 kilos capacity per resident, however this will vary dependent on the type of home. A nursing or dementia home may have more laundry per resident whereas residential homes may have a lower requirement.*
soiled and infected items. This way, your team can easily select the appropriate programs in the laundry room, ensuring proper cleaning and safe disinfection of the linens. Moreover, drying similar loads together optimises the use of residual moisture programs, further reducing drying times.
Following current HTM01-04 guidelines, only "red bag" laundry (e.g. foul and infected items in a red dissolvable bag) needs to be processed at 65 degrees for thermal disinfection. Consider switching to a 40-degree wash (with the appropriate chemical) for standard laundry, which can save you about 20 minutes per cycle. This small change can add up to significant time savings, allowing you to increase throughput in the laundry.
Establishing a sorting practice at the source, such as within residents' rooms, can streamline your laundry process. For example, you could categorise laundry items into textile families such as bedding, towels, clothing, and "red bag"
A well-designed laundry room is crucial for optimal performance. Carefully plan the layout to provide easy access to machines and smooth transportation of laundry. It's recommended to have a clear separation between clean and dirty linen areas, with separate entry and exit points for dirty linen, if possible. A good rule of thumb is to reserve approximately 1/3 of the room for dirty laundry and 2/3 for clean laundry.
On Day 1 of the Care Show this October, Amanda will be hosting a talk at the People Theatre (2:55pm – 3:25pm).
During the talk, she’ll discuss why people, not machines, are the most valuable asset
to your care home’s laundry, as well as why laundry is such a critical function of your operations. At the end, the winners of the 2023 Love Laundry Awards will be revealed!
The WASHCO team can also be found on Stand C35 at the show, where they will be on hand to discuss your care home laundry needs.
WASHCO have a library of handy resources to give you a helping hand with managing your care home’s laundry. Scan the QR code to check it out.
Alternatively, visit washco.co.uk/ free-care-home-resources
Ron Taylor, managing director of Parklands Care Homes, warns Scotland's care home sector is leaning into a precipice

Based in the Highlands of Scotland, Parklands Care Homes, which celebrates its 30th anniversary this year, is on the front line of the challenges facing social care.
This was starkly illustrated when the operator was forced to close Mo Dhachaidh Care Home in Ullapool in March, just six months after it was purchased from Barchester Healthcare.
“It was the most difficult decision I have had to make in 30 years of working in the sector,” Taylor says. “It became clear after we bought Mo Dhacaidh that the costs of operating and upgrading the home were beginning to spiral and were becoming too great to bear.
“Mo Dhacaidh had only 19 beds. The Care Inspectorate had introduced new building guidelines and the redevelopment costs were 200% more than we had anticipated six months earlier. We weren’t generating the revenue to make it sustainable.
“We focus on identifying small, rural economies of 10 to 12,000 people and a feeder population of around 40 to 50,000. Mo Dhacaidh fitted well into that scenario. The problem was that
although we had reduced the reliance on agency staff, the costs of running the home had escalated far too much. It wouldn’t work with a fixed income coming in.”
Mo Dhacaidh highlighted in microcosm the enormous challenges care home operators across Scotland are facing, particularly those in remote rural areas.
“This is the most challenging it has been in my 30 years in the sector,” Taylor notes. “We are suffering 500 to 600% rises in energy costs. Food price inflation is running at 18%, we have soaring interest rates and labour shortages and a lack of government funding.”
With Scottish Care estimating one care home a week is closing, Taylor says there’s urgent need for government intervention to avoid the total collapse of the system.
“The outlook for the sector in Scotland is not good at all,” he warns. “It does feel like we are leaning into a precipice. The lack of interest and support from Scottish ministers is quite staggering. If social care collapses, then the impact on the NHS will be huge. Even at this late stage I would hope that we can convince ministers of the need to invest in social care.
“We look after people at their most
vulnerable and we are blessed to look after people when they reach an old age. It’s an honour and a privilege to do so, but how many care homes are going to close before something is done about it? We can’t understand why the reform of social care hasn’t come up further the agenda. We celebrated the 75th anniversary of the NHS recently, but there was no word of social care being involved. That needs to be looked at as a priority.”

The care chief highlights July’s reluctant acceptance by Scottish Care on behalf of care home operators of a 6% rise in the annual National Care Home Contract (NCHC) as an example of the woefully inadequate government support for the sector.

“I’m delighted we have the NCHC,” Taylor says. “I think we need a framework. Without the NCHC local authorities would negotiate locally themselves and in many places would drive the prices down. It’s good that we have coverage for the NCHC, but the cover itself is very disappointing. We ended up with a 6% increase this year which is frankly quite insulting. In the past two years prices for food and utilities have spiralled out of control and we have other costs with interest rates and labour shortages and the lack of government funding. The current set up
“We need a price reset. We need to look at dependency levels rather than definitions of care. There was a lot more residential care when the NCHC was set up. Now more people are staying at home longer, which in my mind is residential care.”
When pressed, Taylor suggested £1,200 as an appropriate figure to reflect the costs of operators, representing a roughly 50% rise on the £838 for a nursing home and £719 for a residential care home currently on offer.
“The government is looking to provide complex care on the cheap,” Taylor says. “This is cheap hospital care if you ask me. It’s simply not sustainable in its current form. The stark reality is that more homes will close and staff will lose their jobs and older people will suffer.”
Given the current trials facing the sector, Taylor welcome First Minister Humza Yousaf’s decision to delay introduction of a National Care Service after coming into office in March.
The Bill for the legislation, which has encountered widespread opposition, has been delayed to next year in order to address the current challenges facing the sector.
“The First Minister has listened to us and it’s right to delay the introduction of the National Care Service and to reform it,” Taylor notes. “Change on this scale should not be rushed. We agree with the unions that the money would >
“It does feel like we are leaning into a precipice. The lack of interest and support from Scottish ministers is quite staggering.”Eileen Dubh care home
be better spent now in dealing with the immediate problems in social care. The concept is good and the principle is something we very much support. The National Care Service will put social care on a similar footing to the NHS, which is good.
“There needs to be local accountability, but it remains to be seen how it is going to be delivered. We must avoid centralisation at all costs. It’s something that could move forward constructively but not now. It’s being delayed until the government gets more feedback from the sector which is a good thing.”
When asked by Caring Times about what needs to be done by government to support the sector through its current crisis, Taylor cites getting the economy back on track as first and foremost.
“We need the government to get on top of inflation which has been crippling
“There was a lot more residential care when the NCHC was set up. Now more people are staying at home longer, which in my mind is residential care.”
for the last two years,” the care boss says. Secondly, Taylor says additional funding is urgently required to make the sector sustainable and an attractive place to work. “We need Scottish ministers to put their money where their mouth is,” Taylor says. “The First Minister has said that he would like to pay care workers £12 an hour, but there’s no timetable for additional funding on this.
“We have increased our carer rate to £12 an hour and our nurses rate to £20 an hour, which is something we could ill afford to do, but despite no additional funding from the government it was the right thing to do to retain our staff and try to attract new staff. It’s not something we can do on an annual basis but it’s something we need to do to keep our existing staff in the communities in which we operate.
“Ideally we would want to pay our care staff about £15 an hour, but there isn’t the government funding available to enable us to do that. It’s important to acknowledge and reward the fantastic job our care workforce does. We operate in quite a low-wage economy so if we can help with the cost of living let’s do it.”
Additionally, Taylor says further measures are needed to open overseas markets to the sector, particularly those in rural areas where an adequate local staffing resource is unavailable.
“We’re expanding our overseas recruitment with the new visa
accessibility granted by the government,” says Taylor. “We are a wee bit disappointment by some of the mood music in England about trying to close the visa applications for care workers. In the rural Highlands we need that availability of labour. It just isn’t here, so it’s very important that that remains open for us.
“The local workforce in our locations is just not there in terms of getting people to come forward. We have had Covid and Brexit and a lot of people have taken early retirement and taken advantage of the tax break at 55 and taken money out of their pension. I think we need to look elsewhere and overseas is an obvious attraction. More overseas recruitment needs to be part of the solution.
“We have specific problems in rural Scotland and the labour ability is not there so we need to bring in other people, including from Europe as well as further afield.”
While remaining optimistic about the future of Parklands, with a number of new care homes, independent living services and affordable homes for care workers among plans for the future, Taylor re-emphasised the need for major reform to make the sector sustainable at a national level.
“I am a canny Scot so the cup is half full but half empty,” he concludes. “We need the government to help us drive social care and drive recruitment north

of the border. We don’t have any scheme to help us with international recruitment in Scotland and we badly need that too. We need the national government to get inflation down and create a more stable economy.”
When asked for a response to Taylor's interview, a Scottish government spokesperson told us: “We are committed to working with all partners to improve social care services and know
well the challenges that the adult social care sector faces at this time. These challenges particularly around staffing are exacerbated by Brexit, funding challenges and the cost of living crisis.
“Over the last couple of years we have increased the pay for social care workers by more than 14%. We are looking at how we can plan for, attract, train, employ and nurture the workforce, working with COSLA on consistency of improved pay and conditions, improving access to training and development and ensuring a career in social care is attractive and rewarding.
“We are also continuing to work towards our commitment to increase spend in social care by 25% by the end of this Parliament, an increase of over £840 million.
“The Scottish government is not a party to the negotiations for the National Care Home Contract, but we note that the new agreed rate between the sector and COSLA reflects increased costs, including higher energy costs.”


Townsend Communications’ managing director, William Walter interviews the chair of the Health and Social Care Committee Steve Brine about the pandemic’s effect on adult social care and what’s been learnt from policymakers’ handling of the crisis
"In the case of a future pandemic, the joint report recommended that prominence of social care within the Department of Health and Social Care should be enhanced and ministers must address the relative lack of knowledge of social care within the Department and NHS."

this, the government and NHS England, working with ICSs, must monitor and resolve poor partnership working.
What were the most unforeseen affects of the pandemic on the adult social care sector?
The pandemic put a massive strain on a social care sector already under pressure. Between 2020 and 2021, the Health and Social Care Committee led a joint inquiry with the Science and Technology Committee into lessons learned. We found that while the UK was not alone in suffering significant loss of life in care homes, the tragic scale of loss was among the worst in Europe and could have been mitigated. In particular, staff shortages, the lack of testing, difficulties in obtaining PPE and the design of care settings hampered isolation and infection control and the ability to keep Covid-19 at bay. The pandemic also had a significant and lasting impact on the social care workforce, where staffing gaps have continued to grow.
Are claims that the health service was prioritised over social care during the pandemic justified?
The inquiry found that the lack of priority attached to social care during
the initial phase of the pandemic was illustrative of a long-standing failure to afford social care the same attention as the health service. In the case of a future pandemic, the joint report recommended that prominence of social care within the Department of Health and Social Care should be enhanced and ministers must address the relative lack of knowledge of social care within the Department and NHS.
Post-pandemic, how can policymakers improve the interfunctionality of the health and care services?
Planning for future pandemics should have a more developed and explicit consideration of the intense interaction between the NHS and social care. The committee is optimistic about the newly formed integrated care systems. We hope these will offer a refreshed way of working across health, social care and wider local authority functions and community organisations. However, it is vital that social care is not forgotten, and that ICSs don’t become too NHS-centric. To do
How can the government ensure additional funding for the sector promotes its post-pandemic recovery while also addressing inconsistencies in local care provision?
While additional funding for social care is welcome, long-term reform of the sector is overdue and should be pursued as a matter of urgency. One aspect of reform the committee argued should be prioritised in its workforce report is to end ‘by the minute’ commissioning by local authorities and private providers. This practice is having a damaging impact on the continuity of care offered to people in receipt of social care and the terms and conditions under which workers provide care. Instead, workers should be paid in advance to provide care that is both relational and task-based and is focused on achieving outcomes. Lack of funding also underpins the poor digital capabilities and infrastructure within social care and is preventing the sector from benefiting from the huge potential gains digital can bring.
Head of social care for Unison Gavin Edwards discusses how the adult social care sector suffered during the pandemic and what lessons can be learnt from the experience
Memories of the pandemic are still raw for many, including the thousands of care staff who worked on the front line. Being left with no choice but to make aprons from bin bags, watching helplessly as care home residents died, and living in fear of infecting loved ones are among the harrowing experiences haunting them still.
Social care was treated as a secondclass service and its skilled employees abandoned by the government during Covid.
There was no protective ring around care homes. Ministers systematically neglected staff and the people in their care, exposing them to the virus with grim consequences.
Matt Hancock’s recent evidence to the Covid Inquiry highlights this lack of political accountability. The former health and social care secretary's account of the darkest days of the pandemic was a masterclass in buck-passing, deflection and responsibility dodging. His claim that he had the job title, was accountable, but didn't have the levers to act rings hollow.
When the mood took Matt Hancock, he was perfectly capable of using his influence and authority. Discharging Covid-positive NHS patients into care homes, forcing staff to take the vaccination, banning relatives from visiting. These were all policies he pursued.
Matt Hancock's assertion he was powerless over a care sector left without

enough safety kit, sick pay or adequate testing defies belief. This is a poorly disguised attempt to shirk responsibility for a situation the then secretary of state could have prevented, had the sector been a priority. Powerlessness was Matt Hancock’s choice. He could have made proper sick pay mandatory for all care workers. He could have made sourcing protective kit and testing for all care workers his absolute priority.
Matt Hancock's disastrous failure to keep the care sector from harm is a lesson that radical change is needed. And needed now. That means a National Care Service providing access to quality support for all those who need it. A service on a par with the NHS, delivered by empowered local councils, but where political responsibility stops with the secretary of state. A high-quality care service backed by long-term funding, set at decent levels. A service focused on providing world-class care, not delivering huge profits for shareholders.
All staff in social care would have their wages set nationally, along with holidays, sick pay and other job benefits. Underlying all this would be a proper
workforce plan. But this will take time. Time the sector doesn't have. Care workers need an emergency pay boost now to help keep experienced staff in their posts and encourage others to have careers in care. The staffing crisis won't end otherwise.
Unison recently commissioned a report from the Fabian Society. The response to it has been heartening. It’s had a major impact on the debate by setting out a road map for reform.
Some learn by their mistakes. Others, like this government, look set to carry on repeating them. Social care can no longer be ignored or forgotten. Care staff and those they support deserve a much brighter future.
"There was no protective ring around care homes. Ministers systematically neglected staff and the people in their care, exposing them to the virus with grim consequences."
Gavin Edwards
"All staff in social care would have their wages set nationally, along with holidays, sick pay and other job benefits."
Skills for Care’s annual report highlights the key role of migrant workers in filling the shortfall in the social care workforce
Overseas recruitment played a key role in returning the adult social care workforce to growth in 2022-23 after numbers fell in the previous year, a report has found.
Skills for Care’s annual report ‘Size and structure of the adult social care sector and workforce in England’ found the workforce rose by 1% (20,000) between April 2022 and March 2023 after dropping for the first time on record by around 4% (60,000) in the previous year.
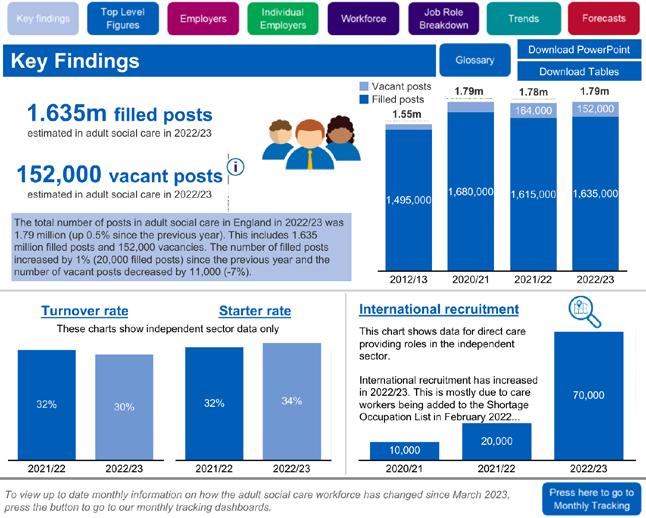
The vacancy rate decreased to 9.9%, or around 152,000, compared with 10.6% (around 164,000) the previous year.
Overseas recruitment played a key role in sustaining employment levels, with around 70,000 people recruited from abroad. Around 58,000 skilled worker
visas were received after adult social care was added to the Shortage Occupation List in February last year.
The level of international recruitment contributed to the rate of new starters increasing from 32% to 34% in the independent sector, with the turnover rate down from 32% to 30%.
Skills for Care said early evidence suggested the turnover rate for international recruits was around half that of people recruited from within the UK.
Oonagh Smyth, chief executive of Skills for Care, said: “It is encouraging that the number of filled posts has gone up and the vacancy rate has come down. Nevertheless, the data shared by employers with our adult social care
workforce data set still show significant pressure on them to find and keep people with the right values needed to work in care.
“It’s positive that we now have a workforce plan for the NHS, which
“Our data support the case for a social care workforce plan, including consideration of terms and conditions to support social care roles to be competitive in local labour markets"
recognises how health and social care are dependent on each other. Our data support the case for a social care workforce plan, including consideration of terms and conditions to support social care roles to be competitive in local labour markets.
“This will help to make sure that we have enough people with the right skills in the right places to support people who draw on care and support now, and for future generations.
“Any workforce plan needs to involve a range of partners as social care is a large and diverse sector. Skills for Care is ready to work with local and national government, employers, people who draw on care and support and our sector partners to help deliver a sustainable plan for the adult social care workforce.”

Unison general secretary Christina McAnea said migrant workers were “propping up the broken system”, adding: “Many overseas care workers have paid extortionate fees to come to the UK. When they get here, many can’t believe what they’ve signed up for.
“Sold an expensive dream, the sad reality for many is a nightmare of terrible treatment, scant training, excessive hours and low pay. The government must hold care providers to account and put a stop to this ill-treatment.
“Ministers must stop with the excuses, get a grip and start clearing up the mess they’ve let care become.”
Association of Directors of Adult Social Services’ joint chief executive, Cathie Williams said: “International
recruitment has been helping to fill some of the gaps, but it’s not a proper, long-term solution to the workforce challenge. We must as a matter of urgency develop a social care workforce plan that attracts people to make rewarding careers in social care. The NHS now has its workforce plan, but we can’t tackle the deep-rooted challenges in the care and health system as a whole without a social care plan too.”
Miriam Deakin, director of policy and strategy at NHS Providers, commented: “While the contribution of overseas workers is invaluable, the sector cannot rely on this in the long term. We desperately need better investment to recruit and retain UK staff to put the sector on a sustainable footing.
“The NHS long-term workforce plan promises to deliver more care at home. A social care workforce plan could ensure we have enough staff in place – with better pay and terms and conditions – to meet growing demand.”
Nadra Ahmed, executive co-chairman of National Care Association and chair of Care Provider Alliance, said: “International recruitment is a shortterm solution to a more long-term and sustainable issue. We call on government to look at our sector as one which requires real investment to ensure that we can deliver the best quality of care to those who need it when they need it.”
Professor Vic Rayner, chief executive of the National Care Forum, said:
“The report shows that the workforce situation in social care remains critical. The small reduction in vacancies is a direct result of the fantastic contribution that our international colleagues have made to support the delivery of social care up and down the country. Over 70,000 workers have joined the English care workforce from other countries, and their presence is a contribution to be celebrated, whilst at the same time recognising it masks a further shrinking of the domestic workforce. The gaping strategic hole created by the absence of a funded workforce plan for social care could not be any clearer, and the government must take action now.”
A Department of Health and Social Care spokesperson said: “With the number of people working in social care increasing and vacancies falling, things are heading in the right direction, but there’s still more to be done.
“The workforce are at the centre of the ‘Next steps to put people at the heart of care’ plan which is backed by £700 million. This includes £250 million for staff to develop their skills through relevant training and progress within their careers with the introduction of the Care Workforce Pathway.
“We are also making available £15 million for 2023/24 to help local areas establish support arrangements for ethical international recruitment in adult social care.”
“The NHS long-term workforce plan promises to deliver more care at home. A social care workforce plan could ensure we have enough staff in place –with better pay and terms and conditions – to meet growing demand.”
and retail sectors, having started her career as a pharmacist and most recently working at Boots in national operational roles, including on Covid-19 test and trace work.
and a half years as quality director and area director with HC-One. He has also been quality consultant and regional support manager for Bupa Care Homes and operations manager with Voyage, as well as spending time as a registered manager for both organisations.


Yorkshire-based heritage furniture brand and luxury care home supplier, Shackletons, appointed Donna Bellingham as chief executive. Bellingham joined following 18 years as chief executive of Parker Knoll, Duresta and Collins & Hayes, all premium furniture brands within the Sofa Brands International stable. Bellingham previously worked in senior executive roles at Marks & Spencer.

Care provider Cornerstone Healthcare Group appointed Gaynor Rhead as commissioning home director and she will spearhead the opening of two homes: Cale View in Wincanton, Somerset and The Burren in Bristol. Rhead has experience of healthcare management.

Orchard Care Homes appointed Eleanor Mercer as group head of marketing and communications. Mercer has 15 years’ multichannel experience having previously led multidisciplinary marketing departments for brands in the retail, fast moving consumer goods and charity sectors.

Home care provider Bluebird Care appointed Jonathan Gardner as chief operating officer and managing director. Gardner has more than 25 years’ experience in healthcare services. He spent more than 25 years as a practising pharmacist after qualifying in 1996, before going on to become managing director of Boots Hearingcare and chief executive of Boots Opticians, with franchise structures and hundreds of practices across the UK.
Camelot Care appointed Sonny Valmiki as deputy manager at Avalon Nursing Home in Bridgwater, Somerset. Valmiki started his career in 1994 in adult general nursing, spending 23 years with the NHS then moving to the care sector. He previously worked as the clinical lead for Harbour Healthcare (previously Majesticare) in Chard.

The Housing and Ageing Alliance appointed Mario Ambrosi, director of communications and marketing at Anchor, as its new chair, replacing Housing Learning & Improvement Network’s chief executive Jeremy Porteus. Sarah Davis, senior policy and practice officer at The Chartered Institute of Housing, was appointed vice-chair.
Liaise, a provider of specialist care services for adults with learning disabilities, mental health and other complex needs, has appointed Emma Sperling as chief operating officer. Sperling has 25 years’ experience in the healthcare

Camelot Care also appointed James Marchant as the group’s new operations manager, overseeing quality and service delivery at four homes in Somerset and Devon. Marchant has worked in the care sector for 32 years and joins from Care South, where he was regional operations manager. Before that he worked for six
Social care and education provider CareTech appointed Steve Bennett as its group human resources director. Bennett has experience of leadership and talent development at Care UK and the Lifeways Group.


The biggest conference for investors and operators in health and social care




The Healthcare Summit will include sessions on social care, where our insightful speakers will cover topics such as CQC assessment, creating businesses, ageing, fee data, new builds, specialist care and investment.
Connect with colleagues and make new contacts in our networking zone, where exhibitors will be showcasing their brands and products.

Tickets are available now –and are free for healthcare providers.*
The event will end with our special guest Alastair Campbell in discussion with an industry expert.

Amanda Narkiewicz, healthcare regulatory partner at Mills & Reeve, explains how to understand the new evidence categories under CQC’s Single Assessment Framework

Under the Care Quality Commission’s new Single Assessment Framework (SAF), care providers’ existing ratings will no longer be used as the main basis for their next inspection. Now evidence collected or given to the CQC can prompt an assessment at any time, marking an end to point-in-time ratings based on periodic inspections.
The CQC will use evidence gathered from both on-site and offsite sources to score services across 34 quality statements based around the statutory fundamental standards and underpinned by between one and six new evidence categories. Together, the quality statements and the evidence categories form the backbone of the new assessment framework. This shift in approach reflects the CQC’s focus on becoming more ‘dynamic’ and ‘data-led’.
The CQC has grouped the different types of evidence it will look at into six categories. Each category sets out the types of evidence the CQC will use to understand the:
• Quality of care being delivered and
• Performance against each quality statement.
The CQC hopes to bring consistency to assessments and to make its judgements more transparent and consistent for providers and other stakeholders.
The six evidence categories cover:
1. People’s experiences
2. Feedback from staff and leaders
3. Feedback from partners
4. Observation
5. Processes
6. Outcomes.
Evidence under the six categories will be collected using a variety of methods from both on-site and off-site sources and updated on a rolling basis over a two-year period or in response to concerns. Sources of evidence within the categories will be wide ranging covering whistleblowing reports, safeguarding
concerns, statutory notifications and feedback from partners in the wider health and care system.
Under the new framework, the number of evidence categories the CQC will consider and the sources of evidence it will collect will vary according to:
• The type or model of service
• The level of assessment (service provider, local authority or integrated care system)
• Whether the assessment is for an existing service or at registration. SAF dispenses with the separate registration process. However, it will be interesting to see what changes the introduction of the evidence categories make to the registration process, with many of the categories difficult to evidence pre-registration. The exception being the processes categories as evidencing policies is a requirement of registration.
Quality statements will be assessed using the evidence, which falls into one of the six categories although not every evidence category applies to every quality statement. The evidence categories will require a renewed focus on how services are manged and how to evidence compliance.
The CQC has said to make clear what it will look at in its assessments, it will set out the key evidence categories it will focus on when assessing a particular quality statement, as there will be different evidence categories
for different types of services. Care providers can expect to receive some examples of the types of evidence required to make it easier to understand what the CQC will look at.
The evidence categories provide care providers with an opportunity to continue to drive improvements in the quality and safety of services, and to demonstrate proactively quality beyond mere compliance – similarly, they provide potential opportunities for differentiation in the sector.
While the exact timeline for implementation remains uncertain beyond ‘later in 2023’, we know care providers are working hard to review their internal processes to ensure these are aligned with the new quality statements and in particular the specific evidence categories relevant to their types of services. Familiarising your compliance team with the evidence categorises will be key to being inspection-ready.
Get in touch with Amanda Narkiewicz if you’d like to find out about Mills & Reeve’s compliance support services and how we can support your care provider transition to the new assessment framework. Call 01223 222267.
"Now evidence collected or given to the CQC can prompt an assessment at any time, marking an end to point-in-time ratings based on periodic inspections."
L e a r n i n g d i s a b i l i t i e s c a r e s t a f f
H e a l t h c a r e a s s i s t a n t
E l d e r l y c a r e s t a f f
S e n i o r c a r e a s s i s t a n t
L i v e i n C a r e r s
D o m i c i l i a r y c a r e s t a f f
M e n t a l h e a l t h c a r e s t a f f
D e m e n t i a c a r e s t a f f
P a l l i a t i v e c a r e s t a f f
Benefits:
Financial Savings: Say goodbye to sky-high agenc embrace budget predictability.
Team Continuity: Establish a dedicated workforce understands your facility's operations and values
Enhanced Quality: Reduced turnover translates t more engaged staff, elevating patient care.

Operational Efficiency: Minimize onboarding and optimising daily operations.

Are you ready to regain control of your staffing costs
dedicated healthcare team? Contact Brits Global Ltd
Phone: +44 1296 487925
Email: info@britsglobal.c
Website: www.britsglobal
You can find us at Health care Sum www.healthcare-summit.co.uk at S
resources?
t future. At nly slashes care. started.
Following the success of the inaugural Care Managers Show this summer, exhibitor CHD Living explains why care home operators should get on board for Volume 2 at ExCeL London in November
Family-run care home operator
CHD Living owns 10 homes spanning residential, nursing, respite, and palliative care, as well as offering home care and rehab services. The operator was one of tens of exhibitors to sign up for the Care Managers Show at NEC Birmingham on 30 June and 1 July.
• Shaleeza Hasham (SH), head of hospitality and communications
• Becs Page (BP), quality assurance and compliance manager
• Helen Aitchison (HA), transformation manager
• Josh Barlow (JB), registered manager, Kings Lodge Care Centre
Why did you decide to exhibit at the Care Managers Show?

SH: We wanted to raise our profile, aid our recruitment, and promote our Adopt a Grandparent partner charity.
Tell us about your experience of the show
JB: It was busier than I thought it was going to be, with a lot more people coming to the stand and having a decent conversation.
BP: We spoke to approximately 400 people across the two days and got the details of 85 new contacts at the show. We have also since received contact from 24 people that we know to be directly as a result of the show, quite a lot looking for jobs and new careers.

SH: There was a lot of scepticism before we went, but the outcomes were really positive and we would want to do it again.
BP: “We spoke to 400 people and we have since received contact from 24 people looking for jobs and new careers”
How did you promote your offering to the attendees from a recruitment perspective?
SH: Because we have so many types of care offerings, we have a good message that we support people in their professional development. For example, we can support a healthcare assistant to become a nurse or a manager, or give people the opportunity to work in specialist care.
BP: We had quite a few interesting conversations about different ways of attracting staff, motivating workforce, and retention.
Was the continuing professional development at the show worth coming for?
BP: The Arden University session on ‘Creating a safety culture’ and the Care Quality Commission session from BKR Care Consultancy were particularly good.
Josh, you were one of the managers interviewed by Davina McCall during the show. How was that?
JB: It felt like a real conversation about being a registered care home manager,

rather than an interview, which took the pressure off. I certainly really enjoyed it and thought she did a great job. It was something that I was glad I said yes to.
You obviously met a lot of registered and aspiring managers; did you meet anyone else interesting?
BP: A lot of new providers came and spoke to us – case managers who were interested in our rehab services and others who were more interested in the nursing and residential side.

HA: We had some people wanting to talk to us almost from a consultancy perspective. They wanted some support for them to offer the same services in their area.
SH: There were also quite a few suppliers who took the opportunity to come and introduce themselves – and we are quite well versed on the supplier side of things, but there were some suppliers I
hadn’t come across, so I think that’s really useful for operators.
JB: I was approached by somebody from Skills for Care after the panel, who said there was a drive around young men who work in care, and they asked if I would be tentatively happy to jump on board with that.
What advice do you have for the care providers exhibiting at the November Managers Show?
SH: Don’t think ‘this is for recruitment, therefore someone from HR needs to go’. You need to look at your people and see who are the real ambassadors for your company – it should be focused on the people and their talent and skills.
JB: It was good to have diversity in the team, because sometimes I was asked questions I didn’t know the answer to. You had other people you could rely on,
so you never lost a potential lead and interaction.
Find out how to join CHD Living in exhibiting at the next instalment of the Care Managers Show.


• 400 conversations
• 85 new contacts
• Join CHD Living at the Care Managers Show London and take your company to the next level.
• Contact Steven Godleman on 07947 947 144 –steven.godleman.nexusgroup.co.uk
– to create a bespoke package.
In our ongoing series, Aaron White, head of business services and sustainability at Oakland Care, outlines small but effective changes care homes can implement to promote sustainability, here focusing on reducing waste

Reducing waste is not only a sensible way to benefit the environment but it can also save you money. Recycling is a great step, but ultimately you are still paying for the items to be collected, so anything you can keep and reuse in a different way will reduce the amount of waste being generated.

Engage with your waste management company to find out where your waste is going. Our company gives us access to a portal which shows us the volume and weight of waste that has been collected from each site and its destination. Map out your waste streams and look at each one to find out whether there’s a better option. General waste is one of the most expensive forms of collection, so making changes could even save you some money.
Composting, for example, is a way to reuse kitchen waste and cardboard. At Oakland Care, we have also carried out upcycling activities with residents, where we have used old pallets to make planters or old plastic bottles to make plant feeders. One of our homes has a scheme which is similar to a Bring and Buy, except there’s no buying involved. Staff bring in items they no longer need, such as clothes, toys and toiletries, and other team members can take what they need. It’s a simple initiative and great for staff wellbeing in these times of high living costs.
At Oakland Care we have reduced the volume of our clinical waste by 50% by investing in a vacuum pack system. A
machine reduces waste to small blocks rather than large bags. This also reduces odour, which is beneficial, especially if your bin store is close to a residential area.
As we are charged per bin, by halving the volume of waste, we have halved the cost of collection. Reducing the number of trucks coming to collect waste also reduces their emissions, which further benefits the environment. An investment of this sort is not necessarily a simple, quick fix, but it shows how far you can go if you want to, and within a year we’ve found it has paid for itself.
When it comes to recycling, at an absolute minimum you should be splitting your standard recycling into cardboard, recyclable plastics, glass and food waste. You need to have separate or split recycling bins at each station inside the care home as well as outside.
Waste oil should be collected by a reputable waste oil collector as it can be recycled and used for fuel. There are sustainable ways of getting rid of batteries, printer cartridges and toners –we have a community battery recycling box in place at each home, which is a completely free service.
Your waste electrical and electronic equipment must be disposed of through a reputable route, it can’t just go into a bin
or skip. Our IT company, for example, is a registered disposer of that kind of waste and even repurposes any parts first.
There are also lots of schemes out there for donating old computer equipment to community projects, or schools in other countries where children need laptops. We donate items like newspapers and old towels and blankets to animal shelters. It’s a great way of repurposing items and avoiding putting them in the general waste bin.
The waste in the general bin should be the minority, not the majority.
“When it comes to recycling, at an absolute minimum you should be splitting your standard recycling into cardboard, recyclable plastics, glass and food waste."
Jonathan Freeman, group sustainability director at CareTech, looks at how consumer demand is increasingly driving the green agenda in care homes

July saw leading climate change experts setting out in the starkest terms their shared concern that action to date to limit global temperature rises to 1.5˚C is falling woefully short of what’s required.
This year has been witness to some of the most serious effects yet of human-induced climate change, from forest fires sweeping across North America, a record-breaking cyclone in southeastern Africa, devastating monsoon flooding in India, to powerful ice storms in the southern US.
Unless decisive, significant action is taken, this is only going to get worse –much worse. Professor Robert Watson of the Tyndall Centre for Climate Change recently stated: “If we don’t [act], we’re going to see more heatwaves, more adverse effects on health, we’re going to see agriculture food production threatened, we’re going to see problems with water quantity and water quality. We’ll see more floods, more sea level rises displacing people on coastal areas, lots of adverse health effects.”
But we all know this, right? And we all want our political leaders to sort it out for us – that’s their job, right?
Meanwhile, back in social care, we have our own immediate concerns to deal with: chronic underfunding, escalating costs, recruitment and retention crises, and ever-demanding regulation. Tackling climate change is just adding new burdens and costs to the bottom line; indeed, The Telegraph recently reported that care operators are closing down services purely down to the costs of ensuring their properties meet carbon reduction requirements being imposed on them. So, thanks for all the doom-and-gloom, Jonathan, but we just need to focus on keeping our business afloat!
A recurrent theme of my articles on sustainability, however, is that as powerful as the moral case for social care providers to tackle their own carbon impacts might be, sustainability has also to prove that there’s an economic business case for action. This is especially true in our social care sector with ever-reducing margins
and ever-increasing complexity. The business case for sustainability often focuses on reducing operating costs. An important aspect that is too often overlooked, however, is the demands of consumers who increasingly expect businesses to play their part in tackling climate change as much as governments. And consumers increasingly factor in an organisation’s values and their commitment to sustainability at the heart of their buying decisions.
Research is increasingly clear on the importance of consumers’ expectations of business in respect of environmental sustainability:
• Recent research by The Economist highlighted that the demand for sustainable products in the UK has increased eightfold over the past five years
• Market researcher Garner reported in 2021 that 73% of UK consumers want to behave more sustainably in the year ahead (and beyond)
• An independent study commissioned by SmartestEnergy revealed that four out of five people describe themselves as likely to choose a brand with a positive approach to environmental sustainability
• Research by Vypr for its 2023 ‘Food for thought’ report revealed 58% of consumers actively or sometimes choose sustainable products when they can.
I don’t often hear social care providers talk about those for whom their organisations care as consumers. But they are. Whether individuals are private funders or their care services or their fees are being met by the state, they are consuming a service. They are able to make a choice about what sort of service they want, how they want to receive that service, how much they are willing to pay for that service, and, in the case of residential care, where they want to receive that service.
The Vypr study also highlighted how individuals are changing their daily routines to become more sustainable. This includes recycling more (58%),
choosing products with less packaging (36%), choosing local produce (27%) and reducing the amount of meat consumed (26%).
The Vypr research also showed two other important aspects to consumer demand relevant to social care:
• 45% of consumers are unaware of practices which consumer brands have adopted to encourage environmental sustainability
• 66% of consumers would be happy to pay more for sustainable products. That is why the recent launch of Autumna’s Go Green initiative is so important and responds so well to the increasing sustainability demands of social care’s consumers. As Autumna states: “Go Green will give care providers the ability to showcase all of their sustainability and green projects to increasingly environmentally-conscious care seekers.”
For me, the argument is very clear. Consumers increasingly demand that the products and services they purchase must be increasingly sustainable, that they want to select organisations that are ethically-driven, and that the services they purchase must support their own increasingly sustainable daily routines. There is absolutely no reason why this should be any different for people choosing their social care providers. To remain competitive, therefore, social care providers must not only adopt environmentally sustainable practices, but ensure that they communicate this to their potential customers.
E
HOSTED BY LORRAINE KELLY
Following the landmark launch event at the NEC Birmingham, join Caring Times at ExCeL London for the largest show in the UK dedicated to care managers. Lorraine Kelly will be our host, with thousands of managers, care groups and sector specialists in attendance.


30 CPD IN FOCUS
Skills for Care discusses the care workforce pathway for adult social care
31 FUNDRAISING
The number of workers The Care Workers’ Charity has supported moves into five figures
32 CT ON THE ROAD
Charlotte Goddard takes a trip to the south coast to talk to Barchester head of interior design Holly Rance about how she brings her visions to life
34 FIVE OF THE BEST
We pick our Top Five foodservice providers
37 NORRMS' BLOG
Norrms McNamara chronicles the day to day experience of living with dementia
38 CHEF OF THE MONTH
John Pomfrett head chef at Barchester’s Iddenshall Hall and Beeston View
39 10 QUESTIONS WITH Raina Jordan, general manager at Signature at Ascot
32 CT ON THE ROAD
Charlotte Goddard takes a trip to the south coast to talk to Barchester head of interior design Holly Rance about how she brings her visions to life

40 CARE FOR TOMORROW
Majesticare pioneers Alexa roll-out in care homes and the NHS Transformation Directorate discusses delivering change
42 BEST PRACTICE
ACI Care director Ravi Sodha says a strong workforce could be key to less expenditure in care homes
43 CREATIVE CARING
Carers demonstrate their creativity through fun and engaging activities
44 CARE MANAGERS SHOW
We look back at July's smash hit event
Skills for Care’s chief executive Oonagh Smyth discusses the care workforce pathway for adult social care and why this is an important step in supporting learning and development for people working in the sector

We’re pleased to be supporting the Department of Health and Social Care (DHSC) in its work developing a new care workforce pathway, supporting people working in adult social care to progress and thrive in their roles.
The care workforce pathway will better articulate what a career in social care means, supporting the development of a consistent understanding of what it is to be a professional working in adult social care.
It will set out the knowledge and skills needed to work in adult social care and establish career stages for progression. This is a vital step in supporting the social care sector to find and keep skilled and passionate people to provide highquality care and support, now and in the future.
Career structures and pathways are key to attracting and keeping people by providing clear opportunities to develop. For care workers, a care workforce pathway will help gain greater recognition for their skills, as well as supporting people to progress based on their individual motivations and skills set.
For employers, it will help with recruiting and retaining the right people by supporting employees in their career development. And for people who draw on care and support, it will ensure high-

quality, compassionate care continues to be provided.
In April we issued a call for evidence asking people who work across social care to share their insights into what the pathway should look like. Thank you to the 500-plus people who took the time to contribute to the call for evidence and provide their valuable insights to help ensure the pathway meets the needs of people working across social care.
Thanks also to everyone who’s been involved in our engagement events, which has included registered managers, nominated individuals, chief executives, directors of adult social services, learning providers, HR leads, large national employers and members of the Care Workers Forum.
The discussions and responses we’ve had about the pathway so far have been enthusiastic, with it being widely viewed as a positive step in the right direction. People have told us they can see how the pathway could help recognise and support the professionalism of people working in social care, influence a shift in the wider perception of the sector, and help to retain and develop staff.
An expert consultation group with stakeholders from across health and social care has been formed, which will provide useful insights and expertise into the content of the pathway as it progresses.
Think Local Act Personal is also working with people who draw on care and support to gather more insights about the values that care workers need to have to deliver high-quality care, as values and behaviours will underpin the pathway.
It’s intended that a first iteration –focused on care and support worker roles – will be available in the autumn, and we look forward to seeing this take shape.
Find out more: skillsforcare.org.uk/ Developing-your-workforce/Careworkforce-pathway-for-adult-social-care. aspx
"For care workers, a care workforce pathway will help gain greater recognition for their skills, as well as supporting people to progress based on their individual motivations and skills set."Oonagh Smyth
Chief executive Karolina Gerlich celebrates as the number of workers The Care Workers’ Charity has supported moves into five figures

The Care Workers’ Charity has reached an incredible milestone by supporting 10,000 care workers across our many grant streams.

We delivered specific Covid-19 support in 2020 and 2021 focused on care workers who were not getting full pay while absent due to Covid or having to shield from it. We have our ongoing crisis grants that support care workers in financial crisis around housing, bills, debt, white goods, transportation, childcare and funerals.
Additionally, our mental health support work enables care workers to selfrefer for therapy as well as attend training courses for mental health first aiders, both delivered via a partner. Among our 10,000 grants, we have worked with some local authorities to deliver support to their local workforce and with care providers to support their teams.
Our 10,000 grants have been delivered by a small team working tirelessly to help people that support the lives of others. We understand and appreciate the work that care workers do, the relationships they have with the people they support and the contribution they make to society and the economy. That’s what drives us to continue our work and keep fundraising and giving grants so care workers may continue with their ever-important work.
We know our grants help care workers stay in their jobs and we see supporting retention in the sector as an essential part of our work.
To continue with our work and to reach our next milestone of 20,000 grants we need your kindness and support. First
of all, huge thanks to all of you who have supported us over time. Without you we couldn’t have supported so many care workers. Second, with demand so high for our services, we need more people to support us, by becoming members and sponsors, participating in our fundraising events, organising their own and telling others to do the same. As a charity with no endowment, we rely on your understanding and goodwill to enable us
to help care workers and continue giving life-changing grants.
We are immensely proud of the impact these grants have had on the lives of care workers, providing them with a lifeline during challenging times. However, we must remember that while the ability to help so many people is something to celebrate, the fact they need help is not. We have much work ahead of us to improve the working conditions of care workers. We will continue to call on the government to reform social care and vastly improve funding to the sector, and finally recognise care workers as skilled professionals that hugely contribute to our society.
To find out how you can support The Care Workers’ Charity, visit: thecareworkerscharity.org.uk
“Everyone is feeling the financial pinch at the moment, and I would encourage anyone who works as a carer… to take a closer look to see if the grant can help them too... getting my car fixed has helped me get back to the job I love” – Elena, Oxfordshire care worker
"If I go and work in a shop somewhere, you have steady hours. Really that was the only option, and I was very close to doing that... It’s really reassuring that carers have got somewhere looking out for them." – A recent grant applicantKarolina Gerlich
Charlotte Goddard took a trip to the south coast to talk to Barchester head of interior design Holly Rance about how she brings her visions to life

When Holly Rance shows up at a Barchester new-build it’s just a shell, but by the time she leaves, it’s become a home. As head of interior design at Barchester, Rance oversees everything from the colour of the walls and carpets to the positioning of the smallest ornament in a corner of a lounge.
When Caring Times visited Bere Grove Care Home in Horndean, near Portsmouth, Rance had been on site for around a week, getting the home ready for opening. This was the end of a twoand-a-half year process, during which she worked closely with the home’s architects on details including the positioning of sockets and radiators.
At any one time Rance might be working on 10 new-builds, all at a different stage of design, as well as overseeing the refurbishment of around eight existing homes. Before she arrives at a new-build Rance knows exactly how every space should look, enabling her to whizz through the home at double-quick
time. “I like to have different heights, different textures, different finishes, so if somebody is sitting for a while just chilling, they have interesting things to look at,” she explains.
Rance has a story about every ornament, picture or piece of furniture, and can tell you how much it cost and where it came from. Animal designs are always a hit, she says. “You may notice a few sausage dogs around because I have one, that is a little nod to my personal life,” she laughs. “I always buy the animals because they end up getting named by residents.” Animal prints are also a favourite, with a textured wallpaper reminiscent of snakeskin decorating one of Bere Grove’s dining rooms.
Rance has been working for the interior design team for 13 years, heading it up for the past six years. She has transformed the look of the organisation’s 200-plus homes with her bold approach, overseeing the adoption of three core colour schemes, known as Windsor (red), Hampton (turquoise) and Buckingham (purple).
Home managers can refer to an evolving manual detailing the accessories, furniture and colours that go with each scheme, if they want to redecorate a lounge area, for example. “I choose bold colours, but they're warm, easy-to-live-with colours,” she explains. “People will be spending a lot of time in the home, and I think they have got to feel really at ease and comfortable.”
The three schemes suit Barchester’s diverse portfolio. “We have some massive buildings with really high ceilings, and the red scheme really suits those kinds of homes,” explains Rance. “The turquoise scheme is more urban, and the purple scheme bridges the gap between
"When I went to hospital as a child, it was so clinical, and I found solace in small things like a rainbow drawn on the wall”
The 60-bed Bere Grove Care Home follows the Buckingham scheme – the key colour is woven through the home to give unity, but a range of accent colours including greys, pinks, golds and blacks ensure it’s not overwhelmingly purple.
Rance combines experience in luxury interior design, including time spent within the superyacht interior industry and designing high-end residential interiors, with a deep passion for the care sector. “Care is in my core,” she says. She is able to draw on her own experiences, as she has a disability herself. “When I went to hospital as a child, it was so clinical, and I found solace in small things like a rainbow drawn on the wall,” she remembers. “I never make the homes feel clinical. If you are feeling unwell, you want your surroundings to be like a big hug.”
Bere Grove has two 15-bed dementia communities, each with their own dining room, lounge and outdoor space. Rance works closely with Barchester’s in-house dementia specialist and spends a lot of time observing how people with dementia use the spaces. Lavatories are set against darker tile colours to make them stand out, for example. “We stick with the same tone of flooring throughout a corridor, because when residents reach another colour, sometimes they can think they are going to fall off a cliff,” she says.
The tour takes in a spa bathroom with a twinkly ceiling and a photographic mural which gives the impression of looking out of a window. Descending to the ground floor, which is a residential community,

we move into a large orangery, with an impressive light fitting.
The annual ‘Tell Barchester’ survey, which is completed by residents, family and staff, gives Rance an insight into design-related likes and dislikes, which she feeds into future homes. “For inspiration, I look at the best of the best, whether that is a hotel or a superyacht, and then I work backwards and find how I can do that within my budget,” she says. Choice and variety are key, with a range of different chairs in lounge areas, for example, so people can choose to have a nap, or sit and chat, or read a book. Bringing the outside indoors was a key inspiration at Bere Grove, with plants, nature-inspired artwork and green fabrics.
Everything that Rance buys for the homes is majority manufactured in the UK. Many of the furnishings are bespoke, including footstools which open up to provide storage space and can double as “softer coffee tables”. “The artworks are framed in Edinburgh, the curtains are made in Darlington, all of this oak furniture comes from Devon,” she says, indicating a solid-looking wooden side table. When she’s not travelling the length and breadth of the UK, Rance can be found in a warehouse in Salisbury, full of fixtures and fittings waiting for a good home. “Having everything stored in one place makes fitting out a home so efficient,” she says. “We can get things at a good price because we can bulk buy – I might buy 100 lovely woollen throws at time.”
Every fabric used in the home is flame retardant, waterproof and antibacterial. “Nothing will get through that fabric at all. It’s just completely bulletproof,” says Rance. “This new paint finish we are using is amazing, the home just needs to wipe it so we are not constantly repainting.”
As well as designing new builds from scratch, Rance is overseeing a rolling programme of refurbishment across Barchester’s existing portfolio. This is often trickier, as she is not presented with a blank canvas but a home with people already living in it, who may have concerns about change. To tackle this, Rance tries to engage residents and families and listen to their concerns and preferences. “When I was in West Abbey, which is in Yeovil, we had pictures of the local area from the 1950s and one guy said ‘I used to live in that street.’ So I put that picture outside his bedroom and every time he was so thrilled to see it,” she recalls.
The team tackles one room at a time, to minimise disruption, and only revamps unoccupied bedrooms. Rance is often moved to tears to see the difference that her revamps make to residents’ quality of life. The impact can be huge, particularly for residents with dementia who are often better able to navigate spaces. In one case a resident who never left their room suddenly started coming to the lounge after a refurbishment.
“I love my job so much because it makes a difference to people,” Rance concludes.
In the first of a new regular feature showcasing the UK’s best care home suppliers we pick our Top Five foodservice providers
apetito’s care home meals service improves labour efficiencies, reduces costs, makes catering for dietary requirements easy and ensures residents enjoy high-quality, nutritious meals.
apetito allows care homes to have transparency of costs, while reducing staffing requirements and meal preparation time without compromising on quality. Its service can more than halve the time spent in the kitchen compared to cooking from scratch.

Staff cook the meals from frozen, meaning that with some initial training, the complexities of managing kitchen staff and time spent in the kitchen can be reduced, allowing staff resources to be devoted back to front line care.
As a provider of care home meals, apetito knows how to help care homes deliver a dining experience that satisfies and nourishes residents, whatever

Foodservice provider Bidfood has a passion for great food and going the extra mile for customers.

With a range of more than 500 carespecific recipes, its team is on hand to provide support in areas such as catering for differing needs and keeping operators up to date with the latest trends.

Bidfood says consistently creating nutritious and delicious meals tailored to residents’ individual requirements isn’t always easy, especially when juggling time, budgets, stock levels and staff skill. So, to support care operators, it has launched Caterers Campus, an online learning platform for Bidfood customers that supports their teams, allowing more time to be focused on residents.
The platform gives teams the opportunity to learn key skills, enabling them to cater to residents better.
their dietary requirements or culinary preference.
With a range of IDDSI compliant texture-modified food and Finger Food Bites range, apetito’s meals enable care homes to bring back dignity and independence to dining for residents living with dysphagia and dementia. apetito knows that one size never fits all when it comes to catering provision within a care home, and tailors its services to individual needs.
“Since moving to apetito, I’m never worried about mealtimes. Now if I get a call from my kitchen team saying they’re unavailable, I don’t feel stressed – I know all the residents, no matter their requirements are always going to have a meal that’s safe, nutritious and that they’ll enjoy.” – Fatma
Makalo, Bridgeside Lodge Care HomeModules include:
• Dysphagia and IDDSI
• Fortification
• Dementia
• Hydration
• Menu planning
• Costing
• Diabetes
• How to understand and calculate profit
“Over the past two years we’ve been accessing the Catering Campus for our chefs and kitchen assistants. This has made a huge difference to the team as many come into care without any previous understanding of the adaptations they need to make for our residents. This is a unique training platform covering the basics and we’ve included it on all our chefs’ and kitchen assistants’ learning pathways and inductions. This is the first place I have found tailored training for them in health and social care. I would highly recommend.” – Samantha Varnals, learning and development manager, Gold Care Homes.
Creed understands catering in the care sector can be challenging work at the best of times. Not only do chefs have to cater for residents’ varying tastes while ensuring meals meet required nutritional standards, they are also required to offer enough variety throughout the day to suit individual needs, while also keeping residents interested in their food to prevent malnutrition.
Creed is more than a foodservice provider and its customers rely on the company to help support them and offer expert advice. Its range of tools, such as Saffron Nutritional Software, menu ideas

EF-group works closely with more than 3,000 care homes, saving them time and money while offering value, efficiency and safety to their day-to-day operations. It stocks everything customers need, from food, drink and cleaning products to medical and sanitary supplies through its supply chain network and manages all orders to invoice process via its simple-touse system, Freshmarkets.
The company understands a top priority for care homes is creating nutritious, fortified food that provide residents with healthy, individual choices, satisfying recommended daily allowance and complying with the Care Quality Commission’s requirements. Its customers can manage budgets and food margins, reduce waste and produce nutritionally balanced meals using the advanced menu planning features in its
The Full Range is a food purchasing business which aims to help independent care and nursing home operators save on food costs while delivering highquality standards for their residents. The company combines market knowledge, manufacturer supported pricing and client spend of more than £42 million per annum to give its customers big company buying power. It adds that as it is 100% supplier funded, its services don’t cost anything.
The Full Range takes a proactive approach to delivering results and is committed to quality and forming strong
and recipes from its Care Asset Hub, and market updates from its Insights specialist, are all intended to help its customers streamline and improve their operations.
Creed services a range of sectors across the foodservice industry with its care customers a priority. It points to its 99.3% service levels, with stock availability and order fulfilment at the forefront.
It employs a dedicated team of care sector specialists, working together to support independent and group care homes to deliver hospitality to their residents, while working to a set budget per head.

HC-One, one of the biggest providers of healthcare in the UK, approached EFgroup as part of its digital transformation programme. Using Freshmarkets and CaterCloud, EF-group changed HCOne’s provision and introduced a fully integrated stock system, budget module and 250 cost-effective recipes with flavour and nutrition.
EF-group can help with controlling cost per resident per day, managing menus and providing insights into allergen and nutritional information. It also helps customers stay on top of food safety compliance and budget handling, including multi-category and multi-supplier ordering. Its systems can take care of operational issues. It also points to its 160 years of procurement and menu management experience in the care and senior living sector.
"Our experience with Saffron and the Creed team has been brilliant. Saffron has made our lives so much easier; we have absolute confidence in the nutritional and allergen information it provides, and Creed are helpful and respond very quickly." –
Lucy Coombs, nutritional advisor, Lilian Faithful Carerelationships with its local and national suppliers. The care sector has been a growing market for the company and it is focused on residents in care and nursing homes being able to enjoy nutritious and delicious meals. It takes the time to understand customers’ businesses and the challenges they face, working with all stakeholders, from owners to chefs, to reach solutions that leave everyone happy.
Customer feedback
“I would recommend EF-group to other clients as nothing is ever too much to ask; the flexibility and adaptability from the team is amazing. The support we have received has been second to none and I wouldn’t look at using anybody else.” – Chris Bonner, executive chef and nutrition and hydration lead at HC-One
Customer feedback
“The Full Range offers an invaluable service for procurement, with no contracts and no hidden costs. They allowed us to analyse our purchases, look at new potential suppliers, and dramatically lowered our costs. The team offers an excellent service including lots of hard work behind the scenes. Resolving issues and offering solutions free up my time to enable me to focus on other areas of the business.” – Chris White, Sunbury Nursing Homes


Vincent has been The White House’s (TWH) facilities manager for more than 30 years. He has overseen TWH’s expansion from the conversion of a detached house in the 1980s into the 30-bed, three-storey, Outstanding-rated, care home it is today.
Although he has been diagnosed with cancer and undergone treatment in recent years, Vincent has still shown up to work between treatments ready to support the home and his colleagues. He regularly escorts the activities team on trips so he can help residents on and off the home’s van. Vincent is much-loved by everyone at the home and makes time to talk to residents and their families ensuring they are happy with the facilities provided for their residents.
He is an extremely talented carpenter and somehow was able to create a dedicated visiting pod during Covid to keep residents and families safe and has even made a bar for the residents’ lounge. Vincent has gone above and beyond in supporting the home and residents over the years.
One of our residents Mary was in the last stages of her life and very latterly suddenly requested her last rites be performed by a vicar from a specific church type. Having called the relevant churches, no one was available and it transpired they were all in a meeting at a church in Tolworth. Hearing this and without even waiting, Vincent jumped onto his motorbike, rode to the church and dramatically interrupted the meeting with his request for a vicar to come and perform the last rites. One of the vicar's readily agreed and followed Vincent back to the home where Mary's last wishes were fulfilled.
Vincent also helped with the very noble cause of fulfilling another dying resident’s wishes. Her wish was to see her son from whom she had been

estranged for a while before she died. Vincent again without being asked got on his motorbike and rode all the way to Staines to see the son and request that he come with him. The son agreed and
they both came back on Vince's bike in time for the mum to see his son before she passed away.
We feel he is well worthy of this award. Thank you.
Ihave said many times that I hate this disease of dementia. Hate is a word that doesn’t figure that high in my vocabulary, apart from when it comes to this illness, but I can now say, hand on heart, I not only hate it but despise it.

It chips away at your self-worth, self-confidence, makes you question everything you have even known and learnt. As it chips away at you, you lose your life skills and how to do the simplest things that come so easy to others without a thought.
It’s the little things like forgetting how to tie your shoelaces – I now wear slipons only – or which way round you used to hold your knife and fork, the time, the day, the date, and so on. With some things it happens so quickly. That’s the frightening part of this disease. Sadly, some lose their life skills at a very rapid rate and some not so rapidly. I have had this disease for over 10 years now. Some call it the long goodbye and I can fully understand why. But it’s when you lose the skill to do something you absolutely love when it becomes absolutely devastating.
It’s no secret around town as they say, how much I love my fishing. It’s something I believe has helped me keep going even at the worst of times and I have been so lucky as the majority of carers that took me fishing were wonderful, but as the years have passed I noticed I was forgetting more and more,
and even though there were carers by my side, not all were fishermen/women. So when it comes to remembering how to put the line on the rod, the floats, and especially the hook, it just got harder and harder, and the last straw was when I forget how to tie the knots. Well, as any fisherman/woman will tell you, you can have the most expensive gear in the world, ‘all the gear, no idea’, but if you can’t tie a knot? Well, you aren’t going to catch any fish are you, and as much as you try and trust the
carer to do so, every time the line snaps or you lose a fish the feeling is just awful as anybody will tell you.
Fishing is something I have done for years; it has given me so much pleasure and I would recommend it to all to de-stress or just kick back and watch the world go by. I fished at the wonderful Town Parks in Paignton and I have made so many friends up there who have even invited me back just to sit and chat with them and watch them pull in the incredible 40 pound-plus catfish they have there. Who knows, one day I may take them up on it but it’s not the same as feeling the rod tip bending over and shouting “fish on!”
As daft at it sounds, I did shed a few tears when I got rid of my fishing gear, and believe me, there was lots of it, but I passed it all on to the wonderful Plymouth British Royal Legion forces veterans who have fallen on hard times. I have been told it’s being used on a weekly basis with great success.
So you see, sometimes you lose a few battles, but I am still convinced I will win the war. I have to be, or what would be the point?
Till next time…
like to live with dementiaNorrms McNamara
Tell us about your background and how you joined Barchester
My interest in food and cooking began with part-time jobs washing up in pubs and restaurants while at school. After leaving I studied hotel and catering management at college and moved into pub management, but my real passion has always been in the kitchen and cooking good honest tasty food, often covering shifts cooking for the restaurants and pubs I managed. So when I was made redundant, the obvious choice for me was to pursue my love for cooking while considering my career. I spent a year working as an agency chef, a time I thoroughly enjoyed, learning lots of different ideas in kitchens in many various businesses, schools, hospitals and homes all over Cheshire. This led me to Barchester Healthcare and Iddenshall Hall in particular. I was booked for a week – that was 15 years ago and counting.
What is special about working at Iddenshall?
Iddenshall Hall has become like a second home for me. I’ve made some very good friends among the residents and staff. There’s a very real community feel about the home. The old manor house itself is fascinating, with nooks and crannies and a very special character. I like to imagine how it was when a family lived here, with kitchens in the cellar and servants’ rooms in the attic, fresh meals from the produce grown in the extensive gardens and maybe cider made from apples out of the orchard.
How do you vary your menu to provide choice for residents?
I try to keep the theme of fresh locally produced and grown food as much as possible, changing our menu to reflect the seasons. Cheshire new potatoes with plenty of butter and a dash of homegrown mint are a seasonal treat. We still use apples from the orchard, but more often for a lovely crumble or apple cobbler rather than scrumpy now.
What does your typical weekly menu look like?
A typical week’s menu here at Iddenshall Hall and Beeston View will see lots of fresh home baking. Our moist fruity carrot cake and sticky toffee puddings with lashings of custard are particular favourites. Meals are mostly traditional, with freshly battered cod or haddock, hearty roast dinners with Yorkshire puddings and all the trimmings, and lighter choices such as home-baked quiches all being enjoyed. We do, however, have more adventurous palates covered, as well with warming moussaka, lamb tagines and home-baked focaccia breads all being tried recently.
What’s your most popular dish? One of our best loved puddings is our trifle. There’s always seconds and rarely any leftovers.
What’s your favourite dish? My own favourite must be our toad in the hole. I like to make individual ones so everyone gets a toad and plenty of hole, with lashings of gravy of course.
How do you meet residents’ nutritional and health needs?
As we are a care and nursing home, our resident’s nutritional needs are something I give a lot of consideration to. Some days people may feel a bit under the weather or not particularly feel like eating. I make sure there’s always something tempting available, be it a fresh fruit platter, a freshly baked cookie or maybe a healthy and nutritious smoothie with yoghurt and honey. I like to be present at mealtimes as much as I can, talking with our guests, getting to know them and their preferences. Making sure everyone is enjoying the food as much as I enjoy making it.
How do you cater for residents living with dementia?
Catering for people living with dementia is a large part of our role here at Beeston View and something I am passionate
about. Sometimes people will not remember they have eaten, or if they are hungry. Smells can be a very good prompt or reminder so we try to get as many aromas and flavours into the home as we can. Baking bread in the ovens and bringing in freshly grilled bacon for breakfast times are great appetite prompts. If a resident wants cornflakes and toast at three o’clock in the morning or two bowls of trifle for breakfast, yes, that’s great too, no problem. They’re happy and comforted and feel a little bit more at home.
How do you make the dining experience special for residents and their families? Mealtimes are not only about our delicious food, they are also a very important social occasion for our community, a time for people to get together, chat about their day, welcome visitors and maybe celebrate a special occasion. We welcome families and visitors regularly, catering for special birthdays and events such as anniversaries, either in our dining rooms or our beautiful conservatory or grounds, weather permitting. We love a good party and have recently hosted an afternoon tea party for one of our families and of course a coronation party for King Charles.
I’m proud of our home here at Iddenshall Hall and I enjoy welcoming old and new residents, visitors and staff. Last year I attended Barchester’s own chef training academy. This year I am passing on the knowledge and skills I have gained to other chefs within the company at our very own training kitchen here at Iddenshall Hall.
 Head chef John Pomfret tells us what’s on the menu at Barchester’s Iddenshall Hall and Beeston View care homes.
Head chef John Pomfret tells us what’s on the menu at Barchester’s Iddenshall Hall and Beeston View care homes.
In our regular feature showcasing our amazing care home managers, we talk to Raina Jordan, general manager at Signature at Ascot

“I am a people person and so working with residents and families from all walks of life and hearing about their lives and experiences, and how they can thrive in care, is amazing. ”
build great relationships with residents. Care is team-orientated, so ensuring you support colleagues is equally a crucial part of the job.
What do you do when life all gets a bit too much?
I have to remind myself that nothing lasts forever and that if I am having a bad day, the next day is likely to be better. I find an open water swim in the ladies’ pond at Hampstead Heath clears the mind and helps me reset.
Why did you join the social care sector?
Like so many people who have worked within our sector, my route into social care began from lived experience. Having seen at first hand an elderly aunt’s difficult move into residential care a few years ago, I wanted to make a positive difference to the emotional journey of residents and families. Knowing that I could support people in a helpful and empathetic way was a key driver behind me working in social care.
What do you enjoy most about your job?
I am a people person and so working with residents and families from all walks of life and hearing about their lives and experiences, and how they can thrive in care, is amazing. I enjoy the variety the role gives me. Each day is completely different and provides a healthy mix of short- and long-term work. For example, on a day-to-day basis I oversee a team of 90 who all have a part to play in caring
for our residents, while also having worked on a future plan to open a new floor at the home.
Who is your social care hero and why?
I love working with an amazing team, every single member is therefore a hero to me. Aside from the wider sector’s outstanding work on a daily basis, its collective effort throughout the pandemic was truly heroic.
What is the one thing you would change about social care?
For everybody to gain swift and timely access to the good-quality care they need; we are all aware of how long the social care waiting lists currently are.
What, in your opinion, makes a great care worker?
Someone who has a big heart, is respectful, and they need to be organised and dynamic. If someone has a passion for caring, then they can
What advice would you give your younger self? Look after your knees!
Which three famous people would you have to dinner and why?
Cleopatra, to find out more about ancient Egypt, Salvador Dali to understand more about how his mind worked and Ricky Gervais – I find him hilarious.
What three items would you bring with you on a desert island?
Scuba equipment, the complete works of the Bronte sisters and an endless supply of teabags.
What is your secret talent?
I used to be able to walk on my knees, unfortunately I didn’t give my younger self the right advice so that talent has now been lost. I have a good knack for remembering lyrics to songs, especially from the 1980s.
Lee
Majesticare’s Cavendish Park in Evesham became the first care home in Europe to adopt Alexa Smart Properties with Amazon and technology partner Ascom in November last year.
Majesticare's chief executive, Angela Boxall, says: “We have always been dedicated to being at the forefront of innovation in care through technology. As a forward thinking organisation we were really excited to see what Alexa could bring to the table. We wanted to make sure it was developing technology and providing data in the right way and for the right reasons to improve care outcome statistics rather than just ignore them.”
Over the past 10 months, the technology has been developed at Cavendish Park with the active input of residents who have been key to compiling an ever-evolving list of commands. The commands are inputted into the system so that they can be answered by Alexa or immediately circulated to members of the care or maintenance teams to attend to. They include: requesting food and beverages; ordering drinks for visitors; ordering breakfast; checking daily menus and activities; calling for assistance; needing something to be fixed; calling a family member, GP or dentist; or speaking to a member of the care home team. Residents can also have fun asking Alexa for the joke of the day or finding out the news or what the weather will be like.
“For our residents to be involved in something so innovative and forward thinking to potentially map out how care can be developed is wonderful,” Boxall says.
As well as enhancing care delivery for residents, Alexa has helped spur conversations and develop friendships in the home. Alongside making phone calls to family and friends more easily, the technology even allows residents to talk to each other in the comfort of their own rooms.

“It’s become a lovely social activity with residents sharing Alexa’s jokes of the day
at breakfast,” Boxall says. “It’s helped to stimulate new conversations with loved ones having a new topic to talk about every day in the home. We went from 3,000 Alexa commands to 9,000 in just four weeks.
“As well as helping us to understand how to continue to develop our care offering, Alexa is building new communities and friendships in the home. It’s created a common conversation piece between residents and even for those who aren’t Alexa’s biggest fans; it’s a great talking point.”
As well as benefiting residents, the technology also helps carers by saving time (see graphic below).
Activities co-ordinator Ellie Lucas says: “I enter our upcoming activities schedules and daily menus on Alexa at the start of each week so residents can easily find out what’s going on and have independence
“It’s brilliant. If I wake up in the middle of the night. I can ask it to play the radio for an hour. It’s lovely. It’s allowed me to call my family as I had difficulty using the telephone”
in planning their day. It’s lovely to hear music in the residents’ rooms. One of our ladies loves to put Classic FM on as soon as she wakes up. Some of our residents would listen to the radio on TV but now if they can’t reach the remote they can just ask Alexa. I love how Alexa has given some of our residents that feeling of empowerment, the ability to ask for what they want, when they want it and know that it’s on the way, especially if it’s time for a cup of tea. It’s helped us as a care team be able to respond to their needs faster and more efficiently.”
Having been the first to get on board with the technology, Boxall has no regrets, adding Majesticare’s Alexa journey was only just beginning.
“The possibilities for Alexa are endless and as an organisation we would not hesitate to be on board for future innovations,” she concludes.
Nick Goodall from the Digitising Social Care programme and Richard Harding at the Science and Technology Facilities Council Hartree Centre discuss how lessons from history can help us understand how to deliver change
What if we told you that in our opinion, data and digital approaches are not the key to solving the challenges of social care? You’d definitely be wondering why there’s so much being made about digital transformation of adult social care.
But before you breathe a sigh of relief at the thought you don’t have to get your head around all that technical stuff, let us explain what we mean.
We believe the key to solving the challenges of the social care sector lies in the hands of the right people using data to make informed decisions about what actions to take. Data gives you information. Wisdom is the ability to understand the data and translate that into actions and insights.
History teaches us valuable lessons. It was not that long ago that the idea of sterilising medical equipment and using antiseptic approaches to care for wounds was considered unusual. Yet thanks to the work of the surgeon Joseph Lister, it’s inconceivable that any care setting would not have infection prevention and control measures in place.
Concerned about the high rate of post-surgical infections and mortality he was seeing, Lister began trialling ways to prevent infection based on observations of his patients. He then used the data he gathered from those observations to test and develop his idea to sterilise surgical equipment and use antiseptic techniques to treat wounds. Lister’s trials led to dramatically improved post-surgical survival rates and the development of the antiseptic system approach to surgical care.
With the increasing number of care providers implementing digital social care records (digital care plans) to support the delivery of safer and more personalised care, there’s never been a better time to start applying the same principles used by Lister and use data to unlock ways to deliver better social care.
Data has the potential to be transformative. Whether it’s artificial intelligence tools to help people navigate the complex world of the care sector, smarter systems to plan home care routes or organise rotas, or even using data to support the next generation of pandemic preparedness responses.
For data to be useful and relevant to the way care is delivered, however, it needs enquiring minds from within the sector. The innovative ideas and new ways to support people drawing on care will come from people working in social care. It’s the people on the front line who know what problems need solving. And it’s data and what it can tell us which holds the key to workable solutions.
What are the questions you need data to help you answer? Maybe start with areas like falls prevention, medication
optimisation or tackling loneliness.
Using data to help us shape how care is delivered also opens new opportunities for career development within the sector. Roles which focus on digital, data and technology (DDaT) are more commonplace in health than social care, but digital transformation is helping to change that.
We don’t know where these ideas will lead, or what positive outcomes there will be for those drawing on social care, so while data is not the answer it’s certainly the stepping stone to finding an answer to the question, what does good care look like in the future?
If you really want to explore the art of the possible, you can read about the £94 million being directed to the National Quantum Computing Centre (nqcc. ac.uk). What challenges might it help us with? Could it help us optimise care?
Closer to home, how might we use AI to solve our care challenges with access to support from the Hartree National Centre for Digital Innovation, leveraging £210 million of investment? Maybe there’s a challenge that you face as part of your role that it could help with?
Have a look at artree.stfc.ac.uk/trainingskills for free, accessible courses on data and what you can do with it. Find out more about our work on digitising social care at: digitisingsocialcare.co.uk
Nick Goodall is senior programme manager at the Digitising Social Care programme and Richard Harding is business development manager at the Science and Technology Facilities Council Hartree Centre.
“History teaches us valuable lessons. It was not that long ago that the idea of sterilising medical equipment and using antiseptic approaches to care for wounds was considered unusual.”The platform for outstanding care management
ACI Care director Ravi Sodha says a strong workforce could be the key to less expenditure in care homes

Care homes in the UK, like many businesses, are grappling with rising costs, but an effective workforce can help significantly mitigate this challenge. While the importance of a dedicated and skilled workforce remains constant, their collaboration in helping to reduce expenditure is needed now more than ever. As a care home director who has experienced the strain first-hand, I firmly believe that competent staff can not only reduce costs but also enhance efficiency and deliver high-quality care.
One of the primary benefits of a strong team is the reduced reliance on agency workers. During busy periods, or when faced with staff shortages, care homes often turn to agency staff to fill the gaps. However, the fees charged by agencies can quickly accumulate and increase the strain on already tight budgets. Carterwood recently reported that the cost of agency staff increased by 228% from January 2021 to September 2022, placing further pressure on a sector heavily affected by the cost of living crisis. By creating a skilled and reliable workforce, care providers can minimise the need for agency recruits, resulting in significant cost savings over time.
Additionally, a proficient staff team can be entrusted with greater control and oversight. Well-trained employees who understand the broader goals and expectations of the care group are better equipped to make informed decisions

regarding resource allocation. This level of control ensures that unnecessary overspending is avoided and greater financial efficiency is achieved. There is often a misconception about how cutting costs can lead to a decline in quality of care, but it’s important to understand that cost-effective solutions can be implemented while still maintaining high standards.
Moreover, investing in technology within a care home holds the potential for substantial cost savings, while also allowing care workers to focus on delivering personable care. By implementing automation and digitalisation, administrative tasks and paperwork can be significantly reduced, leading to time savings and reduced errors. Remote monitoring and telehealth solutions enable virtual consultations and remote health monitoring, which therefore minimises hospital visits, transportation costs, and the need to take carers away from the home environment. A strong workforce can contribute to financial savings, but they must be adequately supported, freeing up their time to fulfil their essential responsibilities. This way, investing in technology not only optimises cost management but also empowers care workers to perform the tasks they were employed to do. Beyond cost considerations, a strong team is essential for delivering highquality care. Care homes exist to provide crucial support and assistance to vulnerable individuals, and the
quality of care they receive is of the utmost importance. Competent staff ensure that residents' needs are promptly and compassionately met. When the quality of care is prioritised, it opens the door for improvements in other areas, including cost-reduction initiatives. While the importance of a strong staffing team is not a new concept, its significance has become even more prominent in the face of rising costs. Care homes must find ways to reduce expenses without compromising the quality of care, making a skilled workforce the key to achieving this delicate balance. By minimising reliance on agency staff, exercising financial control, and maintaining the care environment, care providers can mitigate rising costs and redirect their efforts toward areas such as the development and support of their care team.
“Well-trained employees who understand the broader goals and expectations of the care group are better equipped to make informed decisions regarding resource allocation."Ravi Sodha
Carers have been demonstrating their creativity through fun and innovative events for their residents and visitors to mark Championing Social Care’s Care Home Open Week


Care Home laid on a summer fete. Staff members took on a ‘pie to the face’ challenge to raise money for the National Activity Providers Association and the Care Workers’ Charity. The event raised £1,400.

Dementia nursing home Wren Hall in Selston, Nottinghamshire celebrated Care Home Open Week with a carnival, including traditional games such as a coconut shy. Children from nextdoor nursery Little Wrens judged the carnival float competition and crowned two carnival queens. The home raised £671.80 which will go towards providing engaging activities.

Fun of the fair
Excelcare transformed its care suites with vintage carnival-themed décor and games to mark Care Home Open Week. Visitors and residents took part in activities and won some exciting prizes.

from Hester’s Way Primary School. Mitesh Dhanak, chair of the organising committee of Championing Social Care, founder of Precious Homes and owner of Wentworth Court, said: “We’re delighted with the enthusiasm we’ve seen from care homes to participate in this year’s Care Home Open Week.”

This year’s Thank You Day anthem ‘Thank you for being a friend’ was performed at HC-One’s care home in Chandlers Ford, Hampshire by the Singabout Choir, whose singers are aged between 45 and 85. TV’s Anneka Rice joined them to encourage residents and colleagues to sing along. Thank You Day, an annual event organised by the Together coalition, Care Home Open Week and Music for Dementia joined forces to create musical events across the UK.
Friends of the Elderly’s Redcot care home in Surrey marked Care Home Open Week by opening its own pub, the Redcot Arms. Joyce Douglas, who has lived at Redcot for two years, was the first resident to christen the pub, enjoying a glass of fruit punch served by The Mayor of Haslemere, Councillor Jerome Davidson.
Care UK homes across the country hosted their own festivals for residents, relatives and the local community for Care Home Open Week. Care UK’s Field Lodge in St Ives, Cambridgeshire, ran its own Notting Hill Carnival-themed festival. Residents at Ambleside in Stratford-upon-Avon, woke up to find the home’s garden had been transformed into a Glastonbury-inspired festival site, fit for the ultimate rock ‘n’ rollers. Meanwhile, Bishops Manor in Sutton Coldfield had a Caribbean beach themed festival for locals.
As part of Athena Care Homes’ Care Home Open Week celebrations, the team and residents at Goodwins Hall


Cheltenham’s Wentworth Court care home welcomed visitors from the local community, including Ben the labrador from Pets as Therapy, practitioners from the Everyman Theatre and children
CHD Living’s The Summers in West Molesey and White Gates, in LalehamUpon-Thames, Surrey hosted tea and cakes for visitors, while Abbey Chase in Chertsey, held a cheese and wine event for the local community. CHD Living’s rehabilitation services also hosted professional and education open days to showcase the breadth of support available for those with acquired brain injuries and complex nursing care needs.
More than 4,000 managers, employers and sector specialists gathered at NEC Birmingham for the inaugural Care Managers Show in July.

Hosted by TV star, philanthropist and lifestyle guru Davina McCall, the event proved a hit with managers who packed out presentations and workshops covering five core streams of content: Operational Excellence, Wellbeing, Home Care, Free CPD, and Technology.

McCall entertained visitors on the central entertainment stage in a Q&A focused on challenges facing women in the workplace and her bestseller on dealing with the menopause. She also presented awards to this year’s Care Home Hero winners.
Irish boy band duo Boyzlife brought the house down at lunchtime on both days with a set list packed with Boyzone and Westlife hits.

Managers left the show having broadened their horizons, gained valuable CPD credits, and most importantly, had fun.
The only bespoke event dedicated to the UK’s care managers, the Care Managers Show has already become a must attend event in the social care calendar but don’t take our word it, here’s some of the rave reviews we received on social media:
“Thank you for this event. A show not to miss. We managed to attend both shows. So informative.”
– Dravens Healthcare“A wonderful day at the Caring Times Care Managers Show at the NEC Birmingham where Salima and Ajitha proudly received a Care Home Hero Award on behalf of facilities manager Vincent from Davina McCall.
“Thank you also to Matt from Training 2 Care UK for the incredible dementia virtual reality experience which was so thoughtprovoking and emotional to see and feel what it is really like for people living with dementia.
“And lastly thank you to Keith Duffy and Brian McFadden, original Boyzone members, now Boyzlife for a fabulous performance!”
– The White House Nursing Home
Speakers at the Care Managers Show gave their advice on how managers can best look after their own wellbeing and that of their team

Niki Husher, safeguarding and people business partner at Paragon Skills, gave her tips on supporting your team’s mental health.

1. Looking after yourself is just as important as looking after others – we are told to put the oxygen mask on ourselves in a plane before helping our children.
2. Mental health is a continuum and we can all move up and down it. We can make a positive difference to others by helping them transition back to feeling healthy more quickly.
3. Look out for the signs of poor mental health in your team, including changes in behaviour, avoiding social situations, mood swings and confused thinking or problems concentrating and learning.
4. If you notice someone is struggling, the next step is to start a nonjudgemental conversation. “I can hear you have been going through a tough time. Please tell me more about it so I can understand.”
5. Listen carefully to what they are saying, not what you think they are saying, and try not to interrupt. You might say “Take your time, there is no rush. I know it can be difficult to talk about this.”
6. Allow for periods of silence – what they are trying to explain might be hard to put into words. Leave comments and queries to the end.
7. Paraphrase – “I have heard you say… is that right?”
8. Thank them for sharing – they have been brave.
9. Remind them that they are not alone – one in four adults experience a mental health condition. They can, and will, get better.
10. Make sure they know that support is available.
11. The NHS offers a number of tools to keep you mentally healthy including the Mind Plan which includes personal tips and advice sent by email.
12. Encourage people who are struggling with their mental wellbeing to make a note each day of the things they are grateful for. This can be as simple as having an amazing cheese toastie for lunch. You will end up with a lovely record which will make you smile.
13. Signpost to professional mental health support if necessary, for example if someone is not sleeping or self-harming, suggest they make a GP appointment. You could sit with them while they make it, and check in with them later to make sure they went.
14. Other sources of help include Mind and Calm, which both operate helplines. The NHS offers talking therapies through self-referral although there’s a long waiting list.
15. Crisis support includes Shout, which offers a 24/7 text service with access to a trained counsellor, and the
Samaritans. If someone is in a crisis and poses a risk to themselves or others you should call 999.
Jess Baker, chartered psychologist and author of The Super-Helper Syndrome: A Survival Guide for Compassionate People, gave her tips on how to be kinder to ourselves.
1. Find someone at work who can support you – maybe a manager, a mental health first aider, a trusted colleague or a mentor. Ask for the specific kind of help you need.
2. Make sure you prioritise your needs –nobody else is going to make sure you take your full break, they are more likely to say “can you help me with this?”
3. Book time for yourself in your diary to do things you love to do as if you were booking a meeting with a senior manager or executive. You would prepare for that meeting, you would turn up early, you wouldn’t cancel.
4. Become aware of your self-critical thoughts – this helps us choose how to react to them. Just because your inner critic pipes up, doesn’t mean you have to feel anxious about whatever it wants you to feel anxious about.
5. Practise saying the phrases you would to say to a friend in distress – “I am here for you”, “you are always good enough”, but say them to yourself. Record them on your phone and play it back when caught up in self-criticism.

5. Shift to environmentally friendly cleaning products.
6. Appoint ‘green champions’ to empower staff to create and lead on new initiatives.
7. Set up recycling points in the home for staff, residents and families.
8. Establish cycle-to-work and car sharing schemes for staff members.
9. Offer small rewards such as cereal bars to people who cycle into work.
10. Buy in bulk and co-ordinate deliveries to avoid multiple trips to the home by suppliers.
11. Take residents on community litter picking days.
Leading experts offered top tips on how to do things better in the Operational Excellence stream of the Care Managers Show. Here’s our round-up of some of the best.

Kicking off the show, Aaron White, head of business services at Oakland Care, the UK’s only carbon neutral care home group, offered hands-on tips on how to make your care home more sustainable without having to break the bank.
1. Start small. For example, set up a battery recycling bucket in your reception.
2. Set aside a ‘green day’, ‘green week’ or ‘green month’ where staff, residents and families can all contribute to a range of activities and events.
3. Participate in community tree planting events.
4. Set up biodiversity areas in your homes to provide fun outdoor activities for residents and staff, including cultivating wild flowers, nettle patches, ponds, wormeries, bird feeders, hedgehog tunnels or building bug houses.
12. Invite the Wildlife Trust to give presentations to residents for a fun, educational and different activity.
13. Remove single-use plastic items in the home.
14. Use less red meat in meals. Reduce meat content in spaghetti bolognese, for example, by using more vegetables.
15. Replace old appliances such as ovens to reduce energy consumption.
16. Make sure food waste is collected separately from other waste products.
17. Use food waste for garden compost.
18. Produce digital care home brochures to reduce paper usage.
19. Use paperless digital care planning systems.
20. Hold ‘car boot’ style events where staff and families bring items such as clothing they don’t need anymore.
Founder Bhavna Keane-Rao and care and clinical director Charlie Jones of BKR Care Consultancy offer 10 tips on how to get the most out of your care home inspection.
1. Prepare your team. Carry out mock inspections. Walk around with a piece of paper and write down what your staff members are doing to demonstrate what the CQC will be doing.
2. Know your weakest link. If a staff member is particularly anxious give them a day off on the day of the inspection.
3. Use your provider information return as an opportunity to show how great you are.
4. Send the CQC emails about positive and negative things that happen in the home as they happen to take control of the situation.
5. Document complaints and your responses so that the CQC understands your risk profile and you can get your version of any incident to the regulator first.
6. Start collecting evidence on how you are meeting the quality statements under the new CQC Single Assessment Framework (for more info see cqc.org.uk/assessment/ quality-statements
7. Document ‘magic moments’ as part of your evidence to the CQC.
8. Don’t be fearful. If you make a mistake show how you have learnt from it.
9. If you bring in extra staff, explain to the CQC that you are doing this to free up people to give it the best access to the information it needs.
10. Get your staff to email you during the day about what’s going on during the inspection, so if you have concerns later you have that evidence of feedback.
As digital transformation takes hold, care businesses are realising the positive impact of using digital tools on their performance and ability to navigate financial changes. It is no longer just about preventing failure; digital transformation has become the hallmark for growth and success in the care sector.
One of the key advantages of digital tools, such as care home administration software, is the ability to save time and money. The age-old adage that time is money still holds true, and digital tools offer streamlined processes and automation that can significantly reduce the time spent on tasks. Care providers using care home administration software have reported saving several days each month on common processes like fee adjustments, staff clocking-in, and holiday requests. This time-saving benefit is just the tip of the iceberg, as digital tools offer much more functionality and further opportunities for time and cost savings.
A crucial factor in successfully adopting new technology and processes is having a constant improvement mindset. While manual processes may appear to be working initially, they can become ineffective as times change and businesses need to adapt rapidly. Digital adoption can be driven by the need to fix issues with manual processes, but it is even more powerful when approached proactively as a foundation for building a stronger and thriving business. Implementing change proactively allows
for designing ideal digital solutions, which can lead to positive step changes rather than simply replacing limited manual processes.
The recent challenges faced by businesses, including rising energy costs and inflation, have affected various sectors, including social care. However, evidence shows that care businesses that have embraced technology and implemented digital transformation have weathered the storm with greater success. Whether adopting change proactively or reactively, digital transformation is proving to be rewarding.
Digital software offers the significant benefit of visibility, enabling instant generation of reports on any given topic. Care businesses with access to live reporting can make informed decisions as soon as opportunities or threats arise. This increased agility stabilises business performance, encourages a success mindset, and promotes proactive management. Making smaller course corrections throughout the month becomes easier, reducing implementation time and stress for teams. Utilising digital tools fosters success across the board and goes beyond fixing and preventing issues.
Reducing risk is another crucial advantage of digital tools. Businesses often rely on individuals with extensive knowledge, but this can pose a risk if that person leaves the organisation. Care home administration software acts as a central source of information, accessible to all, with the added safety of backups. It ensures knowledge is not lost or unavailable, even when individuals are out of the business. Digital transformation allows for internal and external risk analysis, identifying potential risks and preparing for their implications. It provides businesses with resilience and performance improvement, enabling them to navigate changes without significant disruptions.
Efficiency is a key factor in addressing
challenges and reacting to pitfalls effectively. Care home administration software streamlines processes and creates room for addressing issues as they arise. This helps to ease time pressures and reduce stress for staff, ultimately leading to a happy and healthy workforce. Increased efficiency, achieved through digital tools, contributes to a successful care business by improving turnover and profit.
Implementing digital tools like care home administration software offers quick and simple efficiency gains. The built-in automations streamline processes from the start, enabling businesses to see immediate returns on their digitisation investment. This low-risk investment yields tangible benefits, making efficiency within reach for care businesses of all sizes and ages.
The care sector is experiencing a growing appetite for improvement and a better way of working. Driven by the goal of betterment, businesses are turning to digital tools with great success. While the pandemic may have prompted the change, the positive mindset towards digitisation is benefiting everyone involved in delivering and receiving care.
The key message is that running an efficient care business is achievable for organisations of all sizes and ages. Digital transformation is accessible to both established and new businesses, and its benefits are tangible for all. By adopting a success mindset, striving for constant improvement, and utilising the wide range of digital tools available, care businesses can strengthen their operations and ensure their continued support for those in need.
In the ever-changing landscape of the care sector, the methods, tools, and materials used to build and grow businesses play a crucial role in their strength and resilience
“Efficiency is a key factor in addressing challenges and reacting to pitfalls effectively.”
of property sold:
Austenwood Nursing Home
Gerrards Cross
35 care home with nursing
Premium Care Group
Mr P Evans
Undisclosed
transfer agent:
Buckinghamshire
of property sold:
transfer agent: Contact person:
Derbyshire
of property sold:


Christie & Co
Jordan Oborne – 07736 615 870
Kingfishers Care Home
Bourne End
35 care home with nursing
Premium Care Group
Mr P Evans
Undisclosed
Christie & Co
Jordan Oborne – 07736 615 870
person:
Devon
Name of property sold:
Hazeldene House Chesterfield

21 residential
Undisclosed
Undisclosed
Undisclosed
Christie & Co
Rosie Turner – 07703 716 156
transfer agent:
Springfield Residential Home Bridestowe, near Okehampton

34 residential
Undisclosed
Stephen and Kathy Byrne
£3,250,000
Christie & Co
Simon Harvey – 07764 241 310
IF YOU’RE THINKING OF SELLING YOUR CARE BUSINESS, SPEAK TO THE EXPERTS: Contact our award-winning team on: 0207 448 8826 | care@christie.com






LOOKING TO SELL? TALK TO THE EXPERTS. We have a large pool of buyers ready to invest in the UK social care sector.





Care Home with Nursing, Lincolnshire


Freehold £1,050,000
Large detached two storey extended property
24 single bedrooms
T: 07764 241 296
Mental Health Care Home, Essex
Freehold £1,800,000
• Registered for 14 residents
• Manager in place
2470399
T: 07736 615 870
Former Residential Home,
Freehold £495,000
Previously registered
• Residential location
5471561
T: 07764 241 328
Closed Care Home, Cornwall
Freehold £495,000
• Terraced property in town centre
• Sub-divided into self-contained flats
3470720
T: 07764 241 310
Freehold £2,250,000

• Registered for 48
• Run under strong management
5771002
T: 07754 559 539
Former Residential Home, West Yorkshire
Freehold £595,000
• Closed 15-bedroom care home
• Suitable for alternative use (STPP)
5471554
T: 07764 241 328
Care Home, North Somerset

Freehold £1,250,000
• Registered for 22
• Run by registered manager
3470723
T: 07764 241 310
Care Home, Devon
Freehold £1,4750,000
• Registered for 24
• Urban town location
If you’re thinking of selling your care business, speak to the experts:
3270357
T: 07764 241 310
care@christie.com 0333 034 1750
