
International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN: 2395-0072


International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN: 2395-0072
Parvathi S J1, Anjana R M2, Ranjit Unnikrishnan I3, Vinitha Lakshmi P4, Parthasarathy B5, Gopal Menon6, Ivy S7, Dhandapaani C G8, Ilankumaran P9, Premkumar B10 Viswanathan Mohan11
1 Vice President, Quality Systems, 2 Managing Director & Senior Consultant Diabetology, 3 Vice Chairman & Senior Consultant Diabetology, 4 Senior Manager- Quality Systems, 5 Consultant Diabetology & Committee Head for Facility, Safety& Security, 6Chief Operating Officer, 7 Nursing Superintendent 8 HOD- Maintenance, 9 HOD – Safety & Security, 10 Security officer, 11 Chairman & Chief consultant Dr. Mohan's Diabetes Specialities Centre & Madras Diabetes Research Foundation, WHO Collaborating Centre for Non-Communicable Diseases Prevention and Control, Chennai, India 1-10 belong to Dr Mohan’s Diabetes Specialities Centre, No. 6B, Conron Smith Road, Gopalapuram, Chennai 600086, Tamil Nadu, India
Abstract
Hospital is a place where safety is of prime importance. Healthcareworkers,patientsandthepublicarevulnerable to injuriesandillnessduetounforeseenhazardsatworkplace [1] . A study was conducted to develop a safe environment by implementing hazard identification, analysing and assessing the risk at a tertiary diabetes centre in Chennai. Hazard identification and Risk Assessment (HIRA) was done at departments of the hospital including the medical, paramedicalandsupportservices. Inthispaper,theproactive measure of risk identification and implementation of control measures was introduced through a step-by-step process. Hazards identified were classified and analyzed for the severity of impact. The process implementation was done for severe impact first, followed by moderate and then minimal impact risk. This was followed by the review of the implementationanditseffectiveness.Inthisprocess,newrisks, if any, were also identified. This implementation has been carried out for 3 years since 2017, and the cycle is being followed till date. Major impact hazards were addressed immediately through suitable risk management techniques, such as reducing the impact of risk, removing the risk, adopting preventive measures, substituting other means of mitigating the risks, etc. The teams were equipped through regular training on HIRA and guided to review risk and preventive measures regularly. This standardisation has imbibedacultureofsafety withinthe organisation. Fromthis exercise, HIRA matrix is prepared and the factors influencing hazards are controlled from time to time thereby reducing incidents and saving costs on damage.
Key Words: Hazard Identification, Risk Assessment, HIRA, Safety, Diabetes hospital
Dr.Mohan’sDiabetesSpecialitiesCentre,(DMDSC),aworld classDiabetesCareCentre wasestablishedinRoyapettah, Chennai, India in September 1991, with an objective of providing comprehensive diabetes care and guidance to patients, to help them lead a full and healthy life despite diabetes. Currently DMDSC has it’s headquarters at Gopalapuram in Chennai and provides complete diabetes careunderoneroof.
About 640,000 patients have been registered since 1991, andspreadacross32citiesandeightstatesofIndiawith50 branches. DMDSC is the largest chain of diabetes centres. Themainaimofthecentreistoensurethatpatientshave accesstodiabetestreatmentasclosetotheirresidenceas possible(www.drmohans.com).Thecentrealsofocuseson increasingtheawarenessofthegeneralpublicwithrespect todiabetesanditscomplications,diabetesmanagementand updates on the newest in the field of diabetes. With the number of branches increasing, we find a surge in the number of people having better access to diabetes management.
1.1 Hazard identification and Risk Assessment (HIRA) technique
Ahazardisanypotential damage,harmoradversehealth effectonaperson(staff,patientorvisitor)orhospitalassets [2] “Hazard” is the cause or circumstances that have the potential to cause injury or illness to humans, property damage,andpollutiontotheenvironmentoracombination ofall[3]and“risk”isthelikelihoodthatthehazardwillcause harm. Safetymeasureshavetobeimplementedbasedonthe identificationofhazardsandassessingtherisksinorderto provide a safe environment in the hospital. It is also the

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN: 2395-0072
responsibilityoftheemployertoensurethesafetyofstaff andforthestafftosafeguardtheemployer’sproperty.The WHO has emphasised the necessity of implementing risk managementprogramsinhospitals.
HIRAisaprocessofsystematicandcrucialreviewofhazards involvingstaff,services,equipmentandenvironmentaiming to identify the prevailing measures to safe guard from dangersandsuggestadditionalcontrolmeasures [4]through elimination, substitution engineering and administrative controlsandPPE[5].Usuallyhazardidentification,estimation ofexposure,andacceptabilityofrisk [6]canbeidentifiedby risk assessment. Preparing a record and continuously monitoringtherisk,identifyingchangesandmakingcertain that the controls are effective are ways in which HIRA is carriedout [5]
InnovationsandnewimplementationsatDMDSC,constitute one of the important path to its success. Many new approaches and strategies are being implemented continuously.Onesuchprocessimplementation isHazard IdentificationandRiskAssessment.AsperNABH5thedition standard,PatientSafetyandQualityImprovementPSQ.1.g; Responsibility of Management ROM 5a, ROM 5b, ROM 5c; Facility Management and Safety FMS 1 a-e mandates the identification and control of risks. At DMDSC, HIRA is not focussed as enforcement, but is instead covered by all departmentsasanessentialrequirement. Inthisreview,the step by step process of HIRA analysis followed till date is covered. The step by step process enables individual employeeunderstandaboutHIRAanditsimplementation,so that,itbecomesanintegralpartoftheirroutinejustnota guideline.
The step by step process of implementation of HIRA is outlinedbelow:
Step 1 Need for HIRA & training on the concept
Patientscomingtothehospitalfortreatment,trustthesafe environmentandbelievethattheirhealthwouldimproveby followingtheinstructionsgivenbythedoctors.Henceitis essentialtoprovideasafeplacetothepeoplewalkinginto thehospital.Itisimpossibletoeliminateallhazards,sothe goalistoeliminateand/orcontrolthehazardswithcritical and high potential risk [7]. Creating awareness among the staffonsafetyconceptsisessentialforthemtoparticipatein this safety culture program. This was done through facilitator (head of the department) training who in turn facilitatedtheirstafftrainingontheHIRAconcept.

Thehazardsandtheriskspertainingtotheactivitieswere identifiedbytheserviceprovidersofmedical,paramedical andsupportservices.Thiswasdonebydiscussionwithstaff abouthazardsintheirworkplaceandinspectionoffacility fromthesafetyperspective[1].Manyhazardswereidentified usingcommonknowledge,suchasslipperyfloor,criss-cross electrical wires, etc. All these inputs were collated by the heads of department and the risk list was finalised. For instance,firehazards,slipsorfallsofpatients,hazardousor toxic materials, unsafe work practises, non-availability of spill kit, working posture (ergonomic), physical working condition,hightemperature,poorlightinglevels,electrical shock [8]
Riskassessmentistheanalysisoftheimpactofthepotential risk.Impactistheextenttowhichsurroundingisaffected. The impact of the risk ‘if occurred’ was evaluated by the team and was classified as severe, moderate and minimal risk.Trainedfacilitators(usuallytheprocessowners)along withtheirteamwereinvolvedintheclassificationofeach risk. This was held through brainstorming by multiple departments through each facilitator for their processes involvingallcategoriesofstaffandtheirexperience [9]
Aftertheidentificationoftheseverityofrisk,thehighrisk points(riskswithsevereimpact)weresegregatedandaction points for control measures or prevention of risk were developed. The appropriateness and feasibility for implementationwerecheckedandtherespectiveteamwere entrustedwiththeexecution.

Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN: 2395-0072
Step 5 Implementation of Risk Control measures
Thecontrolmeasuresplannedwerediscussedwiththeteam forimplementation.Flowchartsweredevelopedwherever necessary. Actions were taken based on the hierarchy of controls such as elimination, substitution, engineering control, administrative control and personal protective equipment [4]. During the implementation, changes in processes, process controls, etc. were discussed with the groundstaff.Theeliminationorreductionofriskwasalso evaluated.Insomecases,whereriskcouldnotbereduced, thepreparednesstohandleriskwaschecked.
Step 6 Monitoring occurrence and review of control
Afterimplementationofthesaidactionplan,theHeadofthe Departmentensuredthattheactionswerefollowedandthe risks were prevented, or occurrence of risk was brought down.Incidentsofoccurrenceweretobereportedpromptly [4] to the safety committee to validate the strength of the control measures and for this a new incident reporting systemwasintroduced.Thisisnowbeingmonitoredfrom timetotimebytheseniorlevelstaff.
Step 7 Standardisation of risk policy and procedure; and review of risk for control measures
The concerned process owners and the service providers wereconsultedforstandardisationduringthereviewofthe respectiveSOP.Thiswaythecontrolmeasuressuchasthe administrative controls and engineering controls which wereimplementedwerestandardised.
Thestep-by-stepprocessofimplementationisexplainedin theflowchartfigureno.1.ThisincludesNeedforHIRAand Training,RiskIdentification,SeverityAnalysis(Analysisof the impact of the risk), Mitigation / Control Measures, Implementation of Risk Mitigation Measures, Monitoring Occurrence and Review of Control and Standardisation of Risk Policy and Procedure. The various departments involvedinidentifyingHIRAwereclassifiedundermedical, paramedicalandsupportservicesasmentionedinTable1.
Table 1: Departments Involved in identifying HIRA
Medicalservices Diabetology unit, Diabetes Eye care Unit, Diabetes Foot clinic, Diabetes Cardiac unit, Diabetes Dental Unit, Diabetes Kidney unit, Psychological counselling,ObesityManagement
Paramedical Lifestyle Management (Fitness/Physio), Surgical unit & Operation theatre (OT), Nursing, Investigations unit, Wound dressing unit, State-of-the-art Clinical Laboratory,Radiologyunit,Nutrition & Dietetics unit, Clinical secretary section,Pharmacy
Support Front office, Home care, Call centre, Security, Maintenance, Catering, Medical records department, Housekeeping,TransportSupplychain management, kids zone, despatch section
A total of 211 risks were identified. Some of the risks identified by the service providers are given in Table 2. While analysing, it was found that certain risks were repetitiveindifferentlocations.Theseriskswereretainedin the list (without being deleted as duplication) since the identifiedactionsforeachriskhadtobeimplementedinthe particularlocationbytheserviceprovider.
Table3describestheHIRAmatrixidentifyingtheimpactof riskasminimal,moderate,severe.Onanalysis,itwasfound that66%oftherisksidentifiedwillhavesevereimpact,26% willhavemoderateimpactand8%minimalimpactwhichis similar to previous studies[5]. From the matrix it was also found that the risk related to medical and paramedical serviceswas26%andsupportservicesriskwas64%.
Table 2: Details of the risks identified
Service type Risk identified
Medical Suddenemergencyofpatientduringthe procedure
Medical Crossinfectionduetonon-sterileinstrument
Medical Lackofexpertupdatedknowledgefor providingthebestclinicalcare
Medical Suddenstoppageofpatientsoftwarewhile operating
Medical Lapseinservicestopatientascriticalalert resultoftestvalueswerenotinformed
Medical BPApparatusnon-functional
Medical Notdispatchingpendingreportsafterfinal consultation
Medical Locallanguagewasnotfamiliarduring consultation
Medical Sterilitynotmaintainedinsurgicaldressing/ OT
Medical Oozingwoundofpatientleadingtocross infection
Medical Crossinfectionduetononsterile environment/handlinginfectiouspatient
Medical Allergictofluoresceindye
Medical AllergictoMydriaticeyedrops
Medical Takingwrongtest
Medical Dispatchofwrongreportstopatients

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN: 2395-0072
Paramedical Radiationtostaffduringexposure
Paramedical ImproperuseofradiationTLDbadges
Paramedical AbnormalHaemogramforstaff
Paramedical Fallofpatientfromcouch
Paramedical Injurywhilecenteringthex-raytube
Paramedical Exposuretopregnantwomen
Paramedical Spillageofbodyfluids
Paramedical Needlestickinjuryduringblooddraw
Paramedical Splashofchemicals
Paramedical Doubleprick/Adversereaction
Paramedical Equipmentbreakdown
Paramedical Lapseinadministeringmedicationorwrong medication
Paramedical Crossinfectionthroughpatientsadmittedfor longduration
Paramedical Issueofexpirymedicinestopatient
Paramedical Dispensingwrongmedicines
Paramedical Medicinesgettingspoiledduetoelectricity fluctuation/breakdown
Paramedical Droppingdownthebottlemedicineswhile arranging/retrieving
Paramedical Patient’sM.No.wronglyenteredinthereport software
Support Lapseincalibration/preventivemaintenance ofequipment
Support DataLeakage
Support Dataaccuracyandperfection
Support IftheGasRangeisnotopenedandclosed properlyitposesrisk
Support Wearandtearofgaspipelinesposesriskto humanandtotheequipment
Support BurnsduetoSteam,duetocontactwithdirect flame
Support Crankycallsatthereception/threatsthrough phone
Support Peopletryingtoenteratnighttimesinto hospitalcampus
Support Safety/protectionofstaffduringtheHome CareTravel
Support Samplespillageinsidecollectionbox
Support Slipperyfloorleadingtofalls
Support Hazardouswastemixedwithnon-infectious waste
Support Crossinfectionthroughpatientsadmittedfor longduration
Support Lackofbackupandrecovery
Support DisasterManagement
Support Malware/Virus
Support ElectricalHazard-Shortcircuitduringpower changeoverEBtoDG&DGtoEB
Support Mechanicalhazardslikemoving/rotating machinerythatcancauseinjury
Support Rainwatergettingintothebuilding
Support Whileclimbinguptherackforretrieving,staff mayfalldown
Support Whileusingthecompressedsystemoffiling stafffingersmaygetjammed
Support Pestattackonthecasesheetsstored
Support StorageofAmmonia
Support Nonavailabilityofoxygencylinders
Support Safetyduringthetravelwhiletransporting staff
Support Attritionofexperiencedemployees
Support Lackoftechnicalknowledgeonproductand Productupdates
Support Theftofcashinstorage
Support Theftofcashintransit
Support UnknownentityposingasDr.Mohan’sand givingnegativeinputstopublicinsocial domain
Table 3 Risk Identification – Examples of different risks added in DMDSC
Figure2describesthefollowingprocess
Elimination – Elimination of the risk is usually the most effectiveriskmanagementmethod. Usuallyitinvolvesacost asitadoptsupgradedtechnologiesandinnovation.
OneexamplegivenintheTable4isexplainedhere:Unsafe exitwaywhileevacuatingpatientsduringemergencywasa risk identified by the security department. When shifting patients to the assembly point during a fire or other emergency,thesteelrampexitwayavailablewasunsafeand

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN: 2395-0072
couldcauseasliporfall,whichwasdangerous.Hencethis was changed to concrete ramp way with good supportive sides and hand rails. A huge investment was involved but totallyeliminatedthisriskandnowprovidesasafetransitto theassemblypoint.
Figure 2 Risk mitigation - Hierarchy of controls Vs Responsibilities
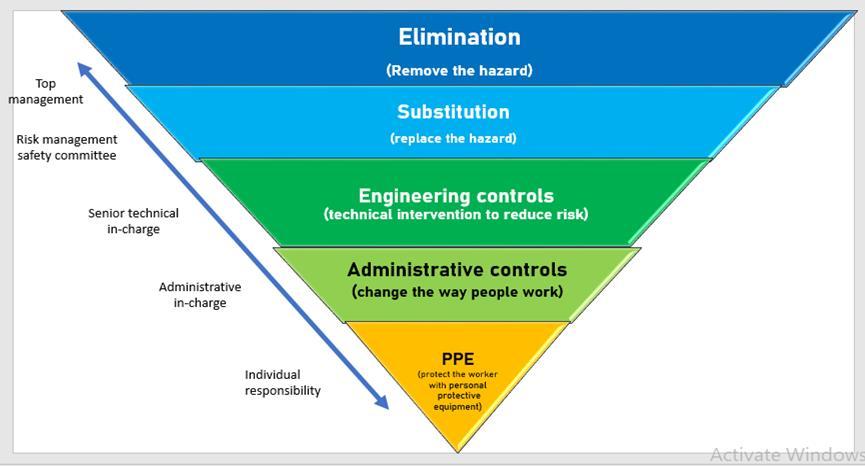
Source:https://www.ccohs.ca/oshanswers/hsprograms/hazard/hierarchy_controls.html
Substitution- Ifeliminationoftheriskisnotpossiblethen substitution will be next control method that should be considered[3],example,achemicalusedforfogging,iffound to be cause eye irritation can be substituted with another chemicalwhichdoesnotcauseirritation.
Engineering controls – theuseofalarmpanel foroxygen supply indicator level, sprinklers with fire alarm system, safety belts for patients to prevent patient fall etc. are examplesofengineeringcontrols. Manyatime,hazardous/ infectiousmaterialscanbediluted/separatedbyrespective technicalemployeessoastomakeithazardfree.
Administrative control – thisdoesnotremoveorreplace the hazard. It minimises the hazard by preventive maintenance program, scheduling work reset program, restricting task to qualified staff, training, developing safe work procedure, emergency preparedness and use of personalprotectiveequipmentasmayberequired.
SomeexamplesaregiveninTable4aalongwiththeaction proposed. Someoftheactionsproposedinclude replacing hazardouschemicalswithsaferones.Eliminatingthosethat could be removed such as mercury from the hospital, providingthestandardchairsbyreplacingtheolderonesfor settingtherightposturesforstafftoavoidergonomicissues, providing adequate lighting in the work environment, installing alarm call system, educating personnel on safe practises,equippingallhospitalequipmentwithproper
Risks Identified Department Name
Impactanalysis Preventive or control measuresproposed
Min Mod Sev
Unsafe exit way while excavating patients during emergenc y Security
Cross infection through patients admitted for a long duration
Nursing
Steel ramp exit way to be changed to concrete ramp way
Good supportive sides withoutgaps
Continuous hand rails for holding
Antiskidflooring
Fluorescent stickers at the bendsandturns
Antiskid stickers in the rampending.
Thoroughcleaningfollowed by fumigation is to be ensured before admitting next patient to the same room.
Training to be held for nursing staff to notify the house-keeping on the long stay
Swabcultureoftheroomto be taken to determine the intensityofcleaningandits validation
Standardisationtobedone–to be added in the HICSOP, Nursing Sop and HousekeepingSOP
Incidur used for foggingall areas causing eye irritation
Issue of expired medicines topatient
Housekeepin g 1.
Substitute to be used for fogging to prevent eye irritationorproceduretobe amendedtopreventstaffto beisolatedduringfogging 2. Fogging to be done after peakhoursandlockareato makeiteffective
3. Photos of the fogging process to be taken and shared to the infection controlcommitteemembers
Pharmacy Medicinerecallfrompatient. Patientistobeexplainedby higherauthorities.
Twomonthspriortoexpiry analertwillhavetobegiven in the system, so that the stock can be immediately separated and sent to supplier.
Training to be given to all pharmaciststodoublecheck beforeissuingthemedicine topatient
Fire Hazard Supply chain Management
Immediate announcement ofCoderedalarm. ERT members to be strengthenedtohandle. Patientstobesafelyshifted. Firecontrolthrough AppropriatenumbersofFire extinguishers, Firealarmpanel, Install water sprinklers in allfloors, Hosewaterpipes
Nominationofsafetyofficer tooversee
Safety rounds at regular intervals
Announcementsystemtoall areas to alert the entire team

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN: 2395-0072
earthingsystems,providingfloorwithelectricalinsulation under power panels, fire alarm systems and fire panels, installingwarningsignsforslipperyfloors,placinganti-skid floorstickertapes,strengtheningthefire-fightingteamand developing firefighting skills through mock drills, training staffonPPEs,handwashstepsetc.Theresponsibilitiesfor implementation (including the designation of the staff responsible)wereassignedasgiveninTable.4b.
It was ensured that the service providers consistently followed up with the implementation team assured That thesewereimplemented.Trainingwasgiventotherelevant and appropriate staff to ensure that the changes in the system were understood by the ground level staff even before implementation. The control measures and the actions taken were recorded and discussed during the committee meeting. Some examples of delegation of this actionpointaregiveninTable4b.
Asa team,thisisreviewed oncein6months tofindoutif thereareanyoccurrences,anditseffectivenessinreducing theriskorifnewpreventivemeasuresareneeded.Thisis nowbeingdoneasaregularpracticeandisreflectedinthe standard operating procedure of the respective service documents.
This study has identified various hazards under medical, paramedical and support services and also the control measures such as elimination, substitution, engineering controls, administrative controls and PPE. It has been observed that some processes carried out in the Hospital unitentailsevereriskwhichrequirescontinuousmonitoring and periodic control measures to be implemented. The majority of risks identified were in the severe impact category and that was identified with respect to support services.
Review of risk is a continuous process. New risks may be identified,newcontrolmeasurescanbeestablishedandnew innovation techniques and engineering controls are being encouraged in the system. However, when these are regularised,itisessentialtostandardisethemandinclude them in the SOPs. This has led to improving the safety measureswhichisreflectedintheSOPandpavesapathto buildingacultureofsafetyamongtheemployees.
Risks Identified Preventiveorcontrol measuresproposed Responsib ility Control established
Unsafe exit way while excavating patients during emergenc
Cross infection through patients admitted for a long duration
Good supportive sides withoutgaps
Continuous hand rails forholding
y Steel ramp exit way to be changed to concrete rampway
Antiskidflooring
Fluorescent stickers at thebendsandturns
Antiskid stickers in the rampending.
Thorough cleaning followed by fumigation before admitting next patients to the same room. Trainingheldtonursing stafftonotifythehousekeepingonthelongstay; HOD assigns for more than30daysstay
Swab culture of the room taken to determine the intensity of cleaning and its validation
Standardisation done –reflectedintheHICSOP, nursingSopandHousekeepingSOP
Incidur used for foggingall areas causing eye irritation
Viroff 753 as a Substitutetobeusedfor fogging to prevent eye irritation
Foggingtobedoneafter peak hours and lock areatomakeiteffective
Photos of the fogging processtobetakenand shared to the infection control committee members
Fire Hazard Announcement system of Code red to all areas toalerttheentireteam ERT members to be strengthenedtohandle. Patients to be safely shifted.
Firecontrolthrough Appropriatenumbersof Fireextinguishers, Firealarmpanel, Install water sprinklers inallfloors, Hosewaterpipes
Nomination of safety officertooversee Safety rounds at regular intervalsMockdrillheld andthesprinklers,hose lines and fire panel checked
Procedurestandardised byreflectinginSecurity andSafetySOP
Chief operating Officer, HODProjects, HOD_ security,
Eliminationoffalls through sides of the steel rails, preventslips
HODNursing and House keeping Process Administrative Engineeringcontrol
HOD_ House keeping, Infection control nurseand HIC committee
HODSecurity & ERT members
Substitution Administrative Process/ engineering control
Engineering control
Table 4 B Risk mitigation - control and preventive measures taken at DMDSC

Volume: 11 Issue: 09 | Sep 2024 www.irjet.net
Benedict’s testused to checksugar is a heating method involves flame and posing a risk of fire hazard
2. Radiation hazard duringx-ray procedure
1. Urinesugaranalysed throughanalyser–urine stripmethod
3. Use of lead apron, lead gonads, lead sheets to protect the staff. Console roombuilttoprotectstaff fromexposure
7. Medicine recall from patient through proper documentation.
8. Patient is called and explained by higher authorities regarding the medicine by higher authorities.
6. Issue of expired medicines topatient
9. Alert for short expiryTwo months. Double checkbeforeissue. Training was given to all pharmacists on double checkbeforeissuing. Alertdevelopedforshort expirymedicines-appears in the system- stock is separated and sent to supplier.
List of short expiry medicines two months prior is taken by HOD to seeifnilexist
Breakdown of critical equipment
Lack of knowledge on latest in field of Diabetesknowledge on diagnosis and treatment
Annual maintenance contract to have the preventive maintenance doneregularly
International Diabetes Updates & certificate courseinEvidencebased Diabetes mellitus. Talks, panel discussions and symposiums on Diabetes updates for all doctors thereby improvising knowledge base on Diabetes and understanding the latest in the field of Diabetes management. Involving doctors in education through you tube and other social media thus encouraging themselves to update in their field. Urging the doctors to participate in external nationalandinternational conferences. Sharing needed knowledge and latest updates through whatsappshare. Development of a tool which can assist in the diagnosis of type of Diabetes. Test results in theappcancustomisethe treatmentofpatientwith Diabetes Introduction of DIANA- an organisation developed tool with artificial intelligence assistingtheconsultantin thediagnosisofpatienton thetypeofDiabetes
HODNursing& HOD–laboratory
4. HODRadiology 5. Engineering control
HODPharmacy and Senior staffPharmacy
Elimination through Administrative control and alert system
Throughthecontinuousprocessofriskreview,HIRAisnow integratedasaregularactivitytopreventriskoccurrence. This study revealed several risks with severe impact and identificationofrelatedactivitiesforwhichcontrolmeasures havebeenrecommendedandimplemented.Implementation process is monitored and followed and the study has regularisedthefacilityandsafetyroundsinthehospitalon monthly basis. Mock drills and continuous training on emergencyhandlinghavealsobeen regularised. Thus,the studyhashelpedthemanagementandemployeestofocus on the safety of the patients, staff and the hospital environment. It also has led to minimizing occupational injuries and accidents. It has assured that the culture of safety is built into the system and is part of the working environment.
Theauthorsfullyacknowledgethemanagementandstaffof DMDSCforentiresupportinimplementingHIRAandthereis noconflictofinterestraisedduringpublishing.
HOD_BME Administrative control
Chairman, Vice Chairman, Managing Director, HOD & senior consultantsDiabetology & Management of the institution alongwithIT team
Administrative control
Eliminationof lackofknowledge ondiagnosis
[1] BiswajeevanSahoo,MukundaSSahoo,JawaharSPillai. “Making our Hospitals a Safe Workplace: Hazard IdentificationandRiskAssessmentataTertiary–Level Public Hospital in Eastern India”, CUREUS, Journal of MedicalScience,16(4);(2024),pp.1-8.
[2] Hazard identification and assessment (2021). https:// www.osha.gov/safety-management/hazardidentification
[3] NIOSH, “Training manual for Safety & Health Officer CertificationProgramme”Malaysia,2005.
[4] https://www.ccohs.ca/oshanswers/hsprograms/hazard /hierarchy_controls
[5] Rajvinder Kour, Ankit Singh, Neha Ahire “An ImplementationstudyonHazardIdentificationandrisk assessment(HIRA)techniqueinthecriticalcareunitof tertiary care hospital”, Indian Journal of Forensic Medicine&Toxicology,October-December,14(4),2020, pp.4018-4026.
[6] British Standards Institution, BS8800: Occupational health and Safety Systems Guide”, British Standards Institution,London,2004.
[7] B K Rout,B K Sikdar “Hazard Identification, Risk Assessment,andControlMeasuresasanEffectiveToolof OccupationalHealthAssessmentofHazardousProcessin anIronOrePelletizingIndustry”,InternationalJournalof

International Research Journal of Engineering and Technology (IRJET) e-ISSN: 2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN: 2395-0072
Occupational Environmental Medicine, 21(2), 2017, pp 56-76.
[8] Bambangsuhardi,PringgoWidyoLaksono,AndhikaAyu V.E,JafriMohd.Rohani,TanShyChing,“Analysisofthe potential hazard identification and risk assessment (HIRA) and Hazard operability study (HAZOP): case study”. International Journal of Engineering and Technology,vol.7(3,24),2018,pp1-7.
[9] Behzad Soranjam, Leila Naghizadeh, Elnaz Rahimi, Mozhgan Etemed, Bahram Kouhnavard, Zeinab Mosavianasl, Amin Babaei pouya “Hospital occupational safety and health risk assessment” PakistanJournalofMedicalHealthSciences,4(2),2020, pp804-807.
© 2024, IRJET | Impact Factor value: 8.315 | ISO 9001:2008 Certified Journal | Page27