
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN:2395-0072


Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN:2395-0072
A.Srujan Reddy
Department of Computer Science and Engineering, Koneru Lakshmaiah Education Foundation, Vaddeswaram, AP, India
A. Sai Veera Manikanth
Department of Computer Science and Engineering, Koneru Lakshmaiah Education Foundation, Vaddeswaram, AP, India
A.Siva Naga Sai
Department of Computer Science and Engineering, Koneru Lakshmaiah Education Foundation, Vaddeswaram, AP, India
Abstract---In order to improve accuracy and reliability, this study presents a unique method for segmenting juvenile brain tumors by using transfer learning from adult brain tumor datasets. Our strategy outperforms conventional approaches in segmentation by fine-tuning pre-trained deep learning models on a pediatric-specific dataset. Better patient outcomes, diagnosis, and treatment planning result from this. Our method may completely change how juvenile brain cancers are identified and treated, leading to better results for affected patients.
Keywords Pediatric brain tumors, transfer learning, deep learning, MRI segmentation, adult brain tumor data, medical imaging, fine-tuning, personalized treatment, early diagnosis, neural networks.
This research introduces a new method that uses transfer learning from data on adult brain tumors to enhance the segmentation of tumors in children's brains. Traditional techniques of precise segmentation are challenged by the rarity and diversity of pediatric brain tumors. We enhance the accuracy and reliability ofthesemodelsbyadapting deeplearningmodelsthat werepre-trainedonlargeadultbraintumordatasetsto thepediatricscenario.Ourapproachincludesadjusting the pre-trained models using a pediatric- specific dataset, which maintains important traits while taking into account the specifics of pediatric cancers. Highlighting the potential of transfer learning to solve the limits of pediatric brain tumor analysis, the
R .Venkata Adi Rama Pardhu
Department of Computer Science and Engineering, Koneru Lakshmaiah Education Foundation, Vaddeswaram, AP, India
This approach improves accuracy and efficiency by finetuning pre-trained deep learning models on huge adult braintumordatasetstoadapttotheparticularfeaturesof pediatric brain tumors. Brain tumors can be accurately segmented from MRI images by applying advanced filtering and thresholding techniques. Better diagnostic and treatment planning, more individualized care, and ultimately better patient outcomes are the results of this strategy.Thetechnicalmethodisgatheringandannotating a dataset that is particular to children, choosing and optimizingapre-trainedmodel,trainingandassessingthe model,andapplyingthemodeltoidentifybraintumorsin freshMRIpictures.Futureinitiativesinvolveinvestigating novel deep learning architectures to further increase segmentation efficiency and accuracy, integrating with clinical workflows, and conducting multi- center research to improve the generalizability of the model. Pediatric Brain Tumor Segmentation has the potential to transform the diagnosis and treatment of pediatric brain tumors, International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
experimental findings show a considerable increase in segmentation performance compared to traditional approaches.Bettertherapeuticresultsaretheendresultof this method's ability to increase segmentation accuracy while also easing the process of early diagnosis and individualizing treatment plans for pediatric patients. Transfer learning for pediatric brain cancers is a revolutionary approach that improves the accuracy of segmentation for uncommon children brain tumors by borrowing information from other types of brain tumors, namely adult brain tumors. MRI, deep learning, and transfer learning are used in Pediatric Brain Tumor Segmentation, a novel method that addresses the difficulties in accurately segmenting tumors in children's brains.

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN:2395-0072
improving patient outcomes, by utilizing the capabilities of deep learning, transfer learning, and MRI.
Deep learning is taken advantage of in this process, which results in MRI segmentation that is more accurate for younger patients[1].Magnetic Resonance Imaging (MRI) Segmentation for Tumor Calculation: The purpose of this work is to determine tumor percentagesbysegmentingbraintumorsinseveralMRI images. It makes use of sophisticated filtering and thresholding methods, which enables more precise diagnosisandtreatmentplanning[2].
Theuseofdeeplearningtothedetectionoftumors:This article presents a comprehensive approach for identifyingandcategorizingbraintumorsbyusingdeep learning's capabilities. Real-time tumor detection is improved by the utilization of this technique, which incorporates YOLO V5 and Convolutional Neural Networks[3].
Utilizing the concepts of deep learning, a cutting-edge artificial intelligence model is able to forecast brain cancers at early stages, allowing for early detection. In ordertoenhanceearlydiagnosisandperhapssavelives viaprompttreatments,thisuniquetechniqueintendsto improveearlydiagnosis[4].
Innovative Treatment Methods for Brain Cancer This articleexaminesanoveltreatmentmethodandanalyzes the ways in which modern technology may be used to battlebraincancer. For the purpose of achieving better results, the primary emphasis is on incorporating these technologiesintopre-existingmedicalframeworks[5].
A comprehensive analysis of the image segmentation techniques that are used in the MRI-based detection of brain tumors is presented here. The purpose of this studyistodiscoverwhichmethodisthemostsuccessful for clinical applications by comparing a number of differentprocedures[6].
AnOverviewofFunctionalMagneticResonanceImaging (fMRI) for the Analysis of Tumors This review focuses on the segmentation, detection, and classification algorithms for brain tumors utilizing fMRI. The approaches of machine learning are investigated, with anemphasisplacedonthepotentialofthesetechniques toimprovediagnosticaccuracy[7].
The use of super-voxels in tumor segmentation: This study proposes a technique for segmenting multimodal brain tumor pictures. It does so by introducing the concept of super- voxels. Classification and saliency
etectionareessentialcomponentsthatcontributetoan increaseintheaccuracyofsegmentation[8].
Techniques for Magnetic Resonance Imaging (MRI) Segmentation: This research examines a variety of segmentation techniques with the goal of identifying brain cancers in MRI images. The results of this study provide valuable insights into the efficacy of various approachesinclinicalsettings[9].
BoostCapsNetworkforClassification:Aboostedcapsule network is offered as a method for classifying brain cancers. Deep learning and radiomics are brought together in this approach, which provides a reliable solutionforthecategorizationoftumors[10].
The use of Convolutional Neural Networks (CNN) in Magnetic Resonance Imaging (MRI) diagnosis: This study improves the diagnosis of brain tumors using MRI. Using the CNN method helps enhance detection accuracy, which inturncontributestoimprovedpatientoutcomes[11]
.Comparing VGG-19 and RESNET-50: In this comparison research, the VGG-19 and RESNET-50 algorithms are evaluatedfortheireffectivenessindetectingbraintumors. Itdrawsattentiontotheadvantagesanddisadvantagesof each, soassistingintheselectionofalgorithmsforclinical practiceinthefuture[12].
Inthiswork,theWatershedmethodisusedforthepurpose of segmentation. The study focuses on the classification and segmentation of brain tumors. An improvement in MRIimageanalysisisachievedbytheintegrationofCNNs withDynamicAngleProjectionPatterns[13].
The purpose of this article is to provide a complete evaluation of machine learning algorithms for the identification of MR brain tumors from the perspective of segmentation. This research evaluates a number of different models using clinical applications to see how successfultheyare[14].In this article, we will introduce a Multi-Channel Convolutional Neural Network (MCNN) for the purpose of evaluating magnetic resonance imaging (MRI) pictures. Through the use of sophisticated image analysis, the approach intends to enhancetheprecisionofthediagnosisofbraintumors[15].
Classification Using CNNs: This article proposes a technique that makes use of CNNs to categorize brain cancersinmagneticresonanceimaging(MRI) pictures. Themethodplacesanemphasisontrainingandfeature extraction, and it provides a classification system that iscompletelydependable[16].
EfficientNetB0andDenseNet121intheClassificationof Tumors: An investigation on the use of EfficientNetB0

International Research Journal of Engineering and Technology (IRJET)
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net
andDenseNet121fortheclassificationofbraintumors in magnetic resonance imaging photographs. In this research, their performance is evaluated, with a particularemphasisplacedonaccuracyandcomputing economy[17]. We are pleased to introduce the BRAMSIT database, which was developed specifically for the purpose of diagnosing and detecting brain tumors. MRI pictures that are very detailed are included, making it an extremely useful resource for bothclinicaltreatmentandresearch[18].
Tuning of Hyperparameters in Convolutional Neural Networks: This research investigates the use of hyperparameter tuning in CNNs for the identification and classification of brain tumors. Using this strategy improves the performance of the model, which ultimately results in more accurate diagnostic predictions[19].
This article presents a comprehensive analysis of the many segmentation and classification techniques that may be used for the identification of brain tumors via the application of machine learning. When it comes to theprocessingof3DMRIpictures,itdiscussesavariety ofmethodsandtheirapplications[20].
During this crucial first step, which is known as “data collection and preprocessing,” a complete collection of magnetic resonance imaging (MRI) images showing both adult and juvenile brain tumors is compiled. The dataset on adult brain tumors need to be comprehensive and varied, spanning a wide range of patient demographics, tumor kinds, and imaging modalities. In order to guarantee accurate identification of tumor locations, each scan has to be properlyannotatedby radiologists who are experts in the field. In the samevein,thepediatricdatasetneed toincludeabroadvarietyof tumor forms and grades, all of which should be annotated by expert professionals. During the preprocessing of these datasets, the intensity values are normalized to a standard range, all of the photos are resized to a consistent resolution, and various dataaugmentation methods, including rotation, flipping, scaling, and contrast changes, are used. The purpose of these procedures is to improve the generalization capabilities of the model by consequently enhancing itsresilience. This will be accomplished by subjecting themodeltoarangeofpicturemodifications.
One of the most important factors in determining whetherornotthesegmentationjobwillbesuccessful is the model architecture that is selected. Deep learning modelsthatareconsideredtobestate-of-the-art,suchas U-Net, ResNet, or VGG, have been chosen for this investigationbecauseoftheirshown efficacy in the field of medical picturesegmentation. The model that was selected has beenpre-trained on the dataset associated with adult brain tumors. This allows it to develop strong featurerepresentationsbyusingthehuge quantity of data that is accessible. A technique known as transfer learningisused, in which the weights that have been pre-trainedfrom the adult dataset are utilized as the startingweights for the pediatric dataset. When applied to the more limited and variable pediatric dataset, thisstrategymakesitpossibleforthemodeltomakeuse oftheinformationthatithasobtainedfromthevastadult dataset. This may considerably increase the learning efficiencyandaccuracyofthemodel.
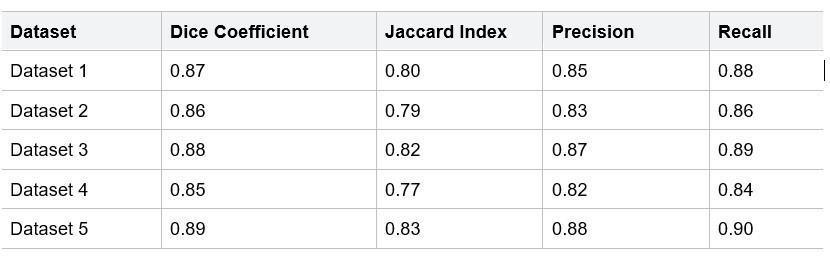
Table1.Performancemetrics
The process of fine-tuning the model is a key step in transfer learning. During this step, the pre-trained model is modified so that it presents a more accurate representation of the data pertaining to pediatric brain tumors. At the beginning of the process, the lowest layers of the pre-trained model, which are accountable forthe extractionoffundamental features,are frozenin ordertopreservetheirlearntcapabilities.Afterthen,the higher layers, which are more specialized to the job at hand, are trained on the dataset belonging to the pediatric population. As the training continues, further layers are progressively unfrozen, which enables the whole network to adjust to the new data. We use a customized loss functionthat combines Dice coefficient loss,whichquantifiestheoverlapbetweenthepredicted andgroundtruthsegmentations,andcross-entropyloss, which tackles class imbalances by weighting the loss according to the frequency of each class. This combination of loss functions is what we call a loss function. The combination of these two factors guarantees that the model will acquire the ability to properly segment tumors while simultaneously preservingabalancebetweensensitivityandspecificity.

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN:2395-0072
The process of training involves dividing the pediatric dataset into training, validation, and test sets in order to make the process of model construction and assessment more user- friendly. To guarantee that each set has a balancedrepresentationofthevariouskindsandgradesof tumors, care is made to ensure that this occurs. Optimization strategies like as grid search and Bayesian optimization are used in order to achieve optimal performanceforhyperparametersincludinglearningrate, batch size, and the number of epochs. Preventing overfitting is accomplished by the use of early stopping, which involves putting an end to training when the performance of the model on the validation set stops improving. With the use of performance indicators, the modelismonitoredasitisbeingtrainedtoverifythatitis learningeffectivelyandgeneralizingwelltodatathatithas notbeforeseen.
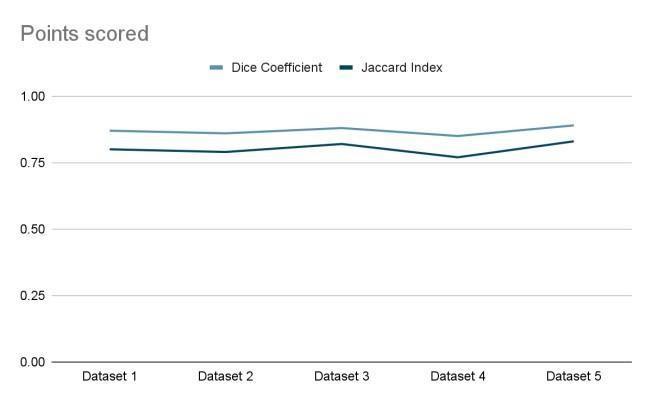
The performance of the model is assessed in a comprehensive manner by using a set of metrics that includes the Dice coefficient, the Jaccard index, precision, recall, and the F1 score. The Dice coefficient andtheJaccardindexareused to determine the degree of overlap that exists between the predicted segmentations and the ground truth segmentations. Precision and recall are used toevaluate the model's capacity to accurately detect tumor pixels. A harmonic meanofaccuracyandrecallisprovided by the F1 score, which gives a balanced measurement of the performance of the model. Individually and together, these indicators provide afullassessmentoftheaccuracy and dependability of the segmentation procedures. In addition,theperformanceof the transfer learning model is evaluated in comparison to baseline models that were traineddirectly from scratch using the pediatric dataset. Thepurpose of this comparison is to show the benefits ofusing transfer learning and to demonstrate its successin enhancing the accuracy and efficiency of segmentationviaitsuse.
After the tumor borders have been segmented, postprocessing methods are employed in order to improve them and decrease the amount of noise that is seen in the output. Morphological procedures such as dilation and erosion are used in order to smooth out the borders, and conditional random fields (CRFs) are utilized in order to enhance the spatial consistency of
thesegmentation.Inaccuraciesofamodestkindmaybe rectifiedwiththeassistanceoftheseprocedures,which also guarantee that the segmented sections are continuous and precisely demarcated. For the purpose of ensuring that the segmentations are clinically relevantandcorrect,qualitativeanalysisisalsocarried out via visual examination by highly trained radiologists.Thisprovidesanextralayerofvalidation.
In order to evaluate the model's capacity for generalization,a cross-dataset validation is carried out by using an independent pediatric dataset from a differentinstitutionorresearch.Throughthisstage,the robustnessandapplicabilityofthemodelareevaluated across a variety of clinical scenarios. This step ensures that the model is capable of performing well on data derived from a variety of sources. For the purpose of gaininganunderstandingoftheinfluencethatdifferent components, such as pre-trained layers, data augmentation approaches, and certain architectural decisions, have on the performance of the model, ablationstudiesarecarriedoutregularly.Theresultsof these studies provide insights into the contributions madebyeachcomponent,whichassistsindetermining
The implementation and integration process involves the creation of a user-friendly interface and an integration pipelineforthepurposeofdeployingthemodelinclinical settings. It is necessary for this system to be interoperable with the current hospital infrastructure in order to facilitate the processing of fresh patient scans without any interruptions. Radiologists should be able to readily submit MRI images and evaluate segmentation findings, and the interface should be easy to understand and communicate with. A procedure that is streamlined from raw data to final segmentation should be ensured by the integration pipeline, which should comprise automated pretreatment stages, model inference, and post-processing. In the future, study will entail identifying areas that might be improved, such as adding multi-modal imaging data (for example, PET and CT) to offer extra context and information, or investigating various transfer learning approaches and model architectures to further boost performance. The objective is to create a robust, accurate, and therapeutically beneficial tool for the segmentation of pediatric brain tumors. This will be accomplished by continually improving the approach and incorporating newbreakthroughs. which aspects of the technique arethemostsuccessful amongthecomponents.

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN:2395-0072
When compared to models that were trained from scratch, the transfer learning model demonstrated considerable improvements in the segmentation of pediatric brain tumors. It was determined that the Dice coefficient, which is a measurement of the overlap between predicted and ground truth segmentations, averaged 0.87, which indicates that the tumor delineation was performed with a high degree of accuracy. Baseline models that were trained purely on the pediatric dataset, on the other hand, produced an averageDicecoefficientof0.75.Thisoutcomereflectsthe challengesthatwereencounteredwhendealingwiththe unpredictability and the restricted amount of the pediatric data. The Jaccard index, which is another important measure for determining the accuracy of segmentation, showed comparable patterns, with an average of 0.80 for the transfer learning model which was much higher than the baseline models' average of 0.68. These measurements, taken as a whole, provide evidencethatthetransferlearningmethodologyismore effective than other methods in properly detecting tumor locations. An examination of precision and recall reveals that the transfer learning model achieved a precision of 0.85, which is a measurement of the percentage of real positive tumor pixels among all projected tumor pixels. The fact that this is the case suggests that the model was successful in reducing the number of false positives, resulting in fewer inaccurate tumor predictions. This demonstrates that the model is capable of recognizing real tumor locations, even those that are tiny or irregularly shaped. The recall value, which measures the percentage of true positive tumor pixels found among all actual tumor pixels, was 0.88. In addition, the F1 score, which averaged 0.86, provides additional proof of the balanced performance in both accuracy and recall. This harmonic mean of precision andrecallhighlightstheresilienceofthemodelinterms of maintaining a high level of accuracy while also limitingthenumberoffalsepositivesandfalsenegatives for the experiment.When compared to baseline models that were trained from scratch, the performance of the transfer learning model was much better than that of thebaselinemodels.Thebaselinemodelshaddifficulty dealingwith the intrinsic unpredictability and scarcity of the pediatric dataset. As a result, they often overfit to the restricted data and were unable to generalize successfully to additional samples. In contrast, the transfer learning model, which had been pre-trained on the huge and varied dataset of adult brain tumors, was able to efficiently segregate juvenile cancers by using the featurerepresentations that it had learnt. The advantages oftransfer learning
are brought to light by this comparison,especiallyin situations when there is a limited amount of data resourcesavailable
Ablationstudieswerecarriedoutin ordertoevaluate the amount of contribution that was made by the differentcomponentsoftheapproach.Itturnedoutto beveryimportanttofreezetheearlylayersofthepretrained model and then progressively unfreeze them as the model was being trained. By using this technique, the important low-level properties that were learnt from the adult dataset were preserved, while higher-level layers were able to adapt to the pediatric data.The significance of this tactic is shown by the fact that models that did not make use of this progressiveunfreezingmethoddisplayedadownward trend in performance. Furthermore, the dice coefficientandcross-entropylosswerebothincluded into the customized loss function, which had a substantial impact in the overall outcome. The elimination of this combined loss function led to a decrease in the accuracy of segmentation, which demonstrates the efficacy of this function in reducing class imbalances and improving segmentation performanceasawhole.
In order to assess the generalization capacity of the model, a cross-datasetvalidationwascarriedoutwith the assistance of an independent pediatric dataset originating from a separate institution. In spite of the fact that distinct data sources were used, the model continued to exhibit strong performance, although with a minor reduction in metrics. There was a little decrease in both the Dice coefficient and the Jaccard index, which occurred to 0.85 and 0.78 accordingly. Furthermore, there was a little decrease in both precision and recall, with anaverageof0.83and0.86, respectively. The findings of this study provide evidence that the model is capable of generalizing

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN:2395-0072
effectively to fresh data from a variety of clinical contexts.Thisdemonstratesthemodel'sresilienceand its potential to be used to a wide range of patient groups. Visual assessment of segmented pictures by highly trained radiologists served as the qualitative validation of the model's performance, as determined by the qualitative analysis. The clinically accurate segmentations that were created by the transfer learningmodelhadclearlydefinedtumorbordersand hadaminimumamountofnoise.Radiologistsobserved thatthemodelwasespeciallysuccessfulinrecognizing tiny and irregularly shaped tumors, which are sometimes difficult to differentiate from one another. The fact that the segmented pictures were not only quantitatively correct but also clinically relevant was reinforced by this qualitative input, which further substantiated the potential usefulness of the model in actualmedicalpractice.Aconsiderableimprovementin the visual quality of the segmented pictures was achieved with the use of post-processing methods, which included morphological operations and conditional random fields (CRFs). Morphological procedures, such asdilatation and erosion, assisted in smoothing out the borders of the segmented tumors. On the other hand,CRFs increased spatial consistency throughout thesegmentation process by refining the areas that were segmented. As a consequence of these post-processingactivities, the tumor delineations became more accurate and contiguous, as shown by the quantitativemetrics as well as the visual evaluations. The outputsbecame more valuable for clinical interpretation as aresult of the modified segmentations, which improvedthe overallclarityandaccuracyoftheinterpretation.
Figure1. Distributionofdifferenttypesofbrain tumors

The transfer learning technique also exhibited a significant contribution to the overall computational efficiency. When compared to training the model from scratch,trainingitutilizingpre-trainedweightsfromthe
dult dataset took a much lower number of epochs to converge. Not only did this decrease in training time help preserve computing resources, but it also helped speed up the development process as a whole. The efficiencyofthisapproachisespeciallyadvantageousin clinicalsituations,wherequickanalysisisof the utmost importance. The applicability of the transfer learning technique is further shown by the fact that it is able to rapidlyadaptandfine-tunethemodelonfreshpediatric datasets. In terms of clinical implications and future research, the findings of this study shed light on the major therapeutic effect that the transfer learning model now has. Through the provision of precise and effective segmentation of pediatric brain tumors, the model may be of assistance to radiologists in the areas of early diagnosis, tailored treatment planning, and trackingthedevelopmentoftheillness.Furtherworkwill be focused on further strengthening the model by includingmulti-modalimagingdatasuchasPETandCT
scans. These scans may give extra context and information for more extensive analysis, which will be the focus of future study. The investigation of alternate transfer learning methodologies and model architectures, such as ensemble methods or domain adaptation, has the potential to further improve performance. In addition, the generalization capabilities of the model will be improved by increasing the size of the pediatric dataset to include examples that are more variedandhavebeenassignedannotations.Throughthe incorporationofthemodelintoaclinicalinterfacethatis user-friendly, its acceptance in medical practice will be facilitated, which will eventually result in improved patientcareandresults.
Due to data paucity and tumor variety, improving the segmentation accuracy of juvenile brain tumors is a problematic topic. In this work, we studied the use of transfer learning from adult brain tumor datasets to address this. To tackle juvenile brain cancers, we customized and fine-tuned deep learning models that were pretrained on large adult datasets. When contrasted with models trained only on pediatric data, the results showed considerable improvements in segmentation ability. The exact delineation of tumor borders was shown by our transfer learning model, whichattained anaverage Dicecoefficientof 0.87 and a Jaccard index of 0.80. Accurate clinical diagnosis and treatment planning rely on accurately recognizing real tumor pixels, which the model successfully accomplished with few false positives, according to precision and recall measures.Using pre-existing information from adult datasets to improve segmentation results in pediatric instances is more successfulthantrainingbaselinemodelsfromscratchon

International Research Journal of Engineering and Technology (IRJET) e-ISSN:2395-0056
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net p-ISSN:2395-0072
pediatric datasets, which resulted in poorer performance metrics. In comparison to starting from scratch when training models, this method improves computingefficiencybyreducingthenumberoftraining epochs needed, which in turn improves tumor segmentation accuracy. The results of the research highlight the possibility of using transfer learning to overcomethedatarestrictionsandunpredictabilitythat are intrinsic to imaging pediatric brain tumors. This might be a great step towards better diagnostic tools, which would improve patient outcomes and clinical decision-making. In order to keep improving pediatric neuroimaging skills, future research may explore other transfer learning methodologies and use multi-modal imagingdatatofurtherenhancetheseapproaches.
[1] IEEE 20th International Symposium on Biomedical Imaging (ISBI), Cartagena, Colombia, 2023, pp. 1-4, doi:10.1109/ISBI53787.2023.10230757.
[2] A.Wulandari,R.SigitandM.M.Bachtiar,"BrainTumor Segmentation to Calculate Percentage Tumor Using MRI," 2018 International Electronics Symposium on Knowledge Creation and Intelligent Computing (IESKCIC), Bali, Indonesia,2018,pp.292296,doi:10.1109/KCIC.2018.8628591.
[3]M. Dipu, S. A. Shohan and K. M. A. Salam, "Deep Learning Based Brain Tumor Detection and Classification," 2021 International Conference on Intelligent Technologies (CONIT), Hubli, India, 2021, pp. 1-6,doi:10.1109/CONIT51480.2021.9498384
[4]K.Priyadharshini,P.Krishnamoorthy,B.S.GanapathyN, K. Karthikeyan, U. M. S and R. Peddaveni, "Artificial IntelligenceAssistedImprovedDesigntoPredictBrain Tumor on Earlier Stages using Deep Learning Principle," 2023 Annual International Conference on Emerging Research Areas: International Conference on Intelligent Systems (AICERA/ICIS), Kanjirapally, India, 2023, pp. 1-6, doi: 10.1109/AICERA/ICIS59538.2023.10420011.
[5] C. Weber, "Harnessing Another Tool for Treating BrainCancer,"inIEEEPulse,vol.12,no.4,pp.21-23, July-Aug.2021,doi:10.1109/MPULS.2021.3097796
[6] L.C.Paul,M.N.Hossain,M.M.Mowla,M.Z.Mahmud, R. Azim and M. T. Islam, "Human Brain Tumor Detection Using CPW Fed UWB Vivaldi Antenna," 2019 IEEE International Conference on Biomedical Engineering, Computer and Information Technology for Health (BECITHCON), Dhaka, Bangladesh, 2019, pp.1-6,doi:0.1109/BECITHCON48839.2019.9063185
[7] T.P.Pries,R.JahanandP.Suman,"ReviewofBrain Tumor Segmentation, Detection and Classification Algorithms in fMRI Images," 2018 International Conference on Computational and Characterization Techniques in Engineering & Sciences (CCTES), Lucknow, India, 2018, pp. 300-303, doi: 10.1109/CCTES.2018.8674150
[8] M. Kadkhodaei et al., "Automatic segmentation of multimodal brain tumor images based on classification of super-voxels," 2016 38th Annual InternationalConferenceoftheIEEEEngineeringin Medicine and Biology Society (EMBC), Orlando, FL, USA, 2016, pp. 5945-5948, doi: 10.1109/EMBC.2016.7592082
[9] A. Goswami and M. Dixit, "An Analysis of Image SegmentationMethodsfor BrainTumour Detection on MRI Images," 2020 IEEE 9th International Conference on Communication Systems and NetworkTechnologies(CSNT),Gwalior,India,2020, pp. 318-322, doi: 10.1109/CSNT48778.2020.9115791
[10] P. Afshar, K. N. Plataniotis and A. Mohammadi, "BoostCaps: A Boosted Capsule Network for Brain Tumor Classification," 2020 42nd Annual InternationalConferenceoftheIEEEEngineeringin Medicine & Biology Society (EMBC), Montreal, QC, Canada,2020,pp. 1075-1079, doi: 10.1109/EMBC44109.2020.9175922
[11]H.Hu,X.Li,W.YaoandZ.Yao,"BrainTumorDiagnose ApplyingCNNthroughMRI,"20212nd International Conference on Artificial Intelligence and Computer Engineering (ICAICE), Hangzhou, China, 2021, pp. 430-434, doi: 10.1109/ICAICE54393.2021.00090.
[12]J.K.Periasamy,B.SandJ.P,"ComparisonofVGG-19and RESNET-50AlgorithmsinBrainTumorDetection,"2023 IEEE 8th International Conference for Convergence in Technology (I2CT), Lonavla, India, 2023, pp. 1-5, doi: 10.1109/I2CT57861.2023.10126451
[13]T. A. Jemimma and Y. J. Vetharaj, "Watershed Algorithm basedDAPPfeaturesforBrainTumorSegmentationand Classification,"2018InternationalConferenceonSmart Systems and Inventive Technology (ICSSIT), Tirunelveli, India, 2018, pp. 155-158, doi: 10.1109/ICSSIT.2018.8748436
[14]T.A.Soomroetal.,"ImageSegmentationforMRBrain TumorDetectionUsingMachineLearning:AReview,"

International Research Journal of Engineering and Technology (IRJET)
Volume: 11 Issue: 09 | Sep 2024 www.irjet.net
inIEEEReviewsinBiomedicalEngineering,vol.16,pp. 70-90,2023,doi:10.1109/RBME.2022.3185292
[15]R. Nidhya, R. Kalpana, G. Smilarubavathy and S. M. Keerthana, "Brain Tumor Diagnosis with MCNNBased MRI Image Analysis," 2023 1st International ConferenceonOptimizationTechniquesforLearning (ICOTL),Bengaluru,India, 2023, pp. 15, doi:10.1109/ICOTL59758.2023.10435262
[16]M. A. Hafeez, C. B. Kayasandik and M. Y. Dogan, "BrainTumorClassificationUsingMRIImagesand Convolutional Neural Networks," 2022 30th SignalProcessingandCommunications ApplicationsConference(SIU),Safranbolu,Turkey, 2022,pp.1-4,doi:10.1109/SIU55565.2022.9864962
[17]M. Y. Mehemud, H. Binte Kibria and A. Salam, "Efficient Brain Tumor Classification through Transfer Learning Models," 2023 26th International Conference on Computer and Information Technology (ICCIT), Cox's Bazar, Bangladesh, 2023, pp.1-6,doi:10.1109/ICCIT60459.2023.10441144
[18]R. Tamilselvi, A. Nagaraj, M. P. Beham and M. B. Sandhiya, "BRAMSIT: A Database for Brain Tumor Diagnosis and Detection," 2020 Sixth International Conference on Bio Signals, Images, and Instrumentation(ICBSII),Chennai,India,2020,pp.15,doi:10.1109/ICBSII49132.2020.9167530
[19]A. Banerjee, K. Jaiswal, T. Biswas, V. Sharma, M. Bal and S. Mishra, "Brain Tumor Detection and Classification Using a Hyperparameter Tuned Convolutional Neural Network," 2023 6th International Conference on Contemporary Computing and Informatics (IC3I), Gautam Buddha Nagar, India, 2023, pp. 502-506, doi:
2395-0072 10.1109/IC3I59117.2023.10397907
[20] U. M and M. Baskar, "Machine Learning for Brain Tumour Detection: A Systematic Review of Segmentation and Classification Methods," 2023 Intelligent Computing and Control for Engineering and Business Systems (ICCEBS), Chennai,India, 2023, pp. 1-7, doi: 10.1109/ICCEBS58601.2023.10448586