S u r g e r y








Welcome to the Department of Surgery Newsletter!

In this newsletter, we will share with you some of the history of the Department of Surgery, provide in-depth profiles of our faculty, and celebrate the accomplishments of the past year
We are constantly striving to improve and innovate maintaining our position on the forefront of surgical advances
Thank you for your interest in our newsletter and I hope you find the information to be informative and useful.
I am extremely proud of all of your accomplishments and continued commitment to academic surgery!
Barish H. Edil, MD Professor & ChairTo learn more about the University of Oklahoma and the Department of Surgery, visit https://medicine.ouhsc.edu/Academic-Departments/Surgery



What began as a program with a single surgery resident developed into a department containing a team of leading surgical experts providing an array of services to the region and an educational environment where residents and fellows thrive
Initially, the University of Oklahoma Health Sciences Center Department of Surgery was attended by surgeons from the Oklahoma City surgical community
However, in 1915 Dr. LeRoy D. Long of McAlester became the first Dean and Professor of Surgery
From the academic year 1920 to 1921, the department accepted its first surgical resident for a year of training, and as the years went on, more were accepted
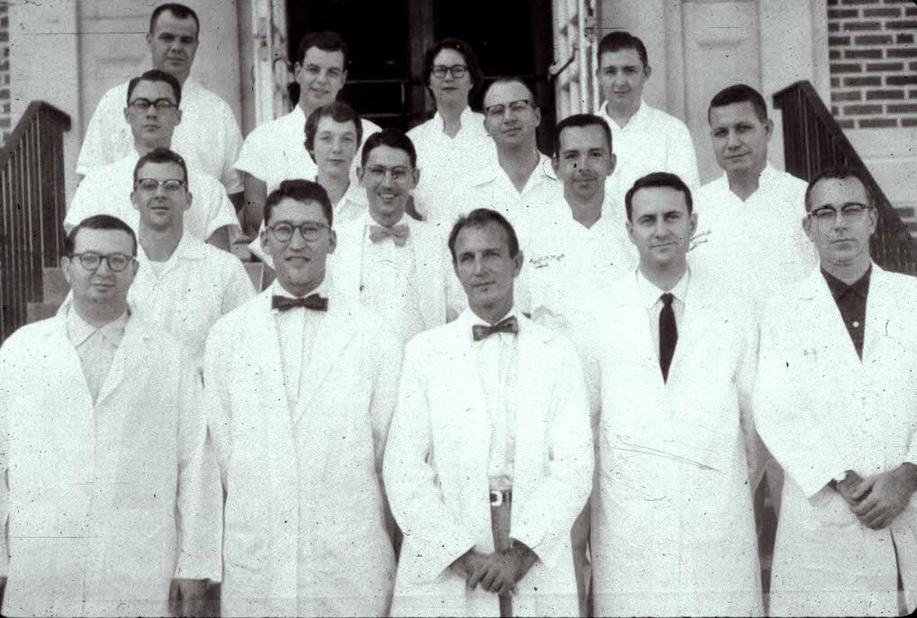
In 1956, Dr John A Schilling became the first full-time Chair of the Department of Surgery
From left to right, standing, Drs William R Richardson and G Rainey Williams; seated, Drs Gilbert S Campbell, Merlin K DuVal Jr , Rene B Menguy, and John A Schilling

Under his tutelage, various surgeons he appointed made up the first original full-time faculty
These faculty members included Dr Merlin K DuVal Jr , Dr Rene B Menguy, Dr Gilbert S Campbell, Dr G Rainey Williams, and Dr William R Richardson
Dr Rainey Williams succeeded Dr Schilling Upon Dr Williams’ retirement, Dr Russell G Postier was named the Chair In 2017 Dr Postier retired, and the current Chair and Professor of Surgery, Dr Barish H Edil, heads the department
Dr John A Schilling was the first full-time Chair of the University of Oklahoma Health Sciences Center Department of Surgery in 1956 Dr Schilling’s career spanned five decades at multiple institutions.
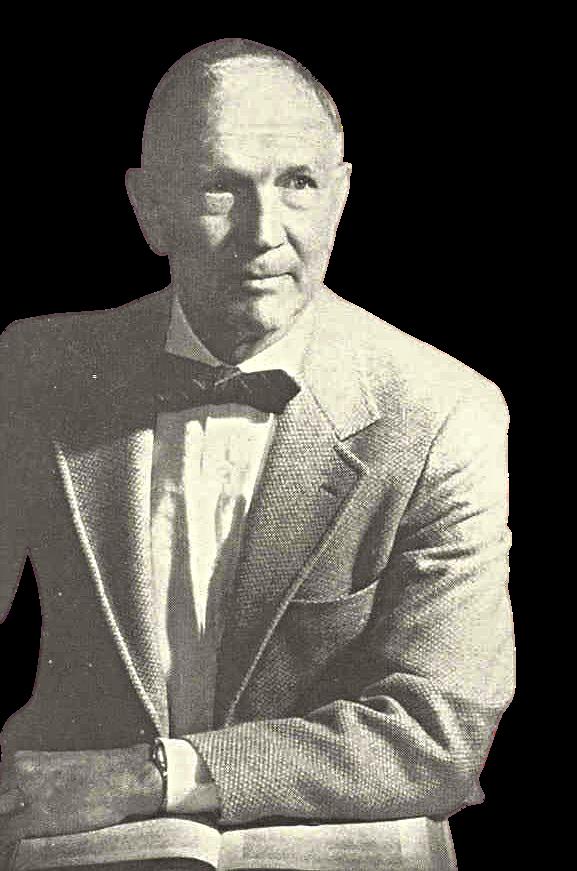
After graduating from Dartmouth in 1937, Dr Schilling attended Harvard Medical School in 1941, the last class to graduate before World War II. Following Harvard, Dr. Schilling worked as a ship’s doctor before completing his residency at the Roosevelt Hospital in New York City
Dr. Schilling was invited to head the Department of Surgery at OU in 1956 and successfully brought various other surgeons to the staff, many of whom ran the department
He remained with the Department for 18 years By the time he left in 1974, Dr. Schilling and his faculty had trained 75 surgeons.
Dr Schilling headed to the University of Washington Department of Surgery before retiring in 1983
Dr Rainey Williams became the new Chair of the Department Surgery following Dr Schilling’s resignation in 1974
Originally from Atlanta, Dr. Williams graduated from Classen High School in 1944, attended the University of Texas from 1944 to 1946, and worked in the Navy V-12 before graduating from the Northwestern University of Medicine in 1950.
Dr Williams completed his General and Thoracic & Cardiovascular Surgery residency at the Johns Hopkins Hospital from 1950 to 1958 Following his residency, Dr Williams joined the first fulltime faculty at the University of Oklahoma Health Sciences Center in July 1958 as an Assistant Professor of Surgery
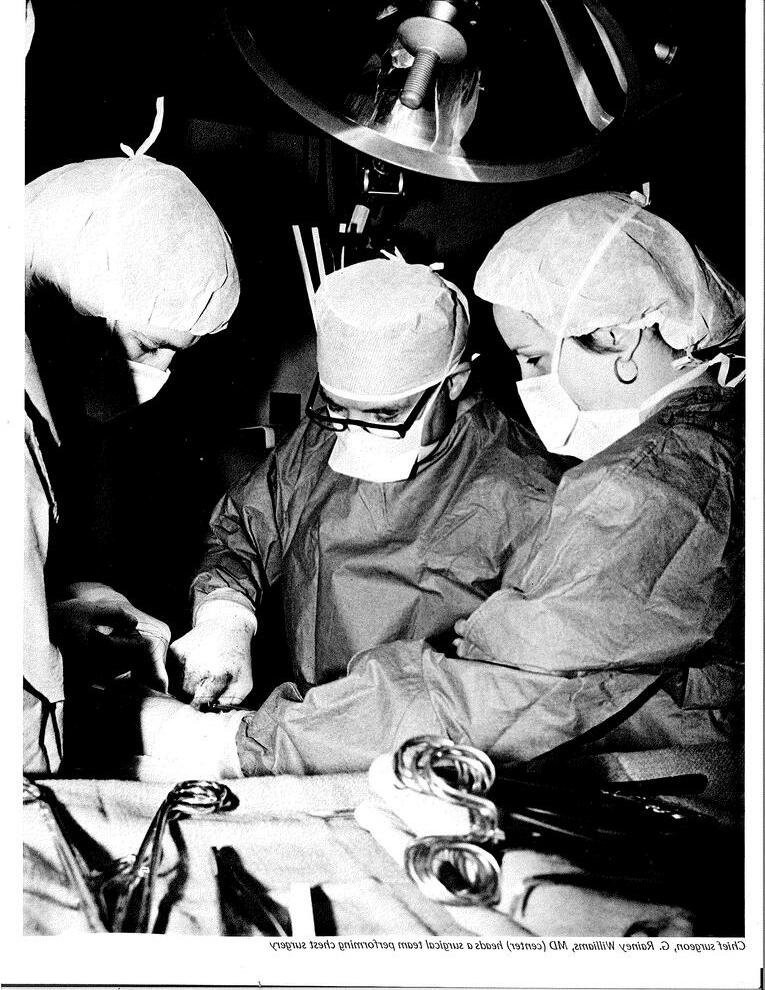
He conducted various research projects, including cardiovascular physiology, which led to him being named a Markle Scholar in 1960 In 1962, he changed the course of his research Eventually, he saved the right arm of OSU basketball player Bob Swaffar
During his time at OU, Dr. Williams performed various general surgeries, lead the Department and educated residents. In 1981, the University offered to make Dr Williams the Dean of the College of Medicine, and though he accepted an interim term as Dean in 1981-1982, he continued leading the Department of Surgery.
Dr Williams retired from his position in 1996 but remained a faculty member until his passing at age 70 in April 1997
Dr Russell Postier became the Chair of the Department of Surgery in 1997 Before taking over the position, Dr Postier was the m 1983 to 1997 He began his service on the
pertise was in gastrointestinal surgery with iary tract and pancreas He attended niversity of Oklahoma College of Medicine ry training at Johns Hopkins University
appointed Interim Executive Dean of the subsequently as the Executive Dean before His dedication to education is most ce of the 91 residents who graduated from his tenure as program director and chair
legacy to ensure all residents and medical st curriculum, research excellence, and changing patient care Dr Postier created M D , Surgical Enrichment Endowed Fund and Postier Lectureship in Pancreas Cancer


Dr Barish Edil became the Chair and Professor of the Department of Surgery in 2017. Dr. Edil completed a Residency in General Surgery and a Research Fellowship in Surgical Oncology at the University of Oklahoma College of Medicine

After completing his residency training, Dr. Edil continued his career as the Assistant Chief of Service at The Johns Hopkins University School of Medicine, receiving a certificate in Surgical Oncology In addition, he completed his postdoctoral training in Cancer Immunology at Johns Hopkins
Dr. Edil remained at Johns Hopkins as an Assistant Professor for the surgery and oncology departments While on the faculty, he performed the first Laparoscopic Pancreaticoduodenectomy (Whipple) operation in the history of the Johns Hopkins Hospital

He later joined the University of Colorado as the first Division Chief of Surgical Oncology While there, Dr Edil was instrumental in pursuing a memorandum of understanding between the CU School of Medicine and the Zhejiang University College of Medicine, one of China’s premier medical institutions, for the transfer of knowledge and sharing of experiences and cutting-edge techniques for pancreas surgery residents and fellows thus promoting the globalization of state-of-the-art healthcare In addition, while at the University of Colorado, Dr. Edil’s team discovered a new cancer vaccine, which is currently being developed for clinical trials.
Dr Edil brings cutting edge knowledge and expertise to the University of Oklahoma with a special interest in pancreas surgery.
Barish H. Edil, MD
Professor/Chair
Jessica Capetillo
Senior Administrative Manager & Executive Assistant
Warren Churchill, MBA, CPA
Senior Clinical Business Administrator
Cheri Parker
Lead Accountant
Mary Sheets
Senior Accountant
Elisabeth Slay, BA
Media Coordinator
Lisa Suriano
Senior Clinical Department Business
Manager
Cardiac, Thoracic & Vascular Surgery
Academic Clinical Faculty
Harold Burkhart, MD
Professor/Division Chief
Klay Buckley
Clinician Educator
Amanda Burris, NP Clinician Educator
Cody Fields Clinician Educator
Joshua Gierman, MD
Associate Professor
Lacy Harville, MD
Assistant Professor Constantine Ionan Clinician Educator
Michael Massoni Clinician Educator
Yuki Nakamura, MD
Assistant Professor
Janelle Nelson Clinician Educator
J. Matthew Reinersman, MD
Assistant Professor
Joni Schroeder, PA
Clinician Educator
Berkeley Stevens Clinician Educator
Carmen Taylor, APRN Clinician Educator
David Vint Clinician Educator
Emily Wilhelm, APRN Clinician Educator
Academic Clinical Support Staff
Jennifer Burks
Administrative Manager
Kristen Earnhardt
Staff Assistant Pediatric Cardiac Surgery
Shelly Jones
Financial Coordinator/Administrative
Assistant
Nashona Ragland
Administrative Manager
Crystal Taylor
Resident Coordinator/ Administrative Assistant
General Surgery / Trauma/Critical Care
Academic Clinical Faculty
Roxie Albrecht, MD Professor/Division Chief
Ann-Marie Alexander, PA Clinician Educator
Scott Blair, DO
Assistant Professor
Mary Margaret Brandt, MD
Professor
Amanda Celii, MD
Assistant Professor
Alisa Cross, MD
Associate Professor Megan Cuoco, PA Clinician Educator
Marielle Del Rosario, PA Clinician Educator
Laura Fischer, MD
Associate Professor
Breanne Fritze, PA Clinician Educator
Kenzee Gambrell, PA Clinician Educator
Lauren Hink, PA Clinician Educator
Ryan Kennedy, MD
Associate Professor
Jason Lees, MD
Professor/Vice Chair of Academic Affairs
Fernando Mier, MD
Assistant Professor Celia Quang-Blair, MD
Assistant Professor
Alexander Raines, MD
Associate Professor
Ashley Richey, NP Clinician Educator
Jessi Siler, PA Clinician Educator
Emily Skinner, PA-C
Associate Professor
Carlee Steele, NP Clinician Educator
Caitlin Stenberg, APRN Clinician Educator
Jacob Steverson, PA-C
Associate Professor
Ronald Taylor, PA-C Clinician Educator
Rachael Thies, NP Clinician Educator
Frank Wood, MD
Assistant Professor
Academic Clinical Support Staff
Amber Fuller
Administrative Assistant Research Faculty
Kenneth Stewart, Ph.D. Assistant Professor Zoona Sarwar Senior Epidemiologist
Ph.D.
BS
Academic Clinical Faculty
Suhair Maqusi, MD Associate Professor/Division Chief
Guilherme Barreiro, MD Assistant Professor
Christian El-Amm, MD Professor
Mark Mims, MD Assistant Professor
Jasmine Ashford Administrative Assistant
Academic Clinical Faculty
Ajay Jain, MD Professor/Division Chief Morgan Bonds, MD Assistant Professor Kristina Booth, MD Associate Professor Steven Carter, MD Assistant Professor Juan Carlos Claros-Sorto, MD Assistant Professor William Dooley, MD Professor Gary D. Dunn, MD Associate Professor Barish Edil, MD Professor/Chair Katherine Morris, MD Professor/Vice Chair of Academic and Research Advancement
Joshy Shabu, NP Clinician Educator
Academic Clinical Faculty Jason Lees, MD Professor/Vice Chair of Academic Affairs
Academic Clinical Support Staff Laura Blackburn, Ed.D. Senior Residency Program CoordinatorSurgery
Nicole Owens, NP Clinician Educator Erin Poole, NP Clinician Educator
The Cardiac, Thoracic, & Vascular Surgery Division of the University of Oklahoma Health Sciences Center Department of Surgery provides patients with highly specialized care from providers dedicated solely to their areas of expertise
Patients receive care from a wellrounded team whose individual members focus on four distinct specialties and a department that combines each area of expertise to create life-saving outcomes for Oklahomans of every age, every day
According to Division Chief Dr Harold Burkhart, recently, U S News and World Report recognized the Division as part of one of the Top 50 Best Children’s Hospitals in the nation for Pediatric Cardiology and Heart Surgery
The surgeons within the Division work closely with the experts at the OU Medicine Cardiovascular Institute, providing people with leading diagnostic, preventive care, and treatment for common and complex ailments

The Division continues to help patients and communities by providing research and education to help reduce and prevent heart and vascular diseases in the state
Over the last year, various surgeons from the Division received honors for their work and grants to further their research
Since 2012, Vascular Surgeon Dr Joshua Gierman, M D , has provided quality care for Oklahoma patients of all ages.
Originally from Michigan, Dr Gierman attended college and medical school in New Orleans before completing his surgical training at the University of Oklahoma College of Medicine and working as a trauma surgeon at OU.
"I did my vascular surgery fellowship in Dallas, and then I came back here in 2012," he said


Dr Gierman explained when he began his medical career, he wasn't planning to become a surgeon.
"When I was going through medical school, I tried not to pigeon-hold myself into some career because I think you set yourself up for disappointment when you do that," he said
However, he always had an interest in the practice, which developed more as he was exposed to it during his education
For Dr Gierman, the best aspect of being a surgeon is helping patients with challenging issues and bettering their lives
"I think the ability to definitively fix problems for patients, and improve the quality of their lives and in some cases save their lives, those are the rewarding things," he said
While he is fond of his profession, Dr Gierman explained it's not without its challenges
"I don't think there's any one thing that makes being a surgeon difficult there are probably many little things that add up to making your life difficult," he said
Despite these hardships, Dr Gierman said bettering patients' lives makes the challenges worthwhile
While he may not perform surgeries entirely unique to the field, Dr Gierman feels he is one of a few doctors to take on challenging vascular surgeries

"I do a lot of thoracic outlet surgery, and I do arteriovenous malformations," he said
Dr Gierman said arteriovenous malformations are benign tumors of blood vessels
The surgeon is proud of his work and that fellow University of Oklahoma employees trust him with their health care
"I think what's unique about vascular surgeons, in general, is that we offer a full service for patients with vascular disease," he said Dr. Gierman is looking forward to divisional growth and expanding the Vascular Surgery program.
"I look forward to working with our colleagues in Tulsa to promote the OU brand of Vascular Surgery throughout the state," he said.
Dr Harville explained when performing a surgery, he acts as the conductor, leading the orchestra of nurses, respiratory technicians, physician’s assistants, and family members, collaborating to produce a work of art

“It is like a big symphony,” Dr Harville said
Dr Harville joined the University of Oklahoma Health Sciences Center Department of Surgery in 2016

Originally from Knoxville, Tennessee, Dr Harville said he grew up knowing he wanted to be a heart surgeon
He began scrubbing into surgeries and working with surgeons when he was 19 years old
“I would drive to Memphis and work with them all summer It started with shadowing, but by the end of five years, they taught me first to assist, harvest vein, and then actually to run the heart and lung machine,” he said
Dr Harville explained he was inspired to become a heart surgeon after reading “The Making of a Surgeon” by William Nolen at 10 years old
Cardiac Surgeon Dr Lacy E Harville III feels he is the maestro in the production that is open heart surgeryIt is like a symphony.
“I was just fascinated by it," he said
Harville attended the University of Tennessee for medical school, and he conducted research on liver transplantation
He explained he worked various rotations and training in liver transplant, cardiac surgery, and general surgery in Houston and San Antonino, Texas
Following his training, Dr Harville returned to his hometown of Knoxville and practiced cardiac surgery for 24 years

During that time, Dr Harville said he helped develop a successful heart education app called Heart Pro 3
"I always liked teaching, and that app was one of the best in the world, and it won all these awards," he said
Dr Harville said working on Heart Pro 3 made him realize his passion for teaching
For the surgeon, there are various aspects he enjoys about being a surgeon
"I like the idea of seeing a patient that has a problem, trying to figure out if surgery is going to make them better, and determining if they are ready for that operation," he said
He also enjoys seeing the patients after their recovery and knowing he helped improve the quality of their lives
"Living longer is not always the best thing, but being able to live your life and be better is," Dr Harville said "And so those are very pleasing "
Dr Harville also finds the technical challenges of surgery appealing
He's also passionate about caring for patients and their families and maintaining communication with the family during an operation
"I have been on the other side when you are waiting for hours, and you did not know if something good or bad is happening," he said
At OU, Dr Harville said he feels grateful for the opportunity to educate residents
“I can hopefully try to impart knowledge and wisdom on them so that they can be better doctors and take better care of my (people),” Harville said
Harville feels navigating the disease process of critically ill patients is challenging as he is responsible for their care and helping them make the difficult decisions of operating or not operating
For Harville, cardiac surgery is an art form in several ways, one being in the act of reconstructing parts of a major organ
“You are trying to rebuild structures within the heart, so that it has the best function for the patient,” he said “If you make a mistake, it can make a big difference, so you ’ ve got to try to achieve perfection all the time ”
Additionally, Harville feels there are various layers to the art of cardiac medicine
“It is an art form to do it a bit, then you cover up your heart, but you get to see it relived because you are seeing patients do things they otherwise would not be able to do,” Harville said “So, it is a different way of viewing the art It is like you have got an art gallery, but you cannot see the painting, but you know they are in there, and they are really good ”
In the future, Harville hopes to continue producing quality surgeries for patients and quality education opportunities for residents

For
The Pittsburgh native explained before coming OU, she attended the University of Scranton for her undergraduate degree, attended medical school in Philadelphia at Thomas Jefferson Medical College, and completed her trauma critical care fellowship at Emory University and Grady Memorial Hospital in Atlanta
Dr Celii explained she was motivated to come to Oklahoma by Dr Alisa Cross who enticed her with exciting tales of different trauma surgeries and cases
"I didn't realize how busy this trauma center was I didn't realize it was the only level-one trauma center in the state," Dr Celii said "I started looking into the hospital and the program and thought it sounded like a great hospital for trauma and a hidden gem "

The medical professional was inspired to become a trauma surgeon after shadowing an emergency room doctor and other surgeons in high school and medical school
 Trauma Surgeon Dr Amanda Celii, the organized chaos within the trauma bay led her to the University of Oklahoma Health Sciences Center Department of Surgery nearly six years ago
Trauma Surgeon Dr Amanda Celii, the organized chaos within the trauma bay led her to the University of Oklahoma Health Sciences Center Department of Surgery nearly six years ago
The controlled chaos is fun to me."
"Hetaughtmehowtosuture,andIsawmyfirstbaby beingborn Isawmyfirstcodeanddeath,andfrom thatexperience,IknewIwantedtodomedicinefor sure,mostlikelymoresurgicalstuff,"shesaid
Dr Celiifurtheredherpassionforsurgerywhenshe wasincollegeafterlearningfromothertypesof surgeons
"WhenIwasaresident,Ijustkindoffellinlovewith trauma Wehadsomesurgeonsthatweretheold schoolsurgeonsthatcoulddoeverything,"Dr Celii said "Sothat'sreallywhatIaspiredtobe"
Dr Celiisaidtraumasurgeonsmustrepairalldifferent areasofthebody
"Traumaprovidesthatunknowneveryday,andI enjoythatchaos Thecontrolledchaosisfuntome," shesaid
Thatchaosisalsooneofthemoredifficultaspectsof hercareer
"Achallengecanalsobenotknowingwhat'scomingin Therearepatternsandthingsyoulookfortotryand makeyourbestjudgmentcallofwhatyouthinkthis person'sinjuriesare,"shesaid "However,knowing exactlywhatyouhavetodoissometimesunclear"
Dr CeliifeelshertimeatGradyandEmory,where chaosiseverywhere,helpedherlearntoembracethe unexpectedandfocusonprovidingthebestpatient care
"Ithinkthatexperiencegavemetheuniqueabilityto cometoOU ItishecticandveryclosetoGradyfrom thepenetratingtraumalevel,andtobeabletostart withminimalneedforextramentoringwasbeneficial," shesaid
WhileattheUniversity,Dr Celiihelpedcreateawhole bloodprogramandatele-traumaprogram
"Ourwholebloodprogramisanewandinnovative producthereatOU Thisallowsustogivetrauma patientsallofthecomponentslostduringbleedingat thesametime,"shesaid Sheexplainedthewholebloodprogramallowsfor improvedhealingoutcomesanddecreasedmortality rates
WearetheonlycenterinOklahomausingthislifesavingproductandoneofahandfulofcenters nationally,"shesaid
Additionally, Dr Celii explained during the COVID-19 pandemic that she began researching and utilizing telemedicine to treat patients
"During this time, as the only level one trauma center in the state, we reviewed our trauma transfers discharged from our emergency department From this, we found a very isolated population of patients that could utilize this new resource and potentially avoid transfer while being able to receive the same evaluation from a subspecialty provider and receive the same care and follow-up," Dr Celii said

The trauma surgeon said the telehealth program helps a rural state such as Oklahoma, that has a stressed trauma system and very few trauma centers
For Dr Celii, trauma surgery both is and isn't an art form because treating trauma is pretty standard but requires the unique ability to see beyond the uniformity
"Trauma surgeons joke that we keep it simple Do ABCDE However, I think there's an art to trauma because there are sometimes such subtle signs of impending badness that you have to be in tune to be able to see," she said
Dr Celii plans to continue developing the whole blood program and telehealth program as well as other projects that will ultimately improve the Division
In November 2019, Trauma and Critical Care Surgeon, Dr Maggie Brandt joined the University of Oklahoma Health Sciences Center Department of Surgery.


Dr Brandt explained she completed most of her medical education training in her hometown of Albuquerque, New Mexico
“I finished my residency in Albuquerque, and then I did my critical care in Rochester, New York, and went to work in Michigan,” she said
Before coming to the University, Dr Brandt practiced for 20 years in Michigan and then decided to transition to Oklahoma after being recruited by Division Chief Dr Roxie Albrecht
Dr Albrecht encouraged Dr Brandt to create a burn care program
“I like doing burns and critical care, and it seemed logical that OU should have the burn center,” she said “To me, trauma and burns go together ”
Dr Brandt said she will always work on ways to further develop the adult burn care program
There's an art and science to it.
“Iwouldlikeustobeaverifiedburnprogram thatcantakecareofprettymuchanybodyin Oklahomathatgetsburned,”shesaid “The ultimategoalistonotsendpeopleoutofthe stateforcare”
Thesurgeonexplainedshewantedtobecome amedicalprofessionalfortheunknownof day-to-daylife
“Ilikesolvingproblems,andIfindthatin surgery,youalwaysknowwhatyouaregoing todo,butyouneverknowwhatyouaregoing todobecausethingscanchange,”Dr Brandt said
Dr Brandtfeelsherpracticeissimilarto polishingsilver,“youstartwithsomethingugly anddirty,andyoudoyourmagic,andviola, youhavesomethingbetterthanwhenwe started”
“Ithasabeginningandanend,”shesaid “Thereisanartandasciencetoit,anditis beingabletostartwithaneventorapromise oraproblemandbeingabletovisualizeitin yourheadandseewheretheresultis”
Dr.Brandtfeelshervastexperiencegivesher adifferentoutlookinherfield.
“Ihavebeendoingthisforaverylongtime, andIhaveseenthingschangeovertime,”she said “Itiscompletelychangingminutebyminute, andwatchingitinevolutioniskindofexciting”
Dr Brandt'sfavoriteaspectofbeinga surgeonisherrelationshipwithapatient “Itisanincrediblyintimaterelationshipwitha person,anditisahugehonorthatpatients trustustotakecareofthem,”shesaid “Now andagain,whenthereisthatflow,and everythingisgoingwell It’smagical”
Dr Brandtsaiditcanbechallengingtobein criticalcareasthereareneverenough resources,andalotoftraumainjuriesare avoidable
“There is so much that happens that truly is preventable, and it is sometimes really disturbing that we just kind of keep doing the same thing over again and expect a different response, ” she said
The General Surgery, Trauma, & Critical Care Division contains a diverse group of surgeons, and Dr. Brandt feels this will help the Division both remain stable and evolve.
“I hope it keeps being a place where those of us who have been around forever and those people who are young and have fresh new ideas are all working together in the same group, ” she said

The medical professionals in the Pediatric Surgery Division are dedicated to providing quality care for children and their families from the first visit to the last
Oklahoma Children's Hospital-OU Health believes in providing quality medical care as the only fully comprehensive children's hospital in the state

According to Dr Catherine Hunter, Division Chief of Pediatric Surgery, the surgeons are board certified and partake in additional training to specialize in the surgical care of infants, children, and young adults
"We treat several congenital anomalies, as well as pediatric tumors, intestinal and thoracic disorders, and care for traumatically injured children," Hunter said "We operate on almost all areas of the body Our patients are as young as 23-24 weeks of gestational age through age 21 "
Dr Hunter explained recently that the Division was recognized in the US News and World Reports Best Children's Hospitals as a top 50 program in Pediatric Gastroenterology and GI Surgery
Additionally, Dr Hunter explained her research group received funding from the Oklahoma Center for Adult Stem Cell Research which is focused on researching necrotizing enterocolitis
"Necrotizing enterocolitis (NEC) is a deadly disease of the newborn and affects five to seven percent of babies in neonatal intensive care units," she said "Prematurity and an abnormal response to bacteria in the gastrointestinal tract contribute to NEC "
Dr Hunter explained not all premature infants develop NEC, and it is this mystery that the group is currently researching
Dr Hunter explained the group conducted three research projects studying necrotizing enterocolitis, including "Experimental Modeling of Necrotizing Enterocolitis in Human Infant Intestinal Enteroids," "A Review of the Diagnosis and Treatment of Necrotizing Enterocolitis," and "Determining Intestinal Permeability using Lucifer Yellow in an ApicalOut Enteroid Model "
The Division also conducted an ethical study entitled "This is Our Lane: A Pilot Study Examining the Surgeon's Role in Social Justice Advocacy," which Dr Hunter said opens a critical dialogue regarding the surgeon's role in directing advocacy efforts that may affect patients

 By Elisabeth Slay
By Elisabeth Slay
Two years ago, Plastic Surgeon Dr Guilherme Barreiro came to the University of Oklahoma Health Sciences Center Department of Surgery to practice his passion for reconstructive surgery and microsurgery
Originally from Brazil, Dr Barreiro completed most of his medical education and training in Brazil and various fellowships worldwide
Dr Barreiro explained he wanted to become a surgeon to positively impact people’s lives
Before coming to the University, he practiced in various places in Brazil but moved to the United States to be with his wife
Dr Barreiro said he enjoys working at an academic institution because he can participate in projects such as clinical research and work with residents
“Bright young minds surround me, ” he said “Sometimes they come up with ideas and questions that are mindblowing ”
For the medical professional, plastic surgery is a complete art form because it is forever evolving

and innovation will shape the future.
“The artistic part of plastic surgery is to be able to develop ways or new techniques where you can achieve good function with good results,” he said

Dr Barreiro said there are similarities between his cases, but also several differences, which he enjoys adapting to
“Even though we are doing breast construction or nose jobs every day Every single patient is different,” he said “The result, the goal, and the face symmetry are all different ”
He loves the artistic elements of plastic surgery but feels it is an extremely challenging profession
“I think the hardships of plastic surgery are similar to the hardships of becoming a surgeon in any area,” he said “Plastic surgery has an extra difficulty because it is such a widespread area from head to toe, and for all ages, you need to be extremely well trained and well dedicated ”
Dr Barreiro said he tries to take an out-of-thebox approach when conducting his surgeries
“I think that creativity and innovation are the things that will shape the future and change the world,” he said “I think that is where I thrive and I try to get everybody around me to get to that level where they are free to think, come up with ideas, and make mistakes ”
Currently, Dr Barreiro is working on robotic plastic surgery to improve flap harvesting techniques and uflap options for reconstructive surgery
“Flaps are tissue that we harvest It can be a transplant from another individual of the same species Still, usually, from the same individual, we harvest areas of excessive tissue to reconstruct areas that are missing,” he said
Dr Barreiro explained there is not a lot of tissue to spare, so it can be challenging to harvest enough for reconstructive surgeries
“Some of them are limited by the surgical techniques we have now ideas I am trying to develop new things to robotics surgery which give a new realm of approach to operating in the body and harvesting new tissues,” Dr Barreiro said
Additionally, the plastic surgeon is working with residents on optimizing results and technical details on reconstructive surgery, flap harvesting, and other areas
“I also have some projects that I am running with bioengineers from OU in Norman to develop new surgical devices for surgery and for monitoring and surgical instruments to help in plastic surgery, ” he said
As time passes, Barreiro hopes the Division will become a recognized center of excellence for plastic surgery
“I think we have all the resources to get there We need to be able to put in some time and organization to get to that point,” Dr Barreiro said
Ten years ago, Division Chief of Plastic Surgery Dr Suhair Maqusi joined the University of Oklahoma Health Sciences Center Department of Surgery

Originally from Jordan, Dr Maqusi moved to the United States after high school
She earned her undergraduate, Master’s, and medical degree at Texas Tech University before completing her general surgery residency at Henry Ford Hospital in Michigan

She then pursued plastic surgery at the University of Illinois, and a hand and microsurgery fellowship at The Kleinert and Kutz Hand Institute in Kentucky
The plastic surgeon said she came to OU to work at an academic institution and to be closer to her home in Lubbock, Texas
“When this job opportunity came about, it was tailored for me I decided to take the opportunity, and ten years later I am still here ” Dr Maqusi said
She explained if she were not a surgeon, she would be an architect Her love for surgery started when she was a child, and it only continued to grow as she got older
In medical school, she was drawn to all surgical specialties and started her path with general surgery followed by plastics
We're the last piece to that puzzle.
For Dr Maqusi, plastic surgery is the ultimate form of art, as it allows her to shape and change things
“The origin of the word plastic surgery is from the Greek word ‘plastikos,’ which means ‘the art of modeling or sculping,’ Dr Maqusi said “What I found appealing about plastic surgery is that it is transforming something that is already there, into something more improved, with a little bit of an artistic touch to it that the patients find very desirable ”
Dr Maqusi finds this extremely rewarding and she explained she was attracted to the specialty because there’s more to it than just cosmetic surgery
“Frequently, we are assisting other surgeons We are assisting in reconstruction after cancer removal, after a major car accident, or with congenital deformities, and we are the last piece to that puzzle that puts things back together,” she said

Dr Maqusi is the first and only female plastic surgeon to join the plastic surgery practice at the University
"Being a part of the Plastics Division at OU has been a great experience and journey,” she said "I have been a part of a great accomplished team that always works together as a unit and strives to be the best ”
Dr Maqusi was named one of the “10 Best Plastic Surgeons” by the American Institute of Plastic Surgeons for 2021 and 2022 and the “Top Plastic and Reconstructive Surgeon” by Top Doctor for 2021 and 2022
Currently, Dr Maqusi is working on various projects, including breast projects, orthopedic surgery, functional muscle revision, and various others
Dr Maqusi said she hopes the Division will become one of the best plastic surgery programs in the nation




The University of Oklahoma Health Sciences Center Surgical Oncology Division provides clinical services at OU Health while educating the surgical oncologists of tomorrow and taking part in advancing the field of medicine through clinical and basic science research
According to Division Chief of Surgical Oncology Dr Ajay Jain, the Division has several active grants in cancer research, autoimmune disease, and other areas
“The grants increase the prestige of the Department, and it shows that we are committed not only to carrying out patient care, but also developing the newest advances in cancer treatment,” he said
Additionally, Dr Jain said the scholarly activity generated through the grants provides an opportunity for students, residents, and faculty to publish, learn how to perform research, and advance their own career goals
There are several active research projects ongoing in the Division by members of the faculty
These include novel fluorescence-based imaging techniques for breast cancer in human patients Additionally, there is ongoing research porcine model of pancreas cancer
“These are genetically modified pigs that develop pancreas cancer within a year when injected surgically into the pancreas with an adenovirus,” Dr Jain said “Using this model, we are investigating novel fluorescencebased methods for early detection of pancreas cancer "
The Division focuses on treating specific diseases so it can ensure high surgical volumes with the greatest quality The types of cancer treated at OU include Breast, Colon, Rectal, and Anal, Hepatobiliary and Pancreas (pancreas, liver, gallbladder, bile ducts), Gastrointestinal (stomach, small bowel, gastrointestinal stromal – GIST) and Cutaneous and Soft Tissue (melanoma, squamous cell, sarcoma)

Recently, Drs Laura Fischer, Fernando Meir, and Alex Raines also joined the Division
They offer advanced, minimally invasive surgical approaches for a variety of benign and malignant diseases
Originally from Lawton, Dr Carter attended OU for his undergrad degree, medical school, and surgical residency Additionally, he attended Baylor University in Dallas for his colorectal surgery fellowship

For Dr Carter, the best aspect of being a surgeon is working in the operating room
“I like anatomy I like doing difficult cases and fixing complex problems,” he said
Dr Carter explained one of the problematic aspects of colorectal surgeries is the high complication rate
“Colorectal surgery has a nationwide complication rate of above 10 percent Dealing with those is a real major challenge,” he said
He said he is currently participating in a multi-institutional study looking at a different way to do bowel anastomosis for Crohn’s disease.
 Colorectal Surgeon Dr Steven Carter came to the University of Oklahoma Health Sciences Center Department of Surgery in 2019 to join the Surgical Oncology Division
Colorectal Surgeon Dr Steven Carter came to the University of Oklahoma Health Sciences Center Department of Surgery in 2019 to join the Surgical Oncology Division
“It is where you remove a piece of intestines and look at a new way to put it back together Hopefully, this novel method can slow down the recurrence of Crohn’s,” he said
Additionally, Dr. Carter explained he is studying ways to decrease post-operative pain following hemorrhoid surgery
Carter is one of the few surgeons in the state who can perform robotic colorectal surgeries including transanal robotic surgery
The surgeon has performed over 400 robotic cases since 2016
When it comes to rectal cancer, Dr Carter said, unlike many other forms of cancer or diseases, the surgeon ’ s volume has been shown to directly impact survival
“The most important factor for survival in rectal cancer is the surgeon, ” he said “If you have rectal cancer, you want to see a colorectal surgeon with a multidisciplinary team ”
A multidisciplinary team includes surgeons, medical oncologists, radiation oncologists, pathologists, radiologists, and ancillary staff such as physical therapists and nutritionists
This team approach is critical in rectal cancer compared to many other cancers This team is currently applying for Rectal Cancer Center of Excellence accreditation
“We are the only ones in the state able to do this We would be one of the few in the entire country The whole point is that it is a team approach,” he said
Dr Carter explained rectal cancer treatment often requires surgery, chemotherapy, and radiation “So, you need all those people talking and forming plans,” he said “I think that’s unique to us ”
Dr Carter said getting the Division its accreditation is the number one priority for the future as it will allow the surgeons such as himself to provide better patient care
Additionally, Carter would like to see the Division offering a colorectal fellowship so future surgeons can continue providing better patient care

 By Elisabeth Slay
By Elisabeth Slay
Before joining the University of Oklahoma Health Sciences Center Department of Surgery faculty in 2018, Surgical Oncologist Dr Juan Claros Sorto began his journey at OU as a resident in 2010

Dr Claros said he is a Breast Surgical Oncologist, which means he is a general surgeon who specializes in breast cancer care
“So, I take care of both malignant and benign breast disease, but the majority of my practice is breast cancer care,” he said
He was born and raised in El Salvador, moved to America at age 16, received a Bachelor’s degree in Science and Biology from William Patterson University, and attended medical school at Mahavir Medical College before completing his residency at OU and his breast cancer fellowship at Texas Tech University
Various aspects inspired Dr Claros to become a surgeon, including the challenge of the specialty and his fathe, who was also a physician
"That lifestyle that he had of waking up early, getting things done early, operating, working, and meeting survivors that he helped cure their cancers molded my decision to go into a surgical oncology field,” he said
It’s removing diseases without anyone seeing it.”
Forthesurgeon,thebestaspectsofbeinga breastsurgicaloncologistarehislong-lasting connectionswithhispatientsandtheirfamilies
“Inothersurgicalspecialties,youdonotgetto knoworinteractwiththepatients,”Dr Claros said.“Withsurgicaloncology,youmeetthem pre-op,beforechemo,afterchemo,post-op, andyouhavetodigdeepintotheirfamily history”
Heexplainedmanytimes,patientswillhave theirfamilieswiththematappointments
“So,yougettoknownotjustthepatientsbut theirfamilies Youreallyneedtofindoutwhat theirsupportsystemwillbe,”hesaid Whilebuildingthatconnectionwithpatientsis oneofthebestaspectsofhisfield,Dr Claros explainedit'salsoastruggle
“Havingpatientsyoungerthanmedyingfroma diseasethatIhavegottentomeetandIhave gottentoknowtheirfamilies,thatischallenging andsomethingIamstilllearninghowtodeal with,”hesaid
Dr Clarosisoneoftheonlybreastoncology surgeonsinOklahomawhospeaksSpanish,and heenjoysprovidingthatsenseofconnectionto hisSpanish-speakingpatients
“Just being able to help our community in my own language, which is their own language, is very rewarding,” he said Dr. Claros feels breast surgical oncology is a form of art because it requires the ability to produce the same results when working with different types of people
He explained each surgery is a new challenge as all breasts vary in size, shape, mass, and more.

“There is an art form at trying to not only remove cancer but doing it in a way where the patient, after all the treatments, can ideally walk out and not notice a difference in their breast size, volume, or shape That’s an art, and you ’ re continuously having to work on, improve on, and develop different techniques to master,” he said “It’s removing diseases without anyone seeing it ”
In the future, Claros hopes the Division and the Department will continue to grow and change.

According to Division Chief Tomasz Kozlowski, the Division increased its ability to perform various transplant surgeries, including liver, kidney, pancreas, living donor kidney transplants, and pediatric liver and kidney transplants

“We are a unique division combining the work of individuals from three different specialties,” Kozlowski said
Four transplant surgeons, two transplant nephrologists, and three transplant
make up the Division
Kozlowski said the Division of Transplantation is developing pilot projects related to acute on chronic alcoholic liver disease as a proinflammatory condition with prothrombotic complications in pre and post-liver transplant settings
Another project under investigation is an attempt of defining a molecular diagnostic panel to differentiate idiopathic pulmonary hypertension from benign fluid overload in organ transplant candidates.
For surgeon Dr Oya Andacoglu the anatomy of a liver is beautiful and the intricacy of transplant operations offers a creative outlet in a profession where perfection is required.
“The operation itself is an art How you do it matters All the details matter That is where art comes in,” Dr Andacoglu said
From monitoring blood pressure to every small detail in the operating room, and how physicians manage patients after the surgery, the medical professional explained performing surgeries is not unlike painting a portrait
“Multiple things add up and dictate your outcome,” She said “You put little details on your painting like a leaf here, a little cloud there, or you put more details into a face, more lines around the eye and it becomes a masterpiece ”
Originally from Turkey, Dr Andacoglu joined the transplant division of the University of Oklahoma Health Sciences Center Department of Surgery in December 2021

Dr Andacoglu was inspired to enter the medical field by her father, a physician, and started observing patients in the ICU and scrubbing in during high school, thus beginning her love for the practice
"I was completely amazed and surgery was such an enticing thing for me, so I had to be a surgeon, ” she said

"Liver anatomy was so amazing to me that I thought I should do something in liver surgery, ” she said
She graduated with Honors from Hacettepe University School of Medicine, in Ankara, Turkey in 2007 and served two years there as a surgical resident before moving to the United States to begin her transplant career
The surgeon attended the University of Pittsburgh Medical Center as a post-doctoral Research Fellow in 2009 and completed her surgical residency at the University of Wisconsin in 2016
Additionally, Dr Andacoglu completed an Abdominal Multi-Organ Transplant and Hepatobiliary Surgery Fellowship at MedStar Transplant Institute at Georgetown University in 2018
She also spent two years in Turkey and worked exclusively in living donor liver transplant surgery
For Dr Andacoglu the best aspect of being a surgeon is the direct impact she has on a patient’s health
“I think surgery is and should be the most humbling job on Earth We are privileged to impact patients’ lives,” she said
Dr Andacoglu stated she is the first female transplant surgeon to practice in Oklahoma, the first female transplant surgery fellow at Georgetown University, and the first Turkish female surgeon to become American Board Certified
In addition to providing quality care, she strives to be a positive role model for young women
“I am very passionate about creating and contributing a truly equal work set up in surgery and in the transplant world,” she said “Women should not be worrying about child care, and family lives while building their careers Similarly, we should not worry about equal pay or leadership opportunities, but we certainly are ”
Dr Andacoglu feels while there have been improvements for women over several decades, more needs to be done
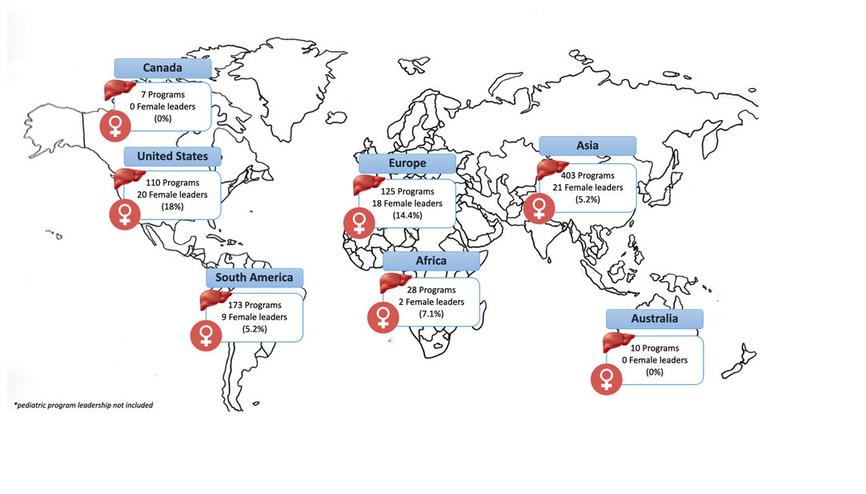
The medical professional stated according to a survey from the International Liver Transplantation Society, which she is a part of, globally only eight percent of women are leaders in liver transplants
Dr Andacoglu is active in various national and international organizations dedicated to providing more opportunities for women and minorities in the medical field
“I am hoping to continue to be a role model, continue to expand leadership in transplant surgery for women and minorities, and to contribute to change things in a better and global way,” she said
To view Gender and Racial Disparity Among Liver Transplantation Professionals: Report of a Global Survey visit:
https://www frontierspartnerships org/articles/10 3 389/ti 2022 10506/full
It
In March of 2021 surgeon, Dr Narendra Battula joined the University of Oklahoma Health Sciences Center Department of Surgery as Surgical Director for the Liver Transplant Division

Dr Battula explained he grew up and attended medical school in India
“I finished my internship and moved to England I did my surgical training including my residency, fellowship, and research at worldrenowned liver transplant centers in the United Kingdom,” he said.
After completing his surgical training in Europe, Dr. Battula moved to America to pursue a multi-organ abdominal transplant fellowship in New Orleans.
He took a job as an Attending at the University of Florida where he practiced for four years before coming to OU Health
Dr Battula was inspired by his colleague Dr Tomasz Kozlowski who encouraged him to join the Division
“He had this project to reshape the transplant program that was not very strong and needed a lot of changes,” he said

“I saw the opportunity and potential to be a part of this growth so I decided to join in ”
Dr Battula said he has helped rebuild the program and feels there has been enormous growth in the Division in the last 18 months
keeps you on your toes.
“It’s a challenging project but it is satisfactory that we have seen this growth,” he said
The medical professional explained that he is qualified to perform various surgeries including liver, kidney, and pancreas transplants as well as hepatobiliary surgeries
Dr Battula said he was inspired to become a surgeon after seeing the complexities of the position and the quick pace process of making decisions regarding patient care

“I like that you can make a huge change in such a short time frame,” he said
While he enjoys his position, he said it is not without its challenges as there are long unsocial hours and years of intense required training
However, Dr Battula said despite the hardships it is worth it to see patients making remarkable recoveries with lifesaving transplant procedures
Dr Battula feels because of his diverse education and training bring him a unique perspective in his field
“I have met people from different cultural backgrounds, worked with personnel with different skill sets, and networked with surgeons from different areas of the world,” he said
For the surgeon, the complexity of multiorgan transplant surgery is what makes it an art form
“You have got to be fast You have got to be precise,” he said “Any wrong move can be unforgiving,” he said.
He explained there is also creativity in the differences between each case.
“Unexpected issues can happen at any time. Although it is somewhat standardized every operation is still unique,” he said. “There are little variations from patient to patient ”
Currently, Dr Battula is working on an organ preservation project he started at the University of Florida
“One of the projects I did was experimenting with oxygenated perfusion solutions for the machine perfusion of organs,” he said
He explained the purpose of this project is to provide a more efficient commercially available solution for organ perfusion as a blood substitute for machine perfusion
The project is still ongoing and Dr Battula and his team are in the process of patenting the technology
In the future, Dr Battula will continue to help the Division evolve and hopes to see it as a leader in transplant surgery throughout the state
“Going forward I want to build a stable program with numbers that will be consistent and with excellent results I want to see the program as the number one choice for patients in the state of Oklahoma,” Battula said
The Department of Surgery Residency Program offers various residency and fellowship training opportunities for future surgeons
The Division is dedicated to teaching and motivating leaders who are committed to practicing the highest quality surgical procedures at every level of care
Three residency programs are offered including general surgery, pediatric surgery, and plastic surgery
Recently, the general surgery residency participated in the launch and beta testing of the Educational Quality Improvement Program (EQIP)
EQIP is a continuous quality improvement program run by program directors for program directors to allow for data-driven innovation in surgical education and to allow data-informed conversations about the future of general surgery
According to Vice Chair of Academic Affairs and Residency Program Director Dr Jason Lees, the Division achieved its third year of a 100 percent American Board of Surgery Board Certified Exam passage rate and currently has zero citations from the Accreditation Council for Graduate Medical Education
“These accomplishments are reflective of the daily efforts of all trainees, the support from our staff, and the instruction provided by faculty,” Dr Lees said
According to the General Surgery Residency Associate Program Director, Dr Kristina Booth, the improvement of the certifying exam scores has been driven by the implementation of three formal opportunities for certifying exam practice
"For many years we have annually hosted a session that is meant to mimic the real event with three rooms and a variety of examiners and topics This allows residents to practice answering back-to-back questions so they get a feel for the speed of the exam as well as practice moving from question to question,” she said
Dr Booth said the second opportunity is an event for PGY5 residents in which faculty examine the residents and then offer feedback on presentation and content to help them hone their oral exam skills while expanding their knowledge
“The most recent addition to our curriculum is examining PGY4 residents twice a year during the department’s Morbidity and Mortality Conference (M&M)
Dr Booth said M&M helps PGY4 residents perform better at the annual mock orals which take place in the Spring and their start in the PGY5 monthly mock orals
“None of these events could be possible were it not for the commitment and availability of the faculty, alumni, and outside practicing surgeons to help ensure our residents are prepared for their certifying exam,” Dr Booth said
Going forward the Education Program will continue to provide the best opportunities to its residents
Don’t be afraid to work hard. Show up. Do your thing.
Husband and wife Drs Connor and Taylor Wilkinson are in the fourth year of their General Surgery Residency at the University of Oklahoma College of Medicine


During their second year, the two met and became a couple
Connor said he was inspired to become a medical professional after witnessing his grandfather go through and survive cancer
“I went to college and thought I wanted to work at a pharmacy because I like organic chemistry,” he said “Then I shadowed a hematologist oncologist, which made me want to attend medical school ”
Connor received his Bachelor’s Degree in Biology at the University of Central Oklahoma and attended the College of Medicine from 2015 to 2019 before beginning his residency
Initially, from Blanchard, Taylor explained she always knew she wanted to be a surgeon
The medical professional graduated with a degree in Chemical Biosciences from OU and received her medical degree at OU College of Medicine before starting her residency
“As I went through medical school and was exposed to various specialties, I was struck by the breadth of skill and knowledge of the general surgeons, ” she said “I wanted to get broad training experience before committing to any specific subspecialty ”
Connor and Taylor got married and are going through their residencies together
They both feel grateful to have the opportunities they do at OU and to be going through the same challenges together
“I feel fortunate that we were able to find a place where we could both obtain great surgical training and be close to home and our families,” Taylor said “It is pretty special to be able to go home and decompress about our work days, difficult operations, and challenging call shifts and know that the other person 100 percent understands ”
Connor and Taylor enjoy the OU community and learning with their fellow residents

“I enjoy the people I love the co-residents I love the faculty. Everyone is willing to help out when needed,” he said.
Taylor loves the family-like atmosphere and support from her colleagues and mentors.
"I enjoy the collegiality with my coresidents. They make spending the long hours at the hospital bearable. This past year I had a baby, and I have felt extremely supported throughout both my pregnancy and the newborn stage by both my coresidents and the faculty here,” Taylor said While going through their residencies, Connor and Taylor are also raising three children
For the couple, one of the more challenging aspects of their residencies is finding the balance between work and personal life
“I think balancing your time is difficult You have friends and family, and you work most of the time, and choosing whom to see when you have your time off is a big challenge,” Connor said
Additionally, Taylor feels one of the biggest struggles for her as she continues her residency is the growth in her level of autonomy and responsibility
“I am constantly self-evaluating while also reminding myself to trust my judgment and do what I know is best for the patients,” she said
Connor advises future residents to learn proper time management and work hard but take care of themselves
"Do not be afraid to work hard Show up Do your thing Take care of your patients Be passionate and find a hobby or something you enjoy doing outside of work,” he said
The father of three explained his favorite pass time is spending time with his children
In the future, Connor wants to have his private general surgery practice in the community and raise his children
Taylor is interested in pursuing a Colorectal Surgery Fellowship after residency
“I hope to have a fulfilling practice where I can make a difference for my patients and create a positive work environment and raise happy and kind children,” she said





 Hayden Bryan University of Oklahoma COMOklahoma City
Caroline Freedle Texas Tech University Health Science Center SOM
Heather Grubbs East Tennessee State University James H Quilen COM
Kaitlin Pardue University of South Alabama COM
Abigail Roberts University of Oklahoma COMTulsa
Hayden Bryan University of Oklahoma COMOklahoma City
Caroline Freedle Texas Tech University Health Science Center SOM
Heather Grubbs East Tennessee State University James H Quilen COM
Kaitlin Pardue University of South Alabama COM
Abigail Roberts University of Oklahoma COMTulsa





 William Patrick Browne University of Oklahoma COMOklahoma City
Coleman Dennis University of Arkansas for Medical Sciences COM
Amy Gin University of Oklahoma COMOklahoma City
Garrett Hauck University of Oklahoma COMOklahoma City
Michael Kutteh University of Oklahoma COMOklahoma City
William Patrick Browne University of Oklahoma COMOklahoma City
Coleman Dennis University of Arkansas for Medical Sciences COM
Amy Gin University of Oklahoma COMOklahoma City
Garrett Hauck University of Oklahoma COMOklahoma City
Michael Kutteh University of Oklahoma COMOklahoma City
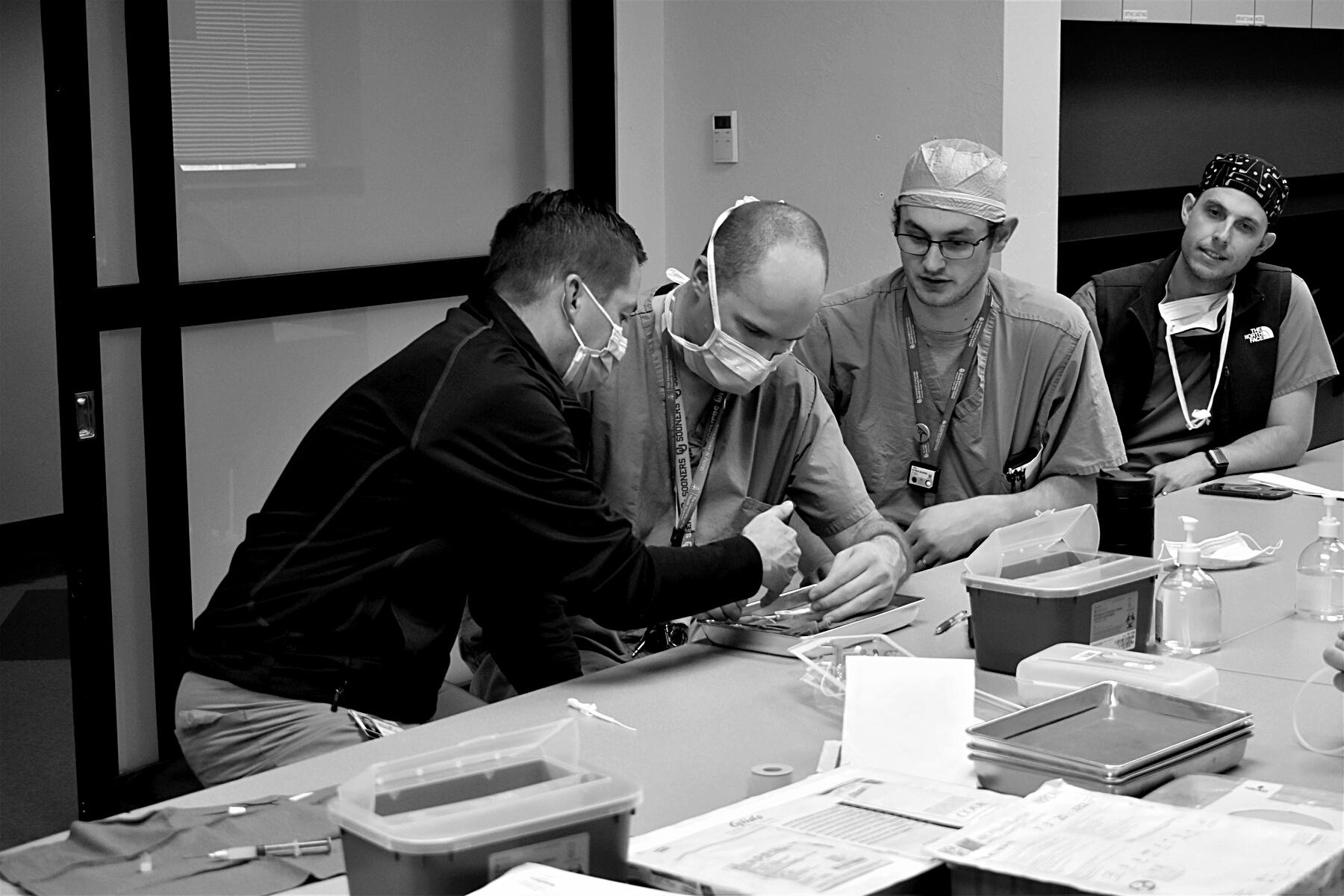
 Dr. Taylor Martin, M.D. received the Outstanding Trauma Resident Award
Dr. Taylor Martin, M.D. received the Outstanding Trauma Resident Award



For the last five years, Assistant Professor for the University of Oklahoma Health Scenes Center Department of Surgery Dr William Berry has studied and researched topics to further the medical field
Dr Berry attended OU as a graduate student from 2006 to 2013 and received his P.H.D. from the University of Oklahoma Health Sciences Center
Dr Berry explained he was inspired to enter the research field as an undergraduate at OU


“I got some research experience research in human subjects and started noticing changes and wanted to know why those changes were occurring,” he said “I wanted to learn what was happening at the cellular and molecular levels ”
Recently, Dr Berry received funding through an NIH grant called the Maximizing Investigators Research Award (MIRA) to continue his studies of peritoneal adhesion tissue, a common complication of intraabdominal surgery
“The surgeons they go in, they open up the belly, remove a tumor, remove an organ, and most times they can do what they do,” he said “If they are moving the tumor, the patient may be fine, or remove an organ, and the patient may be fine, except they may get deleterious scar tissue.”
The researcher explained that scar tissue could cause issues for patients later in their lives.
“We need to have better ways to prevent scar tissue from forming So that is what I study: ways of learning about how the scar tissue forms and then trying to find ways to stop it from forming,” Dr Berry said
The medical professional explained peritoneal adhesion tissue could impact various people, including a new mother undergoing a C-section, patients with digestive issues, and more
Dr Berry’s daughter inspired his study of peritoneal adhesion tissue
“So, my daughter was born with a condition called gastroschisis What that is, is the abdomen does not close on time, and the abdomen is open, and the organs are just kind of out,” he said
“Around 10 to 12 weeks, that closes, and we get a belly button In a subset of kids with gastroschisis, which it is getting more prominent, it will not close on time," he said Dr Berry said his daughter was born around 37 weeks with her intestines on the outside of her body She is living a healthy life at eight years old However, Dr Berry explained that due to the surgery to place her intestines back in her abdomen, his daughter could have health issues in the future
“It was one of those rare circumstances where you are affected directly by something I was interested in studying that and had an opportunity; that is what made me a good fit in the Department of Surgery,” he said
As part of his research, Dr Berry and his team created models of the peritoneal adhesion tissue by utilizing animals
“We do an open (animal) abdominal surgery and cause them to form this tissue,” he said, “And that is how we test to see if we can prevent it from forming ”
Additionally, through IRB protocols, Dr Berry utilizes tissue samples from human patients He can perform these methods through funding provided by his gran
“I could not do this without the grant So, it is five years of funding totaling $1 25 million So, it allows me to have two employees senior level,” he said
Dr Berry explained to receive his grant, he submitted a publication and proposal of his research project, which he feels displays the most artistic element of his field
“We are partly judged on our innovation Innovation is art because you are trying to do something that no one has done before, which is hard,” he said
In the future, Dr Berry hopes to continue his research and find ways to prevent this tissue from forming
“It applies to more than just the adhesion tissue, such as other forms of fibrosis It is a tissue with lots of collagen in it, and there are a lot of diseases which are going to be very similar in how they form,” he said “So, to be able to take what we learn from this and maybe apply it for patients with liver fibrosis or lung fibrosis would be great ”




 Dr Nita Ahuja
Dr Nita Ahuja




 Dr Nita Ahuja
Dr Nita Ahuja












The
Aditi
Bailey
The resident included the following:
Arthur
Maureen
Jackie
Rachael
2021-2022 Chief Residents received their Captain's Chair at the Chief Resident Farewell Breakfast on June 16, 2022. Grimes, M.D., Trauma Surgery and Surgical Critical Care Fellowship - Wake Forest Baptist Medical Center, Winston-Salem, North Carolina Isabella, M D , Colorectal Surgery Fellowship – Louisiana State University Health Sciences Center, New Orleans, Louisiana.
Harold Burkhart, MD
Burge KY, Gunasekaran A, Makoni MM, Mir AM Burkhart HM Chaaban H Clinical Characteristics and Potential Pathogenesis of Cardiac Necrotizing Enterocolitis in Neonates with Congenital Heart Disease: A Narrative Review J Clin Med 2022 Jul 9;11(14):3987 doi: 10 3390/jcm11143987 PMID: 35887751; PMCID: PMC9320426
Burkhart HM Mir A Nakamura Y
Commentary: Diastolic dysfunction and timing of pulmonary valve replacement in tetralogy of Fallot J Thorac Cardiovasc Surg 2022 Mar 5:S00225223(22)00237-9 doi: 10 1016/j jtcvs 2022 02 043 Epub ahead of print PMID: 35337677
Chohan A, Abraham CJ, Ward K, Ponniah K, Salkini A, Burkhart HM, Mir A Isolated ostial left main coronary artery stenosis causing ischemic cardiomyopathy in a child with bicuspid aortic valve: Role of echocardiography in diagnosis and follow-up Ann Pediatr Cardiol 2022 Jan-Feb;15(1):84-86 doi: 10 4103/apc apc 78 21 Epub 2022 Jun 14 PMID: 35847396; PMCID: PMC9280105
Nakamura Y, Burkhart HM Staged unifocalization revisited J Card Surg 2022 Apr;37(4):967-968 doi: 10 1111/jocs 16296 Epub 2022 Feb 9 PMID: 35137983
Nakamura Y, Schwartz R, Mir A, Burkhart HM Tracheobronchial Release for Left Bronchus Compression After Aortic Arch Repair World J Pediatr Congenit Heart Surg 2022 Mar 9:21501351221084303 doi: 10 1177/21501351221084303 Epub ahead of print PMID: 35261322
Ross CJ, Trimble EJ, Johnson EL, Baumwart R, Jolley MA, Mir A, Burkhart HM, Lee CH A pilot investigation of the tricuspid valve annulus in newborns with hypoplastic left heart syndrome JTCVS Open 2022Jun;10:324-339 doi: 10 1016/j xjon 2022 02 015 Epub 2022 Feb 24 PMID: 35937182; PMCID: PMC9354836
J Matthew Reinersman, MD Lindsey, L , Rasmussen, L , Hendrickson L Frech E Bozell S Stewart, K , Kennedy, R , Cross, A , Albrecht R Celii A (2022) Trauma transfers discharged from the emergency department-Is there a role for telemedicine? The Journal of Trauma and Acute Care Surgery 92(4) 656-663 DOI: doi: 10 1097/TA 0000000000003505
Palumbo R Sarwar Z Stewart K Garwe, T , Reinersman, J M (2022) Predictors of Success When Implementing an electromagnetic Navigational Bronchoscopy Program
The Journal of Surgical Research, 274, 248-253 PMID: 35216801 DOI:10 1016/j jss 2022 01 025
Yuki Nakamura, MD Abraham CJ, Salkini A, Burkhart H, Nakamura Y, Mir A Spontaneous thrombus formation in native aortic root in patients with hypoplastic left heart syndrome: clinical presentation, treatment, and outcomes Cardiology in the Young 2022
Burkhart HM, Mir A, Nakamura Y
Commentary: Diastolic dysfunction and timing of pulmonary valve replacement in tetralogy of Fallot J Thorac Cardiovasc Surg 2022 Mar 5:S00225223(22)00237-9
Burkhart HM, Mir A, Nakamura Y
Commentary: Congenitally corrected transposition of the great arteries: Is anatomic repair the preferred approach? J Thorac Cardiovasc Surg, accepted
Carr K Nijres BM Windsor JJ Nakamura Y, Karimi M, Ricci M, Aldoss O Single Center Experience of Hybrid Pulmonary Valve Replacement Using Left Anterior Thoracotomy with Pulmonary Artery Plication in Patients with Large Right Ventricular Outflow Tract J Am Heart Assoc 2022 Jul 19;11(14):e026517
Nakamura Y, Burkhart HM Staged unifocalization revisited J Card Surg 2022 Apr;37(4):967-968
Nakamura Y, Burkhart HM Sinus of Valsalva aneurysm: defining the optimal approach J Card Surg 2022, accepted
Nakamura Y, Schwartz R, Mir A, Burkhart HM Tracheobronchial release for left bronchus compression after aortic arch repair World J Pediatr Congenit Heart Surg 2022 Mar 9:21501351221084303
Roxie Albrecht, MD Harrell, K , Grimes, A , Albrecht, R , Reynolds, J , Ueland, W , Sciarretta, J , Todd, S , Trust, M , Ngoue, M , Thomas, B , Ayuso, S , LaRiccia, A , Spalding, C , Collins, M , Collier, B , Karam, B , De Moya, M , Lesier, M , Chipko, J , Haan, J , Lightwine, K , Cullinane, D , Falank, C , Phillips, R , Temp, M , Alam, H , Udekwu, P , Sanin, G , Hildreth, A , Biffl, W , Schaffer, K , Marshall, G , Muttalib, O , Nahmias, J , Shahi, N , Moulton, S , Maxwell, R (2021)
Management of blunt traumatic abdominal wall hernias: A Western Trauma Association multicenter study The Journal of Trauma and Acute Care Surgery, 91(5), 834-840 DOI: doi: 10 1097/TA 0000000000003250
Lindsey, L , Rasmussen, L , Hendrickson, L , Frech, E , Bozell, S , Stewart, K , Kennedy, R , Cross, A , Albrecht, R , Celii, A (2022) Trauma transfers discharged from the emergency department-Is there a role for telemedicine? The Journal of Trauma and Acute Care Surgery, 92(4), 656-663 DOI: doi: 10 1097/TA 0000000000003505
Amanda Celii, MD
Lindsay MD L J Rasmussen BSN RN, L +, Hendrickson, BS, L S +, Frech, BA E S + Bozell BS S P + Stewart PhD, MPH, K E +, Kennedy, MD, R O + Cross MD A + Albrecht MD R M +, Celii, A + (2021) Trauma
Transfers Discharged From The Emergency Department - Is there a Role for Telemedicine? Journal of Trauma and Acute Care Surgery, 2 DOI:10 1097/TA 0000000000003505
Tracy B M Paterson C W Torres D M , Young, K , Celii, A , Saxe, J M , Kinstedt D P Zielinski M D Camazine, M , Yeh, D D , Gelbard, R B (2021) Prolonged Antibiotics for Common Bile Duct Stones are Associated with Worse Outcomes: Post-hoc Analysis of an EAST MCT National Library of Medicine, 234-240 PMID: 34144566 DOI: 10 1097/TA 0000000000003203
Wandling, M , Cuschieri, J , Kozar, R , O'M, L , Celii, A , Starr, W , Burlew, C C , Todd, S R , Leon, A D , Melntyre, R C , Urban, S , Biffl, W L , Bayat, D , Dunn, J , Peck, K , Rooney, A S , Kornblith, L , Callcut, R A, Lollar, D I , Ambroz, E , Leichtle, S W , Aboutanos, M B , Schroeppel, T , Hennessy, E A , Russo, R , McNutt, M (2021) MultiCenter Validation of the Bowel Injury Predictive Score (BIPS) for the Early Identification of Need to Operate in Blunt Bowel and Mesenteric Injuries Journal of Trauma and Acute Care Surgery DOI: https://doi org/10 1016/j injury 2021 07 026
Alisa Cross, MD Lindsay, MD, L J , Rasmussen, BSN, RN, L S , Hendrickson, BS, L S , Frech, BA, E S , Bozell, BS, S P , Stewart, PhD, MPH, K E , Kennedy, MD, FACS, R O , Cross, MD, FACS, A , Albrecht, MD, FACS, R M , Celii, MD, FACS, A M (2022) Trauma Transfers Discharged from the Emergency Department- Is There a Role for Telemedicine? Journal of Trauma and Acute Care Surgery, 92(4), 656-663 PMID: 34936588 DOI: 10 1097/TA 0000000000003505
McGaha, P , Klingensmith, M , Cross, A M Stewart K Grimes A Horton M Kowdley, G , Patel, Galante, J , P , Delman K Joshi A (2021) Trainee Utilization of the SCORE Curriculum is Associated With Improved ABSITE Performance: A Multi-institutional Study Journal of Surgical Education PMID: 34384730 DOI: https://doi org/10 1016/j jsurg 2021 06 022
Laura Fischer, MD
Parmar, C , Zakeri, R , Abouelazayem, M Shin T Aminian A Mahmoud T Abu-Dayyeh, B , Wee, M , Fischer, L E Daams F Mahawar K (2022) Esophageal and gastric malignancies after bariatric surgery: a retrospective global study Surgery for Obesity and Related Diseases 18(4) 464-472 PMID: 35065887 DOI: doi: 10 1016/j soard 2021 11 024
Ryan Kennedy, MD
Lindsay L Rasmussen L Kennedy R Celii, A # (2022) Trauma Transfers Discharged from the Emergency Department - Is There a Role for Telemedicine? Journal of Trauma and Acute Care Surgery PMID: 34936588 DOI: 10 1097/TA 0000000000003505
Urner M Kennedy R COVID-19
Critical Care Consortium Investigators (2022) Venovenous extracorporeal membrane oxygenation in patients with acute covid-19 associated respiratory failure: comparative effectiveness study BMJ PMID: 35508314 DOI: 10 1136/bmj-2021-068723
Yorkgitis, B K , Berndtson, A , Cross, A M Kennedy R Kochuba M Costantini, T (2022) American Association for the Surgery of Trauma / American College of SurgeonsCommittee on Trauma Clinical Protocol for Inpatient Venous Thromboembolism Prophylaxis after Trauma Journal of Trauma and Acute Care Surgery, 92(3), 597-604 PMID: 34797813 DOI: 10 1097/TA 0000000000003475
Jason Lees, MD Booth, K K , Stewart, K E , Lewis, S L , Garwe, T , Kempenich, J W , Lees, J S (2021) Correlation of Supervised Independence and Performance with Procedure Difficulty amongst Surgical Residents Stratified by Post Graduate Year Journal of Surgical Education, 78(6) PMID: 3452656 DOI: 10 1016/j jsurg 2021 08 002
Biffl, W L , Ball, C G , Moore, E E , Lees, J , Todd, S R , Wydo, S , Privette, A , Weaver, J L , Koenig, S M , Meagher, A , Dultz, L , Udekwu, P O , Harrell, K , Chen, A K , Callcut, R , Kornblith, L , Castelo, M , Schaffer, K B (2021) Don't Mess with the Pancreas! A Multicenter Analysis of the Management of Low-Grade Pancreatic Injuries The Journal of Trauma and Acute Care Surgery PMID: 34039927 DOI: 10 1097/TA 0000000000003293
Kramer, DO, MS, B , Plitt, MD, G , French, PhD, J C , Nygaard, PhD, R M , Cassaro, MD, FACS, S , Edelman, MD, MSHPEd, FACS, D A , Lees, MD, FACS, J , Meier, MD, MEd, FACS, FAAP, A H Joshi MD FACS A R T Johnson, MD, M P , Chavez, MD, J , Hope MD FACS W W Morrissey DO, FACS, S , Gauvin, MD, J M , Puri, MBBS MS FACS R LaFemina MD FACS, J , Kang, MD, H S , Harzman, MD A E Jaafar MD S Chandramouli, MD, M A , Lipman, MD, MHPE FACS FASCRS J M (2022) A Multicenter Analysis of the Early Impact of COVID-19 on Junior
Relles, MD,
Murphy, BBA, S
Ciolkosz, MS, J , Fise, JD, T , Klingensmith, MD, M E , Hickey, MA, M , Brunsvold, MD, M E , Korndorffer, JR MD, J R , Jarman, MD, B T , Smith MD, MPH, D S , Terhune, MD, MBA, K , Kmiec, MHA, K , Harrington, MD, D T , Lees, MD, J , Edhayan, E DiSiena, M , Kent, T , Rubino, M , Prabhu, A , Rosenkranz, K , Brown, C , Edelman, D , Srinivasan, J , Cagir, B , Surick, B , Neville, A , Choi, J N , Yeung, L , Cassaro, S , Iverson, K , Nepomnayshy, D , Namm, J , Dorion, H , Truitt, M , Hope, W , Berman, R, Harzman, A , Kothuru, R , Feinman, M , Hoey, B , Dresner, L , Williams, M , Chojnacki, K , Schroll, R , Nehler, M , Sarosi, G , Porter, M , Kavic, S , LaFemina, J , Kempenich, J , Daley, B , Bailey, C , Chang, L , Hildreth, A , Borgstrom, D , Tuttle, R M , Mpinga, E , Rivera, N , Hai, S Zera R Halverson A Schurr M Bradley, M , Sirsi, S , Fuhrman, G , Brasel, K Palesty A Nehler M R Crandell M Thambi-Pillai, T , O Rourke, A P (2022) EQIP's First Year: A Step Closer to
Alex
Kristina Booth , MD Booth, K K , Stewart, K E , Lewis, S L Garwe T Kempenich J W Lees J S (2021) Correlation of Supervised Independence and Performance with Procedure Difficulty amongst Surgical Residents Stratified by Post Graduate Year Journal of Surgical Education, 78(6) PMID: 3452656 DOI: 10 1016/j jsurg 2021 08 002
Grimes, A D , Stewart, K E , Morris, K T Dunn G D Booth K K Carter S N , Garwe, T , Sarwar, Z , Fischer, L E (2021) The Effect of Body Mass Index on the Creation of an EndColostomy in Rectal Cancer Patients
American Journal of Surgery, 31348211047474 PMID: 34633227 DOI: 10 1177/00031348211047474
William Dooley, MD
EB Finn C Corcoran K Blumencranz LE, Audeh W; NBRST Investigators Group Distinct Neoadjuvant Chemotherapy Response and 5-Year Outcome in Patients With Estrogen Receptor-Positive, Human Epidermal Growth Factor Receptor 2Negative Breast Tumors That Reclassify as Basal-Type by the 80Gene Signature JCO Precis Oncol 2022 Apr;6(1):e2100463 doi: 10 1200/PO 21 00463 PMID: 35476550; PMCID: PMC9200401
Hills, N , Macall, L , Davis, R , Crowell, M , Kamemyama, H , Rui, H , Chervoneva, I , Dooley, W C , Tanaka, T (2021) ASO Author Reflections: Does Prompt Breast-Conserving Surgery Matter? Annals of Surgical Oncology, 28(11), 5906-5906 PMID: 33666812 DOI: DOI: 10 1245/s10434-021-09753-x
Whitworth PW, Beitsch PD, Murray MK, Richards PD, Mislowsky A, Dul CL, Pellicane JV, Baron PL, Rahman RL, Lee LA, Dupree BB, Kelemen PR, Ashikari AY, Budway RJ, LopezPenalver C, Dooley W, Wang S, Dauer P, Menicucci AR, Yoder EB, Finn C, Blumencranz LE, Audeh W Genomic Classification of HER2-Positive Patients With 80-Gene and 70-Gene Signatures Identifies Diversity in Clinical Outcomes With HER2Targeted Neoadjuvant Therapy JCO Precis Oncol 2022 Sep;6:e2200197 doi: 10 1200/PO 22 00197 PMID: 36108259; PMCID: PMC9489196
Whitworth P, Beitsch PD, Pellicane JV, Baron PL, Lee LA, Dul CL, Nash CH 3rd, Murray MK, Richards PD, Gittleman M Budway R Rahman RL Kelemen P, Dooley WC, Rock DT Cowan K Lesnikoski BA Barone JL, Ashikari AY, Dupree B, Wang S Menicucci AR Yoder EB Finn C, Corcoran
Whitworth, MD, P , Beitsch, MD, P , Pellicane, MD, J , Baron, MD, P , Lee, MD, L , Dul, MD, C , Murray, MD, M , Gittleman, MD, M , Budway, MD, R , Rahman, MD, R , Kelemen, MD, P , Dooley, W C , Rock, MD, D , Cowan, MD, PhD, K , Lesnikoski, MD, B -A , Barone, DO, J , Ashikari, MD, A , Dupree, MD, B , Wang, MS, S , Menicucci, DO, A , Yoder, MS, E , Finn, BS, C , Corcoran, MPH, K , Blumencranz, PhD, L , Audeh, MD, MS, W (2022) Distinct Neoadjuvant Chemotherapy Response and 5-Year Outcome in Patients With Estrogen Receptor–Positive, Human Epidermal Growth Factor Receptor 2–Negative Breast Tumors That Reclassify as Basal-Type by the 80-Gene Signature JCO Precision Oncology - An American Society of Clinical Oncology Journal, 6 11 PMID: 35476550 DOI: https://doi org/10 1200/PO 21 00463
Barish Edil, MD M , Ding, D , Qin, T , Wang, H , Liu, Y , Lu J Zhang H Zhao J Wu C -H Javed, A , Wolfgang, C , Guo, S , Chen, Q Zhao W Shi W Zhu F Guo X Li, X , He, R , Xu, S , Edil, B H , Tien, Y -W Jin G Zheng L He J Qin R (2021) New staging classification for pancreatic neuroendocrine neoplasms combining TNM stage and WHO grade classification [] Cancer Lett 2021 Oct 10;518:, 207-213 PMID: 34271105 DOI: 10 1016/j canlet 2021 07 018
Sun, Y , Chen, W , Torphy, R , Yao, S , Zhu G Lin R Lugano R Miller E N , Fijuwara, Y , Bian, L , Zheng, L , A, S Gao F Zhang W Ferrara S E Goodspeed, A E , Dimberg, A , Wang, X -J Edil B H Barnett C C Schulick, R D , Chen, L , Zhu, Y (2021) Blockade of the CD93 pathway normalizes tumor vasculature to facilitate drug delivery and immunotherapy Sci Transl Med 2021 Jul 28;13, (604):eabc8922 PMID: 34321321 DOI: 10 1126/scitranslmed abc8922
Wang, H , Ding, D , Qin, T , Zhang, H , Liu, J , Zhao, J , Wu, C -H , Javed, A , Wolfgang, C , Guo, S , Chen, Q , Zhao, W , Shi, W , Zhu, F , Guo, X , Li, X , Peng, F , He, R , Xu, S , Jin, J , Wu, Y , Nuer, A , Edil, B H , Tien, Y -W , Jin, G , Zheng, L , He, J , Liu, J , Liu, Y , Wang, Qin, R (2021) Prognostic validity of the American joint committee on cancer eighth edition staging system for well-differentiated pancreatic neuroendocrine tumors HPB (Oxford) 2021 Nov :S1365182X(21)01671-3 PMID: 34836754 DOI: 10 1016/j hpb 2021 10 017
Gary Dunn, MD
Lacey McNally, MD
Morgan Bonds, MD Bonds, M M , Garwe, T , Rozich, N , Oluborode, B , Sarwar, Z , Postier, R G , Morris, K T (2021) Risk Factors
Associated With Readmission After Pancreatectomy: A Single-Institution Retrospective Cohort Study The American surgeon, 3134820988824 PMID: 33517699 DOI: 10 1177/0003134820988824
Grimes, A D , Stewart, K E , Morris, K T , Dunn, G D , Booth, K K , Carter, S N , Garwe, T , Sarwar, Z , Fischer, L E (2021) The Effect of Body Mass Index on the Creation of an EndColostomy in Rectal Cancer Patients American Journal of Surgery (31348211047474) PMID: 34633227 DOI: 10 1177/00031348211047474
Xu Y -F Xu X Bhandari K Gin A Rao, C , Morris, K T , Hannafon, B, Ding W -Q (2021) Isolation of ExtraCellular Vesicles in the Context of Pancreatic Adenocarcinomas: Addition of One Stringent Filtration Step Improves Recovery of Specific MicroRNA's PLos One, 16(11), e0259563 PMID: 34784377 DOI: 10 1371/journal pone 0259563
MD Dennahy I S MacCuaig W M Chalfant, H M , Condascse, A ,
J M Claros-Sorto J C Razaq, W ,
J , Squires R A Edil B Jain A McNally, L R (2022) Nanotheranostics for Image-Guided Cancer Treatment MDPI, 14(917) DOI: 10 3390
STARSurg Collaborative and EuroSurg Collaborative Validation of the OAKS prognostic model for acute kidney injury after gastrointestinal surgery
BJS Open 2022 Jan 6;6(1):zrab150 doi: 10 1093/bjsopen/zrab150 PMID: 35179188
STARSurg Collaborative Impact of postoperative acute kidney injury in patients undergoing major gastrointestinal surgery on 1-year survival and renal outcomes: a national mutlicenter cohort study BJS Open 2021 Nov 9;5(6): zrab134 doi:10 1093/bjsopen/zrab134 PMID: 35029656
STARSurg Collaborative Perioperative nonsteroidal anti-inflammatory drugs (NSAID) administration and acute kidney injury (AKI) in major gastrointestinal surgery: a prospective, multicenter, propensity matched cohort study Ann Surg 2022 May 1;275(5):904-910 doi: 10 1097/SLA 0000000000004314 Epub 2020 Oct 14 PMID: 33074883
Oya Andacoglu, MD
Andacoglu, O M , Sabisch, E , Malamutmann, E , Ozbek, U , Emre, A , Tokat, Y , Oezcelik, A (2022) Multicenter living liver donor quality of life survey up to 20 years after donor hepatectomy and association with surgical outcomes Science Direct, 1365-182X(22) PMID: 35817693
DOI: DOI: 10 1016/j hpb 2022 06 007
Andacoglu, O M , Tokat, Y , Malamutmann, E , Adali, G , Emre, A , Oezcelik, A (2022) Outcomes of right lobe donors with BMI≥30 for living donor liver transplantation Clinical Transplantation, 36(7), 1-7 PMID: 35561085 DOI: DOI: 10 1111/ctr 14698
Karadag, H I , Andacoglu, O M , Papadakis, M , Paul, A , Oezcelik, A , Malamutmann, E (2021) Invasive Fungal Infections After Liver Transplantation: A Retrospective Matched Controlled Risk Analysis Annals of Transplantation, 26(E930117) PMID: 34354035 DOI: 10 12659/AOT 930117
Narendra Battula, MD Boominathan, V , Willman, M , Battula, N R , Zarrinpar, A , Duarte, S , "Perfusate Cell-Free DNA Content is a Potential Marker of Cellular Injury During Hypothermic Machine Perfusion of Porcine Kidneys Subject to Prolonged Warm Ischemia", 2022 American Transplant Congress, American Transplant Congress, Virtual, Accepted, Oral Presentation June 5, 2022
Duarte, S , Willman, M , Boominathan, V , Lewis, D , De Faria, W , Vrakas, G , El-Hinnawi, A , Beduschi, T , Battula, N R , Zarrinpar, A , "Cell-Free DNA Concentration in Hypothermic Machine Perfusate is a Potential Rapid Marker for Kidney Graft Quality", 2022 American Transplant Congress, American Transplant Congress, Virtual, Accepted, Oral Presentation June 5, 2022
Zarrinpar, A , Ho, C , Warren, C , Khong J Lee M Duarte S Andreoni, K , Johnson, M , Battula, N R McKimmy D Beduschi T "Artificial Intelligence Based Dosing of Tacrolimus in Liver Transplantation: Prospective, Randomized Phase 2 Trial" 2022 American Transplant Congress, American Transplant Congress Virtual Accepted Oral Presentation June 7, 2022
Christian Castro, MD Clapp, B , Vivar, A , Castro, CM , Kim, J , Gamez, J , Dodoo, C , Davis, B , Rates of readmission and ER visits of publicly vs commercially insured patients in an MBSAQIP accredited center, Texas Tech University Health Sciences Center El Paso (January 2020 – July 2020) Published JSLS March 4, 2022
Ng, G , Castro, CM , Tyroch, AH , Michelson, E , Harper, B , Evaluating the Change in Patterns of Traumatic Injury in the Setting of Pandemic and Social Distancing Restrictions: An Analysis of Texas Trauma Centers, Texas Tech University Health Sciences Center El Paso (June 2020 – July 2021)
Published AJS March 23, 2022
Rachel Davis, MD McCarty, C , Yi, M , Sous, S , Leslie, M , Tariq, E , Dondapati, P , Kameyama, H , Nuguri, S , Hills, N , Wilkerson, M , Davis, R , Mesiya, S , Rui, H , Chervoneva, I , Zhang, R , Tanaka, T Sustained Inflammation of Breast Tumors After Needle Biopsy Pathobiology Pathobiology 2022;19 doi:10 1159/000524668
Published Online Ahead of Print June 1, 2022 Hills
Isabel Dennahy, MD (accepted) Chalfant H, Bonds M, Scott K, Condacse A, Martin WT, Little C, Dennahy IS, Edil BH, McNally LR, Jain A Borderline-resectable pancreatic adenocarcinoma using innovative imaging J Surg Res
Amy Gin-Gossett, MD Xu Y-F, Xu X, Bhandari K, Gin A, Rao CV, Morris KT, et al (Nov 16, 2021)
Isolation of extra-cellular vesicles in the context of pancreatic adenocarcinomas: Addition of one stringent filtration step improves recovery of specific microRNAs PLoS ONE 16(11): e0259563 https://doi org/10 1371/journal pone 0259563
Michael Kutteh, MD Melson AT, O’Brien JC, Kutteh MA, Siatkowski RM A Case of Brain Hamartoma in a Child Leading to Compressive Optic Neuropathy Mimicking Amblyopia J AAPOS 2021 2021;25(6):360-362 doi:10 1016/j jaapos 2021 07 004
Richards Z, Nguyen M, Kutteh MA, Ahmad S, Henson C, Firestone BK, Herman TS, and Herman TD Ocular Malignancies Treated with Iodine-125 Low Dose Rate (LDR) Brachytherapy at a Single High-Volume Institution: A Retrospective Review Medical Dosimetry 2022 doi org/10 1016/j meddos 2022 04 006
Tyler Leiva, MD
Leiva T, Luschen C, Yu Z, Liebe H, Golubkova A, Hunter C J COVID-19related intussusception: A case series and review of the literature Surgical Infections 2022
Samara Lewis, MD
Chotai, P; Watlington, J; Lewis, S; Pyo, T; Abdelgawad, A; Huang, E Pediatric Snakebites: Comparing Patients in Two Geographic Locations in the United States” Journal of Surgical Research September 2021 (PMID: 33965770 DOI: 10 1016/j jss 2021 03 045)
Lewis S; Grimes A; Landman A; Johnson, J; Sarwar, Z; Stewart, K; Kennedy R “Retrospective review of intervention for traumatic blunt spleen injuries in adolescents by trauma center type American Journal of Surgery October 2021 PMID: 34953577 DOI: 10 1016/j amjsurg 2021 12 010 Pub Status: Published
Lewis, S; Sarwar, Z; Stewart, K; Garwe T; Morris K “The Impact of Age on Overall Survival, Nodal Status, and Systemic Inflammatory Markers in Colorectal Cancer Patients ” University of Oklahoma Health Sciences Center Graduate College Thesis: Masters of Science August 2, 2021
Liebe, H; Buonpane, C; Lewis, S; Stewart, K; Garwe, T; Sarwar, Z; Hunter, C “This is Our Lane: The Surgeon’s Role in Social Justice Advocacy” Association of Women Surgeons issue of the Journal of American College of Surgeon November 2021 doi:10 1016/j jamcollsurg 2021 07 1 32 Pub Status: Published
Whitney Taylor Martin, MD
Martin, WT , Steward, K , Sarwar, Z , Kennedy, R , Quang, C , Albrecht, R , Cross, A Clinical Diagnosis of Cholecystitis in Emergency Department Patients with Cholelithiasis Is Indication for Urgent Cholecystectomy: A Comparison of Clinical, Ultrasound, and Pathologic Diagnosis The American Journal of Surgery, Volume 224, Issue 1, Part A, 2022, Pages 8084, ISSN 0002-9610, https://doi org/10 1016/j amjsurg 202 2 02 051
Kimberly Mihalsky, MD
2022 Scientific Session of the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES), Denver, Colorado, 16-19 March 2022 Video Loops Surg Endosc (2022)
Abigail Roberts, MD
Therapy J Clin Images Med Case Rep 2022; 3(3): 1716
Roberts, A “OR” In Blood and Thunder: Musings on the Art of Medicine (Fall 2021, p 73) Poem
Snyder, K B , Raposo-Hadley, A , Evans, C , Farrens, A , Burt, J , Armstrong, G , Garman, J , Wylie, L , & Foxall, M (January 2022) Defense, Disrespect, and #Deadly: A qualitative exploration of precursors to youth violence informed through hospital-based youth violence prevention program follow-up The Journal of Qualitative Criminology and Criminal Justice https://doi org/10 21428/88de04a1 b a7bc0c9 [doi org]
003
Ryan Bynum, MD
Bynum R C , Richman J S , Corey B , Fazendin J M Impact of Faculty Wellbeing on Medical Student Education Manuscript submitted to Global Surgical Education, May 2022
Bynum R C , Richman J S , Corey B , Fazendin J M Impact of Faculty Wellbeing on Medical Student Education Podium Presentation at the 42nd Annual Meeting for Association for Surgical Education at Surgical Education Week, May 2022
Rachel Davis, MD
Davis, R , Mier, F , Lees, J , “A Novel Suction-Irrigation Catheter for Use in Minimally-Invasive Fluid Evacuation”, 2022 SAGES Annual Meeting, Next Big Thing Session, Poster March 18, 2022
Amy Gin- Gossett, MD
Valente, A , Gin, A , Essel, K , Wells, A , Ding, K , Moore, K Exploring associations between tumor mutational burden and clinical benefit of immune checkpoint inhibition in endometrial cancers Western Association of Gynecologic Oncologists Annual Meeting, June 2021
Christopher Jeffery, MD
The Need for Free Nipple Graft Breast Reduction Revisited Pending podium presentation at Plastic Surgery the Meeting 2022 in Boston, MA
The Effects of Cannabinoids on Wound Healing Abstract presented by coauthor at COSM (Combined Otolaryngology Spring Meetings) 2022 in Dallas, TX
Navigational Transthoracic Localization of Small Peripheral Lung Nodules for Resection Podium presentation at American Surgical Congress 2022 in Orlando, FL
Intravenous Ketorolac in a Level I Trauma Center: Is It Safe to Use?
Presented by primary author at Southwestern Surgical Congress in Maui, HI
Tyler Leiva, MD
Academic Surgical Congress Feb 2, 2022Presentation: Caveolin-1 Expression in Neonatal Intestine As A Susceptibility Marker for Necrotizing Enterocolitis Authors: Tyler Leiva MD, Douglas Wood MD & Catherine Hunter MD
University of Oklahoma Pediatrics Research Day March 5, 2022
Poster: COVID-19 Related Intussusception: A Case Report and Literature Review Authors: Tyler Leiva MD Christopher Luschen BS Jonathan Green MD, Heather Liebe MD, Alena Golubkova MD Catherine Hunter MD
American Academy of Cancer Research April 12, 2022 Poster: Genetic metastatic CRC model with in vivo imaging capabilities Authors: Tyler Leiva MD James Griffith BS Shaoxuan Guo BS, Megan Lerner BS, Lacy McNally PhD William Berry PhD Katherine Morris MD
Surgical Infection Society April 24, 2022 Presentation: A comparison of basolateral versus apical out enteroids as a model for necrotizing enterocolitis
Education Trauma Transfers Discharged from the Emergency Department – Is there a Role for Telemedicine? Journal of Trauma and Acute Care Surgery, April 2022
Authors: Heather Liebe MD, Camille Schlegel BS, Xue Cai PhD, Alena Golubkova MD, Tyler Leiva MD, Catherine Hunter MD
American Pediatric Surgical Association May 12, 2022 Poster: Staying Out of The Operating Room: A Historical Exploration of NonOperative Management of Solid Organ Injury in Pediatric Trauma Authors: Tyler Leiva MD, Heather Liebe MD, Alena Golubkova MD, Catherine Hunter MD
Digestive Diseases Week May 22, 2022 Poster: PDGF Signaling Promotes the Formation of Post-operative Peritoneal Adhesions Authors: Tyler Leiva, James Griffith, Megan Lerner, Lorin E Olson, William L Berry
ACS Clinical Congress Conference Oct, 18 2022 Presentation: Caveolin-1 and tight junction expression in human intestine as a susceptibility marker of necrotizing Enterocolitis Authors: Tyler Leiva
Samara Lewis, MD
Lewis S; Retrospective Review of Risk Factors For Splenic Intervention In Adolescents With Blunt Spleen Injuries ACS Clinical Congress Conference, October 18th 2022
Lewis S; Stewart K; Garwe T; Sarwar Z; Morris, K “Effect of Age on Overall Survival in Surgically Resected Colorectal Cancer Patients”
Southwestern Surgical Congress 73rd Annual Meeting April 25th, 2022
Lewis, S; Stewart, K; Garwe, T; Sarwar, Z; Morris K “Effect of Age on Overall Survival Resected Colorectal Cancer Patients” 17th Annual Academic Surgical Congress February 1st, 2022
Liebe H, Lewis S, Golubkova A, Leiva T, Hunter CJ “Elevated Procalcitonin as a Novel Biomarker in Surgical Necrotizing Enterocolitis”, poster, American Pediatric Surgical Association, San Diego, CA, May 12, 2022
The Department of Surgery Annual Research Symposium Presentation: Retrospective Evaluation of Tumor Specific Factors Associated with Neutrophil to Lymphocyte Ratio in Surgically Resected Colorectal Cancer Patients Presenter: Samara Lewis, MD
The Department of Surgery Annual Research Symposium Retrospective Review of Angioembolization in Traumatic Blunt High Grade Liver Injuries in Adolescent Age Children Presenter: Samara Lewis, MD
The Department of Surgery Annual Research Symposium Retrospective Review of Procalcitonin Association with Surgical Necrotizing Enterocolitis Presenter: Samara Lewis, MD
Lindsay Lindsey, MD Revision of Bariatric Procedures have Improvement of Preoperative Comorbidities and Symptoms with Noninferior Weight Loss Compared to Primary Bariatric Surgeries Presidential Grand Rounds, American Society for Metabolic and Bariatric Surgery, June 2022
Cognitive Fitness - Emotional Intelligence Training in the MS3 Surgery Clerkship Association for Surgical Education Conference, 2021
Whitney (Taylor) Martin, MD
Martin, WT , Sarwar, Z , Garwe, T , Stewart, K , Fischer, L , Paniccia, A , Morris, K , Bonds, M , Edil, B (2022)
“Learning Curve of a Laparoscopic Pancreaticoduodenectomy Program at a Second Institution” Academic Surgical Congress Annual Meeting, Orlando, FL Poster & Oral Presentation February 3, 2022
Martin, WT , Steward, K , Sarwar, Z , Kennedy, R , Quang, C , Albrecht, R , Cross, A (in press) “Clinical Diagnosis of Cholecystitis in Emergency Department Patients with Cholelithiasis Is Indication for Cholecystectomy: A Comparison of Clinical, Ultrasound, and Pathologic Diagnosis” OUHSC Annual Research Symposium, Oklahoma City, OK Oral Presentation October, 15 2021
Martin, WT , Sarwar, Z , Garwe, T , Stewart, K , Fischer, L , Paniccia, A , Morris, K , Bonds, M , Edil, B (2022)
“Learning Curve of a Laparoscopic Pancreaticoduodenectomy Program at a Second Institution” OUHSC Annual Research Symposium, Oklahoma City, OK Oral Presentation October 15 2021
Martin, WT , Steward, K , Sarwar, Z , Kennedy R Quang C Albrecht R Cross, A (in press) “Clinical Diagnosis of Cholecystitis in Emergency Department Patients with Cholelithiasis Is Indication for Cholecystectomy: A Comparison of Clinical Ultrasound and Pathologic Diagnosis” SWSC Annual Meeting, Plenary Oral Presentation San Francisco, CA September 1, 2021
Martin, WT Attempting to Bridge the Gap: Comparison of Clinical Characteristics, Ultrasound, And Final Surgical Pathology of Emergency Department Versus Outpatient Clinic Patients Undergoing Cholecystectomy, ACS Clinical Congress Conference 2022 October 17th, 2022
Laparoscopic Resection of a Duodenal Gastrointestinal Stromal Tumor March 2022 Video Presentation, Society of American Gastrointestinal and Endoscopic Surgeons Denver, CO
Poster Presentation, Texas Society for Vascular & Endovascular Surgery 2021 Annual Meeting, Nov 4-6, 2021, Spontaneous Ulnar Artery Pseudoaneurysm: A Case Report Abby Rinchuso, MD; Andrew Murphy, MD; Joshua Gierman, MD
Digital Poster Session, Texas Society for Vascular and Endovascular Surgery Annual Meeting, November 5-6, 2021 “Spontaneous Ulnar Artery Pseudoaneurysm: A Case Report”
Areej Sami, MD
Isabella, J , Stewart, K , Sami, A , Mitchell S Cross B Morris K Carter, S , Cross, A (October, 2022) Enoxaparin Dosing in Surgical Sub-specialty Patients: A Prospective Randomized Controlled Trial to be presented at: American College of Surgeons’ Scientific Forum Clinical Congress; San Diego, CA USA 2022
Trimble, E , Sami, A , Reinersman, J M , Kennedy, R O , Wood, F C (April, 2022) Extracorporeal Membrane Oxygenation as Salvage Therapy in a Newly Diagnosed Human Immunodeficiency Virus Patient with Pneumocystic Pneumonia and Acute Respiratory Distress Syndrome Poster presented at: Southwestern Surgical Congress Meeting; Wingwam, AZ, USA 2022
Katherine Snyder, MD
The Department of Surgery Annual Research Symposium A Hyperinflammatory Response is Associated with Enteroids Generated from Infants with Necrotizing Enterocolitis Compared with Controls Presenter: Katherine B Snyder, MD
Elizabeth Trimble, MD
Trimble, Elizabeth J , Wood, Frank (April, 2022) Extracorporeal Membrane Oxygenation as Salvage Therapy in a Newly Diagnosed Human Immunodeficiency Virus Patient with Pneumocystis Pneumonia and Acute Respiratory Distress Syndrome Podium Presentation presented at: South West Surgical Congress (SWSC) 2022 Annual Meeting; Wigwam, AR, USA
Trimble, Elizabeth J , Reinersman, J Matthew (March, 2022) Definitive Treatment with Custom 3D Printed Titanium Sternal Plate in a Patient with Multiple Failed Chest Wall Reconstructions Poster Presentation presented at: General Thoracic Surgical Club (GTSC) 2022 Annual meeting; Naples, FL, USA
Trimble, Elizabeth J , Booth, Kristina (September, 2021) Comparing Level of Autonomy, Performance and Procedure Difficulty amongst Surgical Residents Stratified by Post Graduate Year across General Surgery Residencies Nationwide Poster Presentation presented at: Academy of Teaching Scholars (ATS) 2021 Health Professions Education Research Virtual Poster Session; Oklahoma City, OK, USA
The Department of Surgery Annual Research Symposium Early Comparison Robotic Bronchoscopy Versus Electromagnetic Navigational Bronchoscopy for Biopsy of Pulmonary Nodules in a Thoracic Surgery Practice Presenter: Elizabeth Joy Trimble MD
$25,000 Ro e: PI
Jason Lees, MD Lees, J (Collaborator), Berry, W L (Principal Investigator), Mechanisms Driving the Formation of PostOperat ve Peritoneal Adhesions, Sponsored by Maximizing Investigators Research Award (MIRA) for Early Stage Investigators (R35Clin cal Trial Optional) Foundation Grant/Contract Number: 1R335GM142786-01
Current Funding (Total Cost per Year): $250,000 00 Total D rect Costs: $1,250,000 00 May 25, 2021 - Present
Katherine Morris, MD Morris,
Development
Rational Design and Synthesis of a Small Mo ecule Dye for Optoacoustic Imaging Role:PI (will be reviewed in February 2023)
Guilherme Barreiro, MD Combined Removable Deep Dermal and Vertical Mattress Stitch: A Novel Surgical Technique to Optimize Suture Strength with Better Skin Edge Eversion and Eliminate Foreign Body Reaction in Reconstructive Surgeries Authors: Bradley Miyake, Colton Ross, Parker Bryant, Henry Marsh, Vijay Raj, Guilherme Barreiro, Chung-Hao Lee
Split Thickness
Designing
Reverse Osteomyocutaneous Medial Tibia Flap for Complex Reconstruction: An Anatomic Study with Clinical Translation Authors: Angel Farinas Bradley Miyake, Vijay Raj, Guilherme Barriero
Anatomical Study of the Sensate Pedicled Anterolateral Thigh (ALT) Flap for Reconstruction of Pelviperineal and Knee Region Defects Authors: Bradley Miyake Henry Marsh, Vijay Raj, Angel Farinas, Guilherme Barreiro
Novelty Design of Chimeric Multiple Perforator Fibula Flap Authors: Angel Farinas Bradley Miyake Henry Marsh, Vijay Raj, Guilherme Barreiro
Reverse Sural Supercharged with
Surgeons at the University of Oklahoma Health Sciences Center are dedicated to excellence in education, research and patient care. We appreciate the generous support of patients and their families, alumni, physicians, friends and businesses

Your gift can help improve a child’s health, award a resident a scholarship, or provide funds for research, equipment, computers, library materials and more Every gift we receive makes a difference, and we sincerely thank you for your generosity
Development Office University of Oklahoma Health Sciences Center P.O. Box 26901 Oklahoma City, OK 73126 405-271-2300